User login
Patients With Hypersensitivity Pneumonitis Want More Disease Information
Adults with hypersensitivity pneumonitis (HP) expressed interest in more knowledge of prognosis, etiology, treatment, and living well with the disease, based on new survey data presented at the American Thoracic Society International Conference.
HP is caused by environmental exposure and is often incurable, and patients are challenged with identifying and mitigating the exposure with limited guidance, wrote Janani Varadarajan, MD, of Weill Cornell Medicine, New York, and colleagues.
Surveys Conducted to Understand Patient Concerns
To better identify patient-perceived HP knowledge gaps and develop educational resources, the researchers assessed 21 adults diagnosed with HP. Patients underwent interviews using nominal group technique (NGT) for group consensus and completed a survey on educational preferences. The mean age of the participants was 69.5 years, and 81% were women.
The researchers conducted five NGTs. Participants were asked two questions: What questions about your HP do you have that keep you awake at night?” and “What information do you want about your HP that you cannot find?” They also voted on responses that were grouped by theme.
The top themes that emerged from the interviews were concerns about natural history and prognosis of HP (28.3%), current treatment options and therapeutic research (22.5%), epidemiology and etiology (17.5%), living well with HP (15.4%), origin and management of symptoms (8.3%), identifying and mitigating exposures (4.6%), and methods of information uptake and dissemination (3.3%).
The findings were limited by the relatively small sample size. However, the results will inform the development of educational materials on the virtual Patient Activated Learning System, the researchers noted in their abstract. “This curriculum will be a component of a larger support intervention that aims to improve patient knowledge, self-efficacy, and HRQOL [health-related quality of life],” they said.
Findings Will Fuel Needed Education
Recognizing more interstitial lung disease (ILD) has led to diagnosing more hypersensitivity pneumonitis, and it is important to keep patients’ concerns in mind, said Aamir Ajmeri, MD, assistant professor of clinical thoracic medicine and surgery at the Lewis Katz School of Medicine at Temple University, Philadelphia, in an interview.
“If patients research ILD online, most of the literature is based on idiopathic pulmonary fibrosis,” he said. “IPF literature can be frightening because patients will see a median 2- to 5-year survival rate from time of diagnosis, the need for lung transplant, and progressive hypoxemia; however, all of this may not be true in HP,” he noted.
“HP is more of a spectrum, but it is more difficult for patient to understand when we say ‘your lungs have reacted to something in your environment,’ and they will ask ‘what can I do to change this?’” Dr. Ajmeri told this news organization. “That is why these types of studies, where we recognize what patients need and how they can learn more about their diagnosis, are very important,” he said.
The study findings were not surprising, Dr. Ajmeri said. “We have a large cohort of patients with HP at Temple Health, and these are the same questions they ask me and my colleagues,” he said. “It can be tough for patients to grasp this diagnosis. We know it is related to something inhaled from the environment, but it may be difficult to pinpoint,” he said.
In patient-centered research, patients can help shed light onto the needs that are unmet for the disease process by asking hypothesis-generating questions, Dr. Ajmeri said. For example, he said he is frequently asked by patients why HP continues to recur after they have remediated a home (potential source of exposure) and been on medication.
“The study was limited in part by the small sample size but captured a good representation of what patients are asking their physicians about,” Dr. Ajmeri said. Although it is always preferable to have more patients, the findings are important, “and the educational materials that they will lead to are greatly needed,” he said.
The study was supported by the Stony Wold-Herbert Fund, the American Lung Association Catalyst Award, and the National Heart, Lung, and Blood Institute. The researchers had no financial conflicts to disclose. Dr. Ajmeri had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Adults with hypersensitivity pneumonitis (HP) expressed interest in more knowledge of prognosis, etiology, treatment, and living well with the disease, based on new survey data presented at the American Thoracic Society International Conference.
HP is caused by environmental exposure and is often incurable, and patients are challenged with identifying and mitigating the exposure with limited guidance, wrote Janani Varadarajan, MD, of Weill Cornell Medicine, New York, and colleagues.
Surveys Conducted to Understand Patient Concerns
To better identify patient-perceived HP knowledge gaps and develop educational resources, the researchers assessed 21 adults diagnosed with HP. Patients underwent interviews using nominal group technique (NGT) for group consensus and completed a survey on educational preferences. The mean age of the participants was 69.5 years, and 81% were women.
The researchers conducted five NGTs. Participants were asked two questions: What questions about your HP do you have that keep you awake at night?” and “What information do you want about your HP that you cannot find?” They also voted on responses that were grouped by theme.
The top themes that emerged from the interviews were concerns about natural history and prognosis of HP (28.3%), current treatment options and therapeutic research (22.5%), epidemiology and etiology (17.5%), living well with HP (15.4%), origin and management of symptoms (8.3%), identifying and mitigating exposures (4.6%), and methods of information uptake and dissemination (3.3%).
The findings were limited by the relatively small sample size. However, the results will inform the development of educational materials on the virtual Patient Activated Learning System, the researchers noted in their abstract. “This curriculum will be a component of a larger support intervention that aims to improve patient knowledge, self-efficacy, and HRQOL [health-related quality of life],” they said.
Findings Will Fuel Needed Education
Recognizing more interstitial lung disease (ILD) has led to diagnosing more hypersensitivity pneumonitis, and it is important to keep patients’ concerns in mind, said Aamir Ajmeri, MD, assistant professor of clinical thoracic medicine and surgery at the Lewis Katz School of Medicine at Temple University, Philadelphia, in an interview.
“If patients research ILD online, most of the literature is based on idiopathic pulmonary fibrosis,” he said. “IPF literature can be frightening because patients will see a median 2- to 5-year survival rate from time of diagnosis, the need for lung transplant, and progressive hypoxemia; however, all of this may not be true in HP,” he noted.
“HP is more of a spectrum, but it is more difficult for patient to understand when we say ‘your lungs have reacted to something in your environment,’ and they will ask ‘what can I do to change this?’” Dr. Ajmeri told this news organization. “That is why these types of studies, where we recognize what patients need and how they can learn more about their diagnosis, are very important,” he said.
The study findings were not surprising, Dr. Ajmeri said. “We have a large cohort of patients with HP at Temple Health, and these are the same questions they ask me and my colleagues,” he said. “It can be tough for patients to grasp this diagnosis. We know it is related to something inhaled from the environment, but it may be difficult to pinpoint,” he said.
In patient-centered research, patients can help shed light onto the needs that are unmet for the disease process by asking hypothesis-generating questions, Dr. Ajmeri said. For example, he said he is frequently asked by patients why HP continues to recur after they have remediated a home (potential source of exposure) and been on medication.
“The study was limited in part by the small sample size but captured a good representation of what patients are asking their physicians about,” Dr. Ajmeri said. Although it is always preferable to have more patients, the findings are important, “and the educational materials that they will lead to are greatly needed,” he said.
The study was supported by the Stony Wold-Herbert Fund, the American Lung Association Catalyst Award, and the National Heart, Lung, and Blood Institute. The researchers had no financial conflicts to disclose. Dr. Ajmeri had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Adults with hypersensitivity pneumonitis (HP) expressed interest in more knowledge of prognosis, etiology, treatment, and living well with the disease, based on new survey data presented at the American Thoracic Society International Conference.
HP is caused by environmental exposure and is often incurable, and patients are challenged with identifying and mitigating the exposure with limited guidance, wrote Janani Varadarajan, MD, of Weill Cornell Medicine, New York, and colleagues.
Surveys Conducted to Understand Patient Concerns
To better identify patient-perceived HP knowledge gaps and develop educational resources, the researchers assessed 21 adults diagnosed with HP. Patients underwent interviews using nominal group technique (NGT) for group consensus and completed a survey on educational preferences. The mean age of the participants was 69.5 years, and 81% were women.
The researchers conducted five NGTs. Participants were asked two questions: What questions about your HP do you have that keep you awake at night?” and “What information do you want about your HP that you cannot find?” They also voted on responses that were grouped by theme.
The top themes that emerged from the interviews were concerns about natural history and prognosis of HP (28.3%), current treatment options and therapeutic research (22.5%), epidemiology and etiology (17.5%), living well with HP (15.4%), origin and management of symptoms (8.3%), identifying and mitigating exposures (4.6%), and methods of information uptake and dissemination (3.3%).
The findings were limited by the relatively small sample size. However, the results will inform the development of educational materials on the virtual Patient Activated Learning System, the researchers noted in their abstract. “This curriculum will be a component of a larger support intervention that aims to improve patient knowledge, self-efficacy, and HRQOL [health-related quality of life],” they said.
Findings Will Fuel Needed Education
Recognizing more interstitial lung disease (ILD) has led to diagnosing more hypersensitivity pneumonitis, and it is important to keep patients’ concerns in mind, said Aamir Ajmeri, MD, assistant professor of clinical thoracic medicine and surgery at the Lewis Katz School of Medicine at Temple University, Philadelphia, in an interview.
“If patients research ILD online, most of the literature is based on idiopathic pulmonary fibrosis,” he said. “IPF literature can be frightening because patients will see a median 2- to 5-year survival rate from time of diagnosis, the need for lung transplant, and progressive hypoxemia; however, all of this may not be true in HP,” he noted.
“HP is more of a spectrum, but it is more difficult for patient to understand when we say ‘your lungs have reacted to something in your environment,’ and they will ask ‘what can I do to change this?’” Dr. Ajmeri told this news organization. “That is why these types of studies, where we recognize what patients need and how they can learn more about their diagnosis, are very important,” he said.
The study findings were not surprising, Dr. Ajmeri said. “We have a large cohort of patients with HP at Temple Health, and these are the same questions they ask me and my colleagues,” he said. “It can be tough for patients to grasp this diagnosis. We know it is related to something inhaled from the environment, but it may be difficult to pinpoint,” he said.
In patient-centered research, patients can help shed light onto the needs that are unmet for the disease process by asking hypothesis-generating questions, Dr. Ajmeri said. For example, he said he is frequently asked by patients why HP continues to recur after they have remediated a home (potential source of exposure) and been on medication.
“The study was limited in part by the small sample size but captured a good representation of what patients are asking their physicians about,” Dr. Ajmeri said. Although it is always preferable to have more patients, the findings are important, “and the educational materials that they will lead to are greatly needed,” he said.
The study was supported by the Stony Wold-Herbert Fund, the American Lung Association Catalyst Award, and the National Heart, Lung, and Blood Institute. The researchers had no financial conflicts to disclose. Dr. Ajmeri had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Why Are We Undertreating So Many Pulmonary Embolisms?
LONG BEACH, CALIFORNIA — A small fraction of patients with pulmonary embolism (PE) who are eligible for advanced therapies are actually getting them, reported investigators who conducted a big data analysis.
“Advanced PE therapy seems to be vulnerable to disparate use, and perhaps underuse,” Sahil Parikh, MD, a cardiovascular interventionalist at the Columbia University Medical Center in New York, said when he presented results from the REAL-PE study at the Society for Cardiovascular Angiography and Interventions (SCAI) 2024 Scientific Sessions.
The underuse of advanced PE therapies is “the controversy,” Dr. Parikh said after his presentation. “It remains unclear what the role of invasive therapy is in the management of so-called high-intermediate–risk people. There isn’t a Class 1 guideline recommendation, and there is a very rapidly evolving trend that we’re increasingly treating these patients invasively,” he said.
“However, if you come to these meetings [such as SCAI], you might think everyone is getting one of these devices, but these data show that’s not the case,” Dr. Parikh said.
The analysis mined deidentified data from Truveta, a collective of health systems that provides regulatory-grade electronic health record data for research.
The researchers accessed data on patients treated with ultrasound-assisted catheter-directed thrombolysis or mechanical thrombectomy, identified from claims codes. Patient characteristics — age, race, ethnicity, sex, comorbidities, and diagnoses — were also accessed for the analysis. Earlier results were published in the January issue of the Journal of the Society for Cardiovascular Angioplasty Interventions.
Less Intervention for Black Patients and Women
White patients were more likely to receive advanced therapy than were Black patients (0.5% vs 0.37%; P = .000), Dr. Parikh reported, and women were less likely to receive advanced therapy than were men (0.41% vs 0.55%; P = .000).
The only discernable differences in outcomes were in major bleeding events in the 7 days after the procedure, which affected more White patients than it did Black patients (13.9% vs 9.3%) and affected more women than it did men (16.6% vs 11.1%).
What’s noteworthy about this study is that it demonstrates the potential of advanced data analytics to identify disparities in care and outcomes, Dr. Parikh said during his presentation. “These analyses provide a means of evaluating disparities in real clinical practice, both in the area of PE and otherwise, and may also be used for real-time monitoring of clinical decision-making and decisional support,” he said. “We do think that both novel and established therapies can benefit equally from similar types of analyses.”
Big Data Signaling Disparities
“That’s where these data are helpful,” Dr. Parikh explained. They provide “a real snapshot of how many procedures are being performed and in what kinds of patients. The low number of patients getting the procedure would suggest that there are probably more patients who would be eligible for treatment based on some of the emerging consensus documents, and they’re not receiving them.”
The data are “hypotheses generating,” Dr. Parikh said in an interview. “These hypotheses have to be evaluated further in more granular databases.”
REAL-PE is also a “clarion call” for clinical trials of investigative devices going forward, he said. “In those trials, we need to endeavor to enroll enough women and men, minority and nonminority patients so that we can make meaningful assessments of differences in efficacy and safety.”
This study is “real proof that big data can be used to provide information on outcomes for patients in a very rapid manner; that’s really exciting,” said Ethan Korngold, MD, chair of structural and interventional cardiology at the Providence Health Institute in Portland, Oregon. “This is an area of great research with great innovation, and it’s proof that, with these type of techniques using artificial intelligence and big data, we can generate data quickly on how we’re doing and what kind of patients we’re reaching.”
Findings like these may also help identify sources of the disparities, Dr. Korngold added.
“This shows we need to be reaching every patient with advanced therapies,” he said. “Different hospitals have different capabilities and different expertise in this area and they reach different patient populations. A lot of the difference in utilization stems from this fact,” he said.
“It just underscores the fact that we need to standardize our treatment approaches, and then we need to reach every person who’s suffering from this disease,” Dr. Korngold said.
A version of this article appeared on Medscape.com.
LONG BEACH, CALIFORNIA — A small fraction of patients with pulmonary embolism (PE) who are eligible for advanced therapies are actually getting them, reported investigators who conducted a big data analysis.
“Advanced PE therapy seems to be vulnerable to disparate use, and perhaps underuse,” Sahil Parikh, MD, a cardiovascular interventionalist at the Columbia University Medical Center in New York, said when he presented results from the REAL-PE study at the Society for Cardiovascular Angiography and Interventions (SCAI) 2024 Scientific Sessions.
The underuse of advanced PE therapies is “the controversy,” Dr. Parikh said after his presentation. “It remains unclear what the role of invasive therapy is in the management of so-called high-intermediate–risk people. There isn’t a Class 1 guideline recommendation, and there is a very rapidly evolving trend that we’re increasingly treating these patients invasively,” he said.
“However, if you come to these meetings [such as SCAI], you might think everyone is getting one of these devices, but these data show that’s not the case,” Dr. Parikh said.
The analysis mined deidentified data from Truveta, a collective of health systems that provides regulatory-grade electronic health record data for research.
The researchers accessed data on patients treated with ultrasound-assisted catheter-directed thrombolysis or mechanical thrombectomy, identified from claims codes. Patient characteristics — age, race, ethnicity, sex, comorbidities, and diagnoses — were also accessed for the analysis. Earlier results were published in the January issue of the Journal of the Society for Cardiovascular Angioplasty Interventions.
Less Intervention for Black Patients and Women
White patients were more likely to receive advanced therapy than were Black patients (0.5% vs 0.37%; P = .000), Dr. Parikh reported, and women were less likely to receive advanced therapy than were men (0.41% vs 0.55%; P = .000).
The only discernable differences in outcomes were in major bleeding events in the 7 days after the procedure, which affected more White patients than it did Black patients (13.9% vs 9.3%) and affected more women than it did men (16.6% vs 11.1%).
What’s noteworthy about this study is that it demonstrates the potential of advanced data analytics to identify disparities in care and outcomes, Dr. Parikh said during his presentation. “These analyses provide a means of evaluating disparities in real clinical practice, both in the area of PE and otherwise, and may also be used for real-time monitoring of clinical decision-making and decisional support,” he said. “We do think that both novel and established therapies can benefit equally from similar types of analyses.”
Big Data Signaling Disparities
“That’s where these data are helpful,” Dr. Parikh explained. They provide “a real snapshot of how many procedures are being performed and in what kinds of patients. The low number of patients getting the procedure would suggest that there are probably more patients who would be eligible for treatment based on some of the emerging consensus documents, and they’re not receiving them.”
The data are “hypotheses generating,” Dr. Parikh said in an interview. “These hypotheses have to be evaluated further in more granular databases.”
REAL-PE is also a “clarion call” for clinical trials of investigative devices going forward, he said. “In those trials, we need to endeavor to enroll enough women and men, minority and nonminority patients so that we can make meaningful assessments of differences in efficacy and safety.”
This study is “real proof that big data can be used to provide information on outcomes for patients in a very rapid manner; that’s really exciting,” said Ethan Korngold, MD, chair of structural and interventional cardiology at the Providence Health Institute in Portland, Oregon. “This is an area of great research with great innovation, and it’s proof that, with these type of techniques using artificial intelligence and big data, we can generate data quickly on how we’re doing and what kind of patients we’re reaching.”
Findings like these may also help identify sources of the disparities, Dr. Korngold added.
“This shows we need to be reaching every patient with advanced therapies,” he said. “Different hospitals have different capabilities and different expertise in this area and they reach different patient populations. A lot of the difference in utilization stems from this fact,” he said.
“It just underscores the fact that we need to standardize our treatment approaches, and then we need to reach every person who’s suffering from this disease,” Dr. Korngold said.
A version of this article appeared on Medscape.com.
LONG BEACH, CALIFORNIA — A small fraction of patients with pulmonary embolism (PE) who are eligible for advanced therapies are actually getting them, reported investigators who conducted a big data analysis.
“Advanced PE therapy seems to be vulnerable to disparate use, and perhaps underuse,” Sahil Parikh, MD, a cardiovascular interventionalist at the Columbia University Medical Center in New York, said when he presented results from the REAL-PE study at the Society for Cardiovascular Angiography and Interventions (SCAI) 2024 Scientific Sessions.
The underuse of advanced PE therapies is “the controversy,” Dr. Parikh said after his presentation. “It remains unclear what the role of invasive therapy is in the management of so-called high-intermediate–risk people. There isn’t a Class 1 guideline recommendation, and there is a very rapidly evolving trend that we’re increasingly treating these patients invasively,” he said.
“However, if you come to these meetings [such as SCAI], you might think everyone is getting one of these devices, but these data show that’s not the case,” Dr. Parikh said.
The analysis mined deidentified data from Truveta, a collective of health systems that provides regulatory-grade electronic health record data for research.
The researchers accessed data on patients treated with ultrasound-assisted catheter-directed thrombolysis or mechanical thrombectomy, identified from claims codes. Patient characteristics — age, race, ethnicity, sex, comorbidities, and diagnoses — were also accessed for the analysis. Earlier results were published in the January issue of the Journal of the Society for Cardiovascular Angioplasty Interventions.
Less Intervention for Black Patients and Women
White patients were more likely to receive advanced therapy than were Black patients (0.5% vs 0.37%; P = .000), Dr. Parikh reported, and women were less likely to receive advanced therapy than were men (0.41% vs 0.55%; P = .000).
The only discernable differences in outcomes were in major bleeding events in the 7 days after the procedure, which affected more White patients than it did Black patients (13.9% vs 9.3%) and affected more women than it did men (16.6% vs 11.1%).
What’s noteworthy about this study is that it demonstrates the potential of advanced data analytics to identify disparities in care and outcomes, Dr. Parikh said during his presentation. “These analyses provide a means of evaluating disparities in real clinical practice, both in the area of PE and otherwise, and may also be used for real-time monitoring of clinical decision-making and decisional support,” he said. “We do think that both novel and established therapies can benefit equally from similar types of analyses.”
Big Data Signaling Disparities
“That’s where these data are helpful,” Dr. Parikh explained. They provide “a real snapshot of how many procedures are being performed and in what kinds of patients. The low number of patients getting the procedure would suggest that there are probably more patients who would be eligible for treatment based on some of the emerging consensus documents, and they’re not receiving them.”
The data are “hypotheses generating,” Dr. Parikh said in an interview. “These hypotheses have to be evaluated further in more granular databases.”
REAL-PE is also a “clarion call” for clinical trials of investigative devices going forward, he said. “In those trials, we need to endeavor to enroll enough women and men, minority and nonminority patients so that we can make meaningful assessments of differences in efficacy and safety.”
This study is “real proof that big data can be used to provide information on outcomes for patients in a very rapid manner; that’s really exciting,” said Ethan Korngold, MD, chair of structural and interventional cardiology at the Providence Health Institute in Portland, Oregon. “This is an area of great research with great innovation, and it’s proof that, with these type of techniques using artificial intelligence and big data, we can generate data quickly on how we’re doing and what kind of patients we’re reaching.”
Findings like these may also help identify sources of the disparities, Dr. Korngold added.
“This shows we need to be reaching every patient with advanced therapies,” he said. “Different hospitals have different capabilities and different expertise in this area and they reach different patient populations. A lot of the difference in utilization stems from this fact,” he said.
“It just underscores the fact that we need to standardize our treatment approaches, and then we need to reach every person who’s suffering from this disease,” Dr. Korngold said.
A version of this article appeared on Medscape.com.
Age, Race, and Insurance Status May Effect Initial Sarcoidosis Severity
presented at the American Thoracic Society’s International Conference 2024.
“We know socioeconomic status plays an important role in health outcomes; however, there is little research into the impact of socioeconomic status on patients with sarcoidosis, particularly with disease severity,” said lead author Joshua Boron, MD, of Virginia Commonwealth University, Richmond, Virginia, in an interview. Identification of patients at higher risk of developing severe lung disease can help clinicians stratify these patients, he said.
Overall, the risk for severe lung disease at initial presentation was nearly three times higher in patients with no insurance than in those with private insurance and nearly three times higher in Black patients than in White patients (odds ratio [OR], 2.97 and 2.83, respectively). In addition, older age was associated with increased risk of fibrosis, with an OR of 1.03 per year increase in age.
No differences in fibrosis at presentation occurred based on sex or median income, and no difference in the likelihood of fibrosis at presentation appeared between patients with Medicaid vs private insurance.
“We were surprised at the degree of risk associated with no insurance,” said Dr. Boron. The researchers also were surprised at the lack of association between higher risk of severe stage lung disease in sarcoidosis patients and zip code estimates of household income as an indicator of socioeconomic status, he said.
For clinical practice, the study findings highlight the potentially increased risk for fibrotic lung disease among patients who are older, uninsured, and African American, said Dr. Boron.
“A limitation of our study was the utilization of zip code based on the US Census Bureau to get an estimation of average household income — a particular limitation in our city because of gentrification over the past few decades,” Dr. Boron said in an interview. “Utilizing area deprivation indices could be a better marker for identifying household income and give a more accurate representation of the true impact of socioeconomic disparities and severity of sarcoidosis at presentation,” he said.
Pinpointing Persistent Disparities
“We know there are multiple sources of disparities in the sarcoidosis population,” said Rohit Gupta, MD, director of the sarcoidosis program at Temple University Hospital, Philadelphia, in an interview.
The current study identified the relationship between several socioeconomic factors and sarcoidosis severity, showing greater disease severity in people experiencing socioeconomic inequalities, said Dr. Gupta, who was not involved in the study.
“I have personally seen this [disparity] in clinic,” said Dr. Gupta. However, supporting data are limited, aside from recent studies published in the last few years by researchers at the Cleveland Clinic and Johns Hopkins University, Baltimore, he said. The current study reflects those previous findings that people suffering from inequality have worse medical care, he added.
Overall, the findings were not surprising, “as we know this cohort of patients have chronic disease and worse morbidity and, in some cases, higher mortality,” but the results reinforce the need to pay closer attention to socioeconomic factors, said Dr. Gupta.
In practice, “we might use these findings as a reminder that when we see these patients for the first time, we should pay closer attention because they might need higher care,” he said. “The study also suggests these patients are coming late to a center of excellence,” he noted. When patients with socioeconomic disparities are seen for sarcoidosis at community hospitals and small centers, providers should keep in mind that their disease might progress faster and, therefore, send them to advanced centers earlier, he said.
The study was limited to the use of data from a single center and by the retrospective design, Dr. Gupta said. “Additional research should focus on building better platforms to understand these disparities,” he emphasized, so clinicians can develop plans not only to identify inequalities but also to address them.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Gupta had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
presented at the American Thoracic Society’s International Conference 2024.
“We know socioeconomic status plays an important role in health outcomes; however, there is little research into the impact of socioeconomic status on patients with sarcoidosis, particularly with disease severity,” said lead author Joshua Boron, MD, of Virginia Commonwealth University, Richmond, Virginia, in an interview. Identification of patients at higher risk of developing severe lung disease can help clinicians stratify these patients, he said.
Overall, the risk for severe lung disease at initial presentation was nearly three times higher in patients with no insurance than in those with private insurance and nearly three times higher in Black patients than in White patients (odds ratio [OR], 2.97 and 2.83, respectively). In addition, older age was associated with increased risk of fibrosis, with an OR of 1.03 per year increase in age.
No differences in fibrosis at presentation occurred based on sex or median income, and no difference in the likelihood of fibrosis at presentation appeared between patients with Medicaid vs private insurance.
“We were surprised at the degree of risk associated with no insurance,” said Dr. Boron. The researchers also were surprised at the lack of association between higher risk of severe stage lung disease in sarcoidosis patients and zip code estimates of household income as an indicator of socioeconomic status, he said.
For clinical practice, the study findings highlight the potentially increased risk for fibrotic lung disease among patients who are older, uninsured, and African American, said Dr. Boron.
“A limitation of our study was the utilization of zip code based on the US Census Bureau to get an estimation of average household income — a particular limitation in our city because of gentrification over the past few decades,” Dr. Boron said in an interview. “Utilizing area deprivation indices could be a better marker for identifying household income and give a more accurate representation of the true impact of socioeconomic disparities and severity of sarcoidosis at presentation,” he said.
Pinpointing Persistent Disparities
“We know there are multiple sources of disparities in the sarcoidosis population,” said Rohit Gupta, MD, director of the sarcoidosis program at Temple University Hospital, Philadelphia, in an interview.
The current study identified the relationship between several socioeconomic factors and sarcoidosis severity, showing greater disease severity in people experiencing socioeconomic inequalities, said Dr. Gupta, who was not involved in the study.
“I have personally seen this [disparity] in clinic,” said Dr. Gupta. However, supporting data are limited, aside from recent studies published in the last few years by researchers at the Cleveland Clinic and Johns Hopkins University, Baltimore, he said. The current study reflects those previous findings that people suffering from inequality have worse medical care, he added.
Overall, the findings were not surprising, “as we know this cohort of patients have chronic disease and worse morbidity and, in some cases, higher mortality,” but the results reinforce the need to pay closer attention to socioeconomic factors, said Dr. Gupta.
In practice, “we might use these findings as a reminder that when we see these patients for the first time, we should pay closer attention because they might need higher care,” he said. “The study also suggests these patients are coming late to a center of excellence,” he noted. When patients with socioeconomic disparities are seen for sarcoidosis at community hospitals and small centers, providers should keep in mind that their disease might progress faster and, therefore, send them to advanced centers earlier, he said.
The study was limited to the use of data from a single center and by the retrospective design, Dr. Gupta said. “Additional research should focus on building better platforms to understand these disparities,” he emphasized, so clinicians can develop plans not only to identify inequalities but also to address them.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Gupta had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
presented at the American Thoracic Society’s International Conference 2024.
“We know socioeconomic status plays an important role in health outcomes; however, there is little research into the impact of socioeconomic status on patients with sarcoidosis, particularly with disease severity,” said lead author Joshua Boron, MD, of Virginia Commonwealth University, Richmond, Virginia, in an interview. Identification of patients at higher risk of developing severe lung disease can help clinicians stratify these patients, he said.
Overall, the risk for severe lung disease at initial presentation was nearly three times higher in patients with no insurance than in those with private insurance and nearly three times higher in Black patients than in White patients (odds ratio [OR], 2.97 and 2.83, respectively). In addition, older age was associated with increased risk of fibrosis, with an OR of 1.03 per year increase in age.
No differences in fibrosis at presentation occurred based on sex or median income, and no difference in the likelihood of fibrosis at presentation appeared between patients with Medicaid vs private insurance.
“We were surprised at the degree of risk associated with no insurance,” said Dr. Boron. The researchers also were surprised at the lack of association between higher risk of severe stage lung disease in sarcoidosis patients and zip code estimates of household income as an indicator of socioeconomic status, he said.
For clinical practice, the study findings highlight the potentially increased risk for fibrotic lung disease among patients who are older, uninsured, and African American, said Dr. Boron.
“A limitation of our study was the utilization of zip code based on the US Census Bureau to get an estimation of average household income — a particular limitation in our city because of gentrification over the past few decades,” Dr. Boron said in an interview. “Utilizing area deprivation indices could be a better marker for identifying household income and give a more accurate representation of the true impact of socioeconomic disparities and severity of sarcoidosis at presentation,” he said.
Pinpointing Persistent Disparities
“We know there are multiple sources of disparities in the sarcoidosis population,” said Rohit Gupta, MD, director of the sarcoidosis program at Temple University Hospital, Philadelphia, in an interview.
The current study identified the relationship between several socioeconomic factors and sarcoidosis severity, showing greater disease severity in people experiencing socioeconomic inequalities, said Dr. Gupta, who was not involved in the study.
“I have personally seen this [disparity] in clinic,” said Dr. Gupta. However, supporting data are limited, aside from recent studies published in the last few years by researchers at the Cleveland Clinic and Johns Hopkins University, Baltimore, he said. The current study reflects those previous findings that people suffering from inequality have worse medical care, he added.
Overall, the findings were not surprising, “as we know this cohort of patients have chronic disease and worse morbidity and, in some cases, higher mortality,” but the results reinforce the need to pay closer attention to socioeconomic factors, said Dr. Gupta.
In practice, “we might use these findings as a reminder that when we see these patients for the first time, we should pay closer attention because they might need higher care,” he said. “The study also suggests these patients are coming late to a center of excellence,” he noted. When patients with socioeconomic disparities are seen for sarcoidosis at community hospitals and small centers, providers should keep in mind that their disease might progress faster and, therefore, send them to advanced centers earlier, he said.
The study was limited to the use of data from a single center and by the retrospective design, Dr. Gupta said. “Additional research should focus on building better platforms to understand these disparities,” he emphasized, so clinicians can develop plans not only to identify inequalities but also to address them.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Gupta had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Educational Tool Reduces Unnecessary Inhaler Use in ILD
Use of an electronic tool contributed to the deprescribing of unnecessary inhalers in patients with interstitial lung disease (ILD), based on data from nearly 200 individuals.
Patients with ILD often have symptoms that overlap with those of obstructive airways diseases, Stephanie Nevison, MD, of the University of Toronto, and colleagues wrote in a study presented at the American Thoracic Society’s international conference.
, they noted.
“Our aim was twofold: To quantify the extent of inappropriate inhaler use in patients with ILD and to discontinue them where appropriate,” the researchers wrote.
“We hypothesized that inappropriate inhaler use in ILD is common and that an electronic initiative would improve deprescribing rates,” they said.
The researchers conducted a quality improvement project in an ILD clinic at a single center. They reviewed 5 months of baseline data for 191 patients with ILD to assess baseline frequency of inappropriate inhaler use, defined as one or more of the following criteria: Reported asthma history, smoking history of > 15 pack/years, emphysema on chest CT, patient-reported benefits from therapy, airflow obstruction, or bronchodilator response on spirometry.
A total of 48 patients (25.1%) were on inhalers, and 15 (7.8%) had no indication for them (9% of new referrals and 7% of follow-up patients). The most-prescribed inhalers for patients with no indication were corticosteroids (10 patients), short-acting beta-agonists (8 patients), and long-acting beta-agonists (7 patients).
None of the patients on inhalers received counseling about discontinuing their use. The results of the baseline assessment were shared with clinicians along with education about reducing unnecessary inhaler use in the form of a prompt linked to electronic medical records to discuss deprescription of unnecessary inhalers.
The electronic intervention was applied in 400 of 518 patient encounters, and the researchers reviewed data over another 5-month period. A total of 99 patients were on inhalers, and 3.3% had no indication (5.3% of new referrals and 3.0% of follow-up patients). In the wake of the intervention, “all patients on unnecessary inhalers were counseled on deprescribing, representing a significant increase compared to the preintervention period,” the researchers wrote.
Intervention Shows Potential to Curb Unnecessary Inhaler Use
More research is needed as the findings were limited by the relatively small sample size and use of data from a single center, the researchers noted.
However, the results suggest that electronic reminders are effective for prompting a review of inhaler use, and deprescribing inappropriate inhalers for patients with ILD could reduce the potential for adverse events associated with their use, they concluded.
The current study is important because some patients with ILD may not benefit from inhaler use, David Mannino, MD, of the University of Kentucky, Lexington, said in an interview. In the study, “I was a bit surprised that only 3.3% of patients had no indication for them; this seems rather low,” said Dr. Mannino, who was not involved in the study.
Use of an electronic system that evaluates patients and flags inappropriate therapy is an effective way to decrease overprescribing of medications, Dr. Mannino told this news organization.
As for additional research, application of the tool used in this study to other pulmonary populations could be interesting and potentially useful, he said.
The study received no outside funding. The researchers and Dr. Mannino had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Use of an electronic tool contributed to the deprescribing of unnecessary inhalers in patients with interstitial lung disease (ILD), based on data from nearly 200 individuals.
Patients with ILD often have symptoms that overlap with those of obstructive airways diseases, Stephanie Nevison, MD, of the University of Toronto, and colleagues wrote in a study presented at the American Thoracic Society’s international conference.
, they noted.
“Our aim was twofold: To quantify the extent of inappropriate inhaler use in patients with ILD and to discontinue them where appropriate,” the researchers wrote.
“We hypothesized that inappropriate inhaler use in ILD is common and that an electronic initiative would improve deprescribing rates,” they said.
The researchers conducted a quality improvement project in an ILD clinic at a single center. They reviewed 5 months of baseline data for 191 patients with ILD to assess baseline frequency of inappropriate inhaler use, defined as one or more of the following criteria: Reported asthma history, smoking history of > 15 pack/years, emphysema on chest CT, patient-reported benefits from therapy, airflow obstruction, or bronchodilator response on spirometry.
A total of 48 patients (25.1%) were on inhalers, and 15 (7.8%) had no indication for them (9% of new referrals and 7% of follow-up patients). The most-prescribed inhalers for patients with no indication were corticosteroids (10 patients), short-acting beta-agonists (8 patients), and long-acting beta-agonists (7 patients).
None of the patients on inhalers received counseling about discontinuing their use. The results of the baseline assessment were shared with clinicians along with education about reducing unnecessary inhaler use in the form of a prompt linked to electronic medical records to discuss deprescription of unnecessary inhalers.
The electronic intervention was applied in 400 of 518 patient encounters, and the researchers reviewed data over another 5-month period. A total of 99 patients were on inhalers, and 3.3% had no indication (5.3% of new referrals and 3.0% of follow-up patients). In the wake of the intervention, “all patients on unnecessary inhalers were counseled on deprescribing, representing a significant increase compared to the preintervention period,” the researchers wrote.
Intervention Shows Potential to Curb Unnecessary Inhaler Use
More research is needed as the findings were limited by the relatively small sample size and use of data from a single center, the researchers noted.
However, the results suggest that electronic reminders are effective for prompting a review of inhaler use, and deprescribing inappropriate inhalers for patients with ILD could reduce the potential for adverse events associated with their use, they concluded.
The current study is important because some patients with ILD may not benefit from inhaler use, David Mannino, MD, of the University of Kentucky, Lexington, said in an interview. In the study, “I was a bit surprised that only 3.3% of patients had no indication for them; this seems rather low,” said Dr. Mannino, who was not involved in the study.
Use of an electronic system that evaluates patients and flags inappropriate therapy is an effective way to decrease overprescribing of medications, Dr. Mannino told this news organization.
As for additional research, application of the tool used in this study to other pulmonary populations could be interesting and potentially useful, he said.
The study received no outside funding. The researchers and Dr. Mannino had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Use of an electronic tool contributed to the deprescribing of unnecessary inhalers in patients with interstitial lung disease (ILD), based on data from nearly 200 individuals.
Patients with ILD often have symptoms that overlap with those of obstructive airways diseases, Stephanie Nevison, MD, of the University of Toronto, and colleagues wrote in a study presented at the American Thoracic Society’s international conference.
, they noted.
“Our aim was twofold: To quantify the extent of inappropriate inhaler use in patients with ILD and to discontinue them where appropriate,” the researchers wrote.
“We hypothesized that inappropriate inhaler use in ILD is common and that an electronic initiative would improve deprescribing rates,” they said.
The researchers conducted a quality improvement project in an ILD clinic at a single center. They reviewed 5 months of baseline data for 191 patients with ILD to assess baseline frequency of inappropriate inhaler use, defined as one or more of the following criteria: Reported asthma history, smoking history of > 15 pack/years, emphysema on chest CT, patient-reported benefits from therapy, airflow obstruction, or bronchodilator response on spirometry.
A total of 48 patients (25.1%) were on inhalers, and 15 (7.8%) had no indication for them (9% of new referrals and 7% of follow-up patients). The most-prescribed inhalers for patients with no indication were corticosteroids (10 patients), short-acting beta-agonists (8 patients), and long-acting beta-agonists (7 patients).
None of the patients on inhalers received counseling about discontinuing their use. The results of the baseline assessment were shared with clinicians along with education about reducing unnecessary inhaler use in the form of a prompt linked to electronic medical records to discuss deprescription of unnecessary inhalers.
The electronic intervention was applied in 400 of 518 patient encounters, and the researchers reviewed data over another 5-month period. A total of 99 patients were on inhalers, and 3.3% had no indication (5.3% of new referrals and 3.0% of follow-up patients). In the wake of the intervention, “all patients on unnecessary inhalers were counseled on deprescribing, representing a significant increase compared to the preintervention period,” the researchers wrote.
Intervention Shows Potential to Curb Unnecessary Inhaler Use
More research is needed as the findings were limited by the relatively small sample size and use of data from a single center, the researchers noted.
However, the results suggest that electronic reminders are effective for prompting a review of inhaler use, and deprescribing inappropriate inhalers for patients with ILD could reduce the potential for adverse events associated with their use, they concluded.
The current study is important because some patients with ILD may not benefit from inhaler use, David Mannino, MD, of the University of Kentucky, Lexington, said in an interview. In the study, “I was a bit surprised that only 3.3% of patients had no indication for them; this seems rather low,” said Dr. Mannino, who was not involved in the study.
Use of an electronic system that evaluates patients and flags inappropriate therapy is an effective way to decrease overprescribing of medications, Dr. Mannino told this news organization.
As for additional research, application of the tool used in this study to other pulmonary populations could be interesting and potentially useful, he said.
The study received no outside funding. The researchers and Dr. Mannino had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
FROM ATS 2024
Use of Hypoglossal Nerve Stimulation for Treating OSA in Military Patient Populations
Obstructive sleep apnea (OSA), the repetitive collapse of posterior oropharynx during sleep resulting in hypoxia and/or arousals from sleep, is the most common form of sleep disordered breathing and a common chronic respiratory disorders among middle-aged adults. OSA can lead to significant health problems, such as worsened cardiometabolic disease and cognitive impairment, which can increase morbidity and mortality.1
The gold standard for OSA diagnosis is polysomnography (PSG), although home sleep studies can be performed for select patients. OSA diagnoses are based on the number of times per hour of sleep a patient’s airway narrows or collapses, reducing or stopping airflow, scored as hypopnea or apnea events, respectively. An Apnea-Hypopnea Index (AHI) score of 5 to 14 events/hour is considered mild OSA, 15 to 30 events/hour moderate OSA, and ≥ 30 events/hour severe OSA.2
Treatment commonly includes positive airway pressure (PAP) but more than one-half of patients are not adherent to continuous PAP (CPAP) treatment after about 90 days.3 Efficacy of treatments vary as a function of disease severity and etiology, which—in addition to the classic presentation of obesity with large neck/narrowupper airway—includes craniofacial abnormalities, altered muscle function in the upper airway, pharyngeal neuropathy, and fluid shifts to the neck.
Background
The American Academy of Sleep Medicine (AASM) estimates that 10% to 17% of adults in the United States have OSA.4 Compared with civilians, the military population generally is younger and healthier. Service members have access to regular health care with yearly physical examinations, exercise scheduled into the workday, and mandatory height/weight and fitness standards. Because obesity is a major risk factor for OSA, and the incidence of obesity is relatively low in the military population (estimated at 18.8% in 2021 vs 39.8% among all US adults aged 20 to 39 years), it might be expected that incidence of OSA would be correspondingly low.5,6 However, there is evidence of a rapidly increasing incidence of OSA in military populations. A 2021 study revealed that OSA incidence rates increased from 11 to 333 per 10,000 between 2005 and 2019 across all military branches and demographics, with the highest rate among Army personnel.7 An earlier study revealed a 600% increase in OSA incidence among Army personnel between 2003 and 2011.8
Several factors likely contributed to this increase, including expanding obesity and greater physician awareness and availability of sleep study centers. Rogers and colleagues found that 40% to 50% of incident OSA diagnoses among military personnel occur within 12 months of separation, suggesting that the secondary gains associated with military disability benefits might motivate OSA evaluation.9 It is possible that secondary gain is a factor because an OSA diagnosis can range from a 0% to 100% disability rating, depending on the severity.10 This disability claim is based on evidence that untreated OSA can negatively affect long-term health and mission readiness.8 For example, untreated OSA can lead to hypertension, which contributes to a long list of adverse health and wellness consequences. Most importantly for the military, OSA has been shown to increase daytime sleepiness and reduce cognitive performance.10
The current first-line treatment for OSA is CPAP, which improves symptoms of daytime sleepiness, hypertension management, and daytime alertness.11 Despite its efficacy, nonadherence rates range from 29% to 83%.12-15 Nonadherence factors include lifestyle changes, adverse effects (eg, nasal congestion), and lack of education on proper use.11 Lifestyle changes needed to increase the likelihood of successful therapy, such as regular sleep schedules and proper CPAP cleaning and maintenance, are difficult for military personnel because of the nature of continuous or sustained operations that might require shift work and/or around-the-clock (ie, 24-hour, 7 days a week) task performance. Traveling with CPAP is an added burden for service members deployed to combat operations (ie, added luggage, weight, maintenance). Although alternate treatments such as oral appliances (ie, custom dental devices) are available, they generally are less effective than CPAP.2 Oral appliances could be a reasonable alternative treatment for some patients who cannot manage their OSA with behavioral modifications and are intolerant or unable to effectively use CPAP. This could include patients in the military who are deployed to austere environments.
Surgically implanted hypoglossal nerve stimulator (HGNS) treatment may provide long-term health benefits to service members. After the device is implanted near the hypoglossal nerve, electrical stimulation causes the tongue to move forward, which opens the airway in the anteroposterior dimension. The most important consideration is the mechanism of airway collapse. HGNS is not effective for patients whose OSA events are caused by circumferential collapse of other airway muscles. The cause of airway collapse is ascertained before surgery with drug-induced sleep endoscopy, a procedure that allows visualization of conformational changes in the upper airway during OSA events.
The US Food and Drug Administration (FDA) approved HGNS in 2014. However, it is not considered a first-line treatment for OSA by the AASM. Original candidate criteria for HGNS included an AHI score of 15 to 65 events/hour, age ≥ 18 years, failed CPAP use, body mass index (BMI) < 32, absence of palatal complete concentric collapse, and central apneas comprising < 25% of total events.16 In June 2023, the FDA expanded approval to increase the upper limit of AHI to 100 events/hour and the BMI to < 40.17
HGNS has been reported to be effective in appropriately selected patients with OSA at tertiary care centers with established multidisciplinary sleep surgical programs. These benefits have not been confirmed in larger, community-based settings, where most of these surgeries occur. In community practice, there is significant confusion among patients and clinicians about the optimal pathway for patient selection and clinical follow-up. Many patients view HGNS as a viable alternative to CPAP, but initially do not understand that it requires surgery. Surgical treatments for OSA, such as HGNS, are appealing because they suggest a 1-time intervention that permanently treats the condition, without need for follow-up or equipment resupply. HGNS might be an appealing treatment option because it is less obtrusive than CPAP and requires fewer resources for set-up and maintenance. Also, it does not cause skin irritation (a possible adverse effect of nightly use of a CPAP mask), allows the individual to sleep in a variety of positions, has less impact on social and sex life, and does not require an electric outlet. In the long term, HGNS might be more cost effective because there is no yearly physician follow-up or equipment resupply and/or maintenance.
The military population has specific demands that impact delivery and effectiveness of health care. Among service members with OSA, CPAP treatment can be challenging because of low adherence, required annual follow-up despite frequent moving cycles that pose a challenge for care continuity, and duty limitations for affected service members (ie, the requirement for a waiver to deploy and potential medical separation if symptoms are not adequately controlled). As the incidence of OSA continues to increase among service members, so does the need for OSA treatment options that are efficacious as CPAP but better tolerated and more suitable for use during military operations. The aim of this review is to assess the effectiveness of HGNS and its potential use by the military OSA patient population.
METHODS
To identify eligible studies, we employed PICOS: Population (patients aged ≥ 18 years with a history of OSA), Intervention (HGNS), Comparator (standard of care PAP therapy), Outcome (AHI or Epworth Sleepiness Scale [ESS], and Study (randomized control trial [RCT] or clinical trial). Studies were excluded if they were not written in English or included pediatric populations. The ESS is a subjective rating scale used to determine and quantify a patient’s level of daytime sleepiness, using a 4-point scale for the likelihood of falling asleep totaled across 8 different situations.18 Daytime sleepiness is considered lower normal(0-5 points), higher normal (6-10 points), mild or moderate excessive (11-15 points), and severe excessive (16-24 points).
Literature Search
We conducted a review of PubMed and Scopus for RCTs and controlled trials published from 2013 to 2023 that included the keywords and phrases: obstructive sleep apnea and either hypoglossal nerve stimulation or upper airway stimulation. The final literature search was performed December 8, 2023.
Two authors independently assessed the titles and abstracts of studies identified in the literature search based on the predefined inclusion criteria. If it was not clear whether an article met inclusion criteria based on its title and/or abstract, the 2 review authors assessed the full text of study and resolved any disagreement through consensus. If consensus was not obtained, a third author was consulted. No duplicates were identified. The PRISMA study selection process is presented in the Figure.
Data extraction was performed by 1 independent reviewer. A second author reviewed the extracted data. Any identified discrepancies were resolved through discussion and consensus. If consensus was not obtained, a third author was consulted. Study data included methods (study design and study objective), participants mean age, inclusion criteria, exclusion criteria, interventions and comparators, and primary study outcomes.
The quality of evidence was assessed using a rating of 1 to 5 based on a modified version of the Oxford Centre for Evidence-based Medicine Levels of Evidence and Grades of Recommendation.19 A rating of 1 indicated a properly powered and conducted RCT, 2 demonstrated a well-designed controlled trial without randomization or prospective comparative cohort trial, 3 designated a case-control study or retrospective cohort study, 4 signified a case series with or without intervention or a cross-sectional study, and 5 denoted an opinion of respected authorities or case reports. Two reviewers independently evaluated the quality of evidence. Any identified discrepancies were resolved through discussion and consensus. If consensus was not obtained, a third review author was consulted.
RESULTS
We identified 30 studies; 19 articles did not meet inclusion criteria. The remaining 11 articles were divided into 4 cohorts. Five articles were based on data from the STAR trial, a multicenter study that included adults with moderate-to-severe OSA and inadequate adherence to CPAP.20-24 Four articles used the same patient selection criteria as the STAR trial for a long-term German postmarket study of upper airway stimulation efficacy with OSA.25-28 The third and fourth cohorts each consist of 31 patients with moderate-to-severe OSA with CPAP nonadherence or failure.29,30 The STAR trial included follow-up at 5 years, and the German-postmarket had a follow-up at3 years. The remaining 2 cohorts have 1-year follow-ups.
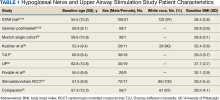
The Scopus review identified 304 studies; 299 did not meet inclusion criteria and 1 was part of the STAR trial.31 The remaining 4 articles were classified as distinct cohorts. Huntley and colleagues included patients from Thomas Jefferson University (TJU) and University of Pittsburgh (UP) academic medical centers.32 The Pordzik and colleagues cohort received implantation at a tertiary medical center, an RCCT, and a 1:1 comparator trial (Table 1).33-35
STAR Trial
This multicenter, prospective, single-group cohort study was conducted in the US, Germany, Belgium, Netherlands, and France. The STAR trial included 126 patients who were not CPAP therapy adherent. Patients were excluded if they had AHI < 20 or > 50, central sleep apnea > 25% of total AHI, anatomical abnormalities that prevent effective assessment of upper-airway stimulation, complete concentric collapse of the retropalatal airway during drug-induced sleep, neuromuscular disease, hypoglossal-nerve palsy, severe restrictive or obstructive pulmonary disease, moderate-to-severe pulmonary arterial hypertension, severe valvular heart disease, New York Heart Association class III or IV heart failure, recent myocardial infarction or severe cardiac arrhythmias (within the past 6 months), persistent uncontrolled hypertension despite medication use, active psychiatric illness, or coexisting nonrespiratory sleep disorders that would confound functional sleep assessment. Primary outcome measures included the AHI and oxygen desaturation index (ODI) with secondary outcomes using the ESS, the Functional Outcomes of Sleep Questionnaire (FOSQ), and the percentage of sleep time with oxygen saturation < 90%. Of 126 patients who received implantation, 71 underwent an overnight PSG evaluation at 5-year follow-up. Mean (SD) AHI at baseline was reduced with HGNS treatment to from 32.0 (11.8) to 12.4 (16.3). Mean (SD) ESS for 92 participants with 2 measurements declined from 11.6 (5.0) at baseline to 6.9 (4.7) at 5-year follow-up.
The STAR trial included a randomized controlled withdrawal study for 46 patients who had a positive response to therapy to evaluate efficacy and durability of upper airway stimulation. Patients were randomly assigned to therapy maintenance or therapy withdrawal groups for ≥ 1 week. The short-term withdrawal effect was assessed using the original trial outcome measures and indicated that both the withdrawal and maintenance groups showed improvements at 12 months compared with the baseline. However, after the randomized withdrawal, the withdrawal group’s outcome measures deteriorated to baseline levels while the maintenance group showed no change. At 18 months of therapy, outcome measures for both groups were similar to those observed with therapy at 12 months.24 The STAR trial included self-reported outcomes at baseline, 12 months, and 24 months that used ESS to measure daytime sleepiness. These results included subsequent STAR trial reports.20-24,31
The German Postmarket Cohort
This multicenter, prospective, single-arm study used selection criteria that were based on those used in the STAR trial and included patients with moderate-to-severe OSA and nonadherence to CPAP. Patients were excluded if they had a BMI > 35, AHI < 15 or > 65; central apnea index > 25% of total AHI; or complete concentric collapse at the velopharynx during drug-induced sleep. Measured outcomes included AHI, ODI, FOSQ, and ESS. Among the 60 participants, 38 received implantation and a 3-year follow-up. Mean (SD) AHI decreased from 31.2 (13.2) at baseline to 13.1 (14.1) at follow-up, while mean (SD) ESS decreased from 12.8 (5.3) at baseline to 6.0 (3.2) at follow-up.25-28
Munich Cohort
This single-center, prospective clinical trial included patients with AHI > 15 and < 65, central apnea index < 25% of total AHI, and nonadherence to CPAP. Patients were excluded if they had a BMI > 35, anatomical abnormalities that would prevent effective assessment of upper-airway stimulation; all other exclusion criteria matched those used in the STAR trial. Among 31 patients who received implants and completed a 1-year follow-up, mean (SD) AHI decreased from 32.9 (11.2) at baseline to 7.1 (5.9) at follow-up and mean (SD) ESS decreased from 12.6 (5.6) at baseline to 5.9 (5.2) at follow-up.29
Kezirian and Colleagues Cohort
This prospective, single-arm, open-label study was conducted at 4 Australian and 4 US sites. Selection criteria included moderate-to-severe OSA with failure of CPAP, AHI of 20 to 100 with ≥ 15 events/hour occurring in sleep that was non-REM (rapid eye movement) sleep, BMI ≤ 40 (Australia) or ≤ 37 (US), and a predominance of hypopneas (≥ 80% of disordered breathing events during sleep). Patients were excluded if they had earlier upper airway surgery, markedly enlarged tonsils, uncontrolled nasal obstruction, severe retrognathia, > 5% central or mixed apneic events, incompletely treated sleep disorders other than OSA, or a major disorder of the pulmonary, cardiac, renal, or nervous systems. Data were reported for 31 patients whose mean (SD) AHI declined from 45.4 (17.5) at baseline to 25.3 (20.6) at 1-year follow-up and mean (SD) ESS score declined from 12.1 (4.6) at baseline to 7.9 (3.8) 1 year later.30
TJU and UP Cohorts
The TJU and UP cohorts are composed of patients who underwent implantation between May 2014 and August 2016 at 2 academic centers.31,32 Selection criteria was consistent with that used in the STAR trial, and patients completed postoperative titration PSG and outpatient follow-up (48 patients at TJU and 49 at UP). Primary outcomes included AHI, ESS, and O2 nadir. Secondary outcomes consisted of surgical success and percentage of patients tolerating optimal titration setting at follow-up. Postoperative outcomes were assessed during the titration PSG. Time from initial ESS to postoperative PSG at TJU was 1.7 years and at UP was 1.9 years. Time from initial AHI to postoperative PSG at TJU was 90.4 days and 85.2 days at UP. At TJU, mean (SD) AHI and ESS dropped from 35.9 (20.8) and 11.1 (3.8), respectively at baseline to 6.3 (11.5) and 5.8 (3.4), respectively at follow-up. At UP, mean (SD) AHI and ESS fell from 35.3 (15.3) and 10.9 (4.9), respectively at baseline to 6.3 (6.1) and 6.6 (4.5), respectively at follow-up. There were no site-related differences in rates of AHI, ESS, or surgical success.31
Pordzik and Colleagues Cohort
This cohort of 29 patients underwent implantation between February 2020 and June 2022 at a tertiary university medical center with both pre- and postoperative PSG. Selection criteria was consistent with that of the German postmarket cohort. Postoperative PSG was completed a mean (SD) 96.3 (27.0) days after device activation. Mean (SD) AHI dropped from 38.6 (12.7) preoperatively to 24.4 (13.3) postoperatively. Notably, this cohort showed a much lower decrease of postoperative AHI than reported by the STAR trial and UP/TJU cohort.33
Stimulation vs Sham Trial
This multicenter, double-blinded, randomized, crossover trial assessed the effect of HGNS (stim) vs sham stimulation (sham) in 86 patients that completed both phases of the trial. Primary outcomes included AHI and ESS. Secondary outcomes included FOSQ. No carryover effect was found during the crossover phase. The difference between the phases was−15.5 (95% CI, −18.3 to −12.8) for AHI and −3.3 (95% CI, −4.4 to −2.2) for ESS.34
Comparator
The comparator study used propensity score matching to compare outcomes of HGNS and PAP therapy. Primary outcomes included sleepiness, AHI, and effectiveness with outcome measures of AHI and ESS collected at baseline and 12 months postimplantation. The article reported that 126 of 227 patients were matched 1:1. Both groups showed improvement in AHI and ESS. Mean (SD) AHI for the HGNS group at baseline started at 33.9 (15.1) and decreased to 8.1 (6.3). Mean (SD) ESS for the HGNS group at baseline was 15.4 (3.5) and decreased to 7.5 (4.7). In the PAP comparator group, mean (SD) baseline AHI was 36.8 (21.6) and at follow-up was 6.6 (8.0) and mean (SD) ESS was 14.6 (3.9) at baseline and 10.8 (5.6) at follow-up.35
DISCUSSION
The current clinical data on HGNS suggest that this treatment is effective in adults with moderate-to-severe OSA and effects are sustained at long-term follow-up, as measured by AHI reduction and improvements in sleep related symptoms and quality of life (Table 2). These results have been consistent across several sites.
The STAR trial included a randomized control withdrawal group, for whom HGNS treatment was withdrawn after the 12-month follow-up, and then restored at 18 months.21 This revealed that withdrawal of HGNS treatment resulted in deterioration of both objective and subjective measures of OSA and sleepiness. The beneficial effects of HGNS were restored when treatment was resumed.24 Additionally, the RCCT revealed that therapeutic stimulation via HGNS significantly reduced subjective and objective measures of OSA.34 These studies provide definitive evidence of HGNS efficacy.
Currently, a diagnosis of OSA on PAP is classified as a 50% military disability rating. This rating is based primarily on epidemiologic evidence that untreated OSA is a costly disease that leads to other chronic illnesses that increases health care utilization.9 HGNS requires an initially invasive procedure and higher upfront costs, but it could result in reduced health care use and long-term costs because of improved adherence to treatment—compared with CPAP—that results in better outcomes.
Limitations to OSA Studies
The reviewed studies have several limitations that warrant caution when determining the possible benefits of HGNS treatment. The primary limitation is the lack of active control groups, therefore precluding a direct comparison of the short- and long-term effectiveness of HGNS vs other treatments (eg, CPAP). This is especially problematic because in the reviewed studies HGNS treatment efficacy is reported as a function of the mean—and SD—percent reduction in the AHI, whereas the efficacy of CPAP treatment usually is defined in terms of “adequacy of titration” as suggested by the AASM.36 It has been reported that with CPAP treatment, 50% to 60% of OSA patients achieve AASM-defined optimal improvement of respiratory disturbance index of < 5/hour during a polysomnographic sleep recording of ≥ 15 minutes duration that includes REM sleep in the supine position.37 In most of the reviewed studies, treatment success was more liberally defined as a decrease of AHI by ≥ 50%, regardless of the resulting AHI. It is notable that among the reviewed HGNS studies, the TJU and UP cohorts achieved the best outcome in short-term follow-up of 2 months with a mean (SD) AHI of 6.3 (11.5) and 6.4 (6.1), respectively. Among those cohortsassessed at a 12-month follow-up, the Munich cohort achieved the best outcome with a mean (SD) AHI of 7.1 (5.9).
Although the metrics reported in the reviewed studies are not directly comparable, the reported findings strongly suggest that HGNS generally is less effective than CPAP. How important are these differences? With findings that HGNS “reliably produces clinically meaningful (positive) effects on daytime sleepiness, daytime functioning, and sleep quality,” does it really matter if the outcome metrics for HGNS are a little less positive than those produced by CPAP?38 For individual military OSA patients the answer is yes. This is because in military operational environments—especially during deployment—sleep restriction is nearly ubiquitous, therefore any mild residual deficits in sleep quality and daytime alertness resulting from nominally adequate, but suboptimal OSA treatment, could be exacerbated by sleep restriction, therefore placing the service member and the mission at increased risk.39
Another limitation is the narrow inclusion criteria these studies employed, which limits the generalizability of the findings. Participants in the reviewed clinical trials were selected from a patient population that was mostly middle-aged, White, and obese or overweight. In a Medical Surveillance Monthly Report study, OSA was found to be highest among service members aged > 40 years, male, obese, and Black/non-Hispanic (although it should be noted that more than one-half of enlisted service members aged ≤ 25 years).40,41 Obesity has been noted as a growing concern for the military as the military population is beginning to mirror the civilian population in terms of being overweight or obese despite height and weight standards. HGNS might not be as successful in military populations with different demographics. Moreover, HGNS has been shown to have greater AHI reduction among those with higher BMI.30 Although obese service members have a 6-fold higher 12-year incidence rate of OSA than service members without obesity, this nevertheless suggests that general level of HGNS efficacy might be lower among the military patient population, because obesity is less prevalent in the military than the general population.9
Ethnicity has been found to be a relevant factor, with the highest incidence rate of OSA among non-Hispanic Black males, a demographic that was underrepresented in cohorts included in this review. Further studies will be needed to determine the extent to which findings from HGNS treatment studies are generalizable to the broader OSA patient population.
HGNS Implementation Challenges
Current impediments to widespread use of HGNS as an OSA treatment include no standardized guidance for titration and follow-on care, which varies based on the resources available. Titrating a new device for HGNS requires experienced sleep technicians who have close relationships with device representatives and can troubleshoot problems. Technical expertise, which currently is rare, is required if there are complications after placement or if adjustments to voltage settings are needed over time. In addition, patients may require multiple specialists making it easy to get lost to follow-up after implantation. This is particularly challenging in a transient community, such as the military, because there is no guarantee that a service member will have access to the same specialty care at the next duty station.
Although some evidence suggests that HGNS is a viable alternative treatment for some patients with OSA, the generalizability of these findings to the military patient population is unclear. Specialized facilities and expertise are needed for the surgical procedure and follow-up requirements, which currently constitute significant logistical constraints. As with any implantable device, there is a risk of complications including infection that could result in medical evacuation from a theater of operations. If the device malfunctions or loses effectiveness in a deployed environment, the service member might not have immediate access to medical support, potentially leading to undertreatment of OSA. In future battlefield scenarios in multidomain operations, prolonged, far-forward field care will become the new normal because the military is not expected to have air superiority or the ability to quickly evacuate service members to a higher level of medical care.42
In deployed environments, the potential limitations of HGNS become increasingly risky for the service member and the overall mission. Considering these factors, it will be important to evaluate the practicality of HGNS as a treatment option in military populations. Military-specific challenges associated with HGNS that require further study, include guidance for patient selection outside academic centers, guidance on long-term postsurgical care and device maintenance, duty limitation and military retention considerations, and limitations in training and combat environments. The military medical community needs to conduct its own studies in appropriately selected service members to guide clinical practice.
CONCLUSIONS
HGNS treatment results in improvement of both AHI and ESS scores and could be a deployable treatment option for military patients with OSA. However, HGNS has not been found to be as effective as CPAP, although the current literature is limited by small sample sizes, homogeneous populations that do not reflect the demographics of the military, and mostly short follow-up periods. Future studies should be focused on collecting data on HGNS from demographic groups that are more representative of the military OSA patient population and identifying the subpopulation of patients who derive the greatest benefit from HGNS, so that this treatment can be better individually targeted. Until data on existing military patients is published, it is not possible to fully weigh risks and benefits in this population and generalize civilian guidance to the military.
1. Cumpston E, Chen P. Sleep Apnea Syndrome. PubMed. Updated September 4, 2023. Published January 2024. https://www.ncbi.nlm.nih.gov/books/NBK564431/
2. American Academy of Sleep Medicine. Obstructive sleep apnea. Accessed November 27, 2023. https://aasm.org/resources/factsheets/sleepapnea.pdf
3. Cowen J, Harrison S, Thom L, et al. Use of historical remote monitoring data to determine predictors of CPAP non-compliance in patients with Osa. Sleep Breath. 2023;27(5):1899-1908. doi:10.1007/s11325-023-02806-3
4. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006-1014. doi:10.1093/aje/kws342
5. Stiegmann RA, Payne CB, Kiel MA, Stahlman SL. Increased Prevalence of Overweight and Obesity and Incidence of Prediabetes and Type 2 Diabetes During the COVID-19 Pandemic, Active Component Service Members, U.S. Armed Forces, 2018 to 2021. MSMR. 2023;30(1):11-18. Published 2023 Jan 20.
6. Adult obesity facts. Centers for Disease Control and Prevention. Updated May 17, 2022. Accessed November 27, 2023. https://www.cdc.gov/obesity/data/adult.html
7. Moore BA, Tison LM, Palacios JG, Peterson AL, Mysliwiec V. Incidence of insomnia and obstructive sleep apnea in active duty United States military service members. Sleep. 2021;44(7):zsab024. doi:10.1093/sleep/zsab024
8. Caldwell JA, Knapik JJ, Shing TL, Kardouni JR, Lieberman HR. The association of insomnia and sleep apnea with deployment and combat exposure in the entire population of US army soldiers from 1997 to 2011: a retrospective cohort investigation. Sleep. 2019;42(8):zsz112. doi:10.1093/sleep/zsz112
9. Rogers AE, Stahlman S, Hunt DJ, Oh GT, Clark LL. Obstructive sleep apnea and associated attrition, active component, U.S. Armed Forces, January 2004-May 2016. MSMR. 2016;23(10):2-11.
10. Veterans Affairs 38 C.F.R. § 4.97-13, Code 6847.
11. Shapiro GK, Shapiro CM. Factors that influence CPAP adherence: an overview. Sleep Breath. 2010;14(4):323-335. doi:10.1007/s11325-010-0391-y
12. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173-178. doi:10.1513/pats.200708-119mg
13. Sin DD, Mayers I, Man GCW, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430-435. doi:10.1378/chest.121.2.430
14. Nowak C, Bourgin P, Portier F, Genty E, Escourrou P, Bobin S. Obstruction nasale et compliance à la ventilation nasale à pression positive [Nasal obstruction and compliance to nasal positive airway pressure]. Ann Otolaryngol Chir Cervicofac. 2003;120(3):161-166.
15. Brin YS, Reuveni H, Greenberg S, Tal A, Tarasiuk A. Determinants affecting initiation of continuous positive airway pressure treatment. Isr Med Assoc J. 2005;7(1):13-18.
16. Suurna MV, Jacobowitz O, Chang J, et al. Improving outcomes of hypoglossal nerve stimulation therapy: current practice, future directions, and research gaps. Proceedings of the 2019 International Sleep Surgery Society Research Forum. J Clin Sleep Med. 2021;17(12):2477-2487. doi:10.5664/jcsm.9542
17. Inspire Medical Systems, Inc. Announces FDA approval for apnea hypopnea index indication expansion and increased body mass index labeling. Inspire Medical Systems, Inc. Accessed July 14, 2023. https://investors.inspiresleep.com/investors/press-releases/press-release-details/2023/Inspire-Medical-Systems-Inc.-Announces-FDA-Approval-for-Apnea-Hypopnea-Index-Indication-Expansion-and-Increased-Body-Mass-Index-Labeling/default.aspx
18. Lapin BR, Bena JF, Walia HK, Moul DE. The Epworth Sleepiness Scale: Validation of one-dimensional factor structure in a large clinical sample. J Clin Sleep Med. 2018;14(08):1293-1301. Published 2018 Aug 15. doi:10.5664/jcsm.7258
19. The Centre for Evidence-Based Medicine. November 25, 2020. http://www.cebm.net/index.aspx?o=5653
20. Strollo PJ Jr, Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370(2):139-149. doi:10.1056/NEJMoa1308659
21. Strollo PJ Jr, Gillespie MB, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: durability of the treatment effect at 18 months. Sleep. 2015;38(10):1593-1598. Published 2015 Oct 1. doi:10.5665/sleep.5054
22. Woodson BT, Soose RJ, Gillespie MB, et al. Three-year outcomes of cranial nerve stimulation for obstructive sleep apnea: the STAR trial. Otolaryngol Head Neck Surg. 2016;154(1):181-188. doi:10.1177/0194599815616618
23. Woodson BT, Strohl KP, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: 5-year outcomes. Otolaryngol Head Neck Surg. 2018;159(1):194-202. doi:10.1177/0194599818762383
24. Woodson BT, Gillespie MB, Soose RJ, et al. Randomized controlled withdrawal study of upper airway stimulation on OSA: short- and long-term effect. Otolaryngol Head Neck Surg. 2014;151(5):880-887. doi:10.1177/0194599814544445
25. Heiser C, Maurer JT, Hofauer B, Sommer JU, Seitz A, Steffen A. Outcomes of upper airway stimulation for obstructive sleep apnea in a multicenter German postmarket study. Otolaryngol Head Neck Surg. 2017;156(2):378-384. doi:10.1177/0194599816683378
26. Steffen A, Sommer JU, Hofauer B, Maurer JT, Hasselbacher K, Heiser C. Outcome after one year of upper airway stimulation for obstructive sleep apnea in a multicenter German post-market study. Laryngoscope. 2018;128(2):509-515. doi:10.1002/lary.26688
27. Steffen A, Sommer UJ, Maurer JT, Abrams N, Hofauer B, Heiser C. Long-term follow-up of the German post-market study for upper airway stimulation for obstructive sleep apnea. Sleep Breath. 2020;24(3):979-984. doi:10.1007/s11325-019-01933-028.
28. Hasselbacher K, Hofauer B, Maurer JT, Heiser C, Steffen A, Sommer JU. Patient-reported outcome: results of the multicenter German post-market study. Eur Arch Otorhinolaryngol. 2018;275(7):1913-1919. doi:10.1007/s00405-018-5017-129.
29. Heiser C, Knopf A, Bas M, Gahleitner C, Hofauer B. Selective upper airway stimulation for obstructive sleep apnea: a single center clinical experience. Eur Arch Otorhinolaryngol. 2017;274(3):1727-1734. doi:10.1007/s00405-016-4297-6
30. Kezirian EJ, Goding GS Jr, Malhotra A, et al. Hypoglossal nerve stimulation improves obstructive sleep apnea: 12-month outcomes. J Sleep Res. 2014;23(1):77-83. doi:10.1111/jsr.12079
31. Soose RJ, Woodson BT, Gillespie MB, et al. Upper airway stimulation for obstructive sleep apnea: self-reported outcomes at 24 months. J Clin Sleep Med. 2016;12(1):43-48. doi:10.5664/jcsm.5390
32. Huntley C, Kaffenberger T, Doghramji K, Soose R, Boon M. Upper airway stimulation for treatment of obstructive sleep apnea: an evaluation and comparison of outcomes at two academic centers. J Clin Sleep Med. 2017;13(9):1075-1079. Published 2017 Sep 15. doi:10.5664/jcsm.6726

33. Pordzik J, Seifen C, Ludwig K, et al. Short-term outcome of unilateral inspiration-coupled hypoglossal nerve stimulation in patients with obstructive sleep apnea. Int J Environ Res Public Health. 2022;19(24):16443. Published 2022 Dec 8. doi:10.3390/ijerph192416443
34. Heiser C, Steffen A, Hofauer B, et al. Effect of upper airway stimulation in patients with obstructive sleep apnea (EFFECT): a randomized controlled crossover trial. J Clin Med. 2021;10(13):2880. Published 2021 Jun 29. doi:10.3390/jcm1013288035.
35. Heiser C, Steffen A, Strollo PJ Jr, Giaie-Miniet C, Vanderveken OM, Hofauer B. Hypoglossal nerve stimulation versus positive airway pressure therapy for obstructive sleep apnea. Sleep Breath. 2023;27(2):693-701. doi:10.1007/s11325-022-02663-6
36. Kushida CA, Chediak A, Berry RB, et al. Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med. 2008;4(2):157-171.
37. Freedman N, Johnson K. Positive airway pressure treatment for obstructive sleep apnea. In: Kryger MH, Roth T, Goldstein CA, Dement WC, eds. Principles and Practice of Sleep Medicine. Elsevier; 2022:1260-1283.
38. Braun M, Stoerzel M, Wollny M, Schoebel C, Ulrich Sommer J, Heiser C. Patient-reported outcomes with hypoglossal nerve stimulation for treatment of obstructive sleep apnea: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2023;280(10):4627-4639. doi:10.1007/s00405-023-08062-1
39. Luxton DD, Greenburg D, Ryan J, Niven A, Wheeler G, Mysliwiec V. Prevalence and impact of short sleep duration in redeployed OIF soldiers. Sleep. 2011;34(9):1189-1195. doi:10.5665/SLEEP.1236
40. Rogers AE, Stahlman S, Hunt DJ, Oh GT, Clark LL. Obstructive sleep apnea and associated attrition, active component, U.S. Armed Forces, January 2004-May 2016. MSMR. 2016;23(10):2-11.
41. Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy. 2017 Demographics: Profile of the Military Community. US Dept of Defense;2017. Accessed April 4, 2024. http://download.militaryonesource.mil/12038/MOS/Reports/2017-demographics-report.pdf
42. Remondelli MH, Remick KN, Shackelford SA, et al. Casualty care implications of large-scale combat operations. J Trauma Acute Care Surg. 2023;95(2S Suppl 1): S180-S184. doi:10.1097/TA.0000000000004063
Obstructive sleep apnea (OSA), the repetitive collapse of posterior oropharynx during sleep resulting in hypoxia and/or arousals from sleep, is the most common form of sleep disordered breathing and a common chronic respiratory disorders among middle-aged adults. OSA can lead to significant health problems, such as worsened cardiometabolic disease and cognitive impairment, which can increase morbidity and mortality.1
The gold standard for OSA diagnosis is polysomnography (PSG), although home sleep studies can be performed for select patients. OSA diagnoses are based on the number of times per hour of sleep a patient’s airway narrows or collapses, reducing or stopping airflow, scored as hypopnea or apnea events, respectively. An Apnea-Hypopnea Index (AHI) score of 5 to 14 events/hour is considered mild OSA, 15 to 30 events/hour moderate OSA, and ≥ 30 events/hour severe OSA.2
Treatment commonly includes positive airway pressure (PAP) but more than one-half of patients are not adherent to continuous PAP (CPAP) treatment after about 90 days.3 Efficacy of treatments vary as a function of disease severity and etiology, which—in addition to the classic presentation of obesity with large neck/narrowupper airway—includes craniofacial abnormalities, altered muscle function in the upper airway, pharyngeal neuropathy, and fluid shifts to the neck.
Background
The American Academy of Sleep Medicine (AASM) estimates that 10% to 17% of adults in the United States have OSA.4 Compared with civilians, the military population generally is younger and healthier. Service members have access to regular health care with yearly physical examinations, exercise scheduled into the workday, and mandatory height/weight and fitness standards. Because obesity is a major risk factor for OSA, and the incidence of obesity is relatively low in the military population (estimated at 18.8% in 2021 vs 39.8% among all US adults aged 20 to 39 years), it might be expected that incidence of OSA would be correspondingly low.5,6 However, there is evidence of a rapidly increasing incidence of OSA in military populations. A 2021 study revealed that OSA incidence rates increased from 11 to 333 per 10,000 between 2005 and 2019 across all military branches and demographics, with the highest rate among Army personnel.7 An earlier study revealed a 600% increase in OSA incidence among Army personnel between 2003 and 2011.8
Several factors likely contributed to this increase, including expanding obesity and greater physician awareness and availability of sleep study centers. Rogers and colleagues found that 40% to 50% of incident OSA diagnoses among military personnel occur within 12 months of separation, suggesting that the secondary gains associated with military disability benefits might motivate OSA evaluation.9 It is possible that secondary gain is a factor because an OSA diagnosis can range from a 0% to 100% disability rating, depending on the severity.10 This disability claim is based on evidence that untreated OSA can negatively affect long-term health and mission readiness.8 For example, untreated OSA can lead to hypertension, which contributes to a long list of adverse health and wellness consequences. Most importantly for the military, OSA has been shown to increase daytime sleepiness and reduce cognitive performance.10
The current first-line treatment for OSA is CPAP, which improves symptoms of daytime sleepiness, hypertension management, and daytime alertness.11 Despite its efficacy, nonadherence rates range from 29% to 83%.12-15 Nonadherence factors include lifestyle changes, adverse effects (eg, nasal congestion), and lack of education on proper use.11 Lifestyle changes needed to increase the likelihood of successful therapy, such as regular sleep schedules and proper CPAP cleaning and maintenance, are difficult for military personnel because of the nature of continuous or sustained operations that might require shift work and/or around-the-clock (ie, 24-hour, 7 days a week) task performance. Traveling with CPAP is an added burden for service members deployed to combat operations (ie, added luggage, weight, maintenance). Although alternate treatments such as oral appliances (ie, custom dental devices) are available, they generally are less effective than CPAP.2 Oral appliances could be a reasonable alternative treatment for some patients who cannot manage their OSA with behavioral modifications and are intolerant or unable to effectively use CPAP. This could include patients in the military who are deployed to austere environments.
Surgically implanted hypoglossal nerve stimulator (HGNS) treatment may provide long-term health benefits to service members. After the device is implanted near the hypoglossal nerve, electrical stimulation causes the tongue to move forward, which opens the airway in the anteroposterior dimension. The most important consideration is the mechanism of airway collapse. HGNS is not effective for patients whose OSA events are caused by circumferential collapse of other airway muscles. The cause of airway collapse is ascertained before surgery with drug-induced sleep endoscopy, a procedure that allows visualization of conformational changes in the upper airway during OSA events.
The US Food and Drug Administration (FDA) approved HGNS in 2014. However, it is not considered a first-line treatment for OSA by the AASM. Original candidate criteria for HGNS included an AHI score of 15 to 65 events/hour, age ≥ 18 years, failed CPAP use, body mass index (BMI) < 32, absence of palatal complete concentric collapse, and central apneas comprising < 25% of total events.16 In June 2023, the FDA expanded approval to increase the upper limit of AHI to 100 events/hour and the BMI to < 40.17
HGNS has been reported to be effective in appropriately selected patients with OSA at tertiary care centers with established multidisciplinary sleep surgical programs. These benefits have not been confirmed in larger, community-based settings, where most of these surgeries occur. In community practice, there is significant confusion among patients and clinicians about the optimal pathway for patient selection and clinical follow-up. Many patients view HGNS as a viable alternative to CPAP, but initially do not understand that it requires surgery. Surgical treatments for OSA, such as HGNS, are appealing because they suggest a 1-time intervention that permanently treats the condition, without need for follow-up or equipment resupply. HGNS might be an appealing treatment option because it is less obtrusive than CPAP and requires fewer resources for set-up and maintenance. Also, it does not cause skin irritation (a possible adverse effect of nightly use of a CPAP mask), allows the individual to sleep in a variety of positions, has less impact on social and sex life, and does not require an electric outlet. In the long term, HGNS might be more cost effective because there is no yearly physician follow-up or equipment resupply and/or maintenance.
The military population has specific demands that impact delivery and effectiveness of health care. Among service members with OSA, CPAP treatment can be challenging because of low adherence, required annual follow-up despite frequent moving cycles that pose a challenge for care continuity, and duty limitations for affected service members (ie, the requirement for a waiver to deploy and potential medical separation if symptoms are not adequately controlled). As the incidence of OSA continues to increase among service members, so does the need for OSA treatment options that are efficacious as CPAP but better tolerated and more suitable for use during military operations. The aim of this review is to assess the effectiveness of HGNS and its potential use by the military OSA patient population.
METHODS
To identify eligible studies, we employed PICOS: Population (patients aged ≥ 18 years with a history of OSA), Intervention (HGNS), Comparator (standard of care PAP therapy), Outcome (AHI or Epworth Sleepiness Scale [ESS], and Study (randomized control trial [RCT] or clinical trial). Studies were excluded if they were not written in English or included pediatric populations. The ESS is a subjective rating scale used to determine and quantify a patient’s level of daytime sleepiness, using a 4-point scale for the likelihood of falling asleep totaled across 8 different situations.18 Daytime sleepiness is considered lower normal(0-5 points), higher normal (6-10 points), mild or moderate excessive (11-15 points), and severe excessive (16-24 points).
Literature Search
We conducted a review of PubMed and Scopus for RCTs and controlled trials published from 2013 to 2023 that included the keywords and phrases: obstructive sleep apnea and either hypoglossal nerve stimulation or upper airway stimulation. The final literature search was performed December 8, 2023.
Two authors independently assessed the titles and abstracts of studies identified in the literature search based on the predefined inclusion criteria. If it was not clear whether an article met inclusion criteria based on its title and/or abstract, the 2 review authors assessed the full text of study and resolved any disagreement through consensus. If consensus was not obtained, a third author was consulted. No duplicates were identified. The PRISMA study selection process is presented in the Figure.
Data extraction was performed by 1 independent reviewer. A second author reviewed the extracted data. Any identified discrepancies were resolved through discussion and consensus. If consensus was not obtained, a third author was consulted. Study data included methods (study design and study objective), participants mean age, inclusion criteria, exclusion criteria, interventions and comparators, and primary study outcomes.
The quality of evidence was assessed using a rating of 1 to 5 based on a modified version of the Oxford Centre for Evidence-based Medicine Levels of Evidence and Grades of Recommendation.19 A rating of 1 indicated a properly powered and conducted RCT, 2 demonstrated a well-designed controlled trial without randomization or prospective comparative cohort trial, 3 designated a case-control study or retrospective cohort study, 4 signified a case series with or without intervention or a cross-sectional study, and 5 denoted an opinion of respected authorities or case reports. Two reviewers independently evaluated the quality of evidence. Any identified discrepancies were resolved through discussion and consensus. If consensus was not obtained, a third review author was consulted.
RESULTS
We identified 30 studies; 19 articles did not meet inclusion criteria. The remaining 11 articles were divided into 4 cohorts. Five articles were based on data from the STAR trial, a multicenter study that included adults with moderate-to-severe OSA and inadequate adherence to CPAP.20-24 Four articles used the same patient selection criteria as the STAR trial for a long-term German postmarket study of upper airway stimulation efficacy with OSA.25-28 The third and fourth cohorts each consist of 31 patients with moderate-to-severe OSA with CPAP nonadherence or failure.29,30 The STAR trial included follow-up at 5 years, and the German-postmarket had a follow-up at3 years. The remaining 2 cohorts have 1-year follow-ups.
The Scopus review identified 304 studies; 299 did not meet inclusion criteria and 1 was part of the STAR trial.31 The remaining 4 articles were classified as distinct cohorts. Huntley and colleagues included patients from Thomas Jefferson University (TJU) and University of Pittsburgh (UP) academic medical centers.32 The Pordzik and colleagues cohort received implantation at a tertiary medical center, an RCCT, and a 1:1 comparator trial (Table 1).33-35
STAR Trial
This multicenter, prospective, single-group cohort study was conducted in the US, Germany, Belgium, Netherlands, and France. The STAR trial included 126 patients who were not CPAP therapy adherent. Patients were excluded if they had AHI < 20 or > 50, central sleep apnea > 25% of total AHI, anatomical abnormalities that prevent effective assessment of upper-airway stimulation, complete concentric collapse of the retropalatal airway during drug-induced sleep, neuromuscular disease, hypoglossal-nerve palsy, severe restrictive or obstructive pulmonary disease, moderate-to-severe pulmonary arterial hypertension, severe valvular heart disease, New York Heart Association class III or IV heart failure, recent myocardial infarction or severe cardiac arrhythmias (within the past 6 months), persistent uncontrolled hypertension despite medication use, active psychiatric illness, or coexisting nonrespiratory sleep disorders that would confound functional sleep assessment. Primary outcome measures included the AHI and oxygen desaturation index (ODI) with secondary outcomes using the ESS, the Functional Outcomes of Sleep Questionnaire (FOSQ), and the percentage of sleep time with oxygen saturation < 90%. Of 126 patients who received implantation, 71 underwent an overnight PSG evaluation at 5-year follow-up. Mean (SD) AHI at baseline was reduced with HGNS treatment to from 32.0 (11.8) to 12.4 (16.3). Mean (SD) ESS for 92 participants with 2 measurements declined from 11.6 (5.0) at baseline to 6.9 (4.7) at 5-year follow-up.
The STAR trial included a randomized controlled withdrawal study for 46 patients who had a positive response to therapy to evaluate efficacy and durability of upper airway stimulation. Patients were randomly assigned to therapy maintenance or therapy withdrawal groups for ≥ 1 week. The short-term withdrawal effect was assessed using the original trial outcome measures and indicated that both the withdrawal and maintenance groups showed improvements at 12 months compared with the baseline. However, after the randomized withdrawal, the withdrawal group’s outcome measures deteriorated to baseline levels while the maintenance group showed no change. At 18 months of therapy, outcome measures for both groups were similar to those observed with therapy at 12 months.24 The STAR trial included self-reported outcomes at baseline, 12 months, and 24 months that used ESS to measure daytime sleepiness. These results included subsequent STAR trial reports.20-24,31
The German Postmarket Cohort
This multicenter, prospective, single-arm study used selection criteria that were based on those used in the STAR trial and included patients with moderate-to-severe OSA and nonadherence to CPAP. Patients were excluded if they had a BMI > 35, AHI < 15 or > 65; central apnea index > 25% of total AHI; or complete concentric collapse at the velopharynx during drug-induced sleep. Measured outcomes included AHI, ODI, FOSQ, and ESS. Among the 60 participants, 38 received implantation and a 3-year follow-up. Mean (SD) AHI decreased from 31.2 (13.2) at baseline to 13.1 (14.1) at follow-up, while mean (SD) ESS decreased from 12.8 (5.3) at baseline to 6.0 (3.2) at follow-up.25-28
Munich Cohort
This single-center, prospective clinical trial included patients with AHI > 15 and < 65, central apnea index < 25% of total AHI, and nonadherence to CPAP. Patients were excluded if they had a BMI > 35, anatomical abnormalities that would prevent effective assessment of upper-airway stimulation; all other exclusion criteria matched those used in the STAR trial. Among 31 patients who received implants and completed a 1-year follow-up, mean (SD) AHI decreased from 32.9 (11.2) at baseline to 7.1 (5.9) at follow-up and mean (SD) ESS decreased from 12.6 (5.6) at baseline to 5.9 (5.2) at follow-up.29
Kezirian and Colleagues Cohort
This prospective, single-arm, open-label study was conducted at 4 Australian and 4 US sites. Selection criteria included moderate-to-severe OSA with failure of CPAP, AHI of 20 to 100 with ≥ 15 events/hour occurring in sleep that was non-REM (rapid eye movement) sleep, BMI ≤ 40 (Australia) or ≤ 37 (US), and a predominance of hypopneas (≥ 80% of disordered breathing events during sleep). Patients were excluded if they had earlier upper airway surgery, markedly enlarged tonsils, uncontrolled nasal obstruction, severe retrognathia, > 5% central or mixed apneic events, incompletely treated sleep disorders other than OSA, or a major disorder of the pulmonary, cardiac, renal, or nervous systems. Data were reported for 31 patients whose mean (SD) AHI declined from 45.4 (17.5) at baseline to 25.3 (20.6) at 1-year follow-up and mean (SD) ESS score declined from 12.1 (4.6) at baseline to 7.9 (3.8) 1 year later.30
TJU and UP Cohorts
The TJU and UP cohorts are composed of patients who underwent implantation between May 2014 and August 2016 at 2 academic centers.31,32 Selection criteria was consistent with that used in the STAR trial, and patients completed postoperative titration PSG and outpatient follow-up (48 patients at TJU and 49 at UP). Primary outcomes included AHI, ESS, and O2 nadir. Secondary outcomes consisted of surgical success and percentage of patients tolerating optimal titration setting at follow-up. Postoperative outcomes were assessed during the titration PSG. Time from initial ESS to postoperative PSG at TJU was 1.7 years and at UP was 1.9 years. Time from initial AHI to postoperative PSG at TJU was 90.4 days and 85.2 days at UP. At TJU, mean (SD) AHI and ESS dropped from 35.9 (20.8) and 11.1 (3.8), respectively at baseline to 6.3 (11.5) and 5.8 (3.4), respectively at follow-up. At UP, mean (SD) AHI and ESS fell from 35.3 (15.3) and 10.9 (4.9), respectively at baseline to 6.3 (6.1) and 6.6 (4.5), respectively at follow-up. There were no site-related differences in rates of AHI, ESS, or surgical success.31
Pordzik and Colleagues Cohort
This cohort of 29 patients underwent implantation between February 2020 and June 2022 at a tertiary university medical center with both pre- and postoperative PSG. Selection criteria was consistent with that of the German postmarket cohort. Postoperative PSG was completed a mean (SD) 96.3 (27.0) days after device activation. Mean (SD) AHI dropped from 38.6 (12.7) preoperatively to 24.4 (13.3) postoperatively. Notably, this cohort showed a much lower decrease of postoperative AHI than reported by the STAR trial and UP/TJU cohort.33
Stimulation vs Sham Trial
This multicenter, double-blinded, randomized, crossover trial assessed the effect of HGNS (stim) vs sham stimulation (sham) in 86 patients that completed both phases of the trial. Primary outcomes included AHI and ESS. Secondary outcomes included FOSQ. No carryover effect was found during the crossover phase. The difference between the phases was−15.5 (95% CI, −18.3 to −12.8) for AHI and −3.3 (95% CI, −4.4 to −2.2) for ESS.34
Comparator
The comparator study used propensity score matching to compare outcomes of HGNS and PAP therapy. Primary outcomes included sleepiness, AHI, and effectiveness with outcome measures of AHI and ESS collected at baseline and 12 months postimplantation. The article reported that 126 of 227 patients were matched 1:1. Both groups showed improvement in AHI and ESS. Mean (SD) AHI for the HGNS group at baseline started at 33.9 (15.1) and decreased to 8.1 (6.3). Mean (SD) ESS for the HGNS group at baseline was 15.4 (3.5) and decreased to 7.5 (4.7). In the PAP comparator group, mean (SD) baseline AHI was 36.8 (21.6) and at follow-up was 6.6 (8.0) and mean (SD) ESS was 14.6 (3.9) at baseline and 10.8 (5.6) at follow-up.35
DISCUSSION
The current clinical data on HGNS suggest that this treatment is effective in adults with moderate-to-severe OSA and effects are sustained at long-term follow-up, as measured by AHI reduction and improvements in sleep related symptoms and quality of life (Table 2). These results have been consistent across several sites.
The STAR trial included a randomized control withdrawal group, for whom HGNS treatment was withdrawn after the 12-month follow-up, and then restored at 18 months.21 This revealed that withdrawal of HGNS treatment resulted in deterioration of both objective and subjective measures of OSA and sleepiness. The beneficial effects of HGNS were restored when treatment was resumed.24 Additionally, the RCCT revealed that therapeutic stimulation via HGNS significantly reduced subjective and objective measures of OSA.34 These studies provide definitive evidence of HGNS efficacy.
Currently, a diagnosis of OSA on PAP is classified as a 50% military disability rating. This rating is based primarily on epidemiologic evidence that untreated OSA is a costly disease that leads to other chronic illnesses that increases health care utilization.9 HGNS requires an initially invasive procedure and higher upfront costs, but it could result in reduced health care use and long-term costs because of improved adherence to treatment—compared with CPAP—that results in better outcomes.
Limitations to OSA Studies
The reviewed studies have several limitations that warrant caution when determining the possible benefits of HGNS treatment. The primary limitation is the lack of active control groups, therefore precluding a direct comparison of the short- and long-term effectiveness of HGNS vs other treatments (eg, CPAP). This is especially problematic because in the reviewed studies HGNS treatment efficacy is reported as a function of the mean—and SD—percent reduction in the AHI, whereas the efficacy of CPAP treatment usually is defined in terms of “adequacy of titration” as suggested by the AASM.36 It has been reported that with CPAP treatment, 50% to 60% of OSA patients achieve AASM-defined optimal improvement of respiratory disturbance index of < 5/hour during a polysomnographic sleep recording of ≥ 15 minutes duration that includes REM sleep in the supine position.37 In most of the reviewed studies, treatment success was more liberally defined as a decrease of AHI by ≥ 50%, regardless of the resulting AHI. It is notable that among the reviewed HGNS studies, the TJU and UP cohorts achieved the best outcome in short-term follow-up of 2 months with a mean (SD) AHI of 6.3 (11.5) and 6.4 (6.1), respectively. Among those cohortsassessed at a 12-month follow-up, the Munich cohort achieved the best outcome with a mean (SD) AHI of 7.1 (5.9).
Although the metrics reported in the reviewed studies are not directly comparable, the reported findings strongly suggest that HGNS generally is less effective than CPAP. How important are these differences? With findings that HGNS “reliably produces clinically meaningful (positive) effects on daytime sleepiness, daytime functioning, and sleep quality,” does it really matter if the outcome metrics for HGNS are a little less positive than those produced by CPAP?38 For individual military OSA patients the answer is yes. This is because in military operational environments—especially during deployment—sleep restriction is nearly ubiquitous, therefore any mild residual deficits in sleep quality and daytime alertness resulting from nominally adequate, but suboptimal OSA treatment, could be exacerbated by sleep restriction, therefore placing the service member and the mission at increased risk.39
Another limitation is the narrow inclusion criteria these studies employed, which limits the generalizability of the findings. Participants in the reviewed clinical trials were selected from a patient population that was mostly middle-aged, White, and obese or overweight. In a Medical Surveillance Monthly Report study, OSA was found to be highest among service members aged > 40 years, male, obese, and Black/non-Hispanic (although it should be noted that more than one-half of enlisted service members aged ≤ 25 years).40,41 Obesity has been noted as a growing concern for the military as the military population is beginning to mirror the civilian population in terms of being overweight or obese despite height and weight standards. HGNS might not be as successful in military populations with different demographics. Moreover, HGNS has been shown to have greater AHI reduction among those with higher BMI.30 Although obese service members have a 6-fold higher 12-year incidence rate of OSA than service members without obesity, this nevertheless suggests that general level of HGNS efficacy might be lower among the military patient population, because obesity is less prevalent in the military than the general population.9
Ethnicity has been found to be a relevant factor, with the highest incidence rate of OSA among non-Hispanic Black males, a demographic that was underrepresented in cohorts included in this review. Further studies will be needed to determine the extent to which findings from HGNS treatment studies are generalizable to the broader OSA patient population.
HGNS Implementation Challenges
Current impediments to widespread use of HGNS as an OSA treatment include no standardized guidance for titration and follow-on care, which varies based on the resources available. Titrating a new device for HGNS requires experienced sleep technicians who have close relationships with device representatives and can troubleshoot problems. Technical expertise, which currently is rare, is required if there are complications after placement or if adjustments to voltage settings are needed over time. In addition, patients may require multiple specialists making it easy to get lost to follow-up after implantation. This is particularly challenging in a transient community, such as the military, because there is no guarantee that a service member will have access to the same specialty care at the next duty station.
Although some evidence suggests that HGNS is a viable alternative treatment for some patients with OSA, the generalizability of these findings to the military patient population is unclear. Specialized facilities and expertise are needed for the surgical procedure and follow-up requirements, which currently constitute significant logistical constraints. As with any implantable device, there is a risk of complications including infection that could result in medical evacuation from a theater of operations. If the device malfunctions or loses effectiveness in a deployed environment, the service member might not have immediate access to medical support, potentially leading to undertreatment of OSA. In future battlefield scenarios in multidomain operations, prolonged, far-forward field care will become the new normal because the military is not expected to have air superiority or the ability to quickly evacuate service members to a higher level of medical care.42
In deployed environments, the potential limitations of HGNS become increasingly risky for the service member and the overall mission. Considering these factors, it will be important to evaluate the practicality of HGNS as a treatment option in military populations. Military-specific challenges associated with HGNS that require further study, include guidance for patient selection outside academic centers, guidance on long-term postsurgical care and device maintenance, duty limitation and military retention considerations, and limitations in training and combat environments. The military medical community needs to conduct its own studies in appropriately selected service members to guide clinical practice.
CONCLUSIONS
HGNS treatment results in improvement of both AHI and ESS scores and could be a deployable treatment option for military patients with OSA. However, HGNS has not been found to be as effective as CPAP, although the current literature is limited by small sample sizes, homogeneous populations that do not reflect the demographics of the military, and mostly short follow-up periods. Future studies should be focused on collecting data on HGNS from demographic groups that are more representative of the military OSA patient population and identifying the subpopulation of patients who derive the greatest benefit from HGNS, so that this treatment can be better individually targeted. Until data on existing military patients is published, it is not possible to fully weigh risks and benefits in this population and generalize civilian guidance to the military.
Obstructive sleep apnea (OSA), the repetitive collapse of posterior oropharynx during sleep resulting in hypoxia and/or arousals from sleep, is the most common form of sleep disordered breathing and a common chronic respiratory disorders among middle-aged adults. OSA can lead to significant health problems, such as worsened cardiometabolic disease and cognitive impairment, which can increase morbidity and mortality.1
The gold standard for OSA diagnosis is polysomnography (PSG), although home sleep studies can be performed for select patients. OSA diagnoses are based on the number of times per hour of sleep a patient’s airway narrows or collapses, reducing or stopping airflow, scored as hypopnea or apnea events, respectively. An Apnea-Hypopnea Index (AHI) score of 5 to 14 events/hour is considered mild OSA, 15 to 30 events/hour moderate OSA, and ≥ 30 events/hour severe OSA.2
Treatment commonly includes positive airway pressure (PAP) but more than one-half of patients are not adherent to continuous PAP (CPAP) treatment after about 90 days.3 Efficacy of treatments vary as a function of disease severity and etiology, which—in addition to the classic presentation of obesity with large neck/narrowupper airway—includes craniofacial abnormalities, altered muscle function in the upper airway, pharyngeal neuropathy, and fluid shifts to the neck.
Background
The American Academy of Sleep Medicine (AASM) estimates that 10% to 17% of adults in the United States have OSA.4 Compared with civilians, the military population generally is younger and healthier. Service members have access to regular health care with yearly physical examinations, exercise scheduled into the workday, and mandatory height/weight and fitness standards. Because obesity is a major risk factor for OSA, and the incidence of obesity is relatively low in the military population (estimated at 18.8% in 2021 vs 39.8% among all US adults aged 20 to 39 years), it might be expected that incidence of OSA would be correspondingly low.5,6 However, there is evidence of a rapidly increasing incidence of OSA in military populations. A 2021 study revealed that OSA incidence rates increased from 11 to 333 per 10,000 between 2005 and 2019 across all military branches and demographics, with the highest rate among Army personnel.7 An earlier study revealed a 600% increase in OSA incidence among Army personnel between 2003 and 2011.8
Several factors likely contributed to this increase, including expanding obesity and greater physician awareness and availability of sleep study centers. Rogers and colleagues found that 40% to 50% of incident OSA diagnoses among military personnel occur within 12 months of separation, suggesting that the secondary gains associated with military disability benefits might motivate OSA evaluation.9 It is possible that secondary gain is a factor because an OSA diagnosis can range from a 0% to 100% disability rating, depending on the severity.10 This disability claim is based on evidence that untreated OSA can negatively affect long-term health and mission readiness.8 For example, untreated OSA can lead to hypertension, which contributes to a long list of adverse health and wellness consequences. Most importantly for the military, OSA has been shown to increase daytime sleepiness and reduce cognitive performance.10
The current first-line treatment for OSA is CPAP, which improves symptoms of daytime sleepiness, hypertension management, and daytime alertness.11 Despite its efficacy, nonadherence rates range from 29% to 83%.12-15 Nonadherence factors include lifestyle changes, adverse effects (eg, nasal congestion), and lack of education on proper use.11 Lifestyle changes needed to increase the likelihood of successful therapy, such as regular sleep schedules and proper CPAP cleaning and maintenance, are difficult for military personnel because of the nature of continuous or sustained operations that might require shift work and/or around-the-clock (ie, 24-hour, 7 days a week) task performance. Traveling with CPAP is an added burden for service members deployed to combat operations (ie, added luggage, weight, maintenance). Although alternate treatments such as oral appliances (ie, custom dental devices) are available, they generally are less effective than CPAP.2 Oral appliances could be a reasonable alternative treatment for some patients who cannot manage their OSA with behavioral modifications and are intolerant or unable to effectively use CPAP. This could include patients in the military who are deployed to austere environments.
Surgically implanted hypoglossal nerve stimulator (HGNS) treatment may provide long-term health benefits to service members. After the device is implanted near the hypoglossal nerve, electrical stimulation causes the tongue to move forward, which opens the airway in the anteroposterior dimension. The most important consideration is the mechanism of airway collapse. HGNS is not effective for patients whose OSA events are caused by circumferential collapse of other airway muscles. The cause of airway collapse is ascertained before surgery with drug-induced sleep endoscopy, a procedure that allows visualization of conformational changes in the upper airway during OSA events.
The US Food and Drug Administration (FDA) approved HGNS in 2014. However, it is not considered a first-line treatment for OSA by the AASM. Original candidate criteria for HGNS included an AHI score of 15 to 65 events/hour, age ≥ 18 years, failed CPAP use, body mass index (BMI) < 32, absence of palatal complete concentric collapse, and central apneas comprising < 25% of total events.16 In June 2023, the FDA expanded approval to increase the upper limit of AHI to 100 events/hour and the BMI to < 40.17
HGNS has been reported to be effective in appropriately selected patients with OSA at tertiary care centers with established multidisciplinary sleep surgical programs. These benefits have not been confirmed in larger, community-based settings, where most of these surgeries occur. In community practice, there is significant confusion among patients and clinicians about the optimal pathway for patient selection and clinical follow-up. Many patients view HGNS as a viable alternative to CPAP, but initially do not understand that it requires surgery. Surgical treatments for OSA, such as HGNS, are appealing because they suggest a 1-time intervention that permanently treats the condition, without need for follow-up or equipment resupply. HGNS might be an appealing treatment option because it is less obtrusive than CPAP and requires fewer resources for set-up and maintenance. Also, it does not cause skin irritation (a possible adverse effect of nightly use of a CPAP mask), allows the individual to sleep in a variety of positions, has less impact on social and sex life, and does not require an electric outlet. In the long term, HGNS might be more cost effective because there is no yearly physician follow-up or equipment resupply and/or maintenance.
The military population has specific demands that impact delivery and effectiveness of health care. Among service members with OSA, CPAP treatment can be challenging because of low adherence, required annual follow-up despite frequent moving cycles that pose a challenge for care continuity, and duty limitations for affected service members (ie, the requirement for a waiver to deploy and potential medical separation if symptoms are not adequately controlled). As the incidence of OSA continues to increase among service members, so does the need for OSA treatment options that are efficacious as CPAP but better tolerated and more suitable for use during military operations. The aim of this review is to assess the effectiveness of HGNS and its potential use by the military OSA patient population.
METHODS
To identify eligible studies, we employed PICOS: Population (patients aged ≥ 18 years with a history of OSA), Intervention (HGNS), Comparator (standard of care PAP therapy), Outcome (AHI or Epworth Sleepiness Scale [ESS], and Study (randomized control trial [RCT] or clinical trial). Studies were excluded if they were not written in English or included pediatric populations. The ESS is a subjective rating scale used to determine and quantify a patient’s level of daytime sleepiness, using a 4-point scale for the likelihood of falling asleep totaled across 8 different situations.18 Daytime sleepiness is considered lower normal(0-5 points), higher normal (6-10 points), mild or moderate excessive (11-15 points), and severe excessive (16-24 points).
Literature Search
We conducted a review of PubMed and Scopus for RCTs and controlled trials published from 2013 to 2023 that included the keywords and phrases: obstructive sleep apnea and either hypoglossal nerve stimulation or upper airway stimulation. The final literature search was performed December 8, 2023.
Two authors independently assessed the titles and abstracts of studies identified in the literature search based on the predefined inclusion criteria. If it was not clear whether an article met inclusion criteria based on its title and/or abstract, the 2 review authors assessed the full text of study and resolved any disagreement through consensus. If consensus was not obtained, a third author was consulted. No duplicates were identified. The PRISMA study selection process is presented in the Figure.
Data extraction was performed by 1 independent reviewer. A second author reviewed the extracted data. Any identified discrepancies were resolved through discussion and consensus. If consensus was not obtained, a third author was consulted. Study data included methods (study design and study objective), participants mean age, inclusion criteria, exclusion criteria, interventions and comparators, and primary study outcomes.
The quality of evidence was assessed using a rating of 1 to 5 based on a modified version of the Oxford Centre for Evidence-based Medicine Levels of Evidence and Grades of Recommendation.19 A rating of 1 indicated a properly powered and conducted RCT, 2 demonstrated a well-designed controlled trial without randomization or prospective comparative cohort trial, 3 designated a case-control study or retrospective cohort study, 4 signified a case series with or without intervention or a cross-sectional study, and 5 denoted an opinion of respected authorities or case reports. Two reviewers independently evaluated the quality of evidence. Any identified discrepancies were resolved through discussion and consensus. If consensus was not obtained, a third review author was consulted.
RESULTS
We identified 30 studies; 19 articles did not meet inclusion criteria. The remaining 11 articles were divided into 4 cohorts. Five articles were based on data from the STAR trial, a multicenter study that included adults with moderate-to-severe OSA and inadequate adherence to CPAP.20-24 Four articles used the same patient selection criteria as the STAR trial for a long-term German postmarket study of upper airway stimulation efficacy with OSA.25-28 The third and fourth cohorts each consist of 31 patients with moderate-to-severe OSA with CPAP nonadherence or failure.29,30 The STAR trial included follow-up at 5 years, and the German-postmarket had a follow-up at3 years. The remaining 2 cohorts have 1-year follow-ups.
The Scopus review identified 304 studies; 299 did not meet inclusion criteria and 1 was part of the STAR trial.31 The remaining 4 articles were classified as distinct cohorts. Huntley and colleagues included patients from Thomas Jefferson University (TJU) and University of Pittsburgh (UP) academic medical centers.32 The Pordzik and colleagues cohort received implantation at a tertiary medical center, an RCCT, and a 1:1 comparator trial (Table 1).33-35
STAR Trial
This multicenter, prospective, single-group cohort study was conducted in the US, Germany, Belgium, Netherlands, and France. The STAR trial included 126 patients who were not CPAP therapy adherent. Patients were excluded if they had AHI < 20 or > 50, central sleep apnea > 25% of total AHI, anatomical abnormalities that prevent effective assessment of upper-airway stimulation, complete concentric collapse of the retropalatal airway during drug-induced sleep, neuromuscular disease, hypoglossal-nerve palsy, severe restrictive or obstructive pulmonary disease, moderate-to-severe pulmonary arterial hypertension, severe valvular heart disease, New York Heart Association class III or IV heart failure, recent myocardial infarction or severe cardiac arrhythmias (within the past 6 months), persistent uncontrolled hypertension despite medication use, active psychiatric illness, or coexisting nonrespiratory sleep disorders that would confound functional sleep assessment. Primary outcome measures included the AHI and oxygen desaturation index (ODI) with secondary outcomes using the ESS, the Functional Outcomes of Sleep Questionnaire (FOSQ), and the percentage of sleep time with oxygen saturation < 90%. Of 126 patients who received implantation, 71 underwent an overnight PSG evaluation at 5-year follow-up. Mean (SD) AHI at baseline was reduced with HGNS treatment to from 32.0 (11.8) to 12.4 (16.3). Mean (SD) ESS for 92 participants with 2 measurements declined from 11.6 (5.0) at baseline to 6.9 (4.7) at 5-year follow-up.
The STAR trial included a randomized controlled withdrawal study for 46 patients who had a positive response to therapy to evaluate efficacy and durability of upper airway stimulation. Patients were randomly assigned to therapy maintenance or therapy withdrawal groups for ≥ 1 week. The short-term withdrawal effect was assessed using the original trial outcome measures and indicated that both the withdrawal and maintenance groups showed improvements at 12 months compared with the baseline. However, after the randomized withdrawal, the withdrawal group’s outcome measures deteriorated to baseline levels while the maintenance group showed no change. At 18 months of therapy, outcome measures for both groups were similar to those observed with therapy at 12 months.24 The STAR trial included self-reported outcomes at baseline, 12 months, and 24 months that used ESS to measure daytime sleepiness. These results included subsequent STAR trial reports.20-24,31
The German Postmarket Cohort
This multicenter, prospective, single-arm study used selection criteria that were based on those used in the STAR trial and included patients with moderate-to-severe OSA and nonadherence to CPAP. Patients were excluded if they had a BMI > 35, AHI < 15 or > 65; central apnea index > 25% of total AHI; or complete concentric collapse at the velopharynx during drug-induced sleep. Measured outcomes included AHI, ODI, FOSQ, and ESS. Among the 60 participants, 38 received implantation and a 3-year follow-up. Mean (SD) AHI decreased from 31.2 (13.2) at baseline to 13.1 (14.1) at follow-up, while mean (SD) ESS decreased from 12.8 (5.3) at baseline to 6.0 (3.2) at follow-up.25-28
Munich Cohort
This single-center, prospective clinical trial included patients with AHI > 15 and < 65, central apnea index < 25% of total AHI, and nonadherence to CPAP. Patients were excluded if they had a BMI > 35, anatomical abnormalities that would prevent effective assessment of upper-airway stimulation; all other exclusion criteria matched those used in the STAR trial. Among 31 patients who received implants and completed a 1-year follow-up, mean (SD) AHI decreased from 32.9 (11.2) at baseline to 7.1 (5.9) at follow-up and mean (SD) ESS decreased from 12.6 (5.6) at baseline to 5.9 (5.2) at follow-up.29
Kezirian and Colleagues Cohort
This prospective, single-arm, open-label study was conducted at 4 Australian and 4 US sites. Selection criteria included moderate-to-severe OSA with failure of CPAP, AHI of 20 to 100 with ≥ 15 events/hour occurring in sleep that was non-REM (rapid eye movement) sleep, BMI ≤ 40 (Australia) or ≤ 37 (US), and a predominance of hypopneas (≥ 80% of disordered breathing events during sleep). Patients were excluded if they had earlier upper airway surgery, markedly enlarged tonsils, uncontrolled nasal obstruction, severe retrognathia, > 5% central or mixed apneic events, incompletely treated sleep disorders other than OSA, or a major disorder of the pulmonary, cardiac, renal, or nervous systems. Data were reported for 31 patients whose mean (SD) AHI declined from 45.4 (17.5) at baseline to 25.3 (20.6) at 1-year follow-up and mean (SD) ESS score declined from 12.1 (4.6) at baseline to 7.9 (3.8) 1 year later.30
TJU and UP Cohorts
The TJU and UP cohorts are composed of patients who underwent implantation between May 2014 and August 2016 at 2 academic centers.31,32 Selection criteria was consistent with that used in the STAR trial, and patients completed postoperative titration PSG and outpatient follow-up (48 patients at TJU and 49 at UP). Primary outcomes included AHI, ESS, and O2 nadir. Secondary outcomes consisted of surgical success and percentage of patients tolerating optimal titration setting at follow-up. Postoperative outcomes were assessed during the titration PSG. Time from initial ESS to postoperative PSG at TJU was 1.7 years and at UP was 1.9 years. Time from initial AHI to postoperative PSG at TJU was 90.4 days and 85.2 days at UP. At TJU, mean (SD) AHI and ESS dropped from 35.9 (20.8) and 11.1 (3.8), respectively at baseline to 6.3 (11.5) and 5.8 (3.4), respectively at follow-up. At UP, mean (SD) AHI and ESS fell from 35.3 (15.3) and 10.9 (4.9), respectively at baseline to 6.3 (6.1) and 6.6 (4.5), respectively at follow-up. There were no site-related differences in rates of AHI, ESS, or surgical success.31
Pordzik and Colleagues Cohort
This cohort of 29 patients underwent implantation between February 2020 and June 2022 at a tertiary university medical center with both pre- and postoperative PSG. Selection criteria was consistent with that of the German postmarket cohort. Postoperative PSG was completed a mean (SD) 96.3 (27.0) days after device activation. Mean (SD) AHI dropped from 38.6 (12.7) preoperatively to 24.4 (13.3) postoperatively. Notably, this cohort showed a much lower decrease of postoperative AHI than reported by the STAR trial and UP/TJU cohort.33
Stimulation vs Sham Trial
This multicenter, double-blinded, randomized, crossover trial assessed the effect of HGNS (stim) vs sham stimulation (sham) in 86 patients that completed both phases of the trial. Primary outcomes included AHI and ESS. Secondary outcomes included FOSQ. No carryover effect was found during the crossover phase. The difference between the phases was−15.5 (95% CI, −18.3 to −12.8) for AHI and −3.3 (95% CI, −4.4 to −2.2) for ESS.34
Comparator
The comparator study used propensity score matching to compare outcomes of HGNS and PAP therapy. Primary outcomes included sleepiness, AHI, and effectiveness with outcome measures of AHI and ESS collected at baseline and 12 months postimplantation. The article reported that 126 of 227 patients were matched 1:1. Both groups showed improvement in AHI and ESS. Mean (SD) AHI for the HGNS group at baseline started at 33.9 (15.1) and decreased to 8.1 (6.3). Mean (SD) ESS for the HGNS group at baseline was 15.4 (3.5) and decreased to 7.5 (4.7). In the PAP comparator group, mean (SD) baseline AHI was 36.8 (21.6) and at follow-up was 6.6 (8.0) and mean (SD) ESS was 14.6 (3.9) at baseline and 10.8 (5.6) at follow-up.35
DISCUSSION
The current clinical data on HGNS suggest that this treatment is effective in adults with moderate-to-severe OSA and effects are sustained at long-term follow-up, as measured by AHI reduction and improvements in sleep related symptoms and quality of life (Table 2). These results have been consistent across several sites.
The STAR trial included a randomized control withdrawal group, for whom HGNS treatment was withdrawn after the 12-month follow-up, and then restored at 18 months.21 This revealed that withdrawal of HGNS treatment resulted in deterioration of both objective and subjective measures of OSA and sleepiness. The beneficial effects of HGNS were restored when treatment was resumed.24 Additionally, the RCCT revealed that therapeutic stimulation via HGNS significantly reduced subjective and objective measures of OSA.34 These studies provide definitive evidence of HGNS efficacy.
Currently, a diagnosis of OSA on PAP is classified as a 50% military disability rating. This rating is based primarily on epidemiologic evidence that untreated OSA is a costly disease that leads to other chronic illnesses that increases health care utilization.9 HGNS requires an initially invasive procedure and higher upfront costs, but it could result in reduced health care use and long-term costs because of improved adherence to treatment—compared with CPAP—that results in better outcomes.
Limitations to OSA Studies
The reviewed studies have several limitations that warrant caution when determining the possible benefits of HGNS treatment. The primary limitation is the lack of active control groups, therefore precluding a direct comparison of the short- and long-term effectiveness of HGNS vs other treatments (eg, CPAP). This is especially problematic because in the reviewed studies HGNS treatment efficacy is reported as a function of the mean—and SD—percent reduction in the AHI, whereas the efficacy of CPAP treatment usually is defined in terms of “adequacy of titration” as suggested by the AASM.36 It has been reported that with CPAP treatment, 50% to 60% of OSA patients achieve AASM-defined optimal improvement of respiratory disturbance index of < 5/hour during a polysomnographic sleep recording of ≥ 15 minutes duration that includes REM sleep in the supine position.37 In most of the reviewed studies, treatment success was more liberally defined as a decrease of AHI by ≥ 50%, regardless of the resulting AHI. It is notable that among the reviewed HGNS studies, the TJU and UP cohorts achieved the best outcome in short-term follow-up of 2 months with a mean (SD) AHI of 6.3 (11.5) and 6.4 (6.1), respectively. Among those cohortsassessed at a 12-month follow-up, the Munich cohort achieved the best outcome with a mean (SD) AHI of 7.1 (5.9).
Although the metrics reported in the reviewed studies are not directly comparable, the reported findings strongly suggest that HGNS generally is less effective than CPAP. How important are these differences? With findings that HGNS “reliably produces clinically meaningful (positive) effects on daytime sleepiness, daytime functioning, and sleep quality,” does it really matter if the outcome metrics for HGNS are a little less positive than those produced by CPAP?38 For individual military OSA patients the answer is yes. This is because in military operational environments—especially during deployment—sleep restriction is nearly ubiquitous, therefore any mild residual deficits in sleep quality and daytime alertness resulting from nominally adequate, but suboptimal OSA treatment, could be exacerbated by sleep restriction, therefore placing the service member and the mission at increased risk.39
Another limitation is the narrow inclusion criteria these studies employed, which limits the generalizability of the findings. Participants in the reviewed clinical trials were selected from a patient population that was mostly middle-aged, White, and obese or overweight. In a Medical Surveillance Monthly Report study, OSA was found to be highest among service members aged > 40 years, male, obese, and Black/non-Hispanic (although it should be noted that more than one-half of enlisted service members aged ≤ 25 years).40,41 Obesity has been noted as a growing concern for the military as the military population is beginning to mirror the civilian population in terms of being overweight or obese despite height and weight standards. HGNS might not be as successful in military populations with different demographics. Moreover, HGNS has been shown to have greater AHI reduction among those with higher BMI.30 Although obese service members have a 6-fold higher 12-year incidence rate of OSA than service members without obesity, this nevertheless suggests that general level of HGNS efficacy might be lower among the military patient population, because obesity is less prevalent in the military than the general population.9
Ethnicity has been found to be a relevant factor, with the highest incidence rate of OSA among non-Hispanic Black males, a demographic that was underrepresented in cohorts included in this review. Further studies will be needed to determine the extent to which findings from HGNS treatment studies are generalizable to the broader OSA patient population.
HGNS Implementation Challenges
Current impediments to widespread use of HGNS as an OSA treatment include no standardized guidance for titration and follow-on care, which varies based on the resources available. Titrating a new device for HGNS requires experienced sleep technicians who have close relationships with device representatives and can troubleshoot problems. Technical expertise, which currently is rare, is required if there are complications after placement or if adjustments to voltage settings are needed over time. In addition, patients may require multiple specialists making it easy to get lost to follow-up after implantation. This is particularly challenging in a transient community, such as the military, because there is no guarantee that a service member will have access to the same specialty care at the next duty station.
Although some evidence suggests that HGNS is a viable alternative treatment for some patients with OSA, the generalizability of these findings to the military patient population is unclear. Specialized facilities and expertise are needed for the surgical procedure and follow-up requirements, which currently constitute significant logistical constraints. As with any implantable device, there is a risk of complications including infection that could result in medical evacuation from a theater of operations. If the device malfunctions or loses effectiveness in a deployed environment, the service member might not have immediate access to medical support, potentially leading to undertreatment of OSA. In future battlefield scenarios in multidomain operations, prolonged, far-forward field care will become the new normal because the military is not expected to have air superiority or the ability to quickly evacuate service members to a higher level of medical care.42
In deployed environments, the potential limitations of HGNS become increasingly risky for the service member and the overall mission. Considering these factors, it will be important to evaluate the practicality of HGNS as a treatment option in military populations. Military-specific challenges associated with HGNS that require further study, include guidance for patient selection outside academic centers, guidance on long-term postsurgical care and device maintenance, duty limitation and military retention considerations, and limitations in training and combat environments. The military medical community needs to conduct its own studies in appropriately selected service members to guide clinical practice.
CONCLUSIONS
HGNS treatment results in improvement of both AHI and ESS scores and could be a deployable treatment option for military patients with OSA. However, HGNS has not been found to be as effective as CPAP, although the current literature is limited by small sample sizes, homogeneous populations that do not reflect the demographics of the military, and mostly short follow-up periods. Future studies should be focused on collecting data on HGNS from demographic groups that are more representative of the military OSA patient population and identifying the subpopulation of patients who derive the greatest benefit from HGNS, so that this treatment can be better individually targeted. Until data on existing military patients is published, it is not possible to fully weigh risks and benefits in this population and generalize civilian guidance to the military.
1. Cumpston E, Chen P. Sleep Apnea Syndrome. PubMed. Updated September 4, 2023. Published January 2024. https://www.ncbi.nlm.nih.gov/books/NBK564431/
2. American Academy of Sleep Medicine. Obstructive sleep apnea. Accessed November 27, 2023. https://aasm.org/resources/factsheets/sleepapnea.pdf
3. Cowen J, Harrison S, Thom L, et al. Use of historical remote monitoring data to determine predictors of CPAP non-compliance in patients with Osa. Sleep Breath. 2023;27(5):1899-1908. doi:10.1007/s11325-023-02806-3
4. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006-1014. doi:10.1093/aje/kws342
5. Stiegmann RA, Payne CB, Kiel MA, Stahlman SL. Increased Prevalence of Overweight and Obesity and Incidence of Prediabetes and Type 2 Diabetes During the COVID-19 Pandemic, Active Component Service Members, U.S. Armed Forces, 2018 to 2021. MSMR. 2023;30(1):11-18. Published 2023 Jan 20.
6. Adult obesity facts. Centers for Disease Control and Prevention. Updated May 17, 2022. Accessed November 27, 2023. https://www.cdc.gov/obesity/data/adult.html
7. Moore BA, Tison LM, Palacios JG, Peterson AL, Mysliwiec V. Incidence of insomnia and obstructive sleep apnea in active duty United States military service members. Sleep. 2021;44(7):zsab024. doi:10.1093/sleep/zsab024
8. Caldwell JA, Knapik JJ, Shing TL, Kardouni JR, Lieberman HR. The association of insomnia and sleep apnea with deployment and combat exposure in the entire population of US army soldiers from 1997 to 2011: a retrospective cohort investigation. Sleep. 2019;42(8):zsz112. doi:10.1093/sleep/zsz112
9. Rogers AE, Stahlman S, Hunt DJ, Oh GT, Clark LL. Obstructive sleep apnea and associated attrition, active component, U.S. Armed Forces, January 2004-May 2016. MSMR. 2016;23(10):2-11.
10. Veterans Affairs 38 C.F.R. § 4.97-13, Code 6847.
11. Shapiro GK, Shapiro CM. Factors that influence CPAP adherence: an overview. Sleep Breath. 2010;14(4):323-335. doi:10.1007/s11325-010-0391-y
12. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173-178. doi:10.1513/pats.200708-119mg
13. Sin DD, Mayers I, Man GCW, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430-435. doi:10.1378/chest.121.2.430
14. Nowak C, Bourgin P, Portier F, Genty E, Escourrou P, Bobin S. Obstruction nasale et compliance à la ventilation nasale à pression positive [Nasal obstruction and compliance to nasal positive airway pressure]. Ann Otolaryngol Chir Cervicofac. 2003;120(3):161-166.
15. Brin YS, Reuveni H, Greenberg S, Tal A, Tarasiuk A. Determinants affecting initiation of continuous positive airway pressure treatment. Isr Med Assoc J. 2005;7(1):13-18.
16. Suurna MV, Jacobowitz O, Chang J, et al. Improving outcomes of hypoglossal nerve stimulation therapy: current practice, future directions, and research gaps. Proceedings of the 2019 International Sleep Surgery Society Research Forum. J Clin Sleep Med. 2021;17(12):2477-2487. doi:10.5664/jcsm.9542
17. Inspire Medical Systems, Inc. Announces FDA approval for apnea hypopnea index indication expansion and increased body mass index labeling. Inspire Medical Systems, Inc. Accessed July 14, 2023. https://investors.inspiresleep.com/investors/press-releases/press-release-details/2023/Inspire-Medical-Systems-Inc.-Announces-FDA-Approval-for-Apnea-Hypopnea-Index-Indication-Expansion-and-Increased-Body-Mass-Index-Labeling/default.aspx
18. Lapin BR, Bena JF, Walia HK, Moul DE. The Epworth Sleepiness Scale: Validation of one-dimensional factor structure in a large clinical sample. J Clin Sleep Med. 2018;14(08):1293-1301. Published 2018 Aug 15. doi:10.5664/jcsm.7258
19. The Centre for Evidence-Based Medicine. November 25, 2020. http://www.cebm.net/index.aspx?o=5653
20. Strollo PJ Jr, Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370(2):139-149. doi:10.1056/NEJMoa1308659
21. Strollo PJ Jr, Gillespie MB, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: durability of the treatment effect at 18 months. Sleep. 2015;38(10):1593-1598. Published 2015 Oct 1. doi:10.5665/sleep.5054
22. Woodson BT, Soose RJ, Gillespie MB, et al. Three-year outcomes of cranial nerve stimulation for obstructive sleep apnea: the STAR trial. Otolaryngol Head Neck Surg. 2016;154(1):181-188. doi:10.1177/0194599815616618
23. Woodson BT, Strohl KP, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: 5-year outcomes. Otolaryngol Head Neck Surg. 2018;159(1):194-202. doi:10.1177/0194599818762383
24. Woodson BT, Gillespie MB, Soose RJ, et al. Randomized controlled withdrawal study of upper airway stimulation on OSA: short- and long-term effect. Otolaryngol Head Neck Surg. 2014;151(5):880-887. doi:10.1177/0194599814544445
25. Heiser C, Maurer JT, Hofauer B, Sommer JU, Seitz A, Steffen A. Outcomes of upper airway stimulation for obstructive sleep apnea in a multicenter German postmarket study. Otolaryngol Head Neck Surg. 2017;156(2):378-384. doi:10.1177/0194599816683378
26. Steffen A, Sommer JU, Hofauer B, Maurer JT, Hasselbacher K, Heiser C. Outcome after one year of upper airway stimulation for obstructive sleep apnea in a multicenter German post-market study. Laryngoscope. 2018;128(2):509-515. doi:10.1002/lary.26688
27. Steffen A, Sommer UJ, Maurer JT, Abrams N, Hofauer B, Heiser C. Long-term follow-up of the German post-market study for upper airway stimulation for obstructive sleep apnea. Sleep Breath. 2020;24(3):979-984. doi:10.1007/s11325-019-01933-028.
28. Hasselbacher K, Hofauer B, Maurer JT, Heiser C, Steffen A, Sommer JU. Patient-reported outcome: results of the multicenter German post-market study. Eur Arch Otorhinolaryngol. 2018;275(7):1913-1919. doi:10.1007/s00405-018-5017-129.
29. Heiser C, Knopf A, Bas M, Gahleitner C, Hofauer B. Selective upper airway stimulation for obstructive sleep apnea: a single center clinical experience. Eur Arch Otorhinolaryngol. 2017;274(3):1727-1734. doi:10.1007/s00405-016-4297-6
30. Kezirian EJ, Goding GS Jr, Malhotra A, et al. Hypoglossal nerve stimulation improves obstructive sleep apnea: 12-month outcomes. J Sleep Res. 2014;23(1):77-83. doi:10.1111/jsr.12079
31. Soose RJ, Woodson BT, Gillespie MB, et al. Upper airway stimulation for obstructive sleep apnea: self-reported outcomes at 24 months. J Clin Sleep Med. 2016;12(1):43-48. doi:10.5664/jcsm.5390
32. Huntley C, Kaffenberger T, Doghramji K, Soose R, Boon M. Upper airway stimulation for treatment of obstructive sleep apnea: an evaluation and comparison of outcomes at two academic centers. J Clin Sleep Med. 2017;13(9):1075-1079. Published 2017 Sep 15. doi:10.5664/jcsm.6726

33. Pordzik J, Seifen C, Ludwig K, et al. Short-term outcome of unilateral inspiration-coupled hypoglossal nerve stimulation in patients with obstructive sleep apnea. Int J Environ Res Public Health. 2022;19(24):16443. Published 2022 Dec 8. doi:10.3390/ijerph192416443
34. Heiser C, Steffen A, Hofauer B, et al. Effect of upper airway stimulation in patients with obstructive sleep apnea (EFFECT): a randomized controlled crossover trial. J Clin Med. 2021;10(13):2880. Published 2021 Jun 29. doi:10.3390/jcm1013288035.
35. Heiser C, Steffen A, Strollo PJ Jr, Giaie-Miniet C, Vanderveken OM, Hofauer B. Hypoglossal nerve stimulation versus positive airway pressure therapy for obstructive sleep apnea. Sleep Breath. 2023;27(2):693-701. doi:10.1007/s11325-022-02663-6
36. Kushida CA, Chediak A, Berry RB, et al. Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med. 2008;4(2):157-171.
37. Freedman N, Johnson K. Positive airway pressure treatment for obstructive sleep apnea. In: Kryger MH, Roth T, Goldstein CA, Dement WC, eds. Principles and Practice of Sleep Medicine. Elsevier; 2022:1260-1283.
38. Braun M, Stoerzel M, Wollny M, Schoebel C, Ulrich Sommer J, Heiser C. Patient-reported outcomes with hypoglossal nerve stimulation for treatment of obstructive sleep apnea: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2023;280(10):4627-4639. doi:10.1007/s00405-023-08062-1
39. Luxton DD, Greenburg D, Ryan J, Niven A, Wheeler G, Mysliwiec V. Prevalence and impact of short sleep duration in redeployed OIF soldiers. Sleep. 2011;34(9):1189-1195. doi:10.5665/SLEEP.1236
40. Rogers AE, Stahlman S, Hunt DJ, Oh GT, Clark LL. Obstructive sleep apnea and associated attrition, active component, U.S. Armed Forces, January 2004-May 2016. MSMR. 2016;23(10):2-11.
41. Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy. 2017 Demographics: Profile of the Military Community. US Dept of Defense;2017. Accessed April 4, 2024. http://download.militaryonesource.mil/12038/MOS/Reports/2017-demographics-report.pdf
42. Remondelli MH, Remick KN, Shackelford SA, et al. Casualty care implications of large-scale combat operations. J Trauma Acute Care Surg. 2023;95(2S Suppl 1): S180-S184. doi:10.1097/TA.0000000000004063
1. Cumpston E, Chen P. Sleep Apnea Syndrome. PubMed. Updated September 4, 2023. Published January 2024. https://www.ncbi.nlm.nih.gov/books/NBK564431/
2. American Academy of Sleep Medicine. Obstructive sleep apnea. Accessed November 27, 2023. https://aasm.org/resources/factsheets/sleepapnea.pdf
3. Cowen J, Harrison S, Thom L, et al. Use of historical remote monitoring data to determine predictors of CPAP non-compliance in patients with Osa. Sleep Breath. 2023;27(5):1899-1908. doi:10.1007/s11325-023-02806-3
4. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006-1014. doi:10.1093/aje/kws342
5. Stiegmann RA, Payne CB, Kiel MA, Stahlman SL. Increased Prevalence of Overweight and Obesity and Incidence of Prediabetes and Type 2 Diabetes During the COVID-19 Pandemic, Active Component Service Members, U.S. Armed Forces, 2018 to 2021. MSMR. 2023;30(1):11-18. Published 2023 Jan 20.
6. Adult obesity facts. Centers for Disease Control and Prevention. Updated May 17, 2022. Accessed November 27, 2023. https://www.cdc.gov/obesity/data/adult.html
7. Moore BA, Tison LM, Palacios JG, Peterson AL, Mysliwiec V. Incidence of insomnia and obstructive sleep apnea in active duty United States military service members. Sleep. 2021;44(7):zsab024. doi:10.1093/sleep/zsab024
8. Caldwell JA, Knapik JJ, Shing TL, Kardouni JR, Lieberman HR. The association of insomnia and sleep apnea with deployment and combat exposure in the entire population of US army soldiers from 1997 to 2011: a retrospective cohort investigation. Sleep. 2019;42(8):zsz112. doi:10.1093/sleep/zsz112
9. Rogers AE, Stahlman S, Hunt DJ, Oh GT, Clark LL. Obstructive sleep apnea and associated attrition, active component, U.S. Armed Forces, January 2004-May 2016. MSMR. 2016;23(10):2-11.
10. Veterans Affairs 38 C.F.R. § 4.97-13, Code 6847.
11. Shapiro GK, Shapiro CM. Factors that influence CPAP adherence: an overview. Sleep Breath. 2010;14(4):323-335. doi:10.1007/s11325-010-0391-y
12. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173-178. doi:10.1513/pats.200708-119mg
13. Sin DD, Mayers I, Man GCW, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430-435. doi:10.1378/chest.121.2.430
14. Nowak C, Bourgin P, Portier F, Genty E, Escourrou P, Bobin S. Obstruction nasale et compliance à la ventilation nasale à pression positive [Nasal obstruction and compliance to nasal positive airway pressure]. Ann Otolaryngol Chir Cervicofac. 2003;120(3):161-166.
15. Brin YS, Reuveni H, Greenberg S, Tal A, Tarasiuk A. Determinants affecting initiation of continuous positive airway pressure treatment. Isr Med Assoc J. 2005;7(1):13-18.
16. Suurna MV, Jacobowitz O, Chang J, et al. Improving outcomes of hypoglossal nerve stimulation therapy: current practice, future directions, and research gaps. Proceedings of the 2019 International Sleep Surgery Society Research Forum. J Clin Sleep Med. 2021;17(12):2477-2487. doi:10.5664/jcsm.9542
17. Inspire Medical Systems, Inc. Announces FDA approval for apnea hypopnea index indication expansion and increased body mass index labeling. Inspire Medical Systems, Inc. Accessed July 14, 2023. https://investors.inspiresleep.com/investors/press-releases/press-release-details/2023/Inspire-Medical-Systems-Inc.-Announces-FDA-Approval-for-Apnea-Hypopnea-Index-Indication-Expansion-and-Increased-Body-Mass-Index-Labeling/default.aspx
18. Lapin BR, Bena JF, Walia HK, Moul DE. The Epworth Sleepiness Scale: Validation of one-dimensional factor structure in a large clinical sample. J Clin Sleep Med. 2018;14(08):1293-1301. Published 2018 Aug 15. doi:10.5664/jcsm.7258
19. The Centre for Evidence-Based Medicine. November 25, 2020. http://www.cebm.net/index.aspx?o=5653
20. Strollo PJ Jr, Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370(2):139-149. doi:10.1056/NEJMoa1308659
21. Strollo PJ Jr, Gillespie MB, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: durability of the treatment effect at 18 months. Sleep. 2015;38(10):1593-1598. Published 2015 Oct 1. doi:10.5665/sleep.5054
22. Woodson BT, Soose RJ, Gillespie MB, et al. Three-year outcomes of cranial nerve stimulation for obstructive sleep apnea: the STAR trial. Otolaryngol Head Neck Surg. 2016;154(1):181-188. doi:10.1177/0194599815616618
23. Woodson BT, Strohl KP, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: 5-year outcomes. Otolaryngol Head Neck Surg. 2018;159(1):194-202. doi:10.1177/0194599818762383
24. Woodson BT, Gillespie MB, Soose RJ, et al. Randomized controlled withdrawal study of upper airway stimulation on OSA: short- and long-term effect. Otolaryngol Head Neck Surg. 2014;151(5):880-887. doi:10.1177/0194599814544445
25. Heiser C, Maurer JT, Hofauer B, Sommer JU, Seitz A, Steffen A. Outcomes of upper airway stimulation for obstructive sleep apnea in a multicenter German postmarket study. Otolaryngol Head Neck Surg. 2017;156(2):378-384. doi:10.1177/0194599816683378
26. Steffen A, Sommer JU, Hofauer B, Maurer JT, Hasselbacher K, Heiser C. Outcome after one year of upper airway stimulation for obstructive sleep apnea in a multicenter German post-market study. Laryngoscope. 2018;128(2):509-515. doi:10.1002/lary.26688
27. Steffen A, Sommer UJ, Maurer JT, Abrams N, Hofauer B, Heiser C. Long-term follow-up of the German post-market study for upper airway stimulation for obstructive sleep apnea. Sleep Breath. 2020;24(3):979-984. doi:10.1007/s11325-019-01933-028.
28. Hasselbacher K, Hofauer B, Maurer JT, Heiser C, Steffen A, Sommer JU. Patient-reported outcome: results of the multicenter German post-market study. Eur Arch Otorhinolaryngol. 2018;275(7):1913-1919. doi:10.1007/s00405-018-5017-129.
29. Heiser C, Knopf A, Bas M, Gahleitner C, Hofauer B. Selective upper airway stimulation for obstructive sleep apnea: a single center clinical experience. Eur Arch Otorhinolaryngol. 2017;274(3):1727-1734. doi:10.1007/s00405-016-4297-6
30. Kezirian EJ, Goding GS Jr, Malhotra A, et al. Hypoglossal nerve stimulation improves obstructive sleep apnea: 12-month outcomes. J Sleep Res. 2014;23(1):77-83. doi:10.1111/jsr.12079
31. Soose RJ, Woodson BT, Gillespie MB, et al. Upper airway stimulation for obstructive sleep apnea: self-reported outcomes at 24 months. J Clin Sleep Med. 2016;12(1):43-48. doi:10.5664/jcsm.5390
32. Huntley C, Kaffenberger T, Doghramji K, Soose R, Boon M. Upper airway stimulation for treatment of obstructive sleep apnea: an evaluation and comparison of outcomes at two academic centers. J Clin Sleep Med. 2017;13(9):1075-1079. Published 2017 Sep 15. doi:10.5664/jcsm.6726

33. Pordzik J, Seifen C, Ludwig K, et al. Short-term outcome of unilateral inspiration-coupled hypoglossal nerve stimulation in patients with obstructive sleep apnea. Int J Environ Res Public Health. 2022;19(24):16443. Published 2022 Dec 8. doi:10.3390/ijerph192416443
34. Heiser C, Steffen A, Hofauer B, et al. Effect of upper airway stimulation in patients with obstructive sleep apnea (EFFECT): a randomized controlled crossover trial. J Clin Med. 2021;10(13):2880. Published 2021 Jun 29. doi:10.3390/jcm1013288035.
35. Heiser C, Steffen A, Strollo PJ Jr, Giaie-Miniet C, Vanderveken OM, Hofauer B. Hypoglossal nerve stimulation versus positive airway pressure therapy for obstructive sleep apnea. Sleep Breath. 2023;27(2):693-701. doi:10.1007/s11325-022-02663-6
36. Kushida CA, Chediak A, Berry RB, et al. Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med. 2008;4(2):157-171.
37. Freedman N, Johnson K. Positive airway pressure treatment for obstructive sleep apnea. In: Kryger MH, Roth T, Goldstein CA, Dement WC, eds. Principles and Practice of Sleep Medicine. Elsevier; 2022:1260-1283.
38. Braun M, Stoerzel M, Wollny M, Schoebel C, Ulrich Sommer J, Heiser C. Patient-reported outcomes with hypoglossal nerve stimulation for treatment of obstructive sleep apnea: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2023;280(10):4627-4639. doi:10.1007/s00405-023-08062-1
39. Luxton DD, Greenburg D, Ryan J, Niven A, Wheeler G, Mysliwiec V. Prevalence and impact of short sleep duration in redeployed OIF soldiers. Sleep. 2011;34(9):1189-1195. doi:10.5665/SLEEP.1236
40. Rogers AE, Stahlman S, Hunt DJ, Oh GT, Clark LL. Obstructive sleep apnea and associated attrition, active component, U.S. Armed Forces, January 2004-May 2016. MSMR. 2016;23(10):2-11.
41. Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy. 2017 Demographics: Profile of the Military Community. US Dept of Defense;2017. Accessed April 4, 2024. http://download.militaryonesource.mil/12038/MOS/Reports/2017-demographics-report.pdf
42. Remondelli MH, Remick KN, Shackelford SA, et al. Casualty care implications of large-scale combat operations. J Trauma Acute Care Surg. 2023;95(2S Suppl 1): S180-S184. doi:10.1097/TA.0000000000004063
Could a Fungal Infection Cause a Future Pandemic?
The principle of resilience and survival is crucial for medically significant fungi. These microorganisms are far from creating the postapocalyptic scenario depicted in TV series like The Last of Us, and much work is necessary to learn more about them. Accurate statistics on fungal infections, accompanied by clinical histories, simple laboratory tests, new antifungals, and a necessary One Health approach are lacking.
The entomopathogenic fungus Ophiocordyceps unilateralis was made notorious by the TV series, but for now, it only manages to control the brains of some ants at will. Luckily, there are no signs that fungi affecting humans are inclined to create zombies.
What is clear is that the world belongs to the kingdom of fungi and that fungi are everywhere. There are already close to 150,000 described species, but millions remain to be discovered. They abound in decomposing organic matter, soil, or animal excrement, including that of bats and pigeons. Some fungi have even managed to find a home in hospitals. Lastly, we must not forget those that establish themselves in the human microbiome.
Given such diversity, it is legitimate to ask whether any of them could be capable of generating new pandemics. Could the forgotten Cryptococcus neoformans, Aspergillus fumigatus, or Histoplasma species, among others, trigger new health emergencies on the scale of the one generated by SARS-CoV-2?
We cannot forget that a coronavirus has already confirmed that reality can surpass fiction. However, Edith Sánchez Paredes, a biologist, doctor in biomedical sciences, and specialist in medical mycology, provided a reassuring response to Medscape Spanish Edition on this point.
“That would be very difficult to see because the way fungal infections are acquired is not from person to person, in most cases,” said Dr. Sánchez Paredes, from the Mycology Unit of the Faculty of Medicine at the National Autonomous University of Mexico.
Close to 300 species have already been classified as pathogenic in humans. Although the numbers are not precise and are increasing, it is estimated that around 1,500,000 people worldwide die each year of systemic fungal infections.
“However, it is important to emphasize that establishment of an infection depends not only on the causal agent. A crucial factor is the host, in this case, the human. Generally, these types of infections will develop in individuals with some deficiency in their immune system. The more deficient the immune response, the more likely a fungal infection may occur,” stated Dr. Sánchez Paredes.
The possibility of a pandemic like the one experienced with SARS-CoV-2 in the short term is remote, but the threat posed by fungal infections persists.
In 2022, the World Health Organization (WHO) defined a priority list of pathogenic fungi, with the aim of guiding actions to control them. It is mentioned there that invasive fungal diseases are on the rise worldwide, particularly in immunocompromised populations.
“Despite the growing concern, fungal infections receive very little attention and resources, leading to a paucity of quality data on fungal disease distribution and antifungal resistance patterns. Consequently, it is impossible to estimate their exact burden,” as stated in the document.
In line with this, an article published in Mycoses in 2022 concluded that fungal infections are neglected diseases in Latin America. Among other difficulties, deficiencies in access to tests such as polymerase chain reaction or serum detection of beta-1,3-D-glucan have been reported there.
In terms of treatments, most countries encounter problems with access to liposomal amphotericin B and new azoles, such as posaconazole and isavuconazole.
“Unfortunately, in Latin America, we suffer from a poor infrastructure for diagnosing fungal infections; likewise, we have limited access to antifungals available in the global market. What’s more, we lack reliable data on the epidemiology of fungal infections in the region, so many times governments are unaware of the true extent of the problem,” said Rogelio de Jesús Treviño Rangel, PhD, a medical microbiologist and expert in clinical mycology, professor, and researcher at the Faculty of Medicine of the Autonomous University of Nuevo León in Mexico.
Need for More Medical Mycology Training
Dr. Fernando Messina is a medical mycologist with the Mycology Unit of the Francisco Javier Muñiz Infectious Diseases Hospital in Buenos Aires, Argentina. He has noted an increase in the number of cases of cryptococcosis, histoplasmosis, and aspergillosis in his daily practice.
“Particularly, pulmonary aspergillosis is steadily increasing. This is because many patients have structural lung alterations that favor the appearance of this mycosis. This is related to the increase in cases of tuberculosis and the rise in life expectancy of patients with chronic obstructive pulmonary disease or other pulmonary or systemic diseases,” Dr. Messina stated.
For Dr. Messina, the main obstacle in current clinical practice is the low level of awareness among nonspecialist physicians regarding the presence of systemic fungal infections, and because these infections are more common than realized, it is vital to consider fungal etiology before starting empirical antibiotic therapy.
“Health professionals usually do not think about mycoses because mycology occupies a very small space in medical education at universities. As the Venezuelan mycologist Gioconda Cunto de San Blas once said, ‘Mycology is the Cinderella of microbiology.’ To change this, we need to give more space to mycoses in undergraduate and postgraduate studies,” Dr. Messina asserted.
He added, “The main challenge is to train professionals with an emphasis on the clinical interpretation of cases. Current medicine has a strong trend toward molecular biology and the use of rapid diagnostic methods, without considering the clinical symptoms or the patient’s history. Determinations are very useful, but it is necessary to interpret the results.”
Dr. Messina sees it as unlikely in the short term for a pandemic to be caused by fungi, but if it were to occur, he believes it would happen in healthcare systems in regions that are not prepared in terms of infrastructure. However, as seen in the health emergency resulting from SARS-CoV-2, he thinks the impact would be mitigated by the performance of healthcare professionals.
“In general, we have the ability to adapt to any adverse situation or change — although it is clear that we need more doctors, biochemists, and microbiologists trained in mycology,” emphasized Dr. Messina.
More than 40 interns pass through Muñiz Hospital each year. They are doctors and biochemists from Argentina, other countries in the region, or even Europe, seeking to enhance their training in mycology. Regarding fungal infection laboratory work, the interest lies in learning to use traditional techniques and innovative molecular methods.
“Rapid diagnostic methods, especially the detection of circulating antigens, have marked a change in the prognosis of deep mycosis in immunocompromised hosts. The possibility of screening and monitoring in this group of patients is very important and has a great benefit,” said Gabriela Santiso, PhD, a biochemist and head of the Mycology Unit of the Francisco Javier Muñiz Infectious Diseases Hospital.
According to Dr. Santiso, the current landscape includes the ability to identify genus and species, which can help in understanding resistance to antifungals. Furthermore, conducting sensitivity tests to these drugs, using standardized commercial methods, also provides timely information for treatment.
But Dr. Santiso warns that Latin America is a vast region with great disparity in human and technological resources. Although most countries in the region have networks facilitating access to timely diagnosis, resources are generally more available in major urban centers.
This often clashes with the epidemiology of most fungal infections. “Let’s not forget that many fungal pathologies affect low-income people who have difficulties accessing health centers, which sometimes turns them into chronic diseases that are hard to treat,” Dr. Santiso pointed out.
In mycology laboratories, the biggest cost is incurred by new diagnostic tests, such as those allowing molecular identification. Conventional methods are not usually expensive, but they require time and effort to train human resources to handle them.
Because new methodologies are not always available or easily accessible throughout the region, Dr. Santiso recommended not neglecting traditional mycological techniques. “Molecular methods, rapid diagnostic methods, and conventional mycology techniques are complementary and not mutually exclusive tests. Continuous training and updating are needed in this area,” she emphasized.
Why Are Resistant Fungal Infections Becoming Increasingly Common?
The first barrier for fungi to cause infection in humans is body temperature; most of them cannot withstand 37 °C. However, they also struggle to evade the immune response that is activated when they try to enter the body.
“We are normally exposed to many of these fungi, almost all the time, but if our immune system is adequate, it may not go beyond a mild infection, in most cases subclinical, which will resolve quickly,” Dr. Sánchez Paredes stated.
However, according to Dr. Sánchez Paredes, if the immune response is weak, “the fungus will have no trouble establishing itself in our organs. Some are even part of our microbiota, such as Candida albicans, which in the face of an imbalance or immunocompromise, can lead to serious infections.”
It is clear that the population at risk for immunosuppression has increased. According to the WHO, this is due to the high prevalence of such diseases as tuberculosis, cancer, and HIV infection, among others.
But the WHO also believes that the increase in fungal infections is related to greater population access to critical care units, invasive procedures, chemotherapy, or immunotherapy treatments.
Furthermore, factors related to the fungus itself and the environment play a role. “These organisms have enzymes, proteins, and other molecules that allow them to survive in the environment in which they normally inhabit. When they face a new and stressful one, they must express other molecules that will allow them to survive. All of this helps them evade elements of the immune system, antifungals, and, of course, body temperature,” according to Dr. Sánchez Paredes.
It is possible that climate change is also behind the noticeable increase in fungal infections and that this crisis may have an even greater impact in the future. The temperature of the environment has increased, and fungi will have to adapt to the planet’s temperature, to the point where body temperature may no longer be a significant barrier for them.
Environmental changes would also be responsible for modifications in the distribution of endemic mycoses, and it is believed that fungi will more frequently find new ecological niches, be able to survive in other environments, and alter distribution zones.
This is what is happening between Mexico and the United States with coccidioidomycosis, or valley fever. “We will begin to see cases of some mycoses where they were not normally seen, so we will have to conduct more studies to confirm that the fungus is inhabiting these new areas or is simply appearing in new sites owing to migration and the great mobility of populations,” Dr. Sánchez Paredes said.
Finally, exposure to environmental factors would partly be responsible for the increasing resistance to first-line antifungals observed in these microorganisms. This seems to be the case with A. fumigatus when exposed to azoles used as fungicides in agriculture.
One Health in Fungal Infections
The increasing resistance to antifungals is a clear testament that human, animal, and environmental health are interconnected. This is why a multidisciplinary approach that adopts the perspective of One Health is necessary for its management.
“The use of fungicides in agriculture, structurally similar to the azoles used in clinics, generates resistance in Aspergillus fumigatus found in the environment. These fungi in humans can be associated with infections that do not respond to first-line treatment,” explained Carlos Arturo Álvarez, an infectious diseases physician and professor at the Faculty of Medicine at the National University of Colombia.
According to Dr. Álvarez, the approach to control them should not only focus on the search for diagnostic methods that allow early detection of antifungal resistance or research on new antifungal treatments. He believes that progress must also be made with strategies that allow for the proper use of antifungals in agriculture.
“Unfortunately, the One Health approach is not yet well implemented in the region, and in my view, there is a lack of articulation in the different sectors. That is, there is a need for true coordination between government offices of agriculture, animal and human health, academia, and international organizations. This is not happening yet, and I believe we are in the initial stage of visibility,” Dr. Álvarez opined.
Veterinary public health is another pillar of the aforementioned approach. For various reasons, animals experience a higher frequency of fungal infections. A few carry and transmit true zoonoses that affect human health, but most often, animals act only as sentinels indicating a potential source of transmission.
Carolina Segundo Zaragoza, PhD, has worked in veterinary mycology for 30 years. She currently heads the veterinary mycology laboratory at the Animal Production Teaching, Research, and Extension Center in Altiplano, under the Faculty of Veterinary Medicine and Animal Husbandry at the National Autonomous University of Mexico. Because she has frequent contact with specialists in human mycology, during her professional career she has received several patient consultations, most of which were for cutaneous mycoses.
“They detect some dermatomycosis and realize that the common factor is owning a companion animal or a production animal with which the patient has contact. Both animals and humans present the same type of lesions, and then comes the question: Who infected whom? I remind them that the main source of infection is the soil and that animals should not be blamed in the first instance,” Dr. Segundo Zaragoza clarified.
She is currently collaborating on a research project analyzing the presence of Coccidioides immitis in the soil. This pathogen is responsible for coccidioidomycosis in dogs and humans, and she sees with satisfaction how these types of initiatives, which include some components of the One Health vision, are becoming more common in Mexico.
“Fortunately, human mycologists are increasingly providing more space for the dissemination of veterinary mycology. So I have had the opportunity to be invited to different forums on medical mycology to present the clinical cases we can have in animals and talk about the research projects we carry out. I have more and more opportunities to conduct joint research with human mycologists and veterinary doctors,” she said.
Dr. Segundo Zaragoza believes that to better implement the One Health vision, standardizing the criteria for detecting, diagnosing, and treating mycoses is necessary. She considers that teamwork will be key to achieving the common goal of safeguarding the well-being and health of humans and animals.
Alarms Sound for Candida auris
The WHO included the yeast Candida auris in its group of pathogens with critical priority, and since 2009, it has raised alarm owing to the ease with which it grows in hospitals. In that setting, C auris is known for its high transmissibility, its ability to cause outbreaks, and the high mortality rate from disseminated infections.
“It has been a concern for the mycological community because it shows resistance to most antifungals used clinically, mainly azoles, but also for causing epidemic outbreaks,” emphasized Dr. Sánchez Paredes.
Its mode of transmission is not very clear, but it has been documented to be present on the skin and persist in hospital materials and furniture. It causes nosocomial infections in critically ill patients, such as those in intensive care, and those with cancer or who have received a transplant.
Risk factors for its development include renal insufficiency, hospital stays of more than 15 days, mechanical ventilation, central lines, use of parenteral nutrition, and presence of sepsis.
As for other mycoses, there are no precise studies reporting global incidence rates, but the trend indicates an increase in the detection of outbreaks in various countries lately — something that began to be visible during the COVID-19 pandemic.
In Mexico, Dr. Treviño Rangel and colleagues from Nuevo León reported the first case of candidemia caused by this agent. It occurred in May 2020 and involved a 58-year-old woman with a history of severe endometriosis and multiple complications in the gastrointestinal tract. The patient’s condition improved favorably thanks to antifungal therapy with caspofungin and liposomal amphotericin B.
However, 3 months after that episode, the group reported an outbreak of C. auris at the same hospital in 12 critically ill patients co-infected with SARS-CoV-2. All were on mechanical ventilation, had peripherally inserted central catheters and urinary catheters, and had a prolonged hospital stay (20-70 days). The mortality in patients with candidemia in this cohort was 83.3%.
Open Ending
As seen in some science fiction series, fungal infections in the region still have an open ending, and Global Action For Fungal Infections (GAFFI) has estimated that with better diagnostics and treatments, deaths caused by fungi could decrease to less than 750,000 per year worldwide.
But if everything continues as is, some aspects of what is to come may resemble the dystopia depicted in The Last of Us. No zombies, but emerging and reemerging fungi in a chaotic distribution, and resistant to all established treatments.
“The risk factors of patients and their immune status, combined with the behavior of mycoses, bring a complicated scenario. But therapeutic failure resulting from multidrug resistance to antifungals could make it catastrophic,” Dr. Sánchez Paredes summarized.
At the moment, there are only four families of drugs capable of counteracting fungal infections — and as mentioned, some are already scarce in Latin America’s hospital pharmacies.
“Historically, fungal infections have been given less importance than those caused by viruses or bacteria. Even in some developed countries, the true extent of morbidity and mortality they present is unknown. This results in less investment in the development of new antifungal molecules because knowledge is lacking about the incidence and prevalence of these diseases,” Dr. Treviño Rangel pointed out.
He added that the main limitation for the development of new drugs is economic. “Unfortunately, not many pharmaceutical companies are willing to invest in the development of new antifungals, and there are no government programs specifically promoting and supporting research into new therapeutic options against these neglected diseases,” he asserted.
Development of vaccines to prevent fungal infections faces the same barriers. Although, according to Dr. Treviño Rangel, the difficulties are compounded by the great similarity between fungal cells and human cells. This makes it possible for harmful cross-reactivity to occur. In addition, because most severe fungal infections occur in individuals with immunosuppression, a vaccine would need to trigger an adequate immune response despite this issue.
Meanwhile, fungi quietly continue to do what they do best: resist and survive. For millions of years, they have mutated and adapted to new environments. Some theories even blame them for the extinction of dinosaurs and the subsequent rise of mammals. They exist on the edge of life and death, decomposing and creating. There is consensus that at the moment, it does not seem feasible for them to generate a pandemic like the one due to SARS-CoV-2, given their transmission mechanism. But who is willing to rule out that this may not happen in the long or medium term?
Dr. Sánchez Paredes, Dr. Treviño Rangel, Dr. Messina, Dr. Santiso, Dr. Álvarez, and Dr. Segundo Zaragoza have declared no relevant financial conflicts of interest.
This story was translated from Medscape Spanish Edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
The principle of resilience and survival is crucial for medically significant fungi. These microorganisms are far from creating the postapocalyptic scenario depicted in TV series like The Last of Us, and much work is necessary to learn more about them. Accurate statistics on fungal infections, accompanied by clinical histories, simple laboratory tests, new antifungals, and a necessary One Health approach are lacking.
The entomopathogenic fungus Ophiocordyceps unilateralis was made notorious by the TV series, but for now, it only manages to control the brains of some ants at will. Luckily, there are no signs that fungi affecting humans are inclined to create zombies.
What is clear is that the world belongs to the kingdom of fungi and that fungi are everywhere. There are already close to 150,000 described species, but millions remain to be discovered. They abound in decomposing organic matter, soil, or animal excrement, including that of bats and pigeons. Some fungi have even managed to find a home in hospitals. Lastly, we must not forget those that establish themselves in the human microbiome.
Given such diversity, it is legitimate to ask whether any of them could be capable of generating new pandemics. Could the forgotten Cryptococcus neoformans, Aspergillus fumigatus, or Histoplasma species, among others, trigger new health emergencies on the scale of the one generated by SARS-CoV-2?
We cannot forget that a coronavirus has already confirmed that reality can surpass fiction. However, Edith Sánchez Paredes, a biologist, doctor in biomedical sciences, and specialist in medical mycology, provided a reassuring response to Medscape Spanish Edition on this point.
“That would be very difficult to see because the way fungal infections are acquired is not from person to person, in most cases,” said Dr. Sánchez Paredes, from the Mycology Unit of the Faculty of Medicine at the National Autonomous University of Mexico.
Close to 300 species have already been classified as pathogenic in humans. Although the numbers are not precise and are increasing, it is estimated that around 1,500,000 people worldwide die each year of systemic fungal infections.
“However, it is important to emphasize that establishment of an infection depends not only on the causal agent. A crucial factor is the host, in this case, the human. Generally, these types of infections will develop in individuals with some deficiency in their immune system. The more deficient the immune response, the more likely a fungal infection may occur,” stated Dr. Sánchez Paredes.
The possibility of a pandemic like the one experienced with SARS-CoV-2 in the short term is remote, but the threat posed by fungal infections persists.
In 2022, the World Health Organization (WHO) defined a priority list of pathogenic fungi, with the aim of guiding actions to control them. It is mentioned there that invasive fungal diseases are on the rise worldwide, particularly in immunocompromised populations.
“Despite the growing concern, fungal infections receive very little attention and resources, leading to a paucity of quality data on fungal disease distribution and antifungal resistance patterns. Consequently, it is impossible to estimate their exact burden,” as stated in the document.
In line with this, an article published in Mycoses in 2022 concluded that fungal infections are neglected diseases in Latin America. Among other difficulties, deficiencies in access to tests such as polymerase chain reaction or serum detection of beta-1,3-D-glucan have been reported there.
In terms of treatments, most countries encounter problems with access to liposomal amphotericin B and new azoles, such as posaconazole and isavuconazole.
“Unfortunately, in Latin America, we suffer from a poor infrastructure for diagnosing fungal infections; likewise, we have limited access to antifungals available in the global market. What’s more, we lack reliable data on the epidemiology of fungal infections in the region, so many times governments are unaware of the true extent of the problem,” said Rogelio de Jesús Treviño Rangel, PhD, a medical microbiologist and expert in clinical mycology, professor, and researcher at the Faculty of Medicine of the Autonomous University of Nuevo León in Mexico.
Need for More Medical Mycology Training
Dr. Fernando Messina is a medical mycologist with the Mycology Unit of the Francisco Javier Muñiz Infectious Diseases Hospital in Buenos Aires, Argentina. He has noted an increase in the number of cases of cryptococcosis, histoplasmosis, and aspergillosis in his daily practice.
“Particularly, pulmonary aspergillosis is steadily increasing. This is because many patients have structural lung alterations that favor the appearance of this mycosis. This is related to the increase in cases of tuberculosis and the rise in life expectancy of patients with chronic obstructive pulmonary disease or other pulmonary or systemic diseases,” Dr. Messina stated.
For Dr. Messina, the main obstacle in current clinical practice is the low level of awareness among nonspecialist physicians regarding the presence of systemic fungal infections, and because these infections are more common than realized, it is vital to consider fungal etiology before starting empirical antibiotic therapy.
“Health professionals usually do not think about mycoses because mycology occupies a very small space in medical education at universities. As the Venezuelan mycologist Gioconda Cunto de San Blas once said, ‘Mycology is the Cinderella of microbiology.’ To change this, we need to give more space to mycoses in undergraduate and postgraduate studies,” Dr. Messina asserted.
He added, “The main challenge is to train professionals with an emphasis on the clinical interpretation of cases. Current medicine has a strong trend toward molecular biology and the use of rapid diagnostic methods, without considering the clinical symptoms or the patient’s history. Determinations are very useful, but it is necessary to interpret the results.”
Dr. Messina sees it as unlikely in the short term for a pandemic to be caused by fungi, but if it were to occur, he believes it would happen in healthcare systems in regions that are not prepared in terms of infrastructure. However, as seen in the health emergency resulting from SARS-CoV-2, he thinks the impact would be mitigated by the performance of healthcare professionals.
“In general, we have the ability to adapt to any adverse situation or change — although it is clear that we need more doctors, biochemists, and microbiologists trained in mycology,” emphasized Dr. Messina.
More than 40 interns pass through Muñiz Hospital each year. They are doctors and biochemists from Argentina, other countries in the region, or even Europe, seeking to enhance their training in mycology. Regarding fungal infection laboratory work, the interest lies in learning to use traditional techniques and innovative molecular methods.
“Rapid diagnostic methods, especially the detection of circulating antigens, have marked a change in the prognosis of deep mycosis in immunocompromised hosts. The possibility of screening and monitoring in this group of patients is very important and has a great benefit,” said Gabriela Santiso, PhD, a biochemist and head of the Mycology Unit of the Francisco Javier Muñiz Infectious Diseases Hospital.
According to Dr. Santiso, the current landscape includes the ability to identify genus and species, which can help in understanding resistance to antifungals. Furthermore, conducting sensitivity tests to these drugs, using standardized commercial methods, also provides timely information for treatment.
But Dr. Santiso warns that Latin America is a vast region with great disparity in human and technological resources. Although most countries in the region have networks facilitating access to timely diagnosis, resources are generally more available in major urban centers.
This often clashes with the epidemiology of most fungal infections. “Let’s not forget that many fungal pathologies affect low-income people who have difficulties accessing health centers, which sometimes turns them into chronic diseases that are hard to treat,” Dr. Santiso pointed out.
In mycology laboratories, the biggest cost is incurred by new diagnostic tests, such as those allowing molecular identification. Conventional methods are not usually expensive, but they require time and effort to train human resources to handle them.
Because new methodologies are not always available or easily accessible throughout the region, Dr. Santiso recommended not neglecting traditional mycological techniques. “Molecular methods, rapid diagnostic methods, and conventional mycology techniques are complementary and not mutually exclusive tests. Continuous training and updating are needed in this area,” she emphasized.
Why Are Resistant Fungal Infections Becoming Increasingly Common?
The first barrier for fungi to cause infection in humans is body temperature; most of them cannot withstand 37 °C. However, they also struggle to evade the immune response that is activated when they try to enter the body.
“We are normally exposed to many of these fungi, almost all the time, but if our immune system is adequate, it may not go beyond a mild infection, in most cases subclinical, which will resolve quickly,” Dr. Sánchez Paredes stated.
However, according to Dr. Sánchez Paredes, if the immune response is weak, “the fungus will have no trouble establishing itself in our organs. Some are even part of our microbiota, such as Candida albicans, which in the face of an imbalance or immunocompromise, can lead to serious infections.”
It is clear that the population at risk for immunosuppression has increased. According to the WHO, this is due to the high prevalence of such diseases as tuberculosis, cancer, and HIV infection, among others.
But the WHO also believes that the increase in fungal infections is related to greater population access to critical care units, invasive procedures, chemotherapy, or immunotherapy treatments.
Furthermore, factors related to the fungus itself and the environment play a role. “These organisms have enzymes, proteins, and other molecules that allow them to survive in the environment in which they normally inhabit. When they face a new and stressful one, they must express other molecules that will allow them to survive. All of this helps them evade elements of the immune system, antifungals, and, of course, body temperature,” according to Dr. Sánchez Paredes.
It is possible that climate change is also behind the noticeable increase in fungal infections and that this crisis may have an even greater impact in the future. The temperature of the environment has increased, and fungi will have to adapt to the planet’s temperature, to the point where body temperature may no longer be a significant barrier for them.
Environmental changes would also be responsible for modifications in the distribution of endemic mycoses, and it is believed that fungi will more frequently find new ecological niches, be able to survive in other environments, and alter distribution zones.
This is what is happening between Mexico and the United States with coccidioidomycosis, or valley fever. “We will begin to see cases of some mycoses where they were not normally seen, so we will have to conduct more studies to confirm that the fungus is inhabiting these new areas or is simply appearing in new sites owing to migration and the great mobility of populations,” Dr. Sánchez Paredes said.
Finally, exposure to environmental factors would partly be responsible for the increasing resistance to first-line antifungals observed in these microorganisms. This seems to be the case with A. fumigatus when exposed to azoles used as fungicides in agriculture.
One Health in Fungal Infections
The increasing resistance to antifungals is a clear testament that human, animal, and environmental health are interconnected. This is why a multidisciplinary approach that adopts the perspective of One Health is necessary for its management.
“The use of fungicides in agriculture, structurally similar to the azoles used in clinics, generates resistance in Aspergillus fumigatus found in the environment. These fungi in humans can be associated with infections that do not respond to first-line treatment,” explained Carlos Arturo Álvarez, an infectious diseases physician and professor at the Faculty of Medicine at the National University of Colombia.
According to Dr. Álvarez, the approach to control them should not only focus on the search for diagnostic methods that allow early detection of antifungal resistance or research on new antifungal treatments. He believes that progress must also be made with strategies that allow for the proper use of antifungals in agriculture.
“Unfortunately, the One Health approach is not yet well implemented in the region, and in my view, there is a lack of articulation in the different sectors. That is, there is a need for true coordination between government offices of agriculture, animal and human health, academia, and international organizations. This is not happening yet, and I believe we are in the initial stage of visibility,” Dr. Álvarez opined.
Veterinary public health is another pillar of the aforementioned approach. For various reasons, animals experience a higher frequency of fungal infections. A few carry and transmit true zoonoses that affect human health, but most often, animals act only as sentinels indicating a potential source of transmission.
Carolina Segundo Zaragoza, PhD, has worked in veterinary mycology for 30 years. She currently heads the veterinary mycology laboratory at the Animal Production Teaching, Research, and Extension Center in Altiplano, under the Faculty of Veterinary Medicine and Animal Husbandry at the National Autonomous University of Mexico. Because she has frequent contact with specialists in human mycology, during her professional career she has received several patient consultations, most of which were for cutaneous mycoses.
“They detect some dermatomycosis and realize that the common factor is owning a companion animal or a production animal with which the patient has contact. Both animals and humans present the same type of lesions, and then comes the question: Who infected whom? I remind them that the main source of infection is the soil and that animals should not be blamed in the first instance,” Dr. Segundo Zaragoza clarified.
She is currently collaborating on a research project analyzing the presence of Coccidioides immitis in the soil. This pathogen is responsible for coccidioidomycosis in dogs and humans, and she sees with satisfaction how these types of initiatives, which include some components of the One Health vision, are becoming more common in Mexico.
“Fortunately, human mycologists are increasingly providing more space for the dissemination of veterinary mycology. So I have had the opportunity to be invited to different forums on medical mycology to present the clinical cases we can have in animals and talk about the research projects we carry out. I have more and more opportunities to conduct joint research with human mycologists and veterinary doctors,” she said.
Dr. Segundo Zaragoza believes that to better implement the One Health vision, standardizing the criteria for detecting, diagnosing, and treating mycoses is necessary. She considers that teamwork will be key to achieving the common goal of safeguarding the well-being and health of humans and animals.
Alarms Sound for Candida auris
The WHO included the yeast Candida auris in its group of pathogens with critical priority, and since 2009, it has raised alarm owing to the ease with which it grows in hospitals. In that setting, C auris is known for its high transmissibility, its ability to cause outbreaks, and the high mortality rate from disseminated infections.
“It has been a concern for the mycological community because it shows resistance to most antifungals used clinically, mainly azoles, but also for causing epidemic outbreaks,” emphasized Dr. Sánchez Paredes.
Its mode of transmission is not very clear, but it has been documented to be present on the skin and persist in hospital materials and furniture. It causes nosocomial infections in critically ill patients, such as those in intensive care, and those with cancer or who have received a transplant.
Risk factors for its development include renal insufficiency, hospital stays of more than 15 days, mechanical ventilation, central lines, use of parenteral nutrition, and presence of sepsis.
As for other mycoses, there are no precise studies reporting global incidence rates, but the trend indicates an increase in the detection of outbreaks in various countries lately — something that began to be visible during the COVID-19 pandemic.
In Mexico, Dr. Treviño Rangel and colleagues from Nuevo León reported the first case of candidemia caused by this agent. It occurred in May 2020 and involved a 58-year-old woman with a history of severe endometriosis and multiple complications in the gastrointestinal tract. The patient’s condition improved favorably thanks to antifungal therapy with caspofungin and liposomal amphotericin B.
However, 3 months after that episode, the group reported an outbreak of C. auris at the same hospital in 12 critically ill patients co-infected with SARS-CoV-2. All were on mechanical ventilation, had peripherally inserted central catheters and urinary catheters, and had a prolonged hospital stay (20-70 days). The mortality in patients with candidemia in this cohort was 83.3%.
Open Ending
As seen in some science fiction series, fungal infections in the region still have an open ending, and Global Action For Fungal Infections (GAFFI) has estimated that with better diagnostics and treatments, deaths caused by fungi could decrease to less than 750,000 per year worldwide.
But if everything continues as is, some aspects of what is to come may resemble the dystopia depicted in The Last of Us. No zombies, but emerging and reemerging fungi in a chaotic distribution, and resistant to all established treatments.
“The risk factors of patients and their immune status, combined with the behavior of mycoses, bring a complicated scenario. But therapeutic failure resulting from multidrug resistance to antifungals could make it catastrophic,” Dr. Sánchez Paredes summarized.
At the moment, there are only four families of drugs capable of counteracting fungal infections — and as mentioned, some are already scarce in Latin America’s hospital pharmacies.
“Historically, fungal infections have been given less importance than those caused by viruses or bacteria. Even in some developed countries, the true extent of morbidity and mortality they present is unknown. This results in less investment in the development of new antifungal molecules because knowledge is lacking about the incidence and prevalence of these diseases,” Dr. Treviño Rangel pointed out.
He added that the main limitation for the development of new drugs is economic. “Unfortunately, not many pharmaceutical companies are willing to invest in the development of new antifungals, and there are no government programs specifically promoting and supporting research into new therapeutic options against these neglected diseases,” he asserted.
Development of vaccines to prevent fungal infections faces the same barriers. Although, according to Dr. Treviño Rangel, the difficulties are compounded by the great similarity between fungal cells and human cells. This makes it possible for harmful cross-reactivity to occur. In addition, because most severe fungal infections occur in individuals with immunosuppression, a vaccine would need to trigger an adequate immune response despite this issue.
Meanwhile, fungi quietly continue to do what they do best: resist and survive. For millions of years, they have mutated and adapted to new environments. Some theories even blame them for the extinction of dinosaurs and the subsequent rise of mammals. They exist on the edge of life and death, decomposing and creating. There is consensus that at the moment, it does not seem feasible for them to generate a pandemic like the one due to SARS-CoV-2, given their transmission mechanism. But who is willing to rule out that this may not happen in the long or medium term?
Dr. Sánchez Paredes, Dr. Treviño Rangel, Dr. Messina, Dr. Santiso, Dr. Álvarez, and Dr. Segundo Zaragoza have declared no relevant financial conflicts of interest.
This story was translated from Medscape Spanish Edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
The principle of resilience and survival is crucial for medically significant fungi. These microorganisms are far from creating the postapocalyptic scenario depicted in TV series like The Last of Us, and much work is necessary to learn more about them. Accurate statistics on fungal infections, accompanied by clinical histories, simple laboratory tests, new antifungals, and a necessary One Health approach are lacking.
The entomopathogenic fungus Ophiocordyceps unilateralis was made notorious by the TV series, but for now, it only manages to control the brains of some ants at will. Luckily, there are no signs that fungi affecting humans are inclined to create zombies.
What is clear is that the world belongs to the kingdom of fungi and that fungi are everywhere. There are already close to 150,000 described species, but millions remain to be discovered. They abound in decomposing organic matter, soil, or animal excrement, including that of bats and pigeons. Some fungi have even managed to find a home in hospitals. Lastly, we must not forget those that establish themselves in the human microbiome.
Given such diversity, it is legitimate to ask whether any of them could be capable of generating new pandemics. Could the forgotten Cryptococcus neoformans, Aspergillus fumigatus, or Histoplasma species, among others, trigger new health emergencies on the scale of the one generated by SARS-CoV-2?
We cannot forget that a coronavirus has already confirmed that reality can surpass fiction. However, Edith Sánchez Paredes, a biologist, doctor in biomedical sciences, and specialist in medical mycology, provided a reassuring response to Medscape Spanish Edition on this point.
“That would be very difficult to see because the way fungal infections are acquired is not from person to person, in most cases,” said Dr. Sánchez Paredes, from the Mycology Unit of the Faculty of Medicine at the National Autonomous University of Mexico.
Close to 300 species have already been classified as pathogenic in humans. Although the numbers are not precise and are increasing, it is estimated that around 1,500,000 people worldwide die each year of systemic fungal infections.
“However, it is important to emphasize that establishment of an infection depends not only on the causal agent. A crucial factor is the host, in this case, the human. Generally, these types of infections will develop in individuals with some deficiency in their immune system. The more deficient the immune response, the more likely a fungal infection may occur,” stated Dr. Sánchez Paredes.
The possibility of a pandemic like the one experienced with SARS-CoV-2 in the short term is remote, but the threat posed by fungal infections persists.
In 2022, the World Health Organization (WHO) defined a priority list of pathogenic fungi, with the aim of guiding actions to control them. It is mentioned there that invasive fungal diseases are on the rise worldwide, particularly in immunocompromised populations.
“Despite the growing concern, fungal infections receive very little attention and resources, leading to a paucity of quality data on fungal disease distribution and antifungal resistance patterns. Consequently, it is impossible to estimate their exact burden,” as stated in the document.
In line with this, an article published in Mycoses in 2022 concluded that fungal infections are neglected diseases in Latin America. Among other difficulties, deficiencies in access to tests such as polymerase chain reaction or serum detection of beta-1,3-D-glucan have been reported there.
In terms of treatments, most countries encounter problems with access to liposomal amphotericin B and new azoles, such as posaconazole and isavuconazole.
“Unfortunately, in Latin America, we suffer from a poor infrastructure for diagnosing fungal infections; likewise, we have limited access to antifungals available in the global market. What’s more, we lack reliable data on the epidemiology of fungal infections in the region, so many times governments are unaware of the true extent of the problem,” said Rogelio de Jesús Treviño Rangel, PhD, a medical microbiologist and expert in clinical mycology, professor, and researcher at the Faculty of Medicine of the Autonomous University of Nuevo León in Mexico.
Need for More Medical Mycology Training
Dr. Fernando Messina is a medical mycologist with the Mycology Unit of the Francisco Javier Muñiz Infectious Diseases Hospital in Buenos Aires, Argentina. He has noted an increase in the number of cases of cryptococcosis, histoplasmosis, and aspergillosis in his daily practice.
“Particularly, pulmonary aspergillosis is steadily increasing. This is because many patients have structural lung alterations that favor the appearance of this mycosis. This is related to the increase in cases of tuberculosis and the rise in life expectancy of patients with chronic obstructive pulmonary disease or other pulmonary or systemic diseases,” Dr. Messina stated.
For Dr. Messina, the main obstacle in current clinical practice is the low level of awareness among nonspecialist physicians regarding the presence of systemic fungal infections, and because these infections are more common than realized, it is vital to consider fungal etiology before starting empirical antibiotic therapy.
“Health professionals usually do not think about mycoses because mycology occupies a very small space in medical education at universities. As the Venezuelan mycologist Gioconda Cunto de San Blas once said, ‘Mycology is the Cinderella of microbiology.’ To change this, we need to give more space to mycoses in undergraduate and postgraduate studies,” Dr. Messina asserted.
He added, “The main challenge is to train professionals with an emphasis on the clinical interpretation of cases. Current medicine has a strong trend toward molecular biology and the use of rapid diagnostic methods, without considering the clinical symptoms or the patient’s history. Determinations are very useful, but it is necessary to interpret the results.”
Dr. Messina sees it as unlikely in the short term for a pandemic to be caused by fungi, but if it were to occur, he believes it would happen in healthcare systems in regions that are not prepared in terms of infrastructure. However, as seen in the health emergency resulting from SARS-CoV-2, he thinks the impact would be mitigated by the performance of healthcare professionals.
“In general, we have the ability to adapt to any adverse situation or change — although it is clear that we need more doctors, biochemists, and microbiologists trained in mycology,” emphasized Dr. Messina.
More than 40 interns pass through Muñiz Hospital each year. They are doctors and biochemists from Argentina, other countries in the region, or even Europe, seeking to enhance their training in mycology. Regarding fungal infection laboratory work, the interest lies in learning to use traditional techniques and innovative molecular methods.
“Rapid diagnostic methods, especially the detection of circulating antigens, have marked a change in the prognosis of deep mycosis in immunocompromised hosts. The possibility of screening and monitoring in this group of patients is very important and has a great benefit,” said Gabriela Santiso, PhD, a biochemist and head of the Mycology Unit of the Francisco Javier Muñiz Infectious Diseases Hospital.
According to Dr. Santiso, the current landscape includes the ability to identify genus and species, which can help in understanding resistance to antifungals. Furthermore, conducting sensitivity tests to these drugs, using standardized commercial methods, also provides timely information for treatment.
But Dr. Santiso warns that Latin America is a vast region with great disparity in human and technological resources. Although most countries in the region have networks facilitating access to timely diagnosis, resources are generally more available in major urban centers.
This often clashes with the epidemiology of most fungal infections. “Let’s not forget that many fungal pathologies affect low-income people who have difficulties accessing health centers, which sometimes turns them into chronic diseases that are hard to treat,” Dr. Santiso pointed out.
In mycology laboratories, the biggest cost is incurred by new diagnostic tests, such as those allowing molecular identification. Conventional methods are not usually expensive, but they require time and effort to train human resources to handle them.
Because new methodologies are not always available or easily accessible throughout the region, Dr. Santiso recommended not neglecting traditional mycological techniques. “Molecular methods, rapid diagnostic methods, and conventional mycology techniques are complementary and not mutually exclusive tests. Continuous training and updating are needed in this area,” she emphasized.
Why Are Resistant Fungal Infections Becoming Increasingly Common?
The first barrier for fungi to cause infection in humans is body temperature; most of them cannot withstand 37 °C. However, they also struggle to evade the immune response that is activated when they try to enter the body.
“We are normally exposed to many of these fungi, almost all the time, but if our immune system is adequate, it may not go beyond a mild infection, in most cases subclinical, which will resolve quickly,” Dr. Sánchez Paredes stated.
However, according to Dr. Sánchez Paredes, if the immune response is weak, “the fungus will have no trouble establishing itself in our organs. Some are even part of our microbiota, such as Candida albicans, which in the face of an imbalance or immunocompromise, can lead to serious infections.”
It is clear that the population at risk for immunosuppression has increased. According to the WHO, this is due to the high prevalence of such diseases as tuberculosis, cancer, and HIV infection, among others.
But the WHO also believes that the increase in fungal infections is related to greater population access to critical care units, invasive procedures, chemotherapy, or immunotherapy treatments.
Furthermore, factors related to the fungus itself and the environment play a role. “These organisms have enzymes, proteins, and other molecules that allow them to survive in the environment in which they normally inhabit. When they face a new and stressful one, they must express other molecules that will allow them to survive. All of this helps them evade elements of the immune system, antifungals, and, of course, body temperature,” according to Dr. Sánchez Paredes.
It is possible that climate change is also behind the noticeable increase in fungal infections and that this crisis may have an even greater impact in the future. The temperature of the environment has increased, and fungi will have to adapt to the planet’s temperature, to the point where body temperature may no longer be a significant barrier for them.
Environmental changes would also be responsible for modifications in the distribution of endemic mycoses, and it is believed that fungi will more frequently find new ecological niches, be able to survive in other environments, and alter distribution zones.
This is what is happening between Mexico and the United States with coccidioidomycosis, or valley fever. “We will begin to see cases of some mycoses where they were not normally seen, so we will have to conduct more studies to confirm that the fungus is inhabiting these new areas or is simply appearing in new sites owing to migration and the great mobility of populations,” Dr. Sánchez Paredes said.
Finally, exposure to environmental factors would partly be responsible for the increasing resistance to first-line antifungals observed in these microorganisms. This seems to be the case with A. fumigatus when exposed to azoles used as fungicides in agriculture.
One Health in Fungal Infections
The increasing resistance to antifungals is a clear testament that human, animal, and environmental health are interconnected. This is why a multidisciplinary approach that adopts the perspective of One Health is necessary for its management.
“The use of fungicides in agriculture, structurally similar to the azoles used in clinics, generates resistance in Aspergillus fumigatus found in the environment. These fungi in humans can be associated with infections that do not respond to first-line treatment,” explained Carlos Arturo Álvarez, an infectious diseases physician and professor at the Faculty of Medicine at the National University of Colombia.
According to Dr. Álvarez, the approach to control them should not only focus on the search for diagnostic methods that allow early detection of antifungal resistance or research on new antifungal treatments. He believes that progress must also be made with strategies that allow for the proper use of antifungals in agriculture.
“Unfortunately, the One Health approach is not yet well implemented in the region, and in my view, there is a lack of articulation in the different sectors. That is, there is a need for true coordination between government offices of agriculture, animal and human health, academia, and international organizations. This is not happening yet, and I believe we are in the initial stage of visibility,” Dr. Álvarez opined.
Veterinary public health is another pillar of the aforementioned approach. For various reasons, animals experience a higher frequency of fungal infections. A few carry and transmit true zoonoses that affect human health, but most often, animals act only as sentinels indicating a potential source of transmission.
Carolina Segundo Zaragoza, PhD, has worked in veterinary mycology for 30 years. She currently heads the veterinary mycology laboratory at the Animal Production Teaching, Research, and Extension Center in Altiplano, under the Faculty of Veterinary Medicine and Animal Husbandry at the National Autonomous University of Mexico. Because she has frequent contact with specialists in human mycology, during her professional career she has received several patient consultations, most of which were for cutaneous mycoses.
“They detect some dermatomycosis and realize that the common factor is owning a companion animal or a production animal with which the patient has contact. Both animals and humans present the same type of lesions, and then comes the question: Who infected whom? I remind them that the main source of infection is the soil and that animals should not be blamed in the first instance,” Dr. Segundo Zaragoza clarified.
She is currently collaborating on a research project analyzing the presence of Coccidioides immitis in the soil. This pathogen is responsible for coccidioidomycosis in dogs and humans, and she sees with satisfaction how these types of initiatives, which include some components of the One Health vision, are becoming more common in Mexico.
“Fortunately, human mycologists are increasingly providing more space for the dissemination of veterinary mycology. So I have had the opportunity to be invited to different forums on medical mycology to present the clinical cases we can have in animals and talk about the research projects we carry out. I have more and more opportunities to conduct joint research with human mycologists and veterinary doctors,” she said.
Dr. Segundo Zaragoza believes that to better implement the One Health vision, standardizing the criteria for detecting, diagnosing, and treating mycoses is necessary. She considers that teamwork will be key to achieving the common goal of safeguarding the well-being and health of humans and animals.
Alarms Sound for Candida auris
The WHO included the yeast Candida auris in its group of pathogens with critical priority, and since 2009, it has raised alarm owing to the ease with which it grows in hospitals. In that setting, C auris is known for its high transmissibility, its ability to cause outbreaks, and the high mortality rate from disseminated infections.
“It has been a concern for the mycological community because it shows resistance to most antifungals used clinically, mainly azoles, but also for causing epidemic outbreaks,” emphasized Dr. Sánchez Paredes.
Its mode of transmission is not very clear, but it has been documented to be present on the skin and persist in hospital materials and furniture. It causes nosocomial infections in critically ill patients, such as those in intensive care, and those with cancer or who have received a transplant.
Risk factors for its development include renal insufficiency, hospital stays of more than 15 days, mechanical ventilation, central lines, use of parenteral nutrition, and presence of sepsis.
As for other mycoses, there are no precise studies reporting global incidence rates, but the trend indicates an increase in the detection of outbreaks in various countries lately — something that began to be visible during the COVID-19 pandemic.
In Mexico, Dr. Treviño Rangel and colleagues from Nuevo León reported the first case of candidemia caused by this agent. It occurred in May 2020 and involved a 58-year-old woman with a history of severe endometriosis and multiple complications in the gastrointestinal tract. The patient’s condition improved favorably thanks to antifungal therapy with caspofungin and liposomal amphotericin B.
However, 3 months after that episode, the group reported an outbreak of C. auris at the same hospital in 12 critically ill patients co-infected with SARS-CoV-2. All were on mechanical ventilation, had peripherally inserted central catheters and urinary catheters, and had a prolonged hospital stay (20-70 days). The mortality in patients with candidemia in this cohort was 83.3%.
Open Ending
As seen in some science fiction series, fungal infections in the region still have an open ending, and Global Action For Fungal Infections (GAFFI) has estimated that with better diagnostics and treatments, deaths caused by fungi could decrease to less than 750,000 per year worldwide.
But if everything continues as is, some aspects of what is to come may resemble the dystopia depicted in The Last of Us. No zombies, but emerging and reemerging fungi in a chaotic distribution, and resistant to all established treatments.
“The risk factors of patients and their immune status, combined with the behavior of mycoses, bring a complicated scenario. But therapeutic failure resulting from multidrug resistance to antifungals could make it catastrophic,” Dr. Sánchez Paredes summarized.
At the moment, there are only four families of drugs capable of counteracting fungal infections — and as mentioned, some are already scarce in Latin America’s hospital pharmacies.
“Historically, fungal infections have been given less importance than those caused by viruses or bacteria. Even in some developed countries, the true extent of morbidity and mortality they present is unknown. This results in less investment in the development of new antifungal molecules because knowledge is lacking about the incidence and prevalence of these diseases,” Dr. Treviño Rangel pointed out.
He added that the main limitation for the development of new drugs is economic. “Unfortunately, not many pharmaceutical companies are willing to invest in the development of new antifungals, and there are no government programs specifically promoting and supporting research into new therapeutic options against these neglected diseases,” he asserted.
Development of vaccines to prevent fungal infections faces the same barriers. Although, according to Dr. Treviño Rangel, the difficulties are compounded by the great similarity between fungal cells and human cells. This makes it possible for harmful cross-reactivity to occur. In addition, because most severe fungal infections occur in individuals with immunosuppression, a vaccine would need to trigger an adequate immune response despite this issue.
Meanwhile, fungi quietly continue to do what they do best: resist and survive. For millions of years, they have mutated and adapted to new environments. Some theories even blame them for the extinction of dinosaurs and the subsequent rise of mammals. They exist on the edge of life and death, decomposing and creating. There is consensus that at the moment, it does not seem feasible for them to generate a pandemic like the one due to SARS-CoV-2, given their transmission mechanism. But who is willing to rule out that this may not happen in the long or medium term?
Dr. Sánchez Paredes, Dr. Treviño Rangel, Dr. Messina, Dr. Santiso, Dr. Álvarez, and Dr. Segundo Zaragoza have declared no relevant financial conflicts of interest.
This story was translated from Medscape Spanish Edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Machine learning meets cardiopulmonary exercise testing
DIFFUSE LUNG DISEASE AND LUNG TRANSPLANT NETWORK
Pulmonary Physiology and Rehabilitation Section
Several studies have explored automation of CPET interpretation, the most notable of which utilized machine learning.1
Recently, Schwendinger et al. investigated the ability of machine learning algorithms to not only categorize (pulmonary-vascular, mechanical-ventilatory, cardiocirculatory, and muscular), but also assign severity scores (0-6) to exercise limitations found in a group of 200 CPETs performed on adult patients referred to a lung clinic in Germany.2 Decision trees were constructed for each of the limitation categories by identifying variables with the lowest Root Mean Square Error (RMSE), which were comparable to agreement within expert interpretations. Combining decision trees allowed for a more comprehensive analysis with identification of multiple abnormalities in the same test.
A major limitation to the study is limited applicability to general patient populations without suspected lung disease. This bias is reflected in the decision tree for cardiovascular limitation that relied on VO2 peak and FEV1 alone. The authors were unable to construct a decision tree for muscular limitations due to a lack of identified cases.
Overall, these results suggest that refinement of machine learning algorithms built with larger heterogeneous data sets and expert interpretation can make CPETs accessible to the nonexpert clinician as long as test quality can be replicated across centers.
–Joseph Russo, MD
Fellow-in-Training
– Fatima Zeba, MD
Member-at-Large
References
1. Portella JJ, Andonian BJ, Brown DE, et al. Using machine learning to identify organ system specific limitations to exercise via cardiopulmonary exercise testing. IEEE J Biomed Health Inform. 2022;26(8):4228-4237.
2. Schwendinger F, Biehler AK, Nagy-Huber M, et al. Using machine learning-based algorithms to identify and quantify exercise limitations in clinical practice: are we there yet? Med Sci Sports Exerc. 2024;56(2):159-169.
DIFFUSE LUNG DISEASE AND LUNG TRANSPLANT NETWORK
Pulmonary Physiology and Rehabilitation Section
Several studies have explored automation of CPET interpretation, the most notable of which utilized machine learning.1
Recently, Schwendinger et al. investigated the ability of machine learning algorithms to not only categorize (pulmonary-vascular, mechanical-ventilatory, cardiocirculatory, and muscular), but also assign severity scores (0-6) to exercise limitations found in a group of 200 CPETs performed on adult patients referred to a lung clinic in Germany.2 Decision trees were constructed for each of the limitation categories by identifying variables with the lowest Root Mean Square Error (RMSE), which were comparable to agreement within expert interpretations. Combining decision trees allowed for a more comprehensive analysis with identification of multiple abnormalities in the same test.
A major limitation to the study is limited applicability to general patient populations without suspected lung disease. This bias is reflected in the decision tree for cardiovascular limitation that relied on VO2 peak and FEV1 alone. The authors were unable to construct a decision tree for muscular limitations due to a lack of identified cases.
Overall, these results suggest that refinement of machine learning algorithms built with larger heterogeneous data sets and expert interpretation can make CPETs accessible to the nonexpert clinician as long as test quality can be replicated across centers.
–Joseph Russo, MD
Fellow-in-Training
– Fatima Zeba, MD
Member-at-Large
References
1. Portella JJ, Andonian BJ, Brown DE, et al. Using machine learning to identify organ system specific limitations to exercise via cardiopulmonary exercise testing. IEEE J Biomed Health Inform. 2022;26(8):4228-4237.
2. Schwendinger F, Biehler AK, Nagy-Huber M, et al. Using machine learning-based algorithms to identify and quantify exercise limitations in clinical practice: are we there yet? Med Sci Sports Exerc. 2024;56(2):159-169.
DIFFUSE LUNG DISEASE AND LUNG TRANSPLANT NETWORK
Pulmonary Physiology and Rehabilitation Section
Several studies have explored automation of CPET interpretation, the most notable of which utilized machine learning.1
Recently, Schwendinger et al. investigated the ability of machine learning algorithms to not only categorize (pulmonary-vascular, mechanical-ventilatory, cardiocirculatory, and muscular), but also assign severity scores (0-6) to exercise limitations found in a group of 200 CPETs performed on adult patients referred to a lung clinic in Germany.2 Decision trees were constructed for each of the limitation categories by identifying variables with the lowest Root Mean Square Error (RMSE), which were comparable to agreement within expert interpretations. Combining decision trees allowed for a more comprehensive analysis with identification of multiple abnormalities in the same test.
A major limitation to the study is limited applicability to general patient populations without suspected lung disease. This bias is reflected in the decision tree for cardiovascular limitation that relied on VO2 peak and FEV1 alone. The authors were unable to construct a decision tree for muscular limitations due to a lack of identified cases.
Overall, these results suggest that refinement of machine learning algorithms built with larger heterogeneous data sets and expert interpretation can make CPETs accessible to the nonexpert clinician as long as test quality can be replicated across centers.
–Joseph Russo, MD
Fellow-in-Training
– Fatima Zeba, MD
Member-at-Large
References
1. Portella JJ, Andonian BJ, Brown DE, et al. Using machine learning to identify organ system specific limitations to exercise via cardiopulmonary exercise testing. IEEE J Biomed Health Inform. 2022;26(8):4228-4237.
2. Schwendinger F, Biehler AK, Nagy-Huber M, et al. Using machine learning-based algorithms to identify and quantify exercise limitations in clinical practice: are we there yet? Med Sci Sports Exerc. 2024;56(2):159-169.
Pulmonary telerehabilitation for COPD: Promising, but more data needed
As COVID-19 cedes its pandemic-scale status to the past, its wake is revealing surprises and raising questions, particularly in relation to pulmonary medicine. The need for isolation at COVID’s outset kept many millions at home, creating conditions favorable for the rapid expansion of technologies that were taken up quickly in telehealth applications. The need was overwhelming. But just how effective telehealth actually is at replacing on-site programs for COPD pulmonary rehab has remained a research challenge, although results from early studies show unmistakable value. Creating conditions conducive to research into the strengths and weaknesses of pulmonary rehab, and determining how research can be applied effectively, remain formidable challenges.
Early studies of telehealth pulmonary rehabilitation have not uncovered any glaring erosion of pulmonary rehabilitation’s well-established benefits. But, at the same time, the relatively young field of pulmonary telerehabilitation for chronic obstructive pulmonary disease (COPD) has lacked coordinated efforts to determine its key practices and the instruments for measuring them, both basic elements for pursuing research questions.
A 2021 American Thoracic Society workshop report (AE Holland, https://doi.org/10.1513/AnnalsATS.202102-146ST) identified essential components of a pulmonary rehabilitation model through an online Delphi process involving about 50 international experts. Components ultimately included those with median scores of 2 or higher (strongly agree or agree that the item is essential) and high consensus (interquartile range, 0). Thirteen essential components fit into four categories (Patient Assessment, Program Components, Method of Delivery and Quality Assurance). The Patient Assessment category included seven items: (1) An initial center-based assessment by a health care professional, (2) An exercise test at the time of assessment, (3) A field exercise test, (4) Quality of life measure, (5) Dyspnea assessment, (6) Nutritional status evaluation, and (7) Occupational status evaluation. The Program Components: (8) Endurance training and (9) Resistance training). The Method of Delivery: (10) An exercise program that is individually prescribed, (11) An exercise program that is individually progressed, and (12) Team includes a health care professional with experience in exercise prescription and progression. The single Quality Assurance item: (13) Health care professionals are trained to deliver the components of the model that is deployed.
Cochrane Library review
2021 “Intervention Review” (“Telerehabilitation for chronic respiratory disease,” https://doi.org/10.1002/14651858.CD013040.pub2). Using their own databases (eg, Cochrane Airways Trials Register) and others, the authors included controlled trials published up to November 30, 2020 with at least 50% of the rehabilitation delivered by telerehabilitation. The authors’ analysis of 15 studies (with 32 reports) including 1904 participants (99% with COPD): “There was probably little or no difference between telerehabilitation and in-person pulmonary rehabilitation for exercise capacity measured as 6-Minute Walking Distance (mean difference 0.06 meters (m), 95% confidence interval (CI) -10.82 m to 10.94 m).” They reached the same conclusion for quality of life, and for breathlessness. Completion of rehabilitation programs, however, was more likely with telerehabilitation at 93% versus 70% for in-person rehabilitation. No adverse effects of telerehabilitation were observed over and above those for in-person or no rehabilitation. An obvious limitation of the findings is that the studies all pre-date COVID-19, which would have introduced very significant disincentives for in-person rehabilitation completion.
An older (2016) international randomized controlled study (Zanaboni et al, https://doi.org/10.1186/s12890-016-0288-z) comparing long-term telerehabilitation or unsupervised treadmill training at home with standard care included 120 participants with COPD and had 2-years of follow-up. Telerehabilitation consisted of individualized treadmill training at home. Participants had scheduled exercise sessions supervised by a physiotherapist via videoconferencing following a standardized protocol. Participants in the unsupervised training group were provided with a treadmill only to perform unsupervised exercise at home. They also received an exercise booklet, a paper exercise diary to record their training sessions, and an individualized training program but without regular review or progression of the program. For the primary outcomes of combined hospitalizations and emergency department presentations, incidence rate of hospitalizations and emergency department presentations was lower with telerehabilitation (1.18 events per person-year; 95% confidence interval [CI], 0.94–1.46) and with unsupervised training group (1.14; 95% CI, 0.92–1.41) than in the control group (1.88; 95% CI, 1.58–2.21; P < .001 compared with intervention groups). Both training groups had better health status at 1-year, and achieved and maintained clinically significant improvements in exercise capacity.
Access to pulmonary rehabilitation
Continuing evidence of clear telerehabilitation benefits is good news, especially in the light of impediments to attendance at in-clinic programs. Although the COVID-provoked disincentives have been diminishing, persisting access issues remain for substantial portions of eligible populations, according to a recent (2024) cross-sectional study (PA Kahn, WA Mathis, doi:10.1001/jamanetworkopen.2023.54867) looking at travel time to pulmonary rehabilitation programs as a marker for pulmonary rehabilitation access. The report, based on US Census designations (lower 48 states and Washington, D.C.) found that while 80.3% of the population lives in urban or suburban areas within a 30-minute drive of a pulmonary rehabilitation program, travel time exceeds that in rural and other sparsely populated areas with more than 14 million people residing in areas demanding more than 1-hour for travel. A further analysis showed also that nearly 30% of American Indian and Alaska Native populations live more than 60 minutes from a pulmonary rehabilitation program.
Aside from the obvious restraints for homebound patients or those lacking transportation or who need medical transport, other common impediments inhibit on-site pulmonary rehabilitation attendance, said Corinne Young, MSN, FNP-C, FCCP. Ms. Young is the director of Advance Practice Provider and Clinical Services for Colorado Springs Pulmonary Consultants, president and founder of the Association of Pulmonary Advance Practice Providers, and a member of the CHEST Physician Editorial Board. “I have some patients who say ‘There’s no way I could do onsite pulmonary rehab because of my knee — or back, or shoulder.’ But in their own home environment they may feel more comfortable. They may be willing to try new things at their own pace, whereas for them a program may feel too regimented.” For others, Ms. Young said, aspects of a formal program are a clear plus factor. “They love to hear their progress at the end of — say a 12-week program — where their virtual respiratory therapist records and reports to them their six-minute walk and other test results. Feedback is a great reinforcer.” Quality of life improvements, Ms. Young commented, were one of the very impressive benefits that appeared in the initial studies of pulmonary rehabilitation for COPD patients. “Being patient-centric, you want to improve quality of life for them as much as possible and we see telerehabilitation as a great opportunity for many,” she added.
“I would like to see head-to-head data on outpatient versus at-home pulmonary rehabilitation on hospitalizations, time to exacerbation and, of course, mortality. We have all that for outpatient rehab, but it would be great to be able to compare them. Knowing that would influence what we recommend, especially for patients who could go either way. Also, you have to assess their motivation and discipline to know who might be more appropriate for unsupervised pulmonary rehabilitation.”
The current reality for Ms. Young is that in her Colorado Springs vicinity, where both in-patient programs are only 15 minutes apart, she knows of no telerehabilitation programs being offered. While there are contract telerehabilitation providers, Young said, and her organization (The Association of Pulmonary Advanced Practice Providers) has been approached by one, none are licensed in Colorado, and telerehabilitation is not a billable service.
“As of yet, I’m not aware of any telemedicine pulmonary rehab available at our institution,” said pulmonologist Mary Jo S. Farmer, MD, PhD, FCCP, Associate Professor of Medicine at UMass Chan Medical School – Baystate, Springfield, MA, and a member of the CHEST Physician Editorial Board. A brief internet search identified a telerehabilitation contract provider available only in Arizona.
Reimbursement will also be a foundational concern, Ms. Young commented. While a physician, nurse practitioner, or physician virtual visit for education may be billable, telerehabilitation reimbursement is new territory. “How that all is going to work out is a big unknown piece,” she said.
Minimal components
Effective pulmonary telerehabilitation programs, Ms. Young said, need to provide exercise with an aerobic device, either a treadmill, a stationary bike or even a Cubii-type under desk foot pedal/elliptical machine, and some resistance training (elastic bands, or weights, for example). “But 50% of pulmonary rehabilitation is education about breathing techniques, purse-lip breathing, and pulmonary nutrition.” Also essential: one-on-one discussion with a qualified medical practitioner who checks on oximeter use, inhaler technique, and titrating oxygen therapy. “At our elevation of 6500 feet, most of our patients are on that.” Optimal frequency of encounters between providers and remote patients has to be elucidated by future research, Ms. Young said.
Ms. Young commented further, “With outpatient pulmonary rehabilitation there often isn’t a lot of one-on-one, but rather a big group of people exercising at the same time. I think actually there may be the potential to have more individualization with pulmonary telerehabilitation. But the barriers, the reimbursement/financial part, and the red tape and bureaucracy have to be worked on.”
As COVID-19 cedes its pandemic-scale status to the past, its wake is revealing surprises and raising questions, particularly in relation to pulmonary medicine. The need for isolation at COVID’s outset kept many millions at home, creating conditions favorable for the rapid expansion of technologies that were taken up quickly in telehealth applications. The need was overwhelming. But just how effective telehealth actually is at replacing on-site programs for COPD pulmonary rehab has remained a research challenge, although results from early studies show unmistakable value. Creating conditions conducive to research into the strengths and weaknesses of pulmonary rehab, and determining how research can be applied effectively, remain formidable challenges.
Early studies of telehealth pulmonary rehabilitation have not uncovered any glaring erosion of pulmonary rehabilitation’s well-established benefits. But, at the same time, the relatively young field of pulmonary telerehabilitation for chronic obstructive pulmonary disease (COPD) has lacked coordinated efforts to determine its key practices and the instruments for measuring them, both basic elements for pursuing research questions.
A 2021 American Thoracic Society workshop report (AE Holland, https://doi.org/10.1513/AnnalsATS.202102-146ST) identified essential components of a pulmonary rehabilitation model through an online Delphi process involving about 50 international experts. Components ultimately included those with median scores of 2 or higher (strongly agree or agree that the item is essential) and high consensus (interquartile range, 0). Thirteen essential components fit into four categories (Patient Assessment, Program Components, Method of Delivery and Quality Assurance). The Patient Assessment category included seven items: (1) An initial center-based assessment by a health care professional, (2) An exercise test at the time of assessment, (3) A field exercise test, (4) Quality of life measure, (5) Dyspnea assessment, (6) Nutritional status evaluation, and (7) Occupational status evaluation. The Program Components: (8) Endurance training and (9) Resistance training). The Method of Delivery: (10) An exercise program that is individually prescribed, (11) An exercise program that is individually progressed, and (12) Team includes a health care professional with experience in exercise prescription and progression. The single Quality Assurance item: (13) Health care professionals are trained to deliver the components of the model that is deployed.
Cochrane Library review
2021 “Intervention Review” (“Telerehabilitation for chronic respiratory disease,” https://doi.org/10.1002/14651858.CD013040.pub2). Using their own databases (eg, Cochrane Airways Trials Register) and others, the authors included controlled trials published up to November 30, 2020 with at least 50% of the rehabilitation delivered by telerehabilitation. The authors’ analysis of 15 studies (with 32 reports) including 1904 participants (99% with COPD): “There was probably little or no difference between telerehabilitation and in-person pulmonary rehabilitation for exercise capacity measured as 6-Minute Walking Distance (mean difference 0.06 meters (m), 95% confidence interval (CI) -10.82 m to 10.94 m).” They reached the same conclusion for quality of life, and for breathlessness. Completion of rehabilitation programs, however, was more likely with telerehabilitation at 93% versus 70% for in-person rehabilitation. No adverse effects of telerehabilitation were observed over and above those for in-person or no rehabilitation. An obvious limitation of the findings is that the studies all pre-date COVID-19, which would have introduced very significant disincentives for in-person rehabilitation completion.
An older (2016) international randomized controlled study (Zanaboni et al, https://doi.org/10.1186/s12890-016-0288-z) comparing long-term telerehabilitation or unsupervised treadmill training at home with standard care included 120 participants with COPD and had 2-years of follow-up. Telerehabilitation consisted of individualized treadmill training at home. Participants had scheduled exercise sessions supervised by a physiotherapist via videoconferencing following a standardized protocol. Participants in the unsupervised training group were provided with a treadmill only to perform unsupervised exercise at home. They also received an exercise booklet, a paper exercise diary to record their training sessions, and an individualized training program but without regular review or progression of the program. For the primary outcomes of combined hospitalizations and emergency department presentations, incidence rate of hospitalizations and emergency department presentations was lower with telerehabilitation (1.18 events per person-year; 95% confidence interval [CI], 0.94–1.46) and with unsupervised training group (1.14; 95% CI, 0.92–1.41) than in the control group (1.88; 95% CI, 1.58–2.21; P < .001 compared with intervention groups). Both training groups had better health status at 1-year, and achieved and maintained clinically significant improvements in exercise capacity.
Access to pulmonary rehabilitation
Continuing evidence of clear telerehabilitation benefits is good news, especially in the light of impediments to attendance at in-clinic programs. Although the COVID-provoked disincentives have been diminishing, persisting access issues remain for substantial portions of eligible populations, according to a recent (2024) cross-sectional study (PA Kahn, WA Mathis, doi:10.1001/jamanetworkopen.2023.54867) looking at travel time to pulmonary rehabilitation programs as a marker for pulmonary rehabilitation access. The report, based on US Census designations (lower 48 states and Washington, D.C.) found that while 80.3% of the population lives in urban or suburban areas within a 30-minute drive of a pulmonary rehabilitation program, travel time exceeds that in rural and other sparsely populated areas with more than 14 million people residing in areas demanding more than 1-hour for travel. A further analysis showed also that nearly 30% of American Indian and Alaska Native populations live more than 60 minutes from a pulmonary rehabilitation program.
Aside from the obvious restraints for homebound patients or those lacking transportation or who need medical transport, other common impediments inhibit on-site pulmonary rehabilitation attendance, said Corinne Young, MSN, FNP-C, FCCP. Ms. Young is the director of Advance Practice Provider and Clinical Services for Colorado Springs Pulmonary Consultants, president and founder of the Association of Pulmonary Advance Practice Providers, and a member of the CHEST Physician Editorial Board. “I have some patients who say ‘There’s no way I could do onsite pulmonary rehab because of my knee — or back, or shoulder.’ But in their own home environment they may feel more comfortable. They may be willing to try new things at their own pace, whereas for them a program may feel too regimented.” For others, Ms. Young said, aspects of a formal program are a clear plus factor. “They love to hear their progress at the end of — say a 12-week program — where their virtual respiratory therapist records and reports to them their six-minute walk and other test results. Feedback is a great reinforcer.” Quality of life improvements, Ms. Young commented, were one of the very impressive benefits that appeared in the initial studies of pulmonary rehabilitation for COPD patients. “Being patient-centric, you want to improve quality of life for them as much as possible and we see telerehabilitation as a great opportunity for many,” she added.
“I would like to see head-to-head data on outpatient versus at-home pulmonary rehabilitation on hospitalizations, time to exacerbation and, of course, mortality. We have all that for outpatient rehab, but it would be great to be able to compare them. Knowing that would influence what we recommend, especially for patients who could go either way. Also, you have to assess their motivation and discipline to know who might be more appropriate for unsupervised pulmonary rehabilitation.”
The current reality for Ms. Young is that in her Colorado Springs vicinity, where both in-patient programs are only 15 minutes apart, she knows of no telerehabilitation programs being offered. While there are contract telerehabilitation providers, Young said, and her organization (The Association of Pulmonary Advanced Practice Providers) has been approached by one, none are licensed in Colorado, and telerehabilitation is not a billable service.
“As of yet, I’m not aware of any telemedicine pulmonary rehab available at our institution,” said pulmonologist Mary Jo S. Farmer, MD, PhD, FCCP, Associate Professor of Medicine at UMass Chan Medical School – Baystate, Springfield, MA, and a member of the CHEST Physician Editorial Board. A brief internet search identified a telerehabilitation contract provider available only in Arizona.
Reimbursement will also be a foundational concern, Ms. Young commented. While a physician, nurse practitioner, or physician virtual visit for education may be billable, telerehabilitation reimbursement is new territory. “How that all is going to work out is a big unknown piece,” she said.
Minimal components
Effective pulmonary telerehabilitation programs, Ms. Young said, need to provide exercise with an aerobic device, either a treadmill, a stationary bike or even a Cubii-type under desk foot pedal/elliptical machine, and some resistance training (elastic bands, or weights, for example). “But 50% of pulmonary rehabilitation is education about breathing techniques, purse-lip breathing, and pulmonary nutrition.” Also essential: one-on-one discussion with a qualified medical practitioner who checks on oximeter use, inhaler technique, and titrating oxygen therapy. “At our elevation of 6500 feet, most of our patients are on that.” Optimal frequency of encounters between providers and remote patients has to be elucidated by future research, Ms. Young said.
Ms. Young commented further, “With outpatient pulmonary rehabilitation there often isn’t a lot of one-on-one, but rather a big group of people exercising at the same time. I think actually there may be the potential to have more individualization with pulmonary telerehabilitation. But the barriers, the reimbursement/financial part, and the red tape and bureaucracy have to be worked on.”
As COVID-19 cedes its pandemic-scale status to the past, its wake is revealing surprises and raising questions, particularly in relation to pulmonary medicine. The need for isolation at COVID’s outset kept many millions at home, creating conditions favorable for the rapid expansion of technologies that were taken up quickly in telehealth applications. The need was overwhelming. But just how effective telehealth actually is at replacing on-site programs for COPD pulmonary rehab has remained a research challenge, although results from early studies show unmistakable value. Creating conditions conducive to research into the strengths and weaknesses of pulmonary rehab, and determining how research can be applied effectively, remain formidable challenges.
Early studies of telehealth pulmonary rehabilitation have not uncovered any glaring erosion of pulmonary rehabilitation’s well-established benefits. But, at the same time, the relatively young field of pulmonary telerehabilitation for chronic obstructive pulmonary disease (COPD) has lacked coordinated efforts to determine its key practices and the instruments for measuring them, both basic elements for pursuing research questions.
A 2021 American Thoracic Society workshop report (AE Holland, https://doi.org/10.1513/AnnalsATS.202102-146ST) identified essential components of a pulmonary rehabilitation model through an online Delphi process involving about 50 international experts. Components ultimately included those with median scores of 2 or higher (strongly agree or agree that the item is essential) and high consensus (interquartile range, 0). Thirteen essential components fit into four categories (Patient Assessment, Program Components, Method of Delivery and Quality Assurance). The Patient Assessment category included seven items: (1) An initial center-based assessment by a health care professional, (2) An exercise test at the time of assessment, (3) A field exercise test, (4) Quality of life measure, (5) Dyspnea assessment, (6) Nutritional status evaluation, and (7) Occupational status evaluation. The Program Components: (8) Endurance training and (9) Resistance training). The Method of Delivery: (10) An exercise program that is individually prescribed, (11) An exercise program that is individually progressed, and (12) Team includes a health care professional with experience in exercise prescription and progression. The single Quality Assurance item: (13) Health care professionals are trained to deliver the components of the model that is deployed.
Cochrane Library review
2021 “Intervention Review” (“Telerehabilitation for chronic respiratory disease,” https://doi.org/10.1002/14651858.CD013040.pub2). Using their own databases (eg, Cochrane Airways Trials Register) and others, the authors included controlled trials published up to November 30, 2020 with at least 50% of the rehabilitation delivered by telerehabilitation. The authors’ analysis of 15 studies (with 32 reports) including 1904 participants (99% with COPD): “There was probably little or no difference between telerehabilitation and in-person pulmonary rehabilitation for exercise capacity measured as 6-Minute Walking Distance (mean difference 0.06 meters (m), 95% confidence interval (CI) -10.82 m to 10.94 m).” They reached the same conclusion for quality of life, and for breathlessness. Completion of rehabilitation programs, however, was more likely with telerehabilitation at 93% versus 70% for in-person rehabilitation. No adverse effects of telerehabilitation were observed over and above those for in-person or no rehabilitation. An obvious limitation of the findings is that the studies all pre-date COVID-19, which would have introduced very significant disincentives for in-person rehabilitation completion.
An older (2016) international randomized controlled study (Zanaboni et al, https://doi.org/10.1186/s12890-016-0288-z) comparing long-term telerehabilitation or unsupervised treadmill training at home with standard care included 120 participants with COPD and had 2-years of follow-up. Telerehabilitation consisted of individualized treadmill training at home. Participants had scheduled exercise sessions supervised by a physiotherapist via videoconferencing following a standardized protocol. Participants in the unsupervised training group were provided with a treadmill only to perform unsupervised exercise at home. They also received an exercise booklet, a paper exercise diary to record their training sessions, and an individualized training program but without regular review or progression of the program. For the primary outcomes of combined hospitalizations and emergency department presentations, incidence rate of hospitalizations and emergency department presentations was lower with telerehabilitation (1.18 events per person-year; 95% confidence interval [CI], 0.94–1.46) and with unsupervised training group (1.14; 95% CI, 0.92–1.41) than in the control group (1.88; 95% CI, 1.58–2.21; P < .001 compared with intervention groups). Both training groups had better health status at 1-year, and achieved and maintained clinically significant improvements in exercise capacity.
Access to pulmonary rehabilitation
Continuing evidence of clear telerehabilitation benefits is good news, especially in the light of impediments to attendance at in-clinic programs. Although the COVID-provoked disincentives have been diminishing, persisting access issues remain for substantial portions of eligible populations, according to a recent (2024) cross-sectional study (PA Kahn, WA Mathis, doi:10.1001/jamanetworkopen.2023.54867) looking at travel time to pulmonary rehabilitation programs as a marker for pulmonary rehabilitation access. The report, based on US Census designations (lower 48 states and Washington, D.C.) found that while 80.3% of the population lives in urban or suburban areas within a 30-minute drive of a pulmonary rehabilitation program, travel time exceeds that in rural and other sparsely populated areas with more than 14 million people residing in areas demanding more than 1-hour for travel. A further analysis showed also that nearly 30% of American Indian and Alaska Native populations live more than 60 minutes from a pulmonary rehabilitation program.
Aside from the obvious restraints for homebound patients or those lacking transportation or who need medical transport, other common impediments inhibit on-site pulmonary rehabilitation attendance, said Corinne Young, MSN, FNP-C, FCCP. Ms. Young is the director of Advance Practice Provider and Clinical Services for Colorado Springs Pulmonary Consultants, president and founder of the Association of Pulmonary Advance Practice Providers, and a member of the CHEST Physician Editorial Board. “I have some patients who say ‘There’s no way I could do onsite pulmonary rehab because of my knee — or back, or shoulder.’ But in their own home environment they may feel more comfortable. They may be willing to try new things at their own pace, whereas for them a program may feel too regimented.” For others, Ms. Young said, aspects of a formal program are a clear plus factor. “They love to hear their progress at the end of — say a 12-week program — where their virtual respiratory therapist records and reports to them their six-minute walk and other test results. Feedback is a great reinforcer.” Quality of life improvements, Ms. Young commented, were one of the very impressive benefits that appeared in the initial studies of pulmonary rehabilitation for COPD patients. “Being patient-centric, you want to improve quality of life for them as much as possible and we see telerehabilitation as a great opportunity for many,” she added.
“I would like to see head-to-head data on outpatient versus at-home pulmonary rehabilitation on hospitalizations, time to exacerbation and, of course, mortality. We have all that for outpatient rehab, but it would be great to be able to compare them. Knowing that would influence what we recommend, especially for patients who could go either way. Also, you have to assess their motivation and discipline to know who might be more appropriate for unsupervised pulmonary rehabilitation.”
The current reality for Ms. Young is that in her Colorado Springs vicinity, where both in-patient programs are only 15 minutes apart, she knows of no telerehabilitation programs being offered. While there are contract telerehabilitation providers, Young said, and her organization (The Association of Pulmonary Advanced Practice Providers) has been approached by one, none are licensed in Colorado, and telerehabilitation is not a billable service.
“As of yet, I’m not aware of any telemedicine pulmonary rehab available at our institution,” said pulmonologist Mary Jo S. Farmer, MD, PhD, FCCP, Associate Professor of Medicine at UMass Chan Medical School – Baystate, Springfield, MA, and a member of the CHEST Physician Editorial Board. A brief internet search identified a telerehabilitation contract provider available only in Arizona.
Reimbursement will also be a foundational concern, Ms. Young commented. While a physician, nurse practitioner, or physician virtual visit for education may be billable, telerehabilitation reimbursement is new territory. “How that all is going to work out is a big unknown piece,” she said.
Minimal components
Effective pulmonary telerehabilitation programs, Ms. Young said, need to provide exercise with an aerobic device, either a treadmill, a stationary bike or even a Cubii-type under desk foot pedal/elliptical machine, and some resistance training (elastic bands, or weights, for example). “But 50% of pulmonary rehabilitation is education about breathing techniques, purse-lip breathing, and pulmonary nutrition.” Also essential: one-on-one discussion with a qualified medical practitioner who checks on oximeter use, inhaler technique, and titrating oxygen therapy. “At our elevation of 6500 feet, most of our patients are on that.” Optimal frequency of encounters between providers and remote patients has to be elucidated by future research, Ms. Young said.
Ms. Young commented further, “With outpatient pulmonary rehabilitation there often isn’t a lot of one-on-one, but rather a big group of people exercising at the same time. I think actually there may be the potential to have more individualization with pulmonary telerehabilitation. But the barriers, the reimbursement/financial part, and the red tape and bureaucracy have to be worked on.”
Military burn pits: Their evidence and implications for respiratory health
Military service is a hazard-ridden profession. It’s easy to recognize the direct dangers from warfighting, such as gunfire and explosions, but the risks from environmental, chemical, and other occupational exposures can be harder to see.
Combustion-based waste management systems, otherwise known as “burn pits,” were used in deployed environments by the US military from the 1990s to the early 2010s. These burn pits were commonly used to eliminate plastics, electronics, munitions, metals, wood, chemicals, and even human waste. At the height of the recent conflicts in Afghanistan, Iraq, and other southwest Asia locations, more than 70% of military installations employed at least one, and nearly 4 million service members were exposed to some degree to their emissions.
Reports of burn pits being related to organic disease have garnered widespread media attention. Initially, this came through anecdotal reports of post-deployment respiratory symptoms. Over time, the conditions attributed to burn pits expanded to include newly diagnosed respiratory diseases and malignancies.
Ultimately, Congress passed the 2022 Promise to Address Comprehensive Toxins (PACT) Act, presumptively linking more than 20 diagnoses to burn pits. The PACT Act provides countless veterans access to low-cost or free medical care for their respective conditions.
What do we know about burn pits and deployment-related respiratory disease?
Data from the Millennium Cohort Study noted an approximately 40% increase in respiratory symptoms among individuals returning from deployment but no increase in the frequency of diagnosed respiratory diseases.1 This study and others definitively established a temporal relationship between deployment and respiratory symptoms. Soon after, a retrospective, observational study of service members with post-deployment respiratory symptoms found a high prevalence of constrictive bronchiolitis (CB) identified by lung biopsy.2 Patients in this group reported exposure to burn pits and a sulfur mine fire in the Mosul area while deployed. Most had normal imaging and pulmonary function testing before biopsy, confounding the clinical significance of the CB finding. The publication of this report led to increased investigation of respiratory function during and after deployment.
In a series of prospective studies that included full pulmonary function testing, impulse oscillometry, cardiopulmonary exercise testing, bronchoscopy, and, occasionally, lung biopsy to evaluate post-deployment dyspnea, only a small minority received a diagnosis of clinically significant lung disease.3,4 Additionally, when comparing spirometry and impulse oscillometry results from before and after deployment, no decline in lung function was observed in a population of service members reporting regular burn pit exposure.5 These studies suggest that at the population level, deployment does not lead to abnormalities in the structure and function of the respiratory system.
The National Academies of Sciences published two separate reviews of burn pit exposure and outcomes in 2011 and 2020.6,7 They found insufficient evidence to support a causal relationship between burn pit exposure and pulmonary disease. They highlighted studies on the composition of emissions from the area surrounding the largest military burn pit in Iraq. Levels of particulate matter, volatile organic compounds, and polycyclic aromatic hydrocarbons were elevated when compared with those of a typical American city but were similar to the pollution levels seen in the region at the time. Given these findings, they suggested ambient air pollution may have contributed more to clinically significant disease than burn pit emissions.
How do we interpret this mixed data?
At the population level, we have yet to find conclusive data directly linking burn pit exposure to the development of any respiratory disease. Does this mean that burn pits are not harmful?
Not necessarily. Research on outcomes related to burn pit exposure is challenging given the heterogeneity in exposure volume. Much of the research is retrospective and subject to recall bias. Relationships may be distorted, and the precision of reported symptoms and exposure levels is altered. Given these challenges, it’s unsurprising that evidence of causality has yet to be proven. In addition, some portion of service members has been diagnosed with respiratory disease that could be related to burn pit exposure.
What is now indisputable is that deployment to southwest Asia leads to an increase in respiratory complaints. Whether veteran respiratory symptoms are due to burn pits, ambient pollution, environmental particulate matter, or dust storms is less clinically relevant. These symptoms require attention, investigation, and management.
What does this mean for the future medical care of service members and veterans?
Many veterans with post-deployment respiratory symptoms undergo extensive evaluations without obtaining a definitive diagnosis. A recent consensus statement on deployment-related respiratory symptoms provides a framework for evaluation in such cases.8 In keeping with that statement, we recommend veterans be referred to centers with expertise in this field, such as the Department of Veterans Affairs (VA) or military health centers, when deployment-related respiratory symptoms are reported. When the evaluation does not lead to a treatable diagnosis, these centers can provide multidisciplinary care to address the symptoms of dyspnea, cough, fatigue, and exercise intolerance to improve functional status.
Despite uncertainty in the evidence or challenges in diagnosis, both the Department of Defense (DoD) and VA remain fully committed to addressing the health concerns of service members and veterans. Notably, the VA has already screened more than 5 million veterans for toxic military exposures in accordance with the PACT Act and is providing ongoing screening and care for veterans with post-deployment respiratory symptoms. Furthermore, the DoD and VA have dedicated large portions of their research budgets to investigating the impacts of exposures during military service and optimizing the care of those with respiratory symptoms. With these commitments to patient care and research, our veterans’ respiratory health can now be optimized, and future risks can be mitigated.
Dr. Haynes is Fellow, Pulmonary and Critical Care Medicine, Walter Reed National Military Medical Center, Assistant Professor of Medicine, Uniformed Services University. Dr. Nations is Pulmonary and Critical Care Medicine, Deputy Chief of Staff for Operations, Washington DC VA Medical Center, Associate Professor of Medicine, Uniformed Services University.
References
1. Smith B, Wong CA, Smith TC, Boyko EJ, Gackstetter GD; Margaret A. K. Ryan for the Millennium Cohort Study Team. Newly reported respiratory symptoms and conditions among military personnel deployed to Iraq and Afghanistan: a prospective population-based study. Am J Epidemiol. 2009;170(11):1433-1442. Preprint. Posted online October 22, 2009. PMID: 19850627. doi: 10.1093/aje/kwp287
2. King MS, Eisenberg R, Newman JH, et al. Constrictive bronchiolitis in soldiers returning from Iraq and Afghanistan. N Engl J Med. 2011;365(3):222-230. Erratum in: N Engl J Med. 2011;365(18):1749. PMID: 21774710; PMCID: PMC3296566. doi: 10.1056/NEJMoa1101388
3. Morris MJ, Dodson DW, Lucero PF, et al. Study of active duty military for pulmonary disease related to environmental deployment exposures (STAMPEDE). Am J Respir Crit Care Med. 2014;190(1):77-84. PMID: 24922562. doi: 10.1164/rccm.201402-0372OC
4. Morris MJ, Walter RJ, McCann ET, et al. Clinical evaluation of deployed military personnel with chronic respiratory symptoms: study of active duty military for pulmonary disease related to environmental deployment exposures (STAMPEDE) III. Chest. 2020;157(6):1559-1567. Preprint. Posted online February 1, 2020. PMID: 32017933. doi: 10.1016/j.chest.2020.01.024
5. Morris MJ, Skabelund AJ, Rawlins FA 3rd, Gallup RA, Aden JK, Holley AB. Study of active duty military personnel for environmental deployment exposures: pre- and post-deployment spirometry (STAMPEDE II). Respir Care. 2019;64(5):536-544. Preprint. Posted online January 8, 2019.PMID: 30622173. doi: 10.4187/respcare.06396
6. Institute of Medicine. Long-Term Health Consequences of Exposure to Burn Pits in Iraq and Afghanistan. The National Academies Press; 2011. https://doi.org/10.17226/13209
7. National Academies of Sciences, Engineering, and Medicine. Respiratory Health Effects of Airborne Hazards Exposures in the Southwest Asia Theater of Military Operations. The National Academies Press; 2020. https://doi.org/10.17226/25837
8. Falvo MJ, Sotolongo AM, Osterholzer JJ, et al. Consensus statements on deployment-related respiratory disease, inclusive of constrictive bronchiolitis: a modified Delphi study. Chest. 2023;163(3):599-609. Preprint. Posted November 4, 2022. PMID: 36343686; PMCID: PMC10154857. doi: 10.1016/j.chest.2022.10.031
Military service is a hazard-ridden profession. It’s easy to recognize the direct dangers from warfighting, such as gunfire and explosions, but the risks from environmental, chemical, and other occupational exposures can be harder to see.
Combustion-based waste management systems, otherwise known as “burn pits,” were used in deployed environments by the US military from the 1990s to the early 2010s. These burn pits were commonly used to eliminate plastics, electronics, munitions, metals, wood, chemicals, and even human waste. At the height of the recent conflicts in Afghanistan, Iraq, and other southwest Asia locations, more than 70% of military installations employed at least one, and nearly 4 million service members were exposed to some degree to their emissions.
Reports of burn pits being related to organic disease have garnered widespread media attention. Initially, this came through anecdotal reports of post-deployment respiratory symptoms. Over time, the conditions attributed to burn pits expanded to include newly diagnosed respiratory diseases and malignancies.
Ultimately, Congress passed the 2022 Promise to Address Comprehensive Toxins (PACT) Act, presumptively linking more than 20 diagnoses to burn pits. The PACT Act provides countless veterans access to low-cost or free medical care for their respective conditions.
What do we know about burn pits and deployment-related respiratory disease?
Data from the Millennium Cohort Study noted an approximately 40% increase in respiratory symptoms among individuals returning from deployment but no increase in the frequency of diagnosed respiratory diseases.1 This study and others definitively established a temporal relationship between deployment and respiratory symptoms. Soon after, a retrospective, observational study of service members with post-deployment respiratory symptoms found a high prevalence of constrictive bronchiolitis (CB) identified by lung biopsy.2 Patients in this group reported exposure to burn pits and a sulfur mine fire in the Mosul area while deployed. Most had normal imaging and pulmonary function testing before biopsy, confounding the clinical significance of the CB finding. The publication of this report led to increased investigation of respiratory function during and after deployment.
In a series of prospective studies that included full pulmonary function testing, impulse oscillometry, cardiopulmonary exercise testing, bronchoscopy, and, occasionally, lung biopsy to evaluate post-deployment dyspnea, only a small minority received a diagnosis of clinically significant lung disease.3,4 Additionally, when comparing spirometry and impulse oscillometry results from before and after deployment, no decline in lung function was observed in a population of service members reporting regular burn pit exposure.5 These studies suggest that at the population level, deployment does not lead to abnormalities in the structure and function of the respiratory system.
The National Academies of Sciences published two separate reviews of burn pit exposure and outcomes in 2011 and 2020.6,7 They found insufficient evidence to support a causal relationship between burn pit exposure and pulmonary disease. They highlighted studies on the composition of emissions from the area surrounding the largest military burn pit in Iraq. Levels of particulate matter, volatile organic compounds, and polycyclic aromatic hydrocarbons were elevated when compared with those of a typical American city but were similar to the pollution levels seen in the region at the time. Given these findings, they suggested ambient air pollution may have contributed more to clinically significant disease than burn pit emissions.
How do we interpret this mixed data?
At the population level, we have yet to find conclusive data directly linking burn pit exposure to the development of any respiratory disease. Does this mean that burn pits are not harmful?
Not necessarily. Research on outcomes related to burn pit exposure is challenging given the heterogeneity in exposure volume. Much of the research is retrospective and subject to recall bias. Relationships may be distorted, and the precision of reported symptoms and exposure levels is altered. Given these challenges, it’s unsurprising that evidence of causality has yet to be proven. In addition, some portion of service members has been diagnosed with respiratory disease that could be related to burn pit exposure.
What is now indisputable is that deployment to southwest Asia leads to an increase in respiratory complaints. Whether veteran respiratory symptoms are due to burn pits, ambient pollution, environmental particulate matter, or dust storms is less clinically relevant. These symptoms require attention, investigation, and management.
What does this mean for the future medical care of service members and veterans?
Many veterans with post-deployment respiratory symptoms undergo extensive evaluations without obtaining a definitive diagnosis. A recent consensus statement on deployment-related respiratory symptoms provides a framework for evaluation in such cases.8 In keeping with that statement, we recommend veterans be referred to centers with expertise in this field, such as the Department of Veterans Affairs (VA) or military health centers, when deployment-related respiratory symptoms are reported. When the evaluation does not lead to a treatable diagnosis, these centers can provide multidisciplinary care to address the symptoms of dyspnea, cough, fatigue, and exercise intolerance to improve functional status.
Despite uncertainty in the evidence or challenges in diagnosis, both the Department of Defense (DoD) and VA remain fully committed to addressing the health concerns of service members and veterans. Notably, the VA has already screened more than 5 million veterans for toxic military exposures in accordance with the PACT Act and is providing ongoing screening and care for veterans with post-deployment respiratory symptoms. Furthermore, the DoD and VA have dedicated large portions of their research budgets to investigating the impacts of exposures during military service and optimizing the care of those with respiratory symptoms. With these commitments to patient care and research, our veterans’ respiratory health can now be optimized, and future risks can be mitigated.
Dr. Haynes is Fellow, Pulmonary and Critical Care Medicine, Walter Reed National Military Medical Center, Assistant Professor of Medicine, Uniformed Services University. Dr. Nations is Pulmonary and Critical Care Medicine, Deputy Chief of Staff for Operations, Washington DC VA Medical Center, Associate Professor of Medicine, Uniformed Services University.
References
1. Smith B, Wong CA, Smith TC, Boyko EJ, Gackstetter GD; Margaret A. K. Ryan for the Millennium Cohort Study Team. Newly reported respiratory symptoms and conditions among military personnel deployed to Iraq and Afghanistan: a prospective population-based study. Am J Epidemiol. 2009;170(11):1433-1442. Preprint. Posted online October 22, 2009. PMID: 19850627. doi: 10.1093/aje/kwp287
2. King MS, Eisenberg R, Newman JH, et al. Constrictive bronchiolitis in soldiers returning from Iraq and Afghanistan. N Engl J Med. 2011;365(3):222-230. Erratum in: N Engl J Med. 2011;365(18):1749. PMID: 21774710; PMCID: PMC3296566. doi: 10.1056/NEJMoa1101388
3. Morris MJ, Dodson DW, Lucero PF, et al. Study of active duty military for pulmonary disease related to environmental deployment exposures (STAMPEDE). Am J Respir Crit Care Med. 2014;190(1):77-84. PMID: 24922562. doi: 10.1164/rccm.201402-0372OC
4. Morris MJ, Walter RJ, McCann ET, et al. Clinical evaluation of deployed military personnel with chronic respiratory symptoms: study of active duty military for pulmonary disease related to environmental deployment exposures (STAMPEDE) III. Chest. 2020;157(6):1559-1567. Preprint. Posted online February 1, 2020. PMID: 32017933. doi: 10.1016/j.chest.2020.01.024
5. Morris MJ, Skabelund AJ, Rawlins FA 3rd, Gallup RA, Aden JK, Holley AB. Study of active duty military personnel for environmental deployment exposures: pre- and post-deployment spirometry (STAMPEDE II). Respir Care. 2019;64(5):536-544. Preprint. Posted online January 8, 2019.PMID: 30622173. doi: 10.4187/respcare.06396
6. Institute of Medicine. Long-Term Health Consequences of Exposure to Burn Pits in Iraq and Afghanistan. The National Academies Press; 2011. https://doi.org/10.17226/13209
7. National Academies of Sciences, Engineering, and Medicine. Respiratory Health Effects of Airborne Hazards Exposures in the Southwest Asia Theater of Military Operations. The National Academies Press; 2020. https://doi.org/10.17226/25837
8. Falvo MJ, Sotolongo AM, Osterholzer JJ, et al. Consensus statements on deployment-related respiratory disease, inclusive of constrictive bronchiolitis: a modified Delphi study. Chest. 2023;163(3):599-609. Preprint. Posted November 4, 2022. PMID: 36343686; PMCID: PMC10154857. doi: 10.1016/j.chest.2022.10.031
Military service is a hazard-ridden profession. It’s easy to recognize the direct dangers from warfighting, such as gunfire and explosions, but the risks from environmental, chemical, and other occupational exposures can be harder to see.
Combustion-based waste management systems, otherwise known as “burn pits,” were used in deployed environments by the US military from the 1990s to the early 2010s. These burn pits were commonly used to eliminate plastics, electronics, munitions, metals, wood, chemicals, and even human waste. At the height of the recent conflicts in Afghanistan, Iraq, and other southwest Asia locations, more than 70% of military installations employed at least one, and nearly 4 million service members were exposed to some degree to their emissions.
Reports of burn pits being related to organic disease have garnered widespread media attention. Initially, this came through anecdotal reports of post-deployment respiratory symptoms. Over time, the conditions attributed to burn pits expanded to include newly diagnosed respiratory diseases and malignancies.
Ultimately, Congress passed the 2022 Promise to Address Comprehensive Toxins (PACT) Act, presumptively linking more than 20 diagnoses to burn pits. The PACT Act provides countless veterans access to low-cost or free medical care for their respective conditions.
What do we know about burn pits and deployment-related respiratory disease?
Data from the Millennium Cohort Study noted an approximately 40% increase in respiratory symptoms among individuals returning from deployment but no increase in the frequency of diagnosed respiratory diseases.1 This study and others definitively established a temporal relationship between deployment and respiratory symptoms. Soon after, a retrospective, observational study of service members with post-deployment respiratory symptoms found a high prevalence of constrictive bronchiolitis (CB) identified by lung biopsy.2 Patients in this group reported exposure to burn pits and a sulfur mine fire in the Mosul area while deployed. Most had normal imaging and pulmonary function testing before biopsy, confounding the clinical significance of the CB finding. The publication of this report led to increased investigation of respiratory function during and after deployment.
In a series of prospective studies that included full pulmonary function testing, impulse oscillometry, cardiopulmonary exercise testing, bronchoscopy, and, occasionally, lung biopsy to evaluate post-deployment dyspnea, only a small minority received a diagnosis of clinically significant lung disease.3,4 Additionally, when comparing spirometry and impulse oscillometry results from before and after deployment, no decline in lung function was observed in a population of service members reporting regular burn pit exposure.5 These studies suggest that at the population level, deployment does not lead to abnormalities in the structure and function of the respiratory system.
The National Academies of Sciences published two separate reviews of burn pit exposure and outcomes in 2011 and 2020.6,7 They found insufficient evidence to support a causal relationship between burn pit exposure and pulmonary disease. They highlighted studies on the composition of emissions from the area surrounding the largest military burn pit in Iraq. Levels of particulate matter, volatile organic compounds, and polycyclic aromatic hydrocarbons were elevated when compared with those of a typical American city but were similar to the pollution levels seen in the region at the time. Given these findings, they suggested ambient air pollution may have contributed more to clinically significant disease than burn pit emissions.
How do we interpret this mixed data?
At the population level, we have yet to find conclusive data directly linking burn pit exposure to the development of any respiratory disease. Does this mean that burn pits are not harmful?
Not necessarily. Research on outcomes related to burn pit exposure is challenging given the heterogeneity in exposure volume. Much of the research is retrospective and subject to recall bias. Relationships may be distorted, and the precision of reported symptoms and exposure levels is altered. Given these challenges, it’s unsurprising that evidence of causality has yet to be proven. In addition, some portion of service members has been diagnosed with respiratory disease that could be related to burn pit exposure.
What is now indisputable is that deployment to southwest Asia leads to an increase in respiratory complaints. Whether veteran respiratory symptoms are due to burn pits, ambient pollution, environmental particulate matter, or dust storms is less clinically relevant. These symptoms require attention, investigation, and management.
What does this mean for the future medical care of service members and veterans?
Many veterans with post-deployment respiratory symptoms undergo extensive evaluations without obtaining a definitive diagnosis. A recent consensus statement on deployment-related respiratory symptoms provides a framework for evaluation in such cases.8 In keeping with that statement, we recommend veterans be referred to centers with expertise in this field, such as the Department of Veterans Affairs (VA) or military health centers, when deployment-related respiratory symptoms are reported. When the evaluation does not lead to a treatable diagnosis, these centers can provide multidisciplinary care to address the symptoms of dyspnea, cough, fatigue, and exercise intolerance to improve functional status.
Despite uncertainty in the evidence or challenges in diagnosis, both the Department of Defense (DoD) and VA remain fully committed to addressing the health concerns of service members and veterans. Notably, the VA has already screened more than 5 million veterans for toxic military exposures in accordance with the PACT Act and is providing ongoing screening and care for veterans with post-deployment respiratory symptoms. Furthermore, the DoD and VA have dedicated large portions of their research budgets to investigating the impacts of exposures during military service and optimizing the care of those with respiratory symptoms. With these commitments to patient care and research, our veterans’ respiratory health can now be optimized, and future risks can be mitigated.
Dr. Haynes is Fellow, Pulmonary and Critical Care Medicine, Walter Reed National Military Medical Center, Assistant Professor of Medicine, Uniformed Services University. Dr. Nations is Pulmonary and Critical Care Medicine, Deputy Chief of Staff for Operations, Washington DC VA Medical Center, Associate Professor of Medicine, Uniformed Services University.
References
1. Smith B, Wong CA, Smith TC, Boyko EJ, Gackstetter GD; Margaret A. K. Ryan for the Millennium Cohort Study Team. Newly reported respiratory symptoms and conditions among military personnel deployed to Iraq and Afghanistan: a prospective population-based study. Am J Epidemiol. 2009;170(11):1433-1442. Preprint. Posted online October 22, 2009. PMID: 19850627. doi: 10.1093/aje/kwp287
2. King MS, Eisenberg R, Newman JH, et al. Constrictive bronchiolitis in soldiers returning from Iraq and Afghanistan. N Engl J Med. 2011;365(3):222-230. Erratum in: N Engl J Med. 2011;365(18):1749. PMID: 21774710; PMCID: PMC3296566. doi: 10.1056/NEJMoa1101388
3. Morris MJ, Dodson DW, Lucero PF, et al. Study of active duty military for pulmonary disease related to environmental deployment exposures (STAMPEDE). Am J Respir Crit Care Med. 2014;190(1):77-84. PMID: 24922562. doi: 10.1164/rccm.201402-0372OC
4. Morris MJ, Walter RJ, McCann ET, et al. Clinical evaluation of deployed military personnel with chronic respiratory symptoms: study of active duty military for pulmonary disease related to environmental deployment exposures (STAMPEDE) III. Chest. 2020;157(6):1559-1567. Preprint. Posted online February 1, 2020. PMID: 32017933. doi: 10.1016/j.chest.2020.01.024
5. Morris MJ, Skabelund AJ, Rawlins FA 3rd, Gallup RA, Aden JK, Holley AB. Study of active duty military personnel for environmental deployment exposures: pre- and post-deployment spirometry (STAMPEDE II). Respir Care. 2019;64(5):536-544. Preprint. Posted online January 8, 2019.PMID: 30622173. doi: 10.4187/respcare.06396
6. Institute of Medicine. Long-Term Health Consequences of Exposure to Burn Pits in Iraq and Afghanistan. The National Academies Press; 2011. https://doi.org/10.17226/13209
7. National Academies of Sciences, Engineering, and Medicine. Respiratory Health Effects of Airborne Hazards Exposures in the Southwest Asia Theater of Military Operations. The National Academies Press; 2020. https://doi.org/10.17226/25837
8. Falvo MJ, Sotolongo AM, Osterholzer JJ, et al. Consensus statements on deployment-related respiratory disease, inclusive of constrictive bronchiolitis: a modified Delphi study. Chest. 2023;163(3):599-609. Preprint. Posted November 4, 2022. PMID: 36343686; PMCID: PMC10154857. doi: 10.1016/j.chest.2022.10.031
AI Tools Could Change Pulmonological Imaging and Prognosis
MADRID — Artificial intelligence (AI) can enhance endobronchial ultrasound (EBUS) image processing and new techniques such as cryoEBUS to achieve significant diagnostic and prognostic breakthroughs in interventional pulmonology and general pulmonology.
Pulmonologists are witnessing a surge in new technologies for endoscopy and pulmonology in general. Some, such as AI, robotic bronchoscopy, radiomics, or improvements in electromagnetic bronchial navigation, are minimally invasive diagnostic techniques that significantly enhance the characterization of lung lesions, said Virginia Pajares, MD, a member of the Catalan Society of Pulmonology and coordinator of the Bronchoscopy Unit at Hospital de Sant Pau in Barcelona, Spain. She spoke at the XLI Pneumological Day of the Catalan Society of Pulmonology in Vilanova i la Geltrú, Spain.
Regarding AI, pulmonologists “already have platforms that enable the calculation of the malignancy risk of lung lesions and mediastinal adenopathies. In addition, some devices that allow for an initial radiological assessment of lung nodules are starting to be used,” said Dr. Pajares.
Radiomics: Histology and Markers
“At an endoscopic level, some studies have confirmed the ability of AI applied to imaging to differentiate between benign and malignant lesions, although currently the studies are limited and in the initial stages,” said Dr. Pajares. “AI in interventional pulmonology will be highly beneficial in image interpretation and patient assessment for those who require more invasive diagnostic techniques or for follow-up.”
Regarding the application of AI in medicine, “we lack knowledge and require specific training, especially concerning the learning curve of different technologies, such as electromagnetic navigation, cryoEBUS, or robotic bronchoscopy, which require significant training efforts,” said Dr. Pajares. “The use of AI without a specific goal, that is, creating a mathematical algorithm and feeding it with clinical patient data without control and validation, can lead to inaccurate conclusions. Additionally, we need to determine how to input patient data into these systems to avoid ethical issues, and, of course, legislation on this matter is essential.”
Electromagnetic Navigation
Bronchial electromagnetic navigation is a bronchoscopic technique that allows access to peripheral lung lesions. “It involves virtual route planning using the patient’s chest CT scan and subsequently performing bronchoscopy with navigation using a dirigible electromagnetic probe that allows access to the lesion,” Dr. Pajares explained. “Currently, we have navigators that can incorporate imaging techniques (fluoroscopy or cone-beam CT) to immediately correct discrepancies observed during navigation.”
These new technologies enable a greater number of precise diagnoses and may bring greater patient safety. Studies like NAVIGATE, which was published in 2022 by Folch and colleagues, confirm the diagnostic possibilities and performance of electromagnetic navigation.
In this prospective study, which followed patients for 24 months, the indications are broad. “Its most common use is as a diagnostic technique for peripheral lung nodules and for marking lung lesions for surgical resection or marking for radiotherapy field fiducial placement,” said Dr. Pajares. “Results are also beginning to be published on the treatment of lung lesions using electromagnetic navigation ablation, demonstrating its safety and efficacy in this area.”
Nonsolid Imaging
The challenges in navigation include “improving the diagnosis of lung lesions that are nonsolid, known as ground glass opacities, and verifying it as an additional treatment option for lung nodules in patients who are not candidates for surgical resection,” said Dr. Pajares.
Tess Kramer, PhD, of Amsterdam University Medical Center, Amsterdam, the Netherlands, advocates for the combined use of different technologies to have a beneficial impact on patients’ clinical outcomes.
Robotic bronchoscopy has been implemented in the United States for several years, enhancing the precision of lung nodule diagnosis. However, “currently, there are no clear differences in the diagnostic performance of robotic bronchoscopy compared with navigation in general. Soon, there will be studies to assess in which type of nodules one technique may be more cost-effective.” No centers in Spain have this technology yet, “although some are already evaluating the acquisition of robotic bronchoscopy; it’s only a matter of time,” said Dr. Pajares.
Improvements in echobronchoscopy technology include high-quality image processors and smaller device calibers with greater angulation to diagnose lesions and hard-to-reach adenopathies. From an imaging perspective, AI, combined with the creation of risk calculators, could enable the prediction of lymph node malignancy.
Moreover, the use of small-caliber cryoprobes (1.1 mm) for obtaining samples of adenopathies (cryoEBUS) has enhanced diagnosis by enabling larger tissue samples. Current studies are being conducted to confirm the utility of cryoEBUS in pathologies requiring extensive molecular and immunohistochemical studies for diagnosing lymphoproliferative syndromes or neoplasms.
In a different context, liquid biopsy, a recent laboratory technology unrelated to bronchoscopy, allows the analysis of blood/pleural fluid samples that were extracted using the aforementioned technologies to locate tumor cells and differentiate between malignancy and benignity.
The Challenge of Pneumonitis
Samantha Aso, MD, a pulmonologist, member of the Catalan Society of Pulmonology, and specialist at the Lung Unit of Bellvitge University Hospital in Barcelona, Spain, discussed the challenge of managing pneumonitis in oncology patients.
Pneumonitis is an inflammation of the lungs that can be secondary to treatments, such as oncological therapy, which is the leading cause in 15%-50% of cases. Most oncological treatments can result in this process, including chemotherapy, chest radiotherapy, targeted therapies, conjugated monoclonal antibodies, and monotherapy.
To date, there is no known idiosyncratic cause of this process, except for autoimmune diseases. Pulmonary fibrosis is believed to be a risk factor. “Patients with interstitial lung disease and pulmonary fibrosis have been found to have a higher mortality risk due to pneumonitis. Consequently, cancer treatment cannot be administered to these patients,” said Dr. Aso.
Pulmonologists face the challenge of managing pneumonitis secondary to monotherapy, which currently is treated with cortisone. Patients respond well to this medication, but after corticosteroid withdrawal, reinflammation may occur. “In pneumonitis patients, oncological treatment (monotherapy) should be suspended while pulmonologists manage the pneumonitis with corticosteroids. However, we are uncertain about how rapidly or slowly to reduce the dosage. We cannot taper these doses as quickly as desired because reinflammation may occur, and to date, there are no alternative treatments apart from corticosteroids,” said Dr. Aso.
She noted that excellent survival results are achieved with monotherapy, but further research is required on the safety of antineoplastic drugs as a secondary endpoint. “Suspending oncological treatment due to pneumonitis means that patients are not receiving adequate cancer treatment, which has a significant psychological impact that also needs to be addressed,” Dr. Aso concluded.
Dr. Pajares and Dr. Aso declared no relevant financial relationships.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
MADRID — Artificial intelligence (AI) can enhance endobronchial ultrasound (EBUS) image processing and new techniques such as cryoEBUS to achieve significant diagnostic and prognostic breakthroughs in interventional pulmonology and general pulmonology.
Pulmonologists are witnessing a surge in new technologies for endoscopy and pulmonology in general. Some, such as AI, robotic bronchoscopy, radiomics, or improvements in electromagnetic bronchial navigation, are minimally invasive diagnostic techniques that significantly enhance the characterization of lung lesions, said Virginia Pajares, MD, a member of the Catalan Society of Pulmonology and coordinator of the Bronchoscopy Unit at Hospital de Sant Pau in Barcelona, Spain. She spoke at the XLI Pneumological Day of the Catalan Society of Pulmonology in Vilanova i la Geltrú, Spain.
Regarding AI, pulmonologists “already have platforms that enable the calculation of the malignancy risk of lung lesions and mediastinal adenopathies. In addition, some devices that allow for an initial radiological assessment of lung nodules are starting to be used,” said Dr. Pajares.
Radiomics: Histology and Markers
“At an endoscopic level, some studies have confirmed the ability of AI applied to imaging to differentiate between benign and malignant lesions, although currently the studies are limited and in the initial stages,” said Dr. Pajares. “AI in interventional pulmonology will be highly beneficial in image interpretation and patient assessment for those who require more invasive diagnostic techniques or for follow-up.”
Regarding the application of AI in medicine, “we lack knowledge and require specific training, especially concerning the learning curve of different technologies, such as electromagnetic navigation, cryoEBUS, or robotic bronchoscopy, which require significant training efforts,” said Dr. Pajares. “The use of AI without a specific goal, that is, creating a mathematical algorithm and feeding it with clinical patient data without control and validation, can lead to inaccurate conclusions. Additionally, we need to determine how to input patient data into these systems to avoid ethical issues, and, of course, legislation on this matter is essential.”
Electromagnetic Navigation
Bronchial electromagnetic navigation is a bronchoscopic technique that allows access to peripheral lung lesions. “It involves virtual route planning using the patient’s chest CT scan and subsequently performing bronchoscopy with navigation using a dirigible electromagnetic probe that allows access to the lesion,” Dr. Pajares explained. “Currently, we have navigators that can incorporate imaging techniques (fluoroscopy or cone-beam CT) to immediately correct discrepancies observed during navigation.”
These new technologies enable a greater number of precise diagnoses and may bring greater patient safety. Studies like NAVIGATE, which was published in 2022 by Folch and colleagues, confirm the diagnostic possibilities and performance of electromagnetic navigation.
In this prospective study, which followed patients for 24 months, the indications are broad. “Its most common use is as a diagnostic technique for peripheral lung nodules and for marking lung lesions for surgical resection or marking for radiotherapy field fiducial placement,” said Dr. Pajares. “Results are also beginning to be published on the treatment of lung lesions using electromagnetic navigation ablation, demonstrating its safety and efficacy in this area.”
Nonsolid Imaging
The challenges in navigation include “improving the diagnosis of lung lesions that are nonsolid, known as ground glass opacities, and verifying it as an additional treatment option for lung nodules in patients who are not candidates for surgical resection,” said Dr. Pajares.
Tess Kramer, PhD, of Amsterdam University Medical Center, Amsterdam, the Netherlands, advocates for the combined use of different technologies to have a beneficial impact on patients’ clinical outcomes.
Robotic bronchoscopy has been implemented in the United States for several years, enhancing the precision of lung nodule diagnosis. However, “currently, there are no clear differences in the diagnostic performance of robotic bronchoscopy compared with navigation in general. Soon, there will be studies to assess in which type of nodules one technique may be more cost-effective.” No centers in Spain have this technology yet, “although some are already evaluating the acquisition of robotic bronchoscopy; it’s only a matter of time,” said Dr. Pajares.
Improvements in echobronchoscopy technology include high-quality image processors and smaller device calibers with greater angulation to diagnose lesions and hard-to-reach adenopathies. From an imaging perspective, AI, combined with the creation of risk calculators, could enable the prediction of lymph node malignancy.
Moreover, the use of small-caliber cryoprobes (1.1 mm) for obtaining samples of adenopathies (cryoEBUS) has enhanced diagnosis by enabling larger tissue samples. Current studies are being conducted to confirm the utility of cryoEBUS in pathologies requiring extensive molecular and immunohistochemical studies for diagnosing lymphoproliferative syndromes or neoplasms.
In a different context, liquid biopsy, a recent laboratory technology unrelated to bronchoscopy, allows the analysis of blood/pleural fluid samples that were extracted using the aforementioned technologies to locate tumor cells and differentiate between malignancy and benignity.
The Challenge of Pneumonitis
Samantha Aso, MD, a pulmonologist, member of the Catalan Society of Pulmonology, and specialist at the Lung Unit of Bellvitge University Hospital in Barcelona, Spain, discussed the challenge of managing pneumonitis in oncology patients.
Pneumonitis is an inflammation of the lungs that can be secondary to treatments, such as oncological therapy, which is the leading cause in 15%-50% of cases. Most oncological treatments can result in this process, including chemotherapy, chest radiotherapy, targeted therapies, conjugated monoclonal antibodies, and monotherapy.
To date, there is no known idiosyncratic cause of this process, except for autoimmune diseases. Pulmonary fibrosis is believed to be a risk factor. “Patients with interstitial lung disease and pulmonary fibrosis have been found to have a higher mortality risk due to pneumonitis. Consequently, cancer treatment cannot be administered to these patients,” said Dr. Aso.
Pulmonologists face the challenge of managing pneumonitis secondary to monotherapy, which currently is treated with cortisone. Patients respond well to this medication, but after corticosteroid withdrawal, reinflammation may occur. “In pneumonitis patients, oncological treatment (monotherapy) should be suspended while pulmonologists manage the pneumonitis with corticosteroids. However, we are uncertain about how rapidly or slowly to reduce the dosage. We cannot taper these doses as quickly as desired because reinflammation may occur, and to date, there are no alternative treatments apart from corticosteroids,” said Dr. Aso.
She noted that excellent survival results are achieved with monotherapy, but further research is required on the safety of antineoplastic drugs as a secondary endpoint. “Suspending oncological treatment due to pneumonitis means that patients are not receiving adequate cancer treatment, which has a significant psychological impact that also needs to be addressed,” Dr. Aso concluded.
Dr. Pajares and Dr. Aso declared no relevant financial relationships.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
MADRID — Artificial intelligence (AI) can enhance endobronchial ultrasound (EBUS) image processing and new techniques such as cryoEBUS to achieve significant diagnostic and prognostic breakthroughs in interventional pulmonology and general pulmonology.
Pulmonologists are witnessing a surge in new technologies for endoscopy and pulmonology in general. Some, such as AI, robotic bronchoscopy, radiomics, or improvements in electromagnetic bronchial navigation, are minimally invasive diagnostic techniques that significantly enhance the characterization of lung lesions, said Virginia Pajares, MD, a member of the Catalan Society of Pulmonology and coordinator of the Bronchoscopy Unit at Hospital de Sant Pau in Barcelona, Spain. She spoke at the XLI Pneumological Day of the Catalan Society of Pulmonology in Vilanova i la Geltrú, Spain.
Regarding AI, pulmonologists “already have platforms that enable the calculation of the malignancy risk of lung lesions and mediastinal adenopathies. In addition, some devices that allow for an initial radiological assessment of lung nodules are starting to be used,” said Dr. Pajares.
Radiomics: Histology and Markers
“At an endoscopic level, some studies have confirmed the ability of AI applied to imaging to differentiate between benign and malignant lesions, although currently the studies are limited and in the initial stages,” said Dr. Pajares. “AI in interventional pulmonology will be highly beneficial in image interpretation and patient assessment for those who require more invasive diagnostic techniques or for follow-up.”
Regarding the application of AI in medicine, “we lack knowledge and require specific training, especially concerning the learning curve of different technologies, such as electromagnetic navigation, cryoEBUS, or robotic bronchoscopy, which require significant training efforts,” said Dr. Pajares. “The use of AI without a specific goal, that is, creating a mathematical algorithm and feeding it with clinical patient data without control and validation, can lead to inaccurate conclusions. Additionally, we need to determine how to input patient data into these systems to avoid ethical issues, and, of course, legislation on this matter is essential.”
Electromagnetic Navigation
Bronchial electromagnetic navigation is a bronchoscopic technique that allows access to peripheral lung lesions. “It involves virtual route planning using the patient’s chest CT scan and subsequently performing bronchoscopy with navigation using a dirigible electromagnetic probe that allows access to the lesion,” Dr. Pajares explained. “Currently, we have navigators that can incorporate imaging techniques (fluoroscopy or cone-beam CT) to immediately correct discrepancies observed during navigation.”
These new technologies enable a greater number of precise diagnoses and may bring greater patient safety. Studies like NAVIGATE, which was published in 2022 by Folch and colleagues, confirm the diagnostic possibilities and performance of electromagnetic navigation.
In this prospective study, which followed patients for 24 months, the indications are broad. “Its most common use is as a diagnostic technique for peripheral lung nodules and for marking lung lesions for surgical resection or marking for radiotherapy field fiducial placement,” said Dr. Pajares. “Results are also beginning to be published on the treatment of lung lesions using electromagnetic navigation ablation, demonstrating its safety and efficacy in this area.”
Nonsolid Imaging
The challenges in navigation include “improving the diagnosis of lung lesions that are nonsolid, known as ground glass opacities, and verifying it as an additional treatment option for lung nodules in patients who are not candidates for surgical resection,” said Dr. Pajares.
Tess Kramer, PhD, of Amsterdam University Medical Center, Amsterdam, the Netherlands, advocates for the combined use of different technologies to have a beneficial impact on patients’ clinical outcomes.
Robotic bronchoscopy has been implemented in the United States for several years, enhancing the precision of lung nodule diagnosis. However, “currently, there are no clear differences in the diagnostic performance of robotic bronchoscopy compared with navigation in general. Soon, there will be studies to assess in which type of nodules one technique may be more cost-effective.” No centers in Spain have this technology yet, “although some are already evaluating the acquisition of robotic bronchoscopy; it’s only a matter of time,” said Dr. Pajares.
Improvements in echobronchoscopy technology include high-quality image processors and smaller device calibers with greater angulation to diagnose lesions and hard-to-reach adenopathies. From an imaging perspective, AI, combined with the creation of risk calculators, could enable the prediction of lymph node malignancy.
Moreover, the use of small-caliber cryoprobes (1.1 mm) for obtaining samples of adenopathies (cryoEBUS) has enhanced diagnosis by enabling larger tissue samples. Current studies are being conducted to confirm the utility of cryoEBUS in pathologies requiring extensive molecular and immunohistochemical studies for diagnosing lymphoproliferative syndromes or neoplasms.
In a different context, liquid biopsy, a recent laboratory technology unrelated to bronchoscopy, allows the analysis of blood/pleural fluid samples that were extracted using the aforementioned technologies to locate tumor cells and differentiate between malignancy and benignity.
The Challenge of Pneumonitis
Samantha Aso, MD, a pulmonologist, member of the Catalan Society of Pulmonology, and specialist at the Lung Unit of Bellvitge University Hospital in Barcelona, Spain, discussed the challenge of managing pneumonitis in oncology patients.
Pneumonitis is an inflammation of the lungs that can be secondary to treatments, such as oncological therapy, which is the leading cause in 15%-50% of cases. Most oncological treatments can result in this process, including chemotherapy, chest radiotherapy, targeted therapies, conjugated monoclonal antibodies, and monotherapy.
To date, there is no known idiosyncratic cause of this process, except for autoimmune diseases. Pulmonary fibrosis is believed to be a risk factor. “Patients with interstitial lung disease and pulmonary fibrosis have been found to have a higher mortality risk due to pneumonitis. Consequently, cancer treatment cannot be administered to these patients,” said Dr. Aso.
Pulmonologists face the challenge of managing pneumonitis secondary to monotherapy, which currently is treated with cortisone. Patients respond well to this medication, but after corticosteroid withdrawal, reinflammation may occur. “In pneumonitis patients, oncological treatment (monotherapy) should be suspended while pulmonologists manage the pneumonitis with corticosteroids. However, we are uncertain about how rapidly or slowly to reduce the dosage. We cannot taper these doses as quickly as desired because reinflammation may occur, and to date, there are no alternative treatments apart from corticosteroids,” said Dr. Aso.
She noted that excellent survival results are achieved with monotherapy, but further research is required on the safety of antineoplastic drugs as a secondary endpoint. “Suspending oncological treatment due to pneumonitis means that patients are not receiving adequate cancer treatment, which has a significant psychological impact that also needs to be addressed,” Dr. Aso concluded.
Dr. Pajares and Dr. Aso declared no relevant financial relationships.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.