User login
Depressed and awkward: Is it more than that?
CASE Treatment-resistant MDD
Ms. P, age 21, presents to the outpatient clinic. She has diagnoses of treatment-resistant major depressive disorder (MDD) and schizoid personality disorder (SPD). Ms. P was diagnosed with MDD 3 years ago after reporting symptoms of prevailing sadness for approximately 8 years, described as feelings of worthlessness, anhedonia, social withdrawal, and decreased hygiene and self-care behaviors, as well as suicidal ideation and self-harm. SPD was diagnosed 1 year earlier based on her “odd” behaviors and disheveled appearance following observation and in collateral with her family. Her odd behaviors are described as spending most of her time alone, preferring solitary activities, and having little contact with people other than her parents.
Ms. P reports that she was previously treated with citalopram, 20 mg/d, bupropion, 150 mg/d, aripiprazole, 3.75 mg/d, topiramate, 100 mg twice daily, and melatonin, 9 mg/d at bedtime, but discontinued follow-up appointments and medications after no significant improvement in symptoms.
[polldaddy:11027942]
The authors’ observations
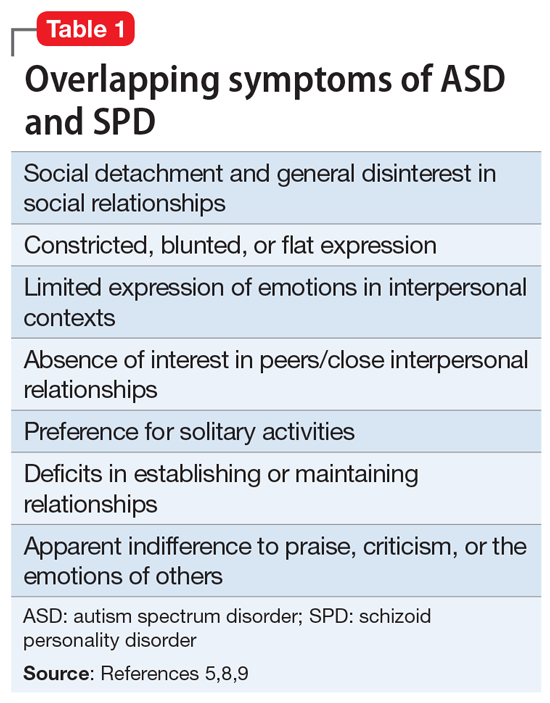
The term “schizoid” first made its debut in the medical community to describe the prodromal social withdrawal and isolation observed in schizophrenia.1 The use of schizoid to describe a personality type first occurred in DSM-III in 1980.2 SPD is a Cluster A personality disorder that groups personalities characterized by common traits that are “odd” or “eccentric” and may resemble the positive and/or negative symptoms of schizophrenia.3,4 Relatively uncommon in clinical settings, SPD includes individuals who do not desire or enjoy close relationships. Those afflicted with SPD will be described as isolated, aloof, and detached from social relationships with others, even immediate family members. Individuals with SPD may appear indifferent to criticism and praise, and may take pleasure in only a few activities. They may exhibit a general absence of affective range, which contributes to their characterization as flat, blunted, or emotionally vacant. SPD is more commonly diagnosed in males and may be present in childhood and adolescence. These children are typified by solitariness, poor peer relationships, and underachievement in school. SPD impacts 3.1% to 4.9% of the United States population and approximately 1% of community populations.5,6
EVALUATION Persistent depressive symptoms
Ms. P is accompanied by her parents for the examination. She reports a chronic, persistent sad mood, hopelessness, anergia, insomnia, anhedonia, and decreased concentration and appetite. She says she experiences episodes of intense worry, along with tension, restlessness, feelings of being on the edge, irritability, and difficulty relaxing. Socially, she is withdrawn, preferring to stay alone in her room most of the day watching YouTube or trying to write stories. She has 2 friends with whom she does not interact with in person, but rather through digital means. Ms. P has never enjoyed attending school and feels “nervous” when she is around people. She has difficulty expressing her thoughts and often looks to her parents for help. Her parents add that getting Ms. P to attend school was a struggle, which resulted in periods of home schooling throughout high school.
The treating team prescribes citalopram, 10 mg/d, and aripiprazole, 2 mg/d. On subsequent follow-up visits, Ms. P’s depression improves with an increase in citalopram to 40 mg/d. Psychotherapy is added to her treatment plan to help address the persistent social deficits, odd behavior, and anxieties.
Continue to: Evaluation Psychological assessment...
EVALUATION Psychological assessment
At her psychotherapy intake appointment with the clinical neuropsychologist, Ms. P is dressed in purple from head to toe and sits clutching her purse and looking at the ground. She is overweight with clean, fitting clothing. Ms. P takes a secondary role during most of the interview, allowing her parents to answer most questions. When asked why she is starting therapy, Ms. P replies, “Well, I’ve been using the bathroom a lot.” She describes a feeling of comfort and calmness while in the restroom. Suddenly, she asks her parents to exit the exam room for a moment. Once they leave, she leans in and whispers, “Have you ever heard of self-sabotage? I think that’s what I’m doing.”
Her mood is euthymic, with a blunted affect. She scores 2 on the Patient Health Questionnaire-9 (PHQ-9) and 10 on the Generalized Anxiety Disorder 7-item scale (GAD-7), which indicates the positive impact of medication on her depressive symptoms but continuing moderate anxious distress. She endorses fear of the night, insomnia, and suicidal ideation. She reports an unusual “constant itching sensation,” resulting in hours of repetitive excoriation. Physical examination reveals several significant scars and scabs covering her bilateral upper and lower extremities. Her vocational history is brief; she had held 2 entry-level customer service positions that lasted <1 year. She was fired due to excessive bathroom use.
As the interview progresses, the intake clinician’s background in neuropsychological assessment facilitates screening for possible developmental disorders. Given the nature of the referral and psychotherapy intake, a full neuropsychological assessment is not conducted. The clinician emphasizes verbal abstraction and theory of mind. Ms. P’s IQ was estimated to be average by Wide Range Achievement Test 4 word reading and interview questions about her academic history. Questions are abstracted from the Autism Diagnostic Observation Schedule, Module 4, to assess for conversation ability, emotional insight, awareness and expression, relationships, and areas of functioning in daily living. Developmental history questions, such as those found on the Adaptive Behavior Assessment System, 3rd edition, help guide developmental information provided by parents in the areas of communication, emotion and eye-gaze, gestures, sensory function, language, social functioning, hygiene behavior, and specific interests.
Ms. P’s mother describes a normal pregnancy and delivery; however, she states that Ms. P was “born with problems,” including difficulty with rooting and sucking, and required gastrointestinal intubation until age 3. Cyclical vomiting followed normal food consumption. Ambulation, language acquisition, toilet training, and hygiene behavior were delayed. Ms. P experienced improvements with early intervention in intensive physical and occupational therapy.
Ms. P’s hygiene is well below average, and she requires cueing from her parents. She attended general education until she reached high school, when she began special education. She was sensitive to sensory stimulation from infancy, with sensory sensitivity to textures. Ms. P continues to report sensory sensitivity and lapses in hygiene.
She has difficulty establishing and maintaining relationships with her peers, and prefers solitary activities. Ms. P has no history of romantic relationships, although she does desire one. When asked about her understanding of various relationships, Ms. P’s responses are stereotyped, such as “I know someone is my friend because they are nice to me” and “People get married because they love each other.” She struggles to offer greater insight into the nuances that form lasting relationships and bonds. Ms. P struggles to imitate and describe the physical and internal cues of several basic emotions (eg, fear, joy, anger).
Her conversational and social skills are assessed by asking her to engage in a conversation with the examiner as if meeting for the first time. Her speech is reciprocal, aprosodic, and delayed. The conversation is one-sided, and the examiner fills in several awkward pauses. Ms. P’s gaze at times is intense and prolonged, especially when responding to questions. She tends to use descriptive statements (eg, “I like your purple pen, I like your shirt”) to engage in conversation, rather than gathering more information through reflective statements, questions, or expressing a shared interest.
Ms. P’s verbal abstraction is screened using questions from the Wechsler Adult Intelligence Scale, 4th edition Similarities subtest, to which she provides several responses within normal limits. Her understanding of colloquial speech is assessed by asking her the meaning of common phrases (eg, “Get knocked down 9 times, get up 10,” “Jack and Jill are 2 peas in a pod”). On many occasions, she is able to limit her response to 1 word, (eg, “resiliency”), demonstrating intact ability to decipher idioms.
[polldaddy:11027971]
The authors’ observations
Upon reflection of Ms. P’s clinical presentation and history of developmental delays, social deficits, sensory sensitivity since infancy, and repetitive behaviors (all which continue to impact her), the clinical team concluded that the diagnosis of autism spectrum disorder (ASD) helps explain the patient’s “odd” behaviors, more so than SPD.
ASD is a heterogenous, complex neuropsychiatric disorder characterized by a persistent deficit in social reciprocity, verbal, and nonverbal communication, and includes a pattern of restricted, repetitive and/or stereotyped behaviors and/or interests.5 The term “autismus” is Greek meaning “self,” and was first used to classify the qualities of “morbid self-admiration” observed in prodromal schizophrenia.7
To properly distinguish these disorders, keep in mind that patients with ASD have repetitive and restricted patterns of behaviors or interests that are not found in SPD, and experience deficits in forming, maintaining, and understanding relationships since they lack those skills, while patients with SPD are more prone to desire solitary activities and limited relationships.5,9
There has been an increased interest in determining why for some patients the diagnosis of ASD is delayed until they reach adulthood. Limited or no access to the patient’s childhood caregiver to obtain a developmental history, as well as generational differences on what constitutes typical childhood behavior, could contribute to a delayed diagnosis of ASD until adulthood. Some patients develop camouflaging strategies that allow them to navigate social expectations to a limited degree, such as learning stock phrases, imitating gestures, and telling anecdotes. Another factor to consider is that co-occurring psychiatric disorders may take center stage when patients present for mental health services.10 Fusar-Poli et al11 investigated the characteristics of patients who received a diagnosis of ASD in adulthood. They found that the median time from the initial clinical evaluation to diagnosis of ASD in adulthood was 11 years. In adults identified with ASD, their cognitive abilities ranged from average to above average, and they required less support. Additionally, they also had higher rates of being previously diagnosed with psychotic disorders and personality disorders.11
It is important to keep in mind that the wide spectrum of autism as currently defined by DSM-5 and its overlap of symptoms with other psychiatric disorders can make the diagnosis challenging for both child and adolescent psychiatrists and adult psychiatrists and might help explain why severe cases of ASD are more readily identified earlier than milder cases of ASD.10
Ms. P’s case is also an example of how women are more likely than men to be overlooked when evaluated for ASD. According to DSM-5, the estimated gender ratio for ASD is believed to be 4:1 (male:female).5 However, upon systematic review and meta-analysis, Loomes et al12 found that the gender ratio may be closer to 3:1 (male:female). These authors suggested that diagnostic bias and a failure of passive case ascertainment to estimate gender ratios as stated by DSM-5 in identifying ASD might explain the lower gender ratio.12 A growing body of evidence suggests that ASD is different in males and females. A 2019 qualitative study by Milner et al13 found that female participants reported using masking and camouflaging strategies to appear neurotypical. Compensatory behaviors were found to be linked to a delay in diagnosis and support for ASD.13
Cognitive ability as measured by IQ has also been found to be a factor in receiving a diagnosis of ASD. In a 2010 secondary analysis of a population-based study of the prevalence of ASD, Giarelli et al14found that girls with cognitive impairments as measured by IQ were less likely to be diagnosed with ASD than boys with cognitive impairment, despite meeting the criteria for ASD. Females tend to exhibit fewer repetitive behaviors than males, and tend to be more likely to show accompanying intellectual disability, which suggests that females with ASD may go unrecognized when they exhibit average intelligence with less impairment of behavior and subtler manifestation of social and communication deficits.15 Consequently, females tend to receive this diagnosis later than males.
Continue to: Treatment...
TREATMENT Adding CBT
At an interdisciplinary session several weeks later that includes Ms. P and her parents, the treatment team discusses the revised diagnoses of ASD and MDD, a treatment recommendation for cognitive-behavioral therapy (CBT), and continued use of medication. At this session, Ms. P discloses that she has not been consistent with her medication regimen since her last appointment, which helps explain the increase in her PHQ-9 score from 2 to 14 and GAD-7 score
[polldaddy:11027990]
The authors’ observations
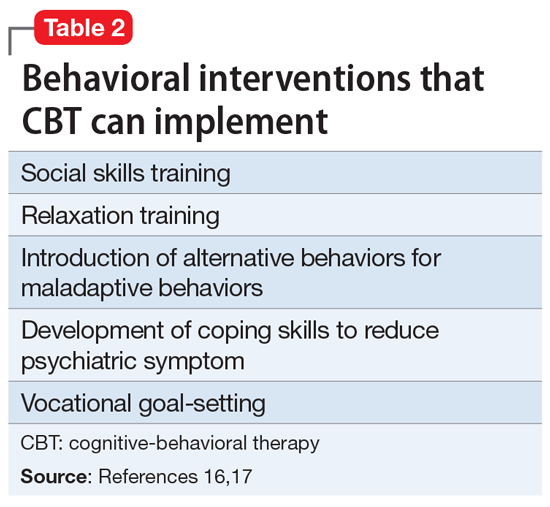
CBT can be helpful in improving medication adherence, developing coping skills, and modifying maladaptive behaviors.
OUTCOME Improvement with psychotherapy
Ms. P and family agree with the team’s recommendations. The aims of Ms. P’s psychotherapy are to maintain medication compliance; implement behavioral modification, vocational rehabilitation, and community engagement; develop social skills; increase functional independence; and develop coping skills for depression and anxiety.
Bottom Line
The prevalence of schizoid personality disorder (SPD) is low, and its symptoms overlap with those of autism spectrum disorder. Therefore, before diagnosing SPD in an adult patient, it is important to obtain a detailed developmental history and include an interdisciplinary team to assess for autism spectrum disorder.
1. Fariba K, Gupta V. Schizoid personality disorder. StatPearls Publishing. Updated June 9, 2021. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK559234/
2. Diagnostic and Statistical Manual of Mental Disorders: DSM-III. 3rd ed rev. American Psychiatric Association; 1987.
3. Esterberg ML, Goulding SM, Walker EF. Cluster A personality disorders: schizotypal, schizoid and paranoid personality disorders in childhood and adolescence. J Psychopathol Behav Assess. 2010;32(4):515-528. doi:10.1007/s10862-010-9183-8
4. Kalus O, Bernstein DP, Siever LJ. Schizoid personality disorder: a review of current status and implications for DSM-IV. Journal of Personality Disorders. 1993;7(1), 43-52.
5. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
6. Eaton NR, Greene AL. Personality disorders: community prevalence and socio-demographic correlates. Curr Opin Psychol. 2018;21:28-32. doi:10.1016/j.copsyc.2017.09.001
7. Vatano
8. Ritsner MS. Handbook of Schizophrenia Spectrum Disorders, Volume I: Conceptual Issues and Neurobiological Advances. Springer; 2011.
9. Cook ML, Zhang Y, Constantino JN. On the continuity between autistic and schizoid personality disorder trait burden: a prospective study in adolescence. J Nerv Ment Dis. 2020;208(2):94-100. doi:10.1097/NMD.0000000000001105
10. Lai MC, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. 2015;2(11):1013-1027. doi:10.1016/S2215-0366(15)00277-1
11. Fusar-Poli L, Brondino N, Politi P, et al. Missed diagnoses and misdiagnoses of adults with autism spectrum disorder. Eur Arch Psychiatry Clin Neurosci. 2020;10.1007/s00406-020-01189-2. doi:10.1007/s00406-020-01189-w
12. Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(6):466-474. doi:10.1016/j.jaac.2017.03.013
13. Milner V, McIntosh H, Colvert E, et al. A qualitative exploration of the female experience of autism spectrum disorder (ASD). J Autism Dev Disord. 2019;49(6):2389-2402. doi:10.1007/s10803-019-03906-4
14. Giarelli E, Wiggins LD, Rice CE, et al. Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disabil Health J. 2010;3(2):107-116. doi:10.1016/j.dhjo.2009.07.001
15. Frazier TW, Georgiades S, Bishop SL, et al. Behavioral and cognitive characteristics of females and males with autism in the Simons Simplex Collection. J Am Acad Child Adolesc Psychiatry. 2014;53(3):329-40.e403. doi:10.1016/j.jaac.2013.12.004
16. Julius RJ, Novitsky MA Jr, et al. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009;15(1):34-44. doi:10.1097/01.pra.0000344917.43780.77
17. Spain D, Sin J, Chalder T, et al. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: a review. Research in Autism Spectrum Disorders. 2015;9, 151-162. https://doi.org/10.1016/j.rasd.2014.10.019
18. Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. J Autism Dev Disord. 2013;43(3):687-694. doi:10.1007/s10803-012-1615-8
CASE Treatment-resistant MDD
Ms. P, age 21, presents to the outpatient clinic. She has diagnoses of treatment-resistant major depressive disorder (MDD) and schizoid personality disorder (SPD). Ms. P was diagnosed with MDD 3 years ago after reporting symptoms of prevailing sadness for approximately 8 years, described as feelings of worthlessness, anhedonia, social withdrawal, and decreased hygiene and self-care behaviors, as well as suicidal ideation and self-harm. SPD was diagnosed 1 year earlier based on her “odd” behaviors and disheveled appearance following observation and in collateral with her family. Her odd behaviors are described as spending most of her time alone, preferring solitary activities, and having little contact with people other than her parents.
Ms. P reports that she was previously treated with citalopram, 20 mg/d, bupropion, 150 mg/d, aripiprazole, 3.75 mg/d, topiramate, 100 mg twice daily, and melatonin, 9 mg/d at bedtime, but discontinued follow-up appointments and medications after no significant improvement in symptoms.
[polldaddy:11027942]
The authors’ observations
The term “schizoid” first made its debut in the medical community to describe the prodromal social withdrawal and isolation observed in schizophrenia.1 The use of schizoid to describe a personality type first occurred in DSM-III in 1980.2 SPD is a Cluster A personality disorder that groups personalities characterized by common traits that are “odd” or “eccentric” and may resemble the positive and/or negative symptoms of schizophrenia.3,4 Relatively uncommon in clinical settings, SPD includes individuals who do not desire or enjoy close relationships. Those afflicted with SPD will be described as isolated, aloof, and detached from social relationships with others, even immediate family members. Individuals with SPD may appear indifferent to criticism and praise, and may take pleasure in only a few activities. They may exhibit a general absence of affective range, which contributes to their characterization as flat, blunted, or emotionally vacant. SPD is more commonly diagnosed in males and may be present in childhood and adolescence. These children are typified by solitariness, poor peer relationships, and underachievement in school. SPD impacts 3.1% to 4.9% of the United States population and approximately 1% of community populations.5,6
EVALUATION Persistent depressive symptoms
Ms. P is accompanied by her parents for the examination. She reports a chronic, persistent sad mood, hopelessness, anergia, insomnia, anhedonia, and decreased concentration and appetite. She says she experiences episodes of intense worry, along with tension, restlessness, feelings of being on the edge, irritability, and difficulty relaxing. Socially, she is withdrawn, preferring to stay alone in her room most of the day watching YouTube or trying to write stories. She has 2 friends with whom she does not interact with in person, but rather through digital means. Ms. P has never enjoyed attending school and feels “nervous” when she is around people. She has difficulty expressing her thoughts and often looks to her parents for help. Her parents add that getting Ms. P to attend school was a struggle, which resulted in periods of home schooling throughout high school.
The treating team prescribes citalopram, 10 mg/d, and aripiprazole, 2 mg/d. On subsequent follow-up visits, Ms. P’s depression improves with an increase in citalopram to 40 mg/d. Psychotherapy is added to her treatment plan to help address the persistent social deficits, odd behavior, and anxieties.
Continue to: Evaluation Psychological assessment...
EVALUATION Psychological assessment
At her psychotherapy intake appointment with the clinical neuropsychologist, Ms. P is dressed in purple from head to toe and sits clutching her purse and looking at the ground. She is overweight with clean, fitting clothing. Ms. P takes a secondary role during most of the interview, allowing her parents to answer most questions. When asked why she is starting therapy, Ms. P replies, “Well, I’ve been using the bathroom a lot.” She describes a feeling of comfort and calmness while in the restroom. Suddenly, she asks her parents to exit the exam room for a moment. Once they leave, she leans in and whispers, “Have you ever heard of self-sabotage? I think that’s what I’m doing.”
Her mood is euthymic, with a blunted affect. She scores 2 on the Patient Health Questionnaire-9 (PHQ-9) and 10 on the Generalized Anxiety Disorder 7-item scale (GAD-7), which indicates the positive impact of medication on her depressive symptoms but continuing moderate anxious distress. She endorses fear of the night, insomnia, and suicidal ideation. She reports an unusual “constant itching sensation,” resulting in hours of repetitive excoriation. Physical examination reveals several significant scars and scabs covering her bilateral upper and lower extremities. Her vocational history is brief; she had held 2 entry-level customer service positions that lasted <1 year. She was fired due to excessive bathroom use.
As the interview progresses, the intake clinician’s background in neuropsychological assessment facilitates screening for possible developmental disorders. Given the nature of the referral and psychotherapy intake, a full neuropsychological assessment is not conducted. The clinician emphasizes verbal abstraction and theory of mind. Ms. P’s IQ was estimated to be average by Wide Range Achievement Test 4 word reading and interview questions about her academic history. Questions are abstracted from the Autism Diagnostic Observation Schedule, Module 4, to assess for conversation ability, emotional insight, awareness and expression, relationships, and areas of functioning in daily living. Developmental history questions, such as those found on the Adaptive Behavior Assessment System, 3rd edition, help guide developmental information provided by parents in the areas of communication, emotion and eye-gaze, gestures, sensory function, language, social functioning, hygiene behavior, and specific interests.
Ms. P’s mother describes a normal pregnancy and delivery; however, she states that Ms. P was “born with problems,” including difficulty with rooting and sucking, and required gastrointestinal intubation until age 3. Cyclical vomiting followed normal food consumption. Ambulation, language acquisition, toilet training, and hygiene behavior were delayed. Ms. P experienced improvements with early intervention in intensive physical and occupational therapy.
Ms. P’s hygiene is well below average, and she requires cueing from her parents. She attended general education until she reached high school, when she began special education. She was sensitive to sensory stimulation from infancy, with sensory sensitivity to textures. Ms. P continues to report sensory sensitivity and lapses in hygiene.
She has difficulty establishing and maintaining relationships with her peers, and prefers solitary activities. Ms. P has no history of romantic relationships, although she does desire one. When asked about her understanding of various relationships, Ms. P’s responses are stereotyped, such as “I know someone is my friend because they are nice to me” and “People get married because they love each other.” She struggles to offer greater insight into the nuances that form lasting relationships and bonds. Ms. P struggles to imitate and describe the physical and internal cues of several basic emotions (eg, fear, joy, anger).
Her conversational and social skills are assessed by asking her to engage in a conversation with the examiner as if meeting for the first time. Her speech is reciprocal, aprosodic, and delayed. The conversation is one-sided, and the examiner fills in several awkward pauses. Ms. P’s gaze at times is intense and prolonged, especially when responding to questions. She tends to use descriptive statements (eg, “I like your purple pen, I like your shirt”) to engage in conversation, rather than gathering more information through reflective statements, questions, or expressing a shared interest.
Ms. P’s verbal abstraction is screened using questions from the Wechsler Adult Intelligence Scale, 4th edition Similarities subtest, to which she provides several responses within normal limits. Her understanding of colloquial speech is assessed by asking her the meaning of common phrases (eg, “Get knocked down 9 times, get up 10,” “Jack and Jill are 2 peas in a pod”). On many occasions, she is able to limit her response to 1 word, (eg, “resiliency”), demonstrating intact ability to decipher idioms.
[polldaddy:11027971]
The authors’ observations
Upon reflection of Ms. P’s clinical presentation and history of developmental delays, social deficits, sensory sensitivity since infancy, and repetitive behaviors (all which continue to impact her), the clinical team concluded that the diagnosis of autism spectrum disorder (ASD) helps explain the patient’s “odd” behaviors, more so than SPD.
ASD is a heterogenous, complex neuropsychiatric disorder characterized by a persistent deficit in social reciprocity, verbal, and nonverbal communication, and includes a pattern of restricted, repetitive and/or stereotyped behaviors and/or interests.5 The term “autismus” is Greek meaning “self,” and was first used to classify the qualities of “morbid self-admiration” observed in prodromal schizophrenia.7
To properly distinguish these disorders, keep in mind that patients with ASD have repetitive and restricted patterns of behaviors or interests that are not found in SPD, and experience deficits in forming, maintaining, and understanding relationships since they lack those skills, while patients with SPD are more prone to desire solitary activities and limited relationships.5,9
There has been an increased interest in determining why for some patients the diagnosis of ASD is delayed until they reach adulthood. Limited or no access to the patient’s childhood caregiver to obtain a developmental history, as well as generational differences on what constitutes typical childhood behavior, could contribute to a delayed diagnosis of ASD until adulthood. Some patients develop camouflaging strategies that allow them to navigate social expectations to a limited degree, such as learning stock phrases, imitating gestures, and telling anecdotes. Another factor to consider is that co-occurring psychiatric disorders may take center stage when patients present for mental health services.10 Fusar-Poli et al11 investigated the characteristics of patients who received a diagnosis of ASD in adulthood. They found that the median time from the initial clinical evaluation to diagnosis of ASD in adulthood was 11 years. In adults identified with ASD, their cognitive abilities ranged from average to above average, and they required less support. Additionally, they also had higher rates of being previously diagnosed with psychotic disorders and personality disorders.11
It is important to keep in mind that the wide spectrum of autism as currently defined by DSM-5 and its overlap of symptoms with other psychiatric disorders can make the diagnosis challenging for both child and adolescent psychiatrists and adult psychiatrists and might help explain why severe cases of ASD are more readily identified earlier than milder cases of ASD.10
Ms. P’s case is also an example of how women are more likely than men to be overlooked when evaluated for ASD. According to DSM-5, the estimated gender ratio for ASD is believed to be 4:1 (male:female).5 However, upon systematic review and meta-analysis, Loomes et al12 found that the gender ratio may be closer to 3:1 (male:female). These authors suggested that diagnostic bias and a failure of passive case ascertainment to estimate gender ratios as stated by DSM-5 in identifying ASD might explain the lower gender ratio.12 A growing body of evidence suggests that ASD is different in males and females. A 2019 qualitative study by Milner et al13 found that female participants reported using masking and camouflaging strategies to appear neurotypical. Compensatory behaviors were found to be linked to a delay in diagnosis and support for ASD.13
Cognitive ability as measured by IQ has also been found to be a factor in receiving a diagnosis of ASD. In a 2010 secondary analysis of a population-based study of the prevalence of ASD, Giarelli et al14found that girls with cognitive impairments as measured by IQ were less likely to be diagnosed with ASD than boys with cognitive impairment, despite meeting the criteria for ASD. Females tend to exhibit fewer repetitive behaviors than males, and tend to be more likely to show accompanying intellectual disability, which suggests that females with ASD may go unrecognized when they exhibit average intelligence with less impairment of behavior and subtler manifestation of social and communication deficits.15 Consequently, females tend to receive this diagnosis later than males.
Continue to: Treatment...
TREATMENT Adding CBT
At an interdisciplinary session several weeks later that includes Ms. P and her parents, the treatment team discusses the revised diagnoses of ASD and MDD, a treatment recommendation for cognitive-behavioral therapy (CBT), and continued use of medication. At this session, Ms. P discloses that she has not been consistent with her medication regimen since her last appointment, which helps explain the increase in her PHQ-9 score from 2 to 14 and GAD-7 score
[polldaddy:11027990]
The authors’ observations
CBT can be helpful in improving medication adherence, developing coping skills, and modifying maladaptive behaviors.
OUTCOME Improvement with psychotherapy
Ms. P and family agree with the team’s recommendations. The aims of Ms. P’s psychotherapy are to maintain medication compliance; implement behavioral modification, vocational rehabilitation, and community engagement; develop social skills; increase functional independence; and develop coping skills for depression and anxiety.
Bottom Line
The prevalence of schizoid personality disorder (SPD) is low, and its symptoms overlap with those of autism spectrum disorder. Therefore, before diagnosing SPD in an adult patient, it is important to obtain a detailed developmental history and include an interdisciplinary team to assess for autism spectrum disorder.
CASE Treatment-resistant MDD
Ms. P, age 21, presents to the outpatient clinic. She has diagnoses of treatment-resistant major depressive disorder (MDD) and schizoid personality disorder (SPD). Ms. P was diagnosed with MDD 3 years ago after reporting symptoms of prevailing sadness for approximately 8 years, described as feelings of worthlessness, anhedonia, social withdrawal, and decreased hygiene and self-care behaviors, as well as suicidal ideation and self-harm. SPD was diagnosed 1 year earlier based on her “odd” behaviors and disheveled appearance following observation and in collateral with her family. Her odd behaviors are described as spending most of her time alone, preferring solitary activities, and having little contact with people other than her parents.
Ms. P reports that she was previously treated with citalopram, 20 mg/d, bupropion, 150 mg/d, aripiprazole, 3.75 mg/d, topiramate, 100 mg twice daily, and melatonin, 9 mg/d at bedtime, but discontinued follow-up appointments and medications after no significant improvement in symptoms.
[polldaddy:11027942]
The authors’ observations
The term “schizoid” first made its debut in the medical community to describe the prodromal social withdrawal and isolation observed in schizophrenia.1 The use of schizoid to describe a personality type first occurred in DSM-III in 1980.2 SPD is a Cluster A personality disorder that groups personalities characterized by common traits that are “odd” or “eccentric” and may resemble the positive and/or negative symptoms of schizophrenia.3,4 Relatively uncommon in clinical settings, SPD includes individuals who do not desire or enjoy close relationships. Those afflicted with SPD will be described as isolated, aloof, and detached from social relationships with others, even immediate family members. Individuals with SPD may appear indifferent to criticism and praise, and may take pleasure in only a few activities. They may exhibit a general absence of affective range, which contributes to their characterization as flat, blunted, or emotionally vacant. SPD is more commonly diagnosed in males and may be present in childhood and adolescence. These children are typified by solitariness, poor peer relationships, and underachievement in school. SPD impacts 3.1% to 4.9% of the United States population and approximately 1% of community populations.5,6
EVALUATION Persistent depressive symptoms
Ms. P is accompanied by her parents for the examination. She reports a chronic, persistent sad mood, hopelessness, anergia, insomnia, anhedonia, and decreased concentration and appetite. She says she experiences episodes of intense worry, along with tension, restlessness, feelings of being on the edge, irritability, and difficulty relaxing. Socially, she is withdrawn, preferring to stay alone in her room most of the day watching YouTube or trying to write stories. She has 2 friends with whom she does not interact with in person, but rather through digital means. Ms. P has never enjoyed attending school and feels “nervous” when she is around people. She has difficulty expressing her thoughts and often looks to her parents for help. Her parents add that getting Ms. P to attend school was a struggle, which resulted in periods of home schooling throughout high school.
The treating team prescribes citalopram, 10 mg/d, and aripiprazole, 2 mg/d. On subsequent follow-up visits, Ms. P’s depression improves with an increase in citalopram to 40 mg/d. Psychotherapy is added to her treatment plan to help address the persistent social deficits, odd behavior, and anxieties.
Continue to: Evaluation Psychological assessment...
EVALUATION Psychological assessment
At her psychotherapy intake appointment with the clinical neuropsychologist, Ms. P is dressed in purple from head to toe and sits clutching her purse and looking at the ground. She is overweight with clean, fitting clothing. Ms. P takes a secondary role during most of the interview, allowing her parents to answer most questions. When asked why she is starting therapy, Ms. P replies, “Well, I’ve been using the bathroom a lot.” She describes a feeling of comfort and calmness while in the restroom. Suddenly, she asks her parents to exit the exam room for a moment. Once they leave, she leans in and whispers, “Have you ever heard of self-sabotage? I think that’s what I’m doing.”
Her mood is euthymic, with a blunted affect. She scores 2 on the Patient Health Questionnaire-9 (PHQ-9) and 10 on the Generalized Anxiety Disorder 7-item scale (GAD-7), which indicates the positive impact of medication on her depressive symptoms but continuing moderate anxious distress. She endorses fear of the night, insomnia, and suicidal ideation. She reports an unusual “constant itching sensation,” resulting in hours of repetitive excoriation. Physical examination reveals several significant scars and scabs covering her bilateral upper and lower extremities. Her vocational history is brief; she had held 2 entry-level customer service positions that lasted <1 year. She was fired due to excessive bathroom use.
As the interview progresses, the intake clinician’s background in neuropsychological assessment facilitates screening for possible developmental disorders. Given the nature of the referral and psychotherapy intake, a full neuropsychological assessment is not conducted. The clinician emphasizes verbal abstraction and theory of mind. Ms. P’s IQ was estimated to be average by Wide Range Achievement Test 4 word reading and interview questions about her academic history. Questions are abstracted from the Autism Diagnostic Observation Schedule, Module 4, to assess for conversation ability, emotional insight, awareness and expression, relationships, and areas of functioning in daily living. Developmental history questions, such as those found on the Adaptive Behavior Assessment System, 3rd edition, help guide developmental information provided by parents in the areas of communication, emotion and eye-gaze, gestures, sensory function, language, social functioning, hygiene behavior, and specific interests.
Ms. P’s mother describes a normal pregnancy and delivery; however, she states that Ms. P was “born with problems,” including difficulty with rooting and sucking, and required gastrointestinal intubation until age 3. Cyclical vomiting followed normal food consumption. Ambulation, language acquisition, toilet training, and hygiene behavior were delayed. Ms. P experienced improvements with early intervention in intensive physical and occupational therapy.
Ms. P’s hygiene is well below average, and she requires cueing from her parents. She attended general education until she reached high school, when she began special education. She was sensitive to sensory stimulation from infancy, with sensory sensitivity to textures. Ms. P continues to report sensory sensitivity and lapses in hygiene.
She has difficulty establishing and maintaining relationships with her peers, and prefers solitary activities. Ms. P has no history of romantic relationships, although she does desire one. When asked about her understanding of various relationships, Ms. P’s responses are stereotyped, such as “I know someone is my friend because they are nice to me” and “People get married because they love each other.” She struggles to offer greater insight into the nuances that form lasting relationships and bonds. Ms. P struggles to imitate and describe the physical and internal cues of several basic emotions (eg, fear, joy, anger).
Her conversational and social skills are assessed by asking her to engage in a conversation with the examiner as if meeting for the first time. Her speech is reciprocal, aprosodic, and delayed. The conversation is one-sided, and the examiner fills in several awkward pauses. Ms. P’s gaze at times is intense and prolonged, especially when responding to questions. She tends to use descriptive statements (eg, “I like your purple pen, I like your shirt”) to engage in conversation, rather than gathering more information through reflective statements, questions, or expressing a shared interest.
Ms. P’s verbal abstraction is screened using questions from the Wechsler Adult Intelligence Scale, 4th edition Similarities subtest, to which she provides several responses within normal limits. Her understanding of colloquial speech is assessed by asking her the meaning of common phrases (eg, “Get knocked down 9 times, get up 10,” “Jack and Jill are 2 peas in a pod”). On many occasions, she is able to limit her response to 1 word, (eg, “resiliency”), demonstrating intact ability to decipher idioms.
[polldaddy:11027971]
The authors’ observations
Upon reflection of Ms. P’s clinical presentation and history of developmental delays, social deficits, sensory sensitivity since infancy, and repetitive behaviors (all which continue to impact her), the clinical team concluded that the diagnosis of autism spectrum disorder (ASD) helps explain the patient’s “odd” behaviors, more so than SPD.
ASD is a heterogenous, complex neuropsychiatric disorder characterized by a persistent deficit in social reciprocity, verbal, and nonverbal communication, and includes a pattern of restricted, repetitive and/or stereotyped behaviors and/or interests.5 The term “autismus” is Greek meaning “self,” and was first used to classify the qualities of “morbid self-admiration” observed in prodromal schizophrenia.7
To properly distinguish these disorders, keep in mind that patients with ASD have repetitive and restricted patterns of behaviors or interests that are not found in SPD, and experience deficits in forming, maintaining, and understanding relationships since they lack those skills, while patients with SPD are more prone to desire solitary activities and limited relationships.5,9
There has been an increased interest in determining why for some patients the diagnosis of ASD is delayed until they reach adulthood. Limited or no access to the patient’s childhood caregiver to obtain a developmental history, as well as generational differences on what constitutes typical childhood behavior, could contribute to a delayed diagnosis of ASD until adulthood. Some patients develop camouflaging strategies that allow them to navigate social expectations to a limited degree, such as learning stock phrases, imitating gestures, and telling anecdotes. Another factor to consider is that co-occurring psychiatric disorders may take center stage when patients present for mental health services.10 Fusar-Poli et al11 investigated the characteristics of patients who received a diagnosis of ASD in adulthood. They found that the median time from the initial clinical evaluation to diagnosis of ASD in adulthood was 11 years. In adults identified with ASD, their cognitive abilities ranged from average to above average, and they required less support. Additionally, they also had higher rates of being previously diagnosed with psychotic disorders and personality disorders.11
It is important to keep in mind that the wide spectrum of autism as currently defined by DSM-5 and its overlap of symptoms with other psychiatric disorders can make the diagnosis challenging for both child and adolescent psychiatrists and adult psychiatrists and might help explain why severe cases of ASD are more readily identified earlier than milder cases of ASD.10
Ms. P’s case is also an example of how women are more likely than men to be overlooked when evaluated for ASD. According to DSM-5, the estimated gender ratio for ASD is believed to be 4:1 (male:female).5 However, upon systematic review and meta-analysis, Loomes et al12 found that the gender ratio may be closer to 3:1 (male:female). These authors suggested that diagnostic bias and a failure of passive case ascertainment to estimate gender ratios as stated by DSM-5 in identifying ASD might explain the lower gender ratio.12 A growing body of evidence suggests that ASD is different in males and females. A 2019 qualitative study by Milner et al13 found that female participants reported using masking and camouflaging strategies to appear neurotypical. Compensatory behaviors were found to be linked to a delay in diagnosis and support for ASD.13
Cognitive ability as measured by IQ has also been found to be a factor in receiving a diagnosis of ASD. In a 2010 secondary analysis of a population-based study of the prevalence of ASD, Giarelli et al14found that girls with cognitive impairments as measured by IQ were less likely to be diagnosed with ASD than boys with cognitive impairment, despite meeting the criteria for ASD. Females tend to exhibit fewer repetitive behaviors than males, and tend to be more likely to show accompanying intellectual disability, which suggests that females with ASD may go unrecognized when they exhibit average intelligence with less impairment of behavior and subtler manifestation of social and communication deficits.15 Consequently, females tend to receive this diagnosis later than males.
Continue to: Treatment...
TREATMENT Adding CBT
At an interdisciplinary session several weeks later that includes Ms. P and her parents, the treatment team discusses the revised diagnoses of ASD and MDD, a treatment recommendation for cognitive-behavioral therapy (CBT), and continued use of medication. At this session, Ms. P discloses that she has not been consistent with her medication regimen since her last appointment, which helps explain the increase in her PHQ-9 score from 2 to 14 and GAD-7 score
[polldaddy:11027990]
The authors’ observations
CBT can be helpful in improving medication adherence, developing coping skills, and modifying maladaptive behaviors.
OUTCOME Improvement with psychotherapy
Ms. P and family agree with the team’s recommendations. The aims of Ms. P’s psychotherapy are to maintain medication compliance; implement behavioral modification, vocational rehabilitation, and community engagement; develop social skills; increase functional independence; and develop coping skills for depression and anxiety.
Bottom Line
The prevalence of schizoid personality disorder (SPD) is low, and its symptoms overlap with those of autism spectrum disorder. Therefore, before diagnosing SPD in an adult patient, it is important to obtain a detailed developmental history and include an interdisciplinary team to assess for autism spectrum disorder.
1. Fariba K, Gupta V. Schizoid personality disorder. StatPearls Publishing. Updated June 9, 2021. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK559234/
2. Diagnostic and Statistical Manual of Mental Disorders: DSM-III. 3rd ed rev. American Psychiatric Association; 1987.
3. Esterberg ML, Goulding SM, Walker EF. Cluster A personality disorders: schizotypal, schizoid and paranoid personality disorders in childhood and adolescence. J Psychopathol Behav Assess. 2010;32(4):515-528. doi:10.1007/s10862-010-9183-8
4. Kalus O, Bernstein DP, Siever LJ. Schizoid personality disorder: a review of current status and implications for DSM-IV. Journal of Personality Disorders. 1993;7(1), 43-52.
5. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
6. Eaton NR, Greene AL. Personality disorders: community prevalence and socio-demographic correlates. Curr Opin Psychol. 2018;21:28-32. doi:10.1016/j.copsyc.2017.09.001
7. Vatano
8. Ritsner MS. Handbook of Schizophrenia Spectrum Disorders, Volume I: Conceptual Issues and Neurobiological Advances. Springer; 2011.
9. Cook ML, Zhang Y, Constantino JN. On the continuity between autistic and schizoid personality disorder trait burden: a prospective study in adolescence. J Nerv Ment Dis. 2020;208(2):94-100. doi:10.1097/NMD.0000000000001105
10. Lai MC, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. 2015;2(11):1013-1027. doi:10.1016/S2215-0366(15)00277-1
11. Fusar-Poli L, Brondino N, Politi P, et al. Missed diagnoses and misdiagnoses of adults with autism spectrum disorder. Eur Arch Psychiatry Clin Neurosci. 2020;10.1007/s00406-020-01189-2. doi:10.1007/s00406-020-01189-w
12. Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(6):466-474. doi:10.1016/j.jaac.2017.03.013
13. Milner V, McIntosh H, Colvert E, et al. A qualitative exploration of the female experience of autism spectrum disorder (ASD). J Autism Dev Disord. 2019;49(6):2389-2402. doi:10.1007/s10803-019-03906-4
14. Giarelli E, Wiggins LD, Rice CE, et al. Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disabil Health J. 2010;3(2):107-116. doi:10.1016/j.dhjo.2009.07.001
15. Frazier TW, Georgiades S, Bishop SL, et al. Behavioral and cognitive characteristics of females and males with autism in the Simons Simplex Collection. J Am Acad Child Adolesc Psychiatry. 2014;53(3):329-40.e403. doi:10.1016/j.jaac.2013.12.004
16. Julius RJ, Novitsky MA Jr, et al. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009;15(1):34-44. doi:10.1097/01.pra.0000344917.43780.77
17. Spain D, Sin J, Chalder T, et al. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: a review. Research in Autism Spectrum Disorders. 2015;9, 151-162. https://doi.org/10.1016/j.rasd.2014.10.019
18. Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. J Autism Dev Disord. 2013;43(3):687-694. doi:10.1007/s10803-012-1615-8
1. Fariba K, Gupta V. Schizoid personality disorder. StatPearls Publishing. Updated June 9, 2021. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK559234/
2. Diagnostic and Statistical Manual of Mental Disorders: DSM-III. 3rd ed rev. American Psychiatric Association; 1987.
3. Esterberg ML, Goulding SM, Walker EF. Cluster A personality disorders: schizotypal, schizoid and paranoid personality disorders in childhood and adolescence. J Psychopathol Behav Assess. 2010;32(4):515-528. doi:10.1007/s10862-010-9183-8
4. Kalus O, Bernstein DP, Siever LJ. Schizoid personality disorder: a review of current status and implications for DSM-IV. Journal of Personality Disorders. 1993;7(1), 43-52.
5. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
6. Eaton NR, Greene AL. Personality disorders: community prevalence and socio-demographic correlates. Curr Opin Psychol. 2018;21:28-32. doi:10.1016/j.copsyc.2017.09.001
7. Vatano
8. Ritsner MS. Handbook of Schizophrenia Spectrum Disorders, Volume I: Conceptual Issues and Neurobiological Advances. Springer; 2011.
9. Cook ML, Zhang Y, Constantino JN. On the continuity between autistic and schizoid personality disorder trait burden: a prospective study in adolescence. J Nerv Ment Dis. 2020;208(2):94-100. doi:10.1097/NMD.0000000000001105
10. Lai MC, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. 2015;2(11):1013-1027. doi:10.1016/S2215-0366(15)00277-1
11. Fusar-Poli L, Brondino N, Politi P, et al. Missed diagnoses and misdiagnoses of adults with autism spectrum disorder. Eur Arch Psychiatry Clin Neurosci. 2020;10.1007/s00406-020-01189-2. doi:10.1007/s00406-020-01189-w
12. Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(6):466-474. doi:10.1016/j.jaac.2017.03.013
13. Milner V, McIntosh H, Colvert E, et al. A qualitative exploration of the female experience of autism spectrum disorder (ASD). J Autism Dev Disord. 2019;49(6):2389-2402. doi:10.1007/s10803-019-03906-4
14. Giarelli E, Wiggins LD, Rice CE, et al. Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disabil Health J. 2010;3(2):107-116. doi:10.1016/j.dhjo.2009.07.001
15. Frazier TW, Georgiades S, Bishop SL, et al. Behavioral and cognitive characteristics of females and males with autism in the Simons Simplex Collection. J Am Acad Child Adolesc Psychiatry. 2014;53(3):329-40.e403. doi:10.1016/j.jaac.2013.12.004
16. Julius RJ, Novitsky MA Jr, et al. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009;15(1):34-44. doi:10.1097/01.pra.0000344917.43780.77
17. Spain D, Sin J, Chalder T, et al. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: a review. Research in Autism Spectrum Disorders. 2015;9, 151-162. https://doi.org/10.1016/j.rasd.2014.10.019
18. Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. J Autism Dev Disord. 2013;43(3):687-694. doi:10.1007/s10803-012-1615-8
The skill of administering IM medications: 3 questions to consider
The intramuscular (IM) route is commonly used to administer medication in various clinical settings. Even when an IM medication is administered appropriately, patient factors such as high subcutaneous tissue, greater body mass index, and gender can lower the success rate of injections.1 A key but infrequently discussed issue is the skill of the individual administering the IM medication. Incorrectly administering an IM medication can lead to complications, such as abscesses, nerve injury, and skeletal muscle fibrosis.2 Poor IM injection technique can impact patient care and safety.1 For example, a poorly administered antipsychotic medication might lead to the patient receiving a subtherapeutic dose, and could prompt a clinician to ask, “Does this agitated patient need more emergent medication because the medication being given is not effective, or because the medication is not being administered properly?”
This article offers 3 questions to ask when clinicians are evaluating how IM medications are being administered in their clinical setting.
1. Who is administering the medication?
Is the person a registered nurse, licensed psychiatric technician, certified nursing assistant, licensed vocational nurse, or medical assistant? What a specific clinician is permitted to do in one state may not be permitted in another state. For example, in the state of Washington, under certain conditions a medical assistant is allowed to administer an IM medication.3
2. What is the individual’s training in administering IM medications?
Has the person been trained in the proper technique, depending on the body location? Is the injection being properly prepared? Is the correct needle gauge being used?
3. What is the individual’s comfort level with administering IM medications?
Is the person comfortable administering medication only when a patient is calm? Or are they comfortable administering medication when a patient is agitated and being physically held or in 4-point restraints, such as in inpatient psychiatric units or emergency departments?
1. Soliman E, Ranjan S, Xu T, et al. A narrative review of the success of intramuscular gluteal injections and its impact in psychiatry. Biodes Manuf. 2018;1(3):161-170.
2. Nicoll LH, Hesby A. Intramuscular injection: an integrative research review and guideline for evidence-based practice. Appl Nurs Res. 2002;15(3):149-162.
3. Washington State Legislature. WAC 246-827-0240. Medical assistant-certified—Administering medications and injections. Accessed January 10, 2022. https://apps.leg.wa.gov/wac/default.aspx?cite=246-827-0240
The intramuscular (IM) route is commonly used to administer medication in various clinical settings. Even when an IM medication is administered appropriately, patient factors such as high subcutaneous tissue, greater body mass index, and gender can lower the success rate of injections.1 A key but infrequently discussed issue is the skill of the individual administering the IM medication. Incorrectly administering an IM medication can lead to complications, such as abscesses, nerve injury, and skeletal muscle fibrosis.2 Poor IM injection technique can impact patient care and safety.1 For example, a poorly administered antipsychotic medication might lead to the patient receiving a subtherapeutic dose, and could prompt a clinician to ask, “Does this agitated patient need more emergent medication because the medication being given is not effective, or because the medication is not being administered properly?”
This article offers 3 questions to ask when clinicians are evaluating how IM medications are being administered in their clinical setting.
1. Who is administering the medication?
Is the person a registered nurse, licensed psychiatric technician, certified nursing assistant, licensed vocational nurse, or medical assistant? What a specific clinician is permitted to do in one state may not be permitted in another state. For example, in the state of Washington, under certain conditions a medical assistant is allowed to administer an IM medication.3
2. What is the individual’s training in administering IM medications?
Has the person been trained in the proper technique, depending on the body location? Is the injection being properly prepared? Is the correct needle gauge being used?
3. What is the individual’s comfort level with administering IM medications?
Is the person comfortable administering medication only when a patient is calm? Or are they comfortable administering medication when a patient is agitated and being physically held or in 4-point restraints, such as in inpatient psychiatric units or emergency departments?
The intramuscular (IM) route is commonly used to administer medication in various clinical settings. Even when an IM medication is administered appropriately, patient factors such as high subcutaneous tissue, greater body mass index, and gender can lower the success rate of injections.1 A key but infrequently discussed issue is the skill of the individual administering the IM medication. Incorrectly administering an IM medication can lead to complications, such as abscesses, nerve injury, and skeletal muscle fibrosis.2 Poor IM injection technique can impact patient care and safety.1 For example, a poorly administered antipsychotic medication might lead to the patient receiving a subtherapeutic dose, and could prompt a clinician to ask, “Does this agitated patient need more emergent medication because the medication being given is not effective, or because the medication is not being administered properly?”
This article offers 3 questions to ask when clinicians are evaluating how IM medications are being administered in their clinical setting.
1. Who is administering the medication?
Is the person a registered nurse, licensed psychiatric technician, certified nursing assistant, licensed vocational nurse, or medical assistant? What a specific clinician is permitted to do in one state may not be permitted in another state. For example, in the state of Washington, under certain conditions a medical assistant is allowed to administer an IM medication.3
2. What is the individual’s training in administering IM medications?
Has the person been trained in the proper technique, depending on the body location? Is the injection being properly prepared? Is the correct needle gauge being used?
3. What is the individual’s comfort level with administering IM medications?
Is the person comfortable administering medication only when a patient is calm? Or are they comfortable administering medication when a patient is agitated and being physically held or in 4-point restraints, such as in inpatient psychiatric units or emergency departments?
1. Soliman E, Ranjan S, Xu T, et al. A narrative review of the success of intramuscular gluteal injections and its impact in psychiatry. Biodes Manuf. 2018;1(3):161-170.
2. Nicoll LH, Hesby A. Intramuscular injection: an integrative research review and guideline for evidence-based practice. Appl Nurs Res. 2002;15(3):149-162.
3. Washington State Legislature. WAC 246-827-0240. Medical assistant-certified—Administering medications and injections. Accessed January 10, 2022. https://apps.leg.wa.gov/wac/default.aspx?cite=246-827-0240
1. Soliman E, Ranjan S, Xu T, et al. A narrative review of the success of intramuscular gluteal injections and its impact in psychiatry. Biodes Manuf. 2018;1(3):161-170.
2. Nicoll LH, Hesby A. Intramuscular injection: an integrative research review and guideline for evidence-based practice. Appl Nurs Res. 2002;15(3):149-162.
3. Washington State Legislature. WAC 246-827-0240. Medical assistant-certified—Administering medications and injections. Accessed January 10, 2022. https://apps.leg.wa.gov/wac/default.aspx?cite=246-827-0240
Brain stimulation for improved memory?
Electrical brain stimulation may have the potential to improve verbal memory, results of a small study of patients with epilepsy suggest.
Investigators observed improvements in patients implanted with a responsive neurostimulation system (RNS) to control seizures, in that the patients had improved word recall when the system was activated.
Beyond epilepsy, “we suspect that our results would be broadly applicable regardless of the underlying condition, for example, memory loss with Alzheimer’s disease or traumatic brain injury,” Zulfi Haneef, MBBS, MD, associate professor of neurology, Baylor College of Medicine, Houston, said in an interview.
“Mental health conditions such as depression or psychosis could also benefit from targeted electrical stimulation. While we focused on enhancing a preferred brain function [such as memory], parallel areas of research may target enhancing function [such as weakness following stroke] or suppressing function [to manage conditions such as chronic pain,]” Dr. Haneef added.
The study was published online Jan. 17, 2022, in Neurosurgery.
As reported by this news organization, Following implantation of the system, patients attend the clinic for adjustments about every 8-12 weeks.
The investigators studied 17 patients with epilepsy and RNS implants who attended the clinic for routine appointments. A clinical neuropsychologist administered the Hopkins Verbal Learning Test–Revised (HVLT-R), a well-validated list-learning measure of memory and verbal learning.
Patients were read a list of 12 semantically related words and asked to recall the list after three different learning trials. Active or sham stimulation was performed for every third word presented for immediate recall.
The investigators found that the HVLT-R delayed recall raw score was higher for the stimulation condition, compared with the nonstimulation condition (paired t-test, P = .04; effect size, d = 0.627).
“The patients were not aware of when the RNS system was being activated. We alternated when patients were undergoing stimulation versus no stimulation, and still found that when patients’ RNS systems were activated, their memory recall score was greater than when there was no stimulation,” Dr. Haneef said in a release.
This suggests the “human memory can be potentially improved by direct electrical brain stimulation at extremely low currents,” Dr. Haneef said in an interview.
Most patients in the study had stimulation of the hippocampus, the brain’s memory center.
“Moving forward we would want to look at how different patterns or standardized stimulation patterns affect memory. Ultimately, the underlying brain rhythms responsible for these changes in brain function need to be understood so that a more targeted and precise application of electrical stimulation can be achieved,” Dr. Haneef said.
The researchers also caution that, for this preliminary study, no follow-up testing was conducted to determine whether the memory improvement was transient and settled back to baseline after a specified period.
However, they note, this study lays the groundwork for larger-scale and extensive studies examining the nuanced effects of brain stimulation on human cognition and memory.
The study was funded by the Mike Hogg Foundation. Dr. Haneef and two coauthors received coverage for travel expenses but no honorarium for a NeuroPace advisory meeting.
A version of this article first appeared on Medscape.com.
Electrical brain stimulation may have the potential to improve verbal memory, results of a small study of patients with epilepsy suggest.
Investigators observed improvements in patients implanted with a responsive neurostimulation system (RNS) to control seizures, in that the patients had improved word recall when the system was activated.
Beyond epilepsy, “we suspect that our results would be broadly applicable regardless of the underlying condition, for example, memory loss with Alzheimer’s disease or traumatic brain injury,” Zulfi Haneef, MBBS, MD, associate professor of neurology, Baylor College of Medicine, Houston, said in an interview.
“Mental health conditions such as depression or psychosis could also benefit from targeted electrical stimulation. While we focused on enhancing a preferred brain function [such as memory], parallel areas of research may target enhancing function [such as weakness following stroke] or suppressing function [to manage conditions such as chronic pain,]” Dr. Haneef added.
The study was published online Jan. 17, 2022, in Neurosurgery.
As reported by this news organization, Following implantation of the system, patients attend the clinic for adjustments about every 8-12 weeks.
The investigators studied 17 patients with epilepsy and RNS implants who attended the clinic for routine appointments. A clinical neuropsychologist administered the Hopkins Verbal Learning Test–Revised (HVLT-R), a well-validated list-learning measure of memory and verbal learning.
Patients were read a list of 12 semantically related words and asked to recall the list after three different learning trials. Active or sham stimulation was performed for every third word presented for immediate recall.
The investigators found that the HVLT-R delayed recall raw score was higher for the stimulation condition, compared with the nonstimulation condition (paired t-test, P = .04; effect size, d = 0.627).
“The patients were not aware of when the RNS system was being activated. We alternated when patients were undergoing stimulation versus no stimulation, and still found that when patients’ RNS systems were activated, their memory recall score was greater than when there was no stimulation,” Dr. Haneef said in a release.
This suggests the “human memory can be potentially improved by direct electrical brain stimulation at extremely low currents,” Dr. Haneef said in an interview.
Most patients in the study had stimulation of the hippocampus, the brain’s memory center.
“Moving forward we would want to look at how different patterns or standardized stimulation patterns affect memory. Ultimately, the underlying brain rhythms responsible for these changes in brain function need to be understood so that a more targeted and precise application of electrical stimulation can be achieved,” Dr. Haneef said.
The researchers also caution that, for this preliminary study, no follow-up testing was conducted to determine whether the memory improvement was transient and settled back to baseline after a specified period.
However, they note, this study lays the groundwork for larger-scale and extensive studies examining the nuanced effects of brain stimulation on human cognition and memory.
The study was funded by the Mike Hogg Foundation. Dr. Haneef and two coauthors received coverage for travel expenses but no honorarium for a NeuroPace advisory meeting.
A version of this article first appeared on Medscape.com.
Electrical brain stimulation may have the potential to improve verbal memory, results of a small study of patients with epilepsy suggest.
Investigators observed improvements in patients implanted with a responsive neurostimulation system (RNS) to control seizures, in that the patients had improved word recall when the system was activated.
Beyond epilepsy, “we suspect that our results would be broadly applicable regardless of the underlying condition, for example, memory loss with Alzheimer’s disease or traumatic brain injury,” Zulfi Haneef, MBBS, MD, associate professor of neurology, Baylor College of Medicine, Houston, said in an interview.
“Mental health conditions such as depression or psychosis could also benefit from targeted electrical stimulation. While we focused on enhancing a preferred brain function [such as memory], parallel areas of research may target enhancing function [such as weakness following stroke] or suppressing function [to manage conditions such as chronic pain,]” Dr. Haneef added.
The study was published online Jan. 17, 2022, in Neurosurgery.
As reported by this news organization, Following implantation of the system, patients attend the clinic for adjustments about every 8-12 weeks.
The investigators studied 17 patients with epilepsy and RNS implants who attended the clinic for routine appointments. A clinical neuropsychologist administered the Hopkins Verbal Learning Test–Revised (HVLT-R), a well-validated list-learning measure of memory and verbal learning.
Patients were read a list of 12 semantically related words and asked to recall the list after three different learning trials. Active or sham stimulation was performed for every third word presented for immediate recall.
The investigators found that the HVLT-R delayed recall raw score was higher for the stimulation condition, compared with the nonstimulation condition (paired t-test, P = .04; effect size, d = 0.627).
“The patients were not aware of when the RNS system was being activated. We alternated when patients were undergoing stimulation versus no stimulation, and still found that when patients’ RNS systems were activated, their memory recall score was greater than when there was no stimulation,” Dr. Haneef said in a release.
This suggests the “human memory can be potentially improved by direct electrical brain stimulation at extremely low currents,” Dr. Haneef said in an interview.
Most patients in the study had stimulation of the hippocampus, the brain’s memory center.
“Moving forward we would want to look at how different patterns or standardized stimulation patterns affect memory. Ultimately, the underlying brain rhythms responsible for these changes in brain function need to be understood so that a more targeted and precise application of electrical stimulation can be achieved,” Dr. Haneef said.
The researchers also caution that, for this preliminary study, no follow-up testing was conducted to determine whether the memory improvement was transient and settled back to baseline after a specified period.
However, they note, this study lays the groundwork for larger-scale and extensive studies examining the nuanced effects of brain stimulation on human cognition and memory.
The study was funded by the Mike Hogg Foundation. Dr. Haneef and two coauthors received coverage for travel expenses but no honorarium for a NeuroPace advisory meeting.
A version of this article first appeared on Medscape.com.
FROM NEUROSURGERY
Identifying and preventing IPV: Are clinicians doing enough?
Violence against women remains a global dilemma in need of attention. Physical violence in particular, is the most prevalent type of violence across all genders, races, and nationalities.
The Centers for Disease Control and Prevention says more than 43 million women and 38 million men report experiencing psychological aggression by an intimate partner in their lifetime. Meanwhile, 11 million women and 5 million men report enduring sexual or physical violence and intimate partner violence (IPV), and/or stalking by an intimate partner during their lifetimes, according to the CDC.1
Women who have endured this kind of violence might present differently from men. Some studies, for example, show a more significant association between mutual violence, depression, and substance use among women than men.2 Studies on the phenomenon of IPV victims/survivors becoming perpetrators of abuse are limited, but that this happens in some cases.
Having a psychiatric disorder is associated with a higher likelihood of being physically violent with a partner.3,4 One recent study of 250 female psychiatric patients who were married and had no history of drug abuse found that almost 68% reported psychological abuse, 52% reported sexual abuse, 38% social abuse, 37% reported economic abuse, and 25% reported physical abuse.5
Given those statistics and trends, it is incumbent upon clinicians – including those in primary care, psychiatry, and emergency medicine – to learn to quickly identify IPV survivors, and to use available prognostic tools to monitor perpetrators and survivors.
COVID pandemic’s influence
Isolation tied to the COVID-19 pandemic has been linked to increased IPV. A study conducted by researchers at the University of California, Davis, suggested that extra stress experienced during the COVID-19 pandemic caused by income loss, and the inability to pay for housing and food exacerbated the prevalence of IPV early during the pandemic.6
That study, where researchers collected in surveys of nearly 400 adults in the beginning in April 2020 for 10 weeks, showed that more services and communication are needed so that frontline health care and food bank workers, for example, in addition to social workers, doctors, and therapists, can spot the signs and ask clients questions about potential IPV. They could then link survivors to pertinent assistance and resources.
Furthermore, multiple factors probably have played a pivotal role in increasing the prevalence of IPV during the COVID-19 pandemic. For instance, disruption to usual health and social services as well as diminished access to support systems, such as shelters, and charity helplines negatively affected the reporting of domestic violence.
Long before the pandemic, over the past decade, international and national bodies have played a crucial role in terms of improving the awareness and response to domestic violence.7,8 In addition, several policies have been introduced in countries around the globe emphasizing the need to inquire routinely about domestic violence. Nevertheless, mental health services often fail to adequately address domestic violence in clinical encounters. A systematic review of domestic violence assessment screening performed in a variety of health care settings found that evidence was insufficient to conclude that routine inquiry improved morbidity and mortality among victims of IPV.9 So the question becomes: How can we get our patients to tell us about these experiences so we can intervene?
Gender differences in perpetuating IPV
Several studies have found that abuse can result in various mental illnesses, such as depression, PTSD, anxiety, and suicidal ideation. Again, men have a disproportionately higher rate of perpetrating IPV, compared with women. This theory has been a source of debate in the academic community for years, but recent research has confirmed that women do perpetuate violence against their partners to some extent.10,11
Some members of the LGBTQ+ community also report experiencing violence from partners, so as clinicians, we also need to raise our awareness about the existence of violence among same-sex couples. In fact, a team of Italian researchers report more than 50% of gay men and almost 75% of lesbian women reported that they had been psychologically abused by a partner.12 More research into this area is needed.
Our role as health care professionals
The U.S. Preventive Services Task Force advises that all clinic visits include regular IPV screening.13 But these screenings are all too rare. In fact, a meta-analysis of 19 trials of more than 1,600 participants showed only 9%-40% of doctors routinely test for IPV.14 That research clearly shows how important it is for all clinicians to execute IPV screening. However, numerous challenges toward screening exist, including personal discomfort, limited time during appointments, insufficient resources, and inadequate training.
One ongoing debate revolves around which clinician should screen for IPV. Should the psychiatrist carry out this role – or perhaps the primary care physician, nurse, or social worker? These issues become even more fraught when clinicians worry about offending the patient – especially if the clinician is a male.15
The bottom line is that physicians should inquire about intimate partner violence, because research indicates that women are more likely to reveal abuse when prompted. In addition, during physician appointments, they can use the physician-patient therapeutic connection to conduct a domestic violence evaluation, give resources to victims, and provide ongoing care. Patients who exhibit treatment resistance, persistent pain, depression, sleeplessness, and headaches should prompt psychiatrists to conduct additional investigations into the likelihood of intimate partner violence and domestic abuse.
W also should be attentive when counseling patients about domestic violence when suggesting life-changing events such as pregnancy, employment loss, separation, or divorce. Similar to the recommendations of the USPSTF that all women and men should be screened for IPV, it is suggested that physicians be conscious of facilitating a conversation and not being overtly judgmental while observing body cues. Using the statements such as “we have been hearing a lot of violence in our community lately” could be a segue to introduce the subject.
Asking the question of whether you are being hit rather than being abused has allowed more women to open up more about domestic violence. While physicians are aware that most victims might recant and often go back to their abusers, victims need to be counseled that the abuse might intensify and lead to death.
For women who perpetuate IPV and survivors of IPV, safety is the priority. Physicians should provide safety options and be the facilitators. Studies have shown that fewer victims get the referral to the supporting agencies when IPV is indicated, which puts their safety at risk. In women who commit IPV, clinicians should assess the role of the individual in an IPV disclosure. There are various treatment modalities, whether the violence is performed through self-defense, bidirectionally, or because of aggression.
With the advancement of technology, web-based training on how to ask for IPV, documentation, acknowledgment, and structured referral increase physicians’ confidence when faced with an IPV disclosure than none.16 Treatment modalities should include medication reconciliation and cognitive-behavioral therapy – focusing on emotion regulation.
Using instruments such as the danger assessment tool can help physicians intervene early, reducing the risk of domestic violence and IPV recurrence instead of using clinical assessment alone.17 Physicians should convey empathy, validate victims, and help, especially when abuse is reported.
Also, it is important to evaluate survivors’ safety. Counseling can help people rebuild their self-esteem. Structured referrals for psychiatric help and support services are needed to help survivors on the long road to recovery.
Training all physicians, regardless of specialty, is essential to improve prompt IPV identification and bring awareness to resources available to survivors when IPV is disclosed. Although we described an association between IPV victims becoming possible perpetrators of IPV, more long-term studies are required to show the various processes that influence IPV perpetration rates, especially by survivors.
We would also like international and national regulatory bodies to increase the awareness of IPV and adequately address IPV with special emphasis on how mental health services should assess, identify, and respond to services for people who are survivors and perpetrators of IPV.
Dr. Kumari, Dr. Otite, Dr. Afzal, Dr. Alcera, and Dr. Doumas are affiliated with Hackensack Meridian Health at Ocean Medical Center, Brick, N.J. They have no conflicts of interest.
References
1. Centers for Disease Control and Prevention. Preventing intimate partner violence. 2020 Oct 9.
2. Yu R et al. PLOS Med. 16(12):e1002995. doi: 10.1371/journal.pmed.1002995.
3. Oram S et al. Epidemiol Psychiatr Sci. 2014 Dec;23(4):361-76.
4. Munro OE and Sellbom M. Pers Ment Health. 2020 Mar 11. doi: 10.1002/pmh.1480.
5. Sahraian A et al. Asian J Psychiatry. 2020 Jun. doi: 10.1016/j.ajp.2020.102062.
6. Nikos-Rose K. “COVID-19 Isolation Linked to Increased Domestic Violence, Researchers Suggest.” 2021 Feb 24. University of California, Davis.
7. World Health Organization. “Responding to intimate partner violence and sexual violence against women.” WHO clinical policy guidelines. 2013.
8. National Institute for Health and Care Excellence. “Domestic violence and abuse: Multi-agency working.” PH50. 2014 Feb 26.
9. Feder GS et al. Arch Intern Med. 2006;166(1):22-37.
10. Gondolf EW. Violence Against Women. 2014 Dec;20(12)1539-46.
11. Hamberger LK and Larsen SE. J Fam Violence. 2015;30(6):699-717.
12. Rollè L et al. Front Psychol. 21 Aug 2018. doi: 10.3389/fpsyg.2018.01506.
13. Paterno MT and Draughon JE. J Midwif Women Health. 2016;61(31):370-5.
14. Kalra N et al. Cochrane Database Syst Rev. 2021 May 31;5(5)CD012423.
15. Larsen SE and Hamberger LK. J Fam Viol. 2015;30:1007-30.
16. Kalra N et al. Cochrane Database Syst Rev. 2017 Feb;2017(2):CD012423.
17. Campbell JC et al. J Interpers Violence. 2009;24(4):653-74.
Violence against women remains a global dilemma in need of attention. Physical violence in particular, is the most prevalent type of violence across all genders, races, and nationalities.
The Centers for Disease Control and Prevention says more than 43 million women and 38 million men report experiencing psychological aggression by an intimate partner in their lifetime. Meanwhile, 11 million women and 5 million men report enduring sexual or physical violence and intimate partner violence (IPV), and/or stalking by an intimate partner during their lifetimes, according to the CDC.1
Women who have endured this kind of violence might present differently from men. Some studies, for example, show a more significant association between mutual violence, depression, and substance use among women than men.2 Studies on the phenomenon of IPV victims/survivors becoming perpetrators of abuse are limited, but that this happens in some cases.
Having a psychiatric disorder is associated with a higher likelihood of being physically violent with a partner.3,4 One recent study of 250 female psychiatric patients who were married and had no history of drug abuse found that almost 68% reported psychological abuse, 52% reported sexual abuse, 38% social abuse, 37% reported economic abuse, and 25% reported physical abuse.5
Given those statistics and trends, it is incumbent upon clinicians – including those in primary care, psychiatry, and emergency medicine – to learn to quickly identify IPV survivors, and to use available prognostic tools to monitor perpetrators and survivors.
COVID pandemic’s influence
Isolation tied to the COVID-19 pandemic has been linked to increased IPV. A study conducted by researchers at the University of California, Davis, suggested that extra stress experienced during the COVID-19 pandemic caused by income loss, and the inability to pay for housing and food exacerbated the prevalence of IPV early during the pandemic.6
That study, where researchers collected in surveys of nearly 400 adults in the beginning in April 2020 for 10 weeks, showed that more services and communication are needed so that frontline health care and food bank workers, for example, in addition to social workers, doctors, and therapists, can spot the signs and ask clients questions about potential IPV. They could then link survivors to pertinent assistance and resources.
Furthermore, multiple factors probably have played a pivotal role in increasing the prevalence of IPV during the COVID-19 pandemic. For instance, disruption to usual health and social services as well as diminished access to support systems, such as shelters, and charity helplines negatively affected the reporting of domestic violence.
Long before the pandemic, over the past decade, international and national bodies have played a crucial role in terms of improving the awareness and response to domestic violence.7,8 In addition, several policies have been introduced in countries around the globe emphasizing the need to inquire routinely about domestic violence. Nevertheless, mental health services often fail to adequately address domestic violence in clinical encounters. A systematic review of domestic violence assessment screening performed in a variety of health care settings found that evidence was insufficient to conclude that routine inquiry improved morbidity and mortality among victims of IPV.9 So the question becomes: How can we get our patients to tell us about these experiences so we can intervene?
Gender differences in perpetuating IPV
Several studies have found that abuse can result in various mental illnesses, such as depression, PTSD, anxiety, and suicidal ideation. Again, men have a disproportionately higher rate of perpetrating IPV, compared with women. This theory has been a source of debate in the academic community for years, but recent research has confirmed that women do perpetuate violence against their partners to some extent.10,11
Some members of the LGBTQ+ community also report experiencing violence from partners, so as clinicians, we also need to raise our awareness about the existence of violence among same-sex couples. In fact, a team of Italian researchers report more than 50% of gay men and almost 75% of lesbian women reported that they had been psychologically abused by a partner.12 More research into this area is needed.
Our role as health care professionals
The U.S. Preventive Services Task Force advises that all clinic visits include regular IPV screening.13 But these screenings are all too rare. In fact, a meta-analysis of 19 trials of more than 1,600 participants showed only 9%-40% of doctors routinely test for IPV.14 That research clearly shows how important it is for all clinicians to execute IPV screening. However, numerous challenges toward screening exist, including personal discomfort, limited time during appointments, insufficient resources, and inadequate training.
One ongoing debate revolves around which clinician should screen for IPV. Should the psychiatrist carry out this role – or perhaps the primary care physician, nurse, or social worker? These issues become even more fraught when clinicians worry about offending the patient – especially if the clinician is a male.15
The bottom line is that physicians should inquire about intimate partner violence, because research indicates that women are more likely to reveal abuse when prompted. In addition, during physician appointments, they can use the physician-patient therapeutic connection to conduct a domestic violence evaluation, give resources to victims, and provide ongoing care. Patients who exhibit treatment resistance, persistent pain, depression, sleeplessness, and headaches should prompt psychiatrists to conduct additional investigations into the likelihood of intimate partner violence and domestic abuse.
W also should be attentive when counseling patients about domestic violence when suggesting life-changing events such as pregnancy, employment loss, separation, or divorce. Similar to the recommendations of the USPSTF that all women and men should be screened for IPV, it is suggested that physicians be conscious of facilitating a conversation and not being overtly judgmental while observing body cues. Using the statements such as “we have been hearing a lot of violence in our community lately” could be a segue to introduce the subject.
Asking the question of whether you are being hit rather than being abused has allowed more women to open up more about domestic violence. While physicians are aware that most victims might recant and often go back to their abusers, victims need to be counseled that the abuse might intensify and lead to death.
For women who perpetuate IPV and survivors of IPV, safety is the priority. Physicians should provide safety options and be the facilitators. Studies have shown that fewer victims get the referral to the supporting agencies when IPV is indicated, which puts their safety at risk. In women who commit IPV, clinicians should assess the role of the individual in an IPV disclosure. There are various treatment modalities, whether the violence is performed through self-defense, bidirectionally, or because of aggression.
With the advancement of technology, web-based training on how to ask for IPV, documentation, acknowledgment, and structured referral increase physicians’ confidence when faced with an IPV disclosure than none.16 Treatment modalities should include medication reconciliation and cognitive-behavioral therapy – focusing on emotion regulation.
Using instruments such as the danger assessment tool can help physicians intervene early, reducing the risk of domestic violence and IPV recurrence instead of using clinical assessment alone.17 Physicians should convey empathy, validate victims, and help, especially when abuse is reported.
Also, it is important to evaluate survivors’ safety. Counseling can help people rebuild their self-esteem. Structured referrals for psychiatric help and support services are needed to help survivors on the long road to recovery.
Training all physicians, regardless of specialty, is essential to improve prompt IPV identification and bring awareness to resources available to survivors when IPV is disclosed. Although we described an association between IPV victims becoming possible perpetrators of IPV, more long-term studies are required to show the various processes that influence IPV perpetration rates, especially by survivors.
We would also like international and national regulatory bodies to increase the awareness of IPV and adequately address IPV with special emphasis on how mental health services should assess, identify, and respond to services for people who are survivors and perpetrators of IPV.
Dr. Kumari, Dr. Otite, Dr. Afzal, Dr. Alcera, and Dr. Doumas are affiliated with Hackensack Meridian Health at Ocean Medical Center, Brick, N.J. They have no conflicts of interest.
References
1. Centers for Disease Control and Prevention. Preventing intimate partner violence. 2020 Oct 9.
2. Yu R et al. PLOS Med. 16(12):e1002995. doi: 10.1371/journal.pmed.1002995.
3. Oram S et al. Epidemiol Psychiatr Sci. 2014 Dec;23(4):361-76.
4. Munro OE and Sellbom M. Pers Ment Health. 2020 Mar 11. doi: 10.1002/pmh.1480.
5. Sahraian A et al. Asian J Psychiatry. 2020 Jun. doi: 10.1016/j.ajp.2020.102062.
6. Nikos-Rose K. “COVID-19 Isolation Linked to Increased Domestic Violence, Researchers Suggest.” 2021 Feb 24. University of California, Davis.
7. World Health Organization. “Responding to intimate partner violence and sexual violence against women.” WHO clinical policy guidelines. 2013.
8. National Institute for Health and Care Excellence. “Domestic violence and abuse: Multi-agency working.” PH50. 2014 Feb 26.
9. Feder GS et al. Arch Intern Med. 2006;166(1):22-37.
10. Gondolf EW. Violence Against Women. 2014 Dec;20(12)1539-46.
11. Hamberger LK and Larsen SE. J Fam Violence. 2015;30(6):699-717.
12. Rollè L et al. Front Psychol. 21 Aug 2018. doi: 10.3389/fpsyg.2018.01506.
13. Paterno MT and Draughon JE. J Midwif Women Health. 2016;61(31):370-5.
14. Kalra N et al. Cochrane Database Syst Rev. 2021 May 31;5(5)CD012423.
15. Larsen SE and Hamberger LK. J Fam Viol. 2015;30:1007-30.
16. Kalra N et al. Cochrane Database Syst Rev. 2017 Feb;2017(2):CD012423.
17. Campbell JC et al. J Interpers Violence. 2009;24(4):653-74.
Violence against women remains a global dilemma in need of attention. Physical violence in particular, is the most prevalent type of violence across all genders, races, and nationalities.
The Centers for Disease Control and Prevention says more than 43 million women and 38 million men report experiencing psychological aggression by an intimate partner in their lifetime. Meanwhile, 11 million women and 5 million men report enduring sexual or physical violence and intimate partner violence (IPV), and/or stalking by an intimate partner during their lifetimes, according to the CDC.1
Women who have endured this kind of violence might present differently from men. Some studies, for example, show a more significant association between mutual violence, depression, and substance use among women than men.2 Studies on the phenomenon of IPV victims/survivors becoming perpetrators of abuse are limited, but that this happens in some cases.
Having a psychiatric disorder is associated with a higher likelihood of being physically violent with a partner.3,4 One recent study of 250 female psychiatric patients who were married and had no history of drug abuse found that almost 68% reported psychological abuse, 52% reported sexual abuse, 38% social abuse, 37% reported economic abuse, and 25% reported physical abuse.5
Given those statistics and trends, it is incumbent upon clinicians – including those in primary care, psychiatry, and emergency medicine – to learn to quickly identify IPV survivors, and to use available prognostic tools to monitor perpetrators and survivors.
COVID pandemic’s influence
Isolation tied to the COVID-19 pandemic has been linked to increased IPV. A study conducted by researchers at the University of California, Davis, suggested that extra stress experienced during the COVID-19 pandemic caused by income loss, and the inability to pay for housing and food exacerbated the prevalence of IPV early during the pandemic.6
That study, where researchers collected in surveys of nearly 400 adults in the beginning in April 2020 for 10 weeks, showed that more services and communication are needed so that frontline health care and food bank workers, for example, in addition to social workers, doctors, and therapists, can spot the signs and ask clients questions about potential IPV. They could then link survivors to pertinent assistance and resources.
Furthermore, multiple factors probably have played a pivotal role in increasing the prevalence of IPV during the COVID-19 pandemic. For instance, disruption to usual health and social services as well as diminished access to support systems, such as shelters, and charity helplines negatively affected the reporting of domestic violence.
Long before the pandemic, over the past decade, international and national bodies have played a crucial role in terms of improving the awareness and response to domestic violence.7,8 In addition, several policies have been introduced in countries around the globe emphasizing the need to inquire routinely about domestic violence. Nevertheless, mental health services often fail to adequately address domestic violence in clinical encounters. A systematic review of domestic violence assessment screening performed in a variety of health care settings found that evidence was insufficient to conclude that routine inquiry improved morbidity and mortality among victims of IPV.9 So the question becomes: How can we get our patients to tell us about these experiences so we can intervene?
Gender differences in perpetuating IPV
Several studies have found that abuse can result in various mental illnesses, such as depression, PTSD, anxiety, and suicidal ideation. Again, men have a disproportionately higher rate of perpetrating IPV, compared with women. This theory has been a source of debate in the academic community for years, but recent research has confirmed that women do perpetuate violence against their partners to some extent.10,11
Some members of the LGBTQ+ community also report experiencing violence from partners, so as clinicians, we also need to raise our awareness about the existence of violence among same-sex couples. In fact, a team of Italian researchers report more than 50% of gay men and almost 75% of lesbian women reported that they had been psychologically abused by a partner.12 More research into this area is needed.
Our role as health care professionals
The U.S. Preventive Services Task Force advises that all clinic visits include regular IPV screening.13 But these screenings are all too rare. In fact, a meta-analysis of 19 trials of more than 1,600 participants showed only 9%-40% of doctors routinely test for IPV.14 That research clearly shows how important it is for all clinicians to execute IPV screening. However, numerous challenges toward screening exist, including personal discomfort, limited time during appointments, insufficient resources, and inadequate training.
One ongoing debate revolves around which clinician should screen for IPV. Should the psychiatrist carry out this role – or perhaps the primary care physician, nurse, or social worker? These issues become even more fraught when clinicians worry about offending the patient – especially if the clinician is a male.15
The bottom line is that physicians should inquire about intimate partner violence, because research indicates that women are more likely to reveal abuse when prompted. In addition, during physician appointments, they can use the physician-patient therapeutic connection to conduct a domestic violence evaluation, give resources to victims, and provide ongoing care. Patients who exhibit treatment resistance, persistent pain, depression, sleeplessness, and headaches should prompt psychiatrists to conduct additional investigations into the likelihood of intimate partner violence and domestic abuse.
W also should be attentive when counseling patients about domestic violence when suggesting life-changing events such as pregnancy, employment loss, separation, or divorce. Similar to the recommendations of the USPSTF that all women and men should be screened for IPV, it is suggested that physicians be conscious of facilitating a conversation and not being overtly judgmental while observing body cues. Using the statements such as “we have been hearing a lot of violence in our community lately” could be a segue to introduce the subject.
Asking the question of whether you are being hit rather than being abused has allowed more women to open up more about domestic violence. While physicians are aware that most victims might recant and often go back to their abusers, victims need to be counseled that the abuse might intensify and lead to death.
For women who perpetuate IPV and survivors of IPV, safety is the priority. Physicians should provide safety options and be the facilitators. Studies have shown that fewer victims get the referral to the supporting agencies when IPV is indicated, which puts their safety at risk. In women who commit IPV, clinicians should assess the role of the individual in an IPV disclosure. There are various treatment modalities, whether the violence is performed through self-defense, bidirectionally, or because of aggression.
With the advancement of technology, web-based training on how to ask for IPV, documentation, acknowledgment, and structured referral increase physicians’ confidence when faced with an IPV disclosure than none.16 Treatment modalities should include medication reconciliation and cognitive-behavioral therapy – focusing on emotion regulation.
Using instruments such as the danger assessment tool can help physicians intervene early, reducing the risk of domestic violence and IPV recurrence instead of using clinical assessment alone.17 Physicians should convey empathy, validate victims, and help, especially when abuse is reported.
Also, it is important to evaluate survivors’ safety. Counseling can help people rebuild their self-esteem. Structured referrals for psychiatric help and support services are needed to help survivors on the long road to recovery.
Training all physicians, regardless of specialty, is essential to improve prompt IPV identification and bring awareness to resources available to survivors when IPV is disclosed. Although we described an association between IPV victims becoming possible perpetrators of IPV, more long-term studies are required to show the various processes that influence IPV perpetration rates, especially by survivors.
We would also like international and national regulatory bodies to increase the awareness of IPV and adequately address IPV with special emphasis on how mental health services should assess, identify, and respond to services for people who are survivors and perpetrators of IPV.
Dr. Kumari, Dr. Otite, Dr. Afzal, Dr. Alcera, and Dr. Doumas are affiliated with Hackensack Meridian Health at Ocean Medical Center, Brick, N.J. They have no conflicts of interest.
References
1. Centers for Disease Control and Prevention. Preventing intimate partner violence. 2020 Oct 9.
2. Yu R et al. PLOS Med. 16(12):e1002995. doi: 10.1371/journal.pmed.1002995.
3. Oram S et al. Epidemiol Psychiatr Sci. 2014 Dec;23(4):361-76.
4. Munro OE and Sellbom M. Pers Ment Health. 2020 Mar 11. doi: 10.1002/pmh.1480.
5. Sahraian A et al. Asian J Psychiatry. 2020 Jun. doi: 10.1016/j.ajp.2020.102062.
6. Nikos-Rose K. “COVID-19 Isolation Linked to Increased Domestic Violence, Researchers Suggest.” 2021 Feb 24. University of California, Davis.
7. World Health Organization. “Responding to intimate partner violence and sexual violence against women.” WHO clinical policy guidelines. 2013.
8. National Institute for Health and Care Excellence. “Domestic violence and abuse: Multi-agency working.” PH50. 2014 Feb 26.
9. Feder GS et al. Arch Intern Med. 2006;166(1):22-37.
10. Gondolf EW. Violence Against Women. 2014 Dec;20(12)1539-46.
11. Hamberger LK and Larsen SE. J Fam Violence. 2015;30(6):699-717.
12. Rollè L et al. Front Psychol. 21 Aug 2018. doi: 10.3389/fpsyg.2018.01506.
13. Paterno MT and Draughon JE. J Midwif Women Health. 2016;61(31):370-5.
14. Kalra N et al. Cochrane Database Syst Rev. 2021 May 31;5(5)CD012423.
15. Larsen SE and Hamberger LK. J Fam Viol. 2015;30:1007-30.
16. Kalra N et al. Cochrane Database Syst Rev. 2017 Feb;2017(2):CD012423.
17. Campbell JC et al. J Interpers Violence. 2009;24(4):653-74.
Siblings of people with bipolar disorder have higher cancer risk
, according to new research from Taiwan.
“To our knowledge, our study is the first to report an increased overall cancer risk as well as increased risks of breast and ectodermal cancer among the unaffected siblings aged < 50 years of patients with bipolar disorder,” Ya-Mei Bai, MD, PhD, of National Yang-Ming University, Taipei, Taiwan, and colleagues write in an article published online in the International Journal of Cancer.
Most, but not all, previous studies have shown a link between bipolar disorder and cancer. Whether the elevated risk of malignancy extends to family members without the mental health condition has not been elucidated.
To investigate, the researchers turned to the National Health Insurance Research Database of Taiwan. They identified 25,356 individuals diagnosed with bipolar disorder by a psychiatrist between 1996 and 2010 and the same number of unaffected siblings, as well as more than 100,000 age-, sex-, income-, and residence-matched controls without severe mental illness.
Compared with the control group, people with bipolar disorder (odds ratio, 1.22) and their unaffected siblings (OR, 1.17) both had a higher risk of developing malignant cancer of any kind. The researchers also found that both groups were at higher risk for breast cancer, with odds ratios of 1.98 in individuals with bipolar disorder and 1.73 in their unaffected siblings.
However, the risk of skin cancer was only high in people with bipolar disorder (OR, 2.70) and not in their siblings (OR, 0.62). And conversely, the risk of kidney cancer was significantly increased in unaffected siblings (OR, 2.45) but not in people with bipolar disorder (OR, 0.47).
When stratified by the embryonic developmental layer from which tumors had originated – ectodermal, mesodermal, or endodermal – the authors observed a significantly increased risk for only ectodermal cancers. In addition, only people under age 50 in both groups (OR, 1.90 for those with bipolar disorder; OR, 1.65 for siblings) were more likely to develop an ectodermal cancer, especially of the breast, compared with the control group. The risks remained elevated after excluding breast cancer but were no longer significant.
When stratified by age, the risk of developing any cancer in both groups also only appeared to be greater for those under age 50 (OR, 1.34 in people with bipolar disorder; OR, 1.32 in siblings) compared with those aged 50 and over (OR, 0.97 and 0.99, respectively). The authors highlighted these figures in the supplemental data set but did not discuss it further in the study beyond a brief mention that “younger patients with bipolar disorder and younger unaffected siblings (< 50 years), but not older ones (≥ 50 years), were more likely to develop any malignancy during the follow-up than matched controls.”
“This paper essentially finds what we have found in our previous work – that people with bipolar disorder have a greater risk of cancer,” said Michael Berk, MBBCh, PhD, a professor of psychiatry at the Deakin University School of Medicine in Geelong, Australia, who published a systematic review and meta-analysis last spring on cancer risk and the role of lithium treatment in bipolar disorder.
“The interesting finding in our work,” Dr. Berk told this news organization, “is that this risk is attenuated by use of lithium but not other agents.”
The Taiwanese researchers propose a “biopsychosocial explanation” for their results, noting that both the nervous system and the breast and skin develop from the ectoderm, and that cancer risk factors such as smoking and obesity are more common in people with bipolar disorder and their unaffected siblings.
“The findings,” they write, “imply a genetic overlap in neurodevelopment and malignancy pathogenesis and may encourage clinicians to closely monitor patients with bipolar disorder and their unaffected siblings for cancer warning signs.”
The authors, however, caution that their study needs validation and had several limitations, including lack of adjustment for drug treatment and lifestyle and environmental factors.
“Our findings may persuade clinicians and researchers to reevaluate the cancer risk among the unaffected siblings of patients with schizophrenia and bipolar disorder because these two severe mental disorders may have a common biopsychosocial pathophysiology,” the team writes.
The study was supported by a grant from Taipei Veterans General Hospital, Yen Tjing Ling Medical Foundation, and the Ministry of Science and Technology, Taiwan.
A version of this article first appeared on Medscape.com.
, according to new research from Taiwan.
“To our knowledge, our study is the first to report an increased overall cancer risk as well as increased risks of breast and ectodermal cancer among the unaffected siblings aged < 50 years of patients with bipolar disorder,” Ya-Mei Bai, MD, PhD, of National Yang-Ming University, Taipei, Taiwan, and colleagues write in an article published online in the International Journal of Cancer.
Most, but not all, previous studies have shown a link between bipolar disorder and cancer. Whether the elevated risk of malignancy extends to family members without the mental health condition has not been elucidated.
To investigate, the researchers turned to the National Health Insurance Research Database of Taiwan. They identified 25,356 individuals diagnosed with bipolar disorder by a psychiatrist between 1996 and 2010 and the same number of unaffected siblings, as well as more than 100,000 age-, sex-, income-, and residence-matched controls without severe mental illness.
Compared with the control group, people with bipolar disorder (odds ratio, 1.22) and their unaffected siblings (OR, 1.17) both had a higher risk of developing malignant cancer of any kind. The researchers also found that both groups were at higher risk for breast cancer, with odds ratios of 1.98 in individuals with bipolar disorder and 1.73 in their unaffected siblings.
However, the risk of skin cancer was only high in people with bipolar disorder (OR, 2.70) and not in their siblings (OR, 0.62). And conversely, the risk of kidney cancer was significantly increased in unaffected siblings (OR, 2.45) but not in people with bipolar disorder (OR, 0.47).
When stratified by the embryonic developmental layer from which tumors had originated – ectodermal, mesodermal, or endodermal – the authors observed a significantly increased risk for only ectodermal cancers. In addition, only people under age 50 in both groups (OR, 1.90 for those with bipolar disorder; OR, 1.65 for siblings) were more likely to develop an ectodermal cancer, especially of the breast, compared with the control group. The risks remained elevated after excluding breast cancer but were no longer significant.
When stratified by age, the risk of developing any cancer in both groups also only appeared to be greater for those under age 50 (OR, 1.34 in people with bipolar disorder; OR, 1.32 in siblings) compared with those aged 50 and over (OR, 0.97 and 0.99, respectively). The authors highlighted these figures in the supplemental data set but did not discuss it further in the study beyond a brief mention that “younger patients with bipolar disorder and younger unaffected siblings (< 50 years), but not older ones (≥ 50 years), were more likely to develop any malignancy during the follow-up than matched controls.”
“This paper essentially finds what we have found in our previous work – that people with bipolar disorder have a greater risk of cancer,” said Michael Berk, MBBCh, PhD, a professor of psychiatry at the Deakin University School of Medicine in Geelong, Australia, who published a systematic review and meta-analysis last spring on cancer risk and the role of lithium treatment in bipolar disorder.
“The interesting finding in our work,” Dr. Berk told this news organization, “is that this risk is attenuated by use of lithium but not other agents.”
The Taiwanese researchers propose a “biopsychosocial explanation” for their results, noting that both the nervous system and the breast and skin develop from the ectoderm, and that cancer risk factors such as smoking and obesity are more common in people with bipolar disorder and their unaffected siblings.
“The findings,” they write, “imply a genetic overlap in neurodevelopment and malignancy pathogenesis and may encourage clinicians to closely monitor patients with bipolar disorder and their unaffected siblings for cancer warning signs.”
The authors, however, caution that their study needs validation and had several limitations, including lack of adjustment for drug treatment and lifestyle and environmental factors.
“Our findings may persuade clinicians and researchers to reevaluate the cancer risk among the unaffected siblings of patients with schizophrenia and bipolar disorder because these two severe mental disorders may have a common biopsychosocial pathophysiology,” the team writes.
The study was supported by a grant from Taipei Veterans General Hospital, Yen Tjing Ling Medical Foundation, and the Ministry of Science and Technology, Taiwan.
A version of this article first appeared on Medscape.com.
, according to new research from Taiwan.
“To our knowledge, our study is the first to report an increased overall cancer risk as well as increased risks of breast and ectodermal cancer among the unaffected siblings aged < 50 years of patients with bipolar disorder,” Ya-Mei Bai, MD, PhD, of National Yang-Ming University, Taipei, Taiwan, and colleagues write in an article published online in the International Journal of Cancer.
Most, but not all, previous studies have shown a link between bipolar disorder and cancer. Whether the elevated risk of malignancy extends to family members without the mental health condition has not been elucidated.
To investigate, the researchers turned to the National Health Insurance Research Database of Taiwan. They identified 25,356 individuals diagnosed with bipolar disorder by a psychiatrist between 1996 and 2010 and the same number of unaffected siblings, as well as more than 100,000 age-, sex-, income-, and residence-matched controls without severe mental illness.
Compared with the control group, people with bipolar disorder (odds ratio, 1.22) and their unaffected siblings (OR, 1.17) both had a higher risk of developing malignant cancer of any kind. The researchers also found that both groups were at higher risk for breast cancer, with odds ratios of 1.98 in individuals with bipolar disorder and 1.73 in their unaffected siblings.
However, the risk of skin cancer was only high in people with bipolar disorder (OR, 2.70) and not in their siblings (OR, 0.62). And conversely, the risk of kidney cancer was significantly increased in unaffected siblings (OR, 2.45) but not in people with bipolar disorder (OR, 0.47).
When stratified by the embryonic developmental layer from which tumors had originated – ectodermal, mesodermal, or endodermal – the authors observed a significantly increased risk for only ectodermal cancers. In addition, only people under age 50 in both groups (OR, 1.90 for those with bipolar disorder; OR, 1.65 for siblings) were more likely to develop an ectodermal cancer, especially of the breast, compared with the control group. The risks remained elevated after excluding breast cancer but were no longer significant.
When stratified by age, the risk of developing any cancer in both groups also only appeared to be greater for those under age 50 (OR, 1.34 in people with bipolar disorder; OR, 1.32 in siblings) compared with those aged 50 and over (OR, 0.97 and 0.99, respectively). The authors highlighted these figures in the supplemental data set but did not discuss it further in the study beyond a brief mention that “younger patients with bipolar disorder and younger unaffected siblings (< 50 years), but not older ones (≥ 50 years), were more likely to develop any malignancy during the follow-up than matched controls.”
“This paper essentially finds what we have found in our previous work – that people with bipolar disorder have a greater risk of cancer,” said Michael Berk, MBBCh, PhD, a professor of psychiatry at the Deakin University School of Medicine in Geelong, Australia, who published a systematic review and meta-analysis last spring on cancer risk and the role of lithium treatment in bipolar disorder.
“The interesting finding in our work,” Dr. Berk told this news organization, “is that this risk is attenuated by use of lithium but not other agents.”
The Taiwanese researchers propose a “biopsychosocial explanation” for their results, noting that both the nervous system and the breast and skin develop from the ectoderm, and that cancer risk factors such as smoking and obesity are more common in people with bipolar disorder and their unaffected siblings.
“The findings,” they write, “imply a genetic overlap in neurodevelopment and malignancy pathogenesis and may encourage clinicians to closely monitor patients with bipolar disorder and their unaffected siblings for cancer warning signs.”
The authors, however, caution that their study needs validation and had several limitations, including lack of adjustment for drug treatment and lifestyle and environmental factors.
“Our findings may persuade clinicians and researchers to reevaluate the cancer risk among the unaffected siblings of patients with schizophrenia and bipolar disorder because these two severe mental disorders may have a common biopsychosocial pathophysiology,” the team writes.
The study was supported by a grant from Taipei Veterans General Hospital, Yen Tjing Ling Medical Foundation, and the Ministry of Science and Technology, Taiwan.
A version of this article first appeared on Medscape.com.
FROM INTERNATIONAL JOURNAL OF CANCER
Family-oriented care in adult psychiatric residency
The Group for the Advancement of Psychiatry’s Committee on the Family published an updated curriculum in October 2021 on family-oriented care. The first curriculum, published in 2006, was nominated as the American Association of Directors of Psychiatric Residency Training model curriculum for family-oriented care. The updated curriculum, produced by the GAP family committee and guests, is shorter and more focused.
The following is a summary of the introduction and the highlights.
Introduction
Use of family systems–based techniques in the diagnosis and care of patients is a key evidence-based tool for psychiatric disorders. However, it is not a current Accreditation Council for Graduate Medical Education Training training requirement, and it is possible to complete psychiatry residency without exposure to this key framework.
Here, we highlight the importance of considering patients through a “family systems” lens and the incorporation of multiple individuals from an individual patient’s identified system in their care.
Current medicine curricula emphasize patient autonomy, one of the core pillars of ethics. Autonomy is the cornerstone of the everyday practice within medicine of communicating all risks, benefits, and alternatives of a proposed treatment to a patient making decisions about desired paths forward. This prevents paternalistic care in which the doctor “knows best” and makes decisions for the patient. Unfortunately, the emphasis of this pillar has morphed over time into the idea that the individual patient is the only person to whom this information should be provided or from whom information should be obtained.
Extensive research proves conclusively that family support, education, and psychoeducation improve both patient and family functioning in medical and psychiatric illness. as well as overlook the opportunity to use the structure and support system around a patient to strengthen their care and improve treatment outcomes.
The network and family dynamics around a patient can be critical to providing accurate information on medication adherence and symptoms, supporting recovery, and handling emergencies. Markedly improved patient outcomes occur when family members are seen as allies and offered support, assessment, and psychoeducation. In fact, the American Psychiatric Association’s Practice Guidelines on the treatment of schizophrenia (2020), major depressive disorder (2010), and bipolar disorder (2002) include the expectation that patients’ family members will be involved in the assessment and treatment of patients. Yet, training in how to incorporate these practices is often minimal or nonexistent during residency.
A family systems orientation is distinguished by its view of the family as a transactional system. Stressful events and problems of an individual member affect the whole family as a functional unit, with ripple effects for all members and their relationships. In turn, the family response – how the family handles problems – contributes significantly to positive adaptation or to individual and relational dysfunction. Thus, individual problems are assessed and addressed in the context of the family, with attention to socioeconomic and other environmental stressors.
A family systems approach is distinguished less by who is in the room and more by the clinician’s attention to relationship systems in assessment and treatment planning. We need to consider how family members may contribute to – and be affected by – problem situations. Most importantly, regardless of the source of difficulties, we involve key family members who can contribute to needed changes. Interventions are aimed at modifying dysfunctional patterns, tapping family resources, and strengthening both individual and family functioning.
A family systemic lens is useful for working with all types of families, for example: refugee families, thinking through child adoption processes, working with families with specific social disadvantages, etc. Incorporating issues of race, gender, and sexual orientation is important in this work, as is working with larger systems such as schools, workplaces, and health care settings.
As opposed to previous viewpoints that family therapy is the only “family” skill to be taught during residency, the GAP committee proposes that psychiatric residents should be trained in skills of family inclusion, support, and psychoeducation, and that these skills should be taught throughout the residency. Our goal is to have residents be able to consider any case through a family systems lens, to understand how patients’ illnesses and their family systems have bidirectional effects on each other, to perform a basic assessment of family system functioning, and to use this information in diagnostic and treatment planning.
Training goals
Systems-based thinking will enable trainees to:
1. Ally with family members to work with the patient to comply with goals of care (for example, taking medications, complying with lifestyle changes, and maintaining sobriety).
- Teachers focus on engagement, joining with families.
2. Help patients understand the influences of their families in their own lives, such as intergenerational transmission of trauma and resilience.
- Teachers focus on the creation of a genogram, and the location of the individual within their family system.
3. Understand that mental health includes the creation and maintenance of healthy relationships.
- Teachers focus on assessing a willingness to listen to others’ points of view and the cocreation of a shared reality and belief system: a belief that relationships can change over time and how to create new family narratives.
4. Understand the impact of illness on the family unit and the impact of the family unit on illness.
- Teachers focus on the concept of a family system, clarifying the roles within the family, including caregiving responsibilities.
5. Assess the family for strengths and weaknesses.
- Teachers focus on how families maintain a healthy emotional climate, allocate roles, decide on rules, problem-solving abilities, and so on.
6. Gather information from multiple informants in the same room.
- Teachers focus on using communication techniques to elicit, guide, and redirect information from multiple individuals of a system with varying perspectives in the same room. Teachers help students understand that there are multiple realities in families and learn how to maintain multidirectional partiality.
Knowledge, skills, and attitudes across all treatment settings
Knowledge: Beginning level
- Healthy family functioning at the various phases of the family life cycle. Systems concepts are applicable to families, multidisciplinary teams in clinical settings, and medical/government organizations. However, family systems are distinguished by deep attachment bonds, specific generational hierarchy, goals of emotional safety and, for many families, child rearing.
- Systemic thinking, unlike a linear cause and effect model, examines the feedback loops by which multiple persons or groups arrive at a specific way of functioning.
- Understanding boundaries, subsystems, and feedback loops is critical to understanding interpersonal connections. Understand how the family affects and is affected by psychiatric and medical illnesses. Impact of interpersonal stress on biological systems. The role of expressed emotion (EE) in psychiatric illness. EE describes the level of criticism, hostility, and emotional overinvolvement in families. It has been studied extensively across the health care spectrum, and cultural variance is significant.
- The components of family psychoeducation, and its associated research in improving patient and family outcomes.
Knowledge: Advanced level
- Principles of adaptive and maladaptive relational functioning in family life and family organization, communication, problem solving, and emotional regulation. Role of family strengths, resilience in reducing vulnerability.
- Couple and family development over the life cycle.
- Understanding multigenerational patterns.
- How age, gender, class, culture, and spirituality affect family life.
- The variety of family forms (for example, single parent, stepfamilies, same-sex parents).
- Special issues in couples and families, including loss, divorce and remarriage, immigration, illness, secrets, affairs, violence, alcohol and substance abuse, sexuality, including LGBTQi. Relationship of families to larger systems, for example, schools, work, health care systems, government agencies.
Skills
- Family-interviewing skills, especially managing high levels of emotion and making room for multiple points of view.
- Promoting resilience, hope, and strength.
- Basic psychoeducation techniques, which includes providing a therapeutic space for emotional processing, providing information about the illness, skills such as better communication, problem-solving, and relapse drill and support.
- Collaborative treatment planning with family members and other helping professionals. Treatment planning should include all members of the system: patient, family members, and members of the treatment team. Good planning establishes a role for family members, helps define criteria for managing emergencies, looks for areas of strength and resilience and provides clear and realistic goals for treatment.
- Knowledge of, and referral to, local and national resources, both in the community and online.
Attitudes
- Appreciate the multiple points of view in a family.
- Interest in family members as people with their own needs and history.
- Including family members as a resource in recovery.
- Understand caregiver burden and rewards and that stress extends to all family members.
Training techniques
Most learning takes place at the level of patient, supervisor, and resident. It is critical that the resident sees faculty members dealing with patients in observed or shared family sessions, and /or sees videos made by faculty or professionally made videos. Attitudes are best learned by modeling.
Areas of focus can include time management, addressing the fear that family sessions may get out of control, and the influence of the residents’ own life experiences and background including potential generational or cultural differences on their assessment and interactions with patient family dynamics. In skill development, our goal is efficient interviewing, history taking, and support in controlling sessions.
It is difficult to specify which techniques are most useful in didactic sessions as each presenter will have a different skill set for engaging the class. The techniques that work best are the ones most comfortable to the presenter. Any technique that gets emotions involved, such as role play, sculpting, discussing movie clips, bringing in family members to discuss their experiences, or self-exploration, will generate the most powerful learning. If time permits, exploration of the resident’s own family, including a genogram, is an exceptionally helpful technique, especially if accompanied by asking the residents to interview their own families.
Adult didactic curriculum
The curriculum represents basic concepts. We have vignettes by the authors, if needed, but it is best if the class, including the supervisor, uses vignettes from their own experiences. Material for use in class is in references, but the class is urged to draw on their own experiences as this supports strength-based teaching. The following are key topics and concepts for each of the training years.
Basic concepts for PGY1 and PGY2
1. Where are you in the family and individual life cycles? What are your experiences with psychiatric illness in family/friends? Open discussion about how individual and family life cycles interact. Draw genograms of s/o in the class or with the supervisor.
2. Healthy family functioning and family resilience. Recommend asking residents to talk to their parents/elders about their lives and family life cycle when they were your age. Open discussion about what makes a healthy resilient family.
3. How do I connect with the family rather than just one person? How do you learn to hold multiple perspectives? How do I try not to take sides/multidirectional partiality? How do I see each person in a positive way? How do I focus on family strengths, rather than focusing on someone behaving badly (which is really hard because it is overlearned in individual therapy).
4. What are the common factors used across all therapies, both individual and family? When is it best to use an individual relational approach versus a family systemic approach?
5. How do I decide if a family needs support or education or family therapy?
6. Psychoeducation: Research, current use and cultural adaptations.
7. Attachment styles and couples therapy.
8. What is the evidence base behind our work?
System practice for PGY 3 and 4
These seminars follow the basic seminars. The focus is on clarification of what systems thinking means. Systems thinking or relational thinking is to be differentiated from systems-based practice. These lectures require knowledge of systemic practice. If there are no local experts, residency programs can reach out to national experts at the Association of Family Psychiatrists, for help with virtual/remote or in-person teaching.
Here is a list of other topics that should be covered:
- Relational formulation, nested subsystems, boundaries, history of these concepts, contributions to the development of family therapy.
- How to define and identify common systems concepts, such as circular patterns, feedback loops, and triangulation. Teach circular questioning. Framing. This concept is the family systems equivalent of insight. How to intervene to effect communication change and behavior change?
- Working at interfaces: community, legal, government, agencies, and so on, and other treaters, consultation. Include systemic and individual racism.
- Understanding the complexity of intimacy.
- Emergency situations. When to report regarding abuse. Dealing with family trauma.
- Varieties of family therapy; assumptions and major concepts.
*The new curriculum was written by The GAP Committee on the Family: Ellen Berman, MD; John Rolland, MD, MPH; John Sargent, MD; and me, and with guests Chayanin Foongsathaporn, MD; Sarah Nguyen, MD, MPH; Neha Sharma, DO; and Jodi Zik, MD. For the full curriculum, which includes residency milestones, site-specific training goals, references, and case studies, please access the Association of Family Psychiatry’s website: www.familypsychiatrists.org.Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
The Group for the Advancement of Psychiatry’s Committee on the Family published an updated curriculum in October 2021 on family-oriented care. The first curriculum, published in 2006, was nominated as the American Association of Directors of Psychiatric Residency Training model curriculum for family-oriented care. The updated curriculum, produced by the GAP family committee and guests, is shorter and more focused.
The following is a summary of the introduction and the highlights.
Introduction
Use of family systems–based techniques in the diagnosis and care of patients is a key evidence-based tool for psychiatric disorders. However, it is not a current Accreditation Council for Graduate Medical Education Training training requirement, and it is possible to complete psychiatry residency without exposure to this key framework.
Here, we highlight the importance of considering patients through a “family systems” lens and the incorporation of multiple individuals from an individual patient’s identified system in their care.
Current medicine curricula emphasize patient autonomy, one of the core pillars of ethics. Autonomy is the cornerstone of the everyday practice within medicine of communicating all risks, benefits, and alternatives of a proposed treatment to a patient making decisions about desired paths forward. This prevents paternalistic care in which the doctor “knows best” and makes decisions for the patient. Unfortunately, the emphasis of this pillar has morphed over time into the idea that the individual patient is the only person to whom this information should be provided or from whom information should be obtained.
Extensive research proves conclusively that family support, education, and psychoeducation improve both patient and family functioning in medical and psychiatric illness. as well as overlook the opportunity to use the structure and support system around a patient to strengthen their care and improve treatment outcomes.
The network and family dynamics around a patient can be critical to providing accurate information on medication adherence and symptoms, supporting recovery, and handling emergencies. Markedly improved patient outcomes occur when family members are seen as allies and offered support, assessment, and psychoeducation. In fact, the American Psychiatric Association’s Practice Guidelines on the treatment of schizophrenia (2020), major depressive disorder (2010), and bipolar disorder (2002) include the expectation that patients’ family members will be involved in the assessment and treatment of patients. Yet, training in how to incorporate these practices is often minimal or nonexistent during residency.
A family systems orientation is distinguished by its view of the family as a transactional system. Stressful events and problems of an individual member affect the whole family as a functional unit, with ripple effects for all members and their relationships. In turn, the family response – how the family handles problems – contributes significantly to positive adaptation or to individual and relational dysfunction. Thus, individual problems are assessed and addressed in the context of the family, with attention to socioeconomic and other environmental stressors.
A family systems approach is distinguished less by who is in the room and more by the clinician’s attention to relationship systems in assessment and treatment planning. We need to consider how family members may contribute to – and be affected by – problem situations. Most importantly, regardless of the source of difficulties, we involve key family members who can contribute to needed changes. Interventions are aimed at modifying dysfunctional patterns, tapping family resources, and strengthening both individual and family functioning.
A family systemic lens is useful for working with all types of families, for example: refugee families, thinking through child adoption processes, working with families with specific social disadvantages, etc. Incorporating issues of race, gender, and sexual orientation is important in this work, as is working with larger systems such as schools, workplaces, and health care settings.
As opposed to previous viewpoints that family therapy is the only “family” skill to be taught during residency, the GAP committee proposes that psychiatric residents should be trained in skills of family inclusion, support, and psychoeducation, and that these skills should be taught throughout the residency. Our goal is to have residents be able to consider any case through a family systems lens, to understand how patients’ illnesses and their family systems have bidirectional effects on each other, to perform a basic assessment of family system functioning, and to use this information in diagnostic and treatment planning.
Training goals
Systems-based thinking will enable trainees to:
1. Ally with family members to work with the patient to comply with goals of care (for example, taking medications, complying with lifestyle changes, and maintaining sobriety).
- Teachers focus on engagement, joining with families.
2. Help patients understand the influences of their families in their own lives, such as intergenerational transmission of trauma and resilience.
- Teachers focus on the creation of a genogram, and the location of the individual within their family system.
3. Understand that mental health includes the creation and maintenance of healthy relationships.
- Teachers focus on assessing a willingness to listen to others’ points of view and the cocreation of a shared reality and belief system: a belief that relationships can change over time and how to create new family narratives.
4. Understand the impact of illness on the family unit and the impact of the family unit on illness.
- Teachers focus on the concept of a family system, clarifying the roles within the family, including caregiving responsibilities.
5. Assess the family for strengths and weaknesses.
- Teachers focus on how families maintain a healthy emotional climate, allocate roles, decide on rules, problem-solving abilities, and so on.
6. Gather information from multiple informants in the same room.
- Teachers focus on using communication techniques to elicit, guide, and redirect information from multiple individuals of a system with varying perspectives in the same room. Teachers help students understand that there are multiple realities in families and learn how to maintain multidirectional partiality.
Knowledge, skills, and attitudes across all treatment settings
Knowledge: Beginning level
- Healthy family functioning at the various phases of the family life cycle. Systems concepts are applicable to families, multidisciplinary teams in clinical settings, and medical/government organizations. However, family systems are distinguished by deep attachment bonds, specific generational hierarchy, goals of emotional safety and, for many families, child rearing.
- Systemic thinking, unlike a linear cause and effect model, examines the feedback loops by which multiple persons or groups arrive at a specific way of functioning.
- Understanding boundaries, subsystems, and feedback loops is critical to understanding interpersonal connections. Understand how the family affects and is affected by psychiatric and medical illnesses. Impact of interpersonal stress on biological systems. The role of expressed emotion (EE) in psychiatric illness. EE describes the level of criticism, hostility, and emotional overinvolvement in families. It has been studied extensively across the health care spectrum, and cultural variance is significant.
- The components of family psychoeducation, and its associated research in improving patient and family outcomes.
Knowledge: Advanced level
- Principles of adaptive and maladaptive relational functioning in family life and family organization, communication, problem solving, and emotional regulation. Role of family strengths, resilience in reducing vulnerability.
- Couple and family development over the life cycle.
- Understanding multigenerational patterns.
- How age, gender, class, culture, and spirituality affect family life.
- The variety of family forms (for example, single parent, stepfamilies, same-sex parents).
- Special issues in couples and families, including loss, divorce and remarriage, immigration, illness, secrets, affairs, violence, alcohol and substance abuse, sexuality, including LGBTQi. Relationship of families to larger systems, for example, schools, work, health care systems, government agencies.
Skills
- Family-interviewing skills, especially managing high levels of emotion and making room for multiple points of view.
- Promoting resilience, hope, and strength.
- Basic psychoeducation techniques, which includes providing a therapeutic space for emotional processing, providing information about the illness, skills such as better communication, problem-solving, and relapse drill and support.
- Collaborative treatment planning with family members and other helping professionals. Treatment planning should include all members of the system: patient, family members, and members of the treatment team. Good planning establishes a role for family members, helps define criteria for managing emergencies, looks for areas of strength and resilience and provides clear and realistic goals for treatment.
- Knowledge of, and referral to, local and national resources, both in the community and online.
Attitudes
- Appreciate the multiple points of view in a family.
- Interest in family members as people with their own needs and history.
- Including family members as a resource in recovery.
- Understand caregiver burden and rewards and that stress extends to all family members.
Training techniques
Most learning takes place at the level of patient, supervisor, and resident. It is critical that the resident sees faculty members dealing with patients in observed or shared family sessions, and /or sees videos made by faculty or professionally made videos. Attitudes are best learned by modeling.
Areas of focus can include time management, addressing the fear that family sessions may get out of control, and the influence of the residents’ own life experiences and background including potential generational or cultural differences on their assessment and interactions with patient family dynamics. In skill development, our goal is efficient interviewing, history taking, and support in controlling sessions.
It is difficult to specify which techniques are most useful in didactic sessions as each presenter will have a different skill set for engaging the class. The techniques that work best are the ones most comfortable to the presenter. Any technique that gets emotions involved, such as role play, sculpting, discussing movie clips, bringing in family members to discuss their experiences, or self-exploration, will generate the most powerful learning. If time permits, exploration of the resident’s own family, including a genogram, is an exceptionally helpful technique, especially if accompanied by asking the residents to interview their own families.
Adult didactic curriculum
The curriculum represents basic concepts. We have vignettes by the authors, if needed, but it is best if the class, including the supervisor, uses vignettes from their own experiences. Material for use in class is in references, but the class is urged to draw on their own experiences as this supports strength-based teaching. The following are key topics and concepts for each of the training years.
Basic concepts for PGY1 and PGY2
1. Where are you in the family and individual life cycles? What are your experiences with psychiatric illness in family/friends? Open discussion about how individual and family life cycles interact. Draw genograms of s/o in the class or with the supervisor.
2. Healthy family functioning and family resilience. Recommend asking residents to talk to their parents/elders about their lives and family life cycle when they were your age. Open discussion about what makes a healthy resilient family.
3. How do I connect with the family rather than just one person? How do you learn to hold multiple perspectives? How do I try not to take sides/multidirectional partiality? How do I see each person in a positive way? How do I focus on family strengths, rather than focusing on someone behaving badly (which is really hard because it is overlearned in individual therapy).
4. What are the common factors used across all therapies, both individual and family? When is it best to use an individual relational approach versus a family systemic approach?
5. How do I decide if a family needs support or education or family therapy?
6. Psychoeducation: Research, current use and cultural adaptations.
7. Attachment styles and couples therapy.
8. What is the evidence base behind our work?
System practice for PGY 3 and 4
These seminars follow the basic seminars. The focus is on clarification of what systems thinking means. Systems thinking or relational thinking is to be differentiated from systems-based practice. These lectures require knowledge of systemic practice. If there are no local experts, residency programs can reach out to national experts at the Association of Family Psychiatrists, for help with virtual/remote or in-person teaching.
Here is a list of other topics that should be covered:
- Relational formulation, nested subsystems, boundaries, history of these concepts, contributions to the development of family therapy.
- How to define and identify common systems concepts, such as circular patterns, feedback loops, and triangulation. Teach circular questioning. Framing. This concept is the family systems equivalent of insight. How to intervene to effect communication change and behavior change?
- Working at interfaces: community, legal, government, agencies, and so on, and other treaters, consultation. Include systemic and individual racism.
- Understanding the complexity of intimacy.
- Emergency situations. When to report regarding abuse. Dealing with family trauma.
- Varieties of family therapy; assumptions and major concepts.
*The new curriculum was written by The GAP Committee on the Family: Ellen Berman, MD; John Rolland, MD, MPH; John Sargent, MD; and me, and with guests Chayanin Foongsathaporn, MD; Sarah Nguyen, MD, MPH; Neha Sharma, DO; and Jodi Zik, MD. For the full curriculum, which includes residency milestones, site-specific training goals, references, and case studies, please access the Association of Family Psychiatry’s website: www.familypsychiatrists.org.Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
The Group for the Advancement of Psychiatry’s Committee on the Family published an updated curriculum in October 2021 on family-oriented care. The first curriculum, published in 2006, was nominated as the American Association of Directors of Psychiatric Residency Training model curriculum for family-oriented care. The updated curriculum, produced by the GAP family committee and guests, is shorter and more focused.
The following is a summary of the introduction and the highlights.
Introduction
Use of family systems–based techniques in the diagnosis and care of patients is a key evidence-based tool for psychiatric disorders. However, it is not a current Accreditation Council for Graduate Medical Education Training training requirement, and it is possible to complete psychiatry residency without exposure to this key framework.
Here, we highlight the importance of considering patients through a “family systems” lens and the incorporation of multiple individuals from an individual patient’s identified system in their care.
Current medicine curricula emphasize patient autonomy, one of the core pillars of ethics. Autonomy is the cornerstone of the everyday practice within medicine of communicating all risks, benefits, and alternatives of a proposed treatment to a patient making decisions about desired paths forward. This prevents paternalistic care in which the doctor “knows best” and makes decisions for the patient. Unfortunately, the emphasis of this pillar has morphed over time into the idea that the individual patient is the only person to whom this information should be provided or from whom information should be obtained.
Extensive research proves conclusively that family support, education, and psychoeducation improve both patient and family functioning in medical and psychiatric illness. as well as overlook the opportunity to use the structure and support system around a patient to strengthen their care and improve treatment outcomes.
The network and family dynamics around a patient can be critical to providing accurate information on medication adherence and symptoms, supporting recovery, and handling emergencies. Markedly improved patient outcomes occur when family members are seen as allies and offered support, assessment, and psychoeducation. In fact, the American Psychiatric Association’s Practice Guidelines on the treatment of schizophrenia (2020), major depressive disorder (2010), and bipolar disorder (2002) include the expectation that patients’ family members will be involved in the assessment and treatment of patients. Yet, training in how to incorporate these practices is often minimal or nonexistent during residency.
A family systems orientation is distinguished by its view of the family as a transactional system. Stressful events and problems of an individual member affect the whole family as a functional unit, with ripple effects for all members and their relationships. In turn, the family response – how the family handles problems – contributes significantly to positive adaptation or to individual and relational dysfunction. Thus, individual problems are assessed and addressed in the context of the family, with attention to socioeconomic and other environmental stressors.
A family systems approach is distinguished less by who is in the room and more by the clinician’s attention to relationship systems in assessment and treatment planning. We need to consider how family members may contribute to – and be affected by – problem situations. Most importantly, regardless of the source of difficulties, we involve key family members who can contribute to needed changes. Interventions are aimed at modifying dysfunctional patterns, tapping family resources, and strengthening both individual and family functioning.
A family systemic lens is useful for working with all types of families, for example: refugee families, thinking through child adoption processes, working with families with specific social disadvantages, etc. Incorporating issues of race, gender, and sexual orientation is important in this work, as is working with larger systems such as schools, workplaces, and health care settings.
As opposed to previous viewpoints that family therapy is the only “family” skill to be taught during residency, the GAP committee proposes that psychiatric residents should be trained in skills of family inclusion, support, and psychoeducation, and that these skills should be taught throughout the residency. Our goal is to have residents be able to consider any case through a family systems lens, to understand how patients’ illnesses and their family systems have bidirectional effects on each other, to perform a basic assessment of family system functioning, and to use this information in diagnostic and treatment planning.
Training goals
Systems-based thinking will enable trainees to:
1. Ally with family members to work with the patient to comply with goals of care (for example, taking medications, complying with lifestyle changes, and maintaining sobriety).
- Teachers focus on engagement, joining with families.
2. Help patients understand the influences of their families in their own lives, such as intergenerational transmission of trauma and resilience.
- Teachers focus on the creation of a genogram, and the location of the individual within their family system.
3. Understand that mental health includes the creation and maintenance of healthy relationships.
- Teachers focus on assessing a willingness to listen to others’ points of view and the cocreation of a shared reality and belief system: a belief that relationships can change over time and how to create new family narratives.
4. Understand the impact of illness on the family unit and the impact of the family unit on illness.
- Teachers focus on the concept of a family system, clarifying the roles within the family, including caregiving responsibilities.
5. Assess the family for strengths and weaknesses.
- Teachers focus on how families maintain a healthy emotional climate, allocate roles, decide on rules, problem-solving abilities, and so on.
6. Gather information from multiple informants in the same room.
- Teachers focus on using communication techniques to elicit, guide, and redirect information from multiple individuals of a system with varying perspectives in the same room. Teachers help students understand that there are multiple realities in families and learn how to maintain multidirectional partiality.
Knowledge, skills, and attitudes across all treatment settings
Knowledge: Beginning level
- Healthy family functioning at the various phases of the family life cycle. Systems concepts are applicable to families, multidisciplinary teams in clinical settings, and medical/government organizations. However, family systems are distinguished by deep attachment bonds, specific generational hierarchy, goals of emotional safety and, for many families, child rearing.
- Systemic thinking, unlike a linear cause and effect model, examines the feedback loops by which multiple persons or groups arrive at a specific way of functioning.
- Understanding boundaries, subsystems, and feedback loops is critical to understanding interpersonal connections. Understand how the family affects and is affected by psychiatric and medical illnesses. Impact of interpersonal stress on biological systems. The role of expressed emotion (EE) in psychiatric illness. EE describes the level of criticism, hostility, and emotional overinvolvement in families. It has been studied extensively across the health care spectrum, and cultural variance is significant.
- The components of family psychoeducation, and its associated research in improving patient and family outcomes.
Knowledge: Advanced level
- Principles of adaptive and maladaptive relational functioning in family life and family organization, communication, problem solving, and emotional regulation. Role of family strengths, resilience in reducing vulnerability.
- Couple and family development over the life cycle.
- Understanding multigenerational patterns.
- How age, gender, class, culture, and spirituality affect family life.
- The variety of family forms (for example, single parent, stepfamilies, same-sex parents).
- Special issues in couples and families, including loss, divorce and remarriage, immigration, illness, secrets, affairs, violence, alcohol and substance abuse, sexuality, including LGBTQi. Relationship of families to larger systems, for example, schools, work, health care systems, government agencies.
Skills
- Family-interviewing skills, especially managing high levels of emotion and making room for multiple points of view.
- Promoting resilience, hope, and strength.
- Basic psychoeducation techniques, which includes providing a therapeutic space for emotional processing, providing information about the illness, skills such as better communication, problem-solving, and relapse drill and support.
- Collaborative treatment planning with family members and other helping professionals. Treatment planning should include all members of the system: patient, family members, and members of the treatment team. Good planning establishes a role for family members, helps define criteria for managing emergencies, looks for areas of strength and resilience and provides clear and realistic goals for treatment.
- Knowledge of, and referral to, local and national resources, both in the community and online.
Attitudes
- Appreciate the multiple points of view in a family.
- Interest in family members as people with their own needs and history.
- Including family members as a resource in recovery.
- Understand caregiver burden and rewards and that stress extends to all family members.
Training techniques
Most learning takes place at the level of patient, supervisor, and resident. It is critical that the resident sees faculty members dealing with patients in observed or shared family sessions, and /or sees videos made by faculty or professionally made videos. Attitudes are best learned by modeling.
Areas of focus can include time management, addressing the fear that family sessions may get out of control, and the influence of the residents’ own life experiences and background including potential generational or cultural differences on their assessment and interactions with patient family dynamics. In skill development, our goal is efficient interviewing, history taking, and support in controlling sessions.
It is difficult to specify which techniques are most useful in didactic sessions as each presenter will have a different skill set for engaging the class. The techniques that work best are the ones most comfortable to the presenter. Any technique that gets emotions involved, such as role play, sculpting, discussing movie clips, bringing in family members to discuss their experiences, or self-exploration, will generate the most powerful learning. If time permits, exploration of the resident’s own family, including a genogram, is an exceptionally helpful technique, especially if accompanied by asking the residents to interview their own families.
Adult didactic curriculum
The curriculum represents basic concepts. We have vignettes by the authors, if needed, but it is best if the class, including the supervisor, uses vignettes from their own experiences. Material for use in class is in references, but the class is urged to draw on their own experiences as this supports strength-based teaching. The following are key topics and concepts for each of the training years.
Basic concepts for PGY1 and PGY2
1. Where are you in the family and individual life cycles? What are your experiences with psychiatric illness in family/friends? Open discussion about how individual and family life cycles interact. Draw genograms of s/o in the class or with the supervisor.
2. Healthy family functioning and family resilience. Recommend asking residents to talk to their parents/elders about their lives and family life cycle when they were your age. Open discussion about what makes a healthy resilient family.
3. How do I connect with the family rather than just one person? How do you learn to hold multiple perspectives? How do I try not to take sides/multidirectional partiality? How do I see each person in a positive way? How do I focus on family strengths, rather than focusing on someone behaving badly (which is really hard because it is overlearned in individual therapy).
4. What are the common factors used across all therapies, both individual and family? When is it best to use an individual relational approach versus a family systemic approach?
5. How do I decide if a family needs support or education or family therapy?
6. Psychoeducation: Research, current use and cultural adaptations.
7. Attachment styles and couples therapy.
8. What is the evidence base behind our work?
System practice for PGY 3 and 4
These seminars follow the basic seminars. The focus is on clarification of what systems thinking means. Systems thinking or relational thinking is to be differentiated from systems-based practice. These lectures require knowledge of systemic practice. If there are no local experts, residency programs can reach out to national experts at the Association of Family Psychiatrists, for help with virtual/remote or in-person teaching.
Here is a list of other topics that should be covered:
- Relational formulation, nested subsystems, boundaries, history of these concepts, contributions to the development of family therapy.
- How to define and identify common systems concepts, such as circular patterns, feedback loops, and triangulation. Teach circular questioning. Framing. This concept is the family systems equivalent of insight. How to intervene to effect communication change and behavior change?
- Working at interfaces: community, legal, government, agencies, and so on, and other treaters, consultation. Include systemic and individual racism.
- Understanding the complexity of intimacy.
- Emergency situations. When to report regarding abuse. Dealing with family trauma.
- Varieties of family therapy; assumptions and major concepts.
*The new curriculum was written by The GAP Committee on the Family: Ellen Berman, MD; John Rolland, MD, MPH; John Sargent, MD; and me, and with guests Chayanin Foongsathaporn, MD; Sarah Nguyen, MD, MPH; Neha Sharma, DO; and Jodi Zik, MD. For the full curriculum, which includes residency milestones, site-specific training goals, references, and case studies, please access the Association of Family Psychiatry’s website: www.familypsychiatrists.org.Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
Despite the stigma, ECT remains a gold standard
For Clayton Lively, electroconvulsive therapy, or ECT, has been a lifesaver.
“ECT was like a last resort to treat mania and psychosis for bipolar disorder,” said the 31-year-old financial firm associate who lives in Silver Spring, Md. “I had tried lots of different medications.”
The first course of treatments – three times per week for several weeks – was in 2005. They helped tremendously. “I came down from my mania,” Mr. Lively said. “The hallucinations stopped. The psychosis disappeared.”
He reached a point where medications and psychotherapy worked again. And for a decade, his condition was under control.
But in 2017, another episode of hallucinations and mania jolted him off course. Intrusive thoughts returned. For instance, while driving, he would visualize veering off the road. The thoughts were jarring, and yet, he couldn’t stop them from recurring.
“I wasn’t sleeping, and it just kind of wreaked havoc on my life,” Mr. Lively recalled. “I ended up being hospitalized again.”
Once again, ECT came to the rescue – and yet again, in 2018. Now, he’s on an effective maintenance regimen, receiving ECT once every 4 weeks, after tapering down from more frequent sessions.
When a combination of antidepressants and psychotherapy fails to control severe mental illness, there’s hope on the horizon. ECT can be a reliably safe and effective option.
For some patients, using it as maintenance therapy makes sense, said Vaughn McCall, MD, editor-in-chief of The Journal of ECT and professor and chairman of psychiatry at the Medical College of Georgia in Augusta. “I would think of it the same way as you have to treat any chronic illness,” such as blood pressure medicine to keep hypertension in check and dialysis to prevent kidney failure.
Despite a cacophony of contrarian voices – mainly from the Church of Scientology – “the number of psychiatrists who see controversy in ECT is vanishingly small,” Dr. McCall said.
In weighing the pros and cons of ECT, he noted that “when you’re trying to decide if it’s worth doing a treatment, you’re looking at the effectiveness on one hand and the side effects on the other hand.”
The answer to that emerges from several scales measuring patients’ quality of life by posing questions such as: “After receiving ECT, are you more able or less able to take care of yourself, to work, and enjoy the company of other people?”
In the end, Dr. McCall said, “we’ve applied these scales in probably half a dozen studies or more, and they always show that the patients’ qualify of life as a group is improved.”
A recent study published in The Lancet Psychiatry provides a significant degree of reassurance that ECT – also called “electroshock” or colloquially just “shock” therapy – does not increase the risk of serious medical side effects. In fact, the study suggests a potential benefit in reducing suicide risk.
First performed in 1938, the treatment has been well documented in the medical literature. But negative portrayals in books and movies, such as the 1975 film “One Flew Over the Cuckoo’s Nest,” have contributed to casting it in an unfavorable light.
“Unfortunately, over the past decades and years, there’s a lot of stigma and fear around the treatment,” said the study’s lead author, Tyler Kaster, MD, a psychiatrist and clinical fellow in brain stimulation at the University of Toronto.
For the study, Canadian investigators reviewed the admission records of 10,000 patients hospitalized for at least 3 days because of a severe depressive episode. Nearly two-thirds of the patients were women, and the average age for the entire group approached 57 years.
While half of the patients underwent ECT, the others received medication and psychotherapy. Researchers found that the group undergoing ECT did not have a heightened risk of death over the next 30 days and were not any more likely to be hospitalized for a medical problem.
Previous ECT comparative studies were at high risk of bias because of their inability to sufficiently account for confounding variables and differences between those who received the treatment and those who did not. The current study employed “rigorous methods with careful attention to bias and confounding to overcome limitations of previous work,” the authors wrote.
They used propensity score matching, which included more than 75 variables, such as measures of cognitive impairment, depression severity, medication use, other illnesses, and use of psychiatric and various medical services, capacity to consent to treatment, and sociodemographic factors.
“This is really a landmark study in terms of showing the medical safety of ECT,” said Mark S. George, MD, professor of psychiatry and neurology at the Medical University of South Carolina, Charleston, who was not involved in the study.
He added that “ECT is a life-saving treatment” for individuals with severe depression. “It’s good that we have this option for our patients.”
The authors highlight that depression is a major cause of illness and disability worldwide, with many individuals failing to achieve remission from initial therapies. Treatment-resistant depression is often described as being nonresponsive “to two or more medication trials of adequate dose and duration from different classes,” they wrote. In these instances, the authors point out, there is little evidence that psychotherapy would be helpful.
“The reason we consider ECT is someone has very severe depression that hasn’t responded to medications and talk therapy,” Dr. Kaster said. “The advantage of ECT is that it’s very effective in those circumstances.”
Of all therapies for treatment-resistant depression, ECT has the highest success rate, with 60% of patients attaining remission, according to the study, which cites prior research.
Compared with neurosurgery, the procedure is not invasive but requires general anesthesia. While the patient is asleep, Dr. Kaster said, the treating clinician places an electrical stimulus on the patient’s scalp, causing a generalized seizure inside the brain that lasts from 15 seconds to 2 minutes.
A course of ECT usually takes a total of 8-12 treatments, delivered two to three times per week over a month to a month and a half, Dr. George said.
Some patients need a new course of ECT if they relapse after several months. Others are unable to control their depression between courses and require repeated doses for maintenance. The time between these ECT sessions varies for each individual, Dr. George said, but is typically one session every 3-4 weeks.
To improve the odds of staying well, patients typically need to continue taking antidepressants and engaging in psychotherapy.
“It helps improve the efficacy of ECT and also down the road helps prevent relapse,” Dr. Kaster said, noting that “depression is, unfortunately, a chronic illness. We don’t have a cure.”
Murat Altinay, MD, associate professor of psychiatry at the Cleveland Clinic and a mood disorders specialist, said his patients generally need to demonstrate a lack of response to at least three or four antidepressants before he considers recommending ECT.
Confusion, short-term memory impairment, and muscle aches and pains may occur after the procedure, but they are relatively mild. Patients are monitored in a recovery room before discharge from the hospital, Dr. Altinay said.
The first few treatments will affect everyday function. After that initial period, however, people can resume most of their daily activities, he said.
“Maybe they won’t be able to work full-time right away, but anecdotally, we have had patients who were able to go back to the workforce relatively quickly or while they’re getting ECT,” Dr. Altinay said.
More significant adverse events are very rare, he noted, although heart rate and blood pressure can become elevated because of the electrical stimulus.
Dr. Altinay said he is pleased that the large-scale journal article has been published to help dispel myths surrounding ECT. While psychiatrists feel that ECT is generally safe and effective, the public maintains a negative view.
“It is an underutilized treatment,” he said. “In the media, it is almost depicted as a barbaric and archaic treatment in psychiatry.”
Patients are afraid of major side effects such as personality changes. Some fear they will forget someone’s birthday or other important factual information, “but that kind of stuff obviously does not happen,” Dr. Altinay said.
Sometimes it’s not only the patients who are hesitant to try ECT; it’s the family members who express concerns, said Irving Reti, MBBS, professor of psychiatry and neuroscience and director of the brain stimulation program at the Johns Hopkins University, Baltimore.
“It varies from one patient to another how agreeable or reluctant or cautious they are about their treatment if the doctor thinks it’s indicated for them,” Dr. Reti said. “Family members’ concerns may be very legitimate but may also be influenced by stigma and misunderstanding about the treatment. They may also not fully appreciate the severity of their loved one’s depression that warrants the administration of ECT.”
Hospitalized patients who are at risk of suicide have benefited from ECT. “It’s very effective,” he said. “I think it’s still the gold standard for severe treatment-resistant depression and also particularly helpful in people who are acutely suicidal.”
Dr. George cautioned that psychiatrists and the public should beware of questionable online sources that attempt to discredit ECT. “A quick Google search will find plenty of nonmedical doctors, many funded through Scientology, who will speak poorly of ECT. But they do not use evidence-based arguments and commonly do not treat patients,” he said.
“All good practicing psychiatrists that I know are in favor of ECT, as it clearly saves lives,” Dr. George added. “We all hope that the future will provide refinements of ECT, or even disruptive technologies that are more effective and with less hassle and will make ECT as we do it now obsolete. But we are not there yet.”
A version of this article first appeared on Medscape.com.
For Clayton Lively, electroconvulsive therapy, or ECT, has been a lifesaver.
“ECT was like a last resort to treat mania and psychosis for bipolar disorder,” said the 31-year-old financial firm associate who lives in Silver Spring, Md. “I had tried lots of different medications.”
The first course of treatments – three times per week for several weeks – was in 2005. They helped tremendously. “I came down from my mania,” Mr. Lively said. “The hallucinations stopped. The psychosis disappeared.”
He reached a point where medications and psychotherapy worked again. And for a decade, his condition was under control.
But in 2017, another episode of hallucinations and mania jolted him off course. Intrusive thoughts returned. For instance, while driving, he would visualize veering off the road. The thoughts were jarring, and yet, he couldn’t stop them from recurring.
“I wasn’t sleeping, and it just kind of wreaked havoc on my life,” Mr. Lively recalled. “I ended up being hospitalized again.”
Once again, ECT came to the rescue – and yet again, in 2018. Now, he’s on an effective maintenance regimen, receiving ECT once every 4 weeks, after tapering down from more frequent sessions.
When a combination of antidepressants and psychotherapy fails to control severe mental illness, there’s hope on the horizon. ECT can be a reliably safe and effective option.
For some patients, using it as maintenance therapy makes sense, said Vaughn McCall, MD, editor-in-chief of The Journal of ECT and professor and chairman of psychiatry at the Medical College of Georgia in Augusta. “I would think of it the same way as you have to treat any chronic illness,” such as blood pressure medicine to keep hypertension in check and dialysis to prevent kidney failure.
Despite a cacophony of contrarian voices – mainly from the Church of Scientology – “the number of psychiatrists who see controversy in ECT is vanishingly small,” Dr. McCall said.
In weighing the pros and cons of ECT, he noted that “when you’re trying to decide if it’s worth doing a treatment, you’re looking at the effectiveness on one hand and the side effects on the other hand.”
The answer to that emerges from several scales measuring patients’ quality of life by posing questions such as: “After receiving ECT, are you more able or less able to take care of yourself, to work, and enjoy the company of other people?”
In the end, Dr. McCall said, “we’ve applied these scales in probably half a dozen studies or more, and they always show that the patients’ qualify of life as a group is improved.”
A recent study published in The Lancet Psychiatry provides a significant degree of reassurance that ECT – also called “electroshock” or colloquially just “shock” therapy – does not increase the risk of serious medical side effects. In fact, the study suggests a potential benefit in reducing suicide risk.
First performed in 1938, the treatment has been well documented in the medical literature. But negative portrayals in books and movies, such as the 1975 film “One Flew Over the Cuckoo’s Nest,” have contributed to casting it in an unfavorable light.
“Unfortunately, over the past decades and years, there’s a lot of stigma and fear around the treatment,” said the study’s lead author, Tyler Kaster, MD, a psychiatrist and clinical fellow in brain stimulation at the University of Toronto.
For the study, Canadian investigators reviewed the admission records of 10,000 patients hospitalized for at least 3 days because of a severe depressive episode. Nearly two-thirds of the patients were women, and the average age for the entire group approached 57 years.
While half of the patients underwent ECT, the others received medication and psychotherapy. Researchers found that the group undergoing ECT did not have a heightened risk of death over the next 30 days and were not any more likely to be hospitalized for a medical problem.
Previous ECT comparative studies were at high risk of bias because of their inability to sufficiently account for confounding variables and differences between those who received the treatment and those who did not. The current study employed “rigorous methods with careful attention to bias and confounding to overcome limitations of previous work,” the authors wrote.
They used propensity score matching, which included more than 75 variables, such as measures of cognitive impairment, depression severity, medication use, other illnesses, and use of psychiatric and various medical services, capacity to consent to treatment, and sociodemographic factors.
“This is really a landmark study in terms of showing the medical safety of ECT,” said Mark S. George, MD, professor of psychiatry and neurology at the Medical University of South Carolina, Charleston, who was not involved in the study.
He added that “ECT is a life-saving treatment” for individuals with severe depression. “It’s good that we have this option for our patients.”
The authors highlight that depression is a major cause of illness and disability worldwide, with many individuals failing to achieve remission from initial therapies. Treatment-resistant depression is often described as being nonresponsive “to two or more medication trials of adequate dose and duration from different classes,” they wrote. In these instances, the authors point out, there is little evidence that psychotherapy would be helpful.
“The reason we consider ECT is someone has very severe depression that hasn’t responded to medications and talk therapy,” Dr. Kaster said. “The advantage of ECT is that it’s very effective in those circumstances.”
Of all therapies for treatment-resistant depression, ECT has the highest success rate, with 60% of patients attaining remission, according to the study, which cites prior research.
Compared with neurosurgery, the procedure is not invasive but requires general anesthesia. While the patient is asleep, Dr. Kaster said, the treating clinician places an electrical stimulus on the patient’s scalp, causing a generalized seizure inside the brain that lasts from 15 seconds to 2 minutes.
A course of ECT usually takes a total of 8-12 treatments, delivered two to three times per week over a month to a month and a half, Dr. George said.
Some patients need a new course of ECT if they relapse after several months. Others are unable to control their depression between courses and require repeated doses for maintenance. The time between these ECT sessions varies for each individual, Dr. George said, but is typically one session every 3-4 weeks.
To improve the odds of staying well, patients typically need to continue taking antidepressants and engaging in psychotherapy.
“It helps improve the efficacy of ECT and also down the road helps prevent relapse,” Dr. Kaster said, noting that “depression is, unfortunately, a chronic illness. We don’t have a cure.”
Murat Altinay, MD, associate professor of psychiatry at the Cleveland Clinic and a mood disorders specialist, said his patients generally need to demonstrate a lack of response to at least three or four antidepressants before he considers recommending ECT.
Confusion, short-term memory impairment, and muscle aches and pains may occur after the procedure, but they are relatively mild. Patients are monitored in a recovery room before discharge from the hospital, Dr. Altinay said.
The first few treatments will affect everyday function. After that initial period, however, people can resume most of their daily activities, he said.
“Maybe they won’t be able to work full-time right away, but anecdotally, we have had patients who were able to go back to the workforce relatively quickly or while they’re getting ECT,” Dr. Altinay said.
More significant adverse events are very rare, he noted, although heart rate and blood pressure can become elevated because of the electrical stimulus.
Dr. Altinay said he is pleased that the large-scale journal article has been published to help dispel myths surrounding ECT. While psychiatrists feel that ECT is generally safe and effective, the public maintains a negative view.
“It is an underutilized treatment,” he said. “In the media, it is almost depicted as a barbaric and archaic treatment in psychiatry.”
Patients are afraid of major side effects such as personality changes. Some fear they will forget someone’s birthday or other important factual information, “but that kind of stuff obviously does not happen,” Dr. Altinay said.
Sometimes it’s not only the patients who are hesitant to try ECT; it’s the family members who express concerns, said Irving Reti, MBBS, professor of psychiatry and neuroscience and director of the brain stimulation program at the Johns Hopkins University, Baltimore.
“It varies from one patient to another how agreeable or reluctant or cautious they are about their treatment if the doctor thinks it’s indicated for them,” Dr. Reti said. “Family members’ concerns may be very legitimate but may also be influenced by stigma and misunderstanding about the treatment. They may also not fully appreciate the severity of their loved one’s depression that warrants the administration of ECT.”
Hospitalized patients who are at risk of suicide have benefited from ECT. “It’s very effective,” he said. “I think it’s still the gold standard for severe treatment-resistant depression and also particularly helpful in people who are acutely suicidal.”
Dr. George cautioned that psychiatrists and the public should beware of questionable online sources that attempt to discredit ECT. “A quick Google search will find plenty of nonmedical doctors, many funded through Scientology, who will speak poorly of ECT. But they do not use evidence-based arguments and commonly do not treat patients,” he said.
“All good practicing psychiatrists that I know are in favor of ECT, as it clearly saves lives,” Dr. George added. “We all hope that the future will provide refinements of ECT, or even disruptive technologies that are more effective and with less hassle and will make ECT as we do it now obsolete. But we are not there yet.”
A version of this article first appeared on Medscape.com.
For Clayton Lively, electroconvulsive therapy, or ECT, has been a lifesaver.
“ECT was like a last resort to treat mania and psychosis for bipolar disorder,” said the 31-year-old financial firm associate who lives in Silver Spring, Md. “I had tried lots of different medications.”
The first course of treatments – three times per week for several weeks – was in 2005. They helped tremendously. “I came down from my mania,” Mr. Lively said. “The hallucinations stopped. The psychosis disappeared.”
He reached a point where medications and psychotherapy worked again. And for a decade, his condition was under control.
But in 2017, another episode of hallucinations and mania jolted him off course. Intrusive thoughts returned. For instance, while driving, he would visualize veering off the road. The thoughts were jarring, and yet, he couldn’t stop them from recurring.
“I wasn’t sleeping, and it just kind of wreaked havoc on my life,” Mr. Lively recalled. “I ended up being hospitalized again.”
Once again, ECT came to the rescue – and yet again, in 2018. Now, he’s on an effective maintenance regimen, receiving ECT once every 4 weeks, after tapering down from more frequent sessions.
When a combination of antidepressants and psychotherapy fails to control severe mental illness, there’s hope on the horizon. ECT can be a reliably safe and effective option.
For some patients, using it as maintenance therapy makes sense, said Vaughn McCall, MD, editor-in-chief of The Journal of ECT and professor and chairman of psychiatry at the Medical College of Georgia in Augusta. “I would think of it the same way as you have to treat any chronic illness,” such as blood pressure medicine to keep hypertension in check and dialysis to prevent kidney failure.
Despite a cacophony of contrarian voices – mainly from the Church of Scientology – “the number of psychiatrists who see controversy in ECT is vanishingly small,” Dr. McCall said.
In weighing the pros and cons of ECT, he noted that “when you’re trying to decide if it’s worth doing a treatment, you’re looking at the effectiveness on one hand and the side effects on the other hand.”
The answer to that emerges from several scales measuring patients’ quality of life by posing questions such as: “After receiving ECT, are you more able or less able to take care of yourself, to work, and enjoy the company of other people?”
In the end, Dr. McCall said, “we’ve applied these scales in probably half a dozen studies or more, and they always show that the patients’ qualify of life as a group is improved.”
A recent study published in The Lancet Psychiatry provides a significant degree of reassurance that ECT – also called “electroshock” or colloquially just “shock” therapy – does not increase the risk of serious medical side effects. In fact, the study suggests a potential benefit in reducing suicide risk.
First performed in 1938, the treatment has been well documented in the medical literature. But negative portrayals in books and movies, such as the 1975 film “One Flew Over the Cuckoo’s Nest,” have contributed to casting it in an unfavorable light.
“Unfortunately, over the past decades and years, there’s a lot of stigma and fear around the treatment,” said the study’s lead author, Tyler Kaster, MD, a psychiatrist and clinical fellow in brain stimulation at the University of Toronto.
For the study, Canadian investigators reviewed the admission records of 10,000 patients hospitalized for at least 3 days because of a severe depressive episode. Nearly two-thirds of the patients were women, and the average age for the entire group approached 57 years.
While half of the patients underwent ECT, the others received medication and psychotherapy. Researchers found that the group undergoing ECT did not have a heightened risk of death over the next 30 days and were not any more likely to be hospitalized for a medical problem.
Previous ECT comparative studies were at high risk of bias because of their inability to sufficiently account for confounding variables and differences between those who received the treatment and those who did not. The current study employed “rigorous methods with careful attention to bias and confounding to overcome limitations of previous work,” the authors wrote.
They used propensity score matching, which included more than 75 variables, such as measures of cognitive impairment, depression severity, medication use, other illnesses, and use of psychiatric and various medical services, capacity to consent to treatment, and sociodemographic factors.
“This is really a landmark study in terms of showing the medical safety of ECT,” said Mark S. George, MD, professor of psychiatry and neurology at the Medical University of South Carolina, Charleston, who was not involved in the study.
He added that “ECT is a life-saving treatment” for individuals with severe depression. “It’s good that we have this option for our patients.”
The authors highlight that depression is a major cause of illness and disability worldwide, with many individuals failing to achieve remission from initial therapies. Treatment-resistant depression is often described as being nonresponsive “to two or more medication trials of adequate dose and duration from different classes,” they wrote. In these instances, the authors point out, there is little evidence that psychotherapy would be helpful.
“The reason we consider ECT is someone has very severe depression that hasn’t responded to medications and talk therapy,” Dr. Kaster said. “The advantage of ECT is that it’s very effective in those circumstances.”
Of all therapies for treatment-resistant depression, ECT has the highest success rate, with 60% of patients attaining remission, according to the study, which cites prior research.
Compared with neurosurgery, the procedure is not invasive but requires general anesthesia. While the patient is asleep, Dr. Kaster said, the treating clinician places an electrical stimulus on the patient’s scalp, causing a generalized seizure inside the brain that lasts from 15 seconds to 2 minutes.
A course of ECT usually takes a total of 8-12 treatments, delivered two to three times per week over a month to a month and a half, Dr. George said.
Some patients need a new course of ECT if they relapse after several months. Others are unable to control their depression between courses and require repeated doses for maintenance. The time between these ECT sessions varies for each individual, Dr. George said, but is typically one session every 3-4 weeks.
To improve the odds of staying well, patients typically need to continue taking antidepressants and engaging in psychotherapy.
“It helps improve the efficacy of ECT and also down the road helps prevent relapse,” Dr. Kaster said, noting that “depression is, unfortunately, a chronic illness. We don’t have a cure.”
Murat Altinay, MD, associate professor of psychiatry at the Cleveland Clinic and a mood disorders specialist, said his patients generally need to demonstrate a lack of response to at least three or four antidepressants before he considers recommending ECT.
Confusion, short-term memory impairment, and muscle aches and pains may occur after the procedure, but they are relatively mild. Patients are monitored in a recovery room before discharge from the hospital, Dr. Altinay said.
The first few treatments will affect everyday function. After that initial period, however, people can resume most of their daily activities, he said.
“Maybe they won’t be able to work full-time right away, but anecdotally, we have had patients who were able to go back to the workforce relatively quickly or while they’re getting ECT,” Dr. Altinay said.
More significant adverse events are very rare, he noted, although heart rate and blood pressure can become elevated because of the electrical stimulus.
Dr. Altinay said he is pleased that the large-scale journal article has been published to help dispel myths surrounding ECT. While psychiatrists feel that ECT is generally safe and effective, the public maintains a negative view.
“It is an underutilized treatment,” he said. “In the media, it is almost depicted as a barbaric and archaic treatment in psychiatry.”
Patients are afraid of major side effects such as personality changes. Some fear they will forget someone’s birthday or other important factual information, “but that kind of stuff obviously does not happen,” Dr. Altinay said.
Sometimes it’s not only the patients who are hesitant to try ECT; it’s the family members who express concerns, said Irving Reti, MBBS, professor of psychiatry and neuroscience and director of the brain stimulation program at the Johns Hopkins University, Baltimore.
“It varies from one patient to another how agreeable or reluctant or cautious they are about their treatment if the doctor thinks it’s indicated for them,” Dr. Reti said. “Family members’ concerns may be very legitimate but may also be influenced by stigma and misunderstanding about the treatment. They may also not fully appreciate the severity of their loved one’s depression that warrants the administration of ECT.”
Hospitalized patients who are at risk of suicide have benefited from ECT. “It’s very effective,” he said. “I think it’s still the gold standard for severe treatment-resistant depression and also particularly helpful in people who are acutely suicidal.”
Dr. George cautioned that psychiatrists and the public should beware of questionable online sources that attempt to discredit ECT. “A quick Google search will find plenty of nonmedical doctors, many funded through Scientology, who will speak poorly of ECT. But they do not use evidence-based arguments and commonly do not treat patients,” he said.
“All good practicing psychiatrists that I know are in favor of ECT, as it clearly saves lives,” Dr. George added. “We all hope that the future will provide refinements of ECT, or even disruptive technologies that are more effective and with less hassle and will make ECT as we do it now obsolete. But we are not there yet.”
A version of this article first appeared on Medscape.com.
Schizophrenia linked to violent behavior, but experts push back
A new meta-analysis suggests the risk for violence is higher in patients with schizophrenia, but some experts beg to differ, calling out study limitations and urging caution when interpreting the findings.
The study suggests patients with schizophrenia spectrum disorder (SSD) are 4.5 times more likely than individuals in the general population to perpetrate violence against others.
While the results showed comorbid substance misuse was associated with a significantly increased risk for violence in those with SSD, data on medication nonadherence, prior exposure to violence, childhood trauma, or other known risk factors were not included in the study.
“I think one of the main implications of this study is that prevention of violence outcomes really should be a focus for clinical services, because these are important outcomes to prevent and many of the factors that increase risk are modifiable, such as substance misuse and treatment adherence,” study coinvestigator Seena Fazel, MD, professor of forensic psychiatry at the University of Oxford (England), said in an interview.
Still, some experts urge caution when interpreting the findings, which they fear could perpetuate stigma against individuals with serious mental illness if not taken in the context of a study that shows association, not causation.
“While potential for violence is certainly a relevant consideration in assessing persons with schizophrenia spectrum disorder, professor emeritus of psychiatry at the State University of New York, Syracuse, who commented on the findings.
The findings were published online Dec. 22, 2021, in JAMA Psychiatry.
No causal link
The meta-analysis included 24 studies involving 51,309 individuals with SSD from 15 countries over 4 decades.
Risk for violence perpetrated by men with schizophrenia was 4.5 times higher (95% confidence interval, 3.6-5.6) than their counterparts in the general population. Among women, the rate was 10.2 times higher (95% CI, 7.1-14.6) versus those without SSD.
The odds of perpetrating sexual offenses (odds ratio, 5.1; 95% CI, 3.8-6.8) and homicide (OR, 17.7; 95% CI, 13.9-22.6) were also increased.
When restricting analysis to studies that used outcomes only from register-based sources, indicating a criminal arrest or conviction, absolute risks of violence perpetration ranged from 2.3% to 24.7% in men with SSD and from 0% to 5.4% in women up to a 35-year follow-up.
“That means that over a 35-year period most men are not going to be involved in these criminal register-based violent outcomes,” Dr. Fazel said. “And at least 90% of the women are not going to have any register-based violent outcomes.”
When accounting for substance use comorbidity, risk for violence perpetration dropped sharply. Those with no substance misuse were 3.5 times more likely than those in the general population to commit acts of violence versus 9.9 times in those with substance misuse comorbidity.
“In these subgroup studies of people with dual diagnoses of schizophrenia and substance misuse, the risk was increased 10-fold,” Dr. Fazel said. “If you look at people without substance misuse comorbidity, there remains a risk there of between three- to fourfold increase. It doesn’t explain the association completely.”
The investigators were quick to point out that this new study identifies an association between SSD and violence, and not causation.
“One important way to consider the association is to think of clinical services for people presenting with a schizophrenia spectrum disorder: Does the evidence suggest that violence is an important enough potential adverse outcome, for a minority of those individuals, such that support for this clinical need should be improved?” study investigator Daniel Whiting, BM BCh, a doctoral research fellow in psychiatry at the University of Oxford, said in an interview. “We highlight this as an implication of the findings.”
Whether the association would change if researchers controlled for substance misuse in both the study and control groups is unknown. Also unclear from this study is what impact other risk factors may have on increasing violent outcomes in individuals with SSD.
Education, treatment adherence important
Dr. Pies pointed out that, “notably, the risk for violence in the study population declined more than sixfold when comorbid substance abuse was excluded from the analysis.”
That aligns with an earlier study conducted in Sweden by Dr. Fazel, which showed that, after controlling for substance misuse, the rate of violent crime among individuals with schizophrenia was only slightly higher than in the general population.
“The fact is that people with schizophrenia who are compliant with proper medication do not commit violent acts any more than those in the general population,” Lynn DeLisi, MD, professor of psychiatry at Harvard Medical School, Boston, and founding editor of Schizophrenia Research, said in a comment.
Indeed, Dr. Fazel’s own research suggests treatment with antipsychotics cuts in half the risk for violent crime by patients with severe mental illness.
“The goal should be education of school officials, families, and primary care physicians to detect this illness early and treat it. Programs that make sure patients comply with medication once they begin it are equally important,” Dr. DeLisi said.
Treatment adherence is important, but the first step toward violence prevention is high-quality risk assessment, said Dr. Fazel. His research team has developed a web-based, free risk calculator shown to help clinicians evaluate the risk that a patient might become violent.
Dr. Pies agreed with the importance of comprehensive, clinical assessments of modifiable risk factors, including substance use, homelessness, medication adherence, and conflictual relationships.
This kind of assessment, “in my experience, is rarely carried out in most evaluations of persons with psychotic symptoms or SSD,” he said.
Perpetuating stigma?
Another concern raised by Dr. Pies and Dr. DeLisi is how the findings might perpetuate stigma toward individuals with serious mental illness. Results from a recently published study showed that, although attitudes toward those with major depression have improved in the United States over the past few decades, stigma toward those with schizophrenia has actually worsened.
The most effective approach to reducing stigma is to “face up to the evidence, then try and prevent the negative outcomes,” Dr. Fazel said.
“The conclusion of this paper is that it’s all pointing toward a strategy toward prevention by developing high-quality risk assessment and then developing high-quality treatment programs that include not just pharmacological treatments but psychosocial treatments and beyond,” he added. “We know that’s the way it works for other disorders as well.”
Although mental illness stigma is a serious problem, Dr. Pies noted, “the risk is not so much that studies of this sort are carried out and then covered in the media, but that they are decontextualized and reduced to ‘bumper sticker’ headlines.”
“The public needs context and perspective,” he said. “It needs to be informed that violent behavior is relatively rare among persons with psychiatric illness, including persons with schizophrenia and related disorders who do not also have a substance use disorder.”
Indeed, some studies have shown that individuals with mental illness are more often the victims of violence than the perpetrators.
“Frankly, the public is much more at risk from the neighborhood lout who drinks heavily and repeatedly starts bar fights than from the average patient with a schizophrenia spectrum disorder,” Dr. Pies said.
Dr. Fazel reported receiving funding from the Wellcome Trust. Dr. DeLisi and Dr. Pies disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new meta-analysis suggests the risk for violence is higher in patients with schizophrenia, but some experts beg to differ, calling out study limitations and urging caution when interpreting the findings.
The study suggests patients with schizophrenia spectrum disorder (SSD) are 4.5 times more likely than individuals in the general population to perpetrate violence against others.
While the results showed comorbid substance misuse was associated with a significantly increased risk for violence in those with SSD, data on medication nonadherence, prior exposure to violence, childhood trauma, or other known risk factors were not included in the study.
“I think one of the main implications of this study is that prevention of violence outcomes really should be a focus for clinical services, because these are important outcomes to prevent and many of the factors that increase risk are modifiable, such as substance misuse and treatment adherence,” study coinvestigator Seena Fazel, MD, professor of forensic psychiatry at the University of Oxford (England), said in an interview.
Still, some experts urge caution when interpreting the findings, which they fear could perpetuate stigma against individuals with serious mental illness if not taken in the context of a study that shows association, not causation.
“While potential for violence is certainly a relevant consideration in assessing persons with schizophrenia spectrum disorder, professor emeritus of psychiatry at the State University of New York, Syracuse, who commented on the findings.
The findings were published online Dec. 22, 2021, in JAMA Psychiatry.
No causal link
The meta-analysis included 24 studies involving 51,309 individuals with SSD from 15 countries over 4 decades.
Risk for violence perpetrated by men with schizophrenia was 4.5 times higher (95% confidence interval, 3.6-5.6) than their counterparts in the general population. Among women, the rate was 10.2 times higher (95% CI, 7.1-14.6) versus those without SSD.
The odds of perpetrating sexual offenses (odds ratio, 5.1; 95% CI, 3.8-6.8) and homicide (OR, 17.7; 95% CI, 13.9-22.6) were also increased.
When restricting analysis to studies that used outcomes only from register-based sources, indicating a criminal arrest or conviction, absolute risks of violence perpetration ranged from 2.3% to 24.7% in men with SSD and from 0% to 5.4% in women up to a 35-year follow-up.
“That means that over a 35-year period most men are not going to be involved in these criminal register-based violent outcomes,” Dr. Fazel said. “And at least 90% of the women are not going to have any register-based violent outcomes.”
When accounting for substance use comorbidity, risk for violence perpetration dropped sharply. Those with no substance misuse were 3.5 times more likely than those in the general population to commit acts of violence versus 9.9 times in those with substance misuse comorbidity.
“In these subgroup studies of people with dual diagnoses of schizophrenia and substance misuse, the risk was increased 10-fold,” Dr. Fazel said. “If you look at people without substance misuse comorbidity, there remains a risk there of between three- to fourfold increase. It doesn’t explain the association completely.”
The investigators were quick to point out that this new study identifies an association between SSD and violence, and not causation.
“One important way to consider the association is to think of clinical services for people presenting with a schizophrenia spectrum disorder: Does the evidence suggest that violence is an important enough potential adverse outcome, for a minority of those individuals, such that support for this clinical need should be improved?” study investigator Daniel Whiting, BM BCh, a doctoral research fellow in psychiatry at the University of Oxford, said in an interview. “We highlight this as an implication of the findings.”
Whether the association would change if researchers controlled for substance misuse in both the study and control groups is unknown. Also unclear from this study is what impact other risk factors may have on increasing violent outcomes in individuals with SSD.
Education, treatment adherence important
Dr. Pies pointed out that, “notably, the risk for violence in the study population declined more than sixfold when comorbid substance abuse was excluded from the analysis.”
That aligns with an earlier study conducted in Sweden by Dr. Fazel, which showed that, after controlling for substance misuse, the rate of violent crime among individuals with schizophrenia was only slightly higher than in the general population.
“The fact is that people with schizophrenia who are compliant with proper medication do not commit violent acts any more than those in the general population,” Lynn DeLisi, MD, professor of psychiatry at Harvard Medical School, Boston, and founding editor of Schizophrenia Research, said in a comment.
Indeed, Dr. Fazel’s own research suggests treatment with antipsychotics cuts in half the risk for violent crime by patients with severe mental illness.
“The goal should be education of school officials, families, and primary care physicians to detect this illness early and treat it. Programs that make sure patients comply with medication once they begin it are equally important,” Dr. DeLisi said.
Treatment adherence is important, but the first step toward violence prevention is high-quality risk assessment, said Dr. Fazel. His research team has developed a web-based, free risk calculator shown to help clinicians evaluate the risk that a patient might become violent.
Dr. Pies agreed with the importance of comprehensive, clinical assessments of modifiable risk factors, including substance use, homelessness, medication adherence, and conflictual relationships.
This kind of assessment, “in my experience, is rarely carried out in most evaluations of persons with psychotic symptoms or SSD,” he said.
Perpetuating stigma?
Another concern raised by Dr. Pies and Dr. DeLisi is how the findings might perpetuate stigma toward individuals with serious mental illness. Results from a recently published study showed that, although attitudes toward those with major depression have improved in the United States over the past few decades, stigma toward those with schizophrenia has actually worsened.
The most effective approach to reducing stigma is to “face up to the evidence, then try and prevent the negative outcomes,” Dr. Fazel said.
“The conclusion of this paper is that it’s all pointing toward a strategy toward prevention by developing high-quality risk assessment and then developing high-quality treatment programs that include not just pharmacological treatments but psychosocial treatments and beyond,” he added. “We know that’s the way it works for other disorders as well.”
Although mental illness stigma is a serious problem, Dr. Pies noted, “the risk is not so much that studies of this sort are carried out and then covered in the media, but that they are decontextualized and reduced to ‘bumper sticker’ headlines.”
“The public needs context and perspective,” he said. “It needs to be informed that violent behavior is relatively rare among persons with psychiatric illness, including persons with schizophrenia and related disorders who do not also have a substance use disorder.”
Indeed, some studies have shown that individuals with mental illness are more often the victims of violence than the perpetrators.
“Frankly, the public is much more at risk from the neighborhood lout who drinks heavily and repeatedly starts bar fights than from the average patient with a schizophrenia spectrum disorder,” Dr. Pies said.
Dr. Fazel reported receiving funding from the Wellcome Trust. Dr. DeLisi and Dr. Pies disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new meta-analysis suggests the risk for violence is higher in patients with schizophrenia, but some experts beg to differ, calling out study limitations and urging caution when interpreting the findings.
The study suggests patients with schizophrenia spectrum disorder (SSD) are 4.5 times more likely than individuals in the general population to perpetrate violence against others.
While the results showed comorbid substance misuse was associated with a significantly increased risk for violence in those with SSD, data on medication nonadherence, prior exposure to violence, childhood trauma, or other known risk factors were not included in the study.
“I think one of the main implications of this study is that prevention of violence outcomes really should be a focus for clinical services, because these are important outcomes to prevent and many of the factors that increase risk are modifiable, such as substance misuse and treatment adherence,” study coinvestigator Seena Fazel, MD, professor of forensic psychiatry at the University of Oxford (England), said in an interview.
Still, some experts urge caution when interpreting the findings, which they fear could perpetuate stigma against individuals with serious mental illness if not taken in the context of a study that shows association, not causation.
“While potential for violence is certainly a relevant consideration in assessing persons with schizophrenia spectrum disorder, professor emeritus of psychiatry at the State University of New York, Syracuse, who commented on the findings.
The findings were published online Dec. 22, 2021, in JAMA Psychiatry.
No causal link
The meta-analysis included 24 studies involving 51,309 individuals with SSD from 15 countries over 4 decades.
Risk for violence perpetrated by men with schizophrenia was 4.5 times higher (95% confidence interval, 3.6-5.6) than their counterparts in the general population. Among women, the rate was 10.2 times higher (95% CI, 7.1-14.6) versus those without SSD.
The odds of perpetrating sexual offenses (odds ratio, 5.1; 95% CI, 3.8-6.8) and homicide (OR, 17.7; 95% CI, 13.9-22.6) were also increased.
When restricting analysis to studies that used outcomes only from register-based sources, indicating a criminal arrest or conviction, absolute risks of violence perpetration ranged from 2.3% to 24.7% in men with SSD and from 0% to 5.4% in women up to a 35-year follow-up.
“That means that over a 35-year period most men are not going to be involved in these criminal register-based violent outcomes,” Dr. Fazel said. “And at least 90% of the women are not going to have any register-based violent outcomes.”
When accounting for substance use comorbidity, risk for violence perpetration dropped sharply. Those with no substance misuse were 3.5 times more likely than those in the general population to commit acts of violence versus 9.9 times in those with substance misuse comorbidity.
“In these subgroup studies of people with dual diagnoses of schizophrenia and substance misuse, the risk was increased 10-fold,” Dr. Fazel said. “If you look at people without substance misuse comorbidity, there remains a risk there of between three- to fourfold increase. It doesn’t explain the association completely.”
The investigators were quick to point out that this new study identifies an association between SSD and violence, and not causation.
“One important way to consider the association is to think of clinical services for people presenting with a schizophrenia spectrum disorder: Does the evidence suggest that violence is an important enough potential adverse outcome, for a minority of those individuals, such that support for this clinical need should be improved?” study investigator Daniel Whiting, BM BCh, a doctoral research fellow in psychiatry at the University of Oxford, said in an interview. “We highlight this as an implication of the findings.”
Whether the association would change if researchers controlled for substance misuse in both the study and control groups is unknown. Also unclear from this study is what impact other risk factors may have on increasing violent outcomes in individuals with SSD.
Education, treatment adherence important
Dr. Pies pointed out that, “notably, the risk for violence in the study population declined more than sixfold when comorbid substance abuse was excluded from the analysis.”
That aligns with an earlier study conducted in Sweden by Dr. Fazel, which showed that, after controlling for substance misuse, the rate of violent crime among individuals with schizophrenia was only slightly higher than in the general population.
“The fact is that people with schizophrenia who are compliant with proper medication do not commit violent acts any more than those in the general population,” Lynn DeLisi, MD, professor of psychiatry at Harvard Medical School, Boston, and founding editor of Schizophrenia Research, said in a comment.
Indeed, Dr. Fazel’s own research suggests treatment with antipsychotics cuts in half the risk for violent crime by patients with severe mental illness.
“The goal should be education of school officials, families, and primary care physicians to detect this illness early and treat it. Programs that make sure patients comply with medication once they begin it are equally important,” Dr. DeLisi said.
Treatment adherence is important, but the first step toward violence prevention is high-quality risk assessment, said Dr. Fazel. His research team has developed a web-based, free risk calculator shown to help clinicians evaluate the risk that a patient might become violent.
Dr. Pies agreed with the importance of comprehensive, clinical assessments of modifiable risk factors, including substance use, homelessness, medication adherence, and conflictual relationships.
This kind of assessment, “in my experience, is rarely carried out in most evaluations of persons with psychotic symptoms or SSD,” he said.
Perpetuating stigma?
Another concern raised by Dr. Pies and Dr. DeLisi is how the findings might perpetuate stigma toward individuals with serious mental illness. Results from a recently published study showed that, although attitudes toward those with major depression have improved in the United States over the past few decades, stigma toward those with schizophrenia has actually worsened.
The most effective approach to reducing stigma is to “face up to the evidence, then try and prevent the negative outcomes,” Dr. Fazel said.
“The conclusion of this paper is that it’s all pointing toward a strategy toward prevention by developing high-quality risk assessment and then developing high-quality treatment programs that include not just pharmacological treatments but psychosocial treatments and beyond,” he added. “We know that’s the way it works for other disorders as well.”
Although mental illness stigma is a serious problem, Dr. Pies noted, “the risk is not so much that studies of this sort are carried out and then covered in the media, but that they are decontextualized and reduced to ‘bumper sticker’ headlines.”
“The public needs context and perspective,” he said. “It needs to be informed that violent behavior is relatively rare among persons with psychiatric illness, including persons with schizophrenia and related disorders who do not also have a substance use disorder.”
Indeed, some studies have shown that individuals with mental illness are more often the victims of violence than the perpetrators.
“Frankly, the public is much more at risk from the neighborhood lout who drinks heavily and repeatedly starts bar fights than from the average patient with a schizophrenia spectrum disorder,” Dr. Pies said.
Dr. Fazel reported receiving funding from the Wellcome Trust. Dr. DeLisi and Dr. Pies disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Effect of vitamin D supplementation in early psychosis
Low vitamin D is common in patients with first-episode psychosis (FEP), but supplementation does not appear to improve mental or physical symptoms, new data show.
“Previous work, our own and others, has shown that people with psychosis, even soon after their first diagnosis, have low vitamin D levels, but it was not known whether supplementing with vitamin D in people with early psychosis would improve health outcomes,” study investigator Fiona Gaughran, MD, with the Institute of Psychiatry, Psychology & Neuroscience, King’s College London, told this news organization.
“While we did not demonstrate a benefit of supplementation over 6 months, these very high rates of vitamin deficiency and insufficiency may have longer-term negative health impacts which we have not measured, so raising awareness of the need to optimize vitamin D in people with psychosis is important,” said Dr. Gaughran.
The results of the randomized clinical trial were published online Dec. 28 in JAMA Network Open.
Thoughtful approach, negative result
Participants included 149 adults within 3 years of a first presentation with a functional psychotic disorder. The cohort’s mean age was 28 years, 60% were men, 44% were Black or of other racial and ethnic minority groups, and 56% were White.
Seventy-five participants were randomly assigned to receive 120,000 IU of cholecalciferol or matching placebo administered by the researchers in monthly doses with an oral syringe.
“We chose a dose of 120,000 IU monthly (equivalent to 4,000 IU daily) which was expected to safely increase vitamin D levels. The regimen was discussed with experts with lived experience, and took into account that a daily preparation would add to the significant medication load that people with psychosis already carry,” said Dr. Gaughran.
Vitamin D supplementation as administered in this study was safe and led to a significant increase in 25-hydroxyvitamin D concentrations.
However, at 6 months (mean difference, 3.57; 95% confidence interval, –1.11 to 8.25; P = .13).
There was also no apparent benefit of vitamin D supplementation on any secondary outcome, including the PANSS subscores of global function and depression or cardiometabolic risk factors.
“With respect to clinical practice, we cannot now recommend monthly treatments with 120,000 IU of cholecalciferol in FEP,” the investigators note.
The prevalence of vitamin D insufficiency and deficiency was high in the population – 74.6% overall and 93.4% among ethnic minorities.
“Thus, the sample was well suited to detecting any potential benefits that may have arisen from correcting this. However, even in this subgroup, there was no evidence to support the guiding hypothesis” that vitamin D supplementation would improve outcomes in patients with early psychosis, the researchers note.
They suggest that future studies examine the association of vitamin D with brain-related outcomes based on periods of treatment longer than 6 months and administered as daily rather than bolus treatments.
“Future public health strategies should acknowledge the high prevalence of vitamin D insufficiency and deficiency in people with psychosis and consider any reasonable adjustments which may be needed to address this over and above general population guidance,” said Dr. Gaughran.
The study was funded by the Stanley Medical Research Institute and received support from the National Institute for Health Research Maudsley Biomedical Research Centre, King’s College London, and the NIHR Applied Research Collaboration South London. Dr. Gaughran reported receiving speaking honoraria from Otsuka Lundbeck outside the submitted work. A complete list of author disclosures is available with the original article.
A version of this article first appeared on Medscape.com.
Low vitamin D is common in patients with first-episode psychosis (FEP), but supplementation does not appear to improve mental or physical symptoms, new data show.
“Previous work, our own and others, has shown that people with psychosis, even soon after their first diagnosis, have low vitamin D levels, but it was not known whether supplementing with vitamin D in people with early psychosis would improve health outcomes,” study investigator Fiona Gaughran, MD, with the Institute of Psychiatry, Psychology & Neuroscience, King’s College London, told this news organization.
“While we did not demonstrate a benefit of supplementation over 6 months, these very high rates of vitamin deficiency and insufficiency may have longer-term negative health impacts which we have not measured, so raising awareness of the need to optimize vitamin D in people with psychosis is important,” said Dr. Gaughran.
The results of the randomized clinical trial were published online Dec. 28 in JAMA Network Open.
Thoughtful approach, negative result
Participants included 149 adults within 3 years of a first presentation with a functional psychotic disorder. The cohort’s mean age was 28 years, 60% were men, 44% were Black or of other racial and ethnic minority groups, and 56% were White.
Seventy-five participants were randomly assigned to receive 120,000 IU of cholecalciferol or matching placebo administered by the researchers in monthly doses with an oral syringe.
“We chose a dose of 120,000 IU monthly (equivalent to 4,000 IU daily) which was expected to safely increase vitamin D levels. The regimen was discussed with experts with lived experience, and took into account that a daily preparation would add to the significant medication load that people with psychosis already carry,” said Dr. Gaughran.
Vitamin D supplementation as administered in this study was safe and led to a significant increase in 25-hydroxyvitamin D concentrations.
However, at 6 months (mean difference, 3.57; 95% confidence interval, –1.11 to 8.25; P = .13).
There was also no apparent benefit of vitamin D supplementation on any secondary outcome, including the PANSS subscores of global function and depression or cardiometabolic risk factors.
“With respect to clinical practice, we cannot now recommend monthly treatments with 120,000 IU of cholecalciferol in FEP,” the investigators note.
The prevalence of vitamin D insufficiency and deficiency was high in the population – 74.6% overall and 93.4% among ethnic minorities.
“Thus, the sample was well suited to detecting any potential benefits that may have arisen from correcting this. However, even in this subgroup, there was no evidence to support the guiding hypothesis” that vitamin D supplementation would improve outcomes in patients with early psychosis, the researchers note.
They suggest that future studies examine the association of vitamin D with brain-related outcomes based on periods of treatment longer than 6 months and administered as daily rather than bolus treatments.
“Future public health strategies should acknowledge the high prevalence of vitamin D insufficiency and deficiency in people with psychosis and consider any reasonable adjustments which may be needed to address this over and above general population guidance,” said Dr. Gaughran.
The study was funded by the Stanley Medical Research Institute and received support from the National Institute for Health Research Maudsley Biomedical Research Centre, King’s College London, and the NIHR Applied Research Collaboration South London. Dr. Gaughran reported receiving speaking honoraria from Otsuka Lundbeck outside the submitted work. A complete list of author disclosures is available with the original article.
A version of this article first appeared on Medscape.com.
Low vitamin D is common in patients with first-episode psychosis (FEP), but supplementation does not appear to improve mental or physical symptoms, new data show.
“Previous work, our own and others, has shown that people with psychosis, even soon after their first diagnosis, have low vitamin D levels, but it was not known whether supplementing with vitamin D in people with early psychosis would improve health outcomes,” study investigator Fiona Gaughran, MD, with the Institute of Psychiatry, Psychology & Neuroscience, King’s College London, told this news organization.
“While we did not demonstrate a benefit of supplementation over 6 months, these very high rates of vitamin deficiency and insufficiency may have longer-term negative health impacts which we have not measured, so raising awareness of the need to optimize vitamin D in people with psychosis is important,” said Dr. Gaughran.
The results of the randomized clinical trial were published online Dec. 28 in JAMA Network Open.
Thoughtful approach, negative result
Participants included 149 adults within 3 years of a first presentation with a functional psychotic disorder. The cohort’s mean age was 28 years, 60% were men, 44% were Black or of other racial and ethnic minority groups, and 56% were White.
Seventy-five participants were randomly assigned to receive 120,000 IU of cholecalciferol or matching placebo administered by the researchers in monthly doses with an oral syringe.
“We chose a dose of 120,000 IU monthly (equivalent to 4,000 IU daily) which was expected to safely increase vitamin D levels. The regimen was discussed with experts with lived experience, and took into account that a daily preparation would add to the significant medication load that people with psychosis already carry,” said Dr. Gaughran.
Vitamin D supplementation as administered in this study was safe and led to a significant increase in 25-hydroxyvitamin D concentrations.
However, at 6 months (mean difference, 3.57; 95% confidence interval, –1.11 to 8.25; P = .13).
There was also no apparent benefit of vitamin D supplementation on any secondary outcome, including the PANSS subscores of global function and depression or cardiometabolic risk factors.
“With respect to clinical practice, we cannot now recommend monthly treatments with 120,000 IU of cholecalciferol in FEP,” the investigators note.
The prevalence of vitamin D insufficiency and deficiency was high in the population – 74.6% overall and 93.4% among ethnic minorities.
“Thus, the sample was well suited to detecting any potential benefits that may have arisen from correcting this. However, even in this subgroup, there was no evidence to support the guiding hypothesis” that vitamin D supplementation would improve outcomes in patients with early psychosis, the researchers note.
They suggest that future studies examine the association of vitamin D with brain-related outcomes based on periods of treatment longer than 6 months and administered as daily rather than bolus treatments.
“Future public health strategies should acknowledge the high prevalence of vitamin D insufficiency and deficiency in people with psychosis and consider any reasonable adjustments which may be needed to address this over and above general population guidance,” said Dr. Gaughran.
The study was funded by the Stanley Medical Research Institute and received support from the National Institute for Health Research Maudsley Biomedical Research Centre, King’s College London, and the NIHR Applied Research Collaboration South London. Dr. Gaughran reported receiving speaking honoraria from Otsuka Lundbeck outside the submitted work. A complete list of author disclosures is available with the original article.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Too close for comfort: When the psychiatrist is stalked
Dr. A has been treating Ms. W, a graduate student, for depression. Ms. W made subtle comments expressing her interest in pursuing a romantic relationship with her psychiatrist. Dr. A gently redirected her, and she seemed to respond appropriately. However, over the past 2 weeks, Dr. A has seen Ms. W at a local park and at the grocery store. Today, Dr. A is startled to see Ms. W at her weekly yoga class. Dr. A plans to ask her supervisor for advice.
Dr. M is a child psychiatrist who spoke at his local school board meeting in support of masking requirements for students during COVID-19. During the discussion, Dr. M shared that, as a psychiatrist, he does not believe it is especially distressing for students to wear masks, and that doing so is a necessary public health measure. On leaving, other parents shouted, “We know who you are and where you live!” The next day, his integrated clinic started receiving threatening and harassing messages, including threats to kill him or his staff if they take part in vaccinating children against COVID-19.
Because of their work, mental health professionals—like other health care professionals—face an elevated risk of being harassed or stalked. Stalking often includes online harassment and may escalate to serious physical violence. Stalking is criminal behavior by a patient and should not be constructed as a “failure to manage transference.” This article explores basic strategies to reduce the risk of harassment and stalking, describes how to recognize early behaviors, and outlines basic steps health care professionals and their employers can take to respond to stalking and harassing behaviors.
Although this article is intended for psychiatrists, it is important to note that all health professionals have significant risk for experiencing stalking or harassment. This is due in part, but not exclusively, to our clinical work. Estimates of how many health professionals experience stalking vary substantially depending upon the study, and differences in methodologies limit easy comparison or extrapolation. More thorough reviews have reported ranges from 2% to 70% among physicians; psychiatrists and other mental health professionals appear to be at greater risk than those in other specialties and the general population.1-3 Physicians who are active on social media may also be at elevated risk.4 Unexpected communications from patients and their family members—especially those with threatening, harassing, or sexualized tones, or involving contact outside of a work setting—can be distressing. These behaviors represent potential harbingers of more dangerous behavior, including physical assault, sexual assault, or homicide. Despite their elevated risk, many psychiatrists are unaware of how to prevent or respond to stalking or harassment.
Recognizing harassment and stalking
Repeated and unwanted contact or communication, regardless of intent, may constitute stalking. Legal definitions vary by jurisdiction and may not align with subjective experiences or understanding of what constitutes stalking.5 At its essence, stalking is repeated harassing behaviors likely to provoke fear in the targeted person. FOUR is a helpful mnemonic when conceptualizing the attributes of stalking: Fixated, Obsessive, Unwanted, and Repetitive.6Table 1 lists examples of common stalking behaviors. Stalking and harassing behavior may be from a known source (eg, a patient, coworker, or paramour), a masked source (ie, someone known to the target but who conceals or obscures their identity), or from otherwise unknown persons. Behaviors that persist after the person engaging in the behaviors has clearly been informed that they are unwanted or inappropriate are especially concerning. Stalking may escalate to include physical or sexual assault and, in some cases, homicide.
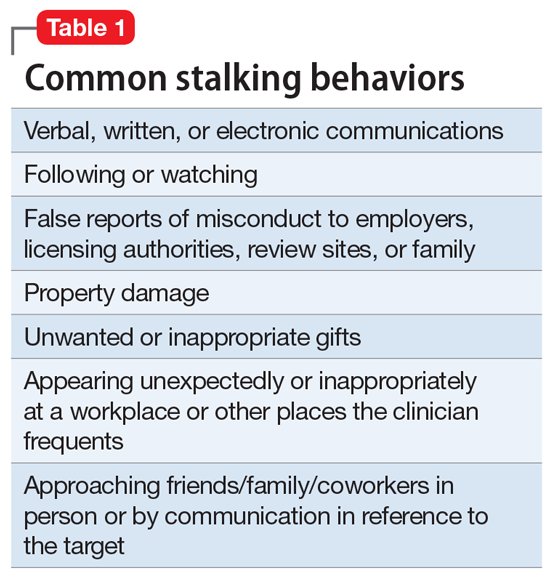
Stalking duration can vary substantially, as can the factors that lead to the cessation of the behavior. Indicators of increased risk for physical violence include unwanted physical presence/following of the target (“approach behaviors”), having a prior violent intimate relationship, property destruction, explicit threats, and having a prior intimate relationship with the target.7
Stalking contact or communication may be unwanted because of the content (eg, sexualized or threatening tone), location (eg, at a professional’s home), or means (eg, through social media). Stalking behaviors are not appropriate in any relationship, including a clinical relationship. They should not be treated as a “failure to manage transference” or in other victim-blaming ways.
There are multiple typologies for stalking behavior. Common motivations for stalking health professionals include resentment or grievance, misjudgment of social boundaries, and delusional fixation, including erotomania.8 Associated psychopathologies vary significantly and, while some may be more amenable to psychiatric treatment than others, psychiatrists should not feel compelled to treat patients who repeatedly violate boundaries, regardless of intent or comorbidity.
Patients are not the exclusive perpetrators of stalking; a recent study found that 4% of physicians surveyed reported current or recent stalking by a current or former intimate partner.9 When a person who is a victim of intimate partner violence is also stalked as part of the abuse, homicide risk increases.10 Workplace homicides of health care professionals are most likely to be committed by a current or former partner or other personal acquaintance, not by a patient.11 Workplace harassment and stalking of health care professionals is especially concerning because this behavior can escalate and endanger coworkers or clients.
Continue to: Risk awareness: Recognize your exposure...
Risk awareness: Recognize your exposure
About 80% of stalking involves some form of technology—often telephone calls but also online or other “cyber” elements.12 One recent survey found the rate of online harassment, including threats of physical and sexual violence, was >20% among physicians who were active on social media.4 Health professionals may be at greater risk of having patients find their personal information simply because patients routinely search online for information about new clinicians. Personal information about a clinician may be readily visible among professional information in search results, or a curious patient may simply scroll further down in the results. For a potential stalker, clicking on a search result linking to a personal social media page may be far easier than finding a home address and going in person—but the action may be just as distressing or risky for the clinician.13 Additionally, items visible in a clinician’s office—or visible in the background of those providing telehealth services from their home—may inadvertently reveal personal information about the clinician, their home, or their family.
Psychiatrists are often in a special position in relation to patients and times of crises. They may be involved in involuntary commitment—or declining an admission when a patient or family wishes it. They may be present at the time of the revelation of a serious diagnosis, abuse, injury, or death. They may be a mandated reporter of child or elder abuse.2 Additionally, physicians may be engaged in discourse on politically charged public health topics.14 These factors may increase their risk of being stalked.
Conducting an online visibility self-assessment can be a useful way to learn what information others can find. Table 2 outlines the steps for completing this exercise. Searching multiple iterations of your current and former names (with and without degrees, titles, and cities) will yield differing results in various search engines. After establishing a baseline of what information is available online, it can be helpful to periodically repeat this exercise, and to set up automated alerts for your name, number(s), email(s), and address(es).
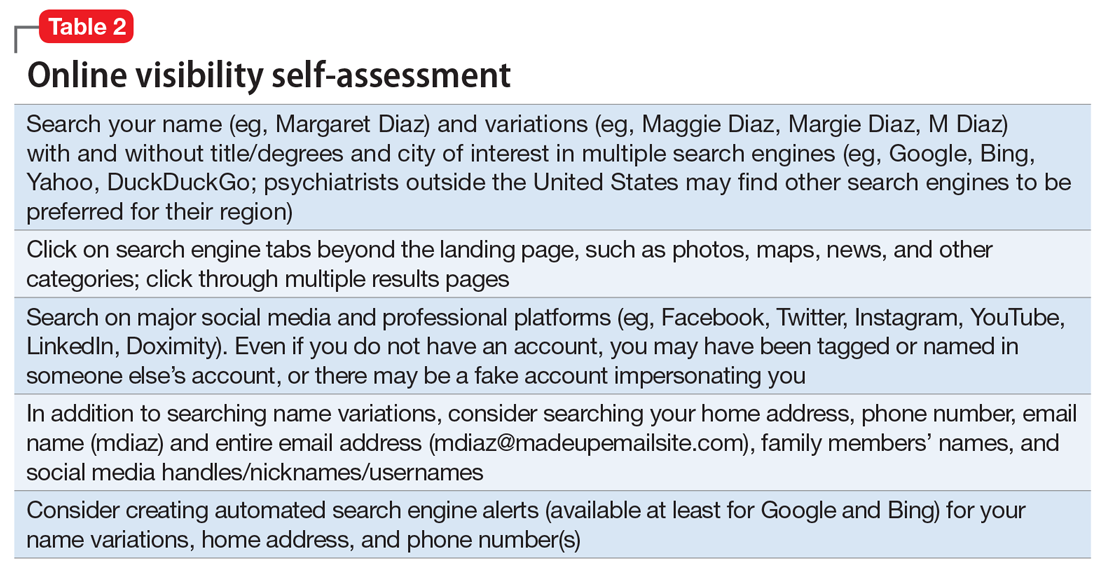
Basic mitigation strategies
In the modern era, being invisible online is impractical and likely impossible—especially for a health care professional. Instead, it may be prudent to limit your public visibility to professional portals (eg, LinkedIn or Doximity) and maximize privacy settings on other platforms. Another basic strategy is to avoid providing personal contact information (your home address, phone number, or personal email) for professional purposes, such as licensing and credentialing, conference submissions, or journal publications. Be aware that driving a visually distinct vehicle—one with vanity plates or distinct bumper stickers, or an exotic sportscar—can make it easier to be recognized and located. A personally recorded voicemail greeting (vs one recorded by, for example, an office manager) may be inappropriately reinforcing for some stalkers.
Workplaces should have an established safety policy that addresses stalking and harassment of employees. Similarly, patients and others should receive clear education on how to contact different staff, including physicians, with consideration of how and when to use electronic health information portals, office numbers, and emails. Workplaces should not disclose staff schedules. For example, a receptionist should say “I’ll have Dr. Diaz return your call when she can” instead of “Dr. Diaz is not in until tomorrow.” Avoid unnecessary location/name signals (eg, a parking spot labeled “Dr. Diaz”). Consider creating alert words or phrases for staff to use to signal they are concerned about their immediate safety—and provide education and training, including drills, to test emergency responses when the words/phrases are used. Leaders and managers should nurture a workplace culture where people are comfortable seeking support if they feel they may be the target of harassment or stalking. Many larger health care organizations have threat management programs, which can play a critical role in preventing, investigating, and responding to stalking of employees. Increasingly, threat management teams are being identified as a best practice in health care settings.15Table 3 summarizes measures to mitigate risk.
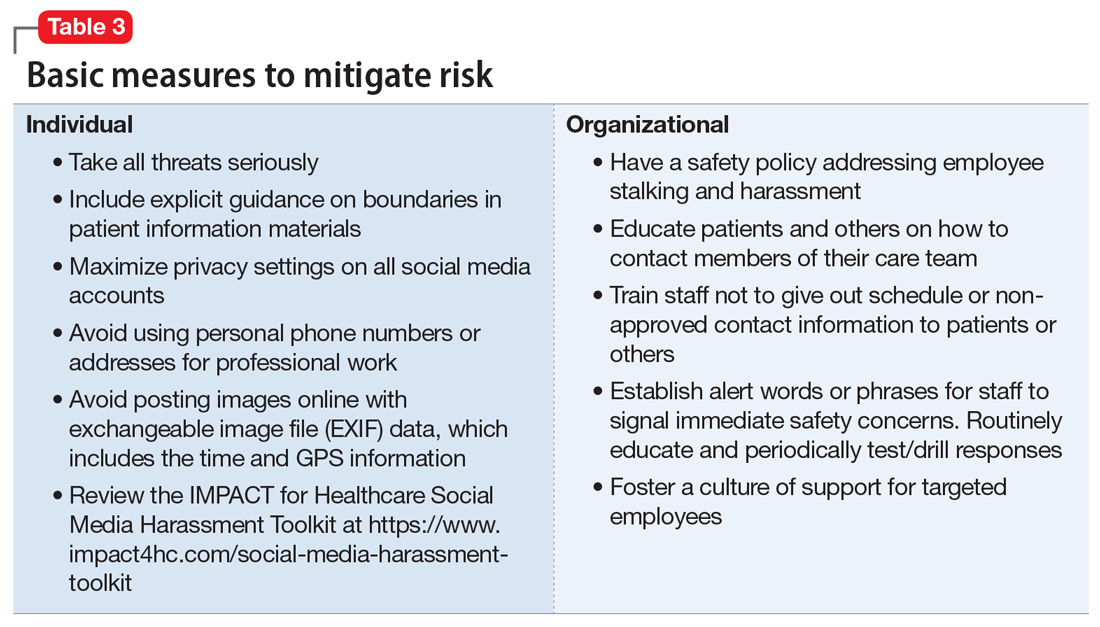
What to do when harassment or stalking occurs
Consulting with subject matter experts is essential. Approach behaviors, stalking patterns, and immediate circumstances vary highly, and so too must responses. A socially inept approach outside of the work setting by a patient may be effectively responded to with a firm explanation of why the behavior was inappropriate and a reiteration of limits. More persistent or serious threats may require taking actions for immediate safety, calling law enforcement or security (who may have the expertise to assist appropriately), or even run/hide/fight measures. Others to notify early on include human resources, supervisors, front desk staff, and coworkers. Although no single measure is always indicated and no single measure will always be effective, consultation with a specialist is always advisable.
Attempting to assess your own risk may be subject to bias and error, even for an experienced forensic psychiatrist. Risk assessment in stalking and harassment cases is complex, nuanced, and beyond the scope of this article; engagement with specialized threat programs or subject matter experts is advisable.15,16 If your medical center or area has police or security officers, engage them early. Risk management, insurers, and legal can also be helpful to consult. Attorneys specializing in harassment, stalking, and domestic violence may be helpful in extreme situations.17Table 417,18 highlights steps to take.
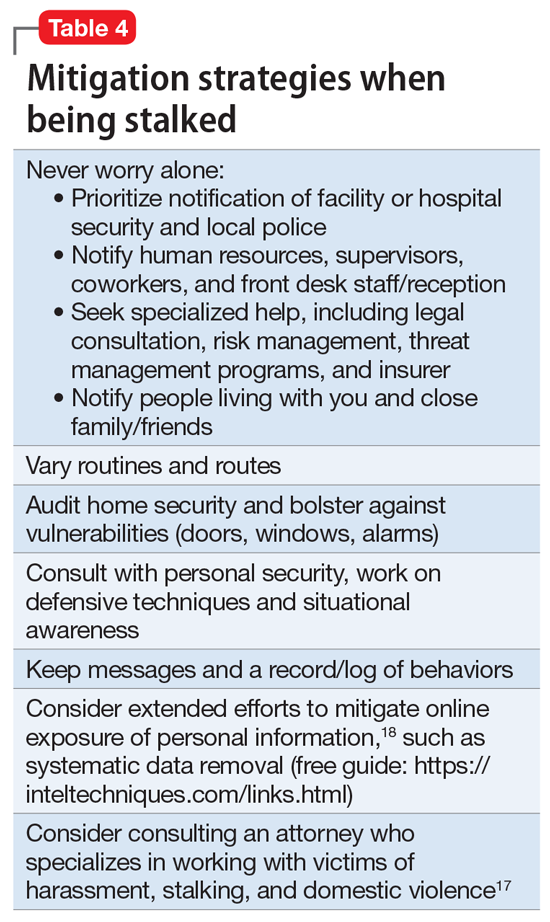
While effective interventions to stop or redirect stalking behavior may vary, some initial considerations include changing established routines (eg, your parking location or daily/weekly patterns such as gym, class, etc.) and letting family and others you live with know what is occurring. Consider implementing and bolstering personal, work, and home security; honing situational awareness skills; and learning advanced situational awareness and self-defense techniques.
Continue to: Clinical documentation and termination of care...
Clinical documentation and termination of care
Repeated and unwanted contact behaviors by a patient may be considered grounds for termination of care by the targeted clinician. Termination may occur through a direct conversation, followed by a mailed letter explaining that the patient’s inappropriate behaviors are the basis for termination. The letter should outline steps for establishing care with another psychiatrist and signing a release to facilitate transfer of records to the next psychiatrist. Ensure that the patient has access to a reasonable supply of medications or refills according to jurisdictional standards for transfer or termination of care.19 While these are common legal standards for termination of care in the United States, clinicians would be well served by appropriate consultation to verify the most appropriate standards for their location.
Documentation of a patient’s behavior should be factual and clear. Under the 21st Century Cures Act, patients often have access to their own electronic records.20 Therefore, clinicians should avoid documenting personal security measures or other information that is not clinically relevant. Communications with legal or risk management should not be documented unless otherwise advised, because such communications may be privileged and may not be clinically relevant.
In some circumstances, continuing to treat a patient who has stalked a member of the current treatment team may be appropriate or necessary. For example, a patient may respond appropriately to redirection after an initial approach behavior and continue to make clinical progress, or may be in a forensic specialty setting with appropriate operational support to continue with treatment.
Ethical dilemmas may arise in underserved areas where there are limited options for psychiatric care and in communicating the reasons for termination to a new clinician. Consultation may help to address these issues. However, as noted before, clinicians should be permitted to discontinue and transfer treatment and should not be compelled to continue to treat a patient who has threatened or harassed them.
Organizational and employer considerations
Victims of stalking have reported that they appreciated explicit support from their supervisor, regular meetings, and measures to reduce potential stalking or violence in the workplace; unsurprisingly, victim blaming and leaving the employee to address the situation on their own were labeled experienced as negative.2 Employers may consider implementing physical security, access controls and panic alarms, and enhancing coworkers’ situational awareness.21 Explicit policies about and attention to reducing workplace violence, including stalking, are always beneficial—and in some settings such policies may be a regulatory requirement.22 Large health care organizations may benefit from developing specialized threat management programs to assist with the evaluation and mitigation of stalking and other workplace violence risks.15,23
Self-care considerations
The impact of stalking can include psychological distress, disruption of work and personal relationships, and false allegations of impropriety. Stalking can make targets feel isolated, violated, and fearful, which makes it challenging to reach out to others for support and safety. It takes time to regain a sense of safety and to find a “new normal,” particularly while experiencing and responding to stalking behavior. Notifying close personal contacts such as family and coworkers about what is occurring (without sharing protected health information) can be helpful for recovery and important for the clinician’s safety. Reaching out for organizational and legal supports is also prudent. It is also important to allow time for, and patience with, a targeted individual’s normal responses, such as decreased work performance, sleep/appetite changes, and hypervigilance, without pathologizing these common stress reactions. Further review of appropriate resources by impacted clinicians is advisable.24-26
1. Nelsen AJ, Johnson RS, Ostermeyer B, et al. The prevalence of physicians who have been stalked: a systematic review. J Am Acad Psychiatry Law. 2015;43(2):177-182.
2. Jutasi C, McEwan TE. Stalking of professionals: a scoping review. Journal of Threat Assessment and Management. 2021;8(3):94-124.
3. Pathé MT, Meloy JR. Commentary: Stalking by patients—psychiatrists’ tales of anger, lust and ignorance. J Am Acad Psychiatry Law. 2013;41(2):200-205.
4. Pendergrast TR, Jain S, Trueger NS, et al. Prevalence of personal attacks and sexual harassment of physicians on social media. JAMA Intern Med. 2021;181(4):550-552.
5. Owens JG. Why definitions matter: stalking victimization in the United States. J Interpers Violence. 2016;31(12):2196-2226.
6. College of Policing. Stalking or harassment. May 2019. Accessed March 8, 2020. https://library.college.police.uk/docs/college-of-policing/Stalking_or_harassment_guidance_200519.pdf
7. McEwan TE, Daffern M, MacKenzie RD, et al. Risk factors for stalking violence, persistence, and recurrence. Journal of Forensic Psychiatry & Psychology. 2017;28(1):3856.
8. Pathé MT, Mullen PE, Purcell R. Patients who stalk doctors: their motives and management. Med J Australia. 2002;176(7):335-338.
9. Reibling ET, Distelberg B, Guptill M, et al. Intimate partner violence experienced by physicians. J Prim Care Community Health. 2020;11:2150132720965077.
10. Matias A, Gonçalves M, Soeiro C, et al. Intimate partner homicide: a meta-analysis of risk factors. Aggression and Violent Behavior. 2019;50:101358.
11. US Bureau of Labor Statistics. Fact sheet. Workplace violence in healthcare, 2018. April 2020. Accessed November 24, 2021. https://www.bls.gov/iif/oshwc/cfoi/workplace-violence-healthcare-2018.htm
12. Truman JL, Morgan RE. Stalking victimization, 2016. Bureau of Justice Statistics, Office of Justice Programs, U.S. Department of Justice. Report No.: NCJ 253526. April 2021. Accessed November 24, 2021. https://bjs.ojp.gov/library/publications/stalking-victimization-2016
13. Reyns BW, Henson B, Fisher BS. Being pursued online: applying cyberlifestyle–routine activities theory to cyberstalking victimization. Criminal Justice and Behavior. 2011;38(11):1149-1169.
14. Stea JN. When promoting knowledge makes you a target. Scientific American Blog Network. March 16, 2020. Accessed November 24, 2021. https://blogs.scientificamerican.com/observations/when-promoting-knowledge-makes-you-a-target/
15. Henkel SJ. Threat assessment strategies to mitigate violence in healthcare. IAHSS Foundation. IAHSS-F RS-19-02. November 2019. Accessed November 24, 2021. https://iahssf.org/assets/IAHSS-Foundation-Threat-Assessment-Strategies-to-Mitigate-Violence-in-Healthcare.pdf
16. McEwan TE. Stalking threat and risk assessment. In: Reid Meloy J, Hoffman J (eds). International Handbook of Threat Assessment. 2nd ed. Oxford University Press; 2021:210-234.
17. Goldberg C. Nobody’s Victim: Fighting Psychos, Stalkers, Pervs, and Trolls. Plume; 2019.
18. Bazzell M. Extreme Privacy: What It Takes to Disappear. 2nd ed. Independently published; 2020.
19. Simon RI, Shuman DW. The doctor-patient relationship. Focus. 2007;5(4):423-431.
20. Department of Health and Human Services. 21st Century Cures Act: Interoperability, Information Blocking, and the ONC Health IT Certification Program Final Rule (To be codified at 45 CFR 170 and 171). Federal Register. 2020;85(85):25642-25961.
21. Sheridan L, North AC, Scott AJ. Stalking in the workplace. Journal of Threat Assessment and Management. 2019;6(2):61-75.
22. The Joint Commission. Workplace Violence Prevention Standards. R3 Report: Requirement, Rationale, Reference. Issue 30. June 18, 2021. Accessed November 24, 2021. https://www.jointcommission.org/-/media/tjc/documents/standards/r3-reports/wpvp-r3-30_revised_06302021.pdf
23. Terry LP. Threat assessment teams. J Healthc Prot Manage. 2015;31(2):23-35.
24. Pathé M. Surviving Stalking. Cambridge University Press; 2002.
25. Noffsinger S. What stalking victims need to restore their mental and somatic health. Current Psychiatry. 2015;14(6):43-47.
26. Mullen P, Whyte S, McIvor R; Psychiatrists’ Support Service, Royal College of Psychiatry. PSS Information Guide: Stalking. Report No. 11. 2017. Accessed November 24, 2021. https://www.rcpsych.ac.uk/docs/default-source/members/supporting-you/pss/pss-guide-11-stalking.pdf?sfvrsn=2f1c7253_2
Dr. A has been treating Ms. W, a graduate student, for depression. Ms. W made subtle comments expressing her interest in pursuing a romantic relationship with her psychiatrist. Dr. A gently redirected her, and she seemed to respond appropriately. However, over the past 2 weeks, Dr. A has seen Ms. W at a local park and at the grocery store. Today, Dr. A is startled to see Ms. W at her weekly yoga class. Dr. A plans to ask her supervisor for advice.
Dr. M is a child psychiatrist who spoke at his local school board meeting in support of masking requirements for students during COVID-19. During the discussion, Dr. M shared that, as a psychiatrist, he does not believe it is especially distressing for students to wear masks, and that doing so is a necessary public health measure. On leaving, other parents shouted, “We know who you are and where you live!” The next day, his integrated clinic started receiving threatening and harassing messages, including threats to kill him or his staff if they take part in vaccinating children against COVID-19.
Because of their work, mental health professionals—like other health care professionals—face an elevated risk of being harassed or stalked. Stalking often includes online harassment and may escalate to serious physical violence. Stalking is criminal behavior by a patient and should not be constructed as a “failure to manage transference.” This article explores basic strategies to reduce the risk of harassment and stalking, describes how to recognize early behaviors, and outlines basic steps health care professionals and their employers can take to respond to stalking and harassing behaviors.
Although this article is intended for psychiatrists, it is important to note that all health professionals have significant risk for experiencing stalking or harassment. This is due in part, but not exclusively, to our clinical work. Estimates of how many health professionals experience stalking vary substantially depending upon the study, and differences in methodologies limit easy comparison or extrapolation. More thorough reviews have reported ranges from 2% to 70% among physicians; psychiatrists and other mental health professionals appear to be at greater risk than those in other specialties and the general population.1-3 Physicians who are active on social media may also be at elevated risk.4 Unexpected communications from patients and their family members—especially those with threatening, harassing, or sexualized tones, or involving contact outside of a work setting—can be distressing. These behaviors represent potential harbingers of more dangerous behavior, including physical assault, sexual assault, or homicide. Despite their elevated risk, many psychiatrists are unaware of how to prevent or respond to stalking or harassment.
Recognizing harassment and stalking
Repeated and unwanted contact or communication, regardless of intent, may constitute stalking. Legal definitions vary by jurisdiction and may not align with subjective experiences or understanding of what constitutes stalking.5 At its essence, stalking is repeated harassing behaviors likely to provoke fear in the targeted person. FOUR is a helpful mnemonic when conceptualizing the attributes of stalking: Fixated, Obsessive, Unwanted, and Repetitive.6Table 1 lists examples of common stalking behaviors. Stalking and harassing behavior may be from a known source (eg, a patient, coworker, or paramour), a masked source (ie, someone known to the target but who conceals or obscures their identity), or from otherwise unknown persons. Behaviors that persist after the person engaging in the behaviors has clearly been informed that they are unwanted or inappropriate are especially concerning. Stalking may escalate to include physical or sexual assault and, in some cases, homicide.
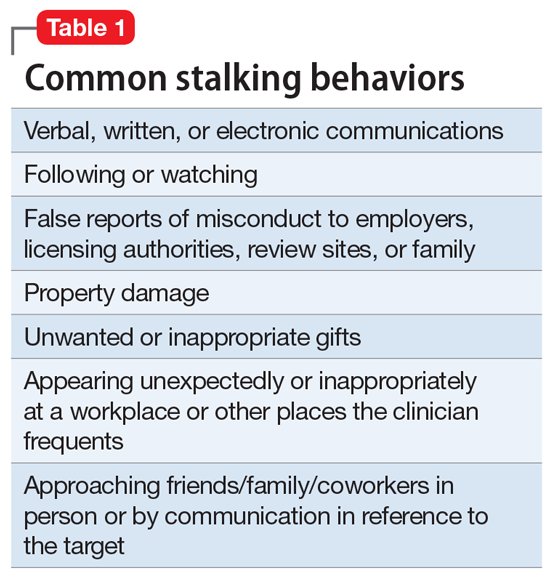
Stalking duration can vary substantially, as can the factors that lead to the cessation of the behavior. Indicators of increased risk for physical violence include unwanted physical presence/following of the target (“approach behaviors”), having a prior violent intimate relationship, property destruction, explicit threats, and having a prior intimate relationship with the target.7
Stalking contact or communication may be unwanted because of the content (eg, sexualized or threatening tone), location (eg, at a professional’s home), or means (eg, through social media). Stalking behaviors are not appropriate in any relationship, including a clinical relationship. They should not be treated as a “failure to manage transference” or in other victim-blaming ways.
There are multiple typologies for stalking behavior. Common motivations for stalking health professionals include resentment or grievance, misjudgment of social boundaries, and delusional fixation, including erotomania.8 Associated psychopathologies vary significantly and, while some may be more amenable to psychiatric treatment than others, psychiatrists should not feel compelled to treat patients who repeatedly violate boundaries, regardless of intent or comorbidity.
Patients are not the exclusive perpetrators of stalking; a recent study found that 4% of physicians surveyed reported current or recent stalking by a current or former intimate partner.9 When a person who is a victim of intimate partner violence is also stalked as part of the abuse, homicide risk increases.10 Workplace homicides of health care professionals are most likely to be committed by a current or former partner or other personal acquaintance, not by a patient.11 Workplace harassment and stalking of health care professionals is especially concerning because this behavior can escalate and endanger coworkers or clients.
Continue to: Risk awareness: Recognize your exposure...
Risk awareness: Recognize your exposure
About 80% of stalking involves some form of technology—often telephone calls but also online or other “cyber” elements.12 One recent survey found the rate of online harassment, including threats of physical and sexual violence, was >20% among physicians who were active on social media.4 Health professionals may be at greater risk of having patients find their personal information simply because patients routinely search online for information about new clinicians. Personal information about a clinician may be readily visible among professional information in search results, or a curious patient may simply scroll further down in the results. For a potential stalker, clicking on a search result linking to a personal social media page may be far easier than finding a home address and going in person—but the action may be just as distressing or risky for the clinician.13 Additionally, items visible in a clinician’s office—or visible in the background of those providing telehealth services from their home—may inadvertently reveal personal information about the clinician, their home, or their family.
Psychiatrists are often in a special position in relation to patients and times of crises. They may be involved in involuntary commitment—or declining an admission when a patient or family wishes it. They may be present at the time of the revelation of a serious diagnosis, abuse, injury, or death. They may be a mandated reporter of child or elder abuse.2 Additionally, physicians may be engaged in discourse on politically charged public health topics.14 These factors may increase their risk of being stalked.
Conducting an online visibility self-assessment can be a useful way to learn what information others can find. Table 2 outlines the steps for completing this exercise. Searching multiple iterations of your current and former names (with and without degrees, titles, and cities) will yield differing results in various search engines. After establishing a baseline of what information is available online, it can be helpful to periodically repeat this exercise, and to set up automated alerts for your name, number(s), email(s), and address(es).
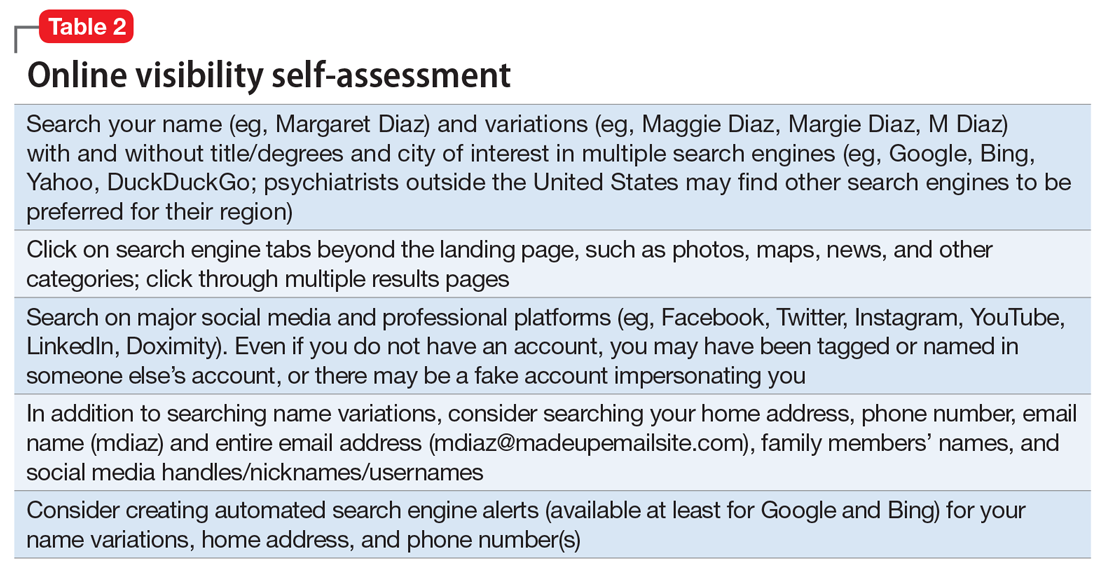
Basic mitigation strategies
In the modern era, being invisible online is impractical and likely impossible—especially for a health care professional. Instead, it may be prudent to limit your public visibility to professional portals (eg, LinkedIn or Doximity) and maximize privacy settings on other platforms. Another basic strategy is to avoid providing personal contact information (your home address, phone number, or personal email) for professional purposes, such as licensing and credentialing, conference submissions, or journal publications. Be aware that driving a visually distinct vehicle—one with vanity plates or distinct bumper stickers, or an exotic sportscar—can make it easier to be recognized and located. A personally recorded voicemail greeting (vs one recorded by, for example, an office manager) may be inappropriately reinforcing for some stalkers.
Workplaces should have an established safety policy that addresses stalking and harassment of employees. Similarly, patients and others should receive clear education on how to contact different staff, including physicians, with consideration of how and when to use electronic health information portals, office numbers, and emails. Workplaces should not disclose staff schedules. For example, a receptionist should say “I’ll have Dr. Diaz return your call when she can” instead of “Dr. Diaz is not in until tomorrow.” Avoid unnecessary location/name signals (eg, a parking spot labeled “Dr. Diaz”). Consider creating alert words or phrases for staff to use to signal they are concerned about their immediate safety—and provide education and training, including drills, to test emergency responses when the words/phrases are used. Leaders and managers should nurture a workplace culture where people are comfortable seeking support if they feel they may be the target of harassment or stalking. Many larger health care organizations have threat management programs, which can play a critical role in preventing, investigating, and responding to stalking of employees. Increasingly, threat management teams are being identified as a best practice in health care settings.15Table 3 summarizes measures to mitigate risk.
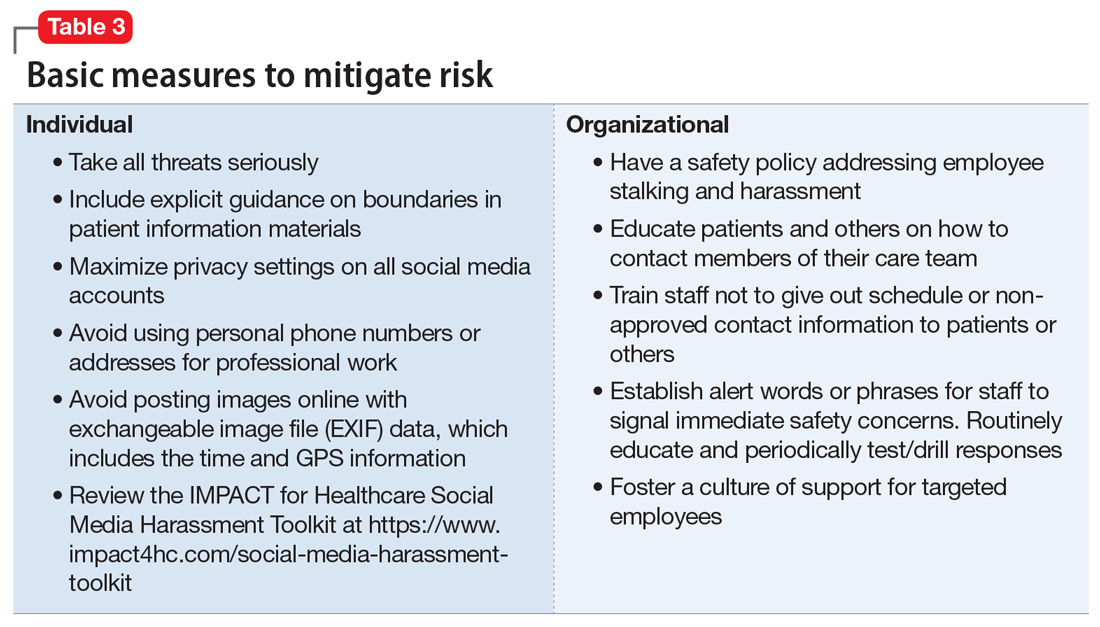
What to do when harassment or stalking occurs
Consulting with subject matter experts is essential. Approach behaviors, stalking patterns, and immediate circumstances vary highly, and so too must responses. A socially inept approach outside of the work setting by a patient may be effectively responded to with a firm explanation of why the behavior was inappropriate and a reiteration of limits. More persistent or serious threats may require taking actions for immediate safety, calling law enforcement or security (who may have the expertise to assist appropriately), or even run/hide/fight measures. Others to notify early on include human resources, supervisors, front desk staff, and coworkers. Although no single measure is always indicated and no single measure will always be effective, consultation with a specialist is always advisable.
Attempting to assess your own risk may be subject to bias and error, even for an experienced forensic psychiatrist. Risk assessment in stalking and harassment cases is complex, nuanced, and beyond the scope of this article; engagement with specialized threat programs or subject matter experts is advisable.15,16 If your medical center or area has police or security officers, engage them early. Risk management, insurers, and legal can also be helpful to consult. Attorneys specializing in harassment, stalking, and domestic violence may be helpful in extreme situations.17Table 417,18 highlights steps to take.
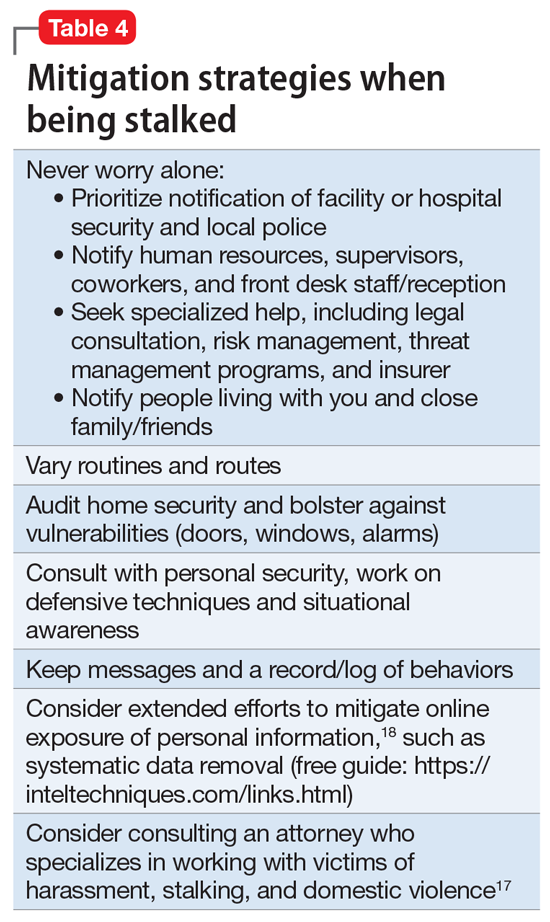
While effective interventions to stop or redirect stalking behavior may vary, some initial considerations include changing established routines (eg, your parking location or daily/weekly patterns such as gym, class, etc.) and letting family and others you live with know what is occurring. Consider implementing and bolstering personal, work, and home security; honing situational awareness skills; and learning advanced situational awareness and self-defense techniques.
Continue to: Clinical documentation and termination of care...
Clinical documentation and termination of care
Repeated and unwanted contact behaviors by a patient may be considered grounds for termination of care by the targeted clinician. Termination may occur through a direct conversation, followed by a mailed letter explaining that the patient’s inappropriate behaviors are the basis for termination. The letter should outline steps for establishing care with another psychiatrist and signing a release to facilitate transfer of records to the next psychiatrist. Ensure that the patient has access to a reasonable supply of medications or refills according to jurisdictional standards for transfer or termination of care.19 While these are common legal standards for termination of care in the United States, clinicians would be well served by appropriate consultation to verify the most appropriate standards for their location.
Documentation of a patient’s behavior should be factual and clear. Under the 21st Century Cures Act, patients often have access to their own electronic records.20 Therefore, clinicians should avoid documenting personal security measures or other information that is not clinically relevant. Communications with legal or risk management should not be documented unless otherwise advised, because such communications may be privileged and may not be clinically relevant.
In some circumstances, continuing to treat a patient who has stalked a member of the current treatment team may be appropriate or necessary. For example, a patient may respond appropriately to redirection after an initial approach behavior and continue to make clinical progress, or may be in a forensic specialty setting with appropriate operational support to continue with treatment.
Ethical dilemmas may arise in underserved areas where there are limited options for psychiatric care and in communicating the reasons for termination to a new clinician. Consultation may help to address these issues. However, as noted before, clinicians should be permitted to discontinue and transfer treatment and should not be compelled to continue to treat a patient who has threatened or harassed them.
Organizational and employer considerations
Victims of stalking have reported that they appreciated explicit support from their supervisor, regular meetings, and measures to reduce potential stalking or violence in the workplace; unsurprisingly, victim blaming and leaving the employee to address the situation on their own were labeled experienced as negative.2 Employers may consider implementing physical security, access controls and panic alarms, and enhancing coworkers’ situational awareness.21 Explicit policies about and attention to reducing workplace violence, including stalking, are always beneficial—and in some settings such policies may be a regulatory requirement.22 Large health care organizations may benefit from developing specialized threat management programs to assist with the evaluation and mitigation of stalking and other workplace violence risks.15,23
Self-care considerations
The impact of stalking can include psychological distress, disruption of work and personal relationships, and false allegations of impropriety. Stalking can make targets feel isolated, violated, and fearful, which makes it challenging to reach out to others for support and safety. It takes time to regain a sense of safety and to find a “new normal,” particularly while experiencing and responding to stalking behavior. Notifying close personal contacts such as family and coworkers about what is occurring (without sharing protected health information) can be helpful for recovery and important for the clinician’s safety. Reaching out for organizational and legal supports is also prudent. It is also important to allow time for, and patience with, a targeted individual’s normal responses, such as decreased work performance, sleep/appetite changes, and hypervigilance, without pathologizing these common stress reactions. Further review of appropriate resources by impacted clinicians is advisable.24-26
Dr. A has been treating Ms. W, a graduate student, for depression. Ms. W made subtle comments expressing her interest in pursuing a romantic relationship with her psychiatrist. Dr. A gently redirected her, and she seemed to respond appropriately. However, over the past 2 weeks, Dr. A has seen Ms. W at a local park and at the grocery store. Today, Dr. A is startled to see Ms. W at her weekly yoga class. Dr. A plans to ask her supervisor for advice.
Dr. M is a child psychiatrist who spoke at his local school board meeting in support of masking requirements for students during COVID-19. During the discussion, Dr. M shared that, as a psychiatrist, he does not believe it is especially distressing for students to wear masks, and that doing so is a necessary public health measure. On leaving, other parents shouted, “We know who you are and where you live!” The next day, his integrated clinic started receiving threatening and harassing messages, including threats to kill him or his staff if they take part in vaccinating children against COVID-19.
Because of their work, mental health professionals—like other health care professionals—face an elevated risk of being harassed or stalked. Stalking often includes online harassment and may escalate to serious physical violence. Stalking is criminal behavior by a patient and should not be constructed as a “failure to manage transference.” This article explores basic strategies to reduce the risk of harassment and stalking, describes how to recognize early behaviors, and outlines basic steps health care professionals and their employers can take to respond to stalking and harassing behaviors.
Although this article is intended for psychiatrists, it is important to note that all health professionals have significant risk for experiencing stalking or harassment. This is due in part, but not exclusively, to our clinical work. Estimates of how many health professionals experience stalking vary substantially depending upon the study, and differences in methodologies limit easy comparison or extrapolation. More thorough reviews have reported ranges from 2% to 70% among physicians; psychiatrists and other mental health professionals appear to be at greater risk than those in other specialties and the general population.1-3 Physicians who are active on social media may also be at elevated risk.4 Unexpected communications from patients and their family members—especially those with threatening, harassing, or sexualized tones, or involving contact outside of a work setting—can be distressing. These behaviors represent potential harbingers of more dangerous behavior, including physical assault, sexual assault, or homicide. Despite their elevated risk, many psychiatrists are unaware of how to prevent or respond to stalking or harassment.
Recognizing harassment and stalking
Repeated and unwanted contact or communication, regardless of intent, may constitute stalking. Legal definitions vary by jurisdiction and may not align with subjective experiences or understanding of what constitutes stalking.5 At its essence, stalking is repeated harassing behaviors likely to provoke fear in the targeted person. FOUR is a helpful mnemonic when conceptualizing the attributes of stalking: Fixated, Obsessive, Unwanted, and Repetitive.6Table 1 lists examples of common stalking behaviors. Stalking and harassing behavior may be from a known source (eg, a patient, coworker, or paramour), a masked source (ie, someone known to the target but who conceals or obscures their identity), or from otherwise unknown persons. Behaviors that persist after the person engaging in the behaviors has clearly been informed that they are unwanted or inappropriate are especially concerning. Stalking may escalate to include physical or sexual assault and, in some cases, homicide.
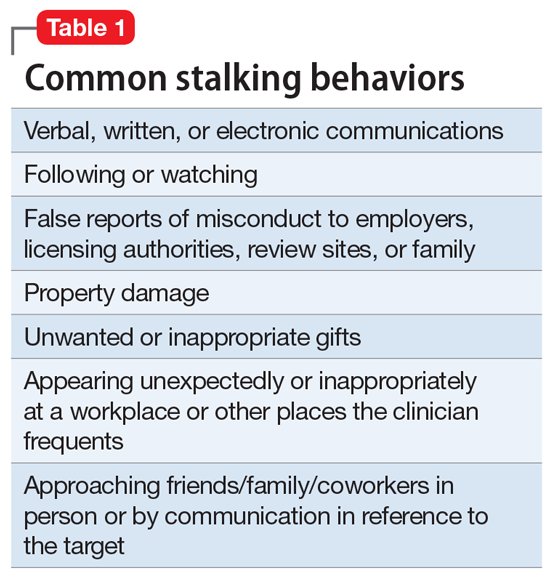
Stalking duration can vary substantially, as can the factors that lead to the cessation of the behavior. Indicators of increased risk for physical violence include unwanted physical presence/following of the target (“approach behaviors”), having a prior violent intimate relationship, property destruction, explicit threats, and having a prior intimate relationship with the target.7
Stalking contact or communication may be unwanted because of the content (eg, sexualized or threatening tone), location (eg, at a professional’s home), or means (eg, through social media). Stalking behaviors are not appropriate in any relationship, including a clinical relationship. They should not be treated as a “failure to manage transference” or in other victim-blaming ways.
There are multiple typologies for stalking behavior. Common motivations for stalking health professionals include resentment or grievance, misjudgment of social boundaries, and delusional fixation, including erotomania.8 Associated psychopathologies vary significantly and, while some may be more amenable to psychiatric treatment than others, psychiatrists should not feel compelled to treat patients who repeatedly violate boundaries, regardless of intent or comorbidity.
Patients are not the exclusive perpetrators of stalking; a recent study found that 4% of physicians surveyed reported current or recent stalking by a current or former intimate partner.9 When a person who is a victim of intimate partner violence is also stalked as part of the abuse, homicide risk increases.10 Workplace homicides of health care professionals are most likely to be committed by a current or former partner or other personal acquaintance, not by a patient.11 Workplace harassment and stalking of health care professionals is especially concerning because this behavior can escalate and endanger coworkers or clients.
Continue to: Risk awareness: Recognize your exposure...
Risk awareness: Recognize your exposure
About 80% of stalking involves some form of technology—often telephone calls but also online or other “cyber” elements.12 One recent survey found the rate of online harassment, including threats of physical and sexual violence, was >20% among physicians who were active on social media.4 Health professionals may be at greater risk of having patients find their personal information simply because patients routinely search online for information about new clinicians. Personal information about a clinician may be readily visible among professional information in search results, or a curious patient may simply scroll further down in the results. For a potential stalker, clicking on a search result linking to a personal social media page may be far easier than finding a home address and going in person—but the action may be just as distressing or risky for the clinician.13 Additionally, items visible in a clinician’s office—or visible in the background of those providing telehealth services from their home—may inadvertently reveal personal information about the clinician, their home, or their family.
Psychiatrists are often in a special position in relation to patients and times of crises. They may be involved in involuntary commitment—or declining an admission when a patient or family wishes it. They may be present at the time of the revelation of a serious diagnosis, abuse, injury, or death. They may be a mandated reporter of child or elder abuse.2 Additionally, physicians may be engaged in discourse on politically charged public health topics.14 These factors may increase their risk of being stalked.
Conducting an online visibility self-assessment can be a useful way to learn what information others can find. Table 2 outlines the steps for completing this exercise. Searching multiple iterations of your current and former names (with and without degrees, titles, and cities) will yield differing results in various search engines. After establishing a baseline of what information is available online, it can be helpful to periodically repeat this exercise, and to set up automated alerts for your name, number(s), email(s), and address(es).
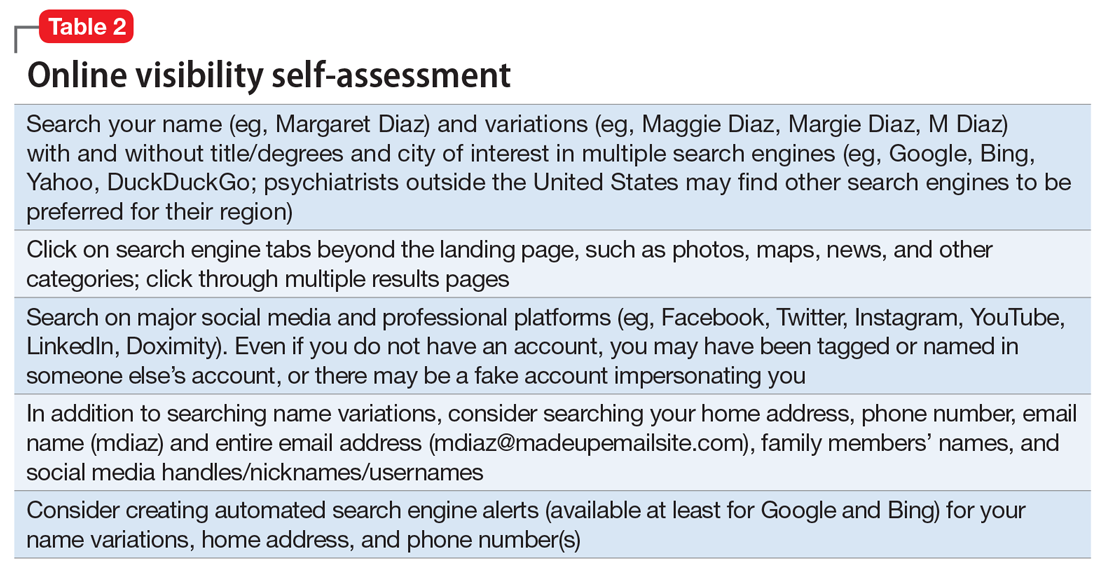
Basic mitigation strategies
In the modern era, being invisible online is impractical and likely impossible—especially for a health care professional. Instead, it may be prudent to limit your public visibility to professional portals (eg, LinkedIn or Doximity) and maximize privacy settings on other platforms. Another basic strategy is to avoid providing personal contact information (your home address, phone number, or personal email) for professional purposes, such as licensing and credentialing, conference submissions, or journal publications. Be aware that driving a visually distinct vehicle—one with vanity plates or distinct bumper stickers, or an exotic sportscar—can make it easier to be recognized and located. A personally recorded voicemail greeting (vs one recorded by, for example, an office manager) may be inappropriately reinforcing for some stalkers.
Workplaces should have an established safety policy that addresses stalking and harassment of employees. Similarly, patients and others should receive clear education on how to contact different staff, including physicians, with consideration of how and when to use electronic health information portals, office numbers, and emails. Workplaces should not disclose staff schedules. For example, a receptionist should say “I’ll have Dr. Diaz return your call when she can” instead of “Dr. Diaz is not in until tomorrow.” Avoid unnecessary location/name signals (eg, a parking spot labeled “Dr. Diaz”). Consider creating alert words or phrases for staff to use to signal they are concerned about their immediate safety—and provide education and training, including drills, to test emergency responses when the words/phrases are used. Leaders and managers should nurture a workplace culture where people are comfortable seeking support if they feel they may be the target of harassment or stalking. Many larger health care organizations have threat management programs, which can play a critical role in preventing, investigating, and responding to stalking of employees. Increasingly, threat management teams are being identified as a best practice in health care settings.15Table 3 summarizes measures to mitigate risk.
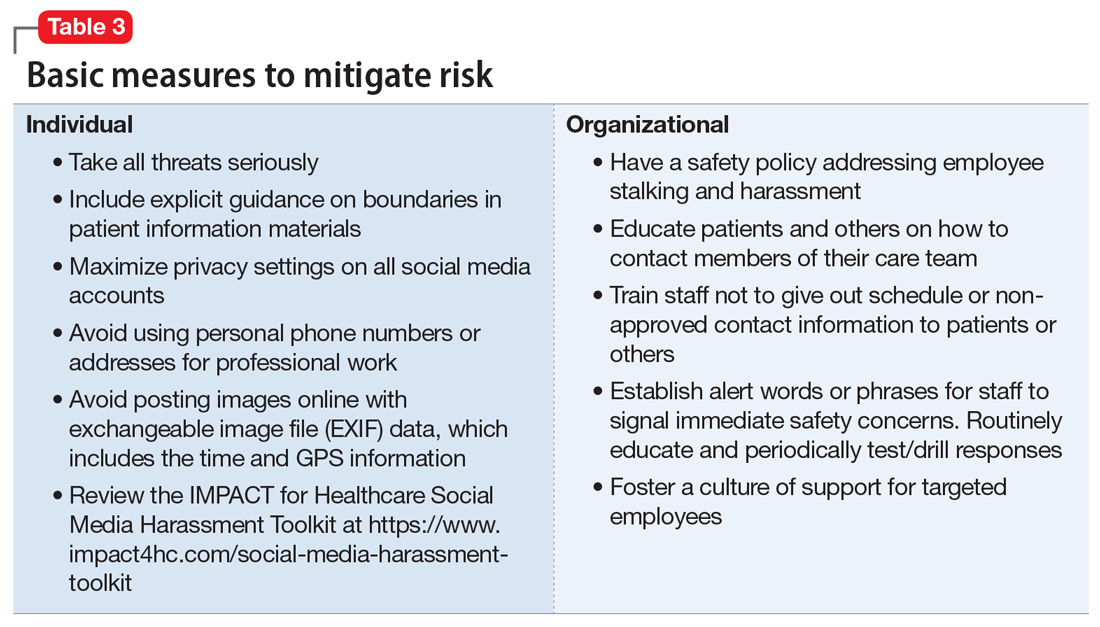
What to do when harassment or stalking occurs
Consulting with subject matter experts is essential. Approach behaviors, stalking patterns, and immediate circumstances vary highly, and so too must responses. A socially inept approach outside of the work setting by a patient may be effectively responded to with a firm explanation of why the behavior was inappropriate and a reiteration of limits. More persistent or serious threats may require taking actions for immediate safety, calling law enforcement or security (who may have the expertise to assist appropriately), or even run/hide/fight measures. Others to notify early on include human resources, supervisors, front desk staff, and coworkers. Although no single measure is always indicated and no single measure will always be effective, consultation with a specialist is always advisable.
Attempting to assess your own risk may be subject to bias and error, even for an experienced forensic psychiatrist. Risk assessment in stalking and harassment cases is complex, nuanced, and beyond the scope of this article; engagement with specialized threat programs or subject matter experts is advisable.15,16 If your medical center or area has police or security officers, engage them early. Risk management, insurers, and legal can also be helpful to consult. Attorneys specializing in harassment, stalking, and domestic violence may be helpful in extreme situations.17Table 417,18 highlights steps to take.
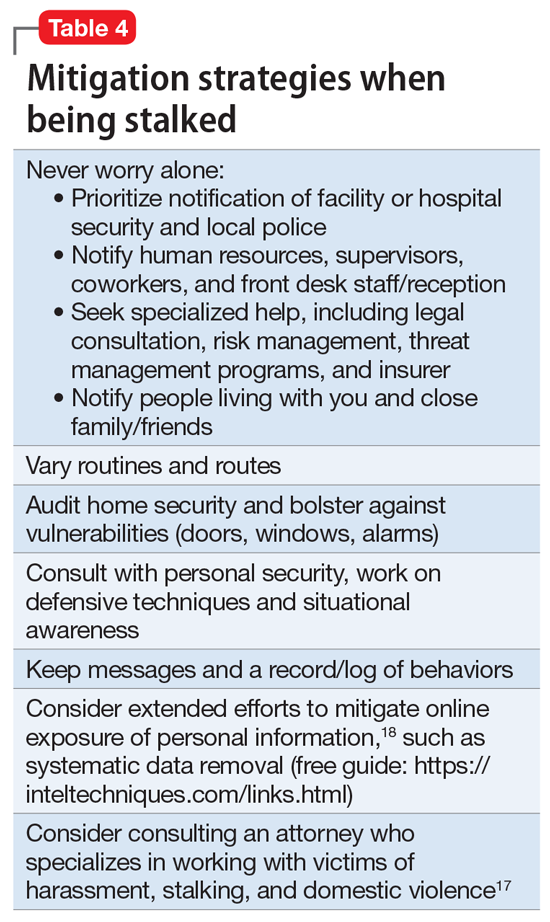
While effective interventions to stop or redirect stalking behavior may vary, some initial considerations include changing established routines (eg, your parking location or daily/weekly patterns such as gym, class, etc.) and letting family and others you live with know what is occurring. Consider implementing and bolstering personal, work, and home security; honing situational awareness skills; and learning advanced situational awareness and self-defense techniques.
Continue to: Clinical documentation and termination of care...
Clinical documentation and termination of care
Repeated and unwanted contact behaviors by a patient may be considered grounds for termination of care by the targeted clinician. Termination may occur through a direct conversation, followed by a mailed letter explaining that the patient’s inappropriate behaviors are the basis for termination. The letter should outline steps for establishing care with another psychiatrist and signing a release to facilitate transfer of records to the next psychiatrist. Ensure that the patient has access to a reasonable supply of medications or refills according to jurisdictional standards for transfer or termination of care.19 While these are common legal standards for termination of care in the United States, clinicians would be well served by appropriate consultation to verify the most appropriate standards for their location.
Documentation of a patient’s behavior should be factual and clear. Under the 21st Century Cures Act, patients often have access to their own electronic records.20 Therefore, clinicians should avoid documenting personal security measures or other information that is not clinically relevant. Communications with legal or risk management should not be documented unless otherwise advised, because such communications may be privileged and may not be clinically relevant.
In some circumstances, continuing to treat a patient who has stalked a member of the current treatment team may be appropriate or necessary. For example, a patient may respond appropriately to redirection after an initial approach behavior and continue to make clinical progress, or may be in a forensic specialty setting with appropriate operational support to continue with treatment.
Ethical dilemmas may arise in underserved areas where there are limited options for psychiatric care and in communicating the reasons for termination to a new clinician. Consultation may help to address these issues. However, as noted before, clinicians should be permitted to discontinue and transfer treatment and should not be compelled to continue to treat a patient who has threatened or harassed them.
Organizational and employer considerations
Victims of stalking have reported that they appreciated explicit support from their supervisor, regular meetings, and measures to reduce potential stalking or violence in the workplace; unsurprisingly, victim blaming and leaving the employee to address the situation on their own were labeled experienced as negative.2 Employers may consider implementing physical security, access controls and panic alarms, and enhancing coworkers’ situational awareness.21 Explicit policies about and attention to reducing workplace violence, including stalking, are always beneficial—and in some settings such policies may be a regulatory requirement.22 Large health care organizations may benefit from developing specialized threat management programs to assist with the evaluation and mitigation of stalking and other workplace violence risks.15,23
Self-care considerations
The impact of stalking can include psychological distress, disruption of work and personal relationships, and false allegations of impropriety. Stalking can make targets feel isolated, violated, and fearful, which makes it challenging to reach out to others for support and safety. It takes time to regain a sense of safety and to find a “new normal,” particularly while experiencing and responding to stalking behavior. Notifying close personal contacts such as family and coworkers about what is occurring (without sharing protected health information) can be helpful for recovery and important for the clinician’s safety. Reaching out for organizational and legal supports is also prudent. It is also important to allow time for, and patience with, a targeted individual’s normal responses, such as decreased work performance, sleep/appetite changes, and hypervigilance, without pathologizing these common stress reactions. Further review of appropriate resources by impacted clinicians is advisable.24-26
1. Nelsen AJ, Johnson RS, Ostermeyer B, et al. The prevalence of physicians who have been stalked: a systematic review. J Am Acad Psychiatry Law. 2015;43(2):177-182.
2. Jutasi C, McEwan TE. Stalking of professionals: a scoping review. Journal of Threat Assessment and Management. 2021;8(3):94-124.
3. Pathé MT, Meloy JR. Commentary: Stalking by patients—psychiatrists’ tales of anger, lust and ignorance. J Am Acad Psychiatry Law. 2013;41(2):200-205.
4. Pendergrast TR, Jain S, Trueger NS, et al. Prevalence of personal attacks and sexual harassment of physicians on social media. JAMA Intern Med. 2021;181(4):550-552.
5. Owens JG. Why definitions matter: stalking victimization in the United States. J Interpers Violence. 2016;31(12):2196-2226.
6. College of Policing. Stalking or harassment. May 2019. Accessed March 8, 2020. https://library.college.police.uk/docs/college-of-policing/Stalking_or_harassment_guidance_200519.pdf
7. McEwan TE, Daffern M, MacKenzie RD, et al. Risk factors for stalking violence, persistence, and recurrence. Journal of Forensic Psychiatry & Psychology. 2017;28(1):3856.
8. Pathé MT, Mullen PE, Purcell R. Patients who stalk doctors: their motives and management. Med J Australia. 2002;176(7):335-338.
9. Reibling ET, Distelberg B, Guptill M, et al. Intimate partner violence experienced by physicians. J Prim Care Community Health. 2020;11:2150132720965077.
10. Matias A, Gonçalves M, Soeiro C, et al. Intimate partner homicide: a meta-analysis of risk factors. Aggression and Violent Behavior. 2019;50:101358.
11. US Bureau of Labor Statistics. Fact sheet. Workplace violence in healthcare, 2018. April 2020. Accessed November 24, 2021. https://www.bls.gov/iif/oshwc/cfoi/workplace-violence-healthcare-2018.htm
12. Truman JL, Morgan RE. Stalking victimization, 2016. Bureau of Justice Statistics, Office of Justice Programs, U.S. Department of Justice. Report No.: NCJ 253526. April 2021. Accessed November 24, 2021. https://bjs.ojp.gov/library/publications/stalking-victimization-2016
13. Reyns BW, Henson B, Fisher BS. Being pursued online: applying cyberlifestyle–routine activities theory to cyberstalking victimization. Criminal Justice and Behavior. 2011;38(11):1149-1169.
14. Stea JN. When promoting knowledge makes you a target. Scientific American Blog Network. March 16, 2020. Accessed November 24, 2021. https://blogs.scientificamerican.com/observations/when-promoting-knowledge-makes-you-a-target/
15. Henkel SJ. Threat assessment strategies to mitigate violence in healthcare. IAHSS Foundation. IAHSS-F RS-19-02. November 2019. Accessed November 24, 2021. https://iahssf.org/assets/IAHSS-Foundation-Threat-Assessment-Strategies-to-Mitigate-Violence-in-Healthcare.pdf
16. McEwan TE. Stalking threat and risk assessment. In: Reid Meloy J, Hoffman J (eds). International Handbook of Threat Assessment. 2nd ed. Oxford University Press; 2021:210-234.
17. Goldberg C. Nobody’s Victim: Fighting Psychos, Stalkers, Pervs, and Trolls. Plume; 2019.
18. Bazzell M. Extreme Privacy: What It Takes to Disappear. 2nd ed. Independently published; 2020.
19. Simon RI, Shuman DW. The doctor-patient relationship. Focus. 2007;5(4):423-431.
20. Department of Health and Human Services. 21st Century Cures Act: Interoperability, Information Blocking, and the ONC Health IT Certification Program Final Rule (To be codified at 45 CFR 170 and 171). Federal Register. 2020;85(85):25642-25961.
21. Sheridan L, North AC, Scott AJ. Stalking in the workplace. Journal of Threat Assessment and Management. 2019;6(2):61-75.
22. The Joint Commission. Workplace Violence Prevention Standards. R3 Report: Requirement, Rationale, Reference. Issue 30. June 18, 2021. Accessed November 24, 2021. https://www.jointcommission.org/-/media/tjc/documents/standards/r3-reports/wpvp-r3-30_revised_06302021.pdf
23. Terry LP. Threat assessment teams. J Healthc Prot Manage. 2015;31(2):23-35.
24. Pathé M. Surviving Stalking. Cambridge University Press; 2002.
25. Noffsinger S. What stalking victims need to restore their mental and somatic health. Current Psychiatry. 2015;14(6):43-47.
26. Mullen P, Whyte S, McIvor R; Psychiatrists’ Support Service, Royal College of Psychiatry. PSS Information Guide: Stalking. Report No. 11. 2017. Accessed November 24, 2021. https://www.rcpsych.ac.uk/docs/default-source/members/supporting-you/pss/pss-guide-11-stalking.pdf?sfvrsn=2f1c7253_2
1. Nelsen AJ, Johnson RS, Ostermeyer B, et al. The prevalence of physicians who have been stalked: a systematic review. J Am Acad Psychiatry Law. 2015;43(2):177-182.
2. Jutasi C, McEwan TE. Stalking of professionals: a scoping review. Journal of Threat Assessment and Management. 2021;8(3):94-124.
3. Pathé MT, Meloy JR. Commentary: Stalking by patients—psychiatrists’ tales of anger, lust and ignorance. J Am Acad Psychiatry Law. 2013;41(2):200-205.
4. Pendergrast TR, Jain S, Trueger NS, et al. Prevalence of personal attacks and sexual harassment of physicians on social media. JAMA Intern Med. 2021;181(4):550-552.
5. Owens JG. Why definitions matter: stalking victimization in the United States. J Interpers Violence. 2016;31(12):2196-2226.
6. College of Policing. Stalking or harassment. May 2019. Accessed March 8, 2020. https://library.college.police.uk/docs/college-of-policing/Stalking_or_harassment_guidance_200519.pdf
7. McEwan TE, Daffern M, MacKenzie RD, et al. Risk factors for stalking violence, persistence, and recurrence. Journal of Forensic Psychiatry & Psychology. 2017;28(1):3856.
8. Pathé MT, Mullen PE, Purcell R. Patients who stalk doctors: their motives and management. Med J Australia. 2002;176(7):335-338.
9. Reibling ET, Distelberg B, Guptill M, et al. Intimate partner violence experienced by physicians. J Prim Care Community Health. 2020;11:2150132720965077.
10. Matias A, Gonçalves M, Soeiro C, et al. Intimate partner homicide: a meta-analysis of risk factors. Aggression and Violent Behavior. 2019;50:101358.
11. US Bureau of Labor Statistics. Fact sheet. Workplace violence in healthcare, 2018. April 2020. Accessed November 24, 2021. https://www.bls.gov/iif/oshwc/cfoi/workplace-violence-healthcare-2018.htm
12. Truman JL, Morgan RE. Stalking victimization, 2016. Bureau of Justice Statistics, Office of Justice Programs, U.S. Department of Justice. Report No.: NCJ 253526. April 2021. Accessed November 24, 2021. https://bjs.ojp.gov/library/publications/stalking-victimization-2016
13. Reyns BW, Henson B, Fisher BS. Being pursued online: applying cyberlifestyle–routine activities theory to cyberstalking victimization. Criminal Justice and Behavior. 2011;38(11):1149-1169.
14. Stea JN. When promoting knowledge makes you a target. Scientific American Blog Network. March 16, 2020. Accessed November 24, 2021. https://blogs.scientificamerican.com/observations/when-promoting-knowledge-makes-you-a-target/
15. Henkel SJ. Threat assessment strategies to mitigate violence in healthcare. IAHSS Foundation. IAHSS-F RS-19-02. November 2019. Accessed November 24, 2021. https://iahssf.org/assets/IAHSS-Foundation-Threat-Assessment-Strategies-to-Mitigate-Violence-in-Healthcare.pdf
16. McEwan TE. Stalking threat and risk assessment. In: Reid Meloy J, Hoffman J (eds). International Handbook of Threat Assessment. 2nd ed. Oxford University Press; 2021:210-234.
17. Goldberg C. Nobody’s Victim: Fighting Psychos, Stalkers, Pervs, and Trolls. Plume; 2019.
18. Bazzell M. Extreme Privacy: What It Takes to Disappear. 2nd ed. Independently published; 2020.
19. Simon RI, Shuman DW. The doctor-patient relationship. Focus. 2007;5(4):423-431.
20. Department of Health and Human Services. 21st Century Cures Act: Interoperability, Information Blocking, and the ONC Health IT Certification Program Final Rule (To be codified at 45 CFR 170 and 171). Federal Register. 2020;85(85):25642-25961.
21. Sheridan L, North AC, Scott AJ. Stalking in the workplace. Journal of Threat Assessment and Management. 2019;6(2):61-75.
22. The Joint Commission. Workplace Violence Prevention Standards. R3 Report: Requirement, Rationale, Reference. Issue 30. June 18, 2021. Accessed November 24, 2021. https://www.jointcommission.org/-/media/tjc/documents/standards/r3-reports/wpvp-r3-30_revised_06302021.pdf
23. Terry LP. Threat assessment teams. J Healthc Prot Manage. 2015;31(2):23-35.
24. Pathé M. Surviving Stalking. Cambridge University Press; 2002.
25. Noffsinger S. What stalking victims need to restore their mental and somatic health. Current Psychiatry. 2015;14(6):43-47.
26. Mullen P, Whyte S, McIvor R; Psychiatrists’ Support Service, Royal College of Psychiatry. PSS Information Guide: Stalking. Report No. 11. 2017. Accessed November 24, 2021. https://www.rcpsych.ac.uk/docs/default-source/members/supporting-you/pss/pss-guide-11-stalking.pdf?sfvrsn=2f1c7253_2