User login
Can high hematocrit predict early shunt thrombosis?
Shunt occlusion has been a well-documented cause of shunt failure in newborns who have had systemic to pulmonary shunt placement, and little has been known about why shunts occlude. However, researchers have reported in a small retrospective study that higher postoperative hematocrit levels immediately after surgery may be predictors of shunt occlusion.
Reporting in the April 2017 issue of The Journal of Thoracic and Cardiovascular Surgery, Brett R. Anderson, MD, of New York-Presbyterian/Morgan Stanley Children’s Hospital, Columbia University Medical Center in New York, and coauthors, found that every 5-point increase in postoperative hematocrit more than doubled an infant’s odds of having early shunt occlusion (J Thorac Cardiovasc Surg. 2017;153:947-55).
“Beginning in the latter half of 2014, we noticed an increase in the incidence of early shunt occlusions in our neonatal cardiac intensive care unit,” Dr. Anderson and coauthors said. So they conducted a retrospective chart review of 80 infants who had undergone systemic to pulmonary shunt placement from January 2010 to July 2015, hypothesizing that increased hematocrit in the early postoperative period might have caused early shunt occlusion. They investigated the association between the first postoperative hematocrit and early shunt occlusion and in-hospital mortality in these patients.
Five patients (6.3%) experienced early shunt occlusion – that is, within 24 hours of placement (actually, within 10 hours of placement). Overall, 12 infants (15%) experienced shunt occlusion. The physicians at New York-Presbyterian do not administer anticoagulation in these patients during the first 12 hours after shunt placement.
The median initial postoperative hematocrit was 41.7%, with a range of 31.7%-55.8%. The survival analysis the researchers performed found that for every 5 additional percentage points, the hazard ratio for early shunt occlusion was 2.7 (P = .007) and 1.74 for any shunt occlusion (P less than .001). Incidentally, four cases of early shunt occlusion occurred in the later study period after 2014, during which the average first postoperative hematocrit was significantly higher than in the pre-2014 study period, 45.3% vs. 41.5% (P = .21), and the odds of early shunt occlusion were 16 times higher (P less than .001). Dr. Anderson and coauthors said the possible explanation for this variation was a switch to a new point-of-care analyzer in 2013.
With regard to mortality, six infants overall (7.4%) died before discharge, and four (5%) within 30 days of shunt placement. No infants with early shunt occlusion died, although two with late shunt occlusion died. Increased inotrope score and first postoperative arterial oxygen tension were the only factors associated with increased mortality. “No significant association was identified between hematocrit and 30-day mortality,” Dr. Anderson and coauthors said.
In the first 24 hours after surgery, 11 infants (13.8%) received packed red blood cell (PRBC) transfusions, seven (8.8%) received platelets, and four (5%) received fresh frozen plasma/cryoprecipitate. Higher postoperative PRBC transfusion volumes were associated with increased odds of mortality (P = .001), but none of these factors were significantly associated with early shunt occlusion.
Dr. Anderson and coauthors acknowledged that shunt occlusion is a “vexing problem” in infants with cyanotic heart disease. While other researchers studied postoperative hematocrit levels and possible associations with outcomes, including shunt occlusion and mortality, the New York-Presbyterian investigators said this is the first study of the first postoperative hematocrit.
Dr. Anderson and coauthors said their findings raise the question about the ideal perioperative prophylactic antithrombotic therapy in these patients. These researchers initiate aspirin therapy 12 hours after surgery if hemostasis is established.
As a result of this study, Dr. Anderson and coauthors instituted a number of practice changes at their center. They include:
• Cardiac anesthesiologists have been asked not to transfuse shunted neonates with hematocrit level of greater than or equal to 35%, and hematocrits are then immediately repeated when a patient returns to the cardiac ICU.
• Patients with hematocrits greater than or equal to 55% get partial exchange transfusions.
• An individualized approach for patients with lower hematocrits who are more cyanotic than expected. This includes a diagnostic echocardiogram, nitric oxide, oxygen and heparin, escalated inotropic support if necessary and sometimes a cautious approach to transfusions if symptoms do not resolve and an acute shunt occlusion if not likely.
Dr. Anderson and coauthors acknowledged limits to their study, most notably its retrospective nature and a small population at a single center, and that large investigations are needed to validate their findings.
Dr. Anderson disclosed receiving salary support from the National Center for Advancing Translational Sciences. Coauthor Jennifer M. Duchon, MDCM, MPH, receives salary support from the National Institute of Allergy and Infectious Disease. The remaining coauthors had no financial relationships to disclose.
In her invited commentary, Nancy S. Ghanayem, MD, of the Medical College of Wisconsin, gives credit to Dr. Anderson and coauthors for introducing the notion that high initial postoperative hematocrit may increase the risk of early shunt thrombosis in newborns, but with a caveat: “we remain somewhat hesitant regarding wholesale acceptance of the validity of the conclusions for several reasons” (J Thorac Cardiovasc Surg. 2017;153:956).
Those reasons include the low number of reported events, failure to list the actual hematocrits of the five patients who experienced early shunt occlusion and the lack of hemodynamic data – the latter of which she called “a significant limitation.”
A patient with low cardiac output, especially one who is cyanotic or has a single ventricle, is at higher risk for thrombosis and more likely to be transfused, “which in this case would potentially be masked by the method of comparing transfused volumes,” Dr. Ghanayem said. The inotrope score, while useful, is not a surrogate for actual cardiac output. She asks, “Accordingly, is early shunt occlusion due predominantly to passenger (corpuscular) overload or to a slow-moving train?”
Dr. Ghanayem had no financial relationships to disclose.
In her invited commentary, Nancy S. Ghanayem, MD, of the Medical College of Wisconsin, gives credit to Dr. Anderson and coauthors for introducing the notion that high initial postoperative hematocrit may increase the risk of early shunt thrombosis in newborns, but with a caveat: “we remain somewhat hesitant regarding wholesale acceptance of the validity of the conclusions for several reasons” (J Thorac Cardiovasc Surg. 2017;153:956).
Those reasons include the low number of reported events, failure to list the actual hematocrits of the five patients who experienced early shunt occlusion and the lack of hemodynamic data – the latter of which she called “a significant limitation.”
A patient with low cardiac output, especially one who is cyanotic or has a single ventricle, is at higher risk for thrombosis and more likely to be transfused, “which in this case would potentially be masked by the method of comparing transfused volumes,” Dr. Ghanayem said. The inotrope score, while useful, is not a surrogate for actual cardiac output. She asks, “Accordingly, is early shunt occlusion due predominantly to passenger (corpuscular) overload or to a slow-moving train?”
Dr. Ghanayem had no financial relationships to disclose.
In her invited commentary, Nancy S. Ghanayem, MD, of the Medical College of Wisconsin, gives credit to Dr. Anderson and coauthors for introducing the notion that high initial postoperative hematocrit may increase the risk of early shunt thrombosis in newborns, but with a caveat: “we remain somewhat hesitant regarding wholesale acceptance of the validity of the conclusions for several reasons” (J Thorac Cardiovasc Surg. 2017;153:956).
Those reasons include the low number of reported events, failure to list the actual hematocrits of the five patients who experienced early shunt occlusion and the lack of hemodynamic data – the latter of which she called “a significant limitation.”
A patient with low cardiac output, especially one who is cyanotic or has a single ventricle, is at higher risk for thrombosis and more likely to be transfused, “which in this case would potentially be masked by the method of comparing transfused volumes,” Dr. Ghanayem said. The inotrope score, while useful, is not a surrogate for actual cardiac output. She asks, “Accordingly, is early shunt occlusion due predominantly to passenger (corpuscular) overload or to a slow-moving train?”
Dr. Ghanayem had no financial relationships to disclose.
Shunt occlusion has been a well-documented cause of shunt failure in newborns who have had systemic to pulmonary shunt placement, and little has been known about why shunts occlude. However, researchers have reported in a small retrospective study that higher postoperative hematocrit levels immediately after surgery may be predictors of shunt occlusion.
Reporting in the April 2017 issue of The Journal of Thoracic and Cardiovascular Surgery, Brett R. Anderson, MD, of New York-Presbyterian/Morgan Stanley Children’s Hospital, Columbia University Medical Center in New York, and coauthors, found that every 5-point increase in postoperative hematocrit more than doubled an infant’s odds of having early shunt occlusion (J Thorac Cardiovasc Surg. 2017;153:947-55).
“Beginning in the latter half of 2014, we noticed an increase in the incidence of early shunt occlusions in our neonatal cardiac intensive care unit,” Dr. Anderson and coauthors said. So they conducted a retrospective chart review of 80 infants who had undergone systemic to pulmonary shunt placement from January 2010 to July 2015, hypothesizing that increased hematocrit in the early postoperative period might have caused early shunt occlusion. They investigated the association between the first postoperative hematocrit and early shunt occlusion and in-hospital mortality in these patients.
Five patients (6.3%) experienced early shunt occlusion – that is, within 24 hours of placement (actually, within 10 hours of placement). Overall, 12 infants (15%) experienced shunt occlusion. The physicians at New York-Presbyterian do not administer anticoagulation in these patients during the first 12 hours after shunt placement.
The median initial postoperative hematocrit was 41.7%, with a range of 31.7%-55.8%. The survival analysis the researchers performed found that for every 5 additional percentage points, the hazard ratio for early shunt occlusion was 2.7 (P = .007) and 1.74 for any shunt occlusion (P less than .001). Incidentally, four cases of early shunt occlusion occurred in the later study period after 2014, during which the average first postoperative hematocrit was significantly higher than in the pre-2014 study period, 45.3% vs. 41.5% (P = .21), and the odds of early shunt occlusion were 16 times higher (P less than .001). Dr. Anderson and coauthors said the possible explanation for this variation was a switch to a new point-of-care analyzer in 2013.
With regard to mortality, six infants overall (7.4%) died before discharge, and four (5%) within 30 days of shunt placement. No infants with early shunt occlusion died, although two with late shunt occlusion died. Increased inotrope score and first postoperative arterial oxygen tension were the only factors associated with increased mortality. “No significant association was identified between hematocrit and 30-day mortality,” Dr. Anderson and coauthors said.
In the first 24 hours after surgery, 11 infants (13.8%) received packed red blood cell (PRBC) transfusions, seven (8.8%) received platelets, and four (5%) received fresh frozen plasma/cryoprecipitate. Higher postoperative PRBC transfusion volumes were associated with increased odds of mortality (P = .001), but none of these factors were significantly associated with early shunt occlusion.
Dr. Anderson and coauthors acknowledged that shunt occlusion is a “vexing problem” in infants with cyanotic heart disease. While other researchers studied postoperative hematocrit levels and possible associations with outcomes, including shunt occlusion and mortality, the New York-Presbyterian investigators said this is the first study of the first postoperative hematocrit.
Dr. Anderson and coauthors said their findings raise the question about the ideal perioperative prophylactic antithrombotic therapy in these patients. These researchers initiate aspirin therapy 12 hours after surgery if hemostasis is established.
As a result of this study, Dr. Anderson and coauthors instituted a number of practice changes at their center. They include:
• Cardiac anesthesiologists have been asked not to transfuse shunted neonates with hematocrit level of greater than or equal to 35%, and hematocrits are then immediately repeated when a patient returns to the cardiac ICU.
• Patients with hematocrits greater than or equal to 55% get partial exchange transfusions.
• An individualized approach for patients with lower hematocrits who are more cyanotic than expected. This includes a diagnostic echocardiogram, nitric oxide, oxygen and heparin, escalated inotropic support if necessary and sometimes a cautious approach to transfusions if symptoms do not resolve and an acute shunt occlusion if not likely.
Dr. Anderson and coauthors acknowledged limits to their study, most notably its retrospective nature and a small population at a single center, and that large investigations are needed to validate their findings.
Dr. Anderson disclosed receiving salary support from the National Center for Advancing Translational Sciences. Coauthor Jennifer M. Duchon, MDCM, MPH, receives salary support from the National Institute of Allergy and Infectious Disease. The remaining coauthors had no financial relationships to disclose.
Shunt occlusion has been a well-documented cause of shunt failure in newborns who have had systemic to pulmonary shunt placement, and little has been known about why shunts occlude. However, researchers have reported in a small retrospective study that higher postoperative hematocrit levels immediately after surgery may be predictors of shunt occlusion.
Reporting in the April 2017 issue of The Journal of Thoracic and Cardiovascular Surgery, Brett R. Anderson, MD, of New York-Presbyterian/Morgan Stanley Children’s Hospital, Columbia University Medical Center in New York, and coauthors, found that every 5-point increase in postoperative hematocrit more than doubled an infant’s odds of having early shunt occlusion (J Thorac Cardiovasc Surg. 2017;153:947-55).
“Beginning in the latter half of 2014, we noticed an increase in the incidence of early shunt occlusions in our neonatal cardiac intensive care unit,” Dr. Anderson and coauthors said. So they conducted a retrospective chart review of 80 infants who had undergone systemic to pulmonary shunt placement from January 2010 to July 2015, hypothesizing that increased hematocrit in the early postoperative period might have caused early shunt occlusion. They investigated the association between the first postoperative hematocrit and early shunt occlusion and in-hospital mortality in these patients.
Five patients (6.3%) experienced early shunt occlusion – that is, within 24 hours of placement (actually, within 10 hours of placement). Overall, 12 infants (15%) experienced shunt occlusion. The physicians at New York-Presbyterian do not administer anticoagulation in these patients during the first 12 hours after shunt placement.
The median initial postoperative hematocrit was 41.7%, with a range of 31.7%-55.8%. The survival analysis the researchers performed found that for every 5 additional percentage points, the hazard ratio for early shunt occlusion was 2.7 (P = .007) and 1.74 for any shunt occlusion (P less than .001). Incidentally, four cases of early shunt occlusion occurred in the later study period after 2014, during which the average first postoperative hematocrit was significantly higher than in the pre-2014 study period, 45.3% vs. 41.5% (P = .21), and the odds of early shunt occlusion were 16 times higher (P less than .001). Dr. Anderson and coauthors said the possible explanation for this variation was a switch to a new point-of-care analyzer in 2013.
With regard to mortality, six infants overall (7.4%) died before discharge, and four (5%) within 30 days of shunt placement. No infants with early shunt occlusion died, although two with late shunt occlusion died. Increased inotrope score and first postoperative arterial oxygen tension were the only factors associated with increased mortality. “No significant association was identified between hematocrit and 30-day mortality,” Dr. Anderson and coauthors said.
In the first 24 hours after surgery, 11 infants (13.8%) received packed red blood cell (PRBC) transfusions, seven (8.8%) received platelets, and four (5%) received fresh frozen plasma/cryoprecipitate. Higher postoperative PRBC transfusion volumes were associated with increased odds of mortality (P = .001), but none of these factors were significantly associated with early shunt occlusion.
Dr. Anderson and coauthors acknowledged that shunt occlusion is a “vexing problem” in infants with cyanotic heart disease. While other researchers studied postoperative hematocrit levels and possible associations with outcomes, including shunt occlusion and mortality, the New York-Presbyterian investigators said this is the first study of the first postoperative hematocrit.
Dr. Anderson and coauthors said their findings raise the question about the ideal perioperative prophylactic antithrombotic therapy in these patients. These researchers initiate aspirin therapy 12 hours after surgery if hemostasis is established.
As a result of this study, Dr. Anderson and coauthors instituted a number of practice changes at their center. They include:
• Cardiac anesthesiologists have been asked not to transfuse shunted neonates with hematocrit level of greater than or equal to 35%, and hematocrits are then immediately repeated when a patient returns to the cardiac ICU.
• Patients with hematocrits greater than or equal to 55% get partial exchange transfusions.
• An individualized approach for patients with lower hematocrits who are more cyanotic than expected. This includes a diagnostic echocardiogram, nitric oxide, oxygen and heparin, escalated inotropic support if necessary and sometimes a cautious approach to transfusions if symptoms do not resolve and an acute shunt occlusion if not likely.
Dr. Anderson and coauthors acknowledged limits to their study, most notably its retrospective nature and a small population at a single center, and that large investigations are needed to validate their findings.
Dr. Anderson disclosed receiving salary support from the National Center for Advancing Translational Sciences. Coauthor Jennifer M. Duchon, MDCM, MPH, receives salary support from the National Institute of Allergy and Infectious Disease. The remaining coauthors had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Higher hematocrit levels have been associated with early shunt occlusion in newborns having systemic to pulmonary artery shunt placement.
Major finding: For every 5 additional percentage points of hematocrit, an infant’s odds of early shunt occlusion more than doubled (odds ratio, 2.70; P = .009).
Data source: Retrospective study of all newborns who underwent primary systemic to pulmonary artery shunt placement from January 2010 to July 2015 at a single center.
Disclosure: Dr. Anderson receives salary support from the National Center for Advancing Translational Sciences. Coauthor Jennifer M. Duchon, MDCM, MPH, receives salary support from the National Institute of Allergy and Infectious Disease. The remaining coauthors had no financial relationships to disclose.
Liposomal bupivacaine cut need for opioids after gyn surgery
SAN ANTONIO – Liposomal bupivacaine reduced pain after midurethral sling surgery, compared with placebo in a randomized trial, but because of its cost it may be best to keep it in reserve for women who can’t, or shouldn’t, take opioids, said lead investigator Donna Mazloomdoost, MD, a gynecologic surgeon at Good Samaritan Hospital, Cincinnati.
Fifty-four women were randomized to receive liposomal bupivacaine (Exparel) injected into the two trocar paths and the vaginal incision at the end of the procedure; 55 others were injected with normal saline as a placebo.
Fewer women in the liposomal bupivacaine group took narcotics on postop day 2 (12 versus 27, P = .006). However, there was no difference in overall satisfaction with pain control at 1 and 2 weeks follow-up.
Even so, “for this common outpatient surgery, liposomal bupivacaine may be a beneficial addition for pain control,” the investigators concluded.
Liposomal bupivacaine is a local anesthetic with slow release over 72 hours, approved for treatment of postsurgical pain in 2011. “The cost is about $300 at our institution; the charge to the patient is about $1,000,” Dr. Mazloomdoost said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Because of the expense, liposomal bupivacaine is restricted in many hospitals, and gynecologic surgeons are trying to figure out what role it has, if any, in low-pain outpatient procedures like midurethral slings.
“I don’t know if you can justify” routine use for low-pain procedures, “but if you are concerned about opioid” use after surgery – intolerance or addiction – “I would use this,” Dr. Mazloomdoost said.
The investigators expanded 20 mL of liposomal bupivacaine with 10 mL of normal saline for a total of 30 mL. It was split evenly between the two trocar sites and the vaginal epithelium; 10 mL was injected in each of the three sites shortly before the intervention women were roused from anesthesia. The needle was inserted as deeply as possible, and liposomal bupivacaine was injected as the needle was drawn back. Because of the viscosity, it takes at least a 25-gauge needle.
Surgeons knew that they were injecting liposomal bupivacaine instead of saline because of the thickness and color, but they weren’t the ones collecting data, and the women were blinded to the treatment.
Patients were a mean age of 52 years. The mean body mass index was 29.2 kg/m2 in the liposomal bupivacaine group, and 31.6 kg/m2 in the placebo group; there were otherwise no significant demographic differences. Fifty-two women in the liposomal bupivacaine group received midazolam during anesthesia induction versus 44 women receiving placebo, but there were no significant differences in operating time or the number of women in each group who had concomitant anterior or urethrocele repairs, and no differences in urinary retention, time to first bowel movement – about 2 days – or adverse events. The most common adverse events in both groups were nausea/vomiting, headache, and itching.
Women in both groups received intravenous acetaminophen before anesthesia induction, and ketorolac before leaving the operating room; 10 mL of lidocaine with epinephrine was injected into the trocar paths and vaginal epithelium prior to the first incision.
The investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Liposomal bupivacaine reduced pain after midurethral sling surgery, compared with placebo in a randomized trial, but because of its cost it may be best to keep it in reserve for women who can’t, or shouldn’t, take opioids, said lead investigator Donna Mazloomdoost, MD, a gynecologic surgeon at Good Samaritan Hospital, Cincinnati.
Fifty-four women were randomized to receive liposomal bupivacaine (Exparel) injected into the two trocar paths and the vaginal incision at the end of the procedure; 55 others were injected with normal saline as a placebo.
Fewer women in the liposomal bupivacaine group took narcotics on postop day 2 (12 versus 27, P = .006). However, there was no difference in overall satisfaction with pain control at 1 and 2 weeks follow-up.
Even so, “for this common outpatient surgery, liposomal bupivacaine may be a beneficial addition for pain control,” the investigators concluded.
Liposomal bupivacaine is a local anesthetic with slow release over 72 hours, approved for treatment of postsurgical pain in 2011. “The cost is about $300 at our institution; the charge to the patient is about $1,000,” Dr. Mazloomdoost said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Because of the expense, liposomal bupivacaine is restricted in many hospitals, and gynecologic surgeons are trying to figure out what role it has, if any, in low-pain outpatient procedures like midurethral slings.
“I don’t know if you can justify” routine use for low-pain procedures, “but if you are concerned about opioid” use after surgery – intolerance or addiction – “I would use this,” Dr. Mazloomdoost said.
The investigators expanded 20 mL of liposomal bupivacaine with 10 mL of normal saline for a total of 30 mL. It was split evenly between the two trocar sites and the vaginal epithelium; 10 mL was injected in each of the three sites shortly before the intervention women were roused from anesthesia. The needle was inserted as deeply as possible, and liposomal bupivacaine was injected as the needle was drawn back. Because of the viscosity, it takes at least a 25-gauge needle.
Surgeons knew that they were injecting liposomal bupivacaine instead of saline because of the thickness and color, but they weren’t the ones collecting data, and the women were blinded to the treatment.
Patients were a mean age of 52 years. The mean body mass index was 29.2 kg/m2 in the liposomal bupivacaine group, and 31.6 kg/m2 in the placebo group; there were otherwise no significant demographic differences. Fifty-two women in the liposomal bupivacaine group received midazolam during anesthesia induction versus 44 women receiving placebo, but there were no significant differences in operating time or the number of women in each group who had concomitant anterior or urethrocele repairs, and no differences in urinary retention, time to first bowel movement – about 2 days – or adverse events. The most common adverse events in both groups were nausea/vomiting, headache, and itching.
Women in both groups received intravenous acetaminophen before anesthesia induction, and ketorolac before leaving the operating room; 10 mL of lidocaine with epinephrine was injected into the trocar paths and vaginal epithelium prior to the first incision.
The investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Liposomal bupivacaine reduced pain after midurethral sling surgery, compared with placebo in a randomized trial, but because of its cost it may be best to keep it in reserve for women who can’t, or shouldn’t, take opioids, said lead investigator Donna Mazloomdoost, MD, a gynecologic surgeon at Good Samaritan Hospital, Cincinnati.
Fifty-four women were randomized to receive liposomal bupivacaine (Exparel) injected into the two trocar paths and the vaginal incision at the end of the procedure; 55 others were injected with normal saline as a placebo.
Fewer women in the liposomal bupivacaine group took narcotics on postop day 2 (12 versus 27, P = .006). However, there was no difference in overall satisfaction with pain control at 1 and 2 weeks follow-up.
Even so, “for this common outpatient surgery, liposomal bupivacaine may be a beneficial addition for pain control,” the investigators concluded.
Liposomal bupivacaine is a local anesthetic with slow release over 72 hours, approved for treatment of postsurgical pain in 2011. “The cost is about $300 at our institution; the charge to the patient is about $1,000,” Dr. Mazloomdoost said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Because of the expense, liposomal bupivacaine is restricted in many hospitals, and gynecologic surgeons are trying to figure out what role it has, if any, in low-pain outpatient procedures like midurethral slings.
“I don’t know if you can justify” routine use for low-pain procedures, “but if you are concerned about opioid” use after surgery – intolerance or addiction – “I would use this,” Dr. Mazloomdoost said.
The investigators expanded 20 mL of liposomal bupivacaine with 10 mL of normal saline for a total of 30 mL. It was split evenly between the two trocar sites and the vaginal epithelium; 10 mL was injected in each of the three sites shortly before the intervention women were roused from anesthesia. The needle was inserted as deeply as possible, and liposomal bupivacaine was injected as the needle was drawn back. Because of the viscosity, it takes at least a 25-gauge needle.
Surgeons knew that they were injecting liposomal bupivacaine instead of saline because of the thickness and color, but they weren’t the ones collecting data, and the women were blinded to the treatment.
Patients were a mean age of 52 years. The mean body mass index was 29.2 kg/m2 in the liposomal bupivacaine group, and 31.6 kg/m2 in the placebo group; there were otherwise no significant demographic differences. Fifty-two women in the liposomal bupivacaine group received midazolam during anesthesia induction versus 44 women receiving placebo, but there were no significant differences in operating time or the number of women in each group who had concomitant anterior or urethrocele repairs, and no differences in urinary retention, time to first bowel movement – about 2 days – or adverse events. The most common adverse events in both groups were nausea/vomiting, headache, and itching.
Women in both groups received intravenous acetaminophen before anesthesia induction, and ketorolac before leaving the operating room; 10 mL of lidocaine with epinephrine was injected into the trocar paths and vaginal epithelium prior to the first incision.
The investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
AT SGS 2017
Key clinical point:
Major finding: Pain scores, assessed by diary, were lower in the liposomal bupivacaine group 4 hours after discharge on a 100-mm visual analogue scale (3.5 mm versus 13 mm, P = .014).
Data source: Randomized trial with 109 women at Good Samaritan Hospital, Cincinnati.
Disclosures: The investigators reported having no relevant financial disclosures.
Avoid hysterectomy in POP repairs
SAN ANTONIO – The Systematic Review Group of the Society of Gynecologic Surgeons is suggesting uterine preservation, when not contraindicated, for most pelvic organ prolapse repairs to decrease mesh erosion, operating room time, and blood loss.
The advice is based on a review of 94 original studies, including 12 randomized controlled trials (RCTs) and 41 nonrandomized comparative studies, winnowed down to the strongest work from an original review of 7,324 abstracts through January 2017.
Short-term prolapse outcomes – 12-30 months in most of the studies – “are usually not clinically significant due to uterine preservation,” with the one exception of vaginal hysterectomy with native tissue reconstruction, which the group recommended over laparoscopic sacrohysteropexy, Kate Meriwether, MD, a gynecologic surgeon at the University of Louisville, Ky., said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Hysterectomy for prolapse surgery is common: More than 74,000 hysterectomies are done in the United States each year with prolapse as the main indication. Even so, it’s not always necessary to take out the uterus, and perhaps more than a third of women would prefer to keep theirs, Dr. Meriwether said, speaking on behalf of the SGS Systematic Review Group.
The recommendations from the Systematic Review Group must be sent to the SGS board and the full membership before they can be approved as guidelines.*
The Review Group made a grade A recommendation for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, meaning it was based on high-quality evidence. The rest of the advice came in the form of suggestions, based on moderate grade B evidence, often nonrandomized comparative studies and case reviews.
The Review Group suggested uterine preservation during laparoscopic native tissue prolapse repair to reduce operating room (OR) time and blood loss, and preserve vaginal length, based on four nonrandomized comparison studies using various approaches, with a total of 446 women and up to 3 years’ follow-up. There might be a higher risk of apical recurrence without hysterectomy, but without worsening of prolapse symptoms.
The Review Group also suggested uterine preservation in transvaginal mesh reconstruction for prolapse, based on four RCTs and nine comparison studies with 1,381 women and up to 30 months’ follow-up. The studies found a decreased risk of mesh erosion, reoperating for mesh erosion, blood loss, and postop bleeding, and improved posterior and apical Pelvic Organ Prolapse Quantification scores when women keep their uterus.
However, “the patient should be counseled that there may be increased de novo stress incontinence, overactive bladder,” postop constipation, and shorter vaginal length, Dr. Meriwether said.
Also, “we suggest preservation of the uterus in transvaginal apical native tissue repair of prolapse, as it does not worsen any outcomes and slightly reduces OR time and estimated blood loss,” based on 13 studies, including four RCTs, and a total of 1,449 women followed for up to 26 months, she said.
The Review Group also came out in favor of the Manchester procedure, when available, over vaginal hysterectomy with native tissue suspension, based on one RCT and five nonrandomized studies involving 1,126 women and up to 61 months’ follow-up. The Manchester procedure pushed back the time to prolapse reoperation 9 months in one study, and also decreased transfusions, OR time, and blood loss. It also better preserved perineal length.
The group suggested uterine preservation when considering mesh sacrocolpopexy versus mesh sacrohysteropexy, to reduce mesh erosion, OR time, blood loss, hospital stay, and surgery costs, although there might be a slight worsening of Pelvic Floor Distress Inventory and Pelvic Floor Impact scores. The advice was based on nine nonrandomized comparison studies involving 745 women followed for up to 39 months. There was no difference in prolapse resolution between the two techniques.
The one grade A recommendation, for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, was based on two RCTs with 182 women followed for up to 12 months.
Hysterectomy in those studies significantly reduced the risk of repeat surgery for prolapse and urinary symptoms, shortened OR time, and improved quality of life scores. However, the benefits came at the cost of slightly shorter vaginal length, worse Pelvic Organ Prolapse Quantification point C scores, greater blood loss, and up to a day longer spent in the hospital.
Dr. Meriwether reported having no relevant financial disclosures.
*Correction, 6/8/2017: An earlier version of this story misstated the status of the Systematic Review Group's recommendations. The recommendations have not been approved as official SGS guidelines. Also, the meeting sponsor information was updated.
SAN ANTONIO – The Systematic Review Group of the Society of Gynecologic Surgeons is suggesting uterine preservation, when not contraindicated, for most pelvic organ prolapse repairs to decrease mesh erosion, operating room time, and blood loss.
The advice is based on a review of 94 original studies, including 12 randomized controlled trials (RCTs) and 41 nonrandomized comparative studies, winnowed down to the strongest work from an original review of 7,324 abstracts through January 2017.
Short-term prolapse outcomes – 12-30 months in most of the studies – “are usually not clinically significant due to uterine preservation,” with the one exception of vaginal hysterectomy with native tissue reconstruction, which the group recommended over laparoscopic sacrohysteropexy, Kate Meriwether, MD, a gynecologic surgeon at the University of Louisville, Ky., said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Hysterectomy for prolapse surgery is common: More than 74,000 hysterectomies are done in the United States each year with prolapse as the main indication. Even so, it’s not always necessary to take out the uterus, and perhaps more than a third of women would prefer to keep theirs, Dr. Meriwether said, speaking on behalf of the SGS Systematic Review Group.
The recommendations from the Systematic Review Group must be sent to the SGS board and the full membership before they can be approved as guidelines.*
The Review Group made a grade A recommendation for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, meaning it was based on high-quality evidence. The rest of the advice came in the form of suggestions, based on moderate grade B evidence, often nonrandomized comparative studies and case reviews.
The Review Group suggested uterine preservation during laparoscopic native tissue prolapse repair to reduce operating room (OR) time and blood loss, and preserve vaginal length, based on four nonrandomized comparison studies using various approaches, with a total of 446 women and up to 3 years’ follow-up. There might be a higher risk of apical recurrence without hysterectomy, but without worsening of prolapse symptoms.
The Review Group also suggested uterine preservation in transvaginal mesh reconstruction for prolapse, based on four RCTs and nine comparison studies with 1,381 women and up to 30 months’ follow-up. The studies found a decreased risk of mesh erosion, reoperating for mesh erosion, blood loss, and postop bleeding, and improved posterior and apical Pelvic Organ Prolapse Quantification scores when women keep their uterus.
However, “the patient should be counseled that there may be increased de novo stress incontinence, overactive bladder,” postop constipation, and shorter vaginal length, Dr. Meriwether said.
Also, “we suggest preservation of the uterus in transvaginal apical native tissue repair of prolapse, as it does not worsen any outcomes and slightly reduces OR time and estimated blood loss,” based on 13 studies, including four RCTs, and a total of 1,449 women followed for up to 26 months, she said.
The Review Group also came out in favor of the Manchester procedure, when available, over vaginal hysterectomy with native tissue suspension, based on one RCT and five nonrandomized studies involving 1,126 women and up to 61 months’ follow-up. The Manchester procedure pushed back the time to prolapse reoperation 9 months in one study, and also decreased transfusions, OR time, and blood loss. It also better preserved perineal length.
The group suggested uterine preservation when considering mesh sacrocolpopexy versus mesh sacrohysteropexy, to reduce mesh erosion, OR time, blood loss, hospital stay, and surgery costs, although there might be a slight worsening of Pelvic Floor Distress Inventory and Pelvic Floor Impact scores. The advice was based on nine nonrandomized comparison studies involving 745 women followed for up to 39 months. There was no difference in prolapse resolution between the two techniques.
The one grade A recommendation, for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, was based on two RCTs with 182 women followed for up to 12 months.
Hysterectomy in those studies significantly reduced the risk of repeat surgery for prolapse and urinary symptoms, shortened OR time, and improved quality of life scores. However, the benefits came at the cost of slightly shorter vaginal length, worse Pelvic Organ Prolapse Quantification point C scores, greater blood loss, and up to a day longer spent in the hospital.
Dr. Meriwether reported having no relevant financial disclosures.
*Correction, 6/8/2017: An earlier version of this story misstated the status of the Systematic Review Group's recommendations. The recommendations have not been approved as official SGS guidelines. Also, the meeting sponsor information was updated.
SAN ANTONIO – The Systematic Review Group of the Society of Gynecologic Surgeons is suggesting uterine preservation, when not contraindicated, for most pelvic organ prolapse repairs to decrease mesh erosion, operating room time, and blood loss.
The advice is based on a review of 94 original studies, including 12 randomized controlled trials (RCTs) and 41 nonrandomized comparative studies, winnowed down to the strongest work from an original review of 7,324 abstracts through January 2017.
Short-term prolapse outcomes – 12-30 months in most of the studies – “are usually not clinically significant due to uterine preservation,” with the one exception of vaginal hysterectomy with native tissue reconstruction, which the group recommended over laparoscopic sacrohysteropexy, Kate Meriwether, MD, a gynecologic surgeon at the University of Louisville, Ky., said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Hysterectomy for prolapse surgery is common: More than 74,000 hysterectomies are done in the United States each year with prolapse as the main indication. Even so, it’s not always necessary to take out the uterus, and perhaps more than a third of women would prefer to keep theirs, Dr. Meriwether said, speaking on behalf of the SGS Systematic Review Group.
The recommendations from the Systematic Review Group must be sent to the SGS board and the full membership before they can be approved as guidelines.*
The Review Group made a grade A recommendation for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, meaning it was based on high-quality evidence. The rest of the advice came in the form of suggestions, based on moderate grade B evidence, often nonrandomized comparative studies and case reviews.
The Review Group suggested uterine preservation during laparoscopic native tissue prolapse repair to reduce operating room (OR) time and blood loss, and preserve vaginal length, based on four nonrandomized comparison studies using various approaches, with a total of 446 women and up to 3 years’ follow-up. There might be a higher risk of apical recurrence without hysterectomy, but without worsening of prolapse symptoms.
The Review Group also suggested uterine preservation in transvaginal mesh reconstruction for prolapse, based on four RCTs and nine comparison studies with 1,381 women and up to 30 months’ follow-up. The studies found a decreased risk of mesh erosion, reoperating for mesh erosion, blood loss, and postop bleeding, and improved posterior and apical Pelvic Organ Prolapse Quantification scores when women keep their uterus.
However, “the patient should be counseled that there may be increased de novo stress incontinence, overactive bladder,” postop constipation, and shorter vaginal length, Dr. Meriwether said.
Also, “we suggest preservation of the uterus in transvaginal apical native tissue repair of prolapse, as it does not worsen any outcomes and slightly reduces OR time and estimated blood loss,” based on 13 studies, including four RCTs, and a total of 1,449 women followed for up to 26 months, she said.
The Review Group also came out in favor of the Manchester procedure, when available, over vaginal hysterectomy with native tissue suspension, based on one RCT and five nonrandomized studies involving 1,126 women and up to 61 months’ follow-up. The Manchester procedure pushed back the time to prolapse reoperation 9 months in one study, and also decreased transfusions, OR time, and blood loss. It also better preserved perineal length.
The group suggested uterine preservation when considering mesh sacrocolpopexy versus mesh sacrohysteropexy, to reduce mesh erosion, OR time, blood loss, hospital stay, and surgery costs, although there might be a slight worsening of Pelvic Floor Distress Inventory and Pelvic Floor Impact scores. The advice was based on nine nonrandomized comparison studies involving 745 women followed for up to 39 months. There was no difference in prolapse resolution between the two techniques.
The one grade A recommendation, for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, was based on two RCTs with 182 women followed for up to 12 months.
Hysterectomy in those studies significantly reduced the risk of repeat surgery for prolapse and urinary symptoms, shortened OR time, and improved quality of life scores. However, the benefits came at the cost of slightly shorter vaginal length, worse Pelvic Organ Prolapse Quantification point C scores, greater blood loss, and up to a day longer spent in the hospital.
Dr. Meriwether reported having no relevant financial disclosures.
*Correction, 6/8/2017: An earlier version of this story misstated the status of the Systematic Review Group's recommendations. The recommendations have not been approved as official SGS guidelines. Also, the meeting sponsor information was updated.
OSA tool uncovers risks of postoperative complications
High scores on the symptomless multivariable apnea prediction index (sMVAP) showed a strong correlation with increased risk for postsurgery complications, according to a study approved by the University of Pennsylvania, Philadelphia.
This validation helps assert the benefits of using the sMVAP as a tool to screen for obstructive sleep apnea (OSA) before elective inpatient surgeries, a test that is highly underutilized but very important, wrote M. Melanie Lyons, PhD, of the Center for Sleep and Circadian Neurobiology, University of Pennsylvania, Philadelphia, and her colleagues.
“Most patients having elective surgery are not screened for obstructive sleep apnea, even though OSA is a risk factor for postoperative complications,” wrote Dr. Lyons and her colleagues. “We observe that sMVAP correlates with higher risk for OSA, hypertension, and select postoperative complications, particularly in non-bariatric groups without routine preoperative screening for OSA.”
In a retrospective study of 40,432 patients undergoing elective surgery, high sMVAP scores were strongly correlated with postoperative complications including longer hospital stays (OR = 1.83), stays in the ICU (OR = 1.44), and respiratory complications (OR = 1.85) according to the researchers (Sleep. 2017 Jan 6. doi: 10.1093/sleep/zsw081).
Researchers separated participants into 10 categories according to the type of procedure: bariatric, orthopedic, cardiac, gastrointestinal, genitourinary, neurological, otorhinolaryngology/oral-maxillofacial/ear-nose-throat, pulmonary/thoracic, spine, and vascular.
The sMVAP calculates risk factors for OSA based on gender, age and body mass index, the researchers noted.
Those in the highest sMVAP score quintile were predominantly male (58%), with average age of 61 years, and average BMI of 40.9 kg/m2 (indicating morbid obesity). These patients reported the highest prevalence of having been previously diagnosed with OSA (26%). Comparatively, those patients in the lowest sMVAP quintile reported the lowest prevalence of an OSA diagnosis prior to undergoing their surgeries (9.3%).
Among non–bariatric surgery patients, those undergoing orthopedic procedures showed the highest correlation between complications and sMVAP scores.
The orthopedic surgery category reported a higher percentage of ICU-stay compared with bariatric surgery (14.3% vs 5.4%, P less than .0001), despite 23% of the patients who underwent an orthopedic surgery reporting previous OSA, compared with 50% of those who underwent surgery in the bariatric category.
This difference in previously reported OSA, according to Dr. Lyons and her colleagues, shows another example of the need for sMVAP in non–bariatric surgery preoperative procedure as a way to catch potentially undiagnosed OSA.
“[W]ork by Penn Bariatrics suggests that it is logical that the benefits of rigorous preoperative screening and diagnosis for OSA followed by a tailored team approach toward ensuring compliance toward treatment postoperation ... may be effective in limiting the likelihood of select postoperative complications,” the researchers wrote.
With 9.3% of all patients diagnosed with OSA, and a projected 14%-47% increase in specialty surgeries, there is an urgency in implementation of sMVAP and in conducting further studies, they noted.
This test was limited by the sample population, primarily male commercial truck drivers, the researchers noted. In addition, misclassification of OSA based on weight may have occurred in up to 20% of normal weight patients. Finally, data were collected from one hospital network, so generalizability may be limited.
Dr. M. Melanie Lyons and Dr. Junxin Li, another of the study’s authors, receive grants from the National Institutes of Health. The other authors reported no relevant disclosures.
High scores on the symptomless multivariable apnea prediction index (sMVAP) showed a strong correlation with increased risk for postsurgery complications, according to a study approved by the University of Pennsylvania, Philadelphia.
This validation helps assert the benefits of using the sMVAP as a tool to screen for obstructive sleep apnea (OSA) before elective inpatient surgeries, a test that is highly underutilized but very important, wrote M. Melanie Lyons, PhD, of the Center for Sleep and Circadian Neurobiology, University of Pennsylvania, Philadelphia, and her colleagues.
“Most patients having elective surgery are not screened for obstructive sleep apnea, even though OSA is a risk factor for postoperative complications,” wrote Dr. Lyons and her colleagues. “We observe that sMVAP correlates with higher risk for OSA, hypertension, and select postoperative complications, particularly in non-bariatric groups without routine preoperative screening for OSA.”
In a retrospective study of 40,432 patients undergoing elective surgery, high sMVAP scores were strongly correlated with postoperative complications including longer hospital stays (OR = 1.83), stays in the ICU (OR = 1.44), and respiratory complications (OR = 1.85) according to the researchers (Sleep. 2017 Jan 6. doi: 10.1093/sleep/zsw081).
Researchers separated participants into 10 categories according to the type of procedure: bariatric, orthopedic, cardiac, gastrointestinal, genitourinary, neurological, otorhinolaryngology/oral-maxillofacial/ear-nose-throat, pulmonary/thoracic, spine, and vascular.
The sMVAP calculates risk factors for OSA based on gender, age and body mass index, the researchers noted.
Those in the highest sMVAP score quintile were predominantly male (58%), with average age of 61 years, and average BMI of 40.9 kg/m2 (indicating morbid obesity). These patients reported the highest prevalence of having been previously diagnosed with OSA (26%). Comparatively, those patients in the lowest sMVAP quintile reported the lowest prevalence of an OSA diagnosis prior to undergoing their surgeries (9.3%).
Among non–bariatric surgery patients, those undergoing orthopedic procedures showed the highest correlation between complications and sMVAP scores.
The orthopedic surgery category reported a higher percentage of ICU-stay compared with bariatric surgery (14.3% vs 5.4%, P less than .0001), despite 23% of the patients who underwent an orthopedic surgery reporting previous OSA, compared with 50% of those who underwent surgery in the bariatric category.
This difference in previously reported OSA, according to Dr. Lyons and her colleagues, shows another example of the need for sMVAP in non–bariatric surgery preoperative procedure as a way to catch potentially undiagnosed OSA.
“[W]ork by Penn Bariatrics suggests that it is logical that the benefits of rigorous preoperative screening and diagnosis for OSA followed by a tailored team approach toward ensuring compliance toward treatment postoperation ... may be effective in limiting the likelihood of select postoperative complications,” the researchers wrote.
With 9.3% of all patients diagnosed with OSA, and a projected 14%-47% increase in specialty surgeries, there is an urgency in implementation of sMVAP and in conducting further studies, they noted.
This test was limited by the sample population, primarily male commercial truck drivers, the researchers noted. In addition, misclassification of OSA based on weight may have occurred in up to 20% of normal weight patients. Finally, data were collected from one hospital network, so generalizability may be limited.
Dr. M. Melanie Lyons and Dr. Junxin Li, another of the study’s authors, receive grants from the National Institutes of Health. The other authors reported no relevant disclosures.
High scores on the symptomless multivariable apnea prediction index (sMVAP) showed a strong correlation with increased risk for postsurgery complications, according to a study approved by the University of Pennsylvania, Philadelphia.
This validation helps assert the benefits of using the sMVAP as a tool to screen for obstructive sleep apnea (OSA) before elective inpatient surgeries, a test that is highly underutilized but very important, wrote M. Melanie Lyons, PhD, of the Center for Sleep and Circadian Neurobiology, University of Pennsylvania, Philadelphia, and her colleagues.
“Most patients having elective surgery are not screened for obstructive sleep apnea, even though OSA is a risk factor for postoperative complications,” wrote Dr. Lyons and her colleagues. “We observe that sMVAP correlates with higher risk for OSA, hypertension, and select postoperative complications, particularly in non-bariatric groups without routine preoperative screening for OSA.”
In a retrospective study of 40,432 patients undergoing elective surgery, high sMVAP scores were strongly correlated with postoperative complications including longer hospital stays (OR = 1.83), stays in the ICU (OR = 1.44), and respiratory complications (OR = 1.85) according to the researchers (Sleep. 2017 Jan 6. doi: 10.1093/sleep/zsw081).
Researchers separated participants into 10 categories according to the type of procedure: bariatric, orthopedic, cardiac, gastrointestinal, genitourinary, neurological, otorhinolaryngology/oral-maxillofacial/ear-nose-throat, pulmonary/thoracic, spine, and vascular.
The sMVAP calculates risk factors for OSA based on gender, age and body mass index, the researchers noted.
Those in the highest sMVAP score quintile were predominantly male (58%), with average age of 61 years, and average BMI of 40.9 kg/m2 (indicating morbid obesity). These patients reported the highest prevalence of having been previously diagnosed with OSA (26%). Comparatively, those patients in the lowest sMVAP quintile reported the lowest prevalence of an OSA diagnosis prior to undergoing their surgeries (9.3%).
Among non–bariatric surgery patients, those undergoing orthopedic procedures showed the highest correlation between complications and sMVAP scores.
The orthopedic surgery category reported a higher percentage of ICU-stay compared with bariatric surgery (14.3% vs 5.4%, P less than .0001), despite 23% of the patients who underwent an orthopedic surgery reporting previous OSA, compared with 50% of those who underwent surgery in the bariatric category.
This difference in previously reported OSA, according to Dr. Lyons and her colleagues, shows another example of the need for sMVAP in non–bariatric surgery preoperative procedure as a way to catch potentially undiagnosed OSA.
“[W]ork by Penn Bariatrics suggests that it is logical that the benefits of rigorous preoperative screening and diagnosis for OSA followed by a tailored team approach toward ensuring compliance toward treatment postoperation ... may be effective in limiting the likelihood of select postoperative complications,” the researchers wrote.
With 9.3% of all patients diagnosed with OSA, and a projected 14%-47% increase in specialty surgeries, there is an urgency in implementation of sMVAP and in conducting further studies, they noted.
This test was limited by the sample population, primarily male commercial truck drivers, the researchers noted. In addition, misclassification of OSA based on weight may have occurred in up to 20% of normal weight patients. Finally, data were collected from one hospital network, so generalizability may be limited.
Dr. M. Melanie Lyons and Dr. Junxin Li, another of the study’s authors, receive grants from the National Institutes of Health. The other authors reported no relevant disclosures.
FROM SLEEP
Key clinical point:
Major finding: Patients with high sMVAP scores had increased odds of complications, including extended length of stay (OR = 1.83), ICU stay (OR = 1.44), and respiratory complications (OR = 1.85).
Data source: Retrospective study of 40,432 elective surgery patient records collected from the Hospital of University of Pennsylvania, Pennsylvania Hospital, and Penn Presbyterian Medical Center between July 1, 2011, and June 30, 2014.
Disclosures: Dr. M. Melanie Lyons and Dr. Junxin Li receive grants from the National Institutes of Health. Other authors reported no relevant financial disclosures.
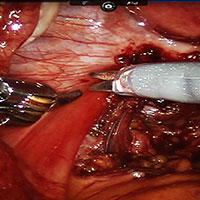
Robot-assisted laparoscopic excision of a rectovaginal endometriotic nodule
A rectovaginal endometriosis (RVE) is the most severe form of endometriosis. The gold standard for diagnosis is laparoscopy with histologic confirmation. A review of the literature suggests that surgery improves up to 70% of symptoms with generally favorable outcomes.
In this video, we provide a general introduction to endometriosis and a discussion of disease treatment options, ranging from hormonal suppression to radical bowel resections. We also illustrate the steps in robot-assisted laparoscopic excision of an RVE nodule:
- identify the borders of the rectosigmoid
- dissect the pararectal spaces
- release the rectosigmoid from its attachment to the RVE nodule
- identify and isolate the ureter(s)
- determine the margins of the nodule
- ensure complete resection.
Excision of an RVE nodule is a technically challenging surgical procedure. Use of the robot for resection is safe and feasible when performed by a trained and experienced surgeon.
I am pleased to bring you this video, and I hope that it is helpful to your practice.
>> Arnold P. Advincula, MD

Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
A rectovaginal endometriosis (RVE) is the most severe form of endometriosis. The gold standard for diagnosis is laparoscopy with histologic confirmation. A review of the literature suggests that surgery improves up to 70% of symptoms with generally favorable outcomes.
In this video, we provide a general introduction to endometriosis and a discussion of disease treatment options, ranging from hormonal suppression to radical bowel resections. We also illustrate the steps in robot-assisted laparoscopic excision of an RVE nodule:
- identify the borders of the rectosigmoid
- dissect the pararectal spaces
- release the rectosigmoid from its attachment to the RVE nodule
- identify and isolate the ureter(s)
- determine the margins of the nodule
- ensure complete resection.
Excision of an RVE nodule is a technically challenging surgical procedure. Use of the robot for resection is safe and feasible when performed by a trained and experienced surgeon.
I am pleased to bring you this video, and I hope that it is helpful to your practice.
>> Arnold P. Advincula, MD

Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
A rectovaginal endometriosis (RVE) is the most severe form of endometriosis. The gold standard for diagnosis is laparoscopy with histologic confirmation. A review of the literature suggests that surgery improves up to 70% of symptoms with generally favorable outcomes.
In this video, we provide a general introduction to endometriosis and a discussion of disease treatment options, ranging from hormonal suppression to radical bowel resections. We also illustrate the steps in robot-assisted laparoscopic excision of an RVE nodule:
- identify the borders of the rectosigmoid
- dissect the pararectal spaces
- release the rectosigmoid from its attachment to the RVE nodule
- identify and isolate the ureter(s)
- determine the margins of the nodule
- ensure complete resection.
Excision of an RVE nodule is a technically challenging surgical procedure. Use of the robot for resection is safe and feasible when performed by a trained and experienced surgeon.
I am pleased to bring you this video, and I hope that it is helpful to your practice.
>> Arnold P. Advincula, MD

Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
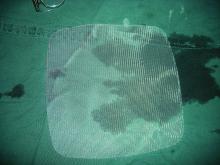
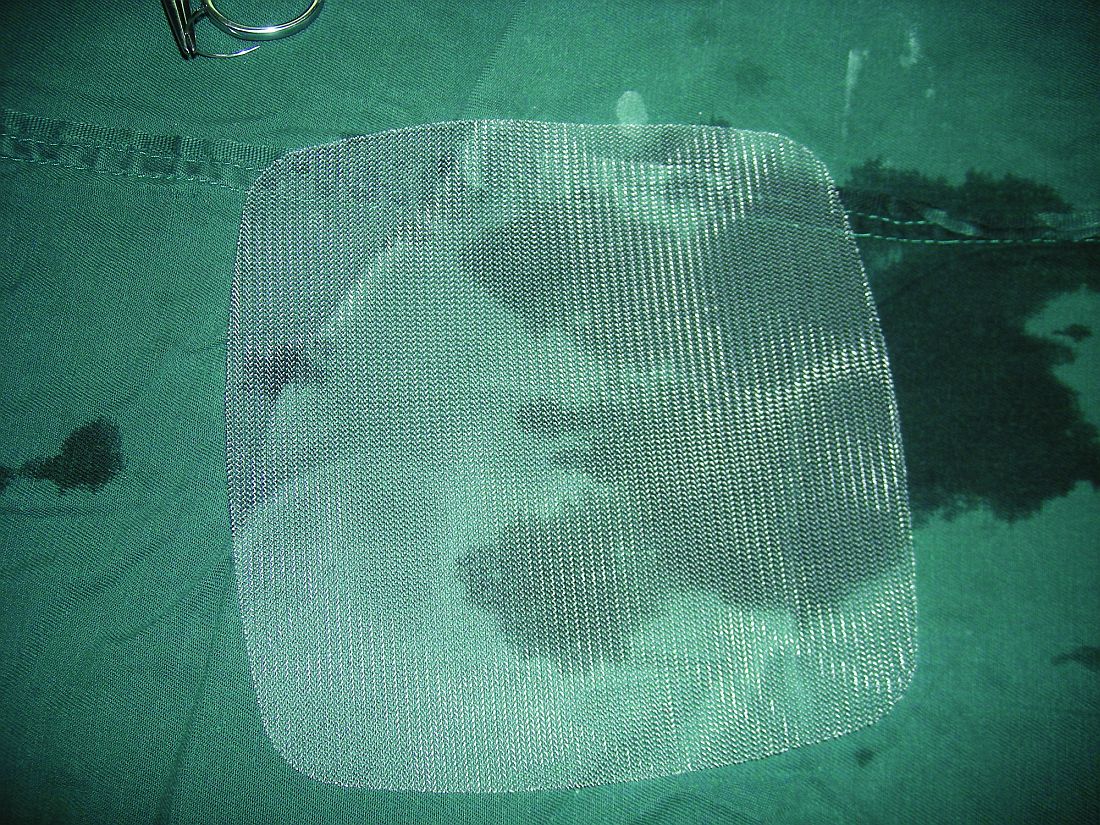
Lightweight mesh reduces erosion risk after sacrocolpopexy
SAN ANTONIO – Compared with heavier mesh types, ultralightweight polypropylene (Restorelle Y) did not increase the risk of mesh erosion after sacrocolpopexy in a retrospective, case-control study.
Delayed–absorbable monofilament polydioxanone suture (PDS) also decreased the risk, compared with nonabsorbable braided suture (Ethibond Excel) for vaginal mesh attachment.
The odds ratio for the ultralightweight polypropylene mesh exposure, versus heavier mesh, was not statistically significant (odds ratio, 2.18; 95% confidence interval, 0.33-14.57), which led to the main study conclusion.
“Mesh choice and suture selection [are] important independent predictors of” erosion, she said at the annual scientific meeting of the Society of Gynecologic Surgeons. “Based on this study, surgeons should consider use of [PDS over nonabsorbable braided suture] to reduce the risk of mesh exposure when using ultralightweight mesh.”
The team also found that prior surgery for incontinence, as well as immediate postoperative complications, which likely impede healing, increase erosion risk. The findings are useful in counseling patients and perhaps guiding follow-up, at least early on. Most of the 133 erosions in the study – out of 1,247 sacrocolpopexies performed at the university from 2003 to2013 – occurred in the first year, usually in the first 3 months.
The 133 women with erosions were randomly matched with 261 women who did not have erosions after sacrocolpopexy. The erosion rate hovered around 9.5% for most years. They shot up to 19% in 2006, the first year of robot-assisted sacrocolpopexies and fell to about 6% in 2011, 4% in 2012, and 2% in 2013, when surgeons started using the ultralightweight mesh.
“Our study also confirmed several known risk factors,” Dr. Durst said, including smoking, stage IV prolapse, nonabsorbable braided suture, and heavyweight polypropylene mesh.
On multivariate regression, prior surgery for incontinence (OR, 2.87; 95% CI, 1.19-6.96), porcine acellular collagen matrix with soft polypropylene mesh (Pelvicol with soft Prolene, OR, 4.95; 95% CI, 1.70-14.42), other polypropylene mesh (OR, 6.73; 95% CI, 1.12-40.63); braided suture for vaginal mesh attachment (OR, 4.52; 95% CI, 1.53-13.37), and immediate perioperative complications (OR, 1.04; 95% CI, 1.58-8.43) all remained independent risk factors for mesh exposure, as did duration of follow-up (OR, 1.04; 95% CI, 1.03-1.06).
There was no industry funding for the study, and the investigators reported having no financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Compared with heavier mesh types, ultralightweight polypropylene (Restorelle Y) did not increase the risk of mesh erosion after sacrocolpopexy in a retrospective, case-control study.
Delayed–absorbable monofilament polydioxanone suture (PDS) also decreased the risk, compared with nonabsorbable braided suture (Ethibond Excel) for vaginal mesh attachment.
The odds ratio for the ultralightweight polypropylene mesh exposure, versus heavier mesh, was not statistically significant (odds ratio, 2.18; 95% confidence interval, 0.33-14.57), which led to the main study conclusion.
“Mesh choice and suture selection [are] important independent predictors of” erosion, she said at the annual scientific meeting of the Society of Gynecologic Surgeons. “Based on this study, surgeons should consider use of [PDS over nonabsorbable braided suture] to reduce the risk of mesh exposure when using ultralightweight mesh.”
The team also found that prior surgery for incontinence, as well as immediate postoperative complications, which likely impede healing, increase erosion risk. The findings are useful in counseling patients and perhaps guiding follow-up, at least early on. Most of the 133 erosions in the study – out of 1,247 sacrocolpopexies performed at the university from 2003 to2013 – occurred in the first year, usually in the first 3 months.
The 133 women with erosions were randomly matched with 261 women who did not have erosions after sacrocolpopexy. The erosion rate hovered around 9.5% for most years. They shot up to 19% in 2006, the first year of robot-assisted sacrocolpopexies and fell to about 6% in 2011, 4% in 2012, and 2% in 2013, when surgeons started using the ultralightweight mesh.
“Our study also confirmed several known risk factors,” Dr. Durst said, including smoking, stage IV prolapse, nonabsorbable braided suture, and heavyweight polypropylene mesh.
On multivariate regression, prior surgery for incontinence (OR, 2.87; 95% CI, 1.19-6.96), porcine acellular collagen matrix with soft polypropylene mesh (Pelvicol with soft Prolene, OR, 4.95; 95% CI, 1.70-14.42), other polypropylene mesh (OR, 6.73; 95% CI, 1.12-40.63); braided suture for vaginal mesh attachment (OR, 4.52; 95% CI, 1.53-13.37), and immediate perioperative complications (OR, 1.04; 95% CI, 1.58-8.43) all remained independent risk factors for mesh exposure, as did duration of follow-up (OR, 1.04; 95% CI, 1.03-1.06).
There was no industry funding for the study, and the investigators reported having no financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Compared with heavier mesh types, ultralightweight polypropylene (Restorelle Y) did not increase the risk of mesh erosion after sacrocolpopexy in a retrospective, case-control study.
Delayed–absorbable monofilament polydioxanone suture (PDS) also decreased the risk, compared with nonabsorbable braided suture (Ethibond Excel) for vaginal mesh attachment.
The odds ratio for the ultralightweight polypropylene mesh exposure, versus heavier mesh, was not statistically significant (odds ratio, 2.18; 95% confidence interval, 0.33-14.57), which led to the main study conclusion.
“Mesh choice and suture selection [are] important independent predictors of” erosion, she said at the annual scientific meeting of the Society of Gynecologic Surgeons. “Based on this study, surgeons should consider use of [PDS over nonabsorbable braided suture] to reduce the risk of mesh exposure when using ultralightweight mesh.”
The team also found that prior surgery for incontinence, as well as immediate postoperative complications, which likely impede healing, increase erosion risk. The findings are useful in counseling patients and perhaps guiding follow-up, at least early on. Most of the 133 erosions in the study – out of 1,247 sacrocolpopexies performed at the university from 2003 to2013 – occurred in the first year, usually in the first 3 months.
The 133 women with erosions were randomly matched with 261 women who did not have erosions after sacrocolpopexy. The erosion rate hovered around 9.5% for most years. They shot up to 19% in 2006, the first year of robot-assisted sacrocolpopexies and fell to about 6% in 2011, 4% in 2012, and 2% in 2013, when surgeons started using the ultralightweight mesh.
“Our study also confirmed several known risk factors,” Dr. Durst said, including smoking, stage IV prolapse, nonabsorbable braided suture, and heavyweight polypropylene mesh.
On multivariate regression, prior surgery for incontinence (OR, 2.87; 95% CI, 1.19-6.96), porcine acellular collagen matrix with soft polypropylene mesh (Pelvicol with soft Prolene, OR, 4.95; 95% CI, 1.70-14.42), other polypropylene mesh (OR, 6.73; 95% CI, 1.12-40.63); braided suture for vaginal mesh attachment (OR, 4.52; 95% CI, 1.53-13.37), and immediate perioperative complications (OR, 1.04; 95% CI, 1.58-8.43) all remained independent risk factors for mesh exposure, as did duration of follow-up (OR, 1.04; 95% CI, 1.03-1.06).
There was no industry funding for the study, and the investigators reported having no financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
AT SGS 2017
Key clinical point:
Major finding: The odds ratio for ultralightweight polypropylene (Restorelle Y) exposure, versus heavier polypropylene mesh, was not statistically significant (OR, 2.18; 95% CI, 0.33-14.57).
Data source: A single-center study matching 133 erosion cases to 261 controls.
Disclosures: There was no industry funding of the study, and the investigators reported no financial disclosures.
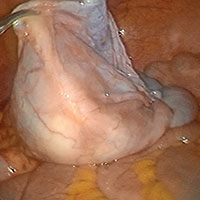
Predicting extraction of an intact uterus in robotic-assisted laparoscopic hysterectomy
SAN ANTONIO – Investigators at the University of Tennessee, Chattanooga, have come up with a simple scoring system to predict if an intact uterus can be delivered vaginally during laparoscopic hysterectomy.
Age greater than 50 years counts as 1 point and uterine length greater than 11 cm, height greater than 8 cm, and width greater than 6.9 cm each count for 3 points. A score of 4 or higher suggests the need for an alternative to vaginal extraction, they reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
The team reviewed 367 robotic-assisted total laparoscopic hysterectomies. An intact uterus was able to be extracted vaginally in 265 cases (72%); minilaparotomy was used for the rest. Uterine length, height, and width were documented from pathology reports. The scoring system correctly classified 94.6% of the cases. Sensitivity was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Factoring in parity, uterine weight, body mass index, procedure indications, tobacco use, and comorbidities did not statistically influence the predictive power.
Gynecologic surgeons “are trying to get specimens out intact” and want to know ahead of time if it’s possible, Dr. Mohling said. “I wanted to create a model that was very reproducible.”
The general benchmark for vaginal delivery of an intact uterus is size below 12 weeks pregnancy, but the University of Tennessee model is more precise, according to Dr. Mohling. “I’ve added this to my counseling,” she said.
There was no external funding for the work and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Investigators at the University of Tennessee, Chattanooga, have come up with a simple scoring system to predict if an intact uterus can be delivered vaginally during laparoscopic hysterectomy.
Age greater than 50 years counts as 1 point and uterine length greater than 11 cm, height greater than 8 cm, and width greater than 6.9 cm each count for 3 points. A score of 4 or higher suggests the need for an alternative to vaginal extraction, they reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
The team reviewed 367 robotic-assisted total laparoscopic hysterectomies. An intact uterus was able to be extracted vaginally in 265 cases (72%); minilaparotomy was used for the rest. Uterine length, height, and width were documented from pathology reports. The scoring system correctly classified 94.6% of the cases. Sensitivity was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Factoring in parity, uterine weight, body mass index, procedure indications, tobacco use, and comorbidities did not statistically influence the predictive power.
Gynecologic surgeons “are trying to get specimens out intact” and want to know ahead of time if it’s possible, Dr. Mohling said. “I wanted to create a model that was very reproducible.”
The general benchmark for vaginal delivery of an intact uterus is size below 12 weeks pregnancy, but the University of Tennessee model is more precise, according to Dr. Mohling. “I’ve added this to my counseling,” she said.
There was no external funding for the work and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Investigators at the University of Tennessee, Chattanooga, have come up with a simple scoring system to predict if an intact uterus can be delivered vaginally during laparoscopic hysterectomy.
Age greater than 50 years counts as 1 point and uterine length greater than 11 cm, height greater than 8 cm, and width greater than 6.9 cm each count for 3 points. A score of 4 or higher suggests the need for an alternative to vaginal extraction, they reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
The team reviewed 367 robotic-assisted total laparoscopic hysterectomies. An intact uterus was able to be extracted vaginally in 265 cases (72%); minilaparotomy was used for the rest. Uterine length, height, and width were documented from pathology reports. The scoring system correctly classified 94.6% of the cases. Sensitivity was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Factoring in parity, uterine weight, body mass index, procedure indications, tobacco use, and comorbidities did not statistically influence the predictive power.
Gynecologic surgeons “are trying to get specimens out intact” and want to know ahead of time if it’s possible, Dr. Mohling said. “I wanted to create a model that was very reproducible.”
The general benchmark for vaginal delivery of an intact uterus is size below 12 weeks pregnancy, but the University of Tennessee model is more precise, according to Dr. Mohling. “I’ve added this to my counseling,” she said.
There was no external funding for the work and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
AT SGS 2017
Key clinical point:
Major finding: The sensitivity of the scoring system was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Data source: Single-center review of 367 robotic total laparoscopic hysterectomies during 2012-2015.
Disclosures: There was no external funding for the work, and the investigators reported having no relevant financial disclosures.
Advanced techniques in cystectomy for mature cystic teratomas

Visit the Society of Gynecologic Surgeons online: sgsonline.org
More videos from SGS:
- Novel classification of labial anatomy and evaluation in the treatment of labial agglutination
- Strategies for prophylactic oophoropexy
- Tips and tricks for open laparoscopy
- Complete colpectomy & colpocleisis: Model for simulation
- Natural orifice sacral colpopexy
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist

Visit the Society of Gynecologic Surgeons online: sgsonline.org
More videos from SGS:
- Novel classification of labial anatomy and evaluation in the treatment of labial agglutination
- Strategies for prophylactic oophoropexy
- Tips and tricks for open laparoscopy
- Complete colpectomy & colpocleisis: Model for simulation
- Natural orifice sacral colpopexy
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist

Visit the Society of Gynecologic Surgeons online: sgsonline.org
More videos from SGS:
- Novel classification of labial anatomy and evaluation in the treatment of labial agglutination
- Strategies for prophylactic oophoropexy
- Tips and tricks for open laparoscopy
- Complete colpectomy & colpocleisis: Model for simulation
- Natural orifice sacral colpopexy
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist
This video is brought to you by
Confirmatory blood typing unnecessary for closed prolapse repairs
SAN ANTONIO – It was safe to skip preoperative blood type and antibody screening before vaginal and robotic apical prolapse surgeries at the University of North Carolina, Chapel Hill, so long as the women didn’t have hemorrhage risk factors.
The rate of blood transfusions was 0.5% for both the 204 women who had vaginal repairs and the 203 women who underwent robotic repairs; the rate of positive antibody tests was 1.6%. Given the 0.4% risk of transfusion reactions in unscreened women, the investigators calculated that the risk of serious transfusion reactions was 1 in 50,000 with closed vaginal prolapse repairs.
“The bottom line for us is that the risk in this situation is very low, even if preop type and screens are not performed, and women hemorrhage. This information provides insight to answer our key clinical question, which was if we should continue to order preop type and screens,” lead investigator Taylor Brueseke, MD, an ob.gyn. fellow at the University of North Carolina, Chapel Hill, said at the annual scientific meeting of the Society of Gynecologic Surgeons.
That question has been on the minds of gynecologic surgeons, and it’s probably never been parsed out before by route of surgery. The American College of Pathologists recommends two blood type and antibody screens from separate venipunctures before surgery. Often, the second, confirmatory test means that women have to come in even earlier on the morning of surgery and deal with another painful blood draw. It also adds a few hundred dollars to the bill.
Every surgeon needs to draw their own line between risks and benefits, Dr. Brueseke said, but it seems reasonable in many cases to skip the second screening for closed repairs. Even if a woman has a transfusion reaction, “it doesn’t mean that the patient is going to die. It’s something that you can deal with,” he said.
However, the team reached a different conclusion for women who undergo open abdominal repairs. Among the 201 cases they reviewed, 10.5% had a transfusion, which translated to a transfusion reaction risk of 1 in 2,645 for unscreened women undergoing open apical prolapse surgery. The higher hemorrhage rate was probably due to concomitant Burch procedures and other open incontinence operations.
For abdominal cases, and for women who have had prior transfusions, surgeries, or anticoagulation, “consider type and screen,” Dr. Brueseke said at the meeting.
In a separate study presented at the conference, more than 50,000 pelvic floor disorder surgeries in the National Surgery Quality Improvement Program database further defined the hemorrhage risk.
Investigators at Ohio State University, Columbus, found that the overall incidence of blood transfusions was low at 1.26%, but open abdominal procedures again increased the risk. Other factors associated with an increased risk of blood transfusion included preoperative hematocrit less than 30%, an American Society of Anesthesiologists physical status score of 3 or higher, concomitant hysterectomy, body mass index below 18.5 kg/m2, age less than 30 and over 65 years, and a history of bleeding disorders.
In the UNC study, the median Pelvic Organ Prolapse Quantification was stage III. Patients with bleeding disorders, anticoagulant use, or combined surgery with other services were excluded.
There was no industry funding for the two studies, and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
A lot of people automatically order type and screen for vaginal prolapse repairs, but we really need to rethink that if there aren’t risk factors that warrant it. I defer to the anesthesiologists because they are the ones who usually want this, but most of the time we screen but don’t use the results. There’s room to improve clinical practice here.
Robert Gutman, MD, is a gynecologic surgeon in Washington, D.C., and the program chair for the 2017 Society of Gynecologic Surgeons annual scientific meeting. He wasn’t involved in the studies presented.
A lot of people automatically order type and screen for vaginal prolapse repairs, but we really need to rethink that if there aren’t risk factors that warrant it. I defer to the anesthesiologists because they are the ones who usually want this, but most of the time we screen but don’t use the results. There’s room to improve clinical practice here.
Robert Gutman, MD, is a gynecologic surgeon in Washington, D.C., and the program chair for the 2017 Society of Gynecologic Surgeons annual scientific meeting. He wasn’t involved in the studies presented.
A lot of people automatically order type and screen for vaginal prolapse repairs, but we really need to rethink that if there aren’t risk factors that warrant it. I defer to the anesthesiologists because they are the ones who usually want this, but most of the time we screen but don’t use the results. There’s room to improve clinical practice here.
Robert Gutman, MD, is a gynecologic surgeon in Washington, D.C., and the program chair for the 2017 Society of Gynecologic Surgeons annual scientific meeting. He wasn’t involved in the studies presented.
SAN ANTONIO – It was safe to skip preoperative blood type and antibody screening before vaginal and robotic apical prolapse surgeries at the University of North Carolina, Chapel Hill, so long as the women didn’t have hemorrhage risk factors.
The rate of blood transfusions was 0.5% for both the 204 women who had vaginal repairs and the 203 women who underwent robotic repairs; the rate of positive antibody tests was 1.6%. Given the 0.4% risk of transfusion reactions in unscreened women, the investigators calculated that the risk of serious transfusion reactions was 1 in 50,000 with closed vaginal prolapse repairs.
“The bottom line for us is that the risk in this situation is very low, even if preop type and screens are not performed, and women hemorrhage. This information provides insight to answer our key clinical question, which was if we should continue to order preop type and screens,” lead investigator Taylor Brueseke, MD, an ob.gyn. fellow at the University of North Carolina, Chapel Hill, said at the annual scientific meeting of the Society of Gynecologic Surgeons.
That question has been on the minds of gynecologic surgeons, and it’s probably never been parsed out before by route of surgery. The American College of Pathologists recommends two blood type and antibody screens from separate venipunctures before surgery. Often, the second, confirmatory test means that women have to come in even earlier on the morning of surgery and deal with another painful blood draw. It also adds a few hundred dollars to the bill.
Every surgeon needs to draw their own line between risks and benefits, Dr. Brueseke said, but it seems reasonable in many cases to skip the second screening for closed repairs. Even if a woman has a transfusion reaction, “it doesn’t mean that the patient is going to die. It’s something that you can deal with,” he said.
However, the team reached a different conclusion for women who undergo open abdominal repairs. Among the 201 cases they reviewed, 10.5% had a transfusion, which translated to a transfusion reaction risk of 1 in 2,645 for unscreened women undergoing open apical prolapse surgery. The higher hemorrhage rate was probably due to concomitant Burch procedures and other open incontinence operations.
For abdominal cases, and for women who have had prior transfusions, surgeries, or anticoagulation, “consider type and screen,” Dr. Brueseke said at the meeting.
In a separate study presented at the conference, more than 50,000 pelvic floor disorder surgeries in the National Surgery Quality Improvement Program database further defined the hemorrhage risk.
Investigators at Ohio State University, Columbus, found that the overall incidence of blood transfusions was low at 1.26%, but open abdominal procedures again increased the risk. Other factors associated with an increased risk of blood transfusion included preoperative hematocrit less than 30%, an American Society of Anesthesiologists physical status score of 3 or higher, concomitant hysterectomy, body mass index below 18.5 kg/m2, age less than 30 and over 65 years, and a history of bleeding disorders.
In the UNC study, the median Pelvic Organ Prolapse Quantification was stage III. Patients with bleeding disorders, anticoagulant use, or combined surgery with other services were excluded.
There was no industry funding for the two studies, and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – It was safe to skip preoperative blood type and antibody screening before vaginal and robotic apical prolapse surgeries at the University of North Carolina, Chapel Hill, so long as the women didn’t have hemorrhage risk factors.
The rate of blood transfusions was 0.5% for both the 204 women who had vaginal repairs and the 203 women who underwent robotic repairs; the rate of positive antibody tests was 1.6%. Given the 0.4% risk of transfusion reactions in unscreened women, the investigators calculated that the risk of serious transfusion reactions was 1 in 50,000 with closed vaginal prolapse repairs.
“The bottom line for us is that the risk in this situation is very low, even if preop type and screens are not performed, and women hemorrhage. This information provides insight to answer our key clinical question, which was if we should continue to order preop type and screens,” lead investigator Taylor Brueseke, MD, an ob.gyn. fellow at the University of North Carolina, Chapel Hill, said at the annual scientific meeting of the Society of Gynecologic Surgeons.
That question has been on the minds of gynecologic surgeons, and it’s probably never been parsed out before by route of surgery. The American College of Pathologists recommends two blood type and antibody screens from separate venipunctures before surgery. Often, the second, confirmatory test means that women have to come in even earlier on the morning of surgery and deal with another painful blood draw. It also adds a few hundred dollars to the bill.
Every surgeon needs to draw their own line between risks and benefits, Dr. Brueseke said, but it seems reasonable in many cases to skip the second screening for closed repairs. Even if a woman has a transfusion reaction, “it doesn’t mean that the patient is going to die. It’s something that you can deal with,” he said.
However, the team reached a different conclusion for women who undergo open abdominal repairs. Among the 201 cases they reviewed, 10.5% had a transfusion, which translated to a transfusion reaction risk of 1 in 2,645 for unscreened women undergoing open apical prolapse surgery. The higher hemorrhage rate was probably due to concomitant Burch procedures and other open incontinence operations.
For abdominal cases, and for women who have had prior transfusions, surgeries, or anticoagulation, “consider type and screen,” Dr. Brueseke said at the meeting.
In a separate study presented at the conference, more than 50,000 pelvic floor disorder surgeries in the National Surgery Quality Improvement Program database further defined the hemorrhage risk.
Investigators at Ohio State University, Columbus, found that the overall incidence of blood transfusions was low at 1.26%, but open abdominal procedures again increased the risk. Other factors associated with an increased risk of blood transfusion included preoperative hematocrit less than 30%, an American Society of Anesthesiologists physical status score of 3 or higher, concomitant hysterectomy, body mass index below 18.5 kg/m2, age less than 30 and over 65 years, and a history of bleeding disorders.
In the UNC study, the median Pelvic Organ Prolapse Quantification was stage III. Patients with bleeding disorders, anticoagulant use, or combined surgery with other services were excluded.
There was no industry funding for the two studies, and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
Key clinical point:
Major finding: Given the 0.4% risk of transfusion reactions in unscreened women, the risk of serious transfusion reactions was 1 in 50,000 women with closed apical prolapse repairs.
Data source: A review of more than 600 cases of apical prolapse surgery at a single center.
Disclosures: There was no industry funding, and the investigators reported having no relevant financial disclosures.
Long-term durability low for nonmesh vaginal prolapse repair
SAN ANTONIO – At 5-year follow-up, outcomes were slightly better on most measures for transvaginal uterosacral ligament suspension versus transvaginal sacrospinous ligament fixation for apical prolapse, but the differences were not statistically significant, according to the first randomized trial to compare the two techniques.
Quality of life improvements were durable, but the overall 5-year success rate – defined as the absence of descent of the vaginal apex more than one-third into the vagina; anterior or posterior vaginal wall descent beyond the hymen; bothersome vaginal bulge symptoms; and further treatment for prolapse – was 39% in the 109 women randomized to bilateral uterosacral ligament suspension (ULS) and 30% in the 109 women randomized to unilateral sacrospinous ligament fixation (SSLF).
But there was a notable finding in the study. If women failed to meet all the requirements for success at any one visit, they were classified as surgical failures. However, many who missed the mark at one visit met all the requirements for success on other visits, including their last follow-up.
“We don’t think as surgeons that a bulge comes and goes on a yearly basis, but people actually moved in and out of success and failure over time, and that’s new,” Dr. Jelovsek said. “We just don’t understand the dynamic variables of anatomic prolapse, because no one’s looked at it. The assumption of ‘once a failure, always a failure’ may underestimate success rates.”
Nonetheless, using that approach in the study, the investigators found that the anatomic success was 54% in the ULS and 38% in the SSLF groups at 5 years, and 37% of women in the ULS group reported bothersome vaginal bulge symptoms, versus 42% of women with SSLF. A total of 12% of women with ULS and 8% of women with SSLF had undergone POP retreatment at 5 years, either by pessary or secondary surgery but, again, the differences were not statistically significant.
Of the 145 anatomic failures in the study, 41% were stage 3 or 4.
Quality of life improvements, assessed annually by phone, “were maintained over 5 years despite progressive increases in surgical failure rates over time,” with about a 70-point improvement in the Pelvic Organ Prolapse Distress Inventory and similar gains in other measures in both groups, Dr. Jelovsek reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
There were no between-group differences in suture exposure (about 25% in both groups) or sling erosion (about 3%) at 5 years.
There was a difference in granulation tissue: 28.9% with ULS and 18.8% with SSLF (odds ratio with ULS, 1.9; 95% confidence interval 1-3.7). The majority of adverse events occurred within 2 years of surgery.
Early pelvic floor muscle training made no difference in outcomes for the women randomized to it.
The women in the study had stage 2-4 prolapse at baseline. In addition to vaginal suspension surgery, they had vaginal hysterectomies if there was uterine prolapse, and all the women had concomitant retropubic midurethral sling surgery for stress incontinence.
At 2 years, composite success rates were about 60% in both groups (JAMA. 2014 Mar 12;311[10]:1023-34).
The study didn’t identify risk factors for failure, but they would be helpful to know, Dr. Jelovsek said. High-risk women might benefit from a more durable mesh repair. For now at least, “most women say the risk” of pain and other serious mesh complications “completely outweighs the bulge symptoms,” he said.
The trial, an extension of OPTIMAL (Operations and Pelvic Muscle Training in the Management of Apical Support Loss), was conducted at nine U.S. centers in the Pelvic Floor Disorders Network, which is funded by the National Institutes of Health. Dr. Jelovsek reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – At 5-year follow-up, outcomes were slightly better on most measures for transvaginal uterosacral ligament suspension versus transvaginal sacrospinous ligament fixation for apical prolapse, but the differences were not statistically significant, according to the first randomized trial to compare the two techniques.
Quality of life improvements were durable, but the overall 5-year success rate – defined as the absence of descent of the vaginal apex more than one-third into the vagina; anterior or posterior vaginal wall descent beyond the hymen; bothersome vaginal bulge symptoms; and further treatment for prolapse – was 39% in the 109 women randomized to bilateral uterosacral ligament suspension (ULS) and 30% in the 109 women randomized to unilateral sacrospinous ligament fixation (SSLF).
But there was a notable finding in the study. If women failed to meet all the requirements for success at any one visit, they were classified as surgical failures. However, many who missed the mark at one visit met all the requirements for success on other visits, including their last follow-up.
“We don’t think as surgeons that a bulge comes and goes on a yearly basis, but people actually moved in and out of success and failure over time, and that’s new,” Dr. Jelovsek said. “We just don’t understand the dynamic variables of anatomic prolapse, because no one’s looked at it. The assumption of ‘once a failure, always a failure’ may underestimate success rates.”
Nonetheless, using that approach in the study, the investigators found that the anatomic success was 54% in the ULS and 38% in the SSLF groups at 5 years, and 37% of women in the ULS group reported bothersome vaginal bulge symptoms, versus 42% of women with SSLF. A total of 12% of women with ULS and 8% of women with SSLF had undergone POP retreatment at 5 years, either by pessary or secondary surgery but, again, the differences were not statistically significant.
Of the 145 anatomic failures in the study, 41% were stage 3 or 4.
Quality of life improvements, assessed annually by phone, “were maintained over 5 years despite progressive increases in surgical failure rates over time,” with about a 70-point improvement in the Pelvic Organ Prolapse Distress Inventory and similar gains in other measures in both groups, Dr. Jelovsek reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
There were no between-group differences in suture exposure (about 25% in both groups) or sling erosion (about 3%) at 5 years.
There was a difference in granulation tissue: 28.9% with ULS and 18.8% with SSLF (odds ratio with ULS, 1.9; 95% confidence interval 1-3.7). The majority of adverse events occurred within 2 years of surgery.
Early pelvic floor muscle training made no difference in outcomes for the women randomized to it.
The women in the study had stage 2-4 prolapse at baseline. In addition to vaginal suspension surgery, they had vaginal hysterectomies if there was uterine prolapse, and all the women had concomitant retropubic midurethral sling surgery for stress incontinence.
At 2 years, composite success rates were about 60% in both groups (JAMA. 2014 Mar 12;311[10]:1023-34).
The study didn’t identify risk factors for failure, but they would be helpful to know, Dr. Jelovsek said. High-risk women might benefit from a more durable mesh repair. For now at least, “most women say the risk” of pain and other serious mesh complications “completely outweighs the bulge symptoms,” he said.
The trial, an extension of OPTIMAL (Operations and Pelvic Muscle Training in the Management of Apical Support Loss), was conducted at nine U.S. centers in the Pelvic Floor Disorders Network, which is funded by the National Institutes of Health. Dr. Jelovsek reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – At 5-year follow-up, outcomes were slightly better on most measures for transvaginal uterosacral ligament suspension versus transvaginal sacrospinous ligament fixation for apical prolapse, but the differences were not statistically significant, according to the first randomized trial to compare the two techniques.
Quality of life improvements were durable, but the overall 5-year success rate – defined as the absence of descent of the vaginal apex more than one-third into the vagina; anterior or posterior vaginal wall descent beyond the hymen; bothersome vaginal bulge symptoms; and further treatment for prolapse – was 39% in the 109 women randomized to bilateral uterosacral ligament suspension (ULS) and 30% in the 109 women randomized to unilateral sacrospinous ligament fixation (SSLF).
But there was a notable finding in the study. If women failed to meet all the requirements for success at any one visit, they were classified as surgical failures. However, many who missed the mark at one visit met all the requirements for success on other visits, including their last follow-up.
“We don’t think as surgeons that a bulge comes and goes on a yearly basis, but people actually moved in and out of success and failure over time, and that’s new,” Dr. Jelovsek said. “We just don’t understand the dynamic variables of anatomic prolapse, because no one’s looked at it. The assumption of ‘once a failure, always a failure’ may underestimate success rates.”
Nonetheless, using that approach in the study, the investigators found that the anatomic success was 54% in the ULS and 38% in the SSLF groups at 5 years, and 37% of women in the ULS group reported bothersome vaginal bulge symptoms, versus 42% of women with SSLF. A total of 12% of women with ULS and 8% of women with SSLF had undergone POP retreatment at 5 years, either by pessary or secondary surgery but, again, the differences were not statistically significant.
Of the 145 anatomic failures in the study, 41% were stage 3 or 4.
Quality of life improvements, assessed annually by phone, “were maintained over 5 years despite progressive increases in surgical failure rates over time,” with about a 70-point improvement in the Pelvic Organ Prolapse Distress Inventory and similar gains in other measures in both groups, Dr. Jelovsek reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
There were no between-group differences in suture exposure (about 25% in both groups) or sling erosion (about 3%) at 5 years.
There was a difference in granulation tissue: 28.9% with ULS and 18.8% with SSLF (odds ratio with ULS, 1.9; 95% confidence interval 1-3.7). The majority of adverse events occurred within 2 years of surgery.
Early pelvic floor muscle training made no difference in outcomes for the women randomized to it.
The women in the study had stage 2-4 prolapse at baseline. In addition to vaginal suspension surgery, they had vaginal hysterectomies if there was uterine prolapse, and all the women had concomitant retropubic midurethral sling surgery for stress incontinence.
At 2 years, composite success rates were about 60% in both groups (JAMA. 2014 Mar 12;311[10]:1023-34).
The study didn’t identify risk factors for failure, but they would be helpful to know, Dr. Jelovsek said. High-risk women might benefit from a more durable mesh repair. For now at least, “most women say the risk” of pain and other serious mesh complications “completely outweighs the bulge symptoms,” he said.
The trial, an extension of OPTIMAL (Operations and Pelvic Muscle Training in the Management of Apical Support Loss), was conducted at nine U.S. centers in the Pelvic Floor Disorders Network, which is funded by the National Institutes of Health. Dr. Jelovsek reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
Key clinical point:
Major finding: The overall 5-year success rate was 39% in women randomized to bilateral uterosacral ligament suspension and 30% in women randomized to unilateral sacrospinous ligament fixation.
Data source: The first randomized trial to compare the two commonly used techniques was conducted among 218 women at nine U.S. centers in the Pelvic Floor Disorders Network.
Disclosures: The Pelvic Floor Disorders Network is funded by the National Institutes of Health. The lead investigator reported having no relevant financial disclosures.