User login
Mifepristone freed of restrictions for the pandemic
Since evidence shows that medication abortion is extremely safe, why is mifepristone so restricted? And should it be? Mifepristone, used with misoprostol for medication abortion for pregnancies up to 10 weeks’ gestation, is highly regulated in the United States. Going back to 2000, when the Food and Drug Administration approved Mifeprex (brand name of mifepristone), its access was restricted under the FDA Risk Evaluation and Mitigation Strategy (REMS).
REMS is an FDA drug safety program, where certain medications with serious safety concerns are subject to restrictions intended to ensure that the benefits of the medication outweigh its risks. For example, the drug vigabatrin, with a side effect of permanent vision loss, is used to treat epilepsy. The REMS for vigabatrin requires counseling on the risk of vision loss and periodic vision monitoring.
The FDA claims that rare side effects of mifepristone – heavy vaginal bleeding, severe infection, and incomplete abortion – are risks that warrant the REMS, despite the known safety of medication abortion, with less than 1% of patients requiring emergency intervention for heavy vaginal bleeding or infection. The mifepristone REMS requires that the drug is dispensed in a hospital, clinic or medical office by a certified health care provider and not in a pharmacy as is the case with most prescribed medications, and that patients must read and sign the patient agreement form in the physical presence of the dispensing physician and may not receive counseling via telemedicine, for example.
Since FDA approval over 20 years ago, much evidence shows that the REMS is unnecessary and creates a major obstacle to access. Many clinicians cannot meet the REMS requirements. Many women must travel great distances to obtain mifepristone or delay their abortion past the acceptable gestational age for medication abortion.
In spring 2020, at the onset of the COVID-19 pandemic, the Centers for Disease Control and Prevention issued general guidance recommending use of telemedicine to limit in-person medical visits to reduce risk of exposure to the SARS-CoV-2 virus, and to ensure access to medication abortion, the ACLU filed a federal lawsuit against the FDA to suspend the requirement for in-person mifepristone dispensing. In July 2020, a Maryland District Judge granted a preliminary injunction, preventing the FDA from enforcing the in-person dispensing requirement for the duration of the declared public health emergency, allowing telemedicine medication abortion using mail or delivery service for administration of mifepristone. All other REMS requirements remained in effect.
In January 2021, the FDA appealed, seeking to reinstate the REMS. The U.S. Supreme Court, with its conservative majority, ruled to reimpose the REMS. Following this decision, a large coalition of reproductive rights groups petitioned the Biden administration to suspend the mifepristone in-person requirement during the public health emergency of the pandemic. In April 2021, the FDA announced it would use discretion and cease to enforce the in-person dispensing requirement throughout the remainder of the public health emergency.
We applaud the FDA for doing the right thing, taking the advice of numerous scientific and advocacy groups to expand access to mifepristone by at least temporarily nullifying unnecessary and burdensome restrictions that disproportionately affect people of color; young people; and people who live in rural areas, have lower incomes, and/or who are undocumented. We join the voices of numerous colleagues and organizations, including the American College of Obstetricians and Gynecologists, our premier women’s health organization, in calling for a permanent end to the mifepristone REMS.
Dr. Dale is an obstetrics and gynecology specialist in Albuquerque, N.M.; Dr. Black is an obstetrics and gynecology specialist in Albuquerque, N.M., who currently practices at the University of New Mexico Children’s Psychiatric Center, Albuquerque; and Dr. Espey is professor and chair of the department of ob.gyn. and family planning, and fellowship director at the University of New Mexico, Albuquerque.
This article was updated 8/24/21.
Since evidence shows that medication abortion is extremely safe, why is mifepristone so restricted? And should it be? Mifepristone, used with misoprostol for medication abortion for pregnancies up to 10 weeks’ gestation, is highly regulated in the United States. Going back to 2000, when the Food and Drug Administration approved Mifeprex (brand name of mifepristone), its access was restricted under the FDA Risk Evaluation and Mitigation Strategy (REMS).
REMS is an FDA drug safety program, where certain medications with serious safety concerns are subject to restrictions intended to ensure that the benefits of the medication outweigh its risks. For example, the drug vigabatrin, with a side effect of permanent vision loss, is used to treat epilepsy. The REMS for vigabatrin requires counseling on the risk of vision loss and periodic vision monitoring.
The FDA claims that rare side effects of mifepristone – heavy vaginal bleeding, severe infection, and incomplete abortion – are risks that warrant the REMS, despite the known safety of medication abortion, with less than 1% of patients requiring emergency intervention for heavy vaginal bleeding or infection. The mifepristone REMS requires that the drug is dispensed in a hospital, clinic or medical office by a certified health care provider and not in a pharmacy as is the case with most prescribed medications, and that patients must read and sign the patient agreement form in the physical presence of the dispensing physician and may not receive counseling via telemedicine, for example.
Since FDA approval over 20 years ago, much evidence shows that the REMS is unnecessary and creates a major obstacle to access. Many clinicians cannot meet the REMS requirements. Many women must travel great distances to obtain mifepristone or delay their abortion past the acceptable gestational age for medication abortion.
In spring 2020, at the onset of the COVID-19 pandemic, the Centers for Disease Control and Prevention issued general guidance recommending use of telemedicine to limit in-person medical visits to reduce risk of exposure to the SARS-CoV-2 virus, and to ensure access to medication abortion, the ACLU filed a federal lawsuit against the FDA to suspend the requirement for in-person mifepristone dispensing. In July 2020, a Maryland District Judge granted a preliminary injunction, preventing the FDA from enforcing the in-person dispensing requirement for the duration of the declared public health emergency, allowing telemedicine medication abortion using mail or delivery service for administration of mifepristone. All other REMS requirements remained in effect.
In January 2021, the FDA appealed, seeking to reinstate the REMS. The U.S. Supreme Court, with its conservative majority, ruled to reimpose the REMS. Following this decision, a large coalition of reproductive rights groups petitioned the Biden administration to suspend the mifepristone in-person requirement during the public health emergency of the pandemic. In April 2021, the FDA announced it would use discretion and cease to enforce the in-person dispensing requirement throughout the remainder of the public health emergency.
We applaud the FDA for doing the right thing, taking the advice of numerous scientific and advocacy groups to expand access to mifepristone by at least temporarily nullifying unnecessary and burdensome restrictions that disproportionately affect people of color; young people; and people who live in rural areas, have lower incomes, and/or who are undocumented. We join the voices of numerous colleagues and organizations, including the American College of Obstetricians and Gynecologists, our premier women’s health organization, in calling for a permanent end to the mifepristone REMS.
Dr. Dale is an obstetrics and gynecology specialist in Albuquerque, N.M.; Dr. Black is an obstetrics and gynecology specialist in Albuquerque, N.M., who currently practices at the University of New Mexico Children’s Psychiatric Center, Albuquerque; and Dr. Espey is professor and chair of the department of ob.gyn. and family planning, and fellowship director at the University of New Mexico, Albuquerque.
This article was updated 8/24/21.
Since evidence shows that medication abortion is extremely safe, why is mifepristone so restricted? And should it be? Mifepristone, used with misoprostol for medication abortion for pregnancies up to 10 weeks’ gestation, is highly regulated in the United States. Going back to 2000, when the Food and Drug Administration approved Mifeprex (brand name of mifepristone), its access was restricted under the FDA Risk Evaluation and Mitigation Strategy (REMS).
REMS is an FDA drug safety program, where certain medications with serious safety concerns are subject to restrictions intended to ensure that the benefits of the medication outweigh its risks. For example, the drug vigabatrin, with a side effect of permanent vision loss, is used to treat epilepsy. The REMS for vigabatrin requires counseling on the risk of vision loss and periodic vision monitoring.
The FDA claims that rare side effects of mifepristone – heavy vaginal bleeding, severe infection, and incomplete abortion – are risks that warrant the REMS, despite the known safety of medication abortion, with less than 1% of patients requiring emergency intervention for heavy vaginal bleeding or infection. The mifepristone REMS requires that the drug is dispensed in a hospital, clinic or medical office by a certified health care provider and not in a pharmacy as is the case with most prescribed medications, and that patients must read and sign the patient agreement form in the physical presence of the dispensing physician and may not receive counseling via telemedicine, for example.
Since FDA approval over 20 years ago, much evidence shows that the REMS is unnecessary and creates a major obstacle to access. Many clinicians cannot meet the REMS requirements. Many women must travel great distances to obtain mifepristone or delay their abortion past the acceptable gestational age for medication abortion.
In spring 2020, at the onset of the COVID-19 pandemic, the Centers for Disease Control and Prevention issued general guidance recommending use of telemedicine to limit in-person medical visits to reduce risk of exposure to the SARS-CoV-2 virus, and to ensure access to medication abortion, the ACLU filed a federal lawsuit against the FDA to suspend the requirement for in-person mifepristone dispensing. In July 2020, a Maryland District Judge granted a preliminary injunction, preventing the FDA from enforcing the in-person dispensing requirement for the duration of the declared public health emergency, allowing telemedicine medication abortion using mail or delivery service for administration of mifepristone. All other REMS requirements remained in effect.
In January 2021, the FDA appealed, seeking to reinstate the REMS. The U.S. Supreme Court, with its conservative majority, ruled to reimpose the REMS. Following this decision, a large coalition of reproductive rights groups petitioned the Biden administration to suspend the mifepristone in-person requirement during the public health emergency of the pandemic. In April 2021, the FDA announced it would use discretion and cease to enforce the in-person dispensing requirement throughout the remainder of the public health emergency.
We applaud the FDA for doing the right thing, taking the advice of numerous scientific and advocacy groups to expand access to mifepristone by at least temporarily nullifying unnecessary and burdensome restrictions that disproportionately affect people of color; young people; and people who live in rural areas, have lower incomes, and/or who are undocumented. We join the voices of numerous colleagues and organizations, including the American College of Obstetricians and Gynecologists, our premier women’s health organization, in calling for a permanent end to the mifepristone REMS.
Dr. Dale is an obstetrics and gynecology specialist in Albuquerque, N.M.; Dr. Black is an obstetrics and gynecology specialist in Albuquerque, N.M., who currently practices at the University of New Mexico Children’s Psychiatric Center, Albuquerque; and Dr. Espey is professor and chair of the department of ob.gyn. and family planning, and fellowship director at the University of New Mexico, Albuquerque.
This article was updated 8/24/21.
Toward a clearer risk model for postpartum psychosis
Postpartum depression, in many respects, has become a household term. Over the last decade, there has been increasing awareness of the importance of screening for postpartum depression, with increased systematic screening across clinical settings where care is delivered to women during pregnancy and the postpartum period. There have also been greater efforts to identify women who are suffering postpartum depression and to support them with appropriate clinical interventions, whether through psychotherapy and/or pharmacologic therapy. Clinical interventions are supplemented by the increasing awareness of the value of community-based support groups for women who are suffering from postpartum mood and anxiety disorders.
Despite the growing, appropriate focus on recognition and acute treatment of postpartum depression as well as assessing clinical outcomes for those who suffer from postpartum mood and anxiety disorders, less attention has been given to postpartum psychosis, the most severe form of postpartum depression. It is indeed, the least common postpartum psychiatric syndrome (1 in 1,000 births) and comes to public attention when there has been a tragedy during the acute postpartum period such as maternal suicide or infanticide. In this sense, postpartum psychosis is ironically an underappreciated clinical entity across America given its severity, the effect it has on longer-term psychiatric morbidity, and its effect on children and families.
Our group at the Center for Women’s Mental Health has been interested in postpartum psychosis for years and started the Postpartum Psychosis Project in an effort to better understand the phenomenology, course, treatment, outcome, and genomic underpinnings of postpartum psychosis. Risk factors that are well established for postpartum psychosis have been described and overwhelmingly include patients with bipolar disorder. The risk for recurrent postpartum psychosis in women who have had a previous episode is as great as 75%-90% in the absence of prophylactic intervention. With that said, we are extremely interested in understanding the etiology of postpartum psychosis. Various studies over the last 5 years have looked at a whole host of psychosocial as well as neurobiologic variables that may contribute to risk for postpartum psychosis, including dysregulation of the stress axis, heightened inflammation as well as a history of child adversity and heightened experience of stress during the perinatal period.
There have also been anecdotal reports during Virtual Rounds at the Center for Women’s Mental Health of higher recent rates of postpartum psychosis manifesting during the postpartum period. This is a clinical observation and has not been systematically studied. However, one can wonder whether the experience of the pandemic has constituted a stressor for at-risk women, tipping the scales toward women becoming ill, or whether clinicians are seeing this finding more because of our ability to observe it more within the context of the pandemic.
Precise quantification of risk for postpartum psychosis is complicated; as noted, women with bipolar disorder have a predictably high risk for getting ill during the postpartum period and many go on to have clinical courses consistent with recurrent bipolar disorder. However, there are other women who have circumscribed episodes of psychotic illness in the postpartum period who recover and are totally well without any evidence of psychiatric disorder until they have another child, at which time the risk for recurrence of postpartum psychosis is very high. Interest in developing a model of risk that could reliably predict an illness as serious as postpartum psychosis is on the minds of researchers around the world.
One recent study that highlights the multiple factors involved in risk of postpartum psychosis involved a prospective longitudinal study of a group of women who were followed across the peripartum period from the third trimester until 4 weeks postpartum. In this group, 51 women were at increased risk for postpartum psychosis based on their diagnosis of bipolar disorder, schizoaffective disorder, or a previous episode of postpartum psychosis. These women were matched with a control group with no past or current diagnosis of psychiatric disorder or family history of postpartum psychosis. The findings suggested that women at risk for postpartum psychosis who experienced a psychiatric relapse during the first 4 weeks postpartum relative to women at risk who remained well had histories of severe childhood adversity as well as biomarkers consistent with a dysregulated stress axis (a statistically higher daily cortisol level). This is consistent with other data that have implicated the complex role between psychosocial variables as well as neurobiologic variables, such as a dysregulation in the hypothalamic pituitary adrenal axis and other studies that suggest that dysregulated inflammatory status may also drive risk for postpartum psychosis (Hazelgrove K et al. Psychoneuroendocrinology. 2021 Jun. doi: 10.1016/j.psyneuen.2021.105218).
At the end of the day, postpartum psychosis is a psychiatric and obstetrical emergency. In our center, it is rare for women not to be hospitalized with this condition to ensure the safety of the mother as well as her newborn, and to also get her recompensated and functioning as quickly and as significantly as possible. However, an interesting extrapolation of the findings noted by Hazelgrove and colleagues is that it raises the question of what effective treatments might be used to mitigate risk for those at greatest risk for postpartum psychosis. For example, are there other treatments over and above the few effective ones that have been studied as prophylactic pharmacologic interventions that might mitigate risk for recurrence of an illness as serious as postpartum psychosis?
The data suggesting dysregulation of the stress axis as a predictor variable for risk in women vulnerable to postpartum psychosis opens an array of opportunities that are nonpharmacologic, such as mindfulness-based cognitive therapy or other interventions that help to modulate the stress axis. This is a terrific opportunity to have pharmacologic intervention meet nonpharmacologic intervention to potentially mitigate risk for postpartum psychosis with its attendant serious sequelae.
In our own work, where we are evaluating genomic data in an extremely well-characterized group of women with known histories of postpartum psychosis, we are interested to see if we can enhance understanding of the model of risk for postpartum psychosis by factoring in genomic underpinning, history of diagnosis, and psychosocial variables to optimally craft interventions for this population of at-risk women. This brings us one step closer to the future in women’s mental health, to the practice of “precision reproductive psychiatry,” matching interventions to specific presentations across perinatal populations.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at obnews@mdedge.com.
Postpartum depression, in many respects, has become a household term. Over the last decade, there has been increasing awareness of the importance of screening for postpartum depression, with increased systematic screening across clinical settings where care is delivered to women during pregnancy and the postpartum period. There have also been greater efforts to identify women who are suffering postpartum depression and to support them with appropriate clinical interventions, whether through psychotherapy and/or pharmacologic therapy. Clinical interventions are supplemented by the increasing awareness of the value of community-based support groups for women who are suffering from postpartum mood and anxiety disorders.
Despite the growing, appropriate focus on recognition and acute treatment of postpartum depression as well as assessing clinical outcomes for those who suffer from postpartum mood and anxiety disorders, less attention has been given to postpartum psychosis, the most severe form of postpartum depression. It is indeed, the least common postpartum psychiatric syndrome (1 in 1,000 births) and comes to public attention when there has been a tragedy during the acute postpartum period such as maternal suicide or infanticide. In this sense, postpartum psychosis is ironically an underappreciated clinical entity across America given its severity, the effect it has on longer-term psychiatric morbidity, and its effect on children and families.
Our group at the Center for Women’s Mental Health has been interested in postpartum psychosis for years and started the Postpartum Psychosis Project in an effort to better understand the phenomenology, course, treatment, outcome, and genomic underpinnings of postpartum psychosis. Risk factors that are well established for postpartum psychosis have been described and overwhelmingly include patients with bipolar disorder. The risk for recurrent postpartum psychosis in women who have had a previous episode is as great as 75%-90% in the absence of prophylactic intervention. With that said, we are extremely interested in understanding the etiology of postpartum psychosis. Various studies over the last 5 years have looked at a whole host of psychosocial as well as neurobiologic variables that may contribute to risk for postpartum psychosis, including dysregulation of the stress axis, heightened inflammation as well as a history of child adversity and heightened experience of stress during the perinatal period.
There have also been anecdotal reports during Virtual Rounds at the Center for Women’s Mental Health of higher recent rates of postpartum psychosis manifesting during the postpartum period. This is a clinical observation and has not been systematically studied. However, one can wonder whether the experience of the pandemic has constituted a stressor for at-risk women, tipping the scales toward women becoming ill, or whether clinicians are seeing this finding more because of our ability to observe it more within the context of the pandemic.
Precise quantification of risk for postpartum psychosis is complicated; as noted, women with bipolar disorder have a predictably high risk for getting ill during the postpartum period and many go on to have clinical courses consistent with recurrent bipolar disorder. However, there are other women who have circumscribed episodes of psychotic illness in the postpartum period who recover and are totally well without any evidence of psychiatric disorder until they have another child, at which time the risk for recurrence of postpartum psychosis is very high. Interest in developing a model of risk that could reliably predict an illness as serious as postpartum psychosis is on the minds of researchers around the world.
One recent study that highlights the multiple factors involved in risk of postpartum psychosis involved a prospective longitudinal study of a group of women who were followed across the peripartum period from the third trimester until 4 weeks postpartum. In this group, 51 women were at increased risk for postpartum psychosis based on their diagnosis of bipolar disorder, schizoaffective disorder, or a previous episode of postpartum psychosis. These women were matched with a control group with no past or current diagnosis of psychiatric disorder or family history of postpartum psychosis. The findings suggested that women at risk for postpartum psychosis who experienced a psychiatric relapse during the first 4 weeks postpartum relative to women at risk who remained well had histories of severe childhood adversity as well as biomarkers consistent with a dysregulated stress axis (a statistically higher daily cortisol level). This is consistent with other data that have implicated the complex role between psychosocial variables as well as neurobiologic variables, such as a dysregulation in the hypothalamic pituitary adrenal axis and other studies that suggest that dysregulated inflammatory status may also drive risk for postpartum psychosis (Hazelgrove K et al. Psychoneuroendocrinology. 2021 Jun. doi: 10.1016/j.psyneuen.2021.105218).
At the end of the day, postpartum psychosis is a psychiatric and obstetrical emergency. In our center, it is rare for women not to be hospitalized with this condition to ensure the safety of the mother as well as her newborn, and to also get her recompensated and functioning as quickly and as significantly as possible. However, an interesting extrapolation of the findings noted by Hazelgrove and colleagues is that it raises the question of what effective treatments might be used to mitigate risk for those at greatest risk for postpartum psychosis. For example, are there other treatments over and above the few effective ones that have been studied as prophylactic pharmacologic interventions that might mitigate risk for recurrence of an illness as serious as postpartum psychosis?
The data suggesting dysregulation of the stress axis as a predictor variable for risk in women vulnerable to postpartum psychosis opens an array of opportunities that are nonpharmacologic, such as mindfulness-based cognitive therapy or other interventions that help to modulate the stress axis. This is a terrific opportunity to have pharmacologic intervention meet nonpharmacologic intervention to potentially mitigate risk for postpartum psychosis with its attendant serious sequelae.
In our own work, where we are evaluating genomic data in an extremely well-characterized group of women with known histories of postpartum psychosis, we are interested to see if we can enhance understanding of the model of risk for postpartum psychosis by factoring in genomic underpinning, history of diagnosis, and psychosocial variables to optimally craft interventions for this population of at-risk women. This brings us one step closer to the future in women’s mental health, to the practice of “precision reproductive psychiatry,” matching interventions to specific presentations across perinatal populations.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at obnews@mdedge.com.
Postpartum depression, in many respects, has become a household term. Over the last decade, there has been increasing awareness of the importance of screening for postpartum depression, with increased systematic screening across clinical settings where care is delivered to women during pregnancy and the postpartum period. There have also been greater efforts to identify women who are suffering postpartum depression and to support them with appropriate clinical interventions, whether through psychotherapy and/or pharmacologic therapy. Clinical interventions are supplemented by the increasing awareness of the value of community-based support groups for women who are suffering from postpartum mood and anxiety disorders.
Despite the growing, appropriate focus on recognition and acute treatment of postpartum depression as well as assessing clinical outcomes for those who suffer from postpartum mood and anxiety disorders, less attention has been given to postpartum psychosis, the most severe form of postpartum depression. It is indeed, the least common postpartum psychiatric syndrome (1 in 1,000 births) and comes to public attention when there has been a tragedy during the acute postpartum period such as maternal suicide or infanticide. In this sense, postpartum psychosis is ironically an underappreciated clinical entity across America given its severity, the effect it has on longer-term psychiatric morbidity, and its effect on children and families.
Our group at the Center for Women’s Mental Health has been interested in postpartum psychosis for years and started the Postpartum Psychosis Project in an effort to better understand the phenomenology, course, treatment, outcome, and genomic underpinnings of postpartum psychosis. Risk factors that are well established for postpartum psychosis have been described and overwhelmingly include patients with bipolar disorder. The risk for recurrent postpartum psychosis in women who have had a previous episode is as great as 75%-90% in the absence of prophylactic intervention. With that said, we are extremely interested in understanding the etiology of postpartum psychosis. Various studies over the last 5 years have looked at a whole host of psychosocial as well as neurobiologic variables that may contribute to risk for postpartum psychosis, including dysregulation of the stress axis, heightened inflammation as well as a history of child adversity and heightened experience of stress during the perinatal period.
There have also been anecdotal reports during Virtual Rounds at the Center for Women’s Mental Health of higher recent rates of postpartum psychosis manifesting during the postpartum period. This is a clinical observation and has not been systematically studied. However, one can wonder whether the experience of the pandemic has constituted a stressor for at-risk women, tipping the scales toward women becoming ill, or whether clinicians are seeing this finding more because of our ability to observe it more within the context of the pandemic.
Precise quantification of risk for postpartum psychosis is complicated; as noted, women with bipolar disorder have a predictably high risk for getting ill during the postpartum period and many go on to have clinical courses consistent with recurrent bipolar disorder. However, there are other women who have circumscribed episodes of psychotic illness in the postpartum period who recover and are totally well without any evidence of psychiatric disorder until they have another child, at which time the risk for recurrence of postpartum psychosis is very high. Interest in developing a model of risk that could reliably predict an illness as serious as postpartum psychosis is on the minds of researchers around the world.
One recent study that highlights the multiple factors involved in risk of postpartum psychosis involved a prospective longitudinal study of a group of women who were followed across the peripartum period from the third trimester until 4 weeks postpartum. In this group, 51 women were at increased risk for postpartum psychosis based on their diagnosis of bipolar disorder, schizoaffective disorder, or a previous episode of postpartum psychosis. These women were matched with a control group with no past or current diagnosis of psychiatric disorder or family history of postpartum psychosis. The findings suggested that women at risk for postpartum psychosis who experienced a psychiatric relapse during the first 4 weeks postpartum relative to women at risk who remained well had histories of severe childhood adversity as well as biomarkers consistent with a dysregulated stress axis (a statistically higher daily cortisol level). This is consistent with other data that have implicated the complex role between psychosocial variables as well as neurobiologic variables, such as a dysregulation in the hypothalamic pituitary adrenal axis and other studies that suggest that dysregulated inflammatory status may also drive risk for postpartum psychosis (Hazelgrove K et al. Psychoneuroendocrinology. 2021 Jun. doi: 10.1016/j.psyneuen.2021.105218).
At the end of the day, postpartum psychosis is a psychiatric and obstetrical emergency. In our center, it is rare for women not to be hospitalized with this condition to ensure the safety of the mother as well as her newborn, and to also get her recompensated and functioning as quickly and as significantly as possible. However, an interesting extrapolation of the findings noted by Hazelgrove and colleagues is that it raises the question of what effective treatments might be used to mitigate risk for those at greatest risk for postpartum psychosis. For example, are there other treatments over and above the few effective ones that have been studied as prophylactic pharmacologic interventions that might mitigate risk for recurrence of an illness as serious as postpartum psychosis?
The data suggesting dysregulation of the stress axis as a predictor variable for risk in women vulnerable to postpartum psychosis opens an array of opportunities that are nonpharmacologic, such as mindfulness-based cognitive therapy or other interventions that help to modulate the stress axis. This is a terrific opportunity to have pharmacologic intervention meet nonpharmacologic intervention to potentially mitigate risk for postpartum psychosis with its attendant serious sequelae.
In our own work, where we are evaluating genomic data in an extremely well-characterized group of women with known histories of postpartum psychosis, we are interested to see if we can enhance understanding of the model of risk for postpartum psychosis by factoring in genomic underpinning, history of diagnosis, and psychosocial variables to optimally craft interventions for this population of at-risk women. This brings us one step closer to the future in women’s mental health, to the practice of “precision reproductive psychiatry,” matching interventions to specific presentations across perinatal populations.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at obnews@mdedge.com.
Preterm and early term birth linked to an increased risk of autism
Preterm and early birth is associated with an increased risk of autism independent of genetic or environmental factors, according to new research published in Pediatrics.
Although previous studies have linked preterm births to an increased risk of autism – one 2017 study published in Cerebral Cortex found that 27.4% of the children born extremely preterm were diagnosed with autism – Casey Crump, MD, PhD, said potential causality, sex-specific differences, and association with early-term births were still unclear.
“Preterm birth had previously been linked with higher risk of autism; however, several important questions remained unanswered,” said Dr. Crump, professor and vice chair for research at the department of family medicine and community health and professor of epidemiology in the department of population health science and policy at Icahn School of Medicine at Mount Sinai New York. “To our knowledge, [our study] is the largest to date of gestational age at birth in relation to autism, and one of the first to investigate sex-specific differences, early term birth, or the influence of shared familial factors.”
Dr. Crump and colleagues examined data from more than 4 million infants born in Sweden between 1973 and 2013 who were followed-up for autism spectrum disorder identified from nationwide outpatient and inpatient diagnoses through December 2015. Children born between 22 and 27 weeks were considered extremely preterm, those born between 28 and 33 week were characterized as very to moderate preterm, and those born between 34 and 36 weeks were considered late preterm. Early-term births are characterized as infants born between 37 and 38 weeks and children born between 39 and 41 weeks were considered term births.
They found that 6.1% of those born extremely preterm were diagnosed with autism. Meanwhile, autism spectrum disorder prevalences were 2.6% for very to moderate preterm, 1.9% for late preterm, 2.1% for all preterm, and 1.6% for early term, compared with 1.4% for term birth.
The researchers’ analysis showed that preterm and early birth were associated with a significantly increased risk of autism in males and females. Children who were born extremely preterm had an approximately fourfold increased risk of autism. Researchers also found that each additional week of gestation was associated with a 5% lower prevalence of autism spectrum disorder (ASD) on average.
“The elevated risk even in [late preterm] infants is not completely surprising because a number of investigators have shown higher incidences of early cognitive, language motor and impairment, and school problems ... and psychiatric disorders, some of which may extend to adulthood,” Elisabeth McGowan, MD, who was not involved in the study, said in a solicited editorial commentary about the study.
Dr. Crump believes the association between preterm birth and autism may be because of increased inflammatory marker levels. A 2009 study published in Reproductive Sciences found that increased proinflammatory cytokine levels have been associated with the timing and initiation of preterm birth, and also have been detected in the brain and cerebrospinal fluid of individuals with autism “and may play a key role in its pathogenesis,” Dr. Crump said.
“Inflammatory-driven alteration of neuronal connections during critical periods of brain development may be central to the development of autism,” Dr. Crump explained.
However, Dr. Crump said that, although the relative risks of autism were higher in those born preterm, the absolute risk of the condition is low.
“The report by Crump is in many ways a definitive accounting of the elevated rates of ASD in preterm infants,” said Dr. McGowan, associate professor of pediatrics at the Women and Infants Hospital, Providence, R.I. “And although the impact of prematurity on brain development may be part of the causal chain resulting in ASD (or other neurodevelopmental outcomes), these factors are operating in a complex biological landscape, with pathways to ASD outcomes that can be expected to be heterogeneous.”
ASD is a developmental condition that affects about 1 in 54 children, according to the Centers for Disease Control and Prevention. Many children are not diagnosed with ASD until later in childhood, which in some cases delays treatment and early intervention. ASD may be detected as early as 18 months, but the average age of diagnosis for ASD is 4.3 years, according to the CDC.
“Children born prematurely need early evaluation and long-term follow-up to facilitate timely detection and treatment of autism, especially those born at the earliest gestational ages,” Dr. Crump said in an interview. “In patients of all ages, gestational age at birth should be routinely included in history-taking and medical records to help identify in clinical practice those born preterm or early term. Such information can provide additional valuable context for understanding patients’ health and may facilitate earlier evaluation for autism and other neurodevelopmental conditions in those born prematurely.”
Dr. Crump and colleagues said more research is needed to understand the biologic mechanisms linking preterm birth with higher risks of autism, which “may reveal new targets for intervention at critical windows of neurodevelopment to improve the disease trajectory.”
Experts interviewed did not disclose any relevant financial relationships.
Preterm and early birth is associated with an increased risk of autism independent of genetic or environmental factors, according to new research published in Pediatrics.
Although previous studies have linked preterm births to an increased risk of autism – one 2017 study published in Cerebral Cortex found that 27.4% of the children born extremely preterm were diagnosed with autism – Casey Crump, MD, PhD, said potential causality, sex-specific differences, and association with early-term births were still unclear.
“Preterm birth had previously been linked with higher risk of autism; however, several important questions remained unanswered,” said Dr. Crump, professor and vice chair for research at the department of family medicine and community health and professor of epidemiology in the department of population health science and policy at Icahn School of Medicine at Mount Sinai New York. “To our knowledge, [our study] is the largest to date of gestational age at birth in relation to autism, and one of the first to investigate sex-specific differences, early term birth, or the influence of shared familial factors.”
Dr. Crump and colleagues examined data from more than 4 million infants born in Sweden between 1973 and 2013 who were followed-up for autism spectrum disorder identified from nationwide outpatient and inpatient diagnoses through December 2015. Children born between 22 and 27 weeks were considered extremely preterm, those born between 28 and 33 week were characterized as very to moderate preterm, and those born between 34 and 36 weeks were considered late preterm. Early-term births are characterized as infants born between 37 and 38 weeks and children born between 39 and 41 weeks were considered term births.
They found that 6.1% of those born extremely preterm were diagnosed with autism. Meanwhile, autism spectrum disorder prevalences were 2.6% for very to moderate preterm, 1.9% for late preterm, 2.1% for all preterm, and 1.6% for early term, compared with 1.4% for term birth.
The researchers’ analysis showed that preterm and early birth were associated with a significantly increased risk of autism in males and females. Children who were born extremely preterm had an approximately fourfold increased risk of autism. Researchers also found that each additional week of gestation was associated with a 5% lower prevalence of autism spectrum disorder (ASD) on average.
“The elevated risk even in [late preterm] infants is not completely surprising because a number of investigators have shown higher incidences of early cognitive, language motor and impairment, and school problems ... and psychiatric disorders, some of which may extend to adulthood,” Elisabeth McGowan, MD, who was not involved in the study, said in a solicited editorial commentary about the study.
Dr. Crump believes the association between preterm birth and autism may be because of increased inflammatory marker levels. A 2009 study published in Reproductive Sciences found that increased proinflammatory cytokine levels have been associated with the timing and initiation of preterm birth, and also have been detected in the brain and cerebrospinal fluid of individuals with autism “and may play a key role in its pathogenesis,” Dr. Crump said.
“Inflammatory-driven alteration of neuronal connections during critical periods of brain development may be central to the development of autism,” Dr. Crump explained.
However, Dr. Crump said that, although the relative risks of autism were higher in those born preterm, the absolute risk of the condition is low.
“The report by Crump is in many ways a definitive accounting of the elevated rates of ASD in preterm infants,” said Dr. McGowan, associate professor of pediatrics at the Women and Infants Hospital, Providence, R.I. “And although the impact of prematurity on brain development may be part of the causal chain resulting in ASD (or other neurodevelopmental outcomes), these factors are operating in a complex biological landscape, with pathways to ASD outcomes that can be expected to be heterogeneous.”
ASD is a developmental condition that affects about 1 in 54 children, according to the Centers for Disease Control and Prevention. Many children are not diagnosed with ASD until later in childhood, which in some cases delays treatment and early intervention. ASD may be detected as early as 18 months, but the average age of diagnosis for ASD is 4.3 years, according to the CDC.
“Children born prematurely need early evaluation and long-term follow-up to facilitate timely detection and treatment of autism, especially those born at the earliest gestational ages,” Dr. Crump said in an interview. “In patients of all ages, gestational age at birth should be routinely included in history-taking and medical records to help identify in clinical practice those born preterm or early term. Such information can provide additional valuable context for understanding patients’ health and may facilitate earlier evaluation for autism and other neurodevelopmental conditions in those born prematurely.”
Dr. Crump and colleagues said more research is needed to understand the biologic mechanisms linking preterm birth with higher risks of autism, which “may reveal new targets for intervention at critical windows of neurodevelopment to improve the disease trajectory.”
Experts interviewed did not disclose any relevant financial relationships.
Preterm and early birth is associated with an increased risk of autism independent of genetic or environmental factors, according to new research published in Pediatrics.
Although previous studies have linked preterm births to an increased risk of autism – one 2017 study published in Cerebral Cortex found that 27.4% of the children born extremely preterm were diagnosed with autism – Casey Crump, MD, PhD, said potential causality, sex-specific differences, and association with early-term births were still unclear.
“Preterm birth had previously been linked with higher risk of autism; however, several important questions remained unanswered,” said Dr. Crump, professor and vice chair for research at the department of family medicine and community health and professor of epidemiology in the department of population health science and policy at Icahn School of Medicine at Mount Sinai New York. “To our knowledge, [our study] is the largest to date of gestational age at birth in relation to autism, and one of the first to investigate sex-specific differences, early term birth, or the influence of shared familial factors.”
Dr. Crump and colleagues examined data from more than 4 million infants born in Sweden between 1973 and 2013 who were followed-up for autism spectrum disorder identified from nationwide outpatient and inpatient diagnoses through December 2015. Children born between 22 and 27 weeks were considered extremely preterm, those born between 28 and 33 week were characterized as very to moderate preterm, and those born between 34 and 36 weeks were considered late preterm. Early-term births are characterized as infants born between 37 and 38 weeks and children born between 39 and 41 weeks were considered term births.
They found that 6.1% of those born extremely preterm were diagnosed with autism. Meanwhile, autism spectrum disorder prevalences were 2.6% for very to moderate preterm, 1.9% for late preterm, 2.1% for all preterm, and 1.6% for early term, compared with 1.4% for term birth.
The researchers’ analysis showed that preterm and early birth were associated with a significantly increased risk of autism in males and females. Children who were born extremely preterm had an approximately fourfold increased risk of autism. Researchers also found that each additional week of gestation was associated with a 5% lower prevalence of autism spectrum disorder (ASD) on average.
“The elevated risk even in [late preterm] infants is not completely surprising because a number of investigators have shown higher incidences of early cognitive, language motor and impairment, and school problems ... and psychiatric disorders, some of which may extend to adulthood,” Elisabeth McGowan, MD, who was not involved in the study, said in a solicited editorial commentary about the study.
Dr. Crump believes the association between preterm birth and autism may be because of increased inflammatory marker levels. A 2009 study published in Reproductive Sciences found that increased proinflammatory cytokine levels have been associated with the timing and initiation of preterm birth, and also have been detected in the brain and cerebrospinal fluid of individuals with autism “and may play a key role in its pathogenesis,” Dr. Crump said.
“Inflammatory-driven alteration of neuronal connections during critical periods of brain development may be central to the development of autism,” Dr. Crump explained.
However, Dr. Crump said that, although the relative risks of autism were higher in those born preterm, the absolute risk of the condition is low.
“The report by Crump is in many ways a definitive accounting of the elevated rates of ASD in preterm infants,” said Dr. McGowan, associate professor of pediatrics at the Women and Infants Hospital, Providence, R.I. “And although the impact of prematurity on brain development may be part of the causal chain resulting in ASD (or other neurodevelopmental outcomes), these factors are operating in a complex biological landscape, with pathways to ASD outcomes that can be expected to be heterogeneous.”
ASD is a developmental condition that affects about 1 in 54 children, according to the Centers for Disease Control and Prevention. Many children are not diagnosed with ASD until later in childhood, which in some cases delays treatment and early intervention. ASD may be detected as early as 18 months, but the average age of diagnosis for ASD is 4.3 years, according to the CDC.
“Children born prematurely need early evaluation and long-term follow-up to facilitate timely detection and treatment of autism, especially those born at the earliest gestational ages,” Dr. Crump said in an interview. “In patients of all ages, gestational age at birth should be routinely included in history-taking and medical records to help identify in clinical practice those born preterm or early term. Such information can provide additional valuable context for understanding patients’ health and may facilitate earlier evaluation for autism and other neurodevelopmental conditions in those born prematurely.”
Dr. Crump and colleagues said more research is needed to understand the biologic mechanisms linking preterm birth with higher risks of autism, which “may reveal new targets for intervention at critical windows of neurodevelopment to improve the disease trajectory.”
Experts interviewed did not disclose any relevant financial relationships.
FROM PEDIATRICS
‘Reassuring’ findings for second-generation antipsychotics during pregnancy
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
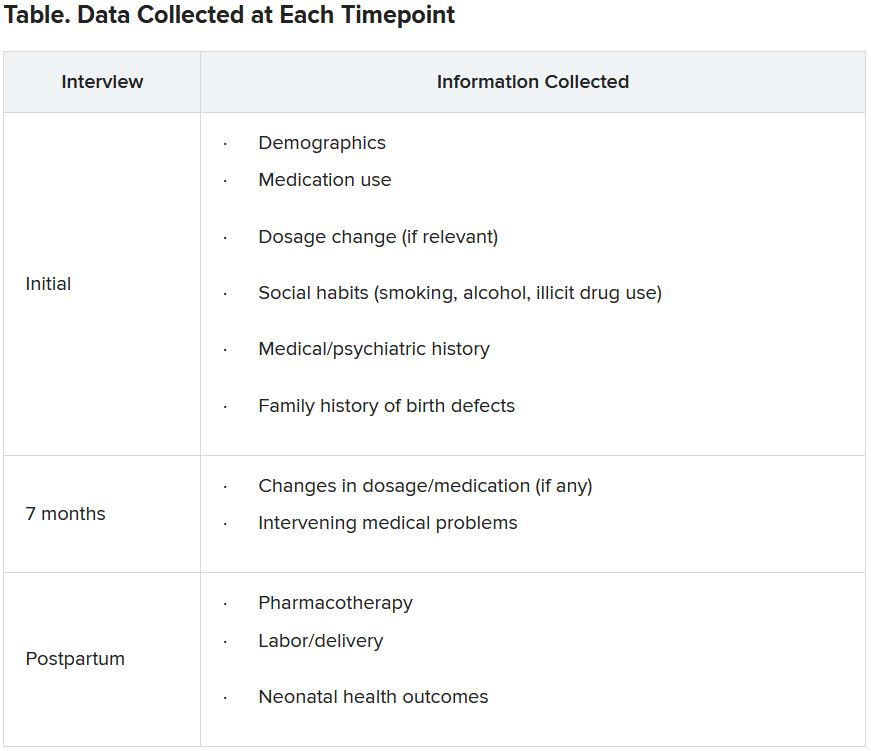
Specific data collected are shown in the following table.
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
One center’s experience delivering monochorionic twins
Between 2005 and 2021, mode of delivery of diamniotic twins at this practice did not significantly differ by chorionicity, researchers affiliated with Maternal Fetal Medicine Associates and the department of obstetrics, gynecology, and reproductive science at Icahn School of Medicine at Mount Sinai, New York reported in Obstetrics & Gynecology.
The study supports a recommendation from the American College of Obstetricians and Gynecologists that vaginal delivery “is a reasonable option in well selected diamniotic twin pregnancies, irrespective of chorionicity, and should be considered, provided that an experienced obstetrician is available,” said Iris Krishna, MD, assistant professor of maternal-fetal medicine at Emory University, Atlanta.
The experience at this practice, however, may not apply to many practices in the United States, said Dr. Krishna, who was not involved in the study.
Of 1,121 diamniotic twin pregnancies included in the analysis, 202 (18%) were monochorionic. The cesarean delivery rate was not significantly different between groups: 61% for monochorionic and 63% for dichorionic pregnancies.
Among women with planned vaginal delivery (101 monochorionic pregnancies and 422 dichorionic pregnancies), the cesarean delivery rate likewise did not significantly differ by chorionicity. Twenty-two percent of the monochorionic pregnancies and 21% of the dichorionic pregnancies in this subgroup had a cesarean delivery.
Among patients with a vaginal delivery of twin A, chorionicity was not associated with mode of delivery for twin B. Combined vaginal-cesarean deliveries occurred less than 1% of the time, and breech extraction of twin B occurred approximately 75% of the time, regardless of chorionicity.
The researchers also compared neonatal outcomes for monochorionic-diamniotic twin pregnancies at or after 34 weeks of gestation, based on the intended mode of delivery (95 women with planned vaginal delivery and 68 with planned cesarean delivery). Neonatal outcomes generally were similar, although the incidence of mechanical ventilation was less common in cases with planned vaginal delivery (7% vs. 21%).
“Our data affirm that an attempt at a vaginal birth for twin pregnancies, without contraindications to vaginal delivery and regardless of chorionicity, is reasonable and achievable,” wrote study author Henry N. Lesser, MD, with the department of obstetrics and gynecology at Sinai Hospital in Baltimore, and colleagues.
The patients with planned cesarean delivery had a contraindication to vaginal delivery or otherwise chose to have a cesarean delivery. The researchers excluded from their analysis pregnancies with intrauterine fetal demise of either twin before labor or planned cesarean delivery.
The study’s reliance on data from a single practice decreases its external validity, the researchers noted. Induction of labor at this center typically occurs at 37 weeks’ gestation for monochorionic twins and at 38 weeks for dichorionic twins, and “senior personnel experienced in intrauterine twin manipulation are always present at delivery,” the study authors said.
The study describes “the experience of a single site with skilled obstetricians following a standardized approach to management of diamniotic twin deliveries,” Dr. Krishna said. “Findings may not be generalizable to many U.S. practices as obstetrics and gynecology residents often lack training in breech extraction or internal podalic version of the second twin. This underscores the importance of a concerted effort by skilled senior physicians to train junior physicians in vaginal delivery of the second twin to improve overall outcomes amongst women with diamniotic twin gestations.”
Michael F. Greene, MD, professor emeritus of obstetrics, gynecology, and reproductive biology at Massachusetts General Hospital, Boston, agreed that the findings are not generalizable to the national population. Approximately 10% of the patients in the study had prepregnancy obesity, whereas doctors practicing in other areas likely encounter higher rates, Dr. Greene said in an interview.
He also wondered about other data points that could be of interest but were not reported, such as the racial or ethnic distribution of the patients, rates of birth defects, the use of instruments to aid delivery, and neonatal outcomes for the dichorionic twins.
Monochorionic pregnancies entail a risk of twin-twin transfusion syndrome and other complications, including an increased likelihood of birth defects.
Dr. Greene is an associate editor with the New England Journal of Medicine, which in 2013 published results from the Twin Birth Study, an international trial where women with dichorionic or monochorionic twins were randomly assigned to planned vaginal delivery or planned cesarean delivery. Outcomes did not significantly differ between groups. In the trial, the rate of cesarean delivery in the group with planned vaginal delivery was 43.8%, and Dr. Greene discussed the implications of the study in an accompanying editorial.
Since then, the obstetrics and gynecology community “has been focusing in recent years on trying to avoid the first cesarean section” when it is safe to do so, Dr. Greene said. “That has become almost a bumper sticker in modern obstetrics.”
And patients should know that it is an option, Dr. Krishna added.
“Women with monochorionic-diamniotic twins should be counseled that with an experienced obstetrician that an attempt at vaginal delivery is not associated with adverse neonatal outcomes when compared with planned cesarean delivery,” Dr. Krishna said.
A study coauthor disclosed serving on the speakers bureau for Natera and Hologic. Dr. Krishna is a member of the editorial advisory board for Ob.Gyn. News.
Between 2005 and 2021, mode of delivery of diamniotic twins at this practice did not significantly differ by chorionicity, researchers affiliated with Maternal Fetal Medicine Associates and the department of obstetrics, gynecology, and reproductive science at Icahn School of Medicine at Mount Sinai, New York reported in Obstetrics & Gynecology.
The study supports a recommendation from the American College of Obstetricians and Gynecologists that vaginal delivery “is a reasonable option in well selected diamniotic twin pregnancies, irrespective of chorionicity, and should be considered, provided that an experienced obstetrician is available,” said Iris Krishna, MD, assistant professor of maternal-fetal medicine at Emory University, Atlanta.
The experience at this practice, however, may not apply to many practices in the United States, said Dr. Krishna, who was not involved in the study.
Of 1,121 diamniotic twin pregnancies included in the analysis, 202 (18%) were monochorionic. The cesarean delivery rate was not significantly different between groups: 61% for monochorionic and 63% for dichorionic pregnancies.
Among women with planned vaginal delivery (101 monochorionic pregnancies and 422 dichorionic pregnancies), the cesarean delivery rate likewise did not significantly differ by chorionicity. Twenty-two percent of the monochorionic pregnancies and 21% of the dichorionic pregnancies in this subgroup had a cesarean delivery.
Among patients with a vaginal delivery of twin A, chorionicity was not associated with mode of delivery for twin B. Combined vaginal-cesarean deliveries occurred less than 1% of the time, and breech extraction of twin B occurred approximately 75% of the time, regardless of chorionicity.
The researchers also compared neonatal outcomes for monochorionic-diamniotic twin pregnancies at or after 34 weeks of gestation, based on the intended mode of delivery (95 women with planned vaginal delivery and 68 with planned cesarean delivery). Neonatal outcomes generally were similar, although the incidence of mechanical ventilation was less common in cases with planned vaginal delivery (7% vs. 21%).
“Our data affirm that an attempt at a vaginal birth for twin pregnancies, without contraindications to vaginal delivery and regardless of chorionicity, is reasonable and achievable,” wrote study author Henry N. Lesser, MD, with the department of obstetrics and gynecology at Sinai Hospital in Baltimore, and colleagues.
The patients with planned cesarean delivery had a contraindication to vaginal delivery or otherwise chose to have a cesarean delivery. The researchers excluded from their analysis pregnancies with intrauterine fetal demise of either twin before labor or planned cesarean delivery.
The study’s reliance on data from a single practice decreases its external validity, the researchers noted. Induction of labor at this center typically occurs at 37 weeks’ gestation for monochorionic twins and at 38 weeks for dichorionic twins, and “senior personnel experienced in intrauterine twin manipulation are always present at delivery,” the study authors said.
The study describes “the experience of a single site with skilled obstetricians following a standardized approach to management of diamniotic twin deliveries,” Dr. Krishna said. “Findings may not be generalizable to many U.S. practices as obstetrics and gynecology residents often lack training in breech extraction or internal podalic version of the second twin. This underscores the importance of a concerted effort by skilled senior physicians to train junior physicians in vaginal delivery of the second twin to improve overall outcomes amongst women with diamniotic twin gestations.”
Michael F. Greene, MD, professor emeritus of obstetrics, gynecology, and reproductive biology at Massachusetts General Hospital, Boston, agreed that the findings are not generalizable to the national population. Approximately 10% of the patients in the study had prepregnancy obesity, whereas doctors practicing in other areas likely encounter higher rates, Dr. Greene said in an interview.
He also wondered about other data points that could be of interest but were not reported, such as the racial or ethnic distribution of the patients, rates of birth defects, the use of instruments to aid delivery, and neonatal outcomes for the dichorionic twins.
Monochorionic pregnancies entail a risk of twin-twin transfusion syndrome and other complications, including an increased likelihood of birth defects.
Dr. Greene is an associate editor with the New England Journal of Medicine, which in 2013 published results from the Twin Birth Study, an international trial where women with dichorionic or monochorionic twins were randomly assigned to planned vaginal delivery or planned cesarean delivery. Outcomes did not significantly differ between groups. In the trial, the rate of cesarean delivery in the group with planned vaginal delivery was 43.8%, and Dr. Greene discussed the implications of the study in an accompanying editorial.
Since then, the obstetrics and gynecology community “has been focusing in recent years on trying to avoid the first cesarean section” when it is safe to do so, Dr. Greene said. “That has become almost a bumper sticker in modern obstetrics.”
And patients should know that it is an option, Dr. Krishna added.
“Women with monochorionic-diamniotic twins should be counseled that with an experienced obstetrician that an attempt at vaginal delivery is not associated with adverse neonatal outcomes when compared with planned cesarean delivery,” Dr. Krishna said.
A study coauthor disclosed serving on the speakers bureau for Natera and Hologic. Dr. Krishna is a member of the editorial advisory board for Ob.Gyn. News.
Between 2005 and 2021, mode of delivery of diamniotic twins at this practice did not significantly differ by chorionicity, researchers affiliated with Maternal Fetal Medicine Associates and the department of obstetrics, gynecology, and reproductive science at Icahn School of Medicine at Mount Sinai, New York reported in Obstetrics & Gynecology.
The study supports a recommendation from the American College of Obstetricians and Gynecologists that vaginal delivery “is a reasonable option in well selected diamniotic twin pregnancies, irrespective of chorionicity, and should be considered, provided that an experienced obstetrician is available,” said Iris Krishna, MD, assistant professor of maternal-fetal medicine at Emory University, Atlanta.
The experience at this practice, however, may not apply to many practices in the United States, said Dr. Krishna, who was not involved in the study.
Of 1,121 diamniotic twin pregnancies included in the analysis, 202 (18%) were monochorionic. The cesarean delivery rate was not significantly different between groups: 61% for monochorionic and 63% for dichorionic pregnancies.
Among women with planned vaginal delivery (101 monochorionic pregnancies and 422 dichorionic pregnancies), the cesarean delivery rate likewise did not significantly differ by chorionicity. Twenty-two percent of the monochorionic pregnancies and 21% of the dichorionic pregnancies in this subgroup had a cesarean delivery.
Among patients with a vaginal delivery of twin A, chorionicity was not associated with mode of delivery for twin B. Combined vaginal-cesarean deliveries occurred less than 1% of the time, and breech extraction of twin B occurred approximately 75% of the time, regardless of chorionicity.
The researchers also compared neonatal outcomes for monochorionic-diamniotic twin pregnancies at or after 34 weeks of gestation, based on the intended mode of delivery (95 women with planned vaginal delivery and 68 with planned cesarean delivery). Neonatal outcomes generally were similar, although the incidence of mechanical ventilation was less common in cases with planned vaginal delivery (7% vs. 21%).
“Our data affirm that an attempt at a vaginal birth for twin pregnancies, without contraindications to vaginal delivery and regardless of chorionicity, is reasonable and achievable,” wrote study author Henry N. Lesser, MD, with the department of obstetrics and gynecology at Sinai Hospital in Baltimore, and colleagues.
The patients with planned cesarean delivery had a contraindication to vaginal delivery or otherwise chose to have a cesarean delivery. The researchers excluded from their analysis pregnancies with intrauterine fetal demise of either twin before labor or planned cesarean delivery.
The study’s reliance on data from a single practice decreases its external validity, the researchers noted. Induction of labor at this center typically occurs at 37 weeks’ gestation for monochorionic twins and at 38 weeks for dichorionic twins, and “senior personnel experienced in intrauterine twin manipulation are always present at delivery,” the study authors said.
The study describes “the experience of a single site with skilled obstetricians following a standardized approach to management of diamniotic twin deliveries,” Dr. Krishna said. “Findings may not be generalizable to many U.S. practices as obstetrics and gynecology residents often lack training in breech extraction or internal podalic version of the second twin. This underscores the importance of a concerted effort by skilled senior physicians to train junior physicians in vaginal delivery of the second twin to improve overall outcomes amongst women with diamniotic twin gestations.”
Michael F. Greene, MD, professor emeritus of obstetrics, gynecology, and reproductive biology at Massachusetts General Hospital, Boston, agreed that the findings are not generalizable to the national population. Approximately 10% of the patients in the study had prepregnancy obesity, whereas doctors practicing in other areas likely encounter higher rates, Dr. Greene said in an interview.
He also wondered about other data points that could be of interest but were not reported, such as the racial or ethnic distribution of the patients, rates of birth defects, the use of instruments to aid delivery, and neonatal outcomes for the dichorionic twins.
Monochorionic pregnancies entail a risk of twin-twin transfusion syndrome and other complications, including an increased likelihood of birth defects.
Dr. Greene is an associate editor with the New England Journal of Medicine, which in 2013 published results from the Twin Birth Study, an international trial where women with dichorionic or monochorionic twins were randomly assigned to planned vaginal delivery or planned cesarean delivery. Outcomes did not significantly differ between groups. In the trial, the rate of cesarean delivery in the group with planned vaginal delivery was 43.8%, and Dr. Greene discussed the implications of the study in an accompanying editorial.
Since then, the obstetrics and gynecology community “has been focusing in recent years on trying to avoid the first cesarean section” when it is safe to do so, Dr. Greene said. “That has become almost a bumper sticker in modern obstetrics.”
And patients should know that it is an option, Dr. Krishna added.
“Women with monochorionic-diamniotic twins should be counseled that with an experienced obstetrician that an attempt at vaginal delivery is not associated with adverse neonatal outcomes when compared with planned cesarean delivery,” Dr. Krishna said.
A study coauthor disclosed serving on the speakers bureau for Natera and Hologic. Dr. Krishna is a member of the editorial advisory board for Ob.Gyn. News.
FROM OBSTETRICS & GYNECOLOGY
Task force affirms routine gestational diabetes testing
Asymptomatic pregnant women with no previous diagnosis of type 1 or 2 diabetes should be screened for gestational diabetes at 24 weeks’ gestation or later, according to an updated recommendation from the U.S. Preventive Services Task Force.
Pregnant individuals who develop gestational diabetes are at increased risk for complications including preeclampsia, fetal macrosomia, and neonatal hypoglycemia, as well as negative long-term outcomes for themselves and their children, wrote lead author Karina W. Davidson, PhD, of Feinstein Institute for Medical Research, Manhasset, N.Y., and colleagues. The statement was published online in JAMA.
The B recommendation and I statement reflect “moderate certainty” that current evidence supports the recommendation in terms of harms versus benefits, and is consistent with the 2014 USPSTF recommendation.
The statement calls for a one-time screening using a glucose tolerance test at or after 24 weeks’ gestation. Although most screening in the United States takes place prior to 28 weeks’ gestation, it can be performed later in patients who begin prenatal care after 28 weeks’ gestation, according to the statement. Data on the harms and benefits of gestational diabetes screening prior to 24 weeks’ gestation are limited, the authors noted. Gestational diabetes was defined as diabetes that develops during pregnancy that is not clearly overt diabetes.
To update the 2014 recommendation, the USPSTF commissioned a systematic review. In 45 prospective studies on the accuracy of gestational diabetes screening, several tests, included oral glucose challenge test, oral glucose tolerance test, and fasting plasma glucose using either a one- or two-step approach were accurate detectors of gestational diabetes; therefore, the USPSTF does not recommend a specific test.
In 13 trials on the impact of treating gestational diabetes on intermediate and health outcomes, treatment was associated with a reduced risk of outcomes, including primary cesarean delivery (but not total cesarean delivery) and preterm delivery, but not with a reduced risk of outcomes including preeclampsia, emergency cesarean delivery, induction of labor, or maternal birth trauma.
The task force also reviewed seven studies of harms associated with screening for gestational diabetes, including three on psychosocial harms, three on hospital experiences, and one of the odds of cesarean delivery after a diagnosis of gestational diabetes. No increase in anxiety or depression occurred following a positive diagnosis or false-positive test result, but data suggested that a gestational diabetes diagnosis may be associated with higher rates of cesarean delivery.
A total of 13 trials evaluated the harms associated with treatment of gestational diabetes, and found no association between treatment and increased risk of several outcomes including severe maternal hypoglycemia, low birth weight, and small for gestational age, and no effect was noted on the number of cesarean deliveries.
Evidence gaps that require additional research include randomized, controlled trials on the effects of gestational diabetes screening on health outcomes, as well as benefits versus harms of screening for pregnant individuals prior to 24 weeks, and studies on the effects of screening in subpopulations of race/ethnicity, age, and socioeconomic factors, according to the task force. Additional research also is needed in areas of maternal health outcomes, long-term outcomes, and the effect on outcomes of one-step versus two-step screening, the USPSTF said.
However, “screening for and detecting gestational diabetes provides a potential opportunity to control blood glucose levels (through lifestyle changes, pharmacological interventions, or both) and reduce the risk of macrosomia and LGA [large for gestational age] infants,” the task force wrote. “In turn, this can prevent associated complications such as primary cesarean delivery, shoulder dystocia, and [neonatal] ICU admissions.”
Support screening with counseling on risk reduction
The USPSTF recommendation is important at this time because “the prevalence of gestational diabetes is increasing secondary to rising rates of obesity,” Iris Krishna, MD, of Emory University, Atlanta, said in an interview.
“In 2014, based on a systematic review of literature, the USPSTF recommended screening all asymptomatic pregnant women for gestational diabetes mellitus [GDM] starting at 24 weeks’ gestation. The recommended gestational age for screening coincides with increasing insulin resistance during pregnancy with advancing gestational age,” Dr. Krishna said.
“An updated systematic review by the USPSTF concluded that existing literature continues to affirm current recommendations of universal screening for GDM at 24 weeks gestation or later. There continues, however, to be no consensus on the optimal approach to screening,” she noted.
“Screening can be performed as a two-step or one-step approach,” said Dr. Krishna. “The two-step approach is commonly used in the United States, and all pregnant women are first screened with a 50-gram oral glucose solution followed by a diagnostic test if they have a positive initial screening.
“Women with risk factors for diabetes, such as prior GDM, obesity, strong family history of diabetes, or history of fetal macrosomia, should be screened early in pregnancy for GDM and have the GDM screen repeated at 24 weeks’ gestation or later if normal in early pregnancy,” Dr. Krishna said. “Pregnant women should be counseled on the importance of diet and exercise and appropriate weight gain in pregnancy to reduce the risk of GDM. Overall, timely diagnosis of gestational diabetes is crucial to improving maternal and fetal pregnancy outcomes.”
The full recommendation statement is also available on the USPSTF website. The research was supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose. Dr. Krishna had no disclosures, but serves on the editorial advisory board of Ob.Gyn News.
Asymptomatic pregnant women with no previous diagnosis of type 1 or 2 diabetes should be screened for gestational diabetes at 24 weeks’ gestation or later, according to an updated recommendation from the U.S. Preventive Services Task Force.
Pregnant individuals who develop gestational diabetes are at increased risk for complications including preeclampsia, fetal macrosomia, and neonatal hypoglycemia, as well as negative long-term outcomes for themselves and their children, wrote lead author Karina W. Davidson, PhD, of Feinstein Institute for Medical Research, Manhasset, N.Y., and colleagues. The statement was published online in JAMA.
The B recommendation and I statement reflect “moderate certainty” that current evidence supports the recommendation in terms of harms versus benefits, and is consistent with the 2014 USPSTF recommendation.
The statement calls for a one-time screening using a glucose tolerance test at or after 24 weeks’ gestation. Although most screening in the United States takes place prior to 28 weeks’ gestation, it can be performed later in patients who begin prenatal care after 28 weeks’ gestation, according to the statement. Data on the harms and benefits of gestational diabetes screening prior to 24 weeks’ gestation are limited, the authors noted. Gestational diabetes was defined as diabetes that develops during pregnancy that is not clearly overt diabetes.
To update the 2014 recommendation, the USPSTF commissioned a systematic review. In 45 prospective studies on the accuracy of gestational diabetes screening, several tests, included oral glucose challenge test, oral glucose tolerance test, and fasting plasma glucose using either a one- or two-step approach were accurate detectors of gestational diabetes; therefore, the USPSTF does not recommend a specific test.
In 13 trials on the impact of treating gestational diabetes on intermediate and health outcomes, treatment was associated with a reduced risk of outcomes, including primary cesarean delivery (but not total cesarean delivery) and preterm delivery, but not with a reduced risk of outcomes including preeclampsia, emergency cesarean delivery, induction of labor, or maternal birth trauma.
The task force also reviewed seven studies of harms associated with screening for gestational diabetes, including three on psychosocial harms, three on hospital experiences, and one of the odds of cesarean delivery after a diagnosis of gestational diabetes. No increase in anxiety or depression occurred following a positive diagnosis or false-positive test result, but data suggested that a gestational diabetes diagnosis may be associated with higher rates of cesarean delivery.
A total of 13 trials evaluated the harms associated with treatment of gestational diabetes, and found no association between treatment and increased risk of several outcomes including severe maternal hypoglycemia, low birth weight, and small for gestational age, and no effect was noted on the number of cesarean deliveries.
Evidence gaps that require additional research include randomized, controlled trials on the effects of gestational diabetes screening on health outcomes, as well as benefits versus harms of screening for pregnant individuals prior to 24 weeks, and studies on the effects of screening in subpopulations of race/ethnicity, age, and socioeconomic factors, according to the task force. Additional research also is needed in areas of maternal health outcomes, long-term outcomes, and the effect on outcomes of one-step versus two-step screening, the USPSTF said.
However, “screening for and detecting gestational diabetes provides a potential opportunity to control blood glucose levels (through lifestyle changes, pharmacological interventions, or both) and reduce the risk of macrosomia and LGA [large for gestational age] infants,” the task force wrote. “In turn, this can prevent associated complications such as primary cesarean delivery, shoulder dystocia, and [neonatal] ICU admissions.”
Support screening with counseling on risk reduction
The USPSTF recommendation is important at this time because “the prevalence of gestational diabetes is increasing secondary to rising rates of obesity,” Iris Krishna, MD, of Emory University, Atlanta, said in an interview.
“In 2014, based on a systematic review of literature, the USPSTF recommended screening all asymptomatic pregnant women for gestational diabetes mellitus [GDM] starting at 24 weeks’ gestation. The recommended gestational age for screening coincides with increasing insulin resistance during pregnancy with advancing gestational age,” Dr. Krishna said.
“An updated systematic review by the USPSTF concluded that existing literature continues to affirm current recommendations of universal screening for GDM at 24 weeks gestation or later. There continues, however, to be no consensus on the optimal approach to screening,” she noted.
“Screening can be performed as a two-step or one-step approach,” said Dr. Krishna. “The two-step approach is commonly used in the United States, and all pregnant women are first screened with a 50-gram oral glucose solution followed by a diagnostic test if they have a positive initial screening.
“Women with risk factors for diabetes, such as prior GDM, obesity, strong family history of diabetes, or history of fetal macrosomia, should be screened early in pregnancy for GDM and have the GDM screen repeated at 24 weeks’ gestation or later if normal in early pregnancy,” Dr. Krishna said. “Pregnant women should be counseled on the importance of diet and exercise and appropriate weight gain in pregnancy to reduce the risk of GDM. Overall, timely diagnosis of gestational diabetes is crucial to improving maternal and fetal pregnancy outcomes.”
The full recommendation statement is also available on the USPSTF website. The research was supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose. Dr. Krishna had no disclosures, but serves on the editorial advisory board of Ob.Gyn News.
Asymptomatic pregnant women with no previous diagnosis of type 1 or 2 diabetes should be screened for gestational diabetes at 24 weeks’ gestation or later, according to an updated recommendation from the U.S. Preventive Services Task Force.
Pregnant individuals who develop gestational diabetes are at increased risk for complications including preeclampsia, fetal macrosomia, and neonatal hypoglycemia, as well as negative long-term outcomes for themselves and their children, wrote lead author Karina W. Davidson, PhD, of Feinstein Institute for Medical Research, Manhasset, N.Y., and colleagues. The statement was published online in JAMA.
The B recommendation and I statement reflect “moderate certainty” that current evidence supports the recommendation in terms of harms versus benefits, and is consistent with the 2014 USPSTF recommendation.
The statement calls for a one-time screening using a glucose tolerance test at or after 24 weeks’ gestation. Although most screening in the United States takes place prior to 28 weeks’ gestation, it can be performed later in patients who begin prenatal care after 28 weeks’ gestation, according to the statement. Data on the harms and benefits of gestational diabetes screening prior to 24 weeks’ gestation are limited, the authors noted. Gestational diabetes was defined as diabetes that develops during pregnancy that is not clearly overt diabetes.
To update the 2014 recommendation, the USPSTF commissioned a systematic review. In 45 prospective studies on the accuracy of gestational diabetes screening, several tests, included oral glucose challenge test, oral glucose tolerance test, and fasting plasma glucose using either a one- or two-step approach were accurate detectors of gestational diabetes; therefore, the USPSTF does not recommend a specific test.
In 13 trials on the impact of treating gestational diabetes on intermediate and health outcomes, treatment was associated with a reduced risk of outcomes, including primary cesarean delivery (but not total cesarean delivery) and preterm delivery, but not with a reduced risk of outcomes including preeclampsia, emergency cesarean delivery, induction of labor, or maternal birth trauma.
The task force also reviewed seven studies of harms associated with screening for gestational diabetes, including three on psychosocial harms, three on hospital experiences, and one of the odds of cesarean delivery after a diagnosis of gestational diabetes. No increase in anxiety or depression occurred following a positive diagnosis or false-positive test result, but data suggested that a gestational diabetes diagnosis may be associated with higher rates of cesarean delivery.
A total of 13 trials evaluated the harms associated with treatment of gestational diabetes, and found no association between treatment and increased risk of several outcomes including severe maternal hypoglycemia, low birth weight, and small for gestational age, and no effect was noted on the number of cesarean deliveries.
Evidence gaps that require additional research include randomized, controlled trials on the effects of gestational diabetes screening on health outcomes, as well as benefits versus harms of screening for pregnant individuals prior to 24 weeks, and studies on the effects of screening in subpopulations of race/ethnicity, age, and socioeconomic factors, according to the task force. Additional research also is needed in areas of maternal health outcomes, long-term outcomes, and the effect on outcomes of one-step versus two-step screening, the USPSTF said.
However, “screening for and detecting gestational diabetes provides a potential opportunity to control blood glucose levels (through lifestyle changes, pharmacological interventions, or both) and reduce the risk of macrosomia and LGA [large for gestational age] infants,” the task force wrote. “In turn, this can prevent associated complications such as primary cesarean delivery, shoulder dystocia, and [neonatal] ICU admissions.”
Support screening with counseling on risk reduction
The USPSTF recommendation is important at this time because “the prevalence of gestational diabetes is increasing secondary to rising rates of obesity,” Iris Krishna, MD, of Emory University, Atlanta, said in an interview.
“In 2014, based on a systematic review of literature, the USPSTF recommended screening all asymptomatic pregnant women for gestational diabetes mellitus [GDM] starting at 24 weeks’ gestation. The recommended gestational age for screening coincides with increasing insulin resistance during pregnancy with advancing gestational age,” Dr. Krishna said.
“An updated systematic review by the USPSTF concluded that existing literature continues to affirm current recommendations of universal screening for GDM at 24 weeks gestation or later. There continues, however, to be no consensus on the optimal approach to screening,” she noted.
“Screening can be performed as a two-step or one-step approach,” said Dr. Krishna. “The two-step approach is commonly used in the United States, and all pregnant women are first screened with a 50-gram oral glucose solution followed by a diagnostic test if they have a positive initial screening.
“Women with risk factors for diabetes, such as prior GDM, obesity, strong family history of diabetes, or history of fetal macrosomia, should be screened early in pregnancy for GDM and have the GDM screen repeated at 24 weeks’ gestation or later if normal in early pregnancy,” Dr. Krishna said. “Pregnant women should be counseled on the importance of diet and exercise and appropriate weight gain in pregnancy to reduce the risk of GDM. Overall, timely diagnosis of gestational diabetes is crucial to improving maternal and fetal pregnancy outcomes.”
The full recommendation statement is also available on the USPSTF website. The research was supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose. Dr. Krishna had no disclosures, but serves on the editorial advisory board of Ob.Gyn News.
FROM JAMA
Medical residents need breastfeeding support too
As working mothers with babies in tow when the COVID-19 crisis struck, countless uncertainties threatened our already precarious work-life balance. We suddenly had many questions:
“If my daycare closes, what will I do for childcare?”
“How do I navigate diaper changes, feedings, and naps with my hectic remote work schedule?”
“If I’m constantly interrupted during the day, should I skip sleep to catch up on work and not let my colleagues down?”
As professionals who work closely with medical trainees, we knew our parenting dilemmas were being experienced even more acutely by our frontline worker colleagues.
Medical training is an increasingly common time to start a family. In a recent study, 34% of trainees in Harvard-affiliated residency programs became parents during training, and another 52% planned to do so. Trainees have higher breastfeeding initiation rates but lower continuation rates than the general population. Early nursing cessation among trainees is well documented nationally and is most often attributed to work-related barriers. These barriers range from insufficient time and limited access to facilities to a lack of support and discrimination by supervisors and peers.
This trend does not discriminate by specialty. Even among training programs known to be “family friendly,” the average duration of nursing is just 4.5 months. Residents of color are disproportionately affected by inadequate support. Studies show that Black parents breastfeed at lower rates than White parents. This has been largely attributed to structural racism and implicit bias, such as Black parents receiving less assistance initiating nursing after delivery. Adequate lactation support and inclusivity are also lacking for transgender parents who choose to breastfeed or chestfeed.
The very nature of residency training, which includes shifts that can span more than 24 hours, conflicts with many health-promoting behaviors like sleeping and eating well. However, its interference with lactation is correlated with gender. Women are disproportionately affected by the negative outcomes of unmet lactation goals. These include work-life imbalance, career dissatisfaction, and negative emotions. In a study of pediatric residents, one in four did not achieve their breastfeeding goals. Respondents reported feeling “sad, devastated, defeated, disappointed, guilty, embarrassed, frustrated, angry, like a failure, and inadequate.” Among physician mothers more broadly, discrimination related to pregnancy, parental leave, and nursing is associated with higher self-reported burnout.
Navigating nursing during residency training has more than just emotional and psychological consequences – it also has professional ones. Pursuing personal lactation goals can delay residency program completion and board certification, influence specialty selection, negatively impact research productivity, impede career advancement, and lead to misgivings about career choice.
Trainees and their families are not the only ones harmed by inadequate support in residency programs. Patients and their families are affected, too. Research suggests that physicians’ personal breastfeeding practices affect the advice they give to patients. Those who receive lactation support are more likely to help patients meet their own goals. In the previously mentioned study of pediatric residents, more than 90% of the 400 respondents said their own or their partner’s nursing experience affected their interaction with lactating patients in their clinic or hospital.
Increased lactation support is a straightforward, low-cost, high-impact intervention. It benefits trainee well-being, satisfaction, workflow, and future patient care. The Accreditation Council for Graduate Medical Education mandated in July 2019 that all residency programs provide adequate lactation facilities – including refrigeration capabilities and proximity for safe patient care. However, to our knowledge, rates of compliance with this new policy and citation for noncompliance have yet to be seen. Regardless, facilities alone are not enough. Residency programs should develop and enforce formal lactation policies.
Several institutions have successfully piloted such policies in recent years. One in particular from the University of Michigan’s surgery residency program inspired the development of a lactation policy within the internal medicine residency at our institution. These policies designate appropriate spaces at each clinical rotation site, clarify that residents are encouraged to take pumping breaks as needed – in coordination with clinical teams so as not to compromise patient care – and communicate support from supervisors.
Our program also established an informal peer mentoring program. Residents with experience pumping at work pair up with newer trainees. The policy benefits residents who wish to chestfeed or breastfeed, normalizes lactation, and empowers trainees by diminishing the need to ask for individual accommodations. It also costs the program nothing.
As more women enter medicine and more trainees become parents during residency, the need for support in this area will only continue to grow. The widespread lack of such resources, and the fact that clean and private facilities are only now being mandated, is symbolic. If even this basic need is rarely acknowledged or met, what other resident needs are being neglected?
A version of this article first appeared on Medscape.com.
As working mothers with babies in tow when the COVID-19 crisis struck, countless uncertainties threatened our already precarious work-life balance. We suddenly had many questions:
“If my daycare closes, what will I do for childcare?”
“How do I navigate diaper changes, feedings, and naps with my hectic remote work schedule?”
“If I’m constantly interrupted during the day, should I skip sleep to catch up on work and not let my colleagues down?”
As professionals who work closely with medical trainees, we knew our parenting dilemmas were being experienced even more acutely by our frontline worker colleagues.
Medical training is an increasingly common time to start a family. In a recent study, 34% of trainees in Harvard-affiliated residency programs became parents during training, and another 52% planned to do so. Trainees have higher breastfeeding initiation rates but lower continuation rates than the general population. Early nursing cessation among trainees is well documented nationally and is most often attributed to work-related barriers. These barriers range from insufficient time and limited access to facilities to a lack of support and discrimination by supervisors and peers.
This trend does not discriminate by specialty. Even among training programs known to be “family friendly,” the average duration of nursing is just 4.5 months. Residents of color are disproportionately affected by inadequate support. Studies show that Black parents breastfeed at lower rates than White parents. This has been largely attributed to structural racism and implicit bias, such as Black parents receiving less assistance initiating nursing after delivery. Adequate lactation support and inclusivity are also lacking for transgender parents who choose to breastfeed or chestfeed.
The very nature of residency training, which includes shifts that can span more than 24 hours, conflicts with many health-promoting behaviors like sleeping and eating well. However, its interference with lactation is correlated with gender. Women are disproportionately affected by the negative outcomes of unmet lactation goals. These include work-life imbalance, career dissatisfaction, and negative emotions. In a study of pediatric residents, one in four did not achieve their breastfeeding goals. Respondents reported feeling “sad, devastated, defeated, disappointed, guilty, embarrassed, frustrated, angry, like a failure, and inadequate.” Among physician mothers more broadly, discrimination related to pregnancy, parental leave, and nursing is associated with higher self-reported burnout.
Navigating nursing during residency training has more than just emotional and psychological consequences – it also has professional ones. Pursuing personal lactation goals can delay residency program completion and board certification, influence specialty selection, negatively impact research productivity, impede career advancement, and lead to misgivings about career choice.
Trainees and their families are not the only ones harmed by inadequate support in residency programs. Patients and their families are affected, too. Research suggests that physicians’ personal breastfeeding practices affect the advice they give to patients. Those who receive lactation support are more likely to help patients meet their own goals. In the previously mentioned study of pediatric residents, more than 90% of the 400 respondents said their own or their partner’s nursing experience affected their interaction with lactating patients in their clinic or hospital.
Increased lactation support is a straightforward, low-cost, high-impact intervention. It benefits trainee well-being, satisfaction, workflow, and future patient care. The Accreditation Council for Graduate Medical Education mandated in July 2019 that all residency programs provide adequate lactation facilities – including refrigeration capabilities and proximity for safe patient care. However, to our knowledge, rates of compliance with this new policy and citation for noncompliance have yet to be seen. Regardless, facilities alone are not enough. Residency programs should develop and enforce formal lactation policies.
Several institutions have successfully piloted such policies in recent years. One in particular from the University of Michigan’s surgery residency program inspired the development of a lactation policy within the internal medicine residency at our institution. These policies designate appropriate spaces at each clinical rotation site, clarify that residents are encouraged to take pumping breaks as needed – in coordination with clinical teams so as not to compromise patient care – and communicate support from supervisors.
Our program also established an informal peer mentoring program. Residents with experience pumping at work pair up with newer trainees. The policy benefits residents who wish to chestfeed or breastfeed, normalizes lactation, and empowers trainees by diminishing the need to ask for individual accommodations. It also costs the program nothing.
As more women enter medicine and more trainees become parents during residency, the need for support in this area will only continue to grow. The widespread lack of such resources, and the fact that clean and private facilities are only now being mandated, is symbolic. If even this basic need is rarely acknowledged or met, what other resident needs are being neglected?
A version of this article first appeared on Medscape.com.
As working mothers with babies in tow when the COVID-19 crisis struck, countless uncertainties threatened our already precarious work-life balance. We suddenly had many questions:
“If my daycare closes, what will I do for childcare?”
“How do I navigate diaper changes, feedings, and naps with my hectic remote work schedule?”
“If I’m constantly interrupted during the day, should I skip sleep to catch up on work and not let my colleagues down?”
As professionals who work closely with medical trainees, we knew our parenting dilemmas were being experienced even more acutely by our frontline worker colleagues.
Medical training is an increasingly common time to start a family. In a recent study, 34% of trainees in Harvard-affiliated residency programs became parents during training, and another 52% planned to do so. Trainees have higher breastfeeding initiation rates but lower continuation rates than the general population. Early nursing cessation among trainees is well documented nationally and is most often attributed to work-related barriers. These barriers range from insufficient time and limited access to facilities to a lack of support and discrimination by supervisors and peers.
This trend does not discriminate by specialty. Even among training programs known to be “family friendly,” the average duration of nursing is just 4.5 months. Residents of color are disproportionately affected by inadequate support. Studies show that Black parents breastfeed at lower rates than White parents. This has been largely attributed to structural racism and implicit bias, such as Black parents receiving less assistance initiating nursing after delivery. Adequate lactation support and inclusivity are also lacking for transgender parents who choose to breastfeed or chestfeed.
The very nature of residency training, which includes shifts that can span more than 24 hours, conflicts with many health-promoting behaviors like sleeping and eating well. However, its interference with lactation is correlated with gender. Women are disproportionately affected by the negative outcomes of unmet lactation goals. These include work-life imbalance, career dissatisfaction, and negative emotions. In a study of pediatric residents, one in four did not achieve their breastfeeding goals. Respondents reported feeling “sad, devastated, defeated, disappointed, guilty, embarrassed, frustrated, angry, like a failure, and inadequate.” Among physician mothers more broadly, discrimination related to pregnancy, parental leave, and nursing is associated with higher self-reported burnout.
Navigating nursing during residency training has more than just emotional and psychological consequences – it also has professional ones. Pursuing personal lactation goals can delay residency program completion and board certification, influence specialty selection, negatively impact research productivity, impede career advancement, and lead to misgivings about career choice.
Trainees and their families are not the only ones harmed by inadequate support in residency programs. Patients and their families are affected, too. Research suggests that physicians’ personal breastfeeding practices affect the advice they give to patients. Those who receive lactation support are more likely to help patients meet their own goals. In the previously mentioned study of pediatric residents, more than 90% of the 400 respondents said their own or their partner’s nursing experience affected their interaction with lactating patients in their clinic or hospital.
Increased lactation support is a straightforward, low-cost, high-impact intervention. It benefits trainee well-being, satisfaction, workflow, and future patient care. The Accreditation Council for Graduate Medical Education mandated in July 2019 that all residency programs provide adequate lactation facilities – including refrigeration capabilities and proximity for safe patient care. However, to our knowledge, rates of compliance with this new policy and citation for noncompliance have yet to be seen. Regardless, facilities alone are not enough. Residency programs should develop and enforce formal lactation policies.
Several institutions have successfully piloted such policies in recent years. One in particular from the University of Michigan’s surgery residency program inspired the development of a lactation policy within the internal medicine residency at our institution. These policies designate appropriate spaces at each clinical rotation site, clarify that residents are encouraged to take pumping breaks as needed – in coordination with clinical teams so as not to compromise patient care – and communicate support from supervisors.
Our program also established an informal peer mentoring program. Residents with experience pumping at work pair up with newer trainees. The policy benefits residents who wish to chestfeed or breastfeed, normalizes lactation, and empowers trainees by diminishing the need to ask for individual accommodations. It also costs the program nothing.
As more women enter medicine and more trainees become parents during residency, the need for support in this area will only continue to grow. The widespread lack of such resources, and the fact that clean and private facilities are only now being mandated, is symbolic. If even this basic need is rarely acknowledged or met, what other resident needs are being neglected?
A version of this article first appeared on Medscape.com.
‘Munchausen by Internet’ crises a warning for all HCPs
A new study documents a handful of cases of women with Munchausen syndrome by Internet who targeted doulas in the United Kingdom during the COVID-19 lockdown.
The five cases were investigated by Kathryn Newns, MSc, DClinPsy, a clinical psychologist in Cambridge, England, who said the cases were brought to her attention by a doula she herself had used for the birth of her own child a decade earlier.
Dr. Newns said she believes these are not isolated cases – either geographically or in terms of the specialty involved.
“I don’t think it is likely that this is only happening in the United Kingdom. And I’m sure it’s not just happening in the doula world,” Dr. Newns told this news organization.
Coinvestigator Marc Feldman, MD, a clinical professor of psychiatry at the University of Alabama, Tuscaloosa, coined the term “Munchausen by Internet” in a 2000 article. The expression refers to use of electronic media to perpetrate hoaxes that reward posers with sympathy, control, or emotional gratification. The hoaxers do not seek financial gain.
“The ease of carrying out Munchausen behaviors makes me think that it must be much more common than it ever was,” Dr. Feldman said in an interview.
He noted that the new DSM-5 will eliminate the terms “Munchausen” and “Munchausen by Internet” and will clarify that “factitious disorder” can be partly or wholly carried out online.
The study was published in the May issue of the Annals of Clinical Psychiatry.
A warning for others
In the past, those with factitious disorder had to go to medical libraries to study up on the ailment they wanted to feign. They would then present to an emergency department or a doctor’s office and act convincingly, Dr. Feldman said.
“Now all you have to do is go to Wikipedia and you can become an expert on a medical ailment within a few minutes,” he added.
In the five cases described in the study, the hoaxers created rich stories, especially in cases 1 and 2. In those cases, the perpetrator turned out to be the same person. Subterfuge “obviously made it much harder to know she wasn’t who she purported to be,” said Dr. Newns.
Dr. Feldman noted that in Munchausen by Internet, there may be some element of truth within the stories.
For health care professionals, “it takes a considerable leap to assume that somebody who’s talking about some dreaded ailment is in fact exaggerating or outright lying,” he said.
In the five cases described in the study, persons contacted doulas, then related traumatic stories and described dramatic, immediate needs. All of the doulas were working remotely because of the COVID-19 pandemic. This likely made it easier for the perpetrators to pull off the hoaxes. The health care professionals agreed to share their experiences in the hopes of warning others.
Elaborate scenarios
The first two cases were ultimately determined to involve one person who had created elaborate scenarios.
In case 1, the hoaxer, who called herself “Jessica,” texted the doula “Charlotte” when she was allegedly 39 weeks’ pregnant. She said she was unable to go to the hospital because of the COVID-19 risks to her husband, who had cystic fibrosis and had recently undergone a heart and lung transplant.
The husband “Jordan” took over communications, using the same WhatsApp number as Jessica, as Jessica went into labor.
Ostensibly, a midwife team had come to Jessica’s and Jordan’s house. When the doula was on the phone with Jordan, she heard Jessica crying, grunting, and screaming, and then, at 2:00 a.m., she heard the sound of a baby crying. A photo of the baby was texted to Charlotte.
Soon, there were many problems. Jessica allegedly had a postpartum hemorrhage, and mother and baby were taken to separate hospitals. The baby was then diagnosed with congenital heart disease.
Over the next week, “midwives” started texting back and forth with Charlotte. The doula began to have doubts and asked a midwife to share a visual communication.
After receiving no response, Charlotte used a video call, got Jessica on screen, and told her she thought there was no baby. Jessica said the baby was real and showed a “growth chart” as proof of the 5-day-old baby’s existence. The birth and baby noises were later determined to be recordings.
Child deaths
After sharing information among themselves on a private Facebook group, the doulas determined that the person in case 2, “Dakota,” was the same woman who was involved in case 1.
In case 2, a doula had spent 2 years supporting Dakota through the deaths of a parent and her baby, who had a congenital defect. A baby-loss charity had also worked with Dakota but could not confirm the baby’s existence.
Dakota had gone so far as to make a video for the doula that showed a hospital room. In a voice-over, Dakota thanks everyone for the support she received as the baby died.
In case 3, “Hannah” texted a doula seeking emotional but not birth support. The doula, Nikki Barrow, has recounted the case on her own blog.
Hannah became desperate when she went into labor. Ms. Barrow remained close via texts, phone, and video calls, even as the baby supposedly died after 3 days. The doula lit a candle for the baby and cried with Hannah.
Ms. Barrow was eventually able to break away from Hannah, saying she was not a bereavement specialist. However, days later, Hannah tracked her down and claimed she had an infection in her heart and did not have much time to live. At that point, Ms. Barrow stopped all contact.
She determined from other doulas that Hannah had been hoaxing doulas for 4 or 5 years. Some had offered to get her help, but she refused and ended all contact.
Multiple COVID crises?
In case 4, a woman sought support on a doula-centered Facebook page and said her partner “Jack” would be in touch. Jack sent the doula hundreds of emails, texts, and WhatsApp messages and then said he was hospitalized with COVID. The woman, “Hayley,” was also soon diagnosed with COVID.
Hayley refused video contact and did not share photos. Drama continued to unfold. She reported that her baby was breach, that she had a second uterus with a second pregnancy simultaneously, and that the baby had COVID.
Hayley also claimed that her partner had come to the hospital, had raped her, and had brandished a gun. When the doula called the police, they did not find Hayley at the hospital or elsewhere.
In case 5, a “grandmother” contacted “Lisa” to find a doula for her daughter-in-law, “Anna.” Hours later, Anna was giving birth, and the baby had to be taken to the hospital because of cardiac and breathing problems. The doula heard nothing more after a few weeks.
However, at least three other doulas said they had supported the same “family.”
Online training program
In all cases, the doulas were not paid for their time. Reports to the police prompted no action because no money had changed hands. Some doulas said they felt bereaved, angry, or “silly” that they had been hoodwinked. All noted how difficult it was to disengage from clients who seemed to be in peril.
Ms. Barrow decided to create an online training program in which doulas are advised on how to stay safe while working online.
DoulaMatch, which matches birth support specialists with women in the United States and Canada, offers tips to help protect doulas from hoaxes.
Kim James, BDT(DONA), ICCE, LCCE, CLE, the owner and operator of DoulaMatch, said the organization is aware of “scammers who waste everyone’s time and have found doulas to be the latest easy targets.”
However, she noted, “I’ve only very occasionally and anecdotally heard about people fabricating a pregnancy for emotional gratification.”
In his 2000 article, Dr. Feldman offers clues to help detect hoaxers. He advises clinicians to be wary of the following:
- Cases in which the length, frequency, and duration of posts are incongruous with the severity of the illness the person is claiming to have; for example, someone who claims to be in submitting detailed posts.
- Near-fatal exacerbations of illness alternating with miraculous recoveries.
- Personal claims that are fantastic, are contradicted by later posts, or are disproved.
- Continual dramatic events occurring in the person’s life, especially when others in a group become the focus of attention.
- Others ostensibly posting on behalf of the individual who have identical patterns of writing, such as making grammatical errors, misspellings, and using stylistic idiosyncrasies.
A version of this article first appeared on Medscape.com.
A new study documents a handful of cases of women with Munchausen syndrome by Internet who targeted doulas in the United Kingdom during the COVID-19 lockdown.
The five cases were investigated by Kathryn Newns, MSc, DClinPsy, a clinical psychologist in Cambridge, England, who said the cases were brought to her attention by a doula she herself had used for the birth of her own child a decade earlier.
Dr. Newns said she believes these are not isolated cases – either geographically or in terms of the specialty involved.
“I don’t think it is likely that this is only happening in the United Kingdom. And I’m sure it’s not just happening in the doula world,” Dr. Newns told this news organization.
Coinvestigator Marc Feldman, MD, a clinical professor of psychiatry at the University of Alabama, Tuscaloosa, coined the term “Munchausen by Internet” in a 2000 article. The expression refers to use of electronic media to perpetrate hoaxes that reward posers with sympathy, control, or emotional gratification. The hoaxers do not seek financial gain.
“The ease of carrying out Munchausen behaviors makes me think that it must be much more common than it ever was,” Dr. Feldman said in an interview.
He noted that the new DSM-5 will eliminate the terms “Munchausen” and “Munchausen by Internet” and will clarify that “factitious disorder” can be partly or wholly carried out online.
The study was published in the May issue of the Annals of Clinical Psychiatry.
A warning for others
In the past, those with factitious disorder had to go to medical libraries to study up on the ailment they wanted to feign. They would then present to an emergency department or a doctor’s office and act convincingly, Dr. Feldman said.
“Now all you have to do is go to Wikipedia and you can become an expert on a medical ailment within a few minutes,” he added.
In the five cases described in the study, the hoaxers created rich stories, especially in cases 1 and 2. In those cases, the perpetrator turned out to be the same person. Subterfuge “obviously made it much harder to know she wasn’t who she purported to be,” said Dr. Newns.
Dr. Feldman noted that in Munchausen by Internet, there may be some element of truth within the stories.
For health care professionals, “it takes a considerable leap to assume that somebody who’s talking about some dreaded ailment is in fact exaggerating or outright lying,” he said.
In the five cases described in the study, persons contacted doulas, then related traumatic stories and described dramatic, immediate needs. All of the doulas were working remotely because of the COVID-19 pandemic. This likely made it easier for the perpetrators to pull off the hoaxes. The health care professionals agreed to share their experiences in the hopes of warning others.
Elaborate scenarios
The first two cases were ultimately determined to involve one person who had created elaborate scenarios.
In case 1, the hoaxer, who called herself “Jessica,” texted the doula “Charlotte” when she was allegedly 39 weeks’ pregnant. She said she was unable to go to the hospital because of the COVID-19 risks to her husband, who had cystic fibrosis and had recently undergone a heart and lung transplant.
The husband “Jordan” took over communications, using the same WhatsApp number as Jessica, as Jessica went into labor.
Ostensibly, a midwife team had come to Jessica’s and Jordan’s house. When the doula was on the phone with Jordan, she heard Jessica crying, grunting, and screaming, and then, at 2:00 a.m., she heard the sound of a baby crying. A photo of the baby was texted to Charlotte.
Soon, there were many problems. Jessica allegedly had a postpartum hemorrhage, and mother and baby were taken to separate hospitals. The baby was then diagnosed with congenital heart disease.
Over the next week, “midwives” started texting back and forth with Charlotte. The doula began to have doubts and asked a midwife to share a visual communication.
After receiving no response, Charlotte used a video call, got Jessica on screen, and told her she thought there was no baby. Jessica said the baby was real and showed a “growth chart” as proof of the 5-day-old baby’s existence. The birth and baby noises were later determined to be recordings.
Child deaths
After sharing information among themselves on a private Facebook group, the doulas determined that the person in case 2, “Dakota,” was the same woman who was involved in case 1.
In case 2, a doula had spent 2 years supporting Dakota through the deaths of a parent and her baby, who had a congenital defect. A baby-loss charity had also worked with Dakota but could not confirm the baby’s existence.
Dakota had gone so far as to make a video for the doula that showed a hospital room. In a voice-over, Dakota thanks everyone for the support she received as the baby died.
In case 3, “Hannah” texted a doula seeking emotional but not birth support. The doula, Nikki Barrow, has recounted the case on her own blog.
Hannah became desperate when she went into labor. Ms. Barrow remained close via texts, phone, and video calls, even as the baby supposedly died after 3 days. The doula lit a candle for the baby and cried with Hannah.
Ms. Barrow was eventually able to break away from Hannah, saying she was not a bereavement specialist. However, days later, Hannah tracked her down and claimed she had an infection in her heart and did not have much time to live. At that point, Ms. Barrow stopped all contact.
She determined from other doulas that Hannah had been hoaxing doulas for 4 or 5 years. Some had offered to get her help, but she refused and ended all contact.
Multiple COVID crises?
In case 4, a woman sought support on a doula-centered Facebook page and said her partner “Jack” would be in touch. Jack sent the doula hundreds of emails, texts, and WhatsApp messages and then said he was hospitalized with COVID. The woman, “Hayley,” was also soon diagnosed with COVID.
Hayley refused video contact and did not share photos. Drama continued to unfold. She reported that her baby was breach, that she had a second uterus with a second pregnancy simultaneously, and that the baby had COVID.
Hayley also claimed that her partner had come to the hospital, had raped her, and had brandished a gun. When the doula called the police, they did not find Hayley at the hospital or elsewhere.
In case 5, a “grandmother” contacted “Lisa” to find a doula for her daughter-in-law, “Anna.” Hours later, Anna was giving birth, and the baby had to be taken to the hospital because of cardiac and breathing problems. The doula heard nothing more after a few weeks.
However, at least three other doulas said they had supported the same “family.”
Online training program
In all cases, the doulas were not paid for their time. Reports to the police prompted no action because no money had changed hands. Some doulas said they felt bereaved, angry, or “silly” that they had been hoodwinked. All noted how difficult it was to disengage from clients who seemed to be in peril.
Ms. Barrow decided to create an online training program in which doulas are advised on how to stay safe while working online.
DoulaMatch, which matches birth support specialists with women in the United States and Canada, offers tips to help protect doulas from hoaxes.
Kim James, BDT(DONA), ICCE, LCCE, CLE, the owner and operator of DoulaMatch, said the organization is aware of “scammers who waste everyone’s time and have found doulas to be the latest easy targets.”
However, she noted, “I’ve only very occasionally and anecdotally heard about people fabricating a pregnancy for emotional gratification.”
In his 2000 article, Dr. Feldman offers clues to help detect hoaxers. He advises clinicians to be wary of the following:
- Cases in which the length, frequency, and duration of posts are incongruous with the severity of the illness the person is claiming to have; for example, someone who claims to be in submitting detailed posts.
- Near-fatal exacerbations of illness alternating with miraculous recoveries.
- Personal claims that are fantastic, are contradicted by later posts, or are disproved.
- Continual dramatic events occurring in the person’s life, especially when others in a group become the focus of attention.
- Others ostensibly posting on behalf of the individual who have identical patterns of writing, such as making grammatical errors, misspellings, and using stylistic idiosyncrasies.
A version of this article first appeared on Medscape.com.
A new study documents a handful of cases of women with Munchausen syndrome by Internet who targeted doulas in the United Kingdom during the COVID-19 lockdown.
The five cases were investigated by Kathryn Newns, MSc, DClinPsy, a clinical psychologist in Cambridge, England, who said the cases were brought to her attention by a doula she herself had used for the birth of her own child a decade earlier.
Dr. Newns said she believes these are not isolated cases – either geographically or in terms of the specialty involved.
“I don’t think it is likely that this is only happening in the United Kingdom. And I’m sure it’s not just happening in the doula world,” Dr. Newns told this news organization.
Coinvestigator Marc Feldman, MD, a clinical professor of psychiatry at the University of Alabama, Tuscaloosa, coined the term “Munchausen by Internet” in a 2000 article. The expression refers to use of electronic media to perpetrate hoaxes that reward posers with sympathy, control, or emotional gratification. The hoaxers do not seek financial gain.
“The ease of carrying out Munchausen behaviors makes me think that it must be much more common than it ever was,” Dr. Feldman said in an interview.
He noted that the new DSM-5 will eliminate the terms “Munchausen” and “Munchausen by Internet” and will clarify that “factitious disorder” can be partly or wholly carried out online.
The study was published in the May issue of the Annals of Clinical Psychiatry.
A warning for others
In the past, those with factitious disorder had to go to medical libraries to study up on the ailment they wanted to feign. They would then present to an emergency department or a doctor’s office and act convincingly, Dr. Feldman said.
“Now all you have to do is go to Wikipedia and you can become an expert on a medical ailment within a few minutes,” he added.
In the five cases described in the study, the hoaxers created rich stories, especially in cases 1 and 2. In those cases, the perpetrator turned out to be the same person. Subterfuge “obviously made it much harder to know she wasn’t who she purported to be,” said Dr. Newns.
Dr. Feldman noted that in Munchausen by Internet, there may be some element of truth within the stories.
For health care professionals, “it takes a considerable leap to assume that somebody who’s talking about some dreaded ailment is in fact exaggerating or outright lying,” he said.
In the five cases described in the study, persons contacted doulas, then related traumatic stories and described dramatic, immediate needs. All of the doulas were working remotely because of the COVID-19 pandemic. This likely made it easier for the perpetrators to pull off the hoaxes. The health care professionals agreed to share their experiences in the hopes of warning others.
Elaborate scenarios
The first two cases were ultimately determined to involve one person who had created elaborate scenarios.
In case 1, the hoaxer, who called herself “Jessica,” texted the doula “Charlotte” when she was allegedly 39 weeks’ pregnant. She said she was unable to go to the hospital because of the COVID-19 risks to her husband, who had cystic fibrosis and had recently undergone a heart and lung transplant.
The husband “Jordan” took over communications, using the same WhatsApp number as Jessica, as Jessica went into labor.
Ostensibly, a midwife team had come to Jessica’s and Jordan’s house. When the doula was on the phone with Jordan, she heard Jessica crying, grunting, and screaming, and then, at 2:00 a.m., she heard the sound of a baby crying. A photo of the baby was texted to Charlotte.
Soon, there were many problems. Jessica allegedly had a postpartum hemorrhage, and mother and baby were taken to separate hospitals. The baby was then diagnosed with congenital heart disease.
Over the next week, “midwives” started texting back and forth with Charlotte. The doula began to have doubts and asked a midwife to share a visual communication.
After receiving no response, Charlotte used a video call, got Jessica on screen, and told her she thought there was no baby. Jessica said the baby was real and showed a “growth chart” as proof of the 5-day-old baby’s existence. The birth and baby noises were later determined to be recordings.
Child deaths
After sharing information among themselves on a private Facebook group, the doulas determined that the person in case 2, “Dakota,” was the same woman who was involved in case 1.
In case 2, a doula had spent 2 years supporting Dakota through the deaths of a parent and her baby, who had a congenital defect. A baby-loss charity had also worked with Dakota but could not confirm the baby’s existence.
Dakota had gone so far as to make a video for the doula that showed a hospital room. In a voice-over, Dakota thanks everyone for the support she received as the baby died.
In case 3, “Hannah” texted a doula seeking emotional but not birth support. The doula, Nikki Barrow, has recounted the case on her own blog.
Hannah became desperate when she went into labor. Ms. Barrow remained close via texts, phone, and video calls, even as the baby supposedly died after 3 days. The doula lit a candle for the baby and cried with Hannah.
Ms. Barrow was eventually able to break away from Hannah, saying she was not a bereavement specialist. However, days later, Hannah tracked her down and claimed she had an infection in her heart and did not have much time to live. At that point, Ms. Barrow stopped all contact.
She determined from other doulas that Hannah had been hoaxing doulas for 4 or 5 years. Some had offered to get her help, but she refused and ended all contact.
Multiple COVID crises?
In case 4, a woman sought support on a doula-centered Facebook page and said her partner “Jack” would be in touch. Jack sent the doula hundreds of emails, texts, and WhatsApp messages and then said he was hospitalized with COVID. The woman, “Hayley,” was also soon diagnosed with COVID.
Hayley refused video contact and did not share photos. Drama continued to unfold. She reported that her baby was breach, that she had a second uterus with a second pregnancy simultaneously, and that the baby had COVID.
Hayley also claimed that her partner had come to the hospital, had raped her, and had brandished a gun. When the doula called the police, they did not find Hayley at the hospital or elsewhere.
In case 5, a “grandmother” contacted “Lisa” to find a doula for her daughter-in-law, “Anna.” Hours later, Anna was giving birth, and the baby had to be taken to the hospital because of cardiac and breathing problems. The doula heard nothing more after a few weeks.
However, at least three other doulas said they had supported the same “family.”
Online training program
In all cases, the doulas were not paid for their time. Reports to the police prompted no action because no money had changed hands. Some doulas said they felt bereaved, angry, or “silly” that they had been hoodwinked. All noted how difficult it was to disengage from clients who seemed to be in peril.
Ms. Barrow decided to create an online training program in which doulas are advised on how to stay safe while working online.
DoulaMatch, which matches birth support specialists with women in the United States and Canada, offers tips to help protect doulas from hoaxes.
Kim James, BDT(DONA), ICCE, LCCE, CLE, the owner and operator of DoulaMatch, said the organization is aware of “scammers who waste everyone’s time and have found doulas to be the latest easy targets.”
However, she noted, “I’ve only very occasionally and anecdotally heard about people fabricating a pregnancy for emotional gratification.”
In his 2000 article, Dr. Feldman offers clues to help detect hoaxers. He advises clinicians to be wary of the following:
- Cases in which the length, frequency, and duration of posts are incongruous with the severity of the illness the person is claiming to have; for example, someone who claims to be in submitting detailed posts.
- Near-fatal exacerbations of illness alternating with miraculous recoveries.
- Personal claims that are fantastic, are contradicted by later posts, or are disproved.
- Continual dramatic events occurring in the person’s life, especially when others in a group become the focus of attention.
- Others ostensibly posting on behalf of the individual who have identical patterns of writing, such as making grammatical errors, misspellings, and using stylistic idiosyncrasies.
A version of this article first appeared on Medscape.com.
New moms latched on to remote breastfeeding help. Will demand wane as pandemic fades?
Madison Cano knew she wanted to breastfeed her son, Theo. But breastfeeding was painful for her. The skin on her breasts was chafed and blistered last July when she returned home from the hospital. And Theo sometimes screamed during feedings.
Ms. Cano, 30, realized she needed help to get the short- and long-term health benefits of breastfeeding for moms and babies. New studies (Am J Obstet Gynecol. 2021 Mar 26. doi: 10.1016/j.ajog.2021.03.023) also have shown that COVID-vaccinated mothers pass protective antibodies on to their newborns. However, Ms. Cano lives in Montrose in western Colorado, 60 miles away from her lactation counselor, Ali Reynolds, in Grand Junction – and it was during the thick of the pandemic.
She messaged Ms. Reynolds on Facebook and took photos and recorded videos of herself breastfeeding so Reynolds could offer advice and encouragement from afar. It worked. She no longer had pain. Ms. Cano is still breastfeeding Theo, who just turned 1.
“I don’t think I would have understood what was happening and been able to work through it without that resource,” said Ms. Cano.
Support for breastfeeding was upended last year, when it no longer seemed safe to take a baby class at the hospital or invite a nurse into one’s home. Hospitals, lactation counselors, and support groups turned to virtual platforms like Zoom or phone calls. That made lactation support accessible to struggling families during the pandemic, said Danielle Harmon, executive director of the United States Lactation Consultant Association.
Today, although lactation specialists have more options to safely meet in person with families after their COVID-19 vaccinations, many are choosing to continue virtual classes, keeping alive the online communities they created and relying on the technology that worked for many families. Virtual options especially help those in remote areas or those with limited transportation access, breastfeeding experts say.
Right before the pandemic, for example, Sandrine Druon typically had one or two moms attend in-person meetings she held for La Leche League of Longmont at the First Evangelical Lutheran Church or at a Ziggi’s Coffee shop. But because they could no longer meet in person, last June she launched two monthly virtual meetings. Now, an online meeting will typically include 9 or 10 moms. She started an online Spanish-speaking meeting in May and parents joined from their homes in several states and even from other countries. She hopes eventually to have a mix of online and in-person meetings.
The virtual switch hasn’t worked for everyone. Ms. Harmon said the logistics of video support remain difficult, along with privacy concerns on platforms that could be hacked. Other lactation experts noted Black and Hispanic mothers are sometimes still left behind. So lactation specialists are trying to learn from the pandemic on what worked – and what didn’t – to reach all kinds of new parents.
Before the pandemic, 84% of U.S. mothers breastfed at least initially, according to 2019 data from the Centers for Disease Control and Prevention, while Colorado had a 93% rate.
The pandemic hasn’t seemed to change the picture, said Stacy Miller, Colorado’s breastfeeding coordinator for the Special Supplemental Nutrition Program for Women, Infants, and Children, shorthanded as WIC. Citing state birth certificate data, Ms. Miller said preliminary breastfeeding rates among families discharged from Colorado hospitals remained similar in the first quarter of 2021 to rates from 2020 or 2019.
Throughout the pandemic, lactation specialists have tried to offer convenient options for parents. St. Joseph Hospital in Denver launched virtual breastfeeding support groups that still occur today, in addition to breastfeeding help during families’ hospital stays, said Katie Halverstadt, the hospital’s clinical nurse manager of lactation and family education.
Last year in North Carolina, experts adapted an in-person prenatal breastfeeding program to an interactive video platform in English and Spanish. A separate effort on New York’s Long Island successfully converted in-person breastfeeding support to phone and video calls in 2020.
To help support parents in Grand Junction, Colo., Ms. Reynolds expanded her private practice, Valley Lactation, by offering virtual appointments while continuing to see some clients in their homes. That hybrid model continues today, although Ms. Reynolds said the demand for virtual or phone appointments has decreased lately as the country reopens.
Paying out-of-pocket for appointments is a hurdle her clients face, said Ms. Reynolds, but she encourages them to submit claims for telehealth or in-person visits to their health insurance companies for reimbursement. Early in the pandemic, telehealth rules were relaxed to encourage more telephone and virtual appointments – many of which have been covered by insurance.
But insurance coverage for lactation support will likely continue to be an issue independent of whether pandemic telehealth rules expire, Ms. Harmon said. While the Affordable Care Act mandates that insurance companies cover lactation support and supplies, such as breast pumps, Ms. Harmon said reimbursement is often spotty. Mirroring Medicaid, insurance providers often cover services only from licensed providers, she said, but just four states – Georgia, New Mexico, Oregon, and Rhode Island – license lactation consultants.
Experts such as Jennifer Schindler-Ruwisch, an assistant professor at Fairfield (Conn.) University, found the pandemic may have exacerbated breastfeeding barriers for those without access to online technology or translation services, among other things. She published one of the first studies in the United States to examine COVID’s effect on lactation services by collecting experiences from lactation support providers in Connecticut, including many working in WIC programs. For income-eligible WIC families, all breastfeeding classes, peer groups and one-on-one consultations are free.
Birdie Johnson, a doula who provides breastfeeding and other postpartum support to Black families as part of Sacred Seeds Black Doula Collective of Colorado, said virtual support groups during the pandemic also did not meet her clients’ needs for connection and interaction. Social media built communities online, particularly by normalizing breastfeeding struggles among Black parents, she said, but obstacles remained.
“COVID brought our community together and at the same time destroyed it,” Ms. Johnson said.
Black parents in the United States already had lower rates of breastfeeding than Asian or White parents, according to 2017 CDC data, and both Black and Hispanic parents have had lower rates of exclusively breastfeeding their babies at 6 months, which is what the American Academy of Pediatrics recommends. Socioeconomics and lack of workplace support have been found to contribute to the gap. Research also has found Black mothers are more likely than White moms to be introduced to infant formula at hospitals.
A scarcity of Black health care providers in lactation, women’s health and pediatrics is a continuing concern, Ms. Johnson said. In Colorado last year, the Colorado Breastfeeding Coalition, the Center for African American Health, Elephant Circle and Families Forward Resource Center held three training sessions for people of color to become lactation specialists, said Ms. Halverstadt, who chairs the coalition.
Jefferson County, which encompasses much of Denver’s western suburbs, is now training at least a dozen Spanish-speaking community members for lactation certification. In addition to classes, the trainees log clinical hours in breastfeeding support, sometimes during virtual meetings of a Spanish-speaking support group called Cuenta Conmigo Lactancia.
“You are more confident and more at ease with someone who knows your language, your culture and who is part of the community,” said Brenda Rodriguez, a dietitian and certified lactation consultant for Jefferson County Public Health, which reaches roughly 400 breastfeeding families each month through its WIC programs.
Angelica Pereda, a maternal and child health registered nurse, is part of that training program. Ms. Pereda, who is Hispanic and bilingual, gave birth to son Ahmias in April 2020 and struggled with breastfeeding because he could not latch on to her breasts. A lactation consultant could not come into her home during the pandemic, and she was skeptical of virtual consultations because of privacy concerns. So she pumped her breast milk and bottle-fed it to her son.
Her experience gave her newfound empathy for families, and she wants to help other Spanish-speaking parents find solutions – whether in person or virtually.
“There is just not enough breastfeeding support in general, but especially when that support is in a different language,” said Ms. Pereda.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Madison Cano knew she wanted to breastfeed her son, Theo. But breastfeeding was painful for her. The skin on her breasts was chafed and blistered last July when she returned home from the hospital. And Theo sometimes screamed during feedings.
Ms. Cano, 30, realized she needed help to get the short- and long-term health benefits of breastfeeding for moms and babies. New studies (Am J Obstet Gynecol. 2021 Mar 26. doi: 10.1016/j.ajog.2021.03.023) also have shown that COVID-vaccinated mothers pass protective antibodies on to their newborns. However, Ms. Cano lives in Montrose in western Colorado, 60 miles away from her lactation counselor, Ali Reynolds, in Grand Junction – and it was during the thick of the pandemic.
She messaged Ms. Reynolds on Facebook and took photos and recorded videos of herself breastfeeding so Reynolds could offer advice and encouragement from afar. It worked. She no longer had pain. Ms. Cano is still breastfeeding Theo, who just turned 1.
“I don’t think I would have understood what was happening and been able to work through it without that resource,” said Ms. Cano.
Support for breastfeeding was upended last year, when it no longer seemed safe to take a baby class at the hospital or invite a nurse into one’s home. Hospitals, lactation counselors, and support groups turned to virtual platforms like Zoom or phone calls. That made lactation support accessible to struggling families during the pandemic, said Danielle Harmon, executive director of the United States Lactation Consultant Association.
Today, although lactation specialists have more options to safely meet in person with families after their COVID-19 vaccinations, many are choosing to continue virtual classes, keeping alive the online communities they created and relying on the technology that worked for many families. Virtual options especially help those in remote areas or those with limited transportation access, breastfeeding experts say.
Right before the pandemic, for example, Sandrine Druon typically had one or two moms attend in-person meetings she held for La Leche League of Longmont at the First Evangelical Lutheran Church or at a Ziggi’s Coffee shop. But because they could no longer meet in person, last June she launched two monthly virtual meetings. Now, an online meeting will typically include 9 or 10 moms. She started an online Spanish-speaking meeting in May and parents joined from their homes in several states and even from other countries. She hopes eventually to have a mix of online and in-person meetings.
The virtual switch hasn’t worked for everyone. Ms. Harmon said the logistics of video support remain difficult, along with privacy concerns on platforms that could be hacked. Other lactation experts noted Black and Hispanic mothers are sometimes still left behind. So lactation specialists are trying to learn from the pandemic on what worked – and what didn’t – to reach all kinds of new parents.
Before the pandemic, 84% of U.S. mothers breastfed at least initially, according to 2019 data from the Centers for Disease Control and Prevention, while Colorado had a 93% rate.
The pandemic hasn’t seemed to change the picture, said Stacy Miller, Colorado’s breastfeeding coordinator for the Special Supplemental Nutrition Program for Women, Infants, and Children, shorthanded as WIC. Citing state birth certificate data, Ms. Miller said preliminary breastfeeding rates among families discharged from Colorado hospitals remained similar in the first quarter of 2021 to rates from 2020 or 2019.
Throughout the pandemic, lactation specialists have tried to offer convenient options for parents. St. Joseph Hospital in Denver launched virtual breastfeeding support groups that still occur today, in addition to breastfeeding help during families’ hospital stays, said Katie Halverstadt, the hospital’s clinical nurse manager of lactation and family education.
Last year in North Carolina, experts adapted an in-person prenatal breastfeeding program to an interactive video platform in English and Spanish. A separate effort on New York’s Long Island successfully converted in-person breastfeeding support to phone and video calls in 2020.
To help support parents in Grand Junction, Colo., Ms. Reynolds expanded her private practice, Valley Lactation, by offering virtual appointments while continuing to see some clients in their homes. That hybrid model continues today, although Ms. Reynolds said the demand for virtual or phone appointments has decreased lately as the country reopens.
Paying out-of-pocket for appointments is a hurdle her clients face, said Ms. Reynolds, but she encourages them to submit claims for telehealth or in-person visits to their health insurance companies for reimbursement. Early in the pandemic, telehealth rules were relaxed to encourage more telephone and virtual appointments – many of which have been covered by insurance.
But insurance coverage for lactation support will likely continue to be an issue independent of whether pandemic telehealth rules expire, Ms. Harmon said. While the Affordable Care Act mandates that insurance companies cover lactation support and supplies, such as breast pumps, Ms. Harmon said reimbursement is often spotty. Mirroring Medicaid, insurance providers often cover services only from licensed providers, she said, but just four states – Georgia, New Mexico, Oregon, and Rhode Island – license lactation consultants.
Experts such as Jennifer Schindler-Ruwisch, an assistant professor at Fairfield (Conn.) University, found the pandemic may have exacerbated breastfeeding barriers for those without access to online technology or translation services, among other things. She published one of the first studies in the United States to examine COVID’s effect on lactation services by collecting experiences from lactation support providers in Connecticut, including many working in WIC programs. For income-eligible WIC families, all breastfeeding classes, peer groups and one-on-one consultations are free.
Birdie Johnson, a doula who provides breastfeeding and other postpartum support to Black families as part of Sacred Seeds Black Doula Collective of Colorado, said virtual support groups during the pandemic also did not meet her clients’ needs for connection and interaction. Social media built communities online, particularly by normalizing breastfeeding struggles among Black parents, she said, but obstacles remained.
“COVID brought our community together and at the same time destroyed it,” Ms. Johnson said.
Black parents in the United States already had lower rates of breastfeeding than Asian or White parents, according to 2017 CDC data, and both Black and Hispanic parents have had lower rates of exclusively breastfeeding their babies at 6 months, which is what the American Academy of Pediatrics recommends. Socioeconomics and lack of workplace support have been found to contribute to the gap. Research also has found Black mothers are more likely than White moms to be introduced to infant formula at hospitals.
A scarcity of Black health care providers in lactation, women’s health and pediatrics is a continuing concern, Ms. Johnson said. In Colorado last year, the Colorado Breastfeeding Coalition, the Center for African American Health, Elephant Circle and Families Forward Resource Center held three training sessions for people of color to become lactation specialists, said Ms. Halverstadt, who chairs the coalition.
Jefferson County, which encompasses much of Denver’s western suburbs, is now training at least a dozen Spanish-speaking community members for lactation certification. In addition to classes, the trainees log clinical hours in breastfeeding support, sometimes during virtual meetings of a Spanish-speaking support group called Cuenta Conmigo Lactancia.
“You are more confident and more at ease with someone who knows your language, your culture and who is part of the community,” said Brenda Rodriguez, a dietitian and certified lactation consultant for Jefferson County Public Health, which reaches roughly 400 breastfeeding families each month through its WIC programs.
Angelica Pereda, a maternal and child health registered nurse, is part of that training program. Ms. Pereda, who is Hispanic and bilingual, gave birth to son Ahmias in April 2020 and struggled with breastfeeding because he could not latch on to her breasts. A lactation consultant could not come into her home during the pandemic, and she was skeptical of virtual consultations because of privacy concerns. So she pumped her breast milk and bottle-fed it to her son.
Her experience gave her newfound empathy for families, and she wants to help other Spanish-speaking parents find solutions – whether in person or virtually.
“There is just not enough breastfeeding support in general, but especially when that support is in a different language,” said Ms. Pereda.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Madison Cano knew she wanted to breastfeed her son, Theo. But breastfeeding was painful for her. The skin on her breasts was chafed and blistered last July when she returned home from the hospital. And Theo sometimes screamed during feedings.
Ms. Cano, 30, realized she needed help to get the short- and long-term health benefits of breastfeeding for moms and babies. New studies (Am J Obstet Gynecol. 2021 Mar 26. doi: 10.1016/j.ajog.2021.03.023) also have shown that COVID-vaccinated mothers pass protective antibodies on to their newborns. However, Ms. Cano lives in Montrose in western Colorado, 60 miles away from her lactation counselor, Ali Reynolds, in Grand Junction – and it was during the thick of the pandemic.
She messaged Ms. Reynolds on Facebook and took photos and recorded videos of herself breastfeeding so Reynolds could offer advice and encouragement from afar. It worked. She no longer had pain. Ms. Cano is still breastfeeding Theo, who just turned 1.
“I don’t think I would have understood what was happening and been able to work through it without that resource,” said Ms. Cano.
Support for breastfeeding was upended last year, when it no longer seemed safe to take a baby class at the hospital or invite a nurse into one’s home. Hospitals, lactation counselors, and support groups turned to virtual platforms like Zoom or phone calls. That made lactation support accessible to struggling families during the pandemic, said Danielle Harmon, executive director of the United States Lactation Consultant Association.
Today, although lactation specialists have more options to safely meet in person with families after their COVID-19 vaccinations, many are choosing to continue virtual classes, keeping alive the online communities they created and relying on the technology that worked for many families. Virtual options especially help those in remote areas or those with limited transportation access, breastfeeding experts say.
Right before the pandemic, for example, Sandrine Druon typically had one or two moms attend in-person meetings she held for La Leche League of Longmont at the First Evangelical Lutheran Church or at a Ziggi’s Coffee shop. But because they could no longer meet in person, last June she launched two monthly virtual meetings. Now, an online meeting will typically include 9 or 10 moms. She started an online Spanish-speaking meeting in May and parents joined from their homes in several states and even from other countries. She hopes eventually to have a mix of online and in-person meetings.
The virtual switch hasn’t worked for everyone. Ms. Harmon said the logistics of video support remain difficult, along with privacy concerns on platforms that could be hacked. Other lactation experts noted Black and Hispanic mothers are sometimes still left behind. So lactation specialists are trying to learn from the pandemic on what worked – and what didn’t – to reach all kinds of new parents.
Before the pandemic, 84% of U.S. mothers breastfed at least initially, according to 2019 data from the Centers for Disease Control and Prevention, while Colorado had a 93% rate.
The pandemic hasn’t seemed to change the picture, said Stacy Miller, Colorado’s breastfeeding coordinator for the Special Supplemental Nutrition Program for Women, Infants, and Children, shorthanded as WIC. Citing state birth certificate data, Ms. Miller said preliminary breastfeeding rates among families discharged from Colorado hospitals remained similar in the first quarter of 2021 to rates from 2020 or 2019.
Throughout the pandemic, lactation specialists have tried to offer convenient options for parents. St. Joseph Hospital in Denver launched virtual breastfeeding support groups that still occur today, in addition to breastfeeding help during families’ hospital stays, said Katie Halverstadt, the hospital’s clinical nurse manager of lactation and family education.
Last year in North Carolina, experts adapted an in-person prenatal breastfeeding program to an interactive video platform in English and Spanish. A separate effort on New York’s Long Island successfully converted in-person breastfeeding support to phone and video calls in 2020.
To help support parents in Grand Junction, Colo., Ms. Reynolds expanded her private practice, Valley Lactation, by offering virtual appointments while continuing to see some clients in their homes. That hybrid model continues today, although Ms. Reynolds said the demand for virtual or phone appointments has decreased lately as the country reopens.
Paying out-of-pocket for appointments is a hurdle her clients face, said Ms. Reynolds, but she encourages them to submit claims for telehealth or in-person visits to their health insurance companies for reimbursement. Early in the pandemic, telehealth rules were relaxed to encourage more telephone and virtual appointments – many of which have been covered by insurance.
But insurance coverage for lactation support will likely continue to be an issue independent of whether pandemic telehealth rules expire, Ms. Harmon said. While the Affordable Care Act mandates that insurance companies cover lactation support and supplies, such as breast pumps, Ms. Harmon said reimbursement is often spotty. Mirroring Medicaid, insurance providers often cover services only from licensed providers, she said, but just four states – Georgia, New Mexico, Oregon, and Rhode Island – license lactation consultants.
Experts such as Jennifer Schindler-Ruwisch, an assistant professor at Fairfield (Conn.) University, found the pandemic may have exacerbated breastfeeding barriers for those without access to online technology or translation services, among other things. She published one of the first studies in the United States to examine COVID’s effect on lactation services by collecting experiences from lactation support providers in Connecticut, including many working in WIC programs. For income-eligible WIC families, all breastfeeding classes, peer groups and one-on-one consultations are free.
Birdie Johnson, a doula who provides breastfeeding and other postpartum support to Black families as part of Sacred Seeds Black Doula Collective of Colorado, said virtual support groups during the pandemic also did not meet her clients’ needs for connection and interaction. Social media built communities online, particularly by normalizing breastfeeding struggles among Black parents, she said, but obstacles remained.
“COVID brought our community together and at the same time destroyed it,” Ms. Johnson said.
Black parents in the United States already had lower rates of breastfeeding than Asian or White parents, according to 2017 CDC data, and both Black and Hispanic parents have had lower rates of exclusively breastfeeding their babies at 6 months, which is what the American Academy of Pediatrics recommends. Socioeconomics and lack of workplace support have been found to contribute to the gap. Research also has found Black mothers are more likely than White moms to be introduced to infant formula at hospitals.
A scarcity of Black health care providers in lactation, women’s health and pediatrics is a continuing concern, Ms. Johnson said. In Colorado last year, the Colorado Breastfeeding Coalition, the Center for African American Health, Elephant Circle and Families Forward Resource Center held three training sessions for people of color to become lactation specialists, said Ms. Halverstadt, who chairs the coalition.
Jefferson County, which encompasses much of Denver’s western suburbs, is now training at least a dozen Spanish-speaking community members for lactation certification. In addition to classes, the trainees log clinical hours in breastfeeding support, sometimes during virtual meetings of a Spanish-speaking support group called Cuenta Conmigo Lactancia.
“You are more confident and more at ease with someone who knows your language, your culture and who is part of the community,” said Brenda Rodriguez, a dietitian and certified lactation consultant for Jefferson County Public Health, which reaches roughly 400 breastfeeding families each month through its WIC programs.
Angelica Pereda, a maternal and child health registered nurse, is part of that training program. Ms. Pereda, who is Hispanic and bilingual, gave birth to son Ahmias in April 2020 and struggled with breastfeeding because he could not latch on to her breasts. A lactation consultant could not come into her home during the pandemic, and she was skeptical of virtual consultations because of privacy concerns. So she pumped her breast milk and bottle-fed it to her son.
Her experience gave her newfound empathy for families, and she wants to help other Spanish-speaking parents find solutions – whether in person or virtually.
“There is just not enough breastfeeding support in general, but especially when that support is in a different language,” said Ms. Pereda.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
ACOG, SMFM urge all pregnant women to get COVID-19 vaccine
The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) strongly recommend that all pregnant women be vaccinated against COVID-19.
Only about 16% of pregnant people have received one or more doses of a COVID-19 vaccine, according to the Centers for Disease Control and Prevention, despite evidence that COVID-19 infection puts pregnant people at an increased risk of severe complications and death.
That CDC report in June also found that vaccination during pregnancy was lowest among Hispanic (11.9%) and non-Hispanic Black women (6%) and women aged 18-24 years (5.5%) and highest among non-Hispanic Asian women (24.7%) and women aged 35-49 years (22.7%).
Linda Eckert, MD, professor of obstetrics and gynecology at University of Washington, Seattle, and a member of ACOG’s immunization expert work group, said in an interview that previously, ACOG has said that pregnant women should have the opportunity to be vaccinated, should they choose it.
Now the urgency has increased, she said: “This is a strong recommendation.”
The recommendation comes after mounting evidence demonstrating that COVID-19 vaccines are safe during pregnancy “from tens of thousands of reporting individuals over the last several months, as well as the current low vaccination rates and concerning increase in cases,” ACOG and SMFM said in the statement.
Both organizations said the timing of the advisory comes amid growing concern about the Delta variant.
CDC Director Rochelle Walensky, MD, has called the variant “one of the most infectious respiratory viruses we know of.”
No evidence of maternal/fetal harm
There is no evidence that COVID-19 vaccines could cause maternal or fetal harm, ACOG stated.
“ACOG encourages its members to enthusiastically recommend vaccination to their patients. This means emphasizing the known safety of the vaccines and the increased risk of severe complications associated with COVID-19 infection, including death, during pregnancy,” said J. Martin Tucker, MD, FACOG, president of ACOG. “It is clear that pregnant people need to feel confident in the decision to choose vaccination, and a strong recommendation from their obstetrician-gynecologist could make a meaningful difference for many pregnant people.”
Pregnant women are considered high risk because of concerns about the effect of COVID-19 during and after pregnancy, and on their offspring.
As this news organization has reported, research published in The BMJ found that pregnant women with COVID-19 may be at higher risk of admission to a hospital intensive care unit.
Preterm birth rates also were found to be higher among pregnant women with COVID-19 than among pregnant women without the disease.
Dr. Eckert said several of her patients have declined the vaccine. Among the reasons are that they don’t want to take any medications while pregnant or that they have heard that effects of the vaccines were not studied in pregnant women.
“Sometimes as I review with them the ongoing data coming in from pregnant individuals and newborns, [these patients] may change their minds and get the vaccine,” Dr. Eckert said.
In some cases, a pregnant patient’s family has pressured the patient not to get the vaccine.
The ACOG/SMFM advice notes that pregnant women who have decided to wait until after delivery to be vaccinated “may be inadvertently exposing themselves to an increased risk of severe illness or death.”
The recommendation extends to those who have already given birth.
“Those who have recently delivered and were not vaccinated during pregnancy are also strongly encouraged to get vaccinated as soon as possible,” the statement reads.
ACOG has developed talking points about the safety and efficacy of COVID-19 vaccines for pregnant patients.
Dr. Eckert disclosed no relevant financial relationships.
The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) strongly recommend that all pregnant women be vaccinated against COVID-19.
Only about 16% of pregnant people have received one or more doses of a COVID-19 vaccine, according to the Centers for Disease Control and Prevention, despite evidence that COVID-19 infection puts pregnant people at an increased risk of severe complications and death.
That CDC report in June also found that vaccination during pregnancy was lowest among Hispanic (11.9%) and non-Hispanic Black women (6%) and women aged 18-24 years (5.5%) and highest among non-Hispanic Asian women (24.7%) and women aged 35-49 years (22.7%).
Linda Eckert, MD, professor of obstetrics and gynecology at University of Washington, Seattle, and a member of ACOG’s immunization expert work group, said in an interview that previously, ACOG has said that pregnant women should have the opportunity to be vaccinated, should they choose it.
Now the urgency has increased, she said: “This is a strong recommendation.”
The recommendation comes after mounting evidence demonstrating that COVID-19 vaccines are safe during pregnancy “from tens of thousands of reporting individuals over the last several months, as well as the current low vaccination rates and concerning increase in cases,” ACOG and SMFM said in the statement.
Both organizations said the timing of the advisory comes amid growing concern about the Delta variant.
CDC Director Rochelle Walensky, MD, has called the variant “one of the most infectious respiratory viruses we know of.”
No evidence of maternal/fetal harm
There is no evidence that COVID-19 vaccines could cause maternal or fetal harm, ACOG stated.
“ACOG encourages its members to enthusiastically recommend vaccination to their patients. This means emphasizing the known safety of the vaccines and the increased risk of severe complications associated with COVID-19 infection, including death, during pregnancy,” said J. Martin Tucker, MD, FACOG, president of ACOG. “It is clear that pregnant people need to feel confident in the decision to choose vaccination, and a strong recommendation from their obstetrician-gynecologist could make a meaningful difference for many pregnant people.”
Pregnant women are considered high risk because of concerns about the effect of COVID-19 during and after pregnancy, and on their offspring.
As this news organization has reported, research published in The BMJ found that pregnant women with COVID-19 may be at higher risk of admission to a hospital intensive care unit.
Preterm birth rates also were found to be higher among pregnant women with COVID-19 than among pregnant women without the disease.
Dr. Eckert said several of her patients have declined the vaccine. Among the reasons are that they don’t want to take any medications while pregnant or that they have heard that effects of the vaccines were not studied in pregnant women.
“Sometimes as I review with them the ongoing data coming in from pregnant individuals and newborns, [these patients] may change their minds and get the vaccine,” Dr. Eckert said.
In some cases, a pregnant patient’s family has pressured the patient not to get the vaccine.
The ACOG/SMFM advice notes that pregnant women who have decided to wait until after delivery to be vaccinated “may be inadvertently exposing themselves to an increased risk of severe illness or death.”
The recommendation extends to those who have already given birth.
“Those who have recently delivered and were not vaccinated during pregnancy are also strongly encouraged to get vaccinated as soon as possible,” the statement reads.
ACOG has developed talking points about the safety and efficacy of COVID-19 vaccines for pregnant patients.
Dr. Eckert disclosed no relevant financial relationships.
The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) strongly recommend that all pregnant women be vaccinated against COVID-19.
Only about 16% of pregnant people have received one or more doses of a COVID-19 vaccine, according to the Centers for Disease Control and Prevention, despite evidence that COVID-19 infection puts pregnant people at an increased risk of severe complications and death.
That CDC report in June also found that vaccination during pregnancy was lowest among Hispanic (11.9%) and non-Hispanic Black women (6%) and women aged 18-24 years (5.5%) and highest among non-Hispanic Asian women (24.7%) and women aged 35-49 years (22.7%).
Linda Eckert, MD, professor of obstetrics and gynecology at University of Washington, Seattle, and a member of ACOG’s immunization expert work group, said in an interview that previously, ACOG has said that pregnant women should have the opportunity to be vaccinated, should they choose it.
Now the urgency has increased, she said: “This is a strong recommendation.”
The recommendation comes after mounting evidence demonstrating that COVID-19 vaccines are safe during pregnancy “from tens of thousands of reporting individuals over the last several months, as well as the current low vaccination rates and concerning increase in cases,” ACOG and SMFM said in the statement.
Both organizations said the timing of the advisory comes amid growing concern about the Delta variant.
CDC Director Rochelle Walensky, MD, has called the variant “one of the most infectious respiratory viruses we know of.”
No evidence of maternal/fetal harm
There is no evidence that COVID-19 vaccines could cause maternal or fetal harm, ACOG stated.
“ACOG encourages its members to enthusiastically recommend vaccination to their patients. This means emphasizing the known safety of the vaccines and the increased risk of severe complications associated with COVID-19 infection, including death, during pregnancy,” said J. Martin Tucker, MD, FACOG, president of ACOG. “It is clear that pregnant people need to feel confident in the decision to choose vaccination, and a strong recommendation from their obstetrician-gynecologist could make a meaningful difference for many pregnant people.”
Pregnant women are considered high risk because of concerns about the effect of COVID-19 during and after pregnancy, and on their offspring.
As this news organization has reported, research published in The BMJ found that pregnant women with COVID-19 may be at higher risk of admission to a hospital intensive care unit.
Preterm birth rates also were found to be higher among pregnant women with COVID-19 than among pregnant women without the disease.
Dr. Eckert said several of her patients have declined the vaccine. Among the reasons are that they don’t want to take any medications while pregnant or that they have heard that effects of the vaccines were not studied in pregnant women.
“Sometimes as I review with them the ongoing data coming in from pregnant individuals and newborns, [these patients] may change their minds and get the vaccine,” Dr. Eckert said.
In some cases, a pregnant patient’s family has pressured the patient not to get the vaccine.
The ACOG/SMFM advice notes that pregnant women who have decided to wait until after delivery to be vaccinated “may be inadvertently exposing themselves to an increased risk of severe illness or death.”
The recommendation extends to those who have already given birth.
“Those who have recently delivered and were not vaccinated during pregnancy are also strongly encouraged to get vaccinated as soon as possible,” the statement reads.
ACOG has developed talking points about the safety and efficacy of COVID-19 vaccines for pregnant patients.
Dr. Eckert disclosed no relevant financial relationships.