User login
Interventional Radiology Treatment for Uterine Fibroids
Interventional approaches are being used as a standard of care more and more to provide image-guided techniques to perform minimally invasive procedures. With this being said, what are some indications and best practices used with interventional radiology for the treatment of uterine fibroids?
Dr. Boone: Interventional radiologists offer minimally invasive non-surgical treatment options for the management of symptomatic uterine fibroids. These approaches include uterine artery embolization or UAE. It may also be called uterine fibroid embolization or UFE. In this procedure, the uterine arteries are embolized with permanent embolic particles to block blood flow to the fibroids.
The goal of this treatment is to shrink the fibroids. It usually leads to a gradual shrinkage of fibroids and can also be particularly effective for reducing bleeding from fibroids. This procedure has been around for more than 20 years and has a lot of data describing its safety and efficacy.
Another treatment, which is non-invasive, but some interventional radiologists offer, is magnetic resonance-guided focused ultrasound. This might also be called high intensity focused ultrasound or HIFU. In this treatment, MRI is used to direct high intensity ultrasound waves onto the fibroid. This focused application of these high intensity ultrasound waves generates heat and leads to coagulative necrosis of the fibroid.
This procedure is newer than uterine artery embolization, but it has some benefits of avoiding ionizing radiation. Although, it can have longer procedure times. For both procedures, the indications are symptomatic uterine fibroids.
The symptoms we're concerned about include menorrhagia, which can result in anemia. There are also “bulk” symptoms, related to the actual bulk of the fibroids, which can cause bladder or bowel dysfunction. Some patients also have protrusion of their abdomen, dysmenorrhea, and infertility.
The goal is to help reduce those symptoms. The Society for Interventional Radiology has published best practices. For expected outcomes, with the uterine artery embolization, it is 50% to 60% reduction in the size of fibroid of the fibroids themselves, 40% to 50% reduction in the size of the uterus, 88% to 92% of reduction of the bulk symptoms.
Every consultation should discuss the range of treatment options—the medical, surgical, and non-surgical or interventional. I wanted to point out that there is a real need for this. The Society for Interventional Radiology commissioned a poll in 2017 of patients–women who had been diagnosed with uterine fibroids—and found that 44% of patients noted never hearing of uterine artery embolization. Eleven percent of these patients believed that hysterectomy was their only treatment option. Further, a recent article from NPR noted concerns about disparities in which women of color, particularly Black women, were not offered or made aware of more minimally invasive options during consultations. Very broad patient education about the range of treatment options is important.
In addition, we want to consider other differential diagnoses that patients may have, such as adenomyosis or rare malignancies. Leiomyosarcoma can present with similar symptoms to uterine fibroids or can even coexist with uterine fibroids. In the case of leiomyosarcoma, the treatment pathway may be completely different, and we don't want to undertreat or delay diagnosis. Other considerations that can have bearing on the selection of treatment can be the number and the size of the fibroids.
To help with the decision-making process, these patients need a complete workup. We want to get lab tests. We want to also make sure they have a complete gynecologic evaluation, which includes an ultrasound and an MRI. Particularly, contrast-enhanced MRI has great accuracy for evaluating fibroid location because we’re imaging the entire pelvis. We can see where everything is and map out our target fibroids.
We can also see the enhancement characteristics of the fibroids. Some fibroids are not just supplied by uterine arteries but ovarian arteries, which can affect the efficacy of the treatment and even some of the risks of the treatment.
What is your role and particularly what is the role of the Nurse Practitioner when thinking about diagnosis and treatment and how do you and the nurse practitioner work together?
Dr. Boone: I would say the specific roles for the physicians and nurse practitioners on an interventional radiology team can vary with a lot of different factors. It could depend on the practice setting, such as, whether you're in a busy academic center or in a small private practice. It can depend on the types of cases we're doing. Even some of the local regulations of the institution and state can come into play. The roles tend to be laid out and specified by the supervising physician based on this context.
For example, ideally, all of that work up and planning is happening in that clinic setting before the patient even comes down to the suite for the procedure. In this setting, nurse practitioners can provide a significant role in obtaining the data that we need. They'll perform the history and physical exam, which helps the team learn about the patients. It helps answer relevant questions: What symptoms is the patient having? What are their wishes for the procedure? What are the things they're hoping to avoid or hoping to get from having the procedure done? They review for those relevant labs and imaging, and in order to recognize the information we don’t have.
The next step is developing the assessment and plan which is usually done in conjunction with the interventional radiologist. This is especially important with new patients. Once that assessment and plan are determined, the nurse practitioner can be helpful in explaining the process in depth to the patient and their family or caregivers while they're in the clinic.
Another important role for nurse practitioners in this setting is the consent. I can talk a little bit more about that later, but informed consent is critical. It can be a pretty extensive discussion, especially if we want to talk about this wide range of treatment options. So that is substantial value added by the nurse practitioner.
The other important role is the follow up visits, which may be almost completely independently by a nurse practitioner. They see patients post-procedure, evaluating how they’re doing and what's changed. This is critical because we need to determine: 1. Have we gotten the result that we want? 2. Do we want to give more time to see changes? and; 3. Do we need to do another procedure? We also want to follow these patients and their response to treatment to look out for something concerning that might raise concern for malignancy, such as the fibroid continuing to grow rapidly. Those follow up visits are also a critical role for NPs.
In the inpatient setting, the attending and senior interventional radiology residents may actually determine the roles and tasks the other team members are going to perform to help the IR service run smoothly. And typically, nurse practitioners and also physician assistants will share many of those responsibilities of running that interventional radiology service outside of the procedure room.
There are also cases where nurse practitioners and physician assistants can have a dedicated role in performing certain procedures. Personally, I've seen physician assistants in these cases, where they were our dedicated bone marrow biopsy providers. Throughout the day, they would do all the bone marrow biopsy cases. Another example I saw was placement of vascular access catheters, whether for ports or dialysis. NPs see many patients throughout the day and perform these procedures. This is helpful because these are very popular procedures and are needed. While those are being done, it frees up time for the other members of the team to do other, more time-consuming, procedures as well.
In all cases, we work closely together. We're sharing this responsibility of patient care. We communicate frequently and it's a valuable team dynamic. NPs are fantastic team members
Dr. Boone, you talked about the treatments and how you work together with NPs. Can you touch on the interventional procedures and the value or benefit over conservative treatments and drugs, particularly, where you receive support or recommendations from nurse practitioners at this stage?
Dr. Boone: Regarding more conservative treatment, there’s expectant management where the patients may not want to undergo an intervention at that time. You’re following the patient and watching for possible worsening of symptoms that may lead to a change in management.
There’s also medical management, which generally gets broken down into hormonal or non-hormonal medications. Among these, there's a lot of different drugs that are available. Among the more frequently used hormonal therapies would be gonadotropin-releasing hormone agonists.
The non-hormonal therapies such as, NSAIDs, or procoagulation medications, like tranexamic acid, are more targeted at symptom control. Particularly, these target the abnormal uterine bleeding and the pain.
For these therapies, the limitations can be side-effect profiles. Sometimes these side effects are just not acceptable to patients. Hormonal therapies like the gonadotropin-releasing hormone agonists create this hypoestrogenic state. Patients may not like having the menopause-like symptoms.
Additionally, medications are more short-term in their benefit. For example, with the cessation of gonadotropin-releasing hormone agonists, the fibroids actually can show rapid rebound growth. Some of the non-surgical interventions can provide longer term benefit, even if they may require re-intervention more frequently compared to surgical interventions.
For interventional radiology, we primarily focus on the procedures. We don't typically manage the medical therapy. These treatment approaches are cultivated more by gynecology or other clinicians.
When it comes to interventional radiology treatment for uterine fibroids in your day-to-day practices, which you've talked a lot about today, what has been your experience in working with Nurse Practitioners overall and where do they, should they or could they potentially add even more value?
Dr. Boone: Nurse practitioners play an integral role on the team and, I think, they provide a lot of value. They have an important role in teaching settings, were they provide continuity of care. They can also greatly impact with teaching of trainees.
In teaching settings, there's a substantial turnover of trainees because -- and this includes residents, medical students, in some cases fellows -- they're rotating between different hospitals every few weeks. Even at the end of the year, the most senior residents, the most experience trainees, leave to go to new jobs. Nurse practitioners on the IR team are a critical source of continuity and consistency for patients and for the rest of the team because they spend the most time on the service and they know the team members well. They also know how to get things done efficiently and really know the system.
They've also honed the skills that trainees, particularly junior residents, are learning. In my experience, I first learned to place and remove tunneled catheters and bone marrow biopsies by spending the day with a physician assistant and a nurse practitioner. Both from the educational standpoint and also consistent, efficient care standpoint, having NPs and PAs on our team is hugely valuable.
Emphasizing that role in teaching is highly valuable. I would encourage nurse practitioners on an IR team with trainees to take ownership of teaching a particular skill or a certain topic, because they're going to bring a different perspective and that's extremely valuable.
Another arena where there's a lot of value, is in the informed consent and patient education portion of patient care. Interventional radiology is not the most familiar medical field for a lot of people. Interventional radiologists also perform a wide array of procedures and they can be very different. Even treatments for the same problem, uterine artery embolization and MRI-guided focused ultrasound, are very different procedures in terms of how they're actually performed.
For example, if you mentioned surgery to most people, there is some idea of what that entails and who performs it. But if you say embolization to most people, they may not entirely understand all those components. For a patient to sufficiently be informed and able to consent, they do need to understand not only their disease and the treatment being offered, but also the risks, the benefits, and the alternatives. They need to understand what to expect from the procedure.
Doing this well can take a substantial amount of time, but it is important. From a physician standpoint, that entails balancing. Along with performing the procedures and reviewing patient imaging as well as other clinical duties this is very challenging. Nurse practitioners can really leverage their expertise in patient communication and education to fill in those knowledge gaps and best serve the patient while also helping the IR service. These are just two of many areas in which NPs can be highly valuable to an IR practice.
1. Kröncke T, David M. MR-Guided Focused Ultrasound in Fibroid Treatment – Results of the 4th Radiological-Gynecological Expert Meeting. Fortschr Röntgenstr. 2019;191(07):626-629. doi:10.1055/a-0884-3143
2. Sridhar D, Kohi M. Updates on MR-Guided Focused Ultrasound for Symptomatic Uterine Fibroids. Semin intervent Radiol. 2018;35(01):017-022. doi:10.1055/s-0038-1636516
3. Kohi MP, Spies JB. Updates on Uterine Artery Embolization. Semin intervent Radiol. 2018;35(1):48-55. doi:10.1055/s-0038-1636521
4. Dariushnia SR, Nikolic B, Stokes LS, Spies JB. Quality Improvement Guidelines for Uterine Artery Embolization for Symptomatic Leiomyomata. Journal of Vascular and Interventional Radiology. 2014;25(11):1737-1747. doi:10.1016/j.jvir.2014.08.029
5. Wise A. Facing invasive treatments for uterine fibroids, Black women advocate for better care. NPR. https://www.npr.org/sections/health-shots/2022/04/10/1087483675/facing-invasive-treatments-for-uterine-fibroids-black-women-advocate-for-better-. Published April 10, 2022. Accessed June 9, 2022.
6. http://fyra.io. SIR Survey Shows Public Awareness Shortcomings for UFE as Treatment Option for Uterine Fibroids. Endovascular Today. Accessed June 9, 2022. https://evtoday.com/news/sir-survey-shows-public-awareness-shortcomings-for-ufe-as-treatment-option-for-uterine-fibroids
Interventional approaches are being used as a standard of care more and more to provide image-guided techniques to perform minimally invasive procedures. With this being said, what are some indications and best practices used with interventional radiology for the treatment of uterine fibroids?
Dr. Boone: Interventional radiologists offer minimally invasive non-surgical treatment options for the management of symptomatic uterine fibroids. These approaches include uterine artery embolization or UAE. It may also be called uterine fibroid embolization or UFE. In this procedure, the uterine arteries are embolized with permanent embolic particles to block blood flow to the fibroids.
The goal of this treatment is to shrink the fibroids. It usually leads to a gradual shrinkage of fibroids and can also be particularly effective for reducing bleeding from fibroids. This procedure has been around for more than 20 years and has a lot of data describing its safety and efficacy.
Another treatment, which is non-invasive, but some interventional radiologists offer, is magnetic resonance-guided focused ultrasound. This might also be called high intensity focused ultrasound or HIFU. In this treatment, MRI is used to direct high intensity ultrasound waves onto the fibroid. This focused application of these high intensity ultrasound waves generates heat and leads to coagulative necrosis of the fibroid.
This procedure is newer than uterine artery embolization, but it has some benefits of avoiding ionizing radiation. Although, it can have longer procedure times. For both procedures, the indications are symptomatic uterine fibroids.
The symptoms we're concerned about include menorrhagia, which can result in anemia. There are also “bulk” symptoms, related to the actual bulk of the fibroids, which can cause bladder or bowel dysfunction. Some patients also have protrusion of their abdomen, dysmenorrhea, and infertility.
The goal is to help reduce those symptoms. The Society for Interventional Radiology has published best practices. For expected outcomes, with the uterine artery embolization, it is 50% to 60% reduction in the size of fibroid of the fibroids themselves, 40% to 50% reduction in the size of the uterus, 88% to 92% of reduction of the bulk symptoms.
Every consultation should discuss the range of treatment options—the medical, surgical, and non-surgical or interventional. I wanted to point out that there is a real need for this. The Society for Interventional Radiology commissioned a poll in 2017 of patients–women who had been diagnosed with uterine fibroids—and found that 44% of patients noted never hearing of uterine artery embolization. Eleven percent of these patients believed that hysterectomy was their only treatment option. Further, a recent article from NPR noted concerns about disparities in which women of color, particularly Black women, were not offered or made aware of more minimally invasive options during consultations. Very broad patient education about the range of treatment options is important.
In addition, we want to consider other differential diagnoses that patients may have, such as adenomyosis or rare malignancies. Leiomyosarcoma can present with similar symptoms to uterine fibroids or can even coexist with uterine fibroids. In the case of leiomyosarcoma, the treatment pathway may be completely different, and we don't want to undertreat or delay diagnosis. Other considerations that can have bearing on the selection of treatment can be the number and the size of the fibroids.
To help with the decision-making process, these patients need a complete workup. We want to get lab tests. We want to also make sure they have a complete gynecologic evaluation, which includes an ultrasound and an MRI. Particularly, contrast-enhanced MRI has great accuracy for evaluating fibroid location because we’re imaging the entire pelvis. We can see where everything is and map out our target fibroids.
We can also see the enhancement characteristics of the fibroids. Some fibroids are not just supplied by uterine arteries but ovarian arteries, which can affect the efficacy of the treatment and even some of the risks of the treatment.
What is your role and particularly what is the role of the Nurse Practitioner when thinking about diagnosis and treatment and how do you and the nurse practitioner work together?
Dr. Boone: I would say the specific roles for the physicians and nurse practitioners on an interventional radiology team can vary with a lot of different factors. It could depend on the practice setting, such as, whether you're in a busy academic center or in a small private practice. It can depend on the types of cases we're doing. Even some of the local regulations of the institution and state can come into play. The roles tend to be laid out and specified by the supervising physician based on this context.
For example, ideally, all of that work up and planning is happening in that clinic setting before the patient even comes down to the suite for the procedure. In this setting, nurse practitioners can provide a significant role in obtaining the data that we need. They'll perform the history and physical exam, which helps the team learn about the patients. It helps answer relevant questions: What symptoms is the patient having? What are their wishes for the procedure? What are the things they're hoping to avoid or hoping to get from having the procedure done? They review for those relevant labs and imaging, and in order to recognize the information we don’t have.
The next step is developing the assessment and plan which is usually done in conjunction with the interventional radiologist. This is especially important with new patients. Once that assessment and plan are determined, the nurse practitioner can be helpful in explaining the process in depth to the patient and their family or caregivers while they're in the clinic.
Another important role for nurse practitioners in this setting is the consent. I can talk a little bit more about that later, but informed consent is critical. It can be a pretty extensive discussion, especially if we want to talk about this wide range of treatment options. So that is substantial value added by the nurse practitioner.
The other important role is the follow up visits, which may be almost completely independently by a nurse practitioner. They see patients post-procedure, evaluating how they’re doing and what's changed. This is critical because we need to determine: 1. Have we gotten the result that we want? 2. Do we want to give more time to see changes? and; 3. Do we need to do another procedure? We also want to follow these patients and their response to treatment to look out for something concerning that might raise concern for malignancy, such as the fibroid continuing to grow rapidly. Those follow up visits are also a critical role for NPs.
In the inpatient setting, the attending and senior interventional radiology residents may actually determine the roles and tasks the other team members are going to perform to help the IR service run smoothly. And typically, nurse practitioners and also physician assistants will share many of those responsibilities of running that interventional radiology service outside of the procedure room.
There are also cases where nurse practitioners and physician assistants can have a dedicated role in performing certain procedures. Personally, I've seen physician assistants in these cases, where they were our dedicated bone marrow biopsy providers. Throughout the day, they would do all the bone marrow biopsy cases. Another example I saw was placement of vascular access catheters, whether for ports or dialysis. NPs see many patients throughout the day and perform these procedures. This is helpful because these are very popular procedures and are needed. While those are being done, it frees up time for the other members of the team to do other, more time-consuming, procedures as well.
In all cases, we work closely together. We're sharing this responsibility of patient care. We communicate frequently and it's a valuable team dynamic. NPs are fantastic team members
Dr. Boone, you talked about the treatments and how you work together with NPs. Can you touch on the interventional procedures and the value or benefit over conservative treatments and drugs, particularly, where you receive support or recommendations from nurse practitioners at this stage?
Dr. Boone: Regarding more conservative treatment, there’s expectant management where the patients may not want to undergo an intervention at that time. You’re following the patient and watching for possible worsening of symptoms that may lead to a change in management.
There’s also medical management, which generally gets broken down into hormonal or non-hormonal medications. Among these, there's a lot of different drugs that are available. Among the more frequently used hormonal therapies would be gonadotropin-releasing hormone agonists.
The non-hormonal therapies such as, NSAIDs, or procoagulation medications, like tranexamic acid, are more targeted at symptom control. Particularly, these target the abnormal uterine bleeding and the pain.
For these therapies, the limitations can be side-effect profiles. Sometimes these side effects are just not acceptable to patients. Hormonal therapies like the gonadotropin-releasing hormone agonists create this hypoestrogenic state. Patients may not like having the menopause-like symptoms.
Additionally, medications are more short-term in their benefit. For example, with the cessation of gonadotropin-releasing hormone agonists, the fibroids actually can show rapid rebound growth. Some of the non-surgical interventions can provide longer term benefit, even if they may require re-intervention more frequently compared to surgical interventions.
For interventional radiology, we primarily focus on the procedures. We don't typically manage the medical therapy. These treatment approaches are cultivated more by gynecology or other clinicians.
When it comes to interventional radiology treatment for uterine fibroids in your day-to-day practices, which you've talked a lot about today, what has been your experience in working with Nurse Practitioners overall and where do they, should they or could they potentially add even more value?
Dr. Boone: Nurse practitioners play an integral role on the team and, I think, they provide a lot of value. They have an important role in teaching settings, were they provide continuity of care. They can also greatly impact with teaching of trainees.
In teaching settings, there's a substantial turnover of trainees because -- and this includes residents, medical students, in some cases fellows -- they're rotating between different hospitals every few weeks. Even at the end of the year, the most senior residents, the most experience trainees, leave to go to new jobs. Nurse practitioners on the IR team are a critical source of continuity and consistency for patients and for the rest of the team because they spend the most time on the service and they know the team members well. They also know how to get things done efficiently and really know the system.
They've also honed the skills that trainees, particularly junior residents, are learning. In my experience, I first learned to place and remove tunneled catheters and bone marrow biopsies by spending the day with a physician assistant and a nurse practitioner. Both from the educational standpoint and also consistent, efficient care standpoint, having NPs and PAs on our team is hugely valuable.
Emphasizing that role in teaching is highly valuable. I would encourage nurse practitioners on an IR team with trainees to take ownership of teaching a particular skill or a certain topic, because they're going to bring a different perspective and that's extremely valuable.
Another arena where there's a lot of value, is in the informed consent and patient education portion of patient care. Interventional radiology is not the most familiar medical field for a lot of people. Interventional radiologists also perform a wide array of procedures and they can be very different. Even treatments for the same problem, uterine artery embolization and MRI-guided focused ultrasound, are very different procedures in terms of how they're actually performed.
For example, if you mentioned surgery to most people, there is some idea of what that entails and who performs it. But if you say embolization to most people, they may not entirely understand all those components. For a patient to sufficiently be informed and able to consent, they do need to understand not only their disease and the treatment being offered, but also the risks, the benefits, and the alternatives. They need to understand what to expect from the procedure.
Doing this well can take a substantial amount of time, but it is important. From a physician standpoint, that entails balancing. Along with performing the procedures and reviewing patient imaging as well as other clinical duties this is very challenging. Nurse practitioners can really leverage their expertise in patient communication and education to fill in those knowledge gaps and best serve the patient while also helping the IR service. These are just two of many areas in which NPs can be highly valuable to an IR practice.
Interventional approaches are being used as a standard of care more and more to provide image-guided techniques to perform minimally invasive procedures. With this being said, what are some indications and best practices used with interventional radiology for the treatment of uterine fibroids?
Dr. Boone: Interventional radiologists offer minimally invasive non-surgical treatment options for the management of symptomatic uterine fibroids. These approaches include uterine artery embolization or UAE. It may also be called uterine fibroid embolization or UFE. In this procedure, the uterine arteries are embolized with permanent embolic particles to block blood flow to the fibroids.
The goal of this treatment is to shrink the fibroids. It usually leads to a gradual shrinkage of fibroids and can also be particularly effective for reducing bleeding from fibroids. This procedure has been around for more than 20 years and has a lot of data describing its safety and efficacy.
Another treatment, which is non-invasive, but some interventional radiologists offer, is magnetic resonance-guided focused ultrasound. This might also be called high intensity focused ultrasound or HIFU. In this treatment, MRI is used to direct high intensity ultrasound waves onto the fibroid. This focused application of these high intensity ultrasound waves generates heat and leads to coagulative necrosis of the fibroid.
This procedure is newer than uterine artery embolization, but it has some benefits of avoiding ionizing radiation. Although, it can have longer procedure times. For both procedures, the indications are symptomatic uterine fibroids.
The symptoms we're concerned about include menorrhagia, which can result in anemia. There are also “bulk” symptoms, related to the actual bulk of the fibroids, which can cause bladder or bowel dysfunction. Some patients also have protrusion of their abdomen, dysmenorrhea, and infertility.
The goal is to help reduce those symptoms. The Society for Interventional Radiology has published best practices. For expected outcomes, with the uterine artery embolization, it is 50% to 60% reduction in the size of fibroid of the fibroids themselves, 40% to 50% reduction in the size of the uterus, 88% to 92% of reduction of the bulk symptoms.
Every consultation should discuss the range of treatment options—the medical, surgical, and non-surgical or interventional. I wanted to point out that there is a real need for this. The Society for Interventional Radiology commissioned a poll in 2017 of patients–women who had been diagnosed with uterine fibroids—and found that 44% of patients noted never hearing of uterine artery embolization. Eleven percent of these patients believed that hysterectomy was their only treatment option. Further, a recent article from NPR noted concerns about disparities in which women of color, particularly Black women, were not offered or made aware of more minimally invasive options during consultations. Very broad patient education about the range of treatment options is important.
In addition, we want to consider other differential diagnoses that patients may have, such as adenomyosis or rare malignancies. Leiomyosarcoma can present with similar symptoms to uterine fibroids or can even coexist with uterine fibroids. In the case of leiomyosarcoma, the treatment pathway may be completely different, and we don't want to undertreat or delay diagnosis. Other considerations that can have bearing on the selection of treatment can be the number and the size of the fibroids.
To help with the decision-making process, these patients need a complete workup. We want to get lab tests. We want to also make sure they have a complete gynecologic evaluation, which includes an ultrasound and an MRI. Particularly, contrast-enhanced MRI has great accuracy for evaluating fibroid location because we’re imaging the entire pelvis. We can see where everything is and map out our target fibroids.
We can also see the enhancement characteristics of the fibroids. Some fibroids are not just supplied by uterine arteries but ovarian arteries, which can affect the efficacy of the treatment and even some of the risks of the treatment.
What is your role and particularly what is the role of the Nurse Practitioner when thinking about diagnosis and treatment and how do you and the nurse practitioner work together?
Dr. Boone: I would say the specific roles for the physicians and nurse practitioners on an interventional radiology team can vary with a lot of different factors. It could depend on the practice setting, such as, whether you're in a busy academic center or in a small private practice. It can depend on the types of cases we're doing. Even some of the local regulations of the institution and state can come into play. The roles tend to be laid out and specified by the supervising physician based on this context.
For example, ideally, all of that work up and planning is happening in that clinic setting before the patient even comes down to the suite for the procedure. In this setting, nurse practitioners can provide a significant role in obtaining the data that we need. They'll perform the history and physical exam, which helps the team learn about the patients. It helps answer relevant questions: What symptoms is the patient having? What are their wishes for the procedure? What are the things they're hoping to avoid or hoping to get from having the procedure done? They review for those relevant labs and imaging, and in order to recognize the information we don’t have.
The next step is developing the assessment and plan which is usually done in conjunction with the interventional radiologist. This is especially important with new patients. Once that assessment and plan are determined, the nurse practitioner can be helpful in explaining the process in depth to the patient and their family or caregivers while they're in the clinic.
Another important role for nurse practitioners in this setting is the consent. I can talk a little bit more about that later, but informed consent is critical. It can be a pretty extensive discussion, especially if we want to talk about this wide range of treatment options. So that is substantial value added by the nurse practitioner.
The other important role is the follow up visits, which may be almost completely independently by a nurse practitioner. They see patients post-procedure, evaluating how they’re doing and what's changed. This is critical because we need to determine: 1. Have we gotten the result that we want? 2. Do we want to give more time to see changes? and; 3. Do we need to do another procedure? We also want to follow these patients and their response to treatment to look out for something concerning that might raise concern for malignancy, such as the fibroid continuing to grow rapidly. Those follow up visits are also a critical role for NPs.
In the inpatient setting, the attending and senior interventional radiology residents may actually determine the roles and tasks the other team members are going to perform to help the IR service run smoothly. And typically, nurse practitioners and also physician assistants will share many of those responsibilities of running that interventional radiology service outside of the procedure room.
There are also cases where nurse practitioners and physician assistants can have a dedicated role in performing certain procedures. Personally, I've seen physician assistants in these cases, where they were our dedicated bone marrow biopsy providers. Throughout the day, they would do all the bone marrow biopsy cases. Another example I saw was placement of vascular access catheters, whether for ports or dialysis. NPs see many patients throughout the day and perform these procedures. This is helpful because these are very popular procedures and are needed. While those are being done, it frees up time for the other members of the team to do other, more time-consuming, procedures as well.
In all cases, we work closely together. We're sharing this responsibility of patient care. We communicate frequently and it's a valuable team dynamic. NPs are fantastic team members
Dr. Boone, you talked about the treatments and how you work together with NPs. Can you touch on the interventional procedures and the value or benefit over conservative treatments and drugs, particularly, where you receive support or recommendations from nurse practitioners at this stage?
Dr. Boone: Regarding more conservative treatment, there’s expectant management where the patients may not want to undergo an intervention at that time. You’re following the patient and watching for possible worsening of symptoms that may lead to a change in management.
There’s also medical management, which generally gets broken down into hormonal or non-hormonal medications. Among these, there's a lot of different drugs that are available. Among the more frequently used hormonal therapies would be gonadotropin-releasing hormone agonists.
The non-hormonal therapies such as, NSAIDs, or procoagulation medications, like tranexamic acid, are more targeted at symptom control. Particularly, these target the abnormal uterine bleeding and the pain.
For these therapies, the limitations can be side-effect profiles. Sometimes these side effects are just not acceptable to patients. Hormonal therapies like the gonadotropin-releasing hormone agonists create this hypoestrogenic state. Patients may not like having the menopause-like symptoms.
Additionally, medications are more short-term in their benefit. For example, with the cessation of gonadotropin-releasing hormone agonists, the fibroids actually can show rapid rebound growth. Some of the non-surgical interventions can provide longer term benefit, even if they may require re-intervention more frequently compared to surgical interventions.
For interventional radiology, we primarily focus on the procedures. We don't typically manage the medical therapy. These treatment approaches are cultivated more by gynecology or other clinicians.
When it comes to interventional radiology treatment for uterine fibroids in your day-to-day practices, which you've talked a lot about today, what has been your experience in working with Nurse Practitioners overall and where do they, should they or could they potentially add even more value?
Dr. Boone: Nurse practitioners play an integral role on the team and, I think, they provide a lot of value. They have an important role in teaching settings, were they provide continuity of care. They can also greatly impact with teaching of trainees.
In teaching settings, there's a substantial turnover of trainees because -- and this includes residents, medical students, in some cases fellows -- they're rotating between different hospitals every few weeks. Even at the end of the year, the most senior residents, the most experience trainees, leave to go to new jobs. Nurse practitioners on the IR team are a critical source of continuity and consistency for patients and for the rest of the team because they spend the most time on the service and they know the team members well. They also know how to get things done efficiently and really know the system.
They've also honed the skills that trainees, particularly junior residents, are learning. In my experience, I first learned to place and remove tunneled catheters and bone marrow biopsies by spending the day with a physician assistant and a nurse practitioner. Both from the educational standpoint and also consistent, efficient care standpoint, having NPs and PAs on our team is hugely valuable.
Emphasizing that role in teaching is highly valuable. I would encourage nurse practitioners on an IR team with trainees to take ownership of teaching a particular skill or a certain topic, because they're going to bring a different perspective and that's extremely valuable.
Another arena where there's a lot of value, is in the informed consent and patient education portion of patient care. Interventional radiology is not the most familiar medical field for a lot of people. Interventional radiologists also perform a wide array of procedures and they can be very different. Even treatments for the same problem, uterine artery embolization and MRI-guided focused ultrasound, are very different procedures in terms of how they're actually performed.
For example, if you mentioned surgery to most people, there is some idea of what that entails and who performs it. But if you say embolization to most people, they may not entirely understand all those components. For a patient to sufficiently be informed and able to consent, they do need to understand not only their disease and the treatment being offered, but also the risks, the benefits, and the alternatives. They need to understand what to expect from the procedure.
Doing this well can take a substantial amount of time, but it is important. From a physician standpoint, that entails balancing. Along with performing the procedures and reviewing patient imaging as well as other clinical duties this is very challenging. Nurse practitioners can really leverage their expertise in patient communication and education to fill in those knowledge gaps and best serve the patient while also helping the IR service. These are just two of many areas in which NPs can be highly valuable to an IR practice.
1. Kröncke T, David M. MR-Guided Focused Ultrasound in Fibroid Treatment – Results of the 4th Radiological-Gynecological Expert Meeting. Fortschr Röntgenstr. 2019;191(07):626-629. doi:10.1055/a-0884-3143
2. Sridhar D, Kohi M. Updates on MR-Guided Focused Ultrasound for Symptomatic Uterine Fibroids. Semin intervent Radiol. 2018;35(01):017-022. doi:10.1055/s-0038-1636516
3. Kohi MP, Spies JB. Updates on Uterine Artery Embolization. Semin intervent Radiol. 2018;35(1):48-55. doi:10.1055/s-0038-1636521
4. Dariushnia SR, Nikolic B, Stokes LS, Spies JB. Quality Improvement Guidelines for Uterine Artery Embolization for Symptomatic Leiomyomata. Journal of Vascular and Interventional Radiology. 2014;25(11):1737-1747. doi:10.1016/j.jvir.2014.08.029
5. Wise A. Facing invasive treatments for uterine fibroids, Black women advocate for better care. NPR. https://www.npr.org/sections/health-shots/2022/04/10/1087483675/facing-invasive-treatments-for-uterine-fibroids-black-women-advocate-for-better-. Published April 10, 2022. Accessed June 9, 2022.
6. http://fyra.io. SIR Survey Shows Public Awareness Shortcomings for UFE as Treatment Option for Uterine Fibroids. Endovascular Today. Accessed June 9, 2022. https://evtoday.com/news/sir-survey-shows-public-awareness-shortcomings-for-ufe-as-treatment-option-for-uterine-fibroids
1. Kröncke T, David M. MR-Guided Focused Ultrasound in Fibroid Treatment – Results of the 4th Radiological-Gynecological Expert Meeting. Fortschr Röntgenstr. 2019;191(07):626-629. doi:10.1055/a-0884-3143
2. Sridhar D, Kohi M. Updates on MR-Guided Focused Ultrasound for Symptomatic Uterine Fibroids. Semin intervent Radiol. 2018;35(01):017-022. doi:10.1055/s-0038-1636516
3. Kohi MP, Spies JB. Updates on Uterine Artery Embolization. Semin intervent Radiol. 2018;35(1):48-55. doi:10.1055/s-0038-1636521
4. Dariushnia SR, Nikolic B, Stokes LS, Spies JB. Quality Improvement Guidelines for Uterine Artery Embolization for Symptomatic Leiomyomata. Journal of Vascular and Interventional Radiology. 2014;25(11):1737-1747. doi:10.1016/j.jvir.2014.08.029
5. Wise A. Facing invasive treatments for uterine fibroids, Black women advocate for better care. NPR. https://www.npr.org/sections/health-shots/2022/04/10/1087483675/facing-invasive-treatments-for-uterine-fibroids-black-women-advocate-for-better-. Published April 10, 2022. Accessed June 9, 2022.
6. http://fyra.io. SIR Survey Shows Public Awareness Shortcomings for UFE as Treatment Option for Uterine Fibroids. Endovascular Today. Accessed June 9, 2022. https://evtoday.com/news/sir-survey-shows-public-awareness-shortcomings-for-ufe-as-treatment-option-for-uterine-fibroids
Tampon shortage linked to supply chain, inflation issues
Social media users have posted about bare shelves and higher costs for months, marking the latest products to face stress under global supply chain concerns after baby formula, cars, and appliances.
Other menstrual products have increased in price as well because of inflation, according to Bloomberg News. The average price for a package of menstrual pads has increased about 8% this year, and the price of a box of tampons has increased about 10%.
Andre Schulten, the chief financial officer for Procter & Gamble, which makes and sells 4.5 billion boxes of Tampax each year, said on a recent earnings call that it has been “costly and highly volatile” to acquire the raw materials needed for production.
Raw materials such as cotton, rayon, and plastic, for instance, have been used to produce personal protective gear during the pandemic, which has led to shortages. The cost of transportation for consumer goods has also nearly tripled, and pandemic policies at ports have led to shipping delays.
Edgewell Personal Care, which makes the brands Playtex and o.b., has had a severe staff shortage at its Delaware facility where tampons are made, according to Time. The FDA has classified tampons as class II medical devices, which require certain quality-control regulations and qualified workers on the assembly line, the news outlet reported.
Representatives for CVS and Walgreens confirmed that they’ve had shortages in recent weeks, according to The Washington Post. Procter & Gamble said it is working with retail partners to make feminine care products more available.
“We understand it is frustrating for consumers when they can’t find what they need,” the company told the newspaper. “We can assure you this is a temporary situation.”
Kimberly-Clark, which makes U by Kotex tampons, told the Post that it “has not experienced a product or supply shortage” in the United States, saying it is “working closely with our retail partners to keep shelves stocked.”
But the shortage may grow worse as the year goes on and the peak season for shipping approaches, the newspaper reported.
“Capacity is only going to get tighter as we move toward the end of the year,” Vaughn Moore, chief executive of AIT Worldwide Logistics, told the Post.
While the situation is being straightened out, gynecologists have recommended against extending supply at home by wearing tampons for longer stretches of time, according to The New York Times. Toxic shock syndrome is a rare but potentially fatal condition that can occur when tampons are worn for more than 8 hours.
There are other options, such as reusable menstrual pads, period underwear, and menstrual cups and discs, the Times reported. But some of these may be less appealing to use, or they may cost too much.
A version of this article first appeared on WebMD.com.
Social media users have posted about bare shelves and higher costs for months, marking the latest products to face stress under global supply chain concerns after baby formula, cars, and appliances.
Other menstrual products have increased in price as well because of inflation, according to Bloomberg News. The average price for a package of menstrual pads has increased about 8% this year, and the price of a box of tampons has increased about 10%.
Andre Schulten, the chief financial officer for Procter & Gamble, which makes and sells 4.5 billion boxes of Tampax each year, said on a recent earnings call that it has been “costly and highly volatile” to acquire the raw materials needed for production.
Raw materials such as cotton, rayon, and plastic, for instance, have been used to produce personal protective gear during the pandemic, which has led to shortages. The cost of transportation for consumer goods has also nearly tripled, and pandemic policies at ports have led to shipping delays.
Edgewell Personal Care, which makes the brands Playtex and o.b., has had a severe staff shortage at its Delaware facility where tampons are made, according to Time. The FDA has classified tampons as class II medical devices, which require certain quality-control regulations and qualified workers on the assembly line, the news outlet reported.
Representatives for CVS and Walgreens confirmed that they’ve had shortages in recent weeks, according to The Washington Post. Procter & Gamble said it is working with retail partners to make feminine care products more available.
“We understand it is frustrating for consumers when they can’t find what they need,” the company told the newspaper. “We can assure you this is a temporary situation.”
Kimberly-Clark, which makes U by Kotex tampons, told the Post that it “has not experienced a product or supply shortage” in the United States, saying it is “working closely with our retail partners to keep shelves stocked.”
But the shortage may grow worse as the year goes on and the peak season for shipping approaches, the newspaper reported.
“Capacity is only going to get tighter as we move toward the end of the year,” Vaughn Moore, chief executive of AIT Worldwide Logistics, told the Post.
While the situation is being straightened out, gynecologists have recommended against extending supply at home by wearing tampons for longer stretches of time, according to The New York Times. Toxic shock syndrome is a rare but potentially fatal condition that can occur when tampons are worn for more than 8 hours.
There are other options, such as reusable menstrual pads, period underwear, and menstrual cups and discs, the Times reported. But some of these may be less appealing to use, or they may cost too much.
A version of this article first appeared on WebMD.com.
Social media users have posted about bare shelves and higher costs for months, marking the latest products to face stress under global supply chain concerns after baby formula, cars, and appliances.
Other menstrual products have increased in price as well because of inflation, according to Bloomberg News. The average price for a package of menstrual pads has increased about 8% this year, and the price of a box of tampons has increased about 10%.
Andre Schulten, the chief financial officer for Procter & Gamble, which makes and sells 4.5 billion boxes of Tampax each year, said on a recent earnings call that it has been “costly and highly volatile” to acquire the raw materials needed for production.
Raw materials such as cotton, rayon, and plastic, for instance, have been used to produce personal protective gear during the pandemic, which has led to shortages. The cost of transportation for consumer goods has also nearly tripled, and pandemic policies at ports have led to shipping delays.
Edgewell Personal Care, which makes the brands Playtex and o.b., has had a severe staff shortage at its Delaware facility where tampons are made, according to Time. The FDA has classified tampons as class II medical devices, which require certain quality-control regulations and qualified workers on the assembly line, the news outlet reported.
Representatives for CVS and Walgreens confirmed that they’ve had shortages in recent weeks, according to The Washington Post. Procter & Gamble said it is working with retail partners to make feminine care products more available.
“We understand it is frustrating for consumers when they can’t find what they need,” the company told the newspaper. “We can assure you this is a temporary situation.”
Kimberly-Clark, which makes U by Kotex tampons, told the Post that it “has not experienced a product or supply shortage” in the United States, saying it is “working closely with our retail partners to keep shelves stocked.”
But the shortage may grow worse as the year goes on and the peak season for shipping approaches, the newspaper reported.
“Capacity is only going to get tighter as we move toward the end of the year,” Vaughn Moore, chief executive of AIT Worldwide Logistics, told the Post.
While the situation is being straightened out, gynecologists have recommended against extending supply at home by wearing tampons for longer stretches of time, according to The New York Times. Toxic shock syndrome is a rare but potentially fatal condition that can occur when tampons are worn for more than 8 hours.
There are other options, such as reusable menstrual pads, period underwear, and menstrual cups and discs, the Times reported. But some of these may be less appealing to use, or they may cost too much.
A version of this article first appeared on WebMD.com.
Hormonal contraceptives protective against suicide?
Contrary to previous analyses, new research suggests.
In a study of more than 800 women younger than age 50 who attempted suicide and more than 3,000 age-matched peers, results showed those who took hormonal contraceptives had a 27% reduced risk for attempted suicide.
Further analysis showed this was confined to women without a history of psychiatric illness and the reduction in risk rose to 43% among those who took combined hormonal contraceptives rather than progestin-only versions.
The protective effect against attempted suicide increased further to 46% if ethinyl estradiol (EE)–containing preparations were used. Moreover, the beneficial effect of contraceptive use increased over time.
The main message is the “current use of hormonal contraceptives is not associated with an increased risk of attempted suicide in our population,” study presenter Elena Toffol, MD, PhD, department of public health, University of Helsinki, told meeting attendees at the European Psychiatric Association 2022 Congress.
Age range differences
Dr. Toffol said there could be “several reasons” why the results are different from those in previous studies, including that the researchers included a “larger age range.” She noted it is known that “older women have a lower rate of attempted suicide and use different types of contraceptives.”
Dr. Toffol said in an interview that, although it’s “hard to estimate any causality” because this is an observational study, it is “tempting to speculate, and it is plausible, that hormones partly play a role with some, but not all, women being more sensitive to hormonal influences.”
However, the results “may also reflect life choices or a protective life status; for example, more stable relationships or more conscious and health-focused behaviors,” she said.
“It may also be that the underlying characteristics of women who are prescribed or opt for certain types of contraceptives are somehow related to their suicidal risk,” she added.
In 2019, the global age-standardized suicide rate was 9.0 per 100,000, which translates into more than 700,000 deaths every year, Dr. Toffol noted.
However, she emphasized the World Health Organization has calculated that, for every adult who dies by suicide, more than 20 people attempt suicide. In addition, data from the U.S. Centers for Disease Control and Prevention indicate that attempted suicides are three times more common among young women than in men.
“What are the reasons for this gender gap?” Dr. Toffol asked during her presentation.
“It is known that the major risk factor for suicidal behavior is a psychiatric disorder, and in particular depression and mood disorders. And depression and mood disorders are more common in women than in men,” she said.
However, there is also “growing interest into the role of biological factors” in the risk for suicide, including hormones and hormonal contraception. Some studies have also suggested that there is an increased risk for depression and “both completed and attempted suicide” after starting hormonal contraception.
Dr. Toffol added that about 70% of European women use some form of contraception and, among Finnish women, 40% choose a hormonal contraceptive.
Nested analysis
The researchers conducted a nested case-control analysis combining 2017 national prescription data on 587,823 women aged 15-49 years with information from general and primary healthcare registers for the years 2018 to 2019.
They were able to identify 818 cases of attempted suicide among the women. These were matched 4:1 with 3,272 age-matched healthy women who acted as the control group. Use of hormonal contraceptives in the previous 180 days was determined for the whole cohort.
Among users of hormonal contraceptives, there were 344 attempted suicides in 2017, at an incidence rate of 0.59 per 1,000 person-years. This compared with 474 attempted suicides among nonusers, at an incidence rate of 0.81 per 1000 person-years.
Kaplan-Meier analysis showed there was a significant difference in rates for attempted suicide among hormonal contraceptive users versus nonusers, at an incidence rate ratio of 0.73 (P < .0001) – and the difference increased over time.
In addition, the incidence of attempted suicide decreased with increasing age, with the highest incidence rate in women aged 15-19 years (1.62 per 1,000 person-years).
Conditional logistic regression analysis that controlled for education, marital status, chronic disease, recent psychiatric hospitalization, and current use of psychotropic medication showed hormonal contraceptive use was not linked to an increased risk of attempted suicide overall, at an odds ratio of 0.79 (95% confidence interval, 0.56-1.11).
However, when they looked specifically at women without a history of psychiatric illness, the association became significant, at an OR of 0.73 for attempted suicide among hormonal contraceptive users (95% CI, 0.58-0.91), while the relationship remained nonsignificant in women with a history of psychiatric disorders.
Further analysis suggested the significant association was confined to women taking combined hormonal contraceptives, at an OR of 0.57 for suicide attempt versus nonusers (95% CI, 0.44-0.75), and those use EE-containing preparations (OR, 0.54; 95% CI, 0.40-0.73).
There was a suggestion in the data that hormonal contraceptives containing desogestrel or drospirenone alongside EE may offer the greatest reduction in attempted suicide risk, but that did not survive multivariate analysis.
Dr. Toffol also noted that they were not able to capture data on use of intrauterine devices in their analysis.
“There is a growing number of municipalities in Finland that are providing free-of-charge contraception to young women” that is often an intrauterine device, she said. The researchers hope to include these women in a future analysis.
‘Age matters’
Commenting on the findings, Alexis C. Edwards, PhD, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said the current study’s findings “made a lot of sense.” Dr. Edwards wasn’t involved with this study but conducted a previous study of 216,702 Swedish women aged 15-22 years that showed use of combination or progestin-only oral contraceptives was associated with an increased risk for suicidal behavior.
She agreed with Dr. Toffol that the “much larger age range” in the new study may have played a role in showing the opposite result.
“The trajectory that we saw if we had been able to continue following the women for longer – which we couldn’t, due to limitations of the registries – [was that] using hormonal contraceptives was going to end up being protective, so I do think that it matters what age you’re looking at,” she said.
Dr. Edwards noted the takeaway from both studies “is that, even if there is a slight increase in risk from using hormonal contraceptives, it’s short lived and it’s probably specific to young women, which is important.”
She suggested the hormonal benefit from extended contraceptive use could come from the regulation of mood, as it offers a “more stable hormonal course than what their body might be putting them through in the absence of using the pill.”
Overall, it is “really lovely to see very well-executed studies on this, providing more empirical evidence on this question, because it is something that’s relevant to anyone who’s potentially going to be using hormonal contraception,” Dr. Edwards said.
Clinical implications?
Andrea Fiorillo, MD, PhD, department of psychiatry, University of Campania “Luigi Vanvitelli,” Naples, Italy, said in a press release that the “striking” findings of the current study need “careful evaluation.”
They also need to be replicated in “different cohorts of women and controlled for the impact of several psychosocial stressors, such as economic upheavals, social insecurity, and uncertainty due to the COVID pandemic,” said Dr. Fiorillo, who was not involved with the research.
Nevertheless, she believes the “clinical implications of the study are obvious and may help to destigmatize the use of hormonal contraceptives.”
The study was funded by the Jane and Aatos Erkko Foundation, the Avohoidon Tsukimis äätiö (Foundation for Primary Care Research), the Yrj ö Jahnsson Foundation, and the Finnish Cultural Foundation. No relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
Contrary to previous analyses, new research suggests.
In a study of more than 800 women younger than age 50 who attempted suicide and more than 3,000 age-matched peers, results showed those who took hormonal contraceptives had a 27% reduced risk for attempted suicide.
Further analysis showed this was confined to women without a history of psychiatric illness and the reduction in risk rose to 43% among those who took combined hormonal contraceptives rather than progestin-only versions.
The protective effect against attempted suicide increased further to 46% if ethinyl estradiol (EE)–containing preparations were used. Moreover, the beneficial effect of contraceptive use increased over time.
The main message is the “current use of hormonal contraceptives is not associated with an increased risk of attempted suicide in our population,” study presenter Elena Toffol, MD, PhD, department of public health, University of Helsinki, told meeting attendees at the European Psychiatric Association 2022 Congress.
Age range differences
Dr. Toffol said there could be “several reasons” why the results are different from those in previous studies, including that the researchers included a “larger age range.” She noted it is known that “older women have a lower rate of attempted suicide and use different types of contraceptives.”
Dr. Toffol said in an interview that, although it’s “hard to estimate any causality” because this is an observational study, it is “tempting to speculate, and it is plausible, that hormones partly play a role with some, but not all, women being more sensitive to hormonal influences.”
However, the results “may also reflect life choices or a protective life status; for example, more stable relationships or more conscious and health-focused behaviors,” she said.
“It may also be that the underlying characteristics of women who are prescribed or opt for certain types of contraceptives are somehow related to their suicidal risk,” she added.
In 2019, the global age-standardized suicide rate was 9.0 per 100,000, which translates into more than 700,000 deaths every year, Dr. Toffol noted.
However, she emphasized the World Health Organization has calculated that, for every adult who dies by suicide, more than 20 people attempt suicide. In addition, data from the U.S. Centers for Disease Control and Prevention indicate that attempted suicides are three times more common among young women than in men.
“What are the reasons for this gender gap?” Dr. Toffol asked during her presentation.
“It is known that the major risk factor for suicidal behavior is a psychiatric disorder, and in particular depression and mood disorders. And depression and mood disorders are more common in women than in men,” she said.
However, there is also “growing interest into the role of biological factors” in the risk for suicide, including hormones and hormonal contraception. Some studies have also suggested that there is an increased risk for depression and “both completed and attempted suicide” after starting hormonal contraception.
Dr. Toffol added that about 70% of European women use some form of contraception and, among Finnish women, 40% choose a hormonal contraceptive.
Nested analysis
The researchers conducted a nested case-control analysis combining 2017 national prescription data on 587,823 women aged 15-49 years with information from general and primary healthcare registers for the years 2018 to 2019.
They were able to identify 818 cases of attempted suicide among the women. These were matched 4:1 with 3,272 age-matched healthy women who acted as the control group. Use of hormonal contraceptives in the previous 180 days was determined for the whole cohort.
Among users of hormonal contraceptives, there were 344 attempted suicides in 2017, at an incidence rate of 0.59 per 1,000 person-years. This compared with 474 attempted suicides among nonusers, at an incidence rate of 0.81 per 1000 person-years.
Kaplan-Meier analysis showed there was a significant difference in rates for attempted suicide among hormonal contraceptive users versus nonusers, at an incidence rate ratio of 0.73 (P < .0001) – and the difference increased over time.
In addition, the incidence of attempted suicide decreased with increasing age, with the highest incidence rate in women aged 15-19 years (1.62 per 1,000 person-years).
Conditional logistic regression analysis that controlled for education, marital status, chronic disease, recent psychiatric hospitalization, and current use of psychotropic medication showed hormonal contraceptive use was not linked to an increased risk of attempted suicide overall, at an odds ratio of 0.79 (95% confidence interval, 0.56-1.11).
However, when they looked specifically at women without a history of psychiatric illness, the association became significant, at an OR of 0.73 for attempted suicide among hormonal contraceptive users (95% CI, 0.58-0.91), while the relationship remained nonsignificant in women with a history of psychiatric disorders.
Further analysis suggested the significant association was confined to women taking combined hormonal contraceptives, at an OR of 0.57 for suicide attempt versus nonusers (95% CI, 0.44-0.75), and those use EE-containing preparations (OR, 0.54; 95% CI, 0.40-0.73).
There was a suggestion in the data that hormonal contraceptives containing desogestrel or drospirenone alongside EE may offer the greatest reduction in attempted suicide risk, but that did not survive multivariate analysis.
Dr. Toffol also noted that they were not able to capture data on use of intrauterine devices in their analysis.
“There is a growing number of municipalities in Finland that are providing free-of-charge contraception to young women” that is often an intrauterine device, she said. The researchers hope to include these women in a future analysis.
‘Age matters’
Commenting on the findings, Alexis C. Edwards, PhD, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said the current study’s findings “made a lot of sense.” Dr. Edwards wasn’t involved with this study but conducted a previous study of 216,702 Swedish women aged 15-22 years that showed use of combination or progestin-only oral contraceptives was associated with an increased risk for suicidal behavior.
She agreed with Dr. Toffol that the “much larger age range” in the new study may have played a role in showing the opposite result.
“The trajectory that we saw if we had been able to continue following the women for longer – which we couldn’t, due to limitations of the registries – [was that] using hormonal contraceptives was going to end up being protective, so I do think that it matters what age you’re looking at,” she said.
Dr. Edwards noted the takeaway from both studies “is that, even if there is a slight increase in risk from using hormonal contraceptives, it’s short lived and it’s probably specific to young women, which is important.”
She suggested the hormonal benefit from extended contraceptive use could come from the regulation of mood, as it offers a “more stable hormonal course than what their body might be putting them through in the absence of using the pill.”
Overall, it is “really lovely to see very well-executed studies on this, providing more empirical evidence on this question, because it is something that’s relevant to anyone who’s potentially going to be using hormonal contraception,” Dr. Edwards said.
Clinical implications?
Andrea Fiorillo, MD, PhD, department of psychiatry, University of Campania “Luigi Vanvitelli,” Naples, Italy, said in a press release that the “striking” findings of the current study need “careful evaluation.”
They also need to be replicated in “different cohorts of women and controlled for the impact of several psychosocial stressors, such as economic upheavals, social insecurity, and uncertainty due to the COVID pandemic,” said Dr. Fiorillo, who was not involved with the research.
Nevertheless, she believes the “clinical implications of the study are obvious and may help to destigmatize the use of hormonal contraceptives.”
The study was funded by the Jane and Aatos Erkko Foundation, the Avohoidon Tsukimis äätiö (Foundation for Primary Care Research), the Yrj ö Jahnsson Foundation, and the Finnish Cultural Foundation. No relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
Contrary to previous analyses, new research suggests.
In a study of more than 800 women younger than age 50 who attempted suicide and more than 3,000 age-matched peers, results showed those who took hormonal contraceptives had a 27% reduced risk for attempted suicide.
Further analysis showed this was confined to women without a history of psychiatric illness and the reduction in risk rose to 43% among those who took combined hormonal contraceptives rather than progestin-only versions.
The protective effect against attempted suicide increased further to 46% if ethinyl estradiol (EE)–containing preparations were used. Moreover, the beneficial effect of contraceptive use increased over time.
The main message is the “current use of hormonal contraceptives is not associated with an increased risk of attempted suicide in our population,” study presenter Elena Toffol, MD, PhD, department of public health, University of Helsinki, told meeting attendees at the European Psychiatric Association 2022 Congress.
Age range differences
Dr. Toffol said there could be “several reasons” why the results are different from those in previous studies, including that the researchers included a “larger age range.” She noted it is known that “older women have a lower rate of attempted suicide and use different types of contraceptives.”
Dr. Toffol said in an interview that, although it’s “hard to estimate any causality” because this is an observational study, it is “tempting to speculate, and it is plausible, that hormones partly play a role with some, but not all, women being more sensitive to hormonal influences.”
However, the results “may also reflect life choices or a protective life status; for example, more stable relationships or more conscious and health-focused behaviors,” she said.
“It may also be that the underlying characteristics of women who are prescribed or opt for certain types of contraceptives are somehow related to their suicidal risk,” she added.
In 2019, the global age-standardized suicide rate was 9.0 per 100,000, which translates into more than 700,000 deaths every year, Dr. Toffol noted.
However, she emphasized the World Health Organization has calculated that, for every adult who dies by suicide, more than 20 people attempt suicide. In addition, data from the U.S. Centers for Disease Control and Prevention indicate that attempted suicides are three times more common among young women than in men.
“What are the reasons for this gender gap?” Dr. Toffol asked during her presentation.
“It is known that the major risk factor for suicidal behavior is a psychiatric disorder, and in particular depression and mood disorders. And depression and mood disorders are more common in women than in men,” she said.
However, there is also “growing interest into the role of biological factors” in the risk for suicide, including hormones and hormonal contraception. Some studies have also suggested that there is an increased risk for depression and “both completed and attempted suicide” after starting hormonal contraception.
Dr. Toffol added that about 70% of European women use some form of contraception and, among Finnish women, 40% choose a hormonal contraceptive.
Nested analysis
The researchers conducted a nested case-control analysis combining 2017 national prescription data on 587,823 women aged 15-49 years with information from general and primary healthcare registers for the years 2018 to 2019.
They were able to identify 818 cases of attempted suicide among the women. These were matched 4:1 with 3,272 age-matched healthy women who acted as the control group. Use of hormonal contraceptives in the previous 180 days was determined for the whole cohort.
Among users of hormonal contraceptives, there were 344 attempted suicides in 2017, at an incidence rate of 0.59 per 1,000 person-years. This compared with 474 attempted suicides among nonusers, at an incidence rate of 0.81 per 1000 person-years.
Kaplan-Meier analysis showed there was a significant difference in rates for attempted suicide among hormonal contraceptive users versus nonusers, at an incidence rate ratio of 0.73 (P < .0001) – and the difference increased over time.
In addition, the incidence of attempted suicide decreased with increasing age, with the highest incidence rate in women aged 15-19 years (1.62 per 1,000 person-years).
Conditional logistic regression analysis that controlled for education, marital status, chronic disease, recent psychiatric hospitalization, and current use of psychotropic medication showed hormonal contraceptive use was not linked to an increased risk of attempted suicide overall, at an odds ratio of 0.79 (95% confidence interval, 0.56-1.11).
However, when they looked specifically at women without a history of psychiatric illness, the association became significant, at an OR of 0.73 for attempted suicide among hormonal contraceptive users (95% CI, 0.58-0.91), while the relationship remained nonsignificant in women with a history of psychiatric disorders.
Further analysis suggested the significant association was confined to women taking combined hormonal contraceptives, at an OR of 0.57 for suicide attempt versus nonusers (95% CI, 0.44-0.75), and those use EE-containing preparations (OR, 0.54; 95% CI, 0.40-0.73).
There was a suggestion in the data that hormonal contraceptives containing desogestrel or drospirenone alongside EE may offer the greatest reduction in attempted suicide risk, but that did not survive multivariate analysis.
Dr. Toffol also noted that they were not able to capture data on use of intrauterine devices in their analysis.
“There is a growing number of municipalities in Finland that are providing free-of-charge contraception to young women” that is often an intrauterine device, she said. The researchers hope to include these women in a future analysis.
‘Age matters’
Commenting on the findings, Alexis C. Edwards, PhD, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said the current study’s findings “made a lot of sense.” Dr. Edwards wasn’t involved with this study but conducted a previous study of 216,702 Swedish women aged 15-22 years that showed use of combination or progestin-only oral contraceptives was associated with an increased risk for suicidal behavior.
She agreed with Dr. Toffol that the “much larger age range” in the new study may have played a role in showing the opposite result.
“The trajectory that we saw if we had been able to continue following the women for longer – which we couldn’t, due to limitations of the registries – [was that] using hormonal contraceptives was going to end up being protective, so I do think that it matters what age you’re looking at,” she said.
Dr. Edwards noted the takeaway from both studies “is that, even if there is a slight increase in risk from using hormonal contraceptives, it’s short lived and it’s probably specific to young women, which is important.”
She suggested the hormonal benefit from extended contraceptive use could come from the regulation of mood, as it offers a “more stable hormonal course than what their body might be putting them through in the absence of using the pill.”
Overall, it is “really lovely to see very well-executed studies on this, providing more empirical evidence on this question, because it is something that’s relevant to anyone who’s potentially going to be using hormonal contraception,” Dr. Edwards said.
Clinical implications?
Andrea Fiorillo, MD, PhD, department of psychiatry, University of Campania “Luigi Vanvitelli,” Naples, Italy, said in a press release that the “striking” findings of the current study need “careful evaluation.”
They also need to be replicated in “different cohorts of women and controlled for the impact of several psychosocial stressors, such as economic upheavals, social insecurity, and uncertainty due to the COVID pandemic,” said Dr. Fiorillo, who was not involved with the research.
Nevertheless, she believes the “clinical implications of the study are obvious and may help to destigmatize the use of hormonal contraceptives.”
The study was funded by the Jane and Aatos Erkko Foundation, the Avohoidon Tsukimis äätiö (Foundation for Primary Care Research), the Yrj ö Jahnsson Foundation, and the Finnish Cultural Foundation. No relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
FROM EPA 2022
Surgeons may underestimate recovery from incontinence operation
Surgeons may significantly underestimate how long it will take women to return to normal activities following sling surgery to correct stress urinary incontinence, a new study has found.
The researchers found that just over 40% of women reported returning to work and other normal activities within 2 weeks of having undergone midurethral sling procedures – a much less optimistic forecast than what surgeons typically provide in these cases.
“This is in contrast to a published survey of physicians that showed the majority of surgeons suggested patients return to work within 2 weeks,” Rui Wang, MD, a fellow in female pelvic medicine and reconstructive surgery at Hartford Hospital, Conn., said in an interview.
Dr. Wang referred to a published survey of 135 physicians that was conducted at a 2018 meeting of the Society of Gynecologic Surgeons. In that survey, 88% of respondents indicated that patients could return to sedentary work within 2 weeks after undergoing sling surgery. Most recommended longer waits before returning to manual labor.
The authors of the survey noted a lack of consensus guidelines and wide variations in recommendations for postoperative restrictions after minimally invasive gynecologic and pelvic reconstructive surgery, which the researchers called a “largely unstudied field.”
Dr. Wang said, “The majority of patients may need more than 2 weeks to return to work and normal activities even following minimally invasive outpatient surgeries such as midurethral sling.”
Dr. Wang is scheduled to present the findings June 18 at the annual meeting of the American Urogynecologic Society.
For the new study, Dr. Wang and a colleague examined how patients answered questions about their activity levels during recovery after sling procedures. The patients were enrolled in the Trial of Mid-Urethral Slings (TOMUS), a randomized controlled trial that compared two types of midurethral slings used for the treatment of stress urinary incontinence: the retropubic midurethral mesh sling and the transobturator midurethral sling. Results of the trial were published in 2010.
Of 597 women enrolled in TOMUS, 441 were included in the new analysis. Patients who underwent another surgery at the same time as their sling procedure were excluded from the analysis.
As part of the trial, patients were asked how many paid workdays they took off after surgery; whether they had returned to full normal activities of daily life, including work, if applicable; and how much time it took for them to fully return to normal activities of daily life, including work.
The researchers found that 183 (41.5%) returned to normal activities within 2 weeks of the procedure. Among those patients, the median recovery time was 6 days. Within 6 weeks of surgery, 308 (70%) had returned to normal activities, including work. After 6 months, 407 (98.3%) were back to their normal routines, the study showed.
Multivariate regression analysis yielded no factor that predicted the timing of returning to normal activity and work. Nor did the researchers observe any significant differences in failure rates and adverse outcomes between patients who returned within 2 weeks or after 2 weeks.
Essential information for patient planning
Dr. Wang said she expects that the findings will help physicians in counseling patients and setting postoperative recovery expectations. “For patients planning elective surgery, one of the most important quality-of-life issues is the time they will need to take off from work and recover,” she said.
Although most patients needed more than 2 weeks to recover, the median paid time off after surgery was 4 days. “Many patients would have taken unpaid days off or used vacation time for their postoperative recovery,” Dr. Wang said.
She added that more research is needed to explore whether that discrepancy disproportionately affects women in jobs with fewer employee benefits. “We did not find that age, race/ethnicity, marital status, occupation, symptom severity, and duration of surgery significantly predicted the timing of return to work or normal activities,” she said. “But are there other factors, such as geographic location, insurance status, [or] income, that may affect this timing?”
Sarah Boyd, MD, an assistant professor in the Division of Female Pelvic Medicine and Reconstructive Surgery at Penn State College of Medicine, Hershey, said the new findings add concrete information that can guide patients in planning their recovery.
“Previously, surgeons could only provide general estimates to these patients based on the experience of their patients,” Dr. Boyd, who was not involved in the study, told this news organization.
The analysis has not been published in a peer-reviewed journal, and Dr. Boyd said that the findings may not pertain to all individuals who undergo midurethral sling procedures, such as people who have had prior surgery for incontinence or those who undergo surgery for other pelvic floor disorders at the same time.
Dr. Wang and Dr. Boyd reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Surgeons may significantly underestimate how long it will take women to return to normal activities following sling surgery to correct stress urinary incontinence, a new study has found.
The researchers found that just over 40% of women reported returning to work and other normal activities within 2 weeks of having undergone midurethral sling procedures – a much less optimistic forecast than what surgeons typically provide in these cases.
“This is in contrast to a published survey of physicians that showed the majority of surgeons suggested patients return to work within 2 weeks,” Rui Wang, MD, a fellow in female pelvic medicine and reconstructive surgery at Hartford Hospital, Conn., said in an interview.
Dr. Wang referred to a published survey of 135 physicians that was conducted at a 2018 meeting of the Society of Gynecologic Surgeons. In that survey, 88% of respondents indicated that patients could return to sedentary work within 2 weeks after undergoing sling surgery. Most recommended longer waits before returning to manual labor.
The authors of the survey noted a lack of consensus guidelines and wide variations in recommendations for postoperative restrictions after minimally invasive gynecologic and pelvic reconstructive surgery, which the researchers called a “largely unstudied field.”
Dr. Wang said, “The majority of patients may need more than 2 weeks to return to work and normal activities even following minimally invasive outpatient surgeries such as midurethral sling.”
Dr. Wang is scheduled to present the findings June 18 at the annual meeting of the American Urogynecologic Society.
For the new study, Dr. Wang and a colleague examined how patients answered questions about their activity levels during recovery after sling procedures. The patients were enrolled in the Trial of Mid-Urethral Slings (TOMUS), a randomized controlled trial that compared two types of midurethral slings used for the treatment of stress urinary incontinence: the retropubic midurethral mesh sling and the transobturator midurethral sling. Results of the trial were published in 2010.
Of 597 women enrolled in TOMUS, 441 were included in the new analysis. Patients who underwent another surgery at the same time as their sling procedure were excluded from the analysis.
As part of the trial, patients were asked how many paid workdays they took off after surgery; whether they had returned to full normal activities of daily life, including work, if applicable; and how much time it took for them to fully return to normal activities of daily life, including work.
The researchers found that 183 (41.5%) returned to normal activities within 2 weeks of the procedure. Among those patients, the median recovery time was 6 days. Within 6 weeks of surgery, 308 (70%) had returned to normal activities, including work. After 6 months, 407 (98.3%) were back to their normal routines, the study showed.
Multivariate regression analysis yielded no factor that predicted the timing of returning to normal activity and work. Nor did the researchers observe any significant differences in failure rates and adverse outcomes between patients who returned within 2 weeks or after 2 weeks.
Essential information for patient planning
Dr. Wang said she expects that the findings will help physicians in counseling patients and setting postoperative recovery expectations. “For patients planning elective surgery, one of the most important quality-of-life issues is the time they will need to take off from work and recover,” she said.
Although most patients needed more than 2 weeks to recover, the median paid time off after surgery was 4 days. “Many patients would have taken unpaid days off or used vacation time for their postoperative recovery,” Dr. Wang said.
She added that more research is needed to explore whether that discrepancy disproportionately affects women in jobs with fewer employee benefits. “We did not find that age, race/ethnicity, marital status, occupation, symptom severity, and duration of surgery significantly predicted the timing of return to work or normal activities,” she said. “But are there other factors, such as geographic location, insurance status, [or] income, that may affect this timing?”
Sarah Boyd, MD, an assistant professor in the Division of Female Pelvic Medicine and Reconstructive Surgery at Penn State College of Medicine, Hershey, said the new findings add concrete information that can guide patients in planning their recovery.
“Previously, surgeons could only provide general estimates to these patients based on the experience of their patients,” Dr. Boyd, who was not involved in the study, told this news organization.
The analysis has not been published in a peer-reviewed journal, and Dr. Boyd said that the findings may not pertain to all individuals who undergo midurethral sling procedures, such as people who have had prior surgery for incontinence or those who undergo surgery for other pelvic floor disorders at the same time.
Dr. Wang and Dr. Boyd reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Surgeons may significantly underestimate how long it will take women to return to normal activities following sling surgery to correct stress urinary incontinence, a new study has found.
The researchers found that just over 40% of women reported returning to work and other normal activities within 2 weeks of having undergone midurethral sling procedures – a much less optimistic forecast than what surgeons typically provide in these cases.
“This is in contrast to a published survey of physicians that showed the majority of surgeons suggested patients return to work within 2 weeks,” Rui Wang, MD, a fellow in female pelvic medicine and reconstructive surgery at Hartford Hospital, Conn., said in an interview.
Dr. Wang referred to a published survey of 135 physicians that was conducted at a 2018 meeting of the Society of Gynecologic Surgeons. In that survey, 88% of respondents indicated that patients could return to sedentary work within 2 weeks after undergoing sling surgery. Most recommended longer waits before returning to manual labor.
The authors of the survey noted a lack of consensus guidelines and wide variations in recommendations for postoperative restrictions after minimally invasive gynecologic and pelvic reconstructive surgery, which the researchers called a “largely unstudied field.”
Dr. Wang said, “The majority of patients may need more than 2 weeks to return to work and normal activities even following minimally invasive outpatient surgeries such as midurethral sling.”
Dr. Wang is scheduled to present the findings June 18 at the annual meeting of the American Urogynecologic Society.
For the new study, Dr. Wang and a colleague examined how patients answered questions about their activity levels during recovery after sling procedures. The patients were enrolled in the Trial of Mid-Urethral Slings (TOMUS), a randomized controlled trial that compared two types of midurethral slings used for the treatment of stress urinary incontinence: the retropubic midurethral mesh sling and the transobturator midurethral sling. Results of the trial were published in 2010.
Of 597 women enrolled in TOMUS, 441 were included in the new analysis. Patients who underwent another surgery at the same time as their sling procedure were excluded from the analysis.
As part of the trial, patients were asked how many paid workdays they took off after surgery; whether they had returned to full normal activities of daily life, including work, if applicable; and how much time it took for them to fully return to normal activities of daily life, including work.
The researchers found that 183 (41.5%) returned to normal activities within 2 weeks of the procedure. Among those patients, the median recovery time was 6 days. Within 6 weeks of surgery, 308 (70%) had returned to normal activities, including work. After 6 months, 407 (98.3%) were back to their normal routines, the study showed.
Multivariate regression analysis yielded no factor that predicted the timing of returning to normal activity and work. Nor did the researchers observe any significant differences in failure rates and adverse outcomes between patients who returned within 2 weeks or after 2 weeks.
Essential information for patient planning
Dr. Wang said she expects that the findings will help physicians in counseling patients and setting postoperative recovery expectations. “For patients planning elective surgery, one of the most important quality-of-life issues is the time they will need to take off from work and recover,” she said.
Although most patients needed more than 2 weeks to recover, the median paid time off after surgery was 4 days. “Many patients would have taken unpaid days off or used vacation time for their postoperative recovery,” Dr. Wang said.
She added that more research is needed to explore whether that discrepancy disproportionately affects women in jobs with fewer employee benefits. “We did not find that age, race/ethnicity, marital status, occupation, symptom severity, and duration of surgery significantly predicted the timing of return to work or normal activities,” she said. “But are there other factors, such as geographic location, insurance status, [or] income, that may affect this timing?”
Sarah Boyd, MD, an assistant professor in the Division of Female Pelvic Medicine and Reconstructive Surgery at Penn State College of Medicine, Hershey, said the new findings add concrete information that can guide patients in planning their recovery.
“Previously, surgeons could only provide general estimates to these patients based on the experience of their patients,” Dr. Boyd, who was not involved in the study, told this news organization.
The analysis has not been published in a peer-reviewed journal, and Dr. Boyd said that the findings may not pertain to all individuals who undergo midurethral sling procedures, such as people who have had prior surgery for incontinence or those who undergo surgery for other pelvic floor disorders at the same time.
Dr. Wang and Dr. Boyd reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AUGS 2022
62-year-old woman • dysuria • dyspareunia • urinary incontinence • Dx?
THE CASE
A 62-year-old postmenopausal woman presented to the clinic as a new patient for her annual physical examination. She reported a 9-year history of symptoms including dysuria, post-void dribbling, dyspareunia, and urinary incontinence on review of systems. Her physical examination revealed an anterior vaginal wall bulge (FIGURE). Results of a urinalysis were negative. The patient was referred to Urology for further evaluation.
THE DIAGNOSIS
A pelvic magnetic resonance imaging (MRI) scan revealed a large periurethral diverticulum with a horseshoe shape.
DISCUSSION
Women are more likely than men to develop urethral diverticulum, and it can manifest at any age, usually in the third through seventh decade.4,5 It was once thought to be more common in Black women, although the literature does not support this.6 Black women are 3 times more likely to be operated on than White women to treat urethral diverticula.7
Unknown origin. Most cases of urethral diverticulum are acquired; the etiology is uncertain.8,9 The assumption is that urethral diverticulum occurs as a result of repeated infection of the periurethral glands with subsequent obstruction, abscess formation, and chronic inflammation.1,2,4 Childbirth trauma, iatrogenic causes, and urethral instrumentation have also been implicated.3,4 In rare cases of congenital urethral diverticula, the diverticula are thought to be remnants of Gartner duct cysts, and yet, incidence in the pediatric population is low.8
Diagnosis is confirmed through physical exam and imaging
The urethral diverticulum manifests anteriorly and palpation of the anterior vaginal wall may reveal a painful mass.10 A split-speculum is used for careful inspection and palpation of the anterior vaginal wall.9 If the diverticulum is found to be firm on palpation, or there is bloody urethral drainage, malignancy (although rare) must be ruled out.4,5 Refer such patients to a urologist or urogynecologist.
Radiologic imaging (eg, ultrasound,
Continue to: Nonspecific symptoms may lead to misdiagnosis
Nonspecific symptoms may lead to misdiagnosis. The symptoms associated with urethral diverticulum are diverse and linked to several differential diagnoses (TABLE).3,4,12 The most common signs and symptoms are pelvic pain, urethral mass, dyspareunia, dysuria, urinary incontinence, and post-void dribbling—all of which are considered nonspecific.3,10,11 These nonspecific symptoms (or even an absence of symptoms), along with a physician’s lack of familiarity with urethral diverticulum, can result in a misdiagnosis or even a delayed diagnosis (up to 5.2 years).3,10
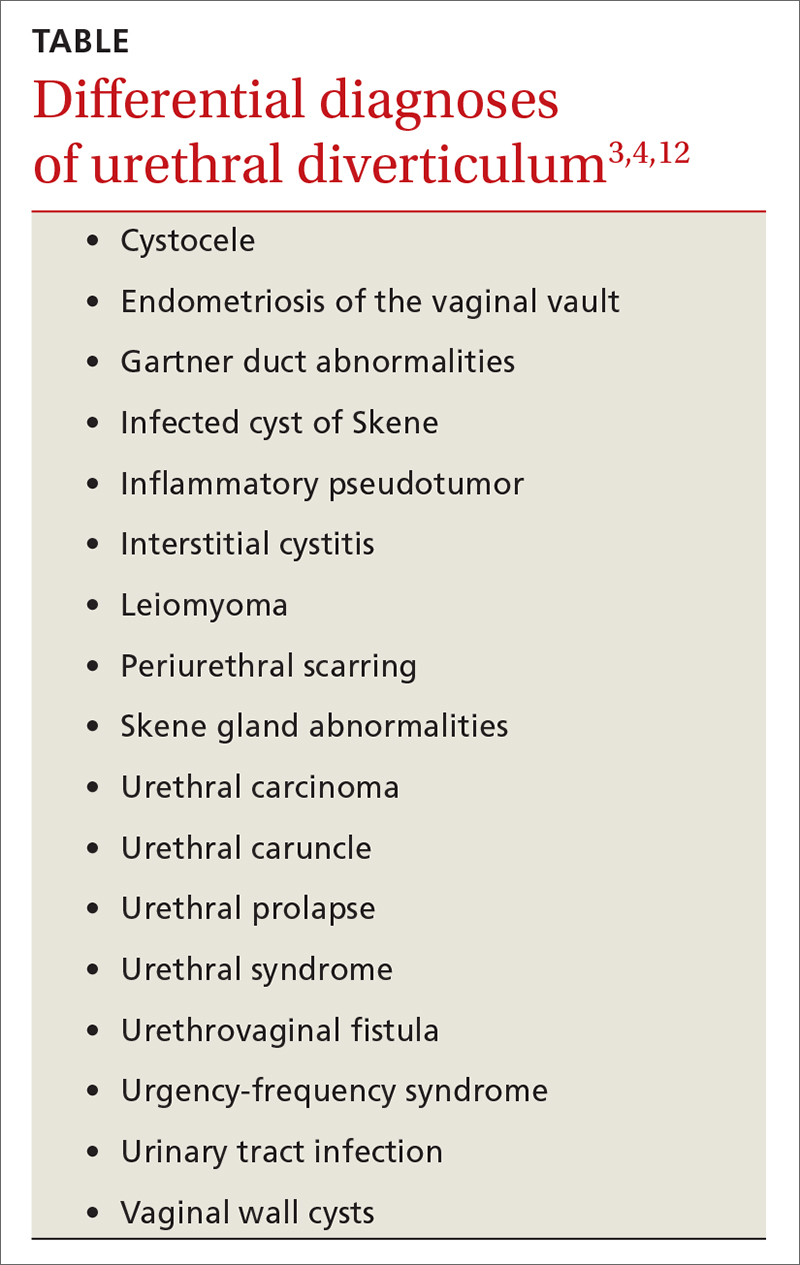
Managing symptoms vs preventing recurrence
Conservative management with antibiotics, anticholinergics, and/or observation is acceptable for patients with mild symptoms and those who are pregnant or who have a current infection or serious comorbidities that preclude surgery.3,9 Complete excision of the urethral diverticulum with reconstruction is considered the most effective surgical management for symptom relief and recurrence prevention.3,4,11,14
Our patient underwent a successful transvaginal suburethral diverticulectomy.
THE TAKEAWAY
The diagnosis of female urethral diverticulum is often delayed or misdiagnosed because symptoms are diverse and nonspecific. One should have a high degree of suspicion for urethral diverticulum in patients with dysuria, dyspareunia, pelvic pain, urinary incontinence, and irritative voiding symptoms who are not responding to conservative management. Ultrasound is an appropriate first-line imaging modality. However, a pelvic MRI is the most sensitive and specific in diagnosing urethral diverticulum.12
CORRESPONDENCE
Folashade Omole, MD, FAAFP, 720 Westview Drive, Atlanta, GA 30310; fomole@msm.edu
1. Billow M, James R, Resnick K, et al. An unusual presentation of a urethral diverticulum as a vaginal wall mass: a case report. J Med Case Rep. 2013;7:171. doi: 10.1186/1752-1947-7-171
2. El-Nashar SA, Bacon MM, Kim-Fine S, et al. Incidence of female urethral diverticulum: a population-based analysis and literature review. Int Urogynecol J. 2014;25:73-79. doi: 10.1007/s00192-013-2155-2
3. Cameron AP. Urethral diverticulum in the female: a meta-analysis of modern series. Minerva Ginecol. 2016;68:186-210.
4. Greiman AK, Rolef J, Rovner ES. Urethral diverticulum: a systematic review. Arab J Urol. 2019;17:49-57. doi: 10.1080/2090598X.2019.1589748
5. Allen D, Mishra V, Pepper W, et al. A single-center experience of symptomatic male urethral diverticula. Urology. 2007;70:650-653. doi: 10.1016/j.urology.2007.06.1111
6. O’Connor E, Iatropoulou D, Hashimoto S, et al. Urethral diverticulum carcinoma in females—a case series and review of the English and Japanese literature. Transl Androl Urol. 2018;7:703-729. doi: 10.21037/tau.2018.07.08
7. Burrows LJ, Howden NL, Meyn L, et al. Surgical procedures for urethral diverticula in women in the United States, 1979-1997. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:158-161. doi: 10.1007/s00192-004-1145-9
8. Riyach O, Ahsaini M, Tazi MF, et al. Female urethral diverticulum: cases report and literature. Ann Surg Innov Res. 2014;8:1. doi: 10.1186/1750-1164-8-1
9. Antosh DD, Gutman RE. Diagnosis and management of female urethral diverticulum. Female Pelvic Med Reconstr Surg. 2011;17:264-271. doi: 10.1097/SPV.0b013e318234a242
10. Romanzi LJ, Groutz A, Blaivas JG. Urethral diverticulum in women: diverse presentations resulting in diagnostic delay and mismanagement. J Urol. 2000;164:428-433.
11. Reeves FA, Inman RD, Chapple CR. Management of symptomatic urethral diverticula in women: a single-centre experience. Eur Urol. 2014;66:164-172. doi: 10.1016/j.eururo.2014.02.041
12. Dwarkasing RS, Dinkelaar W, Hop WCJ, et al. MRI evaluation of urethral diverticula and differential diagnosis in symptomatic women. AJR Am J Roentgenol. 2011;197:676-682. doi: 10.2214/AJR.10.6144
13. Porten S, Kielb S. Diagnosis of female diverticula using magnetic resonance imaging. Adv Urol. 2008;2008:213516. doi: 10.1155/2008/213516
14. Ockrim JL, Allen DJ, Shah PJ, et al. A tertiary experience of urethral diverticulectomy: diagnosis, imaging and surgical outcomes. BJU Int. 2009;103:1550-1554. doi: 10.1111/j.1464-410X.2009.08348.x
THE CASE
A 62-year-old postmenopausal woman presented to the clinic as a new patient for her annual physical examination. She reported a 9-year history of symptoms including dysuria, post-void dribbling, dyspareunia, and urinary incontinence on review of systems. Her physical examination revealed an anterior vaginal wall bulge (FIGURE). Results of a urinalysis were negative. The patient was referred to Urology for further evaluation.
THE DIAGNOSIS
A pelvic magnetic resonance imaging (MRI) scan revealed a large periurethral diverticulum with a horseshoe shape.
DISCUSSION
Women are more likely than men to develop urethral diverticulum, and it can manifest at any age, usually in the third through seventh decade.4,5 It was once thought to be more common in Black women, although the literature does not support this.6 Black women are 3 times more likely to be operated on than White women to treat urethral diverticula.7
Unknown origin. Most cases of urethral diverticulum are acquired; the etiology is uncertain.8,9 The assumption is that urethral diverticulum occurs as a result of repeated infection of the periurethral glands with subsequent obstruction, abscess formation, and chronic inflammation.1,2,4 Childbirth trauma, iatrogenic causes, and urethral instrumentation have also been implicated.3,4 In rare cases of congenital urethral diverticula, the diverticula are thought to be remnants of Gartner duct cysts, and yet, incidence in the pediatric population is low.8
Diagnosis is confirmed through physical exam and imaging
The urethral diverticulum manifests anteriorly and palpation of the anterior vaginal wall may reveal a painful mass.10 A split-speculum is used for careful inspection and palpation of the anterior vaginal wall.9 If the diverticulum is found to be firm on palpation, or there is bloody urethral drainage, malignancy (although rare) must be ruled out.4,5 Refer such patients to a urologist or urogynecologist.
Radiologic imaging (eg, ultrasound,
Continue to: Nonspecific symptoms may lead to misdiagnosis
Nonspecific symptoms may lead to misdiagnosis. The symptoms associated with urethral diverticulum are diverse and linked to several differential diagnoses (TABLE).3,4,12 The most common signs and symptoms are pelvic pain, urethral mass, dyspareunia, dysuria, urinary incontinence, and post-void dribbling—all of which are considered nonspecific.3,10,11 These nonspecific symptoms (or even an absence of symptoms), along with a physician’s lack of familiarity with urethral diverticulum, can result in a misdiagnosis or even a delayed diagnosis (up to 5.2 years).3,10
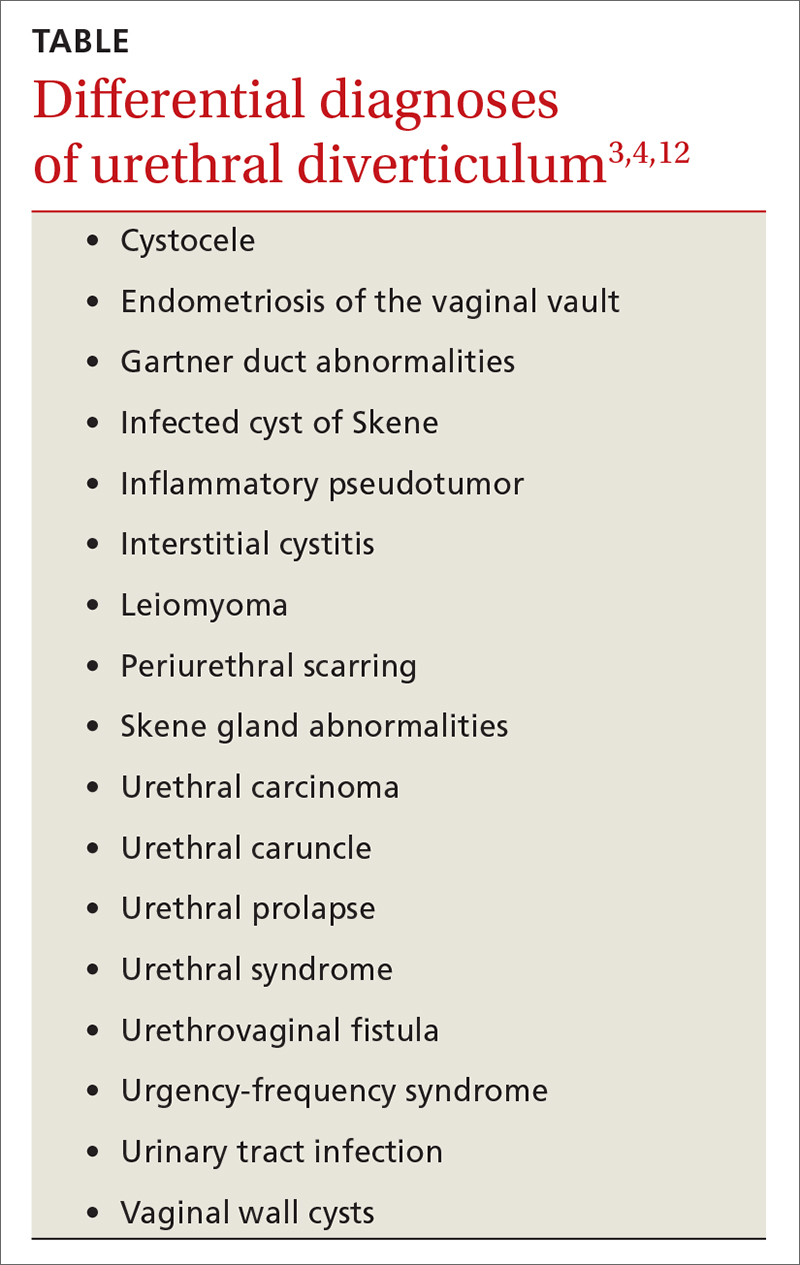
Managing symptoms vs preventing recurrence
Conservative management with antibiotics, anticholinergics, and/or observation is acceptable for patients with mild symptoms and those who are pregnant or who have a current infection or serious comorbidities that preclude surgery.3,9 Complete excision of the urethral diverticulum with reconstruction is considered the most effective surgical management for symptom relief and recurrence prevention.3,4,11,14
Our patient underwent a successful transvaginal suburethral diverticulectomy.
THE TAKEAWAY
The diagnosis of female urethral diverticulum is often delayed or misdiagnosed because symptoms are diverse and nonspecific. One should have a high degree of suspicion for urethral diverticulum in patients with dysuria, dyspareunia, pelvic pain, urinary incontinence, and irritative voiding symptoms who are not responding to conservative management. Ultrasound is an appropriate first-line imaging modality. However, a pelvic MRI is the most sensitive and specific in diagnosing urethral diverticulum.12
CORRESPONDENCE
Folashade Omole, MD, FAAFP, 720 Westview Drive, Atlanta, GA 30310; fomole@msm.edu
THE CASE
A 62-year-old postmenopausal woman presented to the clinic as a new patient for her annual physical examination. She reported a 9-year history of symptoms including dysuria, post-void dribbling, dyspareunia, and urinary incontinence on review of systems. Her physical examination revealed an anterior vaginal wall bulge (FIGURE). Results of a urinalysis were negative. The patient was referred to Urology for further evaluation.
THE DIAGNOSIS
A pelvic magnetic resonance imaging (MRI) scan revealed a large periurethral diverticulum with a horseshoe shape.
DISCUSSION
Women are more likely than men to develop urethral diverticulum, and it can manifest at any age, usually in the third through seventh decade.4,5 It was once thought to be more common in Black women, although the literature does not support this.6 Black women are 3 times more likely to be operated on than White women to treat urethral diverticula.7
Unknown origin. Most cases of urethral diverticulum are acquired; the etiology is uncertain.8,9 The assumption is that urethral diverticulum occurs as a result of repeated infection of the periurethral glands with subsequent obstruction, abscess formation, and chronic inflammation.1,2,4 Childbirth trauma, iatrogenic causes, and urethral instrumentation have also been implicated.3,4 In rare cases of congenital urethral diverticula, the diverticula are thought to be remnants of Gartner duct cysts, and yet, incidence in the pediatric population is low.8
Diagnosis is confirmed through physical exam and imaging
The urethral diverticulum manifests anteriorly and palpation of the anterior vaginal wall may reveal a painful mass.10 A split-speculum is used for careful inspection and palpation of the anterior vaginal wall.9 If the diverticulum is found to be firm on palpation, or there is bloody urethral drainage, malignancy (although rare) must be ruled out.4,5 Refer such patients to a urologist or urogynecologist.
Radiologic imaging (eg, ultrasound,
Continue to: Nonspecific symptoms may lead to misdiagnosis
Nonspecific symptoms may lead to misdiagnosis. The symptoms associated with urethral diverticulum are diverse and linked to several differential diagnoses (TABLE).3,4,12 The most common signs and symptoms are pelvic pain, urethral mass, dyspareunia, dysuria, urinary incontinence, and post-void dribbling—all of which are considered nonspecific.3,10,11 These nonspecific symptoms (or even an absence of symptoms), along with a physician’s lack of familiarity with urethral diverticulum, can result in a misdiagnosis or even a delayed diagnosis (up to 5.2 years).3,10
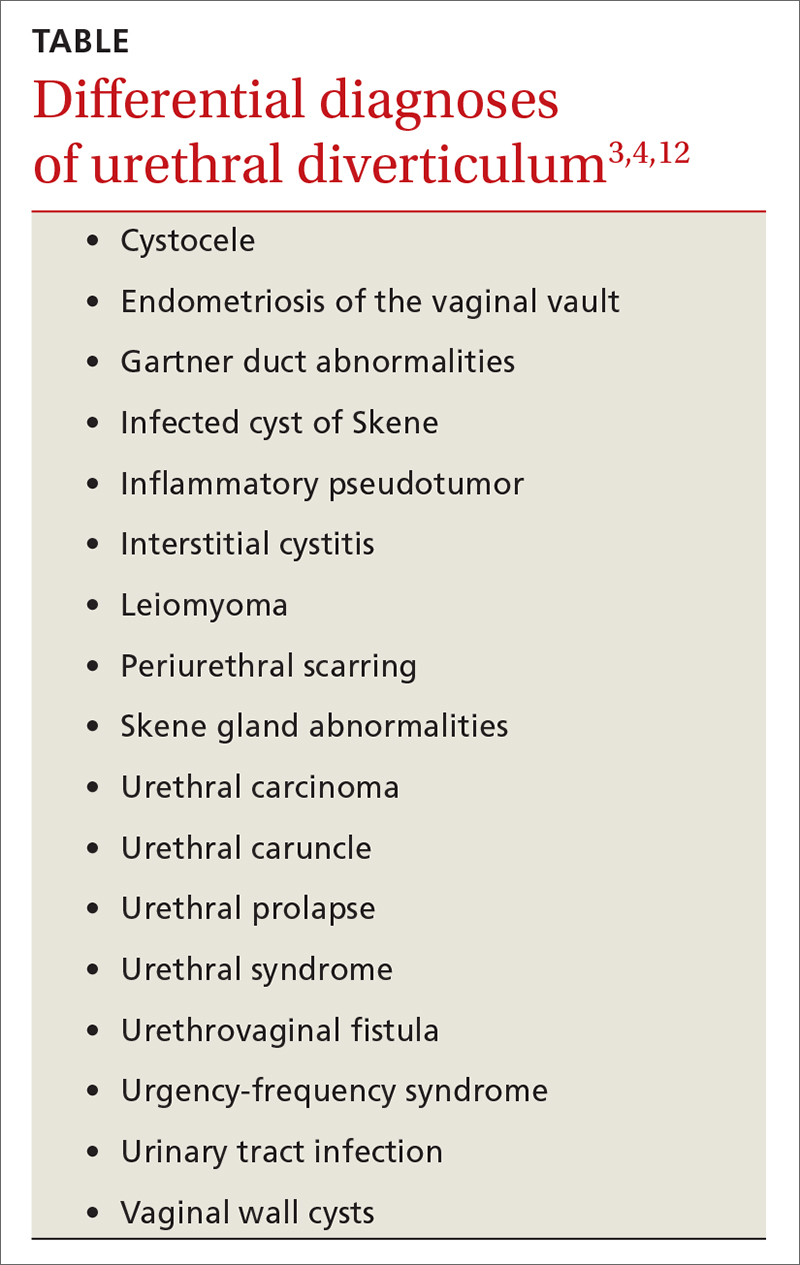
Managing symptoms vs preventing recurrence
Conservative management with antibiotics, anticholinergics, and/or observation is acceptable for patients with mild symptoms and those who are pregnant or who have a current infection or serious comorbidities that preclude surgery.3,9 Complete excision of the urethral diverticulum with reconstruction is considered the most effective surgical management for symptom relief and recurrence prevention.3,4,11,14
Our patient underwent a successful transvaginal suburethral diverticulectomy.
THE TAKEAWAY
The diagnosis of female urethral diverticulum is often delayed or misdiagnosed because symptoms are diverse and nonspecific. One should have a high degree of suspicion for urethral diverticulum in patients with dysuria, dyspareunia, pelvic pain, urinary incontinence, and irritative voiding symptoms who are not responding to conservative management. Ultrasound is an appropriate first-line imaging modality. However, a pelvic MRI is the most sensitive and specific in diagnosing urethral diverticulum.12
CORRESPONDENCE
Folashade Omole, MD, FAAFP, 720 Westview Drive, Atlanta, GA 30310; fomole@msm.edu
1. Billow M, James R, Resnick K, et al. An unusual presentation of a urethral diverticulum as a vaginal wall mass: a case report. J Med Case Rep. 2013;7:171. doi: 10.1186/1752-1947-7-171
2. El-Nashar SA, Bacon MM, Kim-Fine S, et al. Incidence of female urethral diverticulum: a population-based analysis and literature review. Int Urogynecol J. 2014;25:73-79. doi: 10.1007/s00192-013-2155-2
3. Cameron AP. Urethral diverticulum in the female: a meta-analysis of modern series. Minerva Ginecol. 2016;68:186-210.
4. Greiman AK, Rolef J, Rovner ES. Urethral diverticulum: a systematic review. Arab J Urol. 2019;17:49-57. doi: 10.1080/2090598X.2019.1589748
5. Allen D, Mishra V, Pepper W, et al. A single-center experience of symptomatic male urethral diverticula. Urology. 2007;70:650-653. doi: 10.1016/j.urology.2007.06.1111
6. O’Connor E, Iatropoulou D, Hashimoto S, et al. Urethral diverticulum carcinoma in females—a case series and review of the English and Japanese literature. Transl Androl Urol. 2018;7:703-729. doi: 10.21037/tau.2018.07.08
7. Burrows LJ, Howden NL, Meyn L, et al. Surgical procedures for urethral diverticula in women in the United States, 1979-1997. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:158-161. doi: 10.1007/s00192-004-1145-9
8. Riyach O, Ahsaini M, Tazi MF, et al. Female urethral diverticulum: cases report and literature. Ann Surg Innov Res. 2014;8:1. doi: 10.1186/1750-1164-8-1
9. Antosh DD, Gutman RE. Diagnosis and management of female urethral diverticulum. Female Pelvic Med Reconstr Surg. 2011;17:264-271. doi: 10.1097/SPV.0b013e318234a242
10. Romanzi LJ, Groutz A, Blaivas JG. Urethral diverticulum in women: diverse presentations resulting in diagnostic delay and mismanagement. J Urol. 2000;164:428-433.
11. Reeves FA, Inman RD, Chapple CR. Management of symptomatic urethral diverticula in women: a single-centre experience. Eur Urol. 2014;66:164-172. doi: 10.1016/j.eururo.2014.02.041
12. Dwarkasing RS, Dinkelaar W, Hop WCJ, et al. MRI evaluation of urethral diverticula and differential diagnosis in symptomatic women. AJR Am J Roentgenol. 2011;197:676-682. doi: 10.2214/AJR.10.6144
13. Porten S, Kielb S. Diagnosis of female diverticula using magnetic resonance imaging. Adv Urol. 2008;2008:213516. doi: 10.1155/2008/213516
14. Ockrim JL, Allen DJ, Shah PJ, et al. A tertiary experience of urethral diverticulectomy: diagnosis, imaging and surgical outcomes. BJU Int. 2009;103:1550-1554. doi: 10.1111/j.1464-410X.2009.08348.x
1. Billow M, James R, Resnick K, et al. An unusual presentation of a urethral diverticulum as a vaginal wall mass: a case report. J Med Case Rep. 2013;7:171. doi: 10.1186/1752-1947-7-171
2. El-Nashar SA, Bacon MM, Kim-Fine S, et al. Incidence of female urethral diverticulum: a population-based analysis and literature review. Int Urogynecol J. 2014;25:73-79. doi: 10.1007/s00192-013-2155-2
3. Cameron AP. Urethral diverticulum in the female: a meta-analysis of modern series. Minerva Ginecol. 2016;68:186-210.
4. Greiman AK, Rolef J, Rovner ES. Urethral diverticulum: a systematic review. Arab J Urol. 2019;17:49-57. doi: 10.1080/2090598X.2019.1589748
5. Allen D, Mishra V, Pepper W, et al. A single-center experience of symptomatic male urethral diverticula. Urology. 2007;70:650-653. doi: 10.1016/j.urology.2007.06.1111
6. O’Connor E, Iatropoulou D, Hashimoto S, et al. Urethral diverticulum carcinoma in females—a case series and review of the English and Japanese literature. Transl Androl Urol. 2018;7:703-729. doi: 10.21037/tau.2018.07.08
7. Burrows LJ, Howden NL, Meyn L, et al. Surgical procedures for urethral diverticula in women in the United States, 1979-1997. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:158-161. doi: 10.1007/s00192-004-1145-9
8. Riyach O, Ahsaini M, Tazi MF, et al. Female urethral diverticulum: cases report and literature. Ann Surg Innov Res. 2014;8:1. doi: 10.1186/1750-1164-8-1
9. Antosh DD, Gutman RE. Diagnosis and management of female urethral diverticulum. Female Pelvic Med Reconstr Surg. 2011;17:264-271. doi: 10.1097/SPV.0b013e318234a242
10. Romanzi LJ, Groutz A, Blaivas JG. Urethral diverticulum in women: diverse presentations resulting in diagnostic delay and mismanagement. J Urol. 2000;164:428-433.
11. Reeves FA, Inman RD, Chapple CR. Management of symptomatic urethral diverticula in women: a single-centre experience. Eur Urol. 2014;66:164-172. doi: 10.1016/j.eururo.2014.02.041
12. Dwarkasing RS, Dinkelaar W, Hop WCJ, et al. MRI evaluation of urethral diverticula and differential diagnosis in symptomatic women. AJR Am J Roentgenol. 2011;197:676-682. doi: 10.2214/AJR.10.6144
13. Porten S, Kielb S. Diagnosis of female diverticula using magnetic resonance imaging. Adv Urol. 2008;2008:213516. doi: 10.1155/2008/213516
14. Ockrim JL, Allen DJ, Shah PJ, et al. A tertiary experience of urethral diverticulectomy: diagnosis, imaging and surgical outcomes. BJU Int. 2009;103:1550-1554. doi: 10.1111/j.1464-410X.2009.08348.x
How to better identify and manage women with elevated breast cancer risk
Breast cancer is the most common invasive cancer in women in the United States; it is estimated that there will be 287,850 new cases of breast cancer in the United States during 2022 with 43,250 deaths.1 Lives are extended and saved every day because of a robust arsenal of treatments and interventions available to those who have been given a diagnosis of breast cancer. And, of course, lives are also extended and saved when we identify women at risk and provide early interventions. But in busy offices where time is short and there are competing demands on our time, proper assessment of a woman’s risk of breast cancer does not always happen. As a result, women with a higher risk of breast cancer may not be getting appropriate management.2,3
Familiarizing yourself with several risk-assessment tools and knowing when genetic testing is needed can make a big difference. Knowing the timing of mammograms and magnetic resonance imaging (MRI) for women deemed to be at high risk is also key. The following review employs a case-based approach (with an accompanying ALGORITHM) to illustrate how best to identify women who are at heightened risk of breast cancer and maximize their care. We also discuss the chemoprophylaxis regimens that may be used for those at increased risk.
CASE
Rachel P, age 37, presents to establish care. She has an Ashkenazi Jewish background and wonders if she should start doing breast cancer screening before age 40. She has 2 children, ages 4 years and 2 years. Her maternal aunt had unilateral breast cancer at age 54, and her maternal grandmother died of ovarian cancer at age 65.
Risk assessment
The risk assessment process (see ALGORITHM) must start with either the clinician or the patient initiating the discussion about breast cancer risk. The clinician may initiate the discussion with a new patient or at an annual physical examination. The patient may start the discussion because they are experiencing new breast symptoms, have anxiety about developing breast cancer, or have a family member with a new cancer diagnosis.
Risk factors. There are single factors that convey enough risk to automatically designate the patient as high risk (see TABLE 14-9). These factors include having a history of chest radiation between the ages of 10 and 30, a history of breast biopsy with either lobular carcinoma in situ (LCIS) or atypical ductal hyperplasia (ADH), past breast and/or ovarian cancer, and either a family or personal history of a high penetrant genetic variant for breast cancer.4-9
In women with previous chest radiation, breast cancer risk correlates with the total dose of radiation.5 For women with a personal history of breast cancer, the younger the age at diagnosis, the higher the risk of contralateral breast cancer.5 Precancerous changes such as ADH, LCIS, and ductal carcinoma in situ (DCIS) also confer moderate increases in risk. Women with these diagnoses will commonly have follow-up with specialists.
Risk assessment tools. There are several models available to assess a woman’s breast cancer risk (see TABLE 210-12). The Gail model (https://bcrisktool.cancer.gov/) is the oldest, quickest, and most widely known. However, the Gail model only accounts for first-degree relatives diagnosed with breast cancer, may underpredict risk in women with a more extensive family history, and has not been studied in women younger than 35. The International Breast Cancer Intervention Study (IBIS) Risk Evaluation Tool (https://ibis-risk-calculator.magview.com/), commonly referred to as the Tyrer-Cuzick model, incorporates second-degree relatives into the prediction model—although women may not know their full family history. Both the IBIS and the Breast Cancer Surveillance Consortium (BCSC) model (https://tools.bcsc-scc.org/BC5yearRisk/intro.htm) include breast density in the prediction algorithm. The choice of tool depends on clinician comfort and individual patient risk factors. There is no evidence that one model is better than another.10-12

Continue to: CASE
CASE
Ms. P’s clinician starts with an assessment using the Gail model. However, when the result comes back with average risk, the clinician decides to follow up with the Tyrer-Cuzick model in order to incorporate Ms. P’s multiple second-degree relatives with breast and ovarian cancer. (The BCSC model was not used because it only includes first-degree relatives.)
Genetic testing
The National Comprehensive Cancer Network (NCCN) guidelines recommend genetic testing if a woman has a first- or second-degree relative with pancreatic cancer, metastatic prostate cancer, male breast cancer, breast cancer at age 45 or younger, 2 or more breast cancers in a single person, 2 or more people on the same side of the family with at least 1 diagnosed at age 50 or younger, or any relative with ovarian cancer (see TABLE 3).7 Before ordering genetic testing, it is useful to refer the patient to a genetic counselor for a thorough discussion of options.
Results of genetic testing may include high-risk variants, moderate-risk variants, and variants of unknown significance (VUS), or be negative for any variants. High-risk variants for breast cancer include BRCA1, BRCA2, PALB2, and cancer syndrome variants such as TP53, PTEN, STK11, and CDH1.5,6,9,13-15 These high-risk variants confer sufficient risk that women with these mutations are automatically categorized in the high-risk group. It is estimated that high-risk variants account for only 25% of the genetic risk for breast cancer.16
BRCA1/2 and PTEN mutations confer greater than 80% lifetime risk, while other high-risk variants such as TP53, CDH1, and STK11 confer risks between 25% and 40%. These variants are also associated with cancers of other organs, depending on the mutation.17
Moderate-risk variants—ATM and CHEK2—do not confer sufficient risk to elevate women into the high-risk group. However, they do qualify these intermediate-risk women to participate in a specialized management strategy.5,9,13,18
VUS are those for which the associated risk is unclear, but more research may be done to categorize the risk.9 The clinical management of women with VUS usually entails close monitoring.
In an effort to better characterize breast cancer risk using a combination of pathogenic variants found in broad multi-gene cancer predisposition panels, researchers have developed a method to combine risks in a “polygenic risk score” (PRS) that can be used to counsel women (see “What is a polygenic risk score for breast cancer?” on page 203).19-21PRS predicts an additional 18% of genetic risk in women of European descent.21
SIDEBAR
What is a polygenic risk score for breast cancer?
- A polygenic risk score (PRS) is a mathematical method to combine results from a variety of different single nucleotide polymorphisms (SNPs; ie, single base pair variants) into a prediction tool that can estimate a woman’s lifetime risk of breast cancer.
- A PRS may be most accurate in determining risk for women with intermediate pathogenic variants, such as ATM and CHEK2. 19,20
- PRS has not been studied in non-White women.21
Continue to: CASE
CASE
Using the assessment results, the clinician talks to Ms. P about her lifetime risk for breast cancer. The Gail model indicates her lifetime risk is 13.3%, just slightly higher than the average (12.5%), and her 5-year risk is 0.5% (average, 0.4%). The IBIS or Tyrer-Cuzick model, which takes into account her second-degree relatives with breast and ovarian cancer and her Ashkenazi ethnicity (which confers increased risk due to elevated risk of BRCA mutations), predicts her lifetime risk of breast cancer to be 20.4%. This categorizes Ms. P as high risk.
Enhanced screening recommendations for women at high risk
TABLE 48,13,22 summarizes screening recommendations for women deemed to be at high risk for breast cancer. The American Cancer Society (ACS), NCCN, and the American College of Radiology (ACR) recommend that women with at least a 20% lifetime risk have yearly magnetic resonance imaging (MRI) and mammography (staggered so that the patient has 1 test every 6 months) starting 10 years before the age of onset for the youngest affected relative but not before age 30.8 For carriers of high-risk (as well as intermediate-risk) genes, NCCN recommends annual MRI screening starting at age 40.13BRCA1/2 screening includes annual MRI starting at age 25 and annual mammography every 6 months starting at age 30.22 Clinicians should counsel women with moderate risk factors (elevated breast density; personal history of ADH, LCIS, or DCIS) about the potential risks and benefits of enhanced screening and chemoprophylaxis.
Risk-reduction strategies
Chemoprophylaxis
The US Preventive Services Task Force (USPSTF) recommends that all women at increased risk for breast cancer consider chemoprophylaxis (B recommendation)23 based on convincing evidence that 5 years of treatment with either a synthetic estrogen reuptake modulator (SERM) or an aromatase inhibitor (AI) decreases the incidence of estrogen receptor positive breast cancers. (See TABLE 57,23,24 for absolute risk reduction.) There is no benefit for chemoprophylaxis in women at average risk (D recommendation).23 It is unclear whether chemoprophylaxis is indicated in women with moderate increased risk (ie, who do not meet the 20% lifetime risk criteria). Chemoprophylaxis may not be effective in women with BRCA1 mutations, as they often develop triple-negative breast cancers.
Accurate risk assessment and shared decision-making enable the clinician and patient to discuss the potential risks and benefits of chemoprophylaxis.7,24 The USPSTF did not find that any 1 risk prediction tool was better than another to identify women who should be counseled about chemoprophylaxis. Clinicians should counsel all women taking AIs about optimizing bone health with adequate calcium and vitamin D intake and routine bone density tests.
Surgical risk reduction
The NCCN guidelines state that risk-reducing bilateral mastectomy is reserved for individuals with high-risk gene variants and individuals with prior chest radiation between ages 10 and 30.25 NCCN also recommends discussing risk-reducing mastectomy with all women with BRCA mutations.22
Bilateral mastectomy is the most effective method to reduce breast cancer risk and should be discussed after age 25 in women with BRCA mutations and at least 8 years after chest radiation is completed.26 There is a reduction in breast cancer incidence of 90%.25 Breast imaging for screening (mammography or MRI) is not indicated after risk-reducing mastectomy. However, clinical breast examinations of the surgical site are important, because there is a small risk of developing breast cancer in that area.26
Risk-reducing oophorectomy is the standard of care for women with BRCA mutations to reduce the risk of ovarian cancer. It can also reduce the risk of breast cancer in women with BRCA mutations.27
Continue to: CASE
CASE
Based on her risk assessment results, family history, and genetic heritage, Ms. P qualifies for referral to a genetic counselor for discussion of BRCA testing. The clinician discusses adding annual MRI to Ms. P’s breast cancer screening regimen, based on ACS, NCCN, and ACR recommendations, due to her 20.4% lifetime risk. Discussion of whether and when to start chemoprophylaxis is typically based on breast cancer risk, projected benefit, and the potential impact of medication adverse effects. A high-risk woman is eligible for 5 years of chemoprophylaxis (tamoxifen if premenopausal) based on her lifetime risk. The clinician discusses timing with Ms. P, and even though she is finished with childbearing, she would like to wait until she is age 45, which is before the age at which her aunt was given a diagnosis of breast cancer.
Conclusion
Primary care clinicians are well positioned to identify women with an elevated risk of breast cancer and refer them for enhanced screening and chemoprophylaxis (see ALGORITHM). Shared decision-making with the inclusion of patient decision aids (https://decisionaid.ohri.ca/AZsearch.php?criteria=breast+cancer) about genetic testing, chemoprophylaxis, and prophylactic mastectomy or oophorectomy may help women at intermediate or high risk of breast cancer feel empowered to make decisions about their breast—and overall—health.
CORRESPONDENCE
Sarina Schrager, MD, MS, Professor, Department of Family Medicine and Community Health, University of Wisconsin, 1100 Delaplaine Court, Madison, WI 53715; sbschrag@wisc.edu
1. National Cancer Institute. Cancer stat facts: female breast cancer. Accessed May 13, 2022. https://seer.cancer.gov/statfacts/html/breast.html
2. Guerra CE, Sherman M, Armstrong K. Diffusion of breast cancer risk assessment in primary care. J Am Board Fam Med. 2009;22:272-279. doi:10.3122/jabfm.2009.03.080153
3. Hamilton JG, Abdiwahab E, Edwards HM, et al. Primary care providers’ cancer genetic testing-related knowledge, attitudes, and communication behaviors: a systematic review and research agenda. J Gen Intern Med. 2017;32:315-324. doi:10.1007/s11606-016-3943-4
4. Eden KB, Ivlev I, Bensching KL, et al. Use of an online breast cancer risk assessment and patient decision aid in primary care practices. J Womens Health (Larchmt). 2020;29:763-769. doi: 10.1089/jwh.2019.8143
5. Kleibl Z, Kristensen VN. Women at high risk of breast cancer: molecular characteristics, clinical presentation and management. Breast. 2016;28:136-44. doi: 10.1016/j.breast.2016.05.006
6. Sciaraffa T, Guido B, Khan SA, et al. Breast cancer risk assessment and management programs: a practical guide. Breast J. 2020;26:1556-1564. doi: 10.1111/tbj.13967
7. Farkas A, Vanderberg R, Merriam S, et al. Breast cancer chemoprevention: a practical guide for the primary care provider. J Womens Health (Larchmt). 2020;29:46-56. doi: 10.1089/jwh.2018.7643
8. McClintock AH, Golob AL, Laya MB. Breast cancer risk assessment: a step-wise approach for primary care providers on the front lines of shared decision making. Mayo Clin Proc. 2020;95:1268-1275. doi: 10.1016/j.mayocp.2020.04.017
9. Catana A, Apostu AP, Antemie RG. Multi gene panel testing for hereditary breast cancer - is it ready to be used? Med Pharm Rep. 2019;92:220-225. doi: 10.15386/mpr-1083
10. Barke LD, Freivogel ME. Breast cancer risk assessment models and high-risk screening. Radiol Clin North Am. 2017;55:457-474. doi: 10.1016/j.rcl.2016.12.013
11. Amir E, Freedman OC, Seruga B, et al. Assessing women at high risk of breast cancer: a review of risk assessment models. J Natl Cancer Inst. 2010;102:680-91. doi: 10.1093/jnci/djq088
12. Kim G, Bahl M. Assessing risk of breast cancer: a review of risk prediction models. J Breast Imaging. 2021;3:144-155. doi: 10.1093/jbi/wbab001
13. Narod SA. Which genes for hereditary breast cancer? N Engl J Med. 2021;384:471-473. doi: 10.1056/NEJMe2035083
14. Couch FJ, Shimelis H, Hu C, et al. Associations between cancer predisposition testing panel genes and breast cancer. JAMA Oncol. 2017;3:1190-1196. doi: 10.1001/jamaoncol.2017.0424
15. Obeid EI, Hall MJ, Daly MB. Multigene panel testing and breast cancer risk: is it time to scale down? JAMA Oncol. 2017;3:1176-1177. doi: 10.1001/jamaoncol.2017.0342
16. Michailidou K, Lindström S, Dennis J, et al. Association analysis identifies 65 new breast cancer risk loci. Nature. 2017;551:92-94. doi: 10.1038/nature24284
17. Shiovitz S, Korde LA. Genetics of breast cancer: a topic in evolution. Ann Oncol. 2015;26:1291-1299. doi: 10.1093/annonc/mdv022
18. Hu C, Hart SN, Gnanaolivu R, et al. A population-based study of genes previously implicated in breast cancer. N Engl J Med. 2021;384:440-451. doi: 10.1056/NEJMoa2005936
19. Gao C, Polley EC, Hart SN, et al. Risk of breast cancer among carriers of pathogenic variants in breast cancer predisposition genes varies by polygenic risk score. J Clin Oncol. 2021;39:2564-2573. doi: 10.1200/JCO.20.01992
20. Gallagher S, Hughes E, Wagner S, et al. Association of a polygenic risk score with breast cancer among women carriers of high- and moderate-risk breast cancer genes. JAMA Netw Open. 2020;3:e208501. doi: 10.1001/jamanetworkopen.2020.8501
21. Yanes T, Young MA, Meiser B, et al. Clinical applications of polygenic breast cancer risk: a critical review and perspectives of an emerging field. Breast Cancer Res. 2020;22:21. doi: 10.1186/s13058-020-01260-3
22. Schrager S, Torell E, Ledford K, et al. Managing a woman with BRCA mutations? Shared decision-making is key. J Fam Pract. 2020;69:237-243
23. US Preventive Services Task Force; Owens DK, Davidson KW, Krist AH, et al. Medication use to reduce risk of breast cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;322:857-867. doi: 10.1001/jama.2019.11885
24. Pruthi S, Heisey RE, Bevers TB. Chemoprevention for breast cancer. Ann Surg Oncol 2015;22:3230-3235. doi: 10.1245/s10434-015-4715-9
25. Britt KL, Cuzick J, Phillips KA. Key steps for effective breast cancer prevention. Nat Rev Cancer. 2020;20:417-436. doi: 10.1038/s41568-020-0266-x
26. Jatoi I, Kemp Z. Risk-reducing mastectomy. JAMA. 2021;325:1781-1782. doi: 10.1001/jama.2020.22414
27. Choi Y, Terry MB, Daly MB, et al. Association of risk-reducing salpingo-oophorectomy with breast cancer risk in women with BRCA1 and BRCA2 pathogenic variants. JAMA Oncol. 2021;7:585-592. doi:10.1001/jamaoncol.2020.7995
Breast cancer is the most common invasive cancer in women in the United States; it is estimated that there will be 287,850 new cases of breast cancer in the United States during 2022 with 43,250 deaths.1 Lives are extended and saved every day because of a robust arsenal of treatments and interventions available to those who have been given a diagnosis of breast cancer. And, of course, lives are also extended and saved when we identify women at risk and provide early interventions. But in busy offices where time is short and there are competing demands on our time, proper assessment of a woman’s risk of breast cancer does not always happen. As a result, women with a higher risk of breast cancer may not be getting appropriate management.2,3
Familiarizing yourself with several risk-assessment tools and knowing when genetic testing is needed can make a big difference. Knowing the timing of mammograms and magnetic resonance imaging (MRI) for women deemed to be at high risk is also key. The following review employs a case-based approach (with an accompanying ALGORITHM) to illustrate how best to identify women who are at heightened risk of breast cancer and maximize their care. We also discuss the chemoprophylaxis regimens that may be used for those at increased risk.
CASE
Rachel P, age 37, presents to establish care. She has an Ashkenazi Jewish background and wonders if she should start doing breast cancer screening before age 40. She has 2 children, ages 4 years and 2 years. Her maternal aunt had unilateral breast cancer at age 54, and her maternal grandmother died of ovarian cancer at age 65.
Risk assessment
The risk assessment process (see ALGORITHM) must start with either the clinician or the patient initiating the discussion about breast cancer risk. The clinician may initiate the discussion with a new patient or at an annual physical examination. The patient may start the discussion because they are experiencing new breast symptoms, have anxiety about developing breast cancer, or have a family member with a new cancer diagnosis.
Risk factors. There are single factors that convey enough risk to automatically designate the patient as high risk (see TABLE 14-9). These factors include having a history of chest radiation between the ages of 10 and 30, a history of breast biopsy with either lobular carcinoma in situ (LCIS) or atypical ductal hyperplasia (ADH), past breast and/or ovarian cancer, and either a family or personal history of a high penetrant genetic variant for breast cancer.4-9
In women with previous chest radiation, breast cancer risk correlates with the total dose of radiation.5 For women with a personal history of breast cancer, the younger the age at diagnosis, the higher the risk of contralateral breast cancer.5 Precancerous changes such as ADH, LCIS, and ductal carcinoma in situ (DCIS) also confer moderate increases in risk. Women with these diagnoses will commonly have follow-up with specialists.
Risk assessment tools. There are several models available to assess a woman’s breast cancer risk (see TABLE 210-12). The Gail model (https://bcrisktool.cancer.gov/) is the oldest, quickest, and most widely known. However, the Gail model only accounts for first-degree relatives diagnosed with breast cancer, may underpredict risk in women with a more extensive family history, and has not been studied in women younger than 35. The International Breast Cancer Intervention Study (IBIS) Risk Evaluation Tool (https://ibis-risk-calculator.magview.com/), commonly referred to as the Tyrer-Cuzick model, incorporates second-degree relatives into the prediction model—although women may not know their full family history. Both the IBIS and the Breast Cancer Surveillance Consortium (BCSC) model (https://tools.bcsc-scc.org/BC5yearRisk/intro.htm) include breast density in the prediction algorithm. The choice of tool depends on clinician comfort and individual patient risk factors. There is no evidence that one model is better than another.10-12

Continue to: CASE
CASE
Ms. P’s clinician starts with an assessment using the Gail model. However, when the result comes back with average risk, the clinician decides to follow up with the Tyrer-Cuzick model in order to incorporate Ms. P’s multiple second-degree relatives with breast and ovarian cancer. (The BCSC model was not used because it only includes first-degree relatives.)
Genetic testing
The National Comprehensive Cancer Network (NCCN) guidelines recommend genetic testing if a woman has a first- or second-degree relative with pancreatic cancer, metastatic prostate cancer, male breast cancer, breast cancer at age 45 or younger, 2 or more breast cancers in a single person, 2 or more people on the same side of the family with at least 1 diagnosed at age 50 or younger, or any relative with ovarian cancer (see TABLE 3).7 Before ordering genetic testing, it is useful to refer the patient to a genetic counselor for a thorough discussion of options.
Results of genetic testing may include high-risk variants, moderate-risk variants, and variants of unknown significance (VUS), or be negative for any variants. High-risk variants for breast cancer include BRCA1, BRCA2, PALB2, and cancer syndrome variants such as TP53, PTEN, STK11, and CDH1.5,6,9,13-15 These high-risk variants confer sufficient risk that women with these mutations are automatically categorized in the high-risk group. It is estimated that high-risk variants account for only 25% of the genetic risk for breast cancer.16
BRCA1/2 and PTEN mutations confer greater than 80% lifetime risk, while other high-risk variants such as TP53, CDH1, and STK11 confer risks between 25% and 40%. These variants are also associated with cancers of other organs, depending on the mutation.17
Moderate-risk variants—ATM and CHEK2—do not confer sufficient risk to elevate women into the high-risk group. However, they do qualify these intermediate-risk women to participate in a specialized management strategy.5,9,13,18
VUS are those for which the associated risk is unclear, but more research may be done to categorize the risk.9 The clinical management of women with VUS usually entails close monitoring.
In an effort to better characterize breast cancer risk using a combination of pathogenic variants found in broad multi-gene cancer predisposition panels, researchers have developed a method to combine risks in a “polygenic risk score” (PRS) that can be used to counsel women (see “What is a polygenic risk score for breast cancer?” on page 203).19-21PRS predicts an additional 18% of genetic risk in women of European descent.21
SIDEBAR
What is a polygenic risk score for breast cancer?
- A polygenic risk score (PRS) is a mathematical method to combine results from a variety of different single nucleotide polymorphisms (SNPs; ie, single base pair variants) into a prediction tool that can estimate a woman’s lifetime risk of breast cancer.
- A PRS may be most accurate in determining risk for women with intermediate pathogenic variants, such as ATM and CHEK2. 19,20
- PRS has not been studied in non-White women.21
Continue to: CASE
CASE
Using the assessment results, the clinician talks to Ms. P about her lifetime risk for breast cancer. The Gail model indicates her lifetime risk is 13.3%, just slightly higher than the average (12.5%), and her 5-year risk is 0.5% (average, 0.4%). The IBIS or Tyrer-Cuzick model, which takes into account her second-degree relatives with breast and ovarian cancer and her Ashkenazi ethnicity (which confers increased risk due to elevated risk of BRCA mutations), predicts her lifetime risk of breast cancer to be 20.4%. This categorizes Ms. P as high risk.
Enhanced screening recommendations for women at high risk
TABLE 48,13,22 summarizes screening recommendations for women deemed to be at high risk for breast cancer. The American Cancer Society (ACS), NCCN, and the American College of Radiology (ACR) recommend that women with at least a 20% lifetime risk have yearly magnetic resonance imaging (MRI) and mammography (staggered so that the patient has 1 test every 6 months) starting 10 years before the age of onset for the youngest affected relative but not before age 30.8 For carriers of high-risk (as well as intermediate-risk) genes, NCCN recommends annual MRI screening starting at age 40.13BRCA1/2 screening includes annual MRI starting at age 25 and annual mammography every 6 months starting at age 30.22 Clinicians should counsel women with moderate risk factors (elevated breast density; personal history of ADH, LCIS, or DCIS) about the potential risks and benefits of enhanced screening and chemoprophylaxis.
Risk-reduction strategies
Chemoprophylaxis
The US Preventive Services Task Force (USPSTF) recommends that all women at increased risk for breast cancer consider chemoprophylaxis (B recommendation)23 based on convincing evidence that 5 years of treatment with either a synthetic estrogen reuptake modulator (SERM) or an aromatase inhibitor (AI) decreases the incidence of estrogen receptor positive breast cancers. (See TABLE 57,23,24 for absolute risk reduction.) There is no benefit for chemoprophylaxis in women at average risk (D recommendation).23 It is unclear whether chemoprophylaxis is indicated in women with moderate increased risk (ie, who do not meet the 20% lifetime risk criteria). Chemoprophylaxis may not be effective in women with BRCA1 mutations, as they often develop triple-negative breast cancers.
Accurate risk assessment and shared decision-making enable the clinician and patient to discuss the potential risks and benefits of chemoprophylaxis.7,24 The USPSTF did not find that any 1 risk prediction tool was better than another to identify women who should be counseled about chemoprophylaxis. Clinicians should counsel all women taking AIs about optimizing bone health with adequate calcium and vitamin D intake and routine bone density tests.
Surgical risk reduction
The NCCN guidelines state that risk-reducing bilateral mastectomy is reserved for individuals with high-risk gene variants and individuals with prior chest radiation between ages 10 and 30.25 NCCN also recommends discussing risk-reducing mastectomy with all women with BRCA mutations.22
Bilateral mastectomy is the most effective method to reduce breast cancer risk and should be discussed after age 25 in women with BRCA mutations and at least 8 years after chest radiation is completed.26 There is a reduction in breast cancer incidence of 90%.25 Breast imaging for screening (mammography or MRI) is not indicated after risk-reducing mastectomy. However, clinical breast examinations of the surgical site are important, because there is a small risk of developing breast cancer in that area.26
Risk-reducing oophorectomy is the standard of care for women with BRCA mutations to reduce the risk of ovarian cancer. It can also reduce the risk of breast cancer in women with BRCA mutations.27
Continue to: CASE
CASE
Based on her risk assessment results, family history, and genetic heritage, Ms. P qualifies for referral to a genetic counselor for discussion of BRCA testing. The clinician discusses adding annual MRI to Ms. P’s breast cancer screening regimen, based on ACS, NCCN, and ACR recommendations, due to her 20.4% lifetime risk. Discussion of whether and when to start chemoprophylaxis is typically based on breast cancer risk, projected benefit, and the potential impact of medication adverse effects. A high-risk woman is eligible for 5 years of chemoprophylaxis (tamoxifen if premenopausal) based on her lifetime risk. The clinician discusses timing with Ms. P, and even though she is finished with childbearing, she would like to wait until she is age 45, which is before the age at which her aunt was given a diagnosis of breast cancer.
Conclusion
Primary care clinicians are well positioned to identify women with an elevated risk of breast cancer and refer them for enhanced screening and chemoprophylaxis (see ALGORITHM). Shared decision-making with the inclusion of patient decision aids (https://decisionaid.ohri.ca/AZsearch.php?criteria=breast+cancer) about genetic testing, chemoprophylaxis, and prophylactic mastectomy or oophorectomy may help women at intermediate or high risk of breast cancer feel empowered to make decisions about their breast—and overall—health.
CORRESPONDENCE
Sarina Schrager, MD, MS, Professor, Department of Family Medicine and Community Health, University of Wisconsin, 1100 Delaplaine Court, Madison, WI 53715; sbschrag@wisc.edu
Breast cancer is the most common invasive cancer in women in the United States; it is estimated that there will be 287,850 new cases of breast cancer in the United States during 2022 with 43,250 deaths.1 Lives are extended and saved every day because of a robust arsenal of treatments and interventions available to those who have been given a diagnosis of breast cancer. And, of course, lives are also extended and saved when we identify women at risk and provide early interventions. But in busy offices where time is short and there are competing demands on our time, proper assessment of a woman’s risk of breast cancer does not always happen. As a result, women with a higher risk of breast cancer may not be getting appropriate management.2,3
Familiarizing yourself with several risk-assessment tools and knowing when genetic testing is needed can make a big difference. Knowing the timing of mammograms and magnetic resonance imaging (MRI) for women deemed to be at high risk is also key. The following review employs a case-based approach (with an accompanying ALGORITHM) to illustrate how best to identify women who are at heightened risk of breast cancer and maximize their care. We also discuss the chemoprophylaxis regimens that may be used for those at increased risk.
CASE
Rachel P, age 37, presents to establish care. She has an Ashkenazi Jewish background and wonders if she should start doing breast cancer screening before age 40. She has 2 children, ages 4 years and 2 years. Her maternal aunt had unilateral breast cancer at age 54, and her maternal grandmother died of ovarian cancer at age 65.
Risk assessment
The risk assessment process (see ALGORITHM) must start with either the clinician or the patient initiating the discussion about breast cancer risk. The clinician may initiate the discussion with a new patient or at an annual physical examination. The patient may start the discussion because they are experiencing new breast symptoms, have anxiety about developing breast cancer, or have a family member with a new cancer diagnosis.
Risk factors. There are single factors that convey enough risk to automatically designate the patient as high risk (see TABLE 14-9). These factors include having a history of chest radiation between the ages of 10 and 30, a history of breast biopsy with either lobular carcinoma in situ (LCIS) or atypical ductal hyperplasia (ADH), past breast and/or ovarian cancer, and either a family or personal history of a high penetrant genetic variant for breast cancer.4-9
In women with previous chest radiation, breast cancer risk correlates with the total dose of radiation.5 For women with a personal history of breast cancer, the younger the age at diagnosis, the higher the risk of contralateral breast cancer.5 Precancerous changes such as ADH, LCIS, and ductal carcinoma in situ (DCIS) also confer moderate increases in risk. Women with these diagnoses will commonly have follow-up with specialists.
Risk assessment tools. There are several models available to assess a woman’s breast cancer risk (see TABLE 210-12). The Gail model (https://bcrisktool.cancer.gov/) is the oldest, quickest, and most widely known. However, the Gail model only accounts for first-degree relatives diagnosed with breast cancer, may underpredict risk in women with a more extensive family history, and has not been studied in women younger than 35. The International Breast Cancer Intervention Study (IBIS) Risk Evaluation Tool (https://ibis-risk-calculator.magview.com/), commonly referred to as the Tyrer-Cuzick model, incorporates second-degree relatives into the prediction model—although women may not know their full family history. Both the IBIS and the Breast Cancer Surveillance Consortium (BCSC) model (https://tools.bcsc-scc.org/BC5yearRisk/intro.htm) include breast density in the prediction algorithm. The choice of tool depends on clinician comfort and individual patient risk factors. There is no evidence that one model is better than another.10-12

Continue to: CASE
CASE
Ms. P’s clinician starts with an assessment using the Gail model. However, when the result comes back with average risk, the clinician decides to follow up with the Tyrer-Cuzick model in order to incorporate Ms. P’s multiple second-degree relatives with breast and ovarian cancer. (The BCSC model was not used because it only includes first-degree relatives.)
Genetic testing
The National Comprehensive Cancer Network (NCCN) guidelines recommend genetic testing if a woman has a first- or second-degree relative with pancreatic cancer, metastatic prostate cancer, male breast cancer, breast cancer at age 45 or younger, 2 or more breast cancers in a single person, 2 or more people on the same side of the family with at least 1 diagnosed at age 50 or younger, or any relative with ovarian cancer (see TABLE 3).7 Before ordering genetic testing, it is useful to refer the patient to a genetic counselor for a thorough discussion of options.
Results of genetic testing may include high-risk variants, moderate-risk variants, and variants of unknown significance (VUS), or be negative for any variants. High-risk variants for breast cancer include BRCA1, BRCA2, PALB2, and cancer syndrome variants such as TP53, PTEN, STK11, and CDH1.5,6,9,13-15 These high-risk variants confer sufficient risk that women with these mutations are automatically categorized in the high-risk group. It is estimated that high-risk variants account for only 25% of the genetic risk for breast cancer.16
BRCA1/2 and PTEN mutations confer greater than 80% lifetime risk, while other high-risk variants such as TP53, CDH1, and STK11 confer risks between 25% and 40%. These variants are also associated with cancers of other organs, depending on the mutation.17
Moderate-risk variants—ATM and CHEK2—do not confer sufficient risk to elevate women into the high-risk group. However, they do qualify these intermediate-risk women to participate in a specialized management strategy.5,9,13,18
VUS are those for which the associated risk is unclear, but more research may be done to categorize the risk.9 The clinical management of women with VUS usually entails close monitoring.
In an effort to better characterize breast cancer risk using a combination of pathogenic variants found in broad multi-gene cancer predisposition panels, researchers have developed a method to combine risks in a “polygenic risk score” (PRS) that can be used to counsel women (see “What is a polygenic risk score for breast cancer?” on page 203).19-21PRS predicts an additional 18% of genetic risk in women of European descent.21
SIDEBAR
What is a polygenic risk score for breast cancer?
- A polygenic risk score (PRS) is a mathematical method to combine results from a variety of different single nucleotide polymorphisms (SNPs; ie, single base pair variants) into a prediction tool that can estimate a woman’s lifetime risk of breast cancer.
- A PRS may be most accurate in determining risk for women with intermediate pathogenic variants, such as ATM and CHEK2. 19,20
- PRS has not been studied in non-White women.21
Continue to: CASE
CASE
Using the assessment results, the clinician talks to Ms. P about her lifetime risk for breast cancer. The Gail model indicates her lifetime risk is 13.3%, just slightly higher than the average (12.5%), and her 5-year risk is 0.5% (average, 0.4%). The IBIS or Tyrer-Cuzick model, which takes into account her second-degree relatives with breast and ovarian cancer and her Ashkenazi ethnicity (which confers increased risk due to elevated risk of BRCA mutations), predicts her lifetime risk of breast cancer to be 20.4%. This categorizes Ms. P as high risk.
Enhanced screening recommendations for women at high risk
TABLE 48,13,22 summarizes screening recommendations for women deemed to be at high risk for breast cancer. The American Cancer Society (ACS), NCCN, and the American College of Radiology (ACR) recommend that women with at least a 20% lifetime risk have yearly magnetic resonance imaging (MRI) and mammography (staggered so that the patient has 1 test every 6 months) starting 10 years before the age of onset for the youngest affected relative but not before age 30.8 For carriers of high-risk (as well as intermediate-risk) genes, NCCN recommends annual MRI screening starting at age 40.13BRCA1/2 screening includes annual MRI starting at age 25 and annual mammography every 6 months starting at age 30.22 Clinicians should counsel women with moderate risk factors (elevated breast density; personal history of ADH, LCIS, or DCIS) about the potential risks and benefits of enhanced screening and chemoprophylaxis.
Risk-reduction strategies
Chemoprophylaxis
The US Preventive Services Task Force (USPSTF) recommends that all women at increased risk for breast cancer consider chemoprophylaxis (B recommendation)23 based on convincing evidence that 5 years of treatment with either a synthetic estrogen reuptake modulator (SERM) or an aromatase inhibitor (AI) decreases the incidence of estrogen receptor positive breast cancers. (See TABLE 57,23,24 for absolute risk reduction.) There is no benefit for chemoprophylaxis in women at average risk (D recommendation).23 It is unclear whether chemoprophylaxis is indicated in women with moderate increased risk (ie, who do not meet the 20% lifetime risk criteria). Chemoprophylaxis may not be effective in women with BRCA1 mutations, as they often develop triple-negative breast cancers.
Accurate risk assessment and shared decision-making enable the clinician and patient to discuss the potential risks and benefits of chemoprophylaxis.7,24 The USPSTF did not find that any 1 risk prediction tool was better than another to identify women who should be counseled about chemoprophylaxis. Clinicians should counsel all women taking AIs about optimizing bone health with adequate calcium and vitamin D intake and routine bone density tests.
Surgical risk reduction
The NCCN guidelines state that risk-reducing bilateral mastectomy is reserved for individuals with high-risk gene variants and individuals with prior chest radiation between ages 10 and 30.25 NCCN also recommends discussing risk-reducing mastectomy with all women with BRCA mutations.22
Bilateral mastectomy is the most effective method to reduce breast cancer risk and should be discussed after age 25 in women with BRCA mutations and at least 8 years after chest radiation is completed.26 There is a reduction in breast cancer incidence of 90%.25 Breast imaging for screening (mammography or MRI) is not indicated after risk-reducing mastectomy. However, clinical breast examinations of the surgical site are important, because there is a small risk of developing breast cancer in that area.26
Risk-reducing oophorectomy is the standard of care for women with BRCA mutations to reduce the risk of ovarian cancer. It can also reduce the risk of breast cancer in women with BRCA mutations.27
Continue to: CASE
CASE
Based on her risk assessment results, family history, and genetic heritage, Ms. P qualifies for referral to a genetic counselor for discussion of BRCA testing. The clinician discusses adding annual MRI to Ms. P’s breast cancer screening regimen, based on ACS, NCCN, and ACR recommendations, due to her 20.4% lifetime risk. Discussion of whether and when to start chemoprophylaxis is typically based on breast cancer risk, projected benefit, and the potential impact of medication adverse effects. A high-risk woman is eligible for 5 years of chemoprophylaxis (tamoxifen if premenopausal) based on her lifetime risk. The clinician discusses timing with Ms. P, and even though she is finished with childbearing, she would like to wait until she is age 45, which is before the age at which her aunt was given a diagnosis of breast cancer.
Conclusion
Primary care clinicians are well positioned to identify women with an elevated risk of breast cancer and refer them for enhanced screening and chemoprophylaxis (see ALGORITHM). Shared decision-making with the inclusion of patient decision aids (https://decisionaid.ohri.ca/AZsearch.php?criteria=breast+cancer) about genetic testing, chemoprophylaxis, and prophylactic mastectomy or oophorectomy may help women at intermediate or high risk of breast cancer feel empowered to make decisions about their breast—and overall—health.
CORRESPONDENCE
Sarina Schrager, MD, MS, Professor, Department of Family Medicine and Community Health, University of Wisconsin, 1100 Delaplaine Court, Madison, WI 53715; sbschrag@wisc.edu
1. National Cancer Institute. Cancer stat facts: female breast cancer. Accessed May 13, 2022. https://seer.cancer.gov/statfacts/html/breast.html
2. Guerra CE, Sherman M, Armstrong K. Diffusion of breast cancer risk assessment in primary care. J Am Board Fam Med. 2009;22:272-279. doi:10.3122/jabfm.2009.03.080153
3. Hamilton JG, Abdiwahab E, Edwards HM, et al. Primary care providers’ cancer genetic testing-related knowledge, attitudes, and communication behaviors: a systematic review and research agenda. J Gen Intern Med. 2017;32:315-324. doi:10.1007/s11606-016-3943-4
4. Eden KB, Ivlev I, Bensching KL, et al. Use of an online breast cancer risk assessment and patient decision aid in primary care practices. J Womens Health (Larchmt). 2020;29:763-769. doi: 10.1089/jwh.2019.8143
5. Kleibl Z, Kristensen VN. Women at high risk of breast cancer: molecular characteristics, clinical presentation and management. Breast. 2016;28:136-44. doi: 10.1016/j.breast.2016.05.006
6. Sciaraffa T, Guido B, Khan SA, et al. Breast cancer risk assessment and management programs: a practical guide. Breast J. 2020;26:1556-1564. doi: 10.1111/tbj.13967
7. Farkas A, Vanderberg R, Merriam S, et al. Breast cancer chemoprevention: a practical guide for the primary care provider. J Womens Health (Larchmt). 2020;29:46-56. doi: 10.1089/jwh.2018.7643
8. McClintock AH, Golob AL, Laya MB. Breast cancer risk assessment: a step-wise approach for primary care providers on the front lines of shared decision making. Mayo Clin Proc. 2020;95:1268-1275. doi: 10.1016/j.mayocp.2020.04.017
9. Catana A, Apostu AP, Antemie RG. Multi gene panel testing for hereditary breast cancer - is it ready to be used? Med Pharm Rep. 2019;92:220-225. doi: 10.15386/mpr-1083
10. Barke LD, Freivogel ME. Breast cancer risk assessment models and high-risk screening. Radiol Clin North Am. 2017;55:457-474. doi: 10.1016/j.rcl.2016.12.013
11. Amir E, Freedman OC, Seruga B, et al. Assessing women at high risk of breast cancer: a review of risk assessment models. J Natl Cancer Inst. 2010;102:680-91. doi: 10.1093/jnci/djq088
12. Kim G, Bahl M. Assessing risk of breast cancer: a review of risk prediction models. J Breast Imaging. 2021;3:144-155. doi: 10.1093/jbi/wbab001
13. Narod SA. Which genes for hereditary breast cancer? N Engl J Med. 2021;384:471-473. doi: 10.1056/NEJMe2035083
14. Couch FJ, Shimelis H, Hu C, et al. Associations between cancer predisposition testing panel genes and breast cancer. JAMA Oncol. 2017;3:1190-1196. doi: 10.1001/jamaoncol.2017.0424
15. Obeid EI, Hall MJ, Daly MB. Multigene panel testing and breast cancer risk: is it time to scale down? JAMA Oncol. 2017;3:1176-1177. doi: 10.1001/jamaoncol.2017.0342
16. Michailidou K, Lindström S, Dennis J, et al. Association analysis identifies 65 new breast cancer risk loci. Nature. 2017;551:92-94. doi: 10.1038/nature24284
17. Shiovitz S, Korde LA. Genetics of breast cancer: a topic in evolution. Ann Oncol. 2015;26:1291-1299. doi: 10.1093/annonc/mdv022
18. Hu C, Hart SN, Gnanaolivu R, et al. A population-based study of genes previously implicated in breast cancer. N Engl J Med. 2021;384:440-451. doi: 10.1056/NEJMoa2005936
19. Gao C, Polley EC, Hart SN, et al. Risk of breast cancer among carriers of pathogenic variants in breast cancer predisposition genes varies by polygenic risk score. J Clin Oncol. 2021;39:2564-2573. doi: 10.1200/JCO.20.01992
20. Gallagher S, Hughes E, Wagner S, et al. Association of a polygenic risk score with breast cancer among women carriers of high- and moderate-risk breast cancer genes. JAMA Netw Open. 2020;3:e208501. doi: 10.1001/jamanetworkopen.2020.8501
21. Yanes T, Young MA, Meiser B, et al. Clinical applications of polygenic breast cancer risk: a critical review and perspectives of an emerging field. Breast Cancer Res. 2020;22:21. doi: 10.1186/s13058-020-01260-3
22. Schrager S, Torell E, Ledford K, et al. Managing a woman with BRCA mutations? Shared decision-making is key. J Fam Pract. 2020;69:237-243
23. US Preventive Services Task Force; Owens DK, Davidson KW, Krist AH, et al. Medication use to reduce risk of breast cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;322:857-867. doi: 10.1001/jama.2019.11885
24. Pruthi S, Heisey RE, Bevers TB. Chemoprevention for breast cancer. Ann Surg Oncol 2015;22:3230-3235. doi: 10.1245/s10434-015-4715-9
25. Britt KL, Cuzick J, Phillips KA. Key steps for effective breast cancer prevention. Nat Rev Cancer. 2020;20:417-436. doi: 10.1038/s41568-020-0266-x
26. Jatoi I, Kemp Z. Risk-reducing mastectomy. JAMA. 2021;325:1781-1782. doi: 10.1001/jama.2020.22414
27. Choi Y, Terry MB, Daly MB, et al. Association of risk-reducing salpingo-oophorectomy with breast cancer risk in women with BRCA1 and BRCA2 pathogenic variants. JAMA Oncol. 2021;7:585-592. doi:10.1001/jamaoncol.2020.7995
1. National Cancer Institute. Cancer stat facts: female breast cancer. Accessed May 13, 2022. https://seer.cancer.gov/statfacts/html/breast.html
2. Guerra CE, Sherman M, Armstrong K. Diffusion of breast cancer risk assessment in primary care. J Am Board Fam Med. 2009;22:272-279. doi:10.3122/jabfm.2009.03.080153
3. Hamilton JG, Abdiwahab E, Edwards HM, et al. Primary care providers’ cancer genetic testing-related knowledge, attitudes, and communication behaviors: a systematic review and research agenda. J Gen Intern Med. 2017;32:315-324. doi:10.1007/s11606-016-3943-4
4. Eden KB, Ivlev I, Bensching KL, et al. Use of an online breast cancer risk assessment and patient decision aid in primary care practices. J Womens Health (Larchmt). 2020;29:763-769. doi: 10.1089/jwh.2019.8143
5. Kleibl Z, Kristensen VN. Women at high risk of breast cancer: molecular characteristics, clinical presentation and management. Breast. 2016;28:136-44. doi: 10.1016/j.breast.2016.05.006
6. Sciaraffa T, Guido B, Khan SA, et al. Breast cancer risk assessment and management programs: a practical guide. Breast J. 2020;26:1556-1564. doi: 10.1111/tbj.13967
7. Farkas A, Vanderberg R, Merriam S, et al. Breast cancer chemoprevention: a practical guide for the primary care provider. J Womens Health (Larchmt). 2020;29:46-56. doi: 10.1089/jwh.2018.7643
8. McClintock AH, Golob AL, Laya MB. Breast cancer risk assessment: a step-wise approach for primary care providers on the front lines of shared decision making. Mayo Clin Proc. 2020;95:1268-1275. doi: 10.1016/j.mayocp.2020.04.017
9. Catana A, Apostu AP, Antemie RG. Multi gene panel testing for hereditary breast cancer - is it ready to be used? Med Pharm Rep. 2019;92:220-225. doi: 10.15386/mpr-1083
10. Barke LD, Freivogel ME. Breast cancer risk assessment models and high-risk screening. Radiol Clin North Am. 2017;55:457-474. doi: 10.1016/j.rcl.2016.12.013
11. Amir E, Freedman OC, Seruga B, et al. Assessing women at high risk of breast cancer: a review of risk assessment models. J Natl Cancer Inst. 2010;102:680-91. doi: 10.1093/jnci/djq088
12. Kim G, Bahl M. Assessing risk of breast cancer: a review of risk prediction models. J Breast Imaging. 2021;3:144-155. doi: 10.1093/jbi/wbab001
13. Narod SA. Which genes for hereditary breast cancer? N Engl J Med. 2021;384:471-473. doi: 10.1056/NEJMe2035083
14. Couch FJ, Shimelis H, Hu C, et al. Associations between cancer predisposition testing panel genes and breast cancer. JAMA Oncol. 2017;3:1190-1196. doi: 10.1001/jamaoncol.2017.0424
15. Obeid EI, Hall MJ, Daly MB. Multigene panel testing and breast cancer risk: is it time to scale down? JAMA Oncol. 2017;3:1176-1177. doi: 10.1001/jamaoncol.2017.0342
16. Michailidou K, Lindström S, Dennis J, et al. Association analysis identifies 65 new breast cancer risk loci. Nature. 2017;551:92-94. doi: 10.1038/nature24284
17. Shiovitz S, Korde LA. Genetics of breast cancer: a topic in evolution. Ann Oncol. 2015;26:1291-1299. doi: 10.1093/annonc/mdv022
18. Hu C, Hart SN, Gnanaolivu R, et al. A population-based study of genes previously implicated in breast cancer. N Engl J Med. 2021;384:440-451. doi: 10.1056/NEJMoa2005936
19. Gao C, Polley EC, Hart SN, et al. Risk of breast cancer among carriers of pathogenic variants in breast cancer predisposition genes varies by polygenic risk score. J Clin Oncol. 2021;39:2564-2573. doi: 10.1200/JCO.20.01992
20. Gallagher S, Hughes E, Wagner S, et al. Association of a polygenic risk score with breast cancer among women carriers of high- and moderate-risk breast cancer genes. JAMA Netw Open. 2020;3:e208501. doi: 10.1001/jamanetworkopen.2020.8501
21. Yanes T, Young MA, Meiser B, et al. Clinical applications of polygenic breast cancer risk: a critical review and perspectives of an emerging field. Breast Cancer Res. 2020;22:21. doi: 10.1186/s13058-020-01260-3
22. Schrager S, Torell E, Ledford K, et al. Managing a woman with BRCA mutations? Shared decision-making is key. J Fam Pract. 2020;69:237-243
23. US Preventive Services Task Force; Owens DK, Davidson KW, Krist AH, et al. Medication use to reduce risk of breast cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;322:857-867. doi: 10.1001/jama.2019.11885
24. Pruthi S, Heisey RE, Bevers TB. Chemoprevention for breast cancer. Ann Surg Oncol 2015;22:3230-3235. doi: 10.1245/s10434-015-4715-9
25. Britt KL, Cuzick J, Phillips KA. Key steps for effective breast cancer prevention. Nat Rev Cancer. 2020;20:417-436. doi: 10.1038/s41568-020-0266-x
26. Jatoi I, Kemp Z. Risk-reducing mastectomy. JAMA. 2021;325:1781-1782. doi: 10.1001/jama.2020.22414
27. Choi Y, Terry MB, Daly MB, et al. Association of risk-reducing salpingo-oophorectomy with breast cancer risk in women with BRCA1 and BRCA2 pathogenic variants. JAMA Oncol. 2021;7:585-592. doi:10.1001/jamaoncol.2020.7995
PRACTICE RECOMMENDATIONS
› Assess breast cancer risk in all women starting at age 35. C
› Perform enhanced screening in all women with a lifetime risk of breast cancer > 20%. A
› Discuss chemoprevention for all women at elevated risk for breast cancer. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Double morning-after pill dose for women with obesity not effective
Emergency contraception is more likely to fail in women with obesity, but simply doubling the dose of levonorgestrel (LNG)-based contraception does not appear to be effective according to the results of a randomized, controlled trial.
Alison B. Edelman, MD, MPH, of the department of obstetrics & gynecology at Oregon Health & Science University, Portland, led the study published online in Obstetrics & Gynecology.
The researchers included healthy women ages 18-35 with regular menstrual cycles, body mass index (BMI) higher than 30 kg/m2, and weight at least 176 pounds in a randomized study.
After confirming ovulation, researchers monitored participants with transvaginal ultrasonography and blood sampling for progesterone, luteinizing hormone, and estradiol every other day until a dominant follicle 15 mm or greater was seen.
At that point the women received either LNG 1.5 mg or 3 mg and returned for daily monitoring up to 7 days.
Emergency contraception with LNG works by preventing the luteinizing hormone surge, blocking follicle rupture. The researchers had hypothesized that women with obesity might not be getting enough LNG to block the surge after oral dosing.
Previous trials had shown women with obesity had a fourfold higher risk of pregnancy, compared with women with normal BMI taking emergency contraception.
The primary outcome in this trial was whether women had follicle rupture 5 days after dosing.
The authors wrote: “The study had 80% power to detect a 30% difference in the proportion of cycles with at least a 5-day delay in follicle rupture (50% decrease).”
A total of 70 women completed study procedures. The two groups (35 women in each) had similar demographics (mean age, 28 years; BMI, 38).
No differences found between groups
“We found no difference between groups in the proportion of participants without follicle rupture,” the researchers wrote.
More than 5 days after dosing, 51.4% in the lower-dose group did not experience follicle rupture. In the double-dose group 68.6% did not experience rupture but the difference was not significant (P = .14).
Among participants with follicle rupture before 5 days, the time to rupture – the secondary endpoint – also did not differ between groups.
The researchers concluded that more research on the failures of hormonal emergency contraception in women with obesity is needed.
Eve Espey, MD, MPH, distinguished professor and chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque, said in an interview that the study was well designed and the results “form a strong basis for clinical recommendations.”
“Providers should not recommend a higher dose of LNG emergency contraception for patients who are overweight or obese, but rather should counsel patients on the superior effectiveness of ulipristal acetate for those seeking oral emergency contraception as well as the longer time period after unprotected sex – 5 days – that ulipristal maintains its effectiveness.”
“Providers should also counsel patients on the most effective emergency contraception methods, the copper or LNG intrauterine device,” she said.
She said the unique study design of a pharmacodynamic randomized controlled trial adds weight to the findings.
She and the authors noted a limitation is the use of a surrogate outcome, ovulation delay, for ethical and feasibility reasons, instead of the outcome of interest, pregnancy.
The trial was conducted at Oregon Health & Science University and Eastern Virginia Medical School, Norfolk, from June 2017 to February 2021.
Study enrollees were compensated for their time. They were required not to be at risk for pregnancy (abstinent or using a nonhormonal method of contraception).
Dr. Edelman reported receiving honoraria and travel reimbursement from the American College of Obstetricians and Gynecologists, the World Health Organization, and Gynuity for committee activities and honoraria for peer review from the Karolinska Institute. She receives royalties from UpToDate. Several coauthors have received payments for consulting from multiple pharmaceutical companies. These companies and organizations may have a commercial or financial interest in the results of this research and technology. Another was involved in this study as a private consultant and is employed by Gilead Sciences, which was not involved in this research.
Emergency contraception is more likely to fail in women with obesity, but simply doubling the dose of levonorgestrel (LNG)-based contraception does not appear to be effective according to the results of a randomized, controlled trial.
Alison B. Edelman, MD, MPH, of the department of obstetrics & gynecology at Oregon Health & Science University, Portland, led the study published online in Obstetrics & Gynecology.
The researchers included healthy women ages 18-35 with regular menstrual cycles, body mass index (BMI) higher than 30 kg/m2, and weight at least 176 pounds in a randomized study.
After confirming ovulation, researchers monitored participants with transvaginal ultrasonography and blood sampling for progesterone, luteinizing hormone, and estradiol every other day until a dominant follicle 15 mm or greater was seen.
At that point the women received either LNG 1.5 mg or 3 mg and returned for daily monitoring up to 7 days.
Emergency contraception with LNG works by preventing the luteinizing hormone surge, blocking follicle rupture. The researchers had hypothesized that women with obesity might not be getting enough LNG to block the surge after oral dosing.
Previous trials had shown women with obesity had a fourfold higher risk of pregnancy, compared with women with normal BMI taking emergency contraception.
The primary outcome in this trial was whether women had follicle rupture 5 days after dosing.
The authors wrote: “The study had 80% power to detect a 30% difference in the proportion of cycles with at least a 5-day delay in follicle rupture (50% decrease).”
A total of 70 women completed study procedures. The two groups (35 women in each) had similar demographics (mean age, 28 years; BMI, 38).
No differences found between groups
“We found no difference between groups in the proportion of participants without follicle rupture,” the researchers wrote.
More than 5 days after dosing, 51.4% in the lower-dose group did not experience follicle rupture. In the double-dose group 68.6% did not experience rupture but the difference was not significant (P = .14).
Among participants with follicle rupture before 5 days, the time to rupture – the secondary endpoint – also did not differ between groups.
The researchers concluded that more research on the failures of hormonal emergency contraception in women with obesity is needed.
Eve Espey, MD, MPH, distinguished professor and chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque, said in an interview that the study was well designed and the results “form a strong basis for clinical recommendations.”
“Providers should not recommend a higher dose of LNG emergency contraception for patients who are overweight or obese, but rather should counsel patients on the superior effectiveness of ulipristal acetate for those seeking oral emergency contraception as well as the longer time period after unprotected sex – 5 days – that ulipristal maintains its effectiveness.”
“Providers should also counsel patients on the most effective emergency contraception methods, the copper or LNG intrauterine device,” she said.
She said the unique study design of a pharmacodynamic randomized controlled trial adds weight to the findings.
She and the authors noted a limitation is the use of a surrogate outcome, ovulation delay, for ethical and feasibility reasons, instead of the outcome of interest, pregnancy.
The trial was conducted at Oregon Health & Science University and Eastern Virginia Medical School, Norfolk, from June 2017 to February 2021.
Study enrollees were compensated for their time. They were required not to be at risk for pregnancy (abstinent or using a nonhormonal method of contraception).
Dr. Edelman reported receiving honoraria and travel reimbursement from the American College of Obstetricians and Gynecologists, the World Health Organization, and Gynuity for committee activities and honoraria for peer review from the Karolinska Institute. She receives royalties from UpToDate. Several coauthors have received payments for consulting from multiple pharmaceutical companies. These companies and organizations may have a commercial or financial interest in the results of this research and technology. Another was involved in this study as a private consultant and is employed by Gilead Sciences, which was not involved in this research.
Emergency contraception is more likely to fail in women with obesity, but simply doubling the dose of levonorgestrel (LNG)-based contraception does not appear to be effective according to the results of a randomized, controlled trial.
Alison B. Edelman, MD, MPH, of the department of obstetrics & gynecology at Oregon Health & Science University, Portland, led the study published online in Obstetrics & Gynecology.
The researchers included healthy women ages 18-35 with regular menstrual cycles, body mass index (BMI) higher than 30 kg/m2, and weight at least 176 pounds in a randomized study.
After confirming ovulation, researchers monitored participants with transvaginal ultrasonography and blood sampling for progesterone, luteinizing hormone, and estradiol every other day until a dominant follicle 15 mm or greater was seen.
At that point the women received either LNG 1.5 mg or 3 mg and returned for daily monitoring up to 7 days.
Emergency contraception with LNG works by preventing the luteinizing hormone surge, blocking follicle rupture. The researchers had hypothesized that women with obesity might not be getting enough LNG to block the surge after oral dosing.
Previous trials had shown women with obesity had a fourfold higher risk of pregnancy, compared with women with normal BMI taking emergency contraception.
The primary outcome in this trial was whether women had follicle rupture 5 days after dosing.
The authors wrote: “The study had 80% power to detect a 30% difference in the proportion of cycles with at least a 5-day delay in follicle rupture (50% decrease).”
A total of 70 women completed study procedures. The two groups (35 women in each) had similar demographics (mean age, 28 years; BMI, 38).
No differences found between groups
“We found no difference between groups in the proportion of participants without follicle rupture,” the researchers wrote.
More than 5 days after dosing, 51.4% in the lower-dose group did not experience follicle rupture. In the double-dose group 68.6% did not experience rupture but the difference was not significant (P = .14).
Among participants with follicle rupture before 5 days, the time to rupture – the secondary endpoint – also did not differ between groups.
The researchers concluded that more research on the failures of hormonal emergency contraception in women with obesity is needed.
Eve Espey, MD, MPH, distinguished professor and chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque, said in an interview that the study was well designed and the results “form a strong basis for clinical recommendations.”
“Providers should not recommend a higher dose of LNG emergency contraception for patients who are overweight or obese, but rather should counsel patients on the superior effectiveness of ulipristal acetate for those seeking oral emergency contraception as well as the longer time period after unprotected sex – 5 days – that ulipristal maintains its effectiveness.”
“Providers should also counsel patients on the most effective emergency contraception methods, the copper or LNG intrauterine device,” she said.
She said the unique study design of a pharmacodynamic randomized controlled trial adds weight to the findings.
She and the authors noted a limitation is the use of a surrogate outcome, ovulation delay, for ethical and feasibility reasons, instead of the outcome of interest, pregnancy.
The trial was conducted at Oregon Health & Science University and Eastern Virginia Medical School, Norfolk, from June 2017 to February 2021.
Study enrollees were compensated for their time. They were required not to be at risk for pregnancy (abstinent or using a nonhormonal method of contraception).
Dr. Edelman reported receiving honoraria and travel reimbursement from the American College of Obstetricians and Gynecologists, the World Health Organization, and Gynuity for committee activities and honoraria for peer review from the Karolinska Institute. She receives royalties from UpToDate. Several coauthors have received payments for consulting from multiple pharmaceutical companies. These companies and organizations may have a commercial or financial interest in the results of this research and technology. Another was involved in this study as a private consultant and is employed by Gilead Sciences, which was not involved in this research.
FROM OBSTETRICS & GYNECOLOGY
PCOS comes with high morbidity, medication use into late 40s
Women with polycystic ovary syndrome (PCOS) have an increased risk for several diseases and symptoms, many independent of body mass index (BMI), new research indicates.
Some diseases are linked for the first time to PCOS in this study, the authors wrote.
Researchers, led by Linda Kujanpää, MD, of the research unit for pediatrics, dermatology, clinical genetics, obstetrics, and gynecology at University of Oulu (Finland), found the morbidity risk is evident through the late reproductive years.
The paper was published online in Acta Obstetricia et Gynecologica Scandinavica.
This population-based follow-up study investigated comorbidities and medication and health care services use among women with PCOS in Finland at age 46 years via answers to a questionnaire.
The whole PCOS population (n = 280) consisted of women who reported both hirsutism and oligo/amenorrhea at age 31 (4.1%) and/or polycystic ovary morphology/PCOS at age 46 (3.1%), of which 246 replied to the 46-year questionnaire. They were compared with a control group of 1,573 women without PCOS.
Overall morbidity risk was 35% higher than for women without PCOS (risk ratio, 1.35; 95% confidence interval, 1.16-1.57). Medication use was 27% higher (RR, 1.27; 95% CI, 1.08-1.50), and the risk remained after adjusting for BMI.
Diagnoses with increased prevalence in women with PCOS were osteoarthritis, migraine, hypertension, tendinitis, and endometriosis. PCOS was also associated with autoimmune diseases and recurrent upper respiratory tract infections.
“BMI seems not to be solely responsible for the increased morbidity,” the researchers found. The average morbidity score of women with PCOS with a BMI of 25 kg/m2 or higher was similar to that of women with PCOS and lower BMI.
Mindy Christianson, MD, medical director at Johns Hopkins Fertility Center and associate professor of gynecology and obstetrics at Johns Hopkins University, both in Baltimore, said in an interview that the links to diseases independent of BMI are interesting because there’s so much focus on counseling women with PCOS to lose weight.
While that message is still important, it’s important to realize that some related diseases and conditions – such as autoimmune diseases and migraine – are not driven by BMI.
“It really drives home the point that polycystic ovary syndrome is really a chronic medical condition and puts patients at risk for a number of health conditions,” she said. “Having a good primary care physician is important to help them with their overall health.”
Women with PCOS said their health was poor or very poor almost three times more often than did women in the control group.
Surprisingly few studies have looked at overall comorbidity in women with PCOS, the authors wrote.
“This should be of high priority given the high cost to society resulting from PCOS-related morbidity,” they added. As an example, they pointed out that PCOS-related type 2 diabetes alone costs an estimated $1.77 billion in the United States and £237 million ($310 million) each year in the United Kingdom.
Additionally, the focus in previous research has typically been on women in their early or mid-reproductive years, and morbidity burden data in late reproductive years are scarce.
The study population was pulled from the longitudinal Northern Finland Birth Cohort 1966 and included all pregnancies with estimated date of delivery during 1966 in two provinces of Finland (5,889 women).
Dr. Christianson said she hopes this study will spur more research on PCOS, which has been severely underfunded, especially in the United States.
Part of the reason for that is there is a limited number of subspecialists in the country who work with patients with PCOS and do research in the area. PCOS often gets lost in the research priorities of infertility, diabetes, and thyroid disease.
The message in this study that PCOS is not just a fertility issue or an obesity issue but an overall health issue with a substantial cost to the health system may help raise awareness, Dr. Christianson said.
This study was supported by grants from The Finnish Medical Foundation, The Academy of Finland, The Sigrid Juselius Foundation, The Finnish Cultural Foundation, The Jalmari and Rauha Ahokas Foundation, The Päivikki and Sakari Sohlberg Foundation, Genesis Research Trust, The Medical Research Council, University of Oulu, Oulu University Hospital, Ministry of Health and Social Affairs, National Institute for Health and Welfare, Regional Institute of Occupational Health, and the European Regional Development Fund. The Study authors and Dr. Christianson reported no relevant financial relationships.
Women with polycystic ovary syndrome (PCOS) have an increased risk for several diseases and symptoms, many independent of body mass index (BMI), new research indicates.
Some diseases are linked for the first time to PCOS in this study, the authors wrote.
Researchers, led by Linda Kujanpää, MD, of the research unit for pediatrics, dermatology, clinical genetics, obstetrics, and gynecology at University of Oulu (Finland), found the morbidity risk is evident through the late reproductive years.
The paper was published online in Acta Obstetricia et Gynecologica Scandinavica.
This population-based follow-up study investigated comorbidities and medication and health care services use among women with PCOS in Finland at age 46 years via answers to a questionnaire.
The whole PCOS population (n = 280) consisted of women who reported both hirsutism and oligo/amenorrhea at age 31 (4.1%) and/or polycystic ovary morphology/PCOS at age 46 (3.1%), of which 246 replied to the 46-year questionnaire. They were compared with a control group of 1,573 women without PCOS.
Overall morbidity risk was 35% higher than for women without PCOS (risk ratio, 1.35; 95% confidence interval, 1.16-1.57). Medication use was 27% higher (RR, 1.27; 95% CI, 1.08-1.50), and the risk remained after adjusting for BMI.
Diagnoses with increased prevalence in women with PCOS were osteoarthritis, migraine, hypertension, tendinitis, and endometriosis. PCOS was also associated with autoimmune diseases and recurrent upper respiratory tract infections.
“BMI seems not to be solely responsible for the increased morbidity,” the researchers found. The average morbidity score of women with PCOS with a BMI of 25 kg/m2 or higher was similar to that of women with PCOS and lower BMI.
Mindy Christianson, MD, medical director at Johns Hopkins Fertility Center and associate professor of gynecology and obstetrics at Johns Hopkins University, both in Baltimore, said in an interview that the links to diseases independent of BMI are interesting because there’s so much focus on counseling women with PCOS to lose weight.
While that message is still important, it’s important to realize that some related diseases and conditions – such as autoimmune diseases and migraine – are not driven by BMI.
“It really drives home the point that polycystic ovary syndrome is really a chronic medical condition and puts patients at risk for a number of health conditions,” she said. “Having a good primary care physician is important to help them with their overall health.”
Women with PCOS said their health was poor or very poor almost three times more often than did women in the control group.
Surprisingly few studies have looked at overall comorbidity in women with PCOS, the authors wrote.
“This should be of high priority given the high cost to society resulting from PCOS-related morbidity,” they added. As an example, they pointed out that PCOS-related type 2 diabetes alone costs an estimated $1.77 billion in the United States and £237 million ($310 million) each year in the United Kingdom.
Additionally, the focus in previous research has typically been on women in their early or mid-reproductive years, and morbidity burden data in late reproductive years are scarce.
The study population was pulled from the longitudinal Northern Finland Birth Cohort 1966 and included all pregnancies with estimated date of delivery during 1966 in two provinces of Finland (5,889 women).
Dr. Christianson said she hopes this study will spur more research on PCOS, which has been severely underfunded, especially in the United States.
Part of the reason for that is there is a limited number of subspecialists in the country who work with patients with PCOS and do research in the area. PCOS often gets lost in the research priorities of infertility, diabetes, and thyroid disease.
The message in this study that PCOS is not just a fertility issue or an obesity issue but an overall health issue with a substantial cost to the health system may help raise awareness, Dr. Christianson said.
This study was supported by grants from The Finnish Medical Foundation, The Academy of Finland, The Sigrid Juselius Foundation, The Finnish Cultural Foundation, The Jalmari and Rauha Ahokas Foundation, The Päivikki and Sakari Sohlberg Foundation, Genesis Research Trust, The Medical Research Council, University of Oulu, Oulu University Hospital, Ministry of Health and Social Affairs, National Institute for Health and Welfare, Regional Institute of Occupational Health, and the European Regional Development Fund. The Study authors and Dr. Christianson reported no relevant financial relationships.
Women with polycystic ovary syndrome (PCOS) have an increased risk for several diseases and symptoms, many independent of body mass index (BMI), new research indicates.
Some diseases are linked for the first time to PCOS in this study, the authors wrote.
Researchers, led by Linda Kujanpää, MD, of the research unit for pediatrics, dermatology, clinical genetics, obstetrics, and gynecology at University of Oulu (Finland), found the morbidity risk is evident through the late reproductive years.
The paper was published online in Acta Obstetricia et Gynecologica Scandinavica.
This population-based follow-up study investigated comorbidities and medication and health care services use among women with PCOS in Finland at age 46 years via answers to a questionnaire.
The whole PCOS population (n = 280) consisted of women who reported both hirsutism and oligo/amenorrhea at age 31 (4.1%) and/or polycystic ovary morphology/PCOS at age 46 (3.1%), of which 246 replied to the 46-year questionnaire. They were compared with a control group of 1,573 women without PCOS.
Overall morbidity risk was 35% higher than for women without PCOS (risk ratio, 1.35; 95% confidence interval, 1.16-1.57). Medication use was 27% higher (RR, 1.27; 95% CI, 1.08-1.50), and the risk remained after adjusting for BMI.
Diagnoses with increased prevalence in women with PCOS were osteoarthritis, migraine, hypertension, tendinitis, and endometriosis. PCOS was also associated with autoimmune diseases and recurrent upper respiratory tract infections.
“BMI seems not to be solely responsible for the increased morbidity,” the researchers found. The average morbidity score of women with PCOS with a BMI of 25 kg/m2 or higher was similar to that of women with PCOS and lower BMI.
Mindy Christianson, MD, medical director at Johns Hopkins Fertility Center and associate professor of gynecology and obstetrics at Johns Hopkins University, both in Baltimore, said in an interview that the links to diseases independent of BMI are interesting because there’s so much focus on counseling women with PCOS to lose weight.
While that message is still important, it’s important to realize that some related diseases and conditions – such as autoimmune diseases and migraine – are not driven by BMI.
“It really drives home the point that polycystic ovary syndrome is really a chronic medical condition and puts patients at risk for a number of health conditions,” she said. “Having a good primary care physician is important to help them with their overall health.”
Women with PCOS said their health was poor or very poor almost three times more often than did women in the control group.
Surprisingly few studies have looked at overall comorbidity in women with PCOS, the authors wrote.
“This should be of high priority given the high cost to society resulting from PCOS-related morbidity,” they added. As an example, they pointed out that PCOS-related type 2 diabetes alone costs an estimated $1.77 billion in the United States and £237 million ($310 million) each year in the United Kingdom.
Additionally, the focus in previous research has typically been on women in their early or mid-reproductive years, and morbidity burden data in late reproductive years are scarce.
The study population was pulled from the longitudinal Northern Finland Birth Cohort 1966 and included all pregnancies with estimated date of delivery during 1966 in two provinces of Finland (5,889 women).
Dr. Christianson said she hopes this study will spur more research on PCOS, which has been severely underfunded, especially in the United States.
Part of the reason for that is there is a limited number of subspecialists in the country who work with patients with PCOS and do research in the area. PCOS often gets lost in the research priorities of infertility, diabetes, and thyroid disease.
The message in this study that PCOS is not just a fertility issue or an obesity issue but an overall health issue with a substantial cost to the health system may help raise awareness, Dr. Christianson said.
This study was supported by grants from The Finnish Medical Foundation, The Academy of Finland, The Sigrid Juselius Foundation, The Finnish Cultural Foundation, The Jalmari and Rauha Ahokas Foundation, The Päivikki and Sakari Sohlberg Foundation, Genesis Research Trust, The Medical Research Council, University of Oulu, Oulu University Hospital, Ministry of Health and Social Affairs, National Institute for Health and Welfare, Regional Institute of Occupational Health, and the European Regional Development Fund. The Study authors and Dr. Christianson reported no relevant financial relationships.
FROM ACTA OBSTETRICIA ET GYNECOLOGICA SCANDINAVICA
Pregnant women with monkeypox advised to have C-section
The risk of monkeypox infection remains low for the general public, the authors wrote, though cases continue to grow worldwide, particularly in the United Kingdom.
“We are aware infants and children are at greater risk of becoming seriously ill if they do catch monkeypox,” Edward Morris, MBBS, one of the authors and president of the Royal College of Obstetricians and Gynecologists, said in a statement.
“Therefore, to minimize the risk of a baby contracting the virus, we recommend health care professionals discuss the benefits and risks of having a cesarean birth with a pregnant woman or person who has or is suspected of having the virus,” he said.
Dr. Morris and colleagues pulled together existing evidence on monkeypox diagnosis, treatment, and recommended modes of birth for mothers and babies.
“The World Health Organization states there could be adverse consequences for pregnant women and babies if they become infected, including congenital monkeypox, miscarriage, or stillbirth, which is why we have provided clear guidance for health care professionals in this paper,” Dr. Morris said.
The monkeypox virus typically spreads through direct contact, droplets, or contaminated surfaces and objects. But some limited evidence shows that the virus can be passed from a mother to a baby via the placenta, which can lead to congenital monkeypox.
What’s more, mothers may be able to transmit the virus during or after birth. Although no evidence exists around the optimal mode of birth, a pregnant woman with an active monkeypox infection may choose to avoid vaginal delivery to reduce direct contact.
“If genital lesions are identified on a pregnant woman, then a cesarean birth will be recommended,” the authors wrote. “If a pregnant woman or person has suspected or confirmed monkeypox, a caesarean birth will be offered following discussion of the possible risk of neonatal infection, which may be serious.”
After giving birth, close contact can spread the virus as well. To minimize the risk, the authors recommend isolating the baby from family members who have confirmed or suspected monkeypox and carefully monitoring for infection.
Mothers with an active monkeypox infection should also avoid breastfeeding to lower the risk of spreading the virus to their newborn, the authors wrote. But to support breastfeeding after infection, mothers can express and discard milk until the isolation period has passed.
Pregnant women who become infected may also consider getting vaccinated, the authors wrote. Vaccination up to 14 days after exposure doesn’t prevent the disease but can reduce the severity of symptoms. In the current outbreak, public health organizations advised doctors to vaccinate contacts of confirmed cases, including pregnant people.
The data for monkeypox vaccine use in pregnant women is small, the authors wrote, including fewer than 300 women. In previous studies, no adverse outcomes were found. The vaccine is also considered safe for breastfeeding.
“The decision whether to have the vaccine in pregnancy should be a personal choice,” the authors wrote. “Pregnant women and people should be encouraged to discuss the risks and benefits of vaccination, including possible side effects, with a health care professional before making their final decision.”
A version of this article first appeared on Medscape.com.
The risk of monkeypox infection remains low for the general public, the authors wrote, though cases continue to grow worldwide, particularly in the United Kingdom.
“We are aware infants and children are at greater risk of becoming seriously ill if they do catch monkeypox,” Edward Morris, MBBS, one of the authors and president of the Royal College of Obstetricians and Gynecologists, said in a statement.
“Therefore, to minimize the risk of a baby contracting the virus, we recommend health care professionals discuss the benefits and risks of having a cesarean birth with a pregnant woman or person who has or is suspected of having the virus,” he said.
Dr. Morris and colleagues pulled together existing evidence on monkeypox diagnosis, treatment, and recommended modes of birth for mothers and babies.
“The World Health Organization states there could be adverse consequences for pregnant women and babies if they become infected, including congenital monkeypox, miscarriage, or stillbirth, which is why we have provided clear guidance for health care professionals in this paper,” Dr. Morris said.
The monkeypox virus typically spreads through direct contact, droplets, or contaminated surfaces and objects. But some limited evidence shows that the virus can be passed from a mother to a baby via the placenta, which can lead to congenital monkeypox.
What’s more, mothers may be able to transmit the virus during or after birth. Although no evidence exists around the optimal mode of birth, a pregnant woman with an active monkeypox infection may choose to avoid vaginal delivery to reduce direct contact.
“If genital lesions are identified on a pregnant woman, then a cesarean birth will be recommended,” the authors wrote. “If a pregnant woman or person has suspected or confirmed monkeypox, a caesarean birth will be offered following discussion of the possible risk of neonatal infection, which may be serious.”
After giving birth, close contact can spread the virus as well. To minimize the risk, the authors recommend isolating the baby from family members who have confirmed or suspected monkeypox and carefully monitoring for infection.
Mothers with an active monkeypox infection should also avoid breastfeeding to lower the risk of spreading the virus to their newborn, the authors wrote. But to support breastfeeding after infection, mothers can express and discard milk until the isolation period has passed.
Pregnant women who become infected may also consider getting vaccinated, the authors wrote. Vaccination up to 14 days after exposure doesn’t prevent the disease but can reduce the severity of symptoms. In the current outbreak, public health organizations advised doctors to vaccinate contacts of confirmed cases, including pregnant people.
The data for monkeypox vaccine use in pregnant women is small, the authors wrote, including fewer than 300 women. In previous studies, no adverse outcomes were found. The vaccine is also considered safe for breastfeeding.
“The decision whether to have the vaccine in pregnancy should be a personal choice,” the authors wrote. “Pregnant women and people should be encouraged to discuss the risks and benefits of vaccination, including possible side effects, with a health care professional before making their final decision.”
A version of this article first appeared on Medscape.com.
The risk of monkeypox infection remains low for the general public, the authors wrote, though cases continue to grow worldwide, particularly in the United Kingdom.
“We are aware infants and children are at greater risk of becoming seriously ill if they do catch monkeypox,” Edward Morris, MBBS, one of the authors and president of the Royal College of Obstetricians and Gynecologists, said in a statement.
“Therefore, to minimize the risk of a baby contracting the virus, we recommend health care professionals discuss the benefits and risks of having a cesarean birth with a pregnant woman or person who has or is suspected of having the virus,” he said.
Dr. Morris and colleagues pulled together existing evidence on monkeypox diagnosis, treatment, and recommended modes of birth for mothers and babies.
“The World Health Organization states there could be adverse consequences for pregnant women and babies if they become infected, including congenital monkeypox, miscarriage, or stillbirth, which is why we have provided clear guidance for health care professionals in this paper,” Dr. Morris said.
The monkeypox virus typically spreads through direct contact, droplets, or contaminated surfaces and objects. But some limited evidence shows that the virus can be passed from a mother to a baby via the placenta, which can lead to congenital monkeypox.
What’s more, mothers may be able to transmit the virus during or after birth. Although no evidence exists around the optimal mode of birth, a pregnant woman with an active monkeypox infection may choose to avoid vaginal delivery to reduce direct contact.
“If genital lesions are identified on a pregnant woman, then a cesarean birth will be recommended,” the authors wrote. “If a pregnant woman or person has suspected or confirmed monkeypox, a caesarean birth will be offered following discussion of the possible risk of neonatal infection, which may be serious.”
After giving birth, close contact can spread the virus as well. To minimize the risk, the authors recommend isolating the baby from family members who have confirmed or suspected monkeypox and carefully monitoring for infection.
Mothers with an active monkeypox infection should also avoid breastfeeding to lower the risk of spreading the virus to their newborn, the authors wrote. But to support breastfeeding after infection, mothers can express and discard milk until the isolation period has passed.
Pregnant women who become infected may also consider getting vaccinated, the authors wrote. Vaccination up to 14 days after exposure doesn’t prevent the disease but can reduce the severity of symptoms. In the current outbreak, public health organizations advised doctors to vaccinate contacts of confirmed cases, including pregnant people.
The data for monkeypox vaccine use in pregnant women is small, the authors wrote, including fewer than 300 women. In previous studies, no adverse outcomes were found. The vaccine is also considered safe for breastfeeding.
“The decision whether to have the vaccine in pregnancy should be a personal choice,” the authors wrote. “Pregnant women and people should be encouraged to discuss the risks and benefits of vaccination, including possible side effects, with a health care professional before making their final decision.”
A version of this article first appeared on Medscape.com.
FROM ULTRASOUND IN OBSTETRICS & GYNECOLOGY
In utero COVID exposure tied to developmental differences in infants
suggests a small-scale analysis that points to the need for further study and monitoring during pregnancy.
The study included 24 pregnant women, half of whom had COVID-19 during pregnancy, and their offspring. It showed impairments at 6 weeks of age on the social interactive dimension of a neonatal assessment.
“Not all babies born to mothers infected with COVID show neurodevelopmental differences, but our data show that their risk is increased in comparison to those not exposed to COVID in the womb. We need a bigger study to confirm the exact extent of the difference,” said lead researcher Rosa Ayesa Arriola, PhD, Valdecilla Research Institute (IDIVAL), Hospital Universitario Marqués de Valdecilla, Santander, Spain, in a release.
The findings were presented at the virtual European Psychiatric Association 2022 Congress.
Differing responses to cuddling
Coauthor Águeda Castro Quintas, PhD student, Network Centre for Biomedical Research in Mental Health, University of Barcelona, explained that the tests showed the children born to mothers who had COVID-19 during pregnancy reacted “slightly differently to being held, or cuddled.”
“We need to note that these are preliminary results, but this is part of a project following a larger sample of 100 mothers and their babies,” she added. The authors plan to compare their results with those from a similar study.
The group will also monitor infant language and motor development aged between 18 and 42 months.
“This is an ongoing project, and we are at an early stage,” Ms. Castro Quintas said. “We don’t know if these effects will result in any longer-term issues,” but longer-term observation “may help us understand this.”
“Of course, in babies who are so young, there are several things we just can’t measure, such as language skills or cognition,” added coinvestigator Nerea San Martín González, department of evolutionary biology, ecology and environmental sciences, University of Barcelona.
While emphasizing the need for larger sample sizes, she said that “in the meantime, we need to stress the importance of medical monitoring to facilitate a healthy pregnancy.”
The researchers note that the consequences of the COVID-19 pandemic for the newborns of affected mothers remain “unknown.”
However, previous studies of other infections during pregnancy suggest that offspring could be “especially vulnerable,”as the pathophysiological mechanisms of the infection, such as cytokine storms and microcoagulation, “could clearly compromise fetal neurodevelopment.”
To investigate further, they examined the neurodevelopment of infants born both immediately before and during the COVID-19 pandemic, from 2017 to 2021.
Twenty-one women who had COVID-19 during pregnancy were matched with 21 healthy controls. They were studied both during pregnancy and in the postpartum period, completing hormonal and other biochemical tests, salivary tests, movement assessments, and psychological questionnaires, adjusted for various factors.
The team also administered the Brazelton Neonatal Behavioural Assessment Scale (NBAS) to the offspring at 6 weeks of age to evaluate neurologic, social, and behavioral aspects of function.
“We have been especially sensitive in how we have conducted these tests,” said Ms. Castro Quintas. “Each mother and baby were closely examined by clinicians with expert training in the field and in the tests.”
Among those offspring exposed to COVID-19 during pregnancy, there was a significant decrease in scores on the social interactive dimension of the NBAS, particularly if infection occurred before week 20 of gestation.
Other NBAS subscales were not associated with maternal COVID-19 during pregnancy.
More research needed
Commenting on the findings, Livio Provenzi, PhD, a psychologist and researcher in developmental psychobiology at the University of Pavia (Italy), noted there is a “great need” to study the direct and indirect effect of the COVID-19 pandemic on parents and their children. “Pregnancy is a period of life which shapes much of our subsequent development, and exposure to adversity in pregnancy can leave long-lasting biological footprints.”
Dr. Provenzi, who was not involved in the study, added in the release that the findings reinforce “evidence of epigenetic alterations in infants born from mothers exposed to pandemic-related stress during pregnancy.
“It shows we need more large-scale, international research to allow us to understand the developmental effects of this health emergency and to deliver better quality of care to parents and infants.”
The study was funded by the Spanish Ministry of Economy and Competitiveness, Instituto de Salud Carlos III through the University of Barcelona multicenter project and the Government of Cantabria. No relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
suggests a small-scale analysis that points to the need for further study and monitoring during pregnancy.
The study included 24 pregnant women, half of whom had COVID-19 during pregnancy, and their offspring. It showed impairments at 6 weeks of age on the social interactive dimension of a neonatal assessment.
“Not all babies born to mothers infected with COVID show neurodevelopmental differences, but our data show that their risk is increased in comparison to those not exposed to COVID in the womb. We need a bigger study to confirm the exact extent of the difference,” said lead researcher Rosa Ayesa Arriola, PhD, Valdecilla Research Institute (IDIVAL), Hospital Universitario Marqués de Valdecilla, Santander, Spain, in a release.
The findings were presented at the virtual European Psychiatric Association 2022 Congress.
Differing responses to cuddling
Coauthor Águeda Castro Quintas, PhD student, Network Centre for Biomedical Research in Mental Health, University of Barcelona, explained that the tests showed the children born to mothers who had COVID-19 during pregnancy reacted “slightly differently to being held, or cuddled.”
“We need to note that these are preliminary results, but this is part of a project following a larger sample of 100 mothers and their babies,” she added. The authors plan to compare their results with those from a similar study.
The group will also monitor infant language and motor development aged between 18 and 42 months.
“This is an ongoing project, and we are at an early stage,” Ms. Castro Quintas said. “We don’t know if these effects will result in any longer-term issues,” but longer-term observation “may help us understand this.”
“Of course, in babies who are so young, there are several things we just can’t measure, such as language skills or cognition,” added coinvestigator Nerea San Martín González, department of evolutionary biology, ecology and environmental sciences, University of Barcelona.
While emphasizing the need for larger sample sizes, she said that “in the meantime, we need to stress the importance of medical monitoring to facilitate a healthy pregnancy.”
The researchers note that the consequences of the COVID-19 pandemic for the newborns of affected mothers remain “unknown.”
However, previous studies of other infections during pregnancy suggest that offspring could be “especially vulnerable,”as the pathophysiological mechanisms of the infection, such as cytokine storms and microcoagulation, “could clearly compromise fetal neurodevelopment.”
To investigate further, they examined the neurodevelopment of infants born both immediately before and during the COVID-19 pandemic, from 2017 to 2021.
Twenty-one women who had COVID-19 during pregnancy were matched with 21 healthy controls. They were studied both during pregnancy and in the postpartum period, completing hormonal and other biochemical tests, salivary tests, movement assessments, and psychological questionnaires, adjusted for various factors.
The team also administered the Brazelton Neonatal Behavioural Assessment Scale (NBAS) to the offspring at 6 weeks of age to evaluate neurologic, social, and behavioral aspects of function.
“We have been especially sensitive in how we have conducted these tests,” said Ms. Castro Quintas. “Each mother and baby were closely examined by clinicians with expert training in the field and in the tests.”
Among those offspring exposed to COVID-19 during pregnancy, there was a significant decrease in scores on the social interactive dimension of the NBAS, particularly if infection occurred before week 20 of gestation.
Other NBAS subscales were not associated with maternal COVID-19 during pregnancy.
More research needed
Commenting on the findings, Livio Provenzi, PhD, a psychologist and researcher in developmental psychobiology at the University of Pavia (Italy), noted there is a “great need” to study the direct and indirect effect of the COVID-19 pandemic on parents and their children. “Pregnancy is a period of life which shapes much of our subsequent development, and exposure to adversity in pregnancy can leave long-lasting biological footprints.”
Dr. Provenzi, who was not involved in the study, added in the release that the findings reinforce “evidence of epigenetic alterations in infants born from mothers exposed to pandemic-related stress during pregnancy.
“It shows we need more large-scale, international research to allow us to understand the developmental effects of this health emergency and to deliver better quality of care to parents and infants.”
The study was funded by the Spanish Ministry of Economy and Competitiveness, Instituto de Salud Carlos III through the University of Barcelona multicenter project and the Government of Cantabria. No relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
suggests a small-scale analysis that points to the need for further study and monitoring during pregnancy.
The study included 24 pregnant women, half of whom had COVID-19 during pregnancy, and their offspring. It showed impairments at 6 weeks of age on the social interactive dimension of a neonatal assessment.
“Not all babies born to mothers infected with COVID show neurodevelopmental differences, but our data show that their risk is increased in comparison to those not exposed to COVID in the womb. We need a bigger study to confirm the exact extent of the difference,” said lead researcher Rosa Ayesa Arriola, PhD, Valdecilla Research Institute (IDIVAL), Hospital Universitario Marqués de Valdecilla, Santander, Spain, in a release.
The findings were presented at the virtual European Psychiatric Association 2022 Congress.
Differing responses to cuddling
Coauthor Águeda Castro Quintas, PhD student, Network Centre for Biomedical Research in Mental Health, University of Barcelona, explained that the tests showed the children born to mothers who had COVID-19 during pregnancy reacted “slightly differently to being held, or cuddled.”
“We need to note that these are preliminary results, but this is part of a project following a larger sample of 100 mothers and their babies,” she added. The authors plan to compare their results with those from a similar study.
The group will also monitor infant language and motor development aged between 18 and 42 months.
“This is an ongoing project, and we are at an early stage,” Ms. Castro Quintas said. “We don’t know if these effects will result in any longer-term issues,” but longer-term observation “may help us understand this.”
“Of course, in babies who are so young, there are several things we just can’t measure, such as language skills or cognition,” added coinvestigator Nerea San Martín González, department of evolutionary biology, ecology and environmental sciences, University of Barcelona.
While emphasizing the need for larger sample sizes, she said that “in the meantime, we need to stress the importance of medical monitoring to facilitate a healthy pregnancy.”
The researchers note that the consequences of the COVID-19 pandemic for the newborns of affected mothers remain “unknown.”
However, previous studies of other infections during pregnancy suggest that offspring could be “especially vulnerable,”as the pathophysiological mechanisms of the infection, such as cytokine storms and microcoagulation, “could clearly compromise fetal neurodevelopment.”
To investigate further, they examined the neurodevelopment of infants born both immediately before and during the COVID-19 pandemic, from 2017 to 2021.
Twenty-one women who had COVID-19 during pregnancy were matched with 21 healthy controls. They were studied both during pregnancy and in the postpartum period, completing hormonal and other biochemical tests, salivary tests, movement assessments, and psychological questionnaires, adjusted for various factors.
The team also administered the Brazelton Neonatal Behavioural Assessment Scale (NBAS) to the offspring at 6 weeks of age to evaluate neurologic, social, and behavioral aspects of function.
“We have been especially sensitive in how we have conducted these tests,” said Ms. Castro Quintas. “Each mother and baby were closely examined by clinicians with expert training in the field and in the tests.”
Among those offspring exposed to COVID-19 during pregnancy, there was a significant decrease in scores on the social interactive dimension of the NBAS, particularly if infection occurred before week 20 of gestation.
Other NBAS subscales were not associated with maternal COVID-19 during pregnancy.
More research needed
Commenting on the findings, Livio Provenzi, PhD, a psychologist and researcher in developmental psychobiology at the University of Pavia (Italy), noted there is a “great need” to study the direct and indirect effect of the COVID-19 pandemic on parents and their children. “Pregnancy is a period of life which shapes much of our subsequent development, and exposure to adversity in pregnancy can leave long-lasting biological footprints.”
Dr. Provenzi, who was not involved in the study, added in the release that the findings reinforce “evidence of epigenetic alterations in infants born from mothers exposed to pandemic-related stress during pregnancy.
“It shows we need more large-scale, international research to allow us to understand the developmental effects of this health emergency and to deliver better quality of care to parents and infants.”
The study was funded by the Spanish Ministry of Economy and Competitiveness, Instituto de Salud Carlos III through the University of Barcelona multicenter project and the Government of Cantabria. No relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
FROM EPA 2022