User login
PRISm and nonspecific pattern: New insights in lung testing interpretation
The recent statement on interpretive strategies for lung testing uses the acronym PRISm for preserved ratio impaired spirometry. PRISm identifies patients with a normal forced expiratory volume in 1 second/forced vital capacity ratio but abnormal FEV1 and/or FVC (usually both). Most medical students are taught to call this a “restrictive pattern,” and every first-year pulmonary fellow orders full lung volumes when they see it. If total lung capacity (TLC) is normal, PRISm becomes the nonspecific pattern. If TLC is low, then the patient has “true” restriction, and if it’s elevated, then hyperinflation may be present.
The traditional classification scheme for basic spirometry interpretation (normal, restricted, obstructed, or mixed) is simple and conceptually clear. It turns out that many with this pattern won’t have an abnormal TLC, so the name is, in some ways, a misnomer and can be misleading. Enter PRISm, a more descriptive and inclusive term. The phrase also lends itself to a phonetic acronym that is fun to say, easy to remember, and likely to catch on with learners.
Information on occurrence and clinical behavior comes from large cohorts with basic spirometry, but without full lung volumes because PRISm no longer applies once TLC is determined. As may be expected, prevalence varies by the population studied. Estimates for general populations have been in the 7%-12% range; however, one study examining a database of patients with clinical spirometry referrals found a prevalence of 22.3%. Rates may be far higher in low- and middle-income countries. Identified risk factors include sex, tobacco use, and body mass index; the presence of PRISm is associated with respiratory symptoms and mortality. Thus, PRISm is common and it matters.
Along with PRISm, the nonspecific pattern is a new addition, if not a new concept, to the 2022 interpretative strategies statement. As with PRISm, the title is necessarily broad, though far less imaginative. Defined by reductions in FEV1 and FVC and a normal TLC, the nonspecific pattern has classically been considered a marker of early airway disease. The idea is that early, heterogeneous closure of distal segments of the bronchial tree can reduce total volume during a forced expiration before affecting the FEV1/FVC. The fact that the TLC is not a forced maneuver means there is proportionately less effect from more collapsible/susceptible smaller units. More recent data suggest that there are additional causes.
Because the nonspecific pattern requires full lung volumes, we have less population-level data than for PRISm. Estimated prevalence is approximately 9.5% in patients with complete test results. The two most common causes are obesity and airway obstruction, and the pattern is relatively stable over time. Notably, an increase in specific airway resistance or TLC minus alveolar volume difference predicts progression to frank obstruction on spirometry.
The physiologic changes that obesity inflicts on the lung have been well described. Patients with obesity breathe at lower lung volumes and are therefore susceptible to small airway closure at rest and during forced expiration. There is no doubt that the increased recognition of PRISm and the nonspecific pattern is in part related to the worldwide rise in obesity rates.
Key takeaways
In summary, PRISm and the nonspecific pattern are now part of the classification scheme we use for spirometry and full lung volumes, respectively. They should be included in interpretations given their diagnostic and predictive value. Airway disease and obesity are common causes and often coexist with either pattern. Many will not have a true, restrictive lung deficit, and a reductionist approach to interpretation is likely to lead to erroneous diagnoses. There were many important updates included in the 2022 iteration on lung testing interpretation that should not fly under the radar.
Dr. Holley is professor of medicine at Uniformed Services University in Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He disclosed ties with CHEST College, Metapharm, and WebMD.
A version of this article appeared on Medscape.com.
The recent statement on interpretive strategies for lung testing uses the acronym PRISm for preserved ratio impaired spirometry. PRISm identifies patients with a normal forced expiratory volume in 1 second/forced vital capacity ratio but abnormal FEV1 and/or FVC (usually both). Most medical students are taught to call this a “restrictive pattern,” and every first-year pulmonary fellow orders full lung volumes when they see it. If total lung capacity (TLC) is normal, PRISm becomes the nonspecific pattern. If TLC is low, then the patient has “true” restriction, and if it’s elevated, then hyperinflation may be present.
The traditional classification scheme for basic spirometry interpretation (normal, restricted, obstructed, or mixed) is simple and conceptually clear. It turns out that many with this pattern won’t have an abnormal TLC, so the name is, in some ways, a misnomer and can be misleading. Enter PRISm, a more descriptive and inclusive term. The phrase also lends itself to a phonetic acronym that is fun to say, easy to remember, and likely to catch on with learners.
Information on occurrence and clinical behavior comes from large cohorts with basic spirometry, but without full lung volumes because PRISm no longer applies once TLC is determined. As may be expected, prevalence varies by the population studied. Estimates for general populations have been in the 7%-12% range; however, one study examining a database of patients with clinical spirometry referrals found a prevalence of 22.3%. Rates may be far higher in low- and middle-income countries. Identified risk factors include sex, tobacco use, and body mass index; the presence of PRISm is associated with respiratory symptoms and mortality. Thus, PRISm is common and it matters.
Along with PRISm, the nonspecific pattern is a new addition, if not a new concept, to the 2022 interpretative strategies statement. As with PRISm, the title is necessarily broad, though far less imaginative. Defined by reductions in FEV1 and FVC and a normal TLC, the nonspecific pattern has classically been considered a marker of early airway disease. The idea is that early, heterogeneous closure of distal segments of the bronchial tree can reduce total volume during a forced expiration before affecting the FEV1/FVC. The fact that the TLC is not a forced maneuver means there is proportionately less effect from more collapsible/susceptible smaller units. More recent data suggest that there are additional causes.
Because the nonspecific pattern requires full lung volumes, we have less population-level data than for PRISm. Estimated prevalence is approximately 9.5% in patients with complete test results. The two most common causes are obesity and airway obstruction, and the pattern is relatively stable over time. Notably, an increase in specific airway resistance or TLC minus alveolar volume difference predicts progression to frank obstruction on spirometry.
The physiologic changes that obesity inflicts on the lung have been well described. Patients with obesity breathe at lower lung volumes and are therefore susceptible to small airway closure at rest and during forced expiration. There is no doubt that the increased recognition of PRISm and the nonspecific pattern is in part related to the worldwide rise in obesity rates.
Key takeaways
In summary, PRISm and the nonspecific pattern are now part of the classification scheme we use for spirometry and full lung volumes, respectively. They should be included in interpretations given their diagnostic and predictive value. Airway disease and obesity are common causes and often coexist with either pattern. Many will not have a true, restrictive lung deficit, and a reductionist approach to interpretation is likely to lead to erroneous diagnoses. There were many important updates included in the 2022 iteration on lung testing interpretation that should not fly under the radar.
Dr. Holley is professor of medicine at Uniformed Services University in Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He disclosed ties with CHEST College, Metapharm, and WebMD.
A version of this article appeared on Medscape.com.
The recent statement on interpretive strategies for lung testing uses the acronym PRISm for preserved ratio impaired spirometry. PRISm identifies patients with a normal forced expiratory volume in 1 second/forced vital capacity ratio but abnormal FEV1 and/or FVC (usually both). Most medical students are taught to call this a “restrictive pattern,” and every first-year pulmonary fellow orders full lung volumes when they see it. If total lung capacity (TLC) is normal, PRISm becomes the nonspecific pattern. If TLC is low, then the patient has “true” restriction, and if it’s elevated, then hyperinflation may be present.
The traditional classification scheme for basic spirometry interpretation (normal, restricted, obstructed, or mixed) is simple and conceptually clear. It turns out that many with this pattern won’t have an abnormal TLC, so the name is, in some ways, a misnomer and can be misleading. Enter PRISm, a more descriptive and inclusive term. The phrase also lends itself to a phonetic acronym that is fun to say, easy to remember, and likely to catch on with learners.
Information on occurrence and clinical behavior comes from large cohorts with basic spirometry, but without full lung volumes because PRISm no longer applies once TLC is determined. As may be expected, prevalence varies by the population studied. Estimates for general populations have been in the 7%-12% range; however, one study examining a database of patients with clinical spirometry referrals found a prevalence of 22.3%. Rates may be far higher in low- and middle-income countries. Identified risk factors include sex, tobacco use, and body mass index; the presence of PRISm is associated with respiratory symptoms and mortality. Thus, PRISm is common and it matters.
Along with PRISm, the nonspecific pattern is a new addition, if not a new concept, to the 2022 interpretative strategies statement. As with PRISm, the title is necessarily broad, though far less imaginative. Defined by reductions in FEV1 and FVC and a normal TLC, the nonspecific pattern has classically been considered a marker of early airway disease. The idea is that early, heterogeneous closure of distal segments of the bronchial tree can reduce total volume during a forced expiration before affecting the FEV1/FVC. The fact that the TLC is not a forced maneuver means there is proportionately less effect from more collapsible/susceptible smaller units. More recent data suggest that there are additional causes.
Because the nonspecific pattern requires full lung volumes, we have less population-level data than for PRISm. Estimated prevalence is approximately 9.5% in patients with complete test results. The two most common causes are obesity and airway obstruction, and the pattern is relatively stable over time. Notably, an increase in specific airway resistance or TLC minus alveolar volume difference predicts progression to frank obstruction on spirometry.
The physiologic changes that obesity inflicts on the lung have been well described. Patients with obesity breathe at lower lung volumes and are therefore susceptible to small airway closure at rest and during forced expiration. There is no doubt that the increased recognition of PRISm and the nonspecific pattern is in part related to the worldwide rise in obesity rates.
Key takeaways
In summary, PRISm and the nonspecific pattern are now part of the classification scheme we use for spirometry and full lung volumes, respectively. They should be included in interpretations given their diagnostic and predictive value. Airway disease and obesity are common causes and often coexist with either pattern. Many will not have a true, restrictive lung deficit, and a reductionist approach to interpretation is likely to lead to erroneous diagnoses. There were many important updates included in the 2022 iteration on lung testing interpretation that should not fly under the radar.
Dr. Holley is professor of medicine at Uniformed Services University in Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He disclosed ties with CHEST College, Metapharm, and WebMD.
A version of this article appeared on Medscape.com.
Scrubs & Heels Summit 2023: Filling a void for women in GI
.1-3 This gender disparity arises from a multitude of factors including lack of effective mentoring, unequal leadership and career advancement opportunities, and pay inequity. In this context, The Scrubs & Heels Leadership Summit (S&H) was launched in 2022 focused on the professional and personal development of women in gastroenterology.
I had the great pleasure and honor of attending the 2023 summit which took place in February in Rancho Palos Verdes, Calif. There were nearly 200 attendees ranging from trainees to midcareer and senior gastroenterologists and other health care professionals from both academia and private practices across the nation. The weekend course was directed by S&H cofounders, Dr. Aline Charabaty and Dr. Anita Afzali, and cochaired by Dr. Amy Oxentenko and Dr. Aja McCutchen.
The 2-day summit opened with a presentation by Sally Helgesen, author of How Women Rise, describing the 12 common habits that often hold women back in career advancement, promotion, or opportunities. Dr. Aline Charabaty addressed the myth of women needing to fulfill the role of superwoman or have suprahuman abilities. Attendees were challenged to reframe this societal construct and begin to find balance and the reasonable choice to switch to part-time work and, as Dr. Aja McCutch emphasized, dial-down responsibilities to maintain wellness when life has competing priorities.
Dr. Amy Oxentenko shared her personal journey to success and instilled the importance of engaging with community and society at large. We then heard from Dr. Neena Abraham on how to gracefully embrace transitions in our professional lives, whether intentionally sought or natural progressions of a career. She encouraged attendees to control our own narrative and seek challenges that promote growth. We explored different practice models with Dr. Caroline Hwang and learned strategies of switching from academics to private practice or vice versa. We also heard from cofounder Dr. Anita Afzali on becoming a physician executive and the importance of staying connected to patient care when rising in ranks of leadership.
The second day opened with a keynote address delivered by Dr. Marla Dubinsky detailing her journey of becoming a CEO of a publicly-traded company while retaining her role as professor and chief of pediatric gastroenterology in a large academic institution. Attendees were provided with a master class on discovering ways to inspire our inner entrepreneur and highlighted the benefit of physicians, especially women, in being effective business leaders. This talk was followed by a talk by Phil Schoenfeld, MD, FACS, editor-in-chief of Evidence-Based GI for the American College of Gastroenterology. He spoke on the importance of male allyship for women in GI and shared his personal experiences and challenges with allyship.
The summit included a breakout session by Dr. Rashmi Advani designed for residents to hear tips on how to have a successful fellowship match and for fellows to embrace a steep learning curve when starting and included tips for efficiency. Additional breakout sessions included learning ergonomic strategies for positioning and scope-holding, vocal-cord exercises before giving oral presentations, and how to formulate a business plan and negotiate a contract.
We ended the summit with uplifting advice from executive coaches Sonia Narang and Dr. Dawn Sears who taught us the art of leaning into opportunities, mansizing aspirations, finding coconspirators for amplification of female GI leaders, and supporting our colleagues personally and professionally.
Three key takeaway messages:
- Recognize your self-worth and the contributions you bring to your patients and community as a whole.
- Lean into the importance of vocalizing your asks, advocating for yourself, building your brand, and showcasing your accomplishments.
- Be mindful of the balance between the time and energy you dedicate towards goals that bring you recognition and fuel your passion and your mental, physical, and emotional health.
As a trainee, I benefited tremendously from attending and expanding my professional network of mentors, sponsors and colleagues. I am encouraged by this programming and hope to see more of it in the future.
Contributors to this article included: Rashmi Advani, MD2; Anita Afzali, MD3; Aline Charabaty, MD.4
Neither Dr. Syed, nor the article contributors, had financial conflicts of interest associated with this article. The AGA was represented at the Scrubs and Heels Summit as a society partner committed to the advancement of women in GI. AGA is building on years of efforts to bolster leadership, mentorship, and sponsorship among women in GI through its annual women’s leadership conference and most recently with its 2022 regional women in GI workshops held around the country that led to the development of a comprehensive gender equity strategy designed to build an environment of gender equity in the field of GI so that all can thrive.
Institutions and social media handle
1. Santa Clara Valley Medical Center (San Jose, Calif), @noorannemd
2. Cedars Sinai (Los Angeles), @AdvaniRashmiMD
3. University of Cincinnati, @IBD_Afzali
4. Johns Hopkins Medicine (Washington), @DCharabaty
References
Advani R et al. Gender-specific attitudes of internal medicine residents toward gastroenterology. Dig Dis Sci. 2022 Nov;67(11):5044-52.
American Association of Medical Colleges. Diversity in Medicine: Facts and Figures (2019).
Elta GH. The challenges of being a female gastroenterologist. Gastroenterol Clin North Am. 2011 Jun;40(2):441-7.
Burke CA et al. Gender disparity in the practice of gastroenterology: The first 5 years of a career. Am J Gastroenterol 2005;100:259-64
David, Yakira N. et al. Gender-specific factors influencing gastroenterologists to pursue careers in advanced endoscopy: perceptions vs reality. Journal of the American College of Gastroenterology, ACG 116.3 (2021):539-50.
Rabinowitz LG et al. Gender dynamics in education and practice of gastroenterology. Gastrointest Endosc. 2021;93:1047-56.
Rabinowitz LG et al. Survey finds gender disparities impact both women mentors and mentees in gastroenterology. Journal of the American College of Gastroenterology, ACG 2021;116:1876-84.
.1-3 This gender disparity arises from a multitude of factors including lack of effective mentoring, unequal leadership and career advancement opportunities, and pay inequity. In this context, The Scrubs & Heels Leadership Summit (S&H) was launched in 2022 focused on the professional and personal development of women in gastroenterology.
I had the great pleasure and honor of attending the 2023 summit which took place in February in Rancho Palos Verdes, Calif. There were nearly 200 attendees ranging from trainees to midcareer and senior gastroenterologists and other health care professionals from both academia and private practices across the nation. The weekend course was directed by S&H cofounders, Dr. Aline Charabaty and Dr. Anita Afzali, and cochaired by Dr. Amy Oxentenko and Dr. Aja McCutchen.
The 2-day summit opened with a presentation by Sally Helgesen, author of How Women Rise, describing the 12 common habits that often hold women back in career advancement, promotion, or opportunities. Dr. Aline Charabaty addressed the myth of women needing to fulfill the role of superwoman or have suprahuman abilities. Attendees were challenged to reframe this societal construct and begin to find balance and the reasonable choice to switch to part-time work and, as Dr. Aja McCutch emphasized, dial-down responsibilities to maintain wellness when life has competing priorities.
Dr. Amy Oxentenko shared her personal journey to success and instilled the importance of engaging with community and society at large. We then heard from Dr. Neena Abraham on how to gracefully embrace transitions in our professional lives, whether intentionally sought or natural progressions of a career. She encouraged attendees to control our own narrative and seek challenges that promote growth. We explored different practice models with Dr. Caroline Hwang and learned strategies of switching from academics to private practice or vice versa. We also heard from cofounder Dr. Anita Afzali on becoming a physician executive and the importance of staying connected to patient care when rising in ranks of leadership.
The second day opened with a keynote address delivered by Dr. Marla Dubinsky detailing her journey of becoming a CEO of a publicly-traded company while retaining her role as professor and chief of pediatric gastroenterology in a large academic institution. Attendees were provided with a master class on discovering ways to inspire our inner entrepreneur and highlighted the benefit of physicians, especially women, in being effective business leaders. This talk was followed by a talk by Phil Schoenfeld, MD, FACS, editor-in-chief of Evidence-Based GI for the American College of Gastroenterology. He spoke on the importance of male allyship for women in GI and shared his personal experiences and challenges with allyship.
The summit included a breakout session by Dr. Rashmi Advani designed for residents to hear tips on how to have a successful fellowship match and for fellows to embrace a steep learning curve when starting and included tips for efficiency. Additional breakout sessions included learning ergonomic strategies for positioning and scope-holding, vocal-cord exercises before giving oral presentations, and how to formulate a business plan and negotiate a contract.
We ended the summit with uplifting advice from executive coaches Sonia Narang and Dr. Dawn Sears who taught us the art of leaning into opportunities, mansizing aspirations, finding coconspirators for amplification of female GI leaders, and supporting our colleagues personally and professionally.
Three key takeaway messages:
- Recognize your self-worth and the contributions you bring to your patients and community as a whole.
- Lean into the importance of vocalizing your asks, advocating for yourself, building your brand, and showcasing your accomplishments.
- Be mindful of the balance between the time and energy you dedicate towards goals that bring you recognition and fuel your passion and your mental, physical, and emotional health.
As a trainee, I benefited tremendously from attending and expanding my professional network of mentors, sponsors and colleagues. I am encouraged by this programming and hope to see more of it in the future.
Contributors to this article included: Rashmi Advani, MD2; Anita Afzali, MD3; Aline Charabaty, MD.4
Neither Dr. Syed, nor the article contributors, had financial conflicts of interest associated with this article. The AGA was represented at the Scrubs and Heels Summit as a society partner committed to the advancement of women in GI. AGA is building on years of efforts to bolster leadership, mentorship, and sponsorship among women in GI through its annual women’s leadership conference and most recently with its 2022 regional women in GI workshops held around the country that led to the development of a comprehensive gender equity strategy designed to build an environment of gender equity in the field of GI so that all can thrive.
Institutions and social media handle
1. Santa Clara Valley Medical Center (San Jose, Calif), @noorannemd
2. Cedars Sinai (Los Angeles), @AdvaniRashmiMD
3. University of Cincinnati, @IBD_Afzali
4. Johns Hopkins Medicine (Washington), @DCharabaty
References
Advani R et al. Gender-specific attitudes of internal medicine residents toward gastroenterology. Dig Dis Sci. 2022 Nov;67(11):5044-52.
American Association of Medical Colleges. Diversity in Medicine: Facts and Figures (2019).
Elta GH. The challenges of being a female gastroenterologist. Gastroenterol Clin North Am. 2011 Jun;40(2):441-7.
Burke CA et al. Gender disparity in the practice of gastroenterology: The first 5 years of a career. Am J Gastroenterol 2005;100:259-64
David, Yakira N. et al. Gender-specific factors influencing gastroenterologists to pursue careers in advanced endoscopy: perceptions vs reality. Journal of the American College of Gastroenterology, ACG 116.3 (2021):539-50.
Rabinowitz LG et al. Gender dynamics in education and practice of gastroenterology. Gastrointest Endosc. 2021;93:1047-56.
Rabinowitz LG et al. Survey finds gender disparities impact both women mentors and mentees in gastroenterology. Journal of the American College of Gastroenterology, ACG 2021;116:1876-84.
.1-3 This gender disparity arises from a multitude of factors including lack of effective mentoring, unequal leadership and career advancement opportunities, and pay inequity. In this context, The Scrubs & Heels Leadership Summit (S&H) was launched in 2022 focused on the professional and personal development of women in gastroenterology.
I had the great pleasure and honor of attending the 2023 summit which took place in February in Rancho Palos Verdes, Calif. There were nearly 200 attendees ranging from trainees to midcareer and senior gastroenterologists and other health care professionals from both academia and private practices across the nation. The weekend course was directed by S&H cofounders, Dr. Aline Charabaty and Dr. Anita Afzali, and cochaired by Dr. Amy Oxentenko and Dr. Aja McCutchen.
The 2-day summit opened with a presentation by Sally Helgesen, author of How Women Rise, describing the 12 common habits that often hold women back in career advancement, promotion, or opportunities. Dr. Aline Charabaty addressed the myth of women needing to fulfill the role of superwoman or have suprahuman abilities. Attendees were challenged to reframe this societal construct and begin to find balance and the reasonable choice to switch to part-time work and, as Dr. Aja McCutch emphasized, dial-down responsibilities to maintain wellness when life has competing priorities.
Dr. Amy Oxentenko shared her personal journey to success and instilled the importance of engaging with community and society at large. We then heard from Dr. Neena Abraham on how to gracefully embrace transitions in our professional lives, whether intentionally sought or natural progressions of a career. She encouraged attendees to control our own narrative and seek challenges that promote growth. We explored different practice models with Dr. Caroline Hwang and learned strategies of switching from academics to private practice or vice versa. We also heard from cofounder Dr. Anita Afzali on becoming a physician executive and the importance of staying connected to patient care when rising in ranks of leadership.
The second day opened with a keynote address delivered by Dr. Marla Dubinsky detailing her journey of becoming a CEO of a publicly-traded company while retaining her role as professor and chief of pediatric gastroenterology in a large academic institution. Attendees were provided with a master class on discovering ways to inspire our inner entrepreneur and highlighted the benefit of physicians, especially women, in being effective business leaders. This talk was followed by a talk by Phil Schoenfeld, MD, FACS, editor-in-chief of Evidence-Based GI for the American College of Gastroenterology. He spoke on the importance of male allyship for women in GI and shared his personal experiences and challenges with allyship.
The summit included a breakout session by Dr. Rashmi Advani designed for residents to hear tips on how to have a successful fellowship match and for fellows to embrace a steep learning curve when starting and included tips for efficiency. Additional breakout sessions included learning ergonomic strategies for positioning and scope-holding, vocal-cord exercises before giving oral presentations, and how to formulate a business plan and negotiate a contract.
We ended the summit with uplifting advice from executive coaches Sonia Narang and Dr. Dawn Sears who taught us the art of leaning into opportunities, mansizing aspirations, finding coconspirators for amplification of female GI leaders, and supporting our colleagues personally and professionally.
Three key takeaway messages:
- Recognize your self-worth and the contributions you bring to your patients and community as a whole.
- Lean into the importance of vocalizing your asks, advocating for yourself, building your brand, and showcasing your accomplishments.
- Be mindful of the balance between the time and energy you dedicate towards goals that bring you recognition and fuel your passion and your mental, physical, and emotional health.
As a trainee, I benefited tremendously from attending and expanding my professional network of mentors, sponsors and colleagues. I am encouraged by this programming and hope to see more of it in the future.
Contributors to this article included: Rashmi Advani, MD2; Anita Afzali, MD3; Aline Charabaty, MD.4
Neither Dr. Syed, nor the article contributors, had financial conflicts of interest associated with this article. The AGA was represented at the Scrubs and Heels Summit as a society partner committed to the advancement of women in GI. AGA is building on years of efforts to bolster leadership, mentorship, and sponsorship among women in GI through its annual women’s leadership conference and most recently with its 2022 regional women in GI workshops held around the country that led to the development of a comprehensive gender equity strategy designed to build an environment of gender equity in the field of GI so that all can thrive.
Institutions and social media handle
1. Santa Clara Valley Medical Center (San Jose, Calif), @noorannemd
2. Cedars Sinai (Los Angeles), @AdvaniRashmiMD
3. University of Cincinnati, @IBD_Afzali
4. Johns Hopkins Medicine (Washington), @DCharabaty
References
Advani R et al. Gender-specific attitudes of internal medicine residents toward gastroenterology. Dig Dis Sci. 2022 Nov;67(11):5044-52.
American Association of Medical Colleges. Diversity in Medicine: Facts and Figures (2019).
Elta GH. The challenges of being a female gastroenterologist. Gastroenterol Clin North Am. 2011 Jun;40(2):441-7.
Burke CA et al. Gender disparity in the practice of gastroenterology: The first 5 years of a career. Am J Gastroenterol 2005;100:259-64
David, Yakira N. et al. Gender-specific factors influencing gastroenterologists to pursue careers in advanced endoscopy: perceptions vs reality. Journal of the American College of Gastroenterology, ACG 116.3 (2021):539-50.
Rabinowitz LG et al. Gender dynamics in education and practice of gastroenterology. Gastrointest Endosc. 2021;93:1047-56.
Rabinowitz LG et al. Survey finds gender disparities impact both women mentors and mentees in gastroenterology. Journal of the American College of Gastroenterology, ACG 2021;116:1876-84.
A new and completely different pain medicine
This transcript has been edited for clarity.
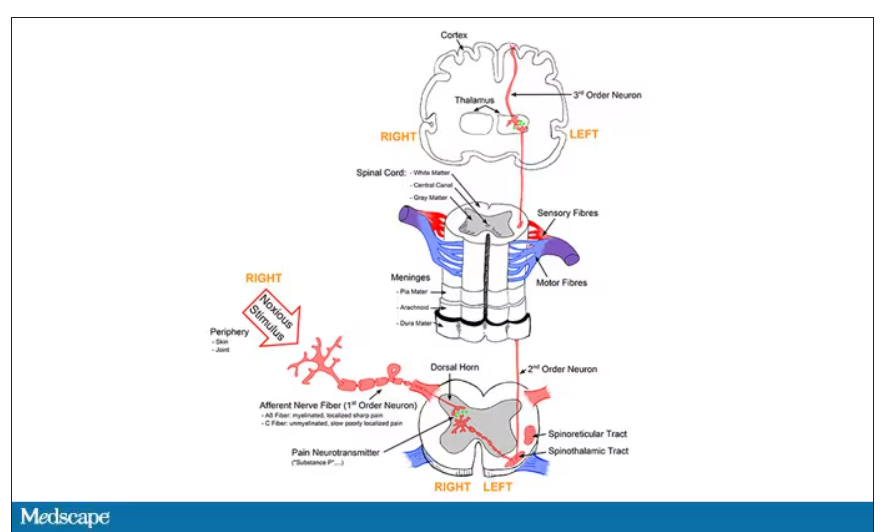
When you stub your toe or get a paper cut on your finger, you feel the pain in that part of your body. It feels like the pain is coming from that place. But, of course, that’s not really what is happening. Pain doesn’t really happen in your toe or your finger. It happens in your brain.
It’s a game of telephone, really. The afferent nerve fiber detects the noxious stimulus, passing that signal to the second-order neuron in the dorsal root ganglia of the spinal cord, which runs it up to the thalamus to be passed to the third-order neuron which brings it to the cortex for localization and conscious perception. It’s not even a very good game of telephone. It takes about 100 ms for a pain signal to get from the hand to the brain – longer from the feet, given the greater distance. You see your foot hit the corner of the coffee table and have just enough time to think: “Oh no!” before the pain hits.
Given the Rube Goldberg nature of the process, it would seem like there are any number of places we could stop pain sensation. And sure, local anesthetics at the site of injury, or even spinal anesthetics, are powerful – if temporary and hard to administer – solutions to acute pain.
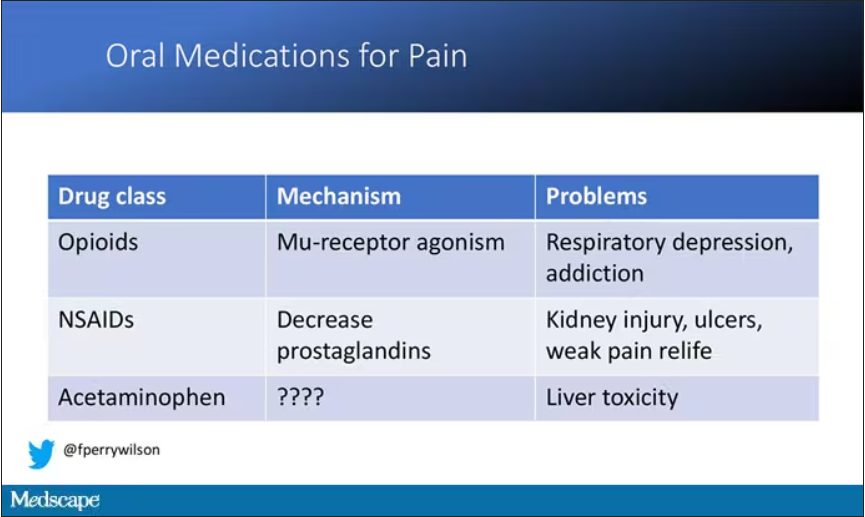
But in our everyday armamentarium, let’s be honest – we essentially have three options: opiates and opioids, which activate the mu-receptors in the brain to dull pain (and cause a host of other nasty side effects); NSAIDs, which block prostaglandin synthesis and thus limit the ability for pain-conducting neurons to get excited; and acetaminophen, which, despite being used for a century, is poorly understood.
But
If you were to zoom in on the connection between that first afferent pain fiber and the secondary nerve in the spinal cord dorsal root ganglion, you would see a receptor called Nav1.8, a voltage-gated sodium channel.
This receptor is a key part of the apparatus that passes information from nerve 1 to nerve 2, but only for fibers that transmit pain signals. In fact, humans with mutations in this receptor that leave it always in the “open” state have a severe pain syndrome. Blocking the receptor, therefore, might reduce pain.
In preclinical work, researchers identified VX-548, which doesn’t have a brand name yet, as a potent blocker of that channel even in nanomolar concentrations. Importantly, the compound was highly selective for that particular channel – about 30,000 times more selective than it was for the other sodium channels in that family.
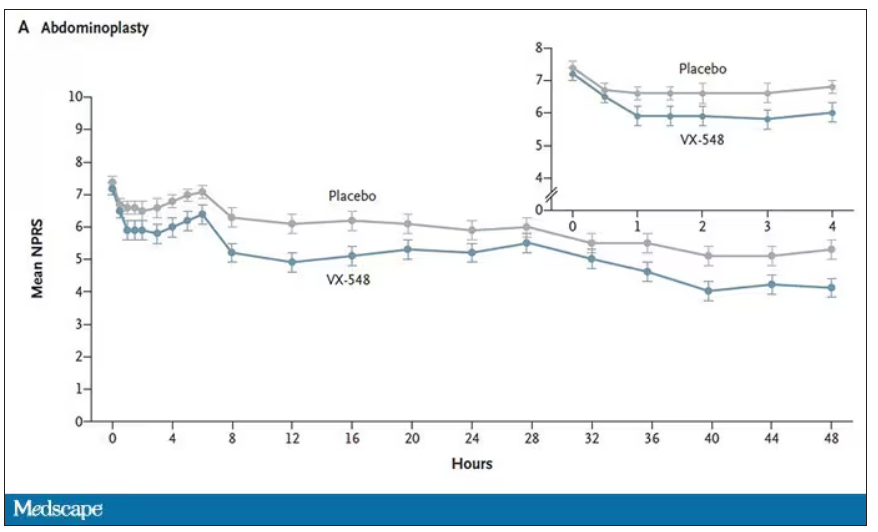
Of course, a highly selective and specific drug does not a blockbuster analgesic make. To determine how this drug would work on humans in pain, they turned to two populations: 303 individuals undergoing abdominoplasty and 274 undergoing bunionectomy, as reported in a new paper in the New England Journal of Medicine.
I know this seems a bit random, but abdominoplasty is quite painful and a good model for soft-tissue pain. Bunionectomy is also quite a painful procedure and a useful model of bone pain. After the surgeries, patients were randomized to several different doses of VX-548, hydrocodone plus acetaminophen, or placebo for 48 hours.
At 19 time points over that 48-hour period, participants were asked to rate their pain on a scale from 0 to 10. The primary outcome was the cumulative pain experienced over the 48 hours. So, higher pain would be worse here, but longer duration of pain would also be worse.
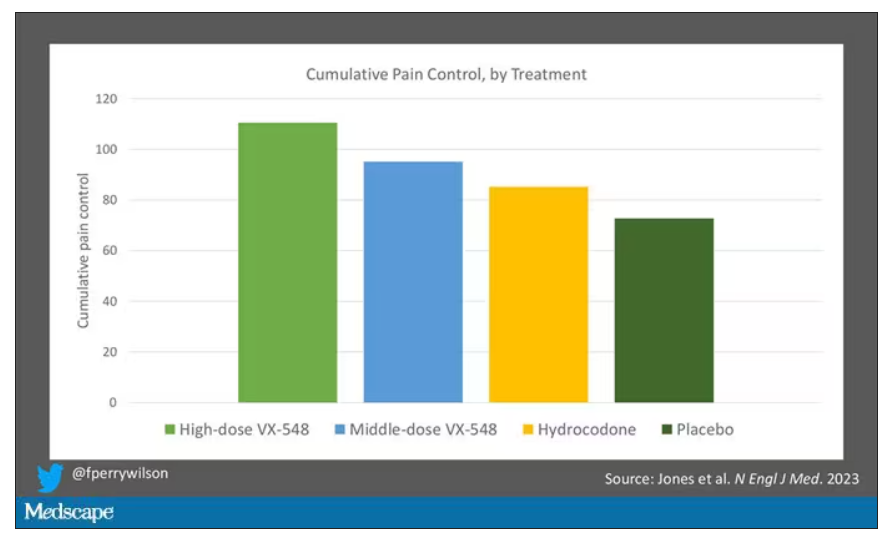
The story of the study is really told in this chart.
Yes, those assigned to the highest dose of VX-548 had a statistically significant lower cumulative amount of pain in the 48 hours after surgery. But the picture is really worth more than the stats here. You can see that the onset of pain relief was fairly quick, and that pain relief was sustained over time. You can also see that this is not a miracle drug. Pain scores were a bit better 48 hours out, but only by about a point and a half.
Placebo isn’t really the fair comparison here; few of us treat our postabdominoplasty patients with placebo, after all. The authors do not formally compare the effect of VX-548 with that of the opioid hydrocodone, for instance. But that doesn’t stop us.
This graph, which I put together from data in the paper, shows pain control across the four randomization categories, with higher numbers indicating more (cumulative) control. While all the active agents do a bit better than placebo, VX-548 at the higher dose appears to do the best. But I should note that 5 mg of hydrocodone may not be an adequate dose for most people.
Yes, I would really have killed for an NSAID arm in this trial. Its absence, given that NSAIDs are a staple of postoperative care, is ... well, let’s just say, notable.
Although not a pain-destroying machine, VX-548 has some other things to recommend it. The receptor is really not found in the brain at all, which suggests that the drug should not carry much risk for dependency, though that has not been formally studied.
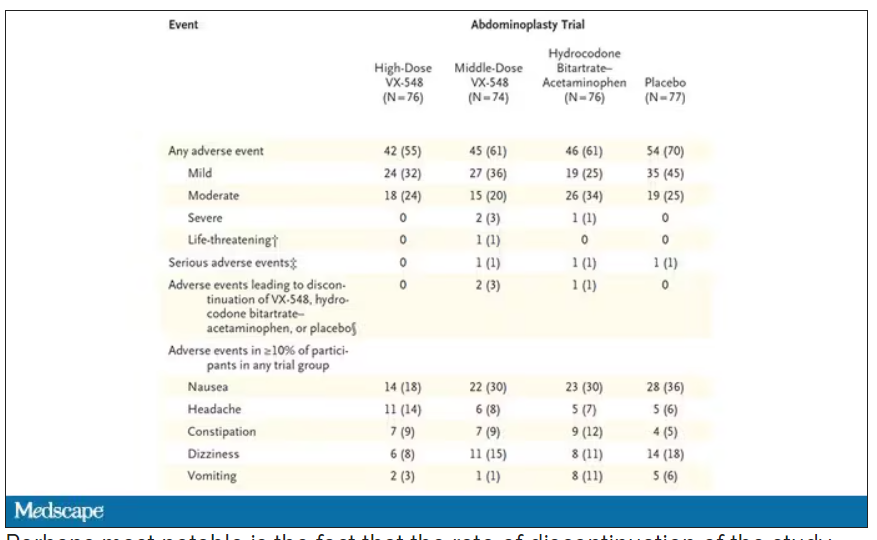
The side effects were generally mild – headache was the most common – and less prevalent than what you see even in the placebo arm.
Perhaps most notable is the fact that the rate of discontinuation of the study drug was lowest in the VX-548 arm. Patients could stop taking the pill they were assigned for any reason, ranging from perceived lack of efficacy to side effects. A low discontinuation rate indicates to me a sort of “voting with your feet” that suggests this might be a well-tolerated and reasonably effective drug.
VX-548 isn’t on the market yet; phase 3 trials are ongoing. But whether it is this particular drug or another in this class, I’m happy to see researchers trying to find new ways to target that most primeval form of suffering: pain.
Dr. Wilson is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Conn. He disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
When you stub your toe or get a paper cut on your finger, you feel the pain in that part of your body. It feels like the pain is coming from that place. But, of course, that’s not really what is happening. Pain doesn’t really happen in your toe or your finger. It happens in your brain.
It’s a game of telephone, really. The afferent nerve fiber detects the noxious stimulus, passing that signal to the second-order neuron in the dorsal root ganglia of the spinal cord, which runs it up to the thalamus to be passed to the third-order neuron which brings it to the cortex for localization and conscious perception. It’s not even a very good game of telephone. It takes about 100 ms for a pain signal to get from the hand to the brain – longer from the feet, given the greater distance. You see your foot hit the corner of the coffee table and have just enough time to think: “Oh no!” before the pain hits.
Given the Rube Goldberg nature of the process, it would seem like there are any number of places we could stop pain sensation. And sure, local anesthetics at the site of injury, or even spinal anesthetics, are powerful – if temporary and hard to administer – solutions to acute pain.
But in our everyday armamentarium, let’s be honest – we essentially have three options: opiates and opioids, which activate the mu-receptors in the brain to dull pain (and cause a host of other nasty side effects); NSAIDs, which block prostaglandin synthesis and thus limit the ability for pain-conducting neurons to get excited; and acetaminophen, which, despite being used for a century, is poorly understood.
But
If you were to zoom in on the connection between that first afferent pain fiber and the secondary nerve in the spinal cord dorsal root ganglion, you would see a receptor called Nav1.8, a voltage-gated sodium channel.
This receptor is a key part of the apparatus that passes information from nerve 1 to nerve 2, but only for fibers that transmit pain signals. In fact, humans with mutations in this receptor that leave it always in the “open” state have a severe pain syndrome. Blocking the receptor, therefore, might reduce pain.
In preclinical work, researchers identified VX-548, which doesn’t have a brand name yet, as a potent blocker of that channel even in nanomolar concentrations. Importantly, the compound was highly selective for that particular channel – about 30,000 times more selective than it was for the other sodium channels in that family.
Of course, a highly selective and specific drug does not a blockbuster analgesic make. To determine how this drug would work on humans in pain, they turned to two populations: 303 individuals undergoing abdominoplasty and 274 undergoing bunionectomy, as reported in a new paper in the New England Journal of Medicine.
I know this seems a bit random, but abdominoplasty is quite painful and a good model for soft-tissue pain. Bunionectomy is also quite a painful procedure and a useful model of bone pain. After the surgeries, patients were randomized to several different doses of VX-548, hydrocodone plus acetaminophen, or placebo for 48 hours.
At 19 time points over that 48-hour period, participants were asked to rate their pain on a scale from 0 to 10. The primary outcome was the cumulative pain experienced over the 48 hours. So, higher pain would be worse here, but longer duration of pain would also be worse.
The story of the study is really told in this chart.
Yes, those assigned to the highest dose of VX-548 had a statistically significant lower cumulative amount of pain in the 48 hours after surgery. But the picture is really worth more than the stats here. You can see that the onset of pain relief was fairly quick, and that pain relief was sustained over time. You can also see that this is not a miracle drug. Pain scores were a bit better 48 hours out, but only by about a point and a half.
Placebo isn’t really the fair comparison here; few of us treat our postabdominoplasty patients with placebo, after all. The authors do not formally compare the effect of VX-548 with that of the opioid hydrocodone, for instance. But that doesn’t stop us.
This graph, which I put together from data in the paper, shows pain control across the four randomization categories, with higher numbers indicating more (cumulative) control. While all the active agents do a bit better than placebo, VX-548 at the higher dose appears to do the best. But I should note that 5 mg of hydrocodone may not be an adequate dose for most people.
Yes, I would really have killed for an NSAID arm in this trial. Its absence, given that NSAIDs are a staple of postoperative care, is ... well, let’s just say, notable.
Although not a pain-destroying machine, VX-548 has some other things to recommend it. The receptor is really not found in the brain at all, which suggests that the drug should not carry much risk for dependency, though that has not been formally studied.
The side effects were generally mild – headache was the most common – and less prevalent than what you see even in the placebo arm.
Perhaps most notable is the fact that the rate of discontinuation of the study drug was lowest in the VX-548 arm. Patients could stop taking the pill they were assigned for any reason, ranging from perceived lack of efficacy to side effects. A low discontinuation rate indicates to me a sort of “voting with your feet” that suggests this might be a well-tolerated and reasonably effective drug.
VX-548 isn’t on the market yet; phase 3 trials are ongoing. But whether it is this particular drug or another in this class, I’m happy to see researchers trying to find new ways to target that most primeval form of suffering: pain.
Dr. Wilson is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Conn. He disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
When you stub your toe or get a paper cut on your finger, you feel the pain in that part of your body. It feels like the pain is coming from that place. But, of course, that’s not really what is happening. Pain doesn’t really happen in your toe or your finger. It happens in your brain.
It’s a game of telephone, really. The afferent nerve fiber detects the noxious stimulus, passing that signal to the second-order neuron in the dorsal root ganglia of the spinal cord, which runs it up to the thalamus to be passed to the third-order neuron which brings it to the cortex for localization and conscious perception. It’s not even a very good game of telephone. It takes about 100 ms for a pain signal to get from the hand to the brain – longer from the feet, given the greater distance. You see your foot hit the corner of the coffee table and have just enough time to think: “Oh no!” before the pain hits.
Given the Rube Goldberg nature of the process, it would seem like there are any number of places we could stop pain sensation. And sure, local anesthetics at the site of injury, or even spinal anesthetics, are powerful – if temporary and hard to administer – solutions to acute pain.
But in our everyday armamentarium, let’s be honest – we essentially have three options: opiates and opioids, which activate the mu-receptors in the brain to dull pain (and cause a host of other nasty side effects); NSAIDs, which block prostaglandin synthesis and thus limit the ability for pain-conducting neurons to get excited; and acetaminophen, which, despite being used for a century, is poorly understood.
But
If you were to zoom in on the connection between that first afferent pain fiber and the secondary nerve in the spinal cord dorsal root ganglion, you would see a receptor called Nav1.8, a voltage-gated sodium channel.
This receptor is a key part of the apparatus that passes information from nerve 1 to nerve 2, but only for fibers that transmit pain signals. In fact, humans with mutations in this receptor that leave it always in the “open” state have a severe pain syndrome. Blocking the receptor, therefore, might reduce pain.
In preclinical work, researchers identified VX-548, which doesn’t have a brand name yet, as a potent blocker of that channel even in nanomolar concentrations. Importantly, the compound was highly selective for that particular channel – about 30,000 times more selective than it was for the other sodium channels in that family.
Of course, a highly selective and specific drug does not a blockbuster analgesic make. To determine how this drug would work on humans in pain, they turned to two populations: 303 individuals undergoing abdominoplasty and 274 undergoing bunionectomy, as reported in a new paper in the New England Journal of Medicine.
I know this seems a bit random, but abdominoplasty is quite painful and a good model for soft-tissue pain. Bunionectomy is also quite a painful procedure and a useful model of bone pain. After the surgeries, patients were randomized to several different doses of VX-548, hydrocodone plus acetaminophen, or placebo for 48 hours.
At 19 time points over that 48-hour period, participants were asked to rate their pain on a scale from 0 to 10. The primary outcome was the cumulative pain experienced over the 48 hours. So, higher pain would be worse here, but longer duration of pain would also be worse.
The story of the study is really told in this chart.
Yes, those assigned to the highest dose of VX-548 had a statistically significant lower cumulative amount of pain in the 48 hours after surgery. But the picture is really worth more than the stats here. You can see that the onset of pain relief was fairly quick, and that pain relief was sustained over time. You can also see that this is not a miracle drug. Pain scores were a bit better 48 hours out, but only by about a point and a half.
Placebo isn’t really the fair comparison here; few of us treat our postabdominoplasty patients with placebo, after all. The authors do not formally compare the effect of VX-548 with that of the opioid hydrocodone, for instance. But that doesn’t stop us.
This graph, which I put together from data in the paper, shows pain control across the four randomization categories, with higher numbers indicating more (cumulative) control. While all the active agents do a bit better than placebo, VX-548 at the higher dose appears to do the best. But I should note that 5 mg of hydrocodone may not be an adequate dose for most people.
Yes, I would really have killed for an NSAID arm in this trial. Its absence, given that NSAIDs are a staple of postoperative care, is ... well, let’s just say, notable.
Although not a pain-destroying machine, VX-548 has some other things to recommend it. The receptor is really not found in the brain at all, which suggests that the drug should not carry much risk for dependency, though that has not been formally studied.
The side effects were generally mild – headache was the most common – and less prevalent than what you see even in the placebo arm.
Perhaps most notable is the fact that the rate of discontinuation of the study drug was lowest in the VX-548 arm. Patients could stop taking the pill they were assigned for any reason, ranging from perceived lack of efficacy to side effects. A low discontinuation rate indicates to me a sort of “voting with your feet” that suggests this might be a well-tolerated and reasonably effective drug.
VX-548 isn’t on the market yet; phase 3 trials are ongoing. But whether it is this particular drug or another in this class, I’m happy to see researchers trying to find new ways to target that most primeval form of suffering: pain.
Dr. Wilson is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Conn. He disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
In 133-vehicle pileup, bleeding paramedic helps while hurt
It seemed like a typical kind of day. I was out the door by 6:00 a.m., heading into work for a shift on I-35 West, my daily commute. It was still dark out. A little bit colder that morning, but nothing us Texans aren’t used to.
I was cruising down the tollway, which is separated from the main highway by a barrier. That stretch has a slight hill and turns to the left. You can’t see anything beyond the hill when you’re at the bottom.
As I made my way up, I spotted brake lights about 400 yards ahead. I eased on my brake, and next thing I knew, I was sliding.
I realized, I’m on black ice.
I was driving a 2011 Toyota FJ Cruiser and I had it all beefed up – lift tires, winch bumpers front and back. I had never had any sort of issue like that.
My ABS brakes kicked in. I slowed, but not fast enough. I saw a wall of crashed cars in front of me.
I was in the left-hand lane, so I turned my steering wheel into the center median. I could hear the whole side of my vehicle scraping against it. I managed to slow down enough to just tap the vehicle in front of me.
I looked in my passenger side-view mirror and saw headlights coming in the right lane. But this car couldn’t slow down. It crashed into the wreckage to my right.
That’s when it sunk in: There was going to be a car coming in my lane, and it might not be able to stop.
I looked in my rear-view mirror and saw headlights. Sparks flying off that center median.
I didn’t know at the time, but it was a fully loaded semi-truck traveling about 60 miles an hour.
I had a split second to think: This is it. This is how it ends. I closed my eyes.
It was the most violent impact I’ve ever experienced in my life.
I had no idea until afterward, but I had slammed into the vehicle in front of me and my SUV did a kind of 360° barrel roll over the median into the northbound lanes, landing wheels down on top of my sheared off roof rack.
Everything stopped. I opened my eyes. All my airbags had deployed. I gently tried moving my arms and legs, and they worked. I couldn’t move my left foot. It was wedged underneath the brake pedal. But I wasn’t in any pain, just very confused and disoriented. I knew I needed to get out of the vehicle.
My door was wedged shut, so I crawled out of the broken window, slipping on the black ice. I realized I had hit a Fort Worth police cruiser, now all smashed up. The driver couldn’t open his door. So, I helped him force it open, got him out of the vehicle, and checked on him. He was fine.
I had no idea how many vehicles and people were involved. I was in so much shock that the only thing I could do was immediately revert back to my training. I was the only first responder there.
I was helping people with lacerations, back and neck issues from the violent impacts. When you’re involved in a mass casualty incident like that, you have to assess which patients will be the most viable and need the most immediate attention. You have greens, yellows, reds, and then blacks – the deceased. Someone who doesn’t have a pulse and isn’t breathing, you can’t necessarily do CPR because you don’t have enough resources. You have to use your best judgment.
Meanwhile, the crashes kept coming. I found out later I was roughly vehicle No. 50 in the pileup; 83 more would follow. I heard them over and over – a crash and then screams from people in their vehicles. Each time a car hit, the entire pileup would move a couple of inches, getting more and more compacted. With that going on, I couldn’t go in there to pull people out. That scene was absolutely unsafe.
It felt like forever, but about 10 minutes later, an ambulance showed up, and I walked over to them. Because I was in my work uniform, they thought I was there on a call.
A couple fire crews came, and a firefighter yelled, “Hey, we need a backboard!” So, I grabbed a backboard from their unit and helped load up a patient. Then I heard somebody screaming, “This patient needs a stretcher!” A woman was having lumbar pain that seemed excruciating. I helped move her from the wreckage and carry her over to the stretcher. I started trying to get as many people as I could out of their cars.
Around this time, one of my supervisors showed up. He thought I was there working. But then he asked me, “Why is your face bleeding? Why do you have blood coming from your nose?” I pointed to my vehicle, and his jaw just dropped. He said, “Okay, you’re done. Go sit in my vehicle over there.”
He put a stop to my helping out, which was probably for the best. Because I actually had a concussion, a bone contusion in my foot, and a severely sprained ankle. The next day, I felt like I had gotten hit by a truck. (I had!) But when you have so much adrenaline pumping, you don’t feel pain or emotion. You don’t really feel anything.
While I was sitting in that vehicle, I called my mom to let her know I was okay. My parents were watching the news, and there was an aerial view of the accident. It was massive – a giant pile of metal stretching 200 or 300 yards. Six people had perished, more than 60 were hurt.
That night, our public information officer reached out to me about doing an interview with NBC. So, I told my story about what happened. Because of the concussion, a lot of it was a blur.
A day later, I got a call on my cell phone and someone said, “This is Tyler from Toyota. We saw the NBC interview. We wanted to let you know, don’t worry about getting a new vehicle. Just tell us what color 4Runner you want.”
My first thought was: Okay, this can’t be real. This doesn’t happen to people like me. But it turned out that it was, and they put me in a brand new vehicle.
Toyota started sending me to events like NASCAR races, putting me up in VIP suites. It was a cool experience. But it’s just surface stuff – it’s never going to erase what happened. The experience left a mark. It took me 6 months to a year to get rid of that feeling of the impact. Every time I tried to fall asleep, the whole scenario would replay in my head.
In EMS, we have a saying: “Every patient is practice for the next one.” That pileup – you can’t train for something like that. We all learned from it, so we can better prepare if anything like that happens again.
Since then, I’ve seen people die in motor vehicle collisions from a lot less than what happened to me. I’m not religious or spiritual, but I believe there must be a reason why I’m still here.
Now I see patients in traffic accidents who are very distraught even though they’re going to be okay. I tell them, “I’m sorry this happened to you. But remember, this is not the end. You are alive. And I’m going to do everything I can to make sure that doesn’t change while you’re with me.”
Trey McDaniel is a paramedic with MedStar Mobile Healthcare in Fort Worth, Tex.
A version of this article first appeared on Medscape.com.
It seemed like a typical kind of day. I was out the door by 6:00 a.m., heading into work for a shift on I-35 West, my daily commute. It was still dark out. A little bit colder that morning, but nothing us Texans aren’t used to.
I was cruising down the tollway, which is separated from the main highway by a barrier. That stretch has a slight hill and turns to the left. You can’t see anything beyond the hill when you’re at the bottom.
As I made my way up, I spotted brake lights about 400 yards ahead. I eased on my brake, and next thing I knew, I was sliding.
I realized, I’m on black ice.
I was driving a 2011 Toyota FJ Cruiser and I had it all beefed up – lift tires, winch bumpers front and back. I had never had any sort of issue like that.
My ABS brakes kicked in. I slowed, but not fast enough. I saw a wall of crashed cars in front of me.
I was in the left-hand lane, so I turned my steering wheel into the center median. I could hear the whole side of my vehicle scraping against it. I managed to slow down enough to just tap the vehicle in front of me.
I looked in my passenger side-view mirror and saw headlights coming in the right lane. But this car couldn’t slow down. It crashed into the wreckage to my right.
That’s when it sunk in: There was going to be a car coming in my lane, and it might not be able to stop.
I looked in my rear-view mirror and saw headlights. Sparks flying off that center median.
I didn’t know at the time, but it was a fully loaded semi-truck traveling about 60 miles an hour.
I had a split second to think: This is it. This is how it ends. I closed my eyes.
It was the most violent impact I’ve ever experienced in my life.
I had no idea until afterward, but I had slammed into the vehicle in front of me and my SUV did a kind of 360° barrel roll over the median into the northbound lanes, landing wheels down on top of my sheared off roof rack.
Everything stopped. I opened my eyes. All my airbags had deployed. I gently tried moving my arms and legs, and they worked. I couldn’t move my left foot. It was wedged underneath the brake pedal. But I wasn’t in any pain, just very confused and disoriented. I knew I needed to get out of the vehicle.
My door was wedged shut, so I crawled out of the broken window, slipping on the black ice. I realized I had hit a Fort Worth police cruiser, now all smashed up. The driver couldn’t open his door. So, I helped him force it open, got him out of the vehicle, and checked on him. He was fine.
I had no idea how many vehicles and people were involved. I was in so much shock that the only thing I could do was immediately revert back to my training. I was the only first responder there.
I was helping people with lacerations, back and neck issues from the violent impacts. When you’re involved in a mass casualty incident like that, you have to assess which patients will be the most viable and need the most immediate attention. You have greens, yellows, reds, and then blacks – the deceased. Someone who doesn’t have a pulse and isn’t breathing, you can’t necessarily do CPR because you don’t have enough resources. You have to use your best judgment.
Meanwhile, the crashes kept coming. I found out later I was roughly vehicle No. 50 in the pileup; 83 more would follow. I heard them over and over – a crash and then screams from people in their vehicles. Each time a car hit, the entire pileup would move a couple of inches, getting more and more compacted. With that going on, I couldn’t go in there to pull people out. That scene was absolutely unsafe.
It felt like forever, but about 10 minutes later, an ambulance showed up, and I walked over to them. Because I was in my work uniform, they thought I was there on a call.
A couple fire crews came, and a firefighter yelled, “Hey, we need a backboard!” So, I grabbed a backboard from their unit and helped load up a patient. Then I heard somebody screaming, “This patient needs a stretcher!” A woman was having lumbar pain that seemed excruciating. I helped move her from the wreckage and carry her over to the stretcher. I started trying to get as many people as I could out of their cars.
Around this time, one of my supervisors showed up. He thought I was there working. But then he asked me, “Why is your face bleeding? Why do you have blood coming from your nose?” I pointed to my vehicle, and his jaw just dropped. He said, “Okay, you’re done. Go sit in my vehicle over there.”
He put a stop to my helping out, which was probably for the best. Because I actually had a concussion, a bone contusion in my foot, and a severely sprained ankle. The next day, I felt like I had gotten hit by a truck. (I had!) But when you have so much adrenaline pumping, you don’t feel pain or emotion. You don’t really feel anything.
While I was sitting in that vehicle, I called my mom to let her know I was okay. My parents were watching the news, and there was an aerial view of the accident. It was massive – a giant pile of metal stretching 200 or 300 yards. Six people had perished, more than 60 were hurt.
That night, our public information officer reached out to me about doing an interview with NBC. So, I told my story about what happened. Because of the concussion, a lot of it was a blur.
A day later, I got a call on my cell phone and someone said, “This is Tyler from Toyota. We saw the NBC interview. We wanted to let you know, don’t worry about getting a new vehicle. Just tell us what color 4Runner you want.”
My first thought was: Okay, this can’t be real. This doesn’t happen to people like me. But it turned out that it was, and they put me in a brand new vehicle.
Toyota started sending me to events like NASCAR races, putting me up in VIP suites. It was a cool experience. But it’s just surface stuff – it’s never going to erase what happened. The experience left a mark. It took me 6 months to a year to get rid of that feeling of the impact. Every time I tried to fall asleep, the whole scenario would replay in my head.
In EMS, we have a saying: “Every patient is practice for the next one.” That pileup – you can’t train for something like that. We all learned from it, so we can better prepare if anything like that happens again.
Since then, I’ve seen people die in motor vehicle collisions from a lot less than what happened to me. I’m not religious or spiritual, but I believe there must be a reason why I’m still here.
Now I see patients in traffic accidents who are very distraught even though they’re going to be okay. I tell them, “I’m sorry this happened to you. But remember, this is not the end. You are alive. And I’m going to do everything I can to make sure that doesn’t change while you’re with me.”
Trey McDaniel is a paramedic with MedStar Mobile Healthcare in Fort Worth, Tex.
A version of this article first appeared on Medscape.com.
It seemed like a typical kind of day. I was out the door by 6:00 a.m., heading into work for a shift on I-35 West, my daily commute. It was still dark out. A little bit colder that morning, but nothing us Texans aren’t used to.
I was cruising down the tollway, which is separated from the main highway by a barrier. That stretch has a slight hill and turns to the left. You can’t see anything beyond the hill when you’re at the bottom.
As I made my way up, I spotted brake lights about 400 yards ahead. I eased on my brake, and next thing I knew, I was sliding.
I realized, I’m on black ice.
I was driving a 2011 Toyota FJ Cruiser and I had it all beefed up – lift tires, winch bumpers front and back. I had never had any sort of issue like that.
My ABS brakes kicked in. I slowed, but not fast enough. I saw a wall of crashed cars in front of me.
I was in the left-hand lane, so I turned my steering wheel into the center median. I could hear the whole side of my vehicle scraping against it. I managed to slow down enough to just tap the vehicle in front of me.
I looked in my passenger side-view mirror and saw headlights coming in the right lane. But this car couldn’t slow down. It crashed into the wreckage to my right.
That’s when it sunk in: There was going to be a car coming in my lane, and it might not be able to stop.
I looked in my rear-view mirror and saw headlights. Sparks flying off that center median.
I didn’t know at the time, but it was a fully loaded semi-truck traveling about 60 miles an hour.
I had a split second to think: This is it. This is how it ends. I closed my eyes.
It was the most violent impact I’ve ever experienced in my life.
I had no idea until afterward, but I had slammed into the vehicle in front of me and my SUV did a kind of 360° barrel roll over the median into the northbound lanes, landing wheels down on top of my sheared off roof rack.
Everything stopped. I opened my eyes. All my airbags had deployed. I gently tried moving my arms and legs, and they worked. I couldn’t move my left foot. It was wedged underneath the brake pedal. But I wasn’t in any pain, just very confused and disoriented. I knew I needed to get out of the vehicle.
My door was wedged shut, so I crawled out of the broken window, slipping on the black ice. I realized I had hit a Fort Worth police cruiser, now all smashed up. The driver couldn’t open his door. So, I helped him force it open, got him out of the vehicle, and checked on him. He was fine.
I had no idea how many vehicles and people were involved. I was in so much shock that the only thing I could do was immediately revert back to my training. I was the only first responder there.
I was helping people with lacerations, back and neck issues from the violent impacts. When you’re involved in a mass casualty incident like that, you have to assess which patients will be the most viable and need the most immediate attention. You have greens, yellows, reds, and then blacks – the deceased. Someone who doesn’t have a pulse and isn’t breathing, you can’t necessarily do CPR because you don’t have enough resources. You have to use your best judgment.
Meanwhile, the crashes kept coming. I found out later I was roughly vehicle No. 50 in the pileup; 83 more would follow. I heard them over and over – a crash and then screams from people in their vehicles. Each time a car hit, the entire pileup would move a couple of inches, getting more and more compacted. With that going on, I couldn’t go in there to pull people out. That scene was absolutely unsafe.
It felt like forever, but about 10 minutes later, an ambulance showed up, and I walked over to them. Because I was in my work uniform, they thought I was there on a call.
A couple fire crews came, and a firefighter yelled, “Hey, we need a backboard!” So, I grabbed a backboard from their unit and helped load up a patient. Then I heard somebody screaming, “This patient needs a stretcher!” A woman was having lumbar pain that seemed excruciating. I helped move her from the wreckage and carry her over to the stretcher. I started trying to get as many people as I could out of their cars.
Around this time, one of my supervisors showed up. He thought I was there working. But then he asked me, “Why is your face bleeding? Why do you have blood coming from your nose?” I pointed to my vehicle, and his jaw just dropped. He said, “Okay, you’re done. Go sit in my vehicle over there.”
He put a stop to my helping out, which was probably for the best. Because I actually had a concussion, a bone contusion in my foot, and a severely sprained ankle. The next day, I felt like I had gotten hit by a truck. (I had!) But when you have so much adrenaline pumping, you don’t feel pain or emotion. You don’t really feel anything.
While I was sitting in that vehicle, I called my mom to let her know I was okay. My parents were watching the news, and there was an aerial view of the accident. It was massive – a giant pile of metal stretching 200 or 300 yards. Six people had perished, more than 60 were hurt.
That night, our public information officer reached out to me about doing an interview with NBC. So, I told my story about what happened. Because of the concussion, a lot of it was a blur.
A day later, I got a call on my cell phone and someone said, “This is Tyler from Toyota. We saw the NBC interview. We wanted to let you know, don’t worry about getting a new vehicle. Just tell us what color 4Runner you want.”
My first thought was: Okay, this can’t be real. This doesn’t happen to people like me. But it turned out that it was, and they put me in a brand new vehicle.
Toyota started sending me to events like NASCAR races, putting me up in VIP suites. It was a cool experience. But it’s just surface stuff – it’s never going to erase what happened. The experience left a mark. It took me 6 months to a year to get rid of that feeling of the impact. Every time I tried to fall asleep, the whole scenario would replay in my head.
In EMS, we have a saying: “Every patient is practice for the next one.” That pileup – you can’t train for something like that. We all learned from it, so we can better prepare if anything like that happens again.
Since then, I’ve seen people die in motor vehicle collisions from a lot less than what happened to me. I’m not religious or spiritual, but I believe there must be a reason why I’m still here.
Now I see patients in traffic accidents who are very distraught even though they’re going to be okay. I tell them, “I’m sorry this happened to you. But remember, this is not the end. You are alive. And I’m going to do everything I can to make sure that doesn’t change while you’re with me.”
Trey McDaniel is a paramedic with MedStar Mobile Healthcare in Fort Worth, Tex.
A version of this article first appeared on Medscape.com.
Obesity: Don’t separate mental health from physical health
“The patient is ready,” the medical assistant informs you while handing you the chart. The chart reads: “Chief complaint: Weight gain/Discuss weight loss options.” You note the normal vital signs other than an increased BMI to 34 from 4 months ago. You knock on the exam room door with your plan half-formulated.
“Come in,” the patient says, almost too softly for you to hear. Shock overtakes you as you enter the room and see something you never imagined. The patient is holding their disconnected head in their lap as they say, “Nice to see you, Doc. I want to do something about my weight.”
You’re baffled at how they are speaking with a disconnected head. Of course, this outlandish patient scenario isn’t real. Or is it?
Patients with mental health concerns don’t literally present with their head disconnected from their bodies. Too often, mental health is treated as separate from physical health, especially regarding weight management and obesity. However, studies have shown an association between mental health and obesity. In this pivotal time of pharmacologic innovation in obesity care, we must also ensure that we effectively address the mental health of our patients with obesity.
Screening
Mental health conditions can look different for everyone. It can be hard to diagnose a mental health condition without validated screening. For example, depression is one of the most common mental health disorders. The U.S. Preventive Services Task Force recommends depression screening in all adults.
The Patient Health Questionnaire-2 (PHQ-2) is one screening tool that can alert doctors and clinicians to potential depression. Patients with obesity have higher rates of depression and other mental health conditions. It’s even more critical to screen for depression and other mental health disorders when prescribing these new medications, given recent reports of suicidal ideation with certain antiobesity medications.
Stigma
Mental health–related stigma can trigger shame and prevent patients from seeking psychological help. Furthermore, compounded stigma in patients with larger bodies (weight bias) and from marginalized communities such as the Black community (racial discrimination) add more barriers to seeking mental health care. When patients seek care for mental health conditions, they may feel more comfortable seeing a primary care physician or other clinician than a mental health professional. Therefore, all physicians and clinicians are integral in normalizing mental health care. Instead of treating mental health as separate from physical health, discussing the bidirectional relationship between mental health conditions and physiologic diseases can help patients understand that having a mental health condition isn’t a choice and facilitate openness to multiple treatment options to improve their quality of life.
Support
Addressing mental health effectively often requires multiple layers of patient support. Support can come from loved ones or community groups. But for severe stress and other mental health conditions, treatment with psychotherapy or psychiatric medications is essential. Unfortunately, even if a patient is willing to see a mental health professional, availability or access may be a challenge. Therefore, other clinicians may have to step in and serve as a bridge to mental health care. It’s also essential to ensure that patients are aware of crisis support lines and online resources for mental health care.
Stress
Having a high level of stress can be harmful physically and can also worsen mental health conditions. Additionally, it can contribute to a higher risk for obesity and can trigger emotional eating. Chronic stress has become so common in society that patients often underestimate how much stress they are under. Assessments like the Holmes-Rahe Stress Inventory can help patients identify and quantify potential stressors. While some stressors are uncontrollable, such as social determinants of health (SDOH), addressing controllable stressors and improving coping mechanisms is possible. For instance, mindfulness and breathwork are easy to follow and relatively accessible for most patients.
Social determinants of health
For a treatment plan to be maximally impactful, we must incorporate SDOH in clinical care. SDOH includes financial instability, safe neighborhoods, and more, and can significantly influence an ideal treatment plan. Furthermore, a high SDOH burden can negatively affect mental health and obesity rates. It’s helpful to incorporate patients’ SDOH burden into treatment planning. Learn how to take action on SDOH.
Empowerment
Patients who address their mental health have taken a courageous step toward health and healing. As mentioned, they may experience gaps in care while awaiting connection to the next steps of their journey, such as starting care with a mental health professional or waiting for a medication to take effect. All clinicians can empower patients about their weight by informing them that:
Food may affect their mood. Studies show that certain foods and eating patterns are associated with high levels of depression and anxiety. Limiting processed foods and increasing fruits, vegetables, and foods high in vitamin D, C, and other nutrients is helpful. Everyone is different, so encourage patients to pay attention to how food uniquely affects their mood by keeping a food/feeling log for 1-3 days.
Move more. Increased physical activity can improve mental health.
Get outdoors. Time in nature is associated with better mental health. Spending as little as 10 minutes outside can be beneficial. It’s important to be aware that SDOH factors such as unsafe environments or limited outdoor access may make this difficult for some patients.
Positive stress-relieving activities. Each person has their own way of reducing stress. It is helpful to remind patients of unhealthy stress relievers such as overeating, drinking alcohol, and smoking, and encourage them to replace those with positive stress relievers.
Spiritual well-being. Spirituality is often overlooked in health care. But studies have shown that incorporating a person’s spirituality may have positive health benefits.
It’s time to stop disconnecting mental health from physical health. Each clinician plays a vital role in treating the whole person. Just as you wouldn’t let a patient with a disconnected head leave the office without addressing it, let’s not leave mental health out when addressing our patients’ weight concerns.
Dr. Gonsahn-Bollie is an integrative obesity specialist focused on individualized solutions for emotional and biological overeating. Connect with her at www.embraceyouweightloss.com or on Instagram @embraceyoumd. Her bestselling book, “Embrace You: Your Guide to Transforming Weight Loss Misconceptions Into Lifelong Wellness,” (Baltimore: Purposely Created Publishing Group, 2019) was Healthline.com’s Best Overall Weight Loss Book of 2022 and one of Livestrong.com’s 8 Best Weight-Loss Books to Read in 2022.
Dr. Gonsahn-Bollie is CEO and Lead Physician, Embrace You Weight and Wellness, Telehealth & Virtual Counseling. She has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“The patient is ready,” the medical assistant informs you while handing you the chart. The chart reads: “Chief complaint: Weight gain/Discuss weight loss options.” You note the normal vital signs other than an increased BMI to 34 from 4 months ago. You knock on the exam room door with your plan half-formulated.
“Come in,” the patient says, almost too softly for you to hear. Shock overtakes you as you enter the room and see something you never imagined. The patient is holding their disconnected head in their lap as they say, “Nice to see you, Doc. I want to do something about my weight.”
You’re baffled at how they are speaking with a disconnected head. Of course, this outlandish patient scenario isn’t real. Or is it?
Patients with mental health concerns don’t literally present with their head disconnected from their bodies. Too often, mental health is treated as separate from physical health, especially regarding weight management and obesity. However, studies have shown an association between mental health and obesity. In this pivotal time of pharmacologic innovation in obesity care, we must also ensure that we effectively address the mental health of our patients with obesity.
Screening
Mental health conditions can look different for everyone. It can be hard to diagnose a mental health condition without validated screening. For example, depression is one of the most common mental health disorders. The U.S. Preventive Services Task Force recommends depression screening in all adults.
The Patient Health Questionnaire-2 (PHQ-2) is one screening tool that can alert doctors and clinicians to potential depression. Patients with obesity have higher rates of depression and other mental health conditions. It’s even more critical to screen for depression and other mental health disorders when prescribing these new medications, given recent reports of suicidal ideation with certain antiobesity medications.
Stigma
Mental health–related stigma can trigger shame and prevent patients from seeking psychological help. Furthermore, compounded stigma in patients with larger bodies (weight bias) and from marginalized communities such as the Black community (racial discrimination) add more barriers to seeking mental health care. When patients seek care for mental health conditions, they may feel more comfortable seeing a primary care physician or other clinician than a mental health professional. Therefore, all physicians and clinicians are integral in normalizing mental health care. Instead of treating mental health as separate from physical health, discussing the bidirectional relationship between mental health conditions and physiologic diseases can help patients understand that having a mental health condition isn’t a choice and facilitate openness to multiple treatment options to improve their quality of life.
Support
Addressing mental health effectively often requires multiple layers of patient support. Support can come from loved ones or community groups. But for severe stress and other mental health conditions, treatment with psychotherapy or psychiatric medications is essential. Unfortunately, even if a patient is willing to see a mental health professional, availability or access may be a challenge. Therefore, other clinicians may have to step in and serve as a bridge to mental health care. It’s also essential to ensure that patients are aware of crisis support lines and online resources for mental health care.
Stress
Having a high level of stress can be harmful physically and can also worsen mental health conditions. Additionally, it can contribute to a higher risk for obesity and can trigger emotional eating. Chronic stress has become so common in society that patients often underestimate how much stress they are under. Assessments like the Holmes-Rahe Stress Inventory can help patients identify and quantify potential stressors. While some stressors are uncontrollable, such as social determinants of health (SDOH), addressing controllable stressors and improving coping mechanisms is possible. For instance, mindfulness and breathwork are easy to follow and relatively accessible for most patients.
Social determinants of health
For a treatment plan to be maximally impactful, we must incorporate SDOH in clinical care. SDOH includes financial instability, safe neighborhoods, and more, and can significantly influence an ideal treatment plan. Furthermore, a high SDOH burden can negatively affect mental health and obesity rates. It’s helpful to incorporate patients’ SDOH burden into treatment planning. Learn how to take action on SDOH.
Empowerment
Patients who address their mental health have taken a courageous step toward health and healing. As mentioned, they may experience gaps in care while awaiting connection to the next steps of their journey, such as starting care with a mental health professional or waiting for a medication to take effect. All clinicians can empower patients about their weight by informing them that:
Food may affect their mood. Studies show that certain foods and eating patterns are associated with high levels of depression and anxiety. Limiting processed foods and increasing fruits, vegetables, and foods high in vitamin D, C, and other nutrients is helpful. Everyone is different, so encourage patients to pay attention to how food uniquely affects their mood by keeping a food/feeling log for 1-3 days.
Move more. Increased physical activity can improve mental health.
Get outdoors. Time in nature is associated with better mental health. Spending as little as 10 minutes outside can be beneficial. It’s important to be aware that SDOH factors such as unsafe environments or limited outdoor access may make this difficult for some patients.
Positive stress-relieving activities. Each person has their own way of reducing stress. It is helpful to remind patients of unhealthy stress relievers such as overeating, drinking alcohol, and smoking, and encourage them to replace those with positive stress relievers.
Spiritual well-being. Spirituality is often overlooked in health care. But studies have shown that incorporating a person’s spirituality may have positive health benefits.
It’s time to stop disconnecting mental health from physical health. Each clinician plays a vital role in treating the whole person. Just as you wouldn’t let a patient with a disconnected head leave the office without addressing it, let’s not leave mental health out when addressing our patients’ weight concerns.
Dr. Gonsahn-Bollie is an integrative obesity specialist focused on individualized solutions for emotional and biological overeating. Connect with her at www.embraceyouweightloss.com or on Instagram @embraceyoumd. Her bestselling book, “Embrace You: Your Guide to Transforming Weight Loss Misconceptions Into Lifelong Wellness,” (Baltimore: Purposely Created Publishing Group, 2019) was Healthline.com’s Best Overall Weight Loss Book of 2022 and one of Livestrong.com’s 8 Best Weight-Loss Books to Read in 2022.
Dr. Gonsahn-Bollie is CEO and Lead Physician, Embrace You Weight and Wellness, Telehealth & Virtual Counseling. She has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“The patient is ready,” the medical assistant informs you while handing you the chart. The chart reads: “Chief complaint: Weight gain/Discuss weight loss options.” You note the normal vital signs other than an increased BMI to 34 from 4 months ago. You knock on the exam room door with your plan half-formulated.
“Come in,” the patient says, almost too softly for you to hear. Shock overtakes you as you enter the room and see something you never imagined. The patient is holding their disconnected head in their lap as they say, “Nice to see you, Doc. I want to do something about my weight.”
You’re baffled at how they are speaking with a disconnected head. Of course, this outlandish patient scenario isn’t real. Or is it?
Patients with mental health concerns don’t literally present with their head disconnected from their bodies. Too often, mental health is treated as separate from physical health, especially regarding weight management and obesity. However, studies have shown an association between mental health and obesity. In this pivotal time of pharmacologic innovation in obesity care, we must also ensure that we effectively address the mental health of our patients with obesity.
Screening
Mental health conditions can look different for everyone. It can be hard to diagnose a mental health condition without validated screening. For example, depression is one of the most common mental health disorders. The U.S. Preventive Services Task Force recommends depression screening in all adults.
The Patient Health Questionnaire-2 (PHQ-2) is one screening tool that can alert doctors and clinicians to potential depression. Patients with obesity have higher rates of depression and other mental health conditions. It’s even more critical to screen for depression and other mental health disorders when prescribing these new medications, given recent reports of suicidal ideation with certain antiobesity medications.
Stigma
Mental health–related stigma can trigger shame and prevent patients from seeking psychological help. Furthermore, compounded stigma in patients with larger bodies (weight bias) and from marginalized communities such as the Black community (racial discrimination) add more barriers to seeking mental health care. When patients seek care for mental health conditions, they may feel more comfortable seeing a primary care physician or other clinician than a mental health professional. Therefore, all physicians and clinicians are integral in normalizing mental health care. Instead of treating mental health as separate from physical health, discussing the bidirectional relationship between mental health conditions and physiologic diseases can help patients understand that having a mental health condition isn’t a choice and facilitate openness to multiple treatment options to improve their quality of life.
Support
Addressing mental health effectively often requires multiple layers of patient support. Support can come from loved ones or community groups. But for severe stress and other mental health conditions, treatment with psychotherapy or psychiatric medications is essential. Unfortunately, even if a patient is willing to see a mental health professional, availability or access may be a challenge. Therefore, other clinicians may have to step in and serve as a bridge to mental health care. It’s also essential to ensure that patients are aware of crisis support lines and online resources for mental health care.
Stress
Having a high level of stress can be harmful physically and can also worsen mental health conditions. Additionally, it can contribute to a higher risk for obesity and can trigger emotional eating. Chronic stress has become so common in society that patients often underestimate how much stress they are under. Assessments like the Holmes-Rahe Stress Inventory can help patients identify and quantify potential stressors. While some stressors are uncontrollable, such as social determinants of health (SDOH), addressing controllable stressors and improving coping mechanisms is possible. For instance, mindfulness and breathwork are easy to follow and relatively accessible for most patients.
Social determinants of health
For a treatment plan to be maximally impactful, we must incorporate SDOH in clinical care. SDOH includes financial instability, safe neighborhoods, and more, and can significantly influence an ideal treatment plan. Furthermore, a high SDOH burden can negatively affect mental health and obesity rates. It’s helpful to incorporate patients’ SDOH burden into treatment planning. Learn how to take action on SDOH.
Empowerment
Patients who address their mental health have taken a courageous step toward health and healing. As mentioned, they may experience gaps in care while awaiting connection to the next steps of their journey, such as starting care with a mental health professional or waiting for a medication to take effect. All clinicians can empower patients about their weight by informing them that:
Food may affect their mood. Studies show that certain foods and eating patterns are associated with high levels of depression and anxiety. Limiting processed foods and increasing fruits, vegetables, and foods high in vitamin D, C, and other nutrients is helpful. Everyone is different, so encourage patients to pay attention to how food uniquely affects their mood by keeping a food/feeling log for 1-3 days.
Move more. Increased physical activity can improve mental health.
Get outdoors. Time in nature is associated with better mental health. Spending as little as 10 minutes outside can be beneficial. It’s important to be aware that SDOH factors such as unsafe environments or limited outdoor access may make this difficult for some patients.
Positive stress-relieving activities. Each person has their own way of reducing stress. It is helpful to remind patients of unhealthy stress relievers such as overeating, drinking alcohol, and smoking, and encourage them to replace those with positive stress relievers.
Spiritual well-being. Spirituality is often overlooked in health care. But studies have shown that incorporating a person’s spirituality may have positive health benefits.
It’s time to stop disconnecting mental health from physical health. Each clinician plays a vital role in treating the whole person. Just as you wouldn’t let a patient with a disconnected head leave the office without addressing it, let’s not leave mental health out when addressing our patients’ weight concerns.
Dr. Gonsahn-Bollie is an integrative obesity specialist focused on individualized solutions for emotional and biological overeating. Connect with her at www.embraceyouweightloss.com or on Instagram @embraceyoumd. Her bestselling book, “Embrace You: Your Guide to Transforming Weight Loss Misconceptions Into Lifelong Wellness,” (Baltimore: Purposely Created Publishing Group, 2019) was Healthline.com’s Best Overall Weight Loss Book of 2022 and one of Livestrong.com’s 8 Best Weight-Loss Books to Read in 2022.
Dr. Gonsahn-Bollie is CEO and Lead Physician, Embrace You Weight and Wellness, Telehealth & Virtual Counseling. She has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Prescribing lifestyle changes: When medicine isn’t enough
In psychiatry, patients come to us with their list of symptoms, often a diagnosis they’ve made themselves, and the expectation that they will be given medication to fix their problem. Their diagnoses are often right on target – people often know if they are depressed or anxious, and Doctor Google may provide useful information.
Sometimes they want a specific medication, one they saw in a TV ad, or one that helped them in the past or has helped someone they know. As psychiatrists have focused more on their strengths as psychopharmacologists and less on psychotherapy, it gets easy for both the patient and the doctor to look to medication, cocktails, and titration as the only thing we do.
“My medicine stopped working,” is a line I commonly hear. Often the patient is on a complicated regimen that has been serving them well, and it seems unlikely that the five psychotropic medications they are taking have suddenly “stopped working.” An obvious exception is the SSRI “poop out” that can occur 6-12 months or more after beginning treatment. In addition, it’s important to make sure patients are taking their medications as prescribed, and that the generic formulations have not changed.
But as rates of mental illness increase, some of it spurred on by difficult times,
This is not to devalue our medications, but to help the patient see symptoms as having multiple factors and give them some means to intervene, in addition to medications. At the beginning of therapy, it is important to “prescribe” lifestyle changes that will facilitate the best possible outcomes.
Nonpharmaceutical prescriptions
Early in my career, people with alcohol use problems were told they needed to be substance free before they were candidates for antidepressants. While we no longer do that, it is still important to emphasize abstinence from addictive substances, and to recommend specific treatment when necessary.
Patients are often reluctant to see their use of alcohol, marijuana (it’s medical! It’s part of wellness!), or their pain medications as part of the problem, and this can be difficult. There have been times, after multiple medications have failed to help their symptoms, when I have said, “If you don’t get treatment for this problem, I am not going to be able to help you feel better” and that has been motivating for the patient.
There are other “prescriptions” to write. Regular sleep is essential for people with mood disorders, and this can be difficult for many patients, especially those who do shift work, or who have regular disruptions to their sleep from noise, pets, and children. Exercise is wonderful for the cardiovascular system, calms anxiety, and maintains strength, endurance, mobility, and quality of life as people age. But it can be a hard sell to people in a mental health crisis.
Nature is healing, and sunshine helps with maintaining circadian rhythms. For those who don’t exercise, I often “prescribe” 20 to 30 minutes a day of walking, preferably outside, during daylight hours, in a park or natural setting. For people with anxiety, it is important to check their caffeine consumption and to suggest ways to moderate it – moving to decaffeinated beverages or titrating down by mixing decaf with caffeinated.
Meditation is something that many people find helpful. For anxious people, it can be very difficult, and I will prescribe a specific instructional video course that I like on the well-being app InsightTimer – Sarah Blondin’s Learn How to Meditate in Seven Days. The sessions are approximately 10 minutes long, and that seems like the right amount of time for a beginner.
When people are very ill and don’t want to go into the hospital, I talk with them about things that happen in the hospital that are helpful, things they can try to mimic at home. In the hospital, patients don’t go to work, they don’t spend hours a day on the computer, and they are given a pass from dealing with the routine stresses of daily life.
I ask them to take time off work, to avoid as much stress as possible, to spend time with loved ones who give them comfort, and to avoid the people who leave them feeling drained or distressed. I ask them to engage in activities they find healing, to eat well, exercise, and avoid social media. In the hospital, I emphasize, they wake patients up in the morning, ask them to get out of bed and engage in therapeutic activities. They are fed and kept from intoxicants.
When it comes to nutrition, we know so little about how food affects mental health. I feel like it can’t hurt to ask people to avoid fast foods, soft drinks, and processed foods, and so I do.
And what about compliance? Of course, not everyone complies; not everyone is interested in making changes and these can be hard changes. I’ve recently started to recommend the book Atomic Habits by James Clear. Sometimes a bit of motivational interviewing can also be helpful in getting people to look at slowly moving toward making changes.
In prescribing lifestyle changes, it is important to offer most of these changes as suggestions, not as things we insist on, or that will leave the patient feeling ashamed if he doesn’t follow through. They should be discussed early in treatment so that patients don’t feel blamed for their illness or relapses. As with all the things we prescribe, some of these behavior changes help some of the people some of the time. Suggesting them, however, makes the strong statement that treating psychiatric disorders can be about more than passively swallowing a pill.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She disclosed no relevant conflicts of interest.
In psychiatry, patients come to us with their list of symptoms, often a diagnosis they’ve made themselves, and the expectation that they will be given medication to fix their problem. Their diagnoses are often right on target – people often know if they are depressed or anxious, and Doctor Google may provide useful information.
Sometimes they want a specific medication, one they saw in a TV ad, or one that helped them in the past or has helped someone they know. As psychiatrists have focused more on their strengths as psychopharmacologists and less on psychotherapy, it gets easy for both the patient and the doctor to look to medication, cocktails, and titration as the only thing we do.
“My medicine stopped working,” is a line I commonly hear. Often the patient is on a complicated regimen that has been serving them well, and it seems unlikely that the five psychotropic medications they are taking have suddenly “stopped working.” An obvious exception is the SSRI “poop out” that can occur 6-12 months or more after beginning treatment. In addition, it’s important to make sure patients are taking their medications as prescribed, and that the generic formulations have not changed.
But as rates of mental illness increase, some of it spurred on by difficult times,
This is not to devalue our medications, but to help the patient see symptoms as having multiple factors and give them some means to intervene, in addition to medications. At the beginning of therapy, it is important to “prescribe” lifestyle changes that will facilitate the best possible outcomes.
Nonpharmaceutical prescriptions
Early in my career, people with alcohol use problems were told they needed to be substance free before they were candidates for antidepressants. While we no longer do that, it is still important to emphasize abstinence from addictive substances, and to recommend specific treatment when necessary.
Patients are often reluctant to see their use of alcohol, marijuana (it’s medical! It’s part of wellness!), or their pain medications as part of the problem, and this can be difficult. There have been times, after multiple medications have failed to help their symptoms, when I have said, “If you don’t get treatment for this problem, I am not going to be able to help you feel better” and that has been motivating for the patient.
There are other “prescriptions” to write. Regular sleep is essential for people with mood disorders, and this can be difficult for many patients, especially those who do shift work, or who have regular disruptions to their sleep from noise, pets, and children. Exercise is wonderful for the cardiovascular system, calms anxiety, and maintains strength, endurance, mobility, and quality of life as people age. But it can be a hard sell to people in a mental health crisis.
Nature is healing, and sunshine helps with maintaining circadian rhythms. For those who don’t exercise, I often “prescribe” 20 to 30 minutes a day of walking, preferably outside, during daylight hours, in a park or natural setting. For people with anxiety, it is important to check their caffeine consumption and to suggest ways to moderate it – moving to decaffeinated beverages or titrating down by mixing decaf with caffeinated.
Meditation is something that many people find helpful. For anxious people, it can be very difficult, and I will prescribe a specific instructional video course that I like on the well-being app InsightTimer – Sarah Blondin’s Learn How to Meditate in Seven Days. The sessions are approximately 10 minutes long, and that seems like the right amount of time for a beginner.
When people are very ill and don’t want to go into the hospital, I talk with them about things that happen in the hospital that are helpful, things they can try to mimic at home. In the hospital, patients don’t go to work, they don’t spend hours a day on the computer, and they are given a pass from dealing with the routine stresses of daily life.
I ask them to take time off work, to avoid as much stress as possible, to spend time with loved ones who give them comfort, and to avoid the people who leave them feeling drained or distressed. I ask them to engage in activities they find healing, to eat well, exercise, and avoid social media. In the hospital, I emphasize, they wake patients up in the morning, ask them to get out of bed and engage in therapeutic activities. They are fed and kept from intoxicants.
When it comes to nutrition, we know so little about how food affects mental health. I feel like it can’t hurt to ask people to avoid fast foods, soft drinks, and processed foods, and so I do.
And what about compliance? Of course, not everyone complies; not everyone is interested in making changes and these can be hard changes. I’ve recently started to recommend the book Atomic Habits by James Clear. Sometimes a bit of motivational interviewing can also be helpful in getting people to look at slowly moving toward making changes.
In prescribing lifestyle changes, it is important to offer most of these changes as suggestions, not as things we insist on, or that will leave the patient feeling ashamed if he doesn’t follow through. They should be discussed early in treatment so that patients don’t feel blamed for their illness or relapses. As with all the things we prescribe, some of these behavior changes help some of the people some of the time. Suggesting them, however, makes the strong statement that treating psychiatric disorders can be about more than passively swallowing a pill.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She disclosed no relevant conflicts of interest.
In psychiatry, patients come to us with their list of symptoms, often a diagnosis they’ve made themselves, and the expectation that they will be given medication to fix their problem. Their diagnoses are often right on target – people often know if they are depressed or anxious, and Doctor Google may provide useful information.
Sometimes they want a specific medication, one they saw in a TV ad, or one that helped them in the past or has helped someone they know. As psychiatrists have focused more on their strengths as psychopharmacologists and less on psychotherapy, it gets easy for both the patient and the doctor to look to medication, cocktails, and titration as the only thing we do.
“My medicine stopped working,” is a line I commonly hear. Often the patient is on a complicated regimen that has been serving them well, and it seems unlikely that the five psychotropic medications they are taking have suddenly “stopped working.” An obvious exception is the SSRI “poop out” that can occur 6-12 months or more after beginning treatment. In addition, it’s important to make sure patients are taking their medications as prescribed, and that the generic formulations have not changed.
But as rates of mental illness increase, some of it spurred on by difficult times,
This is not to devalue our medications, but to help the patient see symptoms as having multiple factors and give them some means to intervene, in addition to medications. At the beginning of therapy, it is important to “prescribe” lifestyle changes that will facilitate the best possible outcomes.
Nonpharmaceutical prescriptions
Early in my career, people with alcohol use problems were told they needed to be substance free before they were candidates for antidepressants. While we no longer do that, it is still important to emphasize abstinence from addictive substances, and to recommend specific treatment when necessary.
Patients are often reluctant to see their use of alcohol, marijuana (it’s medical! It’s part of wellness!), or their pain medications as part of the problem, and this can be difficult. There have been times, after multiple medications have failed to help their symptoms, when I have said, “If you don’t get treatment for this problem, I am not going to be able to help you feel better” and that has been motivating for the patient.
There are other “prescriptions” to write. Regular sleep is essential for people with mood disorders, and this can be difficult for many patients, especially those who do shift work, or who have regular disruptions to their sleep from noise, pets, and children. Exercise is wonderful for the cardiovascular system, calms anxiety, and maintains strength, endurance, mobility, and quality of life as people age. But it can be a hard sell to people in a mental health crisis.
Nature is healing, and sunshine helps with maintaining circadian rhythms. For those who don’t exercise, I often “prescribe” 20 to 30 minutes a day of walking, preferably outside, during daylight hours, in a park or natural setting. For people with anxiety, it is important to check their caffeine consumption and to suggest ways to moderate it – moving to decaffeinated beverages or titrating down by mixing decaf with caffeinated.
Meditation is something that many people find helpful. For anxious people, it can be very difficult, and I will prescribe a specific instructional video course that I like on the well-being app InsightTimer – Sarah Blondin’s Learn How to Meditate in Seven Days. The sessions are approximately 10 minutes long, and that seems like the right amount of time for a beginner.
When people are very ill and don’t want to go into the hospital, I talk with them about things that happen in the hospital that are helpful, things they can try to mimic at home. In the hospital, patients don’t go to work, they don’t spend hours a day on the computer, and they are given a pass from dealing with the routine stresses of daily life.
I ask them to take time off work, to avoid as much stress as possible, to spend time with loved ones who give them comfort, and to avoid the people who leave them feeling drained or distressed. I ask them to engage in activities they find healing, to eat well, exercise, and avoid social media. In the hospital, I emphasize, they wake patients up in the morning, ask them to get out of bed and engage in therapeutic activities. They are fed and kept from intoxicants.
When it comes to nutrition, we know so little about how food affects mental health. I feel like it can’t hurt to ask people to avoid fast foods, soft drinks, and processed foods, and so I do.
And what about compliance? Of course, not everyone complies; not everyone is interested in making changes and these can be hard changes. I’ve recently started to recommend the book Atomic Habits by James Clear. Sometimes a bit of motivational interviewing can also be helpful in getting people to look at slowly moving toward making changes.
In prescribing lifestyle changes, it is important to offer most of these changes as suggestions, not as things we insist on, or that will leave the patient feeling ashamed if he doesn’t follow through. They should be discussed early in treatment so that patients don’t feel blamed for their illness or relapses. As with all the things we prescribe, some of these behavior changes help some of the people some of the time. Suggesting them, however, makes the strong statement that treating psychiatric disorders can be about more than passively swallowing a pill.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She disclosed no relevant conflicts of interest.
Will this trial help solve chronic back pain?
Chronic pain, and back pain in particular, is among the most frequent concerns for patients in the primary care setting. Roughly 8% of adults in the United States say they suffer from chronic low back pain, and many of them say the pain is significant enough to impair their ability to move, work, and otherwise enjoy life. All this, despite decades of research and countless millions in funding to find the optimal approach to treating chronic pain.
As the United States crawls out of the opioid epidemic, a group of pain specialists is hoping to identify effective, personalized approaches to managing back pain. Daniel Clauw, MD, professor of anesthesiology, internal medicine, and psychiatry at the University of Michigan, Ann Arbor, is helping lead the BEST trial. With projected enrollment of nearly 800 patients, BEST will be the largest federally funded clinical trial of interventions to treat chronic low back pain.
In an interview, The interview has been edited for length and clarity.
What are your thoughts on the current state of primary care physicians’ understanding and management of pain?
Primary care physicians need a lot of help in demystifying the diagnosis and treatment of any kind of pain, but back pain is a really good place to start. When it comes to back pain, most primary care physicians are not any more knowledgeable than a layperson.
What has the opioid debacle-cum-tragedy taught you about pain management, particular as regards people with chronic pain?
I don’t feel opioids should ever be used to treat chronic low back pain. The few long-term studies that have been performed using opioids for longer than 3 months suggest that they often make pain worse rather than just failing to make pain better – and we know they are associated with a significantly increased all-cause mortality with increased deaths from myocardial infarction, accidents, and suicides, in addition to overdose.
Given how many patients experience back pain, how did we come to the point at which primary care physicians are so ill equipped?
We’ve had terrible pain curricula in medical schools. To give you an example: I’m one of the leading pain experts in the world and I’m not allowed to teach our medical students their pain curriculum. The students learn about neurophysiology and the anatomy of the nerves, not what’s relevant in pain.
This is notorious in medical school: Curricula are almost impossible to modify and change. So it starts with poor training in medical school. And then, regardless of what education they do or don’t get in medical school, a lot of their education about pain management is through our residencies – mainly in inpatient settings, where you’re really seeing the management of acute pain and not the management of chronic pain.
People get more accustomed to managing acute pain, where opioids are a reasonable option. It’s just that when you start managing subacute or chronic pain, opioids don’t work as well.
The other big problem is that historically, most people trained in medicine think that if you have pain in your elbow, there’s got to be something wrong in your elbow. This third mechanism of pain, central sensitization – or nociplastic pain – the kind of pain that we see in fibromyalgia, headache, and low back pain, where the pain is coming from the brain – that’s confusing to people. People can have pain without any damage or inflammation to that region of the body.
Physicians are trained that if there’s pain, there’s something wrong and we have to do surgery or there’s been some trauma. Most chronic pain is none of that. There’s a big disconnect between how people are trained, and then when they go out and are seeing a tremendous number of people with chronic pain.
What are the different types of pain, and how should they inform clinicians’ understanding about what approaches might work for managing their patients in pain?
The way the central nervous system responds to pain is analogous to the loudness of an electric guitar. You can make an electric guitar louder either by strumming the strings harder or by turning up the amplifier. For many people with fibromyalgia, low back pain, and endometriosis, for example, the problem is really more that the amplifier is turned up too high rather than its being that the guitar is strummed too strongly. That kind of pain where the pain is not due to anatomic damage or inflammation is particularly flummoxing for providers.
Can you explain the design of the new study?
It’s a 13-site study looking at four treatments: enhanced self-care, cognitive-behavioral therapy, physical therapy, and duloxetine. It’s a big precision medicine trial, trying to take everything we’ve learned and putting it all into one big study.
We’re using a SMART design, which randomizes people to two of those treatments, unless they are very much improved from the first treatment. To be eligible for the trial, you have to be able to be randomized to three of the four treatments, and people can’t choose which of the four they get.
We give them one of those treatments for 12 weeks, and at the end of 12 weeks we make the call – “Did you respond or not respond?” – and then we go back to the phenotypic data we collected at the beginning of that trial and say, “What information at baseline that we collected predicts that someone is going to respond better to duloxetine or worse to duloxetine?” And then we create the phenotype that responds best to each of those four treatments.
None of our treatments works so well that someone doesn’t end up getting randomized to a second treatment. About 85% of people so far need a second treatment because they still have enough pain that they want more relief. But the nice thing about that is we’ve already done all the functional brain imaging and all these really expensive and time-consuming things.
We’re hoping to have around 700-800 people total in this trial, which means that around 170 people will get randomized to each of the four initial treatments. No one’s ever done a study that has functional brain imaging and all these other things in it with more than 80 or 100 people. The scale of this is totally unprecedented.
Given that the individual therapies don’t appear to be all that successful on their own, what is your goal?
The primary aim is to match the phenotypic characteristics of a patient with chronic low back pain with treatment response to each of these four treatments. So at the end, we can give clinicians information on which of the patients is going to respond to physical therapy, for instance.
Right now, about one out of three people respond to most treatments for pain. We think by doing a trial like this, we can take treatments that work in one out of three people and make them work in one out of two or two out of three people just by using them in the right people.
How do you differentiate between these types of pain in your study?
We phenotype people by asking them a number of questions. We also do brain imaging, look at their back with MRI, test biomechanics, and then give them four different treatments that we know work in groups of people with low back pain.
We think one of the first parts of the phenotype is, do they have pain just in their back? Or do they have pain in their back plus a lot of other body regions? Because the more body regions that people have pain in, the more likely it is that this is an amplifier problem rather than a guitar problem.
Treatments like physical therapy, surgery, and injections are going to work better for people in whom the pain is a guitar problem rather than an amplifier problem. And drugs like duloxetine, which works in the brain, and cognitive-behavioral therapy are going to work a lot better in the people with pain in multiple sites besides the back.
To pick up on your metaphor, do any symptoms help clinicians differentiate between the guitar and the amplifier?
Sleep problems, fatigue, memory problems, and mood problems are common in patients with chronic pain and are more common with amplifier pain. Because again, those are all central nervous system problems. And so we see that the people that have anxiety, depression, and a lot of distress are more likely to have this kind of pain.
Does medical imaging help?
There’s a terrible relationship between what you see on an MRI of the back and whether someone has pain or how severe the pain is going to be. There’s always going to be individuals that have a lot of anatomic damage who don’t have any pain because they happen to be on the other end of the continuum from fibromyalgia; they’re actually pain-insensitive people.
What are your thoughts about ketamine as a possible treatment for chronic pain?
I have a mentee who’s doing a ketamine trial. We’re doing psilocybin trials in patients with fibromyalgia. Ketamine is such a dirty drug; it has so many different mechanisms of action. It does have some psychedelic effects, but it also is an NMDA blocker. It really has so many different effects.
I think it’s being thrown around like water in settings where we don’t yet know it to be efficacious. Even the data in treatment-refractory depression are pretty weak, but we’re so desperate to do something for those patients. If you’re trying to harness the psychedelic properties of ketamine, I think there’s other psychedelics that are a lot more interesting, which is why we’re using psilocybin for a subset of patients. Most of us in the pain field think that the psychedelics will work best for the people with chronic pain who have a lot of comorbid psychiatric illness, especially the ones with a lot of trauma. These drugs will allow us therapeutically to get at a lot of these patients with the side-by-side psychotherapy that’s being done as people are getting care in the medicalized setting.
Dr. Clauw reported conflicts of interest with Pfizer, Tonix, Theravance, Zynerba, Samumed, Aptinyx, Daiichi Sankyo, Intec, Regeneron, Teva, Lundbeck, Virios, and Cerephex.
A version of this article first appeared on Medscape.com.
Chronic pain, and back pain in particular, is among the most frequent concerns for patients in the primary care setting. Roughly 8% of adults in the United States say they suffer from chronic low back pain, and many of them say the pain is significant enough to impair their ability to move, work, and otherwise enjoy life. All this, despite decades of research and countless millions in funding to find the optimal approach to treating chronic pain.
As the United States crawls out of the opioid epidemic, a group of pain specialists is hoping to identify effective, personalized approaches to managing back pain. Daniel Clauw, MD, professor of anesthesiology, internal medicine, and psychiatry at the University of Michigan, Ann Arbor, is helping lead the BEST trial. With projected enrollment of nearly 800 patients, BEST will be the largest federally funded clinical trial of interventions to treat chronic low back pain.
In an interview, The interview has been edited for length and clarity.
What are your thoughts on the current state of primary care physicians’ understanding and management of pain?
Primary care physicians need a lot of help in demystifying the diagnosis and treatment of any kind of pain, but back pain is a really good place to start. When it comes to back pain, most primary care physicians are not any more knowledgeable than a layperson.
What has the opioid debacle-cum-tragedy taught you about pain management, particular as regards people with chronic pain?
I don’t feel opioids should ever be used to treat chronic low back pain. The few long-term studies that have been performed using opioids for longer than 3 months suggest that they often make pain worse rather than just failing to make pain better – and we know they are associated with a significantly increased all-cause mortality with increased deaths from myocardial infarction, accidents, and suicides, in addition to overdose.
Given how many patients experience back pain, how did we come to the point at which primary care physicians are so ill equipped?
We’ve had terrible pain curricula in medical schools. To give you an example: I’m one of the leading pain experts in the world and I’m not allowed to teach our medical students their pain curriculum. The students learn about neurophysiology and the anatomy of the nerves, not what’s relevant in pain.
This is notorious in medical school: Curricula are almost impossible to modify and change. So it starts with poor training in medical school. And then, regardless of what education they do or don’t get in medical school, a lot of their education about pain management is through our residencies – mainly in inpatient settings, where you’re really seeing the management of acute pain and not the management of chronic pain.
People get more accustomed to managing acute pain, where opioids are a reasonable option. It’s just that when you start managing subacute or chronic pain, opioids don’t work as well.
The other big problem is that historically, most people trained in medicine think that if you have pain in your elbow, there’s got to be something wrong in your elbow. This third mechanism of pain, central sensitization – or nociplastic pain – the kind of pain that we see in fibromyalgia, headache, and low back pain, where the pain is coming from the brain – that’s confusing to people. People can have pain without any damage or inflammation to that region of the body.
Physicians are trained that if there’s pain, there’s something wrong and we have to do surgery or there’s been some trauma. Most chronic pain is none of that. There’s a big disconnect between how people are trained, and then when they go out and are seeing a tremendous number of people with chronic pain.
What are the different types of pain, and how should they inform clinicians’ understanding about what approaches might work for managing their patients in pain?
The way the central nervous system responds to pain is analogous to the loudness of an electric guitar. You can make an electric guitar louder either by strumming the strings harder or by turning up the amplifier. For many people with fibromyalgia, low back pain, and endometriosis, for example, the problem is really more that the amplifier is turned up too high rather than its being that the guitar is strummed too strongly. That kind of pain where the pain is not due to anatomic damage or inflammation is particularly flummoxing for providers.
Can you explain the design of the new study?
It’s a 13-site study looking at four treatments: enhanced self-care, cognitive-behavioral therapy, physical therapy, and duloxetine. It’s a big precision medicine trial, trying to take everything we’ve learned and putting it all into one big study.
We’re using a SMART design, which randomizes people to two of those treatments, unless they are very much improved from the first treatment. To be eligible for the trial, you have to be able to be randomized to three of the four treatments, and people can’t choose which of the four they get.
We give them one of those treatments for 12 weeks, and at the end of 12 weeks we make the call – “Did you respond or not respond?” – and then we go back to the phenotypic data we collected at the beginning of that trial and say, “What information at baseline that we collected predicts that someone is going to respond better to duloxetine or worse to duloxetine?” And then we create the phenotype that responds best to each of those four treatments.
None of our treatments works so well that someone doesn’t end up getting randomized to a second treatment. About 85% of people so far need a second treatment because they still have enough pain that they want more relief. But the nice thing about that is we’ve already done all the functional brain imaging and all these really expensive and time-consuming things.
We’re hoping to have around 700-800 people total in this trial, which means that around 170 people will get randomized to each of the four initial treatments. No one’s ever done a study that has functional brain imaging and all these other things in it with more than 80 or 100 people. The scale of this is totally unprecedented.
Given that the individual therapies don’t appear to be all that successful on their own, what is your goal?
The primary aim is to match the phenotypic characteristics of a patient with chronic low back pain with treatment response to each of these four treatments. So at the end, we can give clinicians information on which of the patients is going to respond to physical therapy, for instance.
Right now, about one out of three people respond to most treatments for pain. We think by doing a trial like this, we can take treatments that work in one out of three people and make them work in one out of two or two out of three people just by using them in the right people.
How do you differentiate between these types of pain in your study?
We phenotype people by asking them a number of questions. We also do brain imaging, look at their back with MRI, test biomechanics, and then give them four different treatments that we know work in groups of people with low back pain.
We think one of the first parts of the phenotype is, do they have pain just in their back? Or do they have pain in their back plus a lot of other body regions? Because the more body regions that people have pain in, the more likely it is that this is an amplifier problem rather than a guitar problem.
Treatments like physical therapy, surgery, and injections are going to work better for people in whom the pain is a guitar problem rather than an amplifier problem. And drugs like duloxetine, which works in the brain, and cognitive-behavioral therapy are going to work a lot better in the people with pain in multiple sites besides the back.
To pick up on your metaphor, do any symptoms help clinicians differentiate between the guitar and the amplifier?
Sleep problems, fatigue, memory problems, and mood problems are common in patients with chronic pain and are more common with amplifier pain. Because again, those are all central nervous system problems. And so we see that the people that have anxiety, depression, and a lot of distress are more likely to have this kind of pain.
Does medical imaging help?
There’s a terrible relationship between what you see on an MRI of the back and whether someone has pain or how severe the pain is going to be. There’s always going to be individuals that have a lot of anatomic damage who don’t have any pain because they happen to be on the other end of the continuum from fibromyalgia; they’re actually pain-insensitive people.
What are your thoughts about ketamine as a possible treatment for chronic pain?
I have a mentee who’s doing a ketamine trial. We’re doing psilocybin trials in patients with fibromyalgia. Ketamine is such a dirty drug; it has so many different mechanisms of action. It does have some psychedelic effects, but it also is an NMDA blocker. It really has so many different effects.
I think it’s being thrown around like water in settings where we don’t yet know it to be efficacious. Even the data in treatment-refractory depression are pretty weak, but we’re so desperate to do something for those patients. If you’re trying to harness the psychedelic properties of ketamine, I think there’s other psychedelics that are a lot more interesting, which is why we’re using psilocybin for a subset of patients. Most of us in the pain field think that the psychedelics will work best for the people with chronic pain who have a lot of comorbid psychiatric illness, especially the ones with a lot of trauma. These drugs will allow us therapeutically to get at a lot of these patients with the side-by-side psychotherapy that’s being done as people are getting care in the medicalized setting.
Dr. Clauw reported conflicts of interest with Pfizer, Tonix, Theravance, Zynerba, Samumed, Aptinyx, Daiichi Sankyo, Intec, Regeneron, Teva, Lundbeck, Virios, and Cerephex.
A version of this article first appeared on Medscape.com.
Chronic pain, and back pain in particular, is among the most frequent concerns for patients in the primary care setting. Roughly 8% of adults in the United States say they suffer from chronic low back pain, and many of them say the pain is significant enough to impair their ability to move, work, and otherwise enjoy life. All this, despite decades of research and countless millions in funding to find the optimal approach to treating chronic pain.
As the United States crawls out of the opioid epidemic, a group of pain specialists is hoping to identify effective, personalized approaches to managing back pain. Daniel Clauw, MD, professor of anesthesiology, internal medicine, and psychiatry at the University of Michigan, Ann Arbor, is helping lead the BEST trial. With projected enrollment of nearly 800 patients, BEST will be the largest federally funded clinical trial of interventions to treat chronic low back pain.
In an interview, The interview has been edited for length and clarity.
What are your thoughts on the current state of primary care physicians’ understanding and management of pain?
Primary care physicians need a lot of help in demystifying the diagnosis and treatment of any kind of pain, but back pain is a really good place to start. When it comes to back pain, most primary care physicians are not any more knowledgeable than a layperson.
What has the opioid debacle-cum-tragedy taught you about pain management, particular as regards people with chronic pain?
I don’t feel opioids should ever be used to treat chronic low back pain. The few long-term studies that have been performed using opioids for longer than 3 months suggest that they often make pain worse rather than just failing to make pain better – and we know they are associated with a significantly increased all-cause mortality with increased deaths from myocardial infarction, accidents, and suicides, in addition to overdose.
Given how many patients experience back pain, how did we come to the point at which primary care physicians are so ill equipped?
We’ve had terrible pain curricula in medical schools. To give you an example: I’m one of the leading pain experts in the world and I’m not allowed to teach our medical students their pain curriculum. The students learn about neurophysiology and the anatomy of the nerves, not what’s relevant in pain.
This is notorious in medical school: Curricula are almost impossible to modify and change. So it starts with poor training in medical school. And then, regardless of what education they do or don’t get in medical school, a lot of their education about pain management is through our residencies – mainly in inpatient settings, where you’re really seeing the management of acute pain and not the management of chronic pain.
People get more accustomed to managing acute pain, where opioids are a reasonable option. It’s just that when you start managing subacute or chronic pain, opioids don’t work as well.
The other big problem is that historically, most people trained in medicine think that if you have pain in your elbow, there’s got to be something wrong in your elbow. This third mechanism of pain, central sensitization – or nociplastic pain – the kind of pain that we see in fibromyalgia, headache, and low back pain, where the pain is coming from the brain – that’s confusing to people. People can have pain without any damage or inflammation to that region of the body.
Physicians are trained that if there’s pain, there’s something wrong and we have to do surgery or there’s been some trauma. Most chronic pain is none of that. There’s a big disconnect between how people are trained, and then when they go out and are seeing a tremendous number of people with chronic pain.
What are the different types of pain, and how should they inform clinicians’ understanding about what approaches might work for managing their patients in pain?
The way the central nervous system responds to pain is analogous to the loudness of an electric guitar. You can make an electric guitar louder either by strumming the strings harder or by turning up the amplifier. For many people with fibromyalgia, low back pain, and endometriosis, for example, the problem is really more that the amplifier is turned up too high rather than its being that the guitar is strummed too strongly. That kind of pain where the pain is not due to anatomic damage or inflammation is particularly flummoxing for providers.
Can you explain the design of the new study?
It’s a 13-site study looking at four treatments: enhanced self-care, cognitive-behavioral therapy, physical therapy, and duloxetine. It’s a big precision medicine trial, trying to take everything we’ve learned and putting it all into one big study.
We’re using a SMART design, which randomizes people to two of those treatments, unless they are very much improved from the first treatment. To be eligible for the trial, you have to be able to be randomized to three of the four treatments, and people can’t choose which of the four they get.
We give them one of those treatments for 12 weeks, and at the end of 12 weeks we make the call – “Did you respond or not respond?” – and then we go back to the phenotypic data we collected at the beginning of that trial and say, “What information at baseline that we collected predicts that someone is going to respond better to duloxetine or worse to duloxetine?” And then we create the phenotype that responds best to each of those four treatments.
None of our treatments works so well that someone doesn’t end up getting randomized to a second treatment. About 85% of people so far need a second treatment because they still have enough pain that they want more relief. But the nice thing about that is we’ve already done all the functional brain imaging and all these really expensive and time-consuming things.
We’re hoping to have around 700-800 people total in this trial, which means that around 170 people will get randomized to each of the four initial treatments. No one’s ever done a study that has functional brain imaging and all these other things in it with more than 80 or 100 people. The scale of this is totally unprecedented.
Given that the individual therapies don’t appear to be all that successful on their own, what is your goal?
The primary aim is to match the phenotypic characteristics of a patient with chronic low back pain with treatment response to each of these four treatments. So at the end, we can give clinicians information on which of the patients is going to respond to physical therapy, for instance.
Right now, about one out of three people respond to most treatments for pain. We think by doing a trial like this, we can take treatments that work in one out of three people and make them work in one out of two or two out of three people just by using them in the right people.
How do you differentiate between these types of pain in your study?
We phenotype people by asking them a number of questions. We also do brain imaging, look at their back with MRI, test biomechanics, and then give them four different treatments that we know work in groups of people with low back pain.
We think one of the first parts of the phenotype is, do they have pain just in their back? Or do they have pain in their back plus a lot of other body regions? Because the more body regions that people have pain in, the more likely it is that this is an amplifier problem rather than a guitar problem.
Treatments like physical therapy, surgery, and injections are going to work better for people in whom the pain is a guitar problem rather than an amplifier problem. And drugs like duloxetine, which works in the brain, and cognitive-behavioral therapy are going to work a lot better in the people with pain in multiple sites besides the back.
To pick up on your metaphor, do any symptoms help clinicians differentiate between the guitar and the amplifier?
Sleep problems, fatigue, memory problems, and mood problems are common in patients with chronic pain and are more common with amplifier pain. Because again, those are all central nervous system problems. And so we see that the people that have anxiety, depression, and a lot of distress are more likely to have this kind of pain.
Does medical imaging help?
There’s a terrible relationship between what you see on an MRI of the back and whether someone has pain or how severe the pain is going to be. There’s always going to be individuals that have a lot of anatomic damage who don’t have any pain because they happen to be on the other end of the continuum from fibromyalgia; they’re actually pain-insensitive people.
What are your thoughts about ketamine as a possible treatment for chronic pain?
I have a mentee who’s doing a ketamine trial. We’re doing psilocybin trials in patients with fibromyalgia. Ketamine is such a dirty drug; it has so many different mechanisms of action. It does have some psychedelic effects, but it also is an NMDA blocker. It really has so many different effects.
I think it’s being thrown around like water in settings where we don’t yet know it to be efficacious. Even the data in treatment-refractory depression are pretty weak, but we’re so desperate to do something for those patients. If you’re trying to harness the psychedelic properties of ketamine, I think there’s other psychedelics that are a lot more interesting, which is why we’re using psilocybin for a subset of patients. Most of us in the pain field think that the psychedelics will work best for the people with chronic pain who have a lot of comorbid psychiatric illness, especially the ones with a lot of trauma. These drugs will allow us therapeutically to get at a lot of these patients with the side-by-side psychotherapy that’s being done as people are getting care in the medicalized setting.
Dr. Clauw reported conflicts of interest with Pfizer, Tonix, Theravance, Zynerba, Samumed, Aptinyx, Daiichi Sankyo, Intec, Regeneron, Teva, Lundbeck, Virios, and Cerephex.
A version of this article first appeared on Medscape.com.
Why doctors should take end-of-life decisions back from insurers, says physician
Sadly, the medical business has descended to this: Some insurers are combing health records to find and target customers with a 50% chance of dying in the next 18 months. Those companies then work to persuade customers to switch into palliative and hospice care.
And more of this automated end-of-life medicine appears to be on the way.
What’s gained is cost savings. What’s lost is empathy and humanity.
Doctor colleagues have warned for decades about the rise of the bean-counters in medicine. Yes, health care is a business, but it should be a higher calling, too. We serve, we heal, we protect, and we comfort.
There are times, however, when the people who try to squeeze the most money out of medicine try to gain too much influence over the people who actually engage in medicine. I think the rise of phone bank boiler rooms, built on business incentives to move patients into cheaper hospice care, should be a bridge too far for our profession.
End-of-life care is one of the most sensitive and emotionally rewarding things a doctor can do. Hospice can be an excellent choice for fully informed patients and families, but we should not be turning over these decisions to artificial intelligence, spreadsheets, and crunchers of big data.
At the same time, we should realize that the end-of-life phone banks have not evolved from nowhere. The reality is that dying is expensive. The last year of life accounts for 13%-25% of all spending on Medicare, according to numerous studies. That’s more than $200 billion a year for just one part of one federal health care program. Much of that money goes to hospitals, where end-of-life patients amass average charges of $6,000 per day.
All this spending runs counter to the wishes of most Americans. According to a Kaiser Family Foundation poll, 9 out of 10 adults say they don’t want their families to be burdened financially by their end-of-life medical care. Given the choice, 7 out of 10 Americans say they want to die at home; fewer than 1 in 10 say they want to die in a hospital.
And far more people (71%) think it’s more important to die without pain or stress than to extend life as long as possible (19%).
It’s crucial for us to get this right. Within 11 years, the U.S. Census projects that seniors will outnumber kids for the first time in history: We’ll have 77 million people age 65 or older and 76.5 million age 18 or under. And many of those seniors have medical and functional conditions that signal they are nearing end of life.
As chief medical officer of a complete senior health company, and as a physician with more than 3 decades of personal experience in geriatrics, I know we can improve the final chapter of life for our older adults and our taxpayers. If medical professionals don’t do a better job with patients at the end of life, then key decisions increasingly will be driven by the money-centered phone banks.
The single biggest improvement is having a frank and direct talk with senior patients about end-of-life wishes. Remarkably, only 1 in 10 Americans say they’ve ever had an end-of-life conversation with their doctor or health care provider – no heartfelt talk about what quality of life looks like under different treatment options. Only half ever discussed the topic with a spouse or loved one.
As a result, the default end-of-life care regimen for many is to extend life at any cost, even though most Americans tell pollsters they don’t truly want that. Doctors must focus on thorough informed consent with patients before major medical crises hurt patient cognition.
Another key is for specialists and general care doctors to do a better job consulting with each other. Two of every 3 seniors have several chronic conditions, or multimorbidities; that status worsens to include 8 of every 10 seniors after age 80. That means seniors often have multiple doctors who work in their own silos and fail to communicate the competing risks and benefits of diagnostic and treatment options. The result is fragmented plans that are difficult to follow and often as likely to harm complex patients as help them.
We all know that 90-year-old people shouldn’t be on 15 drugs, and yet too many are. Big Pharma has made it easy for doctors to add new medications, but I don’t think there’s even a class in medical school to teach clinicians how to trim the medicine list. When a drug is causing side effects, the sad reality is that most doctors add another medication to treat the side effect, as opposed to removing the offending agent. We need to end this practice known as drug cascading.
Doctors need training on how to unwind prescriptions. For example, too many seniors are being prescribed atypical antipsychotics off label for dementia. Overtreatment of geriatric diabetes and hypertension causes weakness and falls. Overprescribing antibiotics for frail patients whose bladders are colonized with bacteria too often leads to colitis. We need to question why our seniors are on so many drugs.
Doctors, patients, and families should be discussing quality of life as much as quantity of life.
I’ve spent my career taking care of older people. It’s rare for me to get a phone call saying an older person died and nobody expected it. We all know that we will die, but we spend so little time talking about it and preparing for it. A great disservice will be done to patients, doctors, and the medical profession if we let the phone banks take over.
Dr. Schneeman is a geriatrician and chief medical officer for Lifespark, a senior health company based in Minneapolis.
A version of this article appeared on Medscape.com.
Sadly, the medical business has descended to this: Some insurers are combing health records to find and target customers with a 50% chance of dying in the next 18 months. Those companies then work to persuade customers to switch into palliative and hospice care.
And more of this automated end-of-life medicine appears to be on the way.
What’s gained is cost savings. What’s lost is empathy and humanity.
Doctor colleagues have warned for decades about the rise of the bean-counters in medicine. Yes, health care is a business, but it should be a higher calling, too. We serve, we heal, we protect, and we comfort.
There are times, however, when the people who try to squeeze the most money out of medicine try to gain too much influence over the people who actually engage in medicine. I think the rise of phone bank boiler rooms, built on business incentives to move patients into cheaper hospice care, should be a bridge too far for our profession.
End-of-life care is one of the most sensitive and emotionally rewarding things a doctor can do. Hospice can be an excellent choice for fully informed patients and families, but we should not be turning over these decisions to artificial intelligence, spreadsheets, and crunchers of big data.
At the same time, we should realize that the end-of-life phone banks have not evolved from nowhere. The reality is that dying is expensive. The last year of life accounts for 13%-25% of all spending on Medicare, according to numerous studies. That’s more than $200 billion a year for just one part of one federal health care program. Much of that money goes to hospitals, where end-of-life patients amass average charges of $6,000 per day.
All this spending runs counter to the wishes of most Americans. According to a Kaiser Family Foundation poll, 9 out of 10 adults say they don’t want their families to be burdened financially by their end-of-life medical care. Given the choice, 7 out of 10 Americans say they want to die at home; fewer than 1 in 10 say they want to die in a hospital.
And far more people (71%) think it’s more important to die without pain or stress than to extend life as long as possible (19%).
It’s crucial for us to get this right. Within 11 years, the U.S. Census projects that seniors will outnumber kids for the first time in history: We’ll have 77 million people age 65 or older and 76.5 million age 18 or under. And many of those seniors have medical and functional conditions that signal they are nearing end of life.
As chief medical officer of a complete senior health company, and as a physician with more than 3 decades of personal experience in geriatrics, I know we can improve the final chapter of life for our older adults and our taxpayers. If medical professionals don’t do a better job with patients at the end of life, then key decisions increasingly will be driven by the money-centered phone banks.
The single biggest improvement is having a frank and direct talk with senior patients about end-of-life wishes. Remarkably, only 1 in 10 Americans say they’ve ever had an end-of-life conversation with their doctor or health care provider – no heartfelt talk about what quality of life looks like under different treatment options. Only half ever discussed the topic with a spouse or loved one.
As a result, the default end-of-life care regimen for many is to extend life at any cost, even though most Americans tell pollsters they don’t truly want that. Doctors must focus on thorough informed consent with patients before major medical crises hurt patient cognition.
Another key is for specialists and general care doctors to do a better job consulting with each other. Two of every 3 seniors have several chronic conditions, or multimorbidities; that status worsens to include 8 of every 10 seniors after age 80. That means seniors often have multiple doctors who work in their own silos and fail to communicate the competing risks and benefits of diagnostic and treatment options. The result is fragmented plans that are difficult to follow and often as likely to harm complex patients as help them.
We all know that 90-year-old people shouldn’t be on 15 drugs, and yet too many are. Big Pharma has made it easy for doctors to add new medications, but I don’t think there’s even a class in medical school to teach clinicians how to trim the medicine list. When a drug is causing side effects, the sad reality is that most doctors add another medication to treat the side effect, as opposed to removing the offending agent. We need to end this practice known as drug cascading.
Doctors need training on how to unwind prescriptions. For example, too many seniors are being prescribed atypical antipsychotics off label for dementia. Overtreatment of geriatric diabetes and hypertension causes weakness and falls. Overprescribing antibiotics for frail patients whose bladders are colonized with bacteria too often leads to colitis. We need to question why our seniors are on so many drugs.
Doctors, patients, and families should be discussing quality of life as much as quantity of life.
I’ve spent my career taking care of older people. It’s rare for me to get a phone call saying an older person died and nobody expected it. We all know that we will die, but we spend so little time talking about it and preparing for it. A great disservice will be done to patients, doctors, and the medical profession if we let the phone banks take over.
Dr. Schneeman is a geriatrician and chief medical officer for Lifespark, a senior health company based in Minneapolis.
A version of this article appeared on Medscape.com.
Sadly, the medical business has descended to this: Some insurers are combing health records to find and target customers with a 50% chance of dying in the next 18 months. Those companies then work to persuade customers to switch into palliative and hospice care.
And more of this automated end-of-life medicine appears to be on the way.
What’s gained is cost savings. What’s lost is empathy and humanity.
Doctor colleagues have warned for decades about the rise of the bean-counters in medicine. Yes, health care is a business, but it should be a higher calling, too. We serve, we heal, we protect, and we comfort.
There are times, however, when the people who try to squeeze the most money out of medicine try to gain too much influence over the people who actually engage in medicine. I think the rise of phone bank boiler rooms, built on business incentives to move patients into cheaper hospice care, should be a bridge too far for our profession.
End-of-life care is one of the most sensitive and emotionally rewarding things a doctor can do. Hospice can be an excellent choice for fully informed patients and families, but we should not be turning over these decisions to artificial intelligence, spreadsheets, and crunchers of big data.
At the same time, we should realize that the end-of-life phone banks have not evolved from nowhere. The reality is that dying is expensive. The last year of life accounts for 13%-25% of all spending on Medicare, according to numerous studies. That’s more than $200 billion a year for just one part of one federal health care program. Much of that money goes to hospitals, where end-of-life patients amass average charges of $6,000 per day.
All this spending runs counter to the wishes of most Americans. According to a Kaiser Family Foundation poll, 9 out of 10 adults say they don’t want their families to be burdened financially by their end-of-life medical care. Given the choice, 7 out of 10 Americans say they want to die at home; fewer than 1 in 10 say they want to die in a hospital.
And far more people (71%) think it’s more important to die without pain or stress than to extend life as long as possible (19%).
It’s crucial for us to get this right. Within 11 years, the U.S. Census projects that seniors will outnumber kids for the first time in history: We’ll have 77 million people age 65 or older and 76.5 million age 18 or under. And many of those seniors have medical and functional conditions that signal they are nearing end of life.
As chief medical officer of a complete senior health company, and as a physician with more than 3 decades of personal experience in geriatrics, I know we can improve the final chapter of life for our older adults and our taxpayers. If medical professionals don’t do a better job with patients at the end of life, then key decisions increasingly will be driven by the money-centered phone banks.
The single biggest improvement is having a frank and direct talk with senior patients about end-of-life wishes. Remarkably, only 1 in 10 Americans say they’ve ever had an end-of-life conversation with their doctor or health care provider – no heartfelt talk about what quality of life looks like under different treatment options. Only half ever discussed the topic with a spouse or loved one.
As a result, the default end-of-life care regimen for many is to extend life at any cost, even though most Americans tell pollsters they don’t truly want that. Doctors must focus on thorough informed consent with patients before major medical crises hurt patient cognition.
Another key is for specialists and general care doctors to do a better job consulting with each other. Two of every 3 seniors have several chronic conditions, or multimorbidities; that status worsens to include 8 of every 10 seniors after age 80. That means seniors often have multiple doctors who work in their own silos and fail to communicate the competing risks and benefits of diagnostic and treatment options. The result is fragmented plans that are difficult to follow and often as likely to harm complex patients as help them.
We all know that 90-year-old people shouldn’t be on 15 drugs, and yet too many are. Big Pharma has made it easy for doctors to add new medications, but I don’t think there’s even a class in medical school to teach clinicians how to trim the medicine list. When a drug is causing side effects, the sad reality is that most doctors add another medication to treat the side effect, as opposed to removing the offending agent. We need to end this practice known as drug cascading.
Doctors need training on how to unwind prescriptions. For example, too many seniors are being prescribed atypical antipsychotics off label for dementia. Overtreatment of geriatric diabetes and hypertension causes weakness and falls. Overprescribing antibiotics for frail patients whose bladders are colonized with bacteria too often leads to colitis. We need to question why our seniors are on so many drugs.
Doctors, patients, and families should be discussing quality of life as much as quantity of life.
I’ve spent my career taking care of older people. It’s rare for me to get a phone call saying an older person died and nobody expected it. We all know that we will die, but we spend so little time talking about it and preparing for it. A great disservice will be done to patients, doctors, and the medical profession if we let the phone banks take over.
Dr. Schneeman is a geriatrician and chief medical officer for Lifespark, a senior health company based in Minneapolis.
A version of this article appeared on Medscape.com.
Who owns your genes?
Who owns your genes? The assumption of any sane person would be that he or she owns his or her own genes. I mean, how dumb a question is that?
Yet, in 2007, Dov Michaeli, MD, PhD, described how an American company had claimed ownership of genetic materials and believed that it had the right to commercialize those naturally occurring bits of DNA. Myriad Genetics began by patenting mutations of BRCA. Dr. Michaeli issued a call for action to support early efforts to pass legislation to restore and preserve individual ownership of one’s own genes. This is a historically important quick read/watch/listen. Give it a click.
In related legislation, the Genetic Information Nondiscrimination Act (GINA), originally introduced by New York Rep. Louise Slaughter in 1995, was ultimately spearheaded by California Rep. Xavier Becerra (now Secretary of Health & Human Services) to passage by the House of Representatives on April 25, 2007, by a vote of 420-9-3. Led by Sen. Edward Kennedy of Massachusetts, it was passed by the Senate on April 24, 2008, by a vote of 95-0. President George W. Bush signed the bill into law on May 21, 2008.
GINA is a landmark piece of legislation that protects Americans. It prohibits employers and health insurers from discriminating against people on the basis of their genetic information, and it also prohibits the use of genetic information in life insurance and long-term care insurance.
Its impact has been immense. GINA has been indispensable in promoting progress in the field of human genetics. By safeguarding individuals against discrimination based on genetic information, it has encouraged broader participation in research, built public trust, and stimulated advancements in genetic testing and personalized medicine. GINA’s impact extends beyond borders and has influenced much of the rest of the world.
As important as GINA was to the field, more was needed. National legislation to protect ownership of genetic materials has, despite many attempts, still not become law in the United States. However, in our system of divided government and balance of power, we also have independent courts.
June 13, 2023, was the 10th anniversary of another landmark event. The legal case is that of the Association for Molecular Pathology v. Myriad Genetics, a Salt Lake City–based biotech company that held patents on isolated DNA sequences associated with breast and ovarian cancer. The AMP, joined by several other organizations and researchers, challenged Myriad’s gene patents, arguing that human genes are naturally occurring and, therefore, should not be subject to patenting. In a unanimous decision, the Supreme Court held that naturally occurring DNA segments are products of nature and therefore are not eligible for patent protection.
This was a pivotal decision in the field of human genetics and had a broad impact on genetic research. The decision clarified that naturally occurring DNA sequences cannot be patented, which means that researchers are free to use these sequences in their research without fear of patent infringement. This has led to a vast increase in the amount of genetic research being conducted, and it has also led to the development of new genetic tests and treatments.
The numbers of genetic research papers published in scientific journals and of genetic tests available to consumers have increased significantly, while the cost of genetic testing has decreased significantly. The AMP v. Myriad decision is likely to continue to have an impact for many years to come.
Thank you, common sense, activist American molecular pathologists, Congress, the President, and the Supreme Court for siding with the people.Dr. Lundbert is editor in chief of Cancer Commons. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Who owns your genes? The assumption of any sane person would be that he or she owns his or her own genes. I mean, how dumb a question is that?
Yet, in 2007, Dov Michaeli, MD, PhD, described how an American company had claimed ownership of genetic materials and believed that it had the right to commercialize those naturally occurring bits of DNA. Myriad Genetics began by patenting mutations of BRCA. Dr. Michaeli issued a call for action to support early efforts to pass legislation to restore and preserve individual ownership of one’s own genes. This is a historically important quick read/watch/listen. Give it a click.
In related legislation, the Genetic Information Nondiscrimination Act (GINA), originally introduced by New York Rep. Louise Slaughter in 1995, was ultimately spearheaded by California Rep. Xavier Becerra (now Secretary of Health & Human Services) to passage by the House of Representatives on April 25, 2007, by a vote of 420-9-3. Led by Sen. Edward Kennedy of Massachusetts, it was passed by the Senate on April 24, 2008, by a vote of 95-0. President George W. Bush signed the bill into law on May 21, 2008.
GINA is a landmark piece of legislation that protects Americans. It prohibits employers and health insurers from discriminating against people on the basis of their genetic information, and it also prohibits the use of genetic information in life insurance and long-term care insurance.
Its impact has been immense. GINA has been indispensable in promoting progress in the field of human genetics. By safeguarding individuals against discrimination based on genetic information, it has encouraged broader participation in research, built public trust, and stimulated advancements in genetic testing and personalized medicine. GINA’s impact extends beyond borders and has influenced much of the rest of the world.
As important as GINA was to the field, more was needed. National legislation to protect ownership of genetic materials has, despite many attempts, still not become law in the United States. However, in our system of divided government and balance of power, we also have independent courts.
June 13, 2023, was the 10th anniversary of another landmark event. The legal case is that of the Association for Molecular Pathology v. Myriad Genetics, a Salt Lake City–based biotech company that held patents on isolated DNA sequences associated with breast and ovarian cancer. The AMP, joined by several other organizations and researchers, challenged Myriad’s gene patents, arguing that human genes are naturally occurring and, therefore, should not be subject to patenting. In a unanimous decision, the Supreme Court held that naturally occurring DNA segments are products of nature and therefore are not eligible for patent protection.
This was a pivotal decision in the field of human genetics and had a broad impact on genetic research. The decision clarified that naturally occurring DNA sequences cannot be patented, which means that researchers are free to use these sequences in their research without fear of patent infringement. This has led to a vast increase in the amount of genetic research being conducted, and it has also led to the development of new genetic tests and treatments.
The numbers of genetic research papers published in scientific journals and of genetic tests available to consumers have increased significantly, while the cost of genetic testing has decreased significantly. The AMP v. Myriad decision is likely to continue to have an impact for many years to come.
Thank you, common sense, activist American molecular pathologists, Congress, the President, and the Supreme Court for siding with the people.Dr. Lundbert is editor in chief of Cancer Commons. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Who owns your genes? The assumption of any sane person would be that he or she owns his or her own genes. I mean, how dumb a question is that?
Yet, in 2007, Dov Michaeli, MD, PhD, described how an American company had claimed ownership of genetic materials and believed that it had the right to commercialize those naturally occurring bits of DNA. Myriad Genetics began by patenting mutations of BRCA. Dr. Michaeli issued a call for action to support early efforts to pass legislation to restore and preserve individual ownership of one’s own genes. This is a historically important quick read/watch/listen. Give it a click.
In related legislation, the Genetic Information Nondiscrimination Act (GINA), originally introduced by New York Rep. Louise Slaughter in 1995, was ultimately spearheaded by California Rep. Xavier Becerra (now Secretary of Health & Human Services) to passage by the House of Representatives on April 25, 2007, by a vote of 420-9-3. Led by Sen. Edward Kennedy of Massachusetts, it was passed by the Senate on April 24, 2008, by a vote of 95-0. President George W. Bush signed the bill into law on May 21, 2008.
GINA is a landmark piece of legislation that protects Americans. It prohibits employers and health insurers from discriminating against people on the basis of their genetic information, and it also prohibits the use of genetic information in life insurance and long-term care insurance.
Its impact has been immense. GINA has been indispensable in promoting progress in the field of human genetics. By safeguarding individuals against discrimination based on genetic information, it has encouraged broader participation in research, built public trust, and stimulated advancements in genetic testing and personalized medicine. GINA’s impact extends beyond borders and has influenced much of the rest of the world.
As important as GINA was to the field, more was needed. National legislation to protect ownership of genetic materials has, despite many attempts, still not become law in the United States. However, in our system of divided government and balance of power, we also have independent courts.
June 13, 2023, was the 10th anniversary of another landmark event. The legal case is that of the Association for Molecular Pathology v. Myriad Genetics, a Salt Lake City–based biotech company that held patents on isolated DNA sequences associated with breast and ovarian cancer. The AMP, joined by several other organizations and researchers, challenged Myriad’s gene patents, arguing that human genes are naturally occurring and, therefore, should not be subject to patenting. In a unanimous decision, the Supreme Court held that naturally occurring DNA segments are products of nature and therefore are not eligible for patent protection.
This was a pivotal decision in the field of human genetics and had a broad impact on genetic research. The decision clarified that naturally occurring DNA sequences cannot be patented, which means that researchers are free to use these sequences in their research without fear of patent infringement. This has led to a vast increase in the amount of genetic research being conducted, and it has also led to the development of new genetic tests and treatments.
The numbers of genetic research papers published in scientific journals and of genetic tests available to consumers have increased significantly, while the cost of genetic testing has decreased significantly. The AMP v. Myriad decision is likely to continue to have an impact for many years to come.
Thank you, common sense, activist American molecular pathologists, Congress, the President, and the Supreme Court for siding with the people.Dr. Lundbert is editor in chief of Cancer Commons. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Ten tips for boosting patient communication
This transcript has been edited for clarity.
Here are 10 ways to improve health communication with patients.
No. 1: Be an active listener
The first tip is to be an active listener and help guide the history-taking process by asking for clarification when needed.
Quickly figure out the patient’s chief complaint. Which symptom is the most severe?
Ask them for symptom-modifying factors, such as onset, duration, frequency, and a pain description. Is the abdominal pain sharp or crampy, dull and achy, or pressure-like? What makes the symptoms better or worse?
As many of us were taught in medical school, 80% of the diagnosis is in a patient’s history and description.
No. 2: Ask questions that resonate with patients
What can we do to help elicit an accurate history from the patient when they’re not providing the needed information or being helpful enough?
The easiest way is to ask your patient in a completely different way but one that resonates with them. For instance, ask how the abdominal pain is affecting their quality of life. That will help focus the history taking and encourage the patient to share details.
Does the pain keep them awake at night? Are they able to eat a normal-sized meal? Or are they forced to eat tiny snacks? Is the pain interfering with work or school?
By providing a framework, the patient will be more passionate about sharing the details of their history.
No. 3: Help patients organize their story
Sometimes, patients provide details in a nonchronological order, jumping all over the place.
A super helpful technique is to explain to the patient that you have a story to write for your computer note, and for them to think back to when they first started noticing their abdominal pain or rectal bleeding symptoms. When were the most-severe episodes? How frequent are the episodes? What’s the volume of their rectal bleeding?
If the patient realizes that you’re trying to write a story synopsis, they will provide information in a much more organized way.
No. 4: Determine patient’s language preference
Quickly determine the patient’s language preference. We want patients to feel extremely comfortable.
Whenever possible, use a certified interpreter. Language phone lines, in-person interpreters, and video conferencing are widely available today. It’s worth investing in this technology so that we can provide the best possible care to immigrants and refugees.
Conversely, avoid using family members as interpreters because they may not be adequately trained in medical vocabulary.
No. 5: Use simple language
When providing explanations, use simple language that your patient can understand and identify with.
For example, use analogies like “the heart is a pump” or the diverticula are thin areas of the colon that can bleed if the blood vessel is too close to the surface.
No. 6: Determine level of medical literacy
Determine your patient’s level of medical literacy. Some of our patients did not graduate from high school. Some patients can’t read very well. Therefore, your discharge instructions and handouts should sometimes be written on a third-grade level.
If patients can’t read, write medication instructions with symbols. Draw a sun for medications that are supposed to be taken in the morning and draw a moon if a medication is supposed to be taken at night.
Always very carefully review the instructions with the patient.
No. 7: Check in with the patient
During the visit, frequently check in with the patient to make sure that they understand what you’re asking or what you’re trying to explain to them.
No. 8: Include family member as patient advocate
If the patient is accompanied by a family member, help them serve in the important role as a patient advocate.
If the family member wants to take notes, encourage them because that provides an awesome value.
Sometimes patients can forget clinic and hospital medical conversations, and that family member might be the key to improving your patient’s health.
No. 9: Follow-up with the patient
If your clinic has the capability, follow up with a patient the next day to make sure that they understood everything.
Check to make sure the patient was able to pick up all of the medications that you prescribed.
Check that laboratory tests are arranged or completed.
Check that important procedures, such as esophagogastroduodenoscopy and colonoscopy, and imaging, such as ultrasounds and CTs, are scheduled.
No. 10: Identify barriers to care
Have fun talking with a patient. Find out what they do for a living. Build a rapport. Listen to their stressors in life.
Try to identify any barriers to care or external stressors, like taking care of a sick parent, which might interfere with their scheduling an important diagnostic colonoscopy for rectal bleeding.
Good luck incorporating these communication strategies into your clinic and hospital work. Together, we can help improve the delivery of health care.
Dr. Levy is a gastroenterologist at the University of Chicago. In 2017, Dr. Levy, a previous Fulbright Fellow in France, also started a gastroenterology clinic for refugees resettling in Chicago. His clinical projects focus on the development of colorectal cancer screening campaigns. Dr. Levy, who recently gave a TEDx Talk about building health education campaigns using music and concerts, organizes Tune It Up: A Concert To Raise Colorectal Cancer Awareness with the American College of Gastroenterology (ACG). He frequently publishes on a variety of gastroenterology topics and serves on ACG’s Public Relations Committee and FDA-Related Matters Committee. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Here are 10 ways to improve health communication with patients.
No. 1: Be an active listener
The first tip is to be an active listener and help guide the history-taking process by asking for clarification when needed.
Quickly figure out the patient’s chief complaint. Which symptom is the most severe?
Ask them for symptom-modifying factors, such as onset, duration, frequency, and a pain description. Is the abdominal pain sharp or crampy, dull and achy, or pressure-like? What makes the symptoms better or worse?
As many of us were taught in medical school, 80% of the diagnosis is in a patient’s history and description.
No. 2: Ask questions that resonate with patients
What can we do to help elicit an accurate history from the patient when they’re not providing the needed information or being helpful enough?
The easiest way is to ask your patient in a completely different way but one that resonates with them. For instance, ask how the abdominal pain is affecting their quality of life. That will help focus the history taking and encourage the patient to share details.
Does the pain keep them awake at night? Are they able to eat a normal-sized meal? Or are they forced to eat tiny snacks? Is the pain interfering with work or school?
By providing a framework, the patient will be more passionate about sharing the details of their history.
No. 3: Help patients organize their story
Sometimes, patients provide details in a nonchronological order, jumping all over the place.
A super helpful technique is to explain to the patient that you have a story to write for your computer note, and for them to think back to when they first started noticing their abdominal pain or rectal bleeding symptoms. When were the most-severe episodes? How frequent are the episodes? What’s the volume of their rectal bleeding?
If the patient realizes that you’re trying to write a story synopsis, they will provide information in a much more organized way.
No. 4: Determine patient’s language preference
Quickly determine the patient’s language preference. We want patients to feel extremely comfortable.
Whenever possible, use a certified interpreter. Language phone lines, in-person interpreters, and video conferencing are widely available today. It’s worth investing in this technology so that we can provide the best possible care to immigrants and refugees.
Conversely, avoid using family members as interpreters because they may not be adequately trained in medical vocabulary.
No. 5: Use simple language
When providing explanations, use simple language that your patient can understand and identify with.
For example, use analogies like “the heart is a pump” or the diverticula are thin areas of the colon that can bleed if the blood vessel is too close to the surface.
No. 6: Determine level of medical literacy
Determine your patient’s level of medical literacy. Some of our patients did not graduate from high school. Some patients can’t read very well. Therefore, your discharge instructions and handouts should sometimes be written on a third-grade level.
If patients can’t read, write medication instructions with symbols. Draw a sun for medications that are supposed to be taken in the morning and draw a moon if a medication is supposed to be taken at night.
Always very carefully review the instructions with the patient.
No. 7: Check in with the patient
During the visit, frequently check in with the patient to make sure that they understand what you’re asking or what you’re trying to explain to them.
No. 8: Include family member as patient advocate
If the patient is accompanied by a family member, help them serve in the important role as a patient advocate.
If the family member wants to take notes, encourage them because that provides an awesome value.
Sometimes patients can forget clinic and hospital medical conversations, and that family member might be the key to improving your patient’s health.
No. 9: Follow-up with the patient
If your clinic has the capability, follow up with a patient the next day to make sure that they understood everything.
Check to make sure the patient was able to pick up all of the medications that you prescribed.
Check that laboratory tests are arranged or completed.
Check that important procedures, such as esophagogastroduodenoscopy and colonoscopy, and imaging, such as ultrasounds and CTs, are scheduled.
No. 10: Identify barriers to care
Have fun talking with a patient. Find out what they do for a living. Build a rapport. Listen to their stressors in life.
Try to identify any barriers to care or external stressors, like taking care of a sick parent, which might interfere with their scheduling an important diagnostic colonoscopy for rectal bleeding.
Good luck incorporating these communication strategies into your clinic and hospital work. Together, we can help improve the delivery of health care.
Dr. Levy is a gastroenterologist at the University of Chicago. In 2017, Dr. Levy, a previous Fulbright Fellow in France, also started a gastroenterology clinic for refugees resettling in Chicago. His clinical projects focus on the development of colorectal cancer screening campaigns. Dr. Levy, who recently gave a TEDx Talk about building health education campaigns using music and concerts, organizes Tune It Up: A Concert To Raise Colorectal Cancer Awareness with the American College of Gastroenterology (ACG). He frequently publishes on a variety of gastroenterology topics and serves on ACG’s Public Relations Committee and FDA-Related Matters Committee. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Here are 10 ways to improve health communication with patients.
No. 1: Be an active listener
The first tip is to be an active listener and help guide the history-taking process by asking for clarification when needed.
Quickly figure out the patient’s chief complaint. Which symptom is the most severe?
Ask them for symptom-modifying factors, such as onset, duration, frequency, and a pain description. Is the abdominal pain sharp or crampy, dull and achy, or pressure-like? What makes the symptoms better or worse?
As many of us were taught in medical school, 80% of the diagnosis is in a patient’s history and description.
No. 2: Ask questions that resonate with patients
What can we do to help elicit an accurate history from the patient when they’re not providing the needed information or being helpful enough?
The easiest way is to ask your patient in a completely different way but one that resonates with them. For instance, ask how the abdominal pain is affecting their quality of life. That will help focus the history taking and encourage the patient to share details.
Does the pain keep them awake at night? Are they able to eat a normal-sized meal? Or are they forced to eat tiny snacks? Is the pain interfering with work or school?
By providing a framework, the patient will be more passionate about sharing the details of their history.
No. 3: Help patients organize their story
Sometimes, patients provide details in a nonchronological order, jumping all over the place.
A super helpful technique is to explain to the patient that you have a story to write for your computer note, and for them to think back to when they first started noticing their abdominal pain or rectal bleeding symptoms. When were the most-severe episodes? How frequent are the episodes? What’s the volume of their rectal bleeding?
If the patient realizes that you’re trying to write a story synopsis, they will provide information in a much more organized way.
No. 4: Determine patient’s language preference
Quickly determine the patient’s language preference. We want patients to feel extremely comfortable.
Whenever possible, use a certified interpreter. Language phone lines, in-person interpreters, and video conferencing are widely available today. It’s worth investing in this technology so that we can provide the best possible care to immigrants and refugees.
Conversely, avoid using family members as interpreters because they may not be adequately trained in medical vocabulary.
No. 5: Use simple language
When providing explanations, use simple language that your patient can understand and identify with.
For example, use analogies like “the heart is a pump” or the diverticula are thin areas of the colon that can bleed if the blood vessel is too close to the surface.
No. 6: Determine level of medical literacy
Determine your patient’s level of medical literacy. Some of our patients did not graduate from high school. Some patients can’t read very well. Therefore, your discharge instructions and handouts should sometimes be written on a third-grade level.
If patients can’t read, write medication instructions with symbols. Draw a sun for medications that are supposed to be taken in the morning and draw a moon if a medication is supposed to be taken at night.
Always very carefully review the instructions with the patient.
No. 7: Check in with the patient
During the visit, frequently check in with the patient to make sure that they understand what you’re asking or what you’re trying to explain to them.
No. 8: Include family member as patient advocate
If the patient is accompanied by a family member, help them serve in the important role as a patient advocate.
If the family member wants to take notes, encourage them because that provides an awesome value.
Sometimes patients can forget clinic and hospital medical conversations, and that family member might be the key to improving your patient’s health.
No. 9: Follow-up with the patient
If your clinic has the capability, follow up with a patient the next day to make sure that they understood everything.
Check to make sure the patient was able to pick up all of the medications that you prescribed.
Check that laboratory tests are arranged or completed.
Check that important procedures, such as esophagogastroduodenoscopy and colonoscopy, and imaging, such as ultrasounds and CTs, are scheduled.
No. 10: Identify barriers to care
Have fun talking with a patient. Find out what they do for a living. Build a rapport. Listen to their stressors in life.
Try to identify any barriers to care or external stressors, like taking care of a sick parent, which might interfere with their scheduling an important diagnostic colonoscopy for rectal bleeding.
Good luck incorporating these communication strategies into your clinic and hospital work. Together, we can help improve the delivery of health care.
Dr. Levy is a gastroenterologist at the University of Chicago. In 2017, Dr. Levy, a previous Fulbright Fellow in France, also started a gastroenterology clinic for refugees resettling in Chicago. His clinical projects focus on the development of colorectal cancer screening campaigns. Dr. Levy, who recently gave a TEDx Talk about building health education campaigns using music and concerts, organizes Tune It Up: A Concert To Raise Colorectal Cancer Awareness with the American College of Gastroenterology (ACG). He frequently publishes on a variety of gastroenterology topics and serves on ACG’s Public Relations Committee and FDA-Related Matters Committee. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.