User login
Top 3 things I learned at the NAMS 2016 annual meeting
- Visit NAMS
- Visit NAMS
- Visit NAMS
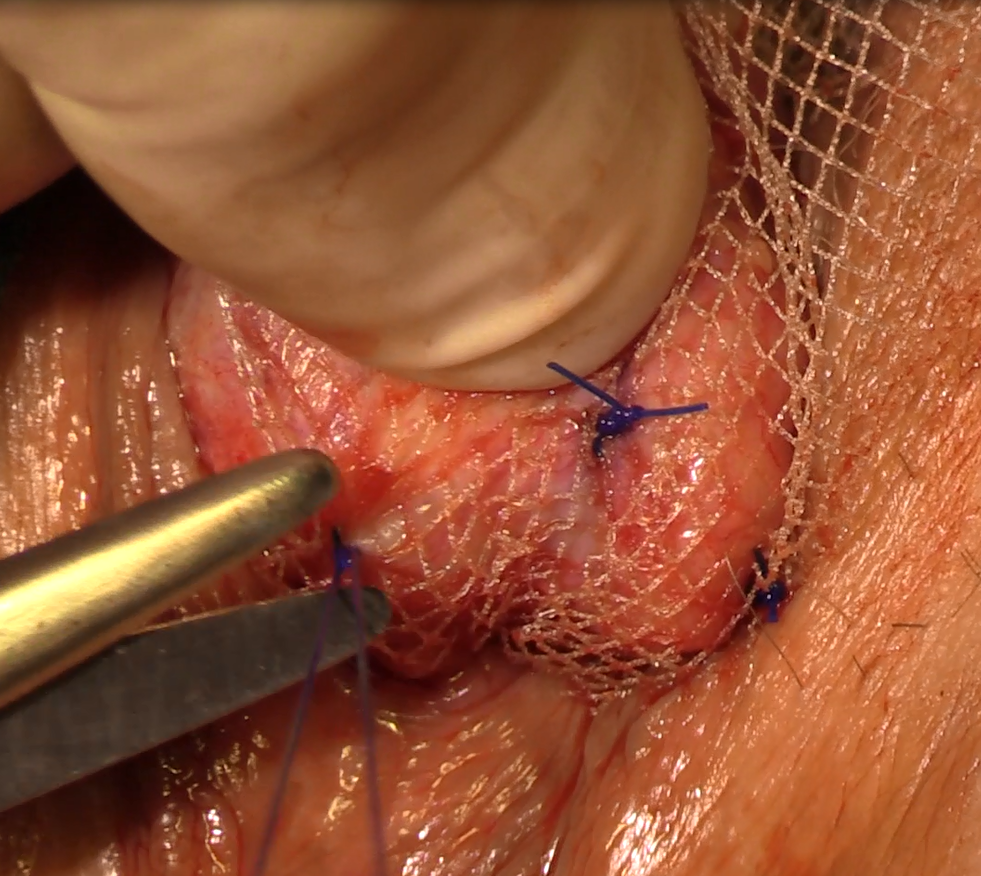
Natural orifice sacral colpopexy
Visit the Society of Gynecologic Surgeons online: sgsonline.org
Related articles:
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist
Visit the Society of Gynecologic Surgeons online: sgsonline.org
Related articles:
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist
Visit the Society of Gynecologic Surgeons online: sgsonline.org
Related articles:
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist
This video brought to you by 
Treating agitation in schizophrenia
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Fibromyalgia management: A multimodal approach
Pulmonary Function Tests
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Allergic Rhinitis
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
COPD: Diagnostic and Treatment Update for the Primary Care Setting
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
TBI scoring system predicts outcomes with only initial head CT findings
WASHINGTON – A simple 8-point scoring system based on head CT accurately predicts mortality, morbidity, and even discharge disposition among patients with a traumatic brain injury (TBI).
In its first clinical study, the Cranial CT Scoring Tool (CCTST) predictive power rivaled both the Glasgow Coma Score (GCS) and the Abbreviated Injury Scale (AIS), Ronnie Mubang, MD, said at the American College of Surgeons’ Clinical Congress.
In addition to adding valuable prognostic information, the CCTST is quick, easy, and completely objective, said Dr. Mubang, of St. Luke’s University Health Network, Bethlehem, Pa.
“The near-universal head CT makes this tool valuable in immediate prognostication and clinical risk assessment for physicians, patients and families. It can serve as a potential adjunct to the Glasgow score and Abbreviated Injury Score for risk assessment,” he said. Of note, the final AIS-Head may not be available until relatively late in the patient’s clinical course, and the GCS has important limitations in terms of outcome prognostication.
The CCTST is an 8-point assessment with one point assigned to each individual cranial CT finding: epidural hematoma, subdural hematoma, subarachnoid hemorrhage, intraventricular hemorrhage, cerebral contusion/ intraparenchymal hemorrhage, skull fracture, brain edema/herniation, and midline shift. The ninth factor is the presence of an external injury to the head.
Dr. Mubang, a fourth-year surgical resident, and his colleagues retrospectively examined the CCTST in 620 patients included in an administrative database at the three-hospital St. Luke’s Regional Trauma Network. Patients were older than 45 years. Half of them underwent neurosurgical intervention within 24 hours of admission and were matched with 310 patients who did not require neurosurgery. The primary clinical endpoint was mortality from head injury. Secondary endpoints included morbidity, hospital and intensive care unit length of stay, and post-discharge destination.
The mean age of the cohort was 73 years. Almost all injuries (99%) were due to blunt force trauma. The mean GCS was 11; the mean Injury Severity Score (ISS) was 24; and the mean AIS – Head score was 4.6, indicating severe to critical level of TBI. Midline shift was significantly greater in the surgical group (0.74 cm vs. 0.29 cm).
Several CT findings were significantly more common in the surgical group, including subdural hematoma (96% vs. 7%); midline shift (74% vs. 29%); brain edema (39% vs. 23%); and epidural hematoma (10% vs. 3%).
As the total CCTST score increased, outcomes worsened accordingly, Dr. Mubang said. Patients with a score of 1-2 had a 20%-30% chance of complications and an approximately 10% chance of injury-related mortality. Patients with higher scores (7-8) had a 60%-75% chance of morbidity and a 55% chance of mortality.
Rising scores correlated well with both hospital and ICU length of stay, with a score of 1-2 associated with a 3-day average stay, and a score of 8 associated with stays exceeding 10 days. The same pattern occurred with overall hospital length of stay: the lowest scores were associated with a stay of about a week, while the highest scores with a stay exceeding 2 weeks.
CCTST was highly associated with discharge disposition. With every additional point, the chance of discharge to home fell. While the majority of patients with scores below 2 were discharged home, no patients with a score of 8 were discharged home.
Finally, the investigators performed a multivariate analysis that controlled for sex; GCS, ISS, and AIS-head scores; time in the trauma bay; and preinjury anticoagulation treatment. The CCTST score was strongly associated with patient mortality (OR 1.31), rivaling both GCS (OR, 1.14) and AIS-Head (OR, 2.68). Neither ISS nor pre-injury anticoagulation predicted mortality. CCTST was also the only variable independently associated with the need for neurosurgical intervention.
The team is planning a multicenter retrospective validation, followed by a prospective observational study in the next 2 years, according to Dr. Stan Stawicki, the senior investigator, also with St. Luke’s. “CCTST offers potential promise to add much needed granularity to our existing TBI clinical assessment paradigm that continues to rely heavily on AIS-Head and GCS,” he said.
Neither Dr. Mubang nor Dr. Stawicki had any financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
WASHINGTON – A simple 8-point scoring system based on head CT accurately predicts mortality, morbidity, and even discharge disposition among patients with a traumatic brain injury (TBI).
In its first clinical study, the Cranial CT Scoring Tool (CCTST) predictive power rivaled both the Glasgow Coma Score (GCS) and the Abbreviated Injury Scale (AIS), Ronnie Mubang, MD, said at the American College of Surgeons’ Clinical Congress.
In addition to adding valuable prognostic information, the CCTST is quick, easy, and completely objective, said Dr. Mubang, of St. Luke’s University Health Network, Bethlehem, Pa.
“The near-universal head CT makes this tool valuable in immediate prognostication and clinical risk assessment for physicians, patients and families. It can serve as a potential adjunct to the Glasgow score and Abbreviated Injury Score for risk assessment,” he said. Of note, the final AIS-Head may not be available until relatively late in the patient’s clinical course, and the GCS has important limitations in terms of outcome prognostication.
The CCTST is an 8-point assessment with one point assigned to each individual cranial CT finding: epidural hematoma, subdural hematoma, subarachnoid hemorrhage, intraventricular hemorrhage, cerebral contusion/ intraparenchymal hemorrhage, skull fracture, brain edema/herniation, and midline shift. The ninth factor is the presence of an external injury to the head.
Dr. Mubang, a fourth-year surgical resident, and his colleagues retrospectively examined the CCTST in 620 patients included in an administrative database at the three-hospital St. Luke’s Regional Trauma Network. Patients were older than 45 years. Half of them underwent neurosurgical intervention within 24 hours of admission and were matched with 310 patients who did not require neurosurgery. The primary clinical endpoint was mortality from head injury. Secondary endpoints included morbidity, hospital and intensive care unit length of stay, and post-discharge destination.
The mean age of the cohort was 73 years. Almost all injuries (99%) were due to blunt force trauma. The mean GCS was 11; the mean Injury Severity Score (ISS) was 24; and the mean AIS – Head score was 4.6, indicating severe to critical level of TBI. Midline shift was significantly greater in the surgical group (0.74 cm vs. 0.29 cm).
Several CT findings were significantly more common in the surgical group, including subdural hematoma (96% vs. 7%); midline shift (74% vs. 29%); brain edema (39% vs. 23%); and epidural hematoma (10% vs. 3%).
As the total CCTST score increased, outcomes worsened accordingly, Dr. Mubang said. Patients with a score of 1-2 had a 20%-30% chance of complications and an approximately 10% chance of injury-related mortality. Patients with higher scores (7-8) had a 60%-75% chance of morbidity and a 55% chance of mortality.
Rising scores correlated well with both hospital and ICU length of stay, with a score of 1-2 associated with a 3-day average stay, and a score of 8 associated with stays exceeding 10 days. The same pattern occurred with overall hospital length of stay: the lowest scores were associated with a stay of about a week, while the highest scores with a stay exceeding 2 weeks.
CCTST was highly associated with discharge disposition. With every additional point, the chance of discharge to home fell. While the majority of patients with scores below 2 were discharged home, no patients with a score of 8 were discharged home.
Finally, the investigators performed a multivariate analysis that controlled for sex; GCS, ISS, and AIS-head scores; time in the trauma bay; and preinjury anticoagulation treatment. The CCTST score was strongly associated with patient mortality (OR 1.31), rivaling both GCS (OR, 1.14) and AIS-Head (OR, 2.68). Neither ISS nor pre-injury anticoagulation predicted mortality. CCTST was also the only variable independently associated with the need for neurosurgical intervention.
The team is planning a multicenter retrospective validation, followed by a prospective observational study in the next 2 years, according to Dr. Stan Stawicki, the senior investigator, also with St. Luke’s. “CCTST offers potential promise to add much needed granularity to our existing TBI clinical assessment paradigm that continues to rely heavily on AIS-Head and GCS,” he said.
Neither Dr. Mubang nor Dr. Stawicki had any financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
WASHINGTON – A simple 8-point scoring system based on head CT accurately predicts mortality, morbidity, and even discharge disposition among patients with a traumatic brain injury (TBI).
In its first clinical study, the Cranial CT Scoring Tool (CCTST) predictive power rivaled both the Glasgow Coma Score (GCS) and the Abbreviated Injury Scale (AIS), Ronnie Mubang, MD, said at the American College of Surgeons’ Clinical Congress.
In addition to adding valuable prognostic information, the CCTST is quick, easy, and completely objective, said Dr. Mubang, of St. Luke’s University Health Network, Bethlehem, Pa.
“The near-universal head CT makes this tool valuable in immediate prognostication and clinical risk assessment for physicians, patients and families. It can serve as a potential adjunct to the Glasgow score and Abbreviated Injury Score for risk assessment,” he said. Of note, the final AIS-Head may not be available until relatively late in the patient’s clinical course, and the GCS has important limitations in terms of outcome prognostication.
The CCTST is an 8-point assessment with one point assigned to each individual cranial CT finding: epidural hematoma, subdural hematoma, subarachnoid hemorrhage, intraventricular hemorrhage, cerebral contusion/ intraparenchymal hemorrhage, skull fracture, brain edema/herniation, and midline shift. The ninth factor is the presence of an external injury to the head.
Dr. Mubang, a fourth-year surgical resident, and his colleagues retrospectively examined the CCTST in 620 patients included in an administrative database at the three-hospital St. Luke’s Regional Trauma Network. Patients were older than 45 years. Half of them underwent neurosurgical intervention within 24 hours of admission and were matched with 310 patients who did not require neurosurgery. The primary clinical endpoint was mortality from head injury. Secondary endpoints included morbidity, hospital and intensive care unit length of stay, and post-discharge destination.
The mean age of the cohort was 73 years. Almost all injuries (99%) were due to blunt force trauma. The mean GCS was 11; the mean Injury Severity Score (ISS) was 24; and the mean AIS – Head score was 4.6, indicating severe to critical level of TBI. Midline shift was significantly greater in the surgical group (0.74 cm vs. 0.29 cm).
Several CT findings were significantly more common in the surgical group, including subdural hematoma (96% vs. 7%); midline shift (74% vs. 29%); brain edema (39% vs. 23%); and epidural hematoma (10% vs. 3%).
As the total CCTST score increased, outcomes worsened accordingly, Dr. Mubang said. Patients with a score of 1-2 had a 20%-30% chance of complications and an approximately 10% chance of injury-related mortality. Patients with higher scores (7-8) had a 60%-75% chance of morbidity and a 55% chance of mortality.
Rising scores correlated well with both hospital and ICU length of stay, with a score of 1-2 associated with a 3-day average stay, and a score of 8 associated with stays exceeding 10 days. The same pattern occurred with overall hospital length of stay: the lowest scores were associated with a stay of about a week, while the highest scores with a stay exceeding 2 weeks.
CCTST was highly associated with discharge disposition. With every additional point, the chance of discharge to home fell. While the majority of patients with scores below 2 were discharged home, no patients with a score of 8 were discharged home.
Finally, the investigators performed a multivariate analysis that controlled for sex; GCS, ISS, and AIS-head scores; time in the trauma bay; and preinjury anticoagulation treatment. The CCTST score was strongly associated with patient mortality (OR 1.31), rivaling both GCS (OR, 1.14) and AIS-Head (OR, 2.68). Neither ISS nor pre-injury anticoagulation predicted mortality. CCTST was also the only variable independently associated with the need for neurosurgical intervention.
The team is planning a multicenter retrospective validation, followed by a prospective observational study in the next 2 years, according to Dr. Stan Stawicki, the senior investigator, also with St. Luke’s. “CCTST offers potential promise to add much needed granularity to our existing TBI clinical assessment paradigm that continues to rely heavily on AIS-Head and GCS,” he said.
Neither Dr. Mubang nor Dr. Stawicki had any financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
AT ACS 2016
Key clinical point:
Major finding: CCTST score was strongly associated with patient mortality (Odds ratio, 1.31), rivaling both the Glasgow Coma Score (OR, 1.14) and the Abbreviated Injury Score – Head (OR, 2.68)Data source: The retrospective database study comprised 620 head trauma patients.
Disclosures: Neither Ronnie Mubang, MD, or Stan Stawicki, MD, had financial disclosures.
Webcast: Contraceptive considerations for women with headache and migraine
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Access Dr. Burkman's Webcasts on contraception:
- Hormonal contraception and risk of venous thromboembolism
- Oral contraceptives and breast cancer: What’s the risk?
- Factors that contribute to overall contraceptive efficacy and risks
- Obesity and contraceptive efficacy and risks
- How to use the CDC's online tools to manage complex cases in contraception
Helpful resources for your practice:
- Book recommendation: Allen RH, Cwiak CA, eds. Contraception for the medically challenging patient. New York, New York: Springer New York; 2014.
- United States Medical Eligibility Criteria for Contraceptive Use, 2016
- United States Medical Eligibility Criteria (US MEC) for Contraceptive Use, 2010
- Summary Chart of US Medical Eligibility for Contraceptive Use
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Access Dr. Burkman's Webcasts on contraception:
- Hormonal contraception and risk of venous thromboembolism
- Oral contraceptives and breast cancer: What’s the risk?
- Factors that contribute to overall contraceptive efficacy and risks
- Obesity and contraceptive efficacy and risks
- How to use the CDC's online tools to manage complex cases in contraception
Helpful resources for your practice:
- Book recommendation: Allen RH, Cwiak CA, eds. Contraception for the medically challenging patient. New York, New York: Springer New York; 2014.
- United States Medical Eligibility Criteria for Contraceptive Use, 2016
- United States Medical Eligibility Criteria (US MEC) for Contraceptive Use, 2010
- Summary Chart of US Medical Eligibility for Contraceptive Use
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Access Dr. Burkman's Webcasts on contraception:
- Hormonal contraception and risk of venous thromboembolism
- Oral contraceptives and breast cancer: What’s the risk?
- Factors that contribute to overall contraceptive efficacy and risks
- Obesity and contraceptive efficacy and risks
- How to use the CDC's online tools to manage complex cases in contraception
Helpful resources for your practice:
- Book recommendation: Allen RH, Cwiak CA, eds. Contraception for the medically challenging patient. New York, New York: Springer New York; 2014.
- United States Medical Eligibility Criteria for Contraceptive Use, 2016
- United States Medical Eligibility Criteria (US MEC) for Contraceptive Use, 2010
- Summary Chart of US Medical Eligibility for Contraceptive Use
Lip Augmentation With Juvéderm Ultra XC