User login
Laparoscopic management of interstitial ectopic pregnancy
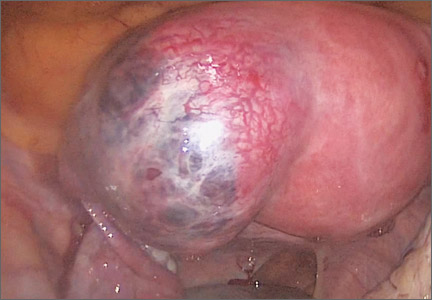
Interstitial ectopic pregnancies, commonly reported as “cornual” ectopic pregnancies, are rare, accounting for only 2% to 3% of all tubal ectopic pregnancies. They can be managed medically with methotrexate or surgically via laparotomy or laparoscopy. Many variations of laparoscopic techniques have been described in the literature but no standardized surgical management has been established.
In this video, we begin by reviewing interstitial ectopic pregnancy and surgical approaches to treatment, with a focus on key surgical techniques and steps for successful laparoscopic management.
We then present the case of a 40-year-old woman (G3P1011) at 7 weeks 2 days gestation with a 5-cm left interstitial ectopic pregnancy who underwent a laparoscopic cornual resection.
We hope this video can serve as a quick reference in your practice for the surgical management of interstitial ectopic pregnancies.

Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Interstitial ectopic pregnancies, commonly reported as “cornual” ectopic pregnancies, are rare, accounting for only 2% to 3% of all tubal ectopic pregnancies. They can be managed medically with methotrexate or surgically via laparotomy or laparoscopy. Many variations of laparoscopic techniques have been described in the literature but no standardized surgical management has been established.
In this video, we begin by reviewing interstitial ectopic pregnancy and surgical approaches to treatment, with a focus on key surgical techniques and steps for successful laparoscopic management.
We then present the case of a 40-year-old woman (G3P1011) at 7 weeks 2 days gestation with a 5-cm left interstitial ectopic pregnancy who underwent a laparoscopic cornual resection.
We hope this video can serve as a quick reference in your practice for the surgical management of interstitial ectopic pregnancies.

Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Interstitial ectopic pregnancies, commonly reported as “cornual” ectopic pregnancies, are rare, accounting for only 2% to 3% of all tubal ectopic pregnancies. They can be managed medically with methotrexate or surgically via laparotomy or laparoscopy. Many variations of laparoscopic techniques have been described in the literature but no standardized surgical management has been established.
In this video, we begin by reviewing interstitial ectopic pregnancy and surgical approaches to treatment, with a focus on key surgical techniques and steps for successful laparoscopic management.
We then present the case of a 40-year-old woman (G3P1011) at 7 weeks 2 days gestation with a 5-cm left interstitial ectopic pregnancy who underwent a laparoscopic cornual resection.
We hope this video can serve as a quick reference in your practice for the surgical management of interstitial ectopic pregnancies.

Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
VIDEO: The coming revolution in brain science
WASHINGTON – What is the chief role of the brain? According to Dr. Henry A. Nasrallah, professor and chair of the department of neurology & psychiatry at Saint Louis University, it is to generate the mind. In this video, recorded at the Summit in Neurology & Psychiatry held by the Global Academy for Medical Education, Dr. Nasrallah explains how neurology and psychiatry, once considered two halves of the same field of study, separated, but are now reuniting. He also discusses what this means for the future of both mind and brain science.
The Global Academy and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
WASHINGTON – What is the chief role of the brain? According to Dr. Henry A. Nasrallah, professor and chair of the department of neurology & psychiatry at Saint Louis University, it is to generate the mind. In this video, recorded at the Summit in Neurology & Psychiatry held by the Global Academy for Medical Education, Dr. Nasrallah explains how neurology and psychiatry, once considered two halves of the same field of study, separated, but are now reuniting. He also discusses what this means for the future of both mind and brain science.
The Global Academy and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
WASHINGTON – What is the chief role of the brain? According to Dr. Henry A. Nasrallah, professor and chair of the department of neurology & psychiatry at Saint Louis University, it is to generate the mind. In this video, recorded at the Summit in Neurology & Psychiatry held by the Global Academy for Medical Education, Dr. Nasrallah explains how neurology and psychiatry, once considered two halves of the same field of study, separated, but are now reuniting. He also discusses what this means for the future of both mind and brain science.
The Global Academy and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
AT THE SUMMIT IN NEUROLOGY & PSYCHIATRY
VIDEO: Watch for anxiety, other symptoms in cannabis users on anti-cannabinoids
WASHINGTON – The physical withdrawal symptoms of cannabis users given anti-cannabinoids resemble those of people withdrawing from opioid use by taking naloxone, according to Dr. Mark S. Gold. In this interview, recorded at the Summit in Neurology & Psychiatry sponsored by the Global Academy for Medical Education, Dr. Gold of the department of psychiatry at Washington University in St. Louis, describes withdrawal from cannabis, including symptoms of anxiety, panic, and confusion. Global Academy and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
WASHINGTON – The physical withdrawal symptoms of cannabis users given anti-cannabinoids resemble those of people withdrawing from opioid use by taking naloxone, according to Dr. Mark S. Gold. In this interview, recorded at the Summit in Neurology & Psychiatry sponsored by the Global Academy for Medical Education, Dr. Gold of the department of psychiatry at Washington University in St. Louis, describes withdrawal from cannabis, including symptoms of anxiety, panic, and confusion. Global Academy and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
WASHINGTON – The physical withdrawal symptoms of cannabis users given anti-cannabinoids resemble those of people withdrawing from opioid use by taking naloxone, according to Dr. Mark S. Gold. In this interview, recorded at the Summit in Neurology & Psychiatry sponsored by the Global Academy for Medical Education, Dr. Gold of the department of psychiatry at Washington University in St. Louis, describes withdrawal from cannabis, including symptoms of anxiety, panic, and confusion. Global Academy and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
AT THE SUMMIT IN NEUROLOGY & PSYCHIATRY
VIDEO: Beware of dehydration, hyperthermia in drug-taking concert-goers, or ‘ravers’*
WASHINGTON – Because “drugs and food compete in the brain for the same reinforcement sites,” people who take drugs while attending festival concerts or rave parties need to be cautious, says Dr. Mark S. Gold, an addiction specialist and the “rock doc” at Woodstock in 1969. “There were a lot of drugs at Woodstock, but no food,” recalled Dr. Gold at the Summit in Neurology & Psychiatry held by the Global Academy for Medical Education. “Sex, drugs, and rock and roll make a person feel like they don’t need to eat,” said Dr. Gold of the department of psychiatry at Washington University in St. Louis. In this video, Dr. Gold shares tips on treating patients who take “club drugs” while attending concerts or raves, including those who suffer from dehydration and hyperthermia as a result.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The Global Academy and this news organization are owned by the same company.
*Correction, 7/16/2015: An earlier version of this story misstated the possible side effects of 'club drug' use at raves or concerts.
On Twitter @whitneymcknight
WASHINGTON – Because “drugs and food compete in the brain for the same reinforcement sites,” people who take drugs while attending festival concerts or rave parties need to be cautious, says Dr. Mark S. Gold, an addiction specialist and the “rock doc” at Woodstock in 1969. “There were a lot of drugs at Woodstock, but no food,” recalled Dr. Gold at the Summit in Neurology & Psychiatry held by the Global Academy for Medical Education. “Sex, drugs, and rock and roll make a person feel like they don’t need to eat,” said Dr. Gold of the department of psychiatry at Washington University in St. Louis. In this video, Dr. Gold shares tips on treating patients who take “club drugs” while attending concerts or raves, including those who suffer from dehydration and hyperthermia as a result.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The Global Academy and this news organization are owned by the same company.
*Correction, 7/16/2015: An earlier version of this story misstated the possible side effects of 'club drug' use at raves or concerts.
On Twitter @whitneymcknight
WASHINGTON – Because “drugs and food compete in the brain for the same reinforcement sites,” people who take drugs while attending festival concerts or rave parties need to be cautious, says Dr. Mark S. Gold, an addiction specialist and the “rock doc” at Woodstock in 1969. “There were a lot of drugs at Woodstock, but no food,” recalled Dr. Gold at the Summit in Neurology & Psychiatry held by the Global Academy for Medical Education. “Sex, drugs, and rock and roll make a person feel like they don’t need to eat,” said Dr. Gold of the department of psychiatry at Washington University in St. Louis. In this video, Dr. Gold shares tips on treating patients who take “club drugs” while attending concerts or raves, including those who suffer from dehydration and hyperthermia as a result.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The Global Academy and this news organization are owned by the same company.
*Correction, 7/16/2015: An earlier version of this story misstated the possible side effects of 'club drug' use at raves or concerts.
On Twitter @whitneymcknight
AT THE SUMMIT IN NEUROLOGY & PSYCHIATRY
VIDEO: Anticipatory guidance can reduce chronic postconcussion syndrome
WASHINGTON – Regardless of the number of tests and tools for helping to diagnose pediatric sports concussions, Dr. Christopher Giza, professor of pediatric neurology and neurosurgery at the University of California, Los Angeles, says it’s important for clinicians to remember that “concussion is a clinical diagnosis.”
In this video interview recorded at Summit in Neurology & Psychiatry, Dr. Giza offers pearls and insights into the latest in sports concussion management. He describes the four “Rs” of treating sports concussions and urges primary care personnel to offer anticipatory guidance to patients and their families. Such guidance can lead to a 20% decrease in chronic postconcussion syndrome in children and adolescents, he said at the meeting held by Global Academy for Medical Education. Global Academy and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
WASHINGTON – Regardless of the number of tests and tools for helping to diagnose pediatric sports concussions, Dr. Christopher Giza, professor of pediatric neurology and neurosurgery at the University of California, Los Angeles, says it’s important for clinicians to remember that “concussion is a clinical diagnosis.”
In this video interview recorded at Summit in Neurology & Psychiatry, Dr. Giza offers pearls and insights into the latest in sports concussion management. He describes the four “Rs” of treating sports concussions and urges primary care personnel to offer anticipatory guidance to patients and their families. Such guidance can lead to a 20% decrease in chronic postconcussion syndrome in children and adolescents, he said at the meeting held by Global Academy for Medical Education. Global Academy and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
WASHINGTON – Regardless of the number of tests and tools for helping to diagnose pediatric sports concussions, Dr. Christopher Giza, professor of pediatric neurology and neurosurgery at the University of California, Los Angeles, says it’s important for clinicians to remember that “concussion is a clinical diagnosis.”
In this video interview recorded at Summit in Neurology & Psychiatry, Dr. Giza offers pearls and insights into the latest in sports concussion management. He describes the four “Rs” of treating sports concussions and urges primary care personnel to offer anticipatory guidance to patients and their families. Such guidance can lead to a 20% decrease in chronic postconcussion syndrome in children and adolescents, he said at the meeting held by Global Academy for Medical Education. Global Academy and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
AT SUMMIT IN NEUROLOGY & PSYCHIATRY
VIDEO: Sometimes, comfort care is best for ruptured AAAs
CHICAGO – Four preoperative variables predict whether or not patients will survive ruptured abdominal aortic aneurysm repairs, according to investigators from Harborview Medical Center in Seattle.
It’s an important finding because until now, it’s been hard to know how they’ll do. Previous risk scores also rely on intraoperative variables, or haven’t been validated for endovascular repair.
Investigator Dr. Ty Garland, chief vascular surgery resident at the University of Washington, explained in a video interview what the four variables are at a meeting hosted by the Society for Vascular Surgery, and why it was so important for a level 1 trauma center like Harborview to identify them.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Four preoperative variables predict whether or not patients will survive ruptured abdominal aortic aneurysm repairs, according to investigators from Harborview Medical Center in Seattle.
It’s an important finding because until now, it’s been hard to know how they’ll do. Previous risk scores also rely on intraoperative variables, or haven’t been validated for endovascular repair.
Investigator Dr. Ty Garland, chief vascular surgery resident at the University of Washington, explained in a video interview what the four variables are at a meeting hosted by the Society for Vascular Surgery, and why it was so important for a level 1 trauma center like Harborview to identify them.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Four preoperative variables predict whether or not patients will survive ruptured abdominal aortic aneurysm repairs, according to investigators from Harborview Medical Center in Seattle.
It’s an important finding because until now, it’s been hard to know how they’ll do. Previous risk scores also rely on intraoperative variables, or haven’t been validated for endovascular repair.
Investigator Dr. Ty Garland, chief vascular surgery resident at the University of Washington, explained in a video interview what the four variables are at a meeting hosted by the Society for Vascular Surgery, and why it was so important for a level 1 trauma center like Harborview to identify them.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE 2015 VASCULAR ANNUAL MEETING
Reducing the duration of untreated psychosis
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO: Could a deep Koebner phenomenon trigger psoriatic arthritis?
ROME – Psoriasis patients with a past history of bone or joint trauma had about 50% higher risk of later developing psoriatic arthritis than did those without a history of trauma in a longitudinal, population-based study of more than 70,000 psoriasis patients in the United Kingdom.
The relationship between trauma and later development of psoriatic arthritis could involve a deep Koebner phenomenon similar to what is observed with the Koebner phenomenon in the skin, suggested lead investigator Dr. Thorvardur Löve in an interview at the European Congress of Rheumatology.
Based on these findings, “one of the things that we are very excited about is the potential to think of strategies and test strategies that might be used in psoriasis patients once they are injured. So should we do anything different in an injured psoriasis patient, for instance, some sort of preventive treatment?” said Dr. Löve of Landspitali University Hospital in Reykjavik, Iceland.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ROME – Psoriasis patients with a past history of bone or joint trauma had about 50% higher risk of later developing psoriatic arthritis than did those without a history of trauma in a longitudinal, population-based study of more than 70,000 psoriasis patients in the United Kingdom.
The relationship between trauma and later development of psoriatic arthritis could involve a deep Koebner phenomenon similar to what is observed with the Koebner phenomenon in the skin, suggested lead investigator Dr. Thorvardur Löve in an interview at the European Congress of Rheumatology.
Based on these findings, “one of the things that we are very excited about is the potential to think of strategies and test strategies that might be used in psoriasis patients once they are injured. So should we do anything different in an injured psoriasis patient, for instance, some sort of preventive treatment?” said Dr. Löve of Landspitali University Hospital in Reykjavik, Iceland.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ROME – Psoriasis patients with a past history of bone or joint trauma had about 50% higher risk of later developing psoriatic arthritis than did those without a history of trauma in a longitudinal, population-based study of more than 70,000 psoriasis patients in the United Kingdom.
The relationship between trauma and later development of psoriatic arthritis could involve a deep Koebner phenomenon similar to what is observed with the Koebner phenomenon in the skin, suggested lead investigator Dr. Thorvardur Löve in an interview at the European Congress of Rheumatology.
Based on these findings, “one of the things that we are very excited about is the potential to think of strategies and test strategies that might be used in psoriasis patients once they are injured. So should we do anything different in an injured psoriasis patient, for instance, some sort of preventive treatment?” said Dr. Löve of Landspitali University Hospital in Reykjavik, Iceland.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE EULAR 2015 CONGRESS