User login
VIDEO: Stem cells may reverse premature menopause, restore fertility
CHICAGO –
Neither of the women had menstruated for about 5 years; both were in premature menopause and wanted desperately to start a family. Estrogen levels began increasing soon after treatment, and night sweats and other symptoms of menopause almost disappeared. After a year, the treated ovary was almost the size of a normal premenopausal ovary. There weren’t any complications or side effects, and both women are now pursuing pregnancy.
The results are “very exciting, very encouraging,” said senior investigator Ayman Al-Hendy, MD, PhD, a gynecology professor at the University of Illinois at Chicago.
“The eggs are there, but they are not active.” Something about the stem cells seems “to activate these eggs to become fertilizable,” he said.
Far more work is planned on the project, and there’s no shortage of volunteers; premature menopause is a devastating diagnosis to young women hoping to start families.
Dr. Al-Hendy explained the procedure and the next steps in a video interview at the Endocrine Society annual meeting.
The work is supported by MD Stem Cells and the National Institutes of Health. Dr. Al-Hendy didn’t have any relevant disclosures.
SOURCE: Al-Hendy A et al. ENDO 2018, Abstract OR33-6.
CHICAGO –
Neither of the women had menstruated for about 5 years; both were in premature menopause and wanted desperately to start a family. Estrogen levels began increasing soon after treatment, and night sweats and other symptoms of menopause almost disappeared. After a year, the treated ovary was almost the size of a normal premenopausal ovary. There weren’t any complications or side effects, and both women are now pursuing pregnancy.
The results are “very exciting, very encouraging,” said senior investigator Ayman Al-Hendy, MD, PhD, a gynecology professor at the University of Illinois at Chicago.
“The eggs are there, but they are not active.” Something about the stem cells seems “to activate these eggs to become fertilizable,” he said.
Far more work is planned on the project, and there’s no shortage of volunteers; premature menopause is a devastating diagnosis to young women hoping to start families.
Dr. Al-Hendy explained the procedure and the next steps in a video interview at the Endocrine Society annual meeting.
The work is supported by MD Stem Cells and the National Institutes of Health. Dr. Al-Hendy didn’t have any relevant disclosures.
SOURCE: Al-Hendy A et al. ENDO 2018, Abstract OR33-6.
CHICAGO –
Neither of the women had menstruated for about 5 years; both were in premature menopause and wanted desperately to start a family. Estrogen levels began increasing soon after treatment, and night sweats and other symptoms of menopause almost disappeared. After a year, the treated ovary was almost the size of a normal premenopausal ovary. There weren’t any complications or side effects, and both women are now pursuing pregnancy.
The results are “very exciting, very encouraging,” said senior investigator Ayman Al-Hendy, MD, PhD, a gynecology professor at the University of Illinois at Chicago.
“The eggs are there, but they are not active.” Something about the stem cells seems “to activate these eggs to become fertilizable,” he said.
Far more work is planned on the project, and there’s no shortage of volunteers; premature menopause is a devastating diagnosis to young women hoping to start families.
Dr. Al-Hendy explained the procedure and the next steps in a video interview at the Endocrine Society annual meeting.
The work is supported by MD Stem Cells and the National Institutes of Health. Dr. Al-Hendy didn’t have any relevant disclosures.
SOURCE: Al-Hendy A et al. ENDO 2018, Abstract OR33-6.
REPORTING FROM ENDO 2018
VIDEO: Fezolinetant drops testosterone levels in PCOS
CHICAGO – currently in development. The proof-of-concept phase 2 trial, which saw no concerning safety signals for the medication, fezolinetant, sets the stage for a larger, and perhaps longer, study to learn more about the neurokinin 3 receptor antagonist’s efficacy against PCOS.
“The primary outcome for this phase 2 trial was to see if we could lower testosterone levels in these PCOS patients,” said Graeme Fraser, PhD, chief scientific officer for Ogeda, discussing the poster he and his colleagues presented at the annual meeting of the Endocrine Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Testosterone levels decreased: Measured at about 3 hours postdose, which is the approximate pharmacokinetic Cmax [maximum serum concentration], there was … a more than 30% decrease in testosterone levels,” said Dr. Fraser. By week 12, he said, “there was a very consistent decrease of 30% of testosterone levels. So that was quite good; we successfully hit the primary outcome.”
At 12 weeks, the higher dose of fezolinetant decreased testosterone by 0.64 nmol/L, compared with the 0.04 nmol/L seen with placebo (P less than .01).
Fezolinetant downregulates the activity of candy neurons in the hypothalamus, said Dr. Fraser in an interview. In turn, gonadotropin-releasing hormone (GNRH) pulse frequency is reduced, lowering luteinizing hormone (LH) levels. Since LH drives testosterone levels, this drops as well – a beneficial effect in PCOS, with its cardinal symptom of hyperandrogenism.
The double-blind, placebo-controlled study was conducted in Western Europe; 73 participants were randomized into three groups: 27 to a placebo group, 23 to a treatment group given 60 mg of fezolinetant once daily, and 23 to a treatment group given 180 mg of fezolinetant once daily. All groups received treatment for 12 weeks.
A total of 26 patients on placebo, 21 on 60-mg fezolinetant, and 17 on 180-mg fezolinetant completed the study. Patients who completed the study were included in the safety analysis, while all who took the study medication were included in the intent-to-treat analysis for primary and secondary outcome measures.
All participants had PCOS with hyperandrogenism, mean age was about 31 years, and about three quarters of enrollees were white, though local regulations restricted the collection of race and ethnicity data in some cases. One secondary outcome measure of the study was how fezolinetant affected the LH:FSH (follicle-stimulating hormone) ratio. “Patients with PCOS tend to have a very high GNRH [gonadotropin-releasing hormone] pulse frequency, which leads to a very high LH:FSH ratio,” said Dr. Fraser.
At baseline, the LH:FSH ratio was about 3. “With treatment, that ratio normalized to about 1, which is where it is in healthy women,” he said. The decrease in LH:FSH ratio occurred in a dose-dependent fashion and was statistically significant (P less than .001 for 180 mg fezolinetant versus placebo).
Dr. Fraser and his collaborators also tracked anti-müllerian hormone (AMH) levels, ovarian volume, and number of follicles. Although the investigators saw trends toward reduction in AMH levels and toward smaller ovarian volumes, these trends weren’t significant. “It was somewhat ambitious, I guess, to consider we’d hit these endpoints within 12 weeks,” he said. There were no serious drug-related adverse events.
“Most importantly, I would say, we did not get an increase in menses frequency, and, of course, that’s an important marker for fertility,” said Dr. Fraser. “There’s a debate in PCOS about whether this disease is driven by a malfunction in the brain or a malfunction in the ovaries. I guess on face value, perhaps this problem is in the ovaries.”
With the trends toward lower AMH and ovarian volumes, the research team is left wondering what would happen if the duration of therapy were extended. “Perhaps, the system would have been reset, and the frequency would have been restored. … So one thought that we have is to prolong the study in future trials and see if that could lead to an increase in fertility in PCOS,” said Dr. Fraser.
Fezolinetant is also being studied for menopause-related hot flashes in the United States and Europe.
Dr. Fraser is an employee of Ogeda, which sponsored the trial. Ogeda is a wholly owned subsidiary of Astelas.
SOURCE: Fraser G et al. ENDO 2018, Abstract SAT-305-LB.
CHICAGO – currently in development. The proof-of-concept phase 2 trial, which saw no concerning safety signals for the medication, fezolinetant, sets the stage for a larger, and perhaps longer, study to learn more about the neurokinin 3 receptor antagonist’s efficacy against PCOS.
“The primary outcome for this phase 2 trial was to see if we could lower testosterone levels in these PCOS patients,” said Graeme Fraser, PhD, chief scientific officer for Ogeda, discussing the poster he and his colleagues presented at the annual meeting of the Endocrine Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Testosterone levels decreased: Measured at about 3 hours postdose, which is the approximate pharmacokinetic Cmax [maximum serum concentration], there was … a more than 30% decrease in testosterone levels,” said Dr. Fraser. By week 12, he said, “there was a very consistent decrease of 30% of testosterone levels. So that was quite good; we successfully hit the primary outcome.”
At 12 weeks, the higher dose of fezolinetant decreased testosterone by 0.64 nmol/L, compared with the 0.04 nmol/L seen with placebo (P less than .01).
Fezolinetant downregulates the activity of candy neurons in the hypothalamus, said Dr. Fraser in an interview. In turn, gonadotropin-releasing hormone (GNRH) pulse frequency is reduced, lowering luteinizing hormone (LH) levels. Since LH drives testosterone levels, this drops as well – a beneficial effect in PCOS, with its cardinal symptom of hyperandrogenism.
The double-blind, placebo-controlled study was conducted in Western Europe; 73 participants were randomized into three groups: 27 to a placebo group, 23 to a treatment group given 60 mg of fezolinetant once daily, and 23 to a treatment group given 180 mg of fezolinetant once daily. All groups received treatment for 12 weeks.
A total of 26 patients on placebo, 21 on 60-mg fezolinetant, and 17 on 180-mg fezolinetant completed the study. Patients who completed the study were included in the safety analysis, while all who took the study medication were included in the intent-to-treat analysis for primary and secondary outcome measures.
All participants had PCOS with hyperandrogenism, mean age was about 31 years, and about three quarters of enrollees were white, though local regulations restricted the collection of race and ethnicity data in some cases. One secondary outcome measure of the study was how fezolinetant affected the LH:FSH (follicle-stimulating hormone) ratio. “Patients with PCOS tend to have a very high GNRH [gonadotropin-releasing hormone] pulse frequency, which leads to a very high LH:FSH ratio,” said Dr. Fraser.
At baseline, the LH:FSH ratio was about 3. “With treatment, that ratio normalized to about 1, which is where it is in healthy women,” he said. The decrease in LH:FSH ratio occurred in a dose-dependent fashion and was statistically significant (P less than .001 for 180 mg fezolinetant versus placebo).
Dr. Fraser and his collaborators also tracked anti-müllerian hormone (AMH) levels, ovarian volume, and number of follicles. Although the investigators saw trends toward reduction in AMH levels and toward smaller ovarian volumes, these trends weren’t significant. “It was somewhat ambitious, I guess, to consider we’d hit these endpoints within 12 weeks,” he said. There were no serious drug-related adverse events.
“Most importantly, I would say, we did not get an increase in menses frequency, and, of course, that’s an important marker for fertility,” said Dr. Fraser. “There’s a debate in PCOS about whether this disease is driven by a malfunction in the brain or a malfunction in the ovaries. I guess on face value, perhaps this problem is in the ovaries.”
With the trends toward lower AMH and ovarian volumes, the research team is left wondering what would happen if the duration of therapy were extended. “Perhaps, the system would have been reset, and the frequency would have been restored. … So one thought that we have is to prolong the study in future trials and see if that could lead to an increase in fertility in PCOS,” said Dr. Fraser.
Fezolinetant is also being studied for menopause-related hot flashes in the United States and Europe.
Dr. Fraser is an employee of Ogeda, which sponsored the trial. Ogeda is a wholly owned subsidiary of Astelas.
SOURCE: Fraser G et al. ENDO 2018, Abstract SAT-305-LB.
CHICAGO – currently in development. The proof-of-concept phase 2 trial, which saw no concerning safety signals for the medication, fezolinetant, sets the stage for a larger, and perhaps longer, study to learn more about the neurokinin 3 receptor antagonist’s efficacy against PCOS.
“The primary outcome for this phase 2 trial was to see if we could lower testosterone levels in these PCOS patients,” said Graeme Fraser, PhD, chief scientific officer for Ogeda, discussing the poster he and his colleagues presented at the annual meeting of the Endocrine Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Testosterone levels decreased: Measured at about 3 hours postdose, which is the approximate pharmacokinetic Cmax [maximum serum concentration], there was … a more than 30% decrease in testosterone levels,” said Dr. Fraser. By week 12, he said, “there was a very consistent decrease of 30% of testosterone levels. So that was quite good; we successfully hit the primary outcome.”
At 12 weeks, the higher dose of fezolinetant decreased testosterone by 0.64 nmol/L, compared with the 0.04 nmol/L seen with placebo (P less than .01).
Fezolinetant downregulates the activity of candy neurons in the hypothalamus, said Dr. Fraser in an interview. In turn, gonadotropin-releasing hormone (GNRH) pulse frequency is reduced, lowering luteinizing hormone (LH) levels. Since LH drives testosterone levels, this drops as well – a beneficial effect in PCOS, with its cardinal symptom of hyperandrogenism.
The double-blind, placebo-controlled study was conducted in Western Europe; 73 participants were randomized into three groups: 27 to a placebo group, 23 to a treatment group given 60 mg of fezolinetant once daily, and 23 to a treatment group given 180 mg of fezolinetant once daily. All groups received treatment for 12 weeks.
A total of 26 patients on placebo, 21 on 60-mg fezolinetant, and 17 on 180-mg fezolinetant completed the study. Patients who completed the study were included in the safety analysis, while all who took the study medication were included in the intent-to-treat analysis for primary and secondary outcome measures.
All participants had PCOS with hyperandrogenism, mean age was about 31 years, and about three quarters of enrollees were white, though local regulations restricted the collection of race and ethnicity data in some cases. One secondary outcome measure of the study was how fezolinetant affected the LH:FSH (follicle-stimulating hormone) ratio. “Patients with PCOS tend to have a very high GNRH [gonadotropin-releasing hormone] pulse frequency, which leads to a very high LH:FSH ratio,” said Dr. Fraser.
At baseline, the LH:FSH ratio was about 3. “With treatment, that ratio normalized to about 1, which is where it is in healthy women,” he said. The decrease in LH:FSH ratio occurred in a dose-dependent fashion and was statistically significant (P less than .001 for 180 mg fezolinetant versus placebo).
Dr. Fraser and his collaborators also tracked anti-müllerian hormone (AMH) levels, ovarian volume, and number of follicles. Although the investigators saw trends toward reduction in AMH levels and toward smaller ovarian volumes, these trends weren’t significant. “It was somewhat ambitious, I guess, to consider we’d hit these endpoints within 12 weeks,” he said. There were no serious drug-related adverse events.
“Most importantly, I would say, we did not get an increase in menses frequency, and, of course, that’s an important marker for fertility,” said Dr. Fraser. “There’s a debate in PCOS about whether this disease is driven by a malfunction in the brain or a malfunction in the ovaries. I guess on face value, perhaps this problem is in the ovaries.”
With the trends toward lower AMH and ovarian volumes, the research team is left wondering what would happen if the duration of therapy were extended. “Perhaps, the system would have been reset, and the frequency would have been restored. … So one thought that we have is to prolong the study in future trials and see if that could lead to an increase in fertility in PCOS,” said Dr. Fraser.
Fezolinetant is also being studied for menopause-related hot flashes in the United States and Europe.
Dr. Fraser is an employee of Ogeda, which sponsored the trial. Ogeda is a wholly owned subsidiary of Astelas.
SOURCE: Fraser G et al. ENDO 2018, Abstract SAT-305-LB.
REPORTING FROM ENDO 2018
Balance risk with reality for pre-conception diabetic counseling
CHICAGO – In particular, “several retrospective studies have shown that the risk for congenital malformations is increased with higher hemoglobin A1c levels,” said Susan Kirk, MD, speaking at a “Meet the Professor” session at the annual meeting of the Endocrine Society.
However, pointed out Dr. Kirk, fact-based counseling about pregnancy risks for women with type 1 or type 2 diabetes can – and should – occur within the framework of a strong and accepting physician-patient relationship.
Most women with diabetes have received pre-conception counseling about the risks of pregnancy with diabetes and the importance of glycemic control. “Despite that, I think many of us are often surprised by the percentage of unplanned pregnancies,” said Dr. Kirk, of the University of Virginia, Charlottesville, in an interview.
“What I have learned is that the desire to become pregnant is so strong, and the contemplation of all the adverse events that can happen … is really scary, not only to the woman but to her partner as well.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Kirk continued, “The more compassion you can show, and the more emphasis that you can place on the fact that she’s most likely to have a healthy baby, the chances are she’ll work with you from the beginning to get her control where she needs to be.”
Target numbers for hemoglobin A1c have become lower over the past several years, with the American Diabetes Association now recommending pre-conception levels below 6.5%. “There’s no randomized controlled trial that defines what that ideal number should be, but with the passage of time and some larger studies, we now know that ‘as close to normal as possible’ should be the goal,” Dr. Kirk said. This means that if women can tolerate the lower blood glucose levels without serious symptoms of hypoglycemia, a level of less than 6% is more preferable still, she said.
In terms of medication management for women with diabetes who become pregnant, physicians need to think about angiotensin converting enzyme inhibitors and statins, both of which are contraindicated for use during pregnancy. If a patient is pregnant or trying for a pregnancy, “I will stop those, and either leave them off all medicine entirely, or transition them to something that’s safe for use during pregnancy,” said Dr. Kirk.
It’s important to know if women have any microvascular complications because these are likely to progress during pregnancy, said Dr. Kirk. “The good news is, it all goes back to where she started before pregnancy after she has the baby,” though pre-existing advanced renal disease or eye disease may still cause concern for permanent damage. “If there are changes in the back of the eye that are suggestive of proliferative retinopathy, she should absolutely try to get that taken care of before she gets pregnant.”
The use of prenatal vitamins is another area where strong evidence is lacking, said Dr. Kirk. What is known is the folic acid supplementation “has been proven beyond a doubt to lower the rate of neural tube complications. And it’s cheap, and it’s easy to take. So any woman who’s even hinting at getting pregnant should be placed on those,” she said.
Dr. Kirk had no financial disclosures.
koakes@frontlinemedcom.com
SOURCE: Kirk S. ENDO 2018, Session M-02-3.
CHICAGO – In particular, “several retrospective studies have shown that the risk for congenital malformations is increased with higher hemoglobin A1c levels,” said Susan Kirk, MD, speaking at a “Meet the Professor” session at the annual meeting of the Endocrine Society.
However, pointed out Dr. Kirk, fact-based counseling about pregnancy risks for women with type 1 or type 2 diabetes can – and should – occur within the framework of a strong and accepting physician-patient relationship.
Most women with diabetes have received pre-conception counseling about the risks of pregnancy with diabetes and the importance of glycemic control. “Despite that, I think many of us are often surprised by the percentage of unplanned pregnancies,” said Dr. Kirk, of the University of Virginia, Charlottesville, in an interview.
“What I have learned is that the desire to become pregnant is so strong, and the contemplation of all the adverse events that can happen … is really scary, not only to the woman but to her partner as well.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Kirk continued, “The more compassion you can show, and the more emphasis that you can place on the fact that she’s most likely to have a healthy baby, the chances are she’ll work with you from the beginning to get her control where she needs to be.”
Target numbers for hemoglobin A1c have become lower over the past several years, with the American Diabetes Association now recommending pre-conception levels below 6.5%. “There’s no randomized controlled trial that defines what that ideal number should be, but with the passage of time and some larger studies, we now know that ‘as close to normal as possible’ should be the goal,” Dr. Kirk said. This means that if women can tolerate the lower blood glucose levels without serious symptoms of hypoglycemia, a level of less than 6% is more preferable still, she said.
In terms of medication management for women with diabetes who become pregnant, physicians need to think about angiotensin converting enzyme inhibitors and statins, both of which are contraindicated for use during pregnancy. If a patient is pregnant or trying for a pregnancy, “I will stop those, and either leave them off all medicine entirely, or transition them to something that’s safe for use during pregnancy,” said Dr. Kirk.
It’s important to know if women have any microvascular complications because these are likely to progress during pregnancy, said Dr. Kirk. “The good news is, it all goes back to where she started before pregnancy after she has the baby,” though pre-existing advanced renal disease or eye disease may still cause concern for permanent damage. “If there are changes in the back of the eye that are suggestive of proliferative retinopathy, she should absolutely try to get that taken care of before she gets pregnant.”
The use of prenatal vitamins is another area where strong evidence is lacking, said Dr. Kirk. What is known is the folic acid supplementation “has been proven beyond a doubt to lower the rate of neural tube complications. And it’s cheap, and it’s easy to take. So any woman who’s even hinting at getting pregnant should be placed on those,” she said.
Dr. Kirk had no financial disclosures.
koakes@frontlinemedcom.com
SOURCE: Kirk S. ENDO 2018, Session M-02-3.
CHICAGO – In particular, “several retrospective studies have shown that the risk for congenital malformations is increased with higher hemoglobin A1c levels,” said Susan Kirk, MD, speaking at a “Meet the Professor” session at the annual meeting of the Endocrine Society.
However, pointed out Dr. Kirk, fact-based counseling about pregnancy risks for women with type 1 or type 2 diabetes can – and should – occur within the framework of a strong and accepting physician-patient relationship.
Most women with diabetes have received pre-conception counseling about the risks of pregnancy with diabetes and the importance of glycemic control. “Despite that, I think many of us are often surprised by the percentage of unplanned pregnancies,” said Dr. Kirk, of the University of Virginia, Charlottesville, in an interview.
“What I have learned is that the desire to become pregnant is so strong, and the contemplation of all the adverse events that can happen … is really scary, not only to the woman but to her partner as well.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Kirk continued, “The more compassion you can show, and the more emphasis that you can place on the fact that she’s most likely to have a healthy baby, the chances are she’ll work with you from the beginning to get her control where she needs to be.”
Target numbers for hemoglobin A1c have become lower over the past several years, with the American Diabetes Association now recommending pre-conception levels below 6.5%. “There’s no randomized controlled trial that defines what that ideal number should be, but with the passage of time and some larger studies, we now know that ‘as close to normal as possible’ should be the goal,” Dr. Kirk said. This means that if women can tolerate the lower blood glucose levels without serious symptoms of hypoglycemia, a level of less than 6% is more preferable still, she said.
In terms of medication management for women with diabetes who become pregnant, physicians need to think about angiotensin converting enzyme inhibitors and statins, both of which are contraindicated for use during pregnancy. If a patient is pregnant or trying for a pregnancy, “I will stop those, and either leave them off all medicine entirely, or transition them to something that’s safe for use during pregnancy,” said Dr. Kirk.
It’s important to know if women have any microvascular complications because these are likely to progress during pregnancy, said Dr. Kirk. “The good news is, it all goes back to where she started before pregnancy after she has the baby,” though pre-existing advanced renal disease or eye disease may still cause concern for permanent damage. “If there are changes in the back of the eye that are suggestive of proliferative retinopathy, she should absolutely try to get that taken care of before she gets pregnant.”
The use of prenatal vitamins is another area where strong evidence is lacking, said Dr. Kirk. What is known is the folic acid supplementation “has been proven beyond a doubt to lower the rate of neural tube complications. And it’s cheap, and it’s easy to take. So any woman who’s even hinting at getting pregnant should be placed on those,” she said.
Dr. Kirk had no financial disclosures.
koakes@frontlinemedcom.com
SOURCE: Kirk S. ENDO 2018, Session M-02-3.
REPORTING FROM ENDO 2018
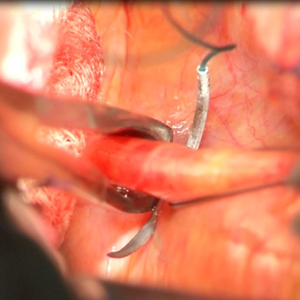
Uterosacral ligament colpopexy: The way we do it
The way we do it

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:
The way we do it
The way we do it
This video is brought to you by
2018 Hidradenitis Suppurativa 4-Part Video Roundtable
Hidradenitis suppurativa (HS) is a chronic, non-contagious skin disease that causes acne-like boils to form in folds of skin, particularly in the axilla and groin areas.
Disclosure: The faculty received modest honoraria from the Custom Programs division of Frontline Medical Communications for their time participating in this roundtable. The faculty was solely responsible for the content presented.
This video roundtable was produced by the Custom Programs division of Frontline Medical Communications. The editorial staff of Dermatology News was not involved in developing the video roundtable.
Hidradenitis suppurativa (HS) is a chronic, non-contagious skin disease that causes acne-like boils to form in folds of skin, particularly in the axilla and groin areas.
Disclosure: The faculty received modest honoraria from the Custom Programs division of Frontline Medical Communications for their time participating in this roundtable. The faculty was solely responsible for the content presented.
This video roundtable was produced by the Custom Programs division of Frontline Medical Communications. The editorial staff of Dermatology News was not involved in developing the video roundtable.
Hidradenitis suppurativa (HS) is a chronic, non-contagious skin disease that causes acne-like boils to form in folds of skin, particularly in the axilla and groin areas.
Disclosure: The faculty received modest honoraria from the Custom Programs division of Frontline Medical Communications for their time participating in this roundtable. The faculty was solely responsible for the content presented.
This video roundtable was produced by the Custom Programs division of Frontline Medical Communications. The editorial staff of Dermatology News was not involved in developing the video roundtable.
VIDEO: Patient vouchers prompt physicians to prescribe top antiplatelet drugs
ORLANDO – Patients who received vouchers to cover copayments were more likely to receive prescriptions for more effective antiplatelet medication, according to data from a multicenter, randomized trial.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“We know that guidelines are very clear; we need to treat patients with antiplatelet therapy for 12 months,” and that the most potent drug, ticagrelor, should be used, Tracy Wang, MD, of Duke University, Durham, N.C., said in a video interview at the annual meeting of the American College of Cardiology. However, in the United States, clopidogrel, though less effective, is prescribed much more often, and many patients discontinue their P2Y12 inhibitor therapy within the first year because of cost, she added.
“We hypothesized that, by reducing the out of pocket costs, treatment would be more evidence driven, rather than driven by what patients could afford,” she said.
The Affordability and Real-World Antiplatelet Treatment Effectiveness After Myocardial Infarction Study (ARTEMIS) included 11,001 MI patients at 301 hospitals across the United States. Patients in the treatment hospital group received a voucher to use at a pharmacy or through a mail-order pharmacy to reduce out of pocket costs. Randomization occurred at the hospital level, and hospital characteristics were similar between the groups.
Overall, patients in the treatment group were significantly more likely to receive a prescription for ticagrelor than clopidogrel (60% vs. 36%); 55% and 32% of patients in the usual care group were prescribed ticagrelor and clopidogrel, respectively. Nonpersistence, defined as a gap in P2Y12-inhibitor use of at least 30 days within 1 year, was significantly lower in the treatment group than it was in the usual care group based on patient reported analysis (13% vs. 16%).
However, the incidence of major adverse cardiac events was roughly 10% in both groups. The similar outcomes may stem from the fact that 28% of patients with vouchers did not fill their prescriptions for reasons that the study did not explore, said Dr. Wang.
All patients had health insurance: 64% private, 42% Medicare, 9% Medicaid. The average age of the patients was 62 years, and 31% were women. Patient demographics and clinical characteristics were similar between the groups.
The vouchers affected choice of treatment but didn’t help clinical outcomes, which suggests that copayment reduction should be part of a broader strategy to help patients with adherence over time, said Dr. Wang.
Next steps for research include taking a subset of patients who are more likely to be nonadherent and at high risk for adverse events and targeting them for additional intervention, she noted.
Discussant Craig J. Beavers, PharmD, of the University of Kentucky College of Pharmacy, Lexington, agreed that a multipronged approach is needed to get patients to take their medicines. “We have to figure out what other barriers there are,” he said. “The real trick is, even if you lead a horse to water, how to get them to drink it,” he said.
The study was funded by AstraZeneca. Dr. Wang disclosed relationships with companies including Gilead Sciences, Merck, and Sanofi Pasteur. Dr. Beavers had no financial conflicts to disclose.
SOURCE: Wang T. ACC 18.
ORLANDO – Patients who received vouchers to cover copayments were more likely to receive prescriptions for more effective antiplatelet medication, according to data from a multicenter, randomized trial.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“We know that guidelines are very clear; we need to treat patients with antiplatelet therapy for 12 months,” and that the most potent drug, ticagrelor, should be used, Tracy Wang, MD, of Duke University, Durham, N.C., said in a video interview at the annual meeting of the American College of Cardiology. However, in the United States, clopidogrel, though less effective, is prescribed much more often, and many patients discontinue their P2Y12 inhibitor therapy within the first year because of cost, she added.
“We hypothesized that, by reducing the out of pocket costs, treatment would be more evidence driven, rather than driven by what patients could afford,” she said.
The Affordability and Real-World Antiplatelet Treatment Effectiveness After Myocardial Infarction Study (ARTEMIS) included 11,001 MI patients at 301 hospitals across the United States. Patients in the treatment hospital group received a voucher to use at a pharmacy or through a mail-order pharmacy to reduce out of pocket costs. Randomization occurred at the hospital level, and hospital characteristics were similar between the groups.
Overall, patients in the treatment group were significantly more likely to receive a prescription for ticagrelor than clopidogrel (60% vs. 36%); 55% and 32% of patients in the usual care group were prescribed ticagrelor and clopidogrel, respectively. Nonpersistence, defined as a gap in P2Y12-inhibitor use of at least 30 days within 1 year, was significantly lower in the treatment group than it was in the usual care group based on patient reported analysis (13% vs. 16%).
However, the incidence of major adverse cardiac events was roughly 10% in both groups. The similar outcomes may stem from the fact that 28% of patients with vouchers did not fill their prescriptions for reasons that the study did not explore, said Dr. Wang.
All patients had health insurance: 64% private, 42% Medicare, 9% Medicaid. The average age of the patients was 62 years, and 31% were women. Patient demographics and clinical characteristics were similar between the groups.
The vouchers affected choice of treatment but didn’t help clinical outcomes, which suggests that copayment reduction should be part of a broader strategy to help patients with adherence over time, said Dr. Wang.
Next steps for research include taking a subset of patients who are more likely to be nonadherent and at high risk for adverse events and targeting them for additional intervention, she noted.
Discussant Craig J. Beavers, PharmD, of the University of Kentucky College of Pharmacy, Lexington, agreed that a multipronged approach is needed to get patients to take their medicines. “We have to figure out what other barriers there are,” he said. “The real trick is, even if you lead a horse to water, how to get them to drink it,” he said.
The study was funded by AstraZeneca. Dr. Wang disclosed relationships with companies including Gilead Sciences, Merck, and Sanofi Pasteur. Dr. Beavers had no financial conflicts to disclose.
SOURCE: Wang T. ACC 18.
ORLANDO – Patients who received vouchers to cover copayments were more likely to receive prescriptions for more effective antiplatelet medication, according to data from a multicenter, randomized trial.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“We know that guidelines are very clear; we need to treat patients with antiplatelet therapy for 12 months,” and that the most potent drug, ticagrelor, should be used, Tracy Wang, MD, of Duke University, Durham, N.C., said in a video interview at the annual meeting of the American College of Cardiology. However, in the United States, clopidogrel, though less effective, is prescribed much more often, and many patients discontinue their P2Y12 inhibitor therapy within the first year because of cost, she added.
“We hypothesized that, by reducing the out of pocket costs, treatment would be more evidence driven, rather than driven by what patients could afford,” she said.
The Affordability and Real-World Antiplatelet Treatment Effectiveness After Myocardial Infarction Study (ARTEMIS) included 11,001 MI patients at 301 hospitals across the United States. Patients in the treatment hospital group received a voucher to use at a pharmacy or through a mail-order pharmacy to reduce out of pocket costs. Randomization occurred at the hospital level, and hospital characteristics were similar between the groups.
Overall, patients in the treatment group were significantly more likely to receive a prescription for ticagrelor than clopidogrel (60% vs. 36%); 55% and 32% of patients in the usual care group were prescribed ticagrelor and clopidogrel, respectively. Nonpersistence, defined as a gap in P2Y12-inhibitor use of at least 30 days within 1 year, was significantly lower in the treatment group than it was in the usual care group based on patient reported analysis (13% vs. 16%).
However, the incidence of major adverse cardiac events was roughly 10% in both groups. The similar outcomes may stem from the fact that 28% of patients with vouchers did not fill their prescriptions for reasons that the study did not explore, said Dr. Wang.
All patients had health insurance: 64% private, 42% Medicare, 9% Medicaid. The average age of the patients was 62 years, and 31% were women. Patient demographics and clinical characteristics were similar between the groups.
The vouchers affected choice of treatment but didn’t help clinical outcomes, which suggests that copayment reduction should be part of a broader strategy to help patients with adherence over time, said Dr. Wang.
Next steps for research include taking a subset of patients who are more likely to be nonadherent and at high risk for adverse events and targeting them for additional intervention, she noted.
Discussant Craig J. Beavers, PharmD, of the University of Kentucky College of Pharmacy, Lexington, agreed that a multipronged approach is needed to get patients to take their medicines. “We have to figure out what other barriers there are,” he said. “The real trick is, even if you lead a horse to water, how to get them to drink it,” he said.
The study was funded by AstraZeneca. Dr. Wang disclosed relationships with companies including Gilead Sciences, Merck, and Sanofi Pasteur. Dr. Beavers had no financial conflicts to disclose.
SOURCE: Wang T. ACC 18.
REPORTING FROM ACC 18
Key clinical point: Physicians were more likely to prescribe ticagrelor after an MI when patients received vouchers.
Major finding: Patients with vouchers received prescriptions for ticagrelor significantly more than clopidogrel (60% vs. 36%).
Study details: The data come from a randomized trial of 301 hospitals in the United States and included 11,001 MI patients.
Disclosures: ARTEMIS was funded by AstraZeneca. Dr. Wang disclosed relationships with companies including Gilead Sciences, Merck, and Sanofi Pasteur. Dr. Beavers had no financial conflicts to disclose.
Source: Wang T. ACC 2018.
VIDEO: Dabigatran effective for myocardial injury after noncardiac surgery
ORLANDO – Treating patients who developed myocardial injury after noncardiac surgery with the anticoagulant dabigatran significantly cut the rate of subsequent major vascular complications in a randomized, multicenter trial with 1,754 patients, a result that gives surgeons and physicians the first evidence-based intervention for treating a common postsurgical condition.
“Because we have not systematically followed noncardiac surgery patients, it’s easy to presume that everyone is okay, but all the epidemiology data show that these patients [who develop myocardial injury after noncardiac surgery] don’t do okay. We need to be aggressive with secondary prophylaxis,” P.J. Devereaux, MD, said at the annual meeting of the American College of Cardiology. “The unfortunate thing is that right now, we don’t do much for these patients,” said Dr. Devereaux, professor of medicine and director of cardiology at McMaster University in Hamilton, Ont.
Results from prior epidemiology studies have shown that, among the roughly 200 million patients who undergo noncardiac surgery worldwide each year, 8% will develop MINS (myocardial injury after noncardiac surgery) (Anesthesiology. 2014 March;120[3]:564-78). The myocardial injury that defines MINS is identified by either an overt MI that meets the universal definition, or an otherwise unexplained rise in serum troponin levels from baseline in the first couple of days after surgery. In the new study, Dr. Devereaux and his associates identified 80% of MINS by a troponin rise and 20% by a diagnosed MI.
The challenge in diagnosing MINS and then administering dabigatran will be implementation of this strategy into routine practice, commented Erin A. Bohula May, MD, a cardiologist at Brigham and Women’s Hospital in Boston. “The problem is, troponin is not routinely measured in postoperative patients. It will be hard to change practice,” she noted.
Dr. Devereaux agreed that a significant barrier is convincing clinicians, especially surgeons, to routinely measure a patient’s troponin levels just before and immediately after surgery. “People are lulled into a false sense of security because patients [who develop MINS] usually don’t have chest pain,” he said in a video interview. “When we first showed that patients with MINS have bad outcomes, that convinced some [surgeons] to measure troponin after surgery. “Showing we can do something about it” is another important step toward fostering more awareness of and interest in diagnosing and treating MINS.
The Management of Myocardial Injury After Noncardiac Surgery Trial (MANAGE) enrolled 1,754 patients at 82 centers in 19 countries. Researchers randomized patients to treatment with either 110 mg dabigatran b.i.d. or placebo. A majority of patients in both arms also received aspirin and a statin, treatments that Dr. Devereaux should be used along with dabigatran in routine practice, based on observational findings, although the efficacy of these drugs for MINS patients has not been tested in randomized studies. The study’s primary endpoint was the incidence of major vascular complications, a composite that included vascular mortality, nonfatal MI, nonfatal and nonhemorrhagic stroke, peripheral arterial thrombosis, amputation, or symptomatic venous thromboembolism.
After an average follow-up of 16 months, the primary endpoint occurred in 11% of the dabigatran-treated patients and in 15% of controls, which represented a 28% risk reduction that was statistically significant. The study’s primary safety endpoint was a composite of life-threatening, major, and critical organ bleeds, which occurred in 3% of the dabigatran-treated patients and in 4% of controls, a nonsignificant difference. The dabigatran-treated patients showed a significant excess of both minor bleeds – 15% compared with 10% in controls – and “nonsignificant” lower gastrointestinal bleeds, 4% with dabigatran and 1% in the controls. The dabigatran-treated patients also had a significantly higher incidence of dyspepsia.
MANAGE was funded by the Population Health Research Institute and had no commercial funding. Dr. Devereaux has received research support from Abbott Diagnostics, Boehringer Ingelheim, Philips Healthcare, and Roche Diagnostics. Dr. May has been a consultant to Daiichi Sankyo, Merck, and Servier and has received research funding from Eisai.
SOURCE: Devereaux P et al. ACC 18.
Dr. Devereaux and his associates are to be congratulated on identifying a new disease entity, MINS (myocardial injury after noncardiac surgery), and now giving us a way to treat it. MINS is extremely common and quite morbid, and there had never before been a trial that studied its treatment. Identifying patients with MINS is extremely important. These are very-high-risk patients, and they are very hard to find. The results from MANAGE give us a way to do something about MINS and an opportunity to improve patient outcomes.
Pamela S. Douglas, MD , is a cardiologist and professor of medicine at Duke University in Durham, N.C. She had no disclosures. She made these comments as a discussant for MANAGE and in an interview.
Dr. Devereaux and his associates are to be congratulated on identifying a new disease entity, MINS (myocardial injury after noncardiac surgery), and now giving us a way to treat it. MINS is extremely common and quite morbid, and there had never before been a trial that studied its treatment. Identifying patients with MINS is extremely important. These are very-high-risk patients, and they are very hard to find. The results from MANAGE give us a way to do something about MINS and an opportunity to improve patient outcomes.
Pamela S. Douglas, MD , is a cardiologist and professor of medicine at Duke University in Durham, N.C. She had no disclosures. She made these comments as a discussant for MANAGE and in an interview.
Dr. Devereaux and his associates are to be congratulated on identifying a new disease entity, MINS (myocardial injury after noncardiac surgery), and now giving us a way to treat it. MINS is extremely common and quite morbid, and there had never before been a trial that studied its treatment. Identifying patients with MINS is extremely important. These are very-high-risk patients, and they are very hard to find. The results from MANAGE give us a way to do something about MINS and an opportunity to improve patient outcomes.
Pamela S. Douglas, MD , is a cardiologist and professor of medicine at Duke University in Durham, N.C. She had no disclosures. She made these comments as a discussant for MANAGE and in an interview.
ORLANDO – Treating patients who developed myocardial injury after noncardiac surgery with the anticoagulant dabigatran significantly cut the rate of subsequent major vascular complications in a randomized, multicenter trial with 1,754 patients, a result that gives surgeons and physicians the first evidence-based intervention for treating a common postsurgical condition.
“Because we have not systematically followed noncardiac surgery patients, it’s easy to presume that everyone is okay, but all the epidemiology data show that these patients [who develop myocardial injury after noncardiac surgery] don’t do okay. We need to be aggressive with secondary prophylaxis,” P.J. Devereaux, MD, said at the annual meeting of the American College of Cardiology. “The unfortunate thing is that right now, we don’t do much for these patients,” said Dr. Devereaux, professor of medicine and director of cardiology at McMaster University in Hamilton, Ont.
Results from prior epidemiology studies have shown that, among the roughly 200 million patients who undergo noncardiac surgery worldwide each year, 8% will develop MINS (myocardial injury after noncardiac surgery) (Anesthesiology. 2014 March;120[3]:564-78). The myocardial injury that defines MINS is identified by either an overt MI that meets the universal definition, or an otherwise unexplained rise in serum troponin levels from baseline in the first couple of days after surgery. In the new study, Dr. Devereaux and his associates identified 80% of MINS by a troponin rise and 20% by a diagnosed MI.
The challenge in diagnosing MINS and then administering dabigatran will be implementation of this strategy into routine practice, commented Erin A. Bohula May, MD, a cardiologist at Brigham and Women’s Hospital in Boston. “The problem is, troponin is not routinely measured in postoperative patients. It will be hard to change practice,” she noted.
Dr. Devereaux agreed that a significant barrier is convincing clinicians, especially surgeons, to routinely measure a patient’s troponin levels just before and immediately after surgery. “People are lulled into a false sense of security because patients [who develop MINS] usually don’t have chest pain,” he said in a video interview. “When we first showed that patients with MINS have bad outcomes, that convinced some [surgeons] to measure troponin after surgery. “Showing we can do something about it” is another important step toward fostering more awareness of and interest in diagnosing and treating MINS.
The Management of Myocardial Injury After Noncardiac Surgery Trial (MANAGE) enrolled 1,754 patients at 82 centers in 19 countries. Researchers randomized patients to treatment with either 110 mg dabigatran b.i.d. or placebo. A majority of patients in both arms also received aspirin and a statin, treatments that Dr. Devereaux should be used along with dabigatran in routine practice, based on observational findings, although the efficacy of these drugs for MINS patients has not been tested in randomized studies. The study’s primary endpoint was the incidence of major vascular complications, a composite that included vascular mortality, nonfatal MI, nonfatal and nonhemorrhagic stroke, peripheral arterial thrombosis, amputation, or symptomatic venous thromboembolism.
After an average follow-up of 16 months, the primary endpoint occurred in 11% of the dabigatran-treated patients and in 15% of controls, which represented a 28% risk reduction that was statistically significant. The study’s primary safety endpoint was a composite of life-threatening, major, and critical organ bleeds, which occurred in 3% of the dabigatran-treated patients and in 4% of controls, a nonsignificant difference. The dabigatran-treated patients showed a significant excess of both minor bleeds – 15% compared with 10% in controls – and “nonsignificant” lower gastrointestinal bleeds, 4% with dabigatran and 1% in the controls. The dabigatran-treated patients also had a significantly higher incidence of dyspepsia.
MANAGE was funded by the Population Health Research Institute and had no commercial funding. Dr. Devereaux has received research support from Abbott Diagnostics, Boehringer Ingelheim, Philips Healthcare, and Roche Diagnostics. Dr. May has been a consultant to Daiichi Sankyo, Merck, and Servier and has received research funding from Eisai.
SOURCE: Devereaux P et al. ACC 18.
ORLANDO – Treating patients who developed myocardial injury after noncardiac surgery with the anticoagulant dabigatran significantly cut the rate of subsequent major vascular complications in a randomized, multicenter trial with 1,754 patients, a result that gives surgeons and physicians the first evidence-based intervention for treating a common postsurgical condition.
“Because we have not systematically followed noncardiac surgery patients, it’s easy to presume that everyone is okay, but all the epidemiology data show that these patients [who develop myocardial injury after noncardiac surgery] don’t do okay. We need to be aggressive with secondary prophylaxis,” P.J. Devereaux, MD, said at the annual meeting of the American College of Cardiology. “The unfortunate thing is that right now, we don’t do much for these patients,” said Dr. Devereaux, professor of medicine and director of cardiology at McMaster University in Hamilton, Ont.
Results from prior epidemiology studies have shown that, among the roughly 200 million patients who undergo noncardiac surgery worldwide each year, 8% will develop MINS (myocardial injury after noncardiac surgery) (Anesthesiology. 2014 March;120[3]:564-78). The myocardial injury that defines MINS is identified by either an overt MI that meets the universal definition, or an otherwise unexplained rise in serum troponin levels from baseline in the first couple of days after surgery. In the new study, Dr. Devereaux and his associates identified 80% of MINS by a troponin rise and 20% by a diagnosed MI.
The challenge in diagnosing MINS and then administering dabigatran will be implementation of this strategy into routine practice, commented Erin A. Bohula May, MD, a cardiologist at Brigham and Women’s Hospital in Boston. “The problem is, troponin is not routinely measured in postoperative patients. It will be hard to change practice,” she noted.
Dr. Devereaux agreed that a significant barrier is convincing clinicians, especially surgeons, to routinely measure a patient’s troponin levels just before and immediately after surgery. “People are lulled into a false sense of security because patients [who develop MINS] usually don’t have chest pain,” he said in a video interview. “When we first showed that patients with MINS have bad outcomes, that convinced some [surgeons] to measure troponin after surgery. “Showing we can do something about it” is another important step toward fostering more awareness of and interest in diagnosing and treating MINS.
The Management of Myocardial Injury After Noncardiac Surgery Trial (MANAGE) enrolled 1,754 patients at 82 centers in 19 countries. Researchers randomized patients to treatment with either 110 mg dabigatran b.i.d. or placebo. A majority of patients in both arms also received aspirin and a statin, treatments that Dr. Devereaux should be used along with dabigatran in routine practice, based on observational findings, although the efficacy of these drugs for MINS patients has not been tested in randomized studies. The study’s primary endpoint was the incidence of major vascular complications, a composite that included vascular mortality, nonfatal MI, nonfatal and nonhemorrhagic stroke, peripheral arterial thrombosis, amputation, or symptomatic venous thromboembolism.
After an average follow-up of 16 months, the primary endpoint occurred in 11% of the dabigatran-treated patients and in 15% of controls, which represented a 28% risk reduction that was statistically significant. The study’s primary safety endpoint was a composite of life-threatening, major, and critical organ bleeds, which occurred in 3% of the dabigatran-treated patients and in 4% of controls, a nonsignificant difference. The dabigatran-treated patients showed a significant excess of both minor bleeds – 15% compared with 10% in controls – and “nonsignificant” lower gastrointestinal bleeds, 4% with dabigatran and 1% in the controls. The dabigatran-treated patients also had a significantly higher incidence of dyspepsia.
MANAGE was funded by the Population Health Research Institute and had no commercial funding. Dr. Devereaux has received research support from Abbott Diagnostics, Boehringer Ingelheim, Philips Healthcare, and Roche Diagnostics. Dr. May has been a consultant to Daiichi Sankyo, Merck, and Servier and has received research funding from Eisai.
SOURCE: Devereaux P et al. ACC 18.
REPORTING FROM ACC 18
Key clinical point: Dabigatran is the first intervention proven to benefit patients with MINS.
Major finding: Major vascular complications occurred in 11% of patients on dabigatran and 15% on placebo.
Study details: MANAGE, a multicenter, randomized trial with 1,754 patients.
Disclosures: MANAGE was funded by the Population Health Research Institute and had no commercial funding. Dr. Devereaux has received research support from Abbott Diagnostics, Boehringer Ingelheim, Philips Healthcare, and Roche Diagnostics. Dr. May has been a consultant to Daiichi Sankyo, Merck, and Servier and has received research funding from Eisai.
Source: Devereaux P et al. ACC 18.
MOMENTUM 3 HeartMate 3 LVAD ‘practice changing’
ORLANDO – of follow-up in patients with advanced heart failure in the large multicenter MOMENTUM 3 trial, Mandeep R. Mehra, MD, reported at the annual meeting of the American College of Cardiology.
HeartMate 3 recipients had a 90% lower risk of undergoing reoperation to replace or remove their device because of malfunction, and a stroke rate half that in the HeartMate II group.
“This was the lowest rate of stroke ever seen in any LVAD trial,” according to Dr. Mehra, medical director of the Brigham and Women’s Hospital Heart and Vascular Center, Boston, and professor of medicine at Harvard Medical School.
“We believe this is a practice-changing result in the field, and that the real implication of our findings is to reassure those who refer or treat patients with advanced heart failure that it is perhaps going to be ignorant not to refer patients for consideration for destination therapy,” he said at a press conference highlighting the MOMENTUM 3 results, also presented in a late-breaking clinical trials session.
The HeartMate 3 is a miniaturized centrifugal-flow device that fits entirely within the chest, whereas the HeartMate II requires creation of a pocket in the abdomen. The HeartMate 3 was designed to prevent pump thrombosis – a common limiting problem with the HeartMate II and other LVADs – by employing three innovations: use of wide blood-flow passages to reduce shear stress and minimize disruption of red blood cells as they pass through the pump; reliance on magnetic levitation technology to create a frictionless pump with no mechanical bearings, which are subject to wear and tear; and incorporation of an artificial fixed pulse that speeds up and slows every 2 seconds in order to minimize blood stasis, which promotes thrombosis, the cardiologist explained in a video interview.
MOMENTUM 3 is the largest-ever randomized trial of LVAD therapy, involving 1,028 advanced heart failure patients at 69 U.S. centers. The study population is a mix of bridge-to-transplant patients and others who weren’t eligible for heart transplantation and are using their device as lifelong destination therapy. In an earlier report on the first 294 patients to reach 6 months of follow-up post implantation, Dr. Mehra and his coinvestigators showed that the HeartMate 3 group had a significantly lower incidence of the composite endpoint of disabling stroke or reoperation to replace or remove the device (N Engl J Med. 2017 Feb 2;376[5]:440-50).
At ACC 2018, he presented the prespecified 2-year analysis of results in the first 366 patients to reach that benchmark. The rate of survival free of disabling stroke or reoperation for device malfunction was 79.5% in the HeartMate 3 group and 60.2% with the HeartMate II, for a highly significant 54% reduction in the risk of bad outcome. Reoperation for device malfunction occurred in 1.6% of HeartMate 3 patients versus 17% of those with a HeartMate II, for a 92% reduction in risk. Two-year survival was 82.8% in the HeartMate 3 group and 76.2% in HeartMate II recipients.
The overall stroke rate was 10% with the HeartMate 3, compared with 19% with the older, axial-flow LVAD. The incidence of disabling stroke was 3% in the HeartMate 3 group and similar at 2% with the HeartMate II; however, nondisabling stroke occurred in only 3% of HeartMate 3 recipients, compared with 14% of patients with the HeartMate II.
“There has always been this notion that, ‘There are so many complications with this device, so let’s suffer with the disease rather than suffer with the pump.’ Now we’re showing that you don’t suffer with the pump as with the earlier-generation devices. I think this is going to open the gates for more referrals and more opportunities for destination therapy in patients who are deemed ineligible for transplant,” Dr. Mehra predicted.
Discussant James L. Janzuzzi Jr., called the MOMENTUM 3 results “a very-much-needed step forward.”
“Perhaps the most dramatic observation in this study is the dramatic reduction in thrombosis events requiring reoperation. In essence, this problem was entirely prevented by the use of this magnetically levitated centrifugal-flow device. Reoperation for thrombosis accounted for two-thirds of the reoperations in the HeartMate II group and the rate was zero in the HeartMate 3 population. Essentially, with this technology we’ve addressed a very important unmet need by reducing the onset of pump thrombosis, which is the precursor to either pump dysfunction or embolic stroke,” commented Dr. Januzzi, professor of medicine at Harvard Medical School, Boston.
Given the 83% survival rate at 2 years in the HeartMate 3 group in the MOMENTUM 3 trial, the on-average 50% survival at 10 years for heart transplant recipients, and the perpetual enormous shortage of donor organs, it’s time to consider a randomized trial of an advanced LVAD such as the HeartMate 3 versus heart transplantation, with quality-of-life outcomes front and center, he asserted.
Dr. Mehra was all for the idea. He noted that within the community of physicians and surgeons who provide care for advanced heart failure patients there is a growing move to replace problematic axial-flow LVADs requiring reoperation with a HeartMate 3 upgrade.
The MOMENTUM 3 trial is funded by Abbott. Dr. Mehra reported receiving research funds from and serving as a consultant to the company.
Simultaneous with his presentation at ACC 2018, the 2-year results of MOMENTUM 3 were published online at NEJM.org (doi: 10.1056/NEJMoa1800866).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SOURCE: Mehra M et al. ACC 18.
ORLANDO – of follow-up in patients with advanced heart failure in the large multicenter MOMENTUM 3 trial, Mandeep R. Mehra, MD, reported at the annual meeting of the American College of Cardiology.
HeartMate 3 recipients had a 90% lower risk of undergoing reoperation to replace or remove their device because of malfunction, and a stroke rate half that in the HeartMate II group.
“This was the lowest rate of stroke ever seen in any LVAD trial,” according to Dr. Mehra, medical director of the Brigham and Women’s Hospital Heart and Vascular Center, Boston, and professor of medicine at Harvard Medical School.
“We believe this is a practice-changing result in the field, and that the real implication of our findings is to reassure those who refer or treat patients with advanced heart failure that it is perhaps going to be ignorant not to refer patients for consideration for destination therapy,” he said at a press conference highlighting the MOMENTUM 3 results, also presented in a late-breaking clinical trials session.
The HeartMate 3 is a miniaturized centrifugal-flow device that fits entirely within the chest, whereas the HeartMate II requires creation of a pocket in the abdomen. The HeartMate 3 was designed to prevent pump thrombosis – a common limiting problem with the HeartMate II and other LVADs – by employing three innovations: use of wide blood-flow passages to reduce shear stress and minimize disruption of red blood cells as they pass through the pump; reliance on magnetic levitation technology to create a frictionless pump with no mechanical bearings, which are subject to wear and tear; and incorporation of an artificial fixed pulse that speeds up and slows every 2 seconds in order to minimize blood stasis, which promotes thrombosis, the cardiologist explained in a video interview.
MOMENTUM 3 is the largest-ever randomized trial of LVAD therapy, involving 1,028 advanced heart failure patients at 69 U.S. centers. The study population is a mix of bridge-to-transplant patients and others who weren’t eligible for heart transplantation and are using their device as lifelong destination therapy. In an earlier report on the first 294 patients to reach 6 months of follow-up post implantation, Dr. Mehra and his coinvestigators showed that the HeartMate 3 group had a significantly lower incidence of the composite endpoint of disabling stroke or reoperation to replace or remove the device (N Engl J Med. 2017 Feb 2;376[5]:440-50).
At ACC 2018, he presented the prespecified 2-year analysis of results in the first 366 patients to reach that benchmark. The rate of survival free of disabling stroke or reoperation for device malfunction was 79.5% in the HeartMate 3 group and 60.2% with the HeartMate II, for a highly significant 54% reduction in the risk of bad outcome. Reoperation for device malfunction occurred in 1.6% of HeartMate 3 patients versus 17% of those with a HeartMate II, for a 92% reduction in risk. Two-year survival was 82.8% in the HeartMate 3 group and 76.2% in HeartMate II recipients.
The overall stroke rate was 10% with the HeartMate 3, compared with 19% with the older, axial-flow LVAD. The incidence of disabling stroke was 3% in the HeartMate 3 group and similar at 2% with the HeartMate II; however, nondisabling stroke occurred in only 3% of HeartMate 3 recipients, compared with 14% of patients with the HeartMate II.
“There has always been this notion that, ‘There are so many complications with this device, so let’s suffer with the disease rather than suffer with the pump.’ Now we’re showing that you don’t suffer with the pump as with the earlier-generation devices. I think this is going to open the gates for more referrals and more opportunities for destination therapy in patients who are deemed ineligible for transplant,” Dr. Mehra predicted.
Discussant James L. Janzuzzi Jr., called the MOMENTUM 3 results “a very-much-needed step forward.”
“Perhaps the most dramatic observation in this study is the dramatic reduction in thrombosis events requiring reoperation. In essence, this problem was entirely prevented by the use of this magnetically levitated centrifugal-flow device. Reoperation for thrombosis accounted for two-thirds of the reoperations in the HeartMate II group and the rate was zero in the HeartMate 3 population. Essentially, with this technology we’ve addressed a very important unmet need by reducing the onset of pump thrombosis, which is the precursor to either pump dysfunction or embolic stroke,” commented Dr. Januzzi, professor of medicine at Harvard Medical School, Boston.
Given the 83% survival rate at 2 years in the HeartMate 3 group in the MOMENTUM 3 trial, the on-average 50% survival at 10 years for heart transplant recipients, and the perpetual enormous shortage of donor organs, it’s time to consider a randomized trial of an advanced LVAD such as the HeartMate 3 versus heart transplantation, with quality-of-life outcomes front and center, he asserted.
Dr. Mehra was all for the idea. He noted that within the community of physicians and surgeons who provide care for advanced heart failure patients there is a growing move to replace problematic axial-flow LVADs requiring reoperation with a HeartMate 3 upgrade.
The MOMENTUM 3 trial is funded by Abbott. Dr. Mehra reported receiving research funds from and serving as a consultant to the company.
Simultaneous with his presentation at ACC 2018, the 2-year results of MOMENTUM 3 were published online at NEJM.org (doi: 10.1056/NEJMoa1800866).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SOURCE: Mehra M et al. ACC 18.
ORLANDO – of follow-up in patients with advanced heart failure in the large multicenter MOMENTUM 3 trial, Mandeep R. Mehra, MD, reported at the annual meeting of the American College of Cardiology.
HeartMate 3 recipients had a 90% lower risk of undergoing reoperation to replace or remove their device because of malfunction, and a stroke rate half that in the HeartMate II group.
“This was the lowest rate of stroke ever seen in any LVAD trial,” according to Dr. Mehra, medical director of the Brigham and Women’s Hospital Heart and Vascular Center, Boston, and professor of medicine at Harvard Medical School.
“We believe this is a practice-changing result in the field, and that the real implication of our findings is to reassure those who refer or treat patients with advanced heart failure that it is perhaps going to be ignorant not to refer patients for consideration for destination therapy,” he said at a press conference highlighting the MOMENTUM 3 results, also presented in a late-breaking clinical trials session.
The HeartMate 3 is a miniaturized centrifugal-flow device that fits entirely within the chest, whereas the HeartMate II requires creation of a pocket in the abdomen. The HeartMate 3 was designed to prevent pump thrombosis – a common limiting problem with the HeartMate II and other LVADs – by employing three innovations: use of wide blood-flow passages to reduce shear stress and minimize disruption of red blood cells as they pass through the pump; reliance on magnetic levitation technology to create a frictionless pump with no mechanical bearings, which are subject to wear and tear; and incorporation of an artificial fixed pulse that speeds up and slows every 2 seconds in order to minimize blood stasis, which promotes thrombosis, the cardiologist explained in a video interview.
MOMENTUM 3 is the largest-ever randomized trial of LVAD therapy, involving 1,028 advanced heart failure patients at 69 U.S. centers. The study population is a mix of bridge-to-transplant patients and others who weren’t eligible for heart transplantation and are using their device as lifelong destination therapy. In an earlier report on the first 294 patients to reach 6 months of follow-up post implantation, Dr. Mehra and his coinvestigators showed that the HeartMate 3 group had a significantly lower incidence of the composite endpoint of disabling stroke or reoperation to replace or remove the device (N Engl J Med. 2017 Feb 2;376[5]:440-50).
At ACC 2018, he presented the prespecified 2-year analysis of results in the first 366 patients to reach that benchmark. The rate of survival free of disabling stroke or reoperation for device malfunction was 79.5% in the HeartMate 3 group and 60.2% with the HeartMate II, for a highly significant 54% reduction in the risk of bad outcome. Reoperation for device malfunction occurred in 1.6% of HeartMate 3 patients versus 17% of those with a HeartMate II, for a 92% reduction in risk. Two-year survival was 82.8% in the HeartMate 3 group and 76.2% in HeartMate II recipients.
The overall stroke rate was 10% with the HeartMate 3, compared with 19% with the older, axial-flow LVAD. The incidence of disabling stroke was 3% in the HeartMate 3 group and similar at 2% with the HeartMate II; however, nondisabling stroke occurred in only 3% of HeartMate 3 recipients, compared with 14% of patients with the HeartMate II.
“There has always been this notion that, ‘There are so many complications with this device, so let’s suffer with the disease rather than suffer with the pump.’ Now we’re showing that you don’t suffer with the pump as with the earlier-generation devices. I think this is going to open the gates for more referrals and more opportunities for destination therapy in patients who are deemed ineligible for transplant,” Dr. Mehra predicted.
Discussant James L. Janzuzzi Jr., called the MOMENTUM 3 results “a very-much-needed step forward.”
“Perhaps the most dramatic observation in this study is the dramatic reduction in thrombosis events requiring reoperation. In essence, this problem was entirely prevented by the use of this magnetically levitated centrifugal-flow device. Reoperation for thrombosis accounted for two-thirds of the reoperations in the HeartMate II group and the rate was zero in the HeartMate 3 population. Essentially, with this technology we’ve addressed a very important unmet need by reducing the onset of pump thrombosis, which is the precursor to either pump dysfunction or embolic stroke,” commented Dr. Januzzi, professor of medicine at Harvard Medical School, Boston.
Given the 83% survival rate at 2 years in the HeartMate 3 group in the MOMENTUM 3 trial, the on-average 50% survival at 10 years for heart transplant recipients, and the perpetual enormous shortage of donor organs, it’s time to consider a randomized trial of an advanced LVAD such as the HeartMate 3 versus heart transplantation, with quality-of-life outcomes front and center, he asserted.
Dr. Mehra was all for the idea. He noted that within the community of physicians and surgeons who provide care for advanced heart failure patients there is a growing move to replace problematic axial-flow LVADs requiring reoperation with a HeartMate 3 upgrade.
The MOMENTUM 3 trial is funded by Abbott. Dr. Mehra reported receiving research funds from and serving as a consultant to the company.
Simultaneous with his presentation at ACC 2018, the 2-year results of MOMENTUM 3 were published online at NEJM.org (doi: 10.1056/NEJMoa1800866).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SOURCE: Mehra M et al. ACC 18.
REPORTING FROM ACC 18
Key clinical point: Landmark trial paves way to much wider use of LVADs as destination therapy.
Major finding: The 2-year rate of survival free of disabling stroke or reoperation to replace or remove a malfunctioning LVAD was 79.5% with the novel HeartMate 3 LVAD, compared with 60.2% with the commonly used HeartMate II axial-flow device.
Study details: This was a randomized, unblinded, multicenter study of more than 1,000 patients with advanced heart failure.
Disclosures: The MOMENTUM 3 trial was funded by Abbott. The presenter reported receiving research grants from and serving as a consultant to the company.
Source: Mehra MR et al. ACC 18.
A Peek at Our March 2018 Issue
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Osteoporosis: Overview, Workup, Diagnosis
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.