User login
Gastroenterology debuts editorial fellowship program
The readership of Gastroenterology includes a broad distribution of stakeholders in digestive health, including those with vested interests in clinical practice, education, policy, clinical investigation, and basic research. One of our most critical constituencies, however, is trainees and early-career GIs. In an effort to support such individuals, our editorial team has developed a freshly minted 1-year editorial fellowship for Gastroenterology. The overarching purpose of this fellowship is to mentor an outstanding trainee for future editorial leadership roles in scientific publishing, as a means to promote the interests of trainee and early-career GI constituencies within the AGA and Gastroenterology. This fellowship is available to exceptional second- or third-year fellows through an application process. The intent of this training is to allow the selected applicant to become intimately involved with Gastroenterology’s entire editorial process, including peer review, editorial oversight, manuscript selection for publication, production, and postpublication activities. Our first fellow, Eric Shah, MD, MBA, was selected from a highly competitive pool of exceptional applicants, and began his fellowship on July 1, 2017.
This year, we have been delighted to work with Dr. Shah as our inaugural Gastroenterology fellow. Dr. Shah has a unique background, having pursued a joint MD and MBA (earning both concurrently), while also following venture-oriented interests in developing GI technology from academia. Dr. Shah began his research career under the mentorship of Mark Pimentel, MD, and Gil Melmed, MD, at Cedars-Sinai as part of a Research Honors Program. Since that time, he has focused on evaluating the comparative efficacy, durability, and harm associated with pharmacotherapy in functional bowel disorders. Dr. Shah was accepted into the GI fellowship training program at the University of Michigan and received a slot on the T32 training grant to study cost-effectiveness and qualitative research techniques to address gaps in the care of functional bowel disorders. His work under the mentorship of William Chey, MD, Ryan Stidham, MD, and Philip S. Schoenfeld, MD, has flourished and culminated in an oral presentation and several posters for DDW 2017, as well as several first-author manuscripts that have been submitted. Dr. Shah has fully embraced the Gastroenterology fellowship and has far surpassed our high expectations for this position.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
In addition to creating an editorial fellowship, our team has also developed other components within the journal that specifically target trainees and early-career GIs. The Mentoring, Education and Training section – initiated in 2011 through the vision and insight of Bishr Omary MD, PhD, and John Del Valle, MD, at the University of Michigan – has been extremely effective in highlighting critical issues relevant to trainees, young faculty, and early-career GIs. Topics have included mentoring advice not only for individuals in academic or private practice careers but also industry careers and midlevel providers. Other topics have included Accreditation Council for Graduate Medical Education milestones, career advancement for clinician-educators, sex and ethnic diversity, and maintenance of certification, as well as guidance regarding nontraditional funding mechanisms such as philanthropy. Potential future topics will include information about major new public and private funding initiatives, comments and input from National Institutes of Health officials, and reports of funding trends relevant to both physician scientists and clinicians. We are fortunate to have Prateek Sharma, MD, lead this section, and his depth of experience as an exceptional mentor has provided the requisite expertise.
Additionally, we offer a reduction in page charges to junior investigators (within 7 years of fellowship) who are the corresponding authors of exceedingly important original Gastroenterology manuscripts. These manuscripts from junior investigators will be highlighted in both print and online versions of Gastroenterology. We are using the journal to expand electronic access to educational offerings for new technologies, training, self-assessment, and practice improvement to establish the AGA as the ultimate resource for junior academicians and practicing physicians. We are also currently integrating Gastroenterology more closely into other AGA educational efforts that target young physicians, such as the AGA Education and Training Committee.
At Gastroenterology, we are acutely aware of the needs and obstacles facing trainees, young faculty, and early-career GIs. We have boldly adopted a multidimensional approach to provide guidance and opportunities to overcome these challenges, including the creation of the nascent Editorial Fellowship. We welcome applications for the next fellowship, which will be announced by the AGA in the spring of 2018!
Dr. Peek is the Mina Wallace Professor of Medicine, Cancer Biology, and Pathology, Microbiology, and Immunology, and director, division of gastroenterology, hepatology and nutrition, Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts of interest.
The readership of Gastroenterology includes a broad distribution of stakeholders in digestive health, including those with vested interests in clinical practice, education, policy, clinical investigation, and basic research. One of our most critical constituencies, however, is trainees and early-career GIs. In an effort to support such individuals, our editorial team has developed a freshly minted 1-year editorial fellowship for Gastroenterology. The overarching purpose of this fellowship is to mentor an outstanding trainee for future editorial leadership roles in scientific publishing, as a means to promote the interests of trainee and early-career GI constituencies within the AGA and Gastroenterology. This fellowship is available to exceptional second- or third-year fellows through an application process. The intent of this training is to allow the selected applicant to become intimately involved with Gastroenterology’s entire editorial process, including peer review, editorial oversight, manuscript selection for publication, production, and postpublication activities. Our first fellow, Eric Shah, MD, MBA, was selected from a highly competitive pool of exceptional applicants, and began his fellowship on July 1, 2017.
This year, we have been delighted to work with Dr. Shah as our inaugural Gastroenterology fellow. Dr. Shah has a unique background, having pursued a joint MD and MBA (earning both concurrently), while also following venture-oriented interests in developing GI technology from academia. Dr. Shah began his research career under the mentorship of Mark Pimentel, MD, and Gil Melmed, MD, at Cedars-Sinai as part of a Research Honors Program. Since that time, he has focused on evaluating the comparative efficacy, durability, and harm associated with pharmacotherapy in functional bowel disorders. Dr. Shah was accepted into the GI fellowship training program at the University of Michigan and received a slot on the T32 training grant to study cost-effectiveness and qualitative research techniques to address gaps in the care of functional bowel disorders. His work under the mentorship of William Chey, MD, Ryan Stidham, MD, and Philip S. Schoenfeld, MD, has flourished and culminated in an oral presentation and several posters for DDW 2017, as well as several first-author manuscripts that have been submitted. Dr. Shah has fully embraced the Gastroenterology fellowship and has far surpassed our high expectations for this position.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
In addition to creating an editorial fellowship, our team has also developed other components within the journal that specifically target trainees and early-career GIs. The Mentoring, Education and Training section – initiated in 2011 through the vision and insight of Bishr Omary MD, PhD, and John Del Valle, MD, at the University of Michigan – has been extremely effective in highlighting critical issues relevant to trainees, young faculty, and early-career GIs. Topics have included mentoring advice not only for individuals in academic or private practice careers but also industry careers and midlevel providers. Other topics have included Accreditation Council for Graduate Medical Education milestones, career advancement for clinician-educators, sex and ethnic diversity, and maintenance of certification, as well as guidance regarding nontraditional funding mechanisms such as philanthropy. Potential future topics will include information about major new public and private funding initiatives, comments and input from National Institutes of Health officials, and reports of funding trends relevant to both physician scientists and clinicians. We are fortunate to have Prateek Sharma, MD, lead this section, and his depth of experience as an exceptional mentor has provided the requisite expertise.
Additionally, we offer a reduction in page charges to junior investigators (within 7 years of fellowship) who are the corresponding authors of exceedingly important original Gastroenterology manuscripts. These manuscripts from junior investigators will be highlighted in both print and online versions of Gastroenterology. We are using the journal to expand electronic access to educational offerings for new technologies, training, self-assessment, and practice improvement to establish the AGA as the ultimate resource for junior academicians and practicing physicians. We are also currently integrating Gastroenterology more closely into other AGA educational efforts that target young physicians, such as the AGA Education and Training Committee.
At Gastroenterology, we are acutely aware of the needs and obstacles facing trainees, young faculty, and early-career GIs. We have boldly adopted a multidimensional approach to provide guidance and opportunities to overcome these challenges, including the creation of the nascent Editorial Fellowship. We welcome applications for the next fellowship, which will be announced by the AGA in the spring of 2018!
Dr. Peek is the Mina Wallace Professor of Medicine, Cancer Biology, and Pathology, Microbiology, and Immunology, and director, division of gastroenterology, hepatology and nutrition, Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts of interest.
The readership of Gastroenterology includes a broad distribution of stakeholders in digestive health, including those with vested interests in clinical practice, education, policy, clinical investigation, and basic research. One of our most critical constituencies, however, is trainees and early-career GIs. In an effort to support such individuals, our editorial team has developed a freshly minted 1-year editorial fellowship for Gastroenterology. The overarching purpose of this fellowship is to mentor an outstanding trainee for future editorial leadership roles in scientific publishing, as a means to promote the interests of trainee and early-career GI constituencies within the AGA and Gastroenterology. This fellowship is available to exceptional second- or third-year fellows through an application process. The intent of this training is to allow the selected applicant to become intimately involved with Gastroenterology’s entire editorial process, including peer review, editorial oversight, manuscript selection for publication, production, and postpublication activities. Our first fellow, Eric Shah, MD, MBA, was selected from a highly competitive pool of exceptional applicants, and began his fellowship on July 1, 2017.
This year, we have been delighted to work with Dr. Shah as our inaugural Gastroenterology fellow. Dr. Shah has a unique background, having pursued a joint MD and MBA (earning both concurrently), while also following venture-oriented interests in developing GI technology from academia. Dr. Shah began his research career under the mentorship of Mark Pimentel, MD, and Gil Melmed, MD, at Cedars-Sinai as part of a Research Honors Program. Since that time, he has focused on evaluating the comparative efficacy, durability, and harm associated with pharmacotherapy in functional bowel disorders. Dr. Shah was accepted into the GI fellowship training program at the University of Michigan and received a slot on the T32 training grant to study cost-effectiveness and qualitative research techniques to address gaps in the care of functional bowel disorders. His work under the mentorship of William Chey, MD, Ryan Stidham, MD, and Philip S. Schoenfeld, MD, has flourished and culminated in an oral presentation and several posters for DDW 2017, as well as several first-author manuscripts that have been submitted. Dr. Shah has fully embraced the Gastroenterology fellowship and has far surpassed our high expectations for this position.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
In addition to creating an editorial fellowship, our team has also developed other components within the journal that specifically target trainees and early-career GIs. The Mentoring, Education and Training section – initiated in 2011 through the vision and insight of Bishr Omary MD, PhD, and John Del Valle, MD, at the University of Michigan – has been extremely effective in highlighting critical issues relevant to trainees, young faculty, and early-career GIs. Topics have included mentoring advice not only for individuals in academic or private practice careers but also industry careers and midlevel providers. Other topics have included Accreditation Council for Graduate Medical Education milestones, career advancement for clinician-educators, sex and ethnic diversity, and maintenance of certification, as well as guidance regarding nontraditional funding mechanisms such as philanthropy. Potential future topics will include information about major new public and private funding initiatives, comments and input from National Institutes of Health officials, and reports of funding trends relevant to both physician scientists and clinicians. We are fortunate to have Prateek Sharma, MD, lead this section, and his depth of experience as an exceptional mentor has provided the requisite expertise.
Additionally, we offer a reduction in page charges to junior investigators (within 7 years of fellowship) who are the corresponding authors of exceedingly important original Gastroenterology manuscripts. These manuscripts from junior investigators will be highlighted in both print and online versions of Gastroenterology. We are using the journal to expand electronic access to educational offerings for new technologies, training, self-assessment, and practice improvement to establish the AGA as the ultimate resource for junior academicians and practicing physicians. We are also currently integrating Gastroenterology more closely into other AGA educational efforts that target young physicians, such as the AGA Education and Training Committee.
At Gastroenterology, we are acutely aware of the needs and obstacles facing trainees, young faculty, and early-career GIs. We have boldly adopted a multidimensional approach to provide guidance and opportunities to overcome these challenges, including the creation of the nascent Editorial Fellowship. We welcome applications for the next fellowship, which will be announced by the AGA in the spring of 2018!
Dr. Peek is the Mina Wallace Professor of Medicine, Cancer Biology, and Pathology, Microbiology, and Immunology, and director, division of gastroenterology, hepatology and nutrition, Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts of interest.
VIDEO: Practice changers out of ASH 2017
ATLANTA – There were a lot of new data presented during the annual meeting of the American Society of Hematology. But what findings could actually change the way you practice?
Robert A. Brodsky, MD, director of the division of hematology at Johns Hopkins University in Baltimore and the moderator for the late-breaking abstract session at ASH, highlighted results from two studies.
Data from the MURANO trial showed robust results for a combination of venetoclax and rituximab in patients with relapsed/refractory chronic lymphocytic leukemia (CLL). At a median follow-up of 23.8 months, median progression-free survival -had not been reached in patients randomized to venetoclax/rituximab, while patients who received bendamustine plus rituximab had a median PFS of 17 months.
The based on the data presented, Dr. Brodsky said.
Another “enormously exciting and practice-changing” finding is that direct oral anticoagulants can be used safely in patients with cancer, Dr. Brodsky said in an interview.
In a randomized, open-label study, 12 months of daily treatment with edoxaban was noninferior to standard subcutaneous therapy with dalteparin for treatment of venous thromboembolism in cancer patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – There were a lot of new data presented during the annual meeting of the American Society of Hematology. But what findings could actually change the way you practice?
Robert A. Brodsky, MD, director of the division of hematology at Johns Hopkins University in Baltimore and the moderator for the late-breaking abstract session at ASH, highlighted results from two studies.
Data from the MURANO trial showed robust results for a combination of venetoclax and rituximab in patients with relapsed/refractory chronic lymphocytic leukemia (CLL). At a median follow-up of 23.8 months, median progression-free survival -had not been reached in patients randomized to venetoclax/rituximab, while patients who received bendamustine plus rituximab had a median PFS of 17 months.
The based on the data presented, Dr. Brodsky said.
Another “enormously exciting and practice-changing” finding is that direct oral anticoagulants can be used safely in patients with cancer, Dr. Brodsky said in an interview.
In a randomized, open-label study, 12 months of daily treatment with edoxaban was noninferior to standard subcutaneous therapy with dalteparin for treatment of venous thromboembolism in cancer patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – There were a lot of new data presented during the annual meeting of the American Society of Hematology. But what findings could actually change the way you practice?
Robert A. Brodsky, MD, director of the division of hematology at Johns Hopkins University in Baltimore and the moderator for the late-breaking abstract session at ASH, highlighted results from two studies.
Data from the MURANO trial showed robust results for a combination of venetoclax and rituximab in patients with relapsed/refractory chronic lymphocytic leukemia (CLL). At a median follow-up of 23.8 months, median progression-free survival -had not been reached in patients randomized to venetoclax/rituximab, while patients who received bendamustine plus rituximab had a median PFS of 17 months.
The based on the data presented, Dr. Brodsky said.
Another “enormously exciting and practice-changing” finding is that direct oral anticoagulants can be used safely in patients with cancer, Dr. Brodsky said in an interview.
In a randomized, open-label study, 12 months of daily treatment with edoxaban was noninferior to standard subcutaneous therapy with dalteparin for treatment of venous thromboembolism in cancer patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
REPORTING FROM ASH 2017
VIDEO: New stroke guideline embraces imaging-guided thrombectomy
LOS ANGELES – When a panel organized by the American Heart Association’s Stroke Council recently revised the group’s guideline for early management of acute ischemic stroke, they were clear on the overarching change they had to make: Incorporate recent evidence collected in two trials that established brain imaging as the way to identify patients eligible for clot removal treatment by thrombectomy, a change in practice that has made this outcome-altering intervention available to more patients.
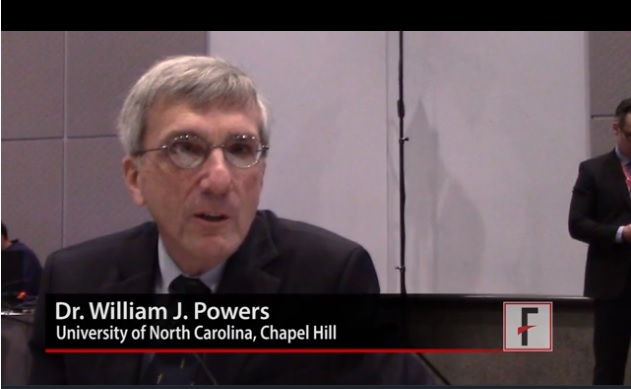
“The major take-home message [of the new guideline] is the extension of the time window for treating acute ischemic stroke,” said William J. Powers, MD, chair of the guideline group (Stroke. 2018 Jan 24. doi: 10.1161/STR.0000000000000158).
Based on recently reported results from the DAWN (N Engl J Med. 2018;378[1]:11-21) and DEFUSE 3 (N Engl J Med. 2018 Jan 24. doi: 10.1056/NEJMoa1713973) trials “we know that there are patients out to 24 hours from their stroke onset who may benefit” from thrombectomy. “This is a major, major change in how we view care for patients with stroke,” Dr. Powers said in a video interview. “Now there’s much more time. Ideally, we’ll see smaller hospitals develop the ability to do the imaging” that makes it possible to select acute ischemic stroke patients eligible for thrombectomy despite a delay of up to 24 hours from their stroke onset to the time of thrombectomy, said Dr. Powers, professor and chair of neurology at the University of North Carolina, Chapel Hill.
The big priority for the stroke community now that this major change in patient selection was incorporated into a U.S. practice guideline will be acting quickly to implement the steps needed to make this change happen, Dr. Powers and others said.
The new guideline will mean “changes in process and systems of care,” agreed Jeffrey L. Saver, MD, professor of neurology and director of the stroke unit at the University of California, Los Angeles. The imaging called for “will be practical at some primary stroke centers but not others,” he said, although most hospitals certified to provide stroke care as primary stroke centers or acute stroke–ready hospitals have a CT scanner that could provide the basic imaging needed to assess many patients. (CT angiography and perfusion CT are more informative for determining thrombectomy eligibility.) But interpretation of the brain images to distinguish patients eligible for thrombectomy from those who aren’t will likely happen at comprehensive stroke centers that perform thrombectomy or by experts using remote image reading.
Dr. Saver expects that the new guideline will translate most quickly into changes in the imaging and transfer protocols that the Joint Commission may now require from hospitals certified as primary stroke centers or acute stroke-ready hospitals, changes that could be in place sometime later in 2018, he predicted. These are steps “that would really help drive system change.”
Dr. Powers and Dr. Furie had no disclosures. Dr. Saver has received research support and personal fees from Medtronic-Abbott and Neuravia.
LOS ANGELES – When a panel organized by the American Heart Association’s Stroke Council recently revised the group’s guideline for early management of acute ischemic stroke, they were clear on the overarching change they had to make: Incorporate recent evidence collected in two trials that established brain imaging as the way to identify patients eligible for clot removal treatment by thrombectomy, a change in practice that has made this outcome-altering intervention available to more patients.
“The major take-home message [of the new guideline] is the extension of the time window for treating acute ischemic stroke,” said William J. Powers, MD, chair of the guideline group (Stroke. 2018 Jan 24. doi: 10.1161/STR.0000000000000158).
Based on recently reported results from the DAWN (N Engl J Med. 2018;378[1]:11-21) and DEFUSE 3 (N Engl J Med. 2018 Jan 24. doi: 10.1056/NEJMoa1713973) trials “we know that there are patients out to 24 hours from their stroke onset who may benefit” from thrombectomy. “This is a major, major change in how we view care for patients with stroke,” Dr. Powers said in a video interview. “Now there’s much more time. Ideally, we’ll see smaller hospitals develop the ability to do the imaging” that makes it possible to select acute ischemic stroke patients eligible for thrombectomy despite a delay of up to 24 hours from their stroke onset to the time of thrombectomy, said Dr. Powers, professor and chair of neurology at the University of North Carolina, Chapel Hill.
The big priority for the stroke community now that this major change in patient selection was incorporated into a U.S. practice guideline will be acting quickly to implement the steps needed to make this change happen, Dr. Powers and others said.
The new guideline will mean “changes in process and systems of care,” agreed Jeffrey L. Saver, MD, professor of neurology and director of the stroke unit at the University of California, Los Angeles. The imaging called for “will be practical at some primary stroke centers but not others,” he said, although most hospitals certified to provide stroke care as primary stroke centers or acute stroke–ready hospitals have a CT scanner that could provide the basic imaging needed to assess many patients. (CT angiography and perfusion CT are more informative for determining thrombectomy eligibility.) But interpretation of the brain images to distinguish patients eligible for thrombectomy from those who aren’t will likely happen at comprehensive stroke centers that perform thrombectomy or by experts using remote image reading.
Dr. Saver expects that the new guideline will translate most quickly into changes in the imaging and transfer protocols that the Joint Commission may now require from hospitals certified as primary stroke centers or acute stroke-ready hospitals, changes that could be in place sometime later in 2018, he predicted. These are steps “that would really help drive system change.”
Dr. Powers and Dr. Furie had no disclosures. Dr. Saver has received research support and personal fees from Medtronic-Abbott and Neuravia.
LOS ANGELES – When a panel organized by the American Heart Association’s Stroke Council recently revised the group’s guideline for early management of acute ischemic stroke, they were clear on the overarching change they had to make: Incorporate recent evidence collected in two trials that established brain imaging as the way to identify patients eligible for clot removal treatment by thrombectomy, a change in practice that has made this outcome-altering intervention available to more patients.
“The major take-home message [of the new guideline] is the extension of the time window for treating acute ischemic stroke,” said William J. Powers, MD, chair of the guideline group (Stroke. 2018 Jan 24. doi: 10.1161/STR.0000000000000158).
Based on recently reported results from the DAWN (N Engl J Med. 2018;378[1]:11-21) and DEFUSE 3 (N Engl J Med. 2018 Jan 24. doi: 10.1056/NEJMoa1713973) trials “we know that there are patients out to 24 hours from their stroke onset who may benefit” from thrombectomy. “This is a major, major change in how we view care for patients with stroke,” Dr. Powers said in a video interview. “Now there’s much more time. Ideally, we’ll see smaller hospitals develop the ability to do the imaging” that makes it possible to select acute ischemic stroke patients eligible for thrombectomy despite a delay of up to 24 hours from their stroke onset to the time of thrombectomy, said Dr. Powers, professor and chair of neurology at the University of North Carolina, Chapel Hill.
The big priority for the stroke community now that this major change in patient selection was incorporated into a U.S. practice guideline will be acting quickly to implement the steps needed to make this change happen, Dr. Powers and others said.
The new guideline will mean “changes in process and systems of care,” agreed Jeffrey L. Saver, MD, professor of neurology and director of the stroke unit at the University of California, Los Angeles. The imaging called for “will be practical at some primary stroke centers but not others,” he said, although most hospitals certified to provide stroke care as primary stroke centers or acute stroke–ready hospitals have a CT scanner that could provide the basic imaging needed to assess many patients. (CT angiography and perfusion CT are more informative for determining thrombectomy eligibility.) But interpretation of the brain images to distinguish patients eligible for thrombectomy from those who aren’t will likely happen at comprehensive stroke centers that perform thrombectomy or by experts using remote image reading.
Dr. Saver expects that the new guideline will translate most quickly into changes in the imaging and transfer protocols that the Joint Commission may now require from hospitals certified as primary stroke centers or acute stroke-ready hospitals, changes that could be in place sometime later in 2018, he predicted. These are steps “that would really help drive system change.”
Dr. Powers and Dr. Furie had no disclosures. Dr. Saver has received research support and personal fees from Medtronic-Abbott and Neuravia.
EXPERT ANALYSIS FROM ISC 2018
Hyaluronic Acid for Lip Rejuvenation



Are you familiar with the use of Tamiflu in pregnant women?
Managing the "Hot" Mess of Thyroiditis
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
VIDEO: Anticoagulant underprescribing common, jeopardizing atrial fib patients
ORLANDO – A high fraction of U.S. patients with atrial fibrillation receive an inappropriately low dosage of an anticoagulant for stroke prevention, often in a misguided attempt to avoid potential bleeding complications.
When physicians “reduce the dose to prevent a bleed they increase the risk for an ischemic stroke,” Elaine M. Hylek, MD, said in a video interview during the annual International AF Symposium.
Recent data on actual anticoagulant dosages prescribed to U.S. patients with atrial fibrillation show that “an unexpectedly high proportion of prescriptions for apixaban (Eliquis), dabigatran (Pradaxa), and rivaroxaban (Xarelto) are given at lower doses,” Dr. Hylek noted at the meeting. The lower-dose formulations with U.S. marketing are only appropriate for patients on apixaban with at least two of the following: serum creatinine 1.5 mg/dL or higher, age 80 years or older, and weight 60 kg or less; patients on dabigatran with moderate renal impairment or treated with dronedarone or systemic ketoconazole; or patients on rivaroxaban with a creatinine clearance of 15-50 mL/min.
For example, in the pivotal trial for apixaban only 5% of atrial fibrillation patients qualified for the lower dosage, yet recent data have shown that, in actual U.S. practice roughly a quarter of patients were on this lower dosage, said Dr. Hylek, professor of medicine at Boston University and director of the thrombosis and anticoagulation service at Boston Medical Center (Curr Med Res Opin. 2016 July;32[7]:1277-79). A second recent report showed that among U.S. patients with atrial fibrillation hospitalized for an ischemic stroke 84% had received inadequate anticoagulation with either subtherapeutic dosages of anticoagulant or no anticoagulant at all (JAMA. 2017 Mar 14;317[10]:1057-67).
Another manifestation of the underprescribing problem are patients with atrial fibrillation treated with aspirin only, an approach proven ineffective for preventing ischemic strokes in these patients, Dr. Hylek said.
Dr. Hylek has been an advisor to or has received honoraria from Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Doasense, Janssen, Medtronic, Pfizer, and Portola, and she has received research funding from Boehringer Ingelheim, Bristol-Myers Squibb, and Janssen.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
ORLANDO – A high fraction of U.S. patients with atrial fibrillation receive an inappropriately low dosage of an anticoagulant for stroke prevention, often in a misguided attempt to avoid potential bleeding complications.
When physicians “reduce the dose to prevent a bleed they increase the risk for an ischemic stroke,” Elaine M. Hylek, MD, said in a video interview during the annual International AF Symposium.
Recent data on actual anticoagulant dosages prescribed to U.S. patients with atrial fibrillation show that “an unexpectedly high proportion of prescriptions for apixaban (Eliquis), dabigatran (Pradaxa), and rivaroxaban (Xarelto) are given at lower doses,” Dr. Hylek noted at the meeting. The lower-dose formulations with U.S. marketing are only appropriate for patients on apixaban with at least two of the following: serum creatinine 1.5 mg/dL or higher, age 80 years or older, and weight 60 kg or less; patients on dabigatran with moderate renal impairment or treated with dronedarone or systemic ketoconazole; or patients on rivaroxaban with a creatinine clearance of 15-50 mL/min.
For example, in the pivotal trial for apixaban only 5% of atrial fibrillation patients qualified for the lower dosage, yet recent data have shown that, in actual U.S. practice roughly a quarter of patients were on this lower dosage, said Dr. Hylek, professor of medicine at Boston University and director of the thrombosis and anticoagulation service at Boston Medical Center (Curr Med Res Opin. 2016 July;32[7]:1277-79). A second recent report showed that among U.S. patients with atrial fibrillation hospitalized for an ischemic stroke 84% had received inadequate anticoagulation with either subtherapeutic dosages of anticoagulant or no anticoagulant at all (JAMA. 2017 Mar 14;317[10]:1057-67).
Another manifestation of the underprescribing problem are patients with atrial fibrillation treated with aspirin only, an approach proven ineffective for preventing ischemic strokes in these patients, Dr. Hylek said.
Dr. Hylek has been an advisor to or has received honoraria from Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Doasense, Janssen, Medtronic, Pfizer, and Portola, and she has received research funding from Boehringer Ingelheim, Bristol-Myers Squibb, and Janssen.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
ORLANDO – A high fraction of U.S. patients with atrial fibrillation receive an inappropriately low dosage of an anticoagulant for stroke prevention, often in a misguided attempt to avoid potential bleeding complications.
When physicians “reduce the dose to prevent a bleed they increase the risk for an ischemic stroke,” Elaine M. Hylek, MD, said in a video interview during the annual International AF Symposium.
Recent data on actual anticoagulant dosages prescribed to U.S. patients with atrial fibrillation show that “an unexpectedly high proportion of prescriptions for apixaban (Eliquis), dabigatran (Pradaxa), and rivaroxaban (Xarelto) are given at lower doses,” Dr. Hylek noted at the meeting. The lower-dose formulations with U.S. marketing are only appropriate for patients on apixaban with at least two of the following: serum creatinine 1.5 mg/dL or higher, age 80 years or older, and weight 60 kg or less; patients on dabigatran with moderate renal impairment or treated with dronedarone or systemic ketoconazole; or patients on rivaroxaban with a creatinine clearance of 15-50 mL/min.
For example, in the pivotal trial for apixaban only 5% of atrial fibrillation patients qualified for the lower dosage, yet recent data have shown that, in actual U.S. practice roughly a quarter of patients were on this lower dosage, said Dr. Hylek, professor of medicine at Boston University and director of the thrombosis and anticoagulation service at Boston Medical Center (Curr Med Res Opin. 2016 July;32[7]:1277-79). A second recent report showed that among U.S. patients with atrial fibrillation hospitalized for an ischemic stroke 84% had received inadequate anticoagulation with either subtherapeutic dosages of anticoagulant or no anticoagulant at all (JAMA. 2017 Mar 14;317[10]:1057-67).
Another manifestation of the underprescribing problem are patients with atrial fibrillation treated with aspirin only, an approach proven ineffective for preventing ischemic strokes in these patients, Dr. Hylek said.
Dr. Hylek has been an advisor to or has received honoraria from Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Doasense, Janssen, Medtronic, Pfizer, and Portola, and she has received research funding from Boehringer Ingelheim, Bristol-Myers Squibb, and Janssen.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM THE AF SYMPOSIUM 2018
Special Populations: New Onset Diabetes in the Elderly
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
Does maternal sleep position affect risk of stillbirth?
WHAT DOES THIS MEAN FOR PRACTICE?
Encourage pregnant patients to not go to sleep in the supine position, especially those who:
- are obese
- have medical complications of pregnancy
- have a history of prior stillbirth
- smoke
- are of advanced maternal age
A Peek at Our January 2018 Issue
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel