User login
Cancer groups offer guidance on musculoskeletal adverse events related to checkpoint inhibitors
Recently released guidelines from two major cancer organizations have provided some of the most comprehensive guidance to date on management of musculoskeletal side effects associated with cancer immunotherapy.
The guidelines, published in February, are a “sorely needed” reference point for the rheumatology community and others who will be encountering patients who experience immune-related adverse events (irAEs), according to Leonard H. Calabrese, DO, the R.J. Fasenmyer Chair of Clinical Immunology at the Cleveland Clinic in Ohio.
“They’re a good first start, given the fact that up until 4 or 5 months ago, there were no endorsed guidelines that included oncologists and rheumatologists,” Dr. Calabrese said of the guidelines, which were collaboratively developed and recently released by both the American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN).
Rheumatologists can add value
“We talk a lot about rheumatologists being aware of these diseases, but it’s been pointed out by some oncologists that unless they’re really knowledgeable and can add considerably to the management, it doesn’t do any good just to be aware of it,” Dr. Calabrese explained. “You need to actually have some procedural knowledge.”
ASCO guidelines also describe a polymyalgia-like syndrome seen in some patients on immune checkpoint inhibitors that according to the guideline authors is characterized by pain, but not true muscle weakness.
In general, the guidelines endorse a stepwise approach, in which milder irAEs can be managed with conservative treatments and without the need to stop the immune checkpoint inhibitor therapy. In contrast, more serious side effects may require more intensive management and either temporary or permanent discontinuation of cancer immunotherapy.
One good example is NCCN’s take on managing inflammatory arthritis.
Mild cases of inflammatory arthritis can be treated with NSAIDs, low-dose prednisone, or intra-articular steroids with no need to stop immune checkpoint inhibitor treatment, according to NCCN guideline authors.
Moderate cases, by contrast, may require holding immunotherapy and treating with prednisone. A rheumatology consult by week 4 is “strongly recommended” if the immune arthritis doesn’t improve, the authors added.
Severe cases may warrant permanent discontinuation of immunotherapy and treatment with methylprednisolone/prednisone, infliximab, or tocilizumab, they added. If the irAE doesn’t improve after 2 weeks, a rheumatology consult should be considered for additional disease-modifying antirheumatic drugs, including methotrexate, leflunomide, or sulfasalazine.
irAEs on the rise
These guidelines are particularly useful for rheumatologists to familiarize themselves with the six Food and Drug Administration–approved immune checkpoint inhibitors, their spectrum of side effects, and how oncologists use the severity of presentation to guide therapy, according to Laura Cappelli, MD.
Understanding irAEs will be increasingly important for rheumatologist as the use of immune checkpoint inhibitors continues to increase, said Dr. Cappelli, who has started a research program at Johns Hopkins to evaluate the rheumatologic adverse effects of these therapies.
Dr. Cappelli said her division sees at least one suspected irAE case per week, most commonly the immune arthritis associated with checkpoint inhibitor therapy.
Likewise, Dr. Calabrese said he is already seeing approximately two new referrals per week for adverse events related to these relatively new therapies.
“It’s far outstripped our notion of what we thought we would be doing,” he said in an interview.
Systems have been set up to encourage interprofessional collaborations, he added, including a “virtual referral clinic” where advanced practitioners working with oncologists communicate with advanced practitioners in each of the specialty areas that are most frequently consulted in order to help facilitate care and triage patients.
In addition, a monthly irAE tumor board was set up to include only cases that have manifest autoimmune or autoinflammatory complications.
“We have a growing group of people who come to this from each area involved, whether it be nephrology, neurology, ophthalmology, gastroenterology, rheumatology, or something else,” Dr. Calabrese said. “That’s been a great learning experience for all of us to talk about these adverse events in real time.”
Critical need for guidance
These guidelines meet a growing need to help practicing clinicians identify and best manage immune-related adverse events, according to Bryan J. Schneider, MD, of the University of Michigan Comprehensive Cancer Center, and vice chair of the NCCN Panel on Management of Immunotherapy-Related Toxicities.
“We’re experienced with chemotherapy, and we are very comfortable with the side effects,” he said. “The immunotherapy story is just an entirely different world because, as I tell patients, the therapies aren’t directly damaging cancer cells like chemotherapy. Instead, they are helping the immune system to identify the cancer cells as abnormal and mount an assault. Proteins on cancer cells may suppress the immune response and these therapies effectively ‘release these brakes’ so the immune system can attack.”
Rheumatologists and those with particular expertise in rheumatologic side effects participated in the development of the ASCO and NCCN guidelines. They include Maria E. Suarez-Almazor, MD, PhD, chief of rheumatology and clinical immunology at the University of Texas MD Anderson Cancer Center, Houston, who served on the ASCO expert panel; Jarushka Naidoo, MBBCh, from the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins, provided expertise in the rheumatologic side effects that were considered by the NCCN panel, according to Dr. Schneider.
Rheumatologist input also informed another set of recommendations on immune checkpoint inhibitor toxicities published several months before the ASCO and NCCN guidelines. The working group for the September 2017 guidelines from the Society for Immunotherapy of Cancer (doi: 10.1186/s40425-017-0300-z) included Dr. Suarez-Almazor, as well as Clifton O. Bingham III, MD, director of the Johns Hopkins Arthritis Center.
Vigilance required
Checkpoint inhibitors have been approved by the FDA to treat a variety of cancers, including melanoma, lung cancer, and Hodgkin lymphoma, as well as lung, liver, kidney, and bladder cancers.
Clinicians managing patients on checkpoint inhibitors should always be vigilant because irAE symptoms can be subtle, according to Julie Brahmer, MD, of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins in Baltimore.
“Everyone has to work as a team, which includes being educated on possible side effects to immunotherapy prior to prescribing it,” said Dr. Brahmer, chair of the ASCO panel and vice chair of the NCCN panel that developed the guidelines.
The guidelines were published Feb. 14 in two documents that are similar in content, but different in format. The ASCO guideline was published in the Journal of Clinical Oncology (doi: 10.1200/JCO.2017.77.6385) and the NCCN Clinical Practice Guidelines in Oncology were posted on the NCCN website.
While the first edition of the guidelines focus specifically on immune checkpoint inhibitors, an update anticipated for 2019 will include guidance on chimeric antigen receptor (CAR) T cell therapy, which is associated with several important side effects, notably cytokine release syndrome.
Recently released guidelines from two major cancer organizations have provided some of the most comprehensive guidance to date on management of musculoskeletal side effects associated with cancer immunotherapy.
The guidelines, published in February, are a “sorely needed” reference point for the rheumatology community and others who will be encountering patients who experience immune-related adverse events (irAEs), according to Leonard H. Calabrese, DO, the R.J. Fasenmyer Chair of Clinical Immunology at the Cleveland Clinic in Ohio.
“They’re a good first start, given the fact that up until 4 or 5 months ago, there were no endorsed guidelines that included oncologists and rheumatologists,” Dr. Calabrese said of the guidelines, which were collaboratively developed and recently released by both the American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN).
Rheumatologists can add value
“We talk a lot about rheumatologists being aware of these diseases, but it’s been pointed out by some oncologists that unless they’re really knowledgeable and can add considerably to the management, it doesn’t do any good just to be aware of it,” Dr. Calabrese explained. “You need to actually have some procedural knowledge.”
ASCO guidelines also describe a polymyalgia-like syndrome seen in some patients on immune checkpoint inhibitors that according to the guideline authors is characterized by pain, but not true muscle weakness.
In general, the guidelines endorse a stepwise approach, in which milder irAEs can be managed with conservative treatments and without the need to stop the immune checkpoint inhibitor therapy. In contrast, more serious side effects may require more intensive management and either temporary or permanent discontinuation of cancer immunotherapy.
One good example is NCCN’s take on managing inflammatory arthritis.
Mild cases of inflammatory arthritis can be treated with NSAIDs, low-dose prednisone, or intra-articular steroids with no need to stop immune checkpoint inhibitor treatment, according to NCCN guideline authors.
Moderate cases, by contrast, may require holding immunotherapy and treating with prednisone. A rheumatology consult by week 4 is “strongly recommended” if the immune arthritis doesn’t improve, the authors added.
Severe cases may warrant permanent discontinuation of immunotherapy and treatment with methylprednisolone/prednisone, infliximab, or tocilizumab, they added. If the irAE doesn’t improve after 2 weeks, a rheumatology consult should be considered for additional disease-modifying antirheumatic drugs, including methotrexate, leflunomide, or sulfasalazine.
irAEs on the rise
These guidelines are particularly useful for rheumatologists to familiarize themselves with the six Food and Drug Administration–approved immune checkpoint inhibitors, their spectrum of side effects, and how oncologists use the severity of presentation to guide therapy, according to Laura Cappelli, MD.
Understanding irAEs will be increasingly important for rheumatologist as the use of immune checkpoint inhibitors continues to increase, said Dr. Cappelli, who has started a research program at Johns Hopkins to evaluate the rheumatologic adverse effects of these therapies.
Dr. Cappelli said her division sees at least one suspected irAE case per week, most commonly the immune arthritis associated with checkpoint inhibitor therapy.
Likewise, Dr. Calabrese said he is already seeing approximately two new referrals per week for adverse events related to these relatively new therapies.
“It’s far outstripped our notion of what we thought we would be doing,” he said in an interview.
Systems have been set up to encourage interprofessional collaborations, he added, including a “virtual referral clinic” where advanced practitioners working with oncologists communicate with advanced practitioners in each of the specialty areas that are most frequently consulted in order to help facilitate care and triage patients.
In addition, a monthly irAE tumor board was set up to include only cases that have manifest autoimmune or autoinflammatory complications.
“We have a growing group of people who come to this from each area involved, whether it be nephrology, neurology, ophthalmology, gastroenterology, rheumatology, or something else,” Dr. Calabrese said. “That’s been a great learning experience for all of us to talk about these adverse events in real time.”
Critical need for guidance
These guidelines meet a growing need to help practicing clinicians identify and best manage immune-related adverse events, according to Bryan J. Schneider, MD, of the University of Michigan Comprehensive Cancer Center, and vice chair of the NCCN Panel on Management of Immunotherapy-Related Toxicities.
“We’re experienced with chemotherapy, and we are very comfortable with the side effects,” he said. “The immunotherapy story is just an entirely different world because, as I tell patients, the therapies aren’t directly damaging cancer cells like chemotherapy. Instead, they are helping the immune system to identify the cancer cells as abnormal and mount an assault. Proteins on cancer cells may suppress the immune response and these therapies effectively ‘release these brakes’ so the immune system can attack.”
Rheumatologists and those with particular expertise in rheumatologic side effects participated in the development of the ASCO and NCCN guidelines. They include Maria E. Suarez-Almazor, MD, PhD, chief of rheumatology and clinical immunology at the University of Texas MD Anderson Cancer Center, Houston, who served on the ASCO expert panel; Jarushka Naidoo, MBBCh, from the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins, provided expertise in the rheumatologic side effects that were considered by the NCCN panel, according to Dr. Schneider.
Rheumatologist input also informed another set of recommendations on immune checkpoint inhibitor toxicities published several months before the ASCO and NCCN guidelines. The working group for the September 2017 guidelines from the Society for Immunotherapy of Cancer (doi: 10.1186/s40425-017-0300-z) included Dr. Suarez-Almazor, as well as Clifton O. Bingham III, MD, director of the Johns Hopkins Arthritis Center.
Vigilance required
Checkpoint inhibitors have been approved by the FDA to treat a variety of cancers, including melanoma, lung cancer, and Hodgkin lymphoma, as well as lung, liver, kidney, and bladder cancers.
Clinicians managing patients on checkpoint inhibitors should always be vigilant because irAE symptoms can be subtle, according to Julie Brahmer, MD, of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins in Baltimore.
“Everyone has to work as a team, which includes being educated on possible side effects to immunotherapy prior to prescribing it,” said Dr. Brahmer, chair of the ASCO panel and vice chair of the NCCN panel that developed the guidelines.
The guidelines were published Feb. 14 in two documents that are similar in content, but different in format. The ASCO guideline was published in the Journal of Clinical Oncology (doi: 10.1200/JCO.2017.77.6385) and the NCCN Clinical Practice Guidelines in Oncology were posted on the NCCN website.
While the first edition of the guidelines focus specifically on immune checkpoint inhibitors, an update anticipated for 2019 will include guidance on chimeric antigen receptor (CAR) T cell therapy, which is associated with several important side effects, notably cytokine release syndrome.
Recently released guidelines from two major cancer organizations have provided some of the most comprehensive guidance to date on management of musculoskeletal side effects associated with cancer immunotherapy.
The guidelines, published in February, are a “sorely needed” reference point for the rheumatology community and others who will be encountering patients who experience immune-related adverse events (irAEs), according to Leonard H. Calabrese, DO, the R.J. Fasenmyer Chair of Clinical Immunology at the Cleveland Clinic in Ohio.
“They’re a good first start, given the fact that up until 4 or 5 months ago, there were no endorsed guidelines that included oncologists and rheumatologists,” Dr. Calabrese said of the guidelines, which were collaboratively developed and recently released by both the American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN).
Rheumatologists can add value
“We talk a lot about rheumatologists being aware of these diseases, but it’s been pointed out by some oncologists that unless they’re really knowledgeable and can add considerably to the management, it doesn’t do any good just to be aware of it,” Dr. Calabrese explained. “You need to actually have some procedural knowledge.”
ASCO guidelines also describe a polymyalgia-like syndrome seen in some patients on immune checkpoint inhibitors that according to the guideline authors is characterized by pain, but not true muscle weakness.
In general, the guidelines endorse a stepwise approach, in which milder irAEs can be managed with conservative treatments and without the need to stop the immune checkpoint inhibitor therapy. In contrast, more serious side effects may require more intensive management and either temporary or permanent discontinuation of cancer immunotherapy.
One good example is NCCN’s take on managing inflammatory arthritis.
Mild cases of inflammatory arthritis can be treated with NSAIDs, low-dose prednisone, or intra-articular steroids with no need to stop immune checkpoint inhibitor treatment, according to NCCN guideline authors.
Moderate cases, by contrast, may require holding immunotherapy and treating with prednisone. A rheumatology consult by week 4 is “strongly recommended” if the immune arthritis doesn’t improve, the authors added.
Severe cases may warrant permanent discontinuation of immunotherapy and treatment with methylprednisolone/prednisone, infliximab, or tocilizumab, they added. If the irAE doesn’t improve after 2 weeks, a rheumatology consult should be considered for additional disease-modifying antirheumatic drugs, including methotrexate, leflunomide, or sulfasalazine.
irAEs on the rise
These guidelines are particularly useful for rheumatologists to familiarize themselves with the six Food and Drug Administration–approved immune checkpoint inhibitors, their spectrum of side effects, and how oncologists use the severity of presentation to guide therapy, according to Laura Cappelli, MD.
Understanding irAEs will be increasingly important for rheumatologist as the use of immune checkpoint inhibitors continues to increase, said Dr. Cappelli, who has started a research program at Johns Hopkins to evaluate the rheumatologic adverse effects of these therapies.
Dr. Cappelli said her division sees at least one suspected irAE case per week, most commonly the immune arthritis associated with checkpoint inhibitor therapy.
Likewise, Dr. Calabrese said he is already seeing approximately two new referrals per week for adverse events related to these relatively new therapies.
“It’s far outstripped our notion of what we thought we would be doing,” he said in an interview.
Systems have been set up to encourage interprofessional collaborations, he added, including a “virtual referral clinic” where advanced practitioners working with oncologists communicate with advanced practitioners in each of the specialty areas that are most frequently consulted in order to help facilitate care and triage patients.
In addition, a monthly irAE tumor board was set up to include only cases that have manifest autoimmune or autoinflammatory complications.
“We have a growing group of people who come to this from each area involved, whether it be nephrology, neurology, ophthalmology, gastroenterology, rheumatology, or something else,” Dr. Calabrese said. “That’s been a great learning experience for all of us to talk about these adverse events in real time.”
Critical need for guidance
These guidelines meet a growing need to help practicing clinicians identify and best manage immune-related adverse events, according to Bryan J. Schneider, MD, of the University of Michigan Comprehensive Cancer Center, and vice chair of the NCCN Panel on Management of Immunotherapy-Related Toxicities.
“We’re experienced with chemotherapy, and we are very comfortable with the side effects,” he said. “The immunotherapy story is just an entirely different world because, as I tell patients, the therapies aren’t directly damaging cancer cells like chemotherapy. Instead, they are helping the immune system to identify the cancer cells as abnormal and mount an assault. Proteins on cancer cells may suppress the immune response and these therapies effectively ‘release these brakes’ so the immune system can attack.”
Rheumatologists and those with particular expertise in rheumatologic side effects participated in the development of the ASCO and NCCN guidelines. They include Maria E. Suarez-Almazor, MD, PhD, chief of rheumatology and clinical immunology at the University of Texas MD Anderson Cancer Center, Houston, who served on the ASCO expert panel; Jarushka Naidoo, MBBCh, from the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins, provided expertise in the rheumatologic side effects that were considered by the NCCN panel, according to Dr. Schneider.
Rheumatologist input also informed another set of recommendations on immune checkpoint inhibitor toxicities published several months before the ASCO and NCCN guidelines. The working group for the September 2017 guidelines from the Society for Immunotherapy of Cancer (doi: 10.1186/s40425-017-0300-z) included Dr. Suarez-Almazor, as well as Clifton O. Bingham III, MD, director of the Johns Hopkins Arthritis Center.
Vigilance required
Checkpoint inhibitors have been approved by the FDA to treat a variety of cancers, including melanoma, lung cancer, and Hodgkin lymphoma, as well as lung, liver, kidney, and bladder cancers.
Clinicians managing patients on checkpoint inhibitors should always be vigilant because irAE symptoms can be subtle, according to Julie Brahmer, MD, of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins in Baltimore.
“Everyone has to work as a team, which includes being educated on possible side effects to immunotherapy prior to prescribing it,” said Dr. Brahmer, chair of the ASCO panel and vice chair of the NCCN panel that developed the guidelines.
The guidelines were published Feb. 14 in two documents that are similar in content, but different in format. The ASCO guideline was published in the Journal of Clinical Oncology (doi: 10.1200/JCO.2017.77.6385) and the NCCN Clinical Practice Guidelines in Oncology were posted on the NCCN website.
While the first edition of the guidelines focus specifically on immune checkpoint inhibitors, an update anticipated for 2019 will include guidance on chimeric antigen receptor (CAR) T cell therapy, which is associated with several important side effects, notably cytokine release syndrome.
In utero exposure to valproate and other AEDs linked to low test scores
In utero exposure to some antiepileptic drugs was linked to decreased educational achievement at the age of 7 years, in results of a matched-case control study.
Compared with controls, children exposed in the womb to sodium valproate alone, or to multiple antiepileptics (AEDs), had lower scores on U.K standardized tests routinely administered to 7-year-olds, according to results published in the Journal of Neurology, Neurosurgery & Psychiatry.
The results provide evidence showing that in utero exposure to some AEDs may lead to developmental issues in children, according to lead author Arron S. Lacey, Wales Epilepsy Research Network, Swansea University Medical School, Swansea, England, and coauthors.
“Women with epilepsy should be informed of this risk, and alternative treatment regimens should be discussed before their pregnancy with a physician that specializes in epilepsy,” Dr. Lacey concluded in a discussion of their study results.
In the United Kingdom, already-stringent guidance on valproate in pregnancy was strengthened on March 23 when the European Medicines Agency announced new measures designed to avoid valproate exposure in pregnancy because of risk of malformations and developmental issues. The measures include a ban on valproate-containing medicines for the treatment of epilepsy during pregnancy unless no other effective treatment is available.
The risks of AEDs, and valproate in particular, in pregnancy have been documented in multiple studies suggesting that exposure may lead to cognitive impairment, neurodevelopmental disorders, and impaired IQ. However, the available data are largely from psychometric studies, Dr. Lacey and colleagues noted in their report. “It is important to know whether the psychometric differences demonstrated in research conditions translate to children in the community,” they wrote.
To address this, Dr. Lacey and coinvestigators conducted a study of standardized academic test results in children in Wales born to mothers with epilepsy who had been prescribed AEDs during pregnancy. They reviewed health records and identified 440 AED-exposed children who had available results for Key Stage 1 tests for mathematics, language, and science at the age of 7 years.
Among children whose mothers had been prescribed valproate during pregnancy, the proportion achieving U.K. minimum standards for all subjects was 12.7% lower than a matched control group, investigators said.
Children of mothers who had been prescribed multiple AEDs had an even lower proportion achieving the minimum standard for all subjects, at 20.7% less than the control group, they added.
By contrast, children whose mothers were prescribed carbamazepine did not have any significant differences in educational achievement, compared with controls.
Some previous studies found as association between exposure to carbamazepine and cognitive impairment, while others found no such association. “Our study supports the latter, with no evidence of decreased educational attainment at school age,” the investigators said in their article.
Some study authors reported competing interests related to Eisai, Sanofi, UCB, and others.
SOURCE: Lacey AS et al. J Neurol Neurosurg Psychiatry. 2018 Mar 25. doi: 10.1136/jnnp-201-317515.
Performing a matched-case control study that links health records and national educational data is an innovative approach to assessing educational achievement in children born to mothers with epilepsy, according to Richard F.M. Chin, MD.
Lacey and colleagues demonstrated that in utero exposure to sodium valproate alone or antiepileptic drugs in combination was associated with significant decreases in educational achievement in national educational tests given to 7-year-old children, Dr Chin wrote in an editorial.
That finding may not seem new, given that multiple previous studies have linked in utero antiepileptic exposure to lower IQ, more frequent behavioral issues, and higher risk of psychiatric disorders. However, previous studies depended on detailed, resource-intensive, one-on-one assessments, or parent responses to questionnaires with potentially biased responses, Dr. Chin said. In contrast, Lacey and colleagues incorporating validated epilepsy diagnoses and made use of already available educational attainment data from the epilepsy cases and matched controls.
Because of that, their results may be more likely than previous studies to be representative of the general population, according to Dr. Chin.
“Such a relatively cost-effective and efficient approach has vast potential to be applicable for a number of other conditions and is at the heart of the emerging health informatics revolution,” he wrote.
Richard F.M. Chin is with the Muir Maxwell Epilepsy Centre, University of Edinburgh, Scotland. These comments are derived from his editorial published in the Journal of Neurology, Neurosurgery & Psychiatry (2018 Mar 25. doi: 10.1136/jnnp-2017-317924 ). Dr. Chin declared no competing interests related to the editorial.
Performing a matched-case control study that links health records and national educational data is an innovative approach to assessing educational achievement in children born to mothers with epilepsy, according to Richard F.M. Chin, MD.
Lacey and colleagues demonstrated that in utero exposure to sodium valproate alone or antiepileptic drugs in combination was associated with significant decreases in educational achievement in national educational tests given to 7-year-old children, Dr Chin wrote in an editorial.
That finding may not seem new, given that multiple previous studies have linked in utero antiepileptic exposure to lower IQ, more frequent behavioral issues, and higher risk of psychiatric disorders. However, previous studies depended on detailed, resource-intensive, one-on-one assessments, or parent responses to questionnaires with potentially biased responses, Dr. Chin said. In contrast, Lacey and colleagues incorporating validated epilepsy diagnoses and made use of already available educational attainment data from the epilepsy cases and matched controls.
Because of that, their results may be more likely than previous studies to be representative of the general population, according to Dr. Chin.
“Such a relatively cost-effective and efficient approach has vast potential to be applicable for a number of other conditions and is at the heart of the emerging health informatics revolution,” he wrote.
Richard F.M. Chin is with the Muir Maxwell Epilepsy Centre, University of Edinburgh, Scotland. These comments are derived from his editorial published in the Journal of Neurology, Neurosurgery & Psychiatry (2018 Mar 25. doi: 10.1136/jnnp-2017-317924 ). Dr. Chin declared no competing interests related to the editorial.
Performing a matched-case control study that links health records and national educational data is an innovative approach to assessing educational achievement in children born to mothers with epilepsy, according to Richard F.M. Chin, MD.
Lacey and colleagues demonstrated that in utero exposure to sodium valproate alone or antiepileptic drugs in combination was associated with significant decreases in educational achievement in national educational tests given to 7-year-old children, Dr Chin wrote in an editorial.
That finding may not seem new, given that multiple previous studies have linked in utero antiepileptic exposure to lower IQ, more frequent behavioral issues, and higher risk of psychiatric disorders. However, previous studies depended on detailed, resource-intensive, one-on-one assessments, or parent responses to questionnaires with potentially biased responses, Dr. Chin said. In contrast, Lacey and colleagues incorporating validated epilepsy diagnoses and made use of already available educational attainment data from the epilepsy cases and matched controls.
Because of that, their results may be more likely than previous studies to be representative of the general population, according to Dr. Chin.
“Such a relatively cost-effective and efficient approach has vast potential to be applicable for a number of other conditions and is at the heart of the emerging health informatics revolution,” he wrote.
Richard F.M. Chin is with the Muir Maxwell Epilepsy Centre, University of Edinburgh, Scotland. These comments are derived from his editorial published in the Journal of Neurology, Neurosurgery & Psychiatry (2018 Mar 25. doi: 10.1136/jnnp-2017-317924 ). Dr. Chin declared no competing interests related to the editorial.
In utero exposure to some antiepileptic drugs was linked to decreased educational achievement at the age of 7 years, in results of a matched-case control study.
Compared with controls, children exposed in the womb to sodium valproate alone, or to multiple antiepileptics (AEDs), had lower scores on U.K standardized tests routinely administered to 7-year-olds, according to results published in the Journal of Neurology, Neurosurgery & Psychiatry.
The results provide evidence showing that in utero exposure to some AEDs may lead to developmental issues in children, according to lead author Arron S. Lacey, Wales Epilepsy Research Network, Swansea University Medical School, Swansea, England, and coauthors.
“Women with epilepsy should be informed of this risk, and alternative treatment regimens should be discussed before their pregnancy with a physician that specializes in epilepsy,” Dr. Lacey concluded in a discussion of their study results.
In the United Kingdom, already-stringent guidance on valproate in pregnancy was strengthened on March 23 when the European Medicines Agency announced new measures designed to avoid valproate exposure in pregnancy because of risk of malformations and developmental issues. The measures include a ban on valproate-containing medicines for the treatment of epilepsy during pregnancy unless no other effective treatment is available.
The risks of AEDs, and valproate in particular, in pregnancy have been documented in multiple studies suggesting that exposure may lead to cognitive impairment, neurodevelopmental disorders, and impaired IQ. However, the available data are largely from psychometric studies, Dr. Lacey and colleagues noted in their report. “It is important to know whether the psychometric differences demonstrated in research conditions translate to children in the community,” they wrote.
To address this, Dr. Lacey and coinvestigators conducted a study of standardized academic test results in children in Wales born to mothers with epilepsy who had been prescribed AEDs during pregnancy. They reviewed health records and identified 440 AED-exposed children who had available results for Key Stage 1 tests for mathematics, language, and science at the age of 7 years.
Among children whose mothers had been prescribed valproate during pregnancy, the proportion achieving U.K. minimum standards for all subjects was 12.7% lower than a matched control group, investigators said.
Children of mothers who had been prescribed multiple AEDs had an even lower proportion achieving the minimum standard for all subjects, at 20.7% less than the control group, they added.
By contrast, children whose mothers were prescribed carbamazepine did not have any significant differences in educational achievement, compared with controls.
Some previous studies found as association between exposure to carbamazepine and cognitive impairment, while others found no such association. “Our study supports the latter, with no evidence of decreased educational attainment at school age,” the investigators said in their article.
Some study authors reported competing interests related to Eisai, Sanofi, UCB, and others.
SOURCE: Lacey AS et al. J Neurol Neurosurg Psychiatry. 2018 Mar 25. doi: 10.1136/jnnp-201-317515.
In utero exposure to some antiepileptic drugs was linked to decreased educational achievement at the age of 7 years, in results of a matched-case control study.
Compared with controls, children exposed in the womb to sodium valproate alone, or to multiple antiepileptics (AEDs), had lower scores on U.K standardized tests routinely administered to 7-year-olds, according to results published in the Journal of Neurology, Neurosurgery & Psychiatry.
The results provide evidence showing that in utero exposure to some AEDs may lead to developmental issues in children, according to lead author Arron S. Lacey, Wales Epilepsy Research Network, Swansea University Medical School, Swansea, England, and coauthors.
“Women with epilepsy should be informed of this risk, and alternative treatment regimens should be discussed before their pregnancy with a physician that specializes in epilepsy,” Dr. Lacey concluded in a discussion of their study results.
In the United Kingdom, already-stringent guidance on valproate in pregnancy was strengthened on March 23 when the European Medicines Agency announced new measures designed to avoid valproate exposure in pregnancy because of risk of malformations and developmental issues. The measures include a ban on valproate-containing medicines for the treatment of epilepsy during pregnancy unless no other effective treatment is available.
The risks of AEDs, and valproate in particular, in pregnancy have been documented in multiple studies suggesting that exposure may lead to cognitive impairment, neurodevelopmental disorders, and impaired IQ. However, the available data are largely from psychometric studies, Dr. Lacey and colleagues noted in their report. “It is important to know whether the psychometric differences demonstrated in research conditions translate to children in the community,” they wrote.
To address this, Dr. Lacey and coinvestigators conducted a study of standardized academic test results in children in Wales born to mothers with epilepsy who had been prescribed AEDs during pregnancy. They reviewed health records and identified 440 AED-exposed children who had available results for Key Stage 1 tests for mathematics, language, and science at the age of 7 years.
Among children whose mothers had been prescribed valproate during pregnancy, the proportion achieving U.K. minimum standards for all subjects was 12.7% lower than a matched control group, investigators said.
Children of mothers who had been prescribed multiple AEDs had an even lower proportion achieving the minimum standard for all subjects, at 20.7% less than the control group, they added.
By contrast, children whose mothers were prescribed carbamazepine did not have any significant differences in educational achievement, compared with controls.
Some previous studies found as association between exposure to carbamazepine and cognitive impairment, while others found no such association. “Our study supports the latter, with no evidence of decreased educational attainment at school age,” the investigators said in their article.
Some study authors reported competing interests related to Eisai, Sanofi, UCB, and others.
SOURCE: Lacey AS et al. J Neurol Neurosurg Psychiatry. 2018 Mar 25. doi: 10.1136/jnnp-201-317515.
FROM THE JOURNAL OF NEUROLOGY, NEUROSURGERY & PSYCHIATRY
Key clinical point: In utero exposure to sodium valproate or to multiple antiepileptic drugs was associated with decreased educational achievement at the age of 7 years.
Major finding: Compared with a control group, the proportion of 7-year-old students achieving U.K. minimum standards for all subjects was 12.7% lower in children born to mothers with epilepsy prescribed valproate during pregnancy.
Study details: An analysis of standardized national test scores for 440 U.K. children who had been born to mothers with epilepsy, compared with test scores for a matched control group.
Disclosures: Some study authors reported competing interests related to Eisai, Sanofi, UCB, and others.
Source: Lacey AS et al. J Neurol Neurosurg Psychiatry. 2018 Mar 25. doi: 10.1136/jnnp-201-317515.
Switching to tenofovir alafenamide may benefit HBV patients
PHILADELPHIA – Tenofovir alafenamide, the newest kid on the block for treatment of chronic hepatitis B, not only has less bone and renal effects than tenofovir disoproxil, but now also appears to improve those parameters in patients switched over from the older tenofovir formulation, according to Paul Kwo, MD.
“Renal function, as well as hip and spine bone mineral density measurements, all improve after you flip,” said Dr. Kwo, director of hepatology at Stanford (Calif.) University.
Dr. Kwo described some of the latest data on the newer tenofovir formulation in a hepatitis B update he gave at the conference, jointly provided by Rutgers and Global Academy for Medical Education.
Tenofovir alafenamide, a nucleoside analogue reverse transcriptase inhibitor, was approved in November 2016 for treatment of adults with chronic hepatitis B virus (HBV) infection and compensated liver disease.
It has similar efficacy to tenofovir disoproxil, with fewer bone and renal effects, according to results of two large international phase 3 trials.
Some of the latest data, presented in October 2017 at The Liver Meeting in Washington, show that switching patients from tenofovir disoproxil to tenofovir alafenamide improved creatinine clearance and increased rates of alanine aminotransferase normalization, with sustained rates of virologic control, over 48 weeks of treatment.
Similar results were seen for bone mineral density. “It goes up over time, and you approach bone mineral density levels that are similar to [levels in] those who are on tenofovir alafenamide long term,” Dr. Kwo said, commenting on results of the study.
Compared with tenofovir disoproxil, tenofovir alafenamide is a slightly different prodrug of tenofovir, according to Dr. Kwo.
The approved dose of tenofovir alafenamide is 25 mg, compared with 300 mg for tenofovir disoproxil. “It’s more stable in the serum, so you don’t need higher levels, and you have fewer off-target effects,” Dr. Kwo said.
The two agents are “Coke and Pepsi” in terms of efficacy, he added, noting that comparative studies showed similar efficacy on endpoints of percentage HBV DNA less than 29 IU/mL and log10 HBV DNA change.
Very low rates of resistance are seen with first-line therapies for chronic hepatitis B, including entecavir and tenofovir disoproxil. “We wouldn’t expect (tenofovir alafenamide) to be any different, but nonetheless the surveillance has to happen,” Dr. Kwo said.
Tenofovir alafenamide is not yet listed in the official recommendations of the American Association for the Study of Liver Diseases, but it is in current guidelines from the European Association for the Study of the Liver.
The published EASL guidelines provide guidance on how tenofovir alafenamide fits into the treatment armamentarium for HBV.
Going by the EASL recommendations, age greater than 60 years, bone disease, and renal alterations are all good reasons to use tenofovir alafenamide as first-line therapy for hepatitis B, according to Dr. Kwo.
Dr. Kwo reported disclosures related to AbbVie, Allergan, Bristol-Myers Squibb, Conatus Pharmaceuticals, Dova Pharmaceuticals, DURECT, Gilead Sciences, Merck, and Shionogi.
Global Academy and this news organization are owned by the same company.
PHILADELPHIA – Tenofovir alafenamide, the newest kid on the block for treatment of chronic hepatitis B, not only has less bone and renal effects than tenofovir disoproxil, but now also appears to improve those parameters in patients switched over from the older tenofovir formulation, according to Paul Kwo, MD.
“Renal function, as well as hip and spine bone mineral density measurements, all improve after you flip,” said Dr. Kwo, director of hepatology at Stanford (Calif.) University.
Dr. Kwo described some of the latest data on the newer tenofovir formulation in a hepatitis B update he gave at the conference, jointly provided by Rutgers and Global Academy for Medical Education.
Tenofovir alafenamide, a nucleoside analogue reverse transcriptase inhibitor, was approved in November 2016 for treatment of adults with chronic hepatitis B virus (HBV) infection and compensated liver disease.
It has similar efficacy to tenofovir disoproxil, with fewer bone and renal effects, according to results of two large international phase 3 trials.
Some of the latest data, presented in October 2017 at The Liver Meeting in Washington, show that switching patients from tenofovir disoproxil to tenofovir alafenamide improved creatinine clearance and increased rates of alanine aminotransferase normalization, with sustained rates of virologic control, over 48 weeks of treatment.
Similar results were seen for bone mineral density. “It goes up over time, and you approach bone mineral density levels that are similar to [levels in] those who are on tenofovir alafenamide long term,” Dr. Kwo said, commenting on results of the study.
Compared with tenofovir disoproxil, tenofovir alafenamide is a slightly different prodrug of tenofovir, according to Dr. Kwo.
The approved dose of tenofovir alafenamide is 25 mg, compared with 300 mg for tenofovir disoproxil. “It’s more stable in the serum, so you don’t need higher levels, and you have fewer off-target effects,” Dr. Kwo said.
The two agents are “Coke and Pepsi” in terms of efficacy, he added, noting that comparative studies showed similar efficacy on endpoints of percentage HBV DNA less than 29 IU/mL and log10 HBV DNA change.
Very low rates of resistance are seen with first-line therapies for chronic hepatitis B, including entecavir and tenofovir disoproxil. “We wouldn’t expect (tenofovir alafenamide) to be any different, but nonetheless the surveillance has to happen,” Dr. Kwo said.
Tenofovir alafenamide is not yet listed in the official recommendations of the American Association for the Study of Liver Diseases, but it is in current guidelines from the European Association for the Study of the Liver.
The published EASL guidelines provide guidance on how tenofovir alafenamide fits into the treatment armamentarium for HBV.
Going by the EASL recommendations, age greater than 60 years, bone disease, and renal alterations are all good reasons to use tenofovir alafenamide as first-line therapy for hepatitis B, according to Dr. Kwo.
Dr. Kwo reported disclosures related to AbbVie, Allergan, Bristol-Myers Squibb, Conatus Pharmaceuticals, Dova Pharmaceuticals, DURECT, Gilead Sciences, Merck, and Shionogi.
Global Academy and this news organization are owned by the same company.
PHILADELPHIA – Tenofovir alafenamide, the newest kid on the block for treatment of chronic hepatitis B, not only has less bone and renal effects than tenofovir disoproxil, but now also appears to improve those parameters in patients switched over from the older tenofovir formulation, according to Paul Kwo, MD.
“Renal function, as well as hip and spine bone mineral density measurements, all improve after you flip,” said Dr. Kwo, director of hepatology at Stanford (Calif.) University.
Dr. Kwo described some of the latest data on the newer tenofovir formulation in a hepatitis B update he gave at the conference, jointly provided by Rutgers and Global Academy for Medical Education.
Tenofovir alafenamide, a nucleoside analogue reverse transcriptase inhibitor, was approved in November 2016 for treatment of adults with chronic hepatitis B virus (HBV) infection and compensated liver disease.
It has similar efficacy to tenofovir disoproxil, with fewer bone and renal effects, according to results of two large international phase 3 trials.
Some of the latest data, presented in October 2017 at The Liver Meeting in Washington, show that switching patients from tenofovir disoproxil to tenofovir alafenamide improved creatinine clearance and increased rates of alanine aminotransferase normalization, with sustained rates of virologic control, over 48 weeks of treatment.
Similar results were seen for bone mineral density. “It goes up over time, and you approach bone mineral density levels that are similar to [levels in] those who are on tenofovir alafenamide long term,” Dr. Kwo said, commenting on results of the study.
Compared with tenofovir disoproxil, tenofovir alafenamide is a slightly different prodrug of tenofovir, according to Dr. Kwo.
The approved dose of tenofovir alafenamide is 25 mg, compared with 300 mg for tenofovir disoproxil. “It’s more stable in the serum, so you don’t need higher levels, and you have fewer off-target effects,” Dr. Kwo said.
The two agents are “Coke and Pepsi” in terms of efficacy, he added, noting that comparative studies showed similar efficacy on endpoints of percentage HBV DNA less than 29 IU/mL and log10 HBV DNA change.
Very low rates of resistance are seen with first-line therapies for chronic hepatitis B, including entecavir and tenofovir disoproxil. “We wouldn’t expect (tenofovir alafenamide) to be any different, but nonetheless the surveillance has to happen,” Dr. Kwo said.
Tenofovir alafenamide is not yet listed in the official recommendations of the American Association for the Study of Liver Diseases, but it is in current guidelines from the European Association for the Study of the Liver.
The published EASL guidelines provide guidance on how tenofovir alafenamide fits into the treatment armamentarium for HBV.
Going by the EASL recommendations, age greater than 60 years, bone disease, and renal alterations are all good reasons to use tenofovir alafenamide as first-line therapy for hepatitis B, according to Dr. Kwo.
Dr. Kwo reported disclosures related to AbbVie, Allergan, Bristol-Myers Squibb, Conatus Pharmaceuticals, Dova Pharmaceuticals, DURECT, Gilead Sciences, Merck, and Shionogi.
Global Academy and this news organization are owned by the same company.
EXPERT ANALYSIS FROM DIGESTIVE DISEASES: NEW ADVANCES
Medical treatment of perianal fistulae often warranted, despite limited evidence
PHILADELPHIA – Perianal fistulae are a common and difficult-to-treat complication of Crohn’s disease that may often require medical therapy, though not all treatment options have robust data supporting their use in this setting, according to Mark T. Osterman, MD.
“Most studies done on fistulae actually didn’t have that as the primary endpoint – it was a secondary endpoint, so they weren’t really designed to look at fistulae, specifically,” said Dr. Osterman, associate professor of medicine in the division of gastroenterology at the University of Pennsylvania in Philadelphia.
Dr. Osterman shared his own approach to medical treatment of perianal fistulae in a presentation he gave at Digestive Diseases: New Advances, jointly provided by Rutgers and Global Academy for Medical Education.
For simple perianal fistula with no rectal inflammation, a fistulotomy is reasonable, but medical treatment may be preferable, Dr. Osterman said.
“I always favor medical therapy because it attacks the root of the problem, which is the immune system,” he explained.
Helpful treatments in this scenario include antibiotics, along with anti–tumor necrosis factor therapy with or without immunomodulators, he said.
Antibiotic use in this setting is based on uncontrolled data, and efficacy is modest at best, according to Dr. Osterman, who noted that the treatments may reduce fistula drainage but likely do not heal fistulae.
The most commonly used antibiotics are metronidazole and ciprofloxacin given for up to 2-4 months, he added.
Infliximab is the drug that has by far the most robust fistula data, and one of only two drugs where a fistula was the primary outcome of the studies, according to Dr. Osterman.
In a randomized trial, infliximab induction treatment more than doubled fistula-related response and remission rates, compared with placebo, he said.
Maintenance infliximab treatment likewise showed an approximate doubling of both response and remission of fistula versus placebo, he added.
While not designed to look at fistulae as a primary outcome, the randomized CHARM study of adalimumab versus placebo for maintenance of Crohn’s disease remission did demonstrate remission rates about twice as high with the use of adalimumab, compared with placebo, in 117 patients who had draining fistulae at baseline, Dr. Osterman recounted.
For patients with complex fistulae, as well as patients with rectal inflammation, a seton and aggressive medical therapy are likely needed, Dr. Osterman said in his presentation.
An advancement flap or medical therapies such as vedolizumab or tacrolimus might be warranted for patients who fail other medical approaches, he added.
Relevant vedolizumab data come from GEMINI 2, a large clinical trial for Crohn’s disease that included 57 patients who had draining fistulas at baseline.
“We see an improvement in remission rates with fistula with vedolizumab, compared to placebo, but again, (GEMINI 2) wasn’t designed to look at fistula, but we do use it,” said Dr. Osterman.
Tacrolimus is the only drug besides infliximab that has randomized data for fistula, according to Dr. Osterman.
In the small randomized study, 48 patients with Crohn’s disease and draining perianal or enterocutaneous fistulae were treated for 10 weeks with oral tacrolimus at 0.2 mg/kg per day or placebo.
Fistula improvement was seen in 43% of tacrolimus-treated patients and 8% of placebo-treated patients (P = .004), while remission was seen in 10% and 8% of those groups, respectively (P = .86), according to published data on the trial.
“[Tacrolimus] showed a nice improvement in response rates, but very similar remission rates,” Dr. Osterman said, “but it does represent an option for us, for our patients.”
Dr. Osterman reported grant/research support from UCB and serving as a consultant for AbbVie, Janssen, Lycera, Merck, Pfizer, Takeda, and UCB.
Global Academy and this news organization are owned by the same company.
PHILADELPHIA – Perianal fistulae are a common and difficult-to-treat complication of Crohn’s disease that may often require medical therapy, though not all treatment options have robust data supporting their use in this setting, according to Mark T. Osterman, MD.
“Most studies done on fistulae actually didn’t have that as the primary endpoint – it was a secondary endpoint, so they weren’t really designed to look at fistulae, specifically,” said Dr. Osterman, associate professor of medicine in the division of gastroenterology at the University of Pennsylvania in Philadelphia.
Dr. Osterman shared his own approach to medical treatment of perianal fistulae in a presentation he gave at Digestive Diseases: New Advances, jointly provided by Rutgers and Global Academy for Medical Education.
For simple perianal fistula with no rectal inflammation, a fistulotomy is reasonable, but medical treatment may be preferable, Dr. Osterman said.
“I always favor medical therapy because it attacks the root of the problem, which is the immune system,” he explained.
Helpful treatments in this scenario include antibiotics, along with anti–tumor necrosis factor therapy with or without immunomodulators, he said.
Antibiotic use in this setting is based on uncontrolled data, and efficacy is modest at best, according to Dr. Osterman, who noted that the treatments may reduce fistula drainage but likely do not heal fistulae.
The most commonly used antibiotics are metronidazole and ciprofloxacin given for up to 2-4 months, he added.
Infliximab is the drug that has by far the most robust fistula data, and one of only two drugs where a fistula was the primary outcome of the studies, according to Dr. Osterman.
In a randomized trial, infliximab induction treatment more than doubled fistula-related response and remission rates, compared with placebo, he said.
Maintenance infliximab treatment likewise showed an approximate doubling of both response and remission of fistula versus placebo, he added.
While not designed to look at fistulae as a primary outcome, the randomized CHARM study of adalimumab versus placebo for maintenance of Crohn’s disease remission did demonstrate remission rates about twice as high with the use of adalimumab, compared with placebo, in 117 patients who had draining fistulae at baseline, Dr. Osterman recounted.
For patients with complex fistulae, as well as patients with rectal inflammation, a seton and aggressive medical therapy are likely needed, Dr. Osterman said in his presentation.
An advancement flap or medical therapies such as vedolizumab or tacrolimus might be warranted for patients who fail other medical approaches, he added.
Relevant vedolizumab data come from GEMINI 2, a large clinical trial for Crohn’s disease that included 57 patients who had draining fistulas at baseline.
“We see an improvement in remission rates with fistula with vedolizumab, compared to placebo, but again, (GEMINI 2) wasn’t designed to look at fistula, but we do use it,” said Dr. Osterman.
Tacrolimus is the only drug besides infliximab that has randomized data for fistula, according to Dr. Osterman.
In the small randomized study, 48 patients with Crohn’s disease and draining perianal or enterocutaneous fistulae were treated for 10 weeks with oral tacrolimus at 0.2 mg/kg per day or placebo.
Fistula improvement was seen in 43% of tacrolimus-treated patients and 8% of placebo-treated patients (P = .004), while remission was seen in 10% and 8% of those groups, respectively (P = .86), according to published data on the trial.
“[Tacrolimus] showed a nice improvement in response rates, but very similar remission rates,” Dr. Osterman said, “but it does represent an option for us, for our patients.”
Dr. Osterman reported grant/research support from UCB and serving as a consultant for AbbVie, Janssen, Lycera, Merck, Pfizer, Takeda, and UCB.
Global Academy and this news organization are owned by the same company.
PHILADELPHIA – Perianal fistulae are a common and difficult-to-treat complication of Crohn’s disease that may often require medical therapy, though not all treatment options have robust data supporting their use in this setting, according to Mark T. Osterman, MD.
“Most studies done on fistulae actually didn’t have that as the primary endpoint – it was a secondary endpoint, so they weren’t really designed to look at fistulae, specifically,” said Dr. Osterman, associate professor of medicine in the division of gastroenterology at the University of Pennsylvania in Philadelphia.
Dr. Osterman shared his own approach to medical treatment of perianal fistulae in a presentation he gave at Digestive Diseases: New Advances, jointly provided by Rutgers and Global Academy for Medical Education.
For simple perianal fistula with no rectal inflammation, a fistulotomy is reasonable, but medical treatment may be preferable, Dr. Osterman said.
“I always favor medical therapy because it attacks the root of the problem, which is the immune system,” he explained.
Helpful treatments in this scenario include antibiotics, along with anti–tumor necrosis factor therapy with or without immunomodulators, he said.
Antibiotic use in this setting is based on uncontrolled data, and efficacy is modest at best, according to Dr. Osterman, who noted that the treatments may reduce fistula drainage but likely do not heal fistulae.
The most commonly used antibiotics are metronidazole and ciprofloxacin given for up to 2-4 months, he added.
Infliximab is the drug that has by far the most robust fistula data, and one of only two drugs where a fistula was the primary outcome of the studies, according to Dr. Osterman.
In a randomized trial, infliximab induction treatment more than doubled fistula-related response and remission rates, compared with placebo, he said.
Maintenance infliximab treatment likewise showed an approximate doubling of both response and remission of fistula versus placebo, he added.
While not designed to look at fistulae as a primary outcome, the randomized CHARM study of adalimumab versus placebo for maintenance of Crohn’s disease remission did demonstrate remission rates about twice as high with the use of adalimumab, compared with placebo, in 117 patients who had draining fistulae at baseline, Dr. Osterman recounted.
For patients with complex fistulae, as well as patients with rectal inflammation, a seton and aggressive medical therapy are likely needed, Dr. Osterman said in his presentation.
An advancement flap or medical therapies such as vedolizumab or tacrolimus might be warranted for patients who fail other medical approaches, he added.
Relevant vedolizumab data come from GEMINI 2, a large clinical trial for Crohn’s disease that included 57 patients who had draining fistulas at baseline.
“We see an improvement in remission rates with fistula with vedolizumab, compared to placebo, but again, (GEMINI 2) wasn’t designed to look at fistula, but we do use it,” said Dr. Osterman.
Tacrolimus is the only drug besides infliximab that has randomized data for fistula, according to Dr. Osterman.
In the small randomized study, 48 patients with Crohn’s disease and draining perianal or enterocutaneous fistulae were treated for 10 weeks with oral tacrolimus at 0.2 mg/kg per day or placebo.
Fistula improvement was seen in 43% of tacrolimus-treated patients and 8% of placebo-treated patients (P = .004), while remission was seen in 10% and 8% of those groups, respectively (P = .86), according to published data on the trial.
“[Tacrolimus] showed a nice improvement in response rates, but very similar remission rates,” Dr. Osterman said, “but it does represent an option for us, for our patients.”
Dr. Osterman reported grant/research support from UCB and serving as a consultant for AbbVie, Janssen, Lycera, Merck, Pfizer, Takeda, and UCB.
Global Academy and this news organization are owned by the same company.
EXPERT ANALYSIS FROM DIGESTIVE DISEASES: NEW ADVANCES
Step-up diet: Less-intensive way to ID eosinophilic esophagitis food triggers?
PHILADELPHIA – While traditional elimination diets for eosinophilic esophagitis are highly restrictive and endoscopically intensive, a new “step-up” approach may offer a superior empiric scheme for identifying food triggers, according to Stuart J. Spechler, MD.
The recently described step-up approach may be preferable to the standard empiric six-food elimination diet, which has a 72% success rate but is challenging to implement, according to Dr. Spechler, chief of the division of gastroenterology, Baylor University Medical Center at Dallas.
“That’s an extremely demanding, time-consuming, inconvenient, and expensive thing to do. It requires at least seven endoscopies, probably more, performed over a period of 42 weeks,” Dr. Spechler said here at Digestive Diseases: New Advances, jointly provided by Rutgers and Global Academy for Medical Education.
In contrast, the step-up approach recently described by Molina-Infante et al. in the Journal of Allergy and Clinical Immunology (2018 Mar 6. doi: 10.1016/j.jaci.2018.02.028) consists of a two-food elimination diet escalated to a four- and six-food elimination diet as needed.
This diet, which the researchers described as a “2-4-6” approach, starts with elimination of milk and wheat, the two most common food triggers for eosinophilic esophagitis. If patients do not respond, eggs and soy/legumes are eliminated, and if that fails, nuts and seafood are eliminated.
Once patients do respond, foods are reintroduced one at a time over 6 weeks with repeat endoscopy and biopsy, according to the report.
Molina-Infante and coauthors further described results of the diet in 220 patients with eosinophilic esophagitis. Of that group, investigators said 90 patients refused dietary therapy.
However, for the remaining 130 patients, 74 responded to the diet, the investigators reported.
Of 74 responders, 56 (43%) achieved remission at the first step in which milk and wheat were eliminated, results show, while an additional 10 had remission after the step up to four-food elimination, and another 8 had remission after the final step up to six-food elimination.
Dr. Spechler said his current take on diet therapy for eosinophilic esophagitis would be to start with the two-food elimination diet.
That first step alone identified about three-quarters of the patients who eventually would respond to the step-up approach in the Molina-Infante study, he observed.
For patients who do not respond and are motivated to continue, Dr. Spechler said he would move up to the four-food elimination diet, which identified about 90% of patients who eventually responded.
However, Dr. Spechler said he would consider the final step-up only in “exceptionally highly motivated” patients, since that step seems to identify very few additional responders.
“They got very little benefit here from going all the way up to a six-food elimination diet,” Dr. Spechler said.
Patient acceptance may be one major barrier to any dietary approach to treatment of eosinophilic esophagitis, regardless of how intensive the approach is.
“Ninety patients just flat-out refused to try the diet, so this is not a popular form of therapy,” Dr. Spechler noted.
However, diet is one of three valid treatment options for patients who do have an established diagnosis of eosinophilic esophagitis, the other two being proton pump inhibitors (PPIs) or 6-8 weeks of topical steroids, according to Dr. Spechler.
“If you’re going to use diet, I think you begin with that two-food elimination diet,“ he said. “Fortunately, most of the patients who don’t respond to diet will respond to PPIs or steroids.”
Dr. Spechler reported disclosures related to Ironwood Pharmaceuticals and Takeda Pharmaceuticals.
Global Academy and this news organization are owned by the same company.
PHILADELPHIA – While traditional elimination diets for eosinophilic esophagitis are highly restrictive and endoscopically intensive, a new “step-up” approach may offer a superior empiric scheme for identifying food triggers, according to Stuart J. Spechler, MD.
The recently described step-up approach may be preferable to the standard empiric six-food elimination diet, which has a 72% success rate but is challenging to implement, according to Dr. Spechler, chief of the division of gastroenterology, Baylor University Medical Center at Dallas.
“That’s an extremely demanding, time-consuming, inconvenient, and expensive thing to do. It requires at least seven endoscopies, probably more, performed over a period of 42 weeks,” Dr. Spechler said here at Digestive Diseases: New Advances, jointly provided by Rutgers and Global Academy for Medical Education.
In contrast, the step-up approach recently described by Molina-Infante et al. in the Journal of Allergy and Clinical Immunology (2018 Mar 6. doi: 10.1016/j.jaci.2018.02.028) consists of a two-food elimination diet escalated to a four- and six-food elimination diet as needed.
This diet, which the researchers described as a “2-4-6” approach, starts with elimination of milk and wheat, the two most common food triggers for eosinophilic esophagitis. If patients do not respond, eggs and soy/legumes are eliminated, and if that fails, nuts and seafood are eliminated.
Once patients do respond, foods are reintroduced one at a time over 6 weeks with repeat endoscopy and biopsy, according to the report.
Molina-Infante and coauthors further described results of the diet in 220 patients with eosinophilic esophagitis. Of that group, investigators said 90 patients refused dietary therapy.
However, for the remaining 130 patients, 74 responded to the diet, the investigators reported.
Of 74 responders, 56 (43%) achieved remission at the first step in which milk and wheat were eliminated, results show, while an additional 10 had remission after the step up to four-food elimination, and another 8 had remission after the final step up to six-food elimination.
Dr. Spechler said his current take on diet therapy for eosinophilic esophagitis would be to start with the two-food elimination diet.
That first step alone identified about three-quarters of the patients who eventually would respond to the step-up approach in the Molina-Infante study, he observed.
For patients who do not respond and are motivated to continue, Dr. Spechler said he would move up to the four-food elimination diet, which identified about 90% of patients who eventually responded.
However, Dr. Spechler said he would consider the final step-up only in “exceptionally highly motivated” patients, since that step seems to identify very few additional responders.
“They got very little benefit here from going all the way up to a six-food elimination diet,” Dr. Spechler said.
Patient acceptance may be one major barrier to any dietary approach to treatment of eosinophilic esophagitis, regardless of how intensive the approach is.
“Ninety patients just flat-out refused to try the diet, so this is not a popular form of therapy,” Dr. Spechler noted.
However, diet is one of three valid treatment options for patients who do have an established diagnosis of eosinophilic esophagitis, the other two being proton pump inhibitors (PPIs) or 6-8 weeks of topical steroids, according to Dr. Spechler.
“If you’re going to use diet, I think you begin with that two-food elimination diet,“ he said. “Fortunately, most of the patients who don’t respond to diet will respond to PPIs or steroids.”
Dr. Spechler reported disclosures related to Ironwood Pharmaceuticals and Takeda Pharmaceuticals.
Global Academy and this news organization are owned by the same company.
PHILADELPHIA – While traditional elimination diets for eosinophilic esophagitis are highly restrictive and endoscopically intensive, a new “step-up” approach may offer a superior empiric scheme for identifying food triggers, according to Stuart J. Spechler, MD.
The recently described step-up approach may be preferable to the standard empiric six-food elimination diet, which has a 72% success rate but is challenging to implement, according to Dr. Spechler, chief of the division of gastroenterology, Baylor University Medical Center at Dallas.
“That’s an extremely demanding, time-consuming, inconvenient, and expensive thing to do. It requires at least seven endoscopies, probably more, performed over a period of 42 weeks,” Dr. Spechler said here at Digestive Diseases: New Advances, jointly provided by Rutgers and Global Academy for Medical Education.
In contrast, the step-up approach recently described by Molina-Infante et al. in the Journal of Allergy and Clinical Immunology (2018 Mar 6. doi: 10.1016/j.jaci.2018.02.028) consists of a two-food elimination diet escalated to a four- and six-food elimination diet as needed.
This diet, which the researchers described as a “2-4-6” approach, starts with elimination of milk and wheat, the two most common food triggers for eosinophilic esophagitis. If patients do not respond, eggs and soy/legumes are eliminated, and if that fails, nuts and seafood are eliminated.
Once patients do respond, foods are reintroduced one at a time over 6 weeks with repeat endoscopy and biopsy, according to the report.
Molina-Infante and coauthors further described results of the diet in 220 patients with eosinophilic esophagitis. Of that group, investigators said 90 patients refused dietary therapy.
However, for the remaining 130 patients, 74 responded to the diet, the investigators reported.
Of 74 responders, 56 (43%) achieved remission at the first step in which milk and wheat were eliminated, results show, while an additional 10 had remission after the step up to four-food elimination, and another 8 had remission after the final step up to six-food elimination.
Dr. Spechler said his current take on diet therapy for eosinophilic esophagitis would be to start with the two-food elimination diet.
That first step alone identified about three-quarters of the patients who eventually would respond to the step-up approach in the Molina-Infante study, he observed.
For patients who do not respond and are motivated to continue, Dr. Spechler said he would move up to the four-food elimination diet, which identified about 90% of patients who eventually responded.
However, Dr. Spechler said he would consider the final step-up only in “exceptionally highly motivated” patients, since that step seems to identify very few additional responders.
“They got very little benefit here from going all the way up to a six-food elimination diet,” Dr. Spechler said.
Patient acceptance may be one major barrier to any dietary approach to treatment of eosinophilic esophagitis, regardless of how intensive the approach is.
“Ninety patients just flat-out refused to try the diet, so this is not a popular form of therapy,” Dr. Spechler noted.
However, diet is one of three valid treatment options for patients who do have an established diagnosis of eosinophilic esophagitis, the other two being proton pump inhibitors (PPIs) or 6-8 weeks of topical steroids, according to Dr. Spechler.
“If you’re going to use diet, I think you begin with that two-food elimination diet,“ he said. “Fortunately, most of the patients who don’t respond to diet will respond to PPIs or steroids.”
Dr. Spechler reported disclosures related to Ironwood Pharmaceuticals and Takeda Pharmaceuticals.
Global Academy and this news organization are owned by the same company.
EXPERT ANALYSIS FROM DIGESTIVE DISEASES: NEW ADVANCES
H. pylori eradication cuts new gastric cancers by half
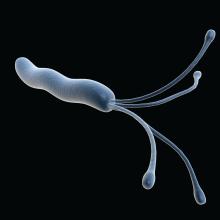
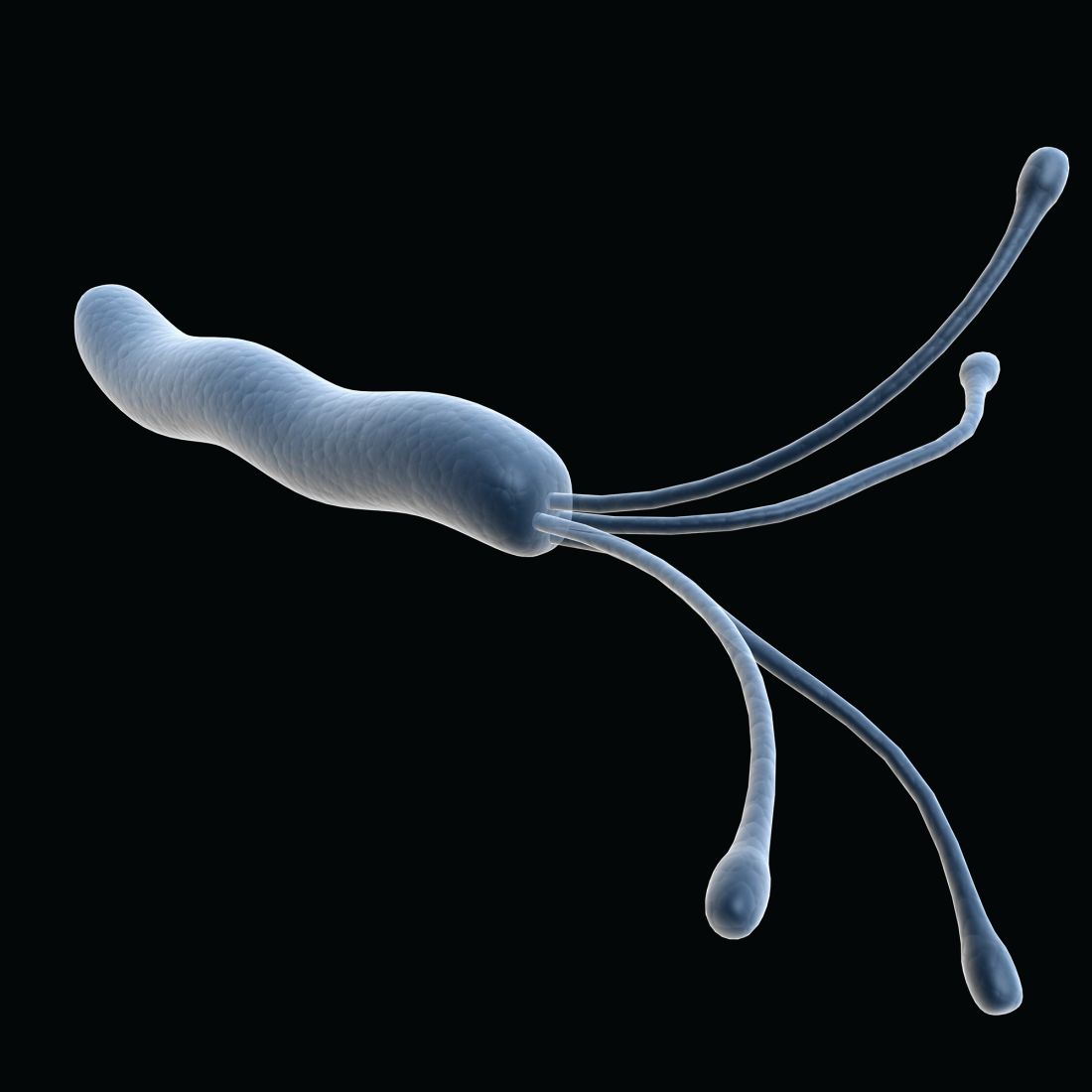
Treatment for Helicobacter pylori infection cut the incidence of new gastric cancers in half among patients undergoing endoscopic resection of early gastric cancer, according to results of a recent randomized, placebo-controlled study.
Patients receiving H. pylori treatment also had greater improvement from baseline in grade of gastric corpus atrophy, compared with patients receiving placebo, according to the study. The results were published in the New England Journal of Medicine.
“We speculate that persistent inflammation of gastric mucosa with H. pylori infection promotes carcinogenesis and also increases tumor growth or invasiveness,” said Il Ju Choi, MD, PhD, of the Center for Gastric Cancer, National Cancer Center, Goyang, South Korea, and coauthors.
Patients with early gastric cancers not at risk for lymph node metastasis may benefit from endoscopic resection. However, these patients are at high risk of developing new gastric cancer, and usually experience glandular atrophy, or advanced loss of mucosal glandular tissue, the authors said.
One nonrandomized study suggested H. pylori eradication could prevent development of subsequent cancers after endoscopic resection, according to the authors, but subsequent open-label trials were inconsistent on whether the treatment reduced cancer incidence.
Accordingly, Dr. Choi and colleagues conducted a prospective, double-blind, placebo-controlled, randomized trial of 470 patients who underwent endoscopic resection for high-grade adenoma or early gastric cancer.
Of 396 patients included in an intention-to-treat analysis, 194 were randomized to receive antibiotics for H. pylori eradication, and 202 received placebo.
Over a median follow-up of 5.9 years, new gastric cancers developed in 14 patients (7.2%) who received treatment, and in 27 patients (13.4%) who received placebo (hazard ratio, 0.50; 95% confidence interval, 0.26-0.94; P = .03).
Histologic analysis, performed in 327 patients, showed that 48.4% of patients in the treatment group had improvement in atrophy grade at the gastric corpus lesser curvature, compared to just 15.0% of the placebo group (P less than .001), the investigators reported.
Mild adverse events were more frequent in the treatment arm (42.0% versus 10.2%; P less than .001), and there were no serious adverse events, they added.
Despite the approximate 50% reduction in incidence of new gastric cancers and histologic improvements, the researchers said that further study would be required to optimize treatment approaches for patients undergoing endoscopic resection for high-grade adenoma or early gastric cancer.
“H. pylori eradication reduces, but cannot completely abolish, the risk of metachronous gastric cancer,” wrote Dr. Choi and colleagues. “Thus, molecular markers, including aberrant methylation at specific genes, might help to identify high-risk patients even after successful eradication.”
The researchers reported that they had nothing to disclose related to the study.
SOURCE: Choi et al. N Engl J Med. 2018 Mar 22. doi: 10.1056/NEJMoa1708423.
The study by Choi and colleagues suggests Helicobacter pylori eradication is effective at stopping the carcinogenic process in patients with severe chronic atrophic gastritis, an advanced precursor lesion to gastric cancer, according to Peter Malfertheiner, MD.
“It is a striking finding that H. pylori eradication may still be effective at this stage, since such therapy decreased the development of gastric cancer by 50% in this trial,” Dr. Malfertheiner wrote in an editorial.
In the randomized, placebo-controlled trial, H. pylori eradication after endoscopic removal of early stage disease effectively prevented metachronous gastric cancers (i.e., those detected on endoscopy at 1-year follow-up or thereafter) with a hazard ratio of 0.50, Dr. Malfertheiner noted.
The results confirm and strengthen previous findings by showing a significant improvement in atrophic gastritis, he added.
“In this endoscopic procedure, removal of early gastric cancer or high-grade adenoma leaves the stomach largely conserved but with the atrophic gastric mucosa remaining in a preneoplastic ‘alarm state,’ ” he noted.
However, the potential link between cancer recurrence and atrophic gastritis was not explored in this particular study report, Dr. Malfertheiner said. Thus, it is unclear whether gastric cancer recurrence was prevented specifically in the subset of patients with atrophic gastritis.
It could be that eradication of H. pylori directly arrests carcinogenic mechanisms directly by ending persistent inflammation, he speculated.
“The beneficial effect may also be mediated by an alteration in the composition of the gastric microbiota because of improvement in the grade of gastric atrophy and a return toward normal gastric acid production,” he added.
Dr. Malfertheiner is with the Clinic of Gastroenterology, Otto von Guericke University, Magdeburg, Germany. These comments are derived from his editorial (N Engl J Med. 2018 Mar 22. doi: 10.1056/NEJMe1800147). Dr. Malfertheiner reported personal fees from Allergan, Biohit, and Infai outside the submitted editorial.
The study by Choi and colleagues suggests Helicobacter pylori eradication is effective at stopping the carcinogenic process in patients with severe chronic atrophic gastritis, an advanced precursor lesion to gastric cancer, according to Peter Malfertheiner, MD.
“It is a striking finding that H. pylori eradication may still be effective at this stage, since such therapy decreased the development of gastric cancer by 50% in this trial,” Dr. Malfertheiner wrote in an editorial.
In the randomized, placebo-controlled trial, H. pylori eradication after endoscopic removal of early stage disease effectively prevented metachronous gastric cancers (i.e., those detected on endoscopy at 1-year follow-up or thereafter) with a hazard ratio of 0.50, Dr. Malfertheiner noted.
The results confirm and strengthen previous findings by showing a significant improvement in atrophic gastritis, he added.
“In this endoscopic procedure, removal of early gastric cancer or high-grade adenoma leaves the stomach largely conserved but with the atrophic gastric mucosa remaining in a preneoplastic ‘alarm state,’ ” he noted.
However, the potential link between cancer recurrence and atrophic gastritis was not explored in this particular study report, Dr. Malfertheiner said. Thus, it is unclear whether gastric cancer recurrence was prevented specifically in the subset of patients with atrophic gastritis.
It could be that eradication of H. pylori directly arrests carcinogenic mechanisms directly by ending persistent inflammation, he speculated.
“The beneficial effect may also be mediated by an alteration in the composition of the gastric microbiota because of improvement in the grade of gastric atrophy and a return toward normal gastric acid production,” he added.
Dr. Malfertheiner is with the Clinic of Gastroenterology, Otto von Guericke University, Magdeburg, Germany. These comments are derived from his editorial (N Engl J Med. 2018 Mar 22. doi: 10.1056/NEJMe1800147). Dr. Malfertheiner reported personal fees from Allergan, Biohit, and Infai outside the submitted editorial.
The study by Choi and colleagues suggests Helicobacter pylori eradication is effective at stopping the carcinogenic process in patients with severe chronic atrophic gastritis, an advanced precursor lesion to gastric cancer, according to Peter Malfertheiner, MD.
“It is a striking finding that H. pylori eradication may still be effective at this stage, since such therapy decreased the development of gastric cancer by 50% in this trial,” Dr. Malfertheiner wrote in an editorial.
In the randomized, placebo-controlled trial, H. pylori eradication after endoscopic removal of early stage disease effectively prevented metachronous gastric cancers (i.e., those detected on endoscopy at 1-year follow-up or thereafter) with a hazard ratio of 0.50, Dr. Malfertheiner noted.
The results confirm and strengthen previous findings by showing a significant improvement in atrophic gastritis, he added.
“In this endoscopic procedure, removal of early gastric cancer or high-grade adenoma leaves the stomach largely conserved but with the atrophic gastric mucosa remaining in a preneoplastic ‘alarm state,’ ” he noted.
However, the potential link between cancer recurrence and atrophic gastritis was not explored in this particular study report, Dr. Malfertheiner said. Thus, it is unclear whether gastric cancer recurrence was prevented specifically in the subset of patients with atrophic gastritis.
It could be that eradication of H. pylori directly arrests carcinogenic mechanisms directly by ending persistent inflammation, he speculated.
“The beneficial effect may also be mediated by an alteration in the composition of the gastric microbiota because of improvement in the grade of gastric atrophy and a return toward normal gastric acid production,” he added.
Dr. Malfertheiner is with the Clinic of Gastroenterology, Otto von Guericke University, Magdeburg, Germany. These comments are derived from his editorial (N Engl J Med. 2018 Mar 22. doi: 10.1056/NEJMe1800147). Dr. Malfertheiner reported personal fees from Allergan, Biohit, and Infai outside the submitted editorial.
Treatment for Helicobacter pylori infection cut the incidence of new gastric cancers in half among patients undergoing endoscopic resection of early gastric cancer, according to results of a recent randomized, placebo-controlled study.
Patients receiving H. pylori treatment also had greater improvement from baseline in grade of gastric corpus atrophy, compared with patients receiving placebo, according to the study. The results were published in the New England Journal of Medicine.
“We speculate that persistent inflammation of gastric mucosa with H. pylori infection promotes carcinogenesis and also increases tumor growth or invasiveness,” said Il Ju Choi, MD, PhD, of the Center for Gastric Cancer, National Cancer Center, Goyang, South Korea, and coauthors.
Patients with early gastric cancers not at risk for lymph node metastasis may benefit from endoscopic resection. However, these patients are at high risk of developing new gastric cancer, and usually experience glandular atrophy, or advanced loss of mucosal glandular tissue, the authors said.
One nonrandomized study suggested H. pylori eradication could prevent development of subsequent cancers after endoscopic resection, according to the authors, but subsequent open-label trials were inconsistent on whether the treatment reduced cancer incidence.
Accordingly, Dr. Choi and colleagues conducted a prospective, double-blind, placebo-controlled, randomized trial of 470 patients who underwent endoscopic resection for high-grade adenoma or early gastric cancer.
Of 396 patients included in an intention-to-treat analysis, 194 were randomized to receive antibiotics for H. pylori eradication, and 202 received placebo.
Over a median follow-up of 5.9 years, new gastric cancers developed in 14 patients (7.2%) who received treatment, and in 27 patients (13.4%) who received placebo (hazard ratio, 0.50; 95% confidence interval, 0.26-0.94; P = .03).
Histologic analysis, performed in 327 patients, showed that 48.4% of patients in the treatment group had improvement in atrophy grade at the gastric corpus lesser curvature, compared to just 15.0% of the placebo group (P less than .001), the investigators reported.
Mild adverse events were more frequent in the treatment arm (42.0% versus 10.2%; P less than .001), and there were no serious adverse events, they added.
Despite the approximate 50% reduction in incidence of new gastric cancers and histologic improvements, the researchers said that further study would be required to optimize treatment approaches for patients undergoing endoscopic resection for high-grade adenoma or early gastric cancer.
“H. pylori eradication reduces, but cannot completely abolish, the risk of metachronous gastric cancer,” wrote Dr. Choi and colleagues. “Thus, molecular markers, including aberrant methylation at specific genes, might help to identify high-risk patients even after successful eradication.”
The researchers reported that they had nothing to disclose related to the study.
SOURCE: Choi et al. N Engl J Med. 2018 Mar 22. doi: 10.1056/NEJMoa1708423.
Treatment for Helicobacter pylori infection cut the incidence of new gastric cancers in half among patients undergoing endoscopic resection of early gastric cancer, according to results of a recent randomized, placebo-controlled study.
Patients receiving H. pylori treatment also had greater improvement from baseline in grade of gastric corpus atrophy, compared with patients receiving placebo, according to the study. The results were published in the New England Journal of Medicine.
“We speculate that persistent inflammation of gastric mucosa with H. pylori infection promotes carcinogenesis and also increases tumor growth or invasiveness,” said Il Ju Choi, MD, PhD, of the Center for Gastric Cancer, National Cancer Center, Goyang, South Korea, and coauthors.
Patients with early gastric cancers not at risk for lymph node metastasis may benefit from endoscopic resection. However, these patients are at high risk of developing new gastric cancer, and usually experience glandular atrophy, or advanced loss of mucosal glandular tissue, the authors said.
One nonrandomized study suggested H. pylori eradication could prevent development of subsequent cancers after endoscopic resection, according to the authors, but subsequent open-label trials were inconsistent on whether the treatment reduced cancer incidence.
Accordingly, Dr. Choi and colleagues conducted a prospective, double-blind, placebo-controlled, randomized trial of 470 patients who underwent endoscopic resection for high-grade adenoma or early gastric cancer.
Of 396 patients included in an intention-to-treat analysis, 194 were randomized to receive antibiotics for H. pylori eradication, and 202 received placebo.
Over a median follow-up of 5.9 years, new gastric cancers developed in 14 patients (7.2%) who received treatment, and in 27 patients (13.4%) who received placebo (hazard ratio, 0.50; 95% confidence interval, 0.26-0.94; P = .03).
Histologic analysis, performed in 327 patients, showed that 48.4% of patients in the treatment group had improvement in atrophy grade at the gastric corpus lesser curvature, compared to just 15.0% of the placebo group (P less than .001), the investigators reported.
Mild adverse events were more frequent in the treatment arm (42.0% versus 10.2%; P less than .001), and there were no serious adverse events, they added.
Despite the approximate 50% reduction in incidence of new gastric cancers and histologic improvements, the researchers said that further study would be required to optimize treatment approaches for patients undergoing endoscopic resection for high-grade adenoma or early gastric cancer.
“H. pylori eradication reduces, but cannot completely abolish, the risk of metachronous gastric cancer,” wrote Dr. Choi and colleagues. “Thus, molecular markers, including aberrant methylation at specific genes, might help to identify high-risk patients even after successful eradication.”
The researchers reported that they had nothing to disclose related to the study.
SOURCE: Choi et al. N Engl J Med. 2018 Mar 22. doi: 10.1056/NEJMoa1708423.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Among patients undergoing endoscopic resection of early gastric cancer, incidence of new gastric cancers was approximately 50% lower for those who received treatment for Helicobacter pylori infection.
Major finding: Over a median follow-up of 5.9 years, new gastric cancers developed in 14 patients (7.2%) who received treatment, and in 27 patients (13.4%) who received placebo (HR, 0.50; 95% CI, 0.26-0.94; P = .03).
Study details: A prospective, double-blind, placebo-controlled, randomized trial of 470 patients who underwent endoscopic resection for high-grade adenoma or early gastric cancer.
Disclosures: The authors reported that they had nothing to disclose related to the study.
Source: Choi et al. N Engl J Med. 2018 Mar 22. doi: 10.1056/NEJMoa1708423.
TACE plus radiotherapy improves outcomes in poor-prognosis hepatocellular carcinoma
Use of transarterial chemoembolization (TACE) plus external beam radiotherapy may improve outcomes in patients with hepatocellular carcinoma (HCC) showing macroscopic vascular invasion, according to results of a recent randomized study.
The TACE plus radiotherapy approach was well tolerated and improved progression-free survival compared with sorafenib treatment, investigators wrote. The report was published in JAMA Oncology.
“The results of this study represent a significant advance in addressing an urgent unmet need in treating patients with advanced HCC,” noted Sang Min Yoon, MD, PhD, of the department of radiation oncology, University of Ulsan College of Medicine, Seoul, Republic of Korea, and coauthors.
Patients with HCC that shows macroscopic vascular invasion are a particularly poor prognosis subset, according to Dr. Yoon and coauthors.
“Sorafenib is the sole treatment option for these patients, with unsatisfactory response and survival benefit,” they wrote.
Building on observational studies suggesting TACE plus external beam therapy may be a promising approach, Dr. Yoon and colleagues initiated a randomized, open-label clinical trial including 90 patients with liver-confined HCC and macroscopic vascular invasion.
Patients were randomized to sorafenib either 400 mg twice daily or TACE every 6 weeks plus radiotherapy starting within 3 weeks of the first TACE, according to the study description.
The primary endpoint, 12-week progression-free survival, was 86.7% for patients receiving TACE plus radiotherapy, versus 34.3% for patients receiving sorafenib (P less than .001).
The TACE plus radiotherapy group also had a significantly longer overall survival (55.0 vs. 43.0 weeks; P = .04), as well as a significantly higher radiologic response rate and significantly longer median time to progression, the authors reported.
Five patients (11.1%) in the TACE plus radiotherapy group were able to undergo curative surgical resection due to downstaging.
The risk of TACE-induced liver failure is a concern based on results of previous studies in patients with HCC and macroscopic vascular invasion, but in this study, there were no discontinuations due to adverse events in the TACE-radiation group, the authors noted.
“Our study may not be large enough to accurately establish the incidence of adverse events,” they wrote. “However, considering the dismal prognosis, the superior efficacy of TACE plus RT vs. sorafenib may justify its use for these patients.”
Dr. Yoon reported no disclosures related to the study. One coauthor reported research funding and advisory board membership with Bayer Healthcare and Gilead Sciences.
SOURCE: Yoon SM et al. 2018 Mar 15 JAMA Oncol. doi: 10.1001/jamaoncol.2017.5847.
Despite some limitations, the research by Yoon and colleagues provides “much-needed prospective data” suggesting that multimodality therapy may improve the dismal prognosis of patients with hepatocellular carcinoma (HCC) with portal venous invasion, according to authors of an editorial on the study.
“Existing treatments demonstrate poor efficacy for HCC with portal venous invasion, with subgroup analyses in early major prospective trials showing modest, if any, benefits of therapy beyond the natural history of the disease,” wrote editorial authors Khashayar Farsad, MD, PhD, Charlotte E. Costentin, MD, and Andrew X. Zhu, MD, PhD.
The data from Yoon et al. not only support a role for locoregional therapy in this challenging patient subgroup, but also suggest external beam radiotherapy is an “asset in the locoregional therapy toolbox,” they wrote.
In the study, use of transarterial chemoembolization (TACE) plus external beam radiotherapy improved the primary endpoint of 12-week progression-free survival versus sorafenib (86.7% versus 34.3%, respectively; P less than .001), among other improved outcomes, they noted.
That is “impressive” but certain caveats must be considered if extrapolating the data from this small study to clinical practice, they added. For example, most of the patients had liver disease related to hepatitis B virus; compared with patients with liver disease related to hepatitis C virus, that subset of patients may have worse outcomes on sorafenib, the authors wrote.
The TACE protocol used in the study included cisplatin, which is not universally used because of availability or practice patterns, they added. Moreover, a median of four treatments were delivered, while many centers use repeat TACE only when needed (e.g., due to residual disease).
Limitations aside, the study results provide prospective evidence that more effective treatment strategies for HCC with portal venous invasion may be established, according to the authors.
“For those of us managing these patients daily in our clinics and procedure suites, it is encouraging to know there is hope ahead,” they said. “Work in this realm is just beginning, highlighting the need for additional prospective studies to validate and optimize these findings in other patient populations.”
Dr. Farsad is with the Charles T. Dotter Department of Interventional Radiology, Oregon Health & Science University, Portland. Dr. Costentin and Dr. Zhu are with Massachusetts General Hospital Cancer Center, Harvard Medical School, Boston. These comments are derived from their editorial (JAMA Oncol. 2018 Mar 15. doi: 10.1001/jamaoncol.2018.0007). The authors reported no conflict of interest disclosures related to their editorial.
Despite some limitations, the research by Yoon and colleagues provides “much-needed prospective data” suggesting that multimodality therapy may improve the dismal prognosis of patients with hepatocellular carcinoma (HCC) with portal venous invasion, according to authors of an editorial on the study.
“Existing treatments demonstrate poor efficacy for HCC with portal venous invasion, with subgroup analyses in early major prospective trials showing modest, if any, benefits of therapy beyond the natural history of the disease,” wrote editorial authors Khashayar Farsad, MD, PhD, Charlotte E. Costentin, MD, and Andrew X. Zhu, MD, PhD.
The data from Yoon et al. not only support a role for locoregional therapy in this challenging patient subgroup, but also suggest external beam radiotherapy is an “asset in the locoregional therapy toolbox,” they wrote.
In the study, use of transarterial chemoembolization (TACE) plus external beam radiotherapy improved the primary endpoint of 12-week progression-free survival versus sorafenib (86.7% versus 34.3%, respectively; P less than .001), among other improved outcomes, they noted.
That is “impressive” but certain caveats must be considered if extrapolating the data from this small study to clinical practice, they added. For example, most of the patients had liver disease related to hepatitis B virus; compared with patients with liver disease related to hepatitis C virus, that subset of patients may have worse outcomes on sorafenib, the authors wrote.
The TACE protocol used in the study included cisplatin, which is not universally used because of availability or practice patterns, they added. Moreover, a median of four treatments were delivered, while many centers use repeat TACE only when needed (e.g., due to residual disease).
Limitations aside, the study results provide prospective evidence that more effective treatment strategies for HCC with portal venous invasion may be established, according to the authors.
“For those of us managing these patients daily in our clinics and procedure suites, it is encouraging to know there is hope ahead,” they said. “Work in this realm is just beginning, highlighting the need for additional prospective studies to validate and optimize these findings in other patient populations.”
Dr. Farsad is with the Charles T. Dotter Department of Interventional Radiology, Oregon Health & Science University, Portland. Dr. Costentin and Dr. Zhu are with Massachusetts General Hospital Cancer Center, Harvard Medical School, Boston. These comments are derived from their editorial (JAMA Oncol. 2018 Mar 15. doi: 10.1001/jamaoncol.2018.0007). The authors reported no conflict of interest disclosures related to their editorial.
Despite some limitations, the research by Yoon and colleagues provides “much-needed prospective data” suggesting that multimodality therapy may improve the dismal prognosis of patients with hepatocellular carcinoma (HCC) with portal venous invasion, according to authors of an editorial on the study.
“Existing treatments demonstrate poor efficacy for HCC with portal venous invasion, with subgroup analyses in early major prospective trials showing modest, if any, benefits of therapy beyond the natural history of the disease,” wrote editorial authors Khashayar Farsad, MD, PhD, Charlotte E. Costentin, MD, and Andrew X. Zhu, MD, PhD.
The data from Yoon et al. not only support a role for locoregional therapy in this challenging patient subgroup, but also suggest external beam radiotherapy is an “asset in the locoregional therapy toolbox,” they wrote.
In the study, use of transarterial chemoembolization (TACE) plus external beam radiotherapy improved the primary endpoint of 12-week progression-free survival versus sorafenib (86.7% versus 34.3%, respectively; P less than .001), among other improved outcomes, they noted.
That is “impressive” but certain caveats must be considered if extrapolating the data from this small study to clinical practice, they added. For example, most of the patients had liver disease related to hepatitis B virus; compared with patients with liver disease related to hepatitis C virus, that subset of patients may have worse outcomes on sorafenib, the authors wrote.
The TACE protocol used in the study included cisplatin, which is not universally used because of availability or practice patterns, they added. Moreover, a median of four treatments were delivered, while many centers use repeat TACE only when needed (e.g., due to residual disease).
Limitations aside, the study results provide prospective evidence that more effective treatment strategies for HCC with portal venous invasion may be established, according to the authors.
“For those of us managing these patients daily in our clinics and procedure suites, it is encouraging to know there is hope ahead,” they said. “Work in this realm is just beginning, highlighting the need for additional prospective studies to validate and optimize these findings in other patient populations.”
Dr. Farsad is with the Charles T. Dotter Department of Interventional Radiology, Oregon Health & Science University, Portland. Dr. Costentin and Dr. Zhu are with Massachusetts General Hospital Cancer Center, Harvard Medical School, Boston. These comments are derived from their editorial (JAMA Oncol. 2018 Mar 15. doi: 10.1001/jamaoncol.2018.0007). The authors reported no conflict of interest disclosures related to their editorial.
Use of transarterial chemoembolization (TACE) plus external beam radiotherapy may improve outcomes in patients with hepatocellular carcinoma (HCC) showing macroscopic vascular invasion, according to results of a recent randomized study.
The TACE plus radiotherapy approach was well tolerated and improved progression-free survival compared with sorafenib treatment, investigators wrote. The report was published in JAMA Oncology.
“The results of this study represent a significant advance in addressing an urgent unmet need in treating patients with advanced HCC,” noted Sang Min Yoon, MD, PhD, of the department of radiation oncology, University of Ulsan College of Medicine, Seoul, Republic of Korea, and coauthors.
Patients with HCC that shows macroscopic vascular invasion are a particularly poor prognosis subset, according to Dr. Yoon and coauthors.
“Sorafenib is the sole treatment option for these patients, with unsatisfactory response and survival benefit,” they wrote.
Building on observational studies suggesting TACE plus external beam therapy may be a promising approach, Dr. Yoon and colleagues initiated a randomized, open-label clinical trial including 90 patients with liver-confined HCC and macroscopic vascular invasion.
Patients were randomized to sorafenib either 400 mg twice daily or TACE every 6 weeks plus radiotherapy starting within 3 weeks of the first TACE, according to the study description.
The primary endpoint, 12-week progression-free survival, was 86.7% for patients receiving TACE plus radiotherapy, versus 34.3% for patients receiving sorafenib (P less than .001).
The TACE plus radiotherapy group also had a significantly longer overall survival (55.0 vs. 43.0 weeks; P = .04), as well as a significantly higher radiologic response rate and significantly longer median time to progression, the authors reported.
Five patients (11.1%) in the TACE plus radiotherapy group were able to undergo curative surgical resection due to downstaging.
The risk of TACE-induced liver failure is a concern based on results of previous studies in patients with HCC and macroscopic vascular invasion, but in this study, there were no discontinuations due to adverse events in the TACE-radiation group, the authors noted.
“Our study may not be large enough to accurately establish the incidence of adverse events,” they wrote. “However, considering the dismal prognosis, the superior efficacy of TACE plus RT vs. sorafenib may justify its use for these patients.”
Dr. Yoon reported no disclosures related to the study. One coauthor reported research funding and advisory board membership with Bayer Healthcare and Gilead Sciences.
SOURCE: Yoon SM et al. 2018 Mar 15 JAMA Oncol. doi: 10.1001/jamaoncol.2017.5847.
Use of transarterial chemoembolization (TACE) plus external beam radiotherapy may improve outcomes in patients with hepatocellular carcinoma (HCC) showing macroscopic vascular invasion, according to results of a recent randomized study.
The TACE plus radiotherapy approach was well tolerated and improved progression-free survival compared with sorafenib treatment, investigators wrote. The report was published in JAMA Oncology.
“The results of this study represent a significant advance in addressing an urgent unmet need in treating patients with advanced HCC,” noted Sang Min Yoon, MD, PhD, of the department of radiation oncology, University of Ulsan College of Medicine, Seoul, Republic of Korea, and coauthors.
Patients with HCC that shows macroscopic vascular invasion are a particularly poor prognosis subset, according to Dr. Yoon and coauthors.
“Sorafenib is the sole treatment option for these patients, with unsatisfactory response and survival benefit,” they wrote.
Building on observational studies suggesting TACE plus external beam therapy may be a promising approach, Dr. Yoon and colleagues initiated a randomized, open-label clinical trial including 90 patients with liver-confined HCC and macroscopic vascular invasion.
Patients were randomized to sorafenib either 400 mg twice daily or TACE every 6 weeks plus radiotherapy starting within 3 weeks of the first TACE, according to the study description.
The primary endpoint, 12-week progression-free survival, was 86.7% for patients receiving TACE plus radiotherapy, versus 34.3% for patients receiving sorafenib (P less than .001).
The TACE plus radiotherapy group also had a significantly longer overall survival (55.0 vs. 43.0 weeks; P = .04), as well as a significantly higher radiologic response rate and significantly longer median time to progression, the authors reported.
Five patients (11.1%) in the TACE plus radiotherapy group were able to undergo curative surgical resection due to downstaging.
The risk of TACE-induced liver failure is a concern based on results of previous studies in patients with HCC and macroscopic vascular invasion, but in this study, there were no discontinuations due to adverse events in the TACE-radiation group, the authors noted.
“Our study may not be large enough to accurately establish the incidence of adverse events,” they wrote. “However, considering the dismal prognosis, the superior efficacy of TACE plus RT vs. sorafenib may justify its use for these patients.”
Dr. Yoon reported no disclosures related to the study. One coauthor reported research funding and advisory board membership with Bayer Healthcare and Gilead Sciences.
SOURCE: Yoon SM et al. 2018 Mar 15 JAMA Oncol. doi: 10.1001/jamaoncol.2017.5847.
FROM JAMA ONCOLOGY
Key clinical point: Use of transarterial chemoembolization (TACE) plus external beam radiotherapy may improve outcomes in patients with hepatocellular carcinoma (HCC) showing macroscopic vascular invasion.
Major finding: Progression-free survival at 12 weeks was 86.7% for patients receiving TACE plus radiotherapy group, versus 34.3% for patients receiving sorafenib (P less than .001).
Study details: A randomized, open-label clinical trial of 90 patients with liver-confined HCC and macroscopic vascular invasion.
Disclosures: One author reported research funding and advisory board membership with Bayer Healthcare and Gilead Sciences.
Source: Yoon SM et al. JAMA Oncol. 2018 Mar 15. doi: 10.1001/jamaoncol.2017.5847.
Allopurinol dose not escalated enough to reduce mortality
An allopurinol dose escalation strategy for patients with gout was associated with a small increase in all-cause mortality when compared against a static dosing strategy, results of a recent observational study show.
Allopurinol dose escalation was also associated with small, but not statistically significant, increases in cardiovascular- and cancer-related mortality, investigators said in a report published in Arthritis & Rheumatology.
Dr. Coburn and his colleagues had hypothesized that dose escalation would instead be associated with lower cause-specific cardiovascular and cancer mortality, compared with static dosing, according to the report.
However, a minority of dose-escalated patients achieved serum urate goal. Thus, inadequate escalation may have obscured any potential mortality benefit associated with the treatment strategy, the investigators suggested.
Current guidelines recommend starting gout patients on a low dose of allopurinol (100 mg/day or less) and then titrating up the dose slowly.
“While randomized, controlled trials of urate-lowering therapies have used static dosing strategies, such strategies are suboptimal and should now be considered unethical,” they wrote.
The researchers’ 10-year, observational, active-comparator study included 6,428 U.S. veterans with gout receiving allopurinol according to a dose escalation strategy, and 6,428 matched individuals not treated with an escalation approach.
Dose escalators had significantly increased all-cause mortality (hazard ratio, 1.08; 95% confidence interval, 1.01-1.17). Similar, but not statistically significant, effect sizes were seen for cardiovascular mortality (HR, 1.08; 95% CI, 0.97-1.21) and cancer mortality (HR, 1.06; 95% CI, 0.88-1.27), the investigators reported.
However, only 10% of dose-escalation patients received allopurinol in doses exceeding 300 mg daily, and only about one-third achieved a serum urate goal of less than 6.0 mg/dL after 2 years, they found.
“Patients receiving urate-lowering therapy dose escalation were only rarely escalated to levels typically required for proper gout control,” the investigators said.
Inadequate dose escalation amounts to “clinical inertia” that limited the ability of the study to show how optimal dose escalation may affect mortality, the investigators said.
“This appears to be particularly relevant since gout patients receiving dose escalation and achieving serum urate goal appeared to have lower cardiovascular mortality in sensitivity analyses,” they noted.
There was a 7% reduction in cardiovascular mortality in a sensitivity analysis limited to dose escalators who achieved goal, though that finding did not reach statistical significance, Dr. Coburn and his coinvestigators reported (HR, 0.93; 95% CI, 0.76-1.14).
“Taken together, these results add to the persistent uncertainty regarding the role of urate-lowering therapy in reducing mortality risk,” the investigators concluded.
The study was supported by a Rheumatology Research Foundation Health Professional Research Preceptorship, a University of Nebraska Medical Center Graduate Fellowship Grant, and the Nebraska Arthritis Outcomes Research Center. No information was provided on author disclosures.
SOURCE: Coburn B et al. Arthritis Rheumatol. 2018 Mar 7. doi: 10.1002/art.40486.
An allopurinol dose escalation strategy for patients with gout was associated with a small increase in all-cause mortality when compared against a static dosing strategy, results of a recent observational study show.
Allopurinol dose escalation was also associated with small, but not statistically significant, increases in cardiovascular- and cancer-related mortality, investigators said in a report published in Arthritis & Rheumatology.
Dr. Coburn and his colleagues had hypothesized that dose escalation would instead be associated with lower cause-specific cardiovascular and cancer mortality, compared with static dosing, according to the report.
However, a minority of dose-escalated patients achieved serum urate goal. Thus, inadequate escalation may have obscured any potential mortality benefit associated with the treatment strategy, the investigators suggested.
Current guidelines recommend starting gout patients on a low dose of allopurinol (100 mg/day or less) and then titrating up the dose slowly.
“While randomized, controlled trials of urate-lowering therapies have used static dosing strategies, such strategies are suboptimal and should now be considered unethical,” they wrote.
The researchers’ 10-year, observational, active-comparator study included 6,428 U.S. veterans with gout receiving allopurinol according to a dose escalation strategy, and 6,428 matched individuals not treated with an escalation approach.
Dose escalators had significantly increased all-cause mortality (hazard ratio, 1.08; 95% confidence interval, 1.01-1.17). Similar, but not statistically significant, effect sizes were seen for cardiovascular mortality (HR, 1.08; 95% CI, 0.97-1.21) and cancer mortality (HR, 1.06; 95% CI, 0.88-1.27), the investigators reported.
However, only 10% of dose-escalation patients received allopurinol in doses exceeding 300 mg daily, and only about one-third achieved a serum urate goal of less than 6.0 mg/dL after 2 years, they found.
“Patients receiving urate-lowering therapy dose escalation were only rarely escalated to levels typically required for proper gout control,” the investigators said.
Inadequate dose escalation amounts to “clinical inertia” that limited the ability of the study to show how optimal dose escalation may affect mortality, the investigators said.
“This appears to be particularly relevant since gout patients receiving dose escalation and achieving serum urate goal appeared to have lower cardiovascular mortality in sensitivity analyses,” they noted.
There was a 7% reduction in cardiovascular mortality in a sensitivity analysis limited to dose escalators who achieved goal, though that finding did not reach statistical significance, Dr. Coburn and his coinvestigators reported (HR, 0.93; 95% CI, 0.76-1.14).
“Taken together, these results add to the persistent uncertainty regarding the role of urate-lowering therapy in reducing mortality risk,” the investigators concluded.
The study was supported by a Rheumatology Research Foundation Health Professional Research Preceptorship, a University of Nebraska Medical Center Graduate Fellowship Grant, and the Nebraska Arthritis Outcomes Research Center. No information was provided on author disclosures.
SOURCE: Coburn B et al. Arthritis Rheumatol. 2018 Mar 7. doi: 10.1002/art.40486.
An allopurinol dose escalation strategy for patients with gout was associated with a small increase in all-cause mortality when compared against a static dosing strategy, results of a recent observational study show.
Allopurinol dose escalation was also associated with small, but not statistically significant, increases in cardiovascular- and cancer-related mortality, investigators said in a report published in Arthritis & Rheumatology.
Dr. Coburn and his colleagues had hypothesized that dose escalation would instead be associated with lower cause-specific cardiovascular and cancer mortality, compared with static dosing, according to the report.
However, a minority of dose-escalated patients achieved serum urate goal. Thus, inadequate escalation may have obscured any potential mortality benefit associated with the treatment strategy, the investigators suggested.
Current guidelines recommend starting gout patients on a low dose of allopurinol (100 mg/day or less) and then titrating up the dose slowly.
“While randomized, controlled trials of urate-lowering therapies have used static dosing strategies, such strategies are suboptimal and should now be considered unethical,” they wrote.
The researchers’ 10-year, observational, active-comparator study included 6,428 U.S. veterans with gout receiving allopurinol according to a dose escalation strategy, and 6,428 matched individuals not treated with an escalation approach.
Dose escalators had significantly increased all-cause mortality (hazard ratio, 1.08; 95% confidence interval, 1.01-1.17). Similar, but not statistically significant, effect sizes were seen for cardiovascular mortality (HR, 1.08; 95% CI, 0.97-1.21) and cancer mortality (HR, 1.06; 95% CI, 0.88-1.27), the investigators reported.
However, only 10% of dose-escalation patients received allopurinol in doses exceeding 300 mg daily, and only about one-third achieved a serum urate goal of less than 6.0 mg/dL after 2 years, they found.
“Patients receiving urate-lowering therapy dose escalation were only rarely escalated to levels typically required for proper gout control,” the investigators said.
Inadequate dose escalation amounts to “clinical inertia” that limited the ability of the study to show how optimal dose escalation may affect mortality, the investigators said.
“This appears to be particularly relevant since gout patients receiving dose escalation and achieving serum urate goal appeared to have lower cardiovascular mortality in sensitivity analyses,” they noted.
There was a 7% reduction in cardiovascular mortality in a sensitivity analysis limited to dose escalators who achieved goal, though that finding did not reach statistical significance, Dr. Coburn and his coinvestigators reported (HR, 0.93; 95% CI, 0.76-1.14).
“Taken together, these results add to the persistent uncertainty regarding the role of urate-lowering therapy in reducing mortality risk,” the investigators concluded.
The study was supported by a Rheumatology Research Foundation Health Professional Research Preceptorship, a University of Nebraska Medical Center Graduate Fellowship Grant, and the Nebraska Arthritis Outcomes Research Center. No information was provided on author disclosures.
SOURCE: Coburn B et al. Arthritis Rheumatol. 2018 Mar 7. doi: 10.1002/art.40486.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point:
Major finding: Patients treated with a dose escalation strategy had a small but statistically significant increase in all-cause mortality, compared with non-escalators (HR, 1.08; 95% CI, 1.01-1.17).
Study details: A 10-year observational, active-comparator study of U.S. veterans with gout who initiated allopurinol, including 6,428 dose escalators and 6,428 non-escalators.
Disclosures: The study was supported by a Rheumatology Research Foundation Health Professional Research Preceptorship, a University of Nebraska Medical Center Graduate Fellowship Grant, and the Nebraska Arthritis Outcomes Research Center. No information was provided on author disclosures.
Source: Coburn B et al. Arthritis Rheumatol. 2018 Mar 7. doi: 10.1002/art.40486.
Children, adolescents with TBI at risk of secondary ADHD
FROM JAMA PEDIATRICS
Children and adolescents with traumatic brain injury (TBI) might be at increased risk of developing attention-deficit/hyperactivity disorder (ADHD) years after the injury, a prospective cohort study published March 19 shows.
Severe TBI was associated with significantly increased risk of new onset ADHD versus controls in the study, which was based on parent-completed assessments done as late as 6.8 years after the initial injury, according to results presented in JAMA Pediatrics.
Although children with severe TBI were at highest risk, those with less severe TBI had about twice the risk of developing ADHD, compared with control subjects who had no brain injury, the study results suggest.
Taken together, the findings suggest a need for long-term monitoring for attention problems, wrote investigator Megan E. Narad, PhD, of Cincinnati Children’s Hospital Medical Center, and her co-authors.
“Physicians and other clinicians should continue to be vigilant in monitoring attention problems in patients with a history of brain injury, even if it has been a number of years since the injury, the injury was moderate in nature, or the patient experienced a predominantly positive recovery,” Dr. Narad and her colleagues wrote.
The results were based on long-term analysis of 187 children who were hospitalized for TBI or orthopedic injury between the ages of 3 and 7 years. That group included 81 children with TBI and 106 with orthopedic injury.
Parents completed assessments soon after the injury, then again at 6 months, 12 months, 18 months, 3.4 years, and 6.8 years afterward, according to the study.
Over the full follow-up period, 48 children (25.7%) met the investigators’ definition of “secondary ADHD,” or onset of ADHD symptoms after an injury. They found that compared with orthopedic injury, the severe TBI was associated with new ADHD (hazard ratio, 3.62; 95% confidence interval, 1.59-8.26), the investigators reported.
In patients with mild or moderate TBI, associations with new onset ADHD did not meet the statistical significance threshol. However, compared with the orthopedic injury group, the risk for ADHD in TBI severity subgroups were up to 4 times higher.
This is not the first study showing an elevated risk of ADHD in TBI patients, but .
“Although most children with severe TBI who developed secondary ADHD did so within the first 18 months after injury, a portion of those with complicated mild and moderate TBI demonstrated new onset of secondary ADHD at the final two assessments, highlighting the importance of continued monitoring even years after TBI,” Dr. Narad and her colleagues wrote.
The study was funded by several sources, including the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the state of Ohio’s Emergency Medical Services.
Dr. Narad reported no relevant disclosures. Other study authors reported disclosures related to Akili Interactive Labs, Multi-Health Systems, Optimal Medicine, and IXICO.
SOURCE: Narad ME et al. JAMA Pediatr. 2018 Mar 19. doi: 10.1001/jamapediatrics.2017.5746.
FROM JAMA PEDIATRICS
Children and adolescents with traumatic brain injury (TBI) might be at increased risk of developing attention-deficit/hyperactivity disorder (ADHD) years after the injury, a prospective cohort study published March 19 shows.
Severe TBI was associated with significantly increased risk of new onset ADHD versus controls in the study, which was based on parent-completed assessments done as late as 6.8 years after the initial injury, according to results presented in JAMA Pediatrics.
Although children with severe TBI were at highest risk, those with less severe TBI had about twice the risk of developing ADHD, compared with control subjects who had no brain injury, the study results suggest.
Taken together, the findings suggest a need for long-term monitoring for attention problems, wrote investigator Megan E. Narad, PhD, of Cincinnati Children’s Hospital Medical Center, and her co-authors.
“Physicians and other clinicians should continue to be vigilant in monitoring attention problems in patients with a history of brain injury, even if it has been a number of years since the injury, the injury was moderate in nature, or the patient experienced a predominantly positive recovery,” Dr. Narad and her colleagues wrote.
The results were based on long-term analysis of 187 children who were hospitalized for TBI or orthopedic injury between the ages of 3 and 7 years. That group included 81 children with TBI and 106 with orthopedic injury.
Parents completed assessments soon after the injury, then again at 6 months, 12 months, 18 months, 3.4 years, and 6.8 years afterward, according to the study.
Over the full follow-up period, 48 children (25.7%) met the investigators’ definition of “secondary ADHD,” or onset of ADHD symptoms after an injury. They found that compared with orthopedic injury, the severe TBI was associated with new ADHD (hazard ratio, 3.62; 95% confidence interval, 1.59-8.26), the investigators reported.
In patients with mild or moderate TBI, associations with new onset ADHD did not meet the statistical significance threshol. However, compared with the orthopedic injury group, the risk for ADHD in TBI severity subgroups were up to 4 times higher.
This is not the first study showing an elevated risk of ADHD in TBI patients, but .
“Although most children with severe TBI who developed secondary ADHD did so within the first 18 months after injury, a portion of those with complicated mild and moderate TBI demonstrated new onset of secondary ADHD at the final two assessments, highlighting the importance of continued monitoring even years after TBI,” Dr. Narad and her colleagues wrote.
The study was funded by several sources, including the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the state of Ohio’s Emergency Medical Services.
Dr. Narad reported no relevant disclosures. Other study authors reported disclosures related to Akili Interactive Labs, Multi-Health Systems, Optimal Medicine, and IXICO.
SOURCE: Narad ME et al. JAMA Pediatr. 2018 Mar 19. doi: 10.1001/jamapediatrics.2017.5746.
FROM JAMA PEDIATRICS
Children and adolescents with traumatic brain injury (TBI) might be at increased risk of developing attention-deficit/hyperactivity disorder (ADHD) years after the injury, a prospective cohort study published March 19 shows.
Severe TBI was associated with significantly increased risk of new onset ADHD versus controls in the study, which was based on parent-completed assessments done as late as 6.8 years after the initial injury, according to results presented in JAMA Pediatrics.
Although children with severe TBI were at highest risk, those with less severe TBI had about twice the risk of developing ADHD, compared with control subjects who had no brain injury, the study results suggest.
Taken together, the findings suggest a need for long-term monitoring for attention problems, wrote investigator Megan E. Narad, PhD, of Cincinnati Children’s Hospital Medical Center, and her co-authors.
“Physicians and other clinicians should continue to be vigilant in monitoring attention problems in patients with a history of brain injury, even if it has been a number of years since the injury, the injury was moderate in nature, or the patient experienced a predominantly positive recovery,” Dr. Narad and her colleagues wrote.
The results were based on long-term analysis of 187 children who were hospitalized for TBI or orthopedic injury between the ages of 3 and 7 years. That group included 81 children with TBI and 106 with orthopedic injury.
Parents completed assessments soon after the injury, then again at 6 months, 12 months, 18 months, 3.4 years, and 6.8 years afterward, according to the study.
Over the full follow-up period, 48 children (25.7%) met the investigators’ definition of “secondary ADHD,” or onset of ADHD symptoms after an injury. They found that compared with orthopedic injury, the severe TBI was associated with new ADHD (hazard ratio, 3.62; 95% confidence interval, 1.59-8.26), the investigators reported.
In patients with mild or moderate TBI, associations with new onset ADHD did not meet the statistical significance threshol. However, compared with the orthopedic injury group, the risk for ADHD in TBI severity subgroups were up to 4 times higher.
This is not the first study showing an elevated risk of ADHD in TBI patients, but .
“Although most children with severe TBI who developed secondary ADHD did so within the first 18 months after injury, a portion of those with complicated mild and moderate TBI demonstrated new onset of secondary ADHD at the final two assessments, highlighting the importance of continued monitoring even years after TBI,” Dr. Narad and her colleagues wrote.
The study was funded by several sources, including the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the state of Ohio’s Emergency Medical Services.
Dr. Narad reported no relevant disclosures. Other study authors reported disclosures related to Akili Interactive Labs, Multi-Health Systems, Optimal Medicine, and IXICO.
SOURCE: Narad ME et al. JAMA Pediatr. 2018 Mar 19. doi: 10.1001/jamapediatrics.2017.5746.
Key clinical point: Children and adolescents with traumatic brain injury (TBI) should continue to be monitored for possible attention problems many years after the injury.
Major finding: In assessments taken up to 6.8 years after injury, severe TBI was associated with secondary ADHD, compared with a control group (hazard ratio, 3.62; 95% confidence interval, 1.59-8.26).
Study details: Analysis of a prospective concurrent cohort study including 187 children aged 3 to 7 years who were hospitalized for TBI or orthopedic injury.
Disclosures: The study was funded by several sources, including the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the state of Ohio’s Emergency Medical Services. The authors reported conflict of interest disclosures related to Akili Interactive Labs, Multi-Health Systems, Optimal Medicine, and IXICO.
Source: Narad ME et al. JAMA Pediatr. 2018 Mar 19. doi:10.1001/jamapediatrics.2017.5746.
Pre-screening could help identify NAFLD biopsy candidates
PHILADELPHIA – When evaluating patients with established non-alcoholic fatty liver disease (NAFLD), using pre-screening criteria may help identify the subset of patients who should be subjected to liver biopsy, according to Vinod K. Rustgi, MD.
The recently described pre-screening criteria include a set of patient and disease characteristics that identify who might be at highest risk for non-alcoholic steatohepatitis (NASH) and fibrosis, said Dr. Rustgi, chief of hepatology at Rutgers Robert Wood Johnson Medical School in New Brunswick, N.J.
“Eighty-five percent of the patients who fall into this category will actually have fibrosis on liver biopsy. So it’s a good way to screen out who you want to actually biopsy,” Dr. Rustgi said at the meeting, jointly provided by Rutgers and Global Academy for Medical Education.
Liver biopsy needs to be considered in patients with NAFLD who are at increased risk of having advanced fibrosis, according to the latest practice guidance on diagnosis and management of NAFLD (Hepatology. 2018 Jan;67[1]:328-57).
While it’s the most accurate means to diagnose and stage severity of NASH, biopsy is invasive, costly, and associated with potential complications, according to a recent Hepatology review article (2017 Dec 9. doi: 10.1002/hep.29721).
Criteria to pinpoint patients at highest risk for NASH and fibrosis could be useful for streamlining clinical trial enrollment and limiting screening failures, according to authors who recently described the pre-screening criteria in the Journal of Hepatology (2018 Feb. doi: 10.1016/j.jhep.2017.10.015).
, or who have a vibration controlled transient elastography (VCTE, FibroScan) score of kPa greater than 8.5, or an AST/ALT ratio greater than 1, among several other criteria described in the article.
“The patients who have a low likelihood of NASH and fibrosis are those who are under the age of 40, who may not be diabetic, who have a elastography score of kPa less than 7, or an AST less than 20,” Dr. Rustgi said of the pre-screening criteria.
In his presentation, Dr. Rustgi provided other notes on when to biopsy as described in the January 2018 practice guidance from Hepatology.
In particular, the guidance states that presence of metabolic syndrome, NAFLD fibrosis score or Fibrosis 4 Score, or liver stiffness measured by VCTE or magnetic resonance elastography might be used to help identify patients at risk for steatohepatitis or advanced fibrosis.
Liver biopsy also should be considered in NAFLD when competing etiologies cannot be excluded except by a liver biopsy, according to the recent guidance.
Dr. Rustgi reported disclosures related to AbbVie, Genfit, and Gilead Sciences.
Global Academy for Medical Education and this news organization are owned by the same company.
PHILADELPHIA – When evaluating patients with established non-alcoholic fatty liver disease (NAFLD), using pre-screening criteria may help identify the subset of patients who should be subjected to liver biopsy, according to Vinod K. Rustgi, MD.
The recently described pre-screening criteria include a set of patient and disease characteristics that identify who might be at highest risk for non-alcoholic steatohepatitis (NASH) and fibrosis, said Dr. Rustgi, chief of hepatology at Rutgers Robert Wood Johnson Medical School in New Brunswick, N.J.
“Eighty-five percent of the patients who fall into this category will actually have fibrosis on liver biopsy. So it’s a good way to screen out who you want to actually biopsy,” Dr. Rustgi said at the meeting, jointly provided by Rutgers and Global Academy for Medical Education.
Liver biopsy needs to be considered in patients with NAFLD who are at increased risk of having advanced fibrosis, according to the latest practice guidance on diagnosis and management of NAFLD (Hepatology. 2018 Jan;67[1]:328-57).
While it’s the most accurate means to diagnose and stage severity of NASH, biopsy is invasive, costly, and associated with potential complications, according to a recent Hepatology review article (2017 Dec 9. doi: 10.1002/hep.29721).
Criteria to pinpoint patients at highest risk for NASH and fibrosis could be useful for streamlining clinical trial enrollment and limiting screening failures, according to authors who recently described the pre-screening criteria in the Journal of Hepatology (2018 Feb. doi: 10.1016/j.jhep.2017.10.015).
, or who have a vibration controlled transient elastography (VCTE, FibroScan) score of kPa greater than 8.5, or an AST/ALT ratio greater than 1, among several other criteria described in the article.
“The patients who have a low likelihood of NASH and fibrosis are those who are under the age of 40, who may not be diabetic, who have a elastography score of kPa less than 7, or an AST less than 20,” Dr. Rustgi said of the pre-screening criteria.
In his presentation, Dr. Rustgi provided other notes on when to biopsy as described in the January 2018 practice guidance from Hepatology.
In particular, the guidance states that presence of metabolic syndrome, NAFLD fibrosis score or Fibrosis 4 Score, or liver stiffness measured by VCTE or magnetic resonance elastography might be used to help identify patients at risk for steatohepatitis or advanced fibrosis.
Liver biopsy also should be considered in NAFLD when competing etiologies cannot be excluded except by a liver biopsy, according to the recent guidance.
Dr. Rustgi reported disclosures related to AbbVie, Genfit, and Gilead Sciences.
Global Academy for Medical Education and this news organization are owned by the same company.
PHILADELPHIA – When evaluating patients with established non-alcoholic fatty liver disease (NAFLD), using pre-screening criteria may help identify the subset of patients who should be subjected to liver biopsy, according to Vinod K. Rustgi, MD.
The recently described pre-screening criteria include a set of patient and disease characteristics that identify who might be at highest risk for non-alcoholic steatohepatitis (NASH) and fibrosis, said Dr. Rustgi, chief of hepatology at Rutgers Robert Wood Johnson Medical School in New Brunswick, N.J.
“Eighty-five percent of the patients who fall into this category will actually have fibrosis on liver biopsy. So it’s a good way to screen out who you want to actually biopsy,” Dr. Rustgi said at the meeting, jointly provided by Rutgers and Global Academy for Medical Education.
Liver biopsy needs to be considered in patients with NAFLD who are at increased risk of having advanced fibrosis, according to the latest practice guidance on diagnosis and management of NAFLD (Hepatology. 2018 Jan;67[1]:328-57).
While it’s the most accurate means to diagnose and stage severity of NASH, biopsy is invasive, costly, and associated with potential complications, according to a recent Hepatology review article (2017 Dec 9. doi: 10.1002/hep.29721).
Criteria to pinpoint patients at highest risk for NASH and fibrosis could be useful for streamlining clinical trial enrollment and limiting screening failures, according to authors who recently described the pre-screening criteria in the Journal of Hepatology (2018 Feb. doi: 10.1016/j.jhep.2017.10.015).
, or who have a vibration controlled transient elastography (VCTE, FibroScan) score of kPa greater than 8.5, or an AST/ALT ratio greater than 1, among several other criteria described in the article.
“The patients who have a low likelihood of NASH and fibrosis are those who are under the age of 40, who may not be diabetic, who have a elastography score of kPa less than 7, or an AST less than 20,” Dr. Rustgi said of the pre-screening criteria.
In his presentation, Dr. Rustgi provided other notes on when to biopsy as described in the January 2018 practice guidance from Hepatology.
In particular, the guidance states that presence of metabolic syndrome, NAFLD fibrosis score or Fibrosis 4 Score, or liver stiffness measured by VCTE or magnetic resonance elastography might be used to help identify patients at risk for steatohepatitis or advanced fibrosis.
Liver biopsy also should be considered in NAFLD when competing etiologies cannot be excluded except by a liver biopsy, according to the recent guidance.
Dr. Rustgi reported disclosures related to AbbVie, Genfit, and Gilead Sciences.
Global Academy for Medical Education and this news organization are owned by the same company.
REPORTING FROM DIGESTIVE DISEASES: NEW ADVANCES