User login
WOSCOPS 20-year follow-up shows impressive statin ‘legacy effect’
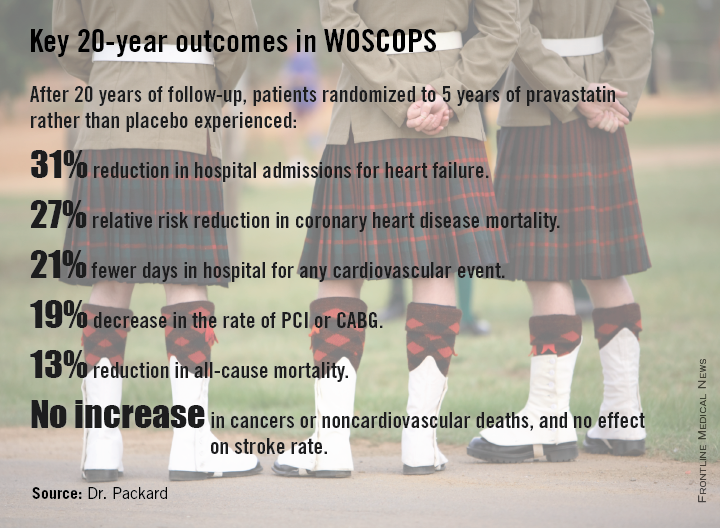
CHICAGO – Five years of statin therapy for primary prevention provided an impressive lifetime benefit expressed as reduced risks of a range of cardiovascular disease outcomes in a 20-year follow-up of the landmark WOSCOPS trial.
“There is a rather remarkable persistence of benefit in terms of risk reduction over a long period. You’ve changed the natural history of the disease in some way by lowering LDL,” Dr. Chris J. Packard said in presenting the 20-year WOSCOPS (West of Scotland Coronary Prevention Study) follow-up at the American Heart Association scientific sessions.
The primary prevention study randomized 6,595 middle-aged Scotsmen with an average baseline LDL cholesterol of 190 mg/dL to 4 years of pravastatin at 40 mg/day or placebo. This was one of the early large statin trials, and publication of the 5-year outcomes showing a 31% reduction in the relative risk of cardiovascular death or MI (N. Engl. J. Med. 1995;333:1301-8) caused a great stir.
At that point, WOSCOPS leaders advised study participants’ primary care physicians to seriously consider putting their patients on long-term statin therapy. However, only an identically low 31% of subjects in each of the two study arms did so.
Because the Scottish national health care system effectively captures all utilization of medical services, Dr. Packard and coinvestigators were able to analyze 20-year outcomes in the former study participants. No other major statin trial has come close in terms of length of reported follow-up.
At 20 years, with the only treatment difference between the two original study arms being that the pravastatin group had been on statin therapy for an additional 5 years, the 20-year coronary heart disease mortality rate in the original statin group was reduced by 27%, compared with the original controls. All-cause mortality was reduced by 13%. And numerous other benefits were noted at 20 years with 5 years of statin therapy.
Indeed, patients treated with pravastatin for 5 years during the trial gained an average of 5 extra years free of nonfatal MI or cardiovascular death at the 20-year mark, he said.
“The average age of the men was 55 years during the trial and 20 years on they’re now 75 years old. This covers the entire period of premature cardiovascular morbidity and mortality. We would argue that this is a good picture of the lifetime benefit, which is different from lifetime risk. This is real events happening to real people, not predictions,” observed Dr. Packard, professor of cardiovascular and medical sciences at the University of Glasgow, Scotland.
The group given pravastatin for 5 years collectively spent 24,038 days in the hospital for any cardiovascular event, compared with 30,342 days for controls.
Particularly noteworthy was the divergence in the risk of heart failure, with 96 cases being diagnosed during 20 years in patients who received 5 years of pravastatin, compared with 128 in controls.
“Heart failure was our biggest surprise,” he said. “We got no result for heart failure at all at 5 years; these were middle-aged men with just high cholesterol, so we didn’t see much in the way of incident heart failure. But extrapolating 20 years, there is a 31% risk reduction in the incidence of hospitalization for heart failure in the statin-treated group, compared to the placebo-treated group. This is a remarkable finding.”
For WOSCOPS participants who got a 20% drop in LDL during 5 years of pravastatin from a baseline of 190 mg/dL, as was typical, the number of patients who needed to be treated (NNT) for 5 years to prevent one cardiovascular hospital admission over a 20-year period was six. Moreover, for every 10 patients on statin therapy for 5 years, an average of 19 hospital days were avoided over the course of 20 years. For patients with a baseline LDL of 120 mg/dL, the NNT was 10, and 12 hospital days were saved over a 20-year period for every 10 patients treated for 5 years.
“This is a real savings to the health service and the health care providers to offset the cost of drugs,” Dr. Packard continued.
He urged physicians to look beyond the initial reports of primary outcomes of the statin clinical trials and take a long-term view.
“If you take a lifetime approach to benefit so you’re looking not only at the first event, but the second event, the third, at heart failure, and at death, you can see tremendous benefits, whereas usually we only focus on the first event. And that’s not the full cost evaluation that you need to do,” according to Dr. Packard.
The overall incidence of cancer during 20 years of follow-up was 24.8% in the initial placebo arm and 24.5% in the pravastatin group, with no differences between the two groups in any type of cancer. Nor did the original pravastatin group show any increase in noncardiovascular mortality.
“This is a very important study – the first study to show a legacy effect, with reduced mortality and a gain of 5 event-free years over 20 years attributable to a 5-year treatment allocation,” said discussant Harvey White of Auckland (New Zealand) City Hospital.
This legacy effect, he added, can be viewed as an ongoing carryover effect related to statin-induced slowing and/or stabilization of existing coronary artery plaque. The mechanism is unknown, Dr. White said, but the key to why the legacy effect was seen in WOSCOPS despite the use of pravastatin – a less potent statin – but not to date in other statin trials may lie in the fact that WOSCOPS was a primary prevention study and its participants had the youngest mean age of all the major statin trials.
“Their plaques may not have been calcified yet and therefore were more able to be modified and stabilized. If you treat very early you might get a bigger effect,” said to Dr. White.
Undercutting that argument, however, was the WOSCOPS finding that the long-term benefits of 5 years of pravastatin were independent of age at treatment, Dr. Packard said.
He believes based upon other studies that statins’ coronary disease prevention benefits are expressed within the first 12 months after starting therapy.
“It suggests that whatever is happening to the pathobiology of atherosclerosis happens within a year, and somehow a statis is introduced into plaque. That’s my guess, that an unstable plaque is reduced to a stable one. People then form a new trajectory going forward and they never catch up. We should think of atherosclerosis as a rate effect rather than something that either happens or doesn’t happen. It’s a rate of happening,” Dr. Packard asserted.
Asked why in the aftermath of the strongly positive 5-year results of WOSCOPS only 31% of patients in each treatment arm were on long-term statin therapy, he replied that 20 years ago in Scotland there really was no push for primary prevention.
“The 4S trial had come out the year before [Lancet 1994;344:1383-9] and placed the focus on secondary prevention. Statins were relatively expensive and everybody was putting their money into secondary prevention. Our health care system, which is socialized, had not put any emphasis at all on primary prevention. We were actually amazed that even 31% got treated,” the physician explained.
Dr. Packard reported serving as a consultant to Merck, Roche, and AstraZeneca.
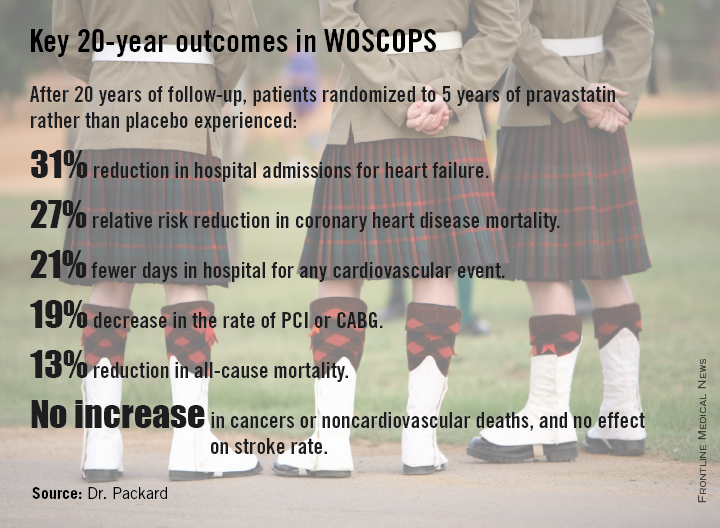
CHICAGO – Five years of statin therapy for primary prevention provided an impressive lifetime benefit expressed as reduced risks of a range of cardiovascular disease outcomes in a 20-year follow-up of the landmark WOSCOPS trial.
“There is a rather remarkable persistence of benefit in terms of risk reduction over a long period. You’ve changed the natural history of the disease in some way by lowering LDL,” Dr. Chris J. Packard said in presenting the 20-year WOSCOPS (West of Scotland Coronary Prevention Study) follow-up at the American Heart Association scientific sessions.
The primary prevention study randomized 6,595 middle-aged Scotsmen with an average baseline LDL cholesterol of 190 mg/dL to 4 years of pravastatin at 40 mg/day or placebo. This was one of the early large statin trials, and publication of the 5-year outcomes showing a 31% reduction in the relative risk of cardiovascular death or MI (N. Engl. J. Med. 1995;333:1301-8) caused a great stir.
At that point, WOSCOPS leaders advised study participants’ primary care physicians to seriously consider putting their patients on long-term statin therapy. However, only an identically low 31% of subjects in each of the two study arms did so.
Because the Scottish national health care system effectively captures all utilization of medical services, Dr. Packard and coinvestigators were able to analyze 20-year outcomes in the former study participants. No other major statin trial has come close in terms of length of reported follow-up.
At 20 years, with the only treatment difference between the two original study arms being that the pravastatin group had been on statin therapy for an additional 5 years, the 20-year coronary heart disease mortality rate in the original statin group was reduced by 27%, compared with the original controls. All-cause mortality was reduced by 13%. And numerous other benefits were noted at 20 years with 5 years of statin therapy.
Indeed, patients treated with pravastatin for 5 years during the trial gained an average of 5 extra years free of nonfatal MI or cardiovascular death at the 20-year mark, he said.
“The average age of the men was 55 years during the trial and 20 years on they’re now 75 years old. This covers the entire period of premature cardiovascular morbidity and mortality. We would argue that this is a good picture of the lifetime benefit, which is different from lifetime risk. This is real events happening to real people, not predictions,” observed Dr. Packard, professor of cardiovascular and medical sciences at the University of Glasgow, Scotland.
The group given pravastatin for 5 years collectively spent 24,038 days in the hospital for any cardiovascular event, compared with 30,342 days for controls.
Particularly noteworthy was the divergence in the risk of heart failure, with 96 cases being diagnosed during 20 years in patients who received 5 years of pravastatin, compared with 128 in controls.
“Heart failure was our biggest surprise,” he said. “We got no result for heart failure at all at 5 years; these were middle-aged men with just high cholesterol, so we didn’t see much in the way of incident heart failure. But extrapolating 20 years, there is a 31% risk reduction in the incidence of hospitalization for heart failure in the statin-treated group, compared to the placebo-treated group. This is a remarkable finding.”
For WOSCOPS participants who got a 20% drop in LDL during 5 years of pravastatin from a baseline of 190 mg/dL, as was typical, the number of patients who needed to be treated (NNT) for 5 years to prevent one cardiovascular hospital admission over a 20-year period was six. Moreover, for every 10 patients on statin therapy for 5 years, an average of 19 hospital days were avoided over the course of 20 years. For patients with a baseline LDL of 120 mg/dL, the NNT was 10, and 12 hospital days were saved over a 20-year period for every 10 patients treated for 5 years.
“This is a real savings to the health service and the health care providers to offset the cost of drugs,” Dr. Packard continued.
He urged physicians to look beyond the initial reports of primary outcomes of the statin clinical trials and take a long-term view.
“If you take a lifetime approach to benefit so you’re looking not only at the first event, but the second event, the third, at heart failure, and at death, you can see tremendous benefits, whereas usually we only focus on the first event. And that’s not the full cost evaluation that you need to do,” according to Dr. Packard.
The overall incidence of cancer during 20 years of follow-up was 24.8% in the initial placebo arm and 24.5% in the pravastatin group, with no differences between the two groups in any type of cancer. Nor did the original pravastatin group show any increase in noncardiovascular mortality.
“This is a very important study – the first study to show a legacy effect, with reduced mortality and a gain of 5 event-free years over 20 years attributable to a 5-year treatment allocation,” said discussant Harvey White of Auckland (New Zealand) City Hospital.
This legacy effect, he added, can be viewed as an ongoing carryover effect related to statin-induced slowing and/or stabilization of existing coronary artery plaque. The mechanism is unknown, Dr. White said, but the key to why the legacy effect was seen in WOSCOPS despite the use of pravastatin – a less potent statin – but not to date in other statin trials may lie in the fact that WOSCOPS was a primary prevention study and its participants had the youngest mean age of all the major statin trials.
“Their plaques may not have been calcified yet and therefore were more able to be modified and stabilized. If you treat very early you might get a bigger effect,” said to Dr. White.
Undercutting that argument, however, was the WOSCOPS finding that the long-term benefits of 5 years of pravastatin were independent of age at treatment, Dr. Packard said.
He believes based upon other studies that statins’ coronary disease prevention benefits are expressed within the first 12 months after starting therapy.
“It suggests that whatever is happening to the pathobiology of atherosclerosis happens within a year, and somehow a statis is introduced into plaque. That’s my guess, that an unstable plaque is reduced to a stable one. People then form a new trajectory going forward and they never catch up. We should think of atherosclerosis as a rate effect rather than something that either happens or doesn’t happen. It’s a rate of happening,” Dr. Packard asserted.
Asked why in the aftermath of the strongly positive 5-year results of WOSCOPS only 31% of patients in each treatment arm were on long-term statin therapy, he replied that 20 years ago in Scotland there really was no push for primary prevention.
“The 4S trial had come out the year before [Lancet 1994;344:1383-9] and placed the focus on secondary prevention. Statins were relatively expensive and everybody was putting their money into secondary prevention. Our health care system, which is socialized, had not put any emphasis at all on primary prevention. We were actually amazed that even 31% got treated,” the physician explained.
Dr. Packard reported serving as a consultant to Merck, Roche, and AstraZeneca.
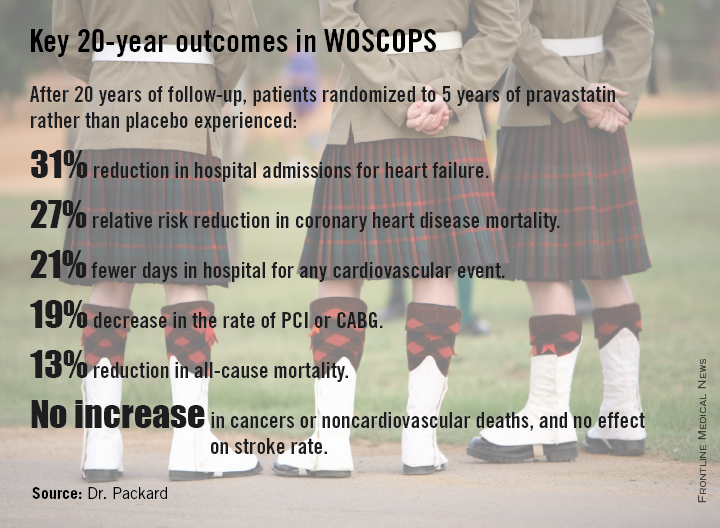
CHICAGO – Five years of statin therapy for primary prevention provided an impressive lifetime benefit expressed as reduced risks of a range of cardiovascular disease outcomes in a 20-year follow-up of the landmark WOSCOPS trial.
“There is a rather remarkable persistence of benefit in terms of risk reduction over a long period. You’ve changed the natural history of the disease in some way by lowering LDL,” Dr. Chris J. Packard said in presenting the 20-year WOSCOPS (West of Scotland Coronary Prevention Study) follow-up at the American Heart Association scientific sessions.
The primary prevention study randomized 6,595 middle-aged Scotsmen with an average baseline LDL cholesterol of 190 mg/dL to 4 years of pravastatin at 40 mg/day or placebo. This was one of the early large statin trials, and publication of the 5-year outcomes showing a 31% reduction in the relative risk of cardiovascular death or MI (N. Engl. J. Med. 1995;333:1301-8) caused a great stir.
At that point, WOSCOPS leaders advised study participants’ primary care physicians to seriously consider putting their patients on long-term statin therapy. However, only an identically low 31% of subjects in each of the two study arms did so.
Because the Scottish national health care system effectively captures all utilization of medical services, Dr. Packard and coinvestigators were able to analyze 20-year outcomes in the former study participants. No other major statin trial has come close in terms of length of reported follow-up.
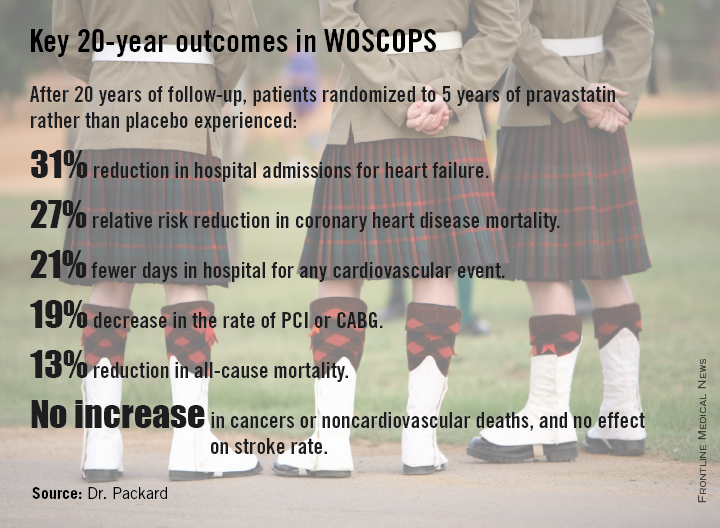
At 20 years, with the only treatment difference between the two original study arms being that the pravastatin group had been on statin therapy for an additional 5 years, the 20-year coronary heart disease mortality rate in the original statin group was reduced by 27%, compared with the original controls. All-cause mortality was reduced by 13%. And numerous other benefits were noted at 20 years with 5 years of statin therapy.
Indeed, patients treated with pravastatin for 5 years during the trial gained an average of 5 extra years free of nonfatal MI or cardiovascular death at the 20-year mark, he said.
“The average age of the men was 55 years during the trial and 20 years on they’re now 75 years old. This covers the entire period of premature cardiovascular morbidity and mortality. We would argue that this is a good picture of the lifetime benefit, which is different from lifetime risk. This is real events happening to real people, not predictions,” observed Dr. Packard, professor of cardiovascular and medical sciences at the University of Glasgow, Scotland.
The group given pravastatin for 5 years collectively spent 24,038 days in the hospital for any cardiovascular event, compared with 30,342 days for controls.
Particularly noteworthy was the divergence in the risk of heart failure, with 96 cases being diagnosed during 20 years in patients who received 5 years of pravastatin, compared with 128 in controls.
“Heart failure was our biggest surprise,” he said. “We got no result for heart failure at all at 5 years; these were middle-aged men with just high cholesterol, so we didn’t see much in the way of incident heart failure. But extrapolating 20 years, there is a 31% risk reduction in the incidence of hospitalization for heart failure in the statin-treated group, compared to the placebo-treated group. This is a remarkable finding.”
For WOSCOPS participants who got a 20% drop in LDL during 5 years of pravastatin from a baseline of 190 mg/dL, as was typical, the number of patients who needed to be treated (NNT) for 5 years to prevent one cardiovascular hospital admission over a 20-year period was six. Moreover, for every 10 patients on statin therapy for 5 years, an average of 19 hospital days were avoided over the course of 20 years. For patients with a baseline LDL of 120 mg/dL, the NNT was 10, and 12 hospital days were saved over a 20-year period for every 10 patients treated for 5 years.
“This is a real savings to the health service and the health care providers to offset the cost of drugs,” Dr. Packard continued.
He urged physicians to look beyond the initial reports of primary outcomes of the statin clinical trials and take a long-term view.
“If you take a lifetime approach to benefit so you’re looking not only at the first event, but the second event, the third, at heart failure, and at death, you can see tremendous benefits, whereas usually we only focus on the first event. And that’s not the full cost evaluation that you need to do,” according to Dr. Packard.
The overall incidence of cancer during 20 years of follow-up was 24.8% in the initial placebo arm and 24.5% in the pravastatin group, with no differences between the two groups in any type of cancer. Nor did the original pravastatin group show any increase in noncardiovascular mortality.
“This is a very important study – the first study to show a legacy effect, with reduced mortality and a gain of 5 event-free years over 20 years attributable to a 5-year treatment allocation,” said discussant Harvey White of Auckland (New Zealand) City Hospital.
This legacy effect, he added, can be viewed as an ongoing carryover effect related to statin-induced slowing and/or stabilization of existing coronary artery plaque. The mechanism is unknown, Dr. White said, but the key to why the legacy effect was seen in WOSCOPS despite the use of pravastatin – a less potent statin – but not to date in other statin trials may lie in the fact that WOSCOPS was a primary prevention study and its participants had the youngest mean age of all the major statin trials.
“Their plaques may not have been calcified yet and therefore were more able to be modified and stabilized. If you treat very early you might get a bigger effect,” said to Dr. White.
Undercutting that argument, however, was the WOSCOPS finding that the long-term benefits of 5 years of pravastatin were independent of age at treatment, Dr. Packard said.
He believes based upon other studies that statins’ coronary disease prevention benefits are expressed within the first 12 months after starting therapy.
“It suggests that whatever is happening to the pathobiology of atherosclerosis happens within a year, and somehow a statis is introduced into plaque. That’s my guess, that an unstable plaque is reduced to a stable one. People then form a new trajectory going forward and they never catch up. We should think of atherosclerosis as a rate effect rather than something that either happens or doesn’t happen. It’s a rate of happening,” Dr. Packard asserted.
Asked why in the aftermath of the strongly positive 5-year results of WOSCOPS only 31% of patients in each treatment arm were on long-term statin therapy, he replied that 20 years ago in Scotland there really was no push for primary prevention.
“The 4S trial had come out the year before [Lancet 1994;344:1383-9] and placed the focus on secondary prevention. Statins were relatively expensive and everybody was putting their money into secondary prevention. Our health care system, which is socialized, had not put any emphasis at all on primary prevention. We were actually amazed that even 31% got treated,” the physician explained.
Dr. Packard reported serving as a consultant to Merck, Roche, and AstraZeneca.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Five years of statin therapy during midlife for primary prevention may reset the clock for atherosclerotic progression, providing persistently lower cardiovascular event rates 20 years later.
Major finding: The number of patients who needed to be treated with pravastatin for 5 years to prevent one cardiovascular hospitalization over a 20-year period was six.
Data source: A 20-year follow-up of the West of Scotland Coronary Prevention Study, in which 6,595 middle-aged men with high cholesterol were randomized to 5 years of pravastatin or placebo.
Disclosures: WOSCOPS was sponsored by Bristol-Myers Squibb. The presenter reported serving as a consultant to Merck, Roche, and AstraZeneca.
Unrecognized MI common with impaired fasting glucose
CHICAGO– Impaired fasting glucose was associated with a doubled risk of asymptomatic or unrecognized myocardial infarction during prospective follow-up of subjects without overt cardiovascular disease in the Multi-Ethnic Study of Atherosclerosis.
The clinical relevance of this finding lies in previous work establishing that asymptomatic, unrecognized MIs are associated with a prognosis as serious as for symptomatic MIs.
“Because of the high prevalence of impaired fasting glucose, the implications of this finding may have ramifications for a large proportion of the adult population,” Dr. Richard B. Stacey observed at the American Heart Association Scientific Sessions.
The magnitude of the risk of unrecognized MI was associated with duration of exposure to abnormal blood glucose levels in the landmark population-based MESA study. Subjects with impaired fasting glucose (IFG) noted on at least three of five biannual examinations conducted over a 10-year period had an adjusted 1.97-fold greater risk of experiencing an unrecognized MI during that time, compared with MESA participants who had normal blood glucose, added Dr. Stacey of Wake Forest University in Winston-Salem, N.C.
He presented two new analyses from the MESA study. One was cross-sectional: Among 4,955 study participants with normal fasting glucose and 930 with IFG upon study enrollment, a baseline 12-lead ECG revealed a prior unrecognized MI in 1.4% of those with normal fasting glucose and 3.2% of those with IFG, a 2.3-fold increase. MESA participants were on average in their mid-60s, and none had clinical cardiovascular disease.
In a multivariate logistic regression analysis fully adjusted for demographics and the standard cardiovascular risk factors as well as body mass index and the use of antihypertensive and lipid-lowering medications, IFG was associated with a 1.63-fold increased risk of prior asymptomatic or unrecognized MI (P < .001).
The other, prospective, longitudinal analysis, included 872 subjects with baseline normal fasting glucose and 545 with IFG, none of whom had evidence of a prior unrecognized MI at entry. This analysis excluded individuals who developed diabetes mellitus, had a clinically recognized MI, or underwent coronary revascularization during follow-up. During 10 years of follow-up, 14.9% of the group who continued to have normal fasting glucose experienced an unrecognized MI, as did 23.8% of those with IFG at entry. The unrecognized MIs were detected either by the presence of pathologic Q waves or minor Q waves with ST-T abnormalities on ECG or by an MRI showing late gadolinium enhancement indicative of myocardial scar.
The MESA study is funded by the National Institutes of Health. Dr. Stacey reported having no financial conflicts.
CHICAGO– Impaired fasting glucose was associated with a doubled risk of asymptomatic or unrecognized myocardial infarction during prospective follow-up of subjects without overt cardiovascular disease in the Multi-Ethnic Study of Atherosclerosis.
The clinical relevance of this finding lies in previous work establishing that asymptomatic, unrecognized MIs are associated with a prognosis as serious as for symptomatic MIs.
“Because of the high prevalence of impaired fasting glucose, the implications of this finding may have ramifications for a large proportion of the adult population,” Dr. Richard B. Stacey observed at the American Heart Association Scientific Sessions.
The magnitude of the risk of unrecognized MI was associated with duration of exposure to abnormal blood glucose levels in the landmark population-based MESA study. Subjects with impaired fasting glucose (IFG) noted on at least three of five biannual examinations conducted over a 10-year period had an adjusted 1.97-fold greater risk of experiencing an unrecognized MI during that time, compared with MESA participants who had normal blood glucose, added Dr. Stacey of Wake Forest University in Winston-Salem, N.C.
He presented two new analyses from the MESA study. One was cross-sectional: Among 4,955 study participants with normal fasting glucose and 930 with IFG upon study enrollment, a baseline 12-lead ECG revealed a prior unrecognized MI in 1.4% of those with normal fasting glucose and 3.2% of those with IFG, a 2.3-fold increase. MESA participants were on average in their mid-60s, and none had clinical cardiovascular disease.
In a multivariate logistic regression analysis fully adjusted for demographics and the standard cardiovascular risk factors as well as body mass index and the use of antihypertensive and lipid-lowering medications, IFG was associated with a 1.63-fold increased risk of prior asymptomatic or unrecognized MI (P < .001).
The other, prospective, longitudinal analysis, included 872 subjects with baseline normal fasting glucose and 545 with IFG, none of whom had evidence of a prior unrecognized MI at entry. This analysis excluded individuals who developed diabetes mellitus, had a clinically recognized MI, or underwent coronary revascularization during follow-up. During 10 years of follow-up, 14.9% of the group who continued to have normal fasting glucose experienced an unrecognized MI, as did 23.8% of those with IFG at entry. The unrecognized MIs were detected either by the presence of pathologic Q waves or minor Q waves with ST-T abnormalities on ECG or by an MRI showing late gadolinium enhancement indicative of myocardial scar.
The MESA study is funded by the National Institutes of Health. Dr. Stacey reported having no financial conflicts.
CHICAGO– Impaired fasting glucose was associated with a doubled risk of asymptomatic or unrecognized myocardial infarction during prospective follow-up of subjects without overt cardiovascular disease in the Multi-Ethnic Study of Atherosclerosis.
The clinical relevance of this finding lies in previous work establishing that asymptomatic, unrecognized MIs are associated with a prognosis as serious as for symptomatic MIs.
“Because of the high prevalence of impaired fasting glucose, the implications of this finding may have ramifications for a large proportion of the adult population,” Dr. Richard B. Stacey observed at the American Heart Association Scientific Sessions.
The magnitude of the risk of unrecognized MI was associated with duration of exposure to abnormal blood glucose levels in the landmark population-based MESA study. Subjects with impaired fasting glucose (IFG) noted on at least three of five biannual examinations conducted over a 10-year period had an adjusted 1.97-fold greater risk of experiencing an unrecognized MI during that time, compared with MESA participants who had normal blood glucose, added Dr. Stacey of Wake Forest University in Winston-Salem, N.C.
He presented two new analyses from the MESA study. One was cross-sectional: Among 4,955 study participants with normal fasting glucose and 930 with IFG upon study enrollment, a baseline 12-lead ECG revealed a prior unrecognized MI in 1.4% of those with normal fasting glucose and 3.2% of those with IFG, a 2.3-fold increase. MESA participants were on average in their mid-60s, and none had clinical cardiovascular disease.
In a multivariate logistic regression analysis fully adjusted for demographics and the standard cardiovascular risk factors as well as body mass index and the use of antihypertensive and lipid-lowering medications, IFG was associated with a 1.63-fold increased risk of prior asymptomatic or unrecognized MI (P < .001).
The other, prospective, longitudinal analysis, included 872 subjects with baseline normal fasting glucose and 545 with IFG, none of whom had evidence of a prior unrecognized MI at entry. This analysis excluded individuals who developed diabetes mellitus, had a clinically recognized MI, or underwent coronary revascularization during follow-up. During 10 years of follow-up, 14.9% of the group who continued to have normal fasting glucose experienced an unrecognized MI, as did 23.8% of those with IFG at entry. The unrecognized MIs were detected either by the presence of pathologic Q waves or minor Q waves with ST-T abnormalities on ECG or by an MRI showing late gadolinium enhancement indicative of myocardial scar.
The MESA study is funded by the National Institutes of Health. Dr. Stacey reported having no financial conflicts.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Consistent impaired fasting glucose may be associated with asymptomatic myocardial infarction.
Major finding: Individuals with impaired fasting glucose on at least three out of five structured clinic visits during 10 years of prospective follow-up were at twice the risk of experiencing an unrecognized MI, compared with those who had normal fasting glucose.
Data source: The Multi-Ethnic Study of Atherosclerosis, a prospective, longitudinal, population-based study.
Disclosures: MESA is funded by the National Institutes of Health. The presenter reported having no financial conflicts.
Bare-metal stent superior safety debunked in DAPT analysis
CHICAGO – Drug-eluting stents were associated with significantly lower risks of both stent thrombosis and major adverse cardio- and cerebrovascular events, compared with bare-metal stents in a prespecified secondary analysis of the landmark Dual Antiplatelet Therapy (DAPT) trial.
“What I’ve learned from this is the myth of the safety of the bare-metal stent: It is not safer. So the concept that we still see in practice every day, where colleagues put in bare-metal stents because they perceive them to be safer and they perceive the optimal duration of dual antiplatelet therapy to be shorter, I’m not sure that’s the right thought process,” Dr. Dean J. Kereiakes said in presenting the study findings at the American Heart Association scientific sessions.
Another eye-opening finding in the secondary analysis was that when it comes to the duration of DAPT after stent placement, be it a drug-eluting stent (DES) or bare-metal stent (BMS), longer appears to be better. A surprising proportion of cases of stent thrombosis in both groups occurred after they stopped DAPT at the 12-month mark.
“Patients who don’t bleed on DAPT should be left on it a long time. I have evolved my thought process such that I’m thinking of this like a statin,” said Dr. Kereiakes, medical director of the Christ Hospital Heart and Vascular Center in Cincinnati.
The DAPT trial included 9,961 patients who underwent percutaneous coronary intervention with one of four types of drug-eluting stent (DES) and 1,687 who got a bare-metal stent (BMS), all of whom received 12 months of DAPT and then were randomized to blinded placebo or an additional 18 months of DAPT. The primary outcome was presented earlier at the AHA meeting and simultaneously published online (N. Engl. J. Med. 2014 [doi:10.1056/NEJMoa1409312]).
The secondary analysis addressed two key questions: Do the risks of stent thrombosis and major adverse cardio- and cerebrovascular events (MACCE) differ between DES and BMS? And does the optimal duration of DAPT differ between the two stent platforms?
Dr. Kereiakes presented a propensity-matched analysis that included 8,308 patients with DES and 1,178 with BMS. The key finding here was that the rate of stent thrombosis was significantly lower in the DES group. This was the case both through the first 12 months of DAPT, where the stent thrombosis rates were 0.7% and 1.7% in the DES and BMS groups, respectively, and at 33 months, where the cumulative stent thrombosis rates were 1.7% and 2.6%.
The MACCE rate – defined as death, MI, or stroke – at 12 months was also significantly lower in the DES group: 5.1%, compared with 6.8% with BMS. The same was true at 33 months, when the rate was 11.4% in the DES group, compared with 13.4% in patients with a BMS. However, because of the smaller sample size of the BMS propensity-matched comparison group, this absolute 2% difference in MACCE at 33 months was sufficient to show DES were noninferior to BMS on this endpoint, but not superior to BMS, the cardiologist continued.
The advantage for DES over BMS in terms of MACCE appeared to be similar across all four DES types utilized in the trial: everolimus-, sirolimus-, paclitaxel-, and zotarolimus-eluting stents. While paclitaxel-eluting stents weren’t significantly better than BMS in terms of stent thrombosis rates, the other three DES types were, and to a comparable degree.
The hazard ratio for stent thrombosis with 30 months of DAPT as compared to 12 months was 0.29 in the DES group and 0.49 in BMS recipients.
“The magnitude of reduction in stent thrombosis risk with the longer, 30-month duration thienopyridine therapy appears consistent for both bare-metal stents and drug-eluting stents,” Dr. Kereiakes said.
There was no significant difference between DES and BMS in the rate of moderate to severe bleeding through 33 months: 4.04% with DES and 3.67% in the BMS group. Stroke rates were similar as well.
Dr. Kereiakes also presented another prespecified secondary analysis from the DAPT trial, this one a comparison of event rates in 1,687 BMS patients randomized to 12 versus 30 months of DAPT. At 33 months’ follow-up, the stent thrombosis rate was 0.5% in BMS patients who got 30 months of DAPT, compared with 1.1% in those who got 12 months of DAPT followed by aspirin plus placebo. The MACCE rate was 4.0% in BMS recipients who received 30 months of DAPT and 4.7% with 12 months.
Discussant Dr. Daniel B. Mark said these secondary analyses of the DAPT trial have brought home for him several key points: First, BMS are not safer than DES from the patient’s viewpoint; second, the risk of stent thrombosis continues after 12 months for both stent platforms; and third, current DAPT regimens can decrease but certainly don’t eliminate either stent thrombosis or non–stent related cardiovascular events.
The late occurrence of stent thromboses between 12 and 30 months in both study arms “really makes us think of this issue of DAPT in a different way than we have in the past,” added Dr. Mark, professor of medicine at Duke University and director of outcomes research at the Duke Clinical Research Institute in Durham, N.C.
He observed that “a perfect storm” of observational evidence arose beginning in 2006 which convinced physicians that BMS were safer – wrongly, as it now turns out.
The conventional wisdom was that BMS had a restenosis problem seen as “a benign nuisance requiring repeat revascularization procedures but having no discernible effect on death or MI,” Dr. Marks said, “while the DES were extremely effective at reducing restenosis but had this stent thrombosis problem” that was viewed in hyperbolic terms in the literature. The DAPT trial has gone a long way towards correcting those misperceptions, he said.
He wondered, however, just how confident Dr. Kereiakes is in the validity of his propensity matching.
“The matching was based on 55 different variables,” Dr. Kereiakes replied. “With all the limitations inherent in propensity-matched analysis, I think this is about as good as it gets.”
Dr. Mark noted that while cardiologists ponder the fine points between DES and BMS, it’s important not to lose sight of the big picture as highlighted in a recent study by Dr. Mark A. Hlatky of Stanford (Calif.) University and coinvestigators. Their analysis of Medicare beneficiaries who underwent either multivessel coronary artery bypass surgery or multivessel percutaneous coronary intervention concluded that the introduction of DES didn’t alter the comparative effectiveness of CABG and PCI. The 5-year survival rate following CABG has been about 10% better than with PCI both in the pre-DES era of BMS and in the DES era. Moreover, the 5-year rate of freedom from MI has been about 18% better with multivessel CABG than multivessel PCI in both stent platform eras (Am. Heart J. 2014;169:149-54).
The DAPT study was supported by more than half a dozen pharmaceutical and medical device companies as well as the U.S. Department of Health and Human Services. Dr. Kereiakes reported receiving payments as an advisor to Boston Scientific and Abbott Vascular. Dr. Marks reported receiving research grants from the National Institutes of Health and serving as a consultant to Somahlution, Milestone, Medtronic, and CardioDx.
CHICAGO – Drug-eluting stents were associated with significantly lower risks of both stent thrombosis and major adverse cardio- and cerebrovascular events, compared with bare-metal stents in a prespecified secondary analysis of the landmark Dual Antiplatelet Therapy (DAPT) trial.
“What I’ve learned from this is the myth of the safety of the bare-metal stent: It is not safer. So the concept that we still see in practice every day, where colleagues put in bare-metal stents because they perceive them to be safer and they perceive the optimal duration of dual antiplatelet therapy to be shorter, I’m not sure that’s the right thought process,” Dr. Dean J. Kereiakes said in presenting the study findings at the American Heart Association scientific sessions.
Another eye-opening finding in the secondary analysis was that when it comes to the duration of DAPT after stent placement, be it a drug-eluting stent (DES) or bare-metal stent (BMS), longer appears to be better. A surprising proportion of cases of stent thrombosis in both groups occurred after they stopped DAPT at the 12-month mark.
“Patients who don’t bleed on DAPT should be left on it a long time. I have evolved my thought process such that I’m thinking of this like a statin,” said Dr. Kereiakes, medical director of the Christ Hospital Heart and Vascular Center in Cincinnati.
The DAPT trial included 9,961 patients who underwent percutaneous coronary intervention with one of four types of drug-eluting stent (DES) and 1,687 who got a bare-metal stent (BMS), all of whom received 12 months of DAPT and then were randomized to blinded placebo or an additional 18 months of DAPT. The primary outcome was presented earlier at the AHA meeting and simultaneously published online (N. Engl. J. Med. 2014 [doi:10.1056/NEJMoa1409312]).
The secondary analysis addressed two key questions: Do the risks of stent thrombosis and major adverse cardio- and cerebrovascular events (MACCE) differ between DES and BMS? And does the optimal duration of DAPT differ between the two stent platforms?
Dr. Kereiakes presented a propensity-matched analysis that included 8,308 patients with DES and 1,178 with BMS. The key finding here was that the rate of stent thrombosis was significantly lower in the DES group. This was the case both through the first 12 months of DAPT, where the stent thrombosis rates were 0.7% and 1.7% in the DES and BMS groups, respectively, and at 33 months, where the cumulative stent thrombosis rates were 1.7% and 2.6%.
The MACCE rate – defined as death, MI, or stroke – at 12 months was also significantly lower in the DES group: 5.1%, compared with 6.8% with BMS. The same was true at 33 months, when the rate was 11.4% in the DES group, compared with 13.4% in patients with a BMS. However, because of the smaller sample size of the BMS propensity-matched comparison group, this absolute 2% difference in MACCE at 33 months was sufficient to show DES were noninferior to BMS on this endpoint, but not superior to BMS, the cardiologist continued.
The advantage for DES over BMS in terms of MACCE appeared to be similar across all four DES types utilized in the trial: everolimus-, sirolimus-, paclitaxel-, and zotarolimus-eluting stents. While paclitaxel-eluting stents weren’t significantly better than BMS in terms of stent thrombosis rates, the other three DES types were, and to a comparable degree.
The hazard ratio for stent thrombosis with 30 months of DAPT as compared to 12 months was 0.29 in the DES group and 0.49 in BMS recipients.
“The magnitude of reduction in stent thrombosis risk with the longer, 30-month duration thienopyridine therapy appears consistent for both bare-metal stents and drug-eluting stents,” Dr. Kereiakes said.
There was no significant difference between DES and BMS in the rate of moderate to severe bleeding through 33 months: 4.04% with DES and 3.67% in the BMS group. Stroke rates were similar as well.
Dr. Kereiakes also presented another prespecified secondary analysis from the DAPT trial, this one a comparison of event rates in 1,687 BMS patients randomized to 12 versus 30 months of DAPT. At 33 months’ follow-up, the stent thrombosis rate was 0.5% in BMS patients who got 30 months of DAPT, compared with 1.1% in those who got 12 months of DAPT followed by aspirin plus placebo. The MACCE rate was 4.0% in BMS recipients who received 30 months of DAPT and 4.7% with 12 months.
Discussant Dr. Daniel B. Mark said these secondary analyses of the DAPT trial have brought home for him several key points: First, BMS are not safer than DES from the patient’s viewpoint; second, the risk of stent thrombosis continues after 12 months for both stent platforms; and third, current DAPT regimens can decrease but certainly don’t eliminate either stent thrombosis or non–stent related cardiovascular events.
The late occurrence of stent thromboses between 12 and 30 months in both study arms “really makes us think of this issue of DAPT in a different way than we have in the past,” added Dr. Mark, professor of medicine at Duke University and director of outcomes research at the Duke Clinical Research Institute in Durham, N.C.
He observed that “a perfect storm” of observational evidence arose beginning in 2006 which convinced physicians that BMS were safer – wrongly, as it now turns out.
The conventional wisdom was that BMS had a restenosis problem seen as “a benign nuisance requiring repeat revascularization procedures but having no discernible effect on death or MI,” Dr. Marks said, “while the DES were extremely effective at reducing restenosis but had this stent thrombosis problem” that was viewed in hyperbolic terms in the literature. The DAPT trial has gone a long way towards correcting those misperceptions, he said.
He wondered, however, just how confident Dr. Kereiakes is in the validity of his propensity matching.
“The matching was based on 55 different variables,” Dr. Kereiakes replied. “With all the limitations inherent in propensity-matched analysis, I think this is about as good as it gets.”
Dr. Mark noted that while cardiologists ponder the fine points between DES and BMS, it’s important not to lose sight of the big picture as highlighted in a recent study by Dr. Mark A. Hlatky of Stanford (Calif.) University and coinvestigators. Their analysis of Medicare beneficiaries who underwent either multivessel coronary artery bypass surgery or multivessel percutaneous coronary intervention concluded that the introduction of DES didn’t alter the comparative effectiveness of CABG and PCI. The 5-year survival rate following CABG has been about 10% better than with PCI both in the pre-DES era of BMS and in the DES era. Moreover, the 5-year rate of freedom from MI has been about 18% better with multivessel CABG than multivessel PCI in both stent platform eras (Am. Heart J. 2014;169:149-54).
The DAPT study was supported by more than half a dozen pharmaceutical and medical device companies as well as the U.S. Department of Health and Human Services. Dr. Kereiakes reported receiving payments as an advisor to Boston Scientific and Abbott Vascular. Dr. Marks reported receiving research grants from the National Institutes of Health and serving as a consultant to Somahlution, Milestone, Medtronic, and CardioDx.
CHICAGO – Drug-eluting stents were associated with significantly lower risks of both stent thrombosis and major adverse cardio- and cerebrovascular events, compared with bare-metal stents in a prespecified secondary analysis of the landmark Dual Antiplatelet Therapy (DAPT) trial.
“What I’ve learned from this is the myth of the safety of the bare-metal stent: It is not safer. So the concept that we still see in practice every day, where colleagues put in bare-metal stents because they perceive them to be safer and they perceive the optimal duration of dual antiplatelet therapy to be shorter, I’m not sure that’s the right thought process,” Dr. Dean J. Kereiakes said in presenting the study findings at the American Heart Association scientific sessions.
Another eye-opening finding in the secondary analysis was that when it comes to the duration of DAPT after stent placement, be it a drug-eluting stent (DES) or bare-metal stent (BMS), longer appears to be better. A surprising proportion of cases of stent thrombosis in both groups occurred after they stopped DAPT at the 12-month mark.
“Patients who don’t bleed on DAPT should be left on it a long time. I have evolved my thought process such that I’m thinking of this like a statin,” said Dr. Kereiakes, medical director of the Christ Hospital Heart and Vascular Center in Cincinnati.
The DAPT trial included 9,961 patients who underwent percutaneous coronary intervention with one of four types of drug-eluting stent (DES) and 1,687 who got a bare-metal stent (BMS), all of whom received 12 months of DAPT and then were randomized to blinded placebo or an additional 18 months of DAPT. The primary outcome was presented earlier at the AHA meeting and simultaneously published online (N. Engl. J. Med. 2014 [doi:10.1056/NEJMoa1409312]).
The secondary analysis addressed two key questions: Do the risks of stent thrombosis and major adverse cardio- and cerebrovascular events (MACCE) differ between DES and BMS? And does the optimal duration of DAPT differ between the two stent platforms?
Dr. Kereiakes presented a propensity-matched analysis that included 8,308 patients with DES and 1,178 with BMS. The key finding here was that the rate of stent thrombosis was significantly lower in the DES group. This was the case both through the first 12 months of DAPT, where the stent thrombosis rates were 0.7% and 1.7% in the DES and BMS groups, respectively, and at 33 months, where the cumulative stent thrombosis rates were 1.7% and 2.6%.
The MACCE rate – defined as death, MI, or stroke – at 12 months was also significantly lower in the DES group: 5.1%, compared with 6.8% with BMS. The same was true at 33 months, when the rate was 11.4% in the DES group, compared with 13.4% in patients with a BMS. However, because of the smaller sample size of the BMS propensity-matched comparison group, this absolute 2% difference in MACCE at 33 months was sufficient to show DES were noninferior to BMS on this endpoint, but not superior to BMS, the cardiologist continued.
The advantage for DES over BMS in terms of MACCE appeared to be similar across all four DES types utilized in the trial: everolimus-, sirolimus-, paclitaxel-, and zotarolimus-eluting stents. While paclitaxel-eluting stents weren’t significantly better than BMS in terms of stent thrombosis rates, the other three DES types were, and to a comparable degree.
The hazard ratio for stent thrombosis with 30 months of DAPT as compared to 12 months was 0.29 in the DES group and 0.49 in BMS recipients.
“The magnitude of reduction in stent thrombosis risk with the longer, 30-month duration thienopyridine therapy appears consistent for both bare-metal stents and drug-eluting stents,” Dr. Kereiakes said.
There was no significant difference between DES and BMS in the rate of moderate to severe bleeding through 33 months: 4.04% with DES and 3.67% in the BMS group. Stroke rates were similar as well.
Dr. Kereiakes also presented another prespecified secondary analysis from the DAPT trial, this one a comparison of event rates in 1,687 BMS patients randomized to 12 versus 30 months of DAPT. At 33 months’ follow-up, the stent thrombosis rate was 0.5% in BMS patients who got 30 months of DAPT, compared with 1.1% in those who got 12 months of DAPT followed by aspirin plus placebo. The MACCE rate was 4.0% in BMS recipients who received 30 months of DAPT and 4.7% with 12 months.
Discussant Dr. Daniel B. Mark said these secondary analyses of the DAPT trial have brought home for him several key points: First, BMS are not safer than DES from the patient’s viewpoint; second, the risk of stent thrombosis continues after 12 months for both stent platforms; and third, current DAPT regimens can decrease but certainly don’t eliminate either stent thrombosis or non–stent related cardiovascular events.
The late occurrence of stent thromboses between 12 and 30 months in both study arms “really makes us think of this issue of DAPT in a different way than we have in the past,” added Dr. Mark, professor of medicine at Duke University and director of outcomes research at the Duke Clinical Research Institute in Durham, N.C.
He observed that “a perfect storm” of observational evidence arose beginning in 2006 which convinced physicians that BMS were safer – wrongly, as it now turns out.
The conventional wisdom was that BMS had a restenosis problem seen as “a benign nuisance requiring repeat revascularization procedures but having no discernible effect on death or MI,” Dr. Marks said, “while the DES were extremely effective at reducing restenosis but had this stent thrombosis problem” that was viewed in hyperbolic terms in the literature. The DAPT trial has gone a long way towards correcting those misperceptions, he said.
He wondered, however, just how confident Dr. Kereiakes is in the validity of his propensity matching.
“The matching was based on 55 different variables,” Dr. Kereiakes replied. “With all the limitations inherent in propensity-matched analysis, I think this is about as good as it gets.”
Dr. Mark noted that while cardiologists ponder the fine points between DES and BMS, it’s important not to lose sight of the big picture as highlighted in a recent study by Dr. Mark A. Hlatky of Stanford (Calif.) University and coinvestigators. Their analysis of Medicare beneficiaries who underwent either multivessel coronary artery bypass surgery or multivessel percutaneous coronary intervention concluded that the introduction of DES didn’t alter the comparative effectiveness of CABG and PCI. The 5-year survival rate following CABG has been about 10% better than with PCI both in the pre-DES era of BMS and in the DES era. Moreover, the 5-year rate of freedom from MI has been about 18% better with multivessel CABG than multivessel PCI in both stent platform eras (Am. Heart J. 2014;169:149-54).
The DAPT study was supported by more than half a dozen pharmaceutical and medical device companies as well as the U.S. Department of Health and Human Services. Dr. Kereiakes reported receiving payments as an advisor to Boston Scientific and Abbott Vascular. Dr. Marks reported receiving research grants from the National Institutes of Health and serving as a consultant to Somahlution, Milestone, Medtronic, and CardioDx.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Bare-metal stents aren’t safer than drug-eluting stents.
Major finding: The stent thrombosis rate in drug-eluting stent recipients through 33 months of follow-up was 1.7%, compared with 2.6% in patients with bare-metal stents.
Data source: A prespecified secondary propensity-matched comparison of stent thrombosis and major cardiovascular and cerebrovascular rates in 8,308 drug-eluting stent recipients and 1,178 bare-metal stent recipients in the Dual Antiplatelet Therapy trial.
Disclosures: DAPT was supported by more than half a dozen pharmaceutical and medical device companies as well as the U.S. Department of Health and Human Services. The presenter reported receiving payments as an advisor to Boston Scientific and Abbott Vascular.
Overanticoagulation in AF boosts dementia risk
CHICAGO – Patients with atrial fibrillation who frequently have a supratherapeutic international normalized ratio are at sharply increased risk for developing dementia, according to a large observational study.
“We postulate that the mechanism is an accumulation of microbleeds in the brain,” Dr. T. Jared Bunch said at the American Heart Association Scientific Sessions.
“In patients with hypertension, a condition that’s extremely common with atrial fibrillation, these repetitive small bleeds are preferentially in the hippocampus, where memory is stored,” added Dr. Bunch, who is medical director for heart rhythm services at the Intermountain Medical Center Heart Institute in Salt Lake City.
He presented a study of 1,031 patients with atrial fibrillation (AF) in Intermountain’s centralized anticoagulation service. All were on dual therapy with warfarin plus aspirin or, much less commonly, another antiplatelet agent. At baseline, their average age was in the early- to mid-70s, and none of the subjects had a history of stroke or any notes in their medical record suggestive of early cognitive decline. At this dedicated anticoagulation center, their INR was measured on a weekly or biweekly basis, as a result of which their average time spent in the therapeutic range of 2.0-3.0 was relatively high at nearly 70%.
The increased risk of dementia in patients with AF has previously been recognized. The association is stronger in patients under age 75 than in those who are older. But the mechanism has been unknown. Dr. Bunch and coinvestigators decided to test their hypothesis that the mechanism involves microbleeds secondary to long-term overanticoagulation by dividing the patients into three groups based upon their percentage of INR measurements above 3.0 during a mean follow-up of more than 4 and up to a maximum of 10 years: 240 patients had a supratherapeutic INR 25% of the time or more; 374 did so less than 10% of the time; and 417 had an elevated INR 10%-24% of the time.
The incidence of dementia diagnosed by a consultant neurologist during follow-up was 5.8% in the group with an INR above 3.0 at least 25% of the time, more than twice the 2.7% rate in patients with a high INR less than 10% of the time. In the middle group, the incidence of dementia was 4.1%. In a multivariate Cox regression analysis, having an INR above 3.0 on at least 25% of occasions was independently associated with a 2.59-fold increased risk of developing dementia, making it by far the most potent risk factor in their analysis.
The next step in their research will be to perform serial brain imaging and volumetric scans, Dr. Bunch said. Also, he and his coworkers are 3 years into an ongoing study looking at the incidence of dementia in AF patients on the various novel oral anticoagulants, where INR is a nonissue. Their hypothesis is the dementia risk will be lower than in patients on warfarin. Dr. Bunch has particularly high hopes for AF patients on apixaban (Eliquis) because it’s known to have a reduced risk of large bleeds, stroke, and GI bleeding; the hope is it will cause fewer cerebral microbleeds as well.
In an interview, the cardiologist said he believes his study showing an increased risk of dementia in AF patients with supratherapeutic INRs on warfarin plus antiplatelet therapy holds several important lessons for AF patients and physicians alike.
For patients, the message is don’t just start taking aspirin on your own because you’ve read it’s good for your heart or may reduce cancer risk; consult your physician.
And for physicians, it’s important to ask all patients on warfarin if they’re using aspirin; many don’t ask. Also, periodically reconsider the need for dual therapy with warfarin and aspirin.
“We find the risks of stroke and bleeding change dynamically over time, so the initial therapy for stroke prevention may not be the ideal therapy after 5-10 years,” Dr. Bunch said.
Lastly, for patients who are overanticoagulated on a substantial percentage of their INR measurements, it’s essential to consider a change in strategy. Either follow their INRs more closely and adjust warfarin dosing accordingly, or switch to one of the novel, more predictable oral anticoagulants, he concluded.
This study was funded internally by Intermountain Healthcare. Dr. Bunch reported having no financial conflicts.
CHICAGO – Patients with atrial fibrillation who frequently have a supratherapeutic international normalized ratio are at sharply increased risk for developing dementia, according to a large observational study.
“We postulate that the mechanism is an accumulation of microbleeds in the brain,” Dr. T. Jared Bunch said at the American Heart Association Scientific Sessions.
“In patients with hypertension, a condition that’s extremely common with atrial fibrillation, these repetitive small bleeds are preferentially in the hippocampus, where memory is stored,” added Dr. Bunch, who is medical director for heart rhythm services at the Intermountain Medical Center Heart Institute in Salt Lake City.
He presented a study of 1,031 patients with atrial fibrillation (AF) in Intermountain’s centralized anticoagulation service. All were on dual therapy with warfarin plus aspirin or, much less commonly, another antiplatelet agent. At baseline, their average age was in the early- to mid-70s, and none of the subjects had a history of stroke or any notes in their medical record suggestive of early cognitive decline. At this dedicated anticoagulation center, their INR was measured on a weekly or biweekly basis, as a result of which their average time spent in the therapeutic range of 2.0-3.0 was relatively high at nearly 70%.
The increased risk of dementia in patients with AF has previously been recognized. The association is stronger in patients under age 75 than in those who are older. But the mechanism has been unknown. Dr. Bunch and coinvestigators decided to test their hypothesis that the mechanism involves microbleeds secondary to long-term overanticoagulation by dividing the patients into three groups based upon their percentage of INR measurements above 3.0 during a mean follow-up of more than 4 and up to a maximum of 10 years: 240 patients had a supratherapeutic INR 25% of the time or more; 374 did so less than 10% of the time; and 417 had an elevated INR 10%-24% of the time.
The incidence of dementia diagnosed by a consultant neurologist during follow-up was 5.8% in the group with an INR above 3.0 at least 25% of the time, more than twice the 2.7% rate in patients with a high INR less than 10% of the time. In the middle group, the incidence of dementia was 4.1%. In a multivariate Cox regression analysis, having an INR above 3.0 on at least 25% of occasions was independently associated with a 2.59-fold increased risk of developing dementia, making it by far the most potent risk factor in their analysis.
The next step in their research will be to perform serial brain imaging and volumetric scans, Dr. Bunch said. Also, he and his coworkers are 3 years into an ongoing study looking at the incidence of dementia in AF patients on the various novel oral anticoagulants, where INR is a nonissue. Their hypothesis is the dementia risk will be lower than in patients on warfarin. Dr. Bunch has particularly high hopes for AF patients on apixaban (Eliquis) because it’s known to have a reduced risk of large bleeds, stroke, and GI bleeding; the hope is it will cause fewer cerebral microbleeds as well.
In an interview, the cardiologist said he believes his study showing an increased risk of dementia in AF patients with supratherapeutic INRs on warfarin plus antiplatelet therapy holds several important lessons for AF patients and physicians alike.
For patients, the message is don’t just start taking aspirin on your own because you’ve read it’s good for your heart or may reduce cancer risk; consult your physician.
And for physicians, it’s important to ask all patients on warfarin if they’re using aspirin; many don’t ask. Also, periodically reconsider the need for dual therapy with warfarin and aspirin.
“We find the risks of stroke and bleeding change dynamically over time, so the initial therapy for stroke prevention may not be the ideal therapy after 5-10 years,” Dr. Bunch said.
Lastly, for patients who are overanticoagulated on a substantial percentage of their INR measurements, it’s essential to consider a change in strategy. Either follow their INRs more closely and adjust warfarin dosing accordingly, or switch to one of the novel, more predictable oral anticoagulants, he concluded.
This study was funded internally by Intermountain Healthcare. Dr. Bunch reported having no financial conflicts.
CHICAGO – Patients with atrial fibrillation who frequently have a supratherapeutic international normalized ratio are at sharply increased risk for developing dementia, according to a large observational study.
“We postulate that the mechanism is an accumulation of microbleeds in the brain,” Dr. T. Jared Bunch said at the American Heart Association Scientific Sessions.
“In patients with hypertension, a condition that’s extremely common with atrial fibrillation, these repetitive small bleeds are preferentially in the hippocampus, where memory is stored,” added Dr. Bunch, who is medical director for heart rhythm services at the Intermountain Medical Center Heart Institute in Salt Lake City.
He presented a study of 1,031 patients with atrial fibrillation (AF) in Intermountain’s centralized anticoagulation service. All were on dual therapy with warfarin plus aspirin or, much less commonly, another antiplatelet agent. At baseline, their average age was in the early- to mid-70s, and none of the subjects had a history of stroke or any notes in their medical record suggestive of early cognitive decline. At this dedicated anticoagulation center, their INR was measured on a weekly or biweekly basis, as a result of which their average time spent in the therapeutic range of 2.0-3.0 was relatively high at nearly 70%.
The increased risk of dementia in patients with AF has previously been recognized. The association is stronger in patients under age 75 than in those who are older. But the mechanism has been unknown. Dr. Bunch and coinvestigators decided to test their hypothesis that the mechanism involves microbleeds secondary to long-term overanticoagulation by dividing the patients into three groups based upon their percentage of INR measurements above 3.0 during a mean follow-up of more than 4 and up to a maximum of 10 years: 240 patients had a supratherapeutic INR 25% of the time or more; 374 did so less than 10% of the time; and 417 had an elevated INR 10%-24% of the time.
The incidence of dementia diagnosed by a consultant neurologist during follow-up was 5.8% in the group with an INR above 3.0 at least 25% of the time, more than twice the 2.7% rate in patients with a high INR less than 10% of the time. In the middle group, the incidence of dementia was 4.1%. In a multivariate Cox regression analysis, having an INR above 3.0 on at least 25% of occasions was independently associated with a 2.59-fold increased risk of developing dementia, making it by far the most potent risk factor in their analysis.
The next step in their research will be to perform serial brain imaging and volumetric scans, Dr. Bunch said. Also, he and his coworkers are 3 years into an ongoing study looking at the incidence of dementia in AF patients on the various novel oral anticoagulants, where INR is a nonissue. Their hypothesis is the dementia risk will be lower than in patients on warfarin. Dr. Bunch has particularly high hopes for AF patients on apixaban (Eliquis) because it’s known to have a reduced risk of large bleeds, stroke, and GI bleeding; the hope is it will cause fewer cerebral microbleeds as well.
In an interview, the cardiologist said he believes his study showing an increased risk of dementia in AF patients with supratherapeutic INRs on warfarin plus antiplatelet therapy holds several important lessons for AF patients and physicians alike.
For patients, the message is don’t just start taking aspirin on your own because you’ve read it’s good for your heart or may reduce cancer risk; consult your physician.
And for physicians, it’s important to ask all patients on warfarin if they’re using aspirin; many don’t ask. Also, periodically reconsider the need for dual therapy with warfarin and aspirin.
“We find the risks of stroke and bleeding change dynamically over time, so the initial therapy for stroke prevention may not be the ideal therapy after 5-10 years,” Dr. Bunch said.
Lastly, for patients who are overanticoagulated on a substantial percentage of their INR measurements, it’s essential to consider a change in strategy. Either follow their INRs more closely and adjust warfarin dosing accordingly, or switch to one of the novel, more predictable oral anticoagulants, he concluded.
This study was funded internally by Intermountain Healthcare. Dr. Bunch reported having no financial conflicts.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: The more time patients with atrial fibrillation who are on warfarin plus aspirin spend with a supratherapeutic INR, the greater their risk of developing dementia.
Major finding: Atrial fibrillation patients on warfarin plus an antiplatelet agent who had an INR above 3.0 on at least 25% of occasions had a 5.8% incidence of dementia during follow-up, compared with a 2.7% incidence in those with a high INR less than 10% of the time.
Data source: This was a retrospective, case-control study involving 1,031 patients with atrial fibrillation on warfarin plus aspirin or another antiplatelet agent followed for a mean of more than 4 years.
Disclosures: This study was funded internally by Intermountain Healthcare. Dr. Bunch reported having no financial conflicts.
Elevated troponin present in 40% with T2D and stable heart disease
CHICAGO– Abnormal levels of high-sensitivity cardiac troponin T are present in 40% of type 2 diabetic patients with stable ischemic heart disease, and they do not bode well, according to a new secondary analysis of the BARI 2D study.
In BARI 2D, an abnormal high-sensitivity cardiac troponin T (hsTnT), defined as 14 ng/L or greater, a powerful marker of ongoing myocardial injury, was independently associated with a doubled 5-year risk of the composite endpoint of cardiovascular death, MI, or stroke. Moreover, and discouragingly so, prompt coronary revascularization did nothing to mitigate that risk, Dr. Brendan M. Everett reported at the American Heart Association Scientific Sessions.
Further, early coronary revascularization did not result in a reduction in abnormal hsTnT at 1 year of follow-up, said Dr. Everett, director of the general cardiology inpatient service at Brigham and Women’s Hospital, Boston.
“To better address the risk represented by an abnormal hsTnT, we need to gain an improved understanding of the biology of troponin release in this population,” he observed. “The fact that we saw an overall decrease of about 0.5% in hemoglobin A1c and an LDL reduction of 16 mg/dL at 1 year and still there was no change in hsTnT leaves me scratching my head. The abnormal hsTnT is clearly a marker of badness, but where is it coming from? Can we address it? Or are we just left to look at it and worry about our patients who have an abnormal hsTnT?”
The BARI 2D trial was designed to learn whether patients with type 2 diabetes and stable ischemic heart disease benefit from prompt coronary revascularization plus intensive medical therapy as compared with intensive medical therapy alone. As previously reported (N. Engl. J. Med. 2009;360:2503-15), this proved not to be the case; prompt revascularization conferred no outcome advantage.
The aim of Dr. Everett’s new secondary analysis of BARI 2D was to learn if the hsTnT assay can be used to identify a subgroup of patients with type 2 diabetes and stable ischemic heart disease who might benefit from prompt coronary revascularization. The rationale was that, in patients with acute coronary syndromes, it’s well established that an abnormal hsTnT is associated with poor prognosis, and such patients would benefit from early revascularization.
The secondary analysis included 2,285 type 2 diabetics with stable ischemic heart disease whose physicians first decided whether they were better candidates for percutaneous coronary intervention or CABG surgery. Patients were then randomized to prompt revascularization by the preferred method plus intensive medical therapy or to intensive medical therapy alone.
Forty percent of participants had an abnormal hsTnT at baseline. Their 5-year rate of the composite primary endpoint of cardiovascular death, MI, or stroke was 27.1%, compared with 12.9% in patients with a baseline hsTnT below 14 ng/mL. After adjusting in a multivariate analysis for various potential confounders – including age, race, and the standard cardiovascular risk factors – the group with an abnormal baseline hsTnT had a 2.09-fold increased risk of a major cardiovascular event.
Early revascularization, regardless of whether by percutaneous coronary intervention or coronary artery bypass graft surgery, provided no benefit no matter what the patient’s baseline hsTnT level. In patients with an hsTnT of 14 ng/L or greater, the 5-year rate of the composite outcome was 26.5% with early revascularization compared with 27.6% with intensive medical therapy. In those with an hsTnT below 14 ng/L, the rate was 11.8% in the early revascularization group and 14% with medical management, a trend favoring prompt revascularization that didn’t achieve statistical significance, according to Dr. Everett.
Of patients with an abnormal hsTnT at baseline, 77% still had an abnormal value at 1 year, regardless of whether they underwent prompt revascularization or intensive medical therapy alone.
Session moderator Dr. Mikhail N. Kosiborod commented that the new BARI 2D substudy highlights a dilemma: “We know that a large population of patients with diabetes, and to some extent those with prediabetes, have elevated hsTnT levels, and we know those patients don’t do well. What we don’t know is what to do about it.”
“What [Dr. Everett’s] study clearly demonstrates is that this does not appear to be driven by epicardial coronary artery disease. If we fix the epicardial CAD, it has absolutely no impact on the outcomes nor on the actual troponin level at follow-up. As far as I can tell, it doesn’t appear to be a glycemic control issue, either. It appears that this is a humoral issue. There are ‘evil humors’ – whatever they are – and we don’t really understand what they are or what to do about it,” said Dr. Kosiborod, professor of medicine at the University of Missouri, Kansas City.
“The truth of the matter is we have no idea what’s causing this low-grade myocardial necrosis, and it’s a hugely important thing,” he continued. “There is absolutely no question that elevated hsTnT, even at very low levels, has a huge impact on subsequent risk of heart failure. We know what the public health effects of heart failure are. And patients with diabetes and heart failure tend to do particularly poorly.”
The BARI 2D trial was funded by the National Institutes of Health. Dr. Everett’s secondary analysis was funded by Roche Diagnostics. He reported receiving research grants from Roche and Novartis.
CHICAGO– Abnormal levels of high-sensitivity cardiac troponin T are present in 40% of type 2 diabetic patients with stable ischemic heart disease, and they do not bode well, according to a new secondary analysis of the BARI 2D study.
In BARI 2D, an abnormal high-sensitivity cardiac troponin T (hsTnT), defined as 14 ng/L or greater, a powerful marker of ongoing myocardial injury, was independently associated with a doubled 5-year risk of the composite endpoint of cardiovascular death, MI, or stroke. Moreover, and discouragingly so, prompt coronary revascularization did nothing to mitigate that risk, Dr. Brendan M. Everett reported at the American Heart Association Scientific Sessions.
Further, early coronary revascularization did not result in a reduction in abnormal hsTnT at 1 year of follow-up, said Dr. Everett, director of the general cardiology inpatient service at Brigham and Women’s Hospital, Boston.
“To better address the risk represented by an abnormal hsTnT, we need to gain an improved understanding of the biology of troponin release in this population,” he observed. “The fact that we saw an overall decrease of about 0.5% in hemoglobin A1c and an LDL reduction of 16 mg/dL at 1 year and still there was no change in hsTnT leaves me scratching my head. The abnormal hsTnT is clearly a marker of badness, but where is it coming from? Can we address it? Or are we just left to look at it and worry about our patients who have an abnormal hsTnT?”
The BARI 2D trial was designed to learn whether patients with type 2 diabetes and stable ischemic heart disease benefit from prompt coronary revascularization plus intensive medical therapy as compared with intensive medical therapy alone. As previously reported (N. Engl. J. Med. 2009;360:2503-15), this proved not to be the case; prompt revascularization conferred no outcome advantage.
The aim of Dr. Everett’s new secondary analysis of BARI 2D was to learn if the hsTnT assay can be used to identify a subgroup of patients with type 2 diabetes and stable ischemic heart disease who might benefit from prompt coronary revascularization. The rationale was that, in patients with acute coronary syndromes, it’s well established that an abnormal hsTnT is associated with poor prognosis, and such patients would benefit from early revascularization.
The secondary analysis included 2,285 type 2 diabetics with stable ischemic heart disease whose physicians first decided whether they were better candidates for percutaneous coronary intervention or CABG surgery. Patients were then randomized to prompt revascularization by the preferred method plus intensive medical therapy or to intensive medical therapy alone.
Forty percent of participants had an abnormal hsTnT at baseline. Their 5-year rate of the composite primary endpoint of cardiovascular death, MI, or stroke was 27.1%, compared with 12.9% in patients with a baseline hsTnT below 14 ng/mL. After adjusting in a multivariate analysis for various potential confounders – including age, race, and the standard cardiovascular risk factors – the group with an abnormal baseline hsTnT had a 2.09-fold increased risk of a major cardiovascular event.
Early revascularization, regardless of whether by percutaneous coronary intervention or coronary artery bypass graft surgery, provided no benefit no matter what the patient’s baseline hsTnT level. In patients with an hsTnT of 14 ng/L or greater, the 5-year rate of the composite outcome was 26.5% with early revascularization compared with 27.6% with intensive medical therapy. In those with an hsTnT below 14 ng/L, the rate was 11.8% in the early revascularization group and 14% with medical management, a trend favoring prompt revascularization that didn’t achieve statistical significance, according to Dr. Everett.
Of patients with an abnormal hsTnT at baseline, 77% still had an abnormal value at 1 year, regardless of whether they underwent prompt revascularization or intensive medical therapy alone.
Session moderator Dr. Mikhail N. Kosiborod commented that the new BARI 2D substudy highlights a dilemma: “We know that a large population of patients with diabetes, and to some extent those with prediabetes, have elevated hsTnT levels, and we know those patients don’t do well. What we don’t know is what to do about it.”
“What [Dr. Everett’s] study clearly demonstrates is that this does not appear to be driven by epicardial coronary artery disease. If we fix the epicardial CAD, it has absolutely no impact on the outcomes nor on the actual troponin level at follow-up. As far as I can tell, it doesn’t appear to be a glycemic control issue, either. It appears that this is a humoral issue. There are ‘evil humors’ – whatever they are – and we don’t really understand what they are or what to do about it,” said Dr. Kosiborod, professor of medicine at the University of Missouri, Kansas City.
“The truth of the matter is we have no idea what’s causing this low-grade myocardial necrosis, and it’s a hugely important thing,” he continued. “There is absolutely no question that elevated hsTnT, even at very low levels, has a huge impact on subsequent risk of heart failure. We know what the public health effects of heart failure are. And patients with diabetes and heart failure tend to do particularly poorly.”
The BARI 2D trial was funded by the National Institutes of Health. Dr. Everett’s secondary analysis was funded by Roche Diagnostics. He reported receiving research grants from Roche and Novartis.
CHICAGO– Abnormal levels of high-sensitivity cardiac troponin T are present in 40% of type 2 diabetic patients with stable ischemic heart disease, and they do not bode well, according to a new secondary analysis of the BARI 2D study.
In BARI 2D, an abnormal high-sensitivity cardiac troponin T (hsTnT), defined as 14 ng/L or greater, a powerful marker of ongoing myocardial injury, was independently associated with a doubled 5-year risk of the composite endpoint of cardiovascular death, MI, or stroke. Moreover, and discouragingly so, prompt coronary revascularization did nothing to mitigate that risk, Dr. Brendan M. Everett reported at the American Heart Association Scientific Sessions.
Further, early coronary revascularization did not result in a reduction in abnormal hsTnT at 1 year of follow-up, said Dr. Everett, director of the general cardiology inpatient service at Brigham and Women’s Hospital, Boston.
“To better address the risk represented by an abnormal hsTnT, we need to gain an improved understanding of the biology of troponin release in this population,” he observed. “The fact that we saw an overall decrease of about 0.5% in hemoglobin A1c and an LDL reduction of 16 mg/dL at 1 year and still there was no change in hsTnT leaves me scratching my head. The abnormal hsTnT is clearly a marker of badness, but where is it coming from? Can we address it? Or are we just left to look at it and worry about our patients who have an abnormal hsTnT?”
The BARI 2D trial was designed to learn whether patients with type 2 diabetes and stable ischemic heart disease benefit from prompt coronary revascularization plus intensive medical therapy as compared with intensive medical therapy alone. As previously reported (N. Engl. J. Med. 2009;360:2503-15), this proved not to be the case; prompt revascularization conferred no outcome advantage.
The aim of Dr. Everett’s new secondary analysis of BARI 2D was to learn if the hsTnT assay can be used to identify a subgroup of patients with type 2 diabetes and stable ischemic heart disease who might benefit from prompt coronary revascularization. The rationale was that, in patients with acute coronary syndromes, it’s well established that an abnormal hsTnT is associated with poor prognosis, and such patients would benefit from early revascularization.
The secondary analysis included 2,285 type 2 diabetics with stable ischemic heart disease whose physicians first decided whether they were better candidates for percutaneous coronary intervention or CABG surgery. Patients were then randomized to prompt revascularization by the preferred method plus intensive medical therapy or to intensive medical therapy alone.
Forty percent of participants had an abnormal hsTnT at baseline. Their 5-year rate of the composite primary endpoint of cardiovascular death, MI, or stroke was 27.1%, compared with 12.9% in patients with a baseline hsTnT below 14 ng/mL. After adjusting in a multivariate analysis for various potential confounders – including age, race, and the standard cardiovascular risk factors – the group with an abnormal baseline hsTnT had a 2.09-fold increased risk of a major cardiovascular event.
Early revascularization, regardless of whether by percutaneous coronary intervention or coronary artery bypass graft surgery, provided no benefit no matter what the patient’s baseline hsTnT level. In patients with an hsTnT of 14 ng/L or greater, the 5-year rate of the composite outcome was 26.5% with early revascularization compared with 27.6% with intensive medical therapy. In those with an hsTnT below 14 ng/L, the rate was 11.8% in the early revascularization group and 14% with medical management, a trend favoring prompt revascularization that didn’t achieve statistical significance, according to Dr. Everett.
Of patients with an abnormal hsTnT at baseline, 77% still had an abnormal value at 1 year, regardless of whether they underwent prompt revascularization or intensive medical therapy alone.
Session moderator Dr. Mikhail N. Kosiborod commented that the new BARI 2D substudy highlights a dilemma: “We know that a large population of patients with diabetes, and to some extent those with prediabetes, have elevated hsTnT levels, and we know those patients don’t do well. What we don’t know is what to do about it.”
“What [Dr. Everett’s] study clearly demonstrates is that this does not appear to be driven by epicardial coronary artery disease. If we fix the epicardial CAD, it has absolutely no impact on the outcomes nor on the actual troponin level at follow-up. As far as I can tell, it doesn’t appear to be a glycemic control issue, either. It appears that this is a humoral issue. There are ‘evil humors’ – whatever they are – and we don’t really understand what they are or what to do about it,” said Dr. Kosiborod, professor of medicine at the University of Missouri, Kansas City.
“The truth of the matter is we have no idea what’s causing this low-grade myocardial necrosis, and it’s a hugely important thing,” he continued. “There is absolutely no question that elevated hsTnT, even at very low levels, has a huge impact on subsequent risk of heart failure. We know what the public health effects of heart failure are. And patients with diabetes and heart failure tend to do particularly poorly.”
The BARI 2D trial was funded by the National Institutes of Health. Dr. Everett’s secondary analysis was funded by Roche Diagnostics. He reported receiving research grants from Roche and Novartis.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Forty percent of patients with type 2 diabetes and stable ischemic heart disease are walking around with abnormal levels of hsTnT, placing them at substantial risk of a major cardiovascular event within 5 years.
Major finding: Prompt coronary revascularization does not reduce this risk, nor does it reduce the elevated troponin T level.
Data source: A secondary analysis of the randomized, prospective BARI 2D study involving 2,285 participants with type 2 diabetes and stable ischemic heart disease.
Disclosures: The BARI 2D study was funded by the National Institutes of Health. This new secondary analysis was funded by a research grant from Roche Diagnostics.
Insulin glargine shows cardiac safety in ORIGIN-ECHO
CHICAGO – Insulin glargine showed no effects on left ventricular mass or function during 3 years of follow-up in dysglycemic patients at high cardiovascular risk in the ORIGIN echocardiographic substudy.
This echocardiographic study of the ORIGIN (Outcome Reduction With an Initial Glargine Intervention) trial, the largest reported study of the effects of exogenous insulin on left ventricular mass and LV systolic and diastolic function, provides reassuring new evidence that insulin glargine is safe from a cardiac standpoint, Dr. Michelle Haroun said at the American Heart Association scientific sessions.
“The key here is that we didn’t see any signal whatsoever to suggest that insulin is putting patients at increased risk. We think that this finding is important. While you need to follow patients for a very long time to detect changes in clinical heart failure outcomes, we think we’d be able to detect subtle changes in endpoints like LV mass over a 3-year period if insulin was of harm to patients,” said Dr. Haroun of the Population Health Research Institute at McMaster University in Hamilton, Ont.
ORIGIN-ECHO involved 564 dysglycemic patients at high cardiovascular risk who were randomized to insulin glargine (Lantus) or standard therapy. All had echocardiograms at baseline and after 3 years of therapy. Participants had to have impaired fasting blood glucose, impaired glucose tolerance, or early type 2 diabetes managed with no more than one oral antiglycemic drug at baseline. This was a group at high cardiovascular risk: 32% had a prior MI, 84% had a history of hypertension, obesity was common, and the average age was 64. However, none of the participants had heart failure at baseline.
The study was undertaken because some of the medications used to treat hyperglycemia are associated with increased risk of heart failure. Regulatory agencies, physicians, and patients want to see evidence of cardiovascular safety, and until ORIGIN-ECHO, the effects of exogenous insulin on LV mass and function hadn’t been well studied.
Baseline LV mass and function values were within normal range and did not change significantly over 3 years of follow-up in either treatment arm. For example, left ventricular mass/height averaged 116 g/m at baseline and 115 g/m after 3 years on insulin glargine, and was comparable at 113 and 114 g/m, respectively, with standard therapy. This was an unexpected finding, according to Dr. Haroun.
“We thought patients with diabetes on standard therapy were going to develop left ventricular hypertrophy over a 3-year follow-up period, and they didn’t. That came as a bit of a surprise to us. We expected to see a lower rate of LVH in the patients on insulin glargine. This patient population was relatively early in their course of diabetes, and we believe our findings suggest that adequate management of cardiovascular risk factors – especially hypertension– and the use of cardioprotective drugs in this population may prevent or delay abnormalities in LV structure and function,” she said.
The primary outcomes of the full ORIGIN study involving more than 12,000 patients have previously been published (N. Engl. J. Med. 2012; 367:319-28). ORIGIN was sponsored by Sanofi. Dr. Haroun reported having no financial conflicts.
CHICAGO – Insulin glargine showed no effects on left ventricular mass or function during 3 years of follow-up in dysglycemic patients at high cardiovascular risk in the ORIGIN echocardiographic substudy.
This echocardiographic study of the ORIGIN (Outcome Reduction With an Initial Glargine Intervention) trial, the largest reported study of the effects of exogenous insulin on left ventricular mass and LV systolic and diastolic function, provides reassuring new evidence that insulin glargine is safe from a cardiac standpoint, Dr. Michelle Haroun said at the American Heart Association scientific sessions.
“The key here is that we didn’t see any signal whatsoever to suggest that insulin is putting patients at increased risk. We think that this finding is important. While you need to follow patients for a very long time to detect changes in clinical heart failure outcomes, we think we’d be able to detect subtle changes in endpoints like LV mass over a 3-year period if insulin was of harm to patients,” said Dr. Haroun of the Population Health Research Institute at McMaster University in Hamilton, Ont.
ORIGIN-ECHO involved 564 dysglycemic patients at high cardiovascular risk who were randomized to insulin glargine (Lantus) or standard therapy. All had echocardiograms at baseline and after 3 years of therapy. Participants had to have impaired fasting blood glucose, impaired glucose tolerance, or early type 2 diabetes managed with no more than one oral antiglycemic drug at baseline. This was a group at high cardiovascular risk: 32% had a prior MI, 84% had a history of hypertension, obesity was common, and the average age was 64. However, none of the participants had heart failure at baseline.
The study was undertaken because some of the medications used to treat hyperglycemia are associated with increased risk of heart failure. Regulatory agencies, physicians, and patients want to see evidence of cardiovascular safety, and until ORIGIN-ECHO, the effects of exogenous insulin on LV mass and function hadn’t been well studied.
Baseline LV mass and function values were within normal range and did not change significantly over 3 years of follow-up in either treatment arm. For example, left ventricular mass/height averaged 116 g/m at baseline and 115 g/m after 3 years on insulin glargine, and was comparable at 113 and 114 g/m, respectively, with standard therapy. This was an unexpected finding, according to Dr. Haroun.
“We thought patients with diabetes on standard therapy were going to develop left ventricular hypertrophy over a 3-year follow-up period, and they didn’t. That came as a bit of a surprise to us. We expected to see a lower rate of LVH in the patients on insulin glargine. This patient population was relatively early in their course of diabetes, and we believe our findings suggest that adequate management of cardiovascular risk factors – especially hypertension– and the use of cardioprotective drugs in this population may prevent or delay abnormalities in LV structure and function,” she said.
The primary outcomes of the full ORIGIN study involving more than 12,000 patients have previously been published (N. Engl. J. Med. 2012; 367:319-28). ORIGIN was sponsored by Sanofi. Dr. Haroun reported having no financial conflicts.
CHICAGO – Insulin glargine showed no effects on left ventricular mass or function during 3 years of follow-up in dysglycemic patients at high cardiovascular risk in the ORIGIN echocardiographic substudy.
This echocardiographic study of the ORIGIN (Outcome Reduction With an Initial Glargine Intervention) trial, the largest reported study of the effects of exogenous insulin on left ventricular mass and LV systolic and diastolic function, provides reassuring new evidence that insulin glargine is safe from a cardiac standpoint, Dr. Michelle Haroun said at the American Heart Association scientific sessions.
“The key here is that we didn’t see any signal whatsoever to suggest that insulin is putting patients at increased risk. We think that this finding is important. While you need to follow patients for a very long time to detect changes in clinical heart failure outcomes, we think we’d be able to detect subtle changes in endpoints like LV mass over a 3-year period if insulin was of harm to patients,” said Dr. Haroun of the Population Health Research Institute at McMaster University in Hamilton, Ont.
ORIGIN-ECHO involved 564 dysglycemic patients at high cardiovascular risk who were randomized to insulin glargine (Lantus) or standard therapy. All had echocardiograms at baseline and after 3 years of therapy. Participants had to have impaired fasting blood glucose, impaired glucose tolerance, or early type 2 diabetes managed with no more than one oral antiglycemic drug at baseline. This was a group at high cardiovascular risk: 32% had a prior MI, 84% had a history of hypertension, obesity was common, and the average age was 64. However, none of the participants had heart failure at baseline.
The study was undertaken because some of the medications used to treat hyperglycemia are associated with increased risk of heart failure. Regulatory agencies, physicians, and patients want to see evidence of cardiovascular safety, and until ORIGIN-ECHO, the effects of exogenous insulin on LV mass and function hadn’t been well studied.
Baseline LV mass and function values were within normal range and did not change significantly over 3 years of follow-up in either treatment arm. For example, left ventricular mass/height averaged 116 g/m at baseline and 115 g/m after 3 years on insulin glargine, and was comparable at 113 and 114 g/m, respectively, with standard therapy. This was an unexpected finding, according to Dr. Haroun.
“We thought patients with diabetes on standard therapy were going to develop left ventricular hypertrophy over a 3-year follow-up period, and they didn’t. That came as a bit of a surprise to us. We expected to see a lower rate of LVH in the patients on insulin glargine. This patient population was relatively early in their course of diabetes, and we believe our findings suggest that adequate management of cardiovascular risk factors – especially hypertension– and the use of cardioprotective drugs in this population may prevent or delay abnormalities in LV structure and function,” she said.
The primary outcomes of the full ORIGIN study involving more than 12,000 patients have previously been published (N. Engl. J. Med. 2012; 367:319-28). ORIGIN was sponsored by Sanofi. Dr. Haroun reported having no financial conflicts.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: The cardiac safety of insulin glargine in dysglycemic patients at high cardiovascular risk has received strong support from a 3-year echocardiographic study.
Major finding: Left ventricular mass over height was 116 g/m at baseline and 115 g/m after 3 years on insulin glargine.
Data source: The ORIGIN-ECHO substudy included 564 dysglycemic patients at high cardiovascular risk who were randomized to 3 years of insulin glargine or standard therapy.
Disclosures: The ORIGIN trial was sponsored by Sanofi. The presenter reported having no financial conflicts.
Open Wide: New Insights Into Burning Mouth Syndrome
AMSTERDAM – The incidence of burning mouth syndrome is considerably lower than previously reported, according to findings from the first population-based study of the disorder.
The age- and gender-adjusted incidence of burning mouth syndrome during 2000-2010 in Olmsted County, Minn., was 11.4 cases per 100,000 person-years, John J. Kohorst reported at the annual congress of the European Academy of Dermatology and Venereology.
Prior epidemiologic studies have reported prevalence rates all over the map, from 1% to 40%, probably in large part because they used a variety of definitions for burning mouth syndrome. The new population-based study focused on disease incidence rather than prevalence utilized a standardized definition for the diagnosis: subjective burning pain of the oral mucosa in the absence of physical findings or an identifiable extraneous cause. All cases had to be diagnosed by a physician participating in the Rochester (Minn.) Epidemiology Project, explained Mr. Kohorst, a medical student at the Mayo Medical School in Rochester.
Because burning mouth syndrome is a diagnosis of exclusion, typically a year or more goes by and three different physicians are consulted before the correct diagnosis is made.
The pathogenesis of burning mouth syndrome remains poorly understood. It is predominantly a disorder affecting postmenopausal women. In the Minnesota study, for example, women accounted for 84% of the 169 individuals diagnosed with new-onset burning mouth syndrome during the study period. The incidence among women was 18.8 cases per 100,000 person-years, compared with 3.7 per 100,000 person-years in men. The incidence climbed sharply after age 50 in both men and women, achieving a peak rate of 70.3 cases per 100,000 person-years among women age 70-79.
Some prior studies have reported a strong association between burning mouth syndrome and smoking that wasn’t evident in the Olmsted County population-based study. Only 11% of the Minnesota patients with new-onset burning mouth syndrome were current smokers and 63% were never-smokers, rates mirroring those of the county’s general population, according to Mr. Kohorst.
Eighty-eight percent of patients reported bilateral as opposed to unilateral mouth pain. The tongue was the sole involved site in 53% of cases. Forty-two percent of patients rated the pain as mild, while 13% characterized it as severe based upon a score of 8 or more on a 10-point scale. Most affected patients described the burning pain as a continuous feature throughout their day.
The next step in this research project will be to investigate the potential role of concurrent disease states and medication use in the incidence and prevalence of burning mouth syndrome in the county’s population, Mr. Kohorst said.
He reported having no financial conflicts regarding this study.
AMSTERDAM – The incidence of burning mouth syndrome is considerably lower than previously reported, according to findings from the first population-based study of the disorder.
The age- and gender-adjusted incidence of burning mouth syndrome during 2000-2010 in Olmsted County, Minn., was 11.4 cases per 100,000 person-years, John J. Kohorst reported at the annual congress of the European Academy of Dermatology and Venereology.
Prior epidemiologic studies have reported prevalence rates all over the map, from 1% to 40%, probably in large part because they used a variety of definitions for burning mouth syndrome. The new population-based study focused on disease incidence rather than prevalence utilized a standardized definition for the diagnosis: subjective burning pain of the oral mucosa in the absence of physical findings or an identifiable extraneous cause. All cases had to be diagnosed by a physician participating in the Rochester (Minn.) Epidemiology Project, explained Mr. Kohorst, a medical student at the Mayo Medical School in Rochester.
Because burning mouth syndrome is a diagnosis of exclusion, typically a year or more goes by and three different physicians are consulted before the correct diagnosis is made.
The pathogenesis of burning mouth syndrome remains poorly understood. It is predominantly a disorder affecting postmenopausal women. In the Minnesota study, for example, women accounted for 84% of the 169 individuals diagnosed with new-onset burning mouth syndrome during the study period. The incidence among women was 18.8 cases per 100,000 person-years, compared with 3.7 per 100,000 person-years in men. The incidence climbed sharply after age 50 in both men and women, achieving a peak rate of 70.3 cases per 100,000 person-years among women age 70-79.
Some prior studies have reported a strong association between burning mouth syndrome and smoking that wasn’t evident in the Olmsted County population-based study. Only 11% of the Minnesota patients with new-onset burning mouth syndrome were current smokers and 63% were never-smokers, rates mirroring those of the county’s general population, according to Mr. Kohorst.
Eighty-eight percent of patients reported bilateral as opposed to unilateral mouth pain. The tongue was the sole involved site in 53% of cases. Forty-two percent of patients rated the pain as mild, while 13% characterized it as severe based upon a score of 8 or more on a 10-point scale. Most affected patients described the burning pain as a continuous feature throughout their day.
The next step in this research project will be to investigate the potential role of concurrent disease states and medication use in the incidence and prevalence of burning mouth syndrome in the county’s population, Mr. Kohorst said.
He reported having no financial conflicts regarding this study.
AMSTERDAM – The incidence of burning mouth syndrome is considerably lower than previously reported, according to findings from the first population-based study of the disorder.
The age- and gender-adjusted incidence of burning mouth syndrome during 2000-2010 in Olmsted County, Minn., was 11.4 cases per 100,000 person-years, John J. Kohorst reported at the annual congress of the European Academy of Dermatology and Venereology.
Prior epidemiologic studies have reported prevalence rates all over the map, from 1% to 40%, probably in large part because they used a variety of definitions for burning mouth syndrome. The new population-based study focused on disease incidence rather than prevalence utilized a standardized definition for the diagnosis: subjective burning pain of the oral mucosa in the absence of physical findings or an identifiable extraneous cause. All cases had to be diagnosed by a physician participating in the Rochester (Minn.) Epidemiology Project, explained Mr. Kohorst, a medical student at the Mayo Medical School in Rochester.
Because burning mouth syndrome is a diagnosis of exclusion, typically a year or more goes by and three different physicians are consulted before the correct diagnosis is made.
The pathogenesis of burning mouth syndrome remains poorly understood. It is predominantly a disorder affecting postmenopausal women. In the Minnesota study, for example, women accounted for 84% of the 169 individuals diagnosed with new-onset burning mouth syndrome during the study period. The incidence among women was 18.8 cases per 100,000 person-years, compared with 3.7 per 100,000 person-years in men. The incidence climbed sharply after age 50 in both men and women, achieving a peak rate of 70.3 cases per 100,000 person-years among women age 70-79.
Some prior studies have reported a strong association between burning mouth syndrome and smoking that wasn’t evident in the Olmsted County population-based study. Only 11% of the Minnesota patients with new-onset burning mouth syndrome were current smokers and 63% were never-smokers, rates mirroring those of the county’s general population, according to Mr. Kohorst.
Eighty-eight percent of patients reported bilateral as opposed to unilateral mouth pain. The tongue was the sole involved site in 53% of cases. Forty-two percent of patients rated the pain as mild, while 13% characterized it as severe based upon a score of 8 or more on a 10-point scale. Most affected patients described the burning pain as a continuous feature throughout their day.
The next step in this research project will be to investigate the potential role of concurrent disease states and medication use in the incidence and prevalence of burning mouth syndrome in the county’s population, Mr. Kohorst said.
He reported having no financial conflicts regarding this study.
AT THE EADV CONGRESS
Open wide: new insights into burning mouth syndrome
AMSTERDAM – The incidence of burning mouth syndrome is considerably lower than previously reported, according to findings from the first population-based study of the disorder.
The age- and gender-adjusted incidence of burning mouth syndrome during 2000-2010 in Olmsted County, Minn., was 11.4 cases per 100,000 person-years, John J. Kohorst reported at the annual congress of the European Academy of Dermatology and Venereology.
Prior epidemiologic studies have reported prevalence rates all over the map, from 1% to 40%, probably in large part because they used a variety of definitions for burning mouth syndrome. The new population-based study focused on disease incidence rather than prevalence utilized a standardized definition for the diagnosis: subjective burning pain of the oral mucosa in the absence of physical findings or an identifiable extraneous cause. All cases had to be diagnosed by a physician participating in the Rochester (Minn.) Epidemiology Project, explained Mr. Kohorst, a medical student at the Mayo Medical School in Rochester.
Because burning mouth syndrome is a diagnosis of exclusion, typically a year or more goes by and three different physicians are consulted before the correct diagnosis is made.
The pathogenesis of burning mouth syndrome remains poorly understood. It is predominantly a disorder affecting postmenopausal women. In the Minnesota study, for example, women accounted for 84% of the 169 individuals diagnosed with new-onset burning mouth syndrome during the study period. The incidence among women was 18.8 cases per 100,000 person-years, compared with 3.7 per 100,000 person-years in men. The incidence climbed sharply after age 50 in both men and women, achieving a peak rate of 70.3 cases per 100,000 person-years among women age 70-79.
Some prior studies have reported a strong association between burning mouth syndrome and smoking that wasn’t evident in the Olmsted County population-based study. Only 11% of the Minnesota patients with new-onset burning mouth syndrome were current smokers and 63% were never-smokers, rates mirroring those of the county’s general population, according to Mr. Kohorst.
Eighty-eight percent of patients reported bilateral as opposed to unilateral mouth pain. The tongue was the sole involved site in 53% of cases. Forty-two percent of patients rated the pain as mild, while 13% characterized it as severe based upon a score of 8 or more on a 10-point scale. Most affected patients described the burning pain as a continuous feature throughout their day.
The next step in this research project will be to investigate the potential role of concurrent disease states and medication use in the incidence and prevalence of burning mouth syndrome in the county’s population, Mr. Kohorst said.
He reported having no financial conflicts regarding this study.
AMSTERDAM – The incidence of burning mouth syndrome is considerably lower than previously reported, according to findings from the first population-based study of the disorder.
The age- and gender-adjusted incidence of burning mouth syndrome during 2000-2010 in Olmsted County, Minn., was 11.4 cases per 100,000 person-years, John J. Kohorst reported at the annual congress of the European Academy of Dermatology and Venereology.
Prior epidemiologic studies have reported prevalence rates all over the map, from 1% to 40%, probably in large part because they used a variety of definitions for burning mouth syndrome. The new population-based study focused on disease incidence rather than prevalence utilized a standardized definition for the diagnosis: subjective burning pain of the oral mucosa in the absence of physical findings or an identifiable extraneous cause. All cases had to be diagnosed by a physician participating in the Rochester (Minn.) Epidemiology Project, explained Mr. Kohorst, a medical student at the Mayo Medical School in Rochester.
Because burning mouth syndrome is a diagnosis of exclusion, typically a year or more goes by and three different physicians are consulted before the correct diagnosis is made.
The pathogenesis of burning mouth syndrome remains poorly understood. It is predominantly a disorder affecting postmenopausal women. In the Minnesota study, for example, women accounted for 84% of the 169 individuals diagnosed with new-onset burning mouth syndrome during the study period. The incidence among women was 18.8 cases per 100,000 person-years, compared with 3.7 per 100,000 person-years in men. The incidence climbed sharply after age 50 in both men and women, achieving a peak rate of 70.3 cases per 100,000 person-years among women age 70-79.
Some prior studies have reported a strong association between burning mouth syndrome and smoking that wasn’t evident in the Olmsted County population-based study. Only 11% of the Minnesota patients with new-onset burning mouth syndrome were current smokers and 63% were never-smokers, rates mirroring those of the county’s general population, according to Mr. Kohorst.
Eighty-eight percent of patients reported bilateral as opposed to unilateral mouth pain. The tongue was the sole involved site in 53% of cases. Forty-two percent of patients rated the pain as mild, while 13% characterized it as severe based upon a score of 8 or more on a 10-point scale. Most affected patients described the burning pain as a continuous feature throughout their day.
The next step in this research project will be to investigate the potential role of concurrent disease states and medication use in the incidence and prevalence of burning mouth syndrome in the county’s population, Mr. Kohorst said.
He reported having no financial conflicts regarding this study.
AMSTERDAM – The incidence of burning mouth syndrome is considerably lower than previously reported, according to findings from the first population-based study of the disorder.
The age- and gender-adjusted incidence of burning mouth syndrome during 2000-2010 in Olmsted County, Minn., was 11.4 cases per 100,000 person-years, John J. Kohorst reported at the annual congress of the European Academy of Dermatology and Venereology.
Prior epidemiologic studies have reported prevalence rates all over the map, from 1% to 40%, probably in large part because they used a variety of definitions for burning mouth syndrome. The new population-based study focused on disease incidence rather than prevalence utilized a standardized definition for the diagnosis: subjective burning pain of the oral mucosa in the absence of physical findings or an identifiable extraneous cause. All cases had to be diagnosed by a physician participating in the Rochester (Minn.) Epidemiology Project, explained Mr. Kohorst, a medical student at the Mayo Medical School in Rochester.
Because burning mouth syndrome is a diagnosis of exclusion, typically a year or more goes by and three different physicians are consulted before the correct diagnosis is made.
The pathogenesis of burning mouth syndrome remains poorly understood. It is predominantly a disorder affecting postmenopausal women. In the Minnesota study, for example, women accounted for 84% of the 169 individuals diagnosed with new-onset burning mouth syndrome during the study period. The incidence among women was 18.8 cases per 100,000 person-years, compared with 3.7 per 100,000 person-years in men. The incidence climbed sharply after age 50 in both men and women, achieving a peak rate of 70.3 cases per 100,000 person-years among women age 70-79.
Some prior studies have reported a strong association between burning mouth syndrome and smoking that wasn’t evident in the Olmsted County population-based study. Only 11% of the Minnesota patients with new-onset burning mouth syndrome were current smokers and 63% were never-smokers, rates mirroring those of the county’s general population, according to Mr. Kohorst.
Eighty-eight percent of patients reported bilateral as opposed to unilateral mouth pain. The tongue was the sole involved site in 53% of cases. Forty-two percent of patients rated the pain as mild, while 13% characterized it as severe based upon a score of 8 or more on a 10-point scale. Most affected patients described the burning pain as a continuous feature throughout their day.
The next step in this research project will be to investigate the potential role of concurrent disease states and medication use in the incidence and prevalence of burning mouth syndrome in the county’s population, Mr. Kohorst said.
He reported having no financial conflicts regarding this study.
AT THE EADV CONGRESS
Key clinical point: Burning mouth syndrome occurs a lot less frequently than previously understood.
Major finding: The incidence of newly diagnosed burning mouth syndrome using standardized criteria in Olmsted County, Minn., during 2000-2010 was 18.8 cases per 100,000 person-years among women and 3.7 in men.
Data source: This first-ever population-based study of burning mouth syndrome was carried out through the Rochester Epidemiology Project.
Disclosures: The Rochester Epidemiology Project is supported by the National Institutes of Health and the Mayo Clinic. Mr. Kohorst reported having no financial conflicts.
Harm-reduction approach to alcoholism gains growing credibility
BERLIN – The harm-reduction concept as an alternative to abstinence as a treatment strategy for alcohol dependence has taken on new legitimacy as a result of the recent approval of nalmefene by the European Medicines Agency.
Nalmefene, an opioid receptor antagonist, received marketing approval across Europe for use specifically in a novel as-needed dosing regimen that is under the patient’s control. One 18-mg tablet is to be taken on days when a patient anticipates a risk of drinking, or if the patient has already started drinking, then as soon as possible.
The indication was granted by European regulators on the strength of three European phase III randomized trials that showed that heavy drinkers who used nalmefene in this way reduced their alcohol consumption to a more normal level. Thus, marketing approval was an implicit endorsement of the harm-reduction strategy.
“I have been praying for this for years and years. I have been strictly against the concept of complete abstinence, because the core of the disease of addiction is relapse. It is just a natural thing that one relapses,” Rainer Spanagel, Ph.D., said at the annual congress of the European College of Neuropsychopharmacology.
“It has been a major mistake to say you are only successful in the field of addiction treatment if there is abstinence. This is an almost unreachable goal. This goal, set out to achieve for decades now, has been almost impossible for most patients to achieve,” added Dr. Spanagel, director of the Institute of Psychopharmacology at the University of Heidelberg (Germany).
Dr. Robert M. Swift noted that most treatment programs in the United States still promote abstinence as the only acceptable treatment outcome. It’s a concept that dates back to the 1800s and was heavily promoted by Alcoholics Anonymous beginning in the early 1900s, a period before there was any viable treatment for alcoholism.
Today, a variety of treatments have proved effective, both psychosocial as well as pharmacologic, but people aren’t receiving them. A large epidemiologic study conducted by the National Institute on Alcohol Abuse and Alcoholism estimated that of 7.9 million Americans who are alcohol dependent, only 2.4 million have ever been diagnosed as such, 1.5 million have ever gotten any treatment for their disorder, and a mere 139,000 have ever received pharmacotherapy.
“There’s this amazing treatment gap,” commented Dr. Swift, professor of psychiatry and associate director of the Center for Alcohol and Addiction Studies at Brown University in Providence, R.I.
The main reason for this huge treatment gap was revealed in a 2012 survey conducted by the U.S. Substance Abuse and Mental Health Services Administration: 49.5% of participants who had not sought treatment for an alcohol problem within the past year even though they needed it and recognized their need for it gave as their reason that they were just not ready to stop drinking completely. This is a group where the harm-reduction strategy makes a great deal of sense, the psychiatrist said.
Harm reduction is based upon evidence that the risk of mortality because of alcohol-related causes rises exponentially as daily consumption climbs above the threshold of hazardous drinking, which has been defined by U.S. public health officials as five drinks per day or 15 per week in men and four per day or eight per week in women. The corollary is that reducing heavy drinking provides exponential health benefits. Investigators at Imperial College, London, have estimated that reducing alcohol intake from 100 g per day to 50 g per day provides an eight-fold reduction in health harms (J. Psychopharmacol. 2014;28:3-7).
“You get a lot of bang for your buck by reducing the amount of alcohol you consume,” Dr. Swift said. “The evidence really is out there that reducing drinking is an effective harm reduction strategy.”
Dr. Wim van den Brink, who led the SENSE trial, a 1-year, phase III, randomized, placebo-controlled study with positive safety and efficacy outcomes for nalmefene as-needed (J. Psychopharmacol. 2014;28:733-44), said one of the strengths of this treatment strategy is that it gives patients responsibility for their drinking and allows them to set their own treatment goals. That enhances the likelihood of successful outcomes.
The harm-reduction approach with as-needed nalmefene also is a way to bring into treatment some of the 50% of problem drinkers who don’t want to stop drinking entirely, added Dr. van den Brink, professor of psychiatry and addiction at the University of Amsterdam and director of the Amsterdam Institute for Addiction Research.
A spokesperson for Lundbeck, which sponsored the SENSE and 6-month ESENSE 1 and ESENSE 2 trials, said the company would not seek marketing approval for nalmefene in the United States because the drug’s remaining duration of patent protection makes it commercially nonviable.
Nalmefene and naltrexone, the latter of which is available in the United States, are both mu opioid receptor antagonists that also affect the delta opioid receptor. However, nalmefene also is a partial agonist at the kappa opioid receptor.
Dr. Swift said both drugs have been shown in preclinical and clinical studies to interrupt multiple biobehavioral mechanisms responsible for initiating and maintaining alcohol dependence. They reduce alcohol craving, block the motivation to drink to relieve stress and anxiety, and might improve impulsivity.
“Naltrexone has been shown not only to affect the rewards of alcohol consumption, it also seems to have direct cognitive and attentional effects in the orbitofrontal cortex. It reduces preoccupation with alcohol and improves attention to non–alcohol related stimuli,” he said. “I think that’s a really important finding and provides a new understanding of how opioid antagonists work.”
The psychiatrist noted that a recent meta-analysis concluded that opioid antagonists are better for reducing heavy drinking than for increasing abstinence (Addiction 2013;108:275-93).
Dr. Swift reported receiving honoraria from Lundbeck and serving as an adviser or consultant to D&B Pharma and CT San Remo. Dr. van den Brink is on the advisory boards of Lundbeck and more than a half-dozen other pharmaceutical companies.
Alcohol use disorders are clinical diagnoses based on a loss of control over alcohol consumption despite adverse consequences. Remission occurs when an individual exerts control over his or her drinking behavior. Abstinence is the safest option, but, paraphrasing Voltaire, the perfect should not be the enemy of the good.
It has long been known that people with a diagnosis of alcohol dependence can moderate their drinking, and that such reductions in consumption reduce end-organ damage and other adverse health consequences. So, it makes complete sense that the opioid antagonists naltrexone or nalmefene that reduce alcohol’s euphoric reward and help alcoholic patients regain control over their drinking should be welcome additions to the pharmacopoeia.
Medicine has long accepted disease-modifying therapies as organ- and lifesaving for other disorders – gold salts and methotrexate for rheumatoid arthritis come to mind. Such remittive agents reduce disease activity without an insistence on complete, total, and lasting cure.
These medications are called effective treatment, and are not burdened by the apologist moniker of “harm reduction.” Effective remittive therapies for alcohol dependence such as naltrexone and nalmefene should not be viewed any differently.
Peter D. Friedmann, M.D., M.P.H., is professor of medicine and professor of health services, policy, and practice at Brown University, Providence, R.I. He has received research support from Alkermes and a speaker’s honorarium from Orexo.
Alcohol use disorders are clinical diagnoses based on a loss of control over alcohol consumption despite adverse consequences. Remission occurs when an individual exerts control over his or her drinking behavior. Abstinence is the safest option, but, paraphrasing Voltaire, the perfect should not be the enemy of the good.
It has long been known that people with a diagnosis of alcohol dependence can moderate their drinking, and that such reductions in consumption reduce end-organ damage and other adverse health consequences. So, it makes complete sense that the opioid antagonists naltrexone or nalmefene that reduce alcohol’s euphoric reward and help alcoholic patients regain control over their drinking should be welcome additions to the pharmacopoeia.
Medicine has long accepted disease-modifying therapies as organ- and lifesaving for other disorders – gold salts and methotrexate for rheumatoid arthritis come to mind. Such remittive agents reduce disease activity without an insistence on complete, total, and lasting cure.
These medications are called effective treatment, and are not burdened by the apologist moniker of “harm reduction.” Effective remittive therapies for alcohol dependence such as naltrexone and nalmefene should not be viewed any differently.
Peter D. Friedmann, M.D., M.P.H., is professor of medicine and professor of health services, policy, and practice at Brown University, Providence, R.I. He has received research support from Alkermes and a speaker’s honorarium from Orexo.
Alcohol use disorders are clinical diagnoses based on a loss of control over alcohol consumption despite adverse consequences. Remission occurs when an individual exerts control over his or her drinking behavior. Abstinence is the safest option, but, paraphrasing Voltaire, the perfect should not be the enemy of the good.
It has long been known that people with a diagnosis of alcohol dependence can moderate their drinking, and that such reductions in consumption reduce end-organ damage and other adverse health consequences. So, it makes complete sense that the opioid antagonists naltrexone or nalmefene that reduce alcohol’s euphoric reward and help alcoholic patients regain control over their drinking should be welcome additions to the pharmacopoeia.
Medicine has long accepted disease-modifying therapies as organ- and lifesaving for other disorders – gold salts and methotrexate for rheumatoid arthritis come to mind. Such remittive agents reduce disease activity without an insistence on complete, total, and lasting cure.
These medications are called effective treatment, and are not burdened by the apologist moniker of “harm reduction.” Effective remittive therapies for alcohol dependence such as naltrexone and nalmefene should not be viewed any differently.
Peter D. Friedmann, M.D., M.P.H., is professor of medicine and professor of health services, policy, and practice at Brown University, Providence, R.I. He has received research support from Alkermes and a speaker’s honorarium from Orexo.
BERLIN – The harm-reduction concept as an alternative to abstinence as a treatment strategy for alcohol dependence has taken on new legitimacy as a result of the recent approval of nalmefene by the European Medicines Agency.
Nalmefene, an opioid receptor antagonist, received marketing approval across Europe for use specifically in a novel as-needed dosing regimen that is under the patient’s control. One 18-mg tablet is to be taken on days when a patient anticipates a risk of drinking, or if the patient has already started drinking, then as soon as possible.
The indication was granted by European regulators on the strength of three European phase III randomized trials that showed that heavy drinkers who used nalmefene in this way reduced their alcohol consumption to a more normal level. Thus, marketing approval was an implicit endorsement of the harm-reduction strategy.
“I have been praying for this for years and years. I have been strictly against the concept of complete abstinence, because the core of the disease of addiction is relapse. It is just a natural thing that one relapses,” Rainer Spanagel, Ph.D., said at the annual congress of the European College of Neuropsychopharmacology.
“It has been a major mistake to say you are only successful in the field of addiction treatment if there is abstinence. This is an almost unreachable goal. This goal, set out to achieve for decades now, has been almost impossible for most patients to achieve,” added Dr. Spanagel, director of the Institute of Psychopharmacology at the University of Heidelberg (Germany).
Dr. Robert M. Swift noted that most treatment programs in the United States still promote abstinence as the only acceptable treatment outcome. It’s a concept that dates back to the 1800s and was heavily promoted by Alcoholics Anonymous beginning in the early 1900s, a period before there was any viable treatment for alcoholism.
Today, a variety of treatments have proved effective, both psychosocial as well as pharmacologic, but people aren’t receiving them. A large epidemiologic study conducted by the National Institute on Alcohol Abuse and Alcoholism estimated that of 7.9 million Americans who are alcohol dependent, only 2.4 million have ever been diagnosed as such, 1.5 million have ever gotten any treatment for their disorder, and a mere 139,000 have ever received pharmacotherapy.
“There’s this amazing treatment gap,” commented Dr. Swift, professor of psychiatry and associate director of the Center for Alcohol and Addiction Studies at Brown University in Providence, R.I.
The main reason for this huge treatment gap was revealed in a 2012 survey conducted by the U.S. Substance Abuse and Mental Health Services Administration: 49.5% of participants who had not sought treatment for an alcohol problem within the past year even though they needed it and recognized their need for it gave as their reason that they were just not ready to stop drinking completely. This is a group where the harm-reduction strategy makes a great deal of sense, the psychiatrist said.
Harm reduction is based upon evidence that the risk of mortality because of alcohol-related causes rises exponentially as daily consumption climbs above the threshold of hazardous drinking, which has been defined by U.S. public health officials as five drinks per day or 15 per week in men and four per day or eight per week in women. The corollary is that reducing heavy drinking provides exponential health benefits. Investigators at Imperial College, London, have estimated that reducing alcohol intake from 100 g per day to 50 g per day provides an eight-fold reduction in health harms (J. Psychopharmacol. 2014;28:3-7).
“You get a lot of bang for your buck by reducing the amount of alcohol you consume,” Dr. Swift said. “The evidence really is out there that reducing drinking is an effective harm reduction strategy.”
Dr. Wim van den Brink, who led the SENSE trial, a 1-year, phase III, randomized, placebo-controlled study with positive safety and efficacy outcomes for nalmefene as-needed (J. Psychopharmacol. 2014;28:733-44), said one of the strengths of this treatment strategy is that it gives patients responsibility for their drinking and allows them to set their own treatment goals. That enhances the likelihood of successful outcomes.
The harm-reduction approach with as-needed nalmefene also is a way to bring into treatment some of the 50% of problem drinkers who don’t want to stop drinking entirely, added Dr. van den Brink, professor of psychiatry and addiction at the University of Amsterdam and director of the Amsterdam Institute for Addiction Research.
A spokesperson for Lundbeck, which sponsored the SENSE and 6-month ESENSE 1 and ESENSE 2 trials, said the company would not seek marketing approval for nalmefene in the United States because the drug’s remaining duration of patent protection makes it commercially nonviable.
Nalmefene and naltrexone, the latter of which is available in the United States, are both mu opioid receptor antagonists that also affect the delta opioid receptor. However, nalmefene also is a partial agonist at the kappa opioid receptor.
Dr. Swift said both drugs have been shown in preclinical and clinical studies to interrupt multiple biobehavioral mechanisms responsible for initiating and maintaining alcohol dependence. They reduce alcohol craving, block the motivation to drink to relieve stress and anxiety, and might improve impulsivity.
“Naltrexone has been shown not only to affect the rewards of alcohol consumption, it also seems to have direct cognitive and attentional effects in the orbitofrontal cortex. It reduces preoccupation with alcohol and improves attention to non–alcohol related stimuli,” he said. “I think that’s a really important finding and provides a new understanding of how opioid antagonists work.”
The psychiatrist noted that a recent meta-analysis concluded that opioid antagonists are better for reducing heavy drinking than for increasing abstinence (Addiction 2013;108:275-93).
Dr. Swift reported receiving honoraria from Lundbeck and serving as an adviser or consultant to D&B Pharma and CT San Remo. Dr. van den Brink is on the advisory boards of Lundbeck and more than a half-dozen other pharmaceutical companies.
BERLIN – The harm-reduction concept as an alternative to abstinence as a treatment strategy for alcohol dependence has taken on new legitimacy as a result of the recent approval of nalmefene by the European Medicines Agency.
Nalmefene, an opioid receptor antagonist, received marketing approval across Europe for use specifically in a novel as-needed dosing regimen that is under the patient’s control. One 18-mg tablet is to be taken on days when a patient anticipates a risk of drinking, or if the patient has already started drinking, then as soon as possible.
The indication was granted by European regulators on the strength of three European phase III randomized trials that showed that heavy drinkers who used nalmefene in this way reduced their alcohol consumption to a more normal level. Thus, marketing approval was an implicit endorsement of the harm-reduction strategy.
“I have been praying for this for years and years. I have been strictly against the concept of complete abstinence, because the core of the disease of addiction is relapse. It is just a natural thing that one relapses,” Rainer Spanagel, Ph.D., said at the annual congress of the European College of Neuropsychopharmacology.
“It has been a major mistake to say you are only successful in the field of addiction treatment if there is abstinence. This is an almost unreachable goal. This goal, set out to achieve for decades now, has been almost impossible for most patients to achieve,” added Dr. Spanagel, director of the Institute of Psychopharmacology at the University of Heidelberg (Germany).
Dr. Robert M. Swift noted that most treatment programs in the United States still promote abstinence as the only acceptable treatment outcome. It’s a concept that dates back to the 1800s and was heavily promoted by Alcoholics Anonymous beginning in the early 1900s, a period before there was any viable treatment for alcoholism.
Today, a variety of treatments have proved effective, both psychosocial as well as pharmacologic, but people aren’t receiving them. A large epidemiologic study conducted by the National Institute on Alcohol Abuse and Alcoholism estimated that of 7.9 million Americans who are alcohol dependent, only 2.4 million have ever been diagnosed as such, 1.5 million have ever gotten any treatment for their disorder, and a mere 139,000 have ever received pharmacotherapy.
“There’s this amazing treatment gap,” commented Dr. Swift, professor of psychiatry and associate director of the Center for Alcohol and Addiction Studies at Brown University in Providence, R.I.
The main reason for this huge treatment gap was revealed in a 2012 survey conducted by the U.S. Substance Abuse and Mental Health Services Administration: 49.5% of participants who had not sought treatment for an alcohol problem within the past year even though they needed it and recognized their need for it gave as their reason that they were just not ready to stop drinking completely. This is a group where the harm-reduction strategy makes a great deal of sense, the psychiatrist said.
Harm reduction is based upon evidence that the risk of mortality because of alcohol-related causes rises exponentially as daily consumption climbs above the threshold of hazardous drinking, which has been defined by U.S. public health officials as five drinks per day or 15 per week in men and four per day or eight per week in women. The corollary is that reducing heavy drinking provides exponential health benefits. Investigators at Imperial College, London, have estimated that reducing alcohol intake from 100 g per day to 50 g per day provides an eight-fold reduction in health harms (J. Psychopharmacol. 2014;28:3-7).
“You get a lot of bang for your buck by reducing the amount of alcohol you consume,” Dr. Swift said. “The evidence really is out there that reducing drinking is an effective harm reduction strategy.”
Dr. Wim van den Brink, who led the SENSE trial, a 1-year, phase III, randomized, placebo-controlled study with positive safety and efficacy outcomes for nalmefene as-needed (J. Psychopharmacol. 2014;28:733-44), said one of the strengths of this treatment strategy is that it gives patients responsibility for their drinking and allows them to set their own treatment goals. That enhances the likelihood of successful outcomes.
The harm-reduction approach with as-needed nalmefene also is a way to bring into treatment some of the 50% of problem drinkers who don’t want to stop drinking entirely, added Dr. van den Brink, professor of psychiatry and addiction at the University of Amsterdam and director of the Amsterdam Institute for Addiction Research.
A spokesperson for Lundbeck, which sponsored the SENSE and 6-month ESENSE 1 and ESENSE 2 trials, said the company would not seek marketing approval for nalmefene in the United States because the drug’s remaining duration of patent protection makes it commercially nonviable.
Nalmefene and naltrexone, the latter of which is available in the United States, are both mu opioid receptor antagonists that also affect the delta opioid receptor. However, nalmefene also is a partial agonist at the kappa opioid receptor.
Dr. Swift said both drugs have been shown in preclinical and clinical studies to interrupt multiple biobehavioral mechanisms responsible for initiating and maintaining alcohol dependence. They reduce alcohol craving, block the motivation to drink to relieve stress and anxiety, and might improve impulsivity.
“Naltrexone has been shown not only to affect the rewards of alcohol consumption, it also seems to have direct cognitive and attentional effects in the orbitofrontal cortex. It reduces preoccupation with alcohol and improves attention to non–alcohol related stimuli,” he said. “I think that’s a really important finding and provides a new understanding of how opioid antagonists work.”
The psychiatrist noted that a recent meta-analysis concluded that opioid antagonists are better for reducing heavy drinking than for increasing abstinence (Addiction 2013;108:275-93).
Dr. Swift reported receiving honoraria from Lundbeck and serving as an adviser or consultant to D&B Pharma and CT San Remo. Dr. van den Brink is on the advisory boards of Lundbeck and more than a half-dozen other pharmaceutical companies.
EXPERT ANALYSIS FROM THE ECNP CONGRESS
Concomitant Depression in Breast Cancer Survivors Doubles Health Care Costs
SAN ANTONIO – Annual health care costs and utilization jump several-fold in nonelderly breast cancer survivors with concomitant depression, according to an analysis from the U.S. military health system.
Analysis of the records of 2,851 breast cancer survivors whose care is provided by the Department of Defense military health system indicated that 15.9% were diagnosed with depression in the time interval within 1 year prior to and 2 years after their cancer diagnosis. These dual-diagnosis patients averaged $15,471 annually in health care costs covering inpatient and outpatient services and outpatient prescriptions in the first years after being diagnosed with breast cancer, compared with $8,297 per year in those without a diagnosis of depression, Diana D. Jeffery, Ph.D., reported at the San Antonio Breast Cancer Symposium.
The mean annual number of hospital admissions was tripled: 0.33 in breast cancer survivors with depression and 0.11 in survivors without depression. The dual-diagosis group averaged 1.94 hospital bed days annually, compared with 0.58 in breast cancer survivors without depression. Breast cancer survivors diagnosed with depression averaged 28 outpatient visits annually, while those without depression averaged 16.5, according to Dr. Jeffery, a senior researcher at the Defense Health Agency in Falls Church, Va.
Fifty percent of the breast cancer survivors were diagnosed with hypertension, making this the most common chronic comorbid condition. A diagnosis of depression, anxiety, adjustment, or stress disorder was present in 37.5% of the breast cancer survivors, making this group of psychiatric diagnoses the second most prevalent comorbidity. Twenty-three percent of the breast cancer survivors had received a diagnosis of heart disease, 20% had diabetes, 16% had asthma or chronic obstructive pulmonary disease, and 17% were obese. No demographic characteristics proved predictive of an increased likelihood of being diagnosed with depression, she said.
Of note, nearly one-half of the patients with depression had been diagnosed with the affective disorder during the year prior to receiving their breast cancer diagnosis.
Dr. Jeffery said that, while these data on health care costs and utilization in breast cancer survivors with concomitant depression are likely to be of particular interest to health plans, they also show what is likely to happen following adoption of the American Society of Clinical Oncology 2014 guidelines on screening and care of depression and anxiety in adults with cancer.
The guidelines recommend that all cancer patients and cancer survivors periodically be evaluated for symptoms of depression and anxiety using validated measures across the trajectory of care to “reduce the human cost of cancer” (J. Clin. Oncol. 2014;32:1605-19).
Adoption of the depression screening guidelines will likely increase the number of breast cancer survivors with a mental health diagnosis, which, as Dr. Jeffery’s study demonstrates, will boost health care costs and utilization. On the other hand, identifying and intervening effectively in patients with mild symptoms that haven’t yet risen to the level that meets diagnostic criteria for clinical depression should yield cost savings as well as quality-of-life benefits, she added.
The Department of Defense military health system, under a health plan known as Tricare, serves 9.5 million beneficiaries in 360 military treatment clinics worldwide. It’s a system with very few restrictions upon medical-ordered cancer follow-up care, according to Dr. Jeffery.
She reported having no financial conflicts regarding this study.
SAN ANTONIO – Annual health care costs and utilization jump several-fold in nonelderly breast cancer survivors with concomitant depression, according to an analysis from the U.S. military health system.
Analysis of the records of 2,851 breast cancer survivors whose care is provided by the Department of Defense military health system indicated that 15.9% were diagnosed with depression in the time interval within 1 year prior to and 2 years after their cancer diagnosis. These dual-diagnosis patients averaged $15,471 annually in health care costs covering inpatient and outpatient services and outpatient prescriptions in the first years after being diagnosed with breast cancer, compared with $8,297 per year in those without a diagnosis of depression, Diana D. Jeffery, Ph.D., reported at the San Antonio Breast Cancer Symposium.
The mean annual number of hospital admissions was tripled: 0.33 in breast cancer survivors with depression and 0.11 in survivors without depression. The dual-diagosis group averaged 1.94 hospital bed days annually, compared with 0.58 in breast cancer survivors without depression. Breast cancer survivors diagnosed with depression averaged 28 outpatient visits annually, while those without depression averaged 16.5, according to Dr. Jeffery, a senior researcher at the Defense Health Agency in Falls Church, Va.
Fifty percent of the breast cancer survivors were diagnosed with hypertension, making this the most common chronic comorbid condition. A diagnosis of depression, anxiety, adjustment, or stress disorder was present in 37.5% of the breast cancer survivors, making this group of psychiatric diagnoses the second most prevalent comorbidity. Twenty-three percent of the breast cancer survivors had received a diagnosis of heart disease, 20% had diabetes, 16% had asthma or chronic obstructive pulmonary disease, and 17% were obese. No demographic characteristics proved predictive of an increased likelihood of being diagnosed with depression, she said.
Of note, nearly one-half of the patients with depression had been diagnosed with the affective disorder during the year prior to receiving their breast cancer diagnosis.
Dr. Jeffery said that, while these data on health care costs and utilization in breast cancer survivors with concomitant depression are likely to be of particular interest to health plans, they also show what is likely to happen following adoption of the American Society of Clinical Oncology 2014 guidelines on screening and care of depression and anxiety in adults with cancer.
The guidelines recommend that all cancer patients and cancer survivors periodically be evaluated for symptoms of depression and anxiety using validated measures across the trajectory of care to “reduce the human cost of cancer” (J. Clin. Oncol. 2014;32:1605-19).
Adoption of the depression screening guidelines will likely increase the number of breast cancer survivors with a mental health diagnosis, which, as Dr. Jeffery’s study demonstrates, will boost health care costs and utilization. On the other hand, identifying and intervening effectively in patients with mild symptoms that haven’t yet risen to the level that meets diagnostic criteria for clinical depression should yield cost savings as well as quality-of-life benefits, she added.
The Department of Defense military health system, under a health plan known as Tricare, serves 9.5 million beneficiaries in 360 military treatment clinics worldwide. It’s a system with very few restrictions upon medical-ordered cancer follow-up care, according to Dr. Jeffery.
She reported having no financial conflicts regarding this study.
SAN ANTONIO – Annual health care costs and utilization jump several-fold in nonelderly breast cancer survivors with concomitant depression, according to an analysis from the U.S. military health system.
Analysis of the records of 2,851 breast cancer survivors whose care is provided by the Department of Defense military health system indicated that 15.9% were diagnosed with depression in the time interval within 1 year prior to and 2 years after their cancer diagnosis. These dual-diagnosis patients averaged $15,471 annually in health care costs covering inpatient and outpatient services and outpatient prescriptions in the first years after being diagnosed with breast cancer, compared with $8,297 per year in those without a diagnosis of depression, Diana D. Jeffery, Ph.D., reported at the San Antonio Breast Cancer Symposium.
The mean annual number of hospital admissions was tripled: 0.33 in breast cancer survivors with depression and 0.11 in survivors without depression. The dual-diagosis group averaged 1.94 hospital bed days annually, compared with 0.58 in breast cancer survivors without depression. Breast cancer survivors diagnosed with depression averaged 28 outpatient visits annually, while those without depression averaged 16.5, according to Dr. Jeffery, a senior researcher at the Defense Health Agency in Falls Church, Va.
Fifty percent of the breast cancer survivors were diagnosed with hypertension, making this the most common chronic comorbid condition. A diagnosis of depression, anxiety, adjustment, or stress disorder was present in 37.5% of the breast cancer survivors, making this group of psychiatric diagnoses the second most prevalent comorbidity. Twenty-three percent of the breast cancer survivors had received a diagnosis of heart disease, 20% had diabetes, 16% had asthma or chronic obstructive pulmonary disease, and 17% were obese. No demographic characteristics proved predictive of an increased likelihood of being diagnosed with depression, she said.
Of note, nearly one-half of the patients with depression had been diagnosed with the affective disorder during the year prior to receiving their breast cancer diagnosis.
Dr. Jeffery said that, while these data on health care costs and utilization in breast cancer survivors with concomitant depression are likely to be of particular interest to health plans, they also show what is likely to happen following adoption of the American Society of Clinical Oncology 2014 guidelines on screening and care of depression and anxiety in adults with cancer.
The guidelines recommend that all cancer patients and cancer survivors periodically be evaluated for symptoms of depression and anxiety using validated measures across the trajectory of care to “reduce the human cost of cancer” (J. Clin. Oncol. 2014;32:1605-19).
Adoption of the depression screening guidelines will likely increase the number of breast cancer survivors with a mental health diagnosis, which, as Dr. Jeffery’s study demonstrates, will boost health care costs and utilization. On the other hand, identifying and intervening effectively in patients with mild symptoms that haven’t yet risen to the level that meets diagnostic criteria for clinical depression should yield cost savings as well as quality-of-life benefits, she added.
The Department of Defense military health system, under a health plan known as Tricare, serves 9.5 million beneficiaries in 360 military treatment clinics worldwide. It’s a system with very few restrictions upon medical-ordered cancer follow-up care, according to Dr. Jeffery.
She reported having no financial conflicts regarding this study.
AT SABCS 2014