User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
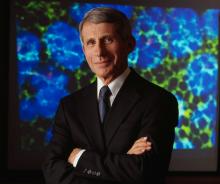
Anthony Fauci faces the ‘perpetual challenge’ of emerging infections
SAN DIEGO – Reflecting on his 33-year career as director of the National Institute of Allergy and Infectious Diseases, Anthony S. Fauci, MD, can say one thing for certain: Emerging and re-emerging infectious diseases in the continental United States are here to stay.
In an article that he and his colleagues published in the Lancet in 2008, they used the term “perpetual challenge” to describe emerging infections, a descriptor that resonates with him to this day.
Global examples of emerging and re-emerging infectious diseases he discussed include dengue, West Nile virus, chikungunya, and carbapenem-resistant Enterobacteriaceae, “which is becoming a progressively more serious problem in hospitalized patients,” said Dr. Fauci, who is also chief of the NIAID Laboratory of Immunoregulation.
“We had a serious challenge with that at our own clinical center in Bethesda just a few years ago,” he noted. Numerous cases of antimicrobial resistance in methicillin-resistant Staphylococcus aureus, Clostridium difficile, and Neisseria gonorrhoeae have been reported.
Dr. Fauci described the Ebola outbreak as “a globally important disease that had ripple effects in the United States that were unpredicted,” referring to the case of the infected man who traveled from Monrovia to Dallas on Sept. 19, 2014, and developed Ebola symptoms 5 days later. Between 2014 and 2016, there were 28,616 cases and 11,310 deaths combined in the countries of Guinea, Sierra Leone, and Liberia.
“There is virtually no health care system in those three countries,” he said. “There’s a distrust in authority, and anything we tried to do as a global health [effort] made things worse. What we’re trying to do now is built sustainable health care issues in countries that don’t have it.”
Of particular concern to public health officials worldwide is getting a lid on Zika virus, a mosquito-borne illness that can be passed from a pregnant woman to her fetus and cause an increased risk of microcephaly, particularly during the first trimester.
“Not only is there microcephaly, there’s a whole host of abnormalities that involve hearing loss, visual abnormalities, and a variety of other issues,” Dr. Fauci said. “There are about 50 countries in the Americas and the Caribbean that have Zika virus transmission.”
According to data from the Centers for Disease Control and Prevention, from Jan. 1, 2015, to March 29, 2017, there were 5,182 reported cases of Zika virus disease in the 50 states and the District of Columbia. The majority of those (4,886) were travel associated, 222 were locally acquired mosquito-borne, 45 were sexually transmitted, 27 congenital, 1 was laboratory acquired, and 1 was unknown.
At the same time, there have been 38,303 cases in the U.S. territories. Of those, 38,156 were locally acquired, and 147 were travel associated. “That’s why there’s such an intense effort to develop a Zika vaccine,” he said.
According to the CDC, as of March 15, 2017, there are 265 cases of locally transmitted cases in Florida: 216 by mosquito and the rest by sexual transmission. “Talk about surprises,” Dr. Fauci said. “Zika is the first mosquito-borne infection that can result in a congenital abnormality, the first mosquito-borne infection that can be sexually transmitted, and now we’re learning more about this problem, which is the reason why it’s very important for us to develop a vaccine.”
A phase I trial of a DNA vaccine developed by the NIH Vaccine Research Center has reached its enrollment goal of 80 patients age 18-35 years. Initial results are expected sometime in the first quarter of 2017. A phase II trial in the United States and Puerto Rico is expected to launch soon.
Dr. Fauci closed his presentation by sharing lessons learned from previous pandemics.
The first lesson is that global surveillance is required. “Namely, know what’s going on in real time,” he said. “That has to be linked to transparency and communication. So that if something happens in China, we don’t find out about it months later, but we know about it in real time.”
Infrastructure and capacity building are also important. “The lack of capacity in West Africa can ultimately have an indirect impact on us here in the United States,” he said.
“Finally, we need to coordinate and collaborate; we need adaptable platforms for vaccines,” Dr. Fauci cautioned. “Importantly, we need a stable funding mechanism such as a public health emergency fund so that we do not have to go scrambling before the Congress when we need emergency funds.”
SAN DIEGO – Reflecting on his 33-year career as director of the National Institute of Allergy and Infectious Diseases, Anthony S. Fauci, MD, can say one thing for certain: Emerging and re-emerging infectious diseases in the continental United States are here to stay.
In an article that he and his colleagues published in the Lancet in 2008, they used the term “perpetual challenge” to describe emerging infections, a descriptor that resonates with him to this day.
Global examples of emerging and re-emerging infectious diseases he discussed include dengue, West Nile virus, chikungunya, and carbapenem-resistant Enterobacteriaceae, “which is becoming a progressively more serious problem in hospitalized patients,” said Dr. Fauci, who is also chief of the NIAID Laboratory of Immunoregulation.
“We had a serious challenge with that at our own clinical center in Bethesda just a few years ago,” he noted. Numerous cases of antimicrobial resistance in methicillin-resistant Staphylococcus aureus, Clostridium difficile, and Neisseria gonorrhoeae have been reported.
Dr. Fauci described the Ebola outbreak as “a globally important disease that had ripple effects in the United States that were unpredicted,” referring to the case of the infected man who traveled from Monrovia to Dallas on Sept. 19, 2014, and developed Ebola symptoms 5 days later. Between 2014 and 2016, there were 28,616 cases and 11,310 deaths combined in the countries of Guinea, Sierra Leone, and Liberia.
“There is virtually no health care system in those three countries,” he said. “There’s a distrust in authority, and anything we tried to do as a global health [effort] made things worse. What we’re trying to do now is built sustainable health care issues in countries that don’t have it.”
Of particular concern to public health officials worldwide is getting a lid on Zika virus, a mosquito-borne illness that can be passed from a pregnant woman to her fetus and cause an increased risk of microcephaly, particularly during the first trimester.
“Not only is there microcephaly, there’s a whole host of abnormalities that involve hearing loss, visual abnormalities, and a variety of other issues,” Dr. Fauci said. “There are about 50 countries in the Americas and the Caribbean that have Zika virus transmission.”
According to data from the Centers for Disease Control and Prevention, from Jan. 1, 2015, to March 29, 2017, there were 5,182 reported cases of Zika virus disease in the 50 states and the District of Columbia. The majority of those (4,886) were travel associated, 222 were locally acquired mosquito-borne, 45 were sexually transmitted, 27 congenital, 1 was laboratory acquired, and 1 was unknown.
At the same time, there have been 38,303 cases in the U.S. territories. Of those, 38,156 were locally acquired, and 147 were travel associated. “That’s why there’s such an intense effort to develop a Zika vaccine,” he said.
According to the CDC, as of March 15, 2017, there are 265 cases of locally transmitted cases in Florida: 216 by mosquito and the rest by sexual transmission. “Talk about surprises,” Dr. Fauci said. “Zika is the first mosquito-borne infection that can result in a congenital abnormality, the first mosquito-borne infection that can be sexually transmitted, and now we’re learning more about this problem, which is the reason why it’s very important for us to develop a vaccine.”
A phase I trial of a DNA vaccine developed by the NIH Vaccine Research Center has reached its enrollment goal of 80 patients age 18-35 years. Initial results are expected sometime in the first quarter of 2017. A phase II trial in the United States and Puerto Rico is expected to launch soon.
Dr. Fauci closed his presentation by sharing lessons learned from previous pandemics.
The first lesson is that global surveillance is required. “Namely, know what’s going on in real time,” he said. “That has to be linked to transparency and communication. So that if something happens in China, we don’t find out about it months later, but we know about it in real time.”
Infrastructure and capacity building are also important. “The lack of capacity in West Africa can ultimately have an indirect impact on us here in the United States,” he said.
“Finally, we need to coordinate and collaborate; we need adaptable platforms for vaccines,” Dr. Fauci cautioned. “Importantly, we need a stable funding mechanism such as a public health emergency fund so that we do not have to go scrambling before the Congress when we need emergency funds.”
SAN DIEGO – Reflecting on his 33-year career as director of the National Institute of Allergy and Infectious Diseases, Anthony S. Fauci, MD, can say one thing for certain: Emerging and re-emerging infectious diseases in the continental United States are here to stay.
In an article that he and his colleagues published in the Lancet in 2008, they used the term “perpetual challenge” to describe emerging infections, a descriptor that resonates with him to this day.
Global examples of emerging and re-emerging infectious diseases he discussed include dengue, West Nile virus, chikungunya, and carbapenem-resistant Enterobacteriaceae, “which is becoming a progressively more serious problem in hospitalized patients,” said Dr. Fauci, who is also chief of the NIAID Laboratory of Immunoregulation.
“We had a serious challenge with that at our own clinical center in Bethesda just a few years ago,” he noted. Numerous cases of antimicrobial resistance in methicillin-resistant Staphylococcus aureus, Clostridium difficile, and Neisseria gonorrhoeae have been reported.
Dr. Fauci described the Ebola outbreak as “a globally important disease that had ripple effects in the United States that were unpredicted,” referring to the case of the infected man who traveled from Monrovia to Dallas on Sept. 19, 2014, and developed Ebola symptoms 5 days later. Between 2014 and 2016, there were 28,616 cases and 11,310 deaths combined in the countries of Guinea, Sierra Leone, and Liberia.
“There is virtually no health care system in those three countries,” he said. “There’s a distrust in authority, and anything we tried to do as a global health [effort] made things worse. What we’re trying to do now is built sustainable health care issues in countries that don’t have it.”
Of particular concern to public health officials worldwide is getting a lid on Zika virus, a mosquito-borne illness that can be passed from a pregnant woman to her fetus and cause an increased risk of microcephaly, particularly during the first trimester.
“Not only is there microcephaly, there’s a whole host of abnormalities that involve hearing loss, visual abnormalities, and a variety of other issues,” Dr. Fauci said. “There are about 50 countries in the Americas and the Caribbean that have Zika virus transmission.”
According to data from the Centers for Disease Control and Prevention, from Jan. 1, 2015, to March 29, 2017, there were 5,182 reported cases of Zika virus disease in the 50 states and the District of Columbia. The majority of those (4,886) were travel associated, 222 were locally acquired mosquito-borne, 45 were sexually transmitted, 27 congenital, 1 was laboratory acquired, and 1 was unknown.
At the same time, there have been 38,303 cases in the U.S. territories. Of those, 38,156 were locally acquired, and 147 were travel associated. “That’s why there’s such an intense effort to develop a Zika vaccine,” he said.
According to the CDC, as of March 15, 2017, there are 265 cases of locally transmitted cases in Florida: 216 by mosquito and the rest by sexual transmission. “Talk about surprises,” Dr. Fauci said. “Zika is the first mosquito-borne infection that can result in a congenital abnormality, the first mosquito-borne infection that can be sexually transmitted, and now we’re learning more about this problem, which is the reason why it’s very important for us to develop a vaccine.”
A phase I trial of a DNA vaccine developed by the NIH Vaccine Research Center has reached its enrollment goal of 80 patients age 18-35 years. Initial results are expected sometime in the first quarter of 2017. A phase II trial in the United States and Puerto Rico is expected to launch soon.
Dr. Fauci closed his presentation by sharing lessons learned from previous pandemics.
The first lesson is that global surveillance is required. “Namely, know what’s going on in real time,” he said. “That has to be linked to transparency and communication. So that if something happens in China, we don’t find out about it months later, but we know about it in real time.”
Infrastructure and capacity building are also important. “The lack of capacity in West Africa can ultimately have an indirect impact on us here in the United States,” he said.
“Finally, we need to coordinate and collaborate; we need adaptable platforms for vaccines,” Dr. Fauci cautioned. “Importantly, we need a stable funding mechanism such as a public health emergency fund so that we do not have to go scrambling before the Congress when we need emergency funds.”
EXPERT ANALYSIS FROM ACP INTERNAL MEDICINE
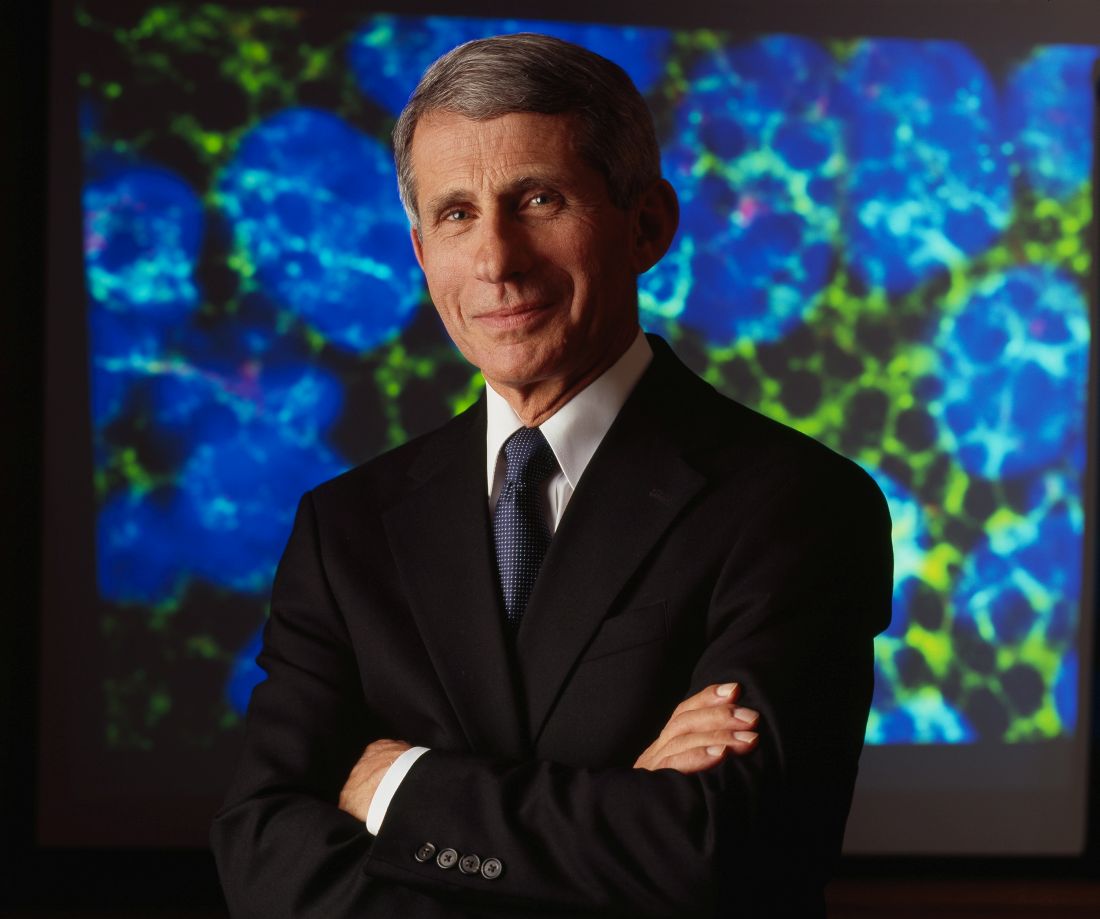
Many patients’ severe asthma remains uncontrolled
ATLANTA – More than half of patients severe asthma have disease that remains uncontrolled at their index date of treatment, and 39% remained uncontrolled at 12 months of follow-up, results from a large single specialty practice study showed.
“Severe asthma accounts for only 5%-10% of all asthma [in] patients but at least half of the health care costs, and it’s a significant burden to those who suffer from it,” study author Brian D. Stone, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
The mean age of patients was 44.4 years, 67% were female, 78% were white, 77% had concomitant rhinitis, 21% had sinusitis, and 44% had allergic sensitivities. The mean baseline prebronchodilation FEV1 and FEV1% predicted were 2.45 L and 79.7%, respectively. The mean baseline ACT score was 17, with 61% of patients having ACT scores of 19 or lower, indicating poor symptom control.
Using National Asthma Education and Prevention Program criteria, the researchers found that 52% of patients had uncontrolled asthma at the index date and 39% remained uncontrolled at 12 months of follow-up. In an effort to better manage their severe asthma, more than one-third of patients on Step 4 therapy and 60% of patients on Step 5 therapy changed their asthma controller medications during follow-up.
“As an asthma specialist, I hoped that more [of these patients] would have come under control. These are the most difficult patients to treat,” said Dr. Stone, who practices at Allergy Partners of San Diego. “It’s a population that deserves special attention, and interventions are probably going to be on multiple levels, depending on what type of severe persistent asthma they have. More therapies are needed.”
He acknowledged certain limitations of the study, including the fact that patients were treated by specialists in allergy, asthma, and immunology and, therefore, may not represent the general population with asthma.
The study was supported by AstraZeneca. Dr. Stone reported having no relevant financial disclosures.
ATLANTA – More than half of patients severe asthma have disease that remains uncontrolled at their index date of treatment, and 39% remained uncontrolled at 12 months of follow-up, results from a large single specialty practice study showed.
“Severe asthma accounts for only 5%-10% of all asthma [in] patients but at least half of the health care costs, and it’s a significant burden to those who suffer from it,” study author Brian D. Stone, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
The mean age of patients was 44.4 years, 67% were female, 78% were white, 77% had concomitant rhinitis, 21% had sinusitis, and 44% had allergic sensitivities. The mean baseline prebronchodilation FEV1 and FEV1% predicted were 2.45 L and 79.7%, respectively. The mean baseline ACT score was 17, with 61% of patients having ACT scores of 19 or lower, indicating poor symptom control.
Using National Asthma Education and Prevention Program criteria, the researchers found that 52% of patients had uncontrolled asthma at the index date and 39% remained uncontrolled at 12 months of follow-up. In an effort to better manage their severe asthma, more than one-third of patients on Step 4 therapy and 60% of patients on Step 5 therapy changed their asthma controller medications during follow-up.
“As an asthma specialist, I hoped that more [of these patients] would have come under control. These are the most difficult patients to treat,” said Dr. Stone, who practices at Allergy Partners of San Diego. “It’s a population that deserves special attention, and interventions are probably going to be on multiple levels, depending on what type of severe persistent asthma they have. More therapies are needed.”
He acknowledged certain limitations of the study, including the fact that patients were treated by specialists in allergy, asthma, and immunology and, therefore, may not represent the general population with asthma.
The study was supported by AstraZeneca. Dr. Stone reported having no relevant financial disclosures.
ATLANTA – More than half of patients severe asthma have disease that remains uncontrolled at their index date of treatment, and 39% remained uncontrolled at 12 months of follow-up, results from a large single specialty practice study showed.
“Severe asthma accounts for only 5%-10% of all asthma [in] patients but at least half of the health care costs, and it’s a significant burden to those who suffer from it,” study author Brian D. Stone, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
The mean age of patients was 44.4 years, 67% were female, 78% were white, 77% had concomitant rhinitis, 21% had sinusitis, and 44% had allergic sensitivities. The mean baseline prebronchodilation FEV1 and FEV1% predicted were 2.45 L and 79.7%, respectively. The mean baseline ACT score was 17, with 61% of patients having ACT scores of 19 or lower, indicating poor symptom control.
Using National Asthma Education and Prevention Program criteria, the researchers found that 52% of patients had uncontrolled asthma at the index date and 39% remained uncontrolled at 12 months of follow-up. In an effort to better manage their severe asthma, more than one-third of patients on Step 4 therapy and 60% of patients on Step 5 therapy changed their asthma controller medications during follow-up.
“As an asthma specialist, I hoped that more [of these patients] would have come under control. These are the most difficult patients to treat,” said Dr. Stone, who practices at Allergy Partners of San Diego. “It’s a population that deserves special attention, and interventions are probably going to be on multiple levels, depending on what type of severe persistent asthma they have. More therapies are needed.”
He acknowledged certain limitations of the study, including the fact that patients were treated by specialists in allergy, asthma, and immunology and, therefore, may not represent the general population with asthma.
The study was supported by AstraZeneca. Dr. Stone reported having no relevant financial disclosures.
AT THE 2017 AAAAI ANNUAL MEETING
Key clinical point:
Major finding: More than half of patients with severe asthma (52%) had uncontrolled disease at the index date of treatment, and 39% remained uncontrolled at 12 months of follow-up.
Data source: A retrospective review of 12,922 patients aged 12 years and older with severe asthma who were treated between Jan. 1, 2010, and April 30, 2016.
Disclosures: The study was supported by AstraZeneca. Dr. Stone reported no relevant financial disclosures.
What happens when a baked egg oral challenge is negative?
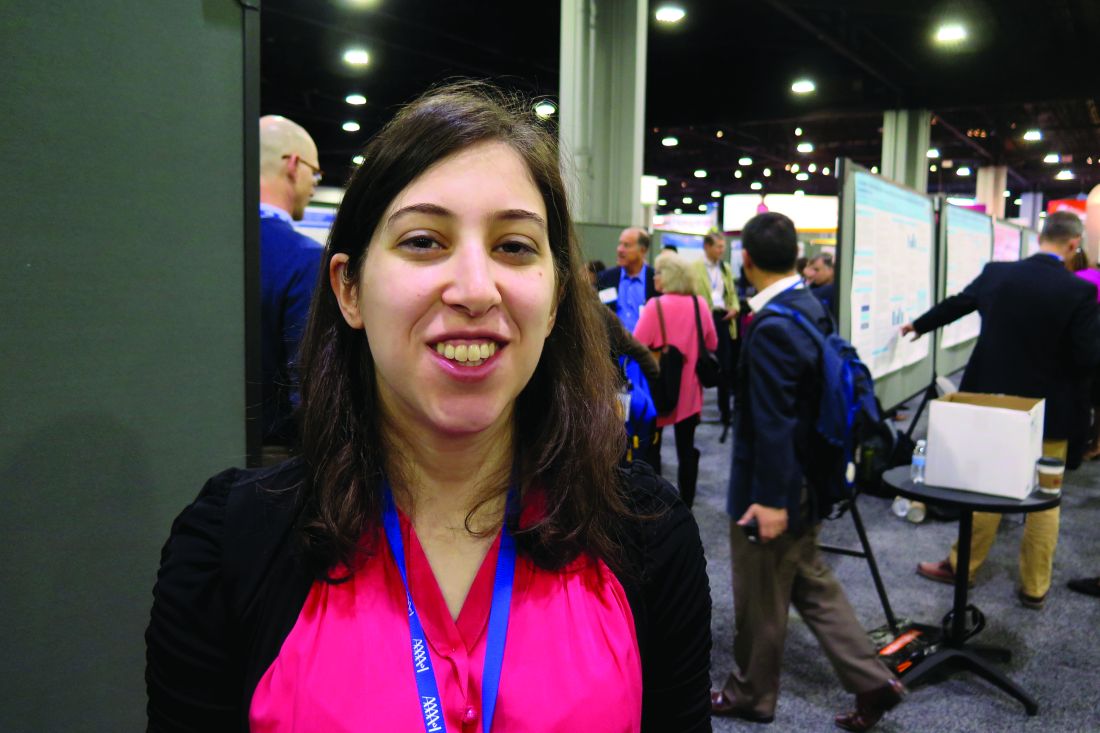
ATLANTA – The majority of patients who had cooked egg exposure following a negative physician-supervised baked egg oral challenge are tolerating cooked egg, according to a retrospective study.
However, no correlation between results and development of tolerance was identified with skin prick testing or serum IgE testing.
To find out, Dr. Peng, a second-year fellow in the department of pediatrics at the University of California, Los Angeles, and her associates identified 22 patients who underwent negative physician-supervised baked egg oral challenges from July 2011 until June 2016. They reviewed medical charts to obtain data on age, clinical history, skin prick test results, and results of serum IgE testing to egg and its components. Next, the researchers contacted patients and their families and invited them to participate in a telephone survey about patterns of baked, cooked, and raw egg exposure and associated reactions, following their negative baked challenge. The patients ranged in age from 10 months to 44 years and their mean age was 7 years.
Dr. Peng presented results from 18 of the 22 patients who were successfully contacted. A mean of 26 months had passed since their baked egg oral challenge. Of these patients, 17 (94%) have had continued exposure to egg while 15 (83%) have shown tolerance to cooked egg. The researchers observed variable patterns of baked egg intake following the negative physician-supervised baked egg challenge. “Some patients are able to tolerate cooked egg rapidly but are not interested in continuing frequent consumption,” Dr. Peng said. “They may say, ‘My 3-year-old doesn’t like scrambled eggs, so I’m not going to keep pushing them.’ They’re not considering themselves egg allergic so their quality of life is much better. I understand that tolerating baked egg is a big deal, as an allergist I want to see them do more, such as tolerating cooked egg.”
When patients were asked about adverse reactions to egg consumption, three (17%) described gastrointestinal symptoms, five (28%) described cutaneous symptoms, and three (17%) described respiratory reactions. Dr. Peng noted that of the three patients who have not achieved tolerance to cooked egg, one patient reported mild reaction to baked egg 2 weeks after the baked egg challenge, while the other two continue to have baked egg exposure but have not yet introduced cooked egg into their diets. “I hope that most pediatricians and family practice physicians consider referral to an allergist if they’re not comfortable introducing a baked egg oral challenge.”
The researchers could not identify any correlation between skin prick or serum IgE test results and development of tolerance to cooked egg. “Data in the literature suggests that serum testing is predictive [of tolerance], but it’s not 100%,” Dr. Peng said.
She reported having no relevant financial disclosures.
ATLANTA – The majority of patients who had cooked egg exposure following a negative physician-supervised baked egg oral challenge are tolerating cooked egg, according to a retrospective study.
However, no correlation between results and development of tolerance was identified with skin prick testing or serum IgE testing.
To find out, Dr. Peng, a second-year fellow in the department of pediatrics at the University of California, Los Angeles, and her associates identified 22 patients who underwent negative physician-supervised baked egg oral challenges from July 2011 until June 2016. They reviewed medical charts to obtain data on age, clinical history, skin prick test results, and results of serum IgE testing to egg and its components. Next, the researchers contacted patients and their families and invited them to participate in a telephone survey about patterns of baked, cooked, and raw egg exposure and associated reactions, following their negative baked challenge. The patients ranged in age from 10 months to 44 years and their mean age was 7 years.
Dr. Peng presented results from 18 of the 22 patients who were successfully contacted. A mean of 26 months had passed since their baked egg oral challenge. Of these patients, 17 (94%) have had continued exposure to egg while 15 (83%) have shown tolerance to cooked egg. The researchers observed variable patterns of baked egg intake following the negative physician-supervised baked egg challenge. “Some patients are able to tolerate cooked egg rapidly but are not interested in continuing frequent consumption,” Dr. Peng said. “They may say, ‘My 3-year-old doesn’t like scrambled eggs, so I’m not going to keep pushing them.’ They’re not considering themselves egg allergic so their quality of life is much better. I understand that tolerating baked egg is a big deal, as an allergist I want to see them do more, such as tolerating cooked egg.”
When patients were asked about adverse reactions to egg consumption, three (17%) described gastrointestinal symptoms, five (28%) described cutaneous symptoms, and three (17%) described respiratory reactions. Dr. Peng noted that of the three patients who have not achieved tolerance to cooked egg, one patient reported mild reaction to baked egg 2 weeks after the baked egg challenge, while the other two continue to have baked egg exposure but have not yet introduced cooked egg into their diets. “I hope that most pediatricians and family practice physicians consider referral to an allergist if they’re not comfortable introducing a baked egg oral challenge.”
The researchers could not identify any correlation between skin prick or serum IgE test results and development of tolerance to cooked egg. “Data in the literature suggests that serum testing is predictive [of tolerance], but it’s not 100%,” Dr. Peng said.
She reported having no relevant financial disclosures.
ATLANTA – The majority of patients who had cooked egg exposure following a negative physician-supervised baked egg oral challenge are tolerating cooked egg, according to a retrospective study.
However, no correlation between results and development of tolerance was identified with skin prick testing or serum IgE testing.
To find out, Dr. Peng, a second-year fellow in the department of pediatrics at the University of California, Los Angeles, and her associates identified 22 patients who underwent negative physician-supervised baked egg oral challenges from July 2011 until June 2016. They reviewed medical charts to obtain data on age, clinical history, skin prick test results, and results of serum IgE testing to egg and its components. Next, the researchers contacted patients and their families and invited them to participate in a telephone survey about patterns of baked, cooked, and raw egg exposure and associated reactions, following their negative baked challenge. The patients ranged in age from 10 months to 44 years and their mean age was 7 years.
Dr. Peng presented results from 18 of the 22 patients who were successfully contacted. A mean of 26 months had passed since their baked egg oral challenge. Of these patients, 17 (94%) have had continued exposure to egg while 15 (83%) have shown tolerance to cooked egg. The researchers observed variable patterns of baked egg intake following the negative physician-supervised baked egg challenge. “Some patients are able to tolerate cooked egg rapidly but are not interested in continuing frequent consumption,” Dr. Peng said. “They may say, ‘My 3-year-old doesn’t like scrambled eggs, so I’m not going to keep pushing them.’ They’re not considering themselves egg allergic so their quality of life is much better. I understand that tolerating baked egg is a big deal, as an allergist I want to see them do more, such as tolerating cooked egg.”
When patients were asked about adverse reactions to egg consumption, three (17%) described gastrointestinal symptoms, five (28%) described cutaneous symptoms, and three (17%) described respiratory reactions. Dr. Peng noted that of the three patients who have not achieved tolerance to cooked egg, one patient reported mild reaction to baked egg 2 weeks after the baked egg challenge, while the other two continue to have baked egg exposure but have not yet introduced cooked egg into their diets. “I hope that most pediatricians and family practice physicians consider referral to an allergist if they’re not comfortable introducing a baked egg oral challenge.”
The researchers could not identify any correlation between skin prick or serum IgE test results and development of tolerance to cooked egg. “Data in the literature suggests that serum testing is predictive [of tolerance], but it’s not 100%,” Dr. Peng said.
She reported having no relevant financial disclosures.
AT THE 2017 AAAAI ANNUAL MEETING
Key clinical point:
Major finding: Following a negative physician-supervised baked egg oral challenge 94% of patients have had continued exposure to egg while 83% have shown tolerance to cooked egg.
Data source: A retrospective review of 22 patients who underwent a physician-supervised negative oral baked egg challenge.
Disclosures: Dr. Peng reported having no relevant financial disclosures.
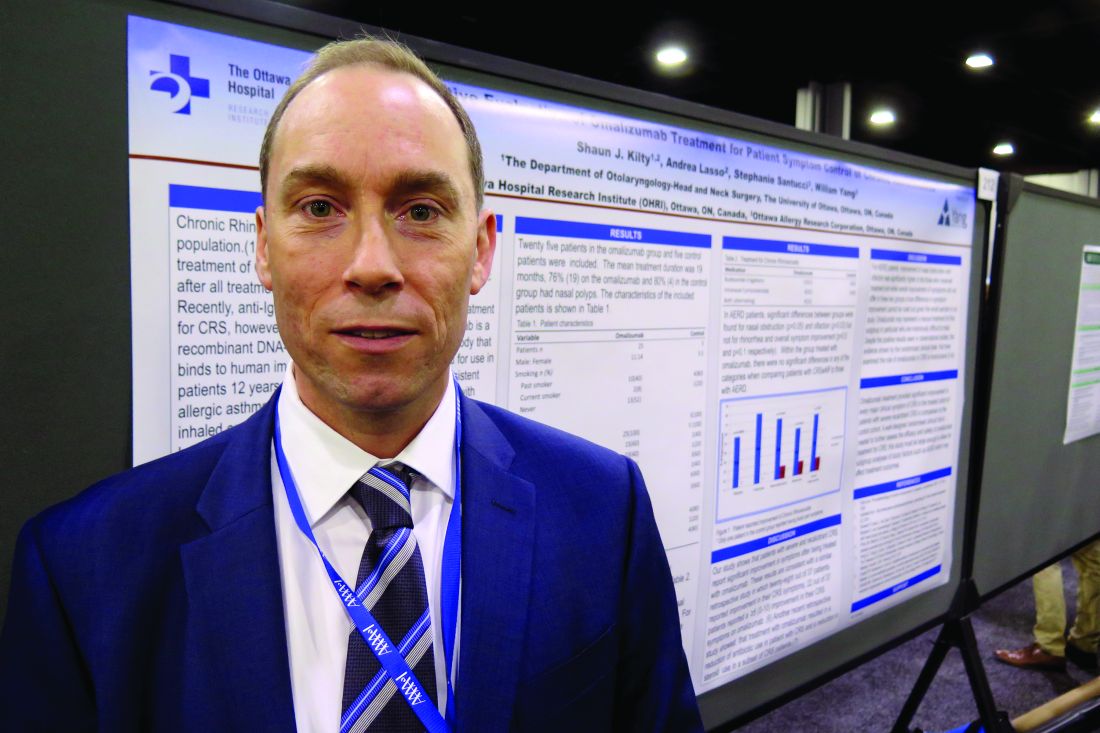
Omalizumab may help chronic rhinosinusitis symptoms
ATLANTA – Patients with severe and recalcitrant chronic rhinosinusitis who were treated with omalizumab reported improvement in symptoms, compared with controls, results from a small single-center study suggested.
A recombinant DNA-derived humanized monoclonal antibody that binds to human IgE, omalizumab is approved for use in patients 12 years or older with moderate to severe persistent asthma and inadequately controlled symptoms with inhaled corticosteroids. Two small randomized controlled trials (J Allergy Clin Immunol. 2013;131[1]:110-6 and Rhinology 2010;48[3]:318-24) have shown that omalizumab reduces polyp size and improves sinus inflammation, Shaun J. Kilty, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
For the current study, Dr. Kilty and his associates evaluated the clinical effect of omalizumab on sinus symptom and disease control in 25 patients with recalcitrant chronic rhinosinusitis (CRS) who were receiving anti-IgE therapy as part of their asthma treatment. Five control patients were included. The researchers used a visual analog scale to measure changes over time among study participants in overall CRS symptoms and major CRS symptoms, including facial pain, nasal obstruction, rhinorrhea, and olfaction. The mean age of the patients was 50 years and 49 years in the omalizumab and control groups, respectively. The mean duration of treatment was 19 months, and most had nasal polyps (76% in the omalizumab group and 80% in the control group).
Dr. Kilty reported that among patients in the omalizumab treatment group, overall symptoms improved by 70%. The individual symptom that improved the most was facial pain (79%), followed by nasal obstruction (70%), rhinorrhea (56%), and olfaction (56%). Among the control group, overall symptoms improved by 17%. Rhinorrhea improved by 16% and nasal obstruction by 15%, but no improvements in facial pain or in olfaction were observed. Symptom improvement was significantly higher for omalizumab-treated patients in every category (P less than .05).
A subset analysis of eight patients in the treatment group and three in the control group who had aspirin-exacerbated respiratory disease (AERD) revealed significant differences between groups for nasal obstruction (P = .05) and olfaction (P = .03), but not for rhinorrhea and overall symptom improvement (P = .5 and P = .1, respectively). “Within the group treated with omalizumab, there were no significant differences in any of the categories when comparing patients with CRS with nasal polyps to those with AERD,” the researchers wrote in their abstract.
“I think there’s a strong enough signal to indicate that this biologic therapy does work in patients with chronic sinusitis with polyps,” Dr. Kilty said. “I think it needs to be better determined exactly what patient cohort is best to use it, and similarly better-structured randomized trials are needed to evaluate the effect of this biologic.”
He reported having no relevant financial disclosures.
ATLANTA – Patients with severe and recalcitrant chronic rhinosinusitis who were treated with omalizumab reported improvement in symptoms, compared with controls, results from a small single-center study suggested.
A recombinant DNA-derived humanized monoclonal antibody that binds to human IgE, omalizumab is approved for use in patients 12 years or older with moderate to severe persistent asthma and inadequately controlled symptoms with inhaled corticosteroids. Two small randomized controlled trials (J Allergy Clin Immunol. 2013;131[1]:110-6 and Rhinology 2010;48[3]:318-24) have shown that omalizumab reduces polyp size and improves sinus inflammation, Shaun J. Kilty, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
For the current study, Dr. Kilty and his associates evaluated the clinical effect of omalizumab on sinus symptom and disease control in 25 patients with recalcitrant chronic rhinosinusitis (CRS) who were receiving anti-IgE therapy as part of their asthma treatment. Five control patients were included. The researchers used a visual analog scale to measure changes over time among study participants in overall CRS symptoms and major CRS symptoms, including facial pain, nasal obstruction, rhinorrhea, and olfaction. The mean age of the patients was 50 years and 49 years in the omalizumab and control groups, respectively. The mean duration of treatment was 19 months, and most had nasal polyps (76% in the omalizumab group and 80% in the control group).
Dr. Kilty reported that among patients in the omalizumab treatment group, overall symptoms improved by 70%. The individual symptom that improved the most was facial pain (79%), followed by nasal obstruction (70%), rhinorrhea (56%), and olfaction (56%). Among the control group, overall symptoms improved by 17%. Rhinorrhea improved by 16% and nasal obstruction by 15%, but no improvements in facial pain or in olfaction were observed. Symptom improvement was significantly higher for omalizumab-treated patients in every category (P less than .05).
A subset analysis of eight patients in the treatment group and three in the control group who had aspirin-exacerbated respiratory disease (AERD) revealed significant differences between groups for nasal obstruction (P = .05) and olfaction (P = .03), but not for rhinorrhea and overall symptom improvement (P = .5 and P = .1, respectively). “Within the group treated with omalizumab, there were no significant differences in any of the categories when comparing patients with CRS with nasal polyps to those with AERD,” the researchers wrote in their abstract.
“I think there’s a strong enough signal to indicate that this biologic therapy does work in patients with chronic sinusitis with polyps,” Dr. Kilty said. “I think it needs to be better determined exactly what patient cohort is best to use it, and similarly better-structured randomized trials are needed to evaluate the effect of this biologic.”
He reported having no relevant financial disclosures.
ATLANTA – Patients with severe and recalcitrant chronic rhinosinusitis who were treated with omalizumab reported improvement in symptoms, compared with controls, results from a small single-center study suggested.
A recombinant DNA-derived humanized monoclonal antibody that binds to human IgE, omalizumab is approved for use in patients 12 years or older with moderate to severe persistent asthma and inadequately controlled symptoms with inhaled corticosteroids. Two small randomized controlled trials (J Allergy Clin Immunol. 2013;131[1]:110-6 and Rhinology 2010;48[3]:318-24) have shown that omalizumab reduces polyp size and improves sinus inflammation, Shaun J. Kilty, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
For the current study, Dr. Kilty and his associates evaluated the clinical effect of omalizumab on sinus symptom and disease control in 25 patients with recalcitrant chronic rhinosinusitis (CRS) who were receiving anti-IgE therapy as part of their asthma treatment. Five control patients were included. The researchers used a visual analog scale to measure changes over time among study participants in overall CRS symptoms and major CRS symptoms, including facial pain, nasal obstruction, rhinorrhea, and olfaction. The mean age of the patients was 50 years and 49 years in the omalizumab and control groups, respectively. The mean duration of treatment was 19 months, and most had nasal polyps (76% in the omalizumab group and 80% in the control group).
Dr. Kilty reported that among patients in the omalizumab treatment group, overall symptoms improved by 70%. The individual symptom that improved the most was facial pain (79%), followed by nasal obstruction (70%), rhinorrhea (56%), and olfaction (56%). Among the control group, overall symptoms improved by 17%. Rhinorrhea improved by 16% and nasal obstruction by 15%, but no improvements in facial pain or in olfaction were observed. Symptom improvement was significantly higher for omalizumab-treated patients in every category (P less than .05).
A subset analysis of eight patients in the treatment group and three in the control group who had aspirin-exacerbated respiratory disease (AERD) revealed significant differences between groups for nasal obstruction (P = .05) and olfaction (P = .03), but not for rhinorrhea and overall symptom improvement (P = .5 and P = .1, respectively). “Within the group treated with omalizumab, there were no significant differences in any of the categories when comparing patients with CRS with nasal polyps to those with AERD,” the researchers wrote in their abstract.
“I think there’s a strong enough signal to indicate that this biologic therapy does work in patients with chronic sinusitis with polyps,” Dr. Kilty said. “I think it needs to be better determined exactly what patient cohort is best to use it, and similarly better-structured randomized trials are needed to evaluate the effect of this biologic.”
He reported having no relevant financial disclosures.
AT 2017 AAAAI ANNUAL MEETING
Key clinical point: In patients with severe chronic rhinosinusitis, omalizumab treatment provided significant improvement in every major clinical symptom of the condition.
Major finding: Among patients in the omalizumab treatment group, overall symptoms improved by 70%.
Data source: A study that evaluated the clinical effect of omalizumab in 25 patients with recalcitrant chronic rhinosinusitis who were receiving anti-IgE therapy as part of their asthma treatment and 5 control patients.
Disclosures: Dr. Kilty reported having no relevant financial disclosures.
A history of asthma exacerbations predicts future exacerbations
ATLANTA – Asthma exacerbations are common, severe events that can be life-threatening and can accelerate loss of lung function. That’s why it’s important to flag high-risk patients in your clinical practice, Nizar N. Jarjour, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Each year in the United States there are 15 million clinic visits, 2 million ED visits, and 500,000 hospitalizations for severe asthma exacerbations. “These exacerbations cause a high cost on the health care system, they lead to loss of work or school, and they’re a burden to patients and certainly to their families,” said Dr. Jarjour, professor of medicine and division head of allergy, pulmonary and critical care at the University of Wisconsin, Madison.
Factors implicated in asthma exacerbation include air pollution, cigarette smoke, occupational exposure, stress, and allergen exposure, but 50%-85% of cases are related to viral upper respiratory infections. “Any respiratory pathogen can precipitate attacks, but rhinoviruses are the most common,” he said. “Seasonal viral [upper respiratory infections] correlate with hospital admissions for asthma, and peak in spring and fall.”
Purported ways that a viral upper respiratory infection can lead to asthma exacerbation include enhanced airway responsiveness, increased eosinophilic airway inflammation in response to antigen, enhanced lower airway neutrophilic inflammation, and direct infection of the lower airway. “There are is an accentuated eosinophilic inflammation in response to allergen challenge when somebody has a cold,” Dr. Jarjour explained. “But the viral infection can actually directly lead to eosinophilic inflammation, perhaps through TSLP [thymic stromal lymphopoietin], interleukin (IL)-25, and IL-33 simulating the ILC2 (type 2 innate lymphoid cells). So there are both accentuating response to allergens as well as direct enhancement of eosinophilic inflammation following viral infection.”
One study that examined airway lavage following experimental infection found that patients had increased numbers of neutrophils in their airway sample (J Allergy Clin Immunol. 2000;105:1169-77). This means that asthma exacerbation triggers neutrophilic inflammation, which relates to the induction of cytokines and chemokines in the upper airway. “We have also demonstrated increased circulation of G-CSF [granulocyte–colony stimulating factor] and nasal IL-8 in the upper airway related to increased neutrophil recruitment,” Dr. Jarjour said.
Host factors associated with asthma exacerbations include altered innate immune response in the form of a defect in production of antiviral cytokines in response to viral infection, and a greater T helper (Th)2/Th1 ratio. Other factors include eosinophilic inflammation and greater levels of specific IgE to dust mite. Baseline data from 709 patients enrolled in the National Heart, Lung, and Blood Institute Severe Asthma Research Program III (SARP-3) showed that three top risk factors for asthma exacerbations are gastroesophageal reflux disease (relative risk (RR) 1.6), greater blood eosinophil count (RR 1.6), and obesity (RR 1.2) (Am J Resp Care Med. 2017; 195:302-13).
Risk factors for exacerbation noted in various epidemiological studies include African American and Hispanic races, poor access to medical care, inadequate chronic control, smoking, allergen sensitivity to cats and dogs, gastroesophageal reflux disease, high body mass index, sinusitis, and uncontrolled eosinophilic inflammation. Key findings from a follow-up study of SARP-3 patients include the fact that the absence of exacerbations on a 12-month recall predicted future stability.
“More importantly, participants with severe disease and two or more exacerbations at baseline had a 75% chance of having an exacerbation in the following year,” Dr. Jarjour said. “This is a call for us to pay more close attention to these patients and is an important fact to keep in mind when designing clinical trials. A history of exacerbations is the best predictor of future exacerbation.”
Dr. Jarjour disclosed that he has received research funding from the National Heart, Lung, and Blood Institute and consulting fees from AstraZeneca and Teva Pharmaceutical. He is a member of the American Board of Internal Medicine–Pulmonary Exam Subcommittee.
ATLANTA – Asthma exacerbations are common, severe events that can be life-threatening and can accelerate loss of lung function. That’s why it’s important to flag high-risk patients in your clinical practice, Nizar N. Jarjour, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Each year in the United States there are 15 million clinic visits, 2 million ED visits, and 500,000 hospitalizations for severe asthma exacerbations. “These exacerbations cause a high cost on the health care system, they lead to loss of work or school, and they’re a burden to patients and certainly to their families,” said Dr. Jarjour, professor of medicine and division head of allergy, pulmonary and critical care at the University of Wisconsin, Madison.
Factors implicated in asthma exacerbation include air pollution, cigarette smoke, occupational exposure, stress, and allergen exposure, but 50%-85% of cases are related to viral upper respiratory infections. “Any respiratory pathogen can precipitate attacks, but rhinoviruses are the most common,” he said. “Seasonal viral [upper respiratory infections] correlate with hospital admissions for asthma, and peak in spring and fall.”
Purported ways that a viral upper respiratory infection can lead to asthma exacerbation include enhanced airway responsiveness, increased eosinophilic airway inflammation in response to antigen, enhanced lower airway neutrophilic inflammation, and direct infection of the lower airway. “There are is an accentuated eosinophilic inflammation in response to allergen challenge when somebody has a cold,” Dr. Jarjour explained. “But the viral infection can actually directly lead to eosinophilic inflammation, perhaps through TSLP [thymic stromal lymphopoietin], interleukin (IL)-25, and IL-33 simulating the ILC2 (type 2 innate lymphoid cells). So there are both accentuating response to allergens as well as direct enhancement of eosinophilic inflammation following viral infection.”
One study that examined airway lavage following experimental infection found that patients had increased numbers of neutrophils in their airway sample (J Allergy Clin Immunol. 2000;105:1169-77). This means that asthma exacerbation triggers neutrophilic inflammation, which relates to the induction of cytokines and chemokines in the upper airway. “We have also demonstrated increased circulation of G-CSF [granulocyte–colony stimulating factor] and nasal IL-8 in the upper airway related to increased neutrophil recruitment,” Dr. Jarjour said.
Host factors associated with asthma exacerbations include altered innate immune response in the form of a defect in production of antiviral cytokines in response to viral infection, and a greater T helper (Th)2/Th1 ratio. Other factors include eosinophilic inflammation and greater levels of specific IgE to dust mite. Baseline data from 709 patients enrolled in the National Heart, Lung, and Blood Institute Severe Asthma Research Program III (SARP-3) showed that three top risk factors for asthma exacerbations are gastroesophageal reflux disease (relative risk (RR) 1.6), greater blood eosinophil count (RR 1.6), and obesity (RR 1.2) (Am J Resp Care Med. 2017; 195:302-13).
Risk factors for exacerbation noted in various epidemiological studies include African American and Hispanic races, poor access to medical care, inadequate chronic control, smoking, allergen sensitivity to cats and dogs, gastroesophageal reflux disease, high body mass index, sinusitis, and uncontrolled eosinophilic inflammation. Key findings from a follow-up study of SARP-3 patients include the fact that the absence of exacerbations on a 12-month recall predicted future stability.
“More importantly, participants with severe disease and two or more exacerbations at baseline had a 75% chance of having an exacerbation in the following year,” Dr. Jarjour said. “This is a call for us to pay more close attention to these patients and is an important fact to keep in mind when designing clinical trials. A history of exacerbations is the best predictor of future exacerbation.”
Dr. Jarjour disclosed that he has received research funding from the National Heart, Lung, and Blood Institute and consulting fees from AstraZeneca and Teva Pharmaceutical. He is a member of the American Board of Internal Medicine–Pulmonary Exam Subcommittee.
ATLANTA – Asthma exacerbations are common, severe events that can be life-threatening and can accelerate loss of lung function. That’s why it’s important to flag high-risk patients in your clinical practice, Nizar N. Jarjour, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Each year in the United States there are 15 million clinic visits, 2 million ED visits, and 500,000 hospitalizations for severe asthma exacerbations. “These exacerbations cause a high cost on the health care system, they lead to loss of work or school, and they’re a burden to patients and certainly to their families,” said Dr. Jarjour, professor of medicine and division head of allergy, pulmonary and critical care at the University of Wisconsin, Madison.
Factors implicated in asthma exacerbation include air pollution, cigarette smoke, occupational exposure, stress, and allergen exposure, but 50%-85% of cases are related to viral upper respiratory infections. “Any respiratory pathogen can precipitate attacks, but rhinoviruses are the most common,” he said. “Seasonal viral [upper respiratory infections] correlate with hospital admissions for asthma, and peak in spring and fall.”
Purported ways that a viral upper respiratory infection can lead to asthma exacerbation include enhanced airway responsiveness, increased eosinophilic airway inflammation in response to antigen, enhanced lower airway neutrophilic inflammation, and direct infection of the lower airway. “There are is an accentuated eosinophilic inflammation in response to allergen challenge when somebody has a cold,” Dr. Jarjour explained. “But the viral infection can actually directly lead to eosinophilic inflammation, perhaps through TSLP [thymic stromal lymphopoietin], interleukin (IL)-25, and IL-33 simulating the ILC2 (type 2 innate lymphoid cells). So there are both accentuating response to allergens as well as direct enhancement of eosinophilic inflammation following viral infection.”
One study that examined airway lavage following experimental infection found that patients had increased numbers of neutrophils in their airway sample (J Allergy Clin Immunol. 2000;105:1169-77). This means that asthma exacerbation triggers neutrophilic inflammation, which relates to the induction of cytokines and chemokines in the upper airway. “We have also demonstrated increased circulation of G-CSF [granulocyte–colony stimulating factor] and nasal IL-8 in the upper airway related to increased neutrophil recruitment,” Dr. Jarjour said.
Host factors associated with asthma exacerbations include altered innate immune response in the form of a defect in production of antiviral cytokines in response to viral infection, and a greater T helper (Th)2/Th1 ratio. Other factors include eosinophilic inflammation and greater levels of specific IgE to dust mite. Baseline data from 709 patients enrolled in the National Heart, Lung, and Blood Institute Severe Asthma Research Program III (SARP-3) showed that three top risk factors for asthma exacerbations are gastroesophageal reflux disease (relative risk (RR) 1.6), greater blood eosinophil count (RR 1.6), and obesity (RR 1.2) (Am J Resp Care Med. 2017; 195:302-13).
Risk factors for exacerbation noted in various epidemiological studies include African American and Hispanic races, poor access to medical care, inadequate chronic control, smoking, allergen sensitivity to cats and dogs, gastroesophageal reflux disease, high body mass index, sinusitis, and uncontrolled eosinophilic inflammation. Key findings from a follow-up study of SARP-3 patients include the fact that the absence of exacerbations on a 12-month recall predicted future stability.
“More importantly, participants with severe disease and two or more exacerbations at baseline had a 75% chance of having an exacerbation in the following year,” Dr. Jarjour said. “This is a call for us to pay more close attention to these patients and is an important fact to keep in mind when designing clinical trials. A history of exacerbations is the best predictor of future exacerbation.”
Dr. Jarjour disclosed that he has received research funding from the National Heart, Lung, and Blood Institute and consulting fees from AstraZeneca and Teva Pharmaceutical. He is a member of the American Board of Internal Medicine–Pulmonary Exam Subcommittee.
Survey eyes trends in care of severe pediatric asthma
ATLANTA – The treatment of pediatric severe acute asthma has changed over the past 21 years, but interspecialty differences in the management of these patients persist, results from a national survey suggest.
“I think it’s good for every ER and ICU department to have a conversation with providers about what to do when these kinds of patients come in,” lead study author Roua Azmeh, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “A lot of ERs are establishing protocols. I think that’s going to be the wave of the future.”
The National Heart, Blood, and Lung Institute Asthma Guidelines, first published in 1991, were most recently revised in 2007. In an effort to observe changes in asthma management in pediatric EDs and ICUs over the past 21 years, and to compare common management strategies, Dr. Azmeh and her associates distributed a 16-question online survey to 144 current program directors of U.S. training programs in pediatric emergency medicine and pediatric critical care. Results were compared to a similar survey that was sent by snail mail to program directors of U.S. training programs in pediatric emergency medicine and pediatric critical care in 1995.
Dr. Azmeh, a fellow in allergy and immunology at the Saint Louis University, reported results from 62 respondents who completed the 2016 questionnaire (43%). For initial management of pediatric acute severe asthma, a greater proportion of program directors in pediatric critical care reported using parenteral corticosteroids, compared with their counterparts in pediatric emergency medicine (85% vs. 32%, respectively; P less than .0001), as well as continuous beta 2-agonists (73% vs. 56%; P less than .05). A majority of overall respondents (98%) did not use theophylline for initial management, but more program directors in pediatric critical care reported using it for treatment failure, compared with their counterparts in pediatric emergency medicine (56% vs. 20%, respectively; P less than .0071). There was a trend among all respondents for more use of heliox for treatment failure than for initial management (13% vs. 6%).
When the researchers compared current survey responses to responses from the 1995 survey, they observed that program training directors across both specialties increased the use of nebulized ipratropium bromide in initial management and treatment failure (17% vs. 69%; P less than .0001 and 33% vs. 42%; P less than .05) and decreased use of theophylline for initial management of severe acute asthma (17% vs. 3%; P less than .05). However, theophylline is still used in treatment failure.
Among respondents to the 2016 survey, program directors in pediatric emergency medicine were less likely than were those in pediatric critical care to use continuous nebulized beta-2 agonists for initial management or to add parenteral selective beta-2 agonists (56% vs. 73% and 12% vs. 21%, respectively; P less than .05). They also were less likely to use theophylline in treatment failure (20% vs. 56%; P less than .05).
Dr. Azmeh reported having no relevant financial disclosures.
Surveys are interesting to establish a trend for what residents and fellows are being taught in emergency rooms and critical care units. The parenteral steroid use difference for the two groups in 2016 may be related to the fact that the emergency room hasn’t decide
Surveys are interesting to establish a trend for what residents and fellows are being taught in emergency rooms and critical care units. The parenteral steroid use difference for the two groups in 2016 may be related to the fact that the emergency room hasn’t decide
Surveys are interesting to establish a trend for what residents and fellows are being taught in emergency rooms and critical care units. The parenteral steroid use difference for the two groups in 2016 may be related to the fact that the emergency room hasn’t decide
ATLANTA – The treatment of pediatric severe acute asthma has changed over the past 21 years, but interspecialty differences in the management of these patients persist, results from a national survey suggest.
“I think it’s good for every ER and ICU department to have a conversation with providers about what to do when these kinds of patients come in,” lead study author Roua Azmeh, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “A lot of ERs are establishing protocols. I think that’s going to be the wave of the future.”
The National Heart, Blood, and Lung Institute Asthma Guidelines, first published in 1991, were most recently revised in 2007. In an effort to observe changes in asthma management in pediatric EDs and ICUs over the past 21 years, and to compare common management strategies, Dr. Azmeh and her associates distributed a 16-question online survey to 144 current program directors of U.S. training programs in pediatric emergency medicine and pediatric critical care. Results were compared to a similar survey that was sent by snail mail to program directors of U.S. training programs in pediatric emergency medicine and pediatric critical care in 1995.
Dr. Azmeh, a fellow in allergy and immunology at the Saint Louis University, reported results from 62 respondents who completed the 2016 questionnaire (43%). For initial management of pediatric acute severe asthma, a greater proportion of program directors in pediatric critical care reported using parenteral corticosteroids, compared with their counterparts in pediatric emergency medicine (85% vs. 32%, respectively; P less than .0001), as well as continuous beta 2-agonists (73% vs. 56%; P less than .05). A majority of overall respondents (98%) did not use theophylline for initial management, but more program directors in pediatric critical care reported using it for treatment failure, compared with their counterparts in pediatric emergency medicine (56% vs. 20%, respectively; P less than .0071). There was a trend among all respondents for more use of heliox for treatment failure than for initial management (13% vs. 6%).
When the researchers compared current survey responses to responses from the 1995 survey, they observed that program training directors across both specialties increased the use of nebulized ipratropium bromide in initial management and treatment failure (17% vs. 69%; P less than .0001 and 33% vs. 42%; P less than .05) and decreased use of theophylline for initial management of severe acute asthma (17% vs. 3%; P less than .05). However, theophylline is still used in treatment failure.
Among respondents to the 2016 survey, program directors in pediatric emergency medicine were less likely than were those in pediatric critical care to use continuous nebulized beta-2 agonists for initial management or to add parenteral selective beta-2 agonists (56% vs. 73% and 12% vs. 21%, respectively; P less than .05). They also were less likely to use theophylline in treatment failure (20% vs. 56%; P less than .05).
Dr. Azmeh reported having no relevant financial disclosures.
ATLANTA – The treatment of pediatric severe acute asthma has changed over the past 21 years, but interspecialty differences in the management of these patients persist, results from a national survey suggest.
“I think it’s good for every ER and ICU department to have a conversation with providers about what to do when these kinds of patients come in,” lead study author Roua Azmeh, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “A lot of ERs are establishing protocols. I think that’s going to be the wave of the future.”
The National Heart, Blood, and Lung Institute Asthma Guidelines, first published in 1991, were most recently revised in 2007. In an effort to observe changes in asthma management in pediatric EDs and ICUs over the past 21 years, and to compare common management strategies, Dr. Azmeh and her associates distributed a 16-question online survey to 144 current program directors of U.S. training programs in pediatric emergency medicine and pediatric critical care. Results were compared to a similar survey that was sent by snail mail to program directors of U.S. training programs in pediatric emergency medicine and pediatric critical care in 1995.
Dr. Azmeh, a fellow in allergy and immunology at the Saint Louis University, reported results from 62 respondents who completed the 2016 questionnaire (43%). For initial management of pediatric acute severe asthma, a greater proportion of program directors in pediatric critical care reported using parenteral corticosteroids, compared with their counterparts in pediatric emergency medicine (85% vs. 32%, respectively; P less than .0001), as well as continuous beta 2-agonists (73% vs. 56%; P less than .05). A majority of overall respondents (98%) did not use theophylline for initial management, but more program directors in pediatric critical care reported using it for treatment failure, compared with their counterparts in pediatric emergency medicine (56% vs. 20%, respectively; P less than .0071). There was a trend among all respondents for more use of heliox for treatment failure than for initial management (13% vs. 6%).
When the researchers compared current survey responses to responses from the 1995 survey, they observed that program training directors across both specialties increased the use of nebulized ipratropium bromide in initial management and treatment failure (17% vs. 69%; P less than .0001 and 33% vs. 42%; P less than .05) and decreased use of theophylline for initial management of severe acute asthma (17% vs. 3%; P less than .05). However, theophylline is still used in treatment failure.
Among respondents to the 2016 survey, program directors in pediatric emergency medicine were less likely than were those in pediatric critical care to use continuous nebulized beta-2 agonists for initial management or to add parenteral selective beta-2 agonists (56% vs. 73% and 12% vs. 21%, respectively; P less than .05). They also were less likely to use theophylline in treatment failure (20% vs. 56%; P less than .05).
Dr. Azmeh reported having no relevant financial disclosures.
Key clinical point:
Major finding: For initial management of pediatric acute severe asthma, a greater proportion of program directors in pediatric critical care reported using parenteral corticosteroids, compared with their counterparts in pediatric emergency medicine (85% vs. 32%, respectively; P less than .0001).
Data source: Results from a 16-question online survey sent to 144 current program directors of U.S. training programs in pediatric emergency medicine and pediatric critical care.
Disclosures: Dr. Azmeh reported having no relevant financial disclosures.
The many faces of formaldehyde contact allergy
ATLANTA – Formaldehyde has various clinical presentations and variable thresholds to trigger allergic contact dermatitis, so it requires a high index of suspicion, according to Salma de la Feld, MD.
It may present as irritant contact dermatitis, allergic contact dermatitis (especially to the hands and face), airborne allergic contact dermatitis, or systemic allergic contact dermatitis (to aspartame).
From most-releasing to least-releasing, these chemicals include quaternium-15, diazolidinyl urea, DMDM hydantoin, imidazolidinyl urea, and bronopol. Exposure can come from personal care products, prescription topical steroids and acne creams, Brazilian hair keratin, cigarettes, and textiles made of blended fabrics, as well as occupations such as a leather handler, surgical nurse, pathology lab worker, and hairdresser.
“Patients can be allergic to either the formaldehyde that [a product] releases or the non–formaldehyde component or both,” said Dr. de la Feld, who is a dermatologist at Emory University, Atlanta.
Recent studies suggest that the formaldehyde allergen should be tested at 2% instead of at 1%. “You do get a few more irritant reactions [with this approach], but you’re also going to catch more people who have a true positive reaction,” she said. “If you see a borderline papule with a little pink, that might be an irritant. You want to test for the formaldehyde releasers. When you do have a positive reaction, you want to have a high index of suspicion. Patients have to be strict in what personal care products they’re using. Some people might be able to tolerate a low concentration of formaldehyde in some products and that magic number differs between patients.”
From a treatment standpoint, Dr. de la Feld advises patients to avoid all formaldehyde releasers and to wear 100% fabrics in an effort to steer clear of textile exposure. “I like to have people be really strict [in their avoidance] when they’re first starting out,” she said. “They don’t like it, but I’ll say, ‘You’re so itchy. Let’s start really strict to get you clear and better.’ Once they’re better and there’s that one moisturizing cream that they really love, then [you] can do a repeat open application test. If nothing happens, it’s probably safe. If [they] start getting red and itchy there, [they] should probably throw away that moisturizer.”
Fragrance
Fragrance, which was named Allergen of the Year in 2007, is another common contact allergen. An estimated 4%-11% of the worldwide population is allergic to fragrance mix, while 1.6%-10.8% is allergic to balsam of Peru. T.R.U.E. tests for the allergen often yield false-negative results. Clinicians who fail to test for fragrance mix 2 will miss about one-third of fragrance allergic contact dermatitis diagnoses. “If the distribution is scattered, you want to be suspicious for fragrance allergy,” Dr. de la Feld said. “Sometimes patients get exposed inadvertently by their significant other or by a family member who is spraying a fragrant product.” Treatment is avoidance. “You want to tell patients to look for products labeled as fragrance free,” she said. “ ‘Unscented’ does not count. When patients tell you that they’re not using any perfume, you want to ask them if they’ve put any on their clothes.”
Systemic contact dermatitis
Dr. de la Feld finished her presentation by discussing systemic contact dermatitis, which she defined as a rash from systemic exposure to an allergen in someone who was previously sensitized. Alternative names for the condition include endogenous contact eczema, systemically-induced contact dermatitis, and internal-external contact-type hypersensitivity. She acknowledged that not all dermatologists believe systemic contact dermatitis to be a true clinical condition, but she does.
“It’s most classically and commonly reported with nickel and balsam of Peru and more slowly with some other allergens,” she said. “It can have multiple clinical presentations, and it’s not always widespread.” The three most common presentations are dyshidrotic hand eczema, sites of prior contact dermatitis (from contact or patch test), and anogenital and/or flexural areas (Baboon syndrome). There are other reports of systemic contact dermatitis presenting as disseminated patchy dermatitis, generalized erythroderma, cheilitis, and lichen planus of the lip.
Dr. de la Feld reported having no relevant financial disclosures.
Correction, 3/28/17: In an earlier version of this article Dr. de la Feld's name was misstated in the photo caption.
ATLANTA – Formaldehyde has various clinical presentations and variable thresholds to trigger allergic contact dermatitis, so it requires a high index of suspicion, according to Salma de la Feld, MD.
It may present as irritant contact dermatitis, allergic contact dermatitis (especially to the hands and face), airborne allergic contact dermatitis, or systemic allergic contact dermatitis (to aspartame).
From most-releasing to least-releasing, these chemicals include quaternium-15, diazolidinyl urea, DMDM hydantoin, imidazolidinyl urea, and bronopol. Exposure can come from personal care products, prescription topical steroids and acne creams, Brazilian hair keratin, cigarettes, and textiles made of blended fabrics, as well as occupations such as a leather handler, surgical nurse, pathology lab worker, and hairdresser.
“Patients can be allergic to either the formaldehyde that [a product] releases or the non–formaldehyde component or both,” said Dr. de la Feld, who is a dermatologist at Emory University, Atlanta.
Recent studies suggest that the formaldehyde allergen should be tested at 2% instead of at 1%. “You do get a few more irritant reactions [with this approach], but you’re also going to catch more people who have a true positive reaction,” she said. “If you see a borderline papule with a little pink, that might be an irritant. You want to test for the formaldehyde releasers. When you do have a positive reaction, you want to have a high index of suspicion. Patients have to be strict in what personal care products they’re using. Some people might be able to tolerate a low concentration of formaldehyde in some products and that magic number differs between patients.”
From a treatment standpoint, Dr. de la Feld advises patients to avoid all formaldehyde releasers and to wear 100% fabrics in an effort to steer clear of textile exposure. “I like to have people be really strict [in their avoidance] when they’re first starting out,” she said. “They don’t like it, but I’ll say, ‘You’re so itchy. Let’s start really strict to get you clear and better.’ Once they’re better and there’s that one moisturizing cream that they really love, then [you] can do a repeat open application test. If nothing happens, it’s probably safe. If [they] start getting red and itchy there, [they] should probably throw away that moisturizer.”
Fragrance
Fragrance, which was named Allergen of the Year in 2007, is another common contact allergen. An estimated 4%-11% of the worldwide population is allergic to fragrance mix, while 1.6%-10.8% is allergic to balsam of Peru. T.R.U.E. tests for the allergen often yield false-negative results. Clinicians who fail to test for fragrance mix 2 will miss about one-third of fragrance allergic contact dermatitis diagnoses. “If the distribution is scattered, you want to be suspicious for fragrance allergy,” Dr. de la Feld said. “Sometimes patients get exposed inadvertently by their significant other or by a family member who is spraying a fragrant product.” Treatment is avoidance. “You want to tell patients to look for products labeled as fragrance free,” she said. “ ‘Unscented’ does not count. When patients tell you that they’re not using any perfume, you want to ask them if they’ve put any on their clothes.”
Systemic contact dermatitis
Dr. de la Feld finished her presentation by discussing systemic contact dermatitis, which she defined as a rash from systemic exposure to an allergen in someone who was previously sensitized. Alternative names for the condition include endogenous contact eczema, systemically-induced contact dermatitis, and internal-external contact-type hypersensitivity. She acknowledged that not all dermatologists believe systemic contact dermatitis to be a true clinical condition, but she does.
“It’s most classically and commonly reported with nickel and balsam of Peru and more slowly with some other allergens,” she said. “It can have multiple clinical presentations, and it’s not always widespread.” The three most common presentations are dyshidrotic hand eczema, sites of prior contact dermatitis (from contact or patch test), and anogenital and/or flexural areas (Baboon syndrome). There are other reports of systemic contact dermatitis presenting as disseminated patchy dermatitis, generalized erythroderma, cheilitis, and lichen planus of the lip.
Dr. de la Feld reported having no relevant financial disclosures.
Correction, 3/28/17: In an earlier version of this article Dr. de la Feld's name was misstated in the photo caption.
ATLANTA – Formaldehyde has various clinical presentations and variable thresholds to trigger allergic contact dermatitis, so it requires a high index of suspicion, according to Salma de la Feld, MD.
It may present as irritant contact dermatitis, allergic contact dermatitis (especially to the hands and face), airborne allergic contact dermatitis, or systemic allergic contact dermatitis (to aspartame).
From most-releasing to least-releasing, these chemicals include quaternium-15, diazolidinyl urea, DMDM hydantoin, imidazolidinyl urea, and bronopol. Exposure can come from personal care products, prescription topical steroids and acne creams, Brazilian hair keratin, cigarettes, and textiles made of blended fabrics, as well as occupations such as a leather handler, surgical nurse, pathology lab worker, and hairdresser.
“Patients can be allergic to either the formaldehyde that [a product] releases or the non–formaldehyde component or both,” said Dr. de la Feld, who is a dermatologist at Emory University, Atlanta.
Recent studies suggest that the formaldehyde allergen should be tested at 2% instead of at 1%. “You do get a few more irritant reactions [with this approach], but you’re also going to catch more people who have a true positive reaction,” she said. “If you see a borderline papule with a little pink, that might be an irritant. You want to test for the formaldehyde releasers. When you do have a positive reaction, you want to have a high index of suspicion. Patients have to be strict in what personal care products they’re using. Some people might be able to tolerate a low concentration of formaldehyde in some products and that magic number differs between patients.”
From a treatment standpoint, Dr. de la Feld advises patients to avoid all formaldehyde releasers and to wear 100% fabrics in an effort to steer clear of textile exposure. “I like to have people be really strict [in their avoidance] when they’re first starting out,” she said. “They don’t like it, but I’ll say, ‘You’re so itchy. Let’s start really strict to get you clear and better.’ Once they’re better and there’s that one moisturizing cream that they really love, then [you] can do a repeat open application test. If nothing happens, it’s probably safe. If [they] start getting red and itchy there, [they] should probably throw away that moisturizer.”
Fragrance
Fragrance, which was named Allergen of the Year in 2007, is another common contact allergen. An estimated 4%-11% of the worldwide population is allergic to fragrance mix, while 1.6%-10.8% is allergic to balsam of Peru. T.R.U.E. tests for the allergen often yield false-negative results. Clinicians who fail to test for fragrance mix 2 will miss about one-third of fragrance allergic contact dermatitis diagnoses. “If the distribution is scattered, you want to be suspicious for fragrance allergy,” Dr. de la Feld said. “Sometimes patients get exposed inadvertently by their significant other or by a family member who is spraying a fragrant product.” Treatment is avoidance. “You want to tell patients to look for products labeled as fragrance free,” she said. “ ‘Unscented’ does not count. When patients tell you that they’re not using any perfume, you want to ask them if they’ve put any on their clothes.”
Systemic contact dermatitis
Dr. de la Feld finished her presentation by discussing systemic contact dermatitis, which she defined as a rash from systemic exposure to an allergen in someone who was previously sensitized. Alternative names for the condition include endogenous contact eczema, systemically-induced contact dermatitis, and internal-external contact-type hypersensitivity. She acknowledged that not all dermatologists believe systemic contact dermatitis to be a true clinical condition, but she does.
“It’s most classically and commonly reported with nickel and balsam of Peru and more slowly with some other allergens,” she said. “It can have multiple clinical presentations, and it’s not always widespread.” The three most common presentations are dyshidrotic hand eczema, sites of prior contact dermatitis (from contact or patch test), and anogenital and/or flexural areas (Baboon syndrome). There are other reports of systemic contact dermatitis presenting as disseminated patchy dermatitis, generalized erythroderma, cheilitis, and lichen planus of the lip.
Dr. de la Feld reported having no relevant financial disclosures.
Correction, 3/28/17: In an earlier version of this article Dr. de la Feld's name was misstated in the photo caption.
EXPERT ANALYSIS AT THE 2017 AAAAI ANNUAL MEETING
Oral agent found promising for subset of chronic rhinosinusitis patients
ATLANTA – The use of dexpramipexole by patients with chronic rhinosinusitis was well tolerated and showed robust and tissue eosinophil–lowering activity, according to results from a small study.
Dexpramipexole is an investigational oral agent that has been studied in previous clinical trials for patients with amyotrophic lateral sclerosis, Calman Prussin, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. The drug did not meet the clinical endpoint for ALS patients, but its investigators noted that it lowered eosinophil counts by about 50%. “It was a serendipitous finding,” said Dr. Prussin, senior director of clinical and translational medicine for Pittsburgh-based Knopp Biosciences. “We do not have a mechanism of action, but we think it’s working on progenitor cells in the bone marrow.”
In all, 16 of the 20 patients completed the trial. Dr. Prussin and his associates found that the baseline eosinophil count fell from 0.525 x 109/L to 0.031 x 109/L at 6 months, a reduction of 94% (P less than.001). “I don’t think any of us expected to see this,” he said, noting that the drug’s maximal eosinophil-lowering effect was maximal after 2 months. No reduction in total polyp score was observed.
Biopsies conducted in 12 of the patients revealed that polyp tissue eosinophilia was reduced from a mean of 233 to 5 eosinophils/high-powered field, a drop of 97% (P = .001). No serious drug-related adverse effects occurred. The most common adverse event was infection (50%), followed by respiratory symptoms (35%) and gastrointestinal disorders (20%).
Knopp Biosciences funded the study. Dr. Prussin is an employee of the company.
ATLANTA – The use of dexpramipexole by patients with chronic rhinosinusitis was well tolerated and showed robust and tissue eosinophil–lowering activity, according to results from a small study.
Dexpramipexole is an investigational oral agent that has been studied in previous clinical trials for patients with amyotrophic lateral sclerosis, Calman Prussin, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. The drug did not meet the clinical endpoint for ALS patients, but its investigators noted that it lowered eosinophil counts by about 50%. “It was a serendipitous finding,” said Dr. Prussin, senior director of clinical and translational medicine for Pittsburgh-based Knopp Biosciences. “We do not have a mechanism of action, but we think it’s working on progenitor cells in the bone marrow.”
In all, 16 of the 20 patients completed the trial. Dr. Prussin and his associates found that the baseline eosinophil count fell from 0.525 x 109/L to 0.031 x 109/L at 6 months, a reduction of 94% (P less than.001). “I don’t think any of us expected to see this,” he said, noting that the drug’s maximal eosinophil-lowering effect was maximal after 2 months. No reduction in total polyp score was observed.
Biopsies conducted in 12 of the patients revealed that polyp tissue eosinophilia was reduced from a mean of 233 to 5 eosinophils/high-powered field, a drop of 97% (P = .001). No serious drug-related adverse effects occurred. The most common adverse event was infection (50%), followed by respiratory symptoms (35%) and gastrointestinal disorders (20%).
Knopp Biosciences funded the study. Dr. Prussin is an employee of the company.
ATLANTA – The use of dexpramipexole by patients with chronic rhinosinusitis was well tolerated and showed robust and tissue eosinophil–lowering activity, according to results from a small study.
Dexpramipexole is an investigational oral agent that has been studied in previous clinical trials for patients with amyotrophic lateral sclerosis, Calman Prussin, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. The drug did not meet the clinical endpoint for ALS patients, but its investigators noted that it lowered eosinophil counts by about 50%. “It was a serendipitous finding,” said Dr. Prussin, senior director of clinical and translational medicine for Pittsburgh-based Knopp Biosciences. “We do not have a mechanism of action, but we think it’s working on progenitor cells in the bone marrow.”
In all, 16 of the 20 patients completed the trial. Dr. Prussin and his associates found that the baseline eosinophil count fell from 0.525 x 109/L to 0.031 x 109/L at 6 months, a reduction of 94% (P less than.001). “I don’t think any of us expected to see this,” he said, noting that the drug’s maximal eosinophil-lowering effect was maximal after 2 months. No reduction in total polyp score was observed.
Biopsies conducted in 12 of the patients revealed that polyp tissue eosinophilia was reduced from a mean of 233 to 5 eosinophils/high-powered field, a drop of 97% (P = .001). No serious drug-related adverse effects occurred. The most common adverse event was infection (50%), followed by respiratory symptoms (35%) and gastrointestinal disorders (20%).
Knopp Biosciences funded the study. Dr. Prussin is an employee of the company.
AT THE 2017 AAAAI ANNUAL MEETING
Key clinical point:
Major finding: The baseline eosinophil count fell from 0.525 x 109/L to 0.031 x 109/L at 6 months, a reduction of 94% (P less than .001).
Data source: Results from a open-label trial in 16 chronic rhinosinusitis patients who received dexpramipexole 150 mg b.i.d. for 6 months.
Disclosures: Knopp Biosciences funded the study. Dr. Prussin is an employee of the company.
Parental perception of asthma may predict future acute visits
ATLANTA – For low-income and minority children with asthma, parents’ perception of a child’s asthma control may be an important predictor of future acute visits, independent of guideline-based criteria for asthma control, judging from the results from a prospective cohort study.
The National Asthma Education and Prevention Program (NAEPP)–based assessment of asthma control incorporates symptoms, nighttime awakenings, and activity interference; short-acting beta 2-agonist use, lung function, and history of exacerbations, “but it does not take into account parental perceptions of asthma control,” lead study author Suzanne Rossi, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “We also know that parental report of symptom frequency and their perception of their child’s asthma control are frequently discordant.”
In an effort to answer these questions, the researchers conducted a prospective cohort study of 150 Baltimore children aged 5-17 years with persistent asthma who had an exacerbation within the past year. After a baseline assessment, clinic visits occurred every 3 months for 1 year. The predictor variable was parental perception of asthma control assessed by the following question: “Do you believe that your child’s asthma was well controlled within the past 4 weeks?” The primary outcome was an acute visit, defined as an unscheduled visit to a physician or an ED visit or a hospitalization. The researchers used generalized estimating equations to relate parental perception of asthma control to future acute visits.
The mean age of patients was 11 years, 57% were male, 91% were African American, and 85% were on public health insurance. In addition, 15% were overweight and 28% were obese. At baseline, patients were using short-acting beta-2 agonists a mean of 4.2 days every 2 weeks, and 96% had an acute visit in the prior 12 months. Only 9% met criteria for well-controlled asthma as defined by NAEPP criteria, 36% were not well controlled, and 55% were poorly controlled.
At the baseline visit, 73% of parents said that their child’s asthma was well controlled, 20% said that it was not well controlled, and 7% were unsure. Of the 136 children who met NAEPP criteria for uncontrolled asthma, 71% had parents who reported that their child’s asthma was well controlled.
The researchers found that on average, children with parents who report uncontrolled asthma were 2.4-fold times more likely to have an acute visit within the next 3 months, compared with children whose parents reported that their child’s asthma was well controlled. The odds ratio remained similar after adjustment for NAEPP-based asthma control, and for age, gender, race, controller medication, insurance, and atopy. Data on hospitalization was excluded because there was insufficient data for analysis.
Dr. Rossi and her associates also found that parental perception of uncontrolled asthma was a predictor of future acute visits among females but not males (odds ratio, 5.3 vs. OR, 1.3, respectively; P = .03), and among those who were overweight or obese but not among those with a normal BMI (OR, 6.2 vs. OR, 1.3; P = .04). Age was not a modifier. She acknowledged certain limitations of the study, including the inability to measure the severity of asthma exacerbation. “Therefore, this primary outcome may reflect parental concern,” Dr. Rossi said. “In addition, these findings may not be generalizable to other pediatric asthma populations. We also had a small sample size for some outcomes such as hospitalization. In terms of future directions, it would be nice to know whether the findings are replicable in other similar populations and in population-based studies. It would be interesting to examine the association with larger study populations to evaluate hospitalizations and to get an assessment of the severity of symptoms associated with the acute visit.”
The National Institute of Allergy and Infectious Diseases, the National Institute of Environmental Health Sciences, and Johns Hopkins University School of Medicine supported the study. Dr. Rossi reported having no financial disclosures.
ATLANTA – For low-income and minority children with asthma, parents’ perception of a child’s asthma control may be an important predictor of future acute visits, independent of guideline-based criteria for asthma control, judging from the results from a prospective cohort study.
The National Asthma Education and Prevention Program (NAEPP)–based assessment of asthma control incorporates symptoms, nighttime awakenings, and activity interference; short-acting beta 2-agonist use, lung function, and history of exacerbations, “but it does not take into account parental perceptions of asthma control,” lead study author Suzanne Rossi, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “We also know that parental report of symptom frequency and their perception of their child’s asthma control are frequently discordant.”
In an effort to answer these questions, the researchers conducted a prospective cohort study of 150 Baltimore children aged 5-17 years with persistent asthma who had an exacerbation within the past year. After a baseline assessment, clinic visits occurred every 3 months for 1 year. The predictor variable was parental perception of asthma control assessed by the following question: “Do you believe that your child’s asthma was well controlled within the past 4 weeks?” The primary outcome was an acute visit, defined as an unscheduled visit to a physician or an ED visit or a hospitalization. The researchers used generalized estimating equations to relate parental perception of asthma control to future acute visits.
The mean age of patients was 11 years, 57% were male, 91% were African American, and 85% were on public health insurance. In addition, 15% were overweight and 28% were obese. At baseline, patients were using short-acting beta-2 agonists a mean of 4.2 days every 2 weeks, and 96% had an acute visit in the prior 12 months. Only 9% met criteria for well-controlled asthma as defined by NAEPP criteria, 36% were not well controlled, and 55% were poorly controlled.
At the baseline visit, 73% of parents said that their child’s asthma was well controlled, 20% said that it was not well controlled, and 7% were unsure. Of the 136 children who met NAEPP criteria for uncontrolled asthma, 71% had parents who reported that their child’s asthma was well controlled.
The researchers found that on average, children with parents who report uncontrolled asthma were 2.4-fold times more likely to have an acute visit within the next 3 months, compared with children whose parents reported that their child’s asthma was well controlled. The odds ratio remained similar after adjustment for NAEPP-based asthma control, and for age, gender, race, controller medication, insurance, and atopy. Data on hospitalization was excluded because there was insufficient data for analysis.
Dr. Rossi and her associates also found that parental perception of uncontrolled asthma was a predictor of future acute visits among females but not males (odds ratio, 5.3 vs. OR, 1.3, respectively; P = .03), and among those who were overweight or obese but not among those with a normal BMI (OR, 6.2 vs. OR, 1.3; P = .04). Age was not a modifier. She acknowledged certain limitations of the study, including the inability to measure the severity of asthma exacerbation. “Therefore, this primary outcome may reflect parental concern,” Dr. Rossi said. “In addition, these findings may not be generalizable to other pediatric asthma populations. We also had a small sample size for some outcomes such as hospitalization. In terms of future directions, it would be nice to know whether the findings are replicable in other similar populations and in population-based studies. It would be interesting to examine the association with larger study populations to evaluate hospitalizations and to get an assessment of the severity of symptoms associated with the acute visit.”
The National Institute of Allergy and Infectious Diseases, the National Institute of Environmental Health Sciences, and Johns Hopkins University School of Medicine supported the study. Dr. Rossi reported having no financial disclosures.
ATLANTA – For low-income and minority children with asthma, parents’ perception of a child’s asthma control may be an important predictor of future acute visits, independent of guideline-based criteria for asthma control, judging from the results from a prospective cohort study.
The National Asthma Education and Prevention Program (NAEPP)–based assessment of asthma control incorporates symptoms, nighttime awakenings, and activity interference; short-acting beta 2-agonist use, lung function, and history of exacerbations, “but it does not take into account parental perceptions of asthma control,” lead study author Suzanne Rossi, MD, said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “We also know that parental report of symptom frequency and their perception of their child’s asthma control are frequently discordant.”
In an effort to answer these questions, the researchers conducted a prospective cohort study of 150 Baltimore children aged 5-17 years with persistent asthma who had an exacerbation within the past year. After a baseline assessment, clinic visits occurred every 3 months for 1 year. The predictor variable was parental perception of asthma control assessed by the following question: “Do you believe that your child’s asthma was well controlled within the past 4 weeks?” The primary outcome was an acute visit, defined as an unscheduled visit to a physician or an ED visit or a hospitalization. The researchers used generalized estimating equations to relate parental perception of asthma control to future acute visits.
The mean age of patients was 11 years, 57% were male, 91% were African American, and 85% were on public health insurance. In addition, 15% were overweight and 28% were obese. At baseline, patients were using short-acting beta-2 agonists a mean of 4.2 days every 2 weeks, and 96% had an acute visit in the prior 12 months. Only 9% met criteria for well-controlled asthma as defined by NAEPP criteria, 36% were not well controlled, and 55% were poorly controlled.
At the baseline visit, 73% of parents said that their child’s asthma was well controlled, 20% said that it was not well controlled, and 7% were unsure. Of the 136 children who met NAEPP criteria for uncontrolled asthma, 71% had parents who reported that their child’s asthma was well controlled.
The researchers found that on average, children with parents who report uncontrolled asthma were 2.4-fold times more likely to have an acute visit within the next 3 months, compared with children whose parents reported that their child’s asthma was well controlled. The odds ratio remained similar after adjustment for NAEPP-based asthma control, and for age, gender, race, controller medication, insurance, and atopy. Data on hospitalization was excluded because there was insufficient data for analysis.
Dr. Rossi and her associates also found that parental perception of uncontrolled asthma was a predictor of future acute visits among females but not males (odds ratio, 5.3 vs. OR, 1.3, respectively; P = .03), and among those who were overweight or obese but not among those with a normal BMI (OR, 6.2 vs. OR, 1.3; P = .04). Age was not a modifier. She acknowledged certain limitations of the study, including the inability to measure the severity of asthma exacerbation. “Therefore, this primary outcome may reflect parental concern,” Dr. Rossi said. “In addition, these findings may not be generalizable to other pediatric asthma populations. We also had a small sample size for some outcomes such as hospitalization. In terms of future directions, it would be nice to know whether the findings are replicable in other similar populations and in population-based studies. It would be interesting to examine the association with larger study populations to evaluate hospitalizations and to get an assessment of the severity of symptoms associated with the acute visit.”
The National Institute of Allergy and Infectious Diseases, the National Institute of Environmental Health Sciences, and Johns Hopkins University School of Medicine supported the study. Dr. Rossi reported having no financial disclosures.
AT THE 2017 AAAAI ANNUAL MEETING
Key clinical point:
Major finding: Children whose parents reported uncontrolled asthma were 2.4-fold times more likely to have an acute visit within the next 3 months, compared with children whose parents reported that their child’s asthma was well controlled.
Data source: A prospective cohort study of 150 Baltimore children aged 5-17 years with persistent asthma who had an exacerbation within the past year.
Disclosures: The National Institute of Allergy and Infectious Diseases, the National Institute of Environmental Health Sciences, and Johns Hopkins University School of Medicine supported the study. Dr. Rossi reported having no financial disclosures.
Survey finds chronic rhinosinusitis common, burdensome
ATLANTA – Results from a large cross-sectional survey of adults who meet diagnostic symptom criteria for chronic rhinosinusitis (CRS) reveal that most report suffering significant symptoms, high rates of physician visits, and dissatisfaction with current intranasal steroid sprays.
“Chronic rhinosinusitis is common, it’s severe, and people are seeking a lot of medical care,” study author Ramy A. Mahmoud, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “It’s causing a lot of disruption in their lives, and they’re not satisfied with currently available intranasal steroids.”
In an effort to better characterize the prevalence and burden of illness in adults with symptoms of CRS, Dr. Mahmoud and his associates conducted a population-based survey of 10,336 U.S. adults drawn from a representative general panel of 4.3 million. They recruited participants via websites, email, phone, online communities, and social networks and collected information about nasal symptoms, frequency, duration, and severity/bother of nasal symptoms and health care use and treatments.
The researchers found that almost 12% of survey respondents self-reported symptoms that met diagnostic criteria for CRS. Of these, 63.5% were classified as having severe CRS without known nasal polyps (CRSsNP), 27% had moderate CRSsNP, and 9.6% had CRS with known nasal polyps (CRSwNP). In addition, 87%-99% of patients reported seeing a physician for their symptoms and/or taking a prescription medicine for their CRS symptoms in the past year. In fact, 60% of CRSwNP patients, 58% of severe CRSsNP patients, and 33% of moderate CRSsNP patients said they made more than five physician visits in the past year for nose and sinus symptoms.
The frequency of key CRS symptoms was similar in patients with and without nasal polyps, except that those with severe CRSsNP reported higher rates of facial pain/pressure (in the range of 60%-65%) and loss of smell/taste (46%-56%). The most frequently reported core symptoms were nasal congestion (94%-97%) and drainage (89%-92%). Despite currently available treatment options, up to 46% of CRS patients reported that they remain “extremely” affected by symptoms, and 79% of all CRS patients expressed concern about flare-ups. In addition, a large proportion of respondents expressed frustration with the inadequate symptom relief produced by their current intranasal corticosteroid (87% of CRSwNP patients, 86% of severe CRSsNP patients, and 63% of moderate CRSsNP patients).
Dr. Mahmoud said that the findings indicate a role for more and/or improved treatment options to meet the needs of this patient population. “People who have CRS have it pretty bad,” he said. “Very few people are not seeking a lot of medical care for their symptoms.”
The study was funded by OptiNose.
ATLANTA – Results from a large cross-sectional survey of adults who meet diagnostic symptom criteria for chronic rhinosinusitis (CRS) reveal that most report suffering significant symptoms, high rates of physician visits, and dissatisfaction with current intranasal steroid sprays.
“Chronic rhinosinusitis is common, it’s severe, and people are seeking a lot of medical care,” study author Ramy A. Mahmoud, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “It’s causing a lot of disruption in their lives, and they’re not satisfied with currently available intranasal steroids.”
In an effort to better characterize the prevalence and burden of illness in adults with symptoms of CRS, Dr. Mahmoud and his associates conducted a population-based survey of 10,336 U.S. adults drawn from a representative general panel of 4.3 million. They recruited participants via websites, email, phone, online communities, and social networks and collected information about nasal symptoms, frequency, duration, and severity/bother of nasal symptoms and health care use and treatments.
The researchers found that almost 12% of survey respondents self-reported symptoms that met diagnostic criteria for CRS. Of these, 63.5% were classified as having severe CRS without known nasal polyps (CRSsNP), 27% had moderate CRSsNP, and 9.6% had CRS with known nasal polyps (CRSwNP). In addition, 87%-99% of patients reported seeing a physician for their symptoms and/or taking a prescription medicine for their CRS symptoms in the past year. In fact, 60% of CRSwNP patients, 58% of severe CRSsNP patients, and 33% of moderate CRSsNP patients said they made more than five physician visits in the past year for nose and sinus symptoms.
The frequency of key CRS symptoms was similar in patients with and without nasal polyps, except that those with severe CRSsNP reported higher rates of facial pain/pressure (in the range of 60%-65%) and loss of smell/taste (46%-56%). The most frequently reported core symptoms were nasal congestion (94%-97%) and drainage (89%-92%). Despite currently available treatment options, up to 46% of CRS patients reported that they remain “extremely” affected by symptoms, and 79% of all CRS patients expressed concern about flare-ups. In addition, a large proportion of respondents expressed frustration with the inadequate symptom relief produced by their current intranasal corticosteroid (87% of CRSwNP patients, 86% of severe CRSsNP patients, and 63% of moderate CRSsNP patients).
Dr. Mahmoud said that the findings indicate a role for more and/or improved treatment options to meet the needs of this patient population. “People who have CRS have it pretty bad,” he said. “Very few people are not seeking a lot of medical care for their symptoms.”
The study was funded by OptiNose.
ATLANTA – Results from a large cross-sectional survey of adults who meet diagnostic symptom criteria for chronic rhinosinusitis (CRS) reveal that most report suffering significant symptoms, high rates of physician visits, and dissatisfaction with current intranasal steroid sprays.
“Chronic rhinosinusitis is common, it’s severe, and people are seeking a lot of medical care,” study author Ramy A. Mahmoud, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “It’s causing a lot of disruption in their lives, and they’re not satisfied with currently available intranasal steroids.”
In an effort to better characterize the prevalence and burden of illness in adults with symptoms of CRS, Dr. Mahmoud and his associates conducted a population-based survey of 10,336 U.S. adults drawn from a representative general panel of 4.3 million. They recruited participants via websites, email, phone, online communities, and social networks and collected information about nasal symptoms, frequency, duration, and severity/bother of nasal symptoms and health care use and treatments.
The researchers found that almost 12% of survey respondents self-reported symptoms that met diagnostic criteria for CRS. Of these, 63.5% were classified as having severe CRS without known nasal polyps (CRSsNP), 27% had moderate CRSsNP, and 9.6% had CRS with known nasal polyps (CRSwNP). In addition, 87%-99% of patients reported seeing a physician for their symptoms and/or taking a prescription medicine for their CRS symptoms in the past year. In fact, 60% of CRSwNP patients, 58% of severe CRSsNP patients, and 33% of moderate CRSsNP patients said they made more than five physician visits in the past year for nose and sinus symptoms.
The frequency of key CRS symptoms was similar in patients with and without nasal polyps, except that those with severe CRSsNP reported higher rates of facial pain/pressure (in the range of 60%-65%) and loss of smell/taste (46%-56%). The most frequently reported core symptoms were nasal congestion (94%-97%) and drainage (89%-92%). Despite currently available treatment options, up to 46% of CRS patients reported that they remain “extremely” affected by symptoms, and 79% of all CRS patients expressed concern about flare-ups. In addition, a large proportion of respondents expressed frustration with the inadequate symptom relief produced by their current intranasal corticosteroid (87% of CRSwNP patients, 86% of severe CRSsNP patients, and 63% of moderate CRSsNP patients).
Dr. Mahmoud said that the findings indicate a role for more and/or improved treatment options to meet the needs of this patient population. “People who have CRS have it pretty bad,” he said. “Very few people are not seeking a lot of medical care for their symptoms.”
The study was funded by OptiNose.
AT 2017 AAAAI ANNUAL MEETING
Key clinical point:
Major finding: Nearly 12% of survey respondents self-reported symptoms that met diagnostic criteria for CRS.
Data source: A population-based survey of 10,336 US adults drawn from a representative general panel of 4.3 million.
Disclosures: The study was funded by OptiNose.