User login
M. Alexander Otto began his reporting career early in 1999 covering the pharmaceutical industry for a national pharmacists' magazine and freelancing for the Washington Post and other newspapers. He then joined BNA, now part of Bloomberg News, covering health law and the protection of people and animals in medical research. Alex next worked for the McClatchy Company. Based on his work, Alex won a year-long Knight Science Journalism Fellowship to MIT in 2008-2009. He joined the company shortly thereafter. Alex has a newspaper journalism degree from Syracuse (N.Y.) University and a master's degree in medical science -- a physician assistant degree -- from George Washington University. Alex is based in Seattle.
Less pain, quicker discharge with post-TORS dexamethasone
SEATTLE – A longer course of dexamethasone was a bit better than the usual single intraoperative dose for controlling pain and dysphagia after transoral robotic surgery in a randomized trial from the Oregon Health and Science University, Portland.
Thirty-five subjects were randomized to the standard 10-mg intraoperative dexamethasone dose plus 8 mg every 8 hours for up to 4 days; 33 others were randomized to the intraoperative dose plus placebo. All the subjects had transoral robotic surgery (TORS) resection for T1 or T2 oropharyngeal squamous cell carcinoma, either partial pharyngectomy/radical tonsillectomy, base of tongue resection, or both.
The dexamethasone group had significantly less pain on postop day 3 (about 1.5 points less on the 10-point visual analogue scale) and were discharged, on average, a day earlier. They also advanced more quickly toward solid food at 1- and 3-weeks’ follow-up. “They were much more likely to be on a full-soft diet, while the placebo group was mostly still on purees, and just starting into soft foods,” said lead investigator Daniel Clayburgh, MD, a head and neck cancer specialist at the university.
Otherwise, however, the extra dexamethasone wasn’t much help; pain scores were the same in both groups for the first couple days after surgery and at follow-up, and both groups used the same amount of post-op opioids. Other than food tolerance, dysphagia metrics were pretty much the same.
“I was actually anticipating a little bit more of a benefit, but there are potentially some benefits to extended corticosteroid courses after TORS. It’s safe, and well tolerated so long as you screen out diabetes and other problems with hyperglycemia,” as was done in the study, he said. “It does decrease post-op length of stay and may provide a modest decrease in post-op pain, and may slightly accelerate advancement of dietary consistency,” Dr. Clayburgh said at the International Conference on Head and Neck Cancer, held by the American Head and Neck Society.
Although he and his colleagues are mulling over what to do with the findings in light of other initiatives to reduce post-TORS pain, they are now likely to extend dexamethasone courses when significant post-op pain seems likely, and doing so is not otherwise contraindicated, he said.
Intraoperative corticosteroids are now routine for TORS, based on the strength of benefit in the tonsillectomy literature. The team decided to try an extended course because “being rather simple minded surgeons, we thought that if one dose is good, more should be better,” Dr. Clayburgh said.
The dexamethasone group was slightly younger than the placebo group (56 vs. 61 years) but otherwise similar; most were men. In addition to patients with hyperglycemia issues, those with confounders for post-op speech and swallowing recovery were among those excluded from the trial. Subjects required nasogastric feeding tubes for a median of 6.5 days postoperatively, lost a mean of 10 pounds in the first 2 post-op weeks, and were hospitalized for a mean of about 5 days. Dexamethasone was delivered orally or by nasogastric tube.
There was no external funding for the study, and Dr. Clayburgh had no relevant financial disclosures.
SEATTLE – A longer course of dexamethasone was a bit better than the usual single intraoperative dose for controlling pain and dysphagia after transoral robotic surgery in a randomized trial from the Oregon Health and Science University, Portland.
Thirty-five subjects were randomized to the standard 10-mg intraoperative dexamethasone dose plus 8 mg every 8 hours for up to 4 days; 33 others were randomized to the intraoperative dose plus placebo. All the subjects had transoral robotic surgery (TORS) resection for T1 or T2 oropharyngeal squamous cell carcinoma, either partial pharyngectomy/radical tonsillectomy, base of tongue resection, or both.
The dexamethasone group had significantly less pain on postop day 3 (about 1.5 points less on the 10-point visual analogue scale) and were discharged, on average, a day earlier. They also advanced more quickly toward solid food at 1- and 3-weeks’ follow-up. “They were much more likely to be on a full-soft diet, while the placebo group was mostly still on purees, and just starting into soft foods,” said lead investigator Daniel Clayburgh, MD, a head and neck cancer specialist at the university.
Otherwise, however, the extra dexamethasone wasn’t much help; pain scores were the same in both groups for the first couple days after surgery and at follow-up, and both groups used the same amount of post-op opioids. Other than food tolerance, dysphagia metrics were pretty much the same.
“I was actually anticipating a little bit more of a benefit, but there are potentially some benefits to extended corticosteroid courses after TORS. It’s safe, and well tolerated so long as you screen out diabetes and other problems with hyperglycemia,” as was done in the study, he said. “It does decrease post-op length of stay and may provide a modest decrease in post-op pain, and may slightly accelerate advancement of dietary consistency,” Dr. Clayburgh said at the International Conference on Head and Neck Cancer, held by the American Head and Neck Society.
Although he and his colleagues are mulling over what to do with the findings in light of other initiatives to reduce post-TORS pain, they are now likely to extend dexamethasone courses when significant post-op pain seems likely, and doing so is not otherwise contraindicated, he said.
Intraoperative corticosteroids are now routine for TORS, based on the strength of benefit in the tonsillectomy literature. The team decided to try an extended course because “being rather simple minded surgeons, we thought that if one dose is good, more should be better,” Dr. Clayburgh said.
The dexamethasone group was slightly younger than the placebo group (56 vs. 61 years) but otherwise similar; most were men. In addition to patients with hyperglycemia issues, those with confounders for post-op speech and swallowing recovery were among those excluded from the trial. Subjects required nasogastric feeding tubes for a median of 6.5 days postoperatively, lost a mean of 10 pounds in the first 2 post-op weeks, and were hospitalized for a mean of about 5 days. Dexamethasone was delivered orally or by nasogastric tube.
There was no external funding for the study, and Dr. Clayburgh had no relevant financial disclosures.
SEATTLE – A longer course of dexamethasone was a bit better than the usual single intraoperative dose for controlling pain and dysphagia after transoral robotic surgery in a randomized trial from the Oregon Health and Science University, Portland.
Thirty-five subjects were randomized to the standard 10-mg intraoperative dexamethasone dose plus 8 mg every 8 hours for up to 4 days; 33 others were randomized to the intraoperative dose plus placebo. All the subjects had transoral robotic surgery (TORS) resection for T1 or T2 oropharyngeal squamous cell carcinoma, either partial pharyngectomy/radical tonsillectomy, base of tongue resection, or both.
The dexamethasone group had significantly less pain on postop day 3 (about 1.5 points less on the 10-point visual analogue scale) and were discharged, on average, a day earlier. They also advanced more quickly toward solid food at 1- and 3-weeks’ follow-up. “They were much more likely to be on a full-soft diet, while the placebo group was mostly still on purees, and just starting into soft foods,” said lead investigator Daniel Clayburgh, MD, a head and neck cancer specialist at the university.
Otherwise, however, the extra dexamethasone wasn’t much help; pain scores were the same in both groups for the first couple days after surgery and at follow-up, and both groups used the same amount of post-op opioids. Other than food tolerance, dysphagia metrics were pretty much the same.
“I was actually anticipating a little bit more of a benefit, but there are potentially some benefits to extended corticosteroid courses after TORS. It’s safe, and well tolerated so long as you screen out diabetes and other problems with hyperglycemia,” as was done in the study, he said. “It does decrease post-op length of stay and may provide a modest decrease in post-op pain, and may slightly accelerate advancement of dietary consistency,” Dr. Clayburgh said at the International Conference on Head and Neck Cancer, held by the American Head and Neck Society.
Although he and his colleagues are mulling over what to do with the findings in light of other initiatives to reduce post-TORS pain, they are now likely to extend dexamethasone courses when significant post-op pain seems likely, and doing so is not otherwise contraindicated, he said.
Intraoperative corticosteroids are now routine for TORS, based on the strength of benefit in the tonsillectomy literature. The team decided to try an extended course because “being rather simple minded surgeons, we thought that if one dose is good, more should be better,” Dr. Clayburgh said.
The dexamethasone group was slightly younger than the placebo group (56 vs. 61 years) but otherwise similar; most were men. In addition to patients with hyperglycemia issues, those with confounders for post-op speech and swallowing recovery were among those excluded from the trial. Subjects required nasogastric feeding tubes for a median of 6.5 days postoperatively, lost a mean of 10 pounds in the first 2 post-op weeks, and were hospitalized for a mean of about 5 days. Dexamethasone was delivered orally or by nasogastric tube.
There was no external funding for the study, and Dr. Clayburgh had no relevant financial disclosures.
AT AHNS 2016
Key clinical point: A longer course of dexamethasone is a bit better than the usual single intraoperative dose for controlling pain and dysphagia after transoral robotic surgery.
Major finding: The dexamethasone group had significantly less pain on post-op day 3 (about 1.5 points less on the 10-point visual analogue scale) and were discharged, on average, a day earlier. They also advanced more quickly toward solid food at 1- and 3-weeks’ follow-up.
Data source: A randomized trial of 68 TORS patients.
Disclosures: There was no external funding for the study, and the lead investigator had no relevant financial disclosures.
Donor NK cells elicited complete remissions in four of nine AML patients
Four of nine acute myeloid leukemia patients went into complete remission – and a fifth responded – after being transfused with donor natural killer cells in a phase I study from Washington University in St. Louis.
The natural killer (NK) cells had been differentiated into “memorylike” NK cells by brief exposure to interleukin (IL) 12, 15, and 18 prior to transfusion. Although NK cells have traditionally been considered part of the innate immune system, it’s become clear recently that they have some adaptive abilities. The cytokine exposure in the St. Louis study seemed, in a sense, to train NK cells to remember and attack acute myeloid leukemia (AML).
The treated cells had enhanced interferon gamma production and cytotoxicity against AML cells in vitro. Once in the patients, they “proliferated extensively” and demonstrated robust responses against leukemia targets. Preactivation of NK cells with IL-12, IL-15, and IL-18 promotes “potent antileukemia functionality in vitro and in vivo and thus represent[s] a promising immunotherapy strategy for AML,” said investigators led by Rizwan Romee, MD, of the oncology division and clinical director of the haploidentical transplant program at Washington University (Sci Transl Med. 2016 Sep. 21. doi: 10.1126/scitranslmed.aaf2341).
NK cell therapy is an emerging treatment for AML, but it’s been unclear, at least until now, how best to maximize the cells’ anti-AML effect before transfer.
Prior studies have tried IL-2 or IL-15 overnight, which does increase NK cell functional capacity, but the effect is rapidly lost after transfer into patients.
That didn’t seem to be much of a problem when NK cells were differentiated into memorylike cells. “The longer-lasting increase in functional capacity ... combined with improved AML recognition, [enhanced] in vivo expansion and antileukemia responses, result[ed] in a several week ‘window of opportunity’ to attack AML blasts.” the authors said.
For safety, the initial cell dose was a tenth or twentieth of the typical adoptive NK cell dose. Even so, the memorylike cells consistently expanded to become greater than 90% of blood and most of bone marrow NK cells, which was “remarkable,” they said.
The National Cancer Institute and others funded the work. The authors had no disclosures.
Four of nine acute myeloid leukemia patients went into complete remission – and a fifth responded – after being transfused with donor natural killer cells in a phase I study from Washington University in St. Louis.
The natural killer (NK) cells had been differentiated into “memorylike” NK cells by brief exposure to interleukin (IL) 12, 15, and 18 prior to transfusion. Although NK cells have traditionally been considered part of the innate immune system, it’s become clear recently that they have some adaptive abilities. The cytokine exposure in the St. Louis study seemed, in a sense, to train NK cells to remember and attack acute myeloid leukemia (AML).
The treated cells had enhanced interferon gamma production and cytotoxicity against AML cells in vitro. Once in the patients, they “proliferated extensively” and demonstrated robust responses against leukemia targets. Preactivation of NK cells with IL-12, IL-15, and IL-18 promotes “potent antileukemia functionality in vitro and in vivo and thus represent[s] a promising immunotherapy strategy for AML,” said investigators led by Rizwan Romee, MD, of the oncology division and clinical director of the haploidentical transplant program at Washington University (Sci Transl Med. 2016 Sep. 21. doi: 10.1126/scitranslmed.aaf2341).
NK cell therapy is an emerging treatment for AML, but it’s been unclear, at least until now, how best to maximize the cells’ anti-AML effect before transfer.
Prior studies have tried IL-2 or IL-15 overnight, which does increase NK cell functional capacity, but the effect is rapidly lost after transfer into patients.
That didn’t seem to be much of a problem when NK cells were differentiated into memorylike cells. “The longer-lasting increase in functional capacity ... combined with improved AML recognition, [enhanced] in vivo expansion and antileukemia responses, result[ed] in a several week ‘window of opportunity’ to attack AML blasts.” the authors said.
For safety, the initial cell dose was a tenth or twentieth of the typical adoptive NK cell dose. Even so, the memorylike cells consistently expanded to become greater than 90% of blood and most of bone marrow NK cells, which was “remarkable,” they said.
The National Cancer Institute and others funded the work. The authors had no disclosures.
Four of nine acute myeloid leukemia patients went into complete remission – and a fifth responded – after being transfused with donor natural killer cells in a phase I study from Washington University in St. Louis.
The natural killer (NK) cells had been differentiated into “memorylike” NK cells by brief exposure to interleukin (IL) 12, 15, and 18 prior to transfusion. Although NK cells have traditionally been considered part of the innate immune system, it’s become clear recently that they have some adaptive abilities. The cytokine exposure in the St. Louis study seemed, in a sense, to train NK cells to remember and attack acute myeloid leukemia (AML).
The treated cells had enhanced interferon gamma production and cytotoxicity against AML cells in vitro. Once in the patients, they “proliferated extensively” and demonstrated robust responses against leukemia targets. Preactivation of NK cells with IL-12, IL-15, and IL-18 promotes “potent antileukemia functionality in vitro and in vivo and thus represent[s] a promising immunotherapy strategy for AML,” said investigators led by Rizwan Romee, MD, of the oncology division and clinical director of the haploidentical transplant program at Washington University (Sci Transl Med. 2016 Sep. 21. doi: 10.1126/scitranslmed.aaf2341).
NK cell therapy is an emerging treatment for AML, but it’s been unclear, at least until now, how best to maximize the cells’ anti-AML effect before transfer.
Prior studies have tried IL-2 or IL-15 overnight, which does increase NK cell functional capacity, but the effect is rapidly lost after transfer into patients.
That didn’t seem to be much of a problem when NK cells were differentiated into memorylike cells. “The longer-lasting increase in functional capacity ... combined with improved AML recognition, [enhanced] in vivo expansion and antileukemia responses, result[ed] in a several week ‘window of opportunity’ to attack AML blasts.” the authors said.
For safety, the initial cell dose was a tenth or twentieth of the typical adoptive NK cell dose. Even so, the memorylike cells consistently expanded to become greater than 90% of blood and most of bone marrow NK cells, which was “remarkable,” they said.
The National Cancer Institute and others funded the work. The authors had no disclosures.
FROM SCIENCE TRANSLATIONAL MEDICINE
Endobariatrics: Coming to a clinic near you
SAN DIEGO – Device companies are working hard to bring obesity management to the endoscopy suite.
The field is called endobariatrics, and its goal is to fill the gap between surgery and pharmacotherapy. Drugs and lifestyle counseling don’t work for all patients, but many patients resist having surgery. These devices are meant to fill the need for nonsurgical, “noninvasive” solutions to obesity management.
Endobariatrics has the potential to be a boon for both obese patients and gastroenterology practices. Surgeons, however, approach these innovations with caution, due in part to past experiences of rescuing patients with failed devices. “Some innovations get disseminated without adequate studies to demonstrate whether they are superior, or even equal in efficacy and safety to, well-established procedures for the same condition. Even when they have been conducted, negative studies showing no difference may end up being rejected by journals and not published,” noted Karen Deveney, MD, FACS, professor of surgery, vice-chair for education in the department of surgery at Oregon Health & Science University, Portland, and co-Editor of ACS Surgery News.
Several new investigational devices and approaches were showcased at the annual Digestive Disease Week; some “are beginning to approach the kind of results we see with surgical techniques,” said Steven Edmundowicz, MD, medical director of the University of Colorado Digestive Health Center, Aurora.
“We are seeing a tremendous amount of development in this space, but it’s early, and we have to be cautious,” he said. There have already been a few disappointments, including the EndoBarrier, a fluoropolymer liner anchored in the duodenal bulb and unfurled down the duodenum to block food absorption. A key U.S. trial was recently halted due to liver abscesses.
Dr. Edmundowicz reviewed the latest developments presented at DDW.Self-assembling magnets for dual-path enteral anastomoses
The goal of the GI Windows system is to create a partial jejunoileal, side to side bypass without surgery. A 28-mm magnet ring is introduced to the ileum by colonoscopy, and a second ring to the jejunum by endoscopy. The rings snap together and tissue caught between them dies from pressure necrosis, leaving patients with a jejunoileal communication. Once food reaches that point, it either diverts through the anastomosis or continues past it down the digestive track. The magnets pass after the anastomosis forms in a week or so.
In a 6-month feasibility study from the Czech Republic, 10 obese patients lost 28.3% of their excess weight without diet restrictions. Those with diabetes had a mean hemoglobin A1c drop of 1.8%, and normalization of fasting blood glucose levels. The procedure took just over an hour and a half after the first five cases.
“I am very excited about [this]; I really want to see where the data are going,” Dr. Edmundowicz said.
Duodenal mucosal resurfacing
The idea of the Revita System (Fractyl) is to ablate “diabetic mucosa” in the duodenum so that normal mucosa can replace it. Saline is injected endoscopically under a portion of the duodenal mucosa to lift it off the muscularis; once isolated, the mucosa is destroyed – some in the audience thought “cooked” was a better word – by exposure to a hot water balloon catheter threaded into the lumen.
Thirty-nine overweight or obese type 2 diabetics had a 1.2% improvement at 6 months from a baseline hemoglobin A1c of 9.6% in a series from Santiago, Chile. Weight loss was modest in the trial; the system is being developed for type 2 diabetics.
There is some histologic support for the notion of a diabetic mucosa with both structural and hormonal aberrations, but it’s unclear if it’s a sign or cause of sickness. Even so, “the mucosa regenerates” and won’t be diabetic “for a while” after the procedure, said investigator Manoel Galvao Neto, MD, of the Gastro Obeso Center, São Paulo.
Gastric balloons
Inflating a balloon in the stomach to make people feel full isn’t new, but the notion of putting the balloon into a capsule that patients can swallow and inflating it through a tether is a more recent notion.
The Obalon Therapeutics is one such device. In an unblinded, sham-controlled trial with 336 obese patients, subjects who got the 250-mL, nitrogen-filled Obalons – most received three – lost about 3% more of their total body weight at 24 weeks than those who did not. Although swallowed, Obalon is removed endoscopically. Meanwhile, 34 obese patients who swallowed the 550-mL, fluid-filled Elipse balloon (Allurion) had a total body weight loss of 9.5% and mean excess weight loss of 37.2% at 4 months, by which time Elipse deflates on its own and passes without endoscopic retrieval.
“This is a very promising approach. I am very excited about digested balloons,” said Dr. Edmundowicz, an investigator in the Obalon study.
Endoscopic sleeve gastroplasty
Endoscopic sleeve gastroplasty duplicates sleeve gastrectomy with stitches placed endoscopically to seal off the greater curvature of the stomach; functionally, patients are left with a narrow sleeve of a stomach. In a multicenter series presented at DDW, 242 patients had a mean total body weight loss of 19.8% at 18 months, with a low incidence of complications. “Weight loss appears to be continuing,” Dr. Edmundowicz said. Investigators used the Apollo OverStitch (Apollo Endosurgery) to place the sutures.
Aspiration therapy
With Food and Drug Administration approval on June 14, AspireAssist (Aspire Bariatrics) is probably the best known of the newer approaches. Patients drain a portion of their meals through an endoscopically placed percutaneous gastrostomy tube a half hour or so after eating. It takes 5-10 minutes. The agency is eager to keep it out of the hands of bulimics.
One-year data were reported at DDW; 111 obese AspireAssist subjects lost a mean of 37.2% of their excess weight versus 13% in 60 patients randomized to lifestyle counseling alone.
“It may not be aesthetically pleasing, but it certainly works. It’s a viable technology,” said Dr. Edmundowicz, who was an investigator.
The studies were funded by companies developing the devices and techniques. Dr. Edmundowicz has stock options, or is a consultant or researcher, Aspire, Obalon, GI Dynamics, Elira, and other firms.
Caveat emptor, all over again
Although many of these innovations will eventually achieve acceptable clinical results in trials and be adopted by both gastroenterologists and surgeons, a note of caution is in order, argues Tyler G. Hughes, MD, FACS, is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, coeditor of ACS Surgery News.
“The recent uptick in ‘non-surgical’ obesity treatment reverberates as history gets ready to repeat itself. If surgeons don’t take the lead, two things are likely to happen. First, ‘interventionists,’ ignorant of the lessons of yesterday will introduce foreign bodies into the soft GI tract only to see these ‘safe’ devices create surgical havoc or malabsorptive disasters. Second, instead of doing a complete spectrum of obesity procedures, surgeons will be left with the worst cases and fixing complications while the ‘interventionist’ (and I do not limit that to gastroenterologists) do the easy cases at prices three times the cost of the old way. Will this really benefit the patients?
Rather than permitting a race to the newest unproven device to satisfy public clamor, while conveniently making a tidy profit for anyone able to claim the title ‘interventionist,’ bariatric surgeons need to grab the endoscope with both hands and do the research and reporting for these new procedures. It starts with the need for every surgical resident to be proficient with the GI endoscopes and ends with surgeons seeing surgery in a wider view than through an incision,” Dr. Hughes said.
SAN DIEGO – Device companies are working hard to bring obesity management to the endoscopy suite.
The field is called endobariatrics, and its goal is to fill the gap between surgery and pharmacotherapy. Drugs and lifestyle counseling don’t work for all patients, but many patients resist having surgery. These devices are meant to fill the need for nonsurgical, “noninvasive” solutions to obesity management.
Endobariatrics has the potential to be a boon for both obese patients and gastroenterology practices. Surgeons, however, approach these innovations with caution, due in part to past experiences of rescuing patients with failed devices. “Some innovations get disseminated without adequate studies to demonstrate whether they are superior, or even equal in efficacy and safety to, well-established procedures for the same condition. Even when they have been conducted, negative studies showing no difference may end up being rejected by journals and not published,” noted Karen Deveney, MD, FACS, professor of surgery, vice-chair for education in the department of surgery at Oregon Health & Science University, Portland, and co-Editor of ACS Surgery News.
Several new investigational devices and approaches were showcased at the annual Digestive Disease Week; some “are beginning to approach the kind of results we see with surgical techniques,” said Steven Edmundowicz, MD, medical director of the University of Colorado Digestive Health Center, Aurora.
“We are seeing a tremendous amount of development in this space, but it’s early, and we have to be cautious,” he said. There have already been a few disappointments, including the EndoBarrier, a fluoropolymer liner anchored in the duodenal bulb and unfurled down the duodenum to block food absorption. A key U.S. trial was recently halted due to liver abscesses.
Dr. Edmundowicz reviewed the latest developments presented at DDW.Self-assembling magnets for dual-path enteral anastomoses
The goal of the GI Windows system is to create a partial jejunoileal, side to side bypass without surgery. A 28-mm magnet ring is introduced to the ileum by colonoscopy, and a second ring to the jejunum by endoscopy. The rings snap together and tissue caught between them dies from pressure necrosis, leaving patients with a jejunoileal communication. Once food reaches that point, it either diverts through the anastomosis or continues past it down the digestive track. The magnets pass after the anastomosis forms in a week or so.
In a 6-month feasibility study from the Czech Republic, 10 obese patients lost 28.3% of their excess weight without diet restrictions. Those with diabetes had a mean hemoglobin A1c drop of 1.8%, and normalization of fasting blood glucose levels. The procedure took just over an hour and a half after the first five cases.
“I am very excited about [this]; I really want to see where the data are going,” Dr. Edmundowicz said.
Duodenal mucosal resurfacing
The idea of the Revita System (Fractyl) is to ablate “diabetic mucosa” in the duodenum so that normal mucosa can replace it. Saline is injected endoscopically under a portion of the duodenal mucosa to lift it off the muscularis; once isolated, the mucosa is destroyed – some in the audience thought “cooked” was a better word – by exposure to a hot water balloon catheter threaded into the lumen.
Thirty-nine overweight or obese type 2 diabetics had a 1.2% improvement at 6 months from a baseline hemoglobin A1c of 9.6% in a series from Santiago, Chile. Weight loss was modest in the trial; the system is being developed for type 2 diabetics.
There is some histologic support for the notion of a diabetic mucosa with both structural and hormonal aberrations, but it’s unclear if it’s a sign or cause of sickness. Even so, “the mucosa regenerates” and won’t be diabetic “for a while” after the procedure, said investigator Manoel Galvao Neto, MD, of the Gastro Obeso Center, São Paulo.
Gastric balloons
Inflating a balloon in the stomach to make people feel full isn’t new, but the notion of putting the balloon into a capsule that patients can swallow and inflating it through a tether is a more recent notion.
The Obalon Therapeutics is one such device. In an unblinded, sham-controlled trial with 336 obese patients, subjects who got the 250-mL, nitrogen-filled Obalons – most received three – lost about 3% more of their total body weight at 24 weeks than those who did not. Although swallowed, Obalon is removed endoscopically. Meanwhile, 34 obese patients who swallowed the 550-mL, fluid-filled Elipse balloon (Allurion) had a total body weight loss of 9.5% and mean excess weight loss of 37.2% at 4 months, by which time Elipse deflates on its own and passes without endoscopic retrieval.
“This is a very promising approach. I am very excited about digested balloons,” said Dr. Edmundowicz, an investigator in the Obalon study.
Endoscopic sleeve gastroplasty
Endoscopic sleeve gastroplasty duplicates sleeve gastrectomy with stitches placed endoscopically to seal off the greater curvature of the stomach; functionally, patients are left with a narrow sleeve of a stomach. In a multicenter series presented at DDW, 242 patients had a mean total body weight loss of 19.8% at 18 months, with a low incidence of complications. “Weight loss appears to be continuing,” Dr. Edmundowicz said. Investigators used the Apollo OverStitch (Apollo Endosurgery) to place the sutures.
Aspiration therapy
With Food and Drug Administration approval on June 14, AspireAssist (Aspire Bariatrics) is probably the best known of the newer approaches. Patients drain a portion of their meals through an endoscopically placed percutaneous gastrostomy tube a half hour or so after eating. It takes 5-10 minutes. The agency is eager to keep it out of the hands of bulimics.
One-year data were reported at DDW; 111 obese AspireAssist subjects lost a mean of 37.2% of their excess weight versus 13% in 60 patients randomized to lifestyle counseling alone.
“It may not be aesthetically pleasing, but it certainly works. It’s a viable technology,” said Dr. Edmundowicz, who was an investigator.
The studies were funded by companies developing the devices and techniques. Dr. Edmundowicz has stock options, or is a consultant or researcher, Aspire, Obalon, GI Dynamics, Elira, and other firms.
Caveat emptor, all over again
Although many of these innovations will eventually achieve acceptable clinical results in trials and be adopted by both gastroenterologists and surgeons, a note of caution is in order, argues Tyler G. Hughes, MD, FACS, is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, coeditor of ACS Surgery News.
“The recent uptick in ‘non-surgical’ obesity treatment reverberates as history gets ready to repeat itself. If surgeons don’t take the lead, two things are likely to happen. First, ‘interventionists,’ ignorant of the lessons of yesterday will introduce foreign bodies into the soft GI tract only to see these ‘safe’ devices create surgical havoc or malabsorptive disasters. Second, instead of doing a complete spectrum of obesity procedures, surgeons will be left with the worst cases and fixing complications while the ‘interventionist’ (and I do not limit that to gastroenterologists) do the easy cases at prices three times the cost of the old way. Will this really benefit the patients?
Rather than permitting a race to the newest unproven device to satisfy public clamor, while conveniently making a tidy profit for anyone able to claim the title ‘interventionist,’ bariatric surgeons need to grab the endoscope with both hands and do the research and reporting for these new procedures. It starts with the need for every surgical resident to be proficient with the GI endoscopes and ends with surgeons seeing surgery in a wider view than through an incision,” Dr. Hughes said.
SAN DIEGO – Device companies are working hard to bring obesity management to the endoscopy suite.
The field is called endobariatrics, and its goal is to fill the gap between surgery and pharmacotherapy. Drugs and lifestyle counseling don’t work for all patients, but many patients resist having surgery. These devices are meant to fill the need for nonsurgical, “noninvasive” solutions to obesity management.
Endobariatrics has the potential to be a boon for both obese patients and gastroenterology practices. Surgeons, however, approach these innovations with caution, due in part to past experiences of rescuing patients with failed devices. “Some innovations get disseminated without adequate studies to demonstrate whether they are superior, or even equal in efficacy and safety to, well-established procedures for the same condition. Even when they have been conducted, negative studies showing no difference may end up being rejected by journals and not published,” noted Karen Deveney, MD, FACS, professor of surgery, vice-chair for education in the department of surgery at Oregon Health & Science University, Portland, and co-Editor of ACS Surgery News.
Several new investigational devices and approaches were showcased at the annual Digestive Disease Week; some “are beginning to approach the kind of results we see with surgical techniques,” said Steven Edmundowicz, MD, medical director of the University of Colorado Digestive Health Center, Aurora.
“We are seeing a tremendous amount of development in this space, but it’s early, and we have to be cautious,” he said. There have already been a few disappointments, including the EndoBarrier, a fluoropolymer liner anchored in the duodenal bulb and unfurled down the duodenum to block food absorption. A key U.S. trial was recently halted due to liver abscesses.
Dr. Edmundowicz reviewed the latest developments presented at DDW.Self-assembling magnets for dual-path enteral anastomoses
The goal of the GI Windows system is to create a partial jejunoileal, side to side bypass without surgery. A 28-mm magnet ring is introduced to the ileum by colonoscopy, and a second ring to the jejunum by endoscopy. The rings snap together and tissue caught between them dies from pressure necrosis, leaving patients with a jejunoileal communication. Once food reaches that point, it either diverts through the anastomosis or continues past it down the digestive track. The magnets pass after the anastomosis forms in a week or so.
In a 6-month feasibility study from the Czech Republic, 10 obese patients lost 28.3% of their excess weight without diet restrictions. Those with diabetes had a mean hemoglobin A1c drop of 1.8%, and normalization of fasting blood glucose levels. The procedure took just over an hour and a half after the first five cases.
“I am very excited about [this]; I really want to see where the data are going,” Dr. Edmundowicz said.
Duodenal mucosal resurfacing
The idea of the Revita System (Fractyl) is to ablate “diabetic mucosa” in the duodenum so that normal mucosa can replace it. Saline is injected endoscopically under a portion of the duodenal mucosa to lift it off the muscularis; once isolated, the mucosa is destroyed – some in the audience thought “cooked” was a better word – by exposure to a hot water balloon catheter threaded into the lumen.
Thirty-nine overweight or obese type 2 diabetics had a 1.2% improvement at 6 months from a baseline hemoglobin A1c of 9.6% in a series from Santiago, Chile. Weight loss was modest in the trial; the system is being developed for type 2 diabetics.
There is some histologic support for the notion of a diabetic mucosa with both structural and hormonal aberrations, but it’s unclear if it’s a sign or cause of sickness. Even so, “the mucosa regenerates” and won’t be diabetic “for a while” after the procedure, said investigator Manoel Galvao Neto, MD, of the Gastro Obeso Center, São Paulo.
Gastric balloons
Inflating a balloon in the stomach to make people feel full isn’t new, but the notion of putting the balloon into a capsule that patients can swallow and inflating it through a tether is a more recent notion.
The Obalon Therapeutics is one such device. In an unblinded, sham-controlled trial with 336 obese patients, subjects who got the 250-mL, nitrogen-filled Obalons – most received three – lost about 3% more of their total body weight at 24 weeks than those who did not. Although swallowed, Obalon is removed endoscopically. Meanwhile, 34 obese patients who swallowed the 550-mL, fluid-filled Elipse balloon (Allurion) had a total body weight loss of 9.5% and mean excess weight loss of 37.2% at 4 months, by which time Elipse deflates on its own and passes without endoscopic retrieval.
“This is a very promising approach. I am very excited about digested balloons,” said Dr. Edmundowicz, an investigator in the Obalon study.
Endoscopic sleeve gastroplasty
Endoscopic sleeve gastroplasty duplicates sleeve gastrectomy with stitches placed endoscopically to seal off the greater curvature of the stomach; functionally, patients are left with a narrow sleeve of a stomach. In a multicenter series presented at DDW, 242 patients had a mean total body weight loss of 19.8% at 18 months, with a low incidence of complications. “Weight loss appears to be continuing,” Dr. Edmundowicz said. Investigators used the Apollo OverStitch (Apollo Endosurgery) to place the sutures.
Aspiration therapy
With Food and Drug Administration approval on June 14, AspireAssist (Aspire Bariatrics) is probably the best known of the newer approaches. Patients drain a portion of their meals through an endoscopically placed percutaneous gastrostomy tube a half hour or so after eating. It takes 5-10 minutes. The agency is eager to keep it out of the hands of bulimics.
One-year data were reported at DDW; 111 obese AspireAssist subjects lost a mean of 37.2% of their excess weight versus 13% in 60 patients randomized to lifestyle counseling alone.
“It may not be aesthetically pleasing, but it certainly works. It’s a viable technology,” said Dr. Edmundowicz, who was an investigator.
The studies were funded by companies developing the devices and techniques. Dr. Edmundowicz has stock options, or is a consultant or researcher, Aspire, Obalon, GI Dynamics, Elira, and other firms.
Caveat emptor, all over again
Although many of these innovations will eventually achieve acceptable clinical results in trials and be adopted by both gastroenterologists and surgeons, a note of caution is in order, argues Tyler G. Hughes, MD, FACS, is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, coeditor of ACS Surgery News.
“The recent uptick in ‘non-surgical’ obesity treatment reverberates as history gets ready to repeat itself. If surgeons don’t take the lead, two things are likely to happen. First, ‘interventionists,’ ignorant of the lessons of yesterday will introduce foreign bodies into the soft GI tract only to see these ‘safe’ devices create surgical havoc or malabsorptive disasters. Second, instead of doing a complete spectrum of obesity procedures, surgeons will be left with the worst cases and fixing complications while the ‘interventionist’ (and I do not limit that to gastroenterologists) do the easy cases at prices three times the cost of the old way. Will this really benefit the patients?
Rather than permitting a race to the newest unproven device to satisfy public clamor, while conveniently making a tidy profit for anyone able to claim the title ‘interventionist,’ bariatric surgeons need to grab the endoscope with both hands and do the research and reporting for these new procedures. It starts with the need for every surgical resident to be proficient with the GI endoscopes and ends with surgeons seeing surgery in a wider view than through an incision,” Dr. Hughes said.
AT DDW 2016
September 2016: Click for Credit
Here are 5 articles in the August issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Women With BRCA1 Mutations at Higher Risk for Endometrial Cancers
To take the posttest, go to: http://bit.ly/2t6SPIY
Expires June 30, 2017
VITALSKey clinical point: Clinicians may wish to discuss the option of hysterectomy at the time of salpingo-oophorectomy in women with deleterious BRCA1 mutations.
Major finding: Among women with BRCA1 but not BRCA2 mutations there was increased risk for serous/serous-like endometrial carcinomas.
Data source: Prospective multicenter follow-up study of 1,083 women with BRCA mutations who underwent salpingo-oophorectomy without hysterectomy.
Disclosures: The study was supported by grants from the Department of Defense, National Institutes of Health, and public and private foundations. Coauthor Robert Soslow, MD, disclosed consulting for EMD Serono. No others reported conflicts of interest. The editorialists reported no conflicts of interest related to the study.
2. Cochrane Review: Topical Steroid—Vitamin D Combo Best for Scalp Psoriasis
To take the posttest, go to: http://bit.ly/2sIyLNI
Expires July 14, 2017
VITALSKey clinical point: The combination of a topical steroid and topical vitamin D is marginally better but with a similar safety profile to steroids alone as a treatment for psoriasis on the scalp.
Major finding: The combination of a topical steroid and vitamin D showed a small but statistically significant advantage over steroids alone, and a greater advantage over vitamin D alone.
Data source: A systematic review of 59 randomized controlled studies in 11,561 patients.
Disclosures: The study was supported by the Universidade Federal de São Paulo, Brazil; the Universidade Federal do Rio Grande do Norte, Brazil; and the National Institute for Health Research, United Kingdom. Six authors and one clinical referee declared speakers' fees, research grants, and funding from the pharmaceutical industry. One author had no conflicts of interest to disclose.
3. Study Finds Emergence of Azithromycin-resistant Gonorrhea
To take the posttest, go to: http://bit.ly/2u1nMmb
Expires July 16, 2017
VITALSKey clinical point:Resistance to azithromycin is emerging among patients diagnosed with gonorrhea.
Major finding: Among patients with gonorrhea, resistance to azithromycin increased from 0.6% in 2013 to 2.5% in 2014, predominantly in the Midwest.
Data source: An analysis of 5,093 Neisseria gonorrhoeae isolates from 27 clinics as part of the CDC's Gonococcal Isolate Surveillance Project.
Disclosures: The researchers had no financial disclosures.
4. Statins Improve Ovarian Cancer Survival
To take the posttest, go to: http://bit.ly/2t6swCF
Expires June 16, 2017
VITALSKey clinical point: The risk of all-cause mortality in ovarian cancer patients on statin therapy was reduced by one-third.
Major finding: Mean survival in a large cohort of women with stage III ovarian cancer was 5.8 months longer among those on statin therapy.
Data source: A retrospective study of 1,510 women diagnosed with epithelial ovarian cancer during 2007-2009.
Disclosures: Dr. Vogel reported having no financial conflicts regarding this study, conducted without commercial support.
5. Common Surgeries Linked to Chronic Opioid Use Among Opioid-naive Patients
To take the posttest, go to: http://bit.ly/2ub9fFg
Expires June 18, 2017
VITALSKey clinical point: Common surgeries increase the risk of chronic opioid use in opioid-naive adults, especially among those using antidepressants or benzodiazepines before their operations, and those with substance abuse histories.
Major finding: After adjustment for potential confounders, knee replacement increased the risk fivefold; open cholecystectomy almost fourfold; and total hip replacement and simple mastectomy almost threefold.
Data source: Insurance claims of more than 18 million people.
Disclosures: The authors had no disclosures. The work was funded in part by the Foundation for Anesthesia Education and Research and the Anesthesia Quality Institute. Claims data came from MarketScan (Truven Health Analytics).
Here are 5 articles in the August issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Women With BRCA1 Mutations at Higher Risk for Endometrial Cancers
To take the posttest, go to: http://bit.ly/2t6SPIY
Expires June 30, 2017
VITALSKey clinical point: Clinicians may wish to discuss the option of hysterectomy at the time of salpingo-oophorectomy in women with deleterious BRCA1 mutations.
Major finding: Among women with BRCA1 but not BRCA2 mutations there was increased risk for serous/serous-like endometrial carcinomas.
Data source: Prospective multicenter follow-up study of 1,083 women with BRCA mutations who underwent salpingo-oophorectomy without hysterectomy.
Disclosures: The study was supported by grants from the Department of Defense, National Institutes of Health, and public and private foundations. Coauthor Robert Soslow, MD, disclosed consulting for EMD Serono. No others reported conflicts of interest. The editorialists reported no conflicts of interest related to the study.
2. Cochrane Review: Topical Steroid—Vitamin D Combo Best for Scalp Psoriasis
To take the posttest, go to: http://bit.ly/2sIyLNI
Expires July 14, 2017
VITALSKey clinical point: The combination of a topical steroid and topical vitamin D is marginally better but with a similar safety profile to steroids alone as a treatment for psoriasis on the scalp.
Major finding: The combination of a topical steroid and vitamin D showed a small but statistically significant advantage over steroids alone, and a greater advantage over vitamin D alone.
Data source: A systematic review of 59 randomized controlled studies in 11,561 patients.
Disclosures: The study was supported by the Universidade Federal de São Paulo, Brazil; the Universidade Federal do Rio Grande do Norte, Brazil; and the National Institute for Health Research, United Kingdom. Six authors and one clinical referee declared speakers' fees, research grants, and funding from the pharmaceutical industry. One author had no conflicts of interest to disclose.
3. Study Finds Emergence of Azithromycin-resistant Gonorrhea
To take the posttest, go to: http://bit.ly/2u1nMmb
Expires July 16, 2017
VITALSKey clinical point:Resistance to azithromycin is emerging among patients diagnosed with gonorrhea.
Major finding: Among patients with gonorrhea, resistance to azithromycin increased from 0.6% in 2013 to 2.5% in 2014, predominantly in the Midwest.
Data source: An analysis of 5,093 Neisseria gonorrhoeae isolates from 27 clinics as part of the CDC's Gonococcal Isolate Surveillance Project.
Disclosures: The researchers had no financial disclosures.
4. Statins Improve Ovarian Cancer Survival
To take the posttest, go to: http://bit.ly/2t6swCF
Expires June 16, 2017
VITALSKey clinical point: The risk of all-cause mortality in ovarian cancer patients on statin therapy was reduced by one-third.
Major finding: Mean survival in a large cohort of women with stage III ovarian cancer was 5.8 months longer among those on statin therapy.
Data source: A retrospective study of 1,510 women diagnosed with epithelial ovarian cancer during 2007-2009.
Disclosures: Dr. Vogel reported having no financial conflicts regarding this study, conducted without commercial support.
5. Common Surgeries Linked to Chronic Opioid Use Among Opioid-naive Patients
To take the posttest, go to: http://bit.ly/2ub9fFg
Expires June 18, 2017
VITALSKey clinical point: Common surgeries increase the risk of chronic opioid use in opioid-naive adults, especially among those using antidepressants or benzodiazepines before their operations, and those with substance abuse histories.
Major finding: After adjustment for potential confounders, knee replacement increased the risk fivefold; open cholecystectomy almost fourfold; and total hip replacement and simple mastectomy almost threefold.
Data source: Insurance claims of more than 18 million people.
Disclosures: The authors had no disclosures. The work was funded in part by the Foundation for Anesthesia Education and Research and the Anesthesia Quality Institute. Claims data came from MarketScan (Truven Health Analytics).
Here are 5 articles in the August issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Women With BRCA1 Mutations at Higher Risk for Endometrial Cancers
To take the posttest, go to: http://bit.ly/2t6SPIY
Expires June 30, 2017
VITALSKey clinical point: Clinicians may wish to discuss the option of hysterectomy at the time of salpingo-oophorectomy in women with deleterious BRCA1 mutations.
Major finding: Among women with BRCA1 but not BRCA2 mutations there was increased risk for serous/serous-like endometrial carcinomas.
Data source: Prospective multicenter follow-up study of 1,083 women with BRCA mutations who underwent salpingo-oophorectomy without hysterectomy.
Disclosures: The study was supported by grants from the Department of Defense, National Institutes of Health, and public and private foundations. Coauthor Robert Soslow, MD, disclosed consulting for EMD Serono. No others reported conflicts of interest. The editorialists reported no conflicts of interest related to the study.
2. Cochrane Review: Topical Steroid—Vitamin D Combo Best for Scalp Psoriasis
To take the posttest, go to: http://bit.ly/2sIyLNI
Expires July 14, 2017
VITALSKey clinical point: The combination of a topical steroid and topical vitamin D is marginally better but with a similar safety profile to steroids alone as a treatment for psoriasis on the scalp.
Major finding: The combination of a topical steroid and vitamin D showed a small but statistically significant advantage over steroids alone, and a greater advantage over vitamin D alone.
Data source: A systematic review of 59 randomized controlled studies in 11,561 patients.
Disclosures: The study was supported by the Universidade Federal de São Paulo, Brazil; the Universidade Federal do Rio Grande do Norte, Brazil; and the National Institute for Health Research, United Kingdom. Six authors and one clinical referee declared speakers' fees, research grants, and funding from the pharmaceutical industry. One author had no conflicts of interest to disclose.
3. Study Finds Emergence of Azithromycin-resistant Gonorrhea
To take the posttest, go to: http://bit.ly/2u1nMmb
Expires July 16, 2017
VITALSKey clinical point:Resistance to azithromycin is emerging among patients diagnosed with gonorrhea.
Major finding: Among patients with gonorrhea, resistance to azithromycin increased from 0.6% in 2013 to 2.5% in 2014, predominantly in the Midwest.
Data source: An analysis of 5,093 Neisseria gonorrhoeae isolates from 27 clinics as part of the CDC's Gonococcal Isolate Surveillance Project.
Disclosures: The researchers had no financial disclosures.
4. Statins Improve Ovarian Cancer Survival
To take the posttest, go to: http://bit.ly/2t6swCF
Expires June 16, 2017
VITALSKey clinical point: The risk of all-cause mortality in ovarian cancer patients on statin therapy was reduced by one-third.
Major finding: Mean survival in a large cohort of women with stage III ovarian cancer was 5.8 months longer among those on statin therapy.
Data source: A retrospective study of 1,510 women diagnosed with epithelial ovarian cancer during 2007-2009.
Disclosures: Dr. Vogel reported having no financial conflicts regarding this study, conducted without commercial support.
5. Common Surgeries Linked to Chronic Opioid Use Among Opioid-naive Patients
To take the posttest, go to: http://bit.ly/2ub9fFg
Expires June 18, 2017
VITALSKey clinical point: Common surgeries increase the risk of chronic opioid use in opioid-naive adults, especially among those using antidepressants or benzodiazepines before their operations, and those with substance abuse histories.
Major finding: After adjustment for potential confounders, knee replacement increased the risk fivefold; open cholecystectomy almost fourfold; and total hip replacement and simple mastectomy almost threefold.
Data source: Insurance claims of more than 18 million people.
Disclosures: The authors had no disclosures. The work was funded in part by the Foundation for Anesthesia Education and Research and the Anesthesia Quality Institute. Claims data came from MarketScan (Truven Health Analytics).
Hospitals increase CRE risk when they share patients
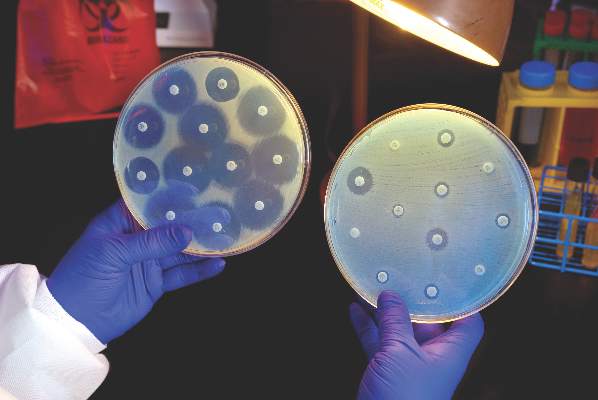
The more hospitals share patients, the more likely they are to have a problem with carbapenem-resistant Enterobacteriaceae (CRE), especially if long-term acute care hospitals (LTACHs) are in the mix, according to a state-wide investigation from Illinois.
Greater hospital centrality was independently associated with higher rates overall, and sharing four or more patients with a long-term acute care hospital (LTACH) in the 3-month study window doubled the rate of CRE cases.
Although it’s possible that was because of chance (P = 0.11), the link between LTACHs and CRE “is consistent with prior analyses that have shown the central role LTACHs have in” spreading the organism, said the researchers, led by Michael Ray of the Illinois Department of Public Health (Clin Infect Dis. 2016 Aug 2. pii: ciw461).
Patients often spend weeks in LTACH facilities for ongoing, serious health problems. The severity of illness, long stay, and sometimes chronic antibiotic use increase the risk of CRE exposure, and the team found that many LTACH patients are colonized.
“These findings have immediate public health implications. … Early interventions should be focused on the most connected facilities, as well as those with strong connections to LTACHs.” When one hospital has an outbreak, facilities that share its patients need to swing into action screening new admissions and taking other steps to prevent regional spread, the team said.
Meanwhile, “state-wide patient-sharing data, which are now increasingly available through sources like the Healthcare Cost and Utilization Project, provide an important way to assess hospital risk of CRE exposure based on its position in regional patient-sharing networks,” they noted. “Public health can play a critical role in identifying tightly connected hospitals and educating personnel at such facilities about their risk and need for enhanced infection control interventions.”
The team came to their conclusions after linking Illinois’ drug-resistant organisms registry with admissions data for 185 hospitals. About half reported at least one CRE case over 3 months, with a mean of 3.5 cases per hospital.
There was an average of 64 patient-sharing connections per facility, with a minimum of one connection and a maximum of 145 connections. Each additional patient two hospitals shared corresponded to a 3% increase in the CRE rate in urban facilities and a 6% increase in rural ones. The investigators didn’t explain the discrepancy, except to note that rural areas don’t have LTACHs.
Almost two-thirds of hospitals reporting CRE were in Chicago-area counties; almost half had shared at least one patient with an LTACH, and 21% had shared four or more.
CRE cases were an average of 64 years old, and equally distributed between men and women and black and white patients.
The Centers for Disease Control and Prevention funded the work. The authors had no disclosures.
The more hospitals share patients, the more likely they are to have a problem with carbapenem-resistant Enterobacteriaceae (CRE), especially if long-term acute care hospitals (LTACHs) are in the mix, according to a state-wide investigation from Illinois.
Greater hospital centrality was independently associated with higher rates overall, and sharing four or more patients with a long-term acute care hospital (LTACH) in the 3-month study window doubled the rate of CRE cases.
Although it’s possible that was because of chance (P = 0.11), the link between LTACHs and CRE “is consistent with prior analyses that have shown the central role LTACHs have in” spreading the organism, said the researchers, led by Michael Ray of the Illinois Department of Public Health (Clin Infect Dis. 2016 Aug 2. pii: ciw461).
Patients often spend weeks in LTACH facilities for ongoing, serious health problems. The severity of illness, long stay, and sometimes chronic antibiotic use increase the risk of CRE exposure, and the team found that many LTACH patients are colonized.
“These findings have immediate public health implications. … Early interventions should be focused on the most connected facilities, as well as those with strong connections to LTACHs.” When one hospital has an outbreak, facilities that share its patients need to swing into action screening new admissions and taking other steps to prevent regional spread, the team said.
Meanwhile, “state-wide patient-sharing data, which are now increasingly available through sources like the Healthcare Cost and Utilization Project, provide an important way to assess hospital risk of CRE exposure based on its position in regional patient-sharing networks,” they noted. “Public health can play a critical role in identifying tightly connected hospitals and educating personnel at such facilities about their risk and need for enhanced infection control interventions.”
The team came to their conclusions after linking Illinois’ drug-resistant organisms registry with admissions data for 185 hospitals. About half reported at least one CRE case over 3 months, with a mean of 3.5 cases per hospital.
There was an average of 64 patient-sharing connections per facility, with a minimum of one connection and a maximum of 145 connections. Each additional patient two hospitals shared corresponded to a 3% increase in the CRE rate in urban facilities and a 6% increase in rural ones. The investigators didn’t explain the discrepancy, except to note that rural areas don’t have LTACHs.
Almost two-thirds of hospitals reporting CRE were in Chicago-area counties; almost half had shared at least one patient with an LTACH, and 21% had shared four or more.
CRE cases were an average of 64 years old, and equally distributed between men and women and black and white patients.
The Centers for Disease Control and Prevention funded the work. The authors had no disclosures.
The more hospitals share patients, the more likely they are to have a problem with carbapenem-resistant Enterobacteriaceae (CRE), especially if long-term acute care hospitals (LTACHs) are in the mix, according to a state-wide investigation from Illinois.
Greater hospital centrality was independently associated with higher rates overall, and sharing four or more patients with a long-term acute care hospital (LTACH) in the 3-month study window doubled the rate of CRE cases.
Although it’s possible that was because of chance (P = 0.11), the link between LTACHs and CRE “is consistent with prior analyses that have shown the central role LTACHs have in” spreading the organism, said the researchers, led by Michael Ray of the Illinois Department of Public Health (Clin Infect Dis. 2016 Aug 2. pii: ciw461).
Patients often spend weeks in LTACH facilities for ongoing, serious health problems. The severity of illness, long stay, and sometimes chronic antibiotic use increase the risk of CRE exposure, and the team found that many LTACH patients are colonized.
“These findings have immediate public health implications. … Early interventions should be focused on the most connected facilities, as well as those with strong connections to LTACHs.” When one hospital has an outbreak, facilities that share its patients need to swing into action screening new admissions and taking other steps to prevent regional spread, the team said.
Meanwhile, “state-wide patient-sharing data, which are now increasingly available through sources like the Healthcare Cost and Utilization Project, provide an important way to assess hospital risk of CRE exposure based on its position in regional patient-sharing networks,” they noted. “Public health can play a critical role in identifying tightly connected hospitals and educating personnel at such facilities about their risk and need for enhanced infection control interventions.”
The team came to their conclusions after linking Illinois’ drug-resistant organisms registry with admissions data for 185 hospitals. About half reported at least one CRE case over 3 months, with a mean of 3.5 cases per hospital.
There was an average of 64 patient-sharing connections per facility, with a minimum of one connection and a maximum of 145 connections. Each additional patient two hospitals shared corresponded to a 3% increase in the CRE rate in urban facilities and a 6% increase in rural ones. The investigators didn’t explain the discrepancy, except to note that rural areas don’t have LTACHs.
Almost two-thirds of hospitals reporting CRE were in Chicago-area counties; almost half had shared at least one patient with an LTACH, and 21% had shared four or more.
CRE cases were an average of 64 years old, and equally distributed between men and women and black and white patients.
The Centers for Disease Control and Prevention funded the work. The authors had no disclosures.
FROM CLINICAL INFECTIOUS DISEASES
Key clinical point: The more hospitals share patients, the more likely they are to have a problem with CRE, especially if long-term acute care hospitals are in the mix.
Major finding: Sharing four or more patients with a long-term acute care hospital in the 3-month study window doubled the rate of CRE cases (P = 0.11).
Data source: 185 Illinois hospitals.
Disclosures: The Centers for Disease Control and Prevention funded the work. The authors had no disclosures.
Studies suggest moving SNAP outside of Alzheimer’s framework
Two studies from JAMA Neurology raise doubts about whether suspected non-Alzheimer’s pathophysiology – a brain biomarker construct suspected by some to be an Alzheimer’s disease precursor – truly belongs on the Alzheimer’s spectrum.
A team from Washington University in St. Louis concluded that neurodegeneration in isolation without beta-amyloid deposition – the definition of suspected non-Alzheimer’s pathophysiology (SNAP) – “often represents comorbid influences rather than emerging” Alzheimer’s disease (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2642).
A team from Harvard Medical School in Boston came to a similar conclusion, finding that patterns of neurodegeneration in brain regions vulnerable to Alzheimer’s disease (AD) “are not specific to AD processes among [clinically normal] individuals. Instead, multiple causes likely contribute to the biomarker construct of SNAP” (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2237).
The relationship between SNAP and AD is, for now, mostly of concern to researchers. SNAP was originally linked to cerebral vascular disease and other age-related problems, but since it was proposed a few years ago as an addition to the National Institute on Aging (NIA)–Alzheimer’s Association’s research criteria for preclinical AD, it’s been unclear how – or if – it really fits. The two research groups tackled the issue.
Patients in stage 1 of the NIA scheme have biomarker evidence of amyloid deposition without neurodegeneration (ND); stage 2 patients have both. Stage 3 adds cognitive decline to the amyloid and ND signs. SNAP captures cognitively normal patients with ND but no evidence of amyloid deposition.
Over a period of 9 years, the St. Louis team split 174 cognitively normal adults – about equal numbers of men and women with an average age of 66 – into the four groups at baseline, plus a fifth: no evidence of ND or amyloid. Amyloid deposition was assessed by positron emission tomography, and ND was assessed by both hippocampal volume loss on MRI and cerebrospinal fluid levels of the AD-linked tau protein.
Amyloid accumulation and hippocampal loss were greater in the later NIA stages than in either SNAP or biomarker-free subjects. Among the 34 SNAP patients (20%), only about 5 went on to deposit amyloid.
“The rates of [amyloid] accumulation and loss of hippocampal volume in individuals with SNAP were indistinguishable from those without any pathologic features at baseline. … SNAP appears most likely to capture inherent individual variability in brain structure or to represent comorbid pathologic features rather than early emerging AD. Low hippocampal volumes or elevated levels of [tau protein] in isolation may not accurately represent ongoing neurodegenerative processes,” said investigators led by Brian Gordon, PhD.
Meanwhile, in the Harvard study, only “a small subset” of the 64 SNAP patients went on to rapid cognitive decline. SNAP seems to be “heterogeneous, and further biomarker refinement will be necessary to characterize this group,” said investigators led by Elizabeth Mormino, PhD.
The Harvard team split 247 clinically normal individuals – a bit more women than men this time, with an average age of 74 years – into NIA categories, SNAP, and patients with no ND or amyloid biomarkers. Hippocampal volume was again assessed by MRI; positron emission tomography scans were used to assess amyloid deposition, but also regional brain tau protein levels and other pathologies, and there was serial cognitive testing. The study started in 2010 and is ongoing, with subjects evaluated yearly.
SNAP patients had less pathology and better ongoing cognitive function than peers in the accepted NIA categories, and had levels of amyloid deposition no greater than biomarker-free subjects. Tau protein “levels in the medial and inferior temporal lobes were indistinguishable between” the two groups.
SNAP patients did slightly worse on serial cognitive tests, but these findings were driven mostly by two SNAP patients who declined faster than the others. (The study by Dr. Gordon and his associates did not report cognitive outcomes.)
Overall, “clinically normal adults with SNAP,” the Harvard group said, “did not exhibit evidence of elevated tau levels, which suggests that this biomarker construct does not represent amyloid-independent tauopathy,” one of the bridges proposed from SNAP to AD.
“SNAP is likely heterogeneous,” with only a subset of patients at risk “for short-term decline. Future refinement of biomarkers will be necessary to subclassify this group and determine the biologic correlates of ND markers.” SNAP does not “appear to be specific to AD,” and is likely influenced by “age-related pathologic processes, the normal aging process, and [individual] differences,” the investigators said.
When asked to comment on the studies, Richard J. Caselli, MD, professor of neurology at the Mayo Clinic, Scottsdale, Ariz., noted that the Mormino study’s findings of a flattened test-retest effect on the serial cognitive tests seemed to be a sensitive cognitive correlate of SNAP, and consistent with the previously reported increased rate of decline in MCI [mild cognitive impairment] patients with SNAP relative to both preclinical stage 0 and preclinical stage 1 (Neurology. 2015 Feb 13;84[5]:508-15).
Overall, the two studies support SNAP as a “generally non-AD heterogeneous diagnosis that does in fact exhibit greater cognitive decline with age, even if subtle in the Mormino study, with an increased risk of MCI and dementia. If we look at the neuropathology of AD cases, we find similar additional pathologies, so maybe SNAP is that minus the AD piece,” said Dr. Caselli, who was not involved in either study.
The heterogeneity explains “our difficulties understanding” the nature of SNAP, Sylvia Villeneuve, PhD, said in an editorial to the Harvard study (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2842).
“Given that the cognitive and brain profile of most SNAP individuals are stable over time, some authors have suggested that neurodegeneration should not be a defining feature of SNAP. … Part of what we capture as SNAP represents a tail of the normal aging distribution,” said Dr. Villeneuve of McGill University in Montreal. “A better comprehension of the biomarkers used to characterize SNAP will be important, with an awareness of the limitations of bimodal markers” – the yes/no answers used for NIA and SNAP classification – “especially those with cutoffs that do not have a biological basis.”
Both studies were funded at least in part by the National Institutes of Health. Dr. Gordon reported research work with Avid Radiopharmaceuticals; Dr. Mormino had no industry disclosures. Other investigators in both projects reported ties to several companies, including Eli Lilly, Janssen, AbbVie, Roche, and Pfizer. Dr. Villeneuve had no disclosures.
The authors have provided a valuable contribution to an area that is receiving increasing attention. While they seem to ascribe small hippocampal volumes to variability in anatomic brain development, it may be that in older individuals, this is more appropriately ascribed to variability in non-Alzheimer’s disease pathologies, resistance to age-related neurodegeneration, or both – all of which should have slow rates of atrophy.
The authors recommended that the field shift from using hippocampal volume as a neurodegenerative measure to using a summary volumetric signature selective for Alzheimer’s disease. This seems justified, although not because hippocampal volume loss with increasing age represents individual variation in brain development. We recommend an Alzheimer’s disease signature (cortical) thickness measure because cortical thickness, unlike volume, is not dependent on head size. Thus, thickness does not need to be adjusted for variation in head size, which imparts a sex effect to all volume adjustments.
Clifford Jack, MD, is a professor of radiology at the Mayo Clinic in Rochester, Minn. He is an originator of the concept of suspected non-Alzheimer’s pathophysiology (SNAP) and also the National Institute on Aging–Alzheimer’s Association’s research criteria for preclinical Alzheimer’s disease. He is a consultant for Eli Lilly and owns stock in Johnson and Johnson. His commentary is adapted from his editorial accompanying the report from Dr. Gordon and his associates (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2843).
The authors have provided a valuable contribution to an area that is receiving increasing attention. While they seem to ascribe small hippocampal volumes to variability in anatomic brain development, it may be that in older individuals, this is more appropriately ascribed to variability in non-Alzheimer’s disease pathologies, resistance to age-related neurodegeneration, or both – all of which should have slow rates of atrophy.
The authors recommended that the field shift from using hippocampal volume as a neurodegenerative measure to using a summary volumetric signature selective for Alzheimer’s disease. This seems justified, although not because hippocampal volume loss with increasing age represents individual variation in brain development. We recommend an Alzheimer’s disease signature (cortical) thickness measure because cortical thickness, unlike volume, is not dependent on head size. Thus, thickness does not need to be adjusted for variation in head size, which imparts a sex effect to all volume adjustments.
Clifford Jack, MD, is a professor of radiology at the Mayo Clinic in Rochester, Minn. He is an originator of the concept of suspected non-Alzheimer’s pathophysiology (SNAP) and also the National Institute on Aging–Alzheimer’s Association’s research criteria for preclinical Alzheimer’s disease. He is a consultant for Eli Lilly and owns stock in Johnson and Johnson. His commentary is adapted from his editorial accompanying the report from Dr. Gordon and his associates (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2843).
The authors have provided a valuable contribution to an area that is receiving increasing attention. While they seem to ascribe small hippocampal volumes to variability in anatomic brain development, it may be that in older individuals, this is more appropriately ascribed to variability in non-Alzheimer’s disease pathologies, resistance to age-related neurodegeneration, or both – all of which should have slow rates of atrophy.
The authors recommended that the field shift from using hippocampal volume as a neurodegenerative measure to using a summary volumetric signature selective for Alzheimer’s disease. This seems justified, although not because hippocampal volume loss with increasing age represents individual variation in brain development. We recommend an Alzheimer’s disease signature (cortical) thickness measure because cortical thickness, unlike volume, is not dependent on head size. Thus, thickness does not need to be adjusted for variation in head size, which imparts a sex effect to all volume adjustments.
Clifford Jack, MD, is a professor of radiology at the Mayo Clinic in Rochester, Minn. He is an originator of the concept of suspected non-Alzheimer’s pathophysiology (SNAP) and also the National Institute on Aging–Alzheimer’s Association’s research criteria for preclinical Alzheimer’s disease. He is a consultant for Eli Lilly and owns stock in Johnson and Johnson. His commentary is adapted from his editorial accompanying the report from Dr. Gordon and his associates (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2843).
Two studies from JAMA Neurology raise doubts about whether suspected non-Alzheimer’s pathophysiology – a brain biomarker construct suspected by some to be an Alzheimer’s disease precursor – truly belongs on the Alzheimer’s spectrum.
A team from Washington University in St. Louis concluded that neurodegeneration in isolation without beta-amyloid deposition – the definition of suspected non-Alzheimer’s pathophysiology (SNAP) – “often represents comorbid influences rather than emerging” Alzheimer’s disease (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2642).
A team from Harvard Medical School in Boston came to a similar conclusion, finding that patterns of neurodegeneration in brain regions vulnerable to Alzheimer’s disease (AD) “are not specific to AD processes among [clinically normal] individuals. Instead, multiple causes likely contribute to the biomarker construct of SNAP” (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2237).
The relationship between SNAP and AD is, for now, mostly of concern to researchers. SNAP was originally linked to cerebral vascular disease and other age-related problems, but since it was proposed a few years ago as an addition to the National Institute on Aging (NIA)–Alzheimer’s Association’s research criteria for preclinical AD, it’s been unclear how – or if – it really fits. The two research groups tackled the issue.
Patients in stage 1 of the NIA scheme have biomarker evidence of amyloid deposition without neurodegeneration (ND); stage 2 patients have both. Stage 3 adds cognitive decline to the amyloid and ND signs. SNAP captures cognitively normal patients with ND but no evidence of amyloid deposition.
Over a period of 9 years, the St. Louis team split 174 cognitively normal adults – about equal numbers of men and women with an average age of 66 – into the four groups at baseline, plus a fifth: no evidence of ND or amyloid. Amyloid deposition was assessed by positron emission tomography, and ND was assessed by both hippocampal volume loss on MRI and cerebrospinal fluid levels of the AD-linked tau protein.
Amyloid accumulation and hippocampal loss were greater in the later NIA stages than in either SNAP or biomarker-free subjects. Among the 34 SNAP patients (20%), only about 5 went on to deposit amyloid.
“The rates of [amyloid] accumulation and loss of hippocampal volume in individuals with SNAP were indistinguishable from those without any pathologic features at baseline. … SNAP appears most likely to capture inherent individual variability in brain structure or to represent comorbid pathologic features rather than early emerging AD. Low hippocampal volumes or elevated levels of [tau protein] in isolation may not accurately represent ongoing neurodegenerative processes,” said investigators led by Brian Gordon, PhD.
Meanwhile, in the Harvard study, only “a small subset” of the 64 SNAP patients went on to rapid cognitive decline. SNAP seems to be “heterogeneous, and further biomarker refinement will be necessary to characterize this group,” said investigators led by Elizabeth Mormino, PhD.
The Harvard team split 247 clinically normal individuals – a bit more women than men this time, with an average age of 74 years – into NIA categories, SNAP, and patients with no ND or amyloid biomarkers. Hippocampal volume was again assessed by MRI; positron emission tomography scans were used to assess amyloid deposition, but also regional brain tau protein levels and other pathologies, and there was serial cognitive testing. The study started in 2010 and is ongoing, with subjects evaluated yearly.
SNAP patients had less pathology and better ongoing cognitive function than peers in the accepted NIA categories, and had levels of amyloid deposition no greater than biomarker-free subjects. Tau protein “levels in the medial and inferior temporal lobes were indistinguishable between” the two groups.
SNAP patients did slightly worse on serial cognitive tests, but these findings were driven mostly by two SNAP patients who declined faster than the others. (The study by Dr. Gordon and his associates did not report cognitive outcomes.)
Overall, “clinically normal adults with SNAP,” the Harvard group said, “did not exhibit evidence of elevated tau levels, which suggests that this biomarker construct does not represent amyloid-independent tauopathy,” one of the bridges proposed from SNAP to AD.
“SNAP is likely heterogeneous,” with only a subset of patients at risk “for short-term decline. Future refinement of biomarkers will be necessary to subclassify this group and determine the biologic correlates of ND markers.” SNAP does not “appear to be specific to AD,” and is likely influenced by “age-related pathologic processes, the normal aging process, and [individual] differences,” the investigators said.
When asked to comment on the studies, Richard J. Caselli, MD, professor of neurology at the Mayo Clinic, Scottsdale, Ariz., noted that the Mormino study’s findings of a flattened test-retest effect on the serial cognitive tests seemed to be a sensitive cognitive correlate of SNAP, and consistent with the previously reported increased rate of decline in MCI [mild cognitive impairment] patients with SNAP relative to both preclinical stage 0 and preclinical stage 1 (Neurology. 2015 Feb 13;84[5]:508-15).
Overall, the two studies support SNAP as a “generally non-AD heterogeneous diagnosis that does in fact exhibit greater cognitive decline with age, even if subtle in the Mormino study, with an increased risk of MCI and dementia. If we look at the neuropathology of AD cases, we find similar additional pathologies, so maybe SNAP is that minus the AD piece,” said Dr. Caselli, who was not involved in either study.
The heterogeneity explains “our difficulties understanding” the nature of SNAP, Sylvia Villeneuve, PhD, said in an editorial to the Harvard study (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2842).
“Given that the cognitive and brain profile of most SNAP individuals are stable over time, some authors have suggested that neurodegeneration should not be a defining feature of SNAP. … Part of what we capture as SNAP represents a tail of the normal aging distribution,” said Dr. Villeneuve of McGill University in Montreal. “A better comprehension of the biomarkers used to characterize SNAP will be important, with an awareness of the limitations of bimodal markers” – the yes/no answers used for NIA and SNAP classification – “especially those with cutoffs that do not have a biological basis.”
Both studies were funded at least in part by the National Institutes of Health. Dr. Gordon reported research work with Avid Radiopharmaceuticals; Dr. Mormino had no industry disclosures. Other investigators in both projects reported ties to several companies, including Eli Lilly, Janssen, AbbVie, Roche, and Pfizer. Dr. Villeneuve had no disclosures.
Two studies from JAMA Neurology raise doubts about whether suspected non-Alzheimer’s pathophysiology – a brain biomarker construct suspected by some to be an Alzheimer’s disease precursor – truly belongs on the Alzheimer’s spectrum.
A team from Washington University in St. Louis concluded that neurodegeneration in isolation without beta-amyloid deposition – the definition of suspected non-Alzheimer’s pathophysiology (SNAP) – “often represents comorbid influences rather than emerging” Alzheimer’s disease (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2642).
A team from Harvard Medical School in Boston came to a similar conclusion, finding that patterns of neurodegeneration in brain regions vulnerable to Alzheimer’s disease (AD) “are not specific to AD processes among [clinically normal] individuals. Instead, multiple causes likely contribute to the biomarker construct of SNAP” (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2237).
The relationship between SNAP and AD is, for now, mostly of concern to researchers. SNAP was originally linked to cerebral vascular disease and other age-related problems, but since it was proposed a few years ago as an addition to the National Institute on Aging (NIA)–Alzheimer’s Association’s research criteria for preclinical AD, it’s been unclear how – or if – it really fits. The two research groups tackled the issue.
Patients in stage 1 of the NIA scheme have biomarker evidence of amyloid deposition without neurodegeneration (ND); stage 2 patients have both. Stage 3 adds cognitive decline to the amyloid and ND signs. SNAP captures cognitively normal patients with ND but no evidence of amyloid deposition.
Over a period of 9 years, the St. Louis team split 174 cognitively normal adults – about equal numbers of men and women with an average age of 66 – into the four groups at baseline, plus a fifth: no evidence of ND or amyloid. Amyloid deposition was assessed by positron emission tomography, and ND was assessed by both hippocampal volume loss on MRI and cerebrospinal fluid levels of the AD-linked tau protein.
Amyloid accumulation and hippocampal loss were greater in the later NIA stages than in either SNAP or biomarker-free subjects. Among the 34 SNAP patients (20%), only about 5 went on to deposit amyloid.
“The rates of [amyloid] accumulation and loss of hippocampal volume in individuals with SNAP were indistinguishable from those without any pathologic features at baseline. … SNAP appears most likely to capture inherent individual variability in brain structure or to represent comorbid pathologic features rather than early emerging AD. Low hippocampal volumes or elevated levels of [tau protein] in isolation may not accurately represent ongoing neurodegenerative processes,” said investigators led by Brian Gordon, PhD.
Meanwhile, in the Harvard study, only “a small subset” of the 64 SNAP patients went on to rapid cognitive decline. SNAP seems to be “heterogeneous, and further biomarker refinement will be necessary to characterize this group,” said investigators led by Elizabeth Mormino, PhD.
The Harvard team split 247 clinically normal individuals – a bit more women than men this time, with an average age of 74 years – into NIA categories, SNAP, and patients with no ND or amyloid biomarkers. Hippocampal volume was again assessed by MRI; positron emission tomography scans were used to assess amyloid deposition, but also regional brain tau protein levels and other pathologies, and there was serial cognitive testing. The study started in 2010 and is ongoing, with subjects evaluated yearly.
SNAP patients had less pathology and better ongoing cognitive function than peers in the accepted NIA categories, and had levels of amyloid deposition no greater than biomarker-free subjects. Tau protein “levels in the medial and inferior temporal lobes were indistinguishable between” the two groups.
SNAP patients did slightly worse on serial cognitive tests, but these findings were driven mostly by two SNAP patients who declined faster than the others. (The study by Dr. Gordon and his associates did not report cognitive outcomes.)
Overall, “clinically normal adults with SNAP,” the Harvard group said, “did not exhibit evidence of elevated tau levels, which suggests that this biomarker construct does not represent amyloid-independent tauopathy,” one of the bridges proposed from SNAP to AD.
“SNAP is likely heterogeneous,” with only a subset of patients at risk “for short-term decline. Future refinement of biomarkers will be necessary to subclassify this group and determine the biologic correlates of ND markers.” SNAP does not “appear to be specific to AD,” and is likely influenced by “age-related pathologic processes, the normal aging process, and [individual] differences,” the investigators said.
When asked to comment on the studies, Richard J. Caselli, MD, professor of neurology at the Mayo Clinic, Scottsdale, Ariz., noted that the Mormino study’s findings of a flattened test-retest effect on the serial cognitive tests seemed to be a sensitive cognitive correlate of SNAP, and consistent with the previously reported increased rate of decline in MCI [mild cognitive impairment] patients with SNAP relative to both preclinical stage 0 and preclinical stage 1 (Neurology. 2015 Feb 13;84[5]:508-15).
Overall, the two studies support SNAP as a “generally non-AD heterogeneous diagnosis that does in fact exhibit greater cognitive decline with age, even if subtle in the Mormino study, with an increased risk of MCI and dementia. If we look at the neuropathology of AD cases, we find similar additional pathologies, so maybe SNAP is that minus the AD piece,” said Dr. Caselli, who was not involved in either study.
The heterogeneity explains “our difficulties understanding” the nature of SNAP, Sylvia Villeneuve, PhD, said in an editorial to the Harvard study (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2842).
“Given that the cognitive and brain profile of most SNAP individuals are stable over time, some authors have suggested that neurodegeneration should not be a defining feature of SNAP. … Part of what we capture as SNAP represents a tail of the normal aging distribution,” said Dr. Villeneuve of McGill University in Montreal. “A better comprehension of the biomarkers used to characterize SNAP will be important, with an awareness of the limitations of bimodal markers” – the yes/no answers used for NIA and SNAP classification – “especially those with cutoffs that do not have a biological basis.”
Both studies were funded at least in part by the National Institutes of Health. Dr. Gordon reported research work with Avid Radiopharmaceuticals; Dr. Mormino had no industry disclosures. Other investigators in both projects reported ties to several companies, including Eli Lilly, Janssen, AbbVie, Roche, and Pfizer. Dr. Villeneuve had no disclosures.
FROM JAMA NEUROLOGY
Key clinical point: Two studies from JAMA Neurology raise doubts about whether suspected non-Alzheimer’s pathophysiology truly belongs on the Alzheimer’s spectrum.
Major finding: SNAP patients had less pathology and better ongoing cognitive function than peers in the accepted NIA categories and had levels of amyloid deposition no greater than biomarker-free subjects.
Data source: One longitudinal study from Harvard Medical School, Boston, and one from Washington University, St. Louis.
Disclosures: Both studies were funded at least in part by the National Institutes of Health. One lead investigator reported research work with Avid Radiopharmaceuticals; the other had no industry disclosures. Other investigators in both projects reported ties to several companies, including Eli Lilly, Janssen, AbbVie, Roche, and Pfizer.
Integrated PrEP and ART prevents HIV transmission in couples
In committed couples, HIV transmission from positive partners dropped from an expected incidence of more than 5% to less than 0.5% per year when the uninfected partner used pre-exposure prophylaxis (PrEP) for the first 6 months of the infected partner’s antiretroviral therapy, according to a study in PLOS Medicine.
The open-label demonstration project on which the study reports involved 1,013 heterosexual HIV-1–serodiscordant couples in Kenya and Uganda (PLOS Med. 2016 Aug 23. doi: 10.1371/journal.pmed.1002099).
“To our knowledge, this study is one of the first and one of the largest demonstration projects to provide PrEP to a priority population at risk for HIV-1 outside of a clinical trial setting, and the findings demonstrate the feasibility and impact of using PrEP as a bridging strategy to sustained HIV-1 protection by ART [antiretroviral therapy]” in serodiscordant couples, said investigators led by Jared Baeten, MD, of the department of global health at the University of Washington, Seattle. Wide-scale roll-out “could have substantial effects in reducing the global burden of new HIV-1 infections,” Dr. Baeten and his coauthors concluded.
PrEP kept uninfected partners safe until ART reliably suppressed viral loads at about 6 months. Adherence to the regimen was about 85%, which was higher than in some clinical trials, perhaps because couples were being offered “a strategy with demonstrated safety and efficacy” instead of unproven products and placebo. Couples also recognized their elevated HIV risk, the research team said.
It was good to find out that the approach works in real-world settings in Africa, Dr. Baeten and his associates said, where the majority of the 2 million people infected each year live. Follow-up was less frequent than in trials, with brief counseling sessions “equivalent to what would be expected in public health settings” and HIV tests about every 4 months over a median of about a year. “This study shows that a practical delivery approach ... can virtually eliminate HIV1- transmission,” the researchers said.
There were just two HIV transmissions in the study, both in women with self-reported and objective evidence of interrupted PrEP use. Overall, the transmission incidence was 0.2/100 person-years. The investigators estimated there would have been 40 transmissions – 5.2/100 person-years – without the intervention.
Couples were recruited by community outreach in four cities and towns – Kisumu and Thika in Kenya, and Kabwohe and Kampala in Uganda. The investigators targeted couples at high risk for transmission, including those reporting unprotected sex and infected partners with plasma HIV-1 RNA levels of 50,000 copies/mL or more.
Almost all were married and living together. They reported a median of six sex acts per month, many unprotected. Partners were a median of about 30 years old, and 67% of uninfected partners were men.
The preferred ART regimen was tenofovir disoproxil fumarate (TDF), lamivudine, and efavirenz, with zidovudine and nevirapine as alternatives. PrEP was a combination emtricitabine/TDF 200 mg/300 mg once daily; it was provided at the study sites since PrEP was otherwise unavailable in Kenya and Uganda.
The National Institutes of Health, Bill and Melinda Gates Foundation, and U.S. Agency for International Development funded the work. Gilead Sciences donated the TDF for PrEP. Dr. Baeten had no disclosures; another author reported funding from Gilead for a TDF pharmacokinetics study, and has a patent pending for a formulation different from the drug used in the study.
In committed couples, HIV transmission from positive partners dropped from an expected incidence of more than 5% to less than 0.5% per year when the uninfected partner used pre-exposure prophylaxis (PrEP) for the first 6 months of the infected partner’s antiretroviral therapy, according to a study in PLOS Medicine.
The open-label demonstration project on which the study reports involved 1,013 heterosexual HIV-1–serodiscordant couples in Kenya and Uganda (PLOS Med. 2016 Aug 23. doi: 10.1371/journal.pmed.1002099).
“To our knowledge, this study is one of the first and one of the largest demonstration projects to provide PrEP to a priority population at risk for HIV-1 outside of a clinical trial setting, and the findings demonstrate the feasibility and impact of using PrEP as a bridging strategy to sustained HIV-1 protection by ART [antiretroviral therapy]” in serodiscordant couples, said investigators led by Jared Baeten, MD, of the department of global health at the University of Washington, Seattle. Wide-scale roll-out “could have substantial effects in reducing the global burden of new HIV-1 infections,” Dr. Baeten and his coauthors concluded.
PrEP kept uninfected partners safe until ART reliably suppressed viral loads at about 6 months. Adherence to the regimen was about 85%, which was higher than in some clinical trials, perhaps because couples were being offered “a strategy with demonstrated safety and efficacy” instead of unproven products and placebo. Couples also recognized their elevated HIV risk, the research team said.
It was good to find out that the approach works in real-world settings in Africa, Dr. Baeten and his associates said, where the majority of the 2 million people infected each year live. Follow-up was less frequent than in trials, with brief counseling sessions “equivalent to what would be expected in public health settings” and HIV tests about every 4 months over a median of about a year. “This study shows that a practical delivery approach ... can virtually eliminate HIV1- transmission,” the researchers said.
There were just two HIV transmissions in the study, both in women with self-reported and objective evidence of interrupted PrEP use. Overall, the transmission incidence was 0.2/100 person-years. The investigators estimated there would have been 40 transmissions – 5.2/100 person-years – without the intervention.
Couples were recruited by community outreach in four cities and towns – Kisumu and Thika in Kenya, and Kabwohe and Kampala in Uganda. The investigators targeted couples at high risk for transmission, including those reporting unprotected sex and infected partners with plasma HIV-1 RNA levels of 50,000 copies/mL or more.
Almost all were married and living together. They reported a median of six sex acts per month, many unprotected. Partners were a median of about 30 years old, and 67% of uninfected partners were men.
The preferred ART regimen was tenofovir disoproxil fumarate (TDF), lamivudine, and efavirenz, with zidovudine and nevirapine as alternatives. PrEP was a combination emtricitabine/TDF 200 mg/300 mg once daily; it was provided at the study sites since PrEP was otherwise unavailable in Kenya and Uganda.
The National Institutes of Health, Bill and Melinda Gates Foundation, and U.S. Agency for International Development funded the work. Gilead Sciences donated the TDF for PrEP. Dr. Baeten had no disclosures; another author reported funding from Gilead for a TDF pharmacokinetics study, and has a patent pending for a formulation different from the drug used in the study.
In committed couples, HIV transmission from positive partners dropped from an expected incidence of more than 5% to less than 0.5% per year when the uninfected partner used pre-exposure prophylaxis (PrEP) for the first 6 months of the infected partner’s antiretroviral therapy, according to a study in PLOS Medicine.
The open-label demonstration project on which the study reports involved 1,013 heterosexual HIV-1–serodiscordant couples in Kenya and Uganda (PLOS Med. 2016 Aug 23. doi: 10.1371/journal.pmed.1002099).
“To our knowledge, this study is one of the first and one of the largest demonstration projects to provide PrEP to a priority population at risk for HIV-1 outside of a clinical trial setting, and the findings demonstrate the feasibility and impact of using PrEP as a bridging strategy to sustained HIV-1 protection by ART [antiretroviral therapy]” in serodiscordant couples, said investigators led by Jared Baeten, MD, of the department of global health at the University of Washington, Seattle. Wide-scale roll-out “could have substantial effects in reducing the global burden of new HIV-1 infections,” Dr. Baeten and his coauthors concluded.
PrEP kept uninfected partners safe until ART reliably suppressed viral loads at about 6 months. Adherence to the regimen was about 85%, which was higher than in some clinical trials, perhaps because couples were being offered “a strategy with demonstrated safety and efficacy” instead of unproven products and placebo. Couples also recognized their elevated HIV risk, the research team said.
It was good to find out that the approach works in real-world settings in Africa, Dr. Baeten and his associates said, where the majority of the 2 million people infected each year live. Follow-up was less frequent than in trials, with brief counseling sessions “equivalent to what would be expected in public health settings” and HIV tests about every 4 months over a median of about a year. “This study shows that a practical delivery approach ... can virtually eliminate HIV1- transmission,” the researchers said.
There were just two HIV transmissions in the study, both in women with self-reported and objective evidence of interrupted PrEP use. Overall, the transmission incidence was 0.2/100 person-years. The investigators estimated there would have been 40 transmissions – 5.2/100 person-years – without the intervention.
Couples were recruited by community outreach in four cities and towns – Kisumu and Thika in Kenya, and Kabwohe and Kampala in Uganda. The investigators targeted couples at high risk for transmission, including those reporting unprotected sex and infected partners with plasma HIV-1 RNA levels of 50,000 copies/mL or more.
Almost all were married and living together. They reported a median of six sex acts per month, many unprotected. Partners were a median of about 30 years old, and 67% of uninfected partners were men.
The preferred ART regimen was tenofovir disoproxil fumarate (TDF), lamivudine, and efavirenz, with zidovudine and nevirapine as alternatives. PrEP was a combination emtricitabine/TDF 200 mg/300 mg once daily; it was provided at the study sites since PrEP was otherwise unavailable in Kenya and Uganda.
The National Institutes of Health, Bill and Melinda Gates Foundation, and U.S. Agency for International Development funded the work. Gilead Sciences donated the TDF for PrEP. Dr. Baeten had no disclosures; another author reported funding from Gilead for a TDF pharmacokinetics study, and has a patent pending for a formulation different from the drug used in the study.
FROM PLOS MEDICINE
Key clinical point: In committed couples, HIV transmission from positive partners dropped from an expected incidence of more than 5% to less than 0.5% per year when the uninfected partner used pre-exposure prophylaxis for the first 6 months of the infected partner’s antiretroviral therapy.
Major finding: The transmission incidence was 0.2/100 person-years. The investigators estimated there would have been 40 transmissions – 5.2/100 person-years – without the intervention.
Data source: Open-label demonstration project with 1,013 heterosexual HIV-1–serodiscordant couples in Kenya and Uganda.
Disclosures: The National Institutes of Health, Bill and Melinda Gates Foundation, and U.S. Agency for International Development funded the work. Gilead Sciences donated the TDF for PrEP. Dr. Baeten had no disclosures; another author reported funding from Gilead for a TDF pharmacokinetics study and has a patent pending for a formulation different from the drug used in the study.
A new model for gout: pharmacy-based care
Something new is being tried to improve gout outcomes in the United States: Pharmacists are being recruited to help manage patients.
People with too-high serum urate levels who agree to extra help are being referred to pharmacists empowered to order blood tests and allopurinol. Pharmacists contact patients by mail or phone, at first, and then maybe automated messages or emails, and educate them about why they need to lower their urate and how to do it. Pharmacists monitor lab results and titrate allopurinol as needed to hit serum urate levels of 6 mg/dL or less. The tune-up usually takes a year, at which point physicians resume ongoing management. The referring doctor is in the background to make sure everything goes okay.
It’s a simple, inexpensive approach that seems to help patients with a serious but notoriously undertreated condition. “It gives them the extra personal attention they might need. They appreciate the extra nudge most of the time,” said Kimberly Low, PharmD, the ambulatory pharmacist in an ongoing study of the approach at Kaiser Permanente Southern California in Pasadena (Contemp Clin Trials. 2016 Jul 20;50:106-15. doi: 10.1016/j.cct.2016.07.019).
“We need to deliver gout care in a more efficient way that doesn’t put it all on primary care,” where almost all gout is managed. “Pharmacy is a possible way to do that,” said Ted Mikuls, MD, a rheumatology professor at the University of Nebraska in Omaha, and senior investigator on the project. Results will be published soon.
The only randomized trial so far was published recently by Kaiser Permanente Northern California. The chance of hitting the 6-mg/dL mark at 6 months almost tripled when a pharmacist was involved. “The next step is to try to get a large-scale program funded using this model” at Kaiser, said lead investigator Robert Goldfien, MD, chair of the Chiefs of Rheumatology for the Permanente Medical Group in Richmond, Calif (Perm J. 2016 Jul 1;20[3]. doi: 10.7812/TPP/15-234).
Other places are turning to pharmacists, too, even when there isn’t a study involved. One of them is the San Diego Veterans Affairs Medical Center. It’s a “huge help; otherwise our clinic would be flooded with gout patients,” said rheumatologist Robert Terkeltaub, MD, who oversees the program.
Patients there are happy to have fewer flares and not to have to drive to the San Diego VA for blood draws; they go to a nearby clinic instead, and “we mail them their medications. We’ve had tremendous success” with pharmacists, and their “charges are affordable. We have treated hundreds of patients this way,” Dr. Terkeltaub said.
There doesn’t seem to be a downside. The only issue is how reimbursements will work. That’s not much of a problem when everyone is in the same health system and on the same electronic health record, with paychecks coming from the same place. Perhaps not surprisingly, large health systems are where the model is taking hold. How it could work with smaller practices and community pharmacists is unclear.
An obvious need
It’s no secret that gout care isn’t very good in the United States, or, really, anywhere else. Gout is a curable or at least imminently manageable condition with the right drugs for flares and lowering urate, but emergency department visits are up; hospitalizations for gout attacks have surpassed rheumatoid arthritis; and allopurinol dosing is routinely too low, if it’s prescribed at all.
Meanwhile, hyperuricemia has been linked to cardiovascular disease and other problems. Some now consider it part of the metabolic syndrome.
There are a lot of reasons why gout care is subpar, but one of them is that primary care providers are just too busy managing diabetes, hypertension, and other problems that seem more important in 10-minute office visits; that’s where pharmacists come in.
“They understand medications, drug-drug, and drug-herb interactions in a way that I don’t,” and also “have access, hopefully, to a more accurate picture of what patients take. I am all thumbs up for any involvement with pharmacists,” said Reid Blackwelder, MD, a recent president of the American Academy of Family Physicians and a family practice professor at East Tennessee State University in Mountain Home, where pharmacists are embedded in primary care.
Gout is a natural fit for pharmacy. Although the pharmacy-gout literature is thin, there have been plenty of reports about pharmacists improving outcomes, saving money, and increasing patient satisfaction when they help family practice and other doctors manage chronic problems. That’s one of the reasons why pharmacists are part of the primary care team in Mountain Home and other places that can afford them. Pharmacist-managed Coumadin clinics are the precedent.
“I think pharmacy is really excited about providing these types of services. Pharmacists managing gout patients is perfectly in line with what is going on now” in the field. “I can’t imagine how” outcomes “are not going to be positive,” said pharmacist Jan Hirsch, PhD, a professor of clinical pharmacy at the University of California, San Diego, where pharmacists are also on primary care teams.
Who’s going to pay?
No one wants a zero-sum game; physicians and pharmacists both need to be paid fairly for their services. The goal is collaborative care, not stealing patients.
Even so, the issue for a lot of primary care providers “will be who pays for this, and who doesn’t get paid when other people do this,” Dr. Blackwelder said.
One option outside of large health systems is for primary care practices to contract with a trusted local pharmacist to come in every few weeks to help with gout and other chronic problems.
Since they would be in the same office as the physician, family doctors could bill under their own name and split the payment with the pharmacist. “I would just contract with [pharmacists] personally,” Dr. Blackwelder said. “That way you don’t have to worry if the pharmacist” is considered “a provider or not” under Medicare Part B.
Meanwhile, Medicare Part D and some commercial plans reimburse for medication management, which is another option for pharmacist payments.
Additional options are likely to emerge, as well. “Payment models are evolving for pharmacists,” Dr. Hirsch said.
Dr. Mikuls disclosed pending research funding from AstraZeneca. Dr. Terkeltaub is a consultant for AstraZeneca, CymaBay, Revive, Relburn, and other companies.
Something new is being tried to improve gout outcomes in the United States: Pharmacists are being recruited to help manage patients.
People with too-high serum urate levels who agree to extra help are being referred to pharmacists empowered to order blood tests and allopurinol. Pharmacists contact patients by mail or phone, at first, and then maybe automated messages or emails, and educate them about why they need to lower their urate and how to do it. Pharmacists monitor lab results and titrate allopurinol as needed to hit serum urate levels of 6 mg/dL or less. The tune-up usually takes a year, at which point physicians resume ongoing management. The referring doctor is in the background to make sure everything goes okay.
It’s a simple, inexpensive approach that seems to help patients with a serious but notoriously undertreated condition. “It gives them the extra personal attention they might need. They appreciate the extra nudge most of the time,” said Kimberly Low, PharmD, the ambulatory pharmacist in an ongoing study of the approach at Kaiser Permanente Southern California in Pasadena (Contemp Clin Trials. 2016 Jul 20;50:106-15. doi: 10.1016/j.cct.2016.07.019).
“We need to deliver gout care in a more efficient way that doesn’t put it all on primary care,” where almost all gout is managed. “Pharmacy is a possible way to do that,” said Ted Mikuls, MD, a rheumatology professor at the University of Nebraska in Omaha, and senior investigator on the project. Results will be published soon.
The only randomized trial so far was published recently by Kaiser Permanente Northern California. The chance of hitting the 6-mg/dL mark at 6 months almost tripled when a pharmacist was involved. “The next step is to try to get a large-scale program funded using this model” at Kaiser, said lead investigator Robert Goldfien, MD, chair of the Chiefs of Rheumatology for the Permanente Medical Group in Richmond, Calif (Perm J. 2016 Jul 1;20[3]. doi: 10.7812/TPP/15-234).
Other places are turning to pharmacists, too, even when there isn’t a study involved. One of them is the San Diego Veterans Affairs Medical Center. It’s a “huge help; otherwise our clinic would be flooded with gout patients,” said rheumatologist Robert Terkeltaub, MD, who oversees the program.
Patients there are happy to have fewer flares and not to have to drive to the San Diego VA for blood draws; they go to a nearby clinic instead, and “we mail them their medications. We’ve had tremendous success” with pharmacists, and their “charges are affordable. We have treated hundreds of patients this way,” Dr. Terkeltaub said.
There doesn’t seem to be a downside. The only issue is how reimbursements will work. That’s not much of a problem when everyone is in the same health system and on the same electronic health record, with paychecks coming from the same place. Perhaps not surprisingly, large health systems are where the model is taking hold. How it could work with smaller practices and community pharmacists is unclear.
An obvious need
It’s no secret that gout care isn’t very good in the United States, or, really, anywhere else. Gout is a curable or at least imminently manageable condition with the right drugs for flares and lowering urate, but emergency department visits are up; hospitalizations for gout attacks have surpassed rheumatoid arthritis; and allopurinol dosing is routinely too low, if it’s prescribed at all.
Meanwhile, hyperuricemia has been linked to cardiovascular disease and other problems. Some now consider it part of the metabolic syndrome.
There are a lot of reasons why gout care is subpar, but one of them is that primary care providers are just too busy managing diabetes, hypertension, and other problems that seem more important in 10-minute office visits; that’s where pharmacists come in.
“They understand medications, drug-drug, and drug-herb interactions in a way that I don’t,” and also “have access, hopefully, to a more accurate picture of what patients take. I am all thumbs up for any involvement with pharmacists,” said Reid Blackwelder, MD, a recent president of the American Academy of Family Physicians and a family practice professor at East Tennessee State University in Mountain Home, where pharmacists are embedded in primary care.
Gout is a natural fit for pharmacy. Although the pharmacy-gout literature is thin, there have been plenty of reports about pharmacists improving outcomes, saving money, and increasing patient satisfaction when they help family practice and other doctors manage chronic problems. That’s one of the reasons why pharmacists are part of the primary care team in Mountain Home and other places that can afford them. Pharmacist-managed Coumadin clinics are the precedent.
“I think pharmacy is really excited about providing these types of services. Pharmacists managing gout patients is perfectly in line with what is going on now” in the field. “I can’t imagine how” outcomes “are not going to be positive,” said pharmacist Jan Hirsch, PhD, a professor of clinical pharmacy at the University of California, San Diego, where pharmacists are also on primary care teams.
Who’s going to pay?
No one wants a zero-sum game; physicians and pharmacists both need to be paid fairly for their services. The goal is collaborative care, not stealing patients.
Even so, the issue for a lot of primary care providers “will be who pays for this, and who doesn’t get paid when other people do this,” Dr. Blackwelder said.
One option outside of large health systems is for primary care practices to contract with a trusted local pharmacist to come in every few weeks to help with gout and other chronic problems.
Since they would be in the same office as the physician, family doctors could bill under their own name and split the payment with the pharmacist. “I would just contract with [pharmacists] personally,” Dr. Blackwelder said. “That way you don’t have to worry if the pharmacist” is considered “a provider or not” under Medicare Part B.
Meanwhile, Medicare Part D and some commercial plans reimburse for medication management, which is another option for pharmacist payments.
Additional options are likely to emerge, as well. “Payment models are evolving for pharmacists,” Dr. Hirsch said.
Dr. Mikuls disclosed pending research funding from AstraZeneca. Dr. Terkeltaub is a consultant for AstraZeneca, CymaBay, Revive, Relburn, and other companies.
Something new is being tried to improve gout outcomes in the United States: Pharmacists are being recruited to help manage patients.
People with too-high serum urate levels who agree to extra help are being referred to pharmacists empowered to order blood tests and allopurinol. Pharmacists contact patients by mail or phone, at first, and then maybe automated messages or emails, and educate them about why they need to lower their urate and how to do it. Pharmacists monitor lab results and titrate allopurinol as needed to hit serum urate levels of 6 mg/dL or less. The tune-up usually takes a year, at which point physicians resume ongoing management. The referring doctor is in the background to make sure everything goes okay.
It’s a simple, inexpensive approach that seems to help patients with a serious but notoriously undertreated condition. “It gives them the extra personal attention they might need. They appreciate the extra nudge most of the time,” said Kimberly Low, PharmD, the ambulatory pharmacist in an ongoing study of the approach at Kaiser Permanente Southern California in Pasadena (Contemp Clin Trials. 2016 Jul 20;50:106-15. doi: 10.1016/j.cct.2016.07.019).
“We need to deliver gout care in a more efficient way that doesn’t put it all on primary care,” where almost all gout is managed. “Pharmacy is a possible way to do that,” said Ted Mikuls, MD, a rheumatology professor at the University of Nebraska in Omaha, and senior investigator on the project. Results will be published soon.
The only randomized trial so far was published recently by Kaiser Permanente Northern California. The chance of hitting the 6-mg/dL mark at 6 months almost tripled when a pharmacist was involved. “The next step is to try to get a large-scale program funded using this model” at Kaiser, said lead investigator Robert Goldfien, MD, chair of the Chiefs of Rheumatology for the Permanente Medical Group in Richmond, Calif (Perm J. 2016 Jul 1;20[3]. doi: 10.7812/TPP/15-234).
Other places are turning to pharmacists, too, even when there isn’t a study involved. One of them is the San Diego Veterans Affairs Medical Center. It’s a “huge help; otherwise our clinic would be flooded with gout patients,” said rheumatologist Robert Terkeltaub, MD, who oversees the program.
Patients there are happy to have fewer flares and not to have to drive to the San Diego VA for blood draws; they go to a nearby clinic instead, and “we mail them their medications. We’ve had tremendous success” with pharmacists, and their “charges are affordable. We have treated hundreds of patients this way,” Dr. Terkeltaub said.
There doesn’t seem to be a downside. The only issue is how reimbursements will work. That’s not much of a problem when everyone is in the same health system and on the same electronic health record, with paychecks coming from the same place. Perhaps not surprisingly, large health systems are where the model is taking hold. How it could work with smaller practices and community pharmacists is unclear.
An obvious need
It’s no secret that gout care isn’t very good in the United States, or, really, anywhere else. Gout is a curable or at least imminently manageable condition with the right drugs for flares and lowering urate, but emergency department visits are up; hospitalizations for gout attacks have surpassed rheumatoid arthritis; and allopurinol dosing is routinely too low, if it’s prescribed at all.
Meanwhile, hyperuricemia has been linked to cardiovascular disease and other problems. Some now consider it part of the metabolic syndrome.
There are a lot of reasons why gout care is subpar, but one of them is that primary care providers are just too busy managing diabetes, hypertension, and other problems that seem more important in 10-minute office visits; that’s where pharmacists come in.
“They understand medications, drug-drug, and drug-herb interactions in a way that I don’t,” and also “have access, hopefully, to a more accurate picture of what patients take. I am all thumbs up for any involvement with pharmacists,” said Reid Blackwelder, MD, a recent president of the American Academy of Family Physicians and a family practice professor at East Tennessee State University in Mountain Home, where pharmacists are embedded in primary care.
Gout is a natural fit for pharmacy. Although the pharmacy-gout literature is thin, there have been plenty of reports about pharmacists improving outcomes, saving money, and increasing patient satisfaction when they help family practice and other doctors manage chronic problems. That’s one of the reasons why pharmacists are part of the primary care team in Mountain Home and other places that can afford them. Pharmacist-managed Coumadin clinics are the precedent.
“I think pharmacy is really excited about providing these types of services. Pharmacists managing gout patients is perfectly in line with what is going on now” in the field. “I can’t imagine how” outcomes “are not going to be positive,” said pharmacist Jan Hirsch, PhD, a professor of clinical pharmacy at the University of California, San Diego, where pharmacists are also on primary care teams.
Who’s going to pay?
No one wants a zero-sum game; physicians and pharmacists both need to be paid fairly for their services. The goal is collaborative care, not stealing patients.
Even so, the issue for a lot of primary care providers “will be who pays for this, and who doesn’t get paid when other people do this,” Dr. Blackwelder said.
One option outside of large health systems is for primary care practices to contract with a trusted local pharmacist to come in every few weeks to help with gout and other chronic problems.
Since they would be in the same office as the physician, family doctors could bill under their own name and split the payment with the pharmacist. “I would just contract with [pharmacists] personally,” Dr. Blackwelder said. “That way you don’t have to worry if the pharmacist” is considered “a provider or not” under Medicare Part B.
Meanwhile, Medicare Part D and some commercial plans reimburse for medication management, which is another option for pharmacist payments.
Additional options are likely to emerge, as well. “Payment models are evolving for pharmacists,” Dr. Hirsch said.
Dr. Mikuls disclosed pending research funding from AstraZeneca. Dr. Terkeltaub is a consultant for AstraZeneca, CymaBay, Revive, Relburn, and other companies.
Clearing tumor bed margins may not improve oral cancer outcomes
SEATTLE – Additional resection to clear positive frozen tumor bed margins in oral cavity squamous cell carcinoma – a common practice in head and neck surgery – does not improve outcomes, investigators report.
In a retrospective review of 406 patients treated with oral cavity squamous cell carcinoma resection, the difference in local recurrence between patients with positive intraoperative frozen tumor bed margins cleared by additional resection (local recurrence in 27%) and those with positive frozen margins that were not cleared (local recurrence in 34%) was not statistically significant.
The team assessed local recurrence rates after dividing their review subjects – 61 years old on average and over half men – into those with negative tumor and tumor bed margins; patients with one positive and the other negative; and patients with both margins positive. Tumor beds were cleared to negative when possible.
The various configurations mattered for prognosis. Local recurrence ranged from 7% when both margins were negative to 65% when both were positive. Cancer recurred in 19% of patients with negative tumor but positive bed margins, and 35% of patients with positive tumor but negative bed margins. “Combining margin groups provides additional prognostic information, [but] the main specimen margin was the strongest predictor of recurrence. Positive margins on the main specimen carry a poor prognosis,” said lead investigator Marisa Buchakjian, MD, at the International Conference on Head and Neck Cancer, held by the American Head and Neck Society.
The study “should influence the use and interpretation of margin data in oral cavity squamous cell carcinoma surgery,” she said, since the majority of head and neck surgeons rely on tumor bed margins for prognosis, and consider positive tumor beds resected to clear pretty much the same as ones that are initially negative.
That approach is probably too simple. Intraoperative frozen tumor bed margins “were unreliable tests of main specimen margins, and would in fact be expected to miss approximately 50%” that are positive, said Dr. Buchakjian of University of Iowa Hospitals and Clinics, Iowa City.
She and her associates concluded that “the concordance between tumor bed and tumor specimen margins is not good ... Cases of main specimen margin involvement with no corresponding findings in tumor bed frozen sections are common; conversely, frozen sections may show involvement, while the main specimen margins are negative. Prognostic information is contained within findings from both the frozen and specimen margins,” and neither should be considered the “true” margin. The tumor margin is an important predictor, even if margins are taken from the tumor bed.
However, “we do not believe that this provides evidence that a known positive margin should not be pursued with additional excision. We emphasize that this study highlights the prognostic importance of margin status and that an involved margin, either on the initial tumor bed frozen sections or the tumor specimen, is associated with worse outcomes regardless of the final margin result,” they said.
The authors had no conflicts of interest, and didn’t report external funding.
SEATTLE – Additional resection to clear positive frozen tumor bed margins in oral cavity squamous cell carcinoma – a common practice in head and neck surgery – does not improve outcomes, investigators report.
In a retrospective review of 406 patients treated with oral cavity squamous cell carcinoma resection, the difference in local recurrence between patients with positive intraoperative frozen tumor bed margins cleared by additional resection (local recurrence in 27%) and those with positive frozen margins that were not cleared (local recurrence in 34%) was not statistically significant.
The team assessed local recurrence rates after dividing their review subjects – 61 years old on average and over half men – into those with negative tumor and tumor bed margins; patients with one positive and the other negative; and patients with both margins positive. Tumor beds were cleared to negative when possible.
The various configurations mattered for prognosis. Local recurrence ranged from 7% when both margins were negative to 65% when both were positive. Cancer recurred in 19% of patients with negative tumor but positive bed margins, and 35% of patients with positive tumor but negative bed margins. “Combining margin groups provides additional prognostic information, [but] the main specimen margin was the strongest predictor of recurrence. Positive margins on the main specimen carry a poor prognosis,” said lead investigator Marisa Buchakjian, MD, at the International Conference on Head and Neck Cancer, held by the American Head and Neck Society.
The study “should influence the use and interpretation of margin data in oral cavity squamous cell carcinoma surgery,” she said, since the majority of head and neck surgeons rely on tumor bed margins for prognosis, and consider positive tumor beds resected to clear pretty much the same as ones that are initially negative.
That approach is probably too simple. Intraoperative frozen tumor bed margins “were unreliable tests of main specimen margins, and would in fact be expected to miss approximately 50%” that are positive, said Dr. Buchakjian of University of Iowa Hospitals and Clinics, Iowa City.
She and her associates concluded that “the concordance between tumor bed and tumor specimen margins is not good ... Cases of main specimen margin involvement with no corresponding findings in tumor bed frozen sections are common; conversely, frozen sections may show involvement, while the main specimen margins are negative. Prognostic information is contained within findings from both the frozen and specimen margins,” and neither should be considered the “true” margin. The tumor margin is an important predictor, even if margins are taken from the tumor bed.
However, “we do not believe that this provides evidence that a known positive margin should not be pursued with additional excision. We emphasize that this study highlights the prognostic importance of margin status and that an involved margin, either on the initial tumor bed frozen sections or the tumor specimen, is associated with worse outcomes regardless of the final margin result,” they said.
The authors had no conflicts of interest, and didn’t report external funding.
SEATTLE – Additional resection to clear positive frozen tumor bed margins in oral cavity squamous cell carcinoma – a common practice in head and neck surgery – does not improve outcomes, investigators report.
In a retrospective review of 406 patients treated with oral cavity squamous cell carcinoma resection, the difference in local recurrence between patients with positive intraoperative frozen tumor bed margins cleared by additional resection (local recurrence in 27%) and those with positive frozen margins that were not cleared (local recurrence in 34%) was not statistically significant.
The team assessed local recurrence rates after dividing their review subjects – 61 years old on average and over half men – into those with negative tumor and tumor bed margins; patients with one positive and the other negative; and patients with both margins positive. Tumor beds were cleared to negative when possible.
The various configurations mattered for prognosis. Local recurrence ranged from 7% when both margins were negative to 65% when both were positive. Cancer recurred in 19% of patients with negative tumor but positive bed margins, and 35% of patients with positive tumor but negative bed margins. “Combining margin groups provides additional prognostic information, [but] the main specimen margin was the strongest predictor of recurrence. Positive margins on the main specimen carry a poor prognosis,” said lead investigator Marisa Buchakjian, MD, at the International Conference on Head and Neck Cancer, held by the American Head and Neck Society.
The study “should influence the use and interpretation of margin data in oral cavity squamous cell carcinoma surgery,” she said, since the majority of head and neck surgeons rely on tumor bed margins for prognosis, and consider positive tumor beds resected to clear pretty much the same as ones that are initially negative.
That approach is probably too simple. Intraoperative frozen tumor bed margins “were unreliable tests of main specimen margins, and would in fact be expected to miss approximately 50%” that are positive, said Dr. Buchakjian of University of Iowa Hospitals and Clinics, Iowa City.
She and her associates concluded that “the concordance between tumor bed and tumor specimen margins is not good ... Cases of main specimen margin involvement with no corresponding findings in tumor bed frozen sections are common; conversely, frozen sections may show involvement, while the main specimen margins are negative. Prognostic information is contained within findings from both the frozen and specimen margins,” and neither should be considered the “true” margin. The tumor margin is an important predictor, even if margins are taken from the tumor bed.
However, “we do not believe that this provides evidence that a known positive margin should not be pursued with additional excision. We emphasize that this study highlights the prognostic importance of margin status and that an involved margin, either on the initial tumor bed frozen sections or the tumor specimen, is associated with worse outcomes regardless of the final margin result,” they said.
The authors had no conflicts of interest, and didn’t report external funding.
AT AHNS 2016
Key clinical point: Additional resection to clear positive frozen tumor bed margins in oral cavity squamous cell carcinoma – a common practice in head and neck surgery – does not improve outcomes.
Major finding: The difference in local recurrence between patients with positive intraoperative frozen tumor bed margins cleared by additional resection (local recurrence in 27%) and those with positive frozen margins that were not cleared (local recurrence in 34%, absolute difference 7%; 95% CI, –8% to 22%) was not statistically significant.
Data source: Review of 406 patients.
Disclosures: The authors had no conflicts of interest, and didn’t report external funding.
Cardiologists underrecognize angina about half the time
Angina is underrecognized by cardiologists in clinic visits, compared with assessments made by the patients themselves, suggesting that a standard screening tool be used to improve accuracy.
Researchers conducted a survey of 1,257 patients and their 155 doctors at 25 cardiology outpatient practices in 19 states. All patients had documented coronary artery disease and completed the Seattle Angina Questionnaire (SAQ) before their office visits to assess angina symptoms and frequency. Right after they left, their cardiologists estimated and recorded their idea of how often their patients had heart pain and what their symptoms were.
Patient and physician estimates didn’t match: 411 patients (33%) reported at least one bout of angina in the previous month, but their physicians estimated a frequency of 14% (173 patients). Heart failure patients were more than three times as likely to have their angina underestimated, and patients who reported a single bout of angina per month were about 70% less likely than those who reported daily or weekly attacks.
Years in practice and the number of angina patients in the case load didn’t seem to make a difference. Patient demographics, atypical symptoms, and comorbidities besides heart failure didn’t either. “Some physicians were much better at recognizing the frequency of patients’ angina,” said lead investigator Suzanne Arnold, MD, a cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Mo., and her associates.
“Evaluation of angina is subject to limitations inherent in history taking, including pre-existing biases and time constraints on the part of physicians and patients. ... Under-recognition of angina by physicians may result in under treatment with revascularization or medications that could improve patients’ quality of life,” and it wastes healthcare dollars, they said.
The team concluded that angina needs to be assessed directly from patients with a standardized survey like the Seattle Angina Questionnaire (SAQ). “We still routinely depend solely on an unstructured interview instead of directly asking patients using standardized assessments,” the investigators noted. “A more systematic approach is needed for eliciting a history and assessing angina in patients with coronary artery disease to appropriately guide further testing and treatment. ... The use of a validated, patient-centered tool for eliciting patients’ angina, such as the SAQ, should be tested in routine clinical care to see if it improves angina recognition, treatment, and outcomes,” the study team said (Circ Cardiovasc Qual Outcomes. 2016 AUG 16;doi: 10.1161/CIRCOUTCOMES.116.002781).
Patients in the study were, on average, 69 years old, and the majority were white men. About 40% reported previous myocardial infarctions, and more than half were stented. Well over three quarters were on beta-blockers for angina.
The senior investigator, John Spertus, MD, holds a copyright on the SAQ used in the study. Gilead Sciences funded the work. Investigators reported ties to Gilead, Abbvie, Genentech, Glumetrics, Maquet, Sanofi, AstraZeneca, Edwards Life Sciences, Roche, St. Jude Medical, Regeneron, Lilly, and ZS Pharma.
Angina is underrecognized by cardiologists in clinic visits, compared with assessments made by the patients themselves, suggesting that a standard screening tool be used to improve accuracy.
Researchers conducted a survey of 1,257 patients and their 155 doctors at 25 cardiology outpatient practices in 19 states. All patients had documented coronary artery disease and completed the Seattle Angina Questionnaire (SAQ) before their office visits to assess angina symptoms and frequency. Right after they left, their cardiologists estimated and recorded their idea of how often their patients had heart pain and what their symptoms were.
Patient and physician estimates didn’t match: 411 patients (33%) reported at least one bout of angina in the previous month, but their physicians estimated a frequency of 14% (173 patients). Heart failure patients were more than three times as likely to have their angina underestimated, and patients who reported a single bout of angina per month were about 70% less likely than those who reported daily or weekly attacks.
Years in practice and the number of angina patients in the case load didn’t seem to make a difference. Patient demographics, atypical symptoms, and comorbidities besides heart failure didn’t either. “Some physicians were much better at recognizing the frequency of patients’ angina,” said lead investigator Suzanne Arnold, MD, a cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Mo., and her associates.
“Evaluation of angina is subject to limitations inherent in history taking, including pre-existing biases and time constraints on the part of physicians and patients. ... Under-recognition of angina by physicians may result in under treatment with revascularization or medications that could improve patients’ quality of life,” and it wastes healthcare dollars, they said.
The team concluded that angina needs to be assessed directly from patients with a standardized survey like the Seattle Angina Questionnaire (SAQ). “We still routinely depend solely on an unstructured interview instead of directly asking patients using standardized assessments,” the investigators noted. “A more systematic approach is needed for eliciting a history and assessing angina in patients with coronary artery disease to appropriately guide further testing and treatment. ... The use of a validated, patient-centered tool for eliciting patients’ angina, such as the SAQ, should be tested in routine clinical care to see if it improves angina recognition, treatment, and outcomes,” the study team said (Circ Cardiovasc Qual Outcomes. 2016 AUG 16;doi: 10.1161/CIRCOUTCOMES.116.002781).
Patients in the study were, on average, 69 years old, and the majority were white men. About 40% reported previous myocardial infarctions, and more than half were stented. Well over three quarters were on beta-blockers for angina.
The senior investigator, John Spertus, MD, holds a copyright on the SAQ used in the study. Gilead Sciences funded the work. Investigators reported ties to Gilead, Abbvie, Genentech, Glumetrics, Maquet, Sanofi, AstraZeneca, Edwards Life Sciences, Roche, St. Jude Medical, Regeneron, Lilly, and ZS Pharma.
Angina is underrecognized by cardiologists in clinic visits, compared with assessments made by the patients themselves, suggesting that a standard screening tool be used to improve accuracy.
Researchers conducted a survey of 1,257 patients and their 155 doctors at 25 cardiology outpatient practices in 19 states. All patients had documented coronary artery disease and completed the Seattle Angina Questionnaire (SAQ) before their office visits to assess angina symptoms and frequency. Right after they left, their cardiologists estimated and recorded their idea of how often their patients had heart pain and what their symptoms were.
Patient and physician estimates didn’t match: 411 patients (33%) reported at least one bout of angina in the previous month, but their physicians estimated a frequency of 14% (173 patients). Heart failure patients were more than three times as likely to have their angina underestimated, and patients who reported a single bout of angina per month were about 70% less likely than those who reported daily or weekly attacks.
Years in practice and the number of angina patients in the case load didn’t seem to make a difference. Patient demographics, atypical symptoms, and comorbidities besides heart failure didn’t either. “Some physicians were much better at recognizing the frequency of patients’ angina,” said lead investigator Suzanne Arnold, MD, a cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Mo., and her associates.
“Evaluation of angina is subject to limitations inherent in history taking, including pre-existing biases and time constraints on the part of physicians and patients. ... Under-recognition of angina by physicians may result in under treatment with revascularization or medications that could improve patients’ quality of life,” and it wastes healthcare dollars, they said.
The team concluded that angina needs to be assessed directly from patients with a standardized survey like the Seattle Angina Questionnaire (SAQ). “We still routinely depend solely on an unstructured interview instead of directly asking patients using standardized assessments,” the investigators noted. “A more systematic approach is needed for eliciting a history and assessing angina in patients with coronary artery disease to appropriately guide further testing and treatment. ... The use of a validated, patient-centered tool for eliciting patients’ angina, such as the SAQ, should be tested in routine clinical care to see if it improves angina recognition, treatment, and outcomes,” the study team said (Circ Cardiovasc Qual Outcomes. 2016 AUG 16;doi: 10.1161/CIRCOUTCOMES.116.002781).
Patients in the study were, on average, 69 years old, and the majority were white men. About 40% reported previous myocardial infarctions, and more than half were stented. Well over three quarters were on beta-blockers for angina.
The senior investigator, John Spertus, MD, holds a copyright on the SAQ used in the study. Gilead Sciences funded the work. Investigators reported ties to Gilead, Abbvie, Genentech, Glumetrics, Maquet, Sanofi, AstraZeneca, Edwards Life Sciences, Roche, St. Jude Medical, Regeneron, Lilly, and ZS Pharma.
FROM CIRCULATION CARDIOVASCULAR QUALITY AND OUTCOMES
Key clinical point: Cardiologists miss angina nearly half of the time.
Major finding: Patient and physician estimates don’t match up; 411 patients (33%) reported at least one bout of angina in the previous month, but their physicians estimated a frequency of 14% (173 patients).
Data source: A survey of 1,257 patients and their 155 doctors at 25 cardiology outpatient practices in 19 states.
Disclosures: The senior investigator, John Spertus, MD, holds a copyright on the Seattle Angina Questionnaire used in the study. Gilead Sciences funded the work. Investigators reported ties to Gilead, Abbvie, Genentech, Glumetrics, Maquet, Sanofi, AstraZeneca, Edwards Life Sciences, Roche, St. Jude Medical, Regeneron, Lilly, and ZS Pharma.