User login
Physician fired after slurs, including ‘cannibalism,’ against Israel
Fidaa Wishah, MD, a pediatric radiologist at Phoenix Children’s Hospital in Arizona, has been fired after the hospital reviewed evidence that included her anti-Israel comments on social media, according to the hospital’s statement.
On May 26, Dr. Wishah posted, “We will uncover your thirst to kill our Palestinian children. … We sense your fear. The fear of your collapse. A state based on atrocity, inhumanity, racism and cannibalism never last long! Hey #israel … your end is coming sooner than you think.”
Phoenix Children’s Hospital did not respond to this news organization’s request for comment but said in a statement to the Jewish News Syndicate : “After a thorough review of the facts related to this matter, this individual is no longer providing care at Phoenix Children’s. All children in the care of Phoenix Children’s receive hope, healing and the best possible health care, regardless of race, color, disability, religion, gender, gender identity, sexual orientation or national origin.”
Dr. Wishah’s profile has been removed from the hospital website. Her LinkedIn profile indicates she had been a pediatric radiology fellow at Stanford (Calif.) University, specializing in advanced magnetic resonance imaging and fetal imaging and had been a senior staff pediatric radiologist at Henry Ford Health System in Detroit.
It wasn’t the first time antisemitic comments have led to the firing of a physician. Last year, this news organization wrote about Lara Kollab, DO, a first-year resident fired for her antisemitic tweets. She was subsequently barred from medicine.
In the same post from May 26, Dr. Wishah also wrote: “We will not be #censored anymore! Bomb our media buildings and we have the phones[.] Bribe the mainstream media and we have our small #socialmedia platforms[.] From our windows ... from our streets ... next the rubble we will expose you to the world[.] We will expose the #massacre and #genocide you #zionists are proud of[.]”
Today, CAIR-AZ, a group whose mission is to “enhance understanding of Islam, protect civil rights, promote justice, and empower American Muslims,” according to its website, announced that it, along with three private law firms, will represent Dr. Wishah in what they referred to as “her wrongful termination case against Phoenix Children’s Hospital.”
The announcement, which mentions that Dr. Wishah was born and raised in Gaza, said, “Dr. Wishah has been a medical doctor since 2010 and has spent the vast majority of her career as a pediatric physician. Despite caring for thousands of children, many of whom are Jewish, she has never been accused of discriminating against any of her patients or colleagues.”
The statement added, “PCH’s decision to terminate Dr. Wishah is shameful and an attack on freedom of speech.”
A version of this article first appeared on Medscape.com.
Fidaa Wishah, MD, a pediatric radiologist at Phoenix Children’s Hospital in Arizona, has been fired after the hospital reviewed evidence that included her anti-Israel comments on social media, according to the hospital’s statement.
On May 26, Dr. Wishah posted, “We will uncover your thirst to kill our Palestinian children. … We sense your fear. The fear of your collapse. A state based on atrocity, inhumanity, racism and cannibalism never last long! Hey #israel … your end is coming sooner than you think.”
Phoenix Children’s Hospital did not respond to this news organization’s request for comment but said in a statement to the Jewish News Syndicate : “After a thorough review of the facts related to this matter, this individual is no longer providing care at Phoenix Children’s. All children in the care of Phoenix Children’s receive hope, healing and the best possible health care, regardless of race, color, disability, religion, gender, gender identity, sexual orientation or national origin.”
Dr. Wishah’s profile has been removed from the hospital website. Her LinkedIn profile indicates she had been a pediatric radiology fellow at Stanford (Calif.) University, specializing in advanced magnetic resonance imaging and fetal imaging and had been a senior staff pediatric radiologist at Henry Ford Health System in Detroit.
It wasn’t the first time antisemitic comments have led to the firing of a physician. Last year, this news organization wrote about Lara Kollab, DO, a first-year resident fired for her antisemitic tweets. She was subsequently barred from medicine.
In the same post from May 26, Dr. Wishah also wrote: “We will not be #censored anymore! Bomb our media buildings and we have the phones[.] Bribe the mainstream media and we have our small #socialmedia platforms[.] From our windows ... from our streets ... next the rubble we will expose you to the world[.] We will expose the #massacre and #genocide you #zionists are proud of[.]”
Today, CAIR-AZ, a group whose mission is to “enhance understanding of Islam, protect civil rights, promote justice, and empower American Muslims,” according to its website, announced that it, along with three private law firms, will represent Dr. Wishah in what they referred to as “her wrongful termination case against Phoenix Children’s Hospital.”
The announcement, which mentions that Dr. Wishah was born and raised in Gaza, said, “Dr. Wishah has been a medical doctor since 2010 and has spent the vast majority of her career as a pediatric physician. Despite caring for thousands of children, many of whom are Jewish, she has never been accused of discriminating against any of her patients or colleagues.”
The statement added, “PCH’s decision to terminate Dr. Wishah is shameful and an attack on freedom of speech.”
A version of this article first appeared on Medscape.com.
Fidaa Wishah, MD, a pediatric radiologist at Phoenix Children’s Hospital in Arizona, has been fired after the hospital reviewed evidence that included her anti-Israel comments on social media, according to the hospital’s statement.
On May 26, Dr. Wishah posted, “We will uncover your thirst to kill our Palestinian children. … We sense your fear. The fear of your collapse. A state based on atrocity, inhumanity, racism and cannibalism never last long! Hey #israel … your end is coming sooner than you think.”
Phoenix Children’s Hospital did not respond to this news organization’s request for comment but said in a statement to the Jewish News Syndicate : “After a thorough review of the facts related to this matter, this individual is no longer providing care at Phoenix Children’s. All children in the care of Phoenix Children’s receive hope, healing and the best possible health care, regardless of race, color, disability, religion, gender, gender identity, sexual orientation or national origin.”
Dr. Wishah’s profile has been removed from the hospital website. Her LinkedIn profile indicates she had been a pediatric radiology fellow at Stanford (Calif.) University, specializing in advanced magnetic resonance imaging and fetal imaging and had been a senior staff pediatric radiologist at Henry Ford Health System in Detroit.
It wasn’t the first time antisemitic comments have led to the firing of a physician. Last year, this news organization wrote about Lara Kollab, DO, a first-year resident fired for her antisemitic tweets. She was subsequently barred from medicine.
In the same post from May 26, Dr. Wishah also wrote: “We will not be #censored anymore! Bomb our media buildings and we have the phones[.] Bribe the mainstream media and we have our small #socialmedia platforms[.] From our windows ... from our streets ... next the rubble we will expose you to the world[.] We will expose the #massacre and #genocide you #zionists are proud of[.]”
Today, CAIR-AZ, a group whose mission is to “enhance understanding of Islam, protect civil rights, promote justice, and empower American Muslims,” according to its website, announced that it, along with three private law firms, will represent Dr. Wishah in what they referred to as “her wrongful termination case against Phoenix Children’s Hospital.”
The announcement, which mentions that Dr. Wishah was born and raised in Gaza, said, “Dr. Wishah has been a medical doctor since 2010 and has spent the vast majority of her career as a pediatric physician. Despite caring for thousands of children, many of whom are Jewish, she has never been accused of discriminating against any of her patients or colleagues.”
The statement added, “PCH’s decision to terminate Dr. Wishah is shameful and an attack on freedom of speech.”
A version of this article first appeared on Medscape.com.
Back-to-school threat: Missed vaccinations in children, teens
U.S. children and adolescents may be at higher risk for vaccine-preventable diseases this fall as vaccination levels have not caught up with prepandemic coverage, according to a study published in Morbidity and Mortality Weekly Report from the Centers for Disease Control and Prevention.
“Pediatric outbreaks of vaccine-preventable diseases have the potential to derail efforts to reopen schools for the 2021-22 academic year and further delay nationwide efforts to return students to the classroom,” wrote Bhavini Patel Murthy, MD, with the immunization services division, National Center for Immunization and Respiratory Diseases, and colleagues.
The number of children getting routine vaccinations plummeted between March and May 2020, compared with the same months in 2019. Although vaccination rates increased again from June 2020 to September 2020, the rebound was not enough to reach prepandemic levels, according to the study.
At the beginning of the June–September 2020 period, the news was good, the authors wrote. After most stay-at-home orders were lifted, the number of weekly routine pediatric vaccinations started to approach, and even surpass, baseline prepandemic levels in most of the 10 jurisdictions studied.
“However,” the authors wrote, “across all age groups and across all vaccine types, none of the jurisdictions demonstrated a sustained or prolonged increase in the number of weekly doses administered above prepandemic administration levels, which would have been necessary to catch up children and adolescents who missed routine vaccinations.”
To overcome the gap, the authors said that clinicians should take the initiative. “Health care providers should assess the vaccination status of all pediatric patients, including adolescents, and contact those who are behind schedule to ensure that all children are fully vaccinated.”
As COVID-19 vaccinations become more readily available to children, the CDC recommends that providers consider giving COVID-19 shots along with other routinely recommended vaccines.
Martha Perry, MD, associate professor and medical director at the University of North Carolina Children’s Primary Care Clinic, Chapel Hill, said in an interview that getting the message out about the need to get children and adolescents caught up may require a national messaging campaign similar to that for COVID-19 vaccinations, as well as opening mass vaccination sites rather than families seeking vaccinations from individual providers.
She noted that, although schools may offer a checks and balances system for required vaccinations, children who are not yet school age depend on families getting individual appointments.
Size of the gaps
The MMWR article shows that the shortfall in vaccinations in June–September 2020, compared with those months the year before are striking.
For children younger than 2 years old and aged 2-6 years, diphtheria, tetanus, and acellular pertussis (DtaP) vaccinations declined an average of 9.1% and 6.7%, respectively.
Among children aged 12-23 months and 2-8 years, MMR vaccinations decreased 8.8% and 11.3%, respectively.
Among children aged 9-12 years and adolescents 13-17 years, human papillomavirus vaccinations decreased an average 12.2% and 28.1%, respectively. Among the same age groups, Tdap vaccinations dropped 21.3% and 30.0%, respectively.
Dr. Perry said that, although all the shortfalls are important, lags in vaccinations for measles and pertussis are particularly alarming in light of outbreaks in recent years.
Additionally, she said, as COVID-19 restrictions are lifting, some of the mitigation strategies, such as mask wearing, that kept other diseases at bay will not be in place, heightening the risk for infection.
The authors chose to measure weekly doses in March–May 2020, and June–September 2020 because many jurisdictions imposed and then lifted stay-at-home orders during these times. They analyzed data from 10 jurisdictions with high-performing information systems (Idaho, Iowa, Louisiana, Michigan, Minnesota, New York City, North Dakota, Oregon, Washington, and Wisconsin).
Adults missing vaccinations as well
Another analysis, commissioned by GlaxoSmithKline and conducted by Avalere Health, calculated 8.8 million missed adolescent vaccine doses and 17.2 million missed adult vaccine doses as a result of the pandemic and ongoing government restrictions and public health measures.
That study examined claims for CDC-recommended vaccines across commercial, managed Medicaid, Medicare Advantage, and Medicare fee-for-service Part B for January–November 2020, compared with the same period in 2019.
It also found that vaccine claims remain well below 2019 levels. Total noninfluenza vaccine claims submissions were down by between 13% and 35% among adolescents and 17% and 40% among adults, compared with the same period in 2019.
Dr. Perry said it will be critical for schools across the nation to enforce their policies on requiring up-to-date vaccinations even if online attendance is offered.
The workforce needed for this will be challenging, she noted.
“We’ve lost a lot of workforce in the health care field in the pandemic for a variety of reasons and it may be challenging to fill those positions,” she said.
She also said the study underlines the importance of each state having a vaccine registry so each provider can determine what vaccinations a child needs.
The study authors and Dr. Perry reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
U.S. children and adolescents may be at higher risk for vaccine-preventable diseases this fall as vaccination levels have not caught up with prepandemic coverage, according to a study published in Morbidity and Mortality Weekly Report from the Centers for Disease Control and Prevention.
“Pediatric outbreaks of vaccine-preventable diseases have the potential to derail efforts to reopen schools for the 2021-22 academic year and further delay nationwide efforts to return students to the classroom,” wrote Bhavini Patel Murthy, MD, with the immunization services division, National Center for Immunization and Respiratory Diseases, and colleagues.
The number of children getting routine vaccinations plummeted between March and May 2020, compared with the same months in 2019. Although vaccination rates increased again from June 2020 to September 2020, the rebound was not enough to reach prepandemic levels, according to the study.
At the beginning of the June–September 2020 period, the news was good, the authors wrote. After most stay-at-home orders were lifted, the number of weekly routine pediatric vaccinations started to approach, and even surpass, baseline prepandemic levels in most of the 10 jurisdictions studied.
“However,” the authors wrote, “across all age groups and across all vaccine types, none of the jurisdictions demonstrated a sustained or prolonged increase in the number of weekly doses administered above prepandemic administration levels, which would have been necessary to catch up children and adolescents who missed routine vaccinations.”
To overcome the gap, the authors said that clinicians should take the initiative. “Health care providers should assess the vaccination status of all pediatric patients, including adolescents, and contact those who are behind schedule to ensure that all children are fully vaccinated.”
As COVID-19 vaccinations become more readily available to children, the CDC recommends that providers consider giving COVID-19 shots along with other routinely recommended vaccines.
Martha Perry, MD, associate professor and medical director at the University of North Carolina Children’s Primary Care Clinic, Chapel Hill, said in an interview that getting the message out about the need to get children and adolescents caught up may require a national messaging campaign similar to that for COVID-19 vaccinations, as well as opening mass vaccination sites rather than families seeking vaccinations from individual providers.
She noted that, although schools may offer a checks and balances system for required vaccinations, children who are not yet school age depend on families getting individual appointments.
Size of the gaps
The MMWR article shows that the shortfall in vaccinations in June–September 2020, compared with those months the year before are striking.
For children younger than 2 years old and aged 2-6 years, diphtheria, tetanus, and acellular pertussis (DtaP) vaccinations declined an average of 9.1% and 6.7%, respectively.
Among children aged 12-23 months and 2-8 years, MMR vaccinations decreased 8.8% and 11.3%, respectively.
Among children aged 9-12 years and adolescents 13-17 years, human papillomavirus vaccinations decreased an average 12.2% and 28.1%, respectively. Among the same age groups, Tdap vaccinations dropped 21.3% and 30.0%, respectively.
Dr. Perry said that, although all the shortfalls are important, lags in vaccinations for measles and pertussis are particularly alarming in light of outbreaks in recent years.
Additionally, she said, as COVID-19 restrictions are lifting, some of the mitigation strategies, such as mask wearing, that kept other diseases at bay will not be in place, heightening the risk for infection.
The authors chose to measure weekly doses in March–May 2020, and June–September 2020 because many jurisdictions imposed and then lifted stay-at-home orders during these times. They analyzed data from 10 jurisdictions with high-performing information systems (Idaho, Iowa, Louisiana, Michigan, Minnesota, New York City, North Dakota, Oregon, Washington, and Wisconsin).
Adults missing vaccinations as well
Another analysis, commissioned by GlaxoSmithKline and conducted by Avalere Health, calculated 8.8 million missed adolescent vaccine doses and 17.2 million missed adult vaccine doses as a result of the pandemic and ongoing government restrictions and public health measures.
That study examined claims for CDC-recommended vaccines across commercial, managed Medicaid, Medicare Advantage, and Medicare fee-for-service Part B for January–November 2020, compared with the same period in 2019.
It also found that vaccine claims remain well below 2019 levels. Total noninfluenza vaccine claims submissions were down by between 13% and 35% among adolescents and 17% and 40% among adults, compared with the same period in 2019.
Dr. Perry said it will be critical for schools across the nation to enforce their policies on requiring up-to-date vaccinations even if online attendance is offered.
The workforce needed for this will be challenging, she noted.
“We’ve lost a lot of workforce in the health care field in the pandemic for a variety of reasons and it may be challenging to fill those positions,” she said.
She also said the study underlines the importance of each state having a vaccine registry so each provider can determine what vaccinations a child needs.
The study authors and Dr. Perry reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
U.S. children and adolescents may be at higher risk for vaccine-preventable diseases this fall as vaccination levels have not caught up with prepandemic coverage, according to a study published in Morbidity and Mortality Weekly Report from the Centers for Disease Control and Prevention.
“Pediatric outbreaks of vaccine-preventable diseases have the potential to derail efforts to reopen schools for the 2021-22 academic year and further delay nationwide efforts to return students to the classroom,” wrote Bhavini Patel Murthy, MD, with the immunization services division, National Center for Immunization and Respiratory Diseases, and colleagues.
The number of children getting routine vaccinations plummeted between March and May 2020, compared with the same months in 2019. Although vaccination rates increased again from June 2020 to September 2020, the rebound was not enough to reach prepandemic levels, according to the study.
At the beginning of the June–September 2020 period, the news was good, the authors wrote. After most stay-at-home orders were lifted, the number of weekly routine pediatric vaccinations started to approach, and even surpass, baseline prepandemic levels in most of the 10 jurisdictions studied.
“However,” the authors wrote, “across all age groups and across all vaccine types, none of the jurisdictions demonstrated a sustained or prolonged increase in the number of weekly doses administered above prepandemic administration levels, which would have been necessary to catch up children and adolescents who missed routine vaccinations.”
To overcome the gap, the authors said that clinicians should take the initiative. “Health care providers should assess the vaccination status of all pediatric patients, including adolescents, and contact those who are behind schedule to ensure that all children are fully vaccinated.”
As COVID-19 vaccinations become more readily available to children, the CDC recommends that providers consider giving COVID-19 shots along with other routinely recommended vaccines.
Martha Perry, MD, associate professor and medical director at the University of North Carolina Children’s Primary Care Clinic, Chapel Hill, said in an interview that getting the message out about the need to get children and adolescents caught up may require a national messaging campaign similar to that for COVID-19 vaccinations, as well as opening mass vaccination sites rather than families seeking vaccinations from individual providers.
She noted that, although schools may offer a checks and balances system for required vaccinations, children who are not yet school age depend on families getting individual appointments.
Size of the gaps
The MMWR article shows that the shortfall in vaccinations in June–September 2020, compared with those months the year before are striking.
For children younger than 2 years old and aged 2-6 years, diphtheria, tetanus, and acellular pertussis (DtaP) vaccinations declined an average of 9.1% and 6.7%, respectively.
Among children aged 12-23 months and 2-8 years, MMR vaccinations decreased 8.8% and 11.3%, respectively.
Among children aged 9-12 years and adolescents 13-17 years, human papillomavirus vaccinations decreased an average 12.2% and 28.1%, respectively. Among the same age groups, Tdap vaccinations dropped 21.3% and 30.0%, respectively.
Dr. Perry said that, although all the shortfalls are important, lags in vaccinations for measles and pertussis are particularly alarming in light of outbreaks in recent years.
Additionally, she said, as COVID-19 restrictions are lifting, some of the mitigation strategies, such as mask wearing, that kept other diseases at bay will not be in place, heightening the risk for infection.
The authors chose to measure weekly doses in March–May 2020, and June–September 2020 because many jurisdictions imposed and then lifted stay-at-home orders during these times. They analyzed data from 10 jurisdictions with high-performing information systems (Idaho, Iowa, Louisiana, Michigan, Minnesota, New York City, North Dakota, Oregon, Washington, and Wisconsin).
Adults missing vaccinations as well
Another analysis, commissioned by GlaxoSmithKline and conducted by Avalere Health, calculated 8.8 million missed adolescent vaccine doses and 17.2 million missed adult vaccine doses as a result of the pandemic and ongoing government restrictions and public health measures.
That study examined claims for CDC-recommended vaccines across commercial, managed Medicaid, Medicare Advantage, and Medicare fee-for-service Part B for January–November 2020, compared with the same period in 2019.
It also found that vaccine claims remain well below 2019 levels. Total noninfluenza vaccine claims submissions were down by between 13% and 35% among adolescents and 17% and 40% among adults, compared with the same period in 2019.
Dr. Perry said it will be critical for schools across the nation to enforce their policies on requiring up-to-date vaccinations even if online attendance is offered.
The workforce needed for this will be challenging, she noted.
“We’ve lost a lot of workforce in the health care field in the pandemic for a variety of reasons and it may be challenging to fill those positions,” she said.
She also said the study underlines the importance of each state having a vaccine registry so each provider can determine what vaccinations a child needs.
The study authors and Dr. Perry reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Remove sex designation from public part of birth certificates, AMA advises
Requiring the designation can lead to discrimination and unnecessary burden on individuals whose current gender identity does not align with their designation at birth when they register for school or sports, adopt, get married, or request personal records.
A person’s sex designation at birth would still be submitted to the U.S. Standard Certificate of Live Birth for medical, public health, and statistical use only, report authors note.
Willie Underwood III, MD, MSc, author of Board Report 15, explained in reference committee testimony that a standard certificate of live birth is critical for uniformly collecting and processing data, but birth certificates are issued by the government to individuals.
Ten states allow gender-neutral designation
According to the report, 48 states (Tennessee and Ohio are the exceptions) and the District of Columbia allow people to amend their sex designation on their birth certificate to reflect their gender identities, but only 10 states allow for a gender-neutral designation, usually “X,” on birth certificates. The U.S. Department of State does not currently offer an option for a gender-neutral designation on U.S. passports.
“Assigning sex using binary variables in the public portion of the birth certificate fails to recognize the medical spectrum of gender identity,” Dr. Underwood said, and it can be used to discriminate.
Jeremy Toler, MD, a delegate from GLMA: Health Professionals Advancing LGBTQ Equality, testified that there is precedent for information to be removed from the public portion of the birth certificates. And much data is collected for each live birth that doesn’t show up on individuals’ birth certificates, he noted.
Dr. Toler said transgender, gender nonbinary, and individuals with differences in sex development can be placed at a disadvantage by the sex label on the birth certificate.
“We unfortunately still live in a world where it is unsafe in many cases for one’s gender to vary from the sex assigned at birth,” Dr. Toler said.
Not having this data on the widely used form will reduce unnecessary reliance on sex as a stand-in for gender, he said, and would “serve as an equalizer” since policies differ by state.
Robert Jackson, MD, an alternate delegate from the American Academy of Cosmetic Surgery, spoke against the measure.
“We as physicians need to report things accurately,” Dr. Jackson said. “All through medical school, residency, and specialty training we were supposed to delegate all of the physical findings of the patient we’re taking care of. I think when the child is born, they do have physical characteristics either male or female, and I think that probably should be on the public record. That’s just my personal opinion.”
Sarah Mae Smith, MD, delegate from California, speaking on behalf of the Women Physicians Section, said removing the sex designation is important for moving toward gender equity.
“We need to recognize [that] gender is not a binary but a spectrum,” she said. “Obligating our patients to jump through numerous administrative hoops to identify as who they are based on a sex assigned at birth primarily on genitalia is not only unnecessary but actively deleterious to their health.”
Race was once public on birth certificates
She noted that the report mentions that previously, information on the race of a person’s parents was included on the public portion of the birth certificate and that information was recognized to facilitate discrimination.
“Thankfully, a change was made to obviate at least that avenue for discriminatory practices,” she said. “Now, likewise, the information on sex assigned at birth is being used to undermine the rights of our transgender, intersex, and nonbinary patients.”
Arlene Seid, MD, MPH, an alternate delegate from the American Association of Public Health Physicians, said the resolution protects the aggregate data “without the discrimination associated with the individual data.”
Sex no longer has a role to play in the jobs people do, she noted, and the designation shouldn’t have to be evaluated for something like a job interview.
“Our society doesn’t need it on an individual basis for most of what occurs in public life,” Dr. Seid said.
Dr. Underwood, Dr. Toler, Dr. Jackson, Dr. Smith, and Dr. Seid declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Requiring the designation can lead to discrimination and unnecessary burden on individuals whose current gender identity does not align with their designation at birth when they register for school or sports, adopt, get married, or request personal records.
A person’s sex designation at birth would still be submitted to the U.S. Standard Certificate of Live Birth for medical, public health, and statistical use only, report authors note.
Willie Underwood III, MD, MSc, author of Board Report 15, explained in reference committee testimony that a standard certificate of live birth is critical for uniformly collecting and processing data, but birth certificates are issued by the government to individuals.
Ten states allow gender-neutral designation
According to the report, 48 states (Tennessee and Ohio are the exceptions) and the District of Columbia allow people to amend their sex designation on their birth certificate to reflect their gender identities, but only 10 states allow for a gender-neutral designation, usually “X,” on birth certificates. The U.S. Department of State does not currently offer an option for a gender-neutral designation on U.S. passports.
“Assigning sex using binary variables in the public portion of the birth certificate fails to recognize the medical spectrum of gender identity,” Dr. Underwood said, and it can be used to discriminate.
Jeremy Toler, MD, a delegate from GLMA: Health Professionals Advancing LGBTQ Equality, testified that there is precedent for information to be removed from the public portion of the birth certificates. And much data is collected for each live birth that doesn’t show up on individuals’ birth certificates, he noted.
Dr. Toler said transgender, gender nonbinary, and individuals with differences in sex development can be placed at a disadvantage by the sex label on the birth certificate.
“We unfortunately still live in a world where it is unsafe in many cases for one’s gender to vary from the sex assigned at birth,” Dr. Toler said.
Not having this data on the widely used form will reduce unnecessary reliance on sex as a stand-in for gender, he said, and would “serve as an equalizer” since policies differ by state.
Robert Jackson, MD, an alternate delegate from the American Academy of Cosmetic Surgery, spoke against the measure.
“We as physicians need to report things accurately,” Dr. Jackson said. “All through medical school, residency, and specialty training we were supposed to delegate all of the physical findings of the patient we’re taking care of. I think when the child is born, they do have physical characteristics either male or female, and I think that probably should be on the public record. That’s just my personal opinion.”
Sarah Mae Smith, MD, delegate from California, speaking on behalf of the Women Physicians Section, said removing the sex designation is important for moving toward gender equity.
“We need to recognize [that] gender is not a binary but a spectrum,” she said. “Obligating our patients to jump through numerous administrative hoops to identify as who they are based on a sex assigned at birth primarily on genitalia is not only unnecessary but actively deleterious to their health.”
Race was once public on birth certificates
She noted that the report mentions that previously, information on the race of a person’s parents was included on the public portion of the birth certificate and that information was recognized to facilitate discrimination.
“Thankfully, a change was made to obviate at least that avenue for discriminatory practices,” she said. “Now, likewise, the information on sex assigned at birth is being used to undermine the rights of our transgender, intersex, and nonbinary patients.”
Arlene Seid, MD, MPH, an alternate delegate from the American Association of Public Health Physicians, said the resolution protects the aggregate data “without the discrimination associated with the individual data.”
Sex no longer has a role to play in the jobs people do, she noted, and the designation shouldn’t have to be evaluated for something like a job interview.
“Our society doesn’t need it on an individual basis for most of what occurs in public life,” Dr. Seid said.
Dr. Underwood, Dr. Toler, Dr. Jackson, Dr. Smith, and Dr. Seid declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Requiring the designation can lead to discrimination and unnecessary burden on individuals whose current gender identity does not align with their designation at birth when they register for school or sports, adopt, get married, or request personal records.
A person’s sex designation at birth would still be submitted to the U.S. Standard Certificate of Live Birth for medical, public health, and statistical use only, report authors note.
Willie Underwood III, MD, MSc, author of Board Report 15, explained in reference committee testimony that a standard certificate of live birth is critical for uniformly collecting and processing data, but birth certificates are issued by the government to individuals.
Ten states allow gender-neutral designation
According to the report, 48 states (Tennessee and Ohio are the exceptions) and the District of Columbia allow people to amend their sex designation on their birth certificate to reflect their gender identities, but only 10 states allow for a gender-neutral designation, usually “X,” on birth certificates. The U.S. Department of State does not currently offer an option for a gender-neutral designation on U.S. passports.
“Assigning sex using binary variables in the public portion of the birth certificate fails to recognize the medical spectrum of gender identity,” Dr. Underwood said, and it can be used to discriminate.
Jeremy Toler, MD, a delegate from GLMA: Health Professionals Advancing LGBTQ Equality, testified that there is precedent for information to be removed from the public portion of the birth certificates. And much data is collected for each live birth that doesn’t show up on individuals’ birth certificates, he noted.
Dr. Toler said transgender, gender nonbinary, and individuals with differences in sex development can be placed at a disadvantage by the sex label on the birth certificate.
“We unfortunately still live in a world where it is unsafe in many cases for one’s gender to vary from the sex assigned at birth,” Dr. Toler said.
Not having this data on the widely used form will reduce unnecessary reliance on sex as a stand-in for gender, he said, and would “serve as an equalizer” since policies differ by state.
Robert Jackson, MD, an alternate delegate from the American Academy of Cosmetic Surgery, spoke against the measure.
“We as physicians need to report things accurately,” Dr. Jackson said. “All through medical school, residency, and specialty training we were supposed to delegate all of the physical findings of the patient we’re taking care of. I think when the child is born, they do have physical characteristics either male or female, and I think that probably should be on the public record. That’s just my personal opinion.”
Sarah Mae Smith, MD, delegate from California, speaking on behalf of the Women Physicians Section, said removing the sex designation is important for moving toward gender equity.
“We need to recognize [that] gender is not a binary but a spectrum,” she said. “Obligating our patients to jump through numerous administrative hoops to identify as who they are based on a sex assigned at birth primarily on genitalia is not only unnecessary but actively deleterious to their health.”
Race was once public on birth certificates
She noted that the report mentions that previously, information on the race of a person’s parents was included on the public portion of the birth certificate and that information was recognized to facilitate discrimination.
“Thankfully, a change was made to obviate at least that avenue for discriminatory practices,” she said. “Now, likewise, the information on sex assigned at birth is being used to undermine the rights of our transgender, intersex, and nonbinary patients.”
Arlene Seid, MD, MPH, an alternate delegate from the American Association of Public Health Physicians, said the resolution protects the aggregate data “without the discrimination associated with the individual data.”
Sex no longer has a role to play in the jobs people do, she noted, and the designation shouldn’t have to be evaluated for something like a job interview.
“Our society doesn’t need it on an individual basis for most of what occurs in public life,” Dr. Seid said.
Dr. Underwood, Dr. Toler, Dr. Jackson, Dr. Smith, and Dr. Seid declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AMA: ‘Excited delirium’ not a legitimate medical diagnosis
Current evidence does not support use of “excited delirium” or “excited delirium syndrome” as a medical diagnosis, the American Medical Association said June 14, and the term should not be used unless clear diagnostic criteria are validated.
The term is disproportionately applied to people of color, “for whom inappropriate and excessive pharmacotherapy continues to be the norm instead of behavioral deescalation,” the report by the AMA’s Council on Science and Public Health stated, and is therefore indicative of systemic racism.
That conclusion was one of many included in CSAPH Report 2, which was adopted June 14 at the special meeting of the AMA House of Delegates.
The AMA also opposes “use of sedative/hypnotic and dissociative agents, including ketamine, as a pharmacologic intervention for agitated individuals in the out-of-hospital setting, when done solely for a law enforcement purpose.”
Medications typically used for restraint include dissociative ketamine, benzodiazepine sedatives such as midazolam, and antipsychotic medications including olanzapine or haloperidol, alone or in combination.
Kenneth Certa, MD, from the American Psychiatric Association, speaking on behalf of the section council on psychiatry, said in a reference committee hearing: “We have been very concerned over the years with the development of the inexact diagnosis of ‘agitated delirium’ or ‘excited delirium,’ especially after having had a number of individuals, more than what’s reported in the press, die by the use of ketamine in the field for this inexact diagnosis.”
Tamaan Osbourne-Roberts, MD, a delegate and CSAPH member, said the diagnosis lacks scientific evidence and is “disproportionately applied to otherwise healthy Black men in their mid-30s and these men are most likely to die from resulting first-responder actions.”
Dr. Osbourne-Roberts testified that deescalation training should be more widely used and that crisis intervention team models in which behavioral health specialists are first deployed to respond to behavioral health emergencies should be more prevalent.
Andrew Rudawsky, MD, an assistant medical director of two emergency departments and delegate from Ohio, speaking as an individual, testified: “I can tell you from first-hand experience that ‘excited delirium’ is very real. These acutely ill, unstable patients have an emergency medical condition best cared for by an emergency medicine physician.”
The report recognizes that drugs used outside a hospital setting by nonphysicians come with significant risks, particularly for those with underlying conditions and in terms of drug–drug interactions.
“I completely agree that medicine should not be practiced by law enforcement,” Dr. Rudawsky said. “I’m gravely concerned by the legal ramifications of stating that this condition doesn’t exist.”
He said he is optimistic that the Diagnostic and Statistical Manual of Mental Disorders (DSM) will be updated to include “excited delirium.”
in medical and mental health emergencies in local communities.
Additionally, the report urges that “administration of any pharmacologic treatments in the out-of-hospital setting be done equitably, in an evidence-based, antiracist, and stigma-free way.”
The report calls on law enforcement and frontline emergency medical service personnel, who are a part of the “dual response” in emergency situations, to engage in training overseen by EMS medical directors. “The training should minimally include deescalation techniques and the appropriate use of pharmacologic intervention for agitated individuals in the out-of-hospital setting,” the report states.
Recommendation on oversight draws controversy
Several commenters were emergency physicians and medical directors who expressed concern that investigation of potential cases of inappropriate pharmacologic intervention would be overseen by nonphysicians.
The CSAPH authors write that independent investigators are appropriate, whereas those in emergency medicine say EMS medical directors should lead oversight.
Stephen Epstein, MD, chair of the section council on emergency medicine, speaking on behalf of the section council, had moved for referral of the portion of the report that deals with oversight of EMS.
“We’re concerned that recommendation 6, by calling for independent investigators, would put nonphysicians in the position of supervising the practice of medicine of a board-approved specialty. This would set an unfortunate precedent for our AMA,” he said.
Dr. Epstein also said the American College of Emergency Physicians will soon release a report on “excited delirium,” which will add key information for debating the issue.
He added that a new report on the safety of ketamine in out-of-hospital use was published just last week in the Annals of Emergency Medicine. The authors reviewed more than 11,000 cases of the pharmacologic intervention over the past 2 years.
“We believe this information may add substantively to the recommendation in this report,” Dr. Epstein said.
Recommendation 6 was referred to the AMA Board for a decision, but the rest of the report was overwhelmingly adopted.
Dr. Certa, Dr. Osbourne-Roberts, Dr. Rudawsky, and Dr. Epstein have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Current evidence does not support use of “excited delirium” or “excited delirium syndrome” as a medical diagnosis, the American Medical Association said June 14, and the term should not be used unless clear diagnostic criteria are validated.
The term is disproportionately applied to people of color, “for whom inappropriate and excessive pharmacotherapy continues to be the norm instead of behavioral deescalation,” the report by the AMA’s Council on Science and Public Health stated, and is therefore indicative of systemic racism.
That conclusion was one of many included in CSAPH Report 2, which was adopted June 14 at the special meeting of the AMA House of Delegates.
The AMA also opposes “use of sedative/hypnotic and dissociative agents, including ketamine, as a pharmacologic intervention for agitated individuals in the out-of-hospital setting, when done solely for a law enforcement purpose.”
Medications typically used for restraint include dissociative ketamine, benzodiazepine sedatives such as midazolam, and antipsychotic medications including olanzapine or haloperidol, alone or in combination.
Kenneth Certa, MD, from the American Psychiatric Association, speaking on behalf of the section council on psychiatry, said in a reference committee hearing: “We have been very concerned over the years with the development of the inexact diagnosis of ‘agitated delirium’ or ‘excited delirium,’ especially after having had a number of individuals, more than what’s reported in the press, die by the use of ketamine in the field for this inexact diagnosis.”
Tamaan Osbourne-Roberts, MD, a delegate and CSAPH member, said the diagnosis lacks scientific evidence and is “disproportionately applied to otherwise healthy Black men in their mid-30s and these men are most likely to die from resulting first-responder actions.”
Dr. Osbourne-Roberts testified that deescalation training should be more widely used and that crisis intervention team models in which behavioral health specialists are first deployed to respond to behavioral health emergencies should be more prevalent.
Andrew Rudawsky, MD, an assistant medical director of two emergency departments and delegate from Ohio, speaking as an individual, testified: “I can tell you from first-hand experience that ‘excited delirium’ is very real. These acutely ill, unstable patients have an emergency medical condition best cared for by an emergency medicine physician.”
The report recognizes that drugs used outside a hospital setting by nonphysicians come with significant risks, particularly for those with underlying conditions and in terms of drug–drug interactions.
“I completely agree that medicine should not be practiced by law enforcement,” Dr. Rudawsky said. “I’m gravely concerned by the legal ramifications of stating that this condition doesn’t exist.”
He said he is optimistic that the Diagnostic and Statistical Manual of Mental Disorders (DSM) will be updated to include “excited delirium.”
in medical and mental health emergencies in local communities.
Additionally, the report urges that “administration of any pharmacologic treatments in the out-of-hospital setting be done equitably, in an evidence-based, antiracist, and stigma-free way.”
The report calls on law enforcement and frontline emergency medical service personnel, who are a part of the “dual response” in emergency situations, to engage in training overseen by EMS medical directors. “The training should minimally include deescalation techniques and the appropriate use of pharmacologic intervention for agitated individuals in the out-of-hospital setting,” the report states.
Recommendation on oversight draws controversy
Several commenters were emergency physicians and medical directors who expressed concern that investigation of potential cases of inappropriate pharmacologic intervention would be overseen by nonphysicians.
The CSAPH authors write that independent investigators are appropriate, whereas those in emergency medicine say EMS medical directors should lead oversight.
Stephen Epstein, MD, chair of the section council on emergency medicine, speaking on behalf of the section council, had moved for referral of the portion of the report that deals with oversight of EMS.
“We’re concerned that recommendation 6, by calling for independent investigators, would put nonphysicians in the position of supervising the practice of medicine of a board-approved specialty. This would set an unfortunate precedent for our AMA,” he said.
Dr. Epstein also said the American College of Emergency Physicians will soon release a report on “excited delirium,” which will add key information for debating the issue.
He added that a new report on the safety of ketamine in out-of-hospital use was published just last week in the Annals of Emergency Medicine. The authors reviewed more than 11,000 cases of the pharmacologic intervention over the past 2 years.
“We believe this information may add substantively to the recommendation in this report,” Dr. Epstein said.
Recommendation 6 was referred to the AMA Board for a decision, but the rest of the report was overwhelmingly adopted.
Dr. Certa, Dr. Osbourne-Roberts, Dr. Rudawsky, and Dr. Epstein have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Current evidence does not support use of “excited delirium” or “excited delirium syndrome” as a medical diagnosis, the American Medical Association said June 14, and the term should not be used unless clear diagnostic criteria are validated.
The term is disproportionately applied to people of color, “for whom inappropriate and excessive pharmacotherapy continues to be the norm instead of behavioral deescalation,” the report by the AMA’s Council on Science and Public Health stated, and is therefore indicative of systemic racism.
That conclusion was one of many included in CSAPH Report 2, which was adopted June 14 at the special meeting of the AMA House of Delegates.
The AMA also opposes “use of sedative/hypnotic and dissociative agents, including ketamine, as a pharmacologic intervention for agitated individuals in the out-of-hospital setting, when done solely for a law enforcement purpose.”
Medications typically used for restraint include dissociative ketamine, benzodiazepine sedatives such as midazolam, and antipsychotic medications including olanzapine or haloperidol, alone or in combination.
Kenneth Certa, MD, from the American Psychiatric Association, speaking on behalf of the section council on psychiatry, said in a reference committee hearing: “We have been very concerned over the years with the development of the inexact diagnosis of ‘agitated delirium’ or ‘excited delirium,’ especially after having had a number of individuals, more than what’s reported in the press, die by the use of ketamine in the field for this inexact diagnosis.”
Tamaan Osbourne-Roberts, MD, a delegate and CSAPH member, said the diagnosis lacks scientific evidence and is “disproportionately applied to otherwise healthy Black men in their mid-30s and these men are most likely to die from resulting first-responder actions.”
Dr. Osbourne-Roberts testified that deescalation training should be more widely used and that crisis intervention team models in which behavioral health specialists are first deployed to respond to behavioral health emergencies should be more prevalent.
Andrew Rudawsky, MD, an assistant medical director of two emergency departments and delegate from Ohio, speaking as an individual, testified: “I can tell you from first-hand experience that ‘excited delirium’ is very real. These acutely ill, unstable patients have an emergency medical condition best cared for by an emergency medicine physician.”
The report recognizes that drugs used outside a hospital setting by nonphysicians come with significant risks, particularly for those with underlying conditions and in terms of drug–drug interactions.
“I completely agree that medicine should not be practiced by law enforcement,” Dr. Rudawsky said. “I’m gravely concerned by the legal ramifications of stating that this condition doesn’t exist.”
He said he is optimistic that the Diagnostic and Statistical Manual of Mental Disorders (DSM) will be updated to include “excited delirium.”
in medical and mental health emergencies in local communities.
Additionally, the report urges that “administration of any pharmacologic treatments in the out-of-hospital setting be done equitably, in an evidence-based, antiracist, and stigma-free way.”
The report calls on law enforcement and frontline emergency medical service personnel, who are a part of the “dual response” in emergency situations, to engage in training overseen by EMS medical directors. “The training should minimally include deescalation techniques and the appropriate use of pharmacologic intervention for agitated individuals in the out-of-hospital setting,” the report states.
Recommendation on oversight draws controversy
Several commenters were emergency physicians and medical directors who expressed concern that investigation of potential cases of inappropriate pharmacologic intervention would be overseen by nonphysicians.
The CSAPH authors write that independent investigators are appropriate, whereas those in emergency medicine say EMS medical directors should lead oversight.
Stephen Epstein, MD, chair of the section council on emergency medicine, speaking on behalf of the section council, had moved for referral of the portion of the report that deals with oversight of EMS.
“We’re concerned that recommendation 6, by calling for independent investigators, would put nonphysicians in the position of supervising the practice of medicine of a board-approved specialty. This would set an unfortunate precedent for our AMA,” he said.
Dr. Epstein also said the American College of Emergency Physicians will soon release a report on “excited delirium,” which will add key information for debating the issue.
He added that a new report on the safety of ketamine in out-of-hospital use was published just last week in the Annals of Emergency Medicine. The authors reviewed more than 11,000 cases of the pharmacologic intervention over the past 2 years.
“We believe this information may add substantively to the recommendation in this report,” Dr. Epstein said.
Recommendation 6 was referred to the AMA Board for a decision, but the rest of the report was overwhelmingly adopted.
Dr. Certa, Dr. Osbourne-Roberts, Dr. Rudawsky, and Dr. Epstein have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Zero-burnout practices often solo, physician-owned
according to an analysis published June 7 in Health Affairs.
The findings may have particular significance in an era when more physicians are being employed by hospitals and health systems, says lead author Samuel T. Edwards, MD, an assistant professor of medicine at Oregon Health & Science University, Portland.
“Market forces and various reform efforts have driven practices to consolidate, and we certainly see some signal here that burnout might be a potential negative consequence of that,” said Dr. Edwards, who is also a staff physician in internal medicine at the Veterans Affairs Portland Health Care System.
30% of practices reported zero burnout
Dr. Edwards told this news organization that he was surprised that 30% of the practices surveyed for this analysis reported zero burnout – meaning no member of the practice reported burnout – because reports of burnout are so pervasive in medicine.
For comparison, in 13% of practices surveyed, more than 40% of practice members reported burnout.
Burnout was assessed with a five-point measure that correlates with the emotional exhaustion scale of the Maslach Burnout Inventory.
It was also surprising, Dr. Edwards said, that practices with some of the heaviest workloads – solo practitioners juggling large numbers of patients, insurance plans, and regulatory requirements – were much more likely than larger practices to report zero burnout.
In this study, solo practices were 5.3 times as likely as practices with 6 to 10 clinicians to report zero burnout (95% confidence interval, 1.25-22.6).
The researchers found no link between burnout and patient volume or the proportion of patients with Medicaid insurance.
“People assume that working harder is associated with more burnout, and there are lots of studies that say that’s true. But in our study, it appears that people work really hard in some settings and are not burned out,” Dr. Edwards said.
He says in small offices, there may be a stronger sense of agency, a sense that everyone is on the same team, and there may be stronger relationships with patients.
The study included survey data from 715 small- to medium-size primary care practices in the United States that participated in the Agency for Healthcare Research and Quality’s EvidenceNOW quality improvement initiative between September 2015 and June 2017.
Zero-burnout practices shared several traits. They were more likely to have “a strong practice culture – one in which teamwork, communication, psychological safety, mindfulness of others, facilitative leadership, and understanding that people make and can learn from mistakes were among the key attributes,” Dr. Edwards and colleagues write.
Burnout higher with ACO participation
Organizations that participated in ACOs and other external primary care transformation projects were more likely to have high burnout rates. Specifically, 29% of these practices reported zero burnout, versus 53% that reported high rates of burnout.
Dr. Edwards said the reasons for that are unclear in this cross-sectional study, but there seemed to be an indication that getting involved in too many demonstration projects might be associated with burnout. He noted that participants in this study were already involved in the EvidenceNOW initiative.
Factors regarding electronic health records (EHRs) were not tied to burnout in this study. Dr. Edwards said they surveyed for both satisfaction with EHRs and EHR features and whether they were linked to zero burnout.
He speculates that this may indicate that by now, practices have adapted to using EHRs, though they continue to be a source of frustration for individual clinicians.
Debora Goetz Goldberg, PhD, MHA, MBA, associate professor at George Mason University, McLean, Virginia, told this news organization that she has found similar results in her research of primary care practices and burnout. She found that health system–owned practices had higher levels of burnout.
“We thought that probably was related to less autonomy and decision-making authority,” she said.
She pointed out that Dr. Edwards and colleagues found that physicians who had more “adaptive reserves” were more likely to have zero burnout. Her research found a similar association.
Such organizations, she explained, have a higher level of organizational development and a culture of innovation. They are more comfortable with change and adapt well.
“They are characterized by teamwork, strong communication, and a culture of learning,” she said.
By contrast, burnout may be higher in health system–owned practices because clinicians may feel they have less control over their work environment and feel a loss of autonomy, according to Dr. Goldberg.
“Moral distress,” which can happen when an individual’s professional values don’t line up with an organization’s values, may also play a part, she said. Physicians may be required to see more patients than they feel they can serve well in a day, for instance.
Reducing burnout may take building a more collaborative leadership style, she said.
No link between burnout and patient volume
The current research also highlighted leadership style as a potential driver of burnout.
Dr. Edwards and colleagues found that one of the strongest associations was between facilitative leadership and low burnout. Zero burnout is associated with participatory decision-making.
“Interestingly, we saw that that kind of leadership could exist in multiple settings,” he said. Health care professionals in smaller practices might know each other better and have a shared mission, but shared decision making can also exist in larger practices, he said.
Higher burnout was associated with traditional leadership models that are hierarchical and that operate with a command-and-control structure, according to the study.
The data may have implications for strategies regarding both the smallest and largest practices.
Initiatives that help small practices remain strong are valuable, especially for communities that depend on those practices, Dr. Edwards said.
The researchers give as an example the funding of primary care practice extension networks, which provide support similar to agricultural extension programs for farmers.
At the same time, “having agency at the practice level about how things work is really important in reducing burnout. So in a large system, finding ways to promote agency at the most local level possible can really help with burnout,” he said.
Dr. Edwards said his team controlled for the fact that mathematically, it’s more likely zero burnout would be reported in a solo practice than in a larger practice.
Every practice in this study, he said, had to have at least three persons who responded to the survey, and responses had to represent three roles – a clinician, a nonclinician staff member, and a clinical staff member. The response rate also had to be 50% within the practice, he explained.
All authors are supported by the Agency for Healthcare Research and Quality. Dr. Edwards was also supported by the Department of Veterans Affairs Health Services Research and Development. Dr. Goldberg has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to an analysis published June 7 in Health Affairs.
The findings may have particular significance in an era when more physicians are being employed by hospitals and health systems, says lead author Samuel T. Edwards, MD, an assistant professor of medicine at Oregon Health & Science University, Portland.
“Market forces and various reform efforts have driven practices to consolidate, and we certainly see some signal here that burnout might be a potential negative consequence of that,” said Dr. Edwards, who is also a staff physician in internal medicine at the Veterans Affairs Portland Health Care System.
30% of practices reported zero burnout
Dr. Edwards told this news organization that he was surprised that 30% of the practices surveyed for this analysis reported zero burnout – meaning no member of the practice reported burnout – because reports of burnout are so pervasive in medicine.
For comparison, in 13% of practices surveyed, more than 40% of practice members reported burnout.
Burnout was assessed with a five-point measure that correlates with the emotional exhaustion scale of the Maslach Burnout Inventory.
It was also surprising, Dr. Edwards said, that practices with some of the heaviest workloads – solo practitioners juggling large numbers of patients, insurance plans, and regulatory requirements – were much more likely than larger practices to report zero burnout.
In this study, solo practices were 5.3 times as likely as practices with 6 to 10 clinicians to report zero burnout (95% confidence interval, 1.25-22.6).
The researchers found no link between burnout and patient volume or the proportion of patients with Medicaid insurance.
“People assume that working harder is associated with more burnout, and there are lots of studies that say that’s true. But in our study, it appears that people work really hard in some settings and are not burned out,” Dr. Edwards said.
He says in small offices, there may be a stronger sense of agency, a sense that everyone is on the same team, and there may be stronger relationships with patients.
The study included survey data from 715 small- to medium-size primary care practices in the United States that participated in the Agency for Healthcare Research and Quality’s EvidenceNOW quality improvement initiative between September 2015 and June 2017.
Zero-burnout practices shared several traits. They were more likely to have “a strong practice culture – one in which teamwork, communication, psychological safety, mindfulness of others, facilitative leadership, and understanding that people make and can learn from mistakes were among the key attributes,” Dr. Edwards and colleagues write.
Burnout higher with ACO participation
Organizations that participated in ACOs and other external primary care transformation projects were more likely to have high burnout rates. Specifically, 29% of these practices reported zero burnout, versus 53% that reported high rates of burnout.
Dr. Edwards said the reasons for that are unclear in this cross-sectional study, but there seemed to be an indication that getting involved in too many demonstration projects might be associated with burnout. He noted that participants in this study were already involved in the EvidenceNOW initiative.
Factors regarding electronic health records (EHRs) were not tied to burnout in this study. Dr. Edwards said they surveyed for both satisfaction with EHRs and EHR features and whether they were linked to zero burnout.
He speculates that this may indicate that by now, practices have adapted to using EHRs, though they continue to be a source of frustration for individual clinicians.
Debora Goetz Goldberg, PhD, MHA, MBA, associate professor at George Mason University, McLean, Virginia, told this news organization that she has found similar results in her research of primary care practices and burnout. She found that health system–owned practices had higher levels of burnout.
“We thought that probably was related to less autonomy and decision-making authority,” she said.
She pointed out that Dr. Edwards and colleagues found that physicians who had more “adaptive reserves” were more likely to have zero burnout. Her research found a similar association.
Such organizations, she explained, have a higher level of organizational development and a culture of innovation. They are more comfortable with change and adapt well.
“They are characterized by teamwork, strong communication, and a culture of learning,” she said.
By contrast, burnout may be higher in health system–owned practices because clinicians may feel they have less control over their work environment and feel a loss of autonomy, according to Dr. Goldberg.
“Moral distress,” which can happen when an individual’s professional values don’t line up with an organization’s values, may also play a part, she said. Physicians may be required to see more patients than they feel they can serve well in a day, for instance.
Reducing burnout may take building a more collaborative leadership style, she said.
No link between burnout and patient volume
The current research also highlighted leadership style as a potential driver of burnout.
Dr. Edwards and colleagues found that one of the strongest associations was between facilitative leadership and low burnout. Zero burnout is associated with participatory decision-making.
“Interestingly, we saw that that kind of leadership could exist in multiple settings,” he said. Health care professionals in smaller practices might know each other better and have a shared mission, but shared decision making can also exist in larger practices, he said.
Higher burnout was associated with traditional leadership models that are hierarchical and that operate with a command-and-control structure, according to the study.
The data may have implications for strategies regarding both the smallest and largest practices.
Initiatives that help small practices remain strong are valuable, especially for communities that depend on those practices, Dr. Edwards said.
The researchers give as an example the funding of primary care practice extension networks, which provide support similar to agricultural extension programs for farmers.
At the same time, “having agency at the practice level about how things work is really important in reducing burnout. So in a large system, finding ways to promote agency at the most local level possible can really help with burnout,” he said.
Dr. Edwards said his team controlled for the fact that mathematically, it’s more likely zero burnout would be reported in a solo practice than in a larger practice.
Every practice in this study, he said, had to have at least three persons who responded to the survey, and responses had to represent three roles – a clinician, a nonclinician staff member, and a clinical staff member. The response rate also had to be 50% within the practice, he explained.
All authors are supported by the Agency for Healthcare Research and Quality. Dr. Edwards was also supported by the Department of Veterans Affairs Health Services Research and Development. Dr. Goldberg has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to an analysis published June 7 in Health Affairs.
The findings may have particular significance in an era when more physicians are being employed by hospitals and health systems, says lead author Samuel T. Edwards, MD, an assistant professor of medicine at Oregon Health & Science University, Portland.
“Market forces and various reform efforts have driven practices to consolidate, and we certainly see some signal here that burnout might be a potential negative consequence of that,” said Dr. Edwards, who is also a staff physician in internal medicine at the Veterans Affairs Portland Health Care System.
30% of practices reported zero burnout
Dr. Edwards told this news organization that he was surprised that 30% of the practices surveyed for this analysis reported zero burnout – meaning no member of the practice reported burnout – because reports of burnout are so pervasive in medicine.
For comparison, in 13% of practices surveyed, more than 40% of practice members reported burnout.
Burnout was assessed with a five-point measure that correlates with the emotional exhaustion scale of the Maslach Burnout Inventory.
It was also surprising, Dr. Edwards said, that practices with some of the heaviest workloads – solo practitioners juggling large numbers of patients, insurance plans, and regulatory requirements – were much more likely than larger practices to report zero burnout.
In this study, solo practices were 5.3 times as likely as practices with 6 to 10 clinicians to report zero burnout (95% confidence interval, 1.25-22.6).
The researchers found no link between burnout and patient volume or the proportion of patients with Medicaid insurance.
“People assume that working harder is associated with more burnout, and there are lots of studies that say that’s true. But in our study, it appears that people work really hard in some settings and are not burned out,” Dr. Edwards said.
He says in small offices, there may be a stronger sense of agency, a sense that everyone is on the same team, and there may be stronger relationships with patients.
The study included survey data from 715 small- to medium-size primary care practices in the United States that participated in the Agency for Healthcare Research and Quality’s EvidenceNOW quality improvement initiative between September 2015 and June 2017.
Zero-burnout practices shared several traits. They were more likely to have “a strong practice culture – one in which teamwork, communication, psychological safety, mindfulness of others, facilitative leadership, and understanding that people make and can learn from mistakes were among the key attributes,” Dr. Edwards and colleagues write.
Burnout higher with ACO participation
Organizations that participated in ACOs and other external primary care transformation projects were more likely to have high burnout rates. Specifically, 29% of these practices reported zero burnout, versus 53% that reported high rates of burnout.
Dr. Edwards said the reasons for that are unclear in this cross-sectional study, but there seemed to be an indication that getting involved in too many demonstration projects might be associated with burnout. He noted that participants in this study were already involved in the EvidenceNOW initiative.
Factors regarding electronic health records (EHRs) were not tied to burnout in this study. Dr. Edwards said they surveyed for both satisfaction with EHRs and EHR features and whether they were linked to zero burnout.
He speculates that this may indicate that by now, practices have adapted to using EHRs, though they continue to be a source of frustration for individual clinicians.
Debora Goetz Goldberg, PhD, MHA, MBA, associate professor at George Mason University, McLean, Virginia, told this news organization that she has found similar results in her research of primary care practices and burnout. She found that health system–owned practices had higher levels of burnout.
“We thought that probably was related to less autonomy and decision-making authority,” she said.
She pointed out that Dr. Edwards and colleagues found that physicians who had more “adaptive reserves” were more likely to have zero burnout. Her research found a similar association.
Such organizations, she explained, have a higher level of organizational development and a culture of innovation. They are more comfortable with change and adapt well.
“They are characterized by teamwork, strong communication, and a culture of learning,” she said.
By contrast, burnout may be higher in health system–owned practices because clinicians may feel they have less control over their work environment and feel a loss of autonomy, according to Dr. Goldberg.
“Moral distress,” which can happen when an individual’s professional values don’t line up with an organization’s values, may also play a part, she said. Physicians may be required to see more patients than they feel they can serve well in a day, for instance.
Reducing burnout may take building a more collaborative leadership style, she said.
No link between burnout and patient volume
The current research also highlighted leadership style as a potential driver of burnout.
Dr. Edwards and colleagues found that one of the strongest associations was between facilitative leadership and low burnout. Zero burnout is associated with participatory decision-making.
“Interestingly, we saw that that kind of leadership could exist in multiple settings,” he said. Health care professionals in smaller practices might know each other better and have a shared mission, but shared decision making can also exist in larger practices, he said.
Higher burnout was associated with traditional leadership models that are hierarchical and that operate with a command-and-control structure, according to the study.
The data may have implications for strategies regarding both the smallest and largest practices.
Initiatives that help small practices remain strong are valuable, especially for communities that depend on those practices, Dr. Edwards said.
The researchers give as an example the funding of primary care practice extension networks, which provide support similar to agricultural extension programs for farmers.
At the same time, “having agency at the practice level about how things work is really important in reducing burnout. So in a large system, finding ways to promote agency at the most local level possible can really help with burnout,” he said.
Dr. Edwards said his team controlled for the fact that mathematically, it’s more likely zero burnout would be reported in a solo practice than in a larger practice.
Every practice in this study, he said, had to have at least three persons who responded to the survey, and responses had to represent three roles – a clinician, a nonclinician staff member, and a clinical staff member. The response rate also had to be 50% within the practice, he explained.
All authors are supported by the Agency for Healthcare Research and Quality. Dr. Edwards was also supported by the Department of Veterans Affairs Health Services Research and Development. Dr. Goldberg has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Concerts may be safe to attend with proper safety precautions: Study
Researchers in Spain have shared heartening results from the first randomized controlled trial to assess risk for COVID-19 transmission at an indoor live music concert.
The study, published May 27 in The Lancet Infectious Diseases, led by virologist Boris Revollo, MD, from the Germans Trias i Pujol University Hospital in Barcelona, included comprehensive safety measures.
It was conducted on Dec. 12, 2020, at a time when local travel restrictions were in place, indoor meetings were limited to six people, and vaccines were not yet available.
All 465 event attendees got same-day SARS-CoV-2 screening with antigen-detecting rapid diagnostic tests before they entered, wore masks throughout, and followed crowd-control measures in the well-ventilated venue, which can hold up to 900 people.
The control group consisted of 495 participants randomly assigned to go home instead of attending the concert after the screening.
None of the attendees tested positive for SARS-CoV-2 infection by polymerase chain reaction (PCR) test 8 days after the 5-hour event, but two in the control group did.
In fact, the study showed that the risk for infection was no higher among those at the concert than it was for those who lived in the same community and did not attend.
The Bayesian estimate for the incidence between the test and control groups was –0.15% (95% confidence Interval, –0.72 to 0.44).
“Our findings pave the way to reactivate cultural activities halted during COVID-19, which could have important sociocultural and economic implications,” the authors wrote.
All wore masks throughout
Among the comprehensive safety measures were that, in addition to testing, all attendees had their temperature checked before gaining access and were given an N95 face mask, which had to be worn at all times inside.
Hand sanitizer was provided in multiple locations, access doors remained open to allow fresh air to circulate, and the coat room was closed to prevent clustering.
There was no mandated distancing, people could sing and dance, and alcohol was available in a bar located in a separate room – and drinks were allowed only in that space.
Rosanna W Peeling, PhD, professor and chair of diagnostic research at the London School of Hygiene and Tropical Medicine in the United Kingdom, and David L. Heymann, MD, of the department of infectious disease epidemiology there, said in an accompanying commentary that there is a great need for studies like this one to help build evidence for a return to normal gatherings.
“So many countries don’t have any policy or any way of doing this because they don’t have the evidence,” Dr. Peeling said in an interview.
The study was well done and a strength was the testing 8 days later, which can be hard to do for similar events when people disperse to locations outside the community where the event or gathering was held, she said.
Study prompts additional questions
Dr. Peeling and Dr. Heymann wrote that the work raises questions such as whether triple-layered masks would have been sufficient. Or how does rapid antigen testing at the entrance compare with molecular screening within 72 hours of entering?
They noted that there are questions around whether existing rapid diagnostic tests are able to detect COVID-19 variants.
Dr. Peeling said that these kinds of results need to be shared and shared more quickly, “if we’re ever going to get out of this pandemic.”
Studies like this are also difficult, she noted, because they may involve non–health sector entities such as city governments and concert organizers working together with researchers.
In addition, the safety measures come at considerable expense and it’s unclear whether those could be employed routinely at such events.
“It’s not really sustainable at sports events with 20,000 people,” Dr. Peeling said.
Infectious disease expert William Schaffner, MD, of Vanderbilt University, Nashville, Tenn., told this news organization that the study results “come a little late to the party.”
If this study had been done in today’s era with authorized vaccines, “it would have been a moot issue,” he said. “The mask is a barrier to transmission, but we now have a much more solid barrier we could put in place, which is vaccination.
“That said, it does reinforce the fact that classical mask wearing does really offer protection even in a crowded venue,” Dr. Schaffner said.
He added that the study was relatively small and he’d like to see it replicated in larger concerts or group gatherings.
Dr. Peeling and Dr. Heymann report no relevant financial relationships. A coauthor is an employee and stockholder of Primavera Sound, sponsor of the study. All other authors declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers in Spain have shared heartening results from the first randomized controlled trial to assess risk for COVID-19 transmission at an indoor live music concert.
The study, published May 27 in The Lancet Infectious Diseases, led by virologist Boris Revollo, MD, from the Germans Trias i Pujol University Hospital in Barcelona, included comprehensive safety measures.
It was conducted on Dec. 12, 2020, at a time when local travel restrictions were in place, indoor meetings were limited to six people, and vaccines were not yet available.
All 465 event attendees got same-day SARS-CoV-2 screening with antigen-detecting rapid diagnostic tests before they entered, wore masks throughout, and followed crowd-control measures in the well-ventilated venue, which can hold up to 900 people.
The control group consisted of 495 participants randomly assigned to go home instead of attending the concert after the screening.
None of the attendees tested positive for SARS-CoV-2 infection by polymerase chain reaction (PCR) test 8 days after the 5-hour event, but two in the control group did.
In fact, the study showed that the risk for infection was no higher among those at the concert than it was for those who lived in the same community and did not attend.
The Bayesian estimate for the incidence between the test and control groups was –0.15% (95% confidence Interval, –0.72 to 0.44).
“Our findings pave the way to reactivate cultural activities halted during COVID-19, which could have important sociocultural and economic implications,” the authors wrote.
All wore masks throughout
Among the comprehensive safety measures were that, in addition to testing, all attendees had their temperature checked before gaining access and were given an N95 face mask, which had to be worn at all times inside.
Hand sanitizer was provided in multiple locations, access doors remained open to allow fresh air to circulate, and the coat room was closed to prevent clustering.
There was no mandated distancing, people could sing and dance, and alcohol was available in a bar located in a separate room – and drinks were allowed only in that space.
Rosanna W Peeling, PhD, professor and chair of diagnostic research at the London School of Hygiene and Tropical Medicine in the United Kingdom, and David L. Heymann, MD, of the department of infectious disease epidemiology there, said in an accompanying commentary that there is a great need for studies like this one to help build evidence for a return to normal gatherings.
“So many countries don’t have any policy or any way of doing this because they don’t have the evidence,” Dr. Peeling said in an interview.
The study was well done and a strength was the testing 8 days later, which can be hard to do for similar events when people disperse to locations outside the community where the event or gathering was held, she said.
Study prompts additional questions
Dr. Peeling and Dr. Heymann wrote that the work raises questions such as whether triple-layered masks would have been sufficient. Or how does rapid antigen testing at the entrance compare with molecular screening within 72 hours of entering?
They noted that there are questions around whether existing rapid diagnostic tests are able to detect COVID-19 variants.
Dr. Peeling said that these kinds of results need to be shared and shared more quickly, “if we’re ever going to get out of this pandemic.”
Studies like this are also difficult, she noted, because they may involve non–health sector entities such as city governments and concert organizers working together with researchers.
In addition, the safety measures come at considerable expense and it’s unclear whether those could be employed routinely at such events.
“It’s not really sustainable at sports events with 20,000 people,” Dr. Peeling said.
Infectious disease expert William Schaffner, MD, of Vanderbilt University, Nashville, Tenn., told this news organization that the study results “come a little late to the party.”
If this study had been done in today’s era with authorized vaccines, “it would have been a moot issue,” he said. “The mask is a barrier to transmission, but we now have a much more solid barrier we could put in place, which is vaccination.
“That said, it does reinforce the fact that classical mask wearing does really offer protection even in a crowded venue,” Dr. Schaffner said.
He added that the study was relatively small and he’d like to see it replicated in larger concerts or group gatherings.
Dr. Peeling and Dr. Heymann report no relevant financial relationships. A coauthor is an employee and stockholder of Primavera Sound, sponsor of the study. All other authors declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers in Spain have shared heartening results from the first randomized controlled trial to assess risk for COVID-19 transmission at an indoor live music concert.
The study, published May 27 in The Lancet Infectious Diseases, led by virologist Boris Revollo, MD, from the Germans Trias i Pujol University Hospital in Barcelona, included comprehensive safety measures.
It was conducted on Dec. 12, 2020, at a time when local travel restrictions were in place, indoor meetings were limited to six people, and vaccines were not yet available.
All 465 event attendees got same-day SARS-CoV-2 screening with antigen-detecting rapid diagnostic tests before they entered, wore masks throughout, and followed crowd-control measures in the well-ventilated venue, which can hold up to 900 people.
The control group consisted of 495 participants randomly assigned to go home instead of attending the concert after the screening.
None of the attendees tested positive for SARS-CoV-2 infection by polymerase chain reaction (PCR) test 8 days after the 5-hour event, but two in the control group did.
In fact, the study showed that the risk for infection was no higher among those at the concert than it was for those who lived in the same community and did not attend.
The Bayesian estimate for the incidence between the test and control groups was –0.15% (95% confidence Interval, –0.72 to 0.44).
“Our findings pave the way to reactivate cultural activities halted during COVID-19, which could have important sociocultural and economic implications,” the authors wrote.
All wore masks throughout
Among the comprehensive safety measures were that, in addition to testing, all attendees had their temperature checked before gaining access and were given an N95 face mask, which had to be worn at all times inside.
Hand sanitizer was provided in multiple locations, access doors remained open to allow fresh air to circulate, and the coat room was closed to prevent clustering.
There was no mandated distancing, people could sing and dance, and alcohol was available in a bar located in a separate room – and drinks were allowed only in that space.
Rosanna W Peeling, PhD, professor and chair of diagnostic research at the London School of Hygiene and Tropical Medicine in the United Kingdom, and David L. Heymann, MD, of the department of infectious disease epidemiology there, said in an accompanying commentary that there is a great need for studies like this one to help build evidence for a return to normal gatherings.
“So many countries don’t have any policy or any way of doing this because they don’t have the evidence,” Dr. Peeling said in an interview.
The study was well done and a strength was the testing 8 days later, which can be hard to do for similar events when people disperse to locations outside the community where the event or gathering was held, she said.
Study prompts additional questions
Dr. Peeling and Dr. Heymann wrote that the work raises questions such as whether triple-layered masks would have been sufficient. Or how does rapid antigen testing at the entrance compare with molecular screening within 72 hours of entering?
They noted that there are questions around whether existing rapid diagnostic tests are able to detect COVID-19 variants.
Dr. Peeling said that these kinds of results need to be shared and shared more quickly, “if we’re ever going to get out of this pandemic.”
Studies like this are also difficult, she noted, because they may involve non–health sector entities such as city governments and concert organizers working together with researchers.
In addition, the safety measures come at considerable expense and it’s unclear whether those could be employed routinely at such events.
“It’s not really sustainable at sports events with 20,000 people,” Dr. Peeling said.
Infectious disease expert William Schaffner, MD, of Vanderbilt University, Nashville, Tenn., told this news organization that the study results “come a little late to the party.”
If this study had been done in today’s era with authorized vaccines, “it would have been a moot issue,” he said. “The mask is a barrier to transmission, but we now have a much more solid barrier we could put in place, which is vaccination.
“That said, it does reinforce the fact that classical mask wearing does really offer protection even in a crowded venue,” Dr. Schaffner said.
He added that the study was relatively small and he’d like to see it replicated in larger concerts or group gatherings.
Dr. Peeling and Dr. Heymann report no relevant financial relationships. A coauthor is an employee and stockholder of Primavera Sound, sponsor of the study. All other authors declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FDA approves ibrexafungerp for vaginal yeast infection
Ibrexafungerp is the first drug approved in a new antifungal class for vulvovaginal candidiasis (VVC) in more than 20 years, the drug’s manufacturer Scynexis said in a press release. It becomes the first and only nonazole treatment for vaginal yeast infections.
The biotechnology company said approval came after positive results from two phase 3 studies in which oral ibrexafungerp demonstrated efficacy and tolerability. The most common reactions observed in clinical trials were diarrhea, nausea, abdominal pain, dizziness, and vomiting.
There are few other treatments for vaginal yeast infections, which is the second most common cause of vaginitis. Those previously approved agents include several topical azole antifungals and oral fluconazole (Diflucan), which, Scynexis said, is the only other orally administered antifungal approved for the treatment of VVC in the United States and has accounted for over more than 90% of prescriptions written for the condition each year.
However, the company noted, oral fluconazole reports a 55% therapeutic cure rate on its label, which now also includes warnings of potential fetal harm, demonstrating the need for new oral options.
The new drug may not fill that need for pregnant women, however, as the company noted that ibrexafungerp should not be used during pregnancy, and administration during pregnancy “may cause fetal harm based on animal studies.”
Because of possible teratogenic effects, the company advised clinicians to verify pregnancy status in females of reproductive potential before prescribing ibrexafungerp and advises effective contraception during treatment.
VVC can come with substantial morbidity, including genital pain, itching and burning, reduced sexual pleasure, and psychological distress.
David Angulo, MD, chief medical officer for Scynexis, said in a statement the tablets brings new benefits.
Dr. Angulo said the drug “has a differentiated fungicidal mechanism of action that kills a broad range of Candida species, including azole-resistant strains. We are working on completing our CANDLE study investigating ibrexafungerp for the prevention of recurrent VVC and expect we will be submitting a supplemental NDA [new drug application] in the first half of 2022.”
Scynexis said it partnered with Amplity Health, a Pennsylvania-based pharmaceutical company, to support U.S. marketing of the drug. The commercial launch will follow the approval.
Ibrexafungerp was granted approval through both the FDA’s Qualified Infectious Disease Product and Fast Track designations. It is expected to be marketed exclusively in the United States for 10 years.
A version of this article first appeared on Medscape.com.
Ibrexafungerp is the first drug approved in a new antifungal class for vulvovaginal candidiasis (VVC) in more than 20 years, the drug’s manufacturer Scynexis said in a press release. It becomes the first and only nonazole treatment for vaginal yeast infections.
The biotechnology company said approval came after positive results from two phase 3 studies in which oral ibrexafungerp demonstrated efficacy and tolerability. The most common reactions observed in clinical trials were diarrhea, nausea, abdominal pain, dizziness, and vomiting.
There are few other treatments for vaginal yeast infections, which is the second most common cause of vaginitis. Those previously approved agents include several topical azole antifungals and oral fluconazole (Diflucan), which, Scynexis said, is the only other orally administered antifungal approved for the treatment of VVC in the United States and has accounted for over more than 90% of prescriptions written for the condition each year.
However, the company noted, oral fluconazole reports a 55% therapeutic cure rate on its label, which now also includes warnings of potential fetal harm, demonstrating the need for new oral options.
The new drug may not fill that need for pregnant women, however, as the company noted that ibrexafungerp should not be used during pregnancy, and administration during pregnancy “may cause fetal harm based on animal studies.”
Because of possible teratogenic effects, the company advised clinicians to verify pregnancy status in females of reproductive potential before prescribing ibrexafungerp and advises effective contraception during treatment.
VVC can come with substantial morbidity, including genital pain, itching and burning, reduced sexual pleasure, and psychological distress.
David Angulo, MD, chief medical officer for Scynexis, said in a statement the tablets brings new benefits.
Dr. Angulo said the drug “has a differentiated fungicidal mechanism of action that kills a broad range of Candida species, including azole-resistant strains. We are working on completing our CANDLE study investigating ibrexafungerp for the prevention of recurrent VVC and expect we will be submitting a supplemental NDA [new drug application] in the first half of 2022.”
Scynexis said it partnered with Amplity Health, a Pennsylvania-based pharmaceutical company, to support U.S. marketing of the drug. The commercial launch will follow the approval.
Ibrexafungerp was granted approval through both the FDA’s Qualified Infectious Disease Product and Fast Track designations. It is expected to be marketed exclusively in the United States for 10 years.
A version of this article first appeared on Medscape.com.
Ibrexafungerp is the first drug approved in a new antifungal class for vulvovaginal candidiasis (VVC) in more than 20 years, the drug’s manufacturer Scynexis said in a press release. It becomes the first and only nonazole treatment for vaginal yeast infections.
The biotechnology company said approval came after positive results from two phase 3 studies in which oral ibrexafungerp demonstrated efficacy and tolerability. The most common reactions observed in clinical trials were diarrhea, nausea, abdominal pain, dizziness, and vomiting.
There are few other treatments for vaginal yeast infections, which is the second most common cause of vaginitis. Those previously approved agents include several topical azole antifungals and oral fluconazole (Diflucan), which, Scynexis said, is the only other orally administered antifungal approved for the treatment of VVC in the United States and has accounted for over more than 90% of prescriptions written for the condition each year.
However, the company noted, oral fluconazole reports a 55% therapeutic cure rate on its label, which now also includes warnings of potential fetal harm, demonstrating the need for new oral options.
The new drug may not fill that need for pregnant women, however, as the company noted that ibrexafungerp should not be used during pregnancy, and administration during pregnancy “may cause fetal harm based on animal studies.”
Because of possible teratogenic effects, the company advised clinicians to verify pregnancy status in females of reproductive potential before prescribing ibrexafungerp and advises effective contraception during treatment.
VVC can come with substantial morbidity, including genital pain, itching and burning, reduced sexual pleasure, and psychological distress.
David Angulo, MD, chief medical officer for Scynexis, said in a statement the tablets brings new benefits.
Dr. Angulo said the drug “has a differentiated fungicidal mechanism of action that kills a broad range of Candida species, including azole-resistant strains. We are working on completing our CANDLE study investigating ibrexafungerp for the prevention of recurrent VVC and expect we will be submitting a supplemental NDA [new drug application] in the first half of 2022.”
Scynexis said it partnered with Amplity Health, a Pennsylvania-based pharmaceutical company, to support U.S. marketing of the drug. The commercial launch will follow the approval.
Ibrexafungerp was granted approval through both the FDA’s Qualified Infectious Disease Product and Fast Track designations. It is expected to be marketed exclusively in the United States for 10 years.
A version of this article first appeared on Medscape.com.
Clean indoor air is vital for infection control
Health workers already know that indoor air quality can be as important to human health as clean water and uncontaminated food. But before the COVID-19 pandemic, its importance in the prevention of respiratory illnesses outside of health circles was only whispered about.
Now, a team of nearly 40 scientists from 14 countries is calling for “a paradigm shift,” so that improvements in indoor air quality are viewed as essential to curb respiratory infections.
Most countries do not have indoor air-quality standards, the scientists point out in their recent report, and those that do often fall short in scope and enforcement.
“We expect everywhere in the world to have clean water flowing from our taps. In most parts of the developed world, it is happening and we take it completely for granted,” said lead investigator Lidia Morawska, PhD, of the International Laboratory for Air Quality and Health at the Queensland University of Technology in Brisbane, Australia.
But bacteria and viruses can circulate freely in the air, and “no one thinks about this, whatsoever, apart from health care facilities,” she said.
A first step is to recognize the risk posed by airborne pathogens, something not yet universally acknowledged. The investigators also want the World Health Organization to extend its guidelines to cover airborne pathogens, and for ventilation standards to include higher airflow and filtration rates.
Germany has been at the forefront of air-quality measures, Dr. Morawska said. Years ago, she observed a monitor showing the carbon dioxide level and relative humidity in the room where she was attending a meeting. The screen was accompanied by red, yellow, and green signals to communicate risk. Such indicators are also commonly displayed in German schools so teachers know when to open the windows or adjust the ventilation.
Monitors show carbon dioxide levels
But this is not yet being done in most other countries, Dr. Morawska said. Levels of carbon dioxide are one measure of indoor air quality, but they serve as a proxy for ventilation, she pointed out. Although the technology is available, sensors that can test a variety of components in a building in real time are not yet affordable.
Dr. Morawska envisions a future where the air quality numbers of the places people frequent are displayed so they know the risk for airborne transmission of respiratory illnesses. And people can begin to expect clean indoor air when they enter a business, office, or entertainment space and request changes when the air quality dips and improvement is needed, she said.
It is a daunting challenge to clean indoor air for several reasons. Air is not containable in the same way water is, which makes it difficult to trace contaminants. And infections transmitted through dirty water and food are usually evident immediately, whereas infections transmitted through airborne pathogens can take days to develop. Plus, the necessary infrastructure changes will be expensive.
However, the initial cost required to change the flow and quality of indoor air might be less than the cost of infections, the scientists pointed out. It is estimated that the global harm caused by COVID-19 alone costs $1 trillion each month.
“In the United States, the yearly cost – direct and indirect – of influenza has been calculated at $11.2 billion. For respiratory infections other than influenza, the yearly cost stood at $40 billion,” the team noted.
“If even half of this was caused by inhalation, we are still talking about massive costs,” said Dr. Morawska.
Bigger is not always better
It is tempting to see the solution as increased ventilation, said Ehsan Mousavi, PhD, assistant professor of construction science and management at Clemson (S.C.) University, who studies indoor air quality and ventilation in hospitals.
“We are ventilating the heck out of hospitals,” he said in an interview. But there is much debate about how much ventilation is the right amount. Too much and “you can blow pathogens into an open wound,” he explained. “Bigger is not always better.”
And there is still debate about the best mix of outside and recirculated air. An increase in the intake of outdoor air can refresh indoor air if it is clean, but that depends on where you live, he pointed out.
The mix used in most standard office buildings is 15% outside air and 85% recirculated air, Dr. Mousavi said. Boosting the percentage of outside air increases costs and energy use.
In fact, it can take five times more energy to ventilate hospital spaces than office spaces, he reported.
Engineers searching for clean-air solutions need to know what particulates are in the air and whether they are harmful to humans, but the sensors currently available can’t identify whether a virus is present in real time.
Samples have to be taken to a lab and, “by the time you know a virus was in the space, the moment is gone,” Dr. Mousavi explained.
More research is needed. “We need a reasonable answer that looks at the problem holistically, not just from the infectious disease perspective,” he said.
Hydrating indoor air
Research is making it clear that health care environments can play a significant role in patient recovery, according to Stephanie Taylor, MD. Dr. Taylor is president of Building4Health, which she founded to help businesses assess the quality of air in their buildings and find solutions. The company uses an algorithm to arrive at a health assessment score.
Air hydration is the most important aspect to target, she said.
Since the 1980s, research has shown that a relative humidity of 40%-60% is healthy for humans, she said. Currently, in an office building in a winter climate, the humidity level is more like 20%.
Canada is the first country to officially recommend the 40%-60% range for senior citizen centers and residential homes.
“Properly hydrated air supports our immune system and prevents skin problems and respiratory problems. It also inactivates many bacteria and viruses,” Dr. Taylor explained. Inhaling dry air compromises the ability of the body to restrict influenza virus infection, researchers showed in a 2019 study.
In the case of COVID-19, as virus particles attach to water molecules, they get bigger and heavier and eventually drop out of the breathing zone and onto surfaces where they can be wiped away, she explained.
But when the particles “are very small – like 5 microns in diameter – and you inhale them, they can lodge deep in the lungs,” she said.
In properly hydrated air, particles will be larger – about 10-20 microns when they attach to the water vapor – so they will get stuck in the nose or the back of the throat, where they can be washed away by mucous and not travel to the lungs.
“Indoor air metrics” can support our health or contribute to disease, “not just over time, but quickly, within minutes or hours,” she said.
No one expects the world’s building stock to suddenly upgrade to the ideal air quality. “But that doesn’t mean we shouldn’t move in that direction,” Dr. Taylor said. Changes can start small and gradually increase.
New research targets indoor air
Humidity is one of the key areas for current research, said Karl Rockne, PhD, director of the environmental engineering program at the National Science Foundation.
“When a virus comes out, it’s not just a naked virus, which is exceptionally small. It’s a virus encapsulated in liquid. And that’s why the humidity is so key. The degree of humidity can determine how fast the water evaporates from the particle,” he said in an interview.
In the wake of COVID-19, his institution is funding more cross-disciplinary research in biology, building science, architecture, and physics, he pointed out.
One such effort involved the development of a sensor that can capture live COVID-19 virus. This so-called “smoking gun,” which proved that the virus can spread through the air, took the combined expertise of professionals in medicine, engineering, and several other disciplines.
Currently, investigators are examining indoor air quality and water supplies in offices that have been left empty during the pandemic, and the effect they will have on human health. And others are looking at the way outside air quality affects indoor air quality, particularly where outdoor air quality is poor, such as in areas experiencing wildfires.
So will COVID-19 be the catalyst that finally drives changes to building design, regulation, and public expectations of air quality in the spaces where we spend close to 90% of our time?
“If not COVID, what else? It affected every country, every sector,” Dr. Morawska said. “There’s enough momentum now to do something about this. And enough realization there is a problem.”
A version of this article first appeared on Medscape.com.
Health workers already know that indoor air quality can be as important to human health as clean water and uncontaminated food. But before the COVID-19 pandemic, its importance in the prevention of respiratory illnesses outside of health circles was only whispered about.
Now, a team of nearly 40 scientists from 14 countries is calling for “a paradigm shift,” so that improvements in indoor air quality are viewed as essential to curb respiratory infections.
Most countries do not have indoor air-quality standards, the scientists point out in their recent report, and those that do often fall short in scope and enforcement.
“We expect everywhere in the world to have clean water flowing from our taps. In most parts of the developed world, it is happening and we take it completely for granted,” said lead investigator Lidia Morawska, PhD, of the International Laboratory for Air Quality and Health at the Queensland University of Technology in Brisbane, Australia.
But bacteria and viruses can circulate freely in the air, and “no one thinks about this, whatsoever, apart from health care facilities,” she said.
A first step is to recognize the risk posed by airborne pathogens, something not yet universally acknowledged. The investigators also want the World Health Organization to extend its guidelines to cover airborne pathogens, and for ventilation standards to include higher airflow and filtration rates.
Germany has been at the forefront of air-quality measures, Dr. Morawska said. Years ago, she observed a monitor showing the carbon dioxide level and relative humidity in the room where she was attending a meeting. The screen was accompanied by red, yellow, and green signals to communicate risk. Such indicators are also commonly displayed in German schools so teachers know when to open the windows or adjust the ventilation.
Monitors show carbon dioxide levels
But this is not yet being done in most other countries, Dr. Morawska said. Levels of carbon dioxide are one measure of indoor air quality, but they serve as a proxy for ventilation, she pointed out. Although the technology is available, sensors that can test a variety of components in a building in real time are not yet affordable.
Dr. Morawska envisions a future where the air quality numbers of the places people frequent are displayed so they know the risk for airborne transmission of respiratory illnesses. And people can begin to expect clean indoor air when they enter a business, office, or entertainment space and request changes when the air quality dips and improvement is needed, she said.
It is a daunting challenge to clean indoor air for several reasons. Air is not containable in the same way water is, which makes it difficult to trace contaminants. And infections transmitted through dirty water and food are usually evident immediately, whereas infections transmitted through airborne pathogens can take days to develop. Plus, the necessary infrastructure changes will be expensive.
However, the initial cost required to change the flow and quality of indoor air might be less than the cost of infections, the scientists pointed out. It is estimated that the global harm caused by COVID-19 alone costs $1 trillion each month.
“In the United States, the yearly cost – direct and indirect – of influenza has been calculated at $11.2 billion. For respiratory infections other than influenza, the yearly cost stood at $40 billion,” the team noted.
“If even half of this was caused by inhalation, we are still talking about massive costs,” said Dr. Morawska.
Bigger is not always better
It is tempting to see the solution as increased ventilation, said Ehsan Mousavi, PhD, assistant professor of construction science and management at Clemson (S.C.) University, who studies indoor air quality and ventilation in hospitals.
“We are ventilating the heck out of hospitals,” he said in an interview. But there is much debate about how much ventilation is the right amount. Too much and “you can blow pathogens into an open wound,” he explained. “Bigger is not always better.”
And there is still debate about the best mix of outside and recirculated air. An increase in the intake of outdoor air can refresh indoor air if it is clean, but that depends on where you live, he pointed out.
The mix used in most standard office buildings is 15% outside air and 85% recirculated air, Dr. Mousavi said. Boosting the percentage of outside air increases costs and energy use.
In fact, it can take five times more energy to ventilate hospital spaces than office spaces, he reported.
Engineers searching for clean-air solutions need to know what particulates are in the air and whether they are harmful to humans, but the sensors currently available can’t identify whether a virus is present in real time.
Samples have to be taken to a lab and, “by the time you know a virus was in the space, the moment is gone,” Dr. Mousavi explained.
More research is needed. “We need a reasonable answer that looks at the problem holistically, not just from the infectious disease perspective,” he said.
Hydrating indoor air
Research is making it clear that health care environments can play a significant role in patient recovery, according to Stephanie Taylor, MD. Dr. Taylor is president of Building4Health, which she founded to help businesses assess the quality of air in their buildings and find solutions. The company uses an algorithm to arrive at a health assessment score.
Air hydration is the most important aspect to target, she said.
Since the 1980s, research has shown that a relative humidity of 40%-60% is healthy for humans, she said. Currently, in an office building in a winter climate, the humidity level is more like 20%.
Canada is the first country to officially recommend the 40%-60% range for senior citizen centers and residential homes.
“Properly hydrated air supports our immune system and prevents skin problems and respiratory problems. It also inactivates many bacteria and viruses,” Dr. Taylor explained. Inhaling dry air compromises the ability of the body to restrict influenza virus infection, researchers showed in a 2019 study.
In the case of COVID-19, as virus particles attach to water molecules, they get bigger and heavier and eventually drop out of the breathing zone and onto surfaces where they can be wiped away, she explained.
But when the particles “are very small – like 5 microns in diameter – and you inhale them, they can lodge deep in the lungs,” she said.
In properly hydrated air, particles will be larger – about 10-20 microns when they attach to the water vapor – so they will get stuck in the nose or the back of the throat, where they can be washed away by mucous and not travel to the lungs.
“Indoor air metrics” can support our health or contribute to disease, “not just over time, but quickly, within minutes or hours,” she said.
No one expects the world’s building stock to suddenly upgrade to the ideal air quality. “But that doesn’t mean we shouldn’t move in that direction,” Dr. Taylor said. Changes can start small and gradually increase.
New research targets indoor air
Humidity is one of the key areas for current research, said Karl Rockne, PhD, director of the environmental engineering program at the National Science Foundation.
“When a virus comes out, it’s not just a naked virus, which is exceptionally small. It’s a virus encapsulated in liquid. And that’s why the humidity is so key. The degree of humidity can determine how fast the water evaporates from the particle,” he said in an interview.
In the wake of COVID-19, his institution is funding more cross-disciplinary research in biology, building science, architecture, and physics, he pointed out.
One such effort involved the development of a sensor that can capture live COVID-19 virus. This so-called “smoking gun,” which proved that the virus can spread through the air, took the combined expertise of professionals in medicine, engineering, and several other disciplines.
Currently, investigators are examining indoor air quality and water supplies in offices that have been left empty during the pandemic, and the effect they will have on human health. And others are looking at the way outside air quality affects indoor air quality, particularly where outdoor air quality is poor, such as in areas experiencing wildfires.
So will COVID-19 be the catalyst that finally drives changes to building design, regulation, and public expectations of air quality in the spaces where we spend close to 90% of our time?
“If not COVID, what else? It affected every country, every sector,” Dr. Morawska said. “There’s enough momentum now to do something about this. And enough realization there is a problem.”
A version of this article first appeared on Medscape.com.
Health workers already know that indoor air quality can be as important to human health as clean water and uncontaminated food. But before the COVID-19 pandemic, its importance in the prevention of respiratory illnesses outside of health circles was only whispered about.
Now, a team of nearly 40 scientists from 14 countries is calling for “a paradigm shift,” so that improvements in indoor air quality are viewed as essential to curb respiratory infections.
Most countries do not have indoor air-quality standards, the scientists point out in their recent report, and those that do often fall short in scope and enforcement.
“We expect everywhere in the world to have clean water flowing from our taps. In most parts of the developed world, it is happening and we take it completely for granted,” said lead investigator Lidia Morawska, PhD, of the International Laboratory for Air Quality and Health at the Queensland University of Technology in Brisbane, Australia.
But bacteria and viruses can circulate freely in the air, and “no one thinks about this, whatsoever, apart from health care facilities,” she said.
A first step is to recognize the risk posed by airborne pathogens, something not yet universally acknowledged. The investigators also want the World Health Organization to extend its guidelines to cover airborne pathogens, and for ventilation standards to include higher airflow and filtration rates.
Germany has been at the forefront of air-quality measures, Dr. Morawska said. Years ago, she observed a monitor showing the carbon dioxide level and relative humidity in the room where she was attending a meeting. The screen was accompanied by red, yellow, and green signals to communicate risk. Such indicators are also commonly displayed in German schools so teachers know when to open the windows or adjust the ventilation.
Monitors show carbon dioxide levels
But this is not yet being done in most other countries, Dr. Morawska said. Levels of carbon dioxide are one measure of indoor air quality, but they serve as a proxy for ventilation, she pointed out. Although the technology is available, sensors that can test a variety of components in a building in real time are not yet affordable.
Dr. Morawska envisions a future where the air quality numbers of the places people frequent are displayed so they know the risk for airborne transmission of respiratory illnesses. And people can begin to expect clean indoor air when they enter a business, office, or entertainment space and request changes when the air quality dips and improvement is needed, she said.
It is a daunting challenge to clean indoor air for several reasons. Air is not containable in the same way water is, which makes it difficult to trace contaminants. And infections transmitted through dirty water and food are usually evident immediately, whereas infections transmitted through airborne pathogens can take days to develop. Plus, the necessary infrastructure changes will be expensive.
However, the initial cost required to change the flow and quality of indoor air might be less than the cost of infections, the scientists pointed out. It is estimated that the global harm caused by COVID-19 alone costs $1 trillion each month.
“In the United States, the yearly cost – direct and indirect – of influenza has been calculated at $11.2 billion. For respiratory infections other than influenza, the yearly cost stood at $40 billion,” the team noted.
“If even half of this was caused by inhalation, we are still talking about massive costs,” said Dr. Morawska.
Bigger is not always better
It is tempting to see the solution as increased ventilation, said Ehsan Mousavi, PhD, assistant professor of construction science and management at Clemson (S.C.) University, who studies indoor air quality and ventilation in hospitals.
“We are ventilating the heck out of hospitals,” he said in an interview. But there is much debate about how much ventilation is the right amount. Too much and “you can blow pathogens into an open wound,” he explained. “Bigger is not always better.”
And there is still debate about the best mix of outside and recirculated air. An increase in the intake of outdoor air can refresh indoor air if it is clean, but that depends on where you live, he pointed out.
The mix used in most standard office buildings is 15% outside air and 85% recirculated air, Dr. Mousavi said. Boosting the percentage of outside air increases costs and energy use.
In fact, it can take five times more energy to ventilate hospital spaces than office spaces, he reported.
Engineers searching for clean-air solutions need to know what particulates are in the air and whether they are harmful to humans, but the sensors currently available can’t identify whether a virus is present in real time.
Samples have to be taken to a lab and, “by the time you know a virus was in the space, the moment is gone,” Dr. Mousavi explained.
More research is needed. “We need a reasonable answer that looks at the problem holistically, not just from the infectious disease perspective,” he said.
Hydrating indoor air
Research is making it clear that health care environments can play a significant role in patient recovery, according to Stephanie Taylor, MD. Dr. Taylor is president of Building4Health, which she founded to help businesses assess the quality of air in their buildings and find solutions. The company uses an algorithm to arrive at a health assessment score.
Air hydration is the most important aspect to target, she said.
Since the 1980s, research has shown that a relative humidity of 40%-60% is healthy for humans, she said. Currently, in an office building in a winter climate, the humidity level is more like 20%.
Canada is the first country to officially recommend the 40%-60% range for senior citizen centers and residential homes.
“Properly hydrated air supports our immune system and prevents skin problems and respiratory problems. It also inactivates many bacteria and viruses,” Dr. Taylor explained. Inhaling dry air compromises the ability of the body to restrict influenza virus infection, researchers showed in a 2019 study.
In the case of COVID-19, as virus particles attach to water molecules, they get bigger and heavier and eventually drop out of the breathing zone and onto surfaces where they can be wiped away, she explained.
But when the particles “are very small – like 5 microns in diameter – and you inhale them, they can lodge deep in the lungs,” she said.
In properly hydrated air, particles will be larger – about 10-20 microns when they attach to the water vapor – so they will get stuck in the nose or the back of the throat, where they can be washed away by mucous and not travel to the lungs.
“Indoor air metrics” can support our health or contribute to disease, “not just over time, but quickly, within minutes or hours,” she said.
No one expects the world’s building stock to suddenly upgrade to the ideal air quality. “But that doesn’t mean we shouldn’t move in that direction,” Dr. Taylor said. Changes can start small and gradually increase.
New research targets indoor air
Humidity is one of the key areas for current research, said Karl Rockne, PhD, director of the environmental engineering program at the National Science Foundation.
“When a virus comes out, it’s not just a naked virus, which is exceptionally small. It’s a virus encapsulated in liquid. And that’s why the humidity is so key. The degree of humidity can determine how fast the water evaporates from the particle,” he said in an interview.
In the wake of COVID-19, his institution is funding more cross-disciplinary research in biology, building science, architecture, and physics, he pointed out.
One such effort involved the development of a sensor that can capture live COVID-19 virus. This so-called “smoking gun,” which proved that the virus can spread through the air, took the combined expertise of professionals in medicine, engineering, and several other disciplines.
Currently, investigators are examining indoor air quality and water supplies in offices that have been left empty during the pandemic, and the effect they will have on human health. And others are looking at the way outside air quality affects indoor air quality, particularly where outdoor air quality is poor, such as in areas experiencing wildfires.
So will COVID-19 be the catalyst that finally drives changes to building design, regulation, and public expectations of air quality in the spaces where we spend close to 90% of our time?
“If not COVID, what else? It affected every country, every sector,” Dr. Morawska said. “There’s enough momentum now to do something about this. And enough realization there is a problem.”
A version of this article first appeared on Medscape.com.
Physicians’ trust in health care leadership drops in pandemic
according to a survey conducted by NORC at the University of Chicago on behalf of the American Board of Internal Medicine Foundation.
Survey results, released May 21, indicate that 30% of physicians say their trust in the U.S. health care system and health care leadership has decreased during the pandemic. Only 18% reported an increase in trust.
Physicians, however, have great trust in their fellow clinicians.
In the survey of 600 physicians, 94% said they trust doctors within their practice; 85% trusted doctors outside of their practice; and 89% trusted nurses. That trust increased during the pandemic, with 41% saying their trust in fellow physicians rose and 37% saying their trust in nurses did.
In a separate survey, NORC asked patients about their trust in various aspects of health care. Among 2,069 respondents, a wide majority reported that they trust doctors (84%) and nurses (85%), but only 64% trusted the health care system as a whole. One in three consumers (32%) said their trust in the health care system decreased during the pandemic, compared with 11% who said their trust increased.
The ABIM Foundation released the research findings on May 21 as part of Building Trust, a national campaign that aims to boost trust among patients, clinicians, system leaders, researchers, and others.
Richard J. Baron, MD, president and chief executive officer of the ABIM Foundation, said in an interview, “Clearly there’s lower trust in health care organization leaders and executives, and that’s troubling.
“Science by itself is not enough,” he said. “Becoming trustworthy has to be a core project of everybody in health care.”
Deterioration in physicians’ trust during the pandemic comes in part from failed promises of adequate personal protective equipment and some physicians’ loss of income as a result of the crisis, Dr. Baron said.
He added that the vaccine rollout was very uneven and that policies as to which elective procedures could be performed were handled differently in different parts of the country.
He also noted that, early on, transparency was lacking as to how many COVID patients hospitals were treating, which may have contributed to the decrease in trust in the system.
Fear of being known as ‘the COVID hospital’
Hospitals were afraid of being known as “the COVID hospital” and losing patients who were afraid to come there, Dr. Baron said.
He said the COVID-19 epidemic exacerbated problems regarding trust, but that trust has been declining for some time. The Building Trust campaign will focus on solutions in breaches of trust as physicians move increasingly toward being employees of huge systems, according to Dr. Baron.
However, trust works both ways, Dr. Baron notes. Physicians can be champions for their health care system or “throw the system under the bus,” he said.
For example, if a patient complains about the appointment system, clinicians who trust their institutions may say the system usually works and that they will try to make sure the patient has a better experience next time. Clinicians without trust may say they agree that the health care system doesn’t know what it is doing, and patients may further lose confidence when physicians validate their complaint, and patients may then go elsewhere.
78% of patients trust primary care doctor
When asked whether they trust their primary care physician, 78% of patients said yes. However, trust in doctors was higher among people who were older (90%), White (82%), or had high income (89%). Among people reporting lower trust, 25% said their physician spends too little time with them, and 14% said their doctor does not know or listen to them.
The survey shows that government agencies have work to do to earn trust. Responses indicate that 43% of physicians said they have “complete trust” in government health care agencies, such as the U.S. Food and Drug Administration and the Centers for Disease Control and Prevention, which is substantially higher than other parts of the health care system. However, trust in agencies declined for 43% of physician respondents and increased for 21%.
Dhruv Khullar, MD, MPP, of the department of health policy and economics at Weill Cornell Medical College in New York, told this news organization the survey results match what he sees anecdotally in medicine – that physicians have been losing trust in the system but not in their colleagues.
He said the sample size of 600 is enough to be influential, though he said he would like to know the response rate, which was not calculated for this survey.
He added that, in large part, physicians’ lack of trust in their systems may come from generally being asked to see more patients and to meet more metrics during the same or shorter periods.
Physicians’ lack of trust in the system can have significant consequences, he said. It can lead to burnout, which has been linked with poorer quality of care and physician turnover, he noted.
COVID-19 led some physicians to wonder whether their system had their best interests at heart, insofar as access to adequate medicines and supplies as well as emotional support were inconsistent, Dr. Khullar said.
He said that to regain trust health care systems need to ask themselves questions in three areas. The first is whether their goals are focused on the best interest of the organization or the best interest of the patient.
“Next is competency,” Dr. Khullar said. “Maybe your motives are right, but are you able to deliver? Are you delivering a good product, whether clinical services or something else?”
The third area is transparency, he said. “Are you going to be honest and forthright in what we’re doing and where we’re going?”
Caroline Pearson, senior vice president of health care strategy for NORC, said the emailed survey was conducted between Dec. 29, 2020, and Feb. 5, 2021, with a health care survey partner that maintains a nationwide panel of physicians across specialties.
She said this report is fairly novel insofar as surveys are more typically conducted regarding patients’ trust of their doctors or of the health care system.
Ms. Pearson said because health care is delivered in teams, understanding the level of trust among the entities helps ensure that care will be delivered effectively and seamlessly with high quality.
“We want our patients to trust our doctors, but we really want doctors to trust each other and trust the hospitals and systems in which they’re working,” she said.
Dr. Baron, Ms. Pearson, and Dr. Khullar report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a survey conducted by NORC at the University of Chicago on behalf of the American Board of Internal Medicine Foundation.
Survey results, released May 21, indicate that 30% of physicians say their trust in the U.S. health care system and health care leadership has decreased during the pandemic. Only 18% reported an increase in trust.
Physicians, however, have great trust in their fellow clinicians.
In the survey of 600 physicians, 94% said they trust doctors within their practice; 85% trusted doctors outside of their practice; and 89% trusted nurses. That trust increased during the pandemic, with 41% saying their trust in fellow physicians rose and 37% saying their trust in nurses did.
In a separate survey, NORC asked patients about their trust in various aspects of health care. Among 2,069 respondents, a wide majority reported that they trust doctors (84%) and nurses (85%), but only 64% trusted the health care system as a whole. One in three consumers (32%) said their trust in the health care system decreased during the pandemic, compared with 11% who said their trust increased.
The ABIM Foundation released the research findings on May 21 as part of Building Trust, a national campaign that aims to boost trust among patients, clinicians, system leaders, researchers, and others.
Richard J. Baron, MD, president and chief executive officer of the ABIM Foundation, said in an interview, “Clearly there’s lower trust in health care organization leaders and executives, and that’s troubling.
“Science by itself is not enough,” he said. “Becoming trustworthy has to be a core project of everybody in health care.”
Deterioration in physicians’ trust during the pandemic comes in part from failed promises of adequate personal protective equipment and some physicians’ loss of income as a result of the crisis, Dr. Baron said.
He added that the vaccine rollout was very uneven and that policies as to which elective procedures could be performed were handled differently in different parts of the country.
He also noted that, early on, transparency was lacking as to how many COVID patients hospitals were treating, which may have contributed to the decrease in trust in the system.
Fear of being known as ‘the COVID hospital’
Hospitals were afraid of being known as “the COVID hospital” and losing patients who were afraid to come there, Dr. Baron said.
He said the COVID-19 epidemic exacerbated problems regarding trust, but that trust has been declining for some time. The Building Trust campaign will focus on solutions in breaches of trust as physicians move increasingly toward being employees of huge systems, according to Dr. Baron.
However, trust works both ways, Dr. Baron notes. Physicians can be champions for their health care system or “throw the system under the bus,” he said.
For example, if a patient complains about the appointment system, clinicians who trust their institutions may say the system usually works and that they will try to make sure the patient has a better experience next time. Clinicians without trust may say they agree that the health care system doesn’t know what it is doing, and patients may further lose confidence when physicians validate their complaint, and patients may then go elsewhere.
78% of patients trust primary care doctor
When asked whether they trust their primary care physician, 78% of patients said yes. However, trust in doctors was higher among people who were older (90%), White (82%), or had high income (89%). Among people reporting lower trust, 25% said their physician spends too little time with them, and 14% said their doctor does not know or listen to them.
The survey shows that government agencies have work to do to earn trust. Responses indicate that 43% of physicians said they have “complete trust” in government health care agencies, such as the U.S. Food and Drug Administration and the Centers for Disease Control and Prevention, which is substantially higher than other parts of the health care system. However, trust in agencies declined for 43% of physician respondents and increased for 21%.
Dhruv Khullar, MD, MPP, of the department of health policy and economics at Weill Cornell Medical College in New York, told this news organization the survey results match what he sees anecdotally in medicine – that physicians have been losing trust in the system but not in their colleagues.
He said the sample size of 600 is enough to be influential, though he said he would like to know the response rate, which was not calculated for this survey.
He added that, in large part, physicians’ lack of trust in their systems may come from generally being asked to see more patients and to meet more metrics during the same or shorter periods.
Physicians’ lack of trust in the system can have significant consequences, he said. It can lead to burnout, which has been linked with poorer quality of care and physician turnover, he noted.
COVID-19 led some physicians to wonder whether their system had their best interests at heart, insofar as access to adequate medicines and supplies as well as emotional support were inconsistent, Dr. Khullar said.
He said that to regain trust health care systems need to ask themselves questions in three areas. The first is whether their goals are focused on the best interest of the organization or the best interest of the patient.
“Next is competency,” Dr. Khullar said. “Maybe your motives are right, but are you able to deliver? Are you delivering a good product, whether clinical services or something else?”
The third area is transparency, he said. “Are you going to be honest and forthright in what we’re doing and where we’re going?”
Caroline Pearson, senior vice president of health care strategy for NORC, said the emailed survey was conducted between Dec. 29, 2020, and Feb. 5, 2021, with a health care survey partner that maintains a nationwide panel of physicians across specialties.
She said this report is fairly novel insofar as surveys are more typically conducted regarding patients’ trust of their doctors or of the health care system.
Ms. Pearson said because health care is delivered in teams, understanding the level of trust among the entities helps ensure that care will be delivered effectively and seamlessly with high quality.
“We want our patients to trust our doctors, but we really want doctors to trust each other and trust the hospitals and systems in which they’re working,” she said.
Dr. Baron, Ms. Pearson, and Dr. Khullar report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a survey conducted by NORC at the University of Chicago on behalf of the American Board of Internal Medicine Foundation.
Survey results, released May 21, indicate that 30% of physicians say their trust in the U.S. health care system and health care leadership has decreased during the pandemic. Only 18% reported an increase in trust.
Physicians, however, have great trust in their fellow clinicians.
In the survey of 600 physicians, 94% said they trust doctors within their practice; 85% trusted doctors outside of their practice; and 89% trusted nurses. That trust increased during the pandemic, with 41% saying their trust in fellow physicians rose and 37% saying their trust in nurses did.
In a separate survey, NORC asked patients about their trust in various aspects of health care. Among 2,069 respondents, a wide majority reported that they trust doctors (84%) and nurses (85%), but only 64% trusted the health care system as a whole. One in three consumers (32%) said their trust in the health care system decreased during the pandemic, compared with 11% who said their trust increased.
The ABIM Foundation released the research findings on May 21 as part of Building Trust, a national campaign that aims to boost trust among patients, clinicians, system leaders, researchers, and others.
Richard J. Baron, MD, president and chief executive officer of the ABIM Foundation, said in an interview, “Clearly there’s lower trust in health care organization leaders and executives, and that’s troubling.
“Science by itself is not enough,” he said. “Becoming trustworthy has to be a core project of everybody in health care.”
Deterioration in physicians’ trust during the pandemic comes in part from failed promises of adequate personal protective equipment and some physicians’ loss of income as a result of the crisis, Dr. Baron said.
He added that the vaccine rollout was very uneven and that policies as to which elective procedures could be performed were handled differently in different parts of the country.
He also noted that, early on, transparency was lacking as to how many COVID patients hospitals were treating, which may have contributed to the decrease in trust in the system.
Fear of being known as ‘the COVID hospital’
Hospitals were afraid of being known as “the COVID hospital” and losing patients who were afraid to come there, Dr. Baron said.
He said the COVID-19 epidemic exacerbated problems regarding trust, but that trust has been declining for some time. The Building Trust campaign will focus on solutions in breaches of trust as physicians move increasingly toward being employees of huge systems, according to Dr. Baron.
However, trust works both ways, Dr. Baron notes. Physicians can be champions for their health care system or “throw the system under the bus,” he said.
For example, if a patient complains about the appointment system, clinicians who trust their institutions may say the system usually works and that they will try to make sure the patient has a better experience next time. Clinicians without trust may say they agree that the health care system doesn’t know what it is doing, and patients may further lose confidence when physicians validate their complaint, and patients may then go elsewhere.
78% of patients trust primary care doctor
When asked whether they trust their primary care physician, 78% of patients said yes. However, trust in doctors was higher among people who were older (90%), White (82%), or had high income (89%). Among people reporting lower trust, 25% said their physician spends too little time with them, and 14% said their doctor does not know or listen to them.
The survey shows that government agencies have work to do to earn trust. Responses indicate that 43% of physicians said they have “complete trust” in government health care agencies, such as the U.S. Food and Drug Administration and the Centers for Disease Control and Prevention, which is substantially higher than other parts of the health care system. However, trust in agencies declined for 43% of physician respondents and increased for 21%.
Dhruv Khullar, MD, MPP, of the department of health policy and economics at Weill Cornell Medical College in New York, told this news organization the survey results match what he sees anecdotally in medicine – that physicians have been losing trust in the system but not in their colleagues.
He said the sample size of 600 is enough to be influential, though he said he would like to know the response rate, which was not calculated for this survey.
He added that, in large part, physicians’ lack of trust in their systems may come from generally being asked to see more patients and to meet more metrics during the same or shorter periods.
Physicians’ lack of trust in the system can have significant consequences, he said. It can lead to burnout, which has been linked with poorer quality of care and physician turnover, he noted.
COVID-19 led some physicians to wonder whether their system had their best interests at heart, insofar as access to adequate medicines and supplies as well as emotional support were inconsistent, Dr. Khullar said.
He said that to regain trust health care systems need to ask themselves questions in three areas. The first is whether their goals are focused on the best interest of the organization or the best interest of the patient.
“Next is competency,” Dr. Khullar said. “Maybe your motives are right, but are you able to deliver? Are you delivering a good product, whether clinical services or something else?”
The third area is transparency, he said. “Are you going to be honest and forthright in what we’re doing and where we’re going?”
Caroline Pearson, senior vice president of health care strategy for NORC, said the emailed survey was conducted between Dec. 29, 2020, and Feb. 5, 2021, with a health care survey partner that maintains a nationwide panel of physicians across specialties.
She said this report is fairly novel insofar as surveys are more typically conducted regarding patients’ trust of their doctors or of the health care system.
Ms. Pearson said because health care is delivered in teams, understanding the level of trust among the entities helps ensure that care will be delivered effectively and seamlessly with high quality.
“We want our patients to trust our doctors, but we really want doctors to trust each other and trust the hospitals and systems in which they’re working,” she said.
Dr. Baron, Ms. Pearson, and Dr. Khullar report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Family physicians’ compensation levels stable in pandemic
to $236,000, up from $234,000 last year, even as many practices saw a decrease in hours and patient visits during the pandemic.
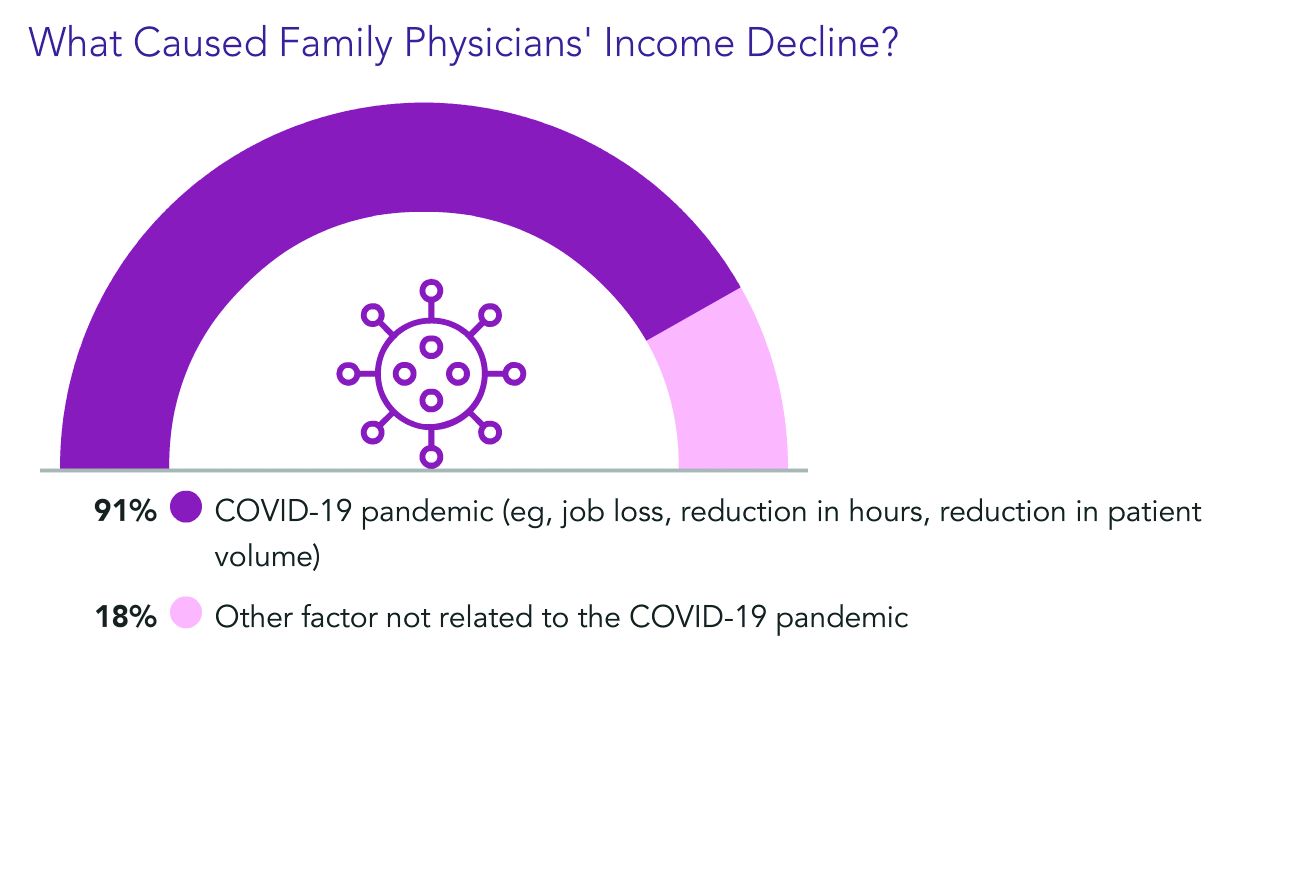
Only pediatricians earned less ($221,000) according to the Medscape Family Physician Compensation Report 2021. Plastic surgeons topped this year’s list, at $526,000, followed by orthopedists, at $511,000, and cardiologists, at $459,000.
Family physicians ranked in the middle of specialties in terms of the percentages of physicians who thought they were fairly compensated: 57% of family physicians said they were fairly paid, and 79% of oncologists said they were. Only 44% of infectious disease physicians said they were fairly compensated.
Survey answers indicate, though, that pay isn’t driving family physicians’ satisfaction.
Only 10% of family physicians in the survey said that “making good money at a job I like” was the most rewarding aspect of the job. The top two answers by far were “gratitude/relationships with patients” (chosen by 34%) and “knowing I’m making the world a better place” (27%). Respondents could choose more than one answer.
Despite the small uptick in earnings overall in the specialty, more than one-third of family physicians (36%) reported a decline in compensation in this year’s survey, which included 18,000 responses from physicians in 29 specialties.
Male family physicians continue to be paid much more than their female colleagues, this year 29% more, widening the gap from 26% last year. Overall, men in primary care earned 27% more than their female colleagues, and male specialists earned 33% more.
As for decline in patients seen in some specialties, family physicians are holding their own.
Whereas pediatricians have seen a drop of 18% in patient visits, family physicians saw a decline of just 5%, from an average of 81 to 77 patients per week.
Most expect return to normal pay within 3 years
Most family physicians (83%) who incurred financial losses this year said they expect that income will return to normal within 3 years. More than one-third of that group (38%) said they expect compensation to get back to normal in the next year.
Almost all of the family physicians who lost income (91%) pointed the finger at COVID-19. Respondents could choose more than one answer, and 18% said other factors were also to blame.
Family physicians averaged $27,000 in incentive bonuses, higher than those in internal medicine, pediatrics, and psychiatry. Orthopedists had by far the highest bonuses, at $116,000.
For family physicians who received a bonus this year, the amount equaled about 12% of their salary, up from 10% last year. Bonuses are usually based on productivity but can also be tied to patient satisfaction, clinical processes, and other factors.
The number of family physicians who achieved more than three-quarters of their potential annual bonus rose to 61% this year, up from 55%.
17 hours a week on administrative tasks
The survey also ranked specialties by the amount of time physicians spent on paperwork and administrative tasks, including participation in professional organizations and clinical reading.
Family physicians fell squarely in the middle, with 17 hours per week spent on such tasks. Infectious disease physicians spent the most time, at 24.2 hours a week, and anesthesiologists spent the least, at 10.1.
Work hours declined for many physicians during the pandemic, and some were furloughed.
But, like most physicians, family physicians are once more working normal hours. They average 49 hours per week, which is slightly more than before the pandemic.
Specialists whose weekly hours are above normal are infectious disease physicians, intensivists, and public health and preventive medicine physicians; all are working 6 to 7 hours a week more than usual, according to the survey responses.
Responses also turned up some uncertainty on the future makeup of patient panels.
Most family physicians (69%) said they would continue to take new and current Medicare/Medicaid patients.
However, close to one-third of family physicians said they would stop treating at least some patients they already have and will not take new ones or haven’t decided yet.
A version of this article first appeared on Medscape.com.
to $236,000, up from $234,000 last year, even as many practices saw a decrease in hours and patient visits during the pandemic.
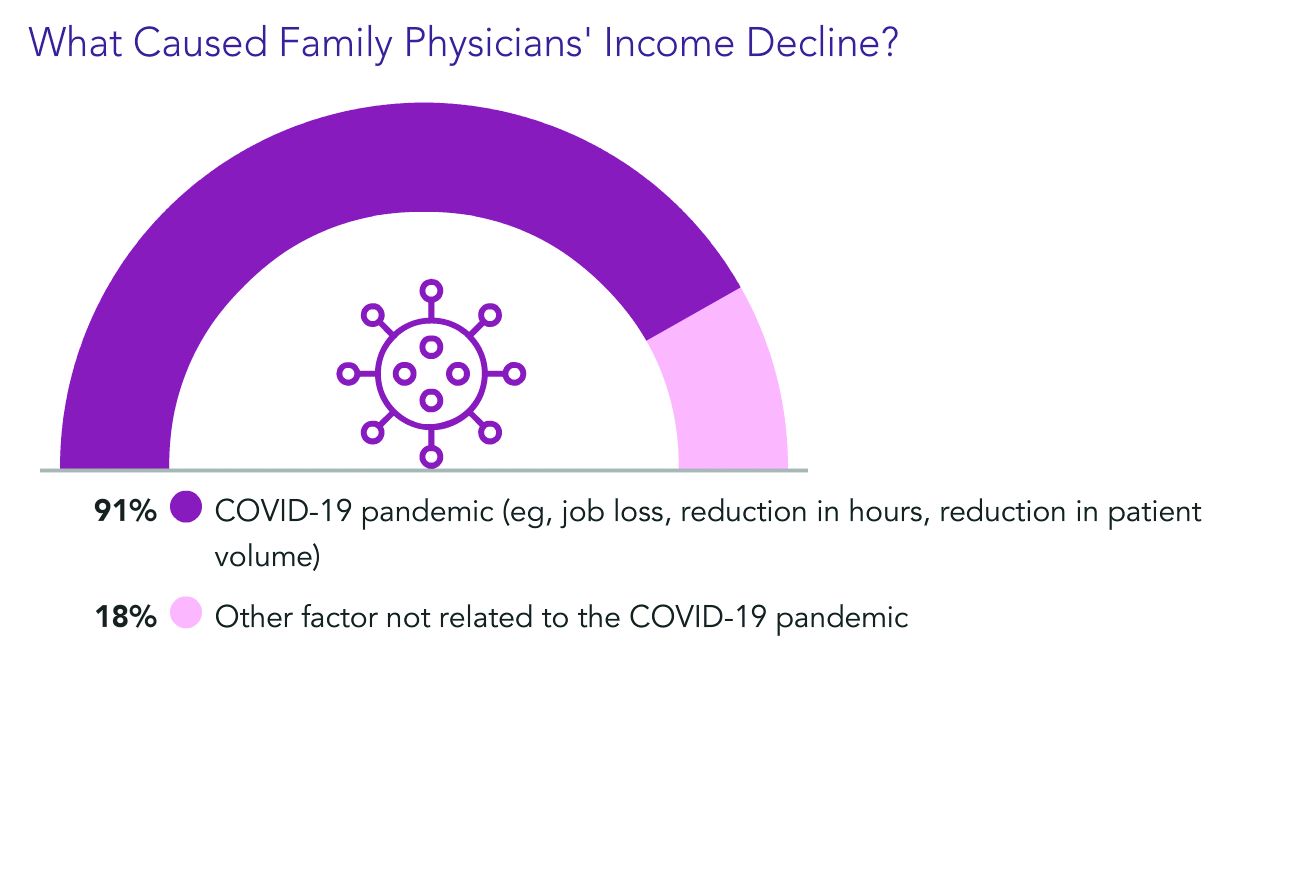
Only pediatricians earned less ($221,000) according to the Medscape Family Physician Compensation Report 2021. Plastic surgeons topped this year’s list, at $526,000, followed by orthopedists, at $511,000, and cardiologists, at $459,000.
Family physicians ranked in the middle of specialties in terms of the percentages of physicians who thought they were fairly compensated: 57% of family physicians said they were fairly paid, and 79% of oncologists said they were. Only 44% of infectious disease physicians said they were fairly compensated.
Survey answers indicate, though, that pay isn’t driving family physicians’ satisfaction.
Only 10% of family physicians in the survey said that “making good money at a job I like” was the most rewarding aspect of the job. The top two answers by far were “gratitude/relationships with patients” (chosen by 34%) and “knowing I’m making the world a better place” (27%). Respondents could choose more than one answer.
Despite the small uptick in earnings overall in the specialty, more than one-third of family physicians (36%) reported a decline in compensation in this year’s survey, which included 18,000 responses from physicians in 29 specialties.
Male family physicians continue to be paid much more than their female colleagues, this year 29% more, widening the gap from 26% last year. Overall, men in primary care earned 27% more than their female colleagues, and male specialists earned 33% more.
As for decline in patients seen in some specialties, family physicians are holding their own.
Whereas pediatricians have seen a drop of 18% in patient visits, family physicians saw a decline of just 5%, from an average of 81 to 77 patients per week.
Most expect return to normal pay within 3 years
Most family physicians (83%) who incurred financial losses this year said they expect that income will return to normal within 3 years. More than one-third of that group (38%) said they expect compensation to get back to normal in the next year.
Almost all of the family physicians who lost income (91%) pointed the finger at COVID-19. Respondents could choose more than one answer, and 18% said other factors were also to blame.
Family physicians averaged $27,000 in incentive bonuses, higher than those in internal medicine, pediatrics, and psychiatry. Orthopedists had by far the highest bonuses, at $116,000.
For family physicians who received a bonus this year, the amount equaled about 12% of their salary, up from 10% last year. Bonuses are usually based on productivity but can also be tied to patient satisfaction, clinical processes, and other factors.
The number of family physicians who achieved more than three-quarters of their potential annual bonus rose to 61% this year, up from 55%.
17 hours a week on administrative tasks
The survey also ranked specialties by the amount of time physicians spent on paperwork and administrative tasks, including participation in professional organizations and clinical reading.
Family physicians fell squarely in the middle, with 17 hours per week spent on such tasks. Infectious disease physicians spent the most time, at 24.2 hours a week, and anesthesiologists spent the least, at 10.1.
Work hours declined for many physicians during the pandemic, and some were furloughed.
But, like most physicians, family physicians are once more working normal hours. They average 49 hours per week, which is slightly more than before the pandemic.
Specialists whose weekly hours are above normal are infectious disease physicians, intensivists, and public health and preventive medicine physicians; all are working 6 to 7 hours a week more than usual, according to the survey responses.
Responses also turned up some uncertainty on the future makeup of patient panels.
Most family physicians (69%) said they would continue to take new and current Medicare/Medicaid patients.
However, close to one-third of family physicians said they would stop treating at least some patients they already have and will not take new ones or haven’t decided yet.
A version of this article first appeared on Medscape.com.
to $236,000, up from $234,000 last year, even as many practices saw a decrease in hours and patient visits during the pandemic.
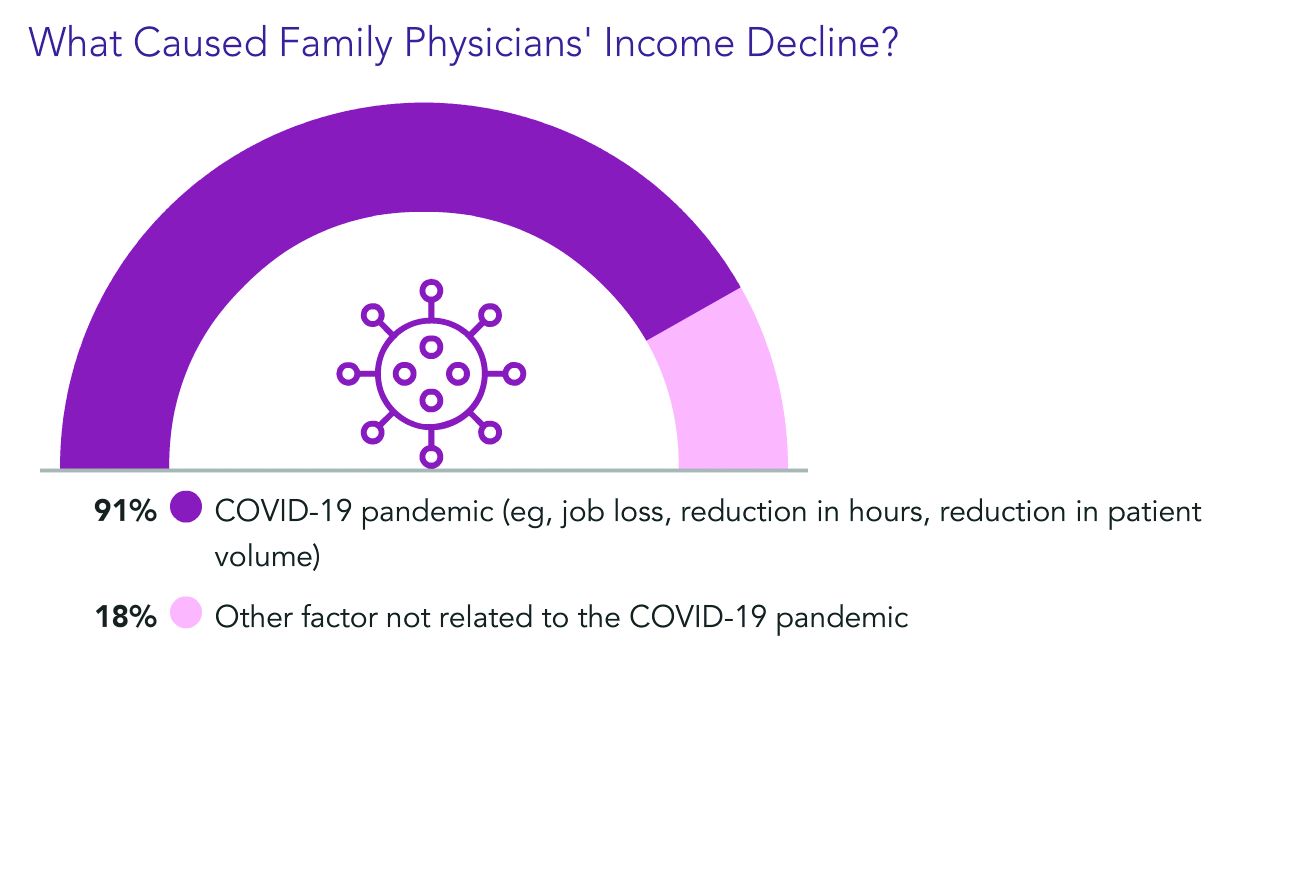
Only pediatricians earned less ($221,000) according to the Medscape Family Physician Compensation Report 2021. Plastic surgeons topped this year’s list, at $526,000, followed by orthopedists, at $511,000, and cardiologists, at $459,000.
Family physicians ranked in the middle of specialties in terms of the percentages of physicians who thought they were fairly compensated: 57% of family physicians said they were fairly paid, and 79% of oncologists said they were. Only 44% of infectious disease physicians said they were fairly compensated.
Survey answers indicate, though, that pay isn’t driving family physicians’ satisfaction.
Only 10% of family physicians in the survey said that “making good money at a job I like” was the most rewarding aspect of the job. The top two answers by far were “gratitude/relationships with patients” (chosen by 34%) and “knowing I’m making the world a better place” (27%). Respondents could choose more than one answer.
Despite the small uptick in earnings overall in the specialty, more than one-third of family physicians (36%) reported a decline in compensation in this year’s survey, which included 18,000 responses from physicians in 29 specialties.
Male family physicians continue to be paid much more than their female colleagues, this year 29% more, widening the gap from 26% last year. Overall, men in primary care earned 27% more than their female colleagues, and male specialists earned 33% more.
As for decline in patients seen in some specialties, family physicians are holding their own.
Whereas pediatricians have seen a drop of 18% in patient visits, family physicians saw a decline of just 5%, from an average of 81 to 77 patients per week.
Most expect return to normal pay within 3 years
Most family physicians (83%) who incurred financial losses this year said they expect that income will return to normal within 3 years. More than one-third of that group (38%) said they expect compensation to get back to normal in the next year.
Almost all of the family physicians who lost income (91%) pointed the finger at COVID-19. Respondents could choose more than one answer, and 18% said other factors were also to blame.
Family physicians averaged $27,000 in incentive bonuses, higher than those in internal medicine, pediatrics, and psychiatry. Orthopedists had by far the highest bonuses, at $116,000.
For family physicians who received a bonus this year, the amount equaled about 12% of their salary, up from 10% last year. Bonuses are usually based on productivity but can also be tied to patient satisfaction, clinical processes, and other factors.
The number of family physicians who achieved more than three-quarters of their potential annual bonus rose to 61% this year, up from 55%.
17 hours a week on administrative tasks
The survey also ranked specialties by the amount of time physicians spent on paperwork and administrative tasks, including participation in professional organizations and clinical reading.
Family physicians fell squarely in the middle, with 17 hours per week spent on such tasks. Infectious disease physicians spent the most time, at 24.2 hours a week, and anesthesiologists spent the least, at 10.1.
Work hours declined for many physicians during the pandemic, and some were furloughed.
But, like most physicians, family physicians are once more working normal hours. They average 49 hours per week, which is slightly more than before the pandemic.
Specialists whose weekly hours are above normal are infectious disease physicians, intensivists, and public health and preventive medicine physicians; all are working 6 to 7 hours a week more than usual, according to the survey responses.
Responses also turned up some uncertainty on the future makeup of patient panels.
Most family physicians (69%) said they would continue to take new and current Medicare/Medicaid patients.
However, close to one-third of family physicians said they would stop treating at least some patients they already have and will not take new ones or haven’t decided yet.
A version of this article first appeared on Medscape.com.

