User login
Autoimmune Disease Risk May Rise Following Cushing Disease Remission After Surgery
Patients with Cushing disease have an increased risk for new-onset autoimmune disease in the 3 years after surgical remission, according to a new retrospective study published on February 20 in Annals of Internal Medicine.
Outcomes for patients with Cushing disease were compared against those with nonfunctioning pituitary adenomas (NFPAs). New-onset autoimmune disease occurred in 10.4% with Cushing disease and 1.6% among patients with NFPA (hazard ratio, 7.80; 95% CI, 2.88-21.10).
“Understanding and recognizing new and recurrent autoimmune disease in this setting is important to avoid misclassifying such patients with glucocorticoid withdrawal syndrome, which could result in failure to treat underlying autoimmune disease, as well as erroneous diagnosis of steroid withdrawal cases,” wrote Dennis Delasi Nyanyo of Massachusetts General Hospital and Harvard Medical School, Boston, and colleagues.
Given the general population’s annual incidence of major autoimmune diseases, estimated at about 100 cases per 100,000 people, and the 3-year incidence of 10.4% found in this study’s cohort, “our findings suggest that Cushing disease remission may trigger development of autoimmune disease,” the authors wrote.
Monitor Patients With Family History of Autoimmune Disease?
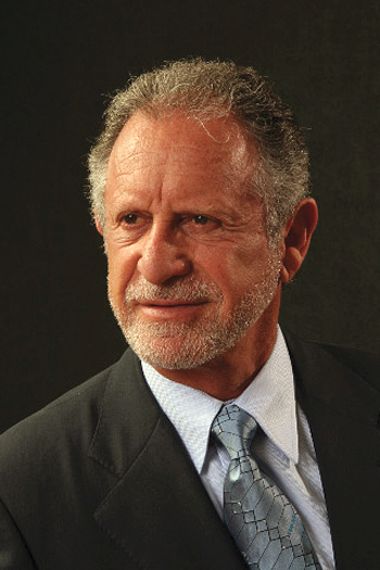
The study results were not necessarily surprising to Anthony P. Heaney, MD, PhD, an endocrinologist and professor of medicine at the University of California, Los Angeles, because past research has raised similar questions. The authors’ suggestion that the rapid postsurgical drop in cortisol that occurs as a result of treating Cushing disease becomes some sort of autoimmune trigger is interesting but remains speculative, Dr. Heaney pointed out.
If future evidence supports that possibility, “it would suggest, in terms of managing those patients in the postoperative setting, that there may be some merit to giving them higher concentrations of glucocorticoids for a short period of time,” Dr. Heaney said, thereby bringing their levels down more gradually rather than taking them off a cliff, in a sense. Or, if more evidence bears out the authors’ hypothesis, another approach might be treating patients with medicine to bring down the cortisol before surgery, though there are challenges to that approach, Dr. Heaney said.
At the same time, those who developed new autoimmune disease remain a small subset of patients with Cushing disease, so such approaches may become only potentially appropriate to consider in patients with risk factors, such as a family history of autoimmune disease.
The researchers conducted a retrospective chart review of adult patients who underwent transsphenoidal surgery for either Cushing disease or NFPA at Massachusetts General Hospital between 2005 and 2019.
The study involved 194 patients with Cushing disease who had postsurgical remission and at least one follow-up visit with a pituitary expert and 92 patients with NFPA who were matched to patients with Cushing disease based on age and sex. The authors regarded autoimmune disease diagnosed within 36 months of the surgery to be temporally associated with Cushing disease remission. Among the autoimmune diseases considered were “rheumatoid arthritis, Sjögren syndrome, systemic lupus erythematosus, autoimmune thyroiditis, celiac disease, psoriasis, vitiligo, autoimmune neuropathy, multiple sclerosis, myasthenia gravis, and ulcerative colitis.”
Patients differed in average body mass index and tumor size, but family history of autoimmune disease was similar in both groups. Average BMI was 34.5 in the Cushing group and 29.5 in the NFPA group. Average tumor size was 5.7 mm in the Cushing group and 21.3 mm in the NFPA group.
Before surgery, 2.9% of patients with Cushing disease and 15.4% of patients with NFPA had central hypothyroidism, and 8% in the Cushing group and 56.8% in the NFPA group had hyperprolactinemia. Central adrenal insufficiency occurred in 11% with NFPA and in all with Cushing disease, by definition.
After surgery, 93.8% in the Cushing group and 16.5% in the NFPA group had adrenal insufficiency. In addition, patients with Cushing disease had lower postsurgical nadir serum cortisol levels (63.8 nmol/L) than those with NFPA (282.3 nmol/L).
Of the 17 patients with Cushing disease — all women — who developed autoimmune disease within 3 years, 6 had a personal history of autoimmune disease and 7 had a family history of it. In addition, 41.2% of them had adrenal insufficiency when they developed the new autoimmune disease. Among the diseases were six autoimmune thyroiditis cases, three Sjögren syndrome cases, and two autoimmune seronegative spondyloarthropathy.
Dr. Heaney said he found it interesting that more than half of the new autoimmune diseases in patients with Cushing disease were related to the thyroid. “In this kind of setting, where you have a patient who has been producing too much steroid over a period of time and then you take that away, it’s almost like you release a brake on the TSH [thyroid-stimulating hormone],” Dr. Heaney said. “So, there’s probably some rebound in TSH that occurs, and that could be driving the thyroiditis, to some extent, that we see in these patients.”
Only one patient with NFPA developed new-onset autoimmune disease, a woman who developed Graves disease 22 months after surgery. When the researchers excluded patients in both groups with central hypothyroidism, new-onset autoimmune disease was still significantly higher (11.4%) in the Cushing group than in the NFPA group (1.9%; HR, 7.02; 95% CI, 2.54-19.39).
Could Postoperative Adrenal Insufficiency Contribute to Risk?
Within the Cushing cohort, those who developed autoimmune disease had a lower BMI (31.8 vs 34.8) and larger tumor size (7.2 vs 5.6 mm) than those who didn’t develop new autoimmune disease. Patients who developed autoimmune disease also had a lower baseline urine free cortisol ratio (2.7 vs 6.3) before surgery and more family history of autoimmune disease (41.2% vs 20.9%) than those who didn’t develop one.
“The higher prevalence of adrenal insufficiency and the lower nadir serum cortisol levels in the Cushing disease group suggest that the postoperative adrenal insufficiency in the Cushing disease group might have contributed to autoimmune disease pathogenesis,” the authors wrote. “This finding is clinically significant because cortisol plays a pivotal role in modulating the immune system.”
Most postoperative management among patients with Cushing disease was similar, with all but one patient receiving 0.5 or 1 mg daily dexamethasone within the first week after surgery. (The one outlier received 5 mg daily prednisone.) However, fewer patients who developed autoimmune disease (17.6%) received supraphysiologic doses of glucocorticoid — equivalent to at least 25 mg hydrocortisone — compared with patients who didn’t develop autoimmune disease (41.8%).
“Although the daily average hydrocortisone equivalent replacement doses within the first month and during long-term follow-up were within the physiologic range in both subgroups, patients with Cushing disease who had autoimmune disease received slightly lower doses of glucocorticoid replacement within the first month after surgery,” the authors reported. “The immediate postoperative period might be a critical window where supraphysiologic glucocorticoids seem to be protective with regard to development of autoimmune disease,” they wrote, though they acknowledged the study’s retrospective design as a limitation in drawing that conclusion.
At the least, they suggested that new symptoms in patients with Cushing disease, particularly those with a family history of autoimmune disease, should prompt investigation of potential autoimmune disease.
Recordati Rare Diseases funded the study. The research was also conducted with support from Harvard Catalyst (the Harvard Clinical and Translational Science Center) as well as financial contributions from Harvard University and its affiliated academic healthcare centers. One author reported holding stocks in Pfizer and Amgen, and another reported receiving consulting fees from Corcept. Dr. Heaney reported receiving institutional grants for trials from Corcept, Ascendis, Crinetics, and Sparrow Pharm; serving on the advisory board for Xeris, Recordati, Corcept, Novo Nordisk, Lundbeck, and Crinetics; and serving as a speaker for Chiesi, Novo Nordisk, and Corcept.
A version of this article appeared on Medscape.com.
Patients with Cushing disease have an increased risk for new-onset autoimmune disease in the 3 years after surgical remission, according to a new retrospective study published on February 20 in Annals of Internal Medicine.
Outcomes for patients with Cushing disease were compared against those with nonfunctioning pituitary adenomas (NFPAs). New-onset autoimmune disease occurred in 10.4% with Cushing disease and 1.6% among patients with NFPA (hazard ratio, 7.80; 95% CI, 2.88-21.10).
“Understanding and recognizing new and recurrent autoimmune disease in this setting is important to avoid misclassifying such patients with glucocorticoid withdrawal syndrome, which could result in failure to treat underlying autoimmune disease, as well as erroneous diagnosis of steroid withdrawal cases,” wrote Dennis Delasi Nyanyo of Massachusetts General Hospital and Harvard Medical School, Boston, and colleagues.
Given the general population’s annual incidence of major autoimmune diseases, estimated at about 100 cases per 100,000 people, and the 3-year incidence of 10.4% found in this study’s cohort, “our findings suggest that Cushing disease remission may trigger development of autoimmune disease,” the authors wrote.
Monitor Patients With Family History of Autoimmune Disease?
The study results were not necessarily surprising to Anthony P. Heaney, MD, PhD, an endocrinologist and professor of medicine at the University of California, Los Angeles, because past research has raised similar questions. The authors’ suggestion that the rapid postsurgical drop in cortisol that occurs as a result of treating Cushing disease becomes some sort of autoimmune trigger is interesting but remains speculative, Dr. Heaney pointed out.
If future evidence supports that possibility, “it would suggest, in terms of managing those patients in the postoperative setting, that there may be some merit to giving them higher concentrations of glucocorticoids for a short period of time,” Dr. Heaney said, thereby bringing their levels down more gradually rather than taking them off a cliff, in a sense. Or, if more evidence bears out the authors’ hypothesis, another approach might be treating patients with medicine to bring down the cortisol before surgery, though there are challenges to that approach, Dr. Heaney said.
At the same time, those who developed new autoimmune disease remain a small subset of patients with Cushing disease, so such approaches may become only potentially appropriate to consider in patients with risk factors, such as a family history of autoimmune disease.
The researchers conducted a retrospective chart review of adult patients who underwent transsphenoidal surgery for either Cushing disease or NFPA at Massachusetts General Hospital between 2005 and 2019.
The study involved 194 patients with Cushing disease who had postsurgical remission and at least one follow-up visit with a pituitary expert and 92 patients with NFPA who were matched to patients with Cushing disease based on age and sex. The authors regarded autoimmune disease diagnosed within 36 months of the surgery to be temporally associated with Cushing disease remission. Among the autoimmune diseases considered were “rheumatoid arthritis, Sjögren syndrome, systemic lupus erythematosus, autoimmune thyroiditis, celiac disease, psoriasis, vitiligo, autoimmune neuropathy, multiple sclerosis, myasthenia gravis, and ulcerative colitis.”
Patients differed in average body mass index and tumor size, but family history of autoimmune disease was similar in both groups. Average BMI was 34.5 in the Cushing group and 29.5 in the NFPA group. Average tumor size was 5.7 mm in the Cushing group and 21.3 mm in the NFPA group.
Before surgery, 2.9% of patients with Cushing disease and 15.4% of patients with NFPA had central hypothyroidism, and 8% in the Cushing group and 56.8% in the NFPA group had hyperprolactinemia. Central adrenal insufficiency occurred in 11% with NFPA and in all with Cushing disease, by definition.
After surgery, 93.8% in the Cushing group and 16.5% in the NFPA group had adrenal insufficiency. In addition, patients with Cushing disease had lower postsurgical nadir serum cortisol levels (63.8 nmol/L) than those with NFPA (282.3 nmol/L).
Of the 17 patients with Cushing disease — all women — who developed autoimmune disease within 3 years, 6 had a personal history of autoimmune disease and 7 had a family history of it. In addition, 41.2% of them had adrenal insufficiency when they developed the new autoimmune disease. Among the diseases were six autoimmune thyroiditis cases, three Sjögren syndrome cases, and two autoimmune seronegative spondyloarthropathy.
Dr. Heaney said he found it interesting that more than half of the new autoimmune diseases in patients with Cushing disease were related to the thyroid. “In this kind of setting, where you have a patient who has been producing too much steroid over a period of time and then you take that away, it’s almost like you release a brake on the TSH [thyroid-stimulating hormone],” Dr. Heaney said. “So, there’s probably some rebound in TSH that occurs, and that could be driving the thyroiditis, to some extent, that we see in these patients.”
Only one patient with NFPA developed new-onset autoimmune disease, a woman who developed Graves disease 22 months after surgery. When the researchers excluded patients in both groups with central hypothyroidism, new-onset autoimmune disease was still significantly higher (11.4%) in the Cushing group than in the NFPA group (1.9%; HR, 7.02; 95% CI, 2.54-19.39).
Could Postoperative Adrenal Insufficiency Contribute to Risk?
Within the Cushing cohort, those who developed autoimmune disease had a lower BMI (31.8 vs 34.8) and larger tumor size (7.2 vs 5.6 mm) than those who didn’t develop new autoimmune disease. Patients who developed autoimmune disease also had a lower baseline urine free cortisol ratio (2.7 vs 6.3) before surgery and more family history of autoimmune disease (41.2% vs 20.9%) than those who didn’t develop one.
“The higher prevalence of adrenal insufficiency and the lower nadir serum cortisol levels in the Cushing disease group suggest that the postoperative adrenal insufficiency in the Cushing disease group might have contributed to autoimmune disease pathogenesis,” the authors wrote. “This finding is clinically significant because cortisol plays a pivotal role in modulating the immune system.”
Most postoperative management among patients with Cushing disease was similar, with all but one patient receiving 0.5 or 1 mg daily dexamethasone within the first week after surgery. (The one outlier received 5 mg daily prednisone.) However, fewer patients who developed autoimmune disease (17.6%) received supraphysiologic doses of glucocorticoid — equivalent to at least 25 mg hydrocortisone — compared with patients who didn’t develop autoimmune disease (41.8%).
“Although the daily average hydrocortisone equivalent replacement doses within the first month and during long-term follow-up were within the physiologic range in both subgroups, patients with Cushing disease who had autoimmune disease received slightly lower doses of glucocorticoid replacement within the first month after surgery,” the authors reported. “The immediate postoperative period might be a critical window where supraphysiologic glucocorticoids seem to be protective with regard to development of autoimmune disease,” they wrote, though they acknowledged the study’s retrospective design as a limitation in drawing that conclusion.
At the least, they suggested that new symptoms in patients with Cushing disease, particularly those with a family history of autoimmune disease, should prompt investigation of potential autoimmune disease.
Recordati Rare Diseases funded the study. The research was also conducted with support from Harvard Catalyst (the Harvard Clinical and Translational Science Center) as well as financial contributions from Harvard University and its affiliated academic healthcare centers. One author reported holding stocks in Pfizer and Amgen, and another reported receiving consulting fees from Corcept. Dr. Heaney reported receiving institutional grants for trials from Corcept, Ascendis, Crinetics, and Sparrow Pharm; serving on the advisory board for Xeris, Recordati, Corcept, Novo Nordisk, Lundbeck, and Crinetics; and serving as a speaker for Chiesi, Novo Nordisk, and Corcept.
A version of this article appeared on Medscape.com.
Patients with Cushing disease have an increased risk for new-onset autoimmune disease in the 3 years after surgical remission, according to a new retrospective study published on February 20 in Annals of Internal Medicine.
Outcomes for patients with Cushing disease were compared against those with nonfunctioning pituitary adenomas (NFPAs). New-onset autoimmune disease occurred in 10.4% with Cushing disease and 1.6% among patients with NFPA (hazard ratio, 7.80; 95% CI, 2.88-21.10).
“Understanding and recognizing new and recurrent autoimmune disease in this setting is important to avoid misclassifying such patients with glucocorticoid withdrawal syndrome, which could result in failure to treat underlying autoimmune disease, as well as erroneous diagnosis of steroid withdrawal cases,” wrote Dennis Delasi Nyanyo of Massachusetts General Hospital and Harvard Medical School, Boston, and colleagues.
Given the general population’s annual incidence of major autoimmune diseases, estimated at about 100 cases per 100,000 people, and the 3-year incidence of 10.4% found in this study’s cohort, “our findings suggest that Cushing disease remission may trigger development of autoimmune disease,” the authors wrote.
Monitor Patients With Family History of Autoimmune Disease?
The study results were not necessarily surprising to Anthony P. Heaney, MD, PhD, an endocrinologist and professor of medicine at the University of California, Los Angeles, because past research has raised similar questions. The authors’ suggestion that the rapid postsurgical drop in cortisol that occurs as a result of treating Cushing disease becomes some sort of autoimmune trigger is interesting but remains speculative, Dr. Heaney pointed out.
If future evidence supports that possibility, “it would suggest, in terms of managing those patients in the postoperative setting, that there may be some merit to giving them higher concentrations of glucocorticoids for a short period of time,” Dr. Heaney said, thereby bringing their levels down more gradually rather than taking them off a cliff, in a sense. Or, if more evidence bears out the authors’ hypothesis, another approach might be treating patients with medicine to bring down the cortisol before surgery, though there are challenges to that approach, Dr. Heaney said.
At the same time, those who developed new autoimmune disease remain a small subset of patients with Cushing disease, so such approaches may become only potentially appropriate to consider in patients with risk factors, such as a family history of autoimmune disease.
The researchers conducted a retrospective chart review of adult patients who underwent transsphenoidal surgery for either Cushing disease or NFPA at Massachusetts General Hospital between 2005 and 2019.
The study involved 194 patients with Cushing disease who had postsurgical remission and at least one follow-up visit with a pituitary expert and 92 patients with NFPA who were matched to patients with Cushing disease based on age and sex. The authors regarded autoimmune disease diagnosed within 36 months of the surgery to be temporally associated with Cushing disease remission. Among the autoimmune diseases considered were “rheumatoid arthritis, Sjögren syndrome, systemic lupus erythematosus, autoimmune thyroiditis, celiac disease, psoriasis, vitiligo, autoimmune neuropathy, multiple sclerosis, myasthenia gravis, and ulcerative colitis.”
Patients differed in average body mass index and tumor size, but family history of autoimmune disease was similar in both groups. Average BMI was 34.5 in the Cushing group and 29.5 in the NFPA group. Average tumor size was 5.7 mm in the Cushing group and 21.3 mm in the NFPA group.
Before surgery, 2.9% of patients with Cushing disease and 15.4% of patients with NFPA had central hypothyroidism, and 8% in the Cushing group and 56.8% in the NFPA group had hyperprolactinemia. Central adrenal insufficiency occurred in 11% with NFPA and in all with Cushing disease, by definition.
After surgery, 93.8% in the Cushing group and 16.5% in the NFPA group had adrenal insufficiency. In addition, patients with Cushing disease had lower postsurgical nadir serum cortisol levels (63.8 nmol/L) than those with NFPA (282.3 nmol/L).
Of the 17 patients with Cushing disease — all women — who developed autoimmune disease within 3 years, 6 had a personal history of autoimmune disease and 7 had a family history of it. In addition, 41.2% of them had adrenal insufficiency when they developed the new autoimmune disease. Among the diseases were six autoimmune thyroiditis cases, three Sjögren syndrome cases, and two autoimmune seronegative spondyloarthropathy.
Dr. Heaney said he found it interesting that more than half of the new autoimmune diseases in patients with Cushing disease were related to the thyroid. “In this kind of setting, where you have a patient who has been producing too much steroid over a period of time and then you take that away, it’s almost like you release a brake on the TSH [thyroid-stimulating hormone],” Dr. Heaney said. “So, there’s probably some rebound in TSH that occurs, and that could be driving the thyroiditis, to some extent, that we see in these patients.”
Only one patient with NFPA developed new-onset autoimmune disease, a woman who developed Graves disease 22 months after surgery. When the researchers excluded patients in both groups with central hypothyroidism, new-onset autoimmune disease was still significantly higher (11.4%) in the Cushing group than in the NFPA group (1.9%; HR, 7.02; 95% CI, 2.54-19.39).
Could Postoperative Adrenal Insufficiency Contribute to Risk?
Within the Cushing cohort, those who developed autoimmune disease had a lower BMI (31.8 vs 34.8) and larger tumor size (7.2 vs 5.6 mm) than those who didn’t develop new autoimmune disease. Patients who developed autoimmune disease also had a lower baseline urine free cortisol ratio (2.7 vs 6.3) before surgery and more family history of autoimmune disease (41.2% vs 20.9%) than those who didn’t develop one.
“The higher prevalence of adrenal insufficiency and the lower nadir serum cortisol levels in the Cushing disease group suggest that the postoperative adrenal insufficiency in the Cushing disease group might have contributed to autoimmune disease pathogenesis,” the authors wrote. “This finding is clinically significant because cortisol plays a pivotal role in modulating the immune system.”
Most postoperative management among patients with Cushing disease was similar, with all but one patient receiving 0.5 or 1 mg daily dexamethasone within the first week after surgery. (The one outlier received 5 mg daily prednisone.) However, fewer patients who developed autoimmune disease (17.6%) received supraphysiologic doses of glucocorticoid — equivalent to at least 25 mg hydrocortisone — compared with patients who didn’t develop autoimmune disease (41.8%).
“Although the daily average hydrocortisone equivalent replacement doses within the first month and during long-term follow-up were within the physiologic range in both subgroups, patients with Cushing disease who had autoimmune disease received slightly lower doses of glucocorticoid replacement within the first month after surgery,” the authors reported. “The immediate postoperative period might be a critical window where supraphysiologic glucocorticoids seem to be protective with regard to development of autoimmune disease,” they wrote, though they acknowledged the study’s retrospective design as a limitation in drawing that conclusion.
At the least, they suggested that new symptoms in patients with Cushing disease, particularly those with a family history of autoimmune disease, should prompt investigation of potential autoimmune disease.
Recordati Rare Diseases funded the study. The research was also conducted with support from Harvard Catalyst (the Harvard Clinical and Translational Science Center) as well as financial contributions from Harvard University and its affiliated academic healthcare centers. One author reported holding stocks in Pfizer and Amgen, and another reported receiving consulting fees from Corcept. Dr. Heaney reported receiving institutional grants for trials from Corcept, Ascendis, Crinetics, and Sparrow Pharm; serving on the advisory board for Xeris, Recordati, Corcept, Novo Nordisk, Lundbeck, and Crinetics; and serving as a speaker for Chiesi, Novo Nordisk, and Corcept.
A version of this article appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
Sepsis mortality greater in Black than White children despite similar interventions
WASHINGTON – , according to research presented at the annual meeting of the American Academy of Pediatrics.
The only other difference between Black and White pediatric patients was the length of hospital stay and the length of time in the ICU among those who died. In both cases, Black children who died spent more time in the hospital and in the ICU, reported Michael H. Stroud, MD, a pediatric critical care physician at the University of Arkansas for Medical Sciences in Little Rock, and his colleagues.
“Further investigations are needed to identify biases, conscious and unconscious, potential socioeconomic factors, and genetic predispositions leading to racial disparities in outcomes of children with pediatric sepsis, severe sepsis, and septic shock,” Dr Stroud and his colleagues said.
Nathan T. Chomilo, MD, adjunct assistant professor of pediatrics at the University of Minnesota, Minneapolis, who was not involved in the study but reviewed it, said the research “builds upon existing evidence that our health care system has work to do to meet its goal of treating patients equitably and provide everyone the opportunity for health.” He found the racial disparity in death particularly striking in 2023. “In the U.S., with all our wealth, knowledge, and resources, very few children should die from this, let alone there be such a stark gap,” Dr. Chomilo wrote.
Racial disparities persist
Dr. Stroud noted that many institutions currently use “automated, real-time, algorithm-based detection of sepsis, severe sepsis, and septic shock incorporated into the electronic medical record,” which leads to earlier recognition and resuscitation and overall better outcomes. Yet racial disparities in sepsis mortality rates persist, and he and his colleagues wanted to explore whether they remained even with these EMR-incorporated systems.
The researchers analyzed data from all patients at Arkansas Children’s Hospital who had sepsis, severe sepsis, or septic shock between January 2018 and April 2022. The hospital uses a best practice advisory (BPA) in the EMR whose activation leads to a bedside huddle and clinical interventions. For this study, the researchers defined a sepsis episode as either a BPA activation or an EMR diagnosis of sepsis, severe sepsis, or septic shock.
Among the 3,514 patients who had a sepsis episode during the study, 60.5% were White (n = 2,126) and 20.9% were Black (n = 736). Overall mortality was 1.65%, but that included 3.13% of Black children versus 1.27% of White children (odds ratio [OR] 2.51, P = .001). No significant differences in mortality were seen in gender or age.
Clinical interventions in the two groups were also similar: Total IV antibiotic days were 23.8 days for Black children and 21.6 days for White children (P = .38); total vasoactive infusion days were 2.2 for Black children and 2.6 for White (P = .18); and extracorporeal membrane oxygenation was necessary for 26.1% of Black children and 18.5% of White children (P = .52).
Length of hospitalization stay, however, was an average 4 days longer for Black children (16.7 days) versus White children (12.7 days) who died (P = .03). ICU stay for Black children who died was also an average 1.9 days longer (7.57 vs. 5.7 days; P = .01). There were no significant differences in the EMR between Black and White patients, however, in the percent who were over the threshold for antibiotic administration and the percent who received an IV fluid bolus.
Contributing factors
Dr. Chomilo said that most BPA systems require staff – including rooming and triage staff, nurses. and physicians – to enter vital signs, order labs, enter the results into the system, and enter other data used by the algorithm. “So even though the time from when those BPA warnings flagged to when clinical interventions were documented didn’t show a significant difference, there are numerous other points along a child’s illness that may be contributing to these numbers,” Dr. Chomilo said.
For example, he pointed out that differences in health insurance coverage could have influenced whether their parent or caregiver was able to bring them in early enough to be diagnosed since studies have revealed disparate access to regular care due to structural racism in the health care system. Studies have also shown disparate rates of patients being triaged or having to wait longer in emergency departments, he added.
“When the child was brought in, how were they triaged? How long did they wait before they had vitals taken? How long until they were seen by a clinician?” Dr. Chomilo said. “Was their care on the inpatient ward the same or different? What was the source of sepsis? Was it all infectious or other issues [since] cancer and autoimmune illnesses can also trigger a sepsis evaluation, for example? Overall, I suspect answers to several of these questions would reveal a disparity due to structural racism that contributed to the ultimate disparity in deaths.”
Other social determinants of health that could have played a role in the outcome disparities here might include the family’s access to transportation options, parental employment or child care options, and nutrition access since baseline nutritional status can be a factor in the outcomes of severe illnesses like sepsis.
”I don’t think this study provided enough information about the potential causative factors to come to any strong conclusions,” Dr. Chomilo said. But it’s important for clinicians to be aware of how biases in the health care system put Black, Indigenous and other communities at higher risk for worse clinical outcomes.
“I would reiterate that clinicians in the hospital can help improve outcomes by being aware of structural racism and structural inequity and how that may contribute to their patient’s risk of severe illness as the decide how to approach their treatment and engaging the patient’s family,” Dr. Chomilo said. “We cannot rely solely on universal tools that don’t take this into account when we are looking to improve clinical outcomes for everyone. Otherwise we will see these gaps persist.”
No external funding sources were noted. Dr. Stroud and Dr. Chomilo had no disclosures.
WASHINGTON – , according to research presented at the annual meeting of the American Academy of Pediatrics.
The only other difference between Black and White pediatric patients was the length of hospital stay and the length of time in the ICU among those who died. In both cases, Black children who died spent more time in the hospital and in the ICU, reported Michael H. Stroud, MD, a pediatric critical care physician at the University of Arkansas for Medical Sciences in Little Rock, and his colleagues.
“Further investigations are needed to identify biases, conscious and unconscious, potential socioeconomic factors, and genetic predispositions leading to racial disparities in outcomes of children with pediatric sepsis, severe sepsis, and septic shock,” Dr Stroud and his colleagues said.
Nathan T. Chomilo, MD, adjunct assistant professor of pediatrics at the University of Minnesota, Minneapolis, who was not involved in the study but reviewed it, said the research “builds upon existing evidence that our health care system has work to do to meet its goal of treating patients equitably and provide everyone the opportunity for health.” He found the racial disparity in death particularly striking in 2023. “In the U.S., with all our wealth, knowledge, and resources, very few children should die from this, let alone there be such a stark gap,” Dr. Chomilo wrote.
Racial disparities persist
Dr. Stroud noted that many institutions currently use “automated, real-time, algorithm-based detection of sepsis, severe sepsis, and septic shock incorporated into the electronic medical record,” which leads to earlier recognition and resuscitation and overall better outcomes. Yet racial disparities in sepsis mortality rates persist, and he and his colleagues wanted to explore whether they remained even with these EMR-incorporated systems.
The researchers analyzed data from all patients at Arkansas Children’s Hospital who had sepsis, severe sepsis, or septic shock between January 2018 and April 2022. The hospital uses a best practice advisory (BPA) in the EMR whose activation leads to a bedside huddle and clinical interventions. For this study, the researchers defined a sepsis episode as either a BPA activation or an EMR diagnosis of sepsis, severe sepsis, or septic shock.
Among the 3,514 patients who had a sepsis episode during the study, 60.5% were White (n = 2,126) and 20.9% were Black (n = 736). Overall mortality was 1.65%, but that included 3.13% of Black children versus 1.27% of White children (odds ratio [OR] 2.51, P = .001). No significant differences in mortality were seen in gender or age.
Clinical interventions in the two groups were also similar: Total IV antibiotic days were 23.8 days for Black children and 21.6 days for White children (P = .38); total vasoactive infusion days were 2.2 for Black children and 2.6 for White (P = .18); and extracorporeal membrane oxygenation was necessary for 26.1% of Black children and 18.5% of White children (P = .52).
Length of hospitalization stay, however, was an average 4 days longer for Black children (16.7 days) versus White children (12.7 days) who died (P = .03). ICU stay for Black children who died was also an average 1.9 days longer (7.57 vs. 5.7 days; P = .01). There were no significant differences in the EMR between Black and White patients, however, in the percent who were over the threshold for antibiotic administration and the percent who received an IV fluid bolus.
Contributing factors
Dr. Chomilo said that most BPA systems require staff – including rooming and triage staff, nurses. and physicians – to enter vital signs, order labs, enter the results into the system, and enter other data used by the algorithm. “So even though the time from when those BPA warnings flagged to when clinical interventions were documented didn’t show a significant difference, there are numerous other points along a child’s illness that may be contributing to these numbers,” Dr. Chomilo said.
For example, he pointed out that differences in health insurance coverage could have influenced whether their parent or caregiver was able to bring them in early enough to be diagnosed since studies have revealed disparate access to regular care due to structural racism in the health care system. Studies have also shown disparate rates of patients being triaged or having to wait longer in emergency departments, he added.
“When the child was brought in, how were they triaged? How long did they wait before they had vitals taken? How long until they were seen by a clinician?” Dr. Chomilo said. “Was their care on the inpatient ward the same or different? What was the source of sepsis? Was it all infectious or other issues [since] cancer and autoimmune illnesses can also trigger a sepsis evaluation, for example? Overall, I suspect answers to several of these questions would reveal a disparity due to structural racism that contributed to the ultimate disparity in deaths.”
Other social determinants of health that could have played a role in the outcome disparities here might include the family’s access to transportation options, parental employment or child care options, and nutrition access since baseline nutritional status can be a factor in the outcomes of severe illnesses like sepsis.
”I don’t think this study provided enough information about the potential causative factors to come to any strong conclusions,” Dr. Chomilo said. But it’s important for clinicians to be aware of how biases in the health care system put Black, Indigenous and other communities at higher risk for worse clinical outcomes.
“I would reiterate that clinicians in the hospital can help improve outcomes by being aware of structural racism and structural inequity and how that may contribute to their patient’s risk of severe illness as the decide how to approach their treatment and engaging the patient’s family,” Dr. Chomilo said. “We cannot rely solely on universal tools that don’t take this into account when we are looking to improve clinical outcomes for everyone. Otherwise we will see these gaps persist.”
No external funding sources were noted. Dr. Stroud and Dr. Chomilo had no disclosures.
WASHINGTON – , according to research presented at the annual meeting of the American Academy of Pediatrics.
The only other difference between Black and White pediatric patients was the length of hospital stay and the length of time in the ICU among those who died. In both cases, Black children who died spent more time in the hospital and in the ICU, reported Michael H. Stroud, MD, a pediatric critical care physician at the University of Arkansas for Medical Sciences in Little Rock, and his colleagues.
“Further investigations are needed to identify biases, conscious and unconscious, potential socioeconomic factors, and genetic predispositions leading to racial disparities in outcomes of children with pediatric sepsis, severe sepsis, and septic shock,” Dr Stroud and his colleagues said.
Nathan T. Chomilo, MD, adjunct assistant professor of pediatrics at the University of Minnesota, Minneapolis, who was not involved in the study but reviewed it, said the research “builds upon existing evidence that our health care system has work to do to meet its goal of treating patients equitably and provide everyone the opportunity for health.” He found the racial disparity in death particularly striking in 2023. “In the U.S., with all our wealth, knowledge, and resources, very few children should die from this, let alone there be such a stark gap,” Dr. Chomilo wrote.
Racial disparities persist
Dr. Stroud noted that many institutions currently use “automated, real-time, algorithm-based detection of sepsis, severe sepsis, and septic shock incorporated into the electronic medical record,” which leads to earlier recognition and resuscitation and overall better outcomes. Yet racial disparities in sepsis mortality rates persist, and he and his colleagues wanted to explore whether they remained even with these EMR-incorporated systems.
The researchers analyzed data from all patients at Arkansas Children’s Hospital who had sepsis, severe sepsis, or septic shock between January 2018 and April 2022. The hospital uses a best practice advisory (BPA) in the EMR whose activation leads to a bedside huddle and clinical interventions. For this study, the researchers defined a sepsis episode as either a BPA activation or an EMR diagnosis of sepsis, severe sepsis, or septic shock.
Among the 3,514 patients who had a sepsis episode during the study, 60.5% were White (n = 2,126) and 20.9% were Black (n = 736). Overall mortality was 1.65%, but that included 3.13% of Black children versus 1.27% of White children (odds ratio [OR] 2.51, P = .001). No significant differences in mortality were seen in gender or age.
Clinical interventions in the two groups were also similar: Total IV antibiotic days were 23.8 days for Black children and 21.6 days for White children (P = .38); total vasoactive infusion days were 2.2 for Black children and 2.6 for White (P = .18); and extracorporeal membrane oxygenation was necessary for 26.1% of Black children and 18.5% of White children (P = .52).
Length of hospitalization stay, however, was an average 4 days longer for Black children (16.7 days) versus White children (12.7 days) who died (P = .03). ICU stay for Black children who died was also an average 1.9 days longer (7.57 vs. 5.7 days; P = .01). There were no significant differences in the EMR between Black and White patients, however, in the percent who were over the threshold for antibiotic administration and the percent who received an IV fluid bolus.
Contributing factors
Dr. Chomilo said that most BPA systems require staff – including rooming and triage staff, nurses. and physicians – to enter vital signs, order labs, enter the results into the system, and enter other data used by the algorithm. “So even though the time from when those BPA warnings flagged to when clinical interventions were documented didn’t show a significant difference, there are numerous other points along a child’s illness that may be contributing to these numbers,” Dr. Chomilo said.
For example, he pointed out that differences in health insurance coverage could have influenced whether their parent or caregiver was able to bring them in early enough to be diagnosed since studies have revealed disparate access to regular care due to structural racism in the health care system. Studies have also shown disparate rates of patients being triaged or having to wait longer in emergency departments, he added.
“When the child was brought in, how were they triaged? How long did they wait before they had vitals taken? How long until they were seen by a clinician?” Dr. Chomilo said. “Was their care on the inpatient ward the same or different? What was the source of sepsis? Was it all infectious or other issues [since] cancer and autoimmune illnesses can also trigger a sepsis evaluation, for example? Overall, I suspect answers to several of these questions would reveal a disparity due to structural racism that contributed to the ultimate disparity in deaths.”
Other social determinants of health that could have played a role in the outcome disparities here might include the family’s access to transportation options, parental employment or child care options, and nutrition access since baseline nutritional status can be a factor in the outcomes of severe illnesses like sepsis.
”I don’t think this study provided enough information about the potential causative factors to come to any strong conclusions,” Dr. Chomilo said. But it’s important for clinicians to be aware of how biases in the health care system put Black, Indigenous and other communities at higher risk for worse clinical outcomes.
“I would reiterate that clinicians in the hospital can help improve outcomes by being aware of structural racism and structural inequity and how that may contribute to their patient’s risk of severe illness as the decide how to approach their treatment and engaging the patient’s family,” Dr. Chomilo said. “We cannot rely solely on universal tools that don’t take this into account when we are looking to improve clinical outcomes for everyone. Otherwise we will see these gaps persist.”
No external funding sources were noted. Dr. Stroud and Dr. Chomilo had no disclosures.
AT AAP 2023
Five times greater suicide risk for trans, gender-diverse teens in ED
WASHINGTON – , according to a study presented at the annual meeting of the American Academy of Pediatrics.
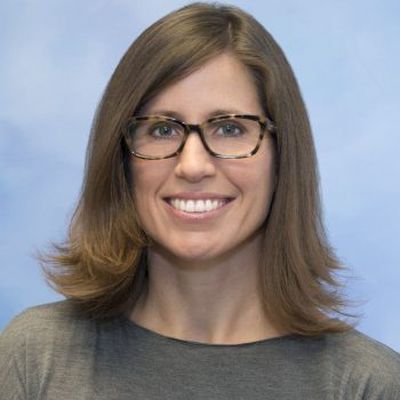
“The take-home message here is this study emphasizes the importance of universal screening to identify gender-diverse youth at risk,” Amanda Burnside, PhD, assistant professor of psychiatry and behavioral sciences at Ann and Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, told attendees. “We really need to develop robust strategies and systems to link better mental health services.”
Suicide rates in transgender and gender-diverse youth are exceptionally high among youth in the U.S., Dr. Burnside said during her presentation. For example, the 2022 LGBTQ health survey from the Trevor Project found that much higher percentages of transgender and gender nonconforming youth had considered suicide in the past year compared with cisgender youth, even within the LGBTQ umbrella. Among nearly 34,000 LGBTQ youth aged 13-24, nearly half of trans females (48%) and more than half of trans males (59%) had considered suicide, compared with 28% of cisgender males and 37% of cisgender females. The rate among nonbinary/genderqueer individuals was 53%, and it was 48% for those questioning their gender.
Current methods of identifying trans and gender-diverse (TGD) youth in the hospital, however, may not actually be capturing the entire population.
“In health care settings, research involving TGD individuals has historically been limited to specialized clinic populations or youth with gender-specific diagnostic codes documented in the electronic medical record,” an approach that “likely significantly underestimates the prevalence of TGD youth in health care settings.” While at least one study has attempted to bridge this gap by searching the EMR for keywords, that study only tried to identify trans youth and not other youth on the gender diversity spectrum, such as nonbinary youth or those questioning their gender identity. Dr. Burnside and her colleagues therefore designed a study that used keywords to identify both trans youth and other gender-diverse youth who visited the ED so they could assess the rate of positive suicide screens in this population.
Underestimating the population at risk?
The researchers conducted a retrospective cross-sectional study of EMR data for all ED visits during which the patient underwent suicide screening. For the period of November 2019 to August 2022, they collected data on the screening results and the patient’s gender identity, age, race/ethnicity, insurance status, chief complaint in the ED and child opportunity index, which assess a youth’s access to resources based on geography. The suicide screener used was the Ask Suicide–Screening Questions (ASQ) tool.
The keywords they looked for in the EMR to identify trans and gender-diverse youth included transgender, pronouns, agender, gender dysphoria, male-to-female, female-to-male, nonbinary, preferred name, and they/them (captured as a complete term, not as “they” and “them” separately).
“If a keyword was present, the surrounding text was extracted and reviewed by two members of our team,” Dr. Burnside explained in her presentation. “We categorized keywords into either indicative of gender-diverse identity or not, and if it wasn’t clear based on the text extracted, we would conduct a manual chart review,” though that only occurred in about 3% of cases, she added.
Among 15,413 ED encounters with a suicide screen, the researchers identified 1,126 of these keywords in the EMR, among which 91.2% were classified as referring to a gender-diverse patient. Nearly all of the words were at least 90% effective in identify a gender-diverse youth, Dr. Burnside said, and all of the 197 instances of “they/them” were classified as gender diverse.
The accuracy was a little lower for the two keywords that appeared most frequently: For “pronouns,” 86.3% of 306 instances were classified as gender diverse, and for “transgender,” 83.1% of 207 instances were classified as gender diverse. Since some providers ask all patients their pronouns, the presence of “pronouns” in the EMR alone did not necessarily indicate the patient was gender diverse, Dr. Burnside said. A common reason the term “transgender” occurred in the EMR of non–gender diverse patients is that the department’s list of crisis resources includes transgender hotlines.
After identifying all the keywords, the researchers determined how many of these occurred in unique ED encounters and removed those with incomplete screening. Overall, they found 565 encounters by 399 gender-diverse individuals who had a suicide screening, representing 4.6% of total visits. This percentage is slightly lower than recent population-based estimates of gender-diverse youth, the researchers noted.
This population ranged from 8 to 23 years old, and 43% were publicly insured. The chief complaint for most of the patients (77.5%) was a mental health one. They were predominantly White (43%) or Hispanic (35%), with 10% Black youth, 4% Asian youth, and 8% youth who were “other” or two or more races. About half (52%) lived in a neighborhood with a “low” or “very low” child opportunity index.
Within this population, 81% of the patients screened positive on the suicide screening, compared with 23% positive screens across all ED visits. One in ten (10%) gender-diverse youth had active suicidal ideation, compared with 3.4% of the rest of the ED patient population. The researchers calculated that gender-diverse youth had 5.35 times greater odds of screening positive than cisgender youth in the ED (95% confidence interval [CI] 8.7-15.92). Further, a quarter (25%) of the trans and gender-diverse youth who screened positive for suicide risk had come to the ED for a primary complaint unrelated to mental health.
“We had a kid who came in because he broke his arm who had active suicidal ideation,” study coauthor Jennifer A. Hoffmann, MD, assistant professor of pediatrics at the Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, mentioned after the presentation. That particular patient even had a suicide plan, but was identified as actively suicidal only because of the screening. In other cases, she said, a youth may come in with self-inflicted injuries, and while those are the primary complaint, they are linked with suicidal ideation.
Among the study’s limitations are that gender identity is not necessarily being systematically assessed during visits, misspellings might have missed some youth, and their search strategy has not yet been externally validated, though they plan to seek that.
“Overall, however, this study did demonstrate that keyword searching is a promising technique to identify and prioritize gender-diverse youth in health services research,” Dr. Burnside said. In addition to showing the feasibility of using a keyword search strategy for identifying gender-diverse youth, Dr. Burnside noted that 31% of the encounters were identified by just one of the keywords they used, “highlighting the importance of using a comprehensive list of keywords to identify gender-diverse youth.”
Uncovering valuable information
Jason Rafferty, MD, MPH, EdM, clinical assistant professor of pediatrics and of psychiatry and human behavior at Brown University, Providence, R.I., who attended the presentation, noted that the study provides information on a population that’s often difficult to get through traditional EMR research methods.
“A lot of medical record systems don’t have uniform ways of capturing [gender diversity], but what we know as providers is that kids are really struggling and that it’s not a surprise that we’re seeing these disparities with suicidality,” Dr. Rafferty said.
The study also provides more discrete estimates by age than what most other current research measures, which tends to be lifetime suicidality as opposed to suicidal thoughts or attempts within the past year, Dr. Rafferty added.
”What this shows is, for adolescents, the risk of suicide is something we need to be paying attention to. Because it’s not that it’s something that only happens in adults, this really dispels a lot of the misquoting of the data that’s out there.” That kind of information is valuable for determining resource allocation, he said. “A disparity like this really underlies the importance of mental health resources in this field,” he said.
Dr. Burnside, Dr. Hoffmann, and Dr. Rafferty had no disclosures, and no external funding sources were noted.
WASHINGTON – , according to a study presented at the annual meeting of the American Academy of Pediatrics.
“The take-home message here is this study emphasizes the importance of universal screening to identify gender-diverse youth at risk,” Amanda Burnside, PhD, assistant professor of psychiatry and behavioral sciences at Ann and Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, told attendees. “We really need to develop robust strategies and systems to link better mental health services.”
Suicide rates in transgender and gender-diverse youth are exceptionally high among youth in the U.S., Dr. Burnside said during her presentation. For example, the 2022 LGBTQ health survey from the Trevor Project found that much higher percentages of transgender and gender nonconforming youth had considered suicide in the past year compared with cisgender youth, even within the LGBTQ umbrella. Among nearly 34,000 LGBTQ youth aged 13-24, nearly half of trans females (48%) and more than half of trans males (59%) had considered suicide, compared with 28% of cisgender males and 37% of cisgender females. The rate among nonbinary/genderqueer individuals was 53%, and it was 48% for those questioning their gender.
Current methods of identifying trans and gender-diverse (TGD) youth in the hospital, however, may not actually be capturing the entire population.
“In health care settings, research involving TGD individuals has historically been limited to specialized clinic populations or youth with gender-specific diagnostic codes documented in the electronic medical record,” an approach that “likely significantly underestimates the prevalence of TGD youth in health care settings.” While at least one study has attempted to bridge this gap by searching the EMR for keywords, that study only tried to identify trans youth and not other youth on the gender diversity spectrum, such as nonbinary youth or those questioning their gender identity. Dr. Burnside and her colleagues therefore designed a study that used keywords to identify both trans youth and other gender-diverse youth who visited the ED so they could assess the rate of positive suicide screens in this population.
Underestimating the population at risk?
The researchers conducted a retrospective cross-sectional study of EMR data for all ED visits during which the patient underwent suicide screening. For the period of November 2019 to August 2022, they collected data on the screening results and the patient’s gender identity, age, race/ethnicity, insurance status, chief complaint in the ED and child opportunity index, which assess a youth’s access to resources based on geography. The suicide screener used was the Ask Suicide–Screening Questions (ASQ) tool.
The keywords they looked for in the EMR to identify trans and gender-diverse youth included transgender, pronouns, agender, gender dysphoria, male-to-female, female-to-male, nonbinary, preferred name, and they/them (captured as a complete term, not as “they” and “them” separately).
“If a keyword was present, the surrounding text was extracted and reviewed by two members of our team,” Dr. Burnside explained in her presentation. “We categorized keywords into either indicative of gender-diverse identity or not, and if it wasn’t clear based on the text extracted, we would conduct a manual chart review,” though that only occurred in about 3% of cases, she added.
Among 15,413 ED encounters with a suicide screen, the researchers identified 1,126 of these keywords in the EMR, among which 91.2% were classified as referring to a gender-diverse patient. Nearly all of the words were at least 90% effective in identify a gender-diverse youth, Dr. Burnside said, and all of the 197 instances of “they/them” were classified as gender diverse.
The accuracy was a little lower for the two keywords that appeared most frequently: For “pronouns,” 86.3% of 306 instances were classified as gender diverse, and for “transgender,” 83.1% of 207 instances were classified as gender diverse. Since some providers ask all patients their pronouns, the presence of “pronouns” in the EMR alone did not necessarily indicate the patient was gender diverse, Dr. Burnside said. A common reason the term “transgender” occurred in the EMR of non–gender diverse patients is that the department’s list of crisis resources includes transgender hotlines.
After identifying all the keywords, the researchers determined how many of these occurred in unique ED encounters and removed those with incomplete screening. Overall, they found 565 encounters by 399 gender-diverse individuals who had a suicide screening, representing 4.6% of total visits. This percentage is slightly lower than recent population-based estimates of gender-diverse youth, the researchers noted.
This population ranged from 8 to 23 years old, and 43% were publicly insured. The chief complaint for most of the patients (77.5%) was a mental health one. They were predominantly White (43%) or Hispanic (35%), with 10% Black youth, 4% Asian youth, and 8% youth who were “other” or two or more races. About half (52%) lived in a neighborhood with a “low” or “very low” child opportunity index.
Within this population, 81% of the patients screened positive on the suicide screening, compared with 23% positive screens across all ED visits. One in ten (10%) gender-diverse youth had active suicidal ideation, compared with 3.4% of the rest of the ED patient population. The researchers calculated that gender-diverse youth had 5.35 times greater odds of screening positive than cisgender youth in the ED (95% confidence interval [CI] 8.7-15.92). Further, a quarter (25%) of the trans and gender-diverse youth who screened positive for suicide risk had come to the ED for a primary complaint unrelated to mental health.
“We had a kid who came in because he broke his arm who had active suicidal ideation,” study coauthor Jennifer A. Hoffmann, MD, assistant professor of pediatrics at the Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, mentioned after the presentation. That particular patient even had a suicide plan, but was identified as actively suicidal only because of the screening. In other cases, she said, a youth may come in with self-inflicted injuries, and while those are the primary complaint, they are linked with suicidal ideation.
Among the study’s limitations are that gender identity is not necessarily being systematically assessed during visits, misspellings might have missed some youth, and their search strategy has not yet been externally validated, though they plan to seek that.
“Overall, however, this study did demonstrate that keyword searching is a promising technique to identify and prioritize gender-diverse youth in health services research,” Dr. Burnside said. In addition to showing the feasibility of using a keyword search strategy for identifying gender-diverse youth, Dr. Burnside noted that 31% of the encounters were identified by just one of the keywords they used, “highlighting the importance of using a comprehensive list of keywords to identify gender-diverse youth.”
Uncovering valuable information
Jason Rafferty, MD, MPH, EdM, clinical assistant professor of pediatrics and of psychiatry and human behavior at Brown University, Providence, R.I., who attended the presentation, noted that the study provides information on a population that’s often difficult to get through traditional EMR research methods.
“A lot of medical record systems don’t have uniform ways of capturing [gender diversity], but what we know as providers is that kids are really struggling and that it’s not a surprise that we’re seeing these disparities with suicidality,” Dr. Rafferty said.
The study also provides more discrete estimates by age than what most other current research measures, which tends to be lifetime suicidality as opposed to suicidal thoughts or attempts within the past year, Dr. Rafferty added.
”What this shows is, for adolescents, the risk of suicide is something we need to be paying attention to. Because it’s not that it’s something that only happens in adults, this really dispels a lot of the misquoting of the data that’s out there.” That kind of information is valuable for determining resource allocation, he said. “A disparity like this really underlies the importance of mental health resources in this field,” he said.
Dr. Burnside, Dr. Hoffmann, and Dr. Rafferty had no disclosures, and no external funding sources were noted.
WASHINGTON – , according to a study presented at the annual meeting of the American Academy of Pediatrics.
“The take-home message here is this study emphasizes the importance of universal screening to identify gender-diverse youth at risk,” Amanda Burnside, PhD, assistant professor of psychiatry and behavioral sciences at Ann and Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, told attendees. “We really need to develop robust strategies and systems to link better mental health services.”
Suicide rates in transgender and gender-diverse youth are exceptionally high among youth in the U.S., Dr. Burnside said during her presentation. For example, the 2022 LGBTQ health survey from the Trevor Project found that much higher percentages of transgender and gender nonconforming youth had considered suicide in the past year compared with cisgender youth, even within the LGBTQ umbrella. Among nearly 34,000 LGBTQ youth aged 13-24, nearly half of trans females (48%) and more than half of trans males (59%) had considered suicide, compared with 28% of cisgender males and 37% of cisgender females. The rate among nonbinary/genderqueer individuals was 53%, and it was 48% for those questioning their gender.
Current methods of identifying trans and gender-diverse (TGD) youth in the hospital, however, may not actually be capturing the entire population.
“In health care settings, research involving TGD individuals has historically been limited to specialized clinic populations or youth with gender-specific diagnostic codes documented in the electronic medical record,” an approach that “likely significantly underestimates the prevalence of TGD youth in health care settings.” While at least one study has attempted to bridge this gap by searching the EMR for keywords, that study only tried to identify trans youth and not other youth on the gender diversity spectrum, such as nonbinary youth or those questioning their gender identity. Dr. Burnside and her colleagues therefore designed a study that used keywords to identify both trans youth and other gender-diverse youth who visited the ED so they could assess the rate of positive suicide screens in this population.
Underestimating the population at risk?
The researchers conducted a retrospective cross-sectional study of EMR data for all ED visits during which the patient underwent suicide screening. For the period of November 2019 to August 2022, they collected data on the screening results and the patient’s gender identity, age, race/ethnicity, insurance status, chief complaint in the ED and child opportunity index, which assess a youth’s access to resources based on geography. The suicide screener used was the Ask Suicide–Screening Questions (ASQ) tool.
The keywords they looked for in the EMR to identify trans and gender-diverse youth included transgender, pronouns, agender, gender dysphoria, male-to-female, female-to-male, nonbinary, preferred name, and they/them (captured as a complete term, not as “they” and “them” separately).
“If a keyword was present, the surrounding text was extracted and reviewed by two members of our team,” Dr. Burnside explained in her presentation. “We categorized keywords into either indicative of gender-diverse identity or not, and if it wasn’t clear based on the text extracted, we would conduct a manual chart review,” though that only occurred in about 3% of cases, she added.
Among 15,413 ED encounters with a suicide screen, the researchers identified 1,126 of these keywords in the EMR, among which 91.2% were classified as referring to a gender-diverse patient. Nearly all of the words were at least 90% effective in identify a gender-diverse youth, Dr. Burnside said, and all of the 197 instances of “they/them” were classified as gender diverse.
The accuracy was a little lower for the two keywords that appeared most frequently: For “pronouns,” 86.3% of 306 instances were classified as gender diverse, and for “transgender,” 83.1% of 207 instances were classified as gender diverse. Since some providers ask all patients their pronouns, the presence of “pronouns” in the EMR alone did not necessarily indicate the patient was gender diverse, Dr. Burnside said. A common reason the term “transgender” occurred in the EMR of non–gender diverse patients is that the department’s list of crisis resources includes transgender hotlines.
After identifying all the keywords, the researchers determined how many of these occurred in unique ED encounters and removed those with incomplete screening. Overall, they found 565 encounters by 399 gender-diverse individuals who had a suicide screening, representing 4.6% of total visits. This percentage is slightly lower than recent population-based estimates of gender-diverse youth, the researchers noted.
This population ranged from 8 to 23 years old, and 43% were publicly insured. The chief complaint for most of the patients (77.5%) was a mental health one. They were predominantly White (43%) or Hispanic (35%), with 10% Black youth, 4% Asian youth, and 8% youth who were “other” or two or more races. About half (52%) lived in a neighborhood with a “low” or “very low” child opportunity index.
Within this population, 81% of the patients screened positive on the suicide screening, compared with 23% positive screens across all ED visits. One in ten (10%) gender-diverse youth had active suicidal ideation, compared with 3.4% of the rest of the ED patient population. The researchers calculated that gender-diverse youth had 5.35 times greater odds of screening positive than cisgender youth in the ED (95% confidence interval [CI] 8.7-15.92). Further, a quarter (25%) of the trans and gender-diverse youth who screened positive for suicide risk had come to the ED for a primary complaint unrelated to mental health.
“We had a kid who came in because he broke his arm who had active suicidal ideation,” study coauthor Jennifer A. Hoffmann, MD, assistant professor of pediatrics at the Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern University, mentioned after the presentation. That particular patient even had a suicide plan, but was identified as actively suicidal only because of the screening. In other cases, she said, a youth may come in with self-inflicted injuries, and while those are the primary complaint, they are linked with suicidal ideation.
Among the study’s limitations are that gender identity is not necessarily being systematically assessed during visits, misspellings might have missed some youth, and their search strategy has not yet been externally validated, though they plan to seek that.
“Overall, however, this study did demonstrate that keyword searching is a promising technique to identify and prioritize gender-diverse youth in health services research,” Dr. Burnside said. In addition to showing the feasibility of using a keyword search strategy for identifying gender-diverse youth, Dr. Burnside noted that 31% of the encounters were identified by just one of the keywords they used, “highlighting the importance of using a comprehensive list of keywords to identify gender-diverse youth.”
Uncovering valuable information
Jason Rafferty, MD, MPH, EdM, clinical assistant professor of pediatrics and of psychiatry and human behavior at Brown University, Providence, R.I., who attended the presentation, noted that the study provides information on a population that’s often difficult to get through traditional EMR research methods.
“A lot of medical record systems don’t have uniform ways of capturing [gender diversity], but what we know as providers is that kids are really struggling and that it’s not a surprise that we’re seeing these disparities with suicidality,” Dr. Rafferty said.
The study also provides more discrete estimates by age than what most other current research measures, which tends to be lifetime suicidality as opposed to suicidal thoughts or attempts within the past year, Dr. Rafferty added.
”What this shows is, for adolescents, the risk of suicide is something we need to be paying attention to. Because it’s not that it’s something that only happens in adults, this really dispels a lot of the misquoting of the data that’s out there.” That kind of information is valuable for determining resource allocation, he said. “A disparity like this really underlies the importance of mental health resources in this field,” he said.
Dr. Burnside, Dr. Hoffmann, and Dr. Rafferty had no disclosures, and no external funding sources were noted.
AT AAP 2023
Teens streaming on Twitch vulnerable to predators
WASHINGTON – Half of youth broadcasting live streams on the online platform Twitch revealed their real-world location, and nearly half provided their name to viewers, according to research presented at the annual meeting of the American Academy of Pediatrics. It took researchers less than 5 minutes – and sometimes as little as 12 seconds – to find minors in different video game categories, suggesting the environment offers opportunities to predators to gain sensitive information about minors, reported Fiona Dubrosa, BS, BA, a visiting scholar at Cohen Children’s Medical Center, New York, and colleagues.
A ‘clandestine, threatening digital environment’
the authors concluded. “The nature of live streaming makes it particularly dangerous, as there is no way to take back information that has been revealed or regulate content or viewers. Parents and pediatricians should be aware of the dangers presented by Twitch and other live-streaming platforms and counsel children on best practices for Internet safety.”
Twitch is an online streaming platform where people can watch creator’s live content, such as music performances or narrating real-time video game playing. The platform requires live streamers to be 13 years old with a valid email address or phone number to create an account, but no age restrictions or identification requirements exist for viewers, “potentially putting minors in danger of being watched, followed, and groomed by predators,” the researchers noted. They added that people following different streamers receive notifications when those streamers are live. Further, “viewers can donate money to streamers, which can make it easier for predators to manipulate, track, and encourage risky behaviors from minors.”
To better understand the risks the platform might pose to minors, the researchers searched for and analyzed popular video game live streams that appeared to be streamed by minors who had their cameras on and their faces visible. Then the researchers noted the name of the video game, the topics discussed by the streamers, the time it took to find minors under each game, and each streamer’s age, name, follower count, location, streaming schedule, and social media links for money donations.
The researchers analyzed 100 Twitch streamers who were minors, who had a combined 1,755,452 million followers. Nearly half the streamers (47%) provided their presumably real names, and half (50%) gave out their location. Nearly two-thirds (64%) linked other social media accounts they had and encouraged viewers to follow them. Detailed schedules of when they would be live were available for 38% of the streamers, and 37% of the minor streamers were accepting money donations.
Only 11% of the discussion on the streams revealed personal details, most often related to trying on different outfits for viewers and talking about real-world locations they liked to visit. The researchers needed anywhere from 12 seconds to 5 minutes to find a minor in each game category.
”Young users clearly feel a false sense of safety on the platform; a significant proportion were willing to reveal personal information despite having no knowledge of who might be listening,” the researchers said. “The donation system provides a menacing avenue for manipulation and continued exploitation of minors. Our findings reveal the need for stricter age limitations for streamers and more stringent identity verification of audience members on Twitch.”
Open-minded parental guidance is warranted
Jenny Radesky, MD, a developmental behavioral pediatrician and media researcher at University of Michigan Medicine, Ann Arbor, was not surprised that many teens live stream on Twitch since it’s a popular platform for video gaming, but she was surprised at how many revealed their locations and other personal details.
“I suspect that they do this to build closeness with their viewers, by seeming more authentic,” said Dr. Radesky, who was not involved in the study. “It is this type of parasocial relationship with influencers and gamers that keeps an audience engaged, and encourages future viewing and purchases.”
Their willingness to share personal details suggests it’s important to conduct qualitative research to find out how teen live streamers think about privacy risks, what privacy settings they can use and choose to use, and how they handle inappropriate contact from adults, Dr. Radesky said.
Meanwhile, parents should talk with their kids in an open-minded way about what platforms they use and what they like and dislike about them. She recommended parents read the Common Sense Media guide about different social platforms ”to understand what attracts kids to content on specific sites, what their pitfalls are, and what types of privacy and safety settings are available.”
“A child or teen is much more likely to be honest about negative experiences online if they think their parent will hear them out – not judge them or take away their tech. No teen wants to talk with a panicky parent,” Dr. Radesky said.
David Hill, MD, a hospitalist pediatrician for Goldsboro Pediatrics in Wayne County, North Carolina, who also specializes in media communication, said that Twitch is just one example of a social media platform where children can encounter a variety of dangers, including sometimes adult predators.
“This just highlights the importance of parents having an ongoing conversation with their children about how they use their social media platforms and ensuring, just as we do with learning to ride a bicycle or learning to drive a car, that they apply some basic rules of safety,” Dr. Hill said. Then it’s important to keep coming back to that conversation “again and again as they grow and change and as those platforms change to ensure that those kids are continuing to apply those rules consistently.
“The best way for parents to keep up is ask your kids,” he said. “They love to share. They love to teach. They love to be in a position to show you something, especially if it’s something that interests them.”
An example of a rule would be setting personal accounts to private, not public, by default, Dr. Radesky said. “When interviewed, teens often say that they feel intruded upon by older people ‘stalking’ them or trying to connect with them on social platforms,” so making an account private can reduce those opportunities.
For teens who specifically want to create content on social platforms, parent oversight is needed, she said, but she acknowledged it can be a lot of work. “This might take the form of talking about what a teen plans to post before they do, expectations for positive behaviors or language, plans for privacy settings (such as public vs. private accounts), and what to do with trolls or hateful comment,” she said. “Parents may want to follow their child’s account to check in on it.”
Useful advice
Dr. Radesky also provided a handful of talking points that pediatricians can use in talking with patients who use these platforms:
- Keep your account private to just your friends and people you want to interact with. There are a lot of people on the Internet that you don’t want intruding upon your social life.
- Maintain your feed and the accounts you follow to keep it positive, entertaining, and not a source of stress or self-doubt. Content creators are always trying to grab your attention in new ways, some of which are rude or dehumanizing, so don’t waste your time on things that bring you down.
- Talk about why you want to post or live stream. Is it to get reactions or feel validated? If so, can you find other ways to feel validated that don’t require performing for other people? Is it to share a special skill? If so, how do you keep your posts creative and community building rather than attention grabbing? And how can you keep your parents involved so that they can help you navigate challenges?”
Ms. Dubrosa and Dr. Hill had no disclosures. Dr. Radesky is a consultant for Melissa & Doug. No information on external funding was provided.
WASHINGTON – Half of youth broadcasting live streams on the online platform Twitch revealed their real-world location, and nearly half provided their name to viewers, according to research presented at the annual meeting of the American Academy of Pediatrics. It took researchers less than 5 minutes – and sometimes as little as 12 seconds – to find minors in different video game categories, suggesting the environment offers opportunities to predators to gain sensitive information about minors, reported Fiona Dubrosa, BS, BA, a visiting scholar at Cohen Children’s Medical Center, New York, and colleagues.
A ‘clandestine, threatening digital environment’
the authors concluded. “The nature of live streaming makes it particularly dangerous, as there is no way to take back information that has been revealed or regulate content or viewers. Parents and pediatricians should be aware of the dangers presented by Twitch and other live-streaming platforms and counsel children on best practices for Internet safety.”
Twitch is an online streaming platform where people can watch creator’s live content, such as music performances or narrating real-time video game playing. The platform requires live streamers to be 13 years old with a valid email address or phone number to create an account, but no age restrictions or identification requirements exist for viewers, “potentially putting minors in danger of being watched, followed, and groomed by predators,” the researchers noted. They added that people following different streamers receive notifications when those streamers are live. Further, “viewers can donate money to streamers, which can make it easier for predators to manipulate, track, and encourage risky behaviors from minors.”
To better understand the risks the platform might pose to minors, the researchers searched for and analyzed popular video game live streams that appeared to be streamed by minors who had their cameras on and their faces visible. Then the researchers noted the name of the video game, the topics discussed by the streamers, the time it took to find minors under each game, and each streamer’s age, name, follower count, location, streaming schedule, and social media links for money donations.
The researchers analyzed 100 Twitch streamers who were minors, who had a combined 1,755,452 million followers. Nearly half the streamers (47%) provided their presumably real names, and half (50%) gave out their location. Nearly two-thirds (64%) linked other social media accounts they had and encouraged viewers to follow them. Detailed schedules of when they would be live were available for 38% of the streamers, and 37% of the minor streamers were accepting money donations.
Only 11% of the discussion on the streams revealed personal details, most often related to trying on different outfits for viewers and talking about real-world locations they liked to visit. The researchers needed anywhere from 12 seconds to 5 minutes to find a minor in each game category.
”Young users clearly feel a false sense of safety on the platform; a significant proportion were willing to reveal personal information despite having no knowledge of who might be listening,” the researchers said. “The donation system provides a menacing avenue for manipulation and continued exploitation of minors. Our findings reveal the need for stricter age limitations for streamers and more stringent identity verification of audience members on Twitch.”
Open-minded parental guidance is warranted
Jenny Radesky, MD, a developmental behavioral pediatrician and media researcher at University of Michigan Medicine, Ann Arbor, was not surprised that many teens live stream on Twitch since it’s a popular platform for video gaming, but she was surprised at how many revealed their locations and other personal details.
“I suspect that they do this to build closeness with their viewers, by seeming more authentic,” said Dr. Radesky, who was not involved in the study. “It is this type of parasocial relationship with influencers and gamers that keeps an audience engaged, and encourages future viewing and purchases.”
Their willingness to share personal details suggests it’s important to conduct qualitative research to find out how teen live streamers think about privacy risks, what privacy settings they can use and choose to use, and how they handle inappropriate contact from adults, Dr. Radesky said.
Meanwhile, parents should talk with their kids in an open-minded way about what platforms they use and what they like and dislike about them. She recommended parents read the Common Sense Media guide about different social platforms ”to understand what attracts kids to content on specific sites, what their pitfalls are, and what types of privacy and safety settings are available.”
“A child or teen is much more likely to be honest about negative experiences online if they think their parent will hear them out – not judge them or take away their tech. No teen wants to talk with a panicky parent,” Dr. Radesky said.
David Hill, MD, a hospitalist pediatrician for Goldsboro Pediatrics in Wayne County, North Carolina, who also specializes in media communication, said that Twitch is just one example of a social media platform where children can encounter a variety of dangers, including sometimes adult predators.
“This just highlights the importance of parents having an ongoing conversation with their children about how they use their social media platforms and ensuring, just as we do with learning to ride a bicycle or learning to drive a car, that they apply some basic rules of safety,” Dr. Hill said. Then it’s important to keep coming back to that conversation “again and again as they grow and change and as those platforms change to ensure that those kids are continuing to apply those rules consistently.
“The best way for parents to keep up is ask your kids,” he said. “They love to share. They love to teach. They love to be in a position to show you something, especially if it’s something that interests them.”
An example of a rule would be setting personal accounts to private, not public, by default, Dr. Radesky said. “When interviewed, teens often say that they feel intruded upon by older people ‘stalking’ them or trying to connect with them on social platforms,” so making an account private can reduce those opportunities.
For teens who specifically want to create content on social platforms, parent oversight is needed, she said, but she acknowledged it can be a lot of work. “This might take the form of talking about what a teen plans to post before they do, expectations for positive behaviors or language, plans for privacy settings (such as public vs. private accounts), and what to do with trolls or hateful comment,” she said. “Parents may want to follow their child’s account to check in on it.”
Useful advice
Dr. Radesky also provided a handful of talking points that pediatricians can use in talking with patients who use these platforms:
- Keep your account private to just your friends and people you want to interact with. There are a lot of people on the Internet that you don’t want intruding upon your social life.
- Maintain your feed and the accounts you follow to keep it positive, entertaining, and not a source of stress or self-doubt. Content creators are always trying to grab your attention in new ways, some of which are rude or dehumanizing, so don’t waste your time on things that bring you down.
- Talk about why you want to post or live stream. Is it to get reactions or feel validated? If so, can you find other ways to feel validated that don’t require performing for other people? Is it to share a special skill? If so, how do you keep your posts creative and community building rather than attention grabbing? And how can you keep your parents involved so that they can help you navigate challenges?”
Ms. Dubrosa and Dr. Hill had no disclosures. Dr. Radesky is a consultant for Melissa & Doug. No information on external funding was provided.
WASHINGTON – Half of youth broadcasting live streams on the online platform Twitch revealed their real-world location, and nearly half provided their name to viewers, according to research presented at the annual meeting of the American Academy of Pediatrics. It took researchers less than 5 minutes – and sometimes as little as 12 seconds – to find minors in different video game categories, suggesting the environment offers opportunities to predators to gain sensitive information about minors, reported Fiona Dubrosa, BS, BA, a visiting scholar at Cohen Children’s Medical Center, New York, and colleagues.
A ‘clandestine, threatening digital environment’
the authors concluded. “The nature of live streaming makes it particularly dangerous, as there is no way to take back information that has been revealed or regulate content or viewers. Parents and pediatricians should be aware of the dangers presented by Twitch and other live-streaming platforms and counsel children on best practices for Internet safety.”
Twitch is an online streaming platform where people can watch creator’s live content, such as music performances or narrating real-time video game playing. The platform requires live streamers to be 13 years old with a valid email address or phone number to create an account, but no age restrictions or identification requirements exist for viewers, “potentially putting minors in danger of being watched, followed, and groomed by predators,” the researchers noted. They added that people following different streamers receive notifications when those streamers are live. Further, “viewers can donate money to streamers, which can make it easier for predators to manipulate, track, and encourage risky behaviors from minors.”
To better understand the risks the platform might pose to minors, the researchers searched for and analyzed popular video game live streams that appeared to be streamed by minors who had their cameras on and their faces visible. Then the researchers noted the name of the video game, the topics discussed by the streamers, the time it took to find minors under each game, and each streamer’s age, name, follower count, location, streaming schedule, and social media links for money donations.
The researchers analyzed 100 Twitch streamers who were minors, who had a combined 1,755,452 million followers. Nearly half the streamers (47%) provided their presumably real names, and half (50%) gave out their location. Nearly two-thirds (64%) linked other social media accounts they had and encouraged viewers to follow them. Detailed schedules of when they would be live were available for 38% of the streamers, and 37% of the minor streamers were accepting money donations.
Only 11% of the discussion on the streams revealed personal details, most often related to trying on different outfits for viewers and talking about real-world locations they liked to visit. The researchers needed anywhere from 12 seconds to 5 minutes to find a minor in each game category.
”Young users clearly feel a false sense of safety on the platform; a significant proportion were willing to reveal personal information despite having no knowledge of who might be listening,” the researchers said. “The donation system provides a menacing avenue for manipulation and continued exploitation of minors. Our findings reveal the need for stricter age limitations for streamers and more stringent identity verification of audience members on Twitch.”
Open-minded parental guidance is warranted
Jenny Radesky, MD, a developmental behavioral pediatrician and media researcher at University of Michigan Medicine, Ann Arbor, was not surprised that many teens live stream on Twitch since it’s a popular platform for video gaming, but she was surprised at how many revealed their locations and other personal details.
“I suspect that they do this to build closeness with their viewers, by seeming more authentic,” said Dr. Radesky, who was not involved in the study. “It is this type of parasocial relationship with influencers and gamers that keeps an audience engaged, and encourages future viewing and purchases.”
Their willingness to share personal details suggests it’s important to conduct qualitative research to find out how teen live streamers think about privacy risks, what privacy settings they can use and choose to use, and how they handle inappropriate contact from adults, Dr. Radesky said.
Meanwhile, parents should talk with their kids in an open-minded way about what platforms they use and what they like and dislike about them. She recommended parents read the Common Sense Media guide about different social platforms ”to understand what attracts kids to content on specific sites, what their pitfalls are, and what types of privacy and safety settings are available.”
“A child or teen is much more likely to be honest about negative experiences online if they think their parent will hear them out – not judge them or take away their tech. No teen wants to talk with a panicky parent,” Dr. Radesky said.
David Hill, MD, a hospitalist pediatrician for Goldsboro Pediatrics in Wayne County, North Carolina, who also specializes in media communication, said that Twitch is just one example of a social media platform where children can encounter a variety of dangers, including sometimes adult predators.
“This just highlights the importance of parents having an ongoing conversation with their children about how they use their social media platforms and ensuring, just as we do with learning to ride a bicycle or learning to drive a car, that they apply some basic rules of safety,” Dr. Hill said. Then it’s important to keep coming back to that conversation “again and again as they grow and change and as those platforms change to ensure that those kids are continuing to apply those rules consistently.
“The best way for parents to keep up is ask your kids,” he said. “They love to share. They love to teach. They love to be in a position to show you something, especially if it’s something that interests them.”
An example of a rule would be setting personal accounts to private, not public, by default, Dr. Radesky said. “When interviewed, teens often say that they feel intruded upon by older people ‘stalking’ them or trying to connect with them on social platforms,” so making an account private can reduce those opportunities.
For teens who specifically want to create content on social platforms, parent oversight is needed, she said, but she acknowledged it can be a lot of work. “This might take the form of talking about what a teen plans to post before they do, expectations for positive behaviors or language, plans for privacy settings (such as public vs. private accounts), and what to do with trolls or hateful comment,” she said. “Parents may want to follow their child’s account to check in on it.”
Useful advice
Dr. Radesky also provided a handful of talking points that pediatricians can use in talking with patients who use these platforms:
- Keep your account private to just your friends and people you want to interact with. There are a lot of people on the Internet that you don’t want intruding upon your social life.
- Maintain your feed and the accounts you follow to keep it positive, entertaining, and not a source of stress or self-doubt. Content creators are always trying to grab your attention in new ways, some of which are rude or dehumanizing, so don’t waste your time on things that bring you down.
- Talk about why you want to post or live stream. Is it to get reactions or feel validated? If so, can you find other ways to feel validated that don’t require performing for other people? Is it to share a special skill? If so, how do you keep your posts creative and community building rather than attention grabbing? And how can you keep your parents involved so that they can help you navigate challenges?”
Ms. Dubrosa and Dr. Hill had no disclosures. Dr. Radesky is a consultant for Melissa & Doug. No information on external funding was provided.
AT AAP 2023
Teens have easy online access to Delta-8 cannabinoid products
WASHINGTON – , researchers reported at the 2023 annual meeting of the American Academy of Pediatrics. Most of the products identified came in bright, colorful, kid-friendly packaging and cost less than $10, the researchers found, and only 2 out of 45 sites had a third-party age verification requirement for purchases.
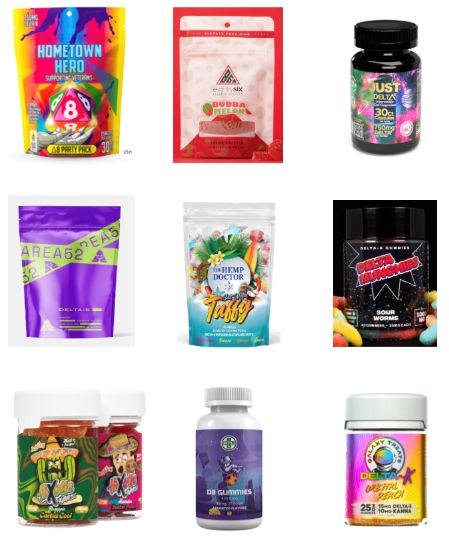
Delta-8 THC, also called D8, is a synthetically produced cannabinoid whose chemical structure and effects are nearly identical to traditional THC, the authors explained, and past research has found that D8 products, such as e-cigarettes, can contain toxic byproducts and contaminants.
”Since D8 is not traditional THC, minors may underestimate its strength and potential danger,” wrote lead author Abhijeet Grewal, BS, a research assistant at Cohen Children’s Medical Center, New York, and senior author Ruth Milanaik, DO, director of the Neonatal Neurodevelopmental Program at Cohen Children’s and a developmental/behavioral pediatrician at Northwell Health, also in New York. “Although traditional THC is a federally banned substance, D8 is legal on a federal level and less restricted on a state by state basis, making it easier for individuals to acquire D8.”
Easily accessible
During the first seven moments of 2021, 77% of reports of accidental exposure occurred in people under age 18, including some children who required ICU admission. The U.S. Food and Drug Administration also received 104 reports of adverse events from products containing D8 between December 2020-February 2022, and more than half of those required medical intervention.
To better understand how easy it is to access D8, the authors collected data on 45 websites they identified that sold D8. The researchers looked for age verification questions for accessing the site, third-party age certification, what kinds of products (edibles, smoke products, or tinctures) were sold, the price and dosage of the cheapest product, and examples of packaging, flavors, marketing claims, and warning statements at each site.
More than a third of the sites (36%) did not ask for customers’ age and almost none of the sites asked for proof: 96% of the sites lacked formal third-party age verification procedures. All but one of the sites sold D8 edibles, and most (82%) sold D8 vaping or smoking products. Only 42% sold tinctures, a mix of concentrated D8 with oil that’s orally consumed.
The cheapest product was priced under $5 on one-third of the sites and under $10 on another third of the sites. The cheapest product was between $10-20 on 16% of the sites while the remaining nine sites’ cheapest product was more than $20. In assessing only the cheapest D8 products on each site, nearly half (47%) contained 51 mg or more of D8, and 20% of the products didn’t report the dosage. Another 22% contained 41-50 mg of D8, and the remaining five products contained 20-40 mg.
Kid-friendly D8
More than half of the D8 products were sold in kid-friendly packaging – packages with bright, colorful designs and fonts that resemble candy or snack food, sometimes cartoon characters or fun items like dice on the packaging. Further, 24% of the websites did not include any warnings or other health information about D8.
“The low prices, high dosages available, and eye-popping packaging make these products extremely attractive to teens who are looking for a high,” the researchers concluded. They advised clinicians to talk with teen patients about the dangers of D8 and advocated for policymakers to more strictly regulate online distributors of D8 products, particularly in requiring age verification procedures and prohibiting kid-friendly packaging.
Megan Moreno, MD, MSEd, MPH, an adolescent medicine physician and researcher at the University of Wisconsin, Madison, School of Medicine and Public Health and UWHealthKids, was particularly struck by how eye-catching the packaging was. “The bright colors and font choices are really designed to attract adolescents,” commented Dr. Moreno, who was not involved in the study. But she was not surprised overall by the findings.
“Other studies have found that the cannabis industry leverages online tools and social media, alongside youth-friendly packaging, to attract youth to their products,” she said. “What is disappointing is that these companies do not use industry standard approaches, such as the alcohol industry, to age-gate their websites.”
It’s important for providers who care for adolescents to ask about substance use but to especially include questions about substances that teens might not think of as “drugs,” such as Delta 8, Dr. Moreno said.
“Prior research on other types of substance such as these has found that teens can think these are less dangerous versions of cannabis, so providing accurate information and asking about these products can prevent harm to kids,” Dr. Moreno said. Although this study focused on websites that sell D8 products, she said that “another important area of influence to consider is social media messaging around these products, which may drive traffic to the purchasing site.” It’s clear this industry is not going to self-regulate without policy changes, Dr. Moreno added, so she noted the importance of advocating for policy that regulates these sites.
Mr. Grewal, Dr. Milanaik and Dr. Moreno had no disclosures. No external funding sources were noted.
WASHINGTON – , researchers reported at the 2023 annual meeting of the American Academy of Pediatrics. Most of the products identified came in bright, colorful, kid-friendly packaging and cost less than $10, the researchers found, and only 2 out of 45 sites had a third-party age verification requirement for purchases.
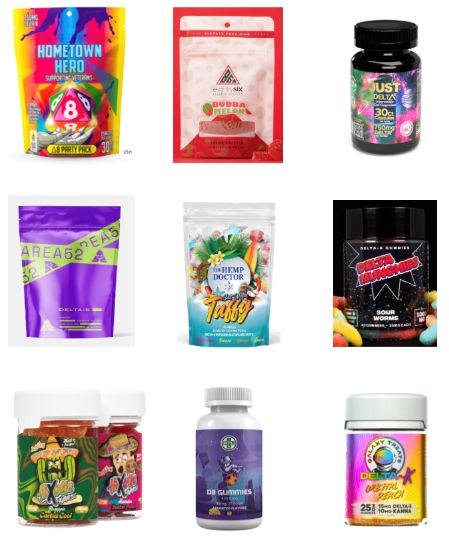
Delta-8 THC, also called D8, is a synthetically produced cannabinoid whose chemical structure and effects are nearly identical to traditional THC, the authors explained, and past research has found that D8 products, such as e-cigarettes, can contain toxic byproducts and contaminants.
”Since D8 is not traditional THC, minors may underestimate its strength and potential danger,” wrote lead author Abhijeet Grewal, BS, a research assistant at Cohen Children’s Medical Center, New York, and senior author Ruth Milanaik, DO, director of the Neonatal Neurodevelopmental Program at Cohen Children’s and a developmental/behavioral pediatrician at Northwell Health, also in New York. “Although traditional THC is a federally banned substance, D8 is legal on a federal level and less restricted on a state by state basis, making it easier for individuals to acquire D8.”
Easily accessible
During the first seven moments of 2021, 77% of reports of accidental exposure occurred in people under age 18, including some children who required ICU admission. The U.S. Food and Drug Administration also received 104 reports of adverse events from products containing D8 between December 2020-February 2022, and more than half of those required medical intervention.
To better understand how easy it is to access D8, the authors collected data on 45 websites they identified that sold D8. The researchers looked for age verification questions for accessing the site, third-party age certification, what kinds of products (edibles, smoke products, or tinctures) were sold, the price and dosage of the cheapest product, and examples of packaging, flavors, marketing claims, and warning statements at each site.
More than a third of the sites (36%) did not ask for customers’ age and almost none of the sites asked for proof: 96% of the sites lacked formal third-party age verification procedures. All but one of the sites sold D8 edibles, and most (82%) sold D8 vaping or smoking products. Only 42% sold tinctures, a mix of concentrated D8 with oil that’s orally consumed.
The cheapest product was priced under $5 on one-third of the sites and under $10 on another third of the sites. The cheapest product was between $10-20 on 16% of the sites while the remaining nine sites’ cheapest product was more than $20. In assessing only the cheapest D8 products on each site, nearly half (47%) contained 51 mg or more of D8, and 20% of the products didn’t report the dosage. Another 22% contained 41-50 mg of D8, and the remaining five products contained 20-40 mg.
Kid-friendly D8
More than half of the D8 products were sold in kid-friendly packaging – packages with bright, colorful designs and fonts that resemble candy or snack food, sometimes cartoon characters or fun items like dice on the packaging. Further, 24% of the websites did not include any warnings or other health information about D8.
“The low prices, high dosages available, and eye-popping packaging make these products extremely attractive to teens who are looking for a high,” the researchers concluded. They advised clinicians to talk with teen patients about the dangers of D8 and advocated for policymakers to more strictly regulate online distributors of D8 products, particularly in requiring age verification procedures and prohibiting kid-friendly packaging.
Megan Moreno, MD, MSEd, MPH, an adolescent medicine physician and researcher at the University of Wisconsin, Madison, School of Medicine and Public Health and UWHealthKids, was particularly struck by how eye-catching the packaging was. “The bright colors and font choices are really designed to attract adolescents,” commented Dr. Moreno, who was not involved in the study. But she was not surprised overall by the findings.
“Other studies have found that the cannabis industry leverages online tools and social media, alongside youth-friendly packaging, to attract youth to their products,” she said. “What is disappointing is that these companies do not use industry standard approaches, such as the alcohol industry, to age-gate their websites.”
It’s important for providers who care for adolescents to ask about substance use but to especially include questions about substances that teens might not think of as “drugs,” such as Delta 8, Dr. Moreno said.
“Prior research on other types of substance such as these has found that teens can think these are less dangerous versions of cannabis, so providing accurate information and asking about these products can prevent harm to kids,” Dr. Moreno said. Although this study focused on websites that sell D8 products, she said that “another important area of influence to consider is social media messaging around these products, which may drive traffic to the purchasing site.” It’s clear this industry is not going to self-regulate without policy changes, Dr. Moreno added, so she noted the importance of advocating for policy that regulates these sites.
Mr. Grewal, Dr. Milanaik and Dr. Moreno had no disclosures. No external funding sources were noted.
WASHINGTON – , researchers reported at the 2023 annual meeting of the American Academy of Pediatrics. Most of the products identified came in bright, colorful, kid-friendly packaging and cost less than $10, the researchers found, and only 2 out of 45 sites had a third-party age verification requirement for purchases.
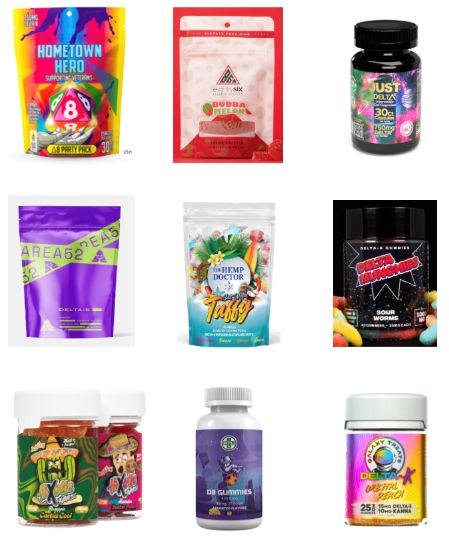
Delta-8 THC, also called D8, is a synthetically produced cannabinoid whose chemical structure and effects are nearly identical to traditional THC, the authors explained, and past research has found that D8 products, such as e-cigarettes, can contain toxic byproducts and contaminants.
”Since D8 is not traditional THC, minors may underestimate its strength and potential danger,” wrote lead author Abhijeet Grewal, BS, a research assistant at Cohen Children’s Medical Center, New York, and senior author Ruth Milanaik, DO, director of the Neonatal Neurodevelopmental Program at Cohen Children’s and a developmental/behavioral pediatrician at Northwell Health, also in New York. “Although traditional THC is a federally banned substance, D8 is legal on a federal level and less restricted on a state by state basis, making it easier for individuals to acquire D8.”
Easily accessible
During the first seven moments of 2021, 77% of reports of accidental exposure occurred in people under age 18, including some children who required ICU admission. The U.S. Food and Drug Administration also received 104 reports of adverse events from products containing D8 between December 2020-February 2022, and more than half of those required medical intervention.
To better understand how easy it is to access D8, the authors collected data on 45 websites they identified that sold D8. The researchers looked for age verification questions for accessing the site, third-party age certification, what kinds of products (edibles, smoke products, or tinctures) were sold, the price and dosage of the cheapest product, and examples of packaging, flavors, marketing claims, and warning statements at each site.
More than a third of the sites (36%) did not ask for customers’ age and almost none of the sites asked for proof: 96% of the sites lacked formal third-party age verification procedures. All but one of the sites sold D8 edibles, and most (82%) sold D8 vaping or smoking products. Only 42% sold tinctures, a mix of concentrated D8 with oil that’s orally consumed.
The cheapest product was priced under $5 on one-third of the sites and under $10 on another third of the sites. The cheapest product was between $10-20 on 16% of the sites while the remaining nine sites’ cheapest product was more than $20. In assessing only the cheapest D8 products on each site, nearly half (47%) contained 51 mg or more of D8, and 20% of the products didn’t report the dosage. Another 22% contained 41-50 mg of D8, and the remaining five products contained 20-40 mg.
Kid-friendly D8
More than half of the D8 products were sold in kid-friendly packaging – packages with bright, colorful designs and fonts that resemble candy or snack food, sometimes cartoon characters or fun items like dice on the packaging. Further, 24% of the websites did not include any warnings or other health information about D8.
“The low prices, high dosages available, and eye-popping packaging make these products extremely attractive to teens who are looking for a high,” the researchers concluded. They advised clinicians to talk with teen patients about the dangers of D8 and advocated for policymakers to more strictly regulate online distributors of D8 products, particularly in requiring age verification procedures and prohibiting kid-friendly packaging.
Megan Moreno, MD, MSEd, MPH, an adolescent medicine physician and researcher at the University of Wisconsin, Madison, School of Medicine and Public Health and UWHealthKids, was particularly struck by how eye-catching the packaging was. “The bright colors and font choices are really designed to attract adolescents,” commented Dr. Moreno, who was not involved in the study. But she was not surprised overall by the findings.
“Other studies have found that the cannabis industry leverages online tools and social media, alongside youth-friendly packaging, to attract youth to their products,” she said. “What is disappointing is that these companies do not use industry standard approaches, such as the alcohol industry, to age-gate their websites.”
It’s important for providers who care for adolescents to ask about substance use but to especially include questions about substances that teens might not think of as “drugs,” such as Delta 8, Dr. Moreno said.
“Prior research on other types of substance such as these has found that teens can think these are less dangerous versions of cannabis, so providing accurate information and asking about these products can prevent harm to kids,” Dr. Moreno said. Although this study focused on websites that sell D8 products, she said that “another important area of influence to consider is social media messaging around these products, which may drive traffic to the purchasing site.” It’s clear this industry is not going to self-regulate without policy changes, Dr. Moreno added, so she noted the importance of advocating for policy that regulates these sites.
Mr. Grewal, Dr. Milanaik and Dr. Moreno had no disclosures. No external funding sources were noted.
At AAP 2023
How clinicians can prepare for and defend against social media attacks
WASHINGTON – The entire video clip is just 15 seconds — 15 seconds that went viral and temporarily upended the entire life and disrupted the medical practice of Nicole Baldwin, MD, a pediatrician in Cincinnati, Ohio, in January 2020. At the annual meeting of the American Academy of Pediatrics, Dr. Baldwin told attendees how her pro-vaccine TikTok video led a horde of anti-vaccine activists to swarm her social media profiles across multiple platforms, leave one-star reviews with false stories about her medical practice on various doctor review sites, and personally threaten her.
The initial response to the video was positive, with 50,000 views in the first 24 hours after the video was posted and more than 1.5 million views the next day. But 2 days after the video was posted, an organized attack that originated on Facebook required Dr. Baldwin to enlist the help of 16 volunteers, working 24/7 for a week, to help ban and block more than 6,000 users on Facebook, Instagram, and TikTok. Just 4 days after she’d posted the video, Dr. Baldwin was reporting personal threats to the police and had begun contacting sites such as Yelp, Google, Healthgrades, Vitals, RateMDs, and WebMD so they could start removing false reviews about her practice.
Today, years after those 2 exhausting, intense weeks of attacks, Dr. Baldwin has found two silver linings in the experience: More people have found her profiles, allowing her to share evidence-based information with an even wider audience, and she can now help other physicians protect themselves and reduce the risk of similar attacks, or at least know how to respond to them if they occur. Dr. Baldwin shared a wealth of tips and resources during her lecture to help pediatricians prepare ahead for the possibility that they will be targeted next, whether the issue is vaccines or another topic.
Online risks and benefits
A Pew survey of U.S. adults in September 2020 found that 41% have personally experienced online harassment, including a quarter of Americans who have experienced severe harassment. More than half of respondents said online harassment and bullying is a major problem – and that was a poll of the entire population, not even just physicians and scientists.
“Now, these numbers would be higher,” Dr. Baldwin said. “A lot has changed in the past 3 years, and the landscape is very different.”
The pandemic contributed to those changes to the landscape, including an increase in harassment of doctors and researchers. A June 2023 study revealed that two-thirds of 359 respondents in an online survey reported harassment on social media, a substantial number even after accounting for selection bias in the individuals who chose to respond to the survey. Although most of the attacks (88%) resulted from the respondent’s advocacy online, nearly half the attacks (45%) were gender based, 27% were based on race/ethnicity, and 13% were based on sexual orientation.
While hateful comments are likely the most common type of online harassment, other types can involve sharing or tagging your profile, creating fake profiles to misrepresent you, fake reviews of your practice, harassing phone calls and hate mail at your office, and doxxing, in which someone online widely shares your personal address, phone number, email, or other contact information.
Despite the risks of all these forms of harassment, Dr. Baldwin emphasized the value of doctors having a social media presence given how much misinformation thrives online. For example, a recent report from the Kaiser Family Foundation revealed how many people weren’t sure whether certain health misinformation claims were true or false. Barely a third of people were sure that COVID-19 vaccines had not caused thousands of deaths in healthy people, and only 22% of people were sure that ivermectin is not an effective treatment for COVID.
“There is so much that we need to be doing and working in these spaces to put evidence-based content out there so that people are not finding all of this crap from everybody else,” Dr. Baldwin said. Having an online presence is particularly important given that the public still has high levels of trust in their doctors, she added.
“They trust their physician, and you may not be their physician online, but I will tell you from experience, when you build a community of followers, you become that trusted source of information for them, and it is so important,” Dr. Baldwin said. “There is room for everybody in this space, and we need all of you.”
Proactive steps for protection
Dr. Baldwin then went through the details of what people should do now to make things easier in the event of an attack later. “The best defense is a good offense,” Dr. Baldwin said, “so make sure all of your accounts are secure.”
She recommended the following steps:
- Use two-factor authentication for all of your logins.
- Use strong, unique passwords for all of your logins.
- Use strong privacy settings on all of your private social media profiles, such as making sure photos are not visible on your personal Facebook account.
- Claim your Google profile and Yelp business profile.
- Claim your doctor and/or business profile on all of the medical review sites where you have one, including Google, Healthgrades, Vitals, RateMDs, and WebMD.
For doctors who are attacked specifically because of pro-vaccine advocacy, Dr. Baldwin recommended contacting Shots Heard Round The World, a site that was created by a physician whose practice was attacked by anti-vaccine activists. The site also has a toolkit that anyone can download for tips on preparing ahead for possible attacks and what to do if you are attacked.
Dr. Baldwin then reviewed how to set up different social media profiles to automatically hide certain comments, including comments with words commonly used by online harassers and trolls:
- Sheep
- Sheeple
- Pharma
- Shill
- Die
- Psychopath
- Clown
- Various curse words
- The clown emoji
In Instagram, go to “Settings and privacy —> Hidden Words” for options on hiding offensive comments and messages and for managing custom words and phrases that should be automatically hidden.
On Facebook, go to “Professional dashboard —> Moderation Assist,” where you can add or edit criteria to automatically hide comments on your Facebook page. In addition to hiding comments with certain keywords, you can hide comments from new accounts, accounts without profile photos, or accounts with no friends or followers.
On TikTok, click the three-line menu icon in the upper right, and choose “Privacy —> Comments —> Filter keywords.”
On the platform formerly known as Twitter, go to “Settings and privacy —> Privacy and safety —> Mute and block —> Muted words.”
On YouTube, under “Manage your community & comments,” select “Learn about comment settings.”
Dr. Baldwin did not discourage doctors from posting about controversial topics, but she said it’s important to know what they are so that you can be prepared for the possibility that a post about one of these topics could lead to online harassment. These hot button topics include vaccines, firearm safety, gender-affirming care, reproductive choice, safe sleep/bedsharing, breastfeeding, and COVID masks.
If you do post on one of these and suspect it could result in harassment, Dr. Baldwin recommends turning on your notifications so you know when attacks begin, alerting your office and call center staff if you think they might receive calls, and, when possible, post your content at a time when you’re more likely to be able to monitor the post. She acknowledged that this last tip isn’t always relevant since attacks can take a few days to start or gain steam.
Defending yourself in an attack
Even after taking all these precautions, it’s not possible to altogether prevent an attack from happening, so Dr. Baldwin provided suggestions on what to do if one occurs, starting with taking a deep breath.
“If you are attacked, first of all, please remain calm, which is a lot easier said than done,” she said. “But know that this too shall pass. These things do come to an end.”
She advises you to get help if you need it, enlisting friends or colleagues to help with moderation and banning/blocking. If necessary, alert your employer to the attack, as attackers may contact your employer. Some people may opt to turn off comments on their post, but doing so “is a really personal decision,” she said. It’s okay to turn off comments if you don’t have the bandwidth or help to deal with them.
However, Dr. Baldwin said she never turns off comments because she wants to be able to ban and block people to reduce the likelihood of a future attack from them, and each comment brings the post higher in the algorithm so that more people are able to see the original content. “So sometimes these things are actually a blessing in disguise,” she said.
If you do have comments turned on, take screenshots of the most egregious or threatening ones and then report them and ban/block them. The screenshots are evidence since blocking will remove the comment.
“Take breaks when you need to,” she said. “Don’t stay up all night” since there are only going to be more in the morning, and if you’re using keywords to help hide many of these comments, that will hide them from your followers while you’re away. She also advised monitoring your online reviews at doctor/practice review sites so you know whether you’re receiving spurious reviews that need to be removed.
Dr. Baldwin also addressed how to handle trolls, the people online who intentionally antagonize others with inflammatory, irrelevant, offensive, or otherwise disruptive comments or content. The No. 1 rule is not to engage – “Don’t feed the trolls” – but Dr. Baldwin acknowledged that she can find that difficult sometimes. So she uses kindness or humor to defuse them or calls them out on their inaccurate information and then thanks them for their engagement. Don’t forget that you are in charge of your own page, so any complaints about “censorship” or infringing “free speech” aren’t relevant.
If the comments are growing out of control and you’re unable to manage them, multiple social media platforms have options for limited interactions or who can comment on your page.
On Instagram under “Settings and privacy,” check out “Limited interactions,” “Comments —> Allow comments from,” and “Tags and mentions” to see ways you can limit who is able to comment, tag or mention your account. If you need a complete break, you can turn off commenting by clicking the three dots in the upper right corner of the post, or make your account temporarily private under “Settings and privacy —> Account privacy.”
On Facebook, click the three dots in the upper right corner of posts to select “Who can comment on your post?” Also, under “Settings —> Privacy —> Your Activity,” you can adjust who sees your future posts. Again, if things are out of control, you can temporarily deactivate your page under “Settings —> Privacy —> Facebook Page information.”
On TikTok, click the three lines in the upper right corner of your profile and select “Privacy —> Comments” to adjust who can comment and to filter comments. Again, you can make your account private under “Settings and privacy —> Privacy —> Private account.”
On the platform formerly known as Twitter, click the three dots in the upper right corner of the tweet to change who can reply to the tweet. If you select “Only people you mentioned,” then no one can reply if you did not mention anyone. You can control tagging under “Settings and privacy —> Privacy and safety —> Audience and tagging.”
If you or your practice receive false reviews on review sites, report the reviews and alert the rating site when you can. In the meantime, lock down your private social media accounts and ensure that no photos of your family are publicly available.
Social media self-care
Dr. Baldwin acknowledged that experiencing a social media attack can be intense and even frightening, but it’s rare and outweighed by the “hundreds and hundreds and hundreds of positive comments all the time.” She also reminded attendees that being on social media doesn’t mean being there all the time.
“Over time, my use of social media has certainly changed. It ebbs and flows,” she said. “There are times when I have a lot of bandwidth and I’m posting a lot, and then I actually have had some struggles with my own mental health, with some anxiety and mild depression, so I took a break from social media for a while. When I came back, I posted about my mental health struggles, and you wouldn’t believe how many people were so appreciative of that.”
Accurate information from a trusted source
Ultimately, Dr. Baldwin sees her work online as an extension of her work educating patients.
“This is where our patients are. They are in your office for maybe 10-15 minutes maybe once a year, but they are on these platforms every single day for hours,” she said. “They need to see this information from medical professionals because there are random people out there that are telling them [misinformation].”
Elizabeth Murray, DO, MBA, an emergency medicine pediatrician at Golisano Children’s Hospital at the University of Rochester, agreed that there’s substantial value in doctors sharing accurate information online.
“Disinformation and misinformation is rampant, and at the end of the day, we know the facts,” Dr. Murray said. “We know what parents want to hear and what they want to learn about, so we need to share that information and get the facts out there.”
Dr. Murray found the session very helpful because there’s so much to learn across different social media platforms and it can feel overwhelming if you aren’t familiar with the tools.
“Social media is always going to be here. We need to learn to live with all of these platforms,” Dr. Murray said. “That’s a skill set. We need to learn the skills and teach our kids the skill set. You never really know what you might put out there that, in your mind is innocent or very science-based, that for whatever reason somebody might take issue with. You might as well be ready because we’re all about prevention in pediatrics.”
There were no funders for the presentation. Dr. Baldwin and Dr. Murray had no disclosures.
WASHINGTON – The entire video clip is just 15 seconds — 15 seconds that went viral and temporarily upended the entire life and disrupted the medical practice of Nicole Baldwin, MD, a pediatrician in Cincinnati, Ohio, in January 2020. At the annual meeting of the American Academy of Pediatrics, Dr. Baldwin told attendees how her pro-vaccine TikTok video led a horde of anti-vaccine activists to swarm her social media profiles across multiple platforms, leave one-star reviews with false stories about her medical practice on various doctor review sites, and personally threaten her.
The initial response to the video was positive, with 50,000 views in the first 24 hours after the video was posted and more than 1.5 million views the next day. But 2 days after the video was posted, an organized attack that originated on Facebook required Dr. Baldwin to enlist the help of 16 volunteers, working 24/7 for a week, to help ban and block more than 6,000 users on Facebook, Instagram, and TikTok. Just 4 days after she’d posted the video, Dr. Baldwin was reporting personal threats to the police and had begun contacting sites such as Yelp, Google, Healthgrades, Vitals, RateMDs, and WebMD so they could start removing false reviews about her practice.
Today, years after those 2 exhausting, intense weeks of attacks, Dr. Baldwin has found two silver linings in the experience: More people have found her profiles, allowing her to share evidence-based information with an even wider audience, and she can now help other physicians protect themselves and reduce the risk of similar attacks, or at least know how to respond to them if they occur. Dr. Baldwin shared a wealth of tips and resources during her lecture to help pediatricians prepare ahead for the possibility that they will be targeted next, whether the issue is vaccines or another topic.
Online risks and benefits
A Pew survey of U.S. adults in September 2020 found that 41% have personally experienced online harassment, including a quarter of Americans who have experienced severe harassment. More than half of respondents said online harassment and bullying is a major problem – and that was a poll of the entire population, not even just physicians and scientists.
“Now, these numbers would be higher,” Dr. Baldwin said. “A lot has changed in the past 3 years, and the landscape is very different.”
The pandemic contributed to those changes to the landscape, including an increase in harassment of doctors and researchers. A June 2023 study revealed that two-thirds of 359 respondents in an online survey reported harassment on social media, a substantial number even after accounting for selection bias in the individuals who chose to respond to the survey. Although most of the attacks (88%) resulted from the respondent’s advocacy online, nearly half the attacks (45%) were gender based, 27% were based on race/ethnicity, and 13% were based on sexual orientation.
While hateful comments are likely the most common type of online harassment, other types can involve sharing or tagging your profile, creating fake profiles to misrepresent you, fake reviews of your practice, harassing phone calls and hate mail at your office, and doxxing, in which someone online widely shares your personal address, phone number, email, or other contact information.
Despite the risks of all these forms of harassment, Dr. Baldwin emphasized the value of doctors having a social media presence given how much misinformation thrives online. For example, a recent report from the Kaiser Family Foundation revealed how many people weren’t sure whether certain health misinformation claims were true or false. Barely a third of people were sure that COVID-19 vaccines had not caused thousands of deaths in healthy people, and only 22% of people were sure that ivermectin is not an effective treatment for COVID.
“There is so much that we need to be doing and working in these spaces to put evidence-based content out there so that people are not finding all of this crap from everybody else,” Dr. Baldwin said. Having an online presence is particularly important given that the public still has high levels of trust in their doctors, she added.
“They trust their physician, and you may not be their physician online, but I will tell you from experience, when you build a community of followers, you become that trusted source of information for them, and it is so important,” Dr. Baldwin said. “There is room for everybody in this space, and we need all of you.”
Proactive steps for protection
Dr. Baldwin then went through the details of what people should do now to make things easier in the event of an attack later. “The best defense is a good offense,” Dr. Baldwin said, “so make sure all of your accounts are secure.”
She recommended the following steps:
- Use two-factor authentication for all of your logins.
- Use strong, unique passwords for all of your logins.
- Use strong privacy settings on all of your private social media profiles, such as making sure photos are not visible on your personal Facebook account.
- Claim your Google profile and Yelp business profile.
- Claim your doctor and/or business profile on all of the medical review sites where you have one, including Google, Healthgrades, Vitals, RateMDs, and WebMD.
For doctors who are attacked specifically because of pro-vaccine advocacy, Dr. Baldwin recommended contacting Shots Heard Round The World, a site that was created by a physician whose practice was attacked by anti-vaccine activists. The site also has a toolkit that anyone can download for tips on preparing ahead for possible attacks and what to do if you are attacked.
Dr. Baldwin then reviewed how to set up different social media profiles to automatically hide certain comments, including comments with words commonly used by online harassers and trolls:
- Sheep
- Sheeple
- Pharma
- Shill
- Die
- Psychopath
- Clown
- Various curse words
- The clown emoji
In Instagram, go to “Settings and privacy —> Hidden Words” for options on hiding offensive comments and messages and for managing custom words and phrases that should be automatically hidden.
On Facebook, go to “Professional dashboard —> Moderation Assist,” where you can add or edit criteria to automatically hide comments on your Facebook page. In addition to hiding comments with certain keywords, you can hide comments from new accounts, accounts without profile photos, or accounts with no friends or followers.
On TikTok, click the three-line menu icon in the upper right, and choose “Privacy —> Comments —> Filter keywords.”
On the platform formerly known as Twitter, go to “Settings and privacy —> Privacy and safety —> Mute and block —> Muted words.”
On YouTube, under “Manage your community & comments,” select “Learn about comment settings.”
Dr. Baldwin did not discourage doctors from posting about controversial topics, but she said it’s important to know what they are so that you can be prepared for the possibility that a post about one of these topics could lead to online harassment. These hot button topics include vaccines, firearm safety, gender-affirming care, reproductive choice, safe sleep/bedsharing, breastfeeding, and COVID masks.
If you do post on one of these and suspect it could result in harassment, Dr. Baldwin recommends turning on your notifications so you know when attacks begin, alerting your office and call center staff if you think they might receive calls, and, when possible, post your content at a time when you’re more likely to be able to monitor the post. She acknowledged that this last tip isn’t always relevant since attacks can take a few days to start or gain steam.
Defending yourself in an attack
Even after taking all these precautions, it’s not possible to altogether prevent an attack from happening, so Dr. Baldwin provided suggestions on what to do if one occurs, starting with taking a deep breath.
“If you are attacked, first of all, please remain calm, which is a lot easier said than done,” she said. “But know that this too shall pass. These things do come to an end.”
She advises you to get help if you need it, enlisting friends or colleagues to help with moderation and banning/blocking. If necessary, alert your employer to the attack, as attackers may contact your employer. Some people may opt to turn off comments on their post, but doing so “is a really personal decision,” she said. It’s okay to turn off comments if you don’t have the bandwidth or help to deal with them.
However, Dr. Baldwin said she never turns off comments because she wants to be able to ban and block people to reduce the likelihood of a future attack from them, and each comment brings the post higher in the algorithm so that more people are able to see the original content. “So sometimes these things are actually a blessing in disguise,” she said.
If you do have comments turned on, take screenshots of the most egregious or threatening ones and then report them and ban/block them. The screenshots are evidence since blocking will remove the comment.
“Take breaks when you need to,” she said. “Don’t stay up all night” since there are only going to be more in the morning, and if you’re using keywords to help hide many of these comments, that will hide them from your followers while you’re away. She also advised monitoring your online reviews at doctor/practice review sites so you know whether you’re receiving spurious reviews that need to be removed.
Dr. Baldwin also addressed how to handle trolls, the people online who intentionally antagonize others with inflammatory, irrelevant, offensive, or otherwise disruptive comments or content. The No. 1 rule is not to engage – “Don’t feed the trolls” – but Dr. Baldwin acknowledged that she can find that difficult sometimes. So she uses kindness or humor to defuse them or calls them out on their inaccurate information and then thanks them for their engagement. Don’t forget that you are in charge of your own page, so any complaints about “censorship” or infringing “free speech” aren’t relevant.
If the comments are growing out of control and you’re unable to manage them, multiple social media platforms have options for limited interactions or who can comment on your page.
On Instagram under “Settings and privacy,” check out “Limited interactions,” “Comments —> Allow comments from,” and “Tags and mentions” to see ways you can limit who is able to comment, tag or mention your account. If you need a complete break, you can turn off commenting by clicking the three dots in the upper right corner of the post, or make your account temporarily private under “Settings and privacy —> Account privacy.”
On Facebook, click the three dots in the upper right corner of posts to select “Who can comment on your post?” Also, under “Settings —> Privacy —> Your Activity,” you can adjust who sees your future posts. Again, if things are out of control, you can temporarily deactivate your page under “Settings —> Privacy —> Facebook Page information.”
On TikTok, click the three lines in the upper right corner of your profile and select “Privacy —> Comments” to adjust who can comment and to filter comments. Again, you can make your account private under “Settings and privacy —> Privacy —> Private account.”
On the platform formerly known as Twitter, click the three dots in the upper right corner of the tweet to change who can reply to the tweet. If you select “Only people you mentioned,” then no one can reply if you did not mention anyone. You can control tagging under “Settings and privacy —> Privacy and safety —> Audience and tagging.”
If you or your practice receive false reviews on review sites, report the reviews and alert the rating site when you can. In the meantime, lock down your private social media accounts and ensure that no photos of your family are publicly available.
Social media self-care
Dr. Baldwin acknowledged that experiencing a social media attack can be intense and even frightening, but it’s rare and outweighed by the “hundreds and hundreds and hundreds of positive comments all the time.” She also reminded attendees that being on social media doesn’t mean being there all the time.
“Over time, my use of social media has certainly changed. It ebbs and flows,” she said. “There are times when I have a lot of bandwidth and I’m posting a lot, and then I actually have had some struggles with my own mental health, with some anxiety and mild depression, so I took a break from social media for a while. When I came back, I posted about my mental health struggles, and you wouldn’t believe how many people were so appreciative of that.”
Accurate information from a trusted source
Ultimately, Dr. Baldwin sees her work online as an extension of her work educating patients.
“This is where our patients are. They are in your office for maybe 10-15 minutes maybe once a year, but they are on these platforms every single day for hours,” she said. “They need to see this information from medical professionals because there are random people out there that are telling them [misinformation].”
Elizabeth Murray, DO, MBA, an emergency medicine pediatrician at Golisano Children’s Hospital at the University of Rochester, agreed that there’s substantial value in doctors sharing accurate information online.
“Disinformation and misinformation is rampant, and at the end of the day, we know the facts,” Dr. Murray said. “We know what parents want to hear and what they want to learn about, so we need to share that information and get the facts out there.”
Dr. Murray found the session very helpful because there’s so much to learn across different social media platforms and it can feel overwhelming if you aren’t familiar with the tools.
“Social media is always going to be here. We need to learn to live with all of these platforms,” Dr. Murray said. “That’s a skill set. We need to learn the skills and teach our kids the skill set. You never really know what you might put out there that, in your mind is innocent or very science-based, that for whatever reason somebody might take issue with. You might as well be ready because we’re all about prevention in pediatrics.”
There were no funders for the presentation. Dr. Baldwin and Dr. Murray had no disclosures.
WASHINGTON – The entire video clip is just 15 seconds — 15 seconds that went viral and temporarily upended the entire life and disrupted the medical practice of Nicole Baldwin, MD, a pediatrician in Cincinnati, Ohio, in January 2020. At the annual meeting of the American Academy of Pediatrics, Dr. Baldwin told attendees how her pro-vaccine TikTok video led a horde of anti-vaccine activists to swarm her social media profiles across multiple platforms, leave one-star reviews with false stories about her medical practice on various doctor review sites, and personally threaten her.
The initial response to the video was positive, with 50,000 views in the first 24 hours after the video was posted and more than 1.5 million views the next day. But 2 days after the video was posted, an organized attack that originated on Facebook required Dr. Baldwin to enlist the help of 16 volunteers, working 24/7 for a week, to help ban and block more than 6,000 users on Facebook, Instagram, and TikTok. Just 4 days after she’d posted the video, Dr. Baldwin was reporting personal threats to the police and had begun contacting sites such as Yelp, Google, Healthgrades, Vitals, RateMDs, and WebMD so they could start removing false reviews about her practice.
Today, years after those 2 exhausting, intense weeks of attacks, Dr. Baldwin has found two silver linings in the experience: More people have found her profiles, allowing her to share evidence-based information with an even wider audience, and she can now help other physicians protect themselves and reduce the risk of similar attacks, or at least know how to respond to them if they occur. Dr. Baldwin shared a wealth of tips and resources during her lecture to help pediatricians prepare ahead for the possibility that they will be targeted next, whether the issue is vaccines or another topic.
Online risks and benefits
A Pew survey of U.S. adults in September 2020 found that 41% have personally experienced online harassment, including a quarter of Americans who have experienced severe harassment. More than half of respondents said online harassment and bullying is a major problem – and that was a poll of the entire population, not even just physicians and scientists.
“Now, these numbers would be higher,” Dr. Baldwin said. “A lot has changed in the past 3 years, and the landscape is very different.”
The pandemic contributed to those changes to the landscape, including an increase in harassment of doctors and researchers. A June 2023 study revealed that two-thirds of 359 respondents in an online survey reported harassment on social media, a substantial number even after accounting for selection bias in the individuals who chose to respond to the survey. Although most of the attacks (88%) resulted from the respondent’s advocacy online, nearly half the attacks (45%) were gender based, 27% were based on race/ethnicity, and 13% were based on sexual orientation.
While hateful comments are likely the most common type of online harassment, other types can involve sharing or tagging your profile, creating fake profiles to misrepresent you, fake reviews of your practice, harassing phone calls and hate mail at your office, and doxxing, in which someone online widely shares your personal address, phone number, email, or other contact information.
Despite the risks of all these forms of harassment, Dr. Baldwin emphasized the value of doctors having a social media presence given how much misinformation thrives online. For example, a recent report from the Kaiser Family Foundation revealed how many people weren’t sure whether certain health misinformation claims were true or false. Barely a third of people were sure that COVID-19 vaccines had not caused thousands of deaths in healthy people, and only 22% of people were sure that ivermectin is not an effective treatment for COVID.
“There is so much that we need to be doing and working in these spaces to put evidence-based content out there so that people are not finding all of this crap from everybody else,” Dr. Baldwin said. Having an online presence is particularly important given that the public still has high levels of trust in their doctors, she added.
“They trust their physician, and you may not be their physician online, but I will tell you from experience, when you build a community of followers, you become that trusted source of information for them, and it is so important,” Dr. Baldwin said. “There is room for everybody in this space, and we need all of you.”
Proactive steps for protection
Dr. Baldwin then went through the details of what people should do now to make things easier in the event of an attack later. “The best defense is a good offense,” Dr. Baldwin said, “so make sure all of your accounts are secure.”
She recommended the following steps:
- Use two-factor authentication for all of your logins.
- Use strong, unique passwords for all of your logins.
- Use strong privacy settings on all of your private social media profiles, such as making sure photos are not visible on your personal Facebook account.
- Claim your Google profile and Yelp business profile.
- Claim your doctor and/or business profile on all of the medical review sites where you have one, including Google, Healthgrades, Vitals, RateMDs, and WebMD.
For doctors who are attacked specifically because of pro-vaccine advocacy, Dr. Baldwin recommended contacting Shots Heard Round The World, a site that was created by a physician whose practice was attacked by anti-vaccine activists. The site also has a toolkit that anyone can download for tips on preparing ahead for possible attacks and what to do if you are attacked.
Dr. Baldwin then reviewed how to set up different social media profiles to automatically hide certain comments, including comments with words commonly used by online harassers and trolls:
- Sheep
- Sheeple
- Pharma
- Shill
- Die
- Psychopath
- Clown
- Various curse words
- The clown emoji
In Instagram, go to “Settings and privacy —> Hidden Words” for options on hiding offensive comments and messages and for managing custom words and phrases that should be automatically hidden.
On Facebook, go to “Professional dashboard —> Moderation Assist,” where you can add or edit criteria to automatically hide comments on your Facebook page. In addition to hiding comments with certain keywords, you can hide comments from new accounts, accounts without profile photos, or accounts with no friends or followers.
On TikTok, click the three-line menu icon in the upper right, and choose “Privacy —> Comments —> Filter keywords.”
On the platform formerly known as Twitter, go to “Settings and privacy —> Privacy and safety —> Mute and block —> Muted words.”
On YouTube, under “Manage your community & comments,” select “Learn about comment settings.”
Dr. Baldwin did not discourage doctors from posting about controversial topics, but she said it’s important to know what they are so that you can be prepared for the possibility that a post about one of these topics could lead to online harassment. These hot button topics include vaccines, firearm safety, gender-affirming care, reproductive choice, safe sleep/bedsharing, breastfeeding, and COVID masks.
If you do post on one of these and suspect it could result in harassment, Dr. Baldwin recommends turning on your notifications so you know when attacks begin, alerting your office and call center staff if you think they might receive calls, and, when possible, post your content at a time when you’re more likely to be able to monitor the post. She acknowledged that this last tip isn’t always relevant since attacks can take a few days to start or gain steam.
Defending yourself in an attack
Even after taking all these precautions, it’s not possible to altogether prevent an attack from happening, so Dr. Baldwin provided suggestions on what to do if one occurs, starting with taking a deep breath.
“If you are attacked, first of all, please remain calm, which is a lot easier said than done,” she said. “But know that this too shall pass. These things do come to an end.”
She advises you to get help if you need it, enlisting friends or colleagues to help with moderation and banning/blocking. If necessary, alert your employer to the attack, as attackers may contact your employer. Some people may opt to turn off comments on their post, but doing so “is a really personal decision,” she said. It’s okay to turn off comments if you don’t have the bandwidth or help to deal with them.
However, Dr. Baldwin said she never turns off comments because she wants to be able to ban and block people to reduce the likelihood of a future attack from them, and each comment brings the post higher in the algorithm so that more people are able to see the original content. “So sometimes these things are actually a blessing in disguise,” she said.
If you do have comments turned on, take screenshots of the most egregious or threatening ones and then report them and ban/block them. The screenshots are evidence since blocking will remove the comment.
“Take breaks when you need to,” she said. “Don’t stay up all night” since there are only going to be more in the morning, and if you’re using keywords to help hide many of these comments, that will hide them from your followers while you’re away. She also advised monitoring your online reviews at doctor/practice review sites so you know whether you’re receiving spurious reviews that need to be removed.
Dr. Baldwin also addressed how to handle trolls, the people online who intentionally antagonize others with inflammatory, irrelevant, offensive, or otherwise disruptive comments or content. The No. 1 rule is not to engage – “Don’t feed the trolls” – but Dr. Baldwin acknowledged that she can find that difficult sometimes. So she uses kindness or humor to defuse them or calls them out on their inaccurate information and then thanks them for their engagement. Don’t forget that you are in charge of your own page, so any complaints about “censorship” or infringing “free speech” aren’t relevant.
If the comments are growing out of control and you’re unable to manage them, multiple social media platforms have options for limited interactions or who can comment on your page.
On Instagram under “Settings and privacy,” check out “Limited interactions,” “Comments —> Allow comments from,” and “Tags and mentions” to see ways you can limit who is able to comment, tag or mention your account. If you need a complete break, you can turn off commenting by clicking the three dots in the upper right corner of the post, or make your account temporarily private under “Settings and privacy —> Account privacy.”
On Facebook, click the three dots in the upper right corner of posts to select “Who can comment on your post?” Also, under “Settings —> Privacy —> Your Activity,” you can adjust who sees your future posts. Again, if things are out of control, you can temporarily deactivate your page under “Settings —> Privacy —> Facebook Page information.”
On TikTok, click the three lines in the upper right corner of your profile and select “Privacy —> Comments” to adjust who can comment and to filter comments. Again, you can make your account private under “Settings and privacy —> Privacy —> Private account.”
On the platform formerly known as Twitter, click the three dots in the upper right corner of the tweet to change who can reply to the tweet. If you select “Only people you mentioned,” then no one can reply if you did not mention anyone. You can control tagging under “Settings and privacy —> Privacy and safety —> Audience and tagging.”
If you or your practice receive false reviews on review sites, report the reviews and alert the rating site when you can. In the meantime, lock down your private social media accounts and ensure that no photos of your family are publicly available.
Social media self-care
Dr. Baldwin acknowledged that experiencing a social media attack can be intense and even frightening, but it’s rare and outweighed by the “hundreds and hundreds and hundreds of positive comments all the time.” She also reminded attendees that being on social media doesn’t mean being there all the time.
“Over time, my use of social media has certainly changed. It ebbs and flows,” she said. “There are times when I have a lot of bandwidth and I’m posting a lot, and then I actually have had some struggles with my own mental health, with some anxiety and mild depression, so I took a break from social media for a while. When I came back, I posted about my mental health struggles, and you wouldn’t believe how many people were so appreciative of that.”
Accurate information from a trusted source
Ultimately, Dr. Baldwin sees her work online as an extension of her work educating patients.
“This is where our patients are. They are in your office for maybe 10-15 minutes maybe once a year, but they are on these platforms every single day for hours,” she said. “They need to see this information from medical professionals because there are random people out there that are telling them [misinformation].”
Elizabeth Murray, DO, MBA, an emergency medicine pediatrician at Golisano Children’s Hospital at the University of Rochester, agreed that there’s substantial value in doctors sharing accurate information online.
“Disinformation and misinformation is rampant, and at the end of the day, we know the facts,” Dr. Murray said. “We know what parents want to hear and what they want to learn about, so we need to share that information and get the facts out there.”
Dr. Murray found the session very helpful because there’s so much to learn across different social media platforms and it can feel overwhelming if you aren’t familiar with the tools.
“Social media is always going to be here. We need to learn to live with all of these platforms,” Dr. Murray said. “That’s a skill set. We need to learn the skills and teach our kids the skill set. You never really know what you might put out there that, in your mind is innocent or very science-based, that for whatever reason somebody might take issue with. You might as well be ready because we’re all about prevention in pediatrics.”
There were no funders for the presentation. Dr. Baldwin and Dr. Murray had no disclosures.
AT AAP 2023
Postmenopausal stress linked to mood, cognitive symptoms
PHILADELPHIA – , according to research presented at the annual meeting of the Menopause Society (formerly the North American Menopause Society).
“This work suggests that markers of hypothalamic-pituitary-axis activation that capture total cortisol secretion over multiple months, [such as] hair cortisol, strongly correlate with cognitive performance on attention and working memory tasks, whereas measures of more acute cortisol, [such as] salivary cortisol, may be more strongly associated with depression symptom severity and verbal learning,” Christina Metcalf, PhD, an assistant professor of psychiatry in the Colorado Center for Women’s Behavioral Health and Wellness at the University of Colorado at Denver, Aurora, told attendees. “Given the associations with chronic stress, there’s a lot of potential here to increase our knowledge about how women are doing and managing stress and life stressors during this life transition,” she said.
The study involved collecting hair and saliva samples from 43 healthy women in late perimenopause or early postmenopause with an average age of 51. The participants were predominantly white and college educated. The hair sample was taken within 2 cm of the scalp, and the saliva samples were collected the day after the hair sample collection, at the start and end of a 30-minute rest period that took place between 2:00 and 3:00 p.m. local time.
All the participants had an intact uterus and at least one ovary. None of the participants were current smokers or had recent alcohol or drug dependence, and none had used hormones within the previous 6 months. The study also excluded women who were pregnant or breastfeeding, who had bleached hair or no hair, who were taking steroids, beta blockers or opioid medication, and who had recently taken NSAIDS.
Measuring hair cortisol more feasible
The study was conducted remotely, with participants using video conferencing to communicate with the study personnel and then completing study procedures at home, including 2 days of cognitive testing with the California Verbal Learning Test – Third Edition and the n-back and continuous performance tasks. The participants also completed the Center for Epidemiologic Studies Depression Scale (CES-D).
Participants with higher levels of hair cortisol and salivary cortisol also had more severe depression symptoms (P < .001). Hair cortisol was also significantly associated with attention and working memory: Women with higher levels had fewer correct answers on the 0-back and 1-back trials (P < .01) and made more mistakes on the 2-back trial (P < .001). They also scored with less specificity on the continuous performance tasks (P = .022).
Although no association existed between hair cortisol levels and verbal learning or verbal memory (P > .05), participants with higher hair cortisol did score worse on the immediate recall trials (P = .034). Salivary cortisol levels, on the other hand, showed no association with memory recall trials, attention or working memory (P > .05).
Measuring cortisol from hair samples is more feasible than using saliva samples and may offer valuable insights regarding hypothalamic-pituitary-axis activity “to consider alongside the cognitive and mental health of late peri-/early postmenopausal women,” Dr. Metcalf told attendees. The next step is to find out whether the hypothalamic-pituitary-axis axis is a modifiable biomarker that can be used to improve executive function.
The study was limited by its small population, its cross-sectional design, and the lack of covariates in the current analyses.
Monitor symptoms in midlife
Hadine Joffe, MD, MSc, a professor of psychiatry and executive director of the Mary Horrigan Connors Center for Women’s Health and Gender Biology at Brigham and Women’s Hospital and Harvard Medical School, both in Boston, said the study findings were not surprising given how common the complaints of stress and depressive symptoms are.
“Mood changes are linked with acute, immediate cortisol levels at the same point in time, and cognitive symptoms were linked to more chronically elevated cortisol levels,” Dr. Joffe said in an interview. “Women and their providers should monitor for these challenging brain symptoms in midlife as they affect performance and quality of life and are linked with changes in the HPA axis as stress biomarkers.”
Because the study is small and has a cross-sectional design, it’s not possible to determine the direction of the associations or to make any inferences about causation, Dr. Joffe said.
“We cannot make the conclusion that stress is adversely affecting mood and cognitive performance given the design limitations. It is possible that mood and cognitive issues contributed to these stress markers,” Dr. Joffe said.“However, it is known that the experience of stress is linked with vulnerability to mood and cognitive symptoms, and also that mood and cognitive symptoms induce significant stress.”
The research was funded by the Menopause Society, Colorado University, the Ludeman Family Center for Women’s Health Research, the National Institute of Mental Health, and the National Institute of Aging. Dr. Metcalf had no disclosures. Dr. Joffe has received grant support from Merck, Pfizer and Sage, and has been a consultant or advisor for Bayer, Merck and Hello Therapeutics.
PHILADELPHIA – , according to research presented at the annual meeting of the Menopause Society (formerly the North American Menopause Society).
“This work suggests that markers of hypothalamic-pituitary-axis activation that capture total cortisol secretion over multiple months, [such as] hair cortisol, strongly correlate with cognitive performance on attention and working memory tasks, whereas measures of more acute cortisol, [such as] salivary cortisol, may be more strongly associated with depression symptom severity and verbal learning,” Christina Metcalf, PhD, an assistant professor of psychiatry in the Colorado Center for Women’s Behavioral Health and Wellness at the University of Colorado at Denver, Aurora, told attendees. “Given the associations with chronic stress, there’s a lot of potential here to increase our knowledge about how women are doing and managing stress and life stressors during this life transition,” she said.
The study involved collecting hair and saliva samples from 43 healthy women in late perimenopause or early postmenopause with an average age of 51. The participants were predominantly white and college educated. The hair sample was taken within 2 cm of the scalp, and the saliva samples were collected the day after the hair sample collection, at the start and end of a 30-minute rest period that took place between 2:00 and 3:00 p.m. local time.
All the participants had an intact uterus and at least one ovary. None of the participants were current smokers or had recent alcohol or drug dependence, and none had used hormones within the previous 6 months. The study also excluded women who were pregnant or breastfeeding, who had bleached hair or no hair, who were taking steroids, beta blockers or opioid medication, and who had recently taken NSAIDS.
Measuring hair cortisol more feasible
The study was conducted remotely, with participants using video conferencing to communicate with the study personnel and then completing study procedures at home, including 2 days of cognitive testing with the California Verbal Learning Test – Third Edition and the n-back and continuous performance tasks. The participants also completed the Center for Epidemiologic Studies Depression Scale (CES-D).
Participants with higher levels of hair cortisol and salivary cortisol also had more severe depression symptoms (P < .001). Hair cortisol was also significantly associated with attention and working memory: Women with higher levels had fewer correct answers on the 0-back and 1-back trials (P < .01) and made more mistakes on the 2-back trial (P < .001). They also scored with less specificity on the continuous performance tasks (P = .022).
Although no association existed between hair cortisol levels and verbal learning or verbal memory (P > .05), participants with higher hair cortisol did score worse on the immediate recall trials (P = .034). Salivary cortisol levels, on the other hand, showed no association with memory recall trials, attention or working memory (P > .05).
Measuring cortisol from hair samples is more feasible than using saliva samples and may offer valuable insights regarding hypothalamic-pituitary-axis activity “to consider alongside the cognitive and mental health of late peri-/early postmenopausal women,” Dr. Metcalf told attendees. The next step is to find out whether the hypothalamic-pituitary-axis axis is a modifiable biomarker that can be used to improve executive function.
The study was limited by its small population, its cross-sectional design, and the lack of covariates in the current analyses.
Monitor symptoms in midlife
Hadine Joffe, MD, MSc, a professor of psychiatry and executive director of the Mary Horrigan Connors Center for Women’s Health and Gender Biology at Brigham and Women’s Hospital and Harvard Medical School, both in Boston, said the study findings were not surprising given how common the complaints of stress and depressive symptoms are.
“Mood changes are linked with acute, immediate cortisol levels at the same point in time, and cognitive symptoms were linked to more chronically elevated cortisol levels,” Dr. Joffe said in an interview. “Women and their providers should monitor for these challenging brain symptoms in midlife as they affect performance and quality of life and are linked with changes in the HPA axis as stress biomarkers.”
Because the study is small and has a cross-sectional design, it’s not possible to determine the direction of the associations or to make any inferences about causation, Dr. Joffe said.
“We cannot make the conclusion that stress is adversely affecting mood and cognitive performance given the design limitations. It is possible that mood and cognitive issues contributed to these stress markers,” Dr. Joffe said.“However, it is known that the experience of stress is linked with vulnerability to mood and cognitive symptoms, and also that mood and cognitive symptoms induce significant stress.”
The research was funded by the Menopause Society, Colorado University, the Ludeman Family Center for Women’s Health Research, the National Institute of Mental Health, and the National Institute of Aging. Dr. Metcalf had no disclosures. Dr. Joffe has received grant support from Merck, Pfizer and Sage, and has been a consultant or advisor for Bayer, Merck and Hello Therapeutics.
PHILADELPHIA – , according to research presented at the annual meeting of the Menopause Society (formerly the North American Menopause Society).
“This work suggests that markers of hypothalamic-pituitary-axis activation that capture total cortisol secretion over multiple months, [such as] hair cortisol, strongly correlate with cognitive performance on attention and working memory tasks, whereas measures of more acute cortisol, [such as] salivary cortisol, may be more strongly associated with depression symptom severity and verbal learning,” Christina Metcalf, PhD, an assistant professor of psychiatry in the Colorado Center for Women’s Behavioral Health and Wellness at the University of Colorado at Denver, Aurora, told attendees. “Given the associations with chronic stress, there’s a lot of potential here to increase our knowledge about how women are doing and managing stress and life stressors during this life transition,” she said.
The study involved collecting hair and saliva samples from 43 healthy women in late perimenopause or early postmenopause with an average age of 51. The participants were predominantly white and college educated. The hair sample was taken within 2 cm of the scalp, and the saliva samples were collected the day after the hair sample collection, at the start and end of a 30-minute rest period that took place between 2:00 and 3:00 p.m. local time.
All the participants had an intact uterus and at least one ovary. None of the participants were current smokers or had recent alcohol or drug dependence, and none had used hormones within the previous 6 months. The study also excluded women who were pregnant or breastfeeding, who had bleached hair or no hair, who were taking steroids, beta blockers or opioid medication, and who had recently taken NSAIDS.
Measuring hair cortisol more feasible
The study was conducted remotely, with participants using video conferencing to communicate with the study personnel and then completing study procedures at home, including 2 days of cognitive testing with the California Verbal Learning Test – Third Edition and the n-back and continuous performance tasks. The participants also completed the Center for Epidemiologic Studies Depression Scale (CES-D).
Participants with higher levels of hair cortisol and salivary cortisol also had more severe depression symptoms (P < .001). Hair cortisol was also significantly associated with attention and working memory: Women with higher levels had fewer correct answers on the 0-back and 1-back trials (P < .01) and made more mistakes on the 2-back trial (P < .001). They also scored with less specificity on the continuous performance tasks (P = .022).
Although no association existed between hair cortisol levels and verbal learning or verbal memory (P > .05), participants with higher hair cortisol did score worse on the immediate recall trials (P = .034). Salivary cortisol levels, on the other hand, showed no association with memory recall trials, attention or working memory (P > .05).
Measuring cortisol from hair samples is more feasible than using saliva samples and may offer valuable insights regarding hypothalamic-pituitary-axis activity “to consider alongside the cognitive and mental health of late peri-/early postmenopausal women,” Dr. Metcalf told attendees. The next step is to find out whether the hypothalamic-pituitary-axis axis is a modifiable biomarker that can be used to improve executive function.
The study was limited by its small population, its cross-sectional design, and the lack of covariates in the current analyses.
Monitor symptoms in midlife
Hadine Joffe, MD, MSc, a professor of psychiatry and executive director of the Mary Horrigan Connors Center for Women’s Health and Gender Biology at Brigham and Women’s Hospital and Harvard Medical School, both in Boston, said the study findings were not surprising given how common the complaints of stress and depressive symptoms are.
“Mood changes are linked with acute, immediate cortisol levels at the same point in time, and cognitive symptoms were linked to more chronically elevated cortisol levels,” Dr. Joffe said in an interview. “Women and their providers should monitor for these challenging brain symptoms in midlife as they affect performance and quality of life and are linked with changes in the HPA axis as stress biomarkers.”
Because the study is small and has a cross-sectional design, it’s not possible to determine the direction of the associations or to make any inferences about causation, Dr. Joffe said.
“We cannot make the conclusion that stress is adversely affecting mood and cognitive performance given the design limitations. It is possible that mood and cognitive issues contributed to these stress markers,” Dr. Joffe said.“However, it is known that the experience of stress is linked with vulnerability to mood and cognitive symptoms, and also that mood and cognitive symptoms induce significant stress.”
The research was funded by the Menopause Society, Colorado University, the Ludeman Family Center for Women’s Health Research, the National Institute of Mental Health, and the National Institute of Aging. Dr. Metcalf had no disclosures. Dr. Joffe has received grant support from Merck, Pfizer and Sage, and has been a consultant or advisor for Bayer, Merck and Hello Therapeutics.
AT NAMS 2023
Fathers’ postpartum depression linked to children’s adversity
WASHINGTON – , according to research presented at the annual meeting of the American Academy of Pediatrics.
The findings held even after taking into account postpartum depression in the child’s mother and other factors that might increase risk of adverse childhood experiences, reported Kristine H. Schmitz, MD, an assistant professor of pediatrics at Robert Wood Johnson Medical School, New Brunswick, N.J.
Paternal postpartum depression has not been studied very well, so it’s difficult to pin down its prevalence, but some research has found rates as high as 25%, Dr. Schmitz told attendees.
”We recognize that it’s very under-recognized and often under-reported, but we also know that it has lots of downstream effects on child outcomes, including difficulties with parenting, difficulties with child behavior, as well as school performance and school attainment and employment,” Dr. Schmitz said.
Paternal depression and adverse childhood experiences
The study involved an analysis of six waves of data from the Future of Families & Child Wellbeing Study, which follows a national cohort of children born in large U.S. cities between 1998 and 2000. The cohort includes an intentional over-representation of unmarried mothers, who make up about 75% of the overall population.
The researchers used the World Health Organization’s Composite International Diagnosis Interview Short Form (CIDI-SF) to assess fathers’ depression when their children were 1 year old. Then the researchers looked at the number of adverse childhood experiences (ACEs) children had at 5 years old.
The analysis was adjusted to account for the child’s sex and the father’s age, race/ethnicity, and education as well as whether he was born inside or outside the United States. The findings were also adjusted for the whether the child’s parents were married or cohabiting, whether the child had low birth weight, whether the birth was covered by Medicaid, and whether the mother had postpartum depression.
Among the 1,933 pairs of fathers and children in the analysis, nearly half the fathers were non-Hispanic Black (48%) and more than half (64%) had a high school education or lower level of education. Medicaid paid for half the children’s births.
Nine percent of the fathers experienced depression during their child’s first year, and 70% of the children had at least one ACE at 5 years old. Two in five children (39%) had two ACEs at age 5, and 21% of children had three ACEs.
Children were twice as likely to have three ACEs at 5 years old if their father had depression during the child’s first year (adjusted odds ratio, 2.04; 95% confidence interval, 1.42-2.93). Paternal depression was also significantly associated with children having one ACE (OR, 2.35; 95% CI, 1.45-3.81) and two ACES (OR, 1.89; 95% CI, 1.35-2.63) at age 5.
The ACE with the highest association with paternal depression was the father’s absence from children’s lives (aOR, 2.65; 95% CI, 1.74-4.04). In addition, children of fathers with depression had 60% greater odds of exposure to substance use (aOR, 1.6; 95% CI, 1.08-2.34).
Children also had greater odds of child maltreatment at age 5 if their father had depression in their child’s first year. Odds were greater for psychological maltreatment (aOR, 1.55; 95% CI, 1.02-2.34), neglect (aOR, 1.63; 95% CI, 1.08-2.46), and physical maltreatment (aOR, 1.56; 95% CI, 1.04-2.35). The researchers did not find any association between paternal depression and the ACEs of sexual maltreatment, maternal depression, incarceration of someone in the home, or violence toward the mother.
”We know that dads play a critical role in the family,” Dr. Schmitz said. “We as pediatricians have a really unique position with families, and we should capitalize on that opportunity to engage with fathers just like we do with mothers and postpartum depression. Hopefully by doing that, we’ll reduce hardships for children and families down the road.”
Dr. Schmitz also said it’s important for pediatricians to advocate at a policy level “to really include dads more explicitly in maternal and child health policy and advocate for better father-focused interventions from father-focused research.” She further acknowledged the stigma that exists around men’s mental health in general and the need to find out the best ways to help overcome that stigma.
‘Concerning’ findings may suggest a need for screening
Jason Terk, MD, a pediatrician practicing in north Texas and past president of the Texas Pediatric Society, was not surprised to see a link between depression in fathers and adversity in their children. Dr. Terk was not involved in the research but noted that the 9% rate of paternal depression seen in the study is similar to national rates of depression in U.S. adults.
“I think that the presence of paternal depression being associated with ACEs in their children in their first 5 years of life is certainly concerning and worthy of intervention for both the fathers and their children,” Dr. Terk said. “The key take-home message for clinicians who care for infants and small children is that the presence of paternal depression should increase awareness of adverse effects on those children. We need to consider screening for this at 12 months of age in much the same way we screen for maternal depression for younger infants.”
Dr. Terk noted one limitation of the study was that it didn’t suggest any specific risk factors pediatricians might look for to increase surveillance of potential depression in fathers.
“Also, unlike maternal depression, in which moms may be connected with their obstetricians if they screen positive on an Edinburgh questionnaire, we will be hard-pressed to know where to refer dads who are found to be depressed when their babies are 12 months old,” Dr. Terk said. “Screening must lead to helpful responses if the screening reveals a problem.”
The research was funded by the Robert Wood Johnson Foundation, the National Institutes of Health, and the Health Resources and Services Administration. Dr. Schmitz had no disclosures. Dr. Terk has been a speaker for Sanofi on a topic unrelated to this research.
WASHINGTON – , according to research presented at the annual meeting of the American Academy of Pediatrics.
The findings held even after taking into account postpartum depression in the child’s mother and other factors that might increase risk of adverse childhood experiences, reported Kristine H. Schmitz, MD, an assistant professor of pediatrics at Robert Wood Johnson Medical School, New Brunswick, N.J.
Paternal postpartum depression has not been studied very well, so it’s difficult to pin down its prevalence, but some research has found rates as high as 25%, Dr. Schmitz told attendees.
”We recognize that it’s very under-recognized and often under-reported, but we also know that it has lots of downstream effects on child outcomes, including difficulties with parenting, difficulties with child behavior, as well as school performance and school attainment and employment,” Dr. Schmitz said.
Paternal depression and adverse childhood experiences
The study involved an analysis of six waves of data from the Future of Families & Child Wellbeing Study, which follows a national cohort of children born in large U.S. cities between 1998 and 2000. The cohort includes an intentional over-representation of unmarried mothers, who make up about 75% of the overall population.
The researchers used the World Health Organization’s Composite International Diagnosis Interview Short Form (CIDI-SF) to assess fathers’ depression when their children were 1 year old. Then the researchers looked at the number of adverse childhood experiences (ACEs) children had at 5 years old.
The analysis was adjusted to account for the child’s sex and the father’s age, race/ethnicity, and education as well as whether he was born inside or outside the United States. The findings were also adjusted for the whether the child’s parents were married or cohabiting, whether the child had low birth weight, whether the birth was covered by Medicaid, and whether the mother had postpartum depression.
Among the 1,933 pairs of fathers and children in the analysis, nearly half the fathers were non-Hispanic Black (48%) and more than half (64%) had a high school education or lower level of education. Medicaid paid for half the children’s births.
Nine percent of the fathers experienced depression during their child’s first year, and 70% of the children had at least one ACE at 5 years old. Two in five children (39%) had two ACEs at age 5, and 21% of children had three ACEs.
Children were twice as likely to have three ACEs at 5 years old if their father had depression during the child’s first year (adjusted odds ratio, 2.04; 95% confidence interval, 1.42-2.93). Paternal depression was also significantly associated with children having one ACE (OR, 2.35; 95% CI, 1.45-3.81) and two ACES (OR, 1.89; 95% CI, 1.35-2.63) at age 5.
The ACE with the highest association with paternal depression was the father’s absence from children’s lives (aOR, 2.65; 95% CI, 1.74-4.04). In addition, children of fathers with depression had 60% greater odds of exposure to substance use (aOR, 1.6; 95% CI, 1.08-2.34).
Children also had greater odds of child maltreatment at age 5 if their father had depression in their child’s first year. Odds were greater for psychological maltreatment (aOR, 1.55; 95% CI, 1.02-2.34), neglect (aOR, 1.63; 95% CI, 1.08-2.46), and physical maltreatment (aOR, 1.56; 95% CI, 1.04-2.35). The researchers did not find any association between paternal depression and the ACEs of sexual maltreatment, maternal depression, incarceration of someone in the home, or violence toward the mother.
”We know that dads play a critical role in the family,” Dr. Schmitz said. “We as pediatricians have a really unique position with families, and we should capitalize on that opportunity to engage with fathers just like we do with mothers and postpartum depression. Hopefully by doing that, we’ll reduce hardships for children and families down the road.”
Dr. Schmitz also said it’s important for pediatricians to advocate at a policy level “to really include dads more explicitly in maternal and child health policy and advocate for better father-focused interventions from father-focused research.” She further acknowledged the stigma that exists around men’s mental health in general and the need to find out the best ways to help overcome that stigma.
‘Concerning’ findings may suggest a need for screening
Jason Terk, MD, a pediatrician practicing in north Texas and past president of the Texas Pediatric Society, was not surprised to see a link between depression in fathers and adversity in their children. Dr. Terk was not involved in the research but noted that the 9% rate of paternal depression seen in the study is similar to national rates of depression in U.S. adults.
“I think that the presence of paternal depression being associated with ACEs in their children in their first 5 years of life is certainly concerning and worthy of intervention for both the fathers and their children,” Dr. Terk said. “The key take-home message for clinicians who care for infants and small children is that the presence of paternal depression should increase awareness of adverse effects on those children. We need to consider screening for this at 12 months of age in much the same way we screen for maternal depression for younger infants.”
Dr. Terk noted one limitation of the study was that it didn’t suggest any specific risk factors pediatricians might look for to increase surveillance of potential depression in fathers.
“Also, unlike maternal depression, in which moms may be connected with their obstetricians if they screen positive on an Edinburgh questionnaire, we will be hard-pressed to know where to refer dads who are found to be depressed when their babies are 12 months old,” Dr. Terk said. “Screening must lead to helpful responses if the screening reveals a problem.”
The research was funded by the Robert Wood Johnson Foundation, the National Institutes of Health, and the Health Resources and Services Administration. Dr. Schmitz had no disclosures. Dr. Terk has been a speaker for Sanofi on a topic unrelated to this research.
WASHINGTON – , according to research presented at the annual meeting of the American Academy of Pediatrics.
The findings held even after taking into account postpartum depression in the child’s mother and other factors that might increase risk of adverse childhood experiences, reported Kristine H. Schmitz, MD, an assistant professor of pediatrics at Robert Wood Johnson Medical School, New Brunswick, N.J.
Paternal postpartum depression has not been studied very well, so it’s difficult to pin down its prevalence, but some research has found rates as high as 25%, Dr. Schmitz told attendees.
”We recognize that it’s very under-recognized and often under-reported, but we also know that it has lots of downstream effects on child outcomes, including difficulties with parenting, difficulties with child behavior, as well as school performance and school attainment and employment,” Dr. Schmitz said.
Paternal depression and adverse childhood experiences
The study involved an analysis of six waves of data from the Future of Families & Child Wellbeing Study, which follows a national cohort of children born in large U.S. cities between 1998 and 2000. The cohort includes an intentional over-representation of unmarried mothers, who make up about 75% of the overall population.
The researchers used the World Health Organization’s Composite International Diagnosis Interview Short Form (CIDI-SF) to assess fathers’ depression when their children were 1 year old. Then the researchers looked at the number of adverse childhood experiences (ACEs) children had at 5 years old.
The analysis was adjusted to account for the child’s sex and the father’s age, race/ethnicity, and education as well as whether he was born inside or outside the United States. The findings were also adjusted for the whether the child’s parents were married or cohabiting, whether the child had low birth weight, whether the birth was covered by Medicaid, and whether the mother had postpartum depression.
Among the 1,933 pairs of fathers and children in the analysis, nearly half the fathers were non-Hispanic Black (48%) and more than half (64%) had a high school education or lower level of education. Medicaid paid for half the children’s births.
Nine percent of the fathers experienced depression during their child’s first year, and 70% of the children had at least one ACE at 5 years old. Two in five children (39%) had two ACEs at age 5, and 21% of children had three ACEs.
Children were twice as likely to have three ACEs at 5 years old if their father had depression during the child’s first year (adjusted odds ratio, 2.04; 95% confidence interval, 1.42-2.93). Paternal depression was also significantly associated with children having one ACE (OR, 2.35; 95% CI, 1.45-3.81) and two ACES (OR, 1.89; 95% CI, 1.35-2.63) at age 5.
The ACE with the highest association with paternal depression was the father’s absence from children’s lives (aOR, 2.65; 95% CI, 1.74-4.04). In addition, children of fathers with depression had 60% greater odds of exposure to substance use (aOR, 1.6; 95% CI, 1.08-2.34).
Children also had greater odds of child maltreatment at age 5 if their father had depression in their child’s first year. Odds were greater for psychological maltreatment (aOR, 1.55; 95% CI, 1.02-2.34), neglect (aOR, 1.63; 95% CI, 1.08-2.46), and physical maltreatment (aOR, 1.56; 95% CI, 1.04-2.35). The researchers did not find any association between paternal depression and the ACEs of sexual maltreatment, maternal depression, incarceration of someone in the home, or violence toward the mother.
”We know that dads play a critical role in the family,” Dr. Schmitz said. “We as pediatricians have a really unique position with families, and we should capitalize on that opportunity to engage with fathers just like we do with mothers and postpartum depression. Hopefully by doing that, we’ll reduce hardships for children and families down the road.”
Dr. Schmitz also said it’s important for pediatricians to advocate at a policy level “to really include dads more explicitly in maternal and child health policy and advocate for better father-focused interventions from father-focused research.” She further acknowledged the stigma that exists around men’s mental health in general and the need to find out the best ways to help overcome that stigma.
‘Concerning’ findings may suggest a need for screening
Jason Terk, MD, a pediatrician practicing in north Texas and past president of the Texas Pediatric Society, was not surprised to see a link between depression in fathers and adversity in their children. Dr. Terk was not involved in the research but noted that the 9% rate of paternal depression seen in the study is similar to national rates of depression in U.S. adults.
“I think that the presence of paternal depression being associated with ACEs in their children in their first 5 years of life is certainly concerning and worthy of intervention for both the fathers and their children,” Dr. Terk said. “The key take-home message for clinicians who care for infants and small children is that the presence of paternal depression should increase awareness of adverse effects on those children. We need to consider screening for this at 12 months of age in much the same way we screen for maternal depression for younger infants.”
Dr. Terk noted one limitation of the study was that it didn’t suggest any specific risk factors pediatricians might look for to increase surveillance of potential depression in fathers.
“Also, unlike maternal depression, in which moms may be connected with their obstetricians if they screen positive on an Edinburgh questionnaire, we will be hard-pressed to know where to refer dads who are found to be depressed when their babies are 12 months old,” Dr. Terk said. “Screening must lead to helpful responses if the screening reveals a problem.”
The research was funded by the Robert Wood Johnson Foundation, the National Institutes of Health, and the Health Resources and Services Administration. Dr. Schmitz had no disclosures. Dr. Terk has been a speaker for Sanofi on a topic unrelated to this research.
AT AAP 2023
Metabolic effects of estetrol are promising in postmenopausal women
PHILADELPHIA – presented at the annual meeting of the Menopause Society (formerly The North American Menopause Society).
Participants taking estetrol experienced a decrease in hemoglobin A1c, fasting plasma glucose, total cholesterol, LDL and lipoprotein as well as an increase in HDL cholesterol, according to the findings presented by Wolf Utian, MD, PhD, DSC, a professor emeritus of reproductive biology at Case Western Reserve University, Cleveland, and medical director emeritus of the Menopause Society.
A separate poster at the conference from the same trial also reported significant improvements from estetrol in quality of life, including that related to vasomotor symptoms, and several psychosocial and sexual functioning areas.
E4 is already available as combination oral contraception and is now being considered for treating vasomotor symptoms, explained Chrisandra Shufelt, MD, professor and chair of general internal of medicine and associate director of the Women’s Health Research Center at Mayo Clinic Florida, who was not involved in the study.
Background on estetrol
E4 is a human fetal liver estrogen produced during pregnancy that’s synthesized from plants for pharmaceutical use, including as the oral contraceptive drospirenone, Dr. Utian told attendees. It’s classified as a native estrogen with selective tissue activity (NEST), he said.
“E4 is a completely different native estrogen with oral administration mimicking the benefits of transdermals and hence safe and effective,” Dr. Utian said in an interview. “It would be a significant new addition to the pharmaceutical armamentarium.”
Two phase 3 trials presented by Dr. Utian at the same conference last year found estetrol reduced the frequency and severity of moderate to severe vasomotor symptoms, and a previous phase 2 trial finding vasomotor and genitourinary symptom benefits suggested it had potential benefits for lipids, carbohydrate metabolism, and bone turnover.
“In summary, E4 at a daily dose of 15 mg exhibited estrogenic effects in the vagina, leading to improved vaginal health and reduced signs of atrophy, emerging as a promising treatment option not only for vasomotor symptoms but also for other significant menopausal symptoms,” Dr. Utian said. “E4 could offer comprehensive relief for women experiencing a range of menopause-related discomforts.”
Dr. Utian also referenced a 2017 trial in which estetrol positively impacted lipid profiles, “lowering low-density lipoprotein cholesterol, increasing high-density lipoprotein cholesterol, and showing minimal influence on triglycerides,” he said. “Importantly, estetrol was associated with a significant decrease in osteocalcin levels in the higher dose groups, suggesting a potential preventive effect on bone loss,” he added. A recent review of the overall evidence on estetrol suggests its use is “promising,” Dr. Utian noted.
Current trial
His current randomized controlled phase 3 trial included postmenopausal women ages 40-65 from 151 sites in 14 countries in Europe, Latin America, and North America, and Russia. Among the 640 participants in the trial, 213 women randomly received 15 mg of estetrol, 213 women received 20 mg of estetrol, and 214 women received a placebo every day for 3 months. All women without hysterectomies also received 200 mg of progesterone once daily for two weeks after completing the estetrol treatment to protect the endometrium.
Researchers took blood samples from the participants at baseline and week 12 to assess total cholesterol, LDL, HDL, the total cholesterol/HDL ratio, triglycerides, lipoprotein A, fasting plasma glucose, insulin, and A1c.
Compared with women in the placebo group, women in both the 15 mg and 20 mg groups saw a statistically significant decrease in lipoprotein A and in the ratio of total cholesterol to HDL, and a statistically significant increase in HDL. Only the women in the 15 mg group saw a statistically significant decrease in LDL and increase in triglycerides; an increase in triglycerides in the 20 mg group did not reach statistical significance.
Statistically significant decreases in fasting plasma glucose and A1c also occurred in both treatment groups, but a decrease in insulin levels and in the homeostasis model-assessment-estimated insulin resistance (HOMA-IR) seen in both treatment arms did not reach significance.
“While the mean changes after 12 weeks from baseline overall were small changes to the cholesterol and blood sugar profiles, they are clinically meaningful because it suggests that E4 does not have any adverse effects to these measures,” Dr. Shufelt said in an interview. “An advantage is that this gives us another hormone option for vasomotor symptoms since it is a native estrogen with selective tissue.”
It’s too early, however, to determine whether estetrol offers benefits in terms of its safety profile, compared with currently available therapies, Dr. Shufelt said.
”These findings of E4 are similar to how oral estradiol changes lipids, which finds an increase in high-density lipoprotein cholesterol, and decreases plasma concentrations of total and low-density lipoprotein cholesterol. an increase in HDL-C and triglycerides and decrease in LDL-C,” she said.
Poster findings also promising
For the findings reported in the poster, researchers assessed quality of life and the clinical meaningfulness of vasomotor symptoms’ reduction at baseline and 12 weeks using the Menopause-Specific Quality of Life (MENQOL) questionnaire and the Clinical Global Impression questionnaire, respectively. They also assessed women’s self-reported genitourinary symptoms, including vaginal dryness, pain during urination, vaginal pain and bleeding related to sex, and vaginal or vulvar irritation or itching. Most of these findings primarily confirmed previous positive effects from E4 in other trials.
Women in both the 15 mg and 20 mg estetrol groups reported a statistically significant improvement at 12 weeks, compared with placebo, in their total MENQOL score and in the vasomotor, psychosocial, and sexual functioning domain scores (P < .05). Those in the 20 mg group also had a statistically significant improvement in their physical domain score (P < .05).
Although numerical improvements in genitourinary symptoms occurred at 12 weeks across all three groups, the only statistically significant difference from baseline occurred in patients taking 15 mg of estetrol, who experienced a decrease in vaginal dryness and vaginal pain during sex (P = .0142 and P = .003, respectively).
The Clinical Global Impression questionnaire asked women at 4 and 12 weeks to rate on a seven-item Likert scale their response to this question: “Rate the total improvement, whether or not in your judgment it is due entirely to drug treatment. Compared to your condition at admission to the study, how much has it changed?” Responses of “very much improved” and “much improved” counted as a clinically meaningful difference.
Compared with 27.9% of patients in the placebo group, 52.9% of patients in the 15 mg group and 59.8% of patients in the 20 mg group rated the weekly frequency of moderate to severe vasomotor symptoms as “much improved” or “very much improved” at 4 weeks (P < .0001). At 12 weeks, those numbers rose to 47% in the placebo group, 73.3% in the 15 mg group and 77.8% in the 20 mg group (P < .0001).
The trial’s primary limitation at this point is having only a 12-week follow-up, Dr. Shufelt said, though a few other questions remain.
“Because the two phase 3 RCTs included hysterectomized and nonhysterectomized women, it was unclear how many women in the study had E4 alone versus E4 with progesterone, as that might play a role in both cholesterol and carbohydrate metabolism,” Dr. Shufelt said. “While baseline data was not presented, it would also be important to know baseline values for the women and confirm that none were on lipid-lowering medications.”
The research was funded by Estetra SRL, an affiliate of Mithra Pharmaceuticals. Dr. Utian is a member of the Mithra and Elektra Scientific Advisory Boards. Dr. Shufelt has no disclosures.
PHILADELPHIA – presented at the annual meeting of the Menopause Society (formerly The North American Menopause Society).
Participants taking estetrol experienced a decrease in hemoglobin A1c, fasting plasma glucose, total cholesterol, LDL and lipoprotein as well as an increase in HDL cholesterol, according to the findings presented by Wolf Utian, MD, PhD, DSC, a professor emeritus of reproductive biology at Case Western Reserve University, Cleveland, and medical director emeritus of the Menopause Society.
A separate poster at the conference from the same trial also reported significant improvements from estetrol in quality of life, including that related to vasomotor symptoms, and several psychosocial and sexual functioning areas.
E4 is already available as combination oral contraception and is now being considered for treating vasomotor symptoms, explained Chrisandra Shufelt, MD, professor and chair of general internal of medicine and associate director of the Women’s Health Research Center at Mayo Clinic Florida, who was not involved in the study.
Background on estetrol
E4 is a human fetal liver estrogen produced during pregnancy that’s synthesized from plants for pharmaceutical use, including as the oral contraceptive drospirenone, Dr. Utian told attendees. It’s classified as a native estrogen with selective tissue activity (NEST), he said.
“E4 is a completely different native estrogen with oral administration mimicking the benefits of transdermals and hence safe and effective,” Dr. Utian said in an interview. “It would be a significant new addition to the pharmaceutical armamentarium.”
Two phase 3 trials presented by Dr. Utian at the same conference last year found estetrol reduced the frequency and severity of moderate to severe vasomotor symptoms, and a previous phase 2 trial finding vasomotor and genitourinary symptom benefits suggested it had potential benefits for lipids, carbohydrate metabolism, and bone turnover.
“In summary, E4 at a daily dose of 15 mg exhibited estrogenic effects in the vagina, leading to improved vaginal health and reduced signs of atrophy, emerging as a promising treatment option not only for vasomotor symptoms but also for other significant menopausal symptoms,” Dr. Utian said. “E4 could offer comprehensive relief for women experiencing a range of menopause-related discomforts.”
Dr. Utian also referenced a 2017 trial in which estetrol positively impacted lipid profiles, “lowering low-density lipoprotein cholesterol, increasing high-density lipoprotein cholesterol, and showing minimal influence on triglycerides,” he said. “Importantly, estetrol was associated with a significant decrease in osteocalcin levels in the higher dose groups, suggesting a potential preventive effect on bone loss,” he added. A recent review of the overall evidence on estetrol suggests its use is “promising,” Dr. Utian noted.
Current trial
His current randomized controlled phase 3 trial included postmenopausal women ages 40-65 from 151 sites in 14 countries in Europe, Latin America, and North America, and Russia. Among the 640 participants in the trial, 213 women randomly received 15 mg of estetrol, 213 women received 20 mg of estetrol, and 214 women received a placebo every day for 3 months. All women without hysterectomies also received 200 mg of progesterone once daily for two weeks after completing the estetrol treatment to protect the endometrium.
Researchers took blood samples from the participants at baseline and week 12 to assess total cholesterol, LDL, HDL, the total cholesterol/HDL ratio, triglycerides, lipoprotein A, fasting plasma glucose, insulin, and A1c.
Compared with women in the placebo group, women in both the 15 mg and 20 mg groups saw a statistically significant decrease in lipoprotein A and in the ratio of total cholesterol to HDL, and a statistically significant increase in HDL. Only the women in the 15 mg group saw a statistically significant decrease in LDL and increase in triglycerides; an increase in triglycerides in the 20 mg group did not reach statistical significance.
Statistically significant decreases in fasting plasma glucose and A1c also occurred in both treatment groups, but a decrease in insulin levels and in the homeostasis model-assessment-estimated insulin resistance (HOMA-IR) seen in both treatment arms did not reach significance.
“While the mean changes after 12 weeks from baseline overall were small changes to the cholesterol and blood sugar profiles, they are clinically meaningful because it suggests that E4 does not have any adverse effects to these measures,” Dr. Shufelt said in an interview. “An advantage is that this gives us another hormone option for vasomotor symptoms since it is a native estrogen with selective tissue.”
It’s too early, however, to determine whether estetrol offers benefits in terms of its safety profile, compared with currently available therapies, Dr. Shufelt said.
”These findings of E4 are similar to how oral estradiol changes lipids, which finds an increase in high-density lipoprotein cholesterol, and decreases plasma concentrations of total and low-density lipoprotein cholesterol. an increase in HDL-C and triglycerides and decrease in LDL-C,” she said.
Poster findings also promising
For the findings reported in the poster, researchers assessed quality of life and the clinical meaningfulness of vasomotor symptoms’ reduction at baseline and 12 weeks using the Menopause-Specific Quality of Life (MENQOL) questionnaire and the Clinical Global Impression questionnaire, respectively. They also assessed women’s self-reported genitourinary symptoms, including vaginal dryness, pain during urination, vaginal pain and bleeding related to sex, and vaginal or vulvar irritation or itching. Most of these findings primarily confirmed previous positive effects from E4 in other trials.
Women in both the 15 mg and 20 mg estetrol groups reported a statistically significant improvement at 12 weeks, compared with placebo, in their total MENQOL score and in the vasomotor, psychosocial, and sexual functioning domain scores (P < .05). Those in the 20 mg group also had a statistically significant improvement in their physical domain score (P < .05).
Although numerical improvements in genitourinary symptoms occurred at 12 weeks across all three groups, the only statistically significant difference from baseline occurred in patients taking 15 mg of estetrol, who experienced a decrease in vaginal dryness and vaginal pain during sex (P = .0142 and P = .003, respectively).
The Clinical Global Impression questionnaire asked women at 4 and 12 weeks to rate on a seven-item Likert scale their response to this question: “Rate the total improvement, whether or not in your judgment it is due entirely to drug treatment. Compared to your condition at admission to the study, how much has it changed?” Responses of “very much improved” and “much improved” counted as a clinically meaningful difference.
Compared with 27.9% of patients in the placebo group, 52.9% of patients in the 15 mg group and 59.8% of patients in the 20 mg group rated the weekly frequency of moderate to severe vasomotor symptoms as “much improved” or “very much improved” at 4 weeks (P < .0001). At 12 weeks, those numbers rose to 47% in the placebo group, 73.3% in the 15 mg group and 77.8% in the 20 mg group (P < .0001).
The trial’s primary limitation at this point is having only a 12-week follow-up, Dr. Shufelt said, though a few other questions remain.
“Because the two phase 3 RCTs included hysterectomized and nonhysterectomized women, it was unclear how many women in the study had E4 alone versus E4 with progesterone, as that might play a role in both cholesterol and carbohydrate metabolism,” Dr. Shufelt said. “While baseline data was not presented, it would also be important to know baseline values for the women and confirm that none were on lipid-lowering medications.”
The research was funded by Estetra SRL, an affiliate of Mithra Pharmaceuticals. Dr. Utian is a member of the Mithra and Elektra Scientific Advisory Boards. Dr. Shufelt has no disclosures.
PHILADELPHIA – presented at the annual meeting of the Menopause Society (formerly The North American Menopause Society).
Participants taking estetrol experienced a decrease in hemoglobin A1c, fasting plasma glucose, total cholesterol, LDL and lipoprotein as well as an increase in HDL cholesterol, according to the findings presented by Wolf Utian, MD, PhD, DSC, a professor emeritus of reproductive biology at Case Western Reserve University, Cleveland, and medical director emeritus of the Menopause Society.
A separate poster at the conference from the same trial also reported significant improvements from estetrol in quality of life, including that related to vasomotor symptoms, and several psychosocial and sexual functioning areas.
E4 is already available as combination oral contraception and is now being considered for treating vasomotor symptoms, explained Chrisandra Shufelt, MD, professor and chair of general internal of medicine and associate director of the Women’s Health Research Center at Mayo Clinic Florida, who was not involved in the study.
Background on estetrol
E4 is a human fetal liver estrogen produced during pregnancy that’s synthesized from plants for pharmaceutical use, including as the oral contraceptive drospirenone, Dr. Utian told attendees. It’s classified as a native estrogen with selective tissue activity (NEST), he said.
“E4 is a completely different native estrogen with oral administration mimicking the benefits of transdermals and hence safe and effective,” Dr. Utian said in an interview. “It would be a significant new addition to the pharmaceutical armamentarium.”
Two phase 3 trials presented by Dr. Utian at the same conference last year found estetrol reduced the frequency and severity of moderate to severe vasomotor symptoms, and a previous phase 2 trial finding vasomotor and genitourinary symptom benefits suggested it had potential benefits for lipids, carbohydrate metabolism, and bone turnover.
“In summary, E4 at a daily dose of 15 mg exhibited estrogenic effects in the vagina, leading to improved vaginal health and reduced signs of atrophy, emerging as a promising treatment option not only for vasomotor symptoms but also for other significant menopausal symptoms,” Dr. Utian said. “E4 could offer comprehensive relief for women experiencing a range of menopause-related discomforts.”
Dr. Utian also referenced a 2017 trial in which estetrol positively impacted lipid profiles, “lowering low-density lipoprotein cholesterol, increasing high-density lipoprotein cholesterol, and showing minimal influence on triglycerides,” he said. “Importantly, estetrol was associated with a significant decrease in osteocalcin levels in the higher dose groups, suggesting a potential preventive effect on bone loss,” he added. A recent review of the overall evidence on estetrol suggests its use is “promising,” Dr. Utian noted.
Current trial
His current randomized controlled phase 3 trial included postmenopausal women ages 40-65 from 151 sites in 14 countries in Europe, Latin America, and North America, and Russia. Among the 640 participants in the trial, 213 women randomly received 15 mg of estetrol, 213 women received 20 mg of estetrol, and 214 women received a placebo every day for 3 months. All women without hysterectomies also received 200 mg of progesterone once daily for two weeks after completing the estetrol treatment to protect the endometrium.
Researchers took blood samples from the participants at baseline and week 12 to assess total cholesterol, LDL, HDL, the total cholesterol/HDL ratio, triglycerides, lipoprotein A, fasting plasma glucose, insulin, and A1c.
Compared with women in the placebo group, women in both the 15 mg and 20 mg groups saw a statistically significant decrease in lipoprotein A and in the ratio of total cholesterol to HDL, and a statistically significant increase in HDL. Only the women in the 15 mg group saw a statistically significant decrease in LDL and increase in triglycerides; an increase in triglycerides in the 20 mg group did not reach statistical significance.
Statistically significant decreases in fasting plasma glucose and A1c also occurred in both treatment groups, but a decrease in insulin levels and in the homeostasis model-assessment-estimated insulin resistance (HOMA-IR) seen in both treatment arms did not reach significance.
“While the mean changes after 12 weeks from baseline overall were small changes to the cholesterol and blood sugar profiles, they are clinically meaningful because it suggests that E4 does not have any adverse effects to these measures,” Dr. Shufelt said in an interview. “An advantage is that this gives us another hormone option for vasomotor symptoms since it is a native estrogen with selective tissue.”
It’s too early, however, to determine whether estetrol offers benefits in terms of its safety profile, compared with currently available therapies, Dr. Shufelt said.
”These findings of E4 are similar to how oral estradiol changes lipids, which finds an increase in high-density lipoprotein cholesterol, and decreases plasma concentrations of total and low-density lipoprotein cholesterol. an increase in HDL-C and triglycerides and decrease in LDL-C,” she said.
Poster findings also promising
For the findings reported in the poster, researchers assessed quality of life and the clinical meaningfulness of vasomotor symptoms’ reduction at baseline and 12 weeks using the Menopause-Specific Quality of Life (MENQOL) questionnaire and the Clinical Global Impression questionnaire, respectively. They also assessed women’s self-reported genitourinary symptoms, including vaginal dryness, pain during urination, vaginal pain and bleeding related to sex, and vaginal or vulvar irritation or itching. Most of these findings primarily confirmed previous positive effects from E4 in other trials.
Women in both the 15 mg and 20 mg estetrol groups reported a statistically significant improvement at 12 weeks, compared with placebo, in their total MENQOL score and in the vasomotor, psychosocial, and sexual functioning domain scores (P < .05). Those in the 20 mg group also had a statistically significant improvement in their physical domain score (P < .05).
Although numerical improvements in genitourinary symptoms occurred at 12 weeks across all three groups, the only statistically significant difference from baseline occurred in patients taking 15 mg of estetrol, who experienced a decrease in vaginal dryness and vaginal pain during sex (P = .0142 and P = .003, respectively).
The Clinical Global Impression questionnaire asked women at 4 and 12 weeks to rate on a seven-item Likert scale their response to this question: “Rate the total improvement, whether or not in your judgment it is due entirely to drug treatment. Compared to your condition at admission to the study, how much has it changed?” Responses of “very much improved” and “much improved” counted as a clinically meaningful difference.
Compared with 27.9% of patients in the placebo group, 52.9% of patients in the 15 mg group and 59.8% of patients in the 20 mg group rated the weekly frequency of moderate to severe vasomotor symptoms as “much improved” or “very much improved” at 4 weeks (P < .0001). At 12 weeks, those numbers rose to 47% in the placebo group, 73.3% in the 15 mg group and 77.8% in the 20 mg group (P < .0001).
The trial’s primary limitation at this point is having only a 12-week follow-up, Dr. Shufelt said, though a few other questions remain.
“Because the two phase 3 RCTs included hysterectomized and nonhysterectomized women, it was unclear how many women in the study had E4 alone versus E4 with progesterone, as that might play a role in both cholesterol and carbohydrate metabolism,” Dr. Shufelt said. “While baseline data was not presented, it would also be important to know baseline values for the women and confirm that none were on lipid-lowering medications.”
The research was funded by Estetra SRL, an affiliate of Mithra Pharmaceuticals. Dr. Utian is a member of the Mithra and Elektra Scientific Advisory Boards. Dr. Shufelt has no disclosures.
AT NAMS 2023
Cannabis use growing among menopausal women
PHILADELPHIA – presented at the annual meeting of the Menopause Society (formerly The North American Menopause Society).
Though most women reported using cannabis for recreational reasons, 13% used it only for medical reasons, most often for chronic pain, anxiety, sleep, and stress.
“These findings highlight the importance of recognizing and discussing cannabis use in the health care setting, and the need for additional research to evaluate the potential harms and/or benefits of use in this vulnerable population,” Carolyn J. Gibson, PhD, MPH, a staff psychologist in women’s health at the San Francisco VA Health Care System and an assistant professor of psychiatry and behavioral sciences at the University of California, San Francisco, told attendees.
As cannabis has become more accessible, with its use legalized in 38 states and Washington, D.C., the proportion of U.S. adults using it has doubled over about a decade, from 6% in 2007 to 12% in 2019, Dr. Gibson said. Further, women aged 50 and older are among the fastest-growing groups of users of cannabis, and it’s being increasingly used – and marketed – for treating menopause-related and aging-related symptoms, including insomnia, anxiety, and chronic pain, she said.
“With these decisions to use cannabis, medically or for these other purposes, there’s this perception that it’s harmless,” Dr. Gibson said. Yet potential health risks associated with cannabis include the usual health effects associated with any kind of smoking as well as dependence in those who use it more frequently and/or develop a tolerance for it. She noted that average THC potency has increased over time, and acute risks for using cannabis with high levels of THC – at least 15% or at least 10 mg – can include anxiety/panic, confusion, disturbing/intrusive thoughts, psychosis, and effects on coordination and cognition. She also acknowledged, however, that most of the data available on risks come from studies of men and younger adults rather than older women.
Given the growing normalization of cannabis use, Dr. Gibson’s team sought to better understand prevalence of use as well as types of use and reasons for use in perimenopasual and postmenopausal women. They analyzed data from a cross-sectional survey of women and gender-diverse members, aged 45-64, of Ipsos KnowledgePanel, an online panel with more than 60,000 participating members in the United States.
All the respondents identified themselves as female at birth and had not used gender-affirming therapy or undergone gender-affirming surgery. The survey included questions on sociodemographics, menopause status, frequency of cannabis use, types of cannabis used, reasons for using cannabis, and use of cannabis in the previous 30 days. The 5,174 respondents were an average 55 years old and predominantly non-Hispanic white (63%), with 13% non-Hispanic Black and 16% Hispanic. Two-thirds of the women reported working full- or part-time (67%) and two-thirds were postmenopausal (68%), with 64% reporting experiencing menopause symptoms.
About two in five respondents (42%) had ever used cannabis in any form, most often smoking it (83%) or consuming edibles (51%). Among those who had ever used it, 30% reported having smoked it daily or nearly daily for at least a year at some point.
Ten percent of respondents had used cannabis in the past month, again primarily smoking (56%) or edibles (52%), though 39% said they used it in more than one form, including vaping, dabbing, or topical use. Nearly half (46%) of the respondents who smoked cannabis recently did not know the THC potency of what they consumed, and just over 20% of those consuming edibles didn’t know the THC potency of what they used. However, about a third of those taking edibles used cannabis with less than 10 mg of THC, and a little over a quarter used edibles with 10 mg of THC.
Within the 10% who had used cannabis in the past month, nearly a third (31%) of respondents – or around 3.1% of the total sample – reported smoking cannabis daily or almost daily, and 19% (or 1.9% of the overall sample) consumed cannabis edibles daily or almost daily.
Most of the respondents who used cannabis said it was for recreational use (62%), but a quarter (25%) reported using it for both recreational and medical reasons, and 13% used it only for medical reasons. The most common reason women used cannabis was to treat chronic pain (28%), followed by nearly as many women reporting cannabis use for anxiety (24%), sleep (22%), and stress (22%). Six percent of women used cannabis specifically for menopause-related sleep and mood problems.
Given the growing use of cannabis in this population and the dearth of data on its effects in older women, Dr. Gibson highlighted the need for research examining the potential benefits and harms of cannabis for menopausal women.
Not risk-free
Susan D. Reed, MD, MPH, MSCP, a professor emeritus of ob.gyn. at the University of Washington, Seattle, and president of the Menopause Society, found the study well-executed and was not surprised by how many respondents had ever used cannabis.
“What did surprise me was that nearly a third reported daily use for at least 1 year and that 38% were medical marijuana users, not just recreational,” Dr. Reed said in an interview. The proportions of women using cannabis for menopausal symptoms or using it daily are concerning, she added.
“These individuals are at risk for dependence and health risks related to marijuana use,” Dr. Reed said. “Providers should always ask patients about OTC products, herbals, supplements, cannabis use, and alternative management of menopausal symptoms to better understand patient preferences for menopausal symptom therapies, so that treatment plans can be discussed with individual patient preferences in mind. We need to start with where the patient is coming from.”
Data presented throughout the conference has shown how people are “disillusioned with the care they are receiving for menopause,” Dr. Reed added. “It is so difficult to distinguish truth from myths based on information gained through social media, family, and friends, and that often is where most people are getting their information.”
Physicians often have not received adequate training on how to provide people with accurate information about menopause and managing menopausal symptoms, so she advises patients and physicians to visit reliable sites such as the Menopause Society, the Swan Study, and My Menoplan.
The research was funded by the Tobacco-Related Disease Research Program and the Veterans Administration. Dr. Gibson has provided unpaid consultation to Astellas Pharmaceuticals. Dr. Reed has received research support from Bayer and receives royalties from UpToDate.
PHILADELPHIA – presented at the annual meeting of the Menopause Society (formerly The North American Menopause Society).
Though most women reported using cannabis for recreational reasons, 13% used it only for medical reasons, most often for chronic pain, anxiety, sleep, and stress.
“These findings highlight the importance of recognizing and discussing cannabis use in the health care setting, and the need for additional research to evaluate the potential harms and/or benefits of use in this vulnerable population,” Carolyn J. Gibson, PhD, MPH, a staff psychologist in women’s health at the San Francisco VA Health Care System and an assistant professor of psychiatry and behavioral sciences at the University of California, San Francisco, told attendees.
As cannabis has become more accessible, with its use legalized in 38 states and Washington, D.C., the proportion of U.S. adults using it has doubled over about a decade, from 6% in 2007 to 12% in 2019, Dr. Gibson said. Further, women aged 50 and older are among the fastest-growing groups of users of cannabis, and it’s being increasingly used – and marketed – for treating menopause-related and aging-related symptoms, including insomnia, anxiety, and chronic pain, she said.
“With these decisions to use cannabis, medically or for these other purposes, there’s this perception that it’s harmless,” Dr. Gibson said. Yet potential health risks associated with cannabis include the usual health effects associated with any kind of smoking as well as dependence in those who use it more frequently and/or develop a tolerance for it. She noted that average THC potency has increased over time, and acute risks for using cannabis with high levels of THC – at least 15% or at least 10 mg – can include anxiety/panic, confusion, disturbing/intrusive thoughts, psychosis, and effects on coordination and cognition. She also acknowledged, however, that most of the data available on risks come from studies of men and younger adults rather than older women.
Given the growing normalization of cannabis use, Dr. Gibson’s team sought to better understand prevalence of use as well as types of use and reasons for use in perimenopasual and postmenopausal women. They analyzed data from a cross-sectional survey of women and gender-diverse members, aged 45-64, of Ipsos KnowledgePanel, an online panel with more than 60,000 participating members in the United States.
All the respondents identified themselves as female at birth and had not used gender-affirming therapy or undergone gender-affirming surgery. The survey included questions on sociodemographics, menopause status, frequency of cannabis use, types of cannabis used, reasons for using cannabis, and use of cannabis in the previous 30 days. The 5,174 respondents were an average 55 years old and predominantly non-Hispanic white (63%), with 13% non-Hispanic Black and 16% Hispanic. Two-thirds of the women reported working full- or part-time (67%) and two-thirds were postmenopausal (68%), with 64% reporting experiencing menopause symptoms.
About two in five respondents (42%) had ever used cannabis in any form, most often smoking it (83%) or consuming edibles (51%). Among those who had ever used it, 30% reported having smoked it daily or nearly daily for at least a year at some point.
Ten percent of respondents had used cannabis in the past month, again primarily smoking (56%) or edibles (52%), though 39% said they used it in more than one form, including vaping, dabbing, or topical use. Nearly half (46%) of the respondents who smoked cannabis recently did not know the THC potency of what they consumed, and just over 20% of those consuming edibles didn’t know the THC potency of what they used. However, about a third of those taking edibles used cannabis with less than 10 mg of THC, and a little over a quarter used edibles with 10 mg of THC.
Within the 10% who had used cannabis in the past month, nearly a third (31%) of respondents – or around 3.1% of the total sample – reported smoking cannabis daily or almost daily, and 19% (or 1.9% of the overall sample) consumed cannabis edibles daily or almost daily.
Most of the respondents who used cannabis said it was for recreational use (62%), but a quarter (25%) reported using it for both recreational and medical reasons, and 13% used it only for medical reasons. The most common reason women used cannabis was to treat chronic pain (28%), followed by nearly as many women reporting cannabis use for anxiety (24%), sleep (22%), and stress (22%). Six percent of women used cannabis specifically for menopause-related sleep and mood problems.
Given the growing use of cannabis in this population and the dearth of data on its effects in older women, Dr. Gibson highlighted the need for research examining the potential benefits and harms of cannabis for menopausal women.
Not risk-free
Susan D. Reed, MD, MPH, MSCP, a professor emeritus of ob.gyn. at the University of Washington, Seattle, and president of the Menopause Society, found the study well-executed and was not surprised by how many respondents had ever used cannabis.
“What did surprise me was that nearly a third reported daily use for at least 1 year and that 38% were medical marijuana users, not just recreational,” Dr. Reed said in an interview. The proportions of women using cannabis for menopausal symptoms or using it daily are concerning, she added.
“These individuals are at risk for dependence and health risks related to marijuana use,” Dr. Reed said. “Providers should always ask patients about OTC products, herbals, supplements, cannabis use, and alternative management of menopausal symptoms to better understand patient preferences for menopausal symptom therapies, so that treatment plans can be discussed with individual patient preferences in mind. We need to start with where the patient is coming from.”
Data presented throughout the conference has shown how people are “disillusioned with the care they are receiving for menopause,” Dr. Reed added. “It is so difficult to distinguish truth from myths based on information gained through social media, family, and friends, and that often is where most people are getting their information.”
Physicians often have not received adequate training on how to provide people with accurate information about menopause and managing menopausal symptoms, so she advises patients and physicians to visit reliable sites such as the Menopause Society, the Swan Study, and My Menoplan.
The research was funded by the Tobacco-Related Disease Research Program and the Veterans Administration. Dr. Gibson has provided unpaid consultation to Astellas Pharmaceuticals. Dr. Reed has received research support from Bayer and receives royalties from UpToDate.
PHILADELPHIA – presented at the annual meeting of the Menopause Society (formerly The North American Menopause Society).
Though most women reported using cannabis for recreational reasons, 13% used it only for medical reasons, most often for chronic pain, anxiety, sleep, and stress.
“These findings highlight the importance of recognizing and discussing cannabis use in the health care setting, and the need for additional research to evaluate the potential harms and/or benefits of use in this vulnerable population,” Carolyn J. Gibson, PhD, MPH, a staff psychologist in women’s health at the San Francisco VA Health Care System and an assistant professor of psychiatry and behavioral sciences at the University of California, San Francisco, told attendees.
As cannabis has become more accessible, with its use legalized in 38 states and Washington, D.C., the proportion of U.S. adults using it has doubled over about a decade, from 6% in 2007 to 12% in 2019, Dr. Gibson said. Further, women aged 50 and older are among the fastest-growing groups of users of cannabis, and it’s being increasingly used – and marketed – for treating menopause-related and aging-related symptoms, including insomnia, anxiety, and chronic pain, she said.
“With these decisions to use cannabis, medically or for these other purposes, there’s this perception that it’s harmless,” Dr. Gibson said. Yet potential health risks associated with cannabis include the usual health effects associated with any kind of smoking as well as dependence in those who use it more frequently and/or develop a tolerance for it. She noted that average THC potency has increased over time, and acute risks for using cannabis with high levels of THC – at least 15% or at least 10 mg – can include anxiety/panic, confusion, disturbing/intrusive thoughts, psychosis, and effects on coordination and cognition. She also acknowledged, however, that most of the data available on risks come from studies of men and younger adults rather than older women.
Given the growing normalization of cannabis use, Dr. Gibson’s team sought to better understand prevalence of use as well as types of use and reasons for use in perimenopasual and postmenopausal women. They analyzed data from a cross-sectional survey of women and gender-diverse members, aged 45-64, of Ipsos KnowledgePanel, an online panel with more than 60,000 participating members in the United States.
All the respondents identified themselves as female at birth and had not used gender-affirming therapy or undergone gender-affirming surgery. The survey included questions on sociodemographics, menopause status, frequency of cannabis use, types of cannabis used, reasons for using cannabis, and use of cannabis in the previous 30 days. The 5,174 respondents were an average 55 years old and predominantly non-Hispanic white (63%), with 13% non-Hispanic Black and 16% Hispanic. Two-thirds of the women reported working full- or part-time (67%) and two-thirds were postmenopausal (68%), with 64% reporting experiencing menopause symptoms.
About two in five respondents (42%) had ever used cannabis in any form, most often smoking it (83%) or consuming edibles (51%). Among those who had ever used it, 30% reported having smoked it daily or nearly daily for at least a year at some point.
Ten percent of respondents had used cannabis in the past month, again primarily smoking (56%) or edibles (52%), though 39% said they used it in more than one form, including vaping, dabbing, or topical use. Nearly half (46%) of the respondents who smoked cannabis recently did not know the THC potency of what they consumed, and just over 20% of those consuming edibles didn’t know the THC potency of what they used. However, about a third of those taking edibles used cannabis with less than 10 mg of THC, and a little over a quarter used edibles with 10 mg of THC.
Within the 10% who had used cannabis in the past month, nearly a third (31%) of respondents – or around 3.1% of the total sample – reported smoking cannabis daily or almost daily, and 19% (or 1.9% of the overall sample) consumed cannabis edibles daily or almost daily.
Most of the respondents who used cannabis said it was for recreational use (62%), but a quarter (25%) reported using it for both recreational and medical reasons, and 13% used it only for medical reasons. The most common reason women used cannabis was to treat chronic pain (28%), followed by nearly as many women reporting cannabis use for anxiety (24%), sleep (22%), and stress (22%). Six percent of women used cannabis specifically for menopause-related sleep and mood problems.
Given the growing use of cannabis in this population and the dearth of data on its effects in older women, Dr. Gibson highlighted the need for research examining the potential benefits and harms of cannabis for menopausal women.
Not risk-free
Susan D. Reed, MD, MPH, MSCP, a professor emeritus of ob.gyn. at the University of Washington, Seattle, and president of the Menopause Society, found the study well-executed and was not surprised by how many respondents had ever used cannabis.
“What did surprise me was that nearly a third reported daily use for at least 1 year and that 38% were medical marijuana users, not just recreational,” Dr. Reed said in an interview. The proportions of women using cannabis for menopausal symptoms or using it daily are concerning, she added.
“These individuals are at risk for dependence and health risks related to marijuana use,” Dr. Reed said. “Providers should always ask patients about OTC products, herbals, supplements, cannabis use, and alternative management of menopausal symptoms to better understand patient preferences for menopausal symptom therapies, so that treatment plans can be discussed with individual patient preferences in mind. We need to start with where the patient is coming from.”
Data presented throughout the conference has shown how people are “disillusioned with the care they are receiving for menopause,” Dr. Reed added. “It is so difficult to distinguish truth from myths based on information gained through social media, family, and friends, and that often is where most people are getting their information.”
Physicians often have not received adequate training on how to provide people with accurate information about menopause and managing menopausal symptoms, so she advises patients and physicians to visit reliable sites such as the Menopause Society, the Swan Study, and My Menoplan.
The research was funded by the Tobacco-Related Disease Research Program and the Veterans Administration. Dr. Gibson has provided unpaid consultation to Astellas Pharmaceuticals. Dr. Reed has received research support from Bayer and receives royalties from UpToDate.
AT NAMS 2023