User login
Clinical Endocrinology News is an independent news source that provides endocrinologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the endocrinologist's practice. Specialty topics include Diabetes, Lipid & Metabolic Disorders Menopause, Obesity, Osteoporosis, Pediatric Endocrinology, Pituitary, Thyroid & Adrenal Disorders, and Reproductive Endocrinology. Featured content includes Commentaries, Implementin Health Reform, Law & Medicine, and In the Loop, the blog of Clinical Endocrinology News. Clinical Endocrinology News is owned by Frontline Medical Communications.
addict
addicted
addicting
addiction
adult sites
alcohol
antibody
ass
attorney
audit
auditor
babies
babpa
baby
ban
banned
banning
best
bisexual
bitch
bleach
blog
blow job
bondage
boobs
booty
buy
cannabis
certificate
certification
certified
cheap
cheapest
class action
cocaine
cock
counterfeit drug
crack
crap
crime
criminal
cunt
curable
cure
dangerous
dangers
dead
deadly
death
defend
defended
depedent
dependence
dependent
detergent
dick
die
dildo
drug abuse
drug recall
dying
fag
fake
fatal
fatalities
fatality
free
fuck
gangs
gingivitis
guns
hardcore
herbal
herbs
heroin
herpes
home remedies
homo
horny
hypersensitivity
hypoglycemia treatment
illegal drug use
illegal use of prescription
incest
infant
infants
job
ketoacidosis
kill
killer
killing
kinky
law suit
lawsuit
lawyer
lesbian
marijuana
medicine for hypoglycemia
murder
naked
natural
newborn
nigger
noise
nude
nudity
orgy
over the counter
overdosage
overdose
overdosed
overdosing
penis
pimp
pistol
porn
porno
pornographic
pornography
prison
profanity
purchase
purchasing
pussy
queer
rape
rapist
recall
recreational drug
rob
robberies
sale
sales
sex
sexual
shit
shoot
slut
slutty
stole
stolen
store
sue
suicidal
suicide
supplements
supply company
theft
thief
thieves
tit
toddler
toddlers
toxic
toxin
tragedy
treating dka
treating hypoglycemia
treatment for hypoglycemia
vagina
violence
whore
withdrawal
without prescription
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-imn')]
div[contains(@class, 'pane-pub-home-imn')]
div[contains(@class, 'pane-pub-topic-imn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Nonhormonal drug for menopause symptoms passes phase 3 test
A phase 3 trial has associated the neurokinin-3 (NK3)–receptor inhibitor fezolinetant, an oral therapy taken once daily, with substantial control over the symptoms of menopause, according to results of the randomized SKYLIGHT 2 trial.
The nonhormonal therapy has the potential to address an important unmet need, Genevieve Neal-Perry, MD, PhD, said at the annual meeting of the Endocrine Society.
The health risks of hormone therapy (HT) have “caused quite a few women to consider whether hormone replacement is right for them, and, in addition, there are other individuals who have hormone-responsive cancers or other disorders that might prohibit them [from using HT],” Dr. Neal-Perry said.
The NK3 receptor stimulates the thermoregulatory center in the hypothalamus. By blocking the NK3 receptor, vasodilation and other downstream effects are inhibited, explained Dr. Neal-Perry. She credited relatively recent advances in understanding the mechanisms of menopausal symptoms for identifying this and other potentially targetable mediators.
SKYLIGHT 2 trial: Two phases
In the double-blind multinational phase 3 SKYLIGHT 2 trial, 484 otherwise healthy symptomatic menopausal women were randomized to 30 mg of fezolinetant, 45 mg of fezolinetant, or placebo. The 120 participating centers were in North American and Europe.
In the first phase, safety and efficacy were evaluated over 12 weeks. In a second extension phase, placebo patients were rerandomized to one of the fezolinetant study doses. Those on active therapy remained in their assigned groups. All patients were then followed for an additional 40 weeks.
The coprimary endpoints were frequency and severity of moderate to severe vasomotor symptoms as reported by patients using an electronic diary. There were several secondary endpoints, including patient-reported outcomes regarding sleep quality.
As expected from other controlled trials, placebo patients achieved about a 40% reduction in moderate to severe vasomotor symptom frequency over the first 12 weeks. Relative to placebo, symptom frequency declined more quickly and steeply on fezolinetant. By week 12, both achieved reductions of about 60%. Statistical P values for the differences in the three arms were not provided, but Dr. Neal-Perry reported they were significant.
Vasomotor severity, like frequency, is reduced
The change in vasomotor severity, which subjects in the trial rated as better or worse, was also significant. The differences in the severity curves were less, but they separated in favor of the two active treatment arms by about 2 weeks, and the curves continued to show an advantage for fezolinetant over both the first 12 weeks and then the remaining 40 weeks.
Overall, the decline in vasomotor symptom frequency remained on a persistent downward slope on both doses of fezolinetant for the full 52 weeks of the study, so that the reduction at 52 weeks was on the order of 25% greater than that seen at 12 weeks.
At 52 weeks, “you can see that individuals on placebo who were crossed over to an active treatment had a significant reduction in their hot flashes and look very much like those who were randomized to fezolinetant at the beginning of the study,” said Dr. Neal-Perry, who is chair of the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill.
Other outcomes also favored fezolinetant over placebo. For example, a reduction in sleep disturbance observed at 12 weeks was sustained over the full 52 weeks of the study. The reduction in sleep symptoms appeared to be slightly greater on the higher dose, but the benefit at 52 weeks among patients after the crossover was similar on either active arm.
No serious side effects identified
There were no serious drug-related treatment-emergent adverse events in any treatment group. One patient in the placebo arm (< 1%), two patients in the 30-mg fezolinetant arm (1.2%), and five patients in the 45-mg arm (3%) discontinued therapy for an adverse event considered to be treatment related.
“The most common side effect associated with fezolinetant was headache. There were no other side effects that led patients to pull out of the study,” Dr. Neal-Perry reported at the meeting, which was held in Atlanta and virtually.
According to Dr. Neal-Perry the vasomotor symptoms relative to menopause, which occur in almost all women, are moderate to severe in an estimated 35%-45%. Some groups, such as those with an elevated body mass index and African Americans, appear to be at even greater risk. Study enrollment was specifically designed to include these high-risk groups, but the subgroup efficacy data have not yet been analyzed.
Other drugs with a similar mechanism of action have not been brought forward because of concern about elevated liver enzymes, but Dr. Neal-Perry said that this does not appear to be an issue for fezolinetant, which was designed with greater specificity for the NK3 target than previous treatments.
If fezolinetant is approved, Dr. Neal-Perry expects this agent to fulfill an important unmet need because of the limitations of other nonhormonal solutions for control of menopause symptoms.
HT alternatives limited
For control of many menopause symptoms, particularly hot flashes, hormone therapy (HT) is the most efficacious, but Richard J. Santen, MD, emeritus professor and an endocrinologist at the University of Virginia, Charlottesville, agreed there is a need for alternatives.
In addition to those who have contraindications for HT, Dr. Santen said in an interview that this option is not acceptable to others “for a variety of reasons.” The problem is that the alternatives are limited.
“The SSRI agents and gabapentin are alternative nonhormonal agents, but they have side effects and are not as effective,” he said. Hot flashes “can be a major disruptor of quality of life,” so he is intrigued with the positive results achieved with fezolinetant.
“A new drug such as reported at the Endocrine Society meeting would be an important new addition to the armamentarium,” he said.
Dr. Neal-Perry reports no conflicts of interest.
A phase 3 trial has associated the neurokinin-3 (NK3)–receptor inhibitor fezolinetant, an oral therapy taken once daily, with substantial control over the symptoms of menopause, according to results of the randomized SKYLIGHT 2 trial.
The nonhormonal therapy has the potential to address an important unmet need, Genevieve Neal-Perry, MD, PhD, said at the annual meeting of the Endocrine Society.
The health risks of hormone therapy (HT) have “caused quite a few women to consider whether hormone replacement is right for them, and, in addition, there are other individuals who have hormone-responsive cancers or other disorders that might prohibit them [from using HT],” Dr. Neal-Perry said.
The NK3 receptor stimulates the thermoregulatory center in the hypothalamus. By blocking the NK3 receptor, vasodilation and other downstream effects are inhibited, explained Dr. Neal-Perry. She credited relatively recent advances in understanding the mechanisms of menopausal symptoms for identifying this and other potentially targetable mediators.
SKYLIGHT 2 trial: Two phases
In the double-blind multinational phase 3 SKYLIGHT 2 trial, 484 otherwise healthy symptomatic menopausal women were randomized to 30 mg of fezolinetant, 45 mg of fezolinetant, or placebo. The 120 participating centers were in North American and Europe.
In the first phase, safety and efficacy were evaluated over 12 weeks. In a second extension phase, placebo patients were rerandomized to one of the fezolinetant study doses. Those on active therapy remained in their assigned groups. All patients were then followed for an additional 40 weeks.
The coprimary endpoints were frequency and severity of moderate to severe vasomotor symptoms as reported by patients using an electronic diary. There were several secondary endpoints, including patient-reported outcomes regarding sleep quality.
As expected from other controlled trials, placebo patients achieved about a 40% reduction in moderate to severe vasomotor symptom frequency over the first 12 weeks. Relative to placebo, symptom frequency declined more quickly and steeply on fezolinetant. By week 12, both achieved reductions of about 60%. Statistical P values for the differences in the three arms were not provided, but Dr. Neal-Perry reported they were significant.
Vasomotor severity, like frequency, is reduced
The change in vasomotor severity, which subjects in the trial rated as better or worse, was also significant. The differences in the severity curves were less, but they separated in favor of the two active treatment arms by about 2 weeks, and the curves continued to show an advantage for fezolinetant over both the first 12 weeks and then the remaining 40 weeks.
Overall, the decline in vasomotor symptom frequency remained on a persistent downward slope on both doses of fezolinetant for the full 52 weeks of the study, so that the reduction at 52 weeks was on the order of 25% greater than that seen at 12 weeks.
At 52 weeks, “you can see that individuals on placebo who were crossed over to an active treatment had a significant reduction in their hot flashes and look very much like those who were randomized to fezolinetant at the beginning of the study,” said Dr. Neal-Perry, who is chair of the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill.
Other outcomes also favored fezolinetant over placebo. For example, a reduction in sleep disturbance observed at 12 weeks was sustained over the full 52 weeks of the study. The reduction in sleep symptoms appeared to be slightly greater on the higher dose, but the benefit at 52 weeks among patients after the crossover was similar on either active arm.
No serious side effects identified
There were no serious drug-related treatment-emergent adverse events in any treatment group. One patient in the placebo arm (< 1%), two patients in the 30-mg fezolinetant arm (1.2%), and five patients in the 45-mg arm (3%) discontinued therapy for an adverse event considered to be treatment related.
“The most common side effect associated with fezolinetant was headache. There were no other side effects that led patients to pull out of the study,” Dr. Neal-Perry reported at the meeting, which was held in Atlanta and virtually.
According to Dr. Neal-Perry the vasomotor symptoms relative to menopause, which occur in almost all women, are moderate to severe in an estimated 35%-45%. Some groups, such as those with an elevated body mass index and African Americans, appear to be at even greater risk. Study enrollment was specifically designed to include these high-risk groups, but the subgroup efficacy data have not yet been analyzed.
Other drugs with a similar mechanism of action have not been brought forward because of concern about elevated liver enzymes, but Dr. Neal-Perry said that this does not appear to be an issue for fezolinetant, which was designed with greater specificity for the NK3 target than previous treatments.
If fezolinetant is approved, Dr. Neal-Perry expects this agent to fulfill an important unmet need because of the limitations of other nonhormonal solutions for control of menopause symptoms.
HT alternatives limited
For control of many menopause symptoms, particularly hot flashes, hormone therapy (HT) is the most efficacious, but Richard J. Santen, MD, emeritus professor and an endocrinologist at the University of Virginia, Charlottesville, agreed there is a need for alternatives.
In addition to those who have contraindications for HT, Dr. Santen said in an interview that this option is not acceptable to others “for a variety of reasons.” The problem is that the alternatives are limited.
“The SSRI agents and gabapentin are alternative nonhormonal agents, but they have side effects and are not as effective,” he said. Hot flashes “can be a major disruptor of quality of life,” so he is intrigued with the positive results achieved with fezolinetant.
“A new drug such as reported at the Endocrine Society meeting would be an important new addition to the armamentarium,” he said.
Dr. Neal-Perry reports no conflicts of interest.
A phase 3 trial has associated the neurokinin-3 (NK3)–receptor inhibitor fezolinetant, an oral therapy taken once daily, with substantial control over the symptoms of menopause, according to results of the randomized SKYLIGHT 2 trial.
The nonhormonal therapy has the potential to address an important unmet need, Genevieve Neal-Perry, MD, PhD, said at the annual meeting of the Endocrine Society.
The health risks of hormone therapy (HT) have “caused quite a few women to consider whether hormone replacement is right for them, and, in addition, there are other individuals who have hormone-responsive cancers or other disorders that might prohibit them [from using HT],” Dr. Neal-Perry said.
The NK3 receptor stimulates the thermoregulatory center in the hypothalamus. By blocking the NK3 receptor, vasodilation and other downstream effects are inhibited, explained Dr. Neal-Perry. She credited relatively recent advances in understanding the mechanisms of menopausal symptoms for identifying this and other potentially targetable mediators.
SKYLIGHT 2 trial: Two phases
In the double-blind multinational phase 3 SKYLIGHT 2 trial, 484 otherwise healthy symptomatic menopausal women were randomized to 30 mg of fezolinetant, 45 mg of fezolinetant, or placebo. The 120 participating centers were in North American and Europe.
In the first phase, safety and efficacy were evaluated over 12 weeks. In a second extension phase, placebo patients were rerandomized to one of the fezolinetant study doses. Those on active therapy remained in their assigned groups. All patients were then followed for an additional 40 weeks.
The coprimary endpoints were frequency and severity of moderate to severe vasomotor symptoms as reported by patients using an electronic diary. There were several secondary endpoints, including patient-reported outcomes regarding sleep quality.
As expected from other controlled trials, placebo patients achieved about a 40% reduction in moderate to severe vasomotor symptom frequency over the first 12 weeks. Relative to placebo, symptom frequency declined more quickly and steeply on fezolinetant. By week 12, both achieved reductions of about 60%. Statistical P values for the differences in the three arms were not provided, but Dr. Neal-Perry reported they were significant.
Vasomotor severity, like frequency, is reduced
The change in vasomotor severity, which subjects in the trial rated as better or worse, was also significant. The differences in the severity curves were less, but they separated in favor of the two active treatment arms by about 2 weeks, and the curves continued to show an advantage for fezolinetant over both the first 12 weeks and then the remaining 40 weeks.
Overall, the decline in vasomotor symptom frequency remained on a persistent downward slope on both doses of fezolinetant for the full 52 weeks of the study, so that the reduction at 52 weeks was on the order of 25% greater than that seen at 12 weeks.
At 52 weeks, “you can see that individuals on placebo who were crossed over to an active treatment had a significant reduction in their hot flashes and look very much like those who were randomized to fezolinetant at the beginning of the study,” said Dr. Neal-Perry, who is chair of the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill.
Other outcomes also favored fezolinetant over placebo. For example, a reduction in sleep disturbance observed at 12 weeks was sustained over the full 52 weeks of the study. The reduction in sleep symptoms appeared to be slightly greater on the higher dose, but the benefit at 52 weeks among patients after the crossover was similar on either active arm.
No serious side effects identified
There were no serious drug-related treatment-emergent adverse events in any treatment group. One patient in the placebo arm (< 1%), two patients in the 30-mg fezolinetant arm (1.2%), and five patients in the 45-mg arm (3%) discontinued therapy for an adverse event considered to be treatment related.
“The most common side effect associated with fezolinetant was headache. There were no other side effects that led patients to pull out of the study,” Dr. Neal-Perry reported at the meeting, which was held in Atlanta and virtually.
According to Dr. Neal-Perry the vasomotor symptoms relative to menopause, which occur in almost all women, are moderate to severe in an estimated 35%-45%. Some groups, such as those with an elevated body mass index and African Americans, appear to be at even greater risk. Study enrollment was specifically designed to include these high-risk groups, but the subgroup efficacy data have not yet been analyzed.
Other drugs with a similar mechanism of action have not been brought forward because of concern about elevated liver enzymes, but Dr. Neal-Perry said that this does not appear to be an issue for fezolinetant, which was designed with greater specificity for the NK3 target than previous treatments.
If fezolinetant is approved, Dr. Neal-Perry expects this agent to fulfill an important unmet need because of the limitations of other nonhormonal solutions for control of menopause symptoms.
HT alternatives limited
For control of many menopause symptoms, particularly hot flashes, hormone therapy (HT) is the most efficacious, but Richard J. Santen, MD, emeritus professor and an endocrinologist at the University of Virginia, Charlottesville, agreed there is a need for alternatives.
In addition to those who have contraindications for HT, Dr. Santen said in an interview that this option is not acceptable to others “for a variety of reasons.” The problem is that the alternatives are limited.
“The SSRI agents and gabapentin are alternative nonhormonal agents, but they have side effects and are not as effective,” he said. Hot flashes “can be a major disruptor of quality of life,” so he is intrigued with the positive results achieved with fezolinetant.
“A new drug such as reported at the Endocrine Society meeting would be an important new addition to the armamentarium,” he said.
Dr. Neal-Perry reports no conflicts of interest.
FROM ENDO 2022
Exercise of any type boosts type 1 diabetes time in range
Adults with type 1 diabetes had significantly better glycemic control on days they exercised, regardless of exercise type, compared to days when they were inactive, according to a prospective study in nearly 500 individuals.
Different types of exercise, such as aerobic workouts, interval training, or resistance training, may have different immediate glycemic effects in adults with type 1 diabetes (T1D), but the impact of exercise type on the percentage of time diabetes patients maintain glucose in the 70-180 mg/dL range on days when they are active vs. inactive has not been well studied, Zoey Li said in a presentation at the annual scientific sessions of the American Diabetes Association.
In the Type 1 Diabetes Exercise Initiative (T1DEXI) study, Ms. Li and colleagues examined continuous glucose monitoring (CGM) data from 497 adults with T1D. The observational study included self-referred adults aged 18 years and older who had been living with T1D for at least 2 years. Participants were assigned to programs of aerobic exercise (defined as a target heart rate of 70%-80% of age-predicted maximum), interval exercise (defined as an interval heart rate of 80%-90% of age-predicted maximum), or resistance exercise (defined as muscle group fatigue after three sets of eight repetitions).
Participants completed the workouts at home via 30-minute videos at least six times over the 4-week study period. The study design involved an activity goal of at least 150 minutes per week, including the videos and self-reported usual activity, such as walking. The data were collected through an app designed for the study, a heart rate monitor, and a CGM.
The researchers compared glucose levels on days when the participants reported being active compared to days when they were sedentary. The goal of the study was to assess the effect of exercise type on time spent with glucose in the range of 70-180 mg/dL, defined as time in range (TIR).
The mean age of the participants was 37 years; 89% were White. The mean duration of diabetes was 18 years, and the mean hemoglobin A1c was 6.6%. “An astounding 95% were current continuous glucose monitoring [CGM] users,” said Ms. Li, a statistician at the Jaeb Center for Health Research in Tampa, Fla.
A total of 398 participants reported at least one exercise day and one sedentary day, for a total of 1,302 exercise days and 2,470 sedentary days.
Overall, the mean TIR was significantly higher on exercise days compared to sedentary days (75% vs. 70%, P < .001). The median time above 180 mg/dL also was significantly lower on exercise days compared to sedentary days (17% vs. 23%, P < .001), and mean glucose levels were 10 mg/dL lower on exercise days (145 mg/dL vs. 155 mg/dL)
“This all came with a slight hit to their time below range,” Ms. Li noted. The median time below 70 mg/dL was 1.1% on exercise days compared to 0.4% on sedentary days (P < .001). The percentage of days with hypoglycemic events was higher on exercise days compared to sedentary days (47% vs. 40%, P < .001), as they are related to time below 70 mg/dL, she added.
The differences for mean glucose level and TIR between exercise days and sedentary days were significant for each of the three exercise types, Ms. Li said.
“After establishing these glycemic trends, we looked at whether there were any factors that influenced the glycemic differences on exercise vs. sedentary days,” Ms. Li said.
Regardless of exercise type, age, sex, baseline A1c, diabetes duration, body mass index, insulin modality, CGM use, and percentage of time below range in the past 24 hours, there was higher TIR and higher hypoglycemia on exercise days compared to sedentary days.
Although the study was limited in part by the observational design, “with these data, we can better understand the glycemic benefits and disadvantages of exercise in adults with type 1 diabetes,” Ms. Li said.
Don’t forget the negative effects of exercise
“It is well known that the three types of exercise can modulate glucose levels. This can be very useful when attempting to reduce excessively high glucose levels, and when encouraging people to engage in frequent, regular, and consistent physical activity and exercise for general cardiovascular pulmonary and musculoskeletal health,” Helena W. Rodbard, MD, an endocrinologist in private practice in Rockville, Md., said in an interview.
“However, it was not known what effects various types of exercise would have on time in range (70-180 mg/dL) and time below range (< 70 mg/dL) measured over a full 24-hour period in people with type 1 diabetes,” said Dr. Rodbard, who was not involved with the study.
“I was surprised to see that the effect of the three different types of exercise were so similar,” Dr. Rodbard noted. “There had been previous reports suggesting that the time course of glucose could be different for these three types of exercise.”
The current study confirms prior knowledge that exercise can help reduce blood glucose, and increase TIR, said Dr. Rodbard. The study shows that TIR increases by roughly 5-7 percentage points (about 1 hour per day) and reduces mean glucose by 9-13 mg/dL irrespective of the three types of exercise,” she said. “There was a suggestion that the risk of increasing hypoglycemia below 70 mg/dL was less likely for resistance exercise than for the interval or aerobic types of exercise,” she noted.
As for additional research, “This study did not address the various ways in which one can mitigate the potentially deleterious effects of exercise, specifically with reference to rates of hypoglycemia, even mild symptomatic biochemical hypoglycemia,” said Dr. Rodbard. “Since the actual amount of time below 70 mg/dL is usually so small (0.3%-0.7% of the 1,440 minutes in the day, or about 5-10 minutes per day on average), it is difficult to measure and there is considerable variability between different people,” she emphasized. “Finding optimal and robust ways to achieve consistency in the reduction of glucose, between days within subjects, and between subjects, will need further examination of various types of protocols for diet, exercise and insulin administration, and of various methods for education of the patient,” she said.
The study was supported in part by the Leona M. and Harry B. Helmsley Charitable Trust. Ms. Li and Dr. Rodbard had no financial conflicts to disclose. Dr. Rodbard serves on the editorial advisory board of Clinical Endocrinology News.
Adults with type 1 diabetes had significantly better glycemic control on days they exercised, regardless of exercise type, compared to days when they were inactive, according to a prospective study in nearly 500 individuals.
Different types of exercise, such as aerobic workouts, interval training, or resistance training, may have different immediate glycemic effects in adults with type 1 diabetes (T1D), but the impact of exercise type on the percentage of time diabetes patients maintain glucose in the 70-180 mg/dL range on days when they are active vs. inactive has not been well studied, Zoey Li said in a presentation at the annual scientific sessions of the American Diabetes Association.
In the Type 1 Diabetes Exercise Initiative (T1DEXI) study, Ms. Li and colleagues examined continuous glucose monitoring (CGM) data from 497 adults with T1D. The observational study included self-referred adults aged 18 years and older who had been living with T1D for at least 2 years. Participants were assigned to programs of aerobic exercise (defined as a target heart rate of 70%-80% of age-predicted maximum), interval exercise (defined as an interval heart rate of 80%-90% of age-predicted maximum), or resistance exercise (defined as muscle group fatigue after three sets of eight repetitions).
Participants completed the workouts at home via 30-minute videos at least six times over the 4-week study period. The study design involved an activity goal of at least 150 minutes per week, including the videos and self-reported usual activity, such as walking. The data were collected through an app designed for the study, a heart rate monitor, and a CGM.
The researchers compared glucose levels on days when the participants reported being active compared to days when they were sedentary. The goal of the study was to assess the effect of exercise type on time spent with glucose in the range of 70-180 mg/dL, defined as time in range (TIR).
The mean age of the participants was 37 years; 89% were White. The mean duration of diabetes was 18 years, and the mean hemoglobin A1c was 6.6%. “An astounding 95% were current continuous glucose monitoring [CGM] users,” said Ms. Li, a statistician at the Jaeb Center for Health Research in Tampa, Fla.
A total of 398 participants reported at least one exercise day and one sedentary day, for a total of 1,302 exercise days and 2,470 sedentary days.
Overall, the mean TIR was significantly higher on exercise days compared to sedentary days (75% vs. 70%, P < .001). The median time above 180 mg/dL also was significantly lower on exercise days compared to sedentary days (17% vs. 23%, P < .001), and mean glucose levels were 10 mg/dL lower on exercise days (145 mg/dL vs. 155 mg/dL)
“This all came with a slight hit to their time below range,” Ms. Li noted. The median time below 70 mg/dL was 1.1% on exercise days compared to 0.4% on sedentary days (P < .001). The percentage of days with hypoglycemic events was higher on exercise days compared to sedentary days (47% vs. 40%, P < .001), as they are related to time below 70 mg/dL, she added.
The differences for mean glucose level and TIR between exercise days and sedentary days were significant for each of the three exercise types, Ms. Li said.
“After establishing these glycemic trends, we looked at whether there were any factors that influenced the glycemic differences on exercise vs. sedentary days,” Ms. Li said.
Regardless of exercise type, age, sex, baseline A1c, diabetes duration, body mass index, insulin modality, CGM use, and percentage of time below range in the past 24 hours, there was higher TIR and higher hypoglycemia on exercise days compared to sedentary days.
Although the study was limited in part by the observational design, “with these data, we can better understand the glycemic benefits and disadvantages of exercise in adults with type 1 diabetes,” Ms. Li said.
Don’t forget the negative effects of exercise
“It is well known that the three types of exercise can modulate glucose levels. This can be very useful when attempting to reduce excessively high glucose levels, and when encouraging people to engage in frequent, regular, and consistent physical activity and exercise for general cardiovascular pulmonary and musculoskeletal health,” Helena W. Rodbard, MD, an endocrinologist in private practice in Rockville, Md., said in an interview.
“However, it was not known what effects various types of exercise would have on time in range (70-180 mg/dL) and time below range (< 70 mg/dL) measured over a full 24-hour period in people with type 1 diabetes,” said Dr. Rodbard, who was not involved with the study.
“I was surprised to see that the effect of the three different types of exercise were so similar,” Dr. Rodbard noted. “There had been previous reports suggesting that the time course of glucose could be different for these three types of exercise.”
The current study confirms prior knowledge that exercise can help reduce blood glucose, and increase TIR, said Dr. Rodbard. The study shows that TIR increases by roughly 5-7 percentage points (about 1 hour per day) and reduces mean glucose by 9-13 mg/dL irrespective of the three types of exercise,” she said. “There was a suggestion that the risk of increasing hypoglycemia below 70 mg/dL was less likely for resistance exercise than for the interval or aerobic types of exercise,” she noted.
As for additional research, “This study did not address the various ways in which one can mitigate the potentially deleterious effects of exercise, specifically with reference to rates of hypoglycemia, even mild symptomatic biochemical hypoglycemia,” said Dr. Rodbard. “Since the actual amount of time below 70 mg/dL is usually so small (0.3%-0.7% of the 1,440 minutes in the day, or about 5-10 minutes per day on average), it is difficult to measure and there is considerable variability between different people,” she emphasized. “Finding optimal and robust ways to achieve consistency in the reduction of glucose, between days within subjects, and between subjects, will need further examination of various types of protocols for diet, exercise and insulin administration, and of various methods for education of the patient,” she said.
The study was supported in part by the Leona M. and Harry B. Helmsley Charitable Trust. Ms. Li and Dr. Rodbard had no financial conflicts to disclose. Dr. Rodbard serves on the editorial advisory board of Clinical Endocrinology News.
Adults with type 1 diabetes had significantly better glycemic control on days they exercised, regardless of exercise type, compared to days when they were inactive, according to a prospective study in nearly 500 individuals.
Different types of exercise, such as aerobic workouts, interval training, or resistance training, may have different immediate glycemic effects in adults with type 1 diabetes (T1D), but the impact of exercise type on the percentage of time diabetes patients maintain glucose in the 70-180 mg/dL range on days when they are active vs. inactive has not been well studied, Zoey Li said in a presentation at the annual scientific sessions of the American Diabetes Association.
In the Type 1 Diabetes Exercise Initiative (T1DEXI) study, Ms. Li and colleagues examined continuous glucose monitoring (CGM) data from 497 adults with T1D. The observational study included self-referred adults aged 18 years and older who had been living with T1D for at least 2 years. Participants were assigned to programs of aerobic exercise (defined as a target heart rate of 70%-80% of age-predicted maximum), interval exercise (defined as an interval heart rate of 80%-90% of age-predicted maximum), or resistance exercise (defined as muscle group fatigue after three sets of eight repetitions).
Participants completed the workouts at home via 30-minute videos at least six times over the 4-week study period. The study design involved an activity goal of at least 150 minutes per week, including the videos and self-reported usual activity, such as walking. The data were collected through an app designed for the study, a heart rate monitor, and a CGM.
The researchers compared glucose levels on days when the participants reported being active compared to days when they were sedentary. The goal of the study was to assess the effect of exercise type on time spent with glucose in the range of 70-180 mg/dL, defined as time in range (TIR).
The mean age of the participants was 37 years; 89% were White. The mean duration of diabetes was 18 years, and the mean hemoglobin A1c was 6.6%. “An astounding 95% were current continuous glucose monitoring [CGM] users,” said Ms. Li, a statistician at the Jaeb Center for Health Research in Tampa, Fla.
A total of 398 participants reported at least one exercise day and one sedentary day, for a total of 1,302 exercise days and 2,470 sedentary days.
Overall, the mean TIR was significantly higher on exercise days compared to sedentary days (75% vs. 70%, P < .001). The median time above 180 mg/dL also was significantly lower on exercise days compared to sedentary days (17% vs. 23%, P < .001), and mean glucose levels were 10 mg/dL lower on exercise days (145 mg/dL vs. 155 mg/dL)
“This all came with a slight hit to their time below range,” Ms. Li noted. The median time below 70 mg/dL was 1.1% on exercise days compared to 0.4% on sedentary days (P < .001). The percentage of days with hypoglycemic events was higher on exercise days compared to sedentary days (47% vs. 40%, P < .001), as they are related to time below 70 mg/dL, she added.
The differences for mean glucose level and TIR between exercise days and sedentary days were significant for each of the three exercise types, Ms. Li said.
“After establishing these glycemic trends, we looked at whether there were any factors that influenced the glycemic differences on exercise vs. sedentary days,” Ms. Li said.
Regardless of exercise type, age, sex, baseline A1c, diabetes duration, body mass index, insulin modality, CGM use, and percentage of time below range in the past 24 hours, there was higher TIR and higher hypoglycemia on exercise days compared to sedentary days.
Although the study was limited in part by the observational design, “with these data, we can better understand the glycemic benefits and disadvantages of exercise in adults with type 1 diabetes,” Ms. Li said.
Don’t forget the negative effects of exercise
“It is well known that the three types of exercise can modulate glucose levels. This can be very useful when attempting to reduce excessively high glucose levels, and when encouraging people to engage in frequent, regular, and consistent physical activity and exercise for general cardiovascular pulmonary and musculoskeletal health,” Helena W. Rodbard, MD, an endocrinologist in private practice in Rockville, Md., said in an interview.
“However, it was not known what effects various types of exercise would have on time in range (70-180 mg/dL) and time below range (< 70 mg/dL) measured over a full 24-hour period in people with type 1 diabetes,” said Dr. Rodbard, who was not involved with the study.
“I was surprised to see that the effect of the three different types of exercise were so similar,” Dr. Rodbard noted. “There had been previous reports suggesting that the time course of glucose could be different for these three types of exercise.”
The current study confirms prior knowledge that exercise can help reduce blood glucose, and increase TIR, said Dr. Rodbard. The study shows that TIR increases by roughly 5-7 percentage points (about 1 hour per day) and reduces mean glucose by 9-13 mg/dL irrespective of the three types of exercise,” she said. “There was a suggestion that the risk of increasing hypoglycemia below 70 mg/dL was less likely for resistance exercise than for the interval or aerobic types of exercise,” she noted.
As for additional research, “This study did not address the various ways in which one can mitigate the potentially deleterious effects of exercise, specifically with reference to rates of hypoglycemia, even mild symptomatic biochemical hypoglycemia,” said Dr. Rodbard. “Since the actual amount of time below 70 mg/dL is usually so small (0.3%-0.7% of the 1,440 minutes in the day, or about 5-10 minutes per day on average), it is difficult to measure and there is considerable variability between different people,” she emphasized. “Finding optimal and robust ways to achieve consistency in the reduction of glucose, between days within subjects, and between subjects, will need further examination of various types of protocols for diet, exercise and insulin administration, and of various methods for education of the patient,” she said.
The study was supported in part by the Leona M. and Harry B. Helmsley Charitable Trust. Ms. Li and Dr. Rodbard had no financial conflicts to disclose. Dr. Rodbard serves on the editorial advisory board of Clinical Endocrinology News.
FROM ADA 2022
‘Forever chemicals’ linked to hypertension in middle-aged women
In a large, prospective study, researchers found an association between higher blood levels of PFAS and increased risk of hypertension in middle-aged women. Women in the highest tertile of overall PFAS concentrations had a 71% increased risk of developing hypertension.
“Our findings suggest that long-term cumulative exposure, even before midlife, may increase the risk of high blood pressure, and therefore, the benefit of reducing the population exposure to PFAS and potential prevention of high blood pressure and other health conditions would be enormous,” Sung Kyun Park, ScD, MPH, University of Michigan School of Public Health, Ann Arbor, said in an interview.
The study was published online in Hypertension.
Everywhere and forever
“PFAS are forever chemicals as well as everywhere chemicals,” Dr. Park noted.
Possible sources of PFAS exposure run the gamut from nonstick cookware, food wrappers, and waterproof fabrics to cosmetics and drinking water. They have been detected in the blood of most people and have been linked to a variety of health concerns.
“A few studies showed an association between PFAS and hypertension, but those were cross-sectional and examined prevalence of hypertension. It was unclear whether PFAS are associated with the development (incidence) of hypertension,” Dr. Park explained.
For their study, the researchers examined the association between serum concentrations of PFAS and risks of incident hypertension in 1,058 initially normotensive women participating in the Study of Women’s Health Across the Nation-Multi-Pollutant Study (SWAN-MPS). They were followed annually between 1999 and 2017.
During 11,722 person-years of follow-up, 470 of the women developed hypertension, at a rate of 40.1 cases per 1,000 person-years. Hypertension was defined as blood pressure of at least 140 mm Hg systolic or at least 90 mm Hg diastolic or receiving antihypertensive treatment.
Women in the highest tertile of baseline serum concentration of perfluorooctane sulfonate (PFOS) had a 42% higher risk of developing hypertension, compared with peers in the lowest tertile (adjusted hazard ratio, 1.42; 95% confidence interval, 1.19-1.68; P trend = .01).
Similar results were found for perfluorooctanoate (PFOA) and 2-N-ethyl-perfluorooctane sulfonamido acetate (EtFOSAA), with 47% (aHR, 1.47; 95% CI, 1.24-1.75; P trend = .01) and 42% (aHR, 1.42; 95% CI, 1.19-1.70; P trend = .01) higher risks of incident hypertension, comparing the highest to the lowest tertiles.
The risks persisted after adjusting for various factors, including race, study site, education, financial strain, smoking status, alcohol use, total calorie intake, and menopausal status.
In the PFAS “mixture” analysis, women in the highest tertile of overall PFAS concentrations were 71% more likely to develop hypertension during follow-up, compared with women in the lowest tertile (aHR, 1.71; 95% CI, 1.15-2.54; P trend = .008).
“These findings suggest that PFAS might be an underappreciated contributing factor to women’s cardiovascular disease risk,” the researchers write.
They caution that the study only included middle-aged women and that it is unclear whether the findings hold for middle-aged men.
“This is an important question, but the answer is that we do not know,” Dr. Park told this news organization.
“Women become more susceptible to metabolic changes and hypertension risk during the menopausal transition. Our findings suggest that PFAS may play a role in the development of hypertension in women during this critical life stage,” Dr. Park said.
The researchers say more research is needed to confirm and expand the findings and to find ways to reduce PFAS exposure.
“If confirmed in future studies, these findings suggest that understanding human exposure to PFAS and developing effective strategies to reduce PFAS exposure may help prevent the development of hypertension and thereby reduce the global burden of CVD,” the researchers write.
‘The more we learn, the worse it gets’
This is an “interesting” study and shows that “the more we learn about PFAS, the worse it seems to get,” Ankur Shah, MD, division of kidney disease and hypertension, Warren Alpert Medical School of Brown University, Providence, R.I., said in an interview.
“This multisite, multiracial and multiethnic, community-based longitudinal study establishes an association between PFAS and hypertension,” said Dr. Shah, who wasn’t involved in the study.
“This adds to a growing literature base of associations of PFAS with illnesses, including malignancy, thyroid disorders, diabetes, ulcerative colitis, hyperlipidemia, and pregnancy-induced hypertension,” he noted.
Dr. Shah also noted that the authors adjusted for race and ethnicity, study site, education, financial strain, smoking status, environmental tobacco smoke, alcohol consumption, total calorie intake, and menopausal status “and still found a strong association.”
“Still to be determined are both whether PFAS are the causative agent or if there is an unmeasured/unadjusted for entity which has resulted in both increased PFAS exposure and hypertension, as well as if PFAS are causative, if reduction in PFAS exposure would be result in blood pressure reduction,” Dr. Shah added.
The study had no sources of funding. Dr. Park and Dr. Shah have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a large, prospective study, researchers found an association between higher blood levels of PFAS and increased risk of hypertension in middle-aged women. Women in the highest tertile of overall PFAS concentrations had a 71% increased risk of developing hypertension.
“Our findings suggest that long-term cumulative exposure, even before midlife, may increase the risk of high blood pressure, and therefore, the benefit of reducing the population exposure to PFAS and potential prevention of high blood pressure and other health conditions would be enormous,” Sung Kyun Park, ScD, MPH, University of Michigan School of Public Health, Ann Arbor, said in an interview.
The study was published online in Hypertension.
Everywhere and forever
“PFAS are forever chemicals as well as everywhere chemicals,” Dr. Park noted.
Possible sources of PFAS exposure run the gamut from nonstick cookware, food wrappers, and waterproof fabrics to cosmetics and drinking water. They have been detected in the blood of most people and have been linked to a variety of health concerns.
“A few studies showed an association between PFAS and hypertension, but those were cross-sectional and examined prevalence of hypertension. It was unclear whether PFAS are associated with the development (incidence) of hypertension,” Dr. Park explained.
For their study, the researchers examined the association between serum concentrations of PFAS and risks of incident hypertension in 1,058 initially normotensive women participating in the Study of Women’s Health Across the Nation-Multi-Pollutant Study (SWAN-MPS). They were followed annually between 1999 and 2017.
During 11,722 person-years of follow-up, 470 of the women developed hypertension, at a rate of 40.1 cases per 1,000 person-years. Hypertension was defined as blood pressure of at least 140 mm Hg systolic or at least 90 mm Hg diastolic or receiving antihypertensive treatment.
Women in the highest tertile of baseline serum concentration of perfluorooctane sulfonate (PFOS) had a 42% higher risk of developing hypertension, compared with peers in the lowest tertile (adjusted hazard ratio, 1.42; 95% confidence interval, 1.19-1.68; P trend = .01).
Similar results were found for perfluorooctanoate (PFOA) and 2-N-ethyl-perfluorooctane sulfonamido acetate (EtFOSAA), with 47% (aHR, 1.47; 95% CI, 1.24-1.75; P trend = .01) and 42% (aHR, 1.42; 95% CI, 1.19-1.70; P trend = .01) higher risks of incident hypertension, comparing the highest to the lowest tertiles.
The risks persisted after adjusting for various factors, including race, study site, education, financial strain, smoking status, alcohol use, total calorie intake, and menopausal status.
In the PFAS “mixture” analysis, women in the highest tertile of overall PFAS concentrations were 71% more likely to develop hypertension during follow-up, compared with women in the lowest tertile (aHR, 1.71; 95% CI, 1.15-2.54; P trend = .008).
“These findings suggest that PFAS might be an underappreciated contributing factor to women’s cardiovascular disease risk,” the researchers write.
They caution that the study only included middle-aged women and that it is unclear whether the findings hold for middle-aged men.
“This is an important question, but the answer is that we do not know,” Dr. Park told this news organization.
“Women become more susceptible to metabolic changes and hypertension risk during the menopausal transition. Our findings suggest that PFAS may play a role in the development of hypertension in women during this critical life stage,” Dr. Park said.
The researchers say more research is needed to confirm and expand the findings and to find ways to reduce PFAS exposure.
“If confirmed in future studies, these findings suggest that understanding human exposure to PFAS and developing effective strategies to reduce PFAS exposure may help prevent the development of hypertension and thereby reduce the global burden of CVD,” the researchers write.
‘The more we learn, the worse it gets’
This is an “interesting” study and shows that “the more we learn about PFAS, the worse it seems to get,” Ankur Shah, MD, division of kidney disease and hypertension, Warren Alpert Medical School of Brown University, Providence, R.I., said in an interview.
“This multisite, multiracial and multiethnic, community-based longitudinal study establishes an association between PFAS and hypertension,” said Dr. Shah, who wasn’t involved in the study.
“This adds to a growing literature base of associations of PFAS with illnesses, including malignancy, thyroid disorders, diabetes, ulcerative colitis, hyperlipidemia, and pregnancy-induced hypertension,” he noted.
Dr. Shah also noted that the authors adjusted for race and ethnicity, study site, education, financial strain, smoking status, environmental tobacco smoke, alcohol consumption, total calorie intake, and menopausal status “and still found a strong association.”
“Still to be determined are both whether PFAS are the causative agent or if there is an unmeasured/unadjusted for entity which has resulted in both increased PFAS exposure and hypertension, as well as if PFAS are causative, if reduction in PFAS exposure would be result in blood pressure reduction,” Dr. Shah added.
The study had no sources of funding. Dr. Park and Dr. Shah have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a large, prospective study, researchers found an association between higher blood levels of PFAS and increased risk of hypertension in middle-aged women. Women in the highest tertile of overall PFAS concentrations had a 71% increased risk of developing hypertension.
“Our findings suggest that long-term cumulative exposure, even before midlife, may increase the risk of high blood pressure, and therefore, the benefit of reducing the population exposure to PFAS and potential prevention of high blood pressure and other health conditions would be enormous,” Sung Kyun Park, ScD, MPH, University of Michigan School of Public Health, Ann Arbor, said in an interview.
The study was published online in Hypertension.
Everywhere and forever
“PFAS are forever chemicals as well as everywhere chemicals,” Dr. Park noted.
Possible sources of PFAS exposure run the gamut from nonstick cookware, food wrappers, and waterproof fabrics to cosmetics and drinking water. They have been detected in the blood of most people and have been linked to a variety of health concerns.
“A few studies showed an association between PFAS and hypertension, but those were cross-sectional and examined prevalence of hypertension. It was unclear whether PFAS are associated with the development (incidence) of hypertension,” Dr. Park explained.
For their study, the researchers examined the association between serum concentrations of PFAS and risks of incident hypertension in 1,058 initially normotensive women participating in the Study of Women’s Health Across the Nation-Multi-Pollutant Study (SWAN-MPS). They were followed annually between 1999 and 2017.
During 11,722 person-years of follow-up, 470 of the women developed hypertension, at a rate of 40.1 cases per 1,000 person-years. Hypertension was defined as blood pressure of at least 140 mm Hg systolic or at least 90 mm Hg diastolic or receiving antihypertensive treatment.
Women in the highest tertile of baseline serum concentration of perfluorooctane sulfonate (PFOS) had a 42% higher risk of developing hypertension, compared with peers in the lowest tertile (adjusted hazard ratio, 1.42; 95% confidence interval, 1.19-1.68; P trend = .01).
Similar results were found for perfluorooctanoate (PFOA) and 2-N-ethyl-perfluorooctane sulfonamido acetate (EtFOSAA), with 47% (aHR, 1.47; 95% CI, 1.24-1.75; P trend = .01) and 42% (aHR, 1.42; 95% CI, 1.19-1.70; P trend = .01) higher risks of incident hypertension, comparing the highest to the lowest tertiles.
The risks persisted after adjusting for various factors, including race, study site, education, financial strain, smoking status, alcohol use, total calorie intake, and menopausal status.
In the PFAS “mixture” analysis, women in the highest tertile of overall PFAS concentrations were 71% more likely to develop hypertension during follow-up, compared with women in the lowest tertile (aHR, 1.71; 95% CI, 1.15-2.54; P trend = .008).
“These findings suggest that PFAS might be an underappreciated contributing factor to women’s cardiovascular disease risk,” the researchers write.
They caution that the study only included middle-aged women and that it is unclear whether the findings hold for middle-aged men.
“This is an important question, but the answer is that we do not know,” Dr. Park told this news organization.
“Women become more susceptible to metabolic changes and hypertension risk during the menopausal transition. Our findings suggest that PFAS may play a role in the development of hypertension in women during this critical life stage,” Dr. Park said.
The researchers say more research is needed to confirm and expand the findings and to find ways to reduce PFAS exposure.
“If confirmed in future studies, these findings suggest that understanding human exposure to PFAS and developing effective strategies to reduce PFAS exposure may help prevent the development of hypertension and thereby reduce the global burden of CVD,” the researchers write.
‘The more we learn, the worse it gets’
This is an “interesting” study and shows that “the more we learn about PFAS, the worse it seems to get,” Ankur Shah, MD, division of kidney disease and hypertension, Warren Alpert Medical School of Brown University, Providence, R.I., said in an interview.
“This multisite, multiracial and multiethnic, community-based longitudinal study establishes an association between PFAS and hypertension,” said Dr. Shah, who wasn’t involved in the study.
“This adds to a growing literature base of associations of PFAS with illnesses, including malignancy, thyroid disorders, diabetes, ulcerative colitis, hyperlipidemia, and pregnancy-induced hypertension,” he noted.
Dr. Shah also noted that the authors adjusted for race and ethnicity, study site, education, financial strain, smoking status, environmental tobacco smoke, alcohol consumption, total calorie intake, and menopausal status “and still found a strong association.”
“Still to be determined are both whether PFAS are the causative agent or if there is an unmeasured/unadjusted for entity which has resulted in both increased PFAS exposure and hypertension, as well as if PFAS are causative, if reduction in PFAS exposure would be result in blood pressure reduction,” Dr. Shah added.
The study had no sources of funding. Dr. Park and Dr. Shah have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HYPERTENSION
‘DIY’ artificial pancreas systems found to be safe, effective: CREATE trial
NEW ORLEANS – Open-source automated insulin delivery systems appear to be both effective and safe in adults and children, new research finds.
Automated insulin delivery (AID) system, also known as closed-loop systems or an artificial pancreas, link an insulin pump and a continuous glucose monitor (CGM) with an algorithm that automatically adjusts insulin delivery to optimize glycemic control.
Prior to the availability of commercial AID systems, Dana Lewis, a patient with type 1 diabetes, and her partner codeveloped an algorithm that could link older versions of an insulin pump and CGM.
In 2015, they made the code and all related materials open-source, so that anyone who wanted to create their own AID system could do so. Today thousands of people worldwide with type 1 diabetes are using the systems, which are sometimes called “do-it-yourself (DIY)” AID systems although the approach has been community based.
AID systems are not approved by any regulatory body, and despite several nonrandomized studies demonstrating their effectiveness and safety, there is still concern among some health professionals about their safety. In 2019, the U.S. Food and Drug Administration warned against the use of any nonapproved devices or algorithms. (Now, though, at least one open-source AID system algorithm is under FDA review.)
Aimed at addressing those concerns, CREATE (Community Derived Automated Insulin Delivery) is the first randomized controlled clinical trial to compare an open-source AID system to insulin pump therapy and CGM (without any communication between the two) in patients with type 1 diabetes, most of whom were naive to AID systems.
Doctors uncomfortable with open source; study provides reassurance
The findings were presented at the American Diabetes Association scientific sessions by Martin I. de Bock, PhD, a pediatric endocrinologist and senior lecturer at the University of Otago, Christchurch, New Zealand.
The study compared the most commonly used open-source AID system (using the OpenAPS algorithm from a version of AndroidAPS implemented in a smartphone with the DANA-i insulin pump and Dexcom G6 CGM) to any insulin pump plus CGM as a comparator group.
The open-source AID system led to a significant reduction in hemoglobin A1c with no major safety issues.
“The acceptance [among clinicians] of open-source systems is diverse and complicated, [with varying] personal comfort levels of seeing someone using an AID system that has no regulatory approval,” Dr. de Bock told this news organization.
“This is one of the reasons that it was so important to conduct the CREATE trial for the many thousands of open-source AID users. Given that the trial demonstrated safety and efficacy using the most robust scientific methodology available – a long-term randomized controlled trial – it may go some way to provide assurance for providers when they are seeing people using an open-source automated system,” he said.
Asked for comment, session moderator Diana Isaacs, PharmD, CDCES, an endocrine clinical pharmacist at the Cleveland Clinic, told this news organization: “There has been concern that these systems aren’t safe, so showing the safety is important. I think people deserve choice. As long as they’re safe, patients should be able to use what they want to use, and we should support them.”
Dr. Isaacs pointed out that an advantage of open-source systems over current commercial AIDs for patients is the ability to customize glucose targets, but in CREATE, those targets were established in the protocol by the investigators.
“I think it’s nice having the data, although in the trial they had specific requirements. They had a target range and active insulin time that they were recommending. So it’s a little different than true DIY where you don’t really have those guidelines you have to follow. It is exciting, it’s very interesting, but I wouldn’t say it’s a true mirror of the real world.”
Open-source systems improved time-in-range, no safety issues
For the CREATE study, 100 participants were enrolled, including 50 children aged 7-15 years and 50 adults aged 16-70 years. All participants had been using insulin pumps for at least 6 months. Most of the children and about two-thirds of the adults were also using CGMs, but just 6% of the children and 18% of the adults had prior experience with AID systems.
Baseline A1c in children was 7.5% and in adults was 7.7%.
After a 4-week run-in, all patients were randomized to the open-source AID or insulin pump plus CGM for 6 months.
The final group analyzed consisted of 42 patients in the open-source AID group and 53 patients in the comparator group.
The primary outcome, the adjusted mean difference in percent time-in-range (glucose of 70-180 mg/dL) during the final 2 weeks of the 6-month trial, showed a significant difference of 14% (P < .001) with open-source AID compared with pump plus CGM only.
Time-in-range in the open-source AID group rose from 61.2% to 71.2%, while it actually dropped slightly in the comparator group, from 57.7% to 54.5%.
The proportion of patients achieving time-in-range greater than 70% with open-source AID was 60% versus just 15% with pump plus CGM.
Glycemic improvements with open-source AID were significant for adults and children and were greater for those with higher baseline A1c levels. The effect was immediate and sustained throughout the study period, “which is super-pleasing, because there was a worry that the technical burden of open source might be [leading to] dropout, but we didn’t see that. It was sustained right through to the end of the trial,” Dr. de Bock commented.
Hypoglycemic rates didn’t differ between groups, and there were no episodes of severe hypoglycemia or diabetic ketoacidosis.
No more waiting: What is the future of open-source AID?
When the open-source APS was first developed, users coined the motto: “We are not waiting.” But now that the “wait” is over and several commercial AIDs have been approved by regulatory bodies, with others still in the pipeline, will people still use open-source systems?
There are no current data on people moving from DIY to commercial systems. However, Dr. de Bock said, “For most who undertook an open-source option, the precision of the settings that they can use and enjoy would mean that most would likely stick to their open source.”
Dr. Isaacs agrees: “I actually don’t think it’s going to go away in the near future, because the FDA has very specific criteria for where these [formally approved] devices can be in terms of their target ranges and requirements versus with open source you can really customize. So I still think there’s going to be a subset of people who want that customization, who want the lower targets.”
Dana Lewis, the originator of the DIY system and a CREATE coauthor, told this news organization: “I don’t believe there has been a fall-off, and in fact, I think open-source AID has continued to have ongoing uptake as awareness increases about options and as more pumps and CGMs become interoperable with various open-source AID choices.”
“I think uptake increasing is also influenced by the fact that in places like Europe, Asia, and Australia there are in-warranty on-the-market pumps that are compatible and interoperable with open-source AID. I think awareness of AID overall increases uptake of commercial and open source alike,” she said.
“Clinicians, as emphasized in recent position statements, must maintain support of the person with diabetes, irrespective of the mode of treatment they are on. ... Health care providers should be encouraged to learn from the experiences of the people who have stuck with open-source AID or switched, so that they can inform themselves of the relative strengths and benefits of each system,” Dr. de Bock advised.
Ms. Lewis noted: “We are seeing increasing awareness and comfort in endocrinologists from the community perspective, and we do hope that this study helps increase conversation and awareness of the safety and efficacy of open-source AID systems as an option for people with diabetes.”
In fact, the team published an article specifically about clinicians’ experience in CREATE. “The learning curve is similar across AID technology,” she observed.
Findings of a 6-month continuation phase of CREATE, in which all participants used the open-source AID, are scheduled to be presented in September at the European Association for the Study of Diabetes annual meeting.
The study was funded by the Health Research Council of New Zealand, with hardware support from SOOIL Developments, South Korea; Dexcom; and Vodafone New Zealand. Dr. de Bock has reported receiving honoraria and/or research funding from Novo Nordisk, Sanofi, Pfizer, Medtronic, Lilly, Ypsomed, and Dexcom. Dr. Isaacs has reported serving as a consultant for LifeScan, Lilly, and Insulet, and as a speaker for Dexcom, Medtronic, Abbott, and Novo Nordisk. Ms. Lewis has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – Open-source automated insulin delivery systems appear to be both effective and safe in adults and children, new research finds.
Automated insulin delivery (AID) system, also known as closed-loop systems or an artificial pancreas, link an insulin pump and a continuous glucose monitor (CGM) with an algorithm that automatically adjusts insulin delivery to optimize glycemic control.
Prior to the availability of commercial AID systems, Dana Lewis, a patient with type 1 diabetes, and her partner codeveloped an algorithm that could link older versions of an insulin pump and CGM.
In 2015, they made the code and all related materials open-source, so that anyone who wanted to create their own AID system could do so. Today thousands of people worldwide with type 1 diabetes are using the systems, which are sometimes called “do-it-yourself (DIY)” AID systems although the approach has been community based.
AID systems are not approved by any regulatory body, and despite several nonrandomized studies demonstrating their effectiveness and safety, there is still concern among some health professionals about their safety. In 2019, the U.S. Food and Drug Administration warned against the use of any nonapproved devices or algorithms. (Now, though, at least one open-source AID system algorithm is under FDA review.)
Aimed at addressing those concerns, CREATE (Community Derived Automated Insulin Delivery) is the first randomized controlled clinical trial to compare an open-source AID system to insulin pump therapy and CGM (without any communication between the two) in patients with type 1 diabetes, most of whom were naive to AID systems.
Doctors uncomfortable with open source; study provides reassurance
The findings were presented at the American Diabetes Association scientific sessions by Martin I. de Bock, PhD, a pediatric endocrinologist and senior lecturer at the University of Otago, Christchurch, New Zealand.
The study compared the most commonly used open-source AID system (using the OpenAPS algorithm from a version of AndroidAPS implemented in a smartphone with the DANA-i insulin pump and Dexcom G6 CGM) to any insulin pump plus CGM as a comparator group.
The open-source AID system led to a significant reduction in hemoglobin A1c with no major safety issues.
“The acceptance [among clinicians] of open-source systems is diverse and complicated, [with varying] personal comfort levels of seeing someone using an AID system that has no regulatory approval,” Dr. de Bock told this news organization.
“This is one of the reasons that it was so important to conduct the CREATE trial for the many thousands of open-source AID users. Given that the trial demonstrated safety and efficacy using the most robust scientific methodology available – a long-term randomized controlled trial – it may go some way to provide assurance for providers when they are seeing people using an open-source automated system,” he said.
Asked for comment, session moderator Diana Isaacs, PharmD, CDCES, an endocrine clinical pharmacist at the Cleveland Clinic, told this news organization: “There has been concern that these systems aren’t safe, so showing the safety is important. I think people deserve choice. As long as they’re safe, patients should be able to use what they want to use, and we should support them.”
Dr. Isaacs pointed out that an advantage of open-source systems over current commercial AIDs for patients is the ability to customize glucose targets, but in CREATE, those targets were established in the protocol by the investigators.
“I think it’s nice having the data, although in the trial they had specific requirements. They had a target range and active insulin time that they were recommending. So it’s a little different than true DIY where you don’t really have those guidelines you have to follow. It is exciting, it’s very interesting, but I wouldn’t say it’s a true mirror of the real world.”
Open-source systems improved time-in-range, no safety issues
For the CREATE study, 100 participants were enrolled, including 50 children aged 7-15 years and 50 adults aged 16-70 years. All participants had been using insulin pumps for at least 6 months. Most of the children and about two-thirds of the adults were also using CGMs, but just 6% of the children and 18% of the adults had prior experience with AID systems.
Baseline A1c in children was 7.5% and in adults was 7.7%.
After a 4-week run-in, all patients were randomized to the open-source AID or insulin pump plus CGM for 6 months.
The final group analyzed consisted of 42 patients in the open-source AID group and 53 patients in the comparator group.
The primary outcome, the adjusted mean difference in percent time-in-range (glucose of 70-180 mg/dL) during the final 2 weeks of the 6-month trial, showed a significant difference of 14% (P < .001) with open-source AID compared with pump plus CGM only.
Time-in-range in the open-source AID group rose from 61.2% to 71.2%, while it actually dropped slightly in the comparator group, from 57.7% to 54.5%.
The proportion of patients achieving time-in-range greater than 70% with open-source AID was 60% versus just 15% with pump plus CGM.
Glycemic improvements with open-source AID were significant for adults and children and were greater for those with higher baseline A1c levels. The effect was immediate and sustained throughout the study period, “which is super-pleasing, because there was a worry that the technical burden of open source might be [leading to] dropout, but we didn’t see that. It was sustained right through to the end of the trial,” Dr. de Bock commented.
Hypoglycemic rates didn’t differ between groups, and there were no episodes of severe hypoglycemia or diabetic ketoacidosis.
No more waiting: What is the future of open-source AID?
When the open-source APS was first developed, users coined the motto: “We are not waiting.” But now that the “wait” is over and several commercial AIDs have been approved by regulatory bodies, with others still in the pipeline, will people still use open-source systems?
There are no current data on people moving from DIY to commercial systems. However, Dr. de Bock said, “For most who undertook an open-source option, the precision of the settings that they can use and enjoy would mean that most would likely stick to their open source.”
Dr. Isaacs agrees: “I actually don’t think it’s going to go away in the near future, because the FDA has very specific criteria for where these [formally approved] devices can be in terms of their target ranges and requirements versus with open source you can really customize. So I still think there’s going to be a subset of people who want that customization, who want the lower targets.”
Dana Lewis, the originator of the DIY system and a CREATE coauthor, told this news organization: “I don’t believe there has been a fall-off, and in fact, I think open-source AID has continued to have ongoing uptake as awareness increases about options and as more pumps and CGMs become interoperable with various open-source AID choices.”
“I think uptake increasing is also influenced by the fact that in places like Europe, Asia, and Australia there are in-warranty on-the-market pumps that are compatible and interoperable with open-source AID. I think awareness of AID overall increases uptake of commercial and open source alike,” she said.
“Clinicians, as emphasized in recent position statements, must maintain support of the person with diabetes, irrespective of the mode of treatment they are on. ... Health care providers should be encouraged to learn from the experiences of the people who have stuck with open-source AID or switched, so that they can inform themselves of the relative strengths and benefits of each system,” Dr. de Bock advised.
Ms. Lewis noted: “We are seeing increasing awareness and comfort in endocrinologists from the community perspective, and we do hope that this study helps increase conversation and awareness of the safety and efficacy of open-source AID systems as an option for people with diabetes.”
In fact, the team published an article specifically about clinicians’ experience in CREATE. “The learning curve is similar across AID technology,” she observed.
Findings of a 6-month continuation phase of CREATE, in which all participants used the open-source AID, are scheduled to be presented in September at the European Association for the Study of Diabetes annual meeting.
The study was funded by the Health Research Council of New Zealand, with hardware support from SOOIL Developments, South Korea; Dexcom; and Vodafone New Zealand. Dr. de Bock has reported receiving honoraria and/or research funding from Novo Nordisk, Sanofi, Pfizer, Medtronic, Lilly, Ypsomed, and Dexcom. Dr. Isaacs has reported serving as a consultant for LifeScan, Lilly, and Insulet, and as a speaker for Dexcom, Medtronic, Abbott, and Novo Nordisk. Ms. Lewis has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – Open-source automated insulin delivery systems appear to be both effective and safe in adults and children, new research finds.
Automated insulin delivery (AID) system, also known as closed-loop systems or an artificial pancreas, link an insulin pump and a continuous glucose monitor (CGM) with an algorithm that automatically adjusts insulin delivery to optimize glycemic control.
Prior to the availability of commercial AID systems, Dana Lewis, a patient with type 1 diabetes, and her partner codeveloped an algorithm that could link older versions of an insulin pump and CGM.
In 2015, they made the code and all related materials open-source, so that anyone who wanted to create their own AID system could do so. Today thousands of people worldwide with type 1 diabetes are using the systems, which are sometimes called “do-it-yourself (DIY)” AID systems although the approach has been community based.
AID systems are not approved by any regulatory body, and despite several nonrandomized studies demonstrating their effectiveness and safety, there is still concern among some health professionals about their safety. In 2019, the U.S. Food and Drug Administration warned against the use of any nonapproved devices or algorithms. (Now, though, at least one open-source AID system algorithm is under FDA review.)
Aimed at addressing those concerns, CREATE (Community Derived Automated Insulin Delivery) is the first randomized controlled clinical trial to compare an open-source AID system to insulin pump therapy and CGM (without any communication between the two) in patients with type 1 diabetes, most of whom were naive to AID systems.
Doctors uncomfortable with open source; study provides reassurance
The findings were presented at the American Diabetes Association scientific sessions by Martin I. de Bock, PhD, a pediatric endocrinologist and senior lecturer at the University of Otago, Christchurch, New Zealand.
The study compared the most commonly used open-source AID system (using the OpenAPS algorithm from a version of AndroidAPS implemented in a smartphone with the DANA-i insulin pump and Dexcom G6 CGM) to any insulin pump plus CGM as a comparator group.
The open-source AID system led to a significant reduction in hemoglobin A1c with no major safety issues.
“The acceptance [among clinicians] of open-source systems is diverse and complicated, [with varying] personal comfort levels of seeing someone using an AID system that has no regulatory approval,” Dr. de Bock told this news organization.
“This is one of the reasons that it was so important to conduct the CREATE trial for the many thousands of open-source AID users. Given that the trial demonstrated safety and efficacy using the most robust scientific methodology available – a long-term randomized controlled trial – it may go some way to provide assurance for providers when they are seeing people using an open-source automated system,” he said.
Asked for comment, session moderator Diana Isaacs, PharmD, CDCES, an endocrine clinical pharmacist at the Cleveland Clinic, told this news organization: “There has been concern that these systems aren’t safe, so showing the safety is important. I think people deserve choice. As long as they’re safe, patients should be able to use what they want to use, and we should support them.”
Dr. Isaacs pointed out that an advantage of open-source systems over current commercial AIDs for patients is the ability to customize glucose targets, but in CREATE, those targets were established in the protocol by the investigators.
“I think it’s nice having the data, although in the trial they had specific requirements. They had a target range and active insulin time that they were recommending. So it’s a little different than true DIY where you don’t really have those guidelines you have to follow. It is exciting, it’s very interesting, but I wouldn’t say it’s a true mirror of the real world.”
Open-source systems improved time-in-range, no safety issues
For the CREATE study, 100 participants were enrolled, including 50 children aged 7-15 years and 50 adults aged 16-70 years. All participants had been using insulin pumps for at least 6 months. Most of the children and about two-thirds of the adults were also using CGMs, but just 6% of the children and 18% of the adults had prior experience with AID systems.
Baseline A1c in children was 7.5% and in adults was 7.7%.
After a 4-week run-in, all patients were randomized to the open-source AID or insulin pump plus CGM for 6 months.
The final group analyzed consisted of 42 patients in the open-source AID group and 53 patients in the comparator group.
The primary outcome, the adjusted mean difference in percent time-in-range (glucose of 70-180 mg/dL) during the final 2 weeks of the 6-month trial, showed a significant difference of 14% (P < .001) with open-source AID compared with pump plus CGM only.
Time-in-range in the open-source AID group rose from 61.2% to 71.2%, while it actually dropped slightly in the comparator group, from 57.7% to 54.5%.
The proportion of patients achieving time-in-range greater than 70% with open-source AID was 60% versus just 15% with pump plus CGM.
Glycemic improvements with open-source AID were significant for adults and children and were greater for those with higher baseline A1c levels. The effect was immediate and sustained throughout the study period, “which is super-pleasing, because there was a worry that the technical burden of open source might be [leading to] dropout, but we didn’t see that. It was sustained right through to the end of the trial,” Dr. de Bock commented.
Hypoglycemic rates didn’t differ between groups, and there were no episodes of severe hypoglycemia or diabetic ketoacidosis.
No more waiting: What is the future of open-source AID?
When the open-source APS was first developed, users coined the motto: “We are not waiting.” But now that the “wait” is over and several commercial AIDs have been approved by regulatory bodies, with others still in the pipeline, will people still use open-source systems?
There are no current data on people moving from DIY to commercial systems. However, Dr. de Bock said, “For most who undertook an open-source option, the precision of the settings that they can use and enjoy would mean that most would likely stick to their open source.”
Dr. Isaacs agrees: “I actually don’t think it’s going to go away in the near future, because the FDA has very specific criteria for where these [formally approved] devices can be in terms of their target ranges and requirements versus with open source you can really customize. So I still think there’s going to be a subset of people who want that customization, who want the lower targets.”
Dana Lewis, the originator of the DIY system and a CREATE coauthor, told this news organization: “I don’t believe there has been a fall-off, and in fact, I think open-source AID has continued to have ongoing uptake as awareness increases about options and as more pumps and CGMs become interoperable with various open-source AID choices.”
“I think uptake increasing is also influenced by the fact that in places like Europe, Asia, and Australia there are in-warranty on-the-market pumps that are compatible and interoperable with open-source AID. I think awareness of AID overall increases uptake of commercial and open source alike,” she said.
“Clinicians, as emphasized in recent position statements, must maintain support of the person with diabetes, irrespective of the mode of treatment they are on. ... Health care providers should be encouraged to learn from the experiences of the people who have stuck with open-source AID or switched, so that they can inform themselves of the relative strengths and benefits of each system,” Dr. de Bock advised.
Ms. Lewis noted: “We are seeing increasing awareness and comfort in endocrinologists from the community perspective, and we do hope that this study helps increase conversation and awareness of the safety and efficacy of open-source AID systems as an option for people with diabetes.”
In fact, the team published an article specifically about clinicians’ experience in CREATE. “The learning curve is similar across AID technology,” she observed.
Findings of a 6-month continuation phase of CREATE, in which all participants used the open-source AID, are scheduled to be presented in September at the European Association for the Study of Diabetes annual meeting.
The study was funded by the Health Research Council of New Zealand, with hardware support from SOOIL Developments, South Korea; Dexcom; and Vodafone New Zealand. Dr. de Bock has reported receiving honoraria and/or research funding from Novo Nordisk, Sanofi, Pfizer, Medtronic, Lilly, Ypsomed, and Dexcom. Dr. Isaacs has reported serving as a consultant for LifeScan, Lilly, and Insulet, and as a speaker for Dexcom, Medtronic, Abbott, and Novo Nordisk. Ms. Lewis has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ADA 2022
A ‘crisis’ of suicidal thoughts, attempts in transgender youth
Transgender youth are significantly more likely to consider suicide and attempt it, compared with their cisgender peers, new research shows.
In a large population-based study, investigators found the increased risk of suicidality is partly because of bullying and cyberbullying experienced by transgender teens.
The findings are “extremely concerning and should be a wake-up call,” Ian Colman, PhD, with the University of Ottawa School of Epidemiology and Public Health, said in an interview.
Young people who are exploring their sexual identities may suffer from depression and anxiety, both about the reactions of their peers and families, as well as their own sense of self.
“These youth are highly marginalized and stigmatized in many corners of our society, and these findings highlight just how distressing these experiences can be,” Dr. Colman said.
The study was published online in the Canadian Medical Association Journal.
Sevenfold increased risk of attempted suicide
The risk of suicidal thoughts and actions is not well studied in transgender and nonbinary youth.
To expand the evidence base, the researchers analyzed data for 6,800 adolescents aged 15-17 years from the 2019 Canadian Health Survey on Children and Youth.
The sample included 1,130 (16.5%) adolescents who identified as having some degree of same-gender attraction, 265 (4.3%) who were unsure of their attraction (“questioning”), and 50 (0.6%) who were transgender, meaning they identified as being of a gender different from that assigned at birth.
Overall, 980 (14.0%) adolescents reported having thoughts of suicide in the prior year, and 480 (6.8%) had attempted suicide in their life.
Transgender youth were five times more likely to think about suicide and more than seven times more likely to have ever attempted suicide than cisgender, heterosexual peers.
Among cisgender adolescents, girls who were attracted to girls had 3.6 times the risk of suicidal ideation and 3.3 times the risk of having ever attempted suicide, compared with their heterosexual peers.
Teens attracted to multiple genders had more than twice the risk of suicidal ideation and suicide attempt. Youth who were questioning their sexual orientation had twice the risk of having attempted suicide in their lifetime.
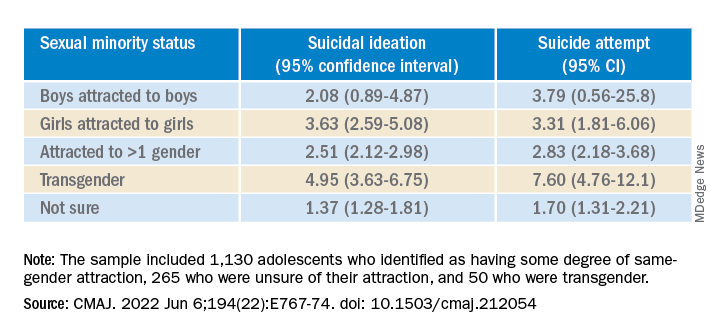
A crisis – with reason for hope
“This is a crisis, and it shows just how much more needs to be done to support transgender young people,” co-author Fae Johnstone, MSW, executive director, Wisdom2Action, who is a trans woman herself, said in the news release.
“Suicide prevention programs specifically targeted to transgender, nonbinary, and sexual minority adolescents, as well as gender-affirming care for transgender adolescents, may help reduce the burden of suicidality among this group,” Ms. Johnstone added.
“The most important thing that parents, teachers, and health care providers can do is to be supportive of these youth,” Dr. Colman told this news organization.
“Providing a safe place where gender and sexual minorities can explore and express themselves is crucial. The first step is to listen and to be compassionate,” Dr. Colman added.
Reached for comment, Jess Ting, MD, director of surgery at the Mount Sinai Center for Transgender Medicine and Surgery, New York, said the data from this study on suicidal thoughts and actions among sexual minority and transgender adolescents “mirror what we see and what we know” about suicidality in trans and nonbinary adults.
“The reasons for this are complex, and it’s hard for someone who doesn’t have a lived experience as a trans or nonbinary person to understand the reasons for suicidality,” he told this news organization.
“But we also know that there are higher rates of anxiety and depression and self-image issues and posttraumatic stress disorder, not to mention outside factors – marginalization, discrimination, violence, abuse. When you add up all these intrinsic and extrinsic factors, it’s not hard to believe that there is a high rate of suicidality,” Dr. Ting said.
“There have been studies that have shown that in children who are supported in their gender identity, the rates of depression and anxiety decreased to almost the same levels as non-trans and nonbinary children, so I think that gives cause for hope,” Dr. Ting added.
The study was funded in part by the Research Council of Norway through its Centres of Excellence funding scheme and by a Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Award. Ms. Johnstone reports consulting fees from Spectrum Waterloo and volunteer participation with the Youth Suicide Prevention Leadership Committee of Ontario. No other competing interests were declared. Dr. Ting has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender youth are significantly more likely to consider suicide and attempt it, compared with their cisgender peers, new research shows.
In a large population-based study, investigators found the increased risk of suicidality is partly because of bullying and cyberbullying experienced by transgender teens.
The findings are “extremely concerning and should be a wake-up call,” Ian Colman, PhD, with the University of Ottawa School of Epidemiology and Public Health, said in an interview.
Young people who are exploring their sexual identities may suffer from depression and anxiety, both about the reactions of their peers and families, as well as their own sense of self.
“These youth are highly marginalized and stigmatized in many corners of our society, and these findings highlight just how distressing these experiences can be,” Dr. Colman said.
The study was published online in the Canadian Medical Association Journal.
Sevenfold increased risk of attempted suicide
The risk of suicidal thoughts and actions is not well studied in transgender and nonbinary youth.
To expand the evidence base, the researchers analyzed data for 6,800 adolescents aged 15-17 years from the 2019 Canadian Health Survey on Children and Youth.
The sample included 1,130 (16.5%) adolescents who identified as having some degree of same-gender attraction, 265 (4.3%) who were unsure of their attraction (“questioning”), and 50 (0.6%) who were transgender, meaning they identified as being of a gender different from that assigned at birth.
Overall, 980 (14.0%) adolescents reported having thoughts of suicide in the prior year, and 480 (6.8%) had attempted suicide in their life.
Transgender youth were five times more likely to think about suicide and more than seven times more likely to have ever attempted suicide than cisgender, heterosexual peers.
Among cisgender adolescents, girls who were attracted to girls had 3.6 times the risk of suicidal ideation and 3.3 times the risk of having ever attempted suicide, compared with their heterosexual peers.
Teens attracted to multiple genders had more than twice the risk of suicidal ideation and suicide attempt. Youth who were questioning their sexual orientation had twice the risk of having attempted suicide in their lifetime.
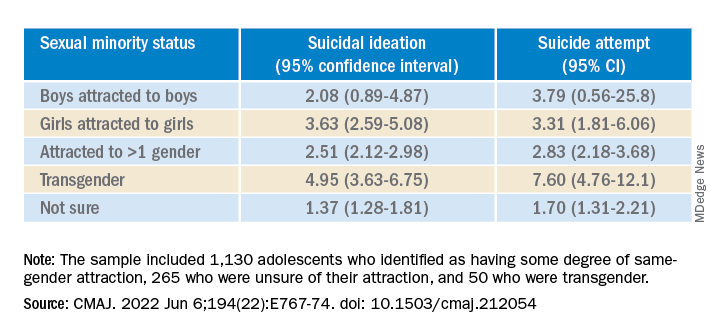
A crisis – with reason for hope
“This is a crisis, and it shows just how much more needs to be done to support transgender young people,” co-author Fae Johnstone, MSW, executive director, Wisdom2Action, who is a trans woman herself, said in the news release.
“Suicide prevention programs specifically targeted to transgender, nonbinary, and sexual minority adolescents, as well as gender-affirming care for transgender adolescents, may help reduce the burden of suicidality among this group,” Ms. Johnstone added.
“The most important thing that parents, teachers, and health care providers can do is to be supportive of these youth,” Dr. Colman told this news organization.
“Providing a safe place where gender and sexual minorities can explore and express themselves is crucial. The first step is to listen and to be compassionate,” Dr. Colman added.
Reached for comment, Jess Ting, MD, director of surgery at the Mount Sinai Center for Transgender Medicine and Surgery, New York, said the data from this study on suicidal thoughts and actions among sexual minority and transgender adolescents “mirror what we see and what we know” about suicidality in trans and nonbinary adults.
“The reasons for this are complex, and it’s hard for someone who doesn’t have a lived experience as a trans or nonbinary person to understand the reasons for suicidality,” he told this news organization.
“But we also know that there are higher rates of anxiety and depression and self-image issues and posttraumatic stress disorder, not to mention outside factors – marginalization, discrimination, violence, abuse. When you add up all these intrinsic and extrinsic factors, it’s not hard to believe that there is a high rate of suicidality,” Dr. Ting said.
“There have been studies that have shown that in children who are supported in their gender identity, the rates of depression and anxiety decreased to almost the same levels as non-trans and nonbinary children, so I think that gives cause for hope,” Dr. Ting added.
The study was funded in part by the Research Council of Norway through its Centres of Excellence funding scheme and by a Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Award. Ms. Johnstone reports consulting fees from Spectrum Waterloo and volunteer participation with the Youth Suicide Prevention Leadership Committee of Ontario. No other competing interests were declared. Dr. Ting has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender youth are significantly more likely to consider suicide and attempt it, compared with their cisgender peers, new research shows.
In a large population-based study, investigators found the increased risk of suicidality is partly because of bullying and cyberbullying experienced by transgender teens.
The findings are “extremely concerning and should be a wake-up call,” Ian Colman, PhD, with the University of Ottawa School of Epidemiology and Public Health, said in an interview.
Young people who are exploring their sexual identities may suffer from depression and anxiety, both about the reactions of their peers and families, as well as their own sense of self.
“These youth are highly marginalized and stigmatized in many corners of our society, and these findings highlight just how distressing these experiences can be,” Dr. Colman said.
The study was published online in the Canadian Medical Association Journal.
Sevenfold increased risk of attempted suicide
The risk of suicidal thoughts and actions is not well studied in transgender and nonbinary youth.
To expand the evidence base, the researchers analyzed data for 6,800 adolescents aged 15-17 years from the 2019 Canadian Health Survey on Children and Youth.
The sample included 1,130 (16.5%) adolescents who identified as having some degree of same-gender attraction, 265 (4.3%) who were unsure of their attraction (“questioning”), and 50 (0.6%) who were transgender, meaning they identified as being of a gender different from that assigned at birth.
Overall, 980 (14.0%) adolescents reported having thoughts of suicide in the prior year, and 480 (6.8%) had attempted suicide in their life.
Transgender youth were five times more likely to think about suicide and more than seven times more likely to have ever attempted suicide than cisgender, heterosexual peers.
Among cisgender adolescents, girls who were attracted to girls had 3.6 times the risk of suicidal ideation and 3.3 times the risk of having ever attempted suicide, compared with their heterosexual peers.
Teens attracted to multiple genders had more than twice the risk of suicidal ideation and suicide attempt. Youth who were questioning their sexual orientation had twice the risk of having attempted suicide in their lifetime.
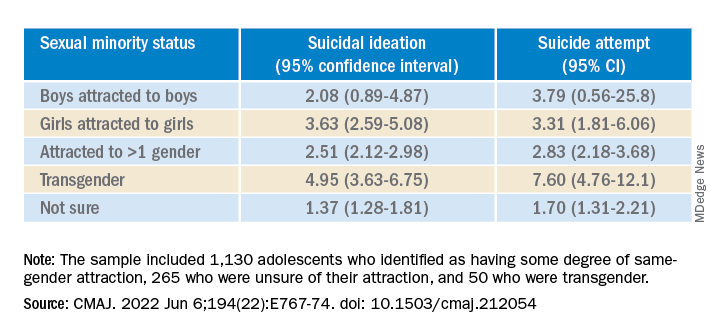
A crisis – with reason for hope
“This is a crisis, and it shows just how much more needs to be done to support transgender young people,” co-author Fae Johnstone, MSW, executive director, Wisdom2Action, who is a trans woman herself, said in the news release.
“Suicide prevention programs specifically targeted to transgender, nonbinary, and sexual minority adolescents, as well as gender-affirming care for transgender adolescents, may help reduce the burden of suicidality among this group,” Ms. Johnstone added.
“The most important thing that parents, teachers, and health care providers can do is to be supportive of these youth,” Dr. Colman told this news organization.
“Providing a safe place where gender and sexual minorities can explore and express themselves is crucial. The first step is to listen and to be compassionate,” Dr. Colman added.
Reached for comment, Jess Ting, MD, director of surgery at the Mount Sinai Center for Transgender Medicine and Surgery, New York, said the data from this study on suicidal thoughts and actions among sexual minority and transgender adolescents “mirror what we see and what we know” about suicidality in trans and nonbinary adults.
“The reasons for this are complex, and it’s hard for someone who doesn’t have a lived experience as a trans or nonbinary person to understand the reasons for suicidality,” he told this news organization.
“But we also know that there are higher rates of anxiety and depression and self-image issues and posttraumatic stress disorder, not to mention outside factors – marginalization, discrimination, violence, abuse. When you add up all these intrinsic and extrinsic factors, it’s not hard to believe that there is a high rate of suicidality,” Dr. Ting said.
“There have been studies that have shown that in children who are supported in their gender identity, the rates of depression and anxiety decreased to almost the same levels as non-trans and nonbinary children, so I think that gives cause for hope,” Dr. Ting added.
The study was funded in part by the Research Council of Norway through its Centres of Excellence funding scheme and by a Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Award. Ms. Johnstone reports consulting fees from Spectrum Waterloo and volunteer participation with the Youth Suicide Prevention Leadership Committee of Ontario. No other competing interests were declared. Dr. Ting has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE CANADIAN MEDICAL ASSOCIATION JOURNAL
New studies show growing number of trans, nonbinary youth in U.S.
Two new studies point to an ever-increasing number of young people in the United States who identify as transgender and nonbinary, with the figures doubling among 18- to 24-year-olds in one institute’s research – from 0.66% of the population in 2016 to 1.3% (398,900) in 2022.
In addition, 1.4% (300,100) of 13- to 17-year-olds identify as trans or nonbinary, according to the report from that group, the Williams Institute at the University of California, Los Angeles, School of Law.
Williams, which conducts independent research on sexual orientation and gender identity law and public policy, did not contain data on 13- to 17-year-olds in its 2016 study, so the growth in that group over the past 5+ years is not as well documented.
Overall, some 1.6 million Americans older than age 13 now identify as transgender, reported the Williams researchers.
And in a new Pew Research Center survey, 2% of adults aged 18-29 identify as transgender and 3% identify as nonbinary, a far greater number than in other age cohorts.
These reports are likely underestimates. The Human Rights Campaign estimates that some 2 million Americans of all ages identify as transgender.
The Pew survey is weighted to be representative but still has limitations, said the organization. The Williams analysis, based on responses to two CDC surveys – the Behavioral Risk Factor Surveillance System (BRFSS) and Youth Risk Behavior Survey (YRBS) – is incomplete, say researchers, because not every state collects data on gender identity.
Transgender identities more predominant among youth
The Williams researchers report that 18.3% of those who identified as trans were 13- to 17-year-olds; that age group makes up 7.6% of the United States population 13 and older.
And despite not having firm figures from earlier reports, they comment: “Youth ages 13-17 comprise a larger share of the transgender-identified population than we previously estimated, currently comprising about 18% of the transgender-identified population in the United State, up from 10% previously.”
About one-quarter of those who identified as trans in the new 2022 report were aged 18-24; that age cohort accounts for 11% of Americans.
The number of older Americans who identify as trans are more proportionate to their representation in the population, according to Williams. Overall, about half of those who said they were trans were aged 25-64; that group accounts for 62% of the overall American population. Some 10% of trans-identified individuals were over age 65. About 20% of Americans are 65 or older, said the researchers.
The Pew research – based on the responses of 10,188 individuals surveyed in May – also found growing numbers of young people who identify as trans. “The share of U.S. adults who are transgender is particularly high among adults younger than 25,” reported Pew in a blog post.
In the 18- to 25-year-old group, 3.1% identified as a trans man or a trans woman, compared with just 0.5% of those ages 25-29.
That compares to 0.3% of those aged 30-49 and 0.2% of those older than 50.
Racial and state-by-state variation
Similar percentages of youth aged 13-17 of all races and ethnicities in the Williams study report they are transgender, ranging from 1% of those who are Asian, to 1.3% of White youth, 1.4% of Black youth, 1.8% of American Indian or Alaska Native, and 1.8% of Latinx youth. The institute reported that 1.5% of biracial and multiracial youth identified as transgender.
The researchers said, however, that “transgender-identified youth and adults appear more likely to report being Latinx and less likely to report being White, as compared to the United States population.”
Transgender individuals live in every state, with the greatest percentage of both youth and adults in the Northeast and West, and lesser percentages in the Midwest and South, reported the Williams Institute.
Williams estimates as many as 3% of 13- to 17-year-olds in New York identify as trans, while just 0.6% of that age group in Wyoming is transgender. A total of 2%-2.5% of those aged 13-17 are transgender in Hawaii, New Mexico, Maryland, and Washington, D.C.
Among the states with higher percentages of trans-identifying 18- to 24-year-olds: Arizona (1.9%), Arkansas (3.6%), Colorado (2%), Delaware (2.4%), Illinois (1.9%), Maryland (1.9%), North Carolina (2.5%), Oklahoma (2.5%), Massachusetts (2.3%), Rhode Island (2.1%), and Washington (2%).
A version of this article first appeared on Medscape.com.
Two new studies point to an ever-increasing number of young people in the United States who identify as transgender and nonbinary, with the figures doubling among 18- to 24-year-olds in one institute’s research – from 0.66% of the population in 2016 to 1.3% (398,900) in 2022.
In addition, 1.4% (300,100) of 13- to 17-year-olds identify as trans or nonbinary, according to the report from that group, the Williams Institute at the University of California, Los Angeles, School of Law.
Williams, which conducts independent research on sexual orientation and gender identity law and public policy, did not contain data on 13- to 17-year-olds in its 2016 study, so the growth in that group over the past 5+ years is not as well documented.
Overall, some 1.6 million Americans older than age 13 now identify as transgender, reported the Williams researchers.
And in a new Pew Research Center survey, 2% of adults aged 18-29 identify as transgender and 3% identify as nonbinary, a far greater number than in other age cohorts.
These reports are likely underestimates. The Human Rights Campaign estimates that some 2 million Americans of all ages identify as transgender.
The Pew survey is weighted to be representative but still has limitations, said the organization. The Williams analysis, based on responses to two CDC surveys – the Behavioral Risk Factor Surveillance System (BRFSS) and Youth Risk Behavior Survey (YRBS) – is incomplete, say researchers, because not every state collects data on gender identity.
Transgender identities more predominant among youth
The Williams researchers report that 18.3% of those who identified as trans were 13- to 17-year-olds; that age group makes up 7.6% of the United States population 13 and older.
And despite not having firm figures from earlier reports, they comment: “Youth ages 13-17 comprise a larger share of the transgender-identified population than we previously estimated, currently comprising about 18% of the transgender-identified population in the United State, up from 10% previously.”
About one-quarter of those who identified as trans in the new 2022 report were aged 18-24; that age cohort accounts for 11% of Americans.
The number of older Americans who identify as trans are more proportionate to their representation in the population, according to Williams. Overall, about half of those who said they were trans were aged 25-64; that group accounts for 62% of the overall American population. Some 10% of trans-identified individuals were over age 65. About 20% of Americans are 65 or older, said the researchers.
The Pew research – based on the responses of 10,188 individuals surveyed in May – also found growing numbers of young people who identify as trans. “The share of U.S. adults who are transgender is particularly high among adults younger than 25,” reported Pew in a blog post.
In the 18- to 25-year-old group, 3.1% identified as a trans man or a trans woman, compared with just 0.5% of those ages 25-29.
That compares to 0.3% of those aged 30-49 and 0.2% of those older than 50.
Racial and state-by-state variation
Similar percentages of youth aged 13-17 of all races and ethnicities in the Williams study report they are transgender, ranging from 1% of those who are Asian, to 1.3% of White youth, 1.4% of Black youth, 1.8% of American Indian or Alaska Native, and 1.8% of Latinx youth. The institute reported that 1.5% of biracial and multiracial youth identified as transgender.
The researchers said, however, that “transgender-identified youth and adults appear more likely to report being Latinx and less likely to report being White, as compared to the United States population.”
Transgender individuals live in every state, with the greatest percentage of both youth and adults in the Northeast and West, and lesser percentages in the Midwest and South, reported the Williams Institute.
Williams estimates as many as 3% of 13- to 17-year-olds in New York identify as trans, while just 0.6% of that age group in Wyoming is transgender. A total of 2%-2.5% of those aged 13-17 are transgender in Hawaii, New Mexico, Maryland, and Washington, D.C.
Among the states with higher percentages of trans-identifying 18- to 24-year-olds: Arizona (1.9%), Arkansas (3.6%), Colorado (2%), Delaware (2.4%), Illinois (1.9%), Maryland (1.9%), North Carolina (2.5%), Oklahoma (2.5%), Massachusetts (2.3%), Rhode Island (2.1%), and Washington (2%).
A version of this article first appeared on Medscape.com.
Two new studies point to an ever-increasing number of young people in the United States who identify as transgender and nonbinary, with the figures doubling among 18- to 24-year-olds in one institute’s research – from 0.66% of the population in 2016 to 1.3% (398,900) in 2022.
In addition, 1.4% (300,100) of 13- to 17-year-olds identify as trans or nonbinary, according to the report from that group, the Williams Institute at the University of California, Los Angeles, School of Law.
Williams, which conducts independent research on sexual orientation and gender identity law and public policy, did not contain data on 13- to 17-year-olds in its 2016 study, so the growth in that group over the past 5+ years is not as well documented.
Overall, some 1.6 million Americans older than age 13 now identify as transgender, reported the Williams researchers.
And in a new Pew Research Center survey, 2% of adults aged 18-29 identify as transgender and 3% identify as nonbinary, a far greater number than in other age cohorts.
These reports are likely underestimates. The Human Rights Campaign estimates that some 2 million Americans of all ages identify as transgender.
The Pew survey is weighted to be representative but still has limitations, said the organization. The Williams analysis, based on responses to two CDC surveys – the Behavioral Risk Factor Surveillance System (BRFSS) and Youth Risk Behavior Survey (YRBS) – is incomplete, say researchers, because not every state collects data on gender identity.
Transgender identities more predominant among youth
The Williams researchers report that 18.3% of those who identified as trans were 13- to 17-year-olds; that age group makes up 7.6% of the United States population 13 and older.
And despite not having firm figures from earlier reports, they comment: “Youth ages 13-17 comprise a larger share of the transgender-identified population than we previously estimated, currently comprising about 18% of the transgender-identified population in the United State, up from 10% previously.”
About one-quarter of those who identified as trans in the new 2022 report were aged 18-24; that age cohort accounts for 11% of Americans.
The number of older Americans who identify as trans are more proportionate to their representation in the population, according to Williams. Overall, about half of those who said they were trans were aged 25-64; that group accounts for 62% of the overall American population. Some 10% of trans-identified individuals were over age 65. About 20% of Americans are 65 or older, said the researchers.
The Pew research – based on the responses of 10,188 individuals surveyed in May – also found growing numbers of young people who identify as trans. “The share of U.S. adults who are transgender is particularly high among adults younger than 25,” reported Pew in a blog post.
In the 18- to 25-year-old group, 3.1% identified as a trans man or a trans woman, compared with just 0.5% of those ages 25-29.
That compares to 0.3% of those aged 30-49 and 0.2% of those older than 50.
Racial and state-by-state variation
Similar percentages of youth aged 13-17 of all races and ethnicities in the Williams study report they are transgender, ranging from 1% of those who are Asian, to 1.3% of White youth, 1.4% of Black youth, 1.8% of American Indian or Alaska Native, and 1.8% of Latinx youth. The institute reported that 1.5% of biracial and multiracial youth identified as transgender.
The researchers said, however, that “transgender-identified youth and adults appear more likely to report being Latinx and less likely to report being White, as compared to the United States population.”
Transgender individuals live in every state, with the greatest percentage of both youth and adults in the Northeast and West, and lesser percentages in the Midwest and South, reported the Williams Institute.
Williams estimates as many as 3% of 13- to 17-year-olds in New York identify as trans, while just 0.6% of that age group in Wyoming is transgender. A total of 2%-2.5% of those aged 13-17 are transgender in Hawaii, New Mexico, Maryland, and Washington, D.C.
Among the states with higher percentages of trans-identifying 18- to 24-year-olds: Arizona (1.9%), Arkansas (3.6%), Colorado (2%), Delaware (2.4%), Illinois (1.9%), Maryland (1.9%), North Carolina (2.5%), Oklahoma (2.5%), Massachusetts (2.3%), Rhode Island (2.1%), and Washington (2%).
A version of this article first appeared on Medscape.com.
Hormonal contraceptives protective against suicide?
Contrary to previous analyses, new research suggests.
In a study of more than 800 women younger than age 50 who attempted suicide and more than 3,000 age-matched peers, results showed those who took hormonal contraceptives had a 27% reduced risk for attempted suicide.
Further analysis showed this was confined to women without a history of psychiatric illness and the reduction in risk rose to 43% among those who took combined hormonal contraceptives rather than progestin-only versions.
The protective effect against attempted suicide increased further to 46% if ethinyl estradiol (EE)–containing preparations were used. Moreover, the beneficial effect of contraceptive use increased over time.
The main message is the “current use of hormonal contraceptives is not associated with an increased risk of attempted suicide in our population,” study presenter Elena Toffol, MD, PhD, department of public health, University of Helsinki, told meeting attendees at the European Psychiatric Association 2022 Congress.
Age range differences
Dr. Toffol said there could be “several reasons” why the results are different from those in previous studies, including that the researchers included a “larger age range.” She noted it is known that “older women have a lower rate of attempted suicide and use different types of contraceptives.”
Dr. Toffol said in an interview that, although it’s “hard to estimate any causality” because this is an observational study, it is “tempting to speculate, and it is plausible, that hormones partly play a role with some, but not all, women being more sensitive to hormonal influences.”
However, the results “may also reflect life choices or a protective life status; for example, more stable relationships or more conscious and health-focused behaviors,” she said.
“It may also be that the underlying characteristics of women who are prescribed or opt for certain types of contraceptives are somehow related to their suicidal risk,” she added.
In 2019, the global age-standardized suicide rate was 9.0 per 100,000, which translates into more than 700,000 deaths every year, Dr. Toffol noted.
However, she emphasized the World Health Organization has calculated that, for every adult who dies by suicide, more than 20 people attempt suicide. In addition, data from the U.S. Centers for Disease Control and Prevention indicate that attempted suicides are three times more common among young women than in men.
“What are the reasons for this gender gap?” Dr. Toffol asked during her presentation.
“It is known that the major risk factor for suicidal behavior is a psychiatric disorder, and in particular depression and mood disorders. And depression and mood disorders are more common in women than in men,” she said.
However, there is also “growing interest into the role of biological factors” in the risk for suicide, including hormones and hormonal contraception. Some studies have also suggested that there is an increased risk for depression and “both completed and attempted suicide” after starting hormonal contraception.
Dr. Toffol added that about 70% of European women use some form of contraception and, among Finnish women, 40% choose a hormonal contraceptive.
Nested analysis
The researchers conducted a nested case-control analysis combining 2017 national prescription data on 587,823 women aged 15-49 years with information from general and primary healthcare registers for the years 2018 to 2019.
They were able to identify 818 cases of attempted suicide among the women. These were matched 4:1 with 3,272 age-matched healthy women who acted as the control group. Use of hormonal contraceptives in the previous 180 days was determined for the whole cohort.
Among users of hormonal contraceptives, there were 344 attempted suicides in 2017, at an incidence rate of 0.59 per 1,000 person-years. This compared with 474 attempted suicides among nonusers, at an incidence rate of 0.81 per 1000 person-years.
Kaplan-Meier analysis showed there was a significant difference in rates for attempted suicide among hormonal contraceptive users versus nonusers, at an incidence rate ratio of 0.73 (P < .0001) – and the difference increased over time.
In addition, the incidence of attempted suicide decreased with increasing age, with the highest incidence rate in women aged 15-19 years (1.62 per 1,000 person-years).
Conditional logistic regression analysis that controlled for education, marital status, chronic disease, recent psychiatric hospitalization, and current use of psychotropic medication showed hormonal contraceptive use was not linked to an increased risk of attempted suicide overall, at an odds ratio of 0.79 (95% confidence interval, 0.56-1.11).
However, when they looked specifically at women without a history of psychiatric illness, the association became significant, at an OR of 0.73 for attempted suicide among hormonal contraceptive users (95% CI, 0.58-0.91), while the relationship remained nonsignificant in women with a history of psychiatric disorders.
Further analysis suggested the significant association was confined to women taking combined hormonal contraceptives, at an OR of 0.57 for suicide attempt versus nonusers (95% CI, 0.44-0.75), and those use EE-containing preparations (OR, 0.54; 95% CI, 0.40-0.73).
There was a suggestion in the data that hormonal contraceptives containing desogestrel or drospirenone alongside EE may offer the greatest reduction in attempted suicide risk, but that did not survive multivariate analysis.
Dr. Toffol also noted that they were not able to capture data on use of intrauterine devices in their analysis.
“There is a growing number of municipalities in Finland that are providing free-of-charge contraception to young women” that is often an intrauterine device, she said. The researchers hope to include these women in a future analysis.
‘Age matters’
Commenting on the findings, Alexis C. Edwards, PhD, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said the current study’s findings “made a lot of sense.” Dr. Edwards wasn’t involved with this study but conducted a previous study of 216,702 Swedish women aged 15-22 years that showed use of combination or progestin-only oral contraceptives was associated with an increased risk for suicidal behavior.
She agreed with Dr. Toffol that the “much larger age range” in the new study may have played a role in showing the opposite result.
“The trajectory that we saw if we had been able to continue following the women for longer – which we couldn’t, due to limitations of the registries – [was that] using hormonal contraceptives was going to end up being protective, so I do think that it matters what age you’re looking at,” she said.
Dr. Edwards noted the takeaway from both studies “is that, even if there is a slight increase in risk from using hormonal contraceptives, it’s short lived and it’s probably specific to young women, which is important.”
She suggested the hormonal benefit from extended contraceptive use could come from the regulation of mood, as it offers a “more stable hormonal course than what their body might be putting them through in the absence of using the pill.”
Overall, it is “really lovely to see very well-executed studies on this, providing more empirical evidence on this question, because it is something that’s relevant to anyone who’s potentially going to be using hormonal contraception,” Dr. Edwards said.
Clinical implications?
Andrea Fiorillo, MD, PhD, department of psychiatry, University of Campania “Luigi Vanvitelli,” Naples, Italy, said in a press release that the “striking” findings of the current study need “careful evaluation.”
They also need to be replicated in “different cohorts of women and controlled for the impact of several psychosocial stressors, such as economic upheavals, social insecurity, and uncertainty due to the COVID pandemic,” said Dr. Fiorillo, who was not involved with the research.
Nevertheless, she believes the “clinical implications of the study are obvious and may help to destigmatize the use of hormonal contraceptives.”
The study was funded by the Jane and Aatos Erkko Foundation, the Avohoidon Tsukimis äätiö (Foundation for Primary Care Research), the Yrj ö Jahnsson Foundation, and the Finnish Cultural Foundation. No relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
Contrary to previous analyses, new research suggests.
In a study of more than 800 women younger than age 50 who attempted suicide and more than 3,000 age-matched peers, results showed those who took hormonal contraceptives had a 27% reduced risk for attempted suicide.
Further analysis showed this was confined to women without a history of psychiatric illness and the reduction in risk rose to 43% among those who took combined hormonal contraceptives rather than progestin-only versions.
The protective effect against attempted suicide increased further to 46% if ethinyl estradiol (EE)–containing preparations were used. Moreover, the beneficial effect of contraceptive use increased over time.
The main message is the “current use of hormonal contraceptives is not associated with an increased risk of attempted suicide in our population,” study presenter Elena Toffol, MD, PhD, department of public health, University of Helsinki, told meeting attendees at the European Psychiatric Association 2022 Congress.
Age range differences
Dr. Toffol said there could be “several reasons” why the results are different from those in previous studies, including that the researchers included a “larger age range.” She noted it is known that “older women have a lower rate of attempted suicide and use different types of contraceptives.”
Dr. Toffol said in an interview that, although it’s “hard to estimate any causality” because this is an observational study, it is “tempting to speculate, and it is plausible, that hormones partly play a role with some, but not all, women being more sensitive to hormonal influences.”
However, the results “may also reflect life choices or a protective life status; for example, more stable relationships or more conscious and health-focused behaviors,” she said.
“It may also be that the underlying characteristics of women who are prescribed or opt for certain types of contraceptives are somehow related to their suicidal risk,” she added.
In 2019, the global age-standardized suicide rate was 9.0 per 100,000, which translates into more than 700,000 deaths every year, Dr. Toffol noted.
However, she emphasized the World Health Organization has calculated that, for every adult who dies by suicide, more than 20 people attempt suicide. In addition, data from the U.S. Centers for Disease Control and Prevention indicate that attempted suicides are three times more common among young women than in men.
“What are the reasons for this gender gap?” Dr. Toffol asked during her presentation.
“It is known that the major risk factor for suicidal behavior is a psychiatric disorder, and in particular depression and mood disorders. And depression and mood disorders are more common in women than in men,” she said.
However, there is also “growing interest into the role of biological factors” in the risk for suicide, including hormones and hormonal contraception. Some studies have also suggested that there is an increased risk for depression and “both completed and attempted suicide” after starting hormonal contraception.
Dr. Toffol added that about 70% of European women use some form of contraception and, among Finnish women, 40% choose a hormonal contraceptive.
Nested analysis
The researchers conducted a nested case-control analysis combining 2017 national prescription data on 587,823 women aged 15-49 years with information from general and primary healthcare registers for the years 2018 to 2019.
They were able to identify 818 cases of attempted suicide among the women. These were matched 4:1 with 3,272 age-matched healthy women who acted as the control group. Use of hormonal contraceptives in the previous 180 days was determined for the whole cohort.
Among users of hormonal contraceptives, there were 344 attempted suicides in 2017, at an incidence rate of 0.59 per 1,000 person-years. This compared with 474 attempted suicides among nonusers, at an incidence rate of 0.81 per 1000 person-years.
Kaplan-Meier analysis showed there was a significant difference in rates for attempted suicide among hormonal contraceptive users versus nonusers, at an incidence rate ratio of 0.73 (P < .0001) – and the difference increased over time.
In addition, the incidence of attempted suicide decreased with increasing age, with the highest incidence rate in women aged 15-19 years (1.62 per 1,000 person-years).
Conditional logistic regression analysis that controlled for education, marital status, chronic disease, recent psychiatric hospitalization, and current use of psychotropic medication showed hormonal contraceptive use was not linked to an increased risk of attempted suicide overall, at an odds ratio of 0.79 (95% confidence interval, 0.56-1.11).
However, when they looked specifically at women without a history of psychiatric illness, the association became significant, at an OR of 0.73 for attempted suicide among hormonal contraceptive users (95% CI, 0.58-0.91), while the relationship remained nonsignificant in women with a history of psychiatric disorders.
Further analysis suggested the significant association was confined to women taking combined hormonal contraceptives, at an OR of 0.57 for suicide attempt versus nonusers (95% CI, 0.44-0.75), and those use EE-containing preparations (OR, 0.54; 95% CI, 0.40-0.73).
There was a suggestion in the data that hormonal contraceptives containing desogestrel or drospirenone alongside EE may offer the greatest reduction in attempted suicide risk, but that did not survive multivariate analysis.
Dr. Toffol also noted that they were not able to capture data on use of intrauterine devices in their analysis.
“There is a growing number of municipalities in Finland that are providing free-of-charge contraception to young women” that is often an intrauterine device, she said. The researchers hope to include these women in a future analysis.
‘Age matters’
Commenting on the findings, Alexis C. Edwards, PhD, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said the current study’s findings “made a lot of sense.” Dr. Edwards wasn’t involved with this study but conducted a previous study of 216,702 Swedish women aged 15-22 years that showed use of combination or progestin-only oral contraceptives was associated with an increased risk for suicidal behavior.
She agreed with Dr. Toffol that the “much larger age range” in the new study may have played a role in showing the opposite result.
“The trajectory that we saw if we had been able to continue following the women for longer – which we couldn’t, due to limitations of the registries – [was that] using hormonal contraceptives was going to end up being protective, so I do think that it matters what age you’re looking at,” she said.
Dr. Edwards noted the takeaway from both studies “is that, even if there is a slight increase in risk from using hormonal contraceptives, it’s short lived and it’s probably specific to young women, which is important.”
She suggested the hormonal benefit from extended contraceptive use could come from the regulation of mood, as it offers a “more stable hormonal course than what their body might be putting them through in the absence of using the pill.”
Overall, it is “really lovely to see very well-executed studies on this, providing more empirical evidence on this question, because it is something that’s relevant to anyone who’s potentially going to be using hormonal contraception,” Dr. Edwards said.
Clinical implications?
Andrea Fiorillo, MD, PhD, department of psychiatry, University of Campania “Luigi Vanvitelli,” Naples, Italy, said in a press release that the “striking” findings of the current study need “careful evaluation.”
They also need to be replicated in “different cohorts of women and controlled for the impact of several psychosocial stressors, such as economic upheavals, social insecurity, and uncertainty due to the COVID pandemic,” said Dr. Fiorillo, who was not involved with the research.
Nevertheless, she believes the “clinical implications of the study are obvious and may help to destigmatize the use of hormonal contraceptives.”
The study was funded by the Jane and Aatos Erkko Foundation, the Avohoidon Tsukimis äätiö (Foundation for Primary Care Research), the Yrj ö Jahnsson Foundation, and the Finnish Cultural Foundation. No relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
Contrary to previous analyses, new research suggests.
In a study of more than 800 women younger than age 50 who attempted suicide and more than 3,000 age-matched peers, results showed those who took hormonal contraceptives had a 27% reduced risk for attempted suicide.
Further analysis showed this was confined to women without a history of psychiatric illness and the reduction in risk rose to 43% among those who took combined hormonal contraceptives rather than progestin-only versions.
The protective effect against attempted suicide increased further to 46% if ethinyl estradiol (EE)–containing preparations were used. Moreover, the beneficial effect of contraceptive use increased over time.
The main message is the “current use of hormonal contraceptives is not associated with an increased risk of attempted suicide in our population,” study presenter Elena Toffol, MD, PhD, department of public health, University of Helsinki, told meeting attendees at the European Psychiatric Association 2022 Congress.
Age range differences
Dr. Toffol said there could be “several reasons” why the results are different from those in previous studies, including that the researchers included a “larger age range.” She noted it is known that “older women have a lower rate of attempted suicide and use different types of contraceptives.”
Dr. Toffol said in an interview that, although it’s “hard to estimate any causality” because this is an observational study, it is “tempting to speculate, and it is plausible, that hormones partly play a role with some, but not all, women being more sensitive to hormonal influences.”
However, the results “may also reflect life choices or a protective life status; for example, more stable relationships or more conscious and health-focused behaviors,” she said.
“It may also be that the underlying characteristics of women who are prescribed or opt for certain types of contraceptives are somehow related to their suicidal risk,” she added.
In 2019, the global age-standardized suicide rate was 9.0 per 100,000, which translates into more than 700,000 deaths every year, Dr. Toffol noted.
However, she emphasized the World Health Organization has calculated that, for every adult who dies by suicide, more than 20 people attempt suicide. In addition, data from the U.S. Centers for Disease Control and Prevention indicate that attempted suicides are three times more common among young women than in men.
“What are the reasons for this gender gap?” Dr. Toffol asked during her presentation.
“It is known that the major risk factor for suicidal behavior is a psychiatric disorder, and in particular depression and mood disorders. And depression and mood disorders are more common in women than in men,” she said.
However, there is also “growing interest into the role of biological factors” in the risk for suicide, including hormones and hormonal contraception. Some studies have also suggested that there is an increased risk for depression and “both completed and attempted suicide” after starting hormonal contraception.
Dr. Toffol added that about 70% of European women use some form of contraception and, among Finnish women, 40% choose a hormonal contraceptive.
Nested analysis
The researchers conducted a nested case-control analysis combining 2017 national prescription data on 587,823 women aged 15-49 years with information from general and primary healthcare registers for the years 2018 to 2019.
They were able to identify 818 cases of attempted suicide among the women. These were matched 4:1 with 3,272 age-matched healthy women who acted as the control group. Use of hormonal contraceptives in the previous 180 days was determined for the whole cohort.
Among users of hormonal contraceptives, there were 344 attempted suicides in 2017, at an incidence rate of 0.59 per 1,000 person-years. This compared with 474 attempted suicides among nonusers, at an incidence rate of 0.81 per 1000 person-years.
Kaplan-Meier analysis showed there was a significant difference in rates for attempted suicide among hormonal contraceptive users versus nonusers, at an incidence rate ratio of 0.73 (P < .0001) – and the difference increased over time.
In addition, the incidence of attempted suicide decreased with increasing age, with the highest incidence rate in women aged 15-19 years (1.62 per 1,000 person-years).
Conditional logistic regression analysis that controlled for education, marital status, chronic disease, recent psychiatric hospitalization, and current use of psychotropic medication showed hormonal contraceptive use was not linked to an increased risk of attempted suicide overall, at an odds ratio of 0.79 (95% confidence interval, 0.56-1.11).
However, when they looked specifically at women without a history of psychiatric illness, the association became significant, at an OR of 0.73 for attempted suicide among hormonal contraceptive users (95% CI, 0.58-0.91), while the relationship remained nonsignificant in women with a history of psychiatric disorders.
Further analysis suggested the significant association was confined to women taking combined hormonal contraceptives, at an OR of 0.57 for suicide attempt versus nonusers (95% CI, 0.44-0.75), and those use EE-containing preparations (OR, 0.54; 95% CI, 0.40-0.73).
There was a suggestion in the data that hormonal contraceptives containing desogestrel or drospirenone alongside EE may offer the greatest reduction in attempted suicide risk, but that did not survive multivariate analysis.
Dr. Toffol also noted that they were not able to capture data on use of intrauterine devices in their analysis.
“There is a growing number of municipalities in Finland that are providing free-of-charge contraception to young women” that is often an intrauterine device, she said. The researchers hope to include these women in a future analysis.
‘Age matters’
Commenting on the findings, Alexis C. Edwards, PhD, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said the current study’s findings “made a lot of sense.” Dr. Edwards wasn’t involved with this study but conducted a previous study of 216,702 Swedish women aged 15-22 years that showed use of combination or progestin-only oral contraceptives was associated with an increased risk for suicidal behavior.
She agreed with Dr. Toffol that the “much larger age range” in the new study may have played a role in showing the opposite result.
“The trajectory that we saw if we had been able to continue following the women for longer – which we couldn’t, due to limitations of the registries – [was that] using hormonal contraceptives was going to end up being protective, so I do think that it matters what age you’re looking at,” she said.
Dr. Edwards noted the takeaway from both studies “is that, even if there is a slight increase in risk from using hormonal contraceptives, it’s short lived and it’s probably specific to young women, which is important.”
She suggested the hormonal benefit from extended contraceptive use could come from the regulation of mood, as it offers a “more stable hormonal course than what their body might be putting them through in the absence of using the pill.”
Overall, it is “really lovely to see very well-executed studies on this, providing more empirical evidence on this question, because it is something that’s relevant to anyone who’s potentially going to be using hormonal contraception,” Dr. Edwards said.
Clinical implications?
Andrea Fiorillo, MD, PhD, department of psychiatry, University of Campania “Luigi Vanvitelli,” Naples, Italy, said in a press release that the “striking” findings of the current study need “careful evaluation.”
They also need to be replicated in “different cohorts of women and controlled for the impact of several psychosocial stressors, such as economic upheavals, social insecurity, and uncertainty due to the COVID pandemic,” said Dr. Fiorillo, who was not involved with the research.
Nevertheless, she believes the “clinical implications of the study are obvious and may help to destigmatize the use of hormonal contraceptives.”
The study was funded by the Jane and Aatos Erkko Foundation, the Avohoidon Tsukimis äätiö (Foundation for Primary Care Research), the Yrj ö Jahnsson Foundation, and the Finnish Cultural Foundation. No relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
FROM EPA 2022
Prediabetes is linked independently to myocardial infarction
Prediabetes is not only a predictor of diabetes and the cardiovascular complications that ensue, but it is also a risk factor by itself for myocardial infarction, according to data drawn from almost 1.8 million patients hospitalized for MI.
“Our study serves as a wakeup call for clinicians and patients to shift the focus to preventing prediabetes, and not just diabetes, said Geethika Thota, MD, at the annual meeting of the Endocrine Society.
There are plenty of data suggesting that prediabetes places patients on a trajectory toward cardiovascular disease. In a meta-analysis of 129 studies published 2 years ago, prediabetes was not only associated with a statistically significant 16% increase in coronary heart disease, but also a 13% increased risk of all-cause mortality relative to those with normoglycemia.
Data drawn from 1.8 million patients
In this study, 1,794,149 weighted patient hospitalizations for MI were drawn from the National Inpatient Sample database. Excluding patients who eventually developed diabetes, roughly 1% of these patients had a history of prediabetes in the past, according to a search of ICD-10 codes.
Before adjustment for other risk factors, prediabetes was linked to a greater than 40% increased odds of MI (odds ratio, 1.41; P < .01). After adjustment for a large array of known MI risk factors – including prior history of MI, dyslipidemia, hypertension, nicotine dependence, and obesity – prediabetes remained an independent risk factor, corresponding with a 25% increased risk of MI (OR, 1.25; P < .01).
A history of prediabetes was also an independent risk factor for percutaneous intervention and coronary artery bypass grafting, with increased risk of 45% and 95%, respectively.
As a retrospective study looking at prediabetes as a risk factor in those who already had a MI, it is possible that not all patients with prediabetes were properly coded, but Dr. Thota said that was unlikely to have been an issue of sufficient magnitude to have affected the major conclusions.
Relevance seen for community care
Although the study was drawn from hospitalized patients, its relevance is for the community setting, where screening and intervention for prediabetes has the potential to alter the risk, according to Dr. Thota.
Most clinicians are likely aware of the value of screening for prediabetes, which was defined in this study as a hemoglobin A1c of 5.7%-6.4%, but Dr. Thota suggested that many might not fully grasp the full scope of goals. Early detection and prevention will prevent diabetes and, by extension, cardiovascular disease, but her data suggest that control of prediabetes with lower cardiovascular risk by a more direct route.
“Despite mounting evidence, many clinicians are unaware that prediabetes is also a major risk factor for atherosclerotic cardiovascular disease,” said Dr. Thota, an internal medicine resident at Saint Peter’s University Hospital, New Brunswick, N.J.
Like diabetes, the prevalence of prediabetes is growing rapidly, according to data from the Centers for Disease Control that Dr. Thota cited. In 2020, the Centers for Disease Control and Prevention estimated that 38% of the adult population have prediabetes. By 2030, one model predicts a further 25% growth.
Screening for hyperglycemia is part of routine patient evaluations at Dr. Thota’s center. In an interview, she said that once a diagnosis of prediabetes is entered in the electronic medical record, the history is carried forward so that changes in status are continually monitored.
Worsening prediabetes should be addressed
“Prediabetes is not treated with medication, at least initially,” Dr. Thota explained. Rather, patients are educated about important lifestyle changes, such as diet and physical activity, that can reverse the diagnosis. However, patients who remain on a path of worsening hyperglycemia are candidates for more intensive lifestyle intervention and might be considered selectively for metformin.
“Early recognition of prediabetes through screening is important,” Dr. Thota emphasized. The benefit for preventing patients from progressing to diabetes is well recognized, but these data provide the basis for incentivizing lifestyle changes in patients with prediabetes by telling them that it can reduce their risk for MI.
These data have an important message, but they are not surprising, according to Deepak L. Bhatt, MD, executive director, interventional cardiovascular programs, Brigham and Women’s Hospital Heart & Vascular Center, Boston.
“In fact, in daily practice we see a substantial percentage of patients with MI who have prediabetes that had not been previously recognized or formally diagnosed,” Dr. Bhatt said in an interview.
“Identifying these patients – preferably prior to coming in with cardiovascular complications – is important both to reduce cardiovascular risk but also to try and prevent progression at diabetes,” he added.
Dr. Bhatt went on to say that this large analysis, confirming that prediabetes is independently associated with MI, should prompt clinicians to screen patients rigorously for this condition.
“At a minimum, such patients would be candidates for intensive lifestyle modification aimed at weight loss and treatment of frequent coexistent conditions, such as hypertension and dyslipidemia,” Dr. Bhatt said.
Dr. Thota reports no potential conflicts of interest. Dr. Bhatt has financial relationships with more than 30 pharmaceutical companies, many of which make products relevant to the management of diabetes and cardiovascular disease.
Prediabetes is not only a predictor of diabetes and the cardiovascular complications that ensue, but it is also a risk factor by itself for myocardial infarction, according to data drawn from almost 1.8 million patients hospitalized for MI.
“Our study serves as a wakeup call for clinicians and patients to shift the focus to preventing prediabetes, and not just diabetes, said Geethika Thota, MD, at the annual meeting of the Endocrine Society.
There are plenty of data suggesting that prediabetes places patients on a trajectory toward cardiovascular disease. In a meta-analysis of 129 studies published 2 years ago, prediabetes was not only associated with a statistically significant 16% increase in coronary heart disease, but also a 13% increased risk of all-cause mortality relative to those with normoglycemia.
Data drawn from 1.8 million patients
In this study, 1,794,149 weighted patient hospitalizations for MI were drawn from the National Inpatient Sample database. Excluding patients who eventually developed diabetes, roughly 1% of these patients had a history of prediabetes in the past, according to a search of ICD-10 codes.
Before adjustment for other risk factors, prediabetes was linked to a greater than 40% increased odds of MI (odds ratio, 1.41; P < .01). After adjustment for a large array of known MI risk factors – including prior history of MI, dyslipidemia, hypertension, nicotine dependence, and obesity – prediabetes remained an independent risk factor, corresponding with a 25% increased risk of MI (OR, 1.25; P < .01).
A history of prediabetes was also an independent risk factor for percutaneous intervention and coronary artery bypass grafting, with increased risk of 45% and 95%, respectively.
As a retrospective study looking at prediabetes as a risk factor in those who already had a MI, it is possible that not all patients with prediabetes were properly coded, but Dr. Thota said that was unlikely to have been an issue of sufficient magnitude to have affected the major conclusions.
Relevance seen for community care
Although the study was drawn from hospitalized patients, its relevance is for the community setting, where screening and intervention for prediabetes has the potential to alter the risk, according to Dr. Thota.
Most clinicians are likely aware of the value of screening for prediabetes, which was defined in this study as a hemoglobin A1c of 5.7%-6.4%, but Dr. Thota suggested that many might not fully grasp the full scope of goals. Early detection and prevention will prevent diabetes and, by extension, cardiovascular disease, but her data suggest that control of prediabetes with lower cardiovascular risk by a more direct route.
“Despite mounting evidence, many clinicians are unaware that prediabetes is also a major risk factor for atherosclerotic cardiovascular disease,” said Dr. Thota, an internal medicine resident at Saint Peter’s University Hospital, New Brunswick, N.J.
Like diabetes, the prevalence of prediabetes is growing rapidly, according to data from the Centers for Disease Control that Dr. Thota cited. In 2020, the Centers for Disease Control and Prevention estimated that 38% of the adult population have prediabetes. By 2030, one model predicts a further 25% growth.
Screening for hyperglycemia is part of routine patient evaluations at Dr. Thota’s center. In an interview, she said that once a diagnosis of prediabetes is entered in the electronic medical record, the history is carried forward so that changes in status are continually monitored.
Worsening prediabetes should be addressed
“Prediabetes is not treated with medication, at least initially,” Dr. Thota explained. Rather, patients are educated about important lifestyle changes, such as diet and physical activity, that can reverse the diagnosis. However, patients who remain on a path of worsening hyperglycemia are candidates for more intensive lifestyle intervention and might be considered selectively for metformin.
“Early recognition of prediabetes through screening is important,” Dr. Thota emphasized. The benefit for preventing patients from progressing to diabetes is well recognized, but these data provide the basis for incentivizing lifestyle changes in patients with prediabetes by telling them that it can reduce their risk for MI.
These data have an important message, but they are not surprising, according to Deepak L. Bhatt, MD, executive director, interventional cardiovascular programs, Brigham and Women’s Hospital Heart & Vascular Center, Boston.
“In fact, in daily practice we see a substantial percentage of patients with MI who have prediabetes that had not been previously recognized or formally diagnosed,” Dr. Bhatt said in an interview.
“Identifying these patients – preferably prior to coming in with cardiovascular complications – is important both to reduce cardiovascular risk but also to try and prevent progression at diabetes,” he added.
Dr. Bhatt went on to say that this large analysis, confirming that prediabetes is independently associated with MI, should prompt clinicians to screen patients rigorously for this condition.
“At a minimum, such patients would be candidates for intensive lifestyle modification aimed at weight loss and treatment of frequent coexistent conditions, such as hypertension and dyslipidemia,” Dr. Bhatt said.
Dr. Thota reports no potential conflicts of interest. Dr. Bhatt has financial relationships with more than 30 pharmaceutical companies, many of which make products relevant to the management of diabetes and cardiovascular disease.
Prediabetes is not only a predictor of diabetes and the cardiovascular complications that ensue, but it is also a risk factor by itself for myocardial infarction, according to data drawn from almost 1.8 million patients hospitalized for MI.
“Our study serves as a wakeup call for clinicians and patients to shift the focus to preventing prediabetes, and not just diabetes, said Geethika Thota, MD, at the annual meeting of the Endocrine Society.
There are plenty of data suggesting that prediabetes places patients on a trajectory toward cardiovascular disease. In a meta-analysis of 129 studies published 2 years ago, prediabetes was not only associated with a statistically significant 16% increase in coronary heart disease, but also a 13% increased risk of all-cause mortality relative to those with normoglycemia.
Data drawn from 1.8 million patients
In this study, 1,794,149 weighted patient hospitalizations for MI were drawn from the National Inpatient Sample database. Excluding patients who eventually developed diabetes, roughly 1% of these patients had a history of prediabetes in the past, according to a search of ICD-10 codes.
Before adjustment for other risk factors, prediabetes was linked to a greater than 40% increased odds of MI (odds ratio, 1.41; P < .01). After adjustment for a large array of known MI risk factors – including prior history of MI, dyslipidemia, hypertension, nicotine dependence, and obesity – prediabetes remained an independent risk factor, corresponding with a 25% increased risk of MI (OR, 1.25; P < .01).
A history of prediabetes was also an independent risk factor for percutaneous intervention and coronary artery bypass grafting, with increased risk of 45% and 95%, respectively.
As a retrospective study looking at prediabetes as a risk factor in those who already had a MI, it is possible that not all patients with prediabetes were properly coded, but Dr. Thota said that was unlikely to have been an issue of sufficient magnitude to have affected the major conclusions.
Relevance seen for community care
Although the study was drawn from hospitalized patients, its relevance is for the community setting, where screening and intervention for prediabetes has the potential to alter the risk, according to Dr. Thota.
Most clinicians are likely aware of the value of screening for prediabetes, which was defined in this study as a hemoglobin A1c of 5.7%-6.4%, but Dr. Thota suggested that many might not fully grasp the full scope of goals. Early detection and prevention will prevent diabetes and, by extension, cardiovascular disease, but her data suggest that control of prediabetes with lower cardiovascular risk by a more direct route.
“Despite mounting evidence, many clinicians are unaware that prediabetes is also a major risk factor for atherosclerotic cardiovascular disease,” said Dr. Thota, an internal medicine resident at Saint Peter’s University Hospital, New Brunswick, N.J.
Like diabetes, the prevalence of prediabetes is growing rapidly, according to data from the Centers for Disease Control that Dr. Thota cited. In 2020, the Centers for Disease Control and Prevention estimated that 38% of the adult population have prediabetes. By 2030, one model predicts a further 25% growth.
Screening for hyperglycemia is part of routine patient evaluations at Dr. Thota’s center. In an interview, she said that once a diagnosis of prediabetes is entered in the electronic medical record, the history is carried forward so that changes in status are continually monitored.
Worsening prediabetes should be addressed
“Prediabetes is not treated with medication, at least initially,” Dr. Thota explained. Rather, patients are educated about important lifestyle changes, such as diet and physical activity, that can reverse the diagnosis. However, patients who remain on a path of worsening hyperglycemia are candidates for more intensive lifestyle intervention and might be considered selectively for metformin.
“Early recognition of prediabetes through screening is important,” Dr. Thota emphasized. The benefit for preventing patients from progressing to diabetes is well recognized, but these data provide the basis for incentivizing lifestyle changes in patients with prediabetes by telling them that it can reduce their risk for MI.
These data have an important message, but they are not surprising, according to Deepak L. Bhatt, MD, executive director, interventional cardiovascular programs, Brigham and Women’s Hospital Heart & Vascular Center, Boston.
“In fact, in daily practice we see a substantial percentage of patients with MI who have prediabetes that had not been previously recognized or formally diagnosed,” Dr. Bhatt said in an interview.
“Identifying these patients – preferably prior to coming in with cardiovascular complications – is important both to reduce cardiovascular risk but also to try and prevent progression at diabetes,” he added.
Dr. Bhatt went on to say that this large analysis, confirming that prediabetes is independently associated with MI, should prompt clinicians to screen patients rigorously for this condition.
“At a minimum, such patients would be candidates for intensive lifestyle modification aimed at weight loss and treatment of frequent coexistent conditions, such as hypertension and dyslipidemia,” Dr. Bhatt said.
Dr. Thota reports no potential conflicts of interest. Dr. Bhatt has financial relationships with more than 30 pharmaceutical companies, many of which make products relevant to the management of diabetes and cardiovascular disease.
FROM ENDO 2022
Avexitide promising for hypoglycemia after weight-loss surgery
Avexitide (Eiger Biopharmaceuticals), a first-in-class glucagonlike peptide (GLP)–1 receptor blocker, significantly reduced hypoglycemia in patients with refractory postbariatric hypoglycemia, new research finds.
Postbariatric hypoglycemia is a complication of bariatric surgery that is estimated to occur in about 29%-34% of people who undergo Roux-en-Y gastric bypass and in 11%-23% of those who undergo vertical sleeve gastrectomy. It typically manifests about 1-3 hours after meals and can lead to severe neuroglycopenic symptoms including blurred vision, confusion, drowsiness, and incoordination.
In addition, more than one-third (37%) with the condition have hypoglycemic unawareness. This can lead to seizures in about 59%, loss of consciousness and hospitalization in 50%, motor vehicle accidents, and even death. More than 90% with the condition consider themselves disabled, and 41% report being unable to work.
There are no currently approved medical treatments for postbariatric hypoglycemia. The standard of care is medical nutrition therapy involving a low-carbohydrate diet with carb restriction and small, frequent mixed meals. If this doesn’t work, off-label stepped pharmacotherapy has been tried, including acarbose (Precose), octreotide (Sandostatin), and diazoxide (Proglycem).
But “these are limited by efficacy and tolerability,” said Marilyn Tan, MD, who presented the findings from the phase 2 trial of avexitide at the annual meeting of the Endocrine Society.
In very severe cases, gastrostomy tubes or bypass reversal are options but those lead to weight regain and incomplete efficacy. “Safe, effective, and targeted therapies are needed urgently for postbariatric hypoglycemia,” said Dr. Tan, of the department of endocrinology at Stanford (Calif.) University.
The pathophysiology isn’t fully understood, but there appears to be an exaggerated GLP-1 response that leads to abnormal insulin secretion and symptomatic hyperinsulinemic hypoglycemia. Avexitide (formerly exendin 9-39), blocks the GLP-1 receptor and mitigates the excessive GLP-1 response, she explained.
Asked to comment, session moderator Michelle Van Name, MD, told this news organization, “This is a problem and it’s important for us to understand more about it and to identify different treatment options so these patients can continue to live their full, healthy lives post bariatric surgery.”
And, avexitide also holds potential for treating congenital hyperinsulinism, “which is a very challenging disease to treat in babies,” noted Dr. Van Name, a pediatric endocrinologist at Yale University, New Haven, Conn.
Drug reduced all levels of hypoglycemia, across surgery types
The study enrolled 14 women and 2 men with severe refractory postbariatric surgery hypoglycemia despite medical nutrition therapy. A majority (9) had undergone Roux-en-Y gastric bypass, 4 had vertical sleeve gastrectomy, 2 gastrectomy, and 1 had Nissen fundoplication. Seven patients (43.7%) had experienced loss of consciousness from hyperinsulinemic hypoglycemia. None had diabetes.
They were randomly assigned to either subcutaneous 45 mg of avexitide twice daily or 90 mg once daily for 14 days each, with a 2-day washout period followed by a switch to the other dose.
Both doses resulted in significant reductions in hypoglycemia as measured by self–blood glucose monitoring. The once-daily dose reduced level 1 hypoglycemia (glucose < 70 mg/dL) by 67.5% and it reduced level 2 (< 54 mg/dL) by 53.3% (P = .0043).
Even greater reductions were seen in severe hypoglycemia (that is, altered mental status/requiring assistance) – by 67.5% for the twice-daily dose (P = .0003) and by 66.1% with the once-daily dose (P = .0003).
“This is consistent with what we’ve seen in prior avexitide trials,” Dr. Tan noted.
More hypoglycemic events were captured using blinded continuous glucose monitoring (CGM), since it picked up episodes of which the patient was unaware. There were significant reductions in percentage time spent in level 1 and level 2 hypoglycemia, as well as in absolute number of hypoglycemic events over 14 days.
Here, the effect was greater with the once-daily 90 mg dose, with reductions of up to 65% in time spent and number of events, but results for the twice-daily dose were also significant, Dr. Tan said.
The drug was effective across all surgical subtypes. Patients who underwent vertical sleeve gastrectomy/gastrectomy had greater rates of hypoglycemia at baseline and “robust responses to avexitide subcutaneous injections. This supports the critical role of GLP-1,” Dr. Tan said.
There were no severe adverse events. The most commonly reported adverse events were diarrhea, headache, bloating, and injection-site reaction/bruising. All were mild and self-limited and resolved without treatment. No participants withdrew from the study.
Eiger Biopharmaceuticals is currently working with the U.S. Food and Drug Administration and the European Medicines Agency to design a phase 3 trial.
The study is an investor-initiated trial with funding from Eiger Biopharmaceuticals. Dr. Tan receives research support from Eiger Biopharmaceuticals as a site investigator. Dr. Van Name is an investigator for a trial sponsored by Provention Bio.
A version of this article first appeared on Medscape.com.
Avexitide (Eiger Biopharmaceuticals), a first-in-class glucagonlike peptide (GLP)–1 receptor blocker, significantly reduced hypoglycemia in patients with refractory postbariatric hypoglycemia, new research finds.
Postbariatric hypoglycemia is a complication of bariatric surgery that is estimated to occur in about 29%-34% of people who undergo Roux-en-Y gastric bypass and in 11%-23% of those who undergo vertical sleeve gastrectomy. It typically manifests about 1-3 hours after meals and can lead to severe neuroglycopenic symptoms including blurred vision, confusion, drowsiness, and incoordination.
In addition, more than one-third (37%) with the condition have hypoglycemic unawareness. This can lead to seizures in about 59%, loss of consciousness and hospitalization in 50%, motor vehicle accidents, and even death. More than 90% with the condition consider themselves disabled, and 41% report being unable to work.
There are no currently approved medical treatments for postbariatric hypoglycemia. The standard of care is medical nutrition therapy involving a low-carbohydrate diet with carb restriction and small, frequent mixed meals. If this doesn’t work, off-label stepped pharmacotherapy has been tried, including acarbose (Precose), octreotide (Sandostatin), and diazoxide (Proglycem).
But “these are limited by efficacy and tolerability,” said Marilyn Tan, MD, who presented the findings from the phase 2 trial of avexitide at the annual meeting of the Endocrine Society.
In very severe cases, gastrostomy tubes or bypass reversal are options but those lead to weight regain and incomplete efficacy. “Safe, effective, and targeted therapies are needed urgently for postbariatric hypoglycemia,” said Dr. Tan, of the department of endocrinology at Stanford (Calif.) University.
The pathophysiology isn’t fully understood, but there appears to be an exaggerated GLP-1 response that leads to abnormal insulin secretion and symptomatic hyperinsulinemic hypoglycemia. Avexitide (formerly exendin 9-39), blocks the GLP-1 receptor and mitigates the excessive GLP-1 response, she explained.
Asked to comment, session moderator Michelle Van Name, MD, told this news organization, “This is a problem and it’s important for us to understand more about it and to identify different treatment options so these patients can continue to live their full, healthy lives post bariatric surgery.”
And, avexitide also holds potential for treating congenital hyperinsulinism, “which is a very challenging disease to treat in babies,” noted Dr. Van Name, a pediatric endocrinologist at Yale University, New Haven, Conn.
Drug reduced all levels of hypoglycemia, across surgery types
The study enrolled 14 women and 2 men with severe refractory postbariatric surgery hypoglycemia despite medical nutrition therapy. A majority (9) had undergone Roux-en-Y gastric bypass, 4 had vertical sleeve gastrectomy, 2 gastrectomy, and 1 had Nissen fundoplication. Seven patients (43.7%) had experienced loss of consciousness from hyperinsulinemic hypoglycemia. None had diabetes.
They were randomly assigned to either subcutaneous 45 mg of avexitide twice daily or 90 mg once daily for 14 days each, with a 2-day washout period followed by a switch to the other dose.
Both doses resulted in significant reductions in hypoglycemia as measured by self–blood glucose monitoring. The once-daily dose reduced level 1 hypoglycemia (glucose < 70 mg/dL) by 67.5% and it reduced level 2 (< 54 mg/dL) by 53.3% (P = .0043).
Even greater reductions were seen in severe hypoglycemia (that is, altered mental status/requiring assistance) – by 67.5% for the twice-daily dose (P = .0003) and by 66.1% with the once-daily dose (P = .0003).
“This is consistent with what we’ve seen in prior avexitide trials,” Dr. Tan noted.
More hypoglycemic events were captured using blinded continuous glucose monitoring (CGM), since it picked up episodes of which the patient was unaware. There were significant reductions in percentage time spent in level 1 and level 2 hypoglycemia, as well as in absolute number of hypoglycemic events over 14 days.
Here, the effect was greater with the once-daily 90 mg dose, with reductions of up to 65% in time spent and number of events, but results for the twice-daily dose were also significant, Dr. Tan said.
The drug was effective across all surgical subtypes. Patients who underwent vertical sleeve gastrectomy/gastrectomy had greater rates of hypoglycemia at baseline and “robust responses to avexitide subcutaneous injections. This supports the critical role of GLP-1,” Dr. Tan said.
There were no severe adverse events. The most commonly reported adverse events were diarrhea, headache, bloating, and injection-site reaction/bruising. All were mild and self-limited and resolved without treatment. No participants withdrew from the study.
Eiger Biopharmaceuticals is currently working with the U.S. Food and Drug Administration and the European Medicines Agency to design a phase 3 trial.
The study is an investor-initiated trial with funding from Eiger Biopharmaceuticals. Dr. Tan receives research support from Eiger Biopharmaceuticals as a site investigator. Dr. Van Name is an investigator for a trial sponsored by Provention Bio.
A version of this article first appeared on Medscape.com.
Avexitide (Eiger Biopharmaceuticals), a first-in-class glucagonlike peptide (GLP)–1 receptor blocker, significantly reduced hypoglycemia in patients with refractory postbariatric hypoglycemia, new research finds.
Postbariatric hypoglycemia is a complication of bariatric surgery that is estimated to occur in about 29%-34% of people who undergo Roux-en-Y gastric bypass and in 11%-23% of those who undergo vertical sleeve gastrectomy. It typically manifests about 1-3 hours after meals and can lead to severe neuroglycopenic symptoms including blurred vision, confusion, drowsiness, and incoordination.
In addition, more than one-third (37%) with the condition have hypoglycemic unawareness. This can lead to seizures in about 59%, loss of consciousness and hospitalization in 50%, motor vehicle accidents, and even death. More than 90% with the condition consider themselves disabled, and 41% report being unable to work.
There are no currently approved medical treatments for postbariatric hypoglycemia. The standard of care is medical nutrition therapy involving a low-carbohydrate diet with carb restriction and small, frequent mixed meals. If this doesn’t work, off-label stepped pharmacotherapy has been tried, including acarbose (Precose), octreotide (Sandostatin), and diazoxide (Proglycem).
But “these are limited by efficacy and tolerability,” said Marilyn Tan, MD, who presented the findings from the phase 2 trial of avexitide at the annual meeting of the Endocrine Society.
In very severe cases, gastrostomy tubes or bypass reversal are options but those lead to weight regain and incomplete efficacy. “Safe, effective, and targeted therapies are needed urgently for postbariatric hypoglycemia,” said Dr. Tan, of the department of endocrinology at Stanford (Calif.) University.
The pathophysiology isn’t fully understood, but there appears to be an exaggerated GLP-1 response that leads to abnormal insulin secretion and symptomatic hyperinsulinemic hypoglycemia. Avexitide (formerly exendin 9-39), blocks the GLP-1 receptor and mitigates the excessive GLP-1 response, she explained.
Asked to comment, session moderator Michelle Van Name, MD, told this news organization, “This is a problem and it’s important for us to understand more about it and to identify different treatment options so these patients can continue to live their full, healthy lives post bariatric surgery.”
And, avexitide also holds potential for treating congenital hyperinsulinism, “which is a very challenging disease to treat in babies,” noted Dr. Van Name, a pediatric endocrinologist at Yale University, New Haven, Conn.
Drug reduced all levels of hypoglycemia, across surgery types
The study enrolled 14 women and 2 men with severe refractory postbariatric surgery hypoglycemia despite medical nutrition therapy. A majority (9) had undergone Roux-en-Y gastric bypass, 4 had vertical sleeve gastrectomy, 2 gastrectomy, and 1 had Nissen fundoplication. Seven patients (43.7%) had experienced loss of consciousness from hyperinsulinemic hypoglycemia. None had diabetes.
They were randomly assigned to either subcutaneous 45 mg of avexitide twice daily or 90 mg once daily for 14 days each, with a 2-day washout period followed by a switch to the other dose.
Both doses resulted in significant reductions in hypoglycemia as measured by self–blood glucose monitoring. The once-daily dose reduced level 1 hypoglycemia (glucose < 70 mg/dL) by 67.5% and it reduced level 2 (< 54 mg/dL) by 53.3% (P = .0043).
Even greater reductions were seen in severe hypoglycemia (that is, altered mental status/requiring assistance) – by 67.5% for the twice-daily dose (P = .0003) and by 66.1% with the once-daily dose (P = .0003).
“This is consistent with what we’ve seen in prior avexitide trials,” Dr. Tan noted.
More hypoglycemic events were captured using blinded continuous glucose monitoring (CGM), since it picked up episodes of which the patient was unaware. There were significant reductions in percentage time spent in level 1 and level 2 hypoglycemia, as well as in absolute number of hypoglycemic events over 14 days.
Here, the effect was greater with the once-daily 90 mg dose, with reductions of up to 65% in time spent and number of events, but results for the twice-daily dose were also significant, Dr. Tan said.
The drug was effective across all surgical subtypes. Patients who underwent vertical sleeve gastrectomy/gastrectomy had greater rates of hypoglycemia at baseline and “robust responses to avexitide subcutaneous injections. This supports the critical role of GLP-1,” Dr. Tan said.
There were no severe adverse events. The most commonly reported adverse events were diarrhea, headache, bloating, and injection-site reaction/bruising. All were mild and self-limited and resolved without treatment. No participants withdrew from the study.
Eiger Biopharmaceuticals is currently working with the U.S. Food and Drug Administration and the European Medicines Agency to design a phase 3 trial.
The study is an investor-initiated trial with funding from Eiger Biopharmaceuticals. Dr. Tan receives research support from Eiger Biopharmaceuticals as a site investigator. Dr. Van Name is an investigator for a trial sponsored by Provention Bio.
A version of this article first appeared on Medscape.com.
FROM ENDO 2022
SGLT2 inhibitors cut AFib risk in real-word analysis
NEW ORLEANS – The case continues to grow for prioritizing a sodium-glucose transporter 2 (SGLT2) inhibitor in patients with type 2 diabetes, as real-world evidence of benefit and safety accumulates on top of the data from randomized trials that first established this class as a management pillar.
Another important effect of these agents gaining increasing currency, on top of their well-established benefits in patients with type 2 diabetes for preventing acute heart failure exacerbations and slowing progression of diabetic kidney disease, is that they cut the incidence of new-onset atrial fibrillation (AFib). That effect was confirmed in an analysis of data from about 300,000 U.S. patients included in recent Medicare records, Elisabetta Patorno, MD, reported at the annual scientific sessions of the American Diabetes Association.
But despite documentation like this, real-world evidence also continues to show limited uptake of SGLT2 inhibitors in U.S. patients with type 2 diabetes. Records from more than 1.3 million patients with type 2 diabetes managed in the Veterans Affairs Healthcare System during 2019 or 2022 documented that just 10% of these patients received an agent from this class, even though all were eligible to receive it, according to findings in a separate report at the meeting.
The AFib analysis analyzed two sets of propensity score–matched Medicare patients during 2013-2018 aged 65 years or older with type 2 diabetes and no history of AFib. One analysis focused on 80,475 matched patients who started on treatment with either an SGLT2 inhibitor or a glucagonlike peptide–1 (GLP-1) receptor agonist, and a second on 74,868 matched patients who began either an SGTL2 inhibitor or a dipeptidyl peptidase–4 (DPP4) inhibitor. In both analyses, matching involved more than 130 variables. In both pair sets, patients at baseline averaged about 72 years old, nearly two-thirds were women, about 8%-9% had heart failure, 77%-80% were on metformin, and 20%-25% were using insulin.
The study’s primary endpoint was the incidence of hospitalization for AFib, which occurred a significant 18% less often in the patients who started on an SGLT2, compared with those who started a DPP4 inhibitor during median follow-up of 6.7 months, and a significant 10% less often, compared with those starting a GLP-1 receptor agonist during a median follow-up of 6.0 months, Elisabetta Patorno, MD, DrPH, reported at the meeting. This worked out to 3.7 fewer hospitalizations for AFib per 1,000 patient-years of follow-up among the people who received an SGLT2 inhibitor, compared with a DPP4 inhibitor, and a decrease of 1.8 hospitalizations/1,000 patient-years when compared against patients in a GLP-1 receptor agonist.
Two secondary outcomes showed significantly fewer episodes of newly diagnosed AFib, and significantly fewer patients initiating AFib treatment among those who received an SGLT2 inhibitor relative to the comparator groups. In addition, these associations were consistent across subgroup analyses that divided patients by their age, sex, history of heart failure, and history of atherosclerotic cardiovascular disease.
AFib effects add to benefits
The findings “suggest that initiation of an SGLT2 inhibitor may be beneficial in older adults with type 2 diabetes who are at risk for AFib,” said Dr. Patorno, a researcher in the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston. “These new findings on AFib may be helpful when weighing the potential risks and benefits of various glucose-lowering drugs in older patients with type 2 diabetes.”
This new evidence follows several prior reports from other research groups of data supporting an AFib benefit from SGLT2 inhibitors. The earlier reports include a post hoc analysis of more than 17,000 patients enrolled in the DECLARE-TIMI 58 cardiovascular outcome trial of dapagliflozin (Farxiga), which showed a 19% relative decrease in the rate of incident AFib or atrial flutter events during a median 4.2 year follow-up.
Other prior reports that found a reduced incidence of AFib events linked with SGLT2 inhibitor treatment include a 2020 meta-analysis based on data from more than 38,000 patients with type 2 diabetes enrolled in any of 16 randomized, controlled trials, which found a 24% relative risk reduction. And an as-yet unpublished report from researchers at the University of Rochester (N.Y.) and their associates presented in November 2021 at the annual scientific sessions of the American Heart Association that documented a significant 24% relative risk reduction in incident AFib events linked to SGLT2 inhibitor treatment in a prospective study of 13,890 patients at several hospitals in Israel or the United States.
Evidence ‘convincing’ in totality
The accumulated evidence for a reduced incidence of AFib when patients were on treatment with an SGLT2 inhibitor are “convincing because it’s real world data that complements what we know from clinical trials,” commented Silvio E. Inzucchi, MD, professor of medicine at Yale University and director of the Yale Medicine Diabetes Center in New Haven, Conn., who was not involved with the study.
“If these drugs reduce heart failure, they may also reduce AFib. Heart failure patients easily slip into AFib,” he noted in an interview, but added that “I don’t think this explains all cases” of the reduced AFib incidence.
Dr. Patorno offered a few other possible mechanisms for the observed effect. The class may work by reducing blood pressure, weight, inflammation, and oxidative stress, mitochondrial dysfunction, atrial remodeling, and AFib susceptibility. These agents are also known to cause natriuresis and diuresis, which could reduce atrial dilation, a mechanism that again relates the AFib effect to the better documented reduction in acute heart failure exacerbations.
“With the diuretic effect, we’d expect less overload at the atrium and less dilation, and the same mechanism would reduce heart failure,” she said in an interview.
“If you reduce preload and afterload you may reduce stress on the ventricle and reduce atrial stretch, and that might have a significant effect on atrial arrhythmia,” agreed Dr. Inzucchi.
EMPRISE produces more real-world evidence
A pair of additional reports at the meeting that Dr. Patorno coauthored provided real-world evidence supporting the dramatic heart failure benefit of the SGLT2 inhibitor empagliflozin (Jardiance) in U.S. patients with type 2 diabetes, compared with alternative drug classes. The EMPRISE study used data from the Medicare, Optum Clinformatics, and MarketScan databases during the period from August 2014, when empagliflozin became available, to September 2019. The study used more than 140 variables to match patients treated with either empagliflozin or a comparator agent.
The results showed that, in an analysis of more than 130,000 matched pairs, treatment with empagliflozin was linked to a significant 30% reduction in the incidence of hospitalization for heart failure, compared with patients treated with a GLP-1 receptor agonist. Analysis of more than 116,000 matched pairs of patients showed that treatment with empagliflozin linked with a significant 29%-50% reduced rate of hospitalization for heart failure, compared with matched patients treated with a DPP4 inhibitor.
These findings “add to the pool of information” on the efficacy of agents from the SGLT2 inhibitor class, Dr. Patorno said in an interview. “We wanted to look at the full range of patients with type 2 diabetes who we see in practice,” rather than the more selected group of patients enrolled in randomized trials.
SGLT2 inhibitor use lags even when cost isn’t an issue
Despite all the accumulated evidence for efficacy and safety of the class, usage remains low, Julio A. Lamprea-Montealegre, MD, PhD, a cardiologist at the University of California, San Francisco, reported in a separate talk at the meeting. The study he presented examined records for 1,319,500 adults with type 2 diabetes managed in the VA Healthcare System during 2019 and 2020. Despite being in a system that “removes the influence of cost,” just 10% of these patients received treatment with an SGLT2 inhibitor, and 7% received treatment with a GLP-1 receptor agonist.
Notably, his analysis further showed that treatment with an SGLT2 inhibitor was especially depressed among patients with an estimated glomerular filtration rate (eGFR) of 30-44 mL/min per 1.73m2. In this subgroup, usage of a drug from this class was at two-thirds of the rate, compared with patients with an eGFR of at least 90 mL/min per 1.73m2. His findings also documented lower rates of use in patients with higher risk for atherosclerotic cardiovascular disease. Dr. Lamprea-Montealegre called this a “treatment paradox,” in which patients likely to get the most benefit from an SGLT2 inhibitor were also less likely to actually receive it.
While his findings from the VA System suggest that drug cost is not the only factor driving underuse, the high price set for the SGLT2 inhibitor drugs that all currently remain on U.S. patents is widely considered an important factor.
“There is a big problem of affordability,” said Dr. Patorno.
“SGLT2 inhibitors should probably be first-line therapy” for many patients with type 2 diabetes, said Dr. Inzucchi. “The only thing holding it back is cost,” a situation that he hopes will dramatically shift once agents from this class become generic and have substantially lower price tags.
The EMPRISE study received funding from Boehringer Ingelheim, the company that markets empagliflozin (Jardiance). Dr. Patorno had no relevant commercial disclosures. Dr. Inzucchi is an adviser to Abbott Diagnostics, Esperion Therapeutics, and vTv Therapeutics, a consultant to Merck and Pfizer, and has other relationships with AstraZeneca, Boehringer Ingelheim, Lexicon, and Novo Nordisk. Dr. Lamprea-Montealegre had received research funding from Bayer.
NEW ORLEANS – The case continues to grow for prioritizing a sodium-glucose transporter 2 (SGLT2) inhibitor in patients with type 2 diabetes, as real-world evidence of benefit and safety accumulates on top of the data from randomized trials that first established this class as a management pillar.
Another important effect of these agents gaining increasing currency, on top of their well-established benefits in patients with type 2 diabetes for preventing acute heart failure exacerbations and slowing progression of diabetic kidney disease, is that they cut the incidence of new-onset atrial fibrillation (AFib). That effect was confirmed in an analysis of data from about 300,000 U.S. patients included in recent Medicare records, Elisabetta Patorno, MD, reported at the annual scientific sessions of the American Diabetes Association.
But despite documentation like this, real-world evidence also continues to show limited uptake of SGLT2 inhibitors in U.S. patients with type 2 diabetes. Records from more than 1.3 million patients with type 2 diabetes managed in the Veterans Affairs Healthcare System during 2019 or 2022 documented that just 10% of these patients received an agent from this class, even though all were eligible to receive it, according to findings in a separate report at the meeting.
The AFib analysis analyzed two sets of propensity score–matched Medicare patients during 2013-2018 aged 65 years or older with type 2 diabetes and no history of AFib. One analysis focused on 80,475 matched patients who started on treatment with either an SGLT2 inhibitor or a glucagonlike peptide–1 (GLP-1) receptor agonist, and a second on 74,868 matched patients who began either an SGTL2 inhibitor or a dipeptidyl peptidase–4 (DPP4) inhibitor. In both analyses, matching involved more than 130 variables. In both pair sets, patients at baseline averaged about 72 years old, nearly two-thirds were women, about 8%-9% had heart failure, 77%-80% were on metformin, and 20%-25% were using insulin.
The study’s primary endpoint was the incidence of hospitalization for AFib, which occurred a significant 18% less often in the patients who started on an SGLT2, compared with those who started a DPP4 inhibitor during median follow-up of 6.7 months, and a significant 10% less often, compared with those starting a GLP-1 receptor agonist during a median follow-up of 6.0 months, Elisabetta Patorno, MD, DrPH, reported at the meeting. This worked out to 3.7 fewer hospitalizations for AFib per 1,000 patient-years of follow-up among the people who received an SGLT2 inhibitor, compared with a DPP4 inhibitor, and a decrease of 1.8 hospitalizations/1,000 patient-years when compared against patients in a GLP-1 receptor agonist.
Two secondary outcomes showed significantly fewer episodes of newly diagnosed AFib, and significantly fewer patients initiating AFib treatment among those who received an SGLT2 inhibitor relative to the comparator groups. In addition, these associations were consistent across subgroup analyses that divided patients by their age, sex, history of heart failure, and history of atherosclerotic cardiovascular disease.
AFib effects add to benefits
The findings “suggest that initiation of an SGLT2 inhibitor may be beneficial in older adults with type 2 diabetes who are at risk for AFib,” said Dr. Patorno, a researcher in the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston. “These new findings on AFib may be helpful when weighing the potential risks and benefits of various glucose-lowering drugs in older patients with type 2 diabetes.”
This new evidence follows several prior reports from other research groups of data supporting an AFib benefit from SGLT2 inhibitors. The earlier reports include a post hoc analysis of more than 17,000 patients enrolled in the DECLARE-TIMI 58 cardiovascular outcome trial of dapagliflozin (Farxiga), which showed a 19% relative decrease in the rate of incident AFib or atrial flutter events during a median 4.2 year follow-up.
Other prior reports that found a reduced incidence of AFib events linked with SGLT2 inhibitor treatment include a 2020 meta-analysis based on data from more than 38,000 patients with type 2 diabetes enrolled in any of 16 randomized, controlled trials, which found a 24% relative risk reduction. And an as-yet unpublished report from researchers at the University of Rochester (N.Y.) and their associates presented in November 2021 at the annual scientific sessions of the American Heart Association that documented a significant 24% relative risk reduction in incident AFib events linked to SGLT2 inhibitor treatment in a prospective study of 13,890 patients at several hospitals in Israel or the United States.
Evidence ‘convincing’ in totality
The accumulated evidence for a reduced incidence of AFib when patients were on treatment with an SGLT2 inhibitor are “convincing because it’s real world data that complements what we know from clinical trials,” commented Silvio E. Inzucchi, MD, professor of medicine at Yale University and director of the Yale Medicine Diabetes Center in New Haven, Conn., who was not involved with the study.
“If these drugs reduce heart failure, they may also reduce AFib. Heart failure patients easily slip into AFib,” he noted in an interview, but added that “I don’t think this explains all cases” of the reduced AFib incidence.
Dr. Patorno offered a few other possible mechanisms for the observed effect. The class may work by reducing blood pressure, weight, inflammation, and oxidative stress, mitochondrial dysfunction, atrial remodeling, and AFib susceptibility. These agents are also known to cause natriuresis and diuresis, which could reduce atrial dilation, a mechanism that again relates the AFib effect to the better documented reduction in acute heart failure exacerbations.
“With the diuretic effect, we’d expect less overload at the atrium and less dilation, and the same mechanism would reduce heart failure,” she said in an interview.
“If you reduce preload and afterload you may reduce stress on the ventricle and reduce atrial stretch, and that might have a significant effect on atrial arrhythmia,” agreed Dr. Inzucchi.
EMPRISE produces more real-world evidence
A pair of additional reports at the meeting that Dr. Patorno coauthored provided real-world evidence supporting the dramatic heart failure benefit of the SGLT2 inhibitor empagliflozin (Jardiance) in U.S. patients with type 2 diabetes, compared with alternative drug classes. The EMPRISE study used data from the Medicare, Optum Clinformatics, and MarketScan databases during the period from August 2014, when empagliflozin became available, to September 2019. The study used more than 140 variables to match patients treated with either empagliflozin or a comparator agent.
The results showed that, in an analysis of more than 130,000 matched pairs, treatment with empagliflozin was linked to a significant 30% reduction in the incidence of hospitalization for heart failure, compared with patients treated with a GLP-1 receptor agonist. Analysis of more than 116,000 matched pairs of patients showed that treatment with empagliflozin linked with a significant 29%-50% reduced rate of hospitalization for heart failure, compared with matched patients treated with a DPP4 inhibitor.
These findings “add to the pool of information” on the efficacy of agents from the SGLT2 inhibitor class, Dr. Patorno said in an interview. “We wanted to look at the full range of patients with type 2 diabetes who we see in practice,” rather than the more selected group of patients enrolled in randomized trials.
SGLT2 inhibitor use lags even when cost isn’t an issue
Despite all the accumulated evidence for efficacy and safety of the class, usage remains low, Julio A. Lamprea-Montealegre, MD, PhD, a cardiologist at the University of California, San Francisco, reported in a separate talk at the meeting. The study he presented examined records for 1,319,500 adults with type 2 diabetes managed in the VA Healthcare System during 2019 and 2020. Despite being in a system that “removes the influence of cost,” just 10% of these patients received treatment with an SGLT2 inhibitor, and 7% received treatment with a GLP-1 receptor agonist.
Notably, his analysis further showed that treatment with an SGLT2 inhibitor was especially depressed among patients with an estimated glomerular filtration rate (eGFR) of 30-44 mL/min per 1.73m2. In this subgroup, usage of a drug from this class was at two-thirds of the rate, compared with patients with an eGFR of at least 90 mL/min per 1.73m2. His findings also documented lower rates of use in patients with higher risk for atherosclerotic cardiovascular disease. Dr. Lamprea-Montealegre called this a “treatment paradox,” in which patients likely to get the most benefit from an SGLT2 inhibitor were also less likely to actually receive it.
While his findings from the VA System suggest that drug cost is not the only factor driving underuse, the high price set for the SGLT2 inhibitor drugs that all currently remain on U.S. patents is widely considered an important factor.
“There is a big problem of affordability,” said Dr. Patorno.
“SGLT2 inhibitors should probably be first-line therapy” for many patients with type 2 diabetes, said Dr. Inzucchi. “The only thing holding it back is cost,” a situation that he hopes will dramatically shift once agents from this class become generic and have substantially lower price tags.
The EMPRISE study received funding from Boehringer Ingelheim, the company that markets empagliflozin (Jardiance). Dr. Patorno had no relevant commercial disclosures. Dr. Inzucchi is an adviser to Abbott Diagnostics, Esperion Therapeutics, and vTv Therapeutics, a consultant to Merck and Pfizer, and has other relationships with AstraZeneca, Boehringer Ingelheim, Lexicon, and Novo Nordisk. Dr. Lamprea-Montealegre had received research funding from Bayer.
NEW ORLEANS – The case continues to grow for prioritizing a sodium-glucose transporter 2 (SGLT2) inhibitor in patients with type 2 diabetes, as real-world evidence of benefit and safety accumulates on top of the data from randomized trials that first established this class as a management pillar.
Another important effect of these agents gaining increasing currency, on top of their well-established benefits in patients with type 2 diabetes for preventing acute heart failure exacerbations and slowing progression of diabetic kidney disease, is that they cut the incidence of new-onset atrial fibrillation (AFib). That effect was confirmed in an analysis of data from about 300,000 U.S. patients included in recent Medicare records, Elisabetta Patorno, MD, reported at the annual scientific sessions of the American Diabetes Association.
But despite documentation like this, real-world evidence also continues to show limited uptake of SGLT2 inhibitors in U.S. patients with type 2 diabetes. Records from more than 1.3 million patients with type 2 diabetes managed in the Veterans Affairs Healthcare System during 2019 or 2022 documented that just 10% of these patients received an agent from this class, even though all were eligible to receive it, according to findings in a separate report at the meeting.
The AFib analysis analyzed two sets of propensity score–matched Medicare patients during 2013-2018 aged 65 years or older with type 2 diabetes and no history of AFib. One analysis focused on 80,475 matched patients who started on treatment with either an SGLT2 inhibitor or a glucagonlike peptide–1 (GLP-1) receptor agonist, and a second on 74,868 matched patients who began either an SGTL2 inhibitor or a dipeptidyl peptidase–4 (DPP4) inhibitor. In both analyses, matching involved more than 130 variables. In both pair sets, patients at baseline averaged about 72 years old, nearly two-thirds were women, about 8%-9% had heart failure, 77%-80% were on metformin, and 20%-25% were using insulin.
The study’s primary endpoint was the incidence of hospitalization for AFib, which occurred a significant 18% less often in the patients who started on an SGLT2, compared with those who started a DPP4 inhibitor during median follow-up of 6.7 months, and a significant 10% less often, compared with those starting a GLP-1 receptor agonist during a median follow-up of 6.0 months, Elisabetta Patorno, MD, DrPH, reported at the meeting. This worked out to 3.7 fewer hospitalizations for AFib per 1,000 patient-years of follow-up among the people who received an SGLT2 inhibitor, compared with a DPP4 inhibitor, and a decrease of 1.8 hospitalizations/1,000 patient-years when compared against patients in a GLP-1 receptor agonist.
Two secondary outcomes showed significantly fewer episodes of newly diagnosed AFib, and significantly fewer patients initiating AFib treatment among those who received an SGLT2 inhibitor relative to the comparator groups. In addition, these associations were consistent across subgroup analyses that divided patients by their age, sex, history of heart failure, and history of atherosclerotic cardiovascular disease.
AFib effects add to benefits
The findings “suggest that initiation of an SGLT2 inhibitor may be beneficial in older adults with type 2 diabetes who are at risk for AFib,” said Dr. Patorno, a researcher in the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston. “These new findings on AFib may be helpful when weighing the potential risks and benefits of various glucose-lowering drugs in older patients with type 2 diabetes.”
This new evidence follows several prior reports from other research groups of data supporting an AFib benefit from SGLT2 inhibitors. The earlier reports include a post hoc analysis of more than 17,000 patients enrolled in the DECLARE-TIMI 58 cardiovascular outcome trial of dapagliflozin (Farxiga), which showed a 19% relative decrease in the rate of incident AFib or atrial flutter events during a median 4.2 year follow-up.
Other prior reports that found a reduced incidence of AFib events linked with SGLT2 inhibitor treatment include a 2020 meta-analysis based on data from more than 38,000 patients with type 2 diabetes enrolled in any of 16 randomized, controlled trials, which found a 24% relative risk reduction. And an as-yet unpublished report from researchers at the University of Rochester (N.Y.) and their associates presented in November 2021 at the annual scientific sessions of the American Heart Association that documented a significant 24% relative risk reduction in incident AFib events linked to SGLT2 inhibitor treatment in a prospective study of 13,890 patients at several hospitals in Israel or the United States.
Evidence ‘convincing’ in totality
The accumulated evidence for a reduced incidence of AFib when patients were on treatment with an SGLT2 inhibitor are “convincing because it’s real world data that complements what we know from clinical trials,” commented Silvio E. Inzucchi, MD, professor of medicine at Yale University and director of the Yale Medicine Diabetes Center in New Haven, Conn., who was not involved with the study.
“If these drugs reduce heart failure, they may also reduce AFib. Heart failure patients easily slip into AFib,” he noted in an interview, but added that “I don’t think this explains all cases” of the reduced AFib incidence.
Dr. Patorno offered a few other possible mechanisms for the observed effect. The class may work by reducing blood pressure, weight, inflammation, and oxidative stress, mitochondrial dysfunction, atrial remodeling, and AFib susceptibility. These agents are also known to cause natriuresis and diuresis, which could reduce atrial dilation, a mechanism that again relates the AFib effect to the better documented reduction in acute heart failure exacerbations.
“With the diuretic effect, we’d expect less overload at the atrium and less dilation, and the same mechanism would reduce heart failure,” she said in an interview.
“If you reduce preload and afterload you may reduce stress on the ventricle and reduce atrial stretch, and that might have a significant effect on atrial arrhythmia,” agreed Dr. Inzucchi.
EMPRISE produces more real-world evidence
A pair of additional reports at the meeting that Dr. Patorno coauthored provided real-world evidence supporting the dramatic heart failure benefit of the SGLT2 inhibitor empagliflozin (Jardiance) in U.S. patients with type 2 diabetes, compared with alternative drug classes. The EMPRISE study used data from the Medicare, Optum Clinformatics, and MarketScan databases during the period from August 2014, when empagliflozin became available, to September 2019. The study used more than 140 variables to match patients treated with either empagliflozin or a comparator agent.
The results showed that, in an analysis of more than 130,000 matched pairs, treatment with empagliflozin was linked to a significant 30% reduction in the incidence of hospitalization for heart failure, compared with patients treated with a GLP-1 receptor agonist. Analysis of more than 116,000 matched pairs of patients showed that treatment with empagliflozin linked with a significant 29%-50% reduced rate of hospitalization for heart failure, compared with matched patients treated with a DPP4 inhibitor.
These findings “add to the pool of information” on the efficacy of agents from the SGLT2 inhibitor class, Dr. Patorno said in an interview. “We wanted to look at the full range of patients with type 2 diabetes who we see in practice,” rather than the more selected group of patients enrolled in randomized trials.
SGLT2 inhibitor use lags even when cost isn’t an issue
Despite all the accumulated evidence for efficacy and safety of the class, usage remains low, Julio A. Lamprea-Montealegre, MD, PhD, a cardiologist at the University of California, San Francisco, reported in a separate talk at the meeting. The study he presented examined records for 1,319,500 adults with type 2 diabetes managed in the VA Healthcare System during 2019 and 2020. Despite being in a system that “removes the influence of cost,” just 10% of these patients received treatment with an SGLT2 inhibitor, and 7% received treatment with a GLP-1 receptor agonist.
Notably, his analysis further showed that treatment with an SGLT2 inhibitor was especially depressed among patients with an estimated glomerular filtration rate (eGFR) of 30-44 mL/min per 1.73m2. In this subgroup, usage of a drug from this class was at two-thirds of the rate, compared with patients with an eGFR of at least 90 mL/min per 1.73m2. His findings also documented lower rates of use in patients with higher risk for atherosclerotic cardiovascular disease. Dr. Lamprea-Montealegre called this a “treatment paradox,” in which patients likely to get the most benefit from an SGLT2 inhibitor were also less likely to actually receive it.
While his findings from the VA System suggest that drug cost is not the only factor driving underuse, the high price set for the SGLT2 inhibitor drugs that all currently remain on U.S. patents is widely considered an important factor.
“There is a big problem of affordability,” said Dr. Patorno.
“SGLT2 inhibitors should probably be first-line therapy” for many patients with type 2 diabetes, said Dr. Inzucchi. “The only thing holding it back is cost,” a situation that he hopes will dramatically shift once agents from this class become generic and have substantially lower price tags.
The EMPRISE study received funding from Boehringer Ingelheim, the company that markets empagliflozin (Jardiance). Dr. Patorno had no relevant commercial disclosures. Dr. Inzucchi is an adviser to Abbott Diagnostics, Esperion Therapeutics, and vTv Therapeutics, a consultant to Merck and Pfizer, and has other relationships with AstraZeneca, Boehringer Ingelheim, Lexicon, and Novo Nordisk. Dr. Lamprea-Montealegre had received research funding from Bayer.
AT ADA 2022









