User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
80% of Americans research recommendations post-visit
Confusion over health information and doctor advice is even higher among people who care for patients than among those who don’t provide care to their loved ones, the nationally representative survey from the AHIMA Foundation found.
The survey also shows that 80% of Americans – and an even higher portion of caregivers – are likely to research medical recommendations online after a doctor’s visit. But 1 in 4 people don’t know how to access their own medical records or find it difficult to do so.
The findings reflect the same low level of health literacy in the U.S. population that earlier surveys did. The results also indicate that little has changed since the Department of Health and Human Services released a National Action Plan to Improve Health Literacy in 2010.
That plan emphasized the need to develop and share accurate health information that helps people make decisions; to promote changes in the health care system that improve health information, communication, informed decision-making, and access to health services; and to increase the sharing and use of evidence-based health literacy practices.
According to the AHIMA Foundation report, 62% of Americans are not sure they understand their doctor’s advice and the health information discussed during a visit. Twenty-four percent say they don’t comprehend any of it, and 31% can’t remember what was said during the visit. Fifteen percent of those surveyed said they were more confused about their health than they were before the encounter with their doctor.
Caregivers have special issues
Forty-three percent of Americans are caregivers, the report notes, and 91% of those play an active role in managing someone else’s health. Millennials (65%) and Gen Xers (50%) are significantly more likely than Gen Zers (39%) and Boomers (20%) to be a caregiver.
Most caregivers have concerns about their loved ones’ ability to manage their own health. Most of them believe that doctors provide enough information, but 38% don’t believe a doctor can communicate effectively with the patient if the caregiver is not present.
Forty-three percent of caretakers don’t think their loved ones can understand medical information on their own. On the other hand, caregivers are more likely than people who don’t provide care to say the doctor confused them and to research the doctor’s advice after an appointment.
For many patients and caregivers, communications break down when they are with their health care provider. Twenty-two percent of Americans say they do not feel comfortable asking their doctor certain health questions. This inability to have a satisfactory dialogue with their doctor means that many patients leave their appointments without getting clear answers to their questions (24%) or without having an opportunity to ask any questions at all (17%).
This is not surprising, considering that a 2018 study found that doctors spend only 11 seconds, on average, listening to patients before interrupting them.
Depending on the internet
Overall, the AHIMA survey found, 42% of Americans research their doctor’s recommendations after an appointment. A higher percentage of caregivers than noncaregiver peers do so (47% vs. 38%). Eighty percent of respondents say they are “likely” to research their doctor’s advice online after a visit.
When they have a medical problem or a question about their condition, just as many Americans (59%) turn to the internet for an answer as contact their doctor directly, the survey found. Twenty-nine percent of the respondents consult friends, family, or colleagues; 23% look up medical records if they’re easily accessible; 19% ask pharmacists for advice; and 6% call an unspecified 800 number.
Americans feel secure in the health information they find on the internet. Among those who go online to look up information, 86% are confident that it is credible. And 42% report feeling relieved that they can find a lot of information about their health concerns. Respondents also say that the information they gather allows them to feel more confident in their doctor’s recommendations (35%) and that they feel better after having learned more on the internet than their doctor had told them (39%). Men are more likely than women to say that their confidence in their doctor’s recommendations increased after doing online research (40% vs. 30%).
Access to health records
Access to medical records would help people better understand their condition or diagnosis. But nearly half of Americans (48%) admit they don’t usually review their medical records until long after an appointment, and 52% say they rarely access their records at all.
One in four Americans say that they don’t know where to go to access their health information or that they didn’t find the process easy. More than half of those who have never had to find their records think the process would be difficult if they had to try.
Eighty-one percent of Americans use an online platform or portal to access their medical records or health information. Two-thirds of Americans who use an online portal trust that their medical information is kept safe and not shared with other people or organizations.
Four in five respondents agree that if they had access to all of their health information, including medical records, recommendations, conditions, and test results, they’d see an improvement in their health management. Fifty-nine percent of them believe they’d also be more confident about understanding their health, and 47% say they’d have greater trust in their doctor’s recommendations. Higher percentages of caregivers than noncaregivers say the same.
Younger people, those with a high school degree or less, and those who earn less than $50,000 are less likely than older, better educated, and more affluent people to understand their doctor’s health information and to ask questions of their providers.
People of color struggle with their relationships with doctors, are less satisfied than white people with the information they receive during visits, and are more likely than white peers to feel that if they had access to all their health information, they’d manage their health better and be more confident in their doctors’ recommendations, the survey found.
A version of this article first appeared on WebMD.com.
Confusion over health information and doctor advice is even higher among people who care for patients than among those who don’t provide care to their loved ones, the nationally representative survey from the AHIMA Foundation found.
The survey also shows that 80% of Americans – and an even higher portion of caregivers – are likely to research medical recommendations online after a doctor’s visit. But 1 in 4 people don’t know how to access their own medical records or find it difficult to do so.
The findings reflect the same low level of health literacy in the U.S. population that earlier surveys did. The results also indicate that little has changed since the Department of Health and Human Services released a National Action Plan to Improve Health Literacy in 2010.
That plan emphasized the need to develop and share accurate health information that helps people make decisions; to promote changes in the health care system that improve health information, communication, informed decision-making, and access to health services; and to increase the sharing and use of evidence-based health literacy practices.
According to the AHIMA Foundation report, 62% of Americans are not sure they understand their doctor’s advice and the health information discussed during a visit. Twenty-four percent say they don’t comprehend any of it, and 31% can’t remember what was said during the visit. Fifteen percent of those surveyed said they were more confused about their health than they were before the encounter with their doctor.
Caregivers have special issues
Forty-three percent of Americans are caregivers, the report notes, and 91% of those play an active role in managing someone else’s health. Millennials (65%) and Gen Xers (50%) are significantly more likely than Gen Zers (39%) and Boomers (20%) to be a caregiver.
Most caregivers have concerns about their loved ones’ ability to manage their own health. Most of them believe that doctors provide enough information, but 38% don’t believe a doctor can communicate effectively with the patient if the caregiver is not present.
Forty-three percent of caretakers don’t think their loved ones can understand medical information on their own. On the other hand, caregivers are more likely than people who don’t provide care to say the doctor confused them and to research the doctor’s advice after an appointment.
For many patients and caregivers, communications break down when they are with their health care provider. Twenty-two percent of Americans say they do not feel comfortable asking their doctor certain health questions. This inability to have a satisfactory dialogue with their doctor means that many patients leave their appointments without getting clear answers to their questions (24%) or without having an opportunity to ask any questions at all (17%).
This is not surprising, considering that a 2018 study found that doctors spend only 11 seconds, on average, listening to patients before interrupting them.
Depending on the internet
Overall, the AHIMA survey found, 42% of Americans research their doctor’s recommendations after an appointment. A higher percentage of caregivers than noncaregiver peers do so (47% vs. 38%). Eighty percent of respondents say they are “likely” to research their doctor’s advice online after a visit.
When they have a medical problem or a question about their condition, just as many Americans (59%) turn to the internet for an answer as contact their doctor directly, the survey found. Twenty-nine percent of the respondents consult friends, family, or colleagues; 23% look up medical records if they’re easily accessible; 19% ask pharmacists for advice; and 6% call an unspecified 800 number.
Americans feel secure in the health information they find on the internet. Among those who go online to look up information, 86% are confident that it is credible. And 42% report feeling relieved that they can find a lot of information about their health concerns. Respondents also say that the information they gather allows them to feel more confident in their doctor’s recommendations (35%) and that they feel better after having learned more on the internet than their doctor had told them (39%). Men are more likely than women to say that their confidence in their doctor’s recommendations increased after doing online research (40% vs. 30%).
Access to health records
Access to medical records would help people better understand their condition or diagnosis. But nearly half of Americans (48%) admit they don’t usually review their medical records until long after an appointment, and 52% say they rarely access their records at all.
One in four Americans say that they don’t know where to go to access their health information or that they didn’t find the process easy. More than half of those who have never had to find their records think the process would be difficult if they had to try.
Eighty-one percent of Americans use an online platform or portal to access their medical records or health information. Two-thirds of Americans who use an online portal trust that their medical information is kept safe and not shared with other people or organizations.
Four in five respondents agree that if they had access to all of their health information, including medical records, recommendations, conditions, and test results, they’d see an improvement in their health management. Fifty-nine percent of them believe they’d also be more confident about understanding their health, and 47% say they’d have greater trust in their doctor’s recommendations. Higher percentages of caregivers than noncaregivers say the same.
Younger people, those with a high school degree or less, and those who earn less than $50,000 are less likely than older, better educated, and more affluent people to understand their doctor’s health information and to ask questions of their providers.
People of color struggle with their relationships with doctors, are less satisfied than white people with the information they receive during visits, and are more likely than white peers to feel that if they had access to all their health information, they’d manage their health better and be more confident in their doctors’ recommendations, the survey found.
A version of this article first appeared on WebMD.com.
Confusion over health information and doctor advice is even higher among people who care for patients than among those who don’t provide care to their loved ones, the nationally representative survey from the AHIMA Foundation found.
The survey also shows that 80% of Americans – and an even higher portion of caregivers – are likely to research medical recommendations online after a doctor’s visit. But 1 in 4 people don’t know how to access their own medical records or find it difficult to do so.
The findings reflect the same low level of health literacy in the U.S. population that earlier surveys did. The results also indicate that little has changed since the Department of Health and Human Services released a National Action Plan to Improve Health Literacy in 2010.
That plan emphasized the need to develop and share accurate health information that helps people make decisions; to promote changes in the health care system that improve health information, communication, informed decision-making, and access to health services; and to increase the sharing and use of evidence-based health literacy practices.
According to the AHIMA Foundation report, 62% of Americans are not sure they understand their doctor’s advice and the health information discussed during a visit. Twenty-four percent say they don’t comprehend any of it, and 31% can’t remember what was said during the visit. Fifteen percent of those surveyed said they were more confused about their health than they were before the encounter with their doctor.
Caregivers have special issues
Forty-three percent of Americans are caregivers, the report notes, and 91% of those play an active role in managing someone else’s health. Millennials (65%) and Gen Xers (50%) are significantly more likely than Gen Zers (39%) and Boomers (20%) to be a caregiver.
Most caregivers have concerns about their loved ones’ ability to manage their own health. Most of them believe that doctors provide enough information, but 38% don’t believe a doctor can communicate effectively with the patient if the caregiver is not present.
Forty-three percent of caretakers don’t think their loved ones can understand medical information on their own. On the other hand, caregivers are more likely than people who don’t provide care to say the doctor confused them and to research the doctor’s advice after an appointment.
For many patients and caregivers, communications break down when they are with their health care provider. Twenty-two percent of Americans say they do not feel comfortable asking their doctor certain health questions. This inability to have a satisfactory dialogue with their doctor means that many patients leave their appointments without getting clear answers to their questions (24%) or without having an opportunity to ask any questions at all (17%).
This is not surprising, considering that a 2018 study found that doctors spend only 11 seconds, on average, listening to patients before interrupting them.
Depending on the internet
Overall, the AHIMA survey found, 42% of Americans research their doctor’s recommendations after an appointment. A higher percentage of caregivers than noncaregiver peers do so (47% vs. 38%). Eighty percent of respondents say they are “likely” to research their doctor’s advice online after a visit.
When they have a medical problem or a question about their condition, just as many Americans (59%) turn to the internet for an answer as contact their doctor directly, the survey found. Twenty-nine percent of the respondents consult friends, family, or colleagues; 23% look up medical records if they’re easily accessible; 19% ask pharmacists for advice; and 6% call an unspecified 800 number.
Americans feel secure in the health information they find on the internet. Among those who go online to look up information, 86% are confident that it is credible. And 42% report feeling relieved that they can find a lot of information about their health concerns. Respondents also say that the information they gather allows them to feel more confident in their doctor’s recommendations (35%) and that they feel better after having learned more on the internet than their doctor had told them (39%). Men are more likely than women to say that their confidence in their doctor’s recommendations increased after doing online research (40% vs. 30%).
Access to health records
Access to medical records would help people better understand their condition or diagnosis. But nearly half of Americans (48%) admit they don’t usually review their medical records until long after an appointment, and 52% say they rarely access their records at all.
One in four Americans say that they don’t know where to go to access their health information or that they didn’t find the process easy. More than half of those who have never had to find their records think the process would be difficult if they had to try.
Eighty-one percent of Americans use an online platform or portal to access their medical records or health information. Two-thirds of Americans who use an online portal trust that their medical information is kept safe and not shared with other people or organizations.
Four in five respondents agree that if they had access to all of their health information, including medical records, recommendations, conditions, and test results, they’d see an improvement in their health management. Fifty-nine percent of them believe they’d also be more confident about understanding their health, and 47% say they’d have greater trust in their doctor’s recommendations. Higher percentages of caregivers than noncaregivers say the same.
Younger people, those with a high school degree or less, and those who earn less than $50,000 are less likely than older, better educated, and more affluent people to understand their doctor’s health information and to ask questions of their providers.
People of color struggle with their relationships with doctors, are less satisfied than white people with the information they receive during visits, and are more likely than white peers to feel that if they had access to all their health information, they’d manage their health better and be more confident in their doctors’ recommendations, the survey found.
A version of this article first appeared on WebMD.com.
Antidepressant may cut COVID-19–related hospitalization, mortality: TOGETHER
The antidepressant fluvoxamine (Luvox) may prevent hospitalization and death in outpatients with COVID-19, new research suggests.
Results from the placebo-controlled, multisite, phase 3 TOGETHER trial showed that in COVID-19 outpatients at high risk for complications, hospitalizations were cut by 66% and deaths were reduced by 91% in those who tolerated fluvoxamine.
“Our trial has found that fluvoxamine, an inexpensive existing drug, reduces the need for advanced disease care in this high-risk population,” wrote the investigators, led by Gilmar Reis, MD, PhD, research division, Cardresearch, Belo Horizonte, Brazil.
The findings were published online Oct. 27 in The Lancet Global Health.
Alternative mechanisms
Fluvoxamine, a selective serotonin reuptake inhibitor (SSRI), is an antidepressant commonly prescribed for obsessive-compulsive disorder.
Besides its known effects on serotonin, the drug acts in other molecular pathways to dampen the production of inflammatory cytokines. Those alternative mechanisms are the ones believed to help patients with COVID-19, said coinvestigator Angela Reiersen, MD, child psychiatrist at Washington University, St. Louis.
Based on cell culture and mouse studies showing effects of the molecule’s binding to the sigma-1 receptor in the endoplasmic reticulum, Dr. Reiersen came up with the idea of testing if fluvoxamine could keep COVID-19 from progressing in newly infected patients.
Dr. Reiersen and psychiatrist Eric Lenze, MD, also from Washington University, led the phase 2 trial that initially suggested fluvoxamine’s promise as an outpatient medication. They are coinvestigators on the new phase 3 adaptive platform trial called TOGETHER, which was conducted by an international team of investigators in Brazil, Canada, and the United States.
For this latest study, researchers at McMaster University, Hamilton, Ont., partnered with the research clinic Cardresearch in Brazil to recruit unvaccinated, high-risk adults within 7 days of developing flu-like symptoms from COVID-19. They analyzed 1,497 newly symptomatic COVID-19 patients at 11 clinical sites in Brazil.
Patients entered the trial between January and August 2021 and were assigned to receive 100 mg fluvoxamine or placebo pills twice a day for 10 days. Investigators monitored participants through 28 days post treatment, noting whether complications developed requiring hospitalization or more than 6 hours of emergency care.
In the placebo group, 119 of 756 patients (15.7%) worsened to this extent. In comparison, 79 of 741 (10.7%) fluvoxamine-treated patients met these primary criteria. This represented a 32% reduction in hospitalizations and emergency visits.
Additional analysis requested
As Lancet Global Health reviewed these findings from the submitted manuscript, journal reviewers requested an additional “pre-protocol analysis” that was not specified in the trial’s original protocol. The request was to examine the subgroup of patients with good adherence (74% of treated group, 82% of placebo group).
Among these three quarters of patients who took at least 80% of their doses, benefits were better.
Fluvoxamine cut serious complications in this group by 66% and reduced mortality by 91%. In the placebo group, 12 people died compared with one who received the study drug.
from complications of the infection.
However, clinicians should note that the drug can cause side effects such as nausea, dizziness, and insomnia, she added. In addition, because it prevents the body from metabolizing caffeine, patients should limit their daily intake to half of a small cup of coffee or one can of soda or one tea while taking the drug.
Previous research has shown that fluvoxamine affects the metabolism of some drugs, such as theophylline, clozapine, olanzapine, and tizanidine.
Despite huge challenges with studying generic drugs as early COVID-19 treatment, the TOGETHER trial shows it is possible to produce quality evidence during a pandemic on a shoestring budget, noted co-principal investigator Edward Mills, PhD, professor in the department of health research methods, evidence, and impact at McMaster University.
To screen more than 12,000 patients and enroll 4,000 to test nine interventions, “our total budget was less than $8 million,” Dr. Mills said. The trial was funded by Fast Grants and the Rainwater Charitable Foundation.
‘A $10 medicine’
Commenting on the findings, David Boulware, MD, MPH, an infectious disease physician-researcher at the University of Minnesota in Minneapolis, noted fluvoxamine is “a $10 medicine that’s available and has a very good safety record.”
By comparison, a 5-day course of Merck’s antiviral molnupiravir, another oral drug that the company says can cut hospitalizations in COVID-19 outpatients, costs $700. However, the data have not been peer reviewed – and molnupiravir is not currently available and has unknown long-term safety implications, Dr. Boulware said.
Pharmaceutical companies typically spend tens of thousands of dollars on a trial evaluating a single drug, he noted.
In addition, the National Institutes of Health’s ACTIV-6 study, a nationwide trial on the effect of fluvoxamine and other repurposed generic drugs on thousands of COVID-19 outpatients, is a $110 million effort, according to Dr. Boulware, who cochairs its steering committee.
ACTIV-6 is currently enrolling outpatients with COVID-19 to test a lower dose of fluvoxamine, at 50 mg twice daily instead of the 100-mg dose used in the TOGETHER trial, as well as ivermectin and inhaled fluticasone. The COVID-OUT trial is also recruiting newly diagnosed COVID-19 patients to test various combinations of fluvoxamine, ivermectin, and the diabetes drug metformin.
Unanswered safety, efficacy questions
In an accompanying editorial in The Lancet Global Health, Otavio Berwanger, MD, cardiologist and clinical trialist, Academic Research Organization, Hospital Israelita Albert Einstein, São Paulo, Brazil, commends the investigators for rapidly generating evidence during the COVID-19 pandemic.
However, despite the important findings, “some questions related to efficacy and safety of fluvoxamine for patients with COVID-19 remain open,” Dr. Berwanger wrote.
The effects of the drug on reducing both mortality and hospitalizations also “still need addressing,” he noted.
“In addition, it remains to be established whether fluvoxamine has an additive effect to other therapies such as monoclonal antibodies and budesonide, and what is the optimal fluvoxamine therapeutic scheme,” wrote Dr. Berwanger.
In an interview, he noted that 74% of the Brazil population have currently received at least one dose of a COVID-19 vaccine and 52% have received two doses. In addition, deaths have gone down from 4,000 per day during the March-April second wave to about 400 per day. “That is still unfortunate and far from ideal,” he said. In total, they have had about 600,000 deaths because of COVID-19.
Asked whether public health authorities are now recommending fluvoxamine as an early treatment for COVID-19 based on the TOGETHER trial data, Dr. Berwanger answered, “Not yet.
“I believe medical and scientific societies will need to critically appraise the manuscript in order to inform their decisions and recommendations. This interesting trial adds another important piece of information in this regard,” he said.
Dr. Reiersen and Dr. Lenze are inventors on a patent application related to methods for treating COVID-19, which was filed by Washington University. Dr. Mills reports no relevant financial relationships, as does Dr. Boulware – except that the TOGETHER trial funders are also funding the University of Minnesota COVID-OUT trial. Dr. Berwanger reports having received research grants outside of the submitted work that were paid to his institution by AstraZeneca, Bayer, Amgen, Servier, Novartis, Pfizer, and Boehringer Ingelheim.
A version of this article first appeared on Medscape.com.
The antidepressant fluvoxamine (Luvox) may prevent hospitalization and death in outpatients with COVID-19, new research suggests.
Results from the placebo-controlled, multisite, phase 3 TOGETHER trial showed that in COVID-19 outpatients at high risk for complications, hospitalizations were cut by 66% and deaths were reduced by 91% in those who tolerated fluvoxamine.
“Our trial has found that fluvoxamine, an inexpensive existing drug, reduces the need for advanced disease care in this high-risk population,” wrote the investigators, led by Gilmar Reis, MD, PhD, research division, Cardresearch, Belo Horizonte, Brazil.
The findings were published online Oct. 27 in The Lancet Global Health.
Alternative mechanisms
Fluvoxamine, a selective serotonin reuptake inhibitor (SSRI), is an antidepressant commonly prescribed for obsessive-compulsive disorder.
Besides its known effects on serotonin, the drug acts in other molecular pathways to dampen the production of inflammatory cytokines. Those alternative mechanisms are the ones believed to help patients with COVID-19, said coinvestigator Angela Reiersen, MD, child psychiatrist at Washington University, St. Louis.
Based on cell culture and mouse studies showing effects of the molecule’s binding to the sigma-1 receptor in the endoplasmic reticulum, Dr. Reiersen came up with the idea of testing if fluvoxamine could keep COVID-19 from progressing in newly infected patients.
Dr. Reiersen and psychiatrist Eric Lenze, MD, also from Washington University, led the phase 2 trial that initially suggested fluvoxamine’s promise as an outpatient medication. They are coinvestigators on the new phase 3 adaptive platform trial called TOGETHER, which was conducted by an international team of investigators in Brazil, Canada, and the United States.
For this latest study, researchers at McMaster University, Hamilton, Ont., partnered with the research clinic Cardresearch in Brazil to recruit unvaccinated, high-risk adults within 7 days of developing flu-like symptoms from COVID-19. They analyzed 1,497 newly symptomatic COVID-19 patients at 11 clinical sites in Brazil.
Patients entered the trial between January and August 2021 and were assigned to receive 100 mg fluvoxamine or placebo pills twice a day for 10 days. Investigators monitored participants through 28 days post treatment, noting whether complications developed requiring hospitalization or more than 6 hours of emergency care.
In the placebo group, 119 of 756 patients (15.7%) worsened to this extent. In comparison, 79 of 741 (10.7%) fluvoxamine-treated patients met these primary criteria. This represented a 32% reduction in hospitalizations and emergency visits.
Additional analysis requested
As Lancet Global Health reviewed these findings from the submitted manuscript, journal reviewers requested an additional “pre-protocol analysis” that was not specified in the trial’s original protocol. The request was to examine the subgroup of patients with good adherence (74% of treated group, 82% of placebo group).
Among these three quarters of patients who took at least 80% of their doses, benefits were better.
Fluvoxamine cut serious complications in this group by 66% and reduced mortality by 91%. In the placebo group, 12 people died compared with one who received the study drug.
from complications of the infection.
However, clinicians should note that the drug can cause side effects such as nausea, dizziness, and insomnia, she added. In addition, because it prevents the body from metabolizing caffeine, patients should limit their daily intake to half of a small cup of coffee or one can of soda or one tea while taking the drug.
Previous research has shown that fluvoxamine affects the metabolism of some drugs, such as theophylline, clozapine, olanzapine, and tizanidine.
Despite huge challenges with studying generic drugs as early COVID-19 treatment, the TOGETHER trial shows it is possible to produce quality evidence during a pandemic on a shoestring budget, noted co-principal investigator Edward Mills, PhD, professor in the department of health research methods, evidence, and impact at McMaster University.
To screen more than 12,000 patients and enroll 4,000 to test nine interventions, “our total budget was less than $8 million,” Dr. Mills said. The trial was funded by Fast Grants and the Rainwater Charitable Foundation.
‘A $10 medicine’
Commenting on the findings, David Boulware, MD, MPH, an infectious disease physician-researcher at the University of Minnesota in Minneapolis, noted fluvoxamine is “a $10 medicine that’s available and has a very good safety record.”
By comparison, a 5-day course of Merck’s antiviral molnupiravir, another oral drug that the company says can cut hospitalizations in COVID-19 outpatients, costs $700. However, the data have not been peer reviewed – and molnupiravir is not currently available and has unknown long-term safety implications, Dr. Boulware said.
Pharmaceutical companies typically spend tens of thousands of dollars on a trial evaluating a single drug, he noted.
In addition, the National Institutes of Health’s ACTIV-6 study, a nationwide trial on the effect of fluvoxamine and other repurposed generic drugs on thousands of COVID-19 outpatients, is a $110 million effort, according to Dr. Boulware, who cochairs its steering committee.
ACTIV-6 is currently enrolling outpatients with COVID-19 to test a lower dose of fluvoxamine, at 50 mg twice daily instead of the 100-mg dose used in the TOGETHER trial, as well as ivermectin and inhaled fluticasone. The COVID-OUT trial is also recruiting newly diagnosed COVID-19 patients to test various combinations of fluvoxamine, ivermectin, and the diabetes drug metformin.
Unanswered safety, efficacy questions
In an accompanying editorial in The Lancet Global Health, Otavio Berwanger, MD, cardiologist and clinical trialist, Academic Research Organization, Hospital Israelita Albert Einstein, São Paulo, Brazil, commends the investigators for rapidly generating evidence during the COVID-19 pandemic.
However, despite the important findings, “some questions related to efficacy and safety of fluvoxamine for patients with COVID-19 remain open,” Dr. Berwanger wrote.
The effects of the drug on reducing both mortality and hospitalizations also “still need addressing,” he noted.
“In addition, it remains to be established whether fluvoxamine has an additive effect to other therapies such as monoclonal antibodies and budesonide, and what is the optimal fluvoxamine therapeutic scheme,” wrote Dr. Berwanger.
In an interview, he noted that 74% of the Brazil population have currently received at least one dose of a COVID-19 vaccine and 52% have received two doses. In addition, deaths have gone down from 4,000 per day during the March-April second wave to about 400 per day. “That is still unfortunate and far from ideal,” he said. In total, they have had about 600,000 deaths because of COVID-19.
Asked whether public health authorities are now recommending fluvoxamine as an early treatment for COVID-19 based on the TOGETHER trial data, Dr. Berwanger answered, “Not yet.
“I believe medical and scientific societies will need to critically appraise the manuscript in order to inform their decisions and recommendations. This interesting trial adds another important piece of information in this regard,” he said.
Dr. Reiersen and Dr. Lenze are inventors on a patent application related to methods for treating COVID-19, which was filed by Washington University. Dr. Mills reports no relevant financial relationships, as does Dr. Boulware – except that the TOGETHER trial funders are also funding the University of Minnesota COVID-OUT trial. Dr. Berwanger reports having received research grants outside of the submitted work that were paid to his institution by AstraZeneca, Bayer, Amgen, Servier, Novartis, Pfizer, and Boehringer Ingelheim.
A version of this article first appeared on Medscape.com.
The antidepressant fluvoxamine (Luvox) may prevent hospitalization and death in outpatients with COVID-19, new research suggests.
Results from the placebo-controlled, multisite, phase 3 TOGETHER trial showed that in COVID-19 outpatients at high risk for complications, hospitalizations were cut by 66% and deaths were reduced by 91% in those who tolerated fluvoxamine.
“Our trial has found that fluvoxamine, an inexpensive existing drug, reduces the need for advanced disease care in this high-risk population,” wrote the investigators, led by Gilmar Reis, MD, PhD, research division, Cardresearch, Belo Horizonte, Brazil.
The findings were published online Oct. 27 in The Lancet Global Health.
Alternative mechanisms
Fluvoxamine, a selective serotonin reuptake inhibitor (SSRI), is an antidepressant commonly prescribed for obsessive-compulsive disorder.
Besides its known effects on serotonin, the drug acts in other molecular pathways to dampen the production of inflammatory cytokines. Those alternative mechanisms are the ones believed to help patients with COVID-19, said coinvestigator Angela Reiersen, MD, child psychiatrist at Washington University, St. Louis.
Based on cell culture and mouse studies showing effects of the molecule’s binding to the sigma-1 receptor in the endoplasmic reticulum, Dr. Reiersen came up with the idea of testing if fluvoxamine could keep COVID-19 from progressing in newly infected patients.
Dr. Reiersen and psychiatrist Eric Lenze, MD, also from Washington University, led the phase 2 trial that initially suggested fluvoxamine’s promise as an outpatient medication. They are coinvestigators on the new phase 3 adaptive platform trial called TOGETHER, which was conducted by an international team of investigators in Brazil, Canada, and the United States.
For this latest study, researchers at McMaster University, Hamilton, Ont., partnered with the research clinic Cardresearch in Brazil to recruit unvaccinated, high-risk adults within 7 days of developing flu-like symptoms from COVID-19. They analyzed 1,497 newly symptomatic COVID-19 patients at 11 clinical sites in Brazil.
Patients entered the trial between January and August 2021 and were assigned to receive 100 mg fluvoxamine or placebo pills twice a day for 10 days. Investigators monitored participants through 28 days post treatment, noting whether complications developed requiring hospitalization or more than 6 hours of emergency care.
In the placebo group, 119 of 756 patients (15.7%) worsened to this extent. In comparison, 79 of 741 (10.7%) fluvoxamine-treated patients met these primary criteria. This represented a 32% reduction in hospitalizations and emergency visits.
Additional analysis requested
As Lancet Global Health reviewed these findings from the submitted manuscript, journal reviewers requested an additional “pre-protocol analysis” that was not specified in the trial’s original protocol. The request was to examine the subgroup of patients with good adherence (74% of treated group, 82% of placebo group).
Among these three quarters of patients who took at least 80% of their doses, benefits were better.
Fluvoxamine cut serious complications in this group by 66% and reduced mortality by 91%. In the placebo group, 12 people died compared with one who received the study drug.
from complications of the infection.
However, clinicians should note that the drug can cause side effects such as nausea, dizziness, and insomnia, she added. In addition, because it prevents the body from metabolizing caffeine, patients should limit their daily intake to half of a small cup of coffee or one can of soda or one tea while taking the drug.
Previous research has shown that fluvoxamine affects the metabolism of some drugs, such as theophylline, clozapine, olanzapine, and tizanidine.
Despite huge challenges with studying generic drugs as early COVID-19 treatment, the TOGETHER trial shows it is possible to produce quality evidence during a pandemic on a shoestring budget, noted co-principal investigator Edward Mills, PhD, professor in the department of health research methods, evidence, and impact at McMaster University.
To screen more than 12,000 patients and enroll 4,000 to test nine interventions, “our total budget was less than $8 million,” Dr. Mills said. The trial was funded by Fast Grants and the Rainwater Charitable Foundation.
‘A $10 medicine’
Commenting on the findings, David Boulware, MD, MPH, an infectious disease physician-researcher at the University of Minnesota in Minneapolis, noted fluvoxamine is “a $10 medicine that’s available and has a very good safety record.”
By comparison, a 5-day course of Merck’s antiviral molnupiravir, another oral drug that the company says can cut hospitalizations in COVID-19 outpatients, costs $700. However, the data have not been peer reviewed – and molnupiravir is not currently available and has unknown long-term safety implications, Dr. Boulware said.
Pharmaceutical companies typically spend tens of thousands of dollars on a trial evaluating a single drug, he noted.
In addition, the National Institutes of Health’s ACTIV-6 study, a nationwide trial on the effect of fluvoxamine and other repurposed generic drugs on thousands of COVID-19 outpatients, is a $110 million effort, according to Dr. Boulware, who cochairs its steering committee.
ACTIV-6 is currently enrolling outpatients with COVID-19 to test a lower dose of fluvoxamine, at 50 mg twice daily instead of the 100-mg dose used in the TOGETHER trial, as well as ivermectin and inhaled fluticasone. The COVID-OUT trial is also recruiting newly diagnosed COVID-19 patients to test various combinations of fluvoxamine, ivermectin, and the diabetes drug metformin.
Unanswered safety, efficacy questions
In an accompanying editorial in The Lancet Global Health, Otavio Berwanger, MD, cardiologist and clinical trialist, Academic Research Organization, Hospital Israelita Albert Einstein, São Paulo, Brazil, commends the investigators for rapidly generating evidence during the COVID-19 pandemic.
However, despite the important findings, “some questions related to efficacy and safety of fluvoxamine for patients with COVID-19 remain open,” Dr. Berwanger wrote.
The effects of the drug on reducing both mortality and hospitalizations also “still need addressing,” he noted.
“In addition, it remains to be established whether fluvoxamine has an additive effect to other therapies such as monoclonal antibodies and budesonide, and what is the optimal fluvoxamine therapeutic scheme,” wrote Dr. Berwanger.
In an interview, he noted that 74% of the Brazil population have currently received at least one dose of a COVID-19 vaccine and 52% have received two doses. In addition, deaths have gone down from 4,000 per day during the March-April second wave to about 400 per day. “That is still unfortunate and far from ideal,” he said. In total, they have had about 600,000 deaths because of COVID-19.
Asked whether public health authorities are now recommending fluvoxamine as an early treatment for COVID-19 based on the TOGETHER trial data, Dr. Berwanger answered, “Not yet.
“I believe medical and scientific societies will need to critically appraise the manuscript in order to inform their decisions and recommendations. This interesting trial adds another important piece of information in this regard,” he said.
Dr. Reiersen and Dr. Lenze are inventors on a patent application related to methods for treating COVID-19, which was filed by Washington University. Dr. Mills reports no relevant financial relationships, as does Dr. Boulware – except that the TOGETHER trial funders are also funding the University of Minnesota COVID-OUT trial. Dr. Berwanger reports having received research grants outside of the submitted work that were paid to his institution by AstraZeneca, Bayer, Amgen, Servier, Novartis, Pfizer, and Boehringer Ingelheim.
A version of this article first appeared on Medscape.com.
Clinicians underprescribe behavior therapy for preschool ADHD
The majority of families of preschool children with a diagnosis of attention-deficit/hyperactivity disorder were not offered behavior therapy as a first-line treatment, according to data from nearly 200 children.
The American Academy of Pediatrics’ current clinical practice guidelines recommend parent training in behavior management (PTBM) as a first-line treatment for children aged 4-5 years diagnosed with attention-deficit/hyperactivity disorder (ADHD) or symptoms of ADHD such as hyperactivity or impulsivity, but data on how well primary care providers follow this recommendation in practice are lacking, wrote Yair Bannett, MD, of Stanford (Calif.) University, and colleagues.
To investigate the rates of PTBM recommendations, the researchers reviewed electronic health records for 22,714 children aged 48-71 months who had at least two visits to any 1 of 10 primary care practices in a California pediatric health network between Oct. 1, 2015, and Dec. 31, 2019. Children with an autism diagnosis were excluded; ADHD-related visits were identified via ADHD diagnosis codes or symptom-level diagnosis codes.
In the study, published in JAMA Pediatrics, 192 children (1%) had either an ADHD diagnosis or ADHD symptoms; of these, 21 (11%) received referrals for PTBM during ADHD-related primary care visits. Records showed an additional 55 patients (29%) had a mention of counseling on PTBM by a primary care provider, including handouts.
PCPs prescribed ADHD medications for 32 children; 9 of these had documented PTBM recommendations, and in 4 cases, the PCPs recommended PTBM before prescribing a first medication.
A majority (73%) of the children were male, 64% were privately insured, 56% had subspecialists involved in their care, and 17% were prescribed ADHD medications (88% of which were stimulants).
In a multivariate analysis, children with public insurance were significantly less likely to receive a PTBM recommendation than were those with private insurance (adjusted relative risk 0.87).
The most common recommendation overall was routine/habit modifications (for 79 children), such as reducing sugar or adding supplements to the diet; improving sleep hygiene; and limiting screen time.
The low rates of PTBM among publicly insured patients in particular highlight the need to identify factors behind disparities in recommended treatments, the researchers noted.
The study findings were limited by several factors including the reliance on primary care provider documentation during the study period and the inclusion only of medical record reviews with diagnostic codes for ADHD, the researchers noted. Further studies beyond a single health care system are needed to assess generalizability, they added.
However, the results present an opportunity for primary care providers to improve adherence to clinical practice guidelines and establish behavioral treatment at an early age to mitigate long-term morbidity, they concluded.
Low rates highlight barriers and opportunities
“We were surprised to find very low rates of documented recommendations for behavioral treatment mentioned by PCPs,” Dr. Bannett said in an interview. The researchers were surprised that recommendations for changes in daily routines and habits, such as reduced sugar intake, regular exercise, better sleep, and reduced screen time, were the most common recommendations for families of children presenting with symptoms of ADHD. “Though these are good recommendations that can support the general health of any young child, there is no evidence to support their benefit in alleviating symptoms of ADHD,” he said.
Dr. Bannett acknowledged the challenge for pediatricians to stay current on where and how families can access this type of behavioral treatment, but the evidence supports behavior therapy over medication in preschool children, he said.
“I think that it is important for primary care clinicians to know that there are options for parent training in behavioral management for both privately and publicly insured patients,” said Dr. Bannett. “In California, for example, parent training programs are offered through county mental health services. In some counties, there are other organizations that offer parent training for underserved populations and those with public insurance,” he said.
Dr. Bannett noted that online treatments, including behavioral treatments, may be possible for some families.
He cited Triple P, an evidence-based curriculum for parent training in behavior management, which offers an online course for parents at triplep-parenting.com, and an online parent training course offered through the CHADD website (chadd.org/parent-to-parent/).
Dr. Bannett noted that the researchers are planning a follow-up study to investigate the reasons behind the low referral rates for PTBM. “A known barrier is the limited availability of therapists who can provide this type of therapy,” Dr. Bannett said. “Research is needed on the effectiveness of online versions of parent training, which can overcome some of the access barriers many families experience,” he added.
“Additionally, since behavioral treatment requires a significant effort on the part of the parents and caregivers, who often are not able to complete the therapy, there is a need for research on ways to enhance parent and family engagement and participation in these important evidence-based treatments,” as well as a need to research ways to increase adherence to evidence-based practices, said Dr. Bannett. “We are currently planning intervention studies that will enhance primary care clinicians’ knowledge and clinical practice; for example, decision support tools in the electronic health record, and up-to-date information about available resources and behavioral therapists in their community that they can share with families,” he said.
Barriers make it difficult to adhere to guidelines
The study authors missed a significant element of the AAP guidelines by failing to acknowledge the extensive accompanying section on barriers to adoption, which details why most pediatricians in clinical practice do not prescribe PTBM, Herschel Lessin, MD, of Children’s Medical Group, Poughkeepsie, N.Y., said in an interview.
“Academically, it is a wonderful article,” said Dr. Lessin, who was a member of the authoring committee of the AAP guidelines and a major contributor to the section on barriers. The AAP guidelines recommend PTBM because it is evidence based, but the barrier section is essential to understanding that this evidence-based recommendation is nearly impossible to follow in real-world clinical practice, he emphasized.
The American Academy of Pediatrics’ “Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents,” published in October of 2019 in Pediatrics, included a full subsection on barriers as to why the guidelines might not be followed in many cases in a real-world setting, and the study authors failed to acknowledge this section and its implications, said Dr. Lessin. Notably, the barriers section was originally published in Pediatrics under a Supplemental Data tab that might easily be overlooked by someone reviewing the main practice guideline recommendations, he said.
In most areas of the country, PTBM is simply unavailable, Dr. Lessin said.
There is a dearth of mental health providers in the United States in general, and “a monstrous shortage of mental health practitioners for young children,” he said. Children in underserved areas barely have access to a medical home, let alone mental health subspecialists, he added.
Even in areas where specialized behavior therapy may be available, it can be prohibitively expensive for all but the wealthiest patients, Dr. Lessin noted. Insurance does not cover this type of behavior therapy, and most mental health professionals don’t accept Medicaid, nor commercial insurance, he said.
“I don’t even bother with those referrals, because they are not available,” said Dr. Lessin. The take-home message is that most community-based pediatricians are not following the guidelines because the barriers are so enormous, he said.
The study was supported by a research grant from the Society of Developmental and Behavioral Pediatrics and salary support through the Instructor Support Program at the department of pediatrics, Lucile Packard Children’s Hospital Stanford, to Dr. Bannett. The researchers had no other financial conflicts to disclose. Dr. Lessin had no financial conflicts to disclose, but serves on the editorial advisory board of Pediatric News.
The majority of families of preschool children with a diagnosis of attention-deficit/hyperactivity disorder were not offered behavior therapy as a first-line treatment, according to data from nearly 200 children.
The American Academy of Pediatrics’ current clinical practice guidelines recommend parent training in behavior management (PTBM) as a first-line treatment for children aged 4-5 years diagnosed with attention-deficit/hyperactivity disorder (ADHD) or symptoms of ADHD such as hyperactivity or impulsivity, but data on how well primary care providers follow this recommendation in practice are lacking, wrote Yair Bannett, MD, of Stanford (Calif.) University, and colleagues.
To investigate the rates of PTBM recommendations, the researchers reviewed electronic health records for 22,714 children aged 48-71 months who had at least two visits to any 1 of 10 primary care practices in a California pediatric health network between Oct. 1, 2015, and Dec. 31, 2019. Children with an autism diagnosis were excluded; ADHD-related visits were identified via ADHD diagnosis codes or symptom-level diagnosis codes.
In the study, published in JAMA Pediatrics, 192 children (1%) had either an ADHD diagnosis or ADHD symptoms; of these, 21 (11%) received referrals for PTBM during ADHD-related primary care visits. Records showed an additional 55 patients (29%) had a mention of counseling on PTBM by a primary care provider, including handouts.
PCPs prescribed ADHD medications for 32 children; 9 of these had documented PTBM recommendations, and in 4 cases, the PCPs recommended PTBM before prescribing a first medication.
A majority (73%) of the children were male, 64% were privately insured, 56% had subspecialists involved in their care, and 17% were prescribed ADHD medications (88% of which were stimulants).
In a multivariate analysis, children with public insurance were significantly less likely to receive a PTBM recommendation than were those with private insurance (adjusted relative risk 0.87).
The most common recommendation overall was routine/habit modifications (for 79 children), such as reducing sugar or adding supplements to the diet; improving sleep hygiene; and limiting screen time.
The low rates of PTBM among publicly insured patients in particular highlight the need to identify factors behind disparities in recommended treatments, the researchers noted.
The study findings were limited by several factors including the reliance on primary care provider documentation during the study period and the inclusion only of medical record reviews with diagnostic codes for ADHD, the researchers noted. Further studies beyond a single health care system are needed to assess generalizability, they added.
However, the results present an opportunity for primary care providers to improve adherence to clinical practice guidelines and establish behavioral treatment at an early age to mitigate long-term morbidity, they concluded.
Low rates highlight barriers and opportunities
“We were surprised to find very low rates of documented recommendations for behavioral treatment mentioned by PCPs,” Dr. Bannett said in an interview. The researchers were surprised that recommendations for changes in daily routines and habits, such as reduced sugar intake, regular exercise, better sleep, and reduced screen time, were the most common recommendations for families of children presenting with symptoms of ADHD. “Though these are good recommendations that can support the general health of any young child, there is no evidence to support their benefit in alleviating symptoms of ADHD,” he said.
Dr. Bannett acknowledged the challenge for pediatricians to stay current on where and how families can access this type of behavioral treatment, but the evidence supports behavior therapy over medication in preschool children, he said.
“I think that it is important for primary care clinicians to know that there are options for parent training in behavioral management for both privately and publicly insured patients,” said Dr. Bannett. “In California, for example, parent training programs are offered through county mental health services. In some counties, there are other organizations that offer parent training for underserved populations and those with public insurance,” he said.
Dr. Bannett noted that online treatments, including behavioral treatments, may be possible for some families.
He cited Triple P, an evidence-based curriculum for parent training in behavior management, which offers an online course for parents at triplep-parenting.com, and an online parent training course offered through the CHADD website (chadd.org/parent-to-parent/).
Dr. Bannett noted that the researchers are planning a follow-up study to investigate the reasons behind the low referral rates for PTBM. “A known barrier is the limited availability of therapists who can provide this type of therapy,” Dr. Bannett said. “Research is needed on the effectiveness of online versions of parent training, which can overcome some of the access barriers many families experience,” he added.
“Additionally, since behavioral treatment requires a significant effort on the part of the parents and caregivers, who often are not able to complete the therapy, there is a need for research on ways to enhance parent and family engagement and participation in these important evidence-based treatments,” as well as a need to research ways to increase adherence to evidence-based practices, said Dr. Bannett. “We are currently planning intervention studies that will enhance primary care clinicians’ knowledge and clinical practice; for example, decision support tools in the electronic health record, and up-to-date information about available resources and behavioral therapists in their community that they can share with families,” he said.
Barriers make it difficult to adhere to guidelines
The study authors missed a significant element of the AAP guidelines by failing to acknowledge the extensive accompanying section on barriers to adoption, which details why most pediatricians in clinical practice do not prescribe PTBM, Herschel Lessin, MD, of Children’s Medical Group, Poughkeepsie, N.Y., said in an interview.
“Academically, it is a wonderful article,” said Dr. Lessin, who was a member of the authoring committee of the AAP guidelines and a major contributor to the section on barriers. The AAP guidelines recommend PTBM because it is evidence based, but the barrier section is essential to understanding that this evidence-based recommendation is nearly impossible to follow in real-world clinical practice, he emphasized.
The American Academy of Pediatrics’ “Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents,” published in October of 2019 in Pediatrics, included a full subsection on barriers as to why the guidelines might not be followed in many cases in a real-world setting, and the study authors failed to acknowledge this section and its implications, said Dr. Lessin. Notably, the barriers section was originally published in Pediatrics under a Supplemental Data tab that might easily be overlooked by someone reviewing the main practice guideline recommendations, he said.
In most areas of the country, PTBM is simply unavailable, Dr. Lessin said.
There is a dearth of mental health providers in the United States in general, and “a monstrous shortage of mental health practitioners for young children,” he said. Children in underserved areas barely have access to a medical home, let alone mental health subspecialists, he added.
Even in areas where specialized behavior therapy may be available, it can be prohibitively expensive for all but the wealthiest patients, Dr. Lessin noted. Insurance does not cover this type of behavior therapy, and most mental health professionals don’t accept Medicaid, nor commercial insurance, he said.
“I don’t even bother with those referrals, because they are not available,” said Dr. Lessin. The take-home message is that most community-based pediatricians are not following the guidelines because the barriers are so enormous, he said.
The study was supported by a research grant from the Society of Developmental and Behavioral Pediatrics and salary support through the Instructor Support Program at the department of pediatrics, Lucile Packard Children’s Hospital Stanford, to Dr. Bannett. The researchers had no other financial conflicts to disclose. Dr. Lessin had no financial conflicts to disclose, but serves on the editorial advisory board of Pediatric News.
The majority of families of preschool children with a diagnosis of attention-deficit/hyperactivity disorder were not offered behavior therapy as a first-line treatment, according to data from nearly 200 children.
The American Academy of Pediatrics’ current clinical practice guidelines recommend parent training in behavior management (PTBM) as a first-line treatment for children aged 4-5 years diagnosed with attention-deficit/hyperactivity disorder (ADHD) or symptoms of ADHD such as hyperactivity or impulsivity, but data on how well primary care providers follow this recommendation in practice are lacking, wrote Yair Bannett, MD, of Stanford (Calif.) University, and colleagues.
To investigate the rates of PTBM recommendations, the researchers reviewed electronic health records for 22,714 children aged 48-71 months who had at least two visits to any 1 of 10 primary care practices in a California pediatric health network between Oct. 1, 2015, and Dec. 31, 2019. Children with an autism diagnosis were excluded; ADHD-related visits were identified via ADHD diagnosis codes or symptom-level diagnosis codes.
In the study, published in JAMA Pediatrics, 192 children (1%) had either an ADHD diagnosis or ADHD symptoms; of these, 21 (11%) received referrals for PTBM during ADHD-related primary care visits. Records showed an additional 55 patients (29%) had a mention of counseling on PTBM by a primary care provider, including handouts.
PCPs prescribed ADHD medications for 32 children; 9 of these had documented PTBM recommendations, and in 4 cases, the PCPs recommended PTBM before prescribing a first medication.
A majority (73%) of the children were male, 64% were privately insured, 56% had subspecialists involved in their care, and 17% were prescribed ADHD medications (88% of which were stimulants).
In a multivariate analysis, children with public insurance were significantly less likely to receive a PTBM recommendation than were those with private insurance (adjusted relative risk 0.87).
The most common recommendation overall was routine/habit modifications (for 79 children), such as reducing sugar or adding supplements to the diet; improving sleep hygiene; and limiting screen time.
The low rates of PTBM among publicly insured patients in particular highlight the need to identify factors behind disparities in recommended treatments, the researchers noted.
The study findings were limited by several factors including the reliance on primary care provider documentation during the study period and the inclusion only of medical record reviews with diagnostic codes for ADHD, the researchers noted. Further studies beyond a single health care system are needed to assess generalizability, they added.
However, the results present an opportunity for primary care providers to improve adherence to clinical practice guidelines and establish behavioral treatment at an early age to mitigate long-term morbidity, they concluded.
Low rates highlight barriers and opportunities
“We were surprised to find very low rates of documented recommendations for behavioral treatment mentioned by PCPs,” Dr. Bannett said in an interview. The researchers were surprised that recommendations for changes in daily routines and habits, such as reduced sugar intake, regular exercise, better sleep, and reduced screen time, were the most common recommendations for families of children presenting with symptoms of ADHD. “Though these are good recommendations that can support the general health of any young child, there is no evidence to support their benefit in alleviating symptoms of ADHD,” he said.
Dr. Bannett acknowledged the challenge for pediatricians to stay current on where and how families can access this type of behavioral treatment, but the evidence supports behavior therapy over medication in preschool children, he said.
“I think that it is important for primary care clinicians to know that there are options for parent training in behavioral management for both privately and publicly insured patients,” said Dr. Bannett. “In California, for example, parent training programs are offered through county mental health services. In some counties, there are other organizations that offer parent training for underserved populations and those with public insurance,” he said.
Dr. Bannett noted that online treatments, including behavioral treatments, may be possible for some families.
He cited Triple P, an evidence-based curriculum for parent training in behavior management, which offers an online course for parents at triplep-parenting.com, and an online parent training course offered through the CHADD website (chadd.org/parent-to-parent/).
Dr. Bannett noted that the researchers are planning a follow-up study to investigate the reasons behind the low referral rates for PTBM. “A known barrier is the limited availability of therapists who can provide this type of therapy,” Dr. Bannett said. “Research is needed on the effectiveness of online versions of parent training, which can overcome some of the access barriers many families experience,” he added.
“Additionally, since behavioral treatment requires a significant effort on the part of the parents and caregivers, who often are not able to complete the therapy, there is a need for research on ways to enhance parent and family engagement and participation in these important evidence-based treatments,” as well as a need to research ways to increase adherence to evidence-based practices, said Dr. Bannett. “We are currently planning intervention studies that will enhance primary care clinicians’ knowledge and clinical practice; for example, decision support tools in the electronic health record, and up-to-date information about available resources and behavioral therapists in their community that they can share with families,” he said.
Barriers make it difficult to adhere to guidelines
The study authors missed a significant element of the AAP guidelines by failing to acknowledge the extensive accompanying section on barriers to adoption, which details why most pediatricians in clinical practice do not prescribe PTBM, Herschel Lessin, MD, of Children’s Medical Group, Poughkeepsie, N.Y., said in an interview.
“Academically, it is a wonderful article,” said Dr. Lessin, who was a member of the authoring committee of the AAP guidelines and a major contributor to the section on barriers. The AAP guidelines recommend PTBM because it is evidence based, but the barrier section is essential to understanding that this evidence-based recommendation is nearly impossible to follow in real-world clinical practice, he emphasized.
The American Academy of Pediatrics’ “Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents,” published in October of 2019 in Pediatrics, included a full subsection on barriers as to why the guidelines might not be followed in many cases in a real-world setting, and the study authors failed to acknowledge this section and its implications, said Dr. Lessin. Notably, the barriers section was originally published in Pediatrics under a Supplemental Data tab that might easily be overlooked by someone reviewing the main practice guideline recommendations, he said.
In most areas of the country, PTBM is simply unavailable, Dr. Lessin said.
There is a dearth of mental health providers in the United States in general, and “a monstrous shortage of mental health practitioners for young children,” he said. Children in underserved areas barely have access to a medical home, let alone mental health subspecialists, he added.
Even in areas where specialized behavior therapy may be available, it can be prohibitively expensive for all but the wealthiest patients, Dr. Lessin noted. Insurance does not cover this type of behavior therapy, and most mental health professionals don’t accept Medicaid, nor commercial insurance, he said.
“I don’t even bother with those referrals, because they are not available,” said Dr. Lessin. The take-home message is that most community-based pediatricians are not following the guidelines because the barriers are so enormous, he said.
The study was supported by a research grant from the Society of Developmental and Behavioral Pediatrics and salary support through the Instructor Support Program at the department of pediatrics, Lucile Packard Children’s Hospital Stanford, to Dr. Bannett. The researchers had no other financial conflicts to disclose. Dr. Lessin had no financial conflicts to disclose, but serves on the editorial advisory board of Pediatric News.
FROM JAMA PEDIATRICS
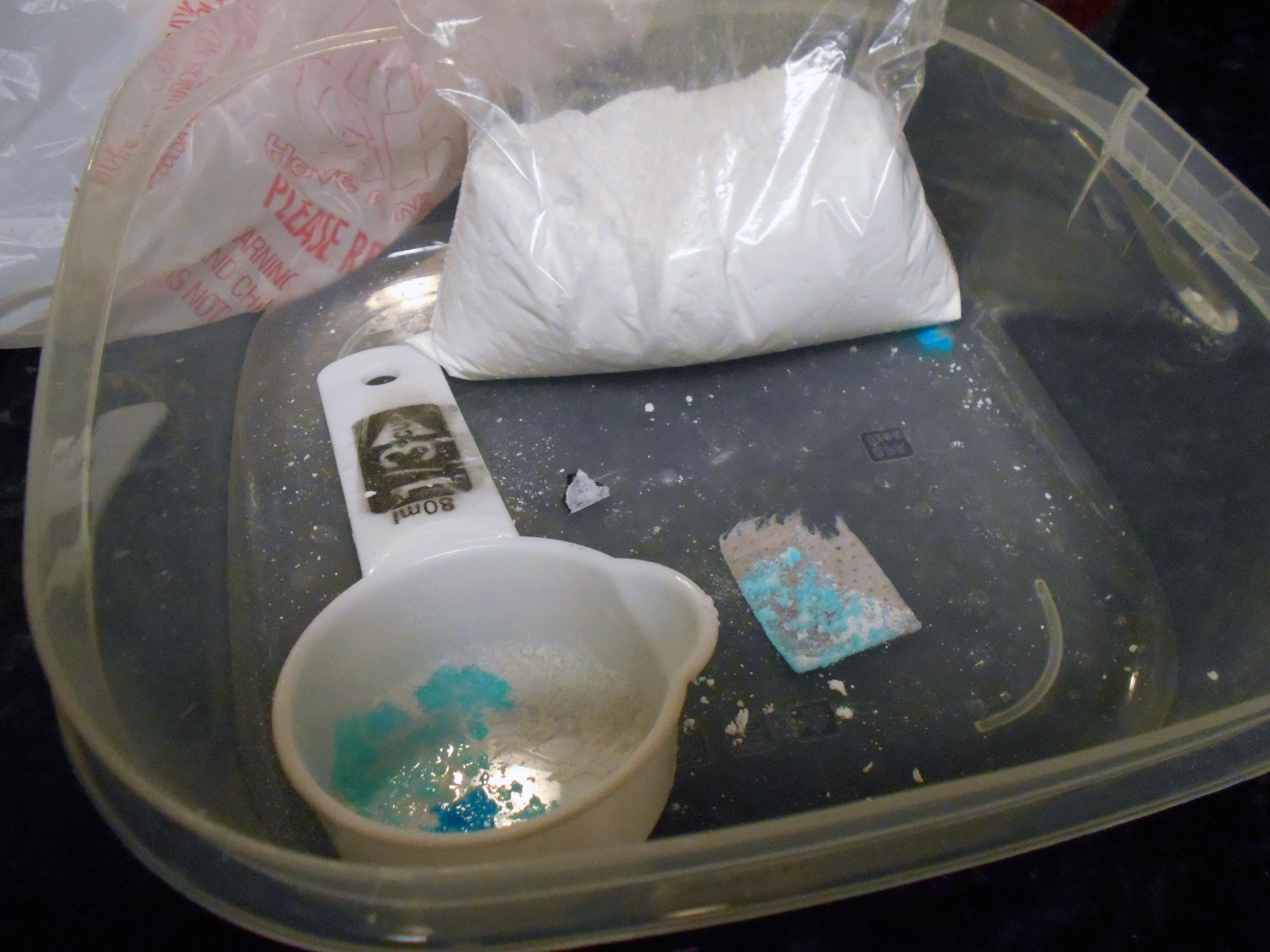
Warn patients about illicit drugs doctored with fentanyl
Fentanyl is now threatening overdoses in patients exposed to essentially any of the full array of recreational drugs – not just opioids – that are being sold illicitly, according to an overview of the problem presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Fentanyl can now be found in cocaine and methamphetamine. At this point, there is really no way to predict what is in a [street] drug,” Edwin A. Salsitz, MD, said at the meeting, sponsored by Medscape Live. He is associate clinical professor of medicine who works in the division of chemical dependency at Mount Sinai Beth Israel Medical Center in New York.
As proof of the frequency with which fentanyl is now being used as an additive, most patients with a drug use disorder, regardless of their drug of choice, are testing positive for fentanyl at Dr. Salsitz’s center. Many of those with positive fentanyl tests are unaware that their drugs had been doctored with this agent.
Relative to drugs sold as an opioid, such as heroin or oxycodone, the fentanyl dose in nonopioid drugs is typically more modest, but Dr. Salsitz pointed out that those expecting cocaine or methamphetamine often “have no heroin tolerance, so they are more vulnerable” to the adverse effects of fentanyl, including an overdose.
Although opioid tolerance might improve the chances for surviving a fentanyl overdose, the toxicology of fentanyl is not the same as other opioids. Death from heroin is typically a result of respiratory depression, but the onset is relatively slow, providing a greater opportunity to administer a reversal agent, such as naloxone.
Fentanyl not only produces respiratory depression but skeletal muscle rigidity. The rapid onset of “wooden chest syndrome” can occur within minutes, making the opportunity for intervention much smaller, Dr. Salsitz said.
To illustrate the phenomenon, Dr. Salsitz recounted a case.
After an argument with his mother, a 26-year-old male with a long history of intravenous drug use went to his bedroom. His mother, responding to the sound of a loud thud, rushed to the bedroom to find her son on the floor with a needle still in his arm. Resuscitation efforts by the mother and by the emergency responders, who arrived quickly, failed.
“The speed of his death made it clear that it was fentanyl related, and the postmortem toxicology confirmed that the exposure involved both heroin and fentanyl,” Dr. Salsitz said.
After the first wave of deaths in the opioid epidemic, which was attributed to inappropriate use of prescription opioids, the second wave was driven by heroin. In that wave, patients who became addicted to prescription opioids but were having more difficulty gaining access to them, turned to far cheaper and readily available street heroin. The third wave, driven by fentanyl, began several years ago when sellers of heroin began adding this synthetic opioid, which is relatively cheap, to intensify the high.
It is not expected to end quickly. The fentanyl added to heroin was never a prescription version. Rather, Dr. Salsitz said, it is synthesized in laboratories in China, Mexico, and the United States. It is relatively easy to produce and compact, which makes it easy to transport.
Exacerbating the risks that fentanyl poses when added to street drugs, even more potent versions, such as carfentanil, are also being added to cocaine, methamphetamines, and other nonopioid illicit drugs. When compared on a per-milligram basis, fentanyl is about 100 times more potent than heroin, but carfentanil is about 100 times more potent than fentanyl, according to Dr. Salsitz.
When the third wave of deaths in the opioid epidemic began around 2013, prescriptions of fentanyl, like many other opioid-type therapies were declining. The “perfect storm” that initiated the opioid epidemic was a product of intense focus on pain control and a misperception that prescription opioids posed a low risk of abuse potential, Dr. Salsitz said. By the time fentanyl was driving opioid deaths, the risks of opioids were widely appreciated and their use for prescription analgesia was declining.
Citing several cases, Dr. Salsitz noted that only 20 years after clinicians were being successfully sued for not offering enough analgesia, they were now going to jail for prescribing these drugs too liberally.
According to Dr. Salsitz, While psychiatrists might not have a role in this issue, Dr. Salsitz did see a role for these specialists in protecting patients from the adverse consequences of using illicit drugs doctored with fentanyl.
Noting that individuals with psychiatric disorders are more likely than the general population to self-medicate with drugs purchased illegally, Dr. Salsitz encouraged psychiatrists “to get involved” in asking about drug use and counseling patients on the risks of fentanyl substitution or additives.
“The message is that no one knows what are in these drugs, anymore,” he said.
In addition to making patients aware that many street drugs are now contaminated with fentanyl, Dr. Salsitz provided some safety tips. He suggested instructing patients to take a low dose of any newly acquired drug to gauge its effect, to avoid taking drugs alone, and to avoid mixing drugs. He also recommended using rapid fentanyl test strips in order to detect fentanyl contamination.
Even for the many psychiatrists who do not feel comfortable managing addiction, Dr. Salsitz recommended a proactive approach to address the current threat.
Test strips as an intervention
The seriousness of fentanyl contamination of illicit drugs, including cocaine and methamphetamine, was corroborated by two investigators at the School of Public Health and the Albert Einstein Medical School of Brown University, Providence, R.I. Brandon D.L. Marshall, PhD, associate professor of epidemiology in the School of Public Health, called fentanyl-contaminated cannabis “extremely rare,” but he said that it is being found in counterfeit prescription pills as well as in crystal methamphetamine and in both crack and powder cocaine.
He also advocated the use of fentanyl test strips.
“Test strips are an efficient, inexpensive, and effective way to determine whether fentanyl or related analogs are present in illicit drugs,” he said, noting that he is involved in a trial designed to determine whether fentanyl test strips can reduce the risk of fatal and nonfatal overdoses.
In a pilot study conducted in Baltimore, 69% of the 103 participants engaged in harm reduction behavior after using a fentanyl test strip and receiving a positive result (Addict Behav. 2020;110:106529). It is notable that 86% of the participants had a least one positive result when using the strips. More than half were surprised by the result.
One of the findings from this study was “that the lasting benefit of fentanyl test strip distribution is the opportunity to engage in discussions around safety and relationship building with historically underserved communities,” said the lead author, Ju Nyeong Park, PhD, assistant professor of medicine and epidemiology at Brown University. She moved to Brown after performing this work at Johns Hopkins University, Baltimore.
Dr. Park noted that “many patients in the community already know that they are using drugs containing fentanyl,” but for those who are concerned and wish to avoid contaminated drugs, fentanyl test strips “are a quick screening tool.” However, while the strips are helpful, she cautioned that they cannot be considered a definitive tool for detecting harm in illicit drugs.
“There may also be other chemicals present in tested drugs that confer risk,” she said.
Medscape Live and this news organization are owned by the same parent company. Dr. Salsitz, Dr. Marshall, and Dr. Park reported no potential conflicts of interest.
Fentanyl is now threatening overdoses in patients exposed to essentially any of the full array of recreational drugs – not just opioids – that are being sold illicitly, according to an overview of the problem presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Fentanyl can now be found in cocaine and methamphetamine. At this point, there is really no way to predict what is in a [street] drug,” Edwin A. Salsitz, MD, said at the meeting, sponsored by Medscape Live. He is associate clinical professor of medicine who works in the division of chemical dependency at Mount Sinai Beth Israel Medical Center in New York.
As proof of the frequency with which fentanyl is now being used as an additive, most patients with a drug use disorder, regardless of their drug of choice, are testing positive for fentanyl at Dr. Salsitz’s center. Many of those with positive fentanyl tests are unaware that their drugs had been doctored with this agent.
Relative to drugs sold as an opioid, such as heroin or oxycodone, the fentanyl dose in nonopioid drugs is typically more modest, but Dr. Salsitz pointed out that those expecting cocaine or methamphetamine often “have no heroin tolerance, so they are more vulnerable” to the adverse effects of fentanyl, including an overdose.
Although opioid tolerance might improve the chances for surviving a fentanyl overdose, the toxicology of fentanyl is not the same as other opioids. Death from heroin is typically a result of respiratory depression, but the onset is relatively slow, providing a greater opportunity to administer a reversal agent, such as naloxone.
Fentanyl not only produces respiratory depression but skeletal muscle rigidity. The rapid onset of “wooden chest syndrome” can occur within minutes, making the opportunity for intervention much smaller, Dr. Salsitz said.
To illustrate the phenomenon, Dr. Salsitz recounted a case.
After an argument with his mother, a 26-year-old male with a long history of intravenous drug use went to his bedroom. His mother, responding to the sound of a loud thud, rushed to the bedroom to find her son on the floor with a needle still in his arm. Resuscitation efforts by the mother and by the emergency responders, who arrived quickly, failed.
“The speed of his death made it clear that it was fentanyl related, and the postmortem toxicology confirmed that the exposure involved both heroin and fentanyl,” Dr. Salsitz said.
After the first wave of deaths in the opioid epidemic, which was attributed to inappropriate use of prescription opioids, the second wave was driven by heroin. In that wave, patients who became addicted to prescription opioids but were having more difficulty gaining access to them, turned to far cheaper and readily available street heroin. The third wave, driven by fentanyl, began several years ago when sellers of heroin began adding this synthetic opioid, which is relatively cheap, to intensify the high.
It is not expected to end quickly. The fentanyl added to heroin was never a prescription version. Rather, Dr. Salsitz said, it is synthesized in laboratories in China, Mexico, and the United States. It is relatively easy to produce and compact, which makes it easy to transport.
Exacerbating the risks that fentanyl poses when added to street drugs, even more potent versions, such as carfentanil, are also being added to cocaine, methamphetamines, and other nonopioid illicit drugs. When compared on a per-milligram basis, fentanyl is about 100 times more potent than heroin, but carfentanil is about 100 times more potent than fentanyl, according to Dr. Salsitz.
When the third wave of deaths in the opioid epidemic began around 2013, prescriptions of fentanyl, like many other opioid-type therapies were declining. The “perfect storm” that initiated the opioid epidemic was a product of intense focus on pain control and a misperception that prescription opioids posed a low risk of abuse potential, Dr. Salsitz said. By the time fentanyl was driving opioid deaths, the risks of opioids were widely appreciated and their use for prescription analgesia was declining.
Citing several cases, Dr. Salsitz noted that only 20 years after clinicians were being successfully sued for not offering enough analgesia, they were now going to jail for prescribing these drugs too liberally.
According to Dr. Salsitz, While psychiatrists might not have a role in this issue, Dr. Salsitz did see a role for these specialists in protecting patients from the adverse consequences of using illicit drugs doctored with fentanyl.
Noting that individuals with psychiatric disorders are more likely than the general population to self-medicate with drugs purchased illegally, Dr. Salsitz encouraged psychiatrists “to get involved” in asking about drug use and counseling patients on the risks of fentanyl substitution or additives.
“The message is that no one knows what are in these drugs, anymore,” he said.
In addition to making patients aware that many street drugs are now contaminated with fentanyl, Dr. Salsitz provided some safety tips. He suggested instructing patients to take a low dose of any newly acquired drug to gauge its effect, to avoid taking drugs alone, and to avoid mixing drugs. He also recommended using rapid fentanyl test strips in order to detect fentanyl contamination.
Even for the many psychiatrists who do not feel comfortable managing addiction, Dr. Salsitz recommended a proactive approach to address the current threat.
Test strips as an intervention
The seriousness of fentanyl contamination of illicit drugs, including cocaine and methamphetamine, was corroborated by two investigators at the School of Public Health and the Albert Einstein Medical School of Brown University, Providence, R.I. Brandon D.L. Marshall, PhD, associate professor of epidemiology in the School of Public Health, called fentanyl-contaminated cannabis “extremely rare,” but he said that it is being found in counterfeit prescription pills as well as in crystal methamphetamine and in both crack and powder cocaine.
He also advocated the use of fentanyl test strips.
“Test strips are an efficient, inexpensive, and effective way to determine whether fentanyl or related analogs are present in illicit drugs,” he said, noting that he is involved in a trial designed to determine whether fentanyl test strips can reduce the risk of fatal and nonfatal overdoses.
In a pilot study conducted in Baltimore, 69% of the 103 participants engaged in harm reduction behavior after using a fentanyl test strip and receiving a positive result (Addict Behav. 2020;110:106529). It is notable that 86% of the participants had a least one positive result when using the strips. More than half were surprised by the result.
One of the findings from this study was “that the lasting benefit of fentanyl test strip distribution is the opportunity to engage in discussions around safety and relationship building with historically underserved communities,” said the lead author, Ju Nyeong Park, PhD, assistant professor of medicine and epidemiology at Brown University. She moved to Brown after performing this work at Johns Hopkins University, Baltimore.
Dr. Park noted that “many patients in the community already know that they are using drugs containing fentanyl,” but for those who are concerned and wish to avoid contaminated drugs, fentanyl test strips “are a quick screening tool.” However, while the strips are helpful, she cautioned that they cannot be considered a definitive tool for detecting harm in illicit drugs.
“There may also be other chemicals present in tested drugs that confer risk,” she said.
Medscape Live and this news organization are owned by the same parent company. Dr. Salsitz, Dr. Marshall, and Dr. Park reported no potential conflicts of interest.
Fentanyl is now threatening overdoses in patients exposed to essentially any of the full array of recreational drugs – not just opioids – that are being sold illicitly, according to an overview of the problem presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Fentanyl can now be found in cocaine and methamphetamine. At this point, there is really no way to predict what is in a [street] drug,” Edwin A. Salsitz, MD, said at the meeting, sponsored by Medscape Live. He is associate clinical professor of medicine who works in the division of chemical dependency at Mount Sinai Beth Israel Medical Center in New York.
As proof of the frequency with which fentanyl is now being used as an additive, most patients with a drug use disorder, regardless of their drug of choice, are testing positive for fentanyl at Dr. Salsitz’s center. Many of those with positive fentanyl tests are unaware that their drugs had been doctored with this agent.
Relative to drugs sold as an opioid, such as heroin or oxycodone, the fentanyl dose in nonopioid drugs is typically more modest, but Dr. Salsitz pointed out that those expecting cocaine or methamphetamine often “have no heroin tolerance, so they are more vulnerable” to the adverse effects of fentanyl, including an overdose.
Although opioid tolerance might improve the chances for surviving a fentanyl overdose, the toxicology of fentanyl is not the same as other opioids. Death from heroin is typically a result of respiratory depression, but the onset is relatively slow, providing a greater opportunity to administer a reversal agent, such as naloxone.
Fentanyl not only produces respiratory depression but skeletal muscle rigidity. The rapid onset of “wooden chest syndrome” can occur within minutes, making the opportunity for intervention much smaller, Dr. Salsitz said.
To illustrate the phenomenon, Dr. Salsitz recounted a case.
After an argument with his mother, a 26-year-old male with a long history of intravenous drug use went to his bedroom. His mother, responding to the sound of a loud thud, rushed to the bedroom to find her son on the floor with a needle still in his arm. Resuscitation efforts by the mother and by the emergency responders, who arrived quickly, failed.
“The speed of his death made it clear that it was fentanyl related, and the postmortem toxicology confirmed that the exposure involved both heroin and fentanyl,” Dr. Salsitz said.
After the first wave of deaths in the opioid epidemic, which was attributed to inappropriate use of prescription opioids, the second wave was driven by heroin. In that wave, patients who became addicted to prescription opioids but were having more difficulty gaining access to them, turned to far cheaper and readily available street heroin. The third wave, driven by fentanyl, began several years ago when sellers of heroin began adding this synthetic opioid, which is relatively cheap, to intensify the high.
It is not expected to end quickly. The fentanyl added to heroin was never a prescription version. Rather, Dr. Salsitz said, it is synthesized in laboratories in China, Mexico, and the United States. It is relatively easy to produce and compact, which makes it easy to transport.
Exacerbating the risks that fentanyl poses when added to street drugs, even more potent versions, such as carfentanil, are also being added to cocaine, methamphetamines, and other nonopioid illicit drugs. When compared on a per-milligram basis, fentanyl is about 100 times more potent than heroin, but carfentanil is about 100 times more potent than fentanyl, according to Dr. Salsitz.
When the third wave of deaths in the opioid epidemic began around 2013, prescriptions of fentanyl, like many other opioid-type therapies were declining. The “perfect storm” that initiated the opioid epidemic was a product of intense focus on pain control and a misperception that prescription opioids posed a low risk of abuse potential, Dr. Salsitz said. By the time fentanyl was driving opioid deaths, the risks of opioids were widely appreciated and their use for prescription analgesia was declining.
Citing several cases, Dr. Salsitz noted that only 20 years after clinicians were being successfully sued for not offering enough analgesia, they were now going to jail for prescribing these drugs too liberally.
According to Dr. Salsitz, While psychiatrists might not have a role in this issue, Dr. Salsitz did see a role for these specialists in protecting patients from the adverse consequences of using illicit drugs doctored with fentanyl.
Noting that individuals with psychiatric disorders are more likely than the general population to self-medicate with drugs purchased illegally, Dr. Salsitz encouraged psychiatrists “to get involved” in asking about drug use and counseling patients on the risks of fentanyl substitution or additives.
“The message is that no one knows what are in these drugs, anymore,” he said.
In addition to making patients aware that many street drugs are now contaminated with fentanyl, Dr. Salsitz provided some safety tips. He suggested instructing patients to take a low dose of any newly acquired drug to gauge its effect, to avoid taking drugs alone, and to avoid mixing drugs. He also recommended using rapid fentanyl test strips in order to detect fentanyl contamination.
Even for the many psychiatrists who do not feel comfortable managing addiction, Dr. Salsitz recommended a proactive approach to address the current threat.
Test strips as an intervention
The seriousness of fentanyl contamination of illicit drugs, including cocaine and methamphetamine, was corroborated by two investigators at the School of Public Health and the Albert Einstein Medical School of Brown University, Providence, R.I. Brandon D.L. Marshall, PhD, associate professor of epidemiology in the School of Public Health, called fentanyl-contaminated cannabis “extremely rare,” but he said that it is being found in counterfeit prescription pills as well as in crystal methamphetamine and in both crack and powder cocaine.
He also advocated the use of fentanyl test strips.
“Test strips are an efficient, inexpensive, and effective way to determine whether fentanyl or related analogs are present in illicit drugs,” he said, noting that he is involved in a trial designed to determine whether fentanyl test strips can reduce the risk of fatal and nonfatal overdoses.
In a pilot study conducted in Baltimore, 69% of the 103 participants engaged in harm reduction behavior after using a fentanyl test strip and receiving a positive result (Addict Behav. 2020;110:106529). It is notable that 86% of the participants had a least one positive result when using the strips. More than half were surprised by the result.
One of the findings from this study was “that the lasting benefit of fentanyl test strip distribution is the opportunity to engage in discussions around safety and relationship building with historically underserved communities,” said the lead author, Ju Nyeong Park, PhD, assistant professor of medicine and epidemiology at Brown University. She moved to Brown after performing this work at Johns Hopkins University, Baltimore.
Dr. Park noted that “many patients in the community already know that they are using drugs containing fentanyl,” but for those who are concerned and wish to avoid contaminated drugs, fentanyl test strips “are a quick screening tool.” However, while the strips are helpful, she cautioned that they cannot be considered a definitive tool for detecting harm in illicit drugs.
“There may also be other chemicals present in tested drugs that confer risk,” she said.
Medscape Live and this news organization are owned by the same parent company. Dr. Salsitz, Dr. Marshall, and Dr. Park reported no potential conflicts of interest.
FROM PSYCHOPHARMACOLOGY UPDATE
Chatbots can improve mental health in vulnerable populations
In this modern age of health care where telemedicine rules, conversational agents (CAs) that use text messaging systems are becoming a major mode of communication.
Many people are familiar with voice-enabled agents, such as Apple’s Siri, Google Now, and Microsoft’s Cortana. However, CAs come in different forms of complexity, ranging from a short message service–based texting platform to an embodied conversational agent (ECA).
ECAs allow participants to interact with a physical or graphical figure that simulates a person in appearance, behavior, and dialect. These are essentially virtual humans, or avatars, who talk with participants. By taking greater advantage of these automated agents, some have projected there may be $11 billion in combined cost savings across a variety of business sectors by 2023.1 The health care field is one sector in which CAs can play an important role. Because of their accessibility, CAs have the potential to improve mental health by combating health care inequities and stigma, encouraging disclosure from participants, and serving as companions during the COVID-19 pandemic.
CAs provide accessible health care for rural, low socioeconomic status (SES), and minority communities in a variety of advantageous ways. For example, one study found that long-term use of a text-based agent that combines motivational interviewing and cognitive-behavioral therapy (CBT) can support smoking cessation in adolescents of low SES.2
CAs can help vulnerable participants advocate for themselves and proactively maintain their mental health through access to health care resources. In specific cases, these agents equalize health care treatment for different populations. Even though some participants live in secluded areas or are blocked by barriers, these text-based agents can still provide self-help intervention for them at any time on an individual basis, regardless of their location or socioeconomic status. Furthermore, they serve as highly cost-effective mental health promotion tools for large populations, some of which might not otherwise be reached by mental health care.
In combating mental illnesses such as depression and anxiety, studies have found that CAs are great treatment tools. For example, participants in an experimental group who received a self-help program based on CBT from a text-based CA named Woebot experienced significantly reduced depression symptoms when compared to the control group of participants, who received only information from a self-help electronic book.3 As a result, CAs might prove successful in treating younger populations who find online tools more feasible and accessible. Often, this population self-identifies depressive and anxiety symptoms without consulting a health care professional. Thus, this tool would prove useful to those who are bothered by the stigma of seeing a mental health professional.
Virtual human–based CAs also encourage participants to disclose more information in a nonjudgmental manner, especially among people with diseases with stigma. CAs use neutral languages, which may be helpful when dealing with stigmatized issues such as HIV, family planning, and abortion care because this heightens confidentiality and privacy. When participants believe that the agent does not “judge” or evaluate their capabilities, this elicits more sensitive information from them. For example, one study found that military service members who believed that they were interacting with a computer rather than a human operator reported lower fear of self-disclosure, displayed more sadness, and were rated by observers as more willing to disclose posttraumatic stress disorder symptoms.4 Additional findings show that participants prefer CAs when topics are highly sensitive and more likely to evoke negative self-admissions.
In what we hope will soon be a post–COVID-19 landscape of medicine, CAs are fast being used on the front lines of health care technology. Empathetic CAs can combat adverse effects of social exclusion during these pressing times. Etsuko Ishii, a researcher affiliated with the Hong Kong University of Science and Technology, and associates demonstrated that a virtual CA was as effective as a COVID-19 companion because it uses natural language processing (NLP) and nonverbal facial expressions to give users the feeling that they are being treated with empathy.5 While minimizing the number of in-person interactions that could potentially spread COVID-19, these agents promote virtual companionship that mirrors natural conversations and provide emotional support with psychological safety as participants express their pent-up thoughts. Not only do these agents help recover mood quickly, but they also have the power to overcome geographic barriers, be constantly available, and alleviate the high demand for mental health care. As a result, CAs have the potential to facilitate better communication and sustain social interactions within the isolated environment the pandemic has created.
CAs can predict, detect, and determine treatment solutions for mental health conditions based on behavioral insights. These agents’ natural language processing also allows them to be powerful therapeutic agents that can serve different communities, particularly for populations with limited access to medical resources. As the use of CAs becomes more integrated into telemedicine, their utility will continue to grow as their proven versatility in many situations expands the boundaries of health care technology.
Ms. Wong, a medical student at New York Institute of Technology College of Osteopathic Medicine in Old Westbury, conducts research related to mental health care services. She disclosed writing a telemental health software platform called Orchid. Dr. Vo, a board-certified psychiatrist, is the medical director of telehealth for the department of child and adolescent psychiatry and behavioral sciences at Children’s Hospital of Philadelphia. She is a faculty member of the University of Pennsylvania, also in Philadelphia. Dr. Vo conducts digital health research focused on using automation and artificial intelligence for suicide risk screening and connecting patients to mental health care services. She disclosed serving as cofounder of Orchid.
References
1. Chatbots: Vendor opportunities & market forecasts 2020-2024. Juniper Research, 2020.
2. Simon P et al. On using chatbots to promote smoking cessation among adolescents of low socioeconomic status, Artificial Intelligence and Work: Association for the Advancement of Artificial Intelligence (AAAI) 2019 Fall Symposium, 2019.
3. Fitzpatrick KK et al. JMIR Mental Health. 2017;4(2):e19.
4. Lucas GM et al. Front Robot AI. 2017 Oct 12. doi: 10.3389/frobt.2017.00051.
5. Ishii E et al. ERICA: An empathetic android companion for COVID-19 quarantine. arXiv preprint arXiv:2106.02325.
In this modern age of health care where telemedicine rules, conversational agents (CAs) that use text messaging systems are becoming a major mode of communication.
Many people are familiar with voice-enabled agents, such as Apple’s Siri, Google Now, and Microsoft’s Cortana. However, CAs come in different forms of complexity, ranging from a short message service–based texting platform to an embodied conversational agent (ECA).
ECAs allow participants to interact with a physical or graphical figure that simulates a person in appearance, behavior, and dialect. These are essentially virtual humans, or avatars, who talk with participants. By taking greater advantage of these automated agents, some have projected there may be $11 billion in combined cost savings across a variety of business sectors by 2023.1 The health care field is one sector in which CAs can play an important role. Because of their accessibility, CAs have the potential to improve mental health by combating health care inequities and stigma, encouraging disclosure from participants, and serving as companions during the COVID-19 pandemic.
CAs provide accessible health care for rural, low socioeconomic status (SES), and minority communities in a variety of advantageous ways. For example, one study found that long-term use of a text-based agent that combines motivational interviewing and cognitive-behavioral therapy (CBT) can support smoking cessation in adolescents of low SES.2
CAs can help vulnerable participants advocate for themselves and proactively maintain their mental health through access to health care resources. In specific cases, these agents equalize health care treatment for different populations. Even though some participants live in secluded areas or are blocked by barriers, these text-based agents can still provide self-help intervention for them at any time on an individual basis, regardless of their location or socioeconomic status. Furthermore, they serve as highly cost-effective mental health promotion tools for large populations, some of which might not otherwise be reached by mental health care.
In combating mental illnesses such as depression and anxiety, studies have found that CAs are great treatment tools. For example, participants in an experimental group who received a self-help program based on CBT from a text-based CA named Woebot experienced significantly reduced depression symptoms when compared to the control group of participants, who received only information from a self-help electronic book.3 As a result, CAs might prove successful in treating younger populations who find online tools more feasible and accessible. Often, this population self-identifies depressive and anxiety symptoms without consulting a health care professional. Thus, this tool would prove useful to those who are bothered by the stigma of seeing a mental health professional.
Virtual human–based CAs also encourage participants to disclose more information in a nonjudgmental manner, especially among people with diseases with stigma. CAs use neutral languages, which may be helpful when dealing with stigmatized issues such as HIV, family planning, and abortion care because this heightens confidentiality and privacy. When participants believe that the agent does not “judge” or evaluate their capabilities, this elicits more sensitive information from them. For example, one study found that military service members who believed that they were interacting with a computer rather than a human operator reported lower fear of self-disclosure, displayed more sadness, and were rated by observers as more willing to disclose posttraumatic stress disorder symptoms.4 Additional findings show that participants prefer CAs when topics are highly sensitive and more likely to evoke negative self-admissions.
In what we hope will soon be a post–COVID-19 landscape of medicine, CAs are fast being used on the front lines of health care technology. Empathetic CAs can combat adverse effects of social exclusion during these pressing times. Etsuko Ishii, a researcher affiliated with the Hong Kong University of Science and Technology, and associates demonstrated that a virtual CA was as effective as a COVID-19 companion because it uses natural language processing (NLP) and nonverbal facial expressions to give users the feeling that they are being treated with empathy.5 While minimizing the number of in-person interactions that could potentially spread COVID-19, these agents promote virtual companionship that mirrors natural conversations and provide emotional support with psychological safety as participants express their pent-up thoughts. Not only do these agents help recover mood quickly, but they also have the power to overcome geographic barriers, be constantly available, and alleviate the high demand for mental health care. As a result, CAs have the potential to facilitate better communication and sustain social interactions within the isolated environment the pandemic has created.
CAs can predict, detect, and determine treatment solutions for mental health conditions based on behavioral insights. These agents’ natural language processing also allows them to be powerful therapeutic agents that can serve different communities, particularly for populations with limited access to medical resources. As the use of CAs becomes more integrated into telemedicine, their utility will continue to grow as their proven versatility in many situations expands the boundaries of health care technology.
Ms. Wong, a medical student at New York Institute of Technology College of Osteopathic Medicine in Old Westbury, conducts research related to mental health care services. She disclosed writing a telemental health software platform called Orchid. Dr. Vo, a board-certified psychiatrist, is the medical director of telehealth for the department of child and adolescent psychiatry and behavioral sciences at Children’s Hospital of Philadelphia. She is a faculty member of the University of Pennsylvania, also in Philadelphia. Dr. Vo conducts digital health research focused on using automation and artificial intelligence for suicide risk screening and connecting patients to mental health care services. She disclosed serving as cofounder of Orchid.
References
1. Chatbots: Vendor opportunities & market forecasts 2020-2024. Juniper Research, 2020.
2. Simon P et al. On using chatbots to promote smoking cessation among adolescents of low socioeconomic status, Artificial Intelligence and Work: Association for the Advancement of Artificial Intelligence (AAAI) 2019 Fall Symposium, 2019.
3. Fitzpatrick KK et al. JMIR Mental Health. 2017;4(2):e19.
4. Lucas GM et al. Front Robot AI. 2017 Oct 12. doi: 10.3389/frobt.2017.00051.
5. Ishii E et al. ERICA: An empathetic android companion for COVID-19 quarantine. arXiv preprint arXiv:2106.02325.
In this modern age of health care where telemedicine rules, conversational agents (CAs) that use text messaging systems are becoming a major mode of communication.
Many people are familiar with voice-enabled agents, such as Apple’s Siri, Google Now, and Microsoft’s Cortana. However, CAs come in different forms of complexity, ranging from a short message service–based texting platform to an embodied conversational agent (ECA).
ECAs allow participants to interact with a physical or graphical figure that simulates a person in appearance, behavior, and dialect. These are essentially virtual humans, or avatars, who talk with participants. By taking greater advantage of these automated agents, some have projected there may be $11 billion in combined cost savings across a variety of business sectors by 2023.1 The health care field is one sector in which CAs can play an important role. Because of their accessibility, CAs have the potential to improve mental health by combating health care inequities and stigma, encouraging disclosure from participants, and serving as companions during the COVID-19 pandemic.
CAs provide accessible health care for rural, low socioeconomic status (SES), and minority communities in a variety of advantageous ways. For example, one study found that long-term use of a text-based agent that combines motivational interviewing and cognitive-behavioral therapy (CBT) can support smoking cessation in adolescents of low SES.2
CAs can help vulnerable participants advocate for themselves and proactively maintain their mental health through access to health care resources. In specific cases, these agents equalize health care treatment for different populations. Even though some participants live in secluded areas or are blocked by barriers, these text-based agents can still provide self-help intervention for them at any time on an individual basis, regardless of their location or socioeconomic status. Furthermore, they serve as highly cost-effective mental health promotion tools for large populations, some of which might not otherwise be reached by mental health care.
In combating mental illnesses such as depression and anxiety, studies have found that CAs are great treatment tools. For example, participants in an experimental group who received a self-help program based on CBT from a text-based CA named Woebot experienced significantly reduced depression symptoms when compared to the control group of participants, who received only information from a self-help electronic book.3 As a result, CAs might prove successful in treating younger populations who find online tools more feasible and accessible. Often, this population self-identifies depressive and anxiety symptoms without consulting a health care professional. Thus, this tool would prove useful to those who are bothered by the stigma of seeing a mental health professional.
Virtual human–based CAs also encourage participants to disclose more information in a nonjudgmental manner, especially among people with diseases with stigma. CAs use neutral languages, which may be helpful when dealing with stigmatized issues such as HIV, family planning, and abortion care because this heightens confidentiality and privacy. When participants believe that the agent does not “judge” or evaluate their capabilities, this elicits more sensitive information from them. For example, one study found that military service members who believed that they were interacting with a computer rather than a human operator reported lower fear of self-disclosure, displayed more sadness, and were rated by observers as more willing to disclose posttraumatic stress disorder symptoms.4 Additional findings show that participants prefer CAs when topics are highly sensitive and more likely to evoke negative self-admissions.
In what we hope will soon be a post–COVID-19 landscape of medicine, CAs are fast being used on the front lines of health care technology. Empathetic CAs can combat adverse effects of social exclusion during these pressing times. Etsuko Ishii, a researcher affiliated with the Hong Kong University of Science and Technology, and associates demonstrated that a virtual CA was as effective as a COVID-19 companion because it uses natural language processing (NLP) and nonverbal facial expressions to give users the feeling that they are being treated with empathy.5 While minimizing the number of in-person interactions that could potentially spread COVID-19, these agents promote virtual companionship that mirrors natural conversations and provide emotional support with psychological safety as participants express their pent-up thoughts. Not only do these agents help recover mood quickly, but they also have the power to overcome geographic barriers, be constantly available, and alleviate the high demand for mental health care. As a result, CAs have the potential to facilitate better communication and sustain social interactions within the isolated environment the pandemic has created.
CAs can predict, detect, and determine treatment solutions for mental health conditions based on behavioral insights. These agents’ natural language processing also allows them to be powerful therapeutic agents that can serve different communities, particularly for populations with limited access to medical resources. As the use of CAs becomes more integrated into telemedicine, their utility will continue to grow as their proven versatility in many situations expands the boundaries of health care technology.
Ms. Wong, a medical student at New York Institute of Technology College of Osteopathic Medicine in Old Westbury, conducts research related to mental health care services. She disclosed writing a telemental health software platform called Orchid. Dr. Vo, a board-certified psychiatrist, is the medical director of telehealth for the department of child and adolescent psychiatry and behavioral sciences at Children’s Hospital of Philadelphia. She is a faculty member of the University of Pennsylvania, also in Philadelphia. Dr. Vo conducts digital health research focused on using automation and artificial intelligence for suicide risk screening and connecting patients to mental health care services. She disclosed serving as cofounder of Orchid.
References
1. Chatbots: Vendor opportunities & market forecasts 2020-2024. Juniper Research, 2020.
2. Simon P et al. On using chatbots to promote smoking cessation among adolescents of low socioeconomic status, Artificial Intelligence and Work: Association for the Advancement of Artificial Intelligence (AAAI) 2019 Fall Symposium, 2019.
3. Fitzpatrick KK et al. JMIR Mental Health. 2017;4(2):e19.
4. Lucas GM et al. Front Robot AI. 2017 Oct 12. doi: 10.3389/frobt.2017.00051.
5. Ishii E et al. ERICA: An empathetic android companion for COVID-19 quarantine. arXiv preprint arXiv:2106.02325.
Spiders, dogs, and PTSD: A virtual treatment for phobias and fear
At Wayne State University’s Stress, Trauma, and Anxiety Research Clinic (STARC) in Michigan, researchers are developing novel interventions for treating some very ancient phobias hardwired into the human brain. By using augmented reality as means of conducting exposure therapy, STARC researchers – including Shantanu Madaboosi, Rakesh Ramaswamy, and Lana Grasser – and STARC director Arash Javanbakht, MD, have produced compelling evidence that they can free patients of their often debilitating fears of spiders, dogs, and snakes. Yet their work doesn’t stop there, and research into treating anxiety and posttraumatic stress disorder among first responders and others with high-stress occupations is ongoing.

This news organization spoke with Dr. Javanbakht, a psychiatrist, about the technological advances that have made this work possible; the future of remote-based psychiatry; and his tarantula colleague, Tony.
Augmenting exposure therapy
How did you begin using artificial intelligence as a way of delivering exposure therapy?
Exposure therapy is a very effective treatment for phobias, obsessive-compulsive disorder, and PTSD. But the problem we had is that, if someone comes to me and says they’re afraid of dogs, snakes, or spiders, I don’t have those in my office. Or, if its social phobia, I can’t create those scenarios. So, despite being such an effective treatment, it’s not utilized as much as it should be.
Several years ago, I saw a TED talk by the CEO of an augmented reality company who happened to be a neuroscientist. I thought the concept was amazing, because it offered a way to overcome those limitations.
Mixed augmented reality allows us to bring all those feared objects to the clinic. I can bring my Labrador to the office for someone who’s afraid of dogs, and they can get the exposure to that one dog. But we know good exposure therapy needs to be generalizable, with as many different breeds of dogs as possible, and is context dependent. If the patient sees a dog in their neighborhood, their fear response may come back. Doing it in a real-life context, and offering as many contexts as possible, makes it more effective.
Augmented reality allows all of these options because you can have as many different types of virtual objects as you want, and the difference between augmented reality and virtual reality is that augmented reality happens in a real-life context. You wear the goggles and you can walk around the environment and track the object, so the context is more realistic.
When did you begin researching augmented reality as a clinical tool?
I became a faculty member here in 2015, right out of my residency training, and I think it was around 2016 or 2017 that we began this work.
I’m very much involved in exposure therapy, utilize it myself, train others, and research how it works and changes the brain. I knew the ins and outs and what would make a better exposure therapy, based on my knowledge of neuroscience.
We spend time thinking about how we can apply these neuroscientific principles in software that can also be easily used by a not very technologically savvy therapist. Because that has been a big barrier when it comes to technology and human use in medicine.
Initially, we had a company create the software for us, but we’ve since brought all the programming inside.
The cool thing about these augmented reality devices is that they have excellent surface mapping. As soon as the person wears the goggles, it automatically maps the surfaces and provides a 3D view of the patient’s environment on the therapist’s computer. Say you’re treating a patient with a fear of spiders. Through drop-down menus, the therapist can choose what type of spider, its color and size, where it should be placed, and the motion. I can choose to move the spider from 6 feet away on the floor to the walls to the ceiling.
Virtual phobias, real fear
A big question for a lot of people was if the spiders are virtual, will they be scary, because it has to be realistic enough to create a fear response for the therapy to work. We use a couple of wires that you can put on a person’s finger and hook them up to a tablet or a cell phone. This provides an online measure of a person’s autonomic sympathetic response.
Like a lie detector test?
Exactly. We put that on their fingers and exposed them to a real-life tarantula and to our virtual tarantulas, and the fear response was no different. That means these do create an objective fear reaction in the body.
We also had people who said, “I know this is not real. I won’t be scared.” And when we started the therapy, it was with a tiny spider 5 meters away from them, and they’d lift their legs off the floor.
With the treatment, we’d come to one room and start with a very little spider, far from them. Then gradually we move them up to bigger, more diverse types of spiders, which are moving around. The patient comes near and tries to touch them.
Then at some point, I’d put a spiderweb on the door, put a few spiders on that, open the door, and have the patient walk through it. They kept walking through this spiderweb.
When they were desensitized to these spiders in this context – and as I said, context is important – we’d go to another room. This was darker, more like a basement, and we’d continue the same thing. That would actually take much less time because they already had desensitized a lot.
In our field, sense of control is very important, especially for when a patient goes home. So at the end, I’d leave the room and talk to the patient via a baby monitor. The patient was surrounded by 20 tarantulas, without the prompt moving around the environment.
Now that they’re desensitized to my virtual spiders, the question is, how would that apply to a real spider? So, we had a real live tarantula, whose name was Tony Stark, because we’re the STARC lab. We’d put Tony at the end of a long hallway before the treatment and see how close the patients could get to him.
It was only one treatment session; nobody’s was longer than 1 hour, and the average treatment time was 38 minutes.
That’s pretty effective.
It’s pretty good, compared with other studies. And I believe this is because of all the components I mentioned: being able to use your real environment; combining it with the real tarantula; the variety of the types of the feared objects; and, of course, giving the patient a sense of autonomy at the end.
Then we had to see how prolonged the effects are. We had them come in 1 week and 1 month after the treatment. I’d remind them of the principles of good exposure therapy and ask them to keep practicing at home between the sessions, looking at pictures and videos. But we never tested who did or did not do it.
After 1 week and 1 month, the effects were either the same or better. A larger number of people at 1 month were able to touch the tarantula than right after treatment.
Treating PTSD in first responders
Did you start with spiders and dogs because those are common fears?
We started with spiders because that worked with the initial goal of creating a prototype. Spiders’ behavior is simple enough for the programming, which takes a lot of time. Another reason for choosing spiders was that we had a lot of other studies of real and virtual reality exposure therapy to compare against.
I think another reason for our success is that, when you do real exposure therapy, you have just one scared tarantula in the corner of their tank, and they don’t listen to you. But my spiders listen to me and do exactly what I tell them.
After our initial success, we obtained more funds to expand it to other phobias. The cool thing is that we don’t need separate software for different phobias. You can choose dogs or snakes, add it to the person’s environment, and decide their behaviors.
We just started a clinical trial using dogs, and another group in Turkey is running a clinical trial with dogs. Eastern Michigan University is working with spiders. And a clinic at the University of Nebraska Medical Center is going to start using them in real-world clinics, not for research.
We have another project whose goal is helping reduce the impact of trauma and also treating PTSD in first responders, who are exposed to a lot of horrible things. Rates of PTSD are around 20%-30% among cops, firefighters, and EMS personnel.
They commonly find it very painful being in crowds because the fight-or-flight instinct in the brain is constantly screening for any sign of threat in their environment. We’re working on them walking into an empty room wearing the goggles, and then their therapist can scale the stimulus up and down.
There’ll be two people in front of you talking to each other, and then another group comes in, and people get louder. People can look at you and talk to you. There’s kids running, Fourth of July fireworks, and other things that might bother someone who’s been involved in gun- or explosion-related traumas. You gradually scale up when the person is next to their therapist.
Another thing we’re doing is related to cardiopulmonary resuscitation. If a young person dies in a CPR situation, that is really painful and traumatic. So, for exposure therapy to that, we’re creating a difficult CPR scenario when that person may die. The responder wears the goggles and basically watches a group of people doing CPR while standing next to a therapist who can help them navigate it and then scale it off.
Another goal is combining this with telemedicine, where the person can do it in their real-life environment. Imagine a person with military trauma. You can put them back in the barracks, connected with their psychiatrists via telemedicine. Then we would put humans in military fatigues near them and have them interact with them to feel comfortable with that situation.
What else is next for you and your group?
The next biggest challenge that we’re tackling is PTSD, because of course creating human-encounter scenarios is much more complicated than spiders and dogs. We’re in the midst of developing this so we can basically bring it to people’s homes.
We’ve been working with some military personnel to see if we can basically give a device to a veteran with PTSD, so they can go home and practice on their own.
There’s another possibility for training. Let’s take the example of a police force, which can have a lot of difficulties and mistakes because of lack of exposure and training. They can wear these goggles, get fully geared up, and be placed in encounters with people of different backgrounds, of different severity, with people who could be severely mentally ill or present different challenges for the officers.
Those situations can teach them a lot. I’m the creator of this thing, but even I’m often surprised by how realistic this technology can be. I find myself interacting with avatars the same way I would if they were real humans. I actually had one of my colleagues, when we started launching the programming with the dogs, immediately jump back. It’s just like the animal brain reacts to them.
Last question: Do you actually interact with Tony, the tarantula?
Oh, Tony is my friend. Unfortunately, he’s not with our lab at this moment. He’s on a sabbatical at Eastern Michigan University for their clinical trials. But yes, I’ve held him. He’s very friendly.
A version of this article first appeared on Medscape.com.
At Wayne State University’s Stress, Trauma, and Anxiety Research Clinic (STARC) in Michigan, researchers are developing novel interventions for treating some very ancient phobias hardwired into the human brain. By using augmented reality as means of conducting exposure therapy, STARC researchers – including Shantanu Madaboosi, Rakesh Ramaswamy, and Lana Grasser – and STARC director Arash Javanbakht, MD, have produced compelling evidence that they can free patients of their often debilitating fears of spiders, dogs, and snakes. Yet their work doesn’t stop there, and research into treating anxiety and posttraumatic stress disorder among first responders and others with high-stress occupations is ongoing.

This news organization spoke with Dr. Javanbakht, a psychiatrist, about the technological advances that have made this work possible; the future of remote-based psychiatry; and his tarantula colleague, Tony.
Augmenting exposure therapy
How did you begin using artificial intelligence as a way of delivering exposure therapy?
Exposure therapy is a very effective treatment for phobias, obsessive-compulsive disorder, and PTSD. But the problem we had is that, if someone comes to me and says they’re afraid of dogs, snakes, or spiders, I don’t have those in my office. Or, if its social phobia, I can’t create those scenarios. So, despite being such an effective treatment, it’s not utilized as much as it should be.
Several years ago, I saw a TED talk by the CEO of an augmented reality company who happened to be a neuroscientist. I thought the concept was amazing, because it offered a way to overcome those limitations.
Mixed augmented reality allows us to bring all those feared objects to the clinic. I can bring my Labrador to the office for someone who’s afraid of dogs, and they can get the exposure to that one dog. But we know good exposure therapy needs to be generalizable, with as many different breeds of dogs as possible, and is context dependent. If the patient sees a dog in their neighborhood, their fear response may come back. Doing it in a real-life context, and offering as many contexts as possible, makes it more effective.
Augmented reality allows all of these options because you can have as many different types of virtual objects as you want, and the difference between augmented reality and virtual reality is that augmented reality happens in a real-life context. You wear the goggles and you can walk around the environment and track the object, so the context is more realistic.
When did you begin researching augmented reality as a clinical tool?
I became a faculty member here in 2015, right out of my residency training, and I think it was around 2016 or 2017 that we began this work.
I’m very much involved in exposure therapy, utilize it myself, train others, and research how it works and changes the brain. I knew the ins and outs and what would make a better exposure therapy, based on my knowledge of neuroscience.
We spend time thinking about how we can apply these neuroscientific principles in software that can also be easily used by a not very technologically savvy therapist. Because that has been a big barrier when it comes to technology and human use in medicine.
Initially, we had a company create the software for us, but we’ve since brought all the programming inside.
The cool thing about these augmented reality devices is that they have excellent surface mapping. As soon as the person wears the goggles, it automatically maps the surfaces and provides a 3D view of the patient’s environment on the therapist’s computer. Say you’re treating a patient with a fear of spiders. Through drop-down menus, the therapist can choose what type of spider, its color and size, where it should be placed, and the motion. I can choose to move the spider from 6 feet away on the floor to the walls to the ceiling.
Virtual phobias, real fear
A big question for a lot of people was if the spiders are virtual, will they be scary, because it has to be realistic enough to create a fear response for the therapy to work. We use a couple of wires that you can put on a person’s finger and hook them up to a tablet or a cell phone. This provides an online measure of a person’s autonomic sympathetic response.
Like a lie detector test?
Exactly. We put that on their fingers and exposed them to a real-life tarantula and to our virtual tarantulas, and the fear response was no different. That means these do create an objective fear reaction in the body.
We also had people who said, “I know this is not real. I won’t be scared.” And when we started the therapy, it was with a tiny spider 5 meters away from them, and they’d lift their legs off the floor.
With the treatment, we’d come to one room and start with a very little spider, far from them. Then gradually we move them up to bigger, more diverse types of spiders, which are moving around. The patient comes near and tries to touch them.
Then at some point, I’d put a spiderweb on the door, put a few spiders on that, open the door, and have the patient walk through it. They kept walking through this spiderweb.
When they were desensitized to these spiders in this context – and as I said, context is important – we’d go to another room. This was darker, more like a basement, and we’d continue the same thing. That would actually take much less time because they already had desensitized a lot.
In our field, sense of control is very important, especially for when a patient goes home. So at the end, I’d leave the room and talk to the patient via a baby monitor. The patient was surrounded by 20 tarantulas, without the prompt moving around the environment.
Now that they’re desensitized to my virtual spiders, the question is, how would that apply to a real spider? So, we had a real live tarantula, whose name was Tony Stark, because we’re the STARC lab. We’d put Tony at the end of a long hallway before the treatment and see how close the patients could get to him.
It was only one treatment session; nobody’s was longer than 1 hour, and the average treatment time was 38 minutes.
That’s pretty effective.
It’s pretty good, compared with other studies. And I believe this is because of all the components I mentioned: being able to use your real environment; combining it with the real tarantula; the variety of the types of the feared objects; and, of course, giving the patient a sense of autonomy at the end.
Then we had to see how prolonged the effects are. We had them come in 1 week and 1 month after the treatment. I’d remind them of the principles of good exposure therapy and ask them to keep practicing at home between the sessions, looking at pictures and videos. But we never tested who did or did not do it.
After 1 week and 1 month, the effects were either the same or better. A larger number of people at 1 month were able to touch the tarantula than right after treatment.
Treating PTSD in first responders
Did you start with spiders and dogs because those are common fears?
We started with spiders because that worked with the initial goal of creating a prototype. Spiders’ behavior is simple enough for the programming, which takes a lot of time. Another reason for choosing spiders was that we had a lot of other studies of real and virtual reality exposure therapy to compare against.
I think another reason for our success is that, when you do real exposure therapy, you have just one scared tarantula in the corner of their tank, and they don’t listen to you. But my spiders listen to me and do exactly what I tell them.
After our initial success, we obtained more funds to expand it to other phobias. The cool thing is that we don’t need separate software for different phobias. You can choose dogs or snakes, add it to the person’s environment, and decide their behaviors.
We just started a clinical trial using dogs, and another group in Turkey is running a clinical trial with dogs. Eastern Michigan University is working with spiders. And a clinic at the University of Nebraska Medical Center is going to start using them in real-world clinics, not for research.
We have another project whose goal is helping reduce the impact of trauma and also treating PTSD in first responders, who are exposed to a lot of horrible things. Rates of PTSD are around 20%-30% among cops, firefighters, and EMS personnel.
They commonly find it very painful being in crowds because the fight-or-flight instinct in the brain is constantly screening for any sign of threat in their environment. We’re working on them walking into an empty room wearing the goggles, and then their therapist can scale the stimulus up and down.
There’ll be two people in front of you talking to each other, and then another group comes in, and people get louder. People can look at you and talk to you. There’s kids running, Fourth of July fireworks, and other things that might bother someone who’s been involved in gun- or explosion-related traumas. You gradually scale up when the person is next to their therapist.
Another thing we’re doing is related to cardiopulmonary resuscitation. If a young person dies in a CPR situation, that is really painful and traumatic. So, for exposure therapy to that, we’re creating a difficult CPR scenario when that person may die. The responder wears the goggles and basically watches a group of people doing CPR while standing next to a therapist who can help them navigate it and then scale it off.
Another goal is combining this with telemedicine, where the person can do it in their real-life environment. Imagine a person with military trauma. You can put them back in the barracks, connected with their psychiatrists via telemedicine. Then we would put humans in military fatigues near them and have them interact with them to feel comfortable with that situation.
What else is next for you and your group?
The next biggest challenge that we’re tackling is PTSD, because of course creating human-encounter scenarios is much more complicated than spiders and dogs. We’re in the midst of developing this so we can basically bring it to people’s homes.
We’ve been working with some military personnel to see if we can basically give a device to a veteran with PTSD, so they can go home and practice on their own.
There’s another possibility for training. Let’s take the example of a police force, which can have a lot of difficulties and mistakes because of lack of exposure and training. They can wear these goggles, get fully geared up, and be placed in encounters with people of different backgrounds, of different severity, with people who could be severely mentally ill or present different challenges for the officers.
Those situations can teach them a lot. I’m the creator of this thing, but even I’m often surprised by how realistic this technology can be. I find myself interacting with avatars the same way I would if they were real humans. I actually had one of my colleagues, when we started launching the programming with the dogs, immediately jump back. It’s just like the animal brain reacts to them.
Last question: Do you actually interact with Tony, the tarantula?
Oh, Tony is my friend. Unfortunately, he’s not with our lab at this moment. He’s on a sabbatical at Eastern Michigan University for their clinical trials. But yes, I’ve held him. He’s very friendly.
A version of this article first appeared on Medscape.com.
At Wayne State University’s Stress, Trauma, and Anxiety Research Clinic (STARC) in Michigan, researchers are developing novel interventions for treating some very ancient phobias hardwired into the human brain. By using augmented reality as means of conducting exposure therapy, STARC researchers – including Shantanu Madaboosi, Rakesh Ramaswamy, and Lana Grasser – and STARC director Arash Javanbakht, MD, have produced compelling evidence that they can free patients of their often debilitating fears of spiders, dogs, and snakes. Yet their work doesn’t stop there, and research into treating anxiety and posttraumatic stress disorder among first responders and others with high-stress occupations is ongoing.

This news organization spoke with Dr. Javanbakht, a psychiatrist, about the technological advances that have made this work possible; the future of remote-based psychiatry; and his tarantula colleague, Tony.
Augmenting exposure therapy
How did you begin using artificial intelligence as a way of delivering exposure therapy?
Exposure therapy is a very effective treatment for phobias, obsessive-compulsive disorder, and PTSD. But the problem we had is that, if someone comes to me and says they’re afraid of dogs, snakes, or spiders, I don’t have those in my office. Or, if its social phobia, I can’t create those scenarios. So, despite being such an effective treatment, it’s not utilized as much as it should be.
Several years ago, I saw a TED talk by the CEO of an augmented reality company who happened to be a neuroscientist. I thought the concept was amazing, because it offered a way to overcome those limitations.
Mixed augmented reality allows us to bring all those feared objects to the clinic. I can bring my Labrador to the office for someone who’s afraid of dogs, and they can get the exposure to that one dog. But we know good exposure therapy needs to be generalizable, with as many different breeds of dogs as possible, and is context dependent. If the patient sees a dog in their neighborhood, their fear response may come back. Doing it in a real-life context, and offering as many contexts as possible, makes it more effective.
Augmented reality allows all of these options because you can have as many different types of virtual objects as you want, and the difference between augmented reality and virtual reality is that augmented reality happens in a real-life context. You wear the goggles and you can walk around the environment and track the object, so the context is more realistic.
When did you begin researching augmented reality as a clinical tool?
I became a faculty member here in 2015, right out of my residency training, and I think it was around 2016 or 2017 that we began this work.
I’m very much involved in exposure therapy, utilize it myself, train others, and research how it works and changes the brain. I knew the ins and outs and what would make a better exposure therapy, based on my knowledge of neuroscience.
We spend time thinking about how we can apply these neuroscientific principles in software that can also be easily used by a not very technologically savvy therapist. Because that has been a big barrier when it comes to technology and human use in medicine.
Initially, we had a company create the software for us, but we’ve since brought all the programming inside.
The cool thing about these augmented reality devices is that they have excellent surface mapping. As soon as the person wears the goggles, it automatically maps the surfaces and provides a 3D view of the patient’s environment on the therapist’s computer. Say you’re treating a patient with a fear of spiders. Through drop-down menus, the therapist can choose what type of spider, its color and size, where it should be placed, and the motion. I can choose to move the spider from 6 feet away on the floor to the walls to the ceiling.
Virtual phobias, real fear
A big question for a lot of people was if the spiders are virtual, will they be scary, because it has to be realistic enough to create a fear response for the therapy to work. We use a couple of wires that you can put on a person’s finger and hook them up to a tablet or a cell phone. This provides an online measure of a person’s autonomic sympathetic response.
Like a lie detector test?
Exactly. We put that on their fingers and exposed them to a real-life tarantula and to our virtual tarantulas, and the fear response was no different. That means these do create an objective fear reaction in the body.
We also had people who said, “I know this is not real. I won’t be scared.” And when we started the therapy, it was with a tiny spider 5 meters away from them, and they’d lift their legs off the floor.
With the treatment, we’d come to one room and start with a very little spider, far from them. Then gradually we move them up to bigger, more diverse types of spiders, which are moving around. The patient comes near and tries to touch them.
Then at some point, I’d put a spiderweb on the door, put a few spiders on that, open the door, and have the patient walk through it. They kept walking through this spiderweb.
When they were desensitized to these spiders in this context – and as I said, context is important – we’d go to another room. This was darker, more like a basement, and we’d continue the same thing. That would actually take much less time because they already had desensitized a lot.
In our field, sense of control is very important, especially for when a patient goes home. So at the end, I’d leave the room and talk to the patient via a baby monitor. The patient was surrounded by 20 tarantulas, without the prompt moving around the environment.
Now that they’re desensitized to my virtual spiders, the question is, how would that apply to a real spider? So, we had a real live tarantula, whose name was Tony Stark, because we’re the STARC lab. We’d put Tony at the end of a long hallway before the treatment and see how close the patients could get to him.
It was only one treatment session; nobody’s was longer than 1 hour, and the average treatment time was 38 minutes.
That’s pretty effective.
It’s pretty good, compared with other studies. And I believe this is because of all the components I mentioned: being able to use your real environment; combining it with the real tarantula; the variety of the types of the feared objects; and, of course, giving the patient a sense of autonomy at the end.
Then we had to see how prolonged the effects are. We had them come in 1 week and 1 month after the treatment. I’d remind them of the principles of good exposure therapy and ask them to keep practicing at home between the sessions, looking at pictures and videos. But we never tested who did or did not do it.
After 1 week and 1 month, the effects were either the same or better. A larger number of people at 1 month were able to touch the tarantula than right after treatment.
Treating PTSD in first responders
Did you start with spiders and dogs because those are common fears?
We started with spiders because that worked with the initial goal of creating a prototype. Spiders’ behavior is simple enough for the programming, which takes a lot of time. Another reason for choosing spiders was that we had a lot of other studies of real and virtual reality exposure therapy to compare against.
I think another reason for our success is that, when you do real exposure therapy, you have just one scared tarantula in the corner of their tank, and they don’t listen to you. But my spiders listen to me and do exactly what I tell them.
After our initial success, we obtained more funds to expand it to other phobias. The cool thing is that we don’t need separate software for different phobias. You can choose dogs or snakes, add it to the person’s environment, and decide their behaviors.
We just started a clinical trial using dogs, and another group in Turkey is running a clinical trial with dogs. Eastern Michigan University is working with spiders. And a clinic at the University of Nebraska Medical Center is going to start using them in real-world clinics, not for research.
We have another project whose goal is helping reduce the impact of trauma and also treating PTSD in first responders, who are exposed to a lot of horrible things. Rates of PTSD are around 20%-30% among cops, firefighters, and EMS personnel.
They commonly find it very painful being in crowds because the fight-or-flight instinct in the brain is constantly screening for any sign of threat in their environment. We’re working on them walking into an empty room wearing the goggles, and then their therapist can scale the stimulus up and down.
There’ll be two people in front of you talking to each other, and then another group comes in, and people get louder. People can look at you and talk to you. There’s kids running, Fourth of July fireworks, and other things that might bother someone who’s been involved in gun- or explosion-related traumas. You gradually scale up when the person is next to their therapist.
Another thing we’re doing is related to cardiopulmonary resuscitation. If a young person dies in a CPR situation, that is really painful and traumatic. So, for exposure therapy to that, we’re creating a difficult CPR scenario when that person may die. The responder wears the goggles and basically watches a group of people doing CPR while standing next to a therapist who can help them navigate it and then scale it off.
Another goal is combining this with telemedicine, where the person can do it in their real-life environment. Imagine a person with military trauma. You can put them back in the barracks, connected with their psychiatrists via telemedicine. Then we would put humans in military fatigues near them and have them interact with them to feel comfortable with that situation.
What else is next for you and your group?
The next biggest challenge that we’re tackling is PTSD, because of course creating human-encounter scenarios is much more complicated than spiders and dogs. We’re in the midst of developing this so we can basically bring it to people’s homes.
We’ve been working with some military personnel to see if we can basically give a device to a veteran with PTSD, so they can go home and practice on their own.
There’s another possibility for training. Let’s take the example of a police force, which can have a lot of difficulties and mistakes because of lack of exposure and training. They can wear these goggles, get fully geared up, and be placed in encounters with people of different backgrounds, of different severity, with people who could be severely mentally ill or present different challenges for the officers.
Those situations can teach them a lot. I’m the creator of this thing, but even I’m often surprised by how realistic this technology can be. I find myself interacting with avatars the same way I would if they were real humans. I actually had one of my colleagues, when we started launching the programming with the dogs, immediately jump back. It’s just like the animal brain reacts to them.
Last question: Do you actually interact with Tony, the tarantula?
Oh, Tony is my friend. Unfortunately, he’s not with our lab at this moment. He’s on a sabbatical at Eastern Michigan University for their clinical trials. But yes, I’ve held him. He’s very friendly.
A version of this article first appeared on Medscape.com.
The devil in the (masking) details
The Devil’s own face covering?
It’s been over a year and a half since the COVID-19 emergency was declared in the United States, and we’ve been starting to wonder what our good friend SARS-CoV-2 has left to give. The collective cynic/optimist in us figures that the insanity can’t last forever, right?
Maybe not forever, but …
A group of parents is suing the Central Bucks (Pa.) School District over school mask mandates, suggesting that the district has no legal authority to enforce such measures. Most of their arguments, Philadelphia Magazine says, are pretty standard stuff: Masks are causing depression, anxiety, and discomfort in their children; masks are a violation of their constitutional rights; and “masks are being used as a control mechanism over the population.”
There are some unusual claims, though. One of the parents, Shannon Harris, said that “wearing masks interferes with their religious duty to spread the word of God and forces them to participate in a satanic ritual,” according to the Philadelphia Inquirer.
Philadelphia Magazine decided to check on that “satanic ritual” claim by asking an expert, in this case a spokesperson for the Church of Satan. The Reverend Raul Antony said that “simply ‘wearing a mask’ is not a Satanic ritual, and anyone that genuinely thinks otherwise is a blithering idiot,” adding that the group’s rituals were available on its website.
COVID, you never let us down.
You’re the (hurricane) wind beneath my wings
Marriage isn’t easy. From finances to everyday stressors like work and children, maintaining a solid relationship is tough. Then a natural disaster shows up on top of everything else, and marriages actually improve, researchers found.
In a study published by Psychological Science, researchers surveyed 231 newlywed couples about the satisfaction of their marriage before and after Hurricane Harvey in 2017. They found after the hurricane couples had a “significant boost” in the satisfaction of their relationship.
One would think something like this would create what researchers call a “stress spillover,” creating a decrease in relationship satisfaction. Destruction to your home or even displacement after a natural disaster seems pretty stressful. But, “a natural disaster can really put things in perspective. People realize how important their partner is to them when they are jolted out of the day-to-day stress of life,” said Hannah Williamson, PhD, the lead author of the study.
And although everyone saw an increase, the biggest jumps in relationship satisfaction belonged to the people who were most unhappy before the hurricane. Unfortunately, the researchers also found that the effects were only temporary and the dissatisfaction came back within a year.
Dr. Williamson thinks there may be something to these findings that can be beneficial from a therapy standpoint where “couples can shift their perspective in a similar way without having to go through a natural disaster.”
Let’s hope she’s right, because the alternative is to seek out a rampaging hurricane every time your relationship is on the rocks, and that just seems impractical after the second or third year.
Not-so-essential oils
Many people use essential oils as a way to unwind and relax. Stressed? Can’t sleep? There’s probably an essential oil for that. However, it seems like these days a lot of things we love and/or think are good for us have a side that’s not so.
According to the Centers for Disease Control and Prevention, a woman from Georgia died from a rare bacteria called Burkholderia pseudomallei. There have been three previous infections in Kansas, Minnesota, and Texas throughout 2021; two of the four infections were in children. Melioidosis, the disease caused by B. pseudomallei, is usually found in southeast Asia and isn’t obvious or easy to diagnose, especially in places like decidedly untropical Minnesota.
The Georgia case was the real break in this medical mystery, as the infection was traced back to a Walmart product called “Better Homes and Gardens Essential Oil Infused Aromatherapy Room Spray with Gemstones” (a very pithy name). The bacteria were in the lavender and chamomile scent. The CDC is investigating all other product scents, and Walmart has recalled all lots of the product.
If you’ve got that particular essential oil, it’s probably for the best that you stop using it. Don’t worry, we’re sure there’s plenty of other essential oil–infused aromatherapy room sprays with gemstones out there for your scent-based needs.
Welcome to the Ministry of Sleep-Deprived Walks
Walking is simple, right? You put one foot in front of the other, and soon you’re walking out the door. Little kids can do it. Even zombies can walk, and they don’t even have brains.
Research from MIT and the University of São Paulo has shown that walking is a little trickier than we might think. One researcher in particular noticed that student volunteers tended to perform worse toward the end of semesters, as project deadlines and multiple exams crashed over their heads and they were deprived of solid sleep schedules.
In a study published in Scientific Reports, our intrepid walking researchers had a collection of students monitor their sleep patterns for 2 weeks; on average, the students got 6 hours per night, though some were able to compensate on weekends. On the final day of a 14-day period, some students pulled all-nighters while the rest were allowed to sleep as usual. Then all students performed a walking test involving keeping time with a metronome.
To absolutely no one’s surprise, the students who performed all-nighters before being tested walked the worst, but between the other students, the ones who compensated for sleep deprivation on weekends did better than those who got 6 hours every night, despite getting a similar amount of sleep overall. This effect persisted even when the compensating students performed their walking tests late in the week, just before they got their weekend beauty sleep.
The moral of the story? Sleep is good, and you should get more of it. But if you can’t, sleep in on weekends. Science has given you permission. All those suburban dads looking to get their teenagers up at 8 in the morning must be sweating right now.
The Devil’s own face covering?
It’s been over a year and a half since the COVID-19 emergency was declared in the United States, and we’ve been starting to wonder what our good friend SARS-CoV-2 has left to give. The collective cynic/optimist in us figures that the insanity can’t last forever, right?
Maybe not forever, but …
A group of parents is suing the Central Bucks (Pa.) School District over school mask mandates, suggesting that the district has no legal authority to enforce such measures. Most of their arguments, Philadelphia Magazine says, are pretty standard stuff: Masks are causing depression, anxiety, and discomfort in their children; masks are a violation of their constitutional rights; and “masks are being used as a control mechanism over the population.”
There are some unusual claims, though. One of the parents, Shannon Harris, said that “wearing masks interferes with their religious duty to spread the word of God and forces them to participate in a satanic ritual,” according to the Philadelphia Inquirer.
Philadelphia Magazine decided to check on that “satanic ritual” claim by asking an expert, in this case a spokesperson for the Church of Satan. The Reverend Raul Antony said that “simply ‘wearing a mask’ is not a Satanic ritual, and anyone that genuinely thinks otherwise is a blithering idiot,” adding that the group’s rituals were available on its website.
COVID, you never let us down.
You’re the (hurricane) wind beneath my wings
Marriage isn’t easy. From finances to everyday stressors like work and children, maintaining a solid relationship is tough. Then a natural disaster shows up on top of everything else, and marriages actually improve, researchers found.
In a study published by Psychological Science, researchers surveyed 231 newlywed couples about the satisfaction of their marriage before and after Hurricane Harvey in 2017. They found after the hurricane couples had a “significant boost” in the satisfaction of their relationship.
One would think something like this would create what researchers call a “stress spillover,” creating a decrease in relationship satisfaction. Destruction to your home or even displacement after a natural disaster seems pretty stressful. But, “a natural disaster can really put things in perspective. People realize how important their partner is to them when they are jolted out of the day-to-day stress of life,” said Hannah Williamson, PhD, the lead author of the study.
And although everyone saw an increase, the biggest jumps in relationship satisfaction belonged to the people who were most unhappy before the hurricane. Unfortunately, the researchers also found that the effects were only temporary and the dissatisfaction came back within a year.
Dr. Williamson thinks there may be something to these findings that can be beneficial from a therapy standpoint where “couples can shift their perspective in a similar way without having to go through a natural disaster.”
Let’s hope she’s right, because the alternative is to seek out a rampaging hurricane every time your relationship is on the rocks, and that just seems impractical after the second or third year.
Not-so-essential oils
Many people use essential oils as a way to unwind and relax. Stressed? Can’t sleep? There’s probably an essential oil for that. However, it seems like these days a lot of things we love and/or think are good for us have a side that’s not so.
According to the Centers for Disease Control and Prevention, a woman from Georgia died from a rare bacteria called Burkholderia pseudomallei. There have been three previous infections in Kansas, Minnesota, and Texas throughout 2021; two of the four infections were in children. Melioidosis, the disease caused by B. pseudomallei, is usually found in southeast Asia and isn’t obvious or easy to diagnose, especially in places like decidedly untropical Minnesota.
The Georgia case was the real break in this medical mystery, as the infection was traced back to a Walmart product called “Better Homes and Gardens Essential Oil Infused Aromatherapy Room Spray with Gemstones” (a very pithy name). The bacteria were in the lavender and chamomile scent. The CDC is investigating all other product scents, and Walmart has recalled all lots of the product.
If you’ve got that particular essential oil, it’s probably for the best that you stop using it. Don’t worry, we’re sure there’s plenty of other essential oil–infused aromatherapy room sprays with gemstones out there for your scent-based needs.
Welcome to the Ministry of Sleep-Deprived Walks
Walking is simple, right? You put one foot in front of the other, and soon you’re walking out the door. Little kids can do it. Even zombies can walk, and they don’t even have brains.
Research from MIT and the University of São Paulo has shown that walking is a little trickier than we might think. One researcher in particular noticed that student volunteers tended to perform worse toward the end of semesters, as project deadlines and multiple exams crashed over their heads and they were deprived of solid sleep schedules.
In a study published in Scientific Reports, our intrepid walking researchers had a collection of students monitor their sleep patterns for 2 weeks; on average, the students got 6 hours per night, though some were able to compensate on weekends. On the final day of a 14-day period, some students pulled all-nighters while the rest were allowed to sleep as usual. Then all students performed a walking test involving keeping time with a metronome.
To absolutely no one’s surprise, the students who performed all-nighters before being tested walked the worst, but between the other students, the ones who compensated for sleep deprivation on weekends did better than those who got 6 hours every night, despite getting a similar amount of sleep overall. This effect persisted even when the compensating students performed their walking tests late in the week, just before they got their weekend beauty sleep.
The moral of the story? Sleep is good, and you should get more of it. But if you can’t, sleep in on weekends. Science has given you permission. All those suburban dads looking to get their teenagers up at 8 in the morning must be sweating right now.
The Devil’s own face covering?
It’s been over a year and a half since the COVID-19 emergency was declared in the United States, and we’ve been starting to wonder what our good friend SARS-CoV-2 has left to give. The collective cynic/optimist in us figures that the insanity can’t last forever, right?
Maybe not forever, but …
A group of parents is suing the Central Bucks (Pa.) School District over school mask mandates, suggesting that the district has no legal authority to enforce such measures. Most of their arguments, Philadelphia Magazine says, are pretty standard stuff: Masks are causing depression, anxiety, and discomfort in their children; masks are a violation of their constitutional rights; and “masks are being used as a control mechanism over the population.”
There are some unusual claims, though. One of the parents, Shannon Harris, said that “wearing masks interferes with their religious duty to spread the word of God and forces them to participate in a satanic ritual,” according to the Philadelphia Inquirer.
Philadelphia Magazine decided to check on that “satanic ritual” claim by asking an expert, in this case a spokesperson for the Church of Satan. The Reverend Raul Antony said that “simply ‘wearing a mask’ is not a Satanic ritual, and anyone that genuinely thinks otherwise is a blithering idiot,” adding that the group’s rituals were available on its website.
COVID, you never let us down.
You’re the (hurricane) wind beneath my wings
Marriage isn’t easy. From finances to everyday stressors like work and children, maintaining a solid relationship is tough. Then a natural disaster shows up on top of everything else, and marriages actually improve, researchers found.
In a study published by Psychological Science, researchers surveyed 231 newlywed couples about the satisfaction of their marriage before and after Hurricane Harvey in 2017. They found after the hurricane couples had a “significant boost” in the satisfaction of their relationship.
One would think something like this would create what researchers call a “stress spillover,” creating a decrease in relationship satisfaction. Destruction to your home or even displacement after a natural disaster seems pretty stressful. But, “a natural disaster can really put things in perspective. People realize how important their partner is to them when they are jolted out of the day-to-day stress of life,” said Hannah Williamson, PhD, the lead author of the study.
And although everyone saw an increase, the biggest jumps in relationship satisfaction belonged to the people who were most unhappy before the hurricane. Unfortunately, the researchers also found that the effects were only temporary and the dissatisfaction came back within a year.
Dr. Williamson thinks there may be something to these findings that can be beneficial from a therapy standpoint where “couples can shift their perspective in a similar way without having to go through a natural disaster.”
Let’s hope she’s right, because the alternative is to seek out a rampaging hurricane every time your relationship is on the rocks, and that just seems impractical after the second or third year.
Not-so-essential oils
Many people use essential oils as a way to unwind and relax. Stressed? Can’t sleep? There’s probably an essential oil for that. However, it seems like these days a lot of things we love and/or think are good for us have a side that’s not so.
According to the Centers for Disease Control and Prevention, a woman from Georgia died from a rare bacteria called Burkholderia pseudomallei. There have been three previous infections in Kansas, Minnesota, and Texas throughout 2021; two of the four infections were in children. Melioidosis, the disease caused by B. pseudomallei, is usually found in southeast Asia and isn’t obvious or easy to diagnose, especially in places like decidedly untropical Minnesota.
The Georgia case was the real break in this medical mystery, as the infection was traced back to a Walmart product called “Better Homes and Gardens Essential Oil Infused Aromatherapy Room Spray with Gemstones” (a very pithy name). The bacteria were in the lavender and chamomile scent. The CDC is investigating all other product scents, and Walmart has recalled all lots of the product.
If you’ve got that particular essential oil, it’s probably for the best that you stop using it. Don’t worry, we’re sure there’s plenty of other essential oil–infused aromatherapy room sprays with gemstones out there for your scent-based needs.
Welcome to the Ministry of Sleep-Deprived Walks
Walking is simple, right? You put one foot in front of the other, and soon you’re walking out the door. Little kids can do it. Even zombies can walk, and they don’t even have brains.
Research from MIT and the University of São Paulo has shown that walking is a little trickier than we might think. One researcher in particular noticed that student volunteers tended to perform worse toward the end of semesters, as project deadlines and multiple exams crashed over their heads and they were deprived of solid sleep schedules.
In a study published in Scientific Reports, our intrepid walking researchers had a collection of students monitor their sleep patterns for 2 weeks; on average, the students got 6 hours per night, though some were able to compensate on weekends. On the final day of a 14-day period, some students pulled all-nighters while the rest were allowed to sleep as usual. Then all students performed a walking test involving keeping time with a metronome.
To absolutely no one’s surprise, the students who performed all-nighters before being tested walked the worst, but between the other students, the ones who compensated for sleep deprivation on weekends did better than those who got 6 hours every night, despite getting a similar amount of sleep overall. This effect persisted even when the compensating students performed their walking tests late in the week, just before they got their weekend beauty sleep.
The moral of the story? Sleep is good, and you should get more of it. But if you can’t, sleep in on weekends. Science has given you permission. All those suburban dads looking to get their teenagers up at 8 in the morning must be sweating right now.
Cannabis use: Messages remain mixed across diagnoses
Marijuana use is now a legal activity in many parts of the United States, but those managing patients with psychiatric disorders are in the difficult position of determining whether this use is helpful, harmful, or irrelevant to the underlying illness on the basis of limited and largely incomplete data, according to an overview of this issue presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
While there is clear evidence that cannabis use relative to the general population “is more prevalent among patients with psychiatric disorders,” it is less certain how often this use is risky, said Diana M. Martinez, MD, professor of psychiatry at Columbia University in New York.
Independent of euphoric effects, cannabis can be perceived by individuals with psychiatric diagnosis as self-medication for feelings of stress, social anxiety, and insomnia, among other symptoms. These are the same reasons why many individuals without psychiatric conditions use cannabis-containing products.
The perception that cannabis use is generally benign presumably explains the successful efforts at legalization, but there are risks for those with or without psychiatric illnesses, Dr. Martinez pointed out at the meeting, sponsored by Medscape Live. Not least, about 20% of regular users of cannabis develop cannabis use disorder (CUD), a condition defined in the DSM-5 as the continued use of cannabis despite adverse consequences, such as dependence.
Impact of severe CUD ‘incapacitating’
“Of those who meet criteria for CUD, 23% have severe CUD, which is an incapacitating form,” reported Dr. Martinez, citing work led by Deborah Hasin, PhD, professor of clinical epidemiology at Columbia University.
However, relative to otherwise healthy individuals, those with a psychiatric diagnosis might face greater benefits or greater risks from cannabis use, according to Dr. Martinez, who cited a 2017 report from the National Academies of Science, Engineering, and Medicine (NASEM).
This report evaluated the potential risks and benefits on the basis of published studies.
There is limited evidence that regular cannabis increases rather than modifies symptoms of mania and hypomania in patients with bipolar disorder, according to the report. The report also cited limited evidence that cannabis use increases severity of posttraumatic stress disorder (PTSD). There was limited evidence of adverse effects on symptoms of anxiety, although this appeared to depend on daily or nearly daily use.
The report found no data of acceptable quality to draw conclusions about the effect of cannabis use on symptoms of depression.
In patients with attention-deficit/hyperactivity disorder (ADHD), “a recent study showed that daily but not occasional use of cannabis increased impulsivity but not inattention, working memory, or verbal intelligence,” said Dr. Martinez, citing a study published this year.
Some evidence also suggests that patients with a psychiatric disorder might benefit from cannabis use, but, again, this evidence is limited. For one example, it includes a potential reduction in symptoms of obsessive-compulsive disorder, Dr. Martinez said.
More support for cannabis in medical disease
Relative to the quality of evidence supporting benefit from cannabis in psychiatric disease, the data appear to be stronger for patients with medical illnesses, such as cancer. For example, Dr. Martinez cited evidence that tetrahydrocannabinol (THC), a major active ingredient in cannabis, improves sleep in the context of a medical illnesses. There is also evidence for anxiolytic effects in patients with a medical illness, although that is weaker.
In patients with or without a psychiatric disorder, marijuana does pose a risk of substance abuse disorder, and it shares the risks of intoxicants, such as inattention leading to increased risk of accidents, including motor vehicle accidents. This pertains to those with or without a psychiatric or medical condition, Dr. Martinez said.
While intermittent light use of cannabis appears to pose no risk or a very low risk of long-term adverse effects on cognition, at least in patients without psychiatric disorders, Dr. Martinez indicated that the risk-benefit ratio for any individual is use dependent. The risk of CUD, for example, increases with the frequency of exposure and the potency of the cannabis.
Empirical evidence for therapeutic role
In published studies, other researchers have expressed interest in a potential therapeutic role of cannabis for psychiatric disorders, but there appears to be a general consensus that the supportive data remain weak. One expert who has written on this topic, Jerome Sarris, PhD, professor of integrative mental health, NICM Health Research Institute, Western Sydney University, Westmead, Australia, said that empirical evidence does support a benefit in selected patients.
“Of course, high THC forms are strongly discouraged in people with schizophrenia or high risk of developing psychotic disorder, or in youths,” Dr. Sarris explained. “However, there is a potential role for use in people with sleep and pain issues, and many find it beneficial to also assist with affective disorder symptoms.”
In a systematic review he led that was published last year, the evidence to support cannabis for psychiatric disorders was characterized as “embryonic.” However, small studies and case reports appear to support benefit for such indications as ADHD if precautions are taken.
“I certainly would not discourage use of prescribed standardized medicinal cannabis therapeutics for all people with psychiatric disorders,” Dr. Sarris said. He suggested that attention should be made to the THC potency and terpene composition of the products that patients with psychiatric disorders are taking.
Marijuana use is now a legal activity in many parts of the United States, but those managing patients with psychiatric disorders are in the difficult position of determining whether this use is helpful, harmful, or irrelevant to the underlying illness on the basis of limited and largely incomplete data, according to an overview of this issue presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
While there is clear evidence that cannabis use relative to the general population “is more prevalent among patients with psychiatric disorders,” it is less certain how often this use is risky, said Diana M. Martinez, MD, professor of psychiatry at Columbia University in New York.
Independent of euphoric effects, cannabis can be perceived by individuals with psychiatric diagnosis as self-medication for feelings of stress, social anxiety, and insomnia, among other symptoms. These are the same reasons why many individuals without psychiatric conditions use cannabis-containing products.
The perception that cannabis use is generally benign presumably explains the successful efforts at legalization, but there are risks for those with or without psychiatric illnesses, Dr. Martinez pointed out at the meeting, sponsored by Medscape Live. Not least, about 20% of regular users of cannabis develop cannabis use disorder (CUD), a condition defined in the DSM-5 as the continued use of cannabis despite adverse consequences, such as dependence.
Impact of severe CUD ‘incapacitating’
“Of those who meet criteria for CUD, 23% have severe CUD, which is an incapacitating form,” reported Dr. Martinez, citing work led by Deborah Hasin, PhD, professor of clinical epidemiology at Columbia University.
However, relative to otherwise healthy individuals, those with a psychiatric diagnosis might face greater benefits or greater risks from cannabis use, according to Dr. Martinez, who cited a 2017 report from the National Academies of Science, Engineering, and Medicine (NASEM).
This report evaluated the potential risks and benefits on the basis of published studies.
There is limited evidence that regular cannabis increases rather than modifies symptoms of mania and hypomania in patients with bipolar disorder, according to the report. The report also cited limited evidence that cannabis use increases severity of posttraumatic stress disorder (PTSD). There was limited evidence of adverse effects on symptoms of anxiety, although this appeared to depend on daily or nearly daily use.
The report found no data of acceptable quality to draw conclusions about the effect of cannabis use on symptoms of depression.
In patients with attention-deficit/hyperactivity disorder (ADHD), “a recent study showed that daily but not occasional use of cannabis increased impulsivity but not inattention, working memory, or verbal intelligence,” said Dr. Martinez, citing a study published this year.
Some evidence also suggests that patients with a psychiatric disorder might benefit from cannabis use, but, again, this evidence is limited. For one example, it includes a potential reduction in symptoms of obsessive-compulsive disorder, Dr. Martinez said.
More support for cannabis in medical disease
Relative to the quality of evidence supporting benefit from cannabis in psychiatric disease, the data appear to be stronger for patients with medical illnesses, such as cancer. For example, Dr. Martinez cited evidence that tetrahydrocannabinol (THC), a major active ingredient in cannabis, improves sleep in the context of a medical illnesses. There is also evidence for anxiolytic effects in patients with a medical illness, although that is weaker.
In patients with or without a psychiatric disorder, marijuana does pose a risk of substance abuse disorder, and it shares the risks of intoxicants, such as inattention leading to increased risk of accidents, including motor vehicle accidents. This pertains to those with or without a psychiatric or medical condition, Dr. Martinez said.
While intermittent light use of cannabis appears to pose no risk or a very low risk of long-term adverse effects on cognition, at least in patients without psychiatric disorders, Dr. Martinez indicated that the risk-benefit ratio for any individual is use dependent. The risk of CUD, for example, increases with the frequency of exposure and the potency of the cannabis.
Empirical evidence for therapeutic role
In published studies, other researchers have expressed interest in a potential therapeutic role of cannabis for psychiatric disorders, but there appears to be a general consensus that the supportive data remain weak. One expert who has written on this topic, Jerome Sarris, PhD, professor of integrative mental health, NICM Health Research Institute, Western Sydney University, Westmead, Australia, said that empirical evidence does support a benefit in selected patients.
“Of course, high THC forms are strongly discouraged in people with schizophrenia or high risk of developing psychotic disorder, or in youths,” Dr. Sarris explained. “However, there is a potential role for use in people with sleep and pain issues, and many find it beneficial to also assist with affective disorder symptoms.”
In a systematic review he led that was published last year, the evidence to support cannabis for psychiatric disorders was characterized as “embryonic.” However, small studies and case reports appear to support benefit for such indications as ADHD if precautions are taken.
“I certainly would not discourage use of prescribed standardized medicinal cannabis therapeutics for all people with psychiatric disorders,” Dr. Sarris said. He suggested that attention should be made to the THC potency and terpene composition of the products that patients with psychiatric disorders are taking.
Marijuana use is now a legal activity in many parts of the United States, but those managing patients with psychiatric disorders are in the difficult position of determining whether this use is helpful, harmful, or irrelevant to the underlying illness on the basis of limited and largely incomplete data, according to an overview of this issue presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
While there is clear evidence that cannabis use relative to the general population “is more prevalent among patients with psychiatric disorders,” it is less certain how often this use is risky, said Diana M. Martinez, MD, professor of psychiatry at Columbia University in New York.
Independent of euphoric effects, cannabis can be perceived by individuals with psychiatric diagnosis as self-medication for feelings of stress, social anxiety, and insomnia, among other symptoms. These are the same reasons why many individuals without psychiatric conditions use cannabis-containing products.
The perception that cannabis use is generally benign presumably explains the successful efforts at legalization, but there are risks for those with or without psychiatric illnesses, Dr. Martinez pointed out at the meeting, sponsored by Medscape Live. Not least, about 20% of regular users of cannabis develop cannabis use disorder (CUD), a condition defined in the DSM-5 as the continued use of cannabis despite adverse consequences, such as dependence.
Impact of severe CUD ‘incapacitating’
“Of those who meet criteria for CUD, 23% have severe CUD, which is an incapacitating form,” reported Dr. Martinez, citing work led by Deborah Hasin, PhD, professor of clinical epidemiology at Columbia University.
However, relative to otherwise healthy individuals, those with a psychiatric diagnosis might face greater benefits or greater risks from cannabis use, according to Dr. Martinez, who cited a 2017 report from the National Academies of Science, Engineering, and Medicine (NASEM).
This report evaluated the potential risks and benefits on the basis of published studies.
There is limited evidence that regular cannabis increases rather than modifies symptoms of mania and hypomania in patients with bipolar disorder, according to the report. The report also cited limited evidence that cannabis use increases severity of posttraumatic stress disorder (PTSD). There was limited evidence of adverse effects on symptoms of anxiety, although this appeared to depend on daily or nearly daily use.
The report found no data of acceptable quality to draw conclusions about the effect of cannabis use on symptoms of depression.
In patients with attention-deficit/hyperactivity disorder (ADHD), “a recent study showed that daily but not occasional use of cannabis increased impulsivity but not inattention, working memory, or verbal intelligence,” said Dr. Martinez, citing a study published this year.
Some evidence also suggests that patients with a psychiatric disorder might benefit from cannabis use, but, again, this evidence is limited. For one example, it includes a potential reduction in symptoms of obsessive-compulsive disorder, Dr. Martinez said.
More support for cannabis in medical disease
Relative to the quality of evidence supporting benefit from cannabis in psychiatric disease, the data appear to be stronger for patients with medical illnesses, such as cancer. For example, Dr. Martinez cited evidence that tetrahydrocannabinol (THC), a major active ingredient in cannabis, improves sleep in the context of a medical illnesses. There is also evidence for anxiolytic effects in patients with a medical illness, although that is weaker.
In patients with or without a psychiatric disorder, marijuana does pose a risk of substance abuse disorder, and it shares the risks of intoxicants, such as inattention leading to increased risk of accidents, including motor vehicle accidents. This pertains to those with or without a psychiatric or medical condition, Dr. Martinez said.
While intermittent light use of cannabis appears to pose no risk or a very low risk of long-term adverse effects on cognition, at least in patients without psychiatric disorders, Dr. Martinez indicated that the risk-benefit ratio for any individual is use dependent. The risk of CUD, for example, increases with the frequency of exposure and the potency of the cannabis.
Empirical evidence for therapeutic role
In published studies, other researchers have expressed interest in a potential therapeutic role of cannabis for psychiatric disorders, but there appears to be a general consensus that the supportive data remain weak. One expert who has written on this topic, Jerome Sarris, PhD, professor of integrative mental health, NICM Health Research Institute, Western Sydney University, Westmead, Australia, said that empirical evidence does support a benefit in selected patients.
“Of course, high THC forms are strongly discouraged in people with schizophrenia or high risk of developing psychotic disorder, or in youths,” Dr. Sarris explained. “However, there is a potential role for use in people with sleep and pain issues, and many find it beneficial to also assist with affective disorder symptoms.”
In a systematic review he led that was published last year, the evidence to support cannabis for psychiatric disorders was characterized as “embryonic.” However, small studies and case reports appear to support benefit for such indications as ADHD if precautions are taken.
“I certainly would not discourage use of prescribed standardized medicinal cannabis therapeutics for all people with psychiatric disorders,” Dr. Sarris said. He suggested that attention should be made to the THC potency and terpene composition of the products that patients with psychiatric disorders are taking.
FROM PSYCHOPHARMACOLOGY UPDATE
FDA panel votes to approve Pfizer’s vaccine for children
Seventeen of the 18 members of the Vaccines and Related Biological Products Advisory Committee (VRBPAC) on Oct. 26 voted to recommend the 10-microgram shot for kids, which is one-third the dose given to adults.
One member, Michael Kurilla, MD, director of the division of clinical innovation at the National Institutes of Health, Bethesda, Md., abstained from voting.
If the FDA follows the recommendation, as it typically does, and issues an Emergency Use Authorization for the vaccine, the shots could be available within days.
After the FDA’s final decision, the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices will meet to make specific recommendations for its use. The CDC committee must stick closely to the conditions for use spelled out in the EUA, so their recommendations are likely to be similar to those made by the FDA. Their next meeting is scheduled for Nov. 2 and 3.
In the end, some on the panel felt uneasy with their decision.
“I voted yes primarily because I wanted to make sure that children who really need this vaccine, the Black and brown children of our country, get the vaccine,” said James Hildreth, MD, PhD, president and CEO of Meharry Medical College in Nashville.
“But to be honest, the best way to protect the health of some children will be to do nothing because they will be just fine,” he said.
Others said they were surprised by how difficult the decision had been.
“This is a much tougher one than we had expected going into it,” said committee member Eric Rubin, MD, editor and chief of the New England Journal of Medicine, during the FDA advisory committee’s meeting.
Ahead of the vote, the committee heard presentations outlining the expected benefits of vaccinating children along with potential risks.
“Children have been greatly impacted by the pandemic,” said Fiona Havers, MD, a medical officer with the CDC in Atlanta who reviewed the epidemiology of COVID-19 in kids.
In the second year of the pandemic, as more seniors have been vaccinated against the virus, COVID cases have largely shifted from older to younger age groups.
So far, there have been more than 1.9 million COVID-19 cases in children ages 5 through 11 in the United States.. Cases in kids saw a big jump in July and August with summer travel, schools reopening, and the dominance of the Delta variant.
And those are just the cases reported to the CDC. Regular testing of anonymous blood samples collected at sites across the United States indicates that 6 times as many kids have had COVID than what is reflected in official counts.
Last winter, blood sample testing showed about 13% of children had antibodies against the virus, suggesting they’d been infected. By this summer, that number had risen to 42%.
That figure clearly made an impression on many members of the committee who asked the FDA’s vaccine reviewers if they had tried to account for immunity from past infections in their modeling. They had not.
Some felt that even with a highly effective vaccine — new data presented by Pfizer showed the children’s dose was 90% effective at preventing symptomatic infections in kids — caution was warranted as much is still unknown about myocarditis, a rare side effect of the mRNA vaccines.
Myocarditis has been more common in younger age groups. It usually goes away over time but requires hospital care. It’s not known if myocarditis could have lingering effects for those who experience it.
There were no cases of myocarditis seen in Pfizer’s studies of the vaccine in children, and no other serious events were seen. Vaccine side effects reported in the Pfizer studies were mostly mild and included fatigue, headache, and pain at the injection site.
“We think we have optimized the immune response and minimized our reactions,” said William Gruber, MD, senior vice president vaccine research and clinical development at Pfizer.
But the studies didn’t include enough participants to pick up rare, but serious adverse events like myocarditis.
“We’re worried about a side effect that we can’t measure yet, but it’s probably real, and we see a benefit that isn’t the same as it is in older age groups,” said Dr. Rubin.
Benefits vs. risks
FDA modeled the benefits and risks for children under a variety of scenarios. The benefits of the vaccines to children very much depend on the amount of transmission in the community.
When transmission is high, the benefits to children — in terms of infections, hospitalizations, ICU admissions — clearly outweigh its risks.
But when COVID-19 rates are low in the community, as they were in June, FDA analysts predicted the vaccines might send more children to the hospital for myocarditis than the virus would.
The FDA noted that kids who are hospitalized for myocarditis tend not to be as ill as children with COVID-19, however.
“If the trends continue the way they are going, the emergency for children is not what we might think it would be. That was my concern,” Dr. Hildreth said.
But others warned against complacency.
“Thinking that this is going to be the end of the wave permanently may be a little overly optimistic,” said committee chairman Arnold Monto, MD, a professor of public health and epidemiology at the University of Michigan, Ann Arbor.
The majority of COVID-19 cases in children are mild. Only about 1% of kids are hospitalized for their infections, according to CDC data. But the rates of hospitalizations in kids are about 3 times higher for people of color — including Blacks, Hispanics, and Native Americans, as compared to Whites and Asian Americans.
Since the start of the pandemic, 94 children ages 5 to 11 have died, making it the eighth leading cause of death for kids this age last year.
More than 5,200 children have developed a delayed complication from their infections called Multi-System Inflammatory Syndrome (MIS-C).
MIS-C can be severe and require hospital care and can lead to myocarditis. Children ages 5 to 11 are the age group at greatest risk for this complication.
Kids can also get long COVID. There’s not a lot of data on how often this happens, though it appears to be less frequent in children than in adults.
But a survey in the United Kingdom found that 7%-8% of kids have symptoms from their infections that last longer than 12 weeks, Dr. Havers said. Symptoms that can linger for kids include fatigue, cough, muscle and joint pain, headaches, and insomnia.
More than 1 million children have been impacted by school closures so far this year, and quarantines have had lasting impacts on learning, social development, and mental health.
Even though kids aren’t usually COVID superspreaders, they can still pass the infection on to others.
“What is clear is that secondary transmission from children, both to other children and to adults, does occur,” Dr. Havers said.
For that reason, they can continue the spread of the virus and give it opportunities to mutate and become more dangerous.
Safety monitoring to continue
Some committee members referenced thousands of letters they had received within the past few days urging them to vote against the vaccine.
Jay Portnoy, MD, a professor of pediatrics at Children’s Mercy Hospital in Kansas City, Mo., said he had personally received about 4,000 emails.
“But I feel like I need to also represent the consumers, the parents that I see every day in the clinic who are terrified of sending their children to school because they’re not protected against COVID,” he said, explaining his vote to recommend authorization.
“Our kids are going to be dealing with this virus for many years to come. It’s going to come repeatedly. Getting this vaccine is just the first step that they can take to protect themselves from having bad outcomes,” Dr. Portnoy said.
Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, reminded members of the committee that there were several government surveillance systems in place to catch any potential safety issues in near real time.
“I really appreciate very much the concern here. The safety monitoring of this vaccine will continue,” Dr. Marks said. “I do view this as one of our greatest responsibilities.”
“I really am so grateful that we had this discussion and voted to approve,” said Capt. Amanda Cohn, MD, chief medical officer at the National Center for Immunization and Respiratory Diseases.
“I think the benefits in this age group really are super important even if they are lower than for other age groups.”
This article was updated 10/27/21.
A version of this article first appeared on WebMD.com.
Seventeen of the 18 members of the Vaccines and Related Biological Products Advisory Committee (VRBPAC) on Oct. 26 voted to recommend the 10-microgram shot for kids, which is one-third the dose given to adults.
One member, Michael Kurilla, MD, director of the division of clinical innovation at the National Institutes of Health, Bethesda, Md., abstained from voting.
If the FDA follows the recommendation, as it typically does, and issues an Emergency Use Authorization for the vaccine, the shots could be available within days.
After the FDA’s final decision, the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices will meet to make specific recommendations for its use. The CDC committee must stick closely to the conditions for use spelled out in the EUA, so their recommendations are likely to be similar to those made by the FDA. Their next meeting is scheduled for Nov. 2 and 3.
In the end, some on the panel felt uneasy with their decision.
“I voted yes primarily because I wanted to make sure that children who really need this vaccine, the Black and brown children of our country, get the vaccine,” said James Hildreth, MD, PhD, president and CEO of Meharry Medical College in Nashville.
“But to be honest, the best way to protect the health of some children will be to do nothing because they will be just fine,” he said.
Others said they were surprised by how difficult the decision had been.
“This is a much tougher one than we had expected going into it,” said committee member Eric Rubin, MD, editor and chief of the New England Journal of Medicine, during the FDA advisory committee’s meeting.
Ahead of the vote, the committee heard presentations outlining the expected benefits of vaccinating children along with potential risks.
“Children have been greatly impacted by the pandemic,” said Fiona Havers, MD, a medical officer with the CDC in Atlanta who reviewed the epidemiology of COVID-19 in kids.
In the second year of the pandemic, as more seniors have been vaccinated against the virus, COVID cases have largely shifted from older to younger age groups.
So far, there have been more than 1.9 million COVID-19 cases in children ages 5 through 11 in the United States.. Cases in kids saw a big jump in July and August with summer travel, schools reopening, and the dominance of the Delta variant.
And those are just the cases reported to the CDC. Regular testing of anonymous blood samples collected at sites across the United States indicates that 6 times as many kids have had COVID than what is reflected in official counts.
Last winter, blood sample testing showed about 13% of children had antibodies against the virus, suggesting they’d been infected. By this summer, that number had risen to 42%.
That figure clearly made an impression on many members of the committee who asked the FDA’s vaccine reviewers if they had tried to account for immunity from past infections in their modeling. They had not.
Some felt that even with a highly effective vaccine — new data presented by Pfizer showed the children’s dose was 90% effective at preventing symptomatic infections in kids — caution was warranted as much is still unknown about myocarditis, a rare side effect of the mRNA vaccines.
Myocarditis has been more common in younger age groups. It usually goes away over time but requires hospital care. It’s not known if myocarditis could have lingering effects for those who experience it.
There were no cases of myocarditis seen in Pfizer’s studies of the vaccine in children, and no other serious events were seen. Vaccine side effects reported in the Pfizer studies were mostly mild and included fatigue, headache, and pain at the injection site.
“We think we have optimized the immune response and minimized our reactions,” said William Gruber, MD, senior vice president vaccine research and clinical development at Pfizer.
But the studies didn’t include enough participants to pick up rare, but serious adverse events like myocarditis.
“We’re worried about a side effect that we can’t measure yet, but it’s probably real, and we see a benefit that isn’t the same as it is in older age groups,” said Dr. Rubin.
Benefits vs. risks
FDA modeled the benefits and risks for children under a variety of scenarios. The benefits of the vaccines to children very much depend on the amount of transmission in the community.
When transmission is high, the benefits to children — in terms of infections, hospitalizations, ICU admissions — clearly outweigh its risks.
But when COVID-19 rates are low in the community, as they were in June, FDA analysts predicted the vaccines might send more children to the hospital for myocarditis than the virus would.
The FDA noted that kids who are hospitalized for myocarditis tend not to be as ill as children with COVID-19, however.
“If the trends continue the way they are going, the emergency for children is not what we might think it would be. That was my concern,” Dr. Hildreth said.
But others warned against complacency.
“Thinking that this is going to be the end of the wave permanently may be a little overly optimistic,” said committee chairman Arnold Monto, MD, a professor of public health and epidemiology at the University of Michigan, Ann Arbor.
The majority of COVID-19 cases in children are mild. Only about 1% of kids are hospitalized for their infections, according to CDC data. But the rates of hospitalizations in kids are about 3 times higher for people of color — including Blacks, Hispanics, and Native Americans, as compared to Whites and Asian Americans.
Since the start of the pandemic, 94 children ages 5 to 11 have died, making it the eighth leading cause of death for kids this age last year.
More than 5,200 children have developed a delayed complication from their infections called Multi-System Inflammatory Syndrome (MIS-C).
MIS-C can be severe and require hospital care and can lead to myocarditis. Children ages 5 to 11 are the age group at greatest risk for this complication.
Kids can also get long COVID. There’s not a lot of data on how often this happens, though it appears to be less frequent in children than in adults.
But a survey in the United Kingdom found that 7%-8% of kids have symptoms from their infections that last longer than 12 weeks, Dr. Havers said. Symptoms that can linger for kids include fatigue, cough, muscle and joint pain, headaches, and insomnia.
More than 1 million children have been impacted by school closures so far this year, and quarantines have had lasting impacts on learning, social development, and mental health.
Even though kids aren’t usually COVID superspreaders, they can still pass the infection on to others.
“What is clear is that secondary transmission from children, both to other children and to adults, does occur,” Dr. Havers said.
For that reason, they can continue the spread of the virus and give it opportunities to mutate and become more dangerous.
Safety monitoring to continue
Some committee members referenced thousands of letters they had received within the past few days urging them to vote against the vaccine.
Jay Portnoy, MD, a professor of pediatrics at Children’s Mercy Hospital in Kansas City, Mo., said he had personally received about 4,000 emails.
“But I feel like I need to also represent the consumers, the parents that I see every day in the clinic who are terrified of sending their children to school because they’re not protected against COVID,” he said, explaining his vote to recommend authorization.
“Our kids are going to be dealing with this virus for many years to come. It’s going to come repeatedly. Getting this vaccine is just the first step that they can take to protect themselves from having bad outcomes,” Dr. Portnoy said.
Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, reminded members of the committee that there were several government surveillance systems in place to catch any potential safety issues in near real time.
“I really appreciate very much the concern here. The safety monitoring of this vaccine will continue,” Dr. Marks said. “I do view this as one of our greatest responsibilities.”
“I really am so grateful that we had this discussion and voted to approve,” said Capt. Amanda Cohn, MD, chief medical officer at the National Center for Immunization and Respiratory Diseases.
“I think the benefits in this age group really are super important even if they are lower than for other age groups.”
This article was updated 10/27/21.
A version of this article first appeared on WebMD.com.
Seventeen of the 18 members of the Vaccines and Related Biological Products Advisory Committee (VRBPAC) on Oct. 26 voted to recommend the 10-microgram shot for kids, which is one-third the dose given to adults.
One member, Michael Kurilla, MD, director of the division of clinical innovation at the National Institutes of Health, Bethesda, Md., abstained from voting.
If the FDA follows the recommendation, as it typically does, and issues an Emergency Use Authorization for the vaccine, the shots could be available within days.
After the FDA’s final decision, the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices will meet to make specific recommendations for its use. The CDC committee must stick closely to the conditions for use spelled out in the EUA, so their recommendations are likely to be similar to those made by the FDA. Their next meeting is scheduled for Nov. 2 and 3.
In the end, some on the panel felt uneasy with their decision.
“I voted yes primarily because I wanted to make sure that children who really need this vaccine, the Black and brown children of our country, get the vaccine,” said James Hildreth, MD, PhD, president and CEO of Meharry Medical College in Nashville.
“But to be honest, the best way to protect the health of some children will be to do nothing because they will be just fine,” he said.
Others said they were surprised by how difficult the decision had been.
“This is a much tougher one than we had expected going into it,” said committee member Eric Rubin, MD, editor and chief of the New England Journal of Medicine, during the FDA advisory committee’s meeting.
Ahead of the vote, the committee heard presentations outlining the expected benefits of vaccinating children along with potential risks.
“Children have been greatly impacted by the pandemic,” said Fiona Havers, MD, a medical officer with the CDC in Atlanta who reviewed the epidemiology of COVID-19 in kids.
In the second year of the pandemic, as more seniors have been vaccinated against the virus, COVID cases have largely shifted from older to younger age groups.
So far, there have been more than 1.9 million COVID-19 cases in children ages 5 through 11 in the United States.. Cases in kids saw a big jump in July and August with summer travel, schools reopening, and the dominance of the Delta variant.
And those are just the cases reported to the CDC. Regular testing of anonymous blood samples collected at sites across the United States indicates that 6 times as many kids have had COVID than what is reflected in official counts.
Last winter, blood sample testing showed about 13% of children had antibodies against the virus, suggesting they’d been infected. By this summer, that number had risen to 42%.
That figure clearly made an impression on many members of the committee who asked the FDA’s vaccine reviewers if they had tried to account for immunity from past infections in their modeling. They had not.
Some felt that even with a highly effective vaccine — new data presented by Pfizer showed the children’s dose was 90% effective at preventing symptomatic infections in kids — caution was warranted as much is still unknown about myocarditis, a rare side effect of the mRNA vaccines.
Myocarditis has been more common in younger age groups. It usually goes away over time but requires hospital care. It’s not known if myocarditis could have lingering effects for those who experience it.
There were no cases of myocarditis seen in Pfizer’s studies of the vaccine in children, and no other serious events were seen. Vaccine side effects reported in the Pfizer studies were mostly mild and included fatigue, headache, and pain at the injection site.
“We think we have optimized the immune response and minimized our reactions,” said William Gruber, MD, senior vice president vaccine research and clinical development at Pfizer.
But the studies didn’t include enough participants to pick up rare, but serious adverse events like myocarditis.
“We’re worried about a side effect that we can’t measure yet, but it’s probably real, and we see a benefit that isn’t the same as it is in older age groups,” said Dr. Rubin.
Benefits vs. risks
FDA modeled the benefits and risks for children under a variety of scenarios. The benefits of the vaccines to children very much depend on the amount of transmission in the community.
When transmission is high, the benefits to children — in terms of infections, hospitalizations, ICU admissions — clearly outweigh its risks.
But when COVID-19 rates are low in the community, as they were in June, FDA analysts predicted the vaccines might send more children to the hospital for myocarditis than the virus would.
The FDA noted that kids who are hospitalized for myocarditis tend not to be as ill as children with COVID-19, however.
“If the trends continue the way they are going, the emergency for children is not what we might think it would be. That was my concern,” Dr. Hildreth said.
But others warned against complacency.
“Thinking that this is going to be the end of the wave permanently may be a little overly optimistic,” said committee chairman Arnold Monto, MD, a professor of public health and epidemiology at the University of Michigan, Ann Arbor.
The majority of COVID-19 cases in children are mild. Only about 1% of kids are hospitalized for their infections, according to CDC data. But the rates of hospitalizations in kids are about 3 times higher for people of color — including Blacks, Hispanics, and Native Americans, as compared to Whites and Asian Americans.
Since the start of the pandemic, 94 children ages 5 to 11 have died, making it the eighth leading cause of death for kids this age last year.
More than 5,200 children have developed a delayed complication from their infections called Multi-System Inflammatory Syndrome (MIS-C).
MIS-C can be severe and require hospital care and can lead to myocarditis. Children ages 5 to 11 are the age group at greatest risk for this complication.
Kids can also get long COVID. There’s not a lot of data on how often this happens, though it appears to be less frequent in children than in adults.
But a survey in the United Kingdom found that 7%-8% of kids have symptoms from their infections that last longer than 12 weeks, Dr. Havers said. Symptoms that can linger for kids include fatigue, cough, muscle and joint pain, headaches, and insomnia.
More than 1 million children have been impacted by school closures so far this year, and quarantines have had lasting impacts on learning, social development, and mental health.
Even though kids aren’t usually COVID superspreaders, they can still pass the infection on to others.
“What is clear is that secondary transmission from children, both to other children and to adults, does occur,” Dr. Havers said.
For that reason, they can continue the spread of the virus and give it opportunities to mutate and become more dangerous.
Safety monitoring to continue
Some committee members referenced thousands of letters they had received within the past few days urging them to vote against the vaccine.
Jay Portnoy, MD, a professor of pediatrics at Children’s Mercy Hospital in Kansas City, Mo., said he had personally received about 4,000 emails.
“But I feel like I need to also represent the consumers, the parents that I see every day in the clinic who are terrified of sending their children to school because they’re not protected against COVID,” he said, explaining his vote to recommend authorization.
“Our kids are going to be dealing with this virus for many years to come. It’s going to come repeatedly. Getting this vaccine is just the first step that they can take to protect themselves from having bad outcomes,” Dr. Portnoy said.
Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, reminded members of the committee that there were several government surveillance systems in place to catch any potential safety issues in near real time.
“I really appreciate very much the concern here. The safety monitoring of this vaccine will continue,” Dr. Marks said. “I do view this as one of our greatest responsibilities.”
“I really am so grateful that we had this discussion and voted to approve,” said Capt. Amanda Cohn, MD, chief medical officer at the National Center for Immunization and Respiratory Diseases.
“I think the benefits in this age group really are super important even if they are lower than for other age groups.”
This article was updated 10/27/21.
A version of this article first appeared on WebMD.com.
Sleep time ‘sweet spot’ to slow cognitive decline identified?
In a longitudinal study, investigators found older adults who slept less than 4.5 hours or more than 6.5 hours a night reported significant cognitive decline over time, but cognitive scores for those with sleep duration in between that range remained stable.
“This really suggests that there’s this middle range, a ‘sweet spot,’ where your sleep is really optimal,” said lead author Brendan Lucey, MD, MSCI, associate professor of neurology and director of the Washington University Sleep Medicine Center, St. Louis.
The study, published online Oct. 20 in Brain, is part of a growing body of research that seeks to determine if sleep can be used as a marker of Alzheimer’s disease progression.
A complex relationship
Studies suggest a strong relationship between sleep patterns and Alzheimer’s disease, which affects nearly 6 million Americans. The challenge, Dr. Lucey said, is unwinding the complex links between sleep, Alzheimer’s disease, and cognitive function.
An earlier study by Dr. Lucey and colleagues found that poor sleep quality is associated with early signs of Alzheimer’s disease, and a report published in September found that elderly people who slept less than 6 hours a night had a greater burden of amyloid beta, a hallmark sign of Alzheimer’s disease.
For this new study, researchers monitored sleep-wake activity over 4-6 nights in 100 participants who underwent annual cognitive assessments and clinical studies, including APOE genotyping, as part of a longitudinal study at the Knight Alzheimer Disease Research Center at Washington University. Participants also provided cerebrospinal fluid (CSF) total tau and amyloid-beta42 and wore a small EEG device on their forehead while they slept.
The majority of participants had a clinical dementia rating (CDR) score of 0, indicating no cognitive impairment. Twelve individuals had a CDR >0, with most reporting mild cognitive impairment.
As expected, CSF analysis showed greater evidence of Alzheimer’s disease pathology in those with a baseline CDR greater than 0.
Changes in cognitive function were measured using a Preclinical Alzheimer Cognitive Composite (PACC) score, a composite of results from a neuropsychological testing battery that included the Free and Cued Selective Reminding Test, the Logical Memory Delayed Recall Test from the Wechsler Memory Scale-Revised, the Digit Symbol Substitution Test from the Wechsler Adult Intelligence Scale-Revised, and the Mini-Mental State Examination.
Researchers found an upside-down U-shaped relationship between PACC scores and sleep duration, with dramatic cognitive decline in those who slept less than 4.5 hours or more than 6.5 hours a night (P < .001 for both). The U-shaped relationship was also found with measures of sleep phases, including time spent in rapid eye movement and in non-REM sleep (P < .001 for both).
The findings persisted even after controlling for confounders that can affect sleep and cognition, such as age, CSF total tau/amyloid-beta-42 ratio, APOE ε4 allele carrier status, years of education, and sex.
Understanding how sleep changes at different stages of Alzheimer’s disease could help researchers determine if sleep can be used as a marker of disease progression, Dr. Lucey said. That could lead to interventions to slow that process.
“We’re not at the point yet where we can say that we need to monitor someone’s sleep time and then do an intervention to see if it would improve their risk for cognitive decline,” said Dr. Lucey, who plans to repeat this sleep study with the same cohort to track changes in sleep patterns and cognitive function over time. “But that’s a question I’m very excited to try to answer.”
A component of cognitive health
Commenting on the findings, Heather Snyder, PhD, vice president of medical and scientific relations for the Alzheimer’s Association, noted that the study adds to a body of evidence linking sleep and cognition, especially how sleep quality can optimize brain function.
“We’ve seen previous research that’s shown poor sleep contributes to dementia risk, as well as research showing sleep duration may play a role in cognition,” she said.
“We also need studies that look at sleep as an intervention for cognitive health,” Dr. Snyder said. “Sleep is an important aspect of our overall health. Clinicians should have conversations with their patients about sleep as part of standard discussions about their health habits and wellness.”
The study was funded by the National Institutes of Health, the American Sleep Medicine Foundation, the Roger and Paula Riney Fund, and the Daniel J. Brennan, MD Fund. Dr. Lucey consults for Merck and Eli Lilly. Dr. Snyder has disclosed no relevant financial relationships. Full disclosures are included in the original article.
A version of this article first appeared on Medscape.com.
In a longitudinal study, investigators found older adults who slept less than 4.5 hours or more than 6.5 hours a night reported significant cognitive decline over time, but cognitive scores for those with sleep duration in between that range remained stable.
“This really suggests that there’s this middle range, a ‘sweet spot,’ where your sleep is really optimal,” said lead author Brendan Lucey, MD, MSCI, associate professor of neurology and director of the Washington University Sleep Medicine Center, St. Louis.
The study, published online Oct. 20 in Brain, is part of a growing body of research that seeks to determine if sleep can be used as a marker of Alzheimer’s disease progression.
A complex relationship
Studies suggest a strong relationship between sleep patterns and Alzheimer’s disease, which affects nearly 6 million Americans. The challenge, Dr. Lucey said, is unwinding the complex links between sleep, Alzheimer’s disease, and cognitive function.
An earlier study by Dr. Lucey and colleagues found that poor sleep quality is associated with early signs of Alzheimer’s disease, and a report published in September found that elderly people who slept less than 6 hours a night had a greater burden of amyloid beta, a hallmark sign of Alzheimer’s disease.
For this new study, researchers monitored sleep-wake activity over 4-6 nights in 100 participants who underwent annual cognitive assessments and clinical studies, including APOE genotyping, as part of a longitudinal study at the Knight Alzheimer Disease Research Center at Washington University. Participants also provided cerebrospinal fluid (CSF) total tau and amyloid-beta42 and wore a small EEG device on their forehead while they slept.
The majority of participants had a clinical dementia rating (CDR) score of 0, indicating no cognitive impairment. Twelve individuals had a CDR >0, with most reporting mild cognitive impairment.
As expected, CSF analysis showed greater evidence of Alzheimer’s disease pathology in those with a baseline CDR greater than 0.
Changes in cognitive function were measured using a Preclinical Alzheimer Cognitive Composite (PACC) score, a composite of results from a neuropsychological testing battery that included the Free and Cued Selective Reminding Test, the Logical Memory Delayed Recall Test from the Wechsler Memory Scale-Revised, the Digit Symbol Substitution Test from the Wechsler Adult Intelligence Scale-Revised, and the Mini-Mental State Examination.
Researchers found an upside-down U-shaped relationship between PACC scores and sleep duration, with dramatic cognitive decline in those who slept less than 4.5 hours or more than 6.5 hours a night (P < .001 for both). The U-shaped relationship was also found with measures of sleep phases, including time spent in rapid eye movement and in non-REM sleep (P < .001 for both).
The findings persisted even after controlling for confounders that can affect sleep and cognition, such as age, CSF total tau/amyloid-beta-42 ratio, APOE ε4 allele carrier status, years of education, and sex.
Understanding how sleep changes at different stages of Alzheimer’s disease could help researchers determine if sleep can be used as a marker of disease progression, Dr. Lucey said. That could lead to interventions to slow that process.
“We’re not at the point yet where we can say that we need to monitor someone’s sleep time and then do an intervention to see if it would improve their risk for cognitive decline,” said Dr. Lucey, who plans to repeat this sleep study with the same cohort to track changes in sleep patterns and cognitive function over time. “But that’s a question I’m very excited to try to answer.”
A component of cognitive health
Commenting on the findings, Heather Snyder, PhD, vice president of medical and scientific relations for the Alzheimer’s Association, noted that the study adds to a body of evidence linking sleep and cognition, especially how sleep quality can optimize brain function.
“We’ve seen previous research that’s shown poor sleep contributes to dementia risk, as well as research showing sleep duration may play a role in cognition,” she said.
“We also need studies that look at sleep as an intervention for cognitive health,” Dr. Snyder said. “Sleep is an important aspect of our overall health. Clinicians should have conversations with their patients about sleep as part of standard discussions about their health habits and wellness.”
The study was funded by the National Institutes of Health, the American Sleep Medicine Foundation, the Roger and Paula Riney Fund, and the Daniel J. Brennan, MD Fund. Dr. Lucey consults for Merck and Eli Lilly. Dr. Snyder has disclosed no relevant financial relationships. Full disclosures are included in the original article.
A version of this article first appeared on Medscape.com.
In a longitudinal study, investigators found older adults who slept less than 4.5 hours or more than 6.5 hours a night reported significant cognitive decline over time, but cognitive scores for those with sleep duration in between that range remained stable.
“This really suggests that there’s this middle range, a ‘sweet spot,’ where your sleep is really optimal,” said lead author Brendan Lucey, MD, MSCI, associate professor of neurology and director of the Washington University Sleep Medicine Center, St. Louis.
The study, published online Oct. 20 in Brain, is part of a growing body of research that seeks to determine if sleep can be used as a marker of Alzheimer’s disease progression.
A complex relationship
Studies suggest a strong relationship between sleep patterns and Alzheimer’s disease, which affects nearly 6 million Americans. The challenge, Dr. Lucey said, is unwinding the complex links between sleep, Alzheimer’s disease, and cognitive function.
An earlier study by Dr. Lucey and colleagues found that poor sleep quality is associated with early signs of Alzheimer’s disease, and a report published in September found that elderly people who slept less than 6 hours a night had a greater burden of amyloid beta, a hallmark sign of Alzheimer’s disease.
For this new study, researchers monitored sleep-wake activity over 4-6 nights in 100 participants who underwent annual cognitive assessments and clinical studies, including APOE genotyping, as part of a longitudinal study at the Knight Alzheimer Disease Research Center at Washington University. Participants also provided cerebrospinal fluid (CSF) total tau and amyloid-beta42 and wore a small EEG device on their forehead while they slept.
The majority of participants had a clinical dementia rating (CDR) score of 0, indicating no cognitive impairment. Twelve individuals had a CDR >0, with most reporting mild cognitive impairment.
As expected, CSF analysis showed greater evidence of Alzheimer’s disease pathology in those with a baseline CDR greater than 0.
Changes in cognitive function were measured using a Preclinical Alzheimer Cognitive Composite (PACC) score, a composite of results from a neuropsychological testing battery that included the Free and Cued Selective Reminding Test, the Logical Memory Delayed Recall Test from the Wechsler Memory Scale-Revised, the Digit Symbol Substitution Test from the Wechsler Adult Intelligence Scale-Revised, and the Mini-Mental State Examination.
Researchers found an upside-down U-shaped relationship between PACC scores and sleep duration, with dramatic cognitive decline in those who slept less than 4.5 hours or more than 6.5 hours a night (P < .001 for both). The U-shaped relationship was also found with measures of sleep phases, including time spent in rapid eye movement and in non-REM sleep (P < .001 for both).
The findings persisted even after controlling for confounders that can affect sleep and cognition, such as age, CSF total tau/amyloid-beta-42 ratio, APOE ε4 allele carrier status, years of education, and sex.
Understanding how sleep changes at different stages of Alzheimer’s disease could help researchers determine if sleep can be used as a marker of disease progression, Dr. Lucey said. That could lead to interventions to slow that process.
“We’re not at the point yet where we can say that we need to monitor someone’s sleep time and then do an intervention to see if it would improve their risk for cognitive decline,” said Dr. Lucey, who plans to repeat this sleep study with the same cohort to track changes in sleep patterns and cognitive function over time. “But that’s a question I’m very excited to try to answer.”
A component of cognitive health
Commenting on the findings, Heather Snyder, PhD, vice president of medical and scientific relations for the Alzheimer’s Association, noted that the study adds to a body of evidence linking sleep and cognition, especially how sleep quality can optimize brain function.
“We’ve seen previous research that’s shown poor sleep contributes to dementia risk, as well as research showing sleep duration may play a role in cognition,” she said.
“We also need studies that look at sleep as an intervention for cognitive health,” Dr. Snyder said. “Sleep is an important aspect of our overall health. Clinicians should have conversations with their patients about sleep as part of standard discussions about their health habits and wellness.”
The study was funded by the National Institutes of Health, the American Sleep Medicine Foundation, the Roger and Paula Riney Fund, and the Daniel J. Brennan, MD Fund. Dr. Lucey consults for Merck and Eli Lilly. Dr. Snyder has disclosed no relevant financial relationships. Full disclosures are included in the original article.
A version of this article first appeared on Medscape.com.
From Brain