User login
Cutis is a peer-reviewed clinical journal for the dermatologist, allergist, and general practitioner published monthly since 1965. Concise clinical articles present the practical side of dermatology, helping physicians to improve patient care. Cutis is referenced in Index Medicus/MEDLINE and is written and edited by industry leaders.
ass lick
assault rifle
balls
ballsac
black jack
bleach
Boko Haram
bondage
causas
cheap
child abuse
cocaine
compulsive behaviors
cost of miracles
cunt
Daech
display network stats
drug paraphernalia
explosion
fart
fda and death
fda AND warn
fda AND warning
fda AND warns
feom
fuck
gambling
gfc
gun
human trafficking
humira AND expensive
illegal
ISIL
ISIS
Islamic caliphate
Islamic state
madvocate
masturbation
mixed martial arts
MMA
molestation
national rifle association
NRA
nsfw
nuccitelli
pedophile
pedophilia
poker
porn
porn
pornography
psychedelic drug
recreational drug
sex slave rings
shit
slot machine
snort
substance abuse
terrorism
terrorist
texarkana
Texas hold 'em
UFC
section[contains(@class, 'nav-hidden')]
section[contains(@class, 'nav-hidden active')
A peer-reviewed, indexed journal for dermatologists with original research, image quizzes, cases and reviews, and columns.
Wound Healing: Cellular Review With Specific Attention to Postamputation Care
Restoring skin integrity and balance after injury is vital for survival, serving as a crucial defense mechanism against potential infections by preventing the entry of harmful pathogens. Moreover, proper healing is essential for restoring normal tissue function, allowing damaged tissues to repair and, in an ideal scenario, regenerate. Timely healing helps reduce the risk for complications, such as chronic wounds, which could lead to more severe issues if left untreated. Additionally, pain relief often is associated with effective wound healing as inflammatory responses diminish during the repair process.
The immune system plays a pivotal role in wound healing, influencing various repair mechanisms and ultimately determining the extent of scarring. Although inflammation is present throughout the repair response, recent studies have challenged the conventional belief of an inverse correlation between the intensity of inflammation and regenerative capacity. Inflammatory signals were found to be crucial for timely repair and fundamental processes in regeneration, possibly presenting a paradigm shift in the understanding of immunology.1-4 The complexities of wound healing are exemplified when evaluating and treating postamputation wounds. To address such a task, one needs a firm understanding of the science behind healing wounds and what can go wrong along the way.
Phases of Wound Healing
Wound healing is a complex process that involves a series of sequential yet overlapping phases, including hemostasis/inflammation, proliferation, and remodeling.
Hemostasis/Inflammation—The initial stage of wound healing involves hemostasis, in which the primary objective is to prevent blood loss and initiate inflammation. Platelets arrive at the wound site, forming a provisional clot that is crucial for subsequent healing phases.4-6 Platelets halt bleeding as well as act as a medium for cell migration and adhesion; they also are a source of growth factors and proinflammatory cytokines that herald the inflammatory response.4-7
Inflammation is characterized by the infiltration of immune cells, particularly neutrophils and macrophages. Neutrophils act as the first line of defense, clearing debris and preventing infection. Macrophages follow, phagocytizing apoptotic cells and releasing growth factors such as tumor necrosis factor α, vascular endothelial growth factor, and matrix metalloprotease 9, which stimulate the next phase.4-6,8 Typically, the hemostasis and inflammatory phase starts approximately 6 to 8 hours after wound origin and lasts 3 to 4 days.4,6,7
Proliferation—Following hemostasis and inflammation, the wound transitions into the proliferation phase, which is marked by the development of granulation tissue—a dynamic amalgamation of fibroblasts, endothelial cells, and inflammatory cells.1,4-8 Fibroblasts play a central role in synthesizing collagen, the primary structural protein in connective tissue. They also orchestrate synthesis of vitronectin, fibronectin, fibrin, and tenascin.4-6,8 Simultaneously, angiogenesis takes place, involving the creation of new blood vessels to supply essential nutrients and oxygen to the healing tissue.4,7,9 Growth factors such as transforming growth factor β and vascular endothelial growth factor coordinate cellular activities and foster tissue repair.4-6,8 The proliferation phase extends over days to weeks, laying the groundwork for subsequent tissue restructuring.
Remodeling—The final stage of wound healing is remodeling, an extended process that may persist for several months or, in some cases, years. Throughout this phase, the initially deposited collagen, predominantly type III collagen, undergoes transformation into mature type I collagen.4-6,8 This transformation is critical for reinstating the tissue’s strength and functionality. The balance between collagen synthesis and degradation is delicate, regulated by matrix metalloproteinases and inhibitors of metalloproteinases.4-8 Fibroblasts, myofibroblasts, and other cells coordinate this intricate process of tissue reorganization.4-7
The eventual outcome of the remodeling phase determines the appearance and functionality of the healed tissue. Any disruption in this phase can lead to complications, such as chronic wounds and hypertrophic scars/keloids.4-6 These abnormal healing processes are characterized by localized inflammation, heightened fibroblast function, and excessive accumulation of the extracellular matrix.4-8
Molecular Mechanisms
Comprehensive investigations—both in vivo and in vitro—have explored the intricate molecular mechanisms involved in heightened wound healing. Transforming growth factor β takes center stage as a crucial factor, prompting the transformation of fibroblasts into myofibroblasts and contributing to the deposition of extracellular matrix.2,4-8,10 Transforming growth factor β activates non-Smad signaling pathways, such as MAPK (mitogen-activated protein kinase) and PI3K (phosphoinositide 3-kinase), influencing processes associated with fibrosis.5,11 Furthermore, microRNAs play a pivotal role in posttranscriptional regulation, influencing both transforming growth factor β signaling and fibroblast behavior.12-16
The involvement of prostaglandins is crucial in wound healing. Prostaglandin E2 plays a notable role and is positively correlated with the rate of wound healing.5 The cyclooxygenase pathway, pivotal for prostaglandin synthesis, becomes a target for inflammation control.4,5,10 Although aspirin and nonsteroidal anti-inflammatory drugs commonly are employed, their impact on wound healing remains controversial, as inhibition of cyclooxygenase may disrupt normal repair processes.5,17,18
Wound healing exhibits variations depending on age. Fetal skin regeneration is marked by the restoration of normal dermal architecture, including adnexal structures, nerves, vessels, and muscle.4-6 The distinctive characteristics of fetal wound healing include a unique profile of growth factors, a diminished inflammatory response, reduced biomechanical stress, and a distinct extracellular matrix composition.19 These factors contribute to a lower propensity for scar formation compared to the healing processes observed in adults. Fetal and adult wound healing differ fundamentally in their extracellular matrix composition, inflammatory cells, and cytokine levels.4-6,19 Adult wounds feature myofibroblasts, which are absent in fetal wounds, contributing to heightened mechanical tension.5 Delving deeper into the biochemical basis of fetal wound healing holds promise for mitigating scar formation in adults.
Takeaways From Other Species
Much of the biochemical knowledge of wound healing, especially regenerative wound healing, is known from other species. Geckos provide a unique model for studying regenerative repair in tails and nonregenerative healing in limbs after amputation. Scar-free wound healing is characterized by rapid wound closure, delayed blood vessel development, and collagen deposition, which contrasts with the hypervascular granulation tissue seen in scarring wounds.20 Scar-free wound healing and regeneration are intrinsic properties of the lizard tail and are unaffected by the location or method of detachment.21
Compared to amphibians with extraordinary regenerative capacity, data suggest the lack of regenerative capacity in mammals may come from a desynchronization of the fine-tuned interplay of progenitor cells such as blastema and differentiated cells.22,23 In mice, the response to amputation is specific to the level: cutting through the distal third of the terminal phalanx elicits a regeneration response, yielding a new digit tip resembling the lost one, while an amputation through the distal third of the intermediate phalanx triggers a wound healing and scarring response.24
Wound Healing Following Limb Amputation
Limb amputation represents a profound change in an individual’s life, impacting daily activities and overall well-being. There are many causes of amputation, but the most common include cardiovascular diseases, diabetes mellitus, cancer, and trauma.25-27 Trauma represents a relatively common cause within the US Military due to the overall young population as well as inherent risks of uniformed service.25,27 Advances in protective gear and combat casualty care have led to an increased number of individuals surviving with extremity injuries requiring amputation, particularly among younger service members, with a subgroup experiencing multiple amputations.27-29
Numerous factors play a crucial role in the healing and function of postamputation wounds. The level of amputation is a key determinant influencing both functional outcomes and the healing process. Achieving a balance between preserving function and removing damaged tissue is essential. A study investigating cardiac function and oxygen consumption in 25 patients with peripheral vascular disease found higher-level amputations resulted in decreased walking speed and cadence, along with increased oxygen consumption per meter walked.30
Selecting the appropriate amputation level is vital to optimize functional outcomes without compromising wound healing. Successful prosthetic limb fitting depends largely on the length of the residual stump to support the body load and suspend the prosthesis. For long bone amputations, maintaining at least 12-cm clearance above the knee joint in transfemoral amputees and 10-cm below the knee joint in transtibial amputees is critical for maximizing functional outcomes.31
Surgical technique also is paramount. The goal is to minimize the risk for pressure ulcers by avoiding bony spurs and muscle imbalances. Shaping the muscle and residual limb is essential for proper prosthesis fitting. Attention to neurovascular structures, such as burying nerve ends to prevent neuropathic pain during prosthesis wear, is crucial.32 In extremity amputations, surgeons often resort to free flap transfer techniques for stump reconstruction. In a study of 31 patients with severe lower extremity injuries undergoing various amputations, the use of latissimus dorsi myocutaneous flaps, alone or in combination with serratus anterior muscle flaps, resulted in fewer instances of deep ulceration and allowed for earlier prosthesis wear.33
Addressing Barriers to Wound Healing
Multiple barriers to successful wound healing are encountered in the amputee population. Amputations from trauma have a less-controlled initiation, which carries with it a higher risk for infection, poor wound healing, and other complications.
Infection—Infection often is one of the first hurdles encountered in postamputation wound healing. Critical first steps in infection prevention include thorough cleaning of soiled traumatic wounds and appropriate tissue debridement coupled with scrupulous sterile technique and postoperative monitoring for signs and symptoms of infection.
In a retrospective study of 223 combat-related major lower extremity amputations (initial and revision) between 2009 and 2015, the use of intrawound antibiotic powder at the time of closure demonstrated a 13% absolute risk reduction in deep infection rates, which was particularly notable in revision amputations, with a number needed to treat of 8 for initial amputations and 4 for revision amputations on previously infected limbs.34 Intra-operative antibiotic powder may represent a cheap and easy consideration for this special population of amputees. Postamputation antibiotic prophylaxis for infection prevention is an area of controversy. For nontraumatic infections, data suggest antibiotic prophylaxis may not decrease infection rates in these patients.35,36
Interestingly, a study by Azarbal et al37 aimed to investigate the correlation between nasal methicillin-resistant Staphylococcus aureus (MRSA) colonization and other patient factors with wound occurrence following major lower extremity amputation. The study found MRSA colonization was associated with higher rates of overall wound occurrence as well as wound occurrence due to wound infection. These data suggest nasal MRSA eradication may improve postoperative wound outcomes after major lower extremity amputation.37
Dressing Choice—The dressing chosen for a residual limb also is of paramount importance following amputation. The personalized and dynamic management of postamputation wounds and skin involves achieving optimal healing through a dressing that sustains appropriate moisture levels, addresses edema, helps prevent contractures, and safeguards the limb.38 From the start, using negative pressure wound dressings after surgical amputation can decrease wound-related complications.39
Topical oxygen therapy following amputation also shows promise. In a retrospective case series by Kalliainen et al,40 topical oxygen therapy applied to 58 wounds in 32 patients over 9 months demonstrated positive outcomes in promoting wound healing, with 38 wounds (66%) healing completely with the use of topical oxygen. Minimal complications and no detrimental effects were observed.40
Current recommendations suggest that non–weight-bearing removable rigid dressings are the superior postoperative management for transtibial amputations compared to soft dressings, offering benefits such as faster healing, reduced limb edema, earlier ambulation, preparatory shaping for prosthetic use, and prevention of knee flexion contractures.41-46 Similarly, adding a silicone liner following amputation significantly reduced the duration of prosthetic rehabilitation compared with a conventional soft dressing program in one study (P<.05).47
Specifically targeting wound edema, a case series by Hoskins et al48 investigated the impact of prostheses with vacuum-assisted suspension on the size of residual limb wounds in individuals with transtibial amputation. Well-fitting sockets with vacuum-assisted suspension did not impede wound healing, and the results suggest the potential for continued prosthesis use during the healing process.48 However, a study by Johannesson et al49 compared the outcomes of transtibial amputation patients using a vacuum-formed rigid dressing and a conventional rigid plaster dressing, finding no significant differences in wound healing, time to prosthetic fitting, or functional outcomes with the prosthesis between the 2 groups. When comparing elastic bandaging, pneumatic prosthesis, and temporary prosthesis on postoperative stump management, temporary prosthesis led to a decrease in stump volume, quicker transition to a permanent prosthesis, and improved quality of life compared with elastic bandaging and pneumatic prosthetics.50
The type of material in dressings may contribute to utility in amputation wounds. Keratin-based wound dressings show promise for wound healing, especially in recalcitrant vascular wounds.51 There also are numerous proprietary wound dressings available for patients, at least one of which has particularly thorough data. In a retrospective study of more than 2 million lower extremity wounds across 644 institutions, a proprietary bioactive human skin allograft (TheraSkin [LifeNet Health]) demonstrated higher healing rates, greater percentage area reductions, lower amputations, reduced recidivism, higher treatment completion, and fewer medical transfers compared with standard of care alone.52
Postamputation Dermatologic Concerns
After the postamputation wound heals, a notable concern is the prevalence of skin diseases affecting residual limbs. The stump site in amputees, marked by a delicate cutaneous landscape vulnerable to skin diseases, faces challenges arising from amputation-induced damage to various structures.53
When integrated into a prosthesis socket, the altered skin must acclimate to a humid environment and endure forces for which it is not well suited, especially during movement.53 Amputation remarkably alters normal tissue perfusion, which can lead to aberrant blood and lymphatic circulation in residual limbs.27,53 This compromised skin, often associated with a history of vascular disease, diabetes mellitus, or malignancy, becomes immunocompromised, heightening the risk for dermatologic issues such as inflammation, infection, and malignancies.53 Unlike the resilient volar skin on palms and soles, stump skin lacks adaptation to withstand the compressive forces generated during ambulation, sometimes leading to skin disease and pain that result in abandonment of the prosthesis.53,54 Mechanical forces on the skin, especially in active patients eager to resume pre-injury lifestyles, contribute to skin breakdown. The dynamic nature of the residual limb, including muscle atrophy, gait changes, and weight fluctuations, complicates the prosthetic fitting process. Prosthesis abandonment remains a challenge, despite modern technologic advancements.
The occurrence of heterotopic ossification (extraskeletal bone formation) is another notable issue in military amputees.27,55-57 Poor prosthetic fit can lead to skin degradation, necessitating further surgery to address mispositioned bone formations. Orthopedic monitoring supplemented by appropriate imaging studies can benefit postamputation patients by detecting and preventing heterotopic ossification in its early stages.
Dermatologic issues, especially among lower limb amputees, are noteworthy, with a substantial percentage experiencing complications related to socket prosthetics, such as heat, sweating, sores, and skin irritation. Up to 41% of patients are seen regularly for a secondary skin disorder following amputation.58 As one might expect, persistent wounds, blisters, ulcers, and abscesses are some of the most typical cutaneous abnormalities affecting residual limbs with prostheses.27,58 More rare skin conditions also are documented in residual limbs, including cutaneous granuloma, verrucous carcinoma, bullous pemphigoid, and angiodermatitis.27,59-61
Treatments offered in the dermatology clinic often are similar to patients who have not had an amputation. For instance, hyperhidrosis can be treated with prescription antiperspirant, topical aluminum chloride, topical glycopyrronium, botulinum toxin, and iontophoresis, which can greatly decrease skin irritation and malodor. Subcutaneous neurotoxins such as botulinum toxin are especially useful for hyperhidrosis following amputation because a single treatment can last 3 to 6 months, whereas topicals must be applied multiple times per day and can be inherently irritating to the skin.27,62 Furthermore, ablative fractional resurfacing lasers also can help stimulate new collagen growth, increase skin mobility on residual limbs, smooth jagged scars, and aid prosthetic fitting.27,63 Perforated prosthetic liners also may be useful to address issues such as excessive sweating, demonstrating improvements in skin health, reduced sweating problems, and potential avoidance of surgical interventions.64
When comorbid skin conditions are at bay, preventive measures for excessive wound healing necessitate early recognition and timely intervention for residual limbs. Preventive techniques encompass the use of silicone gel sheeting, hypoallergenic microporous tape, and intralesional steroid injections.
Psychological Concerns—An overarching issue following amputation is the psychological toll the process imposes on the patient. Psychological concerns, including anxiety and depression, present additional challenges impacting residual limb hygiene and prosthetic maintenance. Chronic wounds are devastating to patients. These patients consistently express feeling ostracized from their community and anxious about unemployment, leaking fluid, or odor from the wound, as well as other social stigmata.62 Depression and anxiety can hinder a patient’s ability to care for their wound and make them more susceptible to the myriad issues that can ensue.
Recent Developments in Wound Healing
Wound healing is ripe for innovation that could assuage ailments that impact patients following amputation. A 2022 study by Abu El Hawa et al65 illustrated advanced progression in wound healing for patients taking statins, even though the statin group had increased age and number of comorbidities compared with patients not taking statins.
Nasseri and Sharifi66 showed the potential of antimicrobial peptides—small proteins with cationic charges and amphipathic structures exhibiting electrostatic interaction with microbial cell membranes—in promoting wound healing, particularly defensins and cathelicidin LL-37.They also discussed innovative delivery systems, such as nanoparticles and electrospun fibrous scaffolds, highlighting their potential as possibly more effective therapeutics than antibiotics, especially in the context of diabetic wound closure.66 Aimed at increased angiogenesis in the proliferative phase, there is evidence that N-acetylcysteine can increase amputation stump perfusion with the goal of better long-term wound healing and more efficient scar formation.67
Stem cell therapy, particularly employing cells from the human amniotic membrane, represents an auspicious avenue for antifibrotic treatment. Amniotic epithelial cells and amniotic mesenchymal cells, with their self-renewal and multilineage differentiation capabilities, exhibit anti-inflammatory and antifibrotic properties.4,5 A study by Dong et al68 aimed to assess the efficacy of cell therapy, particularly differentiated progenitor cell–based graft transplantation or autologous stem cell injection, in treating refractory skin injuries such as nonrevascularizable critical limb ischemic ulcers, venous leg ulcers, and diabetic lower limb ulcers. The findings demonstrated cell therapy effectively reduced the size of ulcers, improved wound closure rates, and decreased major amputation rates compared with standard therapy. Of note, cell therapy had limited impact on alleviating pain in patients with critical limb ischemia-related cutaneous ulcers.68
Final Thoughts
Wound care following amputation is a multidisciplinary endeavor, necessitating collaboration between many health care professionals. Dermatologists play a crucial role in providing routine care as well as addressing wound healing and related skin issues among amputation patients. As the field progresses, dermatologists are well positioned to make notable contributions and ensure enhanced outcomes, resulting in a better quality of life for patients facing the challenges of limb amputation and prosthetic use.
- Brockes JP, Kumar A. Comparative aspects of animal regeneration. Annu Rev Cell Dev Biol. 2008;24:525-549. doi:10.1146/annurev.cellbio.24.110707.175336
- Eming SA, Hammerschmidt M, Krieg T, et al. Interrelation of immunity and tissue repair or regeneration. Semin Cell Dev Biol. 2009;20:517-527. doi:10.1016/j.semcdb.2009.04.009
- Eming SA. Evolution of immune pathways in regeneration and repair: recent concepts and translational perspectives. Semin Immunol. 2014;26:275-276. doi:10.1016/j.smim.2014.09.001
- Bolognia JL, Jorizzo JJ, Schaffer JV, et al. Dermatology. 4th edition. Elsevier; 2018.
- Wang PH, Huang BS, Horng HC, et al. Wound healing. J Chin Med Assoc JCMA. 2018;81:94-101. doi:10.1016/j.jcma.2017.11.002
- Velnar T, Bailey T, Smrkolj V. The wound healing process: an overview of the cellular and molecular mechanisms. J Int Med Res. 2009;37:1528-1542. doi:10.1177/147323000903700531
- Gurtner GC, Werner S, Barrandon Y, et al. Wound repair and regeneration. Nature. 2008;453:314-321. doi:10.1038/nature07039
- Eming SA, Martin P, Tomic-Canic M. Wound repair and regeneration: mechanisms, signaling, and translation. Sci Transl Med. 2014;6:265sr6. doi:10.1126/scitranslmed.3009337
- Eming SA, Brachvogel B, Odorisio T, et al. Regulation of angiogenesis: wound healing as a model. Prog Histochem Cytochem. 2007;42:115-170. doi:10.1016/j.proghi.2007.06.001
- Janis JE, Harrison B. Wound healing: part I. basic science. Plast Reconstr Surg. 2016;138(3 suppl):9S-17S. doi:10.1097/PRS.0000000000002773
- Profyris C, Tziotzios C, Do Vale I. Cutaneous scarring: pathophysiology, molecular mechanisms, and scar reduction therapeutics. part I: the molecular basis of scar formation. J Am Acad Dermatol. 2012;66:1-10; quiz 11-12. doi:10.1016/j.jaad.2011.05.055
- Kwan P, Ding J, Tredget EE. MicroRNA 181b regulates decorin production by dermal fibroblasts and may be a potential therapy for hypertrophic scar. PLoS One. 2015;10:e0123054. doi:10.1371/journal.pone.0123054
- Ben W, Yang Y, Yuan J, et al. Human papillomavirus 16 E6 modulates the expression of host microRNAs in cervical cancer. Taiwan J Obstet Gynecol. 2015;54:364-370. doi:10.1016/j.tjog.2014.06.007
- Yu EH, Tu HF, Wu CH, et al. MicroRNA-21 promotes perineural invasion and impacts survival in patients with oral carcinoma. J Chin Med Assoc JCMA. 2017;80:383-388. doi:10.1016/j.jcma.2017.01.003
- Wen KC, Sung PL, Yen MS, et al. MicroRNAs regulate several functions of normal tissues and malignancies. Taiwan J Obstet Gynecol. 2013;52:465-469. doi:10.1016/j.tjog.2013.10.002
- Babalola O, Mamalis A, Lev-Tov H, et al. The role of microRNAs in skin fibrosis. Arch Dermatol Res. 2013;305:763-776. doi:10.1007/s00403-013-1410-1
- Hofer M, Hoferová Z, Falk M. Pharmacological modulation of radiation damage. does it exist a chance for other substances than hematopoietic growth factors and cytokines? Int J Mol Sci. 2017;18:1385. doi:10.3390/ijms18071385
- Darby IA, Weller CD. Aspirin treatment for chronic wounds: potential beneficial and inhibitory effects. Wound Repair Regen. 2017;25:7-12. doi:10.1111/wrr.12502
- Khalid KA, Nawi AFM, Zulkifli N, et al. Aging and wound healing of the skin: a review of clinical and pathophysiological hallmarks. Life. 2022;12:2142. doi:10.3390/life12122142
- Peacock HM, Gilbert EAB, Vickaryous MK. Scar‐free cutaneous wound healing in the leopard gecko, Eublepharis macularius. J Anat. 2015;227:596-610. doi:10.1111/joa.12368
- Delorme SL, Lungu IM, Vickaryous MK. Scar‐free wound healing and regeneration following tail loss in the leopard gecko, Eublepharis macularius. Anat Rec. 2012;295:1575-1595. doi:10.1002/ar.22490
- Brunauer R, Xia IG, Asrar SN, et al. Aging delays epimorphic regeneration in mice. J Gerontol Ser A Biol Sci Med Sci. 2021;76:1726-1733. doi:10.1093/gerona/glab131
- Dolan CP, Yang TJ, Zimmel K, et al. Epimorphic regeneration of the mouse digit tip is finite. Stem Cell Res Ther. 2022;13:62. doi:10.1186/s13287-022-02741-2
- Simkin J, Han M, Yu L, et al. The mouse digit tip: from wound healing to regeneration. Methods Mol Biol Clifton NJ. 2013;1037:419-435. doi:10.1007/978-1-62703-505-7_24
- Ziegler-Graham K, MacKenzie EJ, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422-429. doi:10.1016/j.apmr.2007.11.005
- Dudek NL, Marks MB, Marshall SC, et al. Dermatologic conditions associated with use of a lower-extremity prosthesis. Arch Phys Med Rehabil. 2005;86:659-663. doi:10.1016/j.apmr.2004.09.003
- Lannan FM, Meyerle JH. The dermatologist’s role in amputee skin care. Cutis. 2019;103:86-90.
- Dougherty AL, Mohrle CR, Galarneau MR, et al. Battlefield extremity injuries in Operation Iraqi Freedom. Injury. 2009;40:772-777. doi:10.1016/j.injury.2009.02.014
- Epstein RA, Heinemann AW, McFarland LV. Quality of life for veterans and servicemembers with major traumatic limb loss from Vietnam and OIF/OEF conflicts. J Rehabil Res Dev. 2010;47:373-385. doi:10.1682/jrrd.2009.03.0023
- Pinzur MS, Gold J, Schwartz D, et al. Energy demands for walking in dysvascular amputees as related to the level of amputation. Orthopedics. 1992;15:1033-1036; discussion 1036-1037. doi:10.3928/0147-7447-19920901-07
- Robinson V, Sansam K, Hirst L, et al. Major lower limb amputation–what, why and how to achieve the best results. Orthop Trauma. 2010;24:276-285. doi:10.1016/j.mporth.2010.03.017
- Lu S, Wang C, Zhong W, et al. Amputation stump revision using a free sural neurocutaneous perforator flap. Ann Plast Surg. 2016;76:83-87. doi:10.1097/SAP.0000000000000211
- Kim SW, Jeon SB, Hwang KT, et al. Coverage of amputation stumps using a latissimus dorsi flap with a serratus anterior muscle flap: a comparative study. Ann Plast Surg. 2016;76:88-93. doi:10.1097/SAP.0000000000000220
- Pavey GJ, Formby PM, Hoyt BW, et al. Intrawound antibiotic powder decreases frequency of deep infection and severity of heterotopic ossification in combat lower extremity amputations. Clin Orthop. 2019;477:802-810. doi:10.1007/s11999.0000000000000090
- Dunkel N, Belaieff W, Assal M, et al. Wound dehiscence and stump infection after lower limb amputation: risk factors and association with antibiotic use. J Orthop Sci Off J Jpn Orthop Assoc. 2012;17:588-594. doi:10.1007/s00776-012-0245-5
- Rubin G, Orbach H, Rinott M, et al. The use of prophylactic antibiotics in treatment of fingertip amputation: a randomized prospective trial. Am J Emerg Med. 2015;33:645-647. doi:10.1016/j.ajem.2015.02.002
- Azarbal AF, Harris S, Mitchell EL, et al. Nasal methicillin-resistant Staphylococcus aureus colonization is associated with increased wound occurrence after major lower extremity amputation. J Vasc Surg. 2015;62:401-405. doi:10.1016/j.jvs.2015.02.052
- Kwasniewski M, Mitchel D. Post amputation skin and wound care. Phys Med Rehabil Clin N Am. 2022;33:857-870. doi:10.1016/j.pmr.2022.06.010
- Chang H, Maldonado TS, Rockman CB, et al. Closed incision negative pressure wound therapy may decrease wound complications in major lower extremity amputations. J Vasc Surg. 2021;73:1041-1047. doi:10.1016/j.jvs.2020.07.061
- Kalliainen LK, Gordillo GM, Schlanger R, et al. Topical oxygen as an adjunct to wound healing: a clinical case series. Pathophysiol Off J Int Soc Pathophysiol. 2003;9:81-87. doi:10.1016/s0928-4680(02)00079-2
- Reichmann JP, Stevens PM, Rheinstein J, et al. Removable rigid dressings for postoperative management of transtibial amputations: a review of published evidence. PM R. 2018;10:516-523. doi:10.1016/j.pmrj.2017.10.002
- MacLean N, Fick GH. The effect of semirigid dressings on below-knee amputations. Phys Ther. 1994;74:668-673. doi:10.1093/ptj/74.7.668
- Koonalinthip N, Sukthongsa A, Janchai S. Comparison of removable rigid dressing and elastic bandage for residual limb maturation in transtibial amputees: a randomized controlled trial. Arch Phys Med Rehabil. 2020;101:1683-1688. doi:10.1016/j.apmr.2020.05.009
- Taylor L, Cavenett S, Stepien JM, et al. Removable rigid dressings: a retrospective case-note audit to determine the validity of post-amputation application. Prosthet Orthot Int. 2008;32:223-230. doi:10.1080/03093640802016795
- Sumpio B, Shine SR, Mahler D, et al. A comparison of immediate postoperative rigid and soft dressings for below-knee amputations. Ann Vasc Surg. 2013;27:774-780. doi:10.1016/j.avsg.2013.03.007
- van Velzen AD, Nederhand MJ, Emmelot CH, et al. Early treatment of trans-tibial amputees: retrospective analysis of early fitting and elastic bandaging. Prosthet Orthot Int. 2005;29:3-12. doi:10.1080/17461550500069588
- Chin T, Toda M. Results of prosthetic rehabilitation on managing transtibial vascular amputation with silicone liner after wound closure. J Int Med Res. 2016;44:957-967. doi:10.1177/0300060516647554
- Hoskins RD, Sutton EE, Kinor D, et al. Using vacuum-assisted suspension to manage residual limb wounds in persons with transtibial amputation: a case series. Prosthet Orthot Int. 2014;38:68-74. doi:10.1177/0309364613487547
- Johannesson A, Larsson GU, Oberg T, et al. Comparison of vacuum-formed removable rigid dressing with conventional rigid dressing after transtibial amputation: similar outcome in a randomized controlled trial involving 27 patients. Acta Orthop. 2008;79:361-369. doi:10.1080/17453670710015265
- Alsancak S, Köse SK, Altınkaynak H. Effect of elastic bandaging and prosthesis on the decrease in stump volume. Acta Orthop Traumatol Turc. 2011;45:14-22. doi:10.3944/AOTT.2011.2365
- Than MP, Smith RA, Hammond C, et al. Keratin-based wound care products for treatment of resistant vascular wounds. J Clin Aesthetic Dermatol. 2012;5:31-35.
- Gurtner GC, Garcia AD, Bakewell K, et al. A retrospective matched‐cohort study of 3994 lower extremity wounds of multiple etiologies across 644 institutions comparing a bioactive human skin allograft, TheraSkin, plus standard of care, to standard of care alone. Int Wound J. 2020;17:55-64. doi:10.1111/iwj.13231
- Buikema KES, Meyerle JH. Amputation stump: privileged harbor for infections, tumors, and immune disorders. Clin Dermatol. 2014;32:670-677. doi:10.1016/j.clindermatol.2014.04.015
- Yang NB, Garza LA, Foote CE, et al. High prevalence of stump dermatoses 38 years or more after amputation. Arch Dermatol. 2012;148:1283-1286. doi:10.1001/archdermatol.2012.3004
- Potter BK, Burns TC, Lacap AP, et al. Heterotopic ossification following traumatic and combat-related amputations. Prevalence, risk factors, and preliminary results of excision. J Bone Joint Surg Am. 2007;89:476-486. doi:10.2106/JBJS.F.00412
- Edwards DS, Kuhn KM, Potter BK, et al. Heterotopic ossification: a review of current understanding, treatment, and future. J Orthop Trauma. 2016;30(suppl 3):S27-S30. doi:10.1097/BOT.0000000000000666
- Tintle SM, Shawen SB, Forsberg JA, et al. Reoperation after combat-related major lower extremity amputations. J Orthop Trauma. 2014;28:232-237. doi:10.1097/BOT.0b013e3182a53130
- Bui KM, Raugi GJ, Nguyen VQ, et al. Skin problems in individuals with lower-limb loss: literature review and proposed classification system. J Rehabil Res Dev. 2009;46:1085-1090. doi:10.1682/jrrd.2009.04.0052
- Turan H, Bas¸kan EB, Adim SB, et al. Acroangiodermatitis in a below-knee amputation stump. Clin Exp Dermatol. 2011;36:560-561. doi:10.1111/j.1365-2230.2011.04037.x
- Lin CH, Ma H, Chung MT, et al. Granulomatous cutaneous lesions associated with risperidone-induced hyperprolactinemia in an amputated upper limb. Int J Dermatol. 2012;51:75-78. doi:10.1111/j.1365-4632.2011.04906.x
- Schwartz RA, Bagley MP, Janniger CK, et al. Verrucous carcinoma of a leg amputation stump. Dermatologica. 1991;182:193-195. doi:10.1159/000247782
- Campanati A, Diotallevi F, Radi G, et al. Efficacy and safety of botulinum toxin B in focal hyperhidrosis: a narrative review. Toxins. 2023;15:147. doi:10.3390/toxins15020147
- Anderson RR, Donelan MB, Hivnor C, et al. Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: consensus report. JAMA Dermatol. 2014;150:187-193. doi:10.1001/jamadermatol.2013.7761
- McGrath M, McCarthy J, Gallego A, et al. The influence of perforated prosthetic liners on residual limb wound healing: a case report. Can Prosthet Orthot J. 2019;2:32723. doi:10.33137/cpoj.v2i1.32723
- Abu El Hawa AA, Klein D, Bekeny JC, et al. The impact of statins on wound healing: an ally in treating the highly comorbid patient. J Wound Care. 2022;31(suppl 2):S36-S41. doi:10.12968/jowc.2022.31.Sup2.S36
- Nasseri S, Sharifi M. Therapeutic potential of antimicrobial peptides for wound healing. Int J Pept Res Ther. 2022;28:38. doi:10.1007/s10989-021-10350-5
- Lee JV, Engel C, Tay S, et al. N-Acetyl-Cysteine treatment after lower extremity amputation improves areas of perfusion defect and wound healing outcomes. J Vasc Surg. 2021;73:39-40. doi:10.1016/j.jvs.2020.12.025
- Dong Y, Yang Q, Sun X. Comprehensive analysis of cell therapy on chronic skin wound healing: a meta-analysis. Hum Gene Ther. 2021;32:787-795. doi:10.1089/hum.2020.275
Restoring skin integrity and balance after injury is vital for survival, serving as a crucial defense mechanism against potential infections by preventing the entry of harmful pathogens. Moreover, proper healing is essential for restoring normal tissue function, allowing damaged tissues to repair and, in an ideal scenario, regenerate. Timely healing helps reduce the risk for complications, such as chronic wounds, which could lead to more severe issues if left untreated. Additionally, pain relief often is associated with effective wound healing as inflammatory responses diminish during the repair process.
The immune system plays a pivotal role in wound healing, influencing various repair mechanisms and ultimately determining the extent of scarring. Although inflammation is present throughout the repair response, recent studies have challenged the conventional belief of an inverse correlation between the intensity of inflammation and regenerative capacity. Inflammatory signals were found to be crucial for timely repair and fundamental processes in regeneration, possibly presenting a paradigm shift in the understanding of immunology.1-4 The complexities of wound healing are exemplified when evaluating and treating postamputation wounds. To address such a task, one needs a firm understanding of the science behind healing wounds and what can go wrong along the way.
Phases of Wound Healing
Wound healing is a complex process that involves a series of sequential yet overlapping phases, including hemostasis/inflammation, proliferation, and remodeling.
Hemostasis/Inflammation—The initial stage of wound healing involves hemostasis, in which the primary objective is to prevent blood loss and initiate inflammation. Platelets arrive at the wound site, forming a provisional clot that is crucial for subsequent healing phases.4-6 Platelets halt bleeding as well as act as a medium for cell migration and adhesion; they also are a source of growth factors and proinflammatory cytokines that herald the inflammatory response.4-7
Inflammation is characterized by the infiltration of immune cells, particularly neutrophils and macrophages. Neutrophils act as the first line of defense, clearing debris and preventing infection. Macrophages follow, phagocytizing apoptotic cells and releasing growth factors such as tumor necrosis factor α, vascular endothelial growth factor, and matrix metalloprotease 9, which stimulate the next phase.4-6,8 Typically, the hemostasis and inflammatory phase starts approximately 6 to 8 hours after wound origin and lasts 3 to 4 days.4,6,7
Proliferation—Following hemostasis and inflammation, the wound transitions into the proliferation phase, which is marked by the development of granulation tissue—a dynamic amalgamation of fibroblasts, endothelial cells, and inflammatory cells.1,4-8 Fibroblasts play a central role in synthesizing collagen, the primary structural protein in connective tissue. They also orchestrate synthesis of vitronectin, fibronectin, fibrin, and tenascin.4-6,8 Simultaneously, angiogenesis takes place, involving the creation of new blood vessels to supply essential nutrients and oxygen to the healing tissue.4,7,9 Growth factors such as transforming growth factor β and vascular endothelial growth factor coordinate cellular activities and foster tissue repair.4-6,8 The proliferation phase extends over days to weeks, laying the groundwork for subsequent tissue restructuring.
Remodeling—The final stage of wound healing is remodeling, an extended process that may persist for several months or, in some cases, years. Throughout this phase, the initially deposited collagen, predominantly type III collagen, undergoes transformation into mature type I collagen.4-6,8 This transformation is critical for reinstating the tissue’s strength and functionality. The balance between collagen synthesis and degradation is delicate, regulated by matrix metalloproteinases and inhibitors of metalloproteinases.4-8 Fibroblasts, myofibroblasts, and other cells coordinate this intricate process of tissue reorganization.4-7
The eventual outcome of the remodeling phase determines the appearance and functionality of the healed tissue. Any disruption in this phase can lead to complications, such as chronic wounds and hypertrophic scars/keloids.4-6 These abnormal healing processes are characterized by localized inflammation, heightened fibroblast function, and excessive accumulation of the extracellular matrix.4-8
Molecular Mechanisms
Comprehensive investigations—both in vivo and in vitro—have explored the intricate molecular mechanisms involved in heightened wound healing. Transforming growth factor β takes center stage as a crucial factor, prompting the transformation of fibroblasts into myofibroblasts and contributing to the deposition of extracellular matrix.2,4-8,10 Transforming growth factor β activates non-Smad signaling pathways, such as MAPK (mitogen-activated protein kinase) and PI3K (phosphoinositide 3-kinase), influencing processes associated with fibrosis.5,11 Furthermore, microRNAs play a pivotal role in posttranscriptional regulation, influencing both transforming growth factor β signaling and fibroblast behavior.12-16
The involvement of prostaglandins is crucial in wound healing. Prostaglandin E2 plays a notable role and is positively correlated with the rate of wound healing.5 The cyclooxygenase pathway, pivotal for prostaglandin synthesis, becomes a target for inflammation control.4,5,10 Although aspirin and nonsteroidal anti-inflammatory drugs commonly are employed, their impact on wound healing remains controversial, as inhibition of cyclooxygenase may disrupt normal repair processes.5,17,18
Wound healing exhibits variations depending on age. Fetal skin regeneration is marked by the restoration of normal dermal architecture, including adnexal structures, nerves, vessels, and muscle.4-6 The distinctive characteristics of fetal wound healing include a unique profile of growth factors, a diminished inflammatory response, reduced biomechanical stress, and a distinct extracellular matrix composition.19 These factors contribute to a lower propensity for scar formation compared to the healing processes observed in adults. Fetal and adult wound healing differ fundamentally in their extracellular matrix composition, inflammatory cells, and cytokine levels.4-6,19 Adult wounds feature myofibroblasts, which are absent in fetal wounds, contributing to heightened mechanical tension.5 Delving deeper into the biochemical basis of fetal wound healing holds promise for mitigating scar formation in adults.
Takeaways From Other Species
Much of the biochemical knowledge of wound healing, especially regenerative wound healing, is known from other species. Geckos provide a unique model for studying regenerative repair in tails and nonregenerative healing in limbs after amputation. Scar-free wound healing is characterized by rapid wound closure, delayed blood vessel development, and collagen deposition, which contrasts with the hypervascular granulation tissue seen in scarring wounds.20 Scar-free wound healing and regeneration are intrinsic properties of the lizard tail and are unaffected by the location or method of detachment.21
Compared to amphibians with extraordinary regenerative capacity, data suggest the lack of regenerative capacity in mammals may come from a desynchronization of the fine-tuned interplay of progenitor cells such as blastema and differentiated cells.22,23 In mice, the response to amputation is specific to the level: cutting through the distal third of the terminal phalanx elicits a regeneration response, yielding a new digit tip resembling the lost one, while an amputation through the distal third of the intermediate phalanx triggers a wound healing and scarring response.24
Wound Healing Following Limb Amputation
Limb amputation represents a profound change in an individual’s life, impacting daily activities and overall well-being. There are many causes of amputation, but the most common include cardiovascular diseases, diabetes mellitus, cancer, and trauma.25-27 Trauma represents a relatively common cause within the US Military due to the overall young population as well as inherent risks of uniformed service.25,27 Advances in protective gear and combat casualty care have led to an increased number of individuals surviving with extremity injuries requiring amputation, particularly among younger service members, with a subgroup experiencing multiple amputations.27-29
Numerous factors play a crucial role in the healing and function of postamputation wounds. The level of amputation is a key determinant influencing both functional outcomes and the healing process. Achieving a balance between preserving function and removing damaged tissue is essential. A study investigating cardiac function and oxygen consumption in 25 patients with peripheral vascular disease found higher-level amputations resulted in decreased walking speed and cadence, along with increased oxygen consumption per meter walked.30
Selecting the appropriate amputation level is vital to optimize functional outcomes without compromising wound healing. Successful prosthetic limb fitting depends largely on the length of the residual stump to support the body load and suspend the prosthesis. For long bone amputations, maintaining at least 12-cm clearance above the knee joint in transfemoral amputees and 10-cm below the knee joint in transtibial amputees is critical for maximizing functional outcomes.31
Surgical technique also is paramount. The goal is to minimize the risk for pressure ulcers by avoiding bony spurs and muscle imbalances. Shaping the muscle and residual limb is essential for proper prosthesis fitting. Attention to neurovascular structures, such as burying nerve ends to prevent neuropathic pain during prosthesis wear, is crucial.32 In extremity amputations, surgeons often resort to free flap transfer techniques for stump reconstruction. In a study of 31 patients with severe lower extremity injuries undergoing various amputations, the use of latissimus dorsi myocutaneous flaps, alone or in combination with serratus anterior muscle flaps, resulted in fewer instances of deep ulceration and allowed for earlier prosthesis wear.33
Addressing Barriers to Wound Healing
Multiple barriers to successful wound healing are encountered in the amputee population. Amputations from trauma have a less-controlled initiation, which carries with it a higher risk for infection, poor wound healing, and other complications.
Infection—Infection often is one of the first hurdles encountered in postamputation wound healing. Critical first steps in infection prevention include thorough cleaning of soiled traumatic wounds and appropriate tissue debridement coupled with scrupulous sterile technique and postoperative monitoring for signs and symptoms of infection.
In a retrospective study of 223 combat-related major lower extremity amputations (initial and revision) between 2009 and 2015, the use of intrawound antibiotic powder at the time of closure demonstrated a 13% absolute risk reduction in deep infection rates, which was particularly notable in revision amputations, with a number needed to treat of 8 for initial amputations and 4 for revision amputations on previously infected limbs.34 Intra-operative antibiotic powder may represent a cheap and easy consideration for this special population of amputees. Postamputation antibiotic prophylaxis for infection prevention is an area of controversy. For nontraumatic infections, data suggest antibiotic prophylaxis may not decrease infection rates in these patients.35,36
Interestingly, a study by Azarbal et al37 aimed to investigate the correlation between nasal methicillin-resistant Staphylococcus aureus (MRSA) colonization and other patient factors with wound occurrence following major lower extremity amputation. The study found MRSA colonization was associated with higher rates of overall wound occurrence as well as wound occurrence due to wound infection. These data suggest nasal MRSA eradication may improve postoperative wound outcomes after major lower extremity amputation.37
Dressing Choice—The dressing chosen for a residual limb also is of paramount importance following amputation. The personalized and dynamic management of postamputation wounds and skin involves achieving optimal healing through a dressing that sustains appropriate moisture levels, addresses edema, helps prevent contractures, and safeguards the limb.38 From the start, using negative pressure wound dressings after surgical amputation can decrease wound-related complications.39
Topical oxygen therapy following amputation also shows promise. In a retrospective case series by Kalliainen et al,40 topical oxygen therapy applied to 58 wounds in 32 patients over 9 months demonstrated positive outcomes in promoting wound healing, with 38 wounds (66%) healing completely with the use of topical oxygen. Minimal complications and no detrimental effects were observed.40
Current recommendations suggest that non–weight-bearing removable rigid dressings are the superior postoperative management for transtibial amputations compared to soft dressings, offering benefits such as faster healing, reduced limb edema, earlier ambulation, preparatory shaping for prosthetic use, and prevention of knee flexion contractures.41-46 Similarly, adding a silicone liner following amputation significantly reduced the duration of prosthetic rehabilitation compared with a conventional soft dressing program in one study (P<.05).47
Specifically targeting wound edema, a case series by Hoskins et al48 investigated the impact of prostheses with vacuum-assisted suspension on the size of residual limb wounds in individuals with transtibial amputation. Well-fitting sockets with vacuum-assisted suspension did not impede wound healing, and the results suggest the potential for continued prosthesis use during the healing process.48 However, a study by Johannesson et al49 compared the outcomes of transtibial amputation patients using a vacuum-formed rigid dressing and a conventional rigid plaster dressing, finding no significant differences in wound healing, time to prosthetic fitting, or functional outcomes with the prosthesis between the 2 groups. When comparing elastic bandaging, pneumatic prosthesis, and temporary prosthesis on postoperative stump management, temporary prosthesis led to a decrease in stump volume, quicker transition to a permanent prosthesis, and improved quality of life compared with elastic bandaging and pneumatic prosthetics.50
The type of material in dressings may contribute to utility in amputation wounds. Keratin-based wound dressings show promise for wound healing, especially in recalcitrant vascular wounds.51 There also are numerous proprietary wound dressings available for patients, at least one of which has particularly thorough data. In a retrospective study of more than 2 million lower extremity wounds across 644 institutions, a proprietary bioactive human skin allograft (TheraSkin [LifeNet Health]) demonstrated higher healing rates, greater percentage area reductions, lower amputations, reduced recidivism, higher treatment completion, and fewer medical transfers compared with standard of care alone.52
Postamputation Dermatologic Concerns
After the postamputation wound heals, a notable concern is the prevalence of skin diseases affecting residual limbs. The stump site in amputees, marked by a delicate cutaneous landscape vulnerable to skin diseases, faces challenges arising from amputation-induced damage to various structures.53
When integrated into a prosthesis socket, the altered skin must acclimate to a humid environment and endure forces for which it is not well suited, especially during movement.53 Amputation remarkably alters normal tissue perfusion, which can lead to aberrant blood and lymphatic circulation in residual limbs.27,53 This compromised skin, often associated with a history of vascular disease, diabetes mellitus, or malignancy, becomes immunocompromised, heightening the risk for dermatologic issues such as inflammation, infection, and malignancies.53 Unlike the resilient volar skin on palms and soles, stump skin lacks adaptation to withstand the compressive forces generated during ambulation, sometimes leading to skin disease and pain that result in abandonment of the prosthesis.53,54 Mechanical forces on the skin, especially in active patients eager to resume pre-injury lifestyles, contribute to skin breakdown. The dynamic nature of the residual limb, including muscle atrophy, gait changes, and weight fluctuations, complicates the prosthetic fitting process. Prosthesis abandonment remains a challenge, despite modern technologic advancements.
The occurrence of heterotopic ossification (extraskeletal bone formation) is another notable issue in military amputees.27,55-57 Poor prosthetic fit can lead to skin degradation, necessitating further surgery to address mispositioned bone formations. Orthopedic monitoring supplemented by appropriate imaging studies can benefit postamputation patients by detecting and preventing heterotopic ossification in its early stages.
Dermatologic issues, especially among lower limb amputees, are noteworthy, with a substantial percentage experiencing complications related to socket prosthetics, such as heat, sweating, sores, and skin irritation. Up to 41% of patients are seen regularly for a secondary skin disorder following amputation.58 As one might expect, persistent wounds, blisters, ulcers, and abscesses are some of the most typical cutaneous abnormalities affecting residual limbs with prostheses.27,58 More rare skin conditions also are documented in residual limbs, including cutaneous granuloma, verrucous carcinoma, bullous pemphigoid, and angiodermatitis.27,59-61
Treatments offered in the dermatology clinic often are similar to patients who have not had an amputation. For instance, hyperhidrosis can be treated with prescription antiperspirant, topical aluminum chloride, topical glycopyrronium, botulinum toxin, and iontophoresis, which can greatly decrease skin irritation and malodor. Subcutaneous neurotoxins such as botulinum toxin are especially useful for hyperhidrosis following amputation because a single treatment can last 3 to 6 months, whereas topicals must be applied multiple times per day and can be inherently irritating to the skin.27,62 Furthermore, ablative fractional resurfacing lasers also can help stimulate new collagen growth, increase skin mobility on residual limbs, smooth jagged scars, and aid prosthetic fitting.27,63 Perforated prosthetic liners also may be useful to address issues such as excessive sweating, demonstrating improvements in skin health, reduced sweating problems, and potential avoidance of surgical interventions.64
When comorbid skin conditions are at bay, preventive measures for excessive wound healing necessitate early recognition and timely intervention for residual limbs. Preventive techniques encompass the use of silicone gel sheeting, hypoallergenic microporous tape, and intralesional steroid injections.
Psychological Concerns—An overarching issue following amputation is the psychological toll the process imposes on the patient. Psychological concerns, including anxiety and depression, present additional challenges impacting residual limb hygiene and prosthetic maintenance. Chronic wounds are devastating to patients. These patients consistently express feeling ostracized from their community and anxious about unemployment, leaking fluid, or odor from the wound, as well as other social stigmata.62 Depression and anxiety can hinder a patient’s ability to care for their wound and make them more susceptible to the myriad issues that can ensue.
Recent Developments in Wound Healing
Wound healing is ripe for innovation that could assuage ailments that impact patients following amputation. A 2022 study by Abu El Hawa et al65 illustrated advanced progression in wound healing for patients taking statins, even though the statin group had increased age and number of comorbidities compared with patients not taking statins.
Nasseri and Sharifi66 showed the potential of antimicrobial peptides—small proteins with cationic charges and amphipathic structures exhibiting electrostatic interaction with microbial cell membranes—in promoting wound healing, particularly defensins and cathelicidin LL-37.They also discussed innovative delivery systems, such as nanoparticles and electrospun fibrous scaffolds, highlighting their potential as possibly more effective therapeutics than antibiotics, especially in the context of diabetic wound closure.66 Aimed at increased angiogenesis in the proliferative phase, there is evidence that N-acetylcysteine can increase amputation stump perfusion with the goal of better long-term wound healing and more efficient scar formation.67
Stem cell therapy, particularly employing cells from the human amniotic membrane, represents an auspicious avenue for antifibrotic treatment. Amniotic epithelial cells and amniotic mesenchymal cells, with their self-renewal and multilineage differentiation capabilities, exhibit anti-inflammatory and antifibrotic properties.4,5 A study by Dong et al68 aimed to assess the efficacy of cell therapy, particularly differentiated progenitor cell–based graft transplantation or autologous stem cell injection, in treating refractory skin injuries such as nonrevascularizable critical limb ischemic ulcers, venous leg ulcers, and diabetic lower limb ulcers. The findings demonstrated cell therapy effectively reduced the size of ulcers, improved wound closure rates, and decreased major amputation rates compared with standard therapy. Of note, cell therapy had limited impact on alleviating pain in patients with critical limb ischemia-related cutaneous ulcers.68
Final Thoughts
Wound care following amputation is a multidisciplinary endeavor, necessitating collaboration between many health care professionals. Dermatologists play a crucial role in providing routine care as well as addressing wound healing and related skin issues among amputation patients. As the field progresses, dermatologists are well positioned to make notable contributions and ensure enhanced outcomes, resulting in a better quality of life for patients facing the challenges of limb amputation and prosthetic use.
Restoring skin integrity and balance after injury is vital for survival, serving as a crucial defense mechanism against potential infections by preventing the entry of harmful pathogens. Moreover, proper healing is essential for restoring normal tissue function, allowing damaged tissues to repair and, in an ideal scenario, regenerate. Timely healing helps reduce the risk for complications, such as chronic wounds, which could lead to more severe issues if left untreated. Additionally, pain relief often is associated with effective wound healing as inflammatory responses diminish during the repair process.
The immune system plays a pivotal role in wound healing, influencing various repair mechanisms and ultimately determining the extent of scarring. Although inflammation is present throughout the repair response, recent studies have challenged the conventional belief of an inverse correlation between the intensity of inflammation and regenerative capacity. Inflammatory signals were found to be crucial for timely repair and fundamental processes in regeneration, possibly presenting a paradigm shift in the understanding of immunology.1-4 The complexities of wound healing are exemplified when evaluating and treating postamputation wounds. To address such a task, one needs a firm understanding of the science behind healing wounds and what can go wrong along the way.
Phases of Wound Healing
Wound healing is a complex process that involves a series of sequential yet overlapping phases, including hemostasis/inflammation, proliferation, and remodeling.
Hemostasis/Inflammation—The initial stage of wound healing involves hemostasis, in which the primary objective is to prevent blood loss and initiate inflammation. Platelets arrive at the wound site, forming a provisional clot that is crucial for subsequent healing phases.4-6 Platelets halt bleeding as well as act as a medium for cell migration and adhesion; they also are a source of growth factors and proinflammatory cytokines that herald the inflammatory response.4-7
Inflammation is characterized by the infiltration of immune cells, particularly neutrophils and macrophages. Neutrophils act as the first line of defense, clearing debris and preventing infection. Macrophages follow, phagocytizing apoptotic cells and releasing growth factors such as tumor necrosis factor α, vascular endothelial growth factor, and matrix metalloprotease 9, which stimulate the next phase.4-6,8 Typically, the hemostasis and inflammatory phase starts approximately 6 to 8 hours after wound origin and lasts 3 to 4 days.4,6,7
Proliferation—Following hemostasis and inflammation, the wound transitions into the proliferation phase, which is marked by the development of granulation tissue—a dynamic amalgamation of fibroblasts, endothelial cells, and inflammatory cells.1,4-8 Fibroblasts play a central role in synthesizing collagen, the primary structural protein in connective tissue. They also orchestrate synthesis of vitronectin, fibronectin, fibrin, and tenascin.4-6,8 Simultaneously, angiogenesis takes place, involving the creation of new blood vessels to supply essential nutrients and oxygen to the healing tissue.4,7,9 Growth factors such as transforming growth factor β and vascular endothelial growth factor coordinate cellular activities and foster tissue repair.4-6,8 The proliferation phase extends over days to weeks, laying the groundwork for subsequent tissue restructuring.
Remodeling—The final stage of wound healing is remodeling, an extended process that may persist for several months or, in some cases, years. Throughout this phase, the initially deposited collagen, predominantly type III collagen, undergoes transformation into mature type I collagen.4-6,8 This transformation is critical for reinstating the tissue’s strength and functionality. The balance between collagen synthesis and degradation is delicate, regulated by matrix metalloproteinases and inhibitors of metalloproteinases.4-8 Fibroblasts, myofibroblasts, and other cells coordinate this intricate process of tissue reorganization.4-7
The eventual outcome of the remodeling phase determines the appearance and functionality of the healed tissue. Any disruption in this phase can lead to complications, such as chronic wounds and hypertrophic scars/keloids.4-6 These abnormal healing processes are characterized by localized inflammation, heightened fibroblast function, and excessive accumulation of the extracellular matrix.4-8
Molecular Mechanisms
Comprehensive investigations—both in vivo and in vitro—have explored the intricate molecular mechanisms involved in heightened wound healing. Transforming growth factor β takes center stage as a crucial factor, prompting the transformation of fibroblasts into myofibroblasts and contributing to the deposition of extracellular matrix.2,4-8,10 Transforming growth factor β activates non-Smad signaling pathways, such as MAPK (mitogen-activated protein kinase) and PI3K (phosphoinositide 3-kinase), influencing processes associated with fibrosis.5,11 Furthermore, microRNAs play a pivotal role in posttranscriptional regulation, influencing both transforming growth factor β signaling and fibroblast behavior.12-16
The involvement of prostaglandins is crucial in wound healing. Prostaglandin E2 plays a notable role and is positively correlated with the rate of wound healing.5 The cyclooxygenase pathway, pivotal for prostaglandin synthesis, becomes a target for inflammation control.4,5,10 Although aspirin and nonsteroidal anti-inflammatory drugs commonly are employed, their impact on wound healing remains controversial, as inhibition of cyclooxygenase may disrupt normal repair processes.5,17,18
Wound healing exhibits variations depending on age. Fetal skin regeneration is marked by the restoration of normal dermal architecture, including adnexal structures, nerves, vessels, and muscle.4-6 The distinctive characteristics of fetal wound healing include a unique profile of growth factors, a diminished inflammatory response, reduced biomechanical stress, and a distinct extracellular matrix composition.19 These factors contribute to a lower propensity for scar formation compared to the healing processes observed in adults. Fetal and adult wound healing differ fundamentally in their extracellular matrix composition, inflammatory cells, and cytokine levels.4-6,19 Adult wounds feature myofibroblasts, which are absent in fetal wounds, contributing to heightened mechanical tension.5 Delving deeper into the biochemical basis of fetal wound healing holds promise for mitigating scar formation in adults.
Takeaways From Other Species
Much of the biochemical knowledge of wound healing, especially regenerative wound healing, is known from other species. Geckos provide a unique model for studying regenerative repair in tails and nonregenerative healing in limbs after amputation. Scar-free wound healing is characterized by rapid wound closure, delayed blood vessel development, and collagen deposition, which contrasts with the hypervascular granulation tissue seen in scarring wounds.20 Scar-free wound healing and regeneration are intrinsic properties of the lizard tail and are unaffected by the location or method of detachment.21
Compared to amphibians with extraordinary regenerative capacity, data suggest the lack of regenerative capacity in mammals may come from a desynchronization of the fine-tuned interplay of progenitor cells such as blastema and differentiated cells.22,23 In mice, the response to amputation is specific to the level: cutting through the distal third of the terminal phalanx elicits a regeneration response, yielding a new digit tip resembling the lost one, while an amputation through the distal third of the intermediate phalanx triggers a wound healing and scarring response.24
Wound Healing Following Limb Amputation
Limb amputation represents a profound change in an individual’s life, impacting daily activities and overall well-being. There are many causes of amputation, but the most common include cardiovascular diseases, diabetes mellitus, cancer, and trauma.25-27 Trauma represents a relatively common cause within the US Military due to the overall young population as well as inherent risks of uniformed service.25,27 Advances in protective gear and combat casualty care have led to an increased number of individuals surviving with extremity injuries requiring amputation, particularly among younger service members, with a subgroup experiencing multiple amputations.27-29
Numerous factors play a crucial role in the healing and function of postamputation wounds. The level of amputation is a key determinant influencing both functional outcomes and the healing process. Achieving a balance between preserving function and removing damaged tissue is essential. A study investigating cardiac function and oxygen consumption in 25 patients with peripheral vascular disease found higher-level amputations resulted in decreased walking speed and cadence, along with increased oxygen consumption per meter walked.30
Selecting the appropriate amputation level is vital to optimize functional outcomes without compromising wound healing. Successful prosthetic limb fitting depends largely on the length of the residual stump to support the body load and suspend the prosthesis. For long bone amputations, maintaining at least 12-cm clearance above the knee joint in transfemoral amputees and 10-cm below the knee joint in transtibial amputees is critical for maximizing functional outcomes.31
Surgical technique also is paramount. The goal is to minimize the risk for pressure ulcers by avoiding bony spurs and muscle imbalances. Shaping the muscle and residual limb is essential for proper prosthesis fitting. Attention to neurovascular structures, such as burying nerve ends to prevent neuropathic pain during prosthesis wear, is crucial.32 In extremity amputations, surgeons often resort to free flap transfer techniques for stump reconstruction. In a study of 31 patients with severe lower extremity injuries undergoing various amputations, the use of latissimus dorsi myocutaneous flaps, alone or in combination with serratus anterior muscle flaps, resulted in fewer instances of deep ulceration and allowed for earlier prosthesis wear.33
Addressing Barriers to Wound Healing
Multiple barriers to successful wound healing are encountered in the amputee population. Amputations from trauma have a less-controlled initiation, which carries with it a higher risk for infection, poor wound healing, and other complications.
Infection—Infection often is one of the first hurdles encountered in postamputation wound healing. Critical first steps in infection prevention include thorough cleaning of soiled traumatic wounds and appropriate tissue debridement coupled with scrupulous sterile technique and postoperative monitoring for signs and symptoms of infection.
In a retrospective study of 223 combat-related major lower extremity amputations (initial and revision) between 2009 and 2015, the use of intrawound antibiotic powder at the time of closure demonstrated a 13% absolute risk reduction in deep infection rates, which was particularly notable in revision amputations, with a number needed to treat of 8 for initial amputations and 4 for revision amputations on previously infected limbs.34 Intra-operative antibiotic powder may represent a cheap and easy consideration for this special population of amputees. Postamputation antibiotic prophylaxis for infection prevention is an area of controversy. For nontraumatic infections, data suggest antibiotic prophylaxis may not decrease infection rates in these patients.35,36
Interestingly, a study by Azarbal et al37 aimed to investigate the correlation between nasal methicillin-resistant Staphylococcus aureus (MRSA) colonization and other patient factors with wound occurrence following major lower extremity amputation. The study found MRSA colonization was associated with higher rates of overall wound occurrence as well as wound occurrence due to wound infection. These data suggest nasal MRSA eradication may improve postoperative wound outcomes after major lower extremity amputation.37
Dressing Choice—The dressing chosen for a residual limb also is of paramount importance following amputation. The personalized and dynamic management of postamputation wounds and skin involves achieving optimal healing through a dressing that sustains appropriate moisture levels, addresses edema, helps prevent contractures, and safeguards the limb.38 From the start, using negative pressure wound dressings after surgical amputation can decrease wound-related complications.39
Topical oxygen therapy following amputation also shows promise. In a retrospective case series by Kalliainen et al,40 topical oxygen therapy applied to 58 wounds in 32 patients over 9 months demonstrated positive outcomes in promoting wound healing, with 38 wounds (66%) healing completely with the use of topical oxygen. Minimal complications and no detrimental effects were observed.40
Current recommendations suggest that non–weight-bearing removable rigid dressings are the superior postoperative management for transtibial amputations compared to soft dressings, offering benefits such as faster healing, reduced limb edema, earlier ambulation, preparatory shaping for prosthetic use, and prevention of knee flexion contractures.41-46 Similarly, adding a silicone liner following amputation significantly reduced the duration of prosthetic rehabilitation compared with a conventional soft dressing program in one study (P<.05).47
Specifically targeting wound edema, a case series by Hoskins et al48 investigated the impact of prostheses with vacuum-assisted suspension on the size of residual limb wounds in individuals with transtibial amputation. Well-fitting sockets with vacuum-assisted suspension did not impede wound healing, and the results suggest the potential for continued prosthesis use during the healing process.48 However, a study by Johannesson et al49 compared the outcomes of transtibial amputation patients using a vacuum-formed rigid dressing and a conventional rigid plaster dressing, finding no significant differences in wound healing, time to prosthetic fitting, or functional outcomes with the prosthesis between the 2 groups. When comparing elastic bandaging, pneumatic prosthesis, and temporary prosthesis on postoperative stump management, temporary prosthesis led to a decrease in stump volume, quicker transition to a permanent prosthesis, and improved quality of life compared with elastic bandaging and pneumatic prosthetics.50
The type of material in dressings may contribute to utility in amputation wounds. Keratin-based wound dressings show promise for wound healing, especially in recalcitrant vascular wounds.51 There also are numerous proprietary wound dressings available for patients, at least one of which has particularly thorough data. In a retrospective study of more than 2 million lower extremity wounds across 644 institutions, a proprietary bioactive human skin allograft (TheraSkin [LifeNet Health]) demonstrated higher healing rates, greater percentage area reductions, lower amputations, reduced recidivism, higher treatment completion, and fewer medical transfers compared with standard of care alone.52
Postamputation Dermatologic Concerns
After the postamputation wound heals, a notable concern is the prevalence of skin diseases affecting residual limbs. The stump site in amputees, marked by a delicate cutaneous landscape vulnerable to skin diseases, faces challenges arising from amputation-induced damage to various structures.53
When integrated into a prosthesis socket, the altered skin must acclimate to a humid environment and endure forces for which it is not well suited, especially during movement.53 Amputation remarkably alters normal tissue perfusion, which can lead to aberrant blood and lymphatic circulation in residual limbs.27,53 This compromised skin, often associated with a history of vascular disease, diabetes mellitus, or malignancy, becomes immunocompromised, heightening the risk for dermatologic issues such as inflammation, infection, and malignancies.53 Unlike the resilient volar skin on palms and soles, stump skin lacks adaptation to withstand the compressive forces generated during ambulation, sometimes leading to skin disease and pain that result in abandonment of the prosthesis.53,54 Mechanical forces on the skin, especially in active patients eager to resume pre-injury lifestyles, contribute to skin breakdown. The dynamic nature of the residual limb, including muscle atrophy, gait changes, and weight fluctuations, complicates the prosthetic fitting process. Prosthesis abandonment remains a challenge, despite modern technologic advancements.
The occurrence of heterotopic ossification (extraskeletal bone formation) is another notable issue in military amputees.27,55-57 Poor prosthetic fit can lead to skin degradation, necessitating further surgery to address mispositioned bone formations. Orthopedic monitoring supplemented by appropriate imaging studies can benefit postamputation patients by detecting and preventing heterotopic ossification in its early stages.
Dermatologic issues, especially among lower limb amputees, are noteworthy, with a substantial percentage experiencing complications related to socket prosthetics, such as heat, sweating, sores, and skin irritation. Up to 41% of patients are seen regularly for a secondary skin disorder following amputation.58 As one might expect, persistent wounds, blisters, ulcers, and abscesses are some of the most typical cutaneous abnormalities affecting residual limbs with prostheses.27,58 More rare skin conditions also are documented in residual limbs, including cutaneous granuloma, verrucous carcinoma, bullous pemphigoid, and angiodermatitis.27,59-61
Treatments offered in the dermatology clinic often are similar to patients who have not had an amputation. For instance, hyperhidrosis can be treated with prescription antiperspirant, topical aluminum chloride, topical glycopyrronium, botulinum toxin, and iontophoresis, which can greatly decrease skin irritation and malodor. Subcutaneous neurotoxins such as botulinum toxin are especially useful for hyperhidrosis following amputation because a single treatment can last 3 to 6 months, whereas topicals must be applied multiple times per day and can be inherently irritating to the skin.27,62 Furthermore, ablative fractional resurfacing lasers also can help stimulate new collagen growth, increase skin mobility on residual limbs, smooth jagged scars, and aid prosthetic fitting.27,63 Perforated prosthetic liners also may be useful to address issues such as excessive sweating, demonstrating improvements in skin health, reduced sweating problems, and potential avoidance of surgical interventions.64
When comorbid skin conditions are at bay, preventive measures for excessive wound healing necessitate early recognition and timely intervention for residual limbs. Preventive techniques encompass the use of silicone gel sheeting, hypoallergenic microporous tape, and intralesional steroid injections.
Psychological Concerns—An overarching issue following amputation is the psychological toll the process imposes on the patient. Psychological concerns, including anxiety and depression, present additional challenges impacting residual limb hygiene and prosthetic maintenance. Chronic wounds are devastating to patients. These patients consistently express feeling ostracized from their community and anxious about unemployment, leaking fluid, or odor from the wound, as well as other social stigmata.62 Depression and anxiety can hinder a patient’s ability to care for their wound and make them more susceptible to the myriad issues that can ensue.
Recent Developments in Wound Healing
Wound healing is ripe for innovation that could assuage ailments that impact patients following amputation. A 2022 study by Abu El Hawa et al65 illustrated advanced progression in wound healing for patients taking statins, even though the statin group had increased age and number of comorbidities compared with patients not taking statins.
Nasseri and Sharifi66 showed the potential of antimicrobial peptides—small proteins with cationic charges and amphipathic structures exhibiting electrostatic interaction with microbial cell membranes—in promoting wound healing, particularly defensins and cathelicidin LL-37.They also discussed innovative delivery systems, such as nanoparticles and electrospun fibrous scaffolds, highlighting their potential as possibly more effective therapeutics than antibiotics, especially in the context of diabetic wound closure.66 Aimed at increased angiogenesis in the proliferative phase, there is evidence that N-acetylcysteine can increase amputation stump perfusion with the goal of better long-term wound healing and more efficient scar formation.67
Stem cell therapy, particularly employing cells from the human amniotic membrane, represents an auspicious avenue for antifibrotic treatment. Amniotic epithelial cells and amniotic mesenchymal cells, with their self-renewal and multilineage differentiation capabilities, exhibit anti-inflammatory and antifibrotic properties.4,5 A study by Dong et al68 aimed to assess the efficacy of cell therapy, particularly differentiated progenitor cell–based graft transplantation or autologous stem cell injection, in treating refractory skin injuries such as nonrevascularizable critical limb ischemic ulcers, venous leg ulcers, and diabetic lower limb ulcers. The findings demonstrated cell therapy effectively reduced the size of ulcers, improved wound closure rates, and decreased major amputation rates compared with standard therapy. Of note, cell therapy had limited impact on alleviating pain in patients with critical limb ischemia-related cutaneous ulcers.68
Final Thoughts
Wound care following amputation is a multidisciplinary endeavor, necessitating collaboration between many health care professionals. Dermatologists play a crucial role in providing routine care as well as addressing wound healing and related skin issues among amputation patients. As the field progresses, dermatologists are well positioned to make notable contributions and ensure enhanced outcomes, resulting in a better quality of life for patients facing the challenges of limb amputation and prosthetic use.
- Brockes JP, Kumar A. Comparative aspects of animal regeneration. Annu Rev Cell Dev Biol. 2008;24:525-549. doi:10.1146/annurev.cellbio.24.110707.175336
- Eming SA, Hammerschmidt M, Krieg T, et al. Interrelation of immunity and tissue repair or regeneration. Semin Cell Dev Biol. 2009;20:517-527. doi:10.1016/j.semcdb.2009.04.009
- Eming SA. Evolution of immune pathways in regeneration and repair: recent concepts and translational perspectives. Semin Immunol. 2014;26:275-276. doi:10.1016/j.smim.2014.09.001
- Bolognia JL, Jorizzo JJ, Schaffer JV, et al. Dermatology. 4th edition. Elsevier; 2018.
- Wang PH, Huang BS, Horng HC, et al. Wound healing. J Chin Med Assoc JCMA. 2018;81:94-101. doi:10.1016/j.jcma.2017.11.002
- Velnar T, Bailey T, Smrkolj V. The wound healing process: an overview of the cellular and molecular mechanisms. J Int Med Res. 2009;37:1528-1542. doi:10.1177/147323000903700531
- Gurtner GC, Werner S, Barrandon Y, et al. Wound repair and regeneration. Nature. 2008;453:314-321. doi:10.1038/nature07039
- Eming SA, Martin P, Tomic-Canic M. Wound repair and regeneration: mechanisms, signaling, and translation. Sci Transl Med. 2014;6:265sr6. doi:10.1126/scitranslmed.3009337
- Eming SA, Brachvogel B, Odorisio T, et al. Regulation of angiogenesis: wound healing as a model. Prog Histochem Cytochem. 2007;42:115-170. doi:10.1016/j.proghi.2007.06.001
- Janis JE, Harrison B. Wound healing: part I. basic science. Plast Reconstr Surg. 2016;138(3 suppl):9S-17S. doi:10.1097/PRS.0000000000002773
- Profyris C, Tziotzios C, Do Vale I. Cutaneous scarring: pathophysiology, molecular mechanisms, and scar reduction therapeutics. part I: the molecular basis of scar formation. J Am Acad Dermatol. 2012;66:1-10; quiz 11-12. doi:10.1016/j.jaad.2011.05.055
- Kwan P, Ding J, Tredget EE. MicroRNA 181b regulates decorin production by dermal fibroblasts and may be a potential therapy for hypertrophic scar. PLoS One. 2015;10:e0123054. doi:10.1371/journal.pone.0123054
- Ben W, Yang Y, Yuan J, et al. Human papillomavirus 16 E6 modulates the expression of host microRNAs in cervical cancer. Taiwan J Obstet Gynecol. 2015;54:364-370. doi:10.1016/j.tjog.2014.06.007
- Yu EH, Tu HF, Wu CH, et al. MicroRNA-21 promotes perineural invasion and impacts survival in patients with oral carcinoma. J Chin Med Assoc JCMA. 2017;80:383-388. doi:10.1016/j.jcma.2017.01.003
- Wen KC, Sung PL, Yen MS, et al. MicroRNAs regulate several functions of normal tissues and malignancies. Taiwan J Obstet Gynecol. 2013;52:465-469. doi:10.1016/j.tjog.2013.10.002
- Babalola O, Mamalis A, Lev-Tov H, et al. The role of microRNAs in skin fibrosis. Arch Dermatol Res. 2013;305:763-776. doi:10.1007/s00403-013-1410-1
- Hofer M, Hoferová Z, Falk M. Pharmacological modulation of radiation damage. does it exist a chance for other substances than hematopoietic growth factors and cytokines? Int J Mol Sci. 2017;18:1385. doi:10.3390/ijms18071385
- Darby IA, Weller CD. Aspirin treatment for chronic wounds: potential beneficial and inhibitory effects. Wound Repair Regen. 2017;25:7-12. doi:10.1111/wrr.12502
- Khalid KA, Nawi AFM, Zulkifli N, et al. Aging and wound healing of the skin: a review of clinical and pathophysiological hallmarks. Life. 2022;12:2142. doi:10.3390/life12122142
- Peacock HM, Gilbert EAB, Vickaryous MK. Scar‐free cutaneous wound healing in the leopard gecko, Eublepharis macularius. J Anat. 2015;227:596-610. doi:10.1111/joa.12368
- Delorme SL, Lungu IM, Vickaryous MK. Scar‐free wound healing and regeneration following tail loss in the leopard gecko, Eublepharis macularius. Anat Rec. 2012;295:1575-1595. doi:10.1002/ar.22490
- Brunauer R, Xia IG, Asrar SN, et al. Aging delays epimorphic regeneration in mice. J Gerontol Ser A Biol Sci Med Sci. 2021;76:1726-1733. doi:10.1093/gerona/glab131
- Dolan CP, Yang TJ, Zimmel K, et al. Epimorphic regeneration of the mouse digit tip is finite. Stem Cell Res Ther. 2022;13:62. doi:10.1186/s13287-022-02741-2
- Simkin J, Han M, Yu L, et al. The mouse digit tip: from wound healing to regeneration. Methods Mol Biol Clifton NJ. 2013;1037:419-435. doi:10.1007/978-1-62703-505-7_24
- Ziegler-Graham K, MacKenzie EJ, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422-429. doi:10.1016/j.apmr.2007.11.005
- Dudek NL, Marks MB, Marshall SC, et al. Dermatologic conditions associated with use of a lower-extremity prosthesis. Arch Phys Med Rehabil. 2005;86:659-663. doi:10.1016/j.apmr.2004.09.003
- Lannan FM, Meyerle JH. The dermatologist’s role in amputee skin care. Cutis. 2019;103:86-90.
- Dougherty AL, Mohrle CR, Galarneau MR, et al. Battlefield extremity injuries in Operation Iraqi Freedom. Injury. 2009;40:772-777. doi:10.1016/j.injury.2009.02.014
- Epstein RA, Heinemann AW, McFarland LV. Quality of life for veterans and servicemembers with major traumatic limb loss from Vietnam and OIF/OEF conflicts. J Rehabil Res Dev. 2010;47:373-385. doi:10.1682/jrrd.2009.03.0023
- Pinzur MS, Gold J, Schwartz D, et al. Energy demands for walking in dysvascular amputees as related to the level of amputation. Orthopedics. 1992;15:1033-1036; discussion 1036-1037. doi:10.3928/0147-7447-19920901-07
- Robinson V, Sansam K, Hirst L, et al. Major lower limb amputation–what, why and how to achieve the best results. Orthop Trauma. 2010;24:276-285. doi:10.1016/j.mporth.2010.03.017
- Lu S, Wang C, Zhong W, et al. Amputation stump revision using a free sural neurocutaneous perforator flap. Ann Plast Surg. 2016;76:83-87. doi:10.1097/SAP.0000000000000211
- Kim SW, Jeon SB, Hwang KT, et al. Coverage of amputation stumps using a latissimus dorsi flap with a serratus anterior muscle flap: a comparative study. Ann Plast Surg. 2016;76:88-93. doi:10.1097/SAP.0000000000000220
- Pavey GJ, Formby PM, Hoyt BW, et al. Intrawound antibiotic powder decreases frequency of deep infection and severity of heterotopic ossification in combat lower extremity amputations. Clin Orthop. 2019;477:802-810. doi:10.1007/s11999.0000000000000090
- Dunkel N, Belaieff W, Assal M, et al. Wound dehiscence and stump infection after lower limb amputation: risk factors and association with antibiotic use. J Orthop Sci Off J Jpn Orthop Assoc. 2012;17:588-594. doi:10.1007/s00776-012-0245-5
- Rubin G, Orbach H, Rinott M, et al. The use of prophylactic antibiotics in treatment of fingertip amputation: a randomized prospective trial. Am J Emerg Med. 2015;33:645-647. doi:10.1016/j.ajem.2015.02.002
- Azarbal AF, Harris S, Mitchell EL, et al. Nasal methicillin-resistant Staphylococcus aureus colonization is associated with increased wound occurrence after major lower extremity amputation. J Vasc Surg. 2015;62:401-405. doi:10.1016/j.jvs.2015.02.052
- Kwasniewski M, Mitchel D. Post amputation skin and wound care. Phys Med Rehabil Clin N Am. 2022;33:857-870. doi:10.1016/j.pmr.2022.06.010
- Chang H, Maldonado TS, Rockman CB, et al. Closed incision negative pressure wound therapy may decrease wound complications in major lower extremity amputations. J Vasc Surg. 2021;73:1041-1047. doi:10.1016/j.jvs.2020.07.061
- Kalliainen LK, Gordillo GM, Schlanger R, et al. Topical oxygen as an adjunct to wound healing: a clinical case series. Pathophysiol Off J Int Soc Pathophysiol. 2003;9:81-87. doi:10.1016/s0928-4680(02)00079-2
- Reichmann JP, Stevens PM, Rheinstein J, et al. Removable rigid dressings for postoperative management of transtibial amputations: a review of published evidence. PM R. 2018;10:516-523. doi:10.1016/j.pmrj.2017.10.002
- MacLean N, Fick GH. The effect of semirigid dressings on below-knee amputations. Phys Ther. 1994;74:668-673. doi:10.1093/ptj/74.7.668
- Koonalinthip N, Sukthongsa A, Janchai S. Comparison of removable rigid dressing and elastic bandage for residual limb maturation in transtibial amputees: a randomized controlled trial. Arch Phys Med Rehabil. 2020;101:1683-1688. doi:10.1016/j.apmr.2020.05.009
- Taylor L, Cavenett S, Stepien JM, et al. Removable rigid dressings: a retrospective case-note audit to determine the validity of post-amputation application. Prosthet Orthot Int. 2008;32:223-230. doi:10.1080/03093640802016795
- Sumpio B, Shine SR, Mahler D, et al. A comparison of immediate postoperative rigid and soft dressings for below-knee amputations. Ann Vasc Surg. 2013;27:774-780. doi:10.1016/j.avsg.2013.03.007
- van Velzen AD, Nederhand MJ, Emmelot CH, et al. Early treatment of trans-tibial amputees: retrospective analysis of early fitting and elastic bandaging. Prosthet Orthot Int. 2005;29:3-12. doi:10.1080/17461550500069588
- Chin T, Toda M. Results of prosthetic rehabilitation on managing transtibial vascular amputation with silicone liner after wound closure. J Int Med Res. 2016;44:957-967. doi:10.1177/0300060516647554
- Hoskins RD, Sutton EE, Kinor D, et al. Using vacuum-assisted suspension to manage residual limb wounds in persons with transtibial amputation: a case series. Prosthet Orthot Int. 2014;38:68-74. doi:10.1177/0309364613487547
- Johannesson A, Larsson GU, Oberg T, et al. Comparison of vacuum-formed removable rigid dressing with conventional rigid dressing after transtibial amputation: similar outcome in a randomized controlled trial involving 27 patients. Acta Orthop. 2008;79:361-369. doi:10.1080/17453670710015265
- Alsancak S, Köse SK, Altınkaynak H. Effect of elastic bandaging and prosthesis on the decrease in stump volume. Acta Orthop Traumatol Turc. 2011;45:14-22. doi:10.3944/AOTT.2011.2365
- Than MP, Smith RA, Hammond C, et al. Keratin-based wound care products for treatment of resistant vascular wounds. J Clin Aesthetic Dermatol. 2012;5:31-35.
- Gurtner GC, Garcia AD, Bakewell K, et al. A retrospective matched‐cohort study of 3994 lower extremity wounds of multiple etiologies across 644 institutions comparing a bioactive human skin allograft, TheraSkin, plus standard of care, to standard of care alone. Int Wound J. 2020;17:55-64. doi:10.1111/iwj.13231
- Buikema KES, Meyerle JH. Amputation stump: privileged harbor for infections, tumors, and immune disorders. Clin Dermatol. 2014;32:670-677. doi:10.1016/j.clindermatol.2014.04.015
- Yang NB, Garza LA, Foote CE, et al. High prevalence of stump dermatoses 38 years or more after amputation. Arch Dermatol. 2012;148:1283-1286. doi:10.1001/archdermatol.2012.3004
- Potter BK, Burns TC, Lacap AP, et al. Heterotopic ossification following traumatic and combat-related amputations. Prevalence, risk factors, and preliminary results of excision. J Bone Joint Surg Am. 2007;89:476-486. doi:10.2106/JBJS.F.00412
- Edwards DS, Kuhn KM, Potter BK, et al. Heterotopic ossification: a review of current understanding, treatment, and future. J Orthop Trauma. 2016;30(suppl 3):S27-S30. doi:10.1097/BOT.0000000000000666
- Tintle SM, Shawen SB, Forsberg JA, et al. Reoperation after combat-related major lower extremity amputations. J Orthop Trauma. 2014;28:232-237. doi:10.1097/BOT.0b013e3182a53130
- Bui KM, Raugi GJ, Nguyen VQ, et al. Skin problems in individuals with lower-limb loss: literature review and proposed classification system. J Rehabil Res Dev. 2009;46:1085-1090. doi:10.1682/jrrd.2009.04.0052
- Turan H, Bas¸kan EB, Adim SB, et al. Acroangiodermatitis in a below-knee amputation stump. Clin Exp Dermatol. 2011;36:560-561. doi:10.1111/j.1365-2230.2011.04037.x
- Lin CH, Ma H, Chung MT, et al. Granulomatous cutaneous lesions associated with risperidone-induced hyperprolactinemia in an amputated upper limb. Int J Dermatol. 2012;51:75-78. doi:10.1111/j.1365-4632.2011.04906.x
- Schwartz RA, Bagley MP, Janniger CK, et al. Verrucous carcinoma of a leg amputation stump. Dermatologica. 1991;182:193-195. doi:10.1159/000247782
- Campanati A, Diotallevi F, Radi G, et al. Efficacy and safety of botulinum toxin B in focal hyperhidrosis: a narrative review. Toxins. 2023;15:147. doi:10.3390/toxins15020147
- Anderson RR, Donelan MB, Hivnor C, et al. Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: consensus report. JAMA Dermatol. 2014;150:187-193. doi:10.1001/jamadermatol.2013.7761
- McGrath M, McCarthy J, Gallego A, et al. The influence of perforated prosthetic liners on residual limb wound healing: a case report. Can Prosthet Orthot J. 2019;2:32723. doi:10.33137/cpoj.v2i1.32723
- Abu El Hawa AA, Klein D, Bekeny JC, et al. The impact of statins on wound healing: an ally in treating the highly comorbid patient. J Wound Care. 2022;31(suppl 2):S36-S41. doi:10.12968/jowc.2022.31.Sup2.S36
- Nasseri S, Sharifi M. Therapeutic potential of antimicrobial peptides for wound healing. Int J Pept Res Ther. 2022;28:38. doi:10.1007/s10989-021-10350-5
- Lee JV, Engel C, Tay S, et al. N-Acetyl-Cysteine treatment after lower extremity amputation improves areas of perfusion defect and wound healing outcomes. J Vasc Surg. 2021;73:39-40. doi:10.1016/j.jvs.2020.12.025
- Dong Y, Yang Q, Sun X. Comprehensive analysis of cell therapy on chronic skin wound healing: a meta-analysis. Hum Gene Ther. 2021;32:787-795. doi:10.1089/hum.2020.275
- Brockes JP, Kumar A. Comparative aspects of animal regeneration. Annu Rev Cell Dev Biol. 2008;24:525-549. doi:10.1146/annurev.cellbio.24.110707.175336
- Eming SA, Hammerschmidt M, Krieg T, et al. Interrelation of immunity and tissue repair or regeneration. Semin Cell Dev Biol. 2009;20:517-527. doi:10.1016/j.semcdb.2009.04.009
- Eming SA. Evolution of immune pathways in regeneration and repair: recent concepts and translational perspectives. Semin Immunol. 2014;26:275-276. doi:10.1016/j.smim.2014.09.001
- Bolognia JL, Jorizzo JJ, Schaffer JV, et al. Dermatology. 4th edition. Elsevier; 2018.
- Wang PH, Huang BS, Horng HC, et al. Wound healing. J Chin Med Assoc JCMA. 2018;81:94-101. doi:10.1016/j.jcma.2017.11.002
- Velnar T, Bailey T, Smrkolj V. The wound healing process: an overview of the cellular and molecular mechanisms. J Int Med Res. 2009;37:1528-1542. doi:10.1177/147323000903700531
- Gurtner GC, Werner S, Barrandon Y, et al. Wound repair and regeneration. Nature. 2008;453:314-321. doi:10.1038/nature07039
- Eming SA, Martin P, Tomic-Canic M. Wound repair and regeneration: mechanisms, signaling, and translation. Sci Transl Med. 2014;6:265sr6. doi:10.1126/scitranslmed.3009337
- Eming SA, Brachvogel B, Odorisio T, et al. Regulation of angiogenesis: wound healing as a model. Prog Histochem Cytochem. 2007;42:115-170. doi:10.1016/j.proghi.2007.06.001
- Janis JE, Harrison B. Wound healing: part I. basic science. Plast Reconstr Surg. 2016;138(3 suppl):9S-17S. doi:10.1097/PRS.0000000000002773
- Profyris C, Tziotzios C, Do Vale I. Cutaneous scarring: pathophysiology, molecular mechanisms, and scar reduction therapeutics. part I: the molecular basis of scar formation. J Am Acad Dermatol. 2012;66:1-10; quiz 11-12. doi:10.1016/j.jaad.2011.05.055
- Kwan P, Ding J, Tredget EE. MicroRNA 181b regulates decorin production by dermal fibroblasts and may be a potential therapy for hypertrophic scar. PLoS One. 2015;10:e0123054. doi:10.1371/journal.pone.0123054
- Ben W, Yang Y, Yuan J, et al. Human papillomavirus 16 E6 modulates the expression of host microRNAs in cervical cancer. Taiwan J Obstet Gynecol. 2015;54:364-370. doi:10.1016/j.tjog.2014.06.007
- Yu EH, Tu HF, Wu CH, et al. MicroRNA-21 promotes perineural invasion and impacts survival in patients with oral carcinoma. J Chin Med Assoc JCMA. 2017;80:383-388. doi:10.1016/j.jcma.2017.01.003
- Wen KC, Sung PL, Yen MS, et al. MicroRNAs regulate several functions of normal tissues and malignancies. Taiwan J Obstet Gynecol. 2013;52:465-469. doi:10.1016/j.tjog.2013.10.002
- Babalola O, Mamalis A, Lev-Tov H, et al. The role of microRNAs in skin fibrosis. Arch Dermatol Res. 2013;305:763-776. doi:10.1007/s00403-013-1410-1
- Hofer M, Hoferová Z, Falk M. Pharmacological modulation of radiation damage. does it exist a chance for other substances than hematopoietic growth factors and cytokines? Int J Mol Sci. 2017;18:1385. doi:10.3390/ijms18071385
- Darby IA, Weller CD. Aspirin treatment for chronic wounds: potential beneficial and inhibitory effects. Wound Repair Regen. 2017;25:7-12. doi:10.1111/wrr.12502
- Khalid KA, Nawi AFM, Zulkifli N, et al. Aging and wound healing of the skin: a review of clinical and pathophysiological hallmarks. Life. 2022;12:2142. doi:10.3390/life12122142
- Peacock HM, Gilbert EAB, Vickaryous MK. Scar‐free cutaneous wound healing in the leopard gecko, Eublepharis macularius. J Anat. 2015;227:596-610. doi:10.1111/joa.12368
- Delorme SL, Lungu IM, Vickaryous MK. Scar‐free wound healing and regeneration following tail loss in the leopard gecko, Eublepharis macularius. Anat Rec. 2012;295:1575-1595. doi:10.1002/ar.22490
- Brunauer R, Xia IG, Asrar SN, et al. Aging delays epimorphic regeneration in mice. J Gerontol Ser A Biol Sci Med Sci. 2021;76:1726-1733. doi:10.1093/gerona/glab131
- Dolan CP, Yang TJ, Zimmel K, et al. Epimorphic regeneration of the mouse digit tip is finite. Stem Cell Res Ther. 2022;13:62. doi:10.1186/s13287-022-02741-2
- Simkin J, Han M, Yu L, et al. The mouse digit tip: from wound healing to regeneration. Methods Mol Biol Clifton NJ. 2013;1037:419-435. doi:10.1007/978-1-62703-505-7_24
- Ziegler-Graham K, MacKenzie EJ, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422-429. doi:10.1016/j.apmr.2007.11.005
- Dudek NL, Marks MB, Marshall SC, et al. Dermatologic conditions associated with use of a lower-extremity prosthesis. Arch Phys Med Rehabil. 2005;86:659-663. doi:10.1016/j.apmr.2004.09.003
- Lannan FM, Meyerle JH. The dermatologist’s role in amputee skin care. Cutis. 2019;103:86-90.
- Dougherty AL, Mohrle CR, Galarneau MR, et al. Battlefield extremity injuries in Operation Iraqi Freedom. Injury. 2009;40:772-777. doi:10.1016/j.injury.2009.02.014
- Epstein RA, Heinemann AW, McFarland LV. Quality of life for veterans and servicemembers with major traumatic limb loss from Vietnam and OIF/OEF conflicts. J Rehabil Res Dev. 2010;47:373-385. doi:10.1682/jrrd.2009.03.0023
- Pinzur MS, Gold J, Schwartz D, et al. Energy demands for walking in dysvascular amputees as related to the level of amputation. Orthopedics. 1992;15:1033-1036; discussion 1036-1037. doi:10.3928/0147-7447-19920901-07
- Robinson V, Sansam K, Hirst L, et al. Major lower limb amputation–what, why and how to achieve the best results. Orthop Trauma. 2010;24:276-285. doi:10.1016/j.mporth.2010.03.017
- Lu S, Wang C, Zhong W, et al. Amputation stump revision using a free sural neurocutaneous perforator flap. Ann Plast Surg. 2016;76:83-87. doi:10.1097/SAP.0000000000000211
- Kim SW, Jeon SB, Hwang KT, et al. Coverage of amputation stumps using a latissimus dorsi flap with a serratus anterior muscle flap: a comparative study. Ann Plast Surg. 2016;76:88-93. doi:10.1097/SAP.0000000000000220
- Pavey GJ, Formby PM, Hoyt BW, et al. Intrawound antibiotic powder decreases frequency of deep infection and severity of heterotopic ossification in combat lower extremity amputations. Clin Orthop. 2019;477:802-810. doi:10.1007/s11999.0000000000000090
- Dunkel N, Belaieff W, Assal M, et al. Wound dehiscence and stump infection after lower limb amputation: risk factors and association with antibiotic use. J Orthop Sci Off J Jpn Orthop Assoc. 2012;17:588-594. doi:10.1007/s00776-012-0245-5
- Rubin G, Orbach H, Rinott M, et al. The use of prophylactic antibiotics in treatment of fingertip amputation: a randomized prospective trial. Am J Emerg Med. 2015;33:645-647. doi:10.1016/j.ajem.2015.02.002
- Azarbal AF, Harris S, Mitchell EL, et al. Nasal methicillin-resistant Staphylococcus aureus colonization is associated with increased wound occurrence after major lower extremity amputation. J Vasc Surg. 2015;62:401-405. doi:10.1016/j.jvs.2015.02.052
- Kwasniewski M, Mitchel D. Post amputation skin and wound care. Phys Med Rehabil Clin N Am. 2022;33:857-870. doi:10.1016/j.pmr.2022.06.010
- Chang H, Maldonado TS, Rockman CB, et al. Closed incision negative pressure wound therapy may decrease wound complications in major lower extremity amputations. J Vasc Surg. 2021;73:1041-1047. doi:10.1016/j.jvs.2020.07.061
- Kalliainen LK, Gordillo GM, Schlanger R, et al. Topical oxygen as an adjunct to wound healing: a clinical case series. Pathophysiol Off J Int Soc Pathophysiol. 2003;9:81-87. doi:10.1016/s0928-4680(02)00079-2
- Reichmann JP, Stevens PM, Rheinstein J, et al. Removable rigid dressings for postoperative management of transtibial amputations: a review of published evidence. PM R. 2018;10:516-523. doi:10.1016/j.pmrj.2017.10.002
- MacLean N, Fick GH. The effect of semirigid dressings on below-knee amputations. Phys Ther. 1994;74:668-673. doi:10.1093/ptj/74.7.668
- Koonalinthip N, Sukthongsa A, Janchai S. Comparison of removable rigid dressing and elastic bandage for residual limb maturation in transtibial amputees: a randomized controlled trial. Arch Phys Med Rehabil. 2020;101:1683-1688. doi:10.1016/j.apmr.2020.05.009
- Taylor L, Cavenett S, Stepien JM, et al. Removable rigid dressings: a retrospective case-note audit to determine the validity of post-amputation application. Prosthet Orthot Int. 2008;32:223-230. doi:10.1080/03093640802016795
- Sumpio B, Shine SR, Mahler D, et al. A comparison of immediate postoperative rigid and soft dressings for below-knee amputations. Ann Vasc Surg. 2013;27:774-780. doi:10.1016/j.avsg.2013.03.007
- van Velzen AD, Nederhand MJ, Emmelot CH, et al. Early treatment of trans-tibial amputees: retrospective analysis of early fitting and elastic bandaging. Prosthet Orthot Int. 2005;29:3-12. doi:10.1080/17461550500069588
- Chin T, Toda M. Results of prosthetic rehabilitation on managing transtibial vascular amputation with silicone liner after wound closure. J Int Med Res. 2016;44:957-967. doi:10.1177/0300060516647554
- Hoskins RD, Sutton EE, Kinor D, et al. Using vacuum-assisted suspension to manage residual limb wounds in persons with transtibial amputation: a case series. Prosthet Orthot Int. 2014;38:68-74. doi:10.1177/0309364613487547
- Johannesson A, Larsson GU, Oberg T, et al. Comparison of vacuum-formed removable rigid dressing with conventional rigid dressing after transtibial amputation: similar outcome in a randomized controlled trial involving 27 patients. Acta Orthop. 2008;79:361-369. doi:10.1080/17453670710015265
- Alsancak S, Köse SK, Altınkaynak H. Effect of elastic bandaging and prosthesis on the decrease in stump volume. Acta Orthop Traumatol Turc. 2011;45:14-22. doi:10.3944/AOTT.2011.2365
- Than MP, Smith RA, Hammond C, et al. Keratin-based wound care products for treatment of resistant vascular wounds. J Clin Aesthetic Dermatol. 2012;5:31-35.
- Gurtner GC, Garcia AD, Bakewell K, et al. A retrospective matched‐cohort study of 3994 lower extremity wounds of multiple etiologies across 644 institutions comparing a bioactive human skin allograft, TheraSkin, plus standard of care, to standard of care alone. Int Wound J. 2020;17:55-64. doi:10.1111/iwj.13231
- Buikema KES, Meyerle JH. Amputation stump: privileged harbor for infections, tumors, and immune disorders. Clin Dermatol. 2014;32:670-677. doi:10.1016/j.clindermatol.2014.04.015
- Yang NB, Garza LA, Foote CE, et al. High prevalence of stump dermatoses 38 years or more after amputation. Arch Dermatol. 2012;148:1283-1286. doi:10.1001/archdermatol.2012.3004
- Potter BK, Burns TC, Lacap AP, et al. Heterotopic ossification following traumatic and combat-related amputations. Prevalence, risk factors, and preliminary results of excision. J Bone Joint Surg Am. 2007;89:476-486. doi:10.2106/JBJS.F.00412
- Edwards DS, Kuhn KM, Potter BK, et al. Heterotopic ossification: a review of current understanding, treatment, and future. J Orthop Trauma. 2016;30(suppl 3):S27-S30. doi:10.1097/BOT.0000000000000666
- Tintle SM, Shawen SB, Forsberg JA, et al. Reoperation after combat-related major lower extremity amputations. J Orthop Trauma. 2014;28:232-237. doi:10.1097/BOT.0b013e3182a53130
- Bui KM, Raugi GJ, Nguyen VQ, et al. Skin problems in individuals with lower-limb loss: literature review and proposed classification system. J Rehabil Res Dev. 2009;46:1085-1090. doi:10.1682/jrrd.2009.04.0052
- Turan H, Bas¸kan EB, Adim SB, et al. Acroangiodermatitis in a below-knee amputation stump. Clin Exp Dermatol. 2011;36:560-561. doi:10.1111/j.1365-2230.2011.04037.x
- Lin CH, Ma H, Chung MT, et al. Granulomatous cutaneous lesions associated with risperidone-induced hyperprolactinemia in an amputated upper limb. Int J Dermatol. 2012;51:75-78. doi:10.1111/j.1365-4632.2011.04906.x
- Schwartz RA, Bagley MP, Janniger CK, et al. Verrucous carcinoma of a leg amputation stump. Dermatologica. 1991;182:193-195. doi:10.1159/000247782
- Campanati A, Diotallevi F, Radi G, et al. Efficacy and safety of botulinum toxin B in focal hyperhidrosis: a narrative review. Toxins. 2023;15:147. doi:10.3390/toxins15020147
- Anderson RR, Donelan MB, Hivnor C, et al. Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: consensus report. JAMA Dermatol. 2014;150:187-193. doi:10.1001/jamadermatol.2013.7761
- McGrath M, McCarthy J, Gallego A, et al. The influence of perforated prosthetic liners on residual limb wound healing: a case report. Can Prosthet Orthot J. 2019;2:32723. doi:10.33137/cpoj.v2i1.32723
- Abu El Hawa AA, Klein D, Bekeny JC, et al. The impact of statins on wound healing: an ally in treating the highly comorbid patient. J Wound Care. 2022;31(suppl 2):S36-S41. doi:10.12968/jowc.2022.31.Sup2.S36
- Nasseri S, Sharifi M. Therapeutic potential of antimicrobial peptides for wound healing. Int J Pept Res Ther. 2022;28:38. doi:10.1007/s10989-021-10350-5
- Lee JV, Engel C, Tay S, et al. N-Acetyl-Cysteine treatment after lower extremity amputation improves areas of perfusion defect and wound healing outcomes. J Vasc Surg. 2021;73:39-40. doi:10.1016/j.jvs.2020.12.025
- Dong Y, Yang Q, Sun X. Comprehensive analysis of cell therapy on chronic skin wound healing: a meta-analysis. Hum Gene Ther. 2021;32:787-795. doi:10.1089/hum.2020.275
Practice Points
- Wound healing in adults is a complex dynamic process that usually takes the greater part of 1 year to completely resolve and is marked by the end of scar formation.
- Postamputation residual limbs are subject to mechanical and biophysical stress to which the overlying skin is not accustomed. Skin treatment aims at mitigating these stresses.
- The major dermatologic barriers to successful wound healing following amputation include infection, skin breakdown, formation of chronic wounds and granulation tissue, heterotopic ossification, and hyperhidrosis.
Tangled Truths: Unraveling the Link Between Frontal Fibrosing Alopecia and Allergic Contact Dermatitis
Frontal fibrosing alopecia (FFA) is an increasingly common diagnosis, especially in middle-aged women, and was first described by Kossard1 in 1994. It is a variant of lichen planopilaris (LPP), a progressive scarring cicatricial alopecia that affects the frontotemporal area of the scalp, eyebrows, and sometimes even body hair.1 Although its etiology remains unclear, genetic causes, drugs, hormones, and environmental exposures—including certain chemicals found in sunscreens—have been implicated in its pathogenesis.2,3 An association between contact allergy to ingredients in personal care products and FFA diagnosis has been suggested; however, there is no evidence of causality to date. In this article, we highlight the potential relationship between contact allergy and FFA as well as clinical considerations for management.
Clinical Features and Diagnosis
Frontal fibrosing alopecia typically manifests with gradual symmetric recession of the frontal hairline leading to bandlike hair loss along the forehead, sometimes extending to the temporal region.4 Some patients may experience symptoms of scalp itching, burning, or tenderness that may precede or accompany the hair loss. Perifollicular erythema may be visible during the early stages and can be visualized on trichoscopy. The affected skin may appear pale and shiny and may have a smooth texture with a distinct lack of follicular openings. Aside from scalp involvement, other manifestations may include lichen planus pigmentosus, facial papules, body hair involvement, hypochromic lesions, diffuse redness on the face and neck, and prominent frontal veins.5 Although most FFA cases have characteristic clinical features and trichoscopic findings, biopsy for histopathologic examination is still recommended to confirm the diagnosis and ensure appropriate treatment.4 Classic histopathologic features include perifollicular lymphocytic inflammation, follicular destruction, and scarring.
Pathophysiology of FFA
The pathogenesis of FFA is thought to involve a variety of triggers, including immune-mediated inflammation, stress, genetics, hormones, and possibly environmental factors.6 Frontal fibrosing alopecia demonstrates considerable upregulation in cytotoxic helper T cells (TH1) and IFN-γ activity resulting in epithelial hair follicle stem cell apoptosis and replacement of normal epithelial tissue with fibrous tissue.7 There is some suspicion of genetic susceptibility in the onset of FFA as suggested by familial reports and genome-wide association studies.8-10 Hormonal and autoimmune factors also have been linked to FFA, including an increased risk for thyroid disease and the postmenopausal rise of androgen levels.6
Allergic Contact Dermatitis and FFA
Although they are 2 distinct conditions with differing etiologies, allergic contact dermatitis (ACD) and FFA may share environmental triggers, especially in susceptible individuals. This may support the coexistence and potential association between ACD and FFA.
In one case report, a woman who developed facial eczema followed by FFA showed positive patch tests to the UV filters drometrizole trisiloxane and ethylhexyl salicylate, which were listed as ingredients in her sunscreens. Avoidance of these allergens reportedly led to notable improvement of the symptoms.11 Case-control studies have found an association between the use of facial sunscreen and risk for FFA.12 A 2016 questionnaire that assessed a wide range of lifestyle, social, and medical factors related to FFA found that the use of sunscreens was significantly higher in patients with FFA than controls (P<.001), pointing to sunscreens as a potential contributing factor, but further research has been inconclusive. A higher frequency of positive patch tests to hydroperoxides of linalool and balsam of Peru (BoP) in patients with FFA have been documented; however, a direct cause cannot be established.2
In a 2020 prospective study conducted at multiple international centers, 65% (13/20) of FFA patients and 37.5% (9/24) of the control group had a positive patch test reaction to one or more allergens (P=.003). The most common allergens that were identified included cobalt chloride (positive in 35% [7/20] of patients with FFA), nickel sulfate (25% [5/20]), and potassium dichromate (15% [3/20]).13 In a recent 2-year cohort study of 42 patients with FFA who were referred for patch testing, the most common allergens included gallates, hydroperoxides of linalool, and other fragrances.14 After a 3-month period of allergen avoidance, 70% (29/42) of patients had decreased scalp erythema on examination, indicating that avoiding relevant allergens may reduce local inflammation. Furthermore, 76.2% (32/42) of patients with FFA showed delayed-type hypersensitivity to allergens found in daily personal care products such as shampoos, sunscreens, and moisturizers, among others.14 Notably, the study lacked a control group. A case-control study of 36 Hispanic women conducted in Mexico also resulted in 83.3% (15/18) of patients with FFA and 55.5% (10/18) of controls having at least 1 positive patch test; in the FFA group, these included iodopropynyl butylcarbamate (16.7% [3/18]) and propolis (16.7% [3/18]).15
Most recently, a retrospective study conducted by Shtaynberger et al16 included 12 patients with LPP or FFA diagnosed via clinical findings or biopsy. It also included an age- and temporally matched control group tested with identical allergens. Among the 12 patients who had FFA/LPP, all had at least 1 allergen identified on patch testing. The most common allergens identified were propolis (positive in 50% [6/12] of patients with FFA/LPP), fragrance mix I (16%), and methylisothiazolinone (16% [2/12]). Follow-up data were available for 9 of these patients, of whom 6 (66.7%) experienced symptom improvement after 6 months of allergen avoidance. Four (44.4%) patients experienced decreased follicular redness or scaling, 2 (22.2%) patients experienced improved scalp pain/itch, 2 (22.2%) patients had stable/improved hair density, and 1 (1.1%) patient had decreased hair shedding. Although this suggests an environmental trigger for FFA/LPP, the authors stated that changes in patient treatment plans could have contributed to their improvement. The study also was limited by its small size and its overall generalizability.16
These studies have underscored the significance of patch testing in individuals diagnosed with FFA and have identified common allergens prevalent in this patient population. They have suggested that patients with FFA are more likely to have positive patch tests, and in some cases patients could experience improvements in scalp pruritus and erythema with allergen avoidance; however, we emphasize that a causal association between contact allergy and FFA remains unproven to date.
Most Common Allergens Pertinent to FFA
Preservatives—In some studies, patients with FFA have had positive patch tests to preservatives such as gallates and methylchloroisothiazolinone/methylisothiazolinone (MCI/MI).14 Gallates are antioxidants that are used in food preservation, pharmaceuticals, and cosmetics due to their ability to inhibit oxidation and rancidity of fats and oils.17 The most common gallates include propyl gallate, octyl gallate, and dodecyl gallate. Propyl gallate is utilized in some waxy or oily cosmetics and personal care items including sunscreens, shampoos, conditioners, bar soaps, facial cleansers, and moisturizers.18 Typically, if patients have a positive patch test to one gallate, they should be advised to avoid all gallate compounds, as they can cross-react.
Similarly, MCI/MI can prevent product degradation through their antibacterial and antifungal properties. This combination of MCI and MI is used as an effective method of prolonging the shelf life of cosmetic products and commonly is found in sunscreens, facial moisturizing creams, shampoos, and conditioners19; it is banned from use in leave-on products in the European Union and Canada due to increased rates of contact allergy.20 In patients with FFA who commonly use facial sunscreen, preservatives can be a potential allergen exposure to consider.
Iodopropynyl butylcarbamate also is a preservative used in cosmetic formulations. Similar to MCI/MI, it is a potent fungicide and bactericide. This allergen can be found in hair care products, bodywashes, and other personal products.21
UV Light–Absorbing Agents—A systematic review and meta-analysis conducted in 2022 showed a significant (P<.001) association between sunscreen use and FFA.22 A majority of allergens identified on patch testing included UVA- and UVB-absorbing agents found in sunscreens and other products including cosmetics,11,12 such as drometrizole trisiloxane, ethylhexyl salicylate, avobenzone, and benzophenone-4. Drometrizole trisiloxane is a photostabilizer and a broad-spectrum UV filter that is not approved for use in sunscreens in the United States.23 It also is effective in stabilizing and preventing the degradation of avobenzone, a commonly used UVA filter.24
Fragrances—Fragrances are present in nearly every personal and cosmetic product, sometimes even in those advertised as being “fragrance free.” Hydroperoxides of linalool, BoP, and fragrance mix are common allergens that are found in a variety of personal care products including perfumes, cosmetics, and even household cleaning supplies.25 Simultaneous positive patch tests to BoP and fragrance mix are common due to shared components. Linalool can be found in various plants such as lavender, rose, bergamot, and jasmine.26 Upon air exposure, linalool auto-oxidizes to form allergenic hydroperoxides of linalool. Among patients with FFA, positive patch test reactions to fragrance chemicals are common and could be attributed to the use of fragranced hair products and facial cosmetics.
Hair Dyes and Bleaches—Allergic reactions to hair dyes and bleaches can result in severe ACD of the head/neck and, in rare cases, scarring alopecia.27 Chemicals found in these products include paraphenylenediamine (PPD) and ammonium persulfate. The most common hair dye allergen, PPD also is used in some rubbers and plastics. Ammonium persulfate is a chemical used in hair bleaches and to deodorize oils. One case study reported a patient with FFA who developed chemically induced vitiligo immediately after the use of a hair color product that contained PPD.28 However, without patch testing to confirm the presence of contact allergy, other patient-specific and environmental risk factors could have contributed to FFA in this case.
A Knot in the Truth
In this endeavor to untangle the truth, it should be remembered that at the time of writing, the purported association between FFA and ACD remains debatable. Contact dermatitis specialists have voiced that the association between FFA and ACD, especially with regard to sunscreen, cannot be supported due to the lack of sufficient evidence.29 A large majority of the research conducted on FFA and ACD is based on case reports and studies limited to a small sample size, and most of these patch test studies lack a control group. Felmingham et al30 noted that the recent epidemiology of FFA aligns with increased sunscreen use. They also highlighted the limitations of the aforementioned studies, which include misclassification of exposures in the control group2 and recall bias in questionnaire participants.2,12 The most pressing limitation that permeates through most of these studies is the temporal ambiguity associated with sunscreen use. A study by Dhana et al31 failed to specify whether increased sunscreen use preceded the diagnosis of FFA or if it stems from the need to protect more exposed skin as a consequence of disease. Broad sunscreen avoidance due to concern for a possible association with hair loss could have detrimental health implications by increasing the risk for photodamage and skin cancer.
FFA Patch Testing
The avoidance of pertinent allergens could be effective in reducing local inflammation, pruritus, and erythema in FFA.9,14,32 At our institution, we selectively patch test patients with FFA when there is a suspected contact allergy. Clinical features that may allude to a potential contact allergy include an erythematous or eczematous dermatitis or symptoms of pruritus along the scalp or eyebrows. If patients recall hair loss or symptoms after using a hair or facial product, then a potential contact allergy to these products could be considered. Patch testing in patients with FFA includes the North American 80 Comprehensive Series and the cosmetic and hairdresser supplemental series, as well as an additional customized panel of 8 allergens as determined by patch testing experts at the University of Massachusetts, Brigham and Women’s Hospital, and Massachusetts General Hospital (private email communication, November 2017). Patch test readings are performed at 48 and 96 or 120 hours. Using the American Contact Dermatitis Society’s Contact Allergen Management Program, patients are provided personalized safe product lists and avoidance strategies are discussed.
Final Interpretation
In a world where cosmetic products are ubiquitous, it is hard to define the potential role of contact allergens in the entangled pathogenesis of FFA and ACD. As evidenced by emerging literature that correlates the 2 conditions and their exacerbating factors, it is important for physicians to have a comprehensive diagnostic approach and heightened awareness for potential allergens at play in FFA (Table). The identification of certain chemicals and preservatives as potential triggers for FFA should emphasize the importance of patch testing in these patients; however, whether the positive reactions are relevant to the pathogenesis or disease course of FFA still is unknown. While these findings begin to unravel the intertwined causes of FFA and ACD, further research encompassing larger cohorts and prospective studies is imperative to solidify these associations, define concrete guidelines, and improve patient outcomes.
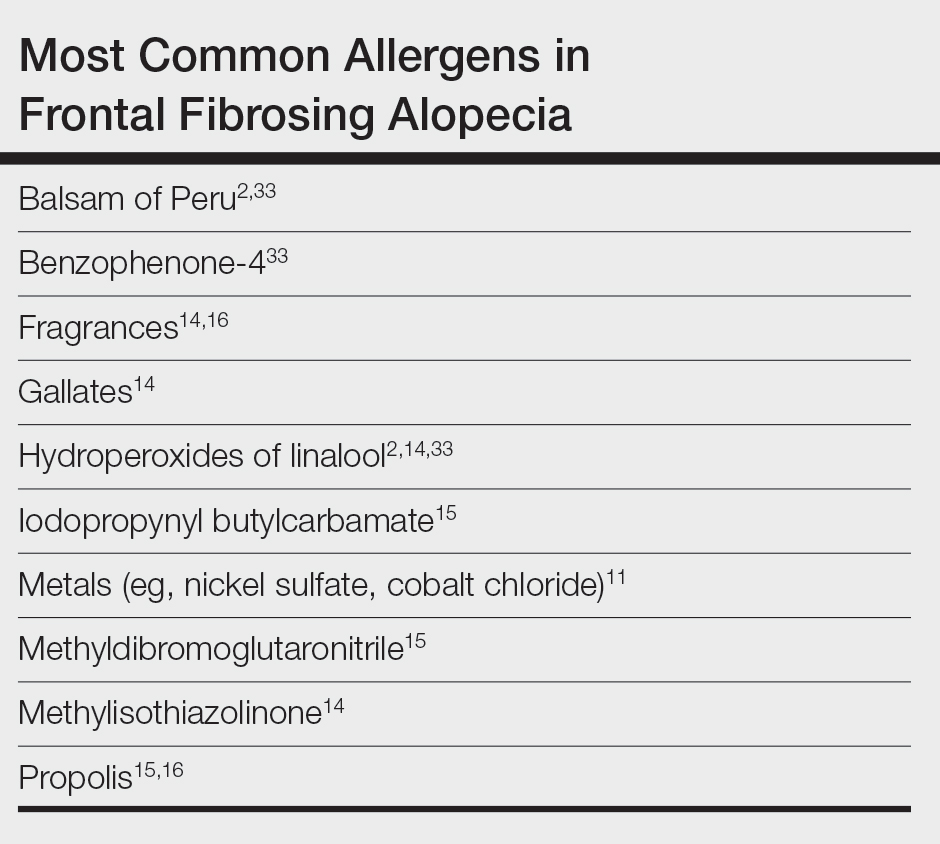
- Kossard S. Postmenopausal frontal fibrosing alopecia: scarring alopecia in a pattern distribution. Arch Dermatol. 1994;130:770-774. doi:10.1001/archderm.1994.01690060100013
- Aldoori N, Dobson K, Holden CR, et al. Frontal fibrosing alopecia: possible association with leave-on facial skin care products and sunscreens; a questionnaire study. Br J Dermatol. 2016;175:762-767. doi:10.1111/bjd.14535
- Debroy Kidambi A, Dobson K, Holmes S, et al. Frontal fibrosing alopecia in men: an association with facial moisturizers and sunscreens. Br J Dermatol. 2017;177:260-261. doi:10.1111/bjd.15311
- Starace M, Orlando G, Iorizzo M, et al. Clinical and dermoscopic approaches to diagnosis of frontal fibrosing alopecia: results from a multicenter study of the International Dermoscopy Society. Dermatol Pract Concept. 2022;12:E2022080. doi:10.5826/dpc.1201a80
- Fechine COC, Valente NYS, Romiti R. Lichen planopilaris and frontal fibrosing alopecia: review and update of diagnostic and therapeutic features. An Bras Dermatol. 2022;97:348-357. doi:10.1016/j.abd.2021.08.008
- Frontal fibrosing alopecia: a review of disease pathogenesis. Front Med (Lausanne). 2022;9:911944. doi:10.3389/fmed.2022.911944
- Del Duca E, Ruano Ruiz J, Pavel AB, et al. Frontal fibrosing alopecia shows robust T helper 1 and Janus kinase 3 skewing. Br J Dermatol. 2020;183:1083-1093. doi:10.1111/bjd.19040
- Tziotzios C, Petridis C, Dand N, et al. Genome-wide association study in frontal fibrosing alopecia identifies four susceptibility loci including HLA-B*07:02. Nat Commun. 2019;10:1150. doi:10.1038/s41467-019-09117-w
- Navarro‐Belmonte MR, Navarro‐López V, Ramírez‐Boscà A, et al. Case series of familial frontal fibrosing alopecia and a review of the literature. J Cosmet Dermatol. 2015;14:64-69. doi:10.1111/jocd.12125
- Cuenca-Barrales C, Ruiz-Villaverde R, Molina-Leyva A. Familial frontal fibrosing alopecia. Sultan Qaboos Univ Med J. 2021;21:E320-E323. doi:10.18295/squmj.2021.21.02.025
- Pastor-Nieto MA, Gatica-Ortega ME. Allergic contact dermatitis to drometrizole trisiloxane in a woman thereafter diagnosed with frontal fibrosing alopecia. Contact Dermatitis. 2023;89:215-217. doi:10.1111/cod.14370
- Moreno-Arrones OM, Saceda-Corralo D, Rodrigues-Barata AR, et al. Risk factors associated with frontal fibrosing alopecia: a multicentre case–control study. Clin Exp Dermatol. 2019;44:404-410. doi:10.1111/ced.13785
- Rudnicka L, Rokni GR, Lotti T, et al. Allergic contact dermatitis in patients with frontal fibrosing alopecia: an international multi-center study. Dermatol Ther. 2020;33:E13560. doi:10.1111/dth.13560
- Prasad S, Marks DH, Burns LJ, et al. Patch testing and contact allergen avoidance in patients with lichen planopilaris and/or frontal fibrosing alopecia: a cohort study. J Am Acad Dermatol. 2020;83:659-661. doi:10.1016/j.jaad.2020.01.026
- Ocampo-Garza SS, Herz-Ruelas ME, Chavez-Alvarez S, et al. Association of frontal fibrosing alopecia and contact allergens in everyday skincare products in Hispanic females: a case-control study. An Bras Dermatol. 2021;96:776-778. doi:10.1016/j.abd.2020.09.013
- Shtaynberger B, Bruder P, Zippin JH. The prevalence of type iv hypersensitivity in patients with lichen planopilaris and frontal fibrosing alopecia. Dermatitis. 2023;34:351-352. doi:10.1097/DER.0000000000000965
- Kahkeshani N, Farzaei F, Fotouhi M, et al. Pharmacological effects of gallic acid in health and diseases: a mechanistic review. Iran J Basic Med Sci. 2019;22:225-237. doi:10.22038/ijbms.2019.32806.7897
- Holcomb ZE, Van Noord MG, Atwater AR. Gallate contact dermatitis: product update and systematic review. Dermatitis. 2017;28:115-127. doi:10.1097/DER.0000000000000263
- Gorris A, Valencak J, Schremser V, et al. Contact allergy to methylisothiazolinone with three clinical presentations in one patient. Contact Dermatitis. 2020;82:162-164. doi:10.1111/cod.13384
- Uter W, Aalto-Korte K, Agner T, et al. The epidemic of methylisothiazolinone contact allergy in Europe: follow-up on changing exposures. J Eur Acad Dermatol Venereol. 2020;34:333-339. doi:10.1111/jdv.15875
- Batista M, Morgado F, Gonçalo M. Patch test reactivity to iodopropynyl butylcarbamate in consecutive patients during a period of 7 years. Contact Dermatitis. 2019;81:54-55. doi:10.1111/cod.13213
- Maghfour J, Ceresnie M, Olson J, et al. The association between frontal fibrosing alopecia, sunscreen, and moisturizers: a systematic review and meta-analysis. J Am Acad Dermatol. 2022;87:395-396. doi:10.1016/j.jaad.2021.12.058
- Drometrizole trisiloxane. PubChem website. Accessed February 21, 2024. https://pubchem.ncbi.nlm.nih.gov/compound/9848888
- Hughes TM, Martin JA, Lewis VJ, et al. Allergic contact dermatitis to drometrizole trisiloxane in a sunscreen with concomitant sensitivities to other sunscreens. Contact Dermatitis. 2005;52:226-227. doi:10.1111/j.0105-1873.2005.0566a.x
- de Groot AC. Myroxylon pereirae resin (balsam of Peru)—a critical review of the literature and assessment of the significance of positive patch test reactions and the usefulness of restrictive diets. Contact Dermatitis. 2019;80:335-353. doi:10.1111/cod.13263
- Sköld M, Börje A, Matura M, et al. Studies on the autoxidation and sensitizing capacity of the fragrance chemical linalool, identifying a linalool hydroperoxide. Contact Dermatitis. 2002;46:267-272. doi:10.1034/j.1600-0536.2002.460504.x
- Dev T, Khan E, Patel U, et al. Cicatricial alopecia following allergic contact dermatitis from hair dyes: a rare clinical presentation. Contact Dermatitis. 2022;86:59-61. doi:10.1111/cod.13974
- De Souza B, Burns L, Senna MM. Frontal fibrosing alopecia preceding the development of vitiligo: a case report. JAAD Case Rep. 2020;6:154-155. doi:10.1016/j.jdcr.2019.12.011
- Abuav R, Shon W. Are sunscreen particles involved in frontal fibrosing alopecia?—a TEM-EDXS analysis on formalin-fixed paraffin-embedded alopecia biopsies (pilot study). Am J Dermatopathol. 2022;44:E135. doi:10.1097/DAD.0000000000002317
- Felmingham C, Yip L, Tam M, et al. Allergy to sunscreen and leave-on facial products is not a likely causative mechanism in frontal fibrosing alopecia: perspective from contact allergy experts. Br J Dermatol. 2020;182:481-482. doi:10.1111/bjd.18380
- Dhana A, Gumedze F, Khumalo N. Regarding “frontal fibrosing alopecia: possible association with leave-on facial skincare products and sunscreens; a questionnaire study.” Br J Dermatol. 2016;176:836-837. doi:10.1111/bjd.15197
- Pastor-Nieto MA, Gatica-Ortega ME, Sánchez-Herreros C, et al. Sensitization to benzyl salicylate and other allergens in patients with frontal fibrosing alopecia. Contact Dermatitis. 2021;84:423-430. doi:10.1111/cod.13763
- Rocha VB, Donati A, Contin LA, et al. Photopatch and patch testing in 63 patients with frontal fibrosing alopecia: a case series. Br J Dermatol. 2018;179:1402-1403. doi:10.1111/bjd.16933
Frontal fibrosing alopecia (FFA) is an increasingly common diagnosis, especially in middle-aged women, and was first described by Kossard1 in 1994. It is a variant of lichen planopilaris (LPP), a progressive scarring cicatricial alopecia that affects the frontotemporal area of the scalp, eyebrows, and sometimes even body hair.1 Although its etiology remains unclear, genetic causes, drugs, hormones, and environmental exposures—including certain chemicals found in sunscreens—have been implicated in its pathogenesis.2,3 An association between contact allergy to ingredients in personal care products and FFA diagnosis has been suggested; however, there is no evidence of causality to date. In this article, we highlight the potential relationship between contact allergy and FFA as well as clinical considerations for management.
Clinical Features and Diagnosis
Frontal fibrosing alopecia typically manifests with gradual symmetric recession of the frontal hairline leading to bandlike hair loss along the forehead, sometimes extending to the temporal region.4 Some patients may experience symptoms of scalp itching, burning, or tenderness that may precede or accompany the hair loss. Perifollicular erythema may be visible during the early stages and can be visualized on trichoscopy. The affected skin may appear pale and shiny and may have a smooth texture with a distinct lack of follicular openings. Aside from scalp involvement, other manifestations may include lichen planus pigmentosus, facial papules, body hair involvement, hypochromic lesions, diffuse redness on the face and neck, and prominent frontal veins.5 Although most FFA cases have characteristic clinical features and trichoscopic findings, biopsy for histopathologic examination is still recommended to confirm the diagnosis and ensure appropriate treatment.4 Classic histopathologic features include perifollicular lymphocytic inflammation, follicular destruction, and scarring.
Pathophysiology of FFA
The pathogenesis of FFA is thought to involve a variety of triggers, including immune-mediated inflammation, stress, genetics, hormones, and possibly environmental factors.6 Frontal fibrosing alopecia demonstrates considerable upregulation in cytotoxic helper T cells (TH1) and IFN-γ activity resulting in epithelial hair follicle stem cell apoptosis and replacement of normal epithelial tissue with fibrous tissue.7 There is some suspicion of genetic susceptibility in the onset of FFA as suggested by familial reports and genome-wide association studies.8-10 Hormonal and autoimmune factors also have been linked to FFA, including an increased risk for thyroid disease and the postmenopausal rise of androgen levels.6
Allergic Contact Dermatitis and FFA
Although they are 2 distinct conditions with differing etiologies, allergic contact dermatitis (ACD) and FFA may share environmental triggers, especially in susceptible individuals. This may support the coexistence and potential association between ACD and FFA.
In one case report, a woman who developed facial eczema followed by FFA showed positive patch tests to the UV filters drometrizole trisiloxane and ethylhexyl salicylate, which were listed as ingredients in her sunscreens. Avoidance of these allergens reportedly led to notable improvement of the symptoms.11 Case-control studies have found an association between the use of facial sunscreen and risk for FFA.12 A 2016 questionnaire that assessed a wide range of lifestyle, social, and medical factors related to FFA found that the use of sunscreens was significantly higher in patients with FFA than controls (P<.001), pointing to sunscreens as a potential contributing factor, but further research has been inconclusive. A higher frequency of positive patch tests to hydroperoxides of linalool and balsam of Peru (BoP) in patients with FFA have been documented; however, a direct cause cannot be established.2
In a 2020 prospective study conducted at multiple international centers, 65% (13/20) of FFA patients and 37.5% (9/24) of the control group had a positive patch test reaction to one or more allergens (P=.003). The most common allergens that were identified included cobalt chloride (positive in 35% [7/20] of patients with FFA), nickel sulfate (25% [5/20]), and potassium dichromate (15% [3/20]).13 In a recent 2-year cohort study of 42 patients with FFA who were referred for patch testing, the most common allergens included gallates, hydroperoxides of linalool, and other fragrances.14 After a 3-month period of allergen avoidance, 70% (29/42) of patients had decreased scalp erythema on examination, indicating that avoiding relevant allergens may reduce local inflammation. Furthermore, 76.2% (32/42) of patients with FFA showed delayed-type hypersensitivity to allergens found in daily personal care products such as shampoos, sunscreens, and moisturizers, among others.14 Notably, the study lacked a control group. A case-control study of 36 Hispanic women conducted in Mexico also resulted in 83.3% (15/18) of patients with FFA and 55.5% (10/18) of controls having at least 1 positive patch test; in the FFA group, these included iodopropynyl butylcarbamate (16.7% [3/18]) and propolis (16.7% [3/18]).15
Most recently, a retrospective study conducted by Shtaynberger et al16 included 12 patients with LPP or FFA diagnosed via clinical findings or biopsy. It also included an age- and temporally matched control group tested with identical allergens. Among the 12 patients who had FFA/LPP, all had at least 1 allergen identified on patch testing. The most common allergens identified were propolis (positive in 50% [6/12] of patients with FFA/LPP), fragrance mix I (16%), and methylisothiazolinone (16% [2/12]). Follow-up data were available for 9 of these patients, of whom 6 (66.7%) experienced symptom improvement after 6 months of allergen avoidance. Four (44.4%) patients experienced decreased follicular redness or scaling, 2 (22.2%) patients experienced improved scalp pain/itch, 2 (22.2%) patients had stable/improved hair density, and 1 (1.1%) patient had decreased hair shedding. Although this suggests an environmental trigger for FFA/LPP, the authors stated that changes in patient treatment plans could have contributed to their improvement. The study also was limited by its small size and its overall generalizability.16
These studies have underscored the significance of patch testing in individuals diagnosed with FFA and have identified common allergens prevalent in this patient population. They have suggested that patients with FFA are more likely to have positive patch tests, and in some cases patients could experience improvements in scalp pruritus and erythema with allergen avoidance; however, we emphasize that a causal association between contact allergy and FFA remains unproven to date.
Most Common Allergens Pertinent to FFA
Preservatives—In some studies, patients with FFA have had positive patch tests to preservatives such as gallates and methylchloroisothiazolinone/methylisothiazolinone (MCI/MI).14 Gallates are antioxidants that are used in food preservation, pharmaceuticals, and cosmetics due to their ability to inhibit oxidation and rancidity of fats and oils.17 The most common gallates include propyl gallate, octyl gallate, and dodecyl gallate. Propyl gallate is utilized in some waxy or oily cosmetics and personal care items including sunscreens, shampoos, conditioners, bar soaps, facial cleansers, and moisturizers.18 Typically, if patients have a positive patch test to one gallate, they should be advised to avoid all gallate compounds, as they can cross-react.
Similarly, MCI/MI can prevent product degradation through their antibacterial and antifungal properties. This combination of MCI and MI is used as an effective method of prolonging the shelf life of cosmetic products and commonly is found in sunscreens, facial moisturizing creams, shampoos, and conditioners19; it is banned from use in leave-on products in the European Union and Canada due to increased rates of contact allergy.20 In patients with FFA who commonly use facial sunscreen, preservatives can be a potential allergen exposure to consider.
Iodopropynyl butylcarbamate also is a preservative used in cosmetic formulations. Similar to MCI/MI, it is a potent fungicide and bactericide. This allergen can be found in hair care products, bodywashes, and other personal products.21
UV Light–Absorbing Agents—A systematic review and meta-analysis conducted in 2022 showed a significant (P<.001) association between sunscreen use and FFA.22 A majority of allergens identified on patch testing included UVA- and UVB-absorbing agents found in sunscreens and other products including cosmetics,11,12 such as drometrizole trisiloxane, ethylhexyl salicylate, avobenzone, and benzophenone-4. Drometrizole trisiloxane is a photostabilizer and a broad-spectrum UV filter that is not approved for use in sunscreens in the United States.23 It also is effective in stabilizing and preventing the degradation of avobenzone, a commonly used UVA filter.24
Fragrances—Fragrances are present in nearly every personal and cosmetic product, sometimes even in those advertised as being “fragrance free.” Hydroperoxides of linalool, BoP, and fragrance mix are common allergens that are found in a variety of personal care products including perfumes, cosmetics, and even household cleaning supplies.25 Simultaneous positive patch tests to BoP and fragrance mix are common due to shared components. Linalool can be found in various plants such as lavender, rose, bergamot, and jasmine.26 Upon air exposure, linalool auto-oxidizes to form allergenic hydroperoxides of linalool. Among patients with FFA, positive patch test reactions to fragrance chemicals are common and could be attributed to the use of fragranced hair products and facial cosmetics.
Hair Dyes and Bleaches—Allergic reactions to hair dyes and bleaches can result in severe ACD of the head/neck and, in rare cases, scarring alopecia.27 Chemicals found in these products include paraphenylenediamine (PPD) and ammonium persulfate. The most common hair dye allergen, PPD also is used in some rubbers and plastics. Ammonium persulfate is a chemical used in hair bleaches and to deodorize oils. One case study reported a patient with FFA who developed chemically induced vitiligo immediately after the use of a hair color product that contained PPD.28 However, without patch testing to confirm the presence of contact allergy, other patient-specific and environmental risk factors could have contributed to FFA in this case.
A Knot in the Truth
In this endeavor to untangle the truth, it should be remembered that at the time of writing, the purported association between FFA and ACD remains debatable. Contact dermatitis specialists have voiced that the association between FFA and ACD, especially with regard to sunscreen, cannot be supported due to the lack of sufficient evidence.29 A large majority of the research conducted on FFA and ACD is based on case reports and studies limited to a small sample size, and most of these patch test studies lack a control group. Felmingham et al30 noted that the recent epidemiology of FFA aligns with increased sunscreen use. They also highlighted the limitations of the aforementioned studies, which include misclassification of exposures in the control group2 and recall bias in questionnaire participants.2,12 The most pressing limitation that permeates through most of these studies is the temporal ambiguity associated with sunscreen use. A study by Dhana et al31 failed to specify whether increased sunscreen use preceded the diagnosis of FFA or if it stems from the need to protect more exposed skin as a consequence of disease. Broad sunscreen avoidance due to concern for a possible association with hair loss could have detrimental health implications by increasing the risk for photodamage and skin cancer.
FFA Patch Testing
The avoidance of pertinent allergens could be effective in reducing local inflammation, pruritus, and erythema in FFA.9,14,32 At our institution, we selectively patch test patients with FFA when there is a suspected contact allergy. Clinical features that may allude to a potential contact allergy include an erythematous or eczematous dermatitis or symptoms of pruritus along the scalp or eyebrows. If patients recall hair loss or symptoms after using a hair or facial product, then a potential contact allergy to these products could be considered. Patch testing in patients with FFA includes the North American 80 Comprehensive Series and the cosmetic and hairdresser supplemental series, as well as an additional customized panel of 8 allergens as determined by patch testing experts at the University of Massachusetts, Brigham and Women’s Hospital, and Massachusetts General Hospital (private email communication, November 2017). Patch test readings are performed at 48 and 96 or 120 hours. Using the American Contact Dermatitis Society’s Contact Allergen Management Program, patients are provided personalized safe product lists and avoidance strategies are discussed.
Final Interpretation
In a world where cosmetic products are ubiquitous, it is hard to define the potential role of contact allergens in the entangled pathogenesis of FFA and ACD. As evidenced by emerging literature that correlates the 2 conditions and their exacerbating factors, it is important for physicians to have a comprehensive diagnostic approach and heightened awareness for potential allergens at play in FFA (Table). The identification of certain chemicals and preservatives as potential triggers for FFA should emphasize the importance of patch testing in these patients; however, whether the positive reactions are relevant to the pathogenesis or disease course of FFA still is unknown. While these findings begin to unravel the intertwined causes of FFA and ACD, further research encompassing larger cohorts and prospective studies is imperative to solidify these associations, define concrete guidelines, and improve patient outcomes.
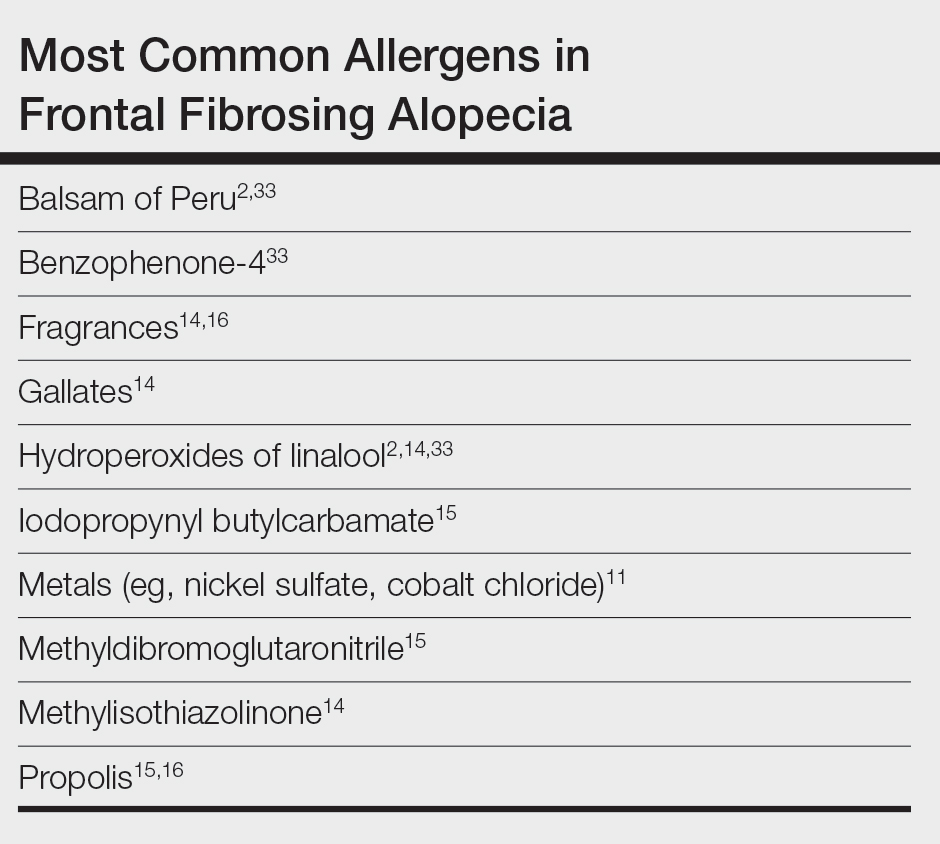
Frontal fibrosing alopecia (FFA) is an increasingly common diagnosis, especially in middle-aged women, and was first described by Kossard1 in 1994. It is a variant of lichen planopilaris (LPP), a progressive scarring cicatricial alopecia that affects the frontotemporal area of the scalp, eyebrows, and sometimes even body hair.1 Although its etiology remains unclear, genetic causes, drugs, hormones, and environmental exposures—including certain chemicals found in sunscreens—have been implicated in its pathogenesis.2,3 An association between contact allergy to ingredients in personal care products and FFA diagnosis has been suggested; however, there is no evidence of causality to date. In this article, we highlight the potential relationship between contact allergy and FFA as well as clinical considerations for management.
Clinical Features and Diagnosis
Frontal fibrosing alopecia typically manifests with gradual symmetric recession of the frontal hairline leading to bandlike hair loss along the forehead, sometimes extending to the temporal region.4 Some patients may experience symptoms of scalp itching, burning, or tenderness that may precede or accompany the hair loss. Perifollicular erythema may be visible during the early stages and can be visualized on trichoscopy. The affected skin may appear pale and shiny and may have a smooth texture with a distinct lack of follicular openings. Aside from scalp involvement, other manifestations may include lichen planus pigmentosus, facial papules, body hair involvement, hypochromic lesions, diffuse redness on the face and neck, and prominent frontal veins.5 Although most FFA cases have characteristic clinical features and trichoscopic findings, biopsy for histopathologic examination is still recommended to confirm the diagnosis and ensure appropriate treatment.4 Classic histopathologic features include perifollicular lymphocytic inflammation, follicular destruction, and scarring.
Pathophysiology of FFA
The pathogenesis of FFA is thought to involve a variety of triggers, including immune-mediated inflammation, stress, genetics, hormones, and possibly environmental factors.6 Frontal fibrosing alopecia demonstrates considerable upregulation in cytotoxic helper T cells (TH1) and IFN-γ activity resulting in epithelial hair follicle stem cell apoptosis and replacement of normal epithelial tissue with fibrous tissue.7 There is some suspicion of genetic susceptibility in the onset of FFA as suggested by familial reports and genome-wide association studies.8-10 Hormonal and autoimmune factors also have been linked to FFA, including an increased risk for thyroid disease and the postmenopausal rise of androgen levels.6
Allergic Contact Dermatitis and FFA
Although they are 2 distinct conditions with differing etiologies, allergic contact dermatitis (ACD) and FFA may share environmental triggers, especially in susceptible individuals. This may support the coexistence and potential association between ACD and FFA.
In one case report, a woman who developed facial eczema followed by FFA showed positive patch tests to the UV filters drometrizole trisiloxane and ethylhexyl salicylate, which were listed as ingredients in her sunscreens. Avoidance of these allergens reportedly led to notable improvement of the symptoms.11 Case-control studies have found an association between the use of facial sunscreen and risk for FFA.12 A 2016 questionnaire that assessed a wide range of lifestyle, social, and medical factors related to FFA found that the use of sunscreens was significantly higher in patients with FFA than controls (P<.001), pointing to sunscreens as a potential contributing factor, but further research has been inconclusive. A higher frequency of positive patch tests to hydroperoxides of linalool and balsam of Peru (BoP) in patients with FFA have been documented; however, a direct cause cannot be established.2
In a 2020 prospective study conducted at multiple international centers, 65% (13/20) of FFA patients and 37.5% (9/24) of the control group had a positive patch test reaction to one or more allergens (P=.003). The most common allergens that were identified included cobalt chloride (positive in 35% [7/20] of patients with FFA), nickel sulfate (25% [5/20]), and potassium dichromate (15% [3/20]).13 In a recent 2-year cohort study of 42 patients with FFA who were referred for patch testing, the most common allergens included gallates, hydroperoxides of linalool, and other fragrances.14 After a 3-month period of allergen avoidance, 70% (29/42) of patients had decreased scalp erythema on examination, indicating that avoiding relevant allergens may reduce local inflammation. Furthermore, 76.2% (32/42) of patients with FFA showed delayed-type hypersensitivity to allergens found in daily personal care products such as shampoos, sunscreens, and moisturizers, among others.14 Notably, the study lacked a control group. A case-control study of 36 Hispanic women conducted in Mexico also resulted in 83.3% (15/18) of patients with FFA and 55.5% (10/18) of controls having at least 1 positive patch test; in the FFA group, these included iodopropynyl butylcarbamate (16.7% [3/18]) and propolis (16.7% [3/18]).15
Most recently, a retrospective study conducted by Shtaynberger et al16 included 12 patients with LPP or FFA diagnosed via clinical findings or biopsy. It also included an age- and temporally matched control group tested with identical allergens. Among the 12 patients who had FFA/LPP, all had at least 1 allergen identified on patch testing. The most common allergens identified were propolis (positive in 50% [6/12] of patients with FFA/LPP), fragrance mix I (16%), and methylisothiazolinone (16% [2/12]). Follow-up data were available for 9 of these patients, of whom 6 (66.7%) experienced symptom improvement after 6 months of allergen avoidance. Four (44.4%) patients experienced decreased follicular redness or scaling, 2 (22.2%) patients experienced improved scalp pain/itch, 2 (22.2%) patients had stable/improved hair density, and 1 (1.1%) patient had decreased hair shedding. Although this suggests an environmental trigger for FFA/LPP, the authors stated that changes in patient treatment plans could have contributed to their improvement. The study also was limited by its small size and its overall generalizability.16
These studies have underscored the significance of patch testing in individuals diagnosed with FFA and have identified common allergens prevalent in this patient population. They have suggested that patients with FFA are more likely to have positive patch tests, and in some cases patients could experience improvements in scalp pruritus and erythema with allergen avoidance; however, we emphasize that a causal association between contact allergy and FFA remains unproven to date.
Most Common Allergens Pertinent to FFA
Preservatives—In some studies, patients with FFA have had positive patch tests to preservatives such as gallates and methylchloroisothiazolinone/methylisothiazolinone (MCI/MI).14 Gallates are antioxidants that are used in food preservation, pharmaceuticals, and cosmetics due to their ability to inhibit oxidation and rancidity of fats and oils.17 The most common gallates include propyl gallate, octyl gallate, and dodecyl gallate. Propyl gallate is utilized in some waxy or oily cosmetics and personal care items including sunscreens, shampoos, conditioners, bar soaps, facial cleansers, and moisturizers.18 Typically, if patients have a positive patch test to one gallate, they should be advised to avoid all gallate compounds, as they can cross-react.
Similarly, MCI/MI can prevent product degradation through their antibacterial and antifungal properties. This combination of MCI and MI is used as an effective method of prolonging the shelf life of cosmetic products and commonly is found in sunscreens, facial moisturizing creams, shampoos, and conditioners19; it is banned from use in leave-on products in the European Union and Canada due to increased rates of contact allergy.20 In patients with FFA who commonly use facial sunscreen, preservatives can be a potential allergen exposure to consider.
Iodopropynyl butylcarbamate also is a preservative used in cosmetic formulations. Similar to MCI/MI, it is a potent fungicide and bactericide. This allergen can be found in hair care products, bodywashes, and other personal products.21
UV Light–Absorbing Agents—A systematic review and meta-analysis conducted in 2022 showed a significant (P<.001) association between sunscreen use and FFA.22 A majority of allergens identified on patch testing included UVA- and UVB-absorbing agents found in sunscreens and other products including cosmetics,11,12 such as drometrizole trisiloxane, ethylhexyl salicylate, avobenzone, and benzophenone-4. Drometrizole trisiloxane is a photostabilizer and a broad-spectrum UV filter that is not approved for use in sunscreens in the United States.23 It also is effective in stabilizing and preventing the degradation of avobenzone, a commonly used UVA filter.24
Fragrances—Fragrances are present in nearly every personal and cosmetic product, sometimes even in those advertised as being “fragrance free.” Hydroperoxides of linalool, BoP, and fragrance mix are common allergens that are found in a variety of personal care products including perfumes, cosmetics, and even household cleaning supplies.25 Simultaneous positive patch tests to BoP and fragrance mix are common due to shared components. Linalool can be found in various plants such as lavender, rose, bergamot, and jasmine.26 Upon air exposure, linalool auto-oxidizes to form allergenic hydroperoxides of linalool. Among patients with FFA, positive patch test reactions to fragrance chemicals are common and could be attributed to the use of fragranced hair products and facial cosmetics.
Hair Dyes and Bleaches—Allergic reactions to hair dyes and bleaches can result in severe ACD of the head/neck and, in rare cases, scarring alopecia.27 Chemicals found in these products include paraphenylenediamine (PPD) and ammonium persulfate. The most common hair dye allergen, PPD also is used in some rubbers and plastics. Ammonium persulfate is a chemical used in hair bleaches and to deodorize oils. One case study reported a patient with FFA who developed chemically induced vitiligo immediately after the use of a hair color product that contained PPD.28 However, without patch testing to confirm the presence of contact allergy, other patient-specific and environmental risk factors could have contributed to FFA in this case.
A Knot in the Truth
In this endeavor to untangle the truth, it should be remembered that at the time of writing, the purported association between FFA and ACD remains debatable. Contact dermatitis specialists have voiced that the association between FFA and ACD, especially with regard to sunscreen, cannot be supported due to the lack of sufficient evidence.29 A large majority of the research conducted on FFA and ACD is based on case reports and studies limited to a small sample size, and most of these patch test studies lack a control group. Felmingham et al30 noted that the recent epidemiology of FFA aligns with increased sunscreen use. They also highlighted the limitations of the aforementioned studies, which include misclassification of exposures in the control group2 and recall bias in questionnaire participants.2,12 The most pressing limitation that permeates through most of these studies is the temporal ambiguity associated with sunscreen use. A study by Dhana et al31 failed to specify whether increased sunscreen use preceded the diagnosis of FFA or if it stems from the need to protect more exposed skin as a consequence of disease. Broad sunscreen avoidance due to concern for a possible association with hair loss could have detrimental health implications by increasing the risk for photodamage and skin cancer.
FFA Patch Testing
The avoidance of pertinent allergens could be effective in reducing local inflammation, pruritus, and erythema in FFA.9,14,32 At our institution, we selectively patch test patients with FFA when there is a suspected contact allergy. Clinical features that may allude to a potential contact allergy include an erythematous or eczematous dermatitis or symptoms of pruritus along the scalp or eyebrows. If patients recall hair loss or symptoms after using a hair or facial product, then a potential contact allergy to these products could be considered. Patch testing in patients with FFA includes the North American 80 Comprehensive Series and the cosmetic and hairdresser supplemental series, as well as an additional customized panel of 8 allergens as determined by patch testing experts at the University of Massachusetts, Brigham and Women’s Hospital, and Massachusetts General Hospital (private email communication, November 2017). Patch test readings are performed at 48 and 96 or 120 hours. Using the American Contact Dermatitis Society’s Contact Allergen Management Program, patients are provided personalized safe product lists and avoidance strategies are discussed.
Final Interpretation
In a world where cosmetic products are ubiquitous, it is hard to define the potential role of contact allergens in the entangled pathogenesis of FFA and ACD. As evidenced by emerging literature that correlates the 2 conditions and their exacerbating factors, it is important for physicians to have a comprehensive diagnostic approach and heightened awareness for potential allergens at play in FFA (Table). The identification of certain chemicals and preservatives as potential triggers for FFA should emphasize the importance of patch testing in these patients; however, whether the positive reactions are relevant to the pathogenesis or disease course of FFA still is unknown. While these findings begin to unravel the intertwined causes of FFA and ACD, further research encompassing larger cohorts and prospective studies is imperative to solidify these associations, define concrete guidelines, and improve patient outcomes.
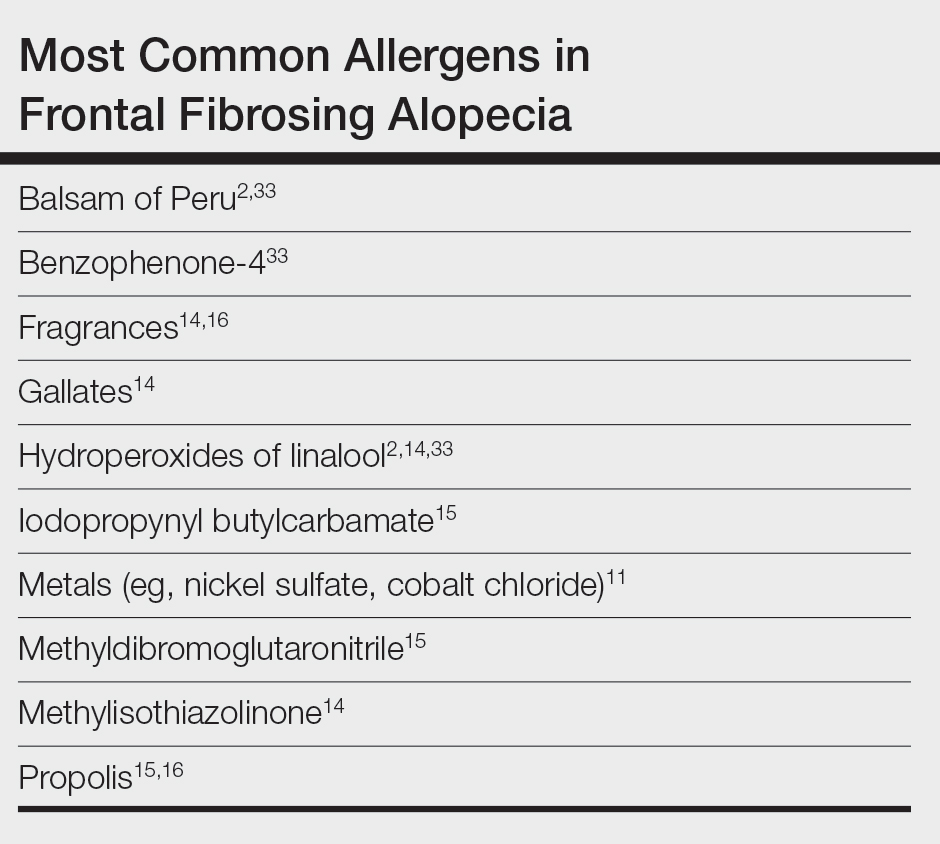
- Kossard S. Postmenopausal frontal fibrosing alopecia: scarring alopecia in a pattern distribution. Arch Dermatol. 1994;130:770-774. doi:10.1001/archderm.1994.01690060100013
- Aldoori N, Dobson K, Holden CR, et al. Frontal fibrosing alopecia: possible association with leave-on facial skin care products and sunscreens; a questionnaire study. Br J Dermatol. 2016;175:762-767. doi:10.1111/bjd.14535
- Debroy Kidambi A, Dobson K, Holmes S, et al. Frontal fibrosing alopecia in men: an association with facial moisturizers and sunscreens. Br J Dermatol. 2017;177:260-261. doi:10.1111/bjd.15311
- Starace M, Orlando G, Iorizzo M, et al. Clinical and dermoscopic approaches to diagnosis of frontal fibrosing alopecia: results from a multicenter study of the International Dermoscopy Society. Dermatol Pract Concept. 2022;12:E2022080. doi:10.5826/dpc.1201a80
- Fechine COC, Valente NYS, Romiti R. Lichen planopilaris and frontal fibrosing alopecia: review and update of diagnostic and therapeutic features. An Bras Dermatol. 2022;97:348-357. doi:10.1016/j.abd.2021.08.008
- Frontal fibrosing alopecia: a review of disease pathogenesis. Front Med (Lausanne). 2022;9:911944. doi:10.3389/fmed.2022.911944
- Del Duca E, Ruano Ruiz J, Pavel AB, et al. Frontal fibrosing alopecia shows robust T helper 1 and Janus kinase 3 skewing. Br J Dermatol. 2020;183:1083-1093. doi:10.1111/bjd.19040
- Tziotzios C, Petridis C, Dand N, et al. Genome-wide association study in frontal fibrosing alopecia identifies four susceptibility loci including HLA-B*07:02. Nat Commun. 2019;10:1150. doi:10.1038/s41467-019-09117-w
- Navarro‐Belmonte MR, Navarro‐López V, Ramírez‐Boscà A, et al. Case series of familial frontal fibrosing alopecia and a review of the literature. J Cosmet Dermatol. 2015;14:64-69. doi:10.1111/jocd.12125
- Cuenca-Barrales C, Ruiz-Villaverde R, Molina-Leyva A. Familial frontal fibrosing alopecia. Sultan Qaboos Univ Med J. 2021;21:E320-E323. doi:10.18295/squmj.2021.21.02.025
- Pastor-Nieto MA, Gatica-Ortega ME. Allergic contact dermatitis to drometrizole trisiloxane in a woman thereafter diagnosed with frontal fibrosing alopecia. Contact Dermatitis. 2023;89:215-217. doi:10.1111/cod.14370
- Moreno-Arrones OM, Saceda-Corralo D, Rodrigues-Barata AR, et al. Risk factors associated with frontal fibrosing alopecia: a multicentre case–control study. Clin Exp Dermatol. 2019;44:404-410. doi:10.1111/ced.13785
- Rudnicka L, Rokni GR, Lotti T, et al. Allergic contact dermatitis in patients with frontal fibrosing alopecia: an international multi-center study. Dermatol Ther. 2020;33:E13560. doi:10.1111/dth.13560
- Prasad S, Marks DH, Burns LJ, et al. Patch testing and contact allergen avoidance in patients with lichen planopilaris and/or frontal fibrosing alopecia: a cohort study. J Am Acad Dermatol. 2020;83:659-661. doi:10.1016/j.jaad.2020.01.026
- Ocampo-Garza SS, Herz-Ruelas ME, Chavez-Alvarez S, et al. Association of frontal fibrosing alopecia and contact allergens in everyday skincare products in Hispanic females: a case-control study. An Bras Dermatol. 2021;96:776-778. doi:10.1016/j.abd.2020.09.013
- Shtaynberger B, Bruder P, Zippin JH. The prevalence of type iv hypersensitivity in patients with lichen planopilaris and frontal fibrosing alopecia. Dermatitis. 2023;34:351-352. doi:10.1097/DER.0000000000000965
- Kahkeshani N, Farzaei F, Fotouhi M, et al. Pharmacological effects of gallic acid in health and diseases: a mechanistic review. Iran J Basic Med Sci. 2019;22:225-237. doi:10.22038/ijbms.2019.32806.7897
- Holcomb ZE, Van Noord MG, Atwater AR. Gallate contact dermatitis: product update and systematic review. Dermatitis. 2017;28:115-127. doi:10.1097/DER.0000000000000263
- Gorris A, Valencak J, Schremser V, et al. Contact allergy to methylisothiazolinone with three clinical presentations in one patient. Contact Dermatitis. 2020;82:162-164. doi:10.1111/cod.13384
- Uter W, Aalto-Korte K, Agner T, et al. The epidemic of methylisothiazolinone contact allergy in Europe: follow-up on changing exposures. J Eur Acad Dermatol Venereol. 2020;34:333-339. doi:10.1111/jdv.15875
- Batista M, Morgado F, Gonçalo M. Patch test reactivity to iodopropynyl butylcarbamate in consecutive patients during a period of 7 years. Contact Dermatitis. 2019;81:54-55. doi:10.1111/cod.13213
- Maghfour J, Ceresnie M, Olson J, et al. The association between frontal fibrosing alopecia, sunscreen, and moisturizers: a systematic review and meta-analysis. J Am Acad Dermatol. 2022;87:395-396. doi:10.1016/j.jaad.2021.12.058
- Drometrizole trisiloxane. PubChem website. Accessed February 21, 2024. https://pubchem.ncbi.nlm.nih.gov/compound/9848888
- Hughes TM, Martin JA, Lewis VJ, et al. Allergic contact dermatitis to drometrizole trisiloxane in a sunscreen with concomitant sensitivities to other sunscreens. Contact Dermatitis. 2005;52:226-227. doi:10.1111/j.0105-1873.2005.0566a.x
- de Groot AC. Myroxylon pereirae resin (balsam of Peru)—a critical review of the literature and assessment of the significance of positive patch test reactions and the usefulness of restrictive diets. Contact Dermatitis. 2019;80:335-353. doi:10.1111/cod.13263
- Sköld M, Börje A, Matura M, et al. Studies on the autoxidation and sensitizing capacity of the fragrance chemical linalool, identifying a linalool hydroperoxide. Contact Dermatitis. 2002;46:267-272. doi:10.1034/j.1600-0536.2002.460504.x
- Dev T, Khan E, Patel U, et al. Cicatricial alopecia following allergic contact dermatitis from hair dyes: a rare clinical presentation. Contact Dermatitis. 2022;86:59-61. doi:10.1111/cod.13974
- De Souza B, Burns L, Senna MM. Frontal fibrosing alopecia preceding the development of vitiligo: a case report. JAAD Case Rep. 2020;6:154-155. doi:10.1016/j.jdcr.2019.12.011
- Abuav R, Shon W. Are sunscreen particles involved in frontal fibrosing alopecia?—a TEM-EDXS analysis on formalin-fixed paraffin-embedded alopecia biopsies (pilot study). Am J Dermatopathol. 2022;44:E135. doi:10.1097/DAD.0000000000002317
- Felmingham C, Yip L, Tam M, et al. Allergy to sunscreen and leave-on facial products is not a likely causative mechanism in frontal fibrosing alopecia: perspective from contact allergy experts. Br J Dermatol. 2020;182:481-482. doi:10.1111/bjd.18380
- Dhana A, Gumedze F, Khumalo N. Regarding “frontal fibrosing alopecia: possible association with leave-on facial skincare products and sunscreens; a questionnaire study.” Br J Dermatol. 2016;176:836-837. doi:10.1111/bjd.15197
- Pastor-Nieto MA, Gatica-Ortega ME, Sánchez-Herreros C, et al. Sensitization to benzyl salicylate and other allergens in patients with frontal fibrosing alopecia. Contact Dermatitis. 2021;84:423-430. doi:10.1111/cod.13763
- Rocha VB, Donati A, Contin LA, et al. Photopatch and patch testing in 63 patients with frontal fibrosing alopecia: a case series. Br J Dermatol. 2018;179:1402-1403. doi:10.1111/bjd.16933
- Kossard S. Postmenopausal frontal fibrosing alopecia: scarring alopecia in a pattern distribution. Arch Dermatol. 1994;130:770-774. doi:10.1001/archderm.1994.01690060100013
- Aldoori N, Dobson K, Holden CR, et al. Frontal fibrosing alopecia: possible association with leave-on facial skin care products and sunscreens; a questionnaire study. Br J Dermatol. 2016;175:762-767. doi:10.1111/bjd.14535
- Debroy Kidambi A, Dobson K, Holmes S, et al. Frontal fibrosing alopecia in men: an association with facial moisturizers and sunscreens. Br J Dermatol. 2017;177:260-261. doi:10.1111/bjd.15311
- Starace M, Orlando G, Iorizzo M, et al. Clinical and dermoscopic approaches to diagnosis of frontal fibrosing alopecia: results from a multicenter study of the International Dermoscopy Society. Dermatol Pract Concept. 2022;12:E2022080. doi:10.5826/dpc.1201a80
- Fechine COC, Valente NYS, Romiti R. Lichen planopilaris and frontal fibrosing alopecia: review and update of diagnostic and therapeutic features. An Bras Dermatol. 2022;97:348-357. doi:10.1016/j.abd.2021.08.008
- Frontal fibrosing alopecia: a review of disease pathogenesis. Front Med (Lausanne). 2022;9:911944. doi:10.3389/fmed.2022.911944
- Del Duca E, Ruano Ruiz J, Pavel AB, et al. Frontal fibrosing alopecia shows robust T helper 1 and Janus kinase 3 skewing. Br J Dermatol. 2020;183:1083-1093. doi:10.1111/bjd.19040
- Tziotzios C, Petridis C, Dand N, et al. Genome-wide association study in frontal fibrosing alopecia identifies four susceptibility loci including HLA-B*07:02. Nat Commun. 2019;10:1150. doi:10.1038/s41467-019-09117-w
- Navarro‐Belmonte MR, Navarro‐López V, Ramírez‐Boscà A, et al. Case series of familial frontal fibrosing alopecia and a review of the literature. J Cosmet Dermatol. 2015;14:64-69. doi:10.1111/jocd.12125
- Cuenca-Barrales C, Ruiz-Villaverde R, Molina-Leyva A. Familial frontal fibrosing alopecia. Sultan Qaboos Univ Med J. 2021;21:E320-E323. doi:10.18295/squmj.2021.21.02.025
- Pastor-Nieto MA, Gatica-Ortega ME. Allergic contact dermatitis to drometrizole trisiloxane in a woman thereafter diagnosed with frontal fibrosing alopecia. Contact Dermatitis. 2023;89:215-217. doi:10.1111/cod.14370
- Moreno-Arrones OM, Saceda-Corralo D, Rodrigues-Barata AR, et al. Risk factors associated with frontal fibrosing alopecia: a multicentre case–control study. Clin Exp Dermatol. 2019;44:404-410. doi:10.1111/ced.13785
- Rudnicka L, Rokni GR, Lotti T, et al. Allergic contact dermatitis in patients with frontal fibrosing alopecia: an international multi-center study. Dermatol Ther. 2020;33:E13560. doi:10.1111/dth.13560
- Prasad S, Marks DH, Burns LJ, et al. Patch testing and contact allergen avoidance in patients with lichen planopilaris and/or frontal fibrosing alopecia: a cohort study. J Am Acad Dermatol. 2020;83:659-661. doi:10.1016/j.jaad.2020.01.026
- Ocampo-Garza SS, Herz-Ruelas ME, Chavez-Alvarez S, et al. Association of frontal fibrosing alopecia and contact allergens in everyday skincare products in Hispanic females: a case-control study. An Bras Dermatol. 2021;96:776-778. doi:10.1016/j.abd.2020.09.013
- Shtaynberger B, Bruder P, Zippin JH. The prevalence of type iv hypersensitivity in patients with lichen planopilaris and frontal fibrosing alopecia. Dermatitis. 2023;34:351-352. doi:10.1097/DER.0000000000000965
- Kahkeshani N, Farzaei F, Fotouhi M, et al. Pharmacological effects of gallic acid in health and diseases: a mechanistic review. Iran J Basic Med Sci. 2019;22:225-237. doi:10.22038/ijbms.2019.32806.7897
- Holcomb ZE, Van Noord MG, Atwater AR. Gallate contact dermatitis: product update and systematic review. Dermatitis. 2017;28:115-127. doi:10.1097/DER.0000000000000263
- Gorris A, Valencak J, Schremser V, et al. Contact allergy to methylisothiazolinone with three clinical presentations in one patient. Contact Dermatitis. 2020;82:162-164. doi:10.1111/cod.13384
- Uter W, Aalto-Korte K, Agner T, et al. The epidemic of methylisothiazolinone contact allergy in Europe: follow-up on changing exposures. J Eur Acad Dermatol Venereol. 2020;34:333-339. doi:10.1111/jdv.15875
- Batista M, Morgado F, Gonçalo M. Patch test reactivity to iodopropynyl butylcarbamate in consecutive patients during a period of 7 years. Contact Dermatitis. 2019;81:54-55. doi:10.1111/cod.13213
- Maghfour J, Ceresnie M, Olson J, et al. The association between frontal fibrosing alopecia, sunscreen, and moisturizers: a systematic review and meta-analysis. J Am Acad Dermatol. 2022;87:395-396. doi:10.1016/j.jaad.2021.12.058
- Drometrizole trisiloxane. PubChem website. Accessed February 21, 2024. https://pubchem.ncbi.nlm.nih.gov/compound/9848888
- Hughes TM, Martin JA, Lewis VJ, et al. Allergic contact dermatitis to drometrizole trisiloxane in a sunscreen with concomitant sensitivities to other sunscreens. Contact Dermatitis. 2005;52:226-227. doi:10.1111/j.0105-1873.2005.0566a.x
- de Groot AC. Myroxylon pereirae resin (balsam of Peru)—a critical review of the literature and assessment of the significance of positive patch test reactions and the usefulness of restrictive diets. Contact Dermatitis. 2019;80:335-353. doi:10.1111/cod.13263
- Sköld M, Börje A, Matura M, et al. Studies on the autoxidation and sensitizing capacity of the fragrance chemical linalool, identifying a linalool hydroperoxide. Contact Dermatitis. 2002;46:267-272. doi:10.1034/j.1600-0536.2002.460504.x
- Dev T, Khan E, Patel U, et al. Cicatricial alopecia following allergic contact dermatitis from hair dyes: a rare clinical presentation. Contact Dermatitis. 2022;86:59-61. doi:10.1111/cod.13974
- De Souza B, Burns L, Senna MM. Frontal fibrosing alopecia preceding the development of vitiligo: a case report. JAAD Case Rep. 2020;6:154-155. doi:10.1016/j.jdcr.2019.12.011
- Abuav R, Shon W. Are sunscreen particles involved in frontal fibrosing alopecia?—a TEM-EDXS analysis on formalin-fixed paraffin-embedded alopecia biopsies (pilot study). Am J Dermatopathol. 2022;44:E135. doi:10.1097/DAD.0000000000002317
- Felmingham C, Yip L, Tam M, et al. Allergy to sunscreen and leave-on facial products is not a likely causative mechanism in frontal fibrosing alopecia: perspective from contact allergy experts. Br J Dermatol. 2020;182:481-482. doi:10.1111/bjd.18380
- Dhana A, Gumedze F, Khumalo N. Regarding “frontal fibrosing alopecia: possible association with leave-on facial skincare products and sunscreens; a questionnaire study.” Br J Dermatol. 2016;176:836-837. doi:10.1111/bjd.15197
- Pastor-Nieto MA, Gatica-Ortega ME, Sánchez-Herreros C, et al. Sensitization to benzyl salicylate and other allergens in patients with frontal fibrosing alopecia. Contact Dermatitis. 2021;84:423-430. doi:10.1111/cod.13763
- Rocha VB, Donati A, Contin LA, et al. Photopatch and patch testing in 63 patients with frontal fibrosing alopecia: a case series. Br J Dermatol. 2018;179:1402-1403. doi:10.1111/bjd.16933
Practice Points
- Frontal fibrosing alopecia (FFA), a variant of lichen planopilaris (LPP), is an increasingly prevalent type of scarring alopecia that may have a closer relationship to contact allergy than was previously understood. However, there is no evidence of a causal association to date.
- When evaluating for FFA/LPP, clinicians should assess for use of cosmetic products or sunscreens that may have a potential impact on the disease course.
E-Consults in Dermatology: A Retrospective Analysis
Dermatologic conditions affect approximately one-third of individuals in the United States.1,2 Nearly 1 in 4 physician office visits in the United States are for skin conditions, and less than one-third of these visits are with dermatologists. Although many of these patients may prefer to see a dermatologist for their concerns, they may not be able to access specialist care.3 The limited supply and urban-focused distribution of dermatologists along with reduced acceptance of state-funded insurance plans and long appointment wait times all pose considerable challenges to individuals seeking dermatologic care.2 Electronic consultations (e-consults) have emerged as a promising solution to overcoming these barriers while providing high-quality dermatologic care to a large diverse patient population.2,4 Although e-consults can be of service to all dermatology patients, this modality may be especially beneficial to underserved populations, such as the uninsured and Medicaid patients—groups that historically have experienced limited access to dermatology care due to the low reimbursement rates and high administrative burdens accompanying care delivery.4 This limited access leads to inequity in care, as timely access to dermatology is associated with improved diagnostic accuracy and disease outcomes.3 E-consult implementation can facilitate timely access for these underserved populations and bypass additional barriers to care such as lack of transportation or time off work. Prior e-consult studies have demonstrated relatively high numbers of Medicaid patients utilizing e-consult services.3,5
Although in-person visits remain the gold standard for diagnosis and treatment of dermatologic conditions, e-consults placed by primary care providers (PCPs) can improve access and help triage patients who require in-person dermatology visits.6 In this study, we conducted a retrospective chart review to characterize the e-consults requested of the dermatology department at a large tertiary care medical center in Winston-Salem, North Carolina.
Methods
The electronic health record (EHR) of Atrium Health Wake Forest Baptist (Winston-Salem, North Carolina) was screened for eligible patients from January 1, 2020, to May 31, 2021. Patients—both adult (aged ≥18 years) and pediatric (aged <18 years)—were included if they underwent a dermatology e-consult within this time frame. Provider notes in the medical records were reviewed to determine the nature of the lesion, how long the dermatologist took to complete the e-consult, whether an in-person appointment was recommended, and whether the patient was seen by dermatology within 90 days of the e-consult. Institutional review board approval was obtained.
For each e-consult, the PCP obtained clinical photographs of the lesion in question either through the EHR mobile application or by having patients upload their own photographs directly to their medical records. The referring PCP then completed a brief template regarding the patient’s clinical question and medical history and then sent the completed information to the consulting dermatologist’s EHR inbox. From there, the dermatologist could view the clinical question, documented photographs, and patient medical record to create a brief consult note with recommendations. The note was then sent back via EHR to the PCP to follow up with the patient. Patients were not charged for the e-consult.

Results
Two hundred fifty-four dermatology e-consults were requested by providers at the study center (eTable), which included 252 unique patients (2 patients had 2 separate e-consults regarding different clinical questions). The median time for completion of the e-consult—from submission of the PCP’s e-consult request to dermatologist completion—was 0.37 days. Fifty-six patients (22.0%) were recommended for an in-person appointment (Figure), 33 (58.9%) of whom ultimately scheduled the in-person appointment, and the median length of time between the completion of the e-consult and the in-person appointment was 16.5 days. The remaining 198 patients (78.0%) were not triaged to receive an in-person appointment following the e-consult,but 2 patients (8.7%) were ultimately seen in-person anyway via other referral pathways, with a median length of 33 days between e-consult completion and the in-person appointment. One hundred seventy-six patients (69.8%) avoided an in-person dermatology visit, although 38 (21.6%) of those patients were fewer than 90 days out from their e-consults at the time of data collection. The 254 e-consults included patients from 50 different zip codes, 49 (98.0%) of which were in North Carolina.

Comment
An e-consult is an asynchronous telehealth modality through which PCPs can request specialty evaluation to provide diagnostic and therapeutic guidance, facilitate PCP-specialist coordination of care, and increase access to specialty care with reduced wait times.7,8 Increased care access is especially important, as specialty referral can decrease overall health care expenditure; however, the demand for specialists often exceeds the availability.8 Our e-consult program drastically reduced the time from patients’ initial presentation at their PCP’s office to dermatologist recommendations for treatment or need for in-person dermatology follow-up.
In our analysis, patients were of different racial, ethnic, and socioeconomic backgrounds and lived across a variety of zip codes, predominantly in central and western North Carolina. Almost three-quarters of the patients resided in zip codes where the average income was less than the North Carolina median household income ($66,196).9 Additionally, 82 patients (32.3%) were uninsured or on Medicaid (eTable). These economically disadvantaged patient populations historically have had limited access to dermatologic care.4 One study showed that privately insured individuals were accepted as new patients by dermatologists 91% of the time compared to a 29.8% acceptance rate for publicly insured individuals.10 Uninsured and Medicaid patients also have to wait 34% longer for an appointment compared to individuals with Medicare or private insurance.2 Considering these patients may already be at an economic disadvantage when it comes to seeing and paying for dermatologic services, e-consults may reduce patient travel and appointment expenses while increasing access to specialty care. Based on a 2020 study, each e-consult generates an estimated savings of $80 out-of-pocket per patient per avoided in-person visit.11
In our study, the most common condition for an e-consult in both adult and pediatric patients was rash, which is consistent with prior e-consult studies.5,11 We found that most e-consult patients were not recommended for an in-person dermatology visit, and for those who were recommended to have an in-person visit, the wait time was reduced (Figure). These results corroborate that e-consults may be used as an important triage tool for determining whether a specialist appointment is indicated as well as a public health tool, as timely evaluation is associated with better dermatologic health care outcomes.3 However, the number of patients who did not present for an in-person appointment in our study may be overestimated, as 38 patients’ (21.6%) e-consults were conducted fewer than 90 days before our data collection. Although none of these patients had been seen in person, it is possible they requested an in-person visit after their medical records were reviewed for this study. Additionally, it is possible patients sought care from outside providers not documented in the EHR.
With regard to the payment model for the e-consult program, Atrium Health Wake Forest Baptist initially piloted the e-consult system through a partnership with the American Academy of Medical Colleges’ Project CORE: Coordinating Optimal Referral Experiences (https://www.aamc.org/what-we-do/mission-areas/health-care/project-core). Grant funding through Project CORE allowed both the referring PCP and the specialist completing the e-consult to each receive approximately 0.5 relative value units in payment for each consult completed. Based on early adoption successes, the institution has created additional internal funding to support the continued expansion of the e-consult system and is incentivized to continue funding, as proper utilization of e-consults improves patient access to timely specialist care, avoids no-shows or last-minute cancellations for specialist appointments, and decreases back-door access to specialist care through the emergency department and urgent care facilities.5 Although 0.5 relative value units is not equivalent compensation to an in-person office visit, our study showed that e-consults can be completed much more quickly and efficiently and do not utilize nursing staff or other office resources.
Conclusion
E-consults are an effective telehealth modality that can increase patients’ access to dermatologic specialty care.
Acknowledgments—The authors thank the Wake Forest University School of Medicine Department of Medical Education and Department of Dermatology (Winston-Salem, North Carolina) for their contributions to this research study as well as the Wake Forest Clinical and Translational Science Institute (Winston-Salem, North Carolina) for their help extracting EHR data.
- Hay RJ, Johns NE, Williams HC, et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Invest Dermatol. 2014;134:1527-1534.
- Naka F, Lu J, Porto A, et al. Impact of dermatology econsults on access to care and skin cancer screening in underserved populations: a model for teledermatology services in community health centers. J Am Acad Dermatol. 2018;78:293-302.
- Mulcahy A, Mehrotra A, Edison K, et al. Variation in dermatologist visits by sociodemographic characteristics. J Am Acad Dermatol. 2017;76:918-924.
- Yang X, Barbieri JS, Kovarik CL. Cost analysis of a store-and-forward teledermatology consult system in Philadelphia. J Am Acad Dermatol. 2019;81:758-764.
- Wang RF, Trinidad J, Lawrence J, et al. Improved patient access and outcomes with the integration of an econsult program (teledermatology) within a large academic medical center. J Am Acad Dermatol. 2020;83:1633-1638.
- Lee KJ, Finnane A, Soyer HP. Recent trends in teledermatology and teledermoscopy. Dermatol Pract Concept. 2018;8:214-223.
- Parikh PJ, Mowrey C, Gallimore J, et al. Evaluating e-consultation implementations based on use and time-line across various specialties. Int J Med Inform. 2017;108:42-48.
- Wasfy JH, Rao SK, Kalwani N, et al. Longer-term impact of cardiology e-consults. Am Heart J. 2016;173:86-93.
- United States Census Bureau. QuickFacts: North Carolina; United States. Accessed February 26, 2024. https://www.census.gov/quickfacts/fact/table/NC,US/PST045222
- Alghothani L, Jacks SK, Vander Horst A, et al. Disparities in access to dermatologic care according to insurance type. Arch Dermatol. 2012;148:956-957.
- Seiger K, Hawryluk EB, Kroshinsky D, et al. Pediatric dermatology econsults: reduced wait times and dermatology office visits. Pediatr Dermatol. 2020;37:804-810.
Dermatologic conditions affect approximately one-third of individuals in the United States.1,2 Nearly 1 in 4 physician office visits in the United States are for skin conditions, and less than one-third of these visits are with dermatologists. Although many of these patients may prefer to see a dermatologist for their concerns, they may not be able to access specialist care.3 The limited supply and urban-focused distribution of dermatologists along with reduced acceptance of state-funded insurance plans and long appointment wait times all pose considerable challenges to individuals seeking dermatologic care.2 Electronic consultations (e-consults) have emerged as a promising solution to overcoming these barriers while providing high-quality dermatologic care to a large diverse patient population.2,4 Although e-consults can be of service to all dermatology patients, this modality may be especially beneficial to underserved populations, such as the uninsured and Medicaid patients—groups that historically have experienced limited access to dermatology care due to the low reimbursement rates and high administrative burdens accompanying care delivery.4 This limited access leads to inequity in care, as timely access to dermatology is associated with improved diagnostic accuracy and disease outcomes.3 E-consult implementation can facilitate timely access for these underserved populations and bypass additional barriers to care such as lack of transportation or time off work. Prior e-consult studies have demonstrated relatively high numbers of Medicaid patients utilizing e-consult services.3,5
Although in-person visits remain the gold standard for diagnosis and treatment of dermatologic conditions, e-consults placed by primary care providers (PCPs) can improve access and help triage patients who require in-person dermatology visits.6 In this study, we conducted a retrospective chart review to characterize the e-consults requested of the dermatology department at a large tertiary care medical center in Winston-Salem, North Carolina.
Methods
The electronic health record (EHR) of Atrium Health Wake Forest Baptist (Winston-Salem, North Carolina) was screened for eligible patients from January 1, 2020, to May 31, 2021. Patients—both adult (aged ≥18 years) and pediatric (aged <18 years)—were included if they underwent a dermatology e-consult within this time frame. Provider notes in the medical records were reviewed to determine the nature of the lesion, how long the dermatologist took to complete the e-consult, whether an in-person appointment was recommended, and whether the patient was seen by dermatology within 90 days of the e-consult. Institutional review board approval was obtained.
For each e-consult, the PCP obtained clinical photographs of the lesion in question either through the EHR mobile application or by having patients upload their own photographs directly to their medical records. The referring PCP then completed a brief template regarding the patient’s clinical question and medical history and then sent the completed information to the consulting dermatologist’s EHR inbox. From there, the dermatologist could view the clinical question, documented photographs, and patient medical record to create a brief consult note with recommendations. The note was then sent back via EHR to the PCP to follow up with the patient. Patients were not charged for the e-consult.

Results
Two hundred fifty-four dermatology e-consults were requested by providers at the study center (eTable), which included 252 unique patients (2 patients had 2 separate e-consults regarding different clinical questions). The median time for completion of the e-consult—from submission of the PCP’s e-consult request to dermatologist completion—was 0.37 days. Fifty-six patients (22.0%) were recommended for an in-person appointment (Figure), 33 (58.9%) of whom ultimately scheduled the in-person appointment, and the median length of time between the completion of the e-consult and the in-person appointment was 16.5 days. The remaining 198 patients (78.0%) were not triaged to receive an in-person appointment following the e-consult,but 2 patients (8.7%) were ultimately seen in-person anyway via other referral pathways, with a median length of 33 days between e-consult completion and the in-person appointment. One hundred seventy-six patients (69.8%) avoided an in-person dermatology visit, although 38 (21.6%) of those patients were fewer than 90 days out from their e-consults at the time of data collection. The 254 e-consults included patients from 50 different zip codes, 49 (98.0%) of which were in North Carolina.

Comment
An e-consult is an asynchronous telehealth modality through which PCPs can request specialty evaluation to provide diagnostic and therapeutic guidance, facilitate PCP-specialist coordination of care, and increase access to specialty care with reduced wait times.7,8 Increased care access is especially important, as specialty referral can decrease overall health care expenditure; however, the demand for specialists often exceeds the availability.8 Our e-consult program drastically reduced the time from patients’ initial presentation at their PCP’s office to dermatologist recommendations for treatment or need for in-person dermatology follow-up.
In our analysis, patients were of different racial, ethnic, and socioeconomic backgrounds and lived across a variety of zip codes, predominantly in central and western North Carolina. Almost three-quarters of the patients resided in zip codes where the average income was less than the North Carolina median household income ($66,196).9 Additionally, 82 patients (32.3%) were uninsured or on Medicaid (eTable). These economically disadvantaged patient populations historically have had limited access to dermatologic care.4 One study showed that privately insured individuals were accepted as new patients by dermatologists 91% of the time compared to a 29.8% acceptance rate for publicly insured individuals.10 Uninsured and Medicaid patients also have to wait 34% longer for an appointment compared to individuals with Medicare or private insurance.2 Considering these patients may already be at an economic disadvantage when it comes to seeing and paying for dermatologic services, e-consults may reduce patient travel and appointment expenses while increasing access to specialty care. Based on a 2020 study, each e-consult generates an estimated savings of $80 out-of-pocket per patient per avoided in-person visit.11
In our study, the most common condition for an e-consult in both adult and pediatric patients was rash, which is consistent with prior e-consult studies.5,11 We found that most e-consult patients were not recommended for an in-person dermatology visit, and for those who were recommended to have an in-person visit, the wait time was reduced (Figure). These results corroborate that e-consults may be used as an important triage tool for determining whether a specialist appointment is indicated as well as a public health tool, as timely evaluation is associated with better dermatologic health care outcomes.3 However, the number of patients who did not present for an in-person appointment in our study may be overestimated, as 38 patients’ (21.6%) e-consults were conducted fewer than 90 days before our data collection. Although none of these patients had been seen in person, it is possible they requested an in-person visit after their medical records were reviewed for this study. Additionally, it is possible patients sought care from outside providers not documented in the EHR.
With regard to the payment model for the e-consult program, Atrium Health Wake Forest Baptist initially piloted the e-consult system through a partnership with the American Academy of Medical Colleges’ Project CORE: Coordinating Optimal Referral Experiences (https://www.aamc.org/what-we-do/mission-areas/health-care/project-core). Grant funding through Project CORE allowed both the referring PCP and the specialist completing the e-consult to each receive approximately 0.5 relative value units in payment for each consult completed. Based on early adoption successes, the institution has created additional internal funding to support the continued expansion of the e-consult system and is incentivized to continue funding, as proper utilization of e-consults improves patient access to timely specialist care, avoids no-shows or last-minute cancellations for specialist appointments, and decreases back-door access to specialist care through the emergency department and urgent care facilities.5 Although 0.5 relative value units is not equivalent compensation to an in-person office visit, our study showed that e-consults can be completed much more quickly and efficiently and do not utilize nursing staff or other office resources.
Conclusion
E-consults are an effective telehealth modality that can increase patients’ access to dermatologic specialty care.
Acknowledgments—The authors thank the Wake Forest University School of Medicine Department of Medical Education and Department of Dermatology (Winston-Salem, North Carolina) for their contributions to this research study as well as the Wake Forest Clinical and Translational Science Institute (Winston-Salem, North Carolina) for their help extracting EHR data.
Dermatologic conditions affect approximately one-third of individuals in the United States.1,2 Nearly 1 in 4 physician office visits in the United States are for skin conditions, and less than one-third of these visits are with dermatologists. Although many of these patients may prefer to see a dermatologist for their concerns, they may not be able to access specialist care.3 The limited supply and urban-focused distribution of dermatologists along with reduced acceptance of state-funded insurance plans and long appointment wait times all pose considerable challenges to individuals seeking dermatologic care.2 Electronic consultations (e-consults) have emerged as a promising solution to overcoming these barriers while providing high-quality dermatologic care to a large diverse patient population.2,4 Although e-consults can be of service to all dermatology patients, this modality may be especially beneficial to underserved populations, such as the uninsured and Medicaid patients—groups that historically have experienced limited access to dermatology care due to the low reimbursement rates and high administrative burdens accompanying care delivery.4 This limited access leads to inequity in care, as timely access to dermatology is associated with improved diagnostic accuracy and disease outcomes.3 E-consult implementation can facilitate timely access for these underserved populations and bypass additional barriers to care such as lack of transportation or time off work. Prior e-consult studies have demonstrated relatively high numbers of Medicaid patients utilizing e-consult services.3,5
Although in-person visits remain the gold standard for diagnosis and treatment of dermatologic conditions, e-consults placed by primary care providers (PCPs) can improve access and help triage patients who require in-person dermatology visits.6 In this study, we conducted a retrospective chart review to characterize the e-consults requested of the dermatology department at a large tertiary care medical center in Winston-Salem, North Carolina.
Methods
The electronic health record (EHR) of Atrium Health Wake Forest Baptist (Winston-Salem, North Carolina) was screened for eligible patients from January 1, 2020, to May 31, 2021. Patients—both adult (aged ≥18 years) and pediatric (aged <18 years)—were included if they underwent a dermatology e-consult within this time frame. Provider notes in the medical records were reviewed to determine the nature of the lesion, how long the dermatologist took to complete the e-consult, whether an in-person appointment was recommended, and whether the patient was seen by dermatology within 90 days of the e-consult. Institutional review board approval was obtained.
For each e-consult, the PCP obtained clinical photographs of the lesion in question either through the EHR mobile application or by having patients upload their own photographs directly to their medical records. The referring PCP then completed a brief template regarding the patient’s clinical question and medical history and then sent the completed information to the consulting dermatologist’s EHR inbox. From there, the dermatologist could view the clinical question, documented photographs, and patient medical record to create a brief consult note with recommendations. The note was then sent back via EHR to the PCP to follow up with the patient. Patients were not charged for the e-consult.

Results
Two hundred fifty-four dermatology e-consults were requested by providers at the study center (eTable), which included 252 unique patients (2 patients had 2 separate e-consults regarding different clinical questions). The median time for completion of the e-consult—from submission of the PCP’s e-consult request to dermatologist completion—was 0.37 days. Fifty-six patients (22.0%) were recommended for an in-person appointment (Figure), 33 (58.9%) of whom ultimately scheduled the in-person appointment, and the median length of time between the completion of the e-consult and the in-person appointment was 16.5 days. The remaining 198 patients (78.0%) were not triaged to receive an in-person appointment following the e-consult,but 2 patients (8.7%) were ultimately seen in-person anyway via other referral pathways, with a median length of 33 days between e-consult completion and the in-person appointment. One hundred seventy-six patients (69.8%) avoided an in-person dermatology visit, although 38 (21.6%) of those patients were fewer than 90 days out from their e-consults at the time of data collection. The 254 e-consults included patients from 50 different zip codes, 49 (98.0%) of which were in North Carolina.

Comment
An e-consult is an asynchronous telehealth modality through which PCPs can request specialty evaluation to provide diagnostic and therapeutic guidance, facilitate PCP-specialist coordination of care, and increase access to specialty care with reduced wait times.7,8 Increased care access is especially important, as specialty referral can decrease overall health care expenditure; however, the demand for specialists often exceeds the availability.8 Our e-consult program drastically reduced the time from patients’ initial presentation at their PCP’s office to dermatologist recommendations for treatment or need for in-person dermatology follow-up.
In our analysis, patients were of different racial, ethnic, and socioeconomic backgrounds and lived across a variety of zip codes, predominantly in central and western North Carolina. Almost three-quarters of the patients resided in zip codes where the average income was less than the North Carolina median household income ($66,196).9 Additionally, 82 patients (32.3%) were uninsured or on Medicaid (eTable). These economically disadvantaged patient populations historically have had limited access to dermatologic care.4 One study showed that privately insured individuals were accepted as new patients by dermatologists 91% of the time compared to a 29.8% acceptance rate for publicly insured individuals.10 Uninsured and Medicaid patients also have to wait 34% longer for an appointment compared to individuals with Medicare or private insurance.2 Considering these patients may already be at an economic disadvantage when it comes to seeing and paying for dermatologic services, e-consults may reduce patient travel and appointment expenses while increasing access to specialty care. Based on a 2020 study, each e-consult generates an estimated savings of $80 out-of-pocket per patient per avoided in-person visit.11
In our study, the most common condition for an e-consult in both adult and pediatric patients was rash, which is consistent with prior e-consult studies.5,11 We found that most e-consult patients were not recommended for an in-person dermatology visit, and for those who were recommended to have an in-person visit, the wait time was reduced (Figure). These results corroborate that e-consults may be used as an important triage tool for determining whether a specialist appointment is indicated as well as a public health tool, as timely evaluation is associated with better dermatologic health care outcomes.3 However, the number of patients who did not present for an in-person appointment in our study may be overestimated, as 38 patients’ (21.6%) e-consults were conducted fewer than 90 days before our data collection. Although none of these patients had been seen in person, it is possible they requested an in-person visit after their medical records were reviewed for this study. Additionally, it is possible patients sought care from outside providers not documented in the EHR.
With regard to the payment model for the e-consult program, Atrium Health Wake Forest Baptist initially piloted the e-consult system through a partnership with the American Academy of Medical Colleges’ Project CORE: Coordinating Optimal Referral Experiences (https://www.aamc.org/what-we-do/mission-areas/health-care/project-core). Grant funding through Project CORE allowed both the referring PCP and the specialist completing the e-consult to each receive approximately 0.5 relative value units in payment for each consult completed. Based on early adoption successes, the institution has created additional internal funding to support the continued expansion of the e-consult system and is incentivized to continue funding, as proper utilization of e-consults improves patient access to timely specialist care, avoids no-shows or last-minute cancellations for specialist appointments, and decreases back-door access to specialist care through the emergency department and urgent care facilities.5 Although 0.5 relative value units is not equivalent compensation to an in-person office visit, our study showed that e-consults can be completed much more quickly and efficiently and do not utilize nursing staff or other office resources.
Conclusion
E-consults are an effective telehealth modality that can increase patients’ access to dermatologic specialty care.
Acknowledgments—The authors thank the Wake Forest University School of Medicine Department of Medical Education and Department of Dermatology (Winston-Salem, North Carolina) for their contributions to this research study as well as the Wake Forest Clinical and Translational Science Institute (Winston-Salem, North Carolina) for their help extracting EHR data.
- Hay RJ, Johns NE, Williams HC, et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Invest Dermatol. 2014;134:1527-1534.
- Naka F, Lu J, Porto A, et al. Impact of dermatology econsults on access to care and skin cancer screening in underserved populations: a model for teledermatology services in community health centers. J Am Acad Dermatol. 2018;78:293-302.
- Mulcahy A, Mehrotra A, Edison K, et al. Variation in dermatologist visits by sociodemographic characteristics. J Am Acad Dermatol. 2017;76:918-924.
- Yang X, Barbieri JS, Kovarik CL. Cost analysis of a store-and-forward teledermatology consult system in Philadelphia. J Am Acad Dermatol. 2019;81:758-764.
- Wang RF, Trinidad J, Lawrence J, et al. Improved patient access and outcomes with the integration of an econsult program (teledermatology) within a large academic medical center. J Am Acad Dermatol. 2020;83:1633-1638.
- Lee KJ, Finnane A, Soyer HP. Recent trends in teledermatology and teledermoscopy. Dermatol Pract Concept. 2018;8:214-223.
- Parikh PJ, Mowrey C, Gallimore J, et al. Evaluating e-consultation implementations based on use and time-line across various specialties. Int J Med Inform. 2017;108:42-48.
- Wasfy JH, Rao SK, Kalwani N, et al. Longer-term impact of cardiology e-consults. Am Heart J. 2016;173:86-93.
- United States Census Bureau. QuickFacts: North Carolina; United States. Accessed February 26, 2024. https://www.census.gov/quickfacts/fact/table/NC,US/PST045222
- Alghothani L, Jacks SK, Vander Horst A, et al. Disparities in access to dermatologic care according to insurance type. Arch Dermatol. 2012;148:956-957.
- Seiger K, Hawryluk EB, Kroshinsky D, et al. Pediatric dermatology econsults: reduced wait times and dermatology office visits. Pediatr Dermatol. 2020;37:804-810.
- Hay RJ, Johns NE, Williams HC, et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Invest Dermatol. 2014;134:1527-1534.
- Naka F, Lu J, Porto A, et al. Impact of dermatology econsults on access to care and skin cancer screening in underserved populations: a model for teledermatology services in community health centers. J Am Acad Dermatol. 2018;78:293-302.
- Mulcahy A, Mehrotra A, Edison K, et al. Variation in dermatologist visits by sociodemographic characteristics. J Am Acad Dermatol. 2017;76:918-924.
- Yang X, Barbieri JS, Kovarik CL. Cost analysis of a store-and-forward teledermatology consult system in Philadelphia. J Am Acad Dermatol. 2019;81:758-764.
- Wang RF, Trinidad J, Lawrence J, et al. Improved patient access and outcomes with the integration of an econsult program (teledermatology) within a large academic medical center. J Am Acad Dermatol. 2020;83:1633-1638.
- Lee KJ, Finnane A, Soyer HP. Recent trends in teledermatology and teledermoscopy. Dermatol Pract Concept. 2018;8:214-223.
- Parikh PJ, Mowrey C, Gallimore J, et al. Evaluating e-consultation implementations based on use and time-line across various specialties. Int J Med Inform. 2017;108:42-48.
- Wasfy JH, Rao SK, Kalwani N, et al. Longer-term impact of cardiology e-consults. Am Heart J. 2016;173:86-93.
- United States Census Bureau. QuickFacts: North Carolina; United States. Accessed February 26, 2024. https://www.census.gov/quickfacts/fact/table/NC,US/PST045222
- Alghothani L, Jacks SK, Vander Horst A, et al. Disparities in access to dermatologic care according to insurance type. Arch Dermatol. 2012;148:956-957.
- Seiger K, Hawryluk EB, Kroshinsky D, et al. Pediatric dermatology econsults: reduced wait times and dermatology office visits. Pediatr Dermatol. 2020;37:804-810.
Practice Points
- Most electronic consult patients may be able to avoid in-person dermatology appointments.
- E-consults can increase patient access to dermatologic specialty care.
Vulvar Lichen Sclerosus: What’s New?
Vulvar lichen sclerosus (VLS) is an underserved area in medicine and dermatology. We discuss updates in VLS, which include the following: (1) development of core outcome domains to include in all future clinical trials, with current efforts focused on determining outcome measurements for each domain; (2) increased understanding of the impact VLS has on quality-of-life (QOL) outcomes; (3) expanded disease associations; (4) clinical and histologic variants, including vestibular sclerosis and nonsclerotic VLS; and (5) updates in management of VLS.
Core Outcomes Measures
The burden of VLS is challenging to quantify, with little agreement among experts.1 Recently there has been a focus on developing scoring scales to measure disease progression and treatment response. Simpson et al2 pioneered the development of a core outcome set to be included in all future clinical trials for genital lichen sclerosus (LS)—clinical (visible) signs, symptoms, and LS-specific QOL.
Although there is no standardized method for assessing disease severity, various scales have been proposed to measure clinical findings in VLS, such as the vulvar architecture severity scale3 as well as the clinical LS score,4 which is the only validated scale to incorporate the signs and architectural changes identified by a 2018 Delphi consensus group of the International Society for the Study of Vulvovaginal Disease.5 Work is ongoing to identify and evaluate outcome measurement instruments for each of the 3 core outcome domains.
Increased Understanding of QOL Impacts
Pain, pruritus, impairment of sexual function, genitourinary complications, architectural changes, and risk for squamous cell carcinoma (SCC) all have been well established as VLS sequelae.6,7 Recent studies have focused on the QOL impact and associations with psychiatric comorbidities. A matched case-control study found that LS was significantly associated with depression and anxiety among US women (P<.001), and individuals with LS had a more than 2-fold increased odds of receiving a diagnosis of depression or anxiety.8
A review evaluating QOL outcomes in LS found that overall QOL was impaired. Female patients reported worse QOL in the work-school domain of the dermatology life quality index compared with male counterparts.9
Finally, a study exploring the experiences of patients living with VLS highlighted the secrecy and stigma of the condition,10 which serves as a call to action to improve the general population’s knowledge about vulvar anatomy and create change in societal attitudes on vulvar conditions.
Although there are several instruments assessing vulvar-specific QOL, most are for patients with vulvar cancer and focus on sexual function. In 2020, Saunderson et al11 published the 15-item vulvar quality of life index (VQLI), which has broad implications for measuring vulvar disease burden and is an important tool for standardizing vulvar disease measurements and outcomes for clinical research.12 The VQLI, though not specific to VLS, consists of 4 domains to assess vulvar QOL including symptoms, anxiety, activities of daily living, and sexuality. Studies have evaluated this scoring system in patients with VLS, with 1 study finding that VQLI correlated with clinician-rated severity scores (P=.01) and overall patient itch/discomfort score (P<.001) in VLS.13,14
Expanded Disease Associations
Lichen sclerosus has a well-known association with vulvar SCC and other autoimmune conditions, including thyroid disease and bullous pemphigoid.15-17 Recent studies also have revealed an association between LS and psoriasis.18 A case-control study from a single center found VLS was associated with elevated body mass index, statin usage, and cholecystectomy.19 Gynecologic pain syndromes, interstitial cystitis, urinary incontinence, and some gastrointestinal tract disorders including celiac disease also have been found to be increased in patients with VLS.20 Finally, the incidence of cutaneous immune-related adverse events such as LS has increased as the use of immune checkpoint therapies as anticancer treatments has expanded.21 Clinicians should be aware of these potential disease associations when caring for patients with VLS.
The incidence of VLS is higher in lower estrogen states throughout the lifespan, and a recent case-control study evaluated the cutaneous hormonal and microbial landscapes in postmenopausal patients (6 patients with VLS; 12 controls).22 Levels of the following cutaneous hormones in the groin were found to be altered in patients with VLS compared with controls: estrone (lower; P=.006), progesterone (higher; P<.0001), and testosterone (lower; P=.02). The authors found that most hormone levels normalized following treatment with a topical steroid. Additionally, bacterial microbiome alterations were seen in patients with VLS compared with controls. Thus, cutaneous sex hormone and skin microbiome alterations may be associated with VLS.22
Updates in Clinical and Histologic Variants
Less-recognized variants of VLS have been characterized in recent years. Vestibular sclerosis is a variant of VLS with unique clinical and histopathologic features; it is characterized by involvement localized to the anterior vestibule and either an absent or sparse lymphocytic infiltrate on histopathology.23,24 Nonsclerotic VLS is a variant with clinical features consistent with VLS that does not exhibit dermal sclerosis on histopathology. Thus, a diagnosis of nonsclerotic VLS requires clinicopathologic correlation. Four nonsclerotic histopathologic subtypes are proposed: lichenoid, hypertrophic lichenoid, dermal fibrosis without acanthosis, and dermal fibrosis with acanthosis.25 Longitudinal studies that correlate duration, signs, and symptoms will be important to further understand these variants.
Management Updates
First-line treatment of VLS still consists of ultrapotent topical corticosteroids with chronic maintenance therapy (usually lifetime) to decrease the risk for SCC and architectural changes.26 However, a survey across social media platforms found steroid phobia is common in patients with VLS (N=865), with approximately 40% of respondents endorsing waiting as long as they could before using topical corticosteroids and stopping as soon as possible.27 Clinicians should be aware of possible patient perceptions in the use of chronic steroids when discussing this therapy.
Randomized controlled trials utilizing fractional CO2 devices for VLS have been performed with conflicting results and no consensus regarding outcome measurement.28,29 Additionally, long-term disease outcomes following laser use have not been investigated. Although there is evidence that both ablative and nonablative devices can improve symptoms and signs, there is no evidence that they offer a cure for a chronic inflammatory skin condition. Current evidence suggests that even for patients undergoing these procedures, maintenance therapy is still essential to prevent sequelae.30 Future studies incorporating standardized outcome measures will be important for assessing the benefits of laser therapy in VLS. Finally, the reasons why topical corticosteroids may fail in an individual patient are multifaceted and should be explored thoroughly when considering laser therapy for VLS.
Studies evaluating the role of systemic therapies for refractory cases of VLS have expanded. A systematic review of systemic therapies for both genital and extragenital LS found oral corticosteroids and methotrexate were the most-reported systemic treatment regimens.31 Use of biologics in LS has been reported, with cases utilizing adalimumab for VLS and dupilumab for extragenital LS. Use of Janus kinase inhibitors including abrocitinib and baricitinib also has been reported for LS.31 A clinical trial to evaluate the safety and efficacy of topical ruxolitinib in VLS was recently completed (ClinicalTrials.govidentifier NCT05593445). Future research studies likely will focus on the safety and efficacy of targeted and steroid-sparing therapies for patients with VLS.
Final Thoughts
Vulvar lichen sclerosus increasingly is becoming recognized as a chronic genital skin condition that impacts QOL and health outcomes, with a need to develop more effective and safe evidence-based therapies. Recent literature has focused on the importance of developing and standardizing disease outcomes; identifying disease associations including the role of cutaneous hormones and microbiome alterations; characterizing histologic and clinical variants; and staying up-to-date on management, including the need for understanding patient perceptions of chronic topical steroid therapy. Each of these are important updates for clinicians to consider when caring for patients with VLS. Future studies likely will focus on elucidating disease etiology and mechanisms to gain a better understanding of VLS pathogenesis and potential targets for therapies as well as implementation of clinical trials that incorporate standardized outcome domains to test efficacy and safety of additional therapies.
- Sheinis M, Green N, Vieira-Baptista P, et al. Adult vulvar lichen sclerosus: can experts agree on the assessment of disease severity? J Low Genit Tract Dis. 2020;24:295-298. doi:10.1097/LGT.0000000000000534
- Simpson RC, Kirtschig G, Selk A, et al. Core outcome domains for lichen sclerosus: a CORALS initiative consensus statement. Br J Dermatol. 2023;188:628-635. doi:10.1093/bjd/ljac145
- Almadori A, Zenner N, Boyle D, et al. Development and validation of a clinical grading scale to assess the vulvar region: the Vulvar Architecture Severity Scale. Aesthet Surg J. 2020;40:1319-1326. doi:10.1093/asj/sjz342
- Erni B, Navarini AA, Huang D, et al. Proposition of a severity scale for lichen sclerosus: the “Clinical Lichen Sclerosus Score.” Dermatol Ther. 2021;34:E14773. doi:10.1111/dth.14773
- Sheinis M, Selk A. Development of the Adult Vulvar Lichen Sclerosus Severity Scale—a Delphi Consensus Exercise for Item Generation. J Low Genit Tract Dis. 2018;22:66-73. doi:10.1097/LGT.0000000000000361
- Mauskar MM, Marathe K, Venkatesan A, et al. Vulvar diseases. J Am Acad Dermatol. 2020;82:1287-1298. doi:10.1016/j.jaad.2019.10.077
- Wijaya M, Lee G, Fischer G. Why do some patients with vulval lichen sclerosus on long-term topical corticosteroid treatment experience ongoing poor quality of life? Australas J Dermatol. 2022;63:463-472. doi:10.1111/ajd.13926
- Fan R, Leasure AC, Maisha FI, et al. Depression and anxiety in patients with lichen sclerosus. JAMA Dermatol. 2022;158:953-954. doi:10.1001/jamadermatol.2022.1964
- Ranum A, Pearson DR. The impact of genital lichen sclerosus and lichen planus on quality of life: a review. Int J Womens Dermatol. 2022;8:E042. doi:10.1097/JW9.0000000000000042
- Arnold S, Fernando S, Rees S. Living with vulval lichen sclerosus: a qualitative interview study. Br J Dermatol. 2022;187:909-918. doi:10.1111/bjd.21777
- Saunderson RB, Harris V, Yeh R, et al. Vulvar quality of life index (VQLI)—a simple tool to measure quality of life in patients with vulvar disease. Australas J Dermatol. 2020;61:152-157. doi:10.1111/ajd.13235
- Pyle HJ, Evans JC, Vandergriff TW, et al. Vulvar lichen sclerosus clinical severity scales and histopathologic correlation: a case series. Am J Dermatopathol. 2023;45:588-592. doi:10.1097/DAD.0000000000002471
- Wijaya M, Lee G, Fischer G. Quality of life of women with untreated vulval lichen sclerosus assessed with vulval quality of life index (VQLI) [published online January 28, 2021]. Australas J Dermatol. 2021;62:177-182. doi:10.1111/ajd.13530
- Felmingham C, Chan L, Doyle LW, et al. The Vulval Disease Quality of Life Index in women with vulval lichen sclerosus correlates with clinician and symptom scores [published online November 14, 2019]. Australas J Dermatol. 2020;61:110-118. doi:10.1111/ajd.13197
- Walsh ML, Leonard N, Shawki H, et al. Lichen sclerosus and immunobullous disease. J Low Genit Tract Dis. 2012;16:468-470. doi:10.1097/LGT.0b013e31825e9b18
- Chin S, Scurry J, Bradford J, et al. Association of topical corticosteroids with reduced vulvar squamous cell carcinoma recurrence in patients with vulvar lichen sclerosus. JAMA Dermatol. 2020;156:813. doi:10.1001/jamadermatol.2020.1074
- Fan R, Leasure AC, Maisha FI, et al. Thyroid disorders associated with lichen sclerosus: a case–control study in the All of Us Research Program. Br J Dermatol. 2022;187:797-799. doi:10.1111/bjd.21702
- Fan R, Leasure AC, Little AJ, et al. Lichen sclerosus among women with psoriasis: a cross-sectional study in the All of Us research program. J Am Acad Dermatol. 2023;88:1175-1177. doi:10.1016/j.jaad.2022.12.012
- Luu Y, Cheng AL, Reisz C. Elevated body mass index, statin use, and cholecystectomy are associated with vulvar lichen sclerosus: a retrospective, case-control study. J Am Acad Dermatol. 2023;88:1376-1378. doi:10.1016/j.jaad.2023.01.023
- Söderlund JM, Hieta NK, Kurki SH, et al. Comorbidity of urogynecological and gastrointestinal disorders in female patients with lichen sclerosus. J Low Genit Tract Dis. 2023;2:156-160. doi:10.1097/LGT.0000000000000727
- Shin L, Smith J, Shiu J, et al. Association of lichen sclerosus and morphea with immune checkpoint therapy: a systematic review. Int J Womens Dermatol. 2023;9:E070. doi:10.1097/JW9.0000000000000070
- Pyle HJ, Evans JC, Artami M, et al. Assessment of the cutaneous hormone landscapes and microbiomes in vulvar lichen sclerosus [published online February 16, 2024]. J Invest Dermatol. 2024:S0022-202X(24)00111-8. doi:10.1016/j.jid.2024.01.027
- Day T, Burston K, Dennerstein G, et al. Vestibulovaginal sclerosis versus lichen sclerosus. Int J Gynecol Pathol. 2018;37:356-363. doi:10.1097/PGP.0000000000000441
- Croker BA, Scurry JP, Petry FM, et al. Vestibular sclerosis: is this a new, distinct clinicopathological entity? J Low Genit Tract Dis. 2018;22:260-263. doi:10.1097/LGT.0000000000000404
- Day T, Selim MA, Allbritton JI, et al. Nonsclerotic lichen sclerosus: definition of a concept and pathologic description. J Low Genit Tract Dis. 2023;27:358-364. doi:10.1097/LGT.0000000000000760
- Lee A, Bradford J, Fischer G. Long-term management of adult vulvar lichen sclerosus: a prospective cohort study of 507 women. JAMA Dermatol. 2015;151:1061. doi:10.1001/jamadermatol.2015.0643
- Delpero E, Sriharan A, Selk A. Steroid phobia in patients with vulvar lichen sclerosus. J Low Genit Tract Dis. 2023;27:286-290. doi:10.1097/LGT.0000000000000753
- Burkett LS, Siddique M, Zeymo A, et al. Clobetasol compared with fractionated carbon dioxide laser for lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:968-978. doi:10.1097/AOG.0000000000004332
- Mitchell L, Goldstein AT, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:979-987. doi:10.1097/AOG.0000000000004409
- Li HOY, Bailey AMJ, Tan MG, Dover JS. Lasers as an adjuvant for vulvar lichen sclerosus: a systematic review and meta-analysis. J Am Acad Dermatol. 2022;86:694-696. doi:10.1016/j.jaad.2021.02.081
- Hargis A, Ngo M, Kraus CN, et al. Systemic therapy for lichen sclerosus: a systematic review [published online November 4, 2023]. J Low Genit Tract Dis. doi:10.1097/LGT.0000000000000775
Vulvar lichen sclerosus (VLS) is an underserved area in medicine and dermatology. We discuss updates in VLS, which include the following: (1) development of core outcome domains to include in all future clinical trials, with current efforts focused on determining outcome measurements for each domain; (2) increased understanding of the impact VLS has on quality-of-life (QOL) outcomes; (3) expanded disease associations; (4) clinical and histologic variants, including vestibular sclerosis and nonsclerotic VLS; and (5) updates in management of VLS.
Core Outcomes Measures
The burden of VLS is challenging to quantify, with little agreement among experts.1 Recently there has been a focus on developing scoring scales to measure disease progression and treatment response. Simpson et al2 pioneered the development of a core outcome set to be included in all future clinical trials for genital lichen sclerosus (LS)—clinical (visible) signs, symptoms, and LS-specific QOL.
Although there is no standardized method for assessing disease severity, various scales have been proposed to measure clinical findings in VLS, such as the vulvar architecture severity scale3 as well as the clinical LS score,4 which is the only validated scale to incorporate the signs and architectural changes identified by a 2018 Delphi consensus group of the International Society for the Study of Vulvovaginal Disease.5 Work is ongoing to identify and evaluate outcome measurement instruments for each of the 3 core outcome domains.
Increased Understanding of QOL Impacts
Pain, pruritus, impairment of sexual function, genitourinary complications, architectural changes, and risk for squamous cell carcinoma (SCC) all have been well established as VLS sequelae.6,7 Recent studies have focused on the QOL impact and associations with psychiatric comorbidities. A matched case-control study found that LS was significantly associated with depression and anxiety among US women (P<.001), and individuals with LS had a more than 2-fold increased odds of receiving a diagnosis of depression or anxiety.8
A review evaluating QOL outcomes in LS found that overall QOL was impaired. Female patients reported worse QOL in the work-school domain of the dermatology life quality index compared with male counterparts.9
Finally, a study exploring the experiences of patients living with VLS highlighted the secrecy and stigma of the condition,10 which serves as a call to action to improve the general population’s knowledge about vulvar anatomy and create change in societal attitudes on vulvar conditions.
Although there are several instruments assessing vulvar-specific QOL, most are for patients with vulvar cancer and focus on sexual function. In 2020, Saunderson et al11 published the 15-item vulvar quality of life index (VQLI), which has broad implications for measuring vulvar disease burden and is an important tool for standardizing vulvar disease measurements and outcomes for clinical research.12 The VQLI, though not specific to VLS, consists of 4 domains to assess vulvar QOL including symptoms, anxiety, activities of daily living, and sexuality. Studies have evaluated this scoring system in patients with VLS, with 1 study finding that VQLI correlated with clinician-rated severity scores (P=.01) and overall patient itch/discomfort score (P<.001) in VLS.13,14
Expanded Disease Associations
Lichen sclerosus has a well-known association with vulvar SCC and other autoimmune conditions, including thyroid disease and bullous pemphigoid.15-17 Recent studies also have revealed an association between LS and psoriasis.18 A case-control study from a single center found VLS was associated with elevated body mass index, statin usage, and cholecystectomy.19 Gynecologic pain syndromes, interstitial cystitis, urinary incontinence, and some gastrointestinal tract disorders including celiac disease also have been found to be increased in patients with VLS.20 Finally, the incidence of cutaneous immune-related adverse events such as LS has increased as the use of immune checkpoint therapies as anticancer treatments has expanded.21 Clinicians should be aware of these potential disease associations when caring for patients with VLS.
The incidence of VLS is higher in lower estrogen states throughout the lifespan, and a recent case-control study evaluated the cutaneous hormonal and microbial landscapes in postmenopausal patients (6 patients with VLS; 12 controls).22 Levels of the following cutaneous hormones in the groin were found to be altered in patients with VLS compared with controls: estrone (lower; P=.006), progesterone (higher; P<.0001), and testosterone (lower; P=.02). The authors found that most hormone levels normalized following treatment with a topical steroid. Additionally, bacterial microbiome alterations were seen in patients with VLS compared with controls. Thus, cutaneous sex hormone and skin microbiome alterations may be associated with VLS.22
Updates in Clinical and Histologic Variants
Less-recognized variants of VLS have been characterized in recent years. Vestibular sclerosis is a variant of VLS with unique clinical and histopathologic features; it is characterized by involvement localized to the anterior vestibule and either an absent or sparse lymphocytic infiltrate on histopathology.23,24 Nonsclerotic VLS is a variant with clinical features consistent with VLS that does not exhibit dermal sclerosis on histopathology. Thus, a diagnosis of nonsclerotic VLS requires clinicopathologic correlation. Four nonsclerotic histopathologic subtypes are proposed: lichenoid, hypertrophic lichenoid, dermal fibrosis without acanthosis, and dermal fibrosis with acanthosis.25 Longitudinal studies that correlate duration, signs, and symptoms will be important to further understand these variants.
Management Updates
First-line treatment of VLS still consists of ultrapotent topical corticosteroids with chronic maintenance therapy (usually lifetime) to decrease the risk for SCC and architectural changes.26 However, a survey across social media platforms found steroid phobia is common in patients with VLS (N=865), with approximately 40% of respondents endorsing waiting as long as they could before using topical corticosteroids and stopping as soon as possible.27 Clinicians should be aware of possible patient perceptions in the use of chronic steroids when discussing this therapy.
Randomized controlled trials utilizing fractional CO2 devices for VLS have been performed with conflicting results and no consensus regarding outcome measurement.28,29 Additionally, long-term disease outcomes following laser use have not been investigated. Although there is evidence that both ablative and nonablative devices can improve symptoms and signs, there is no evidence that they offer a cure for a chronic inflammatory skin condition. Current evidence suggests that even for patients undergoing these procedures, maintenance therapy is still essential to prevent sequelae.30 Future studies incorporating standardized outcome measures will be important for assessing the benefits of laser therapy in VLS. Finally, the reasons why topical corticosteroids may fail in an individual patient are multifaceted and should be explored thoroughly when considering laser therapy for VLS.
Studies evaluating the role of systemic therapies for refractory cases of VLS have expanded. A systematic review of systemic therapies for both genital and extragenital LS found oral corticosteroids and methotrexate were the most-reported systemic treatment regimens.31 Use of biologics in LS has been reported, with cases utilizing adalimumab for VLS and dupilumab for extragenital LS. Use of Janus kinase inhibitors including abrocitinib and baricitinib also has been reported for LS.31 A clinical trial to evaluate the safety and efficacy of topical ruxolitinib in VLS was recently completed (ClinicalTrials.govidentifier NCT05593445). Future research studies likely will focus on the safety and efficacy of targeted and steroid-sparing therapies for patients with VLS.
Final Thoughts
Vulvar lichen sclerosus increasingly is becoming recognized as a chronic genital skin condition that impacts QOL and health outcomes, with a need to develop more effective and safe evidence-based therapies. Recent literature has focused on the importance of developing and standardizing disease outcomes; identifying disease associations including the role of cutaneous hormones and microbiome alterations; characterizing histologic and clinical variants; and staying up-to-date on management, including the need for understanding patient perceptions of chronic topical steroid therapy. Each of these are important updates for clinicians to consider when caring for patients with VLS. Future studies likely will focus on elucidating disease etiology and mechanisms to gain a better understanding of VLS pathogenesis and potential targets for therapies as well as implementation of clinical trials that incorporate standardized outcome domains to test efficacy and safety of additional therapies.
Vulvar lichen sclerosus (VLS) is an underserved area in medicine and dermatology. We discuss updates in VLS, which include the following: (1) development of core outcome domains to include in all future clinical trials, with current efforts focused on determining outcome measurements for each domain; (2) increased understanding of the impact VLS has on quality-of-life (QOL) outcomes; (3) expanded disease associations; (4) clinical and histologic variants, including vestibular sclerosis and nonsclerotic VLS; and (5) updates in management of VLS.
Core Outcomes Measures
The burden of VLS is challenging to quantify, with little agreement among experts.1 Recently there has been a focus on developing scoring scales to measure disease progression and treatment response. Simpson et al2 pioneered the development of a core outcome set to be included in all future clinical trials for genital lichen sclerosus (LS)—clinical (visible) signs, symptoms, and LS-specific QOL.
Although there is no standardized method for assessing disease severity, various scales have been proposed to measure clinical findings in VLS, such as the vulvar architecture severity scale3 as well as the clinical LS score,4 which is the only validated scale to incorporate the signs and architectural changes identified by a 2018 Delphi consensus group of the International Society for the Study of Vulvovaginal Disease.5 Work is ongoing to identify and evaluate outcome measurement instruments for each of the 3 core outcome domains.
Increased Understanding of QOL Impacts
Pain, pruritus, impairment of sexual function, genitourinary complications, architectural changes, and risk for squamous cell carcinoma (SCC) all have been well established as VLS sequelae.6,7 Recent studies have focused on the QOL impact and associations with psychiatric comorbidities. A matched case-control study found that LS was significantly associated with depression and anxiety among US women (P<.001), and individuals with LS had a more than 2-fold increased odds of receiving a diagnosis of depression or anxiety.8
A review evaluating QOL outcomes in LS found that overall QOL was impaired. Female patients reported worse QOL in the work-school domain of the dermatology life quality index compared with male counterparts.9
Finally, a study exploring the experiences of patients living with VLS highlighted the secrecy and stigma of the condition,10 which serves as a call to action to improve the general population’s knowledge about vulvar anatomy and create change in societal attitudes on vulvar conditions.
Although there are several instruments assessing vulvar-specific QOL, most are for patients with vulvar cancer and focus on sexual function. In 2020, Saunderson et al11 published the 15-item vulvar quality of life index (VQLI), which has broad implications for measuring vulvar disease burden and is an important tool for standardizing vulvar disease measurements and outcomes for clinical research.12 The VQLI, though not specific to VLS, consists of 4 domains to assess vulvar QOL including symptoms, anxiety, activities of daily living, and sexuality. Studies have evaluated this scoring system in patients with VLS, with 1 study finding that VQLI correlated with clinician-rated severity scores (P=.01) and overall patient itch/discomfort score (P<.001) in VLS.13,14
Expanded Disease Associations
Lichen sclerosus has a well-known association with vulvar SCC and other autoimmune conditions, including thyroid disease and bullous pemphigoid.15-17 Recent studies also have revealed an association between LS and psoriasis.18 A case-control study from a single center found VLS was associated with elevated body mass index, statin usage, and cholecystectomy.19 Gynecologic pain syndromes, interstitial cystitis, urinary incontinence, and some gastrointestinal tract disorders including celiac disease also have been found to be increased in patients with VLS.20 Finally, the incidence of cutaneous immune-related adverse events such as LS has increased as the use of immune checkpoint therapies as anticancer treatments has expanded.21 Clinicians should be aware of these potential disease associations when caring for patients with VLS.
The incidence of VLS is higher in lower estrogen states throughout the lifespan, and a recent case-control study evaluated the cutaneous hormonal and microbial landscapes in postmenopausal patients (6 patients with VLS; 12 controls).22 Levels of the following cutaneous hormones in the groin were found to be altered in patients with VLS compared with controls: estrone (lower; P=.006), progesterone (higher; P<.0001), and testosterone (lower; P=.02). The authors found that most hormone levels normalized following treatment with a topical steroid. Additionally, bacterial microbiome alterations were seen in patients with VLS compared with controls. Thus, cutaneous sex hormone and skin microbiome alterations may be associated with VLS.22
Updates in Clinical and Histologic Variants
Less-recognized variants of VLS have been characterized in recent years. Vestibular sclerosis is a variant of VLS with unique clinical and histopathologic features; it is characterized by involvement localized to the anterior vestibule and either an absent or sparse lymphocytic infiltrate on histopathology.23,24 Nonsclerotic VLS is a variant with clinical features consistent with VLS that does not exhibit dermal sclerosis on histopathology. Thus, a diagnosis of nonsclerotic VLS requires clinicopathologic correlation. Four nonsclerotic histopathologic subtypes are proposed: lichenoid, hypertrophic lichenoid, dermal fibrosis without acanthosis, and dermal fibrosis with acanthosis.25 Longitudinal studies that correlate duration, signs, and symptoms will be important to further understand these variants.
Management Updates
First-line treatment of VLS still consists of ultrapotent topical corticosteroids with chronic maintenance therapy (usually lifetime) to decrease the risk for SCC and architectural changes.26 However, a survey across social media platforms found steroid phobia is common in patients with VLS (N=865), with approximately 40% of respondents endorsing waiting as long as they could before using topical corticosteroids and stopping as soon as possible.27 Clinicians should be aware of possible patient perceptions in the use of chronic steroids when discussing this therapy.
Randomized controlled trials utilizing fractional CO2 devices for VLS have been performed with conflicting results and no consensus regarding outcome measurement.28,29 Additionally, long-term disease outcomes following laser use have not been investigated. Although there is evidence that both ablative and nonablative devices can improve symptoms and signs, there is no evidence that they offer a cure for a chronic inflammatory skin condition. Current evidence suggests that even for patients undergoing these procedures, maintenance therapy is still essential to prevent sequelae.30 Future studies incorporating standardized outcome measures will be important for assessing the benefits of laser therapy in VLS. Finally, the reasons why topical corticosteroids may fail in an individual patient are multifaceted and should be explored thoroughly when considering laser therapy for VLS.
Studies evaluating the role of systemic therapies for refractory cases of VLS have expanded. A systematic review of systemic therapies for both genital and extragenital LS found oral corticosteroids and methotrexate were the most-reported systemic treatment regimens.31 Use of biologics in LS has been reported, with cases utilizing adalimumab for VLS and dupilumab for extragenital LS. Use of Janus kinase inhibitors including abrocitinib and baricitinib also has been reported for LS.31 A clinical trial to evaluate the safety and efficacy of topical ruxolitinib in VLS was recently completed (ClinicalTrials.govidentifier NCT05593445). Future research studies likely will focus on the safety and efficacy of targeted and steroid-sparing therapies for patients with VLS.
Final Thoughts
Vulvar lichen sclerosus increasingly is becoming recognized as a chronic genital skin condition that impacts QOL and health outcomes, with a need to develop more effective and safe evidence-based therapies. Recent literature has focused on the importance of developing and standardizing disease outcomes; identifying disease associations including the role of cutaneous hormones and microbiome alterations; characterizing histologic and clinical variants; and staying up-to-date on management, including the need for understanding patient perceptions of chronic topical steroid therapy. Each of these are important updates for clinicians to consider when caring for patients with VLS. Future studies likely will focus on elucidating disease etiology and mechanisms to gain a better understanding of VLS pathogenesis and potential targets for therapies as well as implementation of clinical trials that incorporate standardized outcome domains to test efficacy and safety of additional therapies.
- Sheinis M, Green N, Vieira-Baptista P, et al. Adult vulvar lichen sclerosus: can experts agree on the assessment of disease severity? J Low Genit Tract Dis. 2020;24:295-298. doi:10.1097/LGT.0000000000000534
- Simpson RC, Kirtschig G, Selk A, et al. Core outcome domains for lichen sclerosus: a CORALS initiative consensus statement. Br J Dermatol. 2023;188:628-635. doi:10.1093/bjd/ljac145
- Almadori A, Zenner N, Boyle D, et al. Development and validation of a clinical grading scale to assess the vulvar region: the Vulvar Architecture Severity Scale. Aesthet Surg J. 2020;40:1319-1326. doi:10.1093/asj/sjz342
- Erni B, Navarini AA, Huang D, et al. Proposition of a severity scale for lichen sclerosus: the “Clinical Lichen Sclerosus Score.” Dermatol Ther. 2021;34:E14773. doi:10.1111/dth.14773
- Sheinis M, Selk A. Development of the Adult Vulvar Lichen Sclerosus Severity Scale—a Delphi Consensus Exercise for Item Generation. J Low Genit Tract Dis. 2018;22:66-73. doi:10.1097/LGT.0000000000000361
- Mauskar MM, Marathe K, Venkatesan A, et al. Vulvar diseases. J Am Acad Dermatol. 2020;82:1287-1298. doi:10.1016/j.jaad.2019.10.077
- Wijaya M, Lee G, Fischer G. Why do some patients with vulval lichen sclerosus on long-term topical corticosteroid treatment experience ongoing poor quality of life? Australas J Dermatol. 2022;63:463-472. doi:10.1111/ajd.13926
- Fan R, Leasure AC, Maisha FI, et al. Depression and anxiety in patients with lichen sclerosus. JAMA Dermatol. 2022;158:953-954. doi:10.1001/jamadermatol.2022.1964
- Ranum A, Pearson DR. The impact of genital lichen sclerosus and lichen planus on quality of life: a review. Int J Womens Dermatol. 2022;8:E042. doi:10.1097/JW9.0000000000000042
- Arnold S, Fernando S, Rees S. Living with vulval lichen sclerosus: a qualitative interview study. Br J Dermatol. 2022;187:909-918. doi:10.1111/bjd.21777
- Saunderson RB, Harris V, Yeh R, et al. Vulvar quality of life index (VQLI)—a simple tool to measure quality of life in patients with vulvar disease. Australas J Dermatol. 2020;61:152-157. doi:10.1111/ajd.13235
- Pyle HJ, Evans JC, Vandergriff TW, et al. Vulvar lichen sclerosus clinical severity scales and histopathologic correlation: a case series. Am J Dermatopathol. 2023;45:588-592. doi:10.1097/DAD.0000000000002471
- Wijaya M, Lee G, Fischer G. Quality of life of women with untreated vulval lichen sclerosus assessed with vulval quality of life index (VQLI) [published online January 28, 2021]. Australas J Dermatol. 2021;62:177-182. doi:10.1111/ajd.13530
- Felmingham C, Chan L, Doyle LW, et al. The Vulval Disease Quality of Life Index in women with vulval lichen sclerosus correlates with clinician and symptom scores [published online November 14, 2019]. Australas J Dermatol. 2020;61:110-118. doi:10.1111/ajd.13197
- Walsh ML, Leonard N, Shawki H, et al. Lichen sclerosus and immunobullous disease. J Low Genit Tract Dis. 2012;16:468-470. doi:10.1097/LGT.0b013e31825e9b18
- Chin S, Scurry J, Bradford J, et al. Association of topical corticosteroids with reduced vulvar squamous cell carcinoma recurrence in patients with vulvar lichen sclerosus. JAMA Dermatol. 2020;156:813. doi:10.1001/jamadermatol.2020.1074
- Fan R, Leasure AC, Maisha FI, et al. Thyroid disorders associated with lichen sclerosus: a case–control study in the All of Us Research Program. Br J Dermatol. 2022;187:797-799. doi:10.1111/bjd.21702
- Fan R, Leasure AC, Little AJ, et al. Lichen sclerosus among women with psoriasis: a cross-sectional study in the All of Us research program. J Am Acad Dermatol. 2023;88:1175-1177. doi:10.1016/j.jaad.2022.12.012
- Luu Y, Cheng AL, Reisz C. Elevated body mass index, statin use, and cholecystectomy are associated with vulvar lichen sclerosus: a retrospective, case-control study. J Am Acad Dermatol. 2023;88:1376-1378. doi:10.1016/j.jaad.2023.01.023
- Söderlund JM, Hieta NK, Kurki SH, et al. Comorbidity of urogynecological and gastrointestinal disorders in female patients with lichen sclerosus. J Low Genit Tract Dis. 2023;2:156-160. doi:10.1097/LGT.0000000000000727
- Shin L, Smith J, Shiu J, et al. Association of lichen sclerosus and morphea with immune checkpoint therapy: a systematic review. Int J Womens Dermatol. 2023;9:E070. doi:10.1097/JW9.0000000000000070
- Pyle HJ, Evans JC, Artami M, et al. Assessment of the cutaneous hormone landscapes and microbiomes in vulvar lichen sclerosus [published online February 16, 2024]. J Invest Dermatol. 2024:S0022-202X(24)00111-8. doi:10.1016/j.jid.2024.01.027
- Day T, Burston K, Dennerstein G, et al. Vestibulovaginal sclerosis versus lichen sclerosus. Int J Gynecol Pathol. 2018;37:356-363. doi:10.1097/PGP.0000000000000441
- Croker BA, Scurry JP, Petry FM, et al. Vestibular sclerosis: is this a new, distinct clinicopathological entity? J Low Genit Tract Dis. 2018;22:260-263. doi:10.1097/LGT.0000000000000404
- Day T, Selim MA, Allbritton JI, et al. Nonsclerotic lichen sclerosus: definition of a concept and pathologic description. J Low Genit Tract Dis. 2023;27:358-364. doi:10.1097/LGT.0000000000000760
- Lee A, Bradford J, Fischer G. Long-term management of adult vulvar lichen sclerosus: a prospective cohort study of 507 women. JAMA Dermatol. 2015;151:1061. doi:10.1001/jamadermatol.2015.0643
- Delpero E, Sriharan A, Selk A. Steroid phobia in patients with vulvar lichen sclerosus. J Low Genit Tract Dis. 2023;27:286-290. doi:10.1097/LGT.0000000000000753
- Burkett LS, Siddique M, Zeymo A, et al. Clobetasol compared with fractionated carbon dioxide laser for lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:968-978. doi:10.1097/AOG.0000000000004332
- Mitchell L, Goldstein AT, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:979-987. doi:10.1097/AOG.0000000000004409
- Li HOY, Bailey AMJ, Tan MG, Dover JS. Lasers as an adjuvant for vulvar lichen sclerosus: a systematic review and meta-analysis. J Am Acad Dermatol. 2022;86:694-696. doi:10.1016/j.jaad.2021.02.081
- Hargis A, Ngo M, Kraus CN, et al. Systemic therapy for lichen sclerosus: a systematic review [published online November 4, 2023]. J Low Genit Tract Dis. doi:10.1097/LGT.0000000000000775
- Sheinis M, Green N, Vieira-Baptista P, et al. Adult vulvar lichen sclerosus: can experts agree on the assessment of disease severity? J Low Genit Tract Dis. 2020;24:295-298. doi:10.1097/LGT.0000000000000534
- Simpson RC, Kirtschig G, Selk A, et al. Core outcome domains for lichen sclerosus: a CORALS initiative consensus statement. Br J Dermatol. 2023;188:628-635. doi:10.1093/bjd/ljac145
- Almadori A, Zenner N, Boyle D, et al. Development and validation of a clinical grading scale to assess the vulvar region: the Vulvar Architecture Severity Scale. Aesthet Surg J. 2020;40:1319-1326. doi:10.1093/asj/sjz342
- Erni B, Navarini AA, Huang D, et al. Proposition of a severity scale for lichen sclerosus: the “Clinical Lichen Sclerosus Score.” Dermatol Ther. 2021;34:E14773. doi:10.1111/dth.14773
- Sheinis M, Selk A. Development of the Adult Vulvar Lichen Sclerosus Severity Scale—a Delphi Consensus Exercise for Item Generation. J Low Genit Tract Dis. 2018;22:66-73. doi:10.1097/LGT.0000000000000361
- Mauskar MM, Marathe K, Venkatesan A, et al. Vulvar diseases. J Am Acad Dermatol. 2020;82:1287-1298. doi:10.1016/j.jaad.2019.10.077
- Wijaya M, Lee G, Fischer G. Why do some patients with vulval lichen sclerosus on long-term topical corticosteroid treatment experience ongoing poor quality of life? Australas J Dermatol. 2022;63:463-472. doi:10.1111/ajd.13926
- Fan R, Leasure AC, Maisha FI, et al. Depression and anxiety in patients with lichen sclerosus. JAMA Dermatol. 2022;158:953-954. doi:10.1001/jamadermatol.2022.1964
- Ranum A, Pearson DR. The impact of genital lichen sclerosus and lichen planus on quality of life: a review. Int J Womens Dermatol. 2022;8:E042. doi:10.1097/JW9.0000000000000042
- Arnold S, Fernando S, Rees S. Living with vulval lichen sclerosus: a qualitative interview study. Br J Dermatol. 2022;187:909-918. doi:10.1111/bjd.21777
- Saunderson RB, Harris V, Yeh R, et al. Vulvar quality of life index (VQLI)—a simple tool to measure quality of life in patients with vulvar disease. Australas J Dermatol. 2020;61:152-157. doi:10.1111/ajd.13235
- Pyle HJ, Evans JC, Vandergriff TW, et al. Vulvar lichen sclerosus clinical severity scales and histopathologic correlation: a case series. Am J Dermatopathol. 2023;45:588-592. doi:10.1097/DAD.0000000000002471
- Wijaya M, Lee G, Fischer G. Quality of life of women with untreated vulval lichen sclerosus assessed with vulval quality of life index (VQLI) [published online January 28, 2021]. Australas J Dermatol. 2021;62:177-182. doi:10.1111/ajd.13530
- Felmingham C, Chan L, Doyle LW, et al. The Vulval Disease Quality of Life Index in women with vulval lichen sclerosus correlates with clinician and symptom scores [published online November 14, 2019]. Australas J Dermatol. 2020;61:110-118. doi:10.1111/ajd.13197
- Walsh ML, Leonard N, Shawki H, et al. Lichen sclerosus and immunobullous disease. J Low Genit Tract Dis. 2012;16:468-470. doi:10.1097/LGT.0b013e31825e9b18
- Chin S, Scurry J, Bradford J, et al. Association of topical corticosteroids with reduced vulvar squamous cell carcinoma recurrence in patients with vulvar lichen sclerosus. JAMA Dermatol. 2020;156:813. doi:10.1001/jamadermatol.2020.1074
- Fan R, Leasure AC, Maisha FI, et al. Thyroid disorders associated with lichen sclerosus: a case–control study in the All of Us Research Program. Br J Dermatol. 2022;187:797-799. doi:10.1111/bjd.21702
- Fan R, Leasure AC, Little AJ, et al. Lichen sclerosus among women with psoriasis: a cross-sectional study in the All of Us research program. J Am Acad Dermatol. 2023;88:1175-1177. doi:10.1016/j.jaad.2022.12.012
- Luu Y, Cheng AL, Reisz C. Elevated body mass index, statin use, and cholecystectomy are associated with vulvar lichen sclerosus: a retrospective, case-control study. J Am Acad Dermatol. 2023;88:1376-1378. doi:10.1016/j.jaad.2023.01.023
- Söderlund JM, Hieta NK, Kurki SH, et al. Comorbidity of urogynecological and gastrointestinal disorders in female patients with lichen sclerosus. J Low Genit Tract Dis. 2023;2:156-160. doi:10.1097/LGT.0000000000000727
- Shin L, Smith J, Shiu J, et al. Association of lichen sclerosus and morphea with immune checkpoint therapy: a systematic review. Int J Womens Dermatol. 2023;9:E070. doi:10.1097/JW9.0000000000000070
- Pyle HJ, Evans JC, Artami M, et al. Assessment of the cutaneous hormone landscapes and microbiomes in vulvar lichen sclerosus [published online February 16, 2024]. J Invest Dermatol. 2024:S0022-202X(24)00111-8. doi:10.1016/j.jid.2024.01.027
- Day T, Burston K, Dennerstein G, et al. Vestibulovaginal sclerosis versus lichen sclerosus. Int J Gynecol Pathol. 2018;37:356-363. doi:10.1097/PGP.0000000000000441
- Croker BA, Scurry JP, Petry FM, et al. Vestibular sclerosis: is this a new, distinct clinicopathological entity? J Low Genit Tract Dis. 2018;22:260-263. doi:10.1097/LGT.0000000000000404
- Day T, Selim MA, Allbritton JI, et al. Nonsclerotic lichen sclerosus: definition of a concept and pathologic description. J Low Genit Tract Dis. 2023;27:358-364. doi:10.1097/LGT.0000000000000760
- Lee A, Bradford J, Fischer G. Long-term management of adult vulvar lichen sclerosus: a prospective cohort study of 507 women. JAMA Dermatol. 2015;151:1061. doi:10.1001/jamadermatol.2015.0643
- Delpero E, Sriharan A, Selk A. Steroid phobia in patients with vulvar lichen sclerosus. J Low Genit Tract Dis. 2023;27:286-290. doi:10.1097/LGT.0000000000000753
- Burkett LS, Siddique M, Zeymo A, et al. Clobetasol compared with fractionated carbon dioxide laser for lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:968-978. doi:10.1097/AOG.0000000000004332
- Mitchell L, Goldstein AT, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:979-987. doi:10.1097/AOG.0000000000004409
- Li HOY, Bailey AMJ, Tan MG, Dover JS. Lasers as an adjuvant for vulvar lichen sclerosus: a systematic review and meta-analysis. J Am Acad Dermatol. 2022;86:694-696. doi:10.1016/j.jaad.2021.02.081
- Hargis A, Ngo M, Kraus CN, et al. Systemic therapy for lichen sclerosus: a systematic review [published online November 4, 2023]. J Low Genit Tract Dis. doi:10.1097/LGT.0000000000000775
How to Optimize Epidermal Approximation During Wound Suturing Using a Smartphone Camera
Practice Gap
Precise wound approximation during cutaneous suturing is of vital importance for optimal closure and long-term scar outcomes. Although buried dermal sutures achieve wound-edge approximation and eversion, meticulous placement of epidermal sutures allows for fine-tuning of the wound edges through epidermal approximation, eversion, and the correction of minor height discrepancies (step-offs).
Several percutaneous suture techniques and materials are available to dermatologic surgeons. However, precise, gap- and tension-free approximation of the wound edges is desired for prompt re-epithelialization and a barely visible scar.1,2
Epidermal sutures should be placed under minimal tension to align the papillary dermis and epidermis precisely. The dermatologic surgeon can evaluate the effectiveness of their suturing technique by carefully examining the closure for visibility of the bilateral wound edges, which should show equally if approximation is precise; small gaps between the wound edges (undesired); or dermal bleeding, which is a manifestation of inaccurate approximation.
Advances in smartphone camera technology have led to high-quality photography in a variety of settings. Although smartphone photography often is used for documentation purposes in health care, we recommend incorporating it as a quality-control checkpoint for objective evaluation, allowing the dermatologic surgeon to scrutinize the wound edges and refine their surgical technique to improve scar outcomes.
The Technique
After suturing the wound closed, we routinely use a 12-megapixel smartphone camera (up to 2× optical zoom) to photograph the closed wound at 1× or 2× magnification to capture more details and use the zoom function to further evaluate the wound edges close-up (Figure). In any area where inadequate epidermal approximation is noted on the photograph, an additional stitch can be placed. Photography can be repeated until ideal reapproximation occurs.
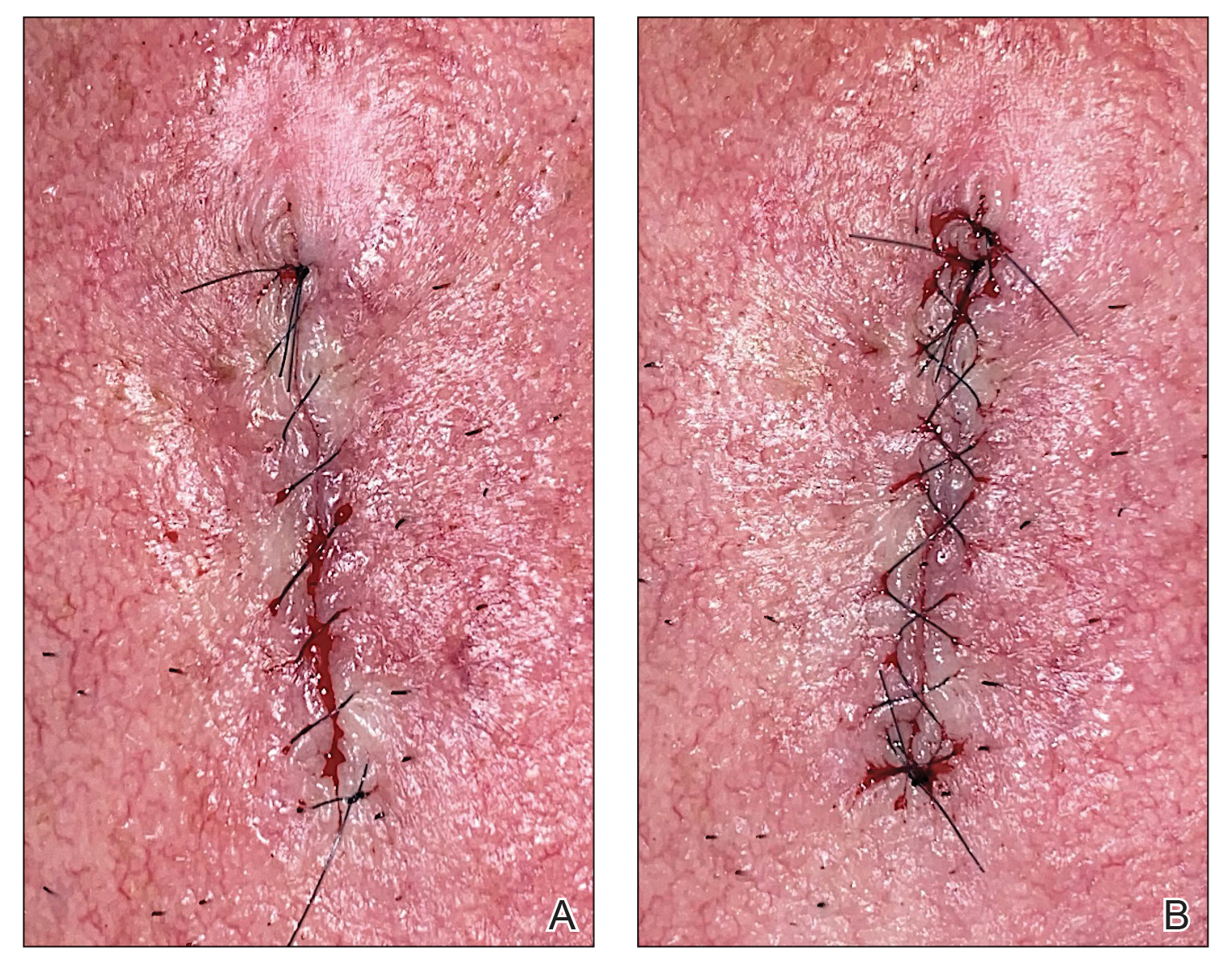
Practice Implications
Most smartphones released in recent years have a 12-megapixel camera, making them more easily accessible than surgical loupes. Additionally, surgical loupes are expensive, come with a learning curve, and can be intimidating to new or inexperienced surgeons or dermatology residents. Because virtually every dermatologic surgeon has access to a smartphone and snapping an image takes no more than a few seconds, we believe this technique is a valuable new self-assessment tool for dermatologic surgeons. It may be particularly valuable to dermatology residents and new/inexperienced surgeons looking to improve their techniques and scar outcomes.
- Perry AW, McShane RH. Fine-tuning of the skin edges in the closure of surgical wounds. Controlling inversion and eversion with the path of the needle—the right stitch at the right time. J Dermatol Surg Oncol. 1981;7:471-476. doi:10.1111/j.1524-4725.1981.tb00680.x
- Miller CJ, Antunes MB, Sobanko JF. Surgical technique for optimal outcomes: part II. repairing tissue: suturing. J Am Acad Dermatol. 2015;72:389-402. doi:10.1016/j.jaad.2014.08.006
Practice Gap
Precise wound approximation during cutaneous suturing is of vital importance for optimal closure and long-term scar outcomes. Although buried dermal sutures achieve wound-edge approximation and eversion, meticulous placement of epidermal sutures allows for fine-tuning of the wound edges through epidermal approximation, eversion, and the correction of minor height discrepancies (step-offs).
Several percutaneous suture techniques and materials are available to dermatologic surgeons. However, precise, gap- and tension-free approximation of the wound edges is desired for prompt re-epithelialization and a barely visible scar.1,2
Epidermal sutures should be placed under minimal tension to align the papillary dermis and epidermis precisely. The dermatologic surgeon can evaluate the effectiveness of their suturing technique by carefully examining the closure for visibility of the bilateral wound edges, which should show equally if approximation is precise; small gaps between the wound edges (undesired); or dermal bleeding, which is a manifestation of inaccurate approximation.
Advances in smartphone camera technology have led to high-quality photography in a variety of settings. Although smartphone photography often is used for documentation purposes in health care, we recommend incorporating it as a quality-control checkpoint for objective evaluation, allowing the dermatologic surgeon to scrutinize the wound edges and refine their surgical technique to improve scar outcomes.
The Technique
After suturing the wound closed, we routinely use a 12-megapixel smartphone camera (up to 2× optical zoom) to photograph the closed wound at 1× or 2× magnification to capture more details and use the zoom function to further evaluate the wound edges close-up (Figure). In any area where inadequate epidermal approximation is noted on the photograph, an additional stitch can be placed. Photography can be repeated until ideal reapproximation occurs.
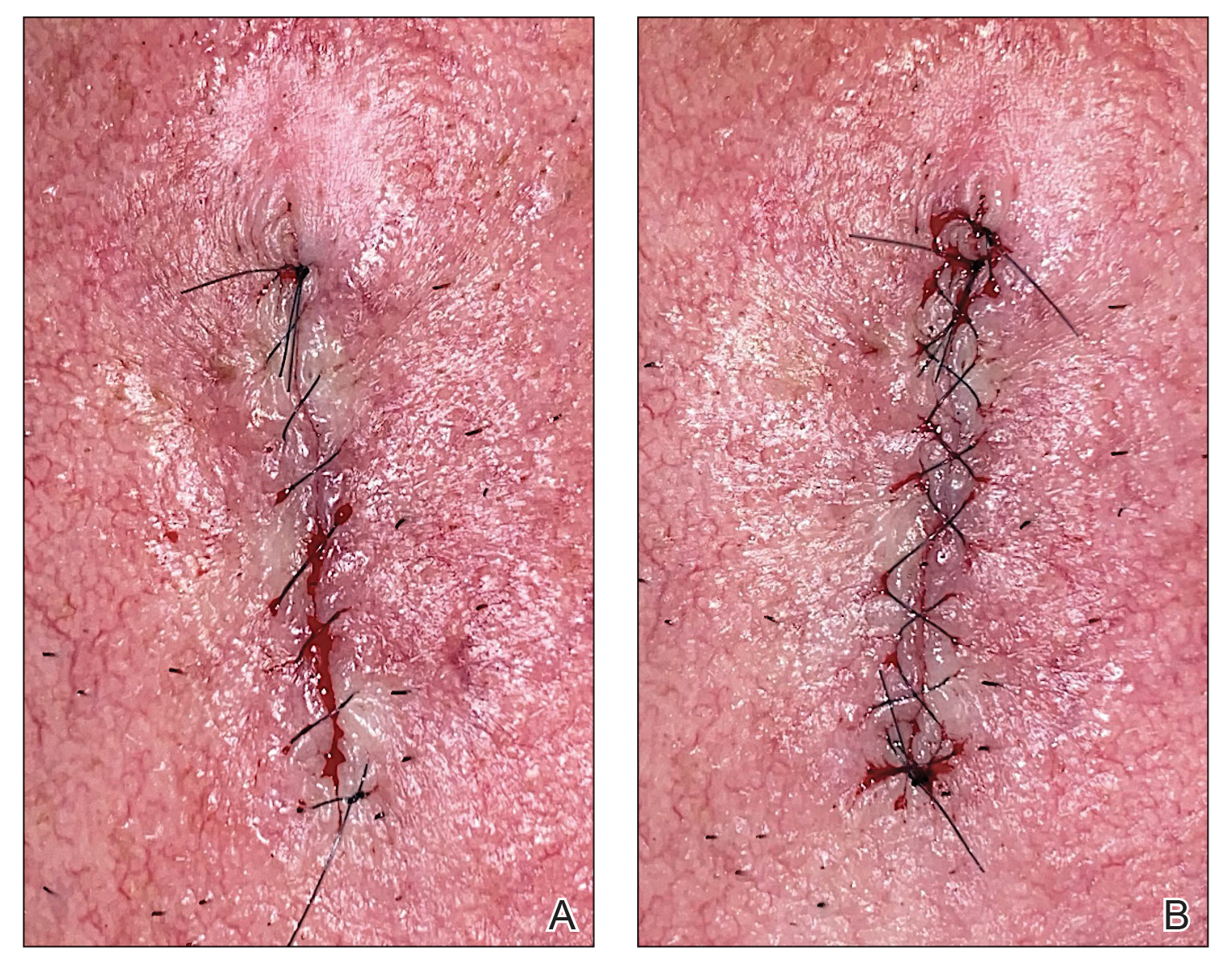
Practice Implications
Most smartphones released in recent years have a 12-megapixel camera, making them more easily accessible than surgical loupes. Additionally, surgical loupes are expensive, come with a learning curve, and can be intimidating to new or inexperienced surgeons or dermatology residents. Because virtually every dermatologic surgeon has access to a smartphone and snapping an image takes no more than a few seconds, we believe this technique is a valuable new self-assessment tool for dermatologic surgeons. It may be particularly valuable to dermatology residents and new/inexperienced surgeons looking to improve their techniques and scar outcomes.
Practice Gap
Precise wound approximation during cutaneous suturing is of vital importance for optimal closure and long-term scar outcomes. Although buried dermal sutures achieve wound-edge approximation and eversion, meticulous placement of epidermal sutures allows for fine-tuning of the wound edges through epidermal approximation, eversion, and the correction of minor height discrepancies (step-offs).
Several percutaneous suture techniques and materials are available to dermatologic surgeons. However, precise, gap- and tension-free approximation of the wound edges is desired for prompt re-epithelialization and a barely visible scar.1,2
Epidermal sutures should be placed under minimal tension to align the papillary dermis and epidermis precisely. The dermatologic surgeon can evaluate the effectiveness of their suturing technique by carefully examining the closure for visibility of the bilateral wound edges, which should show equally if approximation is precise; small gaps between the wound edges (undesired); or dermal bleeding, which is a manifestation of inaccurate approximation.
Advances in smartphone camera technology have led to high-quality photography in a variety of settings. Although smartphone photography often is used for documentation purposes in health care, we recommend incorporating it as a quality-control checkpoint for objective evaluation, allowing the dermatologic surgeon to scrutinize the wound edges and refine their surgical technique to improve scar outcomes.
The Technique
After suturing the wound closed, we routinely use a 12-megapixel smartphone camera (up to 2× optical zoom) to photograph the closed wound at 1× or 2× magnification to capture more details and use the zoom function to further evaluate the wound edges close-up (Figure). In any area where inadequate epidermal approximation is noted on the photograph, an additional stitch can be placed. Photography can be repeated until ideal reapproximation occurs.
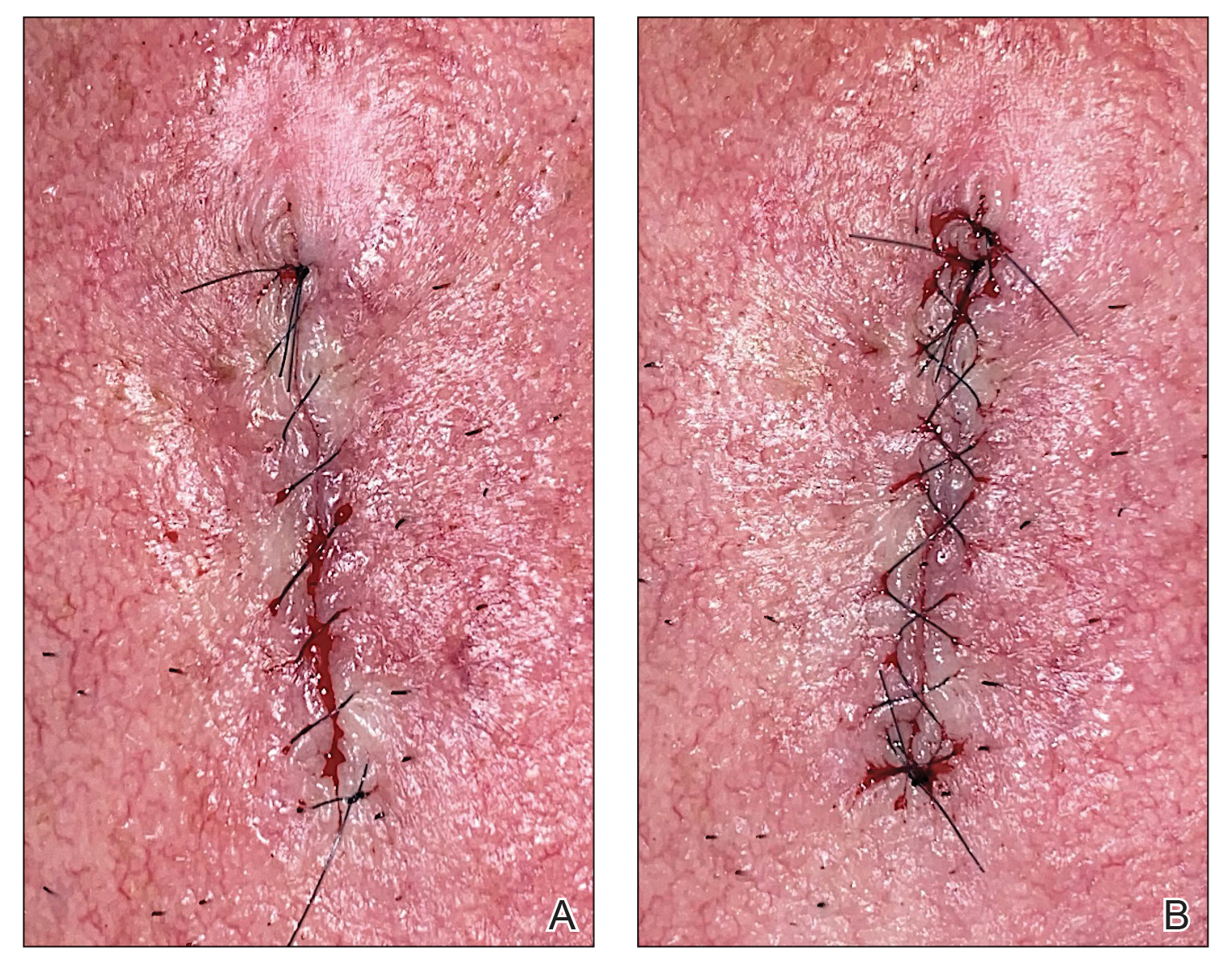
Practice Implications
Most smartphones released in recent years have a 12-megapixel camera, making them more easily accessible than surgical loupes. Additionally, surgical loupes are expensive, come with a learning curve, and can be intimidating to new or inexperienced surgeons or dermatology residents. Because virtually every dermatologic surgeon has access to a smartphone and snapping an image takes no more than a few seconds, we believe this technique is a valuable new self-assessment tool for dermatologic surgeons. It may be particularly valuable to dermatology residents and new/inexperienced surgeons looking to improve their techniques and scar outcomes.
- Perry AW, McShane RH. Fine-tuning of the skin edges in the closure of surgical wounds. Controlling inversion and eversion with the path of the needle—the right stitch at the right time. J Dermatol Surg Oncol. 1981;7:471-476. doi:10.1111/j.1524-4725.1981.tb00680.x
- Miller CJ, Antunes MB, Sobanko JF. Surgical technique for optimal outcomes: part II. repairing tissue: suturing. J Am Acad Dermatol. 2015;72:389-402. doi:10.1016/j.jaad.2014.08.006
- Perry AW, McShane RH. Fine-tuning of the skin edges in the closure of surgical wounds. Controlling inversion and eversion with the path of the needle—the right stitch at the right time. J Dermatol Surg Oncol. 1981;7:471-476. doi:10.1111/j.1524-4725.1981.tb00680.x
- Miller CJ, Antunes MB, Sobanko JF. Surgical technique for optimal outcomes: part II. repairing tissue: suturing. J Am Acad Dermatol. 2015;72:389-402. doi:10.1016/j.jaad.2014.08.006
Brown Plaque in the Axilla Following Immobilization of the Arm
The Diagnosis: Granular Parakeratosis
Histopathology demonstrated diffuse parakeratosis with retention of keratohyalin granules throughout the stratum corneum consistent with a diagnosis of granular parakeratosis (Figure), a rare benign cutaneous condition that is thought to occur due to a defect in epidermal differentiation. The lesion resolved without additional treatment.
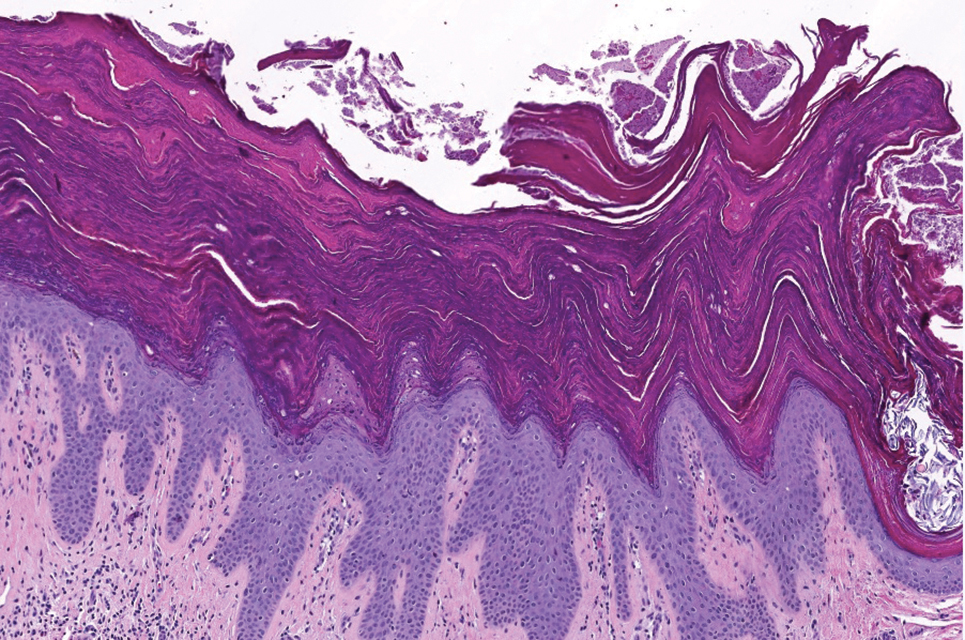
The pathogenesis of granular parakeratosis is unclear, but a reactive process in which locoregional irritation or occlusion prompts increased cell turnover and prevention of profilaggrin breakdown has been proposed.1,2 The diagnosis is linked to various precipitating agents, most commonly topical products (eg, zinc oxide, antiperspirants) and products with benzalkonium chloride (eg, laundry rinses). These agents are thought to cause retention of keratohyalin granules in the stratum corneum during epidermal differentiation.1,2
Most affected patients are middle-aged women (mean age at diagnosis, 37.8 years).2 Patients present with eruptions of erythematous, brown, hyperkeratotic patches and papules that coalesce into plaques.1,2 These lesions can be pruritic and painful or asymptomatic. They often manifest bilaterally in intertriginous sites, most commonly the axillae, groin, or inguinal folds.1,2
Treatment involves identification and removal of potential triggers including changing antiperspirants, limiting use of irritating agents (eg, topical products with strong fragrances), and reducing heat and moisture in the affected areas. If the lesion persists, stepwise treatment can be initiated with topical agents (eg, corticosteroids, vitamin D analogues, retinoids, keratolytics, calcineurin inhibitors) followed by systemic medications (eg, antibiotics, isotretinoin, antifungals, dexamethasone) and procedures (eg, botulinum toxin injections, surgery, laser, cryotherapy).1,2
Unilateral granular parakeratosis, as seen in our patient, is an uncommon manifestation. Our case supports the theory that occlusion is a precipitating factor for this condition, given persistent axillary exposure to heat, sweat, and friction in the setting of limb immobilization.3
Granular parakeratosis is a challenge to diagnose due to clinical overlap with several other cutaneous conditions; histopathologic confirmation is required. Fox- Fordyce disease is a rare condition that is thought to result from keratin buildup or occlusion of apocrine or apoeccrine sweat ducts leading to duct rupture and surrounding inflammation.4 Common triggers include laser hair removal, hormonal changes, and living conditions that promote hot and humid environments.5 It can manifest similarly to granular parakeratosis, with eruptions of multiple red-violet papules that appear bilaterally in aprocine gland–rich areas, including the axillae and less commonly the genital, periareolar, thoracic, abdominal, and facial areas.4,5 However, most patients with Fox-Fordyce disease tend to be younger females (aged 13–35 years) with severely pruritic lesions,4,5 unlike our patient. In addition, histopathology shows hyperkeratosis, hair follicle plugging, and sweat gland and duct dilation.4
Seborrheic keratoses are common benign epidermal tumors caused by an overproliferation of immature keratinocytes.6,7 Similar to granular parakeratosis, they commonly manifest in older adults as hyperpigmented, well-demarcated, verrucous plaques with a hyperkeratotic surface.6 However, they are more common on the face, neck, trunk, and extremities, and they tend to be asymptomatic, differentiating them from granular parakerosis.6 Histopathology demonstrates a papillomatous epidermal surface, large capillaries in the dermal papillae, and intraepidermal and pseudohorn epidermal cysts.7
Inverse lichen planus, a variant of lichen planus, is a rare inflammatory condition that involves the lysis of basal keratinocytes by CD8+ lymphocytes.8 Similar to granular parakeratosis, lichen planus commonly affects middle-aged women (aged 30–60 years), and this particular variant manifests with asymptomatic or mildly pruritic, hyperpigmented patches and plaques in intertriginous areas. Although it also shows hyperkeratosis on histopathology, it can be differentiated from granular parakeratosis by the additional findings of epidermal hypergranulosis, sawtooth acanthosis of rete ridges, apoptotic keratinocytes in the dermoepidermal junction, and lymphocytic infiltrate in the upper dermis.8
Hailey-Hailey disease (also known as familial benign pemphigus) is a rare condition caused by an autosomaldominant mutation affecting intracellular calcium signaling that impairs keratinocyte adhesion.9 Similar to granular parakeratosis, it is most common in middle-aged adults (aged 30–40 years) and manifests as pruritic and burning lesions in symmetric intertriginous areas that also can be triggered by heat and sweating. However, patients present with recurrent blistering and vesicular lesions that may lead to erosions and secondary infections, which reduced clinical suspicion for this diagnosis in our patient. Histopathology shows suprabasilar and intraepidermal clefts, full-thickness acantholysis, protruding dermal papillae, and a perivascular lymphocytic infiltrate in the superficial dermis.9
- Ding CY, Liu H, Khachemoune A. Granular parakeratosis: a comprehensive review and a critical reappraisal. Am J Clin Dermatol. 2015;16:495-500. doi:10.1007/s40257-015-0148-2
- Ip KH, Li A. Clinical features, histology, and treatment outcomes of granular parakeratosis: a systematic review. Int J Dermatol. 2022;61:973-978. doi:10.1111/ijd.16107
- Mehregan DA, Thomas JE, Mehregan DR. Intertriginous granular parakeratosis. J Am Acad Dermatol. 1998;39:495-496. doi:10.1016/s0190-9622(98)70333-0
- Kamada A, Saga K, Jimbow K. Apoeccrine sweat duct obstruction as a cause for Fox-Fordyce disease. J Am Acad Dermatol. 2003;48:453-455. doi:10.1067/mjd.2003.93
- Salloum A, Bouferraa Y, Bazzi N, et al. Pathophysiology, clinical findings, and management of Fox-Fordyce disease: a systematic review. J Cosmet Dermatol. 2022;21:482-500. doi:10.1111/jocd.14135
- Sun MD, Halpern AC. Advances in the etiology, detection, and clinical management of seborrheic keratoses. Dermatology. 2022;238:205-217. doi:10.1159/000517070
- Minagawa A. Dermoscopy-pathology relationship in seborrheic keratosis. J Dermatol. 2017;44:518-524. doi:10.1111/1346-8138.13657
- Weston G, Payette M. Update on lichen planus and its clinical variants [published online September 16, 2015]. Int J Womens Dermatol. 2015;1:140-149. doi:10.1016/j.ijwd.2015.04.001
- Ben Lagha I, Ashack K, Khachemoune A. Hailey-Hailey disease: an update review with a focus on treatment data. Am J Clin Dermatol. 2020;21:49-68. doi:10.1007/s40257-019-00477-z
The Diagnosis: Granular Parakeratosis
Histopathology demonstrated diffuse parakeratosis with retention of keratohyalin granules throughout the stratum corneum consistent with a diagnosis of granular parakeratosis (Figure), a rare benign cutaneous condition that is thought to occur due to a defect in epidermal differentiation. The lesion resolved without additional treatment.
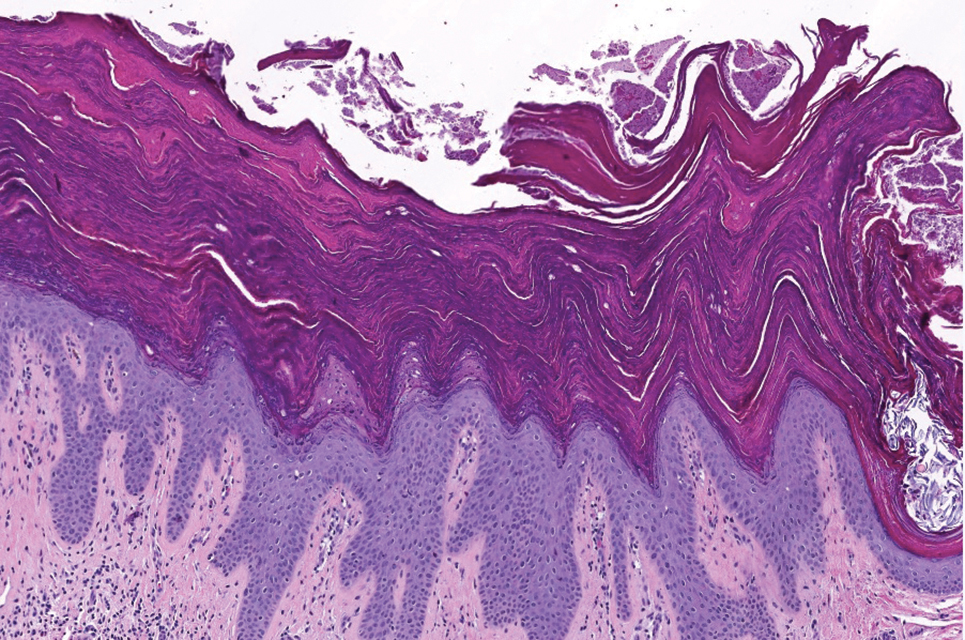
The pathogenesis of granular parakeratosis is unclear, but a reactive process in which locoregional irritation or occlusion prompts increased cell turnover and prevention of profilaggrin breakdown has been proposed.1,2 The diagnosis is linked to various precipitating agents, most commonly topical products (eg, zinc oxide, antiperspirants) and products with benzalkonium chloride (eg, laundry rinses). These agents are thought to cause retention of keratohyalin granules in the stratum corneum during epidermal differentiation.1,2
Most affected patients are middle-aged women (mean age at diagnosis, 37.8 years).2 Patients present with eruptions of erythematous, brown, hyperkeratotic patches and papules that coalesce into plaques.1,2 These lesions can be pruritic and painful or asymptomatic. They often manifest bilaterally in intertriginous sites, most commonly the axillae, groin, or inguinal folds.1,2
Treatment involves identification and removal of potential triggers including changing antiperspirants, limiting use of irritating agents (eg, topical products with strong fragrances), and reducing heat and moisture in the affected areas. If the lesion persists, stepwise treatment can be initiated with topical agents (eg, corticosteroids, vitamin D analogues, retinoids, keratolytics, calcineurin inhibitors) followed by systemic medications (eg, antibiotics, isotretinoin, antifungals, dexamethasone) and procedures (eg, botulinum toxin injections, surgery, laser, cryotherapy).1,2
Unilateral granular parakeratosis, as seen in our patient, is an uncommon manifestation. Our case supports the theory that occlusion is a precipitating factor for this condition, given persistent axillary exposure to heat, sweat, and friction in the setting of limb immobilization.3
Granular parakeratosis is a challenge to diagnose due to clinical overlap with several other cutaneous conditions; histopathologic confirmation is required. Fox- Fordyce disease is a rare condition that is thought to result from keratin buildup or occlusion of apocrine or apoeccrine sweat ducts leading to duct rupture and surrounding inflammation.4 Common triggers include laser hair removal, hormonal changes, and living conditions that promote hot and humid environments.5 It can manifest similarly to granular parakeratosis, with eruptions of multiple red-violet papules that appear bilaterally in aprocine gland–rich areas, including the axillae and less commonly the genital, periareolar, thoracic, abdominal, and facial areas.4,5 However, most patients with Fox-Fordyce disease tend to be younger females (aged 13–35 years) with severely pruritic lesions,4,5 unlike our patient. In addition, histopathology shows hyperkeratosis, hair follicle plugging, and sweat gland and duct dilation.4
Seborrheic keratoses are common benign epidermal tumors caused by an overproliferation of immature keratinocytes.6,7 Similar to granular parakeratosis, they commonly manifest in older adults as hyperpigmented, well-demarcated, verrucous plaques with a hyperkeratotic surface.6 However, they are more common on the face, neck, trunk, and extremities, and they tend to be asymptomatic, differentiating them from granular parakerosis.6 Histopathology demonstrates a papillomatous epidermal surface, large capillaries in the dermal papillae, and intraepidermal and pseudohorn epidermal cysts.7
Inverse lichen planus, a variant of lichen planus, is a rare inflammatory condition that involves the lysis of basal keratinocytes by CD8+ lymphocytes.8 Similar to granular parakeratosis, lichen planus commonly affects middle-aged women (aged 30–60 years), and this particular variant manifests with asymptomatic or mildly pruritic, hyperpigmented patches and plaques in intertriginous areas. Although it also shows hyperkeratosis on histopathology, it can be differentiated from granular parakeratosis by the additional findings of epidermal hypergranulosis, sawtooth acanthosis of rete ridges, apoptotic keratinocytes in the dermoepidermal junction, and lymphocytic infiltrate in the upper dermis.8
Hailey-Hailey disease (also known as familial benign pemphigus) is a rare condition caused by an autosomaldominant mutation affecting intracellular calcium signaling that impairs keratinocyte adhesion.9 Similar to granular parakeratosis, it is most common in middle-aged adults (aged 30–40 years) and manifests as pruritic and burning lesions in symmetric intertriginous areas that also can be triggered by heat and sweating. However, patients present with recurrent blistering and vesicular lesions that may lead to erosions and secondary infections, which reduced clinical suspicion for this diagnosis in our patient. Histopathology shows suprabasilar and intraepidermal clefts, full-thickness acantholysis, protruding dermal papillae, and a perivascular lymphocytic infiltrate in the superficial dermis.9
The Diagnosis: Granular Parakeratosis
Histopathology demonstrated diffuse parakeratosis with retention of keratohyalin granules throughout the stratum corneum consistent with a diagnosis of granular parakeratosis (Figure), a rare benign cutaneous condition that is thought to occur due to a defect in epidermal differentiation. The lesion resolved without additional treatment.
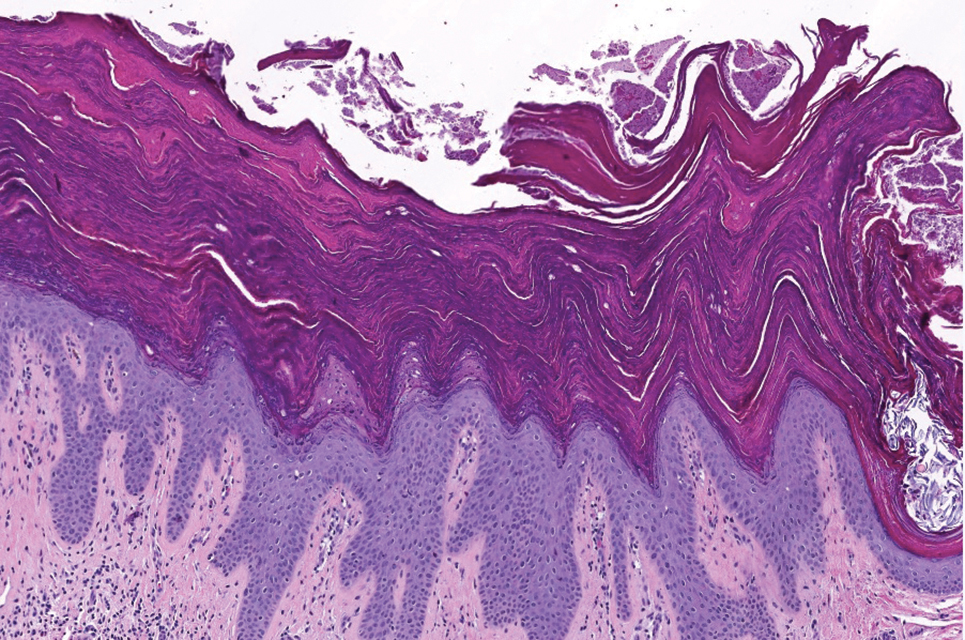
The pathogenesis of granular parakeratosis is unclear, but a reactive process in which locoregional irritation or occlusion prompts increased cell turnover and prevention of profilaggrin breakdown has been proposed.1,2 The diagnosis is linked to various precipitating agents, most commonly topical products (eg, zinc oxide, antiperspirants) and products with benzalkonium chloride (eg, laundry rinses). These agents are thought to cause retention of keratohyalin granules in the stratum corneum during epidermal differentiation.1,2
Most affected patients are middle-aged women (mean age at diagnosis, 37.8 years).2 Patients present with eruptions of erythematous, brown, hyperkeratotic patches and papules that coalesce into plaques.1,2 These lesions can be pruritic and painful or asymptomatic. They often manifest bilaterally in intertriginous sites, most commonly the axillae, groin, or inguinal folds.1,2
Treatment involves identification and removal of potential triggers including changing antiperspirants, limiting use of irritating agents (eg, topical products with strong fragrances), and reducing heat and moisture in the affected areas. If the lesion persists, stepwise treatment can be initiated with topical agents (eg, corticosteroids, vitamin D analogues, retinoids, keratolytics, calcineurin inhibitors) followed by systemic medications (eg, antibiotics, isotretinoin, antifungals, dexamethasone) and procedures (eg, botulinum toxin injections, surgery, laser, cryotherapy).1,2
Unilateral granular parakeratosis, as seen in our patient, is an uncommon manifestation. Our case supports the theory that occlusion is a precipitating factor for this condition, given persistent axillary exposure to heat, sweat, and friction in the setting of limb immobilization.3
Granular parakeratosis is a challenge to diagnose due to clinical overlap with several other cutaneous conditions; histopathologic confirmation is required. Fox- Fordyce disease is a rare condition that is thought to result from keratin buildup or occlusion of apocrine or apoeccrine sweat ducts leading to duct rupture and surrounding inflammation.4 Common triggers include laser hair removal, hormonal changes, and living conditions that promote hot and humid environments.5 It can manifest similarly to granular parakeratosis, with eruptions of multiple red-violet papules that appear bilaterally in aprocine gland–rich areas, including the axillae and less commonly the genital, periareolar, thoracic, abdominal, and facial areas.4,5 However, most patients with Fox-Fordyce disease tend to be younger females (aged 13–35 years) with severely pruritic lesions,4,5 unlike our patient. In addition, histopathology shows hyperkeratosis, hair follicle plugging, and sweat gland and duct dilation.4
Seborrheic keratoses are common benign epidermal tumors caused by an overproliferation of immature keratinocytes.6,7 Similar to granular parakeratosis, they commonly manifest in older adults as hyperpigmented, well-demarcated, verrucous plaques with a hyperkeratotic surface.6 However, they are more common on the face, neck, trunk, and extremities, and they tend to be asymptomatic, differentiating them from granular parakerosis.6 Histopathology demonstrates a papillomatous epidermal surface, large capillaries in the dermal papillae, and intraepidermal and pseudohorn epidermal cysts.7
Inverse lichen planus, a variant of lichen planus, is a rare inflammatory condition that involves the lysis of basal keratinocytes by CD8+ lymphocytes.8 Similar to granular parakeratosis, lichen planus commonly affects middle-aged women (aged 30–60 years), and this particular variant manifests with asymptomatic or mildly pruritic, hyperpigmented patches and plaques in intertriginous areas. Although it also shows hyperkeratosis on histopathology, it can be differentiated from granular parakeratosis by the additional findings of epidermal hypergranulosis, sawtooth acanthosis of rete ridges, apoptotic keratinocytes in the dermoepidermal junction, and lymphocytic infiltrate in the upper dermis.8
Hailey-Hailey disease (also known as familial benign pemphigus) is a rare condition caused by an autosomaldominant mutation affecting intracellular calcium signaling that impairs keratinocyte adhesion.9 Similar to granular parakeratosis, it is most common in middle-aged adults (aged 30–40 years) and manifests as pruritic and burning lesions in symmetric intertriginous areas that also can be triggered by heat and sweating. However, patients present with recurrent blistering and vesicular lesions that may lead to erosions and secondary infections, which reduced clinical suspicion for this diagnosis in our patient. Histopathology shows suprabasilar and intraepidermal clefts, full-thickness acantholysis, protruding dermal papillae, and a perivascular lymphocytic infiltrate in the superficial dermis.9
- Ding CY, Liu H, Khachemoune A. Granular parakeratosis: a comprehensive review and a critical reappraisal. Am J Clin Dermatol. 2015;16:495-500. doi:10.1007/s40257-015-0148-2
- Ip KH, Li A. Clinical features, histology, and treatment outcomes of granular parakeratosis: a systematic review. Int J Dermatol. 2022;61:973-978. doi:10.1111/ijd.16107
- Mehregan DA, Thomas JE, Mehregan DR. Intertriginous granular parakeratosis. J Am Acad Dermatol. 1998;39:495-496. doi:10.1016/s0190-9622(98)70333-0
- Kamada A, Saga K, Jimbow K. Apoeccrine sweat duct obstruction as a cause for Fox-Fordyce disease. J Am Acad Dermatol. 2003;48:453-455. doi:10.1067/mjd.2003.93
- Salloum A, Bouferraa Y, Bazzi N, et al. Pathophysiology, clinical findings, and management of Fox-Fordyce disease: a systematic review. J Cosmet Dermatol. 2022;21:482-500. doi:10.1111/jocd.14135
- Sun MD, Halpern AC. Advances in the etiology, detection, and clinical management of seborrheic keratoses. Dermatology. 2022;238:205-217. doi:10.1159/000517070
- Minagawa A. Dermoscopy-pathology relationship in seborrheic keratosis. J Dermatol. 2017;44:518-524. doi:10.1111/1346-8138.13657
- Weston G, Payette M. Update on lichen planus and its clinical variants [published online September 16, 2015]. Int J Womens Dermatol. 2015;1:140-149. doi:10.1016/j.ijwd.2015.04.001
- Ben Lagha I, Ashack K, Khachemoune A. Hailey-Hailey disease: an update review with a focus on treatment data. Am J Clin Dermatol. 2020;21:49-68. doi:10.1007/s40257-019-00477-z
- Ding CY, Liu H, Khachemoune A. Granular parakeratosis: a comprehensive review and a critical reappraisal. Am J Clin Dermatol. 2015;16:495-500. doi:10.1007/s40257-015-0148-2
- Ip KH, Li A. Clinical features, histology, and treatment outcomes of granular parakeratosis: a systematic review. Int J Dermatol. 2022;61:973-978. doi:10.1111/ijd.16107
- Mehregan DA, Thomas JE, Mehregan DR. Intertriginous granular parakeratosis. J Am Acad Dermatol. 1998;39:495-496. doi:10.1016/s0190-9622(98)70333-0
- Kamada A, Saga K, Jimbow K. Apoeccrine sweat duct obstruction as a cause for Fox-Fordyce disease. J Am Acad Dermatol. 2003;48:453-455. doi:10.1067/mjd.2003.93
- Salloum A, Bouferraa Y, Bazzi N, et al. Pathophysiology, clinical findings, and management of Fox-Fordyce disease: a systematic review. J Cosmet Dermatol. 2022;21:482-500. doi:10.1111/jocd.14135
- Sun MD, Halpern AC. Advances in the etiology, detection, and clinical management of seborrheic keratoses. Dermatology. 2022;238:205-217. doi:10.1159/000517070
- Minagawa A. Dermoscopy-pathology relationship in seborrheic keratosis. J Dermatol. 2017;44:518-524. doi:10.1111/1346-8138.13657
- Weston G, Payette M. Update on lichen planus and its clinical variants [published online September 16, 2015]. Int J Womens Dermatol. 2015;1:140-149. doi:10.1016/j.ijwd.2015.04.001
- Ben Lagha I, Ashack K, Khachemoune A. Hailey-Hailey disease: an update review with a focus on treatment data. Am J Clin Dermatol. 2020;21:49-68. doi:10.1007/s40257-019-00477-z
A 62-year-old woman presented to our clinic for evaluation of a brown plaque in the left axilla of 2 weeks’ duration. She had a history of a rotator cuff injury and adhesive capsulitis several months prior that required immobilization of the left arm in a shoulder orthosis for several months. After the sling was removed, she noticed the lesion and reported mild cutaneous pain. Physical examination revealed a 1.5-cm, verrucous, red-brown plaque in the left axillary vault. A shave biopsy of the plaque was performed.

Photoexposed Rash in an Older Adult
The Diagnosis: Pellagra
The patient was diagnosed with pellagra based on the clinical and laboratory findings. He was discharged with nicotinamide 250 mg and folic acid 5 mg supplementation daily. After 3 months, all symptoms resolved.
Pellagra is a condition usually associated with the 4 Ds: dermatitis; diarrhea; dementia; and, if untreated, death.1 The word pellagra is derived from the Italian terms pelle and agra, which mean skin and rough, respectively.2 Spanish physician Gasper Casal first described pellagra in 1762 after observing the disease in poorer peasants in Asturias who mainly relied on maize and rarely consumed fresh meat.1,2 Joseph Goldberger conducted research in the early 20th century, provoking the disease in jail prisoners by modifying their diets. However, it was not until 1926 that Goldberger discovered the true cause of the illness to be a poor diet and named what would become known as nicotinamide as the pellagra preventative factor.1,2 Niacin (vitamin B3), the deficient molecule in pellagra, also is known as nicotinic acid, nicotinamide, or niacinamide. It is a water-soluble vitamin that is converted into nicotinamide-adenine-dinucleotide (NAD) and its phosphate NADP.1,2 It has been hypothesized that pellagra symptoms arise from insufficient amounts of NAD and NADP, making the body unable to support cellular energy transfer processes.3
Pellagra manifests 50 to 60 days after starting a diet low in niacin. Niacin and nicotinamide are absorbed from the digested food to the stomach through a sodiumdependent mechanism, and then nicotinamide may be transformed into nicotinic acid with microsomal deamidation.3 Niacin may be obtained from one’s diet or produced from tryptophan. Foods with the highest amounts of niacin include liver, poultry, fish, eggs, milk, pork, mushrooms, avocados, almonds, and legumes.1,3 Coffee also contains trigonelline, which may be transformed into nicotinic acid when roasted, increasing the niacin level by 30 times.3 Approximately 60 mg of dietary tryptophan is needed to produce up to 1 mg of niacin in the presence of B2 and B6 vitamins. This mechanism provides approximately half of the needs for niacin.3 Insufficient dietary intake of niacin or the essential amino acid tryptophan can cause pellagra (primary pellagra), which is a concern in resource-limited countries. Alternatively, the body may not be able to properly utilize niacin for metabolic processes (secondary pellagra), which occurs more frequently in developed countries.1 Secondary pellagra also may be caused by alcoholism, colitis, cirrhosis, carcinoid tumors, Hartnup disease, or gastrointestinal tuberculosis, as these conditions prevent niacin from being consumed, absorbed, or processed. Certain medications can cause pellagra by interfering with the tryptophan-niacin pathway, including isoniazid, 5-fluorouracil, pyrazinamide, 6-mercaptopurine, hydantoins, ethionamide, phenobarbital, azathioprine, and chloramphenicol.2
The clinical manifestations of pellagra are diverse because it affects tissues with high turnover rates. Clinical features of pellagra include symmetric photosensitive skin eruptions, gastrointestinal tract symptoms, and neurologic and mental disorders.3 The first signs of pellagra may include muscle weakness, digestive concerns, and psychological or emotional discomfort.2 Pellagra dermatitis manifests as an acute or intermittent, bilaterally symmetrical eruption on sun-exposed areas and is markedly distinct from healthy skin.3 Some individuals may experience vesiculation and bullae development (wet pellagra). The erythema is first brilliant red then turns into a cinnamon-brown color. Over time, the skin becomes thickened, scaly, cracked, and hyperpigmented.1 The dryness of the skin likely is due to a remarkable decrease in wax ester and sebaceous gland atrophy seen on histopathology.4 Pellagra most frequently affects the back of the hands (77%–97% of cases), which can extend upward to create the so-called pellagra glove or gauntlet.3 It is common to see symmetrical eruptions in the shape of a butterfly following an anatomical pattern innervated by the trigeminal nerve, which resembles lupus erythematosus on the face. Another common manifestation is Casal necklace, a well-marginated eruption frequently seen on the front of the neck (Figure).2 On the foot, lesions often do not develop close to the malleoli but rather terminate distally on the backs of the toes. Sometimes a boot pattern may form that covers the front and back of the leg.1-3

The pathophysiology of photosensitivity in pellagra was hypothesized by Karthikeyan and Thappa.3 They discovered an excessive synthesis of a phototoxic substance, kynurenic acid, and a deficiency in urocanic acid, which normally protects the skin by absorbing light in the UVB range. Niacin deprivation leads to the production of kynurenic acid through the tryptophan-kynurenine-nicotinic acid pathway and reduces the amount of urocanic acid by affecting the enzyme histidase in the stratum corneum.1-3 In one-third of patients, pellagra affects the oral mucosa, causing characteristic symptoms such as glossitis, angular stomatitis, and cheilitis.2 In nearly 50% of patients, poor appetite, nausea, epigastric discomfort, diarrhea, and excessive salivation are present. Most of the gastrointestinal tract is affected by mucosal inflammation and atrophy, which can cause malnutrition and cachexia due to anorexia and malabsorptive diarrhea.2 Headache, irritability, poor concentration, hallucinations, photophobia, tremor, and depression are some of the neuropsychiatric symptoms. Patients experience delirium and disorientation as pellagra progresses, followed by a comatose state and ultimately death.2
The patient’s history and physical examination are used to make the diagnosis, with particular attention to the patient’s dietary details. The diagnosis is made in part ex juvantibus by seeing how the patient responds to higher niacin doses. Anemia, hypoproteinemia, elevated blood calcium, reduced serum potassium and phosphorus, abnormal liver function tests, and elevated serum porphyrin levels also indicate pellagra. Niacin 300 mg in divided doses for up to 4 weeks has been recommended by the World Health Organization to treat pellagra.5 The flushing seen with niacin administration is not linked to the usage of nicotinamide. The recommended nicotinamide dosage for adults is 100 mg orally every 6 hours until most acute symptoms have disappeared, followed by oral administration of 50 mg every 8 to 12 hours until all skin lesions have healed.2
Among the differential diagnoses, necrolytic migratory erythema is characterized by an episodic eruption of crusted, erosive, annular erythematous plaques with blister development, which occurs in 70% of patients with glucagonoma syndrome. The perioral region, perineum, lower belly, thighs, and distal extremities are the usual locations.6,7 Laboratory test results include elevated fasting serum glucagon (>1000 ng/L) and normocytic anemia, which aided in ruling out this diagnosis in our patient. Generalized acute cutaneous lupus erythematosus may appear as a broad morbilliform eruption. The hands frequently exhibit erythema and edema, especially across the dorsal and interphalangeal regions.8 Other typical findings of systemic lupus erythematosus such as antinuclear antibody were not seen in our patient, making this diagnosis unlikely. Porphyria cutanea tarda also must be considered in the differential diagnosis. The hepatic deficiency of uroporphyrinogen decarboxylase is the primary cause of this condition. Although it is characterized by blistering lesions, patients more frequently describe increased skin fragility in sun-exposed regions. Hypertrichosis, hyperpigmentation or hypopigmentation, hirsutism, or scarring may appear in the later stage of the disease.9 Phototoxic reaction was ruled out because the patient spent most of the time at home, and no new drugs had been prescribed in the previous months.
- Prabhu D, Dawe RS, Mponda K. Pellagra a review exploring causes and mechanisms, including isoniazid-induced pellagra. Photodermatol Photoimmunol Photomed. 2021;37:99-104. doi:10.1111 /phpp.12659
- Hegyi J, Schwartz RA, Hegyi V. Pellagra: dermatitis, dementia, and diarrhea. Int J Dermatol. 2004;43:1-5. doi:10.1111/j.1365-4632.2004.01959.x
- Karthikeyan K, Thappa DM. Pellagra and skin. Int J Dermatol. 2002;41:476-481. doi:10.1046/j.1365-4362.2002.01551.x
- Dogliotti M, Liebowitz M, Downing DT, et al. Nutritional influences of pellagra on sebum composition. Br J Dermatol. 1977;97:25-28. doi:10.1111/j.1365-2133.1977.tb15423.x
- World Health Organization. Pellagra and Its Prevention and Control in Major Emergencies. Published February 23, 2000. Accessed February 15, 2024. https://www.who.int/publications/i/item/WHO-NHD-00.10
- Liu JW, Qian YT, Ma DL. Necrolytic migratory erythema. JAMA Dermatol. 2019;155:1180. doi:10.1001/jamadermatol.2019.1658
- Tolliver S, Graham J, Kaffenberger BH. A review of cutaneous manifestations within glucagonoma syndrome: necrolytic migratory erythema. Int J Dermatol. 2018;57:642-645. doi:10.1111/ijd.13947
- Walling HW, Sontheimer RD. Cutaneous lupus erythematosus: issues in diagnosis and treatment. Am J Clin Dermatol. 2009;10:365-381. doi:10.2165/11310780-000000000-00000
- Singal AK. Porphyria cutanea tarda: recent update. Mol Genet Metab. 2019;128:271-281. doi:10.1016/j.ymgme.2019.01.004
The Diagnosis: Pellagra
The patient was diagnosed with pellagra based on the clinical and laboratory findings. He was discharged with nicotinamide 250 mg and folic acid 5 mg supplementation daily. After 3 months, all symptoms resolved.
Pellagra is a condition usually associated with the 4 Ds: dermatitis; diarrhea; dementia; and, if untreated, death.1 The word pellagra is derived from the Italian terms pelle and agra, which mean skin and rough, respectively.2 Spanish physician Gasper Casal first described pellagra in 1762 after observing the disease in poorer peasants in Asturias who mainly relied on maize and rarely consumed fresh meat.1,2 Joseph Goldberger conducted research in the early 20th century, provoking the disease in jail prisoners by modifying their diets. However, it was not until 1926 that Goldberger discovered the true cause of the illness to be a poor diet and named what would become known as nicotinamide as the pellagra preventative factor.1,2 Niacin (vitamin B3), the deficient molecule in pellagra, also is known as nicotinic acid, nicotinamide, or niacinamide. It is a water-soluble vitamin that is converted into nicotinamide-adenine-dinucleotide (NAD) and its phosphate NADP.1,2 It has been hypothesized that pellagra symptoms arise from insufficient amounts of NAD and NADP, making the body unable to support cellular energy transfer processes.3
Pellagra manifests 50 to 60 days after starting a diet low in niacin. Niacin and nicotinamide are absorbed from the digested food to the stomach through a sodiumdependent mechanism, and then nicotinamide may be transformed into nicotinic acid with microsomal deamidation.3 Niacin may be obtained from one’s diet or produced from tryptophan. Foods with the highest amounts of niacin include liver, poultry, fish, eggs, milk, pork, mushrooms, avocados, almonds, and legumes.1,3 Coffee also contains trigonelline, which may be transformed into nicotinic acid when roasted, increasing the niacin level by 30 times.3 Approximately 60 mg of dietary tryptophan is needed to produce up to 1 mg of niacin in the presence of B2 and B6 vitamins. This mechanism provides approximately half of the needs for niacin.3 Insufficient dietary intake of niacin or the essential amino acid tryptophan can cause pellagra (primary pellagra), which is a concern in resource-limited countries. Alternatively, the body may not be able to properly utilize niacin for metabolic processes (secondary pellagra), which occurs more frequently in developed countries.1 Secondary pellagra also may be caused by alcoholism, colitis, cirrhosis, carcinoid tumors, Hartnup disease, or gastrointestinal tuberculosis, as these conditions prevent niacin from being consumed, absorbed, or processed. Certain medications can cause pellagra by interfering with the tryptophan-niacin pathway, including isoniazid, 5-fluorouracil, pyrazinamide, 6-mercaptopurine, hydantoins, ethionamide, phenobarbital, azathioprine, and chloramphenicol.2
The clinical manifestations of pellagra are diverse because it affects tissues with high turnover rates. Clinical features of pellagra include symmetric photosensitive skin eruptions, gastrointestinal tract symptoms, and neurologic and mental disorders.3 The first signs of pellagra may include muscle weakness, digestive concerns, and psychological or emotional discomfort.2 Pellagra dermatitis manifests as an acute or intermittent, bilaterally symmetrical eruption on sun-exposed areas and is markedly distinct from healthy skin.3 Some individuals may experience vesiculation and bullae development (wet pellagra). The erythema is first brilliant red then turns into a cinnamon-brown color. Over time, the skin becomes thickened, scaly, cracked, and hyperpigmented.1 The dryness of the skin likely is due to a remarkable decrease in wax ester and sebaceous gland atrophy seen on histopathology.4 Pellagra most frequently affects the back of the hands (77%–97% of cases), which can extend upward to create the so-called pellagra glove or gauntlet.3 It is common to see symmetrical eruptions in the shape of a butterfly following an anatomical pattern innervated by the trigeminal nerve, which resembles lupus erythematosus on the face. Another common manifestation is Casal necklace, a well-marginated eruption frequently seen on the front of the neck (Figure).2 On the foot, lesions often do not develop close to the malleoli but rather terminate distally on the backs of the toes. Sometimes a boot pattern may form that covers the front and back of the leg.1-3

The pathophysiology of photosensitivity in pellagra was hypothesized by Karthikeyan and Thappa.3 They discovered an excessive synthesis of a phototoxic substance, kynurenic acid, and a deficiency in urocanic acid, which normally protects the skin by absorbing light in the UVB range. Niacin deprivation leads to the production of kynurenic acid through the tryptophan-kynurenine-nicotinic acid pathway and reduces the amount of urocanic acid by affecting the enzyme histidase in the stratum corneum.1-3 In one-third of patients, pellagra affects the oral mucosa, causing characteristic symptoms such as glossitis, angular stomatitis, and cheilitis.2 In nearly 50% of patients, poor appetite, nausea, epigastric discomfort, diarrhea, and excessive salivation are present. Most of the gastrointestinal tract is affected by mucosal inflammation and atrophy, which can cause malnutrition and cachexia due to anorexia and malabsorptive diarrhea.2 Headache, irritability, poor concentration, hallucinations, photophobia, tremor, and depression are some of the neuropsychiatric symptoms. Patients experience delirium and disorientation as pellagra progresses, followed by a comatose state and ultimately death.2
The patient’s history and physical examination are used to make the diagnosis, with particular attention to the patient’s dietary details. The diagnosis is made in part ex juvantibus by seeing how the patient responds to higher niacin doses. Anemia, hypoproteinemia, elevated blood calcium, reduced serum potassium and phosphorus, abnormal liver function tests, and elevated serum porphyrin levels also indicate pellagra. Niacin 300 mg in divided doses for up to 4 weeks has been recommended by the World Health Organization to treat pellagra.5 The flushing seen with niacin administration is not linked to the usage of nicotinamide. The recommended nicotinamide dosage for adults is 100 mg orally every 6 hours until most acute symptoms have disappeared, followed by oral administration of 50 mg every 8 to 12 hours until all skin lesions have healed.2
Among the differential diagnoses, necrolytic migratory erythema is characterized by an episodic eruption of crusted, erosive, annular erythematous plaques with blister development, which occurs in 70% of patients with glucagonoma syndrome. The perioral region, perineum, lower belly, thighs, and distal extremities are the usual locations.6,7 Laboratory test results include elevated fasting serum glucagon (>1000 ng/L) and normocytic anemia, which aided in ruling out this diagnosis in our patient. Generalized acute cutaneous lupus erythematosus may appear as a broad morbilliform eruption. The hands frequently exhibit erythema and edema, especially across the dorsal and interphalangeal regions.8 Other typical findings of systemic lupus erythematosus such as antinuclear antibody were not seen in our patient, making this diagnosis unlikely. Porphyria cutanea tarda also must be considered in the differential diagnosis. The hepatic deficiency of uroporphyrinogen decarboxylase is the primary cause of this condition. Although it is characterized by blistering lesions, patients more frequently describe increased skin fragility in sun-exposed regions. Hypertrichosis, hyperpigmentation or hypopigmentation, hirsutism, or scarring may appear in the later stage of the disease.9 Phototoxic reaction was ruled out because the patient spent most of the time at home, and no new drugs had been prescribed in the previous months.
The Diagnosis: Pellagra
The patient was diagnosed with pellagra based on the clinical and laboratory findings. He was discharged with nicotinamide 250 mg and folic acid 5 mg supplementation daily. After 3 months, all symptoms resolved.
Pellagra is a condition usually associated with the 4 Ds: dermatitis; diarrhea; dementia; and, if untreated, death.1 The word pellagra is derived from the Italian terms pelle and agra, which mean skin and rough, respectively.2 Spanish physician Gasper Casal first described pellagra in 1762 after observing the disease in poorer peasants in Asturias who mainly relied on maize and rarely consumed fresh meat.1,2 Joseph Goldberger conducted research in the early 20th century, provoking the disease in jail prisoners by modifying their diets. However, it was not until 1926 that Goldberger discovered the true cause of the illness to be a poor diet and named what would become known as nicotinamide as the pellagra preventative factor.1,2 Niacin (vitamin B3), the deficient molecule in pellagra, also is known as nicotinic acid, nicotinamide, or niacinamide. It is a water-soluble vitamin that is converted into nicotinamide-adenine-dinucleotide (NAD) and its phosphate NADP.1,2 It has been hypothesized that pellagra symptoms arise from insufficient amounts of NAD and NADP, making the body unable to support cellular energy transfer processes.3
Pellagra manifests 50 to 60 days after starting a diet low in niacin. Niacin and nicotinamide are absorbed from the digested food to the stomach through a sodiumdependent mechanism, and then nicotinamide may be transformed into nicotinic acid with microsomal deamidation.3 Niacin may be obtained from one’s diet or produced from tryptophan. Foods with the highest amounts of niacin include liver, poultry, fish, eggs, milk, pork, mushrooms, avocados, almonds, and legumes.1,3 Coffee also contains trigonelline, which may be transformed into nicotinic acid when roasted, increasing the niacin level by 30 times.3 Approximately 60 mg of dietary tryptophan is needed to produce up to 1 mg of niacin in the presence of B2 and B6 vitamins. This mechanism provides approximately half of the needs for niacin.3 Insufficient dietary intake of niacin or the essential amino acid tryptophan can cause pellagra (primary pellagra), which is a concern in resource-limited countries. Alternatively, the body may not be able to properly utilize niacin for metabolic processes (secondary pellagra), which occurs more frequently in developed countries.1 Secondary pellagra also may be caused by alcoholism, colitis, cirrhosis, carcinoid tumors, Hartnup disease, or gastrointestinal tuberculosis, as these conditions prevent niacin from being consumed, absorbed, or processed. Certain medications can cause pellagra by interfering with the tryptophan-niacin pathway, including isoniazid, 5-fluorouracil, pyrazinamide, 6-mercaptopurine, hydantoins, ethionamide, phenobarbital, azathioprine, and chloramphenicol.2
The clinical manifestations of pellagra are diverse because it affects tissues with high turnover rates. Clinical features of pellagra include symmetric photosensitive skin eruptions, gastrointestinal tract symptoms, and neurologic and mental disorders.3 The first signs of pellagra may include muscle weakness, digestive concerns, and psychological or emotional discomfort.2 Pellagra dermatitis manifests as an acute or intermittent, bilaterally symmetrical eruption on sun-exposed areas and is markedly distinct from healthy skin.3 Some individuals may experience vesiculation and bullae development (wet pellagra). The erythema is first brilliant red then turns into a cinnamon-brown color. Over time, the skin becomes thickened, scaly, cracked, and hyperpigmented.1 The dryness of the skin likely is due to a remarkable decrease in wax ester and sebaceous gland atrophy seen on histopathology.4 Pellagra most frequently affects the back of the hands (77%–97% of cases), which can extend upward to create the so-called pellagra glove or gauntlet.3 It is common to see symmetrical eruptions in the shape of a butterfly following an anatomical pattern innervated by the trigeminal nerve, which resembles lupus erythematosus on the face. Another common manifestation is Casal necklace, a well-marginated eruption frequently seen on the front of the neck (Figure).2 On the foot, lesions often do not develop close to the malleoli but rather terminate distally on the backs of the toes. Sometimes a boot pattern may form that covers the front and back of the leg.1-3

The pathophysiology of photosensitivity in pellagra was hypothesized by Karthikeyan and Thappa.3 They discovered an excessive synthesis of a phototoxic substance, kynurenic acid, and a deficiency in urocanic acid, which normally protects the skin by absorbing light in the UVB range. Niacin deprivation leads to the production of kynurenic acid through the tryptophan-kynurenine-nicotinic acid pathway and reduces the amount of urocanic acid by affecting the enzyme histidase in the stratum corneum.1-3 In one-third of patients, pellagra affects the oral mucosa, causing characteristic symptoms such as glossitis, angular stomatitis, and cheilitis.2 In nearly 50% of patients, poor appetite, nausea, epigastric discomfort, diarrhea, and excessive salivation are present. Most of the gastrointestinal tract is affected by mucosal inflammation and atrophy, which can cause malnutrition and cachexia due to anorexia and malabsorptive diarrhea.2 Headache, irritability, poor concentration, hallucinations, photophobia, tremor, and depression are some of the neuropsychiatric symptoms. Patients experience delirium and disorientation as pellagra progresses, followed by a comatose state and ultimately death.2
The patient’s history and physical examination are used to make the diagnosis, with particular attention to the patient’s dietary details. The diagnosis is made in part ex juvantibus by seeing how the patient responds to higher niacin doses. Anemia, hypoproteinemia, elevated blood calcium, reduced serum potassium and phosphorus, abnormal liver function tests, and elevated serum porphyrin levels also indicate pellagra. Niacin 300 mg in divided doses for up to 4 weeks has been recommended by the World Health Organization to treat pellagra.5 The flushing seen with niacin administration is not linked to the usage of nicotinamide. The recommended nicotinamide dosage for adults is 100 mg orally every 6 hours until most acute symptoms have disappeared, followed by oral administration of 50 mg every 8 to 12 hours until all skin lesions have healed.2
Among the differential diagnoses, necrolytic migratory erythema is characterized by an episodic eruption of crusted, erosive, annular erythematous plaques with blister development, which occurs in 70% of patients with glucagonoma syndrome. The perioral region, perineum, lower belly, thighs, and distal extremities are the usual locations.6,7 Laboratory test results include elevated fasting serum glucagon (>1000 ng/L) and normocytic anemia, which aided in ruling out this diagnosis in our patient. Generalized acute cutaneous lupus erythematosus may appear as a broad morbilliform eruption. The hands frequently exhibit erythema and edema, especially across the dorsal and interphalangeal regions.8 Other typical findings of systemic lupus erythematosus such as antinuclear antibody were not seen in our patient, making this diagnosis unlikely. Porphyria cutanea tarda also must be considered in the differential diagnosis. The hepatic deficiency of uroporphyrinogen decarboxylase is the primary cause of this condition. Although it is characterized by blistering lesions, patients more frequently describe increased skin fragility in sun-exposed regions. Hypertrichosis, hyperpigmentation or hypopigmentation, hirsutism, or scarring may appear in the later stage of the disease.9 Phototoxic reaction was ruled out because the patient spent most of the time at home, and no new drugs had been prescribed in the previous months.
- Prabhu D, Dawe RS, Mponda K. Pellagra a review exploring causes and mechanisms, including isoniazid-induced pellagra. Photodermatol Photoimmunol Photomed. 2021;37:99-104. doi:10.1111 /phpp.12659
- Hegyi J, Schwartz RA, Hegyi V. Pellagra: dermatitis, dementia, and diarrhea. Int J Dermatol. 2004;43:1-5. doi:10.1111/j.1365-4632.2004.01959.x
- Karthikeyan K, Thappa DM. Pellagra and skin. Int J Dermatol. 2002;41:476-481. doi:10.1046/j.1365-4362.2002.01551.x
- Dogliotti M, Liebowitz M, Downing DT, et al. Nutritional influences of pellagra on sebum composition. Br J Dermatol. 1977;97:25-28. doi:10.1111/j.1365-2133.1977.tb15423.x
- World Health Organization. Pellagra and Its Prevention and Control in Major Emergencies. Published February 23, 2000. Accessed February 15, 2024. https://www.who.int/publications/i/item/WHO-NHD-00.10
- Liu JW, Qian YT, Ma DL. Necrolytic migratory erythema. JAMA Dermatol. 2019;155:1180. doi:10.1001/jamadermatol.2019.1658
- Tolliver S, Graham J, Kaffenberger BH. A review of cutaneous manifestations within glucagonoma syndrome: necrolytic migratory erythema. Int J Dermatol. 2018;57:642-645. doi:10.1111/ijd.13947
- Walling HW, Sontheimer RD. Cutaneous lupus erythematosus: issues in diagnosis and treatment. Am J Clin Dermatol. 2009;10:365-381. doi:10.2165/11310780-000000000-00000
- Singal AK. Porphyria cutanea tarda: recent update. Mol Genet Metab. 2019;128:271-281. doi:10.1016/j.ymgme.2019.01.004
- Prabhu D, Dawe RS, Mponda K. Pellagra a review exploring causes and mechanisms, including isoniazid-induced pellagra. Photodermatol Photoimmunol Photomed. 2021;37:99-104. doi:10.1111 /phpp.12659
- Hegyi J, Schwartz RA, Hegyi V. Pellagra: dermatitis, dementia, and diarrhea. Int J Dermatol. 2004;43:1-5. doi:10.1111/j.1365-4632.2004.01959.x
- Karthikeyan K, Thappa DM. Pellagra and skin. Int J Dermatol. 2002;41:476-481. doi:10.1046/j.1365-4362.2002.01551.x
- Dogliotti M, Liebowitz M, Downing DT, et al. Nutritional influences of pellagra on sebum composition. Br J Dermatol. 1977;97:25-28. doi:10.1111/j.1365-2133.1977.tb15423.x
- World Health Organization. Pellagra and Its Prevention and Control in Major Emergencies. Published February 23, 2000. Accessed February 15, 2024. https://www.who.int/publications/i/item/WHO-NHD-00.10
- Liu JW, Qian YT, Ma DL. Necrolytic migratory erythema. JAMA Dermatol. 2019;155:1180. doi:10.1001/jamadermatol.2019.1658
- Tolliver S, Graham J, Kaffenberger BH. A review of cutaneous manifestations within glucagonoma syndrome: necrolytic migratory erythema. Int J Dermatol. 2018;57:642-645. doi:10.1111/ijd.13947
- Walling HW, Sontheimer RD. Cutaneous lupus erythematosus: issues in diagnosis and treatment. Am J Clin Dermatol. 2009;10:365-381. doi:10.2165/11310780-000000000-00000
- Singal AK. Porphyria cutanea tarda: recent update. Mol Genet Metab. 2019;128:271-281. doi:10.1016/j.ymgme.2019.01.004
A 66-year-old man presented with an intermittent pruriginous symmetric rash on the dorsal aspects of the arms, legs, and upper chest of 4 months' duration. The patient’s hands, forearms, and neck were diffusely hyperpigmented, dry, cracked, and scaling with a ring of peripheral erythema. He also experienced recurrent photosensitivity reactions on the legs. His poor clinical condition including confusion and diarrhea hindered intake of a balanced diet. He also reported a history of excessive alcohol use. The patient’s vital signs were normal, and Doppler ultrasonography ruled out deep venous thrombosis of the lower legs. A complete blood cell count showed anemia with decreased hemoglobin levels (117 g/L [reference range, 140–180 g/L]) and increased mean corpuscular volume (107.1 fL [reference range, 80–100 fL]). Additionally, low serum levels of albumin, folate, and vitamin B12 were noted. The patient had been taking hydrochlorothiazide and salicylic acid for hypertension with no recent changes in his medication regimen.

Herpes Zoster and Varicella Encephalitis Following the Recombinant Zoster Vaccine
To the Editor:
Reported adverse effects following the recombinant zoster vaccine (RZV) include pyrexia, myalgia, and fatigue.1 We report the case of a patient who developed herpes zoster and subsequent varicella encephalitis within 8 days of receiving the second dose of the RZV.
A 75-year-old man presented to the emergency department with burning pain and pruritus involving the left hip and calf 2 days after receiving the second dose of the RZV. He had a history of chronic lymphocytic leukemia (CLL) and was being clinically monitored. He received the first dose of the RZV without complication 3 months prior. In the emergency department, he was diagnosed with “nerve pain,” given acetaminophen, and discharged home; however, he continued to have worsening pain 8 days later followed by a vesicular eruption that wrapped around the left leg and was concentrated on the inner thigh/groin area in a dermatomal distribution. His primary care physician diagnosed him with herpes zoster and prescribed valacyclovir 1000 mg every 8 hours for 7 days. Two days later, the patient developed weakness and confusion and returned to the emergency department. Upon admission, computed tomography and magnetic resonance imaging/magnetic resonance angiography of the brain was normal. A lumbar puncture confirmed varicella encephalitis via a polymerase chain reaction assay. He was treated with intravenous acyclovir and discharged to a rehabilitation facility. His course was further complicated by a subarachnoid hemorrhage and normal pressure hydrocephalus. He did not require a shunt but continues to have memory impairment, weakness, and cognitive impairment. He is steadily improving with rehabilitative services.
The RZV is an inactivated vaccine composed of the varicella-zoster virus (VZV) glycoprotein E antigen and an adjuvant, AS01B, that boosts both innate and adaptive immunity.2 It was approved by the US Food and Drug Administration in 2017 for prevention of herpes zoster in adults aged 50 years or older. It requires 2 separate injections administered 2 to 6 months apart. Its efficacy for the prevention of cutaneous herpes zoster and postherpetic neuralgia is 97% and 80% to 91%, respectively. It was developed to improve on the existing zoster vaccine live, which contains a live attenuated virus, with efficacy ranging from 38% to 70%.3
The Centers for Disease Control and Prevention initially recommended the RZV for immunocompetent individuals or those taking low-dose immunosuppressant medications as well those who have recovered from an immunocompromising illness. In immunocompetent patients, reported adverse effects include injection site pain and redness, headache, myalgia, fatigue, shivering, fever, and gastrointestinal tract symptoms; however, when the vaccine first came out, many of the studies excluded patients with CLL.4 Our patient’s herpes zoster and varicella encephalitis occurred following administration of the second dose of the RZV. Herpes zoster occurs from declining VZV-specific cell-mediated immunity. Given that the vaccine contains inactive virus, it is unlikely that our patient’s infection was the direct result of dissemination of the virus contained within the vaccine. The RZV specifically generates T-cell responses to the glycoprotein E subunit of VZV, which is thought to be responsible for the high levels of VZV-specific memory T cells with the RZV compared to the zoster vaccine live.5 However, this response does not occur until after the second dose of RZV. Although our patient already had 1 dose of RZV, it was unlikely that he had a substantial number of glycoprotein E and VZV-specific memory T cells to combat virus reactivation. Additionally, his CLL, though mild, may have resulted in an aberrant T-cell response in the presence of already low VZV-specific lymphocytes, allowing for reactivation and dissemination of the virus. Since then, there has been more of an emphasis on looking at the immunogenicity elicited by the vaccine in patients with CLL—both those who are treatment naive and those treated with Bruton tyrosine kinase inhibitors. Both groups of patients have demonstrated reduced immunogenicity in response to RZV, leaving the opportunity for viral reactivation in this patient population.6,7
The safety of the RZV has now been demonstrated in patients with CLL.7 However, even after RZV vaccination, patients with CLL are still at risk for herpes zoster reactivation and may have an aberrant response due to immune cell dysregulation. Our case demonstrates the need to increase monitoring of CLL patients for signs of viral reactivation and shift our focus to providing antiviral therapy quickly after symptom occurrence.
- Centers for Disease Control and Prevention. Shingles: about the vaccine. Updated January 24, 2022. Accessed February 7, 2024. https://www.cdc.gov/vaccines/vpd/shingles/hcp/shingrix/about-vaccine.html
- Dooling KL, Guo A, Patel M, et al. Recommendations of the advisory committee on immunization practices for use of herpes zoster vaccines. MMWR Morb Mortal Wkly Rep. 2018;67:103-108. doi:10.15585/mmwr.mm6703a5external icon
- Hunter P, Fryhofer SA, Szilagyi PG. Vaccination of adults in general medical practice. Mayo Clin Proc. 2020;95:169-183. doi:10.1016/j.mayocp.2019.02.024
- Dagnew AF, Ilhan O, Lee WS, et al. Immunogenicity and safety of the adjuvanted recombinant zoster vaccine in adults with haematological malignancies: a phase 3, randomised, clinical trial and post-hoc efficacy analysis [published correction appears in Lancet Infect Dis. 2020;20:E1]. Lancet Infect Dis. 2019;19:988-1000. doi:10.1016/S1473-3099(19)30163-X
- Levin MJ, Kroehl ME, Johnson MJ, et al. Th1 memory differentiates recombinant from live herpes zoster vaccines. J Clin Invest. 2018;128:4429-4440.
- Pleyer C, Laing KJ, Ali MA, et al. BTK inhibitors impair humoral and cellular responses to recombinant zoster vaccine in CLL. Blood Adv. 2022;6:1732-1740. doi:10.1182/bloodadvances.2021006574
- Pleyer C, Cohen J, Soto S, et al. Response to the Shingrix varicella zoster virus (VZV) vaccine in patients with chronic lymphocytic leukemia (CLL) that are treatment naive or treated with a Bruton’s tyrosine kinase inhibitor (BTK-I). Blood. 2019;134(suppl 1):3053. doi:10.1182/blood-2019-121675
To the Editor:
Reported adverse effects following the recombinant zoster vaccine (RZV) include pyrexia, myalgia, and fatigue.1 We report the case of a patient who developed herpes zoster and subsequent varicella encephalitis within 8 days of receiving the second dose of the RZV.
A 75-year-old man presented to the emergency department with burning pain and pruritus involving the left hip and calf 2 days after receiving the second dose of the RZV. He had a history of chronic lymphocytic leukemia (CLL) and was being clinically monitored. He received the first dose of the RZV without complication 3 months prior. In the emergency department, he was diagnosed with “nerve pain,” given acetaminophen, and discharged home; however, he continued to have worsening pain 8 days later followed by a vesicular eruption that wrapped around the left leg and was concentrated on the inner thigh/groin area in a dermatomal distribution. His primary care physician diagnosed him with herpes zoster and prescribed valacyclovir 1000 mg every 8 hours for 7 days. Two days later, the patient developed weakness and confusion and returned to the emergency department. Upon admission, computed tomography and magnetic resonance imaging/magnetic resonance angiography of the brain was normal. A lumbar puncture confirmed varicella encephalitis via a polymerase chain reaction assay. He was treated with intravenous acyclovir and discharged to a rehabilitation facility. His course was further complicated by a subarachnoid hemorrhage and normal pressure hydrocephalus. He did not require a shunt but continues to have memory impairment, weakness, and cognitive impairment. He is steadily improving with rehabilitative services.
The RZV is an inactivated vaccine composed of the varicella-zoster virus (VZV) glycoprotein E antigen and an adjuvant, AS01B, that boosts both innate and adaptive immunity.2 It was approved by the US Food and Drug Administration in 2017 for prevention of herpes zoster in adults aged 50 years or older. It requires 2 separate injections administered 2 to 6 months apart. Its efficacy for the prevention of cutaneous herpes zoster and postherpetic neuralgia is 97% and 80% to 91%, respectively. It was developed to improve on the existing zoster vaccine live, which contains a live attenuated virus, with efficacy ranging from 38% to 70%.3
The Centers for Disease Control and Prevention initially recommended the RZV for immunocompetent individuals or those taking low-dose immunosuppressant medications as well those who have recovered from an immunocompromising illness. In immunocompetent patients, reported adverse effects include injection site pain and redness, headache, myalgia, fatigue, shivering, fever, and gastrointestinal tract symptoms; however, when the vaccine first came out, many of the studies excluded patients with CLL.4 Our patient’s herpes zoster and varicella encephalitis occurred following administration of the second dose of the RZV. Herpes zoster occurs from declining VZV-specific cell-mediated immunity. Given that the vaccine contains inactive virus, it is unlikely that our patient’s infection was the direct result of dissemination of the virus contained within the vaccine. The RZV specifically generates T-cell responses to the glycoprotein E subunit of VZV, which is thought to be responsible for the high levels of VZV-specific memory T cells with the RZV compared to the zoster vaccine live.5 However, this response does not occur until after the second dose of RZV. Although our patient already had 1 dose of RZV, it was unlikely that he had a substantial number of glycoprotein E and VZV-specific memory T cells to combat virus reactivation. Additionally, his CLL, though mild, may have resulted in an aberrant T-cell response in the presence of already low VZV-specific lymphocytes, allowing for reactivation and dissemination of the virus. Since then, there has been more of an emphasis on looking at the immunogenicity elicited by the vaccine in patients with CLL—both those who are treatment naive and those treated with Bruton tyrosine kinase inhibitors. Both groups of patients have demonstrated reduced immunogenicity in response to RZV, leaving the opportunity for viral reactivation in this patient population.6,7
The safety of the RZV has now been demonstrated in patients with CLL.7 However, even after RZV vaccination, patients with CLL are still at risk for herpes zoster reactivation and may have an aberrant response due to immune cell dysregulation. Our case demonstrates the need to increase monitoring of CLL patients for signs of viral reactivation and shift our focus to providing antiviral therapy quickly after symptom occurrence.
To the Editor:
Reported adverse effects following the recombinant zoster vaccine (RZV) include pyrexia, myalgia, and fatigue.1 We report the case of a patient who developed herpes zoster and subsequent varicella encephalitis within 8 days of receiving the second dose of the RZV.
A 75-year-old man presented to the emergency department with burning pain and pruritus involving the left hip and calf 2 days after receiving the second dose of the RZV. He had a history of chronic lymphocytic leukemia (CLL) and was being clinically monitored. He received the first dose of the RZV without complication 3 months prior. In the emergency department, he was diagnosed with “nerve pain,” given acetaminophen, and discharged home; however, he continued to have worsening pain 8 days later followed by a vesicular eruption that wrapped around the left leg and was concentrated on the inner thigh/groin area in a dermatomal distribution. His primary care physician diagnosed him with herpes zoster and prescribed valacyclovir 1000 mg every 8 hours for 7 days. Two days later, the patient developed weakness and confusion and returned to the emergency department. Upon admission, computed tomography and magnetic resonance imaging/magnetic resonance angiography of the brain was normal. A lumbar puncture confirmed varicella encephalitis via a polymerase chain reaction assay. He was treated with intravenous acyclovir and discharged to a rehabilitation facility. His course was further complicated by a subarachnoid hemorrhage and normal pressure hydrocephalus. He did not require a shunt but continues to have memory impairment, weakness, and cognitive impairment. He is steadily improving with rehabilitative services.
The RZV is an inactivated vaccine composed of the varicella-zoster virus (VZV) glycoprotein E antigen and an adjuvant, AS01B, that boosts both innate and adaptive immunity.2 It was approved by the US Food and Drug Administration in 2017 for prevention of herpes zoster in adults aged 50 years or older. It requires 2 separate injections administered 2 to 6 months apart. Its efficacy for the prevention of cutaneous herpes zoster and postherpetic neuralgia is 97% and 80% to 91%, respectively. It was developed to improve on the existing zoster vaccine live, which contains a live attenuated virus, with efficacy ranging from 38% to 70%.3
The Centers for Disease Control and Prevention initially recommended the RZV for immunocompetent individuals or those taking low-dose immunosuppressant medications as well those who have recovered from an immunocompromising illness. In immunocompetent patients, reported adverse effects include injection site pain and redness, headache, myalgia, fatigue, shivering, fever, and gastrointestinal tract symptoms; however, when the vaccine first came out, many of the studies excluded patients with CLL.4 Our patient’s herpes zoster and varicella encephalitis occurred following administration of the second dose of the RZV. Herpes zoster occurs from declining VZV-specific cell-mediated immunity. Given that the vaccine contains inactive virus, it is unlikely that our patient’s infection was the direct result of dissemination of the virus contained within the vaccine. The RZV specifically generates T-cell responses to the glycoprotein E subunit of VZV, which is thought to be responsible for the high levels of VZV-specific memory T cells with the RZV compared to the zoster vaccine live.5 However, this response does not occur until after the second dose of RZV. Although our patient already had 1 dose of RZV, it was unlikely that he had a substantial number of glycoprotein E and VZV-specific memory T cells to combat virus reactivation. Additionally, his CLL, though mild, may have resulted in an aberrant T-cell response in the presence of already low VZV-specific lymphocytes, allowing for reactivation and dissemination of the virus. Since then, there has been more of an emphasis on looking at the immunogenicity elicited by the vaccine in patients with CLL—both those who are treatment naive and those treated with Bruton tyrosine kinase inhibitors. Both groups of patients have demonstrated reduced immunogenicity in response to RZV, leaving the opportunity for viral reactivation in this patient population.6,7
The safety of the RZV has now been demonstrated in patients with CLL.7 However, even after RZV vaccination, patients with CLL are still at risk for herpes zoster reactivation and may have an aberrant response due to immune cell dysregulation. Our case demonstrates the need to increase monitoring of CLL patients for signs of viral reactivation and shift our focus to providing antiviral therapy quickly after symptom occurrence.
- Centers for Disease Control and Prevention. Shingles: about the vaccine. Updated January 24, 2022. Accessed February 7, 2024. https://www.cdc.gov/vaccines/vpd/shingles/hcp/shingrix/about-vaccine.html
- Dooling KL, Guo A, Patel M, et al. Recommendations of the advisory committee on immunization practices for use of herpes zoster vaccines. MMWR Morb Mortal Wkly Rep. 2018;67:103-108. doi:10.15585/mmwr.mm6703a5external icon
- Hunter P, Fryhofer SA, Szilagyi PG. Vaccination of adults in general medical practice. Mayo Clin Proc. 2020;95:169-183. doi:10.1016/j.mayocp.2019.02.024
- Dagnew AF, Ilhan O, Lee WS, et al. Immunogenicity and safety of the adjuvanted recombinant zoster vaccine in adults with haematological malignancies: a phase 3, randomised, clinical trial and post-hoc efficacy analysis [published correction appears in Lancet Infect Dis. 2020;20:E1]. Lancet Infect Dis. 2019;19:988-1000. doi:10.1016/S1473-3099(19)30163-X
- Levin MJ, Kroehl ME, Johnson MJ, et al. Th1 memory differentiates recombinant from live herpes zoster vaccines. J Clin Invest. 2018;128:4429-4440.
- Pleyer C, Laing KJ, Ali MA, et al. BTK inhibitors impair humoral and cellular responses to recombinant zoster vaccine in CLL. Blood Adv. 2022;6:1732-1740. doi:10.1182/bloodadvances.2021006574
- Pleyer C, Cohen J, Soto S, et al. Response to the Shingrix varicella zoster virus (VZV) vaccine in patients with chronic lymphocytic leukemia (CLL) that are treatment naive or treated with a Bruton’s tyrosine kinase inhibitor (BTK-I). Blood. 2019;134(suppl 1):3053. doi:10.1182/blood-2019-121675
- Centers for Disease Control and Prevention. Shingles: about the vaccine. Updated January 24, 2022. Accessed February 7, 2024. https://www.cdc.gov/vaccines/vpd/shingles/hcp/shingrix/about-vaccine.html
- Dooling KL, Guo A, Patel M, et al. Recommendations of the advisory committee on immunization practices for use of herpes zoster vaccines. MMWR Morb Mortal Wkly Rep. 2018;67:103-108. doi:10.15585/mmwr.mm6703a5external icon
- Hunter P, Fryhofer SA, Szilagyi PG. Vaccination of adults in general medical practice. Mayo Clin Proc. 2020;95:169-183. doi:10.1016/j.mayocp.2019.02.024
- Dagnew AF, Ilhan O, Lee WS, et al. Immunogenicity and safety of the adjuvanted recombinant zoster vaccine in adults with haematological malignancies: a phase 3, randomised, clinical trial and post-hoc efficacy analysis [published correction appears in Lancet Infect Dis. 2020;20:E1]. Lancet Infect Dis. 2019;19:988-1000. doi:10.1016/S1473-3099(19)30163-X
- Levin MJ, Kroehl ME, Johnson MJ, et al. Th1 memory differentiates recombinant from live herpes zoster vaccines. J Clin Invest. 2018;128:4429-4440.
- Pleyer C, Laing KJ, Ali MA, et al. BTK inhibitors impair humoral and cellular responses to recombinant zoster vaccine in CLL. Blood Adv. 2022;6:1732-1740. doi:10.1182/bloodadvances.2021006574
- Pleyer C, Cohen J, Soto S, et al. Response to the Shingrix varicella zoster virus (VZV) vaccine in patients with chronic lymphocytic leukemia (CLL) that are treatment naive or treated with a Bruton’s tyrosine kinase inhibitor (BTK-I). Blood. 2019;134(suppl 1):3053. doi:10.1182/blood-2019-121675
Practice Points
- Patients with chronic lymphocytic leukemia (CLL) are at risk for herpes zoster reactivation even with vaccination due to a decreased immune response. These patients may have an aberrant response due to immune cell dysregulation.
- It is important to increase monitoring of CLL patients for signs of viral reactivation and shift the focus to providing antiviral therapy quickly if herpes zoster symptoms occur.
Rapidly Progressive Necrotizing Myositis Mimicking Pyoderma Gangrenosum
To the Editor:
Necrotizing myositis (NM) is an exceedingly rare necrotizing soft-tissue infection (NSTI) that is characterized by skeletal muscle involvement. β -Hemolytic streptococci, such as Streptococcus pyogenes , are the most common causative organisms. The overall prevalence and incidence of NM is unknown. A review of the literature by Adams et al 2 identified only 21 cases between 1900 and 1985.
Timely treatment of this infection leads to improved outcomes, but diagnosis can be challenging due to the ambiguous presentation of NM and lack of specific cutaneous changes.3 Clinical manifestations including bullae, blisters, vesicles, and petechiae become more prominent as infection progresses.4 If NM is suspected due to cutaneous manifestations, it is imperative that the underlying cause be identified; for example, NM must be distinguished from the overlapping presentation of pyoderma gangrenosum (PG). Because NM has nearly 100% mortality without prompt surgical intervention, early identification is critical.5 Herein, we report a case of NM that illustrates the correlation of clinical, histological, and imaging findings required to diagnose this potentially fatal infection.
An 80-year-old man presented to the emergency department with worsening pain, edema, and spreading redness of the right wrist over the last 5 weeks. He had a history of atopic dermatitis that was refractory to topical steroids and methotrexate; he was dependent on an oral steroid (prednisone 30 mg/d) for symptom control. The patient reported minor trauma to the area after performing home renovations. He received numerous rounds of oral antibiotics as an outpatient for presumed cellulitis and reported he was “getting better” but that the signs and symptoms of the condition grew worse after outpatient arthrocentesis. Dermatology was consulted to evaluate for a necrotizing neutrophilic dermatosis such as PG.
At the current presentation, the patient was tachycardic and afebrile (temperature, 98.2 °F [36.8 °C]). Physical examination revealed large, exquisitely tender, ill-defined necrotic ulceration of the right wrist with purulent debris and diffuse edema (Figure 1). Sequential evaluation at 6-hour intervals revealed notably increasing purulence, edema, and tenderness. Interconnected sinus tracts that extended to the fascial plane were observed.

Laboratory workup was notable for a markedly elevated C-reactive protein level of 18.9 mg/dL (reference range, 0–0.8 mg/dL) and an elevated white blood cell count of 19.92×109/L (reference range, 4.5–11.0×109/L). Blood and tissue cultures were positive for methicillin-sensitive Staphylococcus aureus. Computed tomography and magnetic resonance imaging (MRI) prior to biopsy demonstrated findings consistent with extensive subcutaneous and intramuscular areas of loculation and foci of gas (Figure 2). These findings were consistent with intramuscular involvement. A punch biopsy revealed a necrotic epidermis filled with neutrophilic pustules and a dense dermal infiltrate of neutrophilic inflammation consistent with infection (Figure 3).
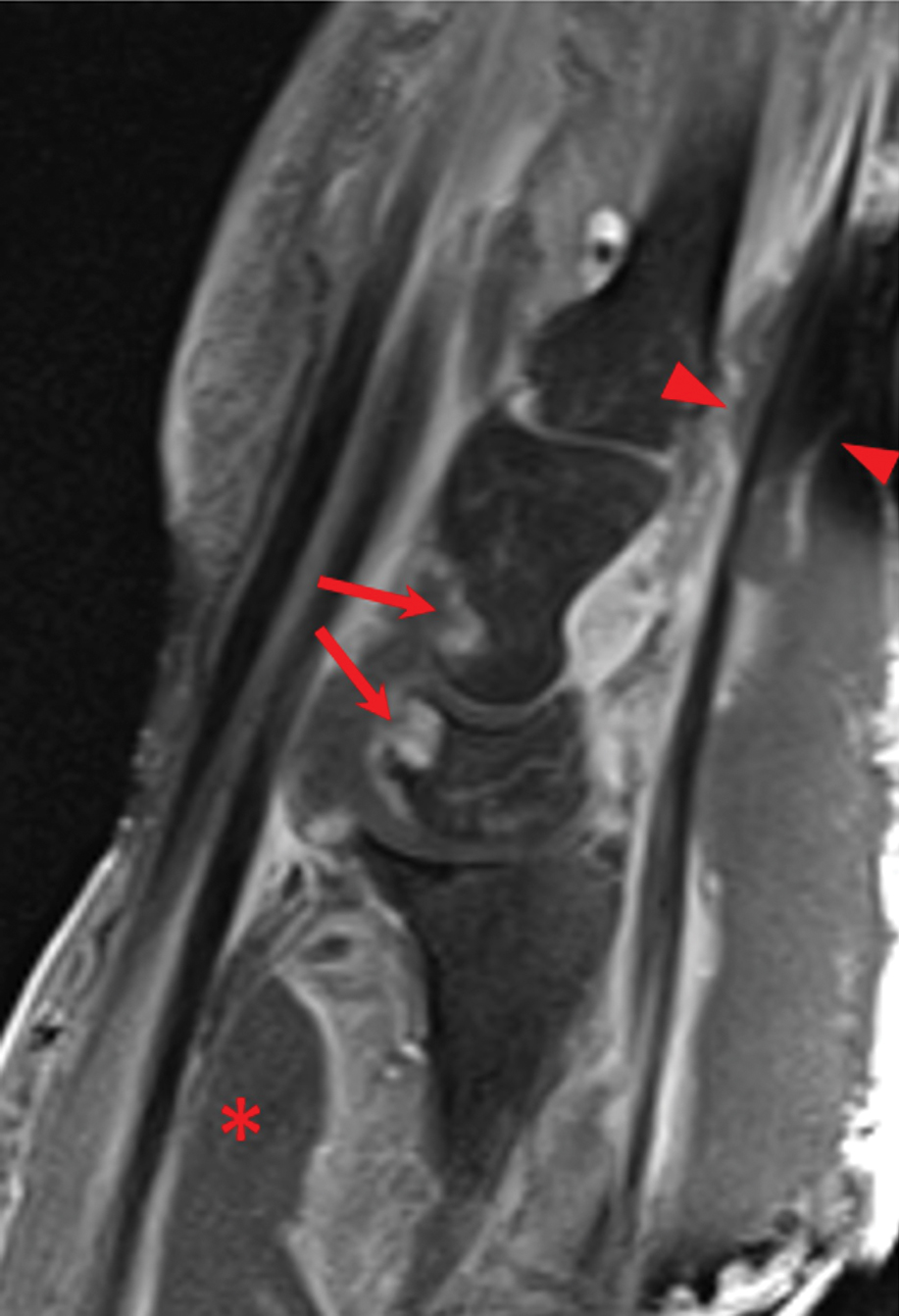
Emergency surgery was performed with debridement of necrotic tissue and muscle. Postoperatively, he became more clinically stable after being placed on cefazolin through a peripherally inserted central catheter. He underwent 4 additional washouts over the ensuing month, as well as tendon reconstructions, a radial forearm flap, and reverse radial forearm flap reconstruction of the forearm. At the time of publication, there has been no recurrence. The patient’s atopic dermatitis is well controlled on dupilumab and topical fluocinonide alone, with a recent IgA level of 1 g/L and a body surface area measurement of 2%. Dupilumab was started 3 months after surgery.
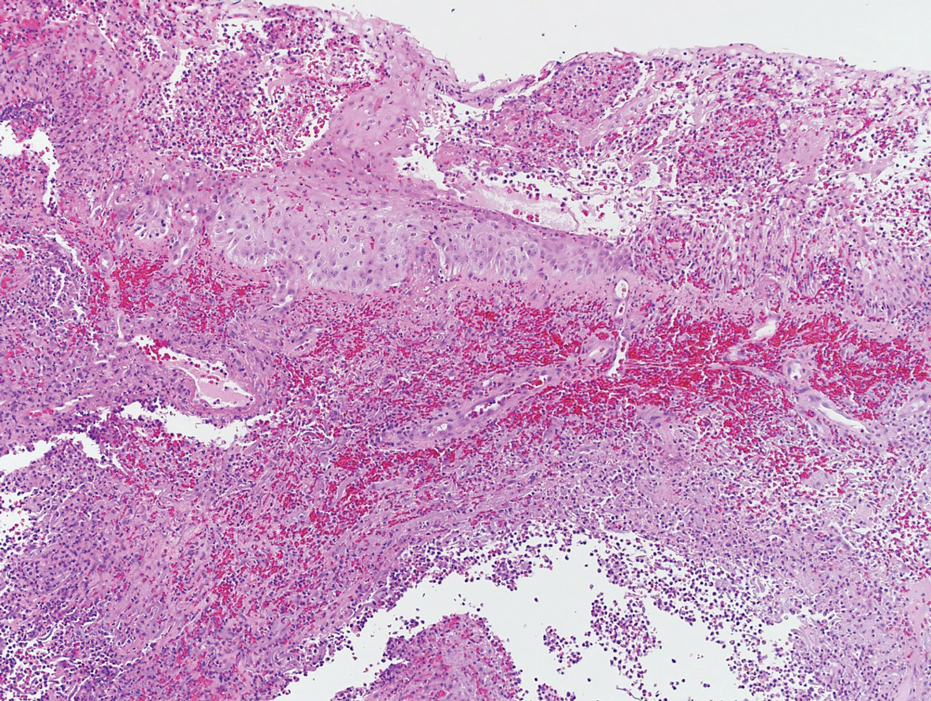
Necrotizing myositis is a rare, rapidly progressive infection involving muscle that can manifest as superficial cutaneous involvement. The clinical manifestation of NM is harder to recognize than other NSTIs such as necrotizing fasciitis, likely due to the initial prodromal phase of NM, which consists of nonspecific constitutional symptoms.3 Systemic findings such as tachycardia, fever, hypotension, and shock occur in only 10% to 40% of NM patients.4,5
In our patient, clues of NM included fulfillment of criteria for systemic inflammatory response syndrome at admission and a presumed source of infection; taken together, these findings should lead to a diagnosis of sepsis until otherwise proven. The patient also reported pain that was not proportional to the skin findings, which suggested an NSTI. His lack of constitutional symptoms may have been due to the effects of prednisone, which was changed to dupilumab during hospitalization.
The clinical and histological findings of NM are nonspecific. Clinical findings include skin discoloration with bullae, blisters, vesicles, or petechiae.4 Our case adds to the descriptive morphology by including marked edema with ulceration, progressive purulence, and interconnected sinuses tracking to the fascial plane. Histologic findings can include confluent necrosis extending from the epidermis to the underlying muscle with dense neutrophilic inflammation. Notably, these findings can mirror necrotizing neutrophilic dermatoses in the absence of an infectious cause. Failure to recognize simple systemic inflammatory response syndrome criteria in NM patients due to slow treatment response or incorrect treatment can can lead to loss of a limb or death.
Workup reveals overlap with necrotizing neutrophilic dermatoses including PG, which is the prototypical neutrophilic dermatosis. Morphologically, PG presents as an ulcer with a purple and undermined border, often having developed from an initial papule, vesicle, or pustule. A neutrophilic infiltrate of the ulcer edge is the major criterion required to diagnose PG6; minor criteria include a positive pathergy test, history of inflammatory arthritis or inflammatory bowel disease, and exclusion of infection.6 When compared directly to an NSTI such as NM, the most important variable that sets PG apart is the absence of bacterial growth on blood and tissue cultures.7
Imaging studies can aid in the clinical diagnosis of NM and help distinguish the disease from PG. Computed tomography and MRI may demonstrate hallmarks of extensive necrotizing infection, such as gas formation and consequent fascial swelling, thickening and edema of involved muscle, and subfascial fluid collection.3,4 Distinct from NM, imaging findings in PG are more subtle, suggesting cellulitic inflammation with edema.8 A defining radiographic feature of NM can be foci of gas within muscle or fascia, though absence of this finding does not exclude NM.1,4
In conclusion, NM is a rare intramuscular infection that can be difficult to diagnose due to its nonspecific presentation and lack of constitutional symptoms. Dermatologists should maintain a high level of suspicion for NM in the setting of rapidly progressive clinical findings; accurate diagnosis requires a multimodal approach with complete correlation of clinical, histological, and imaging findings. Computed tomography and MRI can heighten the approach, even when necrotizing neutrophilic dermatoses and NM have similar clinical and histological appearances. Once a diagnosis of NM is established, prompt surgical and medical intervention improves the prognosis.
- Stevens DL, Baddour LM. Necrotizing soft tissue infections. UpToDate. Updated October 7, 2022. Accessed February 13, 2024. https://www.uptodate.com/contents/necrotizing-soft-tissue-infections?search=Necrotizing%20soft%20tissue%20infections&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
- Adams EM, Gudmundsson S, Yocum DE, et al. Streptococcal myositis. Arch Intern Med . 1985;145:1020-1023.
- Khanna A, Gurusinghe D, Taylor D. Necrotizing myositis: highlighting the hidden depths—case series and review of the literature. ANZ J Surg . 2020;90:130-134. doi:10.1111/ans.15429
- Boinpally H, Howell RS, Ram B, et al. Necrotizing myositis: a rare necrotizing soft tissue infection involving muscle. Wounds . 2018;30:E116-E120.
- Anaya DA, Dellinger EP. Necrotizing soft-tissue infection: diagnosis and management. Clin Infect Dis . 2007;44:705-710. doi:10.1086/511638
- Maverakis E, Ma C, Shinkai K, et al. Diagnostic criteria of ulcerative pyoderma gangrenosum: a Delphi consensus of international experts. JAMA Dermatol . 2018;154:461-466. doi:10.1001/jamadermatol.2017.5980
- Sanchez IM, Lowenstein S, Johnson KA, et al. Clinical features of neutrophilic dermatosis variants resembling necrotizing fasciitis. JAMA Dermatol . 2019;155:79-84. doi:10.1001/jamadermatol.2018.3890
- Demirdover C, Geyik A, Vayvada H. Necrotising fasciitis or pyoderma gangrenosum: a fatal dilemma. Int Wound J . 2019;16:1347-1353. doi:10.1111/iwj.13196
To the Editor:
Necrotizing myositis (NM) is an exceedingly rare necrotizing soft-tissue infection (NSTI) that is characterized by skeletal muscle involvement. β -Hemolytic streptococci, such as Streptococcus pyogenes , are the most common causative organisms. The overall prevalence and incidence of NM is unknown. A review of the literature by Adams et al 2 identified only 21 cases between 1900 and 1985.
Timely treatment of this infection leads to improved outcomes, but diagnosis can be challenging due to the ambiguous presentation of NM and lack of specific cutaneous changes.3 Clinical manifestations including bullae, blisters, vesicles, and petechiae become more prominent as infection progresses.4 If NM is suspected due to cutaneous manifestations, it is imperative that the underlying cause be identified; for example, NM must be distinguished from the overlapping presentation of pyoderma gangrenosum (PG). Because NM has nearly 100% mortality without prompt surgical intervention, early identification is critical.5 Herein, we report a case of NM that illustrates the correlation of clinical, histological, and imaging findings required to diagnose this potentially fatal infection.
An 80-year-old man presented to the emergency department with worsening pain, edema, and spreading redness of the right wrist over the last 5 weeks. He had a history of atopic dermatitis that was refractory to topical steroids and methotrexate; he was dependent on an oral steroid (prednisone 30 mg/d) for symptom control. The patient reported minor trauma to the area after performing home renovations. He received numerous rounds of oral antibiotics as an outpatient for presumed cellulitis and reported he was “getting better” but that the signs and symptoms of the condition grew worse after outpatient arthrocentesis. Dermatology was consulted to evaluate for a necrotizing neutrophilic dermatosis such as PG.
At the current presentation, the patient was tachycardic and afebrile (temperature, 98.2 °F [36.8 °C]). Physical examination revealed large, exquisitely tender, ill-defined necrotic ulceration of the right wrist with purulent debris and diffuse edema (Figure 1). Sequential evaluation at 6-hour intervals revealed notably increasing purulence, edema, and tenderness. Interconnected sinus tracts that extended to the fascial plane were observed.

Laboratory workup was notable for a markedly elevated C-reactive protein level of 18.9 mg/dL (reference range, 0–0.8 mg/dL) and an elevated white blood cell count of 19.92×109/L (reference range, 4.5–11.0×109/L). Blood and tissue cultures were positive for methicillin-sensitive Staphylococcus aureus. Computed tomography and magnetic resonance imaging (MRI) prior to biopsy demonstrated findings consistent with extensive subcutaneous and intramuscular areas of loculation and foci of gas (Figure 2). These findings were consistent with intramuscular involvement. A punch biopsy revealed a necrotic epidermis filled with neutrophilic pustules and a dense dermal infiltrate of neutrophilic inflammation consistent with infection (Figure 3).
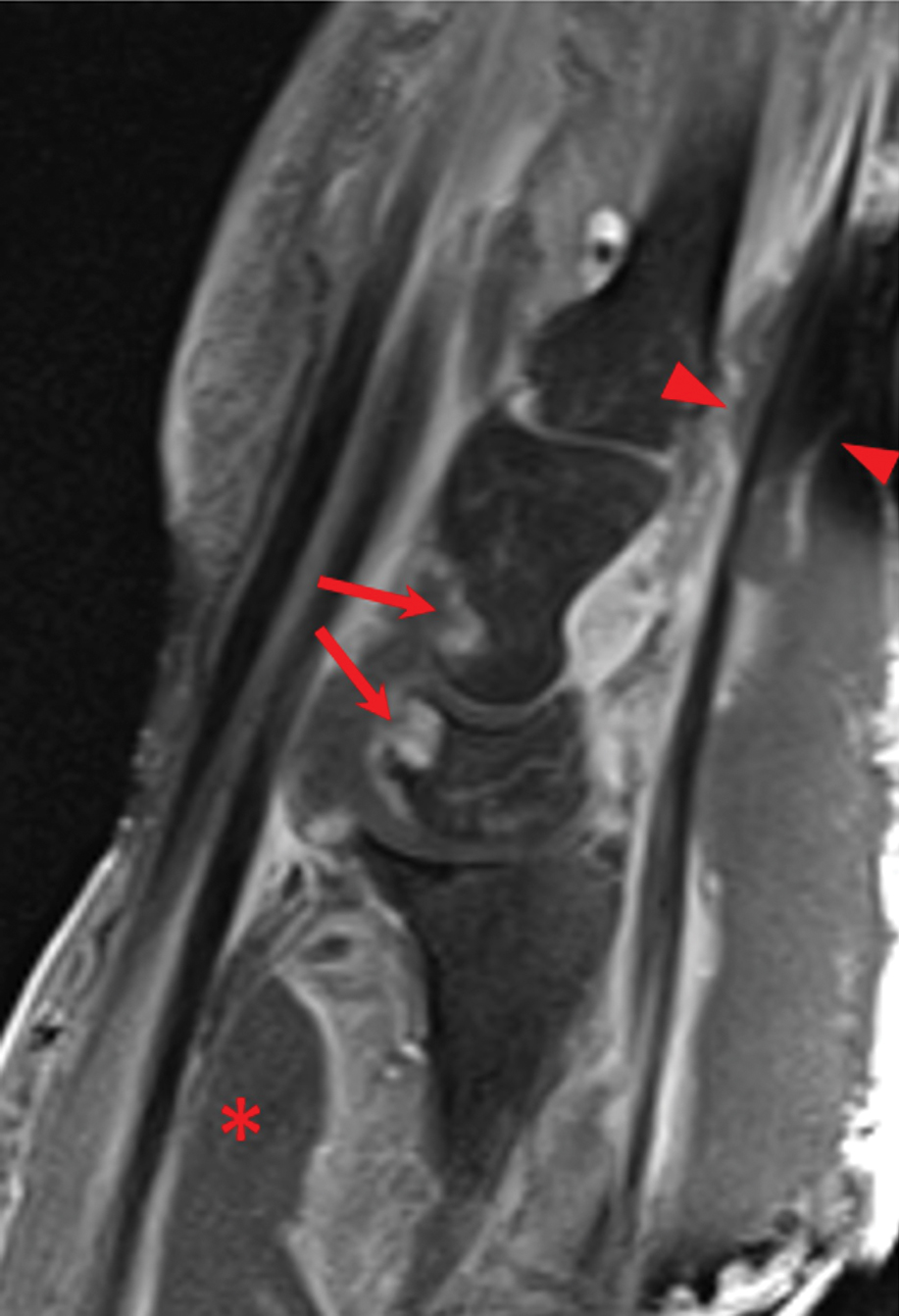
Emergency surgery was performed with debridement of necrotic tissue and muscle. Postoperatively, he became more clinically stable after being placed on cefazolin through a peripherally inserted central catheter. He underwent 4 additional washouts over the ensuing month, as well as tendon reconstructions, a radial forearm flap, and reverse radial forearm flap reconstruction of the forearm. At the time of publication, there has been no recurrence. The patient’s atopic dermatitis is well controlled on dupilumab and topical fluocinonide alone, with a recent IgA level of 1 g/L and a body surface area measurement of 2%. Dupilumab was started 3 months after surgery.
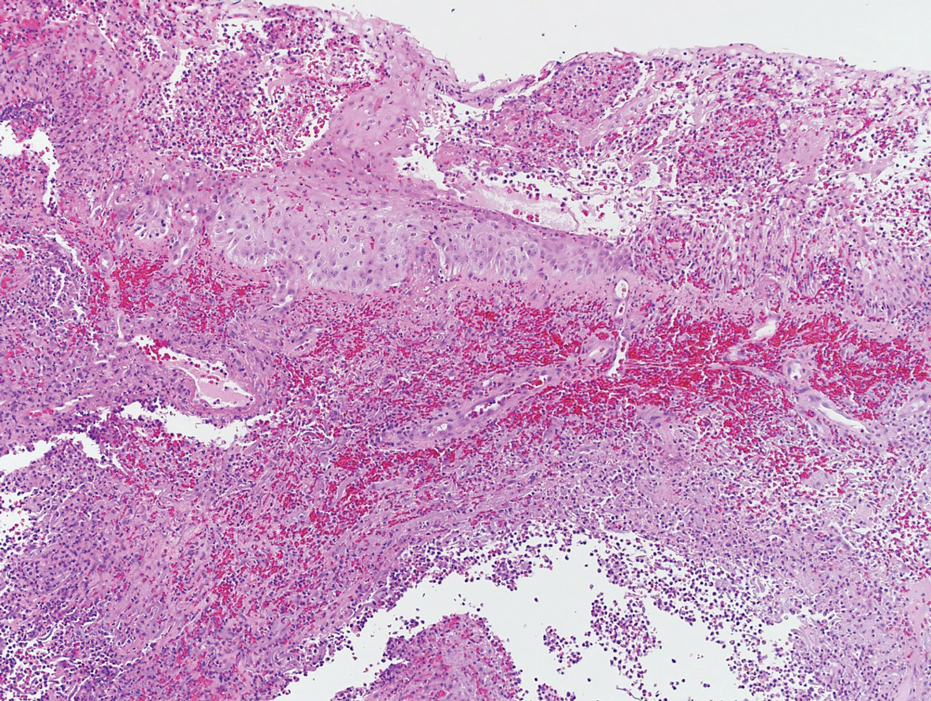
Necrotizing myositis is a rare, rapidly progressive infection involving muscle that can manifest as superficial cutaneous involvement. The clinical manifestation of NM is harder to recognize than other NSTIs such as necrotizing fasciitis, likely due to the initial prodromal phase of NM, which consists of nonspecific constitutional symptoms.3 Systemic findings such as tachycardia, fever, hypotension, and shock occur in only 10% to 40% of NM patients.4,5
In our patient, clues of NM included fulfillment of criteria for systemic inflammatory response syndrome at admission and a presumed source of infection; taken together, these findings should lead to a diagnosis of sepsis until otherwise proven. The patient also reported pain that was not proportional to the skin findings, which suggested an NSTI. His lack of constitutional symptoms may have been due to the effects of prednisone, which was changed to dupilumab during hospitalization.
The clinical and histological findings of NM are nonspecific. Clinical findings include skin discoloration with bullae, blisters, vesicles, or petechiae.4 Our case adds to the descriptive morphology by including marked edema with ulceration, progressive purulence, and interconnected sinuses tracking to the fascial plane. Histologic findings can include confluent necrosis extending from the epidermis to the underlying muscle with dense neutrophilic inflammation. Notably, these findings can mirror necrotizing neutrophilic dermatoses in the absence of an infectious cause. Failure to recognize simple systemic inflammatory response syndrome criteria in NM patients due to slow treatment response or incorrect treatment can can lead to loss of a limb or death.
Workup reveals overlap with necrotizing neutrophilic dermatoses including PG, which is the prototypical neutrophilic dermatosis. Morphologically, PG presents as an ulcer with a purple and undermined border, often having developed from an initial papule, vesicle, or pustule. A neutrophilic infiltrate of the ulcer edge is the major criterion required to diagnose PG6; minor criteria include a positive pathergy test, history of inflammatory arthritis or inflammatory bowel disease, and exclusion of infection.6 When compared directly to an NSTI such as NM, the most important variable that sets PG apart is the absence of bacterial growth on blood and tissue cultures.7
Imaging studies can aid in the clinical diagnosis of NM and help distinguish the disease from PG. Computed tomography and MRI may demonstrate hallmarks of extensive necrotizing infection, such as gas formation and consequent fascial swelling, thickening and edema of involved muscle, and subfascial fluid collection.3,4 Distinct from NM, imaging findings in PG are more subtle, suggesting cellulitic inflammation with edema.8 A defining radiographic feature of NM can be foci of gas within muscle or fascia, though absence of this finding does not exclude NM.1,4
In conclusion, NM is a rare intramuscular infection that can be difficult to diagnose due to its nonspecific presentation and lack of constitutional symptoms. Dermatologists should maintain a high level of suspicion for NM in the setting of rapidly progressive clinical findings; accurate diagnosis requires a multimodal approach with complete correlation of clinical, histological, and imaging findings. Computed tomography and MRI can heighten the approach, even when necrotizing neutrophilic dermatoses and NM have similar clinical and histological appearances. Once a diagnosis of NM is established, prompt surgical and medical intervention improves the prognosis.
To the Editor:
Necrotizing myositis (NM) is an exceedingly rare necrotizing soft-tissue infection (NSTI) that is characterized by skeletal muscle involvement. β -Hemolytic streptococci, such as Streptococcus pyogenes , are the most common causative organisms. The overall prevalence and incidence of NM is unknown. A review of the literature by Adams et al 2 identified only 21 cases between 1900 and 1985.
Timely treatment of this infection leads to improved outcomes, but diagnosis can be challenging due to the ambiguous presentation of NM and lack of specific cutaneous changes.3 Clinical manifestations including bullae, blisters, vesicles, and petechiae become more prominent as infection progresses.4 If NM is suspected due to cutaneous manifestations, it is imperative that the underlying cause be identified; for example, NM must be distinguished from the overlapping presentation of pyoderma gangrenosum (PG). Because NM has nearly 100% mortality without prompt surgical intervention, early identification is critical.5 Herein, we report a case of NM that illustrates the correlation of clinical, histological, and imaging findings required to diagnose this potentially fatal infection.
An 80-year-old man presented to the emergency department with worsening pain, edema, and spreading redness of the right wrist over the last 5 weeks. He had a history of atopic dermatitis that was refractory to topical steroids and methotrexate; he was dependent on an oral steroid (prednisone 30 mg/d) for symptom control. The patient reported minor trauma to the area after performing home renovations. He received numerous rounds of oral antibiotics as an outpatient for presumed cellulitis and reported he was “getting better” but that the signs and symptoms of the condition grew worse after outpatient arthrocentesis. Dermatology was consulted to evaluate for a necrotizing neutrophilic dermatosis such as PG.
At the current presentation, the patient was tachycardic and afebrile (temperature, 98.2 °F [36.8 °C]). Physical examination revealed large, exquisitely tender, ill-defined necrotic ulceration of the right wrist with purulent debris and diffuse edema (Figure 1). Sequential evaluation at 6-hour intervals revealed notably increasing purulence, edema, and tenderness. Interconnected sinus tracts that extended to the fascial plane were observed.

Laboratory workup was notable for a markedly elevated C-reactive protein level of 18.9 mg/dL (reference range, 0–0.8 mg/dL) and an elevated white blood cell count of 19.92×109/L (reference range, 4.5–11.0×109/L). Blood and tissue cultures were positive for methicillin-sensitive Staphylococcus aureus. Computed tomography and magnetic resonance imaging (MRI) prior to biopsy demonstrated findings consistent with extensive subcutaneous and intramuscular areas of loculation and foci of gas (Figure 2). These findings were consistent with intramuscular involvement. A punch biopsy revealed a necrotic epidermis filled with neutrophilic pustules and a dense dermal infiltrate of neutrophilic inflammation consistent with infection (Figure 3).
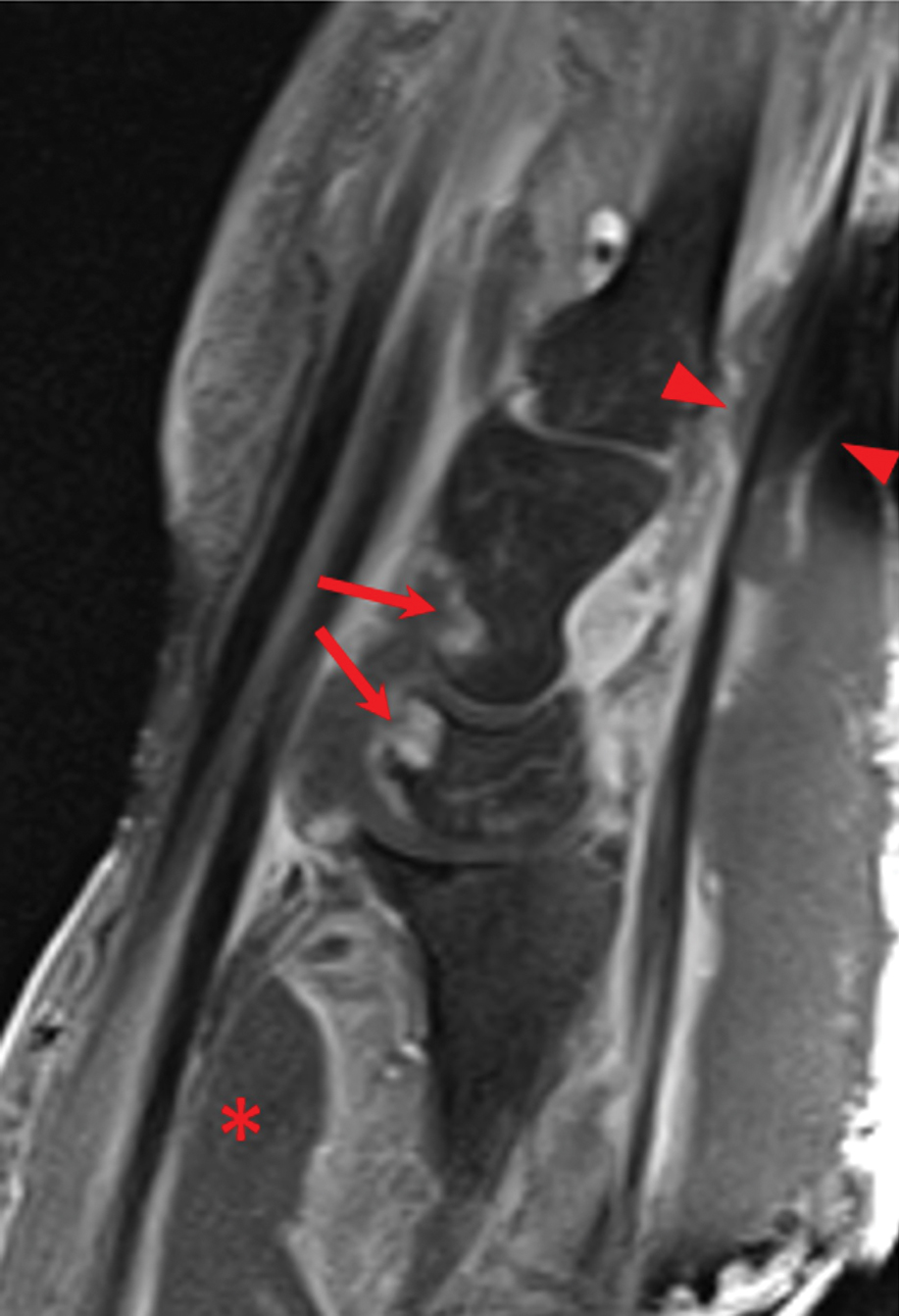
Emergency surgery was performed with debridement of necrotic tissue and muscle. Postoperatively, he became more clinically stable after being placed on cefazolin through a peripherally inserted central catheter. He underwent 4 additional washouts over the ensuing month, as well as tendon reconstructions, a radial forearm flap, and reverse radial forearm flap reconstruction of the forearm. At the time of publication, there has been no recurrence. The patient’s atopic dermatitis is well controlled on dupilumab and topical fluocinonide alone, with a recent IgA level of 1 g/L and a body surface area measurement of 2%. Dupilumab was started 3 months after surgery.
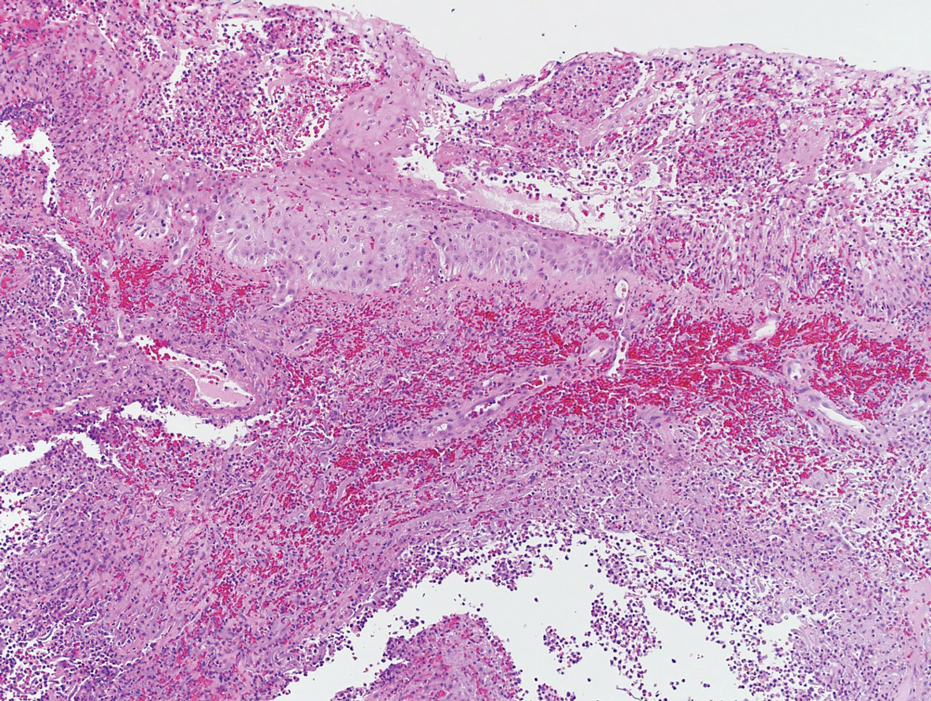
Necrotizing myositis is a rare, rapidly progressive infection involving muscle that can manifest as superficial cutaneous involvement. The clinical manifestation of NM is harder to recognize than other NSTIs such as necrotizing fasciitis, likely due to the initial prodromal phase of NM, which consists of nonspecific constitutional symptoms.3 Systemic findings such as tachycardia, fever, hypotension, and shock occur in only 10% to 40% of NM patients.4,5
In our patient, clues of NM included fulfillment of criteria for systemic inflammatory response syndrome at admission and a presumed source of infection; taken together, these findings should lead to a diagnosis of sepsis until otherwise proven. The patient also reported pain that was not proportional to the skin findings, which suggested an NSTI. His lack of constitutional symptoms may have been due to the effects of prednisone, which was changed to dupilumab during hospitalization.
The clinical and histological findings of NM are nonspecific. Clinical findings include skin discoloration with bullae, blisters, vesicles, or petechiae.4 Our case adds to the descriptive morphology by including marked edema with ulceration, progressive purulence, and interconnected sinuses tracking to the fascial plane. Histologic findings can include confluent necrosis extending from the epidermis to the underlying muscle with dense neutrophilic inflammation. Notably, these findings can mirror necrotizing neutrophilic dermatoses in the absence of an infectious cause. Failure to recognize simple systemic inflammatory response syndrome criteria in NM patients due to slow treatment response or incorrect treatment can can lead to loss of a limb or death.
Workup reveals overlap with necrotizing neutrophilic dermatoses including PG, which is the prototypical neutrophilic dermatosis. Morphologically, PG presents as an ulcer with a purple and undermined border, often having developed from an initial papule, vesicle, or pustule. A neutrophilic infiltrate of the ulcer edge is the major criterion required to diagnose PG6; minor criteria include a positive pathergy test, history of inflammatory arthritis or inflammatory bowel disease, and exclusion of infection.6 When compared directly to an NSTI such as NM, the most important variable that sets PG apart is the absence of bacterial growth on blood and tissue cultures.7
Imaging studies can aid in the clinical diagnosis of NM and help distinguish the disease from PG. Computed tomography and MRI may demonstrate hallmarks of extensive necrotizing infection, such as gas formation and consequent fascial swelling, thickening and edema of involved muscle, and subfascial fluid collection.3,4 Distinct from NM, imaging findings in PG are more subtle, suggesting cellulitic inflammation with edema.8 A defining radiographic feature of NM can be foci of gas within muscle or fascia, though absence of this finding does not exclude NM.1,4
In conclusion, NM is a rare intramuscular infection that can be difficult to diagnose due to its nonspecific presentation and lack of constitutional symptoms. Dermatologists should maintain a high level of suspicion for NM in the setting of rapidly progressive clinical findings; accurate diagnosis requires a multimodal approach with complete correlation of clinical, histological, and imaging findings. Computed tomography and MRI can heighten the approach, even when necrotizing neutrophilic dermatoses and NM have similar clinical and histological appearances. Once a diagnosis of NM is established, prompt surgical and medical intervention improves the prognosis.
- Stevens DL, Baddour LM. Necrotizing soft tissue infections. UpToDate. Updated October 7, 2022. Accessed February 13, 2024. https://www.uptodate.com/contents/necrotizing-soft-tissue-infections?search=Necrotizing%20soft%20tissue%20infections&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
- Adams EM, Gudmundsson S, Yocum DE, et al. Streptococcal myositis. Arch Intern Med . 1985;145:1020-1023.
- Khanna A, Gurusinghe D, Taylor D. Necrotizing myositis: highlighting the hidden depths—case series and review of the literature. ANZ J Surg . 2020;90:130-134. doi:10.1111/ans.15429
- Boinpally H, Howell RS, Ram B, et al. Necrotizing myositis: a rare necrotizing soft tissue infection involving muscle. Wounds . 2018;30:E116-E120.
- Anaya DA, Dellinger EP. Necrotizing soft-tissue infection: diagnosis and management. Clin Infect Dis . 2007;44:705-710. doi:10.1086/511638
- Maverakis E, Ma C, Shinkai K, et al. Diagnostic criteria of ulcerative pyoderma gangrenosum: a Delphi consensus of international experts. JAMA Dermatol . 2018;154:461-466. doi:10.1001/jamadermatol.2017.5980
- Sanchez IM, Lowenstein S, Johnson KA, et al. Clinical features of neutrophilic dermatosis variants resembling necrotizing fasciitis. JAMA Dermatol . 2019;155:79-84. doi:10.1001/jamadermatol.2018.3890
- Demirdover C, Geyik A, Vayvada H. Necrotising fasciitis or pyoderma gangrenosum: a fatal dilemma. Int Wound J . 2019;16:1347-1353. doi:10.1111/iwj.13196
- Stevens DL, Baddour LM. Necrotizing soft tissue infections. UpToDate. Updated October 7, 2022. Accessed February 13, 2024. https://www.uptodate.com/contents/necrotizing-soft-tissue-infections?search=Necrotizing%20soft%20tissue%20infections&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
- Adams EM, Gudmundsson S, Yocum DE, et al. Streptococcal myositis. Arch Intern Med . 1985;145:1020-1023.
- Khanna A, Gurusinghe D, Taylor D. Necrotizing myositis: highlighting the hidden depths—case series and review of the literature. ANZ J Surg . 2020;90:130-134. doi:10.1111/ans.15429
- Boinpally H, Howell RS, Ram B, et al. Necrotizing myositis: a rare necrotizing soft tissue infection involving muscle. Wounds . 2018;30:E116-E120.
- Anaya DA, Dellinger EP. Necrotizing soft-tissue infection: diagnosis and management. Clin Infect Dis . 2007;44:705-710. doi:10.1086/511638
- Maverakis E, Ma C, Shinkai K, et al. Diagnostic criteria of ulcerative pyoderma gangrenosum: a Delphi consensus of international experts. JAMA Dermatol . 2018;154:461-466. doi:10.1001/jamadermatol.2017.5980
- Sanchez IM, Lowenstein S, Johnson KA, et al. Clinical features of neutrophilic dermatosis variants resembling necrotizing fasciitis. JAMA Dermatol . 2019;155:79-84. doi:10.1001/jamadermatol.2018.3890
- Demirdover C, Geyik A, Vayvada H. Necrotising fasciitis or pyoderma gangrenosum: a fatal dilemma. Int Wound J . 2019;16:1347-1353. doi:10.1111/iwj.13196
Practice Points
- The accurate diagnosis of necrotizing myositis (NM) requires a multimodal approach with complete clinical, histological, and radiographic correlation.
- Necrotizing myositis can manifest as violaceous erythematous plaques, bullae, blisters, or vesicles with petechiae, marked edema with ulceration, progressive purulence, and interconnected sinuses tracking to the fascial plane.
- The differential diagnosis of NM includes pyoderma gangrenosum.



