User login
Cardiology News is an independent news source that provides cardiologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on cardiology and the cardiologist's practice. Cardiology News Digital Network is the online destination and multimedia properties of Cardiology News, the independent news publication for cardiologists. Cardiology news is the leading source of news and commentary about clinical developments in cardiology as well as health care policy and regulations that affect the cardiologist's practice. Cardiology News Digital Network is owned by Frontline Medical Communications.
Remission or Not, Biologics May Mitigate Cardiovascular Risks of RA
TOPLINE:
, suggesting that biologics may reduce cardiovascular risk in RA even if remission is not achieved.
METHODOLOGY:
- Studies reported reduced cardiovascular risk in patients with RA who respond to tumor necrosis factor inhibitors but not in nonresponders, highlighting the importance of controlling inflammation for cardiovascular protection.
- Researchers assessed whether bDMARDs modify the impact of disease activity and systemic inflammation on cardiovascular risk in 4370 patients (mean age, 55 years) with RA without cardiovascular disease from a 10-country observational cohort.
- The severity of RA disease activity was assessed using C-reactive protein (CRP) levels and 28-joint Disease Activity Score based on CRP (DAS28-CRP).
- Endpoints were time to first MACE — a composite of cardiovascular death, myocardial infarction, and stroke — and time to first ischemic cardiovascular event (iCVE) — a composite of MACE plus revascularization, angina, transient ischemic attack, and peripheral arterial disease.
TAKEAWAY:
- The interaction between use of bDMARD and DAS28-CRP (P = .017) or CRP (P = .011) was significant for MACE.
- Each unit increase in DAS28-CRP increased the risk for MACE in bDMARD nonusers (hazard ratio [HR], 1.21; P = .002) but not in users.
- The per log unit increase in CRP was associated with a risk for MACE in bDMARD nonusers (HR, 1.16; P = .009) but not in users.
- No interaction was observed between bDMARD use and DAS28-CRP or CRP for the iCVE risk.
IN PRACTICE:
“This may indicate additional bDMARD-specific benefits directly on arterial wall inflammation and atherosclerotic plaque anatomy, stability, and biology, independently of systemic inflammation,” the authors wrote.
SOURCE:
The study, led by George Athanasios Karpouzas, MD, The Lundquist Institute, Torrance, California, was published online in RMD Open.
LIMITATIONS:
Patients with a particular interest in RA-associated cardiovascular disease were included, which may have introduced referral bias and affected the generalizability of the findings. Standard definitions were used for selected outcomes; however, differences in the reporting of outcomes may be plausible. Some patients were evaluated prospectively, while others were evaluated retrospectively, leading to differences in surveillance.
DISCLOSURES:
The study was supported by Pfizer. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
, suggesting that biologics may reduce cardiovascular risk in RA even if remission is not achieved.
METHODOLOGY:
- Studies reported reduced cardiovascular risk in patients with RA who respond to tumor necrosis factor inhibitors but not in nonresponders, highlighting the importance of controlling inflammation for cardiovascular protection.
- Researchers assessed whether bDMARDs modify the impact of disease activity and systemic inflammation on cardiovascular risk in 4370 patients (mean age, 55 years) with RA without cardiovascular disease from a 10-country observational cohort.
- The severity of RA disease activity was assessed using C-reactive protein (CRP) levels and 28-joint Disease Activity Score based on CRP (DAS28-CRP).
- Endpoints were time to first MACE — a composite of cardiovascular death, myocardial infarction, and stroke — and time to first ischemic cardiovascular event (iCVE) — a composite of MACE plus revascularization, angina, transient ischemic attack, and peripheral arterial disease.
TAKEAWAY:
- The interaction between use of bDMARD and DAS28-CRP (P = .017) or CRP (P = .011) was significant for MACE.
- Each unit increase in DAS28-CRP increased the risk for MACE in bDMARD nonusers (hazard ratio [HR], 1.21; P = .002) but not in users.
- The per log unit increase in CRP was associated with a risk for MACE in bDMARD nonusers (HR, 1.16; P = .009) but not in users.
- No interaction was observed between bDMARD use and DAS28-CRP or CRP for the iCVE risk.
IN PRACTICE:
“This may indicate additional bDMARD-specific benefits directly on arterial wall inflammation and atherosclerotic plaque anatomy, stability, and biology, independently of systemic inflammation,” the authors wrote.
SOURCE:
The study, led by George Athanasios Karpouzas, MD, The Lundquist Institute, Torrance, California, was published online in RMD Open.
LIMITATIONS:
Patients with a particular interest in RA-associated cardiovascular disease were included, which may have introduced referral bias and affected the generalizability of the findings. Standard definitions were used for selected outcomes; however, differences in the reporting of outcomes may be plausible. Some patients were evaluated prospectively, while others were evaluated retrospectively, leading to differences in surveillance.
DISCLOSURES:
The study was supported by Pfizer. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
, suggesting that biologics may reduce cardiovascular risk in RA even if remission is not achieved.
METHODOLOGY:
- Studies reported reduced cardiovascular risk in patients with RA who respond to tumor necrosis factor inhibitors but not in nonresponders, highlighting the importance of controlling inflammation for cardiovascular protection.
- Researchers assessed whether bDMARDs modify the impact of disease activity and systemic inflammation on cardiovascular risk in 4370 patients (mean age, 55 years) with RA without cardiovascular disease from a 10-country observational cohort.
- The severity of RA disease activity was assessed using C-reactive protein (CRP) levels and 28-joint Disease Activity Score based on CRP (DAS28-CRP).
- Endpoints were time to first MACE — a composite of cardiovascular death, myocardial infarction, and stroke — and time to first ischemic cardiovascular event (iCVE) — a composite of MACE plus revascularization, angina, transient ischemic attack, and peripheral arterial disease.
TAKEAWAY:
- The interaction between use of bDMARD and DAS28-CRP (P = .017) or CRP (P = .011) was significant for MACE.
- Each unit increase in DAS28-CRP increased the risk for MACE in bDMARD nonusers (hazard ratio [HR], 1.21; P = .002) but not in users.
- The per log unit increase in CRP was associated with a risk for MACE in bDMARD nonusers (HR, 1.16; P = .009) but not in users.
- No interaction was observed between bDMARD use and DAS28-CRP or CRP for the iCVE risk.
IN PRACTICE:
“This may indicate additional bDMARD-specific benefits directly on arterial wall inflammation and atherosclerotic plaque anatomy, stability, and biology, independently of systemic inflammation,” the authors wrote.
SOURCE:
The study, led by George Athanasios Karpouzas, MD, The Lundquist Institute, Torrance, California, was published online in RMD Open.
LIMITATIONS:
Patients with a particular interest in RA-associated cardiovascular disease were included, which may have introduced referral bias and affected the generalizability of the findings. Standard definitions were used for selected outcomes; however, differences in the reporting of outcomes may be plausible. Some patients were evaluated prospectively, while others were evaluated retrospectively, leading to differences in surveillance.
DISCLOSURES:
The study was supported by Pfizer. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
These Four Factors Account for 18 Years of Life Expectancy
This transcript has been edited for clarity.
Two individuals in the United States are celebrating their 30th birthdays. It’s a good day. They are entering the prime of their lives. One is a married White woman with a university degree. The other is a never-married White man with a high school diploma.
How many more years of life can these two individuals look forward to?
There’s a fairly dramatic difference. The man can expect 37.1 more years of life on average, living to be about 67. The woman can expect to live to age 85. That’s a life-expectancy discrepancy of 18 years based solely on gender, education, and marital status.
I’m using these cases to illustrate the extremes of life expectancy across four key social determinants of health: sex, race, marital status, and education. We all have some sense of how these factors play out in terms of health, but a new study suggests that it’s actually quite a bit more complicated than we thought.
Let me start by acknowledging my own bias here. As a clinical researcher, I sometimes find it hard to appreciate the value of actuarial-type studies that look at life expectancy (or any metric, really) between groups defined by marital status, for example. I’m never quite sure what to do with the conclusion. Married people live longer, the headline says. Okay, but as a doctor, what am I supposed to do about that? Encourage my patients to settle down and commit? Studies showing that women live longer than men or that White people live longer than Black people are also hard for me to incorporate into my practice. These are not easily changeable states.
But studies examining these groups are a reasonable starting point to ask more relevant questions. Why do women live longer than men? Is it behavioral (men take more risks and are less likely to see doctors)? Or is it hormonal (estrogen has a lot of protective effects that testosterone does not)? Or is it something else?
Integrating these social determinants of health into a cohesive story is a bit harder than it might seem, as this study, appearing in BMJ Open, illustrates.
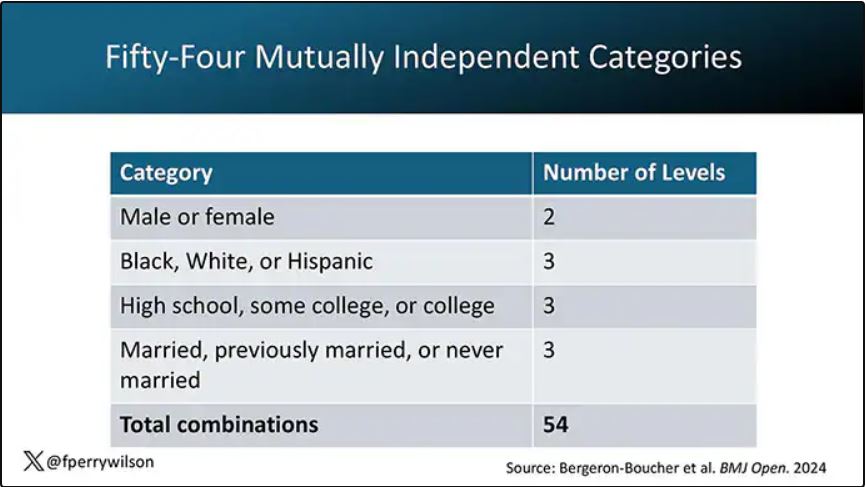
In the context of this study, every person in America can be placed into one of 54 mutually exclusive groups. You can be male or female. You can be Black, White, or Hispanic. You can have a high school diploma or less, an associate degree, or a college degree; and you can be married, previously married, or never married.
Of course, this does not capture the beautiful tapestry that is American life, but let’s give them a pass. They are working with data from the American Community Survey, which contains 8634 people — the statistics would run into trouble with more granular divisions. This survey can be population weighted, so you can scale up the results to reasonably represent the population of the United States.
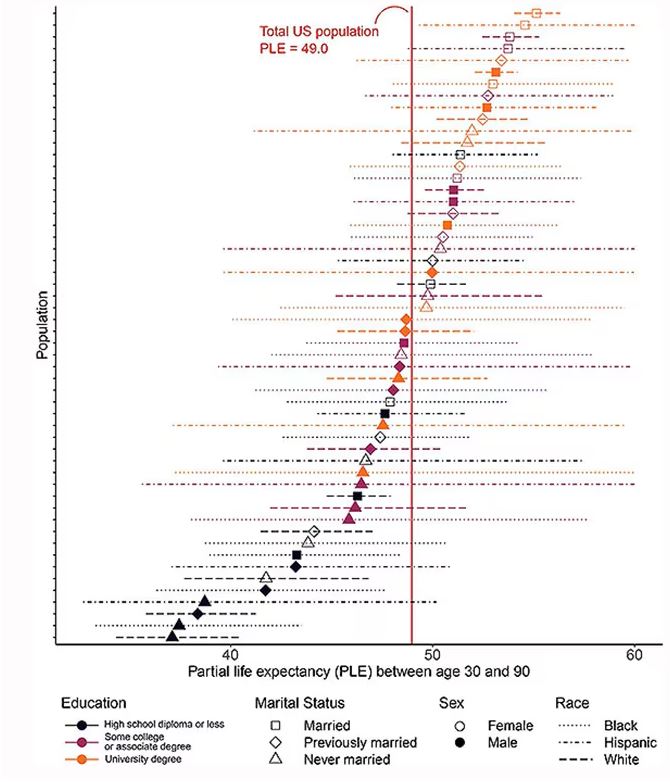
The survey collected data on the four broad categories of sex, race, education, and marital status and linked those survey results to the Multiple Cause of Death dataset from the CDC. From there, it’s a pretty simple task to rank the 54 categories in order from longest to shortest life expectancy, as you can see here.
But that’s not really the interesting part of this study. Sure, there is a lot of variation; it’s interesting that these four factors explain about 18 years’ difference in life expectancy in this country. What strikes me here, actually, is the lack of an entirely consistent message across this spectrum.
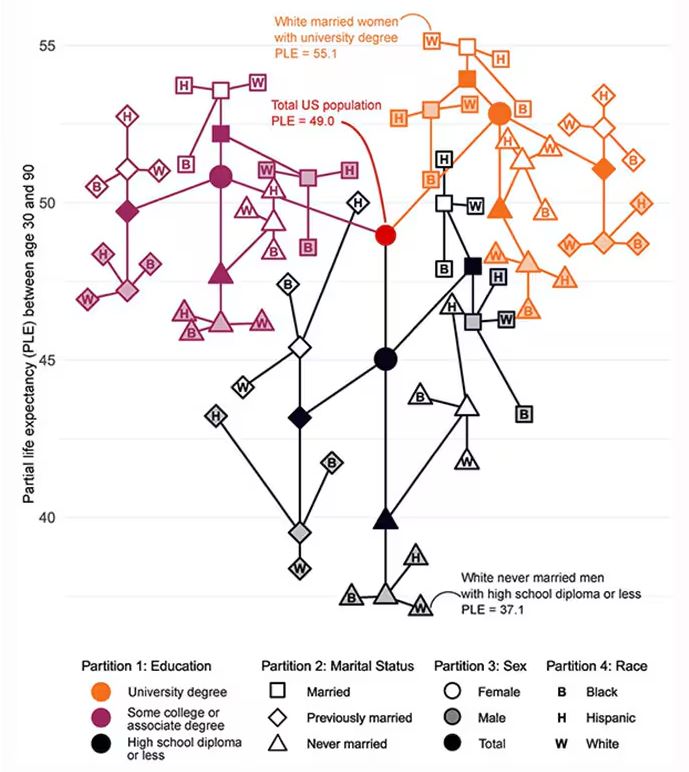
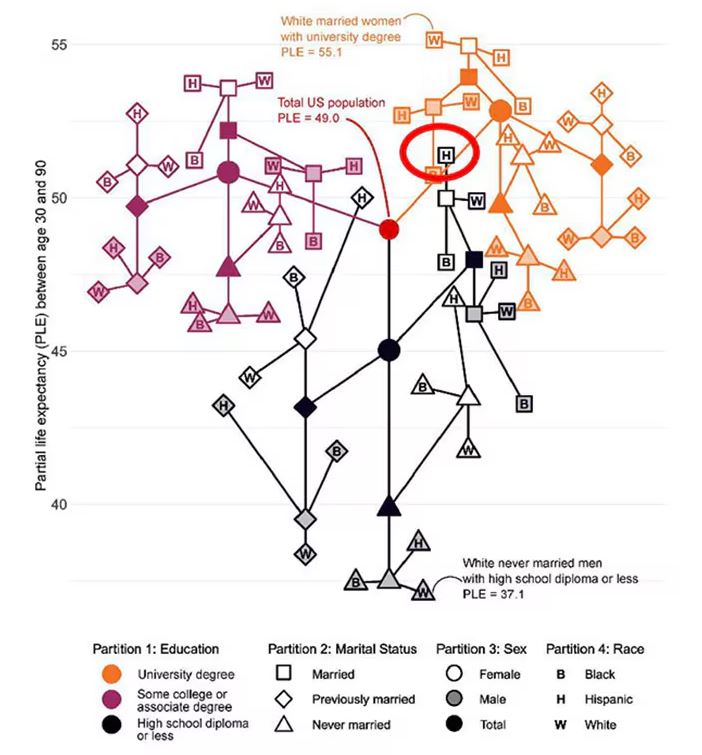
Let me walk you through the second figure in this paper, because this nicely illustrates the surprising heterogeneity that exists here.
This may seem overwhelming, but basically, shapes that are higher up on the Y-axis represent the groups with longer life expectancy.
You can tell, for example, that shapes that are black in color (groups with high school educations or less) are generally lower. But not universally so. This box represents married, Hispanic females who do quite well in terms of life expectancy, even at that lower educational level.
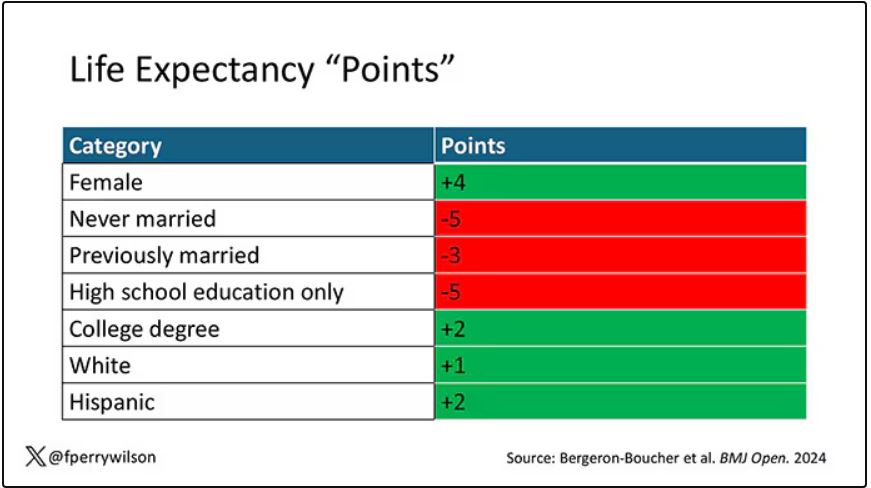
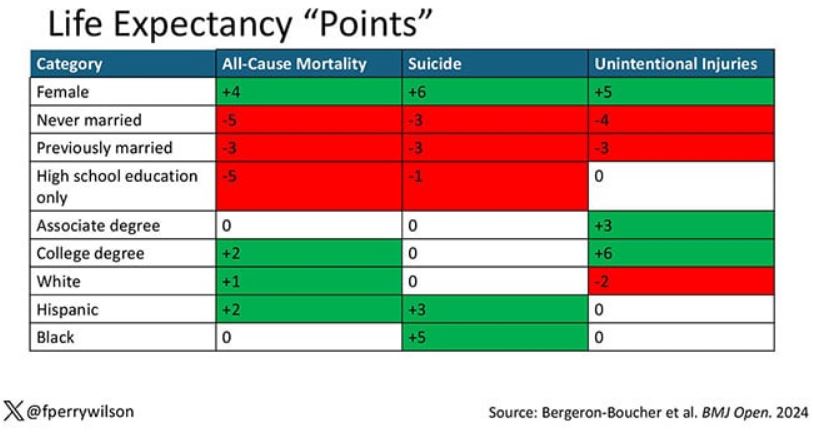
The authors quantify this phenomenon by creating a mortality risk score that integrates these findings. It looks something like this, with 0 being average morality for the United States.
As you can see, you get a bunch of points for being female, but you lose a bunch for not being married. Education plays a large role, with a big hit for those who have a high school diploma or less, and a bonus for those with a college degree. Race plays a relatively more minor role.
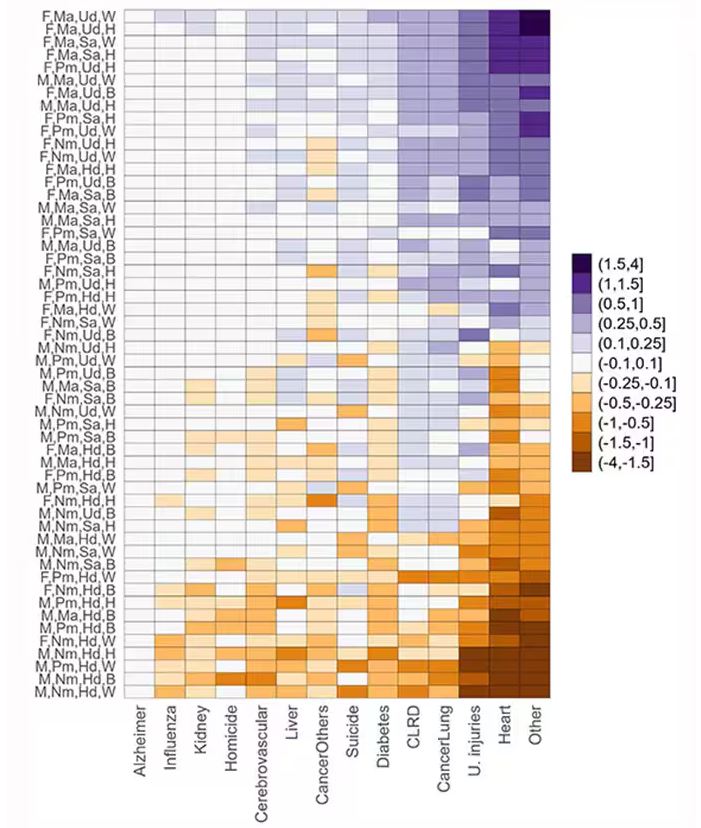
This is all very interesting, but as I said at the beginning, this isn’t terribly useful to me as a physician. More important is figuring out why these differences exist. And there are some clues in the study data, particularly when we examine causes of death. This figure ranks those 54 groups again, from the married, White, college-educated females down to the never-married, White, high school–educated males. The boxes show how much more or less likely this group is to die of a given condition than the general population.
Looking at the bottom groups, you can see a dramatically increased risk for death from unintentional injuries, heart disease, and lung cancer. You see an increased risk for suicide as well. In the upper tiers, the only place where risk seems higher than expected is for the category of “other cancers,” reminding us that many types of cancer do not respect definitions of socioeconomic status.
You can even update the risk-scoring system to reflect the risk for different causes of death. You can see here how White people, for example, are at higher risk for death from unintentional injuries relative to other populations, despite having a lower mortality overall.
So maybe, through cause of death, we get a little closer to the answer of why. But this paper is really just a start. Its primary effect should be to surprise us — that in a country as wealthy as the United States, such dramatic variation exists based on factors that, with the exception of sex, I suppose, are not really biological. Which means that to find the why, we may need to turn from physiology to sociology.
Dr. Wilson is associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Two individuals in the United States are celebrating their 30th birthdays. It’s a good day. They are entering the prime of their lives. One is a married White woman with a university degree. The other is a never-married White man with a high school diploma.
How many more years of life can these two individuals look forward to?
There’s a fairly dramatic difference. The man can expect 37.1 more years of life on average, living to be about 67. The woman can expect to live to age 85. That’s a life-expectancy discrepancy of 18 years based solely on gender, education, and marital status.
I’m using these cases to illustrate the extremes of life expectancy across four key social determinants of health: sex, race, marital status, and education. We all have some sense of how these factors play out in terms of health, but a new study suggests that it’s actually quite a bit more complicated than we thought.
Let me start by acknowledging my own bias here. As a clinical researcher, I sometimes find it hard to appreciate the value of actuarial-type studies that look at life expectancy (or any metric, really) between groups defined by marital status, for example. I’m never quite sure what to do with the conclusion. Married people live longer, the headline says. Okay, but as a doctor, what am I supposed to do about that? Encourage my patients to settle down and commit? Studies showing that women live longer than men or that White people live longer than Black people are also hard for me to incorporate into my practice. These are not easily changeable states.
But studies examining these groups are a reasonable starting point to ask more relevant questions. Why do women live longer than men? Is it behavioral (men take more risks and are less likely to see doctors)? Or is it hormonal (estrogen has a lot of protective effects that testosterone does not)? Or is it something else?
Integrating these social determinants of health into a cohesive story is a bit harder than it might seem, as this study, appearing in BMJ Open, illustrates.
In the context of this study, every person in America can be placed into one of 54 mutually exclusive groups. You can be male or female. You can be Black, White, or Hispanic. You can have a high school diploma or less, an associate degree, or a college degree; and you can be married, previously married, or never married.
Of course, this does not capture the beautiful tapestry that is American life, but let’s give them a pass. They are working with data from the American Community Survey, which contains 8634 people — the statistics would run into trouble with more granular divisions. This survey can be population weighted, so you can scale up the results to reasonably represent the population of the United States.
The survey collected data on the four broad categories of sex, race, education, and marital status and linked those survey results to the Multiple Cause of Death dataset from the CDC. From there, it’s a pretty simple task to rank the 54 categories in order from longest to shortest life expectancy, as you can see here.
But that’s not really the interesting part of this study. Sure, there is a lot of variation; it’s interesting that these four factors explain about 18 years’ difference in life expectancy in this country. What strikes me here, actually, is the lack of an entirely consistent message across this spectrum.
Let me walk you through the second figure in this paper, because this nicely illustrates the surprising heterogeneity that exists here.
This may seem overwhelming, but basically, shapes that are higher up on the Y-axis represent the groups with longer life expectancy.
You can tell, for example, that shapes that are black in color (groups with high school educations or less) are generally lower. But not universally so. This box represents married, Hispanic females who do quite well in terms of life expectancy, even at that lower educational level.
The authors quantify this phenomenon by creating a mortality risk score that integrates these findings. It looks something like this, with 0 being average morality for the United States.
As you can see, you get a bunch of points for being female, but you lose a bunch for not being married. Education plays a large role, with a big hit for those who have a high school diploma or less, and a bonus for those with a college degree. Race plays a relatively more minor role.
This is all very interesting, but as I said at the beginning, this isn’t terribly useful to me as a physician. More important is figuring out why these differences exist. And there are some clues in the study data, particularly when we examine causes of death. This figure ranks those 54 groups again, from the married, White, college-educated females down to the never-married, White, high school–educated males. The boxes show how much more or less likely this group is to die of a given condition than the general population.
Looking at the bottom groups, you can see a dramatically increased risk for death from unintentional injuries, heart disease, and lung cancer. You see an increased risk for suicide as well. In the upper tiers, the only place where risk seems higher than expected is for the category of “other cancers,” reminding us that many types of cancer do not respect definitions of socioeconomic status.
You can even update the risk-scoring system to reflect the risk for different causes of death. You can see here how White people, for example, are at higher risk for death from unintentional injuries relative to other populations, despite having a lower mortality overall.
So maybe, through cause of death, we get a little closer to the answer of why. But this paper is really just a start. Its primary effect should be to surprise us — that in a country as wealthy as the United States, such dramatic variation exists based on factors that, with the exception of sex, I suppose, are not really biological. Which means that to find the why, we may need to turn from physiology to sociology.
Dr. Wilson is associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Two individuals in the United States are celebrating their 30th birthdays. It’s a good day. They are entering the prime of their lives. One is a married White woman with a university degree. The other is a never-married White man with a high school diploma.
How many more years of life can these two individuals look forward to?
There’s a fairly dramatic difference. The man can expect 37.1 more years of life on average, living to be about 67. The woman can expect to live to age 85. That’s a life-expectancy discrepancy of 18 years based solely on gender, education, and marital status.
I’m using these cases to illustrate the extremes of life expectancy across four key social determinants of health: sex, race, marital status, and education. We all have some sense of how these factors play out in terms of health, but a new study suggests that it’s actually quite a bit more complicated than we thought.
Let me start by acknowledging my own bias here. As a clinical researcher, I sometimes find it hard to appreciate the value of actuarial-type studies that look at life expectancy (or any metric, really) between groups defined by marital status, for example. I’m never quite sure what to do with the conclusion. Married people live longer, the headline says. Okay, but as a doctor, what am I supposed to do about that? Encourage my patients to settle down and commit? Studies showing that women live longer than men or that White people live longer than Black people are also hard for me to incorporate into my practice. These are not easily changeable states.
But studies examining these groups are a reasonable starting point to ask more relevant questions. Why do women live longer than men? Is it behavioral (men take more risks and are less likely to see doctors)? Or is it hormonal (estrogen has a lot of protective effects that testosterone does not)? Or is it something else?
Integrating these social determinants of health into a cohesive story is a bit harder than it might seem, as this study, appearing in BMJ Open, illustrates.
In the context of this study, every person in America can be placed into one of 54 mutually exclusive groups. You can be male or female. You can be Black, White, or Hispanic. You can have a high school diploma or less, an associate degree, or a college degree; and you can be married, previously married, or never married.
Of course, this does not capture the beautiful tapestry that is American life, but let’s give them a pass. They are working with data from the American Community Survey, which contains 8634 people — the statistics would run into trouble with more granular divisions. This survey can be population weighted, so you can scale up the results to reasonably represent the population of the United States.
The survey collected data on the four broad categories of sex, race, education, and marital status and linked those survey results to the Multiple Cause of Death dataset from the CDC. From there, it’s a pretty simple task to rank the 54 categories in order from longest to shortest life expectancy, as you can see here.
But that’s not really the interesting part of this study. Sure, there is a lot of variation; it’s interesting that these four factors explain about 18 years’ difference in life expectancy in this country. What strikes me here, actually, is the lack of an entirely consistent message across this spectrum.
Let me walk you through the second figure in this paper, because this nicely illustrates the surprising heterogeneity that exists here.
This may seem overwhelming, but basically, shapes that are higher up on the Y-axis represent the groups with longer life expectancy.
You can tell, for example, that shapes that are black in color (groups with high school educations or less) are generally lower. But not universally so. This box represents married, Hispanic females who do quite well in terms of life expectancy, even at that lower educational level.
The authors quantify this phenomenon by creating a mortality risk score that integrates these findings. It looks something like this, with 0 being average morality for the United States.
As you can see, you get a bunch of points for being female, but you lose a bunch for not being married. Education plays a large role, with a big hit for those who have a high school diploma or less, and a bonus for those with a college degree. Race plays a relatively more minor role.
This is all very interesting, but as I said at the beginning, this isn’t terribly useful to me as a physician. More important is figuring out why these differences exist. And there are some clues in the study data, particularly when we examine causes of death. This figure ranks those 54 groups again, from the married, White, college-educated females down to the never-married, White, high school–educated males. The boxes show how much more or less likely this group is to die of a given condition than the general population.
Looking at the bottom groups, you can see a dramatically increased risk for death from unintentional injuries, heart disease, and lung cancer. You see an increased risk for suicide as well. In the upper tiers, the only place where risk seems higher than expected is for the category of “other cancers,” reminding us that many types of cancer do not respect definitions of socioeconomic status.
You can even update the risk-scoring system to reflect the risk for different causes of death. You can see here how White people, for example, are at higher risk for death from unintentional injuries relative to other populations, despite having a lower mortality overall.
So maybe, through cause of death, we get a little closer to the answer of why. But this paper is really just a start. Its primary effect should be to surprise us — that in a country as wealthy as the United States, such dramatic variation exists based on factors that, with the exception of sex, I suppose, are not really biological. Which means that to find the why, we may need to turn from physiology to sociology.
Dr. Wilson is associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Xanthelasma Not Linked to Heart Diseases, Study Finds
TOPLINE:
Xanthelasma palpebrarum, characterized by yellowish plaques on the eyelids, is not associated with increased rates of dyslipidemia or cardiovascular disease.
METHODOLOGY:
- Researchers conducted a case-control study at a single tertiary care center in Israel and analyzed data from 35,452 individuals (mean age, 52.2 years; 69% men) who underwent medical screening from 2001 to 2020.
- They compared 203 patients with xanthelasma palpebrarum with 2030 individuals without the disease (control).
- Primary outcomes were prevalence of dyslipidemia and cardiovascular disease between the two groups.
TAKEAWAY:
- Lipid profiles were similar between the two groups, with no difference in total cholesterol, high- and low-density lipoprotein, and triglyceride levels (all P > .05).
- The prevalence of dyslipidemia was similar for patients with xanthelasma palpebrarum and controls (46% vs 42%, respectively; P = .29), as was the incidence of cardiovascular disease (8.9% vs 10%, respectively; P = .56).
- The incidence of diabetes (P = .13), cerebrovascular accidents (P > .99), ischemic heart disease (P = .73), and hypertension (P = .56) were not significantly different between the two groups.
IN PRACTICE:
“Our study conducted on a large population of individuals undergoing comprehensive ophthalmic and systemic screening tests did not find a significant association between xanthelasma palpebrarum and an increased prevalence of lipid abnormalities or cardiovascular disease,” the authors wrote.
SOURCE:
The study was led by Yael Lustig, MD, of the Goldschleger Eye Institute at Sheba Medical Center, in Ramat Gan, Israel. It was published online on August 5, 2024, in Ophthalmology.
LIMITATIONS:
The retrospective nature of the study and the single-center design may have limited the generalizability of the findings. The study population was self-selected, potentially introducing selection bias. Lack of histopathologic examination could have affected the accuracy of the diagnosis.
DISCLOSURES:
No funding sources were disclosed for this study. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Xanthelasma palpebrarum, characterized by yellowish plaques on the eyelids, is not associated with increased rates of dyslipidemia or cardiovascular disease.
METHODOLOGY:
- Researchers conducted a case-control study at a single tertiary care center in Israel and analyzed data from 35,452 individuals (mean age, 52.2 years; 69% men) who underwent medical screening from 2001 to 2020.
- They compared 203 patients with xanthelasma palpebrarum with 2030 individuals without the disease (control).
- Primary outcomes were prevalence of dyslipidemia and cardiovascular disease between the two groups.
TAKEAWAY:
- Lipid profiles were similar between the two groups, with no difference in total cholesterol, high- and low-density lipoprotein, and triglyceride levels (all P > .05).
- The prevalence of dyslipidemia was similar for patients with xanthelasma palpebrarum and controls (46% vs 42%, respectively; P = .29), as was the incidence of cardiovascular disease (8.9% vs 10%, respectively; P = .56).
- The incidence of diabetes (P = .13), cerebrovascular accidents (P > .99), ischemic heart disease (P = .73), and hypertension (P = .56) were not significantly different between the two groups.
IN PRACTICE:
“Our study conducted on a large population of individuals undergoing comprehensive ophthalmic and systemic screening tests did not find a significant association between xanthelasma palpebrarum and an increased prevalence of lipid abnormalities or cardiovascular disease,” the authors wrote.
SOURCE:
The study was led by Yael Lustig, MD, of the Goldschleger Eye Institute at Sheba Medical Center, in Ramat Gan, Israel. It was published online on August 5, 2024, in Ophthalmology.
LIMITATIONS:
The retrospective nature of the study and the single-center design may have limited the generalizability of the findings. The study population was self-selected, potentially introducing selection bias. Lack of histopathologic examination could have affected the accuracy of the diagnosis.
DISCLOSURES:
No funding sources were disclosed for this study. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Xanthelasma palpebrarum, characterized by yellowish plaques on the eyelids, is not associated with increased rates of dyslipidemia or cardiovascular disease.
METHODOLOGY:
- Researchers conducted a case-control study at a single tertiary care center in Israel and analyzed data from 35,452 individuals (mean age, 52.2 years; 69% men) who underwent medical screening from 2001 to 2020.
- They compared 203 patients with xanthelasma palpebrarum with 2030 individuals without the disease (control).
- Primary outcomes were prevalence of dyslipidemia and cardiovascular disease between the two groups.
TAKEAWAY:
- Lipid profiles were similar between the two groups, with no difference in total cholesterol, high- and low-density lipoprotein, and triglyceride levels (all P > .05).
- The prevalence of dyslipidemia was similar for patients with xanthelasma palpebrarum and controls (46% vs 42%, respectively; P = .29), as was the incidence of cardiovascular disease (8.9% vs 10%, respectively; P = .56).
- The incidence of diabetes (P = .13), cerebrovascular accidents (P > .99), ischemic heart disease (P = .73), and hypertension (P = .56) were not significantly different between the two groups.
IN PRACTICE:
“Our study conducted on a large population of individuals undergoing comprehensive ophthalmic and systemic screening tests did not find a significant association between xanthelasma palpebrarum and an increased prevalence of lipid abnormalities or cardiovascular disease,” the authors wrote.
SOURCE:
The study was led by Yael Lustig, MD, of the Goldschleger Eye Institute at Sheba Medical Center, in Ramat Gan, Israel. It was published online on August 5, 2024, in Ophthalmology.
LIMITATIONS:
The retrospective nature of the study and the single-center design may have limited the generalizability of the findings. The study population was self-selected, potentially introducing selection bias. Lack of histopathologic examination could have affected the accuracy of the diagnosis.
DISCLOSURES:
No funding sources were disclosed for this study. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
New Study Links Sweetener to Heart Risk: What to Know
Is going sugar free really good advice for patients with cardiometabolic risk factors?
That’s the question raised by new Cleveland Clinic research, which suggests that consuming erythritol, a sweetener widely found in sugar-free and keto food products, could spur a prothrombotic response.
In the study, published in Arteriosclerosis, Thrombosis, and Vascular Biology, 10 healthy participants ate 30 grams of erythritol. Thirty minutes later, their blood showed enhanced platelet aggregation and increased markers of platelet responsiveness and activation.
Specifically, the researchers saw enhanced stimulus-dependent release of serotonin (a marker of platelet dense granules) and CXCL4 (a platelet alpha-granule marker).
“ With every single person, you see a prothrombotic effect with every single test that we did,” said study author Stanley Hazen, MD, PhD, chair of the Department of Cardiovascular & Metabolic Sciences at Cleveland Clinic in Ohio. By contrast, participants who ate 30 grams of glucose saw no such effect.
The erythritol itself does not activate the platelets, Dr. Hazen said, rather it lowers the threshold for triggering a response. This could make someone more prone to clotting, raising heart attack and stroke risk over time.
Though the mechanism is unknown, Dr. Hazen has an idea.
“There appears to be a receptor on platelets that is recognizing and sensing these sugar alcohols,” Dr. Hazen said, “much in the same way your taste bud for sweet is a receptor for recognizing a glucose or sugar molecule.”
“We’re very interested in trying to figure out what the receptor is,” Dr. Hazen said, “because I think that then becomes a very interesting potential target for further investigation and study into how this is linked to causing heart disease.”
The Past and Future of Erythritol Research
In 2001, the Food and Drug Administration classified erythritol as a “generally recognized as safe” food additive. A sugar alcohol that occurs naturally in foods like melon and grapes, erythritol is also manufactured by fermenting sugars. It’s about 70% as sweet as table sugar. Humans also produce small amounts of erythritol naturally: Our blood cells make it from glucose via the pentose phosphate pathway.
Previous research from Dr. Hazen’s group linked erythritol to a risk for major adverse cardiovascular events and clotting.
“Based on their previous study, I think this was a really important study to do in healthy individuals,” said Martha Field, PhD, assistant professor in the Division of Nutritional Sciences at Cornell University, Ithaca, New York, who was not involved in the study.
The earlier paper analyzed blood samples from participants with unknown erythritol intake, including some taken before the sweetener, and it was as widespread as it is today. That made disentangling the effects of eating erythritol vs naturally producing it more difficult.
By showing that eating erythritol raises markers associated with thrombosis, the new paper reinforces the importance of thinking about and developing a deeper understanding of what we put into our bodies.
“This paper was conducted in healthy individuals — might this be particularly dangerous for individuals who are at increased risk of clotting?” asked Dr. Field. “There are lots of genetic polymorphisms that increase your risk for clotting disorders or your propensity to form thrombosis.”
Field would like to see similar analyses of xylitol and sorbitol, other sugar alcohols found in sugar-free foods. And she called for more studies on erythritol that look at lower erythritol consumption over longer time periods.
Registered dietitian nutritionist Valisa E. Hedrick, PhD, agreed: Much more work is needed in this area, particularly in higher-risk groups, such as those with prediabetes and diabetes, said Dr. Hedrick, an associate professor in the Department of Human Nutrition, Foods, and Exercise at Virginia Tech, Blacksburg, who was not involved in the study.
“Because this study was conducted in healthy individuals, the impact of a small dose of glucose was negligible, as their body can effectively regulate blood glucose levels,” she said. “Because high blood glucose concentrations have also been shown to increase platelet reactivity, and consequently increase thrombosis potential, individuals who are not able to regulate their blood glucose levels, such as those with prediabetes and diabetes, could potentially see a similar effect on the body as erythritol when consuming large amounts of sugar.”
At the same time, “individuals with diabetes or prediabetes may be more inclined to consume erythritol as an alternative to sugar,” Dr. Hedrick added. “It will be important to design studies that include these individuals to determine if erythritol has an additive adverse effect on cardiac event risk.”
Criticism and Impact
Critics have suggested the 30-gram dose of erythritol ingested by study participants is unrealistic. Dr. Hazen said that it’s not.
Erythritol is often recommended as a one-to-one sugar replacement. And you could top 30 grams with a few servings of erythritol-sweetened ice cream or soda, Dr. Hazen said.
“The dose that we used, it’s on the high end, but it’s well within a physiologically relevant level,” he said.
Still others say the results are only relevant for people with preexisting heart trouble. But Dr. Hazen said they matter for the masses.
“I think there’s a significant health concern at a population level that this work is underscoring,” he said.
After all, heart disease risk factors like obesity, hypertension, diabetes, and smoking are common and quickly add up.
“If you look at middle-aged America, most people who experience a heart attack or stroke do not know that they have coronary artery disease, and the first recognition of it is that event,” Dr. Hazen said.
For now, Dr. Hazen recommends eating real sugar in moderation. He hopes future research will reveal a nonnutritive sweetener that doesn’t activate platelets.
The Bigger Picture
The new research adds yet another piece to the puzzle of whether nonnutritive sweeteners are better than sugar.
“I think these results are concerning,” said JoAnn E. Manson, MD, chief of the Division of Preventive Medicine at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School, both in Boston, Massachusetts. They “ may help explain the surprising results in some observational studies that artificial sweeteners are linked to an increased risk of cardiovascular disease.”
Dr. Manson, who was not involved in the new study, has conducted other research linking artificial sweetener use with stroke risk.
In an upcoming randomized clinical study, her team is comparing head-to-head sugar-sweetened beverages, drinks sweetened with calorie-free substitutes, and water to determine which is best for a range of cardiometabolic outcomes.
“We need more research on this question,” she said, “because these artificial sweeteners are commonly used, and many people are assuming that their health outcomes will be better with the artificial sweeteners than with sugar-sweetened products.”
A version of this article first appeared on Medscape.com.
Is going sugar free really good advice for patients with cardiometabolic risk factors?
That’s the question raised by new Cleveland Clinic research, which suggests that consuming erythritol, a sweetener widely found in sugar-free and keto food products, could spur a prothrombotic response.
In the study, published in Arteriosclerosis, Thrombosis, and Vascular Biology, 10 healthy participants ate 30 grams of erythritol. Thirty minutes later, their blood showed enhanced platelet aggregation and increased markers of platelet responsiveness and activation.
Specifically, the researchers saw enhanced stimulus-dependent release of serotonin (a marker of platelet dense granules) and CXCL4 (a platelet alpha-granule marker).
“ With every single person, you see a prothrombotic effect with every single test that we did,” said study author Stanley Hazen, MD, PhD, chair of the Department of Cardiovascular & Metabolic Sciences at Cleveland Clinic in Ohio. By contrast, participants who ate 30 grams of glucose saw no such effect.
The erythritol itself does not activate the platelets, Dr. Hazen said, rather it lowers the threshold for triggering a response. This could make someone more prone to clotting, raising heart attack and stroke risk over time.
Though the mechanism is unknown, Dr. Hazen has an idea.
“There appears to be a receptor on platelets that is recognizing and sensing these sugar alcohols,” Dr. Hazen said, “much in the same way your taste bud for sweet is a receptor for recognizing a glucose or sugar molecule.”
“We’re very interested in trying to figure out what the receptor is,” Dr. Hazen said, “because I think that then becomes a very interesting potential target for further investigation and study into how this is linked to causing heart disease.”
The Past and Future of Erythritol Research
In 2001, the Food and Drug Administration classified erythritol as a “generally recognized as safe” food additive. A sugar alcohol that occurs naturally in foods like melon and grapes, erythritol is also manufactured by fermenting sugars. It’s about 70% as sweet as table sugar. Humans also produce small amounts of erythritol naturally: Our blood cells make it from glucose via the pentose phosphate pathway.
Previous research from Dr. Hazen’s group linked erythritol to a risk for major adverse cardiovascular events and clotting.
“Based on their previous study, I think this was a really important study to do in healthy individuals,” said Martha Field, PhD, assistant professor in the Division of Nutritional Sciences at Cornell University, Ithaca, New York, who was not involved in the study.
The earlier paper analyzed blood samples from participants with unknown erythritol intake, including some taken before the sweetener, and it was as widespread as it is today. That made disentangling the effects of eating erythritol vs naturally producing it more difficult.
By showing that eating erythritol raises markers associated with thrombosis, the new paper reinforces the importance of thinking about and developing a deeper understanding of what we put into our bodies.
“This paper was conducted in healthy individuals — might this be particularly dangerous for individuals who are at increased risk of clotting?” asked Dr. Field. “There are lots of genetic polymorphisms that increase your risk for clotting disorders or your propensity to form thrombosis.”
Field would like to see similar analyses of xylitol and sorbitol, other sugar alcohols found in sugar-free foods. And she called for more studies on erythritol that look at lower erythritol consumption over longer time periods.
Registered dietitian nutritionist Valisa E. Hedrick, PhD, agreed: Much more work is needed in this area, particularly in higher-risk groups, such as those with prediabetes and diabetes, said Dr. Hedrick, an associate professor in the Department of Human Nutrition, Foods, and Exercise at Virginia Tech, Blacksburg, who was not involved in the study.
“Because this study was conducted in healthy individuals, the impact of a small dose of glucose was negligible, as their body can effectively regulate blood glucose levels,” she said. “Because high blood glucose concentrations have also been shown to increase platelet reactivity, and consequently increase thrombosis potential, individuals who are not able to regulate their blood glucose levels, such as those with prediabetes and diabetes, could potentially see a similar effect on the body as erythritol when consuming large amounts of sugar.”
At the same time, “individuals with diabetes or prediabetes may be more inclined to consume erythritol as an alternative to sugar,” Dr. Hedrick added. “It will be important to design studies that include these individuals to determine if erythritol has an additive adverse effect on cardiac event risk.”
Criticism and Impact
Critics have suggested the 30-gram dose of erythritol ingested by study participants is unrealistic. Dr. Hazen said that it’s not.
Erythritol is often recommended as a one-to-one sugar replacement. And you could top 30 grams with a few servings of erythritol-sweetened ice cream or soda, Dr. Hazen said.
“The dose that we used, it’s on the high end, but it’s well within a physiologically relevant level,” he said.
Still others say the results are only relevant for people with preexisting heart trouble. But Dr. Hazen said they matter for the masses.
“I think there’s a significant health concern at a population level that this work is underscoring,” he said.
After all, heart disease risk factors like obesity, hypertension, diabetes, and smoking are common and quickly add up.
“If you look at middle-aged America, most people who experience a heart attack or stroke do not know that they have coronary artery disease, and the first recognition of it is that event,” Dr. Hazen said.
For now, Dr. Hazen recommends eating real sugar in moderation. He hopes future research will reveal a nonnutritive sweetener that doesn’t activate platelets.
The Bigger Picture
The new research adds yet another piece to the puzzle of whether nonnutritive sweeteners are better than sugar.
“I think these results are concerning,” said JoAnn E. Manson, MD, chief of the Division of Preventive Medicine at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School, both in Boston, Massachusetts. They “ may help explain the surprising results in some observational studies that artificial sweeteners are linked to an increased risk of cardiovascular disease.”
Dr. Manson, who was not involved in the new study, has conducted other research linking artificial sweetener use with stroke risk.
In an upcoming randomized clinical study, her team is comparing head-to-head sugar-sweetened beverages, drinks sweetened with calorie-free substitutes, and water to determine which is best for a range of cardiometabolic outcomes.
“We need more research on this question,” she said, “because these artificial sweeteners are commonly used, and many people are assuming that their health outcomes will be better with the artificial sweeteners than with sugar-sweetened products.”
A version of this article first appeared on Medscape.com.
Is going sugar free really good advice for patients with cardiometabolic risk factors?
That’s the question raised by new Cleveland Clinic research, which suggests that consuming erythritol, a sweetener widely found in sugar-free and keto food products, could spur a prothrombotic response.
In the study, published in Arteriosclerosis, Thrombosis, and Vascular Biology, 10 healthy participants ate 30 grams of erythritol. Thirty minutes later, their blood showed enhanced platelet aggregation and increased markers of platelet responsiveness and activation.
Specifically, the researchers saw enhanced stimulus-dependent release of serotonin (a marker of platelet dense granules) and CXCL4 (a platelet alpha-granule marker).
“ With every single person, you see a prothrombotic effect with every single test that we did,” said study author Stanley Hazen, MD, PhD, chair of the Department of Cardiovascular & Metabolic Sciences at Cleveland Clinic in Ohio. By contrast, participants who ate 30 grams of glucose saw no such effect.
The erythritol itself does not activate the platelets, Dr. Hazen said, rather it lowers the threshold for triggering a response. This could make someone more prone to clotting, raising heart attack and stroke risk over time.
Though the mechanism is unknown, Dr. Hazen has an idea.
“There appears to be a receptor on platelets that is recognizing and sensing these sugar alcohols,” Dr. Hazen said, “much in the same way your taste bud for sweet is a receptor for recognizing a glucose or sugar molecule.”
“We’re very interested in trying to figure out what the receptor is,” Dr. Hazen said, “because I think that then becomes a very interesting potential target for further investigation and study into how this is linked to causing heart disease.”
The Past and Future of Erythritol Research
In 2001, the Food and Drug Administration classified erythritol as a “generally recognized as safe” food additive. A sugar alcohol that occurs naturally in foods like melon and grapes, erythritol is also manufactured by fermenting sugars. It’s about 70% as sweet as table sugar. Humans also produce small amounts of erythritol naturally: Our blood cells make it from glucose via the pentose phosphate pathway.
Previous research from Dr. Hazen’s group linked erythritol to a risk for major adverse cardiovascular events and clotting.
“Based on their previous study, I think this was a really important study to do in healthy individuals,” said Martha Field, PhD, assistant professor in the Division of Nutritional Sciences at Cornell University, Ithaca, New York, who was not involved in the study.
The earlier paper analyzed blood samples from participants with unknown erythritol intake, including some taken before the sweetener, and it was as widespread as it is today. That made disentangling the effects of eating erythritol vs naturally producing it more difficult.
By showing that eating erythritol raises markers associated with thrombosis, the new paper reinforces the importance of thinking about and developing a deeper understanding of what we put into our bodies.
“This paper was conducted in healthy individuals — might this be particularly dangerous for individuals who are at increased risk of clotting?” asked Dr. Field. “There are lots of genetic polymorphisms that increase your risk for clotting disorders or your propensity to form thrombosis.”
Field would like to see similar analyses of xylitol and sorbitol, other sugar alcohols found in sugar-free foods. And she called for more studies on erythritol that look at lower erythritol consumption over longer time periods.
Registered dietitian nutritionist Valisa E. Hedrick, PhD, agreed: Much more work is needed in this area, particularly in higher-risk groups, such as those with prediabetes and diabetes, said Dr. Hedrick, an associate professor in the Department of Human Nutrition, Foods, and Exercise at Virginia Tech, Blacksburg, who was not involved in the study.
“Because this study was conducted in healthy individuals, the impact of a small dose of glucose was negligible, as their body can effectively regulate blood glucose levels,” she said. “Because high blood glucose concentrations have also been shown to increase platelet reactivity, and consequently increase thrombosis potential, individuals who are not able to regulate their blood glucose levels, such as those with prediabetes and diabetes, could potentially see a similar effect on the body as erythritol when consuming large amounts of sugar.”
At the same time, “individuals with diabetes or prediabetes may be more inclined to consume erythritol as an alternative to sugar,” Dr. Hedrick added. “It will be important to design studies that include these individuals to determine if erythritol has an additive adverse effect on cardiac event risk.”
Criticism and Impact
Critics have suggested the 30-gram dose of erythritol ingested by study participants is unrealistic. Dr. Hazen said that it’s not.
Erythritol is often recommended as a one-to-one sugar replacement. And you could top 30 grams with a few servings of erythritol-sweetened ice cream or soda, Dr. Hazen said.
“The dose that we used, it’s on the high end, but it’s well within a physiologically relevant level,” he said.
Still others say the results are only relevant for people with preexisting heart trouble. But Dr. Hazen said they matter for the masses.
“I think there’s a significant health concern at a population level that this work is underscoring,” he said.
After all, heart disease risk factors like obesity, hypertension, diabetes, and smoking are common and quickly add up.
“If you look at middle-aged America, most people who experience a heart attack or stroke do not know that they have coronary artery disease, and the first recognition of it is that event,” Dr. Hazen said.
For now, Dr. Hazen recommends eating real sugar in moderation. He hopes future research will reveal a nonnutritive sweetener that doesn’t activate platelets.
The Bigger Picture
The new research adds yet another piece to the puzzle of whether nonnutritive sweeteners are better than sugar.
“I think these results are concerning,” said JoAnn E. Manson, MD, chief of the Division of Preventive Medicine at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School, both in Boston, Massachusetts. They “ may help explain the surprising results in some observational studies that artificial sweeteners are linked to an increased risk of cardiovascular disease.”
Dr. Manson, who was not involved in the new study, has conducted other research linking artificial sweetener use with stroke risk.
In an upcoming randomized clinical study, her team is comparing head-to-head sugar-sweetened beverages, drinks sweetened with calorie-free substitutes, and water to determine which is best for a range of cardiometabolic outcomes.
“We need more research on this question,” she said, “because these artificial sweeteners are commonly used, and many people are assuming that their health outcomes will be better with the artificial sweeteners than with sugar-sweetened products.”
A version of this article first appeared on Medscape.com.
FROM ARTERIOSCLEROSIS, THROMBOSIS, AND VASCULAR BIOLOGY
Did Statin Decision-Making Just Get Harder?
The new American Heart Association Predicting Risk of cardiovascular disease EVENTs (PREVENT) equation outperforms the standard pooled cohort equation (PCE). But there is a problem. A big one, actually.
The new score incorporates kidney function and social situation, and it eliminates race from the estimate. It was derived from larger, more modern datasets and can be applied to younger adults.
Two luminaries in preventive cardiology recently called the PREVENT calculator a “substantial improvement over the PCE in terms of accuracy and precision of risk estimates over the entire population and within demographic subgroups.”
Now to the Problem of PREVENT vs PCE
A recent study comparing PREVENT and PCE found that the PREVENT equation would assign lower 10-year risks to millions of US adults.
The authors estimated that the more accurate calculator would result in an estimated 14 million adults no longer reaching the statin eligibility risk threshold of 7.5% over 10 years. Nearly 3 million adults would also not reach the threshold for blood pressure therapy.
Because statins and blood pressure drugs reduce cardiac events, the authors further estimated that more than 100,000 excess myocardial infarctions (MIs) would occur if the PREVENT equation was used along with the current risk thresholds for statin eligibility.
The change in eligibility induced by PREVENT would affect more men than women and a greater proportion of Black adults than White adults.
The Tension of Arbitrary Thresholds
Modern cardiac therapeutics are amazing, but it’s still better to prevent an event than to treat it.
Statin drugs reduce cardiac risk by about 20%-25% at all absolute risks. American experts chose a 10-year risk of 7.5% as the threshold where statin benefit exceed risk. The USPSTF chose 10%. But the thresholds are arbitrary and derived only by opinion.
If your frame is population health, the more patients who take statins, the fewer cardiac events there will be. Anything that reduces statin use increases cardiac events.
The tension occurs because a more accurate equation decreases the number of people who meet eligibility for primary prevention therapy and therefore increases the number of cardiac events.
I write from the perspective of both a clinician and a possible patient. As a clinician, patients often ask me whether they should take a statin. (Sadly, most have not had a risk-based discussion with their clinician. But that is another column.)
The incidence of MI or stroke in a population has no effect on either of these scenarios. I see three broad categories of patients: minimizers, maximizers, and those in between.
I am a minimizer. I don’t worry much about heart disease. First, I won’t ignore symptoms, and I know that we have great treatments. Second, my wife, Staci, practiced hospice and palliative care medicine, and this taught me that worrying about one specific disease is folly. In the next decade, I, like anyone my age, could have many other bad things happen: cancer, trauma, infection, etc. Given these competing risks for serious disease, a PREVENT-calculated risk of 4% or a PCE-calculated risk of 8% makes no difference. I don’t like pills, and, with risks in this range, I decline statin drugs.
Then there are the maximizers. This person wants to avoid heart disease. Maybe they have family or friends who had terrible cardiac events. This person will maximize everything to avoid heart disease. The calculated 10-year risk makes little difference to a maximizer. Whether it is 4% or 8% matters not. They will take a statin or blood pressure drugs to reduce risk to as low as possible.
There are people between minimizers and maximizers. I am not sure that there are that many truly undecided people, but I challenge you to translate a difference of a few percent over a decade to them. I feel comfortable with numbers but struggle to sort out these small absolute differences over such a long time frame.
Other Issues With Risk-Based Decisions
Venk Murthy, MD, PhD, from the University of Michigan, wrote on X about two other issues with a risk-based decision. One is that it does not consider life-years lost. If a 50-year-old person has a fatal MI, that counts as one event. But in life-years lost, that one event is much worse than a fatal MI in a 79-year-old. Cardiac prevention, therefore, may have a greater effect in lower-risk younger people.
Another point Dr. Murthy made is that risk and benefit are driven by many different preferences and rare events. Minimizers and maximizers come to the decision with widely disparate preferences. Risk-based decisions treat patients as if they were automatons who make decisions based simply on calculated probabilities. Clinicians know how untrue that is.
Conclusion
If you carry forward the logic of being disturbed by the estimate of more MIs using the PREVENT score, then you could justify putting statins in the water — because that would reduce population estimates of MIs.
I am not disturbed by the PREVENT score. Clinicians treat individuals, not populations. Individuals want a more accurate score. They don’t need expert-based thresholds. Clinician and patient can discuss the evidence and come up with an agreeable decision, one that is concordant with a person’s goals. The next patient may have a different decision despite seeing the same evidence.
The tension created by this comparative study exposes the gap between population health and basic clinical care. I don’t think clinicians need to worry about populations.
Dr. Mandrola, a clinical electrophysiologist at Baptist Medical Associates, Louisville, Kentucky, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
The new American Heart Association Predicting Risk of cardiovascular disease EVENTs (PREVENT) equation outperforms the standard pooled cohort equation (PCE). But there is a problem. A big one, actually.
The new score incorporates kidney function and social situation, and it eliminates race from the estimate. It was derived from larger, more modern datasets and can be applied to younger adults.
Two luminaries in preventive cardiology recently called the PREVENT calculator a “substantial improvement over the PCE in terms of accuracy and precision of risk estimates over the entire population and within demographic subgroups.”
Now to the Problem of PREVENT vs PCE
A recent study comparing PREVENT and PCE found that the PREVENT equation would assign lower 10-year risks to millions of US adults.
The authors estimated that the more accurate calculator would result in an estimated 14 million adults no longer reaching the statin eligibility risk threshold of 7.5% over 10 years. Nearly 3 million adults would also not reach the threshold for blood pressure therapy.
Because statins and blood pressure drugs reduce cardiac events, the authors further estimated that more than 100,000 excess myocardial infarctions (MIs) would occur if the PREVENT equation was used along with the current risk thresholds for statin eligibility.
The change in eligibility induced by PREVENT would affect more men than women and a greater proportion of Black adults than White adults.
The Tension of Arbitrary Thresholds
Modern cardiac therapeutics are amazing, but it’s still better to prevent an event than to treat it.
Statin drugs reduce cardiac risk by about 20%-25% at all absolute risks. American experts chose a 10-year risk of 7.5% as the threshold where statin benefit exceed risk. The USPSTF chose 10%. But the thresholds are arbitrary and derived only by opinion.
If your frame is population health, the more patients who take statins, the fewer cardiac events there will be. Anything that reduces statin use increases cardiac events.
The tension occurs because a more accurate equation decreases the number of people who meet eligibility for primary prevention therapy and therefore increases the number of cardiac events.
I write from the perspective of both a clinician and a possible patient. As a clinician, patients often ask me whether they should take a statin. (Sadly, most have not had a risk-based discussion with their clinician. But that is another column.)
The incidence of MI or stroke in a population has no effect on either of these scenarios. I see three broad categories of patients: minimizers, maximizers, and those in between.
I am a minimizer. I don’t worry much about heart disease. First, I won’t ignore symptoms, and I know that we have great treatments. Second, my wife, Staci, practiced hospice and palliative care medicine, and this taught me that worrying about one specific disease is folly. In the next decade, I, like anyone my age, could have many other bad things happen: cancer, trauma, infection, etc. Given these competing risks for serious disease, a PREVENT-calculated risk of 4% or a PCE-calculated risk of 8% makes no difference. I don’t like pills, and, with risks in this range, I decline statin drugs.
Then there are the maximizers. This person wants to avoid heart disease. Maybe they have family or friends who had terrible cardiac events. This person will maximize everything to avoid heart disease. The calculated 10-year risk makes little difference to a maximizer. Whether it is 4% or 8% matters not. They will take a statin or blood pressure drugs to reduce risk to as low as possible.
There are people between minimizers and maximizers. I am not sure that there are that many truly undecided people, but I challenge you to translate a difference of a few percent over a decade to them. I feel comfortable with numbers but struggle to sort out these small absolute differences over such a long time frame.
Other Issues With Risk-Based Decisions
Venk Murthy, MD, PhD, from the University of Michigan, wrote on X about two other issues with a risk-based decision. One is that it does not consider life-years lost. If a 50-year-old person has a fatal MI, that counts as one event. But in life-years lost, that one event is much worse than a fatal MI in a 79-year-old. Cardiac prevention, therefore, may have a greater effect in lower-risk younger people.
Another point Dr. Murthy made is that risk and benefit are driven by many different preferences and rare events. Minimizers and maximizers come to the decision with widely disparate preferences. Risk-based decisions treat patients as if they were automatons who make decisions based simply on calculated probabilities. Clinicians know how untrue that is.
Conclusion
If you carry forward the logic of being disturbed by the estimate of more MIs using the PREVENT score, then you could justify putting statins in the water — because that would reduce population estimates of MIs.
I am not disturbed by the PREVENT score. Clinicians treat individuals, not populations. Individuals want a more accurate score. They don’t need expert-based thresholds. Clinician and patient can discuss the evidence and come up with an agreeable decision, one that is concordant with a person’s goals. The next patient may have a different decision despite seeing the same evidence.
The tension created by this comparative study exposes the gap between population health and basic clinical care. I don’t think clinicians need to worry about populations.
Dr. Mandrola, a clinical electrophysiologist at Baptist Medical Associates, Louisville, Kentucky, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
The new American Heart Association Predicting Risk of cardiovascular disease EVENTs (PREVENT) equation outperforms the standard pooled cohort equation (PCE). But there is a problem. A big one, actually.
The new score incorporates kidney function and social situation, and it eliminates race from the estimate. It was derived from larger, more modern datasets and can be applied to younger adults.
Two luminaries in preventive cardiology recently called the PREVENT calculator a “substantial improvement over the PCE in terms of accuracy and precision of risk estimates over the entire population and within demographic subgroups.”
Now to the Problem of PREVENT vs PCE
A recent study comparing PREVENT and PCE found that the PREVENT equation would assign lower 10-year risks to millions of US adults.
The authors estimated that the more accurate calculator would result in an estimated 14 million adults no longer reaching the statin eligibility risk threshold of 7.5% over 10 years. Nearly 3 million adults would also not reach the threshold for blood pressure therapy.
Because statins and blood pressure drugs reduce cardiac events, the authors further estimated that more than 100,000 excess myocardial infarctions (MIs) would occur if the PREVENT equation was used along with the current risk thresholds for statin eligibility.
The change in eligibility induced by PREVENT would affect more men than women and a greater proportion of Black adults than White adults.
The Tension of Arbitrary Thresholds
Modern cardiac therapeutics are amazing, but it’s still better to prevent an event than to treat it.
Statin drugs reduce cardiac risk by about 20%-25% at all absolute risks. American experts chose a 10-year risk of 7.5% as the threshold where statin benefit exceed risk. The USPSTF chose 10%. But the thresholds are arbitrary and derived only by opinion.
If your frame is population health, the more patients who take statins, the fewer cardiac events there will be. Anything that reduces statin use increases cardiac events.
The tension occurs because a more accurate equation decreases the number of people who meet eligibility for primary prevention therapy and therefore increases the number of cardiac events.
I write from the perspective of both a clinician and a possible patient. As a clinician, patients often ask me whether they should take a statin. (Sadly, most have not had a risk-based discussion with their clinician. But that is another column.)
The incidence of MI or stroke in a population has no effect on either of these scenarios. I see three broad categories of patients: minimizers, maximizers, and those in between.
I am a minimizer. I don’t worry much about heart disease. First, I won’t ignore symptoms, and I know that we have great treatments. Second, my wife, Staci, practiced hospice and palliative care medicine, and this taught me that worrying about one specific disease is folly. In the next decade, I, like anyone my age, could have many other bad things happen: cancer, trauma, infection, etc. Given these competing risks for serious disease, a PREVENT-calculated risk of 4% or a PCE-calculated risk of 8% makes no difference. I don’t like pills, and, with risks in this range, I decline statin drugs.
Then there are the maximizers. This person wants to avoid heart disease. Maybe they have family or friends who had terrible cardiac events. This person will maximize everything to avoid heart disease. The calculated 10-year risk makes little difference to a maximizer. Whether it is 4% or 8% matters not. They will take a statin or blood pressure drugs to reduce risk to as low as possible.
There are people between minimizers and maximizers. I am not sure that there are that many truly undecided people, but I challenge you to translate a difference of a few percent over a decade to them. I feel comfortable with numbers but struggle to sort out these small absolute differences over such a long time frame.
Other Issues With Risk-Based Decisions
Venk Murthy, MD, PhD, from the University of Michigan, wrote on X about two other issues with a risk-based decision. One is that it does not consider life-years lost. If a 50-year-old person has a fatal MI, that counts as one event. But in life-years lost, that one event is much worse than a fatal MI in a 79-year-old. Cardiac prevention, therefore, may have a greater effect in lower-risk younger people.
Another point Dr. Murthy made is that risk and benefit are driven by many different preferences and rare events. Minimizers and maximizers come to the decision with widely disparate preferences. Risk-based decisions treat patients as if they were automatons who make decisions based simply on calculated probabilities. Clinicians know how untrue that is.
Conclusion
If you carry forward the logic of being disturbed by the estimate of more MIs using the PREVENT score, then you could justify putting statins in the water — because that would reduce population estimates of MIs.
I am not disturbed by the PREVENT score. Clinicians treat individuals, not populations. Individuals want a more accurate score. They don’t need expert-based thresholds. Clinician and patient can discuss the evidence and come up with an agreeable decision, one that is concordant with a person’s goals. The next patient may have a different decision despite seeing the same evidence.
The tension created by this comparative study exposes the gap between population health and basic clinical care. I don’t think clinicians need to worry about populations.
Dr. Mandrola, a clinical electrophysiologist at Baptist Medical Associates, Louisville, Kentucky, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
On Second Thought: The Truth About Beta-Blockers
This transcript has been edited for clarity.
Giving patients a beta-blocker after a myocardial infarction is standard of care. It’s in the guidelines. It’s one of the performance measures used by the American College of Cardiology (ACC) and the American Heart Association (AHA). If you aren’t putting your post–acute coronary syndrome (ACS) patients on a beta-blocker, the ACC and the AHA both think you suck.
They are very disappointed in you, just like your mother was when you told her you didn’t want to become a surgeon because you don’t like waking up early, your hands shake when you get nervous, it’s not your fault, there’s nothing you can do about it, so just leave me alone!
The data on beta-blockers are decades old. In the time before stents, statins, angiotensin-converting enzyme inhibitors, and dual antiplatelet therapy, when patients either died or got better on their own, beta-blockers showed major benefits. Studies like the Norwegian Multicenter Study Group, the BHAT trial, and the ISIS-1 trial proved the benefits of beta blockade. These studies date back to the 1980s, when you could call a study ISIS without controversy.
It was a simpler time, when all you had to worry about was the Cold War, apartheid, and the global AIDS pandemic. It was a time when doctors smoked in their offices, and patients had bigger infarcts that caused large scars and systolic dysfunction. That world is no longer our world, except for the war, the global pandemic, and the out-of-control gas prices.
The reality is that, before troponins, we probably missed most small heart attacks. Now, most infarcts are small, and most patients walk away from their heart attacks with essentially normal hearts. Do beta-blockers still matter? If you’re a fan of Cochrane reviews, the answer is yes.
In 2021, Cochrane published a review of beta-blockers in patients without heart failure after myocardial infarction (MI). The authors of that analysis concluded, after the usual caveats about heterogeneity, potential bias, and the whims of a random universe, that, yes, beta-blockers do reduce mortality. The risk ratio for max all-cause mortality was 0.81.
What does that mean practically? The absolute risk was reduced from 10.9% to 8.7%, a 2.2–percentage point absolute decrease and about a 20% relative drop. A little math gives us a third number: 46. That’s the number needed to treat. If you think about how many patients you admit during a typical week of critical care unit with an MI, a number needed to treat of 46 is a pretty good trade-off for a fairly inexpensive medication with fairly minimal side effects.
Of course, these are the same people who claim that masks don’t stop the spread of COVID-19. Sure, were they the only people who thought that handwashing was the best way to stop a respiratory virus? No. We all believed that fantasy for far longer than we should have. Not everybody can bat a thousand, if by batting a thousand, you mean reflecting on how your words will impact on a broader population primed to believe misinformation because of the increasingly toxic social media environment and worsening politicization and radicalization of our politics.
By the way, if any of you want to come to Canada, you can stay with me. Things are incrementally better here. In this day and age, incrementally better is the best we can hope for.
Here’s the wrinkle with the Cochrane beta-blocker review: Many of the studies took place before early revascularization became the norm and before our current armamentarium of drugs became standard of care.
Back in the day, bed rest and the power of positive thinking were the mainstays of cardiac treatment. Also, many of these studies mixed together ST-segment MI (STEMI) and non-STEMI patients, so you’re obviously going to see more benefits in STEMI patients who are at higher risk. Some of them used intravenous (IV) beta-blockers right away, whereas some were looking only at oral beta-blockers started days after the infarct.
We don’t use IV beta-blockers that much anymore because of the risk for shock.
Also, some studies had short-term follow-up where the benefits were less pronounced, and some studies used doses and types of beta-blockers rarely used today. Some of the studies had a mix of coronary and heart failure patients, which muddies the water because the heart failure patients would clearly benefit from being on a beta-blocker.
Basically, the data are not definitive because they are old and don’t reflect our current standard of care. The data contain a heterogeneous mix of patients that aren’t really relevant to the question that we’re asking. The question we’re asking is, should you put all your post-MI patients on a beta-blocker routinely, even if they don’t have heart failure?
The REDUCE-AMI trial is the first of a few trials testing, or to be more accurate, retesting, whether beta-blockers are useful after an MI. BETAMI, REBOOT, DANBLOCK— you’ll be hearing these names in the next few years, either because the studies get published or because they’re the Twitter handles of people harassing you online. Either/or. (By the way, I’ll be cold in my grave before I call it X.)
For now, REDUCE-AMI is the first across the finish line, and at least in cardiology, finishing first is a good thing. This study enrolled patients with ACS, both STEMI and non-STEMI, with a post-MI ejection fraction ≥ 50%, and the result was nothing. The risk ratio for all-cause mortality was 0.94 and was not statistically significant.
In absolute terms, that’s a reduction from 4.1% to 3.9%, or a 0.2–percentage point decrease; this translates into a number needed to treat of 500, which is 10 times higher than what the Cochrane review found. That’s if you assume that there is, in fact, a small benefit amidst all the statistical noise, which there probably isn’t.
Now, studies like this can never rule out small effects, either positive or negative, so maybe there is a small benefit from using beta-blockers. If it’s there, it’s really small. Do beta-blockers work? Well, yes, obviously, for heart failure and atrial fibrillation — which, let’s face it, are not exactly rare and often coexist in patients with heart disease. They probably aren’t that great as blood pressure pills, but that’s a story for another day and another video.
Yes, beta-blockers are useful pills, and they are standard of care, just maybe not for post-MI patients with normal ejection fractions because they probably don’t really need them. They worked in the pre-stent, pre-aspirin, pre-anything era.
That’s not our world anymore. Things change. It’s not the 1980s. That’s why I don’t have a mullet, and that’s why you need to update your kitchen.
Dr. Labos, a cardiologist at Kirkland Medical Center, Montreal, Quebec, Canada, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Giving patients a beta-blocker after a myocardial infarction is standard of care. It’s in the guidelines. It’s one of the performance measures used by the American College of Cardiology (ACC) and the American Heart Association (AHA). If you aren’t putting your post–acute coronary syndrome (ACS) patients on a beta-blocker, the ACC and the AHA both think you suck.
They are very disappointed in you, just like your mother was when you told her you didn’t want to become a surgeon because you don’t like waking up early, your hands shake when you get nervous, it’s not your fault, there’s nothing you can do about it, so just leave me alone!
The data on beta-blockers are decades old. In the time before stents, statins, angiotensin-converting enzyme inhibitors, and dual antiplatelet therapy, when patients either died or got better on their own, beta-blockers showed major benefits. Studies like the Norwegian Multicenter Study Group, the BHAT trial, and the ISIS-1 trial proved the benefits of beta blockade. These studies date back to the 1980s, when you could call a study ISIS without controversy.
It was a simpler time, when all you had to worry about was the Cold War, apartheid, and the global AIDS pandemic. It was a time when doctors smoked in their offices, and patients had bigger infarcts that caused large scars and systolic dysfunction. That world is no longer our world, except for the war, the global pandemic, and the out-of-control gas prices.
The reality is that, before troponins, we probably missed most small heart attacks. Now, most infarcts are small, and most patients walk away from their heart attacks with essentially normal hearts. Do beta-blockers still matter? If you’re a fan of Cochrane reviews, the answer is yes.
In 2021, Cochrane published a review of beta-blockers in patients without heart failure after myocardial infarction (MI). The authors of that analysis concluded, after the usual caveats about heterogeneity, potential bias, and the whims of a random universe, that, yes, beta-blockers do reduce mortality. The risk ratio for max all-cause mortality was 0.81.
What does that mean practically? The absolute risk was reduced from 10.9% to 8.7%, a 2.2–percentage point absolute decrease and about a 20% relative drop. A little math gives us a third number: 46. That’s the number needed to treat. If you think about how many patients you admit during a typical week of critical care unit with an MI, a number needed to treat of 46 is a pretty good trade-off for a fairly inexpensive medication with fairly minimal side effects.
Of course, these are the same people who claim that masks don’t stop the spread of COVID-19. Sure, were they the only people who thought that handwashing was the best way to stop a respiratory virus? No. We all believed that fantasy for far longer than we should have. Not everybody can bat a thousand, if by batting a thousand, you mean reflecting on how your words will impact on a broader population primed to believe misinformation because of the increasingly toxic social media environment and worsening politicization and radicalization of our politics.
By the way, if any of you want to come to Canada, you can stay with me. Things are incrementally better here. In this day and age, incrementally better is the best we can hope for.
Here’s the wrinkle with the Cochrane beta-blocker review: Many of the studies took place before early revascularization became the norm and before our current armamentarium of drugs became standard of care.
Back in the day, bed rest and the power of positive thinking were the mainstays of cardiac treatment. Also, many of these studies mixed together ST-segment MI (STEMI) and non-STEMI patients, so you’re obviously going to see more benefits in STEMI patients who are at higher risk. Some of them used intravenous (IV) beta-blockers right away, whereas some were looking only at oral beta-blockers started days after the infarct.
We don’t use IV beta-blockers that much anymore because of the risk for shock.
Also, some studies had short-term follow-up where the benefits were less pronounced, and some studies used doses and types of beta-blockers rarely used today. Some of the studies had a mix of coronary and heart failure patients, which muddies the water because the heart failure patients would clearly benefit from being on a beta-blocker.
Basically, the data are not definitive because they are old and don’t reflect our current standard of care. The data contain a heterogeneous mix of patients that aren’t really relevant to the question that we’re asking. The question we’re asking is, should you put all your post-MI patients on a beta-blocker routinely, even if they don’t have heart failure?
The REDUCE-AMI trial is the first of a few trials testing, or to be more accurate, retesting, whether beta-blockers are useful after an MI. BETAMI, REBOOT, DANBLOCK— you’ll be hearing these names in the next few years, either because the studies get published or because they’re the Twitter handles of people harassing you online. Either/or. (By the way, I’ll be cold in my grave before I call it X.)
For now, REDUCE-AMI is the first across the finish line, and at least in cardiology, finishing first is a good thing. This study enrolled patients with ACS, both STEMI and non-STEMI, with a post-MI ejection fraction ≥ 50%, and the result was nothing. The risk ratio for all-cause mortality was 0.94 and was not statistically significant.
In absolute terms, that’s a reduction from 4.1% to 3.9%, or a 0.2–percentage point decrease; this translates into a number needed to treat of 500, which is 10 times higher than what the Cochrane review found. That’s if you assume that there is, in fact, a small benefit amidst all the statistical noise, which there probably isn’t.
Now, studies like this can never rule out small effects, either positive or negative, so maybe there is a small benefit from using beta-blockers. If it’s there, it’s really small. Do beta-blockers work? Well, yes, obviously, for heart failure and atrial fibrillation — which, let’s face it, are not exactly rare and often coexist in patients with heart disease. They probably aren’t that great as blood pressure pills, but that’s a story for another day and another video.
Yes, beta-blockers are useful pills, and they are standard of care, just maybe not for post-MI patients with normal ejection fractions because they probably don’t really need them. They worked in the pre-stent, pre-aspirin, pre-anything era.
That’s not our world anymore. Things change. It’s not the 1980s. That’s why I don’t have a mullet, and that’s why you need to update your kitchen.
Dr. Labos, a cardiologist at Kirkland Medical Center, Montreal, Quebec, Canada, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Giving patients a beta-blocker after a myocardial infarction is standard of care. It’s in the guidelines. It’s one of the performance measures used by the American College of Cardiology (ACC) and the American Heart Association (AHA). If you aren’t putting your post–acute coronary syndrome (ACS) patients on a beta-blocker, the ACC and the AHA both think you suck.
They are very disappointed in you, just like your mother was when you told her you didn’t want to become a surgeon because you don’t like waking up early, your hands shake when you get nervous, it’s not your fault, there’s nothing you can do about it, so just leave me alone!
The data on beta-blockers are decades old. In the time before stents, statins, angiotensin-converting enzyme inhibitors, and dual antiplatelet therapy, when patients either died or got better on their own, beta-blockers showed major benefits. Studies like the Norwegian Multicenter Study Group, the BHAT trial, and the ISIS-1 trial proved the benefits of beta blockade. These studies date back to the 1980s, when you could call a study ISIS without controversy.
It was a simpler time, when all you had to worry about was the Cold War, apartheid, and the global AIDS pandemic. It was a time when doctors smoked in their offices, and patients had bigger infarcts that caused large scars and systolic dysfunction. That world is no longer our world, except for the war, the global pandemic, and the out-of-control gas prices.
The reality is that, before troponins, we probably missed most small heart attacks. Now, most infarcts are small, and most patients walk away from their heart attacks with essentially normal hearts. Do beta-blockers still matter? If you’re a fan of Cochrane reviews, the answer is yes.
In 2021, Cochrane published a review of beta-blockers in patients without heart failure after myocardial infarction (MI). The authors of that analysis concluded, after the usual caveats about heterogeneity, potential bias, and the whims of a random universe, that, yes, beta-blockers do reduce mortality. The risk ratio for max all-cause mortality was 0.81.
What does that mean practically? The absolute risk was reduced from 10.9% to 8.7%, a 2.2–percentage point absolute decrease and about a 20% relative drop. A little math gives us a third number: 46. That’s the number needed to treat. If you think about how many patients you admit during a typical week of critical care unit with an MI, a number needed to treat of 46 is a pretty good trade-off for a fairly inexpensive medication with fairly minimal side effects.
Of course, these are the same people who claim that masks don’t stop the spread of COVID-19. Sure, were they the only people who thought that handwashing was the best way to stop a respiratory virus? No. We all believed that fantasy for far longer than we should have. Not everybody can bat a thousand, if by batting a thousand, you mean reflecting on how your words will impact on a broader population primed to believe misinformation because of the increasingly toxic social media environment and worsening politicization and radicalization of our politics.
By the way, if any of you want to come to Canada, you can stay with me. Things are incrementally better here. In this day and age, incrementally better is the best we can hope for.
Here’s the wrinkle with the Cochrane beta-blocker review: Many of the studies took place before early revascularization became the norm and before our current armamentarium of drugs became standard of care.
Back in the day, bed rest and the power of positive thinking were the mainstays of cardiac treatment. Also, many of these studies mixed together ST-segment MI (STEMI) and non-STEMI patients, so you’re obviously going to see more benefits in STEMI patients who are at higher risk. Some of them used intravenous (IV) beta-blockers right away, whereas some were looking only at oral beta-blockers started days after the infarct.
We don’t use IV beta-blockers that much anymore because of the risk for shock.
Also, some studies had short-term follow-up where the benefits were less pronounced, and some studies used doses and types of beta-blockers rarely used today. Some of the studies had a mix of coronary and heart failure patients, which muddies the water because the heart failure patients would clearly benefit from being on a beta-blocker.
Basically, the data are not definitive because they are old and don’t reflect our current standard of care. The data contain a heterogeneous mix of patients that aren’t really relevant to the question that we’re asking. The question we’re asking is, should you put all your post-MI patients on a beta-blocker routinely, even if they don’t have heart failure?
The REDUCE-AMI trial is the first of a few trials testing, or to be more accurate, retesting, whether beta-blockers are useful after an MI. BETAMI, REBOOT, DANBLOCK— you’ll be hearing these names in the next few years, either because the studies get published or because they’re the Twitter handles of people harassing you online. Either/or. (By the way, I’ll be cold in my grave before I call it X.)
For now, REDUCE-AMI is the first across the finish line, and at least in cardiology, finishing first is a good thing. This study enrolled patients with ACS, both STEMI and non-STEMI, with a post-MI ejection fraction ≥ 50%, and the result was nothing. The risk ratio for all-cause mortality was 0.94 and was not statistically significant.
In absolute terms, that’s a reduction from 4.1% to 3.9%, or a 0.2–percentage point decrease; this translates into a number needed to treat of 500, which is 10 times higher than what the Cochrane review found. That’s if you assume that there is, in fact, a small benefit amidst all the statistical noise, which there probably isn’t.
Now, studies like this can never rule out small effects, either positive or negative, so maybe there is a small benefit from using beta-blockers. If it’s there, it’s really small. Do beta-blockers work? Well, yes, obviously, for heart failure and atrial fibrillation — which, let’s face it, are not exactly rare and often coexist in patients with heart disease. They probably aren’t that great as blood pressure pills, but that’s a story for another day and another video.
Yes, beta-blockers are useful pills, and they are standard of care, just maybe not for post-MI patients with normal ejection fractions because they probably don’t really need them. They worked in the pre-stent, pre-aspirin, pre-anything era.
That’s not our world anymore. Things change. It’s not the 1980s. That’s why I don’t have a mullet, and that’s why you need to update your kitchen.
Dr. Labos, a cardiologist at Kirkland Medical Center, Montreal, Quebec, Canada, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
New Guidance on Genetic Testing for Kidney Disease
A new consensus statement recommended genetic testing for all categories of kidney diseases whenever a genetic cause is suspected and offered guidance on who to test, which tests are the most useful, and how to talk to patients about results.
The statement, published online in the American Journal of Kidney Diseases, is the work of four dozen authors — including patients, nephrologists, experts in clinical and laboratory genetics, kidney pathology, genetic counseling, and ethics. The experts were brought together by the National Kidney Foundation (NKF) with the goal of broadening use and understanding of the tests.
About 10% or more of kidney diseases in adults and 70% of selected chronic kidney diseases (CKDs) in children have genetic causes. But nephrologists have reported a lack of education about genetic testing, and other barriers to wider use, including limited access to testing, cost, insurance coverage, and a small number of genetic counselors who are versed in kidney genetics.
Genetic testing “in the kidney field is a little less developed than in other fields,” said co–lead author Nora Franceschini, MD, MPH, a professor of epidemiology at the University of North Carolina Gillings School of Global Public Health, Chapel Hill, and a nephrologist who studies the genetic epidemiology of hypertension and kidney and cardiovascular diseases.
There are already many known variants that play a role in various kidney diseases and more are on the horizon, Dr. Franceschini told this news organization. More genetic tests will be available in the near future. “The workforce needs to be prepared,” she said.
The statement is an initial step that gets clinicians thinking about testing in a more systematic way, said Dr. Franceschini. “Genetic testing is just another test that physicians can use to complete the story when evaluating patients.
“I think clinicians are ready to implement” testing, said Dr. Franceschini. “We just need to have better guidance.”
Who, When, What to Test
The NKF statement is not the first to try to address gaps in use and knowledge. A European Renal Association Working Group published guidelines in 2022.
The NKF Working Group came up with 56 recommendations and separate algorithms to guide testing for adult and pediatric individuals who are considered at-risk (and currently asymptomatic) and for those who already have clinical disease.
Testing can help determine a cause if there’s an atypical clinical presentation, and it can help avoid biopsies, said the group. Tests can also guide choice of therapy.
For at-risk individuals, there are two broad situations in which testing might be considered: In family members of a patient who already has kidney disease and in potential kidney donors. But testing at-risk children younger than 18 years should only be done if there is an intervention available that could prevent, treat, or slow progression of disease, said the authors.
For patients with an established genetic diagnosis, at-risk family members should be tested with the known single-gene variant diagnostic instead of a broad panel, said the group.
Single-gene variant testing is most appropriate in situations when clinical disease is already evident or when there is known genetic disease in the family, according to the NKF panel. A large diagnostic panel that covers the many common genetic causes of kidney disease is recommended for the majority of patients.
The group recommended that apolipoprotein L1 (APOL1) testing should be included in gene panels for CKD, and it should be offered to any patient “with clinical findings suggestive of APOL1-association nephropathy, regardless of race and ethnicity.”
High-risk APOL1 genotypes confer a 5- to 10-fold increased risk for CKD and are found in one out of seven individuals of African ancestry, which means the focus has largely been on testing those with that ancestry.
However, with many unknowns about APOL1, the NKF panel did not want to “profile” individuals and suggest that testing should not be based on skin color or race/ethnicity, said Dr. Franceschini.
In addition, only about 10% of those with the variant develop disease, so testing is not currently warranted for those who do not already have kidney disease, said the group.
They also recommended against the use of polygenic risk scores, saying that there are not enough data from diverse populations in genome-wide association studies for kidney disease or on their clinical utility.
More Education Needed; Many Barriers
The authors acknowledged that nephrologists generally receive little education in genetics and lack support for interpreting and discussing results.
“Nephrologists should be provided with training and best practice resources to interpret genetic testing and discuss the results with individuals and their families,” they wrote, adding that there’s a need for genomic medicine boards at academic centers that would be available to help nephrologists interpret results and plot clinical management.
The group did not, however, cite some of the other barriers to adoption of testing, including a limited number of sites offering testing, cost, and lack of insurance coverage for the diagnostics.
Medicare may cover genetic testing for kidney disease when an individual has symptoms and there is a Food and Drug Administration–approved test. Joseph Vassalotti, MD, chief medical officer for the NKF, said private insurance may cover the testing if the nephrologist deems it medically necessary, but that he usually confirms coverage before initiating testing. The often-used Renasight panel, which tests for 385 genes related to kidney diseases, costs $300-$400 out of pocket, Dr. Vassalotti told this news organization.
In a survey of 149 nephrologists conducted in 2021, both users (46%) and nonusers of the tests (69%) said that high cost was the most significant perceived barrier to implementing widespread testing. A third of users and almost two thirds of nonusers said that poor availability or lack of ease of testing was the second most significant barrier.
Clinics that test for kidney genes “are largely confined to large academic centers and some specialty clinics,” said Dominic Raj, MD, the Bert B. Brooks chair, and Divya Shankaranarayanan, MD, director of the Kidney Precision Medicine Clinic, both at George Washington University School of Medicine & Health Sciences, Washington, DC, in an email.
Testing is also limited by cultural barriers, lack of genetic literacy, and patients’ concerns that a positive result could lead to a loss of health insurance coverage, said Dr. Raj and Dr. Shankaranarayanan.
Paper Will Help Expand Use
A lack of consensus has also held back expansion. The new statement “may lead to increased and possibly judicious utilization of genetic testing in nephrology practices,” said Dr. Raj and Dr. Shankaranarayanan. “Most importantly, the panel has given specific guidance as to what type of genetic test platform is likely to yield the best and most cost-effective yield.”
The most effective use is “in monogenic kidney diseases and to a lesser extent in oligogenic kidney disease,” said Dr. Raj and Dr. Shankaranarayanan, adding that testing is of less-certain utility in polygenic kidney diseases, “where complex genetic and epigenetic factors determine the phenotype.”
Genetic testing might be especially useful “in atypical clinical presentations” and can help clinicians avoid unnecessary expensive and extensive investigations when multiple organ systems are involved, they said.
“Most importantly, [testing] might prevent unnecessary and potentially harmful treatment and enable targeted specific treatment, when available,” said Dr. Raj and Dr. Shankaranarayanan.
Dr. Franceschini and Dr. Shankaranarayanan reported no relevant financial relationships. Dr. Raj disclosed that he received consulting fees and honoraria from Novo Nordisk and is a national leader for the company’s Zeus trial, studying whether ziltivekimab reduces the risk for cardiovascular events in cardiovascular disease, CKD, and inflammation. He also participated in a study of Natera’s Renasight, a 385-gene panel for kidney disease.
A version of this article first appeared on Medscape.com.
A new consensus statement recommended genetic testing for all categories of kidney diseases whenever a genetic cause is suspected and offered guidance on who to test, which tests are the most useful, and how to talk to patients about results.
The statement, published online in the American Journal of Kidney Diseases, is the work of four dozen authors — including patients, nephrologists, experts in clinical and laboratory genetics, kidney pathology, genetic counseling, and ethics. The experts were brought together by the National Kidney Foundation (NKF) with the goal of broadening use and understanding of the tests.
About 10% or more of kidney diseases in adults and 70% of selected chronic kidney diseases (CKDs) in children have genetic causes. But nephrologists have reported a lack of education about genetic testing, and other barriers to wider use, including limited access to testing, cost, insurance coverage, and a small number of genetic counselors who are versed in kidney genetics.
Genetic testing “in the kidney field is a little less developed than in other fields,” said co–lead author Nora Franceschini, MD, MPH, a professor of epidemiology at the University of North Carolina Gillings School of Global Public Health, Chapel Hill, and a nephrologist who studies the genetic epidemiology of hypertension and kidney and cardiovascular diseases.
There are already many known variants that play a role in various kidney diseases and more are on the horizon, Dr. Franceschini told this news organization. More genetic tests will be available in the near future. “The workforce needs to be prepared,” she said.
The statement is an initial step that gets clinicians thinking about testing in a more systematic way, said Dr. Franceschini. “Genetic testing is just another test that physicians can use to complete the story when evaluating patients.
“I think clinicians are ready to implement” testing, said Dr. Franceschini. “We just need to have better guidance.”
Who, When, What to Test
The NKF statement is not the first to try to address gaps in use and knowledge. A European Renal Association Working Group published guidelines in 2022.
The NKF Working Group came up with 56 recommendations and separate algorithms to guide testing for adult and pediatric individuals who are considered at-risk (and currently asymptomatic) and for those who already have clinical disease.
Testing can help determine a cause if there’s an atypical clinical presentation, and it can help avoid biopsies, said the group. Tests can also guide choice of therapy.
For at-risk individuals, there are two broad situations in which testing might be considered: In family members of a patient who already has kidney disease and in potential kidney donors. But testing at-risk children younger than 18 years should only be done if there is an intervention available that could prevent, treat, or slow progression of disease, said the authors.
For patients with an established genetic diagnosis, at-risk family members should be tested with the known single-gene variant diagnostic instead of a broad panel, said the group.
Single-gene variant testing is most appropriate in situations when clinical disease is already evident or when there is known genetic disease in the family, according to the NKF panel. A large diagnostic panel that covers the many common genetic causes of kidney disease is recommended for the majority of patients.
The group recommended that apolipoprotein L1 (APOL1) testing should be included in gene panels for CKD, and it should be offered to any patient “with clinical findings suggestive of APOL1-association nephropathy, regardless of race and ethnicity.”
High-risk APOL1 genotypes confer a 5- to 10-fold increased risk for CKD and are found in one out of seven individuals of African ancestry, which means the focus has largely been on testing those with that ancestry.
However, with many unknowns about APOL1, the NKF panel did not want to “profile” individuals and suggest that testing should not be based on skin color or race/ethnicity, said Dr. Franceschini.
In addition, only about 10% of those with the variant develop disease, so testing is not currently warranted for those who do not already have kidney disease, said the group.
They also recommended against the use of polygenic risk scores, saying that there are not enough data from diverse populations in genome-wide association studies for kidney disease or on their clinical utility.
More Education Needed; Many Barriers
The authors acknowledged that nephrologists generally receive little education in genetics and lack support for interpreting and discussing results.
“Nephrologists should be provided with training and best practice resources to interpret genetic testing and discuss the results with individuals and their families,” they wrote, adding that there’s a need for genomic medicine boards at academic centers that would be available to help nephrologists interpret results and plot clinical management.
The group did not, however, cite some of the other barriers to adoption of testing, including a limited number of sites offering testing, cost, and lack of insurance coverage for the diagnostics.
Medicare may cover genetic testing for kidney disease when an individual has symptoms and there is a Food and Drug Administration–approved test. Joseph Vassalotti, MD, chief medical officer for the NKF, said private insurance may cover the testing if the nephrologist deems it medically necessary, but that he usually confirms coverage before initiating testing. The often-used Renasight panel, which tests for 385 genes related to kidney diseases, costs $300-$400 out of pocket, Dr. Vassalotti told this news organization.
In a survey of 149 nephrologists conducted in 2021, both users (46%) and nonusers of the tests (69%) said that high cost was the most significant perceived barrier to implementing widespread testing. A third of users and almost two thirds of nonusers said that poor availability or lack of ease of testing was the second most significant barrier.
Clinics that test for kidney genes “are largely confined to large academic centers and some specialty clinics,” said Dominic Raj, MD, the Bert B. Brooks chair, and Divya Shankaranarayanan, MD, director of the Kidney Precision Medicine Clinic, both at George Washington University School of Medicine & Health Sciences, Washington, DC, in an email.
Testing is also limited by cultural barriers, lack of genetic literacy, and patients’ concerns that a positive result could lead to a loss of health insurance coverage, said Dr. Raj and Dr. Shankaranarayanan.
Paper Will Help Expand Use
A lack of consensus has also held back expansion. The new statement “may lead to increased and possibly judicious utilization of genetic testing in nephrology practices,” said Dr. Raj and Dr. Shankaranarayanan. “Most importantly, the panel has given specific guidance as to what type of genetic test platform is likely to yield the best and most cost-effective yield.”
The most effective use is “in monogenic kidney diseases and to a lesser extent in oligogenic kidney disease,” said Dr. Raj and Dr. Shankaranarayanan, adding that testing is of less-certain utility in polygenic kidney diseases, “where complex genetic and epigenetic factors determine the phenotype.”
Genetic testing might be especially useful “in atypical clinical presentations” and can help clinicians avoid unnecessary expensive and extensive investigations when multiple organ systems are involved, they said.
“Most importantly, [testing] might prevent unnecessary and potentially harmful treatment and enable targeted specific treatment, when available,” said Dr. Raj and Dr. Shankaranarayanan.
Dr. Franceschini and Dr. Shankaranarayanan reported no relevant financial relationships. Dr. Raj disclosed that he received consulting fees and honoraria from Novo Nordisk and is a national leader for the company’s Zeus trial, studying whether ziltivekimab reduces the risk for cardiovascular events in cardiovascular disease, CKD, and inflammation. He also participated in a study of Natera’s Renasight, a 385-gene panel for kidney disease.
A version of this article first appeared on Medscape.com.
A new consensus statement recommended genetic testing for all categories of kidney diseases whenever a genetic cause is suspected and offered guidance on who to test, which tests are the most useful, and how to talk to patients about results.
The statement, published online in the American Journal of Kidney Diseases, is the work of four dozen authors — including patients, nephrologists, experts in clinical and laboratory genetics, kidney pathology, genetic counseling, and ethics. The experts were brought together by the National Kidney Foundation (NKF) with the goal of broadening use and understanding of the tests.
About 10% or more of kidney diseases in adults and 70% of selected chronic kidney diseases (CKDs) in children have genetic causes. But nephrologists have reported a lack of education about genetic testing, and other barriers to wider use, including limited access to testing, cost, insurance coverage, and a small number of genetic counselors who are versed in kidney genetics.
Genetic testing “in the kidney field is a little less developed than in other fields,” said co–lead author Nora Franceschini, MD, MPH, a professor of epidemiology at the University of North Carolina Gillings School of Global Public Health, Chapel Hill, and a nephrologist who studies the genetic epidemiology of hypertension and kidney and cardiovascular diseases.
There are already many known variants that play a role in various kidney diseases and more are on the horizon, Dr. Franceschini told this news organization. More genetic tests will be available in the near future. “The workforce needs to be prepared,” she said.
The statement is an initial step that gets clinicians thinking about testing in a more systematic way, said Dr. Franceschini. “Genetic testing is just another test that physicians can use to complete the story when evaluating patients.
“I think clinicians are ready to implement” testing, said Dr. Franceschini. “We just need to have better guidance.”
Who, When, What to Test
The NKF statement is not the first to try to address gaps in use and knowledge. A European Renal Association Working Group published guidelines in 2022.
The NKF Working Group came up with 56 recommendations and separate algorithms to guide testing for adult and pediatric individuals who are considered at-risk (and currently asymptomatic) and for those who already have clinical disease.
Testing can help determine a cause if there’s an atypical clinical presentation, and it can help avoid biopsies, said the group. Tests can also guide choice of therapy.
For at-risk individuals, there are two broad situations in which testing might be considered: In family members of a patient who already has kidney disease and in potential kidney donors. But testing at-risk children younger than 18 years should only be done if there is an intervention available that could prevent, treat, or slow progression of disease, said the authors.
For patients with an established genetic diagnosis, at-risk family members should be tested with the known single-gene variant diagnostic instead of a broad panel, said the group.
Single-gene variant testing is most appropriate in situations when clinical disease is already evident or when there is known genetic disease in the family, according to the NKF panel. A large diagnostic panel that covers the many common genetic causes of kidney disease is recommended for the majority of patients.
The group recommended that apolipoprotein L1 (APOL1) testing should be included in gene panels for CKD, and it should be offered to any patient “with clinical findings suggestive of APOL1-association nephropathy, regardless of race and ethnicity.”
High-risk APOL1 genotypes confer a 5- to 10-fold increased risk for CKD and are found in one out of seven individuals of African ancestry, which means the focus has largely been on testing those with that ancestry.
However, with many unknowns about APOL1, the NKF panel did not want to “profile” individuals and suggest that testing should not be based on skin color or race/ethnicity, said Dr. Franceschini.
In addition, only about 10% of those with the variant develop disease, so testing is not currently warranted for those who do not already have kidney disease, said the group.
They also recommended against the use of polygenic risk scores, saying that there are not enough data from diverse populations in genome-wide association studies for kidney disease or on their clinical utility.
More Education Needed; Many Barriers
The authors acknowledged that nephrologists generally receive little education in genetics and lack support for interpreting and discussing results.
“Nephrologists should be provided with training and best practice resources to interpret genetic testing and discuss the results with individuals and their families,” they wrote, adding that there’s a need for genomic medicine boards at academic centers that would be available to help nephrologists interpret results and plot clinical management.
The group did not, however, cite some of the other barriers to adoption of testing, including a limited number of sites offering testing, cost, and lack of insurance coverage for the diagnostics.
Medicare may cover genetic testing for kidney disease when an individual has symptoms and there is a Food and Drug Administration–approved test. Joseph Vassalotti, MD, chief medical officer for the NKF, said private insurance may cover the testing if the nephrologist deems it medically necessary, but that he usually confirms coverage before initiating testing. The often-used Renasight panel, which tests for 385 genes related to kidney diseases, costs $300-$400 out of pocket, Dr. Vassalotti told this news organization.
In a survey of 149 nephrologists conducted in 2021, both users (46%) and nonusers of the tests (69%) said that high cost was the most significant perceived barrier to implementing widespread testing. A third of users and almost two thirds of nonusers said that poor availability or lack of ease of testing was the second most significant barrier.
Clinics that test for kidney genes “are largely confined to large academic centers and some specialty clinics,” said Dominic Raj, MD, the Bert B. Brooks chair, and Divya Shankaranarayanan, MD, director of the Kidney Precision Medicine Clinic, both at George Washington University School of Medicine & Health Sciences, Washington, DC, in an email.
Testing is also limited by cultural barriers, lack of genetic literacy, and patients’ concerns that a positive result could lead to a loss of health insurance coverage, said Dr. Raj and Dr. Shankaranarayanan.
Paper Will Help Expand Use
A lack of consensus has also held back expansion. The new statement “may lead to increased and possibly judicious utilization of genetic testing in nephrology practices,” said Dr. Raj and Dr. Shankaranarayanan. “Most importantly, the panel has given specific guidance as to what type of genetic test platform is likely to yield the best and most cost-effective yield.”
The most effective use is “in monogenic kidney diseases and to a lesser extent in oligogenic kidney disease,” said Dr. Raj and Dr. Shankaranarayanan, adding that testing is of less-certain utility in polygenic kidney diseases, “where complex genetic and epigenetic factors determine the phenotype.”
Genetic testing might be especially useful “in atypical clinical presentations” and can help clinicians avoid unnecessary expensive and extensive investigations when multiple organ systems are involved, they said.
“Most importantly, [testing] might prevent unnecessary and potentially harmful treatment and enable targeted specific treatment, when available,” said Dr. Raj and Dr. Shankaranarayanan.
Dr. Franceschini and Dr. Shankaranarayanan reported no relevant financial relationships. Dr. Raj disclosed that he received consulting fees and honoraria from Novo Nordisk and is a national leader for the company’s Zeus trial, studying whether ziltivekimab reduces the risk for cardiovascular events in cardiovascular disease, CKD, and inflammation. He also participated in a study of Natera’s Renasight, a 385-gene panel for kidney disease.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF KIDNEY DISEASES
Weight Loss in Obesity May Create ‘Positive’ Hormone Changes
TOPLINE:
In middle-aged patients with severe obesity, changes in endogenous sex hormones may be proportional to the amount of weight loss after bariatric surgery and dietary intervention, leading to an improved hormonal balance, with more pronounced androgen changes in women.
METHODOLOGY:
- Obesity-related hormonal imbalances are common among those seeking weight loss treatment.
- This prospective observational study evaluated the incremental effect of weight loss by three bariatric procedures and a dietary intervention on endogenous sex hormones in men and women over 3 years.
- The study included 61 adults (median age, 50.9 years; baseline mean body mass index, 40.2; 72% women) from obesity clinics and private bariatric services in Sydney, Australia, between 2009 and 2012, who underwent bariatric surgery or received dietary interventions based on their probability of diabetes remission.
- The researchers evaluated weight loss and hormone levels at baseline and at 6, 12, 24, and 36 months.
- Changes in hormones were also compared among patients who received dietary intervention and those who underwent bariatric procedures such as Roux-en-Y gastric bypass, sleeve gastrectomy, and laparoscopic gastric banding.
TAKEAWAY:
- In women, testosterone levels decreased and sex hormone–binding globulin (SHBG) levels increased at 6 months; these changes were maintained at 24 and 36 months and remained statistically significant when controlled for age and menopausal status.
- In men, testosterone levels were significantly higher at 12, 24, and 36 months, and SHBG levels increased at 12 and 24 months. There were no differences in the estradiol levels among men and women.
- Women who underwent Roux-en-Y gastric bypass surgery experienced the greatest weight loss and the largest reduction (54%) in testosterone levels (P = .004), and sleeve gastrectomy led to an increase of 51% in SHBG levels (P = .0001), all compared with dietary interventions. In men, there were no differences in testosterone and SHBG levels between the diet and surgical groups.
IN PRACTICE:
“Ongoing monitoring of hormone levels and metabolic parameters is crucial for patients undergoing bariatric procedures to ensure long-term optimal health outcomes,” the authors wrote.
SOURCE:
This study was led by Malgorzata M. Brzozowska, MD, PhD, UNSW Sydney, Sydney, Australia, and was published online in the International Journal of Obesity.
LIMITATIONS:
The main limitations were a small sample size, lack of randomization, and absence of data on clinical outcomes related to hormone changes. Additionally, the researchers did not evaluate women for polycystic ovary syndrome or menstrual irregularities, and the clinical significance of testosterone reductions within the normal range remains unknown.
DISCLOSURES:
The study was funded by the National Health and Medical Research Council. Some authors have received honoraria and consulting and research support from various pharmaceutical companies.
A version of this article first appeared on Medscape.com.
TOPLINE:
In middle-aged patients with severe obesity, changes in endogenous sex hormones may be proportional to the amount of weight loss after bariatric surgery and dietary intervention, leading to an improved hormonal balance, with more pronounced androgen changes in women.
METHODOLOGY:
- Obesity-related hormonal imbalances are common among those seeking weight loss treatment.
- This prospective observational study evaluated the incremental effect of weight loss by three bariatric procedures and a dietary intervention on endogenous sex hormones in men and women over 3 years.
- The study included 61 adults (median age, 50.9 years; baseline mean body mass index, 40.2; 72% women) from obesity clinics and private bariatric services in Sydney, Australia, between 2009 and 2012, who underwent bariatric surgery or received dietary interventions based on their probability of diabetes remission.
- The researchers evaluated weight loss and hormone levels at baseline and at 6, 12, 24, and 36 months.
- Changes in hormones were also compared among patients who received dietary intervention and those who underwent bariatric procedures such as Roux-en-Y gastric bypass, sleeve gastrectomy, and laparoscopic gastric banding.
TAKEAWAY:
- In women, testosterone levels decreased and sex hormone–binding globulin (SHBG) levels increased at 6 months; these changes were maintained at 24 and 36 months and remained statistically significant when controlled for age and menopausal status.
- In men, testosterone levels were significantly higher at 12, 24, and 36 months, and SHBG levels increased at 12 and 24 months. There were no differences in the estradiol levels among men and women.
- Women who underwent Roux-en-Y gastric bypass surgery experienced the greatest weight loss and the largest reduction (54%) in testosterone levels (P = .004), and sleeve gastrectomy led to an increase of 51% in SHBG levels (P = .0001), all compared with dietary interventions. In men, there were no differences in testosterone and SHBG levels between the diet and surgical groups.
IN PRACTICE:
“Ongoing monitoring of hormone levels and metabolic parameters is crucial for patients undergoing bariatric procedures to ensure long-term optimal health outcomes,” the authors wrote.
SOURCE:
This study was led by Malgorzata M. Brzozowska, MD, PhD, UNSW Sydney, Sydney, Australia, and was published online in the International Journal of Obesity.
LIMITATIONS:
The main limitations were a small sample size, lack of randomization, and absence of data on clinical outcomes related to hormone changes. Additionally, the researchers did not evaluate women for polycystic ovary syndrome or menstrual irregularities, and the clinical significance of testosterone reductions within the normal range remains unknown.
DISCLOSURES:
The study was funded by the National Health and Medical Research Council. Some authors have received honoraria and consulting and research support from various pharmaceutical companies.
A version of this article first appeared on Medscape.com.
TOPLINE:
In middle-aged patients with severe obesity, changes in endogenous sex hormones may be proportional to the amount of weight loss after bariatric surgery and dietary intervention, leading to an improved hormonal balance, with more pronounced androgen changes in women.
METHODOLOGY:
- Obesity-related hormonal imbalances are common among those seeking weight loss treatment.
- This prospective observational study evaluated the incremental effect of weight loss by three bariatric procedures and a dietary intervention on endogenous sex hormones in men and women over 3 years.
- The study included 61 adults (median age, 50.9 years; baseline mean body mass index, 40.2; 72% women) from obesity clinics and private bariatric services in Sydney, Australia, between 2009 and 2012, who underwent bariatric surgery or received dietary interventions based on their probability of diabetes remission.
- The researchers evaluated weight loss and hormone levels at baseline and at 6, 12, 24, and 36 months.
- Changes in hormones were also compared among patients who received dietary intervention and those who underwent bariatric procedures such as Roux-en-Y gastric bypass, sleeve gastrectomy, and laparoscopic gastric banding.
TAKEAWAY:
- In women, testosterone levels decreased and sex hormone–binding globulin (SHBG) levels increased at 6 months; these changes were maintained at 24 and 36 months and remained statistically significant when controlled for age and menopausal status.
- In men, testosterone levels were significantly higher at 12, 24, and 36 months, and SHBG levels increased at 12 and 24 months. There were no differences in the estradiol levels among men and women.
- Women who underwent Roux-en-Y gastric bypass surgery experienced the greatest weight loss and the largest reduction (54%) in testosterone levels (P = .004), and sleeve gastrectomy led to an increase of 51% in SHBG levels (P = .0001), all compared with dietary interventions. In men, there were no differences in testosterone and SHBG levels between the diet and surgical groups.
IN PRACTICE:
“Ongoing monitoring of hormone levels and metabolic parameters is crucial for patients undergoing bariatric procedures to ensure long-term optimal health outcomes,” the authors wrote.
SOURCE:
This study was led by Malgorzata M. Brzozowska, MD, PhD, UNSW Sydney, Sydney, Australia, and was published online in the International Journal of Obesity.
LIMITATIONS:
The main limitations were a small sample size, lack of randomization, and absence of data on clinical outcomes related to hormone changes. Additionally, the researchers did not evaluate women for polycystic ovary syndrome or menstrual irregularities, and the clinical significance of testosterone reductions within the normal range remains unknown.
DISCLOSURES:
The study was funded by the National Health and Medical Research Council. Some authors have received honoraria and consulting and research support from various pharmaceutical companies.
A version of this article first appeared on Medscape.com.
Study Links Melasma With Comorbidities, Races, Ethnicities
TOPLINE:
A study found significant associations between melasma and several comorbidities, including hypertension and hormonal contraception use, which were the most common.
METHODOLOGY:
- Melasma predominantly affects young women of color and often worsens in hyperestrogen states; understanding the association with comorbidities can improve surveillance and treatment strategies.
- Researchers evaluated 41,283 patients with melasma (mean age, 48.8 years; 93% women) from the TriNetX database and an equal number of matched control individuals.
- The main outcome was comorbidities including allergic rhinitis, atopic dermatitis, anticonvulsants, diabetes, hormonal contraceptives, hypothyroidism, hypertension, lupus, rosacea, skin cancer, and malignancy.
TAKEAWAY:
- Among those with melasma, 25% had hypertension and 24% used hormonal contraception, the two most commonly associated risk factors identified.
- Rosacea (odds ratio [OR], 5.1), atopic dermatitis (OR, 3.3), lupus (OR, 2.5), history of skin cancer (OR, 2.5), and history of internal malignancy (OR, 2.1) were associated with the highest risk of developing melasma (P < .01 for all).
- Asian (OR, 2.0; P < .01) and “other/unknown” races (OR, 1.7; P < .01) and Hispanic ethnicity (OR, 1.3; P < .01) were also significantly associated with melasma, while the odds were slightly lower among White, Black/African American, and “not Hispanic” groups (ORs, 0.8; P < .01 for all groups).
IN PRACTICE:
the authors wrote.
SOURCE:
The study, led by Ajay N. Sharma, MD, MBA, of the Department of Dermatology at the University of California, Irvine, was published online in Journal of Drugs in Dermatology.
LIMITATIONS:
The study limitations included the retrospective design, potential misclassification of diagnoses, and the inability to establish causality.
DISCLOSURES:
The study did not disclose any funding sources. The authors declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
A study found significant associations between melasma and several comorbidities, including hypertension and hormonal contraception use, which were the most common.
METHODOLOGY:
- Melasma predominantly affects young women of color and often worsens in hyperestrogen states; understanding the association with comorbidities can improve surveillance and treatment strategies.
- Researchers evaluated 41,283 patients with melasma (mean age, 48.8 years; 93% women) from the TriNetX database and an equal number of matched control individuals.
- The main outcome was comorbidities including allergic rhinitis, atopic dermatitis, anticonvulsants, diabetes, hormonal contraceptives, hypothyroidism, hypertension, lupus, rosacea, skin cancer, and malignancy.
TAKEAWAY:
- Among those with melasma, 25% had hypertension and 24% used hormonal contraception, the two most commonly associated risk factors identified.
- Rosacea (odds ratio [OR], 5.1), atopic dermatitis (OR, 3.3), lupus (OR, 2.5), history of skin cancer (OR, 2.5), and history of internal malignancy (OR, 2.1) were associated with the highest risk of developing melasma (P < .01 for all).
- Asian (OR, 2.0; P < .01) and “other/unknown” races (OR, 1.7; P < .01) and Hispanic ethnicity (OR, 1.3; P < .01) were also significantly associated with melasma, while the odds were slightly lower among White, Black/African American, and “not Hispanic” groups (ORs, 0.8; P < .01 for all groups).
IN PRACTICE:
the authors wrote.
SOURCE:
The study, led by Ajay N. Sharma, MD, MBA, of the Department of Dermatology at the University of California, Irvine, was published online in Journal of Drugs in Dermatology.
LIMITATIONS:
The study limitations included the retrospective design, potential misclassification of diagnoses, and the inability to establish causality.
DISCLOSURES:
The study did not disclose any funding sources. The authors declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
A study found significant associations between melasma and several comorbidities, including hypertension and hormonal contraception use, which were the most common.
METHODOLOGY:
- Melasma predominantly affects young women of color and often worsens in hyperestrogen states; understanding the association with comorbidities can improve surveillance and treatment strategies.
- Researchers evaluated 41,283 patients with melasma (mean age, 48.8 years; 93% women) from the TriNetX database and an equal number of matched control individuals.
- The main outcome was comorbidities including allergic rhinitis, atopic dermatitis, anticonvulsants, diabetes, hormonal contraceptives, hypothyroidism, hypertension, lupus, rosacea, skin cancer, and malignancy.
TAKEAWAY:
- Among those with melasma, 25% had hypertension and 24% used hormonal contraception, the two most commonly associated risk factors identified.
- Rosacea (odds ratio [OR], 5.1), atopic dermatitis (OR, 3.3), lupus (OR, 2.5), history of skin cancer (OR, 2.5), and history of internal malignancy (OR, 2.1) were associated with the highest risk of developing melasma (P < .01 for all).
- Asian (OR, 2.0; P < .01) and “other/unknown” races (OR, 1.7; P < .01) and Hispanic ethnicity (OR, 1.3; P < .01) were also significantly associated with melasma, while the odds were slightly lower among White, Black/African American, and “not Hispanic” groups (ORs, 0.8; P < .01 for all groups).
IN PRACTICE:
the authors wrote.
SOURCE:
The study, led by Ajay N. Sharma, MD, MBA, of the Department of Dermatology at the University of California, Irvine, was published online in Journal of Drugs in Dermatology.
LIMITATIONS:
The study limitations included the retrospective design, potential misclassification of diagnoses, and the inability to establish causality.
DISCLOSURES:
The study did not disclose any funding sources. The authors declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
Government Accuses Health System of Paying Docs Outrageous Salaries for Patient Referrals
Strapped for cash and searching for new profits, Tennessee-based Erlanger Health System illegally paid excessive salaries to physicians in exchange for patient referrals, the US government alleged in a federal lawsuit.
Erlanger changed its compensation model to entice revenue-generating doctors, paying some two to three times the median salary for their specialty, according to the complaint.
The physicians in turn referred numerous patients to Erlanger, and the health system submitted claims to Medicare for the referred services in violation of the Stark Law, according to the suit, filed in US District Court for the Western District of North Carolina.
The government’s complaint “serves as a warning” to healthcare providers who try to boost profits through improper financial arrangements with referring physicians, said Tamala E. Miles, Special Agent in Charge for the US Department of Health and Human Services (HHS) Office of Inspector General (OIG).
In a statement provided to this news organization, Erlanger denied the allegations and said it would “vigorously” defend the lawsuit.
“Erlanger paid physicians based on amounts that outside experts advised was fair market value,” Erlanger officials said in the statement. “Erlanger did not pay for referrals. A complete picture of the facts will demonstrate that the allegations lack merit and tell a very different story than what the government now claims.”
The Erlanger case is a reminder to physicians to consult their own knowledgeable advisors when considering financial arrangements with hospitals, said William Sarraille, JD, adjunct professor for the University of Maryland Francis King Carey School of Law in Baltimore and a regulatory consultant.
“There is a tendency by physicians when contracting ... to rely on [hospitals’] perceived compliance and legal expertise,” Mr. Sarraille told this news organization. “This case illustrates the risks in doing so. Sometimes bigger doesn’t translate into more sophisticated or more effective from a compliance perspective.”
Stark Law Prohibits Kickbacks
The Stark Law prohibits hospitals from billing the Centers for Medicare & Medicaid Services (CMS) for services referred by a physician with whom the hospital has an improper financial relationship.
CMS paid Erlanger about $27.8 million for claims stemming from the improper financial arrangements, the government contends.
“HHS-OIG will continue to investigate such deals to prevent financial arrangements that could compromise impartial medical judgment, increase healthcare costs, and erode public trust in the healthcare system,” Ms. Miles said in a statement.
Suit: Health System’s Money Woes Led to Illegal Arrangements
Erlanger’s financial troubles allegedly started after a previous run-in with the US government over false claims.
In 2005, Erlanger Health System agreed to pay the government $40 million to resolve allegations that it knowingly submitted false claims to Medicare, according to the government’s complaint. At the time, Erlanger entered into a Corporate Integrity Agreement (CIA) with the OIG that required Erlanger to put controls in place to ensure its financial relationships did not violate the Stark Law.
Erlanger’s agreement with OIG ended in 2010. Over the next 3 years, the health system lost nearly $32 million and in fiscal year 2013, had only 65 days of cash on hand, according to the government’s lawsuit.
Beginning in 2013, Erlanger allegedly implemented a strategy to increase profits by employing more physicians, particularly specialists from competing hospitals whose patients would need costly hospital stays, according to the complaint.
Once hired, Erlanger’s physicians were expected to treat patients at Erlanger’s hospitals and refer them to other providers within the health system, the suit claims. Erlanger also relaxed or eliminated the oversight and controls on physician compensation put in place under the CIA. For example, Erlanger’s CEO signed some compensation contracts before its chief compliance officer could review them and no longer allowed the compliance officer to vote on whether to approve compensation arrangements, according to the complaint.
Erlanger also changed its compensation model to include large salaries for medical director and academic positions and allegedly paid such salaries to physicians without ensuring the required work was performed. As a result, Erlanger physicians with profitable referrals were among the highest paid in the nation for their specialties, the government claims. For example, according to the complaint:
- Erlanger paid an electrophysiologist an annual clinical salary of $816,701, a medical director salary of $101,080, an academic salary of $59,322, and a productivity incentive based on work relative value units (wRVUs). The medical director and academic salaries paid were near the 90th percentile of comparable salaries in the specialty.
- The health system paid a neurosurgeon a base salary of $654,735, a productivity incentive based on wRVUs, and payments for excess call coverage ranging from $400 to $1000 per 24-hour shift. In 2016, the neurosurgeon made $500,000 in excess call payments.
- Erlanger paid a cardiothoracic surgeon a base clinical salary of $1,070,000, a sign-on bonus of $150,000, a retention bonus of $100,000 (payable in the 4th year of the contract), and a program incentive of up to $150,000 per year.
In addition, Erlanger ignored patient safety concerns about some of its high revenue-generating physicians, the government claims.
For instance, Erlanger received multiple complaints that a cardiothoracic surgeon was misusing an expensive form of life support in which pumps and oxygenators take over heart and lung function. Overuse of the equipment prolonged patients’ hospital stays and increased the hospital fees generated by the surgeon, according to the complaint. Staff also raised concerns about the cardiothoracic surgeon’s patient outcomes.
But Erlanger disregarded the concerns and in 2018, increased the cardiothoracic surgeon’s retention bonus from $100,000 to $250,000, the suit alleges. A year later, the health system increased his base salary from $1,070,000 to $1,195,000.
Health care compensation and billing consultants alerted Erlanger that it was overpaying salaries and handing out bonuses based on measures that overstated the work physicians were performing, but Erlanger ignored the warnings, according to the complaint.
Administrators allegedly resisted efforts by the chief compliance officer to hire an outside consultant to review its compensation models. Erlanger fired the compliance officer in 2019.
The former chief compliance officer and another administrator filed a whistleblower lawsuit against Erlanger in 2021. The two administrators are relators in the government’s July 2024 lawsuit.
How to Protect Yourself From Illegal Hospital Deals
The Erlanger case is the latest in a series of recent complaints by the federal government involving financial arrangements between hospitals and physicians.
In December 2023, Indianapolis-based Community Health Network Inc. agreed to pay the government $345 million to resolve claims that it paid physicians above fair market value and awarded bonuses tied to referrals in violation of the Stark Law.
Also in 2023, Saginaw, Michigan–based Covenant HealthCare and two physicians paid the government $69 million to settle allegations that administrators engaged in improper financial arrangements with referring physicians and a physician-owned investment group. In another 2023 case, Massachusetts Eye and Ear in Boston agreed to pay $5.7 million to resolve claims that some of its physician compensation plans violated the Stark Law.
Before you enter into a financial arrangement with a hospital, it’s also important to examine what percentile the aggregate compensation would reflect, law professor Mr. Sarraille said. The Erlanger case highlights federal officials’ suspicion of compensation, in aggregate, that exceeds the 90th percentile and increased attention to compensation that exceeds the 75th percentile, he said.
To research compensation levels, doctors can review the Medical Group Management Association’s annual compensation report or search its compensation data.
Before signing any contracts, Mr. Sarraille suggests, physicians should also consider whether the hospital shares the same values. Ask physicians at the hospital what they have to say about the hospital’s culture, vision, and values. Have physicians left the hospital after their practices were acquired? Consider speaking with them to learn why.
Keep in mind that a doctor’s reputation could be impacted by a compliance complaint, regardless of whether it’s directed at the hospital and not the employed physician, Mr. Sarraille said.
“The [Erlanger] complaint focuses on the compensation of specific, named physicians saying they were wildly overcompensated,” he said. “The implication is that they sold their referral power in exchange for a pay day. It’s a bad look, no matter how the case evolves from here.”
Physicians could also face their own liability risk under the Stark Law and False Claims Act, depending on the circumstances. In the event of related quality-of-care issues, medical liability could come into play, Mr. Sarraille noted. In such cases, plaintiffs’ attorneys may see an opportunity to boost their claims with allegations that the patient harm was a function of “chasing compensation dollars,” Mr. Sarraille said.
“Where that happens, plaintiff lawyers see the potential for crippling punitive damages, which might not be covered by an insurer,” he said.
A version of this article appeared on Medscape.com.
Strapped for cash and searching for new profits, Tennessee-based Erlanger Health System illegally paid excessive salaries to physicians in exchange for patient referrals, the US government alleged in a federal lawsuit.
Erlanger changed its compensation model to entice revenue-generating doctors, paying some two to three times the median salary for their specialty, according to the complaint.
The physicians in turn referred numerous patients to Erlanger, and the health system submitted claims to Medicare for the referred services in violation of the Stark Law, according to the suit, filed in US District Court for the Western District of North Carolina.
The government’s complaint “serves as a warning” to healthcare providers who try to boost profits through improper financial arrangements with referring physicians, said Tamala E. Miles, Special Agent in Charge for the US Department of Health and Human Services (HHS) Office of Inspector General (OIG).
In a statement provided to this news organization, Erlanger denied the allegations and said it would “vigorously” defend the lawsuit.
“Erlanger paid physicians based on amounts that outside experts advised was fair market value,” Erlanger officials said in the statement. “Erlanger did not pay for referrals. A complete picture of the facts will demonstrate that the allegations lack merit and tell a very different story than what the government now claims.”
The Erlanger case is a reminder to physicians to consult their own knowledgeable advisors when considering financial arrangements with hospitals, said William Sarraille, JD, adjunct professor for the University of Maryland Francis King Carey School of Law in Baltimore and a regulatory consultant.
“There is a tendency by physicians when contracting ... to rely on [hospitals’] perceived compliance and legal expertise,” Mr. Sarraille told this news organization. “This case illustrates the risks in doing so. Sometimes bigger doesn’t translate into more sophisticated or more effective from a compliance perspective.”
Stark Law Prohibits Kickbacks
The Stark Law prohibits hospitals from billing the Centers for Medicare & Medicaid Services (CMS) for services referred by a physician with whom the hospital has an improper financial relationship.
CMS paid Erlanger about $27.8 million for claims stemming from the improper financial arrangements, the government contends.
“HHS-OIG will continue to investigate such deals to prevent financial arrangements that could compromise impartial medical judgment, increase healthcare costs, and erode public trust in the healthcare system,” Ms. Miles said in a statement.
Suit: Health System’s Money Woes Led to Illegal Arrangements
Erlanger’s financial troubles allegedly started after a previous run-in with the US government over false claims.
In 2005, Erlanger Health System agreed to pay the government $40 million to resolve allegations that it knowingly submitted false claims to Medicare, according to the government’s complaint. At the time, Erlanger entered into a Corporate Integrity Agreement (CIA) with the OIG that required Erlanger to put controls in place to ensure its financial relationships did not violate the Stark Law.
Erlanger’s agreement with OIG ended in 2010. Over the next 3 years, the health system lost nearly $32 million and in fiscal year 2013, had only 65 days of cash on hand, according to the government’s lawsuit.
Beginning in 2013, Erlanger allegedly implemented a strategy to increase profits by employing more physicians, particularly specialists from competing hospitals whose patients would need costly hospital stays, according to the complaint.
Once hired, Erlanger’s physicians were expected to treat patients at Erlanger’s hospitals and refer them to other providers within the health system, the suit claims. Erlanger also relaxed or eliminated the oversight and controls on physician compensation put in place under the CIA. For example, Erlanger’s CEO signed some compensation contracts before its chief compliance officer could review them and no longer allowed the compliance officer to vote on whether to approve compensation arrangements, according to the complaint.
Erlanger also changed its compensation model to include large salaries for medical director and academic positions and allegedly paid such salaries to physicians without ensuring the required work was performed. As a result, Erlanger physicians with profitable referrals were among the highest paid in the nation for their specialties, the government claims. For example, according to the complaint:
- Erlanger paid an electrophysiologist an annual clinical salary of $816,701, a medical director salary of $101,080, an academic salary of $59,322, and a productivity incentive based on work relative value units (wRVUs). The medical director and academic salaries paid were near the 90th percentile of comparable salaries in the specialty.
- The health system paid a neurosurgeon a base salary of $654,735, a productivity incentive based on wRVUs, and payments for excess call coverage ranging from $400 to $1000 per 24-hour shift. In 2016, the neurosurgeon made $500,000 in excess call payments.
- Erlanger paid a cardiothoracic surgeon a base clinical salary of $1,070,000, a sign-on bonus of $150,000, a retention bonus of $100,000 (payable in the 4th year of the contract), and a program incentive of up to $150,000 per year.
In addition, Erlanger ignored patient safety concerns about some of its high revenue-generating physicians, the government claims.
For instance, Erlanger received multiple complaints that a cardiothoracic surgeon was misusing an expensive form of life support in which pumps and oxygenators take over heart and lung function. Overuse of the equipment prolonged patients’ hospital stays and increased the hospital fees generated by the surgeon, according to the complaint. Staff also raised concerns about the cardiothoracic surgeon’s patient outcomes.
But Erlanger disregarded the concerns and in 2018, increased the cardiothoracic surgeon’s retention bonus from $100,000 to $250,000, the suit alleges. A year later, the health system increased his base salary from $1,070,000 to $1,195,000.
Health care compensation and billing consultants alerted Erlanger that it was overpaying salaries and handing out bonuses based on measures that overstated the work physicians were performing, but Erlanger ignored the warnings, according to the complaint.
Administrators allegedly resisted efforts by the chief compliance officer to hire an outside consultant to review its compensation models. Erlanger fired the compliance officer in 2019.
The former chief compliance officer and another administrator filed a whistleblower lawsuit against Erlanger in 2021. The two administrators are relators in the government’s July 2024 lawsuit.
How to Protect Yourself From Illegal Hospital Deals
The Erlanger case is the latest in a series of recent complaints by the federal government involving financial arrangements between hospitals and physicians.
In December 2023, Indianapolis-based Community Health Network Inc. agreed to pay the government $345 million to resolve claims that it paid physicians above fair market value and awarded bonuses tied to referrals in violation of the Stark Law.
Also in 2023, Saginaw, Michigan–based Covenant HealthCare and two physicians paid the government $69 million to settle allegations that administrators engaged in improper financial arrangements with referring physicians and a physician-owned investment group. In another 2023 case, Massachusetts Eye and Ear in Boston agreed to pay $5.7 million to resolve claims that some of its physician compensation plans violated the Stark Law.
Before you enter into a financial arrangement with a hospital, it’s also important to examine what percentile the aggregate compensation would reflect, law professor Mr. Sarraille said. The Erlanger case highlights federal officials’ suspicion of compensation, in aggregate, that exceeds the 90th percentile and increased attention to compensation that exceeds the 75th percentile, he said.
To research compensation levels, doctors can review the Medical Group Management Association’s annual compensation report or search its compensation data.
Before signing any contracts, Mr. Sarraille suggests, physicians should also consider whether the hospital shares the same values. Ask physicians at the hospital what they have to say about the hospital’s culture, vision, and values. Have physicians left the hospital after their practices were acquired? Consider speaking with them to learn why.
Keep in mind that a doctor’s reputation could be impacted by a compliance complaint, regardless of whether it’s directed at the hospital and not the employed physician, Mr. Sarraille said.
“The [Erlanger] complaint focuses on the compensation of specific, named physicians saying they were wildly overcompensated,” he said. “The implication is that they sold their referral power in exchange for a pay day. It’s a bad look, no matter how the case evolves from here.”
Physicians could also face their own liability risk under the Stark Law and False Claims Act, depending on the circumstances. In the event of related quality-of-care issues, medical liability could come into play, Mr. Sarraille noted. In such cases, plaintiffs’ attorneys may see an opportunity to boost their claims with allegations that the patient harm was a function of “chasing compensation dollars,” Mr. Sarraille said.
“Where that happens, plaintiff lawyers see the potential for crippling punitive damages, which might not be covered by an insurer,” he said.
A version of this article appeared on Medscape.com.
Strapped for cash and searching for new profits, Tennessee-based Erlanger Health System illegally paid excessive salaries to physicians in exchange for patient referrals, the US government alleged in a federal lawsuit.
Erlanger changed its compensation model to entice revenue-generating doctors, paying some two to three times the median salary for their specialty, according to the complaint.
The physicians in turn referred numerous patients to Erlanger, and the health system submitted claims to Medicare for the referred services in violation of the Stark Law, according to the suit, filed in US District Court for the Western District of North Carolina.
The government’s complaint “serves as a warning” to healthcare providers who try to boost profits through improper financial arrangements with referring physicians, said Tamala E. Miles, Special Agent in Charge for the US Department of Health and Human Services (HHS) Office of Inspector General (OIG).
In a statement provided to this news organization, Erlanger denied the allegations and said it would “vigorously” defend the lawsuit.
“Erlanger paid physicians based on amounts that outside experts advised was fair market value,” Erlanger officials said in the statement. “Erlanger did not pay for referrals. A complete picture of the facts will demonstrate that the allegations lack merit and tell a very different story than what the government now claims.”
The Erlanger case is a reminder to physicians to consult their own knowledgeable advisors when considering financial arrangements with hospitals, said William Sarraille, JD, adjunct professor for the University of Maryland Francis King Carey School of Law in Baltimore and a regulatory consultant.
“There is a tendency by physicians when contracting ... to rely on [hospitals’] perceived compliance and legal expertise,” Mr. Sarraille told this news organization. “This case illustrates the risks in doing so. Sometimes bigger doesn’t translate into more sophisticated or more effective from a compliance perspective.”
Stark Law Prohibits Kickbacks
The Stark Law prohibits hospitals from billing the Centers for Medicare & Medicaid Services (CMS) for services referred by a physician with whom the hospital has an improper financial relationship.
CMS paid Erlanger about $27.8 million for claims stemming from the improper financial arrangements, the government contends.
“HHS-OIG will continue to investigate such deals to prevent financial arrangements that could compromise impartial medical judgment, increase healthcare costs, and erode public trust in the healthcare system,” Ms. Miles said in a statement.
Suit: Health System’s Money Woes Led to Illegal Arrangements
Erlanger’s financial troubles allegedly started after a previous run-in with the US government over false claims.
In 2005, Erlanger Health System agreed to pay the government $40 million to resolve allegations that it knowingly submitted false claims to Medicare, according to the government’s complaint. At the time, Erlanger entered into a Corporate Integrity Agreement (CIA) with the OIG that required Erlanger to put controls in place to ensure its financial relationships did not violate the Stark Law.
Erlanger’s agreement with OIG ended in 2010. Over the next 3 years, the health system lost nearly $32 million and in fiscal year 2013, had only 65 days of cash on hand, according to the government’s lawsuit.
Beginning in 2013, Erlanger allegedly implemented a strategy to increase profits by employing more physicians, particularly specialists from competing hospitals whose patients would need costly hospital stays, according to the complaint.
Once hired, Erlanger’s physicians were expected to treat patients at Erlanger’s hospitals and refer them to other providers within the health system, the suit claims. Erlanger also relaxed or eliminated the oversight and controls on physician compensation put in place under the CIA. For example, Erlanger’s CEO signed some compensation contracts before its chief compliance officer could review them and no longer allowed the compliance officer to vote on whether to approve compensation arrangements, according to the complaint.
Erlanger also changed its compensation model to include large salaries for medical director and academic positions and allegedly paid such salaries to physicians without ensuring the required work was performed. As a result, Erlanger physicians with profitable referrals were among the highest paid in the nation for their specialties, the government claims. For example, according to the complaint:
- Erlanger paid an electrophysiologist an annual clinical salary of $816,701, a medical director salary of $101,080, an academic salary of $59,322, and a productivity incentive based on work relative value units (wRVUs). The medical director and academic salaries paid were near the 90th percentile of comparable salaries in the specialty.
- The health system paid a neurosurgeon a base salary of $654,735, a productivity incentive based on wRVUs, and payments for excess call coverage ranging from $400 to $1000 per 24-hour shift. In 2016, the neurosurgeon made $500,000 in excess call payments.
- Erlanger paid a cardiothoracic surgeon a base clinical salary of $1,070,000, a sign-on bonus of $150,000, a retention bonus of $100,000 (payable in the 4th year of the contract), and a program incentive of up to $150,000 per year.
In addition, Erlanger ignored patient safety concerns about some of its high revenue-generating physicians, the government claims.
For instance, Erlanger received multiple complaints that a cardiothoracic surgeon was misusing an expensive form of life support in which pumps and oxygenators take over heart and lung function. Overuse of the equipment prolonged patients’ hospital stays and increased the hospital fees generated by the surgeon, according to the complaint. Staff also raised concerns about the cardiothoracic surgeon’s patient outcomes.
But Erlanger disregarded the concerns and in 2018, increased the cardiothoracic surgeon’s retention bonus from $100,000 to $250,000, the suit alleges. A year later, the health system increased his base salary from $1,070,000 to $1,195,000.
Health care compensation and billing consultants alerted Erlanger that it was overpaying salaries and handing out bonuses based on measures that overstated the work physicians were performing, but Erlanger ignored the warnings, according to the complaint.
Administrators allegedly resisted efforts by the chief compliance officer to hire an outside consultant to review its compensation models. Erlanger fired the compliance officer in 2019.
The former chief compliance officer and another administrator filed a whistleblower lawsuit against Erlanger in 2021. The two administrators are relators in the government’s July 2024 lawsuit.
How to Protect Yourself From Illegal Hospital Deals
The Erlanger case is the latest in a series of recent complaints by the federal government involving financial arrangements between hospitals and physicians.
In December 2023, Indianapolis-based Community Health Network Inc. agreed to pay the government $345 million to resolve claims that it paid physicians above fair market value and awarded bonuses tied to referrals in violation of the Stark Law.
Also in 2023, Saginaw, Michigan–based Covenant HealthCare and two physicians paid the government $69 million to settle allegations that administrators engaged in improper financial arrangements with referring physicians and a physician-owned investment group. In another 2023 case, Massachusetts Eye and Ear in Boston agreed to pay $5.7 million to resolve claims that some of its physician compensation plans violated the Stark Law.
Before you enter into a financial arrangement with a hospital, it’s also important to examine what percentile the aggregate compensation would reflect, law professor Mr. Sarraille said. The Erlanger case highlights federal officials’ suspicion of compensation, in aggregate, that exceeds the 90th percentile and increased attention to compensation that exceeds the 75th percentile, he said.
To research compensation levels, doctors can review the Medical Group Management Association’s annual compensation report or search its compensation data.
Before signing any contracts, Mr. Sarraille suggests, physicians should also consider whether the hospital shares the same values. Ask physicians at the hospital what they have to say about the hospital’s culture, vision, and values. Have physicians left the hospital after their practices were acquired? Consider speaking with them to learn why.
Keep in mind that a doctor’s reputation could be impacted by a compliance complaint, regardless of whether it’s directed at the hospital and not the employed physician, Mr. Sarraille said.
“The [Erlanger] complaint focuses on the compensation of specific, named physicians saying they were wildly overcompensated,” he said. “The implication is that they sold their referral power in exchange for a pay day. It’s a bad look, no matter how the case evolves from here.”
Physicians could also face their own liability risk under the Stark Law and False Claims Act, depending on the circumstances. In the event of related quality-of-care issues, medical liability could come into play, Mr. Sarraille noted. In such cases, plaintiffs’ attorneys may see an opportunity to boost their claims with allegations that the patient harm was a function of “chasing compensation dollars,” Mr. Sarraille said.
“Where that happens, plaintiff lawyers see the potential for crippling punitive damages, which might not be covered by an insurer,” he said.
A version of this article appeared on Medscape.com.