User login
Agrees that OC use clearly reduces mortality
Agrees that OC use clearly reduces mortality
Recent evidence from long-term observations of hundreds of thousands of women, in 10 European countries, clearly demonstrated that the use of oral contraceptives (OCs) reduced mortality by roughly 10%.1,2 Newer OCs increase women’s overall survival.
In comparison, reducing obesity by 5 body mass index points would reduce mortality by only 5%, from 1.05 to 1.3
Dr. Stavros Saripanidis
Thessaloniki, Greece
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Merritt MA, Riboli E, Murphy N, et al. Reproductive factors and risk of mortality in the European Prospective Investigation into Cancer and Nutrition: a cohort study. BMC Med. 2015;13:252.
- Iversen L, Sivasubramaniam S, Lee AJ, Fielding S, Hannaford PC. Lifetime cancer risk and combined oral contraceptives: the Royal College of General Practitioners’ Oral Contraception Study. Am J Obstet Gynecol. 2017;216(6):580.e1–580.e9.
- Aune D, Sen A, Prasad M, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ. 2016;353:i2156.
Agrees that OC use clearly reduces mortality
Recent evidence from long-term observations of hundreds of thousands of women, in 10 European countries, clearly demonstrated that the use of oral contraceptives (OCs) reduced mortality by roughly 10%.1,2 Newer OCs increase women’s overall survival.
In comparison, reducing obesity by 5 body mass index points would reduce mortality by only 5%, from 1.05 to 1.3
Dr. Stavros Saripanidis
Thessaloniki, Greece
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Agrees that OC use clearly reduces mortality
Recent evidence from long-term observations of hundreds of thousands of women, in 10 European countries, clearly demonstrated that the use of oral contraceptives (OCs) reduced mortality by roughly 10%.1,2 Newer OCs increase women’s overall survival.
In comparison, reducing obesity by 5 body mass index points would reduce mortality by only 5%, from 1.05 to 1.3
Dr. Stavros Saripanidis
Thessaloniki, Greece
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Merritt MA, Riboli E, Murphy N, et al. Reproductive factors and risk of mortality in the European Prospective Investigation into Cancer and Nutrition: a cohort study. BMC Med. 2015;13:252.
- Iversen L, Sivasubramaniam S, Lee AJ, Fielding S, Hannaford PC. Lifetime cancer risk and combined oral contraceptives: the Royal College of General Practitioners’ Oral Contraception Study. Am J Obstet Gynecol. 2017;216(6):580.e1–580.e9.
- Aune D, Sen A, Prasad M, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ. 2016;353:i2156.
- Merritt MA, Riboli E, Murphy N, et al. Reproductive factors and risk of mortality in the European Prospective Investigation into Cancer and Nutrition: a cohort study. BMC Med. 2015;13:252.
- Iversen L, Sivasubramaniam S, Lee AJ, Fielding S, Hannaford PC. Lifetime cancer risk and combined oral contraceptives: the Royal College of General Practitioners’ Oral Contraception Study. Am J Obstet Gynecol. 2017;216(6):580.e1–580.e9.
- Aune D, Sen A, Prasad M, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ. 2016;353:i2156.
Dehydration in terminal illness: Which path forward?
CASE 1
A 94-year-old white woman, who had been in excellent health (other than pernicious anemia, treated with monthly cyanocobalamin injections), suddenly developed gastrointestinal distress 2 weeks earlier. A work-up performed by her physician revealed advanced pancreatic cancer.
Over the next 2 weeks, she experienced pain and nausea. A left-sided fistula developed externally at her flank that drained feces and induced considerable discomfort. An indwelling drain was placed, which provided some relief, but the patient’s dyspepsia, pain, and nausea escalated.
One month into her disease course, an oncologist reported on her potential treatment options and prognosis. Her life expectancy was about 3 months without treatment. This could be extended by 1 to 2 months with extensive surgical and chemotherapeutic interventions, but would further diminish her quality of life. The patient declined further treatment.
Her clinical status declined, and her quality of life significantly deteriorated. At 3 months, she felt life had lost meaning and was not worth living. She began asking for a morphine overdose, stating a desire to end her life.
After several discussions with the oncologist, one of the patient’s adult children suggested that her mother stop eating and drinking in order to diminish discomfort and hasten her demise. This plan was adopted, and the patient declined food and drank only enough to swish for oral comfort.
CASE 2
An 83-year-old woman with advanced Parkinson’s disease had become increasingly disabled. Her gait and motor skills were dramatically and progressively compromised. Pharmacotherapy yielded only transient improvement and considerable adverse effects of choreiform hyperkinesia and hallucinations, which were troublesome and embarrassing. Her social, physical, and personal well-being declined to the point that she was placed in a nursing home.
Despite this help, worsening parkinsonism progressively diminished her physical capacity. She became largely bedridden and developed decubitus ulcerations, especially at the coccyx, which produced severe pain and distress.
Continue to: The confluence of pain...
The confluence of pain, bedfastness, constipation, and social isolation yielded a loss of interest and joy in life. The patient required assistance with almost every aspect of daily life, including eating. As the illness progressed, she prayed at night that God would “take her.” Each morning, she spoke of disappointment upon reawakening. She overtly expressed her lack of desire to live to her family. Medical interventions were increasingly ineffective.
After repeated family and physician discussions had focused on her death wishes, one adult daughter recommended her mother stop eating and drinking; her food intake was already minimal. Although she did not endorse this plan verbally, the patient’s oral intake significantly diminished. Within 2 weeks, her physical state had declined, and she died one night during sleep.
Adequate hydration is stressed in physician education and practice. A conventional expectation to normalize fluid balance is important to restore health and improve well-being. In addition to being good medical practice, it can also show patients (and their families) that we care about their well-being.1-3
Treating dehydration in individuals with terminal illness is controversial from both medical and ethical standpoints. While the natural tendency of physicians is to restore full hydration to their patients, in select cases of imminent death, being fully hydrated may prolong discomfort.1,2 Emphasis in this population should be consistently placed on improving comfort care and quality of life, rather than prolonging life or delaying death.3-5
Continue to: A multifactorial, patient-based decision
A multifactorial, patient-based decision
Years ago, before the advent of hospitalizing people with terminal illnesses, dying at home amongst loved ones was believed to be peaceful. Nevertheless, questions arise about the practical vs ethical approach to caring for patients with terminal illness.2 Sometimes it is difficult to find a balance between potential health care benefits and the burdens induced by medical, legal, moral, and/or social pressures. Our medical communities and the general population uphold preserving dignity at the end of life, which is supported by organizations such as Compassion & Choices (a nonprofit group that seeks to improve and expand options for end of life care; https://www.compassionandchoices.org).
Allowing for voluntary, patient-determined dehydration in those with terminal illness can offer greater comfort than maintaining the physiologic degrees of fluid balance. There are 3 key considerations to bear in mind:
- Hydration is usually a standard part of quality medical care.1
- Selectively allowing dehydration in patients who are dying can facilitate comfort.1-5
- Dehydration may be a deliberate strategy to hasten death.6
When is dehydration appropriate?
Hydration is not favored whenever doing so may increase discomfort and prolong pain without meaningful life.3 In people with terminal illness, hydration may reduce quality of life.7
The data support dehydration in certain patients. A randomized controlled trial involving 129 patients receiving hospice care compared parenteral hydration with placebo, documenting that rehydration did not improve symptoms or quality of life; there was no significant difference between patients who were hydrated and those who were dehydrated.7 In fact, dehydration may even yield greater patient comfort.8
Case reports, retrospective chart reviews, and testimonials from health care professionals have reported that being less hydrated can diminish nausea, vomiting, diarrhea, ascites, edema, and urinary or bowel incontinence, with less skin breakdown.8 Hydration, on the other hand, may exacerbate dyspnea, coughing, and choking, increasing the need for suctioning.
Continue to: A component of palliative care
A component of palliative care. When death is imminent, palliation becomes key. Pain may be more manageable with less fluids, an important goal for this population.6,8 Dehydration is associated with an accumulation of opioids throughout body fluid volumes, which may decrease pain, consciousness, and/or agony.2 Pharmacotherapies might also have greater efficacy in a dehydrated patient.9 In addition, tissue shrinkage might mitigate pain from tumors, especially those in confined spaces.8
Hospice care and palliative medicine confirm that routine hydration is not always advisable; allowing for dehydration is a conventional practice, especially in older adults with terminal illness.7 However, do not deny access to liquids if a patient wants them, and never force unwanted fluids by any route.8 Facilitate oral care in the form of swishing fluids, elective drinking, or providing mouth lubrication for any patients selectively allowed to become dehydrated.3,8
The role of the physician in decision-making
Patients with terminal illness sometimes do not want fluids and may actively decline food and drink.10 This can be emotionally distressing for family members and/or caregivers to witness. Physicians can address this concern by compassionately explaining: “I know you are concerned that your relative is not eating or drinking, but there is no indication that hydration or parenteral feeding will improve function or quality of life.”10 This can generate a discussion between physicians and families by acknowledging concerns, relieving distress, and leading to what is ultimately best for the patient.
Implications for practice: Individualized autonomy
Physicians must identify patients who wish to die by purposely becoming dehydrated and uphold the important physician obligation to hydrate those with a recoverable illness. Allowing for a moderate degree of dehydration might provide greater comfort in select people with terminal illness. Some individuals for whom life has lost meaning may choose dehydration as a means to hasten their departure.4-6 Allowing individualized autonomy over life and death choices is part of a physician’s obligation to their patients. It can be difficult for caregivers, but it is medically indicated to comply with a patient’s desire for comfort when death is imminent.
Providing palliation as a priority over treatment is sometimes challenging, but comfort care takes preference and is always coordinated with the person’s own wishes. Facilitating dehydration removes assisted-suicide issues or requests and thus affords everyone involved more emotional comfort. An advantage of this method is that a decisional patient maintains full control over the direction of their choices and helps preserve dignity during the end of life.
CORRESPONDENCE
Steven Lippmann, MD, Department of Psychiatry, University of Louisville School of Medicine, 401 East Chestnut Street, Suite 610, Louisville, KY 40202; sblipp01@louisville.edu
1. Burge FI. Dehydration and provision of fluids in palliative care. What is the evidence? Can Fam Physician. 1996;42:2383-2388.
2. Printz LA. Is withholding hydration a valid comfort measure in the terminally ill? Geriatrics. 1988;43:84-88.
3. Lippmann S. Palliative dehydration. Prim Care Companion CNS Disord. 2015;17: doi: 10.4088/PCC.15101797.
4. Bernat JL, Gert B, Mogielnicki RP. Patient refusal of hydration and nutrition: an alternative to physician-assisted suicide or voluntary active euthanasia. Arch Intern Med. 1993;153:2723-2728.
5. Sullivan RJ. Accepting death without artificial nutrition or hydration. J Gen Intern Med.1993;8:220-224.
6. Miller FG, Meier DE. Voluntary death: a comparison of terminal dehydration and physician-assisted suicide. Ann Intern Med. 1998;128:559-562.
7. Bruera E, Hui D, Dalal S, et al. Parenteral hydration in patients with advanced cancer: a multicenter, double-blind, placebo-controlled randomized trial. J Clin Oncol. 2013;31:111-118.
8. Forrow L, Smith HS. Pain management in end of life: palliative care. In: Warfield CA, Bajwa ZH, ed. Principles and Practice of Pain Management. 2nd ed. New York, NY: McGraw-Hill; 2004.
9. Zerwekh JV. The dehydration question. Nursing. 1983;13:47-51.
10. Bailey F, Harman S. Palliative care: The last hours and days of life. www.uptodate.com. September, 2016. Accessed on September 11, 2018.
CASE 1
A 94-year-old white woman, who had been in excellent health (other than pernicious anemia, treated with monthly cyanocobalamin injections), suddenly developed gastrointestinal distress 2 weeks earlier. A work-up performed by her physician revealed advanced pancreatic cancer.
Over the next 2 weeks, she experienced pain and nausea. A left-sided fistula developed externally at her flank that drained feces and induced considerable discomfort. An indwelling drain was placed, which provided some relief, but the patient’s dyspepsia, pain, and nausea escalated.
One month into her disease course, an oncologist reported on her potential treatment options and prognosis. Her life expectancy was about 3 months without treatment. This could be extended by 1 to 2 months with extensive surgical and chemotherapeutic interventions, but would further diminish her quality of life. The patient declined further treatment.
Her clinical status declined, and her quality of life significantly deteriorated. At 3 months, she felt life had lost meaning and was not worth living. She began asking for a morphine overdose, stating a desire to end her life.
After several discussions with the oncologist, one of the patient’s adult children suggested that her mother stop eating and drinking in order to diminish discomfort and hasten her demise. This plan was adopted, and the patient declined food and drank only enough to swish for oral comfort.
CASE 2
An 83-year-old woman with advanced Parkinson’s disease had become increasingly disabled. Her gait and motor skills were dramatically and progressively compromised. Pharmacotherapy yielded only transient improvement and considerable adverse effects of choreiform hyperkinesia and hallucinations, which were troublesome and embarrassing. Her social, physical, and personal well-being declined to the point that she was placed in a nursing home.
Despite this help, worsening parkinsonism progressively diminished her physical capacity. She became largely bedridden and developed decubitus ulcerations, especially at the coccyx, which produced severe pain and distress.
Continue to: The confluence of pain...
The confluence of pain, bedfastness, constipation, and social isolation yielded a loss of interest and joy in life. The patient required assistance with almost every aspect of daily life, including eating. As the illness progressed, she prayed at night that God would “take her.” Each morning, she spoke of disappointment upon reawakening. She overtly expressed her lack of desire to live to her family. Medical interventions were increasingly ineffective.
After repeated family and physician discussions had focused on her death wishes, one adult daughter recommended her mother stop eating and drinking; her food intake was already minimal. Although she did not endorse this plan verbally, the patient’s oral intake significantly diminished. Within 2 weeks, her physical state had declined, and she died one night during sleep.
Adequate hydration is stressed in physician education and practice. A conventional expectation to normalize fluid balance is important to restore health and improve well-being. In addition to being good medical practice, it can also show patients (and their families) that we care about their well-being.1-3
Treating dehydration in individuals with terminal illness is controversial from both medical and ethical standpoints. While the natural tendency of physicians is to restore full hydration to their patients, in select cases of imminent death, being fully hydrated may prolong discomfort.1,2 Emphasis in this population should be consistently placed on improving comfort care and quality of life, rather than prolonging life or delaying death.3-5
Continue to: A multifactorial, patient-based decision
A multifactorial, patient-based decision
Years ago, before the advent of hospitalizing people with terminal illnesses, dying at home amongst loved ones was believed to be peaceful. Nevertheless, questions arise about the practical vs ethical approach to caring for patients with terminal illness.2 Sometimes it is difficult to find a balance between potential health care benefits and the burdens induced by medical, legal, moral, and/or social pressures. Our medical communities and the general population uphold preserving dignity at the end of life, which is supported by organizations such as Compassion & Choices (a nonprofit group that seeks to improve and expand options for end of life care; https://www.compassionandchoices.org).
Allowing for voluntary, patient-determined dehydration in those with terminal illness can offer greater comfort than maintaining the physiologic degrees of fluid balance. There are 3 key considerations to bear in mind:
- Hydration is usually a standard part of quality medical care.1
- Selectively allowing dehydration in patients who are dying can facilitate comfort.1-5
- Dehydration may be a deliberate strategy to hasten death.6
When is dehydration appropriate?
Hydration is not favored whenever doing so may increase discomfort and prolong pain without meaningful life.3 In people with terminal illness, hydration may reduce quality of life.7
The data support dehydration in certain patients. A randomized controlled trial involving 129 patients receiving hospice care compared parenteral hydration with placebo, documenting that rehydration did not improve symptoms or quality of life; there was no significant difference between patients who were hydrated and those who were dehydrated.7 In fact, dehydration may even yield greater patient comfort.8
Case reports, retrospective chart reviews, and testimonials from health care professionals have reported that being less hydrated can diminish nausea, vomiting, diarrhea, ascites, edema, and urinary or bowel incontinence, with less skin breakdown.8 Hydration, on the other hand, may exacerbate dyspnea, coughing, and choking, increasing the need for suctioning.
Continue to: A component of palliative care
A component of palliative care. When death is imminent, palliation becomes key. Pain may be more manageable with less fluids, an important goal for this population.6,8 Dehydration is associated with an accumulation of opioids throughout body fluid volumes, which may decrease pain, consciousness, and/or agony.2 Pharmacotherapies might also have greater efficacy in a dehydrated patient.9 In addition, tissue shrinkage might mitigate pain from tumors, especially those in confined spaces.8
Hospice care and palliative medicine confirm that routine hydration is not always advisable; allowing for dehydration is a conventional practice, especially in older adults with terminal illness.7 However, do not deny access to liquids if a patient wants them, and never force unwanted fluids by any route.8 Facilitate oral care in the form of swishing fluids, elective drinking, or providing mouth lubrication for any patients selectively allowed to become dehydrated.3,8
The role of the physician in decision-making
Patients with terminal illness sometimes do not want fluids and may actively decline food and drink.10 This can be emotionally distressing for family members and/or caregivers to witness. Physicians can address this concern by compassionately explaining: “I know you are concerned that your relative is not eating or drinking, but there is no indication that hydration or parenteral feeding will improve function or quality of life.”10 This can generate a discussion between physicians and families by acknowledging concerns, relieving distress, and leading to what is ultimately best for the patient.
Implications for practice: Individualized autonomy
Physicians must identify patients who wish to die by purposely becoming dehydrated and uphold the important physician obligation to hydrate those with a recoverable illness. Allowing for a moderate degree of dehydration might provide greater comfort in select people with terminal illness. Some individuals for whom life has lost meaning may choose dehydration as a means to hasten their departure.4-6 Allowing individualized autonomy over life and death choices is part of a physician’s obligation to their patients. It can be difficult for caregivers, but it is medically indicated to comply with a patient’s desire for comfort when death is imminent.
Providing palliation as a priority over treatment is sometimes challenging, but comfort care takes preference and is always coordinated with the person’s own wishes. Facilitating dehydration removes assisted-suicide issues or requests and thus affords everyone involved more emotional comfort. An advantage of this method is that a decisional patient maintains full control over the direction of their choices and helps preserve dignity during the end of life.
CORRESPONDENCE
Steven Lippmann, MD, Department of Psychiatry, University of Louisville School of Medicine, 401 East Chestnut Street, Suite 610, Louisville, KY 40202; sblipp01@louisville.edu
CASE 1
A 94-year-old white woman, who had been in excellent health (other than pernicious anemia, treated with monthly cyanocobalamin injections), suddenly developed gastrointestinal distress 2 weeks earlier. A work-up performed by her physician revealed advanced pancreatic cancer.
Over the next 2 weeks, she experienced pain and nausea. A left-sided fistula developed externally at her flank that drained feces and induced considerable discomfort. An indwelling drain was placed, which provided some relief, but the patient’s dyspepsia, pain, and nausea escalated.
One month into her disease course, an oncologist reported on her potential treatment options and prognosis. Her life expectancy was about 3 months without treatment. This could be extended by 1 to 2 months with extensive surgical and chemotherapeutic interventions, but would further diminish her quality of life. The patient declined further treatment.
Her clinical status declined, and her quality of life significantly deteriorated. At 3 months, she felt life had lost meaning and was not worth living. She began asking for a morphine overdose, stating a desire to end her life.
After several discussions with the oncologist, one of the patient’s adult children suggested that her mother stop eating and drinking in order to diminish discomfort and hasten her demise. This plan was adopted, and the patient declined food and drank only enough to swish for oral comfort.
CASE 2
An 83-year-old woman with advanced Parkinson’s disease had become increasingly disabled. Her gait and motor skills were dramatically and progressively compromised. Pharmacotherapy yielded only transient improvement and considerable adverse effects of choreiform hyperkinesia and hallucinations, which were troublesome and embarrassing. Her social, physical, and personal well-being declined to the point that she was placed in a nursing home.
Despite this help, worsening parkinsonism progressively diminished her physical capacity. She became largely bedridden and developed decubitus ulcerations, especially at the coccyx, which produced severe pain and distress.
Continue to: The confluence of pain...
The confluence of pain, bedfastness, constipation, and social isolation yielded a loss of interest and joy in life. The patient required assistance with almost every aspect of daily life, including eating. As the illness progressed, she prayed at night that God would “take her.” Each morning, she spoke of disappointment upon reawakening. She overtly expressed her lack of desire to live to her family. Medical interventions were increasingly ineffective.
After repeated family and physician discussions had focused on her death wishes, one adult daughter recommended her mother stop eating and drinking; her food intake was already minimal. Although she did not endorse this plan verbally, the patient’s oral intake significantly diminished. Within 2 weeks, her physical state had declined, and she died one night during sleep.
Adequate hydration is stressed in physician education and practice. A conventional expectation to normalize fluid balance is important to restore health and improve well-being. In addition to being good medical practice, it can also show patients (and their families) that we care about their well-being.1-3
Treating dehydration in individuals with terminal illness is controversial from both medical and ethical standpoints. While the natural tendency of physicians is to restore full hydration to their patients, in select cases of imminent death, being fully hydrated may prolong discomfort.1,2 Emphasis in this population should be consistently placed on improving comfort care and quality of life, rather than prolonging life or delaying death.3-5
Continue to: A multifactorial, patient-based decision
A multifactorial, patient-based decision
Years ago, before the advent of hospitalizing people with terminal illnesses, dying at home amongst loved ones was believed to be peaceful. Nevertheless, questions arise about the practical vs ethical approach to caring for patients with terminal illness.2 Sometimes it is difficult to find a balance between potential health care benefits and the burdens induced by medical, legal, moral, and/or social pressures. Our medical communities and the general population uphold preserving dignity at the end of life, which is supported by organizations such as Compassion & Choices (a nonprofit group that seeks to improve and expand options for end of life care; https://www.compassionandchoices.org).
Allowing for voluntary, patient-determined dehydration in those with terminal illness can offer greater comfort than maintaining the physiologic degrees of fluid balance. There are 3 key considerations to bear in mind:
- Hydration is usually a standard part of quality medical care.1
- Selectively allowing dehydration in patients who are dying can facilitate comfort.1-5
- Dehydration may be a deliberate strategy to hasten death.6
When is dehydration appropriate?
Hydration is not favored whenever doing so may increase discomfort and prolong pain without meaningful life.3 In people with terminal illness, hydration may reduce quality of life.7
The data support dehydration in certain patients. A randomized controlled trial involving 129 patients receiving hospice care compared parenteral hydration with placebo, documenting that rehydration did not improve symptoms or quality of life; there was no significant difference between patients who were hydrated and those who were dehydrated.7 In fact, dehydration may even yield greater patient comfort.8
Case reports, retrospective chart reviews, and testimonials from health care professionals have reported that being less hydrated can diminish nausea, vomiting, diarrhea, ascites, edema, and urinary or bowel incontinence, with less skin breakdown.8 Hydration, on the other hand, may exacerbate dyspnea, coughing, and choking, increasing the need for suctioning.
Continue to: A component of palliative care
A component of palliative care. When death is imminent, palliation becomes key. Pain may be more manageable with less fluids, an important goal for this population.6,8 Dehydration is associated with an accumulation of opioids throughout body fluid volumes, which may decrease pain, consciousness, and/or agony.2 Pharmacotherapies might also have greater efficacy in a dehydrated patient.9 In addition, tissue shrinkage might mitigate pain from tumors, especially those in confined spaces.8
Hospice care and palliative medicine confirm that routine hydration is not always advisable; allowing for dehydration is a conventional practice, especially in older adults with terminal illness.7 However, do not deny access to liquids if a patient wants them, and never force unwanted fluids by any route.8 Facilitate oral care in the form of swishing fluids, elective drinking, or providing mouth lubrication for any patients selectively allowed to become dehydrated.3,8
The role of the physician in decision-making
Patients with terminal illness sometimes do not want fluids and may actively decline food and drink.10 This can be emotionally distressing for family members and/or caregivers to witness. Physicians can address this concern by compassionately explaining: “I know you are concerned that your relative is not eating or drinking, but there is no indication that hydration or parenteral feeding will improve function or quality of life.”10 This can generate a discussion between physicians and families by acknowledging concerns, relieving distress, and leading to what is ultimately best for the patient.
Implications for practice: Individualized autonomy
Physicians must identify patients who wish to die by purposely becoming dehydrated and uphold the important physician obligation to hydrate those with a recoverable illness. Allowing for a moderate degree of dehydration might provide greater comfort in select people with terminal illness. Some individuals for whom life has lost meaning may choose dehydration as a means to hasten their departure.4-6 Allowing individualized autonomy over life and death choices is part of a physician’s obligation to their patients. It can be difficult for caregivers, but it is medically indicated to comply with a patient’s desire for comfort when death is imminent.
Providing palliation as a priority over treatment is sometimes challenging, but comfort care takes preference and is always coordinated with the person’s own wishes. Facilitating dehydration removes assisted-suicide issues or requests and thus affords everyone involved more emotional comfort. An advantage of this method is that a decisional patient maintains full control over the direction of their choices and helps preserve dignity during the end of life.
CORRESPONDENCE
Steven Lippmann, MD, Department of Psychiatry, University of Louisville School of Medicine, 401 East Chestnut Street, Suite 610, Louisville, KY 40202; sblipp01@louisville.edu
1. Burge FI. Dehydration and provision of fluids in palliative care. What is the evidence? Can Fam Physician. 1996;42:2383-2388.
2. Printz LA. Is withholding hydration a valid comfort measure in the terminally ill? Geriatrics. 1988;43:84-88.
3. Lippmann S. Palliative dehydration. Prim Care Companion CNS Disord. 2015;17: doi: 10.4088/PCC.15101797.
4. Bernat JL, Gert B, Mogielnicki RP. Patient refusal of hydration and nutrition: an alternative to physician-assisted suicide or voluntary active euthanasia. Arch Intern Med. 1993;153:2723-2728.
5. Sullivan RJ. Accepting death without artificial nutrition or hydration. J Gen Intern Med.1993;8:220-224.
6. Miller FG, Meier DE. Voluntary death: a comparison of terminal dehydration and physician-assisted suicide. Ann Intern Med. 1998;128:559-562.
7. Bruera E, Hui D, Dalal S, et al. Parenteral hydration in patients with advanced cancer: a multicenter, double-blind, placebo-controlled randomized trial. J Clin Oncol. 2013;31:111-118.
8. Forrow L, Smith HS. Pain management in end of life: palliative care. In: Warfield CA, Bajwa ZH, ed. Principles and Practice of Pain Management. 2nd ed. New York, NY: McGraw-Hill; 2004.
9. Zerwekh JV. The dehydration question. Nursing. 1983;13:47-51.
10. Bailey F, Harman S. Palliative care: The last hours and days of life. www.uptodate.com. September, 2016. Accessed on September 11, 2018.
1. Burge FI. Dehydration and provision of fluids in palliative care. What is the evidence? Can Fam Physician. 1996;42:2383-2388.
2. Printz LA. Is withholding hydration a valid comfort measure in the terminally ill? Geriatrics. 1988;43:84-88.
3. Lippmann S. Palliative dehydration. Prim Care Companion CNS Disord. 2015;17: doi: 10.4088/PCC.15101797.
4. Bernat JL, Gert B, Mogielnicki RP. Patient refusal of hydration and nutrition: an alternative to physician-assisted suicide or voluntary active euthanasia. Arch Intern Med. 1993;153:2723-2728.
5. Sullivan RJ. Accepting death without artificial nutrition or hydration. J Gen Intern Med.1993;8:220-224.
6. Miller FG, Meier DE. Voluntary death: a comparison of terminal dehydration and physician-assisted suicide. Ann Intern Med. 1998;128:559-562.
7. Bruera E, Hui D, Dalal S, et al. Parenteral hydration in patients with advanced cancer: a multicenter, double-blind, placebo-controlled randomized trial. J Clin Oncol. 2013;31:111-118.
8. Forrow L, Smith HS. Pain management in end of life: palliative care. In: Warfield CA, Bajwa ZH, ed. Principles and Practice of Pain Management. 2nd ed. New York, NY: McGraw-Hill; 2004.
9. Zerwekh JV. The dehydration question. Nursing. 1983;13:47-51.
10. Bailey F, Harman S. Palliative care: The last hours and days of life. www.uptodate.com. September, 2016. Accessed on September 11, 2018.
Use metrics for populations, not individuals
Use metrics for populations, not individuals
Dr. Kanofsky’s commentary on CD metrics is 100% correct. As an ethical question for physicians and society alike, I would ask, is applying metrics to physicians even moral?
As an ObGyn for most of 4 decades, my approach to obstetrics has not changed. In some years, my CD rate was very low, and in others my rate was average. Women must be treated as individuals. Although the industrial revolution increased quality and decreased costs in manufacturing, I do not believe that we can or should apply those principles to our patients.
Government regulators, insurance companies, and many physician leaders have lost sight of the Oath of Maimonides, which states, “May the love of my art actuate me at all times; may neither avarice nor miserliness…engage my mind,”1 as well as Hippocrates’ ancient observation, “Whatsoever house I may enter, my visit shall be for the convenience and advantage of the patient.”2 In addition, in the modern version of the Hippocratic Oath that most schools use today, physicians swear to “apply, for the benefit of the sick, all measures [that] are required...”3—not to the benefit of the government, the federal budget, or an accountable care organization (ACO).
Clearly, the informed consent of a 42-year-old who had in vitro fertilization and has a floating presentation with a low Bishop score and an estimated fetal weight of 4,000 at 40 6/7 weeks must include not only the risks of primary CD but also the risks of a long labor that may result in a CD, the occasional risk of shoulder dystocia, or third- or fourth-degree extension. Not having had a case of shoulder dystocia or a third- or fourth-degree in more than a decade clearly justifies my rationale.
The morbidity of a multiple repeat CD or even a primary CD in an obese woman is significantly more risky than a non-labored elective CD in a woman of normal weight who plans to have only 1 or 2 children. We must individualize our care. Metrics are for populations, not individuals.
Health economists who aggressively advocate lower cesarean rates accept stillbirths and babies with hypoxic ischemic encephalopathy, cerebral palsy, or Erb’s palsy as long as governmental expenditures are lowered. Do the parents of these children get a vote? The majority of practicing physicians like myself feel more aligned with the Hippocratic Oath and the Oath of Maimonides. We believe that we have a moral, ethical, and medical responsibility to the individual patient and not to an ACO or government bean counter.
I would suggest an overarching theme: choice—the freedom to make our own intelligent decisions based on reasonable data and interpretation of the medical literature.
One size does not fit all. So why do those pushing comparative metrics tell us there is only one way to practice obstetrics?
Howard C. Mandel, MD
Los Angeles, California
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Tan SY, Yeow ME. Moses Maimonides (1135–1204): rabbi, philosopher, physician. Singapore Med J. 2002;43(11):551–553.
- Copland J, ed. The Hippocratic Oath. In: The London Medical Repository, Monthly Journal, and Review, Volume III. 1825;23:258.
- Tyson P. The Hippocratic Oath today. Nova. March 27, 2001. http://www.pbs.org/wgbh/nova/body/hippocratic-oath-today.html. Accessed September 21, 2018.
Use metrics for populations, not individuals
Dr. Kanofsky’s commentary on CD metrics is 100% correct. As an ethical question for physicians and society alike, I would ask, is applying metrics to physicians even moral?
As an ObGyn for most of 4 decades, my approach to obstetrics has not changed. In some years, my CD rate was very low, and in others my rate was average. Women must be treated as individuals. Although the industrial revolution increased quality and decreased costs in manufacturing, I do not believe that we can or should apply those principles to our patients.
Government regulators, insurance companies, and many physician leaders have lost sight of the Oath of Maimonides, which states, “May the love of my art actuate me at all times; may neither avarice nor miserliness…engage my mind,”1 as well as Hippocrates’ ancient observation, “Whatsoever house I may enter, my visit shall be for the convenience and advantage of the patient.”2 In addition, in the modern version of the Hippocratic Oath that most schools use today, physicians swear to “apply, for the benefit of the sick, all measures [that] are required...”3—not to the benefit of the government, the federal budget, or an accountable care organization (ACO).
Clearly, the informed consent of a 42-year-old who had in vitro fertilization and has a floating presentation with a low Bishop score and an estimated fetal weight of 4,000 at 40 6/7 weeks must include not only the risks of primary CD but also the risks of a long labor that may result in a CD, the occasional risk of shoulder dystocia, or third- or fourth-degree extension. Not having had a case of shoulder dystocia or a third- or fourth-degree in more than a decade clearly justifies my rationale.
The morbidity of a multiple repeat CD or even a primary CD in an obese woman is significantly more risky than a non-labored elective CD in a woman of normal weight who plans to have only 1 or 2 children. We must individualize our care. Metrics are for populations, not individuals.
Health economists who aggressively advocate lower cesarean rates accept stillbirths and babies with hypoxic ischemic encephalopathy, cerebral palsy, or Erb’s palsy as long as governmental expenditures are lowered. Do the parents of these children get a vote? The majority of practicing physicians like myself feel more aligned with the Hippocratic Oath and the Oath of Maimonides. We believe that we have a moral, ethical, and medical responsibility to the individual patient and not to an ACO or government bean counter.
I would suggest an overarching theme: choice—the freedom to make our own intelligent decisions based on reasonable data and interpretation of the medical literature.
One size does not fit all. So why do those pushing comparative metrics tell us there is only one way to practice obstetrics?
Howard C. Mandel, MD
Los Angeles, California
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Use metrics for populations, not individuals
Dr. Kanofsky’s commentary on CD metrics is 100% correct. As an ethical question for physicians and society alike, I would ask, is applying metrics to physicians even moral?
As an ObGyn for most of 4 decades, my approach to obstetrics has not changed. In some years, my CD rate was very low, and in others my rate was average. Women must be treated as individuals. Although the industrial revolution increased quality and decreased costs in manufacturing, I do not believe that we can or should apply those principles to our patients.
Government regulators, insurance companies, and many physician leaders have lost sight of the Oath of Maimonides, which states, “May the love of my art actuate me at all times; may neither avarice nor miserliness…engage my mind,”1 as well as Hippocrates’ ancient observation, “Whatsoever house I may enter, my visit shall be for the convenience and advantage of the patient.”2 In addition, in the modern version of the Hippocratic Oath that most schools use today, physicians swear to “apply, for the benefit of the sick, all measures [that] are required...”3—not to the benefit of the government, the federal budget, or an accountable care organization (ACO).
Clearly, the informed consent of a 42-year-old who had in vitro fertilization and has a floating presentation with a low Bishop score and an estimated fetal weight of 4,000 at 40 6/7 weeks must include not only the risks of primary CD but also the risks of a long labor that may result in a CD, the occasional risk of shoulder dystocia, or third- or fourth-degree extension. Not having had a case of shoulder dystocia or a third- or fourth-degree in more than a decade clearly justifies my rationale.
The morbidity of a multiple repeat CD or even a primary CD in an obese woman is significantly more risky than a non-labored elective CD in a woman of normal weight who plans to have only 1 or 2 children. We must individualize our care. Metrics are for populations, not individuals.
Health economists who aggressively advocate lower cesarean rates accept stillbirths and babies with hypoxic ischemic encephalopathy, cerebral palsy, or Erb’s palsy as long as governmental expenditures are lowered. Do the parents of these children get a vote? The majority of practicing physicians like myself feel more aligned with the Hippocratic Oath and the Oath of Maimonides. We believe that we have a moral, ethical, and medical responsibility to the individual patient and not to an ACO or government bean counter.
I would suggest an overarching theme: choice—the freedom to make our own intelligent decisions based on reasonable data and interpretation of the medical literature.
One size does not fit all. So why do those pushing comparative metrics tell us there is only one way to practice obstetrics?
Howard C. Mandel, MD
Los Angeles, California
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Tan SY, Yeow ME. Moses Maimonides (1135–1204): rabbi, philosopher, physician. Singapore Med J. 2002;43(11):551–553.
- Copland J, ed. The Hippocratic Oath. In: The London Medical Repository, Monthly Journal, and Review, Volume III. 1825;23:258.
- Tyson P. The Hippocratic Oath today. Nova. March 27, 2001. http://www.pbs.org/wgbh/nova/body/hippocratic-oath-today.html. Accessed September 21, 2018.
- Tan SY, Yeow ME. Moses Maimonides (1135–1204): rabbi, philosopher, physician. Singapore Med J. 2002;43(11):551–553.
- Copland J, ed. The Hippocratic Oath. In: The London Medical Repository, Monthly Journal, and Review, Volume III. 1825;23:258.
- Tyson P. The Hippocratic Oath today. Nova. March 27, 2001. http://www.pbs.org/wgbh/nova/body/hippocratic-oath-today.html. Accessed September 21, 2018.
A (former) skeptic’s view of bariatric surgery
Because of the high prevalence of obesity and diabetes, bariatric surgery has become very popular. In the United States alone, there were an estimated 228,000 weight loss surgical procedures performed in 2017.1
But I must confess that for many years, I was skeptical about the value of surgery to treat obesity. Yes, everyone who had a bariatric procedure lost weight, but did the long-term benefits really outweigh the harms? I wondered if most people gradually gained back the weight they lost. And the harms can be significant, including dumping syndrome, hypoglycemia, and malabsorption—in addition to the potential for surgical complications and repeat surgery. And, I must confess that my views were likely affected by the death of a friend from complications of gastric bypass 25 years ago.
My skepticism, however, has changed to cautious optimism for carefully selected patients. I say this because we now have long-term follow-up studies demonstrating the value of bariatric procedures—especially for people with type 2 diabetes.
Most studies have been cohort studies that compare results to similar patients with obesity who did not have surgery, and the outcomes have been consistently better in patients who underwent surgery. Two recent meta-analyses summarized these results; one for all patients with obesity and the other for patients with type 2 diabetes.
Continue to: The first meta-analysis
The first meta-analysis included 11 randomized trials, 4 nonrandomized controlled trials, and 17 cohort studies and showed probable reductions in all-cause mortality and possible reductions in cancer and cardiovascular events.2 The second demonstrated significant improvements in microvascular and macrovascular disease and reduced mortality.3 The data were limited, however, because of the lack of large randomized trials with long-term follow-up.
The Stampede trial is one of a few bariatric surgery randomized trials focusing on patients with diabetes.4 The 5-year follow-up results are impressive. Nearly 30% of patients who had gastric bypass and 23% who had sleeve gastrectomy had an A1C ≤6 at 5 years compared to only 5% of those treated medically. Some patients discontinued all medications for diabetes, hypertension, and hyperlipidemia.
There is now adequate research to show that bariatric surgery provides significant benefits to properly selected patients who understand the risks. I no longer hesitate to refer patients for bariatric surgery who have been unsuccessful with weight loss—despite their best efforts.
Where do you stand?
1. American Society for Metabolic and Bariatric Surgery. Estimate of bariatric surgery numbers, 2011-2017. https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers. Accessed September 18, 2018.
2. Zhou X, Yu J, Li L, et al. Effects of bariatric surgery on mortality, cardiovascular events, and cancer outcomes in obese patients: systematic review and meta-analysis. Obes Surg. 2016;26:2590-2601.
3. Sheng B, Truong K, Spitler H, et al. The long-term effects of bariatric surgery on type 2 diabetes remission, microvascular and macrovascular complications, and mortality: a systematic review and meta-analysis. Obes Surg. 2017;27:2724-2732.
4. Schauer PR, Bhatt DL, Kirwan JP; STAMPEDE Investigators. Bariatric surgery versus intensive medical therapy for diabetes - 5-year outcomes. N Engl J Med. 2017;376:641-651.
Because of the high prevalence of obesity and diabetes, bariatric surgery has become very popular. In the United States alone, there were an estimated 228,000 weight loss surgical procedures performed in 2017.1
But I must confess that for many years, I was skeptical about the value of surgery to treat obesity. Yes, everyone who had a bariatric procedure lost weight, but did the long-term benefits really outweigh the harms? I wondered if most people gradually gained back the weight they lost. And the harms can be significant, including dumping syndrome, hypoglycemia, and malabsorption—in addition to the potential for surgical complications and repeat surgery. And, I must confess that my views were likely affected by the death of a friend from complications of gastric bypass 25 years ago.
My skepticism, however, has changed to cautious optimism for carefully selected patients. I say this because we now have long-term follow-up studies demonstrating the value of bariatric procedures—especially for people with type 2 diabetes.
Most studies have been cohort studies that compare results to similar patients with obesity who did not have surgery, and the outcomes have been consistently better in patients who underwent surgery. Two recent meta-analyses summarized these results; one for all patients with obesity and the other for patients with type 2 diabetes.
Continue to: The first meta-analysis
The first meta-analysis included 11 randomized trials, 4 nonrandomized controlled trials, and 17 cohort studies and showed probable reductions in all-cause mortality and possible reductions in cancer and cardiovascular events.2 The second demonstrated significant improvements in microvascular and macrovascular disease and reduced mortality.3 The data were limited, however, because of the lack of large randomized trials with long-term follow-up.
The Stampede trial is one of a few bariatric surgery randomized trials focusing on patients with diabetes.4 The 5-year follow-up results are impressive. Nearly 30% of patients who had gastric bypass and 23% who had sleeve gastrectomy had an A1C ≤6 at 5 years compared to only 5% of those treated medically. Some patients discontinued all medications for diabetes, hypertension, and hyperlipidemia.
There is now adequate research to show that bariatric surgery provides significant benefits to properly selected patients who understand the risks. I no longer hesitate to refer patients for bariatric surgery who have been unsuccessful with weight loss—despite their best efforts.
Where do you stand?
Because of the high prevalence of obesity and diabetes, bariatric surgery has become very popular. In the United States alone, there were an estimated 228,000 weight loss surgical procedures performed in 2017.1
But I must confess that for many years, I was skeptical about the value of surgery to treat obesity. Yes, everyone who had a bariatric procedure lost weight, but did the long-term benefits really outweigh the harms? I wondered if most people gradually gained back the weight they lost. And the harms can be significant, including dumping syndrome, hypoglycemia, and malabsorption—in addition to the potential for surgical complications and repeat surgery. And, I must confess that my views were likely affected by the death of a friend from complications of gastric bypass 25 years ago.
My skepticism, however, has changed to cautious optimism for carefully selected patients. I say this because we now have long-term follow-up studies demonstrating the value of bariatric procedures—especially for people with type 2 diabetes.
Most studies have been cohort studies that compare results to similar patients with obesity who did not have surgery, and the outcomes have been consistently better in patients who underwent surgery. Two recent meta-analyses summarized these results; one for all patients with obesity and the other for patients with type 2 diabetes.
Continue to: The first meta-analysis
The first meta-analysis included 11 randomized trials, 4 nonrandomized controlled trials, and 17 cohort studies and showed probable reductions in all-cause mortality and possible reductions in cancer and cardiovascular events.2 The second demonstrated significant improvements in microvascular and macrovascular disease and reduced mortality.3 The data were limited, however, because of the lack of large randomized trials with long-term follow-up.
The Stampede trial is one of a few bariatric surgery randomized trials focusing on patients with diabetes.4 The 5-year follow-up results are impressive. Nearly 30% of patients who had gastric bypass and 23% who had sleeve gastrectomy had an A1C ≤6 at 5 years compared to only 5% of those treated medically. Some patients discontinued all medications for diabetes, hypertension, and hyperlipidemia.
There is now adequate research to show that bariatric surgery provides significant benefits to properly selected patients who understand the risks. I no longer hesitate to refer patients for bariatric surgery who have been unsuccessful with weight loss—despite their best efforts.
Where do you stand?
1. American Society for Metabolic and Bariatric Surgery. Estimate of bariatric surgery numbers, 2011-2017. https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers. Accessed September 18, 2018.
2. Zhou X, Yu J, Li L, et al. Effects of bariatric surgery on mortality, cardiovascular events, and cancer outcomes in obese patients: systematic review and meta-analysis. Obes Surg. 2016;26:2590-2601.
3. Sheng B, Truong K, Spitler H, et al. The long-term effects of bariatric surgery on type 2 diabetes remission, microvascular and macrovascular complications, and mortality: a systematic review and meta-analysis. Obes Surg. 2017;27:2724-2732.
4. Schauer PR, Bhatt DL, Kirwan JP; STAMPEDE Investigators. Bariatric surgery versus intensive medical therapy for diabetes - 5-year outcomes. N Engl J Med. 2017;376:641-651.
1. American Society for Metabolic and Bariatric Surgery. Estimate of bariatric surgery numbers, 2011-2017. https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers. Accessed September 18, 2018.
2. Zhou X, Yu J, Li L, et al. Effects of bariatric surgery on mortality, cardiovascular events, and cancer outcomes in obese patients: systematic review and meta-analysis. Obes Surg. 2016;26:2590-2601.
3. Sheng B, Truong K, Spitler H, et al. The long-term effects of bariatric surgery on type 2 diabetes remission, microvascular and macrovascular complications, and mortality: a systematic review and meta-analysis. Obes Surg. 2017;27:2724-2732.
4. Schauer PR, Bhatt DL, Kirwan JP; STAMPEDE Investigators. Bariatric surgery versus intensive medical therapy for diabetes - 5-year outcomes. N Engl J Med. 2017;376:641-651.
Laparoscopic suturing is an option
Laparoscopic suturing is an option
Dr. Lum presented a nicely produced video demonstrating various strategies aimed at facilitating total laparoscopic hysterectomy (TLH) of the very large uterus. Her patient’s evaluation included magnetic resonance imaging. In the video, she demonstrates a variety of interventions, including the use of a preoperative gonadotropin–releasing hormone (GNRH) agonist and immediate perioperative radial artery–uterine artery embolization. Intraoperative techniques include use of ureteral stents and securing the uterine arteries at their origins.
Clearly, TLH of a huge uterus is a technical challenge. However, I’d like to suggest that a relatively basic and important skill would greatly assist in such procedures and likely obviate the need for a GNRH agonist and/or uterine artery embolization. The vessel-sealing devices shown in the video are generally not capable of sealing such large vessels adequately, and this is what leads to the massive hemorrhaging that often occurs.
Laparoscopic suturing with extracorporeal knot tying can be used effectively to control the extremely large vessels associated with a huge uterus. The judicious placement of sutures can completely control such vessels and prevent bleeding from both proximal and distal ends when 2 sutures are placed and the vessels are transected between the stitches. Many laparoscopic surgeons have come to rely on bipolar energy or ultrasonic devices to coagulate vessels. But when dealing with huge vessels, a return to basics using laparoscopic suturing will greatly benefit the patient and the surgeon by reducing blood loss and operative time.
David L. Zisow, MD
Baltimore, Maryland
Dr. Lum responds
I thank Dr. Zisow for his thoughtful comments. I agree that laparoscopic suturing is an essential skill that can be utilized to suture ligate vessels. If we consider the basics of an open hysterectomy, the uterine artery is clamped first, then suture ligated. When approaching a very large vessel during TLH, I would be concerned that a simple suture around a large vessel might tear through and cause more bleeding. To mitigate this risk, the vessel can be clamped with a grasper first, similar to the approach in an open hysterectomy. However, once a vessel is compressed, a sealing device can usually work just as well as a suture. It becomes a matter of preference and cost.
During hysterectomy of a very large uterus, a big challenge is managing bleeding of the uterus itself during manipulation from above. Bleeding from the vascular sinuses of the myometrium can be brisk and obscure visualization, potentially leading to laparotomy conversion. A common misconception is that uterine artery embolization is equivalent to suturing the uterine arteries. In actuality, the goal of a uterine artery embolization is to embolize the distal branches of the uterine arteries, which can help with any potential bleeding from the uterus itself during hysterectomy.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Laparoscopic suturing is an option
Dr. Lum presented a nicely produced video demonstrating various strategies aimed at facilitating total laparoscopic hysterectomy (TLH) of the very large uterus. Her patient’s evaluation included magnetic resonance imaging. In the video, she demonstrates a variety of interventions, including the use of a preoperative gonadotropin–releasing hormone (GNRH) agonist and immediate perioperative radial artery–uterine artery embolization. Intraoperative techniques include use of ureteral stents and securing the uterine arteries at their origins.
Clearly, TLH of a huge uterus is a technical challenge. However, I’d like to suggest that a relatively basic and important skill would greatly assist in such procedures and likely obviate the need for a GNRH agonist and/or uterine artery embolization. The vessel-sealing devices shown in the video are generally not capable of sealing such large vessels adequately, and this is what leads to the massive hemorrhaging that often occurs.
Laparoscopic suturing with extracorporeal knot tying can be used effectively to control the extremely large vessels associated with a huge uterus. The judicious placement of sutures can completely control such vessels and prevent bleeding from both proximal and distal ends when 2 sutures are placed and the vessels are transected between the stitches. Many laparoscopic surgeons have come to rely on bipolar energy or ultrasonic devices to coagulate vessels. But when dealing with huge vessels, a return to basics using laparoscopic suturing will greatly benefit the patient and the surgeon by reducing blood loss and operative time.
David L. Zisow, MD
Baltimore, Maryland
Dr. Lum responds
I thank Dr. Zisow for his thoughtful comments. I agree that laparoscopic suturing is an essential skill that can be utilized to suture ligate vessels. If we consider the basics of an open hysterectomy, the uterine artery is clamped first, then suture ligated. When approaching a very large vessel during TLH, I would be concerned that a simple suture around a large vessel might tear through and cause more bleeding. To mitigate this risk, the vessel can be clamped with a grasper first, similar to the approach in an open hysterectomy. However, once a vessel is compressed, a sealing device can usually work just as well as a suture. It becomes a matter of preference and cost.
During hysterectomy of a very large uterus, a big challenge is managing bleeding of the uterus itself during manipulation from above. Bleeding from the vascular sinuses of the myometrium can be brisk and obscure visualization, potentially leading to laparotomy conversion. A common misconception is that uterine artery embolization is equivalent to suturing the uterine arteries. In actuality, the goal of a uterine artery embolization is to embolize the distal branches of the uterine arteries, which can help with any potential bleeding from the uterus itself during hysterectomy.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Laparoscopic suturing is an option
Dr. Lum presented a nicely produced video demonstrating various strategies aimed at facilitating total laparoscopic hysterectomy (TLH) of the very large uterus. Her patient’s evaluation included magnetic resonance imaging. In the video, she demonstrates a variety of interventions, including the use of a preoperative gonadotropin–releasing hormone (GNRH) agonist and immediate perioperative radial artery–uterine artery embolization. Intraoperative techniques include use of ureteral stents and securing the uterine arteries at their origins.
Clearly, TLH of a huge uterus is a technical challenge. However, I’d like to suggest that a relatively basic and important skill would greatly assist in such procedures and likely obviate the need for a GNRH agonist and/or uterine artery embolization. The vessel-sealing devices shown in the video are generally not capable of sealing such large vessels adequately, and this is what leads to the massive hemorrhaging that often occurs.
Laparoscopic suturing with extracorporeal knot tying can be used effectively to control the extremely large vessels associated with a huge uterus. The judicious placement of sutures can completely control such vessels and prevent bleeding from both proximal and distal ends when 2 sutures are placed and the vessels are transected between the stitches. Many laparoscopic surgeons have come to rely on bipolar energy or ultrasonic devices to coagulate vessels. But when dealing with huge vessels, a return to basics using laparoscopic suturing will greatly benefit the patient and the surgeon by reducing blood loss and operative time.
David L. Zisow, MD
Baltimore, Maryland
Dr. Lum responds
I thank Dr. Zisow for his thoughtful comments. I agree that laparoscopic suturing is an essential skill that can be utilized to suture ligate vessels. If we consider the basics of an open hysterectomy, the uterine artery is clamped first, then suture ligated. When approaching a very large vessel during TLH, I would be concerned that a simple suture around a large vessel might tear through and cause more bleeding. To mitigate this risk, the vessel can be clamped with a grasper first, similar to the approach in an open hysterectomy. However, once a vessel is compressed, a sealing device can usually work just as well as a suture. It becomes a matter of preference and cost.
During hysterectomy of a very large uterus, a big challenge is managing bleeding of the uterus itself during manipulation from above. Bleeding from the vascular sinuses of the myometrium can be brisk and obscure visualization, potentially leading to laparotomy conversion. A common misconception is that uterine artery embolization is equivalent to suturing the uterine arteries. In actuality, the goal of a uterine artery embolization is to embolize the distal branches of the uterine arteries, which can help with any potential bleeding from the uterus itself during hysterectomy.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Chronic diarrhea in a 64-year-old woman
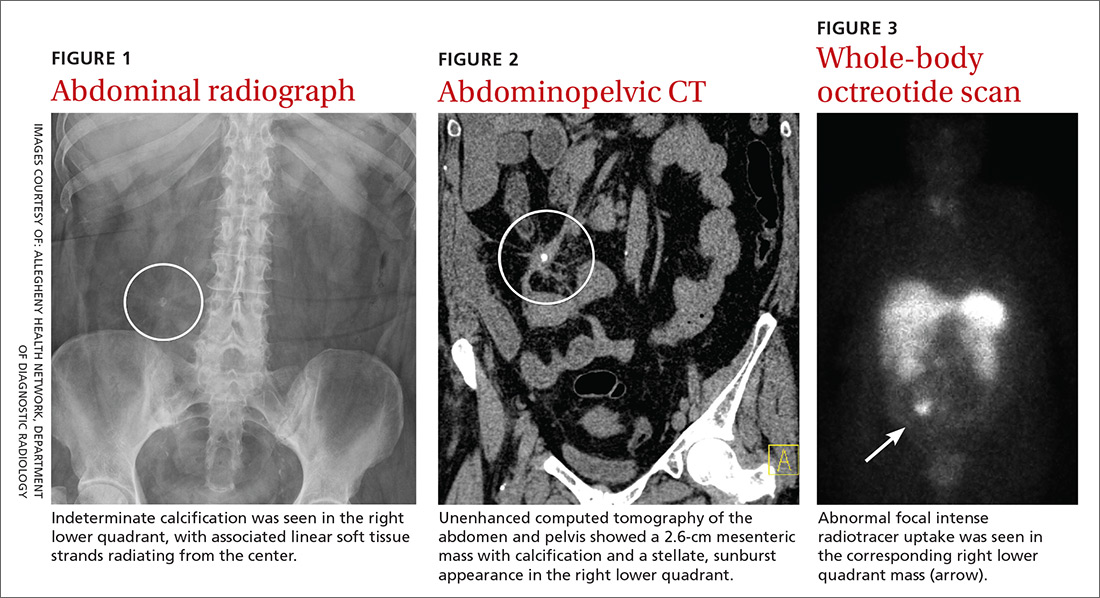
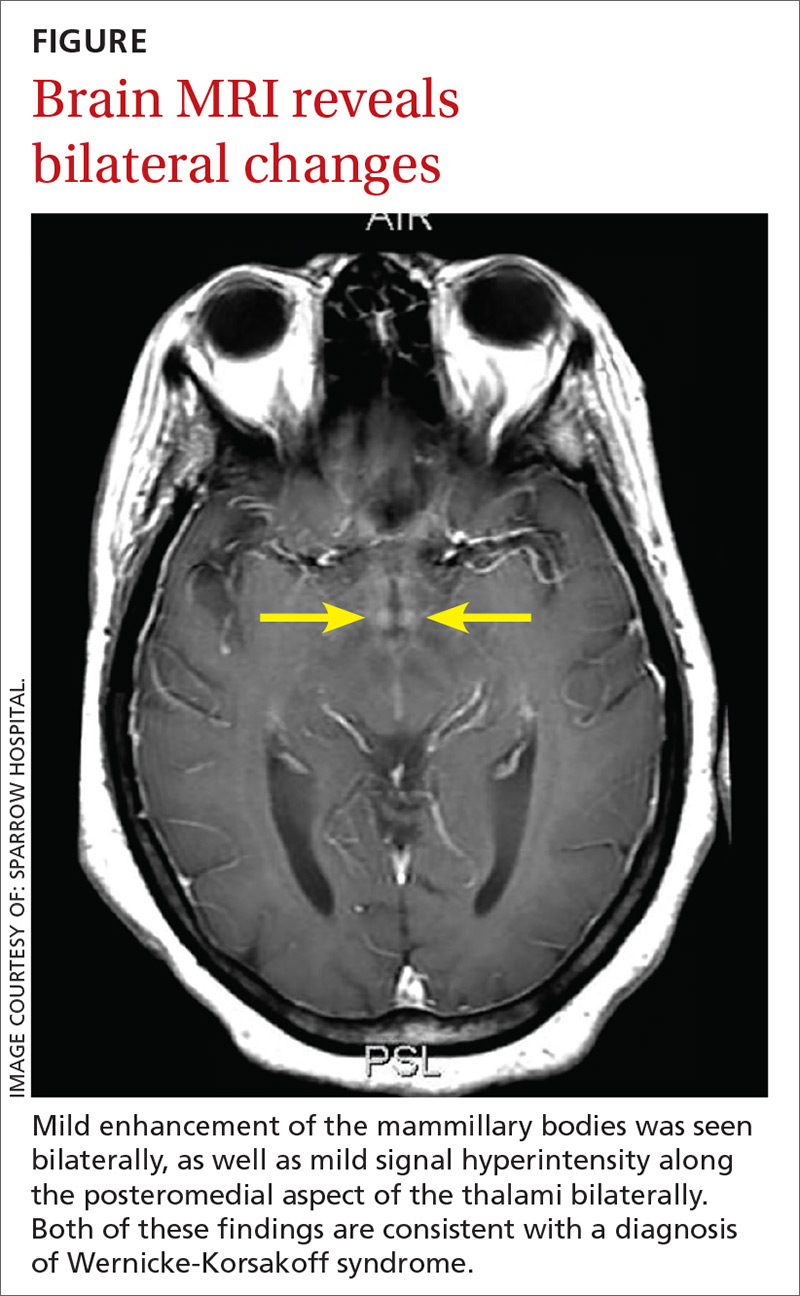
A 64-year-old woman with no significant medical history presented to the emergency department with worsening intermittent abdominal pain and chronic diarrhea, which had increased in frequency over the prior 3 months. She had taken loperamide, which yielded mild symptomatic relief. A complete metabolic panel revealed no significant abnormalities, with a normal inflammatory marker and erythrocyte sedimentation rate (ESR).
Physical examination revealed mild tenderness to palpation over the right hemiabdomen, but no rebound tenderness or guarding. An abdominal radiograph (FIGURE 1), computed tomography (CT) without contrast of the abdomen and pelvis (FIGURE 2), and a whole-body octreotide scan (FIGURE 3) were ordered.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Carcinoid tumor
Based on the patient’s symptoms and imaging studies, we suspected that she had a carcinoid tumor with mesenteric involvement. The CT showed a 2.6-cm mesenteric mass with a characteristic sunburst pattern and desmoplastic stranding, as well as numerous prominent retroperitoneal lymph nodes, suggestive of nodal involvement. The octreotide scan showed abnormal focal intense radiotracer uptake in the corresponding right lower quadrant mass, which confirmed our suspicion. There was no evidence of hepatic metastasis on the CT or octreotide scan.
Most common locations
Carcinoid tumors are the most common type of neuroendocrine tumors and are derived primarily from serotonin-producing enterochromaffin cells.1 These slow-growing, well-differentiated tumors usually originate in the gastrointestinal and bronchopulmonary tracts (67.5% and 25.3%, respectively), with uncommon primary sites involving the mesentery, ovaries, and kidneys.2 Generally, carcinoid tumors that arise in the mesentery are metastatic, often from an occult primary site. It has been reported that 40% to 80% of midgut carcinoid tumors spread to the mesentery.3
Carcinoid tumors are estimated to occur in 1.9 individuals per 100,000 annually.4 Traditionally, the appendix was cited as the most common location for these tumors. However, more recently, Modlin et al2 conducted a comprehensive analysis of epidemiologic data from the 13,715 carcinoid tumors registered in the National Cancer Institute database. Over the more than 25-year study period (1973-1999), Modlin and colleagues found a significant change in the distribution of gastrointestinal carcinoid tumors, with the incidence rates of small bowel (41.8%) and rectal carcinoids (27.4%) increasing, while appendiceal carcinoids decreased (24.1%).2
Gastrointestinal complications can arise from metastasis
Small bowel carcinoid tumors often manifest with intermittent abdominal pain, which can be caused by fibrosis of the mesentery, intestinal obstruction, or kinking of the bowel. Less common is the constellation of diarrhea, cutaneous flushing, and asthma seen with carcinoid syndrome. The prevalence of this syndrome is mediated by various humoral factors, the most notable of which is serotonin.
Continue to: Patients with carcinoid syndrome...
Patients with carcinoid syndrome often have metastasis to the liver, where serotonin is normally metabolized. This metastasis allows serotonin and other vasoactive substances to bypass hepatic metabolic degradation, resulting in the aforementioned symptoms. Carcinoid syndrome can also occur without hepatic metastasis in the setting of nodal involvement, which enables direct hormone release into the systemic circulation.5
Carcinoid syndrome affects fewer than 10% of patients with carcinoid tumors.6 Therefore, although carcinoid tumor should be suspected in patients with suggestive symptoms, other diagnoses must be considered.
Other disorders to consider on work-up
Chronic diarrhea and colicky abdominal pain are nonspecific features also associated with conditions such as inflammatory bowel disease and celiac disease, necessitating further work-up to elucidate the diagnosis.
Inflammatory bowel disease often involves elevated inflammatory markers, such as increased ESR and C-reactive protein.
Ulcerative colitis can show thickened and inflamed bowel walls on CT, with cross-sectional target appearance due to transmural involvement.
Continue to: Crohn's disease
Crohn’s disease usually affects the terminal ileum. CT is useful for identifying complications such as strictures/fistulas and abscesses.
Celiac disease involves elevated endomysial antibody and human tissue transglutaminase antibody. On CT, a characteristic jejunoileal fold pattern reversal can be seen.
A 24-hour urine test + imaging studies
The most useful diagnostic test for carcinoid tumor is the 24-hour urinary test for 5-hydroxyindoleacetic acid (5-HIAA), the metabolic end-product of serotonin. The normal rate of 5-HIAA excretion ranges from 3 to 15 mg/d, whereas the rates of patients with carcinoid tumors may have elevated levels.7
What you’ll see. On CT scan, a carcinoid tumor affecting the mesentery appears as a soft tissue mass with calcification and desmoplastic stranding, which produces a “sunburst” appearance. Another diagnostic tool is the octreotide scan, which is considered the test of choice due to its high sensitivity for detection of the tumor and metastases.8 The increase in somatostatin receptors seen with carcinoid tumors allows not only imaging by octreotide scan but also therapy using octreotide with larger doses of therapeutic radioactive agents.
Continue to: If tumor is operable, surgery is curative
If tumor is operable, surgery is curative
Surgery is the only curative therapy and is the mainstay of treatment for carcinoid tumors. Local segmental resection is generally adequate for tumors <2 cm without nodal involvement. However, tumors >2 cm with regional mesentery metastasis and nodal involvement require wide excision of the bowel and mesentery with lymph node dissection because of the associated higher incidence of metastasis.9 If the tumor has metastasized to the liver and is considered inoperable, radiolabeled octreotide or 131I-metaiodobenzylguanidine are potential treatment options for arresting tumor growth and improving survival rates.10
Our patient underwent an uncomplicated surgical resection of the mesenteric carcinoid tumor and adjacent small bowel, as well as lymph node dissection. Intraoperatively, there was no evidence of tumor elsewhere in the abdomen or pelvis, including the liver, ovaries, and other solid organs, suggesting probable metastasis from an occult primary site. The patient had an unremarkable postoperative course and was reported to be asymptomatic on follow-up.
CORRESPONDENCE
Don N. Nguyen, MD, MHA, Dept. of Diagnostic Radiology, 320 E. North Ave., Pittsburgh, PA 15212; Nguyendn3@gmail.com
1. Pinchot SN, Holen K, Sippel RS, et al. Carcinoid tumors. Oncologist. 2008;13:1255-1269.
2. Modlin M, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003; 97:934-959.
3. Park I-S, Kye B-H, Kim H-S, et al. Primary mesenteric carcinoid tumor. J Korean Surg Soc. 2013;84:114-117.
4. Crocetti E, Paci E. Malignant carcinoids in the USA, SEER 1992–1999: an epidemiological study with 6830 cases. Eur J Cancer Prev. 2003;12:191-194.
5. Sonnet S, Wiesner W. Flush symptoms caused by a mesenteric carcinoid without liver metastases. JBR-BTR. 2002;85:254-256.
6. Levy AD, Sobin L. Gastrointestinal carcinoids: imaging features with clinicopathologic comparison. RadioGraphics. 2007;27:237-257.
7. Maroun J, Kocha W, Kvols L, et al. Guidelines for the diagnosis and management of carcinoid tumours. Part 1: the gastrointestinal tract. A statement from a Canadian National Carcinoid Expert Group. Curr Oncol. 2006;13:67-76.
8. Woodside KJ, Townsend CM, Mark Evers B. Current management of gastrointestinal carcinoid tumors. J Gastrointest Surg. 2004;8:742-756.
9. de Vries H, Verschueren RC, Willemse PH, et al. Diagnostic, surgical and medical aspect of the midgut carcinoids. Cancer Treat Rev. 2002;28:11-25.
10. Akerstrom G, Hellman P, Hessman O, et al. Management of midgut carcinoids. J Surg Oncol. 2005;89:161-169.
A 64-year-old woman with no significant medical history presented to the emergency department with worsening intermittent abdominal pain and chronic diarrhea, which had increased in frequency over the prior 3 months. She had taken loperamide, which yielded mild symptomatic relief. A complete metabolic panel revealed no significant abnormalities, with a normal inflammatory marker and erythrocyte sedimentation rate (ESR).
Physical examination revealed mild tenderness to palpation over the right hemiabdomen, but no rebound tenderness or guarding. An abdominal radiograph (FIGURE 1), computed tomography (CT) without contrast of the abdomen and pelvis (FIGURE 2), and a whole-body octreotide scan (FIGURE 3) were ordered.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Carcinoid tumor
Based on the patient’s symptoms and imaging studies, we suspected that she had a carcinoid tumor with mesenteric involvement. The CT showed a 2.6-cm mesenteric mass with a characteristic sunburst pattern and desmoplastic stranding, as well as numerous prominent retroperitoneal lymph nodes, suggestive of nodal involvement. The octreotide scan showed abnormal focal intense radiotracer uptake in the corresponding right lower quadrant mass, which confirmed our suspicion. There was no evidence of hepatic metastasis on the CT or octreotide scan.
Most common locations
Carcinoid tumors are the most common type of neuroendocrine tumors and are derived primarily from serotonin-producing enterochromaffin cells.1 These slow-growing, well-differentiated tumors usually originate in the gastrointestinal and bronchopulmonary tracts (67.5% and 25.3%, respectively), with uncommon primary sites involving the mesentery, ovaries, and kidneys.2 Generally, carcinoid tumors that arise in the mesentery are metastatic, often from an occult primary site. It has been reported that 40% to 80% of midgut carcinoid tumors spread to the mesentery.3
Carcinoid tumors are estimated to occur in 1.9 individuals per 100,000 annually.4 Traditionally, the appendix was cited as the most common location for these tumors. However, more recently, Modlin et al2 conducted a comprehensive analysis of epidemiologic data from the 13,715 carcinoid tumors registered in the National Cancer Institute database. Over the more than 25-year study period (1973-1999), Modlin and colleagues found a significant change in the distribution of gastrointestinal carcinoid tumors, with the incidence rates of small bowel (41.8%) and rectal carcinoids (27.4%) increasing, while appendiceal carcinoids decreased (24.1%).2
Gastrointestinal complications can arise from metastasis
Small bowel carcinoid tumors often manifest with intermittent abdominal pain, which can be caused by fibrosis of the mesentery, intestinal obstruction, or kinking of the bowel. Less common is the constellation of diarrhea, cutaneous flushing, and asthma seen with carcinoid syndrome. The prevalence of this syndrome is mediated by various humoral factors, the most notable of which is serotonin.
Continue to: Patients with carcinoid syndrome...
Patients with carcinoid syndrome often have metastasis to the liver, where serotonin is normally metabolized. This metastasis allows serotonin and other vasoactive substances to bypass hepatic metabolic degradation, resulting in the aforementioned symptoms. Carcinoid syndrome can also occur without hepatic metastasis in the setting of nodal involvement, which enables direct hormone release into the systemic circulation.5
Carcinoid syndrome affects fewer than 10% of patients with carcinoid tumors.6 Therefore, although carcinoid tumor should be suspected in patients with suggestive symptoms, other diagnoses must be considered.
Other disorders to consider on work-up
Chronic diarrhea and colicky abdominal pain are nonspecific features also associated with conditions such as inflammatory bowel disease and celiac disease, necessitating further work-up to elucidate the diagnosis.
Inflammatory bowel disease often involves elevated inflammatory markers, such as increased ESR and C-reactive protein.
Ulcerative colitis can show thickened and inflamed bowel walls on CT, with cross-sectional target appearance due to transmural involvement.
Continue to: Crohn's disease
Crohn’s disease usually affects the terminal ileum. CT is useful for identifying complications such as strictures/fistulas and abscesses.
Celiac disease involves elevated endomysial antibody and human tissue transglutaminase antibody. On CT, a characteristic jejunoileal fold pattern reversal can be seen.
A 24-hour urine test + imaging studies
The most useful diagnostic test for carcinoid tumor is the 24-hour urinary test for 5-hydroxyindoleacetic acid (5-HIAA), the metabolic end-product of serotonin. The normal rate of 5-HIAA excretion ranges from 3 to 15 mg/d, whereas the rates of patients with carcinoid tumors may have elevated levels.7
What you’ll see. On CT scan, a carcinoid tumor affecting the mesentery appears as a soft tissue mass with calcification and desmoplastic stranding, which produces a “sunburst” appearance. Another diagnostic tool is the octreotide scan, which is considered the test of choice due to its high sensitivity for detection of the tumor and metastases.8 The increase in somatostatin receptors seen with carcinoid tumors allows not only imaging by octreotide scan but also therapy using octreotide with larger doses of therapeutic radioactive agents.
Continue to: If tumor is operable, surgery is curative
If tumor is operable, surgery is curative
Surgery is the only curative therapy and is the mainstay of treatment for carcinoid tumors. Local segmental resection is generally adequate for tumors <2 cm without nodal involvement. However, tumors >2 cm with regional mesentery metastasis and nodal involvement require wide excision of the bowel and mesentery with lymph node dissection because of the associated higher incidence of metastasis.9 If the tumor has metastasized to the liver and is considered inoperable, radiolabeled octreotide or 131I-metaiodobenzylguanidine are potential treatment options for arresting tumor growth and improving survival rates.10
Our patient underwent an uncomplicated surgical resection of the mesenteric carcinoid tumor and adjacent small bowel, as well as lymph node dissection. Intraoperatively, there was no evidence of tumor elsewhere in the abdomen or pelvis, including the liver, ovaries, and other solid organs, suggesting probable metastasis from an occult primary site. The patient had an unremarkable postoperative course and was reported to be asymptomatic on follow-up.
CORRESPONDENCE
Don N. Nguyen, MD, MHA, Dept. of Diagnostic Radiology, 320 E. North Ave., Pittsburgh, PA 15212; Nguyendn3@gmail.com
A 64-year-old woman with no significant medical history presented to the emergency department with worsening intermittent abdominal pain and chronic diarrhea, which had increased in frequency over the prior 3 months. She had taken loperamide, which yielded mild symptomatic relief. A complete metabolic panel revealed no significant abnormalities, with a normal inflammatory marker and erythrocyte sedimentation rate (ESR).
Physical examination revealed mild tenderness to palpation over the right hemiabdomen, but no rebound tenderness or guarding. An abdominal radiograph (FIGURE 1), computed tomography (CT) without contrast of the abdomen and pelvis (FIGURE 2), and a whole-body octreotide scan (FIGURE 3) were ordered.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Carcinoid tumor
Based on the patient’s symptoms and imaging studies, we suspected that she had a carcinoid tumor with mesenteric involvement. The CT showed a 2.6-cm mesenteric mass with a characteristic sunburst pattern and desmoplastic stranding, as well as numerous prominent retroperitoneal lymph nodes, suggestive of nodal involvement. The octreotide scan showed abnormal focal intense radiotracer uptake in the corresponding right lower quadrant mass, which confirmed our suspicion. There was no evidence of hepatic metastasis on the CT or octreotide scan.
Most common locations
Carcinoid tumors are the most common type of neuroendocrine tumors and are derived primarily from serotonin-producing enterochromaffin cells.1 These slow-growing, well-differentiated tumors usually originate in the gastrointestinal and bronchopulmonary tracts (67.5% and 25.3%, respectively), with uncommon primary sites involving the mesentery, ovaries, and kidneys.2 Generally, carcinoid tumors that arise in the mesentery are metastatic, often from an occult primary site. It has been reported that 40% to 80% of midgut carcinoid tumors spread to the mesentery.3
Carcinoid tumors are estimated to occur in 1.9 individuals per 100,000 annually.4 Traditionally, the appendix was cited as the most common location for these tumors. However, more recently, Modlin et al2 conducted a comprehensive analysis of epidemiologic data from the 13,715 carcinoid tumors registered in the National Cancer Institute database. Over the more than 25-year study period (1973-1999), Modlin and colleagues found a significant change in the distribution of gastrointestinal carcinoid tumors, with the incidence rates of small bowel (41.8%) and rectal carcinoids (27.4%) increasing, while appendiceal carcinoids decreased (24.1%).2
Gastrointestinal complications can arise from metastasis
Small bowel carcinoid tumors often manifest with intermittent abdominal pain, which can be caused by fibrosis of the mesentery, intestinal obstruction, or kinking of the bowel. Less common is the constellation of diarrhea, cutaneous flushing, and asthma seen with carcinoid syndrome. The prevalence of this syndrome is mediated by various humoral factors, the most notable of which is serotonin.
Continue to: Patients with carcinoid syndrome...
Patients with carcinoid syndrome often have metastasis to the liver, where serotonin is normally metabolized. This metastasis allows serotonin and other vasoactive substances to bypass hepatic metabolic degradation, resulting in the aforementioned symptoms. Carcinoid syndrome can also occur without hepatic metastasis in the setting of nodal involvement, which enables direct hormone release into the systemic circulation.5
Carcinoid syndrome affects fewer than 10% of patients with carcinoid tumors.6 Therefore, although carcinoid tumor should be suspected in patients with suggestive symptoms, other diagnoses must be considered.
Other disorders to consider on work-up
Chronic diarrhea and colicky abdominal pain are nonspecific features also associated with conditions such as inflammatory bowel disease and celiac disease, necessitating further work-up to elucidate the diagnosis.
Inflammatory bowel disease often involves elevated inflammatory markers, such as increased ESR and C-reactive protein.
Ulcerative colitis can show thickened and inflamed bowel walls on CT, with cross-sectional target appearance due to transmural involvement.
Continue to: Crohn's disease
Crohn’s disease usually affects the terminal ileum. CT is useful for identifying complications such as strictures/fistulas and abscesses.
Celiac disease involves elevated endomysial antibody and human tissue transglutaminase antibody. On CT, a characteristic jejunoileal fold pattern reversal can be seen.
A 24-hour urine test + imaging studies
The most useful diagnostic test for carcinoid tumor is the 24-hour urinary test for 5-hydroxyindoleacetic acid (5-HIAA), the metabolic end-product of serotonin. The normal rate of 5-HIAA excretion ranges from 3 to 15 mg/d, whereas the rates of patients with carcinoid tumors may have elevated levels.7
What you’ll see. On CT scan, a carcinoid tumor affecting the mesentery appears as a soft tissue mass with calcification and desmoplastic stranding, which produces a “sunburst” appearance. Another diagnostic tool is the octreotide scan, which is considered the test of choice due to its high sensitivity for detection of the tumor and metastases.8 The increase in somatostatin receptors seen with carcinoid tumors allows not only imaging by octreotide scan but also therapy using octreotide with larger doses of therapeutic radioactive agents.
Continue to: If tumor is operable, surgery is curative
If tumor is operable, surgery is curative
Surgery is the only curative therapy and is the mainstay of treatment for carcinoid tumors. Local segmental resection is generally adequate for tumors <2 cm without nodal involvement. However, tumors >2 cm with regional mesentery metastasis and nodal involvement require wide excision of the bowel and mesentery with lymph node dissection because of the associated higher incidence of metastasis.9 If the tumor has metastasized to the liver and is considered inoperable, radiolabeled octreotide or 131I-metaiodobenzylguanidine are potential treatment options for arresting tumor growth and improving survival rates.10
Our patient underwent an uncomplicated surgical resection of the mesenteric carcinoid tumor and adjacent small bowel, as well as lymph node dissection. Intraoperatively, there was no evidence of tumor elsewhere in the abdomen or pelvis, including the liver, ovaries, and other solid organs, suggesting probable metastasis from an occult primary site. The patient had an unremarkable postoperative course and was reported to be asymptomatic on follow-up.
CORRESPONDENCE
Don N. Nguyen, MD, MHA, Dept. of Diagnostic Radiology, 320 E. North Ave., Pittsburgh, PA 15212; Nguyendn3@gmail.com
1. Pinchot SN, Holen K, Sippel RS, et al. Carcinoid tumors. Oncologist. 2008;13:1255-1269.
2. Modlin M, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003; 97:934-959.
3. Park I-S, Kye B-H, Kim H-S, et al. Primary mesenteric carcinoid tumor. J Korean Surg Soc. 2013;84:114-117.
4. Crocetti E, Paci E. Malignant carcinoids in the USA, SEER 1992–1999: an epidemiological study with 6830 cases. Eur J Cancer Prev. 2003;12:191-194.
5. Sonnet S, Wiesner W. Flush symptoms caused by a mesenteric carcinoid without liver metastases. JBR-BTR. 2002;85:254-256.
6. Levy AD, Sobin L. Gastrointestinal carcinoids: imaging features with clinicopathologic comparison. RadioGraphics. 2007;27:237-257.
7. Maroun J, Kocha W, Kvols L, et al. Guidelines for the diagnosis and management of carcinoid tumours. Part 1: the gastrointestinal tract. A statement from a Canadian National Carcinoid Expert Group. Curr Oncol. 2006;13:67-76.
8. Woodside KJ, Townsend CM, Mark Evers B. Current management of gastrointestinal carcinoid tumors. J Gastrointest Surg. 2004;8:742-756.
9. de Vries H, Verschueren RC, Willemse PH, et al. Diagnostic, surgical and medical aspect of the midgut carcinoids. Cancer Treat Rev. 2002;28:11-25.
10. Akerstrom G, Hellman P, Hessman O, et al. Management of midgut carcinoids. J Surg Oncol. 2005;89:161-169.
1. Pinchot SN, Holen K, Sippel RS, et al. Carcinoid tumors. Oncologist. 2008;13:1255-1269.
2. Modlin M, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003; 97:934-959.
3. Park I-S, Kye B-H, Kim H-S, et al. Primary mesenteric carcinoid tumor. J Korean Surg Soc. 2013;84:114-117.
4. Crocetti E, Paci E. Malignant carcinoids in the USA, SEER 1992–1999: an epidemiological study with 6830 cases. Eur J Cancer Prev. 2003;12:191-194.
5. Sonnet S, Wiesner W. Flush symptoms caused by a mesenteric carcinoid without liver metastases. JBR-BTR. 2002;85:254-256.
6. Levy AD, Sobin L. Gastrointestinal carcinoids: imaging features with clinicopathologic comparison. RadioGraphics. 2007;27:237-257.
7. Maroun J, Kocha W, Kvols L, et al. Guidelines for the diagnosis and management of carcinoid tumours. Part 1: the gastrointestinal tract. A statement from a Canadian National Carcinoid Expert Group. Curr Oncol. 2006;13:67-76.
8. Woodside KJ, Townsend CM, Mark Evers B. Current management of gastrointestinal carcinoid tumors. J Gastrointest Surg. 2004;8:742-756.
9. de Vries H, Verschueren RC, Willemse PH, et al. Diagnostic, surgical and medical aspect of the midgut carcinoids. Cancer Treat Rev. 2002;28:11-25.
10. Akerstrom G, Hellman P, Hessman O, et al. Management of midgut carcinoids. J Surg Oncol. 2005;89:161-169.
Nausea and vomiting • sensitivity to smell • history of hypertension and alcohol abuse • Dx?
THE CASE
A 57-year-old woman presented to a family physician with acute encephalopathy and complaints of recent gastritis. She reported a 2-month history of nausea, vomiting, decreased oral intake, and extreme sensitivity to smell. The patient had a history of hypertension, and a family member privately disclosed to the FP that she also had a history of alcohol abuse. The patient was taking lorazepam daily, as needed, for anxiety.
On initial assessment, the patient was alert, but not oriented to time or situation. She was ataxic and agitated but did not exhibit pupillary constriction or tremor. The FP sent her to the emergency department (ED).
After being assessed in the ED, the patient was admitted. Over the course of several days, she showed worsening mentation; she persistently believed she was in Chicago, her childhood home. On memory testing, she was unable to recall any of 3 objects after 5 minutes. She exhibited horizontal nystagmus and dysmetria bilaterally and continued to be ataxic, requiring 2-point assistance. Her agitation was managed nonpharmacologically.
A work-up was performed, which included laboratory testing, a urinalysis, and computed tomography (CT) of the head. A comprehensive metabolic panel, complete blood count, and thyroid stimulating hormone test were unremarkable except for electrolyte disturbances, with a sodium level of 158 mEq/L and a potassium level of 2.6 mEq/L (reference ranges: 135-145 mEq/L and 3.5-5 mEq/L, respectively).
Her blood alcohol level was zero, and not surprisingly given her use of lorazepam, a urine drug screen was positive for benzodiazepines. The urinalysis results were consistent with a urinary tract infection (UTI), for which she was treated with an antibiotic. A carbohydrate-deficient transferrin test may have been useful to establish chronic alcohol abuse, but was not ordered. The head CT was negative.
After a few days with fluids and electrolyte replacement, the patient’s electrolytes normalized.
THE DIAGNOSIS
The differential diagnosis included sepsis, metabolic encephalopathy, and alcoholic encephalopathy. Given that the patient’s urine drug screen was positive, benzodiazepine withdrawal was also considered a plausible explanation for her continued cognitive disturbances. (It was surmised that she had likely taken her last lorazepam several days prior.) However, the lack of other signs of withdrawal prompted further investigation.
Continue to: Since her encephalopathy...
Since her encephalopathy, ataxia, and nystagmus persisted, magnetic resonance imaging (MRI) of the brain was performed on Day 3 of hospitalization (FIGURE). A lumbar puncture and an electroencephalogram were also considered but were not performed because the MRI results revealed bilateral enhancement of the m
DISCUSSION
WKS is the concurrence of Wernicke’s encephalopathy (an acute, life-threatening condition marked by ataxia, confusion, and ocular signs) and Korsakoff’s psychosis (a long-term, debilitating amnestic syndrome). WKS is a neuropsychiatric disorder in which patients experience profound short-term amnesia; it is precipitated by thiamine deficiency (defined as a whole blood thiamine level <0.7 ng/ml1).The link to thiamine was confirmed during World War II, when thiamine treatment resolved symptoms in starving prisoners. If recognized early, treatment of thiamine deficiency can prevent long-term morbidity from WKS.
Etiology of thiamine deficiency
Our patient’s alcohol abuse placed her at risk for WKS, and her olfactory aversion to certain foods was a diagnostic clue. In this case, we inadvertently administered dextrose with antibiotics for the UTI prior to administering thiamine; this exacerbated the thiamine deficiency because glucose and thiamine compete for the same substrate.
Is alcohol abuse always to blame for WKS?
The quantity and type of alcohol that results in the development of WKS has not been well studied, but the Caine diagnostic criteria defines chronic alcoholism as the consumption of 80 g/d of ethanol (8 drinks/d).2 While WKS is commonly associated with alcoholism, other causative conditions may be overlooked. Other associated illnesses include acquired immune deficiency syndrome (AIDS), cancer, hyperemesis gravidarum, prolonged total parenteral nutrition, and psychiatric illnesses such as eating disorders and schizophrenia. Procedures such as gastric bypass and dialysis can also precipitate WKS.3
Men and women are both at risk of developing WKS. A lack of consumption of thiamine-rich sources such as cereals, rice, and legumes puts patients at risk for WKS. The recommended dietary allowance of thiamine increases with age and may be higher for obese patients.4
Continue to: Suspect thiamine deficiency and obstain a thorough history
Suspect thiamine deficiency and obtain a thorough history
A high index of suspicion for thiamine deficiency is essential for diagnosis of WKS. History of alcohol use should be obtained, including quantity, frequency, pattern, duration, and time of last use. Physicians should assess nutrition and ask about vomiting and diarrhea. It is important to collaborate with the patient’s family and friends and inquire into other substance misuse.5
Since WKS targets the dorsomedial thalamus, which is responsible for olfactory processing, patients may complain of a distorted perception of smell.6 On physical examination, look for signs of protein-calorie malnutrition, including cheilitis, glossitis, and bleeding gums; signs of alcohol abuse, such as hepatomegaly; and evidence of injuries or poor self-care.5
Varied presentation leads to under- and misdiagnosis
Diagnosis of WKS can be difficult due to the varied presentation; there is a broad spectrum of clinical features. The clinical triad of mental status change, ophthalmoplegia, and gait ataxia is present in as few as 10% of cases.3 Mental status changes may include a global confusional state ranging from disorientation, apathy, anxiety, fear, and mild memory impairment to pronounced amnesia. Ophthalmoplegia can include nystagmus, ocular palsies, retinal hemorrhages, scotoma, or photophobia; and ataxia can range from a mild gait abnormality to an inability to stand.7 This varied presentation ultimately leads to underdiagnosis and misdiagnosis.
MRI findings are also varied in WKS. However, the mammillary bodies are involved in many cases, where atrophy of these structures have high specificity. The dorsomedial thalamus is associated with the reported impairment in memory and can be identified antemortem on MRI.3 There is no quantifiable evidence of how much thiamine should be used to prevent WKS. However, thiamine should be given before the administration of glucose whenever WKS is considered.
Our patient. Despite the administration of thiamine (100 mg parenterally for 5 d, followed by oral thiamine 300 mg/d indefinitely), our patient’s memory and cognition remained unchanged. She underwent intensive inpatient rehabilitation for 2 months and was eventually placed in long-term nursing care.
Continue to: THE TAKEAWAY
THE TAKEAWAY
A high index of suspicion is crucial to prevent possible long-term neurologic sequelae in WKS. Appropriate care starts at the beginning, with the patient’s story.
CORRESPONDENCE
Romith Naug, MD, 15 St. Andrew Street, Unit 601, Brockville, ON Canada K6V0B8; Romith.naug@gmail.com.
1. Doshi S, Velpandian T, Seth S, et al. Prevalence of thiamine deficiency in heart failure patients on long-term diuretic therapy. J Prac Cardiovasc Sci. 2015;1:25-29.
2. Caine D, Halliday GM, Kril JJ, et al. Operational criteria for the classification of chronic alcoholics: identification of Wernicke’s encephalopathy. J Neurol Neurosurg Psychiatry. 1997;62:51-60.
3. Donnino MW, Vega J, Miller J, et al. Myths and misconceptions of Wernicke’s encephalopathy: what every emergency physician should know. Ann Emerg Med. 2007;50:715-721.
4. Kerns J, Arundel C, Chawla LS. Thiamin deficiency in people with obesity. Adv Nutr. 2015;6:147-153.
5. Latt N, Dore G. Thiamine in the treatment of Wernicke encephalopathy in patients with alcohol use disorders. Intern Med J. 2014;44:911-915.
6. Wilson DA, Xu W, Sadrian B, et al. Cortical odor processing in health and disease. Prog Brain Res. 2014;208:275-305.
7. Isenberg-Grzeda E, Kutner HE, Nicolson SE. Wernicke-Korsakoff syndrome: under-recognized and under-treated. Psychosomatics. 2012;53:507-516.
THE CASE
A 57-year-old woman presented to a family physician with acute encephalopathy and complaints of recent gastritis. She reported a 2-month history of nausea, vomiting, decreased oral intake, and extreme sensitivity to smell. The patient had a history of hypertension, and a family member privately disclosed to the FP that she also had a history of alcohol abuse. The patient was taking lorazepam daily, as needed, for anxiety.
On initial assessment, the patient was alert, but not oriented to time or situation. She was ataxic and agitated but did not exhibit pupillary constriction or tremor. The FP sent her to the emergency department (ED).
After being assessed in the ED, the patient was admitted. Over the course of several days, she showed worsening mentation; she persistently believed she was in Chicago, her childhood home. On memory testing, she was unable to recall any of 3 objects after 5 minutes. She exhibited horizontal nystagmus and dysmetria bilaterally and continued to be ataxic, requiring 2-point assistance. Her agitation was managed nonpharmacologically.
A work-up was performed, which included laboratory testing, a urinalysis, and computed tomography (CT) of the head. A comprehensive metabolic panel, complete blood count, and thyroid stimulating hormone test were unremarkable except for electrolyte disturbances, with a sodium level of 158 mEq/L and a potassium level of 2.6 mEq/L (reference ranges: 135-145 mEq/L and 3.5-5 mEq/L, respectively).
Her blood alcohol level was zero, and not surprisingly given her use of lorazepam, a urine drug screen was positive for benzodiazepines. The urinalysis results were consistent with a urinary tract infection (UTI), for which she was treated with an antibiotic. A carbohydrate-deficient transferrin test may have been useful to establish chronic alcohol abuse, but was not ordered. The head CT was negative.
After a few days with fluids and electrolyte replacement, the patient’s electrolytes normalized.
THE DIAGNOSIS
The differential diagnosis included sepsis, metabolic encephalopathy, and alcoholic encephalopathy. Given that the patient’s urine drug screen was positive, benzodiazepine withdrawal was also considered a plausible explanation for her continued cognitive disturbances. (It was surmised that she had likely taken her last lorazepam several days prior.) However, the lack of other signs of withdrawal prompted further investigation.
Continue to: Since her encephalopathy...
Since her encephalopathy, ataxia, and nystagmus persisted, magnetic resonance imaging (MRI) of the brain was performed on Day 3 of hospitalization (FIGURE). A lumbar puncture and an electroencephalogram were also considered but were not performed because the MRI results revealed bilateral enhancement of the m
DISCUSSION
WKS is the concurrence of Wernicke’s encephalopathy (an acute, life-threatening condition marked by ataxia, confusion, and ocular signs) and Korsakoff’s psychosis (a long-term, debilitating amnestic syndrome). WKS is a neuropsychiatric disorder in which patients experience profound short-term amnesia; it is precipitated by thiamine deficiency (defined as a whole blood thiamine level <0.7 ng/ml1).The link to thiamine was confirmed during World War II, when thiamine treatment resolved symptoms in starving prisoners. If recognized early, treatment of thiamine deficiency can prevent long-term morbidity from WKS.
Etiology of thiamine deficiency
Our patient’s alcohol abuse placed her at risk for WKS, and her olfactory aversion to certain foods was a diagnostic clue. In this case, we inadvertently administered dextrose with antibiotics for the UTI prior to administering thiamine; this exacerbated the thiamine deficiency because glucose and thiamine compete for the same substrate.
Is alcohol abuse always to blame for WKS?
The quantity and type of alcohol that results in the development of WKS has not been well studied, but the Caine diagnostic criteria defines chronic alcoholism as the consumption of 80 g/d of ethanol (8 drinks/d).2 While WKS is commonly associated with alcoholism, other causative conditions may be overlooked. Other associated illnesses include acquired immune deficiency syndrome (AIDS), cancer, hyperemesis gravidarum, prolonged total parenteral nutrition, and psychiatric illnesses such as eating disorders and schizophrenia. Procedures such as gastric bypass and dialysis can also precipitate WKS.3
Men and women are both at risk of developing WKS. A lack of consumption of thiamine-rich sources such as cereals, rice, and legumes puts patients at risk for WKS. The recommended dietary allowance of thiamine increases with age and may be higher for obese patients.4
Continue to: Suspect thiamine deficiency and obstain a thorough history
Suspect thiamine deficiency and obtain a thorough history
A high index of suspicion for thiamine deficiency is essential for diagnosis of WKS. History of alcohol use should be obtained, including quantity, frequency, pattern, duration, and time of last use. Physicians should assess nutrition and ask about vomiting and diarrhea. It is important to collaborate with the patient’s family and friends and inquire into other substance misuse.5
Since WKS targets the dorsomedial thalamus, which is responsible for olfactory processing, patients may complain of a distorted perception of smell.6 On physical examination, look for signs of protein-calorie malnutrition, including cheilitis, glossitis, and bleeding gums; signs of alcohol abuse, such as hepatomegaly; and evidence of injuries or poor self-care.5
Varied presentation leads to under- and misdiagnosis
Diagnosis of WKS can be difficult due to the varied presentation; there is a broad spectrum of clinical features. The clinical triad of mental status change, ophthalmoplegia, and gait ataxia is present in as few as 10% of cases.3 Mental status changes may include a global confusional state ranging from disorientation, apathy, anxiety, fear, and mild memory impairment to pronounced amnesia. Ophthalmoplegia can include nystagmus, ocular palsies, retinal hemorrhages, scotoma, or photophobia; and ataxia can range from a mild gait abnormality to an inability to stand.7 This varied presentation ultimately leads to underdiagnosis and misdiagnosis.
MRI findings are also varied in WKS. However, the mammillary bodies are involved in many cases, where atrophy of these structures have high specificity. The dorsomedial thalamus is associated with the reported impairment in memory and can be identified antemortem on MRI.3 There is no quantifiable evidence of how much thiamine should be used to prevent WKS. However, thiamine should be given before the administration of glucose whenever WKS is considered.
Our patient. Despite the administration of thiamine (100 mg parenterally for 5 d, followed by oral thiamine 300 mg/d indefinitely), our patient’s memory and cognition remained unchanged. She underwent intensive inpatient rehabilitation for 2 months and was eventually placed in long-term nursing care.
Continue to: THE TAKEAWAY
THE TAKEAWAY
A high index of suspicion is crucial to prevent possible long-term neurologic sequelae in WKS. Appropriate care starts at the beginning, with the patient’s story.
CORRESPONDENCE
Romith Naug, MD, 15 St. Andrew Street, Unit 601, Brockville, ON Canada K6V0B8; Romith.naug@gmail.com.
THE CASE
A 57-year-old woman presented to a family physician with acute encephalopathy and complaints of recent gastritis. She reported a 2-month history of nausea, vomiting, decreased oral intake, and extreme sensitivity to smell. The patient had a history of hypertension, and a family member privately disclosed to the FP that she also had a history of alcohol abuse. The patient was taking lorazepam daily, as needed, for anxiety.
On initial assessment, the patient was alert, but not oriented to time or situation. She was ataxic and agitated but did not exhibit pupillary constriction or tremor. The FP sent her to the emergency department (ED).
After being assessed in the ED, the patient was admitted. Over the course of several days, she showed worsening mentation; she persistently believed she was in Chicago, her childhood home. On memory testing, she was unable to recall any of 3 objects after 5 minutes. She exhibited horizontal nystagmus and dysmetria bilaterally and continued to be ataxic, requiring 2-point assistance. Her agitation was managed nonpharmacologically.
A work-up was performed, which included laboratory testing, a urinalysis, and computed tomography (CT) of the head. A comprehensive metabolic panel, complete blood count, and thyroid stimulating hormone test were unremarkable except for electrolyte disturbances, with a sodium level of 158 mEq/L and a potassium level of 2.6 mEq/L (reference ranges: 135-145 mEq/L and 3.5-5 mEq/L, respectively).
Her blood alcohol level was zero, and not surprisingly given her use of lorazepam, a urine drug screen was positive for benzodiazepines. The urinalysis results were consistent with a urinary tract infection (UTI), for which she was treated with an antibiotic. A carbohydrate-deficient transferrin test may have been useful to establish chronic alcohol abuse, but was not ordered. The head CT was negative.
After a few days with fluids and electrolyte replacement, the patient’s electrolytes normalized.
THE DIAGNOSIS
The differential diagnosis included sepsis, metabolic encephalopathy, and alcoholic encephalopathy. Given that the patient’s urine drug screen was positive, benzodiazepine withdrawal was also considered a plausible explanation for her continued cognitive disturbances. (It was surmised that she had likely taken her last lorazepam several days prior.) However, the lack of other signs of withdrawal prompted further investigation.
Continue to: Since her encephalopathy...
Since her encephalopathy, ataxia, and nystagmus persisted, magnetic resonance imaging (MRI) of the brain was performed on Day 3 of hospitalization (FIGURE). A lumbar puncture and an electroencephalogram were also considered but were not performed because the MRI results revealed bilateral enhancement of the m
DISCUSSION
WKS is the concurrence of Wernicke’s encephalopathy (an acute, life-threatening condition marked by ataxia, confusion, and ocular signs) and Korsakoff’s psychosis (a long-term, debilitating amnestic syndrome). WKS is a neuropsychiatric disorder in which patients experience profound short-term amnesia; it is precipitated by thiamine deficiency (defined as a whole blood thiamine level <0.7 ng/ml1).The link to thiamine was confirmed during World War II, when thiamine treatment resolved symptoms in starving prisoners. If recognized early, treatment of thiamine deficiency can prevent long-term morbidity from WKS.
Etiology of thiamine deficiency
Our patient’s alcohol abuse placed her at risk for WKS, and her olfactory aversion to certain foods was a diagnostic clue. In this case, we inadvertently administered dextrose with antibiotics for the UTI prior to administering thiamine; this exacerbated the thiamine deficiency because glucose and thiamine compete for the same substrate.
Is alcohol abuse always to blame for WKS?
The quantity and type of alcohol that results in the development of WKS has not been well studied, but the Caine diagnostic criteria defines chronic alcoholism as the consumption of 80 g/d of ethanol (8 drinks/d).2 While WKS is commonly associated with alcoholism, other causative conditions may be overlooked. Other associated illnesses include acquired immune deficiency syndrome (AIDS), cancer, hyperemesis gravidarum, prolonged total parenteral nutrition, and psychiatric illnesses such as eating disorders and schizophrenia. Procedures such as gastric bypass and dialysis can also precipitate WKS.3
Men and women are both at risk of developing WKS. A lack of consumption of thiamine-rich sources such as cereals, rice, and legumes puts patients at risk for WKS. The recommended dietary allowance of thiamine increases with age and may be higher for obese patients.4
Continue to: Suspect thiamine deficiency and obstain a thorough history
Suspect thiamine deficiency and obtain a thorough history
A high index of suspicion for thiamine deficiency is essential for diagnosis of WKS. History of alcohol use should be obtained, including quantity, frequency, pattern, duration, and time of last use. Physicians should assess nutrition and ask about vomiting and diarrhea. It is important to collaborate with the patient’s family and friends and inquire into other substance misuse.5
Since WKS targets the dorsomedial thalamus, which is responsible for olfactory processing, patients may complain of a distorted perception of smell.6 On physical examination, look for signs of protein-calorie malnutrition, including cheilitis, glossitis, and bleeding gums; signs of alcohol abuse, such as hepatomegaly; and evidence of injuries or poor self-care.5
Varied presentation leads to under- and misdiagnosis
Diagnosis of WKS can be difficult due to the varied presentation; there is a broad spectrum of clinical features. The clinical triad of mental status change, ophthalmoplegia, and gait ataxia is present in as few as 10% of cases.3 Mental status changes may include a global confusional state ranging from disorientation, apathy, anxiety, fear, and mild memory impairment to pronounced amnesia. Ophthalmoplegia can include nystagmus, ocular palsies, retinal hemorrhages, scotoma, or photophobia; and ataxia can range from a mild gait abnormality to an inability to stand.7 This varied presentation ultimately leads to underdiagnosis and misdiagnosis.
MRI findings are also varied in WKS. However, the mammillary bodies are involved in many cases, where atrophy of these structures have high specificity. The dorsomedial thalamus is associated with the reported impairment in memory and can be identified antemortem on MRI.3 There is no quantifiable evidence of how much thiamine should be used to prevent WKS. However, thiamine should be given before the administration of glucose whenever WKS is considered.
Our patient. Despite the administration of thiamine (100 mg parenterally for 5 d, followed by oral thiamine 300 mg/d indefinitely), our patient’s memory and cognition remained unchanged. She underwent intensive inpatient rehabilitation for 2 months and was eventually placed in long-term nursing care.
Continue to: THE TAKEAWAY
THE TAKEAWAY
A high index of suspicion is crucial to prevent possible long-term neurologic sequelae in WKS. Appropriate care starts at the beginning, with the patient’s story.
CORRESPONDENCE
Romith Naug, MD, 15 St. Andrew Street, Unit 601, Brockville, ON Canada K6V0B8; Romith.naug@gmail.com.
1. Doshi S, Velpandian T, Seth S, et al. Prevalence of thiamine deficiency in heart failure patients on long-term diuretic therapy. J Prac Cardiovasc Sci. 2015;1:25-29.
2. Caine D, Halliday GM, Kril JJ, et al. Operational criteria for the classification of chronic alcoholics: identification of Wernicke’s encephalopathy. J Neurol Neurosurg Psychiatry. 1997;62:51-60.
3. Donnino MW, Vega J, Miller J, et al. Myths and misconceptions of Wernicke’s encephalopathy: what every emergency physician should know. Ann Emerg Med. 2007;50:715-721.
4. Kerns J, Arundel C, Chawla LS. Thiamin deficiency in people with obesity. Adv Nutr. 2015;6:147-153.
5. Latt N, Dore G. Thiamine in the treatment of Wernicke encephalopathy in patients with alcohol use disorders. Intern Med J. 2014;44:911-915.
6. Wilson DA, Xu W, Sadrian B, et al. Cortical odor processing in health and disease. Prog Brain Res. 2014;208:275-305.
7. Isenberg-Grzeda E, Kutner HE, Nicolson SE. Wernicke-Korsakoff syndrome: under-recognized and under-treated. Psychosomatics. 2012;53:507-516.
1. Doshi S, Velpandian T, Seth S, et al. Prevalence of thiamine deficiency in heart failure patients on long-term diuretic therapy. J Prac Cardiovasc Sci. 2015;1:25-29.
2. Caine D, Halliday GM, Kril JJ, et al. Operational criteria for the classification of chronic alcoholics: identification of Wernicke’s encephalopathy. J Neurol Neurosurg Psychiatry. 1997;62:51-60.
3. Donnino MW, Vega J, Miller J, et al. Myths and misconceptions of Wernicke’s encephalopathy: what every emergency physician should know. Ann Emerg Med. 2007;50:715-721.
4. Kerns J, Arundel C, Chawla LS. Thiamin deficiency in people with obesity. Adv Nutr. 2015;6:147-153.
5. Latt N, Dore G. Thiamine in the treatment of Wernicke encephalopathy in patients with alcohol use disorders. Intern Med J. 2014;44:911-915.
6. Wilson DA, Xu W, Sadrian B, et al. Cortical odor processing in health and disease. Prog Brain Res. 2014;208:275-305.
7. Isenberg-Grzeda E, Kutner HE, Nicolson SE. Wernicke-Korsakoff syndrome: under-recognized and under-treated. Psychosomatics. 2012;53:507-516.
How to treat complicated grief
THE CASE
Al* is a 48-year-old patient whose wife, Vera, died of complications from chronic illness 14 months ago. Al thinks about Vera constantly and says he still has difficulty accepting that she is gone. He does not leave the house much anymore and continues to set a place for her at the kitchen table on special occasions. He says, “Some nights in bed, I swear I can hear her in the living room.”
How would you proceed with this patient?
* The names of the patient and his spouse have been changed to protect their identities.
After the loss of a loved one, grief is a natural response to the separation and stress that go along with the death. Most people, after suffering a loss, experience distress that varies in intensity and gradually decreases over time. Thus, the grieving individual does not act as they would normally if they were not bereaved. However, gains are generally made month by month, and most people adjust to the grief and adapt their lives after some time dealing with the absence of the loved one.1
There’s grief, and then there’s complicated grief
For about 2% to 4% of the population who have experienced a significant loss, complicated grief is an issue.2 As its hallmark, complicated grief exceeds the typical amount of time (6-12 months) that people need to recover from a loss. Prevalence has been estimated at 10% to 20% among grieving individuals for whom the death being grieved was that of a romantic partner or child.2 At increased risk for this disorder are women older than 60 years, patients diagnosed with depression or substance abuse, individuals under financial strain, and those who have experienced a violent or sudden loss.3
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) has conceptualized complicated grief with the name, persistent complex bereavement disorder (PCBD).4 While the guidelines for the definition are still in progress, several specified symptoms must have been present for at least 6 months to a year or more (TABLE 14). For instance, the patient has been ruminating about the death, has been unable to accept the death, or has felt shocked or numb. They may also experience anger, have difficulty trusting others, and be preoccupied with the deceased (eg, sense they can hear their lost loved one, feel the loved one’s pain for them). Symptoms of PCBD may also include experiencing vivid reminders of the loss and avoiding situations that bring up thoughts about the death.4 (Of note: A grief diagnosis in ICD-10 is captured by the code F43.21; however, there is no specific code for complicated grief or PCBD.)
PCBD is a “condition for further study” in DSM-5; it was omitted from DSM-IV only after much debate. One reason for its omission was concern that clinicians might “pathologize” grief more than it needs to be.5 Grief is regarded as a natural process that might be stymied by a formal diagnosis leading to medical treatment.
Shifting the grief diagnosis paradigm
One new development is that recently bereaved patients can be diagnosed with depression if they meet the criteria for that diagnosis. In the past, someone who met criteria for major depression would be excluded from that diagnosis if the depression ensued from grief. DSM-5 no longer makes that distinction.4 Given this diagnostic shift, one might wonder about the difference between PCBD and depression, particularly if the patient is a grieving individual with a current diagnosis of depression.5
Continue to: Differences between PCBD and major depression
Differences between PCBD and major depression. While antidepressant medication is helpful for patients with moderate-to-severe depression, it has thus far been less helpful for those solely experiencing complicated grief.6 The same holds true for traditional psychotherapy. While family physicians can confidently refer people to psychotherapy for depression, it is not as efficacious as focused therapy designed for those with PCBD.6
Other differences between PCBD and major depression involve the constructs of guilt and yearning. Depressed patients typically feel guilty about a number of things, while those with complicated grief have specific death-focused guilt.7 Depressed people generally do not yearn, while those with grief yearn for their loved one. Finally, and most concerning to clinicians, some patients with PCBD have suicidal thoughts.8 While such thoughts in depression are often linked to hopelessness, suicidal thoughts for grieving individuals are generally driven by a desire to be reunited with the deceased loved one.
While these differences may help in making treatment decisions, there can be overlap between depression and complicated grief. As with many mental health diagnoses, major depression and PCBD are not mutually exclusive.4
The role of hospice. Another factor sometimes associated with complicated grief is any hindrance to the survivor’s ability to communicate or say goodbye to the loved one at the end of life.9 This may be avoided if the loved one is in hospice care and is not subjected to procedures that impair communication (ie, ventilator use, sedation). Medicare requires that certified hospice programs offer bereavement services for 1 year following patient death.10 Some hospice providers even offer bereavement services to those not enrolled in hospice. However, evidence indicates that only about 30% of bereaved caregivers take advantage of hospice bereavement services.11 Family physicians may help patients during this process by providing an early referral to hospice services and recommending bereavement counseling. Referral to hospice care can also facilitate discussions that the patient may need to have with the physician or others regarding spirituality. Hospital chaplains can also be referred or get involved with patients and family upon request.
Assessment focal points and tools
As is the case with most mental health concerns, primary care is at the forefront of early assessment. Evaluation of grief is an ongoing process and is multifactorial. One focus is the intensity of the grief. Is the patient reacting to the loss in a way that is disproportionately severe when compared with others who grieve? Another factor is the time elapsed since the loss. If the loss was more than 6 months ago, the patient should have made some progress. Assess grieving patients at around 6 months post-loss to determine how they are handling grief. As mentioned, DSM-5 has criteria for PCBD that providers can use in determining a patient’s grief status. Also needed are assessments for the other DSM-5 issues often associated with loss: depression and post-traumatic stress disorder.
Continue to: While no clinical measure is perfect...
While no clinical measure is perfect, there are tools that can help in assessing patients for the possibility of complicated grief (TABLE 2). Also keep in mind that no measure can make a diagnosis of PCBD, as it is a clinical judgment, not a score on a scale. Furthermore, there is no measure that can accurately predict future complicated grief.6 In most busy practices, the Brief Grief Questionnaire (http://www.massgeneral.org/psychiatry/assets/Brief_Grief_Questionnaire.pdf ) would be the easiest tool to administer, but a case could be made for any of the measures.
Treatment
The literature base emphasizes that PCBD treatment requires a different focus than that applied to uncomplicated grief. And while most people with major depression will respond to medication and psychotherapy, there are provisos to keep in mind when depression is associated with complicated grief.
Complicated grief treatment (CGT) has been studied extensively.6 This treatment combines some of the tenets of evidence-based PTSD treatments, interpersonal therapy for grief, and cognitive behavioral therapy. CGT is generally an individual treatment, although group therapy using some of its tenets can also be effective. According to complicated grief researchers, tasks to accomplish in CGT include establishing a “new normal” following the loss, promoting self-regulation in the grieving, building social connections, and setting aspirational goals for the future.6 Other goals are to revisit the world, tell stories of the past, and relive old memories in a more positive light. Common suggestions in CGT that run parallel to conventional thoughts on dealing with grief include increasing time outside the home, getting more involved interpersonally, and increasing mindfulness-based practices.
A second-line evidence-based treatment for PCBD is the use of selective serotonin-reuptake inhibitors (SSRIs).6 Some studies have found benefit from SSRI treatment, although the findings are preliminary and modest.12 One observational study examined patients who had recently experienced loss and were receiving CGT with or without medication. Researchers found that CGT with medication (citalopram) led to a 61% positive response rate while CGT alone led to a 41% response rate.13 Thus, findings revealed some benefit to combining an antidepressant with CGT, indicating that SSRIs may be helpful as an adjunct treatment.
THE CASE
Al was treated for complicated grief by his family physician and a psychologist for approximately a year. He responded well to an SSRI and received psychotherapy that focused on the tenets of CGT. Prior to his last psychotherapy visit, he reported leaving the house regularly to dine at restaurants and meet up with co-workers after hours. He said, “I still miss Vera quite a bit, but I know that I feel better.”
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu
1. Cozza SJ, Fisher JE, Mauro C, et al. Performance of DSM-5 persistent complex bereavement disorder criteria in a community sample of bereaved military family members. Am J Psychiatry. 2016;173:919-929.
2. Kersting A, Brähler E, Glaesmer H, et al. Prevalence of complicated grief in a representative population-based sample. J Affect Disord. 2011;131:339-343.
3. Fujisawa D, Miyashita M, Nakajima S, et al. Prevalence and determinants of complicated grief in general population. J Affect Disord. 2010;127:352-358.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: APA Press; 2013.
5. Shear MK, Simon N, Wall M, et al. Complicated grief and related issues for DSM-5. Depress Anxiety. 2011;28:103-117.
6. Shear MK. Clinical Practice. Complicated grief. N Engl J Med. 2015;372:153-160.
7. Wolfelt AD. Counseling Skills for Companioning the Mourner: The Fundamentals of Effective Grief Counseling. Fort Collins, CO: Companion Press; 2016.
8. Szanto K, Shear MK, Houck PR, et al. Indirect self-destructive behavior and overt suicidality in patients with complicated grief. J Clin Psychiatry. 2006;67:233-239.
9. Otani H, Yoshida S, Morita T, et al. Meaningful communication before death, but not present at the time of death itself, is associated with better outcomes on measures of depression and complicated grief among bereaved family members of cancer patients. J Pain Symptom Manage. 2017;54:273-279.
10. CMS. Medicare benefit policy manual: coverage of hospice services under hospital insurance. www.cms.gov/Regulations-and-guidance/Guidance/Manuals/downloads/bp102c09.pdf. Accessed February 25, 2018.
11. Cherlin E, Barry LC, Prigerson H, et al. Bereavement services for family caregivers: how often used, why, and why not. J Palliat Med. 2007;10:148–158.
12. Bui E, Nidal-Vicens M, Simon NM. Pharmacologic approaches to the treatment of complicated grief: rationale and a brief review of the literature. Dialogues Clin Neurosci. 2012;14:149-157.
13. Shear MK, Reynolds CF 3rd, Simon NM, et al. Optimizing treatment of complicated grief: a randomized clinical trial. JAMA Psychiatry. 2016;73:685-694.
THE CASE
Al* is a 48-year-old patient whose wife, Vera, died of complications from chronic illness 14 months ago. Al thinks about Vera constantly and says he still has difficulty accepting that she is gone. He does not leave the house much anymore and continues to set a place for her at the kitchen table on special occasions. He says, “Some nights in bed, I swear I can hear her in the living room.”
How would you proceed with this patient?
* The names of the patient and his spouse have been changed to protect their identities.
After the loss of a loved one, grief is a natural response to the separation and stress that go along with the death. Most people, after suffering a loss, experience distress that varies in intensity and gradually decreases over time. Thus, the grieving individual does not act as they would normally if they were not bereaved. However, gains are generally made month by month, and most people adjust to the grief and adapt their lives after some time dealing with the absence of the loved one.1
There’s grief, and then there’s complicated grief
For about 2% to 4% of the population who have experienced a significant loss, complicated grief is an issue.2 As its hallmark, complicated grief exceeds the typical amount of time (6-12 months) that people need to recover from a loss. Prevalence has been estimated at 10% to 20% among grieving individuals for whom the death being grieved was that of a romantic partner or child.2 At increased risk for this disorder are women older than 60 years, patients diagnosed with depression or substance abuse, individuals under financial strain, and those who have experienced a violent or sudden loss.3
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) has conceptualized complicated grief with the name, persistent complex bereavement disorder (PCBD).4 While the guidelines for the definition are still in progress, several specified symptoms must have been present for at least 6 months to a year or more (TABLE 14). For instance, the patient has been ruminating about the death, has been unable to accept the death, or has felt shocked or numb. They may also experience anger, have difficulty trusting others, and be preoccupied with the deceased (eg, sense they can hear their lost loved one, feel the loved one’s pain for them). Symptoms of PCBD may also include experiencing vivid reminders of the loss and avoiding situations that bring up thoughts about the death.4 (Of note: A grief diagnosis in ICD-10 is captured by the code F43.21; however, there is no specific code for complicated grief or PCBD.)
PCBD is a “condition for further study” in DSM-5; it was omitted from DSM-IV only after much debate. One reason for its omission was concern that clinicians might “pathologize” grief more than it needs to be.5 Grief is regarded as a natural process that might be stymied by a formal diagnosis leading to medical treatment.
Shifting the grief diagnosis paradigm
One new development is that recently bereaved patients can be diagnosed with depression if they meet the criteria for that diagnosis. In the past, someone who met criteria for major depression would be excluded from that diagnosis if the depression ensued from grief. DSM-5 no longer makes that distinction.4 Given this diagnostic shift, one might wonder about the difference between PCBD and depression, particularly if the patient is a grieving individual with a current diagnosis of depression.5
Continue to: Differences between PCBD and major depression
Differences between PCBD and major depression. While antidepressant medication is helpful for patients with moderate-to-severe depression, it has thus far been less helpful for those solely experiencing complicated grief.6 The same holds true for traditional psychotherapy. While family physicians can confidently refer people to psychotherapy for depression, it is not as efficacious as focused therapy designed for those with PCBD.6
Other differences between PCBD and major depression involve the constructs of guilt and yearning. Depressed patients typically feel guilty about a number of things, while those with complicated grief have specific death-focused guilt.7 Depressed people generally do not yearn, while those with grief yearn for their loved one. Finally, and most concerning to clinicians, some patients with PCBD have suicidal thoughts.8 While such thoughts in depression are often linked to hopelessness, suicidal thoughts for grieving individuals are generally driven by a desire to be reunited with the deceased loved one.
While these differences may help in making treatment decisions, there can be overlap between depression and complicated grief. As with many mental health diagnoses, major depression and PCBD are not mutually exclusive.4
The role of hospice. Another factor sometimes associated with complicated grief is any hindrance to the survivor’s ability to communicate or say goodbye to the loved one at the end of life.9 This may be avoided if the loved one is in hospice care and is not subjected to procedures that impair communication (ie, ventilator use, sedation). Medicare requires that certified hospice programs offer bereavement services for 1 year following patient death.10 Some hospice providers even offer bereavement services to those not enrolled in hospice. However, evidence indicates that only about 30% of bereaved caregivers take advantage of hospice bereavement services.11 Family physicians may help patients during this process by providing an early referral to hospice services and recommending bereavement counseling. Referral to hospice care can also facilitate discussions that the patient may need to have with the physician or others regarding spirituality. Hospital chaplains can also be referred or get involved with patients and family upon request.
Assessment focal points and tools
As is the case with most mental health concerns, primary care is at the forefront of early assessment. Evaluation of grief is an ongoing process and is multifactorial. One focus is the intensity of the grief. Is the patient reacting to the loss in a way that is disproportionately severe when compared with others who grieve? Another factor is the time elapsed since the loss. If the loss was more than 6 months ago, the patient should have made some progress. Assess grieving patients at around 6 months post-loss to determine how they are handling grief. As mentioned, DSM-5 has criteria for PCBD that providers can use in determining a patient’s grief status. Also needed are assessments for the other DSM-5 issues often associated with loss: depression and post-traumatic stress disorder.
Continue to: While no clinical measure is perfect...
While no clinical measure is perfect, there are tools that can help in assessing patients for the possibility of complicated grief (TABLE 2). Also keep in mind that no measure can make a diagnosis of PCBD, as it is a clinical judgment, not a score on a scale. Furthermore, there is no measure that can accurately predict future complicated grief.6 In most busy practices, the Brief Grief Questionnaire (http://www.massgeneral.org/psychiatry/assets/Brief_Grief_Questionnaire.pdf ) would be the easiest tool to administer, but a case could be made for any of the measures.
Treatment
The literature base emphasizes that PCBD treatment requires a different focus than that applied to uncomplicated grief. And while most people with major depression will respond to medication and psychotherapy, there are provisos to keep in mind when depression is associated with complicated grief.
Complicated grief treatment (CGT) has been studied extensively.6 This treatment combines some of the tenets of evidence-based PTSD treatments, interpersonal therapy for grief, and cognitive behavioral therapy. CGT is generally an individual treatment, although group therapy using some of its tenets can also be effective. According to complicated grief researchers, tasks to accomplish in CGT include establishing a “new normal” following the loss, promoting self-regulation in the grieving, building social connections, and setting aspirational goals for the future.6 Other goals are to revisit the world, tell stories of the past, and relive old memories in a more positive light. Common suggestions in CGT that run parallel to conventional thoughts on dealing with grief include increasing time outside the home, getting more involved interpersonally, and increasing mindfulness-based practices.
A second-line evidence-based treatment for PCBD is the use of selective serotonin-reuptake inhibitors (SSRIs).6 Some studies have found benefit from SSRI treatment, although the findings are preliminary and modest.12 One observational study examined patients who had recently experienced loss and were receiving CGT with or without medication. Researchers found that CGT with medication (citalopram) led to a 61% positive response rate while CGT alone led to a 41% response rate.13 Thus, findings revealed some benefit to combining an antidepressant with CGT, indicating that SSRIs may be helpful as an adjunct treatment.
THE CASE
Al was treated for complicated grief by his family physician and a psychologist for approximately a year. He responded well to an SSRI and received psychotherapy that focused on the tenets of CGT. Prior to his last psychotherapy visit, he reported leaving the house regularly to dine at restaurants and meet up with co-workers after hours. He said, “I still miss Vera quite a bit, but I know that I feel better.”
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu
THE CASE
Al* is a 48-year-old patient whose wife, Vera, died of complications from chronic illness 14 months ago. Al thinks about Vera constantly and says he still has difficulty accepting that she is gone. He does not leave the house much anymore and continues to set a place for her at the kitchen table on special occasions. He says, “Some nights in bed, I swear I can hear her in the living room.”
How would you proceed with this patient?
* The names of the patient and his spouse have been changed to protect their identities.
After the loss of a loved one, grief is a natural response to the separation and stress that go along with the death. Most people, after suffering a loss, experience distress that varies in intensity and gradually decreases over time. Thus, the grieving individual does not act as they would normally if they were not bereaved. However, gains are generally made month by month, and most people adjust to the grief and adapt their lives after some time dealing with the absence of the loved one.1
There’s grief, and then there’s complicated grief
For about 2% to 4% of the population who have experienced a significant loss, complicated grief is an issue.2 As its hallmark, complicated grief exceeds the typical amount of time (6-12 months) that people need to recover from a loss. Prevalence has been estimated at 10% to 20% among grieving individuals for whom the death being grieved was that of a romantic partner or child.2 At increased risk for this disorder are women older than 60 years, patients diagnosed with depression or substance abuse, individuals under financial strain, and those who have experienced a violent or sudden loss.3
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) has conceptualized complicated grief with the name, persistent complex bereavement disorder (PCBD).4 While the guidelines for the definition are still in progress, several specified symptoms must have been present for at least 6 months to a year or more (TABLE 14). For instance, the patient has been ruminating about the death, has been unable to accept the death, or has felt shocked or numb. They may also experience anger, have difficulty trusting others, and be preoccupied with the deceased (eg, sense they can hear their lost loved one, feel the loved one’s pain for them). Symptoms of PCBD may also include experiencing vivid reminders of the loss and avoiding situations that bring up thoughts about the death.4 (Of note: A grief diagnosis in ICD-10 is captured by the code F43.21; however, there is no specific code for complicated grief or PCBD.)
PCBD is a “condition for further study” in DSM-5; it was omitted from DSM-IV only after much debate. One reason for its omission was concern that clinicians might “pathologize” grief more than it needs to be.5 Grief is regarded as a natural process that might be stymied by a formal diagnosis leading to medical treatment.
Shifting the grief diagnosis paradigm
One new development is that recently bereaved patients can be diagnosed with depression if they meet the criteria for that diagnosis. In the past, someone who met criteria for major depression would be excluded from that diagnosis if the depression ensued from grief. DSM-5 no longer makes that distinction.4 Given this diagnostic shift, one might wonder about the difference between PCBD and depression, particularly if the patient is a grieving individual with a current diagnosis of depression.5
Continue to: Differences between PCBD and major depression
Differences between PCBD and major depression. While antidepressant medication is helpful for patients with moderate-to-severe depression, it has thus far been less helpful for those solely experiencing complicated grief.6 The same holds true for traditional psychotherapy. While family physicians can confidently refer people to psychotherapy for depression, it is not as efficacious as focused therapy designed for those with PCBD.6
Other differences between PCBD and major depression involve the constructs of guilt and yearning. Depressed patients typically feel guilty about a number of things, while those with complicated grief have specific death-focused guilt.7 Depressed people generally do not yearn, while those with grief yearn for their loved one. Finally, and most concerning to clinicians, some patients with PCBD have suicidal thoughts.8 While such thoughts in depression are often linked to hopelessness, suicidal thoughts for grieving individuals are generally driven by a desire to be reunited with the deceased loved one.
While these differences may help in making treatment decisions, there can be overlap between depression and complicated grief. As with many mental health diagnoses, major depression and PCBD are not mutually exclusive.4
The role of hospice. Another factor sometimes associated with complicated grief is any hindrance to the survivor’s ability to communicate or say goodbye to the loved one at the end of life.9 This may be avoided if the loved one is in hospice care and is not subjected to procedures that impair communication (ie, ventilator use, sedation). Medicare requires that certified hospice programs offer bereavement services for 1 year following patient death.10 Some hospice providers even offer bereavement services to those not enrolled in hospice. However, evidence indicates that only about 30% of bereaved caregivers take advantage of hospice bereavement services.11 Family physicians may help patients during this process by providing an early referral to hospice services and recommending bereavement counseling. Referral to hospice care can also facilitate discussions that the patient may need to have with the physician or others regarding spirituality. Hospital chaplains can also be referred or get involved with patients and family upon request.
Assessment focal points and tools
As is the case with most mental health concerns, primary care is at the forefront of early assessment. Evaluation of grief is an ongoing process and is multifactorial. One focus is the intensity of the grief. Is the patient reacting to the loss in a way that is disproportionately severe when compared with others who grieve? Another factor is the time elapsed since the loss. If the loss was more than 6 months ago, the patient should have made some progress. Assess grieving patients at around 6 months post-loss to determine how they are handling grief. As mentioned, DSM-5 has criteria for PCBD that providers can use in determining a patient’s grief status. Also needed are assessments for the other DSM-5 issues often associated with loss: depression and post-traumatic stress disorder.
Continue to: While no clinical measure is perfect...
While no clinical measure is perfect, there are tools that can help in assessing patients for the possibility of complicated grief (TABLE 2). Also keep in mind that no measure can make a diagnosis of PCBD, as it is a clinical judgment, not a score on a scale. Furthermore, there is no measure that can accurately predict future complicated grief.6 In most busy practices, the Brief Grief Questionnaire (http://www.massgeneral.org/psychiatry/assets/Brief_Grief_Questionnaire.pdf ) would be the easiest tool to administer, but a case could be made for any of the measures.
Treatment
The literature base emphasizes that PCBD treatment requires a different focus than that applied to uncomplicated grief. And while most people with major depression will respond to medication and psychotherapy, there are provisos to keep in mind when depression is associated with complicated grief.
Complicated grief treatment (CGT) has been studied extensively.6 This treatment combines some of the tenets of evidence-based PTSD treatments, interpersonal therapy for grief, and cognitive behavioral therapy. CGT is generally an individual treatment, although group therapy using some of its tenets can also be effective. According to complicated grief researchers, tasks to accomplish in CGT include establishing a “new normal” following the loss, promoting self-regulation in the grieving, building social connections, and setting aspirational goals for the future.6 Other goals are to revisit the world, tell stories of the past, and relive old memories in a more positive light. Common suggestions in CGT that run parallel to conventional thoughts on dealing with grief include increasing time outside the home, getting more involved interpersonally, and increasing mindfulness-based practices.
A second-line evidence-based treatment for PCBD is the use of selective serotonin-reuptake inhibitors (SSRIs).6 Some studies have found benefit from SSRI treatment, although the findings are preliminary and modest.12 One observational study examined patients who had recently experienced loss and were receiving CGT with or without medication. Researchers found that CGT with medication (citalopram) led to a 61% positive response rate while CGT alone led to a 41% response rate.13 Thus, findings revealed some benefit to combining an antidepressant with CGT, indicating that SSRIs may be helpful as an adjunct treatment.
THE CASE
Al was treated for complicated grief by his family physician and a psychologist for approximately a year. He responded well to an SSRI and received psychotherapy that focused on the tenets of CGT. Prior to his last psychotherapy visit, he reported leaving the house regularly to dine at restaurants and meet up with co-workers after hours. He said, “I still miss Vera quite a bit, but I know that I feel better.”
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu
1. Cozza SJ, Fisher JE, Mauro C, et al. Performance of DSM-5 persistent complex bereavement disorder criteria in a community sample of bereaved military family members. Am J Psychiatry. 2016;173:919-929.
2. Kersting A, Brähler E, Glaesmer H, et al. Prevalence of complicated grief in a representative population-based sample. J Affect Disord. 2011;131:339-343.
3. Fujisawa D, Miyashita M, Nakajima S, et al. Prevalence and determinants of complicated grief in general population. J Affect Disord. 2010;127:352-358.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: APA Press; 2013.
5. Shear MK, Simon N, Wall M, et al. Complicated grief and related issues for DSM-5. Depress Anxiety. 2011;28:103-117.
6. Shear MK. Clinical Practice. Complicated grief. N Engl J Med. 2015;372:153-160.
7. Wolfelt AD. Counseling Skills for Companioning the Mourner: The Fundamentals of Effective Grief Counseling. Fort Collins, CO: Companion Press; 2016.
8. Szanto K, Shear MK, Houck PR, et al. Indirect self-destructive behavior and overt suicidality in patients with complicated grief. J Clin Psychiatry. 2006;67:233-239.
9. Otani H, Yoshida S, Morita T, et al. Meaningful communication before death, but not present at the time of death itself, is associated with better outcomes on measures of depression and complicated grief among bereaved family members of cancer patients. J Pain Symptom Manage. 2017;54:273-279.
10. CMS. Medicare benefit policy manual: coverage of hospice services under hospital insurance. www.cms.gov/Regulations-and-guidance/Guidance/Manuals/downloads/bp102c09.pdf. Accessed February 25, 2018.
11. Cherlin E, Barry LC, Prigerson H, et al. Bereavement services for family caregivers: how often used, why, and why not. J Palliat Med. 2007;10:148–158.
12. Bui E, Nidal-Vicens M, Simon NM. Pharmacologic approaches to the treatment of complicated grief: rationale and a brief review of the literature. Dialogues Clin Neurosci. 2012;14:149-157.
13. Shear MK, Reynolds CF 3rd, Simon NM, et al. Optimizing treatment of complicated grief: a randomized clinical trial. JAMA Psychiatry. 2016;73:685-694.
1. Cozza SJ, Fisher JE, Mauro C, et al. Performance of DSM-5 persistent complex bereavement disorder criteria in a community sample of bereaved military family members. Am J Psychiatry. 2016;173:919-929.
2. Kersting A, Brähler E, Glaesmer H, et al. Prevalence of complicated grief in a representative population-based sample. J Affect Disord. 2011;131:339-343.
3. Fujisawa D, Miyashita M, Nakajima S, et al. Prevalence and determinants of complicated grief in general population. J Affect Disord. 2010;127:352-358.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: APA Press; 2013.
5. Shear MK, Simon N, Wall M, et al. Complicated grief and related issues for DSM-5. Depress Anxiety. 2011;28:103-117.
6. Shear MK. Clinical Practice. Complicated grief. N Engl J Med. 2015;372:153-160.
7. Wolfelt AD. Counseling Skills for Companioning the Mourner: The Fundamentals of Effective Grief Counseling. Fort Collins, CO: Companion Press; 2016.
8. Szanto K, Shear MK, Houck PR, et al. Indirect self-destructive behavior and overt suicidality in patients with complicated grief. J Clin Psychiatry. 2006;67:233-239.
9. Otani H, Yoshida S, Morita T, et al. Meaningful communication before death, but not present at the time of death itself, is associated with better outcomes on measures of depression and complicated grief among bereaved family members of cancer patients. J Pain Symptom Manage. 2017;54:273-279.
10. CMS. Medicare benefit policy manual: coverage of hospice services under hospital insurance. www.cms.gov/Regulations-and-guidance/Guidance/Manuals/downloads/bp102c09.pdf. Accessed February 25, 2018.
11. Cherlin E, Barry LC, Prigerson H, et al. Bereavement services for family caregivers: how often used, why, and why not. J Palliat Med. 2007;10:148–158.
12. Bui E, Nidal-Vicens M, Simon NM. Pharmacologic approaches to the treatment of complicated grief: rationale and a brief review of the literature. Dialogues Clin Neurosci. 2012;14:149-157.
13. Shear MK, Reynolds CF 3rd, Simon NM, et al. Optimizing treatment of complicated grief: a randomized clinical trial. JAMA Psychiatry. 2016;73:685-694.
No significant VTE risk for women taking noncyclic COCs
Women who use combined oral contraceptives (COC) without hormone-free or low-dose hormone intervals have a slightly elevated, but not statistically significant, risk of venous thromboembolism (VTE), compared with women who use cyclic COCs, according to research published in JAMA Internal Medicine.
Jie Li, PhD, from the Center for Drug Evaluation and Research, and colleagues performed a retrospective cohort study of 733,007 women aged 18-50 years in the Sentinel Distributed Database from 2007 to 2015 who received low-dose extended and continuous cycle (210,691 women; mean age, 30 years) COCs or cyclic COCs (522,316 women; mean age, 29 years). Continuous cycle COCs were defined as an 84/7 cycle or a 365/0 cycle, while cyclic COCs were 21/7 cycles.
The researchers noted some baseline differences between the two groups, with gynecologic conditions occurring in 40% of the noncyclic group, compared with 32% in the cyclic group; cardiovascular and metabolic conditions occurring in 7% of noncyclic women, compared with 5% of cyclic women; inflammatory disease occurring in 3% of noncyclic women, compared with 2% of cyclic women; and a slightly higher rate of health care services use in the noncyclic group, compared with the cyclic group.
Dr. Li and associates found 228 cases of VTE in the noncyclic group and 297 cases in the cyclic group, with an incidence rate of 1.54 (95% confidence interval, 1.34-1.74) per 1,000 person-years for noncyclic users and 0.83 (95% CI, 0.74-0.93) per 1,000 person-years for cyclic users (crude hazard ratio, 1.84; 95% CI, 1.53-2.21).
However, propensity score matching lowered the incidence rate to 1.44 (95% CI, 1.24-1.64) per 1,000 person-years for the noncyclic group and raised it to 1.09 (95% CI, 0.92-1.27) per 1,000 person-years for the cyclic group, for an adjusted hazard ratio of 1.32 (95% CI, 1.07-1.64), which does not show “strong evidence” of VTE risk based on a small absolute risk difference of 0.27 cases per 1,000 persons, the researchers said. They added that there might be residual or unmeasured confounding, perhaps for potential concurrent medication use or incompletely measured covariates.
“Accordingly, we do not recommend selective prescribing of COCs based on the cyclic and continuous/extended type,” Dr. Li and colleagues wrote. “Clinicians should prescribe COCs based on patients’ individual risk factors and preferences.”
The Sentinel Initiative is funded by a contract from the Department of Health and Human Services. The authors reported no relevant conflicts of interest.
SOURCE: Li J et al. JAMA Intern Med. 2018 Oct 1. doi: 10.1001/jamainternmed.2018.4251.
Women who use combined oral contraceptives (COC) without hormone-free or low-dose hormone intervals have a slightly elevated, but not statistically significant, risk of venous thromboembolism (VTE), compared with women who use cyclic COCs, according to research published in JAMA Internal Medicine.
Jie Li, PhD, from the Center for Drug Evaluation and Research, and colleagues performed a retrospective cohort study of 733,007 women aged 18-50 years in the Sentinel Distributed Database from 2007 to 2015 who received low-dose extended and continuous cycle (210,691 women; mean age, 30 years) COCs or cyclic COCs (522,316 women; mean age, 29 years). Continuous cycle COCs were defined as an 84/7 cycle or a 365/0 cycle, while cyclic COCs were 21/7 cycles.
The researchers noted some baseline differences between the two groups, with gynecologic conditions occurring in 40% of the noncyclic group, compared with 32% in the cyclic group; cardiovascular and metabolic conditions occurring in 7% of noncyclic women, compared with 5% of cyclic women; inflammatory disease occurring in 3% of noncyclic women, compared with 2% of cyclic women; and a slightly higher rate of health care services use in the noncyclic group, compared with the cyclic group.
Dr. Li and associates found 228 cases of VTE in the noncyclic group and 297 cases in the cyclic group, with an incidence rate of 1.54 (95% confidence interval, 1.34-1.74) per 1,000 person-years for noncyclic users and 0.83 (95% CI, 0.74-0.93) per 1,000 person-years for cyclic users (crude hazard ratio, 1.84; 95% CI, 1.53-2.21).
However, propensity score matching lowered the incidence rate to 1.44 (95% CI, 1.24-1.64) per 1,000 person-years for the noncyclic group and raised it to 1.09 (95% CI, 0.92-1.27) per 1,000 person-years for the cyclic group, for an adjusted hazard ratio of 1.32 (95% CI, 1.07-1.64), which does not show “strong evidence” of VTE risk based on a small absolute risk difference of 0.27 cases per 1,000 persons, the researchers said. They added that there might be residual or unmeasured confounding, perhaps for potential concurrent medication use or incompletely measured covariates.
“Accordingly, we do not recommend selective prescribing of COCs based on the cyclic and continuous/extended type,” Dr. Li and colleagues wrote. “Clinicians should prescribe COCs based on patients’ individual risk factors and preferences.”
The Sentinel Initiative is funded by a contract from the Department of Health and Human Services. The authors reported no relevant conflicts of interest.
SOURCE: Li J et al. JAMA Intern Med. 2018 Oct 1. doi: 10.1001/jamainternmed.2018.4251.
Women who use combined oral contraceptives (COC) without hormone-free or low-dose hormone intervals have a slightly elevated, but not statistically significant, risk of venous thromboembolism (VTE), compared with women who use cyclic COCs, according to research published in JAMA Internal Medicine.
Jie Li, PhD, from the Center for Drug Evaluation and Research, and colleagues performed a retrospective cohort study of 733,007 women aged 18-50 years in the Sentinel Distributed Database from 2007 to 2015 who received low-dose extended and continuous cycle (210,691 women; mean age, 30 years) COCs or cyclic COCs (522,316 women; mean age, 29 years). Continuous cycle COCs were defined as an 84/7 cycle or a 365/0 cycle, while cyclic COCs were 21/7 cycles.
The researchers noted some baseline differences between the two groups, with gynecologic conditions occurring in 40% of the noncyclic group, compared with 32% in the cyclic group; cardiovascular and metabolic conditions occurring in 7% of noncyclic women, compared with 5% of cyclic women; inflammatory disease occurring in 3% of noncyclic women, compared with 2% of cyclic women; and a slightly higher rate of health care services use in the noncyclic group, compared with the cyclic group.
Dr. Li and associates found 228 cases of VTE in the noncyclic group and 297 cases in the cyclic group, with an incidence rate of 1.54 (95% confidence interval, 1.34-1.74) per 1,000 person-years for noncyclic users and 0.83 (95% CI, 0.74-0.93) per 1,000 person-years for cyclic users (crude hazard ratio, 1.84; 95% CI, 1.53-2.21).
However, propensity score matching lowered the incidence rate to 1.44 (95% CI, 1.24-1.64) per 1,000 person-years for the noncyclic group and raised it to 1.09 (95% CI, 0.92-1.27) per 1,000 person-years for the cyclic group, for an adjusted hazard ratio of 1.32 (95% CI, 1.07-1.64), which does not show “strong evidence” of VTE risk based on a small absolute risk difference of 0.27 cases per 1,000 persons, the researchers said. They added that there might be residual or unmeasured confounding, perhaps for potential concurrent medication use or incompletely measured covariates.
“Accordingly, we do not recommend selective prescribing of COCs based on the cyclic and continuous/extended type,” Dr. Li and colleagues wrote. “Clinicians should prescribe COCs based on patients’ individual risk factors and preferences.”
The Sentinel Initiative is funded by a contract from the Department of Health and Human Services. The authors reported no relevant conflicts of interest.
SOURCE: Li J et al. JAMA Intern Med. 2018 Oct 1. doi: 10.1001/jamainternmed.2018.4251.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Continuous or extended cycle combined oral contraceptive (COC) use was associated with a slightly elevated, but not statistically significant, risk of venous thromboembolism.
Major finding: The adjusted hazard ratio for women taking continuous/extended COCs was 1.32 (95% confidence interval, 1.07-1.74), compared with women taking noncyclic COCs, but the absolute risk difference between the two groups was low (0.27 per 1,000 persons).
Study details: A retrospective cohort study of 210,691 women with continuous/extended COC use and 522,316 women with cyclic COC use.
Disclosures: The Sentinel Initiative is funded by a contract from the Department of Health and Human Services. The authors reported no relevant conflicts of interest.
Source: Li J et al. JAMA Intern Med. 2018 Oct 1. doi:10.1001/jamainternmed.2018.4251.
First reported case of induced resistance to tisagenlecleucel
Unintentional transduction of a single leukemic B cell appears to have induced resistance to CTL019 (tisagenlecleucel, Kymriah) therapy, a recent case study suggests.
A total of 9 months after receiving a seemingly successful CD19-targeted chimeric antigen receptor (CAR) T-cell (CTL019; tisagenlecleucel) infusion, a 20-year-old man with B-cell acute lymphoblastic leukemia (B-ALL) had a frank relapse, with more than 90% bone marrow infiltration of CAR-transduced B-cell leukemia cells. Further investigation showed that the CAR gene had unintentionally been added to a solitary leukemic B cell during the CAR T-cell manufacturing process, reported Marco Ruella, MD, of the University of Pennsylvania, Philadelphia.
“The transduction of a single leukemic cell with an anti-CD19 CAR lentivirus during CTL019 manufacturing is sufficient to mediate resistance through masking of the CD19 epitope. This is a rare event, as this is the only case out of 369 patients reported worldwide at the time of publication. ... These findings illustrate the need for improved manufacturing technologies that can purge residual contaminating tumor cells from engineered T cells,” the authors wrote in Nature Medicine.
The findings also confirm the cancer stem cell hypothesis in humans, “given that clonal analysis indicated that the relapse and subsequent death of the patient were attributed to the progeny of a single leukemic blast cell with extensive replicative capacity, both in culture and in vivo,” they wrote.
Initially, “the infused CTL019 cells displayed the typical pattern of in vivo engraftment and expansion by CAR19-specific flow cytometry, followed by decline to an undetectable level in the peripheral blood” of the affected patient, the authors wrote. “The expansion and contraction phases and long-term persistence of CAR T cells were confirmed via qPCR using CAR-specific primers.” The patient was in complete remission at day 28.
However, they added, routine peripheral blood monitoring with quantitative polymerase chain reaction for CAR-specific sequences identified “the emergence of a second expansion phase of CAR cells starting at day 252, which did not correlate with re-expansion of CAR + T cells by flow cytometry.” Frank relapse soon followed.
Analysis confirmed “that the lack of detection of CD19 by flow cytometry was due to CAR19 binding in cis to CD19 on the surface of leukemic blasts, thus masking the epitope from detection by standard flow cytometry,” the authors wrote.
Study funding was provided by Bristol-Myers Squibb, Novartis, the National Institutes of Health, and others. Dr. Ruella and several of his colleagues work under a research collaboration involving the University of Pennsylvania and the Novartis Institutes of Biomedical Research and are inventors of intellectual property licensed by the University of Pennsylvania to Novartis.
SOURCE: Ruella M et al. Nat Med. 2018 Oct 1. doi: 10.1038/s41591-018-0201-9.
Unintentional transduction of a single leukemic B cell appears to have induced resistance to CTL019 (tisagenlecleucel, Kymriah) therapy, a recent case study suggests.
A total of 9 months after receiving a seemingly successful CD19-targeted chimeric antigen receptor (CAR) T-cell (CTL019; tisagenlecleucel) infusion, a 20-year-old man with B-cell acute lymphoblastic leukemia (B-ALL) had a frank relapse, with more than 90% bone marrow infiltration of CAR-transduced B-cell leukemia cells. Further investigation showed that the CAR gene had unintentionally been added to a solitary leukemic B cell during the CAR T-cell manufacturing process, reported Marco Ruella, MD, of the University of Pennsylvania, Philadelphia.
“The transduction of a single leukemic cell with an anti-CD19 CAR lentivirus during CTL019 manufacturing is sufficient to mediate resistance through masking of the CD19 epitope. This is a rare event, as this is the only case out of 369 patients reported worldwide at the time of publication. ... These findings illustrate the need for improved manufacturing technologies that can purge residual contaminating tumor cells from engineered T cells,” the authors wrote in Nature Medicine.
The findings also confirm the cancer stem cell hypothesis in humans, “given that clonal analysis indicated that the relapse and subsequent death of the patient were attributed to the progeny of a single leukemic blast cell with extensive replicative capacity, both in culture and in vivo,” they wrote.
Initially, “the infused CTL019 cells displayed the typical pattern of in vivo engraftment and expansion by CAR19-specific flow cytometry, followed by decline to an undetectable level in the peripheral blood” of the affected patient, the authors wrote. “The expansion and contraction phases and long-term persistence of CAR T cells were confirmed via qPCR using CAR-specific primers.” The patient was in complete remission at day 28.
However, they added, routine peripheral blood monitoring with quantitative polymerase chain reaction for CAR-specific sequences identified “the emergence of a second expansion phase of CAR cells starting at day 252, which did not correlate with re-expansion of CAR + T cells by flow cytometry.” Frank relapse soon followed.
Analysis confirmed “that the lack of detection of CD19 by flow cytometry was due to CAR19 binding in cis to CD19 on the surface of leukemic blasts, thus masking the epitope from detection by standard flow cytometry,” the authors wrote.
Study funding was provided by Bristol-Myers Squibb, Novartis, the National Institutes of Health, and others. Dr. Ruella and several of his colleagues work under a research collaboration involving the University of Pennsylvania and the Novartis Institutes of Biomedical Research and are inventors of intellectual property licensed by the University of Pennsylvania to Novartis.
SOURCE: Ruella M et al. Nat Med. 2018 Oct 1. doi: 10.1038/s41591-018-0201-9.
Unintentional transduction of a single leukemic B cell appears to have induced resistance to CTL019 (tisagenlecleucel, Kymriah) therapy, a recent case study suggests.
A total of 9 months after receiving a seemingly successful CD19-targeted chimeric antigen receptor (CAR) T-cell (CTL019; tisagenlecleucel) infusion, a 20-year-old man with B-cell acute lymphoblastic leukemia (B-ALL) had a frank relapse, with more than 90% bone marrow infiltration of CAR-transduced B-cell leukemia cells. Further investigation showed that the CAR gene had unintentionally been added to a solitary leukemic B cell during the CAR T-cell manufacturing process, reported Marco Ruella, MD, of the University of Pennsylvania, Philadelphia.
“The transduction of a single leukemic cell with an anti-CD19 CAR lentivirus during CTL019 manufacturing is sufficient to mediate resistance through masking of the CD19 epitope. This is a rare event, as this is the only case out of 369 patients reported worldwide at the time of publication. ... These findings illustrate the need for improved manufacturing technologies that can purge residual contaminating tumor cells from engineered T cells,” the authors wrote in Nature Medicine.
The findings also confirm the cancer stem cell hypothesis in humans, “given that clonal analysis indicated that the relapse and subsequent death of the patient were attributed to the progeny of a single leukemic blast cell with extensive replicative capacity, both in culture and in vivo,” they wrote.
Initially, “the infused CTL019 cells displayed the typical pattern of in vivo engraftment and expansion by CAR19-specific flow cytometry, followed by decline to an undetectable level in the peripheral blood” of the affected patient, the authors wrote. “The expansion and contraction phases and long-term persistence of CAR T cells were confirmed via qPCR using CAR-specific primers.” The patient was in complete remission at day 28.
However, they added, routine peripheral blood monitoring with quantitative polymerase chain reaction for CAR-specific sequences identified “the emergence of a second expansion phase of CAR cells starting at day 252, which did not correlate with re-expansion of CAR + T cells by flow cytometry.” Frank relapse soon followed.
Analysis confirmed “that the lack of detection of CD19 by flow cytometry was due to CAR19 binding in cis to CD19 on the surface of leukemic blasts, thus masking the epitope from detection by standard flow cytometry,” the authors wrote.
Study funding was provided by Bristol-Myers Squibb, Novartis, the National Institutes of Health, and others. Dr. Ruella and several of his colleagues work under a research collaboration involving the University of Pennsylvania and the Novartis Institutes of Biomedical Research and are inventors of intellectual property licensed by the University of Pennsylvania to Novartis.
SOURCE: Ruella M et al. Nat Med. 2018 Oct 1. doi: 10.1038/s41591-018-0201-9.
FROM NATURE MEDICINE
Key clinical point: Unintentional transduction of a single leukemic B cell induced resistance to CTL019 (tisagenlecleucel) therapy.
Major finding: A patient with B-cell acute lymphoblastic leukemia (B-ALL) had frank relapse 9 months after a CTL019 infusion, with more than 90% bone marrow infiltration of chimeric antigen receptor–transduced B-cell leukemia cells.
Study details: A case study of a 20-year-old male with B-ALL undergoing CTL019 therapy.
Disclosures: Study funding was provided by Bristol-Myers Squibb, Novartis, the National Institutes of Health, and others. Dr. Ruella and several of his colleagues work under a research collaboration involving the University of Pennsylvania and the Novartis Institutes of Biomedical Research and are inventors of intellectual property licensed by the University of Pennsylvania to Novartis.
Source: Ruella M et al. Nat Med. 2018 Oct 1. doi: 10.1038/s41591-018-0201-9.