User login
How US healthcare compares to other countries
The US has similar healthcare utilization as other high-income countries but spends more and tends to have worse health outcomes, according to a new study.
In 2016, the US spent 17.8% of its gross domestic product on healthcare. For 10 other high-income countries, spending ranged from 9.6% to 12.4%.
However, sizes of physician and nursing workforces were comparable between the countries, numbers of hospital discharges were similar, and lengths of hospital stay were lower in the US than in most other countries.
Meanwhile, the US had the lowest life expectancy and the highest rate of infant mortality.
This research was published in JAMA.
“There’s been a lot of interest in international comparisons between America and other high-income countries, and there’s been a lot of vagueness about why exactly our [US] spending is so much higher and our health outcomes are not necessarily better and often worse,” said study author Ashish K. Jha, MD, of Harvard T. H. Chan School of Public Health in Boston, Massachusetts.
“This study really tries to fill in gaps, I think, across a wide range of issues, from structural capacity to utilization to prices to outcomes.”
For this study, Dr Jha and his colleagues analyzed recent healthcare data, primarily from 2013 to 2016. The team compared differences in healthcare spending, performance, and structural features between the US and 10 high-income countries—UK, Canada, Germany, Australia, Japan, Sweden, France, Netherlands, Switzerland, and Denmark.
Spending
In 2016, healthcare spending, as a percentage of gross domestic product, was as follows:
US—17.8%
Switzerland—12.4%
Sweden—11.9%
Germany—11.3%
France—11%
Japan—10.9%
Denmark—10.8%
Netherlands—10.5%
Canada—10.3%
UK—9.7%
Australia—9.6%.
“The big differences in spending really seem to be driven by prices,” Dr Jha said, noting that salaries for doctors and nurses, administrative expenditures, and pharmaceutical costs are “much higher” in the US.
The total spending on pharmaceuticals per capita was $1443 in the US but ranged from $466 (Netherlands) to $939 (Switzerland) in the other countries.
Administrative costs accounted for 8% of the total national health expenditure in the US but 1% (France, Japan) to 3% (Germany) in the other countries.
Outpatient care expenditures ranged from 22% (Netherlands) to 42% (US). Inpatient care expenditures ranged from 17% (Canada) to 32% (Netherlands), with 19% for the US. And expenditures for medical goods ranged from 10% (Denmark) to 20% (Germany), with the US at 14%.
Physicians’ and nurses’ salaries were higher in the US than other countries. For example, generalist physicians earned $218,173 in the US in 2016 but anywhere from $86,607 (Sweden) to $154,126 (Germany) in the other countries.
Utilization
Although US doctors and nurses earned more than their counterparts in comparator countries, there were no substantial between-country differences in the size of the physician and nursing workforces.
The number of working physicians for every 1000 people ranged from 2.1 (UK) to 4.3 (Switzerland), with the US at 2.6. The number of working nurses for every 1000 people ranged from 8.2 (UK) to 17.4 (Switzerland), with 11.1 for the US.
The US had comparable numbers of hospital beds as some of the other countries. The range was 2.5 (Sweden) to 13.2 (Japan) beds per 1000 people, with the US at 2.8.
The US ranked 6th when it came to hospital discharges for acute myocardial infarction (AMI, 192 per 100,000 people; range, 89 to 287), mental and behavioral issues (679 per 100,000 people; range, 119 to 1719), pneumonia (365 per 100,000 people; range, 187 to 567), and chronic obstructive pulmonary disease (230 per 100,000 people; range, 45 to 352).
The US had greater utilization of computed tomography than the other countries, with 245 examinations per 1000 people (range for other countries, 79 to 231). And US utilization of magnetic resonance imaging was higher than most countries, with 118 examinations per 1000 people (range, 41 to 131).
However, the US ranked on the lower end of the spectrum for length of hospital stay. The length of stay for a “normal delivery” childbirth ranged from a median of 1.5 days (UK) to 5.7 days (Japan), with the US clocking in at 2 days. The median length of stay for AMI ranged from a median of 3.9 days (Netherlands) to 10.3 days (Germany), with the US at 5.4 days.
“So much of the debate about healthcare these days is about over-utilization—that somehow our health system is uniquely bad at avoiding unnecessary services,” Dr Jha said. “I think these data really put that argument to rest. Except for a few pockets, utilization is not really different between us and these high-income Northern European countries, so maybe we need to spend a little less time focusing on that and a little bit more time focusing on prices of our healthcare system.”
Outcomes
The US ranked on the lower end of the spectrum for some mortality outcomes. Thirty-day stroke mortality per 1000 patients ranged from 4.2 in the US to 10 in Canada. Thirty-day AMI mortality per 1000 ranged from 4.1 (Australia) to 8.7 (Germany), with the US at 5.5.
However, infant mortality was highest in the US, at 5.8 deaths per 1000 live births (range for other countries, 2.1 to 5.1). And life expectancy was lowest in the US, at 78.8 years (range for other countries, 80.7 to 83.9).
The researchers noted that the US had the highest percentage of overweight or obese individuals age 15 and older, at 70.1% (range for other countries, 23.8% to 63.4%), but a low percentage of smokers (11.4%; range, 11.2% to 22.4%) and moderate alcohol consumption (8.8 L per capita; range, 7.2 to 11.9).
Limitations of this study include some differences in approaches to collecting and standardizing data across countries, as well as missing data for some countries.
The US has similar healthcare utilization as other high-income countries but spends more and tends to have worse health outcomes, according to a new study.
In 2016, the US spent 17.8% of its gross domestic product on healthcare. For 10 other high-income countries, spending ranged from 9.6% to 12.4%.
However, sizes of physician and nursing workforces were comparable between the countries, numbers of hospital discharges were similar, and lengths of hospital stay were lower in the US than in most other countries.
Meanwhile, the US had the lowest life expectancy and the highest rate of infant mortality.
This research was published in JAMA.
“There’s been a lot of interest in international comparisons between America and other high-income countries, and there’s been a lot of vagueness about why exactly our [US] spending is so much higher and our health outcomes are not necessarily better and often worse,” said study author Ashish K. Jha, MD, of Harvard T. H. Chan School of Public Health in Boston, Massachusetts.
“This study really tries to fill in gaps, I think, across a wide range of issues, from structural capacity to utilization to prices to outcomes.”
For this study, Dr Jha and his colleagues analyzed recent healthcare data, primarily from 2013 to 2016. The team compared differences in healthcare spending, performance, and structural features between the US and 10 high-income countries—UK, Canada, Germany, Australia, Japan, Sweden, France, Netherlands, Switzerland, and Denmark.
Spending
In 2016, healthcare spending, as a percentage of gross domestic product, was as follows:
US—17.8%
Switzerland—12.4%
Sweden—11.9%
Germany—11.3%
France—11%
Japan—10.9%
Denmark—10.8%
Netherlands—10.5%
Canada—10.3%
UK—9.7%
Australia—9.6%.
“The big differences in spending really seem to be driven by prices,” Dr Jha said, noting that salaries for doctors and nurses, administrative expenditures, and pharmaceutical costs are “much higher” in the US.
The total spending on pharmaceuticals per capita was $1443 in the US but ranged from $466 (Netherlands) to $939 (Switzerland) in the other countries.
Administrative costs accounted for 8% of the total national health expenditure in the US but 1% (France, Japan) to 3% (Germany) in the other countries.
Outpatient care expenditures ranged from 22% (Netherlands) to 42% (US). Inpatient care expenditures ranged from 17% (Canada) to 32% (Netherlands), with 19% for the US. And expenditures for medical goods ranged from 10% (Denmark) to 20% (Germany), with the US at 14%.
Physicians’ and nurses’ salaries were higher in the US than other countries. For example, generalist physicians earned $218,173 in the US in 2016 but anywhere from $86,607 (Sweden) to $154,126 (Germany) in the other countries.
Utilization
Although US doctors and nurses earned more than their counterparts in comparator countries, there were no substantial between-country differences in the size of the physician and nursing workforces.
The number of working physicians for every 1000 people ranged from 2.1 (UK) to 4.3 (Switzerland), with the US at 2.6. The number of working nurses for every 1000 people ranged from 8.2 (UK) to 17.4 (Switzerland), with 11.1 for the US.
The US had comparable numbers of hospital beds as some of the other countries. The range was 2.5 (Sweden) to 13.2 (Japan) beds per 1000 people, with the US at 2.8.
The US ranked 6th when it came to hospital discharges for acute myocardial infarction (AMI, 192 per 100,000 people; range, 89 to 287), mental and behavioral issues (679 per 100,000 people; range, 119 to 1719), pneumonia (365 per 100,000 people; range, 187 to 567), and chronic obstructive pulmonary disease (230 per 100,000 people; range, 45 to 352).
The US had greater utilization of computed tomography than the other countries, with 245 examinations per 1000 people (range for other countries, 79 to 231). And US utilization of magnetic resonance imaging was higher than most countries, with 118 examinations per 1000 people (range, 41 to 131).
However, the US ranked on the lower end of the spectrum for length of hospital stay. The length of stay for a “normal delivery” childbirth ranged from a median of 1.5 days (UK) to 5.7 days (Japan), with the US clocking in at 2 days. The median length of stay for AMI ranged from a median of 3.9 days (Netherlands) to 10.3 days (Germany), with the US at 5.4 days.
“So much of the debate about healthcare these days is about over-utilization—that somehow our health system is uniquely bad at avoiding unnecessary services,” Dr Jha said. “I think these data really put that argument to rest. Except for a few pockets, utilization is not really different between us and these high-income Northern European countries, so maybe we need to spend a little less time focusing on that and a little bit more time focusing on prices of our healthcare system.”
Outcomes
The US ranked on the lower end of the spectrum for some mortality outcomes. Thirty-day stroke mortality per 1000 patients ranged from 4.2 in the US to 10 in Canada. Thirty-day AMI mortality per 1000 ranged from 4.1 (Australia) to 8.7 (Germany), with the US at 5.5.
However, infant mortality was highest in the US, at 5.8 deaths per 1000 live births (range for other countries, 2.1 to 5.1). And life expectancy was lowest in the US, at 78.8 years (range for other countries, 80.7 to 83.9).
The researchers noted that the US had the highest percentage of overweight or obese individuals age 15 and older, at 70.1% (range for other countries, 23.8% to 63.4%), but a low percentage of smokers (11.4%; range, 11.2% to 22.4%) and moderate alcohol consumption (8.8 L per capita; range, 7.2 to 11.9).
Limitations of this study include some differences in approaches to collecting and standardizing data across countries, as well as missing data for some countries.
The US has similar healthcare utilization as other high-income countries but spends more and tends to have worse health outcomes, according to a new study.
In 2016, the US spent 17.8% of its gross domestic product on healthcare. For 10 other high-income countries, spending ranged from 9.6% to 12.4%.
However, sizes of physician and nursing workforces were comparable between the countries, numbers of hospital discharges were similar, and lengths of hospital stay were lower in the US than in most other countries.
Meanwhile, the US had the lowest life expectancy and the highest rate of infant mortality.
This research was published in JAMA.
“There’s been a lot of interest in international comparisons between America and other high-income countries, and there’s been a lot of vagueness about why exactly our [US] spending is so much higher and our health outcomes are not necessarily better and often worse,” said study author Ashish K. Jha, MD, of Harvard T. H. Chan School of Public Health in Boston, Massachusetts.
“This study really tries to fill in gaps, I think, across a wide range of issues, from structural capacity to utilization to prices to outcomes.”
For this study, Dr Jha and his colleagues analyzed recent healthcare data, primarily from 2013 to 2016. The team compared differences in healthcare spending, performance, and structural features between the US and 10 high-income countries—UK, Canada, Germany, Australia, Japan, Sweden, France, Netherlands, Switzerland, and Denmark.
Spending
In 2016, healthcare spending, as a percentage of gross domestic product, was as follows:
US—17.8%
Switzerland—12.4%
Sweden—11.9%
Germany—11.3%
France—11%
Japan—10.9%
Denmark—10.8%
Netherlands—10.5%
Canada—10.3%
UK—9.7%
Australia—9.6%.
“The big differences in spending really seem to be driven by prices,” Dr Jha said, noting that salaries for doctors and nurses, administrative expenditures, and pharmaceutical costs are “much higher” in the US.
The total spending on pharmaceuticals per capita was $1443 in the US but ranged from $466 (Netherlands) to $939 (Switzerland) in the other countries.
Administrative costs accounted for 8% of the total national health expenditure in the US but 1% (France, Japan) to 3% (Germany) in the other countries.
Outpatient care expenditures ranged from 22% (Netherlands) to 42% (US). Inpatient care expenditures ranged from 17% (Canada) to 32% (Netherlands), with 19% for the US. And expenditures for medical goods ranged from 10% (Denmark) to 20% (Germany), with the US at 14%.
Physicians’ and nurses’ salaries were higher in the US than other countries. For example, generalist physicians earned $218,173 in the US in 2016 but anywhere from $86,607 (Sweden) to $154,126 (Germany) in the other countries.
Utilization
Although US doctors and nurses earned more than their counterparts in comparator countries, there were no substantial between-country differences in the size of the physician and nursing workforces.
The number of working physicians for every 1000 people ranged from 2.1 (UK) to 4.3 (Switzerland), with the US at 2.6. The number of working nurses for every 1000 people ranged from 8.2 (UK) to 17.4 (Switzerland), with 11.1 for the US.
The US had comparable numbers of hospital beds as some of the other countries. The range was 2.5 (Sweden) to 13.2 (Japan) beds per 1000 people, with the US at 2.8.
The US ranked 6th when it came to hospital discharges for acute myocardial infarction (AMI, 192 per 100,000 people; range, 89 to 287), mental and behavioral issues (679 per 100,000 people; range, 119 to 1719), pneumonia (365 per 100,000 people; range, 187 to 567), and chronic obstructive pulmonary disease (230 per 100,000 people; range, 45 to 352).
The US had greater utilization of computed tomography than the other countries, with 245 examinations per 1000 people (range for other countries, 79 to 231). And US utilization of magnetic resonance imaging was higher than most countries, with 118 examinations per 1000 people (range, 41 to 131).
However, the US ranked on the lower end of the spectrum for length of hospital stay. The length of stay for a “normal delivery” childbirth ranged from a median of 1.5 days (UK) to 5.7 days (Japan), with the US clocking in at 2 days. The median length of stay for AMI ranged from a median of 3.9 days (Netherlands) to 10.3 days (Germany), with the US at 5.4 days.
“So much of the debate about healthcare these days is about over-utilization—that somehow our health system is uniquely bad at avoiding unnecessary services,” Dr Jha said. “I think these data really put that argument to rest. Except for a few pockets, utilization is not really different between us and these high-income Northern European countries, so maybe we need to spend a little less time focusing on that and a little bit more time focusing on prices of our healthcare system.”
Outcomes
The US ranked on the lower end of the spectrum for some mortality outcomes. Thirty-day stroke mortality per 1000 patients ranged from 4.2 in the US to 10 in Canada. Thirty-day AMI mortality per 1000 ranged from 4.1 (Australia) to 8.7 (Germany), with the US at 5.5.
However, infant mortality was highest in the US, at 5.8 deaths per 1000 live births (range for other countries, 2.1 to 5.1). And life expectancy was lowest in the US, at 78.8 years (range for other countries, 80.7 to 83.9).
The researchers noted that the US had the highest percentage of overweight or obese individuals age 15 and older, at 70.1% (range for other countries, 23.8% to 63.4%), but a low percentage of smokers (11.4%; range, 11.2% to 22.4%) and moderate alcohol consumption (8.8 L per capita; range, 7.2 to 11.9).
Limitations of this study include some differences in approaches to collecting and standardizing data across countries, as well as missing data for some countries.
DSCs ‘promising’ for severe acute GVHD
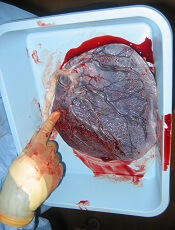
Placenta-derived decidua stromal cells (DSCs) can treat severe acute graft-versus-host disease (GVHD), according to a small study.
When given in the optimal way, DSCs produced GVHD responses in all patients, and the 1-year survival rate was 76%.
Steroid-refractory (SR) patients who received DSCs had superior 1-year survival rates compared to SR historical controls and SR patients who received mesenchymal stem cells (MSCs).
Olle Ringdén, MD, PhD, of Karolinska Institutet in Huddinge, Sweden, and his colleagues reported these findings in STEM CELLS Translational Medicine.
“There were a couple of things that led us to be curious about [DSCs as a treatment for GVHD],” Dr Ringdén said. “First, placenta plays an important role in helping the mother’s body tolerate the developing fetus.”
“[S]econd, placenta has been used in Africa for 100 years to successfully treat burn injuries. This speaks somewhat to its effectiveness and safety. We also found that placenta-derived DSCs are immunosuppressive in vitro and in vivo, which led us to wonder if they might cure severe acute GVHD.”
To test their theory, the team conducted a study of 38 patients with severe acute GVHD, including 25 SR patients.
The patients received DSCs in 1 of 2 groups. In group 1 (n=17), DSCs were infused in buffer supplemented with 10% AB plasma. In group 2 (n=21), the buffer was supplemented with 5% albumin.
Group 1 received significantly fewer infusions than group 2—1 (range, 1-5) and 2 (range, 1-6), respectively (P=0.002). But group 1 had a significantly higher median cell dose—2.0 x 106 DSCs/kg (range, 0.9-2.8) vs 1.2 x 106 DSCs/kg (range, 0.9-2.9; P<0.001).
Cell passage was significantly lower in group 1 than group 2—2 (range, 2-4) and 4 (range, 2-4), respectively (P<0.001). And cell viability was significantly lower in group 1 than 2—90% (range, 70-97) and 95% (range, 69-100), respectively (P<0.001).
Patients
There were no significant differences in baseline characteristics between groups 1 and 2. The median ages were 54.5 (range, 0.9-65.6) and 48.9 (range, 1.6-72.4), respectively.
Most patients were male (9 in group 1 and 16 in group 2), and most had malignant disease (14 and 17, respectively).
The most common graft source was peripheral blood stem cells (14 in group 1 and 16 in group 2), and most patients had a matched, unrelated donor (10 and 14, respectively).
Most patients received reduced-intensity conditioning (9 in group 1 and 17 in group 2) and GVHD prophylaxis with cyclosporine/methotrexate (13 in both groups).
All cases of GVHD were localized to the gut. Fifteen patients in each group had grade 3 GVHD. Two patients in group 1 and 6 in group 2 had grade 2 GVHD.
Results
Responses and survival rates were superior in group 2, but there was no significant difference in relapse or chronic GVHD between the groups.
In group 1, 7 patients did not respond, 5 had a partial response, and 5 had a complete response. In group 2, all patients responded, 10 with a partial response and 11 with a complete response (between-group difference, P=0.01).
The 1-year survival rate was 47% in group 1 and 76% in group 2 (P=0.016). The rate of GVHD-related mortality was 41% and 5%, respectively (P=0.003).
The cumulative incidence of chronic GVHD at 1.5 years was 36% in group 1 and 31% in group 2. The relapse rate was 29% and 18%, respectively.
The researchers compared SR patients in groups 1 (n=13) and 2 (n=11) to SR patients treated with bone marrow-derived MSCs (n=15) and SR historical controls (n=32).
The 1-year survival rate was 73% in SR group 2, which was significantly higher than the 31% survival rate in SR group 1 (P=0.02), the 20% rate in SR MSC recipients (P=0.0015), and the 3% rate in SR historical controls (P<0.001).
Severe adverse events in the DSC recipients included relapse (n=8), pneumonia (n=5), proven or probable invasive fungal infection (n=6), bacterial infection (n=2), graft failure (n=3), multiple organ failure (n=1), viral infection (n=2), central nervous system complications (n=2), septicemia (n=2), skin squamous cell carcinoma (n=2), and acute pancreatitis (n=1).
Causes of death in DSC recipients included acute GVHD (n=9), relapse (n=2), bacterial infection (n=2), invasive fungal infection (n=1), liver failure (n=1), hemorrhage (n=1), and secondary malignancy (n=1).
“Collectively, we think these data demonstrate that DSCs are a promising treatment for severe acute GVHD,” Dr Ringdén said. “But it was a small patient group, so, to further assess safety and efficacy, a larger, prospective trial will be necessary.”
“If an effective therapy for severe acute GVHD is indeed found and validated, it will increase the usefulness of stem cell transplantation with a possible broadening of indications.”
Placenta-derived decidua stromal cells (DSCs) can treat severe acute graft-versus-host disease (GVHD), according to a small study.
When given in the optimal way, DSCs produced GVHD responses in all patients, and the 1-year survival rate was 76%.
Steroid-refractory (SR) patients who received DSCs had superior 1-year survival rates compared to SR historical controls and SR patients who received mesenchymal stem cells (MSCs).
Olle Ringdén, MD, PhD, of Karolinska Institutet in Huddinge, Sweden, and his colleagues reported these findings in STEM CELLS Translational Medicine.
“There were a couple of things that led us to be curious about [DSCs as a treatment for GVHD],” Dr Ringdén said. “First, placenta plays an important role in helping the mother’s body tolerate the developing fetus.”
“[S]econd, placenta has been used in Africa for 100 years to successfully treat burn injuries. This speaks somewhat to its effectiveness and safety. We also found that placenta-derived DSCs are immunosuppressive in vitro and in vivo, which led us to wonder if they might cure severe acute GVHD.”
To test their theory, the team conducted a study of 38 patients with severe acute GVHD, including 25 SR patients.
The patients received DSCs in 1 of 2 groups. In group 1 (n=17), DSCs were infused in buffer supplemented with 10% AB plasma. In group 2 (n=21), the buffer was supplemented with 5% albumin.
Group 1 received significantly fewer infusions than group 2—1 (range, 1-5) and 2 (range, 1-6), respectively (P=0.002). But group 1 had a significantly higher median cell dose—2.0 x 106 DSCs/kg (range, 0.9-2.8) vs 1.2 x 106 DSCs/kg (range, 0.9-2.9; P<0.001).
Cell passage was significantly lower in group 1 than group 2—2 (range, 2-4) and 4 (range, 2-4), respectively (P<0.001). And cell viability was significantly lower in group 1 than 2—90% (range, 70-97) and 95% (range, 69-100), respectively (P<0.001).
Patients
There were no significant differences in baseline characteristics between groups 1 and 2. The median ages were 54.5 (range, 0.9-65.6) and 48.9 (range, 1.6-72.4), respectively.
Most patients were male (9 in group 1 and 16 in group 2), and most had malignant disease (14 and 17, respectively).
The most common graft source was peripheral blood stem cells (14 in group 1 and 16 in group 2), and most patients had a matched, unrelated donor (10 and 14, respectively).
Most patients received reduced-intensity conditioning (9 in group 1 and 17 in group 2) and GVHD prophylaxis with cyclosporine/methotrexate (13 in both groups).
All cases of GVHD were localized to the gut. Fifteen patients in each group had grade 3 GVHD. Two patients in group 1 and 6 in group 2 had grade 2 GVHD.
Results
Responses and survival rates were superior in group 2, but there was no significant difference in relapse or chronic GVHD between the groups.
In group 1, 7 patients did not respond, 5 had a partial response, and 5 had a complete response. In group 2, all patients responded, 10 with a partial response and 11 with a complete response (between-group difference, P=0.01).
The 1-year survival rate was 47% in group 1 and 76% in group 2 (P=0.016). The rate of GVHD-related mortality was 41% and 5%, respectively (P=0.003).
The cumulative incidence of chronic GVHD at 1.5 years was 36% in group 1 and 31% in group 2. The relapse rate was 29% and 18%, respectively.
The researchers compared SR patients in groups 1 (n=13) and 2 (n=11) to SR patients treated with bone marrow-derived MSCs (n=15) and SR historical controls (n=32).
The 1-year survival rate was 73% in SR group 2, which was significantly higher than the 31% survival rate in SR group 1 (P=0.02), the 20% rate in SR MSC recipients (P=0.0015), and the 3% rate in SR historical controls (P<0.001).
Severe adverse events in the DSC recipients included relapse (n=8), pneumonia (n=5), proven or probable invasive fungal infection (n=6), bacterial infection (n=2), graft failure (n=3), multiple organ failure (n=1), viral infection (n=2), central nervous system complications (n=2), septicemia (n=2), skin squamous cell carcinoma (n=2), and acute pancreatitis (n=1).
Causes of death in DSC recipients included acute GVHD (n=9), relapse (n=2), bacterial infection (n=2), invasive fungal infection (n=1), liver failure (n=1), hemorrhage (n=1), and secondary malignancy (n=1).
“Collectively, we think these data demonstrate that DSCs are a promising treatment for severe acute GVHD,” Dr Ringdén said. “But it was a small patient group, so, to further assess safety and efficacy, a larger, prospective trial will be necessary.”
“If an effective therapy for severe acute GVHD is indeed found and validated, it will increase the usefulness of stem cell transplantation with a possible broadening of indications.”
Placenta-derived decidua stromal cells (DSCs) can treat severe acute graft-versus-host disease (GVHD), according to a small study.
When given in the optimal way, DSCs produced GVHD responses in all patients, and the 1-year survival rate was 76%.
Steroid-refractory (SR) patients who received DSCs had superior 1-year survival rates compared to SR historical controls and SR patients who received mesenchymal stem cells (MSCs).
Olle Ringdén, MD, PhD, of Karolinska Institutet in Huddinge, Sweden, and his colleagues reported these findings in STEM CELLS Translational Medicine.
“There were a couple of things that led us to be curious about [DSCs as a treatment for GVHD],” Dr Ringdén said. “First, placenta plays an important role in helping the mother’s body tolerate the developing fetus.”
“[S]econd, placenta has been used in Africa for 100 years to successfully treat burn injuries. This speaks somewhat to its effectiveness and safety. We also found that placenta-derived DSCs are immunosuppressive in vitro and in vivo, which led us to wonder if they might cure severe acute GVHD.”
To test their theory, the team conducted a study of 38 patients with severe acute GVHD, including 25 SR patients.
The patients received DSCs in 1 of 2 groups. In group 1 (n=17), DSCs were infused in buffer supplemented with 10% AB plasma. In group 2 (n=21), the buffer was supplemented with 5% albumin.
Group 1 received significantly fewer infusions than group 2—1 (range, 1-5) and 2 (range, 1-6), respectively (P=0.002). But group 1 had a significantly higher median cell dose—2.0 x 106 DSCs/kg (range, 0.9-2.8) vs 1.2 x 106 DSCs/kg (range, 0.9-2.9; P<0.001).
Cell passage was significantly lower in group 1 than group 2—2 (range, 2-4) and 4 (range, 2-4), respectively (P<0.001). And cell viability was significantly lower in group 1 than 2—90% (range, 70-97) and 95% (range, 69-100), respectively (P<0.001).
Patients
There were no significant differences in baseline characteristics between groups 1 and 2. The median ages were 54.5 (range, 0.9-65.6) and 48.9 (range, 1.6-72.4), respectively.
Most patients were male (9 in group 1 and 16 in group 2), and most had malignant disease (14 and 17, respectively).
The most common graft source was peripheral blood stem cells (14 in group 1 and 16 in group 2), and most patients had a matched, unrelated donor (10 and 14, respectively).
Most patients received reduced-intensity conditioning (9 in group 1 and 17 in group 2) and GVHD prophylaxis with cyclosporine/methotrexate (13 in both groups).
All cases of GVHD were localized to the gut. Fifteen patients in each group had grade 3 GVHD. Two patients in group 1 and 6 in group 2 had grade 2 GVHD.
Results
Responses and survival rates were superior in group 2, but there was no significant difference in relapse or chronic GVHD between the groups.
In group 1, 7 patients did not respond, 5 had a partial response, and 5 had a complete response. In group 2, all patients responded, 10 with a partial response and 11 with a complete response (between-group difference, P=0.01).
The 1-year survival rate was 47% in group 1 and 76% in group 2 (P=0.016). The rate of GVHD-related mortality was 41% and 5%, respectively (P=0.003).
The cumulative incidence of chronic GVHD at 1.5 years was 36% in group 1 and 31% in group 2. The relapse rate was 29% and 18%, respectively.
The researchers compared SR patients in groups 1 (n=13) and 2 (n=11) to SR patients treated with bone marrow-derived MSCs (n=15) and SR historical controls (n=32).
The 1-year survival rate was 73% in SR group 2, which was significantly higher than the 31% survival rate in SR group 1 (P=0.02), the 20% rate in SR MSC recipients (P=0.0015), and the 3% rate in SR historical controls (P<0.001).
Severe adverse events in the DSC recipients included relapse (n=8), pneumonia (n=5), proven or probable invasive fungal infection (n=6), bacterial infection (n=2), graft failure (n=3), multiple organ failure (n=1), viral infection (n=2), central nervous system complications (n=2), septicemia (n=2), skin squamous cell carcinoma (n=2), and acute pancreatitis (n=1).
Causes of death in DSC recipients included acute GVHD (n=9), relapse (n=2), bacterial infection (n=2), invasive fungal infection (n=1), liver failure (n=1), hemorrhage (n=1), and secondary malignancy (n=1).
“Collectively, we think these data demonstrate that DSCs are a promising treatment for severe acute GVHD,” Dr Ringdén said. “But it was a small patient group, so, to further assess safety and efficacy, a larger, prospective trial will be necessary.”
“If an effective therapy for severe acute GVHD is indeed found and validated, it will increase the usefulness of stem cell transplantation with a possible broadening of indications.”
Clopidogrel proves noninferior to Plavix
Generic clopidogrel is noninferior to the brand-name antiplatelet drug Plavix, according to research published in Circulation: Cardiovascular Quality and Outcomes.
When a Canadian health system switched from prescribing Plavix to generic clopidogrel, patients with acute coronary syndrome (ACS) were no more likely to die or experience ACS recurrence within a year.
In addition, there were no significant differences between the Plavix and clopidogrel groups in the percentage of patients who were hospitalized for any reason, had a stroke or transient ischemic attack, or experienced bleeding.
“People can safely use generic clopidogrel,” said study author Dennis T. Ko, MD, of the Institute for Clinical Evaluative Sciences in Toronto, Ontario, Canada.
“This large and real-world study should be reassuring to physicians and healthcare organizations who have been concerned about changing what is prescribed.”
Dr Ko and his colleagues compared outcomes in patients who were prescribed clopidogrel after hospitalization for ACS in Ontario, Canada, where the Ministry of Health began to automatically substitute generic clopidogrel for Plavix once the brand name drug’s patent expired in 2012.
Between 2009 and 2014, 12,643 patients were prescribed Plavix, and 11,887 were prescribed generic clopidogrel.
“There are quite a few different generic brands,” said study author Cynthia Jackevicius, PharmD, of Western University of Health Sciences in Pomona, California.
“In this study, we considered them as a group but later found no differences in outcome when we compared between different generics.”
Results
The study’s primary outcome—a composite of death and hospitalization for ACS at 1 year—was met by 17.6% of patients prescribed Plavix and 17.9% of patients prescribed clopidogrel. The hazard ratio (HR) was 1.02 (95% confidence interval [CI], 0.96–1.08; P=0.005 for noninferiority, P=0.619 for superiority).
The 1-year mortality rate was 10.5% in the Plavix group and 11.2% in the clopidogrel group (HR=1.07; 95% CI, 0.99–1.15, P=0.210 for noninferiority, P=0.114 for superiority).
And hospitalization for ACS occurred in 9.7% and 9.2%, respectively (HR=0.94; 95% CI, 0.87–1.03, P<0.001 for noninferiority, P=0.190 for superiority).
Hospitalization for any reason occurred in 39.4% of patients in the Plavix group and 39.8% of those in the clopidogrel group (HR=1.02; 95% CI, 0.97–1.06, P<0.001 for noninferiority, P=0.482 for superiority).
Hospitalization for stroke or transient ischemic attack occurred in 1.5% and 1.4%, respectively (HR=0.92; 95% CI, 0.74–1.15, P=0.056 for noninferiority, P=0.455 for superiority).
And hospitalization for bleeding occurred in 2.3% and 2.7%, respectively (HR=1.17; 95% CI, 0.99–1.39, P=0.772 for noninferiority, P=0.063 for superiority).
The researchers noted that, in 2010, Plavix cost about $2.58 Canadian dollars per pill. It was projected to cost the Ontario Drug Benefit Program $72.8 million by 2012.
By switching to generic clopidogrel, which costs $0.39 per pill in 2018, the expense was $19 million Canadian dollars.
“Plavix was one of the most commonly used drugs in cardiology,” Dr Ko said, “so switching to generics can reduce a lot of cost for individuals and health systems.”
Generic clopidogrel is noninferior to the brand-name antiplatelet drug Plavix, according to research published in Circulation: Cardiovascular Quality and Outcomes.
When a Canadian health system switched from prescribing Plavix to generic clopidogrel, patients with acute coronary syndrome (ACS) were no more likely to die or experience ACS recurrence within a year.
In addition, there were no significant differences between the Plavix and clopidogrel groups in the percentage of patients who were hospitalized for any reason, had a stroke or transient ischemic attack, or experienced bleeding.
“People can safely use generic clopidogrel,” said study author Dennis T. Ko, MD, of the Institute for Clinical Evaluative Sciences in Toronto, Ontario, Canada.
“This large and real-world study should be reassuring to physicians and healthcare organizations who have been concerned about changing what is prescribed.”
Dr Ko and his colleagues compared outcomes in patients who were prescribed clopidogrel after hospitalization for ACS in Ontario, Canada, where the Ministry of Health began to automatically substitute generic clopidogrel for Plavix once the brand name drug’s patent expired in 2012.
Between 2009 and 2014, 12,643 patients were prescribed Plavix, and 11,887 were prescribed generic clopidogrel.
“There are quite a few different generic brands,” said study author Cynthia Jackevicius, PharmD, of Western University of Health Sciences in Pomona, California.
“In this study, we considered them as a group but later found no differences in outcome when we compared between different generics.”
Results
The study’s primary outcome—a composite of death and hospitalization for ACS at 1 year—was met by 17.6% of patients prescribed Plavix and 17.9% of patients prescribed clopidogrel. The hazard ratio (HR) was 1.02 (95% confidence interval [CI], 0.96–1.08; P=0.005 for noninferiority, P=0.619 for superiority).
The 1-year mortality rate was 10.5% in the Plavix group and 11.2% in the clopidogrel group (HR=1.07; 95% CI, 0.99–1.15, P=0.210 for noninferiority, P=0.114 for superiority).
And hospitalization for ACS occurred in 9.7% and 9.2%, respectively (HR=0.94; 95% CI, 0.87–1.03, P<0.001 for noninferiority, P=0.190 for superiority).
Hospitalization for any reason occurred in 39.4% of patients in the Plavix group and 39.8% of those in the clopidogrel group (HR=1.02; 95% CI, 0.97–1.06, P<0.001 for noninferiority, P=0.482 for superiority).
Hospitalization for stroke or transient ischemic attack occurred in 1.5% and 1.4%, respectively (HR=0.92; 95% CI, 0.74–1.15, P=0.056 for noninferiority, P=0.455 for superiority).
And hospitalization for bleeding occurred in 2.3% and 2.7%, respectively (HR=1.17; 95% CI, 0.99–1.39, P=0.772 for noninferiority, P=0.063 for superiority).
The researchers noted that, in 2010, Plavix cost about $2.58 Canadian dollars per pill. It was projected to cost the Ontario Drug Benefit Program $72.8 million by 2012.
By switching to generic clopidogrel, which costs $0.39 per pill in 2018, the expense was $19 million Canadian dollars.
“Plavix was one of the most commonly used drugs in cardiology,” Dr Ko said, “so switching to generics can reduce a lot of cost for individuals and health systems.”
Generic clopidogrel is noninferior to the brand-name antiplatelet drug Plavix, according to research published in Circulation: Cardiovascular Quality and Outcomes.
When a Canadian health system switched from prescribing Plavix to generic clopidogrel, patients with acute coronary syndrome (ACS) were no more likely to die or experience ACS recurrence within a year.
In addition, there were no significant differences between the Plavix and clopidogrel groups in the percentage of patients who were hospitalized for any reason, had a stroke or transient ischemic attack, or experienced bleeding.
“People can safely use generic clopidogrel,” said study author Dennis T. Ko, MD, of the Institute for Clinical Evaluative Sciences in Toronto, Ontario, Canada.
“This large and real-world study should be reassuring to physicians and healthcare organizations who have been concerned about changing what is prescribed.”
Dr Ko and his colleagues compared outcomes in patients who were prescribed clopidogrel after hospitalization for ACS in Ontario, Canada, where the Ministry of Health began to automatically substitute generic clopidogrel for Plavix once the brand name drug’s patent expired in 2012.
Between 2009 and 2014, 12,643 patients were prescribed Plavix, and 11,887 were prescribed generic clopidogrel.
“There are quite a few different generic brands,” said study author Cynthia Jackevicius, PharmD, of Western University of Health Sciences in Pomona, California.
“In this study, we considered them as a group but later found no differences in outcome when we compared between different generics.”
Results
The study’s primary outcome—a composite of death and hospitalization for ACS at 1 year—was met by 17.6% of patients prescribed Plavix and 17.9% of patients prescribed clopidogrel. The hazard ratio (HR) was 1.02 (95% confidence interval [CI], 0.96–1.08; P=0.005 for noninferiority, P=0.619 for superiority).
The 1-year mortality rate was 10.5% in the Plavix group and 11.2% in the clopidogrel group (HR=1.07; 95% CI, 0.99–1.15, P=0.210 for noninferiority, P=0.114 for superiority).
And hospitalization for ACS occurred in 9.7% and 9.2%, respectively (HR=0.94; 95% CI, 0.87–1.03, P<0.001 for noninferiority, P=0.190 for superiority).
Hospitalization for any reason occurred in 39.4% of patients in the Plavix group and 39.8% of those in the clopidogrel group (HR=1.02; 95% CI, 0.97–1.06, P<0.001 for noninferiority, P=0.482 for superiority).
Hospitalization for stroke or transient ischemic attack occurred in 1.5% and 1.4%, respectively (HR=0.92; 95% CI, 0.74–1.15, P=0.056 for noninferiority, P=0.455 for superiority).
And hospitalization for bleeding occurred in 2.3% and 2.7%, respectively (HR=1.17; 95% CI, 0.99–1.39, P=0.772 for noninferiority, P=0.063 for superiority).
The researchers noted that, in 2010, Plavix cost about $2.58 Canadian dollars per pill. It was projected to cost the Ontario Drug Benefit Program $72.8 million by 2012.
By switching to generic clopidogrel, which costs $0.39 per pill in 2018, the expense was $19 million Canadian dollars.
“Plavix was one of the most commonly used drugs in cardiology,” Dr Ko said, “so switching to generics can reduce a lot of cost for individuals and health systems.”
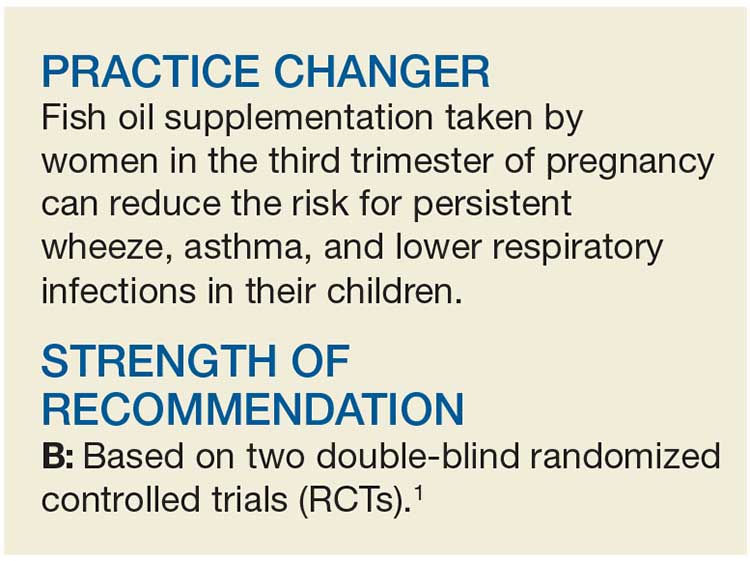
Does Fish Oil During Pregnancy Help Prevent Asthma in Kids?
A 24-year-old G2P1 at 24 weeks’ gestation presents to your clinic for a routine prenatal visit. Her older daughter has asthma, and she wants to know if there is anything she can do to reduce her second child’s risk for it. What do you recommend?
Asthma is the most common chronic disease in children in resource-rich countries such as the United States.2 According to the CDC, 8.4% of children were diagnosed with asthma in 2015.3
Omega-3 fatty acids, found naturally in fish oil, are thought to confer anti-inflammatory properties that offer protection against asthma. Clinical trials have shown that fish oil supplementation in pregnancy results in higher levels of omega-3 fatty acids, along with anti-inflammatory changes, in offspring.4 Previous epidemiologic studies have also found that consumption of omega-3 fatty acids decreases the risk for atopy and asthma in offspring.5,6
A Cochrane review published in 2015, however, concluded that omega-3 supplementation during pregnancy had no benefit on wheeze or asthma in offspring.7 Five RCTs were included in the analysis. The largest trial, by Palmer et al, which included 706 women, showed no benefit for supplementation.8 The second largest, by Olsen et al, which included 533 women, did show a benefit (hazard ratio [HR], 0.37; number needed to treat [NNT], 19.6).9
These results, however, were limited by heterogeneity in the amount of fish oil supplemented and duration of follow-up. For example, the children in the Palmer study were followed only until age 3, which is around the time that asthma can be formally diagnosed—potentially leading to underreporting.8 In addition, the diagnosis of asthma was based on parent report of three episodes of wheezing, use of daily asthma medication, or use of a national registry—all of which can underestimate the incidence of asthma. The reported rate of childhood asthma with IgE-sensitization (rate without sensitization was not reported) was 1.8% in both study groups—much lower than the CDC’s rate of 8.4%, suggesting underdiagnosis.3,8 Due to these biases and other potential confounders, no firm conclusions can be drawn from the Cochrane review.
STUDY SUMMARY
Maternal fish oil supplementation reduces asthma in children
This single-center, double-blind RCT of 736 pregnant women evaluated the effect of 2.4 g/d of n-3 long-chain polyunsaturated fatty acids (eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA]) or placebo (olive oil), starting at an estimated gestational age of 24 to 26 weeks, on wheeze or asthma incidence in their offspring.1
Eligible women were between 22 and 26 weeks’ pregnant at the time of recruitment. Exclusion criteria included supplementation of 600 IU/d or more of vitamin D, or having any endocrine, cardiac, or renal disorders. The investigators randomized the women in a 1:1 ratio to either fish oil or placebo. Maternal EPA and DHA blood levels were tested at the time of randomization and one week after birth.
The primary outcome was persistent wheeze or asthma (after age 3, persistent wheeze was termed asthma), determined based on daily diary recordings of five episodes of troublesome lung symptoms within the past six months (each lasting for at least three consecutive days); rescue use of inhaled ß2-agonists; and/or relapse after a three-month course of inhaled glucocorticoids. Secondary outcomes included reduced incidence of respiratory tract infections, asthma exacerbations, eczema, and allergic sensitization.
In total, 695 offspring were included in the study, with 95.5% follow-up at three years and 93.1% at five. The children had scheduled pediatric visits at 1 week; at one, three, six, 12, 18, 24, 30, and 36 months; and at 4 and 5 years. They also had acute visits for any pulmonary, allergic, or dermatologic symptoms that arose.
Results. The investigators found that the children of mothers who took fish oil had a lower risk for persistent wheeze or asthma at ages 3 to 5, compared to those who received placebo (16.9% vs 23.7%; HR, 0.69; NNT, 14.7). But this effect was significant only in the children whose mothers had baseline EPA and DHA levels in the lowest third (17.5% vs 34.1%; HR, 0.46; NNT, 5.6). Similarly, fish oil supplementation had a greater benefit in children whose mothers had consumed the least EPA and DHA before the start of the study (18.5% vs 32.4%; HR, 0.55; NNT, 7.2).
As for the secondary outcomes, only a reduction in lower respiratory infections was associated with fish oil supplementation compared with placebo (38.8% vs 45.5%; HR, 0.77; NNT, 14.9). There was no reduction in asthma exacerbations, eczema, or risk for sensitization in the fish oil group.
WHAT’S NEW?
Study adds fuel to the fire
This study strengthens the case for fish oil supplementation during pregnancy to reduce the risk for asthma in offspring, despite the recent Cochrane review that showed no benefit.1,7 The Palmer study used a much lower amount of omega-3s (900 mg/d fish oil vs 2,400 mg/d in the current trial).1,8 Olsen et al supplemented with a greater amount of omega-3s (2,700 mg/d) and did find a benefit.9 The NNT from the Olsen study (19.6) is consistent with that of the current investigation, suggesting that a higher dosage may be necessary to prevent the onset of asthma.
Additionally, this study followed children for a longer period than did the Palmer study, which may have led to more accurate diagnoses of asthma.1,8 Lastly, the diagnosis of asthma in the Palmer study was based on parent survey data and use of daily asthma medicine rather than on daily diary cards, which are often more accurate.
Consider fish consumption. Both this study and the Olsen trial were performed in Denmark.1,9 While Denmark and the United States have had a relatively similar level of fish consumption since the 1990s, women in Denmark may eat a higher proportion of oily fish than women in the United States, given the more common inclusion of mackerel and herring in their diet.10 Thus, the effect of supplementation may be more pronounced in women in the US.
CAVEATS
Ideal dose? Which women to treat?
The FDA currently recommends 8 to 12 oz of fish per week for pregnant women, but there are no guidelines on the ideal amount of fish oil to be consumed.11 The Palmer study, using 900 mg/d of fish oil, did not show a benefit, whereas there did appear to be a benefit in this study (2,400 mg/d) and the Olsen study (2,700 mg/d).1,8,9 Further research is needed to determine the optimal dosage.
The decreased risk for persistent wheeze or asthma was seen only in the children of women whose EPA and DHA blood levels were in the lowest third of the study population. Thus, only women whose blood levels are low to begin with will likely benefit from this intervention. Currently, EPA and DHA levels are not routinely checked, but there may be some benefit to doing so.
One proxy for blood levels is maternal intake of fish at baseline. The investigators found that there was an association between dietary intake of fish and blood levels of EPA and DHA (r, 0.32).1 Therefore, additional screening questions to gauge fish consumption would be useful to identify women most likely to benefit from supplementation.
CHALLENGES TO IMPLEMENTATION
Multiple pills, additional cost
Since omega-3 fatty acids are relatively safe and the NNT in the general population is low, it may be worth supplementing all pregnant women, even without a commercially available blood test for EPA or DHA. Nevertheless, some women may find it challenging to take up to four additional pills per day for 13 or more weeks. Also, there is an associated cost with these supplements, although it is low.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2018. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2018;67[2]: 100-102).
1. Bisgaard H, Stokholm J, Chawes BL, et al. Fish oil-derived fatty acids in pregnancy and wheeze and asthma in offspring. N Engl J Med. 2016;375(26):2530-2539.
2. Masoli M, Fabian D, Holt S, et al. The global burden of asthma: executive summary of the GINA Dissemination Committee Report. Allergy. 2004;59(5):469-478.
3. CDC . Asthma. www.cdc.gov/asthma/most_recent_data.htm. Accessed February 1, 2018.
4. Miyata J, Arita M. Role of omega-3 fatty acids and their metabolites in asthma and allergic diseases. Allergol Int. 2015;64(1):27-34.
5. Salam MT, Li YF, Langholz B, et al. Maternal fish consumption during pregnancy and risk of early childhood asthma. J Asthma. 2005;42(6):513-518.
6. Calvani M, Alessandri C, Sopo SM, et al. Consumption of fish, butter and margarine during pregnancy and development of allergic sensitizations in the offspring: role of maternal atopy. Pediatr Allergy Immunol. 2006;17(2):94-102.
7. Gunaratne AW, Makrides M, Collins CT. Maternal prenatal and/or postnatal n-3 long chain polyunsaturated fatty acids (LCPUFA) supplementation for preventing allergies in early childhood. Cochrane Database Syst Rev. 2015;22(7): CD010085.
8. Palmer D, Sullivan T, Gold M, et al. Randomized controlled trial of fish oil supplementation in pregnancy on childhood allergies. Allergy. 2013;68:1370-1376.
9. Olsen SF, Østerdal ML, Salvig JD, et al. Fish oil intake compared with olive oil intake in late pregnancy and asthma in the offspring: 16 y of registry-based follow-up from a randomized controlled trial. Am J Clin Nutr. 2008;88(1): 167-175.
10. Helgi Library. Fish consumption per capita by country. www.helgilibrary.com/indicators/fish-consumption-per-capita/. Accessed February 1, 2018.
11. FDA Advice About Eating Fish, From the Environmental Protection Agency and Food and Drug Administration; Revised Fish Advice; Availability. Fed Regist. 2017;82:6571-6574.
A 24-year-old G2P1 at 24 weeks’ gestation presents to your clinic for a routine prenatal visit. Her older daughter has asthma, and she wants to know if there is anything she can do to reduce her second child’s risk for it. What do you recommend?
Asthma is the most common chronic disease in children in resource-rich countries such as the United States.2 According to the CDC, 8.4% of children were diagnosed with asthma in 2015.3
Omega-3 fatty acids, found naturally in fish oil, are thought to confer anti-inflammatory properties that offer protection against asthma. Clinical trials have shown that fish oil supplementation in pregnancy results in higher levels of omega-3 fatty acids, along with anti-inflammatory changes, in offspring.4 Previous epidemiologic studies have also found that consumption of omega-3 fatty acids decreases the risk for atopy and asthma in offspring.5,6
A Cochrane review published in 2015, however, concluded that omega-3 supplementation during pregnancy had no benefit on wheeze or asthma in offspring.7 Five RCTs were included in the analysis. The largest trial, by Palmer et al, which included 706 women, showed no benefit for supplementation.8 The second largest, by Olsen et al, which included 533 women, did show a benefit (hazard ratio [HR], 0.37; number needed to treat [NNT], 19.6).9
These results, however, were limited by heterogeneity in the amount of fish oil supplemented and duration of follow-up. For example, the children in the Palmer study were followed only until age 3, which is around the time that asthma can be formally diagnosed—potentially leading to underreporting.8 In addition, the diagnosis of asthma was based on parent report of three episodes of wheezing, use of daily asthma medication, or use of a national registry—all of which can underestimate the incidence of asthma. The reported rate of childhood asthma with IgE-sensitization (rate without sensitization was not reported) was 1.8% in both study groups—much lower than the CDC’s rate of 8.4%, suggesting underdiagnosis.3,8 Due to these biases and other potential confounders, no firm conclusions can be drawn from the Cochrane review.
STUDY SUMMARY
Maternal fish oil supplementation reduces asthma in children
This single-center, double-blind RCT of 736 pregnant women evaluated the effect of 2.4 g/d of n-3 long-chain polyunsaturated fatty acids (eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA]) or placebo (olive oil), starting at an estimated gestational age of 24 to 26 weeks, on wheeze or asthma incidence in their offspring.1
Eligible women were between 22 and 26 weeks’ pregnant at the time of recruitment. Exclusion criteria included supplementation of 600 IU/d or more of vitamin D, or having any endocrine, cardiac, or renal disorders. The investigators randomized the women in a 1:1 ratio to either fish oil or placebo. Maternal EPA and DHA blood levels were tested at the time of randomization and one week after birth.
The primary outcome was persistent wheeze or asthma (after age 3, persistent wheeze was termed asthma), determined based on daily diary recordings of five episodes of troublesome lung symptoms within the past six months (each lasting for at least three consecutive days); rescue use of inhaled ß2-agonists; and/or relapse after a three-month course of inhaled glucocorticoids. Secondary outcomes included reduced incidence of respiratory tract infections, asthma exacerbations, eczema, and allergic sensitization.
In total, 695 offspring were included in the study, with 95.5% follow-up at three years and 93.1% at five. The children had scheduled pediatric visits at 1 week; at one, three, six, 12, 18, 24, 30, and 36 months; and at 4 and 5 years. They also had acute visits for any pulmonary, allergic, or dermatologic symptoms that arose.
Results. The investigators found that the children of mothers who took fish oil had a lower risk for persistent wheeze or asthma at ages 3 to 5, compared to those who received placebo (16.9% vs 23.7%; HR, 0.69; NNT, 14.7). But this effect was significant only in the children whose mothers had baseline EPA and DHA levels in the lowest third (17.5% vs 34.1%; HR, 0.46; NNT, 5.6). Similarly, fish oil supplementation had a greater benefit in children whose mothers had consumed the least EPA and DHA before the start of the study (18.5% vs 32.4%; HR, 0.55; NNT, 7.2).
As for the secondary outcomes, only a reduction in lower respiratory infections was associated with fish oil supplementation compared with placebo (38.8% vs 45.5%; HR, 0.77; NNT, 14.9). There was no reduction in asthma exacerbations, eczema, or risk for sensitization in the fish oil group.
WHAT’S NEW?
Study adds fuel to the fire
This study strengthens the case for fish oil supplementation during pregnancy to reduce the risk for asthma in offspring, despite the recent Cochrane review that showed no benefit.1,7 The Palmer study used a much lower amount of omega-3s (900 mg/d fish oil vs 2,400 mg/d in the current trial).1,8 Olsen et al supplemented with a greater amount of omega-3s (2,700 mg/d) and did find a benefit.9 The NNT from the Olsen study (19.6) is consistent with that of the current investigation, suggesting that a higher dosage may be necessary to prevent the onset of asthma.
Additionally, this study followed children for a longer period than did the Palmer study, which may have led to more accurate diagnoses of asthma.1,8 Lastly, the diagnosis of asthma in the Palmer study was based on parent survey data and use of daily asthma medicine rather than on daily diary cards, which are often more accurate.
Consider fish consumption. Both this study and the Olsen trial were performed in Denmark.1,9 While Denmark and the United States have had a relatively similar level of fish consumption since the 1990s, women in Denmark may eat a higher proportion of oily fish than women in the United States, given the more common inclusion of mackerel and herring in their diet.10 Thus, the effect of supplementation may be more pronounced in women in the US.
CAVEATS
Ideal dose? Which women to treat?
The FDA currently recommends 8 to 12 oz of fish per week for pregnant women, but there are no guidelines on the ideal amount of fish oil to be consumed.11 The Palmer study, using 900 mg/d of fish oil, did not show a benefit, whereas there did appear to be a benefit in this study (2,400 mg/d) and the Olsen study (2,700 mg/d).1,8,9 Further research is needed to determine the optimal dosage.
The decreased risk for persistent wheeze or asthma was seen only in the children of women whose EPA and DHA blood levels were in the lowest third of the study population. Thus, only women whose blood levels are low to begin with will likely benefit from this intervention. Currently, EPA and DHA levels are not routinely checked, but there may be some benefit to doing so.
One proxy for blood levels is maternal intake of fish at baseline. The investigators found that there was an association between dietary intake of fish and blood levels of EPA and DHA (r, 0.32).1 Therefore, additional screening questions to gauge fish consumption would be useful to identify women most likely to benefit from supplementation.
CHALLENGES TO IMPLEMENTATION
Multiple pills, additional cost
Since omega-3 fatty acids are relatively safe and the NNT in the general population is low, it may be worth supplementing all pregnant women, even without a commercially available blood test for EPA or DHA. Nevertheless, some women may find it challenging to take up to four additional pills per day for 13 or more weeks. Also, there is an associated cost with these supplements, although it is low.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2018. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2018;67[2]: 100-102).
A 24-year-old G2P1 at 24 weeks’ gestation presents to your clinic for a routine prenatal visit. Her older daughter has asthma, and she wants to know if there is anything she can do to reduce her second child’s risk for it. What do you recommend?
Asthma is the most common chronic disease in children in resource-rich countries such as the United States.2 According to the CDC, 8.4% of children were diagnosed with asthma in 2015.3
Omega-3 fatty acids, found naturally in fish oil, are thought to confer anti-inflammatory properties that offer protection against asthma. Clinical trials have shown that fish oil supplementation in pregnancy results in higher levels of omega-3 fatty acids, along with anti-inflammatory changes, in offspring.4 Previous epidemiologic studies have also found that consumption of omega-3 fatty acids decreases the risk for atopy and asthma in offspring.5,6
A Cochrane review published in 2015, however, concluded that omega-3 supplementation during pregnancy had no benefit on wheeze or asthma in offspring.7 Five RCTs were included in the analysis. The largest trial, by Palmer et al, which included 706 women, showed no benefit for supplementation.8 The second largest, by Olsen et al, which included 533 women, did show a benefit (hazard ratio [HR], 0.37; number needed to treat [NNT], 19.6).9
These results, however, were limited by heterogeneity in the amount of fish oil supplemented and duration of follow-up. For example, the children in the Palmer study were followed only until age 3, which is around the time that asthma can be formally diagnosed—potentially leading to underreporting.8 In addition, the diagnosis of asthma was based on parent report of three episodes of wheezing, use of daily asthma medication, or use of a national registry—all of which can underestimate the incidence of asthma. The reported rate of childhood asthma with IgE-sensitization (rate without sensitization was not reported) was 1.8% in both study groups—much lower than the CDC’s rate of 8.4%, suggesting underdiagnosis.3,8 Due to these biases and other potential confounders, no firm conclusions can be drawn from the Cochrane review.
STUDY SUMMARY
Maternal fish oil supplementation reduces asthma in children
This single-center, double-blind RCT of 736 pregnant women evaluated the effect of 2.4 g/d of n-3 long-chain polyunsaturated fatty acids (eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA]) or placebo (olive oil), starting at an estimated gestational age of 24 to 26 weeks, on wheeze or asthma incidence in their offspring.1
Eligible women were between 22 and 26 weeks’ pregnant at the time of recruitment. Exclusion criteria included supplementation of 600 IU/d or more of vitamin D, or having any endocrine, cardiac, or renal disorders. The investigators randomized the women in a 1:1 ratio to either fish oil or placebo. Maternal EPA and DHA blood levels were tested at the time of randomization and one week after birth.
The primary outcome was persistent wheeze or asthma (after age 3, persistent wheeze was termed asthma), determined based on daily diary recordings of five episodes of troublesome lung symptoms within the past six months (each lasting for at least three consecutive days); rescue use of inhaled ß2-agonists; and/or relapse after a three-month course of inhaled glucocorticoids. Secondary outcomes included reduced incidence of respiratory tract infections, asthma exacerbations, eczema, and allergic sensitization.
In total, 695 offspring were included in the study, with 95.5% follow-up at three years and 93.1% at five. The children had scheduled pediatric visits at 1 week; at one, three, six, 12, 18, 24, 30, and 36 months; and at 4 and 5 years. They also had acute visits for any pulmonary, allergic, or dermatologic symptoms that arose.
Results. The investigators found that the children of mothers who took fish oil had a lower risk for persistent wheeze or asthma at ages 3 to 5, compared to those who received placebo (16.9% vs 23.7%; HR, 0.69; NNT, 14.7). But this effect was significant only in the children whose mothers had baseline EPA and DHA levels in the lowest third (17.5% vs 34.1%; HR, 0.46; NNT, 5.6). Similarly, fish oil supplementation had a greater benefit in children whose mothers had consumed the least EPA and DHA before the start of the study (18.5% vs 32.4%; HR, 0.55; NNT, 7.2).
As for the secondary outcomes, only a reduction in lower respiratory infections was associated with fish oil supplementation compared with placebo (38.8% vs 45.5%; HR, 0.77; NNT, 14.9). There was no reduction in asthma exacerbations, eczema, or risk for sensitization in the fish oil group.
WHAT’S NEW?
Study adds fuel to the fire
This study strengthens the case for fish oil supplementation during pregnancy to reduce the risk for asthma in offspring, despite the recent Cochrane review that showed no benefit.1,7 The Palmer study used a much lower amount of omega-3s (900 mg/d fish oil vs 2,400 mg/d in the current trial).1,8 Olsen et al supplemented with a greater amount of omega-3s (2,700 mg/d) and did find a benefit.9 The NNT from the Olsen study (19.6) is consistent with that of the current investigation, suggesting that a higher dosage may be necessary to prevent the onset of asthma.
Additionally, this study followed children for a longer period than did the Palmer study, which may have led to more accurate diagnoses of asthma.1,8 Lastly, the diagnosis of asthma in the Palmer study was based on parent survey data and use of daily asthma medicine rather than on daily diary cards, which are often more accurate.
Consider fish consumption. Both this study and the Olsen trial were performed in Denmark.1,9 While Denmark and the United States have had a relatively similar level of fish consumption since the 1990s, women in Denmark may eat a higher proportion of oily fish than women in the United States, given the more common inclusion of mackerel and herring in their diet.10 Thus, the effect of supplementation may be more pronounced in women in the US.
CAVEATS
Ideal dose? Which women to treat?
The FDA currently recommends 8 to 12 oz of fish per week for pregnant women, but there are no guidelines on the ideal amount of fish oil to be consumed.11 The Palmer study, using 900 mg/d of fish oil, did not show a benefit, whereas there did appear to be a benefit in this study (2,400 mg/d) and the Olsen study (2,700 mg/d).1,8,9 Further research is needed to determine the optimal dosage.
The decreased risk for persistent wheeze or asthma was seen only in the children of women whose EPA and DHA blood levels were in the lowest third of the study population. Thus, only women whose blood levels are low to begin with will likely benefit from this intervention. Currently, EPA and DHA levels are not routinely checked, but there may be some benefit to doing so.
One proxy for blood levels is maternal intake of fish at baseline. The investigators found that there was an association between dietary intake of fish and blood levels of EPA and DHA (r, 0.32).1 Therefore, additional screening questions to gauge fish consumption would be useful to identify women most likely to benefit from supplementation.
CHALLENGES TO IMPLEMENTATION
Multiple pills, additional cost
Since omega-3 fatty acids are relatively safe and the NNT in the general population is low, it may be worth supplementing all pregnant women, even without a commercially available blood test for EPA or DHA. Nevertheless, some women may find it challenging to take up to four additional pills per day for 13 or more weeks. Also, there is an associated cost with these supplements, although it is low.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2018. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2018;67[2]: 100-102).
1. Bisgaard H, Stokholm J, Chawes BL, et al. Fish oil-derived fatty acids in pregnancy and wheeze and asthma in offspring. N Engl J Med. 2016;375(26):2530-2539.
2. Masoli M, Fabian D, Holt S, et al. The global burden of asthma: executive summary of the GINA Dissemination Committee Report. Allergy. 2004;59(5):469-478.
3. CDC . Asthma. www.cdc.gov/asthma/most_recent_data.htm. Accessed February 1, 2018.
4. Miyata J, Arita M. Role of omega-3 fatty acids and their metabolites in asthma and allergic diseases. Allergol Int. 2015;64(1):27-34.
5. Salam MT, Li YF, Langholz B, et al. Maternal fish consumption during pregnancy and risk of early childhood asthma. J Asthma. 2005;42(6):513-518.
6. Calvani M, Alessandri C, Sopo SM, et al. Consumption of fish, butter and margarine during pregnancy and development of allergic sensitizations in the offspring: role of maternal atopy. Pediatr Allergy Immunol. 2006;17(2):94-102.
7. Gunaratne AW, Makrides M, Collins CT. Maternal prenatal and/or postnatal n-3 long chain polyunsaturated fatty acids (LCPUFA) supplementation for preventing allergies in early childhood. Cochrane Database Syst Rev. 2015;22(7): CD010085.
8. Palmer D, Sullivan T, Gold M, et al. Randomized controlled trial of fish oil supplementation in pregnancy on childhood allergies. Allergy. 2013;68:1370-1376.
9. Olsen SF, Østerdal ML, Salvig JD, et al. Fish oil intake compared with olive oil intake in late pregnancy and asthma in the offspring: 16 y of registry-based follow-up from a randomized controlled trial. Am J Clin Nutr. 2008;88(1): 167-175.
10. Helgi Library. Fish consumption per capita by country. www.helgilibrary.com/indicators/fish-consumption-per-capita/. Accessed February 1, 2018.
11. FDA Advice About Eating Fish, From the Environmental Protection Agency and Food and Drug Administration; Revised Fish Advice; Availability. Fed Regist. 2017;82:6571-6574.
1. Bisgaard H, Stokholm J, Chawes BL, et al. Fish oil-derived fatty acids in pregnancy and wheeze and asthma in offspring. N Engl J Med. 2016;375(26):2530-2539.
2. Masoli M, Fabian D, Holt S, et al. The global burden of asthma: executive summary of the GINA Dissemination Committee Report. Allergy. 2004;59(5):469-478.
3. CDC . Asthma. www.cdc.gov/asthma/most_recent_data.htm. Accessed February 1, 2018.
4. Miyata J, Arita M. Role of omega-3 fatty acids and their metabolites in asthma and allergic diseases. Allergol Int. 2015;64(1):27-34.
5. Salam MT, Li YF, Langholz B, et al. Maternal fish consumption during pregnancy and risk of early childhood asthma. J Asthma. 2005;42(6):513-518.
6. Calvani M, Alessandri C, Sopo SM, et al. Consumption of fish, butter and margarine during pregnancy and development of allergic sensitizations in the offspring: role of maternal atopy. Pediatr Allergy Immunol. 2006;17(2):94-102.
7. Gunaratne AW, Makrides M, Collins CT. Maternal prenatal and/or postnatal n-3 long chain polyunsaturated fatty acids (LCPUFA) supplementation for preventing allergies in early childhood. Cochrane Database Syst Rev. 2015;22(7): CD010085.
8. Palmer D, Sullivan T, Gold M, et al. Randomized controlled trial of fish oil supplementation in pregnancy on childhood allergies. Allergy. 2013;68:1370-1376.
9. Olsen SF, Østerdal ML, Salvig JD, et al. Fish oil intake compared with olive oil intake in late pregnancy and asthma in the offspring: 16 y of registry-based follow-up from a randomized controlled trial. Am J Clin Nutr. 2008;88(1): 167-175.
10. Helgi Library. Fish consumption per capita by country. www.helgilibrary.com/indicators/fish-consumption-per-capita/. Accessed February 1, 2018.
11. FDA Advice About Eating Fish, From the Environmental Protection Agency and Food and Drug Administration; Revised Fish Advice; Availability. Fed Regist. 2017;82:6571-6574.
Quick Byte: U.S. health care can still innovate
“The United States health care system has many problems, but it also promotes more innovation than its counterparts in other nations. … It has more clinical trials than any other country. It has the most Nobel laureates in physiology or medicine. It has won more patents. At least one publication ranks it No. 1 in overall scientific innovation. … The nation’s innovation advantage arises from a first-class research university system, along with robust intellectual property laws and significant public and private investment in research and development. Perhaps most important, this country offers a large market in which patients, organizations, and government spend a lot on health and companies are able to profit greatly from health care innovation.”
Reference
1. Carroll AE et al. “Can the U.S. repair its health care while keeping its innovation edge?” The New York Times. Oct 9, 2017.
. Accessed Oct 10, 2017.
“The United States health care system has many problems, but it also promotes more innovation than its counterparts in other nations. … It has more clinical trials than any other country. It has the most Nobel laureates in physiology or medicine. It has won more patents. At least one publication ranks it No. 1 in overall scientific innovation. … The nation’s innovation advantage arises from a first-class research university system, along with robust intellectual property laws and significant public and private investment in research and development. Perhaps most important, this country offers a large market in which patients, organizations, and government spend a lot on health and companies are able to profit greatly from health care innovation.”
Reference
1. Carroll AE et al. “Can the U.S. repair its health care while keeping its innovation edge?” The New York Times. Oct 9, 2017.
. Accessed Oct 10, 2017.
“The United States health care system has many problems, but it also promotes more innovation than its counterparts in other nations. … It has more clinical trials than any other country. It has the most Nobel laureates in physiology or medicine. It has won more patents. At least one publication ranks it No. 1 in overall scientific innovation. … The nation’s innovation advantage arises from a first-class research university system, along with robust intellectual property laws and significant public and private investment in research and development. Perhaps most important, this country offers a large market in which patients, organizations, and government spend a lot on health and companies are able to profit greatly from health care innovation.”
Reference
1. Carroll AE et al. “Can the U.S. repair its health care while keeping its innovation edge?” The New York Times. Oct 9, 2017.
. Accessed Oct 10, 2017.
KD025 shows promise for steroid-dependent cGVHD
SALT LAKE CITY – KD025, an orally available Rho-associated coiled-coil kinase 2–selective inhibitor, is demonstrating encouraging activity and safety in patients with steroid-dependent or refractory chronic graft-versus-host disease (cGVHD) in a phase 2a clinical trial.
Initial results from the ongoing open-label trial known as KD025-208 showed that 11 of 17 patients (65%) and 11 of 16 patients (69%) enrolled in 200-mg daily and 200-mg twice-daily dose cohorts, respectively, had a clinical response with no reported treatment-related serious adverse events at any evaluation time point, Aleksandr Lazaryan, MD, PhD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
The median duration of treatment in the 200-mg daily group (cohort 1) was 37 weeks, and in the 200-mg twice-daily group (cohort 2) was 28 weeks. At last follow-up, eight patients remained active in each cohort, and these patients had a median treatment duration of 53 and 38 weeks, respectively, he said.
In cohort 1, four patients went off the study because of cGVHD progression, and five withdrew, including two who experienced recurrence of their underlying hematologic malignancy. In cohort 2, 7 of the 16 patients experienced progression of cGVHD, he noted.
Patients in cohorts 1 and 2 had a median age of 52 years and had received at least 2 months of steroid treatment and no more than 3 prior lines of therapy. They were comparable with respect to baseline characteristics, including median time to and duration of GVHD, time from diagnosis to enrollment, median prednisone dose, and median number of prior therapies. They had involvement of various – and often multiple – organ systems: 58% had four or more systems affected at the time of enrollment, and 21% had five or more systems affected.
“This, in a way, reflects a real-life mix of the cGVHD population of patients, with some of those patients having advanced cGVHD,” said Dr. Lazaryan.
Responses were observed across all affected organ systems, with complete responses documented in the upper and lower gastrointestinal tracts. About 75% of patients in cohort 1 who had multiple organ systems involved at enrollment demonstrated responses in at least four organ systems.
Furthermore, the responses were rapid: 68% of responses occurred in the first 8 weeks of treatment and appeared durable, Dr. Lazaryan said, noting that 7 of the 17 patients in cohort 1 had sustained responses for more than 20 weeks, and 3 patients had sustained responses for more than 32 weeks.
“The durability data continue to mature in this trial,” he added.
The adverse events that occurred were consistent with what would be expected for the cGVHD patient population treated with steroids, he said, reporting that no patients discontinued treatment because of infection, no opportunistic or fungal infections have been reported to date, and no treatment-related serious adverse events were reported.
Steroid dose reductions were experienced by 40% and 26% of patients in cohorts 1 and 2, respectively. The dose reductions were achieved in both KD025 responders and nonresponders, he noted.
Overall, four patients (12%) were able to discontinue steroids, and 80% in both cohorts experienced reductions in background tacrolimus.
In addition, up to 65% of patients in cohort 1 achieved a greater than seven point reduction on the Lee cGVHD Symptom Scale, with both responders and nonresponders experiencing improvement on this endpoint.
Chronic GVHD remains a leading cause of post-transplant morbidity and mortality. KD025, which is currently in phase 2 development for inflammatory fibrotic disease, has been shown in preclinical models to down-regulate T helper 17 cells and T follicular helper cells while up-regulating anti-inflammatory regulatory T cells, thereby potentially correcting the immunological imbalance seen in cGVHD, Dr. Lazaryan said.
Analysis is ongoing in this study, including in a third cohort of patients treated with 200 mg of KD025 four times daily, which recently completed accrual. An expansion cohort, at a dose yet to be determined, will include approximately 40 patients, he noted.
The trial is sponsored by Kadmon. Dr. Lazaryan reported advisory board membership and consultancy for GLyPharma Therapeutic.
sworcester@frontlinemedcom.com
SOURCE: Lazaryan A et al. 2018 BMT Tandem Meetings, Abstract 38.
SALT LAKE CITY – KD025, an orally available Rho-associated coiled-coil kinase 2–selective inhibitor, is demonstrating encouraging activity and safety in patients with steroid-dependent or refractory chronic graft-versus-host disease (cGVHD) in a phase 2a clinical trial.
Initial results from the ongoing open-label trial known as KD025-208 showed that 11 of 17 patients (65%) and 11 of 16 patients (69%) enrolled in 200-mg daily and 200-mg twice-daily dose cohorts, respectively, had a clinical response with no reported treatment-related serious adverse events at any evaluation time point, Aleksandr Lazaryan, MD, PhD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
The median duration of treatment in the 200-mg daily group (cohort 1) was 37 weeks, and in the 200-mg twice-daily group (cohort 2) was 28 weeks. At last follow-up, eight patients remained active in each cohort, and these patients had a median treatment duration of 53 and 38 weeks, respectively, he said.
In cohort 1, four patients went off the study because of cGVHD progression, and five withdrew, including two who experienced recurrence of their underlying hematologic malignancy. In cohort 2, 7 of the 16 patients experienced progression of cGVHD, he noted.
Patients in cohorts 1 and 2 had a median age of 52 years and had received at least 2 months of steroid treatment and no more than 3 prior lines of therapy. They were comparable with respect to baseline characteristics, including median time to and duration of GVHD, time from diagnosis to enrollment, median prednisone dose, and median number of prior therapies. They had involvement of various – and often multiple – organ systems: 58% had four or more systems affected at the time of enrollment, and 21% had five or more systems affected.
“This, in a way, reflects a real-life mix of the cGVHD population of patients, with some of those patients having advanced cGVHD,” said Dr. Lazaryan.
Responses were observed across all affected organ systems, with complete responses documented in the upper and lower gastrointestinal tracts. About 75% of patients in cohort 1 who had multiple organ systems involved at enrollment demonstrated responses in at least four organ systems.
Furthermore, the responses were rapid: 68% of responses occurred in the first 8 weeks of treatment and appeared durable, Dr. Lazaryan said, noting that 7 of the 17 patients in cohort 1 had sustained responses for more than 20 weeks, and 3 patients had sustained responses for more than 32 weeks.
“The durability data continue to mature in this trial,” he added.
The adverse events that occurred were consistent with what would be expected for the cGVHD patient population treated with steroids, he said, reporting that no patients discontinued treatment because of infection, no opportunistic or fungal infections have been reported to date, and no treatment-related serious adverse events were reported.
Steroid dose reductions were experienced by 40% and 26% of patients in cohorts 1 and 2, respectively. The dose reductions were achieved in both KD025 responders and nonresponders, he noted.
Overall, four patients (12%) were able to discontinue steroids, and 80% in both cohorts experienced reductions in background tacrolimus.
In addition, up to 65% of patients in cohort 1 achieved a greater than seven point reduction on the Lee cGVHD Symptom Scale, with both responders and nonresponders experiencing improvement on this endpoint.
Chronic GVHD remains a leading cause of post-transplant morbidity and mortality. KD025, which is currently in phase 2 development for inflammatory fibrotic disease, has been shown in preclinical models to down-regulate T helper 17 cells and T follicular helper cells while up-regulating anti-inflammatory regulatory T cells, thereby potentially correcting the immunological imbalance seen in cGVHD, Dr. Lazaryan said.
Analysis is ongoing in this study, including in a third cohort of patients treated with 200 mg of KD025 four times daily, which recently completed accrual. An expansion cohort, at a dose yet to be determined, will include approximately 40 patients, he noted.
The trial is sponsored by Kadmon. Dr. Lazaryan reported advisory board membership and consultancy for GLyPharma Therapeutic.
sworcester@frontlinemedcom.com
SOURCE: Lazaryan A et al. 2018 BMT Tandem Meetings, Abstract 38.
SALT LAKE CITY – KD025, an orally available Rho-associated coiled-coil kinase 2–selective inhibitor, is demonstrating encouraging activity and safety in patients with steroid-dependent or refractory chronic graft-versus-host disease (cGVHD) in a phase 2a clinical trial.
Initial results from the ongoing open-label trial known as KD025-208 showed that 11 of 17 patients (65%) and 11 of 16 patients (69%) enrolled in 200-mg daily and 200-mg twice-daily dose cohorts, respectively, had a clinical response with no reported treatment-related serious adverse events at any evaluation time point, Aleksandr Lazaryan, MD, PhD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
The median duration of treatment in the 200-mg daily group (cohort 1) was 37 weeks, and in the 200-mg twice-daily group (cohort 2) was 28 weeks. At last follow-up, eight patients remained active in each cohort, and these patients had a median treatment duration of 53 and 38 weeks, respectively, he said.
In cohort 1, four patients went off the study because of cGVHD progression, and five withdrew, including two who experienced recurrence of their underlying hematologic malignancy. In cohort 2, 7 of the 16 patients experienced progression of cGVHD, he noted.
Patients in cohorts 1 and 2 had a median age of 52 years and had received at least 2 months of steroid treatment and no more than 3 prior lines of therapy. They were comparable with respect to baseline characteristics, including median time to and duration of GVHD, time from diagnosis to enrollment, median prednisone dose, and median number of prior therapies. They had involvement of various – and often multiple – organ systems: 58% had four or more systems affected at the time of enrollment, and 21% had five or more systems affected.
“This, in a way, reflects a real-life mix of the cGVHD population of patients, with some of those patients having advanced cGVHD,” said Dr. Lazaryan.
Responses were observed across all affected organ systems, with complete responses documented in the upper and lower gastrointestinal tracts. About 75% of patients in cohort 1 who had multiple organ systems involved at enrollment demonstrated responses in at least four organ systems.
Furthermore, the responses were rapid: 68% of responses occurred in the first 8 weeks of treatment and appeared durable, Dr. Lazaryan said, noting that 7 of the 17 patients in cohort 1 had sustained responses for more than 20 weeks, and 3 patients had sustained responses for more than 32 weeks.
“The durability data continue to mature in this trial,” he added.
The adverse events that occurred were consistent with what would be expected for the cGVHD patient population treated with steroids, he said, reporting that no patients discontinued treatment because of infection, no opportunistic or fungal infections have been reported to date, and no treatment-related serious adverse events were reported.
Steroid dose reductions were experienced by 40% and 26% of patients in cohorts 1 and 2, respectively. The dose reductions were achieved in both KD025 responders and nonresponders, he noted.
Overall, four patients (12%) were able to discontinue steroids, and 80% in both cohorts experienced reductions in background tacrolimus.
In addition, up to 65% of patients in cohort 1 achieved a greater than seven point reduction on the Lee cGVHD Symptom Scale, with both responders and nonresponders experiencing improvement on this endpoint.
Chronic GVHD remains a leading cause of post-transplant morbidity and mortality. KD025, which is currently in phase 2 development for inflammatory fibrotic disease, has been shown in preclinical models to down-regulate T helper 17 cells and T follicular helper cells while up-regulating anti-inflammatory regulatory T cells, thereby potentially correcting the immunological imbalance seen in cGVHD, Dr. Lazaryan said.
Analysis is ongoing in this study, including in a third cohort of patients treated with 200 mg of KD025 four times daily, which recently completed accrual. An expansion cohort, at a dose yet to be determined, will include approximately 40 patients, he noted.
The trial is sponsored by Kadmon. Dr. Lazaryan reported advisory board membership and consultancy for GLyPharma Therapeutic.
sworcester@frontlinemedcom.com
SOURCE: Lazaryan A et al. 2018 BMT Tandem Meetings, Abstract 38.
REPORTING FROM THE 2018 BMT TANDEM MEETINGS
Key clinical point:
Major finding: Clinical response rates in cohorts 1 and 2 were 65% and 69%, respectively.
Study details: Preliminary findings in 33 patients from a phase 2a trial.
Disclosures: The trial is sponsored by Kadmon. Dr. Lazaryan reported advisory board membership and consultancy for GLyPharma Therapeutic.
Source: Lazaryan A et al. 2018 BMT Tandem Meetings, Abstract 38.
Minor differences with electric and manual aspiration of molar pregnancy
Manual vacuum aspiration of molar pregnancy achieves similar outcomes to electric vacuum aspiration, although it may lead to a lower incidence of uterine synechia, according to a paper published in the April edition of Obstetrics & Gynecology.
While electric vacuum aspiration of molar pregnancy is the dominant technique in North America, in other parts of the world, such as Brazil, manual vacuum aspiration is far more commonly used.
In a retrospective cohort study, researchers looked at outcomes for 1,727 patients with molar pregnancy; 1,206 of these patients underwent electric vacuum aspiration, and 521 underwent manual vacuum aspiration.
Patients who underwent electric vacuum aspiration had significantly shorter operative times (25.3 minutes vs. 34.2 minutes; P less than .001) and showed a greater drop in hemoglobin levels after evacuation (–0.3 g/dL vs. –0.19 g/dL; P less than .001), compared with those who underwent manual vacuum aspiration.
The electric procedure was also associated with a significantly higher risk of intrauterine adhesions after the procedure, compared with the manual vacuum aspiration (5.2% vs. 1.2%; P less than .001).
Lilian Padrón, MD, of the Trophoblastic Disease Center at the Rio de Janeiro Federal University and coauthors commented that the vacuum pressure is about 100 mm Hg higher in the electric technique than it is in the manual technique, which may be responsible for the greater risk of synechia.
However, there were no significant differences seen between the two groups in the risk of developing postmolar gestational trophoblastic neoplasia (14.2% with electric vs. 17.3% with manual; P = .074) nor in the presence of metastatic disease (19.9% vs. 17.8%; P = .082) or the need for multiagent chemotherapy.
Around 13% of patients had incomplete uterine evacuation, but the risk was similar between electric and manual vacuum aspiration.
“In our sample, formed exclusively by patients with molar pregnancy, the rate of complete uterine emptying did not reach 90% with either technique,” the authors wrote. “This may reflect not only the greater amount of molar trophoblastic tissue, compared with an abortion, but also the invasiveness of molar trophoblastic cells into the maternal decidua.”
There were nine cases of uterine perforation in the electric vacuum aspiration group (0.7%), and none in the manual group, although the difference was not statistically significant.
“Although differences in rates of uterine perforation as well as prolonged length of stay were not statistically different between the groups,” the authors wrote, “both of these were rare events, and we lacked sufficient power to detect differences in rare outcomes.”
No conflicts of interest were declared.
SOURCE: Padrón L et al. Obstet Gynecol. 2018;131:652-9.
Manual vacuum aspiration of molar pregnancy achieves similar outcomes to electric vacuum aspiration, although it may lead to a lower incidence of uterine synechia, according to a paper published in the April edition of Obstetrics & Gynecology.
While electric vacuum aspiration of molar pregnancy is the dominant technique in North America, in other parts of the world, such as Brazil, manual vacuum aspiration is far more commonly used.
In a retrospective cohort study, researchers looked at outcomes for 1,727 patients with molar pregnancy; 1,206 of these patients underwent electric vacuum aspiration, and 521 underwent manual vacuum aspiration.
Patients who underwent electric vacuum aspiration had significantly shorter operative times (25.3 minutes vs. 34.2 minutes; P less than .001) and showed a greater drop in hemoglobin levels after evacuation (–0.3 g/dL vs. –0.19 g/dL; P less than .001), compared with those who underwent manual vacuum aspiration.
The electric procedure was also associated with a significantly higher risk of intrauterine adhesions after the procedure, compared with the manual vacuum aspiration (5.2% vs. 1.2%; P less than .001).
Lilian Padrón, MD, of the Trophoblastic Disease Center at the Rio de Janeiro Federal University and coauthors commented that the vacuum pressure is about 100 mm Hg higher in the electric technique than it is in the manual technique, which may be responsible for the greater risk of synechia.
However, there were no significant differences seen between the two groups in the risk of developing postmolar gestational trophoblastic neoplasia (14.2% with electric vs. 17.3% with manual; P = .074) nor in the presence of metastatic disease (19.9% vs. 17.8%; P = .082) or the need for multiagent chemotherapy.
Around 13% of patients had incomplete uterine evacuation, but the risk was similar between electric and manual vacuum aspiration.
“In our sample, formed exclusively by patients with molar pregnancy, the rate of complete uterine emptying did not reach 90% with either technique,” the authors wrote. “This may reflect not only the greater amount of molar trophoblastic tissue, compared with an abortion, but also the invasiveness of molar trophoblastic cells into the maternal decidua.”
There were nine cases of uterine perforation in the electric vacuum aspiration group (0.7%), and none in the manual group, although the difference was not statistically significant.
“Although differences in rates of uterine perforation as well as prolonged length of stay were not statistically different between the groups,” the authors wrote, “both of these were rare events, and we lacked sufficient power to detect differences in rare outcomes.”
No conflicts of interest were declared.
SOURCE: Padrón L et al. Obstet Gynecol. 2018;131:652-9.
Manual vacuum aspiration of molar pregnancy achieves similar outcomes to electric vacuum aspiration, although it may lead to a lower incidence of uterine synechia, according to a paper published in the April edition of Obstetrics & Gynecology.
While electric vacuum aspiration of molar pregnancy is the dominant technique in North America, in other parts of the world, such as Brazil, manual vacuum aspiration is far more commonly used.
In a retrospective cohort study, researchers looked at outcomes for 1,727 patients with molar pregnancy; 1,206 of these patients underwent electric vacuum aspiration, and 521 underwent manual vacuum aspiration.
Patients who underwent electric vacuum aspiration had significantly shorter operative times (25.3 minutes vs. 34.2 minutes; P less than .001) and showed a greater drop in hemoglobin levels after evacuation (–0.3 g/dL vs. –0.19 g/dL; P less than .001), compared with those who underwent manual vacuum aspiration.
The electric procedure was also associated with a significantly higher risk of intrauterine adhesions after the procedure, compared with the manual vacuum aspiration (5.2% vs. 1.2%; P less than .001).
Lilian Padrón, MD, of the Trophoblastic Disease Center at the Rio de Janeiro Federal University and coauthors commented that the vacuum pressure is about 100 mm Hg higher in the electric technique than it is in the manual technique, which may be responsible for the greater risk of synechia.
However, there were no significant differences seen between the two groups in the risk of developing postmolar gestational trophoblastic neoplasia (14.2% with electric vs. 17.3% with manual; P = .074) nor in the presence of metastatic disease (19.9% vs. 17.8%; P = .082) or the need for multiagent chemotherapy.
Around 13% of patients had incomplete uterine evacuation, but the risk was similar between electric and manual vacuum aspiration.
“In our sample, formed exclusively by patients with molar pregnancy, the rate of complete uterine emptying did not reach 90% with either technique,” the authors wrote. “This may reflect not only the greater amount of molar trophoblastic tissue, compared with an abortion, but also the invasiveness of molar trophoblastic cells into the maternal decidua.”
There were nine cases of uterine perforation in the electric vacuum aspiration group (0.7%), and none in the manual group, although the difference was not statistically significant.
“Although differences in rates of uterine perforation as well as prolonged length of stay were not statistically different between the groups,” the authors wrote, “both of these were rare events, and we lacked sufficient power to detect differences in rare outcomes.”
No conflicts of interest were declared.
SOURCE: Padrón L et al. Obstet Gynecol. 2018;131:652-9.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: Manual vacuum aspiration of molar pregnancy achieves similar outcomes to electric vacuum aspiration, although it may lead to a lower incidence of uterine synechia.
Major finding: Electric vacuum aspiration of molar pregnancy is associated with a higher risk of synechia than manual vacuum aspiration.
Data source: A retrospective cohort study in 1,727 patients with molar pregnancy.
Disclosures: No conflicts of interest were declared.
Source: Padrón L et al. Obstet Gynecol. 2018;131:652-9.
FDA meeting on medical devices for sleep apnea scheduled
In a statement sent to members, CHEST invited all to attend this open meeting, which will be held at the FDA White Oak Campus in Silver Spring, Md.
In a statement sent to members, CHEST invited all to attend this open meeting, which will be held at the FDA White Oak Campus in Silver Spring, Md.
In a statement sent to members, CHEST invited all to attend this open meeting, which will be held at the FDA White Oak Campus in Silver Spring, Md.
SGS 2018: SGS Fellow Scholar provides daily coverage of annual meeting
3/13/18. DAY 3 AT SGS
A busy day gets underway
During a busy morning scientific session, Dr. Amit Sood (@amitsoodMD) delivered the TeLinde lecture, titled "Building resilience," which he defined as doing well when you should not be doing well. He walked meeting attendees through a few exercises, including practicing morning gratitude and finding curious moments. He received a well-deserved standing ovation.
After a quick lunch, the group reconvened for a riveting panel discussion regarding the future of ObGyn in the session, "What is the future of gynecologic surgery and the subspecialties?" Dr. Eric Sokol moderated the discussion, and the panelists included Dr. Carl Zimmerman representing general gynecology, Dr. Dee Fenner from urogynecology, Dr. Arnold Advincula from minimally invasive gynecologic surgery (MIGS), Dr. Javier Magrina from gynecologic oncology, and Dr. Wilma Larsen representing the American Board of Obstetrics and Gynecology (ABOG). Many opinions were shared, including the possibility of allowing residents to choose a track in obstetrics or gynecology. Clearly there is a lot to explore in the future of our field. As a MIGS fellow, it was great to hear Dr. Advincula define our specialty as "non-malignant, advanced pelvic surgery."
The FMIGS Young Alumni Network then met to hear Dr. Samar Nahas give a talk on "Life as you see it, from all the struggles to all the success." She gave an inspiring overview of her life and encouraged those in attendance to keep searching for their next goal in life, whether it be academic, career-related, family, or personal.
Taking in Orlando sun and fun
The afternoon was free for leisure, and many meeting attendees took advantage of the activities offered, including a golf tournament as well as ziplining at nearby Gatorland. Others, like myself, simply took the opportunity to enjoy the sun and warm weather in Orlando, especially while there was a nor'easter occurring back home.
SGS' Got Talent was the festive evening activity on the agenda, during which a competitive talent show occurred. Attendees were able to vote for their favorites while giving donations to the organization Surgeons Helping Advance Research & Education (SHARE). Highlights included a Disney sing-along and a rousing medley of Michael Jackson songs sung on the kazoo.
See you next year!
Tomorrow is the last day of #SGS2018. I look forward to returning to my MIGS fellowship at Bridgeport Hospital in Bridgeport, Connecticut, and sharing all that I have learned. Thank you to Dr. Nancy Frankel, SGS, and OBG Management and all the sponsors supporting the Fellow Scholar program for allowing us trainees to take part in this excellent conference! I am looking forward to #SGS2019 in Tucson, Arizona.
3/12/18. DAY 2 AT SGS
Something for everyone at Day 2 SGS sessions
This morning’s Scientific Sessions began with the Keynote address by Dr. James Merlino, President and Chief Medical Officer, Strategic Consulting, at Press Ganey, who spoke on “Patient Experience: It Is Not About Making People Happy.” Dr. Merlino opened with a personal anecdote about an experience he had with a poor hospital outcome. He reminded us that showing empathy can make a huge difference in patients’ perspectives on their experience and that “an engaged culture is essential to high performance.” He also emphasized that all physicians are leaders and that our involvement in patient safety and decreasing errors is essential.
Surgeons debate best approach for POP
Another highlight of the Scientific Sessions was the debate moderated by Dr. Peter Rosenblatt on “Optimal Surgical Management of Stage 3 and 4 Pelvic Organ Prolapse.” Drs. Rebecca Rogers, Patrick Culligan, and Vincent Lucente participated. The consensus was that Dr. Rogers won over the crowd, convincing us that native tissue repair is the answer. Excellent job by all the panelists for an informative—and entertaining—debate!
Focus on fellows
Immediately following the third Scientific Session, the fellows convened at the Fellows’ Pelvic Research Network (FPRN)® meeting. After a quick joint session during which Dr. Donna Mazloomdoost gave an informative talk on the grant process at the National Institute of Child Health and Human Development (NICHD), the MIGS fellows broke out to review projects that are currently recruiting new sites and to hear a new proposal for a collaborative multicenter study.
President’s events
Evening activities included the President’s Awards Ceremony and the President’s Reception. Awards Ceremony notable moments included the “Honor your Mentor” session, during which the honored individuals were each recognized. Dr. Ralph Chesson then received the inaugural “Mentor of the Year” award, to much applause. Fellow/Resident awards were up next. Dr. Christina Jones received the President’s Award–Prize Paper for her oral presentation, “Liposomal bupivacaine efficacy for postoperative pain following posterior vaginal surgery: a randomized, double-blind, placebo-controlled trial.” Congratulations! The day concluded with the President’s Reception, where the food, drink, and conversation were plentiful.
Get appy
Finally, conference attendees were able to plan their meeting on their smartphones using the Event Pilot App, which also had a running Twitter thread under the hashtag #SGS2018. A Twitter scavenger hunt was also underway, with #speculumsunday, #maskmembermonday, and #trocartuesday. During this event attendees are encouraged to find the “object of the day,” Tweet a response to a prompt, and then bring the object to the social media booth to receive a prize.
Stay tuned to @ChrisTierneyMD for more live updates from #SGS2018.

3/11/18. DAY 1 AT SGS
Good morning from sunny Orlando!
It was a very early morning, due to the conveniently timed daylight savings to start the Annual Scientific Meeting of the Society of Gynecologic Surgeons (SGS). First on the agenda was the postgraduate (PG) course, “Endometriosis: Contemporary Approaches to Diagnosis and Treatment” led by Dr. Rosanne Kho. Excellent talks were given and reminded us that, as a specialty, we have made great strides in advancing the diagnosis and treatment of endometriosis. Nevertheless, there is much work to be done in developing a better classification system, including identifying markers that can help stratify the extent of disease.
A highlight was a question from the audience regarding the important facets of a physical exam in diagnosing deep endometriosis. Dr. Mauricio Abrao reviewed his strategy, which included palpating for adnexal masses, pain, or nodules in the cul-de-sac and evaluating trigger points along the psoas muscle. Dr. Scott Young, a radiologist, then provided some key signs to look for in pelvic magnetic resonance imaging and endovaginal ultrasound in diagnosing deep endometriosis. He reminded all of us that a partnership with an excellent radiology department is key in diagnosing and treating deep endometriosis effectively. Dr. Tommaso Falcone then gave an excellent overview of anatomy in relation to deep endometriosis, teaching us all about the different layers of the retroperitoneum.
An afternoon of simulation
After a quick break, it was on to the next course: “Train the Trainer: Comprehensive Hysterectomy Simulation Course for Educators.” Dr. Christine Vaccaro headed this interactive session, and started us off with a reminder that “simulation is the future, and we need to jump on board!” Unfortunately for trainees, the overall number of hysterectomies performed during residency are decreasing secondary to medical management available for abnormal uterine bleeding and the fact that the 4 years of ObGyn residency have a heavy focus on obstetrics. Therefore, it was great to hear Dr. Vaccaro say that the American Board of Obstetrics and Gynecology (ABOG) is requiring Fundamentals of Laparoscopic Surgery (FLSTM) training for those seeking board certification. Attendees of this session included a combination of trainers and trainees, so to speak, and we took turns rotating around models for abdominal, vaginal, laparoscopic, and robotic hysterectomies. I took the opportunity to learn some tips and tricks from experts like Dr. Ernie Lockrow during a simulated laparoscopic myomectomy, in which the struggle felt very real.
Mix and mingle
Other PG courses offered and attended throughout the day included: “Surgical Coding: Working through the Entire Procedure,” “Variations in the Management of the Vaginal Apex during Reconstructive Pelvic Surgery,” Gynecologic Care of Girls and Young Women Born with Urogenital Anomalies,” and “Social Media, Medicine and your Digital Footprint.” SGS Fellow Scholars were then invited to the “Senior Members Engaging Young Learners” event, designed to connect senior SGS members with residents and fellows. Here, residents and fellows mingled with distinguished faculty, many of them with red badges on their nametags, indicating 20 years of membership with SGS. I learned firsthand that connections are very easy to make in this friendly group, where everyone is willing to introduce you to someone who will help advance your career. After this, we moved straight onto the Welcome Reception, where conversations and connections continued.
I look forward to a full day tomorrow! Stay tuned to @ChrisTierneyMD for live updates from #SGS2018.

3/13/18. DAY 3 AT SGS
A busy day gets underway
During a busy morning scientific session, Dr. Amit Sood (@amitsoodMD) delivered the TeLinde lecture, titled "Building resilience," which he defined as doing well when you should not be doing well. He walked meeting attendees through a few exercises, including practicing morning gratitude and finding curious moments. He received a well-deserved standing ovation.
After a quick lunch, the group reconvened for a riveting panel discussion regarding the future of ObGyn in the session, "What is the future of gynecologic surgery and the subspecialties?" Dr. Eric Sokol moderated the discussion, and the panelists included Dr. Carl Zimmerman representing general gynecology, Dr. Dee Fenner from urogynecology, Dr. Arnold Advincula from minimally invasive gynecologic surgery (MIGS), Dr. Javier Magrina from gynecologic oncology, and Dr. Wilma Larsen representing the American Board of Obstetrics and Gynecology (ABOG). Many opinions were shared, including the possibility of allowing residents to choose a track in obstetrics or gynecology. Clearly there is a lot to explore in the future of our field. As a MIGS fellow, it was great to hear Dr. Advincula define our specialty as "non-malignant, advanced pelvic surgery."
The FMIGS Young Alumni Network then met to hear Dr. Samar Nahas give a talk on "Life as you see it, from all the struggles to all the success." She gave an inspiring overview of her life and encouraged those in attendance to keep searching for their next goal in life, whether it be academic, career-related, family, or personal.
Taking in Orlando sun and fun
The afternoon was free for leisure, and many meeting attendees took advantage of the activities offered, including a golf tournament as well as ziplining at nearby Gatorland. Others, like myself, simply took the opportunity to enjoy the sun and warm weather in Orlando, especially while there was a nor'easter occurring back home.
SGS' Got Talent was the festive evening activity on the agenda, during which a competitive talent show occurred. Attendees were able to vote for their favorites while giving donations to the organization Surgeons Helping Advance Research & Education (SHARE). Highlights included a Disney sing-along and a rousing medley of Michael Jackson songs sung on the kazoo.
See you next year!
Tomorrow is the last day of #SGS2018. I look forward to returning to my MIGS fellowship at Bridgeport Hospital in Bridgeport, Connecticut, and sharing all that I have learned. Thank you to Dr. Nancy Frankel, SGS, and OBG Management and all the sponsors supporting the Fellow Scholar program for allowing us trainees to take part in this excellent conference! I am looking forward to #SGS2019 in Tucson, Arizona.
3/12/18. DAY 2 AT SGS
Something for everyone at Day 2 SGS sessions
This morning’s Scientific Sessions began with the Keynote address by Dr. James Merlino, President and Chief Medical Officer, Strategic Consulting, at Press Ganey, who spoke on “Patient Experience: It Is Not About Making People Happy.” Dr. Merlino opened with a personal anecdote about an experience he had with a poor hospital outcome. He reminded us that showing empathy can make a huge difference in patients’ perspectives on their experience and that “an engaged culture is essential to high performance.” He also emphasized that all physicians are leaders and that our involvement in patient safety and decreasing errors is essential.
Surgeons debate best approach for POP
Another highlight of the Scientific Sessions was the debate moderated by Dr. Peter Rosenblatt on “Optimal Surgical Management of Stage 3 and 4 Pelvic Organ Prolapse.” Drs. Rebecca Rogers, Patrick Culligan, and Vincent Lucente participated. The consensus was that Dr. Rogers won over the crowd, convincing us that native tissue repair is the answer. Excellent job by all the panelists for an informative—and entertaining—debate!
Focus on fellows
Immediately following the third Scientific Session, the fellows convened at the Fellows’ Pelvic Research Network (FPRN)® meeting. After a quick joint session during which Dr. Donna Mazloomdoost gave an informative talk on the grant process at the National Institute of Child Health and Human Development (NICHD), the MIGS fellows broke out to review projects that are currently recruiting new sites and to hear a new proposal for a collaborative multicenter study.
President’s events
Evening activities included the President’s Awards Ceremony and the President’s Reception. Awards Ceremony notable moments included the “Honor your Mentor” session, during which the honored individuals were each recognized. Dr. Ralph Chesson then received the inaugural “Mentor of the Year” award, to much applause. Fellow/Resident awards were up next. Dr. Christina Jones received the President’s Award–Prize Paper for her oral presentation, “Liposomal bupivacaine efficacy for postoperative pain following posterior vaginal surgery: a randomized, double-blind, placebo-controlled trial.” Congratulations! The day concluded with the President’s Reception, where the food, drink, and conversation were plentiful.
Get appy
Finally, conference attendees were able to plan their meeting on their smartphones using the Event Pilot App, which also had a running Twitter thread under the hashtag #SGS2018. A Twitter scavenger hunt was also underway, with #speculumsunday, #maskmembermonday, and #trocartuesday. During this event attendees are encouraged to find the “object of the day,” Tweet a response to a prompt, and then bring the object to the social media booth to receive a prize.
Stay tuned to @ChrisTierneyMD for more live updates from #SGS2018.

3/11/18. DAY 1 AT SGS
Good morning from sunny Orlando!
It was a very early morning, due to the conveniently timed daylight savings to start the Annual Scientific Meeting of the Society of Gynecologic Surgeons (SGS). First on the agenda was the postgraduate (PG) course, “Endometriosis: Contemporary Approaches to Diagnosis and Treatment” led by Dr. Rosanne Kho. Excellent talks were given and reminded us that, as a specialty, we have made great strides in advancing the diagnosis and treatment of endometriosis. Nevertheless, there is much work to be done in developing a better classification system, including identifying markers that can help stratify the extent of disease.
A highlight was a question from the audience regarding the important facets of a physical exam in diagnosing deep endometriosis. Dr. Mauricio Abrao reviewed his strategy, which included palpating for adnexal masses, pain, or nodules in the cul-de-sac and evaluating trigger points along the psoas muscle. Dr. Scott Young, a radiologist, then provided some key signs to look for in pelvic magnetic resonance imaging and endovaginal ultrasound in diagnosing deep endometriosis. He reminded all of us that a partnership with an excellent radiology department is key in diagnosing and treating deep endometriosis effectively. Dr. Tommaso Falcone then gave an excellent overview of anatomy in relation to deep endometriosis, teaching us all about the different layers of the retroperitoneum.
An afternoon of simulation
After a quick break, it was on to the next course: “Train the Trainer: Comprehensive Hysterectomy Simulation Course for Educators.” Dr. Christine Vaccaro headed this interactive session, and started us off with a reminder that “simulation is the future, and we need to jump on board!” Unfortunately for trainees, the overall number of hysterectomies performed during residency are decreasing secondary to medical management available for abnormal uterine bleeding and the fact that the 4 years of ObGyn residency have a heavy focus on obstetrics. Therefore, it was great to hear Dr. Vaccaro say that the American Board of Obstetrics and Gynecology (ABOG) is requiring Fundamentals of Laparoscopic Surgery (FLSTM) training for those seeking board certification. Attendees of this session included a combination of trainers and trainees, so to speak, and we took turns rotating around models for abdominal, vaginal, laparoscopic, and robotic hysterectomies. I took the opportunity to learn some tips and tricks from experts like Dr. Ernie Lockrow during a simulated laparoscopic myomectomy, in which the struggle felt very real.
Mix and mingle
Other PG courses offered and attended throughout the day included: “Surgical Coding: Working through the Entire Procedure,” “Variations in the Management of the Vaginal Apex during Reconstructive Pelvic Surgery,” Gynecologic Care of Girls and Young Women Born with Urogenital Anomalies,” and “Social Media, Medicine and your Digital Footprint.” SGS Fellow Scholars were then invited to the “Senior Members Engaging Young Learners” event, designed to connect senior SGS members with residents and fellows. Here, residents and fellows mingled with distinguished faculty, many of them with red badges on their nametags, indicating 20 years of membership with SGS. I learned firsthand that connections are very easy to make in this friendly group, where everyone is willing to introduce you to someone who will help advance your career. After this, we moved straight onto the Welcome Reception, where conversations and connections continued.
I look forward to a full day tomorrow! Stay tuned to @ChrisTierneyMD for live updates from #SGS2018.

3/13/18. DAY 3 AT SGS
A busy day gets underway
During a busy morning scientific session, Dr. Amit Sood (@amitsoodMD) delivered the TeLinde lecture, titled "Building resilience," which he defined as doing well when you should not be doing well. He walked meeting attendees through a few exercises, including practicing morning gratitude and finding curious moments. He received a well-deserved standing ovation.
After a quick lunch, the group reconvened for a riveting panel discussion regarding the future of ObGyn in the session, "What is the future of gynecologic surgery and the subspecialties?" Dr. Eric Sokol moderated the discussion, and the panelists included Dr. Carl Zimmerman representing general gynecology, Dr. Dee Fenner from urogynecology, Dr. Arnold Advincula from minimally invasive gynecologic surgery (MIGS), Dr. Javier Magrina from gynecologic oncology, and Dr. Wilma Larsen representing the American Board of Obstetrics and Gynecology (ABOG). Many opinions were shared, including the possibility of allowing residents to choose a track in obstetrics or gynecology. Clearly there is a lot to explore in the future of our field. As a MIGS fellow, it was great to hear Dr. Advincula define our specialty as "non-malignant, advanced pelvic surgery."
The FMIGS Young Alumni Network then met to hear Dr. Samar Nahas give a talk on "Life as you see it, from all the struggles to all the success." She gave an inspiring overview of her life and encouraged those in attendance to keep searching for their next goal in life, whether it be academic, career-related, family, or personal.
Taking in Orlando sun and fun
The afternoon was free for leisure, and many meeting attendees took advantage of the activities offered, including a golf tournament as well as ziplining at nearby Gatorland. Others, like myself, simply took the opportunity to enjoy the sun and warm weather in Orlando, especially while there was a nor'easter occurring back home.
SGS' Got Talent was the festive evening activity on the agenda, during which a competitive talent show occurred. Attendees were able to vote for their favorites while giving donations to the organization Surgeons Helping Advance Research & Education (SHARE). Highlights included a Disney sing-along and a rousing medley of Michael Jackson songs sung on the kazoo.
See you next year!
Tomorrow is the last day of #SGS2018. I look forward to returning to my MIGS fellowship at Bridgeport Hospital in Bridgeport, Connecticut, and sharing all that I have learned. Thank you to Dr. Nancy Frankel, SGS, and OBG Management and all the sponsors supporting the Fellow Scholar program for allowing us trainees to take part in this excellent conference! I am looking forward to #SGS2019 in Tucson, Arizona.
3/12/18. DAY 2 AT SGS
Something for everyone at Day 2 SGS sessions
This morning’s Scientific Sessions began with the Keynote address by Dr. James Merlino, President and Chief Medical Officer, Strategic Consulting, at Press Ganey, who spoke on “Patient Experience: It Is Not About Making People Happy.” Dr. Merlino opened with a personal anecdote about an experience he had with a poor hospital outcome. He reminded us that showing empathy can make a huge difference in patients’ perspectives on their experience and that “an engaged culture is essential to high performance.” He also emphasized that all physicians are leaders and that our involvement in patient safety and decreasing errors is essential.
Surgeons debate best approach for POP
Another highlight of the Scientific Sessions was the debate moderated by Dr. Peter Rosenblatt on “Optimal Surgical Management of Stage 3 and 4 Pelvic Organ Prolapse.” Drs. Rebecca Rogers, Patrick Culligan, and Vincent Lucente participated. The consensus was that Dr. Rogers won over the crowd, convincing us that native tissue repair is the answer. Excellent job by all the panelists for an informative—and entertaining—debate!
Focus on fellows
Immediately following the third Scientific Session, the fellows convened at the Fellows’ Pelvic Research Network (FPRN)® meeting. After a quick joint session during which Dr. Donna Mazloomdoost gave an informative talk on the grant process at the National Institute of Child Health and Human Development (NICHD), the MIGS fellows broke out to review projects that are currently recruiting new sites and to hear a new proposal for a collaborative multicenter study.
President’s events
Evening activities included the President’s Awards Ceremony and the President’s Reception. Awards Ceremony notable moments included the “Honor your Mentor” session, during which the honored individuals were each recognized. Dr. Ralph Chesson then received the inaugural “Mentor of the Year” award, to much applause. Fellow/Resident awards were up next. Dr. Christina Jones received the President’s Award–Prize Paper for her oral presentation, “Liposomal bupivacaine efficacy for postoperative pain following posterior vaginal surgery: a randomized, double-blind, placebo-controlled trial.” Congratulations! The day concluded with the President’s Reception, where the food, drink, and conversation were plentiful.
Get appy
Finally, conference attendees were able to plan their meeting on their smartphones using the Event Pilot App, which also had a running Twitter thread under the hashtag #SGS2018. A Twitter scavenger hunt was also underway, with #speculumsunday, #maskmembermonday, and #trocartuesday. During this event attendees are encouraged to find the “object of the day,” Tweet a response to a prompt, and then bring the object to the social media booth to receive a prize.
Stay tuned to @ChrisTierneyMD for more live updates from #SGS2018.

3/11/18. DAY 1 AT SGS
Good morning from sunny Orlando!
It was a very early morning, due to the conveniently timed daylight savings to start the Annual Scientific Meeting of the Society of Gynecologic Surgeons (SGS). First on the agenda was the postgraduate (PG) course, “Endometriosis: Contemporary Approaches to Diagnosis and Treatment” led by Dr. Rosanne Kho. Excellent talks were given and reminded us that, as a specialty, we have made great strides in advancing the diagnosis and treatment of endometriosis. Nevertheless, there is much work to be done in developing a better classification system, including identifying markers that can help stratify the extent of disease.
A highlight was a question from the audience regarding the important facets of a physical exam in diagnosing deep endometriosis. Dr. Mauricio Abrao reviewed his strategy, which included palpating for adnexal masses, pain, or nodules in the cul-de-sac and evaluating trigger points along the psoas muscle. Dr. Scott Young, a radiologist, then provided some key signs to look for in pelvic magnetic resonance imaging and endovaginal ultrasound in diagnosing deep endometriosis. He reminded all of us that a partnership with an excellent radiology department is key in diagnosing and treating deep endometriosis effectively. Dr. Tommaso Falcone then gave an excellent overview of anatomy in relation to deep endometriosis, teaching us all about the different layers of the retroperitoneum.
An afternoon of simulation
After a quick break, it was on to the next course: “Train the Trainer: Comprehensive Hysterectomy Simulation Course for Educators.” Dr. Christine Vaccaro headed this interactive session, and started us off with a reminder that “simulation is the future, and we need to jump on board!” Unfortunately for trainees, the overall number of hysterectomies performed during residency are decreasing secondary to medical management available for abnormal uterine bleeding and the fact that the 4 years of ObGyn residency have a heavy focus on obstetrics. Therefore, it was great to hear Dr. Vaccaro say that the American Board of Obstetrics and Gynecology (ABOG) is requiring Fundamentals of Laparoscopic Surgery (FLSTM) training for those seeking board certification. Attendees of this session included a combination of trainers and trainees, so to speak, and we took turns rotating around models for abdominal, vaginal, laparoscopic, and robotic hysterectomies. I took the opportunity to learn some tips and tricks from experts like Dr. Ernie Lockrow during a simulated laparoscopic myomectomy, in which the struggle felt very real.
Mix and mingle
Other PG courses offered and attended throughout the day included: “Surgical Coding: Working through the Entire Procedure,” “Variations in the Management of the Vaginal Apex during Reconstructive Pelvic Surgery,” Gynecologic Care of Girls and Young Women Born with Urogenital Anomalies,” and “Social Media, Medicine and your Digital Footprint.” SGS Fellow Scholars were then invited to the “Senior Members Engaging Young Learners” event, designed to connect senior SGS members with residents and fellows. Here, residents and fellows mingled with distinguished faculty, many of them with red badges on their nametags, indicating 20 years of membership with SGS. I learned firsthand that connections are very easy to make in this friendly group, where everyone is willing to introduce you to someone who will help advance your career. After this, we moved straight onto the Welcome Reception, where conversations and connections continued.
I look forward to a full day tomorrow! Stay tuned to @ChrisTierneyMD for live updates from #SGS2018.

Depression risks identified in women
The same group of women was significantly more likely to have minor depression, compared with those who were not depressed, if they had less than a high school education or asthma or if they smoked, reported Nan Guo, PhD, and her associates at Stanford (Calif.) University.
The adjusted relative risk for major depression was a significant 2.49 for women if they had government, state, or military insurance, compared with the reference group – those who had private insurance. Women with no insurance had an adjusted RR of 1.84, which did not reach statistical significance, they said.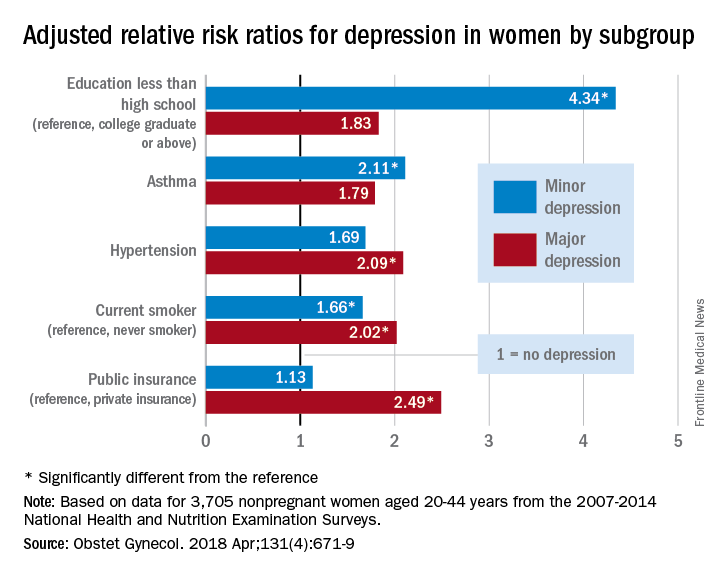
Education was a major area of difference between women with minor depression and those with no depression. Compared with the reference group – college graduate or above – adjusted RRs for minor depression were 4.34 for those with less than a high school education, 2.92 for those with a high school education, and 2.59 for women with some college or an associate degree. Women with asthma were 2.11 times as likely to have minor depression as those without asthma, and current smokers had an RR of 1.66 for minor depression, compared with never smokers, the investigators said.
The study was supported by funding from Stanford University. One investigator received an award from the National Institute of Child Health and Human Development. The investigators did not report any potential conflicts of interest.
The same group of women was significantly more likely to have minor depression, compared with those who were not depressed, if they had less than a high school education or asthma or if they smoked, reported Nan Guo, PhD, and her associates at Stanford (Calif.) University.
The adjusted relative risk for major depression was a significant 2.49 for women if they had government, state, or military insurance, compared with the reference group – those who had private insurance. Women with no insurance had an adjusted RR of 1.84, which did not reach statistical significance, they said.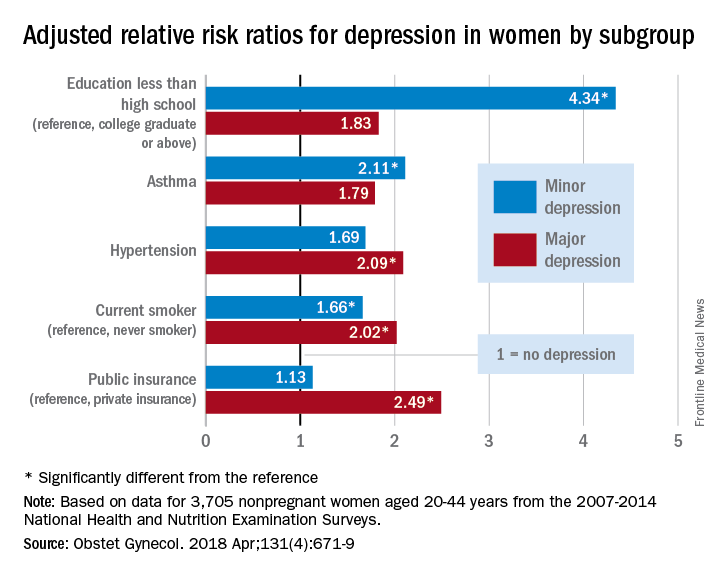
Education was a major area of difference between women with minor depression and those with no depression. Compared with the reference group – college graduate or above – adjusted RRs for minor depression were 4.34 for those with less than a high school education, 2.92 for those with a high school education, and 2.59 for women with some college or an associate degree. Women with asthma were 2.11 times as likely to have minor depression as those without asthma, and current smokers had an RR of 1.66 for minor depression, compared with never smokers, the investigators said.
The study was supported by funding from Stanford University. One investigator received an award from the National Institute of Child Health and Human Development. The investigators did not report any potential conflicts of interest.
The same group of women was significantly more likely to have minor depression, compared with those who were not depressed, if they had less than a high school education or asthma or if they smoked, reported Nan Guo, PhD, and her associates at Stanford (Calif.) University.
The adjusted relative risk for major depression was a significant 2.49 for women if they had government, state, or military insurance, compared with the reference group – those who had private insurance. Women with no insurance had an adjusted RR of 1.84, which did not reach statistical significance, they said.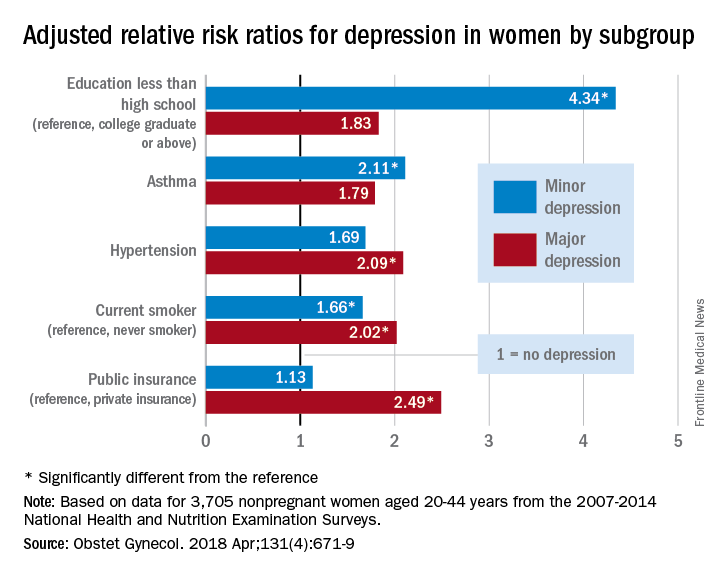
Education was a major area of difference between women with minor depression and those with no depression. Compared with the reference group – college graduate or above – adjusted RRs for minor depression were 4.34 for those with less than a high school education, 2.92 for those with a high school education, and 2.59 for women with some college or an associate degree. Women with asthma were 2.11 times as likely to have minor depression as those without asthma, and current smokers had an RR of 1.66 for minor depression, compared with never smokers, the investigators said.
The study was supported by funding from Stanford University. One investigator received an award from the National Institute of Child Health and Human Development. The investigators did not report any potential conflicts of interest.
FROM OBSTETRICS & GYNECOLOGY