User login
In myeloma, third ASCT is a viable option
A third autologous stem cell transplantation (ASCT) is feasible and provides clinical benefit to patients with relapsed multiple myeloma, according to findings from a retrospective study.
The benefits appear to be most pronounced in patients who had a long duration of response to the previous ASCT, the researchers wrote in Biology of Blood and Marrow Transplantation.
“A salvage third ASCT is of value for patients with relapsed multiple myeloma,” Laurent Garderet, MD, of the department of hematology, Hôpital Saint Antoine, Paris, and coauthors wrote in the report.
A third transplantation is most commonly used in patients who relapse following tandem ASCT. Less often, it is done in patients who receive upfront ASCT, relapse, undergo a second ASCT, and relapse again.
“The first scenario gives much better results, due in part to a better remission status at the third ASCT with no signs of increased [second primary malignancy],” the researchers wrote.
In that group, median overall survival was greater than 5 years if the relapse occurred 3 years or more after the initial tandem ASCT, study results show.
The retrospective analysis, based on European Society for Blood and Marrow Transplantation data, included 570 patients who had undergone a third ASCT between 1997 and 2010. Of that group, 482 patients (81%) received the third transplantation after tandem ASCT and subsequent relapse, and 88 (15%) received it after second relapse.
After third ASCT, overall survival was 33 months in the larger tandem transplant group with 61 months of follow-up, and 15 months in the smaller group of patients who received two salvage ASCTs after 48 months of follow-up.
Median progression-free survival was 13 and 8 months for the tandem ASCT and two-salvage–ASCT groups, respectively, while 100-day nonrelapse mortality was 4% and 7%, respectively.
For both groups, better outcomes were associated with longer duration of remission after the second ASCT, the researchers reported.
Moreover, the time from second ASCT to relapse was the only favorable prognostic factor associated with survival after third ASCT in a multivariate analysis of the patients who relapsed following tandem transplant. The hazard ratio for relapse occurring between 18 and 36 months vs. within 18 months was 0.62 (95% confidence interval, 0.47-0.82; P = .01); for relapse after 36 months, the HR was 0.35 (95% CI, 0.25-0.49; P less than .001).
The researchers acknowledged that, beyond transplant, treatment of myeloma has changed substantially in recent years and could change the clinical picture for patients undergoing a third ASCT.
“The availability of novel agents may further improve the response to a third ASCT, rather than impairing its usefulness in the salvage setting, by enhancing the depth of response before ASCT, which could result in improved durability of the outcome,” they wrote.
The researchers reported having no financial disclosures related to this study.
SOURCE: Garderet L et al. Biol Blood Marrow Transplant. 2018 Feb 3. doi: 10.1016/j.bbmt.2018.01.035.
A third autologous stem cell transplantation (ASCT) is feasible and provides clinical benefit to patients with relapsed multiple myeloma, according to findings from a retrospective study.
The benefits appear to be most pronounced in patients who had a long duration of response to the previous ASCT, the researchers wrote in Biology of Blood and Marrow Transplantation.
“A salvage third ASCT is of value for patients with relapsed multiple myeloma,” Laurent Garderet, MD, of the department of hematology, Hôpital Saint Antoine, Paris, and coauthors wrote in the report.
A third transplantation is most commonly used in patients who relapse following tandem ASCT. Less often, it is done in patients who receive upfront ASCT, relapse, undergo a second ASCT, and relapse again.
“The first scenario gives much better results, due in part to a better remission status at the third ASCT with no signs of increased [second primary malignancy],” the researchers wrote.
In that group, median overall survival was greater than 5 years if the relapse occurred 3 years or more after the initial tandem ASCT, study results show.
The retrospective analysis, based on European Society for Blood and Marrow Transplantation data, included 570 patients who had undergone a third ASCT between 1997 and 2010. Of that group, 482 patients (81%) received the third transplantation after tandem ASCT and subsequent relapse, and 88 (15%) received it after second relapse.
After third ASCT, overall survival was 33 months in the larger tandem transplant group with 61 months of follow-up, and 15 months in the smaller group of patients who received two salvage ASCTs after 48 months of follow-up.
Median progression-free survival was 13 and 8 months for the tandem ASCT and two-salvage–ASCT groups, respectively, while 100-day nonrelapse mortality was 4% and 7%, respectively.
For both groups, better outcomes were associated with longer duration of remission after the second ASCT, the researchers reported.
Moreover, the time from second ASCT to relapse was the only favorable prognostic factor associated with survival after third ASCT in a multivariate analysis of the patients who relapsed following tandem transplant. The hazard ratio for relapse occurring between 18 and 36 months vs. within 18 months was 0.62 (95% confidence interval, 0.47-0.82; P = .01); for relapse after 36 months, the HR was 0.35 (95% CI, 0.25-0.49; P less than .001).
The researchers acknowledged that, beyond transplant, treatment of myeloma has changed substantially in recent years and could change the clinical picture for patients undergoing a third ASCT.
“The availability of novel agents may further improve the response to a third ASCT, rather than impairing its usefulness in the salvage setting, by enhancing the depth of response before ASCT, which could result in improved durability of the outcome,” they wrote.
The researchers reported having no financial disclosures related to this study.
SOURCE: Garderet L et al. Biol Blood Marrow Transplant. 2018 Feb 3. doi: 10.1016/j.bbmt.2018.01.035.
A third autologous stem cell transplantation (ASCT) is feasible and provides clinical benefit to patients with relapsed multiple myeloma, according to findings from a retrospective study.
The benefits appear to be most pronounced in patients who had a long duration of response to the previous ASCT, the researchers wrote in Biology of Blood and Marrow Transplantation.
“A salvage third ASCT is of value for patients with relapsed multiple myeloma,” Laurent Garderet, MD, of the department of hematology, Hôpital Saint Antoine, Paris, and coauthors wrote in the report.
A third transplantation is most commonly used in patients who relapse following tandem ASCT. Less often, it is done in patients who receive upfront ASCT, relapse, undergo a second ASCT, and relapse again.
“The first scenario gives much better results, due in part to a better remission status at the third ASCT with no signs of increased [second primary malignancy],” the researchers wrote.
In that group, median overall survival was greater than 5 years if the relapse occurred 3 years or more after the initial tandem ASCT, study results show.
The retrospective analysis, based on European Society for Blood and Marrow Transplantation data, included 570 patients who had undergone a third ASCT between 1997 and 2010. Of that group, 482 patients (81%) received the third transplantation after tandem ASCT and subsequent relapse, and 88 (15%) received it after second relapse.
After third ASCT, overall survival was 33 months in the larger tandem transplant group with 61 months of follow-up, and 15 months in the smaller group of patients who received two salvage ASCTs after 48 months of follow-up.
Median progression-free survival was 13 and 8 months for the tandem ASCT and two-salvage–ASCT groups, respectively, while 100-day nonrelapse mortality was 4% and 7%, respectively.
For both groups, better outcomes were associated with longer duration of remission after the second ASCT, the researchers reported.
Moreover, the time from second ASCT to relapse was the only favorable prognostic factor associated with survival after third ASCT in a multivariate analysis of the patients who relapsed following tandem transplant. The hazard ratio for relapse occurring between 18 and 36 months vs. within 18 months was 0.62 (95% confidence interval, 0.47-0.82; P = .01); for relapse after 36 months, the HR was 0.35 (95% CI, 0.25-0.49; P less than .001).
The researchers acknowledged that, beyond transplant, treatment of myeloma has changed substantially in recent years and could change the clinical picture for patients undergoing a third ASCT.
“The availability of novel agents may further improve the response to a third ASCT, rather than impairing its usefulness in the salvage setting, by enhancing the depth of response before ASCT, which could result in improved durability of the outcome,” they wrote.
The researchers reported having no financial disclosures related to this study.
SOURCE: Garderet L et al. Biol Blood Marrow Transplant. 2018 Feb 3. doi: 10.1016/j.bbmt.2018.01.035.
FROM BIOLOGY OF BLOOD AND MARROW TRANSPLANTATION
Key clinical point:
Major finding: Relapse-free interval was a favorable prognostic factor and significantly correlated with overall survival (P less than .001) in patients who underwent a third ASCT.
Study details: A retrospective analysis of European Society for Blood and Marrow Transplantation data including 570 patients who had undergone a third ASCT between 1997 and 2010.
Disclosures: The study authors reported having no financial disclosures related to the study.
Source: Garderet L et al. Biol Blood Marrow Transplant. 2018 Feb 3. doi: 10.1016/j.bbmt.2018.01.035.
Variants in one gene account for 7% of juvenile myoclonic epilepsy cases
An extremely rare genetic variant that affects the maturation, migration, and death of neurons appears to be responsible for about 7% of cases of juvenile myoclonic epilepsy.
Variants of the intestinal-cell kinase gene (ICK) occurred in 12 members of a family affected by the disorder and were confirmed in 22 of 310 additional patients, Julia N. Bailey, PhD, of the University of California, Los Angeles, and her colleagues reported in the March 15 issue of the New England Journal of Medicine.
“We report striking variation with respect to epilepsy phenotypes both within and among families,” the team wrote. “Of 34 affected nonproband family members, 5 (15%) had juvenile myoclonic epilepsy, 10 (29%) had myoclonic-tonic-clonic seizures, 4 (12%) had pyknoleptic petit mal seizures alone or with myoclonic-tonic-clonic seizures, 4 (12%) had febrile seizures alone or with absence seizures or myoclonias, and 11 (32%) were clinically asymptomatic but had polyspikes or focal spikes on EEG. These results strongly suggest that ICK is pleiotropic ... and that epistatic loci with different genes are present in affected family members and interact with ICK and contribute to pleiotropism and clinical heterogeneity.”
Despite the misnomer of intestinal-cell kinase, ICK “is ubiquitous and is expressed in all tissues,” senior study author Antonio Delgado-Escueta, MD, professor of neurology at UCLA, noted in an interview. He said the brain dysplasia, or microdysgenesis, that occurs in patients with juvenile myoclonic epilepsy (JME) “is very subtle, diagnosed mainly microscopically, and has neuronal cells that migrated from periventricular zones to the wrong places in wrong layers of the cortical gray matter and even the white matter of the brain. The cells can also be abnormally large and bunch up as a thicker gray matter. On voxel-based brain MRI ... focal thickenings of these abnormally migrated cells can also be partly explained by decreased pruning of cells and circuits (apoptosis).”
The gene encoding for ICK is located close to EFHC1 on chromosome 6p12. EFHC1, which encodes for a calcium-binging protein, has been implicated in JME. Dr. Bailey and her colleagues examined whether several genes in close proximity to EFHC1 also influenced that risk.
The investigators drew data from the GENESS (Genetic Epilepsies Studies) consortium, which has study sites in the United States, Mexico, Honduras, Brazil, and Japan. The current study from the databank analyzed information from 334 families with genetic generalized epilepsies. Among these, 310 patients had adolescent-onset myoclonic seizures and polyspike waves, or had a diagnosis of JME.
The team first performed an exome-wide analysis of four affected members of a large family with genetic JME. They observed the same variants in all four patients, then ran the screen in all 37 family members. Next, they screened these candidate genes in all 334 of the GENESS families and calculated risk scores for JME.
A linkage analysis confirmed two candidate genes on chromosome 6p12.1. Further analyses pinpointed a single variant: K305T on the ICK gene. This was present in each of the 12 affected members and 3 unaffected members of the initial family examined. Of those affected, three had JME, two had myoclonic-tonic-clonic convulsions only, two had febrile convulsions plus childhood absence seizures or neonatal myoclonus, one had febrile convulsions only, and four had polyspikes on EEG and were clinically asymptomatic.
“These results genetically implicated K305T as an autosomal dominant, possibly disease-causing trait,” the authors noted.
ICK variants were also present in 24 of the 310 database patients who had JME (8%). Of these, nine belonged to families with other affected members. The team tested 24 ICK variants for pathogenicity and determined that 13 exerted significant JME risk, with odds ratios exceeding 5.0.
When the team looked for these 24 variants in the Genome Aggregation Database (gnomAD), the found that 12 were present but extremely rare, and 8 were absent. They also found an additional ICK variant in a Mexican patient who was in gnomAD. Interestingly, that variant was a benign polymorphism in Africans.
Dr. Bailey and her colleagues thus concluded that 21 ICK variants accounted for 7% of the JME among the 310 cases examined.
The team also conducted a series of in vitro and in vivo mouse experiments. They determined that ICK variants impaired the migration of neuronal progenitor cells and lowered their mitotic index. ICK transgenic mice under light sedation displayed muscle movements similar to human myoclonic seizures that occur upon awakening. These mice also displayed diffuse polyspike brain waves on EEG recordings.
“The data we obtained through the use of electroporated slices of mouse brain support the conclusion that those pathogenic variants in ICK cause 7% of cases of juvenile myoclonic epilepsy by disrupting mitosis, neuroblast migration, and apoptosis,” they concluded.
The study was funded by a number of private and public grants from within the United States and other countries. Several authors are coholders of patents on EFHC1-based diagnostic and therapeutics that have been licensed to Athena Diagnostics. Several authors also reported receiving honoraria from various pharmaceutical companies.
SOURCE: Bailey J et al. N Engl J Med. 2018;378:1018-28
An extremely rare genetic variant that affects the maturation, migration, and death of neurons appears to be responsible for about 7% of cases of juvenile myoclonic epilepsy.
Variants of the intestinal-cell kinase gene (ICK) occurred in 12 members of a family affected by the disorder and were confirmed in 22 of 310 additional patients, Julia N. Bailey, PhD, of the University of California, Los Angeles, and her colleagues reported in the March 15 issue of the New England Journal of Medicine.
“We report striking variation with respect to epilepsy phenotypes both within and among families,” the team wrote. “Of 34 affected nonproband family members, 5 (15%) had juvenile myoclonic epilepsy, 10 (29%) had myoclonic-tonic-clonic seizures, 4 (12%) had pyknoleptic petit mal seizures alone or with myoclonic-tonic-clonic seizures, 4 (12%) had febrile seizures alone or with absence seizures or myoclonias, and 11 (32%) were clinically asymptomatic but had polyspikes or focal spikes on EEG. These results strongly suggest that ICK is pleiotropic ... and that epistatic loci with different genes are present in affected family members and interact with ICK and contribute to pleiotropism and clinical heterogeneity.”
Despite the misnomer of intestinal-cell kinase, ICK “is ubiquitous and is expressed in all tissues,” senior study author Antonio Delgado-Escueta, MD, professor of neurology at UCLA, noted in an interview. He said the brain dysplasia, or microdysgenesis, that occurs in patients with juvenile myoclonic epilepsy (JME) “is very subtle, diagnosed mainly microscopically, and has neuronal cells that migrated from periventricular zones to the wrong places in wrong layers of the cortical gray matter and even the white matter of the brain. The cells can also be abnormally large and bunch up as a thicker gray matter. On voxel-based brain MRI ... focal thickenings of these abnormally migrated cells can also be partly explained by decreased pruning of cells and circuits (apoptosis).”
The gene encoding for ICK is located close to EFHC1 on chromosome 6p12. EFHC1, which encodes for a calcium-binging protein, has been implicated in JME. Dr. Bailey and her colleagues examined whether several genes in close proximity to EFHC1 also influenced that risk.
The investigators drew data from the GENESS (Genetic Epilepsies Studies) consortium, which has study sites in the United States, Mexico, Honduras, Brazil, and Japan. The current study from the databank analyzed information from 334 families with genetic generalized epilepsies. Among these, 310 patients had adolescent-onset myoclonic seizures and polyspike waves, or had a diagnosis of JME.
The team first performed an exome-wide analysis of four affected members of a large family with genetic JME. They observed the same variants in all four patients, then ran the screen in all 37 family members. Next, they screened these candidate genes in all 334 of the GENESS families and calculated risk scores for JME.
A linkage analysis confirmed two candidate genes on chromosome 6p12.1. Further analyses pinpointed a single variant: K305T on the ICK gene. This was present in each of the 12 affected members and 3 unaffected members of the initial family examined. Of those affected, three had JME, two had myoclonic-tonic-clonic convulsions only, two had febrile convulsions plus childhood absence seizures or neonatal myoclonus, one had febrile convulsions only, and four had polyspikes on EEG and were clinically asymptomatic.
“These results genetically implicated K305T as an autosomal dominant, possibly disease-causing trait,” the authors noted.
ICK variants were also present in 24 of the 310 database patients who had JME (8%). Of these, nine belonged to families with other affected members. The team tested 24 ICK variants for pathogenicity and determined that 13 exerted significant JME risk, with odds ratios exceeding 5.0.
When the team looked for these 24 variants in the Genome Aggregation Database (gnomAD), the found that 12 were present but extremely rare, and 8 were absent. They also found an additional ICK variant in a Mexican patient who was in gnomAD. Interestingly, that variant was a benign polymorphism in Africans.
Dr. Bailey and her colleagues thus concluded that 21 ICK variants accounted for 7% of the JME among the 310 cases examined.
The team also conducted a series of in vitro and in vivo mouse experiments. They determined that ICK variants impaired the migration of neuronal progenitor cells and lowered their mitotic index. ICK transgenic mice under light sedation displayed muscle movements similar to human myoclonic seizures that occur upon awakening. These mice also displayed diffuse polyspike brain waves on EEG recordings.
“The data we obtained through the use of electroporated slices of mouse brain support the conclusion that those pathogenic variants in ICK cause 7% of cases of juvenile myoclonic epilepsy by disrupting mitosis, neuroblast migration, and apoptosis,” they concluded.
The study was funded by a number of private and public grants from within the United States and other countries. Several authors are coholders of patents on EFHC1-based diagnostic and therapeutics that have been licensed to Athena Diagnostics. Several authors also reported receiving honoraria from various pharmaceutical companies.
SOURCE: Bailey J et al. N Engl J Med. 2018;378:1018-28
An extremely rare genetic variant that affects the maturation, migration, and death of neurons appears to be responsible for about 7% of cases of juvenile myoclonic epilepsy.
Variants of the intestinal-cell kinase gene (ICK) occurred in 12 members of a family affected by the disorder and were confirmed in 22 of 310 additional patients, Julia N. Bailey, PhD, of the University of California, Los Angeles, and her colleagues reported in the March 15 issue of the New England Journal of Medicine.
“We report striking variation with respect to epilepsy phenotypes both within and among families,” the team wrote. “Of 34 affected nonproband family members, 5 (15%) had juvenile myoclonic epilepsy, 10 (29%) had myoclonic-tonic-clonic seizures, 4 (12%) had pyknoleptic petit mal seizures alone or with myoclonic-tonic-clonic seizures, 4 (12%) had febrile seizures alone or with absence seizures or myoclonias, and 11 (32%) were clinically asymptomatic but had polyspikes or focal spikes on EEG. These results strongly suggest that ICK is pleiotropic ... and that epistatic loci with different genes are present in affected family members and interact with ICK and contribute to pleiotropism and clinical heterogeneity.”
Despite the misnomer of intestinal-cell kinase, ICK “is ubiquitous and is expressed in all tissues,” senior study author Antonio Delgado-Escueta, MD, professor of neurology at UCLA, noted in an interview. He said the brain dysplasia, or microdysgenesis, that occurs in patients with juvenile myoclonic epilepsy (JME) “is very subtle, diagnosed mainly microscopically, and has neuronal cells that migrated from periventricular zones to the wrong places in wrong layers of the cortical gray matter and even the white matter of the brain. The cells can also be abnormally large and bunch up as a thicker gray matter. On voxel-based brain MRI ... focal thickenings of these abnormally migrated cells can also be partly explained by decreased pruning of cells and circuits (apoptosis).”
The gene encoding for ICK is located close to EFHC1 on chromosome 6p12. EFHC1, which encodes for a calcium-binging protein, has been implicated in JME. Dr. Bailey and her colleagues examined whether several genes in close proximity to EFHC1 also influenced that risk.
The investigators drew data from the GENESS (Genetic Epilepsies Studies) consortium, which has study sites in the United States, Mexico, Honduras, Brazil, and Japan. The current study from the databank analyzed information from 334 families with genetic generalized epilepsies. Among these, 310 patients had adolescent-onset myoclonic seizures and polyspike waves, or had a diagnosis of JME.
The team first performed an exome-wide analysis of four affected members of a large family with genetic JME. They observed the same variants in all four patients, then ran the screen in all 37 family members. Next, they screened these candidate genes in all 334 of the GENESS families and calculated risk scores for JME.
A linkage analysis confirmed two candidate genes on chromosome 6p12.1. Further analyses pinpointed a single variant: K305T on the ICK gene. This was present in each of the 12 affected members and 3 unaffected members of the initial family examined. Of those affected, three had JME, two had myoclonic-tonic-clonic convulsions only, two had febrile convulsions plus childhood absence seizures or neonatal myoclonus, one had febrile convulsions only, and four had polyspikes on EEG and were clinically asymptomatic.
“These results genetically implicated K305T as an autosomal dominant, possibly disease-causing trait,” the authors noted.
ICK variants were also present in 24 of the 310 database patients who had JME (8%). Of these, nine belonged to families with other affected members. The team tested 24 ICK variants for pathogenicity and determined that 13 exerted significant JME risk, with odds ratios exceeding 5.0.
When the team looked for these 24 variants in the Genome Aggregation Database (gnomAD), the found that 12 were present but extremely rare, and 8 were absent. They also found an additional ICK variant in a Mexican patient who was in gnomAD. Interestingly, that variant was a benign polymorphism in Africans.
Dr. Bailey and her colleagues thus concluded that 21 ICK variants accounted for 7% of the JME among the 310 cases examined.
The team also conducted a series of in vitro and in vivo mouse experiments. They determined that ICK variants impaired the migration of neuronal progenitor cells and lowered their mitotic index. ICK transgenic mice under light sedation displayed muscle movements similar to human myoclonic seizures that occur upon awakening. These mice also displayed diffuse polyspike brain waves on EEG recordings.
“The data we obtained through the use of electroporated slices of mouse brain support the conclusion that those pathogenic variants in ICK cause 7% of cases of juvenile myoclonic epilepsy by disrupting mitosis, neuroblast migration, and apoptosis,” they concluded.
The study was funded by a number of private and public grants from within the United States and other countries. Several authors are coholders of patents on EFHC1-based diagnostic and therapeutics that have been licensed to Athena Diagnostics. Several authors also reported receiving honoraria from various pharmaceutical companies.
SOURCE: Bailey J et al. N Engl J Med. 2018;378:1018-28
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: ICK variants account for 7% of JME cases.
Study details: Genetic studies comprising one family and 310 epilepsy cases in a database.
Disclosures: The study was funded by a number of private and public grants from within the United States and other countries. Several authors are coholders of patents on EFHC1-based diagnostic and therapeutics that have been licensed to Athena Diagnostics. Several authors also reported receiving honoraria from various pharmaceutical companies.
Source: Bailey J et al. N Engl J Med. 2018;378:1018-28.
Vaccine priming determines teen susceptibility to pertussis
It is the initial type of pertussis vaccine given in infancy – acellular or whole cell – that primes the immune system and determines how soon adolescents become susceptible to pertussis, regardless of later acellular booster vaccination, noted the authors of a new study.
The IgG4 subclass proportion for IgG4-specific antibodies remained lower in patients who had whole-cell pertussis (wP) priming in infancy, even though they had received acellular pertussis booster vaccinations at ages 4 and 9 years, compared with patients who underwent acellular pertussis (aP) priming in infancy. This was true for all vaccine antigens, other than filamentous hemagglutinin and tetanus, 1 year after the preadolescent booster, noted researcher Saskia van der Lee of the National Institute for Public Health and the Environment, Bilthoven, The Netherlands, and her associates.
“ compared to aP-primed children, even after booster vaccinations. This is in line with epidemiological data indicating that adolescents, after aP vaccination in infancy, are more susceptible to pertussis, compared with wP-primed adolescents, though wP-primed individuals become also susceptible over time,” the researchers said.
In addition, children primed with DTwP vaccines have a more Th1-skewed response for pertussis vaccine antigens after receiving a DTap booster vaccine or clinical infection with Bordetella pertussis, whereas children primed with DTaP have a more mixed pertussis-specific Th1/Th2 response, the researchers said. So “new adjuvants that skew the immune response towards a Th1 profile are desired” for better protection against pertussis over time.
SOURCE: van der Lee S et al. Vaccine. 2018 Jan 4;36(2):220-6.
It is the initial type of pertussis vaccine given in infancy – acellular or whole cell – that primes the immune system and determines how soon adolescents become susceptible to pertussis, regardless of later acellular booster vaccination, noted the authors of a new study.
The IgG4 subclass proportion for IgG4-specific antibodies remained lower in patients who had whole-cell pertussis (wP) priming in infancy, even though they had received acellular pertussis booster vaccinations at ages 4 and 9 years, compared with patients who underwent acellular pertussis (aP) priming in infancy. This was true for all vaccine antigens, other than filamentous hemagglutinin and tetanus, 1 year after the preadolescent booster, noted researcher Saskia van der Lee of the National Institute for Public Health and the Environment, Bilthoven, The Netherlands, and her associates.
“ compared to aP-primed children, even after booster vaccinations. This is in line with epidemiological data indicating that adolescents, after aP vaccination in infancy, are more susceptible to pertussis, compared with wP-primed adolescents, though wP-primed individuals become also susceptible over time,” the researchers said.
In addition, children primed with DTwP vaccines have a more Th1-skewed response for pertussis vaccine antigens after receiving a DTap booster vaccine or clinical infection with Bordetella pertussis, whereas children primed with DTaP have a more mixed pertussis-specific Th1/Th2 response, the researchers said. So “new adjuvants that skew the immune response towards a Th1 profile are desired” for better protection against pertussis over time.
SOURCE: van der Lee S et al. Vaccine. 2018 Jan 4;36(2):220-6.
It is the initial type of pertussis vaccine given in infancy – acellular or whole cell – that primes the immune system and determines how soon adolescents become susceptible to pertussis, regardless of later acellular booster vaccination, noted the authors of a new study.
The IgG4 subclass proportion for IgG4-specific antibodies remained lower in patients who had whole-cell pertussis (wP) priming in infancy, even though they had received acellular pertussis booster vaccinations at ages 4 and 9 years, compared with patients who underwent acellular pertussis (aP) priming in infancy. This was true for all vaccine antigens, other than filamentous hemagglutinin and tetanus, 1 year after the preadolescent booster, noted researcher Saskia van der Lee of the National Institute for Public Health and the Environment, Bilthoven, The Netherlands, and her associates.
“ compared to aP-primed children, even after booster vaccinations. This is in line with epidemiological data indicating that adolescents, after aP vaccination in infancy, are more susceptible to pertussis, compared with wP-primed adolescents, though wP-primed individuals become also susceptible over time,” the researchers said.
In addition, children primed with DTwP vaccines have a more Th1-skewed response for pertussis vaccine antigens after receiving a DTap booster vaccine or clinical infection with Bordetella pertussis, whereas children primed with DTaP have a more mixed pertussis-specific Th1/Th2 response, the researchers said. So “new adjuvants that skew the immune response towards a Th1 profile are desired” for better protection against pertussis over time.
SOURCE: van der Lee S et al. Vaccine. 2018 Jan 4;36(2):220-6.
FROM VACCINE
Congenital Heart Disease Is Associated With a Higher Risk of Dementia
Congenital heart disease (CHD) is associated with an increased risk of dementia, especially early onset dementia, according to research published online ahead of print February 12 in Circulation. A particularly increased risk of dementia was observed among middle-aged adults with CHD and signs of early onset dementia, the authors noted.
“These results support the importance of understanding the risk of adverse long-term neurologic outcomes in the growing and aging population with CHD,” said Carina N. Bagge, a medical student at Aarhus University Hospital in Aarhus, Denmark, and colleagues.
Examining Dementia Risk in Patients With CHD
CHD occurs in six to 10 per 1,000 live births and represents the most common group of congenital defects. Dementia is the sixth most common cause of death in the United States. Although neurodevelopmental deficits among infants and children with CHD are well studied, research on long-term neurologic outcomes in adults with CHD is limited. Based on the increased incidence of neurodevelopmental impairments and associated risk factors for dementia among patients with CHD, Ms. Bagge and colleagues hypothesized that the risk of dementia is higher in adults with CHD than in the general population.
To test this hypothesis, the authors performed a nationwide, population-based cohort study in Denmark using linked medical registries that included data from all Danish hospitals. They identified all adults who received a diagnosis of CHD between 1963 and 1974 (before age 15) and between 1977 and 2012 (at any age). For each patient with CHD, 10 individuals from the general population were matched by sex and birth year,
The primary outcome was a first-time hospital diagnosis of all-cause dementia in the inpatient or outpatient clinic setting. Investigators categorized dementia diagnoses as Alzheimer’s disease, vascular dementia, or other dementias.
CHD Severity Correlated With Increased Risk of Dementia
The investigators identified 10,632 adults with CHD and 103,403 adults from the general population;46% were male in both cohorts. The cumulative incidence of dementia was 4% at age 80 in both cohorts. The overall hazard ratio (HR) of dementia was 1.6 among adults with CHD, compared with the general population. The HR of dementia was 1.4 among patients with CHD without extracardiac defects, 1.5 among patients with mild-to-moderate CHD, and 2.0 for patients with severe CHD, including univentricular hearts. Finally, the HR for early-onset dementia (ie, onset younger than age 65) was 2.6, and the HR for late-onset dementia was 1.3 among patients with CHD.
“These results cannot be directly applied to young adults diagnosed with CHD in the present eras. However, it is important to recognize healthcare needs and risk factors affecting the larger number of middle-aged and older adults currently living with CHD,” said Ms. Bagge and colleagues.
—Erica Tricarico
Suggested Reading
Bagge CN, Henderson VW, Laursen HB, et al. Risk of dementia in adults with congenital heart disease: population-based cohort study. Circulation. 2018 Feb 12 [Epub ahead of print].
Congenital heart disease (CHD) is associated with an increased risk of dementia, especially early onset dementia, according to research published online ahead of print February 12 in Circulation. A particularly increased risk of dementia was observed among middle-aged adults with CHD and signs of early onset dementia, the authors noted.
“These results support the importance of understanding the risk of adverse long-term neurologic outcomes in the growing and aging population with CHD,” said Carina N. Bagge, a medical student at Aarhus University Hospital in Aarhus, Denmark, and colleagues.
Examining Dementia Risk in Patients With CHD
CHD occurs in six to 10 per 1,000 live births and represents the most common group of congenital defects. Dementia is the sixth most common cause of death in the United States. Although neurodevelopmental deficits among infants and children with CHD are well studied, research on long-term neurologic outcomes in adults with CHD is limited. Based on the increased incidence of neurodevelopmental impairments and associated risk factors for dementia among patients with CHD, Ms. Bagge and colleagues hypothesized that the risk of dementia is higher in adults with CHD than in the general population.
To test this hypothesis, the authors performed a nationwide, population-based cohort study in Denmark using linked medical registries that included data from all Danish hospitals. They identified all adults who received a diagnosis of CHD between 1963 and 1974 (before age 15) and between 1977 and 2012 (at any age). For each patient with CHD, 10 individuals from the general population were matched by sex and birth year,
The primary outcome was a first-time hospital diagnosis of all-cause dementia in the inpatient or outpatient clinic setting. Investigators categorized dementia diagnoses as Alzheimer’s disease, vascular dementia, or other dementias.
CHD Severity Correlated With Increased Risk of Dementia
The investigators identified 10,632 adults with CHD and 103,403 adults from the general population;46% were male in both cohorts. The cumulative incidence of dementia was 4% at age 80 in both cohorts. The overall hazard ratio (HR) of dementia was 1.6 among adults with CHD, compared with the general population. The HR of dementia was 1.4 among patients with CHD without extracardiac defects, 1.5 among patients with mild-to-moderate CHD, and 2.0 for patients with severe CHD, including univentricular hearts. Finally, the HR for early-onset dementia (ie, onset younger than age 65) was 2.6, and the HR for late-onset dementia was 1.3 among patients with CHD.
“These results cannot be directly applied to young adults diagnosed with CHD in the present eras. However, it is important to recognize healthcare needs and risk factors affecting the larger number of middle-aged and older adults currently living with CHD,” said Ms. Bagge and colleagues.
—Erica Tricarico
Suggested Reading
Bagge CN, Henderson VW, Laursen HB, et al. Risk of dementia in adults with congenital heart disease: population-based cohort study. Circulation. 2018 Feb 12 [Epub ahead of print].
Congenital heart disease (CHD) is associated with an increased risk of dementia, especially early onset dementia, according to research published online ahead of print February 12 in Circulation. A particularly increased risk of dementia was observed among middle-aged adults with CHD and signs of early onset dementia, the authors noted.
“These results support the importance of understanding the risk of adverse long-term neurologic outcomes in the growing and aging population with CHD,” said Carina N. Bagge, a medical student at Aarhus University Hospital in Aarhus, Denmark, and colleagues.
Examining Dementia Risk in Patients With CHD
CHD occurs in six to 10 per 1,000 live births and represents the most common group of congenital defects. Dementia is the sixth most common cause of death in the United States. Although neurodevelopmental deficits among infants and children with CHD are well studied, research on long-term neurologic outcomes in adults with CHD is limited. Based on the increased incidence of neurodevelopmental impairments and associated risk factors for dementia among patients with CHD, Ms. Bagge and colleagues hypothesized that the risk of dementia is higher in adults with CHD than in the general population.
To test this hypothesis, the authors performed a nationwide, population-based cohort study in Denmark using linked medical registries that included data from all Danish hospitals. They identified all adults who received a diagnosis of CHD between 1963 and 1974 (before age 15) and between 1977 and 2012 (at any age). For each patient with CHD, 10 individuals from the general population were matched by sex and birth year,
The primary outcome was a first-time hospital diagnosis of all-cause dementia in the inpatient or outpatient clinic setting. Investigators categorized dementia diagnoses as Alzheimer’s disease, vascular dementia, or other dementias.
CHD Severity Correlated With Increased Risk of Dementia
The investigators identified 10,632 adults with CHD and 103,403 adults from the general population;46% were male in both cohorts. The cumulative incidence of dementia was 4% at age 80 in both cohorts. The overall hazard ratio (HR) of dementia was 1.6 among adults with CHD, compared with the general population. The HR of dementia was 1.4 among patients with CHD without extracardiac defects, 1.5 among patients with mild-to-moderate CHD, and 2.0 for patients with severe CHD, including univentricular hearts. Finally, the HR for early-onset dementia (ie, onset younger than age 65) was 2.6, and the HR for late-onset dementia was 1.3 among patients with CHD.
“These results cannot be directly applied to young adults diagnosed with CHD in the present eras. However, it is important to recognize healthcare needs and risk factors affecting the larger number of middle-aged and older adults currently living with CHD,” said Ms. Bagge and colleagues.
—Erica Tricarico
Suggested Reading
Bagge CN, Henderson VW, Laursen HB, et al. Risk of dementia in adults with congenital heart disease: population-based cohort study. Circulation. 2018 Feb 12 [Epub ahead of print].
Personalizing Seizure Mapping with a Computer Algorithm
A software algorithm has the potential to increase the likelihood of achieving freedom from seizures after epilepsy surgery suggests an analysis of 3 illustrative case studies.
- Researchers from the University of South Florida created the algorithm to individualize the mapping of patients’ epilepsy networks.
- The computer program combines noninvasive EEG source localization with nonconcurrent resting state functional MRI.
- Investigators used scalp EEG and resting state fMRI to gather data on a healthy control subject, a patient with right temporal lobe epilepsy (TLE), and one with bitemporal seizure onset.
- Results from the healthy subject found symmetrical global connectivity.
- The patient with right TLE had asymmetry in global connectivity and very little connectivity ipsolaterial to the epileptogenic cortex.
- The patient who had bitemporal lobe epilepsy had symmetrical global connectivity and a network of correlating activity in the cortex that was localized in the epileptogenic tissue of both temporal lobes.
Neal EG, Maciver S, Vale FL. Multimodal, noninvasive seizure network mapping software: A novel tool for preoperative epilepsy evaluation. Epilepsy Behav. 2018; 81:25-32. https://doi.org/10.1016/j.yebeh.2018.01.033
A software algorithm has the potential to increase the likelihood of achieving freedom from seizures after epilepsy surgery suggests an analysis of 3 illustrative case studies.
- Researchers from the University of South Florida created the algorithm to individualize the mapping of patients’ epilepsy networks.
- The computer program combines noninvasive EEG source localization with nonconcurrent resting state functional MRI.
- Investigators used scalp EEG and resting state fMRI to gather data on a healthy control subject, a patient with right temporal lobe epilepsy (TLE), and one with bitemporal seizure onset.
- Results from the healthy subject found symmetrical global connectivity.
- The patient with right TLE had asymmetry in global connectivity and very little connectivity ipsolaterial to the epileptogenic cortex.
- The patient who had bitemporal lobe epilepsy had symmetrical global connectivity and a network of correlating activity in the cortex that was localized in the epileptogenic tissue of both temporal lobes.
Neal EG, Maciver S, Vale FL. Multimodal, noninvasive seizure network mapping software: A novel tool for preoperative epilepsy evaluation. Epilepsy Behav. 2018; 81:25-32. https://doi.org/10.1016/j.yebeh.2018.01.033
A software algorithm has the potential to increase the likelihood of achieving freedom from seizures after epilepsy surgery suggests an analysis of 3 illustrative case studies.
- Researchers from the University of South Florida created the algorithm to individualize the mapping of patients’ epilepsy networks.
- The computer program combines noninvasive EEG source localization with nonconcurrent resting state functional MRI.
- Investigators used scalp EEG and resting state fMRI to gather data on a healthy control subject, a patient with right temporal lobe epilepsy (TLE), and one with bitemporal seizure onset.
- Results from the healthy subject found symmetrical global connectivity.
- The patient with right TLE had asymmetry in global connectivity and very little connectivity ipsolaterial to the epileptogenic cortex.
- The patient who had bitemporal lobe epilepsy had symmetrical global connectivity and a network of correlating activity in the cortex that was localized in the epileptogenic tissue of both temporal lobes.
Neal EG, Maciver S, Vale FL. Multimodal, noninvasive seizure network mapping software: A novel tool for preoperative epilepsy evaluation. Epilepsy Behav. 2018; 81:25-32. https://doi.org/10.1016/j.yebeh.2018.01.033
Using Quantitative EEG Spectrograms to Detect Seizure Subtypes
Using quantitative EEG (QEEG) can help differentiate among several types of seizures suggests an analysis of 562 seizures among 58 patitents.
- Investigators from Montefiore Medical Center and Albert Einstein College of Medicine in New York evaluated the sensitivity of the Persyst 12 QEEG spectrograms for detecting focal, focal with secondary generalized, and generalized onset seizures.
- Patients included in the analysis had 2 or more seizures successfully recorded during continuous EEG monitoring in the ICU or epilepsy monitoring unit from July 2016 to January 2017.
- QEEG spectrograms detected seizures with a sensitivity of 43% to 72%.
- Asymmetry spectrograms generated the highest sensitivity for detecting local seizures (94%).
- FFT spectrograms were most sensitive for diagnosing secondarily generalized seizures (84%).
- Seizure detection trend was most sensitive for generalized onset seizures (79%).
Goenka A, Boro A, Yozawitz E. Comparative sensitivity of quantitative EEG (QEEG) spectrograms for detecting seizure subtypes. Seizures. 2018;55:70-75.
Using quantitative EEG (QEEG) can help differentiate among several types of seizures suggests an analysis of 562 seizures among 58 patitents.
- Investigators from Montefiore Medical Center and Albert Einstein College of Medicine in New York evaluated the sensitivity of the Persyst 12 QEEG spectrograms for detecting focal, focal with secondary generalized, and generalized onset seizures.
- Patients included in the analysis had 2 or more seizures successfully recorded during continuous EEG monitoring in the ICU or epilepsy monitoring unit from July 2016 to January 2017.
- QEEG spectrograms detected seizures with a sensitivity of 43% to 72%.
- Asymmetry spectrograms generated the highest sensitivity for detecting local seizures (94%).
- FFT spectrograms were most sensitive for diagnosing secondarily generalized seizures (84%).
- Seizure detection trend was most sensitive for generalized onset seizures (79%).
Goenka A, Boro A, Yozawitz E. Comparative sensitivity of quantitative EEG (QEEG) spectrograms for detecting seizure subtypes. Seizures. 2018;55:70-75.
Using quantitative EEG (QEEG) can help differentiate among several types of seizures suggests an analysis of 562 seizures among 58 patitents.
- Investigators from Montefiore Medical Center and Albert Einstein College of Medicine in New York evaluated the sensitivity of the Persyst 12 QEEG spectrograms for detecting focal, focal with secondary generalized, and generalized onset seizures.
- Patients included in the analysis had 2 or more seizures successfully recorded during continuous EEG monitoring in the ICU or epilepsy monitoring unit from July 2016 to January 2017.
- QEEG spectrograms detected seizures with a sensitivity of 43% to 72%.
- Asymmetry spectrograms generated the highest sensitivity for detecting local seizures (94%).
- FFT spectrograms were most sensitive for diagnosing secondarily generalized seizures (84%).
- Seizure detection trend was most sensitive for generalized onset seizures (79%).
Goenka A, Boro A, Yozawitz E. Comparative sensitivity of quantitative EEG (QEEG) spectrograms for detecting seizure subtypes. Seizures. 2018;55:70-75.
Cognitive Impairment Linked to Depression in Epilepsy
Cognitive impairment affects 40% of adult patients with epilepsy and is associated with mental depression, seizure frequency, and the number of adverse effects of antiepileptic drugs, according to an analysis of a Cleveland Clinic database.
- Adults with epilepsy enrolled in the Cleveland Clinic Knowledge Program Data Registry from January to May 2015 were included in the analysis.
- The patients had completed several assessment scales, including the Aldenkamp–Baker Neuropsychological Assessment Schedule (ABNAS), the Patient Health Questionnaire (PHQ-9), the Generalized Anxiety Disorder scale (GAD-7), and the Quality of Life in Epilepsy questionnaire.
- Since topiramate poses a high risk of cognitive impairment, it was used as the basis for the evaluation.
- 270 of 670 patients (40%) reported cognitive impairment, with PHQ-9 scores, the number of adverse drug effects and the frequency of seizures most closely associated with such impairment., suggesting that these three variables could be used as predictors.
Feldman L, Lapin B, Busch RM, et al. Evaluating subjective cognitive impairment in the adult epilepsy clinic: Effects of depression, number of antiepileptic medications, and seizure frequency. Epilepsy Behav. 2018; 81:18-24.
Cognitive impairment affects 40% of adult patients with epilepsy and is associated with mental depression, seizure frequency, and the number of adverse effects of antiepileptic drugs, according to an analysis of a Cleveland Clinic database.
- Adults with epilepsy enrolled in the Cleveland Clinic Knowledge Program Data Registry from January to May 2015 were included in the analysis.
- The patients had completed several assessment scales, including the Aldenkamp–Baker Neuropsychological Assessment Schedule (ABNAS), the Patient Health Questionnaire (PHQ-9), the Generalized Anxiety Disorder scale (GAD-7), and the Quality of Life in Epilepsy questionnaire.
- Since topiramate poses a high risk of cognitive impairment, it was used as the basis for the evaluation.
- 270 of 670 patients (40%) reported cognitive impairment, with PHQ-9 scores, the number of adverse drug effects and the frequency of seizures most closely associated with such impairment., suggesting that these three variables could be used as predictors.
Feldman L, Lapin B, Busch RM, et al. Evaluating subjective cognitive impairment in the adult epilepsy clinic: Effects of depression, number of antiepileptic medications, and seizure frequency. Epilepsy Behav. 2018; 81:18-24.
Cognitive impairment affects 40% of adult patients with epilepsy and is associated with mental depression, seizure frequency, and the number of adverse effects of antiepileptic drugs, according to an analysis of a Cleveland Clinic database.
- Adults with epilepsy enrolled in the Cleveland Clinic Knowledge Program Data Registry from January to May 2015 were included in the analysis.
- The patients had completed several assessment scales, including the Aldenkamp–Baker Neuropsychological Assessment Schedule (ABNAS), the Patient Health Questionnaire (PHQ-9), the Generalized Anxiety Disorder scale (GAD-7), and the Quality of Life in Epilepsy questionnaire.
- Since topiramate poses a high risk of cognitive impairment, it was used as the basis for the evaluation.
- 270 of 670 patients (40%) reported cognitive impairment, with PHQ-9 scores, the number of adverse drug effects and the frequency of seizures most closely associated with such impairment., suggesting that these three variables could be used as predictors.
Feldman L, Lapin B, Busch RM, et al. Evaluating subjective cognitive impairment in the adult epilepsy clinic: Effects of depression, number of antiepileptic medications, and seizure frequency. Epilepsy Behav. 2018; 81:18-24.
Time to rethink MCL treatment, trial design
Classic mantle cell lymphoma (cMCL) has long been treated as a uniformly aggressive disease in need of similarly aggressive treatment, but that approach may be leading to overtreatment, according to one expert.
“The cMCL encompasses a broad category of lymphomas with highly variable clinical behaviors. A contemporary categorization of cMCL as a predominantly aggressive entity is misleading, as only an estimated 20% to 25% of patients with cMCL present with a symptomatic or aggressively behaving disease,” Leonid L. Yavorkovsky, MD, PhD, of the Kaiser Permanente San Jose Medical Center (Calif.), wrote in a commentary in JAMA Oncology.
While groups like the National Comprehensive Cancer Network and the European Society for Medical Oncology recommend that only older patients and those with significant comorbidities should be exempted from intensive therapy, Dr. Yavorkovsky said to identify asymptomatic patients who might be able to safely delay aggressive treatment. He also called for more risk-adapted patient assignment to cMCL clinical trials.
“The failure to recognize the erratic nature of cMCL in clinical studies may confound the outcome gains and, ultimately, undermine the ensuing treatment recommendations,” Dr. Yavorkovsky wrote.
Read his full commentary in JAMA Oncology.
mschneider@frontlinemedcom.com
SOURCE: Yavorkovsky L, JAMA Oncology. 2018 Mar 1. doi: 10.1001/jamaoncol.2017.5685.
Classic mantle cell lymphoma (cMCL) has long been treated as a uniformly aggressive disease in need of similarly aggressive treatment, but that approach may be leading to overtreatment, according to one expert.
“The cMCL encompasses a broad category of lymphomas with highly variable clinical behaviors. A contemporary categorization of cMCL as a predominantly aggressive entity is misleading, as only an estimated 20% to 25% of patients with cMCL present with a symptomatic or aggressively behaving disease,” Leonid L. Yavorkovsky, MD, PhD, of the Kaiser Permanente San Jose Medical Center (Calif.), wrote in a commentary in JAMA Oncology.
While groups like the National Comprehensive Cancer Network and the European Society for Medical Oncology recommend that only older patients and those with significant comorbidities should be exempted from intensive therapy, Dr. Yavorkovsky said to identify asymptomatic patients who might be able to safely delay aggressive treatment. He also called for more risk-adapted patient assignment to cMCL clinical trials.
“The failure to recognize the erratic nature of cMCL in clinical studies may confound the outcome gains and, ultimately, undermine the ensuing treatment recommendations,” Dr. Yavorkovsky wrote.
Read his full commentary in JAMA Oncology.
mschneider@frontlinemedcom.com
SOURCE: Yavorkovsky L, JAMA Oncology. 2018 Mar 1. doi: 10.1001/jamaoncol.2017.5685.
Classic mantle cell lymphoma (cMCL) has long been treated as a uniformly aggressive disease in need of similarly aggressive treatment, but that approach may be leading to overtreatment, according to one expert.
“The cMCL encompasses a broad category of lymphomas with highly variable clinical behaviors. A contemporary categorization of cMCL as a predominantly aggressive entity is misleading, as only an estimated 20% to 25% of patients with cMCL present with a symptomatic or aggressively behaving disease,” Leonid L. Yavorkovsky, MD, PhD, of the Kaiser Permanente San Jose Medical Center (Calif.), wrote in a commentary in JAMA Oncology.
While groups like the National Comprehensive Cancer Network and the European Society for Medical Oncology recommend that only older patients and those with significant comorbidities should be exempted from intensive therapy, Dr. Yavorkovsky said to identify asymptomatic patients who might be able to safely delay aggressive treatment. He also called for more risk-adapted patient assignment to cMCL clinical trials.
“The failure to recognize the erratic nature of cMCL in clinical studies may confound the outcome gains and, ultimately, undermine the ensuing treatment recommendations,” Dr. Yavorkovsky wrote.
Read his full commentary in JAMA Oncology.
mschneider@frontlinemedcom.com
SOURCE: Yavorkovsky L, JAMA Oncology. 2018 Mar 1. doi: 10.1001/jamaoncol.2017.5685.
FROM JAMA ONCOLOGY
CPT and relative value changes that may affect reimbursement to your ObGyn practice
Another year brings changes to Current Procedural Terminology (CPT) codes (which are developed and copyrighted by the American Medical Association) in the form of additions and revisions, and payments related to resource-based relative value scale (RBRVS) revisions for selected services. As of January 1, 2018, 2 new Category I codes pertain to laparoscopic treatments for gynecologic cancer, and the 4 existing codes for colporrhaphy have been revised to include cystourethroscopy. New Category III codes include 4 for fetal magnetocardiography and 1 for transvaginal tactile imaging. Medicare also has reevaluated certain relative value units (RVUs) in outpatient and facility settings.
New and revised Category I codes
Laparoscopic treatments for gynecologic cancer. Technologic advances in performing laparoscopic procedures have allowed for more extensive laparoscopic surgery for various gynecologic cancers and, to this end, 2 new codes have been added.
First, a new code was added to capture comprehensive laparoscopic surgical staging for gynecologic cancer. This new code, 38573, Laparoscopy, surgical; with bilateral total pelvic lymphadenectomy and peri-aortic lymph node sampling, peritoneal washings, peritoneal biopsy(ies), omentectomy, and diaphragmatic washings, including diaphragmatic and other serosal biopsy(ies), when performed, may not be reported with any other code that includes lymphadenectomy, omentectomy, or hysterectomy. It is intended primarily for a stand-alone staging procedure after an initial biopsy shows a gynecologic malignancy such as ovarian cancer. This new code has been valued at 33.59 RVUs.
Second, a new code was added to capture laparoscopic debulking in conjunction with hysterectomy. The new code, 58575, Laparoscopy, surgical, total hysterectomy for resection of malignancy (tumor debulking), with omentectomy including salpingo-oophorectomy, unilateral or bilateral, when performed, has been valued at 53.62 RVUs. The open equivalent to this new code is 58953, Bilateral salpingo-oophorectomy with omentectomy, total abdominal hysterectomy and radical dissection for debulking.
Cystourethroscopy. The revisions involve no longer permitting separate reporting of 52000, Cystourethroscopy (separate procedure), with the colporrhaphy codes 57240−57265. The rationale behind this change was that surgeons were routinely performing cystoscopy at the time of these procedures and therefore it should become part of the surgical procedure. Currently the Medicare National Correct Coding Initiative (NCCI) bundles 52000 with these 4 codes, but only code 57250 allows for the use of a modifier -59 to bypass the edit if the purpose of the cystoscopy was evaluation of a distinct complaint or problem (such as evaluating patient-expressed urinary symptoms prior to the surgery that were investigated at the time of the prolapse surgery). When codes 57240, 57260, or 57265 are billed along with 52000, the cystoscopy will be denied and a modifier -59 cannot be reported to bypass this edit.
New Category III codes
The new Category III codes represent emerging technology, and it is important to report them, rather than an unlisted code, if the procedures described are performed so that data can be collected for later consideration to make these Category I CPT codes. Since these codes are not assigned relative values, the provider will need to let the payer know which existing CPT Category I code most closely represents the work involved.
Fetal magnetocardiography. The new Category III codes for fetal magnetocardiography describe essentially a fetal electrocardiogram (ECG) that would be performed to assess fetal arrhythmias by placing up to 3 leads on the mother’s abdomen. Possible comparison codes for physician work might include 59050, fetal monitoring by consultant during labor; 93000−93010, 12-lead ECG, or 93040−93042, rhythm strip up to 3 leads. However, because the equipment is very expensive, these codes would not capture practice expense and the physician would have to negotiate a reasonable reimbursement level with the payer, if the magnetocardiography was a covered service. The new codes are as follows:
- 0475T, Recording of fetal magnetic cardiac signal using at least 3 channels; patient recording and storage, data scanning with signal extraction, technical analysis and result, as well as supervision, review, and interpretation of report by a physician or other qualified health care professional
- 0476T, Recording of fetal magnetic cardiac signal using at least 3 channels; patient recording, data scanning, with raw electronic signal transfer of data and storage
- 0477T, Recording of fetal magnetic cardiac signal using at least 3 channels; signal extraction, technical analysis, and result.
Transvaginal tactile imaging. The new Category III code, 0487T, Biomechanical mapping, transvaginal, with report, describes the use of a pressure sensor probe inserted into the vaginal canal to measure and collect data on pelvic muscle strength, elasticity, tissue integrity, and tone. These data produce images in real time that are mapped to produce a report for physician review, interpretation, and report. The data allow quantification of pelvic floor dysfunction and may be useful in determining the most appropriate treatment (whether surgical or medical) for this gynecologic condition. The procedure uses a transvaginal probe like an ultrasound, so using 76830, transvaginal ultrasound, would not be unreasonable as a comparison code as a start.
Medicare relative value changes
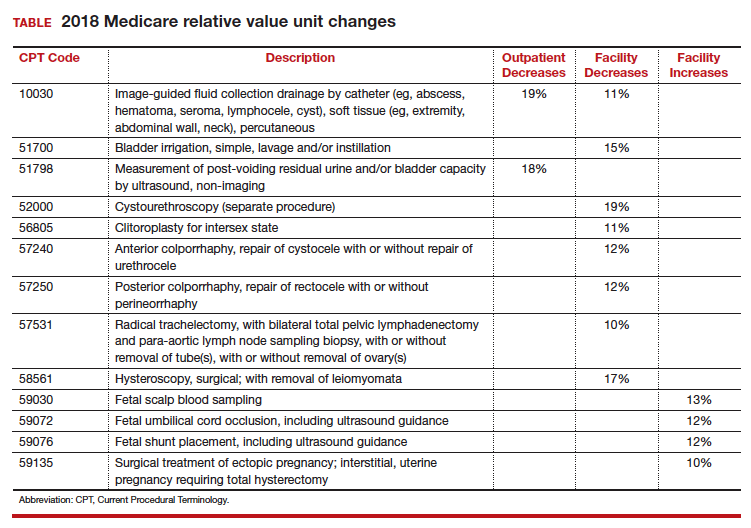
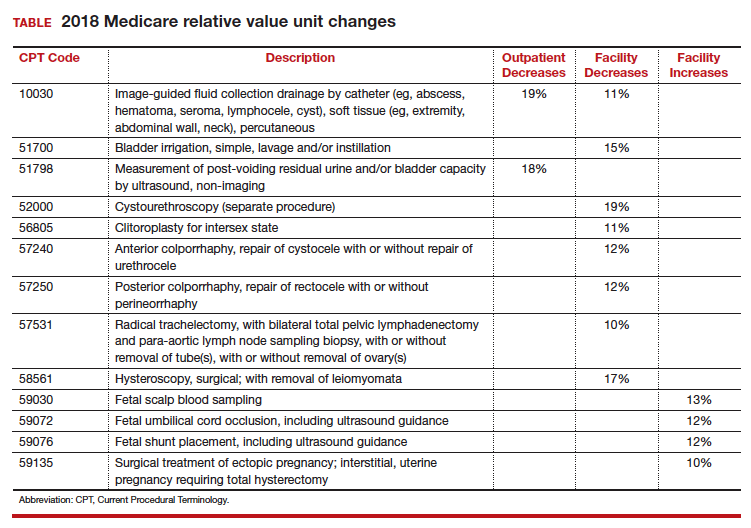
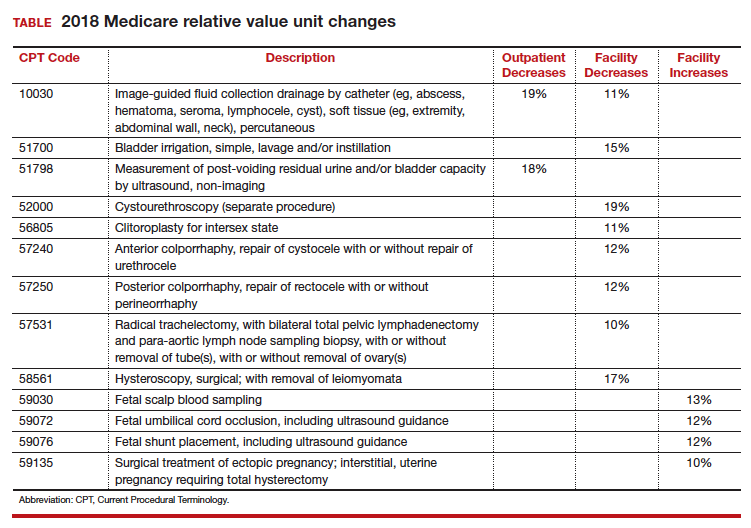
Every year, Medicare reevaluates potentially misvalued CPT codes and this year was no exception. The TABLE represents the winners and losers for codes in the outpatient and facility settings that have increased or decreased RVUs by more than 10%.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Another year brings changes to Current Procedural Terminology (CPT) codes (which are developed and copyrighted by the American Medical Association) in the form of additions and revisions, and payments related to resource-based relative value scale (RBRVS) revisions for selected services. As of January 1, 2018, 2 new Category I codes pertain to laparoscopic treatments for gynecologic cancer, and the 4 existing codes for colporrhaphy have been revised to include cystourethroscopy. New Category III codes include 4 for fetal magnetocardiography and 1 for transvaginal tactile imaging. Medicare also has reevaluated certain relative value units (RVUs) in outpatient and facility settings.
New and revised Category I codes
Laparoscopic treatments for gynecologic cancer. Technologic advances in performing laparoscopic procedures have allowed for more extensive laparoscopic surgery for various gynecologic cancers and, to this end, 2 new codes have been added.
First, a new code was added to capture comprehensive laparoscopic surgical staging for gynecologic cancer. This new code, 38573, Laparoscopy, surgical; with bilateral total pelvic lymphadenectomy and peri-aortic lymph node sampling, peritoneal washings, peritoneal biopsy(ies), omentectomy, and diaphragmatic washings, including diaphragmatic and other serosal biopsy(ies), when performed, may not be reported with any other code that includes lymphadenectomy, omentectomy, or hysterectomy. It is intended primarily for a stand-alone staging procedure after an initial biopsy shows a gynecologic malignancy such as ovarian cancer. This new code has been valued at 33.59 RVUs.
Second, a new code was added to capture laparoscopic debulking in conjunction with hysterectomy. The new code, 58575, Laparoscopy, surgical, total hysterectomy for resection of malignancy (tumor debulking), with omentectomy including salpingo-oophorectomy, unilateral or bilateral, when performed, has been valued at 53.62 RVUs. The open equivalent to this new code is 58953, Bilateral salpingo-oophorectomy with omentectomy, total abdominal hysterectomy and radical dissection for debulking.
Cystourethroscopy. The revisions involve no longer permitting separate reporting of 52000, Cystourethroscopy (separate procedure), with the colporrhaphy codes 57240−57265. The rationale behind this change was that surgeons were routinely performing cystoscopy at the time of these procedures and therefore it should become part of the surgical procedure. Currently the Medicare National Correct Coding Initiative (NCCI) bundles 52000 with these 4 codes, but only code 57250 allows for the use of a modifier -59 to bypass the edit if the purpose of the cystoscopy was evaluation of a distinct complaint or problem (such as evaluating patient-expressed urinary symptoms prior to the surgery that were investigated at the time of the prolapse surgery). When codes 57240, 57260, or 57265 are billed along with 52000, the cystoscopy will be denied and a modifier -59 cannot be reported to bypass this edit.
New Category III codes
The new Category III codes represent emerging technology, and it is important to report them, rather than an unlisted code, if the procedures described are performed so that data can be collected for later consideration to make these Category I CPT codes. Since these codes are not assigned relative values, the provider will need to let the payer know which existing CPT Category I code most closely represents the work involved.
Fetal magnetocardiography. The new Category III codes for fetal magnetocardiography describe essentially a fetal electrocardiogram (ECG) that would be performed to assess fetal arrhythmias by placing up to 3 leads on the mother’s abdomen. Possible comparison codes for physician work might include 59050, fetal monitoring by consultant during labor; 93000−93010, 12-lead ECG, or 93040−93042, rhythm strip up to 3 leads. However, because the equipment is very expensive, these codes would not capture practice expense and the physician would have to negotiate a reasonable reimbursement level with the payer, if the magnetocardiography was a covered service. The new codes are as follows:
- 0475T, Recording of fetal magnetic cardiac signal using at least 3 channels; patient recording and storage, data scanning with signal extraction, technical analysis and result, as well as supervision, review, and interpretation of report by a physician or other qualified health care professional
- 0476T, Recording of fetal magnetic cardiac signal using at least 3 channels; patient recording, data scanning, with raw electronic signal transfer of data and storage
- 0477T, Recording of fetal magnetic cardiac signal using at least 3 channels; signal extraction, technical analysis, and result.
Transvaginal tactile imaging. The new Category III code, 0487T, Biomechanical mapping, transvaginal, with report, describes the use of a pressure sensor probe inserted into the vaginal canal to measure and collect data on pelvic muscle strength, elasticity, tissue integrity, and tone. These data produce images in real time that are mapped to produce a report for physician review, interpretation, and report. The data allow quantification of pelvic floor dysfunction and may be useful in determining the most appropriate treatment (whether surgical or medical) for this gynecologic condition. The procedure uses a transvaginal probe like an ultrasound, so using 76830, transvaginal ultrasound, would not be unreasonable as a comparison code as a start.
Medicare relative value changes
Every year, Medicare reevaluates potentially misvalued CPT codes and this year was no exception. The TABLE represents the winners and losers for codes in the outpatient and facility settings that have increased or decreased RVUs by more than 10%.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Another year brings changes to Current Procedural Terminology (CPT) codes (which are developed and copyrighted by the American Medical Association) in the form of additions and revisions, and payments related to resource-based relative value scale (RBRVS) revisions for selected services. As of January 1, 2018, 2 new Category I codes pertain to laparoscopic treatments for gynecologic cancer, and the 4 existing codes for colporrhaphy have been revised to include cystourethroscopy. New Category III codes include 4 for fetal magnetocardiography and 1 for transvaginal tactile imaging. Medicare also has reevaluated certain relative value units (RVUs) in outpatient and facility settings.
New and revised Category I codes
Laparoscopic treatments for gynecologic cancer. Technologic advances in performing laparoscopic procedures have allowed for more extensive laparoscopic surgery for various gynecologic cancers and, to this end, 2 new codes have been added.
First, a new code was added to capture comprehensive laparoscopic surgical staging for gynecologic cancer. This new code, 38573, Laparoscopy, surgical; with bilateral total pelvic lymphadenectomy and peri-aortic lymph node sampling, peritoneal washings, peritoneal biopsy(ies), omentectomy, and diaphragmatic washings, including diaphragmatic and other serosal biopsy(ies), when performed, may not be reported with any other code that includes lymphadenectomy, omentectomy, or hysterectomy. It is intended primarily for a stand-alone staging procedure after an initial biopsy shows a gynecologic malignancy such as ovarian cancer. This new code has been valued at 33.59 RVUs.
Second, a new code was added to capture laparoscopic debulking in conjunction with hysterectomy. The new code, 58575, Laparoscopy, surgical, total hysterectomy for resection of malignancy (tumor debulking), with omentectomy including salpingo-oophorectomy, unilateral or bilateral, when performed, has been valued at 53.62 RVUs. The open equivalent to this new code is 58953, Bilateral salpingo-oophorectomy with omentectomy, total abdominal hysterectomy and radical dissection for debulking.
Cystourethroscopy. The revisions involve no longer permitting separate reporting of 52000, Cystourethroscopy (separate procedure), with the colporrhaphy codes 57240−57265. The rationale behind this change was that surgeons were routinely performing cystoscopy at the time of these procedures and therefore it should become part of the surgical procedure. Currently the Medicare National Correct Coding Initiative (NCCI) bundles 52000 with these 4 codes, but only code 57250 allows for the use of a modifier -59 to bypass the edit if the purpose of the cystoscopy was evaluation of a distinct complaint or problem (such as evaluating patient-expressed urinary symptoms prior to the surgery that were investigated at the time of the prolapse surgery). When codes 57240, 57260, or 57265 are billed along with 52000, the cystoscopy will be denied and a modifier -59 cannot be reported to bypass this edit.
New Category III codes
The new Category III codes represent emerging technology, and it is important to report them, rather than an unlisted code, if the procedures described are performed so that data can be collected for later consideration to make these Category I CPT codes. Since these codes are not assigned relative values, the provider will need to let the payer know which existing CPT Category I code most closely represents the work involved.
Fetal magnetocardiography. The new Category III codes for fetal magnetocardiography describe essentially a fetal electrocardiogram (ECG) that would be performed to assess fetal arrhythmias by placing up to 3 leads on the mother’s abdomen. Possible comparison codes for physician work might include 59050, fetal monitoring by consultant during labor; 93000−93010, 12-lead ECG, or 93040−93042, rhythm strip up to 3 leads. However, because the equipment is very expensive, these codes would not capture practice expense and the physician would have to negotiate a reasonable reimbursement level with the payer, if the magnetocardiography was a covered service. The new codes are as follows:
- 0475T, Recording of fetal magnetic cardiac signal using at least 3 channels; patient recording and storage, data scanning with signal extraction, technical analysis and result, as well as supervision, review, and interpretation of report by a physician or other qualified health care professional
- 0476T, Recording of fetal magnetic cardiac signal using at least 3 channels; patient recording, data scanning, with raw electronic signal transfer of data and storage
- 0477T, Recording of fetal magnetic cardiac signal using at least 3 channels; signal extraction, technical analysis, and result.
Transvaginal tactile imaging. The new Category III code, 0487T, Biomechanical mapping, transvaginal, with report, describes the use of a pressure sensor probe inserted into the vaginal canal to measure and collect data on pelvic muscle strength, elasticity, tissue integrity, and tone. These data produce images in real time that are mapped to produce a report for physician review, interpretation, and report. The data allow quantification of pelvic floor dysfunction and may be useful in determining the most appropriate treatment (whether surgical or medical) for this gynecologic condition. The procedure uses a transvaginal probe like an ultrasound, so using 76830, transvaginal ultrasound, would not be unreasonable as a comparison code as a start.
Medicare relative value changes
Every year, Medicare reevaluates potentially misvalued CPT codes and this year was no exception. The TABLE represents the winners and losers for codes in the outpatient and facility settings that have increased or decreased RVUs by more than 10%.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Alcohol dependence may accelerate aging, frontal cortical deficits
Alcoholism compounds age-associated volume deficits in the frontal cortex, independent of the additional effects of drug dependence or hepatitis C infection, suggests new research published March 14 in JAMA Psychiatry.
Edith V. Sullivan, PhD, and her coauthors reported the results of a 14-year longitudinal study that used magnetic resonance imaging to examine the brains of 116 participants with alcohol dependence and 96 age-matched controls.
They found that participants with alcohol dependence as defined by the DSM-IV had significantly greater gray matter volume deficits in their frontal, temporal, parietal, cingulate and insular cortices, compared with controls – most prominently in the frontal subregions – with the only exception being the occipital lobe. When age was taken into account, age-related volume deficits were seen in the control group in five of the six cortical regions, but the alcoholism group showed a significantly greater deficit in the precentral and superior frontal cortex.
Dr. Sullivan, of the department of psychiatry and behavioral sciences at Stanford (Calif.) University, and her coauthors said the presence of age-alcoholism interactions puts older alcohol-dependent individuals at greater risk of age-associated functional compromise, even if their excessive drinking starts later in life.
More than half of individuals in the alcoholism group (54.5%) also reported drug dependence. The imaging showed that participants with alcohol use disorder who also reported opiate or cocaine use had smaller frontal cortex volumes compared with those who were not drug users. However, the non–drug-dependent participants in the group still showed deficits in precentral, supplementary motor and medial cortices volumes, compared with controls.
“These findings in alcohol-dependent and control participants, examined 1 to 8 times or more during intervals of 1 week to 12.5 years, representing, to our knowledge, the largest and longest-studied group to date, support our study hypotheses regarding alcoholism-associated accelerated aging and cortical volume deficits independent of drug dependence or HCV infection comorbidity,” the authors wrote.
“We observed a selectivity of frontal cortex to age-alcoholism interaction beyond normal aging effects and independent of deficits related to drug dependence.”
, compared with those with alcoholism alone and compared with controls. “Thus, HCV infection, while having focal effects on frontal brain systems, targeted frontally based systems also vulnerable to chronic and extensive alcohol consumption,” the authors wrote. “Whether the compounded untoward effects of alcoholism and HCV infection on brain structure can be ameliorated with successful treatment of the infection remains to be determined.”
Dr. Sullivan and her coauthors cited several limitations. For example, non–alcohol-dependent or HCV-infected comparison groups were not available for analysis.
The study was supported by the National Institute on Alcohol Abuse and Alcoholism, and the Moldow Women’s Hope and Heal Fund. No conflicts of interest were declared.
SOURCE: Sullivan EV et al. JAMA Psychiatry. 2018 Mar 14. doi: 10.1001/jamapsychiatry.2018.0021.
With an aging population that is also showing significant increases in alcohol use and misuse, studies of the interaction between alcohol and aging and the brain are highly significant. The most compelling finding of this study is the impact of that interaction on the frontal cortex volume, because of the key role this region of the brain plays in executive function.
Deficits in frontal cortical volume associated with aging are hypothesized to also result in impulsivity and compulsivity, which opens up the possibility of greater vulnerability to alcohol use disorder later in life. So as excessive alcohol consumption contributes to this aging process, this aging process also might contribute to excessive drinking in the elderly as a form of self-medication of the negative emotional states associated with aging.
“The study ... provides compelling evidence that alcohol misuse during later adulthood could confer a greater risk of deficits in frontal lobe function beyond the deficits that typically occur with aging,” wrote George F. Koob, PhD.
Given this, it is critical that strategies be explored and implemented aimed at addressing the misuse of alcohol by older drinkers. “As Yoda might say, ‘Protect their brains, we must.’ ”
George F. Koob, PhD, is affiliated with the National Institute on Alcohol Abuse and Alcoholism at the National Institutes of Health, Rockville, Md. These comments are taken from an editorial (JAMA Psychiatry. 2018 March 14. doi: 10.1001/jamapsychiatry.2018.0009). No conflicts of interest were declared.
With an aging population that is also showing significant increases in alcohol use and misuse, studies of the interaction between alcohol and aging and the brain are highly significant. The most compelling finding of this study is the impact of that interaction on the frontal cortex volume, because of the key role this region of the brain plays in executive function.
Deficits in frontal cortical volume associated with aging are hypothesized to also result in impulsivity and compulsivity, which opens up the possibility of greater vulnerability to alcohol use disorder later in life. So as excessive alcohol consumption contributes to this aging process, this aging process also might contribute to excessive drinking in the elderly as a form of self-medication of the negative emotional states associated with aging.
“The study ... provides compelling evidence that alcohol misuse during later adulthood could confer a greater risk of deficits in frontal lobe function beyond the deficits that typically occur with aging,” wrote George F. Koob, PhD.
Given this, it is critical that strategies be explored and implemented aimed at addressing the misuse of alcohol by older drinkers. “As Yoda might say, ‘Protect their brains, we must.’ ”
George F. Koob, PhD, is affiliated with the National Institute on Alcohol Abuse and Alcoholism at the National Institutes of Health, Rockville, Md. These comments are taken from an editorial (JAMA Psychiatry. 2018 March 14. doi: 10.1001/jamapsychiatry.2018.0009). No conflicts of interest were declared.
With an aging population that is also showing significant increases in alcohol use and misuse, studies of the interaction between alcohol and aging and the brain are highly significant. The most compelling finding of this study is the impact of that interaction on the frontal cortex volume, because of the key role this region of the brain plays in executive function.
Deficits in frontal cortical volume associated with aging are hypothesized to also result in impulsivity and compulsivity, which opens up the possibility of greater vulnerability to alcohol use disorder later in life. So as excessive alcohol consumption contributes to this aging process, this aging process also might contribute to excessive drinking in the elderly as a form of self-medication of the negative emotional states associated with aging.
“The study ... provides compelling evidence that alcohol misuse during later adulthood could confer a greater risk of deficits in frontal lobe function beyond the deficits that typically occur with aging,” wrote George F. Koob, PhD.
Given this, it is critical that strategies be explored and implemented aimed at addressing the misuse of alcohol by older drinkers. “As Yoda might say, ‘Protect their brains, we must.’ ”
George F. Koob, PhD, is affiliated with the National Institute on Alcohol Abuse and Alcoholism at the National Institutes of Health, Rockville, Md. These comments are taken from an editorial (JAMA Psychiatry. 2018 March 14. doi: 10.1001/jamapsychiatry.2018.0009). No conflicts of interest were declared.
Alcoholism compounds age-associated volume deficits in the frontal cortex, independent of the additional effects of drug dependence or hepatitis C infection, suggests new research published March 14 in JAMA Psychiatry.
Edith V. Sullivan, PhD, and her coauthors reported the results of a 14-year longitudinal study that used magnetic resonance imaging to examine the brains of 116 participants with alcohol dependence and 96 age-matched controls.
They found that participants with alcohol dependence as defined by the DSM-IV had significantly greater gray matter volume deficits in their frontal, temporal, parietal, cingulate and insular cortices, compared with controls – most prominently in the frontal subregions – with the only exception being the occipital lobe. When age was taken into account, age-related volume deficits were seen in the control group in five of the six cortical regions, but the alcoholism group showed a significantly greater deficit in the precentral and superior frontal cortex.
Dr. Sullivan, of the department of psychiatry and behavioral sciences at Stanford (Calif.) University, and her coauthors said the presence of age-alcoholism interactions puts older alcohol-dependent individuals at greater risk of age-associated functional compromise, even if their excessive drinking starts later in life.
More than half of individuals in the alcoholism group (54.5%) also reported drug dependence. The imaging showed that participants with alcohol use disorder who also reported opiate or cocaine use had smaller frontal cortex volumes compared with those who were not drug users. However, the non–drug-dependent participants in the group still showed deficits in precentral, supplementary motor and medial cortices volumes, compared with controls.
“These findings in alcohol-dependent and control participants, examined 1 to 8 times or more during intervals of 1 week to 12.5 years, representing, to our knowledge, the largest and longest-studied group to date, support our study hypotheses regarding alcoholism-associated accelerated aging and cortical volume deficits independent of drug dependence or HCV infection comorbidity,” the authors wrote.
“We observed a selectivity of frontal cortex to age-alcoholism interaction beyond normal aging effects and independent of deficits related to drug dependence.”
, compared with those with alcoholism alone and compared with controls. “Thus, HCV infection, while having focal effects on frontal brain systems, targeted frontally based systems also vulnerable to chronic and extensive alcohol consumption,” the authors wrote. “Whether the compounded untoward effects of alcoholism and HCV infection on brain structure can be ameliorated with successful treatment of the infection remains to be determined.”
Dr. Sullivan and her coauthors cited several limitations. For example, non–alcohol-dependent or HCV-infected comparison groups were not available for analysis.
The study was supported by the National Institute on Alcohol Abuse and Alcoholism, and the Moldow Women’s Hope and Heal Fund. No conflicts of interest were declared.
SOURCE: Sullivan EV et al. JAMA Psychiatry. 2018 Mar 14. doi: 10.1001/jamapsychiatry.2018.0021.
Alcoholism compounds age-associated volume deficits in the frontal cortex, independent of the additional effects of drug dependence or hepatitis C infection, suggests new research published March 14 in JAMA Psychiatry.
Edith V. Sullivan, PhD, and her coauthors reported the results of a 14-year longitudinal study that used magnetic resonance imaging to examine the brains of 116 participants with alcohol dependence and 96 age-matched controls.
They found that participants with alcohol dependence as defined by the DSM-IV had significantly greater gray matter volume deficits in their frontal, temporal, parietal, cingulate and insular cortices, compared with controls – most prominently in the frontal subregions – with the only exception being the occipital lobe. When age was taken into account, age-related volume deficits were seen in the control group in five of the six cortical regions, but the alcoholism group showed a significantly greater deficit in the precentral and superior frontal cortex.
Dr. Sullivan, of the department of psychiatry and behavioral sciences at Stanford (Calif.) University, and her coauthors said the presence of age-alcoholism interactions puts older alcohol-dependent individuals at greater risk of age-associated functional compromise, even if their excessive drinking starts later in life.
More than half of individuals in the alcoholism group (54.5%) also reported drug dependence. The imaging showed that participants with alcohol use disorder who also reported opiate or cocaine use had smaller frontal cortex volumes compared with those who were not drug users. However, the non–drug-dependent participants in the group still showed deficits in precentral, supplementary motor and medial cortices volumes, compared with controls.
“These findings in alcohol-dependent and control participants, examined 1 to 8 times or more during intervals of 1 week to 12.5 years, representing, to our knowledge, the largest and longest-studied group to date, support our study hypotheses regarding alcoholism-associated accelerated aging and cortical volume deficits independent of drug dependence or HCV infection comorbidity,” the authors wrote.
“We observed a selectivity of frontal cortex to age-alcoholism interaction beyond normal aging effects and independent of deficits related to drug dependence.”
, compared with those with alcoholism alone and compared with controls. “Thus, HCV infection, while having focal effects on frontal brain systems, targeted frontally based systems also vulnerable to chronic and extensive alcohol consumption,” the authors wrote. “Whether the compounded untoward effects of alcoholism and HCV infection on brain structure can be ameliorated with successful treatment of the infection remains to be determined.”
Dr. Sullivan and her coauthors cited several limitations. For example, non–alcohol-dependent or HCV-infected comparison groups were not available for analysis.
The study was supported by the National Institute on Alcohol Abuse and Alcoholism, and the Moldow Women’s Hope and Heal Fund. No conflicts of interest were declared.
SOURCE: Sullivan EV et al. JAMA Psychiatry. 2018 Mar 14. doi: 10.1001/jamapsychiatry.2018.0021.
FROM JAMA PSYCHIATRY
Key clinical point: Older alcohol-dependent patients are at greater risk of functional compromise, even if their excessive drinking starts later in life.
Major finding: Individuals with alcohol use disorder show significantly greater deficits in the precentral and superior frontal cortex, compared with age-matched controls.
Data source: Longitudinal study of 116 participants with alcohol dependence and 96 age-matched controls.
Disclosures: The U.S. National Institute on Alcohol Abuse and Alcoholism, and the Moldow Women’s Hope and Heal Fund supported the study. No conflicts of interest were declared.
Source: Sullivan EV et al. JAMA Psychiatry. 2018 Mar 14. doi: 10.1001/jamapsychiatry.2018.0021.