User login
Blood products unharmed by drone trips

products attached to a
S900-model drone.
Photo courtesy of
Johns Hopkins Medicine
A proof-of-concept study suggests that large bags of blood products can maintain temperature and cellular integrity when transported by drones.
Researchers say these findings, published in Transfusion, add to evidence that remotely piloted drones are an effective, safe, and timely way to quickly get blood products to remote accident or natural catastrophe sites, or other time-sensitive destinations.
“For rural areas that lack access to nearby clinics, or that may lack the infrastructure for collecting blood products or transporting them on their own, drones can provide that access,” said study author Timothy Amukele, MD, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
Drones also can help in urban centers to improve distribution of blood products and the quality of care, he added.
Dr Amukele and his colleagues previously studied the impact of drone transportation on the chemical, hematological, and microbial makeup of drone-flown blood samples and found that none were negatively affected.
Study design, methods
In the new study, the team examined the effects of drone transportation on larger amounts of blood products used for transfusion, which have significantly more complex handling, transport, and storage requirements compared to blood samples for laboratory testing.
The researchers purchased 6 units of red blood cells (RBCs), 6 units of platelets, and 6 units of unthawed plasma from the American Red Cross. They then packed the units into a 5-quart cooler, 2 to 3 units at a time, in keeping with weight restrictions for the transport drone.
The cooler was then attached to a commercial S900-model drone. This particular drone model comes equipped with a camera mount, which the team removed and replaced with the cooler.
For each test, the drone was flown by remote control a distance of approximately 13 to 20 kilometers (8 to 12 miles) while 100 meters (328 feet) above ground. This flight took up to 26.5 minutes.
The researchers designed the test to maintain temperature for the RBCs, platelets, and plasma units. They used wet ice, pre-calibrated thermal packs, and dry ice for each type of blood product, respectively.
Temperature monitoring was constant, keeping with transport and storage requirements for blood components.
The team conducted the tests in an unpopulated area, and a certified, ground-based pilot flew the drone.
Following flight, all units were transported to The Johns Hopkins Hospital and compared to blood products that had not taken a drone trip.
Results
Dr Amukele and his colleagues checked the RBCs for signs of hemolysis. They checked the platelets for changes in pH, the number of platelets, and mean platelet volume. And they checked the plasma units for evidence of air bubbles, which would indicate thawing.
The researchers found no evidence of hemolysis in the control RBCs or the RBCs that had taken the drone flight.
There was no significant difference in pH, platelet counts, or mean platelet volume between control and drone-flown platelets.
And there was no apparent change in the size or shape of air bubbles in the plasma units before and after drone flight.
However, the researchers did find that, for all flown units, there was a decrease in temperature of between 1.5°C and 4°C during the course of the flight. They said the cause of this decrease was probably the ambient temperature in the case of the platelet units, the wet ice in the case of the RBCs, and the dry ice in the case of the plasma.
The team also found an up to 2°C difference between individual flights for both the RBCs and the plasma units. They said this difference is likely due to the differences in the amounts of wet and dry ice placed in the cooler.
The researchers are planning further and larger studies in the US and overseas, and they hope to test methods of active cooling, such as programming a cooler to maintain a specific temperature.
“My vision is that, in the future, when a first responder arrives to the scene of an accident, he or she can test the victim’s blood type right on the spot and send for a drone to bring the correct blood product,” Dr Amukele said.
Funding for this study was provided by Peter Kovler of the Blum-Kovler Foundation. ![]()

products attached to a
S900-model drone.
Photo courtesy of
Johns Hopkins Medicine
A proof-of-concept study suggests that large bags of blood products can maintain temperature and cellular integrity when transported by drones.
Researchers say these findings, published in Transfusion, add to evidence that remotely piloted drones are an effective, safe, and timely way to quickly get blood products to remote accident or natural catastrophe sites, or other time-sensitive destinations.
“For rural areas that lack access to nearby clinics, or that may lack the infrastructure for collecting blood products or transporting them on their own, drones can provide that access,” said study author Timothy Amukele, MD, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
Drones also can help in urban centers to improve distribution of blood products and the quality of care, he added.
Dr Amukele and his colleagues previously studied the impact of drone transportation on the chemical, hematological, and microbial makeup of drone-flown blood samples and found that none were negatively affected.
Study design, methods
In the new study, the team examined the effects of drone transportation on larger amounts of blood products used for transfusion, which have significantly more complex handling, transport, and storage requirements compared to blood samples for laboratory testing.
The researchers purchased 6 units of red blood cells (RBCs), 6 units of platelets, and 6 units of unthawed plasma from the American Red Cross. They then packed the units into a 5-quart cooler, 2 to 3 units at a time, in keeping with weight restrictions for the transport drone.
The cooler was then attached to a commercial S900-model drone. This particular drone model comes equipped with a camera mount, which the team removed and replaced with the cooler.
For each test, the drone was flown by remote control a distance of approximately 13 to 20 kilometers (8 to 12 miles) while 100 meters (328 feet) above ground. This flight took up to 26.5 minutes.
The researchers designed the test to maintain temperature for the RBCs, platelets, and plasma units. They used wet ice, pre-calibrated thermal packs, and dry ice for each type of blood product, respectively.
Temperature monitoring was constant, keeping with transport and storage requirements for blood components.
The team conducted the tests in an unpopulated area, and a certified, ground-based pilot flew the drone.
Following flight, all units were transported to The Johns Hopkins Hospital and compared to blood products that had not taken a drone trip.
Results
Dr Amukele and his colleagues checked the RBCs for signs of hemolysis. They checked the platelets for changes in pH, the number of platelets, and mean platelet volume. And they checked the plasma units for evidence of air bubbles, which would indicate thawing.
The researchers found no evidence of hemolysis in the control RBCs or the RBCs that had taken the drone flight.
There was no significant difference in pH, platelet counts, or mean platelet volume between control and drone-flown platelets.
And there was no apparent change in the size or shape of air bubbles in the plasma units before and after drone flight.
However, the researchers did find that, for all flown units, there was a decrease in temperature of between 1.5°C and 4°C during the course of the flight. They said the cause of this decrease was probably the ambient temperature in the case of the platelet units, the wet ice in the case of the RBCs, and the dry ice in the case of the plasma.
The team also found an up to 2°C difference between individual flights for both the RBCs and the plasma units. They said this difference is likely due to the differences in the amounts of wet and dry ice placed in the cooler.
The researchers are planning further and larger studies in the US and overseas, and they hope to test methods of active cooling, such as programming a cooler to maintain a specific temperature.
“My vision is that, in the future, when a first responder arrives to the scene of an accident, he or she can test the victim’s blood type right on the spot and send for a drone to bring the correct blood product,” Dr Amukele said.
Funding for this study was provided by Peter Kovler of the Blum-Kovler Foundation. ![]()

products attached to a
S900-model drone.
Photo courtesy of
Johns Hopkins Medicine
A proof-of-concept study suggests that large bags of blood products can maintain temperature and cellular integrity when transported by drones.
Researchers say these findings, published in Transfusion, add to evidence that remotely piloted drones are an effective, safe, and timely way to quickly get blood products to remote accident or natural catastrophe sites, or other time-sensitive destinations.
“For rural areas that lack access to nearby clinics, or that may lack the infrastructure for collecting blood products or transporting them on their own, drones can provide that access,” said study author Timothy Amukele, MD, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
Drones also can help in urban centers to improve distribution of blood products and the quality of care, he added.
Dr Amukele and his colleagues previously studied the impact of drone transportation on the chemical, hematological, and microbial makeup of drone-flown blood samples and found that none were negatively affected.
Study design, methods
In the new study, the team examined the effects of drone transportation on larger amounts of blood products used for transfusion, which have significantly more complex handling, transport, and storage requirements compared to blood samples for laboratory testing.
The researchers purchased 6 units of red blood cells (RBCs), 6 units of platelets, and 6 units of unthawed plasma from the American Red Cross. They then packed the units into a 5-quart cooler, 2 to 3 units at a time, in keeping with weight restrictions for the transport drone.
The cooler was then attached to a commercial S900-model drone. This particular drone model comes equipped with a camera mount, which the team removed and replaced with the cooler.
For each test, the drone was flown by remote control a distance of approximately 13 to 20 kilometers (8 to 12 miles) while 100 meters (328 feet) above ground. This flight took up to 26.5 minutes.
The researchers designed the test to maintain temperature for the RBCs, platelets, and plasma units. They used wet ice, pre-calibrated thermal packs, and dry ice for each type of blood product, respectively.
Temperature monitoring was constant, keeping with transport and storage requirements for blood components.
The team conducted the tests in an unpopulated area, and a certified, ground-based pilot flew the drone.
Following flight, all units were transported to The Johns Hopkins Hospital and compared to blood products that had not taken a drone trip.
Results
Dr Amukele and his colleagues checked the RBCs for signs of hemolysis. They checked the platelets for changes in pH, the number of platelets, and mean platelet volume. And they checked the plasma units for evidence of air bubbles, which would indicate thawing.
The researchers found no evidence of hemolysis in the control RBCs or the RBCs that had taken the drone flight.
There was no significant difference in pH, platelet counts, or mean platelet volume between control and drone-flown platelets.
And there was no apparent change in the size or shape of air bubbles in the plasma units before and after drone flight.
However, the researchers did find that, for all flown units, there was a decrease in temperature of between 1.5°C and 4°C during the course of the flight. They said the cause of this decrease was probably the ambient temperature in the case of the platelet units, the wet ice in the case of the RBCs, and the dry ice in the case of the plasma.
The team also found an up to 2°C difference between individual flights for both the RBCs and the plasma units. They said this difference is likely due to the differences in the amounts of wet and dry ice placed in the cooler.
The researchers are planning further and larger studies in the US and overseas, and they hope to test methods of active cooling, such as programming a cooler to maintain a specific temperature.
“My vision is that, in the future, when a first responder arrives to the scene of an accident, he or she can test the victim’s blood type right on the spot and send for a drone to bring the correct blood product,” Dr Amukele said.
Funding for this study was provided by Peter Kovler of the Blum-Kovler Foundation. ![]()
EC grants venetoclax conditional approval for CLL

(US version, Venclexta)
Photo courtesy of Abbvie
The European Commission (EC) has granted conditional marketing authorization for the oral BCL-2 inhibitor venetoclax (Venclyxto™) to treat certain patients with chronic lymphocytic leukemia (CLL).
The drug is now approved as monotherapy to treat adults with CLL who have 17p deletion or TP53 mutation and are unsuitable for or have failed a B-cell receptor pathway inhibitor.
Venetoclax is also approved as monotherapy to treat CLL in the absence of 17p deletion or TP53 mutation in adults who have failed both chemoimmunotherapy and a B-cell receptor pathway inhibitor.
Venetoclax is the first BCL-2 inhibitor authorized for use in Europe.
Conditional marketing authorization represents an expedited path for approval. The EC grants conditional marketing authorization to products whose benefits are thought to outweigh their risks, products that address unmet needs, and products that are expected to provide a significant public health benefit.
Conditional marketing authorization is granted before pivotal registration studies of a product are completed, but the company developing the product is required to complete post-marketing studies showing that the product provides a clinical benefit.
Venetoclax is being developed by AbbVie and Genentech, a member of the Roche Group. The drug is jointly commercialized by the companies in the US and by AbbVie outside of the US.
Phase 2 trials
Venetoclax has produced high objective response rates (ORR) in two phase 2 trials of CLL patients.
In one of these trials, researchers tested venetoclax in 107 patients with previously treated CLL and 17p deletion. The results were published in The Lancet Oncology in June.
The ORR in this trial was 79%. At the time of analysis, the median duration of response had not been reached. The same was true for progression-free survival and overall survival.
The progression-free survival estimate for 12 months was 72%, and the overall survival estimate was 87%.
The incidence of treatment-emergent adverse events was 96%, and the incidence of serious adverse events was 55%.
Grade 3 laboratory tumor lysis syndrome (TLS) was reported in 5 patients. Three of these patients continued on venetoclax, but 2 patients required a dose interruption of 1 day each.
In the second trial, researchers tested venetoclax in 64 patients with CLL who had failed treatment with ibrutinib and/or idelalisib. Results from this trial were presented at the 2016 ASH Annual Meeting.
The ORR was 67%. At 11.8 months of follow-up, the median duration of response, progression-free survival, and overall survival had not been reached. The estimated 12-month progression-free survival was 80%.
The incidence of adverse events was 100%, and the incidence of serious adverse events was 53%. No clinical TLS was observed, but 1 patient met Howard criteria for laboratory TLS. ![]()

(US version, Venclexta)
Photo courtesy of Abbvie
The European Commission (EC) has granted conditional marketing authorization for the oral BCL-2 inhibitor venetoclax (Venclyxto™) to treat certain patients with chronic lymphocytic leukemia (CLL).
The drug is now approved as monotherapy to treat adults with CLL who have 17p deletion or TP53 mutation and are unsuitable for or have failed a B-cell receptor pathway inhibitor.
Venetoclax is also approved as monotherapy to treat CLL in the absence of 17p deletion or TP53 mutation in adults who have failed both chemoimmunotherapy and a B-cell receptor pathway inhibitor.
Venetoclax is the first BCL-2 inhibitor authorized for use in Europe.
Conditional marketing authorization represents an expedited path for approval. The EC grants conditional marketing authorization to products whose benefits are thought to outweigh their risks, products that address unmet needs, and products that are expected to provide a significant public health benefit.
Conditional marketing authorization is granted before pivotal registration studies of a product are completed, but the company developing the product is required to complete post-marketing studies showing that the product provides a clinical benefit.
Venetoclax is being developed by AbbVie and Genentech, a member of the Roche Group. The drug is jointly commercialized by the companies in the US and by AbbVie outside of the US.
Phase 2 trials
Venetoclax has produced high objective response rates (ORR) in two phase 2 trials of CLL patients.
In one of these trials, researchers tested venetoclax in 107 patients with previously treated CLL and 17p deletion. The results were published in The Lancet Oncology in June.
The ORR in this trial was 79%. At the time of analysis, the median duration of response had not been reached. The same was true for progression-free survival and overall survival.
The progression-free survival estimate for 12 months was 72%, and the overall survival estimate was 87%.
The incidence of treatment-emergent adverse events was 96%, and the incidence of serious adverse events was 55%.
Grade 3 laboratory tumor lysis syndrome (TLS) was reported in 5 patients. Three of these patients continued on venetoclax, but 2 patients required a dose interruption of 1 day each.
In the second trial, researchers tested venetoclax in 64 patients with CLL who had failed treatment with ibrutinib and/or idelalisib. Results from this trial were presented at the 2016 ASH Annual Meeting.
The ORR was 67%. At 11.8 months of follow-up, the median duration of response, progression-free survival, and overall survival had not been reached. The estimated 12-month progression-free survival was 80%.
The incidence of adverse events was 100%, and the incidence of serious adverse events was 53%. No clinical TLS was observed, but 1 patient met Howard criteria for laboratory TLS. ![]()

(US version, Venclexta)
Photo courtesy of Abbvie
The European Commission (EC) has granted conditional marketing authorization for the oral BCL-2 inhibitor venetoclax (Venclyxto™) to treat certain patients with chronic lymphocytic leukemia (CLL).
The drug is now approved as monotherapy to treat adults with CLL who have 17p deletion or TP53 mutation and are unsuitable for or have failed a B-cell receptor pathway inhibitor.
Venetoclax is also approved as monotherapy to treat CLL in the absence of 17p deletion or TP53 mutation in adults who have failed both chemoimmunotherapy and a B-cell receptor pathway inhibitor.
Venetoclax is the first BCL-2 inhibitor authorized for use in Europe.
Conditional marketing authorization represents an expedited path for approval. The EC grants conditional marketing authorization to products whose benefits are thought to outweigh their risks, products that address unmet needs, and products that are expected to provide a significant public health benefit.
Conditional marketing authorization is granted before pivotal registration studies of a product are completed, but the company developing the product is required to complete post-marketing studies showing that the product provides a clinical benefit.
Venetoclax is being developed by AbbVie and Genentech, a member of the Roche Group. The drug is jointly commercialized by the companies in the US and by AbbVie outside of the US.
Phase 2 trials
Venetoclax has produced high objective response rates (ORR) in two phase 2 trials of CLL patients.
In one of these trials, researchers tested venetoclax in 107 patients with previously treated CLL and 17p deletion. The results were published in The Lancet Oncology in June.
The ORR in this trial was 79%. At the time of analysis, the median duration of response had not been reached. The same was true for progression-free survival and overall survival.
The progression-free survival estimate for 12 months was 72%, and the overall survival estimate was 87%.
The incidence of treatment-emergent adverse events was 96%, and the incidence of serious adverse events was 55%.
Grade 3 laboratory tumor lysis syndrome (TLS) was reported in 5 patients. Three of these patients continued on venetoclax, but 2 patients required a dose interruption of 1 day each.
In the second trial, researchers tested venetoclax in 64 patients with CLL who had failed treatment with ibrutinib and/or idelalisib. Results from this trial were presented at the 2016 ASH Annual Meeting.
The ORR was 67%. At 11.8 months of follow-up, the median duration of response, progression-free survival, and overall survival had not been reached. The estimated 12-month progression-free survival was 80%.
The incidence of adverse events was 100%, and the incidence of serious adverse events was 53%. No clinical TLS was observed, but 1 patient met Howard criteria for laboratory TLS. ![]()
Drug produces responses in ‘challenging’ patients

© Todd Buchanan 2016
SAN DIEGO—The oral BCL-2 inhibitor venetoclax can produce high objective response rates (ORRs) in chronic lymphocytic leukemia (CLL) patients who have failed treatment with at least one B-cell receptor inhibitor, according to investigators.
In a phase 2 study, venetoclax produced an ORR of 67% among all patients enrolled.
The drug produced a 70% ORR among patients who had failed treatment with ibrutinib and a 62% ORR among patients who had failed idelalisib.
“This represents the first prospective study in this patient population and does demonstrate high rates of durable responses, certainly making [venetoclax] a very viable option for a challenging group of patients to treat,” said study investigator Jeffrey Jones, MD, of The Ohio State University in Columbus.
Dr Jones presented results from this trial at the 2016 ASH Annual Meeting (abstract 637*). This study is sponsored by AbbVie in collaboration with Genentech/Roche.
The trial enrolled patients with CLL who relapsed after or were refractory to ibrutinib (arm A) or idelalisib (arm B). At the time of the data cut-off, 64 patients had been enrolled and treated with venetoclax, including 43 patients in arm A and 21 in arm B.
Patients received venetoclax via a recommended dose-titration schedule—20 mg once daily in week 1, 50 mg daily in week 2, 100 mg daily in week 3, 200 mg daily in week 4, and 400 mg daily from week 5 onward. Patients continued to receive the drug until disease progression or unacceptable toxicity.
To mitigate the risk of tumor lysis syndrome (TLS), patients received prophylaxis with uric acid lowering agents and hydration starting at least 72 hours before the first dose of venetoclax.
Patients with a high tumor burden were hospitalized for the first 20 mg dose and the first 50 mg dose, and they received intravenous hydration and rasburicase. Laboratory values were monitored at the first dose and all dose increases.
Patient characteristics: Arm A
Among patients who had failed ibrutinib, the median age was 66 (range, 48-80). Forty-nine percent of the patients had del(17p), and 35% had bulky nodal disease (5 cm or greater).
The median number of prior treatments was 4 (range, 1-12). All patients had received ibrutinib, but 9% had also received idelalisib. Ninety-one percent of patients were refractory to ibrutinib, and 5% were refractory to idelalisib.
The median time on ibrutinib was 17 months (range, 1-56), and the median time on idelalisib was 10 months (range, 2-31).
Patient characteristics: Arm B
Among patients who had failed idelalisib, the median age was 68 (range, 56-85). Ten percent of patients had del(17p), and 52% had bulky nodal disease (5 cm or greater).
The median number of prior treatments was 3 (range, 1-11). All patients had received idelalisib, but 24% had also received ibrutinib. Sixty-seven percent of patients were refractory to idelalisib, and 10% were refractory to ibrutinib.
The median time on idelalisib was 8 months (range, 1-27), and the median time on ibrutinib was 6 months (range, 2-11).
Results: Arm A
The median time on study in arm A was 13 months (range, 0.1-18). Eighteen patients in this arm discontinued the study—12 due to disease progression, 3 due to adverse events (AEs), 2 due to stem cell transplant, and 1 patient withdrew consent.
The ORR was 70% according to an independent review committee (IRC) and 67% according to investigators.
The rate of complete response (CR) was 0%, and the rate of CR with incomplete bone marrow recovery (CRi) was 2% according to the IRC. According to investigators, the CR rate was 5%, and the CRi rate was 2%.
Sixty-seven percent of patients had a partial response (PR) according to the IRC, and 56% had a PR according to investigators.
Results: Arm B
The median time on study in arm B was 9 months (range, 1.3-16). Four patients in this arm discontinued the study—3 related to disease progression and 1 for an “other” reason.
The ORR was 62% according to the IRC and 57% according to investigators.
The rate of CR/CRi was 0% according to the IRC. According to investigators, the CR rate was 10%, and the CRi rate was 5%.
Sixty-two percent of patients had a PR according to the IRC, and 43% had a PR according to investigators.
Results: Overall
The ORR was 67% according to the IRC and 64% according to investigators.
Forty-five percent of patient samples analyzed (14/31) demonstrated minimal residual disease (MRD) negativity in the peripheral blood between weeks 24 and 48. Five patients with sustained MRD negativity had bone marrow evaluations, and 1 was MRD negative.
At 11.8 months of follow-up, the median duration of response, progression-free survival, and overall survival had not been reached. The estimated 12-month progression-free survival for all patients was 80%.
“Venetoclax has been well-tolerated,” Dr Jones noted. “The toxicity profile in this study is consistent with previous reports. Most of the toxicity has been cytopenias, which can be managed with dose adjustments or supportive care interventions, such as G-CSF.”
All 64 patients experienced an AE. Common AEs were neutropenia (58%), thrombocytopenia (44%), diarrhea (42%), nausea (41%), anemia (36%), fatigue (31%), decreased white blood cell count (22%), and hyperphosphatemia (22%).
Eighty-three percent of patients had grade 3/4 AEs, including neutropenia (45%), thrombocytopenia (28%), anemia (22%), decreased white blood cell count (13%), febrile neutropenia (11%), and pneumonia (11%).
Fifty-three percent of patients had serious AEs, including febrile neutropenia (9%), pneumonia (8%), multi-organ failure (3%), septic shock (3%), and increased potassium (3%).
There were no cases of clinical TLS. However, 1 patient with high tumor burden met Howard criteria for laboratory TLS. ![]()
*Information presented at the meeting differs from the abstract.

© Todd Buchanan 2016
SAN DIEGO—The oral BCL-2 inhibitor venetoclax can produce high objective response rates (ORRs) in chronic lymphocytic leukemia (CLL) patients who have failed treatment with at least one B-cell receptor inhibitor, according to investigators.
In a phase 2 study, venetoclax produced an ORR of 67% among all patients enrolled.
The drug produced a 70% ORR among patients who had failed treatment with ibrutinib and a 62% ORR among patients who had failed idelalisib.
“This represents the first prospective study in this patient population and does demonstrate high rates of durable responses, certainly making [venetoclax] a very viable option for a challenging group of patients to treat,” said study investigator Jeffrey Jones, MD, of The Ohio State University in Columbus.
Dr Jones presented results from this trial at the 2016 ASH Annual Meeting (abstract 637*). This study is sponsored by AbbVie in collaboration with Genentech/Roche.
The trial enrolled patients with CLL who relapsed after or were refractory to ibrutinib (arm A) or idelalisib (arm B). At the time of the data cut-off, 64 patients had been enrolled and treated with venetoclax, including 43 patients in arm A and 21 in arm B.
Patients received venetoclax via a recommended dose-titration schedule—20 mg once daily in week 1, 50 mg daily in week 2, 100 mg daily in week 3, 200 mg daily in week 4, and 400 mg daily from week 5 onward. Patients continued to receive the drug until disease progression or unacceptable toxicity.
To mitigate the risk of tumor lysis syndrome (TLS), patients received prophylaxis with uric acid lowering agents and hydration starting at least 72 hours before the first dose of venetoclax.
Patients with a high tumor burden were hospitalized for the first 20 mg dose and the first 50 mg dose, and they received intravenous hydration and rasburicase. Laboratory values were monitored at the first dose and all dose increases.
Patient characteristics: Arm A
Among patients who had failed ibrutinib, the median age was 66 (range, 48-80). Forty-nine percent of the patients had del(17p), and 35% had bulky nodal disease (5 cm or greater).
The median number of prior treatments was 4 (range, 1-12). All patients had received ibrutinib, but 9% had also received idelalisib. Ninety-one percent of patients were refractory to ibrutinib, and 5% were refractory to idelalisib.
The median time on ibrutinib was 17 months (range, 1-56), and the median time on idelalisib was 10 months (range, 2-31).
Patient characteristics: Arm B
Among patients who had failed idelalisib, the median age was 68 (range, 56-85). Ten percent of patients had del(17p), and 52% had bulky nodal disease (5 cm or greater).
The median number of prior treatments was 3 (range, 1-11). All patients had received idelalisib, but 24% had also received ibrutinib. Sixty-seven percent of patients were refractory to idelalisib, and 10% were refractory to ibrutinib.
The median time on idelalisib was 8 months (range, 1-27), and the median time on ibrutinib was 6 months (range, 2-11).
Results: Arm A
The median time on study in arm A was 13 months (range, 0.1-18). Eighteen patients in this arm discontinued the study—12 due to disease progression, 3 due to adverse events (AEs), 2 due to stem cell transplant, and 1 patient withdrew consent.
The ORR was 70% according to an independent review committee (IRC) and 67% according to investigators.
The rate of complete response (CR) was 0%, and the rate of CR with incomplete bone marrow recovery (CRi) was 2% according to the IRC. According to investigators, the CR rate was 5%, and the CRi rate was 2%.
Sixty-seven percent of patients had a partial response (PR) according to the IRC, and 56% had a PR according to investigators.
Results: Arm B
The median time on study in arm B was 9 months (range, 1.3-16). Four patients in this arm discontinued the study—3 related to disease progression and 1 for an “other” reason.
The ORR was 62% according to the IRC and 57% according to investigators.
The rate of CR/CRi was 0% according to the IRC. According to investigators, the CR rate was 10%, and the CRi rate was 5%.
Sixty-two percent of patients had a PR according to the IRC, and 43% had a PR according to investigators.
Results: Overall
The ORR was 67% according to the IRC and 64% according to investigators.
Forty-five percent of patient samples analyzed (14/31) demonstrated minimal residual disease (MRD) negativity in the peripheral blood between weeks 24 and 48. Five patients with sustained MRD negativity had bone marrow evaluations, and 1 was MRD negative.
At 11.8 months of follow-up, the median duration of response, progression-free survival, and overall survival had not been reached. The estimated 12-month progression-free survival for all patients was 80%.
“Venetoclax has been well-tolerated,” Dr Jones noted. “The toxicity profile in this study is consistent with previous reports. Most of the toxicity has been cytopenias, which can be managed with dose adjustments or supportive care interventions, such as G-CSF.”
All 64 patients experienced an AE. Common AEs were neutropenia (58%), thrombocytopenia (44%), diarrhea (42%), nausea (41%), anemia (36%), fatigue (31%), decreased white blood cell count (22%), and hyperphosphatemia (22%).
Eighty-three percent of patients had grade 3/4 AEs, including neutropenia (45%), thrombocytopenia (28%), anemia (22%), decreased white blood cell count (13%), febrile neutropenia (11%), and pneumonia (11%).
Fifty-three percent of patients had serious AEs, including febrile neutropenia (9%), pneumonia (8%), multi-organ failure (3%), septic shock (3%), and increased potassium (3%).
There were no cases of clinical TLS. However, 1 patient with high tumor burden met Howard criteria for laboratory TLS. ![]()
*Information presented at the meeting differs from the abstract.

© Todd Buchanan 2016
SAN DIEGO—The oral BCL-2 inhibitor venetoclax can produce high objective response rates (ORRs) in chronic lymphocytic leukemia (CLL) patients who have failed treatment with at least one B-cell receptor inhibitor, according to investigators.
In a phase 2 study, venetoclax produced an ORR of 67% among all patients enrolled.
The drug produced a 70% ORR among patients who had failed treatment with ibrutinib and a 62% ORR among patients who had failed idelalisib.
“This represents the first prospective study in this patient population and does demonstrate high rates of durable responses, certainly making [venetoclax] a very viable option for a challenging group of patients to treat,” said study investigator Jeffrey Jones, MD, of The Ohio State University in Columbus.
Dr Jones presented results from this trial at the 2016 ASH Annual Meeting (abstract 637*). This study is sponsored by AbbVie in collaboration with Genentech/Roche.
The trial enrolled patients with CLL who relapsed after or were refractory to ibrutinib (arm A) or idelalisib (arm B). At the time of the data cut-off, 64 patients had been enrolled and treated with venetoclax, including 43 patients in arm A and 21 in arm B.
Patients received venetoclax via a recommended dose-titration schedule—20 mg once daily in week 1, 50 mg daily in week 2, 100 mg daily in week 3, 200 mg daily in week 4, and 400 mg daily from week 5 onward. Patients continued to receive the drug until disease progression or unacceptable toxicity.
To mitigate the risk of tumor lysis syndrome (TLS), patients received prophylaxis with uric acid lowering agents and hydration starting at least 72 hours before the first dose of venetoclax.
Patients with a high tumor burden were hospitalized for the first 20 mg dose and the first 50 mg dose, and they received intravenous hydration and rasburicase. Laboratory values were monitored at the first dose and all dose increases.
Patient characteristics: Arm A
Among patients who had failed ibrutinib, the median age was 66 (range, 48-80). Forty-nine percent of the patients had del(17p), and 35% had bulky nodal disease (5 cm or greater).
The median number of prior treatments was 4 (range, 1-12). All patients had received ibrutinib, but 9% had also received idelalisib. Ninety-one percent of patients were refractory to ibrutinib, and 5% were refractory to idelalisib.
The median time on ibrutinib was 17 months (range, 1-56), and the median time on idelalisib was 10 months (range, 2-31).
Patient characteristics: Arm B
Among patients who had failed idelalisib, the median age was 68 (range, 56-85). Ten percent of patients had del(17p), and 52% had bulky nodal disease (5 cm or greater).
The median number of prior treatments was 3 (range, 1-11). All patients had received idelalisib, but 24% had also received ibrutinib. Sixty-seven percent of patients were refractory to idelalisib, and 10% were refractory to ibrutinib.
The median time on idelalisib was 8 months (range, 1-27), and the median time on ibrutinib was 6 months (range, 2-11).
Results: Arm A
The median time on study in arm A was 13 months (range, 0.1-18). Eighteen patients in this arm discontinued the study—12 due to disease progression, 3 due to adverse events (AEs), 2 due to stem cell transplant, and 1 patient withdrew consent.
The ORR was 70% according to an independent review committee (IRC) and 67% according to investigators.
The rate of complete response (CR) was 0%, and the rate of CR with incomplete bone marrow recovery (CRi) was 2% according to the IRC. According to investigators, the CR rate was 5%, and the CRi rate was 2%.
Sixty-seven percent of patients had a partial response (PR) according to the IRC, and 56% had a PR according to investigators.
Results: Arm B
The median time on study in arm B was 9 months (range, 1.3-16). Four patients in this arm discontinued the study—3 related to disease progression and 1 for an “other” reason.
The ORR was 62% according to the IRC and 57% according to investigators.
The rate of CR/CRi was 0% according to the IRC. According to investigators, the CR rate was 10%, and the CRi rate was 5%.
Sixty-two percent of patients had a PR according to the IRC, and 43% had a PR according to investigators.
Results: Overall
The ORR was 67% according to the IRC and 64% according to investigators.
Forty-five percent of patient samples analyzed (14/31) demonstrated minimal residual disease (MRD) negativity in the peripheral blood between weeks 24 and 48. Five patients with sustained MRD negativity had bone marrow evaluations, and 1 was MRD negative.
At 11.8 months of follow-up, the median duration of response, progression-free survival, and overall survival had not been reached. The estimated 12-month progression-free survival for all patients was 80%.
“Venetoclax has been well-tolerated,” Dr Jones noted. “The toxicity profile in this study is consistent with previous reports. Most of the toxicity has been cytopenias, which can be managed with dose adjustments or supportive care interventions, such as G-CSF.”
All 64 patients experienced an AE. Common AEs were neutropenia (58%), thrombocytopenia (44%), diarrhea (42%), nausea (41%), anemia (36%), fatigue (31%), decreased white blood cell count (22%), and hyperphosphatemia (22%).
Eighty-three percent of patients had grade 3/4 AEs, including neutropenia (45%), thrombocytopenia (28%), anemia (22%), decreased white blood cell count (13%), febrile neutropenia (11%), and pneumonia (11%).
Fifty-three percent of patients had serious AEs, including febrile neutropenia (9%), pneumonia (8%), multi-organ failure (3%), septic shock (3%), and increased potassium (3%).
There were no cases of clinical TLS. However, 1 patient with high tumor burden met Howard criteria for laboratory TLS. ![]()
*Information presented at the meeting differs from the abstract.
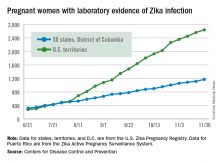
New Zika cases in pregnant women continue to drop
There were 136 new cases of pregnant women with laboratory evidence of Zika infection reported during the 2-week period ending Nov. 30, along with four liveborn infants with Zika-related birth defects, according to the Centers for Disease Control and Prevention.
The CDC did not report new totals for pregnant women and pregnancy outcomes for the week ending Nov. 23, so the most recent data release covers the 2-week period from Nov. 17-30. That 2-week total was barely more than the 124 reported for the week ending Nov. 10.
The four infants born with Zika-related birth defects were all born in the 50 states and D.C., as the CDC is no longer reporting adverse pregnancy outcomes for the territories because Puerto Rico is not using the same “inclusion criteria to monitor brain abnormalities and other adverse pregnancy outcomes.” As of Sept. 29 – the date of the last territorial report – there had been one liveborn infant and one pregnancy loss related to Zika. There were no new pregnancy losses with Zika-related birth defects in the states/D.C., so that number remains at five, while the total number of liveborn infants with Zika-related birth defects is now 32, the CDC reported.
Zika-related birth defects reported by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
The pregnancy-related figures for states, territories, and D.C. reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System.
There were 136 new cases of pregnant women with laboratory evidence of Zika infection reported during the 2-week period ending Nov. 30, along with four liveborn infants with Zika-related birth defects, according to the Centers for Disease Control and Prevention.
The CDC did not report new totals for pregnant women and pregnancy outcomes for the week ending Nov. 23, so the most recent data release covers the 2-week period from Nov. 17-30. That 2-week total was barely more than the 124 reported for the week ending Nov. 10.
The four infants born with Zika-related birth defects were all born in the 50 states and D.C., as the CDC is no longer reporting adverse pregnancy outcomes for the territories because Puerto Rico is not using the same “inclusion criteria to monitor brain abnormalities and other adverse pregnancy outcomes.” As of Sept. 29 – the date of the last territorial report – there had been one liveborn infant and one pregnancy loss related to Zika. There were no new pregnancy losses with Zika-related birth defects in the states/D.C., so that number remains at five, while the total number of liveborn infants with Zika-related birth defects is now 32, the CDC reported.
Zika-related birth defects reported by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
The pregnancy-related figures for states, territories, and D.C. reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System.
There were 136 new cases of pregnant women with laboratory evidence of Zika infection reported during the 2-week period ending Nov. 30, along with four liveborn infants with Zika-related birth defects, according to the Centers for Disease Control and Prevention.
The CDC did not report new totals for pregnant women and pregnancy outcomes for the week ending Nov. 23, so the most recent data release covers the 2-week period from Nov. 17-30. That 2-week total was barely more than the 124 reported for the week ending Nov. 10.
The four infants born with Zika-related birth defects were all born in the 50 states and D.C., as the CDC is no longer reporting adverse pregnancy outcomes for the territories because Puerto Rico is not using the same “inclusion criteria to monitor brain abnormalities and other adverse pregnancy outcomes.” As of Sept. 29 – the date of the last territorial report – there had been one liveborn infant and one pregnancy loss related to Zika. There were no new pregnancy losses with Zika-related birth defects in the states/D.C., so that number remains at five, while the total number of liveborn infants with Zika-related birth defects is now 32, the CDC reported.
Zika-related birth defects reported by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
The pregnancy-related figures for states, territories, and D.C. reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System.
VIDEO: No improvement in pCR with dual ER and HER2 inhibition
SAN ANTONIO – Breast cancers that are positive for the estrogen receptor (ER) and human epidermal growth factor receptor–2 (HER2) are less likely than ER-negative/HER2-positive tumors to respond to dual anti-HER2 therapy, suggesting that the estrogen receptor may act as a pathway of resistance to anti-HER2 treatment.
The National Surgical Adjuvant Breast and Bowel Project (NSABP) B-52 trial was designed to test the hypothesis that concurrent inhibition of both ER and HER2 added to chemotherapy with a platinum compound and a taxane will overcome resistance to treatment and improve pathologic complete response (pCR) rates in patients with ER-positive/HER2-positive breast cancer.
In a video interview at the San Antonio Breast Cancer Symposium, Mothaffar F. Rimawi, MD, discusses the trial results, which failed to show a significant difference in pCR rates between women who received chemotherapy with estrogen deprivation or chemotherapy alone. However, the trial still provided important information about the interplay between hormonal and HER2 receptors, and may inform future clinical trials examining reduction in tumor burden as a prognostic measure, says Dr. Rimawi from the Breast Center at Baylor College of Medicine, Houston.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN ANTONIO – Breast cancers that are positive for the estrogen receptor (ER) and human epidermal growth factor receptor–2 (HER2) are less likely than ER-negative/HER2-positive tumors to respond to dual anti-HER2 therapy, suggesting that the estrogen receptor may act as a pathway of resistance to anti-HER2 treatment.
The National Surgical Adjuvant Breast and Bowel Project (NSABP) B-52 trial was designed to test the hypothesis that concurrent inhibition of both ER and HER2 added to chemotherapy with a platinum compound and a taxane will overcome resistance to treatment and improve pathologic complete response (pCR) rates in patients with ER-positive/HER2-positive breast cancer.
In a video interview at the San Antonio Breast Cancer Symposium, Mothaffar F. Rimawi, MD, discusses the trial results, which failed to show a significant difference in pCR rates between women who received chemotherapy with estrogen deprivation or chemotherapy alone. However, the trial still provided important information about the interplay between hormonal and HER2 receptors, and may inform future clinical trials examining reduction in tumor burden as a prognostic measure, says Dr. Rimawi from the Breast Center at Baylor College of Medicine, Houston.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN ANTONIO – Breast cancers that are positive for the estrogen receptor (ER) and human epidermal growth factor receptor–2 (HER2) are less likely than ER-negative/HER2-positive tumors to respond to dual anti-HER2 therapy, suggesting that the estrogen receptor may act as a pathway of resistance to anti-HER2 treatment.
The National Surgical Adjuvant Breast and Bowel Project (NSABP) B-52 trial was designed to test the hypothesis that concurrent inhibition of both ER and HER2 added to chemotherapy with a platinum compound and a taxane will overcome resistance to treatment and improve pathologic complete response (pCR) rates in patients with ER-positive/HER2-positive breast cancer.
In a video interview at the San Antonio Breast Cancer Symposium, Mothaffar F. Rimawi, MD, discusses the trial results, which failed to show a significant difference in pCR rates between women who received chemotherapy with estrogen deprivation or chemotherapy alone. However, the trial still provided important information about the interplay between hormonal and HER2 receptors, and may inform future clinical trials examining reduction in tumor burden as a prognostic measure, says Dr. Rimawi from the Breast Center at Baylor College of Medicine, Houston.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SABCS 2016
VIDEO: Tips & Strategies for the Hospital Medicine Job Search
Dr. Thomas Frederickson, Dr. Benjamin Frizner, and Dr. Darlene Tad-y are all experienced at hiring and mentoring hospitalists at all career stages. They offer tips and strategies for assessing opportunity and negotiating your ideal HM job.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Thomas Frederickson, Dr. Benjamin Frizner, and Dr. Darlene Tad-y are all experienced at hiring and mentoring hospitalists at all career stages. They offer tips and strategies for assessing opportunity and negotiating your ideal HM job.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Thomas Frederickson, Dr. Benjamin Frizner, and Dr. Darlene Tad-y are all experienced at hiring and mentoring hospitalists at all career stages. They offer tips and strategies for assessing opportunity and negotiating your ideal HM job.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
1967 at a glance
• The Early and Periodic Screening, Diagnostic and Treatment (EPSDT) program was enacted as the child health component of Medicaid. Children under 21 years enrolled in Medicaid are entitled to EPSDT benefits, and states must cover a “broad array of preventive and treatment services.”
• By 1967, all states had laws requiring that physicians report child abuse.
• Field trials of experimental respiratory syncytial virus vaccines were performed but stalled. Currently, 65 RSV vaccines are being studied, and 13 are in phase III trials.
• The World Health Association declared a war on smallpox with a worldwide vaccination campaign. Twelve years later the disease was eradicated.
• The Public Health Service issued the second Surgeon General’s report on the health consequences of smoking.
• The first heart transplant was performed by Christian Barnard.
• The Early and Periodic Screening, Diagnostic and Treatment (EPSDT) program was enacted as the child health component of Medicaid. Children under 21 years enrolled in Medicaid are entitled to EPSDT benefits, and states must cover a “broad array of preventive and treatment services.”
• By 1967, all states had laws requiring that physicians report child abuse.
• Field trials of experimental respiratory syncytial virus vaccines were performed but stalled. Currently, 65 RSV vaccines are being studied, and 13 are in phase III trials.
• The World Health Association declared a war on smallpox with a worldwide vaccination campaign. Twelve years later the disease was eradicated.
• The Public Health Service issued the second Surgeon General’s report on the health consequences of smoking.
• The first heart transplant was performed by Christian Barnard.
• The Early and Periodic Screening, Diagnostic and Treatment (EPSDT) program was enacted as the child health component of Medicaid. Children under 21 years enrolled in Medicaid are entitled to EPSDT benefits, and states must cover a “broad array of preventive and treatment services.”
• By 1967, all states had laws requiring that physicians report child abuse.
• Field trials of experimental respiratory syncytial virus vaccines were performed but stalled. Currently, 65 RSV vaccines are being studied, and 13 are in phase III trials.
• The World Health Association declared a war on smallpox with a worldwide vaccination campaign. Twelve years later the disease was eradicated.
• The Public Health Service issued the second Surgeon General’s report on the health consequences of smoking.
• The first heart transplant was performed by Christian Barnard.
A look back at 1967
As Pediatric News celebrates 50 years of publication, we’re taking a look back at our first year: 1967.
A review of the 1967 issues of the journal Pediatrics offers a snapshot of the state of the science and some surprising similarities with pediatric medicine today.
A commentary in the November issue entitled “Pediatrics at a Crossroad” described an accelerating trend toward pediatric group practice and noted that full-time hospital employment of pediatricians was an emerging pattern of pediatric practice. The author, Richard Smith, MD, of the University of Florida, Gainesville, expressed concern about certain practices, such as the wide employment of antibiotics for uncomplicated respiratory infections and “routine use of gamma globulin in community hospital nurseries supposedly to treat sepsis or its regular injection in putatively allergic children.” He also was concerned about a quality gap in pediatric specialty education (Pediatrics. 1967 Nov;40[5]:783-7).
Articles of interest in the infectious disease area included an article demonstrating the response of infants to trivalent polio vaccine (Dec;40[6]:980-5); a new antibody test for rubella (Dec;40[5]:787-8, 789-97); and a live attenuated mumps vaccine (Dec;40[5]:798-803). And as we deal with emerging infectious diseases on a large scale, a fatal case of dengue hemorrhagic fever was reported in an American child (Dec;40[5]:804-7).
In a commentary, Starkey D. Davis, MD, and Ralph J. Wedgwood, MD, of the University of Washington, Seattle, said that the annual tuberculosis infection rate was low and falling, and that new cases were decreasing. Sufficient beds were available to isolate infectious cases, and effective chemotherapy made most cases noninfectious quickly. Isoniazid was cheap and effective, and it decreased complications of asymptomatic primary tuberculosis in children by 85%. “Pediatricians can expect to see tuberculosis in children become a medical curiosity in this country as infection rates continue to fall, if isoniazid prophylaxis is energetically used,” they predicted (Jun;39[6]:809-10).
D. Holdaway of the Royal Victoria Infirmary in Newcastle Upon Tyne, England, and associates reported on 211 children with acute bronchiolitis and 295 controls with nonrespiratory illness. Of the children with bronchiolitis, 59% had respiratory syncytial virus (RSV), compared with 1% of the controls, which confirmed the etiological significance of RSV in bronchiolitis, the researchers said. They also maintained that “oxygen is vitally important in bronchiolitis and there is little conclusive evidence that any other therapy is consistently or even occasionally useful” (Jun;39[6]:924-8).
In a commentary, Leon Eisenberg, MD, of the division of child psychiatry at the Johns Hopkins Hospital, Baltimore, called for more training in child development for pediatricians (May;39[5];645-7). Today, pediatricians are calling for more training in child psychiatry.
A report by the American Academy of Pediatrics Committee on Nutrition on obesity in childhood was prescient. They said, despite much research, that “our ignorance concerning the etiology, pathogenesis, and treatment is remarkable” (Sep;40[3]:455-67). The committee acknowledged that morbidity and mortality for diabetes and cardiovascular disease were higher in obese adults than in those of average weight, and that obese children tended to remain obese as adults. The committee also wrote that no treatments had achieved more than minor success of weight reduction. It suggested prevention of weight gain as the likely best approach, with initiation by the pediatrician in high-risk families – advice that still holds true today 50 years later.
Throughout 2017, Pediatric News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including changes in child psychiatry, pediatric dermatology, and infectious disease medicine, changes in residency training, and the transformation of the well-child visit. Look for these articles and more special features on the pages of Pediatric News and here online.
As Pediatric News celebrates 50 years of publication, we’re taking a look back at our first year: 1967.
A review of the 1967 issues of the journal Pediatrics offers a snapshot of the state of the science and some surprising similarities with pediatric medicine today.
A commentary in the November issue entitled “Pediatrics at a Crossroad” described an accelerating trend toward pediatric group practice and noted that full-time hospital employment of pediatricians was an emerging pattern of pediatric practice. The author, Richard Smith, MD, of the University of Florida, Gainesville, expressed concern about certain practices, such as the wide employment of antibiotics for uncomplicated respiratory infections and “routine use of gamma globulin in community hospital nurseries supposedly to treat sepsis or its regular injection in putatively allergic children.” He also was concerned about a quality gap in pediatric specialty education (Pediatrics. 1967 Nov;40[5]:783-7).
Articles of interest in the infectious disease area included an article demonstrating the response of infants to trivalent polio vaccine (Dec;40[6]:980-5); a new antibody test for rubella (Dec;40[5]:787-8, 789-97); and a live attenuated mumps vaccine (Dec;40[5]:798-803). And as we deal with emerging infectious diseases on a large scale, a fatal case of dengue hemorrhagic fever was reported in an American child (Dec;40[5]:804-7).
In a commentary, Starkey D. Davis, MD, and Ralph J. Wedgwood, MD, of the University of Washington, Seattle, said that the annual tuberculosis infection rate was low and falling, and that new cases were decreasing. Sufficient beds were available to isolate infectious cases, and effective chemotherapy made most cases noninfectious quickly. Isoniazid was cheap and effective, and it decreased complications of asymptomatic primary tuberculosis in children by 85%. “Pediatricians can expect to see tuberculosis in children become a medical curiosity in this country as infection rates continue to fall, if isoniazid prophylaxis is energetically used,” they predicted (Jun;39[6]:809-10).
D. Holdaway of the Royal Victoria Infirmary in Newcastle Upon Tyne, England, and associates reported on 211 children with acute bronchiolitis and 295 controls with nonrespiratory illness. Of the children with bronchiolitis, 59% had respiratory syncytial virus (RSV), compared with 1% of the controls, which confirmed the etiological significance of RSV in bronchiolitis, the researchers said. They also maintained that “oxygen is vitally important in bronchiolitis and there is little conclusive evidence that any other therapy is consistently or even occasionally useful” (Jun;39[6]:924-8).
In a commentary, Leon Eisenberg, MD, of the division of child psychiatry at the Johns Hopkins Hospital, Baltimore, called for more training in child development for pediatricians (May;39[5];645-7). Today, pediatricians are calling for more training in child psychiatry.
A report by the American Academy of Pediatrics Committee on Nutrition on obesity in childhood was prescient. They said, despite much research, that “our ignorance concerning the etiology, pathogenesis, and treatment is remarkable” (Sep;40[3]:455-67). The committee acknowledged that morbidity and mortality for diabetes and cardiovascular disease were higher in obese adults than in those of average weight, and that obese children tended to remain obese as adults. The committee also wrote that no treatments had achieved more than minor success of weight reduction. It suggested prevention of weight gain as the likely best approach, with initiation by the pediatrician in high-risk families – advice that still holds true today 50 years later.
Throughout 2017, Pediatric News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including changes in child psychiatry, pediatric dermatology, and infectious disease medicine, changes in residency training, and the transformation of the well-child visit. Look for these articles and more special features on the pages of Pediatric News and here online.
As Pediatric News celebrates 50 years of publication, we’re taking a look back at our first year: 1967.
A review of the 1967 issues of the journal Pediatrics offers a snapshot of the state of the science and some surprising similarities with pediatric medicine today.
A commentary in the November issue entitled “Pediatrics at a Crossroad” described an accelerating trend toward pediatric group practice and noted that full-time hospital employment of pediatricians was an emerging pattern of pediatric practice. The author, Richard Smith, MD, of the University of Florida, Gainesville, expressed concern about certain practices, such as the wide employment of antibiotics for uncomplicated respiratory infections and “routine use of gamma globulin in community hospital nurseries supposedly to treat sepsis or its regular injection in putatively allergic children.” He also was concerned about a quality gap in pediatric specialty education (Pediatrics. 1967 Nov;40[5]:783-7).
Articles of interest in the infectious disease area included an article demonstrating the response of infants to trivalent polio vaccine (Dec;40[6]:980-5); a new antibody test for rubella (Dec;40[5]:787-8, 789-97); and a live attenuated mumps vaccine (Dec;40[5]:798-803). And as we deal with emerging infectious diseases on a large scale, a fatal case of dengue hemorrhagic fever was reported in an American child (Dec;40[5]:804-7).
In a commentary, Starkey D. Davis, MD, and Ralph J. Wedgwood, MD, of the University of Washington, Seattle, said that the annual tuberculosis infection rate was low and falling, and that new cases were decreasing. Sufficient beds were available to isolate infectious cases, and effective chemotherapy made most cases noninfectious quickly. Isoniazid was cheap and effective, and it decreased complications of asymptomatic primary tuberculosis in children by 85%. “Pediatricians can expect to see tuberculosis in children become a medical curiosity in this country as infection rates continue to fall, if isoniazid prophylaxis is energetically used,” they predicted (Jun;39[6]:809-10).
D. Holdaway of the Royal Victoria Infirmary in Newcastle Upon Tyne, England, and associates reported on 211 children with acute bronchiolitis and 295 controls with nonrespiratory illness. Of the children with bronchiolitis, 59% had respiratory syncytial virus (RSV), compared with 1% of the controls, which confirmed the etiological significance of RSV in bronchiolitis, the researchers said. They also maintained that “oxygen is vitally important in bronchiolitis and there is little conclusive evidence that any other therapy is consistently or even occasionally useful” (Jun;39[6]:924-8).
In a commentary, Leon Eisenberg, MD, of the division of child psychiatry at the Johns Hopkins Hospital, Baltimore, called for more training in child development for pediatricians (May;39[5];645-7). Today, pediatricians are calling for more training in child psychiatry.
A report by the American Academy of Pediatrics Committee on Nutrition on obesity in childhood was prescient. They said, despite much research, that “our ignorance concerning the etiology, pathogenesis, and treatment is remarkable” (Sep;40[3]:455-67). The committee acknowledged that morbidity and mortality for diabetes and cardiovascular disease were higher in obese adults than in those of average weight, and that obese children tended to remain obese as adults. The committee also wrote that no treatments had achieved more than minor success of weight reduction. It suggested prevention of weight gain as the likely best approach, with initiation by the pediatrician in high-risk families – advice that still holds true today 50 years later.
Throughout 2017, Pediatric News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including changes in child psychiatry, pediatric dermatology, and infectious disease medicine, changes in residency training, and the transformation of the well-child visit. Look for these articles and more special features on the pages of Pediatric News and here online.
Addition of calcipotriene to 5-FU increases efficacy, tolerability as AK treatment
A combined formulation of calcipotriol and 5-fluorouracil (5-FU) outperformed 5-FU alone in reducing the number of actinic keratoses (AKs), with a shorter treatment course and less inflammation than typically seen with 5-FU alone, researchers reported in a study published online in November.
5-FU is effective, but it produces crusting and significant irritation, and is temporarily disfiguring, creating discomfort and inconvenience that often leads to poor patient compliance with treatment.
After demonstrating that the combined treatment reduces AKs in mice, they conducted the study of 131 patients with AKs, randomized to treatment with a cream containing 5% 5-FU and 0.005% calcipotriol, or Vaseline plus 5% 5-FU alone. Participants applied the treatments twice per day for 4 days.
Eight weeks after treatment, the combination group had a mean 87.8% reduction in the number of AKs on the face, compared with 26.3% of the 5-FU controls. The treatment group also had better responses on the scalp (a mean 76.4% reduction in AKs versus 5.7%), right upper extremity (68.8% versus 9.6%), and left upper extremity (79% versus 16.3%). All differences were statistically significant (P less than .0001 for all comparisons).
“The greater efficacy of calcipotriol plus 5-FU versus Vaseline plus 5-FU treatment in eliminating actinic keratoses remained highly significant after controlling for the baseline actinic keratosis count, age, and sex of the participants,” they wrote (J Clin Invest. 2016 Nov 21. pii: 89820. doi: 10.1172/JCI89820).
Significantly more of those in the combination group has skin redness during treatment, and 39% experienced a burning sensation on treated skin, compared with 13% of the 5-FU treated group. The rate of scaling and itching of treated skin during treatment was similar, and no patients had crusting or wounding of the treated skin.
“It was incredibly well tolerated. There wasn’t as much discomfort or crusting to where people had to stop. And patients who had used 5-FU in the past preferred this shorter treatment course as well as the type and amount of inflammation they had,” compared with their previous experience, Lynn Cornelius, MD, professor and chief of dermatology, Washington University, Saint Louis, said in an interview. “And it was more efficacious,” added Dr. Cornelius, who was one of the study authors.
The trial was investigator initiated. Two authors received grants from the American Skin Association, the Dermatology Foundation, the Burroughs Wellcome Fund, the American Philosophical Society, the La Roche-Posay Research Foundation, and the National Institutes of Health; three investigators were supported by an NIH grant. Dr. Cornelius reported having no financial disclosures.
A combined formulation of calcipotriol and 5-fluorouracil (5-FU) outperformed 5-FU alone in reducing the number of actinic keratoses (AKs), with a shorter treatment course and less inflammation than typically seen with 5-FU alone, researchers reported in a study published online in November.
5-FU is effective, but it produces crusting and significant irritation, and is temporarily disfiguring, creating discomfort and inconvenience that often leads to poor patient compliance with treatment.
After demonstrating that the combined treatment reduces AKs in mice, they conducted the study of 131 patients with AKs, randomized to treatment with a cream containing 5% 5-FU and 0.005% calcipotriol, or Vaseline plus 5% 5-FU alone. Participants applied the treatments twice per day for 4 days.
Eight weeks after treatment, the combination group had a mean 87.8% reduction in the number of AKs on the face, compared with 26.3% of the 5-FU controls. The treatment group also had better responses on the scalp (a mean 76.4% reduction in AKs versus 5.7%), right upper extremity (68.8% versus 9.6%), and left upper extremity (79% versus 16.3%). All differences were statistically significant (P less than .0001 for all comparisons).
“The greater efficacy of calcipotriol plus 5-FU versus Vaseline plus 5-FU treatment in eliminating actinic keratoses remained highly significant after controlling for the baseline actinic keratosis count, age, and sex of the participants,” they wrote (J Clin Invest. 2016 Nov 21. pii: 89820. doi: 10.1172/JCI89820).
Significantly more of those in the combination group has skin redness during treatment, and 39% experienced a burning sensation on treated skin, compared with 13% of the 5-FU treated group. The rate of scaling and itching of treated skin during treatment was similar, and no patients had crusting or wounding of the treated skin.
“It was incredibly well tolerated. There wasn’t as much discomfort or crusting to where people had to stop. And patients who had used 5-FU in the past preferred this shorter treatment course as well as the type and amount of inflammation they had,” compared with their previous experience, Lynn Cornelius, MD, professor and chief of dermatology, Washington University, Saint Louis, said in an interview. “And it was more efficacious,” added Dr. Cornelius, who was one of the study authors.
The trial was investigator initiated. Two authors received grants from the American Skin Association, the Dermatology Foundation, the Burroughs Wellcome Fund, the American Philosophical Society, the La Roche-Posay Research Foundation, and the National Institutes of Health; three investigators were supported by an NIH grant. Dr. Cornelius reported having no financial disclosures.
A combined formulation of calcipotriol and 5-fluorouracil (5-FU) outperformed 5-FU alone in reducing the number of actinic keratoses (AKs), with a shorter treatment course and less inflammation than typically seen with 5-FU alone, researchers reported in a study published online in November.
5-FU is effective, but it produces crusting and significant irritation, and is temporarily disfiguring, creating discomfort and inconvenience that often leads to poor patient compliance with treatment.
After demonstrating that the combined treatment reduces AKs in mice, they conducted the study of 131 patients with AKs, randomized to treatment with a cream containing 5% 5-FU and 0.005% calcipotriol, or Vaseline plus 5% 5-FU alone. Participants applied the treatments twice per day for 4 days.
Eight weeks after treatment, the combination group had a mean 87.8% reduction in the number of AKs on the face, compared with 26.3% of the 5-FU controls. The treatment group also had better responses on the scalp (a mean 76.4% reduction in AKs versus 5.7%), right upper extremity (68.8% versus 9.6%), and left upper extremity (79% versus 16.3%). All differences were statistically significant (P less than .0001 for all comparisons).
“The greater efficacy of calcipotriol plus 5-FU versus Vaseline plus 5-FU treatment in eliminating actinic keratoses remained highly significant after controlling for the baseline actinic keratosis count, age, and sex of the participants,” they wrote (J Clin Invest. 2016 Nov 21. pii: 89820. doi: 10.1172/JCI89820).
Significantly more of those in the combination group has skin redness during treatment, and 39% experienced a burning sensation on treated skin, compared with 13% of the 5-FU treated group. The rate of scaling and itching of treated skin during treatment was similar, and no patients had crusting or wounding of the treated skin.
“It was incredibly well tolerated. There wasn’t as much discomfort or crusting to where people had to stop. And patients who had used 5-FU in the past preferred this shorter treatment course as well as the type and amount of inflammation they had,” compared with their previous experience, Lynn Cornelius, MD, professor and chief of dermatology, Washington University, Saint Louis, said in an interview. “And it was more efficacious,” added Dr. Cornelius, who was one of the study authors.
The trial was investigator initiated. Two authors received grants from the American Skin Association, the Dermatology Foundation, the Burroughs Wellcome Fund, the American Philosophical Society, the La Roche-Posay Research Foundation, and the National Institutes of Health; three investigators were supported by an NIH grant. Dr. Cornelius reported having no financial disclosures.
FROM THE JOURNAL OF CLINICAL INVESTIGATION
Key clinical point:
Major finding: The combination cream reduced the number of AKs on the face by 87.8%, compared with 5-FU alone.
Data source: A randomized, placebo controlled trial of 131 subjects with AKs.
Disclosures: The trial was investigator initiated. Two authors received grants from the American Skin Association, the Dermatology Foundation, the Burroughs Wellcome Fund, the American Philosophical Society, the La Roche-Posay Research Foundation, and the National Institutes of Health; three investigators were supported by an NIH grant. Dr. Cornelius reported having no financial disclosures.
Make the Diagnosis - December 2016
Acute generalized exanthematous pustulosis (AGEP)
Acute generalized exanthematous pustulosis (AGEP) is a fairly rare condition, with a reported incidence of one to five cases per million people per year. AGEP affects both sexes, but with a slight female predominance. Although the median age of occurrence is 56 years, people of all ages can develop AGEP. In approximately 90% of cases, AGEP is caused by a drug reaction, with the most common culprits being antibiotics, diltiazem, and antimalarials.
Fever, leukocytosis with an elevated neutrophil count ( greater than 7,000/microL), and mild eosinophilia are commonly observed during the acute phase of AGEP. Systemic involvement is fairly uncommon, with a study of 58 cases exhibiting organ involvement in 17% of patients. When systemic involvement was observed, hepatic, pulmonary, and renal dysfunction were most common. Hepatic dysfunction can result in elevated transaminase levels in some patients. Similarly, reduced creatinine clearance may be observed because of renal involvement.

The management of AGEP involves removal of the offending agent. Antiseptic solutions and moist dressings may be used during the pustular phase to prevent infection. Emollients can aid in restoring skin barrier function during the desquamation phase. Antibiotics are not necessary prophylactically and should be avoided unless infection occurs. Pruritus and inflammation may be treated with topical corticosteroids in prolonged cases. Systemic corticosteroids are generally unwarranted as AGEP is a self-limited condition that is known to spontaneously resolve with the removal of the causative drug.
This case and photo were submitted by Natasha Cowan, BS, University of California, San Diego, and Brooke Resh Sateesh MD, San Diego Family Dermatology.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to dermnews@frontlinemedcom.com.
Acute generalized exanthematous pustulosis (AGEP)
Acute generalized exanthematous pustulosis (AGEP) is a fairly rare condition, with a reported incidence of one to five cases per million people per year. AGEP affects both sexes, but with a slight female predominance. Although the median age of occurrence is 56 years, people of all ages can develop AGEP. In approximately 90% of cases, AGEP is caused by a drug reaction, with the most common culprits being antibiotics, diltiazem, and antimalarials.
Fever, leukocytosis with an elevated neutrophil count ( greater than 7,000/microL), and mild eosinophilia are commonly observed during the acute phase of AGEP. Systemic involvement is fairly uncommon, with a study of 58 cases exhibiting organ involvement in 17% of patients. When systemic involvement was observed, hepatic, pulmonary, and renal dysfunction were most common. Hepatic dysfunction can result in elevated transaminase levels in some patients. Similarly, reduced creatinine clearance may be observed because of renal involvement.

The management of AGEP involves removal of the offending agent. Antiseptic solutions and moist dressings may be used during the pustular phase to prevent infection. Emollients can aid in restoring skin barrier function during the desquamation phase. Antibiotics are not necessary prophylactically and should be avoided unless infection occurs. Pruritus and inflammation may be treated with topical corticosteroids in prolonged cases. Systemic corticosteroids are generally unwarranted as AGEP is a self-limited condition that is known to spontaneously resolve with the removal of the causative drug.
This case and photo were submitted by Natasha Cowan, BS, University of California, San Diego, and Brooke Resh Sateesh MD, San Diego Family Dermatology.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to dermnews@frontlinemedcom.com.
Acute generalized exanthematous pustulosis (AGEP)
Acute generalized exanthematous pustulosis (AGEP) is a fairly rare condition, with a reported incidence of one to five cases per million people per year. AGEP affects both sexes, but with a slight female predominance. Although the median age of occurrence is 56 years, people of all ages can develop AGEP. In approximately 90% of cases, AGEP is caused by a drug reaction, with the most common culprits being antibiotics, diltiazem, and antimalarials.
Fever, leukocytosis with an elevated neutrophil count ( greater than 7,000/microL), and mild eosinophilia are commonly observed during the acute phase of AGEP. Systemic involvement is fairly uncommon, with a study of 58 cases exhibiting organ involvement in 17% of patients. When systemic involvement was observed, hepatic, pulmonary, and renal dysfunction were most common. Hepatic dysfunction can result in elevated transaminase levels in some patients. Similarly, reduced creatinine clearance may be observed because of renal involvement.

The management of AGEP involves removal of the offending agent. Antiseptic solutions and moist dressings may be used during the pustular phase to prevent infection. Emollients can aid in restoring skin barrier function during the desquamation phase. Antibiotics are not necessary prophylactically and should be avoided unless infection occurs. Pruritus and inflammation may be treated with topical corticosteroids in prolonged cases. Systemic corticosteroids are generally unwarranted as AGEP is a self-limited condition that is known to spontaneously resolve with the removal of the causative drug.
This case and photo were submitted by Natasha Cowan, BS, University of California, San Diego, and Brooke Resh Sateesh MD, San Diego Family Dermatology.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to dermnews@frontlinemedcom.com.
A 27 year old female presented with pustules on her upper extremities and bilateral antecubital fossa. She also had superficial desquamation with underlying erythema on her torso. Five days prior to presentation, she underwent rhinoplasty for a deviated nasal septum. She received cefazolin during the surgery. One day post surgery, she developed lesions on her arms that then spread to her chest and back. She was treated in the emergency room with prednisone, famotidine (Pepcid), and diphenhydramine (Benadryl). She returned to the emergency department 4 days later and was treated with vancomycin, piperacillin/tazobactam, and clindamycin for possible toxic shock syndrome. She was admitted to the hospital and dermatology was consulted. Her liver function tests and eosinophil count were normal.