User login
Medicare annual wellness visit remains underused
TORONTO – The annual Medicare wellness visit offers patients and their doctors the chance to review a variety of health concerns, and includes a cognitive health checkup. It’s free for patients and fully reimbursable for physicians. But the visit is far underused, averaging about 14% uptake each year across the United States, according to Pamela Mink, PhD.
Dr. Mink and her colleagues at Minneapolis, Minn.–based Allina Health examined which patients used the visit during 2011-2015 in the Allina Health system. They found annual increases in usage, but by the end of the 5-year period it had been used at least once by only 44% of eligible patients despite some considerable outreach efforts. Those who did were most often white or Asian women who lived in urban areas and were younger than 74 years.
“There’s a real opportunity for tracking and identifying cognitive health issues early here, and it’s being missed,” Dr. Mink said during a press briefing at the Alzheimer’s Association International Conference 2016. “Improving this situation is going to require leadership from health systems, the clinicians administering the visit, and the patients themselves. It’s basic education: Clinicians need to know it’s reimbursable. Patients need to know it’s free, and that it’s a valuable opportunity to address health issues – including any cognitive impairment that may be developing – early.”
Dr. Mink is employed by Allina Health as a senior scientist.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @alz_gal
TORONTO – The annual Medicare wellness visit offers patients and their doctors the chance to review a variety of health concerns, and includes a cognitive health checkup. It’s free for patients and fully reimbursable for physicians. But the visit is far underused, averaging about 14% uptake each year across the United States, according to Pamela Mink, PhD.
Dr. Mink and her colleagues at Minneapolis, Minn.–based Allina Health examined which patients used the visit during 2011-2015 in the Allina Health system. They found annual increases in usage, but by the end of the 5-year period it had been used at least once by only 44% of eligible patients despite some considerable outreach efforts. Those who did were most often white or Asian women who lived in urban areas and were younger than 74 years.
“There’s a real opportunity for tracking and identifying cognitive health issues early here, and it’s being missed,” Dr. Mink said during a press briefing at the Alzheimer’s Association International Conference 2016. “Improving this situation is going to require leadership from health systems, the clinicians administering the visit, and the patients themselves. It’s basic education: Clinicians need to know it’s reimbursable. Patients need to know it’s free, and that it’s a valuable opportunity to address health issues – including any cognitive impairment that may be developing – early.”
Dr. Mink is employed by Allina Health as a senior scientist.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @alz_gal
TORONTO – The annual Medicare wellness visit offers patients and their doctors the chance to review a variety of health concerns, and includes a cognitive health checkup. It’s free for patients and fully reimbursable for physicians. But the visit is far underused, averaging about 14% uptake each year across the United States, according to Pamela Mink, PhD.
Dr. Mink and her colleagues at Minneapolis, Minn.–based Allina Health examined which patients used the visit during 2011-2015 in the Allina Health system. They found annual increases in usage, but by the end of the 5-year period it had been used at least once by only 44% of eligible patients despite some considerable outreach efforts. Those who did were most often white or Asian women who lived in urban areas and were younger than 74 years.
“There’s a real opportunity for tracking and identifying cognitive health issues early here, and it’s being missed,” Dr. Mink said during a press briefing at the Alzheimer’s Association International Conference 2016. “Improving this situation is going to require leadership from health systems, the clinicians administering the visit, and the patients themselves. It’s basic education: Clinicians need to know it’s reimbursable. Patients need to know it’s free, and that it’s a valuable opportunity to address health issues – including any cognitive impairment that may be developing – early.”
Dr. Mink is employed by Allina Health as a senior scientist.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @alz_gal
AT AAIC 2016
Congenital craniofacial deformities
1. This youngster is being followed for symptoms related to his right-sided cranial asymmetry noted at birth, including neurologic impairment (sensorineural hearing loss and visual problems including strabismus) and breathing problems; developmental delay and/or intellectual disability; and hydrocephalus. The hands and feet are normal.
Source: By Michael L. Kaufman at the English language Wikipedia, CC BY-SA 3.0
Diagnosis: Craniosynostosis, also known as acrocephalosyndactyly, is a condition in which the skull sutures close prematurely. This can cause pressure to build up inside the head and skull or facial bones, leading to a misshapen head and distinctive facial features—ocular hypertelorism, proptosis, midface hypoplasia, small beaked nose, and prognathism—and occasionally abnormal fingers and toes.
Mutations of the FGFR gene, which regulates the fibroblast growth factor receptor protein, are responsible for the eight disorders comprising the FGFR-related craniosynostosis spectrum. The protein plays an important role in bone growth, particularly during embryonic development. For example, this protein signals certain immature cells in the developing embryo to become bone cells in the head, hands, feet, and other tissues.
For more information, see Robin NH, MD, Falk MJ, Haldeman-Englert CR. FGFR-related craniosynostosis syndromes. In: GeneReviews® [Internet]. Pagon RA, Adam MP, Ardinger HH, et al, eds. Seattle: University of Washington, Seattle; 1993-2016.
For the next photograph, proceed to the next page >>
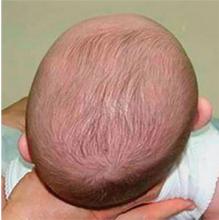
2. This infant presents with a misshapen cranium, most notably the flattened area on the posterior right side. His history includes limited passive neck rotation at birth, preferential head orientation, supine sleep position, and lower activity level.
Source: Wikimedia Commons; By Medical advises - http://larece.ru/?p=27115, CC BY-SA 3.0
Diagnosis: Plagiocephaly, literally means "oblique head" (from the Greek "plagio" for oblique and "cephale" for head). The incidence in infants at 7 to 12 weeks of age is estimated to be 46.6%. Of all infants with plagiocephaly, 63.2% are affected on the right side and 78.3% have a mild form.
For more information, see “Helmets for Positional Skull Deformities: A Good Idea or Not?” Clin Rev. 2015;25(2):16,18.
For the next photograph, proceed to the next page >>
3. An adolescent patient presents with marked facial asymmetry, present since birth. The auricular tissue on the left side is malformed; on the right side, low set. The right midface is underdeveloped with micrognathia and chin deviation, resulting in malocclusion.
Source: Wikimedia Commons
Diagnosis: Craniofacial microsomia, possibly caused by bleeding in the temporal area during gestation, describes a spectrum of cranial and facial abnormalities. After Down syndrome, it is the most common congenital syndrome, occurring in approximately 1 in 3,500 to 4,500 live births. In about two-thirds of cases, abnormalities differ from one side to the other.
These individuals typically demonstrate one-sided maxillary or mandibular hypoplasia, which can cause dental problems and difficulties with feeding and speech. In cases of severe mandibular hypoplasia, breathing may also be affected.
Abnormalities affecting one or both ears may range from preauricular tags to an underdeveloped or absent external ear or a closed or absent ear canal; these patients may experience hearing loss. Microphthalmia, occurring less frequently, may result in vision loss.
For more information, see Heike CL, Luquetti DV, Hing AV. Craniofacial microsomia overview. In: Pagon RA, Adam MP, Ardinger HH, et al, eds. GeneReviews® [Internet]. Seattle: University of Washington, Seattle; 1993-2016.
For the next photograph, proceed to the next page >>
4. A 4-month-old boy is brought in by his mother for evaluation of a “birthmark” on his forehead that has become more prominent with time. The child complains a bit when the lesion is touched.
His mother gives a history of a normal full-term pregnancy with an uneventful delivery. Other than the skin lesion, there have been no other known problems with the child’s health.
Diagnosis: Most first-year medical students could tell you this was a case of an infantile hemangioma—but within the past five years, the categorization and treatment of hemangiomas have changed rapidly.
Hemangiomas are benign and usually self-involuting vascular tumors. They are distinct from the family of permanent congenital vascular lesions, such as port wine stains. About 80% occur on the face or neck and more commonly in females. Those that occur near the skin’s surface tend to be bright red, while those of deeper origin are more bluish. Hemangiomas can also manifest in extracutaneous areas (eg, the liver); these are usually detected via imaging.
For more information, see “A New Approach to “Birthmarks” Clin Rev. 2016;26(3):W1.
RELATED ARTICLE:
Infantile Hemangiomas Increasing, Linked to Prematurity, Low Birth Weight Bruce Jancin, Family Practice News Digital Network
1. This youngster is being followed for symptoms related to his right-sided cranial asymmetry noted at birth, including neurologic impairment (sensorineural hearing loss and visual problems including strabismus) and breathing problems; developmental delay and/or intellectual disability; and hydrocephalus. The hands and feet are normal.
Source: By Michael L. Kaufman at the English language Wikipedia, CC BY-SA 3.0
Diagnosis: Craniosynostosis, also known as acrocephalosyndactyly, is a condition in which the skull sutures close prematurely. This can cause pressure to build up inside the head and skull or facial bones, leading to a misshapen head and distinctive facial features—ocular hypertelorism, proptosis, midface hypoplasia, small beaked nose, and prognathism—and occasionally abnormal fingers and toes.
Mutations of the FGFR gene, which regulates the fibroblast growth factor receptor protein, are responsible for the eight disorders comprising the FGFR-related craniosynostosis spectrum. The protein plays an important role in bone growth, particularly during embryonic development. For example, this protein signals certain immature cells in the developing embryo to become bone cells in the head, hands, feet, and other tissues.
For more information, see Robin NH, MD, Falk MJ, Haldeman-Englert CR. FGFR-related craniosynostosis syndromes. In: GeneReviews® [Internet]. Pagon RA, Adam MP, Ardinger HH, et al, eds. Seattle: University of Washington, Seattle; 1993-2016.
For the next photograph, proceed to the next page >>
2. This infant presents with a misshapen cranium, most notably the flattened area on the posterior right side. His history includes limited passive neck rotation at birth, preferential head orientation, supine sleep position, and lower activity level.
Source: Wikimedia Commons; By Medical advises - http://larece.ru/?p=27115, CC BY-SA 3.0
Diagnosis: Plagiocephaly, literally means "oblique head" (from the Greek "plagio" for oblique and "cephale" for head). The incidence in infants at 7 to 12 weeks of age is estimated to be 46.6%. Of all infants with plagiocephaly, 63.2% are affected on the right side and 78.3% have a mild form.
For more information, see “Helmets for Positional Skull Deformities: A Good Idea or Not?” Clin Rev. 2015;25(2):16,18.
For the next photograph, proceed to the next page >>
3. An adolescent patient presents with marked facial asymmetry, present since birth. The auricular tissue on the left side is malformed; on the right side, low set. The right midface is underdeveloped with micrognathia and chin deviation, resulting in malocclusion.
Source: Wikimedia Commons
Diagnosis: Craniofacial microsomia, possibly caused by bleeding in the temporal area during gestation, describes a spectrum of cranial and facial abnormalities. After Down syndrome, it is the most common congenital syndrome, occurring in approximately 1 in 3,500 to 4,500 live births. In about two-thirds of cases, abnormalities differ from one side to the other.
These individuals typically demonstrate one-sided maxillary or mandibular hypoplasia, which can cause dental problems and difficulties with feeding and speech. In cases of severe mandibular hypoplasia, breathing may also be affected.
Abnormalities affecting one or both ears may range from preauricular tags to an underdeveloped or absent external ear or a closed or absent ear canal; these patients may experience hearing loss. Microphthalmia, occurring less frequently, may result in vision loss.
For more information, see Heike CL, Luquetti DV, Hing AV. Craniofacial microsomia overview. In: Pagon RA, Adam MP, Ardinger HH, et al, eds. GeneReviews® [Internet]. Seattle: University of Washington, Seattle; 1993-2016.
For the next photograph, proceed to the next page >>
4. A 4-month-old boy is brought in by his mother for evaluation of a “birthmark” on his forehead that has become more prominent with time. The child complains a bit when the lesion is touched.
His mother gives a history of a normal full-term pregnancy with an uneventful delivery. Other than the skin lesion, there have been no other known problems with the child’s health.
Diagnosis: Most first-year medical students could tell you this was a case of an infantile hemangioma—but within the past five years, the categorization and treatment of hemangiomas have changed rapidly.
Hemangiomas are benign and usually self-involuting vascular tumors. They are distinct from the family of permanent congenital vascular lesions, such as port wine stains. About 80% occur on the face or neck and more commonly in females. Those that occur near the skin’s surface tend to be bright red, while those of deeper origin are more bluish. Hemangiomas can also manifest in extracutaneous areas (eg, the liver); these are usually detected via imaging.
For more information, see “A New Approach to “Birthmarks” Clin Rev. 2016;26(3):W1.
RELATED ARTICLE:
Infantile Hemangiomas Increasing, Linked to Prematurity, Low Birth Weight Bruce Jancin, Family Practice News Digital Network
1. This youngster is being followed for symptoms related to his right-sided cranial asymmetry noted at birth, including neurologic impairment (sensorineural hearing loss and visual problems including strabismus) and breathing problems; developmental delay and/or intellectual disability; and hydrocephalus. The hands and feet are normal.
Source: By Michael L. Kaufman at the English language Wikipedia, CC BY-SA 3.0
Diagnosis: Craniosynostosis, also known as acrocephalosyndactyly, is a condition in which the skull sutures close prematurely. This can cause pressure to build up inside the head and skull or facial bones, leading to a misshapen head and distinctive facial features—ocular hypertelorism, proptosis, midface hypoplasia, small beaked nose, and prognathism—and occasionally abnormal fingers and toes.
Mutations of the FGFR gene, which regulates the fibroblast growth factor receptor protein, are responsible for the eight disorders comprising the FGFR-related craniosynostosis spectrum. The protein plays an important role in bone growth, particularly during embryonic development. For example, this protein signals certain immature cells in the developing embryo to become bone cells in the head, hands, feet, and other tissues.
For more information, see Robin NH, MD, Falk MJ, Haldeman-Englert CR. FGFR-related craniosynostosis syndromes. In: GeneReviews® [Internet]. Pagon RA, Adam MP, Ardinger HH, et al, eds. Seattle: University of Washington, Seattle; 1993-2016.
For the next photograph, proceed to the next page >>
2. This infant presents with a misshapen cranium, most notably the flattened area on the posterior right side. His history includes limited passive neck rotation at birth, preferential head orientation, supine sleep position, and lower activity level.
Source: Wikimedia Commons; By Medical advises - http://larece.ru/?p=27115, CC BY-SA 3.0
Diagnosis: Plagiocephaly, literally means "oblique head" (from the Greek "plagio" for oblique and "cephale" for head). The incidence in infants at 7 to 12 weeks of age is estimated to be 46.6%. Of all infants with plagiocephaly, 63.2% are affected on the right side and 78.3% have a mild form.
For more information, see “Helmets for Positional Skull Deformities: A Good Idea or Not?” Clin Rev. 2015;25(2):16,18.
For the next photograph, proceed to the next page >>
3. An adolescent patient presents with marked facial asymmetry, present since birth. The auricular tissue on the left side is malformed; on the right side, low set. The right midface is underdeveloped with micrognathia and chin deviation, resulting in malocclusion.
Source: Wikimedia Commons
Diagnosis: Craniofacial microsomia, possibly caused by bleeding in the temporal area during gestation, describes a spectrum of cranial and facial abnormalities. After Down syndrome, it is the most common congenital syndrome, occurring in approximately 1 in 3,500 to 4,500 live births. In about two-thirds of cases, abnormalities differ from one side to the other.
These individuals typically demonstrate one-sided maxillary or mandibular hypoplasia, which can cause dental problems and difficulties with feeding and speech. In cases of severe mandibular hypoplasia, breathing may also be affected.
Abnormalities affecting one or both ears may range from preauricular tags to an underdeveloped or absent external ear or a closed or absent ear canal; these patients may experience hearing loss. Microphthalmia, occurring less frequently, may result in vision loss.
For more information, see Heike CL, Luquetti DV, Hing AV. Craniofacial microsomia overview. In: Pagon RA, Adam MP, Ardinger HH, et al, eds. GeneReviews® [Internet]. Seattle: University of Washington, Seattle; 1993-2016.
For the next photograph, proceed to the next page >>
4. A 4-month-old boy is brought in by his mother for evaluation of a “birthmark” on his forehead that has become more prominent with time. The child complains a bit when the lesion is touched.
His mother gives a history of a normal full-term pregnancy with an uneventful delivery. Other than the skin lesion, there have been no other known problems with the child’s health.
Diagnosis: Most first-year medical students could tell you this was a case of an infantile hemangioma—but within the past five years, the categorization and treatment of hemangiomas have changed rapidly.
Hemangiomas are benign and usually self-involuting vascular tumors. They are distinct from the family of permanent congenital vascular lesions, such as port wine stains. About 80% occur on the face or neck and more commonly in females. Those that occur near the skin’s surface tend to be bright red, while those of deeper origin are more bluish. Hemangiomas can also manifest in extracutaneous areas (eg, the liver); these are usually detected via imaging.
For more information, see “A New Approach to “Birthmarks” Clin Rev. 2016;26(3):W1.
RELATED ARTICLE:
Infantile Hemangiomas Increasing, Linked to Prematurity, Low Birth Weight Bruce Jancin, Family Practice News Digital Network
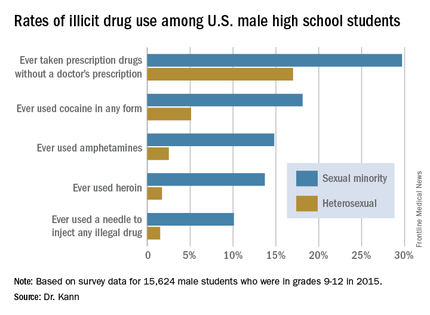
Gay and Bisexual Male High Schoolers Have High Injected Drug Use
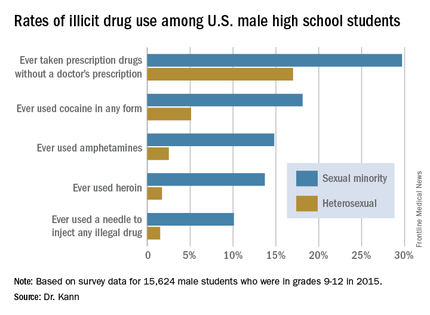
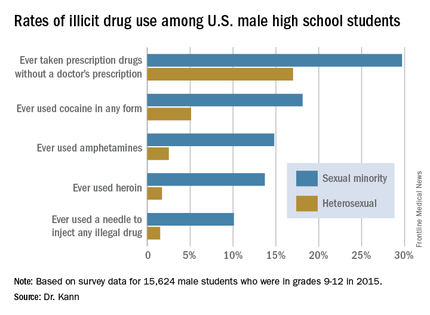
DURBAN, SOUTH AFRICA – The first-ever nationally representative survey on sexual identity and behaviors in U.S. male high school students has exposed a high prevalence of illicit injected drug use among those who have sex with males or with both males and females.
About 10% of high school boys who identify as gay or bisexual reported having ever used a needle to inject any illegal drug into their bodies, compared with 1.5% of high school boys who identify as heterosexual.
“This is a cause for great concern because of the efficiency with which injected drug use transmits not only HIV but hepatitis and other diseases,” Laura Kann, PhD, said in reporting the results of the 2015 National Youth Risk Behavior Survey (YRBS) at the 21st International AIDS Conference.
Dr. Kann of the Centers for Disease Control and Prevention’s division of adolescent and school health directs the YRBS, an annual, multiple-choice, anonymous voluntary survey that addresses six areas of risk: behaviors that contribute to unintentional injuries and violence, tobacco use, alcohol and other drug use, sexual behaviors, inadequate physical activity, and unhealthy diet behaviors.
The 2015 survey was the first ever to include questions regarding sexual identity and behaviors.
“Twenty-two percent of all new HIV diagnoses in the U.S. occur in 13- to 24-year-olds. Most occur in males who have sex with males. This makes young males an important focus for HIV prevention efforts,” Dr. Kann said.
Yet until the 2015 YRBS, no reliable estimates existed regarding the number of gay or bisexual male high school students. “Reducing HIV infection among young sexual minority males is key to reducing HIV infection in the U.S.,” she said. “It’s hard to respond appropriately to a population that has not been counted.”
The 15,624 male students in public and private school grades 9-12 who participated in the YRBS were demographically representative of the nation’s roughly 8 million male high schoolers.
About 2% of male students identified themselves as gay, another 2.4% declared themselves bisexual, 93.1% said they were heterosexual, and 2.6% were unsure. With regard to sexual behaviors, 53.3% of respondents indicated they had sexual contact with females only, 1.3% with males only, and 1.9% with both males and females; 43.6% reported they hadn’t ever had sexual contact. Respondents could interpret “sexual contact” as they wished, ranging from kissing and hugging to intercourse.
Large differences in illicit drug use behaviors were found between the sexual minorities – that is, males who had sexual contact with males or with females as well as males – and those with only heterosexual contacts.
“We need to conduct new research on injected drug use among young males who have sex with males and determine what can be done to minimize, if not eliminate, this very high-risk behavior that is occurring at alarming rates,” Dr. Kann said.
The sexual minority students were also more likely to have engaged in various forms of noninjected illicit drug use known to boost the risk of HIV infection indirectly by increasing the likelihood of having unsafe sex. The sexual minority males had significantly higher rates of having ever used cocaine in any form, of having ever used amphetamines, and of having taken prescription drugs without a physician’s prescription. For instance, 14.8% of sexual minority males reported ever using amphetamines, compared with 2.5% of heterosexual males surveyed.
She noted that the YRBS results provided no evidence that the disparity in HIV diagnoses between young males who have sex with males and young males who have sex with females are caused by differences in the prevalence of HIV-related sexual behaviors. There were no statistically significant differences between heterosexual and sexual minority students in rates of ever having had sexual intercourse, having had intercourse with four or more persons, having sexual activity currently, or having used a condom at last intercourse.
Dr. Kann called for more research in the neglected area of social issues affecting young sexual minority males that likely increase their sense of marginalization and may promote behaviors placing them at increased risk for HIV acquisition.
“Many young males who have sex with males suffer from social isolation, stress from self-concealment and from coming out, discrimination, and even hatred, which may occur at home, at school, and in communities among both their peers and the adults responsible for their care and protection,” she said. “These factors may lead to harmful coping behaviors, such as drug use, that can further increase risk for HIV infection. It’s hard to imagine how even the best intervention technology will be able to eliminate the disparities in HIV diagnosis unless these social issues are addressed first and foremost.”
One clinician from New York rose from the audience to chastise the CDC for taking decades to incorporate questions about sexual minority youth into the YRBS.
“It’s important for the rest of the world to know how long it took the U.S. to collect this data. It’s not right. For those of you in the rest of the world who struggle to get information about your youth, don’t think that America is way ahead of you because it took us a long time,” she said.
Dr. Kann noted that such data have been collected for some time by some state and city public health agencies. As local officials began clamoring for a more comprehensive national picture, “it reached a tipping point” at the CDC.
Dr. Kann reported having no relevant financial conflicts.
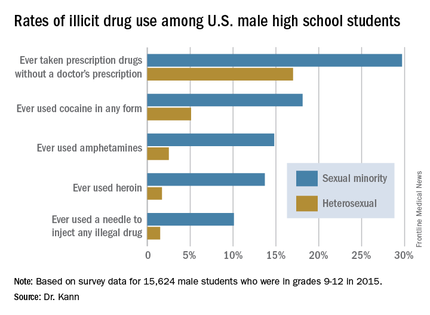
DURBAN, SOUTH AFRICA – The first-ever nationally representative survey on sexual identity and behaviors in U.S. male high school students has exposed a high prevalence of illicit injected drug use among those who have sex with males or with both males and females.
About 10% of high school boys who identify as gay or bisexual reported having ever used a needle to inject any illegal drug into their bodies, compared with 1.5% of high school boys who identify as heterosexual.
“This is a cause for great concern because of the efficiency with which injected drug use transmits not only HIV but hepatitis and other diseases,” Laura Kann, PhD, said in reporting the results of the 2015 National Youth Risk Behavior Survey (YRBS) at the 21st International AIDS Conference.
Dr. Kann of the Centers for Disease Control and Prevention’s division of adolescent and school health directs the YRBS, an annual, multiple-choice, anonymous voluntary survey that addresses six areas of risk: behaviors that contribute to unintentional injuries and violence, tobacco use, alcohol and other drug use, sexual behaviors, inadequate physical activity, and unhealthy diet behaviors.
The 2015 survey was the first ever to include questions regarding sexual identity and behaviors.
“Twenty-two percent of all new HIV diagnoses in the U.S. occur in 13- to 24-year-olds. Most occur in males who have sex with males. This makes young males an important focus for HIV prevention efforts,” Dr. Kann said.
Yet until the 2015 YRBS, no reliable estimates existed regarding the number of gay or bisexual male high school students. “Reducing HIV infection among young sexual minority males is key to reducing HIV infection in the U.S.,” she said. “It’s hard to respond appropriately to a population that has not been counted.”
The 15,624 male students in public and private school grades 9-12 who participated in the YRBS were demographically representative of the nation’s roughly 8 million male high schoolers.
About 2% of male students identified themselves as gay, another 2.4% declared themselves bisexual, 93.1% said they were heterosexual, and 2.6% were unsure. With regard to sexual behaviors, 53.3% of respondents indicated they had sexual contact with females only, 1.3% with males only, and 1.9% with both males and females; 43.6% reported they hadn’t ever had sexual contact. Respondents could interpret “sexual contact” as they wished, ranging from kissing and hugging to intercourse.
Large differences in illicit drug use behaviors were found between the sexual minorities – that is, males who had sexual contact with males or with females as well as males – and those with only heterosexual contacts.
“We need to conduct new research on injected drug use among young males who have sex with males and determine what can be done to minimize, if not eliminate, this very high-risk behavior that is occurring at alarming rates,” Dr. Kann said.
The sexual minority students were also more likely to have engaged in various forms of noninjected illicit drug use known to boost the risk of HIV infection indirectly by increasing the likelihood of having unsafe sex. The sexual minority males had significantly higher rates of having ever used cocaine in any form, of having ever used amphetamines, and of having taken prescription drugs without a physician’s prescription. For instance, 14.8% of sexual minority males reported ever using amphetamines, compared with 2.5% of heterosexual males surveyed.
She noted that the YRBS results provided no evidence that the disparity in HIV diagnoses between young males who have sex with males and young males who have sex with females are caused by differences in the prevalence of HIV-related sexual behaviors. There were no statistically significant differences between heterosexual and sexual minority students in rates of ever having had sexual intercourse, having had intercourse with four or more persons, having sexual activity currently, or having used a condom at last intercourse.
Dr. Kann called for more research in the neglected area of social issues affecting young sexual minority males that likely increase their sense of marginalization and may promote behaviors placing them at increased risk for HIV acquisition.
“Many young males who have sex with males suffer from social isolation, stress from self-concealment and from coming out, discrimination, and even hatred, which may occur at home, at school, and in communities among both their peers and the adults responsible for their care and protection,” she said. “These factors may lead to harmful coping behaviors, such as drug use, that can further increase risk for HIV infection. It’s hard to imagine how even the best intervention technology will be able to eliminate the disparities in HIV diagnosis unless these social issues are addressed first and foremost.”
One clinician from New York rose from the audience to chastise the CDC for taking decades to incorporate questions about sexual minority youth into the YRBS.
“It’s important for the rest of the world to know how long it took the U.S. to collect this data. It’s not right. For those of you in the rest of the world who struggle to get information about your youth, don’t think that America is way ahead of you because it took us a long time,” she said.
Dr. Kann noted that such data have been collected for some time by some state and city public health agencies. As local officials began clamoring for a more comprehensive national picture, “it reached a tipping point” at the CDC.
Dr. Kann reported having no relevant financial conflicts.
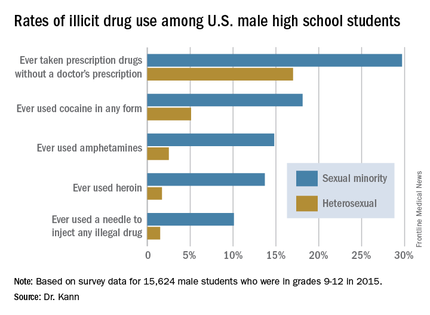
DURBAN, SOUTH AFRICA – The first-ever nationally representative survey on sexual identity and behaviors in U.S. male high school students has exposed a high prevalence of illicit injected drug use among those who have sex with males or with both males and females.
About 10% of high school boys who identify as gay or bisexual reported having ever used a needle to inject any illegal drug into their bodies, compared with 1.5% of high school boys who identify as heterosexual.
“This is a cause for great concern because of the efficiency with which injected drug use transmits not only HIV but hepatitis and other diseases,” Laura Kann, PhD, said in reporting the results of the 2015 National Youth Risk Behavior Survey (YRBS) at the 21st International AIDS Conference.
Dr. Kann of the Centers for Disease Control and Prevention’s division of adolescent and school health directs the YRBS, an annual, multiple-choice, anonymous voluntary survey that addresses six areas of risk: behaviors that contribute to unintentional injuries and violence, tobacco use, alcohol and other drug use, sexual behaviors, inadequate physical activity, and unhealthy diet behaviors.
The 2015 survey was the first ever to include questions regarding sexual identity and behaviors.
“Twenty-two percent of all new HIV diagnoses in the U.S. occur in 13- to 24-year-olds. Most occur in males who have sex with males. This makes young males an important focus for HIV prevention efforts,” Dr. Kann said.
Yet until the 2015 YRBS, no reliable estimates existed regarding the number of gay or bisexual male high school students. “Reducing HIV infection among young sexual minority males is key to reducing HIV infection in the U.S.,” she said. “It’s hard to respond appropriately to a population that has not been counted.”
The 15,624 male students in public and private school grades 9-12 who participated in the YRBS were demographically representative of the nation’s roughly 8 million male high schoolers.
About 2% of male students identified themselves as gay, another 2.4% declared themselves bisexual, 93.1% said they were heterosexual, and 2.6% were unsure. With regard to sexual behaviors, 53.3% of respondents indicated they had sexual contact with females only, 1.3% with males only, and 1.9% with both males and females; 43.6% reported they hadn’t ever had sexual contact. Respondents could interpret “sexual contact” as they wished, ranging from kissing and hugging to intercourse.
Large differences in illicit drug use behaviors were found between the sexual minorities – that is, males who had sexual contact with males or with females as well as males – and those with only heterosexual contacts.
“We need to conduct new research on injected drug use among young males who have sex with males and determine what can be done to minimize, if not eliminate, this very high-risk behavior that is occurring at alarming rates,” Dr. Kann said.
The sexual minority students were also more likely to have engaged in various forms of noninjected illicit drug use known to boost the risk of HIV infection indirectly by increasing the likelihood of having unsafe sex. The sexual minority males had significantly higher rates of having ever used cocaine in any form, of having ever used amphetamines, and of having taken prescription drugs without a physician’s prescription. For instance, 14.8% of sexual minority males reported ever using amphetamines, compared with 2.5% of heterosexual males surveyed.
She noted that the YRBS results provided no evidence that the disparity in HIV diagnoses between young males who have sex with males and young males who have sex with females are caused by differences in the prevalence of HIV-related sexual behaviors. There were no statistically significant differences between heterosexual and sexual minority students in rates of ever having had sexual intercourse, having had intercourse with four or more persons, having sexual activity currently, or having used a condom at last intercourse.
Dr. Kann called for more research in the neglected area of social issues affecting young sexual minority males that likely increase their sense of marginalization and may promote behaviors placing them at increased risk for HIV acquisition.
“Many young males who have sex with males suffer from social isolation, stress from self-concealment and from coming out, discrimination, and even hatred, which may occur at home, at school, and in communities among both their peers and the adults responsible for their care and protection,” she said. “These factors may lead to harmful coping behaviors, such as drug use, that can further increase risk for HIV infection. It’s hard to imagine how even the best intervention technology will be able to eliminate the disparities in HIV diagnosis unless these social issues are addressed first and foremost.”
One clinician from New York rose from the audience to chastise the CDC for taking decades to incorporate questions about sexual minority youth into the YRBS.
“It’s important for the rest of the world to know how long it took the U.S. to collect this data. It’s not right. For those of you in the rest of the world who struggle to get information about your youth, don’t think that America is way ahead of you because it took us a long time,” she said.
Dr. Kann noted that such data have been collected for some time by some state and city public health agencies. As local officials began clamoring for a more comprehensive national picture, “it reached a tipping point” at the CDC.
Dr. Kann reported having no relevant financial conflicts.
AT AIDS 2016
Gay and bisexual male high schoolers have high injected drug use
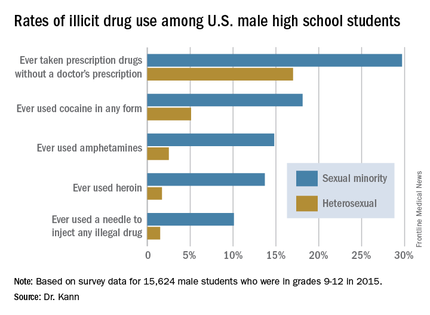
DURBAN, SOUTH AFRICA – The first-ever nationally representative survey on sexual identity and behaviors in U.S. male high school students has exposed a high prevalence of illicit injected drug use among those who have sex with males or with both males and females.
About 10% of high school boys who identify as gay or bisexual reported having ever used a needle to inject any illegal drug into their bodies, compared with 1.5% of high school boys who identify as heterosexual.
“This is a cause for great concern because of the efficiency with which injected drug use transmits not only HIV but hepatitis and other diseases,” Laura Kann, PhD, said in reporting the results of the 2015 National Youth Risk Behavior Survey (YRBS) at the 21st International AIDS Conference.
Dr. Kann of the Centers for Disease Control and Prevention’s division of adolescent and school health directs the YRBS, an annual, multiple-choice, anonymous voluntary survey that addresses six areas of risk: behaviors that contribute to unintentional injuries and violence, tobacco use, alcohol and other drug use, sexual behaviors, inadequate physical activity, and unhealthy diet behaviors.
The 2015 survey was the first ever to include questions regarding sexual identity and behaviors.
“Twenty-two percent of all new HIV diagnoses in the U.S. occur in 13- to 24-year-olds. Most occur in males who have sex with males. This makes young males an important focus for HIV prevention efforts,” Dr. Kann said.
Yet until the 2015 YRBS, no reliable estimates existed regarding the number of gay or bisexual male high school students. “Reducing HIV infection among young sexual minority males is key to reducing HIV infection in the U.S.,” she said. “It’s hard to respond appropriately to a population that has not been counted.”
The 15,624 male students in public and private school grades 9-12 who participated in the YRBS were demographically representative of the nation’s roughly 8 million male high schoolers.
About 2% of male students identified themselves as gay, another 2.4% declared themselves bisexual, 93.1% said they were heterosexual, and 2.6% were unsure. With regard to sexual behaviors, 53.3% of respondents indicated they had sexual contact with females only, 1.3% with males only, and 1.9% with both males and females; 43.6% reported they hadn’t ever had sexual contact. Respondents could interpret “sexual contact” as they wished, ranging from kissing and hugging to intercourse.
Large differences in illicit drug use behaviors were found between the sexual minorities – that is, males who had sexual contact with males or with females as well as males – and those with only heterosexual contacts.
“We need to conduct new research on injected drug use among young males who have sex with males and determine what can be done to minimize, if not eliminate, this very high-risk behavior that is occurring at alarming rates,” Dr. Kann said.
The sexual minority students were also more likely to have engaged in various forms of noninjected illicit drug use known to boost the risk of HIV infection indirectly by increasing the likelihood of having unsafe sex. The sexual minority males had significantly higher rates of having ever used cocaine in any form, of having ever used amphetamines, and of having taken prescription drugs without a physician’s prescription. For instance, 14.8% of sexual minority males reported ever using amphetamines, compared with 2.5% of heterosexual males surveyed.
She noted that the YRBS results provided no evidence that the disparity in HIV diagnoses between young males who have sex with males and young males who have sex with females are caused by differences in the prevalence of HIV-related sexual behaviors. There were no statistically significant differences between heterosexual and sexual minority students in rates of ever having had sexual intercourse, having had intercourse with four or more persons, having sexual activity currently, or having used a condom at last intercourse.
Dr. Kann called for more research in the neglected area of social issues affecting young sexual minority males that likely increase their sense of marginalization and may promote behaviors placing them at increased risk for HIV acquisition.
“Many young males who have sex with males suffer from social isolation, stress from self-concealment and from coming out, discrimination, and even hatred, which may occur at home, at school, and in communities among both their peers and the adults responsible for their care and protection,” she said. “These factors may lead to harmful coping behaviors, such as drug use, that can further increase risk for HIV infection. It’s hard to imagine how even the best intervention technology will be able to eliminate the disparities in HIV diagnosis unless these social issues are addressed first and foremost.”
One clinician from New York rose from the audience to chastise the CDC for taking decades to incorporate questions about sexual minority youth into the YRBS.
“It’s important for the rest of the world to know how long it took the U.S. to collect this data. It’s not right. For those of you in the rest of the world who struggle to get information about your youth, don’t think that America is way ahead of you because it took us a long time,” she said.
Dr. Kann noted that such data have been collected for some time by some state and city public health agencies. As local officials began clamoring for a more comprehensive national picture, “it reached a tipping point” at the CDC.
Dr. Kann reported having no relevant financial conflicts.
DURBAN, SOUTH AFRICA – The first-ever nationally representative survey on sexual identity and behaviors in U.S. male high school students has exposed a high prevalence of illicit injected drug use among those who have sex with males or with both males and females.
About 10% of high school boys who identify as gay or bisexual reported having ever used a needle to inject any illegal drug into their bodies, compared with 1.5% of high school boys who identify as heterosexual.
“This is a cause for great concern because of the efficiency with which injected drug use transmits not only HIV but hepatitis and other diseases,” Laura Kann, PhD, said in reporting the results of the 2015 National Youth Risk Behavior Survey (YRBS) at the 21st International AIDS Conference.
Dr. Kann of the Centers for Disease Control and Prevention’s division of adolescent and school health directs the YRBS, an annual, multiple-choice, anonymous voluntary survey that addresses six areas of risk: behaviors that contribute to unintentional injuries and violence, tobacco use, alcohol and other drug use, sexual behaviors, inadequate physical activity, and unhealthy diet behaviors.
The 2015 survey was the first ever to include questions regarding sexual identity and behaviors.
“Twenty-two percent of all new HIV diagnoses in the U.S. occur in 13- to 24-year-olds. Most occur in males who have sex with males. This makes young males an important focus for HIV prevention efforts,” Dr. Kann said.
Yet until the 2015 YRBS, no reliable estimates existed regarding the number of gay or bisexual male high school students. “Reducing HIV infection among young sexual minority males is key to reducing HIV infection in the U.S.,” she said. “It’s hard to respond appropriately to a population that has not been counted.”
The 15,624 male students in public and private school grades 9-12 who participated in the YRBS were demographically representative of the nation’s roughly 8 million male high schoolers.
About 2% of male students identified themselves as gay, another 2.4% declared themselves bisexual, 93.1% said they were heterosexual, and 2.6% were unsure. With regard to sexual behaviors, 53.3% of respondents indicated they had sexual contact with females only, 1.3% with males only, and 1.9% with both males and females; 43.6% reported they hadn’t ever had sexual contact. Respondents could interpret “sexual contact” as they wished, ranging from kissing and hugging to intercourse.
Large differences in illicit drug use behaviors were found between the sexual minorities – that is, males who had sexual contact with males or with females as well as males – and those with only heterosexual contacts.
“We need to conduct new research on injected drug use among young males who have sex with males and determine what can be done to minimize, if not eliminate, this very high-risk behavior that is occurring at alarming rates,” Dr. Kann said.
The sexual minority students were also more likely to have engaged in various forms of noninjected illicit drug use known to boost the risk of HIV infection indirectly by increasing the likelihood of having unsafe sex. The sexual minority males had significantly higher rates of having ever used cocaine in any form, of having ever used amphetamines, and of having taken prescription drugs without a physician’s prescription. For instance, 14.8% of sexual minority males reported ever using amphetamines, compared with 2.5% of heterosexual males surveyed.
She noted that the YRBS results provided no evidence that the disparity in HIV diagnoses between young males who have sex with males and young males who have sex with females are caused by differences in the prevalence of HIV-related sexual behaviors. There were no statistically significant differences between heterosexual and sexual minority students in rates of ever having had sexual intercourse, having had intercourse with four or more persons, having sexual activity currently, or having used a condom at last intercourse.
Dr. Kann called for more research in the neglected area of social issues affecting young sexual minority males that likely increase their sense of marginalization and may promote behaviors placing them at increased risk for HIV acquisition.
“Many young males who have sex with males suffer from social isolation, stress from self-concealment and from coming out, discrimination, and even hatred, which may occur at home, at school, and in communities among both their peers and the adults responsible for their care and protection,” she said. “These factors may lead to harmful coping behaviors, such as drug use, that can further increase risk for HIV infection. It’s hard to imagine how even the best intervention technology will be able to eliminate the disparities in HIV diagnosis unless these social issues are addressed first and foremost.”
One clinician from New York rose from the audience to chastise the CDC for taking decades to incorporate questions about sexual minority youth into the YRBS.
“It’s important for the rest of the world to know how long it took the U.S. to collect this data. It’s not right. For those of you in the rest of the world who struggle to get information about your youth, don’t think that America is way ahead of you because it took us a long time,” she said.
Dr. Kann noted that such data have been collected for some time by some state and city public health agencies. As local officials began clamoring for a more comprehensive national picture, “it reached a tipping point” at the CDC.
Dr. Kann reported having no relevant financial conflicts.
DURBAN, SOUTH AFRICA – The first-ever nationally representative survey on sexual identity and behaviors in U.S. male high school students has exposed a high prevalence of illicit injected drug use among those who have sex with males or with both males and females.
About 10% of high school boys who identify as gay or bisexual reported having ever used a needle to inject any illegal drug into their bodies, compared with 1.5% of high school boys who identify as heterosexual.
“This is a cause for great concern because of the efficiency with which injected drug use transmits not only HIV but hepatitis and other diseases,” Laura Kann, PhD, said in reporting the results of the 2015 National Youth Risk Behavior Survey (YRBS) at the 21st International AIDS Conference.
Dr. Kann of the Centers for Disease Control and Prevention’s division of adolescent and school health directs the YRBS, an annual, multiple-choice, anonymous voluntary survey that addresses six areas of risk: behaviors that contribute to unintentional injuries and violence, tobacco use, alcohol and other drug use, sexual behaviors, inadequate physical activity, and unhealthy diet behaviors.
The 2015 survey was the first ever to include questions regarding sexual identity and behaviors.
“Twenty-two percent of all new HIV diagnoses in the U.S. occur in 13- to 24-year-olds. Most occur in males who have sex with males. This makes young males an important focus for HIV prevention efforts,” Dr. Kann said.
Yet until the 2015 YRBS, no reliable estimates existed regarding the number of gay or bisexual male high school students. “Reducing HIV infection among young sexual minority males is key to reducing HIV infection in the U.S.,” she said. “It’s hard to respond appropriately to a population that has not been counted.”
The 15,624 male students in public and private school grades 9-12 who participated in the YRBS were demographically representative of the nation’s roughly 8 million male high schoolers.
About 2% of male students identified themselves as gay, another 2.4% declared themselves bisexual, 93.1% said they were heterosexual, and 2.6% were unsure. With regard to sexual behaviors, 53.3% of respondents indicated they had sexual contact with females only, 1.3% with males only, and 1.9% with both males and females; 43.6% reported they hadn’t ever had sexual contact. Respondents could interpret “sexual contact” as they wished, ranging from kissing and hugging to intercourse.
Large differences in illicit drug use behaviors were found between the sexual minorities – that is, males who had sexual contact with males or with females as well as males – and those with only heterosexual contacts.
“We need to conduct new research on injected drug use among young males who have sex with males and determine what can be done to minimize, if not eliminate, this very high-risk behavior that is occurring at alarming rates,” Dr. Kann said.
The sexual minority students were also more likely to have engaged in various forms of noninjected illicit drug use known to boost the risk of HIV infection indirectly by increasing the likelihood of having unsafe sex. The sexual minority males had significantly higher rates of having ever used cocaine in any form, of having ever used amphetamines, and of having taken prescription drugs without a physician’s prescription. For instance, 14.8% of sexual minority males reported ever using amphetamines, compared with 2.5% of heterosexual males surveyed.
She noted that the YRBS results provided no evidence that the disparity in HIV diagnoses between young males who have sex with males and young males who have sex with females are caused by differences in the prevalence of HIV-related sexual behaviors. There were no statistically significant differences between heterosexual and sexual minority students in rates of ever having had sexual intercourse, having had intercourse with four or more persons, having sexual activity currently, or having used a condom at last intercourse.
Dr. Kann called for more research in the neglected area of social issues affecting young sexual minority males that likely increase their sense of marginalization and may promote behaviors placing them at increased risk for HIV acquisition.
“Many young males who have sex with males suffer from social isolation, stress from self-concealment and from coming out, discrimination, and even hatred, which may occur at home, at school, and in communities among both their peers and the adults responsible for their care and protection,” she said. “These factors may lead to harmful coping behaviors, such as drug use, that can further increase risk for HIV infection. It’s hard to imagine how even the best intervention technology will be able to eliminate the disparities in HIV diagnosis unless these social issues are addressed first and foremost.”
One clinician from New York rose from the audience to chastise the CDC for taking decades to incorporate questions about sexual minority youth into the YRBS.
“It’s important for the rest of the world to know how long it took the U.S. to collect this data. It’s not right. For those of you in the rest of the world who struggle to get information about your youth, don’t think that America is way ahead of you because it took us a long time,” she said.
Dr. Kann noted that such data have been collected for some time by some state and city public health agencies. As local officials began clamoring for a more comprehensive national picture, “it reached a tipping point” at the CDC.
Dr. Kann reported having no relevant financial conflicts.
AT AIDS 2016
Key clinical point: Male U.S. students in grades 9-12 who identify themselves as sexual minorities have markedly higher rates of illicit drug use than their heterosexual peers.
Major finding: A total of 4.4% of U.S. male high school students identify themselves as gay or bisexual, and they are about sevenfold more likely than heterosexual students to have ever injected illegal drugs.
Data source: A national population-based survey of 15,624 male students in grades 9-12.
Disclosures: The presenter is an employee of the Centers for Disease Control and Prevention, which sponsored the annual Youth Risk Behavior Survey.
VIDEO: Medicare pays billions for potentially avoidable hospital admissions in dementia patients
TORONTO – In 2013, Medicare spent $2.6 billion on potentially avoidable hospitalizations for patients with Alzheimer’s disease and other dementias.
About half of these hospital visits – each of which cost Medicare around $7,000 – were for conditions that could have been effectively managed in primary care settings, Pei-Jung Lin, PhD, said at the Alzheimer’s Association International Conference 2016.
Half of the admissions were for chronic illnesses such as diabetes, hypertension, and asthma that are often poorly controlled as dementia progresses. The other half was for acute illnesses, said Dr. Lin, director of the Center for the Evaluation of Value and Risk in Health at Tufts University, Boston. But these admissions for acute conditions involved problems that could be treated on an outpatient basis if they’d been caught early – urinary tract infections, pneumonias, and dehydration.
“In 2013, 1 in 10 Alzheimer’s disease patients had at least one potentially avoidable hospitalization, and 1 in 7 hospital admissions among these patients (14%) was for a potentially avoidable condition,” she said during a press briefing.
Although the financial finding is striking, it isn’t the whole story, Dr. Lin said. Hospitalizations put patients at increased risk for infections, confusion, and delirium – any of which can initiate a downward clinical spiral that results in more intervention, more stress, and more cost.
“Not only are these incidences expensive, they can be dangerous for our patients. Being in the hospital is stressful for someone with little grasp of reality. Patients can become even more confused and disoriented. They’re at risk for hospital-acquired infections, which increase costs and caregiver stress, and decrease patient quality of life,” she said.
Dr. Lin and her team looked for potentially avoidable hospitalizations filed in 2013 among 2.75 million patients with Alzheimer’s and other dementias. The acute conditions included in the analysis were bacterial pneumonia, urinary tract infection, and dehydration, and chronic conditions were diabetes, cardiovascular diseases, and respiratory conditions.
About half these admissions (188,870; 47%) were for acute conditions, while the rest were for chronic conditions. About half of all the admissions also occurred in patients with late-stage disease, and these were the most expensive ones. Admissions for these late-stage patients accounted for 59% of the expenditures and cost Medicare $1.53 billion in 2013.
Claims data don’t offer the kind of details that allow a case-by-case review of how the admissions could have been prevented. But one message comes through loud and clear, Dr. Lin said.
“Comorbidity management is simply not optimal among many of our patients with Alzheimer’s disease. Many of these admissions, and much of this cost, could have been prevented with better ambulatory care and early, effective treatment.”
Dr. Richard Caselli, professor of neurology at the Mayo Clinic, Scottsdale, Ariz., commented on these issues in a video interview.
Dr. Lin had no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @alz_gal
TORONTO – In 2013, Medicare spent $2.6 billion on potentially avoidable hospitalizations for patients with Alzheimer’s disease and other dementias.
About half of these hospital visits – each of which cost Medicare around $7,000 – were for conditions that could have been effectively managed in primary care settings, Pei-Jung Lin, PhD, said at the Alzheimer’s Association International Conference 2016.
Half of the admissions were for chronic illnesses such as diabetes, hypertension, and asthma that are often poorly controlled as dementia progresses. The other half was for acute illnesses, said Dr. Lin, director of the Center for the Evaluation of Value and Risk in Health at Tufts University, Boston. But these admissions for acute conditions involved problems that could be treated on an outpatient basis if they’d been caught early – urinary tract infections, pneumonias, and dehydration.
“In 2013, 1 in 10 Alzheimer’s disease patients had at least one potentially avoidable hospitalization, and 1 in 7 hospital admissions among these patients (14%) was for a potentially avoidable condition,” she said during a press briefing.
Although the financial finding is striking, it isn’t the whole story, Dr. Lin said. Hospitalizations put patients at increased risk for infections, confusion, and delirium – any of which can initiate a downward clinical spiral that results in more intervention, more stress, and more cost.
“Not only are these incidences expensive, they can be dangerous for our patients. Being in the hospital is stressful for someone with little grasp of reality. Patients can become even more confused and disoriented. They’re at risk for hospital-acquired infections, which increase costs and caregiver stress, and decrease patient quality of life,” she said.
Dr. Lin and her team looked for potentially avoidable hospitalizations filed in 2013 among 2.75 million patients with Alzheimer’s and other dementias. The acute conditions included in the analysis were bacterial pneumonia, urinary tract infection, and dehydration, and chronic conditions were diabetes, cardiovascular diseases, and respiratory conditions.
About half these admissions (188,870; 47%) were for acute conditions, while the rest were for chronic conditions. About half of all the admissions also occurred in patients with late-stage disease, and these were the most expensive ones. Admissions for these late-stage patients accounted for 59% of the expenditures and cost Medicare $1.53 billion in 2013.
Claims data don’t offer the kind of details that allow a case-by-case review of how the admissions could have been prevented. But one message comes through loud and clear, Dr. Lin said.
“Comorbidity management is simply not optimal among many of our patients with Alzheimer’s disease. Many of these admissions, and much of this cost, could have been prevented with better ambulatory care and early, effective treatment.”
Dr. Richard Caselli, professor of neurology at the Mayo Clinic, Scottsdale, Ariz., commented on these issues in a video interview.
Dr. Lin had no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @alz_gal
TORONTO – In 2013, Medicare spent $2.6 billion on potentially avoidable hospitalizations for patients with Alzheimer’s disease and other dementias.
About half of these hospital visits – each of which cost Medicare around $7,000 – were for conditions that could have been effectively managed in primary care settings, Pei-Jung Lin, PhD, said at the Alzheimer’s Association International Conference 2016.
Half of the admissions were for chronic illnesses such as diabetes, hypertension, and asthma that are often poorly controlled as dementia progresses. The other half was for acute illnesses, said Dr. Lin, director of the Center for the Evaluation of Value and Risk in Health at Tufts University, Boston. But these admissions for acute conditions involved problems that could be treated on an outpatient basis if they’d been caught early – urinary tract infections, pneumonias, and dehydration.
“In 2013, 1 in 10 Alzheimer’s disease patients had at least one potentially avoidable hospitalization, and 1 in 7 hospital admissions among these patients (14%) was for a potentially avoidable condition,” she said during a press briefing.
Although the financial finding is striking, it isn’t the whole story, Dr. Lin said. Hospitalizations put patients at increased risk for infections, confusion, and delirium – any of which can initiate a downward clinical spiral that results in more intervention, more stress, and more cost.
“Not only are these incidences expensive, they can be dangerous for our patients. Being in the hospital is stressful for someone with little grasp of reality. Patients can become even more confused and disoriented. They’re at risk for hospital-acquired infections, which increase costs and caregiver stress, and decrease patient quality of life,” she said.
Dr. Lin and her team looked for potentially avoidable hospitalizations filed in 2013 among 2.75 million patients with Alzheimer’s and other dementias. The acute conditions included in the analysis were bacterial pneumonia, urinary tract infection, and dehydration, and chronic conditions were diabetes, cardiovascular diseases, and respiratory conditions.
About half these admissions (188,870; 47%) were for acute conditions, while the rest were for chronic conditions. About half of all the admissions also occurred in patients with late-stage disease, and these were the most expensive ones. Admissions for these late-stage patients accounted for 59% of the expenditures and cost Medicare $1.53 billion in 2013.
Claims data don’t offer the kind of details that allow a case-by-case review of how the admissions could have been prevented. But one message comes through loud and clear, Dr. Lin said.
“Comorbidity management is simply not optimal among many of our patients with Alzheimer’s disease. Many of these admissions, and much of this cost, could have been prevented with better ambulatory care and early, effective treatment.”
Dr. Richard Caselli, professor of neurology at the Mayo Clinic, Scottsdale, Ariz., commented on these issues in a video interview.
Dr. Lin had no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @alz_gal
AT AAIC 2016
Key clinical point: Billions are being spent on potentially avoidable hospitalizations for people with Alzheimer’s disease and other dementias.
Major finding: In 2013, Medicare spent $2.6 billion on possibly avoidable hospitalizations for acute and chronic illnesses that could have been prevented with better primary care.
Data source: The study included 2013 Medicare claims data on 2.75 million patients with Alzheimer’s and other dementias.
Disclosures: Dr. Lin had no financial disclosures.
USPSTF: Visual skin cancer screening lacks supporting evidence
The benefits and harms of visual screen cancer screening exams for asymptomatic adults can’t be adequately assessed with current evidence, according to a new recommendation from the U.S. Preventive Services Task Force.
“Evidence is inadequate to reliably conclude that early detection of skin cancer through visual skin examination by a clinician reduces morbidity or mortality,” according to the statement published online July 26 in JAMA (2016;316[4]:429-435. doi:10.1001/jama.2016.8465).
Approximately 76,400 adults in the United States will develop melanoma, and more than 10,000 will die from it, according to the USPSTF. However, more than 98% of skin cancer cases in the United States are basal and squamous cell carcinoma, which have much lower morbidity and mortality rates, noted the USPSTF researchers, led by Kirsten Bibbins-Domingo, MD, PhD, of the University of California, San Francisco.
The current statement updates the USPSTF’s 2009 recommendation, which also found insufficient evidence to assess the harms and benefits of visual skin cancer screening in asymptomatic adults with no history of premalignant or malignant skin lesions. However, the current recommendation eliminates a statement about patients’ skin self-exams.
According to the USPSTF, evidence is “adequate” that a clinician’s visual skin exam has “modest sensitivity and specificity for detecting melanoma,” but evidence is inconsistent to support the ability of a visual skin exam to detect nonmelanoma skin cancer.
The USPSTF commissioned an evidence review that included 11 studies previously reviewed and 2 additional studies conducted since 2009. The two new studies included one that evaluated skin cancer screening performed by dermatologists or plastic surgeons and one that evaluated skin cancer screening performed by primary care physicians. Sensitivity and specificity in the two studies ranged from 40% to 70% and from 86% to 98%, respectively.
“None of the studies could draw reliable conclusions as to whether screening performed by any of the clinical specialties differed in diagnostic accuracy,” the researchers noted. In addition, “no [randomized controlled trial] has directly evaluated the effectiveness of the clinical visual skin examination for reducing skin cancer morbidity and mortality,” they wrote.
The recommendation was accompanied by several editorials published online July 26 in JAMA journals.
In JAMA, Hensin Tsao, MD, PhD, of Massachusetts General Hospital, Boston, and Martin Weinstock, MD, PhD, of Brown University, Providence, R.I., noted that the USPSTF considered the possibility of including information from high-quality case-control studies in lieu of randomized controlled trials, which have been difficult to conduct in skin cancer screening. “The evidentiary standard needs to be further refined to be appropriate to the modest magnitude of potential harms of a properly performed skin cancer screening,” they wrote (JAMA. 2016;316:398-400). Dr. Tsao disclosed an honorarium from Lubax.
In JAMA Dermatology, Susan Swetter, MD, of the Veterans Affairs Palo Alto (Calif.) Health Care System; Alan C. Geller, MPH, of Harvard School of Public Health, Boston; and Allan C. Halpern, MD, of Memorial Sloan Kettering Cancer Center, New York, wrote about ways to promote broader uptake of skin cancer screening. “Alternative models should be explored to bundle skin screening with other preventive services (e.g., blood pressure measurements or flu shots) and to engage advanced practice providers (e.g., nurse practitioners and physician assistants) to promote screening among individuals with less access to dermatologists,” they wrote (JAMA Dermatol. 2016. doi: 10.1001/jamadermatol.2016.2606).
In JAMA Oncology, Vinayak K. Nahar, MD, of the University of Mississippi Medical Center, Jackson; Jonathan E. Mayer, MD, of Johns Hopkins University, Baltimore; and Jane M. Grant-Kels, MD, of the University of Connecticut, Farmington, addressed concerns over performing more biopsies. “The USPSTF also raises concern over the number needed to biopsy to detect 1 case of melanoma. In weighing these data, one must also consider that many of the nonmelanomas biopsied were likely severely atypical nevi that have their own risk of malignant transformation. Although difficult to quantify, there is some benefit to removing a severely atypical nevus, both for risk of transformation and for a patient’s peace of mind,” they wrote (JAMA Oncol. 2016. doi: 10.1001/jamaoncol.2016.2440).
In JAMA Internal Medicine, Eleni Linos, MD, of the University of California, San Francisco; Kenneth A. Katz, MD, of Kaiser Permanente, San Francisco; and Graham A. Colditz, MD, of Washington University, St. Louis, cautioned that the USPSTF recommendations shouldn’t be interpreted as minimizing the importance of skin cancer. “Instead, the report should motivate us to improve the evidence base for identifying groups of people in whom the benefits of screening might outweigh risks,” they wrote. “Meanwhile, we should also fully implement skin cancer primary prevention by eliminating indoor tanning exposure, especially among youths, and increasing the use of sun-protection strategies that work” (JAMA Intern. Med. 2016. doi: 10.1001/jamaintermed.2016.5008).
The recommendations are not an official position of the U.S. Department of Health and Human Services or the Agency for Healthcare Research and Quality.
“The American Academy of Dermatology is disappointed with this recommendation, as dermatologists know that skin cancer screenings can save lives, yet we acknowledge the need for additional research on the benefits and harms of skin cancer screening in the primary care setting,” Dr. Abel Torres, president of the American Academy of Dermatology, said in a statement responding to the USPSTF skin cancer screening recommendations.
“It is important for the public to understand that the USPSTF is not recommending against skin cancer screenings; it means the group did not find conclusive evidence to make a recommendation one way or another,” Dr. Torres said. “The public should know that this recommendation does not apply to individuals with suspicious skin lesions and those with an increased skin cancer risk, and it does not address the practice of skin self-exams.”
“The AAD encourages everyone to serve as their own health advocate by regularly conducting skin self-exams. Individuals who notice any unusual spots on their skin, including those that are changing, itching, or bleeding, should make an appointment with a board-certified dermatologist. In addition, individuals with an increased risk of melanoma – including men older than 50; people with more than 50 moles, or large or unusual moles; individuals with fair skin; and those with a history of skin cancer – should talk to a dermatologist about how often they should receive a skin exam from a doctor.”
Dr. Abel Torres is president of the American Academy of Dermatology. The comments are taken from his AAD statement on USPSTF Recommendation on Skin Cancer Screening issued on July 26, 2016.
“The American Academy of Dermatology is disappointed with this recommendation, as dermatologists know that skin cancer screenings can save lives, yet we acknowledge the need for additional research on the benefits and harms of skin cancer screening in the primary care setting,” Dr. Abel Torres, president of the American Academy of Dermatology, said in a statement responding to the USPSTF skin cancer screening recommendations.
“It is important for the public to understand that the USPSTF is not recommending against skin cancer screenings; it means the group did not find conclusive evidence to make a recommendation one way or another,” Dr. Torres said. “The public should know that this recommendation does not apply to individuals with suspicious skin lesions and those with an increased skin cancer risk, and it does not address the practice of skin self-exams.”
“The AAD encourages everyone to serve as their own health advocate by regularly conducting skin self-exams. Individuals who notice any unusual spots on their skin, including those that are changing, itching, or bleeding, should make an appointment with a board-certified dermatologist. In addition, individuals with an increased risk of melanoma – including men older than 50; people with more than 50 moles, or large or unusual moles; individuals with fair skin; and those with a history of skin cancer – should talk to a dermatologist about how often they should receive a skin exam from a doctor.”
Dr. Abel Torres is president of the American Academy of Dermatology. The comments are taken from his AAD statement on USPSTF Recommendation on Skin Cancer Screening issued on July 26, 2016.
“The American Academy of Dermatology is disappointed with this recommendation, as dermatologists know that skin cancer screenings can save lives, yet we acknowledge the need for additional research on the benefits and harms of skin cancer screening in the primary care setting,” Dr. Abel Torres, president of the American Academy of Dermatology, said in a statement responding to the USPSTF skin cancer screening recommendations.
“It is important for the public to understand that the USPSTF is not recommending against skin cancer screenings; it means the group did not find conclusive evidence to make a recommendation one way or another,” Dr. Torres said. “The public should know that this recommendation does not apply to individuals with suspicious skin lesions and those with an increased skin cancer risk, and it does not address the practice of skin self-exams.”
“The AAD encourages everyone to serve as their own health advocate by regularly conducting skin self-exams. Individuals who notice any unusual spots on their skin, including those that are changing, itching, or bleeding, should make an appointment with a board-certified dermatologist. In addition, individuals with an increased risk of melanoma – including men older than 50; people with more than 50 moles, or large or unusual moles; individuals with fair skin; and those with a history of skin cancer – should talk to a dermatologist about how often they should receive a skin exam from a doctor.”
Dr. Abel Torres is president of the American Academy of Dermatology. The comments are taken from his AAD statement on USPSTF Recommendation on Skin Cancer Screening issued on July 26, 2016.
The benefits and harms of visual screen cancer screening exams for asymptomatic adults can’t be adequately assessed with current evidence, according to a new recommendation from the U.S. Preventive Services Task Force.
“Evidence is inadequate to reliably conclude that early detection of skin cancer through visual skin examination by a clinician reduces morbidity or mortality,” according to the statement published online July 26 in JAMA (2016;316[4]:429-435. doi:10.1001/jama.2016.8465).
Approximately 76,400 adults in the United States will develop melanoma, and more than 10,000 will die from it, according to the USPSTF. However, more than 98% of skin cancer cases in the United States are basal and squamous cell carcinoma, which have much lower morbidity and mortality rates, noted the USPSTF researchers, led by Kirsten Bibbins-Domingo, MD, PhD, of the University of California, San Francisco.
The current statement updates the USPSTF’s 2009 recommendation, which also found insufficient evidence to assess the harms and benefits of visual skin cancer screening in asymptomatic adults with no history of premalignant or malignant skin lesions. However, the current recommendation eliminates a statement about patients’ skin self-exams.
According to the USPSTF, evidence is “adequate” that a clinician’s visual skin exam has “modest sensitivity and specificity for detecting melanoma,” but evidence is inconsistent to support the ability of a visual skin exam to detect nonmelanoma skin cancer.
The USPSTF commissioned an evidence review that included 11 studies previously reviewed and 2 additional studies conducted since 2009. The two new studies included one that evaluated skin cancer screening performed by dermatologists or plastic surgeons and one that evaluated skin cancer screening performed by primary care physicians. Sensitivity and specificity in the two studies ranged from 40% to 70% and from 86% to 98%, respectively.
“None of the studies could draw reliable conclusions as to whether screening performed by any of the clinical specialties differed in diagnostic accuracy,” the researchers noted. In addition, “no [randomized controlled trial] has directly evaluated the effectiveness of the clinical visual skin examination for reducing skin cancer morbidity and mortality,” they wrote.
The recommendation was accompanied by several editorials published online July 26 in JAMA journals.
In JAMA, Hensin Tsao, MD, PhD, of Massachusetts General Hospital, Boston, and Martin Weinstock, MD, PhD, of Brown University, Providence, R.I., noted that the USPSTF considered the possibility of including information from high-quality case-control studies in lieu of randomized controlled trials, which have been difficult to conduct in skin cancer screening. “The evidentiary standard needs to be further refined to be appropriate to the modest magnitude of potential harms of a properly performed skin cancer screening,” they wrote (JAMA. 2016;316:398-400). Dr. Tsao disclosed an honorarium from Lubax.
In JAMA Dermatology, Susan Swetter, MD, of the Veterans Affairs Palo Alto (Calif.) Health Care System; Alan C. Geller, MPH, of Harvard School of Public Health, Boston; and Allan C. Halpern, MD, of Memorial Sloan Kettering Cancer Center, New York, wrote about ways to promote broader uptake of skin cancer screening. “Alternative models should be explored to bundle skin screening with other preventive services (e.g., blood pressure measurements or flu shots) and to engage advanced practice providers (e.g., nurse practitioners and physician assistants) to promote screening among individuals with less access to dermatologists,” they wrote (JAMA Dermatol. 2016. doi: 10.1001/jamadermatol.2016.2606).
In JAMA Oncology, Vinayak K. Nahar, MD, of the University of Mississippi Medical Center, Jackson; Jonathan E. Mayer, MD, of Johns Hopkins University, Baltimore; and Jane M. Grant-Kels, MD, of the University of Connecticut, Farmington, addressed concerns over performing more biopsies. “The USPSTF also raises concern over the number needed to biopsy to detect 1 case of melanoma. In weighing these data, one must also consider that many of the nonmelanomas biopsied were likely severely atypical nevi that have their own risk of malignant transformation. Although difficult to quantify, there is some benefit to removing a severely atypical nevus, both for risk of transformation and for a patient’s peace of mind,” they wrote (JAMA Oncol. 2016. doi: 10.1001/jamaoncol.2016.2440).
In JAMA Internal Medicine, Eleni Linos, MD, of the University of California, San Francisco; Kenneth A. Katz, MD, of Kaiser Permanente, San Francisco; and Graham A. Colditz, MD, of Washington University, St. Louis, cautioned that the USPSTF recommendations shouldn’t be interpreted as minimizing the importance of skin cancer. “Instead, the report should motivate us to improve the evidence base for identifying groups of people in whom the benefits of screening might outweigh risks,” they wrote. “Meanwhile, we should also fully implement skin cancer primary prevention by eliminating indoor tanning exposure, especially among youths, and increasing the use of sun-protection strategies that work” (JAMA Intern. Med. 2016. doi: 10.1001/jamaintermed.2016.5008).
The recommendations are not an official position of the U.S. Department of Health and Human Services or the Agency for Healthcare Research and Quality.
The benefits and harms of visual screen cancer screening exams for asymptomatic adults can’t be adequately assessed with current evidence, according to a new recommendation from the U.S. Preventive Services Task Force.
“Evidence is inadequate to reliably conclude that early detection of skin cancer through visual skin examination by a clinician reduces morbidity or mortality,” according to the statement published online July 26 in JAMA (2016;316[4]:429-435. doi:10.1001/jama.2016.8465).
Approximately 76,400 adults in the United States will develop melanoma, and more than 10,000 will die from it, according to the USPSTF. However, more than 98% of skin cancer cases in the United States are basal and squamous cell carcinoma, which have much lower morbidity and mortality rates, noted the USPSTF researchers, led by Kirsten Bibbins-Domingo, MD, PhD, of the University of California, San Francisco.
The current statement updates the USPSTF’s 2009 recommendation, which also found insufficient evidence to assess the harms and benefits of visual skin cancer screening in asymptomatic adults with no history of premalignant or malignant skin lesions. However, the current recommendation eliminates a statement about patients’ skin self-exams.
According to the USPSTF, evidence is “adequate” that a clinician’s visual skin exam has “modest sensitivity and specificity for detecting melanoma,” but evidence is inconsistent to support the ability of a visual skin exam to detect nonmelanoma skin cancer.
The USPSTF commissioned an evidence review that included 11 studies previously reviewed and 2 additional studies conducted since 2009. The two new studies included one that evaluated skin cancer screening performed by dermatologists or plastic surgeons and one that evaluated skin cancer screening performed by primary care physicians. Sensitivity and specificity in the two studies ranged from 40% to 70% and from 86% to 98%, respectively.
“None of the studies could draw reliable conclusions as to whether screening performed by any of the clinical specialties differed in diagnostic accuracy,” the researchers noted. In addition, “no [randomized controlled trial] has directly evaluated the effectiveness of the clinical visual skin examination for reducing skin cancer morbidity and mortality,” they wrote.
The recommendation was accompanied by several editorials published online July 26 in JAMA journals.
In JAMA, Hensin Tsao, MD, PhD, of Massachusetts General Hospital, Boston, and Martin Weinstock, MD, PhD, of Brown University, Providence, R.I., noted that the USPSTF considered the possibility of including information from high-quality case-control studies in lieu of randomized controlled trials, which have been difficult to conduct in skin cancer screening. “The evidentiary standard needs to be further refined to be appropriate to the modest magnitude of potential harms of a properly performed skin cancer screening,” they wrote (JAMA. 2016;316:398-400). Dr. Tsao disclosed an honorarium from Lubax.
In JAMA Dermatology, Susan Swetter, MD, of the Veterans Affairs Palo Alto (Calif.) Health Care System; Alan C. Geller, MPH, of Harvard School of Public Health, Boston; and Allan C. Halpern, MD, of Memorial Sloan Kettering Cancer Center, New York, wrote about ways to promote broader uptake of skin cancer screening. “Alternative models should be explored to bundle skin screening with other preventive services (e.g., blood pressure measurements or flu shots) and to engage advanced practice providers (e.g., nurse practitioners and physician assistants) to promote screening among individuals with less access to dermatologists,” they wrote (JAMA Dermatol. 2016. doi: 10.1001/jamadermatol.2016.2606).
In JAMA Oncology, Vinayak K. Nahar, MD, of the University of Mississippi Medical Center, Jackson; Jonathan E. Mayer, MD, of Johns Hopkins University, Baltimore; and Jane M. Grant-Kels, MD, of the University of Connecticut, Farmington, addressed concerns over performing more biopsies. “The USPSTF also raises concern over the number needed to biopsy to detect 1 case of melanoma. In weighing these data, one must also consider that many of the nonmelanomas biopsied were likely severely atypical nevi that have their own risk of malignant transformation. Although difficult to quantify, there is some benefit to removing a severely atypical nevus, both for risk of transformation and for a patient’s peace of mind,” they wrote (JAMA Oncol. 2016. doi: 10.1001/jamaoncol.2016.2440).
In JAMA Internal Medicine, Eleni Linos, MD, of the University of California, San Francisco; Kenneth A. Katz, MD, of Kaiser Permanente, San Francisco; and Graham A. Colditz, MD, of Washington University, St. Louis, cautioned that the USPSTF recommendations shouldn’t be interpreted as minimizing the importance of skin cancer. “Instead, the report should motivate us to improve the evidence base for identifying groups of people in whom the benefits of screening might outweigh risks,” they wrote. “Meanwhile, we should also fully implement skin cancer primary prevention by eliminating indoor tanning exposure, especially among youths, and increasing the use of sun-protection strategies that work” (JAMA Intern. Med. 2016. doi: 10.1001/jamaintermed.2016.5008).
The recommendations are not an official position of the U.S. Department of Health and Human Services or the Agency for Healthcare Research and Quality.
FROM JAMA
Measure Hospitalist Engagement with SHM’s Engagement Benchmarking Service
One of the most important questions for leaders of HM groups is, “How can I measure the level of engagement of my hospitalists?” Measuring hospitalist engagement can be difficult, and many leaders are not satisfied with the tools they currently have at their disposal.
SHM has developed an Engagement Benchmarking Service to analyze engagement of hospitalists. The service evaluates relationships with leaders, care quality, autonomy, effective motivation, burnout risk, and more. You can see your standardization score in the various domains and where it falls within the national benchmark to help you determine what is working well and identify areas for improvement in your hospital medicine group.
Recruiting ends soon. Ensure hospitalists are engaged in your hospital medicine group by registering now for the next cohort at www.hospitalmedicine.org/pmad3.
One of the most important questions for leaders of HM groups is, “How can I measure the level of engagement of my hospitalists?” Measuring hospitalist engagement can be difficult, and many leaders are not satisfied with the tools they currently have at their disposal.
SHM has developed an Engagement Benchmarking Service to analyze engagement of hospitalists. The service evaluates relationships with leaders, care quality, autonomy, effective motivation, burnout risk, and more. You can see your standardization score in the various domains and where it falls within the national benchmark to help you determine what is working well and identify areas for improvement in your hospital medicine group.
Recruiting ends soon. Ensure hospitalists are engaged in your hospital medicine group by registering now for the next cohort at www.hospitalmedicine.org/pmad3.
One of the most important questions for leaders of HM groups is, “How can I measure the level of engagement of my hospitalists?” Measuring hospitalist engagement can be difficult, and many leaders are not satisfied with the tools they currently have at their disposal.
SHM has developed an Engagement Benchmarking Service to analyze engagement of hospitalists. The service evaluates relationships with leaders, care quality, autonomy, effective motivation, burnout risk, and more. You can see your standardization score in the various domains and where it falls within the national benchmark to help you determine what is working well and identify areas for improvement in your hospital medicine group.
Recruiting ends soon. Ensure hospitalists are engaged in your hospital medicine group by registering now for the next cohort at www.hospitalmedicine.org/pmad3.
SHM Leadership Academy: Learning Awaits in Mastering Teamwork Course
As the SHM Leadership Academy’s course director, I always find time to visit the Mastering Teamwork course because each year, even though it’s slightly different, it’s still exciting. In past meetings, I’ve learned from talented faculty how lessons in college football relate to practice, been provided guidance on how to recognize what makes me tick, and heard firsthand perspective on large-scale medical events like 9/11, Hurricane Katrina, and even the Boston Marathon tragedy. I always learn a few new things. As they say, repetition is the mother of learning, and the Mastering Teamwork course never fails to make that learning a lot of fun.
As a professor of medicine, I’ve always liked learning. But I truly enjoy learning when it’s fun and exciting. To me, this mixture of academia and excitement is the epitome of Mastering Teamwork. When two of the faculty, Mark Williams, MD, MHM, and Amit Prachand, MEng, needed to teach about teamwork, they decided to develop an interactive session. While in Hawaii, they constructed a “river” out of cardboard and props for Mastering Teamwork participants to navigate. It was a hands-on lesson in group dynamics. It was educational and, most of all, a hoot.
Kay Cannon, MBA, taught me that the skills I used in previous job levels may not be the drivers of my success in today’s job (or tomorrow’s), and Jeffrey Wiese, MD, MHM, and Lenny Marcus, PhD, are two of the best storytellers I know and have me on the edge of my seat every time I hear them speak. Their life experiences make excellent fodder for hospitalist leadership pearls and are more riveting than Downton Abbey (or whatever drama is your favorite).
I look forward to seeing everyone at Disney’s BoardWalk Inn in Lake Buena Vista, Florida, from October 24 to 27 to experience what I know will be a memorable, enjoyable learning experience for all.
To register, visit www.shmleadershipacademy.org. TH
Dr. Howell is SHM’s senior physician advisor and course director for SHM’s Leadership Academy.
As the SHM Leadership Academy’s course director, I always find time to visit the Mastering Teamwork course because each year, even though it’s slightly different, it’s still exciting. In past meetings, I’ve learned from talented faculty how lessons in college football relate to practice, been provided guidance on how to recognize what makes me tick, and heard firsthand perspective on large-scale medical events like 9/11, Hurricane Katrina, and even the Boston Marathon tragedy. I always learn a few new things. As they say, repetition is the mother of learning, and the Mastering Teamwork course never fails to make that learning a lot of fun.
As a professor of medicine, I’ve always liked learning. But I truly enjoy learning when it’s fun and exciting. To me, this mixture of academia and excitement is the epitome of Mastering Teamwork. When two of the faculty, Mark Williams, MD, MHM, and Amit Prachand, MEng, needed to teach about teamwork, they decided to develop an interactive session. While in Hawaii, they constructed a “river” out of cardboard and props for Mastering Teamwork participants to navigate. It was a hands-on lesson in group dynamics. It was educational and, most of all, a hoot.
Kay Cannon, MBA, taught me that the skills I used in previous job levels may not be the drivers of my success in today’s job (or tomorrow’s), and Jeffrey Wiese, MD, MHM, and Lenny Marcus, PhD, are two of the best storytellers I know and have me on the edge of my seat every time I hear them speak. Their life experiences make excellent fodder for hospitalist leadership pearls and are more riveting than Downton Abbey (or whatever drama is your favorite).
I look forward to seeing everyone at Disney’s BoardWalk Inn in Lake Buena Vista, Florida, from October 24 to 27 to experience what I know will be a memorable, enjoyable learning experience for all.
To register, visit www.shmleadershipacademy.org. TH
Dr. Howell is SHM’s senior physician advisor and course director for SHM’s Leadership Academy.
As the SHM Leadership Academy’s course director, I always find time to visit the Mastering Teamwork course because each year, even though it’s slightly different, it’s still exciting. In past meetings, I’ve learned from talented faculty how lessons in college football relate to practice, been provided guidance on how to recognize what makes me tick, and heard firsthand perspective on large-scale medical events like 9/11, Hurricane Katrina, and even the Boston Marathon tragedy. I always learn a few new things. As they say, repetition is the mother of learning, and the Mastering Teamwork course never fails to make that learning a lot of fun.
As a professor of medicine, I’ve always liked learning. But I truly enjoy learning when it’s fun and exciting. To me, this mixture of academia and excitement is the epitome of Mastering Teamwork. When two of the faculty, Mark Williams, MD, MHM, and Amit Prachand, MEng, needed to teach about teamwork, they decided to develop an interactive session. While in Hawaii, they constructed a “river” out of cardboard and props for Mastering Teamwork participants to navigate. It was a hands-on lesson in group dynamics. It was educational and, most of all, a hoot.
Kay Cannon, MBA, taught me that the skills I used in previous job levels may not be the drivers of my success in today’s job (or tomorrow’s), and Jeffrey Wiese, MD, MHM, and Lenny Marcus, PhD, are two of the best storytellers I know and have me on the edge of my seat every time I hear them speak. Their life experiences make excellent fodder for hospitalist leadership pearls and are more riveting than Downton Abbey (or whatever drama is your favorite).
I look forward to seeing everyone at Disney’s BoardWalk Inn in Lake Buena Vista, Florida, from October 24 to 27 to experience what I know will be a memorable, enjoyable learning experience for all.
To register, visit www.shmleadershipacademy.org. TH
Dr. Howell is SHM’s senior physician advisor and course director for SHM’s Leadership Academy.
Long-term health burden of Hodgkin lymphoma treatment

Photo courtesy of St. Jude
Children’s Research Hospital
and Seth Dixon
New research has shown that survivors of pediatric Hodgkin lymphoma (HL) are more likely to have chronic cardiovascular conditions than adults who did not have cancer in childhood.
And cardiovascular conditions are more severe among HL survivors than the general population.
Investigators believe this research, published in The Lancet Oncology, should aid efforts to reduce and better manage the late effects of cancer treatment.
For this study, the investigators used a measurement called “cumulative burden” to better capture the distribution and magnitude of chronic disease in childhood cancer survivors.
The metric showed that, by age 50, HL survivors had more than twice as many cardiovascular problems as adults who had not had cancer as children. HL survivors were also 5 times more likely to have severe, life-threatening, or fatal heart conditions.
“With cure rates for pediatric cancer at historic highs, the question becomes, ‘What is the legacy of that cure?’” said study author Nickhill Bhakta, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“We are doing a better job of keeping patients alive, but are we doing a better job at addressing the chronic diseases that are sometimes the price of that cure? Cumulative burden is a new tool for studying chronic illness in childhood cancer survivors or any patient population with significant morbidity, such as diabetes or HIV/AIDS.”
Unlike statistical methods that count health conditions once at diagnosis, cumulative burden tracks individuals’ multiple, recurring treatment-related health conditions.
Dr Bhakta and his colleagues focused on calculating the cumulative burden of cardiovascular disease in 670 pediatric HL survivors. The subjects were at least 18 years old and had survived at least 10 years beyond their cancer diagnoses.
The participants had been assessed for 22 chronic cardiovascular conditions, including heart attacks, hypertension, arrhythmias, and structural heart defects. Investigators used those and other clinical findings to calculate the cumulative burden by tracking the incidence and severity of cardiovascular disease.
The team also determined the cumulative burden for a comparison group of 272 community volunteers who underwent the same health assessments. The volunteers were similar in age and gender to the HL survivors but had no history of childhood cancer.
The analysis showed that the cumulative burden of cardiovascular disease, including severe and life-threatening conditions, was greater among HL survivors at 30 and 50 years of age than among the comparison group. In fact, the cumulative burden of the most serious heart problems, including heart attacks, was similar for 30-year-old HL survivors and 50-year-old community volunteers.
At age 50, 45.5% of HL survivors had developed at least one grade 3-5 cardiovascular condition, compared to 15.7% of the control subjects.
The HL survivors had a cumulative burden of 430.6 grade 1-5 cardiovascular conditions per 100 individuals and 100.8 grade 3-5 cardiovascular conditions per 100 individuals. In comparison, controls had 227.4 grade 1-5 conditions and 17.0 grade 3-5 conditions per 100 individuals.
The investigators noted that severe, chronic heart conditions became more common with age in both groups, but serious problems accumulated more rapidly in HL survivors.
“Survivors tended to have more severe disease across the lifespan and likely need an individualized screening and treatment plan,” Dr Bhakta said.
He added that the results of this study highlight trade-offs to consider in designing future clinical trials. For example, the investigators found that reducing the dose of anthracyclines will lower the rate, but not the severity, of cardiovascular disease in pediatric and young adult HL survivors.
In contrast, lowering the heart radiation dose will not significantly lower the rate of cardiovascular disease, but it will reduce the severity.
“Cumulative burden provides us with a global view of tradeoffs between different treatment late effects that must be considered when designing new interventions,” Dr Bhakta concluded. ![]()

Photo courtesy of St. Jude
Children’s Research Hospital
and Seth Dixon
New research has shown that survivors of pediatric Hodgkin lymphoma (HL) are more likely to have chronic cardiovascular conditions than adults who did not have cancer in childhood.
And cardiovascular conditions are more severe among HL survivors than the general population.
Investigators believe this research, published in The Lancet Oncology, should aid efforts to reduce and better manage the late effects of cancer treatment.
For this study, the investigators used a measurement called “cumulative burden” to better capture the distribution and magnitude of chronic disease in childhood cancer survivors.
The metric showed that, by age 50, HL survivors had more than twice as many cardiovascular problems as adults who had not had cancer as children. HL survivors were also 5 times more likely to have severe, life-threatening, or fatal heart conditions.
“With cure rates for pediatric cancer at historic highs, the question becomes, ‘What is the legacy of that cure?’” said study author Nickhill Bhakta, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“We are doing a better job of keeping patients alive, but are we doing a better job at addressing the chronic diseases that are sometimes the price of that cure? Cumulative burden is a new tool for studying chronic illness in childhood cancer survivors or any patient population with significant morbidity, such as diabetes or HIV/AIDS.”
Unlike statistical methods that count health conditions once at diagnosis, cumulative burden tracks individuals’ multiple, recurring treatment-related health conditions.
Dr Bhakta and his colleagues focused on calculating the cumulative burden of cardiovascular disease in 670 pediatric HL survivors. The subjects were at least 18 years old and had survived at least 10 years beyond their cancer diagnoses.
The participants had been assessed for 22 chronic cardiovascular conditions, including heart attacks, hypertension, arrhythmias, and structural heart defects. Investigators used those and other clinical findings to calculate the cumulative burden by tracking the incidence and severity of cardiovascular disease.
The team also determined the cumulative burden for a comparison group of 272 community volunteers who underwent the same health assessments. The volunteers were similar in age and gender to the HL survivors but had no history of childhood cancer.
The analysis showed that the cumulative burden of cardiovascular disease, including severe and life-threatening conditions, was greater among HL survivors at 30 and 50 years of age than among the comparison group. In fact, the cumulative burden of the most serious heart problems, including heart attacks, was similar for 30-year-old HL survivors and 50-year-old community volunteers.
At age 50, 45.5% of HL survivors had developed at least one grade 3-5 cardiovascular condition, compared to 15.7% of the control subjects.
The HL survivors had a cumulative burden of 430.6 grade 1-5 cardiovascular conditions per 100 individuals and 100.8 grade 3-5 cardiovascular conditions per 100 individuals. In comparison, controls had 227.4 grade 1-5 conditions and 17.0 grade 3-5 conditions per 100 individuals.
The investigators noted that severe, chronic heart conditions became more common with age in both groups, but serious problems accumulated more rapidly in HL survivors.
“Survivors tended to have more severe disease across the lifespan and likely need an individualized screening and treatment plan,” Dr Bhakta said.
He added that the results of this study highlight trade-offs to consider in designing future clinical trials. For example, the investigators found that reducing the dose of anthracyclines will lower the rate, but not the severity, of cardiovascular disease in pediatric and young adult HL survivors.
In contrast, lowering the heart radiation dose will not significantly lower the rate of cardiovascular disease, but it will reduce the severity.
“Cumulative burden provides us with a global view of tradeoffs between different treatment late effects that must be considered when designing new interventions,” Dr Bhakta concluded. ![]()

Photo courtesy of St. Jude
Children’s Research Hospital
and Seth Dixon
New research has shown that survivors of pediatric Hodgkin lymphoma (HL) are more likely to have chronic cardiovascular conditions than adults who did not have cancer in childhood.
And cardiovascular conditions are more severe among HL survivors than the general population.
Investigators believe this research, published in The Lancet Oncology, should aid efforts to reduce and better manage the late effects of cancer treatment.
For this study, the investigators used a measurement called “cumulative burden” to better capture the distribution and magnitude of chronic disease in childhood cancer survivors.
The metric showed that, by age 50, HL survivors had more than twice as many cardiovascular problems as adults who had not had cancer as children. HL survivors were also 5 times more likely to have severe, life-threatening, or fatal heart conditions.
“With cure rates for pediatric cancer at historic highs, the question becomes, ‘What is the legacy of that cure?’” said study author Nickhill Bhakta, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“We are doing a better job of keeping patients alive, but are we doing a better job at addressing the chronic diseases that are sometimes the price of that cure? Cumulative burden is a new tool for studying chronic illness in childhood cancer survivors or any patient population with significant morbidity, such as diabetes or HIV/AIDS.”
Unlike statistical methods that count health conditions once at diagnosis, cumulative burden tracks individuals’ multiple, recurring treatment-related health conditions.
Dr Bhakta and his colleagues focused on calculating the cumulative burden of cardiovascular disease in 670 pediatric HL survivors. The subjects were at least 18 years old and had survived at least 10 years beyond their cancer diagnoses.
The participants had been assessed for 22 chronic cardiovascular conditions, including heart attacks, hypertension, arrhythmias, and structural heart defects. Investigators used those and other clinical findings to calculate the cumulative burden by tracking the incidence and severity of cardiovascular disease.
The team also determined the cumulative burden for a comparison group of 272 community volunteers who underwent the same health assessments. The volunteers were similar in age and gender to the HL survivors but had no history of childhood cancer.
The analysis showed that the cumulative burden of cardiovascular disease, including severe and life-threatening conditions, was greater among HL survivors at 30 and 50 years of age than among the comparison group. In fact, the cumulative burden of the most serious heart problems, including heart attacks, was similar for 30-year-old HL survivors and 50-year-old community volunteers.
At age 50, 45.5% of HL survivors had developed at least one grade 3-5 cardiovascular condition, compared to 15.7% of the control subjects.
The HL survivors had a cumulative burden of 430.6 grade 1-5 cardiovascular conditions per 100 individuals and 100.8 grade 3-5 cardiovascular conditions per 100 individuals. In comparison, controls had 227.4 grade 1-5 conditions and 17.0 grade 3-5 conditions per 100 individuals.
The investigators noted that severe, chronic heart conditions became more common with age in both groups, but serious problems accumulated more rapidly in HL survivors.
“Survivors tended to have more severe disease across the lifespan and likely need an individualized screening and treatment plan,” Dr Bhakta said.
He added that the results of this study highlight trade-offs to consider in designing future clinical trials. For example, the investigators found that reducing the dose of anthracyclines will lower the rate, but not the severity, of cardiovascular disease in pediatric and young adult HL survivors.
In contrast, lowering the heart radiation dose will not significantly lower the rate of cardiovascular disease, but it will reduce the severity.
“Cumulative burden provides us with a global view of tradeoffs between different treatment late effects that must be considered when designing new interventions,” Dr Bhakta concluded. ![]()
FDA clears kit for monitoring molecular response in CML

Photo by Juan D. Alfonso
The US Food and Drug Administration (FDA) has granted premarket clearance for the QuantideX® qPCR BCR-ABL IS Kit, a tool used to monitor molecular response (MR) in patients with chronic myeloid leukemia (CML).
The product is a quantitative polymerase chain reaction (qPCR)-based in vitro diagnostic test that quantifies BCR-ABL1 and ABL1 transcripts in total RNA from the whole blood of t(9;22)-positive CML patients expressing e13a2 and/or e14a2 fusion transcripts.
The QuantideX® qPCR BCR-ABL IS Kit is not designed to diagnose CML or monitor rare transcripts resulting from t(9;22).
The kit was cleared to run on the Applied Biosystems® 7500 Fast DX Real-Time PCR Instrument. Results are reported in International Scale (IS) values.
The QuantideX® qPCR BCR-ABL IS Kit was subjected to analytic and clinical review through the FDA’s de novo 510(k) premarket review pathway and secured clearance with a limit of detection of MR 4.7/0.002% IS (4.7 log molecular reduction from 100% IS).
The limit of detection was determined using real human RNA, not human-derived cell lines, ensuring that the assay reproducibly detects BCR-ABL1 RNA in at least 95% of patients at MR 4.7.
“In evaluating the QuantideX® qPCR BCR-ABL IS Kit, we confirmed the high level of sensitivity achieved for human clinical samples measured in our laboratory at MR 4.7 (0.002% IS),” said Y. Lynn. Wang, MD, PhD, of the University of Chicago Comprehensive Cancer Center.
“The configuration of the assay—multiplexed, single-lot reagents, efficient workflow, and direct IS reporting—provided the robustness, sensitivity, and data quality we believe to be unprecedented in the market today. The high level of sensitivity will contribute to the assessment of the depth and duration of clinical response to [tyrosine kinase inhibitors] and experimental therapies.”
The QuantideX® qPCR BCR-ABL IS Kit is now available for order in the US and Europe. The kit is a product of Asuragen, Inc. ![]()

Photo by Juan D. Alfonso
The US Food and Drug Administration (FDA) has granted premarket clearance for the QuantideX® qPCR BCR-ABL IS Kit, a tool used to monitor molecular response (MR) in patients with chronic myeloid leukemia (CML).
The product is a quantitative polymerase chain reaction (qPCR)-based in vitro diagnostic test that quantifies BCR-ABL1 and ABL1 transcripts in total RNA from the whole blood of t(9;22)-positive CML patients expressing e13a2 and/or e14a2 fusion transcripts.
The QuantideX® qPCR BCR-ABL IS Kit is not designed to diagnose CML or monitor rare transcripts resulting from t(9;22).
The kit was cleared to run on the Applied Biosystems® 7500 Fast DX Real-Time PCR Instrument. Results are reported in International Scale (IS) values.
The QuantideX® qPCR BCR-ABL IS Kit was subjected to analytic and clinical review through the FDA’s de novo 510(k) premarket review pathway and secured clearance with a limit of detection of MR 4.7/0.002% IS (4.7 log molecular reduction from 100% IS).
The limit of detection was determined using real human RNA, not human-derived cell lines, ensuring that the assay reproducibly detects BCR-ABL1 RNA in at least 95% of patients at MR 4.7.
“In evaluating the QuantideX® qPCR BCR-ABL IS Kit, we confirmed the high level of sensitivity achieved for human clinical samples measured in our laboratory at MR 4.7 (0.002% IS),” said Y. Lynn. Wang, MD, PhD, of the University of Chicago Comprehensive Cancer Center.
“The configuration of the assay—multiplexed, single-lot reagents, efficient workflow, and direct IS reporting—provided the robustness, sensitivity, and data quality we believe to be unprecedented in the market today. The high level of sensitivity will contribute to the assessment of the depth and duration of clinical response to [tyrosine kinase inhibitors] and experimental therapies.”
The QuantideX® qPCR BCR-ABL IS Kit is now available for order in the US and Europe. The kit is a product of Asuragen, Inc. ![]()

Photo by Juan D. Alfonso
The US Food and Drug Administration (FDA) has granted premarket clearance for the QuantideX® qPCR BCR-ABL IS Kit, a tool used to monitor molecular response (MR) in patients with chronic myeloid leukemia (CML).
The product is a quantitative polymerase chain reaction (qPCR)-based in vitro diagnostic test that quantifies BCR-ABL1 and ABL1 transcripts in total RNA from the whole blood of t(9;22)-positive CML patients expressing e13a2 and/or e14a2 fusion transcripts.
The QuantideX® qPCR BCR-ABL IS Kit is not designed to diagnose CML or monitor rare transcripts resulting from t(9;22).
The kit was cleared to run on the Applied Biosystems® 7500 Fast DX Real-Time PCR Instrument. Results are reported in International Scale (IS) values.
The QuantideX® qPCR BCR-ABL IS Kit was subjected to analytic and clinical review through the FDA’s de novo 510(k) premarket review pathway and secured clearance with a limit of detection of MR 4.7/0.002% IS (4.7 log molecular reduction from 100% IS).
The limit of detection was determined using real human RNA, not human-derived cell lines, ensuring that the assay reproducibly detects BCR-ABL1 RNA in at least 95% of patients at MR 4.7.
“In evaluating the QuantideX® qPCR BCR-ABL IS Kit, we confirmed the high level of sensitivity achieved for human clinical samples measured in our laboratory at MR 4.7 (0.002% IS),” said Y. Lynn. Wang, MD, PhD, of the University of Chicago Comprehensive Cancer Center.
“The configuration of the assay—multiplexed, single-lot reagents, efficient workflow, and direct IS reporting—provided the robustness, sensitivity, and data quality we believe to be unprecedented in the market today. The high level of sensitivity will contribute to the assessment of the depth and duration of clinical response to [tyrosine kinase inhibitors] and experimental therapies.”
The QuantideX® qPCR BCR-ABL IS Kit is now available for order in the US and Europe. The kit is a product of Asuragen, Inc. ![]()