User login
New HER2-testing guidelines result in more women eligible for HER2-directed treatment
New guidelines for immunohistochemistry (IHC) and fluorescent in situ hybridization (FISH) pathology testing categorize more breast cancers as “equivocal” regarding HER2 positivity and ultimately lead to identifying more of them as HER2 positive, investigators reported online in Journal of Clinical Oncology.
The American Society of Clinical Oncology and the College of American Pathologists released updated IHC and FISH guidelines in 2013, after the Food and Drug Administration approved the initial set of such guidelines in 1998 and ASCO/CAP issued their first such guidelines in 2007. “The intent of the 2013 guidelines was to decrease the number of equivocal [cancers],” said Mithun Vinod Shah, MD, PhD, of the Mayo Clinic, Rochester Minn., and his associates.
To assess the impact of implementing the new guidelines, the investigators analyzed 2,851 breast cancer samples sent to their cytogenetics laboratory by 139 medical centers for HER2 testing during a 1-year period. They compared the three sets of testing criteria – the FDA, the 2007, and the 2013 guidelines.
According to the 2013 guidelines, 69.7% of the tumors were classified as HER2 negative, 16.1% as HER2 positive, and 14.2% as equivocal. In contrast, the 2007 guidelines classified 85.1% as negative, 11.0% as positive, and 3.9% as equivocal, while the FDA guidelines classified 13.1% as positive and 86.9% as negative (there is no “equivocal” category in the FDA guidelines). Thus, “the final FISH interpretations indicate that by using 2013 guidelines, 358 additional patients were interpreted as positive, compared with the 2007 guidelines and that 298 additional patients were considered positive, compared with the FDA criteria,” Dr. Shah and his associates said.
The 2013 guidelines recommend additional chromosome 17 probe testing (among other strategies) to resolve equivocal results, so the investigators did so with the 405 samples classified as equivocal by the 2013 criteria. This resulted in 52.3% of the 405 equivocal tumors being reclassified as HER2 positive, 8.9% being reclassified as HER2 negative, and 38.8% remaining equivocal. Thus, HER2 positivity in the overall cohort rose significantly to 23.6% using the newest guidelines.
These findings demonstrate that using the 2013 guidelines for IHC and FISH pathology testing identifies more women who are eligible for HER2-directed therapy, the investigators said (J Clin Oncol. 2016 Jul 25. doi: 10.1200/JCO.2015.61.8983).
New guidelines for immunohistochemistry (IHC) and fluorescent in situ hybridization (FISH) pathology testing categorize more breast cancers as “equivocal” regarding HER2 positivity and ultimately lead to identifying more of them as HER2 positive, investigators reported online in Journal of Clinical Oncology.
The American Society of Clinical Oncology and the College of American Pathologists released updated IHC and FISH guidelines in 2013, after the Food and Drug Administration approved the initial set of such guidelines in 1998 and ASCO/CAP issued their first such guidelines in 2007. “The intent of the 2013 guidelines was to decrease the number of equivocal [cancers],” said Mithun Vinod Shah, MD, PhD, of the Mayo Clinic, Rochester Minn., and his associates.
To assess the impact of implementing the new guidelines, the investigators analyzed 2,851 breast cancer samples sent to their cytogenetics laboratory by 139 medical centers for HER2 testing during a 1-year period. They compared the three sets of testing criteria – the FDA, the 2007, and the 2013 guidelines.
According to the 2013 guidelines, 69.7% of the tumors were classified as HER2 negative, 16.1% as HER2 positive, and 14.2% as equivocal. In contrast, the 2007 guidelines classified 85.1% as negative, 11.0% as positive, and 3.9% as equivocal, while the FDA guidelines classified 13.1% as positive and 86.9% as negative (there is no “equivocal” category in the FDA guidelines). Thus, “the final FISH interpretations indicate that by using 2013 guidelines, 358 additional patients were interpreted as positive, compared with the 2007 guidelines and that 298 additional patients were considered positive, compared with the FDA criteria,” Dr. Shah and his associates said.
The 2013 guidelines recommend additional chromosome 17 probe testing (among other strategies) to resolve equivocal results, so the investigators did so with the 405 samples classified as equivocal by the 2013 criteria. This resulted in 52.3% of the 405 equivocal tumors being reclassified as HER2 positive, 8.9% being reclassified as HER2 negative, and 38.8% remaining equivocal. Thus, HER2 positivity in the overall cohort rose significantly to 23.6% using the newest guidelines.
These findings demonstrate that using the 2013 guidelines for IHC and FISH pathology testing identifies more women who are eligible for HER2-directed therapy, the investigators said (J Clin Oncol. 2016 Jul 25. doi: 10.1200/JCO.2015.61.8983).
New guidelines for immunohistochemistry (IHC) and fluorescent in situ hybridization (FISH) pathology testing categorize more breast cancers as “equivocal” regarding HER2 positivity and ultimately lead to identifying more of them as HER2 positive, investigators reported online in Journal of Clinical Oncology.
The American Society of Clinical Oncology and the College of American Pathologists released updated IHC and FISH guidelines in 2013, after the Food and Drug Administration approved the initial set of such guidelines in 1998 and ASCO/CAP issued their first such guidelines in 2007. “The intent of the 2013 guidelines was to decrease the number of equivocal [cancers],” said Mithun Vinod Shah, MD, PhD, of the Mayo Clinic, Rochester Minn., and his associates.
To assess the impact of implementing the new guidelines, the investigators analyzed 2,851 breast cancer samples sent to their cytogenetics laboratory by 139 medical centers for HER2 testing during a 1-year period. They compared the three sets of testing criteria – the FDA, the 2007, and the 2013 guidelines.
According to the 2013 guidelines, 69.7% of the tumors were classified as HER2 negative, 16.1% as HER2 positive, and 14.2% as equivocal. In contrast, the 2007 guidelines classified 85.1% as negative, 11.0% as positive, and 3.9% as equivocal, while the FDA guidelines classified 13.1% as positive and 86.9% as negative (there is no “equivocal” category in the FDA guidelines). Thus, “the final FISH interpretations indicate that by using 2013 guidelines, 358 additional patients were interpreted as positive, compared with the 2007 guidelines and that 298 additional patients were considered positive, compared with the FDA criteria,” Dr. Shah and his associates said.
The 2013 guidelines recommend additional chromosome 17 probe testing (among other strategies) to resolve equivocal results, so the investigators did so with the 405 samples classified as equivocal by the 2013 criteria. This resulted in 52.3% of the 405 equivocal tumors being reclassified as HER2 positive, 8.9% being reclassified as HER2 negative, and 38.8% remaining equivocal. Thus, HER2 positivity in the overall cohort rose significantly to 23.6% using the newest guidelines.
These findings demonstrate that using the 2013 guidelines for IHC and FISH pathology testing identifies more women who are eligible for HER2-directed therapy, the investigators said (J Clin Oncol. 2016 Jul 25. doi: 10.1200/JCO.2015.61.8983).
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: New IHC and FISH pathology guidelines categorize more breast cancers as “equivocal” regarding HER2 positivity and ultimately lead to identifying more of them as HER2 positive.
Major finding: By using 2013 guidelines, 358 additional tumors were interpreted as positive, compared with the 2007 guidelines and 298 additional tumors were considered positive, compared with the FDA criteria.
Data source: A cohort study involving 2,851 breast cancer samples analyzed according to three different pathology guidelines during a 1-year period.
Disclosures: This study was supported by the Mayo Clinic. Dr. Shah reported having no relevant financial disclosures; his associates reported ties to Merck, Hospira, Ariad Pharmaceuticals, Abbott Molecular, and Genome Diagnostics.
Study shows faster increase in obesity prevalence among cancer survivors
From 1997 to 2014, cancer survivors had a significantly faster increase in obesity prevalence compared with adults without a history of cancer, investigators found.
Furthermore, the elevated annual increase in rates of obesity was more pronounced in women, in breast and colorectal cancer survivors, and in non-Hispanic blacks.
Cancer patients may be at an increased risk for weight gain caused by specific cancer treatments such as chemotherapy, steroid modifications, and various hormone therapies, especially in “hormonally and metabolically driven cancers such as breast and colorectal cancer,” wrote Heather Greenlee, ND, PhD, of Columbia University, New York, and her associates (J Clin Oncol. 2016 July 25. doi: 10.1200/JCO.2016.66.4391). “To better inform future research on obesity and cancer survival and to inform the planning and implementation of weight loss interventions in cancer survivors, we compared trends from 1997 to 2014 in obesity prevalence in U.S. adults with and without a history of cancer,” the researchers explained.
Obesity prevalence and trends were evaluated through the National Health Interview Survey, an ongoing cross-sectional survey of the health status, health care access, and behaviors of the U.S. civilian population conducted by the National Center for Health Statistics.
For the current study, surveys from a total of 538,969 adults aged 18-85 years with (n = 32,447) or without (n = 506,522) a history of cancer were analyzed. Participants provided self-reported height and weight measures from which body mass index was calculated. Obesity was defined as a BMI of 30 kg/m2 or higher for non-Asians and 27.5 kg/m2 or higher for Asians. Participants also self-reported sex, race, and cancer history.
Overall, the prevalence of obesity consistently increased from 1997 to 2014. Among cancer survivors, the prevalence of obesity increased from 22.4% to 31.7% while in adults without a history of cancer, prevalence increased from 20.9% to 29.5%.
The annual increase in the rate of obesity was significantly greater in both women and men with a history of cancer (2.9% and 2.8% respectively) compared with those without a history of cancer (2.3% and 2.4%, P less than .001 for all).
The elevated annual increase in rates of obesity was even higher in colorectal (3.1% in women and 3.7% in men) and breast (3.0%) cancer survivors compared with adults without a history of cancer, but was lower in prostate cancer survivors (2.1%; P = .001 for all).
“These findings call for public health planning of effective and scalable weight management and control programs for cancer survivors, especially for breast and colorectal cancer survivors and for non-Hispanic blacks,” the investigators concluded.
The National Cancer Institute funded the study. Dr. Greenlee and one other investigator reported serving in advisory roles for EHE International.
On Twitter @jessnicolecraig
From 1997 to 2014, cancer survivors had a significantly faster increase in obesity prevalence compared with adults without a history of cancer, investigators found.
Furthermore, the elevated annual increase in rates of obesity was more pronounced in women, in breast and colorectal cancer survivors, and in non-Hispanic blacks.
Cancer patients may be at an increased risk for weight gain caused by specific cancer treatments such as chemotherapy, steroid modifications, and various hormone therapies, especially in “hormonally and metabolically driven cancers such as breast and colorectal cancer,” wrote Heather Greenlee, ND, PhD, of Columbia University, New York, and her associates (J Clin Oncol. 2016 July 25. doi: 10.1200/JCO.2016.66.4391). “To better inform future research on obesity and cancer survival and to inform the planning and implementation of weight loss interventions in cancer survivors, we compared trends from 1997 to 2014 in obesity prevalence in U.S. adults with and without a history of cancer,” the researchers explained.
Obesity prevalence and trends were evaluated through the National Health Interview Survey, an ongoing cross-sectional survey of the health status, health care access, and behaviors of the U.S. civilian population conducted by the National Center for Health Statistics.
For the current study, surveys from a total of 538,969 adults aged 18-85 years with (n = 32,447) or without (n = 506,522) a history of cancer were analyzed. Participants provided self-reported height and weight measures from which body mass index was calculated. Obesity was defined as a BMI of 30 kg/m2 or higher for non-Asians and 27.5 kg/m2 or higher for Asians. Participants also self-reported sex, race, and cancer history.
Overall, the prevalence of obesity consistently increased from 1997 to 2014. Among cancer survivors, the prevalence of obesity increased from 22.4% to 31.7% while in adults without a history of cancer, prevalence increased from 20.9% to 29.5%.
The annual increase in the rate of obesity was significantly greater in both women and men with a history of cancer (2.9% and 2.8% respectively) compared with those without a history of cancer (2.3% and 2.4%, P less than .001 for all).
The elevated annual increase in rates of obesity was even higher in colorectal (3.1% in women and 3.7% in men) and breast (3.0%) cancer survivors compared with adults without a history of cancer, but was lower in prostate cancer survivors (2.1%; P = .001 for all).
“These findings call for public health planning of effective and scalable weight management and control programs for cancer survivors, especially for breast and colorectal cancer survivors and for non-Hispanic blacks,” the investigators concluded.
The National Cancer Institute funded the study. Dr. Greenlee and one other investigator reported serving in advisory roles for EHE International.
On Twitter @jessnicolecraig
From 1997 to 2014, cancer survivors had a significantly faster increase in obesity prevalence compared with adults without a history of cancer, investigators found.
Furthermore, the elevated annual increase in rates of obesity was more pronounced in women, in breast and colorectal cancer survivors, and in non-Hispanic blacks.
Cancer patients may be at an increased risk for weight gain caused by specific cancer treatments such as chemotherapy, steroid modifications, and various hormone therapies, especially in “hormonally and metabolically driven cancers such as breast and colorectal cancer,” wrote Heather Greenlee, ND, PhD, of Columbia University, New York, and her associates (J Clin Oncol. 2016 July 25. doi: 10.1200/JCO.2016.66.4391). “To better inform future research on obesity and cancer survival and to inform the planning and implementation of weight loss interventions in cancer survivors, we compared trends from 1997 to 2014 in obesity prevalence in U.S. adults with and without a history of cancer,” the researchers explained.
Obesity prevalence and trends were evaluated through the National Health Interview Survey, an ongoing cross-sectional survey of the health status, health care access, and behaviors of the U.S. civilian population conducted by the National Center for Health Statistics.
For the current study, surveys from a total of 538,969 adults aged 18-85 years with (n = 32,447) or without (n = 506,522) a history of cancer were analyzed. Participants provided self-reported height and weight measures from which body mass index was calculated. Obesity was defined as a BMI of 30 kg/m2 or higher for non-Asians and 27.5 kg/m2 or higher for Asians. Participants also self-reported sex, race, and cancer history.
Overall, the prevalence of obesity consistently increased from 1997 to 2014. Among cancer survivors, the prevalence of obesity increased from 22.4% to 31.7% while in adults without a history of cancer, prevalence increased from 20.9% to 29.5%.
The annual increase in the rate of obesity was significantly greater in both women and men with a history of cancer (2.9% and 2.8% respectively) compared with those without a history of cancer (2.3% and 2.4%, P less than .001 for all).
The elevated annual increase in rates of obesity was even higher in colorectal (3.1% in women and 3.7% in men) and breast (3.0%) cancer survivors compared with adults without a history of cancer, but was lower in prostate cancer survivors (2.1%; P = .001 for all).
“These findings call for public health planning of effective and scalable weight management and control programs for cancer survivors, especially for breast and colorectal cancer survivors and for non-Hispanic blacks,” the investigators concluded.
The National Cancer Institute funded the study. Dr. Greenlee and one other investigator reported serving in advisory roles for EHE International.
On Twitter @jessnicolecraig
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Cancer survivors had a significantly faster increase in obesity prevalence compared with adults without a history of cancer.
Major finding: The annual increase in the rate of obesity was significantly higher in both women and men with a history of cancer (2.9% and 2.8% respectively) compared with those without a history of cancer (2.3% and 2.4%, P less than .001 for all).
Data source: National Health Interview Survey responses from 538,969 adults aged 18-85 years with (n = 32,447) or without (n = 506,522) a history of cancer.
Disclosures: The National Cancer Institute funded the study. Dr. Greenlee and one other investigator reported serving in advisory roles for EHE International.
Overweight, obesity increase risk of cardiotoxicity from anthracyclines
Being overweight or obese was significantly associated with a greater risk of developing cardiotoxicity among breast cancer patients treated with anthracyclines and/or trastuzumab, investigators found.
Anthracyclines, a class of anticancer agents widely used to treat many cancer types, have a known association with cardiotoxicity. Furthermore, people who are overweight or obese have an increased risk for developing cardiovascular diseases. The purpose of this study was to “explore in greater depth the influence of overweight and obesity as aggravating factors in the development of cardiotoxicity” specifically among patients who received anthracycline and/or trastuzumab as part of their cancer treatment and were therefore at increased risk of experiencing cardiac-related adverse events, wrote Charles Guenancia, MD, PhD, of University Hospital, Dijon Cedex, France, and his associates (J Clin Oncol. 2016 July 25. doi: 10.1200/JCO.2016.67.4846).
These results are from a meta-analysis of 15 published prospective or retrospective cohort studies that investigated or otherwise reported data on the association between overweight and/or obesity and cardiotoxicity resulting from anthracycline and/or trastuzumab use for treating localized or metastatic breast cancer. Together, the 15 studies represented a total of 8,745 breast cancer patients.
Overall, the mean rate of cardiotoxicity was 17% (95% confidence interval, 11%-25%). Patients treated with anthracyclines only (n = 3,898) had a mean rate of cardiotoxicity of 20% (95% CI, 5%-43%) while patients treated with trastuzumab with or without anthracyclines (n = 4,847) had a lower mean rate of cardiotoxicity at 16% (95% CI, 10%-24%).Paired meta-analysis revealed that overweight, defined as a body mass index score of 25 to 29.9, was associated with increased risk of cardiotoxicity with an odds ratio of 1.15 (95% CI, 0.83-1.58). Obesity, defined as a body mass index score of 30 or greater, was associated with a greater risk of cardiotoxicity with an odds ratio of 1.47 (95% CI, 0.95-2.28).
The association between body mass index and the risk of cardiotoxicity did not differ significantly by drug regimen (anthracyclines alone or sequential anthracyclines and trastuzumab).
This study’s funding source was not listed. Dr. Guenancia and one other investigator reported serving in advisory roles and/or receiving financial compensation from various companies.
On Twitter @jessnicolecraig
Being overweight or obese was significantly associated with a greater risk of developing cardiotoxicity among breast cancer patients treated with anthracyclines and/or trastuzumab, investigators found.
Anthracyclines, a class of anticancer agents widely used to treat many cancer types, have a known association with cardiotoxicity. Furthermore, people who are overweight or obese have an increased risk for developing cardiovascular diseases. The purpose of this study was to “explore in greater depth the influence of overweight and obesity as aggravating factors in the development of cardiotoxicity” specifically among patients who received anthracycline and/or trastuzumab as part of their cancer treatment and were therefore at increased risk of experiencing cardiac-related adverse events, wrote Charles Guenancia, MD, PhD, of University Hospital, Dijon Cedex, France, and his associates (J Clin Oncol. 2016 July 25. doi: 10.1200/JCO.2016.67.4846).
These results are from a meta-analysis of 15 published prospective or retrospective cohort studies that investigated or otherwise reported data on the association between overweight and/or obesity and cardiotoxicity resulting from anthracycline and/or trastuzumab use for treating localized or metastatic breast cancer. Together, the 15 studies represented a total of 8,745 breast cancer patients.
Overall, the mean rate of cardiotoxicity was 17% (95% confidence interval, 11%-25%). Patients treated with anthracyclines only (n = 3,898) had a mean rate of cardiotoxicity of 20% (95% CI, 5%-43%) while patients treated with trastuzumab with or without anthracyclines (n = 4,847) had a lower mean rate of cardiotoxicity at 16% (95% CI, 10%-24%).Paired meta-analysis revealed that overweight, defined as a body mass index score of 25 to 29.9, was associated with increased risk of cardiotoxicity with an odds ratio of 1.15 (95% CI, 0.83-1.58). Obesity, defined as a body mass index score of 30 or greater, was associated with a greater risk of cardiotoxicity with an odds ratio of 1.47 (95% CI, 0.95-2.28).
The association between body mass index and the risk of cardiotoxicity did not differ significantly by drug regimen (anthracyclines alone or sequential anthracyclines and trastuzumab).
This study’s funding source was not listed. Dr. Guenancia and one other investigator reported serving in advisory roles and/or receiving financial compensation from various companies.
On Twitter @jessnicolecraig
Being overweight or obese was significantly associated with a greater risk of developing cardiotoxicity among breast cancer patients treated with anthracyclines and/or trastuzumab, investigators found.
Anthracyclines, a class of anticancer agents widely used to treat many cancer types, have a known association with cardiotoxicity. Furthermore, people who are overweight or obese have an increased risk for developing cardiovascular diseases. The purpose of this study was to “explore in greater depth the influence of overweight and obesity as aggravating factors in the development of cardiotoxicity” specifically among patients who received anthracycline and/or trastuzumab as part of their cancer treatment and were therefore at increased risk of experiencing cardiac-related adverse events, wrote Charles Guenancia, MD, PhD, of University Hospital, Dijon Cedex, France, and his associates (J Clin Oncol. 2016 July 25. doi: 10.1200/JCO.2016.67.4846).
These results are from a meta-analysis of 15 published prospective or retrospective cohort studies that investigated or otherwise reported data on the association between overweight and/or obesity and cardiotoxicity resulting from anthracycline and/or trastuzumab use for treating localized or metastatic breast cancer. Together, the 15 studies represented a total of 8,745 breast cancer patients.
Overall, the mean rate of cardiotoxicity was 17% (95% confidence interval, 11%-25%). Patients treated with anthracyclines only (n = 3,898) had a mean rate of cardiotoxicity of 20% (95% CI, 5%-43%) while patients treated with trastuzumab with or without anthracyclines (n = 4,847) had a lower mean rate of cardiotoxicity at 16% (95% CI, 10%-24%).Paired meta-analysis revealed that overweight, defined as a body mass index score of 25 to 29.9, was associated with increased risk of cardiotoxicity with an odds ratio of 1.15 (95% CI, 0.83-1.58). Obesity, defined as a body mass index score of 30 or greater, was associated with a greater risk of cardiotoxicity with an odds ratio of 1.47 (95% CI, 0.95-2.28).
The association between body mass index and the risk of cardiotoxicity did not differ significantly by drug regimen (anthracyclines alone or sequential anthracyclines and trastuzumab).
This study’s funding source was not listed. Dr. Guenancia and one other investigator reported serving in advisory roles and/or receiving financial compensation from various companies.
On Twitter @jessnicolecraig
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Being overweight or obese was significantly associated with a greater risk of developing cardiotoxicity among breast cancer patients treated with anthracycline and/or trastuzumab.
Major finding: Being overweight was associated with increased risk of cardiotoxicity with an odds ratio of 1.15 (95% CI, 0.83-1.58). Obesity was associated with a greater risk of cardiotoxicity with an odds ratio of 1.47 (95% CI, 0.95-2.28).
Data source: A meta-analysis of 15 studies that investigated or otherwise reported data on the association between overweight and/or obesity and cardiotoxicity resulting from anthracyclines and/or trastuzumab use for treating breast cancer.
Disclosures: This study’s funding source was not identified. Dr. Guenancia and one other investigator reported serving in advisory roles and/or receiving financial compensation from various companies.
ASCO: Always screen cancer survivors for chronic pain
All adult cancer survivors should be screened for chronic pain at every visit, according to the American Society of Clinical Oncology’s first clinical practice guideline for managing this patient population, published July 25 in the Journal of Clinical Oncology.
An estimated 14 million adults with a history of cancer are living in the United States alone, and the prevalence of chronic pain related to their malignancy is reported to be as high as 40%. Yet most health care providers “haven’t been trained to recognize or treat long-term pain associated with cancer,” Judith A. Paice, PhD, RN, said in a press statement accompanying the release of the new guideline.
Existing guidelines focus on the acute pain of cancer and its treatment, or on acute pain related to advanced cancer, said Dr. Paice, cochair of the expert panel that developed the guideline and research professor of hematology/oncology at Northwestern University, Chicago.
The chronic pain addressed in the new guideline document can be related to the malignancy itself or to its treatment. Surgery, chemotherapy, hormone therapy, radiation treatment, and stem-cell transplantation can induce dozens of pain-producing complications, including osteonecrosis, bone fractures, peripheral or central nerve damage, fistulas, lymphedema, arthralgias, and myelopathy. The pain can develop months or years after diagnosis, significantly impacting patients’ quality of life well after treatment is completed.
“This guideline will help clinicians identify pain early and develop comprehensive treatment plans using a broad range of approaches,” Dr. Paice said in the statement.
The panel that developed the guideline comprised experts in medical oncology, hematology, pain medicine, palliative care, hospice, radiation oncology, social work, rehabilitation, psychology, and anesthesiology. They performed a systematic review of the literature and based their recommendations on 35 meta-analyses, 9 randomized controlled trials, 19 comparative studies, and expert consensus.
Some key recommendations include the following:
• Screen all survivors of adult cancers for chronic pain using both a physical exam and an in-depth interview that covers physical, functional, psychological, social, and spiritual aspects of pain, as well as the patient’s treatment history and comorbid conditions. The guideline includes a list of 36 common pain syndromes resulting from cancer treatments.
• Monitor patients at every visit for late-onset treatment effects that can produce pain, just as they are monitored for recurrent disease and secondary malignancy. Some cancer survivors may not recognize that their current pain is related to past disease or its treatments, or may consider it an untreatable complication that they have to endure.
• Consider the entire range of pain medicines – not just opioid analgesics – including NSAIDs, acetaminophen, and selected antidepressants and anticonvulsants with analgesic efficacy. The panel noted that some cancer survivors with chronic pain may benefit from other drugs, including muscle relaxants, benzodiazepines, N-methyl-D-aspartate receptor blockers, alpha-2 agonists, and neutraceuticals and botanicals. But they urged caution since the efficacy of these agents has not been fully established.
Consider nonmedical treatments such as physical, occupational, and recreation therapy; exercise; orthotics; ultrasound; massage; acupuncture; cognitive behavioral therapy; relaxation therapy; and TENS or other types of nerve stimulation.
Consider medical cannabis or cannabinoids as an adjuvant but not a first-line pain treatment, being sure to follow specific state regulations.
Consider a trial of opioids only for carefully selected patients who don’t respond to more conservative management. Weigh potential risks against benefits and employ universal precautions to minimize abuse and addiction, and be cautious in coprescribing other centrally-acting agents (J Clin Oncol. 2016 July 25. doi: 10.1200/JCO.2016.68.5206).
The full clinical practice guideline and other clinical tools and resources are available at www.asco.org/chronic-pai-guideline.
The guideline development process was supported by ASCO. Dr. Paice reported having no relevant financial disclosures; some of her associates reported financial ties to industry sources.
All adult cancer survivors should be screened for chronic pain at every visit, according to the American Society of Clinical Oncology’s first clinical practice guideline for managing this patient population, published July 25 in the Journal of Clinical Oncology.
An estimated 14 million adults with a history of cancer are living in the United States alone, and the prevalence of chronic pain related to their malignancy is reported to be as high as 40%. Yet most health care providers “haven’t been trained to recognize or treat long-term pain associated with cancer,” Judith A. Paice, PhD, RN, said in a press statement accompanying the release of the new guideline.
Existing guidelines focus on the acute pain of cancer and its treatment, or on acute pain related to advanced cancer, said Dr. Paice, cochair of the expert panel that developed the guideline and research professor of hematology/oncology at Northwestern University, Chicago.
The chronic pain addressed in the new guideline document can be related to the malignancy itself or to its treatment. Surgery, chemotherapy, hormone therapy, radiation treatment, and stem-cell transplantation can induce dozens of pain-producing complications, including osteonecrosis, bone fractures, peripheral or central nerve damage, fistulas, lymphedema, arthralgias, and myelopathy. The pain can develop months or years after diagnosis, significantly impacting patients’ quality of life well after treatment is completed.
“This guideline will help clinicians identify pain early and develop comprehensive treatment plans using a broad range of approaches,” Dr. Paice said in the statement.
The panel that developed the guideline comprised experts in medical oncology, hematology, pain medicine, palliative care, hospice, radiation oncology, social work, rehabilitation, psychology, and anesthesiology. They performed a systematic review of the literature and based their recommendations on 35 meta-analyses, 9 randomized controlled trials, 19 comparative studies, and expert consensus.
Some key recommendations include the following:
• Screen all survivors of adult cancers for chronic pain using both a physical exam and an in-depth interview that covers physical, functional, psychological, social, and spiritual aspects of pain, as well as the patient’s treatment history and comorbid conditions. The guideline includes a list of 36 common pain syndromes resulting from cancer treatments.
• Monitor patients at every visit for late-onset treatment effects that can produce pain, just as they are monitored for recurrent disease and secondary malignancy. Some cancer survivors may not recognize that their current pain is related to past disease or its treatments, or may consider it an untreatable complication that they have to endure.
• Consider the entire range of pain medicines – not just opioid analgesics – including NSAIDs, acetaminophen, and selected antidepressants and anticonvulsants with analgesic efficacy. The panel noted that some cancer survivors with chronic pain may benefit from other drugs, including muscle relaxants, benzodiazepines, N-methyl-D-aspartate receptor blockers, alpha-2 agonists, and neutraceuticals and botanicals. But they urged caution since the efficacy of these agents has not been fully established.
Consider nonmedical treatments such as physical, occupational, and recreation therapy; exercise; orthotics; ultrasound; massage; acupuncture; cognitive behavioral therapy; relaxation therapy; and TENS or other types of nerve stimulation.
Consider medical cannabis or cannabinoids as an adjuvant but not a first-line pain treatment, being sure to follow specific state regulations.
Consider a trial of opioids only for carefully selected patients who don’t respond to more conservative management. Weigh potential risks against benefits and employ universal precautions to minimize abuse and addiction, and be cautious in coprescribing other centrally-acting agents (J Clin Oncol. 2016 July 25. doi: 10.1200/JCO.2016.68.5206).
The full clinical practice guideline and other clinical tools and resources are available at www.asco.org/chronic-pai-guideline.
The guideline development process was supported by ASCO. Dr. Paice reported having no relevant financial disclosures; some of her associates reported financial ties to industry sources.
All adult cancer survivors should be screened for chronic pain at every visit, according to the American Society of Clinical Oncology’s first clinical practice guideline for managing this patient population, published July 25 in the Journal of Clinical Oncology.
An estimated 14 million adults with a history of cancer are living in the United States alone, and the prevalence of chronic pain related to their malignancy is reported to be as high as 40%. Yet most health care providers “haven’t been trained to recognize or treat long-term pain associated with cancer,” Judith A. Paice, PhD, RN, said in a press statement accompanying the release of the new guideline.
Existing guidelines focus on the acute pain of cancer and its treatment, or on acute pain related to advanced cancer, said Dr. Paice, cochair of the expert panel that developed the guideline and research professor of hematology/oncology at Northwestern University, Chicago.
The chronic pain addressed in the new guideline document can be related to the malignancy itself or to its treatment. Surgery, chemotherapy, hormone therapy, radiation treatment, and stem-cell transplantation can induce dozens of pain-producing complications, including osteonecrosis, bone fractures, peripheral or central nerve damage, fistulas, lymphedema, arthralgias, and myelopathy. The pain can develop months or years after diagnosis, significantly impacting patients’ quality of life well after treatment is completed.
“This guideline will help clinicians identify pain early and develop comprehensive treatment plans using a broad range of approaches,” Dr. Paice said in the statement.
The panel that developed the guideline comprised experts in medical oncology, hematology, pain medicine, palliative care, hospice, radiation oncology, social work, rehabilitation, psychology, and anesthesiology. They performed a systematic review of the literature and based their recommendations on 35 meta-analyses, 9 randomized controlled trials, 19 comparative studies, and expert consensus.
Some key recommendations include the following:
• Screen all survivors of adult cancers for chronic pain using both a physical exam and an in-depth interview that covers physical, functional, psychological, social, and spiritual aspects of pain, as well as the patient’s treatment history and comorbid conditions. The guideline includes a list of 36 common pain syndromes resulting from cancer treatments.
• Monitor patients at every visit for late-onset treatment effects that can produce pain, just as they are monitored for recurrent disease and secondary malignancy. Some cancer survivors may not recognize that their current pain is related to past disease or its treatments, or may consider it an untreatable complication that they have to endure.
• Consider the entire range of pain medicines – not just opioid analgesics – including NSAIDs, acetaminophen, and selected antidepressants and anticonvulsants with analgesic efficacy. The panel noted that some cancer survivors with chronic pain may benefit from other drugs, including muscle relaxants, benzodiazepines, N-methyl-D-aspartate receptor blockers, alpha-2 agonists, and neutraceuticals and botanicals. But they urged caution since the efficacy of these agents has not been fully established.
Consider nonmedical treatments such as physical, occupational, and recreation therapy; exercise; orthotics; ultrasound; massage; acupuncture; cognitive behavioral therapy; relaxation therapy; and TENS or other types of nerve stimulation.
Consider medical cannabis or cannabinoids as an adjuvant but not a first-line pain treatment, being sure to follow specific state regulations.
Consider a trial of opioids only for carefully selected patients who don’t respond to more conservative management. Weigh potential risks against benefits and employ universal precautions to minimize abuse and addiction, and be cautious in coprescribing other centrally-acting agents (J Clin Oncol. 2016 July 25. doi: 10.1200/JCO.2016.68.5206).
The full clinical practice guideline and other clinical tools and resources are available at www.asco.org/chronic-pai-guideline.
The guideline development process was supported by ASCO. Dr. Paice reported having no relevant financial disclosures; some of her associates reported financial ties to industry sources.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Screen all survivors of adult cancers for chronic pain at every visit.
Major finding: An estimated 14 million adults with a history of cancer are living in the United States alone, and the prevalence of chronic pain related to their malignancy is reported to be as high as 40%.
Data source: The first ASCO clinical practice guideline for managing chronic pain in survivors of adult cancers.
Disclosures: This work was supported by ASCO. Dr. Paice reported having no relevant financial disclosures; some of her associates reported financial ties to industry.
Cervical cancer screening: How our approach may change
› Screen for cervical cancer in women ages 21 to 29 using cytology alone every 3 years. For women ages 30 to 65, screening with a combination of cytology and human papillomavirus (HPV) testing every 5 years is the preferred option. A
› Be aware of the alternative guideline proposed by several specialty organizations: All women ages 25 to 64 should receive primary HPV screening every 3 years with the FDA-approved HPV test. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
If the cervical cytology report you receive for a woman in her mid-20s is negative, how soon would you plan to repeat testing? Recommendations from the United States Preventive Services Task Force (USPSTF) and other leading organizations advise a combination of cytology and human papillomavirus (HPV) testing at specified intervals depending on a patient’s age. However, a study published in 2015 analyzed data from a statewide registry on provider behavior and found a wide array of screening intervals in practice and infrequent use of HPV testing.1 Clearly, adherence to published guidelines has been inconsistent.
Now, recommendations by several specialty groups are evolving based on newer evidence regarding HPV testing. These alternative guidelines recommend primary high-risk HPV testing for all women. This change is the topic of much national debate and is being researched for the USPSTF’s 2018 update on cervical cancer screening.
In this article, I review the USPSTF’s present recommendations and look ahead to how “best practices” for cervical cancer screening may be changing.
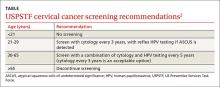
Current cervical cancer screening guidelines
Many subspecialty organizations and government agencies publish cervical cancer screening guidelines. The USPSTF guidelines, reviewed here, are evidence based, frequently updated, and widely used by primary care providers (TABLE).2,3 These guidelines recommend initiating cytology testing at age 21 and, if results are normal, repeating every 3 years. Reflex HPV testing is recommended if cytology results reveal atypical squamous cells of undetermined significance (ASCUS). For women ages 30 to 65, the preferred option is to undergo a combination of cytology and HPV testing every 5 years.2 Women older than 65 may discontinue screening.2 HPV immunization status does not affect USPSTF recommendations. Nationwide rates of HPV vaccination among females ages 13 to 17 vary among states, from ≤49% to ≥70%.4
What the guidelines do, and do not, cover. The USPSTF screening intervals apply as long as testing results are normal.2 These guidelines apply to all women regardless of the age at which they began sexual activity. These guidelines do not apply to women who have had abnormal cytology or HPV results and have not undergone adequate follow-up to ensure their lesion has cleared.5 These guidelines also do not apply to women who are immunosuppressed, who were exposed to diethylstilbestrol (DES) in utero, who have had a hysterectomy for non-oncologic reasons, or who have had cervical cancer.5 A woman may stop routine screening after age 65 if she has had adequate follow-up including either 3 negative cytology samples or 2 negative co-tests (cytology and HPV test) in the last 10 years.6 A woman may also discontinue screening if she has had a total hysterectomy and has no history of cervical dysplasia.7
Evidence behind the guidelines. The USPSTF guidelines were updated to their current state in 2012 reflecting a growing body of evidence that, for women 30 years and older, detection of cervical intraepithelial neoplasia (CIN) 3+ lesions improves with HPV co-testing. The supporting studies also found that the risk of a high-grade lesion appearing 5 years following co-testing was equivalent to the risk seen with cytology samples alone taken at 3-year intervals.8 The sensitivity of a single cytology test is only about 50%.9 A patient’s risk of cervical cancer 18 months after 3 negative cytology tests is about 1.5/100,000.10 The risk at 36 months following 3 negative cytology results is about 4.5/100,000. Annual screening would require almost 100,000 women to be screened to detect 3 additional cases of cervical cancer.10
Additional benefits of the updated USPSTF guidelines. The updated strategy decreases the number of visits for patients and the number of colposcopies, minimizing harm and patient anxiety. The current management algorithms also recommend more conservative management of women in their early 20s who have reported abnormal cytology, as the likelihood of their lesion clearing within 12 to 24 months is high.5 The recommendation does not call for high-risk HPV testing of women ages 21 to 29 because the infection is highly prevalent in this age group and is also likely to clear before any significant pathology arises. This avoids unnecessary and potentially harmful treatment of younger women.11
What about the alternative screening guideline?
In early 2015, the American Society for Colposcopy and Cervical Pathology (ASCCP) and the Society of Gynecologic Oncology (SGO) co-sponsored an expert panel representing several specialty societies. The panel released interim guidelines for cervical cancer screening reflecting a growing body of evidence that favors HPV testing as the primary modality.12 Additionally, in January 2016, these guidelines received an evidence-level B rating from the American Congress of Obstetricians and Gynecologists.13 Primary HPV screening is also the topic of research and discussion for USPSTF’s pending 2018 update of cervical cancer screening strategies.14
The alternative algorithm from the ASCCP and SGO recommends cervical cancer screening with HPV testing alone starting at the age of 25 and, if results are negative, repeating at 3-year intervals.12 If a patient tests positive for any of the 14 identified high-risk HPV types, reflex cytology is indicated with a referral for colposcopy if an abnormality is identified.12 If the cytology result is normal, follow-up with another HPV test in 12 months is recommended.12
Over the last 12 years, multiple international studies have demonstrated the efficacy of high-risk HPV testing in primary screening for cervical cancer.15 The most recent study conducted in the United States from 2008 to 2011—Addressing THE Need for Advanced HPV Diagnostics (ATHENA)—enrolled 42,000 women older than 25 years to compare the screening modalities of cytology alone, cytology and HPV testing combined, and HPV testing alone.16 The purpose of the study was to determine the safety of the cobas HPV test as a co-test and as a primary screening modality in women older than 25 years. (Many HPV tests are commercially available, but only the cobas HPV test is FDA-approved for primary screening.12)
ATHENA researchers concluded that HPV testing was more sensitive than cytology, but less specific.16 The researchers also concluded that adding cytology to the HPV test increased the sensitivity by less than 5% and that HPV was better at detecting CIN 2+ lesions than cytology alone.12,16 Another recently published study conducted at a tertiary care hospital with a smaller sample (1000 patients) corroborated the ATHENA results.17
For patients in their late 20s, this alternative strategy may increase the number of subsequent colposcopies. However, during the clinical trials just described, the absolute number of colposcopies needed to detect high-grade disease was the same as seen with the current guidelines. This finding indicates that, with the current algorithm, clinically significant pathology due to high-risk HPV may be missed in the 25-to-29 age group.8
Looking ahead. The alternative screening strategy is already being adopted in Australia, the Netherlands, and the United Kingdom.15 For providers in the United States considering this alternative strategy, the recommendation is to initiate cervical cancer screening with cytology alone at age 21, manage results appropriately, and then transition the patient to primary HPV testing with the FDA-approved test at age 25.12 This recommendation may be modified in the future. However the guidelines might change, patients will benefit only if the guidelines are implemented consistently in practice.
CORRESPONDENCE
Sabrina Hofmeister, DO, 1121 E. North Ave, Milwaukee, WI 53212; shofmeister@mcw.edu.
1. Kim JJ, Campos NG, Sy S, et al. Inefficiencies and high-value improvements in U.S. cervical cancer screening practice: a cost-effective analysis. Ann Intern Med. 2015;163:589-597.
2. Moyer VA; U.S. Preventive Services Task Force. Screening for cervical cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;156:880-891.
3. U.S. Preventive Services Task Force. Understanding How the USPSTF Works: USPSTF 101. Available at: http://www.uspreventiveservicestaskforce.org/Page/Name/understanding-how-the-uspstf-works. Accessed June 8, 2016.
4. Reagan-Steiner S, Yankey D, Jeyarajah J, et al; Centers for Disease Control and Prevention. National, regional, state, and selected local vaccination coverage among adolescents aged 13-17 years—United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64:784-792.
5. Saslow D, Solomon D, Lawson HW, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. J Low Genit Tract Dis. 2012;16:175-204.
6. Vesco KK, Whitlock EP, Eder M, et al. Risk factors and other epidemiologic considerations for cervical cancer screening: a narrative review for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;155:687-697.
7. Khan MJ, Massad LS, Kinney W, et al. A common clinical dilemma: management of abnormal vaginal cytology and human papilloma virus test results. J Low Genit Tract Dis. 2016;20:119-125.
8. Wright TC, Stoler MH, Behrens CM, et al. Primary cervical cancer screening with human papillomavirus: end of study results from the ATHENA study using HPV as the first-line screening test. Gynecol Oncol. 2015;136:189-197.
9. Naucler P, Ryd W, Törnberg S, et al. Human papillomavirus and Papanicolaou tests to screen for cervical cancer. N Engl J Med. 2007;357:1589-1597.
10. Sawaya GF, Sung HY, Kinney W, et al. Cervical cancer after multiple negative tests in long-term members of a prepaid health plan. Acta Cytol. 2005;49:391-397.
11. Dunne EF, Unger ER, Sternberg M, et al. Prevalence of HPV infection among females in the United States. JAMA. 2007;297:813-819.
12. Huh WK, Ault KA, Chelmow D, et al. Use of primary high-risk HPV testing for cervical cancer screening: interim clinical guidance. J Low Genit Tract Dis. 2015;19:91-96.
13. American Congress of Obstetricians and Gynecologists. Practice Bulletin No. 157: Cervical cancer screening and prevention. Obstet Gynecol. 2016;127:e1-e20.
14. U.S. Preventive Services Task Force. Final Research Plan: Cervical Cancer: Screening. October 2015. Available at: http://www.uspreventiveservicestaskforce.org/Page/Document/final-research-plan/cervical-cancer-screening2. Accessed June 22, 2016.
15. Ronco G, Dillner J, Elfström KM, et al; International HPV Working Group. Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled trials. Lancet. 2014;383:524-532.
16. Stoler MH, Wright TC Jr, Sharma A, et al. High-risk human papilloma virus testing in women with ASC-US cytology: results from the ATHENA HPV study. Am J Clin Path. 2011;135:468-475.
17. Choi JW, Kim Y, Lee JH, et al. The clinical performance of primary HPV screening, primary HPV screening plus cytology cotesting, and cytology alone at a tertiary care hospital. Cancer Cytopathol. 2016;124:144-152.
› Screen for cervical cancer in women ages 21 to 29 using cytology alone every 3 years. For women ages 30 to 65, screening with a combination of cytology and human papillomavirus (HPV) testing every 5 years is the preferred option. A
› Be aware of the alternative guideline proposed by several specialty organizations: All women ages 25 to 64 should receive primary HPV screening every 3 years with the FDA-approved HPV test. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
If the cervical cytology report you receive for a woman in her mid-20s is negative, how soon would you plan to repeat testing? Recommendations from the United States Preventive Services Task Force (USPSTF) and other leading organizations advise a combination of cytology and human papillomavirus (HPV) testing at specified intervals depending on a patient’s age. However, a study published in 2015 analyzed data from a statewide registry on provider behavior and found a wide array of screening intervals in practice and infrequent use of HPV testing.1 Clearly, adherence to published guidelines has been inconsistent.
Now, recommendations by several specialty groups are evolving based on newer evidence regarding HPV testing. These alternative guidelines recommend primary high-risk HPV testing for all women. This change is the topic of much national debate and is being researched for the USPSTF’s 2018 update on cervical cancer screening.
In this article, I review the USPSTF’s present recommendations and look ahead to how “best practices” for cervical cancer screening may be changing.
Current cervical cancer screening guidelines
Many subspecialty organizations and government agencies publish cervical cancer screening guidelines. The USPSTF guidelines, reviewed here, are evidence based, frequently updated, and widely used by primary care providers (TABLE).2,3 These guidelines recommend initiating cytology testing at age 21 and, if results are normal, repeating every 3 years. Reflex HPV testing is recommended if cytology results reveal atypical squamous cells of undetermined significance (ASCUS). For women ages 30 to 65, the preferred option is to undergo a combination of cytology and HPV testing every 5 years.2 Women older than 65 may discontinue screening.2 HPV immunization status does not affect USPSTF recommendations. Nationwide rates of HPV vaccination among females ages 13 to 17 vary among states, from ≤49% to ≥70%.4
What the guidelines do, and do not, cover. The USPSTF screening intervals apply as long as testing results are normal.2 These guidelines apply to all women regardless of the age at which they began sexual activity. These guidelines do not apply to women who have had abnormal cytology or HPV results and have not undergone adequate follow-up to ensure their lesion has cleared.5 These guidelines also do not apply to women who are immunosuppressed, who were exposed to diethylstilbestrol (DES) in utero, who have had a hysterectomy for non-oncologic reasons, or who have had cervical cancer.5 A woman may stop routine screening after age 65 if she has had adequate follow-up including either 3 negative cytology samples or 2 negative co-tests (cytology and HPV test) in the last 10 years.6 A woman may also discontinue screening if she has had a total hysterectomy and has no history of cervical dysplasia.7
Evidence behind the guidelines. The USPSTF guidelines were updated to their current state in 2012 reflecting a growing body of evidence that, for women 30 years and older, detection of cervical intraepithelial neoplasia (CIN) 3+ lesions improves with HPV co-testing. The supporting studies also found that the risk of a high-grade lesion appearing 5 years following co-testing was equivalent to the risk seen with cytology samples alone taken at 3-year intervals.8 The sensitivity of a single cytology test is only about 50%.9 A patient’s risk of cervical cancer 18 months after 3 negative cytology tests is about 1.5/100,000.10 The risk at 36 months following 3 negative cytology results is about 4.5/100,000. Annual screening would require almost 100,000 women to be screened to detect 3 additional cases of cervical cancer.10
Additional benefits of the updated USPSTF guidelines. The updated strategy decreases the number of visits for patients and the number of colposcopies, minimizing harm and patient anxiety. The current management algorithms also recommend more conservative management of women in their early 20s who have reported abnormal cytology, as the likelihood of their lesion clearing within 12 to 24 months is high.5 The recommendation does not call for high-risk HPV testing of women ages 21 to 29 because the infection is highly prevalent in this age group and is also likely to clear before any significant pathology arises. This avoids unnecessary and potentially harmful treatment of younger women.11
What about the alternative screening guideline?
In early 2015, the American Society for Colposcopy and Cervical Pathology (ASCCP) and the Society of Gynecologic Oncology (SGO) co-sponsored an expert panel representing several specialty societies. The panel released interim guidelines for cervical cancer screening reflecting a growing body of evidence that favors HPV testing as the primary modality.12 Additionally, in January 2016, these guidelines received an evidence-level B rating from the American Congress of Obstetricians and Gynecologists.13 Primary HPV screening is also the topic of research and discussion for USPSTF’s pending 2018 update of cervical cancer screening strategies.14
The alternative algorithm from the ASCCP and SGO recommends cervical cancer screening with HPV testing alone starting at the age of 25 and, if results are negative, repeating at 3-year intervals.12 If a patient tests positive for any of the 14 identified high-risk HPV types, reflex cytology is indicated with a referral for colposcopy if an abnormality is identified.12 If the cytology result is normal, follow-up with another HPV test in 12 months is recommended.12
Over the last 12 years, multiple international studies have demonstrated the efficacy of high-risk HPV testing in primary screening for cervical cancer.15 The most recent study conducted in the United States from 2008 to 2011—Addressing THE Need for Advanced HPV Diagnostics (ATHENA)—enrolled 42,000 women older than 25 years to compare the screening modalities of cytology alone, cytology and HPV testing combined, and HPV testing alone.16 The purpose of the study was to determine the safety of the cobas HPV test as a co-test and as a primary screening modality in women older than 25 years. (Many HPV tests are commercially available, but only the cobas HPV test is FDA-approved for primary screening.12)
ATHENA researchers concluded that HPV testing was more sensitive than cytology, but less specific.16 The researchers also concluded that adding cytology to the HPV test increased the sensitivity by less than 5% and that HPV was better at detecting CIN 2+ lesions than cytology alone.12,16 Another recently published study conducted at a tertiary care hospital with a smaller sample (1000 patients) corroborated the ATHENA results.17
For patients in their late 20s, this alternative strategy may increase the number of subsequent colposcopies. However, during the clinical trials just described, the absolute number of colposcopies needed to detect high-grade disease was the same as seen with the current guidelines. This finding indicates that, with the current algorithm, clinically significant pathology due to high-risk HPV may be missed in the 25-to-29 age group.8
Looking ahead. The alternative screening strategy is already being adopted in Australia, the Netherlands, and the United Kingdom.15 For providers in the United States considering this alternative strategy, the recommendation is to initiate cervical cancer screening with cytology alone at age 21, manage results appropriately, and then transition the patient to primary HPV testing with the FDA-approved test at age 25.12 This recommendation may be modified in the future. However the guidelines might change, patients will benefit only if the guidelines are implemented consistently in practice.
CORRESPONDENCE
Sabrina Hofmeister, DO, 1121 E. North Ave, Milwaukee, WI 53212; shofmeister@mcw.edu.
› Screen for cervical cancer in women ages 21 to 29 using cytology alone every 3 years. For women ages 30 to 65, screening with a combination of cytology and human papillomavirus (HPV) testing every 5 years is the preferred option. A
› Be aware of the alternative guideline proposed by several specialty organizations: All women ages 25 to 64 should receive primary HPV screening every 3 years with the FDA-approved HPV test. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
If the cervical cytology report you receive for a woman in her mid-20s is negative, how soon would you plan to repeat testing? Recommendations from the United States Preventive Services Task Force (USPSTF) and other leading organizations advise a combination of cytology and human papillomavirus (HPV) testing at specified intervals depending on a patient’s age. However, a study published in 2015 analyzed data from a statewide registry on provider behavior and found a wide array of screening intervals in practice and infrequent use of HPV testing.1 Clearly, adherence to published guidelines has been inconsistent.
Now, recommendations by several specialty groups are evolving based on newer evidence regarding HPV testing. These alternative guidelines recommend primary high-risk HPV testing for all women. This change is the topic of much national debate and is being researched for the USPSTF’s 2018 update on cervical cancer screening.
In this article, I review the USPSTF’s present recommendations and look ahead to how “best practices” for cervical cancer screening may be changing.
Current cervical cancer screening guidelines
Many subspecialty organizations and government agencies publish cervical cancer screening guidelines. The USPSTF guidelines, reviewed here, are evidence based, frequently updated, and widely used by primary care providers (TABLE).2,3 These guidelines recommend initiating cytology testing at age 21 and, if results are normal, repeating every 3 years. Reflex HPV testing is recommended if cytology results reveal atypical squamous cells of undetermined significance (ASCUS). For women ages 30 to 65, the preferred option is to undergo a combination of cytology and HPV testing every 5 years.2 Women older than 65 may discontinue screening.2 HPV immunization status does not affect USPSTF recommendations. Nationwide rates of HPV vaccination among females ages 13 to 17 vary among states, from ≤49% to ≥70%.4
What the guidelines do, and do not, cover. The USPSTF screening intervals apply as long as testing results are normal.2 These guidelines apply to all women regardless of the age at which they began sexual activity. These guidelines do not apply to women who have had abnormal cytology or HPV results and have not undergone adequate follow-up to ensure their lesion has cleared.5 These guidelines also do not apply to women who are immunosuppressed, who were exposed to diethylstilbestrol (DES) in utero, who have had a hysterectomy for non-oncologic reasons, or who have had cervical cancer.5 A woman may stop routine screening after age 65 if she has had adequate follow-up including either 3 negative cytology samples or 2 negative co-tests (cytology and HPV test) in the last 10 years.6 A woman may also discontinue screening if she has had a total hysterectomy and has no history of cervical dysplasia.7
Evidence behind the guidelines. The USPSTF guidelines were updated to their current state in 2012 reflecting a growing body of evidence that, for women 30 years and older, detection of cervical intraepithelial neoplasia (CIN) 3+ lesions improves with HPV co-testing. The supporting studies also found that the risk of a high-grade lesion appearing 5 years following co-testing was equivalent to the risk seen with cytology samples alone taken at 3-year intervals.8 The sensitivity of a single cytology test is only about 50%.9 A patient’s risk of cervical cancer 18 months after 3 negative cytology tests is about 1.5/100,000.10 The risk at 36 months following 3 negative cytology results is about 4.5/100,000. Annual screening would require almost 100,000 women to be screened to detect 3 additional cases of cervical cancer.10
Additional benefits of the updated USPSTF guidelines. The updated strategy decreases the number of visits for patients and the number of colposcopies, minimizing harm and patient anxiety. The current management algorithms also recommend more conservative management of women in their early 20s who have reported abnormal cytology, as the likelihood of their lesion clearing within 12 to 24 months is high.5 The recommendation does not call for high-risk HPV testing of women ages 21 to 29 because the infection is highly prevalent in this age group and is also likely to clear before any significant pathology arises. This avoids unnecessary and potentially harmful treatment of younger women.11
What about the alternative screening guideline?
In early 2015, the American Society for Colposcopy and Cervical Pathology (ASCCP) and the Society of Gynecologic Oncology (SGO) co-sponsored an expert panel representing several specialty societies. The panel released interim guidelines for cervical cancer screening reflecting a growing body of evidence that favors HPV testing as the primary modality.12 Additionally, in January 2016, these guidelines received an evidence-level B rating from the American Congress of Obstetricians and Gynecologists.13 Primary HPV screening is also the topic of research and discussion for USPSTF’s pending 2018 update of cervical cancer screening strategies.14
The alternative algorithm from the ASCCP and SGO recommends cervical cancer screening with HPV testing alone starting at the age of 25 and, if results are negative, repeating at 3-year intervals.12 If a patient tests positive for any of the 14 identified high-risk HPV types, reflex cytology is indicated with a referral for colposcopy if an abnormality is identified.12 If the cytology result is normal, follow-up with another HPV test in 12 months is recommended.12
Over the last 12 years, multiple international studies have demonstrated the efficacy of high-risk HPV testing in primary screening for cervical cancer.15 The most recent study conducted in the United States from 2008 to 2011—Addressing THE Need for Advanced HPV Diagnostics (ATHENA)—enrolled 42,000 women older than 25 years to compare the screening modalities of cytology alone, cytology and HPV testing combined, and HPV testing alone.16 The purpose of the study was to determine the safety of the cobas HPV test as a co-test and as a primary screening modality in women older than 25 years. (Many HPV tests are commercially available, but only the cobas HPV test is FDA-approved for primary screening.12)
ATHENA researchers concluded that HPV testing was more sensitive than cytology, but less specific.16 The researchers also concluded that adding cytology to the HPV test increased the sensitivity by less than 5% and that HPV was better at detecting CIN 2+ lesions than cytology alone.12,16 Another recently published study conducted at a tertiary care hospital with a smaller sample (1000 patients) corroborated the ATHENA results.17
For patients in their late 20s, this alternative strategy may increase the number of subsequent colposcopies. However, during the clinical trials just described, the absolute number of colposcopies needed to detect high-grade disease was the same as seen with the current guidelines. This finding indicates that, with the current algorithm, clinically significant pathology due to high-risk HPV may be missed in the 25-to-29 age group.8
Looking ahead. The alternative screening strategy is already being adopted in Australia, the Netherlands, and the United Kingdom.15 For providers in the United States considering this alternative strategy, the recommendation is to initiate cervical cancer screening with cytology alone at age 21, manage results appropriately, and then transition the patient to primary HPV testing with the FDA-approved test at age 25.12 This recommendation may be modified in the future. However the guidelines might change, patients will benefit only if the guidelines are implemented consistently in practice.
CORRESPONDENCE
Sabrina Hofmeister, DO, 1121 E. North Ave, Milwaukee, WI 53212; shofmeister@mcw.edu.
1. Kim JJ, Campos NG, Sy S, et al. Inefficiencies and high-value improvements in U.S. cervical cancer screening practice: a cost-effective analysis. Ann Intern Med. 2015;163:589-597.
2. Moyer VA; U.S. Preventive Services Task Force. Screening for cervical cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;156:880-891.
3. U.S. Preventive Services Task Force. Understanding How the USPSTF Works: USPSTF 101. Available at: http://www.uspreventiveservicestaskforce.org/Page/Name/understanding-how-the-uspstf-works. Accessed June 8, 2016.
4. Reagan-Steiner S, Yankey D, Jeyarajah J, et al; Centers for Disease Control and Prevention. National, regional, state, and selected local vaccination coverage among adolescents aged 13-17 years—United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64:784-792.
5. Saslow D, Solomon D, Lawson HW, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. J Low Genit Tract Dis. 2012;16:175-204.
6. Vesco KK, Whitlock EP, Eder M, et al. Risk factors and other epidemiologic considerations for cervical cancer screening: a narrative review for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;155:687-697.
7. Khan MJ, Massad LS, Kinney W, et al. A common clinical dilemma: management of abnormal vaginal cytology and human papilloma virus test results. J Low Genit Tract Dis. 2016;20:119-125.
8. Wright TC, Stoler MH, Behrens CM, et al. Primary cervical cancer screening with human papillomavirus: end of study results from the ATHENA study using HPV as the first-line screening test. Gynecol Oncol. 2015;136:189-197.
9. Naucler P, Ryd W, Törnberg S, et al. Human papillomavirus and Papanicolaou tests to screen for cervical cancer. N Engl J Med. 2007;357:1589-1597.
10. Sawaya GF, Sung HY, Kinney W, et al. Cervical cancer after multiple negative tests in long-term members of a prepaid health plan. Acta Cytol. 2005;49:391-397.
11. Dunne EF, Unger ER, Sternberg M, et al. Prevalence of HPV infection among females in the United States. JAMA. 2007;297:813-819.
12. Huh WK, Ault KA, Chelmow D, et al. Use of primary high-risk HPV testing for cervical cancer screening: interim clinical guidance. J Low Genit Tract Dis. 2015;19:91-96.
13. American Congress of Obstetricians and Gynecologists. Practice Bulletin No. 157: Cervical cancer screening and prevention. Obstet Gynecol. 2016;127:e1-e20.
14. U.S. Preventive Services Task Force. Final Research Plan: Cervical Cancer: Screening. October 2015. Available at: http://www.uspreventiveservicestaskforce.org/Page/Document/final-research-plan/cervical-cancer-screening2. Accessed June 22, 2016.
15. Ronco G, Dillner J, Elfström KM, et al; International HPV Working Group. Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled trials. Lancet. 2014;383:524-532.
16. Stoler MH, Wright TC Jr, Sharma A, et al. High-risk human papilloma virus testing in women with ASC-US cytology: results from the ATHENA HPV study. Am J Clin Path. 2011;135:468-475.
17. Choi JW, Kim Y, Lee JH, et al. The clinical performance of primary HPV screening, primary HPV screening plus cytology cotesting, and cytology alone at a tertiary care hospital. Cancer Cytopathol. 2016;124:144-152.
1. Kim JJ, Campos NG, Sy S, et al. Inefficiencies and high-value improvements in U.S. cervical cancer screening practice: a cost-effective analysis. Ann Intern Med. 2015;163:589-597.
2. Moyer VA; U.S. Preventive Services Task Force. Screening for cervical cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;156:880-891.
3. U.S. Preventive Services Task Force. Understanding How the USPSTF Works: USPSTF 101. Available at: http://www.uspreventiveservicestaskforce.org/Page/Name/understanding-how-the-uspstf-works. Accessed June 8, 2016.
4. Reagan-Steiner S, Yankey D, Jeyarajah J, et al; Centers for Disease Control and Prevention. National, regional, state, and selected local vaccination coverage among adolescents aged 13-17 years—United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64:784-792.
5. Saslow D, Solomon D, Lawson HW, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. J Low Genit Tract Dis. 2012;16:175-204.
6. Vesco KK, Whitlock EP, Eder M, et al. Risk factors and other epidemiologic considerations for cervical cancer screening: a narrative review for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;155:687-697.
7. Khan MJ, Massad LS, Kinney W, et al. A common clinical dilemma: management of abnormal vaginal cytology and human papilloma virus test results. J Low Genit Tract Dis. 2016;20:119-125.
8. Wright TC, Stoler MH, Behrens CM, et al. Primary cervical cancer screening with human papillomavirus: end of study results from the ATHENA study using HPV as the first-line screening test. Gynecol Oncol. 2015;136:189-197.
9. Naucler P, Ryd W, Törnberg S, et al. Human papillomavirus and Papanicolaou tests to screen for cervical cancer. N Engl J Med. 2007;357:1589-1597.
10. Sawaya GF, Sung HY, Kinney W, et al. Cervical cancer after multiple negative tests in long-term members of a prepaid health plan. Acta Cytol. 2005;49:391-397.
11. Dunne EF, Unger ER, Sternberg M, et al. Prevalence of HPV infection among females in the United States. JAMA. 2007;297:813-819.
12. Huh WK, Ault KA, Chelmow D, et al. Use of primary high-risk HPV testing for cervical cancer screening: interim clinical guidance. J Low Genit Tract Dis. 2015;19:91-96.
13. American Congress of Obstetricians and Gynecologists. Practice Bulletin No. 157: Cervical cancer screening and prevention. Obstet Gynecol. 2016;127:e1-e20.
14. U.S. Preventive Services Task Force. Final Research Plan: Cervical Cancer: Screening. October 2015. Available at: http://www.uspreventiveservicestaskforce.org/Page/Document/final-research-plan/cervical-cancer-screening2. Accessed June 22, 2016.
15. Ronco G, Dillner J, Elfström KM, et al; International HPV Working Group. Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled trials. Lancet. 2014;383:524-532.
16. Stoler MH, Wright TC Jr, Sharma A, et al. High-risk human papilloma virus testing in women with ASC-US cytology: results from the ATHENA HPV study. Am J Clin Path. 2011;135:468-475.
17. Choi JW, Kim Y, Lee JH, et al. The clinical performance of primary HPV screening, primary HPV screening plus cytology cotesting, and cytology alone at a tertiary care hospital. Cancer Cytopathol. 2016;124:144-152.
The drive to cut readmissions after bariatric surgery continues with DROP project
SAN DIEGO – John Morton, MD, started his bariatric surgery career about the same time that demand for gastric bypass and other bariatric procedures began to skyrocket. But a troubling trend emerged.
“About 10-15 years ago, bariatric surgery had a problem when it came to mortality,” Dr. Morton said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “You can’t move forward without looking back.”
A 2005 study of early mortality among Medicare beneficiaries undergoing bariatric procedures found a 30-day mortality of 9% and a 1-year mortality of 21% (JAMA 2005 Oct. 19;294[15]:1903-8). Such data prompted Dr. Morton and other leaders in the field to push for accreditation in the field. In 2012, the ACS Bariatric Surgery Center Network program and the American Society for Metabolic and Bariatric Surgery (ASMBS) Bariatric Centers of Excellence program were extended accreditation in the joint Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). As a result, the mortality rate among patients undergoing bariatric procedures has dropped nearly 10-fold and now stands at 1 out of 1,000, said Dr. Morton, chief of bariatric and minimally invasive surgery at Stanford (Calif.) University. “That’s been a real success story for us,” he said. “Part of it has been the accreditation program, having the resources in place to accomplish those goals.”
Of the 802 participating centers in MBSAQIP, 647 are accredited. “One of the reasons we see such good results at accredited centers is the fact that they work as a multidisciplinary team, where you have the nutritionist, the psychologist, the internist, and the anesthesiologist working together,” said Dr. Morton, immediate past president of the American Society for Metabolic and Bariatric Surgery. “When you have that team, it allows you to marshal your resources, do appropriate risk assessment, and get those processes in place to have the very best outcomes.”
In an effort to reduce hospital readmissions among bariatric surgery patients, MBSAQIP launched a national project called Decreasing Readmissions through Opportunities Provided (DROP), which currently has 129 participating hospitals. “If you drill down on the reasons for bariatric surgery readmissions, many are preventable: dehydration, nausea, medication side effects, and patient expectations,” Dr. Morton said. “I have a formula called the Morton Formula: happiness equals reality divided by expectations. If you set expectations accordingly, you’ll get a happier patient. If my patients know they’re going to be discharged in 1 day, they can plan accordingly.”
These concepts were adopted from a study that Dr. Morton and his associates carried out at Stanford Health Care in an effort to reduce readmissions for complications within 30 days to below the national average. It involved “straightforward” strategy including improving patient education, discharge planning, and giving patients a direct phone number to call. “Anybody who has called a health center and has had to go through that phone tree knows how difficult that can be, so we provide a direct number,” he said. “The postop phone call is critical, because that’s a way to nip readmissions in the bud. We do same-day appointments so they come and see us in the clinic rather than going to the ER and getting the enormous workup. Infusion centers are our best friend, because many of these patients come in dehydrated.”
After implementing these strategies, the rate of readmission for complications at Stanford fell from 8% to 2.5%. This led to the creation of a readmission bundle for the DROP project with steps for preoperative, intraoperative, and postoperative aspects of care. For example, preoperatively, “we make sure that they have a postop appointment made [and] rather than waiting to give them a prescription when they get discharged, we make sure that they have those prescriptions earlier at the preoperative visit,” he said. “They are provided the clinic phone number and patients watch video vignettes from all members of the team: surgeon, nurse, nutritionist, pharmacist, and psychologist. Rather than the education being dependent on [the surgeon’s schedule], they can get the same dose of education and even watch these over and over again if they want to.”
Surgeons who participate in the DROP project also stratify high-risk patients by consulting with their primary care physicians and case managers to achieve optimal outcomes. They address modifiable risk factors. “Weight gain prior to bariatric surgery is not ideal, so we want to address that, and have a hemoglobin A1c of less than 10%,” Dr. Morton said. Patients receive a “HELP” card, which instructs them to contact the treating clinic if they have abdominal pain, dehydration, nausea and vomiting, diarrhea, and fatigue.
The inpatient part of the bundle includes a “clinical roadmap” with a fixed length of stay. “There are expectations every single day about what’s going to happen to their care,” Dr. Morton said. “We give them a water bottle with the logo of the hospital. It’s a reminder for them to stay hydrated. They have a nutritional consult and they go through a checklist before they get discharged.”
The postoperative component of the DROP bundle includes a phone call to the patient following discharge. “They also get an appointment with a nutritionist within a month of surgery,” he said. “We treat readmissions seriously, like a complication.”
Data from a study of 18,296 primary bariatric surgery patients gleaned from 2012 ACS-NSQIP Participant Use Data Files found a 30-day readmission rate of 5.2% (Am J Surg 2016 Jul;212[1]:76-80). Compared with the patients’ counterparts who did not require readmission within 30 days, risk factors for those who did included body mass index greater than 50 kg/m2 (30.2% vs. 24.6%, respectively; P = .001); longer operative time (132 vs. 115 minutes; P = .001); length of stay greater than 4 days (9.57% vs. 3.36%; P = .001); surgical site infection (15.5% vs. 1.15%; P less than .001); urinary tract infection (3.15% vs. .65%; P less than .001), and deep vein thrombosis (3.58% vs. .13%; P less than .001). Common reasons for readmissions were GI-related (45%), dietary (33.5%), and bleeding (6.57%). Dr. Morton went on to report preliminary findings from 19,648 cases included in the DROP project, which began collecting data in March 2015 and has a yearlong goal of reducing national admission rates by 20%. The preintervention readmission rate was 4.79%. By the end of October 2015 the readmission rate had dropped to 4.30%. “One of the things we realized is that the hospitals with the higher readmission rates were the ones who had the greatest improvement,” Dr. Morton said. “They went from about 8% down to about 5.51%. We anticipate that for each quarter that we do this, we’ll continue to see improvement.”
Individual center results were made available in late January 2016 and reviewed with mentors. “They also received aggregated reports to see how they stacked up others as a benchmark,” Dr. Morton said.
Final results from DROP are expected to be released later in 2016.
Dr. Morton reported having no financial disclosures.
AGA Resource
The AGA Center for Gut Microbiome Research and Education was created to serve as a virtual “home” for AGA activities related to the gut microbiome. The center is focused on advancing gut microbiome research, educating AGA members and other stakeholders on the latest microbiome breakthroughs, and working with FDA and others to ensure that emerging microbiome-based treatments are safe and appropriately evaluated. Learn more at http://www.gastro.org/about/initiatives/aga-center-for-gut-microbiome-research-education.
SAN DIEGO – John Morton, MD, started his bariatric surgery career about the same time that demand for gastric bypass and other bariatric procedures began to skyrocket. But a troubling trend emerged.
“About 10-15 years ago, bariatric surgery had a problem when it came to mortality,” Dr. Morton said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “You can’t move forward without looking back.”
A 2005 study of early mortality among Medicare beneficiaries undergoing bariatric procedures found a 30-day mortality of 9% and a 1-year mortality of 21% (JAMA 2005 Oct. 19;294[15]:1903-8). Such data prompted Dr. Morton and other leaders in the field to push for accreditation in the field. In 2012, the ACS Bariatric Surgery Center Network program and the American Society for Metabolic and Bariatric Surgery (ASMBS) Bariatric Centers of Excellence program were extended accreditation in the joint Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). As a result, the mortality rate among patients undergoing bariatric procedures has dropped nearly 10-fold and now stands at 1 out of 1,000, said Dr. Morton, chief of bariatric and minimally invasive surgery at Stanford (Calif.) University. “That’s been a real success story for us,” he said. “Part of it has been the accreditation program, having the resources in place to accomplish those goals.”
Of the 802 participating centers in MBSAQIP, 647 are accredited. “One of the reasons we see such good results at accredited centers is the fact that they work as a multidisciplinary team, where you have the nutritionist, the psychologist, the internist, and the anesthesiologist working together,” said Dr. Morton, immediate past president of the American Society for Metabolic and Bariatric Surgery. “When you have that team, it allows you to marshal your resources, do appropriate risk assessment, and get those processes in place to have the very best outcomes.”
In an effort to reduce hospital readmissions among bariatric surgery patients, MBSAQIP launched a national project called Decreasing Readmissions through Opportunities Provided (DROP), which currently has 129 participating hospitals. “If you drill down on the reasons for bariatric surgery readmissions, many are preventable: dehydration, nausea, medication side effects, and patient expectations,” Dr. Morton said. “I have a formula called the Morton Formula: happiness equals reality divided by expectations. If you set expectations accordingly, you’ll get a happier patient. If my patients know they’re going to be discharged in 1 day, they can plan accordingly.”
These concepts were adopted from a study that Dr. Morton and his associates carried out at Stanford Health Care in an effort to reduce readmissions for complications within 30 days to below the national average. It involved “straightforward” strategy including improving patient education, discharge planning, and giving patients a direct phone number to call. “Anybody who has called a health center and has had to go through that phone tree knows how difficult that can be, so we provide a direct number,” he said. “The postop phone call is critical, because that’s a way to nip readmissions in the bud. We do same-day appointments so they come and see us in the clinic rather than going to the ER and getting the enormous workup. Infusion centers are our best friend, because many of these patients come in dehydrated.”
After implementing these strategies, the rate of readmission for complications at Stanford fell from 8% to 2.5%. This led to the creation of a readmission bundle for the DROP project with steps for preoperative, intraoperative, and postoperative aspects of care. For example, preoperatively, “we make sure that they have a postop appointment made [and] rather than waiting to give them a prescription when they get discharged, we make sure that they have those prescriptions earlier at the preoperative visit,” he said. “They are provided the clinic phone number and patients watch video vignettes from all members of the team: surgeon, nurse, nutritionist, pharmacist, and psychologist. Rather than the education being dependent on [the surgeon’s schedule], they can get the same dose of education and even watch these over and over again if they want to.”
Surgeons who participate in the DROP project also stratify high-risk patients by consulting with their primary care physicians and case managers to achieve optimal outcomes. They address modifiable risk factors. “Weight gain prior to bariatric surgery is not ideal, so we want to address that, and have a hemoglobin A1c of less than 10%,” Dr. Morton said. Patients receive a “HELP” card, which instructs them to contact the treating clinic if they have abdominal pain, dehydration, nausea and vomiting, diarrhea, and fatigue.
The inpatient part of the bundle includes a “clinical roadmap” with a fixed length of stay. “There are expectations every single day about what’s going to happen to their care,” Dr. Morton said. “We give them a water bottle with the logo of the hospital. It’s a reminder for them to stay hydrated. They have a nutritional consult and they go through a checklist before they get discharged.”
The postoperative component of the DROP bundle includes a phone call to the patient following discharge. “They also get an appointment with a nutritionist within a month of surgery,” he said. “We treat readmissions seriously, like a complication.”
Data from a study of 18,296 primary bariatric surgery patients gleaned from 2012 ACS-NSQIP Participant Use Data Files found a 30-day readmission rate of 5.2% (Am J Surg 2016 Jul;212[1]:76-80). Compared with the patients’ counterparts who did not require readmission within 30 days, risk factors for those who did included body mass index greater than 50 kg/m2 (30.2% vs. 24.6%, respectively; P = .001); longer operative time (132 vs. 115 minutes; P = .001); length of stay greater than 4 days (9.57% vs. 3.36%; P = .001); surgical site infection (15.5% vs. 1.15%; P less than .001); urinary tract infection (3.15% vs. .65%; P less than .001), and deep vein thrombosis (3.58% vs. .13%; P less than .001). Common reasons for readmissions were GI-related (45%), dietary (33.5%), and bleeding (6.57%). Dr. Morton went on to report preliminary findings from 19,648 cases included in the DROP project, which began collecting data in March 2015 and has a yearlong goal of reducing national admission rates by 20%. The preintervention readmission rate was 4.79%. By the end of October 2015 the readmission rate had dropped to 4.30%. “One of the things we realized is that the hospitals with the higher readmission rates were the ones who had the greatest improvement,” Dr. Morton said. “They went from about 8% down to about 5.51%. We anticipate that for each quarter that we do this, we’ll continue to see improvement.”
Individual center results were made available in late January 2016 and reviewed with mentors. “They also received aggregated reports to see how they stacked up others as a benchmark,” Dr. Morton said.
Final results from DROP are expected to be released later in 2016.
Dr. Morton reported having no financial disclosures.
AGA Resource
The AGA Center for Gut Microbiome Research and Education was created to serve as a virtual “home” for AGA activities related to the gut microbiome. The center is focused on advancing gut microbiome research, educating AGA members and other stakeholders on the latest microbiome breakthroughs, and working with FDA and others to ensure that emerging microbiome-based treatments are safe and appropriately evaluated. Learn more at http://www.gastro.org/about/initiatives/aga-center-for-gut-microbiome-research-education.
SAN DIEGO – John Morton, MD, started his bariatric surgery career about the same time that demand for gastric bypass and other bariatric procedures began to skyrocket. But a troubling trend emerged.
“About 10-15 years ago, bariatric surgery had a problem when it came to mortality,” Dr. Morton said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “You can’t move forward without looking back.”
A 2005 study of early mortality among Medicare beneficiaries undergoing bariatric procedures found a 30-day mortality of 9% and a 1-year mortality of 21% (JAMA 2005 Oct. 19;294[15]:1903-8). Such data prompted Dr. Morton and other leaders in the field to push for accreditation in the field. In 2012, the ACS Bariatric Surgery Center Network program and the American Society for Metabolic and Bariatric Surgery (ASMBS) Bariatric Centers of Excellence program were extended accreditation in the joint Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). As a result, the mortality rate among patients undergoing bariatric procedures has dropped nearly 10-fold and now stands at 1 out of 1,000, said Dr. Morton, chief of bariatric and minimally invasive surgery at Stanford (Calif.) University. “That’s been a real success story for us,” he said. “Part of it has been the accreditation program, having the resources in place to accomplish those goals.”
Of the 802 participating centers in MBSAQIP, 647 are accredited. “One of the reasons we see such good results at accredited centers is the fact that they work as a multidisciplinary team, where you have the nutritionist, the psychologist, the internist, and the anesthesiologist working together,” said Dr. Morton, immediate past president of the American Society for Metabolic and Bariatric Surgery. “When you have that team, it allows you to marshal your resources, do appropriate risk assessment, and get those processes in place to have the very best outcomes.”
In an effort to reduce hospital readmissions among bariatric surgery patients, MBSAQIP launched a national project called Decreasing Readmissions through Opportunities Provided (DROP), which currently has 129 participating hospitals. “If you drill down on the reasons for bariatric surgery readmissions, many are preventable: dehydration, nausea, medication side effects, and patient expectations,” Dr. Morton said. “I have a formula called the Morton Formula: happiness equals reality divided by expectations. If you set expectations accordingly, you’ll get a happier patient. If my patients know they’re going to be discharged in 1 day, they can plan accordingly.”
These concepts were adopted from a study that Dr. Morton and his associates carried out at Stanford Health Care in an effort to reduce readmissions for complications within 30 days to below the national average. It involved “straightforward” strategy including improving patient education, discharge planning, and giving patients a direct phone number to call. “Anybody who has called a health center and has had to go through that phone tree knows how difficult that can be, so we provide a direct number,” he said. “The postop phone call is critical, because that’s a way to nip readmissions in the bud. We do same-day appointments so they come and see us in the clinic rather than going to the ER and getting the enormous workup. Infusion centers are our best friend, because many of these patients come in dehydrated.”
After implementing these strategies, the rate of readmission for complications at Stanford fell from 8% to 2.5%. This led to the creation of a readmission bundle for the DROP project with steps for preoperative, intraoperative, and postoperative aspects of care. For example, preoperatively, “we make sure that they have a postop appointment made [and] rather than waiting to give them a prescription when they get discharged, we make sure that they have those prescriptions earlier at the preoperative visit,” he said. “They are provided the clinic phone number and patients watch video vignettes from all members of the team: surgeon, nurse, nutritionist, pharmacist, and psychologist. Rather than the education being dependent on [the surgeon’s schedule], they can get the same dose of education and even watch these over and over again if they want to.”
Surgeons who participate in the DROP project also stratify high-risk patients by consulting with their primary care physicians and case managers to achieve optimal outcomes. They address modifiable risk factors. “Weight gain prior to bariatric surgery is not ideal, so we want to address that, and have a hemoglobin A1c of less than 10%,” Dr. Morton said. Patients receive a “HELP” card, which instructs them to contact the treating clinic if they have abdominal pain, dehydration, nausea and vomiting, diarrhea, and fatigue.
The inpatient part of the bundle includes a “clinical roadmap” with a fixed length of stay. “There are expectations every single day about what’s going to happen to their care,” Dr. Morton said. “We give them a water bottle with the logo of the hospital. It’s a reminder for them to stay hydrated. They have a nutritional consult and they go through a checklist before they get discharged.”
The postoperative component of the DROP bundle includes a phone call to the patient following discharge. “They also get an appointment with a nutritionist within a month of surgery,” he said. “We treat readmissions seriously, like a complication.”
Data from a study of 18,296 primary bariatric surgery patients gleaned from 2012 ACS-NSQIP Participant Use Data Files found a 30-day readmission rate of 5.2% (Am J Surg 2016 Jul;212[1]:76-80). Compared with the patients’ counterparts who did not require readmission within 30 days, risk factors for those who did included body mass index greater than 50 kg/m2 (30.2% vs. 24.6%, respectively; P = .001); longer operative time (132 vs. 115 minutes; P = .001); length of stay greater than 4 days (9.57% vs. 3.36%; P = .001); surgical site infection (15.5% vs. 1.15%; P less than .001); urinary tract infection (3.15% vs. .65%; P less than .001), and deep vein thrombosis (3.58% vs. .13%; P less than .001). Common reasons for readmissions were GI-related (45%), dietary (33.5%), and bleeding (6.57%). Dr. Morton went on to report preliminary findings from 19,648 cases included in the DROP project, which began collecting data in March 2015 and has a yearlong goal of reducing national admission rates by 20%. The preintervention readmission rate was 4.79%. By the end of October 2015 the readmission rate had dropped to 4.30%. “One of the things we realized is that the hospitals with the higher readmission rates were the ones who had the greatest improvement,” Dr. Morton said. “They went from about 8% down to about 5.51%. We anticipate that for each quarter that we do this, we’ll continue to see improvement.”
Individual center results were made available in late January 2016 and reviewed with mentors. “They also received aggregated reports to see how they stacked up others as a benchmark,” Dr. Morton said.
Final results from DROP are expected to be released later in 2016.
Dr. Morton reported having no financial disclosures.
AGA Resource
The AGA Center for Gut Microbiome Research and Education was created to serve as a virtual “home” for AGA activities related to the gut microbiome. The center is focused on advancing gut microbiome research, educating AGA members and other stakeholders on the latest microbiome breakthroughs, and working with FDA and others to ensure that emerging microbiome-based treatments are safe and appropriately evaluated. Learn more at http://www.gastro.org/about/initiatives/aga-center-for-gut-microbiome-research-education.
EXPERT ANALYSIS AT THE ACS NSQIP NATIONAL CONFERENCE
The drive to cut readmissions after bariatric surgery continues with DROP project
SAN DIEGO – John Morton, MD, started his bariatric surgery career about the same time that demand for gastric bypass and other bariatric procedures began to skyrocket. But a troubling trend emerged.
“About 10-15 years ago, bariatric surgery had a problem when it came to mortality,” Dr. Morton said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “You can’t move forward without looking back.”
A 2005 study of early mortality among Medicare beneficiaries undergoing bariatric procedures found a 30-day mortality of 9% and a 1-year mortality of 21% (JAMA 2005 Oct. 19;294[15]:1903-8). Such data prompted Dr. Morton and other leaders in the field to push for accreditation in the field. In 2012, the ACS Bariatric Surgery Center Network program and the American Society for Metabolic and Bariatric Surgery (ASMBS) Bariatric Centers of Excellence program were extended accreditation in the joint Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). As a result, the mortality rate among patients undergoing bariatric procedures has dropped nearly 10-fold and now stands at 1 out of 1,000, said Dr. Morton, chief of bariatric and minimally invasive surgery at Stanford (Calif.) University. “That’s been a real success story for us,” he said. “Part of it has been the accreditation program, having the resources in place to accomplish those goals.”
Of the 802 participating centers in MBSAQIP, 647 are accredited. “One of the reasons we see such good results at accredited centers is the fact that they work as a multidisciplinary team, where you have the nutritionist, the psychologist, the internist, and the anesthesiologist working together,” said Dr. Morton, immediate past president of the American Society for Metabolic and Bariatric Surgery. “When you have that team, it allows you to marshal your resources, do appropriate risk assessment, and get those processes in place to have the very best outcomes.”
In an effort to reduce hospital readmissions among bariatric surgery patients, MBSAQIP launched a national project called Decreasing Readmissions through Opportunities Provided (DROP), which currently has 129 participating hospitals. “If you drill down on the reasons for bariatric surgery readmissions, many are preventable: dehydration, nausea, medication side effects, and patient expectations,” Dr. Morton said. “I have a formula called the Morton Formula: happiness equals reality divided by expectations. If you set expectations accordingly, you’ll get a happier patient. If my patients know they’re going to be discharged in 1 day, they can plan accordingly.”
These concepts were adopted from a study that Dr. Morton and his associates carried out at Stanford Health Care in an effort to reduce readmissions for complications within 30 days to below the national average. It involved “straightforward” strategy including improving patient education, discharge planning, and giving patients a direct phone number to call. “Anybody who has called a health center and has had to go through that phone tree knows how difficult that can be, so we provide a direct number,” he said. “The postop phone call is critical, because that’s a way to nip readmissions in the bud. We do same-day appointments so they come and see us in the clinic rather than going to the ER and getting the enormous workup. Infusion centers are our best friend, because many of these patients come in dehydrated.”
After implementing these strategies, the rate of readmission for complications at Stanford fell from 8% to 2.5%. This led to the creation of a readmission bundle for the DROP project with steps for preoperative, intraoperative, and postoperative aspects of care. For example, preoperatively, “we make sure that they have a postop appointment made [and] rather than waiting to give them a prescription when they get discharged, we make sure that they have those prescriptions earlier at the preoperative visit,” he said. “They are provided the clinic phone number and patients watch video vignettes from all members of the team: surgeon, nurse, nutritionist, pharmacist, and psychologist. Rather than the education being dependent on [the surgeon’s schedule], they can get the same dose of education and even watch these over and over again if they want to.”
Surgeons who participate in the DROP project also stratify high-risk patients by consulting with their primary care physicians and case managers to achieve optimal outcomes. They address modifiable risk factors. “Weight gain prior to bariatric surgery is not ideal, so we want to address that, and have a hemoglobin A1c of less than 10%,” Dr. Morton said. Patients receive a “HELP” card, which instructs them to contact the treating clinic if they have abdominal pain, dehydration, nausea and vomiting, diarrhea, and fatigue.
The inpatient part of the bundle includes a “clinical roadmap” with a fixed length of stay. “There are expectations every single day about what’s going to happen to their care,” Dr. Morton said. “We give them a water bottle with the logo of the hospital. It’s a reminder for them to stay hydrated. They have a nutritional consult and they go through a checklist before they get discharged.”
The postoperative component of the DROP bundle includes a phone call to the patient following discharge. “They also get an appointment with a nutritionist within a month of surgery,” he said. “We treat readmissions seriously, like a complication.”
Data from a study of 18,296 primary bariatric surgery patients gleaned from 2012 ACS-NSQIP Participant Use Data Files found a 30-day readmission rate of 5.2% (Am J Surg 2016 Jul;212[1]:76-80). Compared with the patients’ counterparts who did not require readmission within 30 days, risk factors for those who did included body mass index greater than 50 kg/m2 (30.2% vs. 24.6%, respectively; P = .001); longer operative time (132 vs. 115 minutes; P = .001); length of stay greater than 4 days (9.57% vs. 3.36%; P = .001); surgical site infection (15.5% vs. 1.15%; P less than .001); urinary tract infection (3.15% vs. .65%; P less than .001), and deep vein thrombosis (3.58% vs. .13%; P less than .001). Common reasons for readmissions were GI-related (45%), dietary (33.5%), and bleeding (6.57%). Dr. Morton went on to report preliminary findings from 19,648 cases included in the DROP project, which began collecting data in March 2015 and has a yearlong goal of reducing national admission rates by 20%. The preintervention readmission rate was 4.79%. By the end of October 2015 the readmission rate had dropped to 4.30%. “One of the things we realized is that the hospitals with the higher readmission rates were the ones who had the greatest improvement,” Dr. Morton said. “They went from about 8% down to about 5.51%. We anticipate that for each quarter that we do this, we’ll continue to see improvement.”
Individual center results were made available in late January 2016 and reviewed with mentors. “They also received aggregated reports to see how they stacked up others as a benchmark,” Dr. Morton said.
Final results from DROP are expected to be released later in 2016.
Dr. Morton reported having no financial disclosures.
SAN DIEGO – John Morton, MD, started his bariatric surgery career about the same time that demand for gastric bypass and other bariatric procedures began to skyrocket. But a troubling trend emerged.
“About 10-15 years ago, bariatric surgery had a problem when it came to mortality,” Dr. Morton said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “You can’t move forward without looking back.”
A 2005 study of early mortality among Medicare beneficiaries undergoing bariatric procedures found a 30-day mortality of 9% and a 1-year mortality of 21% (JAMA 2005 Oct. 19;294[15]:1903-8). Such data prompted Dr. Morton and other leaders in the field to push for accreditation in the field. In 2012, the ACS Bariatric Surgery Center Network program and the American Society for Metabolic and Bariatric Surgery (ASMBS) Bariatric Centers of Excellence program were extended accreditation in the joint Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). As a result, the mortality rate among patients undergoing bariatric procedures has dropped nearly 10-fold and now stands at 1 out of 1,000, said Dr. Morton, chief of bariatric and minimally invasive surgery at Stanford (Calif.) University. “That’s been a real success story for us,” he said. “Part of it has been the accreditation program, having the resources in place to accomplish those goals.”
Of the 802 participating centers in MBSAQIP, 647 are accredited. “One of the reasons we see such good results at accredited centers is the fact that they work as a multidisciplinary team, where you have the nutritionist, the psychologist, the internist, and the anesthesiologist working together,” said Dr. Morton, immediate past president of the American Society for Metabolic and Bariatric Surgery. “When you have that team, it allows you to marshal your resources, do appropriate risk assessment, and get those processes in place to have the very best outcomes.”
In an effort to reduce hospital readmissions among bariatric surgery patients, MBSAQIP launched a national project called Decreasing Readmissions through Opportunities Provided (DROP), which currently has 129 participating hospitals. “If you drill down on the reasons for bariatric surgery readmissions, many are preventable: dehydration, nausea, medication side effects, and patient expectations,” Dr. Morton said. “I have a formula called the Morton Formula: happiness equals reality divided by expectations. If you set expectations accordingly, you’ll get a happier patient. If my patients know they’re going to be discharged in 1 day, they can plan accordingly.”
These concepts were adopted from a study that Dr. Morton and his associates carried out at Stanford Health Care in an effort to reduce readmissions for complications within 30 days to below the national average. It involved “straightforward” strategy including improving patient education, discharge planning, and giving patients a direct phone number to call. “Anybody who has called a health center and has had to go through that phone tree knows how difficult that can be, so we provide a direct number,” he said. “The postop phone call is critical, because that’s a way to nip readmissions in the bud. We do same-day appointments so they come and see us in the clinic rather than going to the ER and getting the enormous workup. Infusion centers are our best friend, because many of these patients come in dehydrated.”
After implementing these strategies, the rate of readmission for complications at Stanford fell from 8% to 2.5%. This led to the creation of a readmission bundle for the DROP project with steps for preoperative, intraoperative, and postoperative aspects of care. For example, preoperatively, “we make sure that they have a postop appointment made [and] rather than waiting to give them a prescription when they get discharged, we make sure that they have those prescriptions earlier at the preoperative visit,” he said. “They are provided the clinic phone number and patients watch video vignettes from all members of the team: surgeon, nurse, nutritionist, pharmacist, and psychologist. Rather than the education being dependent on [the surgeon’s schedule], they can get the same dose of education and even watch these over and over again if they want to.”
Surgeons who participate in the DROP project also stratify high-risk patients by consulting with their primary care physicians and case managers to achieve optimal outcomes. They address modifiable risk factors. “Weight gain prior to bariatric surgery is not ideal, so we want to address that, and have a hemoglobin A1c of less than 10%,” Dr. Morton said. Patients receive a “HELP” card, which instructs them to contact the treating clinic if they have abdominal pain, dehydration, nausea and vomiting, diarrhea, and fatigue.
The inpatient part of the bundle includes a “clinical roadmap” with a fixed length of stay. “There are expectations every single day about what’s going to happen to their care,” Dr. Morton said. “We give them a water bottle with the logo of the hospital. It’s a reminder for them to stay hydrated. They have a nutritional consult and they go through a checklist before they get discharged.”
The postoperative component of the DROP bundle includes a phone call to the patient following discharge. “They also get an appointment with a nutritionist within a month of surgery,” he said. “We treat readmissions seriously, like a complication.”
Data from a study of 18,296 primary bariatric surgery patients gleaned from 2012 ACS-NSQIP Participant Use Data Files found a 30-day readmission rate of 5.2% (Am J Surg 2016 Jul;212[1]:76-80). Compared with the patients’ counterparts who did not require readmission within 30 days, risk factors for those who did included body mass index greater than 50 kg/m2 (30.2% vs. 24.6%, respectively; P = .001); longer operative time (132 vs. 115 minutes; P = .001); length of stay greater than 4 days (9.57% vs. 3.36%; P = .001); surgical site infection (15.5% vs. 1.15%; P less than .001); urinary tract infection (3.15% vs. .65%; P less than .001), and deep vein thrombosis (3.58% vs. .13%; P less than .001). Common reasons for readmissions were GI-related (45%), dietary (33.5%), and bleeding (6.57%). Dr. Morton went on to report preliminary findings from 19,648 cases included in the DROP project, which began collecting data in March 2015 and has a yearlong goal of reducing national admission rates by 20%. The preintervention readmission rate was 4.79%. By the end of October 2015 the readmission rate had dropped to 4.30%. “One of the things we realized is that the hospitals with the higher readmission rates were the ones who had the greatest improvement,” Dr. Morton said. “They went from about 8% down to about 5.51%. We anticipate that for each quarter that we do this, we’ll continue to see improvement.”
Individual center results were made available in late January 2016 and reviewed with mentors. “They also received aggregated reports to see how they stacked up others as a benchmark,” Dr. Morton said.
Final results from DROP are expected to be released later in 2016.
Dr. Morton reported having no financial disclosures.
SAN DIEGO – John Morton, MD, started his bariatric surgery career about the same time that demand for gastric bypass and other bariatric procedures began to skyrocket. But a troubling trend emerged.
“About 10-15 years ago, bariatric surgery had a problem when it came to mortality,” Dr. Morton said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “You can’t move forward without looking back.”
A 2005 study of early mortality among Medicare beneficiaries undergoing bariatric procedures found a 30-day mortality of 9% and a 1-year mortality of 21% (JAMA 2005 Oct. 19;294[15]:1903-8). Such data prompted Dr. Morton and other leaders in the field to push for accreditation in the field. In 2012, the ACS Bariatric Surgery Center Network program and the American Society for Metabolic and Bariatric Surgery (ASMBS) Bariatric Centers of Excellence program were extended accreditation in the joint Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). As a result, the mortality rate among patients undergoing bariatric procedures has dropped nearly 10-fold and now stands at 1 out of 1,000, said Dr. Morton, chief of bariatric and minimally invasive surgery at Stanford (Calif.) University. “That’s been a real success story for us,” he said. “Part of it has been the accreditation program, having the resources in place to accomplish those goals.”
Of the 802 participating centers in MBSAQIP, 647 are accredited. “One of the reasons we see such good results at accredited centers is the fact that they work as a multidisciplinary team, where you have the nutritionist, the psychologist, the internist, and the anesthesiologist working together,” said Dr. Morton, immediate past president of the American Society for Metabolic and Bariatric Surgery. “When you have that team, it allows you to marshal your resources, do appropriate risk assessment, and get those processes in place to have the very best outcomes.”
In an effort to reduce hospital readmissions among bariatric surgery patients, MBSAQIP launched a national project called Decreasing Readmissions through Opportunities Provided (DROP), which currently has 129 participating hospitals. “If you drill down on the reasons for bariatric surgery readmissions, many are preventable: dehydration, nausea, medication side effects, and patient expectations,” Dr. Morton said. “I have a formula called the Morton Formula: happiness equals reality divided by expectations. If you set expectations accordingly, you’ll get a happier patient. If my patients know they’re going to be discharged in 1 day, they can plan accordingly.”
These concepts were adopted from a study that Dr. Morton and his associates carried out at Stanford Health Care in an effort to reduce readmissions for complications within 30 days to below the national average. It involved “straightforward” strategy including improving patient education, discharge planning, and giving patients a direct phone number to call. “Anybody who has called a health center and has had to go through that phone tree knows how difficult that can be, so we provide a direct number,” he said. “The postop phone call is critical, because that’s a way to nip readmissions in the bud. We do same-day appointments so they come and see us in the clinic rather than going to the ER and getting the enormous workup. Infusion centers are our best friend, because many of these patients come in dehydrated.”
After implementing these strategies, the rate of readmission for complications at Stanford fell from 8% to 2.5%. This led to the creation of a readmission bundle for the DROP project with steps for preoperative, intraoperative, and postoperative aspects of care. For example, preoperatively, “we make sure that they have a postop appointment made [and] rather than waiting to give them a prescription when they get discharged, we make sure that they have those prescriptions earlier at the preoperative visit,” he said. “They are provided the clinic phone number and patients watch video vignettes from all members of the team: surgeon, nurse, nutritionist, pharmacist, and psychologist. Rather than the education being dependent on [the surgeon’s schedule], they can get the same dose of education and even watch these over and over again if they want to.”
Surgeons who participate in the DROP project also stratify high-risk patients by consulting with their primary care physicians and case managers to achieve optimal outcomes. They address modifiable risk factors. “Weight gain prior to bariatric surgery is not ideal, so we want to address that, and have a hemoglobin A1c of less than 10%,” Dr. Morton said. Patients receive a “HELP” card, which instructs them to contact the treating clinic if they have abdominal pain, dehydration, nausea and vomiting, diarrhea, and fatigue.
The inpatient part of the bundle includes a “clinical roadmap” with a fixed length of stay. “There are expectations every single day about what’s going to happen to their care,” Dr. Morton said. “We give them a water bottle with the logo of the hospital. It’s a reminder for them to stay hydrated. They have a nutritional consult and they go through a checklist before they get discharged.”
The postoperative component of the DROP bundle includes a phone call to the patient following discharge. “They also get an appointment with a nutritionist within a month of surgery,” he said. “We treat readmissions seriously, like a complication.”
Data from a study of 18,296 primary bariatric surgery patients gleaned from 2012 ACS-NSQIP Participant Use Data Files found a 30-day readmission rate of 5.2% (Am J Surg 2016 Jul;212[1]:76-80). Compared with the patients’ counterparts who did not require readmission within 30 days, risk factors for those who did included body mass index greater than 50 kg/m2 (30.2% vs. 24.6%, respectively; P = .001); longer operative time (132 vs. 115 minutes; P = .001); length of stay greater than 4 days (9.57% vs. 3.36%; P = .001); surgical site infection (15.5% vs. 1.15%; P less than .001); urinary tract infection (3.15% vs. .65%; P less than .001), and deep vein thrombosis (3.58% vs. .13%; P less than .001). Common reasons for readmissions were GI-related (45%), dietary (33.5%), and bleeding (6.57%). Dr. Morton went on to report preliminary findings from 19,648 cases included in the DROP project, which began collecting data in March 2015 and has a yearlong goal of reducing national admission rates by 20%. The preintervention readmission rate was 4.79%. By the end of October 2015 the readmission rate had dropped to 4.30%. “One of the things we realized is that the hospitals with the higher readmission rates were the ones who had the greatest improvement,” Dr. Morton said. “They went from about 8% down to about 5.51%. We anticipate that for each quarter that we do this, we’ll continue to see improvement.”
Individual center results were made available in late January 2016 and reviewed with mentors. “They also received aggregated reports to see how they stacked up others as a benchmark,” Dr. Morton said.
Final results from DROP are expected to be released later in 2016.
Dr. Morton reported having no financial disclosures.
EXPERT ANALYSIS AT THE ACS NSQIP NATIONAL CONFERENCE
Madness and guns
“Bang, bang, you’re dead” has been uttered by millions of American children for generations. It is typical of the ordinary, angry, murderous thoughts of childhood; variations of it are universal. We expect children to learn to control their anger as they grow up and not to play out their angry wishes in reality. Unfortunately, this doesn’t always happen.
Following the many recent dramatic, crazed mass shootings, some commentators have called for restricting gun access for those with mental illness, but psychiatrists have rightly pointed out that murderers, including terror-inducing mass murderers, do not usually have a history of formally diagnosed mental illness. The psychiatrists are right for a reason: The potential for sudden, often unexpected, violence is widespread. This essay will employ a developmental perspective on how people handle anger, and on how we come to distinguish between fantasy and reality, to inform an understanding of gun violence.
Baby hyenas often try to kill their siblings shortly after birth. Human babies do not. They are not only motorically undeveloped, but their emotions appear to be mostly limited to the nonspecific states of distress and satisfaction. Distinct affects, such as anger, differentiate gradually. Babies smile by 2 months. Babies’ specific affection for and loyalty to their caregivers comes along a bit later, hence stranger anxiety commonly appears around 9 months. Facial expressions, sounds, and activity that look specifically like anger, and that occur when babies are frustrated or injured, are observed in the second half of the first year of human life. In the second year of life, feelings such as shame and guilt, which are dependent on the development of a distinct sense of self and other, appear. Shame and guilt, along with loving feelings, help form the basis for consideration of others and for the diminishment of young children’s omnipotence and egocentricity; they become a kind of social “glue,” tempering selfish, angry pursuits and tantrums.
There is a typical developmental sequence of how people come to handle their anger. Younger children express emotions directly, with little restraint; they hit, bite, and scream. Older children should be able to have more impulse control and be able to regulate the motor and verbal expression of their anger to a greater degree. At some point, most also become able to acknowledge their anger and not have to deny it. Adults, in principle, should be able both to inhibit the uncontrolled expression of anger and also, when appropriate, be able to use anger constructively. How tenuous this accomplishment is, and how often adults can function like overgrown children, can be readily observed at children’s sports matches, in which the children are often better behaved than their parents. In short, humans are endowed with the potential for enormous, destructive anger, but also, in our caring for others, a counterbalance to it.
The process of emotional development, and the regulation of anger, is intertwined with the development of the sense of self and of other. Evidence suggests that babies can start to distinguish self and other at birth, but that a full and reliable sense of self and other is a long, complicated developmental process.
The article by pediatrician and psychoanalyst Donald Winnicott, “Transitional Objects and Transitional Phenomena – A Study of the First Not-Me Possession,” one of the most frequently cited papers in the psychoanalytic literature, addresses this process (Int J Psychoanal. 1953;34[2]89-97). While transitional objects are not a human universal, the process of differentiating oneself from others, of finding out what is me and what is not-me, is. According to Dr. Winnicott, learning what is self and what is other assists babies in their related challenges of distinguishing animate from inanimate, wishes from causes, and fantasy from reality. Mother usually appears when I’m distressed – is she a part of me or a separate being? Does she appear because I wish, because I cry, or does she not appear despite my efforts? People never fully complete the developmental distinctions between self and other, and between wishes, fantasies, and magic, as opposed to reality.
Stressful events, such as a sudden loss, for example, commonly prompt a regressive denial of reality: “I don’t believe what I see” can be meant literally. When attending movies, we all “suspend disbelief” and participate, at least vicariously, in wishful magic. Further, although after early childhood, problems understanding material reality are characteristic of psychosis, all people are prone to at least occasional wishful or fearful errors in grasping social reality – we misperceive the meaning and intentions of others.
Combining the understanding of the development of how children handle anger and how they learn to differentiate self and other, and fantasy and reality, leads to an additional, important point. Suppose a person can’t tolerate his own angry wishes and he doesn’t distinguish well between self and other. He can easily attribute his own unwanted hatefulness to others, and he may then want to attack them for it. This process is extremely common, and we are all inclined to it to some degree. As childishly simplistic as it sounds, for humans, there is almost always an us and a them; we are good and they are bad. In addition to directing anger inappropriately at others, people can, of course, turn anger against themselves, and with just as much unreasonableness and venom. However much we grow up, development is never complete. We remain irrational, with a tenuous and incomplete perception of reality.
One would never give a weapon to an infant, but in light of these difficulties with respect to human development, should one give a weapon to an adult?
Whether or not humans have the self-control to possess weapons of great power and destructiveness, weapons are part of our evolution as a species. They have likely contributed to our remarkable success, protecting us from predators and enriching our diets. It is worth noting, however, that small-scale societies such as those we all evolved from often have high murder rates, and that lower rates of intra-societal violence tend to be found in larger, more highly regulated societies. People do not always adequately manage aggression themselves and benefit from external, societal assistance.
We humans all have the capacity to be mad: to be angry, to be crazy, to be crazed with anger. Fantasies of revenge are common when one is angry, and expectable when one has been hurt. Yet, expressions such as “blind with rage” and “seeing red” attest to the challenges to the sense of reality that rage can induce. The crucial distinction between having vengeful wishes and fantasies, and putting them into action, into reality, can crumble quickly. In addition to anger, fear is another emotion that can distort the perception of reality. Regular attention to the news suggests that police, whether they are aware of it or not, are more fearful of black men than of other people. They are more likely to perceive them as being armed and are quicker to shoot. For police and civilians alike, the presence of guns simultaneously requires greater impulse control and makes impulse control more difficult. The more guns, the more fear and anger, the more shootings – a vicious cycle.
Most people who commit crimes with guns, whether a singular “crime of passion” or a mass murder, have been crazed with anger. Some have been known to police as angry individuals with histories of getting into trouble, others not. But most have been angry, isolated individuals with problematic social relationships and little warm or respectful involvement with others to counterbalance their anger. Given the challenges inherent in human development, it is not surprising that in most societies there are a fair number of disaffected, angry, isolated individuals with inadequate realistic emotional regulation.
According to the anthropologist Scott Atran, who has studied both would-be and convicted terrorists, in addition to those individuals who are angry and disturbed, many recruits to terrorism are merely unsettled youth eager to find a sense of identity and belonging in a “band of brothers (and sisters).” He has described the “devoted actor,” who merges his identity with his combat unit and becomes willing to die for his comrades or their cause. These observations are consistent with both anthropological ideas about cultural influences on the sense of self in relation to groups, and with psychoanalytic emphasis on the difficulty of achieving a firm sense of self and other. In fusing with the group and its ideology, one gives up an independent self while feeling that one has gained a sense of self, belonging, and meaning. Whatever the psychological and social picture, it is obvious that the angry, isolated individuals who may regress and explode, and the countless unsettled youth of modern societies, cannot all be identified, tracked, and regulated by society, nor will they all seek help for their troubles. The United States’ decisions to allow massively destructive weapons to anyone and everyone are counter to everything we know about people.
Among many other things, Sigmund Freud is known for highlighting the comment that “The first man to hurl an insult rather than a spear was the founder of civilization.” Anger that is put into words is less destructive than anger put into violent action. From this point of view, the widespread presence of guns undermines civilization. Guns invite putting anger into action rather than conversation – they are a hindrance to impulse control and they shut down discussion. Democracy, a form of civilization contingent on impulse control, discussion, and voting, rather than submission to violent authority, is particularly undermined by guns. Congress should know: It has been so intimidated by the National Rifle Association that it has refused to outlaw private possession of military assault rifles and at the same time has submitted to outlawing the use of federal funds for research about gun violence. Despite this ban on research, there is overwhelming evidence that the presence of a gun in a home is associated not only with significantly increased murder rates, but also, as mental health professionals well know, greatly increased incidence of suicide.
As humans, we all have the ability to control ourselves to some degree. But, we all have the potential to become mad and to lose control. Our internal self-regulation is sometimes insufficient, and we need the restraining influence of our fellow humans. This can be in the form of a comforting word, a warning gesture, a carrot or a stick, or a law. The regulation of guns, assault rifles, and bomb-making materials is a mark of civilization.
Dr. Blum is a psychiatrist and psychoanalyst in private practice in Philadelphia. He teaches in the departments of anthropology and psychiatry at the University of Pennsylvania and at the Psychoanalytic Center of Philadelphia.
“Bang, bang, you’re dead” has been uttered by millions of American children for generations. It is typical of the ordinary, angry, murderous thoughts of childhood; variations of it are universal. We expect children to learn to control their anger as they grow up and not to play out their angry wishes in reality. Unfortunately, this doesn’t always happen.
Following the many recent dramatic, crazed mass shootings, some commentators have called for restricting gun access for those with mental illness, but psychiatrists have rightly pointed out that murderers, including terror-inducing mass murderers, do not usually have a history of formally diagnosed mental illness. The psychiatrists are right for a reason: The potential for sudden, often unexpected, violence is widespread. This essay will employ a developmental perspective on how people handle anger, and on how we come to distinguish between fantasy and reality, to inform an understanding of gun violence.
Baby hyenas often try to kill their siblings shortly after birth. Human babies do not. They are not only motorically undeveloped, but their emotions appear to be mostly limited to the nonspecific states of distress and satisfaction. Distinct affects, such as anger, differentiate gradually. Babies smile by 2 months. Babies’ specific affection for and loyalty to their caregivers comes along a bit later, hence stranger anxiety commonly appears around 9 months. Facial expressions, sounds, and activity that look specifically like anger, and that occur when babies are frustrated or injured, are observed in the second half of the first year of human life. In the second year of life, feelings such as shame and guilt, which are dependent on the development of a distinct sense of self and other, appear. Shame and guilt, along with loving feelings, help form the basis for consideration of others and for the diminishment of young children’s omnipotence and egocentricity; they become a kind of social “glue,” tempering selfish, angry pursuits and tantrums.
There is a typical developmental sequence of how people come to handle their anger. Younger children express emotions directly, with little restraint; they hit, bite, and scream. Older children should be able to have more impulse control and be able to regulate the motor and verbal expression of their anger to a greater degree. At some point, most also become able to acknowledge their anger and not have to deny it. Adults, in principle, should be able both to inhibit the uncontrolled expression of anger and also, when appropriate, be able to use anger constructively. How tenuous this accomplishment is, and how often adults can function like overgrown children, can be readily observed at children’s sports matches, in which the children are often better behaved than their parents. In short, humans are endowed with the potential for enormous, destructive anger, but also, in our caring for others, a counterbalance to it.
The process of emotional development, and the regulation of anger, is intertwined with the development of the sense of self and of other. Evidence suggests that babies can start to distinguish self and other at birth, but that a full and reliable sense of self and other is a long, complicated developmental process.
The article by pediatrician and psychoanalyst Donald Winnicott, “Transitional Objects and Transitional Phenomena – A Study of the First Not-Me Possession,” one of the most frequently cited papers in the psychoanalytic literature, addresses this process (Int J Psychoanal. 1953;34[2]89-97). While transitional objects are not a human universal, the process of differentiating oneself from others, of finding out what is me and what is not-me, is. According to Dr. Winnicott, learning what is self and what is other assists babies in their related challenges of distinguishing animate from inanimate, wishes from causes, and fantasy from reality. Mother usually appears when I’m distressed – is she a part of me or a separate being? Does she appear because I wish, because I cry, or does she not appear despite my efforts? People never fully complete the developmental distinctions between self and other, and between wishes, fantasies, and magic, as opposed to reality.
Stressful events, such as a sudden loss, for example, commonly prompt a regressive denial of reality: “I don’t believe what I see” can be meant literally. When attending movies, we all “suspend disbelief” and participate, at least vicariously, in wishful magic. Further, although after early childhood, problems understanding material reality are characteristic of psychosis, all people are prone to at least occasional wishful or fearful errors in grasping social reality – we misperceive the meaning and intentions of others.
Combining the understanding of the development of how children handle anger and how they learn to differentiate self and other, and fantasy and reality, leads to an additional, important point. Suppose a person can’t tolerate his own angry wishes and he doesn’t distinguish well between self and other. He can easily attribute his own unwanted hatefulness to others, and he may then want to attack them for it. This process is extremely common, and we are all inclined to it to some degree. As childishly simplistic as it sounds, for humans, there is almost always an us and a them; we are good and they are bad. In addition to directing anger inappropriately at others, people can, of course, turn anger against themselves, and with just as much unreasonableness and venom. However much we grow up, development is never complete. We remain irrational, with a tenuous and incomplete perception of reality.
One would never give a weapon to an infant, but in light of these difficulties with respect to human development, should one give a weapon to an adult?
Whether or not humans have the self-control to possess weapons of great power and destructiveness, weapons are part of our evolution as a species. They have likely contributed to our remarkable success, protecting us from predators and enriching our diets. It is worth noting, however, that small-scale societies such as those we all evolved from often have high murder rates, and that lower rates of intra-societal violence tend to be found in larger, more highly regulated societies. People do not always adequately manage aggression themselves and benefit from external, societal assistance.
We humans all have the capacity to be mad: to be angry, to be crazy, to be crazed with anger. Fantasies of revenge are common when one is angry, and expectable when one has been hurt. Yet, expressions such as “blind with rage” and “seeing red” attest to the challenges to the sense of reality that rage can induce. The crucial distinction between having vengeful wishes and fantasies, and putting them into action, into reality, can crumble quickly. In addition to anger, fear is another emotion that can distort the perception of reality. Regular attention to the news suggests that police, whether they are aware of it or not, are more fearful of black men than of other people. They are more likely to perceive them as being armed and are quicker to shoot. For police and civilians alike, the presence of guns simultaneously requires greater impulse control and makes impulse control more difficult. The more guns, the more fear and anger, the more shootings – a vicious cycle.
Most people who commit crimes with guns, whether a singular “crime of passion” or a mass murder, have been crazed with anger. Some have been known to police as angry individuals with histories of getting into trouble, others not. But most have been angry, isolated individuals with problematic social relationships and little warm or respectful involvement with others to counterbalance their anger. Given the challenges inherent in human development, it is not surprising that in most societies there are a fair number of disaffected, angry, isolated individuals with inadequate realistic emotional regulation.
According to the anthropologist Scott Atran, who has studied both would-be and convicted terrorists, in addition to those individuals who are angry and disturbed, many recruits to terrorism are merely unsettled youth eager to find a sense of identity and belonging in a “band of brothers (and sisters).” He has described the “devoted actor,” who merges his identity with his combat unit and becomes willing to die for his comrades or their cause. These observations are consistent with both anthropological ideas about cultural influences on the sense of self in relation to groups, and with psychoanalytic emphasis on the difficulty of achieving a firm sense of self and other. In fusing with the group and its ideology, one gives up an independent self while feeling that one has gained a sense of self, belonging, and meaning. Whatever the psychological and social picture, it is obvious that the angry, isolated individuals who may regress and explode, and the countless unsettled youth of modern societies, cannot all be identified, tracked, and regulated by society, nor will they all seek help for their troubles. The United States’ decisions to allow massively destructive weapons to anyone and everyone are counter to everything we know about people.
Among many other things, Sigmund Freud is known for highlighting the comment that “The first man to hurl an insult rather than a spear was the founder of civilization.” Anger that is put into words is less destructive than anger put into violent action. From this point of view, the widespread presence of guns undermines civilization. Guns invite putting anger into action rather than conversation – they are a hindrance to impulse control and they shut down discussion. Democracy, a form of civilization contingent on impulse control, discussion, and voting, rather than submission to violent authority, is particularly undermined by guns. Congress should know: It has been so intimidated by the National Rifle Association that it has refused to outlaw private possession of military assault rifles and at the same time has submitted to outlawing the use of federal funds for research about gun violence. Despite this ban on research, there is overwhelming evidence that the presence of a gun in a home is associated not only with significantly increased murder rates, but also, as mental health professionals well know, greatly increased incidence of suicide.
As humans, we all have the ability to control ourselves to some degree. But, we all have the potential to become mad and to lose control. Our internal self-regulation is sometimes insufficient, and we need the restraining influence of our fellow humans. This can be in the form of a comforting word, a warning gesture, a carrot or a stick, or a law. The regulation of guns, assault rifles, and bomb-making materials is a mark of civilization.
Dr. Blum is a psychiatrist and psychoanalyst in private practice in Philadelphia. He teaches in the departments of anthropology and psychiatry at the University of Pennsylvania and at the Psychoanalytic Center of Philadelphia.
“Bang, bang, you’re dead” has been uttered by millions of American children for generations. It is typical of the ordinary, angry, murderous thoughts of childhood; variations of it are universal. We expect children to learn to control their anger as they grow up and not to play out their angry wishes in reality. Unfortunately, this doesn’t always happen.
Following the many recent dramatic, crazed mass shootings, some commentators have called for restricting gun access for those with mental illness, but psychiatrists have rightly pointed out that murderers, including terror-inducing mass murderers, do not usually have a history of formally diagnosed mental illness. The psychiatrists are right for a reason: The potential for sudden, often unexpected, violence is widespread. This essay will employ a developmental perspective on how people handle anger, and on how we come to distinguish between fantasy and reality, to inform an understanding of gun violence.
Baby hyenas often try to kill their siblings shortly after birth. Human babies do not. They are not only motorically undeveloped, but their emotions appear to be mostly limited to the nonspecific states of distress and satisfaction. Distinct affects, such as anger, differentiate gradually. Babies smile by 2 months. Babies’ specific affection for and loyalty to their caregivers comes along a bit later, hence stranger anxiety commonly appears around 9 months. Facial expressions, sounds, and activity that look specifically like anger, and that occur when babies are frustrated or injured, are observed in the second half of the first year of human life. In the second year of life, feelings such as shame and guilt, which are dependent on the development of a distinct sense of self and other, appear. Shame and guilt, along with loving feelings, help form the basis for consideration of others and for the diminishment of young children’s omnipotence and egocentricity; they become a kind of social “glue,” tempering selfish, angry pursuits and tantrums.
There is a typical developmental sequence of how people come to handle their anger. Younger children express emotions directly, with little restraint; they hit, bite, and scream. Older children should be able to have more impulse control and be able to regulate the motor and verbal expression of their anger to a greater degree. At some point, most also become able to acknowledge their anger and not have to deny it. Adults, in principle, should be able both to inhibit the uncontrolled expression of anger and also, when appropriate, be able to use anger constructively. How tenuous this accomplishment is, and how often adults can function like overgrown children, can be readily observed at children’s sports matches, in which the children are often better behaved than their parents. In short, humans are endowed with the potential for enormous, destructive anger, but also, in our caring for others, a counterbalance to it.
The process of emotional development, and the regulation of anger, is intertwined with the development of the sense of self and of other. Evidence suggests that babies can start to distinguish self and other at birth, but that a full and reliable sense of self and other is a long, complicated developmental process.
The article by pediatrician and psychoanalyst Donald Winnicott, “Transitional Objects and Transitional Phenomena – A Study of the First Not-Me Possession,” one of the most frequently cited papers in the psychoanalytic literature, addresses this process (Int J Psychoanal. 1953;34[2]89-97). While transitional objects are not a human universal, the process of differentiating oneself from others, of finding out what is me and what is not-me, is. According to Dr. Winnicott, learning what is self and what is other assists babies in their related challenges of distinguishing animate from inanimate, wishes from causes, and fantasy from reality. Mother usually appears when I’m distressed – is she a part of me or a separate being? Does she appear because I wish, because I cry, or does she not appear despite my efforts? People never fully complete the developmental distinctions between self and other, and between wishes, fantasies, and magic, as opposed to reality.
Stressful events, such as a sudden loss, for example, commonly prompt a regressive denial of reality: “I don’t believe what I see” can be meant literally. When attending movies, we all “suspend disbelief” and participate, at least vicariously, in wishful magic. Further, although after early childhood, problems understanding material reality are characteristic of psychosis, all people are prone to at least occasional wishful or fearful errors in grasping social reality – we misperceive the meaning and intentions of others.
Combining the understanding of the development of how children handle anger and how they learn to differentiate self and other, and fantasy and reality, leads to an additional, important point. Suppose a person can’t tolerate his own angry wishes and he doesn’t distinguish well between self and other. He can easily attribute his own unwanted hatefulness to others, and he may then want to attack them for it. This process is extremely common, and we are all inclined to it to some degree. As childishly simplistic as it sounds, for humans, there is almost always an us and a them; we are good and they are bad. In addition to directing anger inappropriately at others, people can, of course, turn anger against themselves, and with just as much unreasonableness and venom. However much we grow up, development is never complete. We remain irrational, with a tenuous and incomplete perception of reality.
One would never give a weapon to an infant, but in light of these difficulties with respect to human development, should one give a weapon to an adult?
Whether or not humans have the self-control to possess weapons of great power and destructiveness, weapons are part of our evolution as a species. They have likely contributed to our remarkable success, protecting us from predators and enriching our diets. It is worth noting, however, that small-scale societies such as those we all evolved from often have high murder rates, and that lower rates of intra-societal violence tend to be found in larger, more highly regulated societies. People do not always adequately manage aggression themselves and benefit from external, societal assistance.
We humans all have the capacity to be mad: to be angry, to be crazy, to be crazed with anger. Fantasies of revenge are common when one is angry, and expectable when one has been hurt. Yet, expressions such as “blind with rage” and “seeing red” attest to the challenges to the sense of reality that rage can induce. The crucial distinction between having vengeful wishes and fantasies, and putting them into action, into reality, can crumble quickly. In addition to anger, fear is another emotion that can distort the perception of reality. Regular attention to the news suggests that police, whether they are aware of it or not, are more fearful of black men than of other people. They are more likely to perceive them as being armed and are quicker to shoot. For police and civilians alike, the presence of guns simultaneously requires greater impulse control and makes impulse control more difficult. The more guns, the more fear and anger, the more shootings – a vicious cycle.
Most people who commit crimes with guns, whether a singular “crime of passion” or a mass murder, have been crazed with anger. Some have been known to police as angry individuals with histories of getting into trouble, others not. But most have been angry, isolated individuals with problematic social relationships and little warm or respectful involvement with others to counterbalance their anger. Given the challenges inherent in human development, it is not surprising that in most societies there are a fair number of disaffected, angry, isolated individuals with inadequate realistic emotional regulation.
According to the anthropologist Scott Atran, who has studied both would-be and convicted terrorists, in addition to those individuals who are angry and disturbed, many recruits to terrorism are merely unsettled youth eager to find a sense of identity and belonging in a “band of brothers (and sisters).” He has described the “devoted actor,” who merges his identity with his combat unit and becomes willing to die for his comrades or their cause. These observations are consistent with both anthropological ideas about cultural influences on the sense of self in relation to groups, and with psychoanalytic emphasis on the difficulty of achieving a firm sense of self and other. In fusing with the group and its ideology, one gives up an independent self while feeling that one has gained a sense of self, belonging, and meaning. Whatever the psychological and social picture, it is obvious that the angry, isolated individuals who may regress and explode, and the countless unsettled youth of modern societies, cannot all be identified, tracked, and regulated by society, nor will they all seek help for their troubles. The United States’ decisions to allow massively destructive weapons to anyone and everyone are counter to everything we know about people.
Among many other things, Sigmund Freud is known for highlighting the comment that “The first man to hurl an insult rather than a spear was the founder of civilization.” Anger that is put into words is less destructive than anger put into violent action. From this point of view, the widespread presence of guns undermines civilization. Guns invite putting anger into action rather than conversation – they are a hindrance to impulse control and they shut down discussion. Democracy, a form of civilization contingent on impulse control, discussion, and voting, rather than submission to violent authority, is particularly undermined by guns. Congress should know: It has been so intimidated by the National Rifle Association that it has refused to outlaw private possession of military assault rifles and at the same time has submitted to outlawing the use of federal funds for research about gun violence. Despite this ban on research, there is overwhelming evidence that the presence of a gun in a home is associated not only with significantly increased murder rates, but also, as mental health professionals well know, greatly increased incidence of suicide.
As humans, we all have the ability to control ourselves to some degree. But, we all have the potential to become mad and to lose control. Our internal self-regulation is sometimes insufficient, and we need the restraining influence of our fellow humans. This can be in the form of a comforting word, a warning gesture, a carrot or a stick, or a law. The regulation of guns, assault rifles, and bomb-making materials is a mark of civilization.
Dr. Blum is a psychiatrist and psychoanalyst in private practice in Philadelphia. He teaches in the departments of anthropology and psychiatry at the University of Pennsylvania and at the Psychoanalytic Center of Philadelphia.
Skin microbiome may differ in unique ways in psoriatic arthritis, psoriasis patients
MIAMI – As patients with psoriasis develop psoriatic arthritis, the abundance of particular genera in the skin microbiome decreases, according to a preliminary study characterizing cutaneous microbiota in these populations.
“The big overall message is there might be a decrease in microbiota diversity as you progress through the disease spectrum,” Julia Manasson, MD, a fellow in the division of rheumatology at New York University said. “This is the first study characterizing the cutaneous microbial compositions of subjects with psoriasis and psoriatic arthritis in both psoriatic lesions and unaffected skin.”
A previous study that revealed changes in gut microbiome between psoriasis and psoriatic arthritis patient stool samples (Arthritis Rheumatol. 2015;67:128-39) prompted the current research, which is “trying to see if the skin has a similar manifestation,” Dr. Manasson said during an oral presentation of her poster at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“The microbiome has been implicated as a potential trigger for inflammation and autoimmune disease,” Dr. Manasson noted.
To investigate a potential role of the skin microbiome, the investigators swabbed lesions and unaffected skin (on a contralateral site) in 29 people with psoriasis and 62 others with psoriatic arthritis. They extracted, amplified, and sequenced DNA from the samples. No participants in the study were on treatment with biologics, disease-modifying antirheumatic drugs, or steroids at the time of assessment. The psoriasis group was 66% men and had an average age of 45 years; the psoriatic arthritis group was 55% men and the average age was 42.
Dr. Manasson and her colleagues calculated the taxonomic relative abundance and contrasted their prevalence among the four skin phenotypes examined: lesions and unaffected skin of psoriasis patients and lesions and unaffected skin of psoriatic arthritis patients. Alpha diversity plots revealed a similar number of operational taxonomic units (OTUs) between psoriasis and psoriatic arthritis samples. Beta diversity analysis showed no distinct clustering or significant difference in microbiota communities among different phenotypes.
“We saw more of a decrease in nonlesional skin and across clinical severity, too,” Dr. Manasson said. “Globally, we didn’t see significant differences [in microbiota present].”
Staphylococcus and Corynebacterium were the predominant bacteria in all samples, but there were also specific genera that were less common in psoriatic arthritis patients and in lesional skin. These less abundant genera included unclassified Bradyrhizobiaceae, Rahnella, unclassified Prevotellaceae, and Parvibaculum.
“It looks like you had some differences between lesion and nonlesional skin,” Alice Gottlieb, MD, chair and dermatologist in chief at Tufts Medical Center in Boston. “In psoriasis, the barrier function is not normal. You may want to look at atopic dermatitis where you clearly have altered barrier function.”
Dr. Manasson said they used a skin swab, so they did not assess barrier function.
“The nonlesional skin may be more interesting to look at,” Dr. Gottlieb added. “If you see a difference in nonlesional skin, it could be more [conclusive].”
Microbiome stability often changes in individuals from week to week, commented Philip Helliwell, DM, PhD, a rheumatologist at the University of Leeds in England and president of GRAPPA. Dr. Manasson said she could assess variability over time in the future. She also would like to evaluate how therapies, including antibiotics, alter the skin microbiome.
Lack of a healthy control group is a potential limitation of the study. Some unanswered questions remain, Dr. Manasson said, such as what are the regional differences in skin microbiota, for example, between a patient’s scalp and forearm? She added, “The most interesting question is what does this actually mean? What are the downstream effects?”
If a decrease in skin microbiome flora diversity is verified in future research as a sign that a patient with psoriasis is at elevated risk for developing psoriatic arthritis, it could help physicians predict who will progress. Currently, about 30% of psoriatic patients go on to develop joint disease, but methods to identify this subpopulation remain elusive.
Dr. Manasson, Dr. Gottlieb, and Dr. Helliwell had no relevant financial disclosures.
MIAMI – As patients with psoriasis develop psoriatic arthritis, the abundance of particular genera in the skin microbiome decreases, according to a preliminary study characterizing cutaneous microbiota in these populations.
“The big overall message is there might be a decrease in microbiota diversity as you progress through the disease spectrum,” Julia Manasson, MD, a fellow in the division of rheumatology at New York University said. “This is the first study characterizing the cutaneous microbial compositions of subjects with psoriasis and psoriatic arthritis in both psoriatic lesions and unaffected skin.”
A previous study that revealed changes in gut microbiome between psoriasis and psoriatic arthritis patient stool samples (Arthritis Rheumatol. 2015;67:128-39) prompted the current research, which is “trying to see if the skin has a similar manifestation,” Dr. Manasson said during an oral presentation of her poster at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“The microbiome has been implicated as a potential trigger for inflammation and autoimmune disease,” Dr. Manasson noted.
To investigate a potential role of the skin microbiome, the investigators swabbed lesions and unaffected skin (on a contralateral site) in 29 people with psoriasis and 62 others with psoriatic arthritis. They extracted, amplified, and sequenced DNA from the samples. No participants in the study were on treatment with biologics, disease-modifying antirheumatic drugs, or steroids at the time of assessment. The psoriasis group was 66% men and had an average age of 45 years; the psoriatic arthritis group was 55% men and the average age was 42.
Dr. Manasson and her colleagues calculated the taxonomic relative abundance and contrasted their prevalence among the four skin phenotypes examined: lesions and unaffected skin of psoriasis patients and lesions and unaffected skin of psoriatic arthritis patients. Alpha diversity plots revealed a similar number of operational taxonomic units (OTUs) between psoriasis and psoriatic arthritis samples. Beta diversity analysis showed no distinct clustering or significant difference in microbiota communities among different phenotypes.
“We saw more of a decrease in nonlesional skin and across clinical severity, too,” Dr. Manasson said. “Globally, we didn’t see significant differences [in microbiota present].”
Staphylococcus and Corynebacterium were the predominant bacteria in all samples, but there were also specific genera that were less common in psoriatic arthritis patients and in lesional skin. These less abundant genera included unclassified Bradyrhizobiaceae, Rahnella, unclassified Prevotellaceae, and Parvibaculum.
“It looks like you had some differences between lesion and nonlesional skin,” Alice Gottlieb, MD, chair and dermatologist in chief at Tufts Medical Center in Boston. “In psoriasis, the barrier function is not normal. You may want to look at atopic dermatitis where you clearly have altered barrier function.”
Dr. Manasson said they used a skin swab, so they did not assess barrier function.
“The nonlesional skin may be more interesting to look at,” Dr. Gottlieb added. “If you see a difference in nonlesional skin, it could be more [conclusive].”
Microbiome stability often changes in individuals from week to week, commented Philip Helliwell, DM, PhD, a rheumatologist at the University of Leeds in England and president of GRAPPA. Dr. Manasson said she could assess variability over time in the future. She also would like to evaluate how therapies, including antibiotics, alter the skin microbiome.
Lack of a healthy control group is a potential limitation of the study. Some unanswered questions remain, Dr. Manasson said, such as what are the regional differences in skin microbiota, for example, between a patient’s scalp and forearm? She added, “The most interesting question is what does this actually mean? What are the downstream effects?”
If a decrease in skin microbiome flora diversity is verified in future research as a sign that a patient with psoriasis is at elevated risk for developing psoriatic arthritis, it could help physicians predict who will progress. Currently, about 30% of psoriatic patients go on to develop joint disease, but methods to identify this subpopulation remain elusive.
Dr. Manasson, Dr. Gottlieb, and Dr. Helliwell had no relevant financial disclosures.
MIAMI – As patients with psoriasis develop psoriatic arthritis, the abundance of particular genera in the skin microbiome decreases, according to a preliminary study characterizing cutaneous microbiota in these populations.
“The big overall message is there might be a decrease in microbiota diversity as you progress through the disease spectrum,” Julia Manasson, MD, a fellow in the division of rheumatology at New York University said. “This is the first study characterizing the cutaneous microbial compositions of subjects with psoriasis and psoriatic arthritis in both psoriatic lesions and unaffected skin.”
A previous study that revealed changes in gut microbiome between psoriasis and psoriatic arthritis patient stool samples (Arthritis Rheumatol. 2015;67:128-39) prompted the current research, which is “trying to see if the skin has a similar manifestation,” Dr. Manasson said during an oral presentation of her poster at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“The microbiome has been implicated as a potential trigger for inflammation and autoimmune disease,” Dr. Manasson noted.
To investigate a potential role of the skin microbiome, the investigators swabbed lesions and unaffected skin (on a contralateral site) in 29 people with psoriasis and 62 others with psoriatic arthritis. They extracted, amplified, and sequenced DNA from the samples. No participants in the study were on treatment with biologics, disease-modifying antirheumatic drugs, or steroids at the time of assessment. The psoriasis group was 66% men and had an average age of 45 years; the psoriatic arthritis group was 55% men and the average age was 42.
Dr. Manasson and her colleagues calculated the taxonomic relative abundance and contrasted their prevalence among the four skin phenotypes examined: lesions and unaffected skin of psoriasis patients and lesions and unaffected skin of psoriatic arthritis patients. Alpha diversity plots revealed a similar number of operational taxonomic units (OTUs) between psoriasis and psoriatic arthritis samples. Beta diversity analysis showed no distinct clustering or significant difference in microbiota communities among different phenotypes.
“We saw more of a decrease in nonlesional skin and across clinical severity, too,” Dr. Manasson said. “Globally, we didn’t see significant differences [in microbiota present].”
Staphylococcus and Corynebacterium were the predominant bacteria in all samples, but there were also specific genera that were less common in psoriatic arthritis patients and in lesional skin. These less abundant genera included unclassified Bradyrhizobiaceae, Rahnella, unclassified Prevotellaceae, and Parvibaculum.
“It looks like you had some differences between lesion and nonlesional skin,” Alice Gottlieb, MD, chair and dermatologist in chief at Tufts Medical Center in Boston. “In psoriasis, the barrier function is not normal. You may want to look at atopic dermatitis where you clearly have altered barrier function.”
Dr. Manasson said they used a skin swab, so they did not assess barrier function.
“The nonlesional skin may be more interesting to look at,” Dr. Gottlieb added. “If you see a difference in nonlesional skin, it could be more [conclusive].”
Microbiome stability often changes in individuals from week to week, commented Philip Helliwell, DM, PhD, a rheumatologist at the University of Leeds in England and president of GRAPPA. Dr. Manasson said she could assess variability over time in the future. She also would like to evaluate how therapies, including antibiotics, alter the skin microbiome.
Lack of a healthy control group is a potential limitation of the study. Some unanswered questions remain, Dr. Manasson said, such as what are the regional differences in skin microbiota, for example, between a patient’s scalp and forearm? She added, “The most interesting question is what does this actually mean? What are the downstream effects?”
If a decrease in skin microbiome flora diversity is verified in future research as a sign that a patient with psoriasis is at elevated risk for developing psoriatic arthritis, it could help physicians predict who will progress. Currently, about 30% of psoriatic patients go on to develop joint disease, but methods to identify this subpopulation remain elusive.
Dr. Manasson, Dr. Gottlieb, and Dr. Helliwell had no relevant financial disclosures.
AT 2016 GRAPPA ANNUAL MEETING
Key clinical point:Changes in skin microbiome diversity in patients with psoriasis might someday help to predict progression to psoriatic arthritis.
Major finding: The abundance of specific genera was decreased in psoriatic arthritis patients and in their lesional skin relative to patients with psoriasis only.
Data source: Comparison of 29 people with psoriasis versus 62 with psoriatic arthritis.
Disclosures: Dr. Manasson, Dr. Gottlieb, and Dr. Helliwell had no relevant disclosures.
Withdrawing Risperidone Spikes Risk for Psychotic Relapse in Hallucinating Alzheimer’s Patients
TORONTO – Hallucinations – especially auditory hallucinations – triple the risk that a risperidone-controlled Alzheimer’s patient with psychoses will relapse if the drug is withdrawn.
“I think the clinical impact we see here is that for patients with hallucinations, and particularly auditory hallucinations, antipsychotic discontinuation should be done very, very cautiously because they do have a very high risk of relapse,” Anjali Patel, DO, said at the Alzheimer’s Association International Conference 2016. “Close monitoring will be necessary and antipsychotic medications promptly reinstated if relapse occurs.”
The findings come from a responder analysis of an open-label study of risperidone (Risperdal) use in Alzheimer’s patients who express neuropsychiatric symptoms. The primary results of the multicenter Antipsychotic Discontinuation in Alzheimer’s Disease (ADAD) trial were published in 2012 (N Engl J Med. 2012;367:1497-507). The 48-week study administered open-label, flexible-dose risperidone for 16 weeks to 180 patients with Alzheimer’s dementia, with agitation and/or aggression. The patients in this study had a mean age of 79 years at baseline. Most (62%) were taking a cholinesterase inhibitor, and many took memantine (35%). Patients commonly used anxiolytics (17%) and antidepressants (24%). The mean Neuropsychiatric Inventory (NPI) score at baseline was 36. Patients were moderately impaired, with a mean Mini Mental State Exam score of 14.
At 16 weeks, patients who had not responded left the study. After 16 weeks of open-label treatment, 110 patients who had responded well continued the dosing schedule for 32 weeks, continued risperidone for 16 weeks and then went on placebo for 16 weeks, or were switched to placebo for 32 weeks. Discontinuation of risperidone was associated with a two- to four-fold increased risk of relapse over 16-32 weeks.
Dr. Patel of Columbia University, New York, presented the preplanned post-hoc analysis that examined the association between the 12 NPI symptom domains and the likelihood of relapse at week 32. In a univariate analysis, only hallucinations posted a significant association with discontinuation of risperidone. Hallucinations of any severity at baseline were present in 43 patients (39%). The relapse rates were similar among patients without baseline hallucinations (35%) and those with mild baseline hallucinations (37%). But 78% of those with severe hallucinations relapsed when risperidone was withdrawn.
Baseline hallucinations remained a strong predictor of relapse in a multivariate model as well, with a risk ratio of 2.96 for relapse among patients who had severe baseline hallucinations, compared with those with mild or no hallucinations. Age, gender, race, and nursing home placement had no significant impact on relapse rate.
Of the 17 patients with any baseline hallucinations who were switched to placebo, 13 (77%) relapsed, compared with 38% of the patients with hallucinations who continued risperidone (risk ratio, 1.98).
The risk for relapse was particularly high when the hallucinations were primarily auditory, Dr. Patel said. “In fact, visual hallucinations were not predictive of relapse.”
Among the 11 patients with severe baseline hallucinations, 10 relapsed when risperidone was withdrawn (91%; RR, 2.88), compared with 57% of patients with severe hallucinations who stayed on the drug (RR, 1.59).
The ADAD trial was funded by the National Institutes of Health and the Department of Veterans Affairs. Dr. Patel had no financial disclosures for the subanalysis.
TORONTO – Hallucinations – especially auditory hallucinations – triple the risk that a risperidone-controlled Alzheimer’s patient with psychoses will relapse if the drug is withdrawn.
“I think the clinical impact we see here is that for patients with hallucinations, and particularly auditory hallucinations, antipsychotic discontinuation should be done very, very cautiously because they do have a very high risk of relapse,” Anjali Patel, DO, said at the Alzheimer’s Association International Conference 2016. “Close monitoring will be necessary and antipsychotic medications promptly reinstated if relapse occurs.”
The findings come from a responder analysis of an open-label study of risperidone (Risperdal) use in Alzheimer’s patients who express neuropsychiatric symptoms. The primary results of the multicenter Antipsychotic Discontinuation in Alzheimer’s Disease (ADAD) trial were published in 2012 (N Engl J Med. 2012;367:1497-507). The 48-week study administered open-label, flexible-dose risperidone for 16 weeks to 180 patients with Alzheimer’s dementia, with agitation and/or aggression. The patients in this study had a mean age of 79 years at baseline. Most (62%) were taking a cholinesterase inhibitor, and many took memantine (35%). Patients commonly used anxiolytics (17%) and antidepressants (24%). The mean Neuropsychiatric Inventory (NPI) score at baseline was 36. Patients were moderately impaired, with a mean Mini Mental State Exam score of 14.
At 16 weeks, patients who had not responded left the study. After 16 weeks of open-label treatment, 110 patients who had responded well continued the dosing schedule for 32 weeks, continued risperidone for 16 weeks and then went on placebo for 16 weeks, or were switched to placebo for 32 weeks. Discontinuation of risperidone was associated with a two- to four-fold increased risk of relapse over 16-32 weeks.
Dr. Patel of Columbia University, New York, presented the preplanned post-hoc analysis that examined the association between the 12 NPI symptom domains and the likelihood of relapse at week 32. In a univariate analysis, only hallucinations posted a significant association with discontinuation of risperidone. Hallucinations of any severity at baseline were present in 43 patients (39%). The relapse rates were similar among patients without baseline hallucinations (35%) and those with mild baseline hallucinations (37%). But 78% of those with severe hallucinations relapsed when risperidone was withdrawn.
Baseline hallucinations remained a strong predictor of relapse in a multivariate model as well, with a risk ratio of 2.96 for relapse among patients who had severe baseline hallucinations, compared with those with mild or no hallucinations. Age, gender, race, and nursing home placement had no significant impact on relapse rate.
Of the 17 patients with any baseline hallucinations who were switched to placebo, 13 (77%) relapsed, compared with 38% of the patients with hallucinations who continued risperidone (risk ratio, 1.98).
The risk for relapse was particularly high when the hallucinations were primarily auditory, Dr. Patel said. “In fact, visual hallucinations were not predictive of relapse.”
Among the 11 patients with severe baseline hallucinations, 10 relapsed when risperidone was withdrawn (91%; RR, 2.88), compared with 57% of patients with severe hallucinations who stayed on the drug (RR, 1.59).
The ADAD trial was funded by the National Institutes of Health and the Department of Veterans Affairs. Dr. Patel had no financial disclosures for the subanalysis.
TORONTO – Hallucinations – especially auditory hallucinations – triple the risk that a risperidone-controlled Alzheimer’s patient with psychoses will relapse if the drug is withdrawn.
“I think the clinical impact we see here is that for patients with hallucinations, and particularly auditory hallucinations, antipsychotic discontinuation should be done very, very cautiously because they do have a very high risk of relapse,” Anjali Patel, DO, said at the Alzheimer’s Association International Conference 2016. “Close monitoring will be necessary and antipsychotic medications promptly reinstated if relapse occurs.”
The findings come from a responder analysis of an open-label study of risperidone (Risperdal) use in Alzheimer’s patients who express neuropsychiatric symptoms. The primary results of the multicenter Antipsychotic Discontinuation in Alzheimer’s Disease (ADAD) trial were published in 2012 (N Engl J Med. 2012;367:1497-507). The 48-week study administered open-label, flexible-dose risperidone for 16 weeks to 180 patients with Alzheimer’s dementia, with agitation and/or aggression. The patients in this study had a mean age of 79 years at baseline. Most (62%) were taking a cholinesterase inhibitor, and many took memantine (35%). Patients commonly used anxiolytics (17%) and antidepressants (24%). The mean Neuropsychiatric Inventory (NPI) score at baseline was 36. Patients were moderately impaired, with a mean Mini Mental State Exam score of 14.
At 16 weeks, patients who had not responded left the study. After 16 weeks of open-label treatment, 110 patients who had responded well continued the dosing schedule for 32 weeks, continued risperidone for 16 weeks and then went on placebo for 16 weeks, or were switched to placebo for 32 weeks. Discontinuation of risperidone was associated with a two- to four-fold increased risk of relapse over 16-32 weeks.
Dr. Patel of Columbia University, New York, presented the preplanned post-hoc analysis that examined the association between the 12 NPI symptom domains and the likelihood of relapse at week 32. In a univariate analysis, only hallucinations posted a significant association with discontinuation of risperidone. Hallucinations of any severity at baseline were present in 43 patients (39%). The relapse rates were similar among patients without baseline hallucinations (35%) and those with mild baseline hallucinations (37%). But 78% of those with severe hallucinations relapsed when risperidone was withdrawn.
Baseline hallucinations remained a strong predictor of relapse in a multivariate model as well, with a risk ratio of 2.96 for relapse among patients who had severe baseline hallucinations, compared with those with mild or no hallucinations. Age, gender, race, and nursing home placement had no significant impact on relapse rate.
Of the 17 patients with any baseline hallucinations who were switched to placebo, 13 (77%) relapsed, compared with 38% of the patients with hallucinations who continued risperidone (risk ratio, 1.98).
The risk for relapse was particularly high when the hallucinations were primarily auditory, Dr. Patel said. “In fact, visual hallucinations were not predictive of relapse.”
Among the 11 patients with severe baseline hallucinations, 10 relapsed when risperidone was withdrawn (91%; RR, 2.88), compared with 57% of patients with severe hallucinations who stayed on the drug (RR, 1.59).
The ADAD trial was funded by the National Institutes of Health and the Department of Veterans Affairs. Dr. Patel had no financial disclosures for the subanalysis.
AT AAIC 2016