User login
Discontinuing Inhaled Corticosteroids in COPD Reduces Risk of Pneumonia
Clinical question: Is discontinuation of inhaled corticosteroids (ICSs) in patients with COPD associated with a decreased risk of pneumonia?
Background: ICSs are used in up to 85% of patients treated for COPD but may be associated with adverse systemic side effects including pneumonia. Trials looking at weaning patients off ICSs and replacing with long-acting bronchodilators have found few adverse outcomes; however, the benefits of discontinuation on adverse events, including pneumonia, have been unclear.
Study design: Case-control study.
Setting: Quebec health systems.
Synopsis: Using the Quebec health insurance databases, a study cohort of 103,386 patients with COPD on ICSs was created. Patients were followed for a mean of 4.9 years; 14,020 patients who were hospitalized for pneumonia or died from pneumonia outside the hospital were matched to control subjects. Discontinuation of ICSs was associated with a 37% decrease in serious pneumonia (relative risk [RR] 0.63; 95% CI, 0.60–0.66). The risk reduction occurred as early as one month after discontinuation of ICSs. Risk reduction was greater with fluticasone (RR 0.58; 95% CI, 0.54–0.61) than with budesonide (RR 0.87; 95% CI, 0.7–0.97).
Population size and follow-up may contribute to why risk reduction in pneumonia was seen in this study but not in other recent randomized trials on discontinuation of ICSs. A limitation of this study was its observational design; however, its results suggest that use of ICSs in COPD patients should be highly selective, as indiscriminate use can subject patients to elevated risk of hospitalization or death from pneumonia.
Bottom line: Discontinuation of ICSs in patients with COPD is associated with a decreased risk of contracting serious pneumonia. This reduction appears greatest with fluticasone.
Citation: Suissa S, Coulombe J, Ernst P. Discontinuation of inhaled corticosteroids in COPD and the risk reduction of pneumonia. Chest. 2015;148(5):1177-1183.
Short Take
Increase in Rates of Prescription Drug Use and Polypharmacy Seen
The percentage of Americans who reported taking prescription medications increased substantially from 1999 to 2012 (51% to 59%), as did the percentage who reported taking at least five prescription medications.
Citation: Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States from 1999-2012. JAMA. 2015;314(17):1818-1830.
Clinical question: Is discontinuation of inhaled corticosteroids (ICSs) in patients with COPD associated with a decreased risk of pneumonia?
Background: ICSs are used in up to 85% of patients treated for COPD but may be associated with adverse systemic side effects including pneumonia. Trials looking at weaning patients off ICSs and replacing with long-acting bronchodilators have found few adverse outcomes; however, the benefits of discontinuation on adverse events, including pneumonia, have been unclear.
Study design: Case-control study.
Setting: Quebec health systems.
Synopsis: Using the Quebec health insurance databases, a study cohort of 103,386 patients with COPD on ICSs was created. Patients were followed for a mean of 4.9 years; 14,020 patients who were hospitalized for pneumonia or died from pneumonia outside the hospital were matched to control subjects. Discontinuation of ICSs was associated with a 37% decrease in serious pneumonia (relative risk [RR] 0.63; 95% CI, 0.60–0.66). The risk reduction occurred as early as one month after discontinuation of ICSs. Risk reduction was greater with fluticasone (RR 0.58; 95% CI, 0.54–0.61) than with budesonide (RR 0.87; 95% CI, 0.7–0.97).
Population size and follow-up may contribute to why risk reduction in pneumonia was seen in this study but not in other recent randomized trials on discontinuation of ICSs. A limitation of this study was its observational design; however, its results suggest that use of ICSs in COPD patients should be highly selective, as indiscriminate use can subject patients to elevated risk of hospitalization or death from pneumonia.
Bottom line: Discontinuation of ICSs in patients with COPD is associated with a decreased risk of contracting serious pneumonia. This reduction appears greatest with fluticasone.
Citation: Suissa S, Coulombe J, Ernst P. Discontinuation of inhaled corticosteroids in COPD and the risk reduction of pneumonia. Chest. 2015;148(5):1177-1183.
Short Take
Increase in Rates of Prescription Drug Use and Polypharmacy Seen
The percentage of Americans who reported taking prescription medications increased substantially from 1999 to 2012 (51% to 59%), as did the percentage who reported taking at least five prescription medications.
Citation: Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States from 1999-2012. JAMA. 2015;314(17):1818-1830.
Clinical question: Is discontinuation of inhaled corticosteroids (ICSs) in patients with COPD associated with a decreased risk of pneumonia?
Background: ICSs are used in up to 85% of patients treated for COPD but may be associated with adverse systemic side effects including pneumonia. Trials looking at weaning patients off ICSs and replacing with long-acting bronchodilators have found few adverse outcomes; however, the benefits of discontinuation on adverse events, including pneumonia, have been unclear.
Study design: Case-control study.
Setting: Quebec health systems.
Synopsis: Using the Quebec health insurance databases, a study cohort of 103,386 patients with COPD on ICSs was created. Patients were followed for a mean of 4.9 years; 14,020 patients who were hospitalized for pneumonia or died from pneumonia outside the hospital were matched to control subjects. Discontinuation of ICSs was associated with a 37% decrease in serious pneumonia (relative risk [RR] 0.63; 95% CI, 0.60–0.66). The risk reduction occurred as early as one month after discontinuation of ICSs. Risk reduction was greater with fluticasone (RR 0.58; 95% CI, 0.54–0.61) than with budesonide (RR 0.87; 95% CI, 0.7–0.97).
Population size and follow-up may contribute to why risk reduction in pneumonia was seen in this study but not in other recent randomized trials on discontinuation of ICSs. A limitation of this study was its observational design; however, its results suggest that use of ICSs in COPD patients should be highly selective, as indiscriminate use can subject patients to elevated risk of hospitalization or death from pneumonia.
Bottom line: Discontinuation of ICSs in patients with COPD is associated with a decreased risk of contracting serious pneumonia. This reduction appears greatest with fluticasone.
Citation: Suissa S, Coulombe J, Ernst P. Discontinuation of inhaled corticosteroids in COPD and the risk reduction of pneumonia. Chest. 2015;148(5):1177-1183.
Short Take
Increase in Rates of Prescription Drug Use and Polypharmacy Seen
The percentage of Americans who reported taking prescription medications increased substantially from 1999 to 2012 (51% to 59%), as did the percentage who reported taking at least five prescription medications.
Citation: Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States from 1999-2012. JAMA. 2015;314(17):1818-1830.
MEDS Score for Sepsis Might Best Predict ED Mortality
Clinical question: Which illness severity score best predicts outcomes in emergency department (ED) patients presenting with infection?
Background: Several scoring models have been developed to predict illness severity and mortality in patients with infection. Some scores were developed specifically for patients with sepsis and others for patients in a general critical care setting. These different scoring models have not been specifically compared and validated in the ED setting in patients with infection of various severities.
Study design: Prospective, observational study.
Setting: Adult ED in a metropolitan tertiary, university-affiliated hospital.
Synopsis: Investigators prospectively identified 8,871 adult inpatients with infection from a single-center ED. Data to calculate five prediction models were collected. The models were:
- Mortality in Emergency Department Sepsis (MEDS) score;
- Acute Physiology and Chronic Health Evaluation II (APACHE II);
- Simplified Acute Physiology Score II (SAPS II);
- Sequential Organ Failure Assessment (SOFA); and
- Severe Sepsis Score (SSS).
Severity score performance was assessed for the overall cohort and for subgroups, including infection without systemic inflammatory response syndrome, sepsis, severe sepsis, and septic shock. The MEDS score best predicted mortality in the cohort, with an area under the receiver operating characteristics curve of 0.92. However, older scoring models such as the APACHE II and SAPS II still discriminated well, especially in patients who were admitted to the ICU. All scores tended to overestimate mortality.
Bottom line: The MEDS score may best predict illness severity in septic patients presenting to the ED, but other scoring models may be better-suited for specific patient populations.
Citation: Williams JM, Greenslade JH, Chu K, Brown AF, Lipman J. Severity scores in emergency department patients with presumed infection: a prospective validation study. Crit Care Med. 2016;44(3):539-547.
Clinical question: Which illness severity score best predicts outcomes in emergency department (ED) patients presenting with infection?
Background: Several scoring models have been developed to predict illness severity and mortality in patients with infection. Some scores were developed specifically for patients with sepsis and others for patients in a general critical care setting. These different scoring models have not been specifically compared and validated in the ED setting in patients with infection of various severities.
Study design: Prospective, observational study.
Setting: Adult ED in a metropolitan tertiary, university-affiliated hospital.
Synopsis: Investigators prospectively identified 8,871 adult inpatients with infection from a single-center ED. Data to calculate five prediction models were collected. The models were:
- Mortality in Emergency Department Sepsis (MEDS) score;
- Acute Physiology and Chronic Health Evaluation II (APACHE II);
- Simplified Acute Physiology Score II (SAPS II);
- Sequential Organ Failure Assessment (SOFA); and
- Severe Sepsis Score (SSS).
Severity score performance was assessed for the overall cohort and for subgroups, including infection without systemic inflammatory response syndrome, sepsis, severe sepsis, and septic shock. The MEDS score best predicted mortality in the cohort, with an area under the receiver operating characteristics curve of 0.92. However, older scoring models such as the APACHE II and SAPS II still discriminated well, especially in patients who were admitted to the ICU. All scores tended to overestimate mortality.
Bottom line: The MEDS score may best predict illness severity in septic patients presenting to the ED, but other scoring models may be better-suited for specific patient populations.
Citation: Williams JM, Greenslade JH, Chu K, Brown AF, Lipman J. Severity scores in emergency department patients with presumed infection: a prospective validation study. Crit Care Med. 2016;44(3):539-547.
Clinical question: Which illness severity score best predicts outcomes in emergency department (ED) patients presenting with infection?
Background: Several scoring models have been developed to predict illness severity and mortality in patients with infection. Some scores were developed specifically for patients with sepsis and others for patients in a general critical care setting. These different scoring models have not been specifically compared and validated in the ED setting in patients with infection of various severities.
Study design: Prospective, observational study.
Setting: Adult ED in a metropolitan tertiary, university-affiliated hospital.
Synopsis: Investigators prospectively identified 8,871 adult inpatients with infection from a single-center ED. Data to calculate five prediction models were collected. The models were:
- Mortality in Emergency Department Sepsis (MEDS) score;
- Acute Physiology and Chronic Health Evaluation II (APACHE II);
- Simplified Acute Physiology Score II (SAPS II);
- Sequential Organ Failure Assessment (SOFA); and
- Severe Sepsis Score (SSS).
Severity score performance was assessed for the overall cohort and for subgroups, including infection without systemic inflammatory response syndrome, sepsis, severe sepsis, and septic shock. The MEDS score best predicted mortality in the cohort, with an area under the receiver operating characteristics curve of 0.92. However, older scoring models such as the APACHE II and SAPS II still discriminated well, especially in patients who were admitted to the ICU. All scores tended to overestimate mortality.
Bottom line: The MEDS score may best predict illness severity in septic patients presenting to the ED, but other scoring models may be better-suited for specific patient populations.
Citation: Williams JM, Greenslade JH, Chu K, Brown AF, Lipman J. Severity scores in emergency department patients with presumed infection: a prospective validation study. Crit Care Med. 2016;44(3):539-547.
Gum Disease is Linked to Faster Cognitive Decline for Alzhemier's Patients
(Reuters Health) - For people with Alzheimer's disease, having gum disease is tied to faster cognitive decline, according to a new study.
"What we have shown is that regardless of the severity of dementia (within this mild to moderate impaired group) that patients with more severe gum disease are declining more rapidly," said senior author Clive Holmes of the University of Southampton in the UK.
In other studies, Holmes and his coauthors have found that conditions such as chest infections, urinary tract infections, rheumatoid arthritis and diabetes are associated with faster disease progression in Alzheimer's, he said.
"We hadn't previously looked at gum disease because MDs tendto leave this in the hands of dentists but it is an important common low grade chronic infection," Holmes told Reuters Health by email.
The researchers observed 60 people with mild to moderate Alzheimer's disease living at home for six months. The participants did not smoke, had not been treated for gum disease within the previous six months, and had at least 10 teeth.
At the start, each participant completed a cognitive assessment, gave a blood sample, was examined by a dental hygienist and their main caregiver was interviewed to provide a medical and dental history. The same tests and interviews were repeated six months later.
Of the 60 people in the study, 22 had moderate to severe gum disease at the beginning of the study. By six months later, one participant had died, three had withdrawn from the study and three were lost to follow-up.
Cognitive score declined more for those who had periodontitis to begin with than for those who did not, the researchers reported February 24 in PLoS One.
According to one theory, cognitive impairment leads to adverse oral health due to inattention to routine oral hygiene and care, said Dr. James M. Noble of the Taub Institute for Research on Alzheimer's Disease and the Aging Brain at Columbia University Medical Center in New York City, who was not part of the new study.
"The second, and the one I'm most intrigued by, is whether or not periodontal disease has an influence on cognitive outcomes of aging, either as an independent risk factor for (new-onset) cognitive impairment including Alzheimer's disease, or more rapid decline once (Alzheimer's disease) has been diagnosed, as was suggested by this study," Noble told Reuters Health by email.
Gum disease may cause chronic low-grade inflammation in the rest of the body, and inflammation is associated with changes in the brain, he said.
"It is known that gum disease is associated with increased markers of inflammation," Holmes said.
But the new study indicates a connection between gum disease and cognitive decline, not necessarily that one causes the other, he said. Further studies need to assess whether treatingthe gum disease would also slow cognitive decline.
"Periodontitis has been associated with heart disease and stroke among other conditions," Noble said. Based on this and other studies, "it seems to be good advice to brush and floss," Noble said.
(Reuters Health) - For people with Alzheimer's disease, having gum disease is tied to faster cognitive decline, according to a new study.
"What we have shown is that regardless of the severity of dementia (within this mild to moderate impaired group) that patients with more severe gum disease are declining more rapidly," said senior author Clive Holmes of the University of Southampton in the UK.
In other studies, Holmes and his coauthors have found that conditions such as chest infections, urinary tract infections, rheumatoid arthritis and diabetes are associated with faster disease progression in Alzheimer's, he said.
"We hadn't previously looked at gum disease because MDs tendto leave this in the hands of dentists but it is an important common low grade chronic infection," Holmes told Reuters Health by email.
The researchers observed 60 people with mild to moderate Alzheimer's disease living at home for six months. The participants did not smoke, had not been treated for gum disease within the previous six months, and had at least 10 teeth.
At the start, each participant completed a cognitive assessment, gave a blood sample, was examined by a dental hygienist and their main caregiver was interviewed to provide a medical and dental history. The same tests and interviews were repeated six months later.
Of the 60 people in the study, 22 had moderate to severe gum disease at the beginning of the study. By six months later, one participant had died, three had withdrawn from the study and three were lost to follow-up.
Cognitive score declined more for those who had periodontitis to begin with than for those who did not, the researchers reported February 24 in PLoS One.
According to one theory, cognitive impairment leads to adverse oral health due to inattention to routine oral hygiene and care, said Dr. James M. Noble of the Taub Institute for Research on Alzheimer's Disease and the Aging Brain at Columbia University Medical Center in New York City, who was not part of the new study.
"The second, and the one I'm most intrigued by, is whether or not periodontal disease has an influence on cognitive outcomes of aging, either as an independent risk factor for (new-onset) cognitive impairment including Alzheimer's disease, or more rapid decline once (Alzheimer's disease) has been diagnosed, as was suggested by this study," Noble told Reuters Health by email.
Gum disease may cause chronic low-grade inflammation in the rest of the body, and inflammation is associated with changes in the brain, he said.
"It is known that gum disease is associated with increased markers of inflammation," Holmes said.
But the new study indicates a connection between gum disease and cognitive decline, not necessarily that one causes the other, he said. Further studies need to assess whether treatingthe gum disease would also slow cognitive decline.
"Periodontitis has been associated with heart disease and stroke among other conditions," Noble said. Based on this and other studies, "it seems to be good advice to brush and floss," Noble said.
(Reuters Health) - For people with Alzheimer's disease, having gum disease is tied to faster cognitive decline, according to a new study.
"What we have shown is that regardless of the severity of dementia (within this mild to moderate impaired group) that patients with more severe gum disease are declining more rapidly," said senior author Clive Holmes of the University of Southampton in the UK.
In other studies, Holmes and his coauthors have found that conditions such as chest infections, urinary tract infections, rheumatoid arthritis and diabetes are associated with faster disease progression in Alzheimer's, he said.
"We hadn't previously looked at gum disease because MDs tendto leave this in the hands of dentists but it is an important common low grade chronic infection," Holmes told Reuters Health by email.
The researchers observed 60 people with mild to moderate Alzheimer's disease living at home for six months. The participants did not smoke, had not been treated for gum disease within the previous six months, and had at least 10 teeth.
At the start, each participant completed a cognitive assessment, gave a blood sample, was examined by a dental hygienist and their main caregiver was interviewed to provide a medical and dental history. The same tests and interviews were repeated six months later.
Of the 60 people in the study, 22 had moderate to severe gum disease at the beginning of the study. By six months later, one participant had died, three had withdrawn from the study and three were lost to follow-up.
Cognitive score declined more for those who had periodontitis to begin with than for those who did not, the researchers reported February 24 in PLoS One.
According to one theory, cognitive impairment leads to adverse oral health due to inattention to routine oral hygiene and care, said Dr. James M. Noble of the Taub Institute for Research on Alzheimer's Disease and the Aging Brain at Columbia University Medical Center in New York City, who was not part of the new study.
"The second, and the one I'm most intrigued by, is whether or not periodontal disease has an influence on cognitive outcomes of aging, either as an independent risk factor for (new-onset) cognitive impairment including Alzheimer's disease, or more rapid decline once (Alzheimer's disease) has been diagnosed, as was suggested by this study," Noble told Reuters Health by email.
Gum disease may cause chronic low-grade inflammation in the rest of the body, and inflammation is associated with changes in the brain, he said.
"It is known that gum disease is associated with increased markers of inflammation," Holmes said.
But the new study indicates a connection between gum disease and cognitive decline, not necessarily that one causes the other, he said. Further studies need to assess whether treatingthe gum disease would also slow cognitive decline.
"Periodontitis has been associated with heart disease and stroke among other conditions," Noble said. Based on this and other studies, "it seems to be good advice to brush and floss," Noble said.
Team traces evolution of malaria

Photo courtesy of
Sesh Sundararaman,
University of Pennsylvania
By studying malaria parasites found in chimpanzees, researchers believe they have gained new insights regarding a malaria parasite that infects humans.
The team used a selective amplification technique to sequence the genomes of 2 divergent Plasmodium species, P reichenowi and P gaboni, from chimpanzee blood.
This revealed clues about the evolution and pathogenicity of P falciparum, the deadliest malaria parasite that affects humans.
The researchers described this work in Nature Communications.
They noted that African apes harbor at least 6 Plasmodium species that have been classified into a separate subgenus, called Laverania. Three of these Laverania species, including P reichenowi and P gaboni, reside in chimps.
Three others—including P praefalciparum, which gave rise to P falciparum—reside in gorillas. The gorilla origin of P falciparum was discovered several years ago by this same group of investigators.
“We want to know why Plasmodium falciparum is so deadly,” said Beatrice Hahn, MD, of the University of Pennsylvania in Philadelphia.
“The answer must lie in the blueprint—the genome—of its chimpanzee and gorilla cousins. We also want to know how and when the gorilla precursor of Plasmodium falciparum jumped into humans and why this happened only once.”
In an attempt to answer these questions, Dr Hahn and her colleagues used their selective amplification method to sequence Laverania genomes.
They used small amounts of unprocessed blood collected during routine health screens of chimpanzees living in sanctuaries. With their technique, the team found they could generate “high-quality” Laverania genome sequences.
The researchers said the chimpanzee parasite genomes contain information about the evolutionary origins of the malaria parasites infecting humans. One of the first things to emerge from genome-wide analyses was that the parasites represent distinct, non-interbreeding species.
In addition, members of each chimpanzee parasite species display about 10 times more genetic diversity than human parasites.
“The chimpanzee parasites really highlight the lack of diversity in Plasmodium falciparum,” said Paul Sharp, PhD, of the University of Edinburgh in the UK.
“This is most likely because these parasites went through a severe bottleneck when first transmitted to humans, perhaps within the past 10,000 years.”
By comparing the different parasite genomes, the researchers found an expansion of a multi-gene family, which governs red blood cell remodeling and therefore helps the parasite to evade host immune cells and clearance by the spleen.
“The remodeling process is a key part of severe malaria pathology in human Plasmodium falciparum infections,” said Julian Rayner, PhD, of the Wellcome Trust Sanger Institute in Cambridge, UK.
“The expansion of this gene family from a single gene in all other Plasmodium parasites to up to 21 genes in Laverania suggests that remodeling evolved early in the radiation of this group of primate parasites and contributed not only to their unique biology but perhaps also to their successful expansion.”
“We also found a short region of the genome, including 2 essential invasion genes, where Plasmodium falciparum was much more different from its close relatives than we expected,” said Lindsey Plenderleith, PhD, of the University of Edinburgh.
Further analysis yielded the surprising finding that this fragment of DNA was horizontally transferred—from one species to another—into the gorilla ancestor of P falciparum.
“It is tempting to speculate that this unusual event somehow predisposed the precursor of Plasmodium falciparum to colonize humans,” Dr Hahn said. “However, this gene transfer clearly is not the entire story.”
Although the origin of P falciparum is considered well-established, nothing is known about the circumstances that led to its emergence.
“Coaxing entire parasite genome sequences out of small quantities of unprocessed ape blood will help us to better understand what happened and whether it can happen again,” said Sesh Sundararaman, an MD/PhD student at the University of Pennsylvania.
The team plans, as a next step, to use their select genome amplification technique to sequence additional ape parasite genomes to identify host-specific interactions and transmission requirements. They believe this would reveal vulnerabilities that might be exploited to combat malaria in humans. ![]()

Photo courtesy of
Sesh Sundararaman,
University of Pennsylvania
By studying malaria parasites found in chimpanzees, researchers believe they have gained new insights regarding a malaria parasite that infects humans.
The team used a selective amplification technique to sequence the genomes of 2 divergent Plasmodium species, P reichenowi and P gaboni, from chimpanzee blood.
This revealed clues about the evolution and pathogenicity of P falciparum, the deadliest malaria parasite that affects humans.
The researchers described this work in Nature Communications.
They noted that African apes harbor at least 6 Plasmodium species that have been classified into a separate subgenus, called Laverania. Three of these Laverania species, including P reichenowi and P gaboni, reside in chimps.
Three others—including P praefalciparum, which gave rise to P falciparum—reside in gorillas. The gorilla origin of P falciparum was discovered several years ago by this same group of investigators.
“We want to know why Plasmodium falciparum is so deadly,” said Beatrice Hahn, MD, of the University of Pennsylvania in Philadelphia.
“The answer must lie in the blueprint—the genome—of its chimpanzee and gorilla cousins. We also want to know how and when the gorilla precursor of Plasmodium falciparum jumped into humans and why this happened only once.”
In an attempt to answer these questions, Dr Hahn and her colleagues used their selective amplification method to sequence Laverania genomes.
They used small amounts of unprocessed blood collected during routine health screens of chimpanzees living in sanctuaries. With their technique, the team found they could generate “high-quality” Laverania genome sequences.
The researchers said the chimpanzee parasite genomes contain information about the evolutionary origins of the malaria parasites infecting humans. One of the first things to emerge from genome-wide analyses was that the parasites represent distinct, non-interbreeding species.
In addition, members of each chimpanzee parasite species display about 10 times more genetic diversity than human parasites.
“The chimpanzee parasites really highlight the lack of diversity in Plasmodium falciparum,” said Paul Sharp, PhD, of the University of Edinburgh in the UK.
“This is most likely because these parasites went through a severe bottleneck when first transmitted to humans, perhaps within the past 10,000 years.”
By comparing the different parasite genomes, the researchers found an expansion of a multi-gene family, which governs red blood cell remodeling and therefore helps the parasite to evade host immune cells and clearance by the spleen.
“The remodeling process is a key part of severe malaria pathology in human Plasmodium falciparum infections,” said Julian Rayner, PhD, of the Wellcome Trust Sanger Institute in Cambridge, UK.
“The expansion of this gene family from a single gene in all other Plasmodium parasites to up to 21 genes in Laverania suggests that remodeling evolved early in the radiation of this group of primate parasites and contributed not only to their unique biology but perhaps also to their successful expansion.”
“We also found a short region of the genome, including 2 essential invasion genes, where Plasmodium falciparum was much more different from its close relatives than we expected,” said Lindsey Plenderleith, PhD, of the University of Edinburgh.
Further analysis yielded the surprising finding that this fragment of DNA was horizontally transferred—from one species to another—into the gorilla ancestor of P falciparum.
“It is tempting to speculate that this unusual event somehow predisposed the precursor of Plasmodium falciparum to colonize humans,” Dr Hahn said. “However, this gene transfer clearly is not the entire story.”
Although the origin of P falciparum is considered well-established, nothing is known about the circumstances that led to its emergence.
“Coaxing entire parasite genome sequences out of small quantities of unprocessed ape blood will help us to better understand what happened and whether it can happen again,” said Sesh Sundararaman, an MD/PhD student at the University of Pennsylvania.
The team plans, as a next step, to use their select genome amplification technique to sequence additional ape parasite genomes to identify host-specific interactions and transmission requirements. They believe this would reveal vulnerabilities that might be exploited to combat malaria in humans. ![]()

Photo courtesy of
Sesh Sundararaman,
University of Pennsylvania
By studying malaria parasites found in chimpanzees, researchers believe they have gained new insights regarding a malaria parasite that infects humans.
The team used a selective amplification technique to sequence the genomes of 2 divergent Plasmodium species, P reichenowi and P gaboni, from chimpanzee blood.
This revealed clues about the evolution and pathogenicity of P falciparum, the deadliest malaria parasite that affects humans.
The researchers described this work in Nature Communications.
They noted that African apes harbor at least 6 Plasmodium species that have been classified into a separate subgenus, called Laverania. Three of these Laverania species, including P reichenowi and P gaboni, reside in chimps.
Three others—including P praefalciparum, which gave rise to P falciparum—reside in gorillas. The gorilla origin of P falciparum was discovered several years ago by this same group of investigators.
“We want to know why Plasmodium falciparum is so deadly,” said Beatrice Hahn, MD, of the University of Pennsylvania in Philadelphia.
“The answer must lie in the blueprint—the genome—of its chimpanzee and gorilla cousins. We also want to know how and when the gorilla precursor of Plasmodium falciparum jumped into humans and why this happened only once.”
In an attempt to answer these questions, Dr Hahn and her colleagues used their selective amplification method to sequence Laverania genomes.
They used small amounts of unprocessed blood collected during routine health screens of chimpanzees living in sanctuaries. With their technique, the team found they could generate “high-quality” Laverania genome sequences.
The researchers said the chimpanzee parasite genomes contain information about the evolutionary origins of the malaria parasites infecting humans. One of the first things to emerge from genome-wide analyses was that the parasites represent distinct, non-interbreeding species.
In addition, members of each chimpanzee parasite species display about 10 times more genetic diversity than human parasites.
“The chimpanzee parasites really highlight the lack of diversity in Plasmodium falciparum,” said Paul Sharp, PhD, of the University of Edinburgh in the UK.
“This is most likely because these parasites went through a severe bottleneck when first transmitted to humans, perhaps within the past 10,000 years.”
By comparing the different parasite genomes, the researchers found an expansion of a multi-gene family, which governs red blood cell remodeling and therefore helps the parasite to evade host immune cells and clearance by the spleen.
“The remodeling process is a key part of severe malaria pathology in human Plasmodium falciparum infections,” said Julian Rayner, PhD, of the Wellcome Trust Sanger Institute in Cambridge, UK.
“The expansion of this gene family from a single gene in all other Plasmodium parasites to up to 21 genes in Laverania suggests that remodeling evolved early in the radiation of this group of primate parasites and contributed not only to their unique biology but perhaps also to their successful expansion.”
“We also found a short region of the genome, including 2 essential invasion genes, where Plasmodium falciparum was much more different from its close relatives than we expected,” said Lindsey Plenderleith, PhD, of the University of Edinburgh.
Further analysis yielded the surprising finding that this fragment of DNA was horizontally transferred—from one species to another—into the gorilla ancestor of P falciparum.
“It is tempting to speculate that this unusual event somehow predisposed the precursor of Plasmodium falciparum to colonize humans,” Dr Hahn said. “However, this gene transfer clearly is not the entire story.”
Although the origin of P falciparum is considered well-established, nothing is known about the circumstances that led to its emergence.
“Coaxing entire parasite genome sequences out of small quantities of unprocessed ape blood will help us to better understand what happened and whether it can happen again,” said Sesh Sundararaman, an MD/PhD student at the University of Pennsylvania.
The team plans, as a next step, to use their select genome amplification technique to sequence additional ape parasite genomes to identify host-specific interactions and transmission requirements. They believe this would reveal vulnerabilities that might be exploited to combat malaria in humans. ![]()
EMA recommends orphan designation for EBV-CTLs

among uninfected cells (blue)
Image courtesy of Benjamin
Chaigne-Delalande
The European Medicines Agency (EMA) has recommended orphan designation for an allogeneic cytotoxic T-lymphocyte product that targets Epstein-Barr virus (EBV-CTLs) as a treatment for patients with EBV post-transplant lymphoproliferative disorder (EBV-PTLD).
The EMA’s opinion has been forwarded to the European Commission (EC), which makes the final decision.
The EC grants orphan designation to products intended to treat, prevent, or diagnose a life-threatening condition affecting up to 5 in 10,000 people in the European Union. The product must provide significant benefit to those affected by the condition.
Orphan designation from the EC provides companies with certain development incentives, including protocol assistance, a type of scientific advice specific for orphan drugs, and 10 years of market exclusivity once the drug is approved for use.
About EBV-CTLs
The EBV-CTL product utilizes a technology in which T cells are collected from the blood of third-party donors and then exposed to EBV antigens.
The activated T cells are then expanded, characterized, and stored for future use in a partially HLA-matched patient, providing an “off-the-shelf,” allogeneic, cellular therapeutic option for patients.
In the context of EBV-PTLD, the EBV-CTLs find the cancer cells expressing EBV and kill them.
Atara Biotherapeutics, Inc., the company developing the EBV-CTL product, is planning to launch a multi-center, early access clinical trial for EBV-CTLs in mid-2016, followed by 2 phase 3 trials in EBV-PTLD later in the year.
Results of a phase 1/2 study of EBV-CTLs were presented at the APHON 37th Annual Conference and Exhibit and at the 2015 ASCO Annual Meeting.
Atara’s EBV-CTL product already has orphan designation in the US for the treatment of patients with EBV-PTLD after hematopoietic stem cell transplant or solid organ transplant. The product has breakthrough designation for this indication as well. ![]()

among uninfected cells (blue)
Image courtesy of Benjamin
Chaigne-Delalande
The European Medicines Agency (EMA) has recommended orphan designation for an allogeneic cytotoxic T-lymphocyte product that targets Epstein-Barr virus (EBV-CTLs) as a treatment for patients with EBV post-transplant lymphoproliferative disorder (EBV-PTLD).
The EMA’s opinion has been forwarded to the European Commission (EC), which makes the final decision.
The EC grants orphan designation to products intended to treat, prevent, or diagnose a life-threatening condition affecting up to 5 in 10,000 people in the European Union. The product must provide significant benefit to those affected by the condition.
Orphan designation from the EC provides companies with certain development incentives, including protocol assistance, a type of scientific advice specific for orphan drugs, and 10 years of market exclusivity once the drug is approved for use.
About EBV-CTLs
The EBV-CTL product utilizes a technology in which T cells are collected from the blood of third-party donors and then exposed to EBV antigens.
The activated T cells are then expanded, characterized, and stored for future use in a partially HLA-matched patient, providing an “off-the-shelf,” allogeneic, cellular therapeutic option for patients.
In the context of EBV-PTLD, the EBV-CTLs find the cancer cells expressing EBV and kill them.
Atara Biotherapeutics, Inc., the company developing the EBV-CTL product, is planning to launch a multi-center, early access clinical trial for EBV-CTLs in mid-2016, followed by 2 phase 3 trials in EBV-PTLD later in the year.
Results of a phase 1/2 study of EBV-CTLs were presented at the APHON 37th Annual Conference and Exhibit and at the 2015 ASCO Annual Meeting.
Atara’s EBV-CTL product already has orphan designation in the US for the treatment of patients with EBV-PTLD after hematopoietic stem cell transplant or solid organ transplant. The product has breakthrough designation for this indication as well. ![]()

among uninfected cells (blue)
Image courtesy of Benjamin
Chaigne-Delalande
The European Medicines Agency (EMA) has recommended orphan designation for an allogeneic cytotoxic T-lymphocyte product that targets Epstein-Barr virus (EBV-CTLs) as a treatment for patients with EBV post-transplant lymphoproliferative disorder (EBV-PTLD).
The EMA’s opinion has been forwarded to the European Commission (EC), which makes the final decision.
The EC grants orphan designation to products intended to treat, prevent, or diagnose a life-threatening condition affecting up to 5 in 10,000 people in the European Union. The product must provide significant benefit to those affected by the condition.
Orphan designation from the EC provides companies with certain development incentives, including protocol assistance, a type of scientific advice specific for orphan drugs, and 10 years of market exclusivity once the drug is approved for use.
About EBV-CTLs
The EBV-CTL product utilizes a technology in which T cells are collected from the blood of third-party donors and then exposed to EBV antigens.
The activated T cells are then expanded, characterized, and stored for future use in a partially HLA-matched patient, providing an “off-the-shelf,” allogeneic, cellular therapeutic option for patients.
In the context of EBV-PTLD, the EBV-CTLs find the cancer cells expressing EBV and kill them.
Atara Biotherapeutics, Inc., the company developing the EBV-CTL product, is planning to launch a multi-center, early access clinical trial for EBV-CTLs in mid-2016, followed by 2 phase 3 trials in EBV-PTLD later in the year.
Results of a phase 1/2 study of EBV-CTLs were presented at the APHON 37th Annual Conference and Exhibit and at the 2015 ASCO Annual Meeting.
Atara’s EBV-CTL product already has orphan designation in the US for the treatment of patients with EBV-PTLD after hematopoietic stem cell transplant or solid organ transplant. The product has breakthrough designation for this indication as well. ![]()
Drug shows early promise for rel/ref NHL

Blinatumomab, a CD19/CD3 bispecific T-cell engager antibody construct, can produce durable responses in patients with relapsed/refractory B-cell non-Hodgkin lymphoma (NHL), according to a phase 1 study.
Among patients who received the maximum-tolerated dose (MTD) of blinatumomab, the overall response rate (ORR) was nearly 70%, and the median duration of response was more than 400 days.
However, there was a high rate of neurologic events, particularly among patients who received higher doses of the drug.
Ralph Bargou, MD, of Wuerzburg University Hospital in Germany, and his colleagues conducted this study and reported the results in the Journal of Clinical Oncology.
The study was supported by Amgen (and Micromet before its acquisition by Amgen), the companies developing blinatumomab.
The study enrolled 76 patients with relapsed/refractory NHL. Most patients (n=52) had indolent NHL. Subtypes included follicular lymphoma (FL, n=28), mantle cell lymphoma (MCL, n=24), diffuse large B-cell lymphoma (DLBCL, n=14), and “other” (n=10).
The “other” category included lymphoplasmacytic lymphoma (n=2), small lymphoplasmacytic lymphoma (n=1), immunocytoma (n=1), Waldenstrom’s macroglobulinemia (n=1), marginal zone NHL (n=1), marginal zone B-cell lymphoma (n=1), marginal zone lymphoma (n=1), chronic lymphocytic leukemia (n=1), and small lymphoplasmacytic lymphoma/chronic lymphocytic leukemia (n=1).
The patients’ median age was 65 (range, 20-80), and the median number of prior treatment regimens was 3 (range, 1-10).
Dosing, toxicity, and discontinuation
This phase 1, dose-escalation study had a 3 + 3 design. Blinatumomab was given over 4 or 8 weeks at 7 different dose levels, ranging from 0.5 μg/m2/day to 90 μg/m2/day.
The researchers found that neurologic events were dose-limiting, and 60 μg/m2/day was the MTD.
Five patients experienced dose-limiting toxicities, including a grade 2 mental disorder (15 μg/m2/day), a case of grade 4 metabolic acidosis due to grand mal seizure (30 μg/m2/day), 2 cases of grade 3 encephalopathy (90 μg/m2/day), and 1 case of grade 3 seizure and aphasia (90 μg/m2/day).
Forty-two patients received treatment in the formal dose-escalation phase. Thirty-four additional patients were recruited to evaluate the antilymphoma activity of blinatumomab and test strategies for mitigating neurologic events at the MTD.
The researchers found that stepwise dosing (5 μg/m2/day to 60 μg/m2/day) plus pentosan polysulfate SP54 (n=3) prompted no treatment discontinuations.
However, single-step (n=5) dosing led to 2 discontinuations, and double-step (n=24) dosing led to 7 discontinuations. All were due to neurologic events.
The most clinically relevant adverse events were neurologic in nature. The overall incidence of these events, regardless of causality, was 71%. The incidence of grade 3 neurologic events was 22%.
Twenty percent of patients experienced serious neurologic events, including encephalopathy (8%), aphasia (4%), and headache (3%). There were no grade 4 or 5 neurologic events.
Response
Among patients treated at the MTD (60 μg/m2/day), the ORR was 69% (24/35). The ORR was 50% at 90 μg/m2/day (2/4), 20% at 15 μg/m2/day (3/15), and 17% at 30 μg/m2/day (1/6).
Complete responses (CRs) occurred in 1 patient at the 15 μg/m2/day dose, 1 at the 30 μg/m2/day dose, 1 at the 90 μg/m2/day dose, and 8 at the 60 μg/m2/day dose. Unconfirmed CRs (CRus) occurred in 5 patients at the 60 μg/m2/day dose.
Among patients who received the MTD, the ORR was 80% in FL patients, 71% in MCL patients, 55% in DLBCL patients, and 50% in the “other” category. There were 6 CR/CRus among FL patients, 3 CR/CRus among MCL patients, and 4 CR/CRus among DLBCL patients.
The median duration of response for patients who received the MTD was 404 days (95% CI, 207 to 1129). The median duration of CR/CRu was 508 days (95% CI, 213 to not estimable). And the median duration of partial response was 185 days (95% CI, 28 to 754).
Nine patients were still in remission at the time of the analysis, and 12 patients had remissions lasting more than 1 year.
“Blinatumomab continues to demonstrate a long duration of response in heavily pretreated non-Hodgkin lymphoma patients,” Dr Bargou said. “Results of the expanded phase 1 experience suggest that blinatumomab has the potential to alter the clinical course of disease in patients with a variety of NHL subtypes.” ![]()

Blinatumomab, a CD19/CD3 bispecific T-cell engager antibody construct, can produce durable responses in patients with relapsed/refractory B-cell non-Hodgkin lymphoma (NHL), according to a phase 1 study.
Among patients who received the maximum-tolerated dose (MTD) of blinatumomab, the overall response rate (ORR) was nearly 70%, and the median duration of response was more than 400 days.
However, there was a high rate of neurologic events, particularly among patients who received higher doses of the drug.
Ralph Bargou, MD, of Wuerzburg University Hospital in Germany, and his colleagues conducted this study and reported the results in the Journal of Clinical Oncology.
The study was supported by Amgen (and Micromet before its acquisition by Amgen), the companies developing blinatumomab.
The study enrolled 76 patients with relapsed/refractory NHL. Most patients (n=52) had indolent NHL. Subtypes included follicular lymphoma (FL, n=28), mantle cell lymphoma (MCL, n=24), diffuse large B-cell lymphoma (DLBCL, n=14), and “other” (n=10).
The “other” category included lymphoplasmacytic lymphoma (n=2), small lymphoplasmacytic lymphoma (n=1), immunocytoma (n=1), Waldenstrom’s macroglobulinemia (n=1), marginal zone NHL (n=1), marginal zone B-cell lymphoma (n=1), marginal zone lymphoma (n=1), chronic lymphocytic leukemia (n=1), and small lymphoplasmacytic lymphoma/chronic lymphocytic leukemia (n=1).
The patients’ median age was 65 (range, 20-80), and the median number of prior treatment regimens was 3 (range, 1-10).
Dosing, toxicity, and discontinuation
This phase 1, dose-escalation study had a 3 + 3 design. Blinatumomab was given over 4 or 8 weeks at 7 different dose levels, ranging from 0.5 μg/m2/day to 90 μg/m2/day.
The researchers found that neurologic events were dose-limiting, and 60 μg/m2/day was the MTD.
Five patients experienced dose-limiting toxicities, including a grade 2 mental disorder (15 μg/m2/day), a case of grade 4 metabolic acidosis due to grand mal seizure (30 μg/m2/day), 2 cases of grade 3 encephalopathy (90 μg/m2/day), and 1 case of grade 3 seizure and aphasia (90 μg/m2/day).
Forty-two patients received treatment in the formal dose-escalation phase. Thirty-four additional patients were recruited to evaluate the antilymphoma activity of blinatumomab and test strategies for mitigating neurologic events at the MTD.
The researchers found that stepwise dosing (5 μg/m2/day to 60 μg/m2/day) plus pentosan polysulfate SP54 (n=3) prompted no treatment discontinuations.
However, single-step (n=5) dosing led to 2 discontinuations, and double-step (n=24) dosing led to 7 discontinuations. All were due to neurologic events.
The most clinically relevant adverse events were neurologic in nature. The overall incidence of these events, regardless of causality, was 71%. The incidence of grade 3 neurologic events was 22%.
Twenty percent of patients experienced serious neurologic events, including encephalopathy (8%), aphasia (4%), and headache (3%). There were no grade 4 or 5 neurologic events.
Response
Among patients treated at the MTD (60 μg/m2/day), the ORR was 69% (24/35). The ORR was 50% at 90 μg/m2/day (2/4), 20% at 15 μg/m2/day (3/15), and 17% at 30 μg/m2/day (1/6).
Complete responses (CRs) occurred in 1 patient at the 15 μg/m2/day dose, 1 at the 30 μg/m2/day dose, 1 at the 90 μg/m2/day dose, and 8 at the 60 μg/m2/day dose. Unconfirmed CRs (CRus) occurred in 5 patients at the 60 μg/m2/day dose.
Among patients who received the MTD, the ORR was 80% in FL patients, 71% in MCL patients, 55% in DLBCL patients, and 50% in the “other” category. There were 6 CR/CRus among FL patients, 3 CR/CRus among MCL patients, and 4 CR/CRus among DLBCL patients.
The median duration of response for patients who received the MTD was 404 days (95% CI, 207 to 1129). The median duration of CR/CRu was 508 days (95% CI, 213 to not estimable). And the median duration of partial response was 185 days (95% CI, 28 to 754).
Nine patients were still in remission at the time of the analysis, and 12 patients had remissions lasting more than 1 year.
“Blinatumomab continues to demonstrate a long duration of response in heavily pretreated non-Hodgkin lymphoma patients,” Dr Bargou said. “Results of the expanded phase 1 experience suggest that blinatumomab has the potential to alter the clinical course of disease in patients with a variety of NHL subtypes.” ![]()

Blinatumomab, a CD19/CD3 bispecific T-cell engager antibody construct, can produce durable responses in patients with relapsed/refractory B-cell non-Hodgkin lymphoma (NHL), according to a phase 1 study.
Among patients who received the maximum-tolerated dose (MTD) of blinatumomab, the overall response rate (ORR) was nearly 70%, and the median duration of response was more than 400 days.
However, there was a high rate of neurologic events, particularly among patients who received higher doses of the drug.
Ralph Bargou, MD, of Wuerzburg University Hospital in Germany, and his colleagues conducted this study and reported the results in the Journal of Clinical Oncology.
The study was supported by Amgen (and Micromet before its acquisition by Amgen), the companies developing blinatumomab.
The study enrolled 76 patients with relapsed/refractory NHL. Most patients (n=52) had indolent NHL. Subtypes included follicular lymphoma (FL, n=28), mantle cell lymphoma (MCL, n=24), diffuse large B-cell lymphoma (DLBCL, n=14), and “other” (n=10).
The “other” category included lymphoplasmacytic lymphoma (n=2), small lymphoplasmacytic lymphoma (n=1), immunocytoma (n=1), Waldenstrom’s macroglobulinemia (n=1), marginal zone NHL (n=1), marginal zone B-cell lymphoma (n=1), marginal zone lymphoma (n=1), chronic lymphocytic leukemia (n=1), and small lymphoplasmacytic lymphoma/chronic lymphocytic leukemia (n=1).
The patients’ median age was 65 (range, 20-80), and the median number of prior treatment regimens was 3 (range, 1-10).
Dosing, toxicity, and discontinuation
This phase 1, dose-escalation study had a 3 + 3 design. Blinatumomab was given over 4 or 8 weeks at 7 different dose levels, ranging from 0.5 μg/m2/day to 90 μg/m2/day.
The researchers found that neurologic events were dose-limiting, and 60 μg/m2/day was the MTD.
Five patients experienced dose-limiting toxicities, including a grade 2 mental disorder (15 μg/m2/day), a case of grade 4 metabolic acidosis due to grand mal seizure (30 μg/m2/day), 2 cases of grade 3 encephalopathy (90 μg/m2/day), and 1 case of grade 3 seizure and aphasia (90 μg/m2/day).
Forty-two patients received treatment in the formal dose-escalation phase. Thirty-four additional patients were recruited to evaluate the antilymphoma activity of blinatumomab and test strategies for mitigating neurologic events at the MTD.
The researchers found that stepwise dosing (5 μg/m2/day to 60 μg/m2/day) plus pentosan polysulfate SP54 (n=3) prompted no treatment discontinuations.
However, single-step (n=5) dosing led to 2 discontinuations, and double-step (n=24) dosing led to 7 discontinuations. All were due to neurologic events.
The most clinically relevant adverse events were neurologic in nature. The overall incidence of these events, regardless of causality, was 71%. The incidence of grade 3 neurologic events was 22%.
Twenty percent of patients experienced serious neurologic events, including encephalopathy (8%), aphasia (4%), and headache (3%). There were no grade 4 or 5 neurologic events.
Response
Among patients treated at the MTD (60 μg/m2/day), the ORR was 69% (24/35). The ORR was 50% at 90 μg/m2/day (2/4), 20% at 15 μg/m2/day (3/15), and 17% at 30 μg/m2/day (1/6).
Complete responses (CRs) occurred in 1 patient at the 15 μg/m2/day dose, 1 at the 30 μg/m2/day dose, 1 at the 90 μg/m2/day dose, and 8 at the 60 μg/m2/day dose. Unconfirmed CRs (CRus) occurred in 5 patients at the 60 μg/m2/day dose.
Among patients who received the MTD, the ORR was 80% in FL patients, 71% in MCL patients, 55% in DLBCL patients, and 50% in the “other” category. There were 6 CR/CRus among FL patients, 3 CR/CRus among MCL patients, and 4 CR/CRus among DLBCL patients.
The median duration of response for patients who received the MTD was 404 days (95% CI, 207 to 1129). The median duration of CR/CRu was 508 days (95% CI, 213 to not estimable). And the median duration of partial response was 185 days (95% CI, 28 to 754).
Nine patients were still in remission at the time of the analysis, and 12 patients had remissions lasting more than 1 year.
“Blinatumomab continues to demonstrate a long duration of response in heavily pretreated non-Hodgkin lymphoma patients,” Dr Bargou said. “Results of the expanded phase 1 experience suggest that blinatumomab has the potential to alter the clinical course of disease in patients with a variety of NHL subtypes.” ![]()
A Double Dose of Trouble
ANSWER
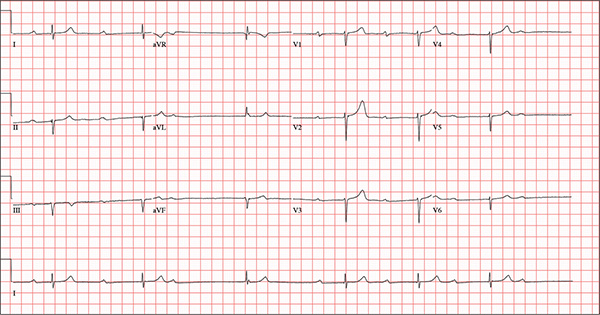
This ECG demonstrates marked sinus bradycardia with a second-degree atrioventricular (AV) block (Mobitz I). Other findings include left-axis deviation, an old inferior MI, and poor R-wave progression.
Second-degree Mobitz I block is present in a 3:1 pattern of progressive prolongation of the PR interval until the third beat, where there is block in the AV node preventing conduction of the P wave to the ventricles. This is typically caused by progressive fatigue within the AV node until block occurs, then the cycle repeats.
Left-axis deviation is evidenced by a QRS axis of –78°. An old inferior MI is signified by the significant Q waves in leads II, III, and aVF. Finally, poor R-wave progression is demonstrated by small R waves in all of the precordial leads.
This ECG represented a significant change from one obtained three months earlier, during a routine outpatient visit. Careful review of the records at the Alzheimer facility revealed that the patient had received twice his usual dose of propranolol on three consecutive days. His rhythm returned to a baseline sinus rhythm (at 68 beats/min) after his ß-blocker was withheld for two days, and no further intervention was needed.
ANSWER
This ECG demonstrates marked sinus bradycardia with a second-degree atrioventricular (AV) block (Mobitz I). Other findings include left-axis deviation, an old inferior MI, and poor R-wave progression.
Second-degree Mobitz I block is present in a 3:1 pattern of progressive prolongation of the PR interval until the third beat, where there is block in the AV node preventing conduction of the P wave to the ventricles. This is typically caused by progressive fatigue within the AV node until block occurs, then the cycle repeats.
Left-axis deviation is evidenced by a QRS axis of –78°. An old inferior MI is signified by the significant Q waves in leads II, III, and aVF. Finally, poor R-wave progression is demonstrated by small R waves in all of the precordial leads.
This ECG represented a significant change from one obtained three months earlier, during a routine outpatient visit. Careful review of the records at the Alzheimer facility revealed that the patient had received twice his usual dose of propranolol on three consecutive days. His rhythm returned to a baseline sinus rhythm (at 68 beats/min) after his ß-blocker was withheld for two days, and no further intervention was needed.
ANSWER
This ECG demonstrates marked sinus bradycardia with a second-degree atrioventricular (AV) block (Mobitz I). Other findings include left-axis deviation, an old inferior MI, and poor R-wave progression.
Second-degree Mobitz I block is present in a 3:1 pattern of progressive prolongation of the PR interval until the third beat, where there is block in the AV node preventing conduction of the P wave to the ventricles. This is typically caused by progressive fatigue within the AV node until block occurs, then the cycle repeats.
Left-axis deviation is evidenced by a QRS axis of –78°. An old inferior MI is signified by the significant Q waves in leads II, III, and aVF. Finally, poor R-wave progression is demonstrated by small R waves in all of the precordial leads.
This ECG represented a significant change from one obtained three months earlier, during a routine outpatient visit. Careful review of the records at the Alzheimer facility revealed that the patient had received twice his usual dose of propranolol on three consecutive days. His rhythm returned to a baseline sinus rhythm (at 68 beats/min) after his ß-blocker was withheld for two days, and no further intervention was needed.
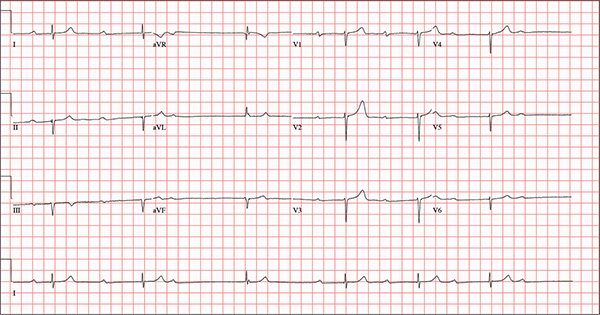
An 82-year-old man is referred from a nearby Alzheimer care facility following an episode of postural hypotension. While trying to get out of bed, he experienced near-syncope, which was observed by a nurse caring for another patient in the same room. The patient was helped back into bed, and the resident care provider was summoned. A careful examination ruled out any injury sustained when the patient’s knees buckled and he fell to the ground. However, he was found to have profound bradycardia with a pulse of 30 beats/min. Emergency medical services were called, and the patient was transported to your facility for further evaluation. You find the patient to be pleasant but mildly confused. He is in no distress. A review of the limited available records shows that he has had Alzheimer disease for four years; it has been relatively stable, with no recent changes in cognition. His history includes an inferior myocardial infarction (MI) at age 68 and hypertension. The latter has been treated with diuretics and ß-blockers, although the doses have not been changed since his MI. Other remarkable items in the history include hypothyroidism, type 2 diabetes, cholecystectomy, and appendectomy. He has significant osteoarthritis in both knees but does not require a cane or other device to ambulate. The patient is a retired iron worker from the local foundry. He is a widower with two adult children who live remotely and do not visit. He was a heavy drinker in his younger years and smoked one to two packs of cigarettes per day until his MI. He has abstained from alcohol and tobacco since his wife’s death six years ago. His medication list includes a daily aspirin, furosemide, potassium chloride, propranolol, and levothyroxine. He is said to be allergic to penicillin, but there is no record of him ever receiving it. The review of systems is difficult to obtain due to the patient’s confusion. He has not had any recent infectious illnesses, according to the accompanying nurse from the Alzheimer facility. Physical exam reveals a disheveled but otherwise pleasant man. He can remember only one out of three words when asked to recite immediately after hearing them. Vital signs include a blood pressure of 86/48 mm Hg; pulse, 40 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 98.4°F. His weight is 163 lb and his height, 66 in. The patient wears corrective lenses and hearing aids, but the batteries in the latter are dead. Regardless, he can hear you if you speak loudly. Pertinent physical findings include scattered crackles in both lung bases, a regularly irregular slow heart rate, a grade III/VI systolic murmur that radiates to the neck, and well-healed surgical scars on the abdomen consistent with the surgeries described in the history. There appear to be no gross focal neurologic findings. An ECG reveals a ventricular rate of 38 beats/min; PR interval, not measured; QRS duration, 78 ms; QT/QTc interval, 434/345 ms; P axis, 25°; R axis, –78°; and T axis, 13°. What is your interpretation of this ECG?
When Trauma Changes the Picture
Answer
The radiograph has several findings. First, there are multiple fractures along the left lateral ribs. Second, there is a small left apical pneumothorax. Most significant, though, is an elevated left hemidiaphragm. There appears to be stomach or possibly bowel protruding into it.
Although a large hiatal hernia could yield similar findings, in the setting of trauma, one must be concerned about a traumatic diaphragmatic hernia. Subsequent CT of the chest, abdomen, and pelvis confirmed a defect within the diaphragm, with a significant portion of the stomach herniating into the left chest.
Surgical consultation was obtained. The patient was admitted and ultimately underwent surgical intervention to repair the problem.
Answer
The radiograph has several findings. First, there are multiple fractures along the left lateral ribs. Second, there is a small left apical pneumothorax. Most significant, though, is an elevated left hemidiaphragm. There appears to be stomach or possibly bowel protruding into it.
Although a large hiatal hernia could yield similar findings, in the setting of trauma, one must be concerned about a traumatic diaphragmatic hernia. Subsequent CT of the chest, abdomen, and pelvis confirmed a defect within the diaphragm, with a significant portion of the stomach herniating into the left chest.
Surgical consultation was obtained. The patient was admitted and ultimately underwent surgical intervention to repair the problem.
Answer
The radiograph has several findings. First, there are multiple fractures along the left lateral ribs. Second, there is a small left apical pneumothorax. Most significant, though, is an elevated left hemidiaphragm. There appears to be stomach or possibly bowel protruding into it.
Although a large hiatal hernia could yield similar findings, in the setting of trauma, one must be concerned about a traumatic diaphragmatic hernia. Subsequent CT of the chest, abdomen, and pelvis confirmed a defect within the diaphragm, with a significant portion of the stomach herniating into the left chest.
Surgical consultation was obtained. The patient was admitted and ultimately underwent surgical intervention to repair the problem.

A 75-year-old man is brought to your emergency center following a fall from his attic. He slipped and fell approximately 10 feet, landing on his left side. He did not hit his head and denies any loss of consciousness. His primary complaint is left-side chest wall pain. Medical history is significant for hypertension, diabetes, reflux, and atrial fibrillation. On primary survey, you note an elderly male who is somewhat uncomfortable but in no obvious distress. His vital signs are stable; O2 saturation is 98% on room air. The patient exhibits moderate tenderness along the anterior lateral aspect of his chest, as well as mild generalized tenderness in his abdomen. Good inspiratory effort is limited secondary to his pain. While you enter orders into the computer, a portable chest radiograph is obtained. What is your impression?
Brain imaging suggests link between stress and cardiovascular events
Stress seems to be a strong driver of cardiovascular events, including heart attack, stroke, and even death.
For the first time, brain imaging has confirmed a link that has long been suspected: Activation of one of the brain’s prime emotional centers, the amygdala, directly correlates with the risk of cardiovascular events.
“This study illustrates a clear relationship between the activity of the amygdala and heart disease,” Dr. Ahmed A. Tawakol said at a press teleconference leading up to the annual meeting of the American College of Cardiology.
“Stress is known to be associated with an increase in the risk of cardiovascular events, and the risk is on par with that exerted by smoking, hypertension, and diabetes, but we don’t address it,” said Dr. Tawakol, codirector of the Cardiac MRI PET CT Program at Massachusetts General Hospital, Boston.
The findings also highlight a possible pathway for this relationship, suggesting that stress-related noradrenalin stimulates extramedullary hematopoiesis, a key driver of inflammation. This can contribute to atherosclerotic inflammation, which increases the likelihood of a heart attack or stroke, said Dr. Tawakol.
His study comprised 293 subjects who had undergone a PET or CT scan for cancer evaluation, but were determined to be cancer free. All scans contained brain and bone imaging data. Dr. Tawakol assessed amygdala and bone marrow activation, and evaluated inflammatory response in arteries.
These findings were then correlated with any cardiovascular events occurring in the next 5 years; the median follow-up was 3.8 years. Events were significantly more common among those with high levels of amygdala activation, occurring in 35% of this group, but in just 5% of those with low activation.
After adjusting for risk factors in the Framingham model, Dr. Tawakol found that high amygdala activation conferred a 14-fold increase in the risk of a cardiovascular event. These were likely to be precipitous as well, he said: The higher the level of activation, the more likely the event was to happen within the first year of follow-up.
He had no financial disclosures.
Stress seems to be a strong driver of cardiovascular events, including heart attack, stroke, and even death.
For the first time, brain imaging has confirmed a link that has long been suspected: Activation of one of the brain’s prime emotional centers, the amygdala, directly correlates with the risk of cardiovascular events.
“This study illustrates a clear relationship between the activity of the amygdala and heart disease,” Dr. Ahmed A. Tawakol said at a press teleconference leading up to the annual meeting of the American College of Cardiology.
“Stress is known to be associated with an increase in the risk of cardiovascular events, and the risk is on par with that exerted by smoking, hypertension, and diabetes, but we don’t address it,” said Dr. Tawakol, codirector of the Cardiac MRI PET CT Program at Massachusetts General Hospital, Boston.
The findings also highlight a possible pathway for this relationship, suggesting that stress-related noradrenalin stimulates extramedullary hematopoiesis, a key driver of inflammation. This can contribute to atherosclerotic inflammation, which increases the likelihood of a heart attack or stroke, said Dr. Tawakol.
His study comprised 293 subjects who had undergone a PET or CT scan for cancer evaluation, but were determined to be cancer free. All scans contained brain and bone imaging data. Dr. Tawakol assessed amygdala and bone marrow activation, and evaluated inflammatory response in arteries.
These findings were then correlated with any cardiovascular events occurring in the next 5 years; the median follow-up was 3.8 years. Events were significantly more common among those with high levels of amygdala activation, occurring in 35% of this group, but in just 5% of those with low activation.
After adjusting for risk factors in the Framingham model, Dr. Tawakol found that high amygdala activation conferred a 14-fold increase in the risk of a cardiovascular event. These were likely to be precipitous as well, he said: The higher the level of activation, the more likely the event was to happen within the first year of follow-up.
He had no financial disclosures.
Stress seems to be a strong driver of cardiovascular events, including heart attack, stroke, and even death.
For the first time, brain imaging has confirmed a link that has long been suspected: Activation of one of the brain’s prime emotional centers, the amygdala, directly correlates with the risk of cardiovascular events.
“This study illustrates a clear relationship between the activity of the amygdala and heart disease,” Dr. Ahmed A. Tawakol said at a press teleconference leading up to the annual meeting of the American College of Cardiology.
“Stress is known to be associated with an increase in the risk of cardiovascular events, and the risk is on par with that exerted by smoking, hypertension, and diabetes, but we don’t address it,” said Dr. Tawakol, codirector of the Cardiac MRI PET CT Program at Massachusetts General Hospital, Boston.
The findings also highlight a possible pathway for this relationship, suggesting that stress-related noradrenalin stimulates extramedullary hematopoiesis, a key driver of inflammation. This can contribute to atherosclerotic inflammation, which increases the likelihood of a heart attack or stroke, said Dr. Tawakol.
His study comprised 293 subjects who had undergone a PET or CT scan for cancer evaluation, but were determined to be cancer free. All scans contained brain and bone imaging data. Dr. Tawakol assessed amygdala and bone marrow activation, and evaluated inflammatory response in arteries.
These findings were then correlated with any cardiovascular events occurring in the next 5 years; the median follow-up was 3.8 years. Events were significantly more common among those with high levels of amygdala activation, occurring in 35% of this group, but in just 5% of those with low activation.
After adjusting for risk factors in the Framingham model, Dr. Tawakol found that high amygdala activation conferred a 14-fold increase in the risk of a cardiovascular event. These were likely to be precipitous as well, he said: The higher the level of activation, the more likely the event was to happen within the first year of follow-up.
He had no financial disclosures.
FROM ACC 16
Key clinical point: Activation of the amygdala, the brain’s fear response center, was directly correlated with the occurrence of cardiovascular events.
Major finding: High amygdala activation conferred a 14-fold increase in the risk of a heart attack, stroke, or cardiac death.
Data source: An imaging study in 293 patients.
Disclosures: Dr. Tawakol had no financial disclosures.
Heart attack patients getting younger, fatter, and less healthy
Despite advances in the prevention and early detection of cardiovascular disease, heart attack patients are getting younger, fatter, and less health conscious.
A look at 10 years’ worth of patient data reveals these and other “alarming trends,” according to Dr. Samir R. Kapadia of the Cleveland Clinic.
“What we found was so very contradictory to what we expected,” he said at a press briefing held in advance of the annual meeting of the American College of Cardiology. “Amazingly, we saw that patients presenting with myocardial infarction were getting younger, and their body mass index was going up. There was more smoking, more hypertension, and more diabetes. And all of this despite our better understanding of cardiovascular risk factors.”
The findings seem to point to a serious gap between gathering scientific knowledge and putting that knowledge into practice.
“We have to extend our efforts and put a lot more into educating patients,” Dr. Kapadia said. “Maybe it’s not enough to just tell people to eat right and exercise – maybe we should also be providing them with a structured program. But this is not just the job of the cardiologist. Primary care physicians have to also have this insight, communicate it to the patients, and get them the resources they need to help prevent heart attacks.”
His retrospective study comprised 3,912 consecutive patients who were treated for ST-segment elevation MI (STEMI) from 1995 to 2014. Data were collected on age, gender, diabetes, hypertension, smoking, lipid levels, chronic renal impairment, and obesity. The group was divided into four epochs: 1995-1999, 2000-2004, 2005-2009, and 2010-2014. The researchers examined these factors both in the entire cohort and in a subset of 1,325 who had a diagnosis of coronary artery disease at the time of their MI.
Patients became significantly younger over the entire study period. In epoch 1, the mean age of the entire cohort was 63.6 years. By epoch 3, this had declined to 60.3 years – a significant drop. The change was also evident in the CAD subset; among these patients, mean age declined from 64.1 years in epoch 1 to 61.8 years in epoch 4.
Tobacco use increased significantly in both groups as well. In the overall cohort, the rate was 27.7% in epoch 1 and 45.4% in epoch 4. In the CAD subset, it rose from 24.6% to 42.7%.
Hypertension in the entire cohort increased from 56.7% to 77.3%. In the CAD subset, it increased from 60.9% to 89%.
Obesity increased in both cohorts in overlapping trends, from about 30% in epoch 1 to 40% in epoch 4.
Diabetes increased as well. In the entire cohort, it rose from 24.6% to 30.6%. In the CAD subset, it rose from 25.4% to 41.5%.
Dr. Kapadia noted that the proportion of patients with at least three major risk factors rose from 65% to 85%, and that the incidence of chronic obstructive pulmonary disease increased from 5% to 12%, although he didn’t break this trend down by group.
He had no financial disclosures.
Despite advances in the prevention and early detection of cardiovascular disease, heart attack patients are getting younger, fatter, and less health conscious.
A look at 10 years’ worth of patient data reveals these and other “alarming trends,” according to Dr. Samir R. Kapadia of the Cleveland Clinic.
“What we found was so very contradictory to what we expected,” he said at a press briefing held in advance of the annual meeting of the American College of Cardiology. “Amazingly, we saw that patients presenting with myocardial infarction were getting younger, and their body mass index was going up. There was more smoking, more hypertension, and more diabetes. And all of this despite our better understanding of cardiovascular risk factors.”
The findings seem to point to a serious gap between gathering scientific knowledge and putting that knowledge into practice.
“We have to extend our efforts and put a lot more into educating patients,” Dr. Kapadia said. “Maybe it’s not enough to just tell people to eat right and exercise – maybe we should also be providing them with a structured program. But this is not just the job of the cardiologist. Primary care physicians have to also have this insight, communicate it to the patients, and get them the resources they need to help prevent heart attacks.”
His retrospective study comprised 3,912 consecutive patients who were treated for ST-segment elevation MI (STEMI) from 1995 to 2014. Data were collected on age, gender, diabetes, hypertension, smoking, lipid levels, chronic renal impairment, and obesity. The group was divided into four epochs: 1995-1999, 2000-2004, 2005-2009, and 2010-2014. The researchers examined these factors both in the entire cohort and in a subset of 1,325 who had a diagnosis of coronary artery disease at the time of their MI.
Patients became significantly younger over the entire study period. In epoch 1, the mean age of the entire cohort was 63.6 years. By epoch 3, this had declined to 60.3 years – a significant drop. The change was also evident in the CAD subset; among these patients, mean age declined from 64.1 years in epoch 1 to 61.8 years in epoch 4.
Tobacco use increased significantly in both groups as well. In the overall cohort, the rate was 27.7% in epoch 1 and 45.4% in epoch 4. In the CAD subset, it rose from 24.6% to 42.7%.
Hypertension in the entire cohort increased from 56.7% to 77.3%. In the CAD subset, it increased from 60.9% to 89%.
Obesity increased in both cohorts in overlapping trends, from about 30% in epoch 1 to 40% in epoch 4.
Diabetes increased as well. In the entire cohort, it rose from 24.6% to 30.6%. In the CAD subset, it rose from 25.4% to 41.5%.
Dr. Kapadia noted that the proportion of patients with at least three major risk factors rose from 65% to 85%, and that the incidence of chronic obstructive pulmonary disease increased from 5% to 12%, although he didn’t break this trend down by group.
He had no financial disclosures.
Despite advances in the prevention and early detection of cardiovascular disease, heart attack patients are getting younger, fatter, and less health conscious.
A look at 10 years’ worth of patient data reveals these and other “alarming trends,” according to Dr. Samir R. Kapadia of the Cleveland Clinic.
“What we found was so very contradictory to what we expected,” he said at a press briefing held in advance of the annual meeting of the American College of Cardiology. “Amazingly, we saw that patients presenting with myocardial infarction were getting younger, and their body mass index was going up. There was more smoking, more hypertension, and more diabetes. And all of this despite our better understanding of cardiovascular risk factors.”
The findings seem to point to a serious gap between gathering scientific knowledge and putting that knowledge into practice.
“We have to extend our efforts and put a lot more into educating patients,” Dr. Kapadia said. “Maybe it’s not enough to just tell people to eat right and exercise – maybe we should also be providing them with a structured program. But this is not just the job of the cardiologist. Primary care physicians have to also have this insight, communicate it to the patients, and get them the resources they need to help prevent heart attacks.”
His retrospective study comprised 3,912 consecutive patients who were treated for ST-segment elevation MI (STEMI) from 1995 to 2014. Data were collected on age, gender, diabetes, hypertension, smoking, lipid levels, chronic renal impairment, and obesity. The group was divided into four epochs: 1995-1999, 2000-2004, 2005-2009, and 2010-2014. The researchers examined these factors both in the entire cohort and in a subset of 1,325 who had a diagnosis of coronary artery disease at the time of their MI.
Patients became significantly younger over the entire study period. In epoch 1, the mean age of the entire cohort was 63.6 years. By epoch 3, this had declined to 60.3 years – a significant drop. The change was also evident in the CAD subset; among these patients, mean age declined from 64.1 years in epoch 1 to 61.8 years in epoch 4.
Tobacco use increased significantly in both groups as well. In the overall cohort, the rate was 27.7% in epoch 1 and 45.4% in epoch 4. In the CAD subset, it rose from 24.6% to 42.7%.
Hypertension in the entire cohort increased from 56.7% to 77.3%. In the CAD subset, it increased from 60.9% to 89%.
Obesity increased in both cohorts in overlapping trends, from about 30% in epoch 1 to 40% in epoch 4.
Diabetes increased as well. In the entire cohort, it rose from 24.6% to 30.6%. In the CAD subset, it rose from 25.4% to 41.5%.
Dr. Kapadia noted that the proportion of patients with at least three major risk factors rose from 65% to 85%, and that the incidence of chronic obstructive pulmonary disease increased from 5% to 12%, although he didn’t break this trend down by group.
He had no financial disclosures.
FROM ACC 16
Key clinical point: Despite advances in understanding heart disease prevention, patients with heart attack are younger and less healthy than they were 10 years ago.
Major finding: Patients are an average of 3 years younger than in 1994, and more are obese and use tobacco.
Data source: A retrospective study of 3,912 patients with acute ST-segment elevation MI.
Disclosures: Dr. Samir Kapadia had no financial disclosures.