User login
Power lines don’t raise leukemia risk in kids
Living near overhead power lines in early life does not increase a child’s risk of developing leukemia, according to a study published in the British Journal of Cancer.
An earlier study using information on childhood leukemia diagnosed between 1962 and 1995 suggested there was an elevated risk for children born within 600 meters of overhead power lines.
But now, updated data indicate that children born after the 1980s don’t have an increased risk.
According to researchers, this strongly suggests there is no direct biological effect of power lines on leukemia risk.
They believe the previous findings could be explained by changes in the characteristics of people living near power lines. The results might also be a chance finding or have resulted from problems with the study design.
“It’s very encouraging to see that, in recent decades, there has been no increased risk of leukemia among children born near overhead power lines,” said lead study author Kathryn Bunch, of the University of Oxford.
“More research is needed to determine precisely why previous evidence suggested a risk prior to 1980, but parents can be reassured from the findings of this study that overhead power lines don’t increase their child’s risk of leukemia.”
Expanding on previous findings
Several years ago, Dr Bunch’s colleagues at the University of Oxford set out to determine if proximity to high-voltage power lines affected the risk of childhood cancers in England and Wales, using data spanning the period from 1962 to 1995.
The team found evidence to suggest a relationship between childhood leukemia risk and the proximity to power lines of the mother’s residence at the time of the child’s birth. This included all 400 kV and 275 kV power lines and a small fraction of 132 kV lines (Draper et al, BMJ 2005).
Dr Bunch and her colleagues decided to extend this study by including more recent data, as well as cases and control subjects from Scotland. The group evaluated 132 kV, 275 kV, and 400 kV power lines and looked at subjects living greater distances from the power lines than those included in the previous study.
The researchers analyzed 53,515 children enrolled in the National Registry of Childhood Tumours from 1962 to 2008 and a group of matched controls.
The team found that, for the entire study period, there was no evidence of an increased risk of leukemia among subjects living closer to power lines. The relative risk of leukemia for children living 0 m to 199 m from power lines, compared with those living 1000 m or more from power lines (for all voltages), was 1.12.
There did appear to be an increased risk of leukemia when the researchers analyzed data according to decade. However, this risk declined over time.
The relative risk of leukemia for children living 0 m to 199 m from power lines, compared with those living 1000 m or more from power lines, was 4.50 in the 1960s, 2.46 in the 1970s, 1.54 in the 1980s, 0.99 in the 1990s, and 0.71 in the 2000s.
The elevated risk in the 1980s was not statistically significant, the researchers noted. They also pointed out that, even in the decades when the risk appears to be present, there is no evidence that it extended beyond the 600 m limit of the original analysis.
The fact that the risk declined over time suggests the leukemia is unlikely to have arisen from any physical effect of the power lines, the researchers said. They believe it’s more likely the result of changing population characteristics. ![]()
Living near overhead power lines in early life does not increase a child’s risk of developing leukemia, according to a study published in the British Journal of Cancer.
An earlier study using information on childhood leukemia diagnosed between 1962 and 1995 suggested there was an elevated risk for children born within 600 meters of overhead power lines.
But now, updated data indicate that children born after the 1980s don’t have an increased risk.
According to researchers, this strongly suggests there is no direct biological effect of power lines on leukemia risk.
They believe the previous findings could be explained by changes in the characteristics of people living near power lines. The results might also be a chance finding or have resulted from problems with the study design.
“It’s very encouraging to see that, in recent decades, there has been no increased risk of leukemia among children born near overhead power lines,” said lead study author Kathryn Bunch, of the University of Oxford.
“More research is needed to determine precisely why previous evidence suggested a risk prior to 1980, but parents can be reassured from the findings of this study that overhead power lines don’t increase their child’s risk of leukemia.”
Expanding on previous findings
Several years ago, Dr Bunch’s colleagues at the University of Oxford set out to determine if proximity to high-voltage power lines affected the risk of childhood cancers in England and Wales, using data spanning the period from 1962 to 1995.
The team found evidence to suggest a relationship between childhood leukemia risk and the proximity to power lines of the mother’s residence at the time of the child’s birth. This included all 400 kV and 275 kV power lines and a small fraction of 132 kV lines (Draper et al, BMJ 2005).
Dr Bunch and her colleagues decided to extend this study by including more recent data, as well as cases and control subjects from Scotland. The group evaluated 132 kV, 275 kV, and 400 kV power lines and looked at subjects living greater distances from the power lines than those included in the previous study.
The researchers analyzed 53,515 children enrolled in the National Registry of Childhood Tumours from 1962 to 2008 and a group of matched controls.
The team found that, for the entire study period, there was no evidence of an increased risk of leukemia among subjects living closer to power lines. The relative risk of leukemia for children living 0 m to 199 m from power lines, compared with those living 1000 m or more from power lines (for all voltages), was 1.12.
There did appear to be an increased risk of leukemia when the researchers analyzed data according to decade. However, this risk declined over time.
The relative risk of leukemia for children living 0 m to 199 m from power lines, compared with those living 1000 m or more from power lines, was 4.50 in the 1960s, 2.46 in the 1970s, 1.54 in the 1980s, 0.99 in the 1990s, and 0.71 in the 2000s.
The elevated risk in the 1980s was not statistically significant, the researchers noted. They also pointed out that, even in the decades when the risk appears to be present, there is no evidence that it extended beyond the 600 m limit of the original analysis.
The fact that the risk declined over time suggests the leukemia is unlikely to have arisen from any physical effect of the power lines, the researchers said. They believe it’s more likely the result of changing population characteristics. ![]()
Living near overhead power lines in early life does not increase a child’s risk of developing leukemia, according to a study published in the British Journal of Cancer.
An earlier study using information on childhood leukemia diagnosed between 1962 and 1995 suggested there was an elevated risk for children born within 600 meters of overhead power lines.
But now, updated data indicate that children born after the 1980s don’t have an increased risk.
According to researchers, this strongly suggests there is no direct biological effect of power lines on leukemia risk.
They believe the previous findings could be explained by changes in the characteristics of people living near power lines. The results might also be a chance finding or have resulted from problems with the study design.
“It’s very encouraging to see that, in recent decades, there has been no increased risk of leukemia among children born near overhead power lines,” said lead study author Kathryn Bunch, of the University of Oxford.
“More research is needed to determine precisely why previous evidence suggested a risk prior to 1980, but parents can be reassured from the findings of this study that overhead power lines don’t increase their child’s risk of leukemia.”
Expanding on previous findings
Several years ago, Dr Bunch’s colleagues at the University of Oxford set out to determine if proximity to high-voltage power lines affected the risk of childhood cancers in England and Wales, using data spanning the period from 1962 to 1995.
The team found evidence to suggest a relationship between childhood leukemia risk and the proximity to power lines of the mother’s residence at the time of the child’s birth. This included all 400 kV and 275 kV power lines and a small fraction of 132 kV lines (Draper et al, BMJ 2005).
Dr Bunch and her colleagues decided to extend this study by including more recent data, as well as cases and control subjects from Scotland. The group evaluated 132 kV, 275 kV, and 400 kV power lines and looked at subjects living greater distances from the power lines than those included in the previous study.
The researchers analyzed 53,515 children enrolled in the National Registry of Childhood Tumours from 1962 to 2008 and a group of matched controls.
The team found that, for the entire study period, there was no evidence of an increased risk of leukemia among subjects living closer to power lines. The relative risk of leukemia for children living 0 m to 199 m from power lines, compared with those living 1000 m or more from power lines (for all voltages), was 1.12.
There did appear to be an increased risk of leukemia when the researchers analyzed data according to decade. However, this risk declined over time.
The relative risk of leukemia for children living 0 m to 199 m from power lines, compared with those living 1000 m or more from power lines, was 4.50 in the 1960s, 2.46 in the 1970s, 1.54 in the 1980s, 0.99 in the 1990s, and 0.71 in the 2000s.
The elevated risk in the 1980s was not statistically significant, the researchers noted. They also pointed out that, even in the decades when the risk appears to be present, there is no evidence that it extended beyond the 600 m limit of the original analysis.
The fact that the risk declined over time suggests the leukemia is unlikely to have arisen from any physical effect of the power lines, the researchers said. They believe it’s more likely the result of changing population characteristics. ![]()
Improving the efficacy of etoposide

after treatment with etoposide
Credit: CNIO
A compound that interferes with the cell cycle can increase the antineoplastic effects of etoposide, according to research published in Cell Reports.
Etoposide works by inhibiting topoisomerase II (TOP2), a protein needed for DNA repair during cell division.
Researchers discovered a relationship between TOP2 and Cdh1, a protein that (along with Cdc20) controls cell division by activating the anaphase-promoting complex/cyclosome (APC/C).
So the team hypothesized that combining etoposide with a compound that inhibits Cdh1 might improve etoposide’s antineoplastic effects. Experiments in cancer cell lines confirmed this theory.
Marcos Malumbres, PhD, of the Spanish National Cancer Research Centre (CNIO) in Madrid, and his colleagues began this research by investigating Cdh1 in vitro and in mouse models.
The team found that a decrease in Cdh1 activity increases cells’ TOP2 levels. So they decided to combine etoposide with a Cdh1 inhibitor and evaluate the effect on cancer cells, which divide more than normal cells and therefore have a greater dependency on TOP2 to maintain DNA integrity.
The researchers tested proTAME, a small molecule that targets APC/C-Cdh1 and APC/C-Cdc20, in combination with etoposide. And they found the drugs had a synergistic effect against cancer cells.
In experiments with a lung cancer cell line (A549) and 2 breast cancer cell lines (HeLa and MCF7), administering proTAME and etoposide together proved more effective than administering either compound alone.
The researchers believe these findings could apply to other malignancies as well. Etoposide has demonstrated activity against a number of cancers, including leukemias, lymphomas, and multiple myeloma.
The team said their next step is to study the etoposide-proTAME combination in patients and investigate the malignancies in which this therapeutic strategy would be most effective.
The researchers also noted that previous studies have shown Cdh1 is inactive in some patients due to various oncogenic mutations. So stratifying patients according to their tumor’s Cdh1 status could optimize treatment with etoposide. ![]()

after treatment with etoposide
Credit: CNIO
A compound that interferes with the cell cycle can increase the antineoplastic effects of etoposide, according to research published in Cell Reports.
Etoposide works by inhibiting topoisomerase II (TOP2), a protein needed for DNA repair during cell division.
Researchers discovered a relationship between TOP2 and Cdh1, a protein that (along with Cdc20) controls cell division by activating the anaphase-promoting complex/cyclosome (APC/C).
So the team hypothesized that combining etoposide with a compound that inhibits Cdh1 might improve etoposide’s antineoplastic effects. Experiments in cancer cell lines confirmed this theory.
Marcos Malumbres, PhD, of the Spanish National Cancer Research Centre (CNIO) in Madrid, and his colleagues began this research by investigating Cdh1 in vitro and in mouse models.
The team found that a decrease in Cdh1 activity increases cells’ TOP2 levels. So they decided to combine etoposide with a Cdh1 inhibitor and evaluate the effect on cancer cells, which divide more than normal cells and therefore have a greater dependency on TOP2 to maintain DNA integrity.
The researchers tested proTAME, a small molecule that targets APC/C-Cdh1 and APC/C-Cdc20, in combination with etoposide. And they found the drugs had a synergistic effect against cancer cells.
In experiments with a lung cancer cell line (A549) and 2 breast cancer cell lines (HeLa and MCF7), administering proTAME and etoposide together proved more effective than administering either compound alone.
The researchers believe these findings could apply to other malignancies as well. Etoposide has demonstrated activity against a number of cancers, including leukemias, lymphomas, and multiple myeloma.
The team said their next step is to study the etoposide-proTAME combination in patients and investigate the malignancies in which this therapeutic strategy would be most effective.
The researchers also noted that previous studies have shown Cdh1 is inactive in some patients due to various oncogenic mutations. So stratifying patients according to their tumor’s Cdh1 status could optimize treatment with etoposide. ![]()

after treatment with etoposide
Credit: CNIO
A compound that interferes with the cell cycle can increase the antineoplastic effects of etoposide, according to research published in Cell Reports.
Etoposide works by inhibiting topoisomerase II (TOP2), a protein needed for DNA repair during cell division.
Researchers discovered a relationship between TOP2 and Cdh1, a protein that (along with Cdc20) controls cell division by activating the anaphase-promoting complex/cyclosome (APC/C).
So the team hypothesized that combining etoposide with a compound that inhibits Cdh1 might improve etoposide’s antineoplastic effects. Experiments in cancer cell lines confirmed this theory.
Marcos Malumbres, PhD, of the Spanish National Cancer Research Centre (CNIO) in Madrid, and his colleagues began this research by investigating Cdh1 in vitro and in mouse models.
The team found that a decrease in Cdh1 activity increases cells’ TOP2 levels. So they decided to combine etoposide with a Cdh1 inhibitor and evaluate the effect on cancer cells, which divide more than normal cells and therefore have a greater dependency on TOP2 to maintain DNA integrity.
The researchers tested proTAME, a small molecule that targets APC/C-Cdh1 and APC/C-Cdc20, in combination with etoposide. And they found the drugs had a synergistic effect against cancer cells.
In experiments with a lung cancer cell line (A549) and 2 breast cancer cell lines (HeLa and MCF7), administering proTAME and etoposide together proved more effective than administering either compound alone.
The researchers believe these findings could apply to other malignancies as well. Etoposide has demonstrated activity against a number of cancers, including leukemias, lymphomas, and multiple myeloma.
The team said their next step is to study the etoposide-proTAME combination in patients and investigate the malignancies in which this therapeutic strategy would be most effective.
The researchers also noted that previous studies have shown Cdh1 is inactive in some patients due to various oncogenic mutations. So stratifying patients according to their tumor’s Cdh1 status could optimize treatment with etoposide. ![]()
National plan to lower HAIs shows signs of success, investigators find

Credit: CDC
New research suggests a federally sponsored plan to decrease the incidence of healthcare-acquired infections (HAIs) in the US was successful in addressing the challenges of prioritizing and coordinating strategies.
The plan has also been associated with reductions in the rates of HAIs, with progress made toward most targets where data are available.
Descriptions of the plan and its initial results appear in a series of articles published in a supplement to the February issue of Medical Care.
“Much progress has been made in raising awareness of and developing strategies for curbing the life-threatening infections that strike patients too often when they are receiving medical care,” said Katherine Kahn, MD, a leader of the project and professor at the Geffen School of Medicine at the University of California, Los Angeles.
“In order to make even more progress, we need to build our systems of care to be safer within and across hospitals, nursing homes, clinics, and community settings.”
In 2009, the US Department of Health and Humans Services released a national plan aimed at preventing HAIs, called “National Action Plan to Prevent Health Care-Associated Infections: Road Map to Elimination.”
Researchers performed an evaluation of the first few years of the plan, reviewing the structure of the effort, as well as the results thus far.
The plan focuses on evidence-based strategies, such as considering the benefits and risks when deciding about the use and duration of treatments like antibiotics.
Most of the prevention initiatives have focused on hospital settings, but the action plan has focused attention on efforts in other care settings, such as outpatient surgery centers, kidney dialysis centers, and long-term care facilities.
The investigators said these efforts have likely contributed to stakeholders’ reported perceptions of greater momentum in adopting strategies to prevent HAIs.
The national plan has generated clinical, political, and financial support for the complex efforts required to eliminate HAIs across federal, regional, state, and local settings.
Despite an influx of federal funding to support elimination of HAIs, the researchers said ongoing dedicated resources will be required to maintain momentum and sustain efforts made to date.
On the other hand, because future funding for efforts to further reduce HAIs is unclear, the investigators said it may be best to incorporate the efforts into the overall movement to improve patient safety. ![]()

Credit: CDC
New research suggests a federally sponsored plan to decrease the incidence of healthcare-acquired infections (HAIs) in the US was successful in addressing the challenges of prioritizing and coordinating strategies.
The plan has also been associated with reductions in the rates of HAIs, with progress made toward most targets where data are available.
Descriptions of the plan and its initial results appear in a series of articles published in a supplement to the February issue of Medical Care.
“Much progress has been made in raising awareness of and developing strategies for curbing the life-threatening infections that strike patients too often when they are receiving medical care,” said Katherine Kahn, MD, a leader of the project and professor at the Geffen School of Medicine at the University of California, Los Angeles.
“In order to make even more progress, we need to build our systems of care to be safer within and across hospitals, nursing homes, clinics, and community settings.”
In 2009, the US Department of Health and Humans Services released a national plan aimed at preventing HAIs, called “National Action Plan to Prevent Health Care-Associated Infections: Road Map to Elimination.”
Researchers performed an evaluation of the first few years of the plan, reviewing the structure of the effort, as well as the results thus far.
The plan focuses on evidence-based strategies, such as considering the benefits and risks when deciding about the use and duration of treatments like antibiotics.
Most of the prevention initiatives have focused on hospital settings, but the action plan has focused attention on efforts in other care settings, such as outpatient surgery centers, kidney dialysis centers, and long-term care facilities.
The investigators said these efforts have likely contributed to stakeholders’ reported perceptions of greater momentum in adopting strategies to prevent HAIs.
The national plan has generated clinical, political, and financial support for the complex efforts required to eliminate HAIs across federal, regional, state, and local settings.
Despite an influx of federal funding to support elimination of HAIs, the researchers said ongoing dedicated resources will be required to maintain momentum and sustain efforts made to date.
On the other hand, because future funding for efforts to further reduce HAIs is unclear, the investigators said it may be best to incorporate the efforts into the overall movement to improve patient safety. ![]()

Credit: CDC
New research suggests a federally sponsored plan to decrease the incidence of healthcare-acquired infections (HAIs) in the US was successful in addressing the challenges of prioritizing and coordinating strategies.
The plan has also been associated with reductions in the rates of HAIs, with progress made toward most targets where data are available.
Descriptions of the plan and its initial results appear in a series of articles published in a supplement to the February issue of Medical Care.
“Much progress has been made in raising awareness of and developing strategies for curbing the life-threatening infections that strike patients too often when they are receiving medical care,” said Katherine Kahn, MD, a leader of the project and professor at the Geffen School of Medicine at the University of California, Los Angeles.
“In order to make even more progress, we need to build our systems of care to be safer within and across hospitals, nursing homes, clinics, and community settings.”
In 2009, the US Department of Health and Humans Services released a national plan aimed at preventing HAIs, called “National Action Plan to Prevent Health Care-Associated Infections: Road Map to Elimination.”
Researchers performed an evaluation of the first few years of the plan, reviewing the structure of the effort, as well as the results thus far.
The plan focuses on evidence-based strategies, such as considering the benefits and risks when deciding about the use and duration of treatments like antibiotics.
Most of the prevention initiatives have focused on hospital settings, but the action plan has focused attention on efforts in other care settings, such as outpatient surgery centers, kidney dialysis centers, and long-term care facilities.
The investigators said these efforts have likely contributed to stakeholders’ reported perceptions of greater momentum in adopting strategies to prevent HAIs.
The national plan has generated clinical, political, and financial support for the complex efforts required to eliminate HAIs across federal, regional, state, and local settings.
Despite an influx of federal funding to support elimination of HAIs, the researchers said ongoing dedicated resources will be required to maintain momentum and sustain efforts made to date.
On the other hand, because future funding for efforts to further reduce HAIs is unclear, the investigators said it may be best to incorporate the efforts into the overall movement to improve patient safety. ![]()
Unique protein found in MM patients

Credit: Rhoda Baer
Researchers say they have discovered a bacterial protein that attaches to virtually any antibody and prevents it from binding to its target.
It appears that this molecule, called mycoplasma protein (or protein M), helps some bacteria evade the immune response and establish long-term infections.
The researchers discovered protein M in samples from multiple myeloma (MM) patients.
And the team believes the protein could be engineered to target cancerous B cells in patients with MM and other B-cell malignancies.
Protein M might also become a target for new antibacterial drugs, and it could prove useful for preparing highly pure antibodies for research and drug manufacturing.
Richard A. Lerner, MD, of The Scripps Research Institute (TSRI) in La Jolla, California, and his colleagues described their discovery of protein M in Science.
The discovery originated from an effort to understand the origin of MM. Clonal B-cell proliferation, as well as MM and lymphomas, can result from chronic infections by organisms such as Escherichia coli, Helicobacter pylori, and hepatitis C virus.
To better understand this process, Dr Lerner and his colleagues investigated mycoplasma, a parasite that infects people chronically and is largely confined to the cell surface.
In a search for factors associated with long-term mycoplasma infection, the team tested samples of antibodies from MM patients’ blood against a variety of mycoplasma species. One of the proteins recognized by the antibodies was from Mycoplasma genitalium, which causes sexually transmitted infections.
To the researchers’ surprise, every antibody sample tested showed reactivity to this protein. But further tests made it clear that these antibody reactions were not in response to mass infection with M genitalium.
Instead, the M genitalium protein, which the team named protein M, appeared to have evolved simply to bind to any antibody it encounters.
“It binds to every antibody generically—capable of hijacking the entire diversity of antibody repertoire—but, at the same time, it blocks the specific interaction between that antibody and its intended biomolecular target,” said Rajesh Grover, PhD, of TSRI.
To better understand how protein M works, the researchers took a structural biology approach. Using X-ray crystallography and other techniques, the team determined the protein’s 3D atomic structure while it was bound to various human antibodies.
Compared to thousands of known structures in the Protein Data Bank, the worldwide structure database, protein M appeared to be unique. The data also revealed that protein M binds to a small, conserved region at the outer tip of every antibody’s antigen-binding arm.
“It likely extends the other end of itself, like a tail, over the antibody’s main antigen-binding region,” said Xueyong Zhu, PhD, of TSRI.
The team is now studying protein M’s function during M genitalium infections. It seems likely that the protein evolved to help M genitalium cope with the immune response, as it has one of the smallest bacterial genomes in nature.
“It appears to represent an elegant evolutionary solution to the special problem that mycoplasma have in evading the adaptive immune system,” Dr Grover said. “The smallest parasitic [bacterium] on planet Earth seems to have evolved the most sophisticated invading molecular machine.”
If protein M is confirmed as a universal “decoy” for antibodies, it will become a target for new drugs, the researchers said. This could make it easier to treat chronic, sometimes silent, infections by M genitalium and any other microbes that have evolved a similar antibody-thwarting defense.
In principle, protein M also could be engineered to target specific groups of B cells, delivering cytotoxic agents to cancerous B cells in patients with MM and lymphomas.
But the most immediate use of protein M, according to the researchers, is likely to be as a tool for grabbing antibodies in test tubes and cell cultures. This would allow the preparation of highly pure antibodies for research and drug manufacturing. Other generic antibody-binding proteins have been put to use in this way, but, so far, it appears that none does the job quite as well as protein M.
“It may be the most useful antibody purification device ever found,” said Dr Lerner, who is now working to commercialize the protein. ![]()

Credit: Rhoda Baer
Researchers say they have discovered a bacterial protein that attaches to virtually any antibody and prevents it from binding to its target.
It appears that this molecule, called mycoplasma protein (or protein M), helps some bacteria evade the immune response and establish long-term infections.
The researchers discovered protein M in samples from multiple myeloma (MM) patients.
And the team believes the protein could be engineered to target cancerous B cells in patients with MM and other B-cell malignancies.
Protein M might also become a target for new antibacterial drugs, and it could prove useful for preparing highly pure antibodies for research and drug manufacturing.
Richard A. Lerner, MD, of The Scripps Research Institute (TSRI) in La Jolla, California, and his colleagues described their discovery of protein M in Science.
The discovery originated from an effort to understand the origin of MM. Clonal B-cell proliferation, as well as MM and lymphomas, can result from chronic infections by organisms such as Escherichia coli, Helicobacter pylori, and hepatitis C virus.
To better understand this process, Dr Lerner and his colleagues investigated mycoplasma, a parasite that infects people chronically and is largely confined to the cell surface.
In a search for factors associated with long-term mycoplasma infection, the team tested samples of antibodies from MM patients’ blood against a variety of mycoplasma species. One of the proteins recognized by the antibodies was from Mycoplasma genitalium, which causes sexually transmitted infections.
To the researchers’ surprise, every antibody sample tested showed reactivity to this protein. But further tests made it clear that these antibody reactions were not in response to mass infection with M genitalium.
Instead, the M genitalium protein, which the team named protein M, appeared to have evolved simply to bind to any antibody it encounters.
“It binds to every antibody generically—capable of hijacking the entire diversity of antibody repertoire—but, at the same time, it blocks the specific interaction between that antibody and its intended biomolecular target,” said Rajesh Grover, PhD, of TSRI.
To better understand how protein M works, the researchers took a structural biology approach. Using X-ray crystallography and other techniques, the team determined the protein’s 3D atomic structure while it was bound to various human antibodies.
Compared to thousands of known structures in the Protein Data Bank, the worldwide structure database, protein M appeared to be unique. The data also revealed that protein M binds to a small, conserved region at the outer tip of every antibody’s antigen-binding arm.
“It likely extends the other end of itself, like a tail, over the antibody’s main antigen-binding region,” said Xueyong Zhu, PhD, of TSRI.
The team is now studying protein M’s function during M genitalium infections. It seems likely that the protein evolved to help M genitalium cope with the immune response, as it has one of the smallest bacterial genomes in nature.
“It appears to represent an elegant evolutionary solution to the special problem that mycoplasma have in evading the adaptive immune system,” Dr Grover said. “The smallest parasitic [bacterium] on planet Earth seems to have evolved the most sophisticated invading molecular machine.”
If protein M is confirmed as a universal “decoy” for antibodies, it will become a target for new drugs, the researchers said. This could make it easier to treat chronic, sometimes silent, infections by M genitalium and any other microbes that have evolved a similar antibody-thwarting defense.
In principle, protein M also could be engineered to target specific groups of B cells, delivering cytotoxic agents to cancerous B cells in patients with MM and lymphomas.
But the most immediate use of protein M, according to the researchers, is likely to be as a tool for grabbing antibodies in test tubes and cell cultures. This would allow the preparation of highly pure antibodies for research and drug manufacturing. Other generic antibody-binding proteins have been put to use in this way, but, so far, it appears that none does the job quite as well as protein M.
“It may be the most useful antibody purification device ever found,” said Dr Lerner, who is now working to commercialize the protein. ![]()

Credit: Rhoda Baer
Researchers say they have discovered a bacterial protein that attaches to virtually any antibody and prevents it from binding to its target.
It appears that this molecule, called mycoplasma protein (or protein M), helps some bacteria evade the immune response and establish long-term infections.
The researchers discovered protein M in samples from multiple myeloma (MM) patients.
And the team believes the protein could be engineered to target cancerous B cells in patients with MM and other B-cell malignancies.
Protein M might also become a target for new antibacterial drugs, and it could prove useful for preparing highly pure antibodies for research and drug manufacturing.
Richard A. Lerner, MD, of The Scripps Research Institute (TSRI) in La Jolla, California, and his colleagues described their discovery of protein M in Science.
The discovery originated from an effort to understand the origin of MM. Clonal B-cell proliferation, as well as MM and lymphomas, can result from chronic infections by organisms such as Escherichia coli, Helicobacter pylori, and hepatitis C virus.
To better understand this process, Dr Lerner and his colleagues investigated mycoplasma, a parasite that infects people chronically and is largely confined to the cell surface.
In a search for factors associated with long-term mycoplasma infection, the team tested samples of antibodies from MM patients’ blood against a variety of mycoplasma species. One of the proteins recognized by the antibodies was from Mycoplasma genitalium, which causes sexually transmitted infections.
To the researchers’ surprise, every antibody sample tested showed reactivity to this protein. But further tests made it clear that these antibody reactions were not in response to mass infection with M genitalium.
Instead, the M genitalium protein, which the team named protein M, appeared to have evolved simply to bind to any antibody it encounters.
“It binds to every antibody generically—capable of hijacking the entire diversity of antibody repertoire—but, at the same time, it blocks the specific interaction between that antibody and its intended biomolecular target,” said Rajesh Grover, PhD, of TSRI.
To better understand how protein M works, the researchers took a structural biology approach. Using X-ray crystallography and other techniques, the team determined the protein’s 3D atomic structure while it was bound to various human antibodies.
Compared to thousands of known structures in the Protein Data Bank, the worldwide structure database, protein M appeared to be unique. The data also revealed that protein M binds to a small, conserved region at the outer tip of every antibody’s antigen-binding arm.
“It likely extends the other end of itself, like a tail, over the antibody’s main antigen-binding region,” said Xueyong Zhu, PhD, of TSRI.
The team is now studying protein M’s function during M genitalium infections. It seems likely that the protein evolved to help M genitalium cope with the immune response, as it has one of the smallest bacterial genomes in nature.
“It appears to represent an elegant evolutionary solution to the special problem that mycoplasma have in evading the adaptive immune system,” Dr Grover said. “The smallest parasitic [bacterium] on planet Earth seems to have evolved the most sophisticated invading molecular machine.”
If protein M is confirmed as a universal “decoy” for antibodies, it will become a target for new drugs, the researchers said. This could make it easier to treat chronic, sometimes silent, infections by M genitalium and any other microbes that have evolved a similar antibody-thwarting defense.
In principle, protein M also could be engineered to target specific groups of B cells, delivering cytotoxic agents to cancerous B cells in patients with MM and lymphomas.
But the most immediate use of protein M, according to the researchers, is likely to be as a tool for grabbing antibodies in test tubes and cell cultures. This would allow the preparation of highly pure antibodies for research and drug manufacturing. Other generic antibody-binding proteins have been put to use in this way, but, so far, it appears that none does the job quite as well as protein M.
“It may be the most useful antibody purification device ever found,” said Dr Lerner, who is now working to commercialize the protein. ![]()
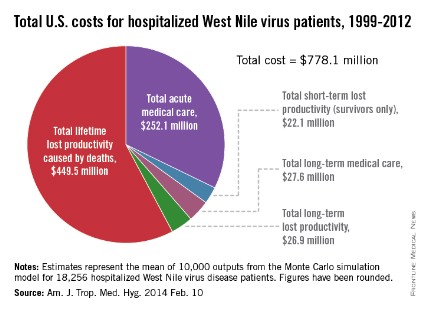
West Nile virus has cost the United States nearly $800 million
Since the West Nile virus was first detected in New York in 1999, hospitalized patients in the United States have cost an estimated $778.1 million in health care expenditures and lost productivity, according to a study published online Feb. 10 in the American Journal of Tropical Medicine and Hygiene.
Of that $778.1 million, the largest share – $449.5 million, or almost 58% – represents mean lifetime lost productivity from deaths caused by infection. Hospitalization for acute illness was estimated at $252.1 million, long-term medical care cost $27.6 million, long-term lost productivity cost $26.9 million, and short-term lost productivity (survivors only) totaled $22.1 million, investigators from the Centers for Disease Control and Prevention reported.
From 1999 through 2012, there were 37,088 cases of West Nile virus disease reported to the CDC’s ArboNET surveillance system, resulting in more than 18,000 hospitalizations and 1,529 deaths, the investigators said (Am. J. Trop. Med. Hyg. 2014 Feb. 10).
They determined the cost of initial hospitalization for 80 patients in a 2003 West Nile virus outbreak in Colorado, then calculated the cost of additional medical care and missed work for 38 patients who had 5 years of follow-up data available after the initial infection. These costs were then extrapolated to the total number of hospitalized cases in the United States since 1999.

Since the West Nile virus was first detected in New York in 1999, hospitalized patients in the United States have cost an estimated $778.1 million in health care expenditures and lost productivity, according to a study published online Feb. 10 in the American Journal of Tropical Medicine and Hygiene.
Of that $778.1 million, the largest share – $449.5 million, or almost 58% – represents mean lifetime lost productivity from deaths caused by infection. Hospitalization for acute illness was estimated at $252.1 million, long-term medical care cost $27.6 million, long-term lost productivity cost $26.9 million, and short-term lost productivity (survivors only) totaled $22.1 million, investigators from the Centers for Disease Control and Prevention reported.
From 1999 through 2012, there were 37,088 cases of West Nile virus disease reported to the CDC’s ArboNET surveillance system, resulting in more than 18,000 hospitalizations and 1,529 deaths, the investigators said (Am. J. Trop. Med. Hyg. 2014 Feb. 10).
They determined the cost of initial hospitalization for 80 patients in a 2003 West Nile virus outbreak in Colorado, then calculated the cost of additional medical care and missed work for 38 patients who had 5 years of follow-up data available after the initial infection. These costs were then extrapolated to the total number of hospitalized cases in the United States since 1999.

Since the West Nile virus was first detected in New York in 1999, hospitalized patients in the United States have cost an estimated $778.1 million in health care expenditures and lost productivity, according to a study published online Feb. 10 in the American Journal of Tropical Medicine and Hygiene.
Of that $778.1 million, the largest share – $449.5 million, or almost 58% – represents mean lifetime lost productivity from deaths caused by infection. Hospitalization for acute illness was estimated at $252.1 million, long-term medical care cost $27.6 million, long-term lost productivity cost $26.9 million, and short-term lost productivity (survivors only) totaled $22.1 million, investigators from the Centers for Disease Control and Prevention reported.
From 1999 through 2012, there were 37,088 cases of West Nile virus disease reported to the CDC’s ArboNET surveillance system, resulting in more than 18,000 hospitalizations and 1,529 deaths, the investigators said (Am. J. Trop. Med. Hyg. 2014 Feb. 10).
They determined the cost of initial hospitalization for 80 patients in a 2003 West Nile virus outbreak in Colorado, then calculated the cost of additional medical care and missed work for 38 patients who had 5 years of follow-up data available after the initial infection. These costs were then extrapolated to the total number of hospitalized cases in the United States since 1999.

FROM AMERICAN JOURNAL OF TROPICAL MEDICINE AND HYGIENE
Treatment of Postoperative Infection After Posterior Spinal Fusion and Instrumentation in a Patient With Neuromuscular Scoliosis
Is There a Role for Arthroscopy in the Treatment of Glenohumeral Arthritis?
This issue of The American Journal of Orthopedics focuses on the treatment of shoulder and elbow pathology in 2014. Treatment of shoulder arthritis in young or high-demand patients remains a significant challenge. Total shoulder arthroplasty (TSA) for glenohumeral arthritis can provide excellent pain relief and improved function in elderly, lower demand patients. In younger or higher demand patients, the long-term outcomes are less favorable—failure rates are higher, and revision surgery outcomes are unpredictable. Sperling and colleagues1 reported a survival rate of only 61% for TSA in patients younger than 50 at 10-year follow-up. In addition, postarthroplasty activity restrictions may be unacceptable for these younger, active patients. Concerns about poor shoulder arthroplasty durability and patient expectations of high activity have led to considerations for nonarthroplastic surgical options for shoulder arthritis in this patient population.
Some consider hemiarthroplasty an appropriate treatment option for shoulder arthritis in young patients and in patients who are too active for TSA, as hemiarthroplasty does not involve implantation of a glenoid component. However, compared with TSA, hemiarthroplasty is generally associated with inferior outcomes. Furthermore, when hemiarthroplasty fails and TSA revision becomes necessary, the outcomes of this revision are often inferior to those of primary TSA in the same population. For these reasons, hemiarthroplasty is considered a less optimal option for primary shoulder arthritis.
Biological resurfacing of the glenoid once was an exciting treatment alternative to TSA. Biological resurfacing includes interposition of soft tissue, whether fascia lata,
Achilles tendon, or lateral meniscus allograft, onto the native glenoid with a hemiarthroplasty of the humerus. Initial short-term outcomes of biological resurfacing were encouraging, but midterm outcomes were unsatisfactory, and attempts to reproduce initial published results were unsuccessful. Biological resurfacing has a very limited role now and is largely reserved for patients with localized humeral head articular cartilage loss with minimal involvement of the glenoid. In general, the glenoid remains the most significant treatment challenge in this group, and, other than for “ream and run” procedures, most biological
solutions for the glenoid are seldom used because of technical difficulty, surgical morbidity, and overall high failure rates.
Arthroscopic treatment of shoulder arthritis has emerged as an alternative to shoulder arthroplasty. Originally reported in 1982, initial attempts consisted mostly of arthroscopic joint lavage and loose body removal.2 More recently, arthroscopic procedures for the treatment of shoulder arthritis have been expanded to include extensive joint debridement with synovectomy and circumferential capsular release, chondroplasty, osteophyte excision, and treatment of associated pathology, such as biceps tendinopathy, subacromial bursitis, acromioclavicular arthrosis, and even neurolysis of the axillary nerve.
Published results of shoulder arthroscopy for arthritis are encouraging. In a recent systematic literature review, Namdari and colleagues3 found a clear trend of significant pain relief and improved function after shoulder arthroscopy for arthritis, despite lack of high-level evidence. Millett and colleagues4 reported 85% survivorship at 2-year follow-up for 30 shoulders (23 men, 6 women; mean age,
52 years). Overall, patients reported significant pain relief with daily activities, athletic or work activity, and ability to rest comfortably. Similarly, Van Thiel and colleagues5 reported excellent pain relief and improved validated shoulder and elbow scores at 27-month follow-up. In both studies, patients with severe joint-space narrowing (<2 mm on radiographs) or severe arthritic deformity had
inferior outcomes, but severity of arthroscopic grade of arthritis was not prognostic of clinical outcomes. Chondroplasty and osteophyte excision were shown to be helpful in reestablishing range-of-motion (ROM) and providing pain relief, but larger osteophytes associated with worse glenohumeral arthritis had poorer outcomes. In general, it should be assumed that, if the humeral head shape is preserved, if glenoid wear is concentric, and if the joint space is visible on radiographs, then the patient is likely to have improved pain and function with arthroscopic treatment.
Properly addressing associated shoulder pain generators at time of arthroscopic surgery is important. Patients with significant arthritic stiffness can have prolonged improvement in ROM and function after arthroscopic debridement and circumferential capsular release. Patients with symptoms of biceps tendinopathy should undergo biceps tenodesis or tenotomy. Acromioclavicular joint pain should
receive a distal clavicle excision. Subacromial debridement should be performed for subacromial symptoms, while acromioplasty can be reserved for type III acromion morphology. With careful preoperative evaluation, the clinician should be able to identify all possible pain generators in the arthritic shoulder and address these concomitantly to optimize pain relief and improved function.
In summary, shoulder arthroscopy should be considered a surgical alternative to shoulder arthroplasty in young or high-demand patients with mild to moderate arthritis. Pathology most responsive to shoulder arthroscopy includes shoulder stiffness caused by capsular tightness, chondral lesion less than 2 cm,3 less severe arthritis with preserved humeral head shape, and properly addressed associated
pathology, such as synovitis, biceps tendinopathy, and subacromial bursitis or acromioclavicular arthrosis. Although high-level evidence is lacking, study trends show improved ROM and pain relief and overall high patient satisfaction at short to midterm follow-up. Ultimately, more data are needed to provide precise surgical indications and prognostic factors. Currently, however, it appears that shoulder arthroscopy can play an important role in the treatment of shoulder arthritis and can provide high satisfaction in appropriately selected patients.
References
1. Sperling JW, Cofield RH, Rowland CM. Neer hemiarthroplasty and Neer
total shoulder arthroplasty in patients fifty years old or less. Long-term
results. J Bone Joint Surg Am. 1998;80(4):464-473.
2. McGinty JB. Arthroscopic removal of loose bodies. Ortho Clin North
Am. 1982;13(2):313-328.
3. Namdari S, Skelley N, Keener JD, Galatz LM, Yamaguchi K. What is the
role of arthroscopic debridement for glenohumeral arthritis? A critical
examination of the literature. Arthroscopy. 2013;29(8):1392-1398.
4. Millett PJ, Horan MP, Pennock AT, Rios D. Comprehensive arthroscopic
management (CAM) procedure: clinical results of a joint-preserving
arthroscopic treatment for young, active patients with advanced shoulder
osteoarthritis. Arthroscopy. 2013;29(3):440-448.
5. Van Thiel GS, Sheehan S, Frank RM, et al. Retrospective analysis of
arthroscopic management of glenohumeral degenerative disease.
Arthroscopy. 2010;26(11):1451-1455.
This issue of The American Journal of Orthopedics focuses on the treatment of shoulder and elbow pathology in 2014. Treatment of shoulder arthritis in young or high-demand patients remains a significant challenge. Total shoulder arthroplasty (TSA) for glenohumeral arthritis can provide excellent pain relief and improved function in elderly, lower demand patients. In younger or higher demand patients, the long-term outcomes are less favorable—failure rates are higher, and revision surgery outcomes are unpredictable. Sperling and colleagues1 reported a survival rate of only 61% for TSA in patients younger than 50 at 10-year follow-up. In addition, postarthroplasty activity restrictions may be unacceptable for these younger, active patients. Concerns about poor shoulder arthroplasty durability and patient expectations of high activity have led to considerations for nonarthroplastic surgical options for shoulder arthritis in this patient population.
Some consider hemiarthroplasty an appropriate treatment option for shoulder arthritis in young patients and in patients who are too active for TSA, as hemiarthroplasty does not involve implantation of a glenoid component. However, compared with TSA, hemiarthroplasty is generally associated with inferior outcomes. Furthermore, when hemiarthroplasty fails and TSA revision becomes necessary, the outcomes of this revision are often inferior to those of primary TSA in the same population. For these reasons, hemiarthroplasty is considered a less optimal option for primary shoulder arthritis.
Biological resurfacing of the glenoid once was an exciting treatment alternative to TSA. Biological resurfacing includes interposition of soft tissue, whether fascia lata,
Achilles tendon, or lateral meniscus allograft, onto the native glenoid with a hemiarthroplasty of the humerus. Initial short-term outcomes of biological resurfacing were encouraging, but midterm outcomes were unsatisfactory, and attempts to reproduce initial published results were unsuccessful. Biological resurfacing has a very limited role now and is largely reserved for patients with localized humeral head articular cartilage loss with minimal involvement of the glenoid. In general, the glenoid remains the most significant treatment challenge in this group, and, other than for “ream and run” procedures, most biological
solutions for the glenoid are seldom used because of technical difficulty, surgical morbidity, and overall high failure rates.
Arthroscopic treatment of shoulder arthritis has emerged as an alternative to shoulder arthroplasty. Originally reported in 1982, initial attempts consisted mostly of arthroscopic joint lavage and loose body removal.2 More recently, arthroscopic procedures for the treatment of shoulder arthritis have been expanded to include extensive joint debridement with synovectomy and circumferential capsular release, chondroplasty, osteophyte excision, and treatment of associated pathology, such as biceps tendinopathy, subacromial bursitis, acromioclavicular arthrosis, and even neurolysis of the axillary nerve.
Published results of shoulder arthroscopy for arthritis are encouraging. In a recent systematic literature review, Namdari and colleagues3 found a clear trend of significant pain relief and improved function after shoulder arthroscopy for arthritis, despite lack of high-level evidence. Millett and colleagues4 reported 85% survivorship at 2-year follow-up for 30 shoulders (23 men, 6 women; mean age,
52 years). Overall, patients reported significant pain relief with daily activities, athletic or work activity, and ability to rest comfortably. Similarly, Van Thiel and colleagues5 reported excellent pain relief and improved validated shoulder and elbow scores at 27-month follow-up. In both studies, patients with severe joint-space narrowing (<2 mm on radiographs) or severe arthritic deformity had
inferior outcomes, but severity of arthroscopic grade of arthritis was not prognostic of clinical outcomes. Chondroplasty and osteophyte excision were shown to be helpful in reestablishing range-of-motion (ROM) and providing pain relief, but larger osteophytes associated with worse glenohumeral arthritis had poorer outcomes. In general, it should be assumed that, if the humeral head shape is preserved, if glenoid wear is concentric, and if the joint space is visible on radiographs, then the patient is likely to have improved pain and function with arthroscopic treatment.
Properly addressing associated shoulder pain generators at time of arthroscopic surgery is important. Patients with significant arthritic stiffness can have prolonged improvement in ROM and function after arthroscopic debridement and circumferential capsular release. Patients with symptoms of biceps tendinopathy should undergo biceps tenodesis or tenotomy. Acromioclavicular joint pain should
receive a distal clavicle excision. Subacromial debridement should be performed for subacromial symptoms, while acromioplasty can be reserved for type III acromion morphology. With careful preoperative evaluation, the clinician should be able to identify all possible pain generators in the arthritic shoulder and address these concomitantly to optimize pain relief and improved function.
In summary, shoulder arthroscopy should be considered a surgical alternative to shoulder arthroplasty in young or high-demand patients with mild to moderate arthritis. Pathology most responsive to shoulder arthroscopy includes shoulder stiffness caused by capsular tightness, chondral lesion less than 2 cm,3 less severe arthritis with preserved humeral head shape, and properly addressed associated
pathology, such as synovitis, biceps tendinopathy, and subacromial bursitis or acromioclavicular arthrosis. Although high-level evidence is lacking, study trends show improved ROM and pain relief and overall high patient satisfaction at short to midterm follow-up. Ultimately, more data are needed to provide precise surgical indications and prognostic factors. Currently, however, it appears that shoulder arthroscopy can play an important role in the treatment of shoulder arthritis and can provide high satisfaction in appropriately selected patients.
References
1. Sperling JW, Cofield RH, Rowland CM. Neer hemiarthroplasty and Neer
total shoulder arthroplasty in patients fifty years old or less. Long-term
results. J Bone Joint Surg Am. 1998;80(4):464-473.
2. McGinty JB. Arthroscopic removal of loose bodies. Ortho Clin North
Am. 1982;13(2):313-328.
3. Namdari S, Skelley N, Keener JD, Galatz LM, Yamaguchi K. What is the
role of arthroscopic debridement for glenohumeral arthritis? A critical
examination of the literature. Arthroscopy. 2013;29(8):1392-1398.
4. Millett PJ, Horan MP, Pennock AT, Rios D. Comprehensive arthroscopic
management (CAM) procedure: clinical results of a joint-preserving
arthroscopic treatment for young, active patients with advanced shoulder
osteoarthritis. Arthroscopy. 2013;29(3):440-448.
5. Van Thiel GS, Sheehan S, Frank RM, et al. Retrospective analysis of
arthroscopic management of glenohumeral degenerative disease.
Arthroscopy. 2010;26(11):1451-1455.
This issue of The American Journal of Orthopedics focuses on the treatment of shoulder and elbow pathology in 2014. Treatment of shoulder arthritis in young or high-demand patients remains a significant challenge. Total shoulder arthroplasty (TSA) for glenohumeral arthritis can provide excellent pain relief and improved function in elderly, lower demand patients. In younger or higher demand patients, the long-term outcomes are less favorable—failure rates are higher, and revision surgery outcomes are unpredictable. Sperling and colleagues1 reported a survival rate of only 61% for TSA in patients younger than 50 at 10-year follow-up. In addition, postarthroplasty activity restrictions may be unacceptable for these younger, active patients. Concerns about poor shoulder arthroplasty durability and patient expectations of high activity have led to considerations for nonarthroplastic surgical options for shoulder arthritis in this patient population.
Some consider hemiarthroplasty an appropriate treatment option for shoulder arthritis in young patients and in patients who are too active for TSA, as hemiarthroplasty does not involve implantation of a glenoid component. However, compared with TSA, hemiarthroplasty is generally associated with inferior outcomes. Furthermore, when hemiarthroplasty fails and TSA revision becomes necessary, the outcomes of this revision are often inferior to those of primary TSA in the same population. For these reasons, hemiarthroplasty is considered a less optimal option for primary shoulder arthritis.
Biological resurfacing of the glenoid once was an exciting treatment alternative to TSA. Biological resurfacing includes interposition of soft tissue, whether fascia lata,
Achilles tendon, or lateral meniscus allograft, onto the native glenoid with a hemiarthroplasty of the humerus. Initial short-term outcomes of biological resurfacing were encouraging, but midterm outcomes were unsatisfactory, and attempts to reproduce initial published results were unsuccessful. Biological resurfacing has a very limited role now and is largely reserved for patients with localized humeral head articular cartilage loss with minimal involvement of the glenoid. In general, the glenoid remains the most significant treatment challenge in this group, and, other than for “ream and run” procedures, most biological
solutions for the glenoid are seldom used because of technical difficulty, surgical morbidity, and overall high failure rates.
Arthroscopic treatment of shoulder arthritis has emerged as an alternative to shoulder arthroplasty. Originally reported in 1982, initial attempts consisted mostly of arthroscopic joint lavage and loose body removal.2 More recently, arthroscopic procedures for the treatment of shoulder arthritis have been expanded to include extensive joint debridement with synovectomy and circumferential capsular release, chondroplasty, osteophyte excision, and treatment of associated pathology, such as biceps tendinopathy, subacromial bursitis, acromioclavicular arthrosis, and even neurolysis of the axillary nerve.
Published results of shoulder arthroscopy for arthritis are encouraging. In a recent systematic literature review, Namdari and colleagues3 found a clear trend of significant pain relief and improved function after shoulder arthroscopy for arthritis, despite lack of high-level evidence. Millett and colleagues4 reported 85% survivorship at 2-year follow-up for 30 shoulders (23 men, 6 women; mean age,
52 years). Overall, patients reported significant pain relief with daily activities, athletic or work activity, and ability to rest comfortably. Similarly, Van Thiel and colleagues5 reported excellent pain relief and improved validated shoulder and elbow scores at 27-month follow-up. In both studies, patients with severe joint-space narrowing (<2 mm on radiographs) or severe arthritic deformity had
inferior outcomes, but severity of arthroscopic grade of arthritis was not prognostic of clinical outcomes. Chondroplasty and osteophyte excision were shown to be helpful in reestablishing range-of-motion (ROM) and providing pain relief, but larger osteophytes associated with worse glenohumeral arthritis had poorer outcomes. In general, it should be assumed that, if the humeral head shape is preserved, if glenoid wear is concentric, and if the joint space is visible on radiographs, then the patient is likely to have improved pain and function with arthroscopic treatment.
Properly addressing associated shoulder pain generators at time of arthroscopic surgery is important. Patients with significant arthritic stiffness can have prolonged improvement in ROM and function after arthroscopic debridement and circumferential capsular release. Patients with symptoms of biceps tendinopathy should undergo biceps tenodesis or tenotomy. Acromioclavicular joint pain should
receive a distal clavicle excision. Subacromial debridement should be performed for subacromial symptoms, while acromioplasty can be reserved for type III acromion morphology. With careful preoperative evaluation, the clinician should be able to identify all possible pain generators in the arthritic shoulder and address these concomitantly to optimize pain relief and improved function.
In summary, shoulder arthroscopy should be considered a surgical alternative to shoulder arthroplasty in young or high-demand patients with mild to moderate arthritis. Pathology most responsive to shoulder arthroscopy includes shoulder stiffness caused by capsular tightness, chondral lesion less than 2 cm,3 less severe arthritis with preserved humeral head shape, and properly addressed associated
pathology, such as synovitis, biceps tendinopathy, and subacromial bursitis or acromioclavicular arthrosis. Although high-level evidence is lacking, study trends show improved ROM and pain relief and overall high patient satisfaction at short to midterm follow-up. Ultimately, more data are needed to provide precise surgical indications and prognostic factors. Currently, however, it appears that shoulder arthroscopy can play an important role in the treatment of shoulder arthritis and can provide high satisfaction in appropriately selected patients.
References
1. Sperling JW, Cofield RH, Rowland CM. Neer hemiarthroplasty and Neer
total shoulder arthroplasty in patients fifty years old or less. Long-term
results. J Bone Joint Surg Am. 1998;80(4):464-473.
2. McGinty JB. Arthroscopic removal of loose bodies. Ortho Clin North
Am. 1982;13(2):313-328.
3. Namdari S, Skelley N, Keener JD, Galatz LM, Yamaguchi K. What is the
role of arthroscopic debridement for glenohumeral arthritis? A critical
examination of the literature. Arthroscopy. 2013;29(8):1392-1398.
4. Millett PJ, Horan MP, Pennock AT, Rios D. Comprehensive arthroscopic
management (CAM) procedure: clinical results of a joint-preserving
arthroscopic treatment for young, active patients with advanced shoulder
osteoarthritis. Arthroscopy. 2013;29(3):440-448.
5. Van Thiel GS, Sheehan S, Frank RM, et al. Retrospective analysis of
arthroscopic management of glenohumeral degenerative disease.
Arthroscopy. 2010;26(11):1451-1455.
Ashiness
Dry skin occurs throughout the year, but for many people it’s most prevalent and problematic in winter. Cold temperatures, low humidity, and strong, harsh winds deplete the skin of its natural lipid layer, which would normally help keep the skin from drying out. Skin of color in particular, can become very flaky, dry, and "ashy" in the winter. Differences in the stratum corneum barrier in skin of color may contribute to the propensity toward ashiness.
The barrier function of the skin depends on the structure of the corneocytes, lipid content, and transepidermal water loss. Compared with skin in white people, black skin has more corneocyte layers and a more compact stratum corneum with greater intercellular cohesiveness. The epidermal barrier in darker skin has been shown to be stronger when exposed to mechanical or chemical challenge. Although the size of the individual corneocytes is the same in black and white skin, the desquamation rate in certain locations is higher in black skin. This is likely due to increased desquamatory enzyme levels such as cathepsin L2 in the lamellar granules of darker pigmented individuals leading to an ashy manifestation of the skin.
Black skin also has the highest sebum content of all ethnicities, but has the lowest ceramide level, and is thus the most susceptible to transepidermal water loss and xerosis of any ethnic group. Of note, one study has shown that the use of a certain type of fatty acid body wash or a synthetic "syndet" bar reduced ashiness.
Although no large, multiethnic group studies have been performed to examine the skin barrier physiologic properties and their relation to clinical signs of disease, these small studies do shed light on some of the ethnic variation in skin barrier function.
In clinical practice, these small variations should play a role in personalized treatment regimens for common conditions such as acne and atopic dermatitis. In my practice, black patients with acne often have high sebum content, but they cannot tolerate drying medications such as benzoyl peroxide because of their skin sensitivity and intolerance to skin drying. These patients often also present with ashy, dry skin in certain areas, and oily, acne-prone skin in other areas, leading to more complex skin care regimens. Understanding these basic concepts can help better tailor our basic skin treatments and education for skin of color patients in the winter and throughout the year.
Sources:
Talakoub L, Wesley NO. Differences in perceptions of beauty and cosmetic procedures performed in ethnic patients. Semin. Cutan. Med. Surg. 2009;28:115-29.
Feng L, Hawkins S. Reduction of "ashiness" in skin of color with a lipid-rich moisturizing body wash. J. Clin. Aesthet. Dermatol. 2011;4:41-4.
Dr. Wesley practices dermatology in Beverly Hills, Calif. Do you have questions about treating patients with dark skin? If so, send them to sknews@frontlinemedcom.com.
Dry skin occurs throughout the year, but for many people it’s most prevalent and problematic in winter. Cold temperatures, low humidity, and strong, harsh winds deplete the skin of its natural lipid layer, which would normally help keep the skin from drying out. Skin of color in particular, can become very flaky, dry, and "ashy" in the winter. Differences in the stratum corneum barrier in skin of color may contribute to the propensity toward ashiness.
The barrier function of the skin depends on the structure of the corneocytes, lipid content, and transepidermal water loss. Compared with skin in white people, black skin has more corneocyte layers and a more compact stratum corneum with greater intercellular cohesiveness. The epidermal barrier in darker skin has been shown to be stronger when exposed to mechanical or chemical challenge. Although the size of the individual corneocytes is the same in black and white skin, the desquamation rate in certain locations is higher in black skin. This is likely due to increased desquamatory enzyme levels such as cathepsin L2 in the lamellar granules of darker pigmented individuals leading to an ashy manifestation of the skin.
Black skin also has the highest sebum content of all ethnicities, but has the lowest ceramide level, and is thus the most susceptible to transepidermal water loss and xerosis of any ethnic group. Of note, one study has shown that the use of a certain type of fatty acid body wash or a synthetic "syndet" bar reduced ashiness.
Although no large, multiethnic group studies have been performed to examine the skin barrier physiologic properties and their relation to clinical signs of disease, these small studies do shed light on some of the ethnic variation in skin barrier function.
In clinical practice, these small variations should play a role in personalized treatment regimens for common conditions such as acne and atopic dermatitis. In my practice, black patients with acne often have high sebum content, but they cannot tolerate drying medications such as benzoyl peroxide because of their skin sensitivity and intolerance to skin drying. These patients often also present with ashy, dry skin in certain areas, and oily, acne-prone skin in other areas, leading to more complex skin care regimens. Understanding these basic concepts can help better tailor our basic skin treatments and education for skin of color patients in the winter and throughout the year.
Sources:
Talakoub L, Wesley NO. Differences in perceptions of beauty and cosmetic procedures performed in ethnic patients. Semin. Cutan. Med. Surg. 2009;28:115-29.
Feng L, Hawkins S. Reduction of "ashiness" in skin of color with a lipid-rich moisturizing body wash. J. Clin. Aesthet. Dermatol. 2011;4:41-4.
Dr. Wesley practices dermatology in Beverly Hills, Calif. Do you have questions about treating patients with dark skin? If so, send them to sknews@frontlinemedcom.com.
Dry skin occurs throughout the year, but for many people it’s most prevalent and problematic in winter. Cold temperatures, low humidity, and strong, harsh winds deplete the skin of its natural lipid layer, which would normally help keep the skin from drying out. Skin of color in particular, can become very flaky, dry, and "ashy" in the winter. Differences in the stratum corneum barrier in skin of color may contribute to the propensity toward ashiness.
The barrier function of the skin depends on the structure of the corneocytes, lipid content, and transepidermal water loss. Compared with skin in white people, black skin has more corneocyte layers and a more compact stratum corneum with greater intercellular cohesiveness. The epidermal barrier in darker skin has been shown to be stronger when exposed to mechanical or chemical challenge. Although the size of the individual corneocytes is the same in black and white skin, the desquamation rate in certain locations is higher in black skin. This is likely due to increased desquamatory enzyme levels such as cathepsin L2 in the lamellar granules of darker pigmented individuals leading to an ashy manifestation of the skin.
Black skin also has the highest sebum content of all ethnicities, but has the lowest ceramide level, and is thus the most susceptible to transepidermal water loss and xerosis of any ethnic group. Of note, one study has shown that the use of a certain type of fatty acid body wash or a synthetic "syndet" bar reduced ashiness.
Although no large, multiethnic group studies have been performed to examine the skin barrier physiologic properties and their relation to clinical signs of disease, these small studies do shed light on some of the ethnic variation in skin barrier function.
In clinical practice, these small variations should play a role in personalized treatment regimens for common conditions such as acne and atopic dermatitis. In my practice, black patients with acne often have high sebum content, but they cannot tolerate drying medications such as benzoyl peroxide because of their skin sensitivity and intolerance to skin drying. These patients often also present with ashy, dry skin in certain areas, and oily, acne-prone skin in other areas, leading to more complex skin care regimens. Understanding these basic concepts can help better tailor our basic skin treatments and education for skin of color patients in the winter and throughout the year.
Sources:
Talakoub L, Wesley NO. Differences in perceptions of beauty and cosmetic procedures performed in ethnic patients. Semin. Cutan. Med. Surg. 2009;28:115-29.
Feng L, Hawkins S. Reduction of "ashiness" in skin of color with a lipid-rich moisturizing body wash. J. Clin. Aesthet. Dermatol. 2011;4:41-4.
Dr. Wesley practices dermatology in Beverly Hills, Calif. Do you have questions about treating patients with dark skin? If so, send them to sknews@frontlinemedcom.com.
Ultrasound and Clinical Evaluation of Soft-Tissue Versus Hardware Biceps Tenodesis: Is Hardware Tenodesis Worth the Cost?
Sequencing reveals therapeutic target for leukemias

of General Medical Sciences
By analyzing the whole genomes of 3-year-old twin sisters—one healthy and one with multi-lineage leukemia (MLL)—researchers have identified a possible therapeutic target for leukemias.
Their research pointed to a molecular pathway involving the gene SETD2, which can mutate in blood cells as DNA is being transcribed and replicated.
The team confirmed the importance of this pathway via follow-up experiments using samples from leukemia patients and mouse models of the disease.
“We reasoned that monozygotic twins discordant for human leukemia would have identical inherited genetic backgrounds and well-matched tissue-specific events,” said Gang Huang, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“This provided a strong basis for comparison and analysis. We identified a gene mutation involving SETD2 that contributes to the initiation and progression of leukemia by promoting the self-renewal potential of leukemia stem cells.”
Dr Huang and his colleagues recounted this discovery in Nature Genetics.
The team showed that the onset of aggressive and acute leukemia is fueled by a spiraling cascade of multiple genetic mutations and chromosomal translocations.
In comparing data from the twins, the researchers identified a chromosomal translocation in the MLL-NRIP3 fusion gene.
When they activated MLL-NRIP3 in mouse models, the animals developed MLL, but it took a long period of time. This suggests that additional epigenetic and molecular events must be involved to induce full-blown leukemia.
The researchers went on to show that activation of MLL-NRIP3 cooperated with the molecular cascade (including mutations in SETD2) to cause leukemia.
The initial clue came when the team was looking for additional genomic alterations in the leukemic cells of the sick twin. They discovered that activation of MLL-NRIP3 started the molecular cascade that led to bi-allelic mutations in SETD2, a tumor suppressor that regulates the histone modification protein H3K36me3.
During transcriptional elongation, SETD2 and H3K36me3 normally mark the zone for accurate gene transcription along the DNA. In the case of the sick twin, the mutations and molecular cascade disrupted the H3K36me3 mark, leading to abnormal transcription and MLL.
To confirm the importance of these findings, the researchers analyzed blood samples from 241 patients—134 with acute myeloid leukemia and 107 with acute lymphoblastic leukemia. This revealed 19 somatic SETD2 mutations in 15 patients (6.2%).
SETD2 mutations were more common in patients with MLL rearrangements than those without—22.6% (6/27) and 4.6% (8/173), respectively. And patients with SETD2 mutations had decreased levels of global H3K36me3.
In follow-up tests on cell cultures of pre-leukemic cells and mouse models, the researchers saw the same progression of genetic mutations and related molecular events fuel the growth of leukemic cells.
The team also noticed that SETD2 mutation activated 2 genes—mTOR and JAK-STAT—that are known to contribute to leukemia and other cancers. So the researchers decided to test 2 mTOR inhibitors—Torin1 and rapamycin—on pre-leukemic cells generated by SETD2 mutations.
That treatment prompted a marked decrease in cell growth, indicating that SETD2 mutations activate numerous molecular pathways to generate leukemia.
Dr Huang said the tests also suggest there are multiple opportunities to find new molecular targets for developing more effective drugs—in particular, those that would target the MLL fusion-SETD2-H3K36me3 pathway to treat acute and aggressive leukemias.
The researchers are following up their current study by identifying additional pathways activated by mutations of SETD2. They also are looking for possible new molecular targets and therapeutic strategies to block disruptions in the SETD2-H3K36me3 pathway. ![]()

of General Medical Sciences
By analyzing the whole genomes of 3-year-old twin sisters—one healthy and one with multi-lineage leukemia (MLL)—researchers have identified a possible therapeutic target for leukemias.
Their research pointed to a molecular pathway involving the gene SETD2, which can mutate in blood cells as DNA is being transcribed and replicated.
The team confirmed the importance of this pathway via follow-up experiments using samples from leukemia patients and mouse models of the disease.
“We reasoned that monozygotic twins discordant for human leukemia would have identical inherited genetic backgrounds and well-matched tissue-specific events,” said Gang Huang, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“This provided a strong basis for comparison and analysis. We identified a gene mutation involving SETD2 that contributes to the initiation and progression of leukemia by promoting the self-renewal potential of leukemia stem cells.”
Dr Huang and his colleagues recounted this discovery in Nature Genetics.
The team showed that the onset of aggressive and acute leukemia is fueled by a spiraling cascade of multiple genetic mutations and chromosomal translocations.
In comparing data from the twins, the researchers identified a chromosomal translocation in the MLL-NRIP3 fusion gene.
When they activated MLL-NRIP3 in mouse models, the animals developed MLL, but it took a long period of time. This suggests that additional epigenetic and molecular events must be involved to induce full-blown leukemia.
The researchers went on to show that activation of MLL-NRIP3 cooperated with the molecular cascade (including mutations in SETD2) to cause leukemia.
The initial clue came when the team was looking for additional genomic alterations in the leukemic cells of the sick twin. They discovered that activation of MLL-NRIP3 started the molecular cascade that led to bi-allelic mutations in SETD2, a tumor suppressor that regulates the histone modification protein H3K36me3.
During transcriptional elongation, SETD2 and H3K36me3 normally mark the zone for accurate gene transcription along the DNA. In the case of the sick twin, the mutations and molecular cascade disrupted the H3K36me3 mark, leading to abnormal transcription and MLL.
To confirm the importance of these findings, the researchers analyzed blood samples from 241 patients—134 with acute myeloid leukemia and 107 with acute lymphoblastic leukemia. This revealed 19 somatic SETD2 mutations in 15 patients (6.2%).
SETD2 mutations were more common in patients with MLL rearrangements than those without—22.6% (6/27) and 4.6% (8/173), respectively. And patients with SETD2 mutations had decreased levels of global H3K36me3.
In follow-up tests on cell cultures of pre-leukemic cells and mouse models, the researchers saw the same progression of genetic mutations and related molecular events fuel the growth of leukemic cells.
The team also noticed that SETD2 mutation activated 2 genes—mTOR and JAK-STAT—that are known to contribute to leukemia and other cancers. So the researchers decided to test 2 mTOR inhibitors—Torin1 and rapamycin—on pre-leukemic cells generated by SETD2 mutations.
That treatment prompted a marked decrease in cell growth, indicating that SETD2 mutations activate numerous molecular pathways to generate leukemia.
Dr Huang said the tests also suggest there are multiple opportunities to find new molecular targets for developing more effective drugs—in particular, those that would target the MLL fusion-SETD2-H3K36me3 pathway to treat acute and aggressive leukemias.
The researchers are following up their current study by identifying additional pathways activated by mutations of SETD2. They also are looking for possible new molecular targets and therapeutic strategies to block disruptions in the SETD2-H3K36me3 pathway. ![]()

of General Medical Sciences
By analyzing the whole genomes of 3-year-old twin sisters—one healthy and one with multi-lineage leukemia (MLL)—researchers have identified a possible therapeutic target for leukemias.
Their research pointed to a molecular pathway involving the gene SETD2, which can mutate in blood cells as DNA is being transcribed and replicated.
The team confirmed the importance of this pathway via follow-up experiments using samples from leukemia patients and mouse models of the disease.
“We reasoned that monozygotic twins discordant for human leukemia would have identical inherited genetic backgrounds and well-matched tissue-specific events,” said Gang Huang, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“This provided a strong basis for comparison and analysis. We identified a gene mutation involving SETD2 that contributes to the initiation and progression of leukemia by promoting the self-renewal potential of leukemia stem cells.”
Dr Huang and his colleagues recounted this discovery in Nature Genetics.
The team showed that the onset of aggressive and acute leukemia is fueled by a spiraling cascade of multiple genetic mutations and chromosomal translocations.
In comparing data from the twins, the researchers identified a chromosomal translocation in the MLL-NRIP3 fusion gene.
When they activated MLL-NRIP3 in mouse models, the animals developed MLL, but it took a long period of time. This suggests that additional epigenetic and molecular events must be involved to induce full-blown leukemia.
The researchers went on to show that activation of MLL-NRIP3 cooperated with the molecular cascade (including mutations in SETD2) to cause leukemia.
The initial clue came when the team was looking for additional genomic alterations in the leukemic cells of the sick twin. They discovered that activation of MLL-NRIP3 started the molecular cascade that led to bi-allelic mutations in SETD2, a tumor suppressor that regulates the histone modification protein H3K36me3.
During transcriptional elongation, SETD2 and H3K36me3 normally mark the zone for accurate gene transcription along the DNA. In the case of the sick twin, the mutations and molecular cascade disrupted the H3K36me3 mark, leading to abnormal transcription and MLL.
To confirm the importance of these findings, the researchers analyzed blood samples from 241 patients—134 with acute myeloid leukemia and 107 with acute lymphoblastic leukemia. This revealed 19 somatic SETD2 mutations in 15 patients (6.2%).
SETD2 mutations were more common in patients with MLL rearrangements than those without—22.6% (6/27) and 4.6% (8/173), respectively. And patients with SETD2 mutations had decreased levels of global H3K36me3.
In follow-up tests on cell cultures of pre-leukemic cells and mouse models, the researchers saw the same progression of genetic mutations and related molecular events fuel the growth of leukemic cells.
The team also noticed that SETD2 mutation activated 2 genes—mTOR and JAK-STAT—that are known to contribute to leukemia and other cancers. So the researchers decided to test 2 mTOR inhibitors—Torin1 and rapamycin—on pre-leukemic cells generated by SETD2 mutations.
That treatment prompted a marked decrease in cell growth, indicating that SETD2 mutations activate numerous molecular pathways to generate leukemia.
Dr Huang said the tests also suggest there are multiple opportunities to find new molecular targets for developing more effective drugs—in particular, those that would target the MLL fusion-SETD2-H3K36me3 pathway to treat acute and aggressive leukemias.
The researchers are following up their current study by identifying additional pathways activated by mutations of SETD2. They also are looking for possible new molecular targets and therapeutic strategies to block disruptions in the SETD2-H3K36me3 pathway. ![]()