User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Patient Navigators for Serious Illnesses Can Now Bill Under New Medicare Codes
In a move that acknowledges the gauntlet the US health system poses for people facing serious and fatal illnesses, Medicare will pay for a new class of workers to help patients manage treatments for conditions like cancer and heart failure.
The 2024 Medicare physician fee schedule includes new billing codes, including G0023, to pay for 60 minutes a month of care coordination by certified or trained auxiliary personnel working under the direction of a clinician.
A diagnosis of cancer or another serious illness takes a toll beyond the physical effects of the disease. Patients often scramble to make adjustments in family and work schedules to manage treatment, said Samyukta Mullangi, MD, MBA, medical director of oncology at Thyme Care, a Nashville, Tennessee–based firm that provides navigation and coordination services to oncology practices and insurers.
“It just really does create a bit of a pressure cooker for patients,” Dr. Mullangi told this news organization.
Medicare has for many years paid for medical professionals to help patients cope with the complexities of disease, such as chronic care management (CCM) provided by physicians, nurses, and physician assistants.
The new principal illness navigation (PIN) payments are intended to pay for work that to date typically has been done by people without medical degrees, including those involved in peer support networks and community health programs. The US Centers for Medicare and Medicaid Services(CMS) expects these navigators will undergo training and work under the supervision of clinicians.
The new navigators may coordinate care transitions between medical settings, follow up with patients after emergency department (ED) visits, or communicate with skilled nursing facilities regarding the psychosocial needs and functional deficits of a patient, among other functions.
CMS expects the new navigators may:
- Conduct assessments to understand a patient’s life story, strengths, needs, goals, preferences, and desired outcomes, including understanding cultural and linguistic factors.
- Provide support to accomplish the clinician’s treatment plan.
- Coordinate the receipt of needed services from healthcare facilities, home- and community-based service providers, and caregivers.
Peers as Navigators
The new navigators can be former patients who have undergone similar treatments for serious diseases, CMS said. This approach sets the new program apart from other care management services Medicare already covers, program officials wrote in the 2024 physician fee schedule.
“For some conditions, patients are best able to engage with the healthcare system and access care if they have assistance from a single, dedicated individual who has ‘lived experience,’ ” according to the rule.
The agency has taken a broad initial approach in defining what kinds of illnesses a patient may have to qualify for services. Patients must have a serious condition that is expected to last at least 3 months, such as cancer, heart failure, or substance use disorder.
But those without a definitive diagnosis may also qualify to receive navigator services.
In the rule, CMS cited a case in which a CT scan identified a suspicious mass in a patient’s colon. A clinician might decide this person would benefit from navigation services due to the potential risks for an undiagnosed illness.
“Regardless of the definitive diagnosis of the mass, presence of a colonic mass for that patient may be a serious high-risk condition that could, for example, cause obstruction and lead the patient to present to the emergency department, as well as be potentially indicative of an underlying life-threatening illness such as colon cancer,” CMS wrote in the rule.
Navigators often start their work when cancer patients are screened and guide them through initial diagnosis, potential surgery, radiation, or chemotherapy, said Sharon Gentry, MSN, RN, a former nurse navigator who is now the editor in chief of the Journal of the Academy of Oncology Nurse & Patient Navigators.
The navigators are meant to be a trusted and continual presence for patients, who otherwise might be left to start anew in finding help at each phase of care.
The navigators “see the whole picture. They see the whole journey the patient takes, from pre-diagnosis all the way through diagnosis care out through survival,” Ms. Gentry said.
Gaining a special Medicare payment for these kinds of services will elevate this work, she said.
Many newer drugs can target specific mechanisms and proteins of cancer. Often, oncology treatment involves testing to find out if mutations are allowing the cancer cells to evade a patient’s immune system.
Checking these biomarkers takes time, however. Patients sometimes become frustrated because they are anxious to begin treatment. Patients may receive inaccurate information from friends or family who went through treatment previously. Navigators can provide knowledge on the current state of care for a patient’s disease, helping them better manage anxieties.
“You have to explain to them that things have changed since the guy you drink coffee with was diagnosed with cancer, and there may be a drug that could target that,” Ms. Gentry said.
Potential Challenges
Initial uptake of the new PIN codes may be slow going, however, as clinicians and health systems may already use well-established codes. These include CCM and principal care management services, which may pay higher rates, Mullangi said.
“There might be sensitivity around not wanting to cannibalize existing programs with a new program,” Dr. Mullangi said.
In addition, many patients will have a copay for the services of principal illness navigators, Dr. Mullangi said.
While many patients have additional insurance that would cover the service, not all do. People with traditional Medicare coverage can sometimes pay 20% of the cost of some medical services.
“I think that may give patients pause, particularly if they’re already feeling the financial burden of a cancer treatment journey,” Dr. Mullangi said.
Pay rates for PIN services involve calculations of regional price differences, which are posted publicly by CMS, and potential added fees for services provided by hospital-affiliated organizations.
Consider payments for code G0023, covering 60 minutes of principal navigation services provided in a single month.
A set reimbursement for patients cared for in independent medical practices exists, with variation for local costs. Medicare’s non-facility price for G0023 would be $102.41 in some parts of Silicon Valley in California, including San Jose. In Arkansas, where costs are lower, reimbursement would be $73.14 for this same service.
Patients who get services covered by code G0023 in independent medical practices would have monthly copays of about $15-$20, depending on where they live.
The tab for patients tends to be higher for these same services if delivered through a medical practice owned by a hospital, as this would trigger the addition of facility fees to the payments made to cover the services. Facility fees are difficult for the public to ascertain before getting a treatment or service.
Dr. Mullangi and Ms. Gentry reported no relevant financial disclosures outside of their employers.
A version of this article first appeared on Medscape.com.
In a move that acknowledges the gauntlet the US health system poses for people facing serious and fatal illnesses, Medicare will pay for a new class of workers to help patients manage treatments for conditions like cancer and heart failure.
The 2024 Medicare physician fee schedule includes new billing codes, including G0023, to pay for 60 minutes a month of care coordination by certified or trained auxiliary personnel working under the direction of a clinician.
A diagnosis of cancer or another serious illness takes a toll beyond the physical effects of the disease. Patients often scramble to make adjustments in family and work schedules to manage treatment, said Samyukta Mullangi, MD, MBA, medical director of oncology at Thyme Care, a Nashville, Tennessee–based firm that provides navigation and coordination services to oncology practices and insurers.
“It just really does create a bit of a pressure cooker for patients,” Dr. Mullangi told this news organization.
Medicare has for many years paid for medical professionals to help patients cope with the complexities of disease, such as chronic care management (CCM) provided by physicians, nurses, and physician assistants.
The new principal illness navigation (PIN) payments are intended to pay for work that to date typically has been done by people without medical degrees, including those involved in peer support networks and community health programs. The US Centers for Medicare and Medicaid Services(CMS) expects these navigators will undergo training and work under the supervision of clinicians.
The new navigators may coordinate care transitions between medical settings, follow up with patients after emergency department (ED) visits, or communicate with skilled nursing facilities regarding the psychosocial needs and functional deficits of a patient, among other functions.
CMS expects the new navigators may:
- Conduct assessments to understand a patient’s life story, strengths, needs, goals, preferences, and desired outcomes, including understanding cultural and linguistic factors.
- Provide support to accomplish the clinician’s treatment plan.
- Coordinate the receipt of needed services from healthcare facilities, home- and community-based service providers, and caregivers.
Peers as Navigators
The new navigators can be former patients who have undergone similar treatments for serious diseases, CMS said. This approach sets the new program apart from other care management services Medicare already covers, program officials wrote in the 2024 physician fee schedule.
“For some conditions, patients are best able to engage with the healthcare system and access care if they have assistance from a single, dedicated individual who has ‘lived experience,’ ” according to the rule.
The agency has taken a broad initial approach in defining what kinds of illnesses a patient may have to qualify for services. Patients must have a serious condition that is expected to last at least 3 months, such as cancer, heart failure, or substance use disorder.
But those without a definitive diagnosis may also qualify to receive navigator services.
In the rule, CMS cited a case in which a CT scan identified a suspicious mass in a patient’s colon. A clinician might decide this person would benefit from navigation services due to the potential risks for an undiagnosed illness.
“Regardless of the definitive diagnosis of the mass, presence of a colonic mass for that patient may be a serious high-risk condition that could, for example, cause obstruction and lead the patient to present to the emergency department, as well as be potentially indicative of an underlying life-threatening illness such as colon cancer,” CMS wrote in the rule.
Navigators often start their work when cancer patients are screened and guide them through initial diagnosis, potential surgery, radiation, or chemotherapy, said Sharon Gentry, MSN, RN, a former nurse navigator who is now the editor in chief of the Journal of the Academy of Oncology Nurse & Patient Navigators.
The navigators are meant to be a trusted and continual presence for patients, who otherwise might be left to start anew in finding help at each phase of care.
The navigators “see the whole picture. They see the whole journey the patient takes, from pre-diagnosis all the way through diagnosis care out through survival,” Ms. Gentry said.
Gaining a special Medicare payment for these kinds of services will elevate this work, she said.
Many newer drugs can target specific mechanisms and proteins of cancer. Often, oncology treatment involves testing to find out if mutations are allowing the cancer cells to evade a patient’s immune system.
Checking these biomarkers takes time, however. Patients sometimes become frustrated because they are anxious to begin treatment. Patients may receive inaccurate information from friends or family who went through treatment previously. Navigators can provide knowledge on the current state of care for a patient’s disease, helping them better manage anxieties.
“You have to explain to them that things have changed since the guy you drink coffee with was diagnosed with cancer, and there may be a drug that could target that,” Ms. Gentry said.
Potential Challenges
Initial uptake of the new PIN codes may be slow going, however, as clinicians and health systems may already use well-established codes. These include CCM and principal care management services, which may pay higher rates, Mullangi said.
“There might be sensitivity around not wanting to cannibalize existing programs with a new program,” Dr. Mullangi said.
In addition, many patients will have a copay for the services of principal illness navigators, Dr. Mullangi said.
While many patients have additional insurance that would cover the service, not all do. People with traditional Medicare coverage can sometimes pay 20% of the cost of some medical services.
“I think that may give patients pause, particularly if they’re already feeling the financial burden of a cancer treatment journey,” Dr. Mullangi said.
Pay rates for PIN services involve calculations of regional price differences, which are posted publicly by CMS, and potential added fees for services provided by hospital-affiliated organizations.
Consider payments for code G0023, covering 60 minutes of principal navigation services provided in a single month.
A set reimbursement for patients cared for in independent medical practices exists, with variation for local costs. Medicare’s non-facility price for G0023 would be $102.41 in some parts of Silicon Valley in California, including San Jose. In Arkansas, where costs are lower, reimbursement would be $73.14 for this same service.
Patients who get services covered by code G0023 in independent medical practices would have monthly copays of about $15-$20, depending on where they live.
The tab for patients tends to be higher for these same services if delivered through a medical practice owned by a hospital, as this would trigger the addition of facility fees to the payments made to cover the services. Facility fees are difficult for the public to ascertain before getting a treatment or service.
Dr. Mullangi and Ms. Gentry reported no relevant financial disclosures outside of their employers.
A version of this article first appeared on Medscape.com.
In a move that acknowledges the gauntlet the US health system poses for people facing serious and fatal illnesses, Medicare will pay for a new class of workers to help patients manage treatments for conditions like cancer and heart failure.
The 2024 Medicare physician fee schedule includes new billing codes, including G0023, to pay for 60 minutes a month of care coordination by certified or trained auxiliary personnel working under the direction of a clinician.
A diagnosis of cancer or another serious illness takes a toll beyond the physical effects of the disease. Patients often scramble to make adjustments in family and work schedules to manage treatment, said Samyukta Mullangi, MD, MBA, medical director of oncology at Thyme Care, a Nashville, Tennessee–based firm that provides navigation and coordination services to oncology practices and insurers.
“It just really does create a bit of a pressure cooker for patients,” Dr. Mullangi told this news organization.
Medicare has for many years paid for medical professionals to help patients cope with the complexities of disease, such as chronic care management (CCM) provided by physicians, nurses, and physician assistants.
The new principal illness navigation (PIN) payments are intended to pay for work that to date typically has been done by people without medical degrees, including those involved in peer support networks and community health programs. The US Centers for Medicare and Medicaid Services(CMS) expects these navigators will undergo training and work under the supervision of clinicians.
The new navigators may coordinate care transitions between medical settings, follow up with patients after emergency department (ED) visits, or communicate with skilled nursing facilities regarding the psychosocial needs and functional deficits of a patient, among other functions.
CMS expects the new navigators may:
- Conduct assessments to understand a patient’s life story, strengths, needs, goals, preferences, and desired outcomes, including understanding cultural and linguistic factors.
- Provide support to accomplish the clinician’s treatment plan.
- Coordinate the receipt of needed services from healthcare facilities, home- and community-based service providers, and caregivers.
Peers as Navigators
The new navigators can be former patients who have undergone similar treatments for serious diseases, CMS said. This approach sets the new program apart from other care management services Medicare already covers, program officials wrote in the 2024 physician fee schedule.
“For some conditions, patients are best able to engage with the healthcare system and access care if they have assistance from a single, dedicated individual who has ‘lived experience,’ ” according to the rule.
The agency has taken a broad initial approach in defining what kinds of illnesses a patient may have to qualify for services. Patients must have a serious condition that is expected to last at least 3 months, such as cancer, heart failure, or substance use disorder.
But those without a definitive diagnosis may also qualify to receive navigator services.
In the rule, CMS cited a case in which a CT scan identified a suspicious mass in a patient’s colon. A clinician might decide this person would benefit from navigation services due to the potential risks for an undiagnosed illness.
“Regardless of the definitive diagnosis of the mass, presence of a colonic mass for that patient may be a serious high-risk condition that could, for example, cause obstruction and lead the patient to present to the emergency department, as well as be potentially indicative of an underlying life-threatening illness such as colon cancer,” CMS wrote in the rule.
Navigators often start their work when cancer patients are screened and guide them through initial diagnosis, potential surgery, radiation, or chemotherapy, said Sharon Gentry, MSN, RN, a former nurse navigator who is now the editor in chief of the Journal of the Academy of Oncology Nurse & Patient Navigators.
The navigators are meant to be a trusted and continual presence for patients, who otherwise might be left to start anew in finding help at each phase of care.
The navigators “see the whole picture. They see the whole journey the patient takes, from pre-diagnosis all the way through diagnosis care out through survival,” Ms. Gentry said.
Gaining a special Medicare payment for these kinds of services will elevate this work, she said.
Many newer drugs can target specific mechanisms and proteins of cancer. Often, oncology treatment involves testing to find out if mutations are allowing the cancer cells to evade a patient’s immune system.
Checking these biomarkers takes time, however. Patients sometimes become frustrated because they are anxious to begin treatment. Patients may receive inaccurate information from friends or family who went through treatment previously. Navigators can provide knowledge on the current state of care for a patient’s disease, helping them better manage anxieties.
“You have to explain to them that things have changed since the guy you drink coffee with was diagnosed with cancer, and there may be a drug that could target that,” Ms. Gentry said.
Potential Challenges
Initial uptake of the new PIN codes may be slow going, however, as clinicians and health systems may already use well-established codes. These include CCM and principal care management services, which may pay higher rates, Mullangi said.
“There might be sensitivity around not wanting to cannibalize existing programs with a new program,” Dr. Mullangi said.
In addition, many patients will have a copay for the services of principal illness navigators, Dr. Mullangi said.
While many patients have additional insurance that would cover the service, not all do. People with traditional Medicare coverage can sometimes pay 20% of the cost of some medical services.
“I think that may give patients pause, particularly if they’re already feeling the financial burden of a cancer treatment journey,” Dr. Mullangi said.
Pay rates for PIN services involve calculations of regional price differences, which are posted publicly by CMS, and potential added fees for services provided by hospital-affiliated organizations.
Consider payments for code G0023, covering 60 minutes of principal navigation services provided in a single month.
A set reimbursement for patients cared for in independent medical practices exists, with variation for local costs. Medicare’s non-facility price for G0023 would be $102.41 in some parts of Silicon Valley in California, including San Jose. In Arkansas, where costs are lower, reimbursement would be $73.14 for this same service.
Patients who get services covered by code G0023 in independent medical practices would have monthly copays of about $15-$20, depending on where they live.
The tab for patients tends to be higher for these same services if delivered through a medical practice owned by a hospital, as this would trigger the addition of facility fees to the payments made to cover the services. Facility fees are difficult for the public to ascertain before getting a treatment or service.
Dr. Mullangi and Ms. Gentry reported no relevant financial disclosures outside of their employers.
A version of this article first appeared on Medscape.com.

Alcohol Use Disorder Therapy Remains Underutilized in Alcohol-Associated Liver Disease
PHILADELPHIA — according to a study presented at the American College of Gastroenterology (ACG) 2024 Annual Scientific Meeting.
In an analysis of commercially insured Americans, AUD medications were prescribed to only 1 in 50 patients with ALD and about 1 in 10 patients with acute alcohol-associated hepatitis (AAH).
“Providers caring for these patients should consider early initiation of this therapy in select cases,” said lead author Alex R. Jones, MD, chief resident of internal medicine at the University of Texas Southwestern Medical Center in Dallas.
“Based on additional analyses looking at the prescriber subspecialty, we didn’t identify any gastroenterologists or hepatologists who prescribed pharmacotherapy,” he said. “This could be a great opportunity for hepatologists to engage in the pharmacologic treatment of AUD.”
Jones and colleagues analyzed 2006-2021 data from IQVIA PharMetrics Plus for Academics, a nationally representative database of commercially insured patients in the United States. They looked for AUD pharmacologic treatment at any time after AUD diagnosis, including prescriptions for gabapentin, naltrexone, topiramate, acamprosate, baclofen, and disulfiram.
Among 28,625 patients with AUD (defined as at least two outpatient codes or at least one inpatient code), 1201 had ALD with cirrhosis and 439 had AAH.
Pharmacologic therapy was prescribed in 3924 (14.5%) patients without ALD, 28 (2.3%) with ALD, and 42 (9.8%) with AAH.
In addition, one-time prescriptions were observed in 1113 (28.4%) patients without ALD, three patients (10.7%) with ALD, and eight patients (18.6%) with AAH.
Overall, 64.5% of the general population consisted of men. About 46% had a psychiatric diagnosis other than substance use disorder (SUD), and 35.7% had a non-AUD SUD.
Patients who received AUD pharmacotherapy tended to be older, at a median age of 45 years, than those aged 42 years without a prescription.
The median time to prescription was 302 days, with no significant differences based on the presence of liver disease.
By medication, gabapentin was prescribed most often (9.4%), followed by oral naltrexone (2.6%) and topiramate (2%). Oral naltrexone was prescribed at a lower rate in patients with ALD and at a higher rate in patients with AAH than in patients without ALD. Baclofen was also prescribed at lower rates in patients with ALD and AAH.
In a multivariable logistic regression analysis, several characteristics were more significantly associated with pharmacologic therapy, such as age ≥ 50 years (adjusted odds ratio [aOR], 1.33), female sex (aOR, 1.31), a non-liver Charlson Comorbidity Index ≥ 3 (aOR, 2.21), and psychiatric comorbidities (aOR, 2.76).
On the other hand, the presence of hepatic decompensation — defined as ascites, hepatic encephalopathy, or bleeding varices — was associated with lower odds of receiving pharmacotherapy (aOR, 0.08). ALD cirrhosis (non-AAH) also had lower odds (aOR, 0.24).
The study was limited by only incorporating patients with commercial insurance, lacking demographic details related to race or ethnicity, and potentially misclassifying patients despite validated definitions of ALD and AUD, Jones said.
As the study couldn’t determine the indications for prescriptions, such as gabapentin use for migraines or diabetes-associated neuropathy, for instance, future studies could look at these precise details, he added.
“It’s important to know we’re underutilizing therapies that we have a lot of information about, such as gabapentin, which is an old medication that we should feel fairly comfortable using,” said Patricia Jones, MD, a hepatologist and associate professor of clinical medicine at the University of Miami Miller School of Medicine, in Florida. Patricia Jones comoderated the plenary session on small intestine, functional, and liver research.
“I also expect that, if a future study reviewed this data and excluded people with valid indications, such as migraines or diabetic neuropathy, we’d see even lower rates of prescription,” she said.
From a clinical perspective, patient communication and clinical decision-making are key, Patricia Jones added, particularly when clinical gastroenterologists and hepatologists may not offer this type of therapy or patients refuse this type of therapy.
“We need to think about our practice patterns and how we can offer therapy,” she said. “In general, we know these medications are very safe. Even though they’re not widely used in people with cirrhosis, there’s not enough evidence to suggest we shouldn’t use them.”
Alex Jones and Patricia Jones reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
PHILADELPHIA — according to a study presented at the American College of Gastroenterology (ACG) 2024 Annual Scientific Meeting.
In an analysis of commercially insured Americans, AUD medications were prescribed to only 1 in 50 patients with ALD and about 1 in 10 patients with acute alcohol-associated hepatitis (AAH).
“Providers caring for these patients should consider early initiation of this therapy in select cases,” said lead author Alex R. Jones, MD, chief resident of internal medicine at the University of Texas Southwestern Medical Center in Dallas.
“Based on additional analyses looking at the prescriber subspecialty, we didn’t identify any gastroenterologists or hepatologists who prescribed pharmacotherapy,” he said. “This could be a great opportunity for hepatologists to engage in the pharmacologic treatment of AUD.”
Jones and colleagues analyzed 2006-2021 data from IQVIA PharMetrics Plus for Academics, a nationally representative database of commercially insured patients in the United States. They looked for AUD pharmacologic treatment at any time after AUD diagnosis, including prescriptions for gabapentin, naltrexone, topiramate, acamprosate, baclofen, and disulfiram.
Among 28,625 patients with AUD (defined as at least two outpatient codes or at least one inpatient code), 1201 had ALD with cirrhosis and 439 had AAH.
Pharmacologic therapy was prescribed in 3924 (14.5%) patients without ALD, 28 (2.3%) with ALD, and 42 (9.8%) with AAH.
In addition, one-time prescriptions were observed in 1113 (28.4%) patients without ALD, three patients (10.7%) with ALD, and eight patients (18.6%) with AAH.
Overall, 64.5% of the general population consisted of men. About 46% had a psychiatric diagnosis other than substance use disorder (SUD), and 35.7% had a non-AUD SUD.
Patients who received AUD pharmacotherapy tended to be older, at a median age of 45 years, than those aged 42 years without a prescription.
The median time to prescription was 302 days, with no significant differences based on the presence of liver disease.
By medication, gabapentin was prescribed most often (9.4%), followed by oral naltrexone (2.6%) and topiramate (2%). Oral naltrexone was prescribed at a lower rate in patients with ALD and at a higher rate in patients with AAH than in patients without ALD. Baclofen was also prescribed at lower rates in patients with ALD and AAH.
In a multivariable logistic regression analysis, several characteristics were more significantly associated with pharmacologic therapy, such as age ≥ 50 years (adjusted odds ratio [aOR], 1.33), female sex (aOR, 1.31), a non-liver Charlson Comorbidity Index ≥ 3 (aOR, 2.21), and psychiatric comorbidities (aOR, 2.76).
On the other hand, the presence of hepatic decompensation — defined as ascites, hepatic encephalopathy, or bleeding varices — was associated with lower odds of receiving pharmacotherapy (aOR, 0.08). ALD cirrhosis (non-AAH) also had lower odds (aOR, 0.24).
The study was limited by only incorporating patients with commercial insurance, lacking demographic details related to race or ethnicity, and potentially misclassifying patients despite validated definitions of ALD and AUD, Jones said.
As the study couldn’t determine the indications for prescriptions, such as gabapentin use for migraines or diabetes-associated neuropathy, for instance, future studies could look at these precise details, he added.
“It’s important to know we’re underutilizing therapies that we have a lot of information about, such as gabapentin, which is an old medication that we should feel fairly comfortable using,” said Patricia Jones, MD, a hepatologist and associate professor of clinical medicine at the University of Miami Miller School of Medicine, in Florida. Patricia Jones comoderated the plenary session on small intestine, functional, and liver research.
“I also expect that, if a future study reviewed this data and excluded people with valid indications, such as migraines or diabetic neuropathy, we’d see even lower rates of prescription,” she said.
From a clinical perspective, patient communication and clinical decision-making are key, Patricia Jones added, particularly when clinical gastroenterologists and hepatologists may not offer this type of therapy or patients refuse this type of therapy.
“We need to think about our practice patterns and how we can offer therapy,” she said. “In general, we know these medications are very safe. Even though they’re not widely used in people with cirrhosis, there’s not enough evidence to suggest we shouldn’t use them.”
Alex Jones and Patricia Jones reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
PHILADELPHIA — according to a study presented at the American College of Gastroenterology (ACG) 2024 Annual Scientific Meeting.
In an analysis of commercially insured Americans, AUD medications were prescribed to only 1 in 50 patients with ALD and about 1 in 10 patients with acute alcohol-associated hepatitis (AAH).
“Providers caring for these patients should consider early initiation of this therapy in select cases,” said lead author Alex R. Jones, MD, chief resident of internal medicine at the University of Texas Southwestern Medical Center in Dallas.
“Based on additional analyses looking at the prescriber subspecialty, we didn’t identify any gastroenterologists or hepatologists who prescribed pharmacotherapy,” he said. “This could be a great opportunity for hepatologists to engage in the pharmacologic treatment of AUD.”
Jones and colleagues analyzed 2006-2021 data from IQVIA PharMetrics Plus for Academics, a nationally representative database of commercially insured patients in the United States. They looked for AUD pharmacologic treatment at any time after AUD diagnosis, including prescriptions for gabapentin, naltrexone, topiramate, acamprosate, baclofen, and disulfiram.
Among 28,625 patients with AUD (defined as at least two outpatient codes or at least one inpatient code), 1201 had ALD with cirrhosis and 439 had AAH.
Pharmacologic therapy was prescribed in 3924 (14.5%) patients without ALD, 28 (2.3%) with ALD, and 42 (9.8%) with AAH.
In addition, one-time prescriptions were observed in 1113 (28.4%) patients without ALD, three patients (10.7%) with ALD, and eight patients (18.6%) with AAH.
Overall, 64.5% of the general population consisted of men. About 46% had a psychiatric diagnosis other than substance use disorder (SUD), and 35.7% had a non-AUD SUD.
Patients who received AUD pharmacotherapy tended to be older, at a median age of 45 years, than those aged 42 years without a prescription.
The median time to prescription was 302 days, with no significant differences based on the presence of liver disease.
By medication, gabapentin was prescribed most often (9.4%), followed by oral naltrexone (2.6%) and topiramate (2%). Oral naltrexone was prescribed at a lower rate in patients with ALD and at a higher rate in patients with AAH than in patients without ALD. Baclofen was also prescribed at lower rates in patients with ALD and AAH.
In a multivariable logistic regression analysis, several characteristics were more significantly associated with pharmacologic therapy, such as age ≥ 50 years (adjusted odds ratio [aOR], 1.33), female sex (aOR, 1.31), a non-liver Charlson Comorbidity Index ≥ 3 (aOR, 2.21), and psychiatric comorbidities (aOR, 2.76).
On the other hand, the presence of hepatic decompensation — defined as ascites, hepatic encephalopathy, or bleeding varices — was associated with lower odds of receiving pharmacotherapy (aOR, 0.08). ALD cirrhosis (non-AAH) also had lower odds (aOR, 0.24).
The study was limited by only incorporating patients with commercial insurance, lacking demographic details related to race or ethnicity, and potentially misclassifying patients despite validated definitions of ALD and AUD, Jones said.
As the study couldn’t determine the indications for prescriptions, such as gabapentin use for migraines or diabetes-associated neuropathy, for instance, future studies could look at these precise details, he added.
“It’s important to know we’re underutilizing therapies that we have a lot of information about, such as gabapentin, which is an old medication that we should feel fairly comfortable using,” said Patricia Jones, MD, a hepatologist and associate professor of clinical medicine at the University of Miami Miller School of Medicine, in Florida. Patricia Jones comoderated the plenary session on small intestine, functional, and liver research.
“I also expect that, if a future study reviewed this data and excluded people with valid indications, such as migraines or diabetic neuropathy, we’d see even lower rates of prescription,” she said.
From a clinical perspective, patient communication and clinical decision-making are key, Patricia Jones added, particularly when clinical gastroenterologists and hepatologists may not offer this type of therapy or patients refuse this type of therapy.
“We need to think about our practice patterns and how we can offer therapy,” she said. “In general, we know these medications are very safe. Even though they’re not widely used in people with cirrhosis, there’s not enough evidence to suggest we shouldn’t use them.”
Alex Jones and Patricia Jones reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM ACG 2024
Canadian Guideline on Managing Opioid Use Disorder Updated
Canada’s National Guideline for the Clinical Management of Opioid Use Disorder (OUD) has been updated to reflect the latest literature. The new document recommends buprenorphine and methadone as first-line treatments for OUD.
Opioid use and OUD remain the leading causes of drug-related death worldwide. In Canada, the number of apparent opioid-related deaths increased from 2831 in 2016 to 8049 in 2023. Despite the expansion of treatment options, including the lifting of restrictions on methadone prescribing in 2018, there has been a substantial surge in opioid-related harms, the authors wrote.
“OUD and opioid-related harms have devastating outcomes for our communities across Canada,” author Ginette Poulin, MD, a family physician at the University of Manitoba in Winnipeg, Manitoba, Canada, said in a statement. “With the growing dangers associated with the illicit market, we need to ensure we are sharing the most relevant therapeutic tools and up-to-date knowledge to help providers and communities address this complex issue.”
The 2024 update, which was drafted by the Canadian Research Initiative in Substance Matters (CRISM), was published in CMAJ.
Expanding Access
The COVID-19 pandemic marked an increase in opioid-related harms, senior author Julie Bruneau, MD, Canada research chair in addiction medicine and professor of family and emergency medicine at the Université de Montréal, in Quebec, Canada, told this news organization. Access to essential services and support for people with OUD became restricted, and the drug supply became toxic and volatile.
“In March 2018, CRISM published the first Canadian national clinical practice guideline to assist clinicians in making informed decisions regarding the clinical management of OUD, and recommendations were made in light of existing evidence on prioritizing available treatments,” said Bruneau.
“This guideline is intended for use by healthcare providers, including physicians, nurse practitioners, pharmacists, clinical psychologists, social workers, medical educators, and clinical care case managers with or without specialized experience in addiction treatment. We hope it will help expand access to evidence-based interventions for people with OUD beyond tertiary care,” she said.
Bruneau added that integrating first-line opioid agonist treatment into primary care could reduce stigma, increase early screening and patient retention, and help reduce Canada’s opioid crisis.
The CRISM guideline development team carried out a comprehensive systematic review of the literature published from January 1, 2017, to September 14, 2023. The team, which included patients with OUD, drafted and graded their recommendations using the Grading of Recommendations, Assessment, Development and Evaluation approach.
“First, OUD management should be based on a patient-centered approach, which includes respect for the patient’s rights, preferences, and dignity,” said Bruneau.
Highlights of the guideline include the following recommendations:
- Buprenorphine, with or without naloxone, and methadone can be used as standard first-line treatment options.
- Opioid agonist treatment with slow-release oral morphine should be made available and offered as a second-line option.
- Patients with OUD should not be offered withdrawal management as stand-alone treatment because it is associated with increased rates of relapse, morbidity, and mortality.
- Psychosocial treatment, interventions, and supports can be offered as adjunct treatments but should not be a mandatory component of standard treatment for OUD and should not prevent access to opioid agonist therapy.
- Harm reduction strategies should be offered as part of the continuum of care for patients with OUD.
- Pregnant people can be offered buprenorphine or methadone as treatment options.
Treating More Patients
“Too many people die from untreated opioid addiction in Canada,” coauthor Peter Selby, MD, director of medical education at the Centre for Addiction and Mental Health, said in a statement. “We have medicines that help people stop using, but too few patients are treated due to stigma and lack of prescribers knowing what to do. These national guidelines help them use proven medications to not only prevent death but also help people recover.”
“That both buprenorphine and methadone are now to be considered first-line therapy for the management of OUD is an important change to the guideline,” said Abhimanyu Sud, MD, PhD, research chair in primary care and population health systems at Humber River Health and assistant professor of family and community medicine at the University of Toronto. He did not participate in drafting the guidelines.
“There is a lot of good evidence that these agents are effective for the management of OUD. We had this idea that methadone was harder or somehow more unsafe than buprenorphine, and that buprenorphine was therefore a safer therapy that should be used more widely. Now we have very high-potency opioids that are circulating, and methadone, as a strong opioid agonist, has an important role to play. Clinical experience has borne that out, and this is reflected in the guidelines,” said Sud.
“When we treat patients who are using fentanyl, for example, or fentanyl analogs, or they’re not sure what they are using because the drug supply has been so contaminated, you sometimes need another agent. Also, a lot of patients do not respond very well to buprenorphine, so for many people, a full agonist like methadone is needed,” he added.
Giving higher priority to slow-release morphine is a good move, and the drug’s use is likely to be safe when administered by a skilled clinician, said Akash Goel, MD, staff physician in the Department of Anesthesiology and Pain Medicine at St. Michael’s Hospital and assistant professor of anesthesiology and pain medicine at the University of Toronto. Goel was not involved in drafting the guideline.
The updated document will empower patients to make informed decisions about their care, he said. “Buprenorphine, for example, may not be the right selection for all patients. The updated guideline recognizes this. So, for patients who are at risk of failing OUD therapy and going back to using, buprenorphine may not be the best option. The new guideline gives patients the opportunity to have a conversation with their healthcare providers and then decide what’s the best way forward for them.”
The guideline was supported by Health Canada and the Canadian Institutes of Health Research (CIHR) via CRISM. Poulin reported receiving honoraria for presentations from the Master Clinician Alliance and Indivior outside this work. Bruneau reported receiving a CIHR research grant and a grant from Health Canada’s Substance Use and Addictions Program. Outside this work, Bruneau received a National Institutes of Health research grant and consulting fees for Gilead Sciences and AbbVie.
A version of this article first appeared on Medscape.com.
Canada’s National Guideline for the Clinical Management of Opioid Use Disorder (OUD) has been updated to reflect the latest literature. The new document recommends buprenorphine and methadone as first-line treatments for OUD.
Opioid use and OUD remain the leading causes of drug-related death worldwide. In Canada, the number of apparent opioid-related deaths increased from 2831 in 2016 to 8049 in 2023. Despite the expansion of treatment options, including the lifting of restrictions on methadone prescribing in 2018, there has been a substantial surge in opioid-related harms, the authors wrote.
“OUD and opioid-related harms have devastating outcomes for our communities across Canada,” author Ginette Poulin, MD, a family physician at the University of Manitoba in Winnipeg, Manitoba, Canada, said in a statement. “With the growing dangers associated with the illicit market, we need to ensure we are sharing the most relevant therapeutic tools and up-to-date knowledge to help providers and communities address this complex issue.”
The 2024 update, which was drafted by the Canadian Research Initiative in Substance Matters (CRISM), was published in CMAJ.
Expanding Access
The COVID-19 pandemic marked an increase in opioid-related harms, senior author Julie Bruneau, MD, Canada research chair in addiction medicine and professor of family and emergency medicine at the Université de Montréal, in Quebec, Canada, told this news organization. Access to essential services and support for people with OUD became restricted, and the drug supply became toxic and volatile.
“In March 2018, CRISM published the first Canadian national clinical practice guideline to assist clinicians in making informed decisions regarding the clinical management of OUD, and recommendations were made in light of existing evidence on prioritizing available treatments,” said Bruneau.
“This guideline is intended for use by healthcare providers, including physicians, nurse practitioners, pharmacists, clinical psychologists, social workers, medical educators, and clinical care case managers with or without specialized experience in addiction treatment. We hope it will help expand access to evidence-based interventions for people with OUD beyond tertiary care,” she said.
Bruneau added that integrating first-line opioid agonist treatment into primary care could reduce stigma, increase early screening and patient retention, and help reduce Canada’s opioid crisis.
The CRISM guideline development team carried out a comprehensive systematic review of the literature published from January 1, 2017, to September 14, 2023. The team, which included patients with OUD, drafted and graded their recommendations using the Grading of Recommendations, Assessment, Development and Evaluation approach.
“First, OUD management should be based on a patient-centered approach, which includes respect for the patient’s rights, preferences, and dignity,” said Bruneau.
Highlights of the guideline include the following recommendations:
- Buprenorphine, with or without naloxone, and methadone can be used as standard first-line treatment options.
- Opioid agonist treatment with slow-release oral morphine should be made available and offered as a second-line option.
- Patients with OUD should not be offered withdrawal management as stand-alone treatment because it is associated with increased rates of relapse, morbidity, and mortality.
- Psychosocial treatment, interventions, and supports can be offered as adjunct treatments but should not be a mandatory component of standard treatment for OUD and should not prevent access to opioid agonist therapy.
- Harm reduction strategies should be offered as part of the continuum of care for patients with OUD.
- Pregnant people can be offered buprenorphine or methadone as treatment options.
Treating More Patients
“Too many people die from untreated opioid addiction in Canada,” coauthor Peter Selby, MD, director of medical education at the Centre for Addiction and Mental Health, said in a statement. “We have medicines that help people stop using, but too few patients are treated due to stigma and lack of prescribers knowing what to do. These national guidelines help them use proven medications to not only prevent death but also help people recover.”
“That both buprenorphine and methadone are now to be considered first-line therapy for the management of OUD is an important change to the guideline,” said Abhimanyu Sud, MD, PhD, research chair in primary care and population health systems at Humber River Health and assistant professor of family and community medicine at the University of Toronto. He did not participate in drafting the guidelines.
“There is a lot of good evidence that these agents are effective for the management of OUD. We had this idea that methadone was harder or somehow more unsafe than buprenorphine, and that buprenorphine was therefore a safer therapy that should be used more widely. Now we have very high-potency opioids that are circulating, and methadone, as a strong opioid agonist, has an important role to play. Clinical experience has borne that out, and this is reflected in the guidelines,” said Sud.
“When we treat patients who are using fentanyl, for example, or fentanyl analogs, or they’re not sure what they are using because the drug supply has been so contaminated, you sometimes need another agent. Also, a lot of patients do not respond very well to buprenorphine, so for many people, a full agonist like methadone is needed,” he added.
Giving higher priority to slow-release morphine is a good move, and the drug’s use is likely to be safe when administered by a skilled clinician, said Akash Goel, MD, staff physician in the Department of Anesthesiology and Pain Medicine at St. Michael’s Hospital and assistant professor of anesthesiology and pain medicine at the University of Toronto. Goel was not involved in drafting the guideline.
The updated document will empower patients to make informed decisions about their care, he said. “Buprenorphine, for example, may not be the right selection for all patients. The updated guideline recognizes this. So, for patients who are at risk of failing OUD therapy and going back to using, buprenorphine may not be the best option. The new guideline gives patients the opportunity to have a conversation with their healthcare providers and then decide what’s the best way forward for them.”
The guideline was supported by Health Canada and the Canadian Institutes of Health Research (CIHR) via CRISM. Poulin reported receiving honoraria for presentations from the Master Clinician Alliance and Indivior outside this work. Bruneau reported receiving a CIHR research grant and a grant from Health Canada’s Substance Use and Addictions Program. Outside this work, Bruneau received a National Institutes of Health research grant and consulting fees for Gilead Sciences and AbbVie.
A version of this article first appeared on Medscape.com.
Canada’s National Guideline for the Clinical Management of Opioid Use Disorder (OUD) has been updated to reflect the latest literature. The new document recommends buprenorphine and methadone as first-line treatments for OUD.
Opioid use and OUD remain the leading causes of drug-related death worldwide. In Canada, the number of apparent opioid-related deaths increased from 2831 in 2016 to 8049 in 2023. Despite the expansion of treatment options, including the lifting of restrictions on methadone prescribing in 2018, there has been a substantial surge in opioid-related harms, the authors wrote.
“OUD and opioid-related harms have devastating outcomes for our communities across Canada,” author Ginette Poulin, MD, a family physician at the University of Manitoba in Winnipeg, Manitoba, Canada, said in a statement. “With the growing dangers associated with the illicit market, we need to ensure we are sharing the most relevant therapeutic tools and up-to-date knowledge to help providers and communities address this complex issue.”
The 2024 update, which was drafted by the Canadian Research Initiative in Substance Matters (CRISM), was published in CMAJ.
Expanding Access
The COVID-19 pandemic marked an increase in opioid-related harms, senior author Julie Bruneau, MD, Canada research chair in addiction medicine and professor of family and emergency medicine at the Université de Montréal, in Quebec, Canada, told this news organization. Access to essential services and support for people with OUD became restricted, and the drug supply became toxic and volatile.
“In March 2018, CRISM published the first Canadian national clinical practice guideline to assist clinicians in making informed decisions regarding the clinical management of OUD, and recommendations were made in light of existing evidence on prioritizing available treatments,” said Bruneau.
“This guideline is intended for use by healthcare providers, including physicians, nurse practitioners, pharmacists, clinical psychologists, social workers, medical educators, and clinical care case managers with or without specialized experience in addiction treatment. We hope it will help expand access to evidence-based interventions for people with OUD beyond tertiary care,” she said.
Bruneau added that integrating first-line opioid agonist treatment into primary care could reduce stigma, increase early screening and patient retention, and help reduce Canada’s opioid crisis.
The CRISM guideline development team carried out a comprehensive systematic review of the literature published from January 1, 2017, to September 14, 2023. The team, which included patients with OUD, drafted and graded their recommendations using the Grading of Recommendations, Assessment, Development and Evaluation approach.
“First, OUD management should be based on a patient-centered approach, which includes respect for the patient’s rights, preferences, and dignity,” said Bruneau.
Highlights of the guideline include the following recommendations:
- Buprenorphine, with or without naloxone, and methadone can be used as standard first-line treatment options.
- Opioid agonist treatment with slow-release oral morphine should be made available and offered as a second-line option.
- Patients with OUD should not be offered withdrawal management as stand-alone treatment because it is associated with increased rates of relapse, morbidity, and mortality.
- Psychosocial treatment, interventions, and supports can be offered as adjunct treatments but should not be a mandatory component of standard treatment for OUD and should not prevent access to opioid agonist therapy.
- Harm reduction strategies should be offered as part of the continuum of care for patients with OUD.
- Pregnant people can be offered buprenorphine or methadone as treatment options.
Treating More Patients
“Too many people die from untreated opioid addiction in Canada,” coauthor Peter Selby, MD, director of medical education at the Centre for Addiction and Mental Health, said in a statement. “We have medicines that help people stop using, but too few patients are treated due to stigma and lack of prescribers knowing what to do. These national guidelines help them use proven medications to not only prevent death but also help people recover.”
“That both buprenorphine and methadone are now to be considered first-line therapy for the management of OUD is an important change to the guideline,” said Abhimanyu Sud, MD, PhD, research chair in primary care and population health systems at Humber River Health and assistant professor of family and community medicine at the University of Toronto. He did not participate in drafting the guidelines.
“There is a lot of good evidence that these agents are effective for the management of OUD. We had this idea that methadone was harder or somehow more unsafe than buprenorphine, and that buprenorphine was therefore a safer therapy that should be used more widely. Now we have very high-potency opioids that are circulating, and methadone, as a strong opioid agonist, has an important role to play. Clinical experience has borne that out, and this is reflected in the guidelines,” said Sud.
“When we treat patients who are using fentanyl, for example, or fentanyl analogs, or they’re not sure what they are using because the drug supply has been so contaminated, you sometimes need another agent. Also, a lot of patients do not respond very well to buprenorphine, so for many people, a full agonist like methadone is needed,” he added.
Giving higher priority to slow-release morphine is a good move, and the drug’s use is likely to be safe when administered by a skilled clinician, said Akash Goel, MD, staff physician in the Department of Anesthesiology and Pain Medicine at St. Michael’s Hospital and assistant professor of anesthesiology and pain medicine at the University of Toronto. Goel was not involved in drafting the guideline.
The updated document will empower patients to make informed decisions about their care, he said. “Buprenorphine, for example, may not be the right selection for all patients. The updated guideline recognizes this. So, for patients who are at risk of failing OUD therapy and going back to using, buprenorphine may not be the best option. The new guideline gives patients the opportunity to have a conversation with their healthcare providers and then decide what’s the best way forward for them.”
The guideline was supported by Health Canada and the Canadian Institutes of Health Research (CIHR) via CRISM. Poulin reported receiving honoraria for presentations from the Master Clinician Alliance and Indivior outside this work. Bruneau reported receiving a CIHR research grant and a grant from Health Canada’s Substance Use and Addictions Program. Outside this work, Bruneau received a National Institutes of Health research grant and consulting fees for Gilead Sciences and AbbVie.
A version of this article first appeared on Medscape.com.
Faster Brain Atrophy Linked to MCI
While some brain atrophy is expected in aging, high levels of atrophy in the white matter and high enlargement in the ventricles are associated with earlier progression from normal cognition to MCI, the study found. The researchers also identified diabetes and atypical levels of amyloid beta protein in the cerebrospinal fluid as risk factors for brain atrophy and MCI.
For their research, published online on JAMA Network Open, Yuto Uchida, MD, PhD, and his colleagues at the Johns Hopkins University School of Medicine in Baltimore, Maryland, looked at data for 185 individuals (mean age, 55.4 years; 63% women) who were cognitively normal at baseline and followed for a median of 20 years.
All had been enrolled in a longitudinal cohort study on biomarkers of cognitive decline conducted at Johns Hopkins. Each participant underwent a median of five structural MRI studies during the follow-up period as well as annual cognitive testing. Altogether 60 individuals developed MCI, with eight of them progressing to dementia.
“We hypothesized that annual rates of change of segmental brain volumes would be associated with vascular risk factors among middle-aged and older adults and that these trends would be associated with the progression from normal cognition to MCI,” Uchida and colleagues wrote.
Uniquely Long Follow-Up
Most longitudinal studies using structural MRI count a decade or less of follow-up, the study authors noted. This makes it difficult to discern whether the annual rates of change of brain volumes are affected by vascular risk factors or are useful in predicting MCI, they said. Individual differences in brain aging make population-based studies less informative.
This study’s long timeframe allowed for tracking of brain changes “on an individual basis, which facilitates the differentiation between interindividual and intraindividual variations and leads to more accurate estimations of rates of brain atrophy,” Uchida and colleagues wrote.
People with high levels of atrophy in the white matter and enlargement in the ventricles saw earlier progression to MCI (hazard ratio [HR], 1.86; 95% CI, 1.24-2.49; P = .001). Diabetes mellitus was associated with progression to MCI (HR, 1.41; 95% CI, 1.06-1.76; P = .04), as was a low CSF Abeta42:Abeta40 ratio (HR, 1.48; 95% CI, 1.09-1.88; P = .04).
People with both diabetes and an abnormal amyloid profile were even more vulnerable to developing MCI (HR, 1.55; 95% CI, 1.13-1.98; P = .03). This indicated “a synergic association of diabetes and amyloid pathology with MCI progression,” Uchida and colleagues wrote, noting that insulin resistance has been shown to promote the formation of amyloid plaques, a hallmark of Alzheimer’s disease.
The findings also underscore that “white matter volume changes are closely associated with cognitive function in aging, suggesting that white matter degeneration may play a crucial role in cognitive decline,” the authors noted.
Uchida and colleagues acknowledged the modest size and imbalanced sex ratio of their study cohort as potential weaknesses, as well as the fact that the imaging technologies had changed over the course of the study. Most of the participants were White with family histories of dementia.
Findings May Lead to Targeted Interventions
In an editorial comment accompanying Uchida and colleagues’ study, Shohei Fujita, MD, PhD, of Massachusetts General Hospital, Boston, said that, while a more diverse population sample would be desirable and should be sought for future studies, the results nonetheless highlight “the potential of long-term longitudinal brain MRI datasets in elucidating the interplay of risk factors underlying cognitive decline and the potential benefits of controlling diabetes to reduce the risk of progression” along the Alzheimer’s disease continuum.
The findings may prove informative, Fujita said, in developing “targeted interventions for those most susceptible to progressive brain changes, potentially combining lifestyle modifications and pharmacological treatments.”
Uchida and colleagues’ study was funded by the Alzheimer’s Association, the National Alzheimer’s Coordinating Center, and the National Institutes of Health. The study’s corresponding author, Kenichi Oishi, disclosed funding from the Richman Family Foundation, Richman, the Sharp Family Foundation, and others. Uchida and Fujita reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
While some brain atrophy is expected in aging, high levels of atrophy in the white matter and high enlargement in the ventricles are associated with earlier progression from normal cognition to MCI, the study found. The researchers also identified diabetes and atypical levels of amyloid beta protein in the cerebrospinal fluid as risk factors for brain atrophy and MCI.
For their research, published online on JAMA Network Open, Yuto Uchida, MD, PhD, and his colleagues at the Johns Hopkins University School of Medicine in Baltimore, Maryland, looked at data for 185 individuals (mean age, 55.4 years; 63% women) who were cognitively normal at baseline and followed for a median of 20 years.
All had been enrolled in a longitudinal cohort study on biomarkers of cognitive decline conducted at Johns Hopkins. Each participant underwent a median of five structural MRI studies during the follow-up period as well as annual cognitive testing. Altogether 60 individuals developed MCI, with eight of them progressing to dementia.
“We hypothesized that annual rates of change of segmental brain volumes would be associated with vascular risk factors among middle-aged and older adults and that these trends would be associated with the progression from normal cognition to MCI,” Uchida and colleagues wrote.
Uniquely Long Follow-Up
Most longitudinal studies using structural MRI count a decade or less of follow-up, the study authors noted. This makes it difficult to discern whether the annual rates of change of brain volumes are affected by vascular risk factors or are useful in predicting MCI, they said. Individual differences in brain aging make population-based studies less informative.
This study’s long timeframe allowed for tracking of brain changes “on an individual basis, which facilitates the differentiation between interindividual and intraindividual variations and leads to more accurate estimations of rates of brain atrophy,” Uchida and colleagues wrote.
People with high levels of atrophy in the white matter and enlargement in the ventricles saw earlier progression to MCI (hazard ratio [HR], 1.86; 95% CI, 1.24-2.49; P = .001). Diabetes mellitus was associated with progression to MCI (HR, 1.41; 95% CI, 1.06-1.76; P = .04), as was a low CSF Abeta42:Abeta40 ratio (HR, 1.48; 95% CI, 1.09-1.88; P = .04).
People with both diabetes and an abnormal amyloid profile were even more vulnerable to developing MCI (HR, 1.55; 95% CI, 1.13-1.98; P = .03). This indicated “a synergic association of diabetes and amyloid pathology with MCI progression,” Uchida and colleagues wrote, noting that insulin resistance has been shown to promote the formation of amyloid plaques, a hallmark of Alzheimer’s disease.
The findings also underscore that “white matter volume changes are closely associated with cognitive function in aging, suggesting that white matter degeneration may play a crucial role in cognitive decline,” the authors noted.
Uchida and colleagues acknowledged the modest size and imbalanced sex ratio of their study cohort as potential weaknesses, as well as the fact that the imaging technologies had changed over the course of the study. Most of the participants were White with family histories of dementia.
Findings May Lead to Targeted Interventions
In an editorial comment accompanying Uchida and colleagues’ study, Shohei Fujita, MD, PhD, of Massachusetts General Hospital, Boston, said that, while a more diverse population sample would be desirable and should be sought for future studies, the results nonetheless highlight “the potential of long-term longitudinal brain MRI datasets in elucidating the interplay of risk factors underlying cognitive decline and the potential benefits of controlling diabetes to reduce the risk of progression” along the Alzheimer’s disease continuum.
The findings may prove informative, Fujita said, in developing “targeted interventions for those most susceptible to progressive brain changes, potentially combining lifestyle modifications and pharmacological treatments.”
Uchida and colleagues’ study was funded by the Alzheimer’s Association, the National Alzheimer’s Coordinating Center, and the National Institutes of Health. The study’s corresponding author, Kenichi Oishi, disclosed funding from the Richman Family Foundation, Richman, the Sharp Family Foundation, and others. Uchida and Fujita reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
While some brain atrophy is expected in aging, high levels of atrophy in the white matter and high enlargement in the ventricles are associated with earlier progression from normal cognition to MCI, the study found. The researchers also identified diabetes and atypical levels of amyloid beta protein in the cerebrospinal fluid as risk factors for brain atrophy and MCI.
For their research, published online on JAMA Network Open, Yuto Uchida, MD, PhD, and his colleagues at the Johns Hopkins University School of Medicine in Baltimore, Maryland, looked at data for 185 individuals (mean age, 55.4 years; 63% women) who were cognitively normal at baseline and followed for a median of 20 years.
All had been enrolled in a longitudinal cohort study on biomarkers of cognitive decline conducted at Johns Hopkins. Each participant underwent a median of five structural MRI studies during the follow-up period as well as annual cognitive testing. Altogether 60 individuals developed MCI, with eight of them progressing to dementia.
“We hypothesized that annual rates of change of segmental brain volumes would be associated with vascular risk factors among middle-aged and older adults and that these trends would be associated with the progression from normal cognition to MCI,” Uchida and colleagues wrote.
Uniquely Long Follow-Up
Most longitudinal studies using structural MRI count a decade or less of follow-up, the study authors noted. This makes it difficult to discern whether the annual rates of change of brain volumes are affected by vascular risk factors or are useful in predicting MCI, they said. Individual differences in brain aging make population-based studies less informative.
This study’s long timeframe allowed for tracking of brain changes “on an individual basis, which facilitates the differentiation between interindividual and intraindividual variations and leads to more accurate estimations of rates of brain atrophy,” Uchida and colleagues wrote.
People with high levels of atrophy in the white matter and enlargement in the ventricles saw earlier progression to MCI (hazard ratio [HR], 1.86; 95% CI, 1.24-2.49; P = .001). Diabetes mellitus was associated with progression to MCI (HR, 1.41; 95% CI, 1.06-1.76; P = .04), as was a low CSF Abeta42:Abeta40 ratio (HR, 1.48; 95% CI, 1.09-1.88; P = .04).
People with both diabetes and an abnormal amyloid profile were even more vulnerable to developing MCI (HR, 1.55; 95% CI, 1.13-1.98; P = .03). This indicated “a synergic association of diabetes and amyloid pathology with MCI progression,” Uchida and colleagues wrote, noting that insulin resistance has been shown to promote the formation of amyloid plaques, a hallmark of Alzheimer’s disease.
The findings also underscore that “white matter volume changes are closely associated with cognitive function in aging, suggesting that white matter degeneration may play a crucial role in cognitive decline,” the authors noted.
Uchida and colleagues acknowledged the modest size and imbalanced sex ratio of their study cohort as potential weaknesses, as well as the fact that the imaging technologies had changed over the course of the study. Most of the participants were White with family histories of dementia.
Findings May Lead to Targeted Interventions
In an editorial comment accompanying Uchida and colleagues’ study, Shohei Fujita, MD, PhD, of Massachusetts General Hospital, Boston, said that, while a more diverse population sample would be desirable and should be sought for future studies, the results nonetheless highlight “the potential of long-term longitudinal brain MRI datasets in elucidating the interplay of risk factors underlying cognitive decline and the potential benefits of controlling diabetes to reduce the risk of progression” along the Alzheimer’s disease continuum.
The findings may prove informative, Fujita said, in developing “targeted interventions for those most susceptible to progressive brain changes, potentially combining lifestyle modifications and pharmacological treatments.”
Uchida and colleagues’ study was funded by the Alzheimer’s Association, the National Alzheimer’s Coordinating Center, and the National Institutes of Health. The study’s corresponding author, Kenichi Oishi, disclosed funding from the Richman Family Foundation, Richman, the Sharp Family Foundation, and others. Uchida and Fujita reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
‘Round Face’: A Viral Term’s Real Diagnostic Implications
“Cortisol” has become a household word, popularized by social media and tagged in videos that garnered nearly 800 million views in 2023. This is linked to the also-trending term “moon face,” which TikTok influencers and others have suggested is caused by high cortisol levels and, conversely, can be reduced through stress reduction.
“When we hear the term ‘moon face,’ we’re typically referring to Cushing syndrome [CS] or treatment with prolonged high-dose glucocorticoids,” said Anat Ben-Shlomo, MD, co-director of the Multidisciplinary Adrenal Program, Pituitary Center, Division of Endocrinology, Diabetes and Metabolism at Cedars-Sinai Medical Center, Los Angeles. Medscape Medical News previously discussed moon face in an article detailing how to diagnose CS.
Ben-Shlomo noted that the labels “moon face” and “moon facies” should be avoided for their potentially derogatory, unprofessional-sounding connotations, and that the preferred terms are “rounded face” or “round plethoric face.”
There are several disorders that can be associated with facial roundness, not all of which relate to elevated cortisol.
“It’s important for clinicians to be able distinguish between presentations due to other pathophysiologies, identify the unique constellation of Cushing-associated signs and symptoms, engage in a differential diagnosis, and treat whatever the condition is appropriately,” Katherine Sherif, MD, professor and vice chair of academic affairs, Department of Medicine, Thomas Jefferson University, Philadelphia, said in an interview.
The Unique Presentation of CS
CS results from “prolonged elevation” in plasma cortisol levels caused by either exogenous steroid use or excess endogenous steroid production.
“The shape of the face isn’t the only feature associated with CS,” Ben-Shlomo said. “There’s central obesity, particularly in the neck, supraclavicular area, chest, and abdomen. You sometimes see a posterior cervical thoracic fat pad, colloquially — but unprofessionally — called a ‘cervical hump.’ Simultaneously, the arms and legs are getting thinner.” The development of a round, plethoric face is common in long-standing significant CS, and a reddening of the skin can appear.
Additional symptoms include hirsutism and acne. “These can also be seen in other conditions, such as PCOS [polycystic ovary syndrome] but, combined with the other facial features, are more suggestive of CS,” Ben-Shlomo said.
Deep, wide purple striae appear in the trunk, breast, upper arms, and thighs, but not in the face, Ben-Shlomo advised. These appear as the fragile, thinning under-skin breaks when the patient gains weight.
Additional metabolic issues that can occur comorbidly include insulin resistance and diabetes, hypertension, osteoporosis, dyslipidemia, ecchymoses, increased susceptibility to infections, mood changes, cognitive dysfunction, low libido, infertility, weakness of muscles in the shoulders and thighs, episodes of bleeding and/or clotting, and an increased risk for heart attacks and strokes, Ben-Shlomo said.
“Not everyone presents with full-blown disease, but if you see any of these symptoms, be suspicious of CS and conduct a biochemical evaluation.” Three screening tests to use as a starting point are recommended by the Pituitary Society’s updated Consensus on Diagnosis and Management of Cushing’s Disease. The tests should be repeated to account for intra-patient variability. If two or all three tests are positive, clinicians should be suspicious of CS and move to additional testing to identify the underlying cause, Ben-Shlomo said.
‘Subclinical’ CS
Ben-Shlomo highlighted a condition called minimal autonomous cortisol secretion (formerly “subclinical CS”). “This condition is found when a person has an adrenal nodule that produces cortisol in excess, however not to levels observed in CS. An abnormal finding on the overnight 1-mg low-dose dexamethasone suppression test (LDDST) will identify this disorder, showing mildly unsuppressed morning cortisol level, while all other tests will be within normal range.”
She described minimal autonomous cortisol secretion as a form of “smoldering CS,” which has become more commonly diagnosed. “The condition needs to be treated because the patient can develop insulin resistance, metabolic syndrome, and osteoporosis over time.”
Once a cause has been determined, the optimal course of action is to take a multidisciplinary approach because CS affects multiple systems.
‘Pseudo-Cushing Syndrome’
A variety of abnormalities of the hypothalamus-pituitary adrenal (HPA) axis can be associated with hypercortisolemia and a rounder facial appearance but aren’t actually CS, Ben-Shlomo said.
Often called “pseudo-Cushing syndrome,” these conditions have recently been renamed “non-neoplastic hypercortisolism” or “physiologic non-neoplastic endogenous hypercortisolism.” They share some clinical and biochemical features of CS, but the hypercortisolemia is usually secondary to other factors. They increase the secretion of hypothalamic corticotropin-releasing hormone, which stimulates adrenocorticotropic hormone (ACTH) and adrenal cortisol secretion.
Identifying PCOS
PCOS is often associated with central obesity, Sherif noted, but not all women with PCOS have overweight or a central distribution of fat.
“Ask about menstrual periods and whether they come monthly,” Sherif advised. “If women using hormonal contraception say they have a regular cycle, ask if their cycle was regular prior to starting contraception. So many women with PCOS are undiagnosed because they started contraception in their teens to ‘regulate their periods’ and never realized they had PCOS.”
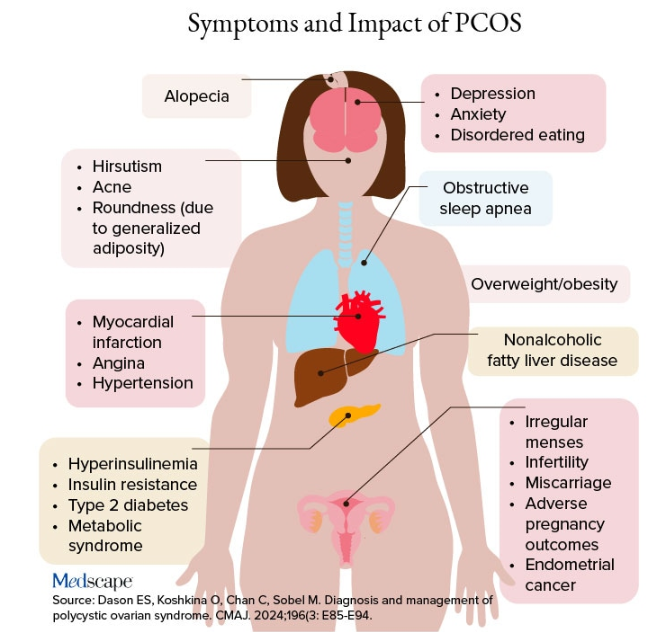
Additional symptoms of PCOS and its impact are found in the figure below.
PCOS is diagnosed when two of the following three Rotterdam criteria are met, and other diagnoses are excluded:
- Irregular menstrual cycles
- Clinical hyperandrogenism or biochemical hyperandrogenism
- Polycystic ovarian morphology on transvaginal ultrasonography or high anti-mullerian hormone (applicable only if patient is ≥ 8 years from menarche)
If PCOS is suspected, further tests can be conducted to confirm or rule out the diagnosis.
Alcohol Abuse: Alcohol abuse stimulates hypothalamic corticotropin-releasing hormone, leading to increased ACTH levels. It’s associated with a higher fasting cortisol level, particularly at 8:30 AM or so, and attributable to impaired cortisol clearance due to alcohol-related hepatic dysfunction. The LDDST will show abnormal cortisol suppression.
Sherif advised asking patients about alcohol use, recommending treatment for alcohol use disorder, and repeating clinical and biochemical workup after patients have discontinued alcohol consumption for ≥ 1 month.
Eating Disorders Mimicking CS: Eating disorders, particularly anorexia nervosa, are associated with endocrine abnormalities, amenorrhea, impaired body temperature regulation, and hypercortisolism, likely due to chronic fasting-related stress. Dysregulation of the HPA axis may linger, even after weight recovery.
It’s unlikely that patients with anorexia will display the “rounded face” associated with hypercortisolism, but some research suggests that anorexia can result in a disproportionate accumulation of central adiposity after recovery from the illness.
Neuropsychiatric Disorders: Major depressive disorder (MDD) is associated with HPA axis hyperactivity, with 20%-30% of patients with MDD showing hypercortisolemia. The post-awakening cortisol surge is more pronounced in those with MDD, and about half of patients with MDD also have high evening cortisol levels, suggesting disrupted diurnal cortisol rhythms.
Some patients with MDD have greater resistance to the feedback action of glucocorticoids on HPA axis activity, with weaker sensitivity often restored by effective pharmacotherapy of the depressive condition. Neuropsychiatric disorders are also associated with reduced activity of cortisol-deactivating enzymes. Posttraumatic stress disorder and anxiety are similarly associated with hypercortisolemia.
Addressing neuropsychiatric conditions with appropriate pharmacotherapy and psychotherapy can restore cortisol levels to normal proportions.
Diabetes, Obesity, and Metabolic Syndrome: Diabetes, obesity, and metabolic syndrome can occur comorbidly with CS, and many patients with these conditions may display both a rounder face, some central adiposity, and hypercortisolemia. For example, obesity is often related to a hyperresponsive HPA axis, with elevated cortisol secretion but normal-to-low circulatory concentrations.
Obesity is associated with increased cortisol reactivity after acute physical and/or psychosocial stressors but preserved pituitary sensitivity to feedback inhibition by the LDDST. When these conditions are appropriately managed with pharmacotherapy and lifestyle changes, cortisol levels should normalize, according to the experts.
Hypothyroidism: Hypothyroidism— Hashimoto disease as well as the subclinical variety — can be associated with weight gain, which may take the form of central obesity. Some research suggests a bidirectional relationship between hypothyroidism and obesity.
“Years ago, we didn’t conduct thyroid tests very often but now they’re easy to do, so we usually catch people with hypothyroidism at the beginning of the condition,” Sherif said. “If the patient’s thyroid hasn’t been checked in a year or so, thyroid hormone testing should be conducted.”
Thyroid disease can easily be managed with the administration of thyroid hormones.
Obstructive Sleep Apnea (OSA): OSA has an impact on HPA axis activation, especially when accompanied by obesity and hypertension. A meta-analysis of 22 studies, encompassing over 600 participants, found that continuous positive airway pressure treatment in patients with OSA reduced cortisol levels as well as blood pressure.
Treatment With Exogenous Corticosteroids: Oral corticosteroid treatment is a cornerstone of therapy in transplant, rheumatic, and autoimmune diseases. The impact of chronic exposure to exogenous glucocorticoids is similar to that with endogenous glucocorticoids.
Sherif said corticosteroid treatment can cause facial roundness in as little as 2 weeks and is characteristic in people taking these agents for longer periods. Although the effects are most pronounced with oral agents, systemic effects can be associated with inhaled corticosteroids as well.
Finding alternative anti-inflammatory treatments is advisable, if possible. The co-administration of metformin might lead to improvements in both the metabolic profile and the clinical outcomes of patients receiving glucocorticoids for inflammatory conditions.
Educating Patients: “There’s much we still don’t know about hypercortisolemia and CS, including the reasons for its impact on metabolic derangement and for the accumulation of fat in particular adipose patterns,” Ben-Shlomo said. “But experienced endocrinologists do know relatively well how to diagnose the condition, distinguish it from other conditions presenting with central obesity or a rounder face, and treat it.”
Given the casual use of the terms “moon face” and “extra cortisol” on social media, it’s important for physicians to educate patients about what elevated cortisol does and doesn’t do, and design treatment strategies accordingly.
Neither Ben-Shlomo nor Sherif reported having any disclosures.
A version of this article appeared on Medscape.com.
“Cortisol” has become a household word, popularized by social media and tagged in videos that garnered nearly 800 million views in 2023. This is linked to the also-trending term “moon face,” which TikTok influencers and others have suggested is caused by high cortisol levels and, conversely, can be reduced through stress reduction.
“When we hear the term ‘moon face,’ we’re typically referring to Cushing syndrome [CS] or treatment with prolonged high-dose glucocorticoids,” said Anat Ben-Shlomo, MD, co-director of the Multidisciplinary Adrenal Program, Pituitary Center, Division of Endocrinology, Diabetes and Metabolism at Cedars-Sinai Medical Center, Los Angeles. Medscape Medical News previously discussed moon face in an article detailing how to diagnose CS.
Ben-Shlomo noted that the labels “moon face” and “moon facies” should be avoided for their potentially derogatory, unprofessional-sounding connotations, and that the preferred terms are “rounded face” or “round plethoric face.”
There are several disorders that can be associated with facial roundness, not all of which relate to elevated cortisol.
“It’s important for clinicians to be able distinguish between presentations due to other pathophysiologies, identify the unique constellation of Cushing-associated signs and symptoms, engage in a differential diagnosis, and treat whatever the condition is appropriately,” Katherine Sherif, MD, professor and vice chair of academic affairs, Department of Medicine, Thomas Jefferson University, Philadelphia, said in an interview.
The Unique Presentation of CS
CS results from “prolonged elevation” in plasma cortisol levels caused by either exogenous steroid use or excess endogenous steroid production.
“The shape of the face isn’t the only feature associated with CS,” Ben-Shlomo said. “There’s central obesity, particularly in the neck, supraclavicular area, chest, and abdomen. You sometimes see a posterior cervical thoracic fat pad, colloquially — but unprofessionally — called a ‘cervical hump.’ Simultaneously, the arms and legs are getting thinner.” The development of a round, plethoric face is common in long-standing significant CS, and a reddening of the skin can appear.
Additional symptoms include hirsutism and acne. “These can also be seen in other conditions, such as PCOS [polycystic ovary syndrome] but, combined with the other facial features, are more suggestive of CS,” Ben-Shlomo said.
Deep, wide purple striae appear in the trunk, breast, upper arms, and thighs, but not in the face, Ben-Shlomo advised. These appear as the fragile, thinning under-skin breaks when the patient gains weight.
Additional metabolic issues that can occur comorbidly include insulin resistance and diabetes, hypertension, osteoporosis, dyslipidemia, ecchymoses, increased susceptibility to infections, mood changes, cognitive dysfunction, low libido, infertility, weakness of muscles in the shoulders and thighs, episodes of bleeding and/or clotting, and an increased risk for heart attacks and strokes, Ben-Shlomo said.
“Not everyone presents with full-blown disease, but if you see any of these symptoms, be suspicious of CS and conduct a biochemical evaluation.” Three screening tests to use as a starting point are recommended by the Pituitary Society’s updated Consensus on Diagnosis and Management of Cushing’s Disease. The tests should be repeated to account for intra-patient variability. If two or all three tests are positive, clinicians should be suspicious of CS and move to additional testing to identify the underlying cause, Ben-Shlomo said.
‘Subclinical’ CS
Ben-Shlomo highlighted a condition called minimal autonomous cortisol secretion (formerly “subclinical CS”). “This condition is found when a person has an adrenal nodule that produces cortisol in excess, however not to levels observed in CS. An abnormal finding on the overnight 1-mg low-dose dexamethasone suppression test (LDDST) will identify this disorder, showing mildly unsuppressed morning cortisol level, while all other tests will be within normal range.”
She described minimal autonomous cortisol secretion as a form of “smoldering CS,” which has become more commonly diagnosed. “The condition needs to be treated because the patient can develop insulin resistance, metabolic syndrome, and osteoporosis over time.”
Once a cause has been determined, the optimal course of action is to take a multidisciplinary approach because CS affects multiple systems.
‘Pseudo-Cushing Syndrome’
A variety of abnormalities of the hypothalamus-pituitary adrenal (HPA) axis can be associated with hypercortisolemia and a rounder facial appearance but aren’t actually CS, Ben-Shlomo said.
Often called “pseudo-Cushing syndrome,” these conditions have recently been renamed “non-neoplastic hypercortisolism” or “physiologic non-neoplastic endogenous hypercortisolism.” They share some clinical and biochemical features of CS, but the hypercortisolemia is usually secondary to other factors. They increase the secretion of hypothalamic corticotropin-releasing hormone, which stimulates adrenocorticotropic hormone (ACTH) and adrenal cortisol secretion.
Identifying PCOS
PCOS is often associated with central obesity, Sherif noted, but not all women with PCOS have overweight or a central distribution of fat.
“Ask about menstrual periods and whether they come monthly,” Sherif advised. “If women using hormonal contraception say they have a regular cycle, ask if their cycle was regular prior to starting contraception. So many women with PCOS are undiagnosed because they started contraception in their teens to ‘regulate their periods’ and never realized they had PCOS.”
Additional symptoms of PCOS and its impact are found in the figure below.
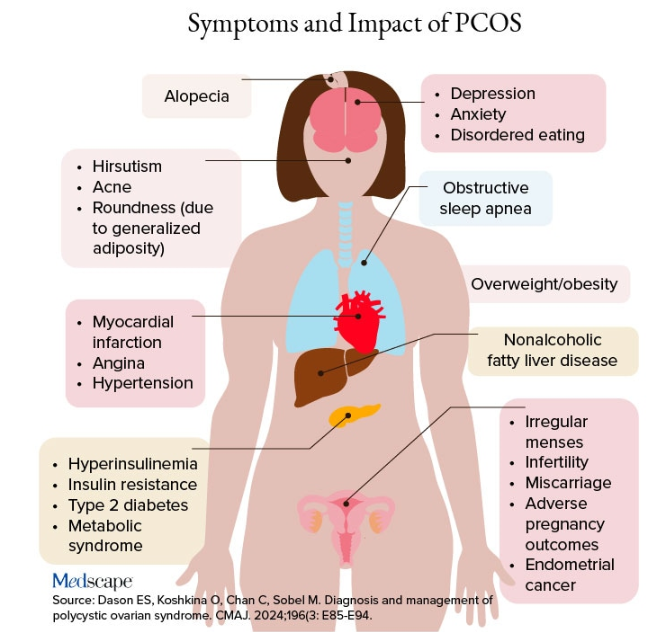
PCOS is diagnosed when two of the following three Rotterdam criteria are met, and other diagnoses are excluded:
- Irregular menstrual cycles
- Clinical hyperandrogenism or biochemical hyperandrogenism
- Polycystic ovarian morphology on transvaginal ultrasonography or high anti-mullerian hormone (applicable only if patient is ≥ 8 years from menarche)
If PCOS is suspected, further tests can be conducted to confirm or rule out the diagnosis.
Alcohol Abuse: Alcohol abuse stimulates hypothalamic corticotropin-releasing hormone, leading to increased ACTH levels. It’s associated with a higher fasting cortisol level, particularly at 8:30 AM or so, and attributable to impaired cortisol clearance due to alcohol-related hepatic dysfunction. The LDDST will show abnormal cortisol suppression.
Sherif advised asking patients about alcohol use, recommending treatment for alcohol use disorder, and repeating clinical and biochemical workup after patients have discontinued alcohol consumption for ≥ 1 month.
Eating Disorders Mimicking CS: Eating disorders, particularly anorexia nervosa, are associated with endocrine abnormalities, amenorrhea, impaired body temperature regulation, and hypercortisolism, likely due to chronic fasting-related stress. Dysregulation of the HPA axis may linger, even after weight recovery.
It’s unlikely that patients with anorexia will display the “rounded face” associated with hypercortisolism, but some research suggests that anorexia can result in a disproportionate accumulation of central adiposity after recovery from the illness.
Neuropsychiatric Disorders: Major depressive disorder (MDD) is associated with HPA axis hyperactivity, with 20%-30% of patients with MDD showing hypercortisolemia. The post-awakening cortisol surge is more pronounced in those with MDD, and about half of patients with MDD also have high evening cortisol levels, suggesting disrupted diurnal cortisol rhythms.
Some patients with MDD have greater resistance to the feedback action of glucocorticoids on HPA axis activity, with weaker sensitivity often restored by effective pharmacotherapy of the depressive condition. Neuropsychiatric disorders are also associated with reduced activity of cortisol-deactivating enzymes. Posttraumatic stress disorder and anxiety are similarly associated with hypercortisolemia.
Addressing neuropsychiatric conditions with appropriate pharmacotherapy and psychotherapy can restore cortisol levels to normal proportions.
Diabetes, Obesity, and Metabolic Syndrome: Diabetes, obesity, and metabolic syndrome can occur comorbidly with CS, and many patients with these conditions may display both a rounder face, some central adiposity, and hypercortisolemia. For example, obesity is often related to a hyperresponsive HPA axis, with elevated cortisol secretion but normal-to-low circulatory concentrations.
Obesity is associated with increased cortisol reactivity after acute physical and/or psychosocial stressors but preserved pituitary sensitivity to feedback inhibition by the LDDST. When these conditions are appropriately managed with pharmacotherapy and lifestyle changes, cortisol levels should normalize, according to the experts.
Hypothyroidism: Hypothyroidism— Hashimoto disease as well as the subclinical variety — can be associated with weight gain, which may take the form of central obesity. Some research suggests a bidirectional relationship between hypothyroidism and obesity.
“Years ago, we didn’t conduct thyroid tests very often but now they’re easy to do, so we usually catch people with hypothyroidism at the beginning of the condition,” Sherif said. “If the patient’s thyroid hasn’t been checked in a year or so, thyroid hormone testing should be conducted.”
Thyroid disease can easily be managed with the administration of thyroid hormones.
Obstructive Sleep Apnea (OSA): OSA has an impact on HPA axis activation, especially when accompanied by obesity and hypertension. A meta-analysis of 22 studies, encompassing over 600 participants, found that continuous positive airway pressure treatment in patients with OSA reduced cortisol levels as well as blood pressure.
Treatment With Exogenous Corticosteroids: Oral corticosteroid treatment is a cornerstone of therapy in transplant, rheumatic, and autoimmune diseases. The impact of chronic exposure to exogenous glucocorticoids is similar to that with endogenous glucocorticoids.
Sherif said corticosteroid treatment can cause facial roundness in as little as 2 weeks and is characteristic in people taking these agents for longer periods. Although the effects are most pronounced with oral agents, systemic effects can be associated with inhaled corticosteroids as well.
Finding alternative anti-inflammatory treatments is advisable, if possible. The co-administration of metformin might lead to improvements in both the metabolic profile and the clinical outcomes of patients receiving glucocorticoids for inflammatory conditions.
Educating Patients: “There’s much we still don’t know about hypercortisolemia and CS, including the reasons for its impact on metabolic derangement and for the accumulation of fat in particular adipose patterns,” Ben-Shlomo said. “But experienced endocrinologists do know relatively well how to diagnose the condition, distinguish it from other conditions presenting with central obesity or a rounder face, and treat it.”
Given the casual use of the terms “moon face” and “extra cortisol” on social media, it’s important for physicians to educate patients about what elevated cortisol does and doesn’t do, and design treatment strategies accordingly.
Neither Ben-Shlomo nor Sherif reported having any disclosures.
A version of this article appeared on Medscape.com.
“Cortisol” has become a household word, popularized by social media and tagged in videos that garnered nearly 800 million views in 2023. This is linked to the also-trending term “moon face,” which TikTok influencers and others have suggested is caused by high cortisol levels and, conversely, can be reduced through stress reduction.
“When we hear the term ‘moon face,’ we’re typically referring to Cushing syndrome [CS] or treatment with prolonged high-dose glucocorticoids,” said Anat Ben-Shlomo, MD, co-director of the Multidisciplinary Adrenal Program, Pituitary Center, Division of Endocrinology, Diabetes and Metabolism at Cedars-Sinai Medical Center, Los Angeles. Medscape Medical News previously discussed moon face in an article detailing how to diagnose CS.
Ben-Shlomo noted that the labels “moon face” and “moon facies” should be avoided for their potentially derogatory, unprofessional-sounding connotations, and that the preferred terms are “rounded face” or “round plethoric face.”
There are several disorders that can be associated with facial roundness, not all of which relate to elevated cortisol.
“It’s important for clinicians to be able distinguish between presentations due to other pathophysiologies, identify the unique constellation of Cushing-associated signs and symptoms, engage in a differential diagnosis, and treat whatever the condition is appropriately,” Katherine Sherif, MD, professor and vice chair of academic affairs, Department of Medicine, Thomas Jefferson University, Philadelphia, said in an interview.
The Unique Presentation of CS
CS results from “prolonged elevation” in plasma cortisol levels caused by either exogenous steroid use or excess endogenous steroid production.
“The shape of the face isn’t the only feature associated with CS,” Ben-Shlomo said. “There’s central obesity, particularly in the neck, supraclavicular area, chest, and abdomen. You sometimes see a posterior cervical thoracic fat pad, colloquially — but unprofessionally — called a ‘cervical hump.’ Simultaneously, the arms and legs are getting thinner.” The development of a round, plethoric face is common in long-standing significant CS, and a reddening of the skin can appear.
Additional symptoms include hirsutism and acne. “These can also be seen in other conditions, such as PCOS [polycystic ovary syndrome] but, combined with the other facial features, are more suggestive of CS,” Ben-Shlomo said.
Deep, wide purple striae appear in the trunk, breast, upper arms, and thighs, but not in the face, Ben-Shlomo advised. These appear as the fragile, thinning under-skin breaks when the patient gains weight.
Additional metabolic issues that can occur comorbidly include insulin resistance and diabetes, hypertension, osteoporosis, dyslipidemia, ecchymoses, increased susceptibility to infections, mood changes, cognitive dysfunction, low libido, infertility, weakness of muscles in the shoulders and thighs, episodes of bleeding and/or clotting, and an increased risk for heart attacks and strokes, Ben-Shlomo said.
“Not everyone presents with full-blown disease, but if you see any of these symptoms, be suspicious of CS and conduct a biochemical evaluation.” Three screening tests to use as a starting point are recommended by the Pituitary Society’s updated Consensus on Diagnosis and Management of Cushing’s Disease. The tests should be repeated to account for intra-patient variability. If two or all three tests are positive, clinicians should be suspicious of CS and move to additional testing to identify the underlying cause, Ben-Shlomo said.
‘Subclinical’ CS
Ben-Shlomo highlighted a condition called minimal autonomous cortisol secretion (formerly “subclinical CS”). “This condition is found when a person has an adrenal nodule that produces cortisol in excess, however not to levels observed in CS. An abnormal finding on the overnight 1-mg low-dose dexamethasone suppression test (LDDST) will identify this disorder, showing mildly unsuppressed morning cortisol level, while all other tests will be within normal range.”
She described minimal autonomous cortisol secretion as a form of “smoldering CS,” which has become more commonly diagnosed. “The condition needs to be treated because the patient can develop insulin resistance, metabolic syndrome, and osteoporosis over time.”
Once a cause has been determined, the optimal course of action is to take a multidisciplinary approach because CS affects multiple systems.
‘Pseudo-Cushing Syndrome’
A variety of abnormalities of the hypothalamus-pituitary adrenal (HPA) axis can be associated with hypercortisolemia and a rounder facial appearance but aren’t actually CS, Ben-Shlomo said.
Often called “pseudo-Cushing syndrome,” these conditions have recently been renamed “non-neoplastic hypercortisolism” or “physiologic non-neoplastic endogenous hypercortisolism.” They share some clinical and biochemical features of CS, but the hypercortisolemia is usually secondary to other factors. They increase the secretion of hypothalamic corticotropin-releasing hormone, which stimulates adrenocorticotropic hormone (ACTH) and adrenal cortisol secretion.
Identifying PCOS
PCOS is often associated with central obesity, Sherif noted, but not all women with PCOS have overweight or a central distribution of fat.
“Ask about menstrual periods and whether they come monthly,” Sherif advised. “If women using hormonal contraception say they have a regular cycle, ask if their cycle was regular prior to starting contraception. So many women with PCOS are undiagnosed because they started contraception in their teens to ‘regulate their periods’ and never realized they had PCOS.”
Additional symptoms of PCOS and its impact are found in the figure below.
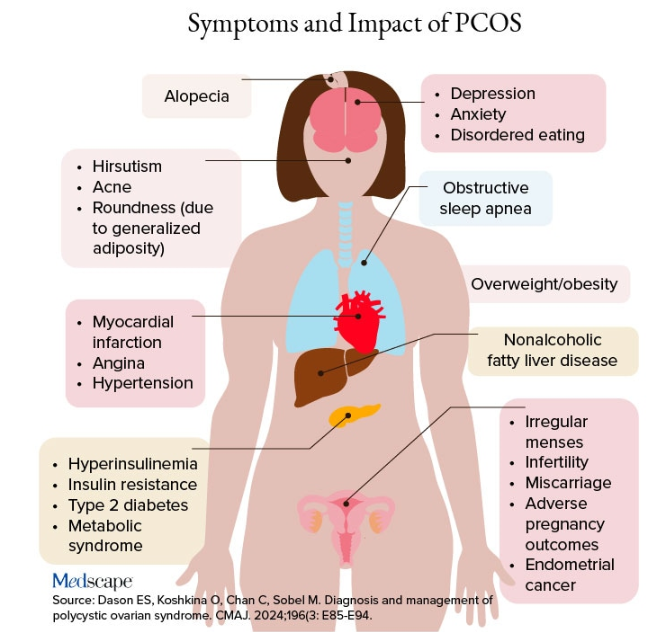
PCOS is diagnosed when two of the following three Rotterdam criteria are met, and other diagnoses are excluded:
- Irregular menstrual cycles
- Clinical hyperandrogenism or biochemical hyperandrogenism
- Polycystic ovarian morphology on transvaginal ultrasonography or high anti-mullerian hormone (applicable only if patient is ≥ 8 years from menarche)
If PCOS is suspected, further tests can be conducted to confirm or rule out the diagnosis.
Alcohol Abuse: Alcohol abuse stimulates hypothalamic corticotropin-releasing hormone, leading to increased ACTH levels. It’s associated with a higher fasting cortisol level, particularly at 8:30 AM or so, and attributable to impaired cortisol clearance due to alcohol-related hepatic dysfunction. The LDDST will show abnormal cortisol suppression.
Sherif advised asking patients about alcohol use, recommending treatment for alcohol use disorder, and repeating clinical and biochemical workup after patients have discontinued alcohol consumption for ≥ 1 month.
Eating Disorders Mimicking CS: Eating disorders, particularly anorexia nervosa, are associated with endocrine abnormalities, amenorrhea, impaired body temperature regulation, and hypercortisolism, likely due to chronic fasting-related stress. Dysregulation of the HPA axis may linger, even after weight recovery.
It’s unlikely that patients with anorexia will display the “rounded face” associated with hypercortisolism, but some research suggests that anorexia can result in a disproportionate accumulation of central adiposity after recovery from the illness.
Neuropsychiatric Disorders: Major depressive disorder (MDD) is associated with HPA axis hyperactivity, with 20%-30% of patients with MDD showing hypercortisolemia. The post-awakening cortisol surge is more pronounced in those with MDD, and about half of patients with MDD also have high evening cortisol levels, suggesting disrupted diurnal cortisol rhythms.
Some patients with MDD have greater resistance to the feedback action of glucocorticoids on HPA axis activity, with weaker sensitivity often restored by effective pharmacotherapy of the depressive condition. Neuropsychiatric disorders are also associated with reduced activity of cortisol-deactivating enzymes. Posttraumatic stress disorder and anxiety are similarly associated with hypercortisolemia.
Addressing neuropsychiatric conditions with appropriate pharmacotherapy and psychotherapy can restore cortisol levels to normal proportions.
Diabetes, Obesity, and Metabolic Syndrome: Diabetes, obesity, and metabolic syndrome can occur comorbidly with CS, and many patients with these conditions may display both a rounder face, some central adiposity, and hypercortisolemia. For example, obesity is often related to a hyperresponsive HPA axis, with elevated cortisol secretion but normal-to-low circulatory concentrations.
Obesity is associated with increased cortisol reactivity after acute physical and/or psychosocial stressors but preserved pituitary sensitivity to feedback inhibition by the LDDST. When these conditions are appropriately managed with pharmacotherapy and lifestyle changes, cortisol levels should normalize, according to the experts.
Hypothyroidism: Hypothyroidism— Hashimoto disease as well as the subclinical variety — can be associated with weight gain, which may take the form of central obesity. Some research suggests a bidirectional relationship between hypothyroidism and obesity.
“Years ago, we didn’t conduct thyroid tests very often but now they’re easy to do, so we usually catch people with hypothyroidism at the beginning of the condition,” Sherif said. “If the patient’s thyroid hasn’t been checked in a year or so, thyroid hormone testing should be conducted.”
Thyroid disease can easily be managed with the administration of thyroid hormones.
Obstructive Sleep Apnea (OSA): OSA has an impact on HPA axis activation, especially when accompanied by obesity and hypertension. A meta-analysis of 22 studies, encompassing over 600 participants, found that continuous positive airway pressure treatment in patients with OSA reduced cortisol levels as well as blood pressure.
Treatment With Exogenous Corticosteroids: Oral corticosteroid treatment is a cornerstone of therapy in transplant, rheumatic, and autoimmune diseases. The impact of chronic exposure to exogenous glucocorticoids is similar to that with endogenous glucocorticoids.
Sherif said corticosteroid treatment can cause facial roundness in as little as 2 weeks and is characteristic in people taking these agents for longer periods. Although the effects are most pronounced with oral agents, systemic effects can be associated with inhaled corticosteroids as well.
Finding alternative anti-inflammatory treatments is advisable, if possible. The co-administration of metformin might lead to improvements in both the metabolic profile and the clinical outcomes of patients receiving glucocorticoids for inflammatory conditions.
Educating Patients: “There’s much we still don’t know about hypercortisolemia and CS, including the reasons for its impact on metabolic derangement and for the accumulation of fat in particular adipose patterns,” Ben-Shlomo said. “But experienced endocrinologists do know relatively well how to diagnose the condition, distinguish it from other conditions presenting with central obesity or a rounder face, and treat it.”
Given the casual use of the terms “moon face” and “extra cortisol” on social media, it’s important for physicians to educate patients about what elevated cortisol does and doesn’t do, and design treatment strategies accordingly.
Neither Ben-Shlomo nor Sherif reported having any disclosures.
A version of this article appeared on Medscape.com.
Postpartum Exercise Reduces Depression and Anxiety Symptoms
TOPLINE:
Postpartum exercise reduces the severity of depressive and anxiety symptoms. Initiating exercise within 12 weeks post partum is linked to greater reductions in depressive symptoms.
METHODOLOGY:
- Researchers conducted a systematic review and meta-analysis including 35 studies with a total of 4072 participants.
- The review included randomized controlled trials and nonrandomized interventions examining the impact of postpartum exercise on depression and anxiety.
- Participants were postpartum individuals within the first year after childbirth, with interventions including various types of exercise.
- Data sources included online databases with data up to January 2024, reference lists, and hand searches.
- The Grading of Recommendations, Assessment, Development, and Evaluation framework was used to assess the certainty of evidence.
TAKEAWAY:
- Postpartum exercise-only interventions resulted in a moderate reduction in the severity of depressive symptoms (standardized mean difference [SMD], –0.52; 95% CI, –0.80 to –0.24).
- Exercise-only interventions were associated with a small reduction in the severity of anxiety symptoms (SMD, –0.25; 95% CI, –0.43 to –0.08).
- Initiating exercise within 12 weeks post partum was associated with a greater reduction in depressive symptoms, compared with starting later.
- Postpartum exercise was associated with a 45% reduction in the odds of developing depression (odds ratio, 0.55; 95% CI, 0.32-0.95).
IN PRACTICE:
“Further investigation should aim to investigate the effects of postpartum exercise in individuals who experienced perinatal complications and in those who had limitations to exercise during pregnancy. Additionally, more investigation is required to address the possible lasting effects of postpartum exercise on maternal mental health as there were very limited studies reporting on this outcome,” the authors of the study wrote.
SOURCE:
This study was led by Margie H. Davenport, University of Alberta in Edmonton, Canada. It was published online in British Journal of Sports Medicine.
LIMITATIONS:
This study’s limitations included high heterogeneity among included studies, small sample sizes in some studies, and the combination of exercise with other interventions in some cases. These factors may have affected the generalizability and precision of the findings.
DISCLOSURES:
This study was funded by the Christenson Professorship in Active Healthy Living. Davenport is funded by a Christenson Professorship in Active Healthy Living. One coauthor is funded by the Université du Québec à Trois-Rivières research chair in physical activity and maternal and neonatal health. No relevant conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Postpartum exercise reduces the severity of depressive and anxiety symptoms. Initiating exercise within 12 weeks post partum is linked to greater reductions in depressive symptoms.
METHODOLOGY:
- Researchers conducted a systematic review and meta-analysis including 35 studies with a total of 4072 participants.
- The review included randomized controlled trials and nonrandomized interventions examining the impact of postpartum exercise on depression and anxiety.
- Participants were postpartum individuals within the first year after childbirth, with interventions including various types of exercise.
- Data sources included online databases with data up to January 2024, reference lists, and hand searches.
- The Grading of Recommendations, Assessment, Development, and Evaluation framework was used to assess the certainty of evidence.
TAKEAWAY:
- Postpartum exercise-only interventions resulted in a moderate reduction in the severity of depressive symptoms (standardized mean difference [SMD], –0.52; 95% CI, –0.80 to –0.24).
- Exercise-only interventions were associated with a small reduction in the severity of anxiety symptoms (SMD, –0.25; 95% CI, –0.43 to –0.08).
- Initiating exercise within 12 weeks post partum was associated with a greater reduction in depressive symptoms, compared with starting later.
- Postpartum exercise was associated with a 45% reduction in the odds of developing depression (odds ratio, 0.55; 95% CI, 0.32-0.95).
IN PRACTICE:
“Further investigation should aim to investigate the effects of postpartum exercise in individuals who experienced perinatal complications and in those who had limitations to exercise during pregnancy. Additionally, more investigation is required to address the possible lasting effects of postpartum exercise on maternal mental health as there were very limited studies reporting on this outcome,” the authors of the study wrote.
SOURCE:
This study was led by Margie H. Davenport, University of Alberta in Edmonton, Canada. It was published online in British Journal of Sports Medicine.
LIMITATIONS:
This study’s limitations included high heterogeneity among included studies, small sample sizes in some studies, and the combination of exercise with other interventions in some cases. These factors may have affected the generalizability and precision of the findings.
DISCLOSURES:
This study was funded by the Christenson Professorship in Active Healthy Living. Davenport is funded by a Christenson Professorship in Active Healthy Living. One coauthor is funded by the Université du Québec à Trois-Rivières research chair in physical activity and maternal and neonatal health. No relevant conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Postpartum exercise reduces the severity of depressive and anxiety symptoms. Initiating exercise within 12 weeks post partum is linked to greater reductions in depressive symptoms.
METHODOLOGY:
- Researchers conducted a systematic review and meta-analysis including 35 studies with a total of 4072 participants.
- The review included randomized controlled trials and nonrandomized interventions examining the impact of postpartum exercise on depression and anxiety.
- Participants were postpartum individuals within the first year after childbirth, with interventions including various types of exercise.
- Data sources included online databases with data up to January 2024, reference lists, and hand searches.
- The Grading of Recommendations, Assessment, Development, and Evaluation framework was used to assess the certainty of evidence.
TAKEAWAY:
- Postpartum exercise-only interventions resulted in a moderate reduction in the severity of depressive symptoms (standardized mean difference [SMD], –0.52; 95% CI, –0.80 to –0.24).
- Exercise-only interventions were associated with a small reduction in the severity of anxiety symptoms (SMD, –0.25; 95% CI, –0.43 to –0.08).
- Initiating exercise within 12 weeks post partum was associated with a greater reduction in depressive symptoms, compared with starting later.
- Postpartum exercise was associated with a 45% reduction in the odds of developing depression (odds ratio, 0.55; 95% CI, 0.32-0.95).
IN PRACTICE:
“Further investigation should aim to investigate the effects of postpartum exercise in individuals who experienced perinatal complications and in those who had limitations to exercise during pregnancy. Additionally, more investigation is required to address the possible lasting effects of postpartum exercise on maternal mental health as there were very limited studies reporting on this outcome,” the authors of the study wrote.
SOURCE:
This study was led by Margie H. Davenport, University of Alberta in Edmonton, Canada. It was published online in British Journal of Sports Medicine.
LIMITATIONS:
This study’s limitations included high heterogeneity among included studies, small sample sizes in some studies, and the combination of exercise with other interventions in some cases. These factors may have affected the generalizability and precision of the findings.
DISCLOSURES:
This study was funded by the Christenson Professorship in Active Healthy Living. Davenport is funded by a Christenson Professorship in Active Healthy Living. One coauthor is funded by the Université du Québec à Trois-Rivières research chair in physical activity and maternal and neonatal health. No relevant conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Do Patients on Anti-Obesity Drugs Decrease Alcohol Use?
SAN ANTONIO —
The findings, from surveys of more than 14,000 participants in WeightWatchers’ telehealth weight management program, were presented on November 6 at the Obesity Society’s Obesity Week 2024 meeting by the company’s Chief Nutrition Officer, Michelle I. Cardel, PhD, RD, based in Gainesville, Florida.
Similar reductions in alcohol consumption were seen in people taking different classes of AOMs, suggesting “an additional mechanism by which AOMs reduce energy intake, and also signal a potential role for these medications to reduce alcohol use,” Cardel said, adding “Clinicians treating individuals for obesity may consider anti-obesity medications particularly among those who report higher alcohol intake.”
Asked to comment, session moderator and obesity researcher Joseph A. Skelton, MD, professor of pediatrics at Wake Forest University School of Medicine, Winston-Salem, North Carolina, said, “I think there are some overlapping pathways there, possibly a reward system or something like that in the brain. I don’t think we know exactly what the end result will be as a potential use of the medications. But there’s a signal that needs to be investigated more.”
Cardel noted that there was one previous large cohort study finding that semaglutide was associated with a lower risk for alcohol use disorder, and another study that analyzed social media threads of people saying they’d quit drinking after starting a GLP-1 drug. But this new study is the first to examine the relationship with different classes of AOMs and to quantify the amount of alcohol consumed.
About Half Reported Reduced Alcohol Consumption, Regardless the AOM Class
The study included 14,053 WeightWatchers’ telehealth program participants who initiated an AOM between January 2022 and August 2023 and refilled the same AOM between October and November 2023. Those who had previously used AOMs before coming to the program or who had undergone bariatric surgery were excluded.
Participants had a mean age of 43 years, were 86% women, were 60% White, and had a mean body mass index of 36. They were surveyed about their weekly alcohol use prior to AOM initiation and again at the time of AOM refill.
At baseline, they were divided into categories of 0 (no alcohol use; n = 6562), category 1 (one to three drinks for women and one to six for men; n = 5948), category 2 (4-6 for women and 7-14 for men; n = 1216), and category 3 (≥ 7 for women and ≥ 15 for men; n = 327).
At the second survey, 24% reported decreased drinking after starting an AOM, 71% reported no change, and 4% reported increased drinking (P < .0001). But when just the 7491 individuals who reported any alcohol use at baseline were included, 45% reported decreased drinking after starting an AOM, 52% reported no change, and only 2% reported increased drinking.
The decrease in drinking with AOM use rose with greater alcohol use at baseline, from 37% for category 1, 76% for category 2, and 91% for category 3. The proportions reporting increased drinking were just 3%, 1%, and 0%, respectively. The adjusted odds ratios (ORs) for decreasing drinking were 5.97 for category 2 (P < .0001) and 19.18 for category 3 (P < .0001) vs category 1.
The proportions reporting reduced drinking were similar across AOM classes: 51% for metformin, 46% for bupropion/naltrexone, 46% for first-generation GLP-1s (Saxenda, Trulicity, and Victoza), and 45% for the second-generation GLP-1 drugs (Mounjaro, Ozempic, Rybelsus, Wegovy, and Zepbound). All were statistically significant at P < .0001.
The highest proportion reporting increased drinking was 4% for bupropion/naltrexone. Compared with women, men were significantly more likely to report decreased drinking with AOM use (adjusted OR, 0.74; P < .001), but there were no differences by race/ethnicity or age.
Compared with those who had overweight, those in obesity classes I, II, and III were all more likely to decrease drinking with AOM use, with adjusted ORs of 1.26 (P = .0045), 1.49 (P < .001), and 1.63 (P < .001), respectively.
Mechanisms Appear Both Biological and Behavioral
During the discussion, Cardel said that qualitative assessments with participants suggest that there are at least two mechanisms behind this phenomenon: One biological and the other intentional.
“What we hear from them is twofold, one, particularly amongst those folks on GLP-1 medications, we’re hearing that physiologically, they feel different with the medications, that their cravings for alcohol are decreased, and that when they do choose to drink that there’s often a very much a negative reinforcement ... I’ve had a patient tell me, ‘I used to be able to have two or three margaritas, and maybe I didn’t feel like the best I’d ever felt in the morning, but I was okay. And now if I have two or three drinks, I will be throwing up for 5 hours, and it’s the worst hangover I’ve ever had in my life.’ And so it very much creates that negative reinforcement loop.”
But at the same time, “folks who are coming to us and seeking these medications are very much on a on a health-based journey. That’s what they tell us. The majority of our patients are there to improve their health. We rarely hear about the vanity or aesthetic part of it. So perhaps it’s that, in terms of trying to improve their health, they’re also trying to reduce their alcohol consumption, either just for their overall health or also as a means of trying to decrease their overall calorie consumption.”
In future research, Cardel said, “we want to examine whether the anti-obesity medications are more successful at reducing alcohol use compared to non-pharmacological weight management interventions, as we know that people often reduce their alcohol consumption on a weight management journey as a means of prioritizing their calories for food and decreasing the calories from alcohol.”
Cardel and all the study coauthors were employees and shareholders at WeightWatchers at the time the research was conducted. Skelton is editor in chief of the journal Childhood Obesity.
A version of this article appeared on Medscape.com.
SAN ANTONIO —
The findings, from surveys of more than 14,000 participants in WeightWatchers’ telehealth weight management program, were presented on November 6 at the Obesity Society’s Obesity Week 2024 meeting by the company’s Chief Nutrition Officer, Michelle I. Cardel, PhD, RD, based in Gainesville, Florida.
Similar reductions in alcohol consumption were seen in people taking different classes of AOMs, suggesting “an additional mechanism by which AOMs reduce energy intake, and also signal a potential role for these medications to reduce alcohol use,” Cardel said, adding “Clinicians treating individuals for obesity may consider anti-obesity medications particularly among those who report higher alcohol intake.”
Asked to comment, session moderator and obesity researcher Joseph A. Skelton, MD, professor of pediatrics at Wake Forest University School of Medicine, Winston-Salem, North Carolina, said, “I think there are some overlapping pathways there, possibly a reward system or something like that in the brain. I don’t think we know exactly what the end result will be as a potential use of the medications. But there’s a signal that needs to be investigated more.”
Cardel noted that there was one previous large cohort study finding that semaglutide was associated with a lower risk for alcohol use disorder, and another study that analyzed social media threads of people saying they’d quit drinking after starting a GLP-1 drug. But this new study is the first to examine the relationship with different classes of AOMs and to quantify the amount of alcohol consumed.
About Half Reported Reduced Alcohol Consumption, Regardless the AOM Class
The study included 14,053 WeightWatchers’ telehealth program participants who initiated an AOM between January 2022 and August 2023 and refilled the same AOM between October and November 2023. Those who had previously used AOMs before coming to the program or who had undergone bariatric surgery were excluded.
Participants had a mean age of 43 years, were 86% women, were 60% White, and had a mean body mass index of 36. They were surveyed about their weekly alcohol use prior to AOM initiation and again at the time of AOM refill.
At baseline, they were divided into categories of 0 (no alcohol use; n = 6562), category 1 (one to three drinks for women and one to six for men; n = 5948), category 2 (4-6 for women and 7-14 for men; n = 1216), and category 3 (≥ 7 for women and ≥ 15 for men; n = 327).
At the second survey, 24% reported decreased drinking after starting an AOM, 71% reported no change, and 4% reported increased drinking (P < .0001). But when just the 7491 individuals who reported any alcohol use at baseline were included, 45% reported decreased drinking after starting an AOM, 52% reported no change, and only 2% reported increased drinking.
The decrease in drinking with AOM use rose with greater alcohol use at baseline, from 37% for category 1, 76% for category 2, and 91% for category 3. The proportions reporting increased drinking were just 3%, 1%, and 0%, respectively. The adjusted odds ratios (ORs) for decreasing drinking were 5.97 for category 2 (P < .0001) and 19.18 for category 3 (P < .0001) vs category 1.
The proportions reporting reduced drinking were similar across AOM classes: 51% for metformin, 46% for bupropion/naltrexone, 46% for first-generation GLP-1s (Saxenda, Trulicity, and Victoza), and 45% for the second-generation GLP-1 drugs (Mounjaro, Ozempic, Rybelsus, Wegovy, and Zepbound). All were statistically significant at P < .0001.
The highest proportion reporting increased drinking was 4% for bupropion/naltrexone. Compared with women, men were significantly more likely to report decreased drinking with AOM use (adjusted OR, 0.74; P < .001), but there were no differences by race/ethnicity or age.
Compared with those who had overweight, those in obesity classes I, II, and III were all more likely to decrease drinking with AOM use, with adjusted ORs of 1.26 (P = .0045), 1.49 (P < .001), and 1.63 (P < .001), respectively.
Mechanisms Appear Both Biological and Behavioral
During the discussion, Cardel said that qualitative assessments with participants suggest that there are at least two mechanisms behind this phenomenon: One biological and the other intentional.
“What we hear from them is twofold, one, particularly amongst those folks on GLP-1 medications, we’re hearing that physiologically, they feel different with the medications, that their cravings for alcohol are decreased, and that when they do choose to drink that there’s often a very much a negative reinforcement ... I’ve had a patient tell me, ‘I used to be able to have two or three margaritas, and maybe I didn’t feel like the best I’d ever felt in the morning, but I was okay. And now if I have two or three drinks, I will be throwing up for 5 hours, and it’s the worst hangover I’ve ever had in my life.’ And so it very much creates that negative reinforcement loop.”
But at the same time, “folks who are coming to us and seeking these medications are very much on a on a health-based journey. That’s what they tell us. The majority of our patients are there to improve their health. We rarely hear about the vanity or aesthetic part of it. So perhaps it’s that, in terms of trying to improve their health, they’re also trying to reduce their alcohol consumption, either just for their overall health or also as a means of trying to decrease their overall calorie consumption.”
In future research, Cardel said, “we want to examine whether the anti-obesity medications are more successful at reducing alcohol use compared to non-pharmacological weight management interventions, as we know that people often reduce their alcohol consumption on a weight management journey as a means of prioritizing their calories for food and decreasing the calories from alcohol.”
Cardel and all the study coauthors were employees and shareholders at WeightWatchers at the time the research was conducted. Skelton is editor in chief of the journal Childhood Obesity.
A version of this article appeared on Medscape.com.
SAN ANTONIO —
The findings, from surveys of more than 14,000 participants in WeightWatchers’ telehealth weight management program, were presented on November 6 at the Obesity Society’s Obesity Week 2024 meeting by the company’s Chief Nutrition Officer, Michelle I. Cardel, PhD, RD, based in Gainesville, Florida.
Similar reductions in alcohol consumption were seen in people taking different classes of AOMs, suggesting “an additional mechanism by which AOMs reduce energy intake, and also signal a potential role for these medications to reduce alcohol use,” Cardel said, adding “Clinicians treating individuals for obesity may consider anti-obesity medications particularly among those who report higher alcohol intake.”
Asked to comment, session moderator and obesity researcher Joseph A. Skelton, MD, professor of pediatrics at Wake Forest University School of Medicine, Winston-Salem, North Carolina, said, “I think there are some overlapping pathways there, possibly a reward system or something like that in the brain. I don’t think we know exactly what the end result will be as a potential use of the medications. But there’s a signal that needs to be investigated more.”
Cardel noted that there was one previous large cohort study finding that semaglutide was associated with a lower risk for alcohol use disorder, and another study that analyzed social media threads of people saying they’d quit drinking after starting a GLP-1 drug. But this new study is the first to examine the relationship with different classes of AOMs and to quantify the amount of alcohol consumed.
About Half Reported Reduced Alcohol Consumption, Regardless the AOM Class
The study included 14,053 WeightWatchers’ telehealth program participants who initiated an AOM between January 2022 and August 2023 and refilled the same AOM between October and November 2023. Those who had previously used AOMs before coming to the program or who had undergone bariatric surgery were excluded.
Participants had a mean age of 43 years, were 86% women, were 60% White, and had a mean body mass index of 36. They were surveyed about their weekly alcohol use prior to AOM initiation and again at the time of AOM refill.
At baseline, they were divided into categories of 0 (no alcohol use; n = 6562), category 1 (one to three drinks for women and one to six for men; n = 5948), category 2 (4-6 for women and 7-14 for men; n = 1216), and category 3 (≥ 7 for women and ≥ 15 for men; n = 327).
At the second survey, 24% reported decreased drinking after starting an AOM, 71% reported no change, and 4% reported increased drinking (P < .0001). But when just the 7491 individuals who reported any alcohol use at baseline were included, 45% reported decreased drinking after starting an AOM, 52% reported no change, and only 2% reported increased drinking.
The decrease in drinking with AOM use rose with greater alcohol use at baseline, from 37% for category 1, 76% for category 2, and 91% for category 3. The proportions reporting increased drinking were just 3%, 1%, and 0%, respectively. The adjusted odds ratios (ORs) for decreasing drinking were 5.97 for category 2 (P < .0001) and 19.18 for category 3 (P < .0001) vs category 1.
The proportions reporting reduced drinking were similar across AOM classes: 51% for metformin, 46% for bupropion/naltrexone, 46% for first-generation GLP-1s (Saxenda, Trulicity, and Victoza), and 45% for the second-generation GLP-1 drugs (Mounjaro, Ozempic, Rybelsus, Wegovy, and Zepbound). All were statistically significant at P < .0001.
The highest proportion reporting increased drinking was 4% for bupropion/naltrexone. Compared with women, men were significantly more likely to report decreased drinking with AOM use (adjusted OR, 0.74; P < .001), but there were no differences by race/ethnicity or age.
Compared with those who had overweight, those in obesity classes I, II, and III were all more likely to decrease drinking with AOM use, with adjusted ORs of 1.26 (P = .0045), 1.49 (P < .001), and 1.63 (P < .001), respectively.
Mechanisms Appear Both Biological and Behavioral
During the discussion, Cardel said that qualitative assessments with participants suggest that there are at least two mechanisms behind this phenomenon: One biological and the other intentional.
“What we hear from them is twofold, one, particularly amongst those folks on GLP-1 medications, we’re hearing that physiologically, they feel different with the medications, that their cravings for alcohol are decreased, and that when they do choose to drink that there’s often a very much a negative reinforcement ... I’ve had a patient tell me, ‘I used to be able to have two or three margaritas, and maybe I didn’t feel like the best I’d ever felt in the morning, but I was okay. And now if I have two or three drinks, I will be throwing up for 5 hours, and it’s the worst hangover I’ve ever had in my life.’ And so it very much creates that negative reinforcement loop.”
But at the same time, “folks who are coming to us and seeking these medications are very much on a on a health-based journey. That’s what they tell us. The majority of our patients are there to improve their health. We rarely hear about the vanity or aesthetic part of it. So perhaps it’s that, in terms of trying to improve their health, they’re also trying to reduce their alcohol consumption, either just for their overall health or also as a means of trying to decrease their overall calorie consumption.”
In future research, Cardel said, “we want to examine whether the anti-obesity medications are more successful at reducing alcohol use compared to non-pharmacological weight management interventions, as we know that people often reduce their alcohol consumption on a weight management journey as a means of prioritizing their calories for food and decreasing the calories from alcohol.”
Cardel and all the study coauthors were employees and shareholders at WeightWatchers at the time the research was conducted. Skelton is editor in chief of the journal Childhood Obesity.
A version of this article appeared on Medscape.com.
FROM OBESITY WEEK 2024
Digital Danger: How Cyberattacks Put Patients at Risk
On September 27, 2024, UMC Health System in Lubbock, Texas, experienced an IT outage because of a cybersecurity incident that temporarily diverted patients to other healthcare facilities. So far, in 2024, there have been 386 cyberattacks on healthcare organizations. These high-impact ransomware attacks disrupt and delay patient care.
In recent years, many healthcare systems, including Scripps Health, Universal Health Services, Vastaamo, Sky Lakes, and the University of Vermont, have paid millions — even tens of millions — to recover data after a cyberattack or data breach. When healthcare systems come under cyber fire, the impact extends far past disrupting workflows and compromising data, patient safety can be also be compromised, vital information may be lost, and imaging and lab results can go missing or be held for ransom, making physicians’ job difficult or impossible.
In fact, cyberattacks on hospitals are far more common than you may realize. A new report issued by Ponemon and Proofpoint found that 92% of healthcare organizations have experienced a cyberattack in the past 12 months. Even more sobering is that about half of the organizations affected suffered disruptions in patient care.
Healthcare Systems = ‘Soft Targets’
Healthcare systems are a “soft target” for hackers for several reasons, pointed out Matthew Radolec, vice president, incident response and cloud operations at Varonis, a data security company. “One, they’re usually an amalgamation of many healthcare systems that are interconnected,” said Radolec. “A lot of hospitals are connected to other hospitals or connected to educational institutions, which means their computer vulnerabilities are shared ... and if they have an issue, it could very easily spread to your network.”
Another factor is the cost of securing data. “[With hospitals], they’ll say that a dollar spent on security is a dollar not spent on patient care,” said Radolec. “So the idea of investing in security is really tough from a budget standpoint…they’re choosing between a new MRI machine or better antivirus, backups, or data security.”
Because of the wealth of private data and healthcare information they maintain, hospitals are considered “high impact” for cybercriminals. Attackers know that if they get a foothold in a hospital, it’s more likely to pay — and pay quickly, Radolec told this news organization. Hospitals are also likely to have cyber insurance to help cover the cost of having their data stolen, encrypted, and ransomed.
The 2024 Microsoft Digital Defense Report also found that the bad actors are more sophisticated and better resourced and can challenge even the best cybersecurity. Improved defenses may not be good enough, and the sheer volume of attacks must be met with effective deterrence and government solutions that impose consequences for cybercriminals.
Vulnerable Users
Whether through a phishing email or text, password attack, or web attack, “the moment a ‘threat actor’ gets into your institution and gets credentials ... that’s the Nirvana state of a threat actor,” warned Ryan Witt, chair of the healthcare customer advisory board and vice president of Industry Solutions at Proofpoint, a cybersecurity platform. “They have those credentials and will go into deep reconnaissance mode. It often takes healthcare up to 6 months to even ascertain whether somebody’s actually in the network.” During that time, the hacker is learning how the institution works, what job functions matter, and how best to plan their attack.
“Attackers are getting in because they’re buying databases of usernames and passwords. And they’re trying them by the millions,” added Radolec. “For a sophisticated actor, all it takes is time and motivation. They have the skills. It’s just a matter of how persistent they want to be.”
Certain hospital staff are also more likely to be targeted by cyberhackers than others. “About 10% of a healthcare organization’s user base is much more vulnerable for all sorts of reasons — how they work, the value of their job title and job function, and therefore their access to systems,” said Witt.
High-profile staff are more likely to be targeted than those in lower-level positions; the so-called “CEO attack” is typical. However, staff in other hospital departments are also subject to cybercriminals, including hospice departments/hospice organizations and research arms of hospitals.
The Impact of Cyberattacks on Patients
Physicians and healthcare execs may have considered cybersecurity more of a compliance issue than a true threat to patients in the past. But this attitude is rapidly changing. “We are starting to see a very clear connection between a cyber event and how it can impact patient care and patient safety,” said Witt.
According to the Proofpoint report, cyber breaches can severely affect patient care. In 2024:
- 56% of respondents saw a delay in patient tests/procedures
- 53% experienced increased patient complications from medical procedures
- 52% noted a longer patient length of stay
- 44% saw an increase in patient transfers to other facilities
- 28% had an increase in mortality rate
What Hospitals and Physicians Can Do
Fortunately, hospitals can take measures to better protect their data and their patients. One strategy is segmenting networks to reduce the amount of data or systems one person or system can access. Educating staff about the dangers of phishing and spoofing emails also help protect organizations from ransomware attacks. Having staff avoid reusing passwords and updating logins and passwords frequently helps.
Most hospitals also need more robust security controls. Physicians and healthcare facilities must also embrace the cybersecurity controls found in other industries, said Witt. “Multifactor authentication is one of those things that can cause us frustration,” he said. “The controls can seem onerous, but they’re really valuable overall…and should become standard practice.”
Doctors can also prepare for a ransomware attack and protect patients by practicing some “old-school” medicine, like using paper systems and maintaining good patient notes — often, those notes are synced locally as well as offsite, so you’d be able to access them even during a data breach. “It’s smart to write prescriptions on pads sometimes,” said Radolec. “Don’t forget how to do those things because that will make you more resilient in the event of a ransomware attack.”
A Continuing Threat
Cyberattacks will continue. “When you look at the high likelihood [of success] and the soft target, you end up with ... a perfect storm,” said Radolec. “Hospitals have a lot of vulnerabilities. They have to keep operations going just to receive income, but also to deliver care to people.”
That means that the burden is on healthcare organizations — including physicians, nurses, staff, and C-level execs — to help keep the “security” in cybersecurity. “We are all part of the cybersecurity defense,” said Witt. Helping to maintain that defense has become a critical aspect of caring for patients.
A version of this article first appeared on Medscape.com.
On September 27, 2024, UMC Health System in Lubbock, Texas, experienced an IT outage because of a cybersecurity incident that temporarily diverted patients to other healthcare facilities. So far, in 2024, there have been 386 cyberattacks on healthcare organizations. These high-impact ransomware attacks disrupt and delay patient care.
In recent years, many healthcare systems, including Scripps Health, Universal Health Services, Vastaamo, Sky Lakes, and the University of Vermont, have paid millions — even tens of millions — to recover data after a cyberattack or data breach. When healthcare systems come under cyber fire, the impact extends far past disrupting workflows and compromising data, patient safety can be also be compromised, vital information may be lost, and imaging and lab results can go missing or be held for ransom, making physicians’ job difficult or impossible.
In fact, cyberattacks on hospitals are far more common than you may realize. A new report issued by Ponemon and Proofpoint found that 92% of healthcare organizations have experienced a cyberattack in the past 12 months. Even more sobering is that about half of the organizations affected suffered disruptions in patient care.
Healthcare Systems = ‘Soft Targets’
Healthcare systems are a “soft target” for hackers for several reasons, pointed out Matthew Radolec, vice president, incident response and cloud operations at Varonis, a data security company. “One, they’re usually an amalgamation of many healthcare systems that are interconnected,” said Radolec. “A lot of hospitals are connected to other hospitals or connected to educational institutions, which means their computer vulnerabilities are shared ... and if they have an issue, it could very easily spread to your network.”
Another factor is the cost of securing data. “[With hospitals], they’ll say that a dollar spent on security is a dollar not spent on patient care,” said Radolec. “So the idea of investing in security is really tough from a budget standpoint…they’re choosing between a new MRI machine or better antivirus, backups, or data security.”
Because of the wealth of private data and healthcare information they maintain, hospitals are considered “high impact” for cybercriminals. Attackers know that if they get a foothold in a hospital, it’s more likely to pay — and pay quickly, Radolec told this news organization. Hospitals are also likely to have cyber insurance to help cover the cost of having their data stolen, encrypted, and ransomed.
The 2024 Microsoft Digital Defense Report also found that the bad actors are more sophisticated and better resourced and can challenge even the best cybersecurity. Improved defenses may not be good enough, and the sheer volume of attacks must be met with effective deterrence and government solutions that impose consequences for cybercriminals.
Vulnerable Users
Whether through a phishing email or text, password attack, or web attack, “the moment a ‘threat actor’ gets into your institution and gets credentials ... that’s the Nirvana state of a threat actor,” warned Ryan Witt, chair of the healthcare customer advisory board and vice president of Industry Solutions at Proofpoint, a cybersecurity platform. “They have those credentials and will go into deep reconnaissance mode. It often takes healthcare up to 6 months to even ascertain whether somebody’s actually in the network.” During that time, the hacker is learning how the institution works, what job functions matter, and how best to plan their attack.
“Attackers are getting in because they’re buying databases of usernames and passwords. And they’re trying them by the millions,” added Radolec. “For a sophisticated actor, all it takes is time and motivation. They have the skills. It’s just a matter of how persistent they want to be.”
Certain hospital staff are also more likely to be targeted by cyberhackers than others. “About 10% of a healthcare organization’s user base is much more vulnerable for all sorts of reasons — how they work, the value of their job title and job function, and therefore their access to systems,” said Witt.
High-profile staff are more likely to be targeted than those in lower-level positions; the so-called “CEO attack” is typical. However, staff in other hospital departments are also subject to cybercriminals, including hospice departments/hospice organizations and research arms of hospitals.
The Impact of Cyberattacks on Patients
Physicians and healthcare execs may have considered cybersecurity more of a compliance issue than a true threat to patients in the past. But this attitude is rapidly changing. “We are starting to see a very clear connection between a cyber event and how it can impact patient care and patient safety,” said Witt.
According to the Proofpoint report, cyber breaches can severely affect patient care. In 2024:
- 56% of respondents saw a delay in patient tests/procedures
- 53% experienced increased patient complications from medical procedures
- 52% noted a longer patient length of stay
- 44% saw an increase in patient transfers to other facilities
- 28% had an increase in mortality rate
What Hospitals and Physicians Can Do
Fortunately, hospitals can take measures to better protect their data and their patients. One strategy is segmenting networks to reduce the amount of data or systems one person or system can access. Educating staff about the dangers of phishing and spoofing emails also help protect organizations from ransomware attacks. Having staff avoid reusing passwords and updating logins and passwords frequently helps.
Most hospitals also need more robust security controls. Physicians and healthcare facilities must also embrace the cybersecurity controls found in other industries, said Witt. “Multifactor authentication is one of those things that can cause us frustration,” he said. “The controls can seem onerous, but they’re really valuable overall…and should become standard practice.”
Doctors can also prepare for a ransomware attack and protect patients by practicing some “old-school” medicine, like using paper systems and maintaining good patient notes — often, those notes are synced locally as well as offsite, so you’d be able to access them even during a data breach. “It’s smart to write prescriptions on pads sometimes,” said Radolec. “Don’t forget how to do those things because that will make you more resilient in the event of a ransomware attack.”
A Continuing Threat
Cyberattacks will continue. “When you look at the high likelihood [of success] and the soft target, you end up with ... a perfect storm,” said Radolec. “Hospitals have a lot of vulnerabilities. They have to keep operations going just to receive income, but also to deliver care to people.”
That means that the burden is on healthcare organizations — including physicians, nurses, staff, and C-level execs — to help keep the “security” in cybersecurity. “We are all part of the cybersecurity defense,” said Witt. Helping to maintain that defense has become a critical aspect of caring for patients.
A version of this article first appeared on Medscape.com.
On September 27, 2024, UMC Health System in Lubbock, Texas, experienced an IT outage because of a cybersecurity incident that temporarily diverted patients to other healthcare facilities. So far, in 2024, there have been 386 cyberattacks on healthcare organizations. These high-impact ransomware attacks disrupt and delay patient care.
In recent years, many healthcare systems, including Scripps Health, Universal Health Services, Vastaamo, Sky Lakes, and the University of Vermont, have paid millions — even tens of millions — to recover data after a cyberattack or data breach. When healthcare systems come under cyber fire, the impact extends far past disrupting workflows and compromising data, patient safety can be also be compromised, vital information may be lost, and imaging and lab results can go missing or be held for ransom, making physicians’ job difficult or impossible.
In fact, cyberattacks on hospitals are far more common than you may realize. A new report issued by Ponemon and Proofpoint found that 92% of healthcare organizations have experienced a cyberattack in the past 12 months. Even more sobering is that about half of the organizations affected suffered disruptions in patient care.
Healthcare Systems = ‘Soft Targets’
Healthcare systems are a “soft target” for hackers for several reasons, pointed out Matthew Radolec, vice president, incident response and cloud operations at Varonis, a data security company. “One, they’re usually an amalgamation of many healthcare systems that are interconnected,” said Radolec. “A lot of hospitals are connected to other hospitals or connected to educational institutions, which means their computer vulnerabilities are shared ... and if they have an issue, it could very easily spread to your network.”
Another factor is the cost of securing data. “[With hospitals], they’ll say that a dollar spent on security is a dollar not spent on patient care,” said Radolec. “So the idea of investing in security is really tough from a budget standpoint…they’re choosing between a new MRI machine or better antivirus, backups, or data security.”
Because of the wealth of private data and healthcare information they maintain, hospitals are considered “high impact” for cybercriminals. Attackers know that if they get a foothold in a hospital, it’s more likely to pay — and pay quickly, Radolec told this news organization. Hospitals are also likely to have cyber insurance to help cover the cost of having their data stolen, encrypted, and ransomed.
The 2024 Microsoft Digital Defense Report also found that the bad actors are more sophisticated and better resourced and can challenge even the best cybersecurity. Improved defenses may not be good enough, and the sheer volume of attacks must be met with effective deterrence and government solutions that impose consequences for cybercriminals.
Vulnerable Users
Whether through a phishing email or text, password attack, or web attack, “the moment a ‘threat actor’ gets into your institution and gets credentials ... that’s the Nirvana state of a threat actor,” warned Ryan Witt, chair of the healthcare customer advisory board and vice president of Industry Solutions at Proofpoint, a cybersecurity platform. “They have those credentials and will go into deep reconnaissance mode. It often takes healthcare up to 6 months to even ascertain whether somebody’s actually in the network.” During that time, the hacker is learning how the institution works, what job functions matter, and how best to plan their attack.
“Attackers are getting in because they’re buying databases of usernames and passwords. And they’re trying them by the millions,” added Radolec. “For a sophisticated actor, all it takes is time and motivation. They have the skills. It’s just a matter of how persistent they want to be.”
Certain hospital staff are also more likely to be targeted by cyberhackers than others. “About 10% of a healthcare organization’s user base is much more vulnerable for all sorts of reasons — how they work, the value of their job title and job function, and therefore their access to systems,” said Witt.
High-profile staff are more likely to be targeted than those in lower-level positions; the so-called “CEO attack” is typical. However, staff in other hospital departments are also subject to cybercriminals, including hospice departments/hospice organizations and research arms of hospitals.
The Impact of Cyberattacks on Patients
Physicians and healthcare execs may have considered cybersecurity more of a compliance issue than a true threat to patients in the past. But this attitude is rapidly changing. “We are starting to see a very clear connection between a cyber event and how it can impact patient care and patient safety,” said Witt.
According to the Proofpoint report, cyber breaches can severely affect patient care. In 2024:
- 56% of respondents saw a delay in patient tests/procedures
- 53% experienced increased patient complications from medical procedures
- 52% noted a longer patient length of stay
- 44% saw an increase in patient transfers to other facilities
- 28% had an increase in mortality rate
What Hospitals and Physicians Can Do
Fortunately, hospitals can take measures to better protect their data and their patients. One strategy is segmenting networks to reduce the amount of data or systems one person or system can access. Educating staff about the dangers of phishing and spoofing emails also help protect organizations from ransomware attacks. Having staff avoid reusing passwords and updating logins and passwords frequently helps.
Most hospitals also need more robust security controls. Physicians and healthcare facilities must also embrace the cybersecurity controls found in other industries, said Witt. “Multifactor authentication is one of those things that can cause us frustration,” he said. “The controls can seem onerous, but they’re really valuable overall…and should become standard practice.”
Doctors can also prepare for a ransomware attack and protect patients by practicing some “old-school” medicine, like using paper systems and maintaining good patient notes — often, those notes are synced locally as well as offsite, so you’d be able to access them even during a data breach. “It’s smart to write prescriptions on pads sometimes,” said Radolec. “Don’t forget how to do those things because that will make you more resilient in the event of a ransomware attack.”
A Continuing Threat
Cyberattacks will continue. “When you look at the high likelihood [of success] and the soft target, you end up with ... a perfect storm,” said Radolec. “Hospitals have a lot of vulnerabilities. They have to keep operations going just to receive income, but also to deliver care to people.”
That means that the burden is on healthcare organizations — including physicians, nurses, staff, and C-level execs — to help keep the “security” in cybersecurity. “We are all part of the cybersecurity defense,” said Witt. Helping to maintain that defense has become a critical aspect of caring for patients.
A version of this article first appeared on Medscape.com.
Postpartum Depression Common After Cesarean Delivery
TOPLINE:
About one in six women experience symptoms of postpartum depression (PPD) 2 months after cesarean delivery, with certain obstetric factors such as emergency cesarean delivery before labor, cesarean delivery after labor induction, lack of social support in the operating room, and severe postoperative pain influencing the risk.
METHODOLOGY:
- Researchers conducted a prospective ancillary cohort study of the Tranexamic Acid for Preventing Postpartum Hemorrhage after Cesarean Delivery (TRAAP2) trial to examine the prevalence of PPD 2 months after cesarean delivery and associated risk factors.
- A total of 2793 women (median age, 33.5 years) were included who had a cesarean delivery at 34 or more weeks of gestation; they completed the Edinburgh Postnatal Depression Scale (EPDS), a self-administered questionnaire, at 2 months after delivery.
- Information about the cesarean delivery, postpartum blood loss, immediate postpartum period, psychiatric history, and memories of delivery and postoperative pain were prospectively collected.
- Medical records were used to obtain details about characteristics of patients; 5.0% had a psychiatric history (2.4% composed of depression).
- The main endpoint was a positive screening for symptoms consistent with this depression — defined as a PPD diagnosis — 2 months after caesarian delivery, with an EPDS score of 13 or higher.
TAKEAWAY:
- The prevalence of a provisional PPD diagnosis at 2 months after cesarean delivery was 16.4% (95% CI, 14.9-18.0) with an EPDS score of 13 or higher and was 23.1% (95% CI, 21.4-24.9%) with a cutoff value of 11 or higher.
- Women who had an emergency cesarean delivery before labor had a higher risk for PPD than those who had a normal cesarean delivery before labor started (adjusted odds ratio [aOR], 1.70; 95% CI, 1.15-2.50); women who had started labor after induction but then had a cesarean delivery also had a higher risk for PPD than those who had a cesarean delivery before going into labor (aOR, 1.36; 95% CI, 1.03-1.84).
- Severe pain during the postpartum stay (aOR, 1.73; 95% CI, 1.32-2.26) and bad memories of delivery (aOR, 1.67; 95% CI, 1.14-2.45) were also risk factors for PPD.
- However, women who had social support in the operating room showed a 27% lower risk for PPD (P = .02).
IN PRACTICE:
“Identifying subgroups of women at risk for PPD based on aspects of their obstetric experience could help to screen for women who might benefit from early screening and interventions,” the authors wrote.
SOURCE:
This study was led by Alizée Froeliger, MD, MPH, of the Department of Obstetrics and Gynecology at Bordeaux University Hospital in France, and was published online in American Journal of Obstetrics & Gynecology.
LIMITATIONS:
The study population was derived from a randomized controlled trial, which may have underestimated the prevalence of PPD. The use of a self-administered questionnaire for PPD screening may not have provided a definitive diagnosis. Moreover, this study did not assess the prevalence of depressive symptoms during pregnancy.
DISCLOSURES:
The TRAAP2 trial was supported by a grant from the French Ministry of Health under its Clinical Research Hospital Program. One author reported carrying out consultancy work and lecturing for Ferring Laboratories, GlaxoSmithKline, and other pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
About one in six women experience symptoms of postpartum depression (PPD) 2 months after cesarean delivery, with certain obstetric factors such as emergency cesarean delivery before labor, cesarean delivery after labor induction, lack of social support in the operating room, and severe postoperative pain influencing the risk.
METHODOLOGY:
- Researchers conducted a prospective ancillary cohort study of the Tranexamic Acid for Preventing Postpartum Hemorrhage after Cesarean Delivery (TRAAP2) trial to examine the prevalence of PPD 2 months after cesarean delivery and associated risk factors.
- A total of 2793 women (median age, 33.5 years) were included who had a cesarean delivery at 34 or more weeks of gestation; they completed the Edinburgh Postnatal Depression Scale (EPDS), a self-administered questionnaire, at 2 months after delivery.
- Information about the cesarean delivery, postpartum blood loss, immediate postpartum period, psychiatric history, and memories of delivery and postoperative pain were prospectively collected.
- Medical records were used to obtain details about characteristics of patients; 5.0% had a psychiatric history (2.4% composed of depression).
- The main endpoint was a positive screening for symptoms consistent with this depression — defined as a PPD diagnosis — 2 months after caesarian delivery, with an EPDS score of 13 or higher.
TAKEAWAY:
- The prevalence of a provisional PPD diagnosis at 2 months after cesarean delivery was 16.4% (95% CI, 14.9-18.0) with an EPDS score of 13 or higher and was 23.1% (95% CI, 21.4-24.9%) with a cutoff value of 11 or higher.
- Women who had an emergency cesarean delivery before labor had a higher risk for PPD than those who had a normal cesarean delivery before labor started (adjusted odds ratio [aOR], 1.70; 95% CI, 1.15-2.50); women who had started labor after induction but then had a cesarean delivery also had a higher risk for PPD than those who had a cesarean delivery before going into labor (aOR, 1.36; 95% CI, 1.03-1.84).
- Severe pain during the postpartum stay (aOR, 1.73; 95% CI, 1.32-2.26) and bad memories of delivery (aOR, 1.67; 95% CI, 1.14-2.45) were also risk factors for PPD.
- However, women who had social support in the operating room showed a 27% lower risk for PPD (P = .02).
IN PRACTICE:
“Identifying subgroups of women at risk for PPD based on aspects of their obstetric experience could help to screen for women who might benefit from early screening and interventions,” the authors wrote.
SOURCE:
This study was led by Alizée Froeliger, MD, MPH, of the Department of Obstetrics and Gynecology at Bordeaux University Hospital in France, and was published online in American Journal of Obstetrics & Gynecology.
LIMITATIONS:
The study population was derived from a randomized controlled trial, which may have underestimated the prevalence of PPD. The use of a self-administered questionnaire for PPD screening may not have provided a definitive diagnosis. Moreover, this study did not assess the prevalence of depressive symptoms during pregnancy.
DISCLOSURES:
The TRAAP2 trial was supported by a grant from the French Ministry of Health under its Clinical Research Hospital Program. One author reported carrying out consultancy work and lecturing for Ferring Laboratories, GlaxoSmithKline, and other pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
About one in six women experience symptoms of postpartum depression (PPD) 2 months after cesarean delivery, with certain obstetric factors such as emergency cesarean delivery before labor, cesarean delivery after labor induction, lack of social support in the operating room, and severe postoperative pain influencing the risk.
METHODOLOGY:
- Researchers conducted a prospective ancillary cohort study of the Tranexamic Acid for Preventing Postpartum Hemorrhage after Cesarean Delivery (TRAAP2) trial to examine the prevalence of PPD 2 months after cesarean delivery and associated risk factors.
- A total of 2793 women (median age, 33.5 years) were included who had a cesarean delivery at 34 or more weeks of gestation; they completed the Edinburgh Postnatal Depression Scale (EPDS), a self-administered questionnaire, at 2 months after delivery.
- Information about the cesarean delivery, postpartum blood loss, immediate postpartum period, psychiatric history, and memories of delivery and postoperative pain were prospectively collected.
- Medical records were used to obtain details about characteristics of patients; 5.0% had a psychiatric history (2.4% composed of depression).
- The main endpoint was a positive screening for symptoms consistent with this depression — defined as a PPD diagnosis — 2 months after caesarian delivery, with an EPDS score of 13 or higher.
TAKEAWAY:
- The prevalence of a provisional PPD diagnosis at 2 months after cesarean delivery was 16.4% (95% CI, 14.9-18.0) with an EPDS score of 13 or higher and was 23.1% (95% CI, 21.4-24.9%) with a cutoff value of 11 or higher.
- Women who had an emergency cesarean delivery before labor had a higher risk for PPD than those who had a normal cesarean delivery before labor started (adjusted odds ratio [aOR], 1.70; 95% CI, 1.15-2.50); women who had started labor after induction but then had a cesarean delivery also had a higher risk for PPD than those who had a cesarean delivery before going into labor (aOR, 1.36; 95% CI, 1.03-1.84).
- Severe pain during the postpartum stay (aOR, 1.73; 95% CI, 1.32-2.26) and bad memories of delivery (aOR, 1.67; 95% CI, 1.14-2.45) were also risk factors for PPD.
- However, women who had social support in the operating room showed a 27% lower risk for PPD (P = .02).
IN PRACTICE:
“Identifying subgroups of women at risk for PPD based on aspects of their obstetric experience could help to screen for women who might benefit from early screening and interventions,” the authors wrote.
SOURCE:
This study was led by Alizée Froeliger, MD, MPH, of the Department of Obstetrics and Gynecology at Bordeaux University Hospital in France, and was published online in American Journal of Obstetrics & Gynecology.
LIMITATIONS:
The study population was derived from a randomized controlled trial, which may have underestimated the prevalence of PPD. The use of a self-administered questionnaire for PPD screening may not have provided a definitive diagnosis. Moreover, this study did not assess the prevalence of depressive symptoms during pregnancy.
DISCLOSURES:
The TRAAP2 trial was supported by a grant from the French Ministry of Health under its Clinical Research Hospital Program. One author reported carrying out consultancy work and lecturing for Ferring Laboratories, GlaxoSmithKline, and other pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
When Your Malpractice Insurer Investigates You: What to Know
When psychiatrist Paul Sartain, MD (not his real name), received a letter from his state’s medical board, he was concerned. A patient’s family complained that he made sexual advances to a young woman he treated for psychotic depression.
“There was absolutely no evidence, and the claims were vague,” he said. “I think the family was angry at me and with the system — the woman had not gotten better.” Sartain reviewed his medical records and then called his malpractice insurer.
The insurer asked about his involvement with the patient’s case, if there was anything credible to the patient’s complaint, and if he had thorough documentation. Then, the carrier offered Sartain his choice of several attorneys who could represent him. The medical board ultimately closed the case with no findings against him, and the patient’s family never sued him.
“If I’m wrongly accused, I’m defended (by the carrier). If I had stolen money or had a sexual relationship with the patient, then you’re acting outside the bounds of what is protected (by the carrier),” he said.
How Medical Board and Malpractice Insurer Investigations Differ
Medical board complaints differ from malpractice claims, in which patients seek damages. The investigation process also varies.
When a patient reports a doctor to a state medical board, they may also sue the doctor for monetary damages in civil court. The medical board responds to patient complaints made directly to them, but it also may also initiate its own investigations. Those can be prompted by a malpractice claim resolution, with a court verdict against the doctor, or a settlement recorded in the National Practitioner Data Bank.
Malpractice insurers may offer limited legal representation for medical board investigations, requiring the doctor to report the medical board issue to them before the doctor takes any action. Often, they will cover up to $50,000 in defense costs but not cover any subsequent medical board fines or required classes or medical board fees.
When a doctor contacts the carrier about a medical board investigation, the carrier may ask for the medical board document and the medical records, said Alex Keoskey, a partner in Frier Levitt’s life sciences group.
The carrier may want to ask about the patient, staff members involved, the doctor’s background, if there have been previous medical board investigations or lawsuits against this doctor, and the doctor’s opinion of the allegations. The doctor should be transparent with the carrier, Keoskey said.
Some carriers conduct more in-depth investigations, examining record-keeping, prescription practices, patient consent processes, and continuing medical education status. That’s because the medical board may inquire about these as well should its own investigation expand.
Not all carriers explore cases like these, even if reimbursing for defense costs, said Karen Frisella, director of professional liability claims at BETA Healthcare Group in California. In her experience, a licensing investigation usually follows a claim resolution that was already worked up by the carrier. If a complaint was made directly to the licensing board without an accompanying liability claim, the carrier’s ability to initiate an investigation on the incident depends on the policy terms or coverage available.
“Typically, a professional liability policy requires that the insured report a claim to trigger coverage. The carrier can’t unilaterally decide to open a claim,” she said. A licensing board investigation is not a claim by definition and therefore does not provide a mechanism for the carrier to open a liability claim file, she added.
If the medical board ultimately restricts the doctor’s license or puts the doctor on probation, that becomes public, and the underwriting department may then look into it.
Malpractice insurers routinely monitor licensing board discipline notices. A reprimand or restrictions on a doctor’s license could trigger a review of the physician’s future insurability and lead to higher premiums or even nonrenewal, Frisella said.
If a carrier investigates a reported claim and determines there are issues with the care rendered, whether there is an accompanying medical board action, that also can affect underwriting decisions, Frisella said.
Who Is Your Attorney Really Working for?
The doctor should understand whose interests the attorney represents. In a medical board claim, the attorney — even if defense is paid by the carrier — represents the doctor.
Frisella said her organization provides pass-through coverage, meaning it reimburses the doctor for medical board defense costs. “Because the carrier isn’t directing the medical board defense, it is not generally privy to the work product.”
If a patient files a malpractice claim, however, the attorney ultimately represents the insurance company.
“The panel counsel who works for the insurer does not work for the doctor, and that’s always important to remember,” Keoskey said. While the attorney will do their best to aggressively defend the doctor, “he’s going to protect the insurer’s interest before the doctor’s.”
Physicians who find any conflict of interest with their insurer should seek counsel.
Such conflicts could include:
- Disagreements over the case’s ultimate worth. For example, a physician might want a case to settle for less than their carrier is willing to pay.
- The legal judgment may exceed the carrier’s policy limits, or there are punitive damages or allegations of criminal acts that the insurer does not cover.
In these cases, the insurance company should recommend the doctor get personal counsel. They will send a reservation of rights letter saying they will defend the doctor for now, but if the facts show the doctor committed some type of misconduct, they may decline coverage, said Keoskey. Some states, including California, require that the carrier pay for this independent counsel.
Unless there is a conflict of interest, though, having a personal attorney just makes the situation more complicated, said Frisella.
A version of this article first appeared on Medscape.com.
When psychiatrist Paul Sartain, MD (not his real name), received a letter from his state’s medical board, he was concerned. A patient’s family complained that he made sexual advances to a young woman he treated for psychotic depression.
“There was absolutely no evidence, and the claims were vague,” he said. “I think the family was angry at me and with the system — the woman had not gotten better.” Sartain reviewed his medical records and then called his malpractice insurer.
The insurer asked about his involvement with the patient’s case, if there was anything credible to the patient’s complaint, and if he had thorough documentation. Then, the carrier offered Sartain his choice of several attorneys who could represent him. The medical board ultimately closed the case with no findings against him, and the patient’s family never sued him.
“If I’m wrongly accused, I’m defended (by the carrier). If I had stolen money or had a sexual relationship with the patient, then you’re acting outside the bounds of what is protected (by the carrier),” he said.
How Medical Board and Malpractice Insurer Investigations Differ
Medical board complaints differ from malpractice claims, in which patients seek damages. The investigation process also varies.
When a patient reports a doctor to a state medical board, they may also sue the doctor for monetary damages in civil court. The medical board responds to patient complaints made directly to them, but it also may also initiate its own investigations. Those can be prompted by a malpractice claim resolution, with a court verdict against the doctor, or a settlement recorded in the National Practitioner Data Bank.
Malpractice insurers may offer limited legal representation for medical board investigations, requiring the doctor to report the medical board issue to them before the doctor takes any action. Often, they will cover up to $50,000 in defense costs but not cover any subsequent medical board fines or required classes or medical board fees.
When a doctor contacts the carrier about a medical board investigation, the carrier may ask for the medical board document and the medical records, said Alex Keoskey, a partner in Frier Levitt’s life sciences group.
The carrier may want to ask about the patient, staff members involved, the doctor’s background, if there have been previous medical board investigations or lawsuits against this doctor, and the doctor’s opinion of the allegations. The doctor should be transparent with the carrier, Keoskey said.
Some carriers conduct more in-depth investigations, examining record-keeping, prescription practices, patient consent processes, and continuing medical education status. That’s because the medical board may inquire about these as well should its own investigation expand.
Not all carriers explore cases like these, even if reimbursing for defense costs, said Karen Frisella, director of professional liability claims at BETA Healthcare Group in California. In her experience, a licensing investigation usually follows a claim resolution that was already worked up by the carrier. If a complaint was made directly to the licensing board without an accompanying liability claim, the carrier’s ability to initiate an investigation on the incident depends on the policy terms or coverage available.
“Typically, a professional liability policy requires that the insured report a claim to trigger coverage. The carrier can’t unilaterally decide to open a claim,” she said. A licensing board investigation is not a claim by definition and therefore does not provide a mechanism for the carrier to open a liability claim file, she added.
If the medical board ultimately restricts the doctor’s license or puts the doctor on probation, that becomes public, and the underwriting department may then look into it.
Malpractice insurers routinely monitor licensing board discipline notices. A reprimand or restrictions on a doctor’s license could trigger a review of the physician’s future insurability and lead to higher premiums or even nonrenewal, Frisella said.
If a carrier investigates a reported claim and determines there are issues with the care rendered, whether there is an accompanying medical board action, that also can affect underwriting decisions, Frisella said.
Who Is Your Attorney Really Working for?
The doctor should understand whose interests the attorney represents. In a medical board claim, the attorney — even if defense is paid by the carrier — represents the doctor.
Frisella said her organization provides pass-through coverage, meaning it reimburses the doctor for medical board defense costs. “Because the carrier isn’t directing the medical board defense, it is not generally privy to the work product.”
If a patient files a malpractice claim, however, the attorney ultimately represents the insurance company.
“The panel counsel who works for the insurer does not work for the doctor, and that’s always important to remember,” Keoskey said. While the attorney will do their best to aggressively defend the doctor, “he’s going to protect the insurer’s interest before the doctor’s.”
Physicians who find any conflict of interest with their insurer should seek counsel.
Such conflicts could include:
- Disagreements over the case’s ultimate worth. For example, a physician might want a case to settle for less than their carrier is willing to pay.
- The legal judgment may exceed the carrier’s policy limits, or there are punitive damages or allegations of criminal acts that the insurer does not cover.
In these cases, the insurance company should recommend the doctor get personal counsel. They will send a reservation of rights letter saying they will defend the doctor for now, but if the facts show the doctor committed some type of misconduct, they may decline coverage, said Keoskey. Some states, including California, require that the carrier pay for this independent counsel.
Unless there is a conflict of interest, though, having a personal attorney just makes the situation more complicated, said Frisella.
A version of this article first appeared on Medscape.com.
When psychiatrist Paul Sartain, MD (not his real name), received a letter from his state’s medical board, he was concerned. A patient’s family complained that he made sexual advances to a young woman he treated for psychotic depression.
“There was absolutely no evidence, and the claims were vague,” he said. “I think the family was angry at me and with the system — the woman had not gotten better.” Sartain reviewed his medical records and then called his malpractice insurer.
The insurer asked about his involvement with the patient’s case, if there was anything credible to the patient’s complaint, and if he had thorough documentation. Then, the carrier offered Sartain his choice of several attorneys who could represent him. The medical board ultimately closed the case with no findings against him, and the patient’s family never sued him.
“If I’m wrongly accused, I’m defended (by the carrier). If I had stolen money or had a sexual relationship with the patient, then you’re acting outside the bounds of what is protected (by the carrier),” he said.
How Medical Board and Malpractice Insurer Investigations Differ
Medical board complaints differ from malpractice claims, in which patients seek damages. The investigation process also varies.
When a patient reports a doctor to a state medical board, they may also sue the doctor for monetary damages in civil court. The medical board responds to patient complaints made directly to them, but it also may also initiate its own investigations. Those can be prompted by a malpractice claim resolution, with a court verdict against the doctor, or a settlement recorded in the National Practitioner Data Bank.
Malpractice insurers may offer limited legal representation for medical board investigations, requiring the doctor to report the medical board issue to them before the doctor takes any action. Often, they will cover up to $50,000 in defense costs but not cover any subsequent medical board fines or required classes or medical board fees.
When a doctor contacts the carrier about a medical board investigation, the carrier may ask for the medical board document and the medical records, said Alex Keoskey, a partner in Frier Levitt’s life sciences group.
The carrier may want to ask about the patient, staff members involved, the doctor’s background, if there have been previous medical board investigations or lawsuits against this doctor, and the doctor’s opinion of the allegations. The doctor should be transparent with the carrier, Keoskey said.
Some carriers conduct more in-depth investigations, examining record-keeping, prescription practices, patient consent processes, and continuing medical education status. That’s because the medical board may inquire about these as well should its own investigation expand.
Not all carriers explore cases like these, even if reimbursing for defense costs, said Karen Frisella, director of professional liability claims at BETA Healthcare Group in California. In her experience, a licensing investigation usually follows a claim resolution that was already worked up by the carrier. If a complaint was made directly to the licensing board without an accompanying liability claim, the carrier’s ability to initiate an investigation on the incident depends on the policy terms or coverage available.
“Typically, a professional liability policy requires that the insured report a claim to trigger coverage. The carrier can’t unilaterally decide to open a claim,” she said. A licensing board investigation is not a claim by definition and therefore does not provide a mechanism for the carrier to open a liability claim file, she added.
If the medical board ultimately restricts the doctor’s license or puts the doctor on probation, that becomes public, and the underwriting department may then look into it.
Malpractice insurers routinely monitor licensing board discipline notices. A reprimand or restrictions on a doctor’s license could trigger a review of the physician’s future insurability and lead to higher premiums or even nonrenewal, Frisella said.
If a carrier investigates a reported claim and determines there are issues with the care rendered, whether there is an accompanying medical board action, that also can affect underwriting decisions, Frisella said.
Who Is Your Attorney Really Working for?
The doctor should understand whose interests the attorney represents. In a medical board claim, the attorney — even if defense is paid by the carrier — represents the doctor.
Frisella said her organization provides pass-through coverage, meaning it reimburses the doctor for medical board defense costs. “Because the carrier isn’t directing the medical board defense, it is not generally privy to the work product.”
If a patient files a malpractice claim, however, the attorney ultimately represents the insurance company.
“The panel counsel who works for the insurer does not work for the doctor, and that’s always important to remember,” Keoskey said. While the attorney will do their best to aggressively defend the doctor, “he’s going to protect the insurer’s interest before the doctor’s.”
Physicians who find any conflict of interest with their insurer should seek counsel.
Such conflicts could include:
- Disagreements over the case’s ultimate worth. For example, a physician might want a case to settle for less than their carrier is willing to pay.
- The legal judgment may exceed the carrier’s policy limits, or there are punitive damages or allegations of criminal acts that the insurer does not cover.
In these cases, the insurance company should recommend the doctor get personal counsel. They will send a reservation of rights letter saying they will defend the doctor for now, but if the facts show the doctor committed some type of misconduct, they may decline coverage, said Keoskey. Some states, including California, require that the carrier pay for this independent counsel.
Unless there is a conflict of interest, though, having a personal attorney just makes the situation more complicated, said Frisella.
A version of this article first appeared on Medscape.com.



