User login
Triple therapy: Boon or bane for high-risk CV patients?
• In a patient with a high risk of reinfarction, thienopyridine therapy (with clopidogrel or prasugrel) should be continued for at least a year. B
• Risk factors for reinfarction and stent thrombosis are the same ones that increase the risk of ACS initially, and include diabetes mellitus, heart failure, smoking, hyperlipidemia, and hypertension. A
• For patients who are good candidates for triple therapy but have an elevated bleeding risk, using a lower dose of aspirin or limiting thienopyridine use to one month may be a reasonable option. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Anthony D, a 61-year-old patient of yours with hypertension and diabetes, is admitted to the hospital with atrial fibrillation and chest pain that radiates to his left arm and hand. On Day 1, he receives aspirin 325 mg and enoxaparin 1 mg/kg; the following day, the patient receives a 600-mg loading dose of clopidogrel prior to catheterization. He undergoes percutaneous coronary intervention and a bare metal stent is placed in his circumflex artery.
The following day, Anthony is ready for discharge and you consider which maintenance drugs to put him on, given that he already takes multiple medications. Is he a candidate for triple therapy?
Triple therapy—the concurrent use of aspirin, a thienopyridine antiplatelet agent, and warfarin—is often prescribed for patients with atrial fibrillation who experience acute coronary syndrome (ACS) or require percutaneous coronary intervention with the placement of a stent (PCI-S). The danger associated with concomitantly treating a patient with 3 agents, each of which has a distinct mechanism that increases bleeding risk, is high, but for carefully selected patients, the benefit may outweigh the risk.
Several studies have evaluated triple therapy and compared it with single or dual therapy (TABLE).1-5 Due to a lack of robust outcome studies, however, the benefits and risks of triple therapy cannot be directly quantified, nor are they generalizable to all potential candidates for triple therapy. Thus, finding the optimal treatment for secondary prevention of ACS or prevention of stent thrombosis in a patient with atrial fibrillation requires an understanding of the potential consequences of triple therapy—and a thorough assessment of the patient’s risk of reinfarction, stroke, and bleeding complications.6-9 To make the best treatment decisions and provide adequate support to patients who were started on triple therapy during a recent hospitalization, here’s what you need to know.
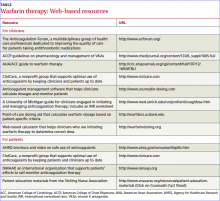
TABLE
Triple therapy: What the studies show
| Study type (N) | Intervention | Efficacy | Bleeding |
|---|---|---|---|
| Retrospective (124)1 | Group 1: Aspirin + clopidogrel + warfarin Group 2: Nontriple therapy | No significant difference | No significant difference in early major bleeding Group 1: Significant increase in late major bleeding |
| Retrospective (373)2 | Group 1: Anticoagulant + antithrombotic therapy* Group 2: Antithrombotic therapy only | Group 1: Significant improvement in efficacy Significant improvement in combination of efficacy and bleeding outcomes | Group 1: Significant improvement in combination of efficacy and bleeding outcomes |
| Cohort (800)3 | Group 1: Warfarin + single antiplatelet agent Group 2: Warfarin + dual antiplatelet therapy | No significant difference in mortality or MI | NR |
| Prospective (359)4 | Group 1: Continued OAC + dual antiplatelet therapy Group 2: Discontinued OAC but continued antiplatelet therapy | No significant difference | Group 1: Significant increase in moderate and severe bleeding |
| Cohort (82,854)5 | Group 1: Warfarin monotherapy Group 2: Aspirin monotherapy Group 3: Clopidogrel monotherapy Group 4: Clopidogrel + aspirin Group 5: Warfarin + aspirin Group 6: Warfarin + clopidogrel Group 7: Warfarin + aspirin + clopidogrel | No significant difference | Groups 6 and 7: Significant increase in crude incidence of bleeding |
| *50% of the participants in Group 1 received triple therapy (aspirin, clopidogrel, and warfarin). MI, myocardial infarction; NR, not reported; OAC, oral anticoagulant. | |||
First, a review of the components
Aspirin, a key component of triple therapy, is the only nonsteroidal anti-inflammatory drug (NSAID) indicated for primary or secondary prevention of cardiovascular events.10,11 The reason: Aspirin is more selective for cyclooxygenase-1 (COX-1) than other NSAIDs and irreversibly inhibits COX enzymes.11 The aspirin-induced decrease in thromboxane production leads to a decline in platelet activation and aggregation, which accounts both for aspirin’s beneficial cardiovascular effects and the associated risk of bleeding—aspirin’s most common adverse effect.12
Most major bleeds linked to aspirin use involve the gastrointestinal (GI) tract, primarily because of the drug’s direct and indirect effects on the GI mucosa.11-14 Aspirin’s toxicities are dose related, but its antiplatelet properties do not appear to be.14
Adding a thienopyridine
Thienopyridine antiplatelet drugs indicated for the secondary prevention of cardiovascular events after ACS or PCI-S include ticlopidine, clopidogrel, and prasugrel.15 Ticlopidine, the first such agent approved in the United States, is rarely used because of potential neutropenia and thrombotic thrombocytopenia purpura.16
Clopidogrel, the most commonly used agent for the purpose of secondary prevention, is the only thienopyridine with trial data for triple therapy.17 Clopidogrel’s antiplatelet effect, however, is highly dependent on specific cytochrome P-450 (CYP) enzymes for conversion to its active metabolite, and can be impaired by genetic variations in CYP 2C19, as well as by medication interactions. This has led to concern about the drug’s efficacy for secondary prevention of ACS.6,17,18 In 2010, the US Food and Drug Administration (FDA) added a black-box warning for clopidogrel, emphasizing the risk of myocardial infarction (MI), stroke, and cardiovascular death in patients with defective CYP 2C19 activity.19
Prasugrel, approved by the FDA in 2009,20 is useful for patients who respond poorly to clopidogrel. In fact, inadequate platelet inhibition with clopidogrel has prompted some physicians to choose prasugrel as a component of triple therapy.
While prasugrel may have greater efficacy compared with clopidogrel in preventing reinfarction, it appears to have a higher bleeding rate.15,17 Because of its bleeding profile, prasugrel is not recommended for patients >75 years unless they are at high risk for MI (prior MI or diabetes), and it is contraindicated for patients with a history of stroke. Caution is needed when prasugrel is prescribed for patients who weigh <132 lb (consider a maintenance dose of 5 mg/d rather than the usual 10 mg/d) or have an increased propensity to bleed.15
Warfarin provides the anticoagulant component of triple therapy
Until late last year, when dabigatran received FDA approval for use in stroke prevention,21 warfarin was the only oral anticoagulant available in the United States. (To learn more about dabigatran, which is not included in this review because of the lack of evidence regarding its use in triple therapy, see “Time to try this warfarin alternative?”.)
Because multiple drug, food, and disease state interactions can interfere with warfarin therapy, frequent monitoring to maintain a target international normalized ratio (INR) is required.22,23 (See Patient on warfarin? Steer clear of these drugs, in “Avoiding drug interactions: Here’s help,” J Fam Pract. 2010;59: 322-329).
Bridge therapy. Warfarin requires several days to reach its full effect, so anticoagulation with a more immediate-acting medication, such as a low-molecular-weight heparin or fondaparinux, is often used until the INR goal is reached.22,23 Thus, there are instances in which patients requiring triple therapy are actually receiving 4 drugs that increase bleeding risk.
When (or whether) to consider triple therapy
While triple therapy may be an option for patients with atrial fibrillation and ACS or PCI-S, there is no validated scoring system to aid in treatment decisions.24 As already noted, selecting the optimal therapy requires an individual assessment of the patient’s risk of reinfarction, stent thrombosis, stroke, and bleeding complications.
Risk factors for reinfarction and stent thrombosis are the same ones that increase the risk of ACS initially, and include diabetes mellitus, heart failure, smoking, hyperlipidemia, and hypertension.10,16 Advanced age; uncontrolled hypertension; chronic conditions such as peripheral vascular disease, anemia, and peptic ulcer disease; and a history of major bleeds are associated with an increased risk of bleeding. 24,25
In a retrospective trial evaluating independent predictors of major bleeding in patients with atrial fibrillation who underwent PCI-S,1 the researchers identified several factors that increased the risk of early major bleeding (within 48 hours of stent placement): the use of a glycoprotein IIb/IIIa inhibitor, stenting of ≥3 vessels, or left main artery disease. Factors that significantly increased the risk of major bleeding more than 48 hours after the procedure included triple therapy, an early major bleed, and baseline anemia.1
Drug combinations: What to consider
In addition to determining whether a patient is a good candidate for triple therapy, it is crucial to consider the choice of drugs. Benefits of prasugrel, compared with clopidogrel, include fewer drug interactions, less resistance to platelet inhibition, more rapid platelet inhibition after an oral loading dose, and higher levels of platelet inhibition during maintenance dosing.15,17
Improved outcomes are another potential benefit, according to TRITON-Thrombolysis in Myocardial Infarction (TIMI) 38,17 a large randomized prospective trial comparing the use of prasugrel with clopidogrel in triple therapy. Among study participants, the primary outcome rate—the combined incidence of death from cardiovascular causes, nonfatal MI, and nonfatal stroke—was 9.9% for those on prasugrel vs 12.1% for the clopidogrel group (hazard ratio [HR]=0.81; 95% confidence interval [CI], 0.73-0.90, P<.001).17 The rate of TIMI major bleeding, however, was higher among those on prasugrel (HR=1.32; 95% CI, 1.03-1.68, P=.03). The evidence suggests that for every 1000 patients treated with prasugrel vs clopidogrel, 24 primary outcomes would be prevented but there would be 10 additional bleeding events.17,26
CASE Anthony D’s risk for stroke, infarction, and stent thrombosis—based on his history of diabetes and hypertension, atrial fibrillation, and PCI-S—and absence of independent bleeding risk factors make him a good candidate for triple therapy. Because the patient is at high risk, the physician starts him on 2 anticoagulants—warfarin (5 mg at bedtime) and enoxaparin (125 mg every 12 hours)—on the evening of his second day in the hospital. On Day 3, clinicians test Anthony’s prothrombin time/international normalized ratio (PT/INR) and P2Y12 function assay, which measure 14.9/1.1 and 8% platelet inhibition, respectively.
The patient is discharged on the following medication schedule: enoxaparin 125 mg every 12 hours, to be discontinued after 3 days; warfarin 5 mg daily, prasugrel 10 mg daily, and aspirin 81 mg daily; metoprolol succinate 100 mg daily; lisinopril 10 mg daily; rosuvastatin 10 mg daily; glyburide-metformin 5 mg/500 mg, 2 tablets twice daily; and insulin glargine 20 units at bedtime.
Safety and efficacy: Do the benefits outweigh the risk?
Safety is central to the continuing controversy surrounding the use of triple therapy.6,9 To date, however, no randomized prospective studies have evaluated its benefits and risks.
Numerous retrospective studies and case series have assessed the risk of bleeding associated with triple therapy.6 Several studies compared triple therapy with dual antiplatelet therapy without anticoagulation, and found a several-fold increase in both major and minor bleeding events in the triple therapy group.6
Few trials have assessed both the safety and the efficacy of triple therapy, however. One exception is a large retrospective trial, published in 2008.2 The researchers found that triple therapy significantly reduced the incidence of major cardiac events (death, acute MI, and target lesion revascularization); all-cause mortality; and major adverse effects (ie, any major cardiovascular event, major bleeding complication, and/or stroke), with no statistically significant increase in major bleeding events compared with patients on antiplatelet therapy without anticoagulation.2
The results of this trial, like those of other studies evaluating triple therapy, were weakened by variance in both the duration of antithrombotic therapy and the drug therapies studied. This limitation was off set, however, by multivariant analysis and well-documented follow-up.2 Despite the researchers’ findings, however, the results of other trials (and our knowledge of the mechanisms of action of the drug components) suggest that triple therapy significantly increases bleeding risk. For patients who would likely benefit from it but face an increased bleeding risk, there are ways to mitigate risk.
Prescribing triple therapy, while mitigating the risks
If bleeding is a serious concern in a patient who would benefit from triple therapy, the drug regimen may be adjusted. Options include:
- targeting a lower INR (2.0-2.5 vs the standard 2.0-3.0).6 While various trials have found a 2.0 to 3.0 range to reduce the risk of stroke, none has compared it with a lower range to evaluate reduction in bleeding risk.27 One potential benefit of trying to maintain a lower INR is the decrease in deviations into the 3.0 to 4.0 range, which is associated with an increased bleeding risk.28 However, lowering the INR target is not supported by any literature.1,18
- using low-dose aspirin therapy after PCI-S
- limiting the thienopyridine component of triple therapy to one month after ACS or PCI-S.6
When the risks of triple therapy outweigh the benefits because of an exceedingly high bleeding risk, single antiplatelet therapy with warfarin is another option to consider.
CASE [H17012] Anthony D’s discharge instructions called for an 81 mg daily dose of aspirin, as opposed to the 325-mg dose for the first 3 months of triple therapy after stent placement recommended by the American College of Cardiology/American Heart Association (ACC/AHA) guidelines for unstable angina/ non-ST segment elevated MI.1 Although the patient had no independent bleeding risk, his physician selected the lower dose of aspirin to mitigate the increased bleeding risk posed by the use of prasugrel as a component of triple therapy.6
Lower aspirin dose. Pharmacodynamic studies support the use of a lower dose of aspirin, finding that serum thromboxane is completely inhibited by a maintenance dose as low as 30 mg/d in healthy individuals and 50 mg/d for those with chronic stable angina.14 Using low-dose aspirin for the secondary prevention of ACS when triple therapy is indicated is likely to reduce GI toxicities as well as bleeding risk.
Reduce the duration of dual antiplatelet therapy. According to the ACC/AHA guidelines, thienopyridine therapy can be limited to one month in patients who are medically managed or have had a bare metal stent placed if there is concern about the patient’s risk of bleeding.6,10 Based on the findings of the one study that found triple therapy to be an independent predictor of major bleeds, this approach seems reasonable.1 It is called into question, however, by another recent trial, which found that patients on dual antiplatelet therapy for one year (vs one month) had a statistically significant improvement in cardiovascular outcomes.16
Before limiting a patient’s thienopyridine therapy to one month, consider his or her risk of reinfarction. If it is high, continuing the thienopyridine for at least one year is likely to provide the most benefit.
The largest triple therapy trial to date compared the efficacy of triple therapy vs dual therapy (a single antiplatelet agent plus warfarin) in patients with ACS and an indication for warfarin therapy.3 This trial found no statistically significant differences in the combined occurrence of death, stroke, unscheduled PCI, and MI between the 2 treatment groups. (Bleeding risk was not evaluated.) Stroke was significantly increased in the group that received therapy with warfarin and a single antiplatelet agent, with this caveat: The occurrence of stroke was so low overall that no conclusions could be reached from this difference.3
One problem with this trial, and with others evaluating triple therapy, has to do with the lack of consistency, as well as the duration. The warfarin and single antiplatelet group, for example, may have included patients who were receiving only warfarin, aspirin, or clopidogrel by 6 months after initiating treatment.3 Thus, although reinfarction or stent thrombosis after ACS or PCI-S typically occurs within the first few months, any triple therapy trial that lasts less than a year is likely to report skewed results. JFP
CORRESPONDENCE
Haley M. Phillippe, PharmD, BCPS, Auburn University Harrison School of Pharmacy, University of Alabama Birmingham School of Medicine?Huntsville, 301 Governors Drive, Huntsville, AL 35801; mccrahl@auburn.edu
1. Manzano-Fernandez S, Pastor FJ, Marin F, et al. Increased major bleeding complications related to triple antithrombotic therapy usage in patients with atrial fibrillation undergoing percutaneous coronary artery stenting. Chest. 2008;134:559-567.
2. Ruiz-Nodar JM, Marin F, Hurtado JA, et al. Anticoagulant and antiplatelet therapy use in 426 patients with atrial fibrillation undergoing percutaneous coronary intervention and stent implantation. J Am Coll Cardiol. 2008;51:818-25.
3. Nguyen MC, Lim YL, Walton A, et al. Combining warfarin and antiplatelet therapy after coronary stenting in the Global Registry of Acute Coronary Events: is it safe and effective to use just one antiplatelet agent? Eur Heart J. 2007;28:1717-1722.
4. Gilard M, Blanchard D, Helft G, et al. Antiplatelet therapy in patients with anticoagulants undergoing percutaneous coronary stenting (from STENTIng and oral anticoagulants [STENTICO]). Am J Cardiol. 2009;104:338-342.
5. Hansen ML, Sorensent R, Clausen MT, et al. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med. 2010;170:1433-1441.
6. Hermosillo AJ, Spinler SA. Aspirin, clopidogrel, and warfarin: is the combination appropriate and effective or inappropriate and too dangerous? Ann Pharmacother 2008;42:790-805.
7. Rothberg MB, Celestin C, Fiore LD, et al. Warfarin plus aspirin after myocardial infarction or the acute coronary syndrome: meta-analysis with estimates of risk and benefit. Ann Intern Med. 2005;143:241-250.
8. Eikelboom JM, Hirsh J. Combined antiplatelet and anticoagulant therapy: clinical benefits and risks. J Thromb Haemost. 2007;5:255-263.
9. Triple antithrombotic therapy Pharm Lett/Prescr Lett. 2009;25:250901.-
10. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. ACC/AHA guideline revision. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction. J Am Coll Cardiol. 2007;50:e1-e157.
11. Furst DE, Ulrich RW. Nonsteroidal anti-inflammatory drugs, disease-modifying antirheumatic drugs, nonopioid analgesics, and drugs used in gout. In: Katzung BG. Basic and Clinical Pharmacology. New York: McGraw Hill; 2008;573-598.
12. Smyth EM, FitzGerald GA. The eicosanoids: prostaglandins, thromboxanes, leukotrienes, and related compounds. In: Katzung BG. Basic and Clinical Pharmacology. New York: McGraw Hill; 2008;293-308.
13. Steinhubl SR, Bhatt DL, Brennan DM, et al. Aspirin to prevent cardiovascular disease: the association of aspirin dose and clopidogrel with thrombosis and bleeding. Ann Intern Med. 2009;150:379-386.
14. Campbell CL, Smyth S, Montalescot G, et al. Aspirin dose for the prevention of cardiovascular disease: a systematic review. JAMA. 2007;297:2018-2024.
15. Lexi-Comp [database online]. Hudson, OH: Lexi-Comp, Inc. Copyright 1978-2007. Available at: http://www.crlonline.com/crlsql/servlet/crlonline. Accessed November 5, 2010.
16. Spinler SA, Rees C. Review of Prasugrel for the secondary prevention of atherothrombosis. J Manag Care Pharm. 2009;15:383-95.
17. Spinler SA, Denus SD, et al. Acute coronary syndromes. In: Dipiro JT, Talbert RL, Yee GC, Pharmacotherapy: A Pathophysiologic Approach. New York: McGraw Hill; 2008;249-277.
18. Plavix [package insert]. Bridgewater, NJ: Bristol-Myers Squibb/ Sanofi Pharmaceuticals Partnership; 2010.
19. US Food and Drug Administration. FDA announces new boxed warning on Plavix. March 12, 2010. Available at: http://www.fda.gov/NewsEvents/Newsroom/Press Announcements/ucm204253.htm. Accessed March 11, 2011.
20. US Food and Drug Administration. FDA approves Effient to reduce the risk of heart attack in angioplasty patients. July 10, 2009. Available at: http://www.fda.gov/NewsEvents/News-room/PressAnnouncements/ucm171497.htm. Accessed March 11, 2011.
21. US Food and Drug Administration. FDA approves Pradaxa to prevent stroke in people with atrial fibrillation. October 19, 2010. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm230241.htm. Accessed March 11, 2011.
22. Ansell J, Hirsh J, Hylek E, et al. Pharmacology and management of the vitamin K antagonists. American College of Chest Physicians Evidence-Based Clinical Guidelines (8Th edition). Chest. 2008;133(suppl):160S-198S.
23. Haines ST, Witt DM, Nutescu EA. Venous thromboembolism. In: Dipiro JT, Talbert RL, Yee GC, et al. Pharmacotherapy: A Pathophysiologic Approach. New York: McGraw Hill; 2008;331-369.
24. Lip G. The balance between stroke prevention and bleeding risk in atrial fibrillation: a delicate balance revisited. Stroke. 2008;39:1406-1408.
25. The Warfarin Antiplatelet Vascular Evaluation Trial Investigators. Oral anticoagulant and antiplatelet therapy and peripheral arterial disease. N Engl J Med. 2007;357:217-227.
26. Schafer JA, Kjesbo NK, Gleason PP. Critical review of prasugrel for formulary decision makers. J Manag Care Pharm. 2009;15:335-343.
27. Singer DE, Albers GW, Dalen JE, et al. Antithrombotic therapy in atrial fibrillation. Chest. 2008;133(suppl):546S-592S.
28. Price MJ. Bedside evaluation of thienopyridine antiplatelet therapy. Circulation. 2009;119:2625-2632.
• In a patient with a high risk of reinfarction, thienopyridine therapy (with clopidogrel or prasugrel) should be continued for at least a year. B
• Risk factors for reinfarction and stent thrombosis are the same ones that increase the risk of ACS initially, and include diabetes mellitus, heart failure, smoking, hyperlipidemia, and hypertension. A
• For patients who are good candidates for triple therapy but have an elevated bleeding risk, using a lower dose of aspirin or limiting thienopyridine use to one month may be a reasonable option. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Anthony D, a 61-year-old patient of yours with hypertension and diabetes, is admitted to the hospital with atrial fibrillation and chest pain that radiates to his left arm and hand. On Day 1, he receives aspirin 325 mg and enoxaparin 1 mg/kg; the following day, the patient receives a 600-mg loading dose of clopidogrel prior to catheterization. He undergoes percutaneous coronary intervention and a bare metal stent is placed in his circumflex artery.
The following day, Anthony is ready for discharge and you consider which maintenance drugs to put him on, given that he already takes multiple medications. Is he a candidate for triple therapy?
Triple therapy—the concurrent use of aspirin, a thienopyridine antiplatelet agent, and warfarin—is often prescribed for patients with atrial fibrillation who experience acute coronary syndrome (ACS) or require percutaneous coronary intervention with the placement of a stent (PCI-S). The danger associated with concomitantly treating a patient with 3 agents, each of which has a distinct mechanism that increases bleeding risk, is high, but for carefully selected patients, the benefit may outweigh the risk.
Several studies have evaluated triple therapy and compared it with single or dual therapy (TABLE).1-5 Due to a lack of robust outcome studies, however, the benefits and risks of triple therapy cannot be directly quantified, nor are they generalizable to all potential candidates for triple therapy. Thus, finding the optimal treatment for secondary prevention of ACS or prevention of stent thrombosis in a patient with atrial fibrillation requires an understanding of the potential consequences of triple therapy—and a thorough assessment of the patient’s risk of reinfarction, stroke, and bleeding complications.6-9 To make the best treatment decisions and provide adequate support to patients who were started on triple therapy during a recent hospitalization, here’s what you need to know.
TABLE
Triple therapy: What the studies show
| Study type (N) | Intervention | Efficacy | Bleeding |
|---|---|---|---|
| Retrospective (124)1 | Group 1: Aspirin + clopidogrel + warfarin Group 2: Nontriple therapy | No significant difference | No significant difference in early major bleeding Group 1: Significant increase in late major bleeding |
| Retrospective (373)2 | Group 1: Anticoagulant + antithrombotic therapy* Group 2: Antithrombotic therapy only | Group 1: Significant improvement in efficacy Significant improvement in combination of efficacy and bleeding outcomes | Group 1: Significant improvement in combination of efficacy and bleeding outcomes |
| Cohort (800)3 | Group 1: Warfarin + single antiplatelet agent Group 2: Warfarin + dual antiplatelet therapy | No significant difference in mortality or MI | NR |
| Prospective (359)4 | Group 1: Continued OAC + dual antiplatelet therapy Group 2: Discontinued OAC but continued antiplatelet therapy | No significant difference | Group 1: Significant increase in moderate and severe bleeding |
| Cohort (82,854)5 | Group 1: Warfarin monotherapy Group 2: Aspirin monotherapy Group 3: Clopidogrel monotherapy Group 4: Clopidogrel + aspirin Group 5: Warfarin + aspirin Group 6: Warfarin + clopidogrel Group 7: Warfarin + aspirin + clopidogrel | No significant difference | Groups 6 and 7: Significant increase in crude incidence of bleeding |
| *50% of the participants in Group 1 received triple therapy (aspirin, clopidogrel, and warfarin). MI, myocardial infarction; NR, not reported; OAC, oral anticoagulant. | |||
First, a review of the components
Aspirin, a key component of triple therapy, is the only nonsteroidal anti-inflammatory drug (NSAID) indicated for primary or secondary prevention of cardiovascular events.10,11 The reason: Aspirin is more selective for cyclooxygenase-1 (COX-1) than other NSAIDs and irreversibly inhibits COX enzymes.11 The aspirin-induced decrease in thromboxane production leads to a decline in platelet activation and aggregation, which accounts both for aspirin’s beneficial cardiovascular effects and the associated risk of bleeding—aspirin’s most common adverse effect.12
Most major bleeds linked to aspirin use involve the gastrointestinal (GI) tract, primarily because of the drug’s direct and indirect effects on the GI mucosa.11-14 Aspirin’s toxicities are dose related, but its antiplatelet properties do not appear to be.14
Adding a thienopyridine
Thienopyridine antiplatelet drugs indicated for the secondary prevention of cardiovascular events after ACS or PCI-S include ticlopidine, clopidogrel, and prasugrel.15 Ticlopidine, the first such agent approved in the United States, is rarely used because of potential neutropenia and thrombotic thrombocytopenia purpura.16
Clopidogrel, the most commonly used agent for the purpose of secondary prevention, is the only thienopyridine with trial data for triple therapy.17 Clopidogrel’s antiplatelet effect, however, is highly dependent on specific cytochrome P-450 (CYP) enzymes for conversion to its active metabolite, and can be impaired by genetic variations in CYP 2C19, as well as by medication interactions. This has led to concern about the drug’s efficacy for secondary prevention of ACS.6,17,18 In 2010, the US Food and Drug Administration (FDA) added a black-box warning for clopidogrel, emphasizing the risk of myocardial infarction (MI), stroke, and cardiovascular death in patients with defective CYP 2C19 activity.19
Prasugrel, approved by the FDA in 2009,20 is useful for patients who respond poorly to clopidogrel. In fact, inadequate platelet inhibition with clopidogrel has prompted some physicians to choose prasugrel as a component of triple therapy.
While prasugrel may have greater efficacy compared with clopidogrel in preventing reinfarction, it appears to have a higher bleeding rate.15,17 Because of its bleeding profile, prasugrel is not recommended for patients >75 years unless they are at high risk for MI (prior MI or diabetes), and it is contraindicated for patients with a history of stroke. Caution is needed when prasugrel is prescribed for patients who weigh <132 lb (consider a maintenance dose of 5 mg/d rather than the usual 10 mg/d) or have an increased propensity to bleed.15
Warfarin provides the anticoagulant component of triple therapy
Until late last year, when dabigatran received FDA approval for use in stroke prevention,21 warfarin was the only oral anticoagulant available in the United States. (To learn more about dabigatran, which is not included in this review because of the lack of evidence regarding its use in triple therapy, see “Time to try this warfarin alternative?”.)
Because multiple drug, food, and disease state interactions can interfere with warfarin therapy, frequent monitoring to maintain a target international normalized ratio (INR) is required.22,23 (See Patient on warfarin? Steer clear of these drugs, in “Avoiding drug interactions: Here’s help,” J Fam Pract. 2010;59: 322-329).
Bridge therapy. Warfarin requires several days to reach its full effect, so anticoagulation with a more immediate-acting medication, such as a low-molecular-weight heparin or fondaparinux, is often used until the INR goal is reached.22,23 Thus, there are instances in which patients requiring triple therapy are actually receiving 4 drugs that increase bleeding risk.
When (or whether) to consider triple therapy
While triple therapy may be an option for patients with atrial fibrillation and ACS or PCI-S, there is no validated scoring system to aid in treatment decisions.24 As already noted, selecting the optimal therapy requires an individual assessment of the patient’s risk of reinfarction, stent thrombosis, stroke, and bleeding complications.
Risk factors for reinfarction and stent thrombosis are the same ones that increase the risk of ACS initially, and include diabetes mellitus, heart failure, smoking, hyperlipidemia, and hypertension.10,16 Advanced age; uncontrolled hypertension; chronic conditions such as peripheral vascular disease, anemia, and peptic ulcer disease; and a history of major bleeds are associated with an increased risk of bleeding. 24,25
In a retrospective trial evaluating independent predictors of major bleeding in patients with atrial fibrillation who underwent PCI-S,1 the researchers identified several factors that increased the risk of early major bleeding (within 48 hours of stent placement): the use of a glycoprotein IIb/IIIa inhibitor, stenting of ≥3 vessels, or left main artery disease. Factors that significantly increased the risk of major bleeding more than 48 hours after the procedure included triple therapy, an early major bleed, and baseline anemia.1
Drug combinations: What to consider
In addition to determining whether a patient is a good candidate for triple therapy, it is crucial to consider the choice of drugs. Benefits of prasugrel, compared with clopidogrel, include fewer drug interactions, less resistance to platelet inhibition, more rapid platelet inhibition after an oral loading dose, and higher levels of platelet inhibition during maintenance dosing.15,17
Improved outcomes are another potential benefit, according to TRITON-Thrombolysis in Myocardial Infarction (TIMI) 38,17 a large randomized prospective trial comparing the use of prasugrel with clopidogrel in triple therapy. Among study participants, the primary outcome rate—the combined incidence of death from cardiovascular causes, nonfatal MI, and nonfatal stroke—was 9.9% for those on prasugrel vs 12.1% for the clopidogrel group (hazard ratio [HR]=0.81; 95% confidence interval [CI], 0.73-0.90, P<.001).17 The rate of TIMI major bleeding, however, was higher among those on prasugrel (HR=1.32; 95% CI, 1.03-1.68, P=.03). The evidence suggests that for every 1000 patients treated with prasugrel vs clopidogrel, 24 primary outcomes would be prevented but there would be 10 additional bleeding events.17,26
CASE Anthony D’s risk for stroke, infarction, and stent thrombosis—based on his history of diabetes and hypertension, atrial fibrillation, and PCI-S—and absence of independent bleeding risk factors make him a good candidate for triple therapy. Because the patient is at high risk, the physician starts him on 2 anticoagulants—warfarin (5 mg at bedtime) and enoxaparin (125 mg every 12 hours)—on the evening of his second day in the hospital. On Day 3, clinicians test Anthony’s prothrombin time/international normalized ratio (PT/INR) and P2Y12 function assay, which measure 14.9/1.1 and 8% platelet inhibition, respectively.
The patient is discharged on the following medication schedule: enoxaparin 125 mg every 12 hours, to be discontinued after 3 days; warfarin 5 mg daily, prasugrel 10 mg daily, and aspirin 81 mg daily; metoprolol succinate 100 mg daily; lisinopril 10 mg daily; rosuvastatin 10 mg daily; glyburide-metformin 5 mg/500 mg, 2 tablets twice daily; and insulin glargine 20 units at bedtime.
Safety and efficacy: Do the benefits outweigh the risk?
Safety is central to the continuing controversy surrounding the use of triple therapy.6,9 To date, however, no randomized prospective studies have evaluated its benefits and risks.
Numerous retrospective studies and case series have assessed the risk of bleeding associated with triple therapy.6 Several studies compared triple therapy with dual antiplatelet therapy without anticoagulation, and found a several-fold increase in both major and minor bleeding events in the triple therapy group.6
Few trials have assessed both the safety and the efficacy of triple therapy, however. One exception is a large retrospective trial, published in 2008.2 The researchers found that triple therapy significantly reduced the incidence of major cardiac events (death, acute MI, and target lesion revascularization); all-cause mortality; and major adverse effects (ie, any major cardiovascular event, major bleeding complication, and/or stroke), with no statistically significant increase in major bleeding events compared with patients on antiplatelet therapy without anticoagulation.2
The results of this trial, like those of other studies evaluating triple therapy, were weakened by variance in both the duration of antithrombotic therapy and the drug therapies studied. This limitation was off set, however, by multivariant analysis and well-documented follow-up.2 Despite the researchers’ findings, however, the results of other trials (and our knowledge of the mechanisms of action of the drug components) suggest that triple therapy significantly increases bleeding risk. For patients who would likely benefit from it but face an increased bleeding risk, there are ways to mitigate risk.
Prescribing triple therapy, while mitigating the risks
If bleeding is a serious concern in a patient who would benefit from triple therapy, the drug regimen may be adjusted. Options include:
- targeting a lower INR (2.0-2.5 vs the standard 2.0-3.0).6 While various trials have found a 2.0 to 3.0 range to reduce the risk of stroke, none has compared it with a lower range to evaluate reduction in bleeding risk.27 One potential benefit of trying to maintain a lower INR is the decrease in deviations into the 3.0 to 4.0 range, which is associated with an increased bleeding risk.28 However, lowering the INR target is not supported by any literature.1,18
- using low-dose aspirin therapy after PCI-S
- limiting the thienopyridine component of triple therapy to one month after ACS or PCI-S.6
When the risks of triple therapy outweigh the benefits because of an exceedingly high bleeding risk, single antiplatelet therapy with warfarin is another option to consider.
CASE [H17012] Anthony D’s discharge instructions called for an 81 mg daily dose of aspirin, as opposed to the 325-mg dose for the first 3 months of triple therapy after stent placement recommended by the American College of Cardiology/American Heart Association (ACC/AHA) guidelines for unstable angina/ non-ST segment elevated MI.1 Although the patient had no independent bleeding risk, his physician selected the lower dose of aspirin to mitigate the increased bleeding risk posed by the use of prasugrel as a component of triple therapy.6
Lower aspirin dose. Pharmacodynamic studies support the use of a lower dose of aspirin, finding that serum thromboxane is completely inhibited by a maintenance dose as low as 30 mg/d in healthy individuals and 50 mg/d for those with chronic stable angina.14 Using low-dose aspirin for the secondary prevention of ACS when triple therapy is indicated is likely to reduce GI toxicities as well as bleeding risk.
Reduce the duration of dual antiplatelet therapy. According to the ACC/AHA guidelines, thienopyridine therapy can be limited to one month in patients who are medically managed or have had a bare metal stent placed if there is concern about the patient’s risk of bleeding.6,10 Based on the findings of the one study that found triple therapy to be an independent predictor of major bleeds, this approach seems reasonable.1 It is called into question, however, by another recent trial, which found that patients on dual antiplatelet therapy for one year (vs one month) had a statistically significant improvement in cardiovascular outcomes.16
Before limiting a patient’s thienopyridine therapy to one month, consider his or her risk of reinfarction. If it is high, continuing the thienopyridine for at least one year is likely to provide the most benefit.
The largest triple therapy trial to date compared the efficacy of triple therapy vs dual therapy (a single antiplatelet agent plus warfarin) in patients with ACS and an indication for warfarin therapy.3 This trial found no statistically significant differences in the combined occurrence of death, stroke, unscheduled PCI, and MI between the 2 treatment groups. (Bleeding risk was not evaluated.) Stroke was significantly increased in the group that received therapy with warfarin and a single antiplatelet agent, with this caveat: The occurrence of stroke was so low overall that no conclusions could be reached from this difference.3
One problem with this trial, and with others evaluating triple therapy, has to do with the lack of consistency, as well as the duration. The warfarin and single antiplatelet group, for example, may have included patients who were receiving only warfarin, aspirin, or clopidogrel by 6 months after initiating treatment.3 Thus, although reinfarction or stent thrombosis after ACS or PCI-S typically occurs within the first few months, any triple therapy trial that lasts less than a year is likely to report skewed results. JFP
CORRESPONDENCE
Haley M. Phillippe, PharmD, BCPS, Auburn University Harrison School of Pharmacy, University of Alabama Birmingham School of Medicine?Huntsville, 301 Governors Drive, Huntsville, AL 35801; mccrahl@auburn.edu
• In a patient with a high risk of reinfarction, thienopyridine therapy (with clopidogrel or prasugrel) should be continued for at least a year. B
• Risk factors for reinfarction and stent thrombosis are the same ones that increase the risk of ACS initially, and include diabetes mellitus, heart failure, smoking, hyperlipidemia, and hypertension. A
• For patients who are good candidates for triple therapy but have an elevated bleeding risk, using a lower dose of aspirin or limiting thienopyridine use to one month may be a reasonable option. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Anthony D, a 61-year-old patient of yours with hypertension and diabetes, is admitted to the hospital with atrial fibrillation and chest pain that radiates to his left arm and hand. On Day 1, he receives aspirin 325 mg and enoxaparin 1 mg/kg; the following day, the patient receives a 600-mg loading dose of clopidogrel prior to catheterization. He undergoes percutaneous coronary intervention and a bare metal stent is placed in his circumflex artery.
The following day, Anthony is ready for discharge and you consider which maintenance drugs to put him on, given that he already takes multiple medications. Is he a candidate for triple therapy?
Triple therapy—the concurrent use of aspirin, a thienopyridine antiplatelet agent, and warfarin—is often prescribed for patients with atrial fibrillation who experience acute coronary syndrome (ACS) or require percutaneous coronary intervention with the placement of a stent (PCI-S). The danger associated with concomitantly treating a patient with 3 agents, each of which has a distinct mechanism that increases bleeding risk, is high, but for carefully selected patients, the benefit may outweigh the risk.
Several studies have evaluated triple therapy and compared it with single or dual therapy (TABLE).1-5 Due to a lack of robust outcome studies, however, the benefits and risks of triple therapy cannot be directly quantified, nor are they generalizable to all potential candidates for triple therapy. Thus, finding the optimal treatment for secondary prevention of ACS or prevention of stent thrombosis in a patient with atrial fibrillation requires an understanding of the potential consequences of triple therapy—and a thorough assessment of the patient’s risk of reinfarction, stroke, and bleeding complications.6-9 To make the best treatment decisions and provide adequate support to patients who were started on triple therapy during a recent hospitalization, here’s what you need to know.
TABLE
Triple therapy: What the studies show
| Study type (N) | Intervention | Efficacy | Bleeding |
|---|---|---|---|
| Retrospective (124)1 | Group 1: Aspirin + clopidogrel + warfarin Group 2: Nontriple therapy | No significant difference | No significant difference in early major bleeding Group 1: Significant increase in late major bleeding |
| Retrospective (373)2 | Group 1: Anticoagulant + antithrombotic therapy* Group 2: Antithrombotic therapy only | Group 1: Significant improvement in efficacy Significant improvement in combination of efficacy and bleeding outcomes | Group 1: Significant improvement in combination of efficacy and bleeding outcomes |
| Cohort (800)3 | Group 1: Warfarin + single antiplatelet agent Group 2: Warfarin + dual antiplatelet therapy | No significant difference in mortality or MI | NR |
| Prospective (359)4 | Group 1: Continued OAC + dual antiplatelet therapy Group 2: Discontinued OAC but continued antiplatelet therapy | No significant difference | Group 1: Significant increase in moderate and severe bleeding |
| Cohort (82,854)5 | Group 1: Warfarin monotherapy Group 2: Aspirin monotherapy Group 3: Clopidogrel monotherapy Group 4: Clopidogrel + aspirin Group 5: Warfarin + aspirin Group 6: Warfarin + clopidogrel Group 7: Warfarin + aspirin + clopidogrel | No significant difference | Groups 6 and 7: Significant increase in crude incidence of bleeding |
| *50% of the participants in Group 1 received triple therapy (aspirin, clopidogrel, and warfarin). MI, myocardial infarction; NR, not reported; OAC, oral anticoagulant. | |||
First, a review of the components
Aspirin, a key component of triple therapy, is the only nonsteroidal anti-inflammatory drug (NSAID) indicated for primary or secondary prevention of cardiovascular events.10,11 The reason: Aspirin is more selective for cyclooxygenase-1 (COX-1) than other NSAIDs and irreversibly inhibits COX enzymes.11 The aspirin-induced decrease in thromboxane production leads to a decline in platelet activation and aggregation, which accounts both for aspirin’s beneficial cardiovascular effects and the associated risk of bleeding—aspirin’s most common adverse effect.12
Most major bleeds linked to aspirin use involve the gastrointestinal (GI) tract, primarily because of the drug’s direct and indirect effects on the GI mucosa.11-14 Aspirin’s toxicities are dose related, but its antiplatelet properties do not appear to be.14
Adding a thienopyridine
Thienopyridine antiplatelet drugs indicated for the secondary prevention of cardiovascular events after ACS or PCI-S include ticlopidine, clopidogrel, and prasugrel.15 Ticlopidine, the first such agent approved in the United States, is rarely used because of potential neutropenia and thrombotic thrombocytopenia purpura.16
Clopidogrel, the most commonly used agent for the purpose of secondary prevention, is the only thienopyridine with trial data for triple therapy.17 Clopidogrel’s antiplatelet effect, however, is highly dependent on specific cytochrome P-450 (CYP) enzymes for conversion to its active metabolite, and can be impaired by genetic variations in CYP 2C19, as well as by medication interactions. This has led to concern about the drug’s efficacy for secondary prevention of ACS.6,17,18 In 2010, the US Food and Drug Administration (FDA) added a black-box warning for clopidogrel, emphasizing the risk of myocardial infarction (MI), stroke, and cardiovascular death in patients with defective CYP 2C19 activity.19
Prasugrel, approved by the FDA in 2009,20 is useful for patients who respond poorly to clopidogrel. In fact, inadequate platelet inhibition with clopidogrel has prompted some physicians to choose prasugrel as a component of triple therapy.
While prasugrel may have greater efficacy compared with clopidogrel in preventing reinfarction, it appears to have a higher bleeding rate.15,17 Because of its bleeding profile, prasugrel is not recommended for patients >75 years unless they are at high risk for MI (prior MI or diabetes), and it is contraindicated for patients with a history of stroke. Caution is needed when prasugrel is prescribed for patients who weigh <132 lb (consider a maintenance dose of 5 mg/d rather than the usual 10 mg/d) or have an increased propensity to bleed.15
Warfarin provides the anticoagulant component of triple therapy
Until late last year, when dabigatran received FDA approval for use in stroke prevention,21 warfarin was the only oral anticoagulant available in the United States. (To learn more about dabigatran, which is not included in this review because of the lack of evidence regarding its use in triple therapy, see “Time to try this warfarin alternative?”.)
Because multiple drug, food, and disease state interactions can interfere with warfarin therapy, frequent monitoring to maintain a target international normalized ratio (INR) is required.22,23 (See Patient on warfarin? Steer clear of these drugs, in “Avoiding drug interactions: Here’s help,” J Fam Pract. 2010;59: 322-329).
Bridge therapy. Warfarin requires several days to reach its full effect, so anticoagulation with a more immediate-acting medication, such as a low-molecular-weight heparin or fondaparinux, is often used until the INR goal is reached.22,23 Thus, there are instances in which patients requiring triple therapy are actually receiving 4 drugs that increase bleeding risk.
When (or whether) to consider triple therapy
While triple therapy may be an option for patients with atrial fibrillation and ACS or PCI-S, there is no validated scoring system to aid in treatment decisions.24 As already noted, selecting the optimal therapy requires an individual assessment of the patient’s risk of reinfarction, stent thrombosis, stroke, and bleeding complications.
Risk factors for reinfarction and stent thrombosis are the same ones that increase the risk of ACS initially, and include diabetes mellitus, heart failure, smoking, hyperlipidemia, and hypertension.10,16 Advanced age; uncontrolled hypertension; chronic conditions such as peripheral vascular disease, anemia, and peptic ulcer disease; and a history of major bleeds are associated with an increased risk of bleeding. 24,25
In a retrospective trial evaluating independent predictors of major bleeding in patients with atrial fibrillation who underwent PCI-S,1 the researchers identified several factors that increased the risk of early major bleeding (within 48 hours of stent placement): the use of a glycoprotein IIb/IIIa inhibitor, stenting of ≥3 vessels, or left main artery disease. Factors that significantly increased the risk of major bleeding more than 48 hours after the procedure included triple therapy, an early major bleed, and baseline anemia.1
Drug combinations: What to consider
In addition to determining whether a patient is a good candidate for triple therapy, it is crucial to consider the choice of drugs. Benefits of prasugrel, compared with clopidogrel, include fewer drug interactions, less resistance to platelet inhibition, more rapid platelet inhibition after an oral loading dose, and higher levels of platelet inhibition during maintenance dosing.15,17
Improved outcomes are another potential benefit, according to TRITON-Thrombolysis in Myocardial Infarction (TIMI) 38,17 a large randomized prospective trial comparing the use of prasugrel with clopidogrel in triple therapy. Among study participants, the primary outcome rate—the combined incidence of death from cardiovascular causes, nonfatal MI, and nonfatal stroke—was 9.9% for those on prasugrel vs 12.1% for the clopidogrel group (hazard ratio [HR]=0.81; 95% confidence interval [CI], 0.73-0.90, P<.001).17 The rate of TIMI major bleeding, however, was higher among those on prasugrel (HR=1.32; 95% CI, 1.03-1.68, P=.03). The evidence suggests that for every 1000 patients treated with prasugrel vs clopidogrel, 24 primary outcomes would be prevented but there would be 10 additional bleeding events.17,26
CASE Anthony D’s risk for stroke, infarction, and stent thrombosis—based on his history of diabetes and hypertension, atrial fibrillation, and PCI-S—and absence of independent bleeding risk factors make him a good candidate for triple therapy. Because the patient is at high risk, the physician starts him on 2 anticoagulants—warfarin (5 mg at bedtime) and enoxaparin (125 mg every 12 hours)—on the evening of his second day in the hospital. On Day 3, clinicians test Anthony’s prothrombin time/international normalized ratio (PT/INR) and P2Y12 function assay, which measure 14.9/1.1 and 8% platelet inhibition, respectively.
The patient is discharged on the following medication schedule: enoxaparin 125 mg every 12 hours, to be discontinued after 3 days; warfarin 5 mg daily, prasugrel 10 mg daily, and aspirin 81 mg daily; metoprolol succinate 100 mg daily; lisinopril 10 mg daily; rosuvastatin 10 mg daily; glyburide-metformin 5 mg/500 mg, 2 tablets twice daily; and insulin glargine 20 units at bedtime.
Safety and efficacy: Do the benefits outweigh the risk?
Safety is central to the continuing controversy surrounding the use of triple therapy.6,9 To date, however, no randomized prospective studies have evaluated its benefits and risks.
Numerous retrospective studies and case series have assessed the risk of bleeding associated with triple therapy.6 Several studies compared triple therapy with dual antiplatelet therapy without anticoagulation, and found a several-fold increase in both major and minor bleeding events in the triple therapy group.6
Few trials have assessed both the safety and the efficacy of triple therapy, however. One exception is a large retrospective trial, published in 2008.2 The researchers found that triple therapy significantly reduced the incidence of major cardiac events (death, acute MI, and target lesion revascularization); all-cause mortality; and major adverse effects (ie, any major cardiovascular event, major bleeding complication, and/or stroke), with no statistically significant increase in major bleeding events compared with patients on antiplatelet therapy without anticoagulation.2
The results of this trial, like those of other studies evaluating triple therapy, were weakened by variance in both the duration of antithrombotic therapy and the drug therapies studied. This limitation was off set, however, by multivariant analysis and well-documented follow-up.2 Despite the researchers’ findings, however, the results of other trials (and our knowledge of the mechanisms of action of the drug components) suggest that triple therapy significantly increases bleeding risk. For patients who would likely benefit from it but face an increased bleeding risk, there are ways to mitigate risk.
Prescribing triple therapy, while mitigating the risks
If bleeding is a serious concern in a patient who would benefit from triple therapy, the drug regimen may be adjusted. Options include:
- targeting a lower INR (2.0-2.5 vs the standard 2.0-3.0).6 While various trials have found a 2.0 to 3.0 range to reduce the risk of stroke, none has compared it with a lower range to evaluate reduction in bleeding risk.27 One potential benefit of trying to maintain a lower INR is the decrease in deviations into the 3.0 to 4.0 range, which is associated with an increased bleeding risk.28 However, lowering the INR target is not supported by any literature.1,18
- using low-dose aspirin therapy after PCI-S
- limiting the thienopyridine component of triple therapy to one month after ACS or PCI-S.6
When the risks of triple therapy outweigh the benefits because of an exceedingly high bleeding risk, single antiplatelet therapy with warfarin is another option to consider.
CASE [H17012] Anthony D’s discharge instructions called for an 81 mg daily dose of aspirin, as opposed to the 325-mg dose for the first 3 months of triple therapy after stent placement recommended by the American College of Cardiology/American Heart Association (ACC/AHA) guidelines for unstable angina/ non-ST segment elevated MI.1 Although the patient had no independent bleeding risk, his physician selected the lower dose of aspirin to mitigate the increased bleeding risk posed by the use of prasugrel as a component of triple therapy.6
Lower aspirin dose. Pharmacodynamic studies support the use of a lower dose of aspirin, finding that serum thromboxane is completely inhibited by a maintenance dose as low as 30 mg/d in healthy individuals and 50 mg/d for those with chronic stable angina.14 Using low-dose aspirin for the secondary prevention of ACS when triple therapy is indicated is likely to reduce GI toxicities as well as bleeding risk.
Reduce the duration of dual antiplatelet therapy. According to the ACC/AHA guidelines, thienopyridine therapy can be limited to one month in patients who are medically managed or have had a bare metal stent placed if there is concern about the patient’s risk of bleeding.6,10 Based on the findings of the one study that found triple therapy to be an independent predictor of major bleeds, this approach seems reasonable.1 It is called into question, however, by another recent trial, which found that patients on dual antiplatelet therapy for one year (vs one month) had a statistically significant improvement in cardiovascular outcomes.16
Before limiting a patient’s thienopyridine therapy to one month, consider his or her risk of reinfarction. If it is high, continuing the thienopyridine for at least one year is likely to provide the most benefit.
The largest triple therapy trial to date compared the efficacy of triple therapy vs dual therapy (a single antiplatelet agent plus warfarin) in patients with ACS and an indication for warfarin therapy.3 This trial found no statistically significant differences in the combined occurrence of death, stroke, unscheduled PCI, and MI between the 2 treatment groups. (Bleeding risk was not evaluated.) Stroke was significantly increased in the group that received therapy with warfarin and a single antiplatelet agent, with this caveat: The occurrence of stroke was so low overall that no conclusions could be reached from this difference.3
One problem with this trial, and with others evaluating triple therapy, has to do with the lack of consistency, as well as the duration. The warfarin and single antiplatelet group, for example, may have included patients who were receiving only warfarin, aspirin, or clopidogrel by 6 months after initiating treatment.3 Thus, although reinfarction or stent thrombosis after ACS or PCI-S typically occurs within the first few months, any triple therapy trial that lasts less than a year is likely to report skewed results. JFP
CORRESPONDENCE
Haley M. Phillippe, PharmD, BCPS, Auburn University Harrison School of Pharmacy, University of Alabama Birmingham School of Medicine?Huntsville, 301 Governors Drive, Huntsville, AL 35801; mccrahl@auburn.edu
1. Manzano-Fernandez S, Pastor FJ, Marin F, et al. Increased major bleeding complications related to triple antithrombotic therapy usage in patients with atrial fibrillation undergoing percutaneous coronary artery stenting. Chest. 2008;134:559-567.
2. Ruiz-Nodar JM, Marin F, Hurtado JA, et al. Anticoagulant and antiplatelet therapy use in 426 patients with atrial fibrillation undergoing percutaneous coronary intervention and stent implantation. J Am Coll Cardiol. 2008;51:818-25.
3. Nguyen MC, Lim YL, Walton A, et al. Combining warfarin and antiplatelet therapy after coronary stenting in the Global Registry of Acute Coronary Events: is it safe and effective to use just one antiplatelet agent? Eur Heart J. 2007;28:1717-1722.
4. Gilard M, Blanchard D, Helft G, et al. Antiplatelet therapy in patients with anticoagulants undergoing percutaneous coronary stenting (from STENTIng and oral anticoagulants [STENTICO]). Am J Cardiol. 2009;104:338-342.
5. Hansen ML, Sorensent R, Clausen MT, et al. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med. 2010;170:1433-1441.
6. Hermosillo AJ, Spinler SA. Aspirin, clopidogrel, and warfarin: is the combination appropriate and effective or inappropriate and too dangerous? Ann Pharmacother 2008;42:790-805.
7. Rothberg MB, Celestin C, Fiore LD, et al. Warfarin plus aspirin after myocardial infarction or the acute coronary syndrome: meta-analysis with estimates of risk and benefit. Ann Intern Med. 2005;143:241-250.
8. Eikelboom JM, Hirsh J. Combined antiplatelet and anticoagulant therapy: clinical benefits and risks. J Thromb Haemost. 2007;5:255-263.
9. Triple antithrombotic therapy Pharm Lett/Prescr Lett. 2009;25:250901.-
10. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. ACC/AHA guideline revision. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction. J Am Coll Cardiol. 2007;50:e1-e157.
11. Furst DE, Ulrich RW. Nonsteroidal anti-inflammatory drugs, disease-modifying antirheumatic drugs, nonopioid analgesics, and drugs used in gout. In: Katzung BG. Basic and Clinical Pharmacology. New York: McGraw Hill; 2008;573-598.
12. Smyth EM, FitzGerald GA. The eicosanoids: prostaglandins, thromboxanes, leukotrienes, and related compounds. In: Katzung BG. Basic and Clinical Pharmacology. New York: McGraw Hill; 2008;293-308.
13. Steinhubl SR, Bhatt DL, Brennan DM, et al. Aspirin to prevent cardiovascular disease: the association of aspirin dose and clopidogrel with thrombosis and bleeding. Ann Intern Med. 2009;150:379-386.
14. Campbell CL, Smyth S, Montalescot G, et al. Aspirin dose for the prevention of cardiovascular disease: a systematic review. JAMA. 2007;297:2018-2024.
15. Lexi-Comp [database online]. Hudson, OH: Lexi-Comp, Inc. Copyright 1978-2007. Available at: http://www.crlonline.com/crlsql/servlet/crlonline. Accessed November 5, 2010.
16. Spinler SA, Rees C. Review of Prasugrel for the secondary prevention of atherothrombosis. J Manag Care Pharm. 2009;15:383-95.
17. Spinler SA, Denus SD, et al. Acute coronary syndromes. In: Dipiro JT, Talbert RL, Yee GC, Pharmacotherapy: A Pathophysiologic Approach. New York: McGraw Hill; 2008;249-277.
18. Plavix [package insert]. Bridgewater, NJ: Bristol-Myers Squibb/ Sanofi Pharmaceuticals Partnership; 2010.
19. US Food and Drug Administration. FDA announces new boxed warning on Plavix. March 12, 2010. Available at: http://www.fda.gov/NewsEvents/Newsroom/Press Announcements/ucm204253.htm. Accessed March 11, 2011.
20. US Food and Drug Administration. FDA approves Effient to reduce the risk of heart attack in angioplasty patients. July 10, 2009. Available at: http://www.fda.gov/NewsEvents/News-room/PressAnnouncements/ucm171497.htm. Accessed March 11, 2011.
21. US Food and Drug Administration. FDA approves Pradaxa to prevent stroke in people with atrial fibrillation. October 19, 2010. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm230241.htm. Accessed March 11, 2011.
22. Ansell J, Hirsh J, Hylek E, et al. Pharmacology and management of the vitamin K antagonists. American College of Chest Physicians Evidence-Based Clinical Guidelines (8Th edition). Chest. 2008;133(suppl):160S-198S.
23. Haines ST, Witt DM, Nutescu EA. Venous thromboembolism. In: Dipiro JT, Talbert RL, Yee GC, et al. Pharmacotherapy: A Pathophysiologic Approach. New York: McGraw Hill; 2008;331-369.
24. Lip G. The balance between stroke prevention and bleeding risk in atrial fibrillation: a delicate balance revisited. Stroke. 2008;39:1406-1408.
25. The Warfarin Antiplatelet Vascular Evaluation Trial Investigators. Oral anticoagulant and antiplatelet therapy and peripheral arterial disease. N Engl J Med. 2007;357:217-227.
26. Schafer JA, Kjesbo NK, Gleason PP. Critical review of prasugrel for formulary decision makers. J Manag Care Pharm. 2009;15:335-343.
27. Singer DE, Albers GW, Dalen JE, et al. Antithrombotic therapy in atrial fibrillation. Chest. 2008;133(suppl):546S-592S.
28. Price MJ. Bedside evaluation of thienopyridine antiplatelet therapy. Circulation. 2009;119:2625-2632.
1. Manzano-Fernandez S, Pastor FJ, Marin F, et al. Increased major bleeding complications related to triple antithrombotic therapy usage in patients with atrial fibrillation undergoing percutaneous coronary artery stenting. Chest. 2008;134:559-567.
2. Ruiz-Nodar JM, Marin F, Hurtado JA, et al. Anticoagulant and antiplatelet therapy use in 426 patients with atrial fibrillation undergoing percutaneous coronary intervention and stent implantation. J Am Coll Cardiol. 2008;51:818-25.
3. Nguyen MC, Lim YL, Walton A, et al. Combining warfarin and antiplatelet therapy after coronary stenting in the Global Registry of Acute Coronary Events: is it safe and effective to use just one antiplatelet agent? Eur Heart J. 2007;28:1717-1722.
4. Gilard M, Blanchard D, Helft G, et al. Antiplatelet therapy in patients with anticoagulants undergoing percutaneous coronary stenting (from STENTIng and oral anticoagulants [STENTICO]). Am J Cardiol. 2009;104:338-342.
5. Hansen ML, Sorensent R, Clausen MT, et al. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med. 2010;170:1433-1441.
6. Hermosillo AJ, Spinler SA. Aspirin, clopidogrel, and warfarin: is the combination appropriate and effective or inappropriate and too dangerous? Ann Pharmacother 2008;42:790-805.
7. Rothberg MB, Celestin C, Fiore LD, et al. Warfarin plus aspirin after myocardial infarction or the acute coronary syndrome: meta-analysis with estimates of risk and benefit. Ann Intern Med. 2005;143:241-250.
8. Eikelboom JM, Hirsh J. Combined antiplatelet and anticoagulant therapy: clinical benefits and risks. J Thromb Haemost. 2007;5:255-263.
9. Triple antithrombotic therapy Pharm Lett/Prescr Lett. 2009;25:250901.-
10. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. ACC/AHA guideline revision. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction. J Am Coll Cardiol. 2007;50:e1-e157.
11. Furst DE, Ulrich RW. Nonsteroidal anti-inflammatory drugs, disease-modifying antirheumatic drugs, nonopioid analgesics, and drugs used in gout. In: Katzung BG. Basic and Clinical Pharmacology. New York: McGraw Hill; 2008;573-598.
12. Smyth EM, FitzGerald GA. The eicosanoids: prostaglandins, thromboxanes, leukotrienes, and related compounds. In: Katzung BG. Basic and Clinical Pharmacology. New York: McGraw Hill; 2008;293-308.
13. Steinhubl SR, Bhatt DL, Brennan DM, et al. Aspirin to prevent cardiovascular disease: the association of aspirin dose and clopidogrel with thrombosis and bleeding. Ann Intern Med. 2009;150:379-386.
14. Campbell CL, Smyth S, Montalescot G, et al. Aspirin dose for the prevention of cardiovascular disease: a systematic review. JAMA. 2007;297:2018-2024.
15. Lexi-Comp [database online]. Hudson, OH: Lexi-Comp, Inc. Copyright 1978-2007. Available at: http://www.crlonline.com/crlsql/servlet/crlonline. Accessed November 5, 2010.
16. Spinler SA, Rees C. Review of Prasugrel for the secondary prevention of atherothrombosis. J Manag Care Pharm. 2009;15:383-95.
17. Spinler SA, Denus SD, et al. Acute coronary syndromes. In: Dipiro JT, Talbert RL, Yee GC, Pharmacotherapy: A Pathophysiologic Approach. New York: McGraw Hill; 2008;249-277.
18. Plavix [package insert]. Bridgewater, NJ: Bristol-Myers Squibb/ Sanofi Pharmaceuticals Partnership; 2010.
19. US Food and Drug Administration. FDA announces new boxed warning on Plavix. March 12, 2010. Available at: http://www.fda.gov/NewsEvents/Newsroom/Press Announcements/ucm204253.htm. Accessed March 11, 2011.
20. US Food and Drug Administration. FDA approves Effient to reduce the risk of heart attack in angioplasty patients. July 10, 2009. Available at: http://www.fda.gov/NewsEvents/News-room/PressAnnouncements/ucm171497.htm. Accessed March 11, 2011.
21. US Food and Drug Administration. FDA approves Pradaxa to prevent stroke in people with atrial fibrillation. October 19, 2010. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm230241.htm. Accessed March 11, 2011.
22. Ansell J, Hirsh J, Hylek E, et al. Pharmacology and management of the vitamin K antagonists. American College of Chest Physicians Evidence-Based Clinical Guidelines (8Th edition). Chest. 2008;133(suppl):160S-198S.
23. Haines ST, Witt DM, Nutescu EA. Venous thromboembolism. In: Dipiro JT, Talbert RL, Yee GC, et al. Pharmacotherapy: A Pathophysiologic Approach. New York: McGraw Hill; 2008;331-369.
24. Lip G. The balance between stroke prevention and bleeding risk in atrial fibrillation: a delicate balance revisited. Stroke. 2008;39:1406-1408.
25. The Warfarin Antiplatelet Vascular Evaluation Trial Investigators. Oral anticoagulant and antiplatelet therapy and peripheral arterial disease. N Engl J Med. 2007;357:217-227.
26. Schafer JA, Kjesbo NK, Gleason PP. Critical review of prasugrel for formulary decision makers. J Manag Care Pharm. 2009;15:335-343.
27. Singer DE, Albers GW, Dalen JE, et al. Antithrombotic therapy in atrial fibrillation. Chest. 2008;133(suppl):546S-592S.
28. Price MJ. Bedside evaluation of thienopyridine antiplatelet therapy. Circulation. 2009;119:2625-2632.
Statin neuropathy?
It took 13 years before an 82-year-old patient learned what had caused the pain and tingling in his feet that he’d been living with all those years.
In 1996 he had a coronary stent insertion, and after the procedure, began taking a beta-blocker and atorvastatin. He subsequently noticed a sensory change in his toes bilaterally. This slowly progressed to paresthesia in the anterior segments of both feet on the plantar and dorsal surfaces.
A nerve conduction study (TABLE) confirmed the presence of a sensorimotor polyneuropathy, despite the fact that he did not have diabetes, or any other condition known to predispose him to polyneuropathy. The patient’s left sural peak latency and amplitude, a measure of sensory nerve action potential (SNAP), was absent. The right sural SNAP demonstrated a mild decrease of the amplitude with a normal distal latency. The left peroneal F wave response (a measure of nerve conduction velocity) was within the upper limits of normal. The left tibial F wave response was normal. The left peroneal and left tibial CMAPs (compound muscle action potentials) were normal.
A nerve biopsy was not considered for this patient because its main use is in the identification of specific lesions that are generally lacking in acquired, distal, symmetrical sensory neuropathy. (Plus, biopsy gives no more information than electrophysiological tests.)1
TABLE
A look at the patient’s nerve conduction results
| Nerve and site | Peak latency (ms) | Amplitude (mV) | Segment | Latency difference (ms) | Distance (mm) | Conduction velocity (m/s) |
|---|---|---|---|---|---|---|
| Sensory nerve conduction | ||||||
| Sural nerve (left) Lower leg | 0.0 | 0.0 | N/A | N/A | N/A | |
| Sural nerve (right) Lower leg | 4.0 | 2 | N/A | N/A | N/A | |
| Motor nerve conduction | ||||||
| Peroneal nerve (left) Ankle | 4.3 | 1.9 | N/A | N/A | N/A | |
| Fibular head | 13.2 | 1.6 | Ankle-fibular head | 8.9 | 358 | 40 |
| Knee | 16.2 | 1.5 | Fibular head-knee | 3.0 | 115 | 38 |
| Tibial nerve (left) Ankle | 4.2 | 2.9 | N/A | N/A | N/A | |
| Popliteal fossa | 15.4 | 2.6 | Ankle-popliteal fossa | 11.2 | 450 | 40 |
| ms, millisecond; m/s, meters/second; mV, millivolt; N/A, not applicable. | ||||||
Connecting the dots years later
Neither the patient’s cardiologist, nor his general physician, was aware of any connection between statins and neuropathy, but the patient stopped taking the drug in 2003. And while the neuropathy never went away, it did subside slightly to a fairly constant level.
In August 2009, because of suboptimal levels of low-density lipoprotein (LDL), high-density lipoprotein (HDL), and C-reactive protein, his cardiologist prescribed simvastatin 5 mg daily.
On the third day, the patient experienced a marked increase of the neuropathy, which extended above his ankles. Cutaneous sensory loss became more extensive and pronounced. He stopped the statin that day, but the paresthesia did not lessen. In addition, he developed intermittent pins and needles in both hands and some instability in his gait. To date, there has been no improvement in his symptoms. Nerve conduction studies were not repeated.
Discussion: The various causes of neuropathy
In 2003, this journal published a question, “Do statins cause myopathy?”2 The item concluded that if they did, the risk was very low, although isolated case reports suggested a myopathy risk for all statins, ranging from benign myalgia to fatal rhabdomyolysis.
It is now widely acknowledged that statins can cause myopathy in as many as 10% of patients taking these drugs.3
The involvement of peripheral nerves bilaterally, usually affecting distal axons of the feet and legs, is the most common form of polyneuropathy and its presentation generally excludes consideration of other forms of neuropathy, such as the mononeuropathies and neuritis. Affected nerves may be sensory, motor, or autonomic.
Symptoms include all varieties of paresthesia, sensory loss, muscle weakness, and pain. The most common cause is diabetes mellitus, which must be the first condition to be excluded. Other conditions, such as vitamin deficiencies, have also been linked with this complication.
Laboratory work-up, aside from blood glucose testing for diabetes, should include routine complete blood count and SMA-12, as well as thyroid profile and vitamin deficiency status (particularly vitamins B12 and B1).
Is a medication—perhaps a statin— to blame?
Numerous drugs are known to be associated with neuropathy.4 These include chemotherapy agents (cisplatin, taxoids), certain antibiotics, nucleoside analogs, dapsone, metronidazole, and certain cardiovascular drugs (amiodarone, hydralazine, statins).4 Recent work has indicated that simvastatin inhibits central nervous system remyelination by blocking progenitor cell differentiation.5 By extension, it probably inhibits progenitor cells in the peripheral nervous system.
The possibility of an association between statins and peripheral neuropathy has expanded from several case reports to a population-based study involving 465,000 subjects.6 More recently, a review of the literature7 concluded that exposure to statins may increase the risk of polyneuropathy and that statins should be considered the cause when other etiologies have been excluded. The authors suggested that the incidence of peripheral neuropathy due to statins is approximately 1 person/14,000 person-years of treatment.
An exposure, a “break,” and another exposure
The reappearance or aggravation of symptoms after cessation of statin therapy and subsequent second exposure has been described in the literature.8 In the case described here, the time between re-exposure and symptoms was suggestive of a T-cell-mediated hypersensitivity reaction. It has been proposed that tumor necrosis factor (TNF)-alpha released by T cells may contribute to the pathogenesis of demyelinating neuropathy.9
Managing this patient’s lipid levels going forward
The patient described in this report is now receiving ezetimibe 10 mg daily, which reduces the absorption of cholesterol from the diet, and niacin 2 g daily, which he can tolerate. His most recent fasting lipid panel showed the following results: cholesterol, 171 mg/dL; LDL cholesterol, calculated, 113 mg/dL; HDL cholesterol, 37 mg/dL; triglycerides, 106 mg/dL; and non-HDL cholesterol, 134 mg/dL.
Controlling the patient’s pain was another matter. Drugs commonly used for paresthesia and pain (including opiates) did not provide relief. Pregabalin (Lyrica) also had little effect. Transcutaneous electrical nerve stimulation did not perceptibly lessen his symptoms, and was also discontinued.
At the present time, this patient is not on any specific treatment for his neuropathy.
CORRESPONDENCE
Walter F. Coulson, MD, Department of Pathology, UCLA, CHS, Los Angeles, CA 90095-1732; wcoulson@mednet.ucla.edu
1. Said G. Indications and usefulness of nerve biopsy. Arch Neurol. 2002;59:1532-1535.
2. Daugird AJ, Crowell K. Do statins cause myopathy? J Fam Pract. 2003;52:973-976.
3. Joy TR, Hegele RA. Narrative review: Statin-related myopathy. Ann Intern Med. 2009;150:858-868.
4. Weimer LH. Medication-induced peripheral neuropathy. Curr Neurosci Rep. 2003;3:86-92.
5. Miron VE, Zehntner SP, Kuhlmann T, et al. Statin therapy inhibits remyelination in the central nervous system. Am J Pathol. 2009;174:1880-1890.
6. Gaist D, Jeppesen U, Andersen M, et al. Statins and risk of polyneuropathy: a case-control study. Neurology. 2002;58:1333-1337.
7. Chong PH, Boskovich A, Stevkovic N, et al. Statin-associated peripheral neuropathy: review of the literature. Pharmacotherapy. 2004;24:1194-1203.
8. Phan T, McLeod JG, Pollard JD, et al. Peripheral neuropathy associated with simvastatin. J Neurol Neurosurg Psychiatry. 1995;58:625-628.
9. Stübgen JP. Tumor necrosis factor–alpha antagonists and neuropathy. Muscle Nerve. 2008;37:281-292.
It took 13 years before an 82-year-old patient learned what had caused the pain and tingling in his feet that he’d been living with all those years.
In 1996 he had a coronary stent insertion, and after the procedure, began taking a beta-blocker and atorvastatin. He subsequently noticed a sensory change in his toes bilaterally. This slowly progressed to paresthesia in the anterior segments of both feet on the plantar and dorsal surfaces.
A nerve conduction study (TABLE) confirmed the presence of a sensorimotor polyneuropathy, despite the fact that he did not have diabetes, or any other condition known to predispose him to polyneuropathy. The patient’s left sural peak latency and amplitude, a measure of sensory nerve action potential (SNAP), was absent. The right sural SNAP demonstrated a mild decrease of the amplitude with a normal distal latency. The left peroneal F wave response (a measure of nerve conduction velocity) was within the upper limits of normal. The left tibial F wave response was normal. The left peroneal and left tibial CMAPs (compound muscle action potentials) were normal.
A nerve biopsy was not considered for this patient because its main use is in the identification of specific lesions that are generally lacking in acquired, distal, symmetrical sensory neuropathy. (Plus, biopsy gives no more information than electrophysiological tests.)1
TABLE
A look at the patient’s nerve conduction results
| Nerve and site | Peak latency (ms) | Amplitude (mV) | Segment | Latency difference (ms) | Distance (mm) | Conduction velocity (m/s) |
|---|---|---|---|---|---|---|
| Sensory nerve conduction | ||||||
| Sural nerve (left) Lower leg | 0.0 | 0.0 | N/A | N/A | N/A | |
| Sural nerve (right) Lower leg | 4.0 | 2 | N/A | N/A | N/A | |
| Motor nerve conduction | ||||||
| Peroneal nerve (left) Ankle | 4.3 | 1.9 | N/A | N/A | N/A | |
| Fibular head | 13.2 | 1.6 | Ankle-fibular head | 8.9 | 358 | 40 |
| Knee | 16.2 | 1.5 | Fibular head-knee | 3.0 | 115 | 38 |
| Tibial nerve (left) Ankle | 4.2 | 2.9 | N/A | N/A | N/A | |
| Popliteal fossa | 15.4 | 2.6 | Ankle-popliteal fossa | 11.2 | 450 | 40 |
| ms, millisecond; m/s, meters/second; mV, millivolt; N/A, not applicable. | ||||||
Connecting the dots years later
Neither the patient’s cardiologist, nor his general physician, was aware of any connection between statins and neuropathy, but the patient stopped taking the drug in 2003. And while the neuropathy never went away, it did subside slightly to a fairly constant level.
In August 2009, because of suboptimal levels of low-density lipoprotein (LDL), high-density lipoprotein (HDL), and C-reactive protein, his cardiologist prescribed simvastatin 5 mg daily.
On the third day, the patient experienced a marked increase of the neuropathy, which extended above his ankles. Cutaneous sensory loss became more extensive and pronounced. He stopped the statin that day, but the paresthesia did not lessen. In addition, he developed intermittent pins and needles in both hands and some instability in his gait. To date, there has been no improvement in his symptoms. Nerve conduction studies were not repeated.
Discussion: The various causes of neuropathy
In 2003, this journal published a question, “Do statins cause myopathy?”2 The item concluded that if they did, the risk was very low, although isolated case reports suggested a myopathy risk for all statins, ranging from benign myalgia to fatal rhabdomyolysis.
It is now widely acknowledged that statins can cause myopathy in as many as 10% of patients taking these drugs.3
The involvement of peripheral nerves bilaterally, usually affecting distal axons of the feet and legs, is the most common form of polyneuropathy and its presentation generally excludes consideration of other forms of neuropathy, such as the mononeuropathies and neuritis. Affected nerves may be sensory, motor, or autonomic.
Symptoms include all varieties of paresthesia, sensory loss, muscle weakness, and pain. The most common cause is diabetes mellitus, which must be the first condition to be excluded. Other conditions, such as vitamin deficiencies, have also been linked with this complication.
Laboratory work-up, aside from blood glucose testing for diabetes, should include routine complete blood count and SMA-12, as well as thyroid profile and vitamin deficiency status (particularly vitamins B12 and B1).
Is a medication—perhaps a statin— to blame?
Numerous drugs are known to be associated with neuropathy.4 These include chemotherapy agents (cisplatin, taxoids), certain antibiotics, nucleoside analogs, dapsone, metronidazole, and certain cardiovascular drugs (amiodarone, hydralazine, statins).4 Recent work has indicated that simvastatin inhibits central nervous system remyelination by blocking progenitor cell differentiation.5 By extension, it probably inhibits progenitor cells in the peripheral nervous system.
The possibility of an association between statins and peripheral neuropathy has expanded from several case reports to a population-based study involving 465,000 subjects.6 More recently, a review of the literature7 concluded that exposure to statins may increase the risk of polyneuropathy and that statins should be considered the cause when other etiologies have been excluded. The authors suggested that the incidence of peripheral neuropathy due to statins is approximately 1 person/14,000 person-years of treatment.
An exposure, a “break,” and another exposure
The reappearance or aggravation of symptoms after cessation of statin therapy and subsequent second exposure has been described in the literature.8 In the case described here, the time between re-exposure and symptoms was suggestive of a T-cell-mediated hypersensitivity reaction. It has been proposed that tumor necrosis factor (TNF)-alpha released by T cells may contribute to the pathogenesis of demyelinating neuropathy.9
Managing this patient’s lipid levels going forward
The patient described in this report is now receiving ezetimibe 10 mg daily, which reduces the absorption of cholesterol from the diet, and niacin 2 g daily, which he can tolerate. His most recent fasting lipid panel showed the following results: cholesterol, 171 mg/dL; LDL cholesterol, calculated, 113 mg/dL; HDL cholesterol, 37 mg/dL; triglycerides, 106 mg/dL; and non-HDL cholesterol, 134 mg/dL.
Controlling the patient’s pain was another matter. Drugs commonly used for paresthesia and pain (including opiates) did not provide relief. Pregabalin (Lyrica) also had little effect. Transcutaneous electrical nerve stimulation did not perceptibly lessen his symptoms, and was also discontinued.
At the present time, this patient is not on any specific treatment for his neuropathy.
CORRESPONDENCE
Walter F. Coulson, MD, Department of Pathology, UCLA, CHS, Los Angeles, CA 90095-1732; wcoulson@mednet.ucla.edu
It took 13 years before an 82-year-old patient learned what had caused the pain and tingling in his feet that he’d been living with all those years.
In 1996 he had a coronary stent insertion, and after the procedure, began taking a beta-blocker and atorvastatin. He subsequently noticed a sensory change in his toes bilaterally. This slowly progressed to paresthesia in the anterior segments of both feet on the plantar and dorsal surfaces.
A nerve conduction study (TABLE) confirmed the presence of a sensorimotor polyneuropathy, despite the fact that he did not have diabetes, or any other condition known to predispose him to polyneuropathy. The patient’s left sural peak latency and amplitude, a measure of sensory nerve action potential (SNAP), was absent. The right sural SNAP demonstrated a mild decrease of the amplitude with a normal distal latency. The left peroneal F wave response (a measure of nerve conduction velocity) was within the upper limits of normal. The left tibial F wave response was normal. The left peroneal and left tibial CMAPs (compound muscle action potentials) were normal.
A nerve biopsy was not considered for this patient because its main use is in the identification of specific lesions that are generally lacking in acquired, distal, symmetrical sensory neuropathy. (Plus, biopsy gives no more information than electrophysiological tests.)1
TABLE
A look at the patient’s nerve conduction results
| Nerve and site | Peak latency (ms) | Amplitude (mV) | Segment | Latency difference (ms) | Distance (mm) | Conduction velocity (m/s) |
|---|---|---|---|---|---|---|
| Sensory nerve conduction | ||||||
| Sural nerve (left) Lower leg | 0.0 | 0.0 | N/A | N/A | N/A | |
| Sural nerve (right) Lower leg | 4.0 | 2 | N/A | N/A | N/A | |
| Motor nerve conduction | ||||||
| Peroneal nerve (left) Ankle | 4.3 | 1.9 | N/A | N/A | N/A | |
| Fibular head | 13.2 | 1.6 | Ankle-fibular head | 8.9 | 358 | 40 |
| Knee | 16.2 | 1.5 | Fibular head-knee | 3.0 | 115 | 38 |
| Tibial nerve (left) Ankle | 4.2 | 2.9 | N/A | N/A | N/A | |
| Popliteal fossa | 15.4 | 2.6 | Ankle-popliteal fossa | 11.2 | 450 | 40 |
| ms, millisecond; m/s, meters/second; mV, millivolt; N/A, not applicable. | ||||||
Connecting the dots years later
Neither the patient’s cardiologist, nor his general physician, was aware of any connection between statins and neuropathy, but the patient stopped taking the drug in 2003. And while the neuropathy never went away, it did subside slightly to a fairly constant level.
In August 2009, because of suboptimal levels of low-density lipoprotein (LDL), high-density lipoprotein (HDL), and C-reactive protein, his cardiologist prescribed simvastatin 5 mg daily.
On the third day, the patient experienced a marked increase of the neuropathy, which extended above his ankles. Cutaneous sensory loss became more extensive and pronounced. He stopped the statin that day, but the paresthesia did not lessen. In addition, he developed intermittent pins and needles in both hands and some instability in his gait. To date, there has been no improvement in his symptoms. Nerve conduction studies were not repeated.
Discussion: The various causes of neuropathy
In 2003, this journal published a question, “Do statins cause myopathy?”2 The item concluded that if they did, the risk was very low, although isolated case reports suggested a myopathy risk for all statins, ranging from benign myalgia to fatal rhabdomyolysis.
It is now widely acknowledged that statins can cause myopathy in as many as 10% of patients taking these drugs.3
The involvement of peripheral nerves bilaterally, usually affecting distal axons of the feet and legs, is the most common form of polyneuropathy and its presentation generally excludes consideration of other forms of neuropathy, such as the mononeuropathies and neuritis. Affected nerves may be sensory, motor, or autonomic.
Symptoms include all varieties of paresthesia, sensory loss, muscle weakness, and pain. The most common cause is diabetes mellitus, which must be the first condition to be excluded. Other conditions, such as vitamin deficiencies, have also been linked with this complication.
Laboratory work-up, aside from blood glucose testing for diabetes, should include routine complete blood count and SMA-12, as well as thyroid profile and vitamin deficiency status (particularly vitamins B12 and B1).
Is a medication—perhaps a statin— to blame?
Numerous drugs are known to be associated with neuropathy.4 These include chemotherapy agents (cisplatin, taxoids), certain antibiotics, nucleoside analogs, dapsone, metronidazole, and certain cardiovascular drugs (amiodarone, hydralazine, statins).4 Recent work has indicated that simvastatin inhibits central nervous system remyelination by blocking progenitor cell differentiation.5 By extension, it probably inhibits progenitor cells in the peripheral nervous system.
The possibility of an association between statins and peripheral neuropathy has expanded from several case reports to a population-based study involving 465,000 subjects.6 More recently, a review of the literature7 concluded that exposure to statins may increase the risk of polyneuropathy and that statins should be considered the cause when other etiologies have been excluded. The authors suggested that the incidence of peripheral neuropathy due to statins is approximately 1 person/14,000 person-years of treatment.
An exposure, a “break,” and another exposure
The reappearance or aggravation of symptoms after cessation of statin therapy and subsequent second exposure has been described in the literature.8 In the case described here, the time between re-exposure and symptoms was suggestive of a T-cell-mediated hypersensitivity reaction. It has been proposed that tumor necrosis factor (TNF)-alpha released by T cells may contribute to the pathogenesis of demyelinating neuropathy.9
Managing this patient’s lipid levels going forward
The patient described in this report is now receiving ezetimibe 10 mg daily, which reduces the absorption of cholesterol from the diet, and niacin 2 g daily, which he can tolerate. His most recent fasting lipid panel showed the following results: cholesterol, 171 mg/dL; LDL cholesterol, calculated, 113 mg/dL; HDL cholesterol, 37 mg/dL; triglycerides, 106 mg/dL; and non-HDL cholesterol, 134 mg/dL.
Controlling the patient’s pain was another matter. Drugs commonly used for paresthesia and pain (including opiates) did not provide relief. Pregabalin (Lyrica) also had little effect. Transcutaneous electrical nerve stimulation did not perceptibly lessen his symptoms, and was also discontinued.
At the present time, this patient is not on any specific treatment for his neuropathy.
CORRESPONDENCE
Walter F. Coulson, MD, Department of Pathology, UCLA, CHS, Los Angeles, CA 90095-1732; wcoulson@mednet.ucla.edu
1. Said G. Indications and usefulness of nerve biopsy. Arch Neurol. 2002;59:1532-1535.
2. Daugird AJ, Crowell K. Do statins cause myopathy? J Fam Pract. 2003;52:973-976.
3. Joy TR, Hegele RA. Narrative review: Statin-related myopathy. Ann Intern Med. 2009;150:858-868.
4. Weimer LH. Medication-induced peripheral neuropathy. Curr Neurosci Rep. 2003;3:86-92.
5. Miron VE, Zehntner SP, Kuhlmann T, et al. Statin therapy inhibits remyelination in the central nervous system. Am J Pathol. 2009;174:1880-1890.
6. Gaist D, Jeppesen U, Andersen M, et al. Statins and risk of polyneuropathy: a case-control study. Neurology. 2002;58:1333-1337.
7. Chong PH, Boskovich A, Stevkovic N, et al. Statin-associated peripheral neuropathy: review of the literature. Pharmacotherapy. 2004;24:1194-1203.
8. Phan T, McLeod JG, Pollard JD, et al. Peripheral neuropathy associated with simvastatin. J Neurol Neurosurg Psychiatry. 1995;58:625-628.
9. Stübgen JP. Tumor necrosis factor–alpha antagonists and neuropathy. Muscle Nerve. 2008;37:281-292.
1. Said G. Indications and usefulness of nerve biopsy. Arch Neurol. 2002;59:1532-1535.
2. Daugird AJ, Crowell K. Do statins cause myopathy? J Fam Pract. 2003;52:973-976.
3. Joy TR, Hegele RA. Narrative review: Statin-related myopathy. Ann Intern Med. 2009;150:858-868.
4. Weimer LH. Medication-induced peripheral neuropathy. Curr Neurosci Rep. 2003;3:86-92.
5. Miron VE, Zehntner SP, Kuhlmann T, et al. Statin therapy inhibits remyelination in the central nervous system. Am J Pathol. 2009;174:1880-1890.
6. Gaist D, Jeppesen U, Andersen M, et al. Statins and risk of polyneuropathy: a case-control study. Neurology. 2002;58:1333-1337.
7. Chong PH, Boskovich A, Stevkovic N, et al. Statin-associated peripheral neuropathy: review of the literature. Pharmacotherapy. 2004;24:1194-1203.
8. Phan T, McLeod JG, Pollard JD, et al. Peripheral neuropathy associated with simvastatin. J Neurol Neurosurg Psychiatry. 1995;58:625-628.
9. Stübgen JP. Tumor necrosis factor–alpha antagonists and neuropathy. Muscle Nerve. 2008;37:281-292.
A new certification for FPs
A new certification process for obstetrics in family medicine has begun under the auspices of the American Board of Physician Specialties (ABPS). The new Board of Certification in Family Medicine Obstetrics (BCFMO) is open to family physicians who have completed a fellowship tract or clinical practice tract in obstetrics. Candidates must complete written and oral examinations and proctor-observed surgical competency testing before receiving certification. To date, 25 family physicians have completed the testing process and received certification. In this article, I describe the genesis of this certification and the process that aspiring applicants can expect.
Working to meet a long-standing need
Twenty-five years ago, board certification was admirable, but not essential to practice medicine. Today it is imperative. In family medicine, most physicians completing residency training seek board certification in that specialty. Many of them then pursue training in fellowships, with recognition usually conferred by a certificate of added qualification. Obstetrics has been such an area of specialized clinical focus in family medicine, especially for those serving rural communities.1,2 And women’s health and routine pregnancy care are an integral part of family medicine and the medical home.3
In 1984, Paul D. Mozley, MD, founded Postgraduate Obstetrics Fellowship Training at the University of Alabama School of Medicine in Tuscaloosa, to address the shortage of obstetric providers in rural and underserved areas and a desire by graduating family medicine residents to obtain additional training in obstetrics. Obstetrics fellowships are usually one year in length and include operative obstetrics with cesarean section and instrumental vaginal delivery, limited gynecologic surgery, and office gynecology.4,5
Family medicine and obstetrics and gynecology organizations have also been working together to continually improve care for obstetric patients. One example is the formation of a Joint Task Force in 1998 by the American Academy of Family Physicians and the American College of Obstetricians and Gynecologists, which developed core educational guidelines in OB/GYN care for training family medicine residents.6 Between 2000 and 2005, parties from both specialties approached a number of national organizations about an examination and certification initiative. Although all organizations were supportive and recognized the need, an examination and certification never materialized.
A like-minded certifying partner emerges
In 2005, I made a formal presentation to the ABPS—one of 3 board-certifying organizations in the United States—proposing a program for examination and board certification of family medicine physicians completing obstetrics fellowships.7 In response, the ABPS created a Task Force for the Certification of Family Physicians Practicing Obstetrics, composed of family physicians and obstetrician/gynecologists. The Task Force conducted a nationwide survey of hospitals, hospital credentialing committees, malpractice insurance carriers, obstetrics fellowship programs, and family physicians regarding the importance of examination and certification, a certificate of added qualification, and a separate board of certification for family physicians practicing obstetrics.8 The aggregate response overwhelmingly favored board certification.
In 2006, responding to the increasingly clear need, the ABPS created the American Board of Family Practice Obstetrics, which is now known as the BCFMO.
What the BcFMO examination entails
From 2006 to 2008, using major textbooks on obstetrics, the BCFMO selected 873 test items that were placed in a bank for review and comment by all board members. The BCFMO then prepared questions of equal competency as the examination in obstetrics and gynecology. Questions of equal competency to both specialties were deemed important to give the certification process validity. Using the same text sources, the Board prepared additional items in a form usable for oral examination. The final written examination comprises 200 questions; the oral examination has 4 questions.
Surgical competency testing
The BCFMO also includes observed surgical competency as part of the process. Documentation of physician competency is emphasized by The Joint Commission. In this part of the testing, a Board-approved local proctor—a family physician practicing obstetrics, a general surgeon who performs cesarean sections, or an obstetrician/ gynecologist—is asked to observe and evaluate the surgical competency of a candidate for examination.
Credentialing for the examinations
Eligible applicants are those who, within the last 5 years, have satisfactorily completed (verified in writing by the fellowship director) a 12-month full-time Obstetrics or Maternal and Child Care Fellowship recognized by the BCFMO (http://www.abpsus.org/userfiles/files/BFMOFellowship.pdf). Applicants who have not completed an obstetrics fellowship but have been actively engaged in the practice of surgical obstetrics for at least 5 years may present a case list of the previous 2 years. All applicants to either tract must have performed a minimum of 100 vaginal deliveries and a verified case list of 50 cesarean sections within the last 5 years.9
Applicants successfully completing the computer-based written examination are required to submit verification of competency in surgical obstetrics described earlier, and then successfully complete the oral examination. The first written examination was administered in May 2009, and the oral examination in September 2009. Subsequent written and oral examinations were administered in 2010.
The next written examination is scheduled for October 2011. Successful completion of the written and oral examinations, surgical proctoring, background check, National Practitioner Data Bank query, and payment of appropriate fees constitute board certification in Family Medicine Obstetrics. Twenty-five family physicians have so far received board certification.
Future of the BCFMO
With its first 2 rounds of examination and certification successfully completed, the BCFMO plans to pursue the following:
- formal ceremony confirming certificate recipients’ diplomat status in the ABPS
- creation of a recertification process
- development of an appeals process
- establishment of an academy, college, or society for fellows
- acceptance by hospitals, malpractice insurance carriers, state medical societies, and licensing commissions
- ABPS accreditation of training programs
- BCFMO membership in the American Medical Association
- BCFMO membership in the Accreditation Council for Graduate Medical Education.
Interested in learning more? Visit http://www.abpsus.org/family-medicine-obstetrics, or call (813) 433-2277.
CORRESPONDENCE
Daniel M. Avery, MD, University of Alabama School of Medicine, Department of Obstetrics and Gynecology, 850 5th Avenue East, Tuscaloosa, AL 35401-7419; davery@cchs.ua.edu
1. Heider A, Neely B, Bell L. Cesarean delivery results in a family medicine residency using a specific training model. Fam Med. 2006;38:103-109.
2. Deutchman M, Connor P, Gobbo R, et al. Outcomes of cesarean sections performed by family physicians and the training they received: a fifteen-year retrospective study. J Am Board Fam Pract. 1995;8:81-90.
3. Larimore WL, Sapolsky BS. Maternity care in family medicine: economics and malpractice. J Fam Pract. 1995;40:153-160.
4. Avery DM, Hooper DE, Garris CE. Minilaparotomy for the surgical management of ectopic pregnancy for family medicine obstetricians. Am J Clin Med. 2009;6:72-73.
5. Avery DM, Hooper DE. Cesarean hysterectomy for family medicine physicians practicing obstetrics. Am J Clin Med. 2009;6:68-71.
6. American Family Physician. Recommended core educational guidelines for family practice residents: maternity and gynecologic care. July 1998. Available at: http://www.aafp.org/afp/980700ap/corematr.html. Accessed March 1, 2009.
7. American Board of Physician Specialties. Annual Leadership Meeting; June 2005;Naples, FL.
8. Avery DM, Garris CE. Board certification versus certificate of added qualification in obstetrics Am J Clin Med. 2006;3:16-18.
9. American Board of Physician Specialties. Family medicine obstetrics eligibility. February 2008. Available at: http://www.abpsus.org/family-medicine-obstetrics-eligibility. Accessed March 1, 2009.
A new certification process for obstetrics in family medicine has begun under the auspices of the American Board of Physician Specialties (ABPS). The new Board of Certification in Family Medicine Obstetrics (BCFMO) is open to family physicians who have completed a fellowship tract or clinical practice tract in obstetrics. Candidates must complete written and oral examinations and proctor-observed surgical competency testing before receiving certification. To date, 25 family physicians have completed the testing process and received certification. In this article, I describe the genesis of this certification and the process that aspiring applicants can expect.
Working to meet a long-standing need
Twenty-five years ago, board certification was admirable, but not essential to practice medicine. Today it is imperative. In family medicine, most physicians completing residency training seek board certification in that specialty. Many of them then pursue training in fellowships, with recognition usually conferred by a certificate of added qualification. Obstetrics has been such an area of specialized clinical focus in family medicine, especially for those serving rural communities.1,2 And women’s health and routine pregnancy care are an integral part of family medicine and the medical home.3
In 1984, Paul D. Mozley, MD, founded Postgraduate Obstetrics Fellowship Training at the University of Alabama School of Medicine in Tuscaloosa, to address the shortage of obstetric providers in rural and underserved areas and a desire by graduating family medicine residents to obtain additional training in obstetrics. Obstetrics fellowships are usually one year in length and include operative obstetrics with cesarean section and instrumental vaginal delivery, limited gynecologic surgery, and office gynecology.4,5
Family medicine and obstetrics and gynecology organizations have also been working together to continually improve care for obstetric patients. One example is the formation of a Joint Task Force in 1998 by the American Academy of Family Physicians and the American College of Obstetricians and Gynecologists, which developed core educational guidelines in OB/GYN care for training family medicine residents.6 Between 2000 and 2005, parties from both specialties approached a number of national organizations about an examination and certification initiative. Although all organizations were supportive and recognized the need, an examination and certification never materialized.
A like-minded certifying partner emerges
In 2005, I made a formal presentation to the ABPS—one of 3 board-certifying organizations in the United States—proposing a program for examination and board certification of family medicine physicians completing obstetrics fellowships.7 In response, the ABPS created a Task Force for the Certification of Family Physicians Practicing Obstetrics, composed of family physicians and obstetrician/gynecologists. The Task Force conducted a nationwide survey of hospitals, hospital credentialing committees, malpractice insurance carriers, obstetrics fellowship programs, and family physicians regarding the importance of examination and certification, a certificate of added qualification, and a separate board of certification for family physicians practicing obstetrics.8 The aggregate response overwhelmingly favored board certification.
In 2006, responding to the increasingly clear need, the ABPS created the American Board of Family Practice Obstetrics, which is now known as the BCFMO.
What the BcFMO examination entails
From 2006 to 2008, using major textbooks on obstetrics, the BCFMO selected 873 test items that were placed in a bank for review and comment by all board members. The BCFMO then prepared questions of equal competency as the examination in obstetrics and gynecology. Questions of equal competency to both specialties were deemed important to give the certification process validity. Using the same text sources, the Board prepared additional items in a form usable for oral examination. The final written examination comprises 200 questions; the oral examination has 4 questions.
Surgical competency testing
The BCFMO also includes observed surgical competency as part of the process. Documentation of physician competency is emphasized by The Joint Commission. In this part of the testing, a Board-approved local proctor—a family physician practicing obstetrics, a general surgeon who performs cesarean sections, or an obstetrician/ gynecologist—is asked to observe and evaluate the surgical competency of a candidate for examination.
Credentialing for the examinations
Eligible applicants are those who, within the last 5 years, have satisfactorily completed (verified in writing by the fellowship director) a 12-month full-time Obstetrics or Maternal and Child Care Fellowship recognized by the BCFMO (http://www.abpsus.org/userfiles/files/BFMOFellowship.pdf). Applicants who have not completed an obstetrics fellowship but have been actively engaged in the practice of surgical obstetrics for at least 5 years may present a case list of the previous 2 years. All applicants to either tract must have performed a minimum of 100 vaginal deliveries and a verified case list of 50 cesarean sections within the last 5 years.9
Applicants successfully completing the computer-based written examination are required to submit verification of competency in surgical obstetrics described earlier, and then successfully complete the oral examination. The first written examination was administered in May 2009, and the oral examination in September 2009. Subsequent written and oral examinations were administered in 2010.
The next written examination is scheduled for October 2011. Successful completion of the written and oral examinations, surgical proctoring, background check, National Practitioner Data Bank query, and payment of appropriate fees constitute board certification in Family Medicine Obstetrics. Twenty-five family physicians have so far received board certification.
Future of the BCFMO
With its first 2 rounds of examination and certification successfully completed, the BCFMO plans to pursue the following:
- formal ceremony confirming certificate recipients’ diplomat status in the ABPS
- creation of a recertification process
- development of an appeals process
- establishment of an academy, college, or society for fellows
- acceptance by hospitals, malpractice insurance carriers, state medical societies, and licensing commissions
- ABPS accreditation of training programs
- BCFMO membership in the American Medical Association
- BCFMO membership in the Accreditation Council for Graduate Medical Education.
Interested in learning more? Visit http://www.abpsus.org/family-medicine-obstetrics, or call (813) 433-2277.
CORRESPONDENCE
Daniel M. Avery, MD, University of Alabama School of Medicine, Department of Obstetrics and Gynecology, 850 5th Avenue East, Tuscaloosa, AL 35401-7419; davery@cchs.ua.edu
A new certification process for obstetrics in family medicine has begun under the auspices of the American Board of Physician Specialties (ABPS). The new Board of Certification in Family Medicine Obstetrics (BCFMO) is open to family physicians who have completed a fellowship tract or clinical practice tract in obstetrics. Candidates must complete written and oral examinations and proctor-observed surgical competency testing before receiving certification. To date, 25 family physicians have completed the testing process and received certification. In this article, I describe the genesis of this certification and the process that aspiring applicants can expect.
Working to meet a long-standing need
Twenty-five years ago, board certification was admirable, but not essential to practice medicine. Today it is imperative. In family medicine, most physicians completing residency training seek board certification in that specialty. Many of them then pursue training in fellowships, with recognition usually conferred by a certificate of added qualification. Obstetrics has been such an area of specialized clinical focus in family medicine, especially for those serving rural communities.1,2 And women’s health and routine pregnancy care are an integral part of family medicine and the medical home.3
In 1984, Paul D. Mozley, MD, founded Postgraduate Obstetrics Fellowship Training at the University of Alabama School of Medicine in Tuscaloosa, to address the shortage of obstetric providers in rural and underserved areas and a desire by graduating family medicine residents to obtain additional training in obstetrics. Obstetrics fellowships are usually one year in length and include operative obstetrics with cesarean section and instrumental vaginal delivery, limited gynecologic surgery, and office gynecology.4,5
Family medicine and obstetrics and gynecology organizations have also been working together to continually improve care for obstetric patients. One example is the formation of a Joint Task Force in 1998 by the American Academy of Family Physicians and the American College of Obstetricians and Gynecologists, which developed core educational guidelines in OB/GYN care for training family medicine residents.6 Between 2000 and 2005, parties from both specialties approached a number of national organizations about an examination and certification initiative. Although all organizations were supportive and recognized the need, an examination and certification never materialized.
A like-minded certifying partner emerges
In 2005, I made a formal presentation to the ABPS—one of 3 board-certifying organizations in the United States—proposing a program for examination and board certification of family medicine physicians completing obstetrics fellowships.7 In response, the ABPS created a Task Force for the Certification of Family Physicians Practicing Obstetrics, composed of family physicians and obstetrician/gynecologists. The Task Force conducted a nationwide survey of hospitals, hospital credentialing committees, malpractice insurance carriers, obstetrics fellowship programs, and family physicians regarding the importance of examination and certification, a certificate of added qualification, and a separate board of certification for family physicians practicing obstetrics.8 The aggregate response overwhelmingly favored board certification.
In 2006, responding to the increasingly clear need, the ABPS created the American Board of Family Practice Obstetrics, which is now known as the BCFMO.
What the BcFMO examination entails
From 2006 to 2008, using major textbooks on obstetrics, the BCFMO selected 873 test items that were placed in a bank for review and comment by all board members. The BCFMO then prepared questions of equal competency as the examination in obstetrics and gynecology. Questions of equal competency to both specialties were deemed important to give the certification process validity. Using the same text sources, the Board prepared additional items in a form usable for oral examination. The final written examination comprises 200 questions; the oral examination has 4 questions.
Surgical competency testing
The BCFMO also includes observed surgical competency as part of the process. Documentation of physician competency is emphasized by The Joint Commission. In this part of the testing, a Board-approved local proctor—a family physician practicing obstetrics, a general surgeon who performs cesarean sections, or an obstetrician/ gynecologist—is asked to observe and evaluate the surgical competency of a candidate for examination.
Credentialing for the examinations
Eligible applicants are those who, within the last 5 years, have satisfactorily completed (verified in writing by the fellowship director) a 12-month full-time Obstetrics or Maternal and Child Care Fellowship recognized by the BCFMO (http://www.abpsus.org/userfiles/files/BFMOFellowship.pdf). Applicants who have not completed an obstetrics fellowship but have been actively engaged in the practice of surgical obstetrics for at least 5 years may present a case list of the previous 2 years. All applicants to either tract must have performed a minimum of 100 vaginal deliveries and a verified case list of 50 cesarean sections within the last 5 years.9
Applicants successfully completing the computer-based written examination are required to submit verification of competency in surgical obstetrics described earlier, and then successfully complete the oral examination. The first written examination was administered in May 2009, and the oral examination in September 2009. Subsequent written and oral examinations were administered in 2010.
The next written examination is scheduled for October 2011. Successful completion of the written and oral examinations, surgical proctoring, background check, National Practitioner Data Bank query, and payment of appropriate fees constitute board certification in Family Medicine Obstetrics. Twenty-five family physicians have so far received board certification.
Future of the BCFMO
With its first 2 rounds of examination and certification successfully completed, the BCFMO plans to pursue the following:
- formal ceremony confirming certificate recipients’ diplomat status in the ABPS
- creation of a recertification process
- development of an appeals process
- establishment of an academy, college, or society for fellows
- acceptance by hospitals, malpractice insurance carriers, state medical societies, and licensing commissions
- ABPS accreditation of training programs
- BCFMO membership in the American Medical Association
- BCFMO membership in the Accreditation Council for Graduate Medical Education.
Interested in learning more? Visit http://www.abpsus.org/family-medicine-obstetrics, or call (813) 433-2277.
CORRESPONDENCE
Daniel M. Avery, MD, University of Alabama School of Medicine, Department of Obstetrics and Gynecology, 850 5th Avenue East, Tuscaloosa, AL 35401-7419; davery@cchs.ua.edu
1. Heider A, Neely B, Bell L. Cesarean delivery results in a family medicine residency using a specific training model. Fam Med. 2006;38:103-109.
2. Deutchman M, Connor P, Gobbo R, et al. Outcomes of cesarean sections performed by family physicians and the training they received: a fifteen-year retrospective study. J Am Board Fam Pract. 1995;8:81-90.
3. Larimore WL, Sapolsky BS. Maternity care in family medicine: economics and malpractice. J Fam Pract. 1995;40:153-160.
4. Avery DM, Hooper DE, Garris CE. Minilaparotomy for the surgical management of ectopic pregnancy for family medicine obstetricians. Am J Clin Med. 2009;6:72-73.
5. Avery DM, Hooper DE. Cesarean hysterectomy for family medicine physicians practicing obstetrics. Am J Clin Med. 2009;6:68-71.
6. American Family Physician. Recommended core educational guidelines for family practice residents: maternity and gynecologic care. July 1998. Available at: http://www.aafp.org/afp/980700ap/corematr.html. Accessed March 1, 2009.
7. American Board of Physician Specialties. Annual Leadership Meeting; June 2005;Naples, FL.
8. Avery DM, Garris CE. Board certification versus certificate of added qualification in obstetrics Am J Clin Med. 2006;3:16-18.
9. American Board of Physician Specialties. Family medicine obstetrics eligibility. February 2008. Available at: http://www.abpsus.org/family-medicine-obstetrics-eligibility. Accessed March 1, 2009.
1. Heider A, Neely B, Bell L. Cesarean delivery results in a family medicine residency using a specific training model. Fam Med. 2006;38:103-109.
2. Deutchman M, Connor P, Gobbo R, et al. Outcomes of cesarean sections performed by family physicians and the training they received: a fifteen-year retrospective study. J Am Board Fam Pract. 1995;8:81-90.
3. Larimore WL, Sapolsky BS. Maternity care in family medicine: economics and malpractice. J Fam Pract. 1995;40:153-160.
4. Avery DM, Hooper DE, Garris CE. Minilaparotomy for the surgical management of ectopic pregnancy for family medicine obstetricians. Am J Clin Med. 2009;6:72-73.
5. Avery DM, Hooper DE. Cesarean hysterectomy for family medicine physicians practicing obstetrics. Am J Clin Med. 2009;6:68-71.
6. American Family Physician. Recommended core educational guidelines for family practice residents: maternity and gynecologic care. July 1998. Available at: http://www.aafp.org/afp/980700ap/corematr.html. Accessed March 1, 2009.
7. American Board of Physician Specialties. Annual Leadership Meeting; June 2005;Naples, FL.
8. Avery DM, Garris CE. Board certification versus certificate of added qualification in obstetrics Am J Clin Med. 2006;3:16-18.
9. American Board of Physician Specialties. Family medicine obstetrics eligibility. February 2008. Available at: http://www.abpsus.org/family-medicine-obstetrics-eligibility. Accessed March 1, 2009.
Patient dismissal: The right way to do it
• Unless a single incident irreparably damaged your relationship with a patient, exhaust all efforts at resolution before deciding on dismissal. C
• Establish policies that help you set limits on problem behavior—eg, drug-seeking or angry outbursts—while continuing to care for the patient. C
• When dismissal is unavoidable, inform the patient in writing that you will be available to handle medical emergencies until he or she has found another physician. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Susan L, a 53-year-old who’d been a patient of Dr. O’s for the past 6 years, received a bill for a visit that had occurred nearly 2 years earlier. She called the office and told the receptionist that she had never been billed for this visit and didn’t think she should have to pay after such a lengthy delay. When she received a past due notice, Susan called and asked to speak to the physician—and to schedule an appointment. She was told that she could do neither until her account was current.
Eventually, the unpaid bill was sent to a collection agency, and Susan received a letter threatening legal action. In response, she sent a letter of her own—certified, return receipt requested—detailing her reason for not paying and threatening to sue Dr. O for abandonment.*
*Adapted from actual cases, with details changed to protect the privacy of the parties involved.
With the national unemployment rate hovering at a record high, unpaid medical bills may be your most pressing problem—and potential grounds for patient dismissal. Judging from a recent survey in which primary care physicians identified nearly one patient in 5 as “difficult,"1 it’s unlikely that nonpayment is the only patient conundrum you face.
Indeed, there are many ways a patient can be difficult, including exhibiting habitual hostility, chronic drug-seeking behavior, or consistent noncompliance; breaking appointments at the last minute; or being a no-show. You may wish you could “fire” the worst off enders but be concerned about professional and ethical responsibilities and the legal risk you might face. Ironically, though, struggling to maintain a chronically stressed physician-patient relationship is often riskier than a well-timed termination.2
The key here, however, is the persistent or extreme nature of the difficulty.3 When a dismissal is prompted by a one-time occurrence or lower-level offense, what constitutes a reasonable response is not always clear-cut.
Under what circumstances is it appropriate to end your relationship with a patient? When you do terminate the relationship, what steps can you take to safeguard the patient and avoid charges of abandonment? Here’s a look at these questions—and some answers.
Professional responsibility: How far does it go?
As a physician, you’ve pledged to “do no harm.” And you’ve likely been taught—as it states in the American College of Physicians (ACP) ethics manual—that you have “a moral duty to care for all patients.” 4 The American Medical Association’s code of ethics cites a similar standard: the obligation to place patients’ welfare above your own interests.5
According to the ACP, the physician-patient relationship should be discontinued only under “exceptional circumstances."6 But not everyone agrees, not only on what constitutes “exceptional,” but on whether that is the correct threshold for termination.
A health care attorney writing in American Medical News, for example, takes a more liberal view. It’s time to dismiss, he asserts, when the doctor-patient relationship doesn’t work.7 By that standard, virtually any ongoing problem could be construed as evidence of an “irreparable breakdown” of the physician-patient relationship (TABLE).
TABLE
Key reasons to "fire" a patient
|
| Sources: Kodner C. FP Essentials. 2008.3 Harris S. Am Med News. 2008.7 |
We can work it out
Legally, a doctor can dismiss a patient for virtually any reason, or fail to give any explanation at all.2 Ethically, dismissal should be your last option, not your first choice.
In a home study course titled “Challenging physician-patient interactions,” the American Academy of Family Physicians (AAFP) advises doctors to be certain they have exhausted every reasonable effort to communicate, set achievable goals, and meet the patient’s needs.3 The steps you take to try to mend a damaged patient relationship, of course, will depend on what caused the rift in the first place. Here are some examples.
Nonpayment. You are not compelled (or expected) to indefinitely continue to treat a patient who’s unable—or unwilling—to pay you, of course. But if he or she is out of work and has fallen on hard times or has a single unpaid bill, discussing the problem and attempting to accommodate the patient’s financial limitations (and establish a realistic payment plan) is a reasonable approach.
Having a billing clerk handle most communications regarding unpaid bills may be a good idea. But when a situation escalates, as in the case of Susan L (CASE 1), foregoing a direct discussion and expecting a subordinate to handle an abrupt patient termination is not (ethically or legally) appropriate.7
Laura K, age 34, had always been a challenging patient. She suffered from a collection of pain-producing maladies, including migraines, fibromyalgia, and low back pain. Controlling her pain required increasing amounts of narcotics, sometimes in doses that exceeded therapeutic recommendations.
Recently she’d begun calling her primary care physician’s office for early refills; more than once, she claimed her prescription had been lost or stolen. When Laura called to report that the oxycodone prescribed 4 days ago had been stolen from her purse and to request a refill, the physician refused to speak with her—and instructed the receptionist to tell her she needed to find another physician.
Laura called several other local physicians, but none was able to see her. She then went to the emergency department. The ED physician evaluated her and offered her a prescription for a mild analgesic, but refused her request for oxycodone.
That night, Laura attempted suicide. Although she survived, she was left with significant neurologic deficits. She sued the physician who had refused to speak to her on a variety of counts of negligence, including a charge of abandonment.
At deposition, experts for the plaintiff testified that refusing to see and evaluate a current patient for her ongoing problems without giving substantial notice constituted abandonment—and was a substantial cause of Laura’s suicide attempt. On the advice of counsel, the physician agreed to a $150,000 settlement.
Drug-seeking. Behavior like that of Laura K (CASE 2), whose requests for narcotics and claims of lost pills or prescriptions occurred with increasing regularity, can’t be ignored. The AAFP course, which states that patients should not be dismissed “on the grounds of drug-seeking behaviors alone,"3 recommends that physicians develop policies for prescribing controlled substances and handling drug-seeking patients. Such a policy—which might include limits on the frequency of renewals and the duration of a single prescription, among other provisions—should be communicated to every patient who seeks opioid analgesics.3 The Federation of State Medical Boards recommends the use of a written agreement, spelling out your responsibilities as well as those of the patient, for individuals at high risk of abuse (http://www.fsmb.org/pdf/2004_grpol_Controlled_Substances.pdf).
While the existence of a policy or written contract may not alter the behavior of a drug-seeking patient, it can prevent you from being caught off -guard or reacting as rashly as Laura K’s physician did. Indeed, Laura’s doctor made 2 key missteps: acting without warning, and expecting a receptionist to deliver the dismissal message.
A better approach, from the AAFP’s perspective, is to calmly maintain the limits you’ve set, remind the patient that you want to help, and offer treatment alternatives, such as nonopioid analgesics.3 Discussions in response to drug-seeking behavior, of course, should always be delivered—and documented—by the physician.
Noncompliance. This is a particularly complex problem, as issues of patient autonomy and physician authority are involved. A case study presented in the AAFP home study course describes the thoughts and feelings of a physician who considered dismissing a pediatric patient because the child’s mother refused to allow him to be vaccinated. The physician ultimately decided to continue to treat the child, after determining that the physician-patient relationship could still be beneficial and planning to revisit the vaccination issue with the mother at a later date.3 (Another physician, faced with a similar issue, wrote a New York Times article about his decision to dismiss a young patient. His reasoning? Accepting the mother’s refusal to allow her son to get a tetanus booster would compromise “my conscience and my professional ethics. I couldn’t do that."8)
Although it is important to recognize the difference between noncompliance and an individual’s right to refuse recommended treatment,9 you, too, may encounter situations in which a patient’s, or parent’s, repeated failure—to follow an agreed-upon therapeutic regimen, perhaps, or adhere to a schedule of visits needed to manage a chronic condition— causes your relationship with the patient to deteriorate to a point where dismissal is warranted. Here, as with other potential causes of dismissal, the patient should be adequately warned, the discussion documented, and action taken only if nothing changes.
Anger. As is the case with drug-seeking, the AAFP course advises physicians to anticipate and develop policies for handling situations in which a patient’s anger escalates and creates a real or perceived threat.3 While this is commonly done in acute care facilities, it is often overlooked in outpatient settings.
Among the issues to address: equipping offices and exam rooms with an emergency call button or intercom, knowing where to position yourself to ensure that you can’t be trapped in a room by a threatening patient, and considering how to respond in a way that defuses—rather than escalates—the anger. Calmly ask the patient what he or she is upset about, listen carefully, and apologize, if appropriate, for your role in the upsetting incident. Then move on to the purpose of the visit, stating, for example, “Now, what brings you in today?” 3
It is crucial to set boundaries (although it’s probably not a good idea to attempt it at the time of the outburst), making it clear, for example, that profanity is not acceptable; directing anger at nurses or other staff members is not permitted; and what the consequences of continued outbursts will be. 3
A single incident that’s grounds for dismissal
Despite the emphasis on resolving problems with patients, there are times when dismissal can and should occur, with little warning and no negotiation. In its home study course, the AAFP describes this as a “sentinel incident"— a single occurrence so egregious that it damages the physician-patient relationship beyond repair.3
A threat of violence or a physical assault itself would rise to that level. Some other examples: a sexual assault or blatant sexual advance, falsifying medical records, and theft or another type of criminal activity carried out in the physician’s office.
When a sentinel incident occurs, the best course is likely to be to forego any attempt at resolution, call the police or your facility’s security officer, and, if appropriate, to immediately prepare to “fire” the patient.
Dismissal without abandonment: Here’s how
In the vast majority of cases, dismissing a patient does not in and of itself constitute patient abandonment. Even if the termination is unduly abrupt, as was the case for Susan (CASE 1) and Laura (CASE 2), it doesn’t constitute abandonment unless the patient is dismissed during a course of treatment and unable to find a physician to provide ongoing care.
Neither was true in Susan’s case, and her threat of a lawsuit based on charges of abandonment never came to fruition. Not so for Laura, who was abruptly terminated during ongoing treatment—and who nonetheless made numerous attempts to find another doctor to care for her, without success. The attorney for Laura’s physician advised that the severe consequences of dismissing without going through the proper channels made a trial defense untenable.
Although most charges of patient abandonment never rise to the level required for a successful lawsuit, attorneys often include it in a litany of charges in an attempt to damage the physician’s credibility with a jury. You can usually avoid that scenario by taking the right steps when you dismiss a patient.
CASE 3 Pregnant patient, rural physician
As part of his rural family medicine practice, Dr. J provided obstetrical care. Dr. J had a partner and they alternated call nights, but his partner did not do OB. Dr. J made it a point, however, to always be on call for his obstetrical patients as they neared delivery. Having no patients imminently due, he took a one-week vacation out of town.
One of his patients went into premature labor and went to the local hospital. Dr. J’s partner was called to attend, but indicated he did not do OB work and advised the emergency physician to call “any obstetrician around.” One obstetrical group covered the region and the on-call physician was at another hospital doing a C-section and requested that the patient be transferred to that hospital for evaluation. After a series of delays, the patient was transferred and delivered a preterm infant who showed signs of neurological injury after a lengthy ICU stay.
The family sued all providers involved on several grounds, including patient abandonment. Plaintiff experts testified that the standard of care would be for Dr. J to be in attendance for such emergencies or, failing that, to provide for adequate coverage of his pregnant patient. They also testified that it was reasonable for the patient to have gone to the local hospital where her delivery was planned and that Dr. J should have arranged for the local OB group to provide emergency coverage. The case concluded with an $800,000 pretrial settlement.
Ensure that dismissal is an option
While we’ve already established that physicians have the legal right to dismiss patients, regardless of the reason, there are instances that make it far more difficult—and legally risky—to do so.
A primary care physician in a rural area is a case in point (CASE 3). If you are the only doctor in the area and the patient has no viable means of getting care from another provider, you may want to reconsider the dismissal. It is far easier to establish that a patient in such an underserved area was abandoned, even— as Dr. J found out—for failing to ensure full coverage during a vacation or leave of absence.
Rural physicians can help prevent charges of abandonment by advising patients of the special call challenges a rural setting presents. Doctors should make sure their patients know what to do if an emergency occurs when the practice is closed or a physician is out of town, and document the discussion in the medical record.
A physician in a staff-model HMO may face similar problems. Unless the HMO has another outpatient clinic in the vicinity, dismissal could leave the patient with no means of receiving affordable health care.
Options in such a case might include asking a colleague at the same clinic to accept a patient whom you would like to dismiss or finding a way to manage the patient’s behavior. If a patient has been excessively angry or threatening in the past, for example, it is often advisable to sit down with the patient (with security nearby) to discuss the parameters of expected behavior and develop a contract for future care. The contract might include a requirement that the patient call in advance so that security can be present when he or she arrives, for example, or that the patient agree to abstain from profanity and threats.
Know the laws in your state. Before you terminate a patient, check with your state medical board or local medical society to make sure your actions will be in compliance with any relevant state rules and regulations.
When you dismiss, cover all bases
Send a letter to the patient by certified mail, return receipt requested, notifying him or her of the dismissal and agreeing to provide emergency care for a reasonable time—typically, 30 days—while the patient seeks another physician. It is advisable, too, to help the patient locate other potential clinicians—by, say, including contact information for your county medical society or the patient’s health insurer’s list of in-network providers, or referring an indigent patient to Medicaid or a sliding scale clinic. It is a good idea to offer to transfer records to the new physician, as well.
It is not mandatory to document the reason for the dismissal in the letter, but some sources recommend that you do so. If you’re uncertain how to proceed, check with legal counsel before you send the letter. (You can find sample dismissal letters at www.ttuhsc.edu/som/clinic/forms/ACForm8.11.A.pdf and in “Terminating a patient: Is it time to part ways?” at http://www.aafp.org/fpm/2005/0900/p34.html.)
The events that led up to the dismissal, however, including any discussions you had with the patient about them, must be documented in the medical record. Put a copy of the letter and the certified mail receipt in the chart, as well. JFP
CORRESPONDENCE John Davenport, MD, JD, 13 Redonda, Irvine, CA 92620; john.y.davenport@kp.org
1. Hinchey SA, Jackson JL. A cohort study assessing difficult patient encounters in a walk-in primary care clinic, predictors and outcomes. J Gen Intern Med. 2011;Jan 25 [Epub ahead of print].
2. Schleiter K. Difficult patient-physician relationships and the risk of medical malpractice litigation. Virtual Mentor. 2009;11:242-246.
3. Kodner C. Challenging physician-patient interactions. FP Essentials. ed 354. AAFP home study. Leawood, Kan: American Academy of Family Physicians; November 2008.
4. Snyder L, Leffler C. Ethics and Human Rights Committee American College of Physicians. Ethics manual: fifth ed. Ann Intern Med. 2005;142:560-582.
5. American Medical Association (AMA). Opinion 10.015. The patient-physician relationship. Code of Medical Ethics. Chicago, Ill: AMA. 2008. Available at: http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion10015.shtml. Accessed February 11, 2011.
6. American College of Physicians. Ethical considerations for the use of patient incentives to promote personal responsibility for health: West Virginia Medicaid and beyond [position paper]. Philadelphia: American College of Physicians; 2010.
7. Harris SM. Take care when firing a patient. Am Med News. February 4, 2008. Available at: http://www.ama-assn.org/amednews/2008/02/04/bica0204.htm. Accessed February 11, 2011.
8. Parikh RK. Showing the patient the door, permanently. New York Times. June 10, 2008. Available at: http://www.nytimes.com/2008/06/10/health/views/10case.html. Accessed February 15, 2011.
9. Summey-Lowman B. Patient non-compliance—a powerful legal defense. Healthcare Risk Manag. 2009;15:1-2.
• Unless a single incident irreparably damaged your relationship with a patient, exhaust all efforts at resolution before deciding on dismissal. C
• Establish policies that help you set limits on problem behavior—eg, drug-seeking or angry outbursts—while continuing to care for the patient. C
• When dismissal is unavoidable, inform the patient in writing that you will be available to handle medical emergencies until he or she has found another physician. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Susan L, a 53-year-old who’d been a patient of Dr. O’s for the past 6 years, received a bill for a visit that had occurred nearly 2 years earlier. She called the office and told the receptionist that she had never been billed for this visit and didn’t think she should have to pay after such a lengthy delay. When she received a past due notice, Susan called and asked to speak to the physician—and to schedule an appointment. She was told that she could do neither until her account was current.
Eventually, the unpaid bill was sent to a collection agency, and Susan received a letter threatening legal action. In response, she sent a letter of her own—certified, return receipt requested—detailing her reason for not paying and threatening to sue Dr. O for abandonment.*
*Adapted from actual cases, with details changed to protect the privacy of the parties involved.
With the national unemployment rate hovering at a record high, unpaid medical bills may be your most pressing problem—and potential grounds for patient dismissal. Judging from a recent survey in which primary care physicians identified nearly one patient in 5 as “difficult,"1 it’s unlikely that nonpayment is the only patient conundrum you face.
Indeed, there are many ways a patient can be difficult, including exhibiting habitual hostility, chronic drug-seeking behavior, or consistent noncompliance; breaking appointments at the last minute; or being a no-show. You may wish you could “fire” the worst off enders but be concerned about professional and ethical responsibilities and the legal risk you might face. Ironically, though, struggling to maintain a chronically stressed physician-patient relationship is often riskier than a well-timed termination.2
The key here, however, is the persistent or extreme nature of the difficulty.3 When a dismissal is prompted by a one-time occurrence or lower-level offense, what constitutes a reasonable response is not always clear-cut.
Under what circumstances is it appropriate to end your relationship with a patient? When you do terminate the relationship, what steps can you take to safeguard the patient and avoid charges of abandonment? Here’s a look at these questions—and some answers.
Professional responsibility: How far does it go?
As a physician, you’ve pledged to “do no harm.” And you’ve likely been taught—as it states in the American College of Physicians (ACP) ethics manual—that you have “a moral duty to care for all patients.” 4 The American Medical Association’s code of ethics cites a similar standard: the obligation to place patients’ welfare above your own interests.5
According to the ACP, the physician-patient relationship should be discontinued only under “exceptional circumstances."6 But not everyone agrees, not only on what constitutes “exceptional,” but on whether that is the correct threshold for termination.
A health care attorney writing in American Medical News, for example, takes a more liberal view. It’s time to dismiss, he asserts, when the doctor-patient relationship doesn’t work.7 By that standard, virtually any ongoing problem could be construed as evidence of an “irreparable breakdown” of the physician-patient relationship (TABLE).
TABLE
Key reasons to "fire" a patient
|
| Sources: Kodner C. FP Essentials. 2008.3 Harris S. Am Med News. 2008.7 |
We can work it out
Legally, a doctor can dismiss a patient for virtually any reason, or fail to give any explanation at all.2 Ethically, dismissal should be your last option, not your first choice.
In a home study course titled “Challenging physician-patient interactions,” the American Academy of Family Physicians (AAFP) advises doctors to be certain they have exhausted every reasonable effort to communicate, set achievable goals, and meet the patient’s needs.3 The steps you take to try to mend a damaged patient relationship, of course, will depend on what caused the rift in the first place. Here are some examples.
Nonpayment. You are not compelled (or expected) to indefinitely continue to treat a patient who’s unable—or unwilling—to pay you, of course. But if he or she is out of work and has fallen on hard times or has a single unpaid bill, discussing the problem and attempting to accommodate the patient’s financial limitations (and establish a realistic payment plan) is a reasonable approach.
Having a billing clerk handle most communications regarding unpaid bills may be a good idea. But when a situation escalates, as in the case of Susan L (CASE 1), foregoing a direct discussion and expecting a subordinate to handle an abrupt patient termination is not (ethically or legally) appropriate.7
Laura K, age 34, had always been a challenging patient. She suffered from a collection of pain-producing maladies, including migraines, fibromyalgia, and low back pain. Controlling her pain required increasing amounts of narcotics, sometimes in doses that exceeded therapeutic recommendations.
Recently she’d begun calling her primary care physician’s office for early refills; more than once, she claimed her prescription had been lost or stolen. When Laura called to report that the oxycodone prescribed 4 days ago had been stolen from her purse and to request a refill, the physician refused to speak with her—and instructed the receptionist to tell her she needed to find another physician.
Laura called several other local physicians, but none was able to see her. She then went to the emergency department. The ED physician evaluated her and offered her a prescription for a mild analgesic, but refused her request for oxycodone.
That night, Laura attempted suicide. Although she survived, she was left with significant neurologic deficits. She sued the physician who had refused to speak to her on a variety of counts of negligence, including a charge of abandonment.
At deposition, experts for the plaintiff testified that refusing to see and evaluate a current patient for her ongoing problems without giving substantial notice constituted abandonment—and was a substantial cause of Laura’s suicide attempt. On the advice of counsel, the physician agreed to a $150,000 settlement.
Drug-seeking. Behavior like that of Laura K (CASE 2), whose requests for narcotics and claims of lost pills or prescriptions occurred with increasing regularity, can’t be ignored. The AAFP course, which states that patients should not be dismissed “on the grounds of drug-seeking behaviors alone,"3 recommends that physicians develop policies for prescribing controlled substances and handling drug-seeking patients. Such a policy—which might include limits on the frequency of renewals and the duration of a single prescription, among other provisions—should be communicated to every patient who seeks opioid analgesics.3 The Federation of State Medical Boards recommends the use of a written agreement, spelling out your responsibilities as well as those of the patient, for individuals at high risk of abuse (http://www.fsmb.org/pdf/2004_grpol_Controlled_Substances.pdf).
While the existence of a policy or written contract may not alter the behavior of a drug-seeking patient, it can prevent you from being caught off -guard or reacting as rashly as Laura K’s physician did. Indeed, Laura’s doctor made 2 key missteps: acting without warning, and expecting a receptionist to deliver the dismissal message.
A better approach, from the AAFP’s perspective, is to calmly maintain the limits you’ve set, remind the patient that you want to help, and offer treatment alternatives, such as nonopioid analgesics.3 Discussions in response to drug-seeking behavior, of course, should always be delivered—and documented—by the physician.
Noncompliance. This is a particularly complex problem, as issues of patient autonomy and physician authority are involved. A case study presented in the AAFP home study course describes the thoughts and feelings of a physician who considered dismissing a pediatric patient because the child’s mother refused to allow him to be vaccinated. The physician ultimately decided to continue to treat the child, after determining that the physician-patient relationship could still be beneficial and planning to revisit the vaccination issue with the mother at a later date.3 (Another physician, faced with a similar issue, wrote a New York Times article about his decision to dismiss a young patient. His reasoning? Accepting the mother’s refusal to allow her son to get a tetanus booster would compromise “my conscience and my professional ethics. I couldn’t do that."8)
Although it is important to recognize the difference between noncompliance and an individual’s right to refuse recommended treatment,9 you, too, may encounter situations in which a patient’s, or parent’s, repeated failure—to follow an agreed-upon therapeutic regimen, perhaps, or adhere to a schedule of visits needed to manage a chronic condition— causes your relationship with the patient to deteriorate to a point where dismissal is warranted. Here, as with other potential causes of dismissal, the patient should be adequately warned, the discussion documented, and action taken only if nothing changes.
Anger. As is the case with drug-seeking, the AAFP course advises physicians to anticipate and develop policies for handling situations in which a patient’s anger escalates and creates a real or perceived threat.3 While this is commonly done in acute care facilities, it is often overlooked in outpatient settings.
Among the issues to address: equipping offices and exam rooms with an emergency call button or intercom, knowing where to position yourself to ensure that you can’t be trapped in a room by a threatening patient, and considering how to respond in a way that defuses—rather than escalates—the anger. Calmly ask the patient what he or she is upset about, listen carefully, and apologize, if appropriate, for your role in the upsetting incident. Then move on to the purpose of the visit, stating, for example, “Now, what brings you in today?” 3
It is crucial to set boundaries (although it’s probably not a good idea to attempt it at the time of the outburst), making it clear, for example, that profanity is not acceptable; directing anger at nurses or other staff members is not permitted; and what the consequences of continued outbursts will be. 3
A single incident that’s grounds for dismissal
Despite the emphasis on resolving problems with patients, there are times when dismissal can and should occur, with little warning and no negotiation. In its home study course, the AAFP describes this as a “sentinel incident"— a single occurrence so egregious that it damages the physician-patient relationship beyond repair.3
A threat of violence or a physical assault itself would rise to that level. Some other examples: a sexual assault or blatant sexual advance, falsifying medical records, and theft or another type of criminal activity carried out in the physician’s office.
When a sentinel incident occurs, the best course is likely to be to forego any attempt at resolution, call the police or your facility’s security officer, and, if appropriate, to immediately prepare to “fire” the patient.
Dismissal without abandonment: Here’s how
In the vast majority of cases, dismissing a patient does not in and of itself constitute patient abandonment. Even if the termination is unduly abrupt, as was the case for Susan (CASE 1) and Laura (CASE 2), it doesn’t constitute abandonment unless the patient is dismissed during a course of treatment and unable to find a physician to provide ongoing care.
Neither was true in Susan’s case, and her threat of a lawsuit based on charges of abandonment never came to fruition. Not so for Laura, who was abruptly terminated during ongoing treatment—and who nonetheless made numerous attempts to find another doctor to care for her, without success. The attorney for Laura’s physician advised that the severe consequences of dismissing without going through the proper channels made a trial defense untenable.
Although most charges of patient abandonment never rise to the level required for a successful lawsuit, attorneys often include it in a litany of charges in an attempt to damage the physician’s credibility with a jury. You can usually avoid that scenario by taking the right steps when you dismiss a patient.
CASE 3 Pregnant patient, rural physician
As part of his rural family medicine practice, Dr. J provided obstetrical care. Dr. J had a partner and they alternated call nights, but his partner did not do OB. Dr. J made it a point, however, to always be on call for his obstetrical patients as they neared delivery. Having no patients imminently due, he took a one-week vacation out of town.
One of his patients went into premature labor and went to the local hospital. Dr. J’s partner was called to attend, but indicated he did not do OB work and advised the emergency physician to call “any obstetrician around.” One obstetrical group covered the region and the on-call physician was at another hospital doing a C-section and requested that the patient be transferred to that hospital for evaluation. After a series of delays, the patient was transferred and delivered a preterm infant who showed signs of neurological injury after a lengthy ICU stay.
The family sued all providers involved on several grounds, including patient abandonment. Plaintiff experts testified that the standard of care would be for Dr. J to be in attendance for such emergencies or, failing that, to provide for adequate coverage of his pregnant patient. They also testified that it was reasonable for the patient to have gone to the local hospital where her delivery was planned and that Dr. J should have arranged for the local OB group to provide emergency coverage. The case concluded with an $800,000 pretrial settlement.
Ensure that dismissal is an option
While we’ve already established that physicians have the legal right to dismiss patients, regardless of the reason, there are instances that make it far more difficult—and legally risky—to do so.
A primary care physician in a rural area is a case in point (CASE 3). If you are the only doctor in the area and the patient has no viable means of getting care from another provider, you may want to reconsider the dismissal. It is far easier to establish that a patient in such an underserved area was abandoned, even— as Dr. J found out—for failing to ensure full coverage during a vacation or leave of absence.
Rural physicians can help prevent charges of abandonment by advising patients of the special call challenges a rural setting presents. Doctors should make sure their patients know what to do if an emergency occurs when the practice is closed or a physician is out of town, and document the discussion in the medical record.
A physician in a staff-model HMO may face similar problems. Unless the HMO has another outpatient clinic in the vicinity, dismissal could leave the patient with no means of receiving affordable health care.
Options in such a case might include asking a colleague at the same clinic to accept a patient whom you would like to dismiss or finding a way to manage the patient’s behavior. If a patient has been excessively angry or threatening in the past, for example, it is often advisable to sit down with the patient (with security nearby) to discuss the parameters of expected behavior and develop a contract for future care. The contract might include a requirement that the patient call in advance so that security can be present when he or she arrives, for example, or that the patient agree to abstain from profanity and threats.
Know the laws in your state. Before you terminate a patient, check with your state medical board or local medical society to make sure your actions will be in compliance with any relevant state rules and regulations.
When you dismiss, cover all bases
Send a letter to the patient by certified mail, return receipt requested, notifying him or her of the dismissal and agreeing to provide emergency care for a reasonable time—typically, 30 days—while the patient seeks another physician. It is advisable, too, to help the patient locate other potential clinicians—by, say, including contact information for your county medical society or the patient’s health insurer’s list of in-network providers, or referring an indigent patient to Medicaid or a sliding scale clinic. It is a good idea to offer to transfer records to the new physician, as well.
It is not mandatory to document the reason for the dismissal in the letter, but some sources recommend that you do so. If you’re uncertain how to proceed, check with legal counsel before you send the letter. (You can find sample dismissal letters at www.ttuhsc.edu/som/clinic/forms/ACForm8.11.A.pdf and in “Terminating a patient: Is it time to part ways?” at http://www.aafp.org/fpm/2005/0900/p34.html.)
The events that led up to the dismissal, however, including any discussions you had with the patient about them, must be documented in the medical record. Put a copy of the letter and the certified mail receipt in the chart, as well. JFP
CORRESPONDENCE John Davenport, MD, JD, 13 Redonda, Irvine, CA 92620; john.y.davenport@kp.org
• Unless a single incident irreparably damaged your relationship with a patient, exhaust all efforts at resolution before deciding on dismissal. C
• Establish policies that help you set limits on problem behavior—eg, drug-seeking or angry outbursts—while continuing to care for the patient. C
• When dismissal is unavoidable, inform the patient in writing that you will be available to handle medical emergencies until he or she has found another physician. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Susan L, a 53-year-old who’d been a patient of Dr. O’s for the past 6 years, received a bill for a visit that had occurred nearly 2 years earlier. She called the office and told the receptionist that she had never been billed for this visit and didn’t think she should have to pay after such a lengthy delay. When she received a past due notice, Susan called and asked to speak to the physician—and to schedule an appointment. She was told that she could do neither until her account was current.
Eventually, the unpaid bill was sent to a collection agency, and Susan received a letter threatening legal action. In response, she sent a letter of her own—certified, return receipt requested—detailing her reason for not paying and threatening to sue Dr. O for abandonment.*
*Adapted from actual cases, with details changed to protect the privacy of the parties involved.
With the national unemployment rate hovering at a record high, unpaid medical bills may be your most pressing problem—and potential grounds for patient dismissal. Judging from a recent survey in which primary care physicians identified nearly one patient in 5 as “difficult,"1 it’s unlikely that nonpayment is the only patient conundrum you face.
Indeed, there are many ways a patient can be difficult, including exhibiting habitual hostility, chronic drug-seeking behavior, or consistent noncompliance; breaking appointments at the last minute; or being a no-show. You may wish you could “fire” the worst off enders but be concerned about professional and ethical responsibilities and the legal risk you might face. Ironically, though, struggling to maintain a chronically stressed physician-patient relationship is often riskier than a well-timed termination.2
The key here, however, is the persistent or extreme nature of the difficulty.3 When a dismissal is prompted by a one-time occurrence or lower-level offense, what constitutes a reasonable response is not always clear-cut.
Under what circumstances is it appropriate to end your relationship with a patient? When you do terminate the relationship, what steps can you take to safeguard the patient and avoid charges of abandonment? Here’s a look at these questions—and some answers.
Professional responsibility: How far does it go?
As a physician, you’ve pledged to “do no harm.” And you’ve likely been taught—as it states in the American College of Physicians (ACP) ethics manual—that you have “a moral duty to care for all patients.” 4 The American Medical Association’s code of ethics cites a similar standard: the obligation to place patients’ welfare above your own interests.5
According to the ACP, the physician-patient relationship should be discontinued only under “exceptional circumstances."6 But not everyone agrees, not only on what constitutes “exceptional,” but on whether that is the correct threshold for termination.
A health care attorney writing in American Medical News, for example, takes a more liberal view. It’s time to dismiss, he asserts, when the doctor-patient relationship doesn’t work.7 By that standard, virtually any ongoing problem could be construed as evidence of an “irreparable breakdown” of the physician-patient relationship (TABLE).
TABLE
Key reasons to "fire" a patient
|
| Sources: Kodner C. FP Essentials. 2008.3 Harris S. Am Med News. 2008.7 |
We can work it out
Legally, a doctor can dismiss a patient for virtually any reason, or fail to give any explanation at all.2 Ethically, dismissal should be your last option, not your first choice.
In a home study course titled “Challenging physician-patient interactions,” the American Academy of Family Physicians (AAFP) advises doctors to be certain they have exhausted every reasonable effort to communicate, set achievable goals, and meet the patient’s needs.3 The steps you take to try to mend a damaged patient relationship, of course, will depend on what caused the rift in the first place. Here are some examples.
Nonpayment. You are not compelled (or expected) to indefinitely continue to treat a patient who’s unable—or unwilling—to pay you, of course. But if he or she is out of work and has fallen on hard times or has a single unpaid bill, discussing the problem and attempting to accommodate the patient’s financial limitations (and establish a realistic payment plan) is a reasonable approach.
Having a billing clerk handle most communications regarding unpaid bills may be a good idea. But when a situation escalates, as in the case of Susan L (CASE 1), foregoing a direct discussion and expecting a subordinate to handle an abrupt patient termination is not (ethically or legally) appropriate.7
Laura K, age 34, had always been a challenging patient. She suffered from a collection of pain-producing maladies, including migraines, fibromyalgia, and low back pain. Controlling her pain required increasing amounts of narcotics, sometimes in doses that exceeded therapeutic recommendations.
Recently she’d begun calling her primary care physician’s office for early refills; more than once, she claimed her prescription had been lost or stolen. When Laura called to report that the oxycodone prescribed 4 days ago had been stolen from her purse and to request a refill, the physician refused to speak with her—and instructed the receptionist to tell her she needed to find another physician.
Laura called several other local physicians, but none was able to see her. She then went to the emergency department. The ED physician evaluated her and offered her a prescription for a mild analgesic, but refused her request for oxycodone.
That night, Laura attempted suicide. Although she survived, she was left with significant neurologic deficits. She sued the physician who had refused to speak to her on a variety of counts of negligence, including a charge of abandonment.
At deposition, experts for the plaintiff testified that refusing to see and evaluate a current patient for her ongoing problems without giving substantial notice constituted abandonment—and was a substantial cause of Laura’s suicide attempt. On the advice of counsel, the physician agreed to a $150,000 settlement.
Drug-seeking. Behavior like that of Laura K (CASE 2), whose requests for narcotics and claims of lost pills or prescriptions occurred with increasing regularity, can’t be ignored. The AAFP course, which states that patients should not be dismissed “on the grounds of drug-seeking behaviors alone,"3 recommends that physicians develop policies for prescribing controlled substances and handling drug-seeking patients. Such a policy—which might include limits on the frequency of renewals and the duration of a single prescription, among other provisions—should be communicated to every patient who seeks opioid analgesics.3 The Federation of State Medical Boards recommends the use of a written agreement, spelling out your responsibilities as well as those of the patient, for individuals at high risk of abuse (http://www.fsmb.org/pdf/2004_grpol_Controlled_Substances.pdf).
While the existence of a policy or written contract may not alter the behavior of a drug-seeking patient, it can prevent you from being caught off -guard or reacting as rashly as Laura K’s physician did. Indeed, Laura’s doctor made 2 key missteps: acting without warning, and expecting a receptionist to deliver the dismissal message.
A better approach, from the AAFP’s perspective, is to calmly maintain the limits you’ve set, remind the patient that you want to help, and offer treatment alternatives, such as nonopioid analgesics.3 Discussions in response to drug-seeking behavior, of course, should always be delivered—and documented—by the physician.
Noncompliance. This is a particularly complex problem, as issues of patient autonomy and physician authority are involved. A case study presented in the AAFP home study course describes the thoughts and feelings of a physician who considered dismissing a pediatric patient because the child’s mother refused to allow him to be vaccinated. The physician ultimately decided to continue to treat the child, after determining that the physician-patient relationship could still be beneficial and planning to revisit the vaccination issue with the mother at a later date.3 (Another physician, faced with a similar issue, wrote a New York Times article about his decision to dismiss a young patient. His reasoning? Accepting the mother’s refusal to allow her son to get a tetanus booster would compromise “my conscience and my professional ethics. I couldn’t do that."8)
Although it is important to recognize the difference between noncompliance and an individual’s right to refuse recommended treatment,9 you, too, may encounter situations in which a patient’s, or parent’s, repeated failure—to follow an agreed-upon therapeutic regimen, perhaps, or adhere to a schedule of visits needed to manage a chronic condition— causes your relationship with the patient to deteriorate to a point where dismissal is warranted. Here, as with other potential causes of dismissal, the patient should be adequately warned, the discussion documented, and action taken only if nothing changes.
Anger. As is the case with drug-seeking, the AAFP course advises physicians to anticipate and develop policies for handling situations in which a patient’s anger escalates and creates a real or perceived threat.3 While this is commonly done in acute care facilities, it is often overlooked in outpatient settings.
Among the issues to address: equipping offices and exam rooms with an emergency call button or intercom, knowing where to position yourself to ensure that you can’t be trapped in a room by a threatening patient, and considering how to respond in a way that defuses—rather than escalates—the anger. Calmly ask the patient what he or she is upset about, listen carefully, and apologize, if appropriate, for your role in the upsetting incident. Then move on to the purpose of the visit, stating, for example, “Now, what brings you in today?” 3
It is crucial to set boundaries (although it’s probably not a good idea to attempt it at the time of the outburst), making it clear, for example, that profanity is not acceptable; directing anger at nurses or other staff members is not permitted; and what the consequences of continued outbursts will be. 3
A single incident that’s grounds for dismissal
Despite the emphasis on resolving problems with patients, there are times when dismissal can and should occur, with little warning and no negotiation. In its home study course, the AAFP describes this as a “sentinel incident"— a single occurrence so egregious that it damages the physician-patient relationship beyond repair.3
A threat of violence or a physical assault itself would rise to that level. Some other examples: a sexual assault or blatant sexual advance, falsifying medical records, and theft or another type of criminal activity carried out in the physician’s office.
When a sentinel incident occurs, the best course is likely to be to forego any attempt at resolution, call the police or your facility’s security officer, and, if appropriate, to immediately prepare to “fire” the patient.
Dismissal without abandonment: Here’s how
In the vast majority of cases, dismissing a patient does not in and of itself constitute patient abandonment. Even if the termination is unduly abrupt, as was the case for Susan (CASE 1) and Laura (CASE 2), it doesn’t constitute abandonment unless the patient is dismissed during a course of treatment and unable to find a physician to provide ongoing care.
Neither was true in Susan’s case, and her threat of a lawsuit based on charges of abandonment never came to fruition. Not so for Laura, who was abruptly terminated during ongoing treatment—and who nonetheless made numerous attempts to find another doctor to care for her, without success. The attorney for Laura’s physician advised that the severe consequences of dismissing without going through the proper channels made a trial defense untenable.
Although most charges of patient abandonment never rise to the level required for a successful lawsuit, attorneys often include it in a litany of charges in an attempt to damage the physician’s credibility with a jury. You can usually avoid that scenario by taking the right steps when you dismiss a patient.
CASE 3 Pregnant patient, rural physician
As part of his rural family medicine practice, Dr. J provided obstetrical care. Dr. J had a partner and they alternated call nights, but his partner did not do OB. Dr. J made it a point, however, to always be on call for his obstetrical patients as they neared delivery. Having no patients imminently due, he took a one-week vacation out of town.
One of his patients went into premature labor and went to the local hospital. Dr. J’s partner was called to attend, but indicated he did not do OB work and advised the emergency physician to call “any obstetrician around.” One obstetrical group covered the region and the on-call physician was at another hospital doing a C-section and requested that the patient be transferred to that hospital for evaluation. After a series of delays, the patient was transferred and delivered a preterm infant who showed signs of neurological injury after a lengthy ICU stay.
The family sued all providers involved on several grounds, including patient abandonment. Plaintiff experts testified that the standard of care would be for Dr. J to be in attendance for such emergencies or, failing that, to provide for adequate coverage of his pregnant patient. They also testified that it was reasonable for the patient to have gone to the local hospital where her delivery was planned and that Dr. J should have arranged for the local OB group to provide emergency coverage. The case concluded with an $800,000 pretrial settlement.
Ensure that dismissal is an option
While we’ve already established that physicians have the legal right to dismiss patients, regardless of the reason, there are instances that make it far more difficult—and legally risky—to do so.
A primary care physician in a rural area is a case in point (CASE 3). If you are the only doctor in the area and the patient has no viable means of getting care from another provider, you may want to reconsider the dismissal. It is far easier to establish that a patient in such an underserved area was abandoned, even— as Dr. J found out—for failing to ensure full coverage during a vacation or leave of absence.
Rural physicians can help prevent charges of abandonment by advising patients of the special call challenges a rural setting presents. Doctors should make sure their patients know what to do if an emergency occurs when the practice is closed or a physician is out of town, and document the discussion in the medical record.
A physician in a staff-model HMO may face similar problems. Unless the HMO has another outpatient clinic in the vicinity, dismissal could leave the patient with no means of receiving affordable health care.
Options in such a case might include asking a colleague at the same clinic to accept a patient whom you would like to dismiss or finding a way to manage the patient’s behavior. If a patient has been excessively angry or threatening in the past, for example, it is often advisable to sit down with the patient (with security nearby) to discuss the parameters of expected behavior and develop a contract for future care. The contract might include a requirement that the patient call in advance so that security can be present when he or she arrives, for example, or that the patient agree to abstain from profanity and threats.
Know the laws in your state. Before you terminate a patient, check with your state medical board or local medical society to make sure your actions will be in compliance with any relevant state rules and regulations.
When you dismiss, cover all bases
Send a letter to the patient by certified mail, return receipt requested, notifying him or her of the dismissal and agreeing to provide emergency care for a reasonable time—typically, 30 days—while the patient seeks another physician. It is advisable, too, to help the patient locate other potential clinicians—by, say, including contact information for your county medical society or the patient’s health insurer’s list of in-network providers, or referring an indigent patient to Medicaid or a sliding scale clinic. It is a good idea to offer to transfer records to the new physician, as well.
It is not mandatory to document the reason for the dismissal in the letter, but some sources recommend that you do so. If you’re uncertain how to proceed, check with legal counsel before you send the letter. (You can find sample dismissal letters at www.ttuhsc.edu/som/clinic/forms/ACForm8.11.A.pdf and in “Terminating a patient: Is it time to part ways?” at http://www.aafp.org/fpm/2005/0900/p34.html.)
The events that led up to the dismissal, however, including any discussions you had with the patient about them, must be documented in the medical record. Put a copy of the letter and the certified mail receipt in the chart, as well. JFP
CORRESPONDENCE John Davenport, MD, JD, 13 Redonda, Irvine, CA 92620; john.y.davenport@kp.org
1. Hinchey SA, Jackson JL. A cohort study assessing difficult patient encounters in a walk-in primary care clinic, predictors and outcomes. J Gen Intern Med. 2011;Jan 25 [Epub ahead of print].
2. Schleiter K. Difficult patient-physician relationships and the risk of medical malpractice litigation. Virtual Mentor. 2009;11:242-246.
3. Kodner C. Challenging physician-patient interactions. FP Essentials. ed 354. AAFP home study. Leawood, Kan: American Academy of Family Physicians; November 2008.
4. Snyder L, Leffler C. Ethics and Human Rights Committee American College of Physicians. Ethics manual: fifth ed. Ann Intern Med. 2005;142:560-582.
5. American Medical Association (AMA). Opinion 10.015. The patient-physician relationship. Code of Medical Ethics. Chicago, Ill: AMA. 2008. Available at: http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion10015.shtml. Accessed February 11, 2011.
6. American College of Physicians. Ethical considerations for the use of patient incentives to promote personal responsibility for health: West Virginia Medicaid and beyond [position paper]. Philadelphia: American College of Physicians; 2010.
7. Harris SM. Take care when firing a patient. Am Med News. February 4, 2008. Available at: http://www.ama-assn.org/amednews/2008/02/04/bica0204.htm. Accessed February 11, 2011.
8. Parikh RK. Showing the patient the door, permanently. New York Times. June 10, 2008. Available at: http://www.nytimes.com/2008/06/10/health/views/10case.html. Accessed February 15, 2011.
9. Summey-Lowman B. Patient non-compliance—a powerful legal defense. Healthcare Risk Manag. 2009;15:1-2.
1. Hinchey SA, Jackson JL. A cohort study assessing difficult patient encounters in a walk-in primary care clinic, predictors and outcomes. J Gen Intern Med. 2011;Jan 25 [Epub ahead of print].
2. Schleiter K. Difficult patient-physician relationships and the risk of medical malpractice litigation. Virtual Mentor. 2009;11:242-246.
3. Kodner C. Challenging physician-patient interactions. FP Essentials. ed 354. AAFP home study. Leawood, Kan: American Academy of Family Physicians; November 2008.
4. Snyder L, Leffler C. Ethics and Human Rights Committee American College of Physicians. Ethics manual: fifth ed. Ann Intern Med. 2005;142:560-582.
5. American Medical Association (AMA). Opinion 10.015. The patient-physician relationship. Code of Medical Ethics. Chicago, Ill: AMA. 2008. Available at: http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion10015.shtml. Accessed February 11, 2011.
6. American College of Physicians. Ethical considerations for the use of patient incentives to promote personal responsibility for health: West Virginia Medicaid and beyond [position paper]. Philadelphia: American College of Physicians; 2010.
7. Harris SM. Take care when firing a patient. Am Med News. February 4, 2008. Available at: http://www.ama-assn.org/amednews/2008/02/04/bica0204.htm. Accessed February 11, 2011.
8. Parikh RK. Showing the patient the door, permanently. New York Times. June 10, 2008. Available at: http://www.nytimes.com/2008/06/10/health/views/10case.html. Accessed February 15, 2011.
9. Summey-Lowman B. Patient non-compliance—a powerful legal defense. Healthcare Risk Manag. 2009;15:1-2.
Is C difficile to blame for your patient’s diarrhea?
• A C difficile diagnosis should be made by one of several widely available testing protocols, including a 2-step method using the common antigen assay to determine whether C difficile is present, followed by an enzyme immunoassay for toxins A and B to improve specificity. B
• Oral metronidazole should be used for initial treatment of mild to moderate C difficile infection, and oral vancomycin and possibly intravenous metronidazole for severe cases. A
• Metronidazole should not be used after an initial recurrence or for long-term therapy because of the risk of neurotoxicity. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Mary S, an 82-year-old patient you recently treated for bronchitis with a 3-day course of levofloxacin, calls your office complaining of diarrhea and abdominal cramps. She describes the diarrhea as nonbloody and particularly foul smelling and asks if she can take loperamide for her symptoms.
If Mary S were your patient, what would you tell her?
The incidence of Clostridium difficile infection (CDI) has been on the rise since 2000, when a common epidemic strain began circulating in North America.1 Although hospitalization or residency in a long-term care facility remains a classic risk factor for CDI, physicians in out-patient settings are increasingly likely to see patients with community-acquired CDI.
Recently updated guidelines from the Society for Health-care Epidemiology of America (SHEA) and the Infectious Diseases Society of America define CDI as the presence of diarrhea (≥3 unformed stools in 24 hours) and either a positive stool test for toxigenic C difficile or its toxins or colonoscopic or histopathologic findings demonstrating pseudomembranous colitis.2 That said, the clinical features of CDI are nonspecific and many patients do not fit the classic profile. So diagnosing CDI requires a high index of suspicion.
The text and tables that follow detail some surprising things about who is likely to develop CDI and which treatment options to employ (and, in some cases, avoid).
Is it CDI? Looking beyond the obvious
Antibiotic use and advanced age, like hospitalization, are classic risk factors for CDI.3 Diarrhea typically begins during or shortly after a course of antibiotics, but may develop as long as 8 weeks after treatment is completed. While any antibiotic, including metronidazole, can precipitate CDI, clindamycin, cephalosporins, extended-spectrum penicillins, and quinolones are most frequently implicated.4 Epidemiologic studies have suggested an association between gastric acid-reducing agents—primarily proton-pump inhibitors—and CDI.4-7 But this link remains controversial, as other investigations have not found a clear relationship.8
In addition to diarrhea, approximately 28% of patients with CDI develop a fever (as high as 104°F); 50% develop leukocytosis (up to 50,000 cells/mcL); and 22% develop abdominal pain, usually localized to the lower quadrants.9 These symptoms, however, are not specific to C difficile, and could be due to a different enteric pathogen, intra-abdominal sepsis, inflammatory bowel disease, or adverse effects of medication, among other causes.9
Markers for severe CDI include age >70 years, leukocyte count >20,000 cells/mcL, albumin level <2.5 g/dL, small-bowel obstruction or ileus, and a computed tomography (CT) scan showing colorectal inflammation.10 Severe CDI can lead to toxic megacolon, bowel perforation, sepsis, and even death.
In addition to considering CDI in patients with nonspecific symptoms, it is important to include it in the differential diagnosis of patients who do not fit the classic profile. In a recent study of patients with CDI at 4 Veterans Affairs facilities, almost half (49%) of those studied had no exposure to antimicrobial drugs. The researchers further found that the median age of patients with CDI was 61 years—younger than that found in previous studies—and that 20% of the cases were community-acquired.11
Consider CDI in children, too. Risk factors for CDI in pediatric patients include disruption of the normal microflora of the gastrointestinal tract, compromised immune status, poor diet, underlying health conditions, concurrent infections, and cancer.12
Diagnostic testing: Consider a 2-step assay
Patients with symptoms suggestive of CDI should undergo laboratory testing to confirm the diagnosis. TABLE 1 lists the tests that are widely available in the United States.3 Only liquid stools should be tested and just one sample should be sent to the lab, as multiple samples do not increase the diagnostic yield.13 In addition, tests should be used only for diagnosis, and not as a “test of cure.” This is because patients can shed C difficile toxin and spores for several weeks after completing treatment, and there are wide variations in the sensitivity of toxin assays.
Infants <1 year old have high rates of asymptomatic toxigenic strains of C difficile, and until 2008, recommendations from SHEA discouraged testing the stools of such young patients. Because of the difficulty in differentiating incidental colonization from true CDI in this patient population, the authors of a recent review suggested using more than one diagnostic approach when testing children <1 year of age.14
We advocate a 2-step assay—that is, testing for both glutamate dehydrogenase (GDH)—an antigen common to all strains of C difficile—and C difficile toxins A and B. The common antigen test is sensitive, but may detect carriers who do not have active disease. The enzyme immunoassay (EIA) for toxins A and B helps to improve specificity. Therefore, positive results of both tests would be considered a positive finding, negative results of both tests would be considered a negative finding, and one positive result with one negative result would require another test for toxin detection.3
The reverse-transcriptase polymerase chain reaction (RT-PCR) assay, which detects the toxin B gene of C difficile, is the newest test for CDI. The RT-PCR assay detects only toxigenic strains of C difficile, and all toxigenic strains produce toxin B, making it more specific than testing for the common antigen. The RT-PCR assay also has better sensitivity than the cytotoxin assay, which also tests for toxin B. The major limitation of the RT-PCR assay is the frequency of false-positive results in hospitalized patients with a high incidence of C difficile colonization.3
Routine laboratory studies, including a complete blood count with differential and a complete metabolic panel, are often useful to ascertain the presence and degree of leukocytosis, dehydration, and other metabolic abnormalities and to test for hypoalbuminemia. Fecal leukocytes can be seen in colitis and may be useful in select cases.
Imaging studies such as radiography, CT, and endoscopy have largely been superseded by lab testing for CDI. Plain radiographs are usually normal in patients with CDI, unless the patient has an ileus or toxic megacolon. CT is useful, however, in suspected cases of fulminant CDI or toxic megacolon, and may reveal colonic-wall thickening, pericolonic stranding, or ascites.9 Colonoscopy is preferred over sigmoidoscopy because up to one-third of patients with pseudomembranous colitis will have involvement of the right colon only.9 However, this test carries the risk of perforation in patients with fulminant colitis.
TABLE 1
Lab tests for C difficile infection
| Test | Substance detected | Time needed | Sensitivity | Specificity |
|---|---|---|---|---|
| Cytotoxin | Toxin B | 1-3 d | 95% | 90%-95% |
| Toxin culture | Toxigenic C difficile† | 3-5 d | >95% | 80%-90% |
| EIA toxin A or A/B | Toxin A or A/B | Hours | 75%-80% | 97%-98% |
| EIA GDH* | C difficile | Hours | 95%-100% | 70%-80% |
| EIA GDH* and toxin A/B | C difficile and C difficile toxin | Hours | 95%-100% | 97%-98% |
| RT-PCR | Toxigenic C difficile† | Hours | >98% | 80%-99% |
| *GDH is the common C difficile antigen. †All toxigenic strains produce toxin B. EIA, enzyme immunoassay; GDH, glutamate dehydrogenase; RT-PCR, reverse-transcriptase polymerase chain reaction. Adapted from: Bartlett JG. Infect Control Hosp Epidemiol. 2010.3 | ||||
Treatment: What to consider, what to avoid
Of the 2 antibiotics most commonly used to treat CDI—metronidazole and vancomycin—only the latter has been approved by the US Food and Drug Administration for this indication. Nevertheless, metronidazole is generally recommended as first-line therapy and has the advantage of being much less expensive than vancomycin. However, an RCT found that oral vancomycin was superior to metronidazole in patients with severe disease.15 The time to resolution of diarrhea may be shorter with oral vancomycin than with metronidazole, as well.16
Recent guidelines suggest that clinicians consider 3 factors in deciding how to treat a first episode of CDI: the patient’s age, peak white blood cell count, and peak serum creatinine level.2 TABLE 2 presents an overview of treatment recommendations for both an initial episode of CDI and recurrences.
Treat severe CDI without delay. For patients with suspected severe CDI, treatment should be started empirically, without waiting for test results. Avoid antiperistaltic agents, which can obscure symptoms and precipitate toxic megacolon.2 Discontinue an antibiotic, if the patient is taking one, as soon as possible after the original infection has been adequately treated. If other infections need to be treated concurrently, we recommend that the course of treatment for CDI be extended until after the other antibiotic regimens have been stopped.
Avoid probiotics in this group. The use of probiotics, both for prevention and to help restore normal bowel flora in patients with CDI, has been advocated for many years. One RCT showed that a yogurt drink containing Lactobacillus and other bacteria reduced the risk of CDI in individuals ≥50 years of age who were taking antibiotics,17 but the guideline development panel recommended against using probiotics until larger trials have been completed.2
Probiotics are not without risk, and several cases of bacteremia have been reported.18,19 Immunocompromised patients appear to be at comparably higher risk, and probiotics should be avoided in this group. Numerous adjunctive agents, including intraluminal toxin binders, biotherapeutic agents, monoclonal antibodies, and a C difficile vaccine, are in various stages of development.2
How to handle recurrences
Relapse rates for CDI range from 6% to 25%,2 and affect patients who receive either vancomycin or metronidazole for the initial treatment. The mechanism relates to either relapse of the original infection or reinfection of susceptible patients with a new strain of C difficile.
Risk of relapse. Elderly patients treated with metronidazole seem to be particularly susceptible to CDI relapse.20 Other risk factors include the administration of non-C difficile antibiotics during or after treatment of CDI, a defective immune response against toxin A, glucocorticoid use, prior stroke, and concurrent use of a proton-pump inhibitor.21-25
TABLE 2 lists tapering and/or pulsed dosing of oral vancomycin as treatment for patients with a second recurrence. We often prescribe the following 6-week regimen, telling patients to take 125 mg vancomycin:
- 4 times a day for one week,
- then 2 times a day for one week,
- then once a day for one week,
- then every other day for one week, and
- finally, every 72 hours for 2 weeks.
Oral metronidazole should not be used beyond the first recurrence or for long-term therapy because of cumulative neurotoxicity, which can be irreversible.2
Management of patients whose CDI recurs after a long course of vancomycin is challenging. Oral rifaximin therapy (400 mg twice a day for 14 days), started immediately at the end of the oral vancomycin course, was shown to cure 7 of 8 patients with multiple relapses.26 Other potential treatment options are oral nitazoxanide, IV tigecycline, or IV immunoglobulin.
CASE You explain to Mary S that diagnostic tests are needed before you can determine whether she can safely take loperamide. When she comes in later that day, you collect a stool sample for C difficile antigen and toxin testing, and order a complete blood count and electrolyte panel.
The patient’s C difficile tests come back positive, her white blood cell count is <15,000 cells/mcL, and her creatinine level is ≤1.5 times her baseline, so you start her on oral metronidazole 500 mg every 8 hours for 14 days. (If the antigen assay had been positive and the toxin negative, you would have either repeated the test or treated Mary S empirically with metronidazole. If the initial antigen assay had been negative, you would have advised her to take the loperamide.)
You schedule a follow-up visit a day or 2 after starting therapy. If the patient is dehydrated or her symptoms have not improved by then, hospitalization may be required.
TABLE 2
Treatment recommendations for C difficile infection
| Clinical description | Clinical evidence | Recommended treatment |
|---|---|---|
| Initial episode (mild or moderate) | Leukocytosis with a white cell count <15,000 cells/mcL and creatinine <1.5 times premorbid level | Metronidazole (oral) 500 mg TID for 10-14 d |
| Initial episode (severe) | Leukocytosis with a white cell count ≥15,000 cells/mcL or creatinine ≥1.5 times premorbid level | Vancomycin (oral) 125 mg QID for 10-14 d |
| Initial episode (severe, complicated) | Hypotension or shock, ileus, megacolon | Vancomycin 500 mg QID (oral or by NG tube) plus metronidazole 500 mg (IV). If complete ileus, consider adding rectal instillation of vancomycin |
| First recurrence | Same as initial episode | |
| Second recurrence | Vancomycin in a tapered and/or pulsed regimen | |
| NG, nasogastric. Adapted from: Cohen SH, et al. Infect Control Hosp Epidemiol. 2010.2 | ||
CORRESPONDENCE
Richard R. Watkins, MD, MS, Division of Infectious Diseases, Akron General Medical Center, 224 West Exchange Street, Suite 290, Akron, OH 44302; rwatkins@agmc.org
1. Gerding DN. Global epidemiology of Clostridium difficile infection in 2010. Infect Control Hosp Epidemiol. 2010;31(suppl 1):S32-S34.
2. Cohen SH, Gerding DH, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31:431-455.
3. Bartlett JG. Detection of Clostridium difficile infection. Infect Control Hosp Epidemiol. 2010;31(suppl 1):S35-S37.
4. Dial S, Alrasadi K, Manoukian C, et al. Risk of Clostridium difficile diarrhea among hospital inpatients prescribed proton pump inhibitors: cohort and case-control studies. CMAJ. 2004;171:33-38.
5. Dial S, Delaney JA, Barkun AN, et al. Use of gastric acid-suppressive agents and the risk of community-acquired Clostridium difficile-associated disease. JAMA. 2005;294:2989-2995.
6. Cunningham R, Dale B, Undy B, et al. Proton pump inhibitors as a risk factor for Clostridium difficile diarrhoea. J Hosp Infect. 2003;54:243-245.
7. Howell MD, Novack V, Grgurich P, et al. Iatrogenic gastric acid suppression and the risk of nosocomial Clostridium difficile infection. Arch Intern Med. 2010;170:784-790.
8. Shah S, Lewis A, Leopold D, et al. Gastric acid suppression does not promote clostridial diarrhoea in the elderly. QJM. 2000;93:175-181.
9. Bartlett JG, Gerding DN. Clinical recognition and diagnosis of Clostridium difficile infection. Clin Infect Dis. 2008;46(suppl 1):S12-S18.
10. Henrich TJ, Krakower D, Bitton A, et al. Clinical risk factors for severe Clostridium difficile-associated disease. Emerg Infect Dis. 2009;15:415-422.
11. Kutty PK, Woods CW, Sena AC, et al. Risk factors for and estimated incidence of community-associated Clostridium difficile infection, North Carolina, USA. Emerg Infect Dis. 2010;16:197-204.
12. Pituch H. Clostridium difficile is no longer just a nosocomial infection or an infection of adults. Int J Antimicrob Agents. 2009;33(suppl 1):S42-S45.
13. Mohan SS, McDermott BP, Parchuri S, et al. Lack of value of repeat stool testing for Clostridium difficile toxin. Am J Med. 2006;119:356.e7-e8.
14. Bryant K, McDonald LC. Clostridium difficile infections in children. Pediatr Infect Dis J. 2009;28:145-146.
15. Zar FA, Bakkanagari SR, Moorthi KM, et al. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45:302-307.
16. Belmares J, Gerding DN, Parada JP, et al. Outcome of metronidazole therapy for Clostridium difficile disease and correlation with a scoring system. J Infect. 2007;55:495-501.
17. Hickson M, D’Souza AL, Muthu N, et al. Use of probiotic Lactobacillus preparation to prevent diarrhoea associated with antibiotics: randomised double blind placebo controlled trial. BMJ. 2007;335:80.-
18. Ledoux D, Labombardi VJ, Karter D. Lactobacillus acidophilus bacteraemia after use of a probiotic in a patient with AIDS and Hodgkin’s disease. Int J STD AIDS. 2006;17:280-282.
19. Hammerman C, Bin-Nun A, Kaplan M. Safety of probiotics: comparison of two popular strains. BMJ. 2006;333:1006-1008.
20. Musher DM, Aslam S, Logan N, et al. Relatively poor outcome after treatment of Clostridium difficile colitis with metronidazole. Clin Infect Dis. 2005;40:1586-1590.
21. Nair S, Yadav D, Corpuz M, et al. Clostridium difficile colitis: factors influencing treatment failure and relapse—a prospective evaluation. Am J Gastroenterol. 1998;93:1873-1876.
22. Garey KW, Sethi S, Yadav Y, et al. Meta-analysis to assess risk factors for recurrent Clostridium difficile infection. J Hosp Infect. 2008;70:298-304.
23. Das R, Feuerstadt P, Brandt LJ. Glucocorticoids are associated with increased risk of short-term mortality in hospitalized patients with Clostridium difficile-associated disease. Am J Gastroenterol. 2010;105:2040-2049.
24. Cadena J, Thompson GR, 3rd, Patterson JE, et al. Clinical predictors and risk factors for relapsing Clostridium difficile infection. Am J Med Sci. 2010;339:350-355.
25. Linsky A, Gupta K, Lawler EV, et al. Proton pump inhibitors and risk for recurrent Clostridium difficile infection. Arch Intern Med. 2010;170:772-778.
26. Johnson S, Schriever C, Galang M, et al. Interruption of recurrent Clostridium difficile-associated diarrhea episodes by serial therapy with vancomycin and rifaximin. Clin Infect Dis. 2007;44:846-848.
• A C difficile diagnosis should be made by one of several widely available testing protocols, including a 2-step method using the common antigen assay to determine whether C difficile is present, followed by an enzyme immunoassay for toxins A and B to improve specificity. B
• Oral metronidazole should be used for initial treatment of mild to moderate C difficile infection, and oral vancomycin and possibly intravenous metronidazole for severe cases. A
• Metronidazole should not be used after an initial recurrence or for long-term therapy because of the risk of neurotoxicity. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Mary S, an 82-year-old patient you recently treated for bronchitis with a 3-day course of levofloxacin, calls your office complaining of diarrhea and abdominal cramps. She describes the diarrhea as nonbloody and particularly foul smelling and asks if she can take loperamide for her symptoms.
If Mary S were your patient, what would you tell her?
The incidence of Clostridium difficile infection (CDI) has been on the rise since 2000, when a common epidemic strain began circulating in North America.1 Although hospitalization or residency in a long-term care facility remains a classic risk factor for CDI, physicians in out-patient settings are increasingly likely to see patients with community-acquired CDI.
Recently updated guidelines from the Society for Health-care Epidemiology of America (SHEA) and the Infectious Diseases Society of America define CDI as the presence of diarrhea (≥3 unformed stools in 24 hours) and either a positive stool test for toxigenic C difficile or its toxins or colonoscopic or histopathologic findings demonstrating pseudomembranous colitis.2 That said, the clinical features of CDI are nonspecific and many patients do not fit the classic profile. So diagnosing CDI requires a high index of suspicion.
The text and tables that follow detail some surprising things about who is likely to develop CDI and which treatment options to employ (and, in some cases, avoid).
Is it CDI? Looking beyond the obvious
Antibiotic use and advanced age, like hospitalization, are classic risk factors for CDI.3 Diarrhea typically begins during or shortly after a course of antibiotics, but may develop as long as 8 weeks after treatment is completed. While any antibiotic, including metronidazole, can precipitate CDI, clindamycin, cephalosporins, extended-spectrum penicillins, and quinolones are most frequently implicated.4 Epidemiologic studies have suggested an association between gastric acid-reducing agents—primarily proton-pump inhibitors—and CDI.4-7 But this link remains controversial, as other investigations have not found a clear relationship.8
In addition to diarrhea, approximately 28% of patients with CDI develop a fever (as high as 104°F); 50% develop leukocytosis (up to 50,000 cells/mcL); and 22% develop abdominal pain, usually localized to the lower quadrants.9 These symptoms, however, are not specific to C difficile, and could be due to a different enteric pathogen, intra-abdominal sepsis, inflammatory bowel disease, or adverse effects of medication, among other causes.9
Markers for severe CDI include age >70 years, leukocyte count >20,000 cells/mcL, albumin level <2.5 g/dL, small-bowel obstruction or ileus, and a computed tomography (CT) scan showing colorectal inflammation.10 Severe CDI can lead to toxic megacolon, bowel perforation, sepsis, and even death.
In addition to considering CDI in patients with nonspecific symptoms, it is important to include it in the differential diagnosis of patients who do not fit the classic profile. In a recent study of patients with CDI at 4 Veterans Affairs facilities, almost half (49%) of those studied had no exposure to antimicrobial drugs. The researchers further found that the median age of patients with CDI was 61 years—younger than that found in previous studies—and that 20% of the cases were community-acquired.11
Consider CDI in children, too. Risk factors for CDI in pediatric patients include disruption of the normal microflora of the gastrointestinal tract, compromised immune status, poor diet, underlying health conditions, concurrent infections, and cancer.12
Diagnostic testing: Consider a 2-step assay
Patients with symptoms suggestive of CDI should undergo laboratory testing to confirm the diagnosis. TABLE 1 lists the tests that are widely available in the United States.3 Only liquid stools should be tested and just one sample should be sent to the lab, as multiple samples do not increase the diagnostic yield.13 In addition, tests should be used only for diagnosis, and not as a “test of cure.” This is because patients can shed C difficile toxin and spores for several weeks after completing treatment, and there are wide variations in the sensitivity of toxin assays.
Infants <1 year old have high rates of asymptomatic toxigenic strains of C difficile, and until 2008, recommendations from SHEA discouraged testing the stools of such young patients. Because of the difficulty in differentiating incidental colonization from true CDI in this patient population, the authors of a recent review suggested using more than one diagnostic approach when testing children <1 year of age.14
We advocate a 2-step assay—that is, testing for both glutamate dehydrogenase (GDH)—an antigen common to all strains of C difficile—and C difficile toxins A and B. The common antigen test is sensitive, but may detect carriers who do not have active disease. The enzyme immunoassay (EIA) for toxins A and B helps to improve specificity. Therefore, positive results of both tests would be considered a positive finding, negative results of both tests would be considered a negative finding, and one positive result with one negative result would require another test for toxin detection.3
The reverse-transcriptase polymerase chain reaction (RT-PCR) assay, which detects the toxin B gene of C difficile, is the newest test for CDI. The RT-PCR assay detects only toxigenic strains of C difficile, and all toxigenic strains produce toxin B, making it more specific than testing for the common antigen. The RT-PCR assay also has better sensitivity than the cytotoxin assay, which also tests for toxin B. The major limitation of the RT-PCR assay is the frequency of false-positive results in hospitalized patients with a high incidence of C difficile colonization.3
Routine laboratory studies, including a complete blood count with differential and a complete metabolic panel, are often useful to ascertain the presence and degree of leukocytosis, dehydration, and other metabolic abnormalities and to test for hypoalbuminemia. Fecal leukocytes can be seen in colitis and may be useful in select cases.
Imaging studies such as radiography, CT, and endoscopy have largely been superseded by lab testing for CDI. Plain radiographs are usually normal in patients with CDI, unless the patient has an ileus or toxic megacolon. CT is useful, however, in suspected cases of fulminant CDI or toxic megacolon, and may reveal colonic-wall thickening, pericolonic stranding, or ascites.9 Colonoscopy is preferred over sigmoidoscopy because up to one-third of patients with pseudomembranous colitis will have involvement of the right colon only.9 However, this test carries the risk of perforation in patients with fulminant colitis.
TABLE 1
Lab tests for C difficile infection
| Test | Substance detected | Time needed | Sensitivity | Specificity |
|---|---|---|---|---|
| Cytotoxin | Toxin B | 1-3 d | 95% | 90%-95% |
| Toxin culture | Toxigenic C difficile† | 3-5 d | >95% | 80%-90% |
| EIA toxin A or A/B | Toxin A or A/B | Hours | 75%-80% | 97%-98% |
| EIA GDH* | C difficile | Hours | 95%-100% | 70%-80% |
| EIA GDH* and toxin A/B | C difficile and C difficile toxin | Hours | 95%-100% | 97%-98% |
| RT-PCR | Toxigenic C difficile† | Hours | >98% | 80%-99% |
| *GDH is the common C difficile antigen. †All toxigenic strains produce toxin B. EIA, enzyme immunoassay; GDH, glutamate dehydrogenase; RT-PCR, reverse-transcriptase polymerase chain reaction. Adapted from: Bartlett JG. Infect Control Hosp Epidemiol. 2010.3 | ||||
Treatment: What to consider, what to avoid
Of the 2 antibiotics most commonly used to treat CDI—metronidazole and vancomycin—only the latter has been approved by the US Food and Drug Administration for this indication. Nevertheless, metronidazole is generally recommended as first-line therapy and has the advantage of being much less expensive than vancomycin. However, an RCT found that oral vancomycin was superior to metronidazole in patients with severe disease.15 The time to resolution of diarrhea may be shorter with oral vancomycin than with metronidazole, as well.16
Recent guidelines suggest that clinicians consider 3 factors in deciding how to treat a first episode of CDI: the patient’s age, peak white blood cell count, and peak serum creatinine level.2 TABLE 2 presents an overview of treatment recommendations for both an initial episode of CDI and recurrences.
Treat severe CDI without delay. For patients with suspected severe CDI, treatment should be started empirically, without waiting for test results. Avoid antiperistaltic agents, which can obscure symptoms and precipitate toxic megacolon.2 Discontinue an antibiotic, if the patient is taking one, as soon as possible after the original infection has been adequately treated. If other infections need to be treated concurrently, we recommend that the course of treatment for CDI be extended until after the other antibiotic regimens have been stopped.
Avoid probiotics in this group. The use of probiotics, both for prevention and to help restore normal bowel flora in patients with CDI, has been advocated for many years. One RCT showed that a yogurt drink containing Lactobacillus and other bacteria reduced the risk of CDI in individuals ≥50 years of age who were taking antibiotics,17 but the guideline development panel recommended against using probiotics until larger trials have been completed.2
Probiotics are not without risk, and several cases of bacteremia have been reported.18,19 Immunocompromised patients appear to be at comparably higher risk, and probiotics should be avoided in this group. Numerous adjunctive agents, including intraluminal toxin binders, biotherapeutic agents, monoclonal antibodies, and a C difficile vaccine, are in various stages of development.2
How to handle recurrences
Relapse rates for CDI range from 6% to 25%,2 and affect patients who receive either vancomycin or metronidazole for the initial treatment. The mechanism relates to either relapse of the original infection or reinfection of susceptible patients with a new strain of C difficile.
Risk of relapse. Elderly patients treated with metronidazole seem to be particularly susceptible to CDI relapse.20 Other risk factors include the administration of non-C difficile antibiotics during or after treatment of CDI, a defective immune response against toxin A, glucocorticoid use, prior stroke, and concurrent use of a proton-pump inhibitor.21-25
TABLE 2 lists tapering and/or pulsed dosing of oral vancomycin as treatment for patients with a second recurrence. We often prescribe the following 6-week regimen, telling patients to take 125 mg vancomycin:
- 4 times a day for one week,
- then 2 times a day for one week,
- then once a day for one week,
- then every other day for one week, and
- finally, every 72 hours for 2 weeks.
Oral metronidazole should not be used beyond the first recurrence or for long-term therapy because of cumulative neurotoxicity, which can be irreversible.2
Management of patients whose CDI recurs after a long course of vancomycin is challenging. Oral rifaximin therapy (400 mg twice a day for 14 days), started immediately at the end of the oral vancomycin course, was shown to cure 7 of 8 patients with multiple relapses.26 Other potential treatment options are oral nitazoxanide, IV tigecycline, or IV immunoglobulin.
CASE You explain to Mary S that diagnostic tests are needed before you can determine whether she can safely take loperamide. When she comes in later that day, you collect a stool sample for C difficile antigen and toxin testing, and order a complete blood count and electrolyte panel.
The patient’s C difficile tests come back positive, her white blood cell count is <15,000 cells/mcL, and her creatinine level is ≤1.5 times her baseline, so you start her on oral metronidazole 500 mg every 8 hours for 14 days. (If the antigen assay had been positive and the toxin negative, you would have either repeated the test or treated Mary S empirically with metronidazole. If the initial antigen assay had been negative, you would have advised her to take the loperamide.)
You schedule a follow-up visit a day or 2 after starting therapy. If the patient is dehydrated or her symptoms have not improved by then, hospitalization may be required.
TABLE 2
Treatment recommendations for C difficile infection
| Clinical description | Clinical evidence | Recommended treatment |
|---|---|---|
| Initial episode (mild or moderate) | Leukocytosis with a white cell count <15,000 cells/mcL and creatinine <1.5 times premorbid level | Metronidazole (oral) 500 mg TID for 10-14 d |
| Initial episode (severe) | Leukocytosis with a white cell count ≥15,000 cells/mcL or creatinine ≥1.5 times premorbid level | Vancomycin (oral) 125 mg QID for 10-14 d |
| Initial episode (severe, complicated) | Hypotension or shock, ileus, megacolon | Vancomycin 500 mg QID (oral or by NG tube) plus metronidazole 500 mg (IV). If complete ileus, consider adding rectal instillation of vancomycin |
| First recurrence | Same as initial episode | |
| Second recurrence | Vancomycin in a tapered and/or pulsed regimen | |
| NG, nasogastric. Adapted from: Cohen SH, et al. Infect Control Hosp Epidemiol. 2010.2 | ||
CORRESPONDENCE
Richard R. Watkins, MD, MS, Division of Infectious Diseases, Akron General Medical Center, 224 West Exchange Street, Suite 290, Akron, OH 44302; rwatkins@agmc.org
• A C difficile diagnosis should be made by one of several widely available testing protocols, including a 2-step method using the common antigen assay to determine whether C difficile is present, followed by an enzyme immunoassay for toxins A and B to improve specificity. B
• Oral metronidazole should be used for initial treatment of mild to moderate C difficile infection, and oral vancomycin and possibly intravenous metronidazole for severe cases. A
• Metronidazole should not be used after an initial recurrence or for long-term therapy because of the risk of neurotoxicity. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Mary S, an 82-year-old patient you recently treated for bronchitis with a 3-day course of levofloxacin, calls your office complaining of diarrhea and abdominal cramps. She describes the diarrhea as nonbloody and particularly foul smelling and asks if she can take loperamide for her symptoms.
If Mary S were your patient, what would you tell her?
The incidence of Clostridium difficile infection (CDI) has been on the rise since 2000, when a common epidemic strain began circulating in North America.1 Although hospitalization or residency in a long-term care facility remains a classic risk factor for CDI, physicians in out-patient settings are increasingly likely to see patients with community-acquired CDI.
Recently updated guidelines from the Society for Health-care Epidemiology of America (SHEA) and the Infectious Diseases Society of America define CDI as the presence of diarrhea (≥3 unformed stools in 24 hours) and either a positive stool test for toxigenic C difficile or its toxins or colonoscopic or histopathologic findings demonstrating pseudomembranous colitis.2 That said, the clinical features of CDI are nonspecific and many patients do not fit the classic profile. So diagnosing CDI requires a high index of suspicion.
The text and tables that follow detail some surprising things about who is likely to develop CDI and which treatment options to employ (and, in some cases, avoid).
Is it CDI? Looking beyond the obvious
Antibiotic use and advanced age, like hospitalization, are classic risk factors for CDI.3 Diarrhea typically begins during or shortly after a course of antibiotics, but may develop as long as 8 weeks after treatment is completed. While any antibiotic, including metronidazole, can precipitate CDI, clindamycin, cephalosporins, extended-spectrum penicillins, and quinolones are most frequently implicated.4 Epidemiologic studies have suggested an association between gastric acid-reducing agents—primarily proton-pump inhibitors—and CDI.4-7 But this link remains controversial, as other investigations have not found a clear relationship.8
In addition to diarrhea, approximately 28% of patients with CDI develop a fever (as high as 104°F); 50% develop leukocytosis (up to 50,000 cells/mcL); and 22% develop abdominal pain, usually localized to the lower quadrants.9 These symptoms, however, are not specific to C difficile, and could be due to a different enteric pathogen, intra-abdominal sepsis, inflammatory bowel disease, or adverse effects of medication, among other causes.9
Markers for severe CDI include age >70 years, leukocyte count >20,000 cells/mcL, albumin level <2.5 g/dL, small-bowel obstruction or ileus, and a computed tomography (CT) scan showing colorectal inflammation.10 Severe CDI can lead to toxic megacolon, bowel perforation, sepsis, and even death.
In addition to considering CDI in patients with nonspecific symptoms, it is important to include it in the differential diagnosis of patients who do not fit the classic profile. In a recent study of patients with CDI at 4 Veterans Affairs facilities, almost half (49%) of those studied had no exposure to antimicrobial drugs. The researchers further found that the median age of patients with CDI was 61 years—younger than that found in previous studies—and that 20% of the cases were community-acquired.11
Consider CDI in children, too. Risk factors for CDI in pediatric patients include disruption of the normal microflora of the gastrointestinal tract, compromised immune status, poor diet, underlying health conditions, concurrent infections, and cancer.12
Diagnostic testing: Consider a 2-step assay
Patients with symptoms suggestive of CDI should undergo laboratory testing to confirm the diagnosis. TABLE 1 lists the tests that are widely available in the United States.3 Only liquid stools should be tested and just one sample should be sent to the lab, as multiple samples do not increase the diagnostic yield.13 In addition, tests should be used only for diagnosis, and not as a “test of cure.” This is because patients can shed C difficile toxin and spores for several weeks after completing treatment, and there are wide variations in the sensitivity of toxin assays.
Infants <1 year old have high rates of asymptomatic toxigenic strains of C difficile, and until 2008, recommendations from SHEA discouraged testing the stools of such young patients. Because of the difficulty in differentiating incidental colonization from true CDI in this patient population, the authors of a recent review suggested using more than one diagnostic approach when testing children <1 year of age.14
We advocate a 2-step assay—that is, testing for both glutamate dehydrogenase (GDH)—an antigen common to all strains of C difficile—and C difficile toxins A and B. The common antigen test is sensitive, but may detect carriers who do not have active disease. The enzyme immunoassay (EIA) for toxins A and B helps to improve specificity. Therefore, positive results of both tests would be considered a positive finding, negative results of both tests would be considered a negative finding, and one positive result with one negative result would require another test for toxin detection.3
The reverse-transcriptase polymerase chain reaction (RT-PCR) assay, which detects the toxin B gene of C difficile, is the newest test for CDI. The RT-PCR assay detects only toxigenic strains of C difficile, and all toxigenic strains produce toxin B, making it more specific than testing for the common antigen. The RT-PCR assay also has better sensitivity than the cytotoxin assay, which also tests for toxin B. The major limitation of the RT-PCR assay is the frequency of false-positive results in hospitalized patients with a high incidence of C difficile colonization.3
Routine laboratory studies, including a complete blood count with differential and a complete metabolic panel, are often useful to ascertain the presence and degree of leukocytosis, dehydration, and other metabolic abnormalities and to test for hypoalbuminemia. Fecal leukocytes can be seen in colitis and may be useful in select cases.
Imaging studies such as radiography, CT, and endoscopy have largely been superseded by lab testing for CDI. Plain radiographs are usually normal in patients with CDI, unless the patient has an ileus or toxic megacolon. CT is useful, however, in suspected cases of fulminant CDI or toxic megacolon, and may reveal colonic-wall thickening, pericolonic stranding, or ascites.9 Colonoscopy is preferred over sigmoidoscopy because up to one-third of patients with pseudomembranous colitis will have involvement of the right colon only.9 However, this test carries the risk of perforation in patients with fulminant colitis.
TABLE 1
Lab tests for C difficile infection
| Test | Substance detected | Time needed | Sensitivity | Specificity |
|---|---|---|---|---|
| Cytotoxin | Toxin B | 1-3 d | 95% | 90%-95% |
| Toxin culture | Toxigenic C difficile† | 3-5 d | >95% | 80%-90% |
| EIA toxin A or A/B | Toxin A or A/B | Hours | 75%-80% | 97%-98% |
| EIA GDH* | C difficile | Hours | 95%-100% | 70%-80% |
| EIA GDH* and toxin A/B | C difficile and C difficile toxin | Hours | 95%-100% | 97%-98% |
| RT-PCR | Toxigenic C difficile† | Hours | >98% | 80%-99% |
| *GDH is the common C difficile antigen. †All toxigenic strains produce toxin B. EIA, enzyme immunoassay; GDH, glutamate dehydrogenase; RT-PCR, reverse-transcriptase polymerase chain reaction. Adapted from: Bartlett JG. Infect Control Hosp Epidemiol. 2010.3 | ||||
Treatment: What to consider, what to avoid
Of the 2 antibiotics most commonly used to treat CDI—metronidazole and vancomycin—only the latter has been approved by the US Food and Drug Administration for this indication. Nevertheless, metronidazole is generally recommended as first-line therapy and has the advantage of being much less expensive than vancomycin. However, an RCT found that oral vancomycin was superior to metronidazole in patients with severe disease.15 The time to resolution of diarrhea may be shorter with oral vancomycin than with metronidazole, as well.16
Recent guidelines suggest that clinicians consider 3 factors in deciding how to treat a first episode of CDI: the patient’s age, peak white blood cell count, and peak serum creatinine level.2 TABLE 2 presents an overview of treatment recommendations for both an initial episode of CDI and recurrences.
Treat severe CDI without delay. For patients with suspected severe CDI, treatment should be started empirically, without waiting for test results. Avoid antiperistaltic agents, which can obscure symptoms and precipitate toxic megacolon.2 Discontinue an antibiotic, if the patient is taking one, as soon as possible after the original infection has been adequately treated. If other infections need to be treated concurrently, we recommend that the course of treatment for CDI be extended until after the other antibiotic regimens have been stopped.
Avoid probiotics in this group. The use of probiotics, both for prevention and to help restore normal bowel flora in patients with CDI, has been advocated for many years. One RCT showed that a yogurt drink containing Lactobacillus and other bacteria reduced the risk of CDI in individuals ≥50 years of age who were taking antibiotics,17 but the guideline development panel recommended against using probiotics until larger trials have been completed.2
Probiotics are not without risk, and several cases of bacteremia have been reported.18,19 Immunocompromised patients appear to be at comparably higher risk, and probiotics should be avoided in this group. Numerous adjunctive agents, including intraluminal toxin binders, biotherapeutic agents, monoclonal antibodies, and a C difficile vaccine, are in various stages of development.2
How to handle recurrences
Relapse rates for CDI range from 6% to 25%,2 and affect patients who receive either vancomycin or metronidazole for the initial treatment. The mechanism relates to either relapse of the original infection or reinfection of susceptible patients with a new strain of C difficile.
Risk of relapse. Elderly patients treated with metronidazole seem to be particularly susceptible to CDI relapse.20 Other risk factors include the administration of non-C difficile antibiotics during or after treatment of CDI, a defective immune response against toxin A, glucocorticoid use, prior stroke, and concurrent use of a proton-pump inhibitor.21-25
TABLE 2 lists tapering and/or pulsed dosing of oral vancomycin as treatment for patients with a second recurrence. We often prescribe the following 6-week regimen, telling patients to take 125 mg vancomycin:
- 4 times a day for one week,
- then 2 times a day for one week,
- then once a day for one week,
- then every other day for one week, and
- finally, every 72 hours for 2 weeks.
Oral metronidazole should not be used beyond the first recurrence or for long-term therapy because of cumulative neurotoxicity, which can be irreversible.2
Management of patients whose CDI recurs after a long course of vancomycin is challenging. Oral rifaximin therapy (400 mg twice a day for 14 days), started immediately at the end of the oral vancomycin course, was shown to cure 7 of 8 patients with multiple relapses.26 Other potential treatment options are oral nitazoxanide, IV tigecycline, or IV immunoglobulin.
CASE You explain to Mary S that diagnostic tests are needed before you can determine whether she can safely take loperamide. When she comes in later that day, you collect a stool sample for C difficile antigen and toxin testing, and order a complete blood count and electrolyte panel.
The patient’s C difficile tests come back positive, her white blood cell count is <15,000 cells/mcL, and her creatinine level is ≤1.5 times her baseline, so you start her on oral metronidazole 500 mg every 8 hours for 14 days. (If the antigen assay had been positive and the toxin negative, you would have either repeated the test or treated Mary S empirically with metronidazole. If the initial antigen assay had been negative, you would have advised her to take the loperamide.)
You schedule a follow-up visit a day or 2 after starting therapy. If the patient is dehydrated or her symptoms have not improved by then, hospitalization may be required.
TABLE 2
Treatment recommendations for C difficile infection
| Clinical description | Clinical evidence | Recommended treatment |
|---|---|---|
| Initial episode (mild or moderate) | Leukocytosis with a white cell count <15,000 cells/mcL and creatinine <1.5 times premorbid level | Metronidazole (oral) 500 mg TID for 10-14 d |
| Initial episode (severe) | Leukocytosis with a white cell count ≥15,000 cells/mcL or creatinine ≥1.5 times premorbid level | Vancomycin (oral) 125 mg QID for 10-14 d |
| Initial episode (severe, complicated) | Hypotension or shock, ileus, megacolon | Vancomycin 500 mg QID (oral or by NG tube) plus metronidazole 500 mg (IV). If complete ileus, consider adding rectal instillation of vancomycin |
| First recurrence | Same as initial episode | |
| Second recurrence | Vancomycin in a tapered and/or pulsed regimen | |
| NG, nasogastric. Adapted from: Cohen SH, et al. Infect Control Hosp Epidemiol. 2010.2 | ||
CORRESPONDENCE
Richard R. Watkins, MD, MS, Division of Infectious Diseases, Akron General Medical Center, 224 West Exchange Street, Suite 290, Akron, OH 44302; rwatkins@agmc.org
1. Gerding DN. Global epidemiology of Clostridium difficile infection in 2010. Infect Control Hosp Epidemiol. 2010;31(suppl 1):S32-S34.
2. Cohen SH, Gerding DH, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31:431-455.
3. Bartlett JG. Detection of Clostridium difficile infection. Infect Control Hosp Epidemiol. 2010;31(suppl 1):S35-S37.
4. Dial S, Alrasadi K, Manoukian C, et al. Risk of Clostridium difficile diarrhea among hospital inpatients prescribed proton pump inhibitors: cohort and case-control studies. CMAJ. 2004;171:33-38.
5. Dial S, Delaney JA, Barkun AN, et al. Use of gastric acid-suppressive agents and the risk of community-acquired Clostridium difficile-associated disease. JAMA. 2005;294:2989-2995.
6. Cunningham R, Dale B, Undy B, et al. Proton pump inhibitors as a risk factor for Clostridium difficile diarrhoea. J Hosp Infect. 2003;54:243-245.
7. Howell MD, Novack V, Grgurich P, et al. Iatrogenic gastric acid suppression and the risk of nosocomial Clostridium difficile infection. Arch Intern Med. 2010;170:784-790.
8. Shah S, Lewis A, Leopold D, et al. Gastric acid suppression does not promote clostridial diarrhoea in the elderly. QJM. 2000;93:175-181.
9. Bartlett JG, Gerding DN. Clinical recognition and diagnosis of Clostridium difficile infection. Clin Infect Dis. 2008;46(suppl 1):S12-S18.
10. Henrich TJ, Krakower D, Bitton A, et al. Clinical risk factors for severe Clostridium difficile-associated disease. Emerg Infect Dis. 2009;15:415-422.
11. Kutty PK, Woods CW, Sena AC, et al. Risk factors for and estimated incidence of community-associated Clostridium difficile infection, North Carolina, USA. Emerg Infect Dis. 2010;16:197-204.
12. Pituch H. Clostridium difficile is no longer just a nosocomial infection or an infection of adults. Int J Antimicrob Agents. 2009;33(suppl 1):S42-S45.
13. Mohan SS, McDermott BP, Parchuri S, et al. Lack of value of repeat stool testing for Clostridium difficile toxin. Am J Med. 2006;119:356.e7-e8.
14. Bryant K, McDonald LC. Clostridium difficile infections in children. Pediatr Infect Dis J. 2009;28:145-146.
15. Zar FA, Bakkanagari SR, Moorthi KM, et al. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45:302-307.
16. Belmares J, Gerding DN, Parada JP, et al. Outcome of metronidazole therapy for Clostridium difficile disease and correlation with a scoring system. J Infect. 2007;55:495-501.
17. Hickson M, D’Souza AL, Muthu N, et al. Use of probiotic Lactobacillus preparation to prevent diarrhoea associated with antibiotics: randomised double blind placebo controlled trial. BMJ. 2007;335:80.-
18. Ledoux D, Labombardi VJ, Karter D. Lactobacillus acidophilus bacteraemia after use of a probiotic in a patient with AIDS and Hodgkin’s disease. Int J STD AIDS. 2006;17:280-282.
19. Hammerman C, Bin-Nun A, Kaplan M. Safety of probiotics: comparison of two popular strains. BMJ. 2006;333:1006-1008.
20. Musher DM, Aslam S, Logan N, et al. Relatively poor outcome after treatment of Clostridium difficile colitis with metronidazole. Clin Infect Dis. 2005;40:1586-1590.
21. Nair S, Yadav D, Corpuz M, et al. Clostridium difficile colitis: factors influencing treatment failure and relapse—a prospective evaluation. Am J Gastroenterol. 1998;93:1873-1876.
22. Garey KW, Sethi S, Yadav Y, et al. Meta-analysis to assess risk factors for recurrent Clostridium difficile infection. J Hosp Infect. 2008;70:298-304.
23. Das R, Feuerstadt P, Brandt LJ. Glucocorticoids are associated with increased risk of short-term mortality in hospitalized patients with Clostridium difficile-associated disease. Am J Gastroenterol. 2010;105:2040-2049.
24. Cadena J, Thompson GR, 3rd, Patterson JE, et al. Clinical predictors and risk factors for relapsing Clostridium difficile infection. Am J Med Sci. 2010;339:350-355.
25. Linsky A, Gupta K, Lawler EV, et al. Proton pump inhibitors and risk for recurrent Clostridium difficile infection. Arch Intern Med. 2010;170:772-778.
26. Johnson S, Schriever C, Galang M, et al. Interruption of recurrent Clostridium difficile-associated diarrhea episodes by serial therapy with vancomycin and rifaximin. Clin Infect Dis. 2007;44:846-848.
1. Gerding DN. Global epidemiology of Clostridium difficile infection in 2010. Infect Control Hosp Epidemiol. 2010;31(suppl 1):S32-S34.
2. Cohen SH, Gerding DH, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31:431-455.
3. Bartlett JG. Detection of Clostridium difficile infection. Infect Control Hosp Epidemiol. 2010;31(suppl 1):S35-S37.
4. Dial S, Alrasadi K, Manoukian C, et al. Risk of Clostridium difficile diarrhea among hospital inpatients prescribed proton pump inhibitors: cohort and case-control studies. CMAJ. 2004;171:33-38.
5. Dial S, Delaney JA, Barkun AN, et al. Use of gastric acid-suppressive agents and the risk of community-acquired Clostridium difficile-associated disease. JAMA. 2005;294:2989-2995.
6. Cunningham R, Dale B, Undy B, et al. Proton pump inhibitors as a risk factor for Clostridium difficile diarrhoea. J Hosp Infect. 2003;54:243-245.
7. Howell MD, Novack V, Grgurich P, et al. Iatrogenic gastric acid suppression and the risk of nosocomial Clostridium difficile infection. Arch Intern Med. 2010;170:784-790.
8. Shah S, Lewis A, Leopold D, et al. Gastric acid suppression does not promote clostridial diarrhoea in the elderly. QJM. 2000;93:175-181.
9. Bartlett JG, Gerding DN. Clinical recognition and diagnosis of Clostridium difficile infection. Clin Infect Dis. 2008;46(suppl 1):S12-S18.
10. Henrich TJ, Krakower D, Bitton A, et al. Clinical risk factors for severe Clostridium difficile-associated disease. Emerg Infect Dis. 2009;15:415-422.
11. Kutty PK, Woods CW, Sena AC, et al. Risk factors for and estimated incidence of community-associated Clostridium difficile infection, North Carolina, USA. Emerg Infect Dis. 2010;16:197-204.
12. Pituch H. Clostridium difficile is no longer just a nosocomial infection or an infection of adults. Int J Antimicrob Agents. 2009;33(suppl 1):S42-S45.
13. Mohan SS, McDermott BP, Parchuri S, et al. Lack of value of repeat stool testing for Clostridium difficile toxin. Am J Med. 2006;119:356.e7-e8.
14. Bryant K, McDonald LC. Clostridium difficile infections in children. Pediatr Infect Dis J. 2009;28:145-146.
15. Zar FA, Bakkanagari SR, Moorthi KM, et al. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45:302-307.
16. Belmares J, Gerding DN, Parada JP, et al. Outcome of metronidazole therapy for Clostridium difficile disease and correlation with a scoring system. J Infect. 2007;55:495-501.
17. Hickson M, D’Souza AL, Muthu N, et al. Use of probiotic Lactobacillus preparation to prevent diarrhoea associated with antibiotics: randomised double blind placebo controlled trial. BMJ. 2007;335:80.-
18. Ledoux D, Labombardi VJ, Karter D. Lactobacillus acidophilus bacteraemia after use of a probiotic in a patient with AIDS and Hodgkin’s disease. Int J STD AIDS. 2006;17:280-282.
19. Hammerman C, Bin-Nun A, Kaplan M. Safety of probiotics: comparison of two popular strains. BMJ. 2006;333:1006-1008.
20. Musher DM, Aslam S, Logan N, et al. Relatively poor outcome after treatment of Clostridium difficile colitis with metronidazole. Clin Infect Dis. 2005;40:1586-1590.
21. Nair S, Yadav D, Corpuz M, et al. Clostridium difficile colitis: factors influencing treatment failure and relapse—a prospective evaluation. Am J Gastroenterol. 1998;93:1873-1876.
22. Garey KW, Sethi S, Yadav Y, et al. Meta-analysis to assess risk factors for recurrent Clostridium difficile infection. J Hosp Infect. 2008;70:298-304.
23. Das R, Feuerstadt P, Brandt LJ. Glucocorticoids are associated with increased risk of short-term mortality in hospitalized patients with Clostridium difficile-associated disease. Am J Gastroenterol. 2010;105:2040-2049.
24. Cadena J, Thompson GR, 3rd, Patterson JE, et al. Clinical predictors and risk factors for relapsing Clostridium difficile infection. Am J Med Sci. 2010;339:350-355.
25. Linsky A, Gupta K, Lawler EV, et al. Proton pump inhibitors and risk for recurrent Clostridium difficile infection. Arch Intern Med. 2010;170:772-778.
26. Johnson S, Schriever C, Galang M, et al. Interruption of recurrent Clostridium difficile-associated diarrhea episodes by serial therapy with vancomycin and rifaximin. Clin Infect Dis. 2007;44:846-848.
How I solved my e-prescribing dilemma
Even with government incentives, I physicians have been slow to make the leap to electronic medical records (EMR) and full electronic prescribing (e-prescribing). My transition to e-prescribing evolved over about a decade, and I was a satisfied e-prescriber—for a while.
Around 2000, I began writing electronic prescriptions using iScribe for Palm handhelds.1 The final transition to full e-prescribing required only a WiFi connection in the office for use with my Palm, and hitting Send to submit the prescription to the pharmacy. iScribe was user friendly and fast. It eliminated pharmacy “callbacks, “ provided printed receipts for charting, and maintained a record of each prescription on the Palm, filed under the patient’s name. A full prescription history for each patient archived on the Palm reduced the need to pull charts for medication questions.
A rude surprise
Then iScribe was acquired by another company whose e-prescribing product, in my opinion, lengthened patient encounters because it required several additional steps to complete a prescription. This was unacceptable to me, and returning to handwritten prescriptions was out of the question. I needed a better solution.
I was disinclined to invest in another e-prescribing product whose tenure could end as abruptly as iScribe’s had. To wit: I recently read about another user-friendly, well-supported medical software program that was scooped up by a larger company selling less functional and more expensive products (while charging for a costly conversion of existing records and delivering poorer customer service).2 And e-prescribing in general has received mixed reviews.3
I briefly considered designing my own prescription writer. A full-featured writer using a relational database, such as Microsoft Access, would be ideal. But developing it would be daunting without software-specific training. The same would be true for spreadsheet software. Adobe Acrobat or word processors with directories or hyperlinks or search functions didn’t seem appropriate.
A welcome surprise
Microsoft Office 2010 software for PC and Mac platforms now includes OneNote, a program new to me. (Price at Costco for Office Home and Student, September 2010, was $119.) OneNote (in which I have no vested interest) is an “electronic notebook” program—a digital version of the multisubject, tabbed binders we all used in school. The user creates tabs, which appear across the top of the notebook interface. Each tab can accommodate as many pages as the user desires, just as in the sections of a paper notebook (FIGURE 1). In OneNote, each page has a title, and the title appears on the page tab on the right side of the screen (left side is an option). Several layers of subpages are also available for each page, similar to subdirectories in a computerized filing system.
FIGURE 1
Tabbed sections
OneNote’s Tabs are visible across the top. Most of the pages on the right side are obscured in this view by the search results window.
First tab: Summary sheet of patient “problems”
Since 2005, my practice has been limited to skin disease and it has been my custom to create paper “problem lists” as a handy method of tracking each patient’s malignancy types, dates, and anatomic locations. I decided to make these lists electronic, using OneNote (FIGURE 2). OneNote allows default templates, whereby clicking on New Page creates a fully formatted page. I used the template to create a derm summary sheet tab. Under that, I created an electronic page for each of the practice’s patients with a malignancy.
These patient pages are rapidly accessible with OneNote’s search box. As each additional letter is entered, the search feature narrows the possible matches. Usually, entering the first couple of letters of the last name presents the desired match in the search window. I then click on the patient’s name and hit Print; the summary is produced faster than the time it would take to find the information in an alphabetized paper notebook.
The advantage of an electronic summary sheet is that it can be updated and printed at each visit. Electronic summary sheets can be designed in any format—eg, a main page with Problems, Medications, Medication Allergies, Social History, Family History, etc, and a second page with a Health Maintenance flow sheet, or whatever makes sense for the clinician’s practice.
With OneNote, tables, graphics, and text with various fonts can be placed anywhere on the page, as can elements created with drawing tools. Pages can be any size: 3x5 card, letter, legal, or endless (like a Web page). OneNote supports “copy and paste” and “drag and drop” from other programs, as well as hyperlinks to documents outside OneNote.
The user can easily design a variety of templates for use in each tab, simply by designing a page and designating a template. One template can be set as the default for that tab. For example, when I click New Page in the Summary tab, a new summary form appears in that section. Pages can be deleted, copied, or moved within and between sections, just as in a word processing program.
FIGURE 2
Summary sheet
Each patient has a page (identifying information at right is covered) that lists his or her chronic/acute problems, as well as malignancies. One can locate the proper page by typing the first few letters of the patient’s last name in the search field.
A second tab for prescriptions
I decided to add a second tab to my notebook: Prescriptions. I designed a prescription template and set that as my default New Page for the prescription section. I created a new page for each of my common prescriptions—eg, doxycycline, minocycline, various topical acne preparations. OneNote’s search function at the top of the pages section is nearly instantaneous and shows all possible matches for a string of characters. Entering “tre” will show all matches with “tretinoin. “ It’s easy, then, to select the preparation of interest, hit Print, and have a printed prescription in seconds. For even greater efficiency, I have created new prescription pages for multiple medications I often use in combination—eg, a morning antimicrobial and an evening retinoid for acne, or compounds such as magic mouthwash (FIGURE 3).
Our office check-in process includes producing printed sticky labels with a patient’s name and address and the current date, which we can affix to things like pictures and pathology slips. So I designed my prescription blank to accommodate such labels. I print prescriptions from my wireless notebook computer to a wireless printer. The nurse affixes a label, I sign the document, and in seconds the patient has a detailed, legible prescription. The only disadvantage with this system is that unlike iScribe, I cannot look up a patient’s prescription history electronically because there is no electronically filed copy saved with the patient’s name. One option would be to enter every patient on a page and put prescriptions as subpages under the patient’s page. But that is more work than I want to do in patient exam rooms during a visit. Instead, I print 2 copies of each prescription, one of which goes into the paper chart.
I populated my Prescriptions tab with my prescription “favorites” before going live. But this can also be done “on the fly. “ You simply enter a new prescription as the need arises. OneNote automatically saves the prescription for future use (unless it’s intentionally deleted).
To produce new prescriptions, I set the Prescription blank as the default template. I click New Page and a blank prescription form appears. So, let’s say that lidocaine gel is not in the prescriber. I search “lido, “ and the ointment and transdermal formulations that have already been entered come up. I click New Page, a blank prescription form appears, and I type the details of the prescription (lidocaine gel 2%, dispense 30 grams, apply 30 to 60 minutes before procedure, refill zero). This prescription is saved automatically and will be available the next time I search “lido. “ Alternatively, an existing prescription can be copied and easily modified, as in copying a “cream” prescription and changing to “ointment” in the copy so both are available for future use.
All sorts of variations are possible: “endocarditis prophylaxis” options could be entered as a list on one prescription form. Before the list is printed, the user could simply check the desired option for that patient. Because OneNote saves all changes automatically, any changes made to the default prescriptions (eg, choosing to give a medication once daily rather than the default of twice daily) are saved automatically. When I make any custom changes, I use the Undo button, which I placed on my Quick Access Toolbar, to easily return to my preferred default status.
FIGURE 3
Prescription page for multiple medications
Medications commonly used together can be combined on a single prescription form. Additional information may be included (and discussed in advance with patients), to reduce formulary callback and preauthorization issues. Alphabetizing the prescriptions is unnecessary, given that the robust search function matches even partial words.
A third tab for patient education
After the success with the Summary sheets and Prescriptions tabs, I added a Patient Ed tab (FIGURE 4). I use handouts liberally to reinforce discussions, to give directions for medication use (eg, retinoids, imiquimod, fluorouracil, permethrin, prednisone), and to educate patients about diseases (eg, dysplastic nevi, melanoma, scabies). Most of this information resides on my computer, and OneNote allows me to rapidly locate and print the documents. I copy the links to patient education files onto corresponding individual OneNote pages, organized by the handouts’ identifying key words.
For example, for the isotretinoin-inflammatory bowel disease information sheet, I created a page called “Isotretinoin - Inflammatory Bowel Disease” in the Patient Education tab. That page contains a hyperlink to the desired document on my computer. The original document can be updated as new information becomes available, and OneNote will always link to the current version. For less commonly used handouts, I can enter key title words in the search box, click on the appropriate page, and print the document.
Because the printer is in the hall 2 steps from each exam room, I can do that faster than the nurse can find these documents in our paper system. This is particularly useful if the information on the possible link between isotretinoin and inflammatory bowel disease is missing from our isotretinoin packet.
FIGURE 4
Patient education tab
OneNote can be used as an indexing aid for patient education materials by simply dragging and dropping into it the links to “original” patient education documents. By clicking on this link, one can go to the information that resides elsewhere, and print out the material for the patient.
Many advantages with this new system
With OneNote, I have elements of a mini-electronic record with summary sheets for patients with malignancies, prescription writing, and patient handouts. In addition, I will not lose this system in a corporate buyout or be charged exorbitant fees to transfer records. Tabs can be password protected for security, and all pages under a tab can be saved in Adobe Acrobat, Microsoft Word, and OneNote formats. Those features help assure security and portability. (This system does not, however, qualify users for government incentives, as it lacks certain functions that are available with a true EMR.)
True e-prescribing—which, for me, included entering patient demographics and offered electronic access to my prescribing history for each patient—is usually an intermediary step for those moving toward full EMR implementation. Using OneNote, I carry a laptop/notebook room to room and print a lot of patient information handouts that otherwise would have to be retrieved from elsewhere.
As a trial, I used the OneNote system along with iScribe’s replacement e-prescribing product for several weeks. My OneNote system was faster. Now, only when patients specifically request e-prescriptions do I use the iScribe replacement product, which, after the corporate merger, has been continued at no charge for 2 to 3 years for existing users. (E-prescribing for Medicare patients at least 25 times in 2011 will qualify users for the Medicare incentive bonus.)
Because the “computer” portion of patient encounters usually occurs at the end of the visit, it does not interfere with the patient-physician relationship. Additionally, my average patient has already been “teched” with a digital scale, digital blood pressure cuff, and digital camera, so a computer is probably one of the more familiar pieces in the technoscape.
OneNote has become a powerful ally in my clinical practice. I thought I had everything I needed with Word, Excel, and Acrobat. But I’m glad I opened OneNote out of curiosity. It’s not only helped me to modernize my patient “problem lists, “ but it’s proven to be the solution to my e-prescribing dilemma.
CORRESPONDENCE
Gary N. Fox, MD, Defiance Clinic, 1400 E. 2nd Street, Defiance, OH 43512; foxgary@yahoo.com
1. Fox GN. Electronic prescribing: drug dealing twenty-first century style. In: Strayer SM, Reynolds PL, Ebell MH, eds. Handhelds in Medicine: A Practical Guide for Clinicians. New York, NY: Springer; 2005.
2. Levine N. Before implementing EMRs, heed words of warning. Dermatology Times. May 2010. Available at: http://www.modernmedicine.com/modernmedicine/Modern+Medicine+Now/Before-implementing-EMRs-heedwords-of-warning/ArticleStandard/Article/detail/666763. Accessed May 28, 2010.
3. Nash K. E-prescribing: a boon or a bane to dermatology practices? Dermatology Times. May 2010. Available at: http://www.modernmedicine.com/modernmedicine/Modern+Medicine+Now/E-prescribing-a-boon-or-a-bane-to-dermatology-prac/ArticleStandard/Article/detail/666779. Accessed May 28, 2010.
Even with government incentives, I physicians have been slow to make the leap to electronic medical records (EMR) and full electronic prescribing (e-prescribing). My transition to e-prescribing evolved over about a decade, and I was a satisfied e-prescriber—for a while.
Around 2000, I began writing electronic prescriptions using iScribe for Palm handhelds.1 The final transition to full e-prescribing required only a WiFi connection in the office for use with my Palm, and hitting Send to submit the prescription to the pharmacy. iScribe was user friendly and fast. It eliminated pharmacy “callbacks, “ provided printed receipts for charting, and maintained a record of each prescription on the Palm, filed under the patient’s name. A full prescription history for each patient archived on the Palm reduced the need to pull charts for medication questions.
A rude surprise
Then iScribe was acquired by another company whose e-prescribing product, in my opinion, lengthened patient encounters because it required several additional steps to complete a prescription. This was unacceptable to me, and returning to handwritten prescriptions was out of the question. I needed a better solution.
I was disinclined to invest in another e-prescribing product whose tenure could end as abruptly as iScribe’s had. To wit: I recently read about another user-friendly, well-supported medical software program that was scooped up by a larger company selling less functional and more expensive products (while charging for a costly conversion of existing records and delivering poorer customer service).2 And e-prescribing in general has received mixed reviews.3
I briefly considered designing my own prescription writer. A full-featured writer using a relational database, such as Microsoft Access, would be ideal. But developing it would be daunting without software-specific training. The same would be true for spreadsheet software. Adobe Acrobat or word processors with directories or hyperlinks or search functions didn’t seem appropriate.
A welcome surprise
Microsoft Office 2010 software for PC and Mac platforms now includes OneNote, a program new to me. (Price at Costco for Office Home and Student, September 2010, was $119.) OneNote (in which I have no vested interest) is an “electronic notebook” program—a digital version of the multisubject, tabbed binders we all used in school. The user creates tabs, which appear across the top of the notebook interface. Each tab can accommodate as many pages as the user desires, just as in the sections of a paper notebook (FIGURE 1). In OneNote, each page has a title, and the title appears on the page tab on the right side of the screen (left side is an option). Several layers of subpages are also available for each page, similar to subdirectories in a computerized filing system.
FIGURE 1
Tabbed sections
OneNote’s Tabs are visible across the top. Most of the pages on the right side are obscured in this view by the search results window.
First tab: Summary sheet of patient “problems”
Since 2005, my practice has been limited to skin disease and it has been my custom to create paper “problem lists” as a handy method of tracking each patient’s malignancy types, dates, and anatomic locations. I decided to make these lists electronic, using OneNote (FIGURE 2). OneNote allows default templates, whereby clicking on New Page creates a fully formatted page. I used the template to create a derm summary sheet tab. Under that, I created an electronic page for each of the practice’s patients with a malignancy.
These patient pages are rapidly accessible with OneNote’s search box. As each additional letter is entered, the search feature narrows the possible matches. Usually, entering the first couple of letters of the last name presents the desired match in the search window. I then click on the patient’s name and hit Print; the summary is produced faster than the time it would take to find the information in an alphabetized paper notebook.
The advantage of an electronic summary sheet is that it can be updated and printed at each visit. Electronic summary sheets can be designed in any format—eg, a main page with Problems, Medications, Medication Allergies, Social History, Family History, etc, and a second page with a Health Maintenance flow sheet, or whatever makes sense for the clinician’s practice.
With OneNote, tables, graphics, and text with various fonts can be placed anywhere on the page, as can elements created with drawing tools. Pages can be any size: 3x5 card, letter, legal, or endless (like a Web page). OneNote supports “copy and paste” and “drag and drop” from other programs, as well as hyperlinks to documents outside OneNote.
The user can easily design a variety of templates for use in each tab, simply by designing a page and designating a template. One template can be set as the default for that tab. For example, when I click New Page in the Summary tab, a new summary form appears in that section. Pages can be deleted, copied, or moved within and between sections, just as in a word processing program.
FIGURE 2
Summary sheet
Each patient has a page (identifying information at right is covered) that lists his or her chronic/acute problems, as well as malignancies. One can locate the proper page by typing the first few letters of the patient’s last name in the search field.
A second tab for prescriptions
I decided to add a second tab to my notebook: Prescriptions. I designed a prescription template and set that as my default New Page for the prescription section. I created a new page for each of my common prescriptions—eg, doxycycline, minocycline, various topical acne preparations. OneNote’s search function at the top of the pages section is nearly instantaneous and shows all possible matches for a string of characters. Entering “tre” will show all matches with “tretinoin. “ It’s easy, then, to select the preparation of interest, hit Print, and have a printed prescription in seconds. For even greater efficiency, I have created new prescription pages for multiple medications I often use in combination—eg, a morning antimicrobial and an evening retinoid for acne, or compounds such as magic mouthwash (FIGURE 3).
Our office check-in process includes producing printed sticky labels with a patient’s name and address and the current date, which we can affix to things like pictures and pathology slips. So I designed my prescription blank to accommodate such labels. I print prescriptions from my wireless notebook computer to a wireless printer. The nurse affixes a label, I sign the document, and in seconds the patient has a detailed, legible prescription. The only disadvantage with this system is that unlike iScribe, I cannot look up a patient’s prescription history electronically because there is no electronically filed copy saved with the patient’s name. One option would be to enter every patient on a page and put prescriptions as subpages under the patient’s page. But that is more work than I want to do in patient exam rooms during a visit. Instead, I print 2 copies of each prescription, one of which goes into the paper chart.
I populated my Prescriptions tab with my prescription “favorites” before going live. But this can also be done “on the fly. “ You simply enter a new prescription as the need arises. OneNote automatically saves the prescription for future use (unless it’s intentionally deleted).
To produce new prescriptions, I set the Prescription blank as the default template. I click New Page and a blank prescription form appears. So, let’s say that lidocaine gel is not in the prescriber. I search “lido, “ and the ointment and transdermal formulations that have already been entered come up. I click New Page, a blank prescription form appears, and I type the details of the prescription (lidocaine gel 2%, dispense 30 grams, apply 30 to 60 minutes before procedure, refill zero). This prescription is saved automatically and will be available the next time I search “lido. “ Alternatively, an existing prescription can be copied and easily modified, as in copying a “cream” prescription and changing to “ointment” in the copy so both are available for future use.
All sorts of variations are possible: “endocarditis prophylaxis” options could be entered as a list on one prescription form. Before the list is printed, the user could simply check the desired option for that patient. Because OneNote saves all changes automatically, any changes made to the default prescriptions (eg, choosing to give a medication once daily rather than the default of twice daily) are saved automatically. When I make any custom changes, I use the Undo button, which I placed on my Quick Access Toolbar, to easily return to my preferred default status.
FIGURE 3
Prescription page for multiple medications
Medications commonly used together can be combined on a single prescription form. Additional information may be included (and discussed in advance with patients), to reduce formulary callback and preauthorization issues. Alphabetizing the prescriptions is unnecessary, given that the robust search function matches even partial words.
A third tab for patient education
After the success with the Summary sheets and Prescriptions tabs, I added a Patient Ed tab (FIGURE 4). I use handouts liberally to reinforce discussions, to give directions for medication use (eg, retinoids, imiquimod, fluorouracil, permethrin, prednisone), and to educate patients about diseases (eg, dysplastic nevi, melanoma, scabies). Most of this information resides on my computer, and OneNote allows me to rapidly locate and print the documents. I copy the links to patient education files onto corresponding individual OneNote pages, organized by the handouts’ identifying key words.
For example, for the isotretinoin-inflammatory bowel disease information sheet, I created a page called “Isotretinoin - Inflammatory Bowel Disease” in the Patient Education tab. That page contains a hyperlink to the desired document on my computer. The original document can be updated as new information becomes available, and OneNote will always link to the current version. For less commonly used handouts, I can enter key title words in the search box, click on the appropriate page, and print the document.
Because the printer is in the hall 2 steps from each exam room, I can do that faster than the nurse can find these documents in our paper system. This is particularly useful if the information on the possible link between isotretinoin and inflammatory bowel disease is missing from our isotretinoin packet.
FIGURE 4
Patient education tab
OneNote can be used as an indexing aid for patient education materials by simply dragging and dropping into it the links to “original” patient education documents. By clicking on this link, one can go to the information that resides elsewhere, and print out the material for the patient.
Many advantages with this new system
With OneNote, I have elements of a mini-electronic record with summary sheets for patients with malignancies, prescription writing, and patient handouts. In addition, I will not lose this system in a corporate buyout or be charged exorbitant fees to transfer records. Tabs can be password protected for security, and all pages under a tab can be saved in Adobe Acrobat, Microsoft Word, and OneNote formats. Those features help assure security and portability. (This system does not, however, qualify users for government incentives, as it lacks certain functions that are available with a true EMR.)
True e-prescribing—which, for me, included entering patient demographics and offered electronic access to my prescribing history for each patient—is usually an intermediary step for those moving toward full EMR implementation. Using OneNote, I carry a laptop/notebook room to room and print a lot of patient information handouts that otherwise would have to be retrieved from elsewhere.
As a trial, I used the OneNote system along with iScribe’s replacement e-prescribing product for several weeks. My OneNote system was faster. Now, only when patients specifically request e-prescriptions do I use the iScribe replacement product, which, after the corporate merger, has been continued at no charge for 2 to 3 years for existing users. (E-prescribing for Medicare patients at least 25 times in 2011 will qualify users for the Medicare incentive bonus.)
Because the “computer” portion of patient encounters usually occurs at the end of the visit, it does not interfere with the patient-physician relationship. Additionally, my average patient has already been “teched” with a digital scale, digital blood pressure cuff, and digital camera, so a computer is probably one of the more familiar pieces in the technoscape.
OneNote has become a powerful ally in my clinical practice. I thought I had everything I needed with Word, Excel, and Acrobat. But I’m glad I opened OneNote out of curiosity. It’s not only helped me to modernize my patient “problem lists, “ but it’s proven to be the solution to my e-prescribing dilemma.
CORRESPONDENCE
Gary N. Fox, MD, Defiance Clinic, 1400 E. 2nd Street, Defiance, OH 43512; foxgary@yahoo.com
Even with government incentives, I physicians have been slow to make the leap to electronic medical records (EMR) and full electronic prescribing (e-prescribing). My transition to e-prescribing evolved over about a decade, and I was a satisfied e-prescriber—for a while.
Around 2000, I began writing electronic prescriptions using iScribe for Palm handhelds.1 The final transition to full e-prescribing required only a WiFi connection in the office for use with my Palm, and hitting Send to submit the prescription to the pharmacy. iScribe was user friendly and fast. It eliminated pharmacy “callbacks, “ provided printed receipts for charting, and maintained a record of each prescription on the Palm, filed under the patient’s name. A full prescription history for each patient archived on the Palm reduced the need to pull charts for medication questions.
A rude surprise
Then iScribe was acquired by another company whose e-prescribing product, in my opinion, lengthened patient encounters because it required several additional steps to complete a prescription. This was unacceptable to me, and returning to handwritten prescriptions was out of the question. I needed a better solution.
I was disinclined to invest in another e-prescribing product whose tenure could end as abruptly as iScribe’s had. To wit: I recently read about another user-friendly, well-supported medical software program that was scooped up by a larger company selling less functional and more expensive products (while charging for a costly conversion of existing records and delivering poorer customer service).2 And e-prescribing in general has received mixed reviews.3
I briefly considered designing my own prescription writer. A full-featured writer using a relational database, such as Microsoft Access, would be ideal. But developing it would be daunting without software-specific training. The same would be true for spreadsheet software. Adobe Acrobat or word processors with directories or hyperlinks or search functions didn’t seem appropriate.
A welcome surprise
Microsoft Office 2010 software for PC and Mac platforms now includes OneNote, a program new to me. (Price at Costco for Office Home and Student, September 2010, was $119.) OneNote (in which I have no vested interest) is an “electronic notebook” program—a digital version of the multisubject, tabbed binders we all used in school. The user creates tabs, which appear across the top of the notebook interface. Each tab can accommodate as many pages as the user desires, just as in the sections of a paper notebook (FIGURE 1). In OneNote, each page has a title, and the title appears on the page tab on the right side of the screen (left side is an option). Several layers of subpages are also available for each page, similar to subdirectories in a computerized filing system.
FIGURE 1
Tabbed sections
OneNote’s Tabs are visible across the top. Most of the pages on the right side are obscured in this view by the search results window.
First tab: Summary sheet of patient “problems”
Since 2005, my practice has been limited to skin disease and it has been my custom to create paper “problem lists” as a handy method of tracking each patient’s malignancy types, dates, and anatomic locations. I decided to make these lists electronic, using OneNote (FIGURE 2). OneNote allows default templates, whereby clicking on New Page creates a fully formatted page. I used the template to create a derm summary sheet tab. Under that, I created an electronic page for each of the practice’s patients with a malignancy.
These patient pages are rapidly accessible with OneNote’s search box. As each additional letter is entered, the search feature narrows the possible matches. Usually, entering the first couple of letters of the last name presents the desired match in the search window. I then click on the patient’s name and hit Print; the summary is produced faster than the time it would take to find the information in an alphabetized paper notebook.
The advantage of an electronic summary sheet is that it can be updated and printed at each visit. Electronic summary sheets can be designed in any format—eg, a main page with Problems, Medications, Medication Allergies, Social History, Family History, etc, and a second page with a Health Maintenance flow sheet, or whatever makes sense for the clinician’s practice.
With OneNote, tables, graphics, and text with various fonts can be placed anywhere on the page, as can elements created with drawing tools. Pages can be any size: 3x5 card, letter, legal, or endless (like a Web page). OneNote supports “copy and paste” and “drag and drop” from other programs, as well as hyperlinks to documents outside OneNote.
The user can easily design a variety of templates for use in each tab, simply by designing a page and designating a template. One template can be set as the default for that tab. For example, when I click New Page in the Summary tab, a new summary form appears in that section. Pages can be deleted, copied, or moved within and between sections, just as in a word processing program.
FIGURE 2
Summary sheet
Each patient has a page (identifying information at right is covered) that lists his or her chronic/acute problems, as well as malignancies. One can locate the proper page by typing the first few letters of the patient’s last name in the search field.
A second tab for prescriptions
I decided to add a second tab to my notebook: Prescriptions. I designed a prescription template and set that as my default New Page for the prescription section. I created a new page for each of my common prescriptions—eg, doxycycline, minocycline, various topical acne preparations. OneNote’s search function at the top of the pages section is nearly instantaneous and shows all possible matches for a string of characters. Entering “tre” will show all matches with “tretinoin. “ It’s easy, then, to select the preparation of interest, hit Print, and have a printed prescription in seconds. For even greater efficiency, I have created new prescription pages for multiple medications I often use in combination—eg, a morning antimicrobial and an evening retinoid for acne, or compounds such as magic mouthwash (FIGURE 3).
Our office check-in process includes producing printed sticky labels with a patient’s name and address and the current date, which we can affix to things like pictures and pathology slips. So I designed my prescription blank to accommodate such labels. I print prescriptions from my wireless notebook computer to a wireless printer. The nurse affixes a label, I sign the document, and in seconds the patient has a detailed, legible prescription. The only disadvantage with this system is that unlike iScribe, I cannot look up a patient’s prescription history electronically because there is no electronically filed copy saved with the patient’s name. One option would be to enter every patient on a page and put prescriptions as subpages under the patient’s page. But that is more work than I want to do in patient exam rooms during a visit. Instead, I print 2 copies of each prescription, one of which goes into the paper chart.
I populated my Prescriptions tab with my prescription “favorites” before going live. But this can also be done “on the fly. “ You simply enter a new prescription as the need arises. OneNote automatically saves the prescription for future use (unless it’s intentionally deleted).
To produce new prescriptions, I set the Prescription blank as the default template. I click New Page and a blank prescription form appears. So, let’s say that lidocaine gel is not in the prescriber. I search “lido, “ and the ointment and transdermal formulations that have already been entered come up. I click New Page, a blank prescription form appears, and I type the details of the prescription (lidocaine gel 2%, dispense 30 grams, apply 30 to 60 minutes before procedure, refill zero). This prescription is saved automatically and will be available the next time I search “lido. “ Alternatively, an existing prescription can be copied and easily modified, as in copying a “cream” prescription and changing to “ointment” in the copy so both are available for future use.
All sorts of variations are possible: “endocarditis prophylaxis” options could be entered as a list on one prescription form. Before the list is printed, the user could simply check the desired option for that patient. Because OneNote saves all changes automatically, any changes made to the default prescriptions (eg, choosing to give a medication once daily rather than the default of twice daily) are saved automatically. When I make any custom changes, I use the Undo button, which I placed on my Quick Access Toolbar, to easily return to my preferred default status.
FIGURE 3
Prescription page for multiple medications
Medications commonly used together can be combined on a single prescription form. Additional information may be included (and discussed in advance with patients), to reduce formulary callback and preauthorization issues. Alphabetizing the prescriptions is unnecessary, given that the robust search function matches even partial words.
A third tab for patient education
After the success with the Summary sheets and Prescriptions tabs, I added a Patient Ed tab (FIGURE 4). I use handouts liberally to reinforce discussions, to give directions for medication use (eg, retinoids, imiquimod, fluorouracil, permethrin, prednisone), and to educate patients about diseases (eg, dysplastic nevi, melanoma, scabies). Most of this information resides on my computer, and OneNote allows me to rapidly locate and print the documents. I copy the links to patient education files onto corresponding individual OneNote pages, organized by the handouts’ identifying key words.
For example, for the isotretinoin-inflammatory bowel disease information sheet, I created a page called “Isotretinoin - Inflammatory Bowel Disease” in the Patient Education tab. That page contains a hyperlink to the desired document on my computer. The original document can be updated as new information becomes available, and OneNote will always link to the current version. For less commonly used handouts, I can enter key title words in the search box, click on the appropriate page, and print the document.
Because the printer is in the hall 2 steps from each exam room, I can do that faster than the nurse can find these documents in our paper system. This is particularly useful if the information on the possible link between isotretinoin and inflammatory bowel disease is missing from our isotretinoin packet.
FIGURE 4
Patient education tab
OneNote can be used as an indexing aid for patient education materials by simply dragging and dropping into it the links to “original” patient education documents. By clicking on this link, one can go to the information that resides elsewhere, and print out the material for the patient.
Many advantages with this new system
With OneNote, I have elements of a mini-electronic record with summary sheets for patients with malignancies, prescription writing, and patient handouts. In addition, I will not lose this system in a corporate buyout or be charged exorbitant fees to transfer records. Tabs can be password protected for security, and all pages under a tab can be saved in Adobe Acrobat, Microsoft Word, and OneNote formats. Those features help assure security and portability. (This system does not, however, qualify users for government incentives, as it lacks certain functions that are available with a true EMR.)
True e-prescribing—which, for me, included entering patient demographics and offered electronic access to my prescribing history for each patient—is usually an intermediary step for those moving toward full EMR implementation. Using OneNote, I carry a laptop/notebook room to room and print a lot of patient information handouts that otherwise would have to be retrieved from elsewhere.
As a trial, I used the OneNote system along with iScribe’s replacement e-prescribing product for several weeks. My OneNote system was faster. Now, only when patients specifically request e-prescriptions do I use the iScribe replacement product, which, after the corporate merger, has been continued at no charge for 2 to 3 years for existing users. (E-prescribing for Medicare patients at least 25 times in 2011 will qualify users for the Medicare incentive bonus.)
Because the “computer” portion of patient encounters usually occurs at the end of the visit, it does not interfere with the patient-physician relationship. Additionally, my average patient has already been “teched” with a digital scale, digital blood pressure cuff, and digital camera, so a computer is probably one of the more familiar pieces in the technoscape.
OneNote has become a powerful ally in my clinical practice. I thought I had everything I needed with Word, Excel, and Acrobat. But I’m glad I opened OneNote out of curiosity. It’s not only helped me to modernize my patient “problem lists, “ but it’s proven to be the solution to my e-prescribing dilemma.
CORRESPONDENCE
Gary N. Fox, MD, Defiance Clinic, 1400 E. 2nd Street, Defiance, OH 43512; foxgary@yahoo.com
1. Fox GN. Electronic prescribing: drug dealing twenty-first century style. In: Strayer SM, Reynolds PL, Ebell MH, eds. Handhelds in Medicine: A Practical Guide for Clinicians. New York, NY: Springer; 2005.
2. Levine N. Before implementing EMRs, heed words of warning. Dermatology Times. May 2010. Available at: http://www.modernmedicine.com/modernmedicine/Modern+Medicine+Now/Before-implementing-EMRs-heedwords-of-warning/ArticleStandard/Article/detail/666763. Accessed May 28, 2010.
3. Nash K. E-prescribing: a boon or a bane to dermatology practices? Dermatology Times. May 2010. Available at: http://www.modernmedicine.com/modernmedicine/Modern+Medicine+Now/E-prescribing-a-boon-or-a-bane-to-dermatology-prac/ArticleStandard/Article/detail/666779. Accessed May 28, 2010.
1. Fox GN. Electronic prescribing: drug dealing twenty-first century style. In: Strayer SM, Reynolds PL, Ebell MH, eds. Handhelds in Medicine: A Practical Guide for Clinicians. New York, NY: Springer; 2005.
2. Levine N. Before implementing EMRs, heed words of warning. Dermatology Times. May 2010. Available at: http://www.modernmedicine.com/modernmedicine/Modern+Medicine+Now/Before-implementing-EMRs-heedwords-of-warning/ArticleStandard/Article/detail/666763. Accessed May 28, 2010.
3. Nash K. E-prescribing: a boon or a bane to dermatology practices? Dermatology Times. May 2010. Available at: http://www.modernmedicine.com/modernmedicine/Modern+Medicine+Now/E-prescribing-a-boon-or-a-bane-to-dermatology-prac/ArticleStandard/Article/detail/666779. Accessed May 28, 2010.
Problem with baby’s hearing? An intervention checklist
• Check hearing screening results for all newborns in your practice. B
• Refer all newborns who fail screening for audiologic and medical evaluation and diagnosis before 3 months of age. B
• Refer infants with diagnosed hearing loss for early intervention services no later than 6 months of age. B
• Educate families about services and resources available to them and their hearing-impaired child. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Congenital permanent hearing loss occurs in about 3 of every 1000 births.1 Undiagnosed hearing loss can result in speech-language, academic, social, and other developmental delays. Until about 20 years ago, most children with hearing loss were not diagnosed until about 3 years of age.2 By that age, opportunities for effective intervention to help these children develop communication skills were often delayed, and many children remained seriously disabled.
In this enlightened age, when newborn hearing screening is nearly universal (92%), the prospects for children with hearing impairments are brighter—but not as bright as they could be.3 That’s because more than half the newborns with positive screens are lost to follow-up.3 Too many remain “lost,” without a diagnosis or access to services, until they show up at school without the language skills they need to keep up, academically or socially, with their classmates.
The medical home can help
The American Academy of Pediatrics (AAP) and the Health Resources Services Administration aggressively promote the concept of the medical home as the best locus for coordinating the care of children with special needs, and the American Academy of Family Physicians (AAFP) has endorsed the medical home concept.2,4 According to the AAFP’s Joint Statement of Principles, the medical home is responsible for coordinating care across all elements of the health care system and the patient’s community.4 Most physicians in a recent survey believed the medical home should be responsible for coordinating services and guiding families in the development of intervention plans for children with hearing loss.5 Family physicians who provide a medical home for infants and young children are in an ideal position to ensure that children with hearing loss are not lost to follow-up and that they receive the services they need to lead healthy lives.
What follow-up entails
According to the 2007 Position Paper of the Joint Committee on Infant Hearing, a body composed of representatives from the AAP, the American Academy of Audiology, the American Speech-Language-Hearing Association, and other professional organizations concerned with hearing loss, an effective program to mitigate the impact of hearing loss should follow this timetable6:
- By 1 month of age, all infants should receive hearing screening. (Of note: In 2008, the US Preventive Services Task Force issued a B recommendation for universal hearing screening of all newborns.7)
- By 3 months of age, hearing loss should be diagnosed.
- Within 1 month of diagnosis, hearing aids should be fitted for infants whose parents choose hearing aids.
- As soon as possible after diagnosis—but no later than 6 months of age—infants with confirmed, permanent hearing loss should receive early intervention services.6
Intervention services should include medical and surgical evaluation, evaluation for hearing aids, and then cochlear implants for those with severe-to-profound hearing loss who do not benefit from hearing aids. Communication assessment and therapy should also be considered. The goal of intervention is to help infants with hearing loss develop communication competence, social skills, emotional well-being, and positive self-esteem.6
The CLINICAL TOOL provides a detailed overview of the early hearing detection and intervention (EHDI) process outlined by the Joint Committee and a checklist of roles and responsibilities for physicians serving as medical homes for children with hearing loss and their families. Unfortunately, many primary caregivers report that their medical training did not prepare them to guide families through this process.8-10 This article is intended to provide the additional information caregivers have requested to help them meet these obligations.
CLINICAL TOOL
The early hearing detection and intervention process6
| Prenatal period | Birth – 1 month | By 3 months | No later than 6 months |
|---|---|---|---|
| Education for parents about the importance of newborn hearing screening and the distinction between screening and diagnosis | Hearing screening for all infants in hospital or at audiologist out-patient facility | Infants with positive screens are diagnosed by an audiologist with auditory brainstem response testing | Physician and parents monitor developmental milestones and experience with hearing aids |
| Auditory brainstem response screening for all NICU infants ≥5 days of age | Hearing loss is ruled out or confirmed | Meeting with family and early intervention personnel to develop an individualized family service plan | |
| Rescreening for all infants with risk factors who are hospitalized within 1 month of discharge | Audiologist shares results with family, medical home, and the early hearing detection and intervention coordinator | Individualized family service plan is in place, as mandated by federal law under the individuals with disabilities education Act | |
| Infants are linked to a medical home before discharge by the hospital | Families are counseled regarding diagnosis and follow-up and given educational materials | Early intervention services are instituted in accordance with the individualized family service plan | |
| Screening results are given to families and to the baby’s medical home | Audiologist recommends treatment in the medical home or referral to an ear, nose, and throat specialist for medical evaluation and treatment | Together, audiologist and family develop expectations for hearing aids | |
| Families are counseled about screening results and follow-up | Audiologist and/or physician provides referrals for genetic counseling and ophthalmologic consultation | If hearing aids are unsuccessful, families are counseled about cochlear implants | |
| Audiologist alerts parents and the medical home that child may need hearing aids and early intervention services | If family wishes, audiologist or medical home makes a referral to a cochlear implant team | ||
| Audiologist or physician counsels parents on the test results, treatments, and communication options: aural-oral, total communication, and sign language | Medical clearance and insurance authorizations are obtained for cochlear implants | ||
| Reports from all involved providers and agencies are transmitted to state early hearing detection and intervention coordinator | |||
| Checklist for family physicians | |||
| ____ Encourage all families to have their baby’s hearing screened | ____ Review screening results | ____ Review audiologic diagnostic evaluation results | ____ Coordinate early intervention services |
| ____ Explain screening procedures | ____ Make referrals for outpatient screening and audiologic diagnostic evaluation by an audiologist | ____ Ensure that an audiologic reevaluation has been completed | ____ Confer with audiologist on child’s progress with hearing aids and consideration of cochlear implants |
| ____ Assess for family history of hearing loss | ____ Ensure all infants hospitalized after discharge are rescreened | ____ Review findings from otolaryngology and audiologic consultations with family | ____ Provide families with basic information about cochlear implants |
| ____ Provide informational materials about newborn hearing screening | ____ Assess risk factors for hearing loss, including congenital and delayed-onset types | ____ Encourage family to comply with professionals’ recommendations and stress importance of keeping appointments | ____ Counsel families about the risks and benefits of cochlear implants |
| ____ Answer family’s questions about newborn screening or hearing loss | ____Ensure that screening results have been transmitted to state early hearing detection and intervention coordinator | ____ Refer for genetic counseling and ophthalmologic consultation | ____ Make referral to cochlear implant team |
| ____ Provide families with preliminary information on amplification and communication options | ____ Encourage families to comply with professionals’ recommendations | ||
| ____Confirm that families have received informational materials on screening and follow-up | ____ Make referral to audiologist for hearing aids | ____Ensure all reports are transmitted to state early hearing detection and intervention coordinator | |
| ____ Ensure hearing aids are fitted within 1 month of diagnosis | ____ Monitor developmental milestones | ||
| ____ Provide medical clearance, insurance authorization, and referral for hearing aids and early intervention services | |||
| ____ Ensure otolaryngology and audiologic results have been transmitted to state early hearing detection and intervention coordinator | |||
| NICU, neonatal intensive care unit. | |||
Getting an early start: Newborn screening
Ideally, intervention should begin before a child is born. When parents come in for prenatal visits, talk to them about the importance of newborn hearing screening. Tell them to expect that their baby will be screened at the birth hospital or at an outpatient audiology facility, and that this screening should be done by the time the baby is 1 month of age.
Tell parents their baby’s hearing will be tested with automated screening equipment that measures otoacoustic emissions from the baby’s ears or auditory brainstem response (ABR) to sound, both measurements that correlate with a child’s hearing and auditory behavior. Infants in well-baby nurseries can be screened by either technology. Infants in neonatal intensive care units (NICUs) for more than 5 days should be screened with ABR technology, which is better able to pick up neural losses.6 NICU babies frequently are at higher risk for neural hearing loss including auditory neuropathy/dyssynchrony, a condition that may account for about 8% of pediatric hearing losses annually.3
Be sure to explain to expectant couples that a positive screen indicates only that a problem may exist. It is not equivalent to a diagnosis of hearing loss, which is usually made by an audiologist.
The medical home’s role. The medical home should make sure that infants who fail an initial or secondary hospital screening and those who were missed or born outside the hospital are referred for outpatient screening. Newborns who fail initial screening should have both ears rescreened before hospital discharge, even if only one ear had failed previously.6 Additionally, any infant readmitted to the hospital within the first month of life who has a condition associated with potential hearing loss should be rescreened before discharge, preferably with an ABR.6 Risk factors associated with permanent-congenital, delayed-onset, or progressive hearing loss in children are listed in the TABLE.
TABLE
Risk indicators associated with hearing loss in childhood
|
| *These indicators are of greater concern for delayed-onset hearing loss. Source: American Academy of Pediatrics, Joint Committee on Infant Hearing. Pediatrics. 2007.6 |
Reporting screening results
Screening results are useful only if they are transmitted to caregivers and families. Breakdowns in transmission are a persistent problem for the early hearing detection and intervention process.2 The process is facilitated when hospitals make sure that all babies and their families are linked to a medical home at the time of discharge.
Hospital personnel should also be responsible for providing screening results to families in a face-to-face meeting. Medical home providers should review screening results again with parents and answer any questions that might have arisen after the initial hospital stay. Screening results should be given to parents in a sensitive manner, and patient education materials should be provided in parents’ native language, written at an appropriate reading level. Because hospital staff may not be trained to do this properly, it is important that medical home providers oversee the process and address any parental concerns.2
Screening results should also be reported by the birth hospital to the state’s EHDI coordinator, part of the national tracking and surveillance system funded by the Centers for Disease Control and Prevention to ensure that all children with hearing loss achieve communication and social skills commensurate with their cognitive abilities. 11 You can find contact information for your state coordinator at www.cdc.gov/ncbddd/ehdi/documents/EHDI_contact.pdf.
Diagnosing hearing loss
When an infant who fails newborn screening testing arrives at the medical home, the urgent next step is to make sure he or she is referred to a pediatric audiologist for a complete audiologic diagnostic evaluation. Advising parents to “wait and see” is not appropriate; researchers have identified that response as a major obstacle to successful follow-up.2 The audiologic evaluation should be done by the time the baby is 3 months of age and should be performed by a pediatric audiologist specializing in diagnosis and management of young children with hearing loss.4-6
Tell parents that, with their approval, the audiologist may fit the baby with hearing aids as early as this visit, as amplification can help even very young infants hear all sounds in the environment, particularly spoken language.
Ongoing monitoring
Family practices serving as medical homes should continue to monitor children who pass their newborn screening but have high-risk factors for delayed-onset hearing loss. Those factors are listed in the TABLE. Refer children at higher risk for an audiologic diagnostic evaluation by 24 to 30 months of age.6 Follow-up on parental concerns about infant hearing or speech and monitor infants’ developmental milestones, auditory skills, and middle ear status using the AAP’s pediatric periodicity schedule.6 Conduct global developmental screenings at 9, 18, and 24 to 30 months of age, and refer for speech-language-hearing evaluations when appropriate.6
The medical home as central referral point
The medical home is a central referral point for the complex needs of children with hearing loss. The physician and all other providers involved in the child’s care should report results of diagnostic evaluations to state EHDI coordinators. The medical home’s continued involvement includes medical clearance for hearing aids, additional consultations, and screenings as necessary to help children receive needed services and keep them from being lost to the system.5,9
Referral for genetic consultation is important, because about half of all autosomal recessive sensorineural hearing losses that are not part of a syndrome are caused by mutations in the Connexin 26 GJB2 gene.12,13 Referral to a pediatric ophthalmologist is similarly important, to identify deficits in visual acuity that frequently co-occur with hearing loss, especially in preterm infants.6 Results of these consultations can assist the physician in guiding families through the intervention process.
Coordination of care among multiple providers is essential. When a family physician’s practice serves as a medical home for a child with hearing loss, the physician should oversee and coordinate the efforts of all stakeholders in the EHDI process; make referrals to, and receive reports from, all providers involved in diagnosis and treatment; and ensure that relevant information is shared. During all phases of the process, the role of the family physician is to encourage families to comply with professionals’ recommendations and to stress the importance of making and keeping scheduled appointments.
Making plans for intervention
Families with children who have any degree of permanent hearing loss in one or both ears are entitled to early intervention services.6 In most states, these services are provided by a multidisciplinary team at no or low cost through a federal grant program. Services can be home- or center-based. They may include, as needed, education for the affected child and family; physical, speech/language, and occupational therapy; and social work and psychotherapy services. The team works with the family to develop an individualized family service plan to document and guide the early intervention process.14
Families with a hearing-impaired child have a range of options to choose from in their search for an approach that is best for the child and most acceptable to them. Communication options span a continuum from emphasis on sign language as used by the deaf community to a variety of oral-aural approaches designed to lead to spoken language. Parental choices are influenced most heavily by the child’s success with hearing aids. Parents need unbiased, culturally sensitive counseling about all available communication options and hearing technologies, so they can make informed choices for their children.6
Answering parents’ questions
To ensure that parents have appropriate expectations for what auditory technology can do for their child, they need to receive information about traditional digital signal processing hearing aids, osseointegrated hearing implant systems (also known as bone-anchored hearing aids), and cochlear implants. They need to know that a trial period will probably be necessary to determine whether hearing aids are appropriate or if cochlear implantation should be considered. Cost of hearing aids and cochlear implants is a serious concern for parents, and for many, it presents a major barrier to obtaining optimal care.2
Many insurance plans cover cochlear implants, but require that children be at least 12 months of age, have bilateral profound sensorineural hearing loss (or severe-to-profound sensorineural hearing loss for those ≥24 months of age), receive minimal benefit from hearing aids, be enrolled in auditory rehabilitative therapy, and possess no medical contraindications.15 Hearing aids and cochlear implants may also be covered for children enrolled in Medicaid or the State Children’s Health Insurance Program.16 However, according to a recent evaluation of hearing screening programs nationwide, public and private insurance policies almost never provide adequate coverage for hearing services.2
As parents consider the options, be sure they are aware that some children younger than 12 months of age are receiving cochlear implants (sometimes in both ears), that stimulation of both ears is being recommended at earlier ages, and that it is also common for children to use a hearing aid in one ear and a cochlear implant in the other.17,18 Distinguishing among hearing loss types and knowing which treatment options are most effective helps physicians counsel families appropriately about making the best decisions for their children. Some physicians have expressed uncertainties about these issues and have requested additional information on this topic.19 Audiologists can help physicians obtain this information and help them to better counsel families about these options.
CORRESPONDENCE
Carole E. Johnson, PhD, AuD, 1199 Haley Center, Auburn University, Auburn, AL 36849; johns19@auburn.edu
1. Vartiainen E, Kemppinen P, Karjalainen S. Prevalence and etiology of bilateral sensorineural hearing impairment in a Finnish childhood population. Int J Pediatr Otorhinolaryngol. 1997;41:175-185.
2. Shulman S, Besculides M, Saltzman A, et al. Evaluation of the universal newborn hearing screening and intervention program. Pediatrics. 2010;126(suppl 1):S19-S27.
3. Centers for Disease Control and Prevention. Early hearing detection and intervention program. Summary of 2006 national EHDI data (version 4). October 2008. Available at: http://www.cdc.gov/ncbdd/ehdi/documents/EHDI_Summ_2006_Web.pdf. Accessed December 23, 2010.
4. AAFP, AAP, ACP, AOA. Joint principles of the patient-centered medical home. February 2007. Available at: www.pcpcc.net/print/14. Accessed December 25, 2010.
5. Dorros C, Kurtzer-White E, Ahlgren M, et al. Medical home for children with hearing loss: physician perspectives and practices. Pediatrics. 2007;120:288-294.
6. American Academy of Pediatrics, Joint Committee on Infant Hearing. Year 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007;120:898-921.
7. US Preventive Services Task Force. Universal screening for hearing loss in newborns: US Preventive Services Task Force recommendation statement. Pediatrics. 2008;122:143-148.
8. Brown NC, James K, Liu J, et al. Newborn hearing screening. An assessment of knowledge, attitudes, and practices among Minnesota physicians. Minn Med. 2006;89:50-54.
9. Moeller MP, White KR, Shisler L. Primary care physicians’ knowledge, attitudes, and practices related to newborn hearing screening. Pediatrics. 2006;118:1357-1370.
10. Johnson CE, Danhauer JL, Granali A, et al. Systematic review of physicians’ knowledge of, participation in, and attitudes toward newborn hearing screening programs. Semin Hear. 2009;30:149-164.
11. Centers for Disease Control and Prevention. Early hearing detection and intervention (EHDI) national goals. Last updated September 17, 2010. Available at: www.cdc.gov/ncbddd/hearingloss/ehdi-goals.html. Accessed December 23, 2010.
12. Kenneson A, Van Naarden K, Boyle C. GJB2 (connexin 26) variants and nonsyndromic sensorineural hearing loss: A HuGe review. Genet Med. 2002;4:258-274.
13. Lerer I, Sagi M, Malamud E, et al. Contribution of connexin 26 mutations to nonsyndromic deafness in Ashkenazi patients and the variable phenotypic effect of the mutation 167delT. Am J Med Genet. 2000;95:53-56.
14. WrightsLaw. Early intervention (Part C of IDEA). Last updated August 16, 2010. Available at: www.wrightslaw.com/info/ei.index.htm. Accessed December 22, 2010.
15. Discolo DM, Hirose K. Pediatric cochlear implants. Am J Audiol. 2002;11:114-118.
16. McManus MA, Levtov R, White KR, et al. Medicaid reimbursement of hearing services for infants and young children. Pediatrics. 2010;126(suppl 1):S34-S42.
17. Papsin BC, Gordon KA. Bilateral cochlear implants should be the standard for children with bilateral sensorineural deafness. Curr Opin Otolaryngol Head Neck Surg. 2008;16:69-74.
18. Beijen JW, Mylanus EA, Leeuw AR, et al. Should a hearing aid in the contralateral ear be recommended for children with a unilateral cochlear implant? Ann Otol Rhinol Laryngol. 2008;117:397-403.
19. Carron JD, Moore RB, Dhaliwal AS. Perceptions of pediatric primary care physicians on congenital hearing loss and cochlear implantation. J Miss State Med Assoc. 2006;47:35-41.
• Check hearing screening results for all newborns in your practice. B
• Refer all newborns who fail screening for audiologic and medical evaluation and diagnosis before 3 months of age. B
• Refer infants with diagnosed hearing loss for early intervention services no later than 6 months of age. B
• Educate families about services and resources available to them and their hearing-impaired child. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Congenital permanent hearing loss occurs in about 3 of every 1000 births.1 Undiagnosed hearing loss can result in speech-language, academic, social, and other developmental delays. Until about 20 years ago, most children with hearing loss were not diagnosed until about 3 years of age.2 By that age, opportunities for effective intervention to help these children develop communication skills were often delayed, and many children remained seriously disabled.
In this enlightened age, when newborn hearing screening is nearly universal (92%), the prospects for children with hearing impairments are brighter—but not as bright as they could be.3 That’s because more than half the newborns with positive screens are lost to follow-up.3 Too many remain “lost,” without a diagnosis or access to services, until they show up at school without the language skills they need to keep up, academically or socially, with their classmates.
The medical home can help
The American Academy of Pediatrics (AAP) and the Health Resources Services Administration aggressively promote the concept of the medical home as the best locus for coordinating the care of children with special needs, and the American Academy of Family Physicians (AAFP) has endorsed the medical home concept.2,4 According to the AAFP’s Joint Statement of Principles, the medical home is responsible for coordinating care across all elements of the health care system and the patient’s community.4 Most physicians in a recent survey believed the medical home should be responsible for coordinating services and guiding families in the development of intervention plans for children with hearing loss.5 Family physicians who provide a medical home for infants and young children are in an ideal position to ensure that children with hearing loss are not lost to follow-up and that they receive the services they need to lead healthy lives.
What follow-up entails
According to the 2007 Position Paper of the Joint Committee on Infant Hearing, a body composed of representatives from the AAP, the American Academy of Audiology, the American Speech-Language-Hearing Association, and other professional organizations concerned with hearing loss, an effective program to mitigate the impact of hearing loss should follow this timetable6:
- By 1 month of age, all infants should receive hearing screening. (Of note: In 2008, the US Preventive Services Task Force issued a B recommendation for universal hearing screening of all newborns.7)
- By 3 months of age, hearing loss should be diagnosed.
- Within 1 month of diagnosis, hearing aids should be fitted for infants whose parents choose hearing aids.
- As soon as possible after diagnosis—but no later than 6 months of age—infants with confirmed, permanent hearing loss should receive early intervention services.6
Intervention services should include medical and surgical evaluation, evaluation for hearing aids, and then cochlear implants for those with severe-to-profound hearing loss who do not benefit from hearing aids. Communication assessment and therapy should also be considered. The goal of intervention is to help infants with hearing loss develop communication competence, social skills, emotional well-being, and positive self-esteem.6
The CLINICAL TOOL provides a detailed overview of the early hearing detection and intervention (EHDI) process outlined by the Joint Committee and a checklist of roles and responsibilities for physicians serving as medical homes for children with hearing loss and their families. Unfortunately, many primary caregivers report that their medical training did not prepare them to guide families through this process.8-10 This article is intended to provide the additional information caregivers have requested to help them meet these obligations.
CLINICAL TOOL
The early hearing detection and intervention process6
| Prenatal period | Birth – 1 month | By 3 months | No later than 6 months |
|---|---|---|---|
| Education for parents about the importance of newborn hearing screening and the distinction between screening and diagnosis | Hearing screening for all infants in hospital or at audiologist out-patient facility | Infants with positive screens are diagnosed by an audiologist with auditory brainstem response testing | Physician and parents monitor developmental milestones and experience with hearing aids |
| Auditory brainstem response screening for all NICU infants ≥5 days of age | Hearing loss is ruled out or confirmed | Meeting with family and early intervention personnel to develop an individualized family service plan | |
| Rescreening for all infants with risk factors who are hospitalized within 1 month of discharge | Audiologist shares results with family, medical home, and the early hearing detection and intervention coordinator | Individualized family service plan is in place, as mandated by federal law under the individuals with disabilities education Act | |
| Infants are linked to a medical home before discharge by the hospital | Families are counseled regarding diagnosis and follow-up and given educational materials | Early intervention services are instituted in accordance with the individualized family service plan | |
| Screening results are given to families and to the baby’s medical home | Audiologist recommends treatment in the medical home or referral to an ear, nose, and throat specialist for medical evaluation and treatment | Together, audiologist and family develop expectations for hearing aids | |
| Families are counseled about screening results and follow-up | Audiologist and/or physician provides referrals for genetic counseling and ophthalmologic consultation | If hearing aids are unsuccessful, families are counseled about cochlear implants | |
| Audiologist alerts parents and the medical home that child may need hearing aids and early intervention services | If family wishes, audiologist or medical home makes a referral to a cochlear implant team | ||
| Audiologist or physician counsels parents on the test results, treatments, and communication options: aural-oral, total communication, and sign language | Medical clearance and insurance authorizations are obtained for cochlear implants | ||
| Reports from all involved providers and agencies are transmitted to state early hearing detection and intervention coordinator | |||
| Checklist for family physicians | |||
| ____ Encourage all families to have their baby’s hearing screened | ____ Review screening results | ____ Review audiologic diagnostic evaluation results | ____ Coordinate early intervention services |
| ____ Explain screening procedures | ____ Make referrals for outpatient screening and audiologic diagnostic evaluation by an audiologist | ____ Ensure that an audiologic reevaluation has been completed | ____ Confer with audiologist on child’s progress with hearing aids and consideration of cochlear implants |
| ____ Assess for family history of hearing loss | ____ Ensure all infants hospitalized after discharge are rescreened | ____ Review findings from otolaryngology and audiologic consultations with family | ____ Provide families with basic information about cochlear implants |
| ____ Provide informational materials about newborn hearing screening | ____ Assess risk factors for hearing loss, including congenital and delayed-onset types | ____ Encourage family to comply with professionals’ recommendations and stress importance of keeping appointments | ____ Counsel families about the risks and benefits of cochlear implants |
| ____ Answer family’s questions about newborn screening or hearing loss | ____Ensure that screening results have been transmitted to state early hearing detection and intervention coordinator | ____ Refer for genetic counseling and ophthalmologic consultation | ____ Make referral to cochlear implant team |
| ____ Provide families with preliminary information on amplification and communication options | ____ Encourage families to comply with professionals’ recommendations | ||
| ____Confirm that families have received informational materials on screening and follow-up | ____ Make referral to audiologist for hearing aids | ____Ensure all reports are transmitted to state early hearing detection and intervention coordinator | |
| ____ Ensure hearing aids are fitted within 1 month of diagnosis | ____ Monitor developmental milestones | ||
| ____ Provide medical clearance, insurance authorization, and referral for hearing aids and early intervention services | |||
| ____ Ensure otolaryngology and audiologic results have been transmitted to state early hearing detection and intervention coordinator | |||
| NICU, neonatal intensive care unit. | |||
Getting an early start: Newborn screening
Ideally, intervention should begin before a child is born. When parents come in for prenatal visits, talk to them about the importance of newborn hearing screening. Tell them to expect that their baby will be screened at the birth hospital or at an outpatient audiology facility, and that this screening should be done by the time the baby is 1 month of age.
Tell parents their baby’s hearing will be tested with automated screening equipment that measures otoacoustic emissions from the baby’s ears or auditory brainstem response (ABR) to sound, both measurements that correlate with a child’s hearing and auditory behavior. Infants in well-baby nurseries can be screened by either technology. Infants in neonatal intensive care units (NICUs) for more than 5 days should be screened with ABR technology, which is better able to pick up neural losses.6 NICU babies frequently are at higher risk for neural hearing loss including auditory neuropathy/dyssynchrony, a condition that may account for about 8% of pediatric hearing losses annually.3
Be sure to explain to expectant couples that a positive screen indicates only that a problem may exist. It is not equivalent to a diagnosis of hearing loss, which is usually made by an audiologist.
The medical home’s role. The medical home should make sure that infants who fail an initial or secondary hospital screening and those who were missed or born outside the hospital are referred for outpatient screening. Newborns who fail initial screening should have both ears rescreened before hospital discharge, even if only one ear had failed previously.6 Additionally, any infant readmitted to the hospital within the first month of life who has a condition associated with potential hearing loss should be rescreened before discharge, preferably with an ABR.6 Risk factors associated with permanent-congenital, delayed-onset, or progressive hearing loss in children are listed in the TABLE.
TABLE
Risk indicators associated with hearing loss in childhood
|
| *These indicators are of greater concern for delayed-onset hearing loss. Source: American Academy of Pediatrics, Joint Committee on Infant Hearing. Pediatrics. 2007.6 |
Reporting screening results
Screening results are useful only if they are transmitted to caregivers and families. Breakdowns in transmission are a persistent problem for the early hearing detection and intervention process.2 The process is facilitated when hospitals make sure that all babies and their families are linked to a medical home at the time of discharge.
Hospital personnel should also be responsible for providing screening results to families in a face-to-face meeting. Medical home providers should review screening results again with parents and answer any questions that might have arisen after the initial hospital stay. Screening results should be given to parents in a sensitive manner, and patient education materials should be provided in parents’ native language, written at an appropriate reading level. Because hospital staff may not be trained to do this properly, it is important that medical home providers oversee the process and address any parental concerns.2
Screening results should also be reported by the birth hospital to the state’s EHDI coordinator, part of the national tracking and surveillance system funded by the Centers for Disease Control and Prevention to ensure that all children with hearing loss achieve communication and social skills commensurate with their cognitive abilities. 11 You can find contact information for your state coordinator at www.cdc.gov/ncbddd/ehdi/documents/EHDI_contact.pdf.
Diagnosing hearing loss
When an infant who fails newborn screening testing arrives at the medical home, the urgent next step is to make sure he or she is referred to a pediatric audiologist for a complete audiologic diagnostic evaluation. Advising parents to “wait and see” is not appropriate; researchers have identified that response as a major obstacle to successful follow-up.2 The audiologic evaluation should be done by the time the baby is 3 months of age and should be performed by a pediatric audiologist specializing in diagnosis and management of young children with hearing loss.4-6
Tell parents that, with their approval, the audiologist may fit the baby with hearing aids as early as this visit, as amplification can help even very young infants hear all sounds in the environment, particularly spoken language.
Ongoing monitoring
Family practices serving as medical homes should continue to monitor children who pass their newborn screening but have high-risk factors for delayed-onset hearing loss. Those factors are listed in the TABLE. Refer children at higher risk for an audiologic diagnostic evaluation by 24 to 30 months of age.6 Follow-up on parental concerns about infant hearing or speech and monitor infants’ developmental milestones, auditory skills, and middle ear status using the AAP’s pediatric periodicity schedule.6 Conduct global developmental screenings at 9, 18, and 24 to 30 months of age, and refer for speech-language-hearing evaluations when appropriate.6
The medical home as central referral point
The medical home is a central referral point for the complex needs of children with hearing loss. The physician and all other providers involved in the child’s care should report results of diagnostic evaluations to state EHDI coordinators. The medical home’s continued involvement includes medical clearance for hearing aids, additional consultations, and screenings as necessary to help children receive needed services and keep them from being lost to the system.5,9
Referral for genetic consultation is important, because about half of all autosomal recessive sensorineural hearing losses that are not part of a syndrome are caused by mutations in the Connexin 26 GJB2 gene.12,13 Referral to a pediatric ophthalmologist is similarly important, to identify deficits in visual acuity that frequently co-occur with hearing loss, especially in preterm infants.6 Results of these consultations can assist the physician in guiding families through the intervention process.
Coordination of care among multiple providers is essential. When a family physician’s practice serves as a medical home for a child with hearing loss, the physician should oversee and coordinate the efforts of all stakeholders in the EHDI process; make referrals to, and receive reports from, all providers involved in diagnosis and treatment; and ensure that relevant information is shared. During all phases of the process, the role of the family physician is to encourage families to comply with professionals’ recommendations and to stress the importance of making and keeping scheduled appointments.
Making plans for intervention
Families with children who have any degree of permanent hearing loss in one or both ears are entitled to early intervention services.6 In most states, these services are provided by a multidisciplinary team at no or low cost through a federal grant program. Services can be home- or center-based. They may include, as needed, education for the affected child and family; physical, speech/language, and occupational therapy; and social work and psychotherapy services. The team works with the family to develop an individualized family service plan to document and guide the early intervention process.14
Families with a hearing-impaired child have a range of options to choose from in their search for an approach that is best for the child and most acceptable to them. Communication options span a continuum from emphasis on sign language as used by the deaf community to a variety of oral-aural approaches designed to lead to spoken language. Parental choices are influenced most heavily by the child’s success with hearing aids. Parents need unbiased, culturally sensitive counseling about all available communication options and hearing technologies, so they can make informed choices for their children.6
Answering parents’ questions
To ensure that parents have appropriate expectations for what auditory technology can do for their child, they need to receive information about traditional digital signal processing hearing aids, osseointegrated hearing implant systems (also known as bone-anchored hearing aids), and cochlear implants. They need to know that a trial period will probably be necessary to determine whether hearing aids are appropriate or if cochlear implantation should be considered. Cost of hearing aids and cochlear implants is a serious concern for parents, and for many, it presents a major barrier to obtaining optimal care.2
Many insurance plans cover cochlear implants, but require that children be at least 12 months of age, have bilateral profound sensorineural hearing loss (or severe-to-profound sensorineural hearing loss for those ≥24 months of age), receive minimal benefit from hearing aids, be enrolled in auditory rehabilitative therapy, and possess no medical contraindications.15 Hearing aids and cochlear implants may also be covered for children enrolled in Medicaid or the State Children’s Health Insurance Program.16 However, according to a recent evaluation of hearing screening programs nationwide, public and private insurance policies almost never provide adequate coverage for hearing services.2
As parents consider the options, be sure they are aware that some children younger than 12 months of age are receiving cochlear implants (sometimes in both ears), that stimulation of both ears is being recommended at earlier ages, and that it is also common for children to use a hearing aid in one ear and a cochlear implant in the other.17,18 Distinguishing among hearing loss types and knowing which treatment options are most effective helps physicians counsel families appropriately about making the best decisions for their children. Some physicians have expressed uncertainties about these issues and have requested additional information on this topic.19 Audiologists can help physicians obtain this information and help them to better counsel families about these options.
CORRESPONDENCE
Carole E. Johnson, PhD, AuD, 1199 Haley Center, Auburn University, Auburn, AL 36849; johns19@auburn.edu
• Check hearing screening results for all newborns in your practice. B
• Refer all newborns who fail screening for audiologic and medical evaluation and diagnosis before 3 months of age. B
• Refer infants with diagnosed hearing loss for early intervention services no later than 6 months of age. B
• Educate families about services and resources available to them and their hearing-impaired child. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Congenital permanent hearing loss occurs in about 3 of every 1000 births.1 Undiagnosed hearing loss can result in speech-language, academic, social, and other developmental delays. Until about 20 years ago, most children with hearing loss were not diagnosed until about 3 years of age.2 By that age, opportunities for effective intervention to help these children develop communication skills were often delayed, and many children remained seriously disabled.
In this enlightened age, when newborn hearing screening is nearly universal (92%), the prospects for children with hearing impairments are brighter—but not as bright as they could be.3 That’s because more than half the newborns with positive screens are lost to follow-up.3 Too many remain “lost,” without a diagnosis or access to services, until they show up at school without the language skills they need to keep up, academically or socially, with their classmates.
The medical home can help
The American Academy of Pediatrics (AAP) and the Health Resources Services Administration aggressively promote the concept of the medical home as the best locus for coordinating the care of children with special needs, and the American Academy of Family Physicians (AAFP) has endorsed the medical home concept.2,4 According to the AAFP’s Joint Statement of Principles, the medical home is responsible for coordinating care across all elements of the health care system and the patient’s community.4 Most physicians in a recent survey believed the medical home should be responsible for coordinating services and guiding families in the development of intervention plans for children with hearing loss.5 Family physicians who provide a medical home for infants and young children are in an ideal position to ensure that children with hearing loss are not lost to follow-up and that they receive the services they need to lead healthy lives.
What follow-up entails
According to the 2007 Position Paper of the Joint Committee on Infant Hearing, a body composed of representatives from the AAP, the American Academy of Audiology, the American Speech-Language-Hearing Association, and other professional organizations concerned with hearing loss, an effective program to mitigate the impact of hearing loss should follow this timetable6:
- By 1 month of age, all infants should receive hearing screening. (Of note: In 2008, the US Preventive Services Task Force issued a B recommendation for universal hearing screening of all newborns.7)
- By 3 months of age, hearing loss should be diagnosed.
- Within 1 month of diagnosis, hearing aids should be fitted for infants whose parents choose hearing aids.
- As soon as possible after diagnosis—but no later than 6 months of age—infants with confirmed, permanent hearing loss should receive early intervention services.6
Intervention services should include medical and surgical evaluation, evaluation for hearing aids, and then cochlear implants for those with severe-to-profound hearing loss who do not benefit from hearing aids. Communication assessment and therapy should also be considered. The goal of intervention is to help infants with hearing loss develop communication competence, social skills, emotional well-being, and positive self-esteem.6
The CLINICAL TOOL provides a detailed overview of the early hearing detection and intervention (EHDI) process outlined by the Joint Committee and a checklist of roles and responsibilities for physicians serving as medical homes for children with hearing loss and their families. Unfortunately, many primary caregivers report that their medical training did not prepare them to guide families through this process.8-10 This article is intended to provide the additional information caregivers have requested to help them meet these obligations.
CLINICAL TOOL
The early hearing detection and intervention process6
| Prenatal period | Birth – 1 month | By 3 months | No later than 6 months |
|---|---|---|---|
| Education for parents about the importance of newborn hearing screening and the distinction between screening and diagnosis | Hearing screening for all infants in hospital or at audiologist out-patient facility | Infants with positive screens are diagnosed by an audiologist with auditory brainstem response testing | Physician and parents monitor developmental milestones and experience with hearing aids |
| Auditory brainstem response screening for all NICU infants ≥5 days of age | Hearing loss is ruled out or confirmed | Meeting with family and early intervention personnel to develop an individualized family service plan | |
| Rescreening for all infants with risk factors who are hospitalized within 1 month of discharge | Audiologist shares results with family, medical home, and the early hearing detection and intervention coordinator | Individualized family service plan is in place, as mandated by federal law under the individuals with disabilities education Act | |
| Infants are linked to a medical home before discharge by the hospital | Families are counseled regarding diagnosis and follow-up and given educational materials | Early intervention services are instituted in accordance with the individualized family service plan | |
| Screening results are given to families and to the baby’s medical home | Audiologist recommends treatment in the medical home or referral to an ear, nose, and throat specialist for medical evaluation and treatment | Together, audiologist and family develop expectations for hearing aids | |
| Families are counseled about screening results and follow-up | Audiologist and/or physician provides referrals for genetic counseling and ophthalmologic consultation | If hearing aids are unsuccessful, families are counseled about cochlear implants | |
| Audiologist alerts parents and the medical home that child may need hearing aids and early intervention services | If family wishes, audiologist or medical home makes a referral to a cochlear implant team | ||
| Audiologist or physician counsels parents on the test results, treatments, and communication options: aural-oral, total communication, and sign language | Medical clearance and insurance authorizations are obtained for cochlear implants | ||
| Reports from all involved providers and agencies are transmitted to state early hearing detection and intervention coordinator | |||
| Checklist for family physicians | |||
| ____ Encourage all families to have their baby’s hearing screened | ____ Review screening results | ____ Review audiologic diagnostic evaluation results | ____ Coordinate early intervention services |
| ____ Explain screening procedures | ____ Make referrals for outpatient screening and audiologic diagnostic evaluation by an audiologist | ____ Ensure that an audiologic reevaluation has been completed | ____ Confer with audiologist on child’s progress with hearing aids and consideration of cochlear implants |
| ____ Assess for family history of hearing loss | ____ Ensure all infants hospitalized after discharge are rescreened | ____ Review findings from otolaryngology and audiologic consultations with family | ____ Provide families with basic information about cochlear implants |
| ____ Provide informational materials about newborn hearing screening | ____ Assess risk factors for hearing loss, including congenital and delayed-onset types | ____ Encourage family to comply with professionals’ recommendations and stress importance of keeping appointments | ____ Counsel families about the risks and benefits of cochlear implants |
| ____ Answer family’s questions about newborn screening or hearing loss | ____Ensure that screening results have been transmitted to state early hearing detection and intervention coordinator | ____ Refer for genetic counseling and ophthalmologic consultation | ____ Make referral to cochlear implant team |
| ____ Provide families with preliminary information on amplification and communication options | ____ Encourage families to comply with professionals’ recommendations | ||
| ____Confirm that families have received informational materials on screening and follow-up | ____ Make referral to audiologist for hearing aids | ____Ensure all reports are transmitted to state early hearing detection and intervention coordinator | |
| ____ Ensure hearing aids are fitted within 1 month of diagnosis | ____ Monitor developmental milestones | ||
| ____ Provide medical clearance, insurance authorization, and referral for hearing aids and early intervention services | |||
| ____ Ensure otolaryngology and audiologic results have been transmitted to state early hearing detection and intervention coordinator | |||
| NICU, neonatal intensive care unit. | |||
Getting an early start: Newborn screening
Ideally, intervention should begin before a child is born. When parents come in for prenatal visits, talk to them about the importance of newborn hearing screening. Tell them to expect that their baby will be screened at the birth hospital or at an outpatient audiology facility, and that this screening should be done by the time the baby is 1 month of age.
Tell parents their baby’s hearing will be tested with automated screening equipment that measures otoacoustic emissions from the baby’s ears or auditory brainstem response (ABR) to sound, both measurements that correlate with a child’s hearing and auditory behavior. Infants in well-baby nurseries can be screened by either technology. Infants in neonatal intensive care units (NICUs) for more than 5 days should be screened with ABR technology, which is better able to pick up neural losses.6 NICU babies frequently are at higher risk for neural hearing loss including auditory neuropathy/dyssynchrony, a condition that may account for about 8% of pediatric hearing losses annually.3
Be sure to explain to expectant couples that a positive screen indicates only that a problem may exist. It is not equivalent to a diagnosis of hearing loss, which is usually made by an audiologist.
The medical home’s role. The medical home should make sure that infants who fail an initial or secondary hospital screening and those who were missed or born outside the hospital are referred for outpatient screening. Newborns who fail initial screening should have both ears rescreened before hospital discharge, even if only one ear had failed previously.6 Additionally, any infant readmitted to the hospital within the first month of life who has a condition associated with potential hearing loss should be rescreened before discharge, preferably with an ABR.6 Risk factors associated with permanent-congenital, delayed-onset, or progressive hearing loss in children are listed in the TABLE.
TABLE
Risk indicators associated with hearing loss in childhood
|
| *These indicators are of greater concern for delayed-onset hearing loss. Source: American Academy of Pediatrics, Joint Committee on Infant Hearing. Pediatrics. 2007.6 |
Reporting screening results
Screening results are useful only if they are transmitted to caregivers and families. Breakdowns in transmission are a persistent problem for the early hearing detection and intervention process.2 The process is facilitated when hospitals make sure that all babies and their families are linked to a medical home at the time of discharge.
Hospital personnel should also be responsible for providing screening results to families in a face-to-face meeting. Medical home providers should review screening results again with parents and answer any questions that might have arisen after the initial hospital stay. Screening results should be given to parents in a sensitive manner, and patient education materials should be provided in parents’ native language, written at an appropriate reading level. Because hospital staff may not be trained to do this properly, it is important that medical home providers oversee the process and address any parental concerns.2
Screening results should also be reported by the birth hospital to the state’s EHDI coordinator, part of the national tracking and surveillance system funded by the Centers for Disease Control and Prevention to ensure that all children with hearing loss achieve communication and social skills commensurate with their cognitive abilities. 11 You can find contact information for your state coordinator at www.cdc.gov/ncbddd/ehdi/documents/EHDI_contact.pdf.
Diagnosing hearing loss
When an infant who fails newborn screening testing arrives at the medical home, the urgent next step is to make sure he or she is referred to a pediatric audiologist for a complete audiologic diagnostic evaluation. Advising parents to “wait and see” is not appropriate; researchers have identified that response as a major obstacle to successful follow-up.2 The audiologic evaluation should be done by the time the baby is 3 months of age and should be performed by a pediatric audiologist specializing in diagnosis and management of young children with hearing loss.4-6
Tell parents that, with their approval, the audiologist may fit the baby with hearing aids as early as this visit, as amplification can help even very young infants hear all sounds in the environment, particularly spoken language.
Ongoing monitoring
Family practices serving as medical homes should continue to monitor children who pass their newborn screening but have high-risk factors for delayed-onset hearing loss. Those factors are listed in the TABLE. Refer children at higher risk for an audiologic diagnostic evaluation by 24 to 30 months of age.6 Follow-up on parental concerns about infant hearing or speech and monitor infants’ developmental milestones, auditory skills, and middle ear status using the AAP’s pediatric periodicity schedule.6 Conduct global developmental screenings at 9, 18, and 24 to 30 months of age, and refer for speech-language-hearing evaluations when appropriate.6
The medical home as central referral point
The medical home is a central referral point for the complex needs of children with hearing loss. The physician and all other providers involved in the child’s care should report results of diagnostic evaluations to state EHDI coordinators. The medical home’s continued involvement includes medical clearance for hearing aids, additional consultations, and screenings as necessary to help children receive needed services and keep them from being lost to the system.5,9
Referral for genetic consultation is important, because about half of all autosomal recessive sensorineural hearing losses that are not part of a syndrome are caused by mutations in the Connexin 26 GJB2 gene.12,13 Referral to a pediatric ophthalmologist is similarly important, to identify deficits in visual acuity that frequently co-occur with hearing loss, especially in preterm infants.6 Results of these consultations can assist the physician in guiding families through the intervention process.
Coordination of care among multiple providers is essential. When a family physician’s practice serves as a medical home for a child with hearing loss, the physician should oversee and coordinate the efforts of all stakeholders in the EHDI process; make referrals to, and receive reports from, all providers involved in diagnosis and treatment; and ensure that relevant information is shared. During all phases of the process, the role of the family physician is to encourage families to comply with professionals’ recommendations and to stress the importance of making and keeping scheduled appointments.
Making plans for intervention
Families with children who have any degree of permanent hearing loss in one or both ears are entitled to early intervention services.6 In most states, these services are provided by a multidisciplinary team at no or low cost through a federal grant program. Services can be home- or center-based. They may include, as needed, education for the affected child and family; physical, speech/language, and occupational therapy; and social work and psychotherapy services. The team works with the family to develop an individualized family service plan to document and guide the early intervention process.14
Families with a hearing-impaired child have a range of options to choose from in their search for an approach that is best for the child and most acceptable to them. Communication options span a continuum from emphasis on sign language as used by the deaf community to a variety of oral-aural approaches designed to lead to spoken language. Parental choices are influenced most heavily by the child’s success with hearing aids. Parents need unbiased, culturally sensitive counseling about all available communication options and hearing technologies, so they can make informed choices for their children.6
Answering parents’ questions
To ensure that parents have appropriate expectations for what auditory technology can do for their child, they need to receive information about traditional digital signal processing hearing aids, osseointegrated hearing implant systems (also known as bone-anchored hearing aids), and cochlear implants. They need to know that a trial period will probably be necessary to determine whether hearing aids are appropriate or if cochlear implantation should be considered. Cost of hearing aids and cochlear implants is a serious concern for parents, and for many, it presents a major barrier to obtaining optimal care.2
Many insurance plans cover cochlear implants, but require that children be at least 12 months of age, have bilateral profound sensorineural hearing loss (or severe-to-profound sensorineural hearing loss for those ≥24 months of age), receive minimal benefit from hearing aids, be enrolled in auditory rehabilitative therapy, and possess no medical contraindications.15 Hearing aids and cochlear implants may also be covered for children enrolled in Medicaid or the State Children’s Health Insurance Program.16 However, according to a recent evaluation of hearing screening programs nationwide, public and private insurance policies almost never provide adequate coverage for hearing services.2
As parents consider the options, be sure they are aware that some children younger than 12 months of age are receiving cochlear implants (sometimes in both ears), that stimulation of both ears is being recommended at earlier ages, and that it is also common for children to use a hearing aid in one ear and a cochlear implant in the other.17,18 Distinguishing among hearing loss types and knowing which treatment options are most effective helps physicians counsel families appropriately about making the best decisions for their children. Some physicians have expressed uncertainties about these issues and have requested additional information on this topic.19 Audiologists can help physicians obtain this information and help them to better counsel families about these options.
CORRESPONDENCE
Carole E. Johnson, PhD, AuD, 1199 Haley Center, Auburn University, Auburn, AL 36849; johns19@auburn.edu
1. Vartiainen E, Kemppinen P, Karjalainen S. Prevalence and etiology of bilateral sensorineural hearing impairment in a Finnish childhood population. Int J Pediatr Otorhinolaryngol. 1997;41:175-185.
2. Shulman S, Besculides M, Saltzman A, et al. Evaluation of the universal newborn hearing screening and intervention program. Pediatrics. 2010;126(suppl 1):S19-S27.
3. Centers for Disease Control and Prevention. Early hearing detection and intervention program. Summary of 2006 national EHDI data (version 4). October 2008. Available at: http://www.cdc.gov/ncbdd/ehdi/documents/EHDI_Summ_2006_Web.pdf. Accessed December 23, 2010.
4. AAFP, AAP, ACP, AOA. Joint principles of the patient-centered medical home. February 2007. Available at: www.pcpcc.net/print/14. Accessed December 25, 2010.
5. Dorros C, Kurtzer-White E, Ahlgren M, et al. Medical home for children with hearing loss: physician perspectives and practices. Pediatrics. 2007;120:288-294.
6. American Academy of Pediatrics, Joint Committee on Infant Hearing. Year 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007;120:898-921.
7. US Preventive Services Task Force. Universal screening for hearing loss in newborns: US Preventive Services Task Force recommendation statement. Pediatrics. 2008;122:143-148.
8. Brown NC, James K, Liu J, et al. Newborn hearing screening. An assessment of knowledge, attitudes, and practices among Minnesota physicians. Minn Med. 2006;89:50-54.
9. Moeller MP, White KR, Shisler L. Primary care physicians’ knowledge, attitudes, and practices related to newborn hearing screening. Pediatrics. 2006;118:1357-1370.
10. Johnson CE, Danhauer JL, Granali A, et al. Systematic review of physicians’ knowledge of, participation in, and attitudes toward newborn hearing screening programs. Semin Hear. 2009;30:149-164.
11. Centers for Disease Control and Prevention. Early hearing detection and intervention (EHDI) national goals. Last updated September 17, 2010. Available at: www.cdc.gov/ncbddd/hearingloss/ehdi-goals.html. Accessed December 23, 2010.
12. Kenneson A, Van Naarden K, Boyle C. GJB2 (connexin 26) variants and nonsyndromic sensorineural hearing loss: A HuGe review. Genet Med. 2002;4:258-274.
13. Lerer I, Sagi M, Malamud E, et al. Contribution of connexin 26 mutations to nonsyndromic deafness in Ashkenazi patients and the variable phenotypic effect of the mutation 167delT. Am J Med Genet. 2000;95:53-56.
14. WrightsLaw. Early intervention (Part C of IDEA). Last updated August 16, 2010. Available at: www.wrightslaw.com/info/ei.index.htm. Accessed December 22, 2010.
15. Discolo DM, Hirose K. Pediatric cochlear implants. Am J Audiol. 2002;11:114-118.
16. McManus MA, Levtov R, White KR, et al. Medicaid reimbursement of hearing services for infants and young children. Pediatrics. 2010;126(suppl 1):S34-S42.
17. Papsin BC, Gordon KA. Bilateral cochlear implants should be the standard for children with bilateral sensorineural deafness. Curr Opin Otolaryngol Head Neck Surg. 2008;16:69-74.
18. Beijen JW, Mylanus EA, Leeuw AR, et al. Should a hearing aid in the contralateral ear be recommended for children with a unilateral cochlear implant? Ann Otol Rhinol Laryngol. 2008;117:397-403.
19. Carron JD, Moore RB, Dhaliwal AS. Perceptions of pediatric primary care physicians on congenital hearing loss and cochlear implantation. J Miss State Med Assoc. 2006;47:35-41.
1. Vartiainen E, Kemppinen P, Karjalainen S. Prevalence and etiology of bilateral sensorineural hearing impairment in a Finnish childhood population. Int J Pediatr Otorhinolaryngol. 1997;41:175-185.
2. Shulman S, Besculides M, Saltzman A, et al. Evaluation of the universal newborn hearing screening and intervention program. Pediatrics. 2010;126(suppl 1):S19-S27.
3. Centers for Disease Control and Prevention. Early hearing detection and intervention program. Summary of 2006 national EHDI data (version 4). October 2008. Available at: http://www.cdc.gov/ncbdd/ehdi/documents/EHDI_Summ_2006_Web.pdf. Accessed December 23, 2010.
4. AAFP, AAP, ACP, AOA. Joint principles of the patient-centered medical home. February 2007. Available at: www.pcpcc.net/print/14. Accessed December 25, 2010.
5. Dorros C, Kurtzer-White E, Ahlgren M, et al. Medical home for children with hearing loss: physician perspectives and practices. Pediatrics. 2007;120:288-294.
6. American Academy of Pediatrics, Joint Committee on Infant Hearing. Year 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007;120:898-921.
7. US Preventive Services Task Force. Universal screening for hearing loss in newborns: US Preventive Services Task Force recommendation statement. Pediatrics. 2008;122:143-148.
8. Brown NC, James K, Liu J, et al. Newborn hearing screening. An assessment of knowledge, attitudes, and practices among Minnesota physicians. Minn Med. 2006;89:50-54.
9. Moeller MP, White KR, Shisler L. Primary care physicians’ knowledge, attitudes, and practices related to newborn hearing screening. Pediatrics. 2006;118:1357-1370.
10. Johnson CE, Danhauer JL, Granali A, et al. Systematic review of physicians’ knowledge of, participation in, and attitudes toward newborn hearing screening programs. Semin Hear. 2009;30:149-164.
11. Centers for Disease Control and Prevention. Early hearing detection and intervention (EHDI) national goals. Last updated September 17, 2010. Available at: www.cdc.gov/ncbddd/hearingloss/ehdi-goals.html. Accessed December 23, 2010.
12. Kenneson A, Van Naarden K, Boyle C. GJB2 (connexin 26) variants and nonsyndromic sensorineural hearing loss: A HuGe review. Genet Med. 2002;4:258-274.
13. Lerer I, Sagi M, Malamud E, et al. Contribution of connexin 26 mutations to nonsyndromic deafness in Ashkenazi patients and the variable phenotypic effect of the mutation 167delT. Am J Med Genet. 2000;95:53-56.
14. WrightsLaw. Early intervention (Part C of IDEA). Last updated August 16, 2010. Available at: www.wrightslaw.com/info/ei.index.htm. Accessed December 22, 2010.
15. Discolo DM, Hirose K. Pediatric cochlear implants. Am J Audiol. 2002;11:114-118.
16. McManus MA, Levtov R, White KR, et al. Medicaid reimbursement of hearing services for infants and young children. Pediatrics. 2010;126(suppl 1):S34-S42.
17. Papsin BC, Gordon KA. Bilateral cochlear implants should be the standard for children with bilateral sensorineural deafness. Curr Opin Otolaryngol Head Neck Surg. 2008;16:69-74.
18. Beijen JW, Mylanus EA, Leeuw AR, et al. Should a hearing aid in the contralateral ear be recommended for children with a unilateral cochlear implant? Ann Otol Rhinol Laryngol. 2008;117:397-403.
19. Carron JD, Moore RB, Dhaliwal AS. Perceptions of pediatric primary care physicians on congenital hearing loss and cochlear implantation. J Miss State Med Assoc. 2006;47:35-41.
Which OC would you choose? Test your skills with these 3 cases
• Before you decide on a particular formulation, ask the patient whether she wishes to menstruate monthly, quarterly, or not at all. C
• Avoid prescribing oral contraceptive pills (OCPs) with a low dose of estrogen for women who are not meticulously compliant, as low-dose pills are associated with a greater failure rate compared with OCPs with higher doses of the hormone. A
• Advise patients to begin taking their OCPs on the same day as their office visit. B
• Remind patients taking progestin-only pills that they must be taken at about the same time every day; even a 3-hour day-to-day variation increases the risk of contraceptive failure. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Like most family physicians, you’ve probably prescribed oral contraceptive pills (OCPs) for countless patients. But are you up to date on the intricacies of dosage and hormone formulations, biphasic and triphasic pills, and non-traditional dosing schedules that allow patients to extend the frequency of—or even avoid—scheduled withdrawal bleeds?
Use the 3 patient scenarios that follow to test your knowledge of today’s OCPs and the text and tables that follow to fill in any details you may be missing. We’ll discuss the best approach for each patient at the end of this article.
CASE 1 Mandy, age 33, comes in asking for OCPs. She is newly married and would like to start a family in 2 or 3 years. The patient—a smoker—previously used a transdermal contraceptive patch.
CASE 2 Julie, age 18, recently became sexually active and would like to start taking OCPs. She will be spending much of the coming year abroad, Julie explains, and would really like to take “the pill that keeps you from getting your period. “ Other than acne, which she is treating with a topical benzyl peroxide/ antibiotic combination, Julie has no health problems—and no medical coverage.
CASE 3 Sandra, age 41, has taken OCPs in the past, but was taken off them after she was hit by a car and sustained a pelvic fracture 2 years ago. A mother of 4, Sandra delivered twins 6 weeks ago. She would like to take OCPs again, but wonders whether the hormones would interfere with nursing.
Is your patient a candidate for an OCP?
Before you prescribe OCPs for these women, or for any patient, there are a number of things to consider. First and foremost, does the patient have any contraindications to hormonal contraceptives related to the risk of adverse vascular events?
Absolute contraindications. Oral contraceptives are contraindicated (TABLE 1) in women older than 35 years who smoke and in women who have uncontrolled hypertension, a past history of venous or arterial vascular complications or a family history of thrombosis, diabetes with end-organ damage, migraine headaches with focal neurologic symptoms, or a history of breast cancer or liver disease.1,2 (A venous thromboembolism [VTE] that occurred in a clinical setting with a clear initiating risk factor—a fractured femur secondary to trauma complicated by a VTE, for example—is not an absolute contraindication to OCP therapy, particularly if it occurred years ago. Such patients may use OCPs if other contraceptive methods are not acceptable.1)
Relative contraindications. Pregnancy is a relative contraindication, as no prescriber would intentionally give a contraceptive medication to a woman known to be pregnant. It is important to note, though, that no harm has been associated with inadvertent use of OCPs during pregnancy.3
Obesity is also a relative contraindication. There is evidence that obese women (body mass index >30 kg/m2) have a higher failure rate with OCPs compared with women who are not overweight. The American College of Obstetricians and Gynecologists (ACOG) recommends nonhormonal contraception for obese patients due to the reduced efficacy of hormonal contraception and increased risk of VTE based on case-control studies.1 An obese patient should not, however, be precluded from using OCPs if her only other option is to use a less effective contraceptive.
Lupus was previously considered a relative contraindication, but recent studies did not find any exacerbation of stable lupus with OCPs.4
Compliance. In determining whether a patient is a candidate for oral contraceptives, you should also discuss the need for daily compliance, the moderate effectiveness of OCPs (which have a 7% failure rate with typical use5), and the importance of refilling the prescription in a timely manner. If the patient indicates that she has trouble following a daily routine, you may want to discuss other contraceptive options.
TABLE 1
Contraindications to oral contraceptives1,2
| Absolute |
| Personal or family history of DVT or PE |
| Uncontrolled hypertension |
| Smoker >35 years of age |
| Migraine with aura |
| Diabetes mellitus with end-organ damage |
| History of breast cancer |
| Liver disease |
| Relative |
| Pregnancy |
| History of DVT/PE from a known cause that is no longer present (eg, healed lower extremity fracture) |
| Obesity |
| DVT, deep vein thrombosis; PE, pulmonary embolism. |
Which OCP? A look at the choices
In determining which OCP to prescribe for a particular patient, there are a number of issues to consider:
- What estrogen dosage and progestin formulation should be used for this patient?
- Should the patient be placed on a mono-phasic, biphasic, triphasic, or quadra-phasic pill?
- How frequently does she want to menstruate?
- Has she taken OCPs before, either for primary contraception or for another condition that the pill is frequently prescribed for, such as dysmenorrhea or premenstrual syndrome? If she has taken OCPs, did she experience any significant adverse effects?
Most commonly prescribed OCPs are a combination of an estrogen and progesterone. Progestin-only OCPs are also available, but are used less frequently than combination pills because they must be taken within a smaller window of time each day to maintain their effectiveness.
Pill formulations
Combination OCPs typically contain the estrogen ethinyl estradiol (EE) or its precursor, mestranol, which is metabolized into EE, and one of the 9 progestins available in the United States.6,7 (An OC approved in May 2010 contains a new estrogen, estradiol valerate [EV], and dienogest, a novel progestin.7)
Categorized according to when they were approved or introduced, progestins include:
- norethindrone, norethindrone acetate (first generation)
- norgestrel, levonorgestrel, ethynodiol diacetate (second generation)
- norgestimate, desogestrel (third generation)
- drospirenone, dienogest (other).6,7
Each progestin differs in its affinity to progesterone, estrogen, and androgen receptors and, therefore, each has a slightly different physiologic effect. The first-generation progestins norethindrone and norethindrone acetate have a shorter half-life compared with those introduced later. While some studies have shown that third-generation progestins have a greater risk of VTE compared with first- and second-generation formulations, others have not found that to be the case. Two recent studies, conducted in the Netherlands and Denmark, did find an increased risk of VTE associated with the third-generation progestin desogestrel.8,9
Drospirenone, one of the more recently approved progestins, should be used with caution in any patient who may be at increased risk of hyperkalemia because of its spironolac-tone-like effects.10 Overall, however, there is little evidence to help guide initial OCP selection based on patient characteristics.
Dosing considerations
Estrogen dosages range from 10 to 50 mcg EE (and from 1 to 3 mg EV); progesterone dosage is ≤1 mg, with the exception of dienogest (2-3 mg). (Pills with higher doses of estrogen were available in the 1960s and 1970s, but were phased out because they carried a greater risk of vascular complications.) Your goal should be to select the lowest effective dosage of estrogen to minimize the risk of adverse effects.
There is a tradeoff, however: The lowest dose pills (10-20 mcg EE) have an increased risk of irregular bleeding, although they also have a reduced risk of minor adverse effects (eg, breast tenderness and headache, among other premenstrual symptoms).11 And, for women who are not meticulously compliant, low-dose pills are associated with a greater failure rate compared with OCPs with higher doses of EE.10
Other than the reduction of premenopausal symptoms, the advantages of pills with a lower dose of estrogen remain largely theoretical. The most serious adverse effects associated with estrogen—deep vein thrombosis (DVT) and pulmonary embolism—may not be significantly different between the lower or higher dose pills, although 2 recent studies found a reduced risk of VTE with lower estrogen doses.8,9
The original OCPs were monophasic, with each active pill having the same amount of estrogen and progesterone. Biphasic pills generally increase in progesterone dose, typically containing one dose for the first 10 days of the pill pack and an increased dose for the next 11 days.
Triphasic pills, designed to mimic the endogenous fluctuation of estrogen and progesterone during the menstrual cycle, have 3 levels of hormones in the active pills. Typically, the progesterone dose is lowest for the first 7 days and then increases on Day 8 and again on Day 15, while the estrogen dose remains constant. In some triphasic formulations, however, the estrogen dose increases and then is reduced in the last 7 days of active pills. (Natazia, the EV/dienogest OCP approved last year, is quadraphasic, featuring 2 different dosages of EV-only pills and 2 different dosages of estrogen/progestin pills.7)
There is no evidence of any advantage of triphasic pills over monophasic pills in terms of effectiveness, bleeding patterns, or discontinuation rates,12 but there is some evidence that biphasic pills result in more adverse effects.13
Frequency of withdrawal bleeds
Traditional OCPs have 21 active pills and 7 days of placebos. Women taking them have a menstrual cycle every 4 weeks during the placebo days. Patients can choose to have less frequent periods or avoid a menstrual cycle altogether either by taking one of the name-brand OCPs designed for extended or continuous dosing (TABLE 2) or by skipping the placebo pills in a traditional OCP regimen and starting the next pill pack immediately after taking the final active pill of the previous pack.
In 2003, a continuous OCP with 30 mcg EE and 0. 015 mg levonorgestrel (Seasonale) was approved. Its pill pack contains 84 mono-phasic active pills, plus 7 days of placebos.14Patients taking Seasonale—which is now available in generic form15—have a menstrual bleed every 3 months. A second 84/7-day OCP with a slightly different formulation (Seasonique) was approved in 2006.16 Patients who follow an 84/7-day regimen have been found to have outcomes that are very similar to those of women using OCPs in the traditional 21/7-day pattern in many respects, including the bleeding pattern, discontinuation rates, and satisfaction reported.17
In 2007, an OCP featuring 365 active pills and no placebo pills was approved (Lybrel).18 The dosage of EE (20 mcg) and levonorgestrel (0. 09 mg) remains constant each day of the year, with the intention that women on this regimen go an entire year without menstruating. No increase in adverse effects has been noted with the use of this OCP. Patients report improved symptomatology, but not a significant reduction in bleeding days compared with cyclic oral contraceptives.19 In fact, a potential downside is the possibility that women on extended or continuous dosing regimens may have more frequent unscheduled bleeding days.
Extended and continuous dosing regimens have benefits for patients with gynecologic conditions responsive to the suppression of menstruation, including endometriosis, dysmenorrhea, and chronic pelvic pain (TABLE 3). In fact, OCPs are often prescribed for these conditions, as well as for acne vul-garis, menorrhagia, premenstrual syndrome, and polycystic ovarian syndrome, as patients taking them have been found to have less difficulty with hormonal withdrawal side effects and no increased risk of adverse events.19
The only problem with extended or continuous dosing is cost (TABLE 4).20 Brand-name OCPs designed as extended-cycle contraceptives are more expensive than generic pills. Similarly, creating a continuous-dosing cycle with a monthly OCP requires more than 13 pill packs a year, and some insurers will not cover the cost of the additional pills.
Currently, no particular OCP or dosing regimen has any evidence-based advantages or indications regarding contraceptive efficacy or bleeding patterns. Until there is ample evidence to show that a particular frequency of withdrawal bleeds has advantages compared with other regimens, the frequency chosen can be at the patient’s and physician’s discretion.
TABLE 2
Traditional vs nontraditional dosing*31
| Oral contraceptive | Combination pills (No.) | Placebos (No.) | Other pills (No.) |
|---|---|---|---|
| Traditional OCP | 21 | 7 | 0 |
| Femcon Fe† | 21 | 7 | 0 |
| Mircette | 21 | 2 | 5 (10 mcg EE) |
| Natazia | 22 | 2 | 2 (3 mg EV); 2 (1 mg EV) |
| Lo Loestrin FE | 24 | 0 | 2 (10 mcg EE); 2 (75 mg ferrous fumarate) |
| Yaz | 24 | 4 | 0 |
| Seasonique | 84 | 0 | 7 (10 mcg EE) |
| Lybrel | 365 | 0 | 0 |
| *A partial list. | |||
| †The tablets are chewable mint-flavored. | |||
| EE, ethinyl estradiol; EV, estradiol valerate; OCP, oral contraceptive pill. | |||
TABLE 3
Noncontraceptive benefits—and risks—of OCPs
| Benefits | Risks |
|---|---|
|
|
| CVA, cerebrovascular accident; CVD, cardiovascular disease; MI, myocardial infarction; OCPs, oral contraceptive pills; PID, pelvic inflammatory disease; PMS, premenstrual syndrome; VTE, venous thromboembolism. | |
TABLE 4
Cost of hormonal contraceptives
| Hormonal contraceptive | Monthly cost | Yearly cost (52 weeks) |
|---|---|---|
| Combination pill (brand name) | $23-$60 | $299-$780 |
| Combination pill (generic) | $8 | $96 |
| Extended-cycle pill | $44-$58 | $578-$753 |
| Progestin-only pill | $19-$61 | $377-$793 |
| Transdermal patch | $90 | $1080 |
| Transvaginal suppository | $77 | $924 |
| Source: Epocrates.com. Accessed January 14, 2011. | ||
Patient preferences, prescribing concerns
In addition to considering OCP characteristics, patient-specific factors and preferences should be taken into account. Before you decide on a particular formulation, ask the patient whether she wishes to menstruate monthly, quarterly, or not at all (and explain that, even with continuous dosing, there will be some breakthrough bleeding). Patients should also be queried about any prior use of—and side effects or difficulty with—oral contraceptives.
For a patient with a history of OCP use, a pill that was previously used successfully is a reasonable starting point. For OCP-naïve patients, physicians may want to prescribe the least costly pill that is compatible with the patient’s health insurer and her preference, as well as your knowledge and comfort level.
How many pill packs to prescribe?
Most women receive 3 pill packs at a time from the pharmacy, although some get only one at a time.21 Yet evidence suggests that dispensing a 12-month supply of hormonal contraceptives at one time significantly increases patient continuation and use of preventive services (Pap smear screening and chlamydia testing, for example), decreases the need for pregnancy testing, and significantly cuts health care costs.21Keep in mind, however, that each pack of traditional pills contains medication for 4 weeks, while a year contains 13 4-week blocks of time. So any prescription written for 12 OCP packs will be insufficient to cover the entire year.
Variation in number and type of placebo
Another consideration: OCPs traditionally come in 28-day pill packs, with the last 7 pills being placebos. The number of active and placebo pills has been modified in some OCPs, in an attempt to decrease the risk of ovulation and unintended pregnancy.
Because some patients develop hormonal withdrawal side effects during the period of time when they’re taking placebos, several OCP formulations have added a small amount of estrogen to some, or all, of the placebos. One variation combines both concepts, featuring 24 active pills (rather than 21, to decrease the risk of ovulation) and 4 placebo pills containing 10 mcg EE (in an attempt to prevent withdrawal effects). Other variations are available, as well.
Although these pills have a greater inhibition of the pituitary-ovarian axis, they do not have better contraceptive efficacy compared with traditional dosing.22 Still, OCPs with such nontraditional regimens may be considered for any patient, and prescribed for women who have had prior success with this type of OCP.
Getting started: What to tell patients
For many years, combination OCPs were started on the Sunday after the onset of the next menses—a method known as conventional start. But there were 3 disadvantages to this: Patients needed to use an additional form of contraception during the first month of OCP therapy, had an increased risk of pregnancy in the first month, and often misunderstood the instructions, frequently starting the pills the Sunday after their period ended, instead of the Sunday after menstrual bleeding began.
The “first day” start came next. Patients were routinely told to begin their pills on the first day of their next menses. This was easily understood and eliminated the need for an additional form of contraception in the first month, but theoretically, a woman could get pregnant while waiting for her next menstrual cycle to start the OCPs.
To address these problems, the newest option is known as the “visit day” or “quick start. “ Advise patients to start the pills on the day of their office visit, either with a sample package or by picking up the OCPs at the pharmacy on the same day. This results in better short-term continuation rates and does not disrupt menstrual bleeding patterns.23,24
Pregnancy test. Prior to the quick start, however, women should have a documented negative pregnancy test (or receive emergency contraception if they have had unprotected intercourse in the last 72 hours). If the patient had unprotected intercourse in the prior 2 weeks, the pregnancy test should be repeated 2 weeks after she starts taking the pill.
OCP timing after a pregnancy
Women who have had a spontaneous or therapeutic abortion <20 weeks’ gestation can start taking combination OCPs immediately. A patient whose pregnancy ended >20 weeks and who is not breastfeeding can use combination OCPs, as well. Because of an increased risk of VTE during the initial postpartum period, however, women should delay the start date until >3 weeks postpartum.25
Breastfeeding considerations. Some women, and some clinicians, fear that combination OCPs reduce both the quantity and quality of breast milk. In fact, low-quality evidence suggests that the pills reduce the quantity of breast milk but do not impair infant growth.26 Studies of OCPs and breastfeeding, although of limited quality, have failed to show specific harm to the infant.
According to ACOG, women who are nursing can begin combination OCPs >6 weeks’ postpartum if breastfeeding is well established and no other form of contraception is acceptable.27 To address concerns about decreased breast milk associated with combination OCPs, however, progestin-only pills are frequently recommended for nursing mothers—and can be started immediately postpartum without any effect on breast milk.25
Progestin-only pills. Because progestin-only pills are taken every day with no placebos, women who take them have unpredictable and irregular menstrual bleeding. In addition, patients need to know that progestin-only pills must be taken at the same time every day; even a 3-hour day-to-day variation increases the risk of contraceptive failure.20
What to do about forgotten pills?
Most women occasionally forget a pill, and it is important to tell them what to do about it (TABLE 5).28,29 Such a discussion is critical to ensure contraceptive effectiveness.
If a patient misses one or 2 pills, she may make them up, using an additional form of contraception for 7 days if she skipped 2 consecutive pills. If she misses 3 consecutive pills, advise her to start a new pill pack, use an additional form of contraception for 7 days, and consider emergency contraception (EC) if she had unprotected sex. A woman who misses 3 pills in a row also needs to be urged to consider a contraceptive method that does not depend on daily compliance29—and to consider EC if she had unprotected intercourse.
The most dangerous pill to forget is the first pill of the next pack. Missing that pill means the patient will have gone 8 days without hormonal treatment—and should use an additional form of contraception until she has taken an active pill for 7 days.
EC should be recommended for patients who forget 2 or more combination OCPs or miss the first pill of the next pack and have unprotected intercourse. Levonorgestrel 0. 75 mg (Plan B) can be taken as 2 doses 12 hours apart or taken together as a single dose (Plan B One Step).30 Patients who are 17 years or older are allowed to buy Plan B over the counter; younger patients require a prescription.
TABLE 5
Forgotten pill(s)? What to tell your patients29
| Missed pill(s) | Instructions |
|---|---|
| Placebo | Skip the pill |
| Active pill <24 hours (1) | Take the pill as soon as you remember |
| Active pill >24 hours and <48 hours (1) | Take the missed pill AND the scheduled pill together |
| Active pills (2) |
|
| Active pills (≥3) |
|
| EC, emergency contraception. | |
What would you prescribe for our 3 patients?
CASE 1: Mandy
You start by strongly suggesting that she stop smoking, explaining that when she reaches age 35, the oral contraceptives will be contra-indicated if she continues to smoke. Because she had previously used a transdermal contraceptive patch without complications, a generic monophasic 30 to 35 mcg EE combination OCP would be a good choice. You schedule a follow-up visit in 3 months to determine how she is adjusting to the pill.
CASE 2: Julie
Julie is interested in continuous dosing but has no health insurance, so you recommend that she use a generic 21/7 combination OCP. Because of her preference for continuous dosing, however, you recommend that she start a new pack every 3 weeks, without taking any of the placebos, and tell her that this may result in improvements in her acne, as well.
CASE 3: Sandra
You reassure Sandra that combination pills have not been found to be harmful to infants, but suggest she consider a progestin-only formulation instead. You talk to her about the importance of meticulous compliance with a progestin-only OCP, which means taking her pill at the same time every day. You also explain that breakthrough bleeding is common with this type of pill, and that you can discuss a combination OCP when she is no longer nursing or if she cannot tolerate the progestin-only pill.
CORRESPONDENCE
Herbert L. Muncie, Jr, MD, 1542 Tulane Avenue, Room 123, New Orleans, LA 70112; hmunci@lsuhsc.edu
1. American College of Obstetricians and Gynecologists. (ACOG) Committee on Practice B. ACOG practice bulletin no. 73: Use of hormonal contraception in women with coexisting medical conditions. Obstet Gynecol. 2006;107:1453-1472.
2. Bezemer ID, van der Meer FJM, Eikenboom JCJ, et al. The value of family history as a risk indicator for venous thrombosis. Arch Intern Med. 2009;169:610-615.
3. Bracken MB. Oral contraception and congenital malformations in offspring: a review and meta-analysis of the prospective studies. Obstet Gynecol. 1990;76:552-557.
4. Petri M, Kim MY, Kalunian KC, et al. Combined oral contraceptives in women with sy stemic lupus erythematosus. N Engl J Med. 2005;353:2550-2558.
5. Trussell J, Vaughan B. Contraceptive failure, method-related discontinuation and resumption of use: results from the 1995 national survey of family growth. Fam Plann Perspect. 1999;31:64-72.
6. Petitti DB. Combination estrogen-progestin oral contraceptives. N Engl J Med. 2003;349:1443-1450.
7. US Food and Drug Administration. FDA approves newcombina-tion product oral contraceptive. May 6, 2010. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm211176.htm. Accessed January 19, 2011.
8. Vlieg AH, Helmerhorst FM, Vandenbroucke JP, et al. The venous thrombotic risk of oral contraceptives, effects of oestrogen dose and progestogen type: results of the MEGA case-control study. BMJ. 2009;339:2921-2928.
9. Lidegaard O, Lokkegaard E, Svendsen AL, et al. Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ. 2009;339:2890-2897.
10. Davis PS, Boatwright EA, Tozer BS, et al. Hormonal contraception update. Mayo ClinProc. 2006;81:949-955.
11. Gallo MF, Nanda K, Grimes DA, et al. 20 mcg versus >20 mcg estrogen combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2005(2);CD003989.-
12. van Vliet HA, Grimes DA, Lopez LM, et al. Triphasic versus monophasic oral contraceptives for contraception. Cochrane Database Syst Rev. 2006(3);003553.-
13. Van Vliet HA, Grimes DA, Helmerhorst FM, Schulz KF. Biphasic versus triphasic oral contraceptives for contraception. Cochrane Database Syst Rev. 2006(3);003283.-
14. US Food and Drug Administration. Office of Women’s Health Update, September-October 2003. Available at: http://www.fda.gov/ForConsumers/ByAudience/ForWomen/ucm118642.htm. Accessed January 19, 2011.
15. US Food and Drug Administration. FDA listing of approved generics as of December 13, 2010. Available at: AG_LISTING_pdf. Accessed January 19, 2011.
16. Drugs.com. FDA approves Seasonique. May 27, 2006. Available at: http://www.drugs.com/newdrugs/fda-approves-duramed-s-seasonique-extended-cycle-oral-contraceptive-1161.html. Accessed January 19, 2011.
17. Edelman AB, Gallo MF, Jensen JT, et al. Continuous or extended cycle vs. cyclic use of combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2005();004695.-
18. US Food and Drug Administration. FDA approves contraceptive for continuous use. May 22, 2007. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2007/ucm108918.htm. Accessed January 19, 2011.
19. Legro RS, Pauli JG, Kunselman AR, et al. Effects of continuous versus cyclical oral contraception: a randomized controlled trial. J Clin Endocrinol Metabol. 2008;93:420-429.
20. Choice of contraceptives. Treatment Guidelines from the Medical Letter. 2007;5:101-108.
21. Foster DG, Parvataneni R, de Bocanegra HT, et al. Number of oral contraceptive pill packages dispensed, method continuation, and costs. Obstet Gynecol. 2006;108:1107-1114.
22. Willis SA, Kuehl TJ, Spiekerman AM, Sulak PJ. Greater inhibition of the pituitary—ovarian axis in oral contraceptive regimens with a shortened hormone-free interval. Contraception. 2006;74:100-103.
23. Westhoff C, Heartwell S, Edwards S, et al. Initiation of oral contraceptives using a quick start compared with a conventional start: A randomized controlled trial. Obstet Gynecol. 2007;109:1270-1276.
24. Edwards SM, Zieman M, Jones K, et al. Initiation of oral contraceptives - start now! J Adolesc Health. 2008;43:432-436.
25. Lesnewski R, Prince L. Initiating hormonal contraception. Am Fam Physician. 2006;74:105-112.
26. Truitt ST, Fraser AB, Grimes DA, et al. Combined hormonal versus nonhormonal versus progestin-only contraception in lactation. Cochrane Database Syst Rev. 2003(2);CD003988.-
27. Queenan JT. Contraception and breast feeding. Clin Obstet Gynecol. 2004;47:734-739.
28. Potter L, Oakley D, de Leon-Wong E, et al. Measuring compliance among oral contraceptive users. Fam Plann Perspect. 1996;28:154-158.
29. PlannedParenthood. Whattodoifyouforgettotakethepill. Available at: http://www.plannedparenthood.org/health-topics/birth-control/if-forget-take-pill-19269.htm. htm. Accessed September 4, 2009.
30. von Hertzen H, Piaggio G, Ding J, et al. Low dose mifepris-tone and two regimens of levonorgestrel for emergency contraception: A WHO multicentre randomised trial. Lancet. 2002;360:1803-1810.
31. Physicians’ Desk Reference. Montvale, NJ: PDR Network; 2010.
32. Hannaford PC, Selvaraj S, Elliott AM, et al. Cancer risk among users of oral contraceptives: cohort data from the royal college of general practitioner’s oral contraception study. BMJ. 2007;335:651.-
33. Lurie G, Thompson P, McDuffie KE, et al. Association of estrogen and progestin potency of oral contraceptives with ovarian carcinoma risk. Obstet Gynecol. 2007;109:597-607.
34. Kiley J, Hammond C. Combined oral contraceptives: A comprehensive review. Clin Obstet Gynecol. 2007;50:868-877.
• Before you decide on a particular formulation, ask the patient whether she wishes to menstruate monthly, quarterly, or not at all. C
• Avoid prescribing oral contraceptive pills (OCPs) with a low dose of estrogen for women who are not meticulously compliant, as low-dose pills are associated with a greater failure rate compared with OCPs with higher doses of the hormone. A
• Advise patients to begin taking their OCPs on the same day as their office visit. B
• Remind patients taking progestin-only pills that they must be taken at about the same time every day; even a 3-hour day-to-day variation increases the risk of contraceptive failure. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Like most family physicians, you’ve probably prescribed oral contraceptive pills (OCPs) for countless patients. But are you up to date on the intricacies of dosage and hormone formulations, biphasic and triphasic pills, and non-traditional dosing schedules that allow patients to extend the frequency of—or even avoid—scheduled withdrawal bleeds?
Use the 3 patient scenarios that follow to test your knowledge of today’s OCPs and the text and tables that follow to fill in any details you may be missing. We’ll discuss the best approach for each patient at the end of this article.
CASE 1 Mandy, age 33, comes in asking for OCPs. She is newly married and would like to start a family in 2 or 3 years. The patient—a smoker—previously used a transdermal contraceptive patch.
CASE 2 Julie, age 18, recently became sexually active and would like to start taking OCPs. She will be spending much of the coming year abroad, Julie explains, and would really like to take “the pill that keeps you from getting your period. “ Other than acne, which she is treating with a topical benzyl peroxide/ antibiotic combination, Julie has no health problems—and no medical coverage.
CASE 3 Sandra, age 41, has taken OCPs in the past, but was taken off them after she was hit by a car and sustained a pelvic fracture 2 years ago. A mother of 4, Sandra delivered twins 6 weeks ago. She would like to take OCPs again, but wonders whether the hormones would interfere with nursing.
Is your patient a candidate for an OCP?
Before you prescribe OCPs for these women, or for any patient, there are a number of things to consider. First and foremost, does the patient have any contraindications to hormonal contraceptives related to the risk of adverse vascular events?
Absolute contraindications. Oral contraceptives are contraindicated (TABLE 1) in women older than 35 years who smoke and in women who have uncontrolled hypertension, a past history of venous or arterial vascular complications or a family history of thrombosis, diabetes with end-organ damage, migraine headaches with focal neurologic symptoms, or a history of breast cancer or liver disease.1,2 (A venous thromboembolism [VTE] that occurred in a clinical setting with a clear initiating risk factor—a fractured femur secondary to trauma complicated by a VTE, for example—is not an absolute contraindication to OCP therapy, particularly if it occurred years ago. Such patients may use OCPs if other contraceptive methods are not acceptable.1)
Relative contraindications. Pregnancy is a relative contraindication, as no prescriber would intentionally give a contraceptive medication to a woman known to be pregnant. It is important to note, though, that no harm has been associated with inadvertent use of OCPs during pregnancy.3
Obesity is also a relative contraindication. There is evidence that obese women (body mass index >30 kg/m2) have a higher failure rate with OCPs compared with women who are not overweight. The American College of Obstetricians and Gynecologists (ACOG) recommends nonhormonal contraception for obese patients due to the reduced efficacy of hormonal contraception and increased risk of VTE based on case-control studies.1 An obese patient should not, however, be precluded from using OCPs if her only other option is to use a less effective contraceptive.
Lupus was previously considered a relative contraindication, but recent studies did not find any exacerbation of stable lupus with OCPs.4
Compliance. In determining whether a patient is a candidate for oral contraceptives, you should also discuss the need for daily compliance, the moderate effectiveness of OCPs (which have a 7% failure rate with typical use5), and the importance of refilling the prescription in a timely manner. If the patient indicates that she has trouble following a daily routine, you may want to discuss other contraceptive options.
TABLE 1
Contraindications to oral contraceptives1,2
| Absolute |
| Personal or family history of DVT or PE |
| Uncontrolled hypertension |
| Smoker >35 years of age |
| Migraine with aura |
| Diabetes mellitus with end-organ damage |
| History of breast cancer |
| Liver disease |
| Relative |
| Pregnancy |
| History of DVT/PE from a known cause that is no longer present (eg, healed lower extremity fracture) |
| Obesity |
| DVT, deep vein thrombosis; PE, pulmonary embolism. |
Which OCP? A look at the choices
In determining which OCP to prescribe for a particular patient, there are a number of issues to consider:
- What estrogen dosage and progestin formulation should be used for this patient?
- Should the patient be placed on a mono-phasic, biphasic, triphasic, or quadra-phasic pill?
- How frequently does she want to menstruate?
- Has she taken OCPs before, either for primary contraception or for another condition that the pill is frequently prescribed for, such as dysmenorrhea or premenstrual syndrome? If she has taken OCPs, did she experience any significant adverse effects?
Most commonly prescribed OCPs are a combination of an estrogen and progesterone. Progestin-only OCPs are also available, but are used less frequently than combination pills because they must be taken within a smaller window of time each day to maintain their effectiveness.
Pill formulations
Combination OCPs typically contain the estrogen ethinyl estradiol (EE) or its precursor, mestranol, which is metabolized into EE, and one of the 9 progestins available in the United States.6,7 (An OC approved in May 2010 contains a new estrogen, estradiol valerate [EV], and dienogest, a novel progestin.7)
Categorized according to when they were approved or introduced, progestins include:
- norethindrone, norethindrone acetate (first generation)
- norgestrel, levonorgestrel, ethynodiol diacetate (second generation)
- norgestimate, desogestrel (third generation)
- drospirenone, dienogest (other).6,7
Each progestin differs in its affinity to progesterone, estrogen, and androgen receptors and, therefore, each has a slightly different physiologic effect. The first-generation progestins norethindrone and norethindrone acetate have a shorter half-life compared with those introduced later. While some studies have shown that third-generation progestins have a greater risk of VTE compared with first- and second-generation formulations, others have not found that to be the case. Two recent studies, conducted in the Netherlands and Denmark, did find an increased risk of VTE associated with the third-generation progestin desogestrel.8,9
Drospirenone, one of the more recently approved progestins, should be used with caution in any patient who may be at increased risk of hyperkalemia because of its spironolac-tone-like effects.10 Overall, however, there is little evidence to help guide initial OCP selection based on patient characteristics.
Dosing considerations
Estrogen dosages range from 10 to 50 mcg EE (and from 1 to 3 mg EV); progesterone dosage is ≤1 mg, with the exception of dienogest (2-3 mg). (Pills with higher doses of estrogen were available in the 1960s and 1970s, but were phased out because they carried a greater risk of vascular complications.) Your goal should be to select the lowest effective dosage of estrogen to minimize the risk of adverse effects.
There is a tradeoff, however: The lowest dose pills (10-20 mcg EE) have an increased risk of irregular bleeding, although they also have a reduced risk of minor adverse effects (eg, breast tenderness and headache, among other premenstrual symptoms).11 And, for women who are not meticulously compliant, low-dose pills are associated with a greater failure rate compared with OCPs with higher doses of EE.10
Other than the reduction of premenopausal symptoms, the advantages of pills with a lower dose of estrogen remain largely theoretical. The most serious adverse effects associated with estrogen—deep vein thrombosis (DVT) and pulmonary embolism—may not be significantly different between the lower or higher dose pills, although 2 recent studies found a reduced risk of VTE with lower estrogen doses.8,9
The original OCPs were monophasic, with each active pill having the same amount of estrogen and progesterone. Biphasic pills generally increase in progesterone dose, typically containing one dose for the first 10 days of the pill pack and an increased dose for the next 11 days.
Triphasic pills, designed to mimic the endogenous fluctuation of estrogen and progesterone during the menstrual cycle, have 3 levels of hormones in the active pills. Typically, the progesterone dose is lowest for the first 7 days and then increases on Day 8 and again on Day 15, while the estrogen dose remains constant. In some triphasic formulations, however, the estrogen dose increases and then is reduced in the last 7 days of active pills. (Natazia, the EV/dienogest OCP approved last year, is quadraphasic, featuring 2 different dosages of EV-only pills and 2 different dosages of estrogen/progestin pills.7)
There is no evidence of any advantage of triphasic pills over monophasic pills in terms of effectiveness, bleeding patterns, or discontinuation rates,12 but there is some evidence that biphasic pills result in more adverse effects.13
Frequency of withdrawal bleeds
Traditional OCPs have 21 active pills and 7 days of placebos. Women taking them have a menstrual cycle every 4 weeks during the placebo days. Patients can choose to have less frequent periods or avoid a menstrual cycle altogether either by taking one of the name-brand OCPs designed for extended or continuous dosing (TABLE 2) or by skipping the placebo pills in a traditional OCP regimen and starting the next pill pack immediately after taking the final active pill of the previous pack.
In 2003, a continuous OCP with 30 mcg EE and 0. 015 mg levonorgestrel (Seasonale) was approved. Its pill pack contains 84 mono-phasic active pills, plus 7 days of placebos.14Patients taking Seasonale—which is now available in generic form15—have a menstrual bleed every 3 months. A second 84/7-day OCP with a slightly different formulation (Seasonique) was approved in 2006.16 Patients who follow an 84/7-day regimen have been found to have outcomes that are very similar to those of women using OCPs in the traditional 21/7-day pattern in many respects, including the bleeding pattern, discontinuation rates, and satisfaction reported.17
In 2007, an OCP featuring 365 active pills and no placebo pills was approved (Lybrel).18 The dosage of EE (20 mcg) and levonorgestrel (0. 09 mg) remains constant each day of the year, with the intention that women on this regimen go an entire year without menstruating. No increase in adverse effects has been noted with the use of this OCP. Patients report improved symptomatology, but not a significant reduction in bleeding days compared with cyclic oral contraceptives.19 In fact, a potential downside is the possibility that women on extended or continuous dosing regimens may have more frequent unscheduled bleeding days.
Extended and continuous dosing regimens have benefits for patients with gynecologic conditions responsive to the suppression of menstruation, including endometriosis, dysmenorrhea, and chronic pelvic pain (TABLE 3). In fact, OCPs are often prescribed for these conditions, as well as for acne vul-garis, menorrhagia, premenstrual syndrome, and polycystic ovarian syndrome, as patients taking them have been found to have less difficulty with hormonal withdrawal side effects and no increased risk of adverse events.19
The only problem with extended or continuous dosing is cost (TABLE 4).20 Brand-name OCPs designed as extended-cycle contraceptives are more expensive than generic pills. Similarly, creating a continuous-dosing cycle with a monthly OCP requires more than 13 pill packs a year, and some insurers will not cover the cost of the additional pills.
Currently, no particular OCP or dosing regimen has any evidence-based advantages or indications regarding contraceptive efficacy or bleeding patterns. Until there is ample evidence to show that a particular frequency of withdrawal bleeds has advantages compared with other regimens, the frequency chosen can be at the patient’s and physician’s discretion.
TABLE 2
Traditional vs nontraditional dosing*31
| Oral contraceptive | Combination pills (No.) | Placebos (No.) | Other pills (No.) |
|---|---|---|---|
| Traditional OCP | 21 | 7 | 0 |
| Femcon Fe† | 21 | 7 | 0 |
| Mircette | 21 | 2 | 5 (10 mcg EE) |
| Natazia | 22 | 2 | 2 (3 mg EV); 2 (1 mg EV) |
| Lo Loestrin FE | 24 | 0 | 2 (10 mcg EE); 2 (75 mg ferrous fumarate) |
| Yaz | 24 | 4 | 0 |
| Seasonique | 84 | 0 | 7 (10 mcg EE) |
| Lybrel | 365 | 0 | 0 |
| *A partial list. | |||
| †The tablets are chewable mint-flavored. | |||
| EE, ethinyl estradiol; EV, estradiol valerate; OCP, oral contraceptive pill. | |||
TABLE 3
Noncontraceptive benefits—and risks—of OCPs
| Benefits | Risks |
|---|---|
|
|
| CVA, cerebrovascular accident; CVD, cardiovascular disease; MI, myocardial infarction; OCPs, oral contraceptive pills; PID, pelvic inflammatory disease; PMS, premenstrual syndrome; VTE, venous thromboembolism. | |
TABLE 4
Cost of hormonal contraceptives
| Hormonal contraceptive | Monthly cost | Yearly cost (52 weeks) |
|---|---|---|
| Combination pill (brand name) | $23-$60 | $299-$780 |
| Combination pill (generic) | $8 | $96 |
| Extended-cycle pill | $44-$58 | $578-$753 |
| Progestin-only pill | $19-$61 | $377-$793 |
| Transdermal patch | $90 | $1080 |
| Transvaginal suppository | $77 | $924 |
| Source: Epocrates.com. Accessed January 14, 2011. | ||
Patient preferences, prescribing concerns
In addition to considering OCP characteristics, patient-specific factors and preferences should be taken into account. Before you decide on a particular formulation, ask the patient whether she wishes to menstruate monthly, quarterly, or not at all (and explain that, even with continuous dosing, there will be some breakthrough bleeding). Patients should also be queried about any prior use of—and side effects or difficulty with—oral contraceptives.
For a patient with a history of OCP use, a pill that was previously used successfully is a reasonable starting point. For OCP-naïve patients, physicians may want to prescribe the least costly pill that is compatible with the patient’s health insurer and her preference, as well as your knowledge and comfort level.
How many pill packs to prescribe?
Most women receive 3 pill packs at a time from the pharmacy, although some get only one at a time.21 Yet evidence suggests that dispensing a 12-month supply of hormonal contraceptives at one time significantly increases patient continuation and use of preventive services (Pap smear screening and chlamydia testing, for example), decreases the need for pregnancy testing, and significantly cuts health care costs.21Keep in mind, however, that each pack of traditional pills contains medication for 4 weeks, while a year contains 13 4-week blocks of time. So any prescription written for 12 OCP packs will be insufficient to cover the entire year.
Variation in number and type of placebo
Another consideration: OCPs traditionally come in 28-day pill packs, with the last 7 pills being placebos. The number of active and placebo pills has been modified in some OCPs, in an attempt to decrease the risk of ovulation and unintended pregnancy.
Because some patients develop hormonal withdrawal side effects during the period of time when they’re taking placebos, several OCP formulations have added a small amount of estrogen to some, or all, of the placebos. One variation combines both concepts, featuring 24 active pills (rather than 21, to decrease the risk of ovulation) and 4 placebo pills containing 10 mcg EE (in an attempt to prevent withdrawal effects). Other variations are available, as well.
Although these pills have a greater inhibition of the pituitary-ovarian axis, they do not have better contraceptive efficacy compared with traditional dosing.22 Still, OCPs with such nontraditional regimens may be considered for any patient, and prescribed for women who have had prior success with this type of OCP.
Getting started: What to tell patients
For many years, combination OCPs were started on the Sunday after the onset of the next menses—a method known as conventional start. But there were 3 disadvantages to this: Patients needed to use an additional form of contraception during the first month of OCP therapy, had an increased risk of pregnancy in the first month, and often misunderstood the instructions, frequently starting the pills the Sunday after their period ended, instead of the Sunday after menstrual bleeding began.
The “first day” start came next. Patients were routinely told to begin their pills on the first day of their next menses. This was easily understood and eliminated the need for an additional form of contraception in the first month, but theoretically, a woman could get pregnant while waiting for her next menstrual cycle to start the OCPs.
To address these problems, the newest option is known as the “visit day” or “quick start. “ Advise patients to start the pills on the day of their office visit, either with a sample package or by picking up the OCPs at the pharmacy on the same day. This results in better short-term continuation rates and does not disrupt menstrual bleeding patterns.23,24
Pregnancy test. Prior to the quick start, however, women should have a documented negative pregnancy test (or receive emergency contraception if they have had unprotected intercourse in the last 72 hours). If the patient had unprotected intercourse in the prior 2 weeks, the pregnancy test should be repeated 2 weeks after she starts taking the pill.
OCP timing after a pregnancy
Women who have had a spontaneous or therapeutic abortion <20 weeks’ gestation can start taking combination OCPs immediately. A patient whose pregnancy ended >20 weeks and who is not breastfeeding can use combination OCPs, as well. Because of an increased risk of VTE during the initial postpartum period, however, women should delay the start date until >3 weeks postpartum.25
Breastfeeding considerations. Some women, and some clinicians, fear that combination OCPs reduce both the quantity and quality of breast milk. In fact, low-quality evidence suggests that the pills reduce the quantity of breast milk but do not impair infant growth.26 Studies of OCPs and breastfeeding, although of limited quality, have failed to show specific harm to the infant.
According to ACOG, women who are nursing can begin combination OCPs >6 weeks’ postpartum if breastfeeding is well established and no other form of contraception is acceptable.27 To address concerns about decreased breast milk associated with combination OCPs, however, progestin-only pills are frequently recommended for nursing mothers—and can be started immediately postpartum without any effect on breast milk.25
Progestin-only pills. Because progestin-only pills are taken every day with no placebos, women who take them have unpredictable and irregular menstrual bleeding. In addition, patients need to know that progestin-only pills must be taken at the same time every day; even a 3-hour day-to-day variation increases the risk of contraceptive failure.20
What to do about forgotten pills?
Most women occasionally forget a pill, and it is important to tell them what to do about it (TABLE 5).28,29 Such a discussion is critical to ensure contraceptive effectiveness.
If a patient misses one or 2 pills, she may make them up, using an additional form of contraception for 7 days if she skipped 2 consecutive pills. If she misses 3 consecutive pills, advise her to start a new pill pack, use an additional form of contraception for 7 days, and consider emergency contraception (EC) if she had unprotected sex. A woman who misses 3 pills in a row also needs to be urged to consider a contraceptive method that does not depend on daily compliance29—and to consider EC if she had unprotected intercourse.
The most dangerous pill to forget is the first pill of the next pack. Missing that pill means the patient will have gone 8 days without hormonal treatment—and should use an additional form of contraception until she has taken an active pill for 7 days.
EC should be recommended for patients who forget 2 or more combination OCPs or miss the first pill of the next pack and have unprotected intercourse. Levonorgestrel 0. 75 mg (Plan B) can be taken as 2 doses 12 hours apart or taken together as a single dose (Plan B One Step).30 Patients who are 17 years or older are allowed to buy Plan B over the counter; younger patients require a prescription.
TABLE 5
Forgotten pill(s)? What to tell your patients29
| Missed pill(s) | Instructions |
|---|---|
| Placebo | Skip the pill |
| Active pill <24 hours (1) | Take the pill as soon as you remember |
| Active pill >24 hours and <48 hours (1) | Take the missed pill AND the scheduled pill together |
| Active pills (2) |
|
| Active pills (≥3) |
|
| EC, emergency contraception. | |
What would you prescribe for our 3 patients?
CASE 1: Mandy
You start by strongly suggesting that she stop smoking, explaining that when she reaches age 35, the oral contraceptives will be contra-indicated if she continues to smoke. Because she had previously used a transdermal contraceptive patch without complications, a generic monophasic 30 to 35 mcg EE combination OCP would be a good choice. You schedule a follow-up visit in 3 months to determine how she is adjusting to the pill.
CASE 2: Julie
Julie is interested in continuous dosing but has no health insurance, so you recommend that she use a generic 21/7 combination OCP. Because of her preference for continuous dosing, however, you recommend that she start a new pack every 3 weeks, without taking any of the placebos, and tell her that this may result in improvements in her acne, as well.
CASE 3: Sandra
You reassure Sandra that combination pills have not been found to be harmful to infants, but suggest she consider a progestin-only formulation instead. You talk to her about the importance of meticulous compliance with a progestin-only OCP, which means taking her pill at the same time every day. You also explain that breakthrough bleeding is common with this type of pill, and that you can discuss a combination OCP when she is no longer nursing or if she cannot tolerate the progestin-only pill.
CORRESPONDENCE
Herbert L. Muncie, Jr, MD, 1542 Tulane Avenue, Room 123, New Orleans, LA 70112; hmunci@lsuhsc.edu
• Before you decide on a particular formulation, ask the patient whether she wishes to menstruate monthly, quarterly, or not at all. C
• Avoid prescribing oral contraceptive pills (OCPs) with a low dose of estrogen for women who are not meticulously compliant, as low-dose pills are associated with a greater failure rate compared with OCPs with higher doses of the hormone. A
• Advise patients to begin taking their OCPs on the same day as their office visit. B
• Remind patients taking progestin-only pills that they must be taken at about the same time every day; even a 3-hour day-to-day variation increases the risk of contraceptive failure. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Like most family physicians, you’ve probably prescribed oral contraceptive pills (OCPs) for countless patients. But are you up to date on the intricacies of dosage and hormone formulations, biphasic and triphasic pills, and non-traditional dosing schedules that allow patients to extend the frequency of—or even avoid—scheduled withdrawal bleeds?
Use the 3 patient scenarios that follow to test your knowledge of today’s OCPs and the text and tables that follow to fill in any details you may be missing. We’ll discuss the best approach for each patient at the end of this article.
CASE 1 Mandy, age 33, comes in asking for OCPs. She is newly married and would like to start a family in 2 or 3 years. The patient—a smoker—previously used a transdermal contraceptive patch.
CASE 2 Julie, age 18, recently became sexually active and would like to start taking OCPs. She will be spending much of the coming year abroad, Julie explains, and would really like to take “the pill that keeps you from getting your period. “ Other than acne, which she is treating with a topical benzyl peroxide/ antibiotic combination, Julie has no health problems—and no medical coverage.
CASE 3 Sandra, age 41, has taken OCPs in the past, but was taken off them after she was hit by a car and sustained a pelvic fracture 2 years ago. A mother of 4, Sandra delivered twins 6 weeks ago. She would like to take OCPs again, but wonders whether the hormones would interfere with nursing.
Is your patient a candidate for an OCP?
Before you prescribe OCPs for these women, or for any patient, there are a number of things to consider. First and foremost, does the patient have any contraindications to hormonal contraceptives related to the risk of adverse vascular events?
Absolute contraindications. Oral contraceptives are contraindicated (TABLE 1) in women older than 35 years who smoke and in women who have uncontrolled hypertension, a past history of venous or arterial vascular complications or a family history of thrombosis, diabetes with end-organ damage, migraine headaches with focal neurologic symptoms, or a history of breast cancer or liver disease.1,2 (A venous thromboembolism [VTE] that occurred in a clinical setting with a clear initiating risk factor—a fractured femur secondary to trauma complicated by a VTE, for example—is not an absolute contraindication to OCP therapy, particularly if it occurred years ago. Such patients may use OCPs if other contraceptive methods are not acceptable.1)
Relative contraindications. Pregnancy is a relative contraindication, as no prescriber would intentionally give a contraceptive medication to a woman known to be pregnant. It is important to note, though, that no harm has been associated with inadvertent use of OCPs during pregnancy.3
Obesity is also a relative contraindication. There is evidence that obese women (body mass index >30 kg/m2) have a higher failure rate with OCPs compared with women who are not overweight. The American College of Obstetricians and Gynecologists (ACOG) recommends nonhormonal contraception for obese patients due to the reduced efficacy of hormonal contraception and increased risk of VTE based on case-control studies.1 An obese patient should not, however, be precluded from using OCPs if her only other option is to use a less effective contraceptive.
Lupus was previously considered a relative contraindication, but recent studies did not find any exacerbation of stable lupus with OCPs.4
Compliance. In determining whether a patient is a candidate for oral contraceptives, you should also discuss the need for daily compliance, the moderate effectiveness of OCPs (which have a 7% failure rate with typical use5), and the importance of refilling the prescription in a timely manner. If the patient indicates that she has trouble following a daily routine, you may want to discuss other contraceptive options.
TABLE 1
Contraindications to oral contraceptives1,2
| Absolute |
| Personal or family history of DVT or PE |
| Uncontrolled hypertension |
| Smoker >35 years of age |
| Migraine with aura |
| Diabetes mellitus with end-organ damage |
| History of breast cancer |
| Liver disease |
| Relative |
| Pregnancy |
| History of DVT/PE from a known cause that is no longer present (eg, healed lower extremity fracture) |
| Obesity |
| DVT, deep vein thrombosis; PE, pulmonary embolism. |
Which OCP? A look at the choices
In determining which OCP to prescribe for a particular patient, there are a number of issues to consider:
- What estrogen dosage and progestin formulation should be used for this patient?
- Should the patient be placed on a mono-phasic, biphasic, triphasic, or quadra-phasic pill?
- How frequently does she want to menstruate?
- Has she taken OCPs before, either for primary contraception or for another condition that the pill is frequently prescribed for, such as dysmenorrhea or premenstrual syndrome? If she has taken OCPs, did she experience any significant adverse effects?
Most commonly prescribed OCPs are a combination of an estrogen and progesterone. Progestin-only OCPs are also available, but are used less frequently than combination pills because they must be taken within a smaller window of time each day to maintain their effectiveness.
Pill formulations
Combination OCPs typically contain the estrogen ethinyl estradiol (EE) or its precursor, mestranol, which is metabolized into EE, and one of the 9 progestins available in the United States.6,7 (An OC approved in May 2010 contains a new estrogen, estradiol valerate [EV], and dienogest, a novel progestin.7)
Categorized according to when they were approved or introduced, progestins include:
- norethindrone, norethindrone acetate (first generation)
- norgestrel, levonorgestrel, ethynodiol diacetate (second generation)
- norgestimate, desogestrel (third generation)
- drospirenone, dienogest (other).6,7
Each progestin differs in its affinity to progesterone, estrogen, and androgen receptors and, therefore, each has a slightly different physiologic effect. The first-generation progestins norethindrone and norethindrone acetate have a shorter half-life compared with those introduced later. While some studies have shown that third-generation progestins have a greater risk of VTE compared with first- and second-generation formulations, others have not found that to be the case. Two recent studies, conducted in the Netherlands and Denmark, did find an increased risk of VTE associated with the third-generation progestin desogestrel.8,9
Drospirenone, one of the more recently approved progestins, should be used with caution in any patient who may be at increased risk of hyperkalemia because of its spironolac-tone-like effects.10 Overall, however, there is little evidence to help guide initial OCP selection based on patient characteristics.
Dosing considerations
Estrogen dosages range from 10 to 50 mcg EE (and from 1 to 3 mg EV); progesterone dosage is ≤1 mg, with the exception of dienogest (2-3 mg). (Pills with higher doses of estrogen were available in the 1960s and 1970s, but were phased out because they carried a greater risk of vascular complications.) Your goal should be to select the lowest effective dosage of estrogen to minimize the risk of adverse effects.
There is a tradeoff, however: The lowest dose pills (10-20 mcg EE) have an increased risk of irregular bleeding, although they also have a reduced risk of minor adverse effects (eg, breast tenderness and headache, among other premenstrual symptoms).11 And, for women who are not meticulously compliant, low-dose pills are associated with a greater failure rate compared with OCPs with higher doses of EE.10
Other than the reduction of premenopausal symptoms, the advantages of pills with a lower dose of estrogen remain largely theoretical. The most serious adverse effects associated with estrogen—deep vein thrombosis (DVT) and pulmonary embolism—may not be significantly different between the lower or higher dose pills, although 2 recent studies found a reduced risk of VTE with lower estrogen doses.8,9
The original OCPs were monophasic, with each active pill having the same amount of estrogen and progesterone. Biphasic pills generally increase in progesterone dose, typically containing one dose for the first 10 days of the pill pack and an increased dose for the next 11 days.
Triphasic pills, designed to mimic the endogenous fluctuation of estrogen and progesterone during the menstrual cycle, have 3 levels of hormones in the active pills. Typically, the progesterone dose is lowest for the first 7 days and then increases on Day 8 and again on Day 15, while the estrogen dose remains constant. In some triphasic formulations, however, the estrogen dose increases and then is reduced in the last 7 days of active pills. (Natazia, the EV/dienogest OCP approved last year, is quadraphasic, featuring 2 different dosages of EV-only pills and 2 different dosages of estrogen/progestin pills.7)
There is no evidence of any advantage of triphasic pills over monophasic pills in terms of effectiveness, bleeding patterns, or discontinuation rates,12 but there is some evidence that biphasic pills result in more adverse effects.13
Frequency of withdrawal bleeds
Traditional OCPs have 21 active pills and 7 days of placebos. Women taking them have a menstrual cycle every 4 weeks during the placebo days. Patients can choose to have less frequent periods or avoid a menstrual cycle altogether either by taking one of the name-brand OCPs designed for extended or continuous dosing (TABLE 2) or by skipping the placebo pills in a traditional OCP regimen and starting the next pill pack immediately after taking the final active pill of the previous pack.
In 2003, a continuous OCP with 30 mcg EE and 0. 015 mg levonorgestrel (Seasonale) was approved. Its pill pack contains 84 mono-phasic active pills, plus 7 days of placebos.14Patients taking Seasonale—which is now available in generic form15—have a menstrual bleed every 3 months. A second 84/7-day OCP with a slightly different formulation (Seasonique) was approved in 2006.16 Patients who follow an 84/7-day regimen have been found to have outcomes that are very similar to those of women using OCPs in the traditional 21/7-day pattern in many respects, including the bleeding pattern, discontinuation rates, and satisfaction reported.17
In 2007, an OCP featuring 365 active pills and no placebo pills was approved (Lybrel).18 The dosage of EE (20 mcg) and levonorgestrel (0. 09 mg) remains constant each day of the year, with the intention that women on this regimen go an entire year without menstruating. No increase in adverse effects has been noted with the use of this OCP. Patients report improved symptomatology, but not a significant reduction in bleeding days compared with cyclic oral contraceptives.19 In fact, a potential downside is the possibility that women on extended or continuous dosing regimens may have more frequent unscheduled bleeding days.
Extended and continuous dosing regimens have benefits for patients with gynecologic conditions responsive to the suppression of menstruation, including endometriosis, dysmenorrhea, and chronic pelvic pain (TABLE 3). In fact, OCPs are often prescribed for these conditions, as well as for acne vul-garis, menorrhagia, premenstrual syndrome, and polycystic ovarian syndrome, as patients taking them have been found to have less difficulty with hormonal withdrawal side effects and no increased risk of adverse events.19
The only problem with extended or continuous dosing is cost (TABLE 4).20 Brand-name OCPs designed as extended-cycle contraceptives are more expensive than generic pills. Similarly, creating a continuous-dosing cycle with a monthly OCP requires more than 13 pill packs a year, and some insurers will not cover the cost of the additional pills.
Currently, no particular OCP or dosing regimen has any evidence-based advantages or indications regarding contraceptive efficacy or bleeding patterns. Until there is ample evidence to show that a particular frequency of withdrawal bleeds has advantages compared with other regimens, the frequency chosen can be at the patient’s and physician’s discretion.
TABLE 2
Traditional vs nontraditional dosing*31
| Oral contraceptive | Combination pills (No.) | Placebos (No.) | Other pills (No.) |
|---|---|---|---|
| Traditional OCP | 21 | 7 | 0 |
| Femcon Fe† | 21 | 7 | 0 |
| Mircette | 21 | 2 | 5 (10 mcg EE) |
| Natazia | 22 | 2 | 2 (3 mg EV); 2 (1 mg EV) |
| Lo Loestrin FE | 24 | 0 | 2 (10 mcg EE); 2 (75 mg ferrous fumarate) |
| Yaz | 24 | 4 | 0 |
| Seasonique | 84 | 0 | 7 (10 mcg EE) |
| Lybrel | 365 | 0 | 0 |
| *A partial list. | |||
| †The tablets are chewable mint-flavored. | |||
| EE, ethinyl estradiol; EV, estradiol valerate; OCP, oral contraceptive pill. | |||
TABLE 3
Noncontraceptive benefits—and risks—of OCPs
| Benefits | Risks |
|---|---|
|
|
| CVA, cerebrovascular accident; CVD, cardiovascular disease; MI, myocardial infarction; OCPs, oral contraceptive pills; PID, pelvic inflammatory disease; PMS, premenstrual syndrome; VTE, venous thromboembolism. | |
TABLE 4
Cost of hormonal contraceptives
| Hormonal contraceptive | Monthly cost | Yearly cost (52 weeks) |
|---|---|---|
| Combination pill (brand name) | $23-$60 | $299-$780 |
| Combination pill (generic) | $8 | $96 |
| Extended-cycle pill | $44-$58 | $578-$753 |
| Progestin-only pill | $19-$61 | $377-$793 |
| Transdermal patch | $90 | $1080 |
| Transvaginal suppository | $77 | $924 |
| Source: Epocrates.com. Accessed January 14, 2011. | ||
Patient preferences, prescribing concerns
In addition to considering OCP characteristics, patient-specific factors and preferences should be taken into account. Before you decide on a particular formulation, ask the patient whether she wishes to menstruate monthly, quarterly, or not at all (and explain that, even with continuous dosing, there will be some breakthrough bleeding). Patients should also be queried about any prior use of—and side effects or difficulty with—oral contraceptives.
For a patient with a history of OCP use, a pill that was previously used successfully is a reasonable starting point. For OCP-naïve patients, physicians may want to prescribe the least costly pill that is compatible with the patient’s health insurer and her preference, as well as your knowledge and comfort level.
How many pill packs to prescribe?
Most women receive 3 pill packs at a time from the pharmacy, although some get only one at a time.21 Yet evidence suggests that dispensing a 12-month supply of hormonal contraceptives at one time significantly increases patient continuation and use of preventive services (Pap smear screening and chlamydia testing, for example), decreases the need for pregnancy testing, and significantly cuts health care costs.21Keep in mind, however, that each pack of traditional pills contains medication for 4 weeks, while a year contains 13 4-week blocks of time. So any prescription written for 12 OCP packs will be insufficient to cover the entire year.
Variation in number and type of placebo
Another consideration: OCPs traditionally come in 28-day pill packs, with the last 7 pills being placebos. The number of active and placebo pills has been modified in some OCPs, in an attempt to decrease the risk of ovulation and unintended pregnancy.
Because some patients develop hormonal withdrawal side effects during the period of time when they’re taking placebos, several OCP formulations have added a small amount of estrogen to some, or all, of the placebos. One variation combines both concepts, featuring 24 active pills (rather than 21, to decrease the risk of ovulation) and 4 placebo pills containing 10 mcg EE (in an attempt to prevent withdrawal effects). Other variations are available, as well.
Although these pills have a greater inhibition of the pituitary-ovarian axis, they do not have better contraceptive efficacy compared with traditional dosing.22 Still, OCPs with such nontraditional regimens may be considered for any patient, and prescribed for women who have had prior success with this type of OCP.
Getting started: What to tell patients
For many years, combination OCPs were started on the Sunday after the onset of the next menses—a method known as conventional start. But there were 3 disadvantages to this: Patients needed to use an additional form of contraception during the first month of OCP therapy, had an increased risk of pregnancy in the first month, and often misunderstood the instructions, frequently starting the pills the Sunday after their period ended, instead of the Sunday after menstrual bleeding began.
The “first day” start came next. Patients were routinely told to begin their pills on the first day of their next menses. This was easily understood and eliminated the need for an additional form of contraception in the first month, but theoretically, a woman could get pregnant while waiting for her next menstrual cycle to start the OCPs.
To address these problems, the newest option is known as the “visit day” or “quick start. “ Advise patients to start the pills on the day of their office visit, either with a sample package or by picking up the OCPs at the pharmacy on the same day. This results in better short-term continuation rates and does not disrupt menstrual bleeding patterns.23,24
Pregnancy test. Prior to the quick start, however, women should have a documented negative pregnancy test (or receive emergency contraception if they have had unprotected intercourse in the last 72 hours). If the patient had unprotected intercourse in the prior 2 weeks, the pregnancy test should be repeated 2 weeks after she starts taking the pill.
OCP timing after a pregnancy
Women who have had a spontaneous or therapeutic abortion <20 weeks’ gestation can start taking combination OCPs immediately. A patient whose pregnancy ended >20 weeks and who is not breastfeeding can use combination OCPs, as well. Because of an increased risk of VTE during the initial postpartum period, however, women should delay the start date until >3 weeks postpartum.25
Breastfeeding considerations. Some women, and some clinicians, fear that combination OCPs reduce both the quantity and quality of breast milk. In fact, low-quality evidence suggests that the pills reduce the quantity of breast milk but do not impair infant growth.26 Studies of OCPs and breastfeeding, although of limited quality, have failed to show specific harm to the infant.
According to ACOG, women who are nursing can begin combination OCPs >6 weeks’ postpartum if breastfeeding is well established and no other form of contraception is acceptable.27 To address concerns about decreased breast milk associated with combination OCPs, however, progestin-only pills are frequently recommended for nursing mothers—and can be started immediately postpartum without any effect on breast milk.25
Progestin-only pills. Because progestin-only pills are taken every day with no placebos, women who take them have unpredictable and irregular menstrual bleeding. In addition, patients need to know that progestin-only pills must be taken at the same time every day; even a 3-hour day-to-day variation increases the risk of contraceptive failure.20
What to do about forgotten pills?
Most women occasionally forget a pill, and it is important to tell them what to do about it (TABLE 5).28,29 Such a discussion is critical to ensure contraceptive effectiveness.
If a patient misses one or 2 pills, she may make them up, using an additional form of contraception for 7 days if she skipped 2 consecutive pills. If she misses 3 consecutive pills, advise her to start a new pill pack, use an additional form of contraception for 7 days, and consider emergency contraception (EC) if she had unprotected sex. A woman who misses 3 pills in a row also needs to be urged to consider a contraceptive method that does not depend on daily compliance29—and to consider EC if she had unprotected intercourse.
The most dangerous pill to forget is the first pill of the next pack. Missing that pill means the patient will have gone 8 days without hormonal treatment—and should use an additional form of contraception until she has taken an active pill for 7 days.
EC should be recommended for patients who forget 2 or more combination OCPs or miss the first pill of the next pack and have unprotected intercourse. Levonorgestrel 0. 75 mg (Plan B) can be taken as 2 doses 12 hours apart or taken together as a single dose (Plan B One Step).30 Patients who are 17 years or older are allowed to buy Plan B over the counter; younger patients require a prescription.
TABLE 5
Forgotten pill(s)? What to tell your patients29
| Missed pill(s) | Instructions |
|---|---|
| Placebo | Skip the pill |
| Active pill <24 hours (1) | Take the pill as soon as you remember |
| Active pill >24 hours and <48 hours (1) | Take the missed pill AND the scheduled pill together |
| Active pills (2) |
|
| Active pills (≥3) |
|
| EC, emergency contraception. | |
What would you prescribe for our 3 patients?
CASE 1: Mandy
You start by strongly suggesting that she stop smoking, explaining that when she reaches age 35, the oral contraceptives will be contra-indicated if she continues to smoke. Because she had previously used a transdermal contraceptive patch without complications, a generic monophasic 30 to 35 mcg EE combination OCP would be a good choice. You schedule a follow-up visit in 3 months to determine how she is adjusting to the pill.
CASE 2: Julie
Julie is interested in continuous dosing but has no health insurance, so you recommend that she use a generic 21/7 combination OCP. Because of her preference for continuous dosing, however, you recommend that she start a new pack every 3 weeks, without taking any of the placebos, and tell her that this may result in improvements in her acne, as well.
CASE 3: Sandra
You reassure Sandra that combination pills have not been found to be harmful to infants, but suggest she consider a progestin-only formulation instead. You talk to her about the importance of meticulous compliance with a progestin-only OCP, which means taking her pill at the same time every day. You also explain that breakthrough bleeding is common with this type of pill, and that you can discuss a combination OCP when she is no longer nursing or if she cannot tolerate the progestin-only pill.
CORRESPONDENCE
Herbert L. Muncie, Jr, MD, 1542 Tulane Avenue, Room 123, New Orleans, LA 70112; hmunci@lsuhsc.edu
1. American College of Obstetricians and Gynecologists. (ACOG) Committee on Practice B. ACOG practice bulletin no. 73: Use of hormonal contraception in women with coexisting medical conditions. Obstet Gynecol. 2006;107:1453-1472.
2. Bezemer ID, van der Meer FJM, Eikenboom JCJ, et al. The value of family history as a risk indicator for venous thrombosis. Arch Intern Med. 2009;169:610-615.
3. Bracken MB. Oral contraception and congenital malformations in offspring: a review and meta-analysis of the prospective studies. Obstet Gynecol. 1990;76:552-557.
4. Petri M, Kim MY, Kalunian KC, et al. Combined oral contraceptives in women with sy stemic lupus erythematosus. N Engl J Med. 2005;353:2550-2558.
5. Trussell J, Vaughan B. Contraceptive failure, method-related discontinuation and resumption of use: results from the 1995 national survey of family growth. Fam Plann Perspect. 1999;31:64-72.
6. Petitti DB. Combination estrogen-progestin oral contraceptives. N Engl J Med. 2003;349:1443-1450.
7. US Food and Drug Administration. FDA approves newcombina-tion product oral contraceptive. May 6, 2010. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm211176.htm. Accessed January 19, 2011.
8. Vlieg AH, Helmerhorst FM, Vandenbroucke JP, et al. The venous thrombotic risk of oral contraceptives, effects of oestrogen dose and progestogen type: results of the MEGA case-control study. BMJ. 2009;339:2921-2928.
9. Lidegaard O, Lokkegaard E, Svendsen AL, et al. Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ. 2009;339:2890-2897.
10. Davis PS, Boatwright EA, Tozer BS, et al. Hormonal contraception update. Mayo ClinProc. 2006;81:949-955.
11. Gallo MF, Nanda K, Grimes DA, et al. 20 mcg versus >20 mcg estrogen combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2005(2);CD003989.-
12. van Vliet HA, Grimes DA, Lopez LM, et al. Triphasic versus monophasic oral contraceptives for contraception. Cochrane Database Syst Rev. 2006(3);003553.-
13. Van Vliet HA, Grimes DA, Helmerhorst FM, Schulz KF. Biphasic versus triphasic oral contraceptives for contraception. Cochrane Database Syst Rev. 2006(3);003283.-
14. US Food and Drug Administration. Office of Women’s Health Update, September-October 2003. Available at: http://www.fda.gov/ForConsumers/ByAudience/ForWomen/ucm118642.htm. Accessed January 19, 2011.
15. US Food and Drug Administration. FDA listing of approved generics as of December 13, 2010. Available at: AG_LISTING_pdf. Accessed January 19, 2011.
16. Drugs.com. FDA approves Seasonique. May 27, 2006. Available at: http://www.drugs.com/newdrugs/fda-approves-duramed-s-seasonique-extended-cycle-oral-contraceptive-1161.html. Accessed January 19, 2011.
17. Edelman AB, Gallo MF, Jensen JT, et al. Continuous or extended cycle vs. cyclic use of combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2005();004695.-
18. US Food and Drug Administration. FDA approves contraceptive for continuous use. May 22, 2007. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2007/ucm108918.htm. Accessed January 19, 2011.
19. Legro RS, Pauli JG, Kunselman AR, et al. Effects of continuous versus cyclical oral contraception: a randomized controlled trial. J Clin Endocrinol Metabol. 2008;93:420-429.
20. Choice of contraceptives. Treatment Guidelines from the Medical Letter. 2007;5:101-108.
21. Foster DG, Parvataneni R, de Bocanegra HT, et al. Number of oral contraceptive pill packages dispensed, method continuation, and costs. Obstet Gynecol. 2006;108:1107-1114.
22. Willis SA, Kuehl TJ, Spiekerman AM, Sulak PJ. Greater inhibition of the pituitary—ovarian axis in oral contraceptive regimens with a shortened hormone-free interval. Contraception. 2006;74:100-103.
23. Westhoff C, Heartwell S, Edwards S, et al. Initiation of oral contraceptives using a quick start compared with a conventional start: A randomized controlled trial. Obstet Gynecol. 2007;109:1270-1276.
24. Edwards SM, Zieman M, Jones K, et al. Initiation of oral contraceptives - start now! J Adolesc Health. 2008;43:432-436.
25. Lesnewski R, Prince L. Initiating hormonal contraception. Am Fam Physician. 2006;74:105-112.
26. Truitt ST, Fraser AB, Grimes DA, et al. Combined hormonal versus nonhormonal versus progestin-only contraception in lactation. Cochrane Database Syst Rev. 2003(2);CD003988.-
27. Queenan JT. Contraception and breast feeding. Clin Obstet Gynecol. 2004;47:734-739.
28. Potter L, Oakley D, de Leon-Wong E, et al. Measuring compliance among oral contraceptive users. Fam Plann Perspect. 1996;28:154-158.
29. PlannedParenthood. Whattodoifyouforgettotakethepill. Available at: http://www.plannedparenthood.org/health-topics/birth-control/if-forget-take-pill-19269.htm. htm. Accessed September 4, 2009.
30. von Hertzen H, Piaggio G, Ding J, et al. Low dose mifepris-tone and two regimens of levonorgestrel for emergency contraception: A WHO multicentre randomised trial. Lancet. 2002;360:1803-1810.
31. Physicians’ Desk Reference. Montvale, NJ: PDR Network; 2010.
32. Hannaford PC, Selvaraj S, Elliott AM, et al. Cancer risk among users of oral contraceptives: cohort data from the royal college of general practitioner’s oral contraception study. BMJ. 2007;335:651.-
33. Lurie G, Thompson P, McDuffie KE, et al. Association of estrogen and progestin potency of oral contraceptives with ovarian carcinoma risk. Obstet Gynecol. 2007;109:597-607.
34. Kiley J, Hammond C. Combined oral contraceptives: A comprehensive review. Clin Obstet Gynecol. 2007;50:868-877.
1. American College of Obstetricians and Gynecologists. (ACOG) Committee on Practice B. ACOG practice bulletin no. 73: Use of hormonal contraception in women with coexisting medical conditions. Obstet Gynecol. 2006;107:1453-1472.
2. Bezemer ID, van der Meer FJM, Eikenboom JCJ, et al. The value of family history as a risk indicator for venous thrombosis. Arch Intern Med. 2009;169:610-615.
3. Bracken MB. Oral contraception and congenital malformations in offspring: a review and meta-analysis of the prospective studies. Obstet Gynecol. 1990;76:552-557.
4. Petri M, Kim MY, Kalunian KC, et al. Combined oral contraceptives in women with sy stemic lupus erythematosus. N Engl J Med. 2005;353:2550-2558.
5. Trussell J, Vaughan B. Contraceptive failure, method-related discontinuation and resumption of use: results from the 1995 national survey of family growth. Fam Plann Perspect. 1999;31:64-72.
6. Petitti DB. Combination estrogen-progestin oral contraceptives. N Engl J Med. 2003;349:1443-1450.
7. US Food and Drug Administration. FDA approves newcombina-tion product oral contraceptive. May 6, 2010. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm211176.htm. Accessed January 19, 2011.
8. Vlieg AH, Helmerhorst FM, Vandenbroucke JP, et al. The venous thrombotic risk of oral contraceptives, effects of oestrogen dose and progestogen type: results of the MEGA case-control study. BMJ. 2009;339:2921-2928.
9. Lidegaard O, Lokkegaard E, Svendsen AL, et al. Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ. 2009;339:2890-2897.
10. Davis PS, Boatwright EA, Tozer BS, et al. Hormonal contraception update. Mayo ClinProc. 2006;81:949-955.
11. Gallo MF, Nanda K, Grimes DA, et al. 20 mcg versus >20 mcg estrogen combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2005(2);CD003989.-
12. van Vliet HA, Grimes DA, Lopez LM, et al. Triphasic versus monophasic oral contraceptives for contraception. Cochrane Database Syst Rev. 2006(3);003553.-
13. Van Vliet HA, Grimes DA, Helmerhorst FM, Schulz KF. Biphasic versus triphasic oral contraceptives for contraception. Cochrane Database Syst Rev. 2006(3);003283.-
14. US Food and Drug Administration. Office of Women’s Health Update, September-October 2003. Available at: http://www.fda.gov/ForConsumers/ByAudience/ForWomen/ucm118642.htm. Accessed January 19, 2011.
15. US Food and Drug Administration. FDA listing of approved generics as of December 13, 2010. Available at: AG_LISTING_pdf. Accessed January 19, 2011.
16. Drugs.com. FDA approves Seasonique. May 27, 2006. Available at: http://www.drugs.com/newdrugs/fda-approves-duramed-s-seasonique-extended-cycle-oral-contraceptive-1161.html. Accessed January 19, 2011.
17. Edelman AB, Gallo MF, Jensen JT, et al. Continuous or extended cycle vs. cyclic use of combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2005();004695.-
18. US Food and Drug Administration. FDA approves contraceptive for continuous use. May 22, 2007. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2007/ucm108918.htm. Accessed January 19, 2011.
19. Legro RS, Pauli JG, Kunselman AR, et al. Effects of continuous versus cyclical oral contraception: a randomized controlled trial. J Clin Endocrinol Metabol. 2008;93:420-429.
20. Choice of contraceptives. Treatment Guidelines from the Medical Letter. 2007;5:101-108.
21. Foster DG, Parvataneni R, de Bocanegra HT, et al. Number of oral contraceptive pill packages dispensed, method continuation, and costs. Obstet Gynecol. 2006;108:1107-1114.
22. Willis SA, Kuehl TJ, Spiekerman AM, Sulak PJ. Greater inhibition of the pituitary—ovarian axis in oral contraceptive regimens with a shortened hormone-free interval. Contraception. 2006;74:100-103.
23. Westhoff C, Heartwell S, Edwards S, et al. Initiation of oral contraceptives using a quick start compared with a conventional start: A randomized controlled trial. Obstet Gynecol. 2007;109:1270-1276.
24. Edwards SM, Zieman M, Jones K, et al. Initiation of oral contraceptives - start now! J Adolesc Health. 2008;43:432-436.
25. Lesnewski R, Prince L. Initiating hormonal contraception. Am Fam Physician. 2006;74:105-112.
26. Truitt ST, Fraser AB, Grimes DA, et al. Combined hormonal versus nonhormonal versus progestin-only contraception in lactation. Cochrane Database Syst Rev. 2003(2);CD003988.-
27. Queenan JT. Contraception and breast feeding. Clin Obstet Gynecol. 2004;47:734-739.
28. Potter L, Oakley D, de Leon-Wong E, et al. Measuring compliance among oral contraceptive users. Fam Plann Perspect. 1996;28:154-158.
29. PlannedParenthood. Whattodoifyouforgettotakethepill. Available at: http://www.plannedparenthood.org/health-topics/birth-control/if-forget-take-pill-19269.htm. htm. Accessed September 4, 2009.
30. von Hertzen H, Piaggio G, Ding J, et al. Low dose mifepris-tone and two regimens of levonorgestrel for emergency contraception: A WHO multicentre randomised trial. Lancet. 2002;360:1803-1810.
31. Physicians’ Desk Reference. Montvale, NJ: PDR Network; 2010.
32. Hannaford PC, Selvaraj S, Elliott AM, et al. Cancer risk among users of oral contraceptives: cohort data from the royal college of general practitioner’s oral contraception study. BMJ. 2007;335:651.-
33. Lurie G, Thompson P, McDuffie KE, et al. Association of estrogen and progestin potency of oral contraceptives with ovarian carcinoma risk. Obstet Gynecol. 2007;109:597-607.
34. Kiley J, Hammond C. Combined oral contraceptives: A comprehensive review. Clin Obstet Gynecol. 2007;50:868-877.
Warfarin therapy: Tips and tools for better control
• INR testing by an anticoagulation management service or private clinician can be reduced to intervals of as long as 4 weeks, but should be more frequent when dosing adjustments occur. B
• Weekly patient self-testing is associated with comparable clinical outcomes to high-quality clinic-based anticoagulation management. A
• Patients who self-test (and report their results) weekly should test more frequently when a change in medication (including herbal remedies and dietary supplements) or diet or an illness occurs. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Approximately 4 million Americans are receiving longterm oral anticoagulation therapy to reduce the risk of primary and secondary thromboembolism.1,2 And, as the population ages, the number of patients on lifelong therapy with warfarin—the only oral anticoagulant available in the United States until dabigatran was approved by the US Food and Drug Administration late last year3—is expected to grow.4
Such patients present a challenge for family physicians. Warfarin is notorious for having both a narrow therapeutic index and numerous drug and dietary interactions.5,6 To safeguard patients on warfarin therapy, frequent, and diligent, monitoring is required.
Engaging patients as participants in their own care can help you decrease the hazards. With that in mind, this article features warfarin treatment tips and tools for both physicians and patients, along with a review of some basic safeguards.
Warfarin therapy: Keeping it safe
Warfarin, a vitamin K antagonist, is used to prevent systemic embolism in patients with prosthetic heart valves, atrial fibrillation, or inherited/acquired thrombophilic disorders; as an adjunct in the prophylaxis of systemic embolism after myocardial infarction (MI); and to reduce the risk of recurrent MI, as well as venous thromboembolism.4,7 Because there is a small but definite risk (1%-2% per year)8 of severe bleeding associated with warfarin, however, therapy should be initiated only when the potential benefits clearly outweigh the risks.
A major contraindication for warfarin therapy is early pregnancy. The anticoagulant is a teratogen, causing deformations of the face (depressed nasal bridge) and bones (stippled epiphyses), neonatal seizures, and spontaneous abortion. If a woman in the first trimester of pregnancy requires anticoagulation, low-molecular-weight heparin should be substituted instead.9
In fact, warfarin is not recommended in the second or third trimesters either, as the use of vitamin K antagonists increases the risk of miscarriages, structural defects, and other adverse outcomes. Nor is warfarin recommended for women who are planning to become pregnant.
Warfarin is also contraindicated in patients for whom the risk of major bleeding outweighs the benefits. Risk factors for warfarin-associated bleeding include renal insufficiency and concomitant antiplatelet therapy, and physicians can use published clinical prediction rules to estimate bleeding risk.10
Dosing considerations
When you start a patient on warfarin therapy, it is important to ensure that therapeutic concentrations are achieved in a timely manner—and that the risk of supra- and subtherapeutic international normalized ratio (INR) values—≥4.0 and <2.0, respectively—is minimized.6
Factors to consider in determining the starting dose include patient-specifi c measures such as age, height, and weight; concomitant medications; and comorbidities. Increasing age, female sex, and a low body mass index all indicate a need for a lower dose.11 A number of Web-based dosing calculators (TABLE) can help clinicians estimate the therapeutic dose in patients who are new to warfarin.
Thyroid activity also affects warfarin dosing requirements.12 Hypothyroidism makes people less responsive to warfarin,13 while hyperthyroidism boosts the anticoagulant effect.14 Several mechanisms have been proposed for this effect, including changes in the rate of breakdown of clotting factors and in the metabolism of warfarin.15,16
Frequency of monitoring. Regardless of the initiation dose, INR values of outpatients should be monitored at least 2 to 3 times a week for the fi rst 7 to 10 days of therapy, or until a stable value is achieved. (In an inpatient setting, INR monitoring is usually performed daily until the therapeutic range has been maintained for ≥2 days.) The target INR level varies from case to case depending on the clinical indicators, but tends to be between 2 and 3 for most patients and between 2.5 and 3.5 for those with mechanical heart valves.17
After stabilization, testing can be reduced to intervals of as long as 4 weeks, althoughevidence suggests that more frequent testing leads to greater time-in-therapeutic range (TTR).18,19 When dosing adjustments are required, the cycle of more frequent monitoring should be repeated until a stable dose response can again be achieved.
Benefits of patient involvement
Patients on warfarin may be managed in one or more of the following 3 methods: (1) with usual care, provided by the patient’s personal physician; (2) by anticoagulation management services (AMSs), specialized programs overseen by physicians, pharmacists, and/or nurses; or (3) by self-testing/self-management, with the help of point-of-care devices that allow patients to monitor their own INR levels and adjust their anticoagulation dose, within certain limits, in consultation with a clinician.4
Many nonrandomized retrospective studies have reported better outcomes in patients whose anticoagulant therapy is managed by an AMS vs management by a primary care physician or specialist alone.7 Compared with usual care, AMS programs have been shown to greatly improve patients’ TTR, thereby reducing hemorrhage or thrombosis as a consequence of excessive or subtherapeutic anticoagulation.4,20,21
Self-testing/self-management—which depends on adequate patient training—has similar benefits: Self-care facilitates more frequent monitoring and empowers patients, and may be a major factor in patient compliance.4 Individuals using their own portable INR monitors and managing their own care have been found to have improved TTRs and a lower frequency of major hemorrhage or thrombosis compared with patients receiving usual care.7,18 The recent THINRS trial randomized 2922 patients to perform weekly self-testing or receive monthly clinic-based testing at an institution with a system for providing anticoagulant care. The study confirmed that patient self-testing is feasible for most warfarin-treated individuals and that weekly home monitoring is as safe and effective as high-quality clinic-based testing.22
Who’s a candidate for self-management?
Various studies have found that, as with insulin-dependent diabetes, most patients who are independent and self-supporting are, in principle, capable of self-management of oral anticoagulation, regardless of education or social status.23,24 The only intellectual requirement is that the patient (or caregiver) grasp the concept of anticoagulant therapy and understand the potential risks. (For more help in determining whether your patient is eligible for self-management, see “Self-monitoring—for which patients?” on page 74.)
The patient must also be willing to actively participate in his or her own care and have sufficient manual dexterity and visual acuity. No previous experience in self-testing or monitoring is necessary.7
INR monitors for patients and physicians
Since the late 1980s, point-of-care devices that measure INR values have made it possible for an increasing number of patients to monitor the anticoagulant eff ects of warfarin without repeat visits to a health care facility. Of the 4 million US residents on warfarin, approximately 60,000 (1.6%) engage in self-testing, according to the International Self-Monitoring Association of Oral Anticoagulated Patients (www.ismaap.org).
One reason may be the cost. Portable monitors are available for approximately $2495, according to Alere Inc., a health management company—a price that may include supplies and training. The expense may not be covered by private insurers. However, in 2008, Medicare began covering the cost of INR monitors (and the testing materials required for their use) for seniors receiving anticoagulation therapy associated with mechanical heart valves, chronic atrial fibrillation, or venous thromboembolism.25 Portable monitoring devices include the following:
CoaguChek (http://www.coaguchek.com). The CoaguChek brand, now in its third generation, features both a monitor (CoaguChek XS) for patient use and a system (CoaguChek XS Plus) for health care professionals. CoaguChek has extended quality control and data management options.
INRatio2 PT/INR Monitor (www.hemosense.com). The HemoSense INRatio2 is a new whole-blood patient monitoring system. The device is well suited for use by both health care professionals and patients.
ProTime PT/INR Monitor (www.protimesystem.com). The ProTime Microcoagulation System is a portable, batteryoperated testing tool designed for both professionals and patients. There are also companies that sell or loan the devices to patients and provide the supplies, training, and support for enrollees engaged in self-testing, including Philips (http://www.inrselftest.com/content) and Roche (https://www.poc.roche.com/poc/home.do).
Preparing patients for self-management In addition to acquiring a monitor, patients interested in self-testing and management need to be aware that the risk of bleeding rises steeply when the INR exceeds 4.0—and the risk of thrombosis increases when INR values fall below 2.0.7
Guard against interactions. Emphasize that numerous environmental factors, such as drugs, diet, alcohol, and various disease states, can alter the pharmacokinetics of warfarin.26 Consequently, INR values need to be measured more frequently than the usual 4-week intervals when a patient taking warfarin adds (orstops taking) virtually any drug, dietary supplement, or herbal remedy, or significantly alters his or her vitamin K intake. Illnesses with a fever, such as infl uenza, or diarrhea and vomiting lasting more than one day, can also aff ect INR levels, and call for more frequent testing and possible adjustments in warfarin dosing.27
Explain that some drugs reduce warfarin’s anticoagulant eff ect by reducing its absorption or enhancing its clearance, while others—including many commonly used antibiotics—enhance the drug’s anticoagulant eff ect by inhibiting its clearance.6,7 Remind patients that the risk of bleeding is high when warfarin is combined with antiplatelet agents such as clopidogrel, aspirin, or nonsteroidal anti-infl ammatory drugs, among other medications.27 And caution them that excessive use of alcohol aff ects the metabolism of warfarin and can elevate the INR.26 (See Patient on warfarin? Steer clear of these drugs, in "Avoiding drug interactions: Here’s help," J Fam Pract. 2010; 59: 322-329.)
Seek medical attention. Patients engaged in self-testing and monitoring also need to be aware of the importance of obtaining treatment for dangerously high or low INR levels and being alert to early indicators of bleeding or other significant adverse effects. Similarly, family physicians who care for such patients need to establish a system to ensure that these individuals are not lost to followup. Whether INR results are transmitted by fax, phone, or e-mail, a patient who leaves a message reporting an INR of 5.6, for example, requires a callback without delay.
Advise patients to watch for signs of warfarin-induced skin necrosis—a rare but serious complication of oral anticoagulant therapy characterized by dusky skin discoloration and pain, typically in an area with significant subcutaneous fat (eg, the breast or abdominal wall). Warfarin necrosis is estimated to occur in 0.01% to 0.1% of patients—primarily women—mostly in the first week of therapy.15 Other serious adverse effects are osteoporosis and purple toe syndrome.1
Patients—and their family members—should also be advised that if the patient is hospitalized, it is critical to let the health care team know that he or she is taking warfarin. Patients should be encouraged to wear a medic alert bracelet, as well.
Warfarin’s effects can be reversed with vitamin K. (See “What to do when warfarin therapy goes too far,” J Fam Pract. 2009;58:346-352.) However, reversal may take 24 hours.7 In patients with life-threatening bleeding (eg, intracranial hemorrhage) and elevated INR, regardless of the magnitude of the elevation, INR should be normalized urgently with fresh frozen plasma, prothrombin complex concentrate, or recombinant factor VIIa supplemented with vitamin K10 mg by slow intravenous infusion.7
CORRESPONDENCE
Michael J. Schwartz, MD, 5 Sunnydale Circle, Swannanoa, NC 28778; ms112@columbia.edu
1. International Self-Monitoring Association of Oral Anticoagulated Patients. We motivate patients to take control of their own oral anticoagulation therapy. Available at: http://www.ismaap.org. Accessed January 12, 2011.
2. Alere Introducing InRatio 2. Available at: www.hemosense. com. Accessed January 25, 2009.
3. US Food and Drug Administration. FDA approves Pradaxa to prevent stroke in people with atrial fibrillation [press release]. October 19, 2010. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm230241.htm. Accessed January 12, 2011.
4. Garcia DA, Witt DM, Hyleck E, et al. Delivery of optimized anticoagulant therapy consensus statement from the Anticoagulant Forum. Ann Pharmacother. 2008;42:979-988.
5. Ansell J, Hirsh J, Poller L, et al. The pharmacology and management of the vitamin K antagonists: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(3 suppl):204S-233S.
6. Holbrook AM, Pereira JA, Labiris R, et al. Systematic overview of warfarin and its drug and food interactions. Arch Intern Med. 2005;165:1095-1106.
7. Ansell J, Hirsh J, Hylek E, et al. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest. 2008;133(6 suppl):160S-198S.
8. Schulman S, Beyth RJ, Kearon C, et al. Hemorrhagic complications of anticoagulant and thrombolytic treatment: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest. 2008;133(6 suppl):257S-299S.
9. Lip GY, Frison L, Halperin JL, et al. Comparative validation of a novel risk score for predicting bleeding risk in anticoagulated patients with atrial fibrillation: the HAS-BLED (Hypertension, Abnormal Renal/Liver Function, Stroke, Bleeding History or Predisposition, Labile INR, Elderly, Drugs/Alcohol Concomitantly) Score. J Am Coll Cardiol. 2011;57:173-180.
10. Beckmann CR. Obstetrics and Gynecology. 4th ed. Baltimore, Md: Lippincott Williams & Wilkins; 2002: 58.
11. Garcia D, Regan S, Crowther M, et al. Warfarin maintenance dosing patterns in clinical practice: implications for safer anticoagulation in the elderly population. Chest. 2005;127:2049-2056.
12. Kurnick D, Loebstein R, Farfel Z, et al. Complex drug-drug-disease interactions between amiodarone, warfarin and the thyroid gland. Medicine. 2004;83:107-113.
13. Stephens MA, Self TH, Lancaster D, et al. Hypothyroidism: effect on warfarin anticoagulation. South Med J. 1989;82:1585-1586.
14. Chute JP, Ryan CP, Sladek G, et al. Exacerbation of warfarin-induced anticoagulation by hyperthyroidism. Endocr Pract. 1997;3:77-79.
15. Kennedy M, Armanious C, Costa M. Dermatologic manifestations of hematologic disease. Emedicine web site. Updated June 25, 2009. Available at: http://emedicine.medscape.com/article/1096183-overview. Accessed January 14, 2011.
16. Kellett HA, Sawers JS, Boulton FE, et al. Problems of anticoagulation with warfarin in hyperthyroidism. Q J Med. 1986;58:43-51.
17. Baglin TP, Keeling DM, Watson HG. Guidelines on oral anticoagulation (warfarin): third edition–2005 update. Br J Haematol. 2006;132:277-285.
18. Horstkotte D, Piper C, Wiemer M. Optimal frequency of patient monitoring and intensity of oral anticoagulation therapy in valvular heart disease. J Thromb Thrombolysis. 1998;5(suppl):19-24.
19. Samsa GP, Matchar DB. Relationship between test frequency and outcomes of anticoagulation: a literature review and commentary with implications for the design of randomized trials of patient self-management. J Thromb Thrombolysis. 2000;9:283-292.
20. Ansell JE, Buttaro ML, Thomas OV, et al. Consensus guidelines for coordinated outpatient oral anticoagulation therapy management. Ann Pharmacother. 1997;31:604-615.
21. Palareti G, Legnani C, Guazzaloca G, et al. Risk factors for highly unstable response to oral anticoagulation: a case-control study. Br J Haematol. 2005;129:72-78.
22. Matchar DB, Jacobson A, Dolor R, et al. for the THINRS Executive Committee and Site Investigators. Effect of home testing of international normalized ratio on clinical events. N Engl J Med. 2010;363:1608-1620.
23. Cromheecke ME, Levi M, Colly LP, et al. Oral anticoagulation self-management and management by a specialist anticoagulation clinic: a randomized cross-over comparison. Lancet. 2000;356:97-102.
24. Heidinger KS, KS Bernardo A, Taborski U, et al. Clinical outcome of self-management of oral anticoagulation in patients with atrial fibrillation or deep vein thrombosis. Thromb Res. 2000;98:287-293.
25. Centers for Medicare and Medicaid Services. CMS manual system. Pub 100-04 Medicare claims processing. Transmittal 1562. July 25, 2008. Available at: http://www.cms.gov/transmittals/downloads/R1562CP.pdf. Accessed January 14, 2011.
26. Weathermon R, Crabb DW. Alcohol and medication interactions. Alcohol Res Health. 1999;23:40-54.
27. Delaney JA, Opatrny L, Brophy JM, et al. Drug interactions between antithrombotic medications and the risk of gastrointestinal bleeding. 2007;177:347-351.
28. Hart RG, Tonarelli SB, Pearce LA. Avoiding central nervous system bleeding during antithrombotic therapy. Stroke. 2005;36:1588-1593.
29. Philips Which patients qualify for PT/INR self-testing? Available at: http://www.inrselftest.com/content/clinicians/which-patients-qualify. Accessed January 13, 2011.
• INR testing by an anticoagulation management service or private clinician can be reduced to intervals of as long as 4 weeks, but should be more frequent when dosing adjustments occur. B
• Weekly patient self-testing is associated with comparable clinical outcomes to high-quality clinic-based anticoagulation management. A
• Patients who self-test (and report their results) weekly should test more frequently when a change in medication (including herbal remedies and dietary supplements) or diet or an illness occurs. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Approximately 4 million Americans are receiving longterm oral anticoagulation therapy to reduce the risk of primary and secondary thromboembolism.1,2 And, as the population ages, the number of patients on lifelong therapy with warfarin—the only oral anticoagulant available in the United States until dabigatran was approved by the US Food and Drug Administration late last year3—is expected to grow.4
Such patients present a challenge for family physicians. Warfarin is notorious for having both a narrow therapeutic index and numerous drug and dietary interactions.5,6 To safeguard patients on warfarin therapy, frequent, and diligent, monitoring is required.
Engaging patients as participants in their own care can help you decrease the hazards. With that in mind, this article features warfarin treatment tips and tools for both physicians and patients, along with a review of some basic safeguards.
Warfarin therapy: Keeping it safe
Warfarin, a vitamin K antagonist, is used to prevent systemic embolism in patients with prosthetic heart valves, atrial fibrillation, or inherited/acquired thrombophilic disorders; as an adjunct in the prophylaxis of systemic embolism after myocardial infarction (MI); and to reduce the risk of recurrent MI, as well as venous thromboembolism.4,7 Because there is a small but definite risk (1%-2% per year)8 of severe bleeding associated with warfarin, however, therapy should be initiated only when the potential benefits clearly outweigh the risks.
A major contraindication for warfarin therapy is early pregnancy. The anticoagulant is a teratogen, causing deformations of the face (depressed nasal bridge) and bones (stippled epiphyses), neonatal seizures, and spontaneous abortion. If a woman in the first trimester of pregnancy requires anticoagulation, low-molecular-weight heparin should be substituted instead.9
In fact, warfarin is not recommended in the second or third trimesters either, as the use of vitamin K antagonists increases the risk of miscarriages, structural defects, and other adverse outcomes. Nor is warfarin recommended for women who are planning to become pregnant.
Warfarin is also contraindicated in patients for whom the risk of major bleeding outweighs the benefits. Risk factors for warfarin-associated bleeding include renal insufficiency and concomitant antiplatelet therapy, and physicians can use published clinical prediction rules to estimate bleeding risk.10
Dosing considerations
When you start a patient on warfarin therapy, it is important to ensure that therapeutic concentrations are achieved in a timely manner—and that the risk of supra- and subtherapeutic international normalized ratio (INR) values—≥4.0 and <2.0, respectively—is minimized.6
Factors to consider in determining the starting dose include patient-specifi c measures such as age, height, and weight; concomitant medications; and comorbidities. Increasing age, female sex, and a low body mass index all indicate a need for a lower dose.11 A number of Web-based dosing calculators (TABLE) can help clinicians estimate the therapeutic dose in patients who are new to warfarin.
Thyroid activity also affects warfarin dosing requirements.12 Hypothyroidism makes people less responsive to warfarin,13 while hyperthyroidism boosts the anticoagulant effect.14 Several mechanisms have been proposed for this effect, including changes in the rate of breakdown of clotting factors and in the metabolism of warfarin.15,16
Frequency of monitoring. Regardless of the initiation dose, INR values of outpatients should be monitored at least 2 to 3 times a week for the fi rst 7 to 10 days of therapy, or until a stable value is achieved. (In an inpatient setting, INR monitoring is usually performed daily until the therapeutic range has been maintained for ≥2 days.) The target INR level varies from case to case depending on the clinical indicators, but tends to be between 2 and 3 for most patients and between 2.5 and 3.5 for those with mechanical heart valves.17
After stabilization, testing can be reduced to intervals of as long as 4 weeks, althoughevidence suggests that more frequent testing leads to greater time-in-therapeutic range (TTR).18,19 When dosing adjustments are required, the cycle of more frequent monitoring should be repeated until a stable dose response can again be achieved.
Benefits of patient involvement
Patients on warfarin may be managed in one or more of the following 3 methods: (1) with usual care, provided by the patient’s personal physician; (2) by anticoagulation management services (AMSs), specialized programs overseen by physicians, pharmacists, and/or nurses; or (3) by self-testing/self-management, with the help of point-of-care devices that allow patients to monitor their own INR levels and adjust their anticoagulation dose, within certain limits, in consultation with a clinician.4
Many nonrandomized retrospective studies have reported better outcomes in patients whose anticoagulant therapy is managed by an AMS vs management by a primary care physician or specialist alone.7 Compared with usual care, AMS programs have been shown to greatly improve patients’ TTR, thereby reducing hemorrhage or thrombosis as a consequence of excessive or subtherapeutic anticoagulation.4,20,21
Self-testing/self-management—which depends on adequate patient training—has similar benefits: Self-care facilitates more frequent monitoring and empowers patients, and may be a major factor in patient compliance.4 Individuals using their own portable INR monitors and managing their own care have been found to have improved TTRs and a lower frequency of major hemorrhage or thrombosis compared with patients receiving usual care.7,18 The recent THINRS trial randomized 2922 patients to perform weekly self-testing or receive monthly clinic-based testing at an institution with a system for providing anticoagulant care. The study confirmed that patient self-testing is feasible for most warfarin-treated individuals and that weekly home monitoring is as safe and effective as high-quality clinic-based testing.22
Who’s a candidate for self-management?
Various studies have found that, as with insulin-dependent diabetes, most patients who are independent and self-supporting are, in principle, capable of self-management of oral anticoagulation, regardless of education or social status.23,24 The only intellectual requirement is that the patient (or caregiver) grasp the concept of anticoagulant therapy and understand the potential risks. (For more help in determining whether your patient is eligible for self-management, see “Self-monitoring—for which patients?” on page 74.)
The patient must also be willing to actively participate in his or her own care and have sufficient manual dexterity and visual acuity. No previous experience in self-testing or monitoring is necessary.7
INR monitors for patients and physicians
Since the late 1980s, point-of-care devices that measure INR values have made it possible for an increasing number of patients to monitor the anticoagulant eff ects of warfarin without repeat visits to a health care facility. Of the 4 million US residents on warfarin, approximately 60,000 (1.6%) engage in self-testing, according to the International Self-Monitoring Association of Oral Anticoagulated Patients (www.ismaap.org).
One reason may be the cost. Portable monitors are available for approximately $2495, according to Alere Inc., a health management company—a price that may include supplies and training. The expense may not be covered by private insurers. However, in 2008, Medicare began covering the cost of INR monitors (and the testing materials required for their use) for seniors receiving anticoagulation therapy associated with mechanical heart valves, chronic atrial fibrillation, or venous thromboembolism.25 Portable monitoring devices include the following:
CoaguChek (http://www.coaguchek.com). The CoaguChek brand, now in its third generation, features both a monitor (CoaguChek XS) for patient use and a system (CoaguChek XS Plus) for health care professionals. CoaguChek has extended quality control and data management options.
INRatio2 PT/INR Monitor (www.hemosense.com). The HemoSense INRatio2 is a new whole-blood patient monitoring system. The device is well suited for use by both health care professionals and patients.
ProTime PT/INR Monitor (www.protimesystem.com). The ProTime Microcoagulation System is a portable, batteryoperated testing tool designed for both professionals and patients. There are also companies that sell or loan the devices to patients and provide the supplies, training, and support for enrollees engaged in self-testing, including Philips (http://www.inrselftest.com/content) and Roche (https://www.poc.roche.com/poc/home.do).
Preparing patients for self-management In addition to acquiring a monitor, patients interested in self-testing and management need to be aware that the risk of bleeding rises steeply when the INR exceeds 4.0—and the risk of thrombosis increases when INR values fall below 2.0.7
Guard against interactions. Emphasize that numerous environmental factors, such as drugs, diet, alcohol, and various disease states, can alter the pharmacokinetics of warfarin.26 Consequently, INR values need to be measured more frequently than the usual 4-week intervals when a patient taking warfarin adds (orstops taking) virtually any drug, dietary supplement, or herbal remedy, or significantly alters his or her vitamin K intake. Illnesses with a fever, such as infl uenza, or diarrhea and vomiting lasting more than one day, can also aff ect INR levels, and call for more frequent testing and possible adjustments in warfarin dosing.27
Explain that some drugs reduce warfarin’s anticoagulant eff ect by reducing its absorption or enhancing its clearance, while others—including many commonly used antibiotics—enhance the drug’s anticoagulant eff ect by inhibiting its clearance.6,7 Remind patients that the risk of bleeding is high when warfarin is combined with antiplatelet agents such as clopidogrel, aspirin, or nonsteroidal anti-infl ammatory drugs, among other medications.27 And caution them that excessive use of alcohol aff ects the metabolism of warfarin and can elevate the INR.26 (See Patient on warfarin? Steer clear of these drugs, in "Avoiding drug interactions: Here’s help," J Fam Pract. 2010; 59: 322-329.)
Seek medical attention. Patients engaged in self-testing and monitoring also need to be aware of the importance of obtaining treatment for dangerously high or low INR levels and being alert to early indicators of bleeding or other significant adverse effects. Similarly, family physicians who care for such patients need to establish a system to ensure that these individuals are not lost to followup. Whether INR results are transmitted by fax, phone, or e-mail, a patient who leaves a message reporting an INR of 5.6, for example, requires a callback without delay.
Advise patients to watch for signs of warfarin-induced skin necrosis—a rare but serious complication of oral anticoagulant therapy characterized by dusky skin discoloration and pain, typically in an area with significant subcutaneous fat (eg, the breast or abdominal wall). Warfarin necrosis is estimated to occur in 0.01% to 0.1% of patients—primarily women—mostly in the first week of therapy.15 Other serious adverse effects are osteoporosis and purple toe syndrome.1
Patients—and their family members—should also be advised that if the patient is hospitalized, it is critical to let the health care team know that he or she is taking warfarin. Patients should be encouraged to wear a medic alert bracelet, as well.
Warfarin’s effects can be reversed with vitamin K. (See “What to do when warfarin therapy goes too far,” J Fam Pract. 2009;58:346-352.) However, reversal may take 24 hours.7 In patients with life-threatening bleeding (eg, intracranial hemorrhage) and elevated INR, regardless of the magnitude of the elevation, INR should be normalized urgently with fresh frozen plasma, prothrombin complex concentrate, or recombinant factor VIIa supplemented with vitamin K10 mg by slow intravenous infusion.7
CORRESPONDENCE
Michael J. Schwartz, MD, 5 Sunnydale Circle, Swannanoa, NC 28778; ms112@columbia.edu
• INR testing by an anticoagulation management service or private clinician can be reduced to intervals of as long as 4 weeks, but should be more frequent when dosing adjustments occur. B
• Weekly patient self-testing is associated with comparable clinical outcomes to high-quality clinic-based anticoagulation management. A
• Patients who self-test (and report their results) weekly should test more frequently when a change in medication (including herbal remedies and dietary supplements) or diet or an illness occurs. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Approximately 4 million Americans are receiving longterm oral anticoagulation therapy to reduce the risk of primary and secondary thromboembolism.1,2 And, as the population ages, the number of patients on lifelong therapy with warfarin—the only oral anticoagulant available in the United States until dabigatran was approved by the US Food and Drug Administration late last year3—is expected to grow.4
Such patients present a challenge for family physicians. Warfarin is notorious for having both a narrow therapeutic index and numerous drug and dietary interactions.5,6 To safeguard patients on warfarin therapy, frequent, and diligent, monitoring is required.
Engaging patients as participants in their own care can help you decrease the hazards. With that in mind, this article features warfarin treatment tips and tools for both physicians and patients, along with a review of some basic safeguards.
Warfarin therapy: Keeping it safe
Warfarin, a vitamin K antagonist, is used to prevent systemic embolism in patients with prosthetic heart valves, atrial fibrillation, or inherited/acquired thrombophilic disorders; as an adjunct in the prophylaxis of systemic embolism after myocardial infarction (MI); and to reduce the risk of recurrent MI, as well as venous thromboembolism.4,7 Because there is a small but definite risk (1%-2% per year)8 of severe bleeding associated with warfarin, however, therapy should be initiated only when the potential benefits clearly outweigh the risks.
A major contraindication for warfarin therapy is early pregnancy. The anticoagulant is a teratogen, causing deformations of the face (depressed nasal bridge) and bones (stippled epiphyses), neonatal seizures, and spontaneous abortion. If a woman in the first trimester of pregnancy requires anticoagulation, low-molecular-weight heparin should be substituted instead.9
In fact, warfarin is not recommended in the second or third trimesters either, as the use of vitamin K antagonists increases the risk of miscarriages, structural defects, and other adverse outcomes. Nor is warfarin recommended for women who are planning to become pregnant.
Warfarin is also contraindicated in patients for whom the risk of major bleeding outweighs the benefits. Risk factors for warfarin-associated bleeding include renal insufficiency and concomitant antiplatelet therapy, and physicians can use published clinical prediction rules to estimate bleeding risk.10
Dosing considerations
When you start a patient on warfarin therapy, it is important to ensure that therapeutic concentrations are achieved in a timely manner—and that the risk of supra- and subtherapeutic international normalized ratio (INR) values—≥4.0 and <2.0, respectively—is minimized.6
Factors to consider in determining the starting dose include patient-specifi c measures such as age, height, and weight; concomitant medications; and comorbidities. Increasing age, female sex, and a low body mass index all indicate a need for a lower dose.11 A number of Web-based dosing calculators (TABLE) can help clinicians estimate the therapeutic dose in patients who are new to warfarin.
Thyroid activity also affects warfarin dosing requirements.12 Hypothyroidism makes people less responsive to warfarin,13 while hyperthyroidism boosts the anticoagulant effect.14 Several mechanisms have been proposed for this effect, including changes in the rate of breakdown of clotting factors and in the metabolism of warfarin.15,16
Frequency of monitoring. Regardless of the initiation dose, INR values of outpatients should be monitored at least 2 to 3 times a week for the fi rst 7 to 10 days of therapy, or until a stable value is achieved. (In an inpatient setting, INR monitoring is usually performed daily until the therapeutic range has been maintained for ≥2 days.) The target INR level varies from case to case depending on the clinical indicators, but tends to be between 2 and 3 for most patients and between 2.5 and 3.5 for those with mechanical heart valves.17
After stabilization, testing can be reduced to intervals of as long as 4 weeks, althoughevidence suggests that more frequent testing leads to greater time-in-therapeutic range (TTR).18,19 When dosing adjustments are required, the cycle of more frequent monitoring should be repeated until a stable dose response can again be achieved.
Benefits of patient involvement
Patients on warfarin may be managed in one or more of the following 3 methods: (1) with usual care, provided by the patient’s personal physician; (2) by anticoagulation management services (AMSs), specialized programs overseen by physicians, pharmacists, and/or nurses; or (3) by self-testing/self-management, with the help of point-of-care devices that allow patients to monitor their own INR levels and adjust their anticoagulation dose, within certain limits, in consultation with a clinician.4
Many nonrandomized retrospective studies have reported better outcomes in patients whose anticoagulant therapy is managed by an AMS vs management by a primary care physician or specialist alone.7 Compared with usual care, AMS programs have been shown to greatly improve patients’ TTR, thereby reducing hemorrhage or thrombosis as a consequence of excessive or subtherapeutic anticoagulation.4,20,21
Self-testing/self-management—which depends on adequate patient training—has similar benefits: Self-care facilitates more frequent monitoring and empowers patients, and may be a major factor in patient compliance.4 Individuals using their own portable INR monitors and managing their own care have been found to have improved TTRs and a lower frequency of major hemorrhage or thrombosis compared with patients receiving usual care.7,18 The recent THINRS trial randomized 2922 patients to perform weekly self-testing or receive monthly clinic-based testing at an institution with a system for providing anticoagulant care. The study confirmed that patient self-testing is feasible for most warfarin-treated individuals and that weekly home monitoring is as safe and effective as high-quality clinic-based testing.22
Who’s a candidate for self-management?
Various studies have found that, as with insulin-dependent diabetes, most patients who are independent and self-supporting are, in principle, capable of self-management of oral anticoagulation, regardless of education or social status.23,24 The only intellectual requirement is that the patient (or caregiver) grasp the concept of anticoagulant therapy and understand the potential risks. (For more help in determining whether your patient is eligible for self-management, see “Self-monitoring—for which patients?” on page 74.)
The patient must also be willing to actively participate in his or her own care and have sufficient manual dexterity and visual acuity. No previous experience in self-testing or monitoring is necessary.7
INR monitors for patients and physicians
Since the late 1980s, point-of-care devices that measure INR values have made it possible for an increasing number of patients to monitor the anticoagulant eff ects of warfarin without repeat visits to a health care facility. Of the 4 million US residents on warfarin, approximately 60,000 (1.6%) engage in self-testing, according to the International Self-Monitoring Association of Oral Anticoagulated Patients (www.ismaap.org).
One reason may be the cost. Portable monitors are available for approximately $2495, according to Alere Inc., a health management company—a price that may include supplies and training. The expense may not be covered by private insurers. However, in 2008, Medicare began covering the cost of INR monitors (and the testing materials required for their use) for seniors receiving anticoagulation therapy associated with mechanical heart valves, chronic atrial fibrillation, or venous thromboembolism.25 Portable monitoring devices include the following:
CoaguChek (http://www.coaguchek.com). The CoaguChek brand, now in its third generation, features both a monitor (CoaguChek XS) for patient use and a system (CoaguChek XS Plus) for health care professionals. CoaguChek has extended quality control and data management options.
INRatio2 PT/INR Monitor (www.hemosense.com). The HemoSense INRatio2 is a new whole-blood patient monitoring system. The device is well suited for use by both health care professionals and patients.
ProTime PT/INR Monitor (www.protimesystem.com). The ProTime Microcoagulation System is a portable, batteryoperated testing tool designed for both professionals and patients. There are also companies that sell or loan the devices to patients and provide the supplies, training, and support for enrollees engaged in self-testing, including Philips (http://www.inrselftest.com/content) and Roche (https://www.poc.roche.com/poc/home.do).
Preparing patients for self-management In addition to acquiring a monitor, patients interested in self-testing and management need to be aware that the risk of bleeding rises steeply when the INR exceeds 4.0—and the risk of thrombosis increases when INR values fall below 2.0.7
Guard against interactions. Emphasize that numerous environmental factors, such as drugs, diet, alcohol, and various disease states, can alter the pharmacokinetics of warfarin.26 Consequently, INR values need to be measured more frequently than the usual 4-week intervals when a patient taking warfarin adds (orstops taking) virtually any drug, dietary supplement, or herbal remedy, or significantly alters his or her vitamin K intake. Illnesses with a fever, such as infl uenza, or diarrhea and vomiting lasting more than one day, can also aff ect INR levels, and call for more frequent testing and possible adjustments in warfarin dosing.27
Explain that some drugs reduce warfarin’s anticoagulant eff ect by reducing its absorption or enhancing its clearance, while others—including many commonly used antibiotics—enhance the drug’s anticoagulant eff ect by inhibiting its clearance.6,7 Remind patients that the risk of bleeding is high when warfarin is combined with antiplatelet agents such as clopidogrel, aspirin, or nonsteroidal anti-infl ammatory drugs, among other medications.27 And caution them that excessive use of alcohol aff ects the metabolism of warfarin and can elevate the INR.26 (See Patient on warfarin? Steer clear of these drugs, in "Avoiding drug interactions: Here’s help," J Fam Pract. 2010; 59: 322-329.)
Seek medical attention. Patients engaged in self-testing and monitoring also need to be aware of the importance of obtaining treatment for dangerously high or low INR levels and being alert to early indicators of bleeding or other significant adverse effects. Similarly, family physicians who care for such patients need to establish a system to ensure that these individuals are not lost to followup. Whether INR results are transmitted by fax, phone, or e-mail, a patient who leaves a message reporting an INR of 5.6, for example, requires a callback without delay.
Advise patients to watch for signs of warfarin-induced skin necrosis—a rare but serious complication of oral anticoagulant therapy characterized by dusky skin discoloration and pain, typically in an area with significant subcutaneous fat (eg, the breast or abdominal wall). Warfarin necrosis is estimated to occur in 0.01% to 0.1% of patients—primarily women—mostly in the first week of therapy.15 Other serious adverse effects are osteoporosis and purple toe syndrome.1
Patients—and their family members—should also be advised that if the patient is hospitalized, it is critical to let the health care team know that he or she is taking warfarin. Patients should be encouraged to wear a medic alert bracelet, as well.
Warfarin’s effects can be reversed with vitamin K. (See “What to do when warfarin therapy goes too far,” J Fam Pract. 2009;58:346-352.) However, reversal may take 24 hours.7 In patients with life-threatening bleeding (eg, intracranial hemorrhage) and elevated INR, regardless of the magnitude of the elevation, INR should be normalized urgently with fresh frozen plasma, prothrombin complex concentrate, or recombinant factor VIIa supplemented with vitamin K10 mg by slow intravenous infusion.7
CORRESPONDENCE
Michael J. Schwartz, MD, 5 Sunnydale Circle, Swannanoa, NC 28778; ms112@columbia.edu
1. International Self-Monitoring Association of Oral Anticoagulated Patients. We motivate patients to take control of their own oral anticoagulation therapy. Available at: http://www.ismaap.org. Accessed January 12, 2011.
2. Alere Introducing InRatio 2. Available at: www.hemosense. com. Accessed January 25, 2009.
3. US Food and Drug Administration. FDA approves Pradaxa to prevent stroke in people with atrial fibrillation [press release]. October 19, 2010. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm230241.htm. Accessed January 12, 2011.
4. Garcia DA, Witt DM, Hyleck E, et al. Delivery of optimized anticoagulant therapy consensus statement from the Anticoagulant Forum. Ann Pharmacother. 2008;42:979-988.
5. Ansell J, Hirsh J, Poller L, et al. The pharmacology and management of the vitamin K antagonists: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(3 suppl):204S-233S.
6. Holbrook AM, Pereira JA, Labiris R, et al. Systematic overview of warfarin and its drug and food interactions. Arch Intern Med. 2005;165:1095-1106.
7. Ansell J, Hirsh J, Hylek E, et al. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest. 2008;133(6 suppl):160S-198S.
8. Schulman S, Beyth RJ, Kearon C, et al. Hemorrhagic complications of anticoagulant and thrombolytic treatment: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest. 2008;133(6 suppl):257S-299S.
9. Lip GY, Frison L, Halperin JL, et al. Comparative validation of a novel risk score for predicting bleeding risk in anticoagulated patients with atrial fibrillation: the HAS-BLED (Hypertension, Abnormal Renal/Liver Function, Stroke, Bleeding History or Predisposition, Labile INR, Elderly, Drugs/Alcohol Concomitantly) Score. J Am Coll Cardiol. 2011;57:173-180.
10. Beckmann CR. Obstetrics and Gynecology. 4th ed. Baltimore, Md: Lippincott Williams & Wilkins; 2002: 58.
11. Garcia D, Regan S, Crowther M, et al. Warfarin maintenance dosing patterns in clinical practice: implications for safer anticoagulation in the elderly population. Chest. 2005;127:2049-2056.
12. Kurnick D, Loebstein R, Farfel Z, et al. Complex drug-drug-disease interactions between amiodarone, warfarin and the thyroid gland. Medicine. 2004;83:107-113.
13. Stephens MA, Self TH, Lancaster D, et al. Hypothyroidism: effect on warfarin anticoagulation. South Med J. 1989;82:1585-1586.
14. Chute JP, Ryan CP, Sladek G, et al. Exacerbation of warfarin-induced anticoagulation by hyperthyroidism. Endocr Pract. 1997;3:77-79.
15. Kennedy M, Armanious C, Costa M. Dermatologic manifestations of hematologic disease. Emedicine web site. Updated June 25, 2009. Available at: http://emedicine.medscape.com/article/1096183-overview. Accessed January 14, 2011.
16. Kellett HA, Sawers JS, Boulton FE, et al. Problems of anticoagulation with warfarin in hyperthyroidism. Q J Med. 1986;58:43-51.
17. Baglin TP, Keeling DM, Watson HG. Guidelines on oral anticoagulation (warfarin): third edition–2005 update. Br J Haematol. 2006;132:277-285.
18. Horstkotte D, Piper C, Wiemer M. Optimal frequency of patient monitoring and intensity of oral anticoagulation therapy in valvular heart disease. J Thromb Thrombolysis. 1998;5(suppl):19-24.
19. Samsa GP, Matchar DB. Relationship between test frequency and outcomes of anticoagulation: a literature review and commentary with implications for the design of randomized trials of patient self-management. J Thromb Thrombolysis. 2000;9:283-292.
20. Ansell JE, Buttaro ML, Thomas OV, et al. Consensus guidelines for coordinated outpatient oral anticoagulation therapy management. Ann Pharmacother. 1997;31:604-615.
21. Palareti G, Legnani C, Guazzaloca G, et al. Risk factors for highly unstable response to oral anticoagulation: a case-control study. Br J Haematol. 2005;129:72-78.
22. Matchar DB, Jacobson A, Dolor R, et al. for the THINRS Executive Committee and Site Investigators. Effect of home testing of international normalized ratio on clinical events. N Engl J Med. 2010;363:1608-1620.
23. Cromheecke ME, Levi M, Colly LP, et al. Oral anticoagulation self-management and management by a specialist anticoagulation clinic: a randomized cross-over comparison. Lancet. 2000;356:97-102.
24. Heidinger KS, KS Bernardo A, Taborski U, et al. Clinical outcome of self-management of oral anticoagulation in patients with atrial fibrillation or deep vein thrombosis. Thromb Res. 2000;98:287-293.
25. Centers for Medicare and Medicaid Services. CMS manual system. Pub 100-04 Medicare claims processing. Transmittal 1562. July 25, 2008. Available at: http://www.cms.gov/transmittals/downloads/R1562CP.pdf. Accessed January 14, 2011.
26. Weathermon R, Crabb DW. Alcohol and medication interactions. Alcohol Res Health. 1999;23:40-54.
27. Delaney JA, Opatrny L, Brophy JM, et al. Drug interactions between antithrombotic medications and the risk of gastrointestinal bleeding. 2007;177:347-351.
28. Hart RG, Tonarelli SB, Pearce LA. Avoiding central nervous system bleeding during antithrombotic therapy. Stroke. 2005;36:1588-1593.
29. Philips Which patients qualify for PT/INR self-testing? Available at: http://www.inrselftest.com/content/clinicians/which-patients-qualify. Accessed January 13, 2011.
1. International Self-Monitoring Association of Oral Anticoagulated Patients. We motivate patients to take control of their own oral anticoagulation therapy. Available at: http://www.ismaap.org. Accessed January 12, 2011.
2. Alere Introducing InRatio 2. Available at: www.hemosense. com. Accessed January 25, 2009.
3. US Food and Drug Administration. FDA approves Pradaxa to prevent stroke in people with atrial fibrillation [press release]. October 19, 2010. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm230241.htm. Accessed January 12, 2011.
4. Garcia DA, Witt DM, Hyleck E, et al. Delivery of optimized anticoagulant therapy consensus statement from the Anticoagulant Forum. Ann Pharmacother. 2008;42:979-988.
5. Ansell J, Hirsh J, Poller L, et al. The pharmacology and management of the vitamin K antagonists: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(3 suppl):204S-233S.
6. Holbrook AM, Pereira JA, Labiris R, et al. Systematic overview of warfarin and its drug and food interactions. Arch Intern Med. 2005;165:1095-1106.
7. Ansell J, Hirsh J, Hylek E, et al. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest. 2008;133(6 suppl):160S-198S.
8. Schulman S, Beyth RJ, Kearon C, et al. Hemorrhagic complications of anticoagulant and thrombolytic treatment: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest. 2008;133(6 suppl):257S-299S.
9. Lip GY, Frison L, Halperin JL, et al. Comparative validation of a novel risk score for predicting bleeding risk in anticoagulated patients with atrial fibrillation: the HAS-BLED (Hypertension, Abnormal Renal/Liver Function, Stroke, Bleeding History or Predisposition, Labile INR, Elderly, Drugs/Alcohol Concomitantly) Score. J Am Coll Cardiol. 2011;57:173-180.
10. Beckmann CR. Obstetrics and Gynecology. 4th ed. Baltimore, Md: Lippincott Williams & Wilkins; 2002: 58.
11. Garcia D, Regan S, Crowther M, et al. Warfarin maintenance dosing patterns in clinical practice: implications for safer anticoagulation in the elderly population. Chest. 2005;127:2049-2056.
12. Kurnick D, Loebstein R, Farfel Z, et al. Complex drug-drug-disease interactions between amiodarone, warfarin and the thyroid gland. Medicine. 2004;83:107-113.
13. Stephens MA, Self TH, Lancaster D, et al. Hypothyroidism: effect on warfarin anticoagulation. South Med J. 1989;82:1585-1586.
14. Chute JP, Ryan CP, Sladek G, et al. Exacerbation of warfarin-induced anticoagulation by hyperthyroidism. Endocr Pract. 1997;3:77-79.
15. Kennedy M, Armanious C, Costa M. Dermatologic manifestations of hematologic disease. Emedicine web site. Updated June 25, 2009. Available at: http://emedicine.medscape.com/article/1096183-overview. Accessed January 14, 2011.
16. Kellett HA, Sawers JS, Boulton FE, et al. Problems of anticoagulation with warfarin in hyperthyroidism. Q J Med. 1986;58:43-51.
17. Baglin TP, Keeling DM, Watson HG. Guidelines on oral anticoagulation (warfarin): third edition–2005 update. Br J Haematol. 2006;132:277-285.
18. Horstkotte D, Piper C, Wiemer M. Optimal frequency of patient monitoring and intensity of oral anticoagulation therapy in valvular heart disease. J Thromb Thrombolysis. 1998;5(suppl):19-24.
19. Samsa GP, Matchar DB. Relationship between test frequency and outcomes of anticoagulation: a literature review and commentary with implications for the design of randomized trials of patient self-management. J Thromb Thrombolysis. 2000;9:283-292.
20. Ansell JE, Buttaro ML, Thomas OV, et al. Consensus guidelines for coordinated outpatient oral anticoagulation therapy management. Ann Pharmacother. 1997;31:604-615.
21. Palareti G, Legnani C, Guazzaloca G, et al. Risk factors for highly unstable response to oral anticoagulation: a case-control study. Br J Haematol. 2005;129:72-78.
22. Matchar DB, Jacobson A, Dolor R, et al. for the THINRS Executive Committee and Site Investigators. Effect of home testing of international normalized ratio on clinical events. N Engl J Med. 2010;363:1608-1620.
23. Cromheecke ME, Levi M, Colly LP, et al. Oral anticoagulation self-management and management by a specialist anticoagulation clinic: a randomized cross-over comparison. Lancet. 2000;356:97-102.
24. Heidinger KS, KS Bernardo A, Taborski U, et al. Clinical outcome of self-management of oral anticoagulation in patients with atrial fibrillation or deep vein thrombosis. Thromb Res. 2000;98:287-293.
25. Centers for Medicare and Medicaid Services. CMS manual system. Pub 100-04 Medicare claims processing. Transmittal 1562. July 25, 2008. Available at: http://www.cms.gov/transmittals/downloads/R1562CP.pdf. Accessed January 14, 2011.
26. Weathermon R, Crabb DW. Alcohol and medication interactions. Alcohol Res Health. 1999;23:40-54.
27. Delaney JA, Opatrny L, Brophy JM, et al. Drug interactions between antithrombotic medications and the risk of gastrointestinal bleeding. 2007;177:347-351.
28. Hart RG, Tonarelli SB, Pearce LA. Avoiding central nervous system bleeding during antithrombotic therapy. Stroke. 2005;36:1588-1593.
29. Philips Which patients qualify for PT/INR self-testing? Available at: http://www.inrselftest.com/content/clinicians/which-patients-qualify. Accessed January 13, 2011.
Texting tendinitis in a teenager
• Consider mobile phone texting as a possible cause of tendinitis in the hand. B
• Advise mobile phone users to text with both hands, take frequent breaks, and not type too fast. C
• Advise users to give proper support to their forearms and back while texting. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
In the United States, 173 billion text messages were sent monthly by 293 million cell phone subscribers, according to mid-year 2010 data.1 That’s about 20 daily text messages per subscriber. According to the Pew Research Center, 82% of US adults are cell phone users and 72% of adult cell phone users send or receive text messages.2 Based on a Kaiser Family Foundation study, cell phone ownership is 85% among 15- to 18-year olds, 69% among 11- to 14-year olds, and 31% among 8- to 10-year olds.3 This study reports that 7th to 12th graders, on average, spend 1 hour and 35 minutes each day texting and send 118 messages. Further, only 14% of these young people say their parents have established any rules about the number of texts they are allowed to send. Additionally, based on this same study, girls, older teens, and non-Hispanic blacks spend more time texting than other groups.
Case presentation
A 14-year-old non-Hispanic white girl, right-hand dominant, visited our rural family practice clinic because of “throbbing right thumb pain” that had gradually worsened over the past week. There was no history of trauma, participation in sports, or thumb/hand problems. She had no fever or other symptoms. She was a healthy high school freshman doing well academically. However, she admitted to texting about 4 hours per day for the last 2 years, which her mother confirmed. She was on her family’s unlimited SMS (short message service) texting plan.
During the examination, the patient sat slouched, holding her mobile phone with her right hand while texting with her right thumb. Tenderness of the right thumb was noted on the lateral aspect of the first proximal phalanx, the first interphalangeal joint, and the first metacarpal, especially along the surface of the extensor pollicis brevis, extensor pollicis longus, and abductor pollicis longus (APL) tendons. We noted local soft tissue swelling and mild erythema, but no nodularity was present. Thumb abduction aggravated the pain, which worsened when encountering resistance. There was no tenderness to palpation in the anatomical snuff box. Finkelstein’s test, Phalen’s test, Tinel’s sign, and Hoffman’s sign were negative.
Radiograph results were normal, with no evidence of acute injury, calcifications, or degenerative disease. Hematologic and biochemical investigations, including complete blood count with differential, erythrocyte sedimentation rate, basic metabolic profile, calcium, phosphate, and magnesium, yielded normal results.
These findings suggested a presumptive diagnosis of texting tendinitis. We managed the patient conservatively with a right thumb spica splint, aspirin as needed (pediatric dosing) for analgesia, and education about the proper application of ice. We also instructed her to modify her mobile phone texting activity.
At 1-month follow-up, the patient reported full resolution of her symptoms. In fact, her pain resolved after only 2 weeks of treatment, at which time she discontinued the splint and aspirin. Her parents had limited her mobile phone texting to 45 minutes per day and disallowed it after 8 pm. Soon thereafter, she switched to instant messaging as a means to stay in touch with her social networks (eg, Facebook, MySpace) while using all of her fingers more comfortably on a larger keyboard.
To our knowledge, this case report is the first one published from the United States describing texting tendinitis in an adolescent.
Injuries from texting: More common than we realize?
In The Medical Journal of Australia, Menz described acute texting tendinitis in a 13-year-old girl involving the abductor or extensor pollicis longus muscle; it resolved with conservative management.4 Ming et al subsequently reported a case of progressive first carpometacarpal joint arthritis due to excessive mobile phone texting in a 48-year-old man who recovered after undergoing an excision arthroplasty of the hand.5 Yoong observed texting tenosynovitis among school children who were sending more than 100 text messages daily.6
Storr et al reported on a 20-year-old woman with de Quervain’s tenosynovitis due to texting with her right thumb, and who later developed symptoms in her left hand after learning how to text with her left thumb.7 Similarly, Ashurst et al described a 48-year-old woman who developed bilateral de Quervain’s tenosynovitis from excessive texting activity.8
These clinical cases and our current report suggest there are variable presentations for texting-induced tendinopathy. As previously discussed by Gross, the mechanism of tendinitis injury involves stressors that are too high in magnitude, too frequent in repetition, or both.9
Recently, Gustafsson et al used an electrogoniometer and surface electromyography to examine thumb movements and muscular loads, respectively, during mobile phone use.10 They found that young adults with musculoskeletal symptoms had higher thumb movement velocities, fewer pauses in thumb movements, and higher APL activity than those without symptoms. Females showed higher thumb velocities, fewer pauses in thumb movements, and greater muscle activity in the APL and extensor digitorum than males. Those with musculoskeletal symptoms were more likely to sit with the head bent forward, to sit without forearm or back support, and to enter text using only one thumb, compared with those without symptoms.
In another study based on surveys administered to college students, Gold et al found that the number of text messages sent daily from handheld devices was associated with self-reports of neck and shoulder discomfort.11
So how can patients avoid injury?
While these cross-sectional studies of Gustafsson and Gold did not track patients with clinically confirmed tendinitis over time to assess the direct impact of specific interventions, the findings are still helpful. They define important risk factors for developing musculoskeletal symptoms, which translate into prevention recommendations for mobile phone users.
Their findings suggest that mobile phone users should:
- limit the duration of daily texting activity
- learn to text with both hands (ie, thumbs) rather than with one hand alone
- take frequent breaks
- avoid typing too fast
- ensure proper support of forearms and backs while texting
- maintain a comfortable posture, avoiding prolonged periods of slouching with the head bent forward.
Our patient incorporated many of these behavioral modifications (in addition to using the spica splint) and fully recovered.
Staying alert to possible texting injury. Using mobile phones for texting has become widespread only relatively recently. Therefore, it may be an underrecognized cause of tendinopathy, especially among young people. By identifying the correct mechanism of overuse injury, you can recommend appropriate behavioral changes for achieving optimal results.
CORRESPONDENCE
Isaiah W. Williams, MS, PA-C, 790 Sunset Avenue #4, Suisun City, CA 94585; iwwilliams16@hotmail.com
1. US wireless quick facts: mid-year figures. Available at: http://www.ctia.org/consumer_info/service/index.cfm/AID/10323. Accessed January 13, 2011.
2. The rise of apps culture. Available at: http://pewintemet.org/~/media//Files/Reports/2010/PIP_Nielsen%20Apps%20 Report.pdf. Accessed January 6, 2011.
3. Rideout VJ, Foehr UG, Roberts DF. Generation M2: media in the lives of 8- to 18-year-olds. A Kaiser Family Foundation study. January 2010. Available at: http://www.kff.org/entmedia/upload/8010.pdf. Accessed January 6, 2011.
4. Menz RJ. “Texting” tendinitis. Med J Aust. 2005;182:308.
5. Ming Z, Pietikainen S, Hanninen O. Excessive texting in pathophysiology of first carpometacarpal joint arthritis. Pathophysiology. 2006;13:269-270.
6. Yoong JK. Mobile phones can be a pain—text messaging tenosynovitis. Hosp Med. 2005;66:370.
7. Storr EF, de Vere Beavis FO, Stringer MD. Texting tenosynovitis. N Z Med J. 2007;120:U2868.
8. Ashurst JV, Turco DA, Lieb BE. Tenosynovitis caused by texting: an emerging disease. J Am Osteopath Assoc. 2010;110:294-296.
9. Gross MT. Chronic tendinitis: pathomechanics of injury, factors affecting the healing response, and treatment. J Orthop SportsPhys Ther. 1992;16:248-261.
10. Gustafsson E, Johnson PW, Hagberg M. Thumb postures and physical loads during mobile phone use-a comparison of young adults with and without musculoskeletal symptoms. J Electromyogr Kinesiol. 2010;20:127-135.
11. Gold JE, Kandadai V, Hanlon A. Text messaging and upper extremity symptoms in college students. Available at: http://apha.confex.com/recording/apha/137am/pdf/free/4db77adf5df9fff0d3caf5cafe28f496/paper201105_1.Pdf. Accessed January 6, 2011.
• Consider mobile phone texting as a possible cause of tendinitis in the hand. B
• Advise mobile phone users to text with both hands, take frequent breaks, and not type too fast. C
• Advise users to give proper support to their forearms and back while texting. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
In the United States, 173 billion text messages were sent monthly by 293 million cell phone subscribers, according to mid-year 2010 data.1 That’s about 20 daily text messages per subscriber. According to the Pew Research Center, 82% of US adults are cell phone users and 72% of adult cell phone users send or receive text messages.2 Based on a Kaiser Family Foundation study, cell phone ownership is 85% among 15- to 18-year olds, 69% among 11- to 14-year olds, and 31% among 8- to 10-year olds.3 This study reports that 7th to 12th graders, on average, spend 1 hour and 35 minutes each day texting and send 118 messages. Further, only 14% of these young people say their parents have established any rules about the number of texts they are allowed to send. Additionally, based on this same study, girls, older teens, and non-Hispanic blacks spend more time texting than other groups.
Case presentation
A 14-year-old non-Hispanic white girl, right-hand dominant, visited our rural family practice clinic because of “throbbing right thumb pain” that had gradually worsened over the past week. There was no history of trauma, participation in sports, or thumb/hand problems. She had no fever or other symptoms. She was a healthy high school freshman doing well academically. However, she admitted to texting about 4 hours per day for the last 2 years, which her mother confirmed. She was on her family’s unlimited SMS (short message service) texting plan.
During the examination, the patient sat slouched, holding her mobile phone with her right hand while texting with her right thumb. Tenderness of the right thumb was noted on the lateral aspect of the first proximal phalanx, the first interphalangeal joint, and the first metacarpal, especially along the surface of the extensor pollicis brevis, extensor pollicis longus, and abductor pollicis longus (APL) tendons. We noted local soft tissue swelling and mild erythema, but no nodularity was present. Thumb abduction aggravated the pain, which worsened when encountering resistance. There was no tenderness to palpation in the anatomical snuff box. Finkelstein’s test, Phalen’s test, Tinel’s sign, and Hoffman’s sign were negative.
Radiograph results were normal, with no evidence of acute injury, calcifications, or degenerative disease. Hematologic and biochemical investigations, including complete blood count with differential, erythrocyte sedimentation rate, basic metabolic profile, calcium, phosphate, and magnesium, yielded normal results.
These findings suggested a presumptive diagnosis of texting tendinitis. We managed the patient conservatively with a right thumb spica splint, aspirin as needed (pediatric dosing) for analgesia, and education about the proper application of ice. We also instructed her to modify her mobile phone texting activity.
At 1-month follow-up, the patient reported full resolution of her symptoms. In fact, her pain resolved after only 2 weeks of treatment, at which time she discontinued the splint and aspirin. Her parents had limited her mobile phone texting to 45 minutes per day and disallowed it after 8 pm. Soon thereafter, she switched to instant messaging as a means to stay in touch with her social networks (eg, Facebook, MySpace) while using all of her fingers more comfortably on a larger keyboard.
To our knowledge, this case report is the first one published from the United States describing texting tendinitis in an adolescent.
Injuries from texting: More common than we realize?
In The Medical Journal of Australia, Menz described acute texting tendinitis in a 13-year-old girl involving the abductor or extensor pollicis longus muscle; it resolved with conservative management.4 Ming et al subsequently reported a case of progressive first carpometacarpal joint arthritis due to excessive mobile phone texting in a 48-year-old man who recovered after undergoing an excision arthroplasty of the hand.5 Yoong observed texting tenosynovitis among school children who were sending more than 100 text messages daily.6
Storr et al reported on a 20-year-old woman with de Quervain’s tenosynovitis due to texting with her right thumb, and who later developed symptoms in her left hand after learning how to text with her left thumb.7 Similarly, Ashurst et al described a 48-year-old woman who developed bilateral de Quervain’s tenosynovitis from excessive texting activity.8
These clinical cases and our current report suggest there are variable presentations for texting-induced tendinopathy. As previously discussed by Gross, the mechanism of tendinitis injury involves stressors that are too high in magnitude, too frequent in repetition, or both.9
Recently, Gustafsson et al used an electrogoniometer and surface electromyography to examine thumb movements and muscular loads, respectively, during mobile phone use.10 They found that young adults with musculoskeletal symptoms had higher thumb movement velocities, fewer pauses in thumb movements, and higher APL activity than those without symptoms. Females showed higher thumb velocities, fewer pauses in thumb movements, and greater muscle activity in the APL and extensor digitorum than males. Those with musculoskeletal symptoms were more likely to sit with the head bent forward, to sit without forearm or back support, and to enter text using only one thumb, compared with those without symptoms.
In another study based on surveys administered to college students, Gold et al found that the number of text messages sent daily from handheld devices was associated with self-reports of neck and shoulder discomfort.11
So how can patients avoid injury?
While these cross-sectional studies of Gustafsson and Gold did not track patients with clinically confirmed tendinitis over time to assess the direct impact of specific interventions, the findings are still helpful. They define important risk factors for developing musculoskeletal symptoms, which translate into prevention recommendations for mobile phone users.
Their findings suggest that mobile phone users should:
- limit the duration of daily texting activity
- learn to text with both hands (ie, thumbs) rather than with one hand alone
- take frequent breaks
- avoid typing too fast
- ensure proper support of forearms and backs while texting
- maintain a comfortable posture, avoiding prolonged periods of slouching with the head bent forward.
Our patient incorporated many of these behavioral modifications (in addition to using the spica splint) and fully recovered.
Staying alert to possible texting injury. Using mobile phones for texting has become widespread only relatively recently. Therefore, it may be an underrecognized cause of tendinopathy, especially among young people. By identifying the correct mechanism of overuse injury, you can recommend appropriate behavioral changes for achieving optimal results.
CORRESPONDENCE
Isaiah W. Williams, MS, PA-C, 790 Sunset Avenue #4, Suisun City, CA 94585; iwwilliams16@hotmail.com
• Consider mobile phone texting as a possible cause of tendinitis in the hand. B
• Advise mobile phone users to text with both hands, take frequent breaks, and not type too fast. C
• Advise users to give proper support to their forearms and back while texting. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
In the United States, 173 billion text messages were sent monthly by 293 million cell phone subscribers, according to mid-year 2010 data.1 That’s about 20 daily text messages per subscriber. According to the Pew Research Center, 82% of US adults are cell phone users and 72% of adult cell phone users send or receive text messages.2 Based on a Kaiser Family Foundation study, cell phone ownership is 85% among 15- to 18-year olds, 69% among 11- to 14-year olds, and 31% among 8- to 10-year olds.3 This study reports that 7th to 12th graders, on average, spend 1 hour and 35 minutes each day texting and send 118 messages. Further, only 14% of these young people say their parents have established any rules about the number of texts they are allowed to send. Additionally, based on this same study, girls, older teens, and non-Hispanic blacks spend more time texting than other groups.
Case presentation
A 14-year-old non-Hispanic white girl, right-hand dominant, visited our rural family practice clinic because of “throbbing right thumb pain” that had gradually worsened over the past week. There was no history of trauma, participation in sports, or thumb/hand problems. She had no fever or other symptoms. She was a healthy high school freshman doing well academically. However, she admitted to texting about 4 hours per day for the last 2 years, which her mother confirmed. She was on her family’s unlimited SMS (short message service) texting plan.
During the examination, the patient sat slouched, holding her mobile phone with her right hand while texting with her right thumb. Tenderness of the right thumb was noted on the lateral aspect of the first proximal phalanx, the first interphalangeal joint, and the first metacarpal, especially along the surface of the extensor pollicis brevis, extensor pollicis longus, and abductor pollicis longus (APL) tendons. We noted local soft tissue swelling and mild erythema, but no nodularity was present. Thumb abduction aggravated the pain, which worsened when encountering resistance. There was no tenderness to palpation in the anatomical snuff box. Finkelstein’s test, Phalen’s test, Tinel’s sign, and Hoffman’s sign were negative.
Radiograph results were normal, with no evidence of acute injury, calcifications, or degenerative disease. Hematologic and biochemical investigations, including complete blood count with differential, erythrocyte sedimentation rate, basic metabolic profile, calcium, phosphate, and magnesium, yielded normal results.
These findings suggested a presumptive diagnosis of texting tendinitis. We managed the patient conservatively with a right thumb spica splint, aspirin as needed (pediatric dosing) for analgesia, and education about the proper application of ice. We also instructed her to modify her mobile phone texting activity.
At 1-month follow-up, the patient reported full resolution of her symptoms. In fact, her pain resolved after only 2 weeks of treatment, at which time she discontinued the splint and aspirin. Her parents had limited her mobile phone texting to 45 minutes per day and disallowed it after 8 pm. Soon thereafter, she switched to instant messaging as a means to stay in touch with her social networks (eg, Facebook, MySpace) while using all of her fingers more comfortably on a larger keyboard.
To our knowledge, this case report is the first one published from the United States describing texting tendinitis in an adolescent.
Injuries from texting: More common than we realize?
In The Medical Journal of Australia, Menz described acute texting tendinitis in a 13-year-old girl involving the abductor or extensor pollicis longus muscle; it resolved with conservative management.4 Ming et al subsequently reported a case of progressive first carpometacarpal joint arthritis due to excessive mobile phone texting in a 48-year-old man who recovered after undergoing an excision arthroplasty of the hand.5 Yoong observed texting tenosynovitis among school children who were sending more than 100 text messages daily.6
Storr et al reported on a 20-year-old woman with de Quervain’s tenosynovitis due to texting with her right thumb, and who later developed symptoms in her left hand after learning how to text with her left thumb.7 Similarly, Ashurst et al described a 48-year-old woman who developed bilateral de Quervain’s tenosynovitis from excessive texting activity.8
These clinical cases and our current report suggest there are variable presentations for texting-induced tendinopathy. As previously discussed by Gross, the mechanism of tendinitis injury involves stressors that are too high in magnitude, too frequent in repetition, or both.9
Recently, Gustafsson et al used an electrogoniometer and surface electromyography to examine thumb movements and muscular loads, respectively, during mobile phone use.10 They found that young adults with musculoskeletal symptoms had higher thumb movement velocities, fewer pauses in thumb movements, and higher APL activity than those without symptoms. Females showed higher thumb velocities, fewer pauses in thumb movements, and greater muscle activity in the APL and extensor digitorum than males. Those with musculoskeletal symptoms were more likely to sit with the head bent forward, to sit without forearm or back support, and to enter text using only one thumb, compared with those without symptoms.
In another study based on surveys administered to college students, Gold et al found that the number of text messages sent daily from handheld devices was associated with self-reports of neck and shoulder discomfort.11
So how can patients avoid injury?
While these cross-sectional studies of Gustafsson and Gold did not track patients with clinically confirmed tendinitis over time to assess the direct impact of specific interventions, the findings are still helpful. They define important risk factors for developing musculoskeletal symptoms, which translate into prevention recommendations for mobile phone users.
Their findings suggest that mobile phone users should:
- limit the duration of daily texting activity
- learn to text with both hands (ie, thumbs) rather than with one hand alone
- take frequent breaks
- avoid typing too fast
- ensure proper support of forearms and backs while texting
- maintain a comfortable posture, avoiding prolonged periods of slouching with the head bent forward.
Our patient incorporated many of these behavioral modifications (in addition to using the spica splint) and fully recovered.
Staying alert to possible texting injury. Using mobile phones for texting has become widespread only relatively recently. Therefore, it may be an underrecognized cause of tendinopathy, especially among young people. By identifying the correct mechanism of overuse injury, you can recommend appropriate behavioral changes for achieving optimal results.
CORRESPONDENCE
Isaiah W. Williams, MS, PA-C, 790 Sunset Avenue #4, Suisun City, CA 94585; iwwilliams16@hotmail.com
1. US wireless quick facts: mid-year figures. Available at: http://www.ctia.org/consumer_info/service/index.cfm/AID/10323. Accessed January 13, 2011.
2. The rise of apps culture. Available at: http://pewintemet.org/~/media//Files/Reports/2010/PIP_Nielsen%20Apps%20 Report.pdf. Accessed January 6, 2011.
3. Rideout VJ, Foehr UG, Roberts DF. Generation M2: media in the lives of 8- to 18-year-olds. A Kaiser Family Foundation study. January 2010. Available at: http://www.kff.org/entmedia/upload/8010.pdf. Accessed January 6, 2011.
4. Menz RJ. “Texting” tendinitis. Med J Aust. 2005;182:308.
5. Ming Z, Pietikainen S, Hanninen O. Excessive texting in pathophysiology of first carpometacarpal joint arthritis. Pathophysiology. 2006;13:269-270.
6. Yoong JK. Mobile phones can be a pain—text messaging tenosynovitis. Hosp Med. 2005;66:370.
7. Storr EF, de Vere Beavis FO, Stringer MD. Texting tenosynovitis. N Z Med J. 2007;120:U2868.
8. Ashurst JV, Turco DA, Lieb BE. Tenosynovitis caused by texting: an emerging disease. J Am Osteopath Assoc. 2010;110:294-296.
9. Gross MT. Chronic tendinitis: pathomechanics of injury, factors affecting the healing response, and treatment. J Orthop SportsPhys Ther. 1992;16:248-261.
10. Gustafsson E, Johnson PW, Hagberg M. Thumb postures and physical loads during mobile phone use-a comparison of young adults with and without musculoskeletal symptoms. J Electromyogr Kinesiol. 2010;20:127-135.
11. Gold JE, Kandadai V, Hanlon A. Text messaging and upper extremity symptoms in college students. Available at: http://apha.confex.com/recording/apha/137am/pdf/free/4db77adf5df9fff0d3caf5cafe28f496/paper201105_1.Pdf. Accessed January 6, 2011.
1. US wireless quick facts: mid-year figures. Available at: http://www.ctia.org/consumer_info/service/index.cfm/AID/10323. Accessed January 13, 2011.
2. The rise of apps culture. Available at: http://pewintemet.org/~/media//Files/Reports/2010/PIP_Nielsen%20Apps%20 Report.pdf. Accessed January 6, 2011.
3. Rideout VJ, Foehr UG, Roberts DF. Generation M2: media in the lives of 8- to 18-year-olds. A Kaiser Family Foundation study. January 2010. Available at: http://www.kff.org/entmedia/upload/8010.pdf. Accessed January 6, 2011.
4. Menz RJ. “Texting” tendinitis. Med J Aust. 2005;182:308.
5. Ming Z, Pietikainen S, Hanninen O. Excessive texting in pathophysiology of first carpometacarpal joint arthritis. Pathophysiology. 2006;13:269-270.
6. Yoong JK. Mobile phones can be a pain—text messaging tenosynovitis. Hosp Med. 2005;66:370.
7. Storr EF, de Vere Beavis FO, Stringer MD. Texting tenosynovitis. N Z Med J. 2007;120:U2868.
8. Ashurst JV, Turco DA, Lieb BE. Tenosynovitis caused by texting: an emerging disease. J Am Osteopath Assoc. 2010;110:294-296.
9. Gross MT. Chronic tendinitis: pathomechanics of injury, factors affecting the healing response, and treatment. J Orthop SportsPhys Ther. 1992;16:248-261.
10. Gustafsson E, Johnson PW, Hagberg M. Thumb postures and physical loads during mobile phone use-a comparison of young adults with and without musculoskeletal symptoms. J Electromyogr Kinesiol. 2010;20:127-135.
11. Gold JE, Kandadai V, Hanlon A. Text messaging and upper extremity symptoms in college students. Available at: http://apha.confex.com/recording/apha/137am/pdf/free/4db77adf5df9fff0d3caf5cafe28f496/paper201105_1.Pdf. Accessed January 6, 2011.