User login
Diabetes Report: The News Isn’t Good
According to the CDC’s recently released National Diabetes Statistics Report, 2014, an additional 3 million people developed diabetes between 2010 and 2012; but nearly 1 in 4 don’t know they have it. The report is based on 2012 data, which show that the number of people with diabetes rose from 26 million in 2010 to 29 million in 2012.
American Indians and Alaska Natives (AI/ANs) are most affected: 16% of AI/ANs aged ≥ 20 years have diabetes, compared with 13% of non-Hispanic blacks, 13% of Hispanics, 9% of Asian Americans, and 8% of non-Hispanic whites. But even those figures don’t tell the whole story. For instance, among AI/AN adults, the rate of diabetes ranges from 6% among Alaska Natives to 24% among American Indians in southern Arizona. Among Hispanic adults, Puerto Ricans (15%) and Mexican Americans (14%) have the highest rates, compared with 9% of Cubans and Central and South Americans. Among Asian Americans, 13% of Asian Indians and 11% of Filipinos have diabetes, vs 4% of Chinese.
Moreover, 1 in 3 American adults has prediabetes—an estimated 86 million. Without weight loss and moderate physical activity, the CDC predicts as many as 30% of American adults will develop diabetes within 5 years.
Diabetes is a public health concern that affects all age groups. According to SEARCH for Diabetes in Youth, a multicenter study, during 2008 and 2009, an estimated 18,436 Americans aged < 20 years were newly diagnosed with type 1 diabetes annually, and 5,089 were newly diagnosed with type 2 diabetes annually.
The physical costs are high. In 2010, diabetes was the seventh leading cause of death in the U.S. and may even have been underreported—only about 35% to 40% of death certificates for people with diabetes listed diabetes anywhere on the certificate. In 2011, hypoglycemia was the first-listed diagnosis for about 282,000 emergency department (ED) visits, and 175,000 ED visits were for hyperglycemic crisis. In 2010, 2,361 adults aged ≥ 20 years died of hyperglycemic crisis. In 2003 to 2006, after adjusting for population age differences, deaths due to cardiovascular disease were nearly doubled among adults aged ≥ 18 years with diagnosed diabetes, compared with adults without diagnosed diabetes. In 2010, diabetes also increased the rates of heart attack and stroke (1.8-fold and 1.5-fold, respectively) and in 2011 was the primary cause of kidney failure in 44% of all new cases.
The costs of care are high, as well. The CDC estimates the total medical costs associated with diabetes and its related complications for 2012 at $245 billion, up from $174 billion in 2010. Average medical expenses among people with diagnosed diabetes ran 2.3 times higher than for people without diabetes.
The report’s estimates were derived from a variety of sources, including CDC, IHS, NIH, and the U.S. Census Bureau; and published studies, including the 2009-2012 National Health and Nutrition Examination Survey (NHANES) and the 2010-2012 National Health Interview Survey (NHIS).
According to the CDC’s recently released National Diabetes Statistics Report, 2014, an additional 3 million people developed diabetes between 2010 and 2012; but nearly 1 in 4 don’t know they have it. The report is based on 2012 data, which show that the number of people with diabetes rose from 26 million in 2010 to 29 million in 2012.
American Indians and Alaska Natives (AI/ANs) are most affected: 16% of AI/ANs aged ≥ 20 years have diabetes, compared with 13% of non-Hispanic blacks, 13% of Hispanics, 9% of Asian Americans, and 8% of non-Hispanic whites. But even those figures don’t tell the whole story. For instance, among AI/AN adults, the rate of diabetes ranges from 6% among Alaska Natives to 24% among American Indians in southern Arizona. Among Hispanic adults, Puerto Ricans (15%) and Mexican Americans (14%) have the highest rates, compared with 9% of Cubans and Central and South Americans. Among Asian Americans, 13% of Asian Indians and 11% of Filipinos have diabetes, vs 4% of Chinese.
Moreover, 1 in 3 American adults has prediabetes—an estimated 86 million. Without weight loss and moderate physical activity, the CDC predicts as many as 30% of American adults will develop diabetes within 5 years.
Diabetes is a public health concern that affects all age groups. According to SEARCH for Diabetes in Youth, a multicenter study, during 2008 and 2009, an estimated 18,436 Americans aged < 20 years were newly diagnosed with type 1 diabetes annually, and 5,089 were newly diagnosed with type 2 diabetes annually.
The physical costs are high. In 2010, diabetes was the seventh leading cause of death in the U.S. and may even have been underreported—only about 35% to 40% of death certificates for people with diabetes listed diabetes anywhere on the certificate. In 2011, hypoglycemia was the first-listed diagnosis for about 282,000 emergency department (ED) visits, and 175,000 ED visits were for hyperglycemic crisis. In 2010, 2,361 adults aged ≥ 20 years died of hyperglycemic crisis. In 2003 to 2006, after adjusting for population age differences, deaths due to cardiovascular disease were nearly doubled among adults aged ≥ 18 years with diagnosed diabetes, compared with adults without diagnosed diabetes. In 2010, diabetes also increased the rates of heart attack and stroke (1.8-fold and 1.5-fold, respectively) and in 2011 was the primary cause of kidney failure in 44% of all new cases.
The costs of care are high, as well. The CDC estimates the total medical costs associated with diabetes and its related complications for 2012 at $245 billion, up from $174 billion in 2010. Average medical expenses among people with diagnosed diabetes ran 2.3 times higher than for people without diabetes.
The report’s estimates were derived from a variety of sources, including CDC, IHS, NIH, and the U.S. Census Bureau; and published studies, including the 2009-2012 National Health and Nutrition Examination Survey (NHANES) and the 2010-2012 National Health Interview Survey (NHIS).
According to the CDC’s recently released National Diabetes Statistics Report, 2014, an additional 3 million people developed diabetes between 2010 and 2012; but nearly 1 in 4 don’t know they have it. The report is based on 2012 data, which show that the number of people with diabetes rose from 26 million in 2010 to 29 million in 2012.
American Indians and Alaska Natives (AI/ANs) are most affected: 16% of AI/ANs aged ≥ 20 years have diabetes, compared with 13% of non-Hispanic blacks, 13% of Hispanics, 9% of Asian Americans, and 8% of non-Hispanic whites. But even those figures don’t tell the whole story. For instance, among AI/AN adults, the rate of diabetes ranges from 6% among Alaska Natives to 24% among American Indians in southern Arizona. Among Hispanic adults, Puerto Ricans (15%) and Mexican Americans (14%) have the highest rates, compared with 9% of Cubans and Central and South Americans. Among Asian Americans, 13% of Asian Indians and 11% of Filipinos have diabetes, vs 4% of Chinese.
Moreover, 1 in 3 American adults has prediabetes—an estimated 86 million. Without weight loss and moderate physical activity, the CDC predicts as many as 30% of American adults will develop diabetes within 5 years.
Diabetes is a public health concern that affects all age groups. According to SEARCH for Diabetes in Youth, a multicenter study, during 2008 and 2009, an estimated 18,436 Americans aged < 20 years were newly diagnosed with type 1 diabetes annually, and 5,089 were newly diagnosed with type 2 diabetes annually.
The physical costs are high. In 2010, diabetes was the seventh leading cause of death in the U.S. and may even have been underreported—only about 35% to 40% of death certificates for people with diabetes listed diabetes anywhere on the certificate. In 2011, hypoglycemia was the first-listed diagnosis for about 282,000 emergency department (ED) visits, and 175,000 ED visits were for hyperglycemic crisis. In 2010, 2,361 adults aged ≥ 20 years died of hyperglycemic crisis. In 2003 to 2006, after adjusting for population age differences, deaths due to cardiovascular disease were nearly doubled among adults aged ≥ 18 years with diagnosed diabetes, compared with adults without diagnosed diabetes. In 2010, diabetes also increased the rates of heart attack and stroke (1.8-fold and 1.5-fold, respectively) and in 2011 was the primary cause of kidney failure in 44% of all new cases.
The costs of care are high, as well. The CDC estimates the total medical costs associated with diabetes and its related complications for 2012 at $245 billion, up from $174 billion in 2010. Average medical expenses among people with diagnosed diabetes ran 2.3 times higher than for people without diabetes.
The report’s estimates were derived from a variety of sources, including CDC, IHS, NIH, and the U.S. Census Bureau; and published studies, including the 2009-2012 National Health and Nutrition Examination Survey (NHANES) and the 2010-2012 National Health Interview Survey (NHIS).
Proper Inpatient Documentation, Coding Essential to Avoid a Medicare Audit
Several years ago we sent a CPT coding auditor 15 chart notes generated by each doctor in our group. Among each doctors’ 15 notes were at least one or two billed as initial hospital care, follow up, discharge, critical care, and so on. This coding expert returned a report showing that, out of all the notes reviewed, a significant portion were not billed at the correct level. Most of the incorrectly billed notes were judged to reflect “up-coding,” and a few were seen as “down-coded.”
This was distressing and hard to believe.
So I took the same set of notes and paid a second coding expert for an independent review. She didn’t know about the first audit but returned a report that showed a nearly identical portion of incorrectly coded notes.
Two independent audits showing nearly the same portion of notes coded incorrectly was alarming. But it was difficult for my partners and me to address, because the auditors didn’t agree on the correct code for many of the notes. In some cases, both flagged a note as incorrectly coded but didn’t agree on the correct code. For a number of the notes, one auditor said the visit was “up-coded,” while the other said it was “down-coded.” There was so little agreement between the two of them that we had a hard time coming up with any firm conclusions about what we should do to improve our performance.
If experts who think about coding all the time can’t agree on the right code for a given note, how can hospitalists be expected to code nearly all of our visits accurately?
RAC: Recovery Audit Contractor
Despite what I believe is poor inter-rater reliability among coding auditors, we need to work diligently to comply with coding guidelines. A 2003 Federal law mandated a program of Recovery Audit Contractors, or RAC for short, to find cases of “up-coding” or other overbilling and require the provider to repay any resulting loss.
A number of companies are in the business of conducting RAC audits (one of them, CGI, is the Canadian company blamed for the failed “Obamacare” exchange websites), and there is a reasonable chance one of these companies has reviewed some of your charges—or those of your hospitalist colleagues.
The RAC auditors review information about your charges, and if they determine that you up-coded or overbilled, they send a “demand letter” summarizing their findings, along with the amount of money they have determined you should pay back. (Theoretically, they could notify you of “under-coding,” so that you can be paid more for past work, but I haven’t yet come across an example of that.)
It is common to appeal the RAC findings, but that can be a long process, and many organizations decide to pay back all the money requested by the RAC as quickly as possible to avoid paying interest on a delayed payment if the appeal is unsuccessful. In the case of a successful appeal, the money previously refunded by the doctor would be returned.
Page 338 of the CMS Fiscal Year 2015 “Justification of Estimates for Appropriations Committees” says that “…about 50 percent of the estimated 43,000 appeals [of adverse RAC audit findings] were fully or partially overturned…” This could mean the RACs are a sort of loose cannon, accusing many providers of overbilling while knowing that some won’t bother to appeal because they don’t understand the process or because the dollar amount involved for a single provider is too small to justify the time and expense of conducting the appeal. In this way, a RAC audit is like the $15 rebate on the last electronic gadget you bought. The seller knows that many people, including me, will fail to do the work required to claim the rebate.
Accuracy Strategies
There are a number of ways to help your group ensure appropriate CPT coding and reduce the chance a RAC will ask for money back.
Education. There are many ways to help providers in your practice understand the elements of documentation and coding. Periodic training classes (e.g. during orientation and annually thereafter) are useful but may not be enough. For me, this is a little like learning a foreign language by going to a couple of classes. Instead, I think “immersion training” is more effective. That might mean a doctor spends a few minutes with a certified coder on most working days for a few weeks. For example, they could meet for 15 minutes near lunchtime and review how the doctor plans to bill visits made that morning. Lastly, consider targeted education for each doctor, based on any problems found in an audit of his/her coding.
Review coding patterns. As I wrote in my August 2007 column, there is value in ensuring that each doctor in the group can see how her coding pattern differs from the group as a whole or any individual in the group. That is, what portion of follow-up visits was billed at the lowest, middle, and highest levels? What about admissions, discharges, and so on? I provided a sample report in that same column.
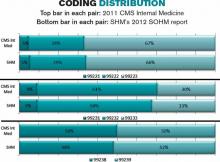
It also is worth taking the time to compare each doctor’s coding pattern to both the CMS Internal Medicine data and SHM’s State of Hospital Medicine report. The accompanying figure shows the most current data sets available.
Keep in mind that the goal is not to simply ensure that your coding pattern matches these external data sets; knowing where yours differs from these sets can suggest where you might want to investigate further or seek additional education.
Coding audits. Having a certified coder audit your performance at least annually is a good idea. It can help uncover areas in which you’d benefit from further review and training, and if, heaven forbid, questions are ever raised about whether you’re intentionally up-coding (fraud), showing that you’re audited regularly could help demonstrate your efforts to code correctly. In the latter case, it is probably more valuable if the audit is done independently of your employer.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Several years ago we sent a CPT coding auditor 15 chart notes generated by each doctor in our group. Among each doctors’ 15 notes were at least one or two billed as initial hospital care, follow up, discharge, critical care, and so on. This coding expert returned a report showing that, out of all the notes reviewed, a significant portion were not billed at the correct level. Most of the incorrectly billed notes were judged to reflect “up-coding,” and a few were seen as “down-coded.”
This was distressing and hard to believe.
So I took the same set of notes and paid a second coding expert for an independent review. She didn’t know about the first audit but returned a report that showed a nearly identical portion of incorrectly coded notes.
Two independent audits showing nearly the same portion of notes coded incorrectly was alarming. But it was difficult for my partners and me to address, because the auditors didn’t agree on the correct code for many of the notes. In some cases, both flagged a note as incorrectly coded but didn’t agree on the correct code. For a number of the notes, one auditor said the visit was “up-coded,” while the other said it was “down-coded.” There was so little agreement between the two of them that we had a hard time coming up with any firm conclusions about what we should do to improve our performance.
If experts who think about coding all the time can’t agree on the right code for a given note, how can hospitalists be expected to code nearly all of our visits accurately?
RAC: Recovery Audit Contractor
Despite what I believe is poor inter-rater reliability among coding auditors, we need to work diligently to comply with coding guidelines. A 2003 Federal law mandated a program of Recovery Audit Contractors, or RAC for short, to find cases of “up-coding” or other overbilling and require the provider to repay any resulting loss.
A number of companies are in the business of conducting RAC audits (one of them, CGI, is the Canadian company blamed for the failed “Obamacare” exchange websites), and there is a reasonable chance one of these companies has reviewed some of your charges—or those of your hospitalist colleagues.
The RAC auditors review information about your charges, and if they determine that you up-coded or overbilled, they send a “demand letter” summarizing their findings, along with the amount of money they have determined you should pay back. (Theoretically, they could notify you of “under-coding,” so that you can be paid more for past work, but I haven’t yet come across an example of that.)
It is common to appeal the RAC findings, but that can be a long process, and many organizations decide to pay back all the money requested by the RAC as quickly as possible to avoid paying interest on a delayed payment if the appeal is unsuccessful. In the case of a successful appeal, the money previously refunded by the doctor would be returned.
Page 338 of the CMS Fiscal Year 2015 “Justification of Estimates for Appropriations Committees” says that “…about 50 percent of the estimated 43,000 appeals [of adverse RAC audit findings] were fully or partially overturned…” This could mean the RACs are a sort of loose cannon, accusing many providers of overbilling while knowing that some won’t bother to appeal because they don’t understand the process or because the dollar amount involved for a single provider is too small to justify the time and expense of conducting the appeal. In this way, a RAC audit is like the $15 rebate on the last electronic gadget you bought. The seller knows that many people, including me, will fail to do the work required to claim the rebate.
Accuracy Strategies
There are a number of ways to help your group ensure appropriate CPT coding and reduce the chance a RAC will ask for money back.
Education. There are many ways to help providers in your practice understand the elements of documentation and coding. Periodic training classes (e.g. during orientation and annually thereafter) are useful but may not be enough. For me, this is a little like learning a foreign language by going to a couple of classes. Instead, I think “immersion training” is more effective. That might mean a doctor spends a few minutes with a certified coder on most working days for a few weeks. For example, they could meet for 15 minutes near lunchtime and review how the doctor plans to bill visits made that morning. Lastly, consider targeted education for each doctor, based on any problems found in an audit of his/her coding.
Review coding patterns. As I wrote in my August 2007 column, there is value in ensuring that each doctor in the group can see how her coding pattern differs from the group as a whole or any individual in the group. That is, what portion of follow-up visits was billed at the lowest, middle, and highest levels? What about admissions, discharges, and so on? I provided a sample report in that same column.
It also is worth taking the time to compare each doctor’s coding pattern to both the CMS Internal Medicine data and SHM’s State of Hospital Medicine report. The accompanying figure shows the most current data sets available.
Keep in mind that the goal is not to simply ensure that your coding pattern matches these external data sets; knowing where yours differs from these sets can suggest where you might want to investigate further or seek additional education.
Coding audits. Having a certified coder audit your performance at least annually is a good idea. It can help uncover areas in which you’d benefit from further review and training, and if, heaven forbid, questions are ever raised about whether you’re intentionally up-coding (fraud), showing that you’re audited regularly could help demonstrate your efforts to code correctly. In the latter case, it is probably more valuable if the audit is done independently of your employer.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Several years ago we sent a CPT coding auditor 15 chart notes generated by each doctor in our group. Among each doctors’ 15 notes were at least one or two billed as initial hospital care, follow up, discharge, critical care, and so on. This coding expert returned a report showing that, out of all the notes reviewed, a significant portion were not billed at the correct level. Most of the incorrectly billed notes were judged to reflect “up-coding,” and a few were seen as “down-coded.”
This was distressing and hard to believe.
So I took the same set of notes and paid a second coding expert for an independent review. She didn’t know about the first audit but returned a report that showed a nearly identical portion of incorrectly coded notes.
Two independent audits showing nearly the same portion of notes coded incorrectly was alarming. But it was difficult for my partners and me to address, because the auditors didn’t agree on the correct code for many of the notes. In some cases, both flagged a note as incorrectly coded but didn’t agree on the correct code. For a number of the notes, one auditor said the visit was “up-coded,” while the other said it was “down-coded.” There was so little agreement between the two of them that we had a hard time coming up with any firm conclusions about what we should do to improve our performance.
If experts who think about coding all the time can’t agree on the right code for a given note, how can hospitalists be expected to code nearly all of our visits accurately?
RAC: Recovery Audit Contractor
Despite what I believe is poor inter-rater reliability among coding auditors, we need to work diligently to comply with coding guidelines. A 2003 Federal law mandated a program of Recovery Audit Contractors, or RAC for short, to find cases of “up-coding” or other overbilling and require the provider to repay any resulting loss.
A number of companies are in the business of conducting RAC audits (one of them, CGI, is the Canadian company blamed for the failed “Obamacare” exchange websites), and there is a reasonable chance one of these companies has reviewed some of your charges—or those of your hospitalist colleagues.
The RAC auditors review information about your charges, and if they determine that you up-coded or overbilled, they send a “demand letter” summarizing their findings, along with the amount of money they have determined you should pay back. (Theoretically, they could notify you of “under-coding,” so that you can be paid more for past work, but I haven’t yet come across an example of that.)
It is common to appeal the RAC findings, but that can be a long process, and many organizations decide to pay back all the money requested by the RAC as quickly as possible to avoid paying interest on a delayed payment if the appeal is unsuccessful. In the case of a successful appeal, the money previously refunded by the doctor would be returned.
Page 338 of the CMS Fiscal Year 2015 “Justification of Estimates for Appropriations Committees” says that “…about 50 percent of the estimated 43,000 appeals [of adverse RAC audit findings] were fully or partially overturned…” This could mean the RACs are a sort of loose cannon, accusing many providers of overbilling while knowing that some won’t bother to appeal because they don’t understand the process or because the dollar amount involved for a single provider is too small to justify the time and expense of conducting the appeal. In this way, a RAC audit is like the $15 rebate on the last electronic gadget you bought. The seller knows that many people, including me, will fail to do the work required to claim the rebate.
Accuracy Strategies
There are a number of ways to help your group ensure appropriate CPT coding and reduce the chance a RAC will ask for money back.
Education. There are many ways to help providers in your practice understand the elements of documentation and coding. Periodic training classes (e.g. during orientation and annually thereafter) are useful but may not be enough. For me, this is a little like learning a foreign language by going to a couple of classes. Instead, I think “immersion training” is more effective. That might mean a doctor spends a few minutes with a certified coder on most working days for a few weeks. For example, they could meet for 15 minutes near lunchtime and review how the doctor plans to bill visits made that morning. Lastly, consider targeted education for each doctor, based on any problems found in an audit of his/her coding.
Review coding patterns. As I wrote in my August 2007 column, there is value in ensuring that each doctor in the group can see how her coding pattern differs from the group as a whole or any individual in the group. That is, what portion of follow-up visits was billed at the lowest, middle, and highest levels? What about admissions, discharges, and so on? I provided a sample report in that same column.
It also is worth taking the time to compare each doctor’s coding pattern to both the CMS Internal Medicine data and SHM’s State of Hospital Medicine report. The accompanying figure shows the most current data sets available.
Keep in mind that the goal is not to simply ensure that your coding pattern matches these external data sets; knowing where yours differs from these sets can suggest where you might want to investigate further or seek additional education.
Coding audits. Having a certified coder audit your performance at least annually is a good idea. It can help uncover areas in which you’d benefit from further review and training, and if, heaven forbid, questions are ever raised about whether you’re intentionally up-coding (fraud), showing that you’re audited regularly could help demonstrate your efforts to code correctly. In the latter case, it is probably more valuable if the audit is done independently of your employer.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Delay in ICD-10 Implementation to Impact Hospitalists, Physicians, Payers
On April 1, President Obama signed into law a bill that again delays a permanent fix of the sustainable growth rate formula, or SGR, the so-called “doc fix.” The bill also contained a surprise provision added by Congress to delay implementation of the switch from ICD-9 to ICD-10. The mandated conversion was supposed to take place by October 1 of this year; its delay will have a range of impacts on everyone from physicians to payers.
Hospitalists and others must weigh their options going forward, as many health systems and groups are already well on their way toward compliance with the 2014 deadline.
At this point, prevailing wisdom is that Congress added the delay as an appeasement to physician groups that would be unhappy about its failure to pass an SGR replacement, says Jeffrey Smith, senior director of federal affairs for CHIME, the College of Healthcare Information Management Executives.
“The appeasement, if in fact that was the motivation, was too little too late,” Smith says, adding Congress “caused a lot of unnecessary chaos.”
For instance, according to Modern Healthcare, executives at Catholic Health Initiatives had already invested millions of dollars updating software programs to handle the coding switch ahead of a new electronic health record system roll-out in 89 of its hospitals, which would not have been ready by the ICD-10 deadline.
“Anyone in the process has to circle the wagons again and reconsider their timelines,” Smith says. “The legislation has punished people trying to do the right thing.”
The transition to ICD-10 is a massive update to the 30-year-old ICD-9 codes, which no longer adequately reflect medical diagnoses, procedures, technology, and knowledge. There are five times more diagnosis codes and 21 times more procedural codes in ICD-10. It’s been on the table for at least a decade, and this was not the first delay.
In 2012, when fewer groups were on their way to compliance, CMS estimated that a one-year push-back of ICD-10 conversion could cost up to $306 million. With the latest delay, the American Health Information Management Association says CMS now estimates those costs between $1 billion and $6.6 billion.
However, according to the American Medical Association, which has actively lobbied to stop ICD-10 altogether, the costs of implementing ICD-10 range from $57,000 for small physician practices to as high as $8 million for large practices.
The increased number of codes, the increased number of characters per code, and the increased specificity require significant planning, training, software updates, and financial investments.
The Medical Group Management Association (MGMA) also pushed for ICD-10 delay, concerned that many groups would not be ready by Oct. 1. MGMA surveys showed as much, says Robert Tennant, senior policy advisor for MGMA.“We were concerned that if everyone has to flip the switch at the same time, there will be huge problems, as there were for healthcare.gov,” Tennant explains.
What MGMA would like to see is more thorough end-to-end testing and staggered roll-outs. Hospitals and health plans should be permitted to start using ICD-10 coding when they're ready, even if ahead of the next deadline, Tennant said. MGMA would also like to see a period of dual coding built in.
The ball is now in CMS' court.
“I think that CMS has within its power … the ability to embolden the industry to be more confident,” Smith says. “Even if it’s not going to require ICD-10 codes [by October 2014], hopefully they are still doing testing, still doing benchmarking, and by the time the deadline rolls around, it will touch every sector of the healthcare economy.”
Hospitalists, Smith says, should be more involved in the conversation going forward, to help maintain the momentum and preserve the investments made by their groups and institutions. Those not ready should push for compliance, rather than finding themselves in the same position a year from now.
Many of the hospital CIOs (chief information officers) he has talked to say that while they are stopping the car, they are keeping the engine running. Some will push for dual coding, even if only internally, because it’s proving to be a valuable tool in understanding their patient populations.
“It’s a frustrating time any time you have to kind of stop something with so much momentum, with hundreds of millions, if not billions, spent in advance of the conversion,” Smith says. “It does nothing to help care in this country to stay on ICD-9. Everybody understands those codes are completely exhausted, and the data we are getting out of it, while workable, is certainly not going to get us where we need to be in terms of transforming healthcare.”
Kelly April Tyrrell is a freelance writer in Madison, Wis.
On April 1, President Obama signed into law a bill that again delays a permanent fix of the sustainable growth rate formula, or SGR, the so-called “doc fix.” The bill also contained a surprise provision added by Congress to delay implementation of the switch from ICD-9 to ICD-10. The mandated conversion was supposed to take place by October 1 of this year; its delay will have a range of impacts on everyone from physicians to payers.
Hospitalists and others must weigh their options going forward, as many health systems and groups are already well on their way toward compliance with the 2014 deadline.
At this point, prevailing wisdom is that Congress added the delay as an appeasement to physician groups that would be unhappy about its failure to pass an SGR replacement, says Jeffrey Smith, senior director of federal affairs for CHIME, the College of Healthcare Information Management Executives.
“The appeasement, if in fact that was the motivation, was too little too late,” Smith says, adding Congress “caused a lot of unnecessary chaos.”
For instance, according to Modern Healthcare, executives at Catholic Health Initiatives had already invested millions of dollars updating software programs to handle the coding switch ahead of a new electronic health record system roll-out in 89 of its hospitals, which would not have been ready by the ICD-10 deadline.
“Anyone in the process has to circle the wagons again and reconsider their timelines,” Smith says. “The legislation has punished people trying to do the right thing.”
The transition to ICD-10 is a massive update to the 30-year-old ICD-9 codes, which no longer adequately reflect medical diagnoses, procedures, technology, and knowledge. There are five times more diagnosis codes and 21 times more procedural codes in ICD-10. It’s been on the table for at least a decade, and this was not the first delay.
In 2012, when fewer groups were on their way to compliance, CMS estimated that a one-year push-back of ICD-10 conversion could cost up to $306 million. With the latest delay, the American Health Information Management Association says CMS now estimates those costs between $1 billion and $6.6 billion.
However, according to the American Medical Association, which has actively lobbied to stop ICD-10 altogether, the costs of implementing ICD-10 range from $57,000 for small physician practices to as high as $8 million for large practices.
The increased number of codes, the increased number of characters per code, and the increased specificity require significant planning, training, software updates, and financial investments.
The Medical Group Management Association (MGMA) also pushed for ICD-10 delay, concerned that many groups would not be ready by Oct. 1. MGMA surveys showed as much, says Robert Tennant, senior policy advisor for MGMA.“We were concerned that if everyone has to flip the switch at the same time, there will be huge problems, as there were for healthcare.gov,” Tennant explains.
What MGMA would like to see is more thorough end-to-end testing and staggered roll-outs. Hospitals and health plans should be permitted to start using ICD-10 coding when they're ready, even if ahead of the next deadline, Tennant said. MGMA would also like to see a period of dual coding built in.
The ball is now in CMS' court.
“I think that CMS has within its power … the ability to embolden the industry to be more confident,” Smith says. “Even if it’s not going to require ICD-10 codes [by October 2014], hopefully they are still doing testing, still doing benchmarking, and by the time the deadline rolls around, it will touch every sector of the healthcare economy.”
Hospitalists, Smith says, should be more involved in the conversation going forward, to help maintain the momentum and preserve the investments made by their groups and institutions. Those not ready should push for compliance, rather than finding themselves in the same position a year from now.
Many of the hospital CIOs (chief information officers) he has talked to say that while they are stopping the car, they are keeping the engine running. Some will push for dual coding, even if only internally, because it’s proving to be a valuable tool in understanding their patient populations.
“It’s a frustrating time any time you have to kind of stop something with so much momentum, with hundreds of millions, if not billions, spent in advance of the conversion,” Smith says. “It does nothing to help care in this country to stay on ICD-9. Everybody understands those codes are completely exhausted, and the data we are getting out of it, while workable, is certainly not going to get us where we need to be in terms of transforming healthcare.”
Kelly April Tyrrell is a freelance writer in Madison, Wis.
On April 1, President Obama signed into law a bill that again delays a permanent fix of the sustainable growth rate formula, or SGR, the so-called “doc fix.” The bill also contained a surprise provision added by Congress to delay implementation of the switch from ICD-9 to ICD-10. The mandated conversion was supposed to take place by October 1 of this year; its delay will have a range of impacts on everyone from physicians to payers.
Hospitalists and others must weigh their options going forward, as many health systems and groups are already well on their way toward compliance with the 2014 deadline.
At this point, prevailing wisdom is that Congress added the delay as an appeasement to physician groups that would be unhappy about its failure to pass an SGR replacement, says Jeffrey Smith, senior director of federal affairs for CHIME, the College of Healthcare Information Management Executives.
“The appeasement, if in fact that was the motivation, was too little too late,” Smith says, adding Congress “caused a lot of unnecessary chaos.”
For instance, according to Modern Healthcare, executives at Catholic Health Initiatives had already invested millions of dollars updating software programs to handle the coding switch ahead of a new electronic health record system roll-out in 89 of its hospitals, which would not have been ready by the ICD-10 deadline.
“Anyone in the process has to circle the wagons again and reconsider their timelines,” Smith says. “The legislation has punished people trying to do the right thing.”
The transition to ICD-10 is a massive update to the 30-year-old ICD-9 codes, which no longer adequately reflect medical diagnoses, procedures, technology, and knowledge. There are five times more diagnosis codes and 21 times more procedural codes in ICD-10. It’s been on the table for at least a decade, and this was not the first delay.
In 2012, when fewer groups were on their way to compliance, CMS estimated that a one-year push-back of ICD-10 conversion could cost up to $306 million. With the latest delay, the American Health Information Management Association says CMS now estimates those costs between $1 billion and $6.6 billion.
However, according to the American Medical Association, which has actively lobbied to stop ICD-10 altogether, the costs of implementing ICD-10 range from $57,000 for small physician practices to as high as $8 million for large practices.
The increased number of codes, the increased number of characters per code, and the increased specificity require significant planning, training, software updates, and financial investments.
The Medical Group Management Association (MGMA) also pushed for ICD-10 delay, concerned that many groups would not be ready by Oct. 1. MGMA surveys showed as much, says Robert Tennant, senior policy advisor for MGMA.“We were concerned that if everyone has to flip the switch at the same time, there will be huge problems, as there were for healthcare.gov,” Tennant explains.
What MGMA would like to see is more thorough end-to-end testing and staggered roll-outs. Hospitals and health plans should be permitted to start using ICD-10 coding when they're ready, even if ahead of the next deadline, Tennant said. MGMA would also like to see a period of dual coding built in.
The ball is now in CMS' court.
“I think that CMS has within its power … the ability to embolden the industry to be more confident,” Smith says. “Even if it’s not going to require ICD-10 codes [by October 2014], hopefully they are still doing testing, still doing benchmarking, and by the time the deadline rolls around, it will touch every sector of the healthcare economy.”
Hospitalists, Smith says, should be more involved in the conversation going forward, to help maintain the momentum and preserve the investments made by their groups and institutions. Those not ready should push for compliance, rather than finding themselves in the same position a year from now.
Many of the hospital CIOs (chief information officers) he has talked to say that while they are stopping the car, they are keeping the engine running. Some will push for dual coding, even if only internally, because it’s proving to be a valuable tool in understanding their patient populations.
“It’s a frustrating time any time you have to kind of stop something with so much momentum, with hundreds of millions, if not billions, spent in advance of the conversion,” Smith says. “It does nothing to help care in this country to stay on ICD-9. Everybody understands those codes are completely exhausted, and the data we are getting out of it, while workable, is certainly not going to get us where we need to be in terms of transforming healthcare.”
Kelly April Tyrrell is a freelance writer in Madison, Wis.
Medicare Rule Change Raises Stakes for Hospital Discharge Planning
When she presents information to hospitalists about the little-known revision to Medicare’s condition of participation for discharge planning by hospitals, most hospitalists have no idea what Amy Boutwell, MD, MPP, is talking about. Even hospitalists who are active in their institutions’ efforts to improve transitions of care out of the hospital setting are unaware of the change, which was published in the Centers for Medicare & Medicaid Services’ Transmittal 87 and became effective July 19, 2013.
“I just don’t hear hospital professionals talking about it,” says Dr. Boutwell, a hospitalist at Newton-Wellesley Hospital and president of Collaborative Healthcare Strategies in Lexington, Mass. “When I say, ‘There are new rules of the road for discharge planning and evaluation,’ many are not aware of it.”
The revised condition states that the hospital must have a discharge planning process that applies to all patients—not just Medicare beneficiaries. Not every patient needs to have a written discharge plan—although this is recommended—but all patients should be screened and, if indicated, evaluated at an early stage of their hospitalization for risk of adverse post-discharge outcomes. Observation patients are not included in this requirement.
The discharge plan is different from a discharge summary document, which must be completed by the inpatient attending physician, not the hospital, and is not directly addressed in the regulation. The regulation does address the need for transfer of essential information to the next provider of care and says the hospital should have a written policy and procedure in place for discharge planning. The policy and procedure should be developed with input from medical staff and approved by the hospital’s governing body.
Any hospitalist participating with a hospital QI team involved in Project BOOST is helping their hospital comply with this condition of participation.
—Mark Williams, MD, FACP, SFHM, principal investigator of SHM’s Project BOOST
Transmittal 87 represents the first major update of the discharge planning regulation (Standard 482.43) and accompanying interpretive guidelines in more than a decade, Dr. Boutwell says. It consolidates and reorganizes 24 “tags” of regulatory language down to 13 and contains blue advisory boxes recommending best practices in discharge planning, drawn from the suggestions of a technical expert panel convened by CMS.
That panel included many of the country’s recognized thought leaders on improving care transitions, such as Mark Williams, MD, FACP, SFHM, principal investigator of SHM’s Project BOOST; Eric Coleman, MD, MPH, head of the University of Colorado’s division of health care policy and research and creator of the widely-adopted Care Transitions Program (caretransitions.org), and Dr. Boutwell, co-founder of the STAAR initiative (www.ihi.org/engage/Initiatives/completed/STAAR).
The new condition raises baseline expectations for discharge planning and elevates care transitions efforts from a quality improvement issue to the realm of regulatory compliance, Dr. Boutwell says.
“This goes way beyond case review,” she adds. “It represents an evolution from discharge planning case by case to a system for improving transitions of care [for the hospital]. I’m impressed.”
The recommendations are consistent with best practices promoted by Project BOOST, STAAR, Project RED [Re-Engineered Discharge], and other national quality initiatives for improving care transitions.
“Any hospitalist participating with a hospital QI team involved in Project BOOST is helping their hospital comply with this condition of participation,” Dr. Williams says.
In the Byzantine structure of federal regulations, Medicare’s conditions of participation are the regulations providers must meet in order to participate in the Medicare program and bill for their services. Condition-level citations, if not resolved, can cause hospitals to be decertified from Medicare. The accompanying interpretive guidelines, with survey protocols, are the playbook to help state auditors and providers know how to interpret and apply the language of the regulations. The suggestions and examples of best practices contained in the new condition are not required of hospitals but, if followed, could increase their likelihood of achieving better patient outcomes and staying in compliance with the regulations on surveys.
“If hospitals were to actually implement all of the CMS advisory practice recommendations contained in this 35-page document, they’d be in really good shape for effectively managing transitions of care,” says Teresa L. Hamblin, RN, MS, a CMS consultant with Joint Commission Resources. “The government has provided robust practice recommendations that are a model for what hospitals can do. I’d advise doing your best to implement these recommendations. Check your current processes using this detailed document for reference.”
Discharge planning starts at admission, Hamblin says. If the hospitalist assumes that responsibility, it becomes easier to leave a paper trail in the patient’s chart. Other important lessons for hospitalists include participation in a multidisciplinary approach to discharge planning (i.e., interdisciplinary rounding) and development of policies and procedures in this area.
“If the hospital has not elected to do a discharge plan on every patient, request this for your own patients and recommend it as a policy,” Hamblin says. “Go the extra mile, making follow-up appointments for your patients, filling prescriptions in house, and calling the patient 24 to 72 hours after discharge.”
Weekend coverage, when case managers typically are not present, is a particular challenge in care transitions.
“Encourage your hospital to provide reliable weekend coverage for discharge planning. Involve the nurses,” Hamblin says. “Anything the hospitalist can do to help the hospital close this gap is important.”
Larry Beresford is a freelance writer in Alameda, Calif.
When she presents information to hospitalists about the little-known revision to Medicare’s condition of participation for discharge planning by hospitals, most hospitalists have no idea what Amy Boutwell, MD, MPP, is talking about. Even hospitalists who are active in their institutions’ efforts to improve transitions of care out of the hospital setting are unaware of the change, which was published in the Centers for Medicare & Medicaid Services’ Transmittal 87 and became effective July 19, 2013.
“I just don’t hear hospital professionals talking about it,” says Dr. Boutwell, a hospitalist at Newton-Wellesley Hospital and president of Collaborative Healthcare Strategies in Lexington, Mass. “When I say, ‘There are new rules of the road for discharge planning and evaluation,’ many are not aware of it.”
The revised condition states that the hospital must have a discharge planning process that applies to all patients—not just Medicare beneficiaries. Not every patient needs to have a written discharge plan—although this is recommended—but all patients should be screened and, if indicated, evaluated at an early stage of their hospitalization for risk of adverse post-discharge outcomes. Observation patients are not included in this requirement.
The discharge plan is different from a discharge summary document, which must be completed by the inpatient attending physician, not the hospital, and is not directly addressed in the regulation. The regulation does address the need for transfer of essential information to the next provider of care and says the hospital should have a written policy and procedure in place for discharge planning. The policy and procedure should be developed with input from medical staff and approved by the hospital’s governing body.
Any hospitalist participating with a hospital QI team involved in Project BOOST is helping their hospital comply with this condition of participation.
—Mark Williams, MD, FACP, SFHM, principal investigator of SHM’s Project BOOST
Transmittal 87 represents the first major update of the discharge planning regulation (Standard 482.43) and accompanying interpretive guidelines in more than a decade, Dr. Boutwell says. It consolidates and reorganizes 24 “tags” of regulatory language down to 13 and contains blue advisory boxes recommending best practices in discharge planning, drawn from the suggestions of a technical expert panel convened by CMS.
That panel included many of the country’s recognized thought leaders on improving care transitions, such as Mark Williams, MD, FACP, SFHM, principal investigator of SHM’s Project BOOST; Eric Coleman, MD, MPH, head of the University of Colorado’s division of health care policy and research and creator of the widely-adopted Care Transitions Program (caretransitions.org), and Dr. Boutwell, co-founder of the STAAR initiative (www.ihi.org/engage/Initiatives/completed/STAAR).
The new condition raises baseline expectations for discharge planning and elevates care transitions efforts from a quality improvement issue to the realm of regulatory compliance, Dr. Boutwell says.
“This goes way beyond case review,” she adds. “It represents an evolution from discharge planning case by case to a system for improving transitions of care [for the hospital]. I’m impressed.”
The recommendations are consistent with best practices promoted by Project BOOST, STAAR, Project RED [Re-Engineered Discharge], and other national quality initiatives for improving care transitions.
“Any hospitalist participating with a hospital QI team involved in Project BOOST is helping their hospital comply with this condition of participation,” Dr. Williams says.
In the Byzantine structure of federal regulations, Medicare’s conditions of participation are the regulations providers must meet in order to participate in the Medicare program and bill for their services. Condition-level citations, if not resolved, can cause hospitals to be decertified from Medicare. The accompanying interpretive guidelines, with survey protocols, are the playbook to help state auditors and providers know how to interpret and apply the language of the regulations. The suggestions and examples of best practices contained in the new condition are not required of hospitals but, if followed, could increase their likelihood of achieving better patient outcomes and staying in compliance with the regulations on surveys.
“If hospitals were to actually implement all of the CMS advisory practice recommendations contained in this 35-page document, they’d be in really good shape for effectively managing transitions of care,” says Teresa L. Hamblin, RN, MS, a CMS consultant with Joint Commission Resources. “The government has provided robust practice recommendations that are a model for what hospitals can do. I’d advise doing your best to implement these recommendations. Check your current processes using this detailed document for reference.”
Discharge planning starts at admission, Hamblin says. If the hospitalist assumes that responsibility, it becomes easier to leave a paper trail in the patient’s chart. Other important lessons for hospitalists include participation in a multidisciplinary approach to discharge planning (i.e., interdisciplinary rounding) and development of policies and procedures in this area.
“If the hospital has not elected to do a discharge plan on every patient, request this for your own patients and recommend it as a policy,” Hamblin says. “Go the extra mile, making follow-up appointments for your patients, filling prescriptions in house, and calling the patient 24 to 72 hours after discharge.”
Weekend coverage, when case managers typically are not present, is a particular challenge in care transitions.
“Encourage your hospital to provide reliable weekend coverage for discharge planning. Involve the nurses,” Hamblin says. “Anything the hospitalist can do to help the hospital close this gap is important.”
Larry Beresford is a freelance writer in Alameda, Calif.
When she presents information to hospitalists about the little-known revision to Medicare’s condition of participation for discharge planning by hospitals, most hospitalists have no idea what Amy Boutwell, MD, MPP, is talking about. Even hospitalists who are active in their institutions’ efforts to improve transitions of care out of the hospital setting are unaware of the change, which was published in the Centers for Medicare & Medicaid Services’ Transmittal 87 and became effective July 19, 2013.
“I just don’t hear hospital professionals talking about it,” says Dr. Boutwell, a hospitalist at Newton-Wellesley Hospital and president of Collaborative Healthcare Strategies in Lexington, Mass. “When I say, ‘There are new rules of the road for discharge planning and evaluation,’ many are not aware of it.”
The revised condition states that the hospital must have a discharge planning process that applies to all patients—not just Medicare beneficiaries. Not every patient needs to have a written discharge plan—although this is recommended—but all patients should be screened and, if indicated, evaluated at an early stage of their hospitalization for risk of adverse post-discharge outcomes. Observation patients are not included in this requirement.
The discharge plan is different from a discharge summary document, which must be completed by the inpatient attending physician, not the hospital, and is not directly addressed in the regulation. The regulation does address the need for transfer of essential information to the next provider of care and says the hospital should have a written policy and procedure in place for discharge planning. The policy and procedure should be developed with input from medical staff and approved by the hospital’s governing body.
Any hospitalist participating with a hospital QI team involved in Project BOOST is helping their hospital comply with this condition of participation.
—Mark Williams, MD, FACP, SFHM, principal investigator of SHM’s Project BOOST
Transmittal 87 represents the first major update of the discharge planning regulation (Standard 482.43) and accompanying interpretive guidelines in more than a decade, Dr. Boutwell says. It consolidates and reorganizes 24 “tags” of regulatory language down to 13 and contains blue advisory boxes recommending best practices in discharge planning, drawn from the suggestions of a technical expert panel convened by CMS.
That panel included many of the country’s recognized thought leaders on improving care transitions, such as Mark Williams, MD, FACP, SFHM, principal investigator of SHM’s Project BOOST; Eric Coleman, MD, MPH, head of the University of Colorado’s division of health care policy and research and creator of the widely-adopted Care Transitions Program (caretransitions.org), and Dr. Boutwell, co-founder of the STAAR initiative (www.ihi.org/engage/Initiatives/completed/STAAR).
The new condition raises baseline expectations for discharge planning and elevates care transitions efforts from a quality improvement issue to the realm of regulatory compliance, Dr. Boutwell says.
“This goes way beyond case review,” she adds. “It represents an evolution from discharge planning case by case to a system for improving transitions of care [for the hospital]. I’m impressed.”
The recommendations are consistent with best practices promoted by Project BOOST, STAAR, Project RED [Re-Engineered Discharge], and other national quality initiatives for improving care transitions.
“Any hospitalist participating with a hospital QI team involved in Project BOOST is helping their hospital comply with this condition of participation,” Dr. Williams says.
In the Byzantine structure of federal regulations, Medicare’s conditions of participation are the regulations providers must meet in order to participate in the Medicare program and bill for their services. Condition-level citations, if not resolved, can cause hospitals to be decertified from Medicare. The accompanying interpretive guidelines, with survey protocols, are the playbook to help state auditors and providers know how to interpret and apply the language of the regulations. The suggestions and examples of best practices contained in the new condition are not required of hospitals but, if followed, could increase their likelihood of achieving better patient outcomes and staying in compliance with the regulations on surveys.
“If hospitals were to actually implement all of the CMS advisory practice recommendations contained in this 35-page document, they’d be in really good shape for effectively managing transitions of care,” says Teresa L. Hamblin, RN, MS, a CMS consultant with Joint Commission Resources. “The government has provided robust practice recommendations that are a model for what hospitals can do. I’d advise doing your best to implement these recommendations. Check your current processes using this detailed document for reference.”
Discharge planning starts at admission, Hamblin says. If the hospitalist assumes that responsibility, it becomes easier to leave a paper trail in the patient’s chart. Other important lessons for hospitalists include participation in a multidisciplinary approach to discharge planning (i.e., interdisciplinary rounding) and development of policies and procedures in this area.
“If the hospital has not elected to do a discharge plan on every patient, request this for your own patients and recommend it as a policy,” Hamblin says. “Go the extra mile, making follow-up appointments for your patients, filling prescriptions in house, and calling the patient 24 to 72 hours after discharge.”
Weekend coverage, when case managers typically are not present, is a particular challenge in care transitions.
“Encourage your hospital to provide reliable weekend coverage for discharge planning. Involve the nurses,” Hamblin says. “Anything the hospitalist can do to help the hospital close this gap is important.”
Larry Beresford is a freelance writer in Alameda, Calif.
SGR Reform, ICD-10 Implementation Delays Frustrate Hospitalists, Physicians
Congress has once again delayed implementation of draconian Medicare cuts tied to the sustainable growth rate (SGR) formula. It was the 17th temporary patch applied to the ailing physician reimbursement program, so the decision caused little surprise.
But with the same legislation—the Protecting Access to Medicare Act of 2014—being used to delay the long-awaited debut of ICD-10, many hospitalists and physicians couldn’t help but wonder whether billing and coding would now be as much of a political football as the SGR fix.1
The upshot: It doesn’t seem that way.
“I think it’s two separate issues,” says Phyllis “PJ” Floyd, RN, BSN, MBA, NE-BC, CCA, director of health information services and clinical documentation improvement at Medical University of South Carolina (MUSC) in Charleston, S.C. “The fact that it was all in one bill, I don’t know that it was well thought out as much as it was, ‘Let’s put the ICD-10 in here at the same time.’
“It was just a few sentences, and then it wasn’t even brought up in the discussion on the floor.”
Four policy wonks interviewed by The Hospitalist concurred that while tying the ICD-10 delay to the SGR issue was an unexpected and frustrating development, the coding system likely will be implemented in the relative short term. Meanwhile, a long-term resolution of the SGR dilemma remains much more elusive.
“For about 12 hours, I felt relief about the ICD-10 [being delayed], and then I just realized, it’s still coming, presumably,” says John Nelson, MD, MHM, a co-founder and past president of SHM and medical director of the hospitalist practice at Overlake Hospital Medical Center in Bellevue, Wash. “[It’s] like a patient who needs surgery and finds out it’s canceled for the day and he’ll have it tomorrow. Well, that’s good for right now, but [he] still has to face this eventually.”
“Doc-Pay” Fix Near?
Congress’ recent decision to delay both an SGR fix and the ICD-10 are troubling to some hospitalists and others for different reasons.
The SGR extension through this year’s end means that physicians do not face a 24% cut to physician payments under Medicare. SHM has long lobbied against temporary patches to the SGR, repeatedly backing legislation that would once and for all scrap the formula and replace it with something sustainable.
The SGR formula was first crafted in 1997, but the now often-delayed cuts were a byproduct of the federal sequester that was included in the Budget Control Act of 2011. At the time, the massive reduction to Medicare payments was tied to political brinksmanship over the country’s debt ceiling. The cuts were implemented as a doomsday scenario that was never likely to actually happen, but despite negotiations over the past three years, no long-term compromise can be found. Paying for the reform remains the main stumbling block.
“I think, this year, Congress was as close as it’s been in a long time to enacting a serious fix, aided by the agreement of major professional societies like the American College of Physicians and American College of Surgeons,” says David Howard, PhD, an associate professor in the department of health policy and management at the Rollins School of Public Health at Emory University in Atlanta. “They were all on board with this solution. ... Who knows, maybe if the economic situation continues to improve [and] tax revenues continue to go up...that will create a more favorable environment for compromise.”
Dr. Howard adds that while Congress might be close to a solution in theory, agreement on how to offset the roughly $100 billion in costs “is just very difficult.” That is why the healthcare professor is pessimistic that a long-term fix is truly at hand.
“The places where Congress might have looked for savings to offset the cost of the doc fix, such as hospital reimbursement rates or payment rates to Medicare Advantage plans—those are exactly the areas that the Affordable Care Act is targeting to pay for insurance expansion,” Dr. Howard adds. “So those areas of savings are not going to be available to offset the cost of the doc fix.”
ICD-10 Delays “Unfair”
The medical coding conundrum presents a different set of issues. The delay in transitioning healthcare providers from the ICD-9 medical coding classification system to the more complicated ICD-10 means the upgraded system is now against an Oct. 1, 2015, deadline. This comes after the Centers for Medicare & Medicaid Services (CMS) already pushed back the original implementation date for ICD-10 by one year.
SHM Public Policy Committee member Joshua Lenchus, DO, RPh, FACP, SFHM, says he thinks most doctors are content with the delay, particularly in light of some estimates that show that only about 20% of physicians “have actually initiated the ICD-10 transition.” But he also notes that it’s unfair to the health systems that have prepared for ICD-10.
“ICD-9 has a little more than 14,000 diagnostic codes and nearly 4,000 procedural codes. That is to be contrasted to ICD-10, which has more than 68,000 diagnostic codes ... and over 72,000 procedural codes,” Dr. Lenchus says. “So, it is not surprising that many take solace in the delay.”
–Dr. Lenchus
Dr. Nelson says the level of frustration for hospitalists is growing; however, the level of disruption for hospitals and health systems is reaching a boiling point.
“Of course, in some places, hospitalists may be the physician lead on ICD-10 efforts, so [they are] very much wrapped up in the problem of ‘What do we do now?’”
The answer, at least to the Coalition for ICD-10, a group of medical/technology trade groups, is to fight to ensure that the delays go no further. In an April letter to CMS Administrator Marilyn Tavenner, the coalition made that case, noting that in 2012, “CMS estimated the cost to the healthcare industry of a one-year delay to be as much as $6.6 billion, or approximately 30% of the $22 billion that CMS estimated had been invested or budgeted for ICD-10 implementation.”2
The letter went on to explain that the disruption and cost will grow each time the ICD-10 deadline is pushed.
“Furthermore, as CMS stated in 2012, implementation costs will continue to increase considerably with every year of a delay,” according to the letter. “The lost opportunity costs of failing to move to a more effective code set also continue to climb every year.”
Stay Engaged, Switch Gears
One of Floyd’s biggest concerns is that the ICD-10 implementation delays will affect physician engagement. The hospitalist groups at MUSC began training for ICD-10 in January 2013; however, the preparation and training were geared toward a 2014 implementation.
“You have to switch gears a little bit,” she says. “What we plan to do now is begin to do heavy auditing, and then from those audits we can give real-time feedback on what we’re doing well and what we’re not doing well. So I think that will be a method for engagement.”
She urges hospitalists, practice leaders, and informatics professionals to discuss ICD-10 not as a theoretical application, but as one tied to reimbursement that will have major impact in the years ahead. To that end, the American Health Information Management Association highlights the fact that the new coding system will result in higher-quality data that can improve performance measures, provide “increased sensitivity” to reimbursement methodologies, and help with stronger public health surveillance.3
“A lot of physicians see this as a hospital issue, and I think that’s why they shy away,” Floyd says. “Now there are some physicians who are interested in how well the hospital does, but the other piece is that it does affect things like [reduced] risk of mortality [and] comparison of data worldwide—those are things that we just have to continue to reiterate … and give them real examples.”
Richard Quinn is a freelance writer in New Jersey.
References
- Govtrack. H.R. 4302: Protecting Access to Medicare Act of 2014. https://www.govtrack.us/congress/bills/113/hr4302. Accessed June 5, 2014.
- Coalition for ICD. Letter to CMS Administrator Tavenner, April 11, 2014. http://coalitionforicd10.wordpress.com/2014/03/26/letter-from-the-coalition-for-icd-10. Accessed June 5, 2014.
- American Health Information Management Association. ICD-10-CM/PCS Transition: Planning and Preparation Checklist. http://journal.ahima.org/wp-content/uploads/ICD10-checklist.pdf. Accessed June 5, 2014.
Congress has once again delayed implementation of draconian Medicare cuts tied to the sustainable growth rate (SGR) formula. It was the 17th temporary patch applied to the ailing physician reimbursement program, so the decision caused little surprise.
But with the same legislation—the Protecting Access to Medicare Act of 2014—being used to delay the long-awaited debut of ICD-10, many hospitalists and physicians couldn’t help but wonder whether billing and coding would now be as much of a political football as the SGR fix.1
The upshot: It doesn’t seem that way.
“I think it’s two separate issues,” says Phyllis “PJ” Floyd, RN, BSN, MBA, NE-BC, CCA, director of health information services and clinical documentation improvement at Medical University of South Carolina (MUSC) in Charleston, S.C. “The fact that it was all in one bill, I don’t know that it was well thought out as much as it was, ‘Let’s put the ICD-10 in here at the same time.’
“It was just a few sentences, and then it wasn’t even brought up in the discussion on the floor.”
Four policy wonks interviewed by The Hospitalist concurred that while tying the ICD-10 delay to the SGR issue was an unexpected and frustrating development, the coding system likely will be implemented in the relative short term. Meanwhile, a long-term resolution of the SGR dilemma remains much more elusive.
“For about 12 hours, I felt relief about the ICD-10 [being delayed], and then I just realized, it’s still coming, presumably,” says John Nelson, MD, MHM, a co-founder and past president of SHM and medical director of the hospitalist practice at Overlake Hospital Medical Center in Bellevue, Wash. “[It’s] like a patient who needs surgery and finds out it’s canceled for the day and he’ll have it tomorrow. Well, that’s good for right now, but [he] still has to face this eventually.”
“Doc-Pay” Fix Near?
Congress’ recent decision to delay both an SGR fix and the ICD-10 are troubling to some hospitalists and others for different reasons.
The SGR extension through this year’s end means that physicians do not face a 24% cut to physician payments under Medicare. SHM has long lobbied against temporary patches to the SGR, repeatedly backing legislation that would once and for all scrap the formula and replace it with something sustainable.
The SGR formula was first crafted in 1997, but the now often-delayed cuts were a byproduct of the federal sequester that was included in the Budget Control Act of 2011. At the time, the massive reduction to Medicare payments was tied to political brinksmanship over the country’s debt ceiling. The cuts were implemented as a doomsday scenario that was never likely to actually happen, but despite negotiations over the past three years, no long-term compromise can be found. Paying for the reform remains the main stumbling block.
“I think, this year, Congress was as close as it’s been in a long time to enacting a serious fix, aided by the agreement of major professional societies like the American College of Physicians and American College of Surgeons,” says David Howard, PhD, an associate professor in the department of health policy and management at the Rollins School of Public Health at Emory University in Atlanta. “They were all on board with this solution. ... Who knows, maybe if the economic situation continues to improve [and] tax revenues continue to go up...that will create a more favorable environment for compromise.”
Dr. Howard adds that while Congress might be close to a solution in theory, agreement on how to offset the roughly $100 billion in costs “is just very difficult.” That is why the healthcare professor is pessimistic that a long-term fix is truly at hand.
“The places where Congress might have looked for savings to offset the cost of the doc fix, such as hospital reimbursement rates or payment rates to Medicare Advantage plans—those are exactly the areas that the Affordable Care Act is targeting to pay for insurance expansion,” Dr. Howard adds. “So those areas of savings are not going to be available to offset the cost of the doc fix.”
ICD-10 Delays “Unfair”
The medical coding conundrum presents a different set of issues. The delay in transitioning healthcare providers from the ICD-9 medical coding classification system to the more complicated ICD-10 means the upgraded system is now against an Oct. 1, 2015, deadline. This comes after the Centers for Medicare & Medicaid Services (CMS) already pushed back the original implementation date for ICD-10 by one year.
SHM Public Policy Committee member Joshua Lenchus, DO, RPh, FACP, SFHM, says he thinks most doctors are content with the delay, particularly in light of some estimates that show that only about 20% of physicians “have actually initiated the ICD-10 transition.” But he also notes that it’s unfair to the health systems that have prepared for ICD-10.
“ICD-9 has a little more than 14,000 diagnostic codes and nearly 4,000 procedural codes. That is to be contrasted to ICD-10, which has more than 68,000 diagnostic codes ... and over 72,000 procedural codes,” Dr. Lenchus says. “So, it is not surprising that many take solace in the delay.”
–Dr. Lenchus
Dr. Nelson says the level of frustration for hospitalists is growing; however, the level of disruption for hospitals and health systems is reaching a boiling point.
“Of course, in some places, hospitalists may be the physician lead on ICD-10 efforts, so [they are] very much wrapped up in the problem of ‘What do we do now?’”
The answer, at least to the Coalition for ICD-10, a group of medical/technology trade groups, is to fight to ensure that the delays go no further. In an April letter to CMS Administrator Marilyn Tavenner, the coalition made that case, noting that in 2012, “CMS estimated the cost to the healthcare industry of a one-year delay to be as much as $6.6 billion, or approximately 30% of the $22 billion that CMS estimated had been invested or budgeted for ICD-10 implementation.”2
The letter went on to explain that the disruption and cost will grow each time the ICD-10 deadline is pushed.
“Furthermore, as CMS stated in 2012, implementation costs will continue to increase considerably with every year of a delay,” according to the letter. “The lost opportunity costs of failing to move to a more effective code set also continue to climb every year.”
Stay Engaged, Switch Gears
One of Floyd’s biggest concerns is that the ICD-10 implementation delays will affect physician engagement. The hospitalist groups at MUSC began training for ICD-10 in January 2013; however, the preparation and training were geared toward a 2014 implementation.
“You have to switch gears a little bit,” she says. “What we plan to do now is begin to do heavy auditing, and then from those audits we can give real-time feedback on what we’re doing well and what we’re not doing well. So I think that will be a method for engagement.”
She urges hospitalists, practice leaders, and informatics professionals to discuss ICD-10 not as a theoretical application, but as one tied to reimbursement that will have major impact in the years ahead. To that end, the American Health Information Management Association highlights the fact that the new coding system will result in higher-quality data that can improve performance measures, provide “increased sensitivity” to reimbursement methodologies, and help with stronger public health surveillance.3
“A lot of physicians see this as a hospital issue, and I think that’s why they shy away,” Floyd says. “Now there are some physicians who are interested in how well the hospital does, but the other piece is that it does affect things like [reduced] risk of mortality [and] comparison of data worldwide—those are things that we just have to continue to reiterate … and give them real examples.”
Richard Quinn is a freelance writer in New Jersey.
References
- Govtrack. H.R. 4302: Protecting Access to Medicare Act of 2014. https://www.govtrack.us/congress/bills/113/hr4302. Accessed June 5, 2014.
- Coalition for ICD. Letter to CMS Administrator Tavenner, April 11, 2014. http://coalitionforicd10.wordpress.com/2014/03/26/letter-from-the-coalition-for-icd-10. Accessed June 5, 2014.
- American Health Information Management Association. ICD-10-CM/PCS Transition: Planning and Preparation Checklist. http://journal.ahima.org/wp-content/uploads/ICD10-checklist.pdf. Accessed June 5, 2014.
Congress has once again delayed implementation of draconian Medicare cuts tied to the sustainable growth rate (SGR) formula. It was the 17th temporary patch applied to the ailing physician reimbursement program, so the decision caused little surprise.
But with the same legislation—the Protecting Access to Medicare Act of 2014—being used to delay the long-awaited debut of ICD-10, many hospitalists and physicians couldn’t help but wonder whether billing and coding would now be as much of a political football as the SGR fix.1
The upshot: It doesn’t seem that way.
“I think it’s two separate issues,” says Phyllis “PJ” Floyd, RN, BSN, MBA, NE-BC, CCA, director of health information services and clinical documentation improvement at Medical University of South Carolina (MUSC) in Charleston, S.C. “The fact that it was all in one bill, I don’t know that it was well thought out as much as it was, ‘Let’s put the ICD-10 in here at the same time.’
“It was just a few sentences, and then it wasn’t even brought up in the discussion on the floor.”
Four policy wonks interviewed by The Hospitalist concurred that while tying the ICD-10 delay to the SGR issue was an unexpected and frustrating development, the coding system likely will be implemented in the relative short term. Meanwhile, a long-term resolution of the SGR dilemma remains much more elusive.
“For about 12 hours, I felt relief about the ICD-10 [being delayed], and then I just realized, it’s still coming, presumably,” says John Nelson, MD, MHM, a co-founder and past president of SHM and medical director of the hospitalist practice at Overlake Hospital Medical Center in Bellevue, Wash. “[It’s] like a patient who needs surgery and finds out it’s canceled for the day and he’ll have it tomorrow. Well, that’s good for right now, but [he] still has to face this eventually.”
“Doc-Pay” Fix Near?
Congress’ recent decision to delay both an SGR fix and the ICD-10 are troubling to some hospitalists and others for different reasons.
The SGR extension through this year’s end means that physicians do not face a 24% cut to physician payments under Medicare. SHM has long lobbied against temporary patches to the SGR, repeatedly backing legislation that would once and for all scrap the formula and replace it with something sustainable.
The SGR formula was first crafted in 1997, but the now often-delayed cuts were a byproduct of the federal sequester that was included in the Budget Control Act of 2011. At the time, the massive reduction to Medicare payments was tied to political brinksmanship over the country’s debt ceiling. The cuts were implemented as a doomsday scenario that was never likely to actually happen, but despite negotiations over the past three years, no long-term compromise can be found. Paying for the reform remains the main stumbling block.
“I think, this year, Congress was as close as it’s been in a long time to enacting a serious fix, aided by the agreement of major professional societies like the American College of Physicians and American College of Surgeons,” says David Howard, PhD, an associate professor in the department of health policy and management at the Rollins School of Public Health at Emory University in Atlanta. “They were all on board with this solution. ... Who knows, maybe if the economic situation continues to improve [and] tax revenues continue to go up...that will create a more favorable environment for compromise.”
Dr. Howard adds that while Congress might be close to a solution in theory, agreement on how to offset the roughly $100 billion in costs “is just very difficult.” That is why the healthcare professor is pessimistic that a long-term fix is truly at hand.
“The places where Congress might have looked for savings to offset the cost of the doc fix, such as hospital reimbursement rates or payment rates to Medicare Advantage plans—those are exactly the areas that the Affordable Care Act is targeting to pay for insurance expansion,” Dr. Howard adds. “So those areas of savings are not going to be available to offset the cost of the doc fix.”
ICD-10 Delays “Unfair”
The medical coding conundrum presents a different set of issues. The delay in transitioning healthcare providers from the ICD-9 medical coding classification system to the more complicated ICD-10 means the upgraded system is now against an Oct. 1, 2015, deadline. This comes after the Centers for Medicare & Medicaid Services (CMS) already pushed back the original implementation date for ICD-10 by one year.
SHM Public Policy Committee member Joshua Lenchus, DO, RPh, FACP, SFHM, says he thinks most doctors are content with the delay, particularly in light of some estimates that show that only about 20% of physicians “have actually initiated the ICD-10 transition.” But he also notes that it’s unfair to the health systems that have prepared for ICD-10.
“ICD-9 has a little more than 14,000 diagnostic codes and nearly 4,000 procedural codes. That is to be contrasted to ICD-10, which has more than 68,000 diagnostic codes ... and over 72,000 procedural codes,” Dr. Lenchus says. “So, it is not surprising that many take solace in the delay.”
–Dr. Lenchus
Dr. Nelson says the level of frustration for hospitalists is growing; however, the level of disruption for hospitals and health systems is reaching a boiling point.
“Of course, in some places, hospitalists may be the physician lead on ICD-10 efforts, so [they are] very much wrapped up in the problem of ‘What do we do now?’”
The answer, at least to the Coalition for ICD-10, a group of medical/technology trade groups, is to fight to ensure that the delays go no further. In an April letter to CMS Administrator Marilyn Tavenner, the coalition made that case, noting that in 2012, “CMS estimated the cost to the healthcare industry of a one-year delay to be as much as $6.6 billion, or approximately 30% of the $22 billion that CMS estimated had been invested or budgeted for ICD-10 implementation.”2
The letter went on to explain that the disruption and cost will grow each time the ICD-10 deadline is pushed.
“Furthermore, as CMS stated in 2012, implementation costs will continue to increase considerably with every year of a delay,” according to the letter. “The lost opportunity costs of failing to move to a more effective code set also continue to climb every year.”
Stay Engaged, Switch Gears
One of Floyd’s biggest concerns is that the ICD-10 implementation delays will affect physician engagement. The hospitalist groups at MUSC began training for ICD-10 in January 2013; however, the preparation and training were geared toward a 2014 implementation.
“You have to switch gears a little bit,” she says. “What we plan to do now is begin to do heavy auditing, and then from those audits we can give real-time feedback on what we’re doing well and what we’re not doing well. So I think that will be a method for engagement.”
She urges hospitalists, practice leaders, and informatics professionals to discuss ICD-10 not as a theoretical application, but as one tied to reimbursement that will have major impact in the years ahead. To that end, the American Health Information Management Association highlights the fact that the new coding system will result in higher-quality data that can improve performance measures, provide “increased sensitivity” to reimbursement methodologies, and help with stronger public health surveillance.3
“A lot of physicians see this as a hospital issue, and I think that’s why they shy away,” Floyd says. “Now there are some physicians who are interested in how well the hospital does, but the other piece is that it does affect things like [reduced] risk of mortality [and] comparison of data worldwide—those are things that we just have to continue to reiterate … and give them real examples.”
Richard Quinn is a freelance writer in New Jersey.
References
- Govtrack. H.R. 4302: Protecting Access to Medicare Act of 2014. https://www.govtrack.us/congress/bills/113/hr4302. Accessed June 5, 2014.
- Coalition for ICD. Letter to CMS Administrator Tavenner, April 11, 2014. http://coalitionforicd10.wordpress.com/2014/03/26/letter-from-the-coalition-for-icd-10. Accessed June 5, 2014.
- American Health Information Management Association. ICD-10-CM/PCS Transition: Planning and Preparation Checklist. http://journal.ahima.org/wp-content/uploads/ICD10-checklist.pdf. Accessed June 5, 2014.
Viral Hepatitis Awareness
As federal, state, and local partners work to “shed light on this hidden [viral hepatitis] epidemic,” the HHS, the Departments of Justice and Housing and Urban Development, and the VA published their joint updated Action Plan for the Prevention, Care and Treatment of Viral Hepatitis (2014-2016).
In 2007, annual deaths in the U.S. due to viral hepatitis outpaced deaths due to human immunodeficiency virus (HIV) for the first time, according to the Centers for Disease Control and Prevention (CDC). Yet “[a]wareness is inexplicably low,” says the World Hepatitis Alliance, a nongovernmental organization. Viral hepatitis is the leading cause of liver cancer and the most common reason for liver transplantation in the U.S. It is also a leading infectious cause of death, killing 12,000 to 18,000 Americans each year.
Between 3.5 and 5.3 million Americans live with chronic viral hepatitis, the CDC says. But advances in treatment of hepatitis C (HCV), more widely available effective vaccines for hepatitis A and B (HBV), and more opportunities for testing for HCV under the Affordable Care Act are having an effect. (There is no vaccine to prevent HCV; the best way to prevent it is to avoid risky behaviors, such as sharing needles, according to the CDC.) With the updated plan, HHS hopes to build on the “substantial progress” made since 2011.
Like the original plan, which was the first comprehensive cross-agency plan to combat viral hepatitis, the updated version has 4 main goals:
- Increase the proportion of people who are aware of the HBV infection from 33% to 66%;
- Increase the proportion of people who are aware of their HCV infection from 45% to 66%;
- Reduce the number of new cases of HCV infection by 25%; and
- Eliminate mother-to-child transmission of HBV.
The updated plan also proposes more than 150 action steps, organized into 6 priority areas: (1) educating providers and communities to reduce viral hepatitis-related health disparities; (2) improving testing, care, and treatment to prevent liver disease and cancer; (3) strengthening surveillance to detect viral hepatitis transmission and disease; (4) eliminating transmission of vaccine-preventable viral hepatitis; (5) reducing viral hepatitis caused by drug use; and (6) protecting patients and workers from health care-associated viral hepatitis.
To assess whether or not an individual should get tested or vaccinated for viral hepatitis, the CDC offers a 5-minute, online personalized Hepatitis Risk Assessment at http://www.cdc.gov/hepatitis/RiskAssessment. For more information on World Hepatitis Day, July 28, 2014, organized by the World Hepatitis Alliance, visit http://www.cdc.gov/hepatitis/WorldHepDay.htm.
As federal, state, and local partners work to “shed light on this hidden [viral hepatitis] epidemic,” the HHS, the Departments of Justice and Housing and Urban Development, and the VA published their joint updated Action Plan for the Prevention, Care and Treatment of Viral Hepatitis (2014-2016).
In 2007, annual deaths in the U.S. due to viral hepatitis outpaced deaths due to human immunodeficiency virus (HIV) for the first time, according to the Centers for Disease Control and Prevention (CDC). Yet “[a]wareness is inexplicably low,” says the World Hepatitis Alliance, a nongovernmental organization. Viral hepatitis is the leading cause of liver cancer and the most common reason for liver transplantation in the U.S. It is also a leading infectious cause of death, killing 12,000 to 18,000 Americans each year.
Between 3.5 and 5.3 million Americans live with chronic viral hepatitis, the CDC says. But advances in treatment of hepatitis C (HCV), more widely available effective vaccines for hepatitis A and B (HBV), and more opportunities for testing for HCV under the Affordable Care Act are having an effect. (There is no vaccine to prevent HCV; the best way to prevent it is to avoid risky behaviors, such as sharing needles, according to the CDC.) With the updated plan, HHS hopes to build on the “substantial progress” made since 2011.
Like the original plan, which was the first comprehensive cross-agency plan to combat viral hepatitis, the updated version has 4 main goals:
- Increase the proportion of people who are aware of the HBV infection from 33% to 66%;
- Increase the proportion of people who are aware of their HCV infection from 45% to 66%;
- Reduce the number of new cases of HCV infection by 25%; and
- Eliminate mother-to-child transmission of HBV.
The updated plan also proposes more than 150 action steps, organized into 6 priority areas: (1) educating providers and communities to reduce viral hepatitis-related health disparities; (2) improving testing, care, and treatment to prevent liver disease and cancer; (3) strengthening surveillance to detect viral hepatitis transmission and disease; (4) eliminating transmission of vaccine-preventable viral hepatitis; (5) reducing viral hepatitis caused by drug use; and (6) protecting patients and workers from health care-associated viral hepatitis.
To assess whether or not an individual should get tested or vaccinated for viral hepatitis, the CDC offers a 5-minute, online personalized Hepatitis Risk Assessment at http://www.cdc.gov/hepatitis/RiskAssessment. For more information on World Hepatitis Day, July 28, 2014, organized by the World Hepatitis Alliance, visit http://www.cdc.gov/hepatitis/WorldHepDay.htm.
As federal, state, and local partners work to “shed light on this hidden [viral hepatitis] epidemic,” the HHS, the Departments of Justice and Housing and Urban Development, and the VA published their joint updated Action Plan for the Prevention, Care and Treatment of Viral Hepatitis (2014-2016).
In 2007, annual deaths in the U.S. due to viral hepatitis outpaced deaths due to human immunodeficiency virus (HIV) for the first time, according to the Centers for Disease Control and Prevention (CDC). Yet “[a]wareness is inexplicably low,” says the World Hepatitis Alliance, a nongovernmental organization. Viral hepatitis is the leading cause of liver cancer and the most common reason for liver transplantation in the U.S. It is also a leading infectious cause of death, killing 12,000 to 18,000 Americans each year.
Between 3.5 and 5.3 million Americans live with chronic viral hepatitis, the CDC says. But advances in treatment of hepatitis C (HCV), more widely available effective vaccines for hepatitis A and B (HBV), and more opportunities for testing for HCV under the Affordable Care Act are having an effect. (There is no vaccine to prevent HCV; the best way to prevent it is to avoid risky behaviors, such as sharing needles, according to the CDC.) With the updated plan, HHS hopes to build on the “substantial progress” made since 2011.
Like the original plan, which was the first comprehensive cross-agency plan to combat viral hepatitis, the updated version has 4 main goals:
- Increase the proportion of people who are aware of the HBV infection from 33% to 66%;
- Increase the proportion of people who are aware of their HCV infection from 45% to 66%;
- Reduce the number of new cases of HCV infection by 25%; and
- Eliminate mother-to-child transmission of HBV.
The updated plan also proposes more than 150 action steps, organized into 6 priority areas: (1) educating providers and communities to reduce viral hepatitis-related health disparities; (2) improving testing, care, and treatment to prevent liver disease and cancer; (3) strengthening surveillance to detect viral hepatitis transmission and disease; (4) eliminating transmission of vaccine-preventable viral hepatitis; (5) reducing viral hepatitis caused by drug use; and (6) protecting patients and workers from health care-associated viral hepatitis.
To assess whether or not an individual should get tested or vaccinated for viral hepatitis, the CDC offers a 5-minute, online personalized Hepatitis Risk Assessment at http://www.cdc.gov/hepatitis/RiskAssessment. For more information on World Hepatitis Day, July 28, 2014, organized by the World Hepatitis Alliance, visit http://www.cdc.gov/hepatitis/WorldHepDay.htm.
Maintenance of certification took center stage at AMA Congress of Delegates
CHICAGO – The American Medical Association should continue to work with the American Board of Medical Specialties to address physicians’ concerns about Maintenance of Certification – that was the consensus at the annual meeting of the AMA House of Delegates.
The AMA’s delegates defeated a resolution that asked the organization to put a moratorium on MOC until it was proven to improve the quality of care and patient outcomes. However, they did agree to a new policy that directs the AMA to:
• Explore with independent entities the feasibility of conducting a study to evaluate the effect MOC requirements and Maintenance of Licensure principles have on workforce, practice costs, patient outcomes, patient safety, and patient access.
• Work with the American Board of Medical Specialties and its 24 member boards to collect data on why physicians choose to maintain or discontinue their board certification.
• Work with the ABMS and the Federation of State Medical Boards to study whether MOC and the principles of Maintenance of Licensure are important factors to physicians when deciding whether to retire and whether they have a direct effect on workforce.
• Oppose making MOC mandatory as a condition of medical licensure, and encourage physicians to strive constantly to improve their care of patients by the means they find most effective.
The new policy applies to both the ABMS MOC process and the Osteopathic Continuous Certification (OCC) process.
Physicians have increasingly voiced their concerns about MOC. Dr. Paul Teirstein, chief of cardiology and director of interventional cardiology for Scripps Clinic in La Jolla, Calif., launched a petition drive to overhaul the American Board of Internal Medicine’s MOC process. The petition has more than 17,000 signatures.
The ABIM says that it is listening to physicians and is making changes in the process, but also recently said that more than 150,000 physicians had participated in its MOC process – making the May 1 deadline to be listed on the ABIM website as having met the MOC criteria.
But anger is still bubbling up, and was expressed at the AMA’s meeting.
"Practicing physicians on the front lines are increasingly burdened, hassled, and confused by the onerous and expensive process of Maintenance of Certification and Maintenance of Licensure," said Dr. James A. Goodyear, a delegate from Pennsylvania.
Dr. Goodyear introduced the resolution to seek a moratorium on the MOC.
But Dr. Darlyne Menscer, a member of the AMA Council on Medical Education, told the delegates that such a moratorium would put a wedge in the close working relationship the AMA has had with the ABMS. "This is more prescriptive than we can commit to as a council, although we definitely do hear the concerns of the House," added Dr. Menscer.
The AMA has been discussing the concerns about MOC with the ABMS, most recently holding a meeting in Chicago in early June.
Dr. Joshua Cohen, a delegate from the American Academy of Neurology, and a member of the AMA Foundation’s Board of Directors, who attended that meeting, also argued against a moratorium. "It would make it impossible for the AMA to improve the process going forward," said Dr. Cohen.
Dr. Chuck Wilson, a pediatrician and delegate from the North Carolina delegation, also opposed any major change in direction for the AMA. He noted that if the AMA was seen as opposed to MOC, it might not be viewed well. "We all want it to be less onerous," said Dr. Wilson. But, he noted, "the Council on Medical Education is working in that direction. Let’s give them a chance to be successful."
In a statement after the HOD meeting, the AMA said that it "continues to ensure the MOC process does not disrupt physician practice or reduce the capacity of the overall physician workforce." Concerns about MOC "center around the need for relevance to the daily practice of physicians and the better integration into physician practices to optimally support learning and improvement."
On Twitter @aliciaault
CHICAGO – The American Medical Association should continue to work with the American Board of Medical Specialties to address physicians’ concerns about Maintenance of Certification – that was the consensus at the annual meeting of the AMA House of Delegates.
The AMA’s delegates defeated a resolution that asked the organization to put a moratorium on MOC until it was proven to improve the quality of care and patient outcomes. However, they did agree to a new policy that directs the AMA to:
• Explore with independent entities the feasibility of conducting a study to evaluate the effect MOC requirements and Maintenance of Licensure principles have on workforce, practice costs, patient outcomes, patient safety, and patient access.
• Work with the American Board of Medical Specialties and its 24 member boards to collect data on why physicians choose to maintain or discontinue their board certification.
• Work with the ABMS and the Federation of State Medical Boards to study whether MOC and the principles of Maintenance of Licensure are important factors to physicians when deciding whether to retire and whether they have a direct effect on workforce.
• Oppose making MOC mandatory as a condition of medical licensure, and encourage physicians to strive constantly to improve their care of patients by the means they find most effective.
The new policy applies to both the ABMS MOC process and the Osteopathic Continuous Certification (OCC) process.
Physicians have increasingly voiced their concerns about MOC. Dr. Paul Teirstein, chief of cardiology and director of interventional cardiology for Scripps Clinic in La Jolla, Calif., launched a petition drive to overhaul the American Board of Internal Medicine’s MOC process. The petition has more than 17,000 signatures.
The ABIM says that it is listening to physicians and is making changes in the process, but also recently said that more than 150,000 physicians had participated in its MOC process – making the May 1 deadline to be listed on the ABIM website as having met the MOC criteria.
But anger is still bubbling up, and was expressed at the AMA’s meeting.
"Practicing physicians on the front lines are increasingly burdened, hassled, and confused by the onerous and expensive process of Maintenance of Certification and Maintenance of Licensure," said Dr. James A. Goodyear, a delegate from Pennsylvania.
Dr. Goodyear introduced the resolution to seek a moratorium on the MOC.
But Dr. Darlyne Menscer, a member of the AMA Council on Medical Education, told the delegates that such a moratorium would put a wedge in the close working relationship the AMA has had with the ABMS. "This is more prescriptive than we can commit to as a council, although we definitely do hear the concerns of the House," added Dr. Menscer.
The AMA has been discussing the concerns about MOC with the ABMS, most recently holding a meeting in Chicago in early June.
Dr. Joshua Cohen, a delegate from the American Academy of Neurology, and a member of the AMA Foundation’s Board of Directors, who attended that meeting, also argued against a moratorium. "It would make it impossible for the AMA to improve the process going forward," said Dr. Cohen.
Dr. Chuck Wilson, a pediatrician and delegate from the North Carolina delegation, also opposed any major change in direction for the AMA. He noted that if the AMA was seen as opposed to MOC, it might not be viewed well. "We all want it to be less onerous," said Dr. Wilson. But, he noted, "the Council on Medical Education is working in that direction. Let’s give them a chance to be successful."
In a statement after the HOD meeting, the AMA said that it "continues to ensure the MOC process does not disrupt physician practice or reduce the capacity of the overall physician workforce." Concerns about MOC "center around the need for relevance to the daily practice of physicians and the better integration into physician practices to optimally support learning and improvement."
On Twitter @aliciaault
CHICAGO – The American Medical Association should continue to work with the American Board of Medical Specialties to address physicians’ concerns about Maintenance of Certification – that was the consensus at the annual meeting of the AMA House of Delegates.
The AMA’s delegates defeated a resolution that asked the organization to put a moratorium on MOC until it was proven to improve the quality of care and patient outcomes. However, they did agree to a new policy that directs the AMA to:
• Explore with independent entities the feasibility of conducting a study to evaluate the effect MOC requirements and Maintenance of Licensure principles have on workforce, practice costs, patient outcomes, patient safety, and patient access.
• Work with the American Board of Medical Specialties and its 24 member boards to collect data on why physicians choose to maintain or discontinue their board certification.
• Work with the ABMS and the Federation of State Medical Boards to study whether MOC and the principles of Maintenance of Licensure are important factors to physicians when deciding whether to retire and whether they have a direct effect on workforce.
• Oppose making MOC mandatory as a condition of medical licensure, and encourage physicians to strive constantly to improve their care of patients by the means they find most effective.
The new policy applies to both the ABMS MOC process and the Osteopathic Continuous Certification (OCC) process.
Physicians have increasingly voiced their concerns about MOC. Dr. Paul Teirstein, chief of cardiology and director of interventional cardiology for Scripps Clinic in La Jolla, Calif., launched a petition drive to overhaul the American Board of Internal Medicine’s MOC process. The petition has more than 17,000 signatures.
The ABIM says that it is listening to physicians and is making changes in the process, but also recently said that more than 150,000 physicians had participated in its MOC process – making the May 1 deadline to be listed on the ABIM website as having met the MOC criteria.
But anger is still bubbling up, and was expressed at the AMA’s meeting.
"Practicing physicians on the front lines are increasingly burdened, hassled, and confused by the onerous and expensive process of Maintenance of Certification and Maintenance of Licensure," said Dr. James A. Goodyear, a delegate from Pennsylvania.
Dr. Goodyear introduced the resolution to seek a moratorium on the MOC.
But Dr. Darlyne Menscer, a member of the AMA Council on Medical Education, told the delegates that such a moratorium would put a wedge in the close working relationship the AMA has had with the ABMS. "This is more prescriptive than we can commit to as a council, although we definitely do hear the concerns of the House," added Dr. Menscer.
The AMA has been discussing the concerns about MOC with the ABMS, most recently holding a meeting in Chicago in early June.
Dr. Joshua Cohen, a delegate from the American Academy of Neurology, and a member of the AMA Foundation’s Board of Directors, who attended that meeting, also argued against a moratorium. "It would make it impossible for the AMA to improve the process going forward," said Dr. Cohen.
Dr. Chuck Wilson, a pediatrician and delegate from the North Carolina delegation, also opposed any major change in direction for the AMA. He noted that if the AMA was seen as opposed to MOC, it might not be viewed well. "We all want it to be less onerous," said Dr. Wilson. But, he noted, "the Council on Medical Education is working in that direction. Let’s give them a chance to be successful."
In a statement after the HOD meeting, the AMA said that it "continues to ensure the MOC process does not disrupt physician practice or reduce the capacity of the overall physician workforce." Concerns about MOC "center around the need for relevance to the daily practice of physicians and the better integration into physician practices to optimally support learning and improvement."
On Twitter @aliciaault
AT THE AMA HOD MEETING
TRICARE Walk-In Service Eliminated
Walk-in service was a “must-have” when TRICARE began nearly 20 years ago. Over the years, TRICARE regional contractors have operated nearly 200 service centers in the U.S., mostly at military hospitals and clinics. But those days are gone, TRICARE says: technology has rendered much of the walk-in service obsolete. So TRICARE recently closed all walk-in customer service in the 50 states as of April 1, 2014, although this feature will still be available for overseas beneficiaries.
The service centers are not as cost-effective or convenient as Internet and toll-free access, TRICARE says. The majority of walk-in visits are for enrollment, billing, primary care manager changes, and general information on benefits and plans, all of which can be handled through websites, mobile applications, or by calling toll-free call centers (see App Corner, p.42). Walk-in customer service is the most expensive option for providing customer support, TRICARE says, costing about $51 million per year. Closing the centers will save about $254 million over 5 years. The closings are part of the DoD’s efforts to manage health care costs without changing benefits, fees, or beneficiary cost-shares.
While they can access TRICARE around-the-clock, beneficiaries can still get personal help if they prefer by calling their regional health care contractor. TRICARE regional contractors will continue beneficiary and military hospital and clinic customer service support. Regional contractors will coordinate with individual military facilities for services, such as briefings and distribution of materials, among other support services.
Walk-in service was a “must-have” when TRICARE began nearly 20 years ago. Over the years, TRICARE regional contractors have operated nearly 200 service centers in the U.S., mostly at military hospitals and clinics. But those days are gone, TRICARE says: technology has rendered much of the walk-in service obsolete. So TRICARE recently closed all walk-in customer service in the 50 states as of April 1, 2014, although this feature will still be available for overseas beneficiaries.
The service centers are not as cost-effective or convenient as Internet and toll-free access, TRICARE says. The majority of walk-in visits are for enrollment, billing, primary care manager changes, and general information on benefits and plans, all of which can be handled through websites, mobile applications, or by calling toll-free call centers (see App Corner, p.42). Walk-in customer service is the most expensive option for providing customer support, TRICARE says, costing about $51 million per year. Closing the centers will save about $254 million over 5 years. The closings are part of the DoD’s efforts to manage health care costs without changing benefits, fees, or beneficiary cost-shares.
While they can access TRICARE around-the-clock, beneficiaries can still get personal help if they prefer by calling their regional health care contractor. TRICARE regional contractors will continue beneficiary and military hospital and clinic customer service support. Regional contractors will coordinate with individual military facilities for services, such as briefings and distribution of materials, among other support services.
Walk-in service was a “must-have” when TRICARE began nearly 20 years ago. Over the years, TRICARE regional contractors have operated nearly 200 service centers in the U.S., mostly at military hospitals and clinics. But those days are gone, TRICARE says: technology has rendered much of the walk-in service obsolete. So TRICARE recently closed all walk-in customer service in the 50 states as of April 1, 2014, although this feature will still be available for overseas beneficiaries.
The service centers are not as cost-effective or convenient as Internet and toll-free access, TRICARE says. The majority of walk-in visits are for enrollment, billing, primary care manager changes, and general information on benefits and plans, all of which can be handled through websites, mobile applications, or by calling toll-free call centers (see App Corner, p.42). Walk-in customer service is the most expensive option for providing customer support, TRICARE says, costing about $51 million per year. Closing the centers will save about $254 million over 5 years. The closings are part of the DoD’s efforts to manage health care costs without changing benefits, fees, or beneficiary cost-shares.
While they can access TRICARE around-the-clock, beneficiaries can still get personal help if they prefer by calling their regional health care contractor. TRICARE regional contractors will continue beneficiary and military hospital and clinic customer service support. Regional contractors will coordinate with individual military facilities for services, such as briefings and distribution of materials, among other support services.
New Clinical Research Network
HHS has established a network of 5 clinical research organizations to design and conduct clinical studies about medical countermeasures—drugs, vaccines, and diagnostic tests—to protect against bioterrorism, pandemics, and other public health emergencies. “Recent disasters, such as Hurricane Sandy, the Deepwater Horizon oil spill, the 2009-H1N1 pandemic, underscored the importance of developing a capability to perform rigorous scientific studies in real time, potentially to shape the response to an unfolding crisis and to support recovery,” said Robin Robinson, PhD, director of the Biomedical Advanced Research and Development Authority (BARDA) in a HHS press release.
Part of the HHS Office of the Assistant Secretary for Preparedness and Response, BARDA will manage the network, coordinating with HHS interagency and industry partners, such as the National Institute of Allergy and Infectious Diseases. The new network will provide a full range of services, including planning, performing, monitoring, and interpreting clinical studies.
BARDA takes a “comprehensive integrated portfolio” approach to the advanced research and development, innovation, acquisition, and manufacturing of vaccines, drugs, therapeutics, diagnostic tools, and nonpharmaceutical products for public health emergency threats, HHS said. For instance, the clinical studies network may use local institutional review boards or the national Public Health Emergency Research Review Board to review multisite studies on health problems arising during a public health emergency. (Both types of boards ensure that appropriate steps are taken to protect the rights and welfare of people participating as subjects.)
Clinical studies will be performed through the network based on proposals provided by network members in response to specific BARDA requests. Five companies have been awarded contracts: EMMES Corporation in Rockville and Technical Resources International, Inc., in Bethesda, both in Maryland; PPD Development, LLC, in Wilmington and Rho Federal Systems Division, Inc., in Chapel Hill, both in North Carolina; and Clinical Research Management, Inc., in Hinckley, Ohio. The contracts include a minimum guarantee of $400,000 over the initial 2 years for access to the clinical research organization’s services. Each contract can be extended for up to 5 years and for a maximum of $100 million.
HHS has established a network of 5 clinical research organizations to design and conduct clinical studies about medical countermeasures—drugs, vaccines, and diagnostic tests—to protect against bioterrorism, pandemics, and other public health emergencies. “Recent disasters, such as Hurricane Sandy, the Deepwater Horizon oil spill, the 2009-H1N1 pandemic, underscored the importance of developing a capability to perform rigorous scientific studies in real time, potentially to shape the response to an unfolding crisis and to support recovery,” said Robin Robinson, PhD, director of the Biomedical Advanced Research and Development Authority (BARDA) in a HHS press release.
Part of the HHS Office of the Assistant Secretary for Preparedness and Response, BARDA will manage the network, coordinating with HHS interagency and industry partners, such as the National Institute of Allergy and Infectious Diseases. The new network will provide a full range of services, including planning, performing, monitoring, and interpreting clinical studies.
BARDA takes a “comprehensive integrated portfolio” approach to the advanced research and development, innovation, acquisition, and manufacturing of vaccines, drugs, therapeutics, diagnostic tools, and nonpharmaceutical products for public health emergency threats, HHS said. For instance, the clinical studies network may use local institutional review boards or the national Public Health Emergency Research Review Board to review multisite studies on health problems arising during a public health emergency. (Both types of boards ensure that appropriate steps are taken to protect the rights and welfare of people participating as subjects.)
Clinical studies will be performed through the network based on proposals provided by network members in response to specific BARDA requests. Five companies have been awarded contracts: EMMES Corporation in Rockville and Technical Resources International, Inc., in Bethesda, both in Maryland; PPD Development, LLC, in Wilmington and Rho Federal Systems Division, Inc., in Chapel Hill, both in North Carolina; and Clinical Research Management, Inc., in Hinckley, Ohio. The contracts include a minimum guarantee of $400,000 over the initial 2 years for access to the clinical research organization’s services. Each contract can be extended for up to 5 years and for a maximum of $100 million.
HHS has established a network of 5 clinical research organizations to design and conduct clinical studies about medical countermeasures—drugs, vaccines, and diagnostic tests—to protect against bioterrorism, pandemics, and other public health emergencies. “Recent disasters, such as Hurricane Sandy, the Deepwater Horizon oil spill, the 2009-H1N1 pandemic, underscored the importance of developing a capability to perform rigorous scientific studies in real time, potentially to shape the response to an unfolding crisis and to support recovery,” said Robin Robinson, PhD, director of the Biomedical Advanced Research and Development Authority (BARDA) in a HHS press release.
Part of the HHS Office of the Assistant Secretary for Preparedness and Response, BARDA will manage the network, coordinating with HHS interagency and industry partners, such as the National Institute of Allergy and Infectious Diseases. The new network will provide a full range of services, including planning, performing, monitoring, and interpreting clinical studies.
BARDA takes a “comprehensive integrated portfolio” approach to the advanced research and development, innovation, acquisition, and manufacturing of vaccines, drugs, therapeutics, diagnostic tools, and nonpharmaceutical products for public health emergency threats, HHS said. For instance, the clinical studies network may use local institutional review boards or the national Public Health Emergency Research Review Board to review multisite studies on health problems arising during a public health emergency. (Both types of boards ensure that appropriate steps are taken to protect the rights and welfare of people participating as subjects.)
Clinical studies will be performed through the network based on proposals provided by network members in response to specific BARDA requests. Five companies have been awarded contracts: EMMES Corporation in Rockville and Technical Resources International, Inc., in Bethesda, both in Maryland; PPD Development, LLC, in Wilmington and Rho Federal Systems Division, Inc., in Chapel Hill, both in North Carolina; and Clinical Research Management, Inc., in Hinckley, Ohio. The contracts include a minimum guarantee of $400,000 over the initial 2 years for access to the clinical research organization’s services. Each contract can be extended for up to 5 years and for a maximum of $100 million.
Bold Ideas Competition
The VA is looking for “big thinkers”—people with “crazy ideas, new approaches, disruptive solutions”—to enter its Industry Innovation Competitions in 2014. The first competition, Targeting Innovations in Veteran Mental Health, is hosted by the VA Center for Innovation (VACI), which is looking to employees, the private sector, entrepreneurs, nonprofit organizations, and academia for new ideas on how to improve the health care experience for veterans. “VA has established a track record as an innovative organization that welcomes new ideas,” said former Secretary of Veterans Affairs Eric K. Shinseki in a VA press release. “The competition represents an important way for us to tap the significant pool of talent and expertise inside and outside of government to improve mental health care and services for our nation’s veterans, their families, and survivors.”
But they also hope to share the “best-of-breed” innovations with the world at large. “With this competition we are focused on challenges that affect a population much larger than our veterans,” said VACI Acting Director Patrick Littlefield. “We anticipate these efforts will benefit a very large community of providers and customers.”
The competition seeks creative solutions in 3 areas of significance to the VA. Entrants are encouraged to propose new ways to respond to veteran mental health challenges, with topics focused on human-centered design. “We want a deep understanding of the users we are developing these programs for, so that the solutions fit with the way people are trying to access services. User-centered design ensures that we’re responsive to the ways communities are living and working now,” said a participant in a Q&A session about the competition.
Entrants are encouraged to consider the “whole lifetime of the veteran,” not focusing on a particular generation or age. The topics include upstream suicide intervention; improving veterans’ receptivity to mental health care to promote treatment, engagement, and participation; and innovative methods of incentivizing behavior to improve mental wellness.
Subject matter experts from VA, other government agencies, and applicable industries review the proposals. Selected innovators work with VACI to design a pilot implementation based on their proposals, after which each project is evaluated. The most successful are eventually rolled out as prototypes in the VA, then nationally. In the first 3 Industry Innovation Competitions, 48 of the nearly 800 ideas submitted across 15 topic areas were selected for awards.
Concept papers will be accepted and reviewed on a rolling basis through May 30, 2016 (as long as funding is available). For more information on the competition, visit http://www.innovation.va.gov.
The VA is looking for “big thinkers”—people with “crazy ideas, new approaches, disruptive solutions”—to enter its Industry Innovation Competitions in 2014. The first competition, Targeting Innovations in Veteran Mental Health, is hosted by the VA Center for Innovation (VACI), which is looking to employees, the private sector, entrepreneurs, nonprofit organizations, and academia for new ideas on how to improve the health care experience for veterans. “VA has established a track record as an innovative organization that welcomes new ideas,” said former Secretary of Veterans Affairs Eric K. Shinseki in a VA press release. “The competition represents an important way for us to tap the significant pool of talent and expertise inside and outside of government to improve mental health care and services for our nation’s veterans, their families, and survivors.”
But they also hope to share the “best-of-breed” innovations with the world at large. “With this competition we are focused on challenges that affect a population much larger than our veterans,” said VACI Acting Director Patrick Littlefield. “We anticipate these efforts will benefit a very large community of providers and customers.”
The competition seeks creative solutions in 3 areas of significance to the VA. Entrants are encouraged to propose new ways to respond to veteran mental health challenges, with topics focused on human-centered design. “We want a deep understanding of the users we are developing these programs for, so that the solutions fit with the way people are trying to access services. User-centered design ensures that we’re responsive to the ways communities are living and working now,” said a participant in a Q&A session about the competition.
Entrants are encouraged to consider the “whole lifetime of the veteran,” not focusing on a particular generation or age. The topics include upstream suicide intervention; improving veterans’ receptivity to mental health care to promote treatment, engagement, and participation; and innovative methods of incentivizing behavior to improve mental wellness.
Subject matter experts from VA, other government agencies, and applicable industries review the proposals. Selected innovators work with VACI to design a pilot implementation based on their proposals, after which each project is evaluated. The most successful are eventually rolled out as prototypes in the VA, then nationally. In the first 3 Industry Innovation Competitions, 48 of the nearly 800 ideas submitted across 15 topic areas were selected for awards.
Concept papers will be accepted and reviewed on a rolling basis through May 30, 2016 (as long as funding is available). For more information on the competition, visit http://www.innovation.va.gov.
The VA is looking for “big thinkers”—people with “crazy ideas, new approaches, disruptive solutions”—to enter its Industry Innovation Competitions in 2014. The first competition, Targeting Innovations in Veteran Mental Health, is hosted by the VA Center for Innovation (VACI), which is looking to employees, the private sector, entrepreneurs, nonprofit organizations, and academia for new ideas on how to improve the health care experience for veterans. “VA has established a track record as an innovative organization that welcomes new ideas,” said former Secretary of Veterans Affairs Eric K. Shinseki in a VA press release. “The competition represents an important way for us to tap the significant pool of talent and expertise inside and outside of government to improve mental health care and services for our nation’s veterans, their families, and survivors.”
But they also hope to share the “best-of-breed” innovations with the world at large. “With this competition we are focused on challenges that affect a population much larger than our veterans,” said VACI Acting Director Patrick Littlefield. “We anticipate these efforts will benefit a very large community of providers and customers.”
The competition seeks creative solutions in 3 areas of significance to the VA. Entrants are encouraged to propose new ways to respond to veteran mental health challenges, with topics focused on human-centered design. “We want a deep understanding of the users we are developing these programs for, so that the solutions fit with the way people are trying to access services. User-centered design ensures that we’re responsive to the ways communities are living and working now,” said a participant in a Q&A session about the competition.
Entrants are encouraged to consider the “whole lifetime of the veteran,” not focusing on a particular generation or age. The topics include upstream suicide intervention; improving veterans’ receptivity to mental health care to promote treatment, engagement, and participation; and innovative methods of incentivizing behavior to improve mental wellness.
Subject matter experts from VA, other government agencies, and applicable industries review the proposals. Selected innovators work with VACI to design a pilot implementation based on their proposals, after which each project is evaluated. The most successful are eventually rolled out as prototypes in the VA, then nationally. In the first 3 Industry Innovation Competitions, 48 of the nearly 800 ideas submitted across 15 topic areas were selected for awards.
Concept papers will be accepted and reviewed on a rolling basis through May 30, 2016 (as long as funding is available). For more information on the competition, visit http://www.innovation.va.gov.