User login
Statins beneficial in elderly, guidelines should be strengthened
Contrary to historical evidence, two new studies show.
“By contrast with previous historical studies, our data show that LDL cholesterol is an important risk factor for myocardial infarction and atherosclerotic cardiovascular disease in a contemporary primary prevention cohort of individuals aged 70 to 100 years,” Borge Nordestgaard, MD, of the University of Copenhagen, and colleagues noted in the first of the two studies, published this week in the Lancet.
“By lowering LDL cholesterol in healthy individuals aged 70-100 years, the potential for preventing myocardial infarctions and atherosclerotic cardiovascular disease is huge, and at a substantially lower number needed to treat when compared with those aged 20-69 years,” they added.
“These findings support the concept of the cumulative burden of LDL cholesterol over one’s lifetime and the progressive increase in risk for atherosclerotic cardiovascular disease, including myocardial infarction, with age,” added Frederick J. Raal, PhD, and Farzahna Mohamed, MB BCh, of the University of the Witwatersrand, Johannesburg, South Africa, in an editorial published with both new studies in the Lancet (2020 Nov 10. doi: 10.1016/S0140-6736[20]32333-3).
The studies underscore the need for clinicians to consider continued risks associated with elevated LDL cholesterol in older age, they stressed, adding that statins are also beneficial for younger persons at risk to prevent conditions from worsening.
“The average age of patients in all the trials analyzed was older than 60 years, an age when atherosclerotic cardiovascular disease is already well established,” the editorialists wrote.
“Lipid-lowering therapy should be initiated at a younger age, preferably before age 40 years, in those at risk to delay the onset of atherosclerosis, rather than try to manage the condition once fully established or advanced,” they stressed.
No RCTs have included patients older than 70
For persons aged 40-75 years, elevated LDL cholesterol levels are a known risk factor for MI and atherosclerotic cardiovascular disease, and there is consensus in guidelines regarding treatment with statins.
However, the risk for people older than 70 is controversial. Some studies show little or no association between elevated LDL cholesterol levels and an increased risk for MI.
Contributing to the uncertainty is that few of the randomized, controlled trials that have investigated the question have included patients aged older than 70 years.
As a consequence, many practice guidelines have noted that the level of evidence in older patients is low, and some organizations have lowered the strength of recommendations regarding the treatment for older patients in comparison with younger patients.
Primary prevention: CV events increase with elevated LDL cholesterol in older age
Dr. Nordestgaard and colleagues studied data on 91,131 people living in Copenhagen who did not have atherosclerotic cardiovascular disease or diabetes at baseline and were not taking statins.
Of the participants, 10,592 were aged 70-79 years, and 3,188 participants were aged 80-100 years.
Over an average follow-up period of 7.7 years, 1,515 participants had a first MI, and 3,389 developed atherosclerotic cardiovascular disease.
In the primary-prevention cohort, after multivariate adjustment, the risk of having a heart attack per 1.0 mmol/L increase in LDL cholesterol was increased in the group overall (hazard ratio, 1.34). The increased risk was observed for all age groups, including those aged 80-100 years (HR, 1.28), 70-79 (HR, 1.25), 60-69 (HR, 1.29), 50-59 (HR, 1.28), and 20-49 (HR, 1.68).
Risk for atherosclerotic cardiovascular disease was also raised per 1.0 mmol/L increase in LDL cholesterol overall (HR, 1.16) and in all age groups, particularly those aged 70-100 years.
Greater elevations in LDL cholesterol (5.0 mmol/L or higher, indicative of possible familial hypercholesterolemia) were associated with a notably higher risk for heart attack after multivariate adjustment in people aged 80-100 (HR, 2.99). Risk was also higher among those aged 70-79 (HR, 1.82).
The highest incidence was in those older than 70. The rate was 8.5 heart attacks per 1,000 people per year among those aged 80-100 and 5.2 heart attacks per 1,000 in those aged 70-79. The rates were 2.5 per 1,000 among those 60-69, 1.8 for those aged 50-59, and 0.8 for those aged 20-49.
“The absolute risk [of cardiovascular events] is of course much higher in the elderly than those under the age of 75, but what was a surprise was how clear our results were on a relative risk scale, that the risk associated with elevated LDL [cholesterol] was as high in people aged 80-100 as the younger patients,” Dr. Nordestgaard said in an interview.
With regard to the benefits of cholesterol-lowering drugs, the study showed that the number needed to prevent one heart attack over 5 years was 80 among those aged 80-100; the number was 439 for people aged 50-59.
With regard to stronger statins, when moderate-intensity statins were used, the number needed to treat to prevent one cardiovascular disease event of any type dropped to 42 for patients aged 80-100. It was 88 for those aged 70-79, 164 for those aged 60-69, 345 for those aged 50-59, and 769 for those aged 20-49.
“The clinical significance of this is that it appears those in older age groups indeed benefit from cholesterol-lowering therapy,” Dr. Nordestgaard said. “I think many people have this idea that LDL [cholesterol] is not important over the age of about 70-75, but that’s not the case.”
“These robust findings are novel,” he and his colleagues stressed.
Despite these observational findings, the South African editorialists noted that “whether lipid-lowering therapy should be initiated for primary prevention in people aged 75 years or older is unclear,” owing to the host of risks and benefits that need to be balanced.
The findings of an ongoing randomized, placebo-controlled trial (STAREE) may answer this question, they wrote. It is investigating primary prevention in 18,000 older patients (≥70 years) who are being randomly assigned to receive atorvastatin 40 mg/d or placebo. The study is seeking to determine whether statin treatment extends the length of a disability-free life, which will be assessed on the basis of survival outside permanent residential care. Results are expected in 2022-2023.
Unequivocal reductions in events in elderly, comparable with younger patients
In the second study (Lancet. 2020 Nov 10. doi: 10.1016/S0140-6736[20]32332-1), Baris Gencer, MD, of Brigham and Women’s Hospital, Boston, =and colleagues evaluated the effects of statins and other cholesterol-lowering drugs, including ezetimibe and proprotein convertase subtilisin/kexin type 9 inhibitors, in older versus younger patients.
The systematic review and meta-analysis of 29 randomized controlled trials, also published in the Lancet, were presented virtually as a poster as part of the 2020 American Heart Association scientific session. It included data on 244,090 patients, including 21,492 aged 75 years and older.
The meta-analysis included studies of cardiovascular outcomes of a guideline-recommended LDL cholesterol–lowering drug, with a median follow-up of at least 2 years and inclusion of data on patients aged 75 years and older.
The results showed that over a median follow-up of 2.2 to 6 years, statin use by older patients was associated with a relative risk reduction of major vascular events of 26% per 1 mmol/L reduction in LDL cholesterol (P = .0019), which was comparable with a risk reduction of 15% per 1 mmol/L reduction in LDL cholesterol for patients younger than 75 years (P = .37, compared with older patients).
Treatment of older patients with LDL cholesterol–lowering drugs was also associated with significantly improved outcomes in cardiovascular death (risk ratio, 0.85), MI (RR, 0.80), stroke (RR, 0.73), and coronary revascularization (RR, 0.80).
“We found an unequivocal reduction in the risk of major vascular events with both statin and nonstatin LDL cholesterol-lowering treatments, which was similar to that seen in younger patients,” the authors wrote.
“Cholesterol-lowering medications are affordable drugs that have reduced risk of heart disease for millions of people worldwide, but until now, their benefits for older people have remained less certain,” said lead author Marc Sabatine, MD, also of Brigham and Women’s Hospital, in a Lancet press release.
“Our analysis indicates that these therapies are as effective in reducing cardiovascular events and deaths in people aged 75 years and over as they are in younger people. We found no offsetting safety concerns, and together, these results should strengthen guideline recommendations for the use of cholesterol-lowering medications, including statin and nonstatin therapy, in elderly people.”
The editorialists agreed: “More than 80% of fatal cardiovascular events occur in individuals older than 65 years, and the incidence of cardiovascular events is increasing in those older than 80 years; therefore, the findings of Gencer and colleagues’ study should encourage the use of lipid-lowering therapy in older patients.”
The authors of the two studies have disclosed no relevant financial relationships. Dr. Raal has received research grants, honoraria, or consulting fees for advisory board membership, professional input, and lectures on lipid-lowering drug therapy from Amgen, Regeneron, Sanofi, Novartis, and the Medicines Company.
A version of this article originally appeared on Medscape.com.
Contrary to historical evidence, two new studies show.
“By contrast with previous historical studies, our data show that LDL cholesterol is an important risk factor for myocardial infarction and atherosclerotic cardiovascular disease in a contemporary primary prevention cohort of individuals aged 70 to 100 years,” Borge Nordestgaard, MD, of the University of Copenhagen, and colleagues noted in the first of the two studies, published this week in the Lancet.
“By lowering LDL cholesterol in healthy individuals aged 70-100 years, the potential for preventing myocardial infarctions and atherosclerotic cardiovascular disease is huge, and at a substantially lower number needed to treat when compared with those aged 20-69 years,” they added.
“These findings support the concept of the cumulative burden of LDL cholesterol over one’s lifetime and the progressive increase in risk for atherosclerotic cardiovascular disease, including myocardial infarction, with age,” added Frederick J. Raal, PhD, and Farzahna Mohamed, MB BCh, of the University of the Witwatersrand, Johannesburg, South Africa, in an editorial published with both new studies in the Lancet (2020 Nov 10. doi: 10.1016/S0140-6736[20]32333-3).
The studies underscore the need for clinicians to consider continued risks associated with elevated LDL cholesterol in older age, they stressed, adding that statins are also beneficial for younger persons at risk to prevent conditions from worsening.
“The average age of patients in all the trials analyzed was older than 60 years, an age when atherosclerotic cardiovascular disease is already well established,” the editorialists wrote.
“Lipid-lowering therapy should be initiated at a younger age, preferably before age 40 years, in those at risk to delay the onset of atherosclerosis, rather than try to manage the condition once fully established or advanced,” they stressed.
No RCTs have included patients older than 70
For persons aged 40-75 years, elevated LDL cholesterol levels are a known risk factor for MI and atherosclerotic cardiovascular disease, and there is consensus in guidelines regarding treatment with statins.
However, the risk for people older than 70 is controversial. Some studies show little or no association between elevated LDL cholesterol levels and an increased risk for MI.
Contributing to the uncertainty is that few of the randomized, controlled trials that have investigated the question have included patients aged older than 70 years.
As a consequence, many practice guidelines have noted that the level of evidence in older patients is low, and some organizations have lowered the strength of recommendations regarding the treatment for older patients in comparison with younger patients.
Primary prevention: CV events increase with elevated LDL cholesterol in older age
Dr. Nordestgaard and colleagues studied data on 91,131 people living in Copenhagen who did not have atherosclerotic cardiovascular disease or diabetes at baseline and were not taking statins.
Of the participants, 10,592 were aged 70-79 years, and 3,188 participants were aged 80-100 years.
Over an average follow-up period of 7.7 years, 1,515 participants had a first MI, and 3,389 developed atherosclerotic cardiovascular disease.
In the primary-prevention cohort, after multivariate adjustment, the risk of having a heart attack per 1.0 mmol/L increase in LDL cholesterol was increased in the group overall (hazard ratio, 1.34). The increased risk was observed for all age groups, including those aged 80-100 years (HR, 1.28), 70-79 (HR, 1.25), 60-69 (HR, 1.29), 50-59 (HR, 1.28), and 20-49 (HR, 1.68).
Risk for atherosclerotic cardiovascular disease was also raised per 1.0 mmol/L increase in LDL cholesterol overall (HR, 1.16) and in all age groups, particularly those aged 70-100 years.
Greater elevations in LDL cholesterol (5.0 mmol/L or higher, indicative of possible familial hypercholesterolemia) were associated with a notably higher risk for heart attack after multivariate adjustment in people aged 80-100 (HR, 2.99). Risk was also higher among those aged 70-79 (HR, 1.82).
The highest incidence was in those older than 70. The rate was 8.5 heart attacks per 1,000 people per year among those aged 80-100 and 5.2 heart attacks per 1,000 in those aged 70-79. The rates were 2.5 per 1,000 among those 60-69, 1.8 for those aged 50-59, and 0.8 for those aged 20-49.
“The absolute risk [of cardiovascular events] is of course much higher in the elderly than those under the age of 75, but what was a surprise was how clear our results were on a relative risk scale, that the risk associated with elevated LDL [cholesterol] was as high in people aged 80-100 as the younger patients,” Dr. Nordestgaard said in an interview.
With regard to the benefits of cholesterol-lowering drugs, the study showed that the number needed to prevent one heart attack over 5 years was 80 among those aged 80-100; the number was 439 for people aged 50-59.
With regard to stronger statins, when moderate-intensity statins were used, the number needed to treat to prevent one cardiovascular disease event of any type dropped to 42 for patients aged 80-100. It was 88 for those aged 70-79, 164 for those aged 60-69, 345 for those aged 50-59, and 769 for those aged 20-49.
“The clinical significance of this is that it appears those in older age groups indeed benefit from cholesterol-lowering therapy,” Dr. Nordestgaard said. “I think many people have this idea that LDL [cholesterol] is not important over the age of about 70-75, but that’s not the case.”
“These robust findings are novel,” he and his colleagues stressed.
Despite these observational findings, the South African editorialists noted that “whether lipid-lowering therapy should be initiated for primary prevention in people aged 75 years or older is unclear,” owing to the host of risks and benefits that need to be balanced.
The findings of an ongoing randomized, placebo-controlled trial (STAREE) may answer this question, they wrote. It is investigating primary prevention in 18,000 older patients (≥70 years) who are being randomly assigned to receive atorvastatin 40 mg/d or placebo. The study is seeking to determine whether statin treatment extends the length of a disability-free life, which will be assessed on the basis of survival outside permanent residential care. Results are expected in 2022-2023.
Unequivocal reductions in events in elderly, comparable with younger patients
In the second study (Lancet. 2020 Nov 10. doi: 10.1016/S0140-6736[20]32332-1), Baris Gencer, MD, of Brigham and Women’s Hospital, Boston, =and colleagues evaluated the effects of statins and other cholesterol-lowering drugs, including ezetimibe and proprotein convertase subtilisin/kexin type 9 inhibitors, in older versus younger patients.
The systematic review and meta-analysis of 29 randomized controlled trials, also published in the Lancet, were presented virtually as a poster as part of the 2020 American Heart Association scientific session. It included data on 244,090 patients, including 21,492 aged 75 years and older.
The meta-analysis included studies of cardiovascular outcomes of a guideline-recommended LDL cholesterol–lowering drug, with a median follow-up of at least 2 years and inclusion of data on patients aged 75 years and older.
The results showed that over a median follow-up of 2.2 to 6 years, statin use by older patients was associated with a relative risk reduction of major vascular events of 26% per 1 mmol/L reduction in LDL cholesterol (P = .0019), which was comparable with a risk reduction of 15% per 1 mmol/L reduction in LDL cholesterol for patients younger than 75 years (P = .37, compared with older patients).
Treatment of older patients with LDL cholesterol–lowering drugs was also associated with significantly improved outcomes in cardiovascular death (risk ratio, 0.85), MI (RR, 0.80), stroke (RR, 0.73), and coronary revascularization (RR, 0.80).
“We found an unequivocal reduction in the risk of major vascular events with both statin and nonstatin LDL cholesterol-lowering treatments, which was similar to that seen in younger patients,” the authors wrote.
“Cholesterol-lowering medications are affordable drugs that have reduced risk of heart disease for millions of people worldwide, but until now, their benefits for older people have remained less certain,” said lead author Marc Sabatine, MD, also of Brigham and Women’s Hospital, in a Lancet press release.
“Our analysis indicates that these therapies are as effective in reducing cardiovascular events and deaths in people aged 75 years and over as they are in younger people. We found no offsetting safety concerns, and together, these results should strengthen guideline recommendations for the use of cholesterol-lowering medications, including statin and nonstatin therapy, in elderly people.”
The editorialists agreed: “More than 80% of fatal cardiovascular events occur in individuals older than 65 years, and the incidence of cardiovascular events is increasing in those older than 80 years; therefore, the findings of Gencer and colleagues’ study should encourage the use of lipid-lowering therapy in older patients.”
The authors of the two studies have disclosed no relevant financial relationships. Dr. Raal has received research grants, honoraria, or consulting fees for advisory board membership, professional input, and lectures on lipid-lowering drug therapy from Amgen, Regeneron, Sanofi, Novartis, and the Medicines Company.
A version of this article originally appeared on Medscape.com.
Contrary to historical evidence, two new studies show.
“By contrast with previous historical studies, our data show that LDL cholesterol is an important risk factor for myocardial infarction and atherosclerotic cardiovascular disease in a contemporary primary prevention cohort of individuals aged 70 to 100 years,” Borge Nordestgaard, MD, of the University of Copenhagen, and colleagues noted in the first of the two studies, published this week in the Lancet.
“By lowering LDL cholesterol in healthy individuals aged 70-100 years, the potential for preventing myocardial infarctions and atherosclerotic cardiovascular disease is huge, and at a substantially lower number needed to treat when compared with those aged 20-69 years,” they added.
“These findings support the concept of the cumulative burden of LDL cholesterol over one’s lifetime and the progressive increase in risk for atherosclerotic cardiovascular disease, including myocardial infarction, with age,” added Frederick J. Raal, PhD, and Farzahna Mohamed, MB BCh, of the University of the Witwatersrand, Johannesburg, South Africa, in an editorial published with both new studies in the Lancet (2020 Nov 10. doi: 10.1016/S0140-6736[20]32333-3).
The studies underscore the need for clinicians to consider continued risks associated with elevated LDL cholesterol in older age, they stressed, adding that statins are also beneficial for younger persons at risk to prevent conditions from worsening.
“The average age of patients in all the trials analyzed was older than 60 years, an age when atherosclerotic cardiovascular disease is already well established,” the editorialists wrote.
“Lipid-lowering therapy should be initiated at a younger age, preferably before age 40 years, in those at risk to delay the onset of atherosclerosis, rather than try to manage the condition once fully established or advanced,” they stressed.
No RCTs have included patients older than 70
For persons aged 40-75 years, elevated LDL cholesterol levels are a known risk factor for MI and atherosclerotic cardiovascular disease, and there is consensus in guidelines regarding treatment with statins.
However, the risk for people older than 70 is controversial. Some studies show little or no association between elevated LDL cholesterol levels and an increased risk for MI.
Contributing to the uncertainty is that few of the randomized, controlled trials that have investigated the question have included patients aged older than 70 years.
As a consequence, many practice guidelines have noted that the level of evidence in older patients is low, and some organizations have lowered the strength of recommendations regarding the treatment for older patients in comparison with younger patients.
Primary prevention: CV events increase with elevated LDL cholesterol in older age
Dr. Nordestgaard and colleagues studied data on 91,131 people living in Copenhagen who did not have atherosclerotic cardiovascular disease or diabetes at baseline and were not taking statins.
Of the participants, 10,592 were aged 70-79 years, and 3,188 participants were aged 80-100 years.
Over an average follow-up period of 7.7 years, 1,515 participants had a first MI, and 3,389 developed atherosclerotic cardiovascular disease.
In the primary-prevention cohort, after multivariate adjustment, the risk of having a heart attack per 1.0 mmol/L increase in LDL cholesterol was increased in the group overall (hazard ratio, 1.34). The increased risk was observed for all age groups, including those aged 80-100 years (HR, 1.28), 70-79 (HR, 1.25), 60-69 (HR, 1.29), 50-59 (HR, 1.28), and 20-49 (HR, 1.68).
Risk for atherosclerotic cardiovascular disease was also raised per 1.0 mmol/L increase in LDL cholesterol overall (HR, 1.16) and in all age groups, particularly those aged 70-100 years.
Greater elevations in LDL cholesterol (5.0 mmol/L or higher, indicative of possible familial hypercholesterolemia) were associated with a notably higher risk for heart attack after multivariate adjustment in people aged 80-100 (HR, 2.99). Risk was also higher among those aged 70-79 (HR, 1.82).
The highest incidence was in those older than 70. The rate was 8.5 heart attacks per 1,000 people per year among those aged 80-100 and 5.2 heart attacks per 1,000 in those aged 70-79. The rates were 2.5 per 1,000 among those 60-69, 1.8 for those aged 50-59, and 0.8 for those aged 20-49.
“The absolute risk [of cardiovascular events] is of course much higher in the elderly than those under the age of 75, but what was a surprise was how clear our results were on a relative risk scale, that the risk associated with elevated LDL [cholesterol] was as high in people aged 80-100 as the younger patients,” Dr. Nordestgaard said in an interview.
With regard to the benefits of cholesterol-lowering drugs, the study showed that the number needed to prevent one heart attack over 5 years was 80 among those aged 80-100; the number was 439 for people aged 50-59.
With regard to stronger statins, when moderate-intensity statins were used, the number needed to treat to prevent one cardiovascular disease event of any type dropped to 42 for patients aged 80-100. It was 88 for those aged 70-79, 164 for those aged 60-69, 345 for those aged 50-59, and 769 for those aged 20-49.
“The clinical significance of this is that it appears those in older age groups indeed benefit from cholesterol-lowering therapy,” Dr. Nordestgaard said. “I think many people have this idea that LDL [cholesterol] is not important over the age of about 70-75, but that’s not the case.”
“These robust findings are novel,” he and his colleagues stressed.
Despite these observational findings, the South African editorialists noted that “whether lipid-lowering therapy should be initiated for primary prevention in people aged 75 years or older is unclear,” owing to the host of risks and benefits that need to be balanced.
The findings of an ongoing randomized, placebo-controlled trial (STAREE) may answer this question, they wrote. It is investigating primary prevention in 18,000 older patients (≥70 years) who are being randomly assigned to receive atorvastatin 40 mg/d or placebo. The study is seeking to determine whether statin treatment extends the length of a disability-free life, which will be assessed on the basis of survival outside permanent residential care. Results are expected in 2022-2023.
Unequivocal reductions in events in elderly, comparable with younger patients
In the second study (Lancet. 2020 Nov 10. doi: 10.1016/S0140-6736[20]32332-1), Baris Gencer, MD, of Brigham and Women’s Hospital, Boston, =and colleagues evaluated the effects of statins and other cholesterol-lowering drugs, including ezetimibe and proprotein convertase subtilisin/kexin type 9 inhibitors, in older versus younger patients.
The systematic review and meta-analysis of 29 randomized controlled trials, also published in the Lancet, were presented virtually as a poster as part of the 2020 American Heart Association scientific session. It included data on 244,090 patients, including 21,492 aged 75 years and older.
The meta-analysis included studies of cardiovascular outcomes of a guideline-recommended LDL cholesterol–lowering drug, with a median follow-up of at least 2 years and inclusion of data on patients aged 75 years and older.
The results showed that over a median follow-up of 2.2 to 6 years, statin use by older patients was associated with a relative risk reduction of major vascular events of 26% per 1 mmol/L reduction in LDL cholesterol (P = .0019), which was comparable with a risk reduction of 15% per 1 mmol/L reduction in LDL cholesterol for patients younger than 75 years (P = .37, compared with older patients).
Treatment of older patients with LDL cholesterol–lowering drugs was also associated with significantly improved outcomes in cardiovascular death (risk ratio, 0.85), MI (RR, 0.80), stroke (RR, 0.73), and coronary revascularization (RR, 0.80).
“We found an unequivocal reduction in the risk of major vascular events with both statin and nonstatin LDL cholesterol-lowering treatments, which was similar to that seen in younger patients,” the authors wrote.
“Cholesterol-lowering medications are affordable drugs that have reduced risk of heart disease for millions of people worldwide, but until now, their benefits for older people have remained less certain,” said lead author Marc Sabatine, MD, also of Brigham and Women’s Hospital, in a Lancet press release.
“Our analysis indicates that these therapies are as effective in reducing cardiovascular events and deaths in people aged 75 years and over as they are in younger people. We found no offsetting safety concerns, and together, these results should strengthen guideline recommendations for the use of cholesterol-lowering medications, including statin and nonstatin therapy, in elderly people.”
The editorialists agreed: “More than 80% of fatal cardiovascular events occur in individuals older than 65 years, and the incidence of cardiovascular events is increasing in those older than 80 years; therefore, the findings of Gencer and colleagues’ study should encourage the use of lipid-lowering therapy in older patients.”
The authors of the two studies have disclosed no relevant financial relationships. Dr. Raal has received research grants, honoraria, or consulting fees for advisory board membership, professional input, and lectures on lipid-lowering drug therapy from Amgen, Regeneron, Sanofi, Novartis, and the Medicines Company.
A version of this article originally appeared on Medscape.com.
Concussion linked to risk for dementia, Parkinson’s disease, and ADHD
new research suggests. Results from a retrospective, population-based cohort study showed that controlling for socioeconomic status and overall health did not significantly affect this association.
The link between concussion and risk for ADHD and for mood and anxiety disorder was stronger in the women than in the men. In addition, having a history of multiple concussions strengthened the association between concussion and subsequent mood and anxiety disorder, dementia, and Parkinson’s disease compared with experiencing just one concussion.
The findings are similar to those of previous studies, noted lead author Marc P. Morissette, PhD, research assistant at the Pan Am Clinic Foundation in Winnipeg, Manitoba, Canada. “The main methodological differences separating our study from previous studies in this area is a focus on concussion-specific injuries identified from medical records and the potential for study participants to have up to 25 years of follow-up data,” said Dr. Morissette.
The findings were published online July 27 in Family Medicine and Community Health, a BMJ journal.
Almost 190,000 participants
Several studies have shown associations between head injury and increased risk for ADHD, depression, anxiety, Alzheimer’s disease, and Parkinson’s disease. However, many of these studies relied on self-reported medical history, included all forms of traumatic brain injury, and failed to adjust for preexisting health conditions.
An improved understanding of concussion and the risks associated with it could help physicians manage their patients’ long-term needs, the investigators noted.
In the current study, the researchers examined anonymized administrative health data collected between the periods of 1990–1991 and 2014–2015 in the Manitoba Population Research Data Repository at the Manitoba Center for Health Policy.
Eligible patients had been diagnosed with concussion in accordance with standard criteria. Participants were excluded if they had been diagnosed with dementia or Parkinson’s disease before the incident concussion during the study period. The investigators matched three control participants to each included patient on the basis of age, sex, and location.
Study outcome was time from index date (date of first concussion) to diagnosis of ADHD, mood and anxiety disorder, dementia, or Parkinson’s disease. The researchers controlled for socioeconomic status using the Socioeconomic Factor Index, version 2 (SEFI2), and for preexisting medical conditions using the Charlson Comorbidity Index (CCI).
The study included 28,021 men (mean age, 25 years) and 19,462 women (mean age, 30 years) in the concussion group and 81,871 men (mean age, 25 years) and 57,159 women (mean age, 30 years) in the control group. Mean SEFI2 score was approximately −0.05, and mean CCI score was approximately 0.2.
Dose effect?
Results showed that concussion was associated with an increased risk for ADHD (hazard ratio [HR], 1.39), mood and anxiety disorder (HR, 1.72), dementia (HR, 1.72), and Parkinson’s disease (HR, 1.57).
After a concussion, the risk of developing ADHD was 28% higher and the risk of developing mood and anxiety disorder was 7% higher among women than among men. Gender was not associated with risk for dementia or Parkinson’s disease after concussion.
Sustaining a second concussion increased the strength of the association with risk for dementia compared with sustaining a single concussion (HR, 1.62). Similarly, sustaining more than three concussions increased the strength of the association with the risk for mood and anxiety disorders (HR for more than three vs one concussion, 1.22) and Parkinson›s disease (HR, 3.27).
A sensitivity analysis found similar associations between concussion and risk for mood and anxiety disorder among all age groups. Younger participants were at greater risk for ADHD, however, and older participants were at greater risk for dementia and Parkinson’s disease.
Increased awareness of concussion and the outcomes of interest, along with improved diagnostic tools, may have influenced the study’s findings, Dr. Morissette noted. “The sex-based differences may be due to either pathophysiological differences in response to concussive injuries or potentially a difference in willingness to seek medical care or share symptoms, concussion-related or otherwise, with a medical professional,” he said.
“We are hopeful that our findings will encourage practitioners to be cognizant of various conditions that may present in individuals who have previously experienced a concussion,” Dr. Morissette added. “If physicians are aware of the various associations identified following a concussion, it may lead to more thorough clinical examination at initial presentation, along with more dedicated care throughout the patient’s life.”
Association versus causation
Commenting on the research, Steven Erickson, MD, sports medicine specialist at Banner–University Medicine Neuroscience Institute, Phoenix, Ariz., noted that although the study showed an association between concussion and subsequent diagnosis of ADHD, anxiety, and Parkinson’s disease, “this association should not be misconstrued as causation.” He added that the study’s conclusions “are just as likely to be due to labeling theory” or a self-fulfilling prophecy.
“Patients diagnosed with ADHD, anxiety, or Parkinson’s disease may recall concussion and associate the two diagnoses; but patients who have not previously been diagnosed with a concussion cannot draw that conclusion,” said Dr. Erickson, who was not involved with the research.
Citing the apparent gender difference in the strength of the association between concussion and the outcomes of interest, Dr. Erickson noted that women are more likely to report symptoms in general “and therefore are more likely to be diagnosed with ADHD and anxiety disorders” because of differences in reporting rather than incidence of disease.
“Further research needs to be done to definitively determine a causal relationship between concussion and any psychiatric or neurologic diagnosis,” Dr. Erickson concluded.
The study was funded by the Pan Am Clinic Foundation. Dr. Morissette and Dr. Erickson have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests. Results from a retrospective, population-based cohort study showed that controlling for socioeconomic status and overall health did not significantly affect this association.
The link between concussion and risk for ADHD and for mood and anxiety disorder was stronger in the women than in the men. In addition, having a history of multiple concussions strengthened the association between concussion and subsequent mood and anxiety disorder, dementia, and Parkinson’s disease compared with experiencing just one concussion.
The findings are similar to those of previous studies, noted lead author Marc P. Morissette, PhD, research assistant at the Pan Am Clinic Foundation in Winnipeg, Manitoba, Canada. “The main methodological differences separating our study from previous studies in this area is a focus on concussion-specific injuries identified from medical records and the potential for study participants to have up to 25 years of follow-up data,” said Dr. Morissette.
The findings were published online July 27 in Family Medicine and Community Health, a BMJ journal.
Almost 190,000 participants
Several studies have shown associations between head injury and increased risk for ADHD, depression, anxiety, Alzheimer’s disease, and Parkinson’s disease. However, many of these studies relied on self-reported medical history, included all forms of traumatic brain injury, and failed to adjust for preexisting health conditions.
An improved understanding of concussion and the risks associated with it could help physicians manage their patients’ long-term needs, the investigators noted.
In the current study, the researchers examined anonymized administrative health data collected between the periods of 1990–1991 and 2014–2015 in the Manitoba Population Research Data Repository at the Manitoba Center for Health Policy.
Eligible patients had been diagnosed with concussion in accordance with standard criteria. Participants were excluded if they had been diagnosed with dementia or Parkinson’s disease before the incident concussion during the study period. The investigators matched three control participants to each included patient on the basis of age, sex, and location.
Study outcome was time from index date (date of first concussion) to diagnosis of ADHD, mood and anxiety disorder, dementia, or Parkinson’s disease. The researchers controlled for socioeconomic status using the Socioeconomic Factor Index, version 2 (SEFI2), and for preexisting medical conditions using the Charlson Comorbidity Index (CCI).
The study included 28,021 men (mean age, 25 years) and 19,462 women (mean age, 30 years) in the concussion group and 81,871 men (mean age, 25 years) and 57,159 women (mean age, 30 years) in the control group. Mean SEFI2 score was approximately −0.05, and mean CCI score was approximately 0.2.
Dose effect?
Results showed that concussion was associated with an increased risk for ADHD (hazard ratio [HR], 1.39), mood and anxiety disorder (HR, 1.72), dementia (HR, 1.72), and Parkinson’s disease (HR, 1.57).
After a concussion, the risk of developing ADHD was 28% higher and the risk of developing mood and anxiety disorder was 7% higher among women than among men. Gender was not associated with risk for dementia or Parkinson’s disease after concussion.
Sustaining a second concussion increased the strength of the association with risk for dementia compared with sustaining a single concussion (HR, 1.62). Similarly, sustaining more than three concussions increased the strength of the association with the risk for mood and anxiety disorders (HR for more than three vs one concussion, 1.22) and Parkinson›s disease (HR, 3.27).
A sensitivity analysis found similar associations between concussion and risk for mood and anxiety disorder among all age groups. Younger participants were at greater risk for ADHD, however, and older participants were at greater risk for dementia and Parkinson’s disease.
Increased awareness of concussion and the outcomes of interest, along with improved diagnostic tools, may have influenced the study’s findings, Dr. Morissette noted. “The sex-based differences may be due to either pathophysiological differences in response to concussive injuries or potentially a difference in willingness to seek medical care or share symptoms, concussion-related or otherwise, with a medical professional,” he said.
“We are hopeful that our findings will encourage practitioners to be cognizant of various conditions that may present in individuals who have previously experienced a concussion,” Dr. Morissette added. “If physicians are aware of the various associations identified following a concussion, it may lead to more thorough clinical examination at initial presentation, along with more dedicated care throughout the patient’s life.”
Association versus causation
Commenting on the research, Steven Erickson, MD, sports medicine specialist at Banner–University Medicine Neuroscience Institute, Phoenix, Ariz., noted that although the study showed an association between concussion and subsequent diagnosis of ADHD, anxiety, and Parkinson’s disease, “this association should not be misconstrued as causation.” He added that the study’s conclusions “are just as likely to be due to labeling theory” or a self-fulfilling prophecy.
“Patients diagnosed with ADHD, anxiety, or Parkinson’s disease may recall concussion and associate the two diagnoses; but patients who have not previously been diagnosed with a concussion cannot draw that conclusion,” said Dr. Erickson, who was not involved with the research.
Citing the apparent gender difference in the strength of the association between concussion and the outcomes of interest, Dr. Erickson noted that women are more likely to report symptoms in general “and therefore are more likely to be diagnosed with ADHD and anxiety disorders” because of differences in reporting rather than incidence of disease.
“Further research needs to be done to definitively determine a causal relationship between concussion and any psychiatric or neurologic diagnosis,” Dr. Erickson concluded.
The study was funded by the Pan Am Clinic Foundation. Dr. Morissette and Dr. Erickson have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests. Results from a retrospective, population-based cohort study showed that controlling for socioeconomic status and overall health did not significantly affect this association.
The link between concussion and risk for ADHD and for mood and anxiety disorder was stronger in the women than in the men. In addition, having a history of multiple concussions strengthened the association between concussion and subsequent mood and anxiety disorder, dementia, and Parkinson’s disease compared with experiencing just one concussion.
The findings are similar to those of previous studies, noted lead author Marc P. Morissette, PhD, research assistant at the Pan Am Clinic Foundation in Winnipeg, Manitoba, Canada. “The main methodological differences separating our study from previous studies in this area is a focus on concussion-specific injuries identified from medical records and the potential for study participants to have up to 25 years of follow-up data,” said Dr. Morissette.
The findings were published online July 27 in Family Medicine and Community Health, a BMJ journal.
Almost 190,000 participants
Several studies have shown associations between head injury and increased risk for ADHD, depression, anxiety, Alzheimer’s disease, and Parkinson’s disease. However, many of these studies relied on self-reported medical history, included all forms of traumatic brain injury, and failed to adjust for preexisting health conditions.
An improved understanding of concussion and the risks associated with it could help physicians manage their patients’ long-term needs, the investigators noted.
In the current study, the researchers examined anonymized administrative health data collected between the periods of 1990–1991 and 2014–2015 in the Manitoba Population Research Data Repository at the Manitoba Center for Health Policy.
Eligible patients had been diagnosed with concussion in accordance with standard criteria. Participants were excluded if they had been diagnosed with dementia or Parkinson’s disease before the incident concussion during the study period. The investigators matched three control participants to each included patient on the basis of age, sex, and location.
Study outcome was time from index date (date of first concussion) to diagnosis of ADHD, mood and anxiety disorder, dementia, or Parkinson’s disease. The researchers controlled for socioeconomic status using the Socioeconomic Factor Index, version 2 (SEFI2), and for preexisting medical conditions using the Charlson Comorbidity Index (CCI).
The study included 28,021 men (mean age, 25 years) and 19,462 women (mean age, 30 years) in the concussion group and 81,871 men (mean age, 25 years) and 57,159 women (mean age, 30 years) in the control group. Mean SEFI2 score was approximately −0.05, and mean CCI score was approximately 0.2.
Dose effect?
Results showed that concussion was associated with an increased risk for ADHD (hazard ratio [HR], 1.39), mood and anxiety disorder (HR, 1.72), dementia (HR, 1.72), and Parkinson’s disease (HR, 1.57).
After a concussion, the risk of developing ADHD was 28% higher and the risk of developing mood and anxiety disorder was 7% higher among women than among men. Gender was not associated with risk for dementia or Parkinson’s disease after concussion.
Sustaining a second concussion increased the strength of the association with risk for dementia compared with sustaining a single concussion (HR, 1.62). Similarly, sustaining more than three concussions increased the strength of the association with the risk for mood and anxiety disorders (HR for more than three vs one concussion, 1.22) and Parkinson›s disease (HR, 3.27).
A sensitivity analysis found similar associations between concussion and risk for mood and anxiety disorder among all age groups. Younger participants were at greater risk for ADHD, however, and older participants were at greater risk for dementia and Parkinson’s disease.
Increased awareness of concussion and the outcomes of interest, along with improved diagnostic tools, may have influenced the study’s findings, Dr. Morissette noted. “The sex-based differences may be due to either pathophysiological differences in response to concussive injuries or potentially a difference in willingness to seek medical care or share symptoms, concussion-related or otherwise, with a medical professional,” he said.
“We are hopeful that our findings will encourage practitioners to be cognizant of various conditions that may present in individuals who have previously experienced a concussion,” Dr. Morissette added. “If physicians are aware of the various associations identified following a concussion, it may lead to more thorough clinical examination at initial presentation, along with more dedicated care throughout the patient’s life.”
Association versus causation
Commenting on the research, Steven Erickson, MD, sports medicine specialist at Banner–University Medicine Neuroscience Institute, Phoenix, Ariz., noted that although the study showed an association between concussion and subsequent diagnosis of ADHD, anxiety, and Parkinson’s disease, “this association should not be misconstrued as causation.” He added that the study’s conclusions “are just as likely to be due to labeling theory” or a self-fulfilling prophecy.
“Patients diagnosed with ADHD, anxiety, or Parkinson’s disease may recall concussion and associate the two diagnoses; but patients who have not previously been diagnosed with a concussion cannot draw that conclusion,” said Dr. Erickson, who was not involved with the research.
Citing the apparent gender difference in the strength of the association between concussion and the outcomes of interest, Dr. Erickson noted that women are more likely to report symptoms in general “and therefore are more likely to be diagnosed with ADHD and anxiety disorders” because of differences in reporting rather than incidence of disease.
“Further research needs to be done to definitively determine a causal relationship between concussion and any psychiatric or neurologic diagnosis,” Dr. Erickson concluded.
The study was funded by the Pan Am Clinic Foundation. Dr. Morissette and Dr. Erickson have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
From Family Medicine and Community Health
Late-onset epilepsy tied to a threefold increased dementia risk
Results of a retrospective analysis show that patients who develop epilepsy at age 67 or older have a threefold increased risk of subsequent dementia versus their counterparts without epilepsy.
“This is an exciting area, as we are finding that just as the risk of seizures is increased in neurodegenerative diseases, the risk of dementia is increased after late-onset epilepsy and seizures,” study investigator Emily L. Johnson, MD, assistant professor of neurology at Johns Hopkins University, Baltimore, said in an interview. “Several other cohort studies are finding similar results, including the Veterans’ Health Study and the Framingham Study,” she added.
The study was published online Oct. 23 in Neurology
Bidirectional relationship?
Previous research has established that dementia is a risk factor for epilepsy, but recent studies also suggest an increased risk of incident dementia among patients with adult-onset epilepsy. Several risk factors for late-onset epilepsy, including diabetes and hypertension, also are risk factors for dementia. However, the effect of late-onset epilepsy on dementia risk in patients with these comorbidities has not been clarified.
To investigate, the researchers examined data from the Atherosclerosis Risk in Communities (ARIC) study. Participants include Black and White men and women from four U.S. communities. Baseline visits in this longitudinal cohort study began between 1987 and 1989, and follow-up included seven additional visits and regular phone calls.
The investigators identified participants with late-onset epilepsy by searching for Medicare claims related to seizures or epilepsy filed between 1991 and 2015. Those with two or more such claims and age of onset of 67 years or greater were considered to have late-onset epilepsy. Participants with preexisting conditions such as brain tumors or multiple sclerosis were excluded.
ARIC participants who presented in person for visits 2, 4, 5, and 6 underwent cognitive testing with the Delayed Word Recall Test, the Digit Symbol Substitution Test, and the Word Fluency Test.
Testing at visits 5 and 6 also included other tests, such as the Mini-Mental State Examination, the Boston Naming test, and the Wechsler Memory Scale-III. Dr. Johnson and colleagues excluded data for visit 7 from the analysis because dementia adjudication was not yet complete.
The researchers identified participants with dementia using data from visits 5 and 6 and ascertained time of dementia onset through participant and informant interviews, phone calls, and hospital discharge data. Participants also were screened for mild cognitive impairment (MCI) at visits 5 and 6.
Data were analyzed using a Cox proportional hazards model and multinomial logistic regression. In subsequent analyses, researchers adjusted the data for age, sex, race, smoking status, alcohol use, hypertension, diabetes, body mass index (BMI), APOE4 status, and prevalent stroke.
The researchers found that of 9,033 study participants, 671 had late-onset epilepsy. The late-onset epilepsy group was older at baseline (56.5 vs. 55.1 years) and more likely to have hypertension (38.9% vs. 33.3%), diabetes (16.1% vs. 9.6%), and two alleles of APOE4 genotype (3.9% vs. 2.5%), compared with those without the disorder.
In all, 1,687 participants developed dementia during follow-up. The rate of incident dementia was 41.6% in participants with late-onset epilepsy and 16.8% in participants without late-onset epilepsy. The adjusted hazard ratio of subsequent dementia in participants with late-onset epilepsy versus those without the disorder was 3.05 (95% confidence interval, 2.65-3.51).
The median time to dementia ascertainment after late-onset epilepsy was 3.66 years.
Counterintuitive finding
The relationship between late-onset epilepsy and subsequent dementia was stronger in patients without stroke. The investigators offered a possible explanation for this counterintuitive finding. “We observed an interaction between [late-onset epilepsy] and stroke, with a lower (but still substantial) association between [late-onset epilepsy] and dementia in those with a history of stroke. This may be due to the known strong association between stroke and dementia, which may wash out the contributions of [late-onset epilepsy] to cognitive impairment,” the researchers wrote.
“There may also be under-capturing of dementia diagnoses among participants with stroke in the ascertainment from [Centers for Medicare & Medicaid Services] codes, as physicians may be reluctant to make a separate code for ‘dementia’ in those with cognitive impairment after stroke,” they added.
When the researchers restricted the analysis only to participants who attended visits 5 and 6 and had late-onset epilepsy ascertainment available, they found that the relative risk ratio for dementia at visit 6 was 2.90 (95% CI, 1.22-6.92; P = .009). The RRR for MCI was 0.97 (95% CI, 0.39-2.38; P = .803). The greater functional impairment in patients with late-onset epilepsy may explain the lack of a relationship between late-onset epilepsy and MCI.
“It will be important for neurologists to be aware of the possibility of cognitive impairment following late-onset epilepsy and to check in with patients and family members to see if there are concerns,” said Dr. Johnson.
“We should also be talking about the importance of lowering other risk factors for dementia by making sure cardiovascular risk factors are controlled and encouraging physical and cognitive activity,” she added.
The results require confirmation in a clinical population, the investigators noted. In addition, future research is necessary to clarify whether seizures directly increase the risk of dementia or whether shared neuropathology between epilepsy and dementia explains the risk.
“In the near future, I plan to enroll participants with late-onset epilepsy in an observational study to better understand factors that may contribute to cognitive change. Collaborations will be key as we seek to further understand what causes these changes and what could be done to prevent them,” Dr. Johnson added.
Strengths and weaknesses
In an accompanying editorial, W. Allen Hauser, MD, professor emeritus of neurology and epidemiology at Columbia University in New York, and colleagues noted that the findings support a bidirectional relationship between dementia and epilepsy, adding that accumulation of amyloid beta peptide is a plausible underlying pathophysiology that may explain this relationship.
Future research should clarify the effect of factors such as seizure type, seizure frequency, and age of onset on the risk of dementia among patients with epilepsy, the editorialists wrote. Such investigations could help elucidate the underlying mechanisms of these conditions and help to improve treatment, they added.
Commenting on the findings, Ilo Leppik, MD, professor of neurology and pharmacy at the University of Minnesota in Minneapolis described the research as “a very well-done study by qualified researchers in the field. … For the last century, medicine has unfortunately become compartmentalized by specialty and then subspecialty. The brain and disorders of the brain do not recognize these silos. … It is not a stretch of the known science to begin to understand that epilepsy and dementia have common anatomical and physiological underpinnings.”
The long period of prospectively gathering data and the measurement of cognitive function through various modalities are among the study’s great strengths, said Dr. Leppik. However, the study’s weakness is its reliance on Medicare claims data, which mainly would reflect convulsive seizures.
“What is missing is how many persons had subtle focal-unaware seizures that may not be identified unless a careful history is taken,” said Dr. Leppik. “Thus, this study likely underestimates the frequency of epilepsy.”
Neurologists who evaluate a person with early dementia should be on the lookout for a history of subtle seizures, said Dr. Leppik. Animal studies suggest treatment with levetiracetam or brivaracetam may slow the course of dementia, and a clinical study in participants with early dementia is underway.
“Treatment with an antiseizure drug may prove to be beneficial, especially if evidence for the presence of subtle epilepsy can be found,” Dr. Leppik added.
Greater collaboration between epileptologists and dementia specialists and larger studies of antiseizure drugs are necessary, he noted. “These studies can incorporate sophisticated structural and biochemical [analyses] to better identify the relationships between brain mechanisms that likely underlie both seizures and dementia. The ultimate promise is that early treatment of seizures may alter the course of dementia,” Dr. Leppik said.
The study by Dr. Johnson and colleagues was supported by a contract from the National Institute on Aging; ARIC from the National Heart, Lung, and Blood Institute; the National Institutes of Health; and the Department of Health & Human Services. The authors and Dr. Leppik have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Results of a retrospective analysis show that patients who develop epilepsy at age 67 or older have a threefold increased risk of subsequent dementia versus their counterparts without epilepsy.
“This is an exciting area, as we are finding that just as the risk of seizures is increased in neurodegenerative diseases, the risk of dementia is increased after late-onset epilepsy and seizures,” study investigator Emily L. Johnson, MD, assistant professor of neurology at Johns Hopkins University, Baltimore, said in an interview. “Several other cohort studies are finding similar results, including the Veterans’ Health Study and the Framingham Study,” she added.
The study was published online Oct. 23 in Neurology
Bidirectional relationship?
Previous research has established that dementia is a risk factor for epilepsy, but recent studies also suggest an increased risk of incident dementia among patients with adult-onset epilepsy. Several risk factors for late-onset epilepsy, including diabetes and hypertension, also are risk factors for dementia. However, the effect of late-onset epilepsy on dementia risk in patients with these comorbidities has not been clarified.
To investigate, the researchers examined data from the Atherosclerosis Risk in Communities (ARIC) study. Participants include Black and White men and women from four U.S. communities. Baseline visits in this longitudinal cohort study began between 1987 and 1989, and follow-up included seven additional visits and regular phone calls.
The investigators identified participants with late-onset epilepsy by searching for Medicare claims related to seizures or epilepsy filed between 1991 and 2015. Those with two or more such claims and age of onset of 67 years or greater were considered to have late-onset epilepsy. Participants with preexisting conditions such as brain tumors or multiple sclerosis were excluded.
ARIC participants who presented in person for visits 2, 4, 5, and 6 underwent cognitive testing with the Delayed Word Recall Test, the Digit Symbol Substitution Test, and the Word Fluency Test.
Testing at visits 5 and 6 also included other tests, such as the Mini-Mental State Examination, the Boston Naming test, and the Wechsler Memory Scale-III. Dr. Johnson and colleagues excluded data for visit 7 from the analysis because dementia adjudication was not yet complete.
The researchers identified participants with dementia using data from visits 5 and 6 and ascertained time of dementia onset through participant and informant interviews, phone calls, and hospital discharge data. Participants also were screened for mild cognitive impairment (MCI) at visits 5 and 6.
Data were analyzed using a Cox proportional hazards model and multinomial logistic regression. In subsequent analyses, researchers adjusted the data for age, sex, race, smoking status, alcohol use, hypertension, diabetes, body mass index (BMI), APOE4 status, and prevalent stroke.
The researchers found that of 9,033 study participants, 671 had late-onset epilepsy. The late-onset epilepsy group was older at baseline (56.5 vs. 55.1 years) and more likely to have hypertension (38.9% vs. 33.3%), diabetes (16.1% vs. 9.6%), and two alleles of APOE4 genotype (3.9% vs. 2.5%), compared with those without the disorder.
In all, 1,687 participants developed dementia during follow-up. The rate of incident dementia was 41.6% in participants with late-onset epilepsy and 16.8% in participants without late-onset epilepsy. The adjusted hazard ratio of subsequent dementia in participants with late-onset epilepsy versus those without the disorder was 3.05 (95% confidence interval, 2.65-3.51).
The median time to dementia ascertainment after late-onset epilepsy was 3.66 years.
Counterintuitive finding
The relationship between late-onset epilepsy and subsequent dementia was stronger in patients without stroke. The investigators offered a possible explanation for this counterintuitive finding. “We observed an interaction between [late-onset epilepsy] and stroke, with a lower (but still substantial) association between [late-onset epilepsy] and dementia in those with a history of stroke. This may be due to the known strong association between stroke and dementia, which may wash out the contributions of [late-onset epilepsy] to cognitive impairment,” the researchers wrote.
“There may also be under-capturing of dementia diagnoses among participants with stroke in the ascertainment from [Centers for Medicare & Medicaid Services] codes, as physicians may be reluctant to make a separate code for ‘dementia’ in those with cognitive impairment after stroke,” they added.
When the researchers restricted the analysis only to participants who attended visits 5 and 6 and had late-onset epilepsy ascertainment available, they found that the relative risk ratio for dementia at visit 6 was 2.90 (95% CI, 1.22-6.92; P = .009). The RRR for MCI was 0.97 (95% CI, 0.39-2.38; P = .803). The greater functional impairment in patients with late-onset epilepsy may explain the lack of a relationship between late-onset epilepsy and MCI.
“It will be important for neurologists to be aware of the possibility of cognitive impairment following late-onset epilepsy and to check in with patients and family members to see if there are concerns,” said Dr. Johnson.
“We should also be talking about the importance of lowering other risk factors for dementia by making sure cardiovascular risk factors are controlled and encouraging physical and cognitive activity,” she added.
The results require confirmation in a clinical population, the investigators noted. In addition, future research is necessary to clarify whether seizures directly increase the risk of dementia or whether shared neuropathology between epilepsy and dementia explains the risk.
“In the near future, I plan to enroll participants with late-onset epilepsy in an observational study to better understand factors that may contribute to cognitive change. Collaborations will be key as we seek to further understand what causes these changes and what could be done to prevent them,” Dr. Johnson added.
Strengths and weaknesses
In an accompanying editorial, W. Allen Hauser, MD, professor emeritus of neurology and epidemiology at Columbia University in New York, and colleagues noted that the findings support a bidirectional relationship between dementia and epilepsy, adding that accumulation of amyloid beta peptide is a plausible underlying pathophysiology that may explain this relationship.
Future research should clarify the effect of factors such as seizure type, seizure frequency, and age of onset on the risk of dementia among patients with epilepsy, the editorialists wrote. Such investigations could help elucidate the underlying mechanisms of these conditions and help to improve treatment, they added.
Commenting on the findings, Ilo Leppik, MD, professor of neurology and pharmacy at the University of Minnesota in Minneapolis described the research as “a very well-done study by qualified researchers in the field. … For the last century, medicine has unfortunately become compartmentalized by specialty and then subspecialty. The brain and disorders of the brain do not recognize these silos. … It is not a stretch of the known science to begin to understand that epilepsy and dementia have common anatomical and physiological underpinnings.”
The long period of prospectively gathering data and the measurement of cognitive function through various modalities are among the study’s great strengths, said Dr. Leppik. However, the study’s weakness is its reliance on Medicare claims data, which mainly would reflect convulsive seizures.
“What is missing is how many persons had subtle focal-unaware seizures that may not be identified unless a careful history is taken,” said Dr. Leppik. “Thus, this study likely underestimates the frequency of epilepsy.”
Neurologists who evaluate a person with early dementia should be on the lookout for a history of subtle seizures, said Dr. Leppik. Animal studies suggest treatment with levetiracetam or brivaracetam may slow the course of dementia, and a clinical study in participants with early dementia is underway.
“Treatment with an antiseizure drug may prove to be beneficial, especially if evidence for the presence of subtle epilepsy can be found,” Dr. Leppik added.
Greater collaboration between epileptologists and dementia specialists and larger studies of antiseizure drugs are necessary, he noted. “These studies can incorporate sophisticated structural and biochemical [analyses] to better identify the relationships between brain mechanisms that likely underlie both seizures and dementia. The ultimate promise is that early treatment of seizures may alter the course of dementia,” Dr. Leppik said.
The study by Dr. Johnson and colleagues was supported by a contract from the National Institute on Aging; ARIC from the National Heart, Lung, and Blood Institute; the National Institutes of Health; and the Department of Health & Human Services. The authors and Dr. Leppik have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Results of a retrospective analysis show that patients who develop epilepsy at age 67 or older have a threefold increased risk of subsequent dementia versus their counterparts without epilepsy.
“This is an exciting area, as we are finding that just as the risk of seizures is increased in neurodegenerative diseases, the risk of dementia is increased after late-onset epilepsy and seizures,” study investigator Emily L. Johnson, MD, assistant professor of neurology at Johns Hopkins University, Baltimore, said in an interview. “Several other cohort studies are finding similar results, including the Veterans’ Health Study and the Framingham Study,” she added.
The study was published online Oct. 23 in Neurology
Bidirectional relationship?
Previous research has established that dementia is a risk factor for epilepsy, but recent studies also suggest an increased risk of incident dementia among patients with adult-onset epilepsy. Several risk factors for late-onset epilepsy, including diabetes and hypertension, also are risk factors for dementia. However, the effect of late-onset epilepsy on dementia risk in patients with these comorbidities has not been clarified.
To investigate, the researchers examined data from the Atherosclerosis Risk in Communities (ARIC) study. Participants include Black and White men and women from four U.S. communities. Baseline visits in this longitudinal cohort study began between 1987 and 1989, and follow-up included seven additional visits and regular phone calls.
The investigators identified participants with late-onset epilepsy by searching for Medicare claims related to seizures or epilepsy filed between 1991 and 2015. Those with two or more such claims and age of onset of 67 years or greater were considered to have late-onset epilepsy. Participants with preexisting conditions such as brain tumors or multiple sclerosis were excluded.
ARIC participants who presented in person for visits 2, 4, 5, and 6 underwent cognitive testing with the Delayed Word Recall Test, the Digit Symbol Substitution Test, and the Word Fluency Test.
Testing at visits 5 and 6 also included other tests, such as the Mini-Mental State Examination, the Boston Naming test, and the Wechsler Memory Scale-III. Dr. Johnson and colleagues excluded data for visit 7 from the analysis because dementia adjudication was not yet complete.
The researchers identified participants with dementia using data from visits 5 and 6 and ascertained time of dementia onset through participant and informant interviews, phone calls, and hospital discharge data. Participants also were screened for mild cognitive impairment (MCI) at visits 5 and 6.
Data were analyzed using a Cox proportional hazards model and multinomial logistic regression. In subsequent analyses, researchers adjusted the data for age, sex, race, smoking status, alcohol use, hypertension, diabetes, body mass index (BMI), APOE4 status, and prevalent stroke.
The researchers found that of 9,033 study participants, 671 had late-onset epilepsy. The late-onset epilepsy group was older at baseline (56.5 vs. 55.1 years) and more likely to have hypertension (38.9% vs. 33.3%), diabetes (16.1% vs. 9.6%), and two alleles of APOE4 genotype (3.9% vs. 2.5%), compared with those without the disorder.
In all, 1,687 participants developed dementia during follow-up. The rate of incident dementia was 41.6% in participants with late-onset epilepsy and 16.8% in participants without late-onset epilepsy. The adjusted hazard ratio of subsequent dementia in participants with late-onset epilepsy versus those without the disorder was 3.05 (95% confidence interval, 2.65-3.51).
The median time to dementia ascertainment after late-onset epilepsy was 3.66 years.
Counterintuitive finding
The relationship between late-onset epilepsy and subsequent dementia was stronger in patients without stroke. The investigators offered a possible explanation for this counterintuitive finding. “We observed an interaction between [late-onset epilepsy] and stroke, with a lower (but still substantial) association between [late-onset epilepsy] and dementia in those with a history of stroke. This may be due to the known strong association between stroke and dementia, which may wash out the contributions of [late-onset epilepsy] to cognitive impairment,” the researchers wrote.
“There may also be under-capturing of dementia diagnoses among participants with stroke in the ascertainment from [Centers for Medicare & Medicaid Services] codes, as physicians may be reluctant to make a separate code for ‘dementia’ in those with cognitive impairment after stroke,” they added.
When the researchers restricted the analysis only to participants who attended visits 5 and 6 and had late-onset epilepsy ascertainment available, they found that the relative risk ratio for dementia at visit 6 was 2.90 (95% CI, 1.22-6.92; P = .009). The RRR for MCI was 0.97 (95% CI, 0.39-2.38; P = .803). The greater functional impairment in patients with late-onset epilepsy may explain the lack of a relationship between late-onset epilepsy and MCI.
“It will be important for neurologists to be aware of the possibility of cognitive impairment following late-onset epilepsy and to check in with patients and family members to see if there are concerns,” said Dr. Johnson.
“We should also be talking about the importance of lowering other risk factors for dementia by making sure cardiovascular risk factors are controlled and encouraging physical and cognitive activity,” she added.
The results require confirmation in a clinical population, the investigators noted. In addition, future research is necessary to clarify whether seizures directly increase the risk of dementia or whether shared neuropathology between epilepsy and dementia explains the risk.
“In the near future, I plan to enroll participants with late-onset epilepsy in an observational study to better understand factors that may contribute to cognitive change. Collaborations will be key as we seek to further understand what causes these changes and what could be done to prevent them,” Dr. Johnson added.
Strengths and weaknesses
In an accompanying editorial, W. Allen Hauser, MD, professor emeritus of neurology and epidemiology at Columbia University in New York, and colleagues noted that the findings support a bidirectional relationship between dementia and epilepsy, adding that accumulation of amyloid beta peptide is a plausible underlying pathophysiology that may explain this relationship.
Future research should clarify the effect of factors such as seizure type, seizure frequency, and age of onset on the risk of dementia among patients with epilepsy, the editorialists wrote. Such investigations could help elucidate the underlying mechanisms of these conditions and help to improve treatment, they added.
Commenting on the findings, Ilo Leppik, MD, professor of neurology and pharmacy at the University of Minnesota in Minneapolis described the research as “a very well-done study by qualified researchers in the field. … For the last century, medicine has unfortunately become compartmentalized by specialty and then subspecialty. The brain and disorders of the brain do not recognize these silos. … It is not a stretch of the known science to begin to understand that epilepsy and dementia have common anatomical and physiological underpinnings.”
The long period of prospectively gathering data and the measurement of cognitive function through various modalities are among the study’s great strengths, said Dr. Leppik. However, the study’s weakness is its reliance on Medicare claims data, which mainly would reflect convulsive seizures.
“What is missing is how many persons had subtle focal-unaware seizures that may not be identified unless a careful history is taken,” said Dr. Leppik. “Thus, this study likely underestimates the frequency of epilepsy.”
Neurologists who evaluate a person with early dementia should be on the lookout for a history of subtle seizures, said Dr. Leppik. Animal studies suggest treatment with levetiracetam or brivaracetam may slow the course of dementia, and a clinical study in participants with early dementia is underway.
“Treatment with an antiseizure drug may prove to be beneficial, especially if evidence for the presence of subtle epilepsy can be found,” Dr. Leppik added.
Greater collaboration between epileptologists and dementia specialists and larger studies of antiseizure drugs are necessary, he noted. “These studies can incorporate sophisticated structural and biochemical [analyses] to better identify the relationships between brain mechanisms that likely underlie both seizures and dementia. The ultimate promise is that early treatment of seizures may alter the course of dementia,” Dr. Leppik said.
The study by Dr. Johnson and colleagues was supported by a contract from the National Institute on Aging; ARIC from the National Heart, Lung, and Blood Institute; the National Institutes of Health; and the Department of Health & Human Services. The authors and Dr. Leppik have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM NEUROLOGY
A skin test for Parkinson’s disease diagnosis?
a new study suggests. For the study, researchers used a chemical assay to detect clumping of the protein alpha-synuclein, a hallmark of Parkinson’s disease, in autopsy skin samples taken from patients who had Parkinson’s disease confirmed by brain pathology and from controls without the disease. The test showed a high degree of sensitivity and specificity for the diagnosis of Parkinson’s disease.
The study was published online in Movement Disorders.
“This test has a lot of promise,” said senior author Anumantha Kanthasamy, PhD, professor of biomedical sciences at Iowa State University in Ames. “At present there are no peripheral biomarkers for Parkinson’s disease. The current diagnosis is just based on symptoms, and the symptoms can be similar to many other neurological diseases,” he added. “It can take many years to establish a correct diagnosis and the accuracy is low even with experienced neurologists.”
If the current results can be replicated in samples from live patients and in those with very early stages of Parkinson’s disease, a skin test could allow early diagnosis and the possibility of starting preventive treatments to slow disease progression before symptoms develop too severely, the researchers suggest.
Sensitive and specific test
The blinded study used a seeding assay – used previously to detect misfolded proteins in prion diseases – to analyze 50 skin samples provided by the Arizona Study of Aging and Neurodegenerative Disorders/Brain and Body Donation Program based at Banner Sun Health Research Institute in Sun City.
Half of the skin samples came from patients with Parkinson’s disease and half came from people without neurologic disease. The protein assay correctly diagnosed 24 out of 25 patients with Parkinson’s disease and only one of the 25 controls had the protein clumping.
“At present, the only way to definitely diagnose Parkinson’s disease is on autopsy – by the detection of alpha-synuclein clumps [Lewy bodies] in the brain,” commented Charles Adler, MD, professor of neurology at Mayo Clinic Arizona in Scottsdale and a coinvestigator of the study. “In our research, we have also seen clumping of alpha-synuclein in many other organs including submandibular gland, colon, skin, heart, and stomach, but in terms of access, the skin is probably the easiest source.”
In this study, “we found this seeding assay for alpha-synuclein clumps to be extremely sensitive and specific in the diagnosis of Parkinson’s disease,” he added. “This is very valuable data as we have samples from patients with autopsy-validated Parkinson’s disease.”
A reliable biomarker?
The researchers are now starting a study in living patients with funding from the National Institutes of Health in which they will repeat the process comparing skin samples from patients with clinically diagnosed Parkinson’s disease and controls.
“We need to know whether analyzing alpha-synuclein clumping in skin biopsies from live patients with Parkinson’s disease would serve as a reliable biomarker for disease progression. Will clumping of this protein in skin samples increase over time and does it correspond with disease progression?” Dr. Adler said.
In future they are also hoping to test individuals who have not yet developed Parkinson’s disease but may have some prodromal type symptoms and to test whether this assay could measure a treatment effect of drug therapy.
Dr. Adler noted that they are currently conducting an autopsy study of skin samples from individuals who did not have clinical Parkinson’s disease when alive but in whom Lewy bodies have been found postmortem.
“This suggests that the disease pathology starts before Parkinson’s symptoms develop, and in the future, if we can diagnose Parkinson’s disease earlier then we may be able to stop progression,” he said.
“There is a long list of compounds that have been studied to try and slow progression but haven’t shown benefits, but by the time patients develop symptoms they already have significant disease and [have] lost most of their dopamine neurons,” he added. “If we could backtrack by 10 years, then these drugs may well make a difference.”
Dr. Adler also noted that currently more advanced patients may undergo invasive procedures such as deep brain stimulation or surgery. “It is of utmost importance that they have an accurate diagnosis before being subjected to such procedures.”
In addition, he pointed out that an accurate test would help the drug development process. “It is vitally important to enroll patients with an accurate diagnosis in clinical trials of new drugs. At present, a large percentage of patients in these trials may not actually have Parkinson’s disease, which makes it very difficult to show a treatment effect.”
Important step, but preliminary
Commenting on the research, James Beck, PhD, chief scientific officer of the Parkinson’s Foundation, said the study “is an important step toward the creation of a new way to potentially diagnose Parkinson’s disease.”
But he cautioned that this is a preliminary study. “To really confirm the possibility of using this approach for diagnosing Parkinson’s disease, a larger study will be necessary. And it will be important to test this in a population with early disease – the most difficult group to accurately diagnose.”
Also commenting on the findings, Beate Ritz, MD, PhD, an epidemiologist at UCLA Fielding School of Public Health in Los Angeles, who is part of a team also working on ways to measure abnormal alpha-synuclein to diagnose Parkinson’s disease, described the current study of skin samples as “pretty nifty.”
“Their research shows clearly that they can distinguish between patients with Parkinson’s disease and controls in this way,” she said. “The big advantage of this study is that they have brain pathology, so they know exactly which individuals had Parkinson’s disease.”
Dr. Ritz is working with Gal Bitan, PhD, from the UCLA Brain Research Institute on a potential blood test to measure abnormal alpha-synuclein.
Dr. Ritz explained that it is not possible to measure alpha-synuclein pathology in regular blood samples as it is expressed normally in red blood cells, but they are measuring the protein and its more toxic phosphorylated form from exosomes, which contain the waste discarded by cells using technology that determines the origin of these exosomes.
“Alpha-synuclein itself is not a problem. It is the way it misfolds that causes toxicity and disrupts the workings of the cell,” Dr. Ritz added. “In Parkinson’s disease, it is particularly toxic to dopaminergic neurons, and in multiple system atrophy, it is toxic to glial cells, so if we can identify the source of the protein then that could be helpful.”
The study was funded by the National Institutes of Health and the US Army Medical Research Materiel Command. The study authors, Dr. Beck, and Dr. Ritz have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
a new study suggests. For the study, researchers used a chemical assay to detect clumping of the protein alpha-synuclein, a hallmark of Parkinson’s disease, in autopsy skin samples taken from patients who had Parkinson’s disease confirmed by brain pathology and from controls without the disease. The test showed a high degree of sensitivity and specificity for the diagnosis of Parkinson’s disease.
The study was published online in Movement Disorders.
“This test has a lot of promise,” said senior author Anumantha Kanthasamy, PhD, professor of biomedical sciences at Iowa State University in Ames. “At present there are no peripheral biomarkers for Parkinson’s disease. The current diagnosis is just based on symptoms, and the symptoms can be similar to many other neurological diseases,” he added. “It can take many years to establish a correct diagnosis and the accuracy is low even with experienced neurologists.”
If the current results can be replicated in samples from live patients and in those with very early stages of Parkinson’s disease, a skin test could allow early diagnosis and the possibility of starting preventive treatments to slow disease progression before symptoms develop too severely, the researchers suggest.
Sensitive and specific test
The blinded study used a seeding assay – used previously to detect misfolded proteins in prion diseases – to analyze 50 skin samples provided by the Arizona Study of Aging and Neurodegenerative Disorders/Brain and Body Donation Program based at Banner Sun Health Research Institute in Sun City.
Half of the skin samples came from patients with Parkinson’s disease and half came from people without neurologic disease. The protein assay correctly diagnosed 24 out of 25 patients with Parkinson’s disease and only one of the 25 controls had the protein clumping.
“At present, the only way to definitely diagnose Parkinson’s disease is on autopsy – by the detection of alpha-synuclein clumps [Lewy bodies] in the brain,” commented Charles Adler, MD, professor of neurology at Mayo Clinic Arizona in Scottsdale and a coinvestigator of the study. “In our research, we have also seen clumping of alpha-synuclein in many other organs including submandibular gland, colon, skin, heart, and stomach, but in terms of access, the skin is probably the easiest source.”
In this study, “we found this seeding assay for alpha-synuclein clumps to be extremely sensitive and specific in the diagnosis of Parkinson’s disease,” he added. “This is very valuable data as we have samples from patients with autopsy-validated Parkinson’s disease.”
A reliable biomarker?
The researchers are now starting a study in living patients with funding from the National Institutes of Health in which they will repeat the process comparing skin samples from patients with clinically diagnosed Parkinson’s disease and controls.
“We need to know whether analyzing alpha-synuclein clumping in skin biopsies from live patients with Parkinson’s disease would serve as a reliable biomarker for disease progression. Will clumping of this protein in skin samples increase over time and does it correspond with disease progression?” Dr. Adler said.
In future they are also hoping to test individuals who have not yet developed Parkinson’s disease but may have some prodromal type symptoms and to test whether this assay could measure a treatment effect of drug therapy.
Dr. Adler noted that they are currently conducting an autopsy study of skin samples from individuals who did not have clinical Parkinson’s disease when alive but in whom Lewy bodies have been found postmortem.
“This suggests that the disease pathology starts before Parkinson’s symptoms develop, and in the future, if we can diagnose Parkinson’s disease earlier then we may be able to stop progression,” he said.
“There is a long list of compounds that have been studied to try and slow progression but haven’t shown benefits, but by the time patients develop symptoms they already have significant disease and [have] lost most of their dopamine neurons,” he added. “If we could backtrack by 10 years, then these drugs may well make a difference.”
Dr. Adler also noted that currently more advanced patients may undergo invasive procedures such as deep brain stimulation or surgery. “It is of utmost importance that they have an accurate diagnosis before being subjected to such procedures.”
In addition, he pointed out that an accurate test would help the drug development process. “It is vitally important to enroll patients with an accurate diagnosis in clinical trials of new drugs. At present, a large percentage of patients in these trials may not actually have Parkinson’s disease, which makes it very difficult to show a treatment effect.”
Important step, but preliminary
Commenting on the research, James Beck, PhD, chief scientific officer of the Parkinson’s Foundation, said the study “is an important step toward the creation of a new way to potentially diagnose Parkinson’s disease.”
But he cautioned that this is a preliminary study. “To really confirm the possibility of using this approach for diagnosing Parkinson’s disease, a larger study will be necessary. And it will be important to test this in a population with early disease – the most difficult group to accurately diagnose.”
Also commenting on the findings, Beate Ritz, MD, PhD, an epidemiologist at UCLA Fielding School of Public Health in Los Angeles, who is part of a team also working on ways to measure abnormal alpha-synuclein to diagnose Parkinson’s disease, described the current study of skin samples as “pretty nifty.”
“Their research shows clearly that they can distinguish between patients with Parkinson’s disease and controls in this way,” she said. “The big advantage of this study is that they have brain pathology, so they know exactly which individuals had Parkinson’s disease.”
Dr. Ritz is working with Gal Bitan, PhD, from the UCLA Brain Research Institute on a potential blood test to measure abnormal alpha-synuclein.
Dr. Ritz explained that it is not possible to measure alpha-synuclein pathology in regular blood samples as it is expressed normally in red blood cells, but they are measuring the protein and its more toxic phosphorylated form from exosomes, which contain the waste discarded by cells using technology that determines the origin of these exosomes.
“Alpha-synuclein itself is not a problem. It is the way it misfolds that causes toxicity and disrupts the workings of the cell,” Dr. Ritz added. “In Parkinson’s disease, it is particularly toxic to dopaminergic neurons, and in multiple system atrophy, it is toxic to glial cells, so if we can identify the source of the protein then that could be helpful.”
The study was funded by the National Institutes of Health and the US Army Medical Research Materiel Command. The study authors, Dr. Beck, and Dr. Ritz have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
a new study suggests. For the study, researchers used a chemical assay to detect clumping of the protein alpha-synuclein, a hallmark of Parkinson’s disease, in autopsy skin samples taken from patients who had Parkinson’s disease confirmed by brain pathology and from controls without the disease. The test showed a high degree of sensitivity and specificity for the diagnosis of Parkinson’s disease.
The study was published online in Movement Disorders.
“This test has a lot of promise,” said senior author Anumantha Kanthasamy, PhD, professor of biomedical sciences at Iowa State University in Ames. “At present there are no peripheral biomarkers for Parkinson’s disease. The current diagnosis is just based on symptoms, and the symptoms can be similar to many other neurological diseases,” he added. “It can take many years to establish a correct diagnosis and the accuracy is low even with experienced neurologists.”
If the current results can be replicated in samples from live patients and in those with very early stages of Parkinson’s disease, a skin test could allow early diagnosis and the possibility of starting preventive treatments to slow disease progression before symptoms develop too severely, the researchers suggest.
Sensitive and specific test
The blinded study used a seeding assay – used previously to detect misfolded proteins in prion diseases – to analyze 50 skin samples provided by the Arizona Study of Aging and Neurodegenerative Disorders/Brain and Body Donation Program based at Banner Sun Health Research Institute in Sun City.
Half of the skin samples came from patients with Parkinson’s disease and half came from people without neurologic disease. The protein assay correctly diagnosed 24 out of 25 patients with Parkinson’s disease and only one of the 25 controls had the protein clumping.
“At present, the only way to definitely diagnose Parkinson’s disease is on autopsy – by the detection of alpha-synuclein clumps [Lewy bodies] in the brain,” commented Charles Adler, MD, professor of neurology at Mayo Clinic Arizona in Scottsdale and a coinvestigator of the study. “In our research, we have also seen clumping of alpha-synuclein in many other organs including submandibular gland, colon, skin, heart, and stomach, but in terms of access, the skin is probably the easiest source.”
In this study, “we found this seeding assay for alpha-synuclein clumps to be extremely sensitive and specific in the diagnosis of Parkinson’s disease,” he added. “This is very valuable data as we have samples from patients with autopsy-validated Parkinson’s disease.”
A reliable biomarker?
The researchers are now starting a study in living patients with funding from the National Institutes of Health in which they will repeat the process comparing skin samples from patients with clinically diagnosed Parkinson’s disease and controls.
“We need to know whether analyzing alpha-synuclein clumping in skin biopsies from live patients with Parkinson’s disease would serve as a reliable biomarker for disease progression. Will clumping of this protein in skin samples increase over time and does it correspond with disease progression?” Dr. Adler said.
In future they are also hoping to test individuals who have not yet developed Parkinson’s disease but may have some prodromal type symptoms and to test whether this assay could measure a treatment effect of drug therapy.
Dr. Adler noted that they are currently conducting an autopsy study of skin samples from individuals who did not have clinical Parkinson’s disease when alive but in whom Lewy bodies have been found postmortem.
“This suggests that the disease pathology starts before Parkinson’s symptoms develop, and in the future, if we can diagnose Parkinson’s disease earlier then we may be able to stop progression,” he said.
“There is a long list of compounds that have been studied to try and slow progression but haven’t shown benefits, but by the time patients develop symptoms they already have significant disease and [have] lost most of their dopamine neurons,” he added. “If we could backtrack by 10 years, then these drugs may well make a difference.”
Dr. Adler also noted that currently more advanced patients may undergo invasive procedures such as deep brain stimulation or surgery. “It is of utmost importance that they have an accurate diagnosis before being subjected to such procedures.”
In addition, he pointed out that an accurate test would help the drug development process. “It is vitally important to enroll patients with an accurate diagnosis in clinical trials of new drugs. At present, a large percentage of patients in these trials may not actually have Parkinson’s disease, which makes it very difficult to show a treatment effect.”
Important step, but preliminary
Commenting on the research, James Beck, PhD, chief scientific officer of the Parkinson’s Foundation, said the study “is an important step toward the creation of a new way to potentially diagnose Parkinson’s disease.”
But he cautioned that this is a preliminary study. “To really confirm the possibility of using this approach for diagnosing Parkinson’s disease, a larger study will be necessary. And it will be important to test this in a population with early disease – the most difficult group to accurately diagnose.”
Also commenting on the findings, Beate Ritz, MD, PhD, an epidemiologist at UCLA Fielding School of Public Health in Los Angeles, who is part of a team also working on ways to measure abnormal alpha-synuclein to diagnose Parkinson’s disease, described the current study of skin samples as “pretty nifty.”
“Their research shows clearly that they can distinguish between patients with Parkinson’s disease and controls in this way,” she said. “The big advantage of this study is that they have brain pathology, so they know exactly which individuals had Parkinson’s disease.”
Dr. Ritz is working with Gal Bitan, PhD, from the UCLA Brain Research Institute on a potential blood test to measure abnormal alpha-synuclein.
Dr. Ritz explained that it is not possible to measure alpha-synuclein pathology in regular blood samples as it is expressed normally in red blood cells, but they are measuring the protein and its more toxic phosphorylated form from exosomes, which contain the waste discarded by cells using technology that determines the origin of these exosomes.
“Alpha-synuclein itself is not a problem. It is the way it misfolds that causes toxicity and disrupts the workings of the cell,” Dr. Ritz added. “In Parkinson’s disease, it is particularly toxic to dopaminergic neurons, and in multiple system atrophy, it is toxic to glial cells, so if we can identify the source of the protein then that could be helpful.”
The study was funded by the National Institutes of Health and the US Army Medical Research Materiel Command. The study authors, Dr. Beck, and Dr. Ritz have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM MOVEMENT DISORDERS
HIT-6 may help track meaningful change in chronic migraine
, recent research suggests.
Using data from the phase 3 PROMISE-2 study, which evaluated intravenous eptinezumab in doses of 100 mg or 300 mg, or placebo every 12 weeks in 1,072 participants for the prevention of chronic migraine, Carrie R. Houts, PhD, director of psychometrics at the Vector Psychometric Group, in Chapel Hill, N.C., and colleagues determined that their finding of 6-point improvement of HIT-6 total score was consistent with other studies. However, they pointed out that little research has been done in evaluating how item-specific scores of HIT-6 impact individuals with chronic migraine. HIT-6 item scores examine whether individuals with headaches experience severe pain, limit their daily activities, have a desire to lie down, feel too tired to do daily activities, felt “fed up or irritated” because of headaches, and feel their headaches limit concentration on work or daily activities.
“The item-specific responder definitions give clinicians and researchers the ability to evaluate and track the impact of headache on specific item-level areas of patients’ lives. These responder definitions provide practical and easily interpreted results that can be used to evaluate treatment benefits over time and to improve clinician-patients communication focus on improvements in key aspects of functioning in individuals with chronic migraine,” Dr. Houts and colleagues wrote in their study, published in the October issue of Headache.
The 6-point value and the 1-2 category improvement values in item-specific scores, they suggested, could be used as a benchmark to help other clinicians and researchers detect meaningful change in individual patients with chronic migraine. Although the user guide for HIT-6 highlights a 5-point change in the total score as clinically meaningful, the authors of the guide do not provide evidence for why the 5-point value signifies clinically meaningful change, they said.
Determining thresholds of clinically meaningful change
In their study, Dr. Houts and colleagues used distribution-based methods to gauge responder values for the HIT-6 total score, while item-specific HIT-6 analyses were measured with Patients’ Global Impression of Change (PGIC), reduction in migraine frequency through monthly migraine days (MMDs), and EuroQol 5 dimensions 5 levels visual analog scale (EQ-5D-5L VAS). The researchers also used HIT-6 values from a literature review and from analyses in PROMISE-2 to calculate “a final chronic migraine-specific responder definition value” between baseline and 12 weeks. Participants in the PROMISE-2 study were mostly women (88.2%) and white (91.0%) with a mean age of 40.5 years.
The literature search revealed responder thresholds for the HIT-6 total score in a range between a decrease of 3 points and 8 points. Within PROMISE-2, the HIT-6 total score responder threshold was found to be between –2.6 and –2.2, which the researchers rounded down to a decrease of 3 points. When taking both sets of responder thresholds into account, the researchers calculated the median responder value as –5.5, which was rounded down to a decrease in 6 points in the HIT-6 total score. “[The estimate] appears most appropriate for discriminating between individuals with chronic migraine who have experienced meaningful change over time and those who have not,” Dr. Houts and colleagues said.
For item-specific HIT-6 scores, the mean score changes were –1 points for categories involving severe pain, limiting activities, lying down, and –2 points for categories involving feeling tired, being fed up or irritated, and limiting concentration.
“Taken together, the current chronic migraine-specific results are consistent with values derived from general headache/migraine samples and suggest that a decrease of 6 points or more on the HIT-6 total score would be considered meaningful to chronic migraine patients,” Dr. Houts and colleagues said. “This would translate to approximately a 4-category change on a single item, change on 2 items of approximately 2 and 3 categories, or a 1-category change on 3 or 4 of the 6 items, depending on the initial category.”
The researchers cautioned that the values outlined in the study “should not be used to determine clinically meaningful difference between treatment groups” and that “future work, similar to that reported here, will identify a chronic migraine-specific clinically meaningful difference between treatment groups value.”
A better measure of chronic migraine?
In an interview, J. D. Bartleson Jr., MD, a retired neurologist with the Mayo Clinic in Rochester, Minn., questioned why HIT-6 criteria was used in the initial PROMISE-2 study. “There is not a lot of difference between the significant and insignificant categories. Chronic migraine may be better measured with pain severity and number of headache days per month,” he said.
,“It may be appropriate to use just 1 or 2 symptoms for evaluating a given patient’s headache burden,” in terms of clinical application of the study for neurologists, Dr. Bartleson said. He emphasized that more research is needed.
This study was funded by H. Lundbeck A/S, which also provided funding of medical writing and editorial support for the manuscript. Three authors report being employees of Vector Psychometric Group at the time of the study, and the company received funding from H. Lundbeck A/S for their time conducting study-related research. Three other authors report relationships with pharmaceutical companies, medical societies, government agencies, and industry related to the study in the form of consultancies, advisory board memberships, honoraria, research support, stock or stock options, and employment. Dr. Bartleson reports no relevant conflicts of interest.
, recent research suggests.
Using data from the phase 3 PROMISE-2 study, which evaluated intravenous eptinezumab in doses of 100 mg or 300 mg, or placebo every 12 weeks in 1,072 participants for the prevention of chronic migraine, Carrie R. Houts, PhD, director of psychometrics at the Vector Psychometric Group, in Chapel Hill, N.C., and colleagues determined that their finding of 6-point improvement of HIT-6 total score was consistent with other studies. However, they pointed out that little research has been done in evaluating how item-specific scores of HIT-6 impact individuals with chronic migraine. HIT-6 item scores examine whether individuals with headaches experience severe pain, limit their daily activities, have a desire to lie down, feel too tired to do daily activities, felt “fed up or irritated” because of headaches, and feel their headaches limit concentration on work or daily activities.
“The item-specific responder definitions give clinicians and researchers the ability to evaluate and track the impact of headache on specific item-level areas of patients’ lives. These responder definitions provide practical and easily interpreted results that can be used to evaluate treatment benefits over time and to improve clinician-patients communication focus on improvements in key aspects of functioning in individuals with chronic migraine,” Dr. Houts and colleagues wrote in their study, published in the October issue of Headache.
The 6-point value and the 1-2 category improvement values in item-specific scores, they suggested, could be used as a benchmark to help other clinicians and researchers detect meaningful change in individual patients with chronic migraine. Although the user guide for HIT-6 highlights a 5-point change in the total score as clinically meaningful, the authors of the guide do not provide evidence for why the 5-point value signifies clinically meaningful change, they said.
Determining thresholds of clinically meaningful change
In their study, Dr. Houts and colleagues used distribution-based methods to gauge responder values for the HIT-6 total score, while item-specific HIT-6 analyses were measured with Patients’ Global Impression of Change (PGIC), reduction in migraine frequency through monthly migraine days (MMDs), and EuroQol 5 dimensions 5 levels visual analog scale (EQ-5D-5L VAS). The researchers also used HIT-6 values from a literature review and from analyses in PROMISE-2 to calculate “a final chronic migraine-specific responder definition value” between baseline and 12 weeks. Participants in the PROMISE-2 study were mostly women (88.2%) and white (91.0%) with a mean age of 40.5 years.
The literature search revealed responder thresholds for the HIT-6 total score in a range between a decrease of 3 points and 8 points. Within PROMISE-2, the HIT-6 total score responder threshold was found to be between –2.6 and –2.2, which the researchers rounded down to a decrease of 3 points. When taking both sets of responder thresholds into account, the researchers calculated the median responder value as –5.5, which was rounded down to a decrease in 6 points in the HIT-6 total score. “[The estimate] appears most appropriate for discriminating between individuals with chronic migraine who have experienced meaningful change over time and those who have not,” Dr. Houts and colleagues said.
For item-specific HIT-6 scores, the mean score changes were –1 points for categories involving severe pain, limiting activities, lying down, and –2 points for categories involving feeling tired, being fed up or irritated, and limiting concentration.
“Taken together, the current chronic migraine-specific results are consistent with values derived from general headache/migraine samples and suggest that a decrease of 6 points or more on the HIT-6 total score would be considered meaningful to chronic migraine patients,” Dr. Houts and colleagues said. “This would translate to approximately a 4-category change on a single item, change on 2 items of approximately 2 and 3 categories, or a 1-category change on 3 or 4 of the 6 items, depending on the initial category.”
The researchers cautioned that the values outlined in the study “should not be used to determine clinically meaningful difference between treatment groups” and that “future work, similar to that reported here, will identify a chronic migraine-specific clinically meaningful difference between treatment groups value.”
A better measure of chronic migraine?
In an interview, J. D. Bartleson Jr., MD, a retired neurologist with the Mayo Clinic in Rochester, Minn., questioned why HIT-6 criteria was used in the initial PROMISE-2 study. “There is not a lot of difference between the significant and insignificant categories. Chronic migraine may be better measured with pain severity and number of headache days per month,” he said.
,“It may be appropriate to use just 1 or 2 symptoms for evaluating a given patient’s headache burden,” in terms of clinical application of the study for neurologists, Dr. Bartleson said. He emphasized that more research is needed.
This study was funded by H. Lundbeck A/S, which also provided funding of medical writing and editorial support for the manuscript. Three authors report being employees of Vector Psychometric Group at the time of the study, and the company received funding from H. Lundbeck A/S for their time conducting study-related research. Three other authors report relationships with pharmaceutical companies, medical societies, government agencies, and industry related to the study in the form of consultancies, advisory board memberships, honoraria, research support, stock or stock options, and employment. Dr. Bartleson reports no relevant conflicts of interest.
, recent research suggests.
Using data from the phase 3 PROMISE-2 study, which evaluated intravenous eptinezumab in doses of 100 mg or 300 mg, or placebo every 12 weeks in 1,072 participants for the prevention of chronic migraine, Carrie R. Houts, PhD, director of psychometrics at the Vector Psychometric Group, in Chapel Hill, N.C., and colleagues determined that their finding of 6-point improvement of HIT-6 total score was consistent with other studies. However, they pointed out that little research has been done in evaluating how item-specific scores of HIT-6 impact individuals with chronic migraine. HIT-6 item scores examine whether individuals with headaches experience severe pain, limit their daily activities, have a desire to lie down, feel too tired to do daily activities, felt “fed up or irritated” because of headaches, and feel their headaches limit concentration on work or daily activities.
“The item-specific responder definitions give clinicians and researchers the ability to evaluate and track the impact of headache on specific item-level areas of patients’ lives. These responder definitions provide practical and easily interpreted results that can be used to evaluate treatment benefits over time and to improve clinician-patients communication focus on improvements in key aspects of functioning in individuals with chronic migraine,” Dr. Houts and colleagues wrote in their study, published in the October issue of Headache.
The 6-point value and the 1-2 category improvement values in item-specific scores, they suggested, could be used as a benchmark to help other clinicians and researchers detect meaningful change in individual patients with chronic migraine. Although the user guide for HIT-6 highlights a 5-point change in the total score as clinically meaningful, the authors of the guide do not provide evidence for why the 5-point value signifies clinically meaningful change, they said.
Determining thresholds of clinically meaningful change
In their study, Dr. Houts and colleagues used distribution-based methods to gauge responder values for the HIT-6 total score, while item-specific HIT-6 analyses were measured with Patients’ Global Impression of Change (PGIC), reduction in migraine frequency through monthly migraine days (MMDs), and EuroQol 5 dimensions 5 levels visual analog scale (EQ-5D-5L VAS). The researchers also used HIT-6 values from a literature review and from analyses in PROMISE-2 to calculate “a final chronic migraine-specific responder definition value” between baseline and 12 weeks. Participants in the PROMISE-2 study were mostly women (88.2%) and white (91.0%) with a mean age of 40.5 years.
The literature search revealed responder thresholds for the HIT-6 total score in a range between a decrease of 3 points and 8 points. Within PROMISE-2, the HIT-6 total score responder threshold was found to be between –2.6 and –2.2, which the researchers rounded down to a decrease of 3 points. When taking both sets of responder thresholds into account, the researchers calculated the median responder value as –5.5, which was rounded down to a decrease in 6 points in the HIT-6 total score. “[The estimate] appears most appropriate for discriminating between individuals with chronic migraine who have experienced meaningful change over time and those who have not,” Dr. Houts and colleagues said.
For item-specific HIT-6 scores, the mean score changes were –1 points for categories involving severe pain, limiting activities, lying down, and –2 points for categories involving feeling tired, being fed up or irritated, and limiting concentration.
“Taken together, the current chronic migraine-specific results are consistent with values derived from general headache/migraine samples and suggest that a decrease of 6 points or more on the HIT-6 total score would be considered meaningful to chronic migraine patients,” Dr. Houts and colleagues said. “This would translate to approximately a 4-category change on a single item, change on 2 items of approximately 2 and 3 categories, or a 1-category change on 3 or 4 of the 6 items, depending on the initial category.”
The researchers cautioned that the values outlined in the study “should not be used to determine clinically meaningful difference between treatment groups” and that “future work, similar to that reported here, will identify a chronic migraine-specific clinically meaningful difference between treatment groups value.”
A better measure of chronic migraine?
In an interview, J. D. Bartleson Jr., MD, a retired neurologist with the Mayo Clinic in Rochester, Minn., questioned why HIT-6 criteria was used in the initial PROMISE-2 study. “There is not a lot of difference between the significant and insignificant categories. Chronic migraine may be better measured with pain severity and number of headache days per month,” he said.
,“It may be appropriate to use just 1 or 2 symptoms for evaluating a given patient’s headache burden,” in terms of clinical application of the study for neurologists, Dr. Bartleson said. He emphasized that more research is needed.
This study was funded by H. Lundbeck A/S, which also provided funding of medical writing and editorial support for the manuscript. Three authors report being employees of Vector Psychometric Group at the time of the study, and the company received funding from H. Lundbeck A/S for their time conducting study-related research. Three other authors report relationships with pharmaceutical companies, medical societies, government agencies, and industry related to the study in the form of consultancies, advisory board memberships, honoraria, research support, stock or stock options, and employment. Dr. Bartleson reports no relevant conflicts of interest.
FROM HEADACHE
Biomarker in the eye may flag neurodegeneration risk
, opening the door to a potential new method of predicting neurodegenerative disease, new research suggests.
In a study of 77 patients undergoing eye surgery for various conditions, more than 70% had more than 20 pg/mL of NfL in their vitreous humor. Higher levels of NfL were associated with higher levels of other biomarkers known to be associated with Alzheimer’s disease, including amyloid-beta and tau proteins.
“The study had three primary findings,” said lead author Manju L. Subramanian, MD, associate professor of ophthalmology at Boston University.
First, the investigators were able to detect levels of NfL in eye fluid; and second, those levels were not in any way correlated to the patient’s clinical eye condition, Dr. Subramanian said. “The third finding was that we were able to correlate those neurofilament light levels with other markers that have been known to be associated with conditions such as Alzheimer’s disease,” she noted.
For Dr. Subramanian, these findings add to the hypothesis that the eye is an extension of the brain. “This is further evidence that the eye might potentially be a proxy for neurodegenerative diseases,” she said. “So finding neurofilament light chain in the eye demonstrates that the eye is not an isolated organ, and things that happen in the body can affect the eye and vice versa.”
The findings were published online Sept. 17 in Alzheimer’s Research & Therapy.
Verge of clinical applicability?
Early diagnosis of neurodegenerative diseases remains a challenge, the investigators noted. As such, there is a palpable need for reliable biomarkers that can help with early diagnosis, prognostic assessment, and measurable response to treatment for Alzheimer’s disease and other neurologic disorders
Recent research has identified NfL as a potential screening tool and some researchers believe it to be on the verge of clinical applicability. In addition, increased levels of the biomarker have been observed in both the cerebrospinal fluid (CSF) and blood of individuals with neurodegeneration and neurological diseases, including Alzheimer’s disease. In previous studies, for example, elevated levels of NfL in CSF and blood have been shown to reliably distinguish between patients with Alzheimer’s disease and healthy volunteers.
Because certain eye diseases have been associated with Alzheimer’s disease in epidemiological studies, they may share common risk factors and pathological mechanisms at the molecular level, the researchers noted. In an earlier study, the current investigators found that cognitive function among patients with eye disease was significantly associated with amyloid-beta and total tau protein levels in the vitreous humor.
Given these connections, the researchers hypothesized that NfL could be identified in the vitreous humor and may be associated with other relevant biomarkers of neuronal origin. “Neurofilament light chain is detectable in the cerebrospinal fluid, but it’s never been tested for detection in the eye,” Dr. Subramanian noted.
In total, vitreous humor samples were collected from 77 unique participants (mean age, 56.2 years; 63% men) as part of the single-center, prospective, cross-sectional cohort study. The researchers aspirated 0.5 to 1.0 ml of undiluted vitreous fluid during vitrectomy, while whole blood was drawn for APOE genotyping.
Immunoassay was used to quantitatively measure for NfL, amyloid-beta, total tau, phosphorylated tau 181 (p-tau181), inflammatory cytokines, chemokines, and vascular proteins in the vitreous humor. The trial’s primary outcome measures were the detection of NfL levels in the vitreous humor, as well as its associations with other proteins.
Significant correlations
Results showed that 55 of the 77 participants (71.4%) had at least 20 pg/ml of NfL protein present in the vitreous humor. The median level was 68.65 pg/ml. Statistically significant associations were found between NfL levels in the vitreous humor and Abeta40, Abeta42, and total tau; higher NfL levels were associated with higher levels of all three biomarkers. On the other hand, NfL levels were not positively associated with increased vitreous levels of p-tau181.
Vitreous NfL concentration was significantly associated with inflammatory cytokines, including interleukin-15, interleukin-16, and monocyte chemoattractant protein-1, as well as vascular proteins such as vascular endothelial growth factor receptor-1, VEGF-C, vascular cell adhesion molecule-1, Tie-2, and intracellular adhesion molecular-1.
Despite these findings, NfL in the vitreous humor was not associated with patients’ clinical ophthalmic conditions or systemic diseases such as hypertension, diabetes, and hyperlipidemia. Similarly, NfL was not significantly associated with APOE genotype E2 and E4, the alleles most commonly associated with Alzheimer’s disease.
Finally, no statistically significant associations were found between NfL and Mini-Mental State Examination (MMSE) scores.
A “first step”
Most research currently examining the role of the eye in neurodegenerative disease is focused on retinal biomarkers imaged by optical coherence tomography, the investigators noted. Although promising, data obtained this way have yielded conflicting results.
Similarly, while the diagnostic potential of the core CSF biomarkers for AD (Abeta40, Abeta42, p-tau, and total tau) is well established, the practical utility of testing CSF for neurodegenerative diseases is limited, wrote the researchers.
As such, an additional biomarker source such as NfL–which is quantifiable and protein-based within eye fluid – has the potential to play an important role in predicting neurodegenerative disease in the clinical setting, they added.
“The holy grail of neurodegenerative-disease diagnosis is early diagnosis. Because if you can implement treatment early, you can slow down and potentially halt the progression of these diseases,” Dr. Subramanian said.
“This study is the first step toward determining if the eye could play a potential role in early diagnosis of conditions such as Alzheimer’s disease,” she added.
That said, Dr. Subramanian was quick to recognize the findings’ preliminary nature and that they do not offer reliable evidence that vitreous NfL levels definitively represent neurodegeneration. As such, the investigators called for more research to validate the association between this type of biomarker with other established biomarkers of neurodegeneration, such as those found in CSF fluid or on MRI and PET scans.
“At this point, we can’t look at eye fluid and say that people have neurodegenerative diseases,” she noted. “The other thing to consider is that vitreous humor is at the back of the eye, so it’s actually a fairly invasive procedure.
“I think the next step is to look at other types of eye fluids such as the aqueous fluid in the front of the eye, or even tear secretions, potentially,” Dr. Subramanian said.
Other study limitations include the lack of an association between NfL levels and MMSE scores and that none of the study participants were actually diagnosed with Alzheimer’s disease. Validation studies are needed to compare vitreous levels of NfL in patients with mild cognitive impairment/AD to normal controls, the investigators noted.
Fascinating but impractical?
Commenting on the findings, Sharon Fekrat, MD, professor of ophthalmology, Duke University, Durham, N.C., agreed that there’s potential importance of the eye in diagnosing neurodegeneration. However, she suggested that vitreous humor may not be the most expedient medium to use.
“I commend the authors for this fascinating work. But practically speaking, if we ultimately want to use intraocular fluid to diagnose Alzheimer’s and perhaps other neurodegeneration, I think aqueous humor might be more practical than the vitreous humor,” said Dr. Fekrat, who was not involved with the research. “What might be even better is to have a device that can be held against the eyeball that measures the levels of various substances inside the eyeball without having to enter the eye,” added Justin Ma, a Duke University medical student working under Dr. Fekrat’s guidance. “It could be similar technology to what’s currently used to measure blood glucose levels,” Mr. Ma added.
The study was supported in part by the National Institute of Aging. Dr. Subramanian, Dr. Fekrat, and Mr. Ma have disclosed no relevant financial relationships. Disclosures for other study authors are listed in the original article.
A version of this article originally appeared on Medscape.com.
, opening the door to a potential new method of predicting neurodegenerative disease, new research suggests.
In a study of 77 patients undergoing eye surgery for various conditions, more than 70% had more than 20 pg/mL of NfL in their vitreous humor. Higher levels of NfL were associated with higher levels of other biomarkers known to be associated with Alzheimer’s disease, including amyloid-beta and tau proteins.
“The study had three primary findings,” said lead author Manju L. Subramanian, MD, associate professor of ophthalmology at Boston University.
First, the investigators were able to detect levels of NfL in eye fluid; and second, those levels were not in any way correlated to the patient’s clinical eye condition, Dr. Subramanian said. “The third finding was that we were able to correlate those neurofilament light levels with other markers that have been known to be associated with conditions such as Alzheimer’s disease,” she noted.
For Dr. Subramanian, these findings add to the hypothesis that the eye is an extension of the brain. “This is further evidence that the eye might potentially be a proxy for neurodegenerative diseases,” she said. “So finding neurofilament light chain in the eye demonstrates that the eye is not an isolated organ, and things that happen in the body can affect the eye and vice versa.”
The findings were published online Sept. 17 in Alzheimer’s Research & Therapy.
Verge of clinical applicability?
Early diagnosis of neurodegenerative diseases remains a challenge, the investigators noted. As such, there is a palpable need for reliable biomarkers that can help with early diagnosis, prognostic assessment, and measurable response to treatment for Alzheimer’s disease and other neurologic disorders
Recent research has identified NfL as a potential screening tool and some researchers believe it to be on the verge of clinical applicability. In addition, increased levels of the biomarker have been observed in both the cerebrospinal fluid (CSF) and blood of individuals with neurodegeneration and neurological diseases, including Alzheimer’s disease. In previous studies, for example, elevated levels of NfL in CSF and blood have been shown to reliably distinguish between patients with Alzheimer’s disease and healthy volunteers.
Because certain eye diseases have been associated with Alzheimer’s disease in epidemiological studies, they may share common risk factors and pathological mechanisms at the molecular level, the researchers noted. In an earlier study, the current investigators found that cognitive function among patients with eye disease was significantly associated with amyloid-beta and total tau protein levels in the vitreous humor.
Given these connections, the researchers hypothesized that NfL could be identified in the vitreous humor and may be associated with other relevant biomarkers of neuronal origin. “Neurofilament light chain is detectable in the cerebrospinal fluid, but it’s never been tested for detection in the eye,” Dr. Subramanian noted.
In total, vitreous humor samples were collected from 77 unique participants (mean age, 56.2 years; 63% men) as part of the single-center, prospective, cross-sectional cohort study. The researchers aspirated 0.5 to 1.0 ml of undiluted vitreous fluid during vitrectomy, while whole blood was drawn for APOE genotyping.
Immunoassay was used to quantitatively measure for NfL, amyloid-beta, total tau, phosphorylated tau 181 (p-tau181), inflammatory cytokines, chemokines, and vascular proteins in the vitreous humor. The trial’s primary outcome measures were the detection of NfL levels in the vitreous humor, as well as its associations with other proteins.
Significant correlations
Results showed that 55 of the 77 participants (71.4%) had at least 20 pg/ml of NfL protein present in the vitreous humor. The median level was 68.65 pg/ml. Statistically significant associations were found between NfL levels in the vitreous humor and Abeta40, Abeta42, and total tau; higher NfL levels were associated with higher levels of all three biomarkers. On the other hand, NfL levels were not positively associated with increased vitreous levels of p-tau181.
Vitreous NfL concentration was significantly associated with inflammatory cytokines, including interleukin-15, interleukin-16, and monocyte chemoattractant protein-1, as well as vascular proteins such as vascular endothelial growth factor receptor-1, VEGF-C, vascular cell adhesion molecule-1, Tie-2, and intracellular adhesion molecular-1.
Despite these findings, NfL in the vitreous humor was not associated with patients’ clinical ophthalmic conditions or systemic diseases such as hypertension, diabetes, and hyperlipidemia. Similarly, NfL was not significantly associated with APOE genotype E2 and E4, the alleles most commonly associated with Alzheimer’s disease.
Finally, no statistically significant associations were found between NfL and Mini-Mental State Examination (MMSE) scores.
A “first step”
Most research currently examining the role of the eye in neurodegenerative disease is focused on retinal biomarkers imaged by optical coherence tomography, the investigators noted. Although promising, data obtained this way have yielded conflicting results.
Similarly, while the diagnostic potential of the core CSF biomarkers for AD (Abeta40, Abeta42, p-tau, and total tau) is well established, the practical utility of testing CSF for neurodegenerative diseases is limited, wrote the researchers.
As such, an additional biomarker source such as NfL–which is quantifiable and protein-based within eye fluid – has the potential to play an important role in predicting neurodegenerative disease in the clinical setting, they added.
“The holy grail of neurodegenerative-disease diagnosis is early diagnosis. Because if you can implement treatment early, you can slow down and potentially halt the progression of these diseases,” Dr. Subramanian said.
“This study is the first step toward determining if the eye could play a potential role in early diagnosis of conditions such as Alzheimer’s disease,” she added.
That said, Dr. Subramanian was quick to recognize the findings’ preliminary nature and that they do not offer reliable evidence that vitreous NfL levels definitively represent neurodegeneration. As such, the investigators called for more research to validate the association between this type of biomarker with other established biomarkers of neurodegeneration, such as those found in CSF fluid or on MRI and PET scans.
“At this point, we can’t look at eye fluid and say that people have neurodegenerative diseases,” she noted. “The other thing to consider is that vitreous humor is at the back of the eye, so it’s actually a fairly invasive procedure.
“I think the next step is to look at other types of eye fluids such as the aqueous fluid in the front of the eye, or even tear secretions, potentially,” Dr. Subramanian said.
Other study limitations include the lack of an association between NfL levels and MMSE scores and that none of the study participants were actually diagnosed with Alzheimer’s disease. Validation studies are needed to compare vitreous levels of NfL in patients with mild cognitive impairment/AD to normal controls, the investigators noted.
Fascinating but impractical?
Commenting on the findings, Sharon Fekrat, MD, professor of ophthalmology, Duke University, Durham, N.C., agreed that there’s potential importance of the eye in diagnosing neurodegeneration. However, she suggested that vitreous humor may not be the most expedient medium to use.
“I commend the authors for this fascinating work. But practically speaking, if we ultimately want to use intraocular fluid to diagnose Alzheimer’s and perhaps other neurodegeneration, I think aqueous humor might be more practical than the vitreous humor,” said Dr. Fekrat, who was not involved with the research. “What might be even better is to have a device that can be held against the eyeball that measures the levels of various substances inside the eyeball without having to enter the eye,” added Justin Ma, a Duke University medical student working under Dr. Fekrat’s guidance. “It could be similar technology to what’s currently used to measure blood glucose levels,” Mr. Ma added.
The study was supported in part by the National Institute of Aging. Dr. Subramanian, Dr. Fekrat, and Mr. Ma have disclosed no relevant financial relationships. Disclosures for other study authors are listed in the original article.
A version of this article originally appeared on Medscape.com.
, opening the door to a potential new method of predicting neurodegenerative disease, new research suggests.
In a study of 77 patients undergoing eye surgery for various conditions, more than 70% had more than 20 pg/mL of NfL in their vitreous humor. Higher levels of NfL were associated with higher levels of other biomarkers known to be associated with Alzheimer’s disease, including amyloid-beta and tau proteins.
“The study had three primary findings,” said lead author Manju L. Subramanian, MD, associate professor of ophthalmology at Boston University.
First, the investigators were able to detect levels of NfL in eye fluid; and second, those levels were not in any way correlated to the patient’s clinical eye condition, Dr. Subramanian said. “The third finding was that we were able to correlate those neurofilament light levels with other markers that have been known to be associated with conditions such as Alzheimer’s disease,” she noted.
For Dr. Subramanian, these findings add to the hypothesis that the eye is an extension of the brain. “This is further evidence that the eye might potentially be a proxy for neurodegenerative diseases,” she said. “So finding neurofilament light chain in the eye demonstrates that the eye is not an isolated organ, and things that happen in the body can affect the eye and vice versa.”
The findings were published online Sept. 17 in Alzheimer’s Research & Therapy.
Verge of clinical applicability?
Early diagnosis of neurodegenerative diseases remains a challenge, the investigators noted. As such, there is a palpable need for reliable biomarkers that can help with early diagnosis, prognostic assessment, and measurable response to treatment for Alzheimer’s disease and other neurologic disorders
Recent research has identified NfL as a potential screening tool and some researchers believe it to be on the verge of clinical applicability. In addition, increased levels of the biomarker have been observed in both the cerebrospinal fluid (CSF) and blood of individuals with neurodegeneration and neurological diseases, including Alzheimer’s disease. In previous studies, for example, elevated levels of NfL in CSF and blood have been shown to reliably distinguish between patients with Alzheimer’s disease and healthy volunteers.
Because certain eye diseases have been associated with Alzheimer’s disease in epidemiological studies, they may share common risk factors and pathological mechanisms at the molecular level, the researchers noted. In an earlier study, the current investigators found that cognitive function among patients with eye disease was significantly associated with amyloid-beta and total tau protein levels in the vitreous humor.
Given these connections, the researchers hypothesized that NfL could be identified in the vitreous humor and may be associated with other relevant biomarkers of neuronal origin. “Neurofilament light chain is detectable in the cerebrospinal fluid, but it’s never been tested for detection in the eye,” Dr. Subramanian noted.
In total, vitreous humor samples were collected from 77 unique participants (mean age, 56.2 years; 63% men) as part of the single-center, prospective, cross-sectional cohort study. The researchers aspirated 0.5 to 1.0 ml of undiluted vitreous fluid during vitrectomy, while whole blood was drawn for APOE genotyping.
Immunoassay was used to quantitatively measure for NfL, amyloid-beta, total tau, phosphorylated tau 181 (p-tau181), inflammatory cytokines, chemokines, and vascular proteins in the vitreous humor. The trial’s primary outcome measures were the detection of NfL levels in the vitreous humor, as well as its associations with other proteins.
Significant correlations
Results showed that 55 of the 77 participants (71.4%) had at least 20 pg/ml of NfL protein present in the vitreous humor. The median level was 68.65 pg/ml. Statistically significant associations were found between NfL levels in the vitreous humor and Abeta40, Abeta42, and total tau; higher NfL levels were associated with higher levels of all three biomarkers. On the other hand, NfL levels were not positively associated with increased vitreous levels of p-tau181.
Vitreous NfL concentration was significantly associated with inflammatory cytokines, including interleukin-15, interleukin-16, and monocyte chemoattractant protein-1, as well as vascular proteins such as vascular endothelial growth factor receptor-1, VEGF-C, vascular cell adhesion molecule-1, Tie-2, and intracellular adhesion molecular-1.
Despite these findings, NfL in the vitreous humor was not associated with patients’ clinical ophthalmic conditions or systemic diseases such as hypertension, diabetes, and hyperlipidemia. Similarly, NfL was not significantly associated with APOE genotype E2 and E4, the alleles most commonly associated with Alzheimer’s disease.
Finally, no statistically significant associations were found between NfL and Mini-Mental State Examination (MMSE) scores.
A “first step”
Most research currently examining the role of the eye in neurodegenerative disease is focused on retinal biomarkers imaged by optical coherence tomography, the investigators noted. Although promising, data obtained this way have yielded conflicting results.
Similarly, while the diagnostic potential of the core CSF biomarkers for AD (Abeta40, Abeta42, p-tau, and total tau) is well established, the practical utility of testing CSF for neurodegenerative diseases is limited, wrote the researchers.
As such, an additional biomarker source such as NfL–which is quantifiable and protein-based within eye fluid – has the potential to play an important role in predicting neurodegenerative disease in the clinical setting, they added.
“The holy grail of neurodegenerative-disease diagnosis is early diagnosis. Because if you can implement treatment early, you can slow down and potentially halt the progression of these diseases,” Dr. Subramanian said.
“This study is the first step toward determining if the eye could play a potential role in early diagnosis of conditions such as Alzheimer’s disease,” she added.
That said, Dr. Subramanian was quick to recognize the findings’ preliminary nature and that they do not offer reliable evidence that vitreous NfL levels definitively represent neurodegeneration. As such, the investigators called for more research to validate the association between this type of biomarker with other established biomarkers of neurodegeneration, such as those found in CSF fluid or on MRI and PET scans.
“At this point, we can’t look at eye fluid and say that people have neurodegenerative diseases,” she noted. “The other thing to consider is that vitreous humor is at the back of the eye, so it’s actually a fairly invasive procedure.
“I think the next step is to look at other types of eye fluids such as the aqueous fluid in the front of the eye, or even tear secretions, potentially,” Dr. Subramanian said.
Other study limitations include the lack of an association between NfL levels and MMSE scores and that none of the study participants were actually diagnosed with Alzheimer’s disease. Validation studies are needed to compare vitreous levels of NfL in patients with mild cognitive impairment/AD to normal controls, the investigators noted.
Fascinating but impractical?
Commenting on the findings, Sharon Fekrat, MD, professor of ophthalmology, Duke University, Durham, N.C., agreed that there’s potential importance of the eye in diagnosing neurodegeneration. However, she suggested that vitreous humor may not be the most expedient medium to use.
“I commend the authors for this fascinating work. But practically speaking, if we ultimately want to use intraocular fluid to diagnose Alzheimer’s and perhaps other neurodegeneration, I think aqueous humor might be more practical than the vitreous humor,” said Dr. Fekrat, who was not involved with the research. “What might be even better is to have a device that can be held against the eyeball that measures the levels of various substances inside the eyeball without having to enter the eye,” added Justin Ma, a Duke University medical student working under Dr. Fekrat’s guidance. “It could be similar technology to what’s currently used to measure blood glucose levels,” Mr. Ma added.
The study was supported in part by the National Institute of Aging. Dr. Subramanian, Dr. Fekrat, and Mr. Ma have disclosed no relevant financial relationships. Disclosures for other study authors are listed in the original article.
A version of this article originally appeared on Medscape.com.
FROM ALZHEIMER’S RESEARCH & THERAPY
Stroke may be the first symptom of COVID-19 in younger patients
new research suggests. Investigators carried out a meta-analysis of data, including 160 patients with COVID-19 and stroke, and found that nearly half of patients under the age of 50 were asymptomatic at the time of stroke onset.
Although younger patients had the highest risk of stroke, the highest risk of death was in patients who were older, had other chronic conditions, and had more severe COVID-19–associated respiratory symptoms.
“One of the most eye-opening findings of this study is that, for patients under 50 years old, many were totally asymptomatic when they had a stroke related to COVID-19, [which] means that, for these patients, the stroke was their first symptom of the disease,” lead author Luciano Sposato, MD, MBA, associate professor and chair in stroke research at Western University, London, Ont.
The study was published online Sept. 15 in Neurology.
Anecdotal reports
“In early April of 2020, we realized that COVID-19 was a highly thrombogenic disease,” said Dr. Sposato. “Almost in parallel, I started to see anecdotal reports in social media of strokes occurring in patients with COVID-19, and there were also very few case reports.”
The investigators “thought it would be a good idea to put all the data together in one paper,” he said, and began by conducting a systematic review of 10 published studies of COVID-19 and stroke (n = 125 patients), which were then pooled with 35 unpublished cases from Canada, the United States, and Iran for a total of 160 cases.
The analysis examined in-hospital mortality rates of patients with stroke and COVID-19.
In addition, the researchers conducted a second review of 150 papers, encompassing a final cohort of 3,306 COVID-19 patients with stroke of any type and 5,322 with ischemic stroke.
“Some studies reported data for only ischemic stroke, and some reported data for all strokes considered together, which resulted in a different number of patients on each meta-analysis, with a lower number of ‘any stroke’ cases,” Dr. Sposato explained. “This review looked at the number of patients who developed a stroke during admission and included thousands of patients.”
Dr. Sposato noted that the first review was conducted on single case reports and small case series “to understand the clinical characteristics of strokes in patients with COVID-19 on an individual patient level,” since “large studies, including hundreds of thousands of patients, usually do not provide the level of detail for a descriptive analysis of the clinical characteristics of a disease.”
Cluster analyses were used to “identify specific clinical phenotypes and their relationship with death.” Patients were stratified into three age groups: <50, 50-70, and >70 years (“young,” “middle aged,” and “older,” respectively). The median age was 65 years and 43% were female.
Mortality ‘remarkably high’
The review showed that 1.8% (95% confidence interval, 0.9%-3.7%) of patients experienced a new stroke, while 1.5% (95% CI, 0.8%-2.8%) of these experienced an ischemic stroke. “These numbers are higher than historical data for other infectious diseases – for example, 0.75% in SARS-CoV-1, 0.78% in sepsis, and 0.2% in influenza,” Dr. Sposato commented.
Moreover, “this number may be an underestimate, given that many patients die without a confirmed diagnosis and that some patients did not come to the emergency department when experiencing mild symptoms during the first months of the pandemic,” he added.
Focusing on the review of 160 patients, the researchers described in-hospital mortality for strokes of all types and for ischemic strokes alone as “remarkably high” (34.4% [95% CI, 27.2%-42.4%] and 35.7% [95% CI, 27.5%-44.8%], respectively), with most deaths occurring among ischemic stroke patients.
“This high mortality rate is higher than the [roughly] 15% to 30% reported for stroke patients without COVID-19 admitted to intensive care units,” Dr. Sposato said.
High-risk phenotype
Many “young” COVID-19 patients (under age 50) who had a stroke (42.9%) had no previous risk factors or comorbidities. Moreover, in almost half of these patients (48.3%), stroke was more likely to occur before the onset of any COVID-19 respiratory symptoms.
Additionally, younger patients showed the highest frequency of elevated cardiac troponin compared with middle-aged and older patients (71.4% vs. 48.4% and 27.8%, respectively). On the other hand, mortality was 67% lower in younger versus older patients (odds ratio, 0.33; 95% CI, 0.12-0.94; P = .039).
Dr. Sposato noted that the proportion of ischemic stroke patients with large-vessel occlusion was “higher than previously reported” for patients with stroke without COVID-19 (47% compared with 29%, respectively).
“We should consider COVID-19 as a new cause or risk factor for stroke. At least, patients with stroke should probably be tested for SARS-CoV-2 infection if they are young and present with a large-vessel occlusion, even in the absence of typical COVID-19 respiratory symptoms,” he suggested.
The researchers identified a “high-risk phenotype” for death for all types of stroke considered together: older age, a higher burden of comorbidities, and severe COVID-19 respiratory symptoms. Patients with all three characteristics had the highest in-hospital mortality rate (58.6%) and a threefold risk of death, compared with the rest of the cohort (OR, 3.52; 95% CI, 1.53-8.09; P = .003).
“Several potential mechanisms can explain the increased risk of stroke among COVID-19 patients, but perhaps the most important one is increased thrombogenesis secondary to an exaggerated inflammatory response,” Dr. Sposato said.
Not just elders
Commenting on the study, Jodi Edwards, PhD, director of the Brain and Heart Nexus Research Program at the University of Ottawa Heart Institute, said the findings are “consistent with and underscore public health messaging emphasizing that COVID-19 does not only affect the elderly and those with underlying health conditions, but can have serious and even fatal consequences at any age.”
Dr. Edwards, who was not involved with the study, emphasized that “adherence to public health recommendations is critical to begin to reduce the rising incidence in younger adults.”
Dr. Sposato acknowledged that the study was small and that there “can be problems associated with a systematic review of case reports, such as publication bias, lack of completeness of data, etc, so more research is needed.”
Dr. Sposato is supported by the Kathleen & Dr. Henry Barnett Research Chair in Stroke Research at Western University, the Edward and Alma Saraydar Neurosciences Fund of the London Health Sciences Foundation, and the Opportunities Fund of the Academic Health Sciences Centre Alternative Funding Plan of the Academic Medical Organization of Southwestern Ontario. Dr. Sposato reported speaker honoraria from Boehringer Ingelheim, Pfizer, Gore, and Bayer and research/quality improvement grants from Boehringer Ingelheim and Bayer. The other authors’ disclosures are listed on the original article. Dr. Edwards has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests. Investigators carried out a meta-analysis of data, including 160 patients with COVID-19 and stroke, and found that nearly half of patients under the age of 50 were asymptomatic at the time of stroke onset.
Although younger patients had the highest risk of stroke, the highest risk of death was in patients who were older, had other chronic conditions, and had more severe COVID-19–associated respiratory symptoms.
“One of the most eye-opening findings of this study is that, for patients under 50 years old, many were totally asymptomatic when they had a stroke related to COVID-19, [which] means that, for these patients, the stroke was their first symptom of the disease,” lead author Luciano Sposato, MD, MBA, associate professor and chair in stroke research at Western University, London, Ont.
The study was published online Sept. 15 in Neurology.
Anecdotal reports
“In early April of 2020, we realized that COVID-19 was a highly thrombogenic disease,” said Dr. Sposato. “Almost in parallel, I started to see anecdotal reports in social media of strokes occurring in patients with COVID-19, and there were also very few case reports.”
The investigators “thought it would be a good idea to put all the data together in one paper,” he said, and began by conducting a systematic review of 10 published studies of COVID-19 and stroke (n = 125 patients), which were then pooled with 35 unpublished cases from Canada, the United States, and Iran for a total of 160 cases.
The analysis examined in-hospital mortality rates of patients with stroke and COVID-19.
In addition, the researchers conducted a second review of 150 papers, encompassing a final cohort of 3,306 COVID-19 patients with stroke of any type and 5,322 with ischemic stroke.
“Some studies reported data for only ischemic stroke, and some reported data for all strokes considered together, which resulted in a different number of patients on each meta-analysis, with a lower number of ‘any stroke’ cases,” Dr. Sposato explained. “This review looked at the number of patients who developed a stroke during admission and included thousands of patients.”
Dr. Sposato noted that the first review was conducted on single case reports and small case series “to understand the clinical characteristics of strokes in patients with COVID-19 on an individual patient level,” since “large studies, including hundreds of thousands of patients, usually do not provide the level of detail for a descriptive analysis of the clinical characteristics of a disease.”
Cluster analyses were used to “identify specific clinical phenotypes and their relationship with death.” Patients were stratified into three age groups: <50, 50-70, and >70 years (“young,” “middle aged,” and “older,” respectively). The median age was 65 years and 43% were female.
Mortality ‘remarkably high’
The review showed that 1.8% (95% confidence interval, 0.9%-3.7%) of patients experienced a new stroke, while 1.5% (95% CI, 0.8%-2.8%) of these experienced an ischemic stroke. “These numbers are higher than historical data for other infectious diseases – for example, 0.75% in SARS-CoV-1, 0.78% in sepsis, and 0.2% in influenza,” Dr. Sposato commented.
Moreover, “this number may be an underestimate, given that many patients die without a confirmed diagnosis and that some patients did not come to the emergency department when experiencing mild symptoms during the first months of the pandemic,” he added.
Focusing on the review of 160 patients, the researchers described in-hospital mortality for strokes of all types and for ischemic strokes alone as “remarkably high” (34.4% [95% CI, 27.2%-42.4%] and 35.7% [95% CI, 27.5%-44.8%], respectively), with most deaths occurring among ischemic stroke patients.
“This high mortality rate is higher than the [roughly] 15% to 30% reported for stroke patients without COVID-19 admitted to intensive care units,” Dr. Sposato said.
High-risk phenotype
Many “young” COVID-19 patients (under age 50) who had a stroke (42.9%) had no previous risk factors or comorbidities. Moreover, in almost half of these patients (48.3%), stroke was more likely to occur before the onset of any COVID-19 respiratory symptoms.
Additionally, younger patients showed the highest frequency of elevated cardiac troponin compared with middle-aged and older patients (71.4% vs. 48.4% and 27.8%, respectively). On the other hand, mortality was 67% lower in younger versus older patients (odds ratio, 0.33; 95% CI, 0.12-0.94; P = .039).
Dr. Sposato noted that the proportion of ischemic stroke patients with large-vessel occlusion was “higher than previously reported” for patients with stroke without COVID-19 (47% compared with 29%, respectively).
“We should consider COVID-19 as a new cause or risk factor for stroke. At least, patients with stroke should probably be tested for SARS-CoV-2 infection if they are young and present with a large-vessel occlusion, even in the absence of typical COVID-19 respiratory symptoms,” he suggested.
The researchers identified a “high-risk phenotype” for death for all types of stroke considered together: older age, a higher burden of comorbidities, and severe COVID-19 respiratory symptoms. Patients with all three characteristics had the highest in-hospital mortality rate (58.6%) and a threefold risk of death, compared with the rest of the cohort (OR, 3.52; 95% CI, 1.53-8.09; P = .003).
“Several potential mechanisms can explain the increased risk of stroke among COVID-19 patients, but perhaps the most important one is increased thrombogenesis secondary to an exaggerated inflammatory response,” Dr. Sposato said.
Not just elders
Commenting on the study, Jodi Edwards, PhD, director of the Brain and Heart Nexus Research Program at the University of Ottawa Heart Institute, said the findings are “consistent with and underscore public health messaging emphasizing that COVID-19 does not only affect the elderly and those with underlying health conditions, but can have serious and even fatal consequences at any age.”
Dr. Edwards, who was not involved with the study, emphasized that “adherence to public health recommendations is critical to begin to reduce the rising incidence in younger adults.”
Dr. Sposato acknowledged that the study was small and that there “can be problems associated with a systematic review of case reports, such as publication bias, lack of completeness of data, etc, so more research is needed.”
Dr. Sposato is supported by the Kathleen & Dr. Henry Barnett Research Chair in Stroke Research at Western University, the Edward and Alma Saraydar Neurosciences Fund of the London Health Sciences Foundation, and the Opportunities Fund of the Academic Health Sciences Centre Alternative Funding Plan of the Academic Medical Organization of Southwestern Ontario. Dr. Sposato reported speaker honoraria from Boehringer Ingelheim, Pfizer, Gore, and Bayer and research/quality improvement grants from Boehringer Ingelheim and Bayer. The other authors’ disclosures are listed on the original article. Dr. Edwards has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests. Investigators carried out a meta-analysis of data, including 160 patients with COVID-19 and stroke, and found that nearly half of patients under the age of 50 were asymptomatic at the time of stroke onset.
Although younger patients had the highest risk of stroke, the highest risk of death was in patients who were older, had other chronic conditions, and had more severe COVID-19–associated respiratory symptoms.
“One of the most eye-opening findings of this study is that, for patients under 50 years old, many were totally asymptomatic when they had a stroke related to COVID-19, [which] means that, for these patients, the stroke was their first symptom of the disease,” lead author Luciano Sposato, MD, MBA, associate professor and chair in stroke research at Western University, London, Ont.
The study was published online Sept. 15 in Neurology.
Anecdotal reports
“In early April of 2020, we realized that COVID-19 was a highly thrombogenic disease,” said Dr. Sposato. “Almost in parallel, I started to see anecdotal reports in social media of strokes occurring in patients with COVID-19, and there were also very few case reports.”
The investigators “thought it would be a good idea to put all the data together in one paper,” he said, and began by conducting a systematic review of 10 published studies of COVID-19 and stroke (n = 125 patients), which were then pooled with 35 unpublished cases from Canada, the United States, and Iran for a total of 160 cases.
The analysis examined in-hospital mortality rates of patients with stroke and COVID-19.
In addition, the researchers conducted a second review of 150 papers, encompassing a final cohort of 3,306 COVID-19 patients with stroke of any type and 5,322 with ischemic stroke.
“Some studies reported data for only ischemic stroke, and some reported data for all strokes considered together, which resulted in a different number of patients on each meta-analysis, with a lower number of ‘any stroke’ cases,” Dr. Sposato explained. “This review looked at the number of patients who developed a stroke during admission and included thousands of patients.”
Dr. Sposato noted that the first review was conducted on single case reports and small case series “to understand the clinical characteristics of strokes in patients with COVID-19 on an individual patient level,” since “large studies, including hundreds of thousands of patients, usually do not provide the level of detail for a descriptive analysis of the clinical characteristics of a disease.”
Cluster analyses were used to “identify specific clinical phenotypes and their relationship with death.” Patients were stratified into three age groups: <50, 50-70, and >70 years (“young,” “middle aged,” and “older,” respectively). The median age was 65 years and 43% were female.
Mortality ‘remarkably high’
The review showed that 1.8% (95% confidence interval, 0.9%-3.7%) of patients experienced a new stroke, while 1.5% (95% CI, 0.8%-2.8%) of these experienced an ischemic stroke. “These numbers are higher than historical data for other infectious diseases – for example, 0.75% in SARS-CoV-1, 0.78% in sepsis, and 0.2% in influenza,” Dr. Sposato commented.
Moreover, “this number may be an underestimate, given that many patients die without a confirmed diagnosis and that some patients did not come to the emergency department when experiencing mild symptoms during the first months of the pandemic,” he added.
Focusing on the review of 160 patients, the researchers described in-hospital mortality for strokes of all types and for ischemic strokes alone as “remarkably high” (34.4% [95% CI, 27.2%-42.4%] and 35.7% [95% CI, 27.5%-44.8%], respectively), with most deaths occurring among ischemic stroke patients.
“This high mortality rate is higher than the [roughly] 15% to 30% reported for stroke patients without COVID-19 admitted to intensive care units,” Dr. Sposato said.
High-risk phenotype
Many “young” COVID-19 patients (under age 50) who had a stroke (42.9%) had no previous risk factors or comorbidities. Moreover, in almost half of these patients (48.3%), stroke was more likely to occur before the onset of any COVID-19 respiratory symptoms.
Additionally, younger patients showed the highest frequency of elevated cardiac troponin compared with middle-aged and older patients (71.4% vs. 48.4% and 27.8%, respectively). On the other hand, mortality was 67% lower in younger versus older patients (odds ratio, 0.33; 95% CI, 0.12-0.94; P = .039).
Dr. Sposato noted that the proportion of ischemic stroke patients with large-vessel occlusion was “higher than previously reported” for patients with stroke without COVID-19 (47% compared with 29%, respectively).
“We should consider COVID-19 as a new cause or risk factor for stroke. At least, patients with stroke should probably be tested for SARS-CoV-2 infection if they are young and present with a large-vessel occlusion, even in the absence of typical COVID-19 respiratory symptoms,” he suggested.
The researchers identified a “high-risk phenotype” for death for all types of stroke considered together: older age, a higher burden of comorbidities, and severe COVID-19 respiratory symptoms. Patients with all three characteristics had the highest in-hospital mortality rate (58.6%) and a threefold risk of death, compared with the rest of the cohort (OR, 3.52; 95% CI, 1.53-8.09; P = .003).
“Several potential mechanisms can explain the increased risk of stroke among COVID-19 patients, but perhaps the most important one is increased thrombogenesis secondary to an exaggerated inflammatory response,” Dr. Sposato said.
Not just elders
Commenting on the study, Jodi Edwards, PhD, director of the Brain and Heart Nexus Research Program at the University of Ottawa Heart Institute, said the findings are “consistent with and underscore public health messaging emphasizing that COVID-19 does not only affect the elderly and those with underlying health conditions, but can have serious and even fatal consequences at any age.”
Dr. Edwards, who was not involved with the study, emphasized that “adherence to public health recommendations is critical to begin to reduce the rising incidence in younger adults.”
Dr. Sposato acknowledged that the study was small and that there “can be problems associated with a systematic review of case reports, such as publication bias, lack of completeness of data, etc, so more research is needed.”
Dr. Sposato is supported by the Kathleen & Dr. Henry Barnett Research Chair in Stroke Research at Western University, the Edward and Alma Saraydar Neurosciences Fund of the London Health Sciences Foundation, and the Opportunities Fund of the Academic Health Sciences Centre Alternative Funding Plan of the Academic Medical Organization of Southwestern Ontario. Dr. Sposato reported speaker honoraria from Boehringer Ingelheim, Pfizer, Gore, and Bayer and research/quality improvement grants from Boehringer Ingelheim and Bayer. The other authors’ disclosures are listed on the original article. Dr. Edwards has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
From Neurology
Nerve damage linked to prone positioning in COVID-19
A new case series describes peripheral nerve injuries associated with this type of positioning and suggests ways to minimize the potential damage.
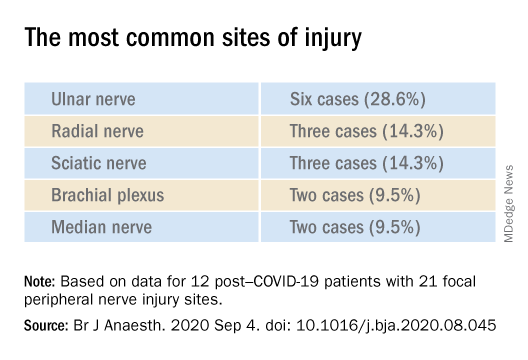
“Physicians should remain aware of increased susceptibility to peripheral nerve damage in patients with severe COVID-19 after prone positioning, since it is surprisingly common among these patients, and should refine standard protocols accordingly to reduce that risk,” said senior author Colin Franz, MD, PhD, director of the Electrodiagnostic Laboratory, Shirley Ryan AbilityLab, Chicago.
The article was published online Sept. 4 in the British Journal of Anaesthesiology.
Unique type of nerve injury
Many patients who are admitted to the intensive care unit with COVID-19 undergo invasive mechanical ventilation because of acute respiratory distress syndrome (ARDS). Clinical guidelines recommend that such patients lie in the prone position 12-16 hours per day.
“Prone positioning for up to 16 hours is a therapy we use for patients with more severe forms of ARDS, and high-level evidence points to mortality benefit in patients with moderate to severe ARDS if [mechanical] ventilation occurs,” said study coauthor James McCauley Walter, MD, of the pulmonary division at Northwestern University, Chicago.
With a “significant number of COVID-19 patients flooding the ICU, we quickly started to prone a lot of them, but if you are in a specific position for multiple hours a day, coupled with the neurotoxic effects of the SARS-CoV-2 virus itself, you may be exposed to a unique type of nerve injury,” he said.
Dr. Walter said that the “incidence of asymmetric neuropathies seems out of proportion to what has been reported in non–COVID-19 settings, which is what caught our attention.”
Many of these patients are discharged to rehabilitation hospitals, and “what we noticed, which was unique about COVID-19 patients coming to our rehab hospital, was that, compared with other patients who had been critically ill with a long hospital stay, there was a significantly higher percentage of COVID-19 patients who had peripheral nerve damage,” Dr. Franz said.
The authors described 12 of these patients who were admitted between April 24 and June 30, 2020 (mean age, 60.3 years; range, 23-80 years). The sample included White, Black, and Hispanic individuals. Eleven of the 12 post–COVID-19 patients with peripheral nerve damage had experienced prone positioning during acute management.
The average number of days patients received mechanical ventilation was 33.6 (range, 12-62 days). The average number of proning sessions was 4.5 (range, 1-16) with an average of 81.2 hours (range, 16-252 hours) spent prone.
A major contributor
Dr. Franz suggested that prone positioning is likely not the only cause of peripheral nerve damage but “may play a big role in these patients who are vulnerable because of viral infection and the critical illness that causes damage and nerve injuries.”
“The first component of lifesaving care for the critically ill in the ICU is intravenous fluids, mechanical ventilation, steroids, and antibiotics for infection,” said Dr. Walter.
“We are trying to come up with ways to place patients in prone position in safer ways, to pay attention to pressure points and areas of injury that we have seen and try to offload them, to see if we can decrease the rate of these injuries,” he added.
The researchers’ article includes a heat map diagram as a “template for where to focus the most efforts, in terms of decreasing pressure,” Dr. Walter said.
“The nerves are accepting too much force for gravely ill COVID-19 patients to handle, so we suggest using the template to determine where extra padding might be needed, or a protocol that might include changes in positioning,” he added.
Dr. Franz described the interventions used for COVID-19 patients with prone positioning–related peripheral nerve damage. “The first step is trying to address the problems one by one, either trying to solve them through exercise or teaching new skills, new ways to compensate, beginning with basic activities, such as getting out of bed and self-care,” he said.
Long-term recovery of nerve injuries depends on how severe the injuries are. Some nerves can slowly regenerate – possibly at the rate of 1 inch per month – which can be a long process, taking between a year and 18 months.
Dr. Franz said that therapies for this condition are “extrapolated from clinical trial work” on promoting nerve regeneration after surgery using electrical stimulation to enable nerves to regrow at a faster rate.
“Regeneration is not only slow, but it may not happen completely, leaving the patient with permanent nerve damage – in fact, based on our experience and what has been reported, the percentage of patients with full recovery is only 10%,” he said.
The most common symptomatic complaint other than lack of movement or feeling is neuropathic pain, “which may require medication to take the edge off the pain,” Dr. Franz added.
Irreversible damage?
Commenting on the study, Tae Chung, MD, of the departments of physical medicine, rehabilitation, and neurology, Johns Hopkins University, Baltimore, said the study “provides one of the first and the largest description of peripheral nerve injury associated with prone positioning for management of ARDS from COVID-19.”
Dr. Chung, who was not involved in the research, noted that “various neurological complications from COVID-19 have been reported, and some of them may result in irreversible neurological damage or delay the recovery from COVID-19 infection,” so “accurate and timely diagnosis of such neurological complications is critical for rehabilitation of the COVID-19 survivors.”
The study received no funding. Dr. Franz, Dr. Walter, study coauthors, and Dr. Chung report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new case series describes peripheral nerve injuries associated with this type of positioning and suggests ways to minimize the potential damage.
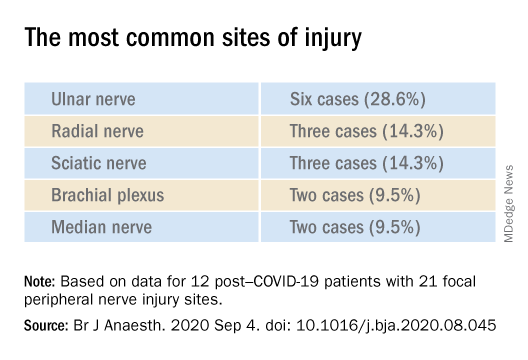
“Physicians should remain aware of increased susceptibility to peripheral nerve damage in patients with severe COVID-19 after prone positioning, since it is surprisingly common among these patients, and should refine standard protocols accordingly to reduce that risk,” said senior author Colin Franz, MD, PhD, director of the Electrodiagnostic Laboratory, Shirley Ryan AbilityLab, Chicago.
The article was published online Sept. 4 in the British Journal of Anaesthesiology.
Unique type of nerve injury
Many patients who are admitted to the intensive care unit with COVID-19 undergo invasive mechanical ventilation because of acute respiratory distress syndrome (ARDS). Clinical guidelines recommend that such patients lie in the prone position 12-16 hours per day.
“Prone positioning for up to 16 hours is a therapy we use for patients with more severe forms of ARDS, and high-level evidence points to mortality benefit in patients with moderate to severe ARDS if [mechanical] ventilation occurs,” said study coauthor James McCauley Walter, MD, of the pulmonary division at Northwestern University, Chicago.
With a “significant number of COVID-19 patients flooding the ICU, we quickly started to prone a lot of them, but if you are in a specific position for multiple hours a day, coupled with the neurotoxic effects of the SARS-CoV-2 virus itself, you may be exposed to a unique type of nerve injury,” he said.
Dr. Walter said that the “incidence of asymmetric neuropathies seems out of proportion to what has been reported in non–COVID-19 settings, which is what caught our attention.”
Many of these patients are discharged to rehabilitation hospitals, and “what we noticed, which was unique about COVID-19 patients coming to our rehab hospital, was that, compared with other patients who had been critically ill with a long hospital stay, there was a significantly higher percentage of COVID-19 patients who had peripheral nerve damage,” Dr. Franz said.
The authors described 12 of these patients who were admitted between April 24 and June 30, 2020 (mean age, 60.3 years; range, 23-80 years). The sample included White, Black, and Hispanic individuals. Eleven of the 12 post–COVID-19 patients with peripheral nerve damage had experienced prone positioning during acute management.
The average number of days patients received mechanical ventilation was 33.6 (range, 12-62 days). The average number of proning sessions was 4.5 (range, 1-16) with an average of 81.2 hours (range, 16-252 hours) spent prone.
A major contributor
Dr. Franz suggested that prone positioning is likely not the only cause of peripheral nerve damage but “may play a big role in these patients who are vulnerable because of viral infection and the critical illness that causes damage and nerve injuries.”
“The first component of lifesaving care for the critically ill in the ICU is intravenous fluids, mechanical ventilation, steroids, and antibiotics for infection,” said Dr. Walter.
“We are trying to come up with ways to place patients in prone position in safer ways, to pay attention to pressure points and areas of injury that we have seen and try to offload them, to see if we can decrease the rate of these injuries,” he added.
The researchers’ article includes a heat map diagram as a “template for where to focus the most efforts, in terms of decreasing pressure,” Dr. Walter said.
“The nerves are accepting too much force for gravely ill COVID-19 patients to handle, so we suggest using the template to determine where extra padding might be needed, or a protocol that might include changes in positioning,” he added.
Dr. Franz described the interventions used for COVID-19 patients with prone positioning–related peripheral nerve damage. “The first step is trying to address the problems one by one, either trying to solve them through exercise or teaching new skills, new ways to compensate, beginning with basic activities, such as getting out of bed and self-care,” he said.
Long-term recovery of nerve injuries depends on how severe the injuries are. Some nerves can slowly regenerate – possibly at the rate of 1 inch per month – which can be a long process, taking between a year and 18 months.
Dr. Franz said that therapies for this condition are “extrapolated from clinical trial work” on promoting nerve regeneration after surgery using electrical stimulation to enable nerves to regrow at a faster rate.
“Regeneration is not only slow, but it may not happen completely, leaving the patient with permanent nerve damage – in fact, based on our experience and what has been reported, the percentage of patients with full recovery is only 10%,” he said.
The most common symptomatic complaint other than lack of movement or feeling is neuropathic pain, “which may require medication to take the edge off the pain,” Dr. Franz added.
Irreversible damage?
Commenting on the study, Tae Chung, MD, of the departments of physical medicine, rehabilitation, and neurology, Johns Hopkins University, Baltimore, said the study “provides one of the first and the largest description of peripheral nerve injury associated with prone positioning for management of ARDS from COVID-19.”
Dr. Chung, who was not involved in the research, noted that “various neurological complications from COVID-19 have been reported, and some of them may result in irreversible neurological damage or delay the recovery from COVID-19 infection,” so “accurate and timely diagnosis of such neurological complications is critical for rehabilitation of the COVID-19 survivors.”
The study received no funding. Dr. Franz, Dr. Walter, study coauthors, and Dr. Chung report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new case series describes peripheral nerve injuries associated with this type of positioning and suggests ways to minimize the potential damage.
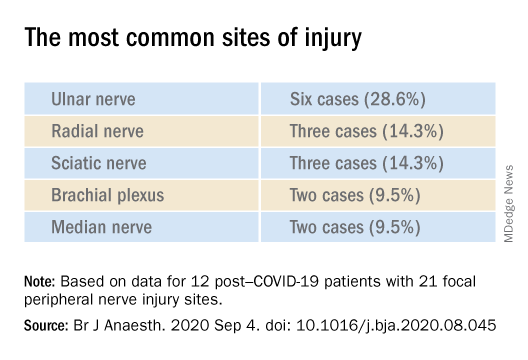
“Physicians should remain aware of increased susceptibility to peripheral nerve damage in patients with severe COVID-19 after prone positioning, since it is surprisingly common among these patients, and should refine standard protocols accordingly to reduce that risk,” said senior author Colin Franz, MD, PhD, director of the Electrodiagnostic Laboratory, Shirley Ryan AbilityLab, Chicago.
The article was published online Sept. 4 in the British Journal of Anaesthesiology.
Unique type of nerve injury
Many patients who are admitted to the intensive care unit with COVID-19 undergo invasive mechanical ventilation because of acute respiratory distress syndrome (ARDS). Clinical guidelines recommend that such patients lie in the prone position 12-16 hours per day.
“Prone positioning for up to 16 hours is a therapy we use for patients with more severe forms of ARDS, and high-level evidence points to mortality benefit in patients with moderate to severe ARDS if [mechanical] ventilation occurs,” said study coauthor James McCauley Walter, MD, of the pulmonary division at Northwestern University, Chicago.
With a “significant number of COVID-19 patients flooding the ICU, we quickly started to prone a lot of them, but if you are in a specific position for multiple hours a day, coupled with the neurotoxic effects of the SARS-CoV-2 virus itself, you may be exposed to a unique type of nerve injury,” he said.
Dr. Walter said that the “incidence of asymmetric neuropathies seems out of proportion to what has been reported in non–COVID-19 settings, which is what caught our attention.”
Many of these patients are discharged to rehabilitation hospitals, and “what we noticed, which was unique about COVID-19 patients coming to our rehab hospital, was that, compared with other patients who had been critically ill with a long hospital stay, there was a significantly higher percentage of COVID-19 patients who had peripheral nerve damage,” Dr. Franz said.
The authors described 12 of these patients who were admitted between April 24 and June 30, 2020 (mean age, 60.3 years; range, 23-80 years). The sample included White, Black, and Hispanic individuals. Eleven of the 12 post–COVID-19 patients with peripheral nerve damage had experienced prone positioning during acute management.
The average number of days patients received mechanical ventilation was 33.6 (range, 12-62 days). The average number of proning sessions was 4.5 (range, 1-16) with an average of 81.2 hours (range, 16-252 hours) spent prone.
A major contributor
Dr. Franz suggested that prone positioning is likely not the only cause of peripheral nerve damage but “may play a big role in these patients who are vulnerable because of viral infection and the critical illness that causes damage and nerve injuries.”
“The first component of lifesaving care for the critically ill in the ICU is intravenous fluids, mechanical ventilation, steroids, and antibiotics for infection,” said Dr. Walter.
“We are trying to come up with ways to place patients in prone position in safer ways, to pay attention to pressure points and areas of injury that we have seen and try to offload them, to see if we can decrease the rate of these injuries,” he added.
The researchers’ article includes a heat map diagram as a “template for where to focus the most efforts, in terms of decreasing pressure,” Dr. Walter said.
“The nerves are accepting too much force for gravely ill COVID-19 patients to handle, so we suggest using the template to determine where extra padding might be needed, or a protocol that might include changes in positioning,” he added.
Dr. Franz described the interventions used for COVID-19 patients with prone positioning–related peripheral nerve damage. “The first step is trying to address the problems one by one, either trying to solve them through exercise or teaching new skills, new ways to compensate, beginning with basic activities, such as getting out of bed and self-care,” he said.
Long-term recovery of nerve injuries depends on how severe the injuries are. Some nerves can slowly regenerate – possibly at the rate of 1 inch per month – which can be a long process, taking between a year and 18 months.
Dr. Franz said that therapies for this condition are “extrapolated from clinical trial work” on promoting nerve regeneration after surgery using electrical stimulation to enable nerves to regrow at a faster rate.
“Regeneration is not only slow, but it may not happen completely, leaving the patient with permanent nerve damage – in fact, based on our experience and what has been reported, the percentage of patients with full recovery is only 10%,” he said.
The most common symptomatic complaint other than lack of movement or feeling is neuropathic pain, “which may require medication to take the edge off the pain,” Dr. Franz added.
Irreversible damage?
Commenting on the study, Tae Chung, MD, of the departments of physical medicine, rehabilitation, and neurology, Johns Hopkins University, Baltimore, said the study “provides one of the first and the largest description of peripheral nerve injury associated with prone positioning for management of ARDS from COVID-19.”
Dr. Chung, who was not involved in the research, noted that “various neurological complications from COVID-19 have been reported, and some of them may result in irreversible neurological damage or delay the recovery from COVID-19 infection,” so “accurate and timely diagnosis of such neurological complications is critical for rehabilitation of the COVID-19 survivors.”
The study received no funding. Dr. Franz, Dr. Walter, study coauthors, and Dr. Chung report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM THE BRITISH JOURNAL OF ANAESTHESIOLOGY
OTC ‘brain boosters’ may pose serious risks, experts say
, new research shows.
“Americans spend more than $600 million on over-the-counter smart pills every year, but we know very little about what is actually in these products,” said Pieter A. Cohen, MD, of the department of medicine at Harvard Medical School, Boston.
“Finding new combinations of drugs [that have] never been tested in humans in over-the-counter brain-boosting supplements is alarming,” said Dr. Cohen.
The study was published online Sept. 23 in Neurology Clinical Practice, a journal of the American Academy of Neurology.
Buyer beware
In a search of the National Institutes of Health Dietary Supplement Label Database and the Natural Medicines Database, Dr. Cohen and colleagues identified 10 supplements labeled as containing omberacetam, aniracetam, phenylpiracetam, or oxiracetam – four analogues of piracetam that are not approved for human use in the United States. Piracetam is also not approved in the United States.
In these 10 products, five unapproved drugs were discovered – omberacetam and aniracetam along with three others (phenibut, vinpocetine and picamilon).
By consuming the recommended serving size of these products, consumers could be exposed to pharmaceutical-level dosages of drugs including a maximum of 40.6 mg omberacetam (typical pharmacologic dose 10 mg), 502 mg of aniracetam (typical pharmacologic dose 200-750 mg), 15.4 mg of phenibut (typical dose 250-500 mg), 4.3 mg of vinpocetine (typical dose 5-40 mg), and 90.1 mg of picamilon (typical dose 50-200 mg), the study team reported.
Several drugs detected in these “smart” pills were not declared on the label, and several declared drugs were not detected in the products. For those products with drug quantities provided on the labels, three-quarters of declared quantities were inaccurate.
Consumers who use these cognitive enhancers could be exposed to amounts of these unapproved drugs that are fourfold greater than pharmaceutical dosages and combinations never tested in humans, the study team says. One product combined three different unapproved drugs and another product contained four different drugs.
“We have previously shown that these products may contain individual foreign drugs, but in our new study we found complex combinations of foreign drugs, up to four different drugs in a single product,” Dr. Cohen said.
The presence of these unapproved drugs in supplements, including at supratherapeutic dosages, suggests “serious risks to consumers and weaknesses in the regulatory framework under which supplements are permitted to be introduced in the U.S.,” Dr. Cohen and colleagues wrote.
“We should counsel our patients to avoid over-the-counter ‘smart pills’ until we can be assured as to the safety and efficacy of these products,” said Dr. Cohen.
Concerning findings
Glen R. Finney, MD, director of the Geisinger Memory and Cognition Program at the Neuroscience Institute, Geisinger Health System, Wilkes-Barre, Penn., said in an interview that two findings are very concerning: the lack of listed ingredients and especially the presence of unlisted drugs at active levels. “What if a person has a sensitivity or allergy to one of the unlisted drugs? This is a safety issue and a consumer issue,” Dr. Finney said.
Despite being widely promoted on television, “over-the-counter supplements are not regulated, so there is no guarantee that they contain what they claim, and there is very little evidence that they help memory and thinking even when they do have the ingredients they claim in the supplement,” said Dr. Finney,
“The best way to stay safe and help memory and thinking is to speak with your health providers about proven treatments that have good safety regulation, so you know what you’re getting, and what you’re getting from it,” Dr. Finney advised.
The study had no targeted funding. Dr. Cohen has collaborated in research with NSF International, received compensation from UptoDate, and received research support from Consumers Union and PEW Charitable Trusts. Dr. Finney has no relevant disclosures.
A version of this article originally appeared on Medscape.com.
, new research shows.
“Americans spend more than $600 million on over-the-counter smart pills every year, but we know very little about what is actually in these products,” said Pieter A. Cohen, MD, of the department of medicine at Harvard Medical School, Boston.
“Finding new combinations of drugs [that have] never been tested in humans in over-the-counter brain-boosting supplements is alarming,” said Dr. Cohen.
The study was published online Sept. 23 in Neurology Clinical Practice, a journal of the American Academy of Neurology.
Buyer beware
In a search of the National Institutes of Health Dietary Supplement Label Database and the Natural Medicines Database, Dr. Cohen and colleagues identified 10 supplements labeled as containing omberacetam, aniracetam, phenylpiracetam, or oxiracetam – four analogues of piracetam that are not approved for human use in the United States. Piracetam is also not approved in the United States.
In these 10 products, five unapproved drugs were discovered – omberacetam and aniracetam along with three others (phenibut, vinpocetine and picamilon).
By consuming the recommended serving size of these products, consumers could be exposed to pharmaceutical-level dosages of drugs including a maximum of 40.6 mg omberacetam (typical pharmacologic dose 10 mg), 502 mg of aniracetam (typical pharmacologic dose 200-750 mg), 15.4 mg of phenibut (typical dose 250-500 mg), 4.3 mg of vinpocetine (typical dose 5-40 mg), and 90.1 mg of picamilon (typical dose 50-200 mg), the study team reported.
Several drugs detected in these “smart” pills were not declared on the label, and several declared drugs were not detected in the products. For those products with drug quantities provided on the labels, three-quarters of declared quantities were inaccurate.
Consumers who use these cognitive enhancers could be exposed to amounts of these unapproved drugs that are fourfold greater than pharmaceutical dosages and combinations never tested in humans, the study team says. One product combined three different unapproved drugs and another product contained four different drugs.
“We have previously shown that these products may contain individual foreign drugs, but in our new study we found complex combinations of foreign drugs, up to four different drugs in a single product,” Dr. Cohen said.
The presence of these unapproved drugs in supplements, including at supratherapeutic dosages, suggests “serious risks to consumers and weaknesses in the regulatory framework under which supplements are permitted to be introduced in the U.S.,” Dr. Cohen and colleagues wrote.
“We should counsel our patients to avoid over-the-counter ‘smart pills’ until we can be assured as to the safety and efficacy of these products,” said Dr. Cohen.
Concerning findings
Glen R. Finney, MD, director of the Geisinger Memory and Cognition Program at the Neuroscience Institute, Geisinger Health System, Wilkes-Barre, Penn., said in an interview that two findings are very concerning: the lack of listed ingredients and especially the presence of unlisted drugs at active levels. “What if a person has a sensitivity or allergy to one of the unlisted drugs? This is a safety issue and a consumer issue,” Dr. Finney said.
Despite being widely promoted on television, “over-the-counter supplements are not regulated, so there is no guarantee that they contain what they claim, and there is very little evidence that they help memory and thinking even when they do have the ingredients they claim in the supplement,” said Dr. Finney,
“The best way to stay safe and help memory and thinking is to speak with your health providers about proven treatments that have good safety regulation, so you know what you’re getting, and what you’re getting from it,” Dr. Finney advised.
The study had no targeted funding. Dr. Cohen has collaborated in research with NSF International, received compensation from UptoDate, and received research support from Consumers Union and PEW Charitable Trusts. Dr. Finney has no relevant disclosures.
A version of this article originally appeared on Medscape.com.
, new research shows.
“Americans spend more than $600 million on over-the-counter smart pills every year, but we know very little about what is actually in these products,” said Pieter A. Cohen, MD, of the department of medicine at Harvard Medical School, Boston.
“Finding new combinations of drugs [that have] never been tested in humans in over-the-counter brain-boosting supplements is alarming,” said Dr. Cohen.
The study was published online Sept. 23 in Neurology Clinical Practice, a journal of the American Academy of Neurology.
Buyer beware
In a search of the National Institutes of Health Dietary Supplement Label Database and the Natural Medicines Database, Dr. Cohen and colleagues identified 10 supplements labeled as containing omberacetam, aniracetam, phenylpiracetam, or oxiracetam – four analogues of piracetam that are not approved for human use in the United States. Piracetam is also not approved in the United States.
In these 10 products, five unapproved drugs were discovered – omberacetam and aniracetam along with three others (phenibut, vinpocetine and picamilon).
By consuming the recommended serving size of these products, consumers could be exposed to pharmaceutical-level dosages of drugs including a maximum of 40.6 mg omberacetam (typical pharmacologic dose 10 mg), 502 mg of aniracetam (typical pharmacologic dose 200-750 mg), 15.4 mg of phenibut (typical dose 250-500 mg), 4.3 mg of vinpocetine (typical dose 5-40 mg), and 90.1 mg of picamilon (typical dose 50-200 mg), the study team reported.
Several drugs detected in these “smart” pills were not declared on the label, and several declared drugs were not detected in the products. For those products with drug quantities provided on the labels, three-quarters of declared quantities were inaccurate.
Consumers who use these cognitive enhancers could be exposed to amounts of these unapproved drugs that are fourfold greater than pharmaceutical dosages and combinations never tested in humans, the study team says. One product combined three different unapproved drugs and another product contained four different drugs.
“We have previously shown that these products may contain individual foreign drugs, but in our new study we found complex combinations of foreign drugs, up to four different drugs in a single product,” Dr. Cohen said.
The presence of these unapproved drugs in supplements, including at supratherapeutic dosages, suggests “serious risks to consumers and weaknesses in the regulatory framework under which supplements are permitted to be introduced in the U.S.,” Dr. Cohen and colleagues wrote.
“We should counsel our patients to avoid over-the-counter ‘smart pills’ until we can be assured as to the safety and efficacy of these products,” said Dr. Cohen.
Concerning findings
Glen R. Finney, MD, director of the Geisinger Memory and Cognition Program at the Neuroscience Institute, Geisinger Health System, Wilkes-Barre, Penn., said in an interview that two findings are very concerning: the lack of listed ingredients and especially the presence of unlisted drugs at active levels. “What if a person has a sensitivity or allergy to one of the unlisted drugs? This is a safety issue and a consumer issue,” Dr. Finney said.
Despite being widely promoted on television, “over-the-counter supplements are not regulated, so there is no guarantee that they contain what they claim, and there is very little evidence that they help memory and thinking even when they do have the ingredients they claim in the supplement,” said Dr. Finney,
“The best way to stay safe and help memory and thinking is to speak with your health providers about proven treatments that have good safety regulation, so you know what you’re getting, and what you’re getting from it,” Dr. Finney advised.
The study had no targeted funding. Dr. Cohen has collaborated in research with NSF International, received compensation from UptoDate, and received research support from Consumers Union and PEW Charitable Trusts. Dr. Finney has no relevant disclosures.
A version of this article originally appeared on Medscape.com.
FROM NEUROLOGY CLINICAL PRACTICE
In MS, serious adverse effects are more common in rituximab versus ocrelizumab
, a new postmarketing analysis finds, and AE-related deaths were not unusual. Serious AEs, and those linked to death, were more common in the rituximab group, although the reported infection rate was higher in the ocrelizumab group.
The analysis, published Aug. 21 in the Multiple Sclerosis Journal, highlights the importance of monitoring patients for infections and encouraging them to do the same, the authors said.
“This report points out the impact of treatments in terms of unrecognized or underappreciated complications,” said Mark Gudesblatt, MD, medical director of the Comprehensive MS Care Center at South Shore Neurologic Associates in Patchogue, N.Y., who reviewed the study findings. “These medications have a significant downside.”
Lead author Natalia Gonzalez Caldito, MD, of the University of Texas Southwestern Medical Center, Dallas, and colleagues analyzed AEs for the drugs in the Food and Drug Administration’s Adverse Event Reporting System. They only included cases in which the drugs were solely used to treat MS and were indicated as the cause of the AEs.
Rituximab (Rituxan) and ocrelizumab (Ocrevus) are both monoclonal antibodies. Rituximab is not FDA approved for MS but is used off label; ocrelizumab is approved for the relapsing forms of MS and primary progressive MS.
The researchers found 623 AE reports and 1,466 total AEs for rituximab and 7,948 and 23,613, respectively, for ocrelizumab. The average ages for the groups were 48.76 versus 43.89, respectively, (P < .001), and 71% in each group were women.
Among total AEs, serious AEs were more common in the rituximab group versus the ocrelizumab group (64.8% vs. 56.3%, respectively, P < .001). Adverse events that caused death were also more common in the rituximab group versus the ocrelizumab group (5.75% vs. 2.11%, P < .001).
Infections and infestations were more common in the ocrelizumab group than the rituximab group (21.93% vs. 11.05%, respectively, P < .001). However, certain AEs were more common in the rituximab group than the ocrelizumab group: Those in the blood and lymphatic system category (2.86% vs. 0.91%, respectively, P < .001), and those in the neoplasms category (4.02% vs. 1.28%, P < .001, respectively).
Researchers found a highly strong association between rituximab and a rare side effects – ear pruritus (itching, 0.8%). They also identified signals for infusion-related reaction (4.82%), throat irritation (4.01%) and throat tightness (1.44%), malignant melanoma (0.8%), breast cancer (1.77%) and neutropenia (2.57%).
Among the ocrelizumab AEs, researchers found the strongest association with oral herpes (2.21%), and they found other signals for herpes zoster (2.89%), urinary tract infection (10.52%), nasopharyngitis (9.79%), infusion-related reaction (4.76%), throat irritation (3.08%), and notably MS relapses (4.1%).
“Additional pharmacovigilance studies are needed to explore and further characterize these findings,” the researchers wrote. “Furthermore, these observations suggest that the AE profile of other second-generation anti-CD20 [monoclonal antibodies] may also differ from those of rituximab and ocrelizumab.”
Dr. Gudesblatt praised the analysis and said the findings make sense. “Use of B-cell–depleting agents lead to accumulative immune deficiency in routine care, which leads to higher rates of infection,” he said. He added that, “in the clinical trials for ocrelizumab, patients with IgG and IgM deficiency were excluded, but there is no advisement to exclude such patients in real care. The rates of infection in those patients with MS who have preexisting immune deficiencies and who are treated with these agents are unknown.”
The prospect of AEs is especially worrisome, he said, since “this information is only short term. Who knows what effect the prolonged use of unopposed B-cell depletion will have on infections in the long run?”
Neurologist Mitchell Wallin, MD, MPH, of George Washington University, Washington, and the University of Maryland, Baltimore County, said in an interview that the analysis is rigorous and especially useful because it includes a wider array of subjects – including those who are older and sicker – than took part in earlier clinical trials. “It’s really important to look at this real-world evidence,” he said, “and basically put this in the back of your head when you follow up with your patients.”
No study funding was reported. The corresponding author reported various disclosures. Dr. Gudesblatt and Dr. Wallin reported no disclosures.
SOURCE: Gonzalez Caldito N et al. Mult Scler J. 2020 Aug 21. doi: 10.1177/1352458520949986.
, a new postmarketing analysis finds, and AE-related deaths were not unusual. Serious AEs, and those linked to death, were more common in the rituximab group, although the reported infection rate was higher in the ocrelizumab group.
The analysis, published Aug. 21 in the Multiple Sclerosis Journal, highlights the importance of monitoring patients for infections and encouraging them to do the same, the authors said.
“This report points out the impact of treatments in terms of unrecognized or underappreciated complications,” said Mark Gudesblatt, MD, medical director of the Comprehensive MS Care Center at South Shore Neurologic Associates in Patchogue, N.Y., who reviewed the study findings. “These medications have a significant downside.”
Lead author Natalia Gonzalez Caldito, MD, of the University of Texas Southwestern Medical Center, Dallas, and colleagues analyzed AEs for the drugs in the Food and Drug Administration’s Adverse Event Reporting System. They only included cases in which the drugs were solely used to treat MS and were indicated as the cause of the AEs.
Rituximab (Rituxan) and ocrelizumab (Ocrevus) are both monoclonal antibodies. Rituximab is not FDA approved for MS but is used off label; ocrelizumab is approved for the relapsing forms of MS and primary progressive MS.
The researchers found 623 AE reports and 1,466 total AEs for rituximab and 7,948 and 23,613, respectively, for ocrelizumab. The average ages for the groups were 48.76 versus 43.89, respectively, (P < .001), and 71% in each group were women.
Among total AEs, serious AEs were more common in the rituximab group versus the ocrelizumab group (64.8% vs. 56.3%, respectively, P < .001). Adverse events that caused death were also more common in the rituximab group versus the ocrelizumab group (5.75% vs. 2.11%, P < .001).
Infections and infestations were more common in the ocrelizumab group than the rituximab group (21.93% vs. 11.05%, respectively, P < .001). However, certain AEs were more common in the rituximab group than the ocrelizumab group: Those in the blood and lymphatic system category (2.86% vs. 0.91%, respectively, P < .001), and those in the neoplasms category (4.02% vs. 1.28%, P < .001, respectively).
Researchers found a highly strong association between rituximab and a rare side effects – ear pruritus (itching, 0.8%). They also identified signals for infusion-related reaction (4.82%), throat irritation (4.01%) and throat tightness (1.44%), malignant melanoma (0.8%), breast cancer (1.77%) and neutropenia (2.57%).
Among the ocrelizumab AEs, researchers found the strongest association with oral herpes (2.21%), and they found other signals for herpes zoster (2.89%), urinary tract infection (10.52%), nasopharyngitis (9.79%), infusion-related reaction (4.76%), throat irritation (3.08%), and notably MS relapses (4.1%).
“Additional pharmacovigilance studies are needed to explore and further characterize these findings,” the researchers wrote. “Furthermore, these observations suggest that the AE profile of other second-generation anti-CD20 [monoclonal antibodies] may also differ from those of rituximab and ocrelizumab.”
Dr. Gudesblatt praised the analysis and said the findings make sense. “Use of B-cell–depleting agents lead to accumulative immune deficiency in routine care, which leads to higher rates of infection,” he said. He added that, “in the clinical trials for ocrelizumab, patients with IgG and IgM deficiency were excluded, but there is no advisement to exclude such patients in real care. The rates of infection in those patients with MS who have preexisting immune deficiencies and who are treated with these agents are unknown.”
The prospect of AEs is especially worrisome, he said, since “this information is only short term. Who knows what effect the prolonged use of unopposed B-cell depletion will have on infections in the long run?”
Neurologist Mitchell Wallin, MD, MPH, of George Washington University, Washington, and the University of Maryland, Baltimore County, said in an interview that the analysis is rigorous and especially useful because it includes a wider array of subjects – including those who are older and sicker – than took part in earlier clinical trials. “It’s really important to look at this real-world evidence,” he said, “and basically put this in the back of your head when you follow up with your patients.”
No study funding was reported. The corresponding author reported various disclosures. Dr. Gudesblatt and Dr. Wallin reported no disclosures.
SOURCE: Gonzalez Caldito N et al. Mult Scler J. 2020 Aug 21. doi: 10.1177/1352458520949986.
, a new postmarketing analysis finds, and AE-related deaths were not unusual. Serious AEs, and those linked to death, were more common in the rituximab group, although the reported infection rate was higher in the ocrelizumab group.
The analysis, published Aug. 21 in the Multiple Sclerosis Journal, highlights the importance of monitoring patients for infections and encouraging them to do the same, the authors said.
“This report points out the impact of treatments in terms of unrecognized or underappreciated complications,” said Mark Gudesblatt, MD, medical director of the Comprehensive MS Care Center at South Shore Neurologic Associates in Patchogue, N.Y., who reviewed the study findings. “These medications have a significant downside.”
Lead author Natalia Gonzalez Caldito, MD, of the University of Texas Southwestern Medical Center, Dallas, and colleagues analyzed AEs for the drugs in the Food and Drug Administration’s Adverse Event Reporting System. They only included cases in which the drugs were solely used to treat MS and were indicated as the cause of the AEs.
Rituximab (Rituxan) and ocrelizumab (Ocrevus) are both monoclonal antibodies. Rituximab is not FDA approved for MS but is used off label; ocrelizumab is approved for the relapsing forms of MS and primary progressive MS.
The researchers found 623 AE reports and 1,466 total AEs for rituximab and 7,948 and 23,613, respectively, for ocrelizumab. The average ages for the groups were 48.76 versus 43.89, respectively, (P < .001), and 71% in each group were women.
Among total AEs, serious AEs were more common in the rituximab group versus the ocrelizumab group (64.8% vs. 56.3%, respectively, P < .001). Adverse events that caused death were also more common in the rituximab group versus the ocrelizumab group (5.75% vs. 2.11%, P < .001).
Infections and infestations were more common in the ocrelizumab group than the rituximab group (21.93% vs. 11.05%, respectively, P < .001). However, certain AEs were more common in the rituximab group than the ocrelizumab group: Those in the blood and lymphatic system category (2.86% vs. 0.91%, respectively, P < .001), and those in the neoplasms category (4.02% vs. 1.28%, P < .001, respectively).
Researchers found a highly strong association between rituximab and a rare side effects – ear pruritus (itching, 0.8%). They also identified signals for infusion-related reaction (4.82%), throat irritation (4.01%) and throat tightness (1.44%), malignant melanoma (0.8%), breast cancer (1.77%) and neutropenia (2.57%).
Among the ocrelizumab AEs, researchers found the strongest association with oral herpes (2.21%), and they found other signals for herpes zoster (2.89%), urinary tract infection (10.52%), nasopharyngitis (9.79%), infusion-related reaction (4.76%), throat irritation (3.08%), and notably MS relapses (4.1%).
“Additional pharmacovigilance studies are needed to explore and further characterize these findings,” the researchers wrote. “Furthermore, these observations suggest that the AE profile of other second-generation anti-CD20 [monoclonal antibodies] may also differ from those of rituximab and ocrelizumab.”
Dr. Gudesblatt praised the analysis and said the findings make sense. “Use of B-cell–depleting agents lead to accumulative immune deficiency in routine care, which leads to higher rates of infection,” he said. He added that, “in the clinical trials for ocrelizumab, patients with IgG and IgM deficiency were excluded, but there is no advisement to exclude such patients in real care. The rates of infection in those patients with MS who have preexisting immune deficiencies and who are treated with these agents are unknown.”
The prospect of AEs is especially worrisome, he said, since “this information is only short term. Who knows what effect the prolonged use of unopposed B-cell depletion will have on infections in the long run?”
Neurologist Mitchell Wallin, MD, MPH, of George Washington University, Washington, and the University of Maryland, Baltimore County, said in an interview that the analysis is rigorous and especially useful because it includes a wider array of subjects – including those who are older and sicker – than took part in earlier clinical trials. “It’s really important to look at this real-world evidence,” he said, “and basically put this in the back of your head when you follow up with your patients.”
No study funding was reported. The corresponding author reported various disclosures. Dr. Gudesblatt and Dr. Wallin reported no disclosures.
SOURCE: Gonzalez Caldito N et al. Mult Scler J. 2020 Aug 21. doi: 10.1177/1352458520949986.
FROM MULTIPLE SCLEROSIS JOURNAL

