User login
Targeted corticosteroids cut GVHD incidence
Short-term low-dose corticosteroid prophylaxis reduces the incidence of graft-vs.-host disease in patients who undergo allogeneic haploidentical stem-cell transplantation to treat hematologic neoplasms, according to a report published online April 18 in the Journal of Clinical Oncology.
The key to selecting patients most likely to benefit from the corticosteroid therapy is to identify those at high risk for graft-vs.-host disease (GVHD) using two biomarkers: high levels of CD56bright natural killer cells in allogeneic grafts or high CD4:CD8 ratios in bone marrow grafts, according to Dr. Ying-Jun Chang of Peking University People’s Hospital, Beijing, and associates.
The investigators performed an open-label trial involving 228 patients aged 15-60 years treated at a single medical center during an 18-month period for acute myeloid leukemia, acute lymphoblastic leukemia, chronic myeloid leukemia, myelodysplastic syndrome, or other hematologic neoplasms. Using the two biomarkers, the patients were categorized as either high or low risk for developing GVHD. They were randomly assigned to three study groups: 72 high-risk patients who received short-term low-dose corticosteroids, 73 high-risk patients who received usual care, and 83 low-risk patients who received usual care.
The cumulative 100-day incidence of acute grade-II to grade-IV GVHD was significantly lower in the high-risk patients who received prophylaxis (21%) than in the high-risk patients who did not receive prophylaxis (48%). In fact, corticosteroids decreased the rate of GVHD so that it was comparable with that in the low-risk patients (26%), Dr. Chang and associates said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.63l.8817).
Moreover, in the high-risk patients the median interval until GVHD developed was 25 days for those who took corticosteroids, compared with only 15 days for those who did not. Median times to myeloid recovery and platelet recovery were significantly shorter for high-risk patients who received corticosteroids than for either of the other study groups. However, 3-year overall survival and leukemia-free survival were comparable among the three study groups.
The short-term low-dose regimen of corticosteroids did not raise the rate of adverse events, including infection, which suggests that it is preferable to standard corticosteroid regimens in this patient population. The incidences of cytomegalovirus or Epstein-Barr virus reactivation, post-transplantation lymphoproliferative disorder, hemorrhagic cystitis, bacteremia, and invasive fungal infections were comparable among the three study groups. Of note, the incidences of osteonecrosis of the femoral head and secondary hypertension were significantly lower among high-risk patients who received corticosteroid prophylaxis than among those who did not.
“These results provide the first test, to our knowledge, of a novel risk-stratification-directed prophylaxis strategy that effectively prevented acute GVHD among patients who were at high risk for GVHD, without unnecessarily exposing patients who were at low risk to excessive toxicity from additional immunosuppressive agents,” Dr. Chang and associates said.
Despite the encouraging results of Chang et al, it would be premature to routinely use corticosteroid prophylaxis to prevent GVHD until further studies are completed.
This study wasn’t sufficiently powered to determine whether corticosteroids reduced treatment-specific mortality or improved overall survival. Future studies must examine these end points, as well as relapse rates, before this method of prophylaxis is widely adopted.
Dr. Edwin P. Alyea is at Dana-Farber Cancer Institute, Boston. He reported having no relevant financial disclosures. Dr. Alyea made these remarks in an editorial accompanying Dr. Chang’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.66.0902).
Despite the encouraging results of Chang et al, it would be premature to routinely use corticosteroid prophylaxis to prevent GVHD until further studies are completed.
This study wasn’t sufficiently powered to determine whether corticosteroids reduced treatment-specific mortality or improved overall survival. Future studies must examine these end points, as well as relapse rates, before this method of prophylaxis is widely adopted.
Dr. Edwin P. Alyea is at Dana-Farber Cancer Institute, Boston. He reported having no relevant financial disclosures. Dr. Alyea made these remarks in an editorial accompanying Dr. Chang’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.66.0902).
Despite the encouraging results of Chang et al, it would be premature to routinely use corticosteroid prophylaxis to prevent GVHD until further studies are completed.
This study wasn’t sufficiently powered to determine whether corticosteroids reduced treatment-specific mortality or improved overall survival. Future studies must examine these end points, as well as relapse rates, before this method of prophylaxis is widely adopted.
Dr. Edwin P. Alyea is at Dana-Farber Cancer Institute, Boston. He reported having no relevant financial disclosures. Dr. Alyea made these remarks in an editorial accompanying Dr. Chang’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.66.0902).
Short-term low-dose corticosteroid prophylaxis reduces the incidence of graft-vs.-host disease in patients who undergo allogeneic haploidentical stem-cell transplantation to treat hematologic neoplasms, according to a report published online April 18 in the Journal of Clinical Oncology.
The key to selecting patients most likely to benefit from the corticosteroid therapy is to identify those at high risk for graft-vs.-host disease (GVHD) using two biomarkers: high levels of CD56bright natural killer cells in allogeneic grafts or high CD4:CD8 ratios in bone marrow grafts, according to Dr. Ying-Jun Chang of Peking University People’s Hospital, Beijing, and associates.
The investigators performed an open-label trial involving 228 patients aged 15-60 years treated at a single medical center during an 18-month period for acute myeloid leukemia, acute lymphoblastic leukemia, chronic myeloid leukemia, myelodysplastic syndrome, or other hematologic neoplasms. Using the two biomarkers, the patients were categorized as either high or low risk for developing GVHD. They were randomly assigned to three study groups: 72 high-risk patients who received short-term low-dose corticosteroids, 73 high-risk patients who received usual care, and 83 low-risk patients who received usual care.
The cumulative 100-day incidence of acute grade-II to grade-IV GVHD was significantly lower in the high-risk patients who received prophylaxis (21%) than in the high-risk patients who did not receive prophylaxis (48%). In fact, corticosteroids decreased the rate of GVHD so that it was comparable with that in the low-risk patients (26%), Dr. Chang and associates said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.63l.8817).
Moreover, in the high-risk patients the median interval until GVHD developed was 25 days for those who took corticosteroids, compared with only 15 days for those who did not. Median times to myeloid recovery and platelet recovery were significantly shorter for high-risk patients who received corticosteroids than for either of the other study groups. However, 3-year overall survival and leukemia-free survival were comparable among the three study groups.
The short-term low-dose regimen of corticosteroids did not raise the rate of adverse events, including infection, which suggests that it is preferable to standard corticosteroid regimens in this patient population. The incidences of cytomegalovirus or Epstein-Barr virus reactivation, post-transplantation lymphoproliferative disorder, hemorrhagic cystitis, bacteremia, and invasive fungal infections were comparable among the three study groups. Of note, the incidences of osteonecrosis of the femoral head and secondary hypertension were significantly lower among high-risk patients who received corticosteroid prophylaxis than among those who did not.
“These results provide the first test, to our knowledge, of a novel risk-stratification-directed prophylaxis strategy that effectively prevented acute GVHD among patients who were at high risk for GVHD, without unnecessarily exposing patients who were at low risk to excessive toxicity from additional immunosuppressive agents,” Dr. Chang and associates said.
Short-term low-dose corticosteroid prophylaxis reduces the incidence of graft-vs.-host disease in patients who undergo allogeneic haploidentical stem-cell transplantation to treat hematologic neoplasms, according to a report published online April 18 in the Journal of Clinical Oncology.
The key to selecting patients most likely to benefit from the corticosteroid therapy is to identify those at high risk for graft-vs.-host disease (GVHD) using two biomarkers: high levels of CD56bright natural killer cells in allogeneic grafts or high CD4:CD8 ratios in bone marrow grafts, according to Dr. Ying-Jun Chang of Peking University People’s Hospital, Beijing, and associates.
The investigators performed an open-label trial involving 228 patients aged 15-60 years treated at a single medical center during an 18-month period for acute myeloid leukemia, acute lymphoblastic leukemia, chronic myeloid leukemia, myelodysplastic syndrome, or other hematologic neoplasms. Using the two biomarkers, the patients were categorized as either high or low risk for developing GVHD. They were randomly assigned to three study groups: 72 high-risk patients who received short-term low-dose corticosteroids, 73 high-risk patients who received usual care, and 83 low-risk patients who received usual care.
The cumulative 100-day incidence of acute grade-II to grade-IV GVHD was significantly lower in the high-risk patients who received prophylaxis (21%) than in the high-risk patients who did not receive prophylaxis (48%). In fact, corticosteroids decreased the rate of GVHD so that it was comparable with that in the low-risk patients (26%), Dr. Chang and associates said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.63l.8817).
Moreover, in the high-risk patients the median interval until GVHD developed was 25 days for those who took corticosteroids, compared with only 15 days for those who did not. Median times to myeloid recovery and platelet recovery were significantly shorter for high-risk patients who received corticosteroids than for either of the other study groups. However, 3-year overall survival and leukemia-free survival were comparable among the three study groups.
The short-term low-dose regimen of corticosteroids did not raise the rate of adverse events, including infection, which suggests that it is preferable to standard corticosteroid regimens in this patient population. The incidences of cytomegalovirus or Epstein-Barr virus reactivation, post-transplantation lymphoproliferative disorder, hemorrhagic cystitis, bacteremia, and invasive fungal infections were comparable among the three study groups. Of note, the incidences of osteonecrosis of the femoral head and secondary hypertension were significantly lower among high-risk patients who received corticosteroid prophylaxis than among those who did not.
“These results provide the first test, to our knowledge, of a novel risk-stratification-directed prophylaxis strategy that effectively prevented acute GVHD among patients who were at high risk for GVHD, without unnecessarily exposing patients who were at low risk to excessive toxicity from additional immunosuppressive agents,” Dr. Chang and associates said.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Short-term low-dose corticosteroid prophylaxis reduces the incidence of the GVHD in patients who undergo haploidentical stem-cell transplantation to treat hematologic neoplasms.
Major finding: The 100-day incidence of acute GVHD was significantly lower in the high-risk patients who received corticosteroid prophylaxis (21%) than in the high-risk patients who did not (48%).
Data source: An open-label randomized controlled trial involving 228 Chinese patients who underwent stem-cell transplantation.
Disclosures: This study was supported by the Beijing Committee of Science and Technology, the National High Technology Research and Development Program of China, and the National Natural Science Foundation of China. Dr. Chang and associates reported having no relevant financial disclosures.
Donor EBV status affects recipient graft-vs-host disease risk
In allogeneic hematopoietic stem-cell transplantation, the donor’s status regarding Epstein-Barr virus affects the recipient’s risk of developing graft-vs-host disease – a “completely new and striking” finding, according to a report published online April 18 in the Journal of Clinical Oncology.
Approximately 80% of the general population has been infected with EBV and carries persistent virus in memory B cells. When viral material is transmitted to stem-cell recipients, it is known to cause posttransplantation lymphoproliferative disorder. Until now, however, no data were available to examine EBV serology’s effect on other posttransplantation outcomes, said Dr. Jan Styczynski of the department of pediatric hematology and oncology at Nicolaus Copernicus University, Bydgoszcz, Poland, and his associates.
They analyzed information in the European Society of Blood and Marrow Transplantation database for 11,364 patients with acute lymphoblastic leukemia or acute myeloblastic leukemia who underwent stem-cell transplantation between 1997 and 2012 and who were followed for approximately 5 years. Most of the donors (82%) were seropositive for EBV. Acute graft-vs-host disease (GVHD) developed in 32% and chronic GVHD developed in 40% of these stem cell–transplant recipients.
The incidence of chronic GVHD was significantly higher when the donor was EBV-seropositive (41%) than when the donor was EBV-seronegative (31%). Similarly, the incidence of acute GVHD was significantly higher when the donor was EBV-seropositive (32% vs 30%), but the magnitude of the difference between the two groups was smaller. The risk for GVHD increased even though patients receiving transplants from EBV-seropositive donors underwent more intensive GVHD prophylaxis than did those who had seronegative donors, the investigators said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.64.2405).
In contrast, the transplant recipients’ EBV status did not affect their risk of developing GVHD.
“Despite the effect of donor EBV serostatus on GVHD, we did not observe a corresponding GVHD-related death rate, and as a result, there was no effect on overall survival, relapse-free survival, relapse incidence, and nonrelapse mortality. However, it should be kept in mind that many other pre- and posttransplantation factors play a role in contributing to final transplantation outcomes,” Dr. Styczynski and his associates noted.
The current recommendation to monitor transplantation recipients for EBV and to give them “preemptive” rituximab to stave off the development of posttransplantation lymphoproliferative disorder might prove useful in also preventing GVHD, they added.
The findings of Dr. Styczynski and his associates raise the possibility that we may be able to prevent or treat GVHD in transplant recipients by controlling EBV infection.
Selecting only EBV-negative donors would be one way to accomplish this, but that would be impractical given the high seroprevalence of EBV in the general population. Depleting memory B cells, the reservoir of EBV infection, using monoclonal antibodies may prove helpful, and these agents might provide additional therapeutic effects. And novel antivirals such as retroviral integrase inhibitors may be more specific at targeting EBV than acyclovir and related agents, which have limited activity against latently infected B cells. These novel drugs, however, are not without risks and adverse effects.
A promising alternative might be to boost immunity to EBV using vaccination or adoptive transfer of ex vivo expanded EBV-specific cytotoxic T cells.
Dr. Katayoun Rezvani and Dr. Richard E. Champlin are with the University of Texas MD Andersen Cancer Center, Houston. Their financial disclosures are available at www.jco.org. They made these remarks in an editorial accompanying Dr. Styczynski’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2016.66.6099).
The findings of Dr. Styczynski and his associates raise the possibility that we may be able to prevent or treat GVHD in transplant recipients by controlling EBV infection.
Selecting only EBV-negative donors would be one way to accomplish this, but that would be impractical given the high seroprevalence of EBV in the general population. Depleting memory B cells, the reservoir of EBV infection, using monoclonal antibodies may prove helpful, and these agents might provide additional therapeutic effects. And novel antivirals such as retroviral integrase inhibitors may be more specific at targeting EBV than acyclovir and related agents, which have limited activity against latently infected B cells. These novel drugs, however, are not without risks and adverse effects.
A promising alternative might be to boost immunity to EBV using vaccination or adoptive transfer of ex vivo expanded EBV-specific cytotoxic T cells.
Dr. Katayoun Rezvani and Dr. Richard E. Champlin are with the University of Texas MD Andersen Cancer Center, Houston. Their financial disclosures are available at www.jco.org. They made these remarks in an editorial accompanying Dr. Styczynski’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2016.66.6099).
The findings of Dr. Styczynski and his associates raise the possibility that we may be able to prevent or treat GVHD in transplant recipients by controlling EBV infection.
Selecting only EBV-negative donors would be one way to accomplish this, but that would be impractical given the high seroprevalence of EBV in the general population. Depleting memory B cells, the reservoir of EBV infection, using monoclonal antibodies may prove helpful, and these agents might provide additional therapeutic effects. And novel antivirals such as retroviral integrase inhibitors may be more specific at targeting EBV than acyclovir and related agents, which have limited activity against latently infected B cells. These novel drugs, however, are not without risks and adverse effects.
A promising alternative might be to boost immunity to EBV using vaccination or adoptive transfer of ex vivo expanded EBV-specific cytotoxic T cells.
Dr. Katayoun Rezvani and Dr. Richard E. Champlin are with the University of Texas MD Andersen Cancer Center, Houston. Their financial disclosures are available at www.jco.org. They made these remarks in an editorial accompanying Dr. Styczynski’s report (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2016.66.6099).
In allogeneic hematopoietic stem-cell transplantation, the donor’s status regarding Epstein-Barr virus affects the recipient’s risk of developing graft-vs-host disease – a “completely new and striking” finding, according to a report published online April 18 in the Journal of Clinical Oncology.
Approximately 80% of the general population has been infected with EBV and carries persistent virus in memory B cells. When viral material is transmitted to stem-cell recipients, it is known to cause posttransplantation lymphoproliferative disorder. Until now, however, no data were available to examine EBV serology’s effect on other posttransplantation outcomes, said Dr. Jan Styczynski of the department of pediatric hematology and oncology at Nicolaus Copernicus University, Bydgoszcz, Poland, and his associates.
They analyzed information in the European Society of Blood and Marrow Transplantation database for 11,364 patients with acute lymphoblastic leukemia or acute myeloblastic leukemia who underwent stem-cell transplantation between 1997 and 2012 and who were followed for approximately 5 years. Most of the donors (82%) were seropositive for EBV. Acute graft-vs-host disease (GVHD) developed in 32% and chronic GVHD developed in 40% of these stem cell–transplant recipients.
The incidence of chronic GVHD was significantly higher when the donor was EBV-seropositive (41%) than when the donor was EBV-seronegative (31%). Similarly, the incidence of acute GVHD was significantly higher when the donor was EBV-seropositive (32% vs 30%), but the magnitude of the difference between the two groups was smaller. The risk for GVHD increased even though patients receiving transplants from EBV-seropositive donors underwent more intensive GVHD prophylaxis than did those who had seronegative donors, the investigators said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.64.2405).
In contrast, the transplant recipients’ EBV status did not affect their risk of developing GVHD.
“Despite the effect of donor EBV serostatus on GVHD, we did not observe a corresponding GVHD-related death rate, and as a result, there was no effect on overall survival, relapse-free survival, relapse incidence, and nonrelapse mortality. However, it should be kept in mind that many other pre- and posttransplantation factors play a role in contributing to final transplantation outcomes,” Dr. Styczynski and his associates noted.
The current recommendation to monitor transplantation recipients for EBV and to give them “preemptive” rituximab to stave off the development of posttransplantation lymphoproliferative disorder might prove useful in also preventing GVHD, they added.
In allogeneic hematopoietic stem-cell transplantation, the donor’s status regarding Epstein-Barr virus affects the recipient’s risk of developing graft-vs-host disease – a “completely new and striking” finding, according to a report published online April 18 in the Journal of Clinical Oncology.
Approximately 80% of the general population has been infected with EBV and carries persistent virus in memory B cells. When viral material is transmitted to stem-cell recipients, it is known to cause posttransplantation lymphoproliferative disorder. Until now, however, no data were available to examine EBV serology’s effect on other posttransplantation outcomes, said Dr. Jan Styczynski of the department of pediatric hematology and oncology at Nicolaus Copernicus University, Bydgoszcz, Poland, and his associates.
They analyzed information in the European Society of Blood and Marrow Transplantation database for 11,364 patients with acute lymphoblastic leukemia or acute myeloblastic leukemia who underwent stem-cell transplantation between 1997 and 2012 and who were followed for approximately 5 years. Most of the donors (82%) were seropositive for EBV. Acute graft-vs-host disease (GVHD) developed in 32% and chronic GVHD developed in 40% of these stem cell–transplant recipients.
The incidence of chronic GVHD was significantly higher when the donor was EBV-seropositive (41%) than when the donor was EBV-seronegative (31%). Similarly, the incidence of acute GVHD was significantly higher when the donor was EBV-seropositive (32% vs 30%), but the magnitude of the difference between the two groups was smaller. The risk for GVHD increased even though patients receiving transplants from EBV-seropositive donors underwent more intensive GVHD prophylaxis than did those who had seronegative donors, the investigators said (J Clin Oncol. 2016 Apr 18. doi: 10.1200/JCO.2015.64.2405).
In contrast, the transplant recipients’ EBV status did not affect their risk of developing GVHD.
“Despite the effect of donor EBV serostatus on GVHD, we did not observe a corresponding GVHD-related death rate, and as a result, there was no effect on overall survival, relapse-free survival, relapse incidence, and nonrelapse mortality. However, it should be kept in mind that many other pre- and posttransplantation factors play a role in contributing to final transplantation outcomes,” Dr. Styczynski and his associates noted.
The current recommendation to monitor transplantation recipients for EBV and to give them “preemptive” rituximab to stave off the development of posttransplantation lymphoproliferative disorder might prove useful in also preventing GVHD, they added.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: In allogeneic hematopoietic stem-cell transplantation, the donor’s EBV status affects the recipient’s risk of developing GVHD.
Major finding: Chronic GVHD was significantly more likely to develop when the donor was EBV-seropositive (41%) than EBV-seronegative (31%).
Data source: A retrospective analysis of data regarding 11,364 European patients with acute leukemia who underwent stem-cell transplantation and were followed for 5 years.
Disclosures: No study sponsor was identified. Dr. Styczynski reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Rigosertib falls short for high-risk myelodysplastic syndromes after failure on azacitidine or decitabine
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
THE LANCET ONCOLOGY
Key clinical point: Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
Major finding: Median overall survival was 8.2 months (95% CI, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group.
Data source: An open-label, randomized controlled trial involving 299 patients at 74 medical centers.
Disclosures: The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society..
Rigosertib falls short for high-risk myelodysplastic syndromes after failure on azacitidine or decitabine
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
THE LANCET ONCOLOGY
Key clinical point: Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
Major finding: Median overall survival was 8.2 months (95% CI, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group.
Data source: An open-label, randomized controlled trial involving 299 patients at 74 medical centers.
Disclosures: The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society..
In myelodysplastic syndrome, improved tool for predicting death after HCT
A new risk-stratification tool goes one better than the standard tools used to predict survival in those undergoing allogeneic hematopoietic cell transplantation (allo HCT) for myelodysplastic syndrome, based on a study published online April 4 in the Journal of Clinical Oncology.
The concordance index for the new risk-stratification tool was modestly better at 0.575, compared with 0.538 for the standard International Prognostic Scoring System (IPSS) and 0.554 for the revised IPSS (IPSS-R), according to Dr. Brian C. Shaffer of Memorial Sloan Kettering Cancer Center, New York, and his colleagues who participate in the Center for International Blood and Marrow Transplant Research (CIBMTR) network.
“The proposed system generally agrees with the IPSS-R in the very high–risk subcategory; however, a significant portion of patients in high- and very high–risk IPSS-R groups were represented in the low- and intermediate-risk proposed scoring subcategories. The 3-year survival in patients classified as high risk with the IPSS-R was 75%; it was 57% in those classified as low or intermediate risk with the proposed system,” the researchers wrote.
Further, the “scoring system uses readily available clinical data and can be calculated quickly, facilitating patient consultation with respect to allo HCT, and may also be used to identify high-risk populations where interventions such as post–allo HCT maintenance therapies may be of benefit,” they wrote (J Clin Oncol. 2016 April 4. doi: 10.1200/JCO.2015.65.0515).
The data were obtained from the CIBMTR, a combined research program of the Medical College of Wisconsin and the National Marrow Donor Program. The CIBMTR comprises a voluntary network of more than 450 transplantation centers worldwide that contribute data on consecutive allo and autologous HCTs to a centralized statistical center.
The researchers applied the prognostic tool to 2,133 patients with MDS undergoing HLA-matched (n = 1,728) or -mismatched (n = 405) allo HCT. Factors prognostic of mortality were identified in a training subset (n = 1,151) of the HLA-matched cohort. A weighted score using these factors was then assigned to the validation cohort of 577 remaining patients undergoing HLA-matched allo HCT as well as to patients undergoing HLA-mismatched allo HCT. The training data set was used to develop a prognostic scoring system, and the validation data set was used to assess the prognostic ability of the scoring system, the researchers noted.
In the scoring system, 1 point was assigned for the following factors: Blood blasts greater than 3%, platelet levels of 50 × 109/L or less at transplantation, Karnofsky performance status less than 90%, comprehensive cytogenetic risk score of poor or very poor, and age 30-49 years. Two points were assigned for monosomal karyotype and age 50 years or older.
Based on the scoring system, 3-year overall survival after transplantation was 71% in patients with scores of 1 point, 49% with scores of 2-3, 41% with scores of 4-5, and 25% with scores of 6 or more. Increasing score was predictive of increased relapse and treatment-related mortality in the HLA-matched set and of relapse in the HLA-mismatched cohort.
To develop the scoring system, the researchers used a model that weighed patient age; sex; and Karnofsky performance status; disease stage at transplantation; comprehensive cytogenetic risk status; bone marrow and peripheral blood blast percentages; hemoglobin, neutrophil, and platelet counts at diagnosis and pretransplantation; lactate dehydrogenase at transplantation; pretransplantation therapy (hypomethylating agents, chemotherapy, neither, or both); time from diagnosis to transplantation; year of transplantation; conditioning regimen and regimen intensity (myeloablative v reduced intensity); donor–recipient sex match or mismatch; graft-versus-host disease prophylaxis; graft type (bone marrow vs. peripheral blood); presence of secondary myelodysplastic syndrome; and unrelated donor vs. related donor.
There were no significant differences in overall survival at 1, 3, and 5 years or in the 3-year incidences of relapse and treatment-related mortality in the training subset and the validation cohort.
Data on somatic mutations have become relevant in myelodysplastic syndrome prognostication and were missing from this analysis, the researchers wrote. “The next generation of prognostic tools will need to account for this information.”
Dr. Shaffer had no relevant financial disclosures.
On Twitter @maryjodales
A new risk-stratification tool goes one better than the standard tools used to predict survival in those undergoing allogeneic hematopoietic cell transplantation (allo HCT) for myelodysplastic syndrome, based on a study published online April 4 in the Journal of Clinical Oncology.
The concordance index for the new risk-stratification tool was modestly better at 0.575, compared with 0.538 for the standard International Prognostic Scoring System (IPSS) and 0.554 for the revised IPSS (IPSS-R), according to Dr. Brian C. Shaffer of Memorial Sloan Kettering Cancer Center, New York, and his colleagues who participate in the Center for International Blood and Marrow Transplant Research (CIBMTR) network.
“The proposed system generally agrees with the IPSS-R in the very high–risk subcategory; however, a significant portion of patients in high- and very high–risk IPSS-R groups were represented in the low- and intermediate-risk proposed scoring subcategories. The 3-year survival in patients classified as high risk with the IPSS-R was 75%; it was 57% in those classified as low or intermediate risk with the proposed system,” the researchers wrote.
Further, the “scoring system uses readily available clinical data and can be calculated quickly, facilitating patient consultation with respect to allo HCT, and may also be used to identify high-risk populations where interventions such as post–allo HCT maintenance therapies may be of benefit,” they wrote (J Clin Oncol. 2016 April 4. doi: 10.1200/JCO.2015.65.0515).
The data were obtained from the CIBMTR, a combined research program of the Medical College of Wisconsin and the National Marrow Donor Program. The CIBMTR comprises a voluntary network of more than 450 transplantation centers worldwide that contribute data on consecutive allo and autologous HCTs to a centralized statistical center.
The researchers applied the prognostic tool to 2,133 patients with MDS undergoing HLA-matched (n = 1,728) or -mismatched (n = 405) allo HCT. Factors prognostic of mortality were identified in a training subset (n = 1,151) of the HLA-matched cohort. A weighted score using these factors was then assigned to the validation cohort of 577 remaining patients undergoing HLA-matched allo HCT as well as to patients undergoing HLA-mismatched allo HCT. The training data set was used to develop a prognostic scoring system, and the validation data set was used to assess the prognostic ability of the scoring system, the researchers noted.
In the scoring system, 1 point was assigned for the following factors: Blood blasts greater than 3%, platelet levels of 50 × 109/L or less at transplantation, Karnofsky performance status less than 90%, comprehensive cytogenetic risk score of poor or very poor, and age 30-49 years. Two points were assigned for monosomal karyotype and age 50 years or older.
Based on the scoring system, 3-year overall survival after transplantation was 71% in patients with scores of 1 point, 49% with scores of 2-3, 41% with scores of 4-5, and 25% with scores of 6 or more. Increasing score was predictive of increased relapse and treatment-related mortality in the HLA-matched set and of relapse in the HLA-mismatched cohort.
To develop the scoring system, the researchers used a model that weighed patient age; sex; and Karnofsky performance status; disease stage at transplantation; comprehensive cytogenetic risk status; bone marrow and peripheral blood blast percentages; hemoglobin, neutrophil, and platelet counts at diagnosis and pretransplantation; lactate dehydrogenase at transplantation; pretransplantation therapy (hypomethylating agents, chemotherapy, neither, or both); time from diagnosis to transplantation; year of transplantation; conditioning regimen and regimen intensity (myeloablative v reduced intensity); donor–recipient sex match or mismatch; graft-versus-host disease prophylaxis; graft type (bone marrow vs. peripheral blood); presence of secondary myelodysplastic syndrome; and unrelated donor vs. related donor.
There were no significant differences in overall survival at 1, 3, and 5 years or in the 3-year incidences of relapse and treatment-related mortality in the training subset and the validation cohort.
Data on somatic mutations have become relevant in myelodysplastic syndrome prognostication and were missing from this analysis, the researchers wrote. “The next generation of prognostic tools will need to account for this information.”
Dr. Shaffer had no relevant financial disclosures.
On Twitter @maryjodales
A new risk-stratification tool goes one better than the standard tools used to predict survival in those undergoing allogeneic hematopoietic cell transplantation (allo HCT) for myelodysplastic syndrome, based on a study published online April 4 in the Journal of Clinical Oncology.
The concordance index for the new risk-stratification tool was modestly better at 0.575, compared with 0.538 for the standard International Prognostic Scoring System (IPSS) and 0.554 for the revised IPSS (IPSS-R), according to Dr. Brian C. Shaffer of Memorial Sloan Kettering Cancer Center, New York, and his colleagues who participate in the Center for International Blood and Marrow Transplant Research (CIBMTR) network.
“The proposed system generally agrees with the IPSS-R in the very high–risk subcategory; however, a significant portion of patients in high- and very high–risk IPSS-R groups were represented in the low- and intermediate-risk proposed scoring subcategories. The 3-year survival in patients classified as high risk with the IPSS-R was 75%; it was 57% in those classified as low or intermediate risk with the proposed system,” the researchers wrote.
Further, the “scoring system uses readily available clinical data and can be calculated quickly, facilitating patient consultation with respect to allo HCT, and may also be used to identify high-risk populations where interventions such as post–allo HCT maintenance therapies may be of benefit,” they wrote (J Clin Oncol. 2016 April 4. doi: 10.1200/JCO.2015.65.0515).
The data were obtained from the CIBMTR, a combined research program of the Medical College of Wisconsin and the National Marrow Donor Program. The CIBMTR comprises a voluntary network of more than 450 transplantation centers worldwide that contribute data on consecutive allo and autologous HCTs to a centralized statistical center.
The researchers applied the prognostic tool to 2,133 patients with MDS undergoing HLA-matched (n = 1,728) or -mismatched (n = 405) allo HCT. Factors prognostic of mortality were identified in a training subset (n = 1,151) of the HLA-matched cohort. A weighted score using these factors was then assigned to the validation cohort of 577 remaining patients undergoing HLA-matched allo HCT as well as to patients undergoing HLA-mismatched allo HCT. The training data set was used to develop a prognostic scoring system, and the validation data set was used to assess the prognostic ability of the scoring system, the researchers noted.
In the scoring system, 1 point was assigned for the following factors: Blood blasts greater than 3%, platelet levels of 50 × 109/L or less at transplantation, Karnofsky performance status less than 90%, comprehensive cytogenetic risk score of poor or very poor, and age 30-49 years. Two points were assigned for monosomal karyotype and age 50 years or older.
Based on the scoring system, 3-year overall survival after transplantation was 71% in patients with scores of 1 point, 49% with scores of 2-3, 41% with scores of 4-5, and 25% with scores of 6 or more. Increasing score was predictive of increased relapse and treatment-related mortality in the HLA-matched set and of relapse in the HLA-mismatched cohort.
To develop the scoring system, the researchers used a model that weighed patient age; sex; and Karnofsky performance status; disease stage at transplantation; comprehensive cytogenetic risk status; bone marrow and peripheral blood blast percentages; hemoglobin, neutrophil, and platelet counts at diagnosis and pretransplantation; lactate dehydrogenase at transplantation; pretransplantation therapy (hypomethylating agents, chemotherapy, neither, or both); time from diagnosis to transplantation; year of transplantation; conditioning regimen and regimen intensity (myeloablative v reduced intensity); donor–recipient sex match or mismatch; graft-versus-host disease prophylaxis; graft type (bone marrow vs. peripheral blood); presence of secondary myelodysplastic syndrome; and unrelated donor vs. related donor.
There were no significant differences in overall survival at 1, 3, and 5 years or in the 3-year incidences of relapse and treatment-related mortality in the training subset and the validation cohort.
Data on somatic mutations have become relevant in myelodysplastic syndrome prognostication and were missing from this analysis, the researchers wrote. “The next generation of prognostic tools will need to account for this information.”
Dr. Shaffer had no relevant financial disclosures.
On Twitter @maryjodales
FROM JCO
Key clinical point: A portion of patients with myelodysplastic syndrome in high- and very high–risk groups of the revised International Prognostic Scoring System (IPSS-R) were represented in the low- and intermediate-risk groups of the proposed scoring subcategories.
Major finding: The 3-year survival in patients classified as high risk with the IPSS-R was 75%; it was 57% in those classified as low or intermediate risk with the proposed system.
Data source: The Center for International Blood and Marrow Transplant Research (CIBMTR), a combined research program of the Medical College of Wisconsin and the National Marrow Donor Program. The CIBMTR comprises a voluntary network of more than 450 transplantation centers worldwide that contribute data on consecutive allo and autologous HCTs to a centralized statistical center.
Disclosures: Dr. Shaffer had no relevant financial disclosures.
Colombia reports first Zika deaths, all in medically compromised patients
AMSTERDAM – Five people with confirmed Zika virus infections have died in Colombia, and all had medical comorbidities, including leukemia, diabetes, sickle cell anemia, and hypertension.
All of the deaths occurred last October in northern and central Colombia, Dr. Alfonso Rodriguez-Morales said at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
Four of the cases were simultaneously published April 7 in the Lancet Infectious Diseases (2016 Apr 7. doi: 10.1016/S1473-3099[16]30006-8). The fifth case occurred in northern Colombia, and was reported in Emerging Infectious Diseases (2016 May. doi: 10.3201/eid2205.151934).
Reports of confirmed Zika-related deaths are rare. Brazil, the only other country to disclose them, has now reported three, said Dr. Rodriguez-Morales of the Universidad Tecnológica de Pereira, Colombia.
“Before the current outbreak in Latin America, Zika virus was not linked to deaths,” he noted. But the eight confirmed Zika-related deaths in South America “call attention to the need for evidence-based guidelines for clinical management of Zika, as well as the possible occurrence of atypical and severe cases, including possibly congenitally related microcephaly.”
Because they all occurred in medically compromised patients, Dr. Rodriguez-Morales also urged clinicians to cast a wary eye on such patients who present with arbovirus-type symptoms, including fever and rash.
From September 2015 to March 2016, Colombia had 58,838 reported cases of Zika. Of those, only 2,361 were lab confirmed. The rest were either diagnosed clinically or were suspected cases, Dr. Rodriguez-Morales said. Although Colombia has a much smaller population than Brazil (49 million vs. 210 million), its Zika case rate is much higher, 120 cases per 100,000 people vs. 34 cases per 100,000 people.
The group of four deaths occurred in central Colombia, and included a 2-year-old girl, a 30-year-old woman, a 61-year-old man, and a 72-year-old woman. All presented with 2-6 days of fever. All were initially suspected to have dengue fever or chikungunya. None tested positive for dengue, but the man was coinfected with chikungunya.
All patients presented with anemia. All but the older man also had severe thrombocytopenia.
The toddler presented with hepatomegaly, mucosal hemorrhage, progressive respiratory collapse, progressive thrombocytopenia, and intravascular coagulation. She died 5 days after symptom onset and was found to have had unrecognized lymphoblastic leukemia.
The 30-year-old woman presented with a severe rash on both arms. She also exhibited coagulation dysfunction, including severe thrombocytopenia and leukopenia that progressed to intracerebral and subarachnoid hemorrhage. She died 12 days after symptom onset. She was determined to have had unrecognized acute myeloid leukemia.
The elderly man had a history of medically controlled hypertension. He experienced mucosal hemorrhage and respiratory distress. He died 7 days after symptom onset. On autopsy, his liver showed necrotic areas, and his spleen indicated a systemic inflammatory response.
The elderly woman had a history of insulin-controlled type 2 diabetes. Her symptoms included gastrointestinal distress, thrombocytopenia, and acute respiratory failure. She died 48 hours after symptom onset; her brain showed edema and ischemic lesions.
The 15-year-old girl in northern Colombia had a 5-year history of sickle cell disease, which, Dr. Rodriguez-Morales pointed out, is a risk factor for arbovirus diseases. However, the patient had never been hospitalized for a vasoocclusive crisis. She presented with a high fever; joint, muscle, and abdominal pain; and jaundice. She was assumed to have dengue virus. Within another day, she had progressed into respiratory failure and was on a ventilator. She died less than 2 days later.
Her autopsy showed hepatic necrosis and severe decrease of splenic lymphoid tissue with splenic sequestration. Systemic inflammation probably triggered a fatal vasoocclusive crisis and splenic sequestration.
Dr. Rodriguez-Morales had no financial disclosures.
AMSTERDAM – Five people with confirmed Zika virus infections have died in Colombia, and all had medical comorbidities, including leukemia, diabetes, sickle cell anemia, and hypertension.
All of the deaths occurred last October in northern and central Colombia, Dr. Alfonso Rodriguez-Morales said at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
Four of the cases were simultaneously published April 7 in the Lancet Infectious Diseases (2016 Apr 7. doi: 10.1016/S1473-3099[16]30006-8). The fifth case occurred in northern Colombia, and was reported in Emerging Infectious Diseases (2016 May. doi: 10.3201/eid2205.151934).
Reports of confirmed Zika-related deaths are rare. Brazil, the only other country to disclose them, has now reported three, said Dr. Rodriguez-Morales of the Universidad Tecnológica de Pereira, Colombia.
“Before the current outbreak in Latin America, Zika virus was not linked to deaths,” he noted. But the eight confirmed Zika-related deaths in South America “call attention to the need for evidence-based guidelines for clinical management of Zika, as well as the possible occurrence of atypical and severe cases, including possibly congenitally related microcephaly.”
Because they all occurred in medically compromised patients, Dr. Rodriguez-Morales also urged clinicians to cast a wary eye on such patients who present with arbovirus-type symptoms, including fever and rash.
From September 2015 to March 2016, Colombia had 58,838 reported cases of Zika. Of those, only 2,361 were lab confirmed. The rest were either diagnosed clinically or were suspected cases, Dr. Rodriguez-Morales said. Although Colombia has a much smaller population than Brazil (49 million vs. 210 million), its Zika case rate is much higher, 120 cases per 100,000 people vs. 34 cases per 100,000 people.
The group of four deaths occurred in central Colombia, and included a 2-year-old girl, a 30-year-old woman, a 61-year-old man, and a 72-year-old woman. All presented with 2-6 days of fever. All were initially suspected to have dengue fever or chikungunya. None tested positive for dengue, but the man was coinfected with chikungunya.
All patients presented with anemia. All but the older man also had severe thrombocytopenia.
The toddler presented with hepatomegaly, mucosal hemorrhage, progressive respiratory collapse, progressive thrombocytopenia, and intravascular coagulation. She died 5 days after symptom onset and was found to have had unrecognized lymphoblastic leukemia.
The 30-year-old woman presented with a severe rash on both arms. She also exhibited coagulation dysfunction, including severe thrombocytopenia and leukopenia that progressed to intracerebral and subarachnoid hemorrhage. She died 12 days after symptom onset. She was determined to have had unrecognized acute myeloid leukemia.
The elderly man had a history of medically controlled hypertension. He experienced mucosal hemorrhage and respiratory distress. He died 7 days after symptom onset. On autopsy, his liver showed necrotic areas, and his spleen indicated a systemic inflammatory response.
The elderly woman had a history of insulin-controlled type 2 diabetes. Her symptoms included gastrointestinal distress, thrombocytopenia, and acute respiratory failure. She died 48 hours after symptom onset; her brain showed edema and ischemic lesions.
The 15-year-old girl in northern Colombia had a 5-year history of sickle cell disease, which, Dr. Rodriguez-Morales pointed out, is a risk factor for arbovirus diseases. However, the patient had never been hospitalized for a vasoocclusive crisis. She presented with a high fever; joint, muscle, and abdominal pain; and jaundice. She was assumed to have dengue virus. Within another day, she had progressed into respiratory failure and was on a ventilator. She died less than 2 days later.
Her autopsy showed hepatic necrosis and severe decrease of splenic lymphoid tissue with splenic sequestration. Systemic inflammation probably triggered a fatal vasoocclusive crisis and splenic sequestration.
Dr. Rodriguez-Morales had no financial disclosures.
AMSTERDAM – Five people with confirmed Zika virus infections have died in Colombia, and all had medical comorbidities, including leukemia, diabetes, sickle cell anemia, and hypertension.
All of the deaths occurred last October in northern and central Colombia, Dr. Alfonso Rodriguez-Morales said at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
Four of the cases were simultaneously published April 7 in the Lancet Infectious Diseases (2016 Apr 7. doi: 10.1016/S1473-3099[16]30006-8). The fifth case occurred in northern Colombia, and was reported in Emerging Infectious Diseases (2016 May. doi: 10.3201/eid2205.151934).
Reports of confirmed Zika-related deaths are rare. Brazil, the only other country to disclose them, has now reported three, said Dr. Rodriguez-Morales of the Universidad Tecnológica de Pereira, Colombia.
“Before the current outbreak in Latin America, Zika virus was not linked to deaths,” he noted. But the eight confirmed Zika-related deaths in South America “call attention to the need for evidence-based guidelines for clinical management of Zika, as well as the possible occurrence of atypical and severe cases, including possibly congenitally related microcephaly.”
Because they all occurred in medically compromised patients, Dr. Rodriguez-Morales also urged clinicians to cast a wary eye on such patients who present with arbovirus-type symptoms, including fever and rash.
From September 2015 to March 2016, Colombia had 58,838 reported cases of Zika. Of those, only 2,361 were lab confirmed. The rest were either diagnosed clinically or were suspected cases, Dr. Rodriguez-Morales said. Although Colombia has a much smaller population than Brazil (49 million vs. 210 million), its Zika case rate is much higher, 120 cases per 100,000 people vs. 34 cases per 100,000 people.
The group of four deaths occurred in central Colombia, and included a 2-year-old girl, a 30-year-old woman, a 61-year-old man, and a 72-year-old woman. All presented with 2-6 days of fever. All were initially suspected to have dengue fever or chikungunya. None tested positive for dengue, but the man was coinfected with chikungunya.
All patients presented with anemia. All but the older man also had severe thrombocytopenia.
The toddler presented with hepatomegaly, mucosal hemorrhage, progressive respiratory collapse, progressive thrombocytopenia, and intravascular coagulation. She died 5 days after symptom onset and was found to have had unrecognized lymphoblastic leukemia.
The 30-year-old woman presented with a severe rash on both arms. She also exhibited coagulation dysfunction, including severe thrombocytopenia and leukopenia that progressed to intracerebral and subarachnoid hemorrhage. She died 12 days after symptom onset. She was determined to have had unrecognized acute myeloid leukemia.
The elderly man had a history of medically controlled hypertension. He experienced mucosal hemorrhage and respiratory distress. He died 7 days after symptom onset. On autopsy, his liver showed necrotic areas, and his spleen indicated a systemic inflammatory response.
The elderly woman had a history of insulin-controlled type 2 diabetes. Her symptoms included gastrointestinal distress, thrombocytopenia, and acute respiratory failure. She died 48 hours after symptom onset; her brain showed edema and ischemic lesions.
The 15-year-old girl in northern Colombia had a 5-year history of sickle cell disease, which, Dr. Rodriguez-Morales pointed out, is a risk factor for arbovirus diseases. However, the patient had never been hospitalized for a vasoocclusive crisis. She presented with a high fever; joint, muscle, and abdominal pain; and jaundice. She was assumed to have dengue virus. Within another day, she had progressed into respiratory failure and was on a ventilator. She died less than 2 days later.
Her autopsy showed hepatic necrosis and severe decrease of splenic lymphoid tissue with splenic sequestration. Systemic inflammation probably triggered a fatal vasoocclusive crisis and splenic sequestration.
Dr. Rodriguez-Morales had no financial disclosures.
AT ECCMID 2016
EMA recommends orphan designation for cancer vaccine

The European Medicines Agency (EMA) has recommended orphan designation for the WT1 cancer vaccine galinpepimut-S as a treatment for patients
with acute myeloid leukemia (AML) and patients with malignant pleural mesothelioma (MPM).
The EMA’s opinion has been forwarded to the European Commission (EC), which makes the final decision.
The EC grants orphan designation to products intended to treat, prevent, or diagnose a life-threatening condition affecting up to 5 in 10,000 people in the European Union. The product must provide significant benefit to those affected by the condition.
Orphan designation from the EC provides companies with certain development incentives, including protocol assistance, a type of scientific advice specific for orphan drugs, and 10 years of market exclusivity once the drug is approved for use.
About the vaccine
The WT1 vaccine consists of 4 modified peptide chains that induce an innate immune response (CD4+/CD8+ T cells) against the WT1 antigen. The vaccine is administered in combination with an adjuvant and an immune modulator to improve the immune response to the target.
Based on the vaccine’s mechanism and the accumulating evidence of activity in mid-stage trials, researchers believe the WT1 vaccine may have the potential to complement currently available therapies by destroying residual tumor cells of cancers in remission and providing ongoing immune surveillance for recurrent tumors.
The WT1 vaccine could potentially target more than 20 cancers that overexpress WT1, many of which are associated with relapse rates of up to 80% or more, as seen in patients with AML and MPM.
The vaccine is being developed by SELLAS Life Sciences Group. The company said that, in a phase 1 study, AML patients treated with the vaccine had a median overall survival of more than 3 years.
In a phase 2 trial of the vaccine, adult AML patients had a median overall survival of around 4 years. Data from the phase 2 trial are scheduled to be presented at the 2016 ASCO Annual Meeting.
SELLAS said it expects to begin a phase 3 trial of the vaccine in AML patients later this year. ![]()

The European Medicines Agency (EMA) has recommended orphan designation for the WT1 cancer vaccine galinpepimut-S as a treatment for patients
with acute myeloid leukemia (AML) and patients with malignant pleural mesothelioma (MPM).
The EMA’s opinion has been forwarded to the European Commission (EC), which makes the final decision.
The EC grants orphan designation to products intended to treat, prevent, or diagnose a life-threatening condition affecting up to 5 in 10,000 people in the European Union. The product must provide significant benefit to those affected by the condition.
Orphan designation from the EC provides companies with certain development incentives, including protocol assistance, a type of scientific advice specific for orphan drugs, and 10 years of market exclusivity once the drug is approved for use.
About the vaccine
The WT1 vaccine consists of 4 modified peptide chains that induce an innate immune response (CD4+/CD8+ T cells) against the WT1 antigen. The vaccine is administered in combination with an adjuvant and an immune modulator to improve the immune response to the target.
Based on the vaccine’s mechanism and the accumulating evidence of activity in mid-stage trials, researchers believe the WT1 vaccine may have the potential to complement currently available therapies by destroying residual tumor cells of cancers in remission and providing ongoing immune surveillance for recurrent tumors.
The WT1 vaccine could potentially target more than 20 cancers that overexpress WT1, many of which are associated with relapse rates of up to 80% or more, as seen in patients with AML and MPM.
The vaccine is being developed by SELLAS Life Sciences Group. The company said that, in a phase 1 study, AML patients treated with the vaccine had a median overall survival of more than 3 years.
In a phase 2 trial of the vaccine, adult AML patients had a median overall survival of around 4 years. Data from the phase 2 trial are scheduled to be presented at the 2016 ASCO Annual Meeting.
SELLAS said it expects to begin a phase 3 trial of the vaccine in AML patients later this year. ![]()

The European Medicines Agency (EMA) has recommended orphan designation for the WT1 cancer vaccine galinpepimut-S as a treatment for patients
with acute myeloid leukemia (AML) and patients with malignant pleural mesothelioma (MPM).
The EMA’s opinion has been forwarded to the European Commission (EC), which makes the final decision.
The EC grants orphan designation to products intended to treat, prevent, or diagnose a life-threatening condition affecting up to 5 in 10,000 people in the European Union. The product must provide significant benefit to those affected by the condition.
Orphan designation from the EC provides companies with certain development incentives, including protocol assistance, a type of scientific advice specific for orphan drugs, and 10 years of market exclusivity once the drug is approved for use.
About the vaccine
The WT1 vaccine consists of 4 modified peptide chains that induce an innate immune response (CD4+/CD8+ T cells) against the WT1 antigen. The vaccine is administered in combination with an adjuvant and an immune modulator to improve the immune response to the target.
Based on the vaccine’s mechanism and the accumulating evidence of activity in mid-stage trials, researchers believe the WT1 vaccine may have the potential to complement currently available therapies by destroying residual tumor cells of cancers in remission and providing ongoing immune surveillance for recurrent tumors.
The WT1 vaccine could potentially target more than 20 cancers that overexpress WT1, many of which are associated with relapse rates of up to 80% or more, as seen in patients with AML and MPM.
The vaccine is being developed by SELLAS Life Sciences Group. The company said that, in a phase 1 study, AML patients treated with the vaccine had a median overall survival of more than 3 years.
In a phase 2 trial of the vaccine, adult AML patients had a median overall survival of around 4 years. Data from the phase 2 trial are scheduled to be presented at the 2016 ASCO Annual Meeting.
SELLAS said it expects to begin a phase 3 trial of the vaccine in AML patients later this year. ![]()
FDA grants product orphan designation for AML

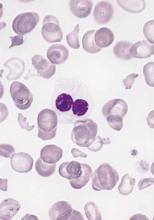
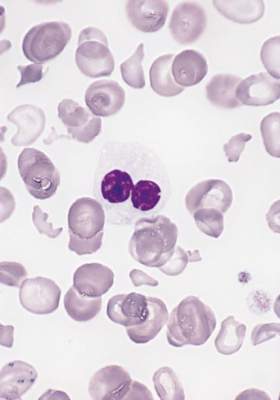
Image by Lance Liotta
The US Food and Drug Administration (FDA) has granted orphan designation for the radioimmunoconjugate Iomab-B to be used as a conditioning agent for patients with relapsed or refractory acute myeloid leukemia (AML) who are undergoing hematopoietic stem cell transplant (HSCT).
Iomab-B is a radioimmunoconjugate consisting of BC8, a novel murine monoclonal antibody, and the radioisotope iodine-131.
BC8 targets CD45, a pan-leukocytic antigen widely expressed on white blood cells. This makes BC8 potentially useful in targeting white blood cells in preparation for HSCT.
When labeled with radioactive isotopes, BC8 carries radioactivity directly to the site of cancerous growth and bone marrow, while avoiding the effects of radiation on most healthy tissues, according to Actinium Pharmaceuticals, Inc., the company developing Iomab-B.
Actinium said Iomab-B has been tested as a myeloconditioning/myeloablative agent in more than 250 patients with incurable hematologic malignancies.
The company has released data from a phase 1/2 trial of Iomab-B in patients with relapsed/refractory AML who are older than 50.
The data show that patients who received Iomab-B before HSCT (n=27) had higher rates of survival at 1 and 2 years than patients who underwent HSCT with conventional myeloablative conditioning (n=10) or chemotherapy (n=61).
One-year survival rates were 30% in the Iomab-B arm and 10% each in the conventional conditioning and chemotherapy arms. Two-year survival rates were 19%, 0%, and 0%, respectively.
Now, Actinium is planning a phase 3 trial of Iomab-B in relapsed/refractory AML patients over the age of 55.
About orphan designation
The FDA grants orphan designation to drugs intended to treat diseases or conditions affecting fewer than 200,000 patients in the US.
The designation provides the drug’s sponsor with various development incentives, including opportunities to apply for research-related tax credits and grant funding, assistance in designing clinical trials, and 7 years of US market exclusivity if the drug is approved. ![]()

Image by Lance Liotta
The US Food and Drug Administration (FDA) has granted orphan designation for the radioimmunoconjugate Iomab-B to be used as a conditioning agent for patients with relapsed or refractory acute myeloid leukemia (AML) who are undergoing hematopoietic stem cell transplant (HSCT).
Iomab-B is a radioimmunoconjugate consisting of BC8, a novel murine monoclonal antibody, and the radioisotope iodine-131.
BC8 targets CD45, a pan-leukocytic antigen widely expressed on white blood cells. This makes BC8 potentially useful in targeting white blood cells in preparation for HSCT.
When labeled with radioactive isotopes, BC8 carries radioactivity directly to the site of cancerous growth and bone marrow, while avoiding the effects of radiation on most healthy tissues, according to Actinium Pharmaceuticals, Inc., the company developing Iomab-B.
Actinium said Iomab-B has been tested as a myeloconditioning/myeloablative agent in more than 250 patients with incurable hematologic malignancies.
The company has released data from a phase 1/2 trial of Iomab-B in patients with relapsed/refractory AML who are older than 50.
The data show that patients who received Iomab-B before HSCT (n=27) had higher rates of survival at 1 and 2 years than patients who underwent HSCT with conventional myeloablative conditioning (n=10) or chemotherapy (n=61).
One-year survival rates were 30% in the Iomab-B arm and 10% each in the conventional conditioning and chemotherapy arms. Two-year survival rates were 19%, 0%, and 0%, respectively.
Now, Actinium is planning a phase 3 trial of Iomab-B in relapsed/refractory AML patients over the age of 55.
About orphan designation
The FDA grants orphan designation to drugs intended to treat diseases or conditions affecting fewer than 200,000 patients in the US.
The designation provides the drug’s sponsor with various development incentives, including opportunities to apply for research-related tax credits and grant funding, assistance in designing clinical trials, and 7 years of US market exclusivity if the drug is approved. ![]()

Image by Lance Liotta
The US Food and Drug Administration (FDA) has granted orphan designation for the radioimmunoconjugate Iomab-B to be used as a conditioning agent for patients with relapsed or refractory acute myeloid leukemia (AML) who are undergoing hematopoietic stem cell transplant (HSCT).
Iomab-B is a radioimmunoconjugate consisting of BC8, a novel murine monoclonal antibody, and the radioisotope iodine-131.
BC8 targets CD45, a pan-leukocytic antigen widely expressed on white blood cells. This makes BC8 potentially useful in targeting white blood cells in preparation for HSCT.
When labeled with radioactive isotopes, BC8 carries radioactivity directly to the site of cancerous growth and bone marrow, while avoiding the effects of radiation on most healthy tissues, according to Actinium Pharmaceuticals, Inc., the company developing Iomab-B.
Actinium said Iomab-B has been tested as a myeloconditioning/myeloablative agent in more than 250 patients with incurable hematologic malignancies.
The company has released data from a phase 1/2 trial of Iomab-B in patients with relapsed/refractory AML who are older than 50.
The data show that patients who received Iomab-B before HSCT (n=27) had higher rates of survival at 1 and 2 years than patients who underwent HSCT with conventional myeloablative conditioning (n=10) or chemotherapy (n=61).
One-year survival rates were 30% in the Iomab-B arm and 10% each in the conventional conditioning and chemotherapy arms. Two-year survival rates were 19%, 0%, and 0%, respectively.
Now, Actinium is planning a phase 3 trial of Iomab-B in relapsed/refractory AML patients over the age of 55.
About orphan designation
The FDA grants orphan designation to drugs intended to treat diseases or conditions affecting fewer than 200,000 patients in the US.
The designation provides the drug’s sponsor with various development incentives, including opportunities to apply for research-related tax credits and grant funding, assistance in designing clinical trials, and 7 years of US market exclusivity if the drug is approved. ![]()
Drug for conditioning AML patients for transplant gets orphan drug designation
A radioimmunotherapeutic drug for conditioning relapsed and refractory acute myeloid leukemia (AML) patients for a hematopoietic stem cell transplant has been granted orphan drug designation by the Food and Drug Administration.
Iomab-B is a radioimmunoconjugate consisting of the murine monoclonal antibody BC8 and an iodine-131 radioisotope. The Fred Hutchinson Cancer Research Center developed BC8 to target CD45, a panleukocytic antigen widely expressed on white blood cells. “When labeled with radioactive isotopes, BC8 carries radioactivity directly to the site of cancerous growth and bone marrow while avoiding effects of radiation on most healthy tissues,” says a statement from Actinium Pharmaceuticals, which would market the drug.
Iomab-B will be tested in a multicenter trial that will include 150 patients over age 55 with refractory and relapsed AML. “There has not been a new drug approved for relapsed and refractory AML patients over the age of 55 in decades and with Iomab-B being the only therapy of its kind, we are pleased to have achieved this important milestone,” Sandesh Seth, executive chairman of Actinium, said in the statement.
A radioimmunotherapeutic drug for conditioning relapsed and refractory acute myeloid leukemia (AML) patients for a hematopoietic stem cell transplant has been granted orphan drug designation by the Food and Drug Administration.
Iomab-B is a radioimmunoconjugate consisting of the murine monoclonal antibody BC8 and an iodine-131 radioisotope. The Fred Hutchinson Cancer Research Center developed BC8 to target CD45, a panleukocytic antigen widely expressed on white blood cells. “When labeled with radioactive isotopes, BC8 carries radioactivity directly to the site of cancerous growth and bone marrow while avoiding effects of radiation on most healthy tissues,” says a statement from Actinium Pharmaceuticals, which would market the drug.
Iomab-B will be tested in a multicenter trial that will include 150 patients over age 55 with refractory and relapsed AML. “There has not been a new drug approved for relapsed and refractory AML patients over the age of 55 in decades and with Iomab-B being the only therapy of its kind, we are pleased to have achieved this important milestone,” Sandesh Seth, executive chairman of Actinium, said in the statement.
A radioimmunotherapeutic drug for conditioning relapsed and refractory acute myeloid leukemia (AML) patients for a hematopoietic stem cell transplant has been granted orphan drug designation by the Food and Drug Administration.
Iomab-B is a radioimmunoconjugate consisting of the murine monoclonal antibody BC8 and an iodine-131 radioisotope. The Fred Hutchinson Cancer Research Center developed BC8 to target CD45, a panleukocytic antigen widely expressed on white blood cells. “When labeled with radioactive isotopes, BC8 carries radioactivity directly to the site of cancerous growth and bone marrow while avoiding effects of radiation on most healthy tissues,” says a statement from Actinium Pharmaceuticals, which would market the drug.
Iomab-B will be tested in a multicenter trial that will include 150 patients over age 55 with refractory and relapsed AML. “There has not been a new drug approved for relapsed and refractory AML patients over the age of 55 in decades and with Iomab-B being the only therapy of its kind, we are pleased to have achieved this important milestone,” Sandesh Seth, executive chairman of Actinium, said in the statement.
Mouse model replicates aggressive AML subtype

Researchers have developed a mouse model of an aggressive type of acute myeloid leukemia (AML) that, they believe, accurately replicates the human form of the disease.
The model replicates AML with co-occurring mutations in FLT3 and DNMT3A.
The researchers said they found that mice with Flt3-ITD and inducible deletion of Dnmt3a developed a rapidly lethal, completely penetrant, and transplantable AML of normal karyotype.
The team described this work in Cancer Discovery.
“Our goal was to create a model that was faithful to the human form of the disease that can be used for preclinical testing of potential cures,” said study author H. Leighton Grimes, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“Previous models were slow, difficult to analyze, and did not accurately represent the human disease. This model is rapid, fully penetrant, and completely spontaneous. We hope that it will open the way for other researchers to join us in attacking this particularly lethal AML subtype.”
Dr Grimes and his colleagues said they were able to look at the disease in a new way with the help of a powerful new core facility utilizing analytical tools related to single-cell RNA sequencing. The team used complementary single-cell analyses to identify the core leukemia-causing stem cells of the tumor.
“Before, researchers were comparing the gene expression patterns of one AML subtype to either normal cells or other AML subtypes,” said study author Sara Meyer, PhD, a fellow in the Grimes lab.
“That approach made it difficult to tease out the specific impact of Dnmt3a mutation. Instead, we isolated the variables and studied only human and murine AML with Flt3 mutation. Comparing Flt3-mutant AML with and without Dnmt3a mutation allowed us to more finely identify those patterns that were specific to the Dnmt3a mutation.”
With that more detailed understanding, the researchers gained new insights into the contributions of the Dnmt3a mutation to the disease.
First, their work confirms suspicions that low-level Dnmt3a activity is cancer-causing. Moreover, they discovered that reduced Dnmt3a function allows genes that are normally expressed only at early development stages of blood cell formation to continue expression at later stages, leading to the development of AML.
The researchers also found that, in mouse tumor cells, rescuing expression of Dnmt3a reversed the leukemia phenotypes and gene expression. But they said more research is warranted to determine if rescuing normal levels of DNMT3A function is a viable method for treating human AML.
The team also identified several potential treatment targets that are unique to this type of AML. In future studies, they plan to proceed with testing potential therapies. ![]()

Researchers have developed a mouse model of an aggressive type of acute myeloid leukemia (AML) that, they believe, accurately replicates the human form of the disease.
The model replicates AML with co-occurring mutations in FLT3 and DNMT3A.
The researchers said they found that mice with Flt3-ITD and inducible deletion of Dnmt3a developed a rapidly lethal, completely penetrant, and transplantable AML of normal karyotype.
The team described this work in Cancer Discovery.
“Our goal was to create a model that was faithful to the human form of the disease that can be used for preclinical testing of potential cures,” said study author H. Leighton Grimes, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“Previous models were slow, difficult to analyze, and did not accurately represent the human disease. This model is rapid, fully penetrant, and completely spontaneous. We hope that it will open the way for other researchers to join us in attacking this particularly lethal AML subtype.”
Dr Grimes and his colleagues said they were able to look at the disease in a new way with the help of a powerful new core facility utilizing analytical tools related to single-cell RNA sequencing. The team used complementary single-cell analyses to identify the core leukemia-causing stem cells of the tumor.
“Before, researchers were comparing the gene expression patterns of one AML subtype to either normal cells or other AML subtypes,” said study author Sara Meyer, PhD, a fellow in the Grimes lab.
“That approach made it difficult to tease out the specific impact of Dnmt3a mutation. Instead, we isolated the variables and studied only human and murine AML with Flt3 mutation. Comparing Flt3-mutant AML with and without Dnmt3a mutation allowed us to more finely identify those patterns that were specific to the Dnmt3a mutation.”
With that more detailed understanding, the researchers gained new insights into the contributions of the Dnmt3a mutation to the disease.
First, their work confirms suspicions that low-level Dnmt3a activity is cancer-causing. Moreover, they discovered that reduced Dnmt3a function allows genes that are normally expressed only at early development stages of blood cell formation to continue expression at later stages, leading to the development of AML.
The researchers also found that, in mouse tumor cells, rescuing expression of Dnmt3a reversed the leukemia phenotypes and gene expression. But they said more research is warranted to determine if rescuing normal levels of DNMT3A function is a viable method for treating human AML.
The team also identified several potential treatment targets that are unique to this type of AML. In future studies, they plan to proceed with testing potential therapies. ![]()

Researchers have developed a mouse model of an aggressive type of acute myeloid leukemia (AML) that, they believe, accurately replicates the human form of the disease.
The model replicates AML with co-occurring mutations in FLT3 and DNMT3A.
The researchers said they found that mice with Flt3-ITD and inducible deletion of Dnmt3a developed a rapidly lethal, completely penetrant, and transplantable AML of normal karyotype.
The team described this work in Cancer Discovery.
“Our goal was to create a model that was faithful to the human form of the disease that can be used for preclinical testing of potential cures,” said study author H. Leighton Grimes, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“Previous models were slow, difficult to analyze, and did not accurately represent the human disease. This model is rapid, fully penetrant, and completely spontaneous. We hope that it will open the way for other researchers to join us in attacking this particularly lethal AML subtype.”
Dr Grimes and his colleagues said they were able to look at the disease in a new way with the help of a powerful new core facility utilizing analytical tools related to single-cell RNA sequencing. The team used complementary single-cell analyses to identify the core leukemia-causing stem cells of the tumor.
“Before, researchers were comparing the gene expression patterns of one AML subtype to either normal cells or other AML subtypes,” said study author Sara Meyer, PhD, a fellow in the Grimes lab.
“That approach made it difficult to tease out the specific impact of Dnmt3a mutation. Instead, we isolated the variables and studied only human and murine AML with Flt3 mutation. Comparing Flt3-mutant AML with and without Dnmt3a mutation allowed us to more finely identify those patterns that were specific to the Dnmt3a mutation.”
With that more detailed understanding, the researchers gained new insights into the contributions of the Dnmt3a mutation to the disease.
First, their work confirms suspicions that low-level Dnmt3a activity is cancer-causing. Moreover, they discovered that reduced Dnmt3a function allows genes that are normally expressed only at early development stages of blood cell formation to continue expression at later stages, leading to the development of AML.
The researchers also found that, in mouse tumor cells, rescuing expression of Dnmt3a reversed the leukemia phenotypes and gene expression. But they said more research is warranted to determine if rescuing normal levels of DNMT3A function is a viable method for treating human AML.
The team also identified several potential treatment targets that are unique to this type of AML. In future studies, they plan to proceed with testing potential therapies. ![]()