User login
Medical students and psychiatry
I have the unfortunate task of trying to teach medical students about psychiatry. I say “unfortunate,” as most of them find psychiatry a difficult art to understand, and they seem reluctant to classify psychiatry as a branch of medicine.
In my efforts to keep things simple, I tell that them psychiatry is one of the most difficult branches of medicine as there are very few objective measures we can rely on to make sense of people’s behavior. Regrettably, the American Psychiatric Association’s Diagnostic and Statistical Manual only seems to confuse them more. So, I remind them that, in medicine, 90%-95% of diagnoses can be obtained from doing a good history, and, if we are lucky a drug level will show drugs in the system, a CT scan without contrast will show cerebral atrophy, or there will be a lab result that will be abnormal and point to a diagnosis. But mostly what they will be seeing is unusual behavior they are unable to classify.
So I identifiable brain damage, psychosis, affective disorders, anxiety disorders, and personality disorders. Under the brain damage category, I include the short- and long-term effects of drugs, major neurocognitive disorders (called dementia before DSM-5), cerebrovascular infarcts, traumatic brain injury, and neurodevelopmental disorders. For their exams and, if they are interested in psychiatry, I tell them to study the DSM. I explain to them that when I was in medical school my dermatology professor told us that if we could recognize the 10 most common dermatologic disorders, we would be able to recognize 90% of the skin disorders we would see. It is similar in psychiatry – thus, my five categories.
However, because I do not want them thinking that only schizophrenia causes psychosis, I let them know that at least 40 different factors cause people to be psychotic indicated by auditory hallucinations. Those 40 factors are: 1) acute alcohol intoxication, 2) alcohol withdrawal, 3) alcoholism, 4) Alzheimer’s disease, 5) benzodiazepine withdrawal, 6) cocaine abuse and addiction, 7) chemical poisoning, 8) dehydration, 9) delirium, 10) dissociative disorders, 11) electrolyte imbalances, 12) encephalopathy of various forms, 13) ecstasy, 14) extreme fatigue, 15) falling asleep, 16) fetal alcohol exposure, 17) grief, 18) hallucinogen use, 19) heroin abuse and dependence, 20) high fever, 21) hyperglycemia, 22) hypoglycemia, 23) intellectual disability, 24) lupus, 25) major depression, 26) mania, 27) methamphetamine use, 28) Parkinson’s disease, 29) phencyclidine, 30) postictal states, 31) posttraumatic stress disorder, 32) schizoid or schizotypal personality disorder, 33) schizophrenia, 34) sleep deprivation, 35) sleep paralysis, 36) solvent abuse, 37) traumatic brain injury, 38) temporal lobe epilepsy, 39) uremia. Lastly, I ask them about No. 40 – “normal” (For example, have you ever been walking down the street and thought you heard someone calling your name, but when you turned around no one was there?). Of course, there are many more causes of psychosis, but keeping it simple makes the principle easier to remember.
Regarding affective disorders, I point out to them, as I did in a previous column, that there is a huge difference between major depressive disorders, unhappiness, or sadness, grief, and demoralization. Regarding anxiety disorders, I let the medical students know that, like personality disorders, there is a lot of comorbidity. Yet, if they can distinguish brain damage, psychosis, and affective disorders from anxiety and personality disorders, that will be good enough.
In keeping with trying to help medical students not make assumptions, I always ask them what’s wrong with people who wash their hands 30 times a day. Invariably, the answer is obsessive-compulsive disorder. So, next I ask: Isn’t it possible that the person who washes his hands 30 times a day is a surgeon – or perhaps a patient with schizophrenia who thinks that Martians are beaming germs to his hands?
I guess I raise this issue because I am concerned with the future of psychiatry, and I think that my approach to medical school education provides a framework that can help students learn how to think about and provide care for psychiatric patients.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital’s Medical/Surgical-Psychiatry Inpatient Unit in Chicago, clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago, former president/CEO of the Community Mental Health Council, and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago. If you have tricks of the medical school teaching trade that you would like to share, email Dr. Bell at cpnews@mededge.com.
I have the unfortunate task of trying to teach medical students about psychiatry. I say “unfortunate,” as most of them find psychiatry a difficult art to understand, and they seem reluctant to classify psychiatry as a branch of medicine.
In my efforts to keep things simple, I tell that them psychiatry is one of the most difficult branches of medicine as there are very few objective measures we can rely on to make sense of people’s behavior. Regrettably, the American Psychiatric Association’s Diagnostic and Statistical Manual only seems to confuse them more. So, I remind them that, in medicine, 90%-95% of diagnoses can be obtained from doing a good history, and, if we are lucky a drug level will show drugs in the system, a CT scan without contrast will show cerebral atrophy, or there will be a lab result that will be abnormal and point to a diagnosis. But mostly what they will be seeing is unusual behavior they are unable to classify.
So I identifiable brain damage, psychosis, affective disorders, anxiety disorders, and personality disorders. Under the brain damage category, I include the short- and long-term effects of drugs, major neurocognitive disorders (called dementia before DSM-5), cerebrovascular infarcts, traumatic brain injury, and neurodevelopmental disorders. For their exams and, if they are interested in psychiatry, I tell them to study the DSM. I explain to them that when I was in medical school my dermatology professor told us that if we could recognize the 10 most common dermatologic disorders, we would be able to recognize 90% of the skin disorders we would see. It is similar in psychiatry – thus, my five categories.
However, because I do not want them thinking that only schizophrenia causes psychosis, I let them know that at least 40 different factors cause people to be psychotic indicated by auditory hallucinations. Those 40 factors are: 1) acute alcohol intoxication, 2) alcohol withdrawal, 3) alcoholism, 4) Alzheimer’s disease, 5) benzodiazepine withdrawal, 6) cocaine abuse and addiction, 7) chemical poisoning, 8) dehydration, 9) delirium, 10) dissociative disorders, 11) electrolyte imbalances, 12) encephalopathy of various forms, 13) ecstasy, 14) extreme fatigue, 15) falling asleep, 16) fetal alcohol exposure, 17) grief, 18) hallucinogen use, 19) heroin abuse and dependence, 20) high fever, 21) hyperglycemia, 22) hypoglycemia, 23) intellectual disability, 24) lupus, 25) major depression, 26) mania, 27) methamphetamine use, 28) Parkinson’s disease, 29) phencyclidine, 30) postictal states, 31) posttraumatic stress disorder, 32) schizoid or schizotypal personality disorder, 33) schizophrenia, 34) sleep deprivation, 35) sleep paralysis, 36) solvent abuse, 37) traumatic brain injury, 38) temporal lobe epilepsy, 39) uremia. Lastly, I ask them about No. 40 – “normal” (For example, have you ever been walking down the street and thought you heard someone calling your name, but when you turned around no one was there?). Of course, there are many more causes of psychosis, but keeping it simple makes the principle easier to remember.
Regarding affective disorders, I point out to them, as I did in a previous column, that there is a huge difference between major depressive disorders, unhappiness, or sadness, grief, and demoralization. Regarding anxiety disorders, I let the medical students know that, like personality disorders, there is a lot of comorbidity. Yet, if they can distinguish brain damage, psychosis, and affective disorders from anxiety and personality disorders, that will be good enough.
In keeping with trying to help medical students not make assumptions, I always ask them what’s wrong with people who wash their hands 30 times a day. Invariably, the answer is obsessive-compulsive disorder. So, next I ask: Isn’t it possible that the person who washes his hands 30 times a day is a surgeon – or perhaps a patient with schizophrenia who thinks that Martians are beaming germs to his hands?
I guess I raise this issue because I am concerned with the future of psychiatry, and I think that my approach to medical school education provides a framework that can help students learn how to think about and provide care for psychiatric patients.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital’s Medical/Surgical-Psychiatry Inpatient Unit in Chicago, clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago, former president/CEO of the Community Mental Health Council, and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago. If you have tricks of the medical school teaching trade that you would like to share, email Dr. Bell at cpnews@mededge.com.
I have the unfortunate task of trying to teach medical students about psychiatry. I say “unfortunate,” as most of them find psychiatry a difficult art to understand, and they seem reluctant to classify psychiatry as a branch of medicine.
In my efforts to keep things simple, I tell that them psychiatry is one of the most difficult branches of medicine as there are very few objective measures we can rely on to make sense of people’s behavior. Regrettably, the American Psychiatric Association’s Diagnostic and Statistical Manual only seems to confuse them more. So, I remind them that, in medicine, 90%-95% of diagnoses can be obtained from doing a good history, and, if we are lucky a drug level will show drugs in the system, a CT scan without contrast will show cerebral atrophy, or there will be a lab result that will be abnormal and point to a diagnosis. But mostly what they will be seeing is unusual behavior they are unable to classify.
So I identifiable brain damage, psychosis, affective disorders, anxiety disorders, and personality disorders. Under the brain damage category, I include the short- and long-term effects of drugs, major neurocognitive disorders (called dementia before DSM-5), cerebrovascular infarcts, traumatic brain injury, and neurodevelopmental disorders. For their exams and, if they are interested in psychiatry, I tell them to study the DSM. I explain to them that when I was in medical school my dermatology professor told us that if we could recognize the 10 most common dermatologic disorders, we would be able to recognize 90% of the skin disorders we would see. It is similar in psychiatry – thus, my five categories.
However, because I do not want them thinking that only schizophrenia causes psychosis, I let them know that at least 40 different factors cause people to be psychotic indicated by auditory hallucinations. Those 40 factors are: 1) acute alcohol intoxication, 2) alcohol withdrawal, 3) alcoholism, 4) Alzheimer’s disease, 5) benzodiazepine withdrawal, 6) cocaine abuse and addiction, 7) chemical poisoning, 8) dehydration, 9) delirium, 10) dissociative disorders, 11) electrolyte imbalances, 12) encephalopathy of various forms, 13) ecstasy, 14) extreme fatigue, 15) falling asleep, 16) fetal alcohol exposure, 17) grief, 18) hallucinogen use, 19) heroin abuse and dependence, 20) high fever, 21) hyperglycemia, 22) hypoglycemia, 23) intellectual disability, 24) lupus, 25) major depression, 26) mania, 27) methamphetamine use, 28) Parkinson’s disease, 29) phencyclidine, 30) postictal states, 31) posttraumatic stress disorder, 32) schizoid or schizotypal personality disorder, 33) schizophrenia, 34) sleep deprivation, 35) sleep paralysis, 36) solvent abuse, 37) traumatic brain injury, 38) temporal lobe epilepsy, 39) uremia. Lastly, I ask them about No. 40 – “normal” (For example, have you ever been walking down the street and thought you heard someone calling your name, but when you turned around no one was there?). Of course, there are many more causes of psychosis, but keeping it simple makes the principle easier to remember.
Regarding affective disorders, I point out to them, as I did in a previous column, that there is a huge difference between major depressive disorders, unhappiness, or sadness, grief, and demoralization. Regarding anxiety disorders, I let the medical students know that, like personality disorders, there is a lot of comorbidity. Yet, if they can distinguish brain damage, psychosis, and affective disorders from anxiety and personality disorders, that will be good enough.
In keeping with trying to help medical students not make assumptions, I always ask them what’s wrong with people who wash their hands 30 times a day. Invariably, the answer is obsessive-compulsive disorder. So, next I ask: Isn’t it possible that the person who washes his hands 30 times a day is a surgeon – or perhaps a patient with schizophrenia who thinks that Martians are beaming germs to his hands?
I guess I raise this issue because I am concerned with the future of psychiatry, and I think that my approach to medical school education provides a framework that can help students learn how to think about and provide care for psychiatric patients.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital’s Medical/Surgical-Psychiatry Inpatient Unit in Chicago, clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago, former president/CEO of the Community Mental Health Council, and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago. If you have tricks of the medical school teaching trade that you would like to share, email Dr. Bell at cpnews@mededge.com.
Use three phases of psychiatric disorders in children to guide treatment
BROOKLYN, N.Y. – , John T. Walkup, MD, said at a pediatric psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
After the onset of symptoms and over the course of time, those with untreated anxiety disorders are at risk for developing impairment in adaptation and coping, and also the development of maladaptive behaviors like substance abuse and suicidal behavior, said Dr. Walkup, chair of the department of psychiatry at Ann and Robert H. Lurie Children’s Hospital of Chicago.
The focus of his presentation was on the treatment of anxiety disorders in children, but Dr. Walkup said the impact of the three-tier progression is likely relevant to any psychiatric disorder that begins in childhood.
In essence, the scope of problems becomes more complicated over time, and without early treatment, children continue to be symptomatic. But they also develop a lifestyle based on avoidance coping and might engage in maladaptive behaviors, Dr. Walkup said. As a result, the complexity of treatment increases substantially beyond just symptom control.
Providing an example, Dr. Walkup described a child of 7 years of age with separation anxiety. If treated at the time symptoms begin, Dr. Walkup explained, cognitive-behavioral therapy and medication would be expected to be both straightforward and highly effective. If left untreated until age 14, the child might accumulate impairment in independent functioning (due to avoidance coping) at a particularly important time in development.
“In those kids, you can reduce their anxiety burden with acute treatments like [cognitive-behavioral therapy] or meds, but now you also have 7 or 8 years of accumulated impairment due to avoidance coping and parental accommodation,” Dr. Walkup said. “If those kids are going to catch up developmentally, they also need life skill support in addition to symptomatic treatment for their anxiety.”
In the case of any pediatric psychiatric disorder, early treatment has the potential to thwart progression to a more complex and treatment-resistant form, but anxiety is a particularly prominent example. In most children, anxiety is relatively easy to control if caught early but a greater challenge when fears are not contained and the child accumulates ongoing impairment.
The obstacle is that many children are not diagnosed at the time of onset, said Dr. Walkup. The solution, he suggested, is better training of pediatricians and other primary care physicians not only to identify those children but to initiate treatment in uncomplicated cases.
“The person who has that longitudinal relationship with the child is their primary care provider, and this is really the person who is going to do the best job in getting to these kids early and initiating treatment,” Dr. Walkup said.
“We have a program in Chicago where we have trained primary care physicians not only to treat anxiety and depression, but we have specifically focused them on the easiest cases in their caseload, the classic phenotypes,” Dr. Walkup reported. Using a collaborative care model, this approach has been effective in building the confidence of primary care clinicians and in reaching children when symptoms are easier to control.
Importantly, anti-anxiety medication delivered in primary care could be sufficient to help children to manage anxiety effectively when parents cooperate in helping their children manage their fears.
“People suggest that we always start with CBT, but there [are no data] to support that. I think it is a conclusion drawn from the fact that CBT works and medication has side effects,” Dr. Walkup said. He appreciates the evidence that CBT is effective, but he cautioned that this therapy is not available everywhere, and pharmacologic therapies may be as or potentially more effective for some anxiety symptoms like anxiety-related physical symptoms.
Conversely, some have expressed the opinion that drugs might be a better option in late adolescence, when the efficacy of CBT appears to diminish, but Dr. Walkup objected to that characterization as well.
“My sense is that if you treat a 7-year-old for symptoms that have lasted a year it’s very different from treating a 17-year-old who has had symptoms for a decade,” Dr. Walkup said. Referring back to the contention that psychiatric disease in children becomes more complicated with a longer duration, this might explain why “you don’t see as much immediate success” with CBT and medication in the older age groups even if this is an effective treatment tool.
Some psychiatric disorders in children, including anxiety, might resolve with age, but early recognition and treatment should be a goal because of the potential to reduce symptoms and avoidance coping, and improve long-term outcomes, Dr. Walkup reported. Ironically, it might not be just anxiety symptoms, but poor adaptation and coping that might be the most important driver of ongoing impairment.
Dr. Walkup has served as an unpaid adviser to the Anxiety Disorders of Association of America. In addition, he has received royalties from Wolters Kluwer for CME activity on childhood anxiety.
This story was updated 2/11/2019.
BROOKLYN, N.Y. – , John T. Walkup, MD, said at a pediatric psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
After the onset of symptoms and over the course of time, those with untreated anxiety disorders are at risk for developing impairment in adaptation and coping, and also the development of maladaptive behaviors like substance abuse and suicidal behavior, said Dr. Walkup, chair of the department of psychiatry at Ann and Robert H. Lurie Children’s Hospital of Chicago.
The focus of his presentation was on the treatment of anxiety disorders in children, but Dr. Walkup said the impact of the three-tier progression is likely relevant to any psychiatric disorder that begins in childhood.
In essence, the scope of problems becomes more complicated over time, and without early treatment, children continue to be symptomatic. But they also develop a lifestyle based on avoidance coping and might engage in maladaptive behaviors, Dr. Walkup said. As a result, the complexity of treatment increases substantially beyond just symptom control.
Providing an example, Dr. Walkup described a child of 7 years of age with separation anxiety. If treated at the time symptoms begin, Dr. Walkup explained, cognitive-behavioral therapy and medication would be expected to be both straightforward and highly effective. If left untreated until age 14, the child might accumulate impairment in independent functioning (due to avoidance coping) at a particularly important time in development.
“In those kids, you can reduce their anxiety burden with acute treatments like [cognitive-behavioral therapy] or meds, but now you also have 7 or 8 years of accumulated impairment due to avoidance coping and parental accommodation,” Dr. Walkup said. “If those kids are going to catch up developmentally, they also need life skill support in addition to symptomatic treatment for their anxiety.”
In the case of any pediatric psychiatric disorder, early treatment has the potential to thwart progression to a more complex and treatment-resistant form, but anxiety is a particularly prominent example. In most children, anxiety is relatively easy to control if caught early but a greater challenge when fears are not contained and the child accumulates ongoing impairment.
The obstacle is that many children are not diagnosed at the time of onset, said Dr. Walkup. The solution, he suggested, is better training of pediatricians and other primary care physicians not only to identify those children but to initiate treatment in uncomplicated cases.
“The person who has that longitudinal relationship with the child is their primary care provider, and this is really the person who is going to do the best job in getting to these kids early and initiating treatment,” Dr. Walkup said.
“We have a program in Chicago where we have trained primary care physicians not only to treat anxiety and depression, but we have specifically focused them on the easiest cases in their caseload, the classic phenotypes,” Dr. Walkup reported. Using a collaborative care model, this approach has been effective in building the confidence of primary care clinicians and in reaching children when symptoms are easier to control.
Importantly, anti-anxiety medication delivered in primary care could be sufficient to help children to manage anxiety effectively when parents cooperate in helping their children manage their fears.
“People suggest that we always start with CBT, but there [are no data] to support that. I think it is a conclusion drawn from the fact that CBT works and medication has side effects,” Dr. Walkup said. He appreciates the evidence that CBT is effective, but he cautioned that this therapy is not available everywhere, and pharmacologic therapies may be as or potentially more effective for some anxiety symptoms like anxiety-related physical symptoms.
Conversely, some have expressed the opinion that drugs might be a better option in late adolescence, when the efficacy of CBT appears to diminish, but Dr. Walkup objected to that characterization as well.
“My sense is that if you treat a 7-year-old for symptoms that have lasted a year it’s very different from treating a 17-year-old who has had symptoms for a decade,” Dr. Walkup said. Referring back to the contention that psychiatric disease in children becomes more complicated with a longer duration, this might explain why “you don’t see as much immediate success” with CBT and medication in the older age groups even if this is an effective treatment tool.
Some psychiatric disorders in children, including anxiety, might resolve with age, but early recognition and treatment should be a goal because of the potential to reduce symptoms and avoidance coping, and improve long-term outcomes, Dr. Walkup reported. Ironically, it might not be just anxiety symptoms, but poor adaptation and coping that might be the most important driver of ongoing impairment.
Dr. Walkup has served as an unpaid adviser to the Anxiety Disorders of Association of America. In addition, he has received royalties from Wolters Kluwer for CME activity on childhood anxiety.
This story was updated 2/11/2019.
BROOKLYN, N.Y. – , John T. Walkup, MD, said at a pediatric psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
After the onset of symptoms and over the course of time, those with untreated anxiety disorders are at risk for developing impairment in adaptation and coping, and also the development of maladaptive behaviors like substance abuse and suicidal behavior, said Dr. Walkup, chair of the department of psychiatry at Ann and Robert H. Lurie Children’s Hospital of Chicago.
The focus of his presentation was on the treatment of anxiety disorders in children, but Dr. Walkup said the impact of the three-tier progression is likely relevant to any psychiatric disorder that begins in childhood.
In essence, the scope of problems becomes more complicated over time, and without early treatment, children continue to be symptomatic. But they also develop a lifestyle based on avoidance coping and might engage in maladaptive behaviors, Dr. Walkup said. As a result, the complexity of treatment increases substantially beyond just symptom control.
Providing an example, Dr. Walkup described a child of 7 years of age with separation anxiety. If treated at the time symptoms begin, Dr. Walkup explained, cognitive-behavioral therapy and medication would be expected to be both straightforward and highly effective. If left untreated until age 14, the child might accumulate impairment in independent functioning (due to avoidance coping) at a particularly important time in development.
“In those kids, you can reduce their anxiety burden with acute treatments like [cognitive-behavioral therapy] or meds, but now you also have 7 or 8 years of accumulated impairment due to avoidance coping and parental accommodation,” Dr. Walkup said. “If those kids are going to catch up developmentally, they also need life skill support in addition to symptomatic treatment for their anxiety.”
In the case of any pediatric psychiatric disorder, early treatment has the potential to thwart progression to a more complex and treatment-resistant form, but anxiety is a particularly prominent example. In most children, anxiety is relatively easy to control if caught early but a greater challenge when fears are not contained and the child accumulates ongoing impairment.
The obstacle is that many children are not diagnosed at the time of onset, said Dr. Walkup. The solution, he suggested, is better training of pediatricians and other primary care physicians not only to identify those children but to initiate treatment in uncomplicated cases.
“The person who has that longitudinal relationship with the child is their primary care provider, and this is really the person who is going to do the best job in getting to these kids early and initiating treatment,” Dr. Walkup said.
“We have a program in Chicago where we have trained primary care physicians not only to treat anxiety and depression, but we have specifically focused them on the easiest cases in their caseload, the classic phenotypes,” Dr. Walkup reported. Using a collaborative care model, this approach has been effective in building the confidence of primary care clinicians and in reaching children when symptoms are easier to control.
Importantly, anti-anxiety medication delivered in primary care could be sufficient to help children to manage anxiety effectively when parents cooperate in helping their children manage their fears.
“People suggest that we always start with CBT, but there [are no data] to support that. I think it is a conclusion drawn from the fact that CBT works and medication has side effects,” Dr. Walkup said. He appreciates the evidence that CBT is effective, but he cautioned that this therapy is not available everywhere, and pharmacologic therapies may be as or potentially more effective for some anxiety symptoms like anxiety-related physical symptoms.
Conversely, some have expressed the opinion that drugs might be a better option in late adolescence, when the efficacy of CBT appears to diminish, but Dr. Walkup objected to that characterization as well.
“My sense is that if you treat a 7-year-old for symptoms that have lasted a year it’s very different from treating a 17-year-old who has had symptoms for a decade,” Dr. Walkup said. Referring back to the contention that psychiatric disease in children becomes more complicated with a longer duration, this might explain why “you don’t see as much immediate success” with CBT and medication in the older age groups even if this is an effective treatment tool.
Some psychiatric disorders in children, including anxiety, might resolve with age, but early recognition and treatment should be a goal because of the potential to reduce symptoms and avoidance coping, and improve long-term outcomes, Dr. Walkup reported. Ironically, it might not be just anxiety symptoms, but poor adaptation and coping that might be the most important driver of ongoing impairment.
Dr. Walkup has served as an unpaid adviser to the Anxiety Disorders of Association of America. In addition, he has received royalties from Wolters Kluwer for CME activity on childhood anxiety.
This story was updated 2/11/2019.
REPORTING FROM THE PSYCHOPHARMACOLOGY UPDATE INSTITUTE
Mental health patients flocking to emergency departments
Emergency department visits in the United States climbed by 15% overall from 2006 to 2014. Over the same time period, ED visits by people with mental health issues soared by 44%, according to a report from the Agency for Health Care Research & Quality.
“The extent to which ERs are now flooded with patients with mental illness is unprecedented,” David R. Rubinow, MD, chairman of the department of psychiatry at the University of North Carolina, Chapel Hill, said in an interview with CNN.
This overflow is “having a really destructive effect on health care delivery in general,” Dr. Rubinow said. “There are ERs now that are repeatedly on diversion – which means they can’t see any more patients – because there are so many patients with mental illness or behavioral problems [who] are populating the ER.”
Physicians such as Mark D. Pearlmutter, MD, are convinced that EDs have become the medical refuge for many people with mental illness. “We are the safety net,” said Dr. Pearlmutter, an emergency physician affiliated with Steward Health Care in Brighton, Mass. Dr. Pearlmutter said some patients he has seen in the ED often have dual diagnoses, such as “substance abuse and depression, for example.”
As a result of this situation, patients with psychiatric needs might not receive the care that they really need, and care might be delayed for patients with other life-threatening conditions. “The ER is not a great place if you’re a mental health patient; the cardiac patients get put in front of you, and you could end up being there for a really long time, said David Morris, PhD, a psychologist at the O’Donnell Brain Institute in Dallas.
, Dr. Pearlmutter suggested. After all, increasingly, primary care physicians are providing mental health care.
Twists on New Year’s resolutions
Some people bring in each new year by shifting their perspectives – without making resolutions.
Tim Ferriss, an entrepreneur known for blogs and podcasts on work and life, engages in what he calls “past year reviews,” where accomplishments are tallied frequently throughout the year in terms of their positive or negative effect, with the latter being ruled out for the coming year. Over a few years, he hopes, the list of negatives will shrink and the positive items will increase, according to a post on the NBC News website.
Instead of making resolutions, Oprah Winfrey keeps a journal that is updated nightly with five things that spark gratitude. “I live in the present moment. I try to find the good that’s going on in any given situation,” Ms. Winfrey said in a 2017 interview. The practice has taught her to be careful in her personal wishes.
Melinda Gates starts the new year with a single word to provide guidance. Past examples include “gentle,” “spacious,” and, last year, “grace.” Her selections, she said, have helped her sharpen her focus on the really important aspects of her life.
“[Grace] even helped me find a beam of peace through the sadness of a friend’s funeral. When I was upset or distressed, I whispered to myself: ‘Grace.’ That’s the power of a well-chosen word of the year. It makes the year better – and it helps me be better, too, she wrote in a recent LinkedIn post.
20-somethings facing challenges
A recent article in the Guardian lamented a life that is not progressing as expected.
“I am 25 and a half, single, unable to pay my rent, and the closest thing I own to a car is a broken skateboard,” wrote Juliana Piskorz. “I’m in the throes of a quarter-life crisis.”
Ms. Piskorz, who said she suffers from anxiety attacks, said her experience of this crisis manifests itself by making her want to run away, start all over, or distract herself from reality.
She is not alone. According to LinkedIn, about three-quarters of people aged 25-33 share this kind of insecurity and doubt. Low self-esteem is an important culprit, according to James Arkell, MD, a psychiatrist affiliated with the Nightingale Hospital London. “Very often, 20-somethings I see here are beautiful, talented, and have the world on a plate, but they don’t like themselves and that’s got to be about society making them feel as if they have to keep up with these unrelenting standards.”
There are other reasons for millennial despair, Ms. Piskorz speculated.
“Our childhood visions for our lives ... are no longer realistic,” she wrote. “Due to unaffordable housing, less job security, and lower incomes, the traditional ‘markers’ of adulthood, such as owning a home, getting married, and having children, are being pushed back. This has left a vacuum between our teenage years and late 20s with many of us feeling we’re navigating a no man’s land with zero clue when we’ll reach the other side.”
Seeking optimism, Ms. Piskorz noted that, as a community, millennials share many positive characteristics that should serve them well.
“We are not afraid to talk about how we feel, although we should probably talk more,” she wrote. “We stand up for the causes that we think matter; we are not afraid to try new things, and we are not willing to live a life half lived.”
Apps monitor teen angst, depression
The smartphone, often seen as a tool that fuels angst, might be a resource that could identify teenagers in trouble.
According to an article in the Washington Post, research is underway on smartphone apps that can decipher the digital footprints left by users during their Internet ramblings.
“As teens scroll through Instagram or Snapchat, tap out texts, or watch YouTube videos, they also leave digital footprints that might offer clues to their psychological well-being,” wrote article author Lindsey Tanner, of the Associated Press. “Changes in typing speed, voice tone, word choice, and how often kids stay home could signal trouble.”
“We are tracking the equivalent of a heartbeat for the human brain,” said Alex Leow, MD, PhD, an app developer, and associate professor of psychiatry and bioengineering at the University of Illinois at Chicago.
The technology is not ready for deployment because of technical glitches and, more importantly, ethical issues concerning the recording and scrutiny of a user’s personal data being roadblocks. Still, with the permission of the user, mood-detecting apps might one day be a smartphone feature. “[Users] could withdraw permission at any time, said Nick B. Allen, PhD, a psychologist at the University of Oregon, Portland, who has helped create an app that is being tested on young people who have attempted suicide.
He said the biggest hurdle is figuring out “what’s the signal and what’s the noise – what is in this enormous amount of data that people accumulate on their phone that is indicative of a mental health crisis.”
Virtues of “intellectual humility”
Intellectual humility is neither a character flaw nor a sign of being a pushover.
Instead, wrote science reporter Brian Resnick in an article posted on Vox.com, “it’s a method of thinking. It’s about entertaining the possibility that you may be wrong and being open to learning from the experience of others. Intellectual humility is about being actively curious about your blind spots.”
In an effort to promote intellectual humility in psychology, two researchers, Tal Yarkoni, PhD, and Christopher F. Chabris, PhD, launched the Loss-of-Confidence project. The project is a safe space where researchers who doubt a previous finding in psychology can recalibrate. “I do think it’s a cultural issue that people are not willing to admit mistakes,” said Julia M. Rohrer, a PhD candidate and personality psychologist at the Max Planck Institute for Human Development in Berlin who joined the team in 2017. “Our broader goal is to gently nudge the whole scientific system and psychology toward a different culture where it’s okay, normalized, and expected for researchers to admit past mistakes and not get penalized for it.”
Put another way, the aim is to foster a culture where intellectually humble, honest, and curious people can thrive. For that to occur, “we all, even the smartest among us, need to better appreciate our cognitive blind spots,” Mr. Resnick wrote. “Our minds are more imperfect and imprecise than we’d often like to admit.”
In a recent paper, Ms. Rohrer and her associates said the Loss-of-Confidence project grew out of an online discussion in the wake of a post by Dana R. Carney, PhD, and associates on power poses. In that post, Dr. Carney explains why she changed her position on the value of power poses, concluding that the data gathered by her lab at the time leading to the power poses theory (Psychol Sci. 2010 Oct 21 [10]:1363-8) were real but flimsy. “My views have been updated to reflect the evidence,” she wrote. “As such, I do not believe that ‘power pose’ effects are real.”
In the Vox.com article, Mr. Resnick wrote that intellectual humility is needed for two reasons. “One is that our culture promotes and rewards overconfidence and arrogance. At the same time, when we are wrong – out of ignorance or error – and realize it, our culture doesn’t make it easy to admit it. Humbling moments too easily can turn into moments of humiliation.”
Emergency department visits in the United States climbed by 15% overall from 2006 to 2014. Over the same time period, ED visits by people with mental health issues soared by 44%, according to a report from the Agency for Health Care Research & Quality.
“The extent to which ERs are now flooded with patients with mental illness is unprecedented,” David R. Rubinow, MD, chairman of the department of psychiatry at the University of North Carolina, Chapel Hill, said in an interview with CNN.
This overflow is “having a really destructive effect on health care delivery in general,” Dr. Rubinow said. “There are ERs now that are repeatedly on diversion – which means they can’t see any more patients – because there are so many patients with mental illness or behavioral problems [who] are populating the ER.”
Physicians such as Mark D. Pearlmutter, MD, are convinced that EDs have become the medical refuge for many people with mental illness. “We are the safety net,” said Dr. Pearlmutter, an emergency physician affiliated with Steward Health Care in Brighton, Mass. Dr. Pearlmutter said some patients he has seen in the ED often have dual diagnoses, such as “substance abuse and depression, for example.”
As a result of this situation, patients with psychiatric needs might not receive the care that they really need, and care might be delayed for patients with other life-threatening conditions. “The ER is not a great place if you’re a mental health patient; the cardiac patients get put in front of you, and you could end up being there for a really long time, said David Morris, PhD, a psychologist at the O’Donnell Brain Institute in Dallas.
, Dr. Pearlmutter suggested. After all, increasingly, primary care physicians are providing mental health care.
Twists on New Year’s resolutions
Some people bring in each new year by shifting their perspectives – without making resolutions.
Tim Ferriss, an entrepreneur known for blogs and podcasts on work and life, engages in what he calls “past year reviews,” where accomplishments are tallied frequently throughout the year in terms of their positive or negative effect, with the latter being ruled out for the coming year. Over a few years, he hopes, the list of negatives will shrink and the positive items will increase, according to a post on the NBC News website.
Instead of making resolutions, Oprah Winfrey keeps a journal that is updated nightly with five things that spark gratitude. “I live in the present moment. I try to find the good that’s going on in any given situation,” Ms. Winfrey said in a 2017 interview. The practice has taught her to be careful in her personal wishes.
Melinda Gates starts the new year with a single word to provide guidance. Past examples include “gentle,” “spacious,” and, last year, “grace.” Her selections, she said, have helped her sharpen her focus on the really important aspects of her life.
“[Grace] even helped me find a beam of peace through the sadness of a friend’s funeral. When I was upset or distressed, I whispered to myself: ‘Grace.’ That’s the power of a well-chosen word of the year. It makes the year better – and it helps me be better, too, she wrote in a recent LinkedIn post.
20-somethings facing challenges
A recent article in the Guardian lamented a life that is not progressing as expected.
“I am 25 and a half, single, unable to pay my rent, and the closest thing I own to a car is a broken skateboard,” wrote Juliana Piskorz. “I’m in the throes of a quarter-life crisis.”
Ms. Piskorz, who said she suffers from anxiety attacks, said her experience of this crisis manifests itself by making her want to run away, start all over, or distract herself from reality.
She is not alone. According to LinkedIn, about three-quarters of people aged 25-33 share this kind of insecurity and doubt. Low self-esteem is an important culprit, according to James Arkell, MD, a psychiatrist affiliated with the Nightingale Hospital London. “Very often, 20-somethings I see here are beautiful, talented, and have the world on a plate, but they don’t like themselves and that’s got to be about society making them feel as if they have to keep up with these unrelenting standards.”
There are other reasons for millennial despair, Ms. Piskorz speculated.
“Our childhood visions for our lives ... are no longer realistic,” she wrote. “Due to unaffordable housing, less job security, and lower incomes, the traditional ‘markers’ of adulthood, such as owning a home, getting married, and having children, are being pushed back. This has left a vacuum between our teenage years and late 20s with many of us feeling we’re navigating a no man’s land with zero clue when we’ll reach the other side.”
Seeking optimism, Ms. Piskorz noted that, as a community, millennials share many positive characteristics that should serve them well.
“We are not afraid to talk about how we feel, although we should probably talk more,” she wrote. “We stand up for the causes that we think matter; we are not afraid to try new things, and we are not willing to live a life half lived.”
Apps monitor teen angst, depression
The smartphone, often seen as a tool that fuels angst, might be a resource that could identify teenagers in trouble.
According to an article in the Washington Post, research is underway on smartphone apps that can decipher the digital footprints left by users during their Internet ramblings.
“As teens scroll through Instagram or Snapchat, tap out texts, or watch YouTube videos, they also leave digital footprints that might offer clues to their psychological well-being,” wrote article author Lindsey Tanner, of the Associated Press. “Changes in typing speed, voice tone, word choice, and how often kids stay home could signal trouble.”
“We are tracking the equivalent of a heartbeat for the human brain,” said Alex Leow, MD, PhD, an app developer, and associate professor of psychiatry and bioengineering at the University of Illinois at Chicago.
The technology is not ready for deployment because of technical glitches and, more importantly, ethical issues concerning the recording and scrutiny of a user’s personal data being roadblocks. Still, with the permission of the user, mood-detecting apps might one day be a smartphone feature. “[Users] could withdraw permission at any time, said Nick B. Allen, PhD, a psychologist at the University of Oregon, Portland, who has helped create an app that is being tested on young people who have attempted suicide.
He said the biggest hurdle is figuring out “what’s the signal and what’s the noise – what is in this enormous amount of data that people accumulate on their phone that is indicative of a mental health crisis.”
Virtues of “intellectual humility”
Intellectual humility is neither a character flaw nor a sign of being a pushover.
Instead, wrote science reporter Brian Resnick in an article posted on Vox.com, “it’s a method of thinking. It’s about entertaining the possibility that you may be wrong and being open to learning from the experience of others. Intellectual humility is about being actively curious about your blind spots.”
In an effort to promote intellectual humility in psychology, two researchers, Tal Yarkoni, PhD, and Christopher F. Chabris, PhD, launched the Loss-of-Confidence project. The project is a safe space where researchers who doubt a previous finding in psychology can recalibrate. “I do think it’s a cultural issue that people are not willing to admit mistakes,” said Julia M. Rohrer, a PhD candidate and personality psychologist at the Max Planck Institute for Human Development in Berlin who joined the team in 2017. “Our broader goal is to gently nudge the whole scientific system and psychology toward a different culture where it’s okay, normalized, and expected for researchers to admit past mistakes and not get penalized for it.”
Put another way, the aim is to foster a culture where intellectually humble, honest, and curious people can thrive. For that to occur, “we all, even the smartest among us, need to better appreciate our cognitive blind spots,” Mr. Resnick wrote. “Our minds are more imperfect and imprecise than we’d often like to admit.”
In a recent paper, Ms. Rohrer and her associates said the Loss-of-Confidence project grew out of an online discussion in the wake of a post by Dana R. Carney, PhD, and associates on power poses. In that post, Dr. Carney explains why she changed her position on the value of power poses, concluding that the data gathered by her lab at the time leading to the power poses theory (Psychol Sci. 2010 Oct 21 [10]:1363-8) were real but flimsy. “My views have been updated to reflect the evidence,” she wrote. “As such, I do not believe that ‘power pose’ effects are real.”
In the Vox.com article, Mr. Resnick wrote that intellectual humility is needed for two reasons. “One is that our culture promotes and rewards overconfidence and arrogance. At the same time, when we are wrong – out of ignorance or error – and realize it, our culture doesn’t make it easy to admit it. Humbling moments too easily can turn into moments of humiliation.”
Emergency department visits in the United States climbed by 15% overall from 2006 to 2014. Over the same time period, ED visits by people with mental health issues soared by 44%, according to a report from the Agency for Health Care Research & Quality.
“The extent to which ERs are now flooded with patients with mental illness is unprecedented,” David R. Rubinow, MD, chairman of the department of psychiatry at the University of North Carolina, Chapel Hill, said in an interview with CNN.
This overflow is “having a really destructive effect on health care delivery in general,” Dr. Rubinow said. “There are ERs now that are repeatedly on diversion – which means they can’t see any more patients – because there are so many patients with mental illness or behavioral problems [who] are populating the ER.”
Physicians such as Mark D. Pearlmutter, MD, are convinced that EDs have become the medical refuge for many people with mental illness. “We are the safety net,” said Dr. Pearlmutter, an emergency physician affiliated with Steward Health Care in Brighton, Mass. Dr. Pearlmutter said some patients he has seen in the ED often have dual diagnoses, such as “substance abuse and depression, for example.”
As a result of this situation, patients with psychiatric needs might not receive the care that they really need, and care might be delayed for patients with other life-threatening conditions. “The ER is not a great place if you’re a mental health patient; the cardiac patients get put in front of you, and you could end up being there for a really long time, said David Morris, PhD, a psychologist at the O’Donnell Brain Institute in Dallas.
, Dr. Pearlmutter suggested. After all, increasingly, primary care physicians are providing mental health care.
Twists on New Year’s resolutions
Some people bring in each new year by shifting their perspectives – without making resolutions.
Tim Ferriss, an entrepreneur known for blogs and podcasts on work and life, engages in what he calls “past year reviews,” where accomplishments are tallied frequently throughout the year in terms of their positive or negative effect, with the latter being ruled out for the coming year. Over a few years, he hopes, the list of negatives will shrink and the positive items will increase, according to a post on the NBC News website.
Instead of making resolutions, Oprah Winfrey keeps a journal that is updated nightly with five things that spark gratitude. “I live in the present moment. I try to find the good that’s going on in any given situation,” Ms. Winfrey said in a 2017 interview. The practice has taught her to be careful in her personal wishes.
Melinda Gates starts the new year with a single word to provide guidance. Past examples include “gentle,” “spacious,” and, last year, “grace.” Her selections, she said, have helped her sharpen her focus on the really important aspects of her life.
“[Grace] even helped me find a beam of peace through the sadness of a friend’s funeral. When I was upset or distressed, I whispered to myself: ‘Grace.’ That’s the power of a well-chosen word of the year. It makes the year better – and it helps me be better, too, she wrote in a recent LinkedIn post.
20-somethings facing challenges
A recent article in the Guardian lamented a life that is not progressing as expected.
“I am 25 and a half, single, unable to pay my rent, and the closest thing I own to a car is a broken skateboard,” wrote Juliana Piskorz. “I’m in the throes of a quarter-life crisis.”
Ms. Piskorz, who said she suffers from anxiety attacks, said her experience of this crisis manifests itself by making her want to run away, start all over, or distract herself from reality.
She is not alone. According to LinkedIn, about three-quarters of people aged 25-33 share this kind of insecurity and doubt. Low self-esteem is an important culprit, according to James Arkell, MD, a psychiatrist affiliated with the Nightingale Hospital London. “Very often, 20-somethings I see here are beautiful, talented, and have the world on a plate, but they don’t like themselves and that’s got to be about society making them feel as if they have to keep up with these unrelenting standards.”
There are other reasons for millennial despair, Ms. Piskorz speculated.
“Our childhood visions for our lives ... are no longer realistic,” she wrote. “Due to unaffordable housing, less job security, and lower incomes, the traditional ‘markers’ of adulthood, such as owning a home, getting married, and having children, are being pushed back. This has left a vacuum between our teenage years and late 20s with many of us feeling we’re navigating a no man’s land with zero clue when we’ll reach the other side.”
Seeking optimism, Ms. Piskorz noted that, as a community, millennials share many positive characteristics that should serve them well.
“We are not afraid to talk about how we feel, although we should probably talk more,” she wrote. “We stand up for the causes that we think matter; we are not afraid to try new things, and we are not willing to live a life half lived.”
Apps monitor teen angst, depression
The smartphone, often seen as a tool that fuels angst, might be a resource that could identify teenagers in trouble.
According to an article in the Washington Post, research is underway on smartphone apps that can decipher the digital footprints left by users during their Internet ramblings.
“As teens scroll through Instagram or Snapchat, tap out texts, or watch YouTube videos, they also leave digital footprints that might offer clues to their psychological well-being,” wrote article author Lindsey Tanner, of the Associated Press. “Changes in typing speed, voice tone, word choice, and how often kids stay home could signal trouble.”
“We are tracking the equivalent of a heartbeat for the human brain,” said Alex Leow, MD, PhD, an app developer, and associate professor of psychiatry and bioengineering at the University of Illinois at Chicago.
The technology is not ready for deployment because of technical glitches and, more importantly, ethical issues concerning the recording and scrutiny of a user’s personal data being roadblocks. Still, with the permission of the user, mood-detecting apps might one day be a smartphone feature. “[Users] could withdraw permission at any time, said Nick B. Allen, PhD, a psychologist at the University of Oregon, Portland, who has helped create an app that is being tested on young people who have attempted suicide.
He said the biggest hurdle is figuring out “what’s the signal and what’s the noise – what is in this enormous amount of data that people accumulate on their phone that is indicative of a mental health crisis.”
Virtues of “intellectual humility”
Intellectual humility is neither a character flaw nor a sign of being a pushover.
Instead, wrote science reporter Brian Resnick in an article posted on Vox.com, “it’s a method of thinking. It’s about entertaining the possibility that you may be wrong and being open to learning from the experience of others. Intellectual humility is about being actively curious about your blind spots.”
In an effort to promote intellectual humility in psychology, two researchers, Tal Yarkoni, PhD, and Christopher F. Chabris, PhD, launched the Loss-of-Confidence project. The project is a safe space where researchers who doubt a previous finding in psychology can recalibrate. “I do think it’s a cultural issue that people are not willing to admit mistakes,” said Julia M. Rohrer, a PhD candidate and personality psychologist at the Max Planck Institute for Human Development in Berlin who joined the team in 2017. “Our broader goal is to gently nudge the whole scientific system and psychology toward a different culture where it’s okay, normalized, and expected for researchers to admit past mistakes and not get penalized for it.”
Put another way, the aim is to foster a culture where intellectually humble, honest, and curious people can thrive. For that to occur, “we all, even the smartest among us, need to better appreciate our cognitive blind spots,” Mr. Resnick wrote. “Our minds are more imperfect and imprecise than we’d often like to admit.”
In a recent paper, Ms. Rohrer and her associates said the Loss-of-Confidence project grew out of an online discussion in the wake of a post by Dana R. Carney, PhD, and associates on power poses. In that post, Dr. Carney explains why she changed her position on the value of power poses, concluding that the data gathered by her lab at the time leading to the power poses theory (Psychol Sci. 2010 Oct 21 [10]:1363-8) were real but flimsy. “My views have been updated to reflect the evidence,” she wrote. “As such, I do not believe that ‘power pose’ effects are real.”
In the Vox.com article, Mr. Resnick wrote that intellectual humility is needed for two reasons. “One is that our culture promotes and rewards overconfidence and arrogance. At the same time, when we are wrong – out of ignorance or error – and realize it, our culture doesn’t make it easy to admit it. Humbling moments too easily can turn into moments of humiliation.”
Single-dose propranolol tied to ‘selective erasure’ of anxiety disorders
BARCELONA – A single 40-mg dose of oral propranolol, judiciously timed, constitutes an outside-the-box yet highly promising treatment for anxiety disorders, and perhaps for posttraumatic stress disorder as well, Marieke Soeter, PhD, said at the annual congress of the European College of Neuropsychopharmacology.
The concept here is that the beta-blocker, when given with a brief therapist-led reactivation of a fear memory, blocks beta-adrenergic receptors in the brain so as to interfere with the specific proteins required for reconsolidation of that memory, thereby disrupting the reconsolidation process and neutralizing subsequent expression of that memory in its toxic form. In effect, timely administration of one dose of propranolol, a drug that readily crosses the blood/brain barrier, achieves pharmacologically induced amnesia regarding the learned fear, explained Dr. Soeter, a clinical psychologist at TNO, the Netherlands Organization for Scientific Research, an independent nonprofit translational research organization.
“It looks like permanent fear erasure. You can never say that something is erased, but we have not been able to get it back,” she said. “Propranolol achieves selective erasure: It targets the emotional component, but knowledge is intact. They know what happened, but they aren’t scared anymore. The fear association is affected, but not the innate fear response to a threat stimulus, so it doesn’t alter reactions to potentially dangerous situations, which is important. If there is a bomb, they still know to run away from it.”
This single-session therapy addressing what psychologists call fear memory reconsolidation is totally outside the box relative to contemporary psychotherapy for anxiety disorders, which typically entails gradual fear extinction learning requiring multiple treatment sessions. But contemporary psychotherapy for anxiety disorders leaves much room for improvement, given that up to 60% of patients experience relapse. That’s probably because the original fear memory remains intact and resurfaces at some point despite initial treatment success, according to Dr. Soeter.
Nearly 2 decades ago, other investigators showed in animal studies that fear memories are not necessarily permanent. Rather, they are modifiable, and even erasable, during the vulnerable period that occurs when the memories are reactivated and become labile.
Later, Dr. Soeter – then at the University of Amsterdam – and her colleagues demonstrated the same phenomenon using Pavlovian fear-conditioning techniques involving pictures and electric shocks in healthy human volunteers. They showed that a dose of propranolol given before memory reactivation blocked the fear response, while nadolol, a beta-blocker that does not cross the blood/brain barrier, did not.
However, since the fear memories they could ethically induce in the psychology laboratory are far less intense than those experienced by patients with anxiety disorders, the researchers next conducted a randomized, double-blind clinical trial in 45 individuals with arachnophobia. Fifteen received 40 mg of propranolol after spending 2 minutes in proximity to a large tarantula, 15 got placebo, and another 15 received propranolol without exposure to a tarantula. One week later, all patients who received propranolol with spider exposure were able to approach and actually pet the tarantula. Pharmacologic disruption of reconsolidation and storage of their fear memory had turned avoidance behavior into approach behavior. This benefit was maintained for at least a year after the brief treatment session (Biol Psychiatry. 2015 Dec 15;78[12]:880-6).
“Interestingly, there was no direct effect of propranolol on spider beliefs. Therefore, do we need treatment that targets the cognitive level? These findings challenge one of the fundamental tenets of cognitive-behavioral therapy that emphasizes changes in cognition as central to behavioral modification,” Dr. Soeter said.
Most recently, she and a coinvestigator have been working to pin down the precise conditions under which memory reconsolidation can be targeted to extinguish fear memories. They have shown in a 30-subject study that the process is both time- and sleep-dependent. The propranolol must be given within roughly an hour before to 1 hour after therapeutic reactivation of the fear memory to be effective. And sleep is an absolute necessity: When subjects were rechallenged 12 hours after memory reactivation and administration of propranolol earlier on the same day, with no opportunity for sleep, there was no therapeutic effect: The disturbing fear memory was elicited. However, when subjects were rechallenged 12 hours after taking propranolol the previous day – that is, after a night’s sleep – the fear memory was gone (Nat Commun. 2018 Apr 3;9[1]:1316. doi: 10.1038/s41467-018-03659-1).
“Postretrieval amnesia requires sleep to happen. ,” Dr. Soeter said. It’s still unclear, however, how much sleep is required. Perhaps a nap will turn out to be sufficient, she said.
Colleagues at the University of Amsterdam are now using single-dose propranolol-based therapy in patients with a wide range of phobias.
“The effects are pretty amazing,” Dr. Soeter said. “Everything is treatable. It’s almost too good to be true, but these are our findings.”
Based upon her favorable anecdotal experience in treating a Dutch military veteran with severe combat-related PTSD of 10 years’ duration which had proved resistant to multiple conventional and unconventional interventions, a pilot study of single-dose propranolol with traumatic memory reactivation is now being planned in patients with war-related PTSD.
“After one pill and a 20-minute session, this veteran with severe chronic PTSD has no more nightmares, insomnia, or alcohol problems, and he now travels the world,” she said.
Her research met with an enthusiastic reception from other speakers at the ECNP session on PTSD. Eric Vermetten, MD, PhD, welcomed the concept that pharmacologic therapy upon reexposure to fearful cues can impede the molecular and cellular cascade required to reestablish fearful memories. This also is the basis for the extremely encouraging, albeit preliminary, clinical data on ketamine, an N-methyl-D-aspartate receptor antagonist, as well as 3,4-Methylenedioxymethamphetamine (MDMA) for therapeutic manipulation of trauma memories.
“Targeting reconsolidation of existing fear memories is worthy of looking into further,” declared Dr. Vermetten, professor of psychiatry at Leiden (the Netherlands) University and a military mental health researcher for the Dutch Ministry of Defense.
New thinking regarding pharmacotherapy for PTSD is sorely needed, he added. He endorsed a consensus statement by the PTSD Psychopharmacology Working Group that decried what was termed a crisis in pharmacotherapy of PTSD (Biol Psychiatry. 2017 Oct 1;82[7]:e51-e59. doi: 10.1016/j.biopsych.2017.03.007. Epub 2017 Mar 14).
“We only have two [Food and Drug Administration]-approved medications for PTSD – sertraline and paroxetine – and they were approved back in 2001,” Dr. Vermetten noted. “Research has stalled, and there is a void in new drug development.”
Dr. Soeter’s study of the time- and sleep-dependent nature of propranolol-induced amnesia was supported by the Netherlands Organization for Scientific Research, where she is employed.
BARCELONA – A single 40-mg dose of oral propranolol, judiciously timed, constitutes an outside-the-box yet highly promising treatment for anxiety disorders, and perhaps for posttraumatic stress disorder as well, Marieke Soeter, PhD, said at the annual congress of the European College of Neuropsychopharmacology.
The concept here is that the beta-blocker, when given with a brief therapist-led reactivation of a fear memory, blocks beta-adrenergic receptors in the brain so as to interfere with the specific proteins required for reconsolidation of that memory, thereby disrupting the reconsolidation process and neutralizing subsequent expression of that memory in its toxic form. In effect, timely administration of one dose of propranolol, a drug that readily crosses the blood/brain barrier, achieves pharmacologically induced amnesia regarding the learned fear, explained Dr. Soeter, a clinical psychologist at TNO, the Netherlands Organization for Scientific Research, an independent nonprofit translational research organization.
“It looks like permanent fear erasure. You can never say that something is erased, but we have not been able to get it back,” she said. “Propranolol achieves selective erasure: It targets the emotional component, but knowledge is intact. They know what happened, but they aren’t scared anymore. The fear association is affected, but not the innate fear response to a threat stimulus, so it doesn’t alter reactions to potentially dangerous situations, which is important. If there is a bomb, they still know to run away from it.”
This single-session therapy addressing what psychologists call fear memory reconsolidation is totally outside the box relative to contemporary psychotherapy for anxiety disorders, which typically entails gradual fear extinction learning requiring multiple treatment sessions. But contemporary psychotherapy for anxiety disorders leaves much room for improvement, given that up to 60% of patients experience relapse. That’s probably because the original fear memory remains intact and resurfaces at some point despite initial treatment success, according to Dr. Soeter.
Nearly 2 decades ago, other investigators showed in animal studies that fear memories are not necessarily permanent. Rather, they are modifiable, and even erasable, during the vulnerable period that occurs when the memories are reactivated and become labile.
Later, Dr. Soeter – then at the University of Amsterdam – and her colleagues demonstrated the same phenomenon using Pavlovian fear-conditioning techniques involving pictures and electric shocks in healthy human volunteers. They showed that a dose of propranolol given before memory reactivation blocked the fear response, while nadolol, a beta-blocker that does not cross the blood/brain barrier, did not.
However, since the fear memories they could ethically induce in the psychology laboratory are far less intense than those experienced by patients with anxiety disorders, the researchers next conducted a randomized, double-blind clinical trial in 45 individuals with arachnophobia. Fifteen received 40 mg of propranolol after spending 2 minutes in proximity to a large tarantula, 15 got placebo, and another 15 received propranolol without exposure to a tarantula. One week later, all patients who received propranolol with spider exposure were able to approach and actually pet the tarantula. Pharmacologic disruption of reconsolidation and storage of their fear memory had turned avoidance behavior into approach behavior. This benefit was maintained for at least a year after the brief treatment session (Biol Psychiatry. 2015 Dec 15;78[12]:880-6).
“Interestingly, there was no direct effect of propranolol on spider beliefs. Therefore, do we need treatment that targets the cognitive level? These findings challenge one of the fundamental tenets of cognitive-behavioral therapy that emphasizes changes in cognition as central to behavioral modification,” Dr. Soeter said.
Most recently, she and a coinvestigator have been working to pin down the precise conditions under which memory reconsolidation can be targeted to extinguish fear memories. They have shown in a 30-subject study that the process is both time- and sleep-dependent. The propranolol must be given within roughly an hour before to 1 hour after therapeutic reactivation of the fear memory to be effective. And sleep is an absolute necessity: When subjects were rechallenged 12 hours after memory reactivation and administration of propranolol earlier on the same day, with no opportunity for sleep, there was no therapeutic effect: The disturbing fear memory was elicited. However, when subjects were rechallenged 12 hours after taking propranolol the previous day – that is, after a night’s sleep – the fear memory was gone (Nat Commun. 2018 Apr 3;9[1]:1316. doi: 10.1038/s41467-018-03659-1).
“Postretrieval amnesia requires sleep to happen. ,” Dr. Soeter said. It’s still unclear, however, how much sleep is required. Perhaps a nap will turn out to be sufficient, she said.
Colleagues at the University of Amsterdam are now using single-dose propranolol-based therapy in patients with a wide range of phobias.
“The effects are pretty amazing,” Dr. Soeter said. “Everything is treatable. It’s almost too good to be true, but these are our findings.”
Based upon her favorable anecdotal experience in treating a Dutch military veteran with severe combat-related PTSD of 10 years’ duration which had proved resistant to multiple conventional and unconventional interventions, a pilot study of single-dose propranolol with traumatic memory reactivation is now being planned in patients with war-related PTSD.
“After one pill and a 20-minute session, this veteran with severe chronic PTSD has no more nightmares, insomnia, or alcohol problems, and he now travels the world,” she said.
Her research met with an enthusiastic reception from other speakers at the ECNP session on PTSD. Eric Vermetten, MD, PhD, welcomed the concept that pharmacologic therapy upon reexposure to fearful cues can impede the molecular and cellular cascade required to reestablish fearful memories. This also is the basis for the extremely encouraging, albeit preliminary, clinical data on ketamine, an N-methyl-D-aspartate receptor antagonist, as well as 3,4-Methylenedioxymethamphetamine (MDMA) for therapeutic manipulation of trauma memories.
“Targeting reconsolidation of existing fear memories is worthy of looking into further,” declared Dr. Vermetten, professor of psychiatry at Leiden (the Netherlands) University and a military mental health researcher for the Dutch Ministry of Defense.
New thinking regarding pharmacotherapy for PTSD is sorely needed, he added. He endorsed a consensus statement by the PTSD Psychopharmacology Working Group that decried what was termed a crisis in pharmacotherapy of PTSD (Biol Psychiatry. 2017 Oct 1;82[7]:e51-e59. doi: 10.1016/j.biopsych.2017.03.007. Epub 2017 Mar 14).
“We only have two [Food and Drug Administration]-approved medications for PTSD – sertraline and paroxetine – and they were approved back in 2001,” Dr. Vermetten noted. “Research has stalled, and there is a void in new drug development.”
Dr. Soeter’s study of the time- and sleep-dependent nature of propranolol-induced amnesia was supported by the Netherlands Organization for Scientific Research, where she is employed.
BARCELONA – A single 40-mg dose of oral propranolol, judiciously timed, constitutes an outside-the-box yet highly promising treatment for anxiety disorders, and perhaps for posttraumatic stress disorder as well, Marieke Soeter, PhD, said at the annual congress of the European College of Neuropsychopharmacology.
The concept here is that the beta-blocker, when given with a brief therapist-led reactivation of a fear memory, blocks beta-adrenergic receptors in the brain so as to interfere with the specific proteins required for reconsolidation of that memory, thereby disrupting the reconsolidation process and neutralizing subsequent expression of that memory in its toxic form. In effect, timely administration of one dose of propranolol, a drug that readily crosses the blood/brain barrier, achieves pharmacologically induced amnesia regarding the learned fear, explained Dr. Soeter, a clinical psychologist at TNO, the Netherlands Organization for Scientific Research, an independent nonprofit translational research organization.
“It looks like permanent fear erasure. You can never say that something is erased, but we have not been able to get it back,” she said. “Propranolol achieves selective erasure: It targets the emotional component, but knowledge is intact. They know what happened, but they aren’t scared anymore. The fear association is affected, but not the innate fear response to a threat stimulus, so it doesn’t alter reactions to potentially dangerous situations, which is important. If there is a bomb, they still know to run away from it.”
This single-session therapy addressing what psychologists call fear memory reconsolidation is totally outside the box relative to contemporary psychotherapy for anxiety disorders, which typically entails gradual fear extinction learning requiring multiple treatment sessions. But contemporary psychotherapy for anxiety disorders leaves much room for improvement, given that up to 60% of patients experience relapse. That’s probably because the original fear memory remains intact and resurfaces at some point despite initial treatment success, according to Dr. Soeter.
Nearly 2 decades ago, other investigators showed in animal studies that fear memories are not necessarily permanent. Rather, they are modifiable, and even erasable, during the vulnerable period that occurs when the memories are reactivated and become labile.
Later, Dr. Soeter – then at the University of Amsterdam – and her colleagues demonstrated the same phenomenon using Pavlovian fear-conditioning techniques involving pictures and electric shocks in healthy human volunteers. They showed that a dose of propranolol given before memory reactivation blocked the fear response, while nadolol, a beta-blocker that does not cross the blood/brain barrier, did not.
However, since the fear memories they could ethically induce in the psychology laboratory are far less intense than those experienced by patients with anxiety disorders, the researchers next conducted a randomized, double-blind clinical trial in 45 individuals with arachnophobia. Fifteen received 40 mg of propranolol after spending 2 minutes in proximity to a large tarantula, 15 got placebo, and another 15 received propranolol without exposure to a tarantula. One week later, all patients who received propranolol with spider exposure were able to approach and actually pet the tarantula. Pharmacologic disruption of reconsolidation and storage of their fear memory had turned avoidance behavior into approach behavior. This benefit was maintained for at least a year after the brief treatment session (Biol Psychiatry. 2015 Dec 15;78[12]:880-6).
“Interestingly, there was no direct effect of propranolol on spider beliefs. Therefore, do we need treatment that targets the cognitive level? These findings challenge one of the fundamental tenets of cognitive-behavioral therapy that emphasizes changes in cognition as central to behavioral modification,” Dr. Soeter said.
Most recently, she and a coinvestigator have been working to pin down the precise conditions under which memory reconsolidation can be targeted to extinguish fear memories. They have shown in a 30-subject study that the process is both time- and sleep-dependent. The propranolol must be given within roughly an hour before to 1 hour after therapeutic reactivation of the fear memory to be effective. And sleep is an absolute necessity: When subjects were rechallenged 12 hours after memory reactivation and administration of propranolol earlier on the same day, with no opportunity for sleep, there was no therapeutic effect: The disturbing fear memory was elicited. However, when subjects were rechallenged 12 hours after taking propranolol the previous day – that is, after a night’s sleep – the fear memory was gone (Nat Commun. 2018 Apr 3;9[1]:1316. doi: 10.1038/s41467-018-03659-1).
“Postretrieval amnesia requires sleep to happen. ,” Dr. Soeter said. It’s still unclear, however, how much sleep is required. Perhaps a nap will turn out to be sufficient, she said.
Colleagues at the University of Amsterdam are now using single-dose propranolol-based therapy in patients with a wide range of phobias.
“The effects are pretty amazing,” Dr. Soeter said. “Everything is treatable. It’s almost too good to be true, but these are our findings.”
Based upon her favorable anecdotal experience in treating a Dutch military veteran with severe combat-related PTSD of 10 years’ duration which had proved resistant to multiple conventional and unconventional interventions, a pilot study of single-dose propranolol with traumatic memory reactivation is now being planned in patients with war-related PTSD.
“After one pill and a 20-minute session, this veteran with severe chronic PTSD has no more nightmares, insomnia, or alcohol problems, and he now travels the world,” she said.
Her research met with an enthusiastic reception from other speakers at the ECNP session on PTSD. Eric Vermetten, MD, PhD, welcomed the concept that pharmacologic therapy upon reexposure to fearful cues can impede the molecular and cellular cascade required to reestablish fearful memories. This also is the basis for the extremely encouraging, albeit preliminary, clinical data on ketamine, an N-methyl-D-aspartate receptor antagonist, as well as 3,4-Methylenedioxymethamphetamine (MDMA) for therapeutic manipulation of trauma memories.
“Targeting reconsolidation of existing fear memories is worthy of looking into further,” declared Dr. Vermetten, professor of psychiatry at Leiden (the Netherlands) University and a military mental health researcher for the Dutch Ministry of Defense.
New thinking regarding pharmacotherapy for PTSD is sorely needed, he added. He endorsed a consensus statement by the PTSD Psychopharmacology Working Group that decried what was termed a crisis in pharmacotherapy of PTSD (Biol Psychiatry. 2017 Oct 1;82[7]:e51-e59. doi: 10.1016/j.biopsych.2017.03.007. Epub 2017 Mar 14).
“We only have two [Food and Drug Administration]-approved medications for PTSD – sertraline and paroxetine – and they were approved back in 2001,” Dr. Vermetten noted. “Research has stalled, and there is a void in new drug development.”
Dr. Soeter’s study of the time- and sleep-dependent nature of propranolol-induced amnesia was supported by the Netherlands Organization for Scientific Research, where she is employed.
REPORTING FROM THE ECNP CONGRESS
Key clinical point: A single 40-mg dose of oral propranolol, judiciously timed, is a highly promising novel treatment for anxiety disorders.
Major finding: The beta-blocker must be given within an hour before to an hour after therapist-facilitated reactivation of the fear memory.
Study details: This study included 30 healthy volunteers who underwent a cued Pavlovian fear-conditioning program.
Disclosures: Dr. Soeter’s study of the time- and sleep-dependent nature of propranolol-induced amnesia was supported by the Netherlands Organization for Scientific Research, where she is employed.
Best of Psychopharmacology: Stimulants, ketamine, benzodiazapines
In this episode we go back to the summer for two master classes on ketamine and stimulants, respectively and we drop in on two conversations between Lorenzo Norris, MD on anxiety and comorbid ADHD as well as a conversation on benzodiazapines. The Psychcast will be back with new content in 2019.
Amazon
Apple
Google
Spotify
In this episode we go back to the summer for two master classes on ketamine and stimulants, respectively and we drop in on two conversations between Lorenzo Norris, MD on anxiety and comorbid ADHD as well as a conversation on benzodiazapines. The Psychcast will be back with new content in 2019.
Amazon
Apple
Google
Spotify
In this episode we go back to the summer for two master classes on ketamine and stimulants, respectively and we drop in on two conversations between Lorenzo Norris, MD on anxiety and comorbid ADHD as well as a conversation on benzodiazapines. The Psychcast will be back with new content in 2019.
Amazon
Apple
Google
Spotify
‘Error neuron’ EEG findings could open up future clinical applications
, and this activity can be tracked through a scalp EEG pattern called error-related negativity, according to findings from experiments carried out during intracranial EEG recordings of candidates for surgical treatment of epilepsy.
“Our results suggest that coordinated neural activity can serve as a substrate for information routing that enables the performance-monitoring system to communicate the need for behavioral control to other brain regions, including those that maintain flexible goal information, such as the lateral prefrontal cortex and the frontal polar cortex,” first author Zhongzheng Fu, a PhD student at the California Institute of Technology in Pasadena, Calif., and Cedars-Sinai Medical Center, Los Angeles, and his colleagues reported in Neuron.
The findings offer insights that could lead to treatments for conditions in which the important executive function task of error self-monitoring is unbalanced, such as obsessive-compulsive disorder and schizophrenia, the authors noted in a press release.
“We discovered that the activity of error neurons correlates with the size of the ERN [error-related negativity],” Mr. Fu said. “This identifies the brain area that causes the ERN and helps explain what it signifies. This new insight might allow doctors to use the ERN as a standard tool to diagnose mental diseases and monitor responses to treatment.”
Error neuron firing and intracranial ERN occurred first in pre-supplementary motor area (pre-SMA), then in the dorsal anterior cingulate cortex (dACC) about 50 ms later, with significant correlations between firing and intracranial ERN in both locations. In dACC, this activity, with error-integrating neuron responses, correlated with magnitude of post-error slowing (PES).
Previous research suggested a link between “the detection of self-generated errors, as reflected in the ERN, with changes in cognitive control, as exhibited behaviorally in PES,” the investigators wrote. “However, several electroencephalogram (EEG) studies have failed to find a significant relationship between PES and ERN.”
The present study involved intracranial EEG of 29 candidates for surgical treatment of epilepsy and scalp EEG of 12 control participants, with each modality measuring activity in the frontal cortex. Both cohorts performed a rapid version of the color-word Stroop task, in which the words “red,” “green,” or “blue” were printed either in corresponding or noncorresponding colors of red, green, or blue. Subjects were presented various color-word combinations while being asked to click one of three buttons indicating the color of the word as quickly as possible. The investigators monitored neuronal activity throughout, discarding responses that were too slow.
As found in previous trials, the subjects demonstrated the “Stroop effect,” which refers to a slower response when word and color are incongruent (224.9 ms difference; P less than .001). As anticipated, correct responses following correct responses were faster than were correct responses following erroneous responses, which defines PES.
In the intracranial EEG group, the investigators isolated 1,171 neurons, of which 618 were located in dACC and 553 in pre-SMA. Using a Poisson regression model and correlations with erroneous responses, the investigators identified 99 “type I” error neurons in dACC and 118 in pre-SMA, based on higher frequency of firing during erroneous responses than during correct responses. At a single-cell level, error neuron mean spike rates were highest when intracranial ERN amplitude was greatest, such that error neuron firing in dACC and pre-SMA had maximal likelihood ratios of 7.9 (P = .01) and 15.1 (P less than .001), respectively. The strength of correlation between intracranial ERN and error neuron firing rate was directly related to PES magnitude exclusively in the dACC (maximum likelihood ratio of 13.9; P = .015). In post-error trials, faster error-integrating neuron firing rates in dACC predicted greater PES (maximal likelihood ratio of 18.3; P less than .001).
The study was funded by the National Institutes of Health, the McKnight Endowment for Neuroscience, and the National Science Foundation. The authors declared no conflicts of interest.
SOURCE: Fu Z et al. Neuron. 2018 Dec 4. doi: 10.1016/j.neuron.2018.11.016
, and this activity can be tracked through a scalp EEG pattern called error-related negativity, according to findings from experiments carried out during intracranial EEG recordings of candidates for surgical treatment of epilepsy.
“Our results suggest that coordinated neural activity can serve as a substrate for information routing that enables the performance-monitoring system to communicate the need for behavioral control to other brain regions, including those that maintain flexible goal information, such as the lateral prefrontal cortex and the frontal polar cortex,” first author Zhongzheng Fu, a PhD student at the California Institute of Technology in Pasadena, Calif., and Cedars-Sinai Medical Center, Los Angeles, and his colleagues reported in Neuron.
The findings offer insights that could lead to treatments for conditions in which the important executive function task of error self-monitoring is unbalanced, such as obsessive-compulsive disorder and schizophrenia, the authors noted in a press release.
“We discovered that the activity of error neurons correlates with the size of the ERN [error-related negativity],” Mr. Fu said. “This identifies the brain area that causes the ERN and helps explain what it signifies. This new insight might allow doctors to use the ERN as a standard tool to diagnose mental diseases and monitor responses to treatment.”
Error neuron firing and intracranial ERN occurred first in pre-supplementary motor area (pre-SMA), then in the dorsal anterior cingulate cortex (dACC) about 50 ms later, with significant correlations between firing and intracranial ERN in both locations. In dACC, this activity, with error-integrating neuron responses, correlated with magnitude of post-error slowing (PES).
Previous research suggested a link between “the detection of self-generated errors, as reflected in the ERN, with changes in cognitive control, as exhibited behaviorally in PES,” the investigators wrote. “However, several electroencephalogram (EEG) studies have failed to find a significant relationship between PES and ERN.”
The present study involved intracranial EEG of 29 candidates for surgical treatment of epilepsy and scalp EEG of 12 control participants, with each modality measuring activity in the frontal cortex. Both cohorts performed a rapid version of the color-word Stroop task, in which the words “red,” “green,” or “blue” were printed either in corresponding or noncorresponding colors of red, green, or blue. Subjects were presented various color-word combinations while being asked to click one of three buttons indicating the color of the word as quickly as possible. The investigators monitored neuronal activity throughout, discarding responses that were too slow.
As found in previous trials, the subjects demonstrated the “Stroop effect,” which refers to a slower response when word and color are incongruent (224.9 ms difference; P less than .001). As anticipated, correct responses following correct responses were faster than were correct responses following erroneous responses, which defines PES.
In the intracranial EEG group, the investigators isolated 1,171 neurons, of which 618 were located in dACC and 553 in pre-SMA. Using a Poisson regression model and correlations with erroneous responses, the investigators identified 99 “type I” error neurons in dACC and 118 in pre-SMA, based on higher frequency of firing during erroneous responses than during correct responses. At a single-cell level, error neuron mean spike rates were highest when intracranial ERN amplitude was greatest, such that error neuron firing in dACC and pre-SMA had maximal likelihood ratios of 7.9 (P = .01) and 15.1 (P less than .001), respectively. The strength of correlation between intracranial ERN and error neuron firing rate was directly related to PES magnitude exclusively in the dACC (maximum likelihood ratio of 13.9; P = .015). In post-error trials, faster error-integrating neuron firing rates in dACC predicted greater PES (maximal likelihood ratio of 18.3; P less than .001).
The study was funded by the National Institutes of Health, the McKnight Endowment for Neuroscience, and the National Science Foundation. The authors declared no conflicts of interest.
SOURCE: Fu Z et al. Neuron. 2018 Dec 4. doi: 10.1016/j.neuron.2018.11.016
, and this activity can be tracked through a scalp EEG pattern called error-related negativity, according to findings from experiments carried out during intracranial EEG recordings of candidates for surgical treatment of epilepsy.
“Our results suggest that coordinated neural activity can serve as a substrate for information routing that enables the performance-monitoring system to communicate the need for behavioral control to other brain regions, including those that maintain flexible goal information, such as the lateral prefrontal cortex and the frontal polar cortex,” first author Zhongzheng Fu, a PhD student at the California Institute of Technology in Pasadena, Calif., and Cedars-Sinai Medical Center, Los Angeles, and his colleagues reported in Neuron.
The findings offer insights that could lead to treatments for conditions in which the important executive function task of error self-monitoring is unbalanced, such as obsessive-compulsive disorder and schizophrenia, the authors noted in a press release.
“We discovered that the activity of error neurons correlates with the size of the ERN [error-related negativity],” Mr. Fu said. “This identifies the brain area that causes the ERN and helps explain what it signifies. This new insight might allow doctors to use the ERN as a standard tool to diagnose mental diseases and monitor responses to treatment.”
Error neuron firing and intracranial ERN occurred first in pre-supplementary motor area (pre-SMA), then in the dorsal anterior cingulate cortex (dACC) about 50 ms later, with significant correlations between firing and intracranial ERN in both locations. In dACC, this activity, with error-integrating neuron responses, correlated with magnitude of post-error slowing (PES).
Previous research suggested a link between “the detection of self-generated errors, as reflected in the ERN, with changes in cognitive control, as exhibited behaviorally in PES,” the investigators wrote. “However, several electroencephalogram (EEG) studies have failed to find a significant relationship between PES and ERN.”
The present study involved intracranial EEG of 29 candidates for surgical treatment of epilepsy and scalp EEG of 12 control participants, with each modality measuring activity in the frontal cortex. Both cohorts performed a rapid version of the color-word Stroop task, in which the words “red,” “green,” or “blue” were printed either in corresponding or noncorresponding colors of red, green, or blue. Subjects were presented various color-word combinations while being asked to click one of three buttons indicating the color of the word as quickly as possible. The investigators monitored neuronal activity throughout, discarding responses that were too slow.
As found in previous trials, the subjects demonstrated the “Stroop effect,” which refers to a slower response when word and color are incongruent (224.9 ms difference; P less than .001). As anticipated, correct responses following correct responses were faster than were correct responses following erroneous responses, which defines PES.
In the intracranial EEG group, the investigators isolated 1,171 neurons, of which 618 were located in dACC and 553 in pre-SMA. Using a Poisson regression model and correlations with erroneous responses, the investigators identified 99 “type I” error neurons in dACC and 118 in pre-SMA, based on higher frequency of firing during erroneous responses than during correct responses. At a single-cell level, error neuron mean spike rates were highest when intracranial ERN amplitude was greatest, such that error neuron firing in dACC and pre-SMA had maximal likelihood ratios of 7.9 (P = .01) and 15.1 (P less than .001), respectively. The strength of correlation between intracranial ERN and error neuron firing rate was directly related to PES magnitude exclusively in the dACC (maximum likelihood ratio of 13.9; P = .015). In post-error trials, faster error-integrating neuron firing rates in dACC predicted greater PES (maximal likelihood ratio of 18.3; P less than .001).
The study was funded by the National Institutes of Health, the McKnight Endowment for Neuroscience, and the National Science Foundation. The authors declared no conflicts of interest.
SOURCE: Fu Z et al. Neuron. 2018 Dec 4. doi: 10.1016/j.neuron.2018.11.016
FROM NEURON
A transgender adolescent with chronic pain, depression, and PTSD
X, a 17-year-old Mexican-American transgender male (assigned female at birth) experienced a traumatic brain injury (TBI) 4 years ago and subsequently developed posttraumatic stress disorder (PTSD). I came to treat X at a pediatric outpatient psychiatric clinic after he developed physiologic dysregulation of his nervous system and began to experience panic attacks, major depressive disorder, and auditory hallucinations. X also developed chronic widespread pain during the next few years, including migraines, abdominal pain, and back pain, which significantly impaired his ability to function socially and academically. X was treated by a child and adolescent psychiatrist who used an integrative approach of traditional and complementary medical practices in a pediatric chronic pain clinic.
X’s treatment course at the pediatric psychiatric clinic included 2 years of field capable mental health services. During this time, fluoxetine was started and titrated up to 40 mg/d to target anxiety and depressive symptoms such as pervasive sadness, poor self-esteem, poor concentration, physiologic arousal, and sleep disruption. Risperidone, 2 mg/d, was temporarily added to address residual mood symptoms and the auditory hallucinations X experienced at school. Neuropsychological testing did not indicate that X had cognitive impairments from the TBI. In the pain clinic, X was encouraged to continue with psychotherapy and the selective serotonin reuptake inhibitor. Another recommendation was to seek out acupuncture and yoga. Over the course of 1 year, X’s pain symptoms began to resolve, and his functioning improved significantly. It was during this year that X came out as transgender, first to his friends, and then to his family and his physicians.
The link between PTSD and chronic pain
X’s PTSD presented as nightmares, hypervigilance, and anxiety, especially when he was in school. He would often describe how his chronic pain symptoms prevented him from functioning academically and socially. I wondered if X’s presentation of PTSD indicated a predisposition for chronic widespread pain symptoms or pain syndromes. This theory could be approximated by an association, but research suggests there is a significant temporal relationship between PTSD and widespread pain symptoms, such as in fibromyalgia.
One multicenter study of patients with fibromyalgia found that the prevalence of comorbid PTSD was 45%.1 In two-thirds of patients with fibromyalgia, traumatic life events and PTSD symptoms preceded the onset of chronic widespread pain, while in roughly one-third, traumatic life events and PTSD symptoms followed the onset of chronic widespread pain.1 This study suggests that PTSD could be viewed as a marker of stress vulnerability in which individuals susceptible to stress are more likely to develop chronic widespread pain and other health problems, including fibromyalgia, when a traumatic event occurs.
Benefits of transgender-specific care
During the course of X’s psychiatric treatment, he eventually revealed that he had been experiencing gender dysphoria for many years. His gender transition was occurring during adolescence; during this time, identity formation is a central developmental task.2 X was not comfortable asking others to use his preferred pronouns until he had physiologically transitioned. Any further delay to accessing transgender-specific services would increase the likelihood of a poor prognosis, both behaviorally and medically, because sexual minority adolescents are 3 to 4 times more likely to meet criteria for an internalizing disorder and 2 to 5 times more likely to meet criteria for externalizing disorders.3 My understanding of the minority stress model raised concerns that if X did not get appropriate treatment, the interdependence of stressors of being a sexual minority as well as an ethnic minority would further burden his mental health.
Now that X had access to transgender-specific care, how would management affect his pain symptoms or response to treatment? While some of his pain symptoms began to remit before he came out as transgender, I considered whether hormone therapy might improve his subjective pain. Little research has been conducted in transgender patients to determine whether sex-steroid administration might alter nociception. One study that examined daily fluctuations of sex hormones in 8 women with fibromyalgia found trends suggesting progesterone and testosterone are inversely associated with pain, with peaks of those hormones occurring on days with lower reported pain.4 A small study of female-to-male transgender patients found that administration of sex steroids was associated with relief from chronic painful conditions (headaches, musculoskeletal pain) in 6 of 16 patients who received testosterone injections.5 What little evidence I found in regards to an association between gender-affirming hormone therapy and chronic pain left me feeling optimistic that hormone therapy would not negatively affect the prognosis of X’s chronic pain.
Another consideration in treating X was the practice of chest binding, the compression of chest tissue for masculine gender expression among people who were assigned female sex at birth. One study found that chest binding can improve mood; decrease suicidality, anxiety, and dysphoria; and increase self-esteem.6 However, 97.2% of participants reported at least one negative outcome they attributed to binding. The most common was back pain (53.8%), which X had been experiencing before he began chest binding. I found it notable that X’s primary doctors in the transgender clinic kept this adverse effect in mind when they recommended that he take breaks and limit daily hours of chest binding to minimize the risk of increased chronic back pain.
This particular case spanned several specialized services and required coordination and careful consideration to address X’s developmental and gender-related needs. X experienced significant symptoms incited by a TBI; however, the manifestation of his chronic pain symptoms were more than likely influenced by several overlapping stressors, including belonging to an ethnic minority, transitioning into adulthood, transitioning publicly as a male, and mood symptoms. While it pleased me to see how X responded positively to the integrative and holistic treatment he received, I remain concerned that simply not enough research exists that addresses how transgender individuals are affected, physically and affectively, by chronic levels of stress attributable to their minority status.
1. Häuser W, Galek A, Erbslöh-Möller B, et al. Posttraumatic stress disorder in fibromyalgia syndrome: prevalence, temporal relationship between posttraumatic stress and fibromyalgia symptoms, and impact on clinical outcome. Pain. 2013;154(8):1216-1223.
2. Erikson EH. Identity: Youth and crisis. New York, NY: W.W. Norton & Company; 1968.
3. Fergusson DM, Horwood LJ, Beautrais AL. Is sexual orientation related to mental health problems and suicidality in young people? Arch Gen Psychiatry. 1999;56(10):876-880.
4. Schertzinger M, Wesson-Sides K, Parkitny L, et al. Daily fluctuations of progesterone and testosterone are associated with fibromyalgia pain severity. J Pain. 2018;19(4):410-417.
5. Aloisi AM, Bachiocco V, Costantino A, et al. Cross-sex hormone administration changes pain in transsexual women and men. Pain. 2007;132(suppl 1):S60-S67.
6. Peitzmeier S, Gardner I, Weinand J et al. Health impact of chest binding among transgender adults: a community-engaged, cross-sectional study. Cult Health Sex. 2017;19(1):64-75.
X, a 17-year-old Mexican-American transgender male (assigned female at birth) experienced a traumatic brain injury (TBI) 4 years ago and subsequently developed posttraumatic stress disorder (PTSD). I came to treat X at a pediatric outpatient psychiatric clinic after he developed physiologic dysregulation of his nervous system and began to experience panic attacks, major depressive disorder, and auditory hallucinations. X also developed chronic widespread pain during the next few years, including migraines, abdominal pain, and back pain, which significantly impaired his ability to function socially and academically. X was treated by a child and adolescent psychiatrist who used an integrative approach of traditional and complementary medical practices in a pediatric chronic pain clinic.
X’s treatment course at the pediatric psychiatric clinic included 2 years of field capable mental health services. During this time, fluoxetine was started and titrated up to 40 mg/d to target anxiety and depressive symptoms such as pervasive sadness, poor self-esteem, poor concentration, physiologic arousal, and sleep disruption. Risperidone, 2 mg/d, was temporarily added to address residual mood symptoms and the auditory hallucinations X experienced at school. Neuropsychological testing did not indicate that X had cognitive impairments from the TBI. In the pain clinic, X was encouraged to continue with psychotherapy and the selective serotonin reuptake inhibitor. Another recommendation was to seek out acupuncture and yoga. Over the course of 1 year, X’s pain symptoms began to resolve, and his functioning improved significantly. It was during this year that X came out as transgender, first to his friends, and then to his family and his physicians.
The link between PTSD and chronic pain
X’s PTSD presented as nightmares, hypervigilance, and anxiety, especially when he was in school. He would often describe how his chronic pain symptoms prevented him from functioning academically and socially. I wondered if X’s presentation of PTSD indicated a predisposition for chronic widespread pain symptoms or pain syndromes. This theory could be approximated by an association, but research suggests there is a significant temporal relationship between PTSD and widespread pain symptoms, such as in fibromyalgia.
One multicenter study of patients with fibromyalgia found that the prevalence of comorbid PTSD was 45%.1 In two-thirds of patients with fibromyalgia, traumatic life events and PTSD symptoms preceded the onset of chronic widespread pain, while in roughly one-third, traumatic life events and PTSD symptoms followed the onset of chronic widespread pain.1 This study suggests that PTSD could be viewed as a marker of stress vulnerability in which individuals susceptible to stress are more likely to develop chronic widespread pain and other health problems, including fibromyalgia, when a traumatic event occurs.
Benefits of transgender-specific care
During the course of X’s psychiatric treatment, he eventually revealed that he had been experiencing gender dysphoria for many years. His gender transition was occurring during adolescence; during this time, identity formation is a central developmental task.2 X was not comfortable asking others to use his preferred pronouns until he had physiologically transitioned. Any further delay to accessing transgender-specific services would increase the likelihood of a poor prognosis, both behaviorally and medically, because sexual minority adolescents are 3 to 4 times more likely to meet criteria for an internalizing disorder and 2 to 5 times more likely to meet criteria for externalizing disorders.3 My understanding of the minority stress model raised concerns that if X did not get appropriate treatment, the interdependence of stressors of being a sexual minority as well as an ethnic minority would further burden his mental health.
Now that X had access to transgender-specific care, how would management affect his pain symptoms or response to treatment? While some of his pain symptoms began to remit before he came out as transgender, I considered whether hormone therapy might improve his subjective pain. Little research has been conducted in transgender patients to determine whether sex-steroid administration might alter nociception. One study that examined daily fluctuations of sex hormones in 8 women with fibromyalgia found trends suggesting progesterone and testosterone are inversely associated with pain, with peaks of those hormones occurring on days with lower reported pain.4 A small study of female-to-male transgender patients found that administration of sex steroids was associated with relief from chronic painful conditions (headaches, musculoskeletal pain) in 6 of 16 patients who received testosterone injections.5 What little evidence I found in regards to an association between gender-affirming hormone therapy and chronic pain left me feeling optimistic that hormone therapy would not negatively affect the prognosis of X’s chronic pain.
Another consideration in treating X was the practice of chest binding, the compression of chest tissue for masculine gender expression among people who were assigned female sex at birth. One study found that chest binding can improve mood; decrease suicidality, anxiety, and dysphoria; and increase self-esteem.6 However, 97.2% of participants reported at least one negative outcome they attributed to binding. The most common was back pain (53.8%), which X had been experiencing before he began chest binding. I found it notable that X’s primary doctors in the transgender clinic kept this adverse effect in mind when they recommended that he take breaks and limit daily hours of chest binding to minimize the risk of increased chronic back pain.
This particular case spanned several specialized services and required coordination and careful consideration to address X’s developmental and gender-related needs. X experienced significant symptoms incited by a TBI; however, the manifestation of his chronic pain symptoms were more than likely influenced by several overlapping stressors, including belonging to an ethnic minority, transitioning into adulthood, transitioning publicly as a male, and mood symptoms. While it pleased me to see how X responded positively to the integrative and holistic treatment he received, I remain concerned that simply not enough research exists that addresses how transgender individuals are affected, physically and affectively, by chronic levels of stress attributable to their minority status.
X, a 17-year-old Mexican-American transgender male (assigned female at birth) experienced a traumatic brain injury (TBI) 4 years ago and subsequently developed posttraumatic stress disorder (PTSD). I came to treat X at a pediatric outpatient psychiatric clinic after he developed physiologic dysregulation of his nervous system and began to experience panic attacks, major depressive disorder, and auditory hallucinations. X also developed chronic widespread pain during the next few years, including migraines, abdominal pain, and back pain, which significantly impaired his ability to function socially and academically. X was treated by a child and adolescent psychiatrist who used an integrative approach of traditional and complementary medical practices in a pediatric chronic pain clinic.
X’s treatment course at the pediatric psychiatric clinic included 2 years of field capable mental health services. During this time, fluoxetine was started and titrated up to 40 mg/d to target anxiety and depressive symptoms such as pervasive sadness, poor self-esteem, poor concentration, physiologic arousal, and sleep disruption. Risperidone, 2 mg/d, was temporarily added to address residual mood symptoms and the auditory hallucinations X experienced at school. Neuropsychological testing did not indicate that X had cognitive impairments from the TBI. In the pain clinic, X was encouraged to continue with psychotherapy and the selective serotonin reuptake inhibitor. Another recommendation was to seek out acupuncture and yoga. Over the course of 1 year, X’s pain symptoms began to resolve, and his functioning improved significantly. It was during this year that X came out as transgender, first to his friends, and then to his family and his physicians.
The link between PTSD and chronic pain
X’s PTSD presented as nightmares, hypervigilance, and anxiety, especially when he was in school. He would often describe how his chronic pain symptoms prevented him from functioning academically and socially. I wondered if X’s presentation of PTSD indicated a predisposition for chronic widespread pain symptoms or pain syndromes. This theory could be approximated by an association, but research suggests there is a significant temporal relationship between PTSD and widespread pain symptoms, such as in fibromyalgia.
One multicenter study of patients with fibromyalgia found that the prevalence of comorbid PTSD was 45%.1 In two-thirds of patients with fibromyalgia, traumatic life events and PTSD symptoms preceded the onset of chronic widespread pain, while in roughly one-third, traumatic life events and PTSD symptoms followed the onset of chronic widespread pain.1 This study suggests that PTSD could be viewed as a marker of stress vulnerability in which individuals susceptible to stress are more likely to develop chronic widespread pain and other health problems, including fibromyalgia, when a traumatic event occurs.
Benefits of transgender-specific care
During the course of X’s psychiatric treatment, he eventually revealed that he had been experiencing gender dysphoria for many years. His gender transition was occurring during adolescence; during this time, identity formation is a central developmental task.2 X was not comfortable asking others to use his preferred pronouns until he had physiologically transitioned. Any further delay to accessing transgender-specific services would increase the likelihood of a poor prognosis, both behaviorally and medically, because sexual minority adolescents are 3 to 4 times more likely to meet criteria for an internalizing disorder and 2 to 5 times more likely to meet criteria for externalizing disorders.3 My understanding of the minority stress model raised concerns that if X did not get appropriate treatment, the interdependence of stressors of being a sexual minority as well as an ethnic minority would further burden his mental health.
Now that X had access to transgender-specific care, how would management affect his pain symptoms or response to treatment? While some of his pain symptoms began to remit before he came out as transgender, I considered whether hormone therapy might improve his subjective pain. Little research has been conducted in transgender patients to determine whether sex-steroid administration might alter nociception. One study that examined daily fluctuations of sex hormones in 8 women with fibromyalgia found trends suggesting progesterone and testosterone are inversely associated with pain, with peaks of those hormones occurring on days with lower reported pain.4 A small study of female-to-male transgender patients found that administration of sex steroids was associated with relief from chronic painful conditions (headaches, musculoskeletal pain) in 6 of 16 patients who received testosterone injections.5 What little evidence I found in regards to an association between gender-affirming hormone therapy and chronic pain left me feeling optimistic that hormone therapy would not negatively affect the prognosis of X’s chronic pain.
Another consideration in treating X was the practice of chest binding, the compression of chest tissue for masculine gender expression among people who were assigned female sex at birth. One study found that chest binding can improve mood; decrease suicidality, anxiety, and dysphoria; and increase self-esteem.6 However, 97.2% of participants reported at least one negative outcome they attributed to binding. The most common was back pain (53.8%), which X had been experiencing before he began chest binding. I found it notable that X’s primary doctors in the transgender clinic kept this adverse effect in mind when they recommended that he take breaks and limit daily hours of chest binding to minimize the risk of increased chronic back pain.
This particular case spanned several specialized services and required coordination and careful consideration to address X’s developmental and gender-related needs. X experienced significant symptoms incited by a TBI; however, the manifestation of his chronic pain symptoms were more than likely influenced by several overlapping stressors, including belonging to an ethnic minority, transitioning into adulthood, transitioning publicly as a male, and mood symptoms. While it pleased me to see how X responded positively to the integrative and holistic treatment he received, I remain concerned that simply not enough research exists that addresses how transgender individuals are affected, physically and affectively, by chronic levels of stress attributable to their minority status.
1. Häuser W, Galek A, Erbslöh-Möller B, et al. Posttraumatic stress disorder in fibromyalgia syndrome: prevalence, temporal relationship between posttraumatic stress and fibromyalgia symptoms, and impact on clinical outcome. Pain. 2013;154(8):1216-1223.
2. Erikson EH. Identity: Youth and crisis. New York, NY: W.W. Norton & Company; 1968.
3. Fergusson DM, Horwood LJ, Beautrais AL. Is sexual orientation related to mental health problems and suicidality in young people? Arch Gen Psychiatry. 1999;56(10):876-880.
4. Schertzinger M, Wesson-Sides K, Parkitny L, et al. Daily fluctuations of progesterone and testosterone are associated with fibromyalgia pain severity. J Pain. 2018;19(4):410-417.
5. Aloisi AM, Bachiocco V, Costantino A, et al. Cross-sex hormone administration changes pain in transsexual women and men. Pain. 2007;132(suppl 1):S60-S67.
6. Peitzmeier S, Gardner I, Weinand J et al. Health impact of chest binding among transgender adults: a community-engaged, cross-sectional study. Cult Health Sex. 2017;19(1):64-75.
1. Häuser W, Galek A, Erbslöh-Möller B, et al. Posttraumatic stress disorder in fibromyalgia syndrome: prevalence, temporal relationship between posttraumatic stress and fibromyalgia symptoms, and impact on clinical outcome. Pain. 2013;154(8):1216-1223.
2. Erikson EH. Identity: Youth and crisis. New York, NY: W.W. Norton & Company; 1968.
3. Fergusson DM, Horwood LJ, Beautrais AL. Is sexual orientation related to mental health problems and suicidality in young people? Arch Gen Psychiatry. 1999;56(10):876-880.
4. Schertzinger M, Wesson-Sides K, Parkitny L, et al. Daily fluctuations of progesterone and testosterone are associated with fibromyalgia pain severity. J Pain. 2018;19(4):410-417.
5. Aloisi AM, Bachiocco V, Costantino A, et al. Cross-sex hormone administration changes pain in transsexual women and men. Pain. 2007;132(suppl 1):S60-S67.
6. Peitzmeier S, Gardner I, Weinand J et al. Health impact of chest binding among transgender adults: a community-engaged, cross-sectional study. Cult Health Sex. 2017;19(1):64-75.
Less-distressed patients driving increase in outpatient services
Adults with less-severe psychological distress contributed to most of the recent increase in outpatient mental health services, based on survey data from nearly 140,000 adults.
“Rising national rates of suicide, opioid misuse, and opioid-related deaths further suggest increasing psychological distress,” wrote Mark Olfson, MD, MPH, of Columbia University, New York, and his colleagues. “However, it is not known whether or to what extent an increase in mental health treatment has occurred in response to rising rates of psychological distress.”
Dr. Olfson and his colleagues reviewed data from the Medical Expenditure Panel Surveys for the years 2004-2005, 2009-2010, and 2014-2015. Overall, 19% of adults received outpatient mental health services in 2004-2005; the percentage increased to 23% in 2014-2015. About half of the study subjects were women, 67% were white, and the average age was 46 years.
The total percentage of adults with serious psychological distress decreased from 5% in 2004-2005 to 4% in 2014-2015, the researchers noted, although those with serious psychological distress had a greater proportionate increase in the use of outpatient services during the study period, from 54% to 68%.
The number of adults with less-serious distress or no distress who were treated with outpatient mental health services increased from 35 million in 2004-2005 to 48 million in 2014-2015, the researchers wrote in JAMA Psychiatry.
The study results were limited by several factors, including the partial reliance on self-reports of mental health care use and on the limitations of the Kessler 6 scale as an assessment of psychological distress. Other limitations included an absence of data on the specific services used and on the effectiveness of treatments. However, the results suggest that, despite increases in outpatient mental health treatment, many adults with serious psychological distress received no mental health care, they wrote. Individuals with more-severe distress might view mental health care less favorably. In addition, the investigators emphasized the need for continued improvement in general medical settings for detecting and treating or referring adults for mental health service.
Dr. Olfson reported no disclosures. One of the coauthors, Steven C. Marcus, PhD, reported receiving consulting fees from several pharmaceutical companies. The study was supported in part by the National Institutes of Health and the New York State Psychiatric Institute. The Medical Expenditure Panel Surveys are sponsored by the Agency for Healthcare Research and Quality.
SOURCE: Olfson M et al. JAMA Psychiatry. 2018 Nov 28. doi: 10.1001/jamapsychiatry.2018.3550.
Adults with less-severe psychological distress contributed to most of the recent increase in outpatient mental health services, based on survey data from nearly 140,000 adults.
“Rising national rates of suicide, opioid misuse, and opioid-related deaths further suggest increasing psychological distress,” wrote Mark Olfson, MD, MPH, of Columbia University, New York, and his colleagues. “However, it is not known whether or to what extent an increase in mental health treatment has occurred in response to rising rates of psychological distress.”
Dr. Olfson and his colleagues reviewed data from the Medical Expenditure Panel Surveys for the years 2004-2005, 2009-2010, and 2014-2015. Overall, 19% of adults received outpatient mental health services in 2004-2005; the percentage increased to 23% in 2014-2015. About half of the study subjects were women, 67% were white, and the average age was 46 years.
The total percentage of adults with serious psychological distress decreased from 5% in 2004-2005 to 4% in 2014-2015, the researchers noted, although those with serious psychological distress had a greater proportionate increase in the use of outpatient services during the study period, from 54% to 68%.
The number of adults with less-serious distress or no distress who were treated with outpatient mental health services increased from 35 million in 2004-2005 to 48 million in 2014-2015, the researchers wrote in JAMA Psychiatry.
The study results were limited by several factors, including the partial reliance on self-reports of mental health care use and on the limitations of the Kessler 6 scale as an assessment of psychological distress. Other limitations included an absence of data on the specific services used and on the effectiveness of treatments. However, the results suggest that, despite increases in outpatient mental health treatment, many adults with serious psychological distress received no mental health care, they wrote. Individuals with more-severe distress might view mental health care less favorably. In addition, the investigators emphasized the need for continued improvement in general medical settings for detecting and treating or referring adults for mental health service.
Dr. Olfson reported no disclosures. One of the coauthors, Steven C. Marcus, PhD, reported receiving consulting fees from several pharmaceutical companies. The study was supported in part by the National Institutes of Health and the New York State Psychiatric Institute. The Medical Expenditure Panel Surveys are sponsored by the Agency for Healthcare Research and Quality.
SOURCE: Olfson M et al. JAMA Psychiatry. 2018 Nov 28. doi: 10.1001/jamapsychiatry.2018.3550.
Adults with less-severe psychological distress contributed to most of the recent increase in outpatient mental health services, based on survey data from nearly 140,000 adults.
“Rising national rates of suicide, opioid misuse, and opioid-related deaths further suggest increasing psychological distress,” wrote Mark Olfson, MD, MPH, of Columbia University, New York, and his colleagues. “However, it is not known whether or to what extent an increase in mental health treatment has occurred in response to rising rates of psychological distress.”
Dr. Olfson and his colleagues reviewed data from the Medical Expenditure Panel Surveys for the years 2004-2005, 2009-2010, and 2014-2015. Overall, 19% of adults received outpatient mental health services in 2004-2005; the percentage increased to 23% in 2014-2015. About half of the study subjects were women, 67% were white, and the average age was 46 years.
The total percentage of adults with serious psychological distress decreased from 5% in 2004-2005 to 4% in 2014-2015, the researchers noted, although those with serious psychological distress had a greater proportionate increase in the use of outpatient services during the study period, from 54% to 68%.
The number of adults with less-serious distress or no distress who were treated with outpatient mental health services increased from 35 million in 2004-2005 to 48 million in 2014-2015, the researchers wrote in JAMA Psychiatry.
The study results were limited by several factors, including the partial reliance on self-reports of mental health care use and on the limitations of the Kessler 6 scale as an assessment of psychological distress. Other limitations included an absence of data on the specific services used and on the effectiveness of treatments. However, the results suggest that, despite increases in outpatient mental health treatment, many adults with serious psychological distress received no mental health care, they wrote. Individuals with more-severe distress might view mental health care less favorably. In addition, the investigators emphasized the need for continued improvement in general medical settings for detecting and treating or referring adults for mental health service.
Dr. Olfson reported no disclosures. One of the coauthors, Steven C. Marcus, PhD, reported receiving consulting fees from several pharmaceutical companies. The study was supported in part by the National Institutes of Health and the New York State Psychiatric Institute. The Medical Expenditure Panel Surveys are sponsored by the Agency for Healthcare Research and Quality.
SOURCE: Olfson M et al. JAMA Psychiatry. 2018 Nov 28. doi: 10.1001/jamapsychiatry.2018.3550.
FROM JAMA PSYCHIATRY
Key clinical point: Overall use of outpatient mental health services is increasing, but most patients report less-severe or no psychological distress.
Major finding: The percentage of U.S. adults receiving outpatient mental health services increased from 19% in 2004-2005 to 23% in 2014-2015.
Study details: The data come from a review of nationally representative surveys taken in 2004-2005, 2009-2010, and 2014-2015 for a total of 139,862 adults aged 18 years and older.
Disclosures: Dr. Olson reported no disclosures. One of the coauthors, Steven C. Marcus, PhD, reported receiving consulting fees from several pharmaceutical companies. The study was supported in part by the National Institutes of Health and the New York State Psychiatric Institute. The Medical Expenditure Panel Surveys are sponsored by the Agency for Healthcare Research and Quality.
Source: Olfson M et al. JAMA Psychiatry. 2018 Nov 28. doi: 10.1001/jamapsychiatry.2018.3550.
Comorbid depression, anxiety linked to doubled risk of diabetes
Comorbid symptoms of anxiety and depression are associated with twice the risk of developing type 2 diabetes, according to a research paper published in the Journal of Affective Disorders.
The researchers sampled 78,025 Dutch adults aged 30-75 years from the Lifelines Cohort Study and assessed them for depressive and anxious symptoms using the Mini-International Neuropsychiatric Interview before sorting them into groups based on whether they had both, depressive symptoms alone, anxious symptoms alone, or neither.
reported Sonya S. Deschênes, PhD, of the department of psychiatry at McGill University, Montreal, and her associates. Furthermore, in an analysis that adjusted for sociodemographic and lifestyle factors and a family history of diabetes, Dr. Deschênes and her associates found that the participants with both kinds of symptoms had an OR of 1.93 (95% CI, 1.21-3.07) of developing type 2 diabetes. Those with only depressive or anxious symptoms alone did not have a statistically significant risk of developing type 2 diabetes.
A limitation cited by the researchers is that a screening tool was used to assess depressive and anxiety symptoms. Also, glycosylated hemoglobin data were available only for a subset of the participants.
Nevertheless, Dr. Deschênes and her associates wrote, the “study extends ... prior findings and suggests that having co-occurring symptoms of [depression] and anxiety is most strongly associated with an increased risk of [type 2 diabetes]. This study also provides further support for the notion that depression with comorbid anxiety symptoms might represent a group with distinct features.”
SOURCE: Deschênes SS et al. J Affect Disorder. 2018 Oct 1. doi: 10.1016/j.jad.2018.05.029.
Comorbid symptoms of anxiety and depression are associated with twice the risk of developing type 2 diabetes, according to a research paper published in the Journal of Affective Disorders.
The researchers sampled 78,025 Dutch adults aged 30-75 years from the Lifelines Cohort Study and assessed them for depressive and anxious symptoms using the Mini-International Neuropsychiatric Interview before sorting them into groups based on whether they had both, depressive symptoms alone, anxious symptoms alone, or neither.
reported Sonya S. Deschênes, PhD, of the department of psychiatry at McGill University, Montreal, and her associates. Furthermore, in an analysis that adjusted for sociodemographic and lifestyle factors and a family history of diabetes, Dr. Deschênes and her associates found that the participants with both kinds of symptoms had an OR of 1.93 (95% CI, 1.21-3.07) of developing type 2 diabetes. Those with only depressive or anxious symptoms alone did not have a statistically significant risk of developing type 2 diabetes.
A limitation cited by the researchers is that a screening tool was used to assess depressive and anxiety symptoms. Also, glycosylated hemoglobin data were available only for a subset of the participants.
Nevertheless, Dr. Deschênes and her associates wrote, the “study extends ... prior findings and suggests that having co-occurring symptoms of [depression] and anxiety is most strongly associated with an increased risk of [type 2 diabetes]. This study also provides further support for the notion that depression with comorbid anxiety symptoms might represent a group with distinct features.”
SOURCE: Deschênes SS et al. J Affect Disorder. 2018 Oct 1. doi: 10.1016/j.jad.2018.05.029.
Comorbid symptoms of anxiety and depression are associated with twice the risk of developing type 2 diabetes, according to a research paper published in the Journal of Affective Disorders.
The researchers sampled 78,025 Dutch adults aged 30-75 years from the Lifelines Cohort Study and assessed them for depressive and anxious symptoms using the Mini-International Neuropsychiatric Interview before sorting them into groups based on whether they had both, depressive symptoms alone, anxious symptoms alone, or neither.
reported Sonya S. Deschênes, PhD, of the department of psychiatry at McGill University, Montreal, and her associates. Furthermore, in an analysis that adjusted for sociodemographic and lifestyle factors and a family history of diabetes, Dr. Deschênes and her associates found that the participants with both kinds of symptoms had an OR of 1.93 (95% CI, 1.21-3.07) of developing type 2 diabetes. Those with only depressive or anxious symptoms alone did not have a statistically significant risk of developing type 2 diabetes.
A limitation cited by the researchers is that a screening tool was used to assess depressive and anxiety symptoms. Also, glycosylated hemoglobin data were available only for a subset of the participants.
Nevertheless, Dr. Deschênes and her associates wrote, the “study extends ... prior findings and suggests that having co-occurring symptoms of [depression] and anxiety is most strongly associated with an increased risk of [type 2 diabetes]. This study also provides further support for the notion that depression with comorbid anxiety symptoms might represent a group with distinct features.”
SOURCE: Deschênes SS et al. J Affect Disorder. 2018 Oct 1. doi: 10.1016/j.jad.2018.05.029.
FROM THE JOURNAL OF AFFECTIVE DISORDERS
Atopic dermatitis hits mental health, quality of life
Atopic dermatitis (AD) places a considerable burden on mental health and quality of life for patients with disease of even moderate severity, according to a cross-sectional study of data from the Atopic Dermatitis in America survey.
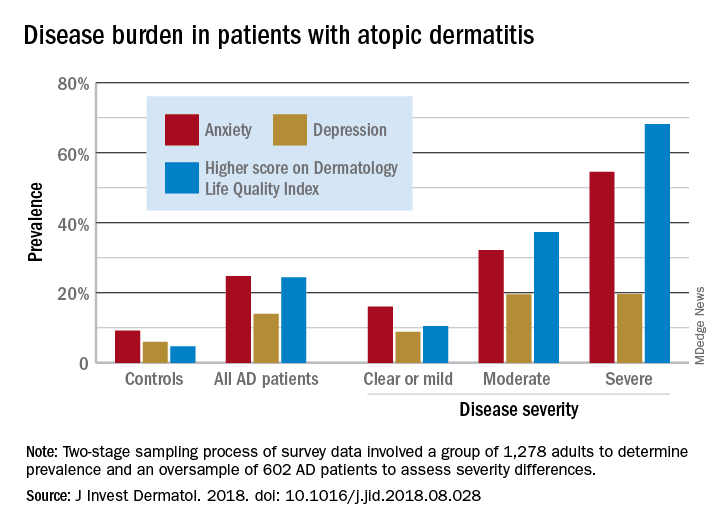
Among adults with severe AD, the mean score on the Dermatology Life Quality Index was 11.4, with a score of 6-30 representing a moderate to large effect on quality of life. The mean for those with moderate disease, 5.9, was just below that range, but 37% of that group did have scores between 6 and 30, Zelma C. Chiesa Fuxench, MD, of the University of Pennsylvania, Philadelphia, and her associates said in the Journal of Investigative Dermatology.
The mean on the Dermatology Life Quality Index for all AD patients was 4.1, with 24% falling into the moderate to large effect range, compared with 1% and 5% for controls. Results were similar on the mental health measure used, the Hospital Anxiety and Depression Scale (HADS). Mean HADS-anxiety scores were 7.0 for all AD patients and 4.7 for controls, and HADS-depression means were 5.8 for AD patients and 3.6 for controls, the investigators reported.
Analysis by disease severity found that 32% of those with moderate AD and almost 56% with severe AD had clinical anxiety (HADS-A score of 11-21), while somewhat lower prevalences were seen for clinical depression (HADS-D score of 11-21): 19.5% for those with moderate AD and 19.7% for patients with severe AD, Dr. Chiesa Fuxench and her associates said.
“An increasing number of studies provide evidence that AD is associated with marked [quality of life] impairment and increased health care costs with higher burden and costs in those with more severe disease. Additional studies should center on exploring those factors associated with AD, and AD disease severity, which lead to increased disease burden in this population,” they wrote.
Respondents to the Atopic Dermatitis in America survey were part of the GfK Knowledge Panel. The study involved a two-stage sampling process: one group of 1,278 adults determined prevalence ,and an oversample of 602 AD patients assessed severity differences.
Dr. Chiesa Fuxench has received research grants from Regeneron, Sanofi, Tioga, and Vanda for work related to atopic dermatitis and has received honoraria for CME work in atopic dermatitis sponsored by educational grants from Regeneron and Sanofi.
SOURCE: J Invest Dermatol. 2018. doi: 10.1016/j.jid.2018.08.028.
Atopic dermatitis (AD) places a considerable burden on mental health and quality of life for patients with disease of even moderate severity, according to a cross-sectional study of data from the Atopic Dermatitis in America survey.
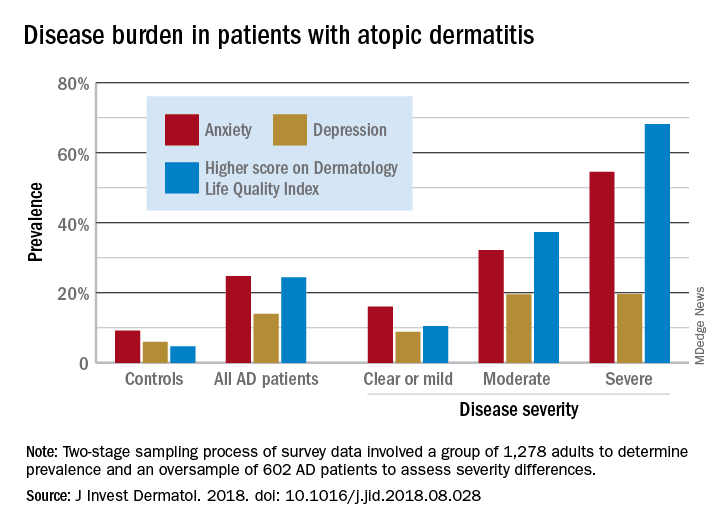
Among adults with severe AD, the mean score on the Dermatology Life Quality Index was 11.4, with a score of 6-30 representing a moderate to large effect on quality of life. The mean for those with moderate disease, 5.9, was just below that range, but 37% of that group did have scores between 6 and 30, Zelma C. Chiesa Fuxench, MD, of the University of Pennsylvania, Philadelphia, and her associates said in the Journal of Investigative Dermatology.
The mean on the Dermatology Life Quality Index for all AD patients was 4.1, with 24% falling into the moderate to large effect range, compared with 1% and 5% for controls. Results were similar on the mental health measure used, the Hospital Anxiety and Depression Scale (HADS). Mean HADS-anxiety scores were 7.0 for all AD patients and 4.7 for controls, and HADS-depression means were 5.8 for AD patients and 3.6 for controls, the investigators reported.
Analysis by disease severity found that 32% of those with moderate AD and almost 56% with severe AD had clinical anxiety (HADS-A score of 11-21), while somewhat lower prevalences were seen for clinical depression (HADS-D score of 11-21): 19.5% for those with moderate AD and 19.7% for patients with severe AD, Dr. Chiesa Fuxench and her associates said.
“An increasing number of studies provide evidence that AD is associated with marked [quality of life] impairment and increased health care costs with higher burden and costs in those with more severe disease. Additional studies should center on exploring those factors associated with AD, and AD disease severity, which lead to increased disease burden in this population,” they wrote.
Respondents to the Atopic Dermatitis in America survey were part of the GfK Knowledge Panel. The study involved a two-stage sampling process: one group of 1,278 adults determined prevalence ,and an oversample of 602 AD patients assessed severity differences.
Dr. Chiesa Fuxench has received research grants from Regeneron, Sanofi, Tioga, and Vanda for work related to atopic dermatitis and has received honoraria for CME work in atopic dermatitis sponsored by educational grants from Regeneron and Sanofi.
SOURCE: J Invest Dermatol. 2018. doi: 10.1016/j.jid.2018.08.028.
Atopic dermatitis (AD) places a considerable burden on mental health and quality of life for patients with disease of even moderate severity, according to a cross-sectional study of data from the Atopic Dermatitis in America survey.
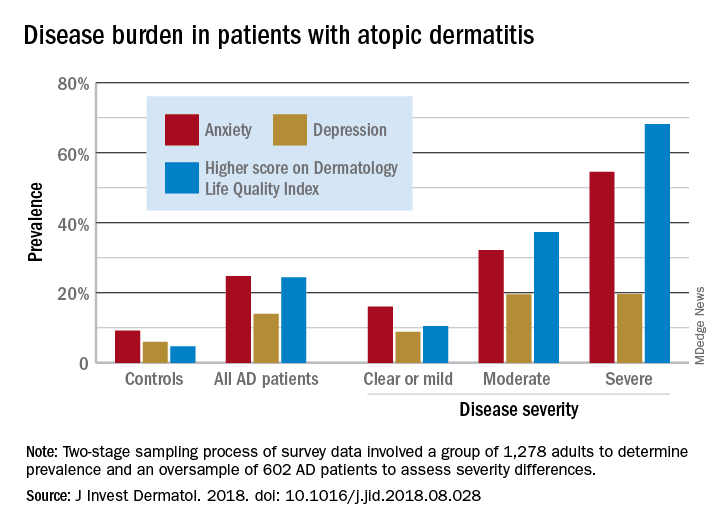
Among adults with severe AD, the mean score on the Dermatology Life Quality Index was 11.4, with a score of 6-30 representing a moderate to large effect on quality of life. The mean for those with moderate disease, 5.9, was just below that range, but 37% of that group did have scores between 6 and 30, Zelma C. Chiesa Fuxench, MD, of the University of Pennsylvania, Philadelphia, and her associates said in the Journal of Investigative Dermatology.
The mean on the Dermatology Life Quality Index for all AD patients was 4.1, with 24% falling into the moderate to large effect range, compared with 1% and 5% for controls. Results were similar on the mental health measure used, the Hospital Anxiety and Depression Scale (HADS). Mean HADS-anxiety scores were 7.0 for all AD patients and 4.7 for controls, and HADS-depression means were 5.8 for AD patients and 3.6 for controls, the investigators reported.
Analysis by disease severity found that 32% of those with moderate AD and almost 56% with severe AD had clinical anxiety (HADS-A score of 11-21), while somewhat lower prevalences were seen for clinical depression (HADS-D score of 11-21): 19.5% for those with moderate AD and 19.7% for patients with severe AD, Dr. Chiesa Fuxench and her associates said.
“An increasing number of studies provide evidence that AD is associated with marked [quality of life] impairment and increased health care costs with higher burden and costs in those with more severe disease. Additional studies should center on exploring those factors associated with AD, and AD disease severity, which lead to increased disease burden in this population,” they wrote.
Respondents to the Atopic Dermatitis in America survey were part of the GfK Knowledge Panel. The study involved a two-stage sampling process: one group of 1,278 adults determined prevalence ,and an oversample of 602 AD patients assessed severity differences.
Dr. Chiesa Fuxench has received research grants from Regeneron, Sanofi, Tioga, and Vanda for work related to atopic dermatitis and has received honoraria for CME work in atopic dermatitis sponsored by educational grants from Regeneron and Sanofi.
SOURCE: J Invest Dermatol. 2018. doi: 10.1016/j.jid.2018.08.028.
FROM THE JOURNAL OF INVESTIGATIVE DERMATOLOGY