User login
SABCS: CREATE-X – Capecitabine is efficacious against residual HER2-negative breast cancer
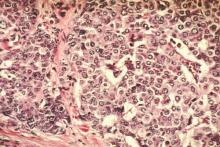
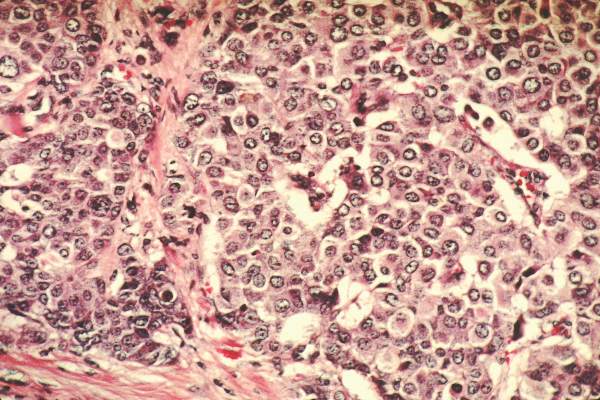
SAN ANTONIO – Adjuvant capecitabine improves outcomes in women with HER2-negative breast cancer who still have invasive disease after neoadjuvant chemotherapy, according to findings of the CREATE-X trial reported at the San Antonio Breast Cancer Symposium.
“Patients with pathologic residual invasive disease after neoadjuvant chemotherapy have a higher risk for relapse,” said presenting author Dr. Masakazu Toi, a professor at Kyoto University Hospital in Japan, and founder and senior director of the Japan Breast Cancer Research Group (JBCRG). But “it is unclear whether postoperative systemic chemotherapy following neoadjuvant chemotherapy is able to prolong survival.”
The phase III trial was conducted among 910 patients with early breast cancer in Japan and Korea who still had positive nodes or didn’t achieve a pathologic complete response after receipt of neoadjuvant chemotherapy that included an anthracycline, a taxane, or both. They were randomized to open-label adjuvant capecitabine (Xeloda) or no capecitabine, in addition to standard therapy.
Results of a preplanned 2-year interim analysis, reported in a session and related press briefing, showed that the risk of disease-free survival events was 30% lower and the risk of death was 40% lower among women given capecitabine than among counterparts not given the drug, prompting early stopping of the trial.
The disease-free survival results were similar in subgroup analyses. In particular, benefit was similar in patients with triple-negative disease, who historically haven’t fared well on this drug.
“The balance of benefit and toxicity would favor the use of capecitabine in [this] post–neoadjuvant chemotherapy situation, but prediction for therapeutic benefit needs to be investigated further,” Dr. Toi concluded. “The cost-effectiveness analysis will be carried out soon,” he added.
Press briefing moderator Dr. Virginia Kaklamani, codirector of the San Antonio Breast Cancer Symposium, as well as professor of medicine in the division of hematology/oncology at the University of Texas, San Antonio, and leader of the Breast Cancer Program, Cancer Therapy & Research Center there, wondered if the results are practice changing.
“On Monday morning, when I see a patient who has residual disease after neoadjuvant chemotherapy, what do I tell her?” she asked.
“I think we need to take care of the reimbursement issue,” Dr. Toi replied, referring to the current lack of U.S. Food and Drug Administration approval of capecitabine for this indication. “But personally, I would like to consider this treatment.”
In the session where the findings were presented, some attendees expressed skepticism about the observed benefit of capecitabine, given previous studies.
This benefit may have been due in part to the fact that in CREATE-X, capecitabine was given largely because it does not have cross-resistance with anthracyclines and taxanes, Dr. Toi speculated.
Attendee Dr. Steven Vogl, an oncologist at the Montefiore Medical Center in New York, proposed that the findings may have different implications for women with estrogen receptor–positive versus triple-negative disease, based on both their likelihood of pathologic complete response (pCR)and the prognostic impact of that response.
“I put it to you that really what this tells us is if we have a triple-negative patient who doesn’t achieve pCR after good neoadjuvant therapy, this [capecitabine] is probably a reasonable option, even though it’s quite toxic, and certainly should be explored further,” he said. “I’m not sure I would go home and treat my ER-positive patients who don’t get a pCR with capecitabine based on this study.”
In the trial, the 2-year disease-free survival rate – the trial’s primary endpoint – was 82.8% with capecitabine and 74.0% without it. The estimated 5-year rates were 74.1% and 67.7%, respectively (hazard ratio, 0.70; P = .005).
Furthermore, the 2-year overall survival rate was 94% with capecitabine and 89.2% without it. The estimated 5-year rates were 89.2% and 83.9%, respectively (HR, 0.60; P less than .01).
Patients in the capecitabine arm were more likely to experience grade 3 or worse neutropenia (7% vs. 2%) and diarrhea (3% vs. less than 1%). And 11% developed grade 3 hand-foot syndrome. However, these toxicities were manageable, according to the investigators.
Dr. Toi disclosed that he receives a research grant from Chugai Pharmaceutical Company. The trial was supported by a grant from Specified Nonprofit Corporation – Advanced Clinical Research Organization (ACRO) and other donations to the Japan Breast Cancer Research Group.
SAN ANTONIO – Adjuvant capecitabine improves outcomes in women with HER2-negative breast cancer who still have invasive disease after neoadjuvant chemotherapy, according to findings of the CREATE-X trial reported at the San Antonio Breast Cancer Symposium.
“Patients with pathologic residual invasive disease after neoadjuvant chemotherapy have a higher risk for relapse,” said presenting author Dr. Masakazu Toi, a professor at Kyoto University Hospital in Japan, and founder and senior director of the Japan Breast Cancer Research Group (JBCRG). But “it is unclear whether postoperative systemic chemotherapy following neoadjuvant chemotherapy is able to prolong survival.”
The phase III trial was conducted among 910 patients with early breast cancer in Japan and Korea who still had positive nodes or didn’t achieve a pathologic complete response after receipt of neoadjuvant chemotherapy that included an anthracycline, a taxane, or both. They were randomized to open-label adjuvant capecitabine (Xeloda) or no capecitabine, in addition to standard therapy.
Results of a preplanned 2-year interim analysis, reported in a session and related press briefing, showed that the risk of disease-free survival events was 30% lower and the risk of death was 40% lower among women given capecitabine than among counterparts not given the drug, prompting early stopping of the trial.
The disease-free survival results were similar in subgroup analyses. In particular, benefit was similar in patients with triple-negative disease, who historically haven’t fared well on this drug.
“The balance of benefit and toxicity would favor the use of capecitabine in [this] post–neoadjuvant chemotherapy situation, but prediction for therapeutic benefit needs to be investigated further,” Dr. Toi concluded. “The cost-effectiveness analysis will be carried out soon,” he added.
Press briefing moderator Dr. Virginia Kaklamani, codirector of the San Antonio Breast Cancer Symposium, as well as professor of medicine in the division of hematology/oncology at the University of Texas, San Antonio, and leader of the Breast Cancer Program, Cancer Therapy & Research Center there, wondered if the results are practice changing.
“On Monday morning, when I see a patient who has residual disease after neoadjuvant chemotherapy, what do I tell her?” she asked.
“I think we need to take care of the reimbursement issue,” Dr. Toi replied, referring to the current lack of U.S. Food and Drug Administration approval of capecitabine for this indication. “But personally, I would like to consider this treatment.”
In the session where the findings were presented, some attendees expressed skepticism about the observed benefit of capecitabine, given previous studies.
This benefit may have been due in part to the fact that in CREATE-X, capecitabine was given largely because it does not have cross-resistance with anthracyclines and taxanes, Dr. Toi speculated.
Attendee Dr. Steven Vogl, an oncologist at the Montefiore Medical Center in New York, proposed that the findings may have different implications for women with estrogen receptor–positive versus triple-negative disease, based on both their likelihood of pathologic complete response (pCR)and the prognostic impact of that response.
“I put it to you that really what this tells us is if we have a triple-negative patient who doesn’t achieve pCR after good neoadjuvant therapy, this [capecitabine] is probably a reasonable option, even though it’s quite toxic, and certainly should be explored further,” he said. “I’m not sure I would go home and treat my ER-positive patients who don’t get a pCR with capecitabine based on this study.”
In the trial, the 2-year disease-free survival rate – the trial’s primary endpoint – was 82.8% with capecitabine and 74.0% without it. The estimated 5-year rates were 74.1% and 67.7%, respectively (hazard ratio, 0.70; P = .005).
Furthermore, the 2-year overall survival rate was 94% with capecitabine and 89.2% without it. The estimated 5-year rates were 89.2% and 83.9%, respectively (HR, 0.60; P less than .01).
Patients in the capecitabine arm were more likely to experience grade 3 or worse neutropenia (7% vs. 2%) and diarrhea (3% vs. less than 1%). And 11% developed grade 3 hand-foot syndrome. However, these toxicities were manageable, according to the investigators.
Dr. Toi disclosed that he receives a research grant from Chugai Pharmaceutical Company. The trial was supported by a grant from Specified Nonprofit Corporation – Advanced Clinical Research Organization (ACRO) and other donations to the Japan Breast Cancer Research Group.
SAN ANTONIO – Adjuvant capecitabine improves outcomes in women with HER2-negative breast cancer who still have invasive disease after neoadjuvant chemotherapy, according to findings of the CREATE-X trial reported at the San Antonio Breast Cancer Symposium.
“Patients with pathologic residual invasive disease after neoadjuvant chemotherapy have a higher risk for relapse,” said presenting author Dr. Masakazu Toi, a professor at Kyoto University Hospital in Japan, and founder and senior director of the Japan Breast Cancer Research Group (JBCRG). But “it is unclear whether postoperative systemic chemotherapy following neoadjuvant chemotherapy is able to prolong survival.”
The phase III trial was conducted among 910 patients with early breast cancer in Japan and Korea who still had positive nodes or didn’t achieve a pathologic complete response after receipt of neoadjuvant chemotherapy that included an anthracycline, a taxane, or both. They were randomized to open-label adjuvant capecitabine (Xeloda) or no capecitabine, in addition to standard therapy.
Results of a preplanned 2-year interim analysis, reported in a session and related press briefing, showed that the risk of disease-free survival events was 30% lower and the risk of death was 40% lower among women given capecitabine than among counterparts not given the drug, prompting early stopping of the trial.
The disease-free survival results were similar in subgroup analyses. In particular, benefit was similar in patients with triple-negative disease, who historically haven’t fared well on this drug.
“The balance of benefit and toxicity would favor the use of capecitabine in [this] post–neoadjuvant chemotherapy situation, but prediction for therapeutic benefit needs to be investigated further,” Dr. Toi concluded. “The cost-effectiveness analysis will be carried out soon,” he added.
Press briefing moderator Dr. Virginia Kaklamani, codirector of the San Antonio Breast Cancer Symposium, as well as professor of medicine in the division of hematology/oncology at the University of Texas, San Antonio, and leader of the Breast Cancer Program, Cancer Therapy & Research Center there, wondered if the results are practice changing.
“On Monday morning, when I see a patient who has residual disease after neoadjuvant chemotherapy, what do I tell her?” she asked.
“I think we need to take care of the reimbursement issue,” Dr. Toi replied, referring to the current lack of U.S. Food and Drug Administration approval of capecitabine for this indication. “But personally, I would like to consider this treatment.”
In the session where the findings were presented, some attendees expressed skepticism about the observed benefit of capecitabine, given previous studies.
This benefit may have been due in part to the fact that in CREATE-X, capecitabine was given largely because it does not have cross-resistance with anthracyclines and taxanes, Dr. Toi speculated.
Attendee Dr. Steven Vogl, an oncologist at the Montefiore Medical Center in New York, proposed that the findings may have different implications for women with estrogen receptor–positive versus triple-negative disease, based on both their likelihood of pathologic complete response (pCR)and the prognostic impact of that response.
“I put it to you that really what this tells us is if we have a triple-negative patient who doesn’t achieve pCR after good neoadjuvant therapy, this [capecitabine] is probably a reasonable option, even though it’s quite toxic, and certainly should be explored further,” he said. “I’m not sure I would go home and treat my ER-positive patients who don’t get a pCR with capecitabine based on this study.”
In the trial, the 2-year disease-free survival rate – the trial’s primary endpoint – was 82.8% with capecitabine and 74.0% without it. The estimated 5-year rates were 74.1% and 67.7%, respectively (hazard ratio, 0.70; P = .005).
Furthermore, the 2-year overall survival rate was 94% with capecitabine and 89.2% without it. The estimated 5-year rates were 89.2% and 83.9%, respectively (HR, 0.60; P less than .01).
Patients in the capecitabine arm were more likely to experience grade 3 or worse neutropenia (7% vs. 2%) and diarrhea (3% vs. less than 1%). And 11% developed grade 3 hand-foot syndrome. However, these toxicities were manageable, according to the investigators.
Dr. Toi disclosed that he receives a research grant from Chugai Pharmaceutical Company. The trial was supported by a grant from Specified Nonprofit Corporation – Advanced Clinical Research Organization (ACRO) and other donations to the Japan Breast Cancer Research Group.
AT SABCS 2015
Key clinical point: Adjuvant capecitabine improves outcomes in women with HER2-negative breast cancer who have residual invasive disease after neoadjuvant chemotherapy.
Major finding: Women in the capecitabine group had better 2-year disease-free survival (82.8% vs. 74.0%) and overall survival (94.0% vs. 89.2%).
Data source: A randomized phase III trial of adjuvant capecitabine in 910 breast cancer patients with HER2-negative pathologic residual invasive disease after neoadjuvant chemotherapy (CREATE-X trial).
Disclosures: Dr. Toi disclosed that he receives a research grant from Chugai Pharmaceutical Company. The trial was supported by a grant from Specified Nonprofit Corporation – Advanced Clinical Research Organization (ACRO) and other donations to the Japan Breast Cancer Research Group.
High risk for getting breast cancer linked with low risk of metastasis
Breast cancer prediction tools were associated with tumor prognosticators such that women with calculated high risk were significantly more likely to be diagnosed with low-grade, estrogen receptor (ER)–positive cancers, according to researchers.
The Tyrer-Cuzick model incorporates hormonal, lifestyle, and reproductive risk factors, as well as family history, into breast cancer risk estimates and was associated with ER status (ER-negative odds ratio, 0.80), grade (grade 3: OR, 0.79), and lymph node involvement (lymph node positive: OR, 0.77), but not tumor size. A polygenic risk score based on 77 single-nucleotide polymorphisms (SNP) variants was associated with ER status (ER-negative: OR, 0.80), tumor size (greater than 40 mm: OR, 0.86), and grade (grade 3: OR, 0.86). Tyrer-Cuzick model associations were observed in women younger than age 50, but not in older women. The polygenic risk score associations held for all age groups.
“Our results support the hypothesis that breast cancer subtypes have different etiologies and highlight the need to identify risk factors separately for distinct breast cancer subtypes and ages of onset. Better knowledge of subtype-specific risk factors and understanding of disease etiology may be vital for the success of primary prevention and screening programs aimed at lowering mortality,” wrote Johanna Holm of the Karolinska Institute, Stockholm, and colleagues (Journ Clin Onc. 2015 Dec 2. doi: 10.1200/JCO.2015.63.0624).
The study evaluated 5,500 female breast cancer patients younger than 80 years diagnosed between 2001 and 2008 in Sweden. In total, 5,232 participants had information on the Tyrer-Cuzick score, 4,927 had information on the polygenic risk score, and 3,488 had a prediagnostic mammographic density measurement.
The researchers assessed three breast cancer prediction tools, the Tyrer-Cuzick–predicted 10-year breast cancer risk score, the polygenic risk score, and mammographic density, to determine if risk estimates differed according to tumor prognosticators and metastasis. Unlike the Tyrer-Cuzick score and polygenic risk score, mammographic densities did not vary according to tumor prognosticators and therefore seem to indicate general breast cancer risk, according to investigators.
Both the Tyrer-Cuzick and polygenic risk scores were associated with favorable tumor prognosticators, and women with high scores in both may be even more likely to have favorable disease outcomes, according to researchers. In support of this finding, the survival analysis showed that women above the median in both risk calculators had decreased risk of distant metastasis.
Breast cancer prediction tools were associated with tumor prognosticators such that women with calculated high risk were significantly more likely to be diagnosed with low-grade, estrogen receptor (ER)–positive cancers, according to researchers.
The Tyrer-Cuzick model incorporates hormonal, lifestyle, and reproductive risk factors, as well as family history, into breast cancer risk estimates and was associated with ER status (ER-negative odds ratio, 0.80), grade (grade 3: OR, 0.79), and lymph node involvement (lymph node positive: OR, 0.77), but not tumor size. A polygenic risk score based on 77 single-nucleotide polymorphisms (SNP) variants was associated with ER status (ER-negative: OR, 0.80), tumor size (greater than 40 mm: OR, 0.86), and grade (grade 3: OR, 0.86). Tyrer-Cuzick model associations were observed in women younger than age 50, but not in older women. The polygenic risk score associations held for all age groups.
“Our results support the hypothesis that breast cancer subtypes have different etiologies and highlight the need to identify risk factors separately for distinct breast cancer subtypes and ages of onset. Better knowledge of subtype-specific risk factors and understanding of disease etiology may be vital for the success of primary prevention and screening programs aimed at lowering mortality,” wrote Johanna Holm of the Karolinska Institute, Stockholm, and colleagues (Journ Clin Onc. 2015 Dec 2. doi: 10.1200/JCO.2015.63.0624).
The study evaluated 5,500 female breast cancer patients younger than 80 years diagnosed between 2001 and 2008 in Sweden. In total, 5,232 participants had information on the Tyrer-Cuzick score, 4,927 had information on the polygenic risk score, and 3,488 had a prediagnostic mammographic density measurement.
The researchers assessed three breast cancer prediction tools, the Tyrer-Cuzick–predicted 10-year breast cancer risk score, the polygenic risk score, and mammographic density, to determine if risk estimates differed according to tumor prognosticators and metastasis. Unlike the Tyrer-Cuzick score and polygenic risk score, mammographic densities did not vary according to tumor prognosticators and therefore seem to indicate general breast cancer risk, according to investigators.
Both the Tyrer-Cuzick and polygenic risk scores were associated with favorable tumor prognosticators, and women with high scores in both may be even more likely to have favorable disease outcomes, according to researchers. In support of this finding, the survival analysis showed that women above the median in both risk calculators had decreased risk of distant metastasis.
Breast cancer prediction tools were associated with tumor prognosticators such that women with calculated high risk were significantly more likely to be diagnosed with low-grade, estrogen receptor (ER)–positive cancers, according to researchers.
The Tyrer-Cuzick model incorporates hormonal, lifestyle, and reproductive risk factors, as well as family history, into breast cancer risk estimates and was associated with ER status (ER-negative odds ratio, 0.80), grade (grade 3: OR, 0.79), and lymph node involvement (lymph node positive: OR, 0.77), but not tumor size. A polygenic risk score based on 77 single-nucleotide polymorphisms (SNP) variants was associated with ER status (ER-negative: OR, 0.80), tumor size (greater than 40 mm: OR, 0.86), and grade (grade 3: OR, 0.86). Tyrer-Cuzick model associations were observed in women younger than age 50, but not in older women. The polygenic risk score associations held for all age groups.
“Our results support the hypothesis that breast cancer subtypes have different etiologies and highlight the need to identify risk factors separately for distinct breast cancer subtypes and ages of onset. Better knowledge of subtype-specific risk factors and understanding of disease etiology may be vital for the success of primary prevention and screening programs aimed at lowering mortality,” wrote Johanna Holm of the Karolinska Institute, Stockholm, and colleagues (Journ Clin Onc. 2015 Dec 2. doi: 10.1200/JCO.2015.63.0624).
The study evaluated 5,500 female breast cancer patients younger than 80 years diagnosed between 2001 and 2008 in Sweden. In total, 5,232 participants had information on the Tyrer-Cuzick score, 4,927 had information on the polygenic risk score, and 3,488 had a prediagnostic mammographic density measurement.
The researchers assessed three breast cancer prediction tools, the Tyrer-Cuzick–predicted 10-year breast cancer risk score, the polygenic risk score, and mammographic density, to determine if risk estimates differed according to tumor prognosticators and metastasis. Unlike the Tyrer-Cuzick score and polygenic risk score, mammographic densities did not vary according to tumor prognosticators and therefore seem to indicate general breast cancer risk, according to investigators.
Both the Tyrer-Cuzick and polygenic risk scores were associated with favorable tumor prognosticators, and women with high scores in both may be even more likely to have favorable disease outcomes, according to researchers. In support of this finding, the survival analysis showed that women above the median in both risk calculators had decreased risk of distant metastasis.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: High risk of breast cancer based on specific prediction models was associated with favorable tumor prognosticators and reduced risk of distant metastasis.
Major finding: The Tyrer-Cuzick model was associated with ER status (ER-negative: OR, 0.80), grade (grade 3: OR, 0.79), and lymph node involvement (lymph node positive: OR, 0.77), but not tumor size; The polygenic risk score was associated with ER status, tumor size, and grade.
Data source: The study evaluated 5,500 female breast cancer patients younger than 80 years diagnosed between 2001 and 2008 in Sweden.
Disclosures: Ms. Holm reported having no disclosures. One of her coauthors reported ties to industry.
Die not yet cast for lymphazurin and methylene blue dye
CHICAGO – Two commonly used dyes produced mixed results in sentinel lymph node mapping of early stage breast cancer in what was described as the highest-powered study to date.
The average number of sentinel lymph nodes identified per person was significantly higher with 1% methylene blue dye than with 1% lymphazurin (2.89 vs. 2.22; P less than .001).
Although there is extensive support for methylene blue as a safe and efficacious alternative to lymphazurin, this finding on the number of sentinel nodes identified is not replicated in any other study, Dr. Vaishali Patel said at the annual clinical congress of the American College of Surgeons. The study was conducted at the McLaren Flint (Mich.) Medical Center. Dr. Sukamal Saha was principal investigator.
On the other hand, lymphazurin identified significantly more additional lymph nodes than methylene blue (mean 4.48 vs. 2.84; P less than .001).
Nodal positivity was also significantly higher with lymphazurin than methylene blue (14.93% vs. 8.85%; P less than .001), which also has not been reported in other trials.
“We think this does offer a true comparison between the two dyes,” Dr. Patel of Detroit Medical Center Sinai-Grace Hospital said. “The volume of dye and technique were consistent for all 651 patients. … with one surgeon performing the injections and one surgeon performing the procedures.” The 651 consecutive patients were randomly assigned based on agent availability to a preoperative injection of lymphazurin (half intraparenchymal and half subareolar in the upper outer quadrant) or an intraoperative injection of methylene blue over 5 minutes (3 ccs intraparenchymal, 1 cc subareolar, and 1 cc intradermal).
The lymphazurin and methylene blue groups were also similar in number (298 patients vs. 353 patients), age (mean 61.6 years vs. 63.5 years), and T stage (in situ 12% vs. 17.8%; T1 64% vs. 65%; T2 23% vs. 17.5%).
In contrast, three smaller, well-established studies that came to different conclusions used four different surgeons and novel techniques to inject their radiocolloid and supervised residents for lymphatic mapping, she noted.
The radiocolloid lymphazurin first demonstrated superiority over methylene blue in 1990, but alternatives continue to be investigated due to frequent nonavailability and a host of adverse events including blue hives, blue discoloration or tattooing, and anaphylaxis.
Lymphazurin also costs 10-12 times more than methylene blue, which was reflected in the study in an average per patient cost of $815 vs. $75 for methylene blue, Dr. Patel said.
The American Society of Breast Surgeons, however, recommends dual-agent mapping using blue dye and a radioisotope in breast cancer to further improve the success in identifying the sentinel lymph nodes. The improvement is likely because of the dual mechanism at play: radiocolloids become entrapped within the lymph node, whereas certain blue dyes bind to interstitial albumin and are taken up by lymphatics, she explained.
The higher number of sentinel lymph nodes in the methylene blue group may be due to its particle size, which is smaller, weighs less, and diffused faster, Dr. Patel suggested.
The higher number of additional lymph nodes captured with lymphazurin may be because of the higher frequency of nodal dissection in this group than in the methylene blue group (25% vs. 16%).
The finding of greater nodal positivity in the lymphazurin group may be related to mechanism of action or the high percentage of patients with T1 disease enrolled in the study. Still, nodal positivity was higher with lymphazurin than methylene blue regardless of T stage, she said.
The lymphazurin group had higher rates than the methylene blue group of pseudohypoxemia (10% vs. 0%; P less than .0001), but blue hives (1.34% vs. 0%; P = .043) and anaphylaxis (.67% vs. 0%; P = .20) were kept in check. Patients were premedicated and early in the series, the surgeon began excising the area of injected blue skin during the primary surgery, Dr. Patel observed.
Despite being diluted, methylene blue was associated with higher rates of seroma (3.4% vs. 1.7%; P = .005) and skin necrosis (2.55% vs. 9%; P = .005).
Discussant Dr. Alyssa Throckmorton of Baptist Memorial Health Care in Memphis pointed out that more recent data show radiocolloid mapping alone is comparable to dual-agent mapping, suggesting that blue dye may not be needed. That said, there have been national shortages of methylene blue as well as lymphazurin.
“I think in surgeons who are going to use blue dye, with the way drug shortages have become in the last few years, you are going to have to be facile and familiar with both types of dye if you are going to use that as part of your clinical practice,” she said.
CHICAGO – Two commonly used dyes produced mixed results in sentinel lymph node mapping of early stage breast cancer in what was described as the highest-powered study to date.
The average number of sentinel lymph nodes identified per person was significantly higher with 1% methylene blue dye than with 1% lymphazurin (2.89 vs. 2.22; P less than .001).
Although there is extensive support for methylene blue as a safe and efficacious alternative to lymphazurin, this finding on the number of sentinel nodes identified is not replicated in any other study, Dr. Vaishali Patel said at the annual clinical congress of the American College of Surgeons. The study was conducted at the McLaren Flint (Mich.) Medical Center. Dr. Sukamal Saha was principal investigator.
On the other hand, lymphazurin identified significantly more additional lymph nodes than methylene blue (mean 4.48 vs. 2.84; P less than .001).
Nodal positivity was also significantly higher with lymphazurin than methylene blue (14.93% vs. 8.85%; P less than .001), which also has not been reported in other trials.
“We think this does offer a true comparison between the two dyes,” Dr. Patel of Detroit Medical Center Sinai-Grace Hospital said. “The volume of dye and technique were consistent for all 651 patients. … with one surgeon performing the injections and one surgeon performing the procedures.” The 651 consecutive patients were randomly assigned based on agent availability to a preoperative injection of lymphazurin (half intraparenchymal and half subareolar in the upper outer quadrant) or an intraoperative injection of methylene blue over 5 minutes (3 ccs intraparenchymal, 1 cc subareolar, and 1 cc intradermal).
The lymphazurin and methylene blue groups were also similar in number (298 patients vs. 353 patients), age (mean 61.6 years vs. 63.5 years), and T stage (in situ 12% vs. 17.8%; T1 64% vs. 65%; T2 23% vs. 17.5%).
In contrast, three smaller, well-established studies that came to different conclusions used four different surgeons and novel techniques to inject their radiocolloid and supervised residents for lymphatic mapping, she noted.
The radiocolloid lymphazurin first demonstrated superiority over methylene blue in 1990, but alternatives continue to be investigated due to frequent nonavailability and a host of adverse events including blue hives, blue discoloration or tattooing, and anaphylaxis.
Lymphazurin also costs 10-12 times more than methylene blue, which was reflected in the study in an average per patient cost of $815 vs. $75 for methylene blue, Dr. Patel said.
The American Society of Breast Surgeons, however, recommends dual-agent mapping using blue dye and a radioisotope in breast cancer to further improve the success in identifying the sentinel lymph nodes. The improvement is likely because of the dual mechanism at play: radiocolloids become entrapped within the lymph node, whereas certain blue dyes bind to interstitial albumin and are taken up by lymphatics, she explained.
The higher number of sentinel lymph nodes in the methylene blue group may be due to its particle size, which is smaller, weighs less, and diffused faster, Dr. Patel suggested.
The higher number of additional lymph nodes captured with lymphazurin may be because of the higher frequency of nodal dissection in this group than in the methylene blue group (25% vs. 16%).
The finding of greater nodal positivity in the lymphazurin group may be related to mechanism of action or the high percentage of patients with T1 disease enrolled in the study. Still, nodal positivity was higher with lymphazurin than methylene blue regardless of T stage, she said.
The lymphazurin group had higher rates than the methylene blue group of pseudohypoxemia (10% vs. 0%; P less than .0001), but blue hives (1.34% vs. 0%; P = .043) and anaphylaxis (.67% vs. 0%; P = .20) were kept in check. Patients were premedicated and early in the series, the surgeon began excising the area of injected blue skin during the primary surgery, Dr. Patel observed.
Despite being diluted, methylene blue was associated with higher rates of seroma (3.4% vs. 1.7%; P = .005) and skin necrosis (2.55% vs. 9%; P = .005).
Discussant Dr. Alyssa Throckmorton of Baptist Memorial Health Care in Memphis pointed out that more recent data show radiocolloid mapping alone is comparable to dual-agent mapping, suggesting that blue dye may not be needed. That said, there have been national shortages of methylene blue as well as lymphazurin.
“I think in surgeons who are going to use blue dye, with the way drug shortages have become in the last few years, you are going to have to be facile and familiar with both types of dye if you are going to use that as part of your clinical practice,” she said.
CHICAGO – Two commonly used dyes produced mixed results in sentinel lymph node mapping of early stage breast cancer in what was described as the highest-powered study to date.
The average number of sentinel lymph nodes identified per person was significantly higher with 1% methylene blue dye than with 1% lymphazurin (2.89 vs. 2.22; P less than .001).
Although there is extensive support for methylene blue as a safe and efficacious alternative to lymphazurin, this finding on the number of sentinel nodes identified is not replicated in any other study, Dr. Vaishali Patel said at the annual clinical congress of the American College of Surgeons. The study was conducted at the McLaren Flint (Mich.) Medical Center. Dr. Sukamal Saha was principal investigator.
On the other hand, lymphazurin identified significantly more additional lymph nodes than methylene blue (mean 4.48 vs. 2.84; P less than .001).
Nodal positivity was also significantly higher with lymphazurin than methylene blue (14.93% vs. 8.85%; P less than .001), which also has not been reported in other trials.
“We think this does offer a true comparison between the two dyes,” Dr. Patel of Detroit Medical Center Sinai-Grace Hospital said. “The volume of dye and technique were consistent for all 651 patients. … with one surgeon performing the injections and one surgeon performing the procedures.” The 651 consecutive patients were randomly assigned based on agent availability to a preoperative injection of lymphazurin (half intraparenchymal and half subareolar in the upper outer quadrant) or an intraoperative injection of methylene blue over 5 minutes (3 ccs intraparenchymal, 1 cc subareolar, and 1 cc intradermal).
The lymphazurin and methylene blue groups were also similar in number (298 patients vs. 353 patients), age (mean 61.6 years vs. 63.5 years), and T stage (in situ 12% vs. 17.8%; T1 64% vs. 65%; T2 23% vs. 17.5%).
In contrast, three smaller, well-established studies that came to different conclusions used four different surgeons and novel techniques to inject their radiocolloid and supervised residents for lymphatic mapping, she noted.
The radiocolloid lymphazurin first demonstrated superiority over methylene blue in 1990, but alternatives continue to be investigated due to frequent nonavailability and a host of adverse events including blue hives, blue discoloration or tattooing, and anaphylaxis.
Lymphazurin also costs 10-12 times more than methylene blue, which was reflected in the study in an average per patient cost of $815 vs. $75 for methylene blue, Dr. Patel said.
The American Society of Breast Surgeons, however, recommends dual-agent mapping using blue dye and a radioisotope in breast cancer to further improve the success in identifying the sentinel lymph nodes. The improvement is likely because of the dual mechanism at play: radiocolloids become entrapped within the lymph node, whereas certain blue dyes bind to interstitial albumin and are taken up by lymphatics, she explained.
The higher number of sentinel lymph nodes in the methylene blue group may be due to its particle size, which is smaller, weighs less, and diffused faster, Dr. Patel suggested.
The higher number of additional lymph nodes captured with lymphazurin may be because of the higher frequency of nodal dissection in this group than in the methylene blue group (25% vs. 16%).
The finding of greater nodal positivity in the lymphazurin group may be related to mechanism of action or the high percentage of patients with T1 disease enrolled in the study. Still, nodal positivity was higher with lymphazurin than methylene blue regardless of T stage, she said.
The lymphazurin group had higher rates than the methylene blue group of pseudohypoxemia (10% vs. 0%; P less than .0001), but blue hives (1.34% vs. 0%; P = .043) and anaphylaxis (.67% vs. 0%; P = .20) were kept in check. Patients were premedicated and early in the series, the surgeon began excising the area of injected blue skin during the primary surgery, Dr. Patel observed.
Despite being diluted, methylene blue was associated with higher rates of seroma (3.4% vs. 1.7%; P = .005) and skin necrosis (2.55% vs. 9%; P = .005).
Discussant Dr. Alyssa Throckmorton of Baptist Memorial Health Care in Memphis pointed out that more recent data show radiocolloid mapping alone is comparable to dual-agent mapping, suggesting that blue dye may not be needed. That said, there have been national shortages of methylene blue as well as lymphazurin.
“I think in surgeons who are going to use blue dye, with the way drug shortages have become in the last few years, you are going to have to be facile and familiar with both types of dye if you are going to use that as part of your clinical practice,” she said.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Contrary to prior studies, lymph node positivity was higher with lymphazurin than methylene blue in patients with early breast cancer.
Major finding: Nodal positivity was 14.93% with lymphazurin vs. 8.85% with methylene blue (P less than .001).
Data source: Prospective study in 651 patients undergoing lymphatic mapping for breast cancer.
Disclosures: Dr. Patel and Dr. Throckmorton reported having no relevant conflicts.
What’s anticipated at SABCS 2015?
FROM SABCS 2015 – A survey of Oncology Practice board members, including Dr. William J. Gradishar, Betsy Bramsen Professor of Breast Oncology, Northwestern University, Chicago, and medical oncologists at the Cleveland Clinic who will be attending the San Antonio Breast Cancer Symposium, revealed several anticipated studies from this year’s symposium, set to begin on Wednesday, Dec. 9. Titles, and links to abstracts if available, are listed below:
• S2-02 The Impact of Adjuvant Denosumab on Disease-Free Survival: Results from 3,425 Postmenopausal Patients of the ABCSG-18 Trial.
• S2-05 Event-free and overall survival following neoadjuvant weekly paclitaxel and dose-dense AC +/-carboplatin and/or bevacizumab in triple-negative breast cancer: Outcomes from CALGB 40603 (Alliance).
• S5-05 Trastuzumab emtansine improves overall survival versus treatment of physician’s choice in patients with previously treated HER2-positive metastatic breast cancer: Final overall survival results from the phase III TH3RESA study.
• S1-05 Prophylactic beta blockade preserves left ventricular ejection fraction in HER2-overexpressing breast cancer patients receiving trastuzumab: Primary results of the MANTICORE randomized controlled trial.
• S1-07 A phase III trial of adjuvant capecitabine in breast cancer patients with HER2-negative pathologic residual invasive disease after neoadjuvant chemotherapy (CREATE-X, JBCRG-04).
• S4-01 Identification of early versus late drivers of breast tumors and metastasis.
• S5-07 Preliminary efficacy and safety of pembrolizumab (MK-3475) in patients with PD-L1–positive, estrogen receptor-positive (ER+)/HER2-negative advanced breast cancer enrolled in KEYNOTE-028.
• S1-09 A comparison of the diagnostic performance of 2D synthetic mammography versus digital breast tomosynthesis in 2,500 patients.
• S6-01 PIK3CA status in circulating tumor DNA (ctDNA) predicts efficacy of buparlisib (BUP) plus fulvestrant (FULV) in postmenopausal women with endocrine-resistant HR+/HER2– advanced breast cancer (BC): First results from the randomized, phase III BELLE-2 trial.
• S5-04 Ten-year follow-up of the BCIRG-006 trial comparing doxorubicin plus cyclophosphamide followed by docetaxel (AC®T) with doxorubicin plus cyclophosphamide followed by docetaxel and trastuzumab (AC®TH) with docetaxel, carboplatin and trastuzumab (TCH) in HER2+ early breast cancer patients.
• S3-05 Higher 10-year overall survival after breast conserving therapy compared to mastectomy in early stage breast cancer: a population-based study with 37,207 patients.
• S1-04 Avelumab (MSB0010718C), an anti-PD-L1 antibody, in patients with locally advanced or metastatic breast cancer: a phase Ib JAVELIN solid tumor trial.
FROM SABCS 2015 – A survey of Oncology Practice board members, including Dr. William J. Gradishar, Betsy Bramsen Professor of Breast Oncology, Northwestern University, Chicago, and medical oncologists at the Cleveland Clinic who will be attending the San Antonio Breast Cancer Symposium, revealed several anticipated studies from this year’s symposium, set to begin on Wednesday, Dec. 9. Titles, and links to abstracts if available, are listed below:
• S2-02 The Impact of Adjuvant Denosumab on Disease-Free Survival: Results from 3,425 Postmenopausal Patients of the ABCSG-18 Trial.
• S2-05 Event-free and overall survival following neoadjuvant weekly paclitaxel and dose-dense AC +/-carboplatin and/or bevacizumab in triple-negative breast cancer: Outcomes from CALGB 40603 (Alliance).
• S5-05 Trastuzumab emtansine improves overall survival versus treatment of physician’s choice in patients with previously treated HER2-positive metastatic breast cancer: Final overall survival results from the phase III TH3RESA study.
• S1-05 Prophylactic beta blockade preserves left ventricular ejection fraction in HER2-overexpressing breast cancer patients receiving trastuzumab: Primary results of the MANTICORE randomized controlled trial.
• S1-07 A phase III trial of adjuvant capecitabine in breast cancer patients with HER2-negative pathologic residual invasive disease after neoadjuvant chemotherapy (CREATE-X, JBCRG-04).
• S4-01 Identification of early versus late drivers of breast tumors and metastasis.
• S5-07 Preliminary efficacy and safety of pembrolizumab (MK-3475) in patients with PD-L1–positive, estrogen receptor-positive (ER+)/HER2-negative advanced breast cancer enrolled in KEYNOTE-028.
• S1-09 A comparison of the diagnostic performance of 2D synthetic mammography versus digital breast tomosynthesis in 2,500 patients.
• S6-01 PIK3CA status in circulating tumor DNA (ctDNA) predicts efficacy of buparlisib (BUP) plus fulvestrant (FULV) in postmenopausal women with endocrine-resistant HR+/HER2– advanced breast cancer (BC): First results from the randomized, phase III BELLE-2 trial.
• S5-04 Ten-year follow-up of the BCIRG-006 trial comparing doxorubicin plus cyclophosphamide followed by docetaxel (AC®T) with doxorubicin plus cyclophosphamide followed by docetaxel and trastuzumab (AC®TH) with docetaxel, carboplatin and trastuzumab (TCH) in HER2+ early breast cancer patients.
• S3-05 Higher 10-year overall survival after breast conserving therapy compared to mastectomy in early stage breast cancer: a population-based study with 37,207 patients.
• S1-04 Avelumab (MSB0010718C), an anti-PD-L1 antibody, in patients with locally advanced or metastatic breast cancer: a phase Ib JAVELIN solid tumor trial.
FROM SABCS 2015 – A survey of Oncology Practice board members, including Dr. William J. Gradishar, Betsy Bramsen Professor of Breast Oncology, Northwestern University, Chicago, and medical oncologists at the Cleveland Clinic who will be attending the San Antonio Breast Cancer Symposium, revealed several anticipated studies from this year’s symposium, set to begin on Wednesday, Dec. 9. Titles, and links to abstracts if available, are listed below:
• S2-02 The Impact of Adjuvant Denosumab on Disease-Free Survival: Results from 3,425 Postmenopausal Patients of the ABCSG-18 Trial.
• S2-05 Event-free and overall survival following neoadjuvant weekly paclitaxel and dose-dense AC +/-carboplatin and/or bevacizumab in triple-negative breast cancer: Outcomes from CALGB 40603 (Alliance).
• S5-05 Trastuzumab emtansine improves overall survival versus treatment of physician’s choice in patients with previously treated HER2-positive metastatic breast cancer: Final overall survival results from the phase III TH3RESA study.
• S1-05 Prophylactic beta blockade preserves left ventricular ejection fraction in HER2-overexpressing breast cancer patients receiving trastuzumab: Primary results of the MANTICORE randomized controlled trial.
• S1-07 A phase III trial of adjuvant capecitabine in breast cancer patients with HER2-negative pathologic residual invasive disease after neoadjuvant chemotherapy (CREATE-X, JBCRG-04).
• S4-01 Identification of early versus late drivers of breast tumors and metastasis.
• S5-07 Preliminary efficacy and safety of pembrolizumab (MK-3475) in patients with PD-L1–positive, estrogen receptor-positive (ER+)/HER2-negative advanced breast cancer enrolled in KEYNOTE-028.
• S1-09 A comparison of the diagnostic performance of 2D synthetic mammography versus digital breast tomosynthesis in 2,500 patients.
• S6-01 PIK3CA status in circulating tumor DNA (ctDNA) predicts efficacy of buparlisib (BUP) plus fulvestrant (FULV) in postmenopausal women with endocrine-resistant HR+/HER2– advanced breast cancer (BC): First results from the randomized, phase III BELLE-2 trial.
• S5-04 Ten-year follow-up of the BCIRG-006 trial comparing doxorubicin plus cyclophosphamide followed by docetaxel (AC®T) with doxorubicin plus cyclophosphamide followed by docetaxel and trastuzumab (AC®TH) with docetaxel, carboplatin and trastuzumab (TCH) in HER2+ early breast cancer patients.
• S3-05 Higher 10-year overall survival after breast conserving therapy compared to mastectomy in early stage breast cancer: a population-based study with 37,207 patients.
• S1-04 Avelumab (MSB0010718C), an anti-PD-L1 antibody, in patients with locally advanced or metastatic breast cancer: a phase Ib JAVELIN solid tumor trial.
Annual screening mammography beginning at age 40 saves the most lives
With the recent publication of new American Cancer Society (ACS) guidelines on breast cancer screening,1 we finally have achieved a consensus. All major organizations, including the US Preventive Services Task Force (USPSTF), agree that the most lives are saved by annual screening beginning at age 40. This is the only science-backed finding of their reviews.
Here is a statement from the USPSTF: “[We] found adequate evidence that mammography screening reduces breast cancer mortality in women ages 40 to 74 years.”2 And from the ACS: “Women should have the opportunity to begin annual screening between the ages of 40 and 44 years.”1
Regrettably, the USPSTF, whose guidelines determine insurance coverage, endangers women by going on to suggest that they can wait until the age of 50 to begin screening and then wait a full 2 years between screens.
The new ACS guidelines have been misreported as recommending the initiation of annual screening at age 45, moving to biennial screening at the age of 55. This misunderstanding arose because the ACS describes annual screening starting at age 40 as a “qualified recommendation.” However, it defines this qualified recommendation as meaning that “The majority of individuals in this situation would want the suggested course of action, but many would not.”1
Why would screening guidelines be based on “what many [women] would not” choose? No one forces women at any age to participate in screening. Each woman, regardless of age, should choose for herself whether or not to participate in screening. In fact, the ACS panel provides no data on what screening option women would prefer. Members of the ACS and USPSTF panels, none of whom provides care for women with breast cancer, injected their own personal biases to qualify what the scientific evidence shows by claiming to have “weighed” benefits against “harms.” Yet they provide no description of the scale that was used. They state only that there are 2 major harms: “false positives” and “overdiagnosis.”
“False positive” is a misnomerRecalls from screening have been called, pejoratively, “false positives,” leading some to believe that women are being told that they have breast cancer when they do not. In reality, most recalled women ultimately are told that there is no reason for concern.
Approximately 10% of US women who undergo screening mammography are recalled—the same percentage as for Pap testing.3 (The ACS and USPSTF panels ignore the benefit for the 90% of women who are reassured by a negative screen.)
Among the women recalled, more than half are told that everything is fine, based on a few extra pictures or an ultrasound. Approximately 25% (2.5% of those screened) are asked to return in 6 months just to be careful, and approximately 20% (2% of women screened) will be advised to undergo imaging-guided needle biopsy using local anesthesia. Among these women, 20% to 40% will be found to have cancer.4
This figure is much higher than in the past, when women had “lumps” surgically removed, only 15% of which were cancer. Most of these lesions were larger and less likely to be cured than screen-detected cancers.5
Panels fail to justify breast cancer deaths that would occur with proposed screening intervalsThe main reason the ACS and USPSTF panels decided to compromise on their recommendations was to try to reduce the number of recalls, yet they never explain how many fewer recalls are equivalent to allowing a death that could have been avoided by annual screening starting at age 40.
The National Cancer Institute’s Cancer Intervention and Surveillance Modeling Network (CISNET)—used by both panels—shows that, if women in their 40s wait until age 50 and then are screened every 2 years (as the USPSTF recommends), as many as 100,000 lives will be lost that could have been saved by annual screening starting at age 40.6 If women wait until age 45 to begin annual screening and then shift to biennial screening at age 55 (as the ACS recommends), more than 38,000 women now in their 40s will die, unnecessarily, as a result.7
Neither panel states how many recalls avoided are equivalent to allowing so many avoidable, premature deaths.
No invasive cancers resolve spontaneouslyThe other alleged harm of screening is “overdiagnosis”—the exaggerated suggestion that mammography screening finds tens of thousands of breast cancers each year that, if left undetected, would disappear on their own.8,9 Such analyses have been shown to be scientifically unsupportable.10–13 In fact, no one has ever seen an invasive breast cancer disappear on its own without therapy. The claim is tens of thousands each year, yet no one has seen a single case.
There certainly are legitimate questions about the need to treat all cases of ductal carcinoma in situ (DCIS). However, if an invasive breast cancer is found during screening and then left alone, it will grow to become a palpable cancer, with lethal capability.
Here are the proven facts about breast cancer screening
- The most lives are saved when annual screening begins at age 40. This fact has been proven by randomized, controlled trials.14,15 All of the data models in CISNET agree that the most lives are saved by annual screening beginning at age 40.16
- There is no scientific or biological reason to use the age of 50 as a threshold for screening. None of the parameters of screening changes abruptly at age 50—or any other age.17
- More than 30,000 new cases of breast cancer occur each year among women in their 40s.18
- More than 40% of years of life lost to breast cancer are among women diagnosed in their 40s.19 The ACS found that the years of life lost to breast cancer for women aged 40 to 44 are the same as for women aged 55 to 59.2
- Despite access to modern therapies, numerous observational studies show that when screening is introduced into the population, the breast cancer death rate goes down, in relation to participation in screening, for women aged 40 and older.20–35
- In the 2 largest Harvard teaching hospitals, more than 70% of women who died from breast cancer were among the 20% who were not participating in screening, including women in their 40s, despite the fact that all had access to modern therapies.36 It is likely that many of the 40,000 women who still die in the United States each year, despite improvements in therapy, were also not participating in screening.
- The death rate from breast cancer remained unchanged from 1940 until screening began in the mid-1980s. Soon after, in 1990, the rate began to fall for the first time in 50 years. Today, 36% fewer women die each year from breast cancer.37 Men with breast cancer have access to the same therapies but, in 1990, the death rate for men began to increase as it began to fall for women. The death rate for men remained elevated until 2005 and then returned to 1990 levels, where it has remained, as the death rate for women has continued to decline.38 Women are being screened, whereas men present with larger and later-stage cancers. Therapy has improved, but the most lives are saved when breast cancer is treated early.
Why not screen only high-risk women? It has been suggested that only high-risk women should participate in screening. However, women who inherit a genetic predisposition account for only about 10% of breast cancers each year.39 If we add to that number other women with family histories or other known risk factors, these cases account for another 15% of cancers.40
Regrettably, high-risk women account for only a quarter of breast cancers diagnosed each year. If only high-risk women are screened, the vast majority of women who develop breast cancer (75%) will not benefit from early detection.
The bottom line Mammography is not perfect. It does not find all cancers and does not find all cancers early enough for a cure. However, there is no universal cure on the horizon, while screening is available today and is saving thousands of lives each year.
All women should have access to, and be encouraged to participate in, annual screening starting at age 40.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Oeffinger KC, Fontham ET, Etzioni R, et al. Breast cancer screening for women at average risk. 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–1614.
- U.S. Preventive Services Task Force. Draft Recommendation Statement. Breast Cancer: Screening [Web page]. Rockville, MD: USPSTF Program Office; 2015. http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementDraft/breast-cancer-screening1. Accessed November 11, 2015.
- Saraiya M, Irwin KL, Carlin L, et al. Cervical cancer screening and management practices among providers in the National Breast and Cervical Cancer Early Detection Program (NBCCEDP). Cancer. 2007;110(5):1024–1032.
- Rosenberg RD, Yankaskas BC, Abraham LA, et al. Performance benchmarks for screening mammography. Radiology. 2006;241(1):55–66.
- Spivey GH, Perry BW, Clark VA, et al. Predicting the risk of cancer at the time of breast biopsy. Am Surg.1982;48(7):326–332.
- Hendrick RE, Helvie MA. USPSTF Guidelines on screening mammography recommendations: science ignored. Am J Roentgenol. 2011; 196(2): W112–116.
- Based on CISNET models. Personal communication: R. Edward Hendrick, PhD.
- Jorgensen KJ, Gotzsche PC. Overdiagnosis in publicly organised mammography screening programmes: systematic review of incidence trends. BMJ. 2009;339:b2587.
- Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012;367(21):1998–2005.
- Puliti D, Duffy SW, Miccinesi G, et al; EUROSCREEN Working Group. Overdiagnosis in mammographic screening for breast cancer in Europe: a literature review. J Med Screen. 2012;19(suppl 1):42–56.
- Kopans DB. Arguments against mammography screening continue to be based on faulty science. Oncologist. 2014;19(2):107–112.
- Helvie MA, Chang JT, Hendrick RE, Banerjee M. Reduction in late-stage breast cancer incidence in the mammography era: implications for overdiagnosis of invasive cancer. Cancer. 2014;120(17):2649–2656.
- Etzioni R, Xia J, Hubbard R, Weiss NS, Gulati R. A reality check for overdiagnosis estimates associated with breast cancer screening. J Natl Cancer Inst. 2014;106(12). doi: 10.1093/jnci/dju315.
- Duffy SW, Tabar L, Smith RA. The mammographicscreening trials: commentary on the recent work by Olsen and Gotzsche. CA Cancer J Clin. 2002;52(2):68–71.
- Hendrick RE, Smith RA, Rutledge JH, Smart CR. Benefit of screening mammography in women ages 40-49: a new meta-analysis of randomized controlled trials. J Natl Cancer Inst Monogr. 1997;22:87–92.
- Mandelblatt JS, Cronin KA, Bailey S, et al; Breast Cancer Working Group of the Cancer Intervention and Surveillance Modeling Network. Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Ann Intern Med. 2009;151(10):738–747.
- Kopans DB, Moore RH, McCarthy KA, et al. Biasing the interpretation of mammography screening data by age grouping: nothing changes abruptly at age 50. Breast J. 1998;4(3):139–145.
- US Census Bureau. 2000 Census Summary File 1 and 2010 Census Summary File 1 show 21,996,493 women ages 40-49 and SEER shows 95.5 cancers per 100,000 for these women, which means 34,578 cancers.
- Shapiro S. Evidence on screening for breast cancer from a randomized trial. Cancer. 1977;39(6 suppl):2772–2278.
- Tabar L, Vitak B, Tony HH, Yen MF, Duffy SW, Smith RA. Beyond randomized controlled trials: organized mammographic screening substantially reduces breast carcinoma mortality. Cancer. 2001;91(9):1724–1731.
- Kopans DB. Beyond randomized, controlled trials: organized mammographic screening substantially reduces breast cancer mortality. Cancer. 2002;94(2):580–581.
- Duffy SW, Tabar L, Chen H, et al. The impact of organized mammography service screening on breast carcinoma mortality in seven Swedish counties. Cancer. 2002;95(3):458–469.
- Otto SJ, Fracheboud J, Looman CWN, et al; National Evaluation Team for Breast Cancer Screening. Initiation of population-based mammography screening in Dutch municipalities and effect on breast-cancer mortality: a systematic review. Lancet. 2003;361(9367):411–417.
- Swedish Organised Service Screening Evaluation Group. Reduction in breast cancer mortality from organized service screening with mammography: 1. Further confirmation with extended data. Cancer Epidemiol Biomarkers Prev. 2006;15(1):45–51.
- Coldman A, Phillips N, Warren L, Kan L. Breast cancer mortality after screening mammography in British Columbia women. Int J Cancer. 2007;120(5):1076–1080.
- Jonsson H, Bordás P, Wallin H, Nyström L, Lenner P. Service screening with mammography in Northern Sweden: effects on breast cancer mortality—an update. J Med Screen. 2007;14(2):87–93.
- Paap E, Holland R, den Heeten GJ, et al. A remarkable reduction of breast cancer deaths in screened versus unscreened women: a case-referent study. Cancer Causes Control. 2010;21(10):1569–1573.
- Otto SJ, Fracheboud J, Verbeek ALM, et al; National Evaluation Team for Breast Cancer Screening. Mammography screening and risk of breast cancer death: a population-based case– control study. Cancer Epidemiol Biomarkers Prev. 2012;21(1):66–73.
- van Schoor G, Moss SM, Otten JD, et al. Increasingly strong reduction in breast cancer mortality due to screening. Br J Cancer. 2011;104(6):910–914.
- Mandelblatt JS, Cronin KA, Bailey S, et al; Breast Cancer Working Group of the Cancer Intervention and Surveillance Modeling Network. Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Ann Intern Med. 2009;151(10):738–747.
- Hellquist BN, Duffy SW, Abdsaleh S, et al. Effectiveness of population-based service screening with mammography for women ages 40 to 49 years: evaluation of the Swedish Mammography Screening in Young Women (SCRY) cohort. Cancer. 2011;117(4):714–722.
- Broeders M, Moss S, Nyström L, et al; EUROSCREEN Working Group. The impact of mammographic screening on breast cancer mortality in Europe: a review of observational studies. J Med Screen. 2012;19(suppl 1):14–25.
- Hofvind S, Ursin G, Tretli S, Sebuødegård S, Møller B. Breast cancer mortality in participants of the Norwegian Breast Cancer Screening Program. Cancer. 2013;119(17):3106–3112.
- Sigurdsson K, Olafsdóttir EJ. Population-based service mammography screening: the Icelandic experience. Breast Cancer (Dove Med Press). 2013;5:17–25.
- Coldman A, Phillips N, Wilson C, et al. Pan- Canadian study of mammography screening and mortality from breast cancer. J Natl Cancer Inst. 2014;106(11):dju261.
- Webb ML, Cady B, Michaelson JS, et al. A failure analysis of invasive breast cancer: most deaths from disease occur in women not regularly screened. Cancer. 2014;120(18):2839–2846.
- DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A. Breast cancer statistics, 2015: Convergence of incidence rates between black and white women. CA Cancer J Clin. 2015 Oct 29. doi: 10.3322/caac.21320.
- National Cancer Institute. Surveillance, Epidemiology, and End Results Program. http://seer.cancer.gov/archive/csr/1975_2010/browse_csr.php?sectionSEL=4&pageSEL=sect_04_table.06.html. Accessed November 16, 2015.
- Claus EB, Schildkraut JM, Thompson WD, Risch NJ. The genetic attributable risk of breast and ovarian cancer. Cancer. 1996;77(11):2318–2324.
- Seidman H, Stellman SD, Mushinski MH. A different perspective on breast cancer risk factors: some implications of nonattributable risk. Cancer. 1982;32(5):301–313.
With the recent publication of new American Cancer Society (ACS) guidelines on breast cancer screening,1 we finally have achieved a consensus. All major organizations, including the US Preventive Services Task Force (USPSTF), agree that the most lives are saved by annual screening beginning at age 40. This is the only science-backed finding of their reviews.
Here is a statement from the USPSTF: “[We] found adequate evidence that mammography screening reduces breast cancer mortality in women ages 40 to 74 years.”2 And from the ACS: “Women should have the opportunity to begin annual screening between the ages of 40 and 44 years.”1
Regrettably, the USPSTF, whose guidelines determine insurance coverage, endangers women by going on to suggest that they can wait until the age of 50 to begin screening and then wait a full 2 years between screens.
The new ACS guidelines have been misreported as recommending the initiation of annual screening at age 45, moving to biennial screening at the age of 55. This misunderstanding arose because the ACS describes annual screening starting at age 40 as a “qualified recommendation.” However, it defines this qualified recommendation as meaning that “The majority of individuals in this situation would want the suggested course of action, but many would not.”1
Why would screening guidelines be based on “what many [women] would not” choose? No one forces women at any age to participate in screening. Each woman, regardless of age, should choose for herself whether or not to participate in screening. In fact, the ACS panel provides no data on what screening option women would prefer. Members of the ACS and USPSTF panels, none of whom provides care for women with breast cancer, injected their own personal biases to qualify what the scientific evidence shows by claiming to have “weighed” benefits against “harms.” Yet they provide no description of the scale that was used. They state only that there are 2 major harms: “false positives” and “overdiagnosis.”
“False positive” is a misnomerRecalls from screening have been called, pejoratively, “false positives,” leading some to believe that women are being told that they have breast cancer when they do not. In reality, most recalled women ultimately are told that there is no reason for concern.
Approximately 10% of US women who undergo screening mammography are recalled—the same percentage as for Pap testing.3 (The ACS and USPSTF panels ignore the benefit for the 90% of women who are reassured by a negative screen.)
Among the women recalled, more than half are told that everything is fine, based on a few extra pictures or an ultrasound. Approximately 25% (2.5% of those screened) are asked to return in 6 months just to be careful, and approximately 20% (2% of women screened) will be advised to undergo imaging-guided needle biopsy using local anesthesia. Among these women, 20% to 40% will be found to have cancer.4
This figure is much higher than in the past, when women had “lumps” surgically removed, only 15% of which were cancer. Most of these lesions were larger and less likely to be cured than screen-detected cancers.5
Panels fail to justify breast cancer deaths that would occur with proposed screening intervalsThe main reason the ACS and USPSTF panels decided to compromise on their recommendations was to try to reduce the number of recalls, yet they never explain how many fewer recalls are equivalent to allowing a death that could have been avoided by annual screening starting at age 40.
The National Cancer Institute’s Cancer Intervention and Surveillance Modeling Network (CISNET)—used by both panels—shows that, if women in their 40s wait until age 50 and then are screened every 2 years (as the USPSTF recommends), as many as 100,000 lives will be lost that could have been saved by annual screening starting at age 40.6 If women wait until age 45 to begin annual screening and then shift to biennial screening at age 55 (as the ACS recommends), more than 38,000 women now in their 40s will die, unnecessarily, as a result.7
Neither panel states how many recalls avoided are equivalent to allowing so many avoidable, premature deaths.
No invasive cancers resolve spontaneouslyThe other alleged harm of screening is “overdiagnosis”—the exaggerated suggestion that mammography screening finds tens of thousands of breast cancers each year that, if left undetected, would disappear on their own.8,9 Such analyses have been shown to be scientifically unsupportable.10–13 In fact, no one has ever seen an invasive breast cancer disappear on its own without therapy. The claim is tens of thousands each year, yet no one has seen a single case.
There certainly are legitimate questions about the need to treat all cases of ductal carcinoma in situ (DCIS). However, if an invasive breast cancer is found during screening and then left alone, it will grow to become a palpable cancer, with lethal capability.
Here are the proven facts about breast cancer screening
- The most lives are saved when annual screening begins at age 40. This fact has been proven by randomized, controlled trials.14,15 All of the data models in CISNET agree that the most lives are saved by annual screening beginning at age 40.16
- There is no scientific or biological reason to use the age of 50 as a threshold for screening. None of the parameters of screening changes abruptly at age 50—or any other age.17
- More than 30,000 new cases of breast cancer occur each year among women in their 40s.18
- More than 40% of years of life lost to breast cancer are among women diagnosed in their 40s.19 The ACS found that the years of life lost to breast cancer for women aged 40 to 44 are the same as for women aged 55 to 59.2
- Despite access to modern therapies, numerous observational studies show that when screening is introduced into the population, the breast cancer death rate goes down, in relation to participation in screening, for women aged 40 and older.20–35
- In the 2 largest Harvard teaching hospitals, more than 70% of women who died from breast cancer were among the 20% who were not participating in screening, including women in their 40s, despite the fact that all had access to modern therapies.36 It is likely that many of the 40,000 women who still die in the United States each year, despite improvements in therapy, were also not participating in screening.
- The death rate from breast cancer remained unchanged from 1940 until screening began in the mid-1980s. Soon after, in 1990, the rate began to fall for the first time in 50 years. Today, 36% fewer women die each year from breast cancer.37 Men with breast cancer have access to the same therapies but, in 1990, the death rate for men began to increase as it began to fall for women. The death rate for men remained elevated until 2005 and then returned to 1990 levels, where it has remained, as the death rate for women has continued to decline.38 Women are being screened, whereas men present with larger and later-stage cancers. Therapy has improved, but the most lives are saved when breast cancer is treated early.
Why not screen only high-risk women? It has been suggested that only high-risk women should participate in screening. However, women who inherit a genetic predisposition account for only about 10% of breast cancers each year.39 If we add to that number other women with family histories or other known risk factors, these cases account for another 15% of cancers.40
Regrettably, high-risk women account for only a quarter of breast cancers diagnosed each year. If only high-risk women are screened, the vast majority of women who develop breast cancer (75%) will not benefit from early detection.
The bottom line Mammography is not perfect. It does not find all cancers and does not find all cancers early enough for a cure. However, there is no universal cure on the horizon, while screening is available today and is saving thousands of lives each year.
All women should have access to, and be encouraged to participate in, annual screening starting at age 40.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
With the recent publication of new American Cancer Society (ACS) guidelines on breast cancer screening,1 we finally have achieved a consensus. All major organizations, including the US Preventive Services Task Force (USPSTF), agree that the most lives are saved by annual screening beginning at age 40. This is the only science-backed finding of their reviews.
Here is a statement from the USPSTF: “[We] found adequate evidence that mammography screening reduces breast cancer mortality in women ages 40 to 74 years.”2 And from the ACS: “Women should have the opportunity to begin annual screening between the ages of 40 and 44 years.”1
Regrettably, the USPSTF, whose guidelines determine insurance coverage, endangers women by going on to suggest that they can wait until the age of 50 to begin screening and then wait a full 2 years between screens.
The new ACS guidelines have been misreported as recommending the initiation of annual screening at age 45, moving to biennial screening at the age of 55. This misunderstanding arose because the ACS describes annual screening starting at age 40 as a “qualified recommendation.” However, it defines this qualified recommendation as meaning that “The majority of individuals in this situation would want the suggested course of action, but many would not.”1
Why would screening guidelines be based on “what many [women] would not” choose? No one forces women at any age to participate in screening. Each woman, regardless of age, should choose for herself whether or not to participate in screening. In fact, the ACS panel provides no data on what screening option women would prefer. Members of the ACS and USPSTF panels, none of whom provides care for women with breast cancer, injected their own personal biases to qualify what the scientific evidence shows by claiming to have “weighed” benefits against “harms.” Yet they provide no description of the scale that was used. They state only that there are 2 major harms: “false positives” and “overdiagnosis.”
“False positive” is a misnomerRecalls from screening have been called, pejoratively, “false positives,” leading some to believe that women are being told that they have breast cancer when they do not. In reality, most recalled women ultimately are told that there is no reason for concern.
Approximately 10% of US women who undergo screening mammography are recalled—the same percentage as for Pap testing.3 (The ACS and USPSTF panels ignore the benefit for the 90% of women who are reassured by a negative screen.)
Among the women recalled, more than half are told that everything is fine, based on a few extra pictures or an ultrasound. Approximately 25% (2.5% of those screened) are asked to return in 6 months just to be careful, and approximately 20% (2% of women screened) will be advised to undergo imaging-guided needle biopsy using local anesthesia. Among these women, 20% to 40% will be found to have cancer.4
This figure is much higher than in the past, when women had “lumps” surgically removed, only 15% of which were cancer. Most of these lesions were larger and less likely to be cured than screen-detected cancers.5
Panels fail to justify breast cancer deaths that would occur with proposed screening intervalsThe main reason the ACS and USPSTF panels decided to compromise on their recommendations was to try to reduce the number of recalls, yet they never explain how many fewer recalls are equivalent to allowing a death that could have been avoided by annual screening starting at age 40.
The National Cancer Institute’s Cancer Intervention and Surveillance Modeling Network (CISNET)—used by both panels—shows that, if women in their 40s wait until age 50 and then are screened every 2 years (as the USPSTF recommends), as many as 100,000 lives will be lost that could have been saved by annual screening starting at age 40.6 If women wait until age 45 to begin annual screening and then shift to biennial screening at age 55 (as the ACS recommends), more than 38,000 women now in their 40s will die, unnecessarily, as a result.7
Neither panel states how many recalls avoided are equivalent to allowing so many avoidable, premature deaths.
No invasive cancers resolve spontaneouslyThe other alleged harm of screening is “overdiagnosis”—the exaggerated suggestion that mammography screening finds tens of thousands of breast cancers each year that, if left undetected, would disappear on their own.8,9 Such analyses have been shown to be scientifically unsupportable.10–13 In fact, no one has ever seen an invasive breast cancer disappear on its own without therapy. The claim is tens of thousands each year, yet no one has seen a single case.
There certainly are legitimate questions about the need to treat all cases of ductal carcinoma in situ (DCIS). However, if an invasive breast cancer is found during screening and then left alone, it will grow to become a palpable cancer, with lethal capability.
Here are the proven facts about breast cancer screening
- The most lives are saved when annual screening begins at age 40. This fact has been proven by randomized, controlled trials.14,15 All of the data models in CISNET agree that the most lives are saved by annual screening beginning at age 40.16
- There is no scientific or biological reason to use the age of 50 as a threshold for screening. None of the parameters of screening changes abruptly at age 50—or any other age.17
- More than 30,000 new cases of breast cancer occur each year among women in their 40s.18
- More than 40% of years of life lost to breast cancer are among women diagnosed in their 40s.19 The ACS found that the years of life lost to breast cancer for women aged 40 to 44 are the same as for women aged 55 to 59.2
- Despite access to modern therapies, numerous observational studies show that when screening is introduced into the population, the breast cancer death rate goes down, in relation to participation in screening, for women aged 40 and older.20–35
- In the 2 largest Harvard teaching hospitals, more than 70% of women who died from breast cancer were among the 20% who were not participating in screening, including women in their 40s, despite the fact that all had access to modern therapies.36 It is likely that many of the 40,000 women who still die in the United States each year, despite improvements in therapy, were also not participating in screening.
- The death rate from breast cancer remained unchanged from 1940 until screening began in the mid-1980s. Soon after, in 1990, the rate began to fall for the first time in 50 years. Today, 36% fewer women die each year from breast cancer.37 Men with breast cancer have access to the same therapies but, in 1990, the death rate for men began to increase as it began to fall for women. The death rate for men remained elevated until 2005 and then returned to 1990 levels, where it has remained, as the death rate for women has continued to decline.38 Women are being screened, whereas men present with larger and later-stage cancers. Therapy has improved, but the most lives are saved when breast cancer is treated early.
Why not screen only high-risk women? It has been suggested that only high-risk women should participate in screening. However, women who inherit a genetic predisposition account for only about 10% of breast cancers each year.39 If we add to that number other women with family histories or other known risk factors, these cases account for another 15% of cancers.40
Regrettably, high-risk women account for only a quarter of breast cancers diagnosed each year. If only high-risk women are screened, the vast majority of women who develop breast cancer (75%) will not benefit from early detection.
The bottom line Mammography is not perfect. It does not find all cancers and does not find all cancers early enough for a cure. However, there is no universal cure on the horizon, while screening is available today and is saving thousands of lives each year.
All women should have access to, and be encouraged to participate in, annual screening starting at age 40.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Oeffinger KC, Fontham ET, Etzioni R, et al. Breast cancer screening for women at average risk. 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–1614.
- U.S. Preventive Services Task Force. Draft Recommendation Statement. Breast Cancer: Screening [Web page]. Rockville, MD: USPSTF Program Office; 2015. http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementDraft/breast-cancer-screening1. Accessed November 11, 2015.
- Saraiya M, Irwin KL, Carlin L, et al. Cervical cancer screening and management practices among providers in the National Breast and Cervical Cancer Early Detection Program (NBCCEDP). Cancer. 2007;110(5):1024–1032.
- Rosenberg RD, Yankaskas BC, Abraham LA, et al. Performance benchmarks for screening mammography. Radiology. 2006;241(1):55–66.
- Spivey GH, Perry BW, Clark VA, et al. Predicting the risk of cancer at the time of breast biopsy. Am Surg.1982;48(7):326–332.
- Hendrick RE, Helvie MA. USPSTF Guidelines on screening mammography recommendations: science ignored. Am J Roentgenol. 2011; 196(2): W112–116.
- Based on CISNET models. Personal communication: R. Edward Hendrick, PhD.
- Jorgensen KJ, Gotzsche PC. Overdiagnosis in publicly organised mammography screening programmes: systematic review of incidence trends. BMJ. 2009;339:b2587.
- Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012;367(21):1998–2005.
- Puliti D, Duffy SW, Miccinesi G, et al; EUROSCREEN Working Group. Overdiagnosis in mammographic screening for breast cancer in Europe: a literature review. J Med Screen. 2012;19(suppl 1):42–56.
- Kopans DB. Arguments against mammography screening continue to be based on faulty science. Oncologist. 2014;19(2):107–112.
- Helvie MA, Chang JT, Hendrick RE, Banerjee M. Reduction in late-stage breast cancer incidence in the mammography era: implications for overdiagnosis of invasive cancer. Cancer. 2014;120(17):2649–2656.
- Etzioni R, Xia J, Hubbard R, Weiss NS, Gulati R. A reality check for overdiagnosis estimates associated with breast cancer screening. J Natl Cancer Inst. 2014;106(12). doi: 10.1093/jnci/dju315.
- Duffy SW, Tabar L, Smith RA. The mammographicscreening trials: commentary on the recent work by Olsen and Gotzsche. CA Cancer J Clin. 2002;52(2):68–71.
- Hendrick RE, Smith RA, Rutledge JH, Smart CR. Benefit of screening mammography in women ages 40-49: a new meta-analysis of randomized controlled trials. J Natl Cancer Inst Monogr. 1997;22:87–92.
- Mandelblatt JS, Cronin KA, Bailey S, et al; Breast Cancer Working Group of the Cancer Intervention and Surveillance Modeling Network. Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Ann Intern Med. 2009;151(10):738–747.
- Kopans DB, Moore RH, McCarthy KA, et al. Biasing the interpretation of mammography screening data by age grouping: nothing changes abruptly at age 50. Breast J. 1998;4(3):139–145.
- US Census Bureau. 2000 Census Summary File 1 and 2010 Census Summary File 1 show 21,996,493 women ages 40-49 and SEER shows 95.5 cancers per 100,000 for these women, which means 34,578 cancers.
- Shapiro S. Evidence on screening for breast cancer from a randomized trial. Cancer. 1977;39(6 suppl):2772–2278.
- Tabar L, Vitak B, Tony HH, Yen MF, Duffy SW, Smith RA. Beyond randomized controlled trials: organized mammographic screening substantially reduces breast carcinoma mortality. Cancer. 2001;91(9):1724–1731.
- Kopans DB. Beyond randomized, controlled trials: organized mammographic screening substantially reduces breast cancer mortality. Cancer. 2002;94(2):580–581.
- Duffy SW, Tabar L, Chen H, et al. The impact of organized mammography service screening on breast carcinoma mortality in seven Swedish counties. Cancer. 2002;95(3):458–469.
- Otto SJ, Fracheboud J, Looman CWN, et al; National Evaluation Team for Breast Cancer Screening. Initiation of population-based mammography screening in Dutch municipalities and effect on breast-cancer mortality: a systematic review. Lancet. 2003;361(9367):411–417.
- Swedish Organised Service Screening Evaluation Group. Reduction in breast cancer mortality from organized service screening with mammography: 1. Further confirmation with extended data. Cancer Epidemiol Biomarkers Prev. 2006;15(1):45–51.
- Coldman A, Phillips N, Warren L, Kan L. Breast cancer mortality after screening mammography in British Columbia women. Int J Cancer. 2007;120(5):1076–1080.
- Jonsson H, Bordás P, Wallin H, Nyström L, Lenner P. Service screening with mammography in Northern Sweden: effects on breast cancer mortality—an update. J Med Screen. 2007;14(2):87–93.
- Paap E, Holland R, den Heeten GJ, et al. A remarkable reduction of breast cancer deaths in screened versus unscreened women: a case-referent study. Cancer Causes Control. 2010;21(10):1569–1573.
- Otto SJ, Fracheboud J, Verbeek ALM, et al; National Evaluation Team for Breast Cancer Screening. Mammography screening and risk of breast cancer death: a population-based case– control study. Cancer Epidemiol Biomarkers Prev. 2012;21(1):66–73.
- van Schoor G, Moss SM, Otten JD, et al. Increasingly strong reduction in breast cancer mortality due to screening. Br J Cancer. 2011;104(6):910–914.
- Mandelblatt JS, Cronin KA, Bailey S, et al; Breast Cancer Working Group of the Cancer Intervention and Surveillance Modeling Network. Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Ann Intern Med. 2009;151(10):738–747.
- Hellquist BN, Duffy SW, Abdsaleh S, et al. Effectiveness of population-based service screening with mammography for women ages 40 to 49 years: evaluation of the Swedish Mammography Screening in Young Women (SCRY) cohort. Cancer. 2011;117(4):714–722.
- Broeders M, Moss S, Nyström L, et al; EUROSCREEN Working Group. The impact of mammographic screening on breast cancer mortality in Europe: a review of observational studies. J Med Screen. 2012;19(suppl 1):14–25.
- Hofvind S, Ursin G, Tretli S, Sebuødegård S, Møller B. Breast cancer mortality in participants of the Norwegian Breast Cancer Screening Program. Cancer. 2013;119(17):3106–3112.
- Sigurdsson K, Olafsdóttir EJ. Population-based service mammography screening: the Icelandic experience. Breast Cancer (Dove Med Press). 2013;5:17–25.
- Coldman A, Phillips N, Wilson C, et al. Pan- Canadian study of mammography screening and mortality from breast cancer. J Natl Cancer Inst. 2014;106(11):dju261.
- Webb ML, Cady B, Michaelson JS, et al. A failure analysis of invasive breast cancer: most deaths from disease occur in women not regularly screened. Cancer. 2014;120(18):2839–2846.
- DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A. Breast cancer statistics, 2015: Convergence of incidence rates between black and white women. CA Cancer J Clin. 2015 Oct 29. doi: 10.3322/caac.21320.
- National Cancer Institute. Surveillance, Epidemiology, and End Results Program. http://seer.cancer.gov/archive/csr/1975_2010/browse_csr.php?sectionSEL=4&pageSEL=sect_04_table.06.html. Accessed November 16, 2015.
- Claus EB, Schildkraut JM, Thompson WD, Risch NJ. The genetic attributable risk of breast and ovarian cancer. Cancer. 1996;77(11):2318–2324.
- Seidman H, Stellman SD, Mushinski MH. A different perspective on breast cancer risk factors: some implications of nonattributable risk. Cancer. 1982;32(5):301–313.
- Oeffinger KC, Fontham ET, Etzioni R, et al. Breast cancer screening for women at average risk. 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–1614.
- U.S. Preventive Services Task Force. Draft Recommendation Statement. Breast Cancer: Screening [Web page]. Rockville, MD: USPSTF Program Office; 2015. http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementDraft/breast-cancer-screening1. Accessed November 11, 2015.
- Saraiya M, Irwin KL, Carlin L, et al. Cervical cancer screening and management practices among providers in the National Breast and Cervical Cancer Early Detection Program (NBCCEDP). Cancer. 2007;110(5):1024–1032.
- Rosenberg RD, Yankaskas BC, Abraham LA, et al. Performance benchmarks for screening mammography. Radiology. 2006;241(1):55–66.
- Spivey GH, Perry BW, Clark VA, et al. Predicting the risk of cancer at the time of breast biopsy. Am Surg.1982;48(7):326–332.
- Hendrick RE, Helvie MA. USPSTF Guidelines on screening mammography recommendations: science ignored. Am J Roentgenol. 2011; 196(2): W112–116.
- Based on CISNET models. Personal communication: R. Edward Hendrick, PhD.
- Jorgensen KJ, Gotzsche PC. Overdiagnosis in publicly organised mammography screening programmes: systematic review of incidence trends. BMJ. 2009;339:b2587.
- Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012;367(21):1998–2005.
- Puliti D, Duffy SW, Miccinesi G, et al; EUROSCREEN Working Group. Overdiagnosis in mammographic screening for breast cancer in Europe: a literature review. J Med Screen. 2012;19(suppl 1):42–56.
- Kopans DB. Arguments against mammography screening continue to be based on faulty science. Oncologist. 2014;19(2):107–112.
- Helvie MA, Chang JT, Hendrick RE, Banerjee M. Reduction in late-stage breast cancer incidence in the mammography era: implications for overdiagnosis of invasive cancer. Cancer. 2014;120(17):2649–2656.
- Etzioni R, Xia J, Hubbard R, Weiss NS, Gulati R. A reality check for overdiagnosis estimates associated with breast cancer screening. J Natl Cancer Inst. 2014;106(12). doi: 10.1093/jnci/dju315.
- Duffy SW, Tabar L, Smith RA. The mammographicscreening trials: commentary on the recent work by Olsen and Gotzsche. CA Cancer J Clin. 2002;52(2):68–71.
- Hendrick RE, Smith RA, Rutledge JH, Smart CR. Benefit of screening mammography in women ages 40-49: a new meta-analysis of randomized controlled trials. J Natl Cancer Inst Monogr. 1997;22:87–92.
- Mandelblatt JS, Cronin KA, Bailey S, et al; Breast Cancer Working Group of the Cancer Intervention and Surveillance Modeling Network. Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Ann Intern Med. 2009;151(10):738–747.
- Kopans DB, Moore RH, McCarthy KA, et al. Biasing the interpretation of mammography screening data by age grouping: nothing changes abruptly at age 50. Breast J. 1998;4(3):139–145.
- US Census Bureau. 2000 Census Summary File 1 and 2010 Census Summary File 1 show 21,996,493 women ages 40-49 and SEER shows 95.5 cancers per 100,000 for these women, which means 34,578 cancers.
- Shapiro S. Evidence on screening for breast cancer from a randomized trial. Cancer. 1977;39(6 suppl):2772–2278.
- Tabar L, Vitak B, Tony HH, Yen MF, Duffy SW, Smith RA. Beyond randomized controlled trials: organized mammographic screening substantially reduces breast carcinoma mortality. Cancer. 2001;91(9):1724–1731.
- Kopans DB. Beyond randomized, controlled trials: organized mammographic screening substantially reduces breast cancer mortality. Cancer. 2002;94(2):580–581.
- Duffy SW, Tabar L, Chen H, et al. The impact of organized mammography service screening on breast carcinoma mortality in seven Swedish counties. Cancer. 2002;95(3):458–469.
- Otto SJ, Fracheboud J, Looman CWN, et al; National Evaluation Team for Breast Cancer Screening. Initiation of population-based mammography screening in Dutch municipalities and effect on breast-cancer mortality: a systematic review. Lancet. 2003;361(9367):411–417.
- Swedish Organised Service Screening Evaluation Group. Reduction in breast cancer mortality from organized service screening with mammography: 1. Further confirmation with extended data. Cancer Epidemiol Biomarkers Prev. 2006;15(1):45–51.
- Coldman A, Phillips N, Warren L, Kan L. Breast cancer mortality after screening mammography in British Columbia women. Int J Cancer. 2007;120(5):1076–1080.
- Jonsson H, Bordás P, Wallin H, Nyström L, Lenner P. Service screening with mammography in Northern Sweden: effects on breast cancer mortality—an update. J Med Screen. 2007;14(2):87–93.
- Paap E, Holland R, den Heeten GJ, et al. A remarkable reduction of breast cancer deaths in screened versus unscreened women: a case-referent study. Cancer Causes Control. 2010;21(10):1569–1573.
- Otto SJ, Fracheboud J, Verbeek ALM, et al; National Evaluation Team for Breast Cancer Screening. Mammography screening and risk of breast cancer death: a population-based case– control study. Cancer Epidemiol Biomarkers Prev. 2012;21(1):66–73.
- van Schoor G, Moss SM, Otten JD, et al. Increasingly strong reduction in breast cancer mortality due to screening. Br J Cancer. 2011;104(6):910–914.
- Mandelblatt JS, Cronin KA, Bailey S, et al; Breast Cancer Working Group of the Cancer Intervention and Surveillance Modeling Network. Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Ann Intern Med. 2009;151(10):738–747.
- Hellquist BN, Duffy SW, Abdsaleh S, et al. Effectiveness of population-based service screening with mammography for women ages 40 to 49 years: evaluation of the Swedish Mammography Screening in Young Women (SCRY) cohort. Cancer. 2011;117(4):714–722.
- Broeders M, Moss S, Nyström L, et al; EUROSCREEN Working Group. The impact of mammographic screening on breast cancer mortality in Europe: a review of observational studies. J Med Screen. 2012;19(suppl 1):14–25.
- Hofvind S, Ursin G, Tretli S, Sebuødegård S, Møller B. Breast cancer mortality in participants of the Norwegian Breast Cancer Screening Program. Cancer. 2013;119(17):3106–3112.
- Sigurdsson K, Olafsdóttir EJ. Population-based service mammography screening: the Icelandic experience. Breast Cancer (Dove Med Press). 2013;5:17–25.
- Coldman A, Phillips N, Wilson C, et al. Pan- Canadian study of mammography screening and mortality from breast cancer. J Natl Cancer Inst. 2014;106(11):dju261.
- Webb ML, Cady B, Michaelson JS, et al. A failure analysis of invasive breast cancer: most deaths from disease occur in women not regularly screened. Cancer. 2014;120(18):2839–2846.
- DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A. Breast cancer statistics, 2015: Convergence of incidence rates between black and white women. CA Cancer J Clin. 2015 Oct 29. doi: 10.3322/caac.21320.
- National Cancer Institute. Surveillance, Epidemiology, and End Results Program. http://seer.cancer.gov/archive/csr/1975_2010/browse_csr.php?sectionSEL=4&pageSEL=sect_04_table.06.html. Accessed November 16, 2015.
- Claus EB, Schildkraut JM, Thompson WD, Risch NJ. The genetic attributable risk of breast and ovarian cancer. Cancer. 1996;77(11):2318–2324.
- Seidman H, Stellman SD, Mushinski MH. A different perspective on breast cancer risk factors: some implications of nonattributable risk. Cancer. 1982;32(5):301–313.
AHA: Older breast cancer patients more likely to die of heart disease than malignancy
ORLANDO – Women diagnosed with localized breast cancer while in their 70s have a higher mortality from cardiovascular disease than from their breast cancer, according to new data from the Women’s Health Initiative.
“Identification and treatment of cardiovascular disease risk factors among older women with breast cancer will likely improve survivorship and should be a high priority, especially for older women with incident localized breast cancer,” Na-Jin Park, Ph.D., said at the American Heart Association scientific sessions.
She presented an analysis that included 101,916 women who were free of cardiovascular disease and breast cancer upon enrollment in the Women’s Health Initiative (WHI) at age 50-79 years during 1993-1998. During follow-up in this prospective cohort study, 4,340 of them developed invasive breast cancer. The diagnosis occurred an average of 5 years into the study, and patients were followed for 10 years afterwards. “Forty-one percent of women with breast cancer already had cardiovascular risk factors at baseline, way before their breast cancer diagnosis,” noted Dr. Park of the University of Pittsburgh.
Among women diagnosed with breast cancer in their 50s, 40% of all deaths were from breast cancer and 15% were caused by cardiovascular disease. In contrast, the cumulative impact of atherosclerosis was far more prominent in women diagnosed with breast cancer at a more advanced age. Indeed, among women diagnosed with breast cancer in their 70s, about 15% of deaths were caused by breast cancer, while 25% resulted from cardiovascular disease.
The number of baseline cardiovascular risk factors present at enrollment in the WHI turned out to be a powerful determinant of the likelihood of acute MI or death as a result of coronary heart disease in participants who developed breast cancer.
Of the 4,340 women who later developed invasive breast cancer, 2,562 were free of hypertension, diabetes, and hypercholesterolemia and were nonsmokers upon enrollment. In an age-adjusted analysis in which this risk factor–free group served as the reference population, the risk of MI after breast cancer diagnosis was increased 1.65-fold in those with a single baseline risk factor, 3.2-fold in those with two, and 5.8-fold in women with three cardiovascular risk factors. Similarly, the breast cancer patients’ risk of CHD death climbed stepwise by 1.78-, 2.28-, and 3.6-fold as the number of baseline cardiovascular risk factors increased from one to three.
The greatest risk was seen in breast cancer patients who at WHI enrollment were current smokers with an additional cardiovascular risk factor. They had a 9.6-fold greater risk of an acute MI after developing breast cancer, compared with breast cancer patients with none of the baseline cardiovascular risk factors. They also had a 7.7-fold increased risk of CHD death.
The WHI was funded by the National Heart, Lung, and Blood Institute. Dr. Park reported having no financial conflicts of interest.
ORLANDO – Women diagnosed with localized breast cancer while in their 70s have a higher mortality from cardiovascular disease than from their breast cancer, according to new data from the Women’s Health Initiative.
“Identification and treatment of cardiovascular disease risk factors among older women with breast cancer will likely improve survivorship and should be a high priority, especially for older women with incident localized breast cancer,” Na-Jin Park, Ph.D., said at the American Heart Association scientific sessions.
She presented an analysis that included 101,916 women who were free of cardiovascular disease and breast cancer upon enrollment in the Women’s Health Initiative (WHI) at age 50-79 years during 1993-1998. During follow-up in this prospective cohort study, 4,340 of them developed invasive breast cancer. The diagnosis occurred an average of 5 years into the study, and patients were followed for 10 years afterwards. “Forty-one percent of women with breast cancer already had cardiovascular risk factors at baseline, way before their breast cancer diagnosis,” noted Dr. Park of the University of Pittsburgh.
Among women diagnosed with breast cancer in their 50s, 40% of all deaths were from breast cancer and 15% were caused by cardiovascular disease. In contrast, the cumulative impact of atherosclerosis was far more prominent in women diagnosed with breast cancer at a more advanced age. Indeed, among women diagnosed with breast cancer in their 70s, about 15% of deaths were caused by breast cancer, while 25% resulted from cardiovascular disease.
The number of baseline cardiovascular risk factors present at enrollment in the WHI turned out to be a powerful determinant of the likelihood of acute MI or death as a result of coronary heart disease in participants who developed breast cancer.
Of the 4,340 women who later developed invasive breast cancer, 2,562 were free of hypertension, diabetes, and hypercholesterolemia and were nonsmokers upon enrollment. In an age-adjusted analysis in which this risk factor–free group served as the reference population, the risk of MI after breast cancer diagnosis was increased 1.65-fold in those with a single baseline risk factor, 3.2-fold in those with two, and 5.8-fold in women with three cardiovascular risk factors. Similarly, the breast cancer patients’ risk of CHD death climbed stepwise by 1.78-, 2.28-, and 3.6-fold as the number of baseline cardiovascular risk factors increased from one to three.
The greatest risk was seen in breast cancer patients who at WHI enrollment were current smokers with an additional cardiovascular risk factor. They had a 9.6-fold greater risk of an acute MI after developing breast cancer, compared with breast cancer patients with none of the baseline cardiovascular risk factors. They also had a 7.7-fold increased risk of CHD death.
The WHI was funded by the National Heart, Lung, and Blood Institute. Dr. Park reported having no financial conflicts of interest.
ORLANDO – Women diagnosed with localized breast cancer while in their 70s have a higher mortality from cardiovascular disease than from their breast cancer, according to new data from the Women’s Health Initiative.
“Identification and treatment of cardiovascular disease risk factors among older women with breast cancer will likely improve survivorship and should be a high priority, especially for older women with incident localized breast cancer,” Na-Jin Park, Ph.D., said at the American Heart Association scientific sessions.
She presented an analysis that included 101,916 women who were free of cardiovascular disease and breast cancer upon enrollment in the Women’s Health Initiative (WHI) at age 50-79 years during 1993-1998. During follow-up in this prospective cohort study, 4,340 of them developed invasive breast cancer. The diagnosis occurred an average of 5 years into the study, and patients were followed for 10 years afterwards. “Forty-one percent of women with breast cancer already had cardiovascular risk factors at baseline, way before their breast cancer diagnosis,” noted Dr. Park of the University of Pittsburgh.
Among women diagnosed with breast cancer in their 50s, 40% of all deaths were from breast cancer and 15% were caused by cardiovascular disease. In contrast, the cumulative impact of atherosclerosis was far more prominent in women diagnosed with breast cancer at a more advanced age. Indeed, among women diagnosed with breast cancer in their 70s, about 15% of deaths were caused by breast cancer, while 25% resulted from cardiovascular disease.
The number of baseline cardiovascular risk factors present at enrollment in the WHI turned out to be a powerful determinant of the likelihood of acute MI or death as a result of coronary heart disease in participants who developed breast cancer.
Of the 4,340 women who later developed invasive breast cancer, 2,562 were free of hypertension, diabetes, and hypercholesterolemia and were nonsmokers upon enrollment. In an age-adjusted analysis in which this risk factor–free group served as the reference population, the risk of MI after breast cancer diagnosis was increased 1.65-fold in those with a single baseline risk factor, 3.2-fold in those with two, and 5.8-fold in women with three cardiovascular risk factors. Similarly, the breast cancer patients’ risk of CHD death climbed stepwise by 1.78-, 2.28-, and 3.6-fold as the number of baseline cardiovascular risk factors increased from one to three.
The greatest risk was seen in breast cancer patients who at WHI enrollment were current smokers with an additional cardiovascular risk factor. They had a 9.6-fold greater risk of an acute MI after developing breast cancer, compared with breast cancer patients with none of the baseline cardiovascular risk factors. They also had a 7.7-fold increased risk of CHD death.
The WHI was funded by the National Heart, Lung, and Blood Institute. Dr. Park reported having no financial conflicts of interest.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Among women diagnosed with breast cancer in their 70s, more will die from cardiovascular disease than from their malignancy.
Major finding: Among women diagnosed with breast cancer in their 70s, only about 15% of deaths were caused by breast cancer, while 25% resulted from cardiovascular disease.
Data source: This prospective cohort analysis from the Women’s Health Initiative included 101,916 women free of cardiovascular disease and breast cancer upon enrollment, of whom 4,340 later developed invasive breast cancer.
Disclosures: The Women’s Health Initiative was funded by the National Heart, Lung, and Blood Institute. The presenter reported having no financial conflicts of interest.
Racial differences found in neoadjuvant chemo, pCR rates for breast cancer
Chemotherapy and neoadjuvant chemotherapy are given more often to non-Hispanic black, Hispanic, and Asian women than to non-Hispanic white women with breast cancer, while black women saw a lower rate of pathological complete response (pCR), according to the results of a new study.
Dr. Brigid Killelea of Yale University, New Haven, Conn., and her colleagues looked at records from nearly 280,000 patients in the National Cancer Data Base who received treatment for stage I-III disease in 2010 and 2011.
In the cohort as a whole, 46% of women received chemotherapy, and, among the majority of patients for whom information on the timing of chemotherapy was available, 23% received neoadjuvant therapy, with non-white women receiving chemotherapy and neoadjuvant chemotherapy more frequently (P less than .001). This could mainly be explained by the advanced age, higher-grade tumors and a larger share of triple-negative and human epidermal growth factor receptor–positive tumors in the non-white women, the investigators said (J Clin Oncol. 2015 Nov. 23. doi: 10.1200/JCO.2015.63.7801).
Of about 18,000 patients in the cohort with known outcomes, 33% had a pathological complete response, Dr. Killelea and her colleagues found. Black women in the study had a lower rate of pCR, compared with white women for estrogen receptor/progesterone receptor–negative, human epidermal growth factor receptor2–positive tumors (43% vs. 54%, P = .001) and for triple-negative tumors (37% vs. 43%, P less than .001) despite adjustment for a large number of clinical and socioeconomic factors. Racial disparities in breast cancer incidence, treatment, and survival have been long reported, and racial disparities in neoadjuvant chemotherapy are important to measure, the investigators wrote, as neoadjuvant chemotherapy allows for initiation of systemic therapy before surgery in patients with locally advanced and/or node-positive disease, among other potential advantages. Meanwhile, pCR has been shown in recent years to be a key prognostic indicator for certain breast cancer subtypes and therefore is also important to measure with regard to race. Dr. Killelea and colleagues concluded that the reasons for the lower pCR rates seen among black women in the study could not be determined, and may involve differences in treatment, chemosensitivity, or socioeconomic factors that they could not control for, but that warranted investigation in future studies. “One hypothesis is that the lower pCR rate reflects undertreatment,” the investigators wrote in their analysis. “Women who were unable to complete chemotherapy or had dose reduction, treatment delays, or less-aggressive chemotherapy regimens would be less likely to have a pCR.”
Chemotherapy and neoadjuvant chemotherapy are given more often to non-Hispanic black, Hispanic, and Asian women than to non-Hispanic white women with breast cancer, while black women saw a lower rate of pathological complete response (pCR), according to the results of a new study.
Dr. Brigid Killelea of Yale University, New Haven, Conn., and her colleagues looked at records from nearly 280,000 patients in the National Cancer Data Base who received treatment for stage I-III disease in 2010 and 2011.
In the cohort as a whole, 46% of women received chemotherapy, and, among the majority of patients for whom information on the timing of chemotherapy was available, 23% received neoadjuvant therapy, with non-white women receiving chemotherapy and neoadjuvant chemotherapy more frequently (P less than .001). This could mainly be explained by the advanced age, higher-grade tumors and a larger share of triple-negative and human epidermal growth factor receptor–positive tumors in the non-white women, the investigators said (J Clin Oncol. 2015 Nov. 23. doi: 10.1200/JCO.2015.63.7801).
Of about 18,000 patients in the cohort with known outcomes, 33% had a pathological complete response, Dr. Killelea and her colleagues found. Black women in the study had a lower rate of pCR, compared with white women for estrogen receptor/progesterone receptor–negative, human epidermal growth factor receptor2–positive tumors (43% vs. 54%, P = .001) and for triple-negative tumors (37% vs. 43%, P less than .001) despite adjustment for a large number of clinical and socioeconomic factors. Racial disparities in breast cancer incidence, treatment, and survival have been long reported, and racial disparities in neoadjuvant chemotherapy are important to measure, the investigators wrote, as neoadjuvant chemotherapy allows for initiation of systemic therapy before surgery in patients with locally advanced and/or node-positive disease, among other potential advantages. Meanwhile, pCR has been shown in recent years to be a key prognostic indicator for certain breast cancer subtypes and therefore is also important to measure with regard to race. Dr. Killelea and colleagues concluded that the reasons for the lower pCR rates seen among black women in the study could not be determined, and may involve differences in treatment, chemosensitivity, or socioeconomic factors that they could not control for, but that warranted investigation in future studies. “One hypothesis is that the lower pCR rate reflects undertreatment,” the investigators wrote in their analysis. “Women who were unable to complete chemotherapy or had dose reduction, treatment delays, or less-aggressive chemotherapy regimens would be less likely to have a pCR.”
Chemotherapy and neoadjuvant chemotherapy are given more often to non-Hispanic black, Hispanic, and Asian women than to non-Hispanic white women with breast cancer, while black women saw a lower rate of pathological complete response (pCR), according to the results of a new study.
Dr. Brigid Killelea of Yale University, New Haven, Conn., and her colleagues looked at records from nearly 280,000 patients in the National Cancer Data Base who received treatment for stage I-III disease in 2010 and 2011.
In the cohort as a whole, 46% of women received chemotherapy, and, among the majority of patients for whom information on the timing of chemotherapy was available, 23% received neoadjuvant therapy, with non-white women receiving chemotherapy and neoadjuvant chemotherapy more frequently (P less than .001). This could mainly be explained by the advanced age, higher-grade tumors and a larger share of triple-negative and human epidermal growth factor receptor–positive tumors in the non-white women, the investigators said (J Clin Oncol. 2015 Nov. 23. doi: 10.1200/JCO.2015.63.7801).
Of about 18,000 patients in the cohort with known outcomes, 33% had a pathological complete response, Dr. Killelea and her colleagues found. Black women in the study had a lower rate of pCR, compared with white women for estrogen receptor/progesterone receptor–negative, human epidermal growth factor receptor2–positive tumors (43% vs. 54%, P = .001) and for triple-negative tumors (37% vs. 43%, P less than .001) despite adjustment for a large number of clinical and socioeconomic factors. Racial disparities in breast cancer incidence, treatment, and survival have been long reported, and racial disparities in neoadjuvant chemotherapy are important to measure, the investigators wrote, as neoadjuvant chemotherapy allows for initiation of systemic therapy before surgery in patients with locally advanced and/or node-positive disease, among other potential advantages. Meanwhile, pCR has been shown in recent years to be a key prognostic indicator for certain breast cancer subtypes and therefore is also important to measure with regard to race. Dr. Killelea and colleagues concluded that the reasons for the lower pCR rates seen among black women in the study could not be determined, and may involve differences in treatment, chemosensitivity, or socioeconomic factors that they could not control for, but that warranted investigation in future studies. “One hypothesis is that the lower pCR rate reflects undertreatment,” the investigators wrote in their analysis. “Women who were unable to complete chemotherapy or had dose reduction, treatment delays, or less-aggressive chemotherapy regimens would be less likely to have a pCR.”
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Non-white Hispanic, Asian, and black women are likelier to receive neoadjuvant chemotherapy than are white women for breast cancers, while black women had lower rates of pathological complete response, compared with white women for some types of cancers.
Major finding: Black women had a lower rate of pCR than did white women for ER/PR-negative, HER2-positive (43% vs. 54%; P = .001) and triple-negative tumors (37% vs. 43%; P less than .001).
Data source: 278,815 women identified in the National Cancer Database diagnosed with stage I-III breast cancer in 2010 and 2011, for whom ethnicity was recorded.
Disclosures: Two authors disclosed relationships with various pharma companies, while the majority reported no relationships to disclose.
No racial disparity in appropriate use of Oncotype DX
Black women with node-positive breast cancer were less likely to receive tumor gene profiling for treatment decision making compared with women of other ethnicities, according to a new study. However, black women who were node negative were just as likely to receive the test as were other women, suggesting that testing protocols for black women are kept closer to guidelines than for other groups.
The genetic test, known as Oncotype DX (ODX), came into wide use a decade ago as a chemotherapy decision-making tool for patients with estrogen receptor–positive, human epidermal growth factor receptor-2–negative breast cancer, stage I or II, with tumors of 0.5 cm or larger. Current guidelines used by public and private insurers, including Medicare, incorporate ODX testing for these patients who are node negative. Still, there is some evidence suggesting a role for ODX for women with up to three positive nodes, and one major clinical trial is underway to determine whether ODX testing is helpful in these patients.
Megan C. Roberts, Ph.D., of the University of North Carolina at Chapel Hill, and her colleagues, looked at data for 1,468 women (609 black) from the population-based, phase III Carolina Breast Cancer Study.
Overall in the cohort, 42% of women received ODX testing, and no racial disparities were seen in the likelihood of ODX testing in node-negative women. For patients with node-positive disease, black women were 46% less likely to receive ODX testing than were nonblack women (adjusted risk ratio 0.54, 95% CI 0.35 to 0.84; P = .006).
“Current medical guidelines do not recommend ODX testing in patients with node-positive, early-stage, ER+ breast cancer,” Dr. Roberts and colleagues wrote in their analysis (J Clin Oncol. 2015 Nov 23. doi: 10.1200/JCO.2015.63.2489).
“Therefore, lower rates of ODX testing among black women in our sample reflect their receipt of more guideline-concordant care than nonblack women with node-positive breast cancer. Thus, differential receipt of ODX testing does not necessarily reflect a racial disparity in the quality of care. This paradox illustrates challenges that will accompany the measurement of disparities in the early adoption of new genetic technologies into clinical practice,” the researchers wrote.
They noted as a study limitations the fact that patient preferences regarding ODX could not be accounted for, and that previous studies have suggested these could differ by race.
Black women with node-positive breast cancer were less likely to receive tumor gene profiling for treatment decision making compared with women of other ethnicities, according to a new study. However, black women who were node negative were just as likely to receive the test as were other women, suggesting that testing protocols for black women are kept closer to guidelines than for other groups.
The genetic test, known as Oncotype DX (ODX), came into wide use a decade ago as a chemotherapy decision-making tool for patients with estrogen receptor–positive, human epidermal growth factor receptor-2–negative breast cancer, stage I or II, with tumors of 0.5 cm or larger. Current guidelines used by public and private insurers, including Medicare, incorporate ODX testing for these patients who are node negative. Still, there is some evidence suggesting a role for ODX for women with up to three positive nodes, and one major clinical trial is underway to determine whether ODX testing is helpful in these patients.
Megan C. Roberts, Ph.D., of the University of North Carolina at Chapel Hill, and her colleagues, looked at data for 1,468 women (609 black) from the population-based, phase III Carolina Breast Cancer Study.
Overall in the cohort, 42% of women received ODX testing, and no racial disparities were seen in the likelihood of ODX testing in node-negative women. For patients with node-positive disease, black women were 46% less likely to receive ODX testing than were nonblack women (adjusted risk ratio 0.54, 95% CI 0.35 to 0.84; P = .006).
“Current medical guidelines do not recommend ODX testing in patients with node-positive, early-stage, ER+ breast cancer,” Dr. Roberts and colleagues wrote in their analysis (J Clin Oncol. 2015 Nov 23. doi: 10.1200/JCO.2015.63.2489).
“Therefore, lower rates of ODX testing among black women in our sample reflect their receipt of more guideline-concordant care than nonblack women with node-positive breast cancer. Thus, differential receipt of ODX testing does not necessarily reflect a racial disparity in the quality of care. This paradox illustrates challenges that will accompany the measurement of disparities in the early adoption of new genetic technologies into clinical practice,” the researchers wrote.
They noted as a study limitations the fact that patient preferences regarding ODX could not be accounted for, and that previous studies have suggested these could differ by race.
Black women with node-positive breast cancer were less likely to receive tumor gene profiling for treatment decision making compared with women of other ethnicities, according to a new study. However, black women who were node negative were just as likely to receive the test as were other women, suggesting that testing protocols for black women are kept closer to guidelines than for other groups.
The genetic test, known as Oncotype DX (ODX), came into wide use a decade ago as a chemotherapy decision-making tool for patients with estrogen receptor–positive, human epidermal growth factor receptor-2–negative breast cancer, stage I or II, with tumors of 0.5 cm or larger. Current guidelines used by public and private insurers, including Medicare, incorporate ODX testing for these patients who are node negative. Still, there is some evidence suggesting a role for ODX for women with up to three positive nodes, and one major clinical trial is underway to determine whether ODX testing is helpful in these patients.
Megan C. Roberts, Ph.D., of the University of North Carolina at Chapel Hill, and her colleagues, looked at data for 1,468 women (609 black) from the population-based, phase III Carolina Breast Cancer Study.
Overall in the cohort, 42% of women received ODX testing, and no racial disparities were seen in the likelihood of ODX testing in node-negative women. For patients with node-positive disease, black women were 46% less likely to receive ODX testing than were nonblack women (adjusted risk ratio 0.54, 95% CI 0.35 to 0.84; P = .006).
“Current medical guidelines do not recommend ODX testing in patients with node-positive, early-stage, ER+ breast cancer,” Dr. Roberts and colleagues wrote in their analysis (J Clin Oncol. 2015 Nov 23. doi: 10.1200/JCO.2015.63.2489).
“Therefore, lower rates of ODX testing among black women in our sample reflect their receipt of more guideline-concordant care than nonblack women with node-positive breast cancer. Thus, differential receipt of ODX testing does not necessarily reflect a racial disparity in the quality of care. This paradox illustrates challenges that will accompany the measurement of disparities in the early adoption of new genetic technologies into clinical practice,” the researchers wrote.
They noted as a study limitations the fact that patient preferences regarding ODX could not be accounted for, and that previous studies have suggested these could differ by race.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: ODX testing is more likely to be administered to nonblack women with node-positive disease than to black women.
Major finding: Black patients with node-positive tumors were 46% less likely to receive ODX testing than were nonblack women (adjusted RR 0.54; 95% CI, 0.35 to 0.84; P = .006).
Data source: Review of data from nearly 1,500 patients from a longitudinal population-based study of 3,000 women with breast cancer in North Carolina, diagnosed from 2008 to 2014.
Disclosures: One author disclosed a consultancy with Salix. All other authors reported no conflicts.
No benefit from dual anti-HER2 blockade in early breast cancer
A dual anti-HER2 blockade with lapatinib and trastuzumab resulted in modest, nonsignificant disease-free survival improvements over adjuvant trastuzumab alone for patients with early human epidermal growth factor 2 (HER2)-positive breast cancer, according to results of the phase III ALTTO trial.
Disease-free survival (DFS) improved slightly with lapatinib and trastuzumab over trastuzumab alone (555 DFS events; hazard ratio, 0.84; 97.5% CI, 0.70-1.02; P = .048). The 4-year overall survival was 95% for lapatinib and trastuzumab and 94% for trastuzumab alone (HR, 0.80; 95% CI, 0.62-1.03; P = .078) (J Clin Oncol. 2015 Nov 23. [doi: 10.1200/JCO.2015.62.1797]).
The marginal benefit observed in lapatinib arms was offset by additional toxicity. The incidence of diarrhea, mostly grade 1 or 2, was higher in the lapatinib arms and was responsible for treatment discontinuation at a rate from 4% to 9% depending on the lapatinib arm. Slightly more than half of the patients in lapatinib arms experienced rash, compared with about 20% in the trastuzumab arm. Primary or secondary cardiac events were rare in any treatment arm.
Previous studies showed benefit from the dual blockade for heavily pretreated patients with advanced disease, particularly in the hormone receptor–negative population.
“We did not expect to observe the degree of toxicity (especially diarrhea), which ultimately reduced the level of enthusiasm for lapatinib in the adjuvant setting,” wrote Dr. Martine J. Piccart-Gebhart, professor of oncology at Université Libre de Bruxelles and director of the medicine department at the Jules Bordet Institute in Brussels, and her colleagues.
The phase III ALTTO (Adjuvant Lapatinib and/or Trastuzumab Treatment Optimization) trial evaluated 8,381 patients with completely excised invasive nonmetastatic HER2-positive breast cancer from 945 sites in 44 countries.
The 4-year overall survival rates of approximately 95% illustrate the steady improvement in clinical outcomes of early breast cancer. The addition of adjuvant lapatinib to trastuzumab produced a modest treatment effect with additional toxicity, and is not clinically meaningful, according to investigators. The standard of care remains trastuzumab for one year.
Research was supported by GlaxoSmithKline and by the National Cancer Institute of the National Institutes of Health. Dr. Piccart-Gebhart reported consulting or advisory roles with Amgen, Astellas, AstraZeneca, Bayer, Eli Lilly, Invivis, Merck Sharp & Dohme, Novartis, Pfizer, Roche/Genentech, Sanofi, Symphogen, Synthon, and Verastem. Several of her coauthors reported ties to industry.
A dual anti-HER2 blockade with lapatinib and trastuzumab resulted in modest, nonsignificant disease-free survival improvements over adjuvant trastuzumab alone for patients with early human epidermal growth factor 2 (HER2)-positive breast cancer, according to results of the phase III ALTTO trial.
Disease-free survival (DFS) improved slightly with lapatinib and trastuzumab over trastuzumab alone (555 DFS events; hazard ratio, 0.84; 97.5% CI, 0.70-1.02; P = .048). The 4-year overall survival was 95% for lapatinib and trastuzumab and 94% for trastuzumab alone (HR, 0.80; 95% CI, 0.62-1.03; P = .078) (J Clin Oncol. 2015 Nov 23. [doi: 10.1200/JCO.2015.62.1797]).
The marginal benefit observed in lapatinib arms was offset by additional toxicity. The incidence of diarrhea, mostly grade 1 or 2, was higher in the lapatinib arms and was responsible for treatment discontinuation at a rate from 4% to 9% depending on the lapatinib arm. Slightly more than half of the patients in lapatinib arms experienced rash, compared with about 20% in the trastuzumab arm. Primary or secondary cardiac events were rare in any treatment arm.
Previous studies showed benefit from the dual blockade for heavily pretreated patients with advanced disease, particularly in the hormone receptor–negative population.
“We did not expect to observe the degree of toxicity (especially diarrhea), which ultimately reduced the level of enthusiasm for lapatinib in the adjuvant setting,” wrote Dr. Martine J. Piccart-Gebhart, professor of oncology at Université Libre de Bruxelles and director of the medicine department at the Jules Bordet Institute in Brussels, and her colleagues.
The phase III ALTTO (Adjuvant Lapatinib and/or Trastuzumab Treatment Optimization) trial evaluated 8,381 patients with completely excised invasive nonmetastatic HER2-positive breast cancer from 945 sites in 44 countries.
The 4-year overall survival rates of approximately 95% illustrate the steady improvement in clinical outcomes of early breast cancer. The addition of adjuvant lapatinib to trastuzumab produced a modest treatment effect with additional toxicity, and is not clinically meaningful, according to investigators. The standard of care remains trastuzumab for one year.
Research was supported by GlaxoSmithKline and by the National Cancer Institute of the National Institutes of Health. Dr. Piccart-Gebhart reported consulting or advisory roles with Amgen, Astellas, AstraZeneca, Bayer, Eli Lilly, Invivis, Merck Sharp & Dohme, Novartis, Pfizer, Roche/Genentech, Sanofi, Symphogen, Synthon, and Verastem. Several of her coauthors reported ties to industry.
A dual anti-HER2 blockade with lapatinib and trastuzumab resulted in modest, nonsignificant disease-free survival improvements over adjuvant trastuzumab alone for patients with early human epidermal growth factor 2 (HER2)-positive breast cancer, according to results of the phase III ALTTO trial.
Disease-free survival (DFS) improved slightly with lapatinib and trastuzumab over trastuzumab alone (555 DFS events; hazard ratio, 0.84; 97.5% CI, 0.70-1.02; P = .048). The 4-year overall survival was 95% for lapatinib and trastuzumab and 94% for trastuzumab alone (HR, 0.80; 95% CI, 0.62-1.03; P = .078) (J Clin Oncol. 2015 Nov 23. [doi: 10.1200/JCO.2015.62.1797]).
The marginal benefit observed in lapatinib arms was offset by additional toxicity. The incidence of diarrhea, mostly grade 1 or 2, was higher in the lapatinib arms and was responsible for treatment discontinuation at a rate from 4% to 9% depending on the lapatinib arm. Slightly more than half of the patients in lapatinib arms experienced rash, compared with about 20% in the trastuzumab arm. Primary or secondary cardiac events were rare in any treatment arm.
Previous studies showed benefit from the dual blockade for heavily pretreated patients with advanced disease, particularly in the hormone receptor–negative population.
“We did not expect to observe the degree of toxicity (especially diarrhea), which ultimately reduced the level of enthusiasm for lapatinib in the adjuvant setting,” wrote Dr. Martine J. Piccart-Gebhart, professor of oncology at Université Libre de Bruxelles and director of the medicine department at the Jules Bordet Institute in Brussels, and her colleagues.
The phase III ALTTO (Adjuvant Lapatinib and/or Trastuzumab Treatment Optimization) trial evaluated 8,381 patients with completely excised invasive nonmetastatic HER2-positive breast cancer from 945 sites in 44 countries.
The 4-year overall survival rates of approximately 95% illustrate the steady improvement in clinical outcomes of early breast cancer. The addition of adjuvant lapatinib to trastuzumab produced a modest treatment effect with additional toxicity, and is not clinically meaningful, according to investigators. The standard of care remains trastuzumab for one year.
Research was supported by GlaxoSmithKline and by the National Cancer Institute of the National Institutes of Health. Dr. Piccart-Gebhart reported consulting or advisory roles with Amgen, Astellas, AstraZeneca, Bayer, Eli Lilly, Invivis, Merck Sharp & Dohme, Novartis, Pfizer, Roche/Genentech, Sanofi, Symphogen, Synthon, and Verastem. Several of her coauthors reported ties to industry.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Adjuvant lapatinib and trastuzumab resulted in similar disease-free survival, compared with trastuzumab alone in early HER2-positive breast cancer.
Major finding: Disease-free survival improved slightly with lapatinib and trastuzumab over trastuzumab alone (555 DFS events; hazard rate 0.84; 97.5% CI, 0.70-1.02; P = .048).
Data source: The phase III Adjuvant Lapatinib and/or Trastuzumab Treatment Optimization (ALTTO) trial evaluated 8,381 patients with completely excised invasive nonmetastatic HER2-positive breast cancer.
Disclosures: Research was supported by GlaxoSmithKline and by the National Cancer Institute of the National Institutes of Health. Dr. Piccart-Gebhart reported consulting or advisory roles with Amgen, Astellas, AstraZeneca, Bayer, Eli Lilly, Invivis, Merck Sharp & Dohme, Novartis, Pfizer, Roche/Genentech, Sanofi, Symphogen, Synthon, and Verastem. Several of her coauthors reported ties to industry.
Antibody drug conjugate induces responses in heavily pretreated TNBC
BOSTON – An antibody conjugated to the active metabolite of irinotecan was associated with a good overall response rate in patients with heavily pretreated triple-negative breast cancer, with lower toxicities than seen with systemic irinotecan therapy, investigators reported.
Among 54 patients with triple-negative breast cancer (TNBC) in a phase II trial who had undergone a median of six prior lines of therapy, treatment with the conjugate, labeled IMMU-132 (sacituzumab govitecan) was associated with a 31.5% overall response rate, including two complete responses, reported Dr. Aditya Bardia of Massachusetts General Hospital, Boston, and his colleagues, at the AACR–NCI–EORTC International Conference on Molecular Targets and Cancer Therapeutics.
The compound consists of a monoclonal antibody (RS7-3G11) targeted to the Trop-2/EGP-1 panepithelial cancer antigen that is conjugated with the active metabolite of irinotecan (SN-38). The antibody has been shown in preclinical studies to bind to human breast, lung, colon, renal, prostate, and urothelial cancer and other solid malignancies. Trop-2 is expressed in more than 80% of triple-negative breast cancers, said coauthor Dr. David M. Goldenberg, chairman of Immunomedics, the maker of the compound.
“What distinguishes this antibody-drug conjugate, or ADC, is that we have used the active metabolite of irinotecan, which is 100 to 1,000 times more toxic than its parent drug, and the reason it’s tolerated is that it’s conjugated to the antibody, and we have shown preclinically that we can deliver approximately 136 times more SN-38 to the cancer cell than if you give irinotecan and measure how much SN-38 gets to the tumor,” he said at a briefing.
The conjugate has good activity in patients who have experienced relapses after multiple prior lines of therapy, and it can be delivered repeatedly over a long course of therapy with toxicities that are manageable, he noted.
The compound was found to have good activity in several solid tumors in a phase I trial, which led to an expanded phase II trial including, as of May 10, 2015, a total of 56 patients with TNBC, 2 of whom had received fewer than three doses of the study drug by the data cutoff, and therefore were not included in the efficacy analysis.
Patients received IMMU-132 intravenously in doses of 8 or 10 mg/kg on days 1 and 8 of each 21-day cycle, which could be repeated until progression or unacceptable toxicity.
Among 54 assessable patients, the overall response rate (percentage change from baseline according to RECIST [Response Evaluation Criteria in Solid Tumors] 1.1 guidelines) was 31.5%, (17 of 54) consisting of 2 confirmed complete responses and 15 partial responses. Additionally, there were 24 cases of stable disease (4 confirmed), 9 of which had a greater than 20% regression of tumor, but had not met the definition of a partial response by the time of the analysis.
The combined clinical benefit rate, a composite of complete and partial responses and stable disease for 6 months or more, was 44%.
Median progression-free survival in an intent to treat analysis was 7 months. Median overall survival had not been reached, with 87% of patients alive at the data cutoff.
Among all patients in the study, including those with TNBC and other tumors, adverse events at the 10 mg/kg dose included diarrhea in 37% (grade 3 or 4 in 6%); Dr. Goldenberg noted that severe diarrhea is one of the common adverse effects of the parent compound irinotecan, earning it a black-box warning. Other common adverse events associated with irinotecan were neutropenia in 26% (grade 3 or 4 in 15%), febrile neutropenia, all grade 3 or 4, in 4%, and anemia in 20% (grade 3/4 in 6%).
“I have to say that for me, SN-38 was a brilliant idea,” commented Dr. Lee J. Helman, a sarcoma specialist at the National Cancer Institute in Bethesda, Md.
He said that the data showing less severe diarrhea with IMMU-132 than with the parent irinotecan are encouraging, because it may allow more patients to benefit from the therapy.
“This is a very active drug, irinotecan. It gets activated to SN-38 through enterohepatic metabolism, and therefore, it has a very difficult toxicity, which is diarrhea. In fact, I’ve had patients who are responding, who have come off the drug because they can’t stand the diarrhea,” he said.
Dr. Helman moderated a briefing in which Dr. Goldenberg presented the data but was not involved in the study.
BOSTON – An antibody conjugated to the active metabolite of irinotecan was associated with a good overall response rate in patients with heavily pretreated triple-negative breast cancer, with lower toxicities than seen with systemic irinotecan therapy, investigators reported.
Among 54 patients with triple-negative breast cancer (TNBC) in a phase II trial who had undergone a median of six prior lines of therapy, treatment with the conjugate, labeled IMMU-132 (sacituzumab govitecan) was associated with a 31.5% overall response rate, including two complete responses, reported Dr. Aditya Bardia of Massachusetts General Hospital, Boston, and his colleagues, at the AACR–NCI–EORTC International Conference on Molecular Targets and Cancer Therapeutics.
The compound consists of a monoclonal antibody (RS7-3G11) targeted to the Trop-2/EGP-1 panepithelial cancer antigen that is conjugated with the active metabolite of irinotecan (SN-38). The antibody has been shown in preclinical studies to bind to human breast, lung, colon, renal, prostate, and urothelial cancer and other solid malignancies. Trop-2 is expressed in more than 80% of triple-negative breast cancers, said coauthor Dr. David M. Goldenberg, chairman of Immunomedics, the maker of the compound.
“What distinguishes this antibody-drug conjugate, or ADC, is that we have used the active metabolite of irinotecan, which is 100 to 1,000 times more toxic than its parent drug, and the reason it’s tolerated is that it’s conjugated to the antibody, and we have shown preclinically that we can deliver approximately 136 times more SN-38 to the cancer cell than if you give irinotecan and measure how much SN-38 gets to the tumor,” he said at a briefing.
The conjugate has good activity in patients who have experienced relapses after multiple prior lines of therapy, and it can be delivered repeatedly over a long course of therapy with toxicities that are manageable, he noted.
The compound was found to have good activity in several solid tumors in a phase I trial, which led to an expanded phase II trial including, as of May 10, 2015, a total of 56 patients with TNBC, 2 of whom had received fewer than three doses of the study drug by the data cutoff, and therefore were not included in the efficacy analysis.
Patients received IMMU-132 intravenously in doses of 8 or 10 mg/kg on days 1 and 8 of each 21-day cycle, which could be repeated until progression or unacceptable toxicity.
Among 54 assessable patients, the overall response rate (percentage change from baseline according to RECIST [Response Evaluation Criteria in Solid Tumors] 1.1 guidelines) was 31.5%, (17 of 54) consisting of 2 confirmed complete responses and 15 partial responses. Additionally, there were 24 cases of stable disease (4 confirmed), 9 of which had a greater than 20% regression of tumor, but had not met the definition of a partial response by the time of the analysis.
The combined clinical benefit rate, a composite of complete and partial responses and stable disease for 6 months or more, was 44%.
Median progression-free survival in an intent to treat analysis was 7 months. Median overall survival had not been reached, with 87% of patients alive at the data cutoff.
Among all patients in the study, including those with TNBC and other tumors, adverse events at the 10 mg/kg dose included diarrhea in 37% (grade 3 or 4 in 6%); Dr. Goldenberg noted that severe diarrhea is one of the common adverse effects of the parent compound irinotecan, earning it a black-box warning. Other common adverse events associated with irinotecan were neutropenia in 26% (grade 3 or 4 in 15%), febrile neutropenia, all grade 3 or 4, in 4%, and anemia in 20% (grade 3/4 in 6%).
“I have to say that for me, SN-38 was a brilliant idea,” commented Dr. Lee J. Helman, a sarcoma specialist at the National Cancer Institute in Bethesda, Md.
He said that the data showing less severe diarrhea with IMMU-132 than with the parent irinotecan are encouraging, because it may allow more patients to benefit from the therapy.
“This is a very active drug, irinotecan. It gets activated to SN-38 through enterohepatic metabolism, and therefore, it has a very difficult toxicity, which is diarrhea. In fact, I’ve had patients who are responding, who have come off the drug because they can’t stand the diarrhea,” he said.
Dr. Helman moderated a briefing in which Dr. Goldenberg presented the data but was not involved in the study.
BOSTON – An antibody conjugated to the active metabolite of irinotecan was associated with a good overall response rate in patients with heavily pretreated triple-negative breast cancer, with lower toxicities than seen with systemic irinotecan therapy, investigators reported.
Among 54 patients with triple-negative breast cancer (TNBC) in a phase II trial who had undergone a median of six prior lines of therapy, treatment with the conjugate, labeled IMMU-132 (sacituzumab govitecan) was associated with a 31.5% overall response rate, including two complete responses, reported Dr. Aditya Bardia of Massachusetts General Hospital, Boston, and his colleagues, at the AACR–NCI–EORTC International Conference on Molecular Targets and Cancer Therapeutics.
The compound consists of a monoclonal antibody (RS7-3G11) targeted to the Trop-2/EGP-1 panepithelial cancer antigen that is conjugated with the active metabolite of irinotecan (SN-38). The antibody has been shown in preclinical studies to bind to human breast, lung, colon, renal, prostate, and urothelial cancer and other solid malignancies. Trop-2 is expressed in more than 80% of triple-negative breast cancers, said coauthor Dr. David M. Goldenberg, chairman of Immunomedics, the maker of the compound.
“What distinguishes this antibody-drug conjugate, or ADC, is that we have used the active metabolite of irinotecan, which is 100 to 1,000 times more toxic than its parent drug, and the reason it’s tolerated is that it’s conjugated to the antibody, and we have shown preclinically that we can deliver approximately 136 times more SN-38 to the cancer cell than if you give irinotecan and measure how much SN-38 gets to the tumor,” he said at a briefing.
The conjugate has good activity in patients who have experienced relapses after multiple prior lines of therapy, and it can be delivered repeatedly over a long course of therapy with toxicities that are manageable, he noted.
The compound was found to have good activity in several solid tumors in a phase I trial, which led to an expanded phase II trial including, as of May 10, 2015, a total of 56 patients with TNBC, 2 of whom had received fewer than three doses of the study drug by the data cutoff, and therefore were not included in the efficacy analysis.
Patients received IMMU-132 intravenously in doses of 8 or 10 mg/kg on days 1 and 8 of each 21-day cycle, which could be repeated until progression or unacceptable toxicity.
Among 54 assessable patients, the overall response rate (percentage change from baseline according to RECIST [Response Evaluation Criteria in Solid Tumors] 1.1 guidelines) was 31.5%, (17 of 54) consisting of 2 confirmed complete responses and 15 partial responses. Additionally, there were 24 cases of stable disease (4 confirmed), 9 of which had a greater than 20% regression of tumor, but had not met the definition of a partial response by the time of the analysis.
The combined clinical benefit rate, a composite of complete and partial responses and stable disease for 6 months or more, was 44%.
Median progression-free survival in an intent to treat analysis was 7 months. Median overall survival had not been reached, with 87% of patients alive at the data cutoff.
Among all patients in the study, including those with TNBC and other tumors, adverse events at the 10 mg/kg dose included diarrhea in 37% (grade 3 or 4 in 6%); Dr. Goldenberg noted that severe diarrhea is one of the common adverse effects of the parent compound irinotecan, earning it a black-box warning. Other common adverse events associated with irinotecan were neutropenia in 26% (grade 3 or 4 in 15%), febrile neutropenia, all grade 3 or 4, in 4%, and anemia in 20% (grade 3/4 in 6%).
“I have to say that for me, SN-38 was a brilliant idea,” commented Dr. Lee J. Helman, a sarcoma specialist at the National Cancer Institute in Bethesda, Md.
He said that the data showing less severe diarrhea with IMMU-132 than with the parent irinotecan are encouraging, because it may allow more patients to benefit from the therapy.
“This is a very active drug, irinotecan. It gets activated to SN-38 through enterohepatic metabolism, and therefore, it has a very difficult toxicity, which is diarrhea. In fact, I’ve had patients who are responding, who have come off the drug because they can’t stand the diarrhea,” he said.
Dr. Helman moderated a briefing in which Dr. Goldenberg presented the data but was not involved in the study.
AT THE AACR–NCI–EORTC
Key clinical point: Conjugating a metabolite of irinotecan to an antibody allows targeted delivery of the otherwise highly toxic drug.
Major finding: The overall response rate in patients with heavily pretreated triple-negative breast cancer was 31%, including two complete responses.
Data source: Phase II open label trial, including a cohort of 56 patients with triple-negative breast cancer.
Disclosures: The study was funded by Immunomedics. Dr. Goldenberg is an officer and chairman of the company. Dr. Bardia and Dr. Helman reported no conflicts of interest.