User login
NICE Rejects Bevacizumab/Capecitabine for Breast Cancer
The cost-effectiveness agency for England and Wales says that it will not recommend bevacizumab in combination with capecitabine to treat advanced metastatic breast cancer.
In new draft guidance issued April 18, the National Institute for Health and Clinical Excellence (NICE) cited insufficient evidence in support of the drug combination, one of two bevacizumab regimens licensed in the European Union for the first-line treatment of advanced metastatic breast cancer.
Roche’s bevacizumab (Avastin) is a humanized monoclonal antibody that blocks vascular endothelial growth factor, reducing blood flow to tumors. The U.S. Food and Drug Administration revoked bevacizumab’s breast cancer indications altogether in November 2011, citing an unfavorable risk-benefit ratio.
The European Medicines Agency did not follow suit, however. Bevacizumab is licensed in Europe in combination with paclitaxel and also with capecitabine, which is used when paclitaxel is judged inappropriate, for advanced metastatic breast cancer.
In February 2011, NICE rejected bevacizumab and paclitaxel for the same indication.
In announcing its decision on bevacizumab and capecitabine, NICE cited uncertainties about overall survival benefit in results from RIBBON-1, a randomized controlled trial of bevacizumab in 1,237 women with advanced breast cancer. In the capecitabine arm of the trial, 615 patients were randomized to capecitabine plus bevacizumab or capecitabine plus placebo.
Although the results showed that capecitabine and bevacizumab prolonged progression-free survival by 2.9 months compared with capecitabine monotherapy, it remained unclear whether that benefit translated into an improvement in overall survival, NICE said, because so many patients on monotherapy crossed over to bevacizumab in the trial’s open-label postprogression phase.
NICE cited in its negative guidance the fact that no quality of life data had been collected in the trial, and that serious adverse reactions were higher with bevacizumab plus capecitabine (36.6%) than with capecitabine plus placebo (22.9%). "In addition, the number of patients with hypertension, proteinuria, sensory neuropathy, and venous thromboembolic events was higher with bevacizumab plus capecitabine compared with capecitabine plus placebo," NICE said in an April 18 press statement about its decision. "The Committee concluded that bevacizumab plus capecitabine had a less favorable toxicity profile than capecitabine plus placebo."
Finally, as in all NICE decisions, there was the question of cost. The manufacturer’s best-case incremental cost-effectiveness ratio (ICER) for bevacizumab plus capecitabine was £82,000 (U.S.$131,400) per quality-adjusted life year gained, and this only for a subgroup of patients. The ICER placed bevacizumab firmly out of NICE’s cost-effectiveness range.
Bevacizumab, which is administered by intravenous infusion, is dosed at 15 mg/kg every 3 weeks, amounting, NICE said, to an average monthly cost of around £3,689 (U.S.$5,913) per patient.
The cost-effectiveness agency for England and Wales says that it will not recommend bevacizumab in combination with capecitabine to treat advanced metastatic breast cancer.
In new draft guidance issued April 18, the National Institute for Health and Clinical Excellence (NICE) cited insufficient evidence in support of the drug combination, one of two bevacizumab regimens licensed in the European Union for the first-line treatment of advanced metastatic breast cancer.
Roche’s bevacizumab (Avastin) is a humanized monoclonal antibody that blocks vascular endothelial growth factor, reducing blood flow to tumors. The U.S. Food and Drug Administration revoked bevacizumab’s breast cancer indications altogether in November 2011, citing an unfavorable risk-benefit ratio.
The European Medicines Agency did not follow suit, however. Bevacizumab is licensed in Europe in combination with paclitaxel and also with capecitabine, which is used when paclitaxel is judged inappropriate, for advanced metastatic breast cancer.
In February 2011, NICE rejected bevacizumab and paclitaxel for the same indication.
In announcing its decision on bevacizumab and capecitabine, NICE cited uncertainties about overall survival benefit in results from RIBBON-1, a randomized controlled trial of bevacizumab in 1,237 women with advanced breast cancer. In the capecitabine arm of the trial, 615 patients were randomized to capecitabine plus bevacizumab or capecitabine plus placebo.
Although the results showed that capecitabine and bevacizumab prolonged progression-free survival by 2.9 months compared with capecitabine monotherapy, it remained unclear whether that benefit translated into an improvement in overall survival, NICE said, because so many patients on monotherapy crossed over to bevacizumab in the trial’s open-label postprogression phase.
NICE cited in its negative guidance the fact that no quality of life data had been collected in the trial, and that serious adverse reactions were higher with bevacizumab plus capecitabine (36.6%) than with capecitabine plus placebo (22.9%). "In addition, the number of patients with hypertension, proteinuria, sensory neuropathy, and venous thromboembolic events was higher with bevacizumab plus capecitabine compared with capecitabine plus placebo," NICE said in an April 18 press statement about its decision. "The Committee concluded that bevacizumab plus capecitabine had a less favorable toxicity profile than capecitabine plus placebo."
Finally, as in all NICE decisions, there was the question of cost. The manufacturer’s best-case incremental cost-effectiveness ratio (ICER) for bevacizumab plus capecitabine was £82,000 (U.S.$131,400) per quality-adjusted life year gained, and this only for a subgroup of patients. The ICER placed bevacizumab firmly out of NICE’s cost-effectiveness range.
Bevacizumab, which is administered by intravenous infusion, is dosed at 15 mg/kg every 3 weeks, amounting, NICE said, to an average monthly cost of around £3,689 (U.S.$5,913) per patient.
The cost-effectiveness agency for England and Wales says that it will not recommend bevacizumab in combination with capecitabine to treat advanced metastatic breast cancer.
In new draft guidance issued April 18, the National Institute for Health and Clinical Excellence (NICE) cited insufficient evidence in support of the drug combination, one of two bevacizumab regimens licensed in the European Union for the first-line treatment of advanced metastatic breast cancer.
Roche’s bevacizumab (Avastin) is a humanized monoclonal antibody that blocks vascular endothelial growth factor, reducing blood flow to tumors. The U.S. Food and Drug Administration revoked bevacizumab’s breast cancer indications altogether in November 2011, citing an unfavorable risk-benefit ratio.
The European Medicines Agency did not follow suit, however. Bevacizumab is licensed in Europe in combination with paclitaxel and also with capecitabine, which is used when paclitaxel is judged inappropriate, for advanced metastatic breast cancer.
In February 2011, NICE rejected bevacizumab and paclitaxel for the same indication.
In announcing its decision on bevacizumab and capecitabine, NICE cited uncertainties about overall survival benefit in results from RIBBON-1, a randomized controlled trial of bevacizumab in 1,237 women with advanced breast cancer. In the capecitabine arm of the trial, 615 patients were randomized to capecitabine plus bevacizumab or capecitabine plus placebo.
Although the results showed that capecitabine and bevacizumab prolonged progression-free survival by 2.9 months compared with capecitabine monotherapy, it remained unclear whether that benefit translated into an improvement in overall survival, NICE said, because so many patients on monotherapy crossed over to bevacizumab in the trial’s open-label postprogression phase.
NICE cited in its negative guidance the fact that no quality of life data had been collected in the trial, and that serious adverse reactions were higher with bevacizumab plus capecitabine (36.6%) than with capecitabine plus placebo (22.9%). "In addition, the number of patients with hypertension, proteinuria, sensory neuropathy, and venous thromboembolic events was higher with bevacizumab plus capecitabine compared with capecitabine plus placebo," NICE said in an April 18 press statement about its decision. "The Committee concluded that bevacizumab plus capecitabine had a less favorable toxicity profile than capecitabine plus placebo."
Finally, as in all NICE decisions, there was the question of cost. The manufacturer’s best-case incremental cost-effectiveness ratio (ICER) for bevacizumab plus capecitabine was £82,000 (U.S.$131,400) per quality-adjusted life year gained, and this only for a subgroup of patients. The ICER placed bevacizumab firmly out of NICE’s cost-effectiveness range.
Bevacizumab, which is administered by intravenous infusion, is dosed at 15 mg/kg every 3 weeks, amounting, NICE said, to an average monthly cost of around £3,689 (U.S.$5,913) per patient.
Trastuzumab Raises Cardiotoxicity Fivefold in Breast Cancer Patients
The risk of cardiotoxicity is five times higher in breast cancer patients given trastuzumab than in those receiving a standard chemotherapy regimen alone, according to a new systematic review from the Cochrane Collaboration.
The review found that regimens containing trastuzumab (Herceptin) significantly increased congestive heart failure and left ventricular ejection fraction (LVEF) decline, with relative risks of 5.11 and 1.83, respectively, in women with HER2-positive early and locally advanced breast cancer (Cochrane Database Syst. Rev. 2012;4 [doi: 10.1002/14651858.CD006243.pub2]).
However, trastuzumab regimens also significantly increased overall and disease-free survival, with hazard ratios of 0.66 and 0.60, respectively, noted Dr. Lorenzo Moja of the University of Milan and his coauthors. All these results were highly significant, with P values ranging from less than .0008 for risk of LVEF decline to less than .00001 for the others.
In a plain-language summary comparing trastuzumab-containing regimens with standard therapy alone in 1,000 women, the investigators wrote that 33 more women would have their lives prolonged with trastuzumab (933 women vs. 900 women with standard therapy alone). However, about 26 in 1,000 women taking trastuzumab would have serious heart toxicity, which is 21 more than the group treated with standard therapy alone.
Trastuzumab’s cardiotoxic effects have been well known, but the magnitude of the effect reported in the systematic review may be larger than what people have thought, commented Dr. Daniel J. Lenihan, director of clinical research in the cardiovascular medicine division at Vanderbilt University, Nashville, Tenn., in an interview.
And that risk may be even greater in the world outside of clinical studies, said Dr. Melinda Telli of Stanford (Calif.) University. The patients in the studies included in the systematic review were younger, and none had baseline cardiac disease, observed Dr. Telli, also in an interview.
Another issue: In practice, oncologists are offering trastuzumab to women at lower risk for cancer recurrence than those in the trials. Thus, she said, "it’s more likely the risks are underestimated in this Cochrane review."
Although the data in the systematic review were previously published, having them encapsulated – along with a number of scenarios outlining potential risks and benefits in women with different cancer recurrence and cardiac risk factors – is a significant addition to the literature, said Dr. Telli.
Cochrane reviews are known for being thorough and balanced. This review began by looking at about 3,900 studies; after applying exclusion criteria, the list was winnowed down to 35 publications that covered 8 randomized controlled clinical trials enrolling 11,991 women. A little more than 7,000 women were assigned to a trastuzumab-containing arm, and 4,971 women to a regimen without trastuzumab. The median age in the trials was 49 years. Pre- and postmenopausal women were included, but those with metastatic disease or preexisting heart conditions were excluded.
The review concluded that high-risk women with few cardiac risk factors would benefit from trastuzumab, while those at lower risk "must be carefully evaluated," adding, "The oncologist should share the decision with the patient concerning whether and how to start the treatment."
Dr. Lenihan said he was concerned that the potential cardiotoxicity might cause oncologists to steer away from trastuzumab. He is a proponent of a multidisciplinary team that involves a cardiologist at the outset of therapy.
If cardiac effects develop, "the key is not to ignore it, but to pay attention," said Dr. Lenihan, who is also president of the International CardiOncology Society USA/Canada.
Early identification enables rapid treatment, which can stabilize or correct the heart issues, he said. That allows patients to return to their cancer therapy.
Dr. Lenihan and his colleagues at Vanderbilt University are currently conducting a study testing various cardiac biomarkers to detect toxicity during chemotherapy.
It is still unknown, however, whether the cardiotoxicity that develops during therapy is ultimately reversible, or becomes a lifelong issue. While the ejection fraction may recover after withdrawal of trastuzumab, at least one study – the Herceptin Adjuvant (HERA) trial – has shown that some women had long-term loss of heart muscle cells, said Dr. Telli.
"So we know that the heart is taking a hit," she said, adding that the trastuzumab damage is not "some sort of reversible thing."
The key, she said, is for oncologists to weigh the risks and benefits individually in each patient.
A targeted therapy, trastuzumab is approved for treatment of HER2-positive breast cancer and of metastatic HER2-positive adenocarcinoma of the stomach or gastroesophageal junction. About 20% of tumors in women with early breast cancer are HER2-positive.
Dr. Telli reported no conflicts of interest. Dr. Lenihan reported receiving consulting fees from Roche and AstraZeneca and research support from Acorda.
The risk of cardiotoxicity is five times higher in breast cancer patients given trastuzumab than in those receiving a standard chemotherapy regimen alone, according to a new systematic review from the Cochrane Collaboration.
The review found that regimens containing trastuzumab (Herceptin) significantly increased congestive heart failure and left ventricular ejection fraction (LVEF) decline, with relative risks of 5.11 and 1.83, respectively, in women with HER2-positive early and locally advanced breast cancer (Cochrane Database Syst. Rev. 2012;4 [doi: 10.1002/14651858.CD006243.pub2]).
However, trastuzumab regimens also significantly increased overall and disease-free survival, with hazard ratios of 0.66 and 0.60, respectively, noted Dr. Lorenzo Moja of the University of Milan and his coauthors. All these results were highly significant, with P values ranging from less than .0008 for risk of LVEF decline to less than .00001 for the others.
In a plain-language summary comparing trastuzumab-containing regimens with standard therapy alone in 1,000 women, the investigators wrote that 33 more women would have their lives prolonged with trastuzumab (933 women vs. 900 women with standard therapy alone). However, about 26 in 1,000 women taking trastuzumab would have serious heart toxicity, which is 21 more than the group treated with standard therapy alone.
Trastuzumab’s cardiotoxic effects have been well known, but the magnitude of the effect reported in the systematic review may be larger than what people have thought, commented Dr. Daniel J. Lenihan, director of clinical research in the cardiovascular medicine division at Vanderbilt University, Nashville, Tenn., in an interview.
And that risk may be even greater in the world outside of clinical studies, said Dr. Melinda Telli of Stanford (Calif.) University. The patients in the studies included in the systematic review were younger, and none had baseline cardiac disease, observed Dr. Telli, also in an interview.
Another issue: In practice, oncologists are offering trastuzumab to women at lower risk for cancer recurrence than those in the trials. Thus, she said, "it’s more likely the risks are underestimated in this Cochrane review."
Although the data in the systematic review were previously published, having them encapsulated – along with a number of scenarios outlining potential risks and benefits in women with different cancer recurrence and cardiac risk factors – is a significant addition to the literature, said Dr. Telli.
Cochrane reviews are known for being thorough and balanced. This review began by looking at about 3,900 studies; after applying exclusion criteria, the list was winnowed down to 35 publications that covered 8 randomized controlled clinical trials enrolling 11,991 women. A little more than 7,000 women were assigned to a trastuzumab-containing arm, and 4,971 women to a regimen without trastuzumab. The median age in the trials was 49 years. Pre- and postmenopausal women were included, but those with metastatic disease or preexisting heart conditions were excluded.
The review concluded that high-risk women with few cardiac risk factors would benefit from trastuzumab, while those at lower risk "must be carefully evaluated," adding, "The oncologist should share the decision with the patient concerning whether and how to start the treatment."
Dr. Lenihan said he was concerned that the potential cardiotoxicity might cause oncologists to steer away from trastuzumab. He is a proponent of a multidisciplinary team that involves a cardiologist at the outset of therapy.
If cardiac effects develop, "the key is not to ignore it, but to pay attention," said Dr. Lenihan, who is also president of the International CardiOncology Society USA/Canada.
Early identification enables rapid treatment, which can stabilize or correct the heart issues, he said. That allows patients to return to their cancer therapy.
Dr. Lenihan and his colleagues at Vanderbilt University are currently conducting a study testing various cardiac biomarkers to detect toxicity during chemotherapy.
It is still unknown, however, whether the cardiotoxicity that develops during therapy is ultimately reversible, or becomes a lifelong issue. While the ejection fraction may recover after withdrawal of trastuzumab, at least one study – the Herceptin Adjuvant (HERA) trial – has shown that some women had long-term loss of heart muscle cells, said Dr. Telli.
"So we know that the heart is taking a hit," she said, adding that the trastuzumab damage is not "some sort of reversible thing."
The key, she said, is for oncologists to weigh the risks and benefits individually in each patient.
A targeted therapy, trastuzumab is approved for treatment of HER2-positive breast cancer and of metastatic HER2-positive adenocarcinoma of the stomach or gastroesophageal junction. About 20% of tumors in women with early breast cancer are HER2-positive.
Dr. Telli reported no conflicts of interest. Dr. Lenihan reported receiving consulting fees from Roche and AstraZeneca and research support from Acorda.
The risk of cardiotoxicity is five times higher in breast cancer patients given trastuzumab than in those receiving a standard chemotherapy regimen alone, according to a new systematic review from the Cochrane Collaboration.
The review found that regimens containing trastuzumab (Herceptin) significantly increased congestive heart failure and left ventricular ejection fraction (LVEF) decline, with relative risks of 5.11 and 1.83, respectively, in women with HER2-positive early and locally advanced breast cancer (Cochrane Database Syst. Rev. 2012;4 [doi: 10.1002/14651858.CD006243.pub2]).
However, trastuzumab regimens also significantly increased overall and disease-free survival, with hazard ratios of 0.66 and 0.60, respectively, noted Dr. Lorenzo Moja of the University of Milan and his coauthors. All these results were highly significant, with P values ranging from less than .0008 for risk of LVEF decline to less than .00001 for the others.
In a plain-language summary comparing trastuzumab-containing regimens with standard therapy alone in 1,000 women, the investigators wrote that 33 more women would have their lives prolonged with trastuzumab (933 women vs. 900 women with standard therapy alone). However, about 26 in 1,000 women taking trastuzumab would have serious heart toxicity, which is 21 more than the group treated with standard therapy alone.
Trastuzumab’s cardiotoxic effects have been well known, but the magnitude of the effect reported in the systematic review may be larger than what people have thought, commented Dr. Daniel J. Lenihan, director of clinical research in the cardiovascular medicine division at Vanderbilt University, Nashville, Tenn., in an interview.
And that risk may be even greater in the world outside of clinical studies, said Dr. Melinda Telli of Stanford (Calif.) University. The patients in the studies included in the systematic review were younger, and none had baseline cardiac disease, observed Dr. Telli, also in an interview.
Another issue: In practice, oncologists are offering trastuzumab to women at lower risk for cancer recurrence than those in the trials. Thus, she said, "it’s more likely the risks are underestimated in this Cochrane review."
Although the data in the systematic review were previously published, having them encapsulated – along with a number of scenarios outlining potential risks and benefits in women with different cancer recurrence and cardiac risk factors – is a significant addition to the literature, said Dr. Telli.
Cochrane reviews are known for being thorough and balanced. This review began by looking at about 3,900 studies; after applying exclusion criteria, the list was winnowed down to 35 publications that covered 8 randomized controlled clinical trials enrolling 11,991 women. A little more than 7,000 women were assigned to a trastuzumab-containing arm, and 4,971 women to a regimen without trastuzumab. The median age in the trials was 49 years. Pre- and postmenopausal women were included, but those with metastatic disease or preexisting heart conditions were excluded.
The review concluded that high-risk women with few cardiac risk factors would benefit from trastuzumab, while those at lower risk "must be carefully evaluated," adding, "The oncologist should share the decision with the patient concerning whether and how to start the treatment."
Dr. Lenihan said he was concerned that the potential cardiotoxicity might cause oncologists to steer away from trastuzumab. He is a proponent of a multidisciplinary team that involves a cardiologist at the outset of therapy.
If cardiac effects develop, "the key is not to ignore it, but to pay attention," said Dr. Lenihan, who is also president of the International CardiOncology Society USA/Canada.
Early identification enables rapid treatment, which can stabilize or correct the heart issues, he said. That allows patients to return to their cancer therapy.
Dr. Lenihan and his colleagues at Vanderbilt University are currently conducting a study testing various cardiac biomarkers to detect toxicity during chemotherapy.
It is still unknown, however, whether the cardiotoxicity that develops during therapy is ultimately reversible, or becomes a lifelong issue. While the ejection fraction may recover after withdrawal of trastuzumab, at least one study – the Herceptin Adjuvant (HERA) trial – has shown that some women had long-term loss of heart muscle cells, said Dr. Telli.
"So we know that the heart is taking a hit," she said, adding that the trastuzumab damage is not "some sort of reversible thing."
The key, she said, is for oncologists to weigh the risks and benefits individually in each patient.
A targeted therapy, trastuzumab is approved for treatment of HER2-positive breast cancer and of metastatic HER2-positive adenocarcinoma of the stomach or gastroesophageal junction. About 20% of tumors in women with early breast cancer are HER2-positive.
Dr. Telli reported no conflicts of interest. Dr. Lenihan reported receiving consulting fees from Roche and AstraZeneca and research support from Acorda.
FROM THE COCHRANE DATABASE OF SYSTEMATIC REVIEWS
Use of Ultrasound Expands Across Surgical Specialties
Ultrasound, a technology that was once mainly in the purview of radiologists, is becoming an integral part of the surgeon’s toolbox.
Across specialties, an increasing number of surgeons are incorporating ultrasound into their practices, whether in the office or in the operating room, especially as procedures become less invasive.
The once-cumbersome machines have gotten smaller over the past three decades, the technology has improved dramatically, and – compared with some other types of imaging – ultrasound is more cost-effective and affordable, experts say.
"It’s a technology that I think is going to expand in use," said Dr. Jay K. Harness, an early adopter of ultrasound in breast surgery and coauthor of the textbook "Ultrasound in Surgical Practice." "I started using it in the 1990s, and it’s like we’ve gone from analog TV to digital."
Dr. Heidi Frankel, chair of American College of Surgeons’ (ACS) National Ultrasound Faculty, compared the developments in use of ultrasound in surgery to laparoscopy.
"Ultimately, the patients and the market pushed the need for it," said Dr. Frankel, professor of surgery at University of Maryland Shock Trauma Center, Baltimore. "Surgeons who didn’t do it had to learn to do it, and it became part of surgical training. I suspect the same thing is going to happen with ultrasound."
And while training and certification requirements vary widely, the surgeons currently using ultrasound predict that guidelines may ultimately become somewhat standardized within and across specialties.
Breast Surgery
Dr. Harness, who is also a member of the ACS National Ultrasound Faculty and the past-president of the American Society of Breast Surgeons (ASBS), was among the first to incorporate ultrasound into his practice. Today, he said, "for the contemporary breast surgeon, [ultrasound] is a fundamental tool ... Ultrasound is our stethoscope."
In breast surgery, ultrasound is an adjunctive tool for the physical exam, said Dr. Harness. It is used for diagnostic biopsy, and it can speed up the diagnostic process. Ultrasound also is used in the operating room, notably for procedures such as lumpectomies. And finally, ultrasound can help guide the placement of partial breast brachyradiation therapy devices.
Breast surgeons can obtain ultrasound certification through ASBS, although becoming certified is not a requirement. "A major goal of the Society’s breast ultrasound certification program is to improve the quality of care for patients with breast disease by encouraging education and training to advance expertise and clinical competency for surgeons who use ultrasound and ultrasound-guided procedures in their practices," according to the ASBS website.
Dr. Harness said that ultrasound combined with other imaging techniques such as MRI provides the most complete imaging possible, given that there’s no single technology that captures everything.
Abdominal Surgery
In the 1980s, not many surgeons used ultrasound in their day-to-day practice and there were few publications on the topic, said Dr. Junji Machi. At that time, x-rays were commonly used to check areas such as the bile duct for stones. "But, it was cumbersome and took 15-30 minutes. So we used ultrasound instead. It was quicker, and the results were accurate," said Dr. Machi, professor of surgery at University of Hawaii, and director of the Abdominal Ultrasound Module at the ACS.
Dr. Machi has published a number of studies on cases and findings, and he uses ultrasound, especially during liver, biliary, and pancreatic surgery.
"For liver surgery, intraoperative ultrasound is a must," he said. "Without it, we consider the procedure suboptimal, because we may miss lesions and cannot perform the best operations."
Among the indications for ultrasound use in abdominal surgery were laparoscopic procedures, which were introduced in the 1990s, he said. "You can see, but not touch, the tissue," said Dr. Machi. "So we needed something to evaluate under the surface. ... With ultrasound, we can see without much dissection."
Surgeons could be discouraged from using ultrasound because the learning curve is steep (usually several months’ experience is needed) and because the equipment is relatively expensive. Yet, "once you learn it, it’s much more cost effective," he said, adding that this imaging technique does not expose the patient and operative team to radiation.
There’s no specialty limitation in the use of ultrasound, and abdominal surgeons can perform it once they master ultrasound. The ACS ultrasound course is an excellent way to learn, said Dr. Machi. Surgeons receive a certificate upon completion of a course.
Indeed, "the training issues are really paramount," said Dr. Ellen Hagopian, who did her liver training in France, and studied with radiologists and surgeons. Ultrasound is used much more frequently in Europe than in the United States, she said. "I sit on the education and training committee of Americas Hepato-Pancreato-Biliary Association [AHPBA], and I think ultrasound training throughout the fellowship programs needs to be more consistent."
Dr. Hagopian, who sits on ACS’s National Ultrasound Faculty board, coordinated and taught the first advanced ultrasound course in hepato-pancreato-biliary surgery at the AHPBA Annual Meeting in March. The course will be given again this year at the ACS Clinical Congress in San Francisco. Surgeons receive a certification of completion.
"Feedback and interest at AHPBA was excellent," said Dr. Hagopian. "There were many more surgeons who wanted to take the course than we could accommodate." She anticipates that similar interest will be shown during the ACS Clinical Congress.
Head and Neck Surgery
"Basically, the best way to evaluate the thyroid gland is ultrasound," said Dr. Robert Sofferman, an otolaryngologist who does thyroid and parathyroid surgery as part of his practice. "It’s cheaper and incredibly accurate."
Dr. Sofferman, professor emeritus of surgery at the University of Vermont in Burlington, said that some 15 years ago, ultrasound machines were too big and didn’t have good resolution. But over time, the equipment has become smaller, better, portable, and less expensive, he said. He predicts that the machines will eventually shrink to the size of an iPad.
"We operate in the neck on a daily basis," said Dr. Sofferman. "Ultrasound is very helpful for us. I couldn’t do my work without it."
Having the imaging available in the office is also convenient for the patients. "We arrange everything before the patient comes in. We do the physical exam. We do the ultrasound exam. We do ultrasound-guided biopsy, so the patient is done in one visit."
He said ultrasound can be used to evaluate the size and characteristics of a tumor before deciding whether to operate or to monitor the tumor’s response to treatment. "It’s a technology that has some advantages. It’s an extension of our physical examination."
It also comes with a few drawbacks. Aside from the price, which can be upwards of $30,000, ultrasound can slow down the day, and it does have a moderate learning curve, according to Dr. Sofferman.
Neither the ACS nor American Association of Otolaryngology-Head and Neck Surgery (AAO-HNS) require certification for the use of ultrasound. However, the ACS offers training in thyroid/parathyroid ultrasound to all surgeons who do neck surgery, either during the annual Clinical Congress or in other courses. Participants who complete training receive certification from the ACS.
Vascular Surgery
Ultrasound is a major component of vascular surgery training and practice, and many vascular surgeons have obtained the Registered Vascular Technologist (RVT) credential from the American Registry for Diagnostic Medical Sonography (ARDMS.)
While the RVT credential has been available since the 1980s, the ARDMS introduced the Registered Physician in Vascular Interpretation (RPVI) credential in 2006 to provide a certification process that focuses more on interpretation of vascular ultrasound tests than on performing the examinations. The RPVI credential is open to all qualified physicians and is not restricted to vascular surgeons.
"The advantage of the RPVI is that it is a national, standardized credential that is available to all physicians with an interest in vascular testing," said Dr. Gene Zierler, a member of the National Ultrasound Faculty and professor of surgery at the University of Washington, Seattle. "So that means it can document expertise in vascular ultrasound across multiple specialties and training programs."
Starting in 2014, the RPVI will be a requirement for vascular surgery board certification, a decision supported by the Society for Vascular Surgery.
Trauma Surgery
Ultrasound is the quickest and most reliable diagnostic tool under emergency conditions, according to Dr. Frankel.
"We work with very time-sensitive injuries. Ultrasound in my specialty is absolutely necessary. We image trauma patients this way. We can’t wait for a radiologist to come in," she said.
Dr. Frankel, who began using ultrasound in 1994, echoed her colleagues who said that technology has improved over time. Her hospital has begun using ultrasound in the intensive care unit, and "our residents are starting to use it early on. And medical students are picking it up," she said.
Whether surgeons are permitted to use ultrasound in the hospital varies by system or institution. Hospitals may require board-certified surgeons to perform a certain number of ultrasound procedures before granting them certification or to show certain certification or credentialing in ultrasound, experts said.
"There’s no science [to show] how many of these procedures I should have done to get credentialed by the hospital to use ultrasound," Dr. Frankel said.
She and other surgeons predicted that the individual surgical societies will ultimately specify the training, certification, or accreditation requirements for performing ultrasound. In the meantime, ultrasound seems to be finding its place in surgery, and surgeons who have been using it say they wouldn’t practice without it.
"It adds to the joy of practicing medicine," said Dr. Sofferman. "It makes it enjoyable for us to be able to see everything. That’s a definite advantage. I couldn’t be as efficient and as accurate without it."
None of the surgeons reported any relevant disclosures.
Ultrasound, a technology that was once mainly in the purview of radiologists, is becoming an integral part of the surgeon’s toolbox.
Across specialties, an increasing number of surgeons are incorporating ultrasound into their practices, whether in the office or in the operating room, especially as procedures become less invasive.
The once-cumbersome machines have gotten smaller over the past three decades, the technology has improved dramatically, and – compared with some other types of imaging – ultrasound is more cost-effective and affordable, experts say.
"It’s a technology that I think is going to expand in use," said Dr. Jay K. Harness, an early adopter of ultrasound in breast surgery and coauthor of the textbook "Ultrasound in Surgical Practice." "I started using it in the 1990s, and it’s like we’ve gone from analog TV to digital."
Dr. Heidi Frankel, chair of American College of Surgeons’ (ACS) National Ultrasound Faculty, compared the developments in use of ultrasound in surgery to laparoscopy.
"Ultimately, the patients and the market pushed the need for it," said Dr. Frankel, professor of surgery at University of Maryland Shock Trauma Center, Baltimore. "Surgeons who didn’t do it had to learn to do it, and it became part of surgical training. I suspect the same thing is going to happen with ultrasound."
And while training and certification requirements vary widely, the surgeons currently using ultrasound predict that guidelines may ultimately become somewhat standardized within and across specialties.
Breast Surgery
Dr. Harness, who is also a member of the ACS National Ultrasound Faculty and the past-president of the American Society of Breast Surgeons (ASBS), was among the first to incorporate ultrasound into his practice. Today, he said, "for the contemporary breast surgeon, [ultrasound] is a fundamental tool ... Ultrasound is our stethoscope."
In breast surgery, ultrasound is an adjunctive tool for the physical exam, said Dr. Harness. It is used for diagnostic biopsy, and it can speed up the diagnostic process. Ultrasound also is used in the operating room, notably for procedures such as lumpectomies. And finally, ultrasound can help guide the placement of partial breast brachyradiation therapy devices.
Breast surgeons can obtain ultrasound certification through ASBS, although becoming certified is not a requirement. "A major goal of the Society’s breast ultrasound certification program is to improve the quality of care for patients with breast disease by encouraging education and training to advance expertise and clinical competency for surgeons who use ultrasound and ultrasound-guided procedures in their practices," according to the ASBS website.
Dr. Harness said that ultrasound combined with other imaging techniques such as MRI provides the most complete imaging possible, given that there’s no single technology that captures everything.
Abdominal Surgery
In the 1980s, not many surgeons used ultrasound in their day-to-day practice and there were few publications on the topic, said Dr. Junji Machi. At that time, x-rays were commonly used to check areas such as the bile duct for stones. "But, it was cumbersome and took 15-30 minutes. So we used ultrasound instead. It was quicker, and the results were accurate," said Dr. Machi, professor of surgery at University of Hawaii, and director of the Abdominal Ultrasound Module at the ACS.
Dr. Machi has published a number of studies on cases and findings, and he uses ultrasound, especially during liver, biliary, and pancreatic surgery.
"For liver surgery, intraoperative ultrasound is a must," he said. "Without it, we consider the procedure suboptimal, because we may miss lesions and cannot perform the best operations."
Among the indications for ultrasound use in abdominal surgery were laparoscopic procedures, which were introduced in the 1990s, he said. "You can see, but not touch, the tissue," said Dr. Machi. "So we needed something to evaluate under the surface. ... With ultrasound, we can see without much dissection."
Surgeons could be discouraged from using ultrasound because the learning curve is steep (usually several months’ experience is needed) and because the equipment is relatively expensive. Yet, "once you learn it, it’s much more cost effective," he said, adding that this imaging technique does not expose the patient and operative team to radiation.
There’s no specialty limitation in the use of ultrasound, and abdominal surgeons can perform it once they master ultrasound. The ACS ultrasound course is an excellent way to learn, said Dr. Machi. Surgeons receive a certificate upon completion of a course.
Indeed, "the training issues are really paramount," said Dr. Ellen Hagopian, who did her liver training in France, and studied with radiologists and surgeons. Ultrasound is used much more frequently in Europe than in the United States, she said. "I sit on the education and training committee of Americas Hepato-Pancreato-Biliary Association [AHPBA], and I think ultrasound training throughout the fellowship programs needs to be more consistent."
Dr. Hagopian, who sits on ACS’s National Ultrasound Faculty board, coordinated and taught the first advanced ultrasound course in hepato-pancreato-biliary surgery at the AHPBA Annual Meeting in March. The course will be given again this year at the ACS Clinical Congress in San Francisco. Surgeons receive a certification of completion.
"Feedback and interest at AHPBA was excellent," said Dr. Hagopian. "There were many more surgeons who wanted to take the course than we could accommodate." She anticipates that similar interest will be shown during the ACS Clinical Congress.
Head and Neck Surgery
"Basically, the best way to evaluate the thyroid gland is ultrasound," said Dr. Robert Sofferman, an otolaryngologist who does thyroid and parathyroid surgery as part of his practice. "It’s cheaper and incredibly accurate."
Dr. Sofferman, professor emeritus of surgery at the University of Vermont in Burlington, said that some 15 years ago, ultrasound machines were too big and didn’t have good resolution. But over time, the equipment has become smaller, better, portable, and less expensive, he said. He predicts that the machines will eventually shrink to the size of an iPad.
"We operate in the neck on a daily basis," said Dr. Sofferman. "Ultrasound is very helpful for us. I couldn’t do my work without it."
Having the imaging available in the office is also convenient for the patients. "We arrange everything before the patient comes in. We do the physical exam. We do the ultrasound exam. We do ultrasound-guided biopsy, so the patient is done in one visit."
He said ultrasound can be used to evaluate the size and characteristics of a tumor before deciding whether to operate or to monitor the tumor’s response to treatment. "It’s a technology that has some advantages. It’s an extension of our physical examination."
It also comes with a few drawbacks. Aside from the price, which can be upwards of $30,000, ultrasound can slow down the day, and it does have a moderate learning curve, according to Dr. Sofferman.
Neither the ACS nor American Association of Otolaryngology-Head and Neck Surgery (AAO-HNS) require certification for the use of ultrasound. However, the ACS offers training in thyroid/parathyroid ultrasound to all surgeons who do neck surgery, either during the annual Clinical Congress or in other courses. Participants who complete training receive certification from the ACS.
Vascular Surgery
Ultrasound is a major component of vascular surgery training and practice, and many vascular surgeons have obtained the Registered Vascular Technologist (RVT) credential from the American Registry for Diagnostic Medical Sonography (ARDMS.)
While the RVT credential has been available since the 1980s, the ARDMS introduced the Registered Physician in Vascular Interpretation (RPVI) credential in 2006 to provide a certification process that focuses more on interpretation of vascular ultrasound tests than on performing the examinations. The RPVI credential is open to all qualified physicians and is not restricted to vascular surgeons.
"The advantage of the RPVI is that it is a national, standardized credential that is available to all physicians with an interest in vascular testing," said Dr. Gene Zierler, a member of the National Ultrasound Faculty and professor of surgery at the University of Washington, Seattle. "So that means it can document expertise in vascular ultrasound across multiple specialties and training programs."
Starting in 2014, the RPVI will be a requirement for vascular surgery board certification, a decision supported by the Society for Vascular Surgery.
Trauma Surgery
Ultrasound is the quickest and most reliable diagnostic tool under emergency conditions, according to Dr. Frankel.
"We work with very time-sensitive injuries. Ultrasound in my specialty is absolutely necessary. We image trauma patients this way. We can’t wait for a radiologist to come in," she said.
Dr. Frankel, who began using ultrasound in 1994, echoed her colleagues who said that technology has improved over time. Her hospital has begun using ultrasound in the intensive care unit, and "our residents are starting to use it early on. And medical students are picking it up," she said.
Whether surgeons are permitted to use ultrasound in the hospital varies by system or institution. Hospitals may require board-certified surgeons to perform a certain number of ultrasound procedures before granting them certification or to show certain certification or credentialing in ultrasound, experts said.
"There’s no science [to show] how many of these procedures I should have done to get credentialed by the hospital to use ultrasound," Dr. Frankel said.
She and other surgeons predicted that the individual surgical societies will ultimately specify the training, certification, or accreditation requirements for performing ultrasound. In the meantime, ultrasound seems to be finding its place in surgery, and surgeons who have been using it say they wouldn’t practice without it.
"It adds to the joy of practicing medicine," said Dr. Sofferman. "It makes it enjoyable for us to be able to see everything. That’s a definite advantage. I couldn’t be as efficient and as accurate without it."
None of the surgeons reported any relevant disclosures.
Ultrasound, a technology that was once mainly in the purview of radiologists, is becoming an integral part of the surgeon’s toolbox.
Across specialties, an increasing number of surgeons are incorporating ultrasound into their practices, whether in the office or in the operating room, especially as procedures become less invasive.
The once-cumbersome machines have gotten smaller over the past three decades, the technology has improved dramatically, and – compared with some other types of imaging – ultrasound is more cost-effective and affordable, experts say.
"It’s a technology that I think is going to expand in use," said Dr. Jay K. Harness, an early adopter of ultrasound in breast surgery and coauthor of the textbook "Ultrasound in Surgical Practice." "I started using it in the 1990s, and it’s like we’ve gone from analog TV to digital."
Dr. Heidi Frankel, chair of American College of Surgeons’ (ACS) National Ultrasound Faculty, compared the developments in use of ultrasound in surgery to laparoscopy.
"Ultimately, the patients and the market pushed the need for it," said Dr. Frankel, professor of surgery at University of Maryland Shock Trauma Center, Baltimore. "Surgeons who didn’t do it had to learn to do it, and it became part of surgical training. I suspect the same thing is going to happen with ultrasound."
And while training and certification requirements vary widely, the surgeons currently using ultrasound predict that guidelines may ultimately become somewhat standardized within and across specialties.
Breast Surgery
Dr. Harness, who is also a member of the ACS National Ultrasound Faculty and the past-president of the American Society of Breast Surgeons (ASBS), was among the first to incorporate ultrasound into his practice. Today, he said, "for the contemporary breast surgeon, [ultrasound] is a fundamental tool ... Ultrasound is our stethoscope."
In breast surgery, ultrasound is an adjunctive tool for the physical exam, said Dr. Harness. It is used for diagnostic biopsy, and it can speed up the diagnostic process. Ultrasound also is used in the operating room, notably for procedures such as lumpectomies. And finally, ultrasound can help guide the placement of partial breast brachyradiation therapy devices.
Breast surgeons can obtain ultrasound certification through ASBS, although becoming certified is not a requirement. "A major goal of the Society’s breast ultrasound certification program is to improve the quality of care for patients with breast disease by encouraging education and training to advance expertise and clinical competency for surgeons who use ultrasound and ultrasound-guided procedures in their practices," according to the ASBS website.
Dr. Harness said that ultrasound combined with other imaging techniques such as MRI provides the most complete imaging possible, given that there’s no single technology that captures everything.
Abdominal Surgery
In the 1980s, not many surgeons used ultrasound in their day-to-day practice and there were few publications on the topic, said Dr. Junji Machi. At that time, x-rays were commonly used to check areas such as the bile duct for stones. "But, it was cumbersome and took 15-30 minutes. So we used ultrasound instead. It was quicker, and the results were accurate," said Dr. Machi, professor of surgery at University of Hawaii, and director of the Abdominal Ultrasound Module at the ACS.
Dr. Machi has published a number of studies on cases and findings, and he uses ultrasound, especially during liver, biliary, and pancreatic surgery.
"For liver surgery, intraoperative ultrasound is a must," he said. "Without it, we consider the procedure suboptimal, because we may miss lesions and cannot perform the best operations."
Among the indications for ultrasound use in abdominal surgery were laparoscopic procedures, which were introduced in the 1990s, he said. "You can see, but not touch, the tissue," said Dr. Machi. "So we needed something to evaluate under the surface. ... With ultrasound, we can see without much dissection."
Surgeons could be discouraged from using ultrasound because the learning curve is steep (usually several months’ experience is needed) and because the equipment is relatively expensive. Yet, "once you learn it, it’s much more cost effective," he said, adding that this imaging technique does not expose the patient and operative team to radiation.
There’s no specialty limitation in the use of ultrasound, and abdominal surgeons can perform it once they master ultrasound. The ACS ultrasound course is an excellent way to learn, said Dr. Machi. Surgeons receive a certificate upon completion of a course.
Indeed, "the training issues are really paramount," said Dr. Ellen Hagopian, who did her liver training in France, and studied with radiologists and surgeons. Ultrasound is used much more frequently in Europe than in the United States, she said. "I sit on the education and training committee of Americas Hepato-Pancreato-Biliary Association [AHPBA], and I think ultrasound training throughout the fellowship programs needs to be more consistent."
Dr. Hagopian, who sits on ACS’s National Ultrasound Faculty board, coordinated and taught the first advanced ultrasound course in hepato-pancreato-biliary surgery at the AHPBA Annual Meeting in March. The course will be given again this year at the ACS Clinical Congress in San Francisco. Surgeons receive a certification of completion.
"Feedback and interest at AHPBA was excellent," said Dr. Hagopian. "There were many more surgeons who wanted to take the course than we could accommodate." She anticipates that similar interest will be shown during the ACS Clinical Congress.
Head and Neck Surgery
"Basically, the best way to evaluate the thyroid gland is ultrasound," said Dr. Robert Sofferman, an otolaryngologist who does thyroid and parathyroid surgery as part of his practice. "It’s cheaper and incredibly accurate."
Dr. Sofferman, professor emeritus of surgery at the University of Vermont in Burlington, said that some 15 years ago, ultrasound machines were too big and didn’t have good resolution. But over time, the equipment has become smaller, better, portable, and less expensive, he said. He predicts that the machines will eventually shrink to the size of an iPad.
"We operate in the neck on a daily basis," said Dr. Sofferman. "Ultrasound is very helpful for us. I couldn’t do my work without it."
Having the imaging available in the office is also convenient for the patients. "We arrange everything before the patient comes in. We do the physical exam. We do the ultrasound exam. We do ultrasound-guided biopsy, so the patient is done in one visit."
He said ultrasound can be used to evaluate the size and characteristics of a tumor before deciding whether to operate or to monitor the tumor’s response to treatment. "It’s a technology that has some advantages. It’s an extension of our physical examination."
It also comes with a few drawbacks. Aside from the price, which can be upwards of $30,000, ultrasound can slow down the day, and it does have a moderate learning curve, according to Dr. Sofferman.
Neither the ACS nor American Association of Otolaryngology-Head and Neck Surgery (AAO-HNS) require certification for the use of ultrasound. However, the ACS offers training in thyroid/parathyroid ultrasound to all surgeons who do neck surgery, either during the annual Clinical Congress or in other courses. Participants who complete training receive certification from the ACS.
Vascular Surgery
Ultrasound is a major component of vascular surgery training and practice, and many vascular surgeons have obtained the Registered Vascular Technologist (RVT) credential from the American Registry for Diagnostic Medical Sonography (ARDMS.)
While the RVT credential has been available since the 1980s, the ARDMS introduced the Registered Physician in Vascular Interpretation (RPVI) credential in 2006 to provide a certification process that focuses more on interpretation of vascular ultrasound tests than on performing the examinations. The RPVI credential is open to all qualified physicians and is not restricted to vascular surgeons.
"The advantage of the RPVI is that it is a national, standardized credential that is available to all physicians with an interest in vascular testing," said Dr. Gene Zierler, a member of the National Ultrasound Faculty and professor of surgery at the University of Washington, Seattle. "So that means it can document expertise in vascular ultrasound across multiple specialties and training programs."
Starting in 2014, the RPVI will be a requirement for vascular surgery board certification, a decision supported by the Society for Vascular Surgery.
Trauma Surgery
Ultrasound is the quickest and most reliable diagnostic tool under emergency conditions, according to Dr. Frankel.
"We work with very time-sensitive injuries. Ultrasound in my specialty is absolutely necessary. We image trauma patients this way. We can’t wait for a radiologist to come in," she said.
Dr. Frankel, who began using ultrasound in 1994, echoed her colleagues who said that technology has improved over time. Her hospital has begun using ultrasound in the intensive care unit, and "our residents are starting to use it early on. And medical students are picking it up," she said.
Whether surgeons are permitted to use ultrasound in the hospital varies by system or institution. Hospitals may require board-certified surgeons to perform a certain number of ultrasound procedures before granting them certification or to show certain certification or credentialing in ultrasound, experts said.
"There’s no science [to show] how many of these procedures I should have done to get credentialed by the hospital to use ultrasound," Dr. Frankel said.
She and other surgeons predicted that the individual surgical societies will ultimately specify the training, certification, or accreditation requirements for performing ultrasound. In the meantime, ultrasound seems to be finding its place in surgery, and surgeons who have been using it say they wouldn’t practice without it.
"It adds to the joy of practicing medicine," said Dr. Sofferman. "It makes it enjoyable for us to be able to see everything. That’s a definite advantage. I couldn’t be as efficient and as accurate without it."
None of the surgeons reported any relevant disclosures.
NCCN: Skip ALND in Some Early Breast Cancer
Axillary lymph node dissection can be skipped in some early-stage breast cancer patients with minimal sentinel node involvement, as well as in those with negative findings on sentinel node biopsy, according to revised clinical practice guidelines issued by the National Comprehensive Cancer Network.
The recommendation that no further axial surgery be considered for certain patients with only one or two involved sentinel lymph nodes reflects an upgrade of the National Comprehensive Cancer Network (NCCN) guideline on sentinel node biopsy to a category 1 recommendation.
The change is based on the findings of recent prospective studies. In particular, the American College of Surgeons Oncology Group (ACOSOG) Z0011 trial, found no survival difference between early-stage breast cancer patients who underwent axillary lymph node dissection [ALND] and those who did not after one or two sentinel nodes were determined to be positive on biopsy (JAMA 2011;305:569-75).
The revised recommendation extends only to those patients with early-stage disease (tumor grades 1 or 2) who undergo breast-conserving surgery and whole-breast radiation and who have not received neoadjuvant chemotherapy, according to the guidelines. A primary objective is to reduce the risk of lymphedema associated with axillary lymph node dissection.
"In the absence of definitive data demonstrating superior survival from the performance of axillary lymph node dissection, patients who have particularly favorable tumors, patients for whom the selection of adjuvant systemic therapy is unlikely to be affected, for the elderly or those with serious comorbid conditions, the performance of axillary lymph node dissection may be considered optional," the guidelines advise.
The update was presented at the NCCN annual meeting in Hollywood, Fla. The Breast Cancer Panel lists potential conflict of interest disclosures on the NCCN website.
Axillary lymph node dissection can be skipped in some early-stage breast cancer patients with minimal sentinel node involvement, as well as in those with negative findings on sentinel node biopsy, according to revised clinical practice guidelines issued by the National Comprehensive Cancer Network.
The recommendation that no further axial surgery be considered for certain patients with only one or two involved sentinel lymph nodes reflects an upgrade of the National Comprehensive Cancer Network (NCCN) guideline on sentinel node biopsy to a category 1 recommendation.
The change is based on the findings of recent prospective studies. In particular, the American College of Surgeons Oncology Group (ACOSOG) Z0011 trial, found no survival difference between early-stage breast cancer patients who underwent axillary lymph node dissection [ALND] and those who did not after one or two sentinel nodes were determined to be positive on biopsy (JAMA 2011;305:569-75).
The revised recommendation extends only to those patients with early-stage disease (tumor grades 1 or 2) who undergo breast-conserving surgery and whole-breast radiation and who have not received neoadjuvant chemotherapy, according to the guidelines. A primary objective is to reduce the risk of lymphedema associated with axillary lymph node dissection.
"In the absence of definitive data demonstrating superior survival from the performance of axillary lymph node dissection, patients who have particularly favorable tumors, patients for whom the selection of adjuvant systemic therapy is unlikely to be affected, for the elderly or those with serious comorbid conditions, the performance of axillary lymph node dissection may be considered optional," the guidelines advise.
The update was presented at the NCCN annual meeting in Hollywood, Fla. The Breast Cancer Panel lists potential conflict of interest disclosures on the NCCN website.
Axillary lymph node dissection can be skipped in some early-stage breast cancer patients with minimal sentinel node involvement, as well as in those with negative findings on sentinel node biopsy, according to revised clinical practice guidelines issued by the National Comprehensive Cancer Network.
The recommendation that no further axial surgery be considered for certain patients with only one or two involved sentinel lymph nodes reflects an upgrade of the National Comprehensive Cancer Network (NCCN) guideline on sentinel node biopsy to a category 1 recommendation.
The change is based on the findings of recent prospective studies. In particular, the American College of Surgeons Oncology Group (ACOSOG) Z0011 trial, found no survival difference between early-stage breast cancer patients who underwent axillary lymph node dissection [ALND] and those who did not after one or two sentinel nodes were determined to be positive on biopsy (JAMA 2011;305:569-75).
The revised recommendation extends only to those patients with early-stage disease (tumor grades 1 or 2) who undergo breast-conserving surgery and whole-breast radiation and who have not received neoadjuvant chemotherapy, according to the guidelines. A primary objective is to reduce the risk of lymphedema associated with axillary lymph node dissection.
"In the absence of definitive data demonstrating superior survival from the performance of axillary lymph node dissection, patients who have particularly favorable tumors, patients for whom the selection of adjuvant systemic therapy is unlikely to be affected, for the elderly or those with serious comorbid conditions, the performance of axillary lymph node dissection may be considered optional," the guidelines advise.
The update was presented at the NCCN annual meeting in Hollywood, Fla. The Breast Cancer Panel lists potential conflict of interest disclosures on the NCCN website.
FROM THE NATIONAL COMPREHENSIVE CANCER NETWORK
Evidence Suggests Pregnancies Can Survive Maternal Cancer Treatment
Emerging data on pregnancy and cancer can now help women and their doctors chart a safer course between effective treatment and protecting the developing fetus.
Two registries – one in the United States and another in Europe – agree: It’s not only possible to save a pregnancy in many situations, but children born to these women appear to be largely unaffected by in utero chemotherapy exposure. The combined studies followed more than 200 exposed children for up to 18 years; neither one found any elevated risk of congenital anomaly or any kind of cognitive or developmental delay.
"This is practice-changing information," Dr. Frédéric Amant, primary author on the European paper, said in an interview. "Until now, physicians were reluctant to administer chemotherapy and usually opted for termination, or at least for a delay in treatment or premature delivery in order to get treatment going," he said.
Dr. Amant’s study leads off a special section on cancer in pregnancy, published in the March issue of Lancet Oncology. The paper examined evidence that both supports and questions the clinical wisdom of treating a disease that threatens two very different patients – an adult woman and the fetus she carries.
Every case is different, depending on the type of cancer, its grade and potential aggressiveness, the stage of pregnancy, and the woman’s own desires, said Dr. Elyce Cardonick, an ob.gyn. at Cooper University Hospital in Camden, N.J., and the lead investigator of the Pregnancy and Cancer Registry.
"With solid tumors you usually have time to do the surgery, get the pathologic diagnosis, and let the patient recover. But if there is leukemia, for instance, you have to move faster. The first question should be ‘Could we delay treatment for this patient if she was not pregnant?’ I don’t want to limit their treatment, but at the same time, it’s true that they might not be getting the most up-to-date treatment – the newest agent on the block – because you would want to go with something there is at least some experience with. But this doesn’t necessarily mean they are going to do worse."
Cancer occurs in about 1 in 1,000 pregnancies, said Dr. Sarah Temkin, a gynecologic oncologist at the University of Maryland, Baltimore. Many of her patients are referred after a routine screening during early pregnancy finds something abnormal, or when a woman with an existing cancer is incidentally found to be pregnant. But signs that might raise a red flag in other situations don’t necessarily alert physicians to danger in pregnant women, she said in an interview. Pregnancy could obfuscate some symptoms, which might be further downplayed in light of a mother’s relatively young age. Breast cancer is a prime example.
"There are two problems, especially for breast cancers, which are the most common ones we see in pregnancy. First, a woman’s breasts are changing anyway during that time. Breast cancer is so rare in women of earlier childbearing age that both the patient and the doctor tend to disregard any new lumps and bumps."
But despite its rarity, cancer in all forms appears to be increasing among pregnant women, she said. This is probably a direct relation to age. "Cancer rates increase with increasing age, and women are becoming mothers at older and older ages."
When cancer coincides with pregnancy, Dr. Temkin views the mother’s health as paramount. "The mother is the person with cancer, and she deserves whatever the standard of care is for that particular cancer – the best care that would be offered to her if she was not pregnant."
Chemotherapy and Fetal Outcomes
To examine long-term neurodevelopmental risks associated with maternal cancer treatment, Dr. Amant, a gynecologic oncologist at the Leuven (Belgium) Cancer Institute, and his colleagues, are following 70 children from the age of 18 months until 18 years. In the newly published interim analysis, the mean follow-up time is 22 months. All the children had intrauterine exposure to chemotherapy, radiation, oncologic surgery, or combinations of these.
The analysis, which also appeared in Lancet Oncology’s special issue, includes data on all the children, including 18 who are now older than 9 years (Lancet Oncol. 2012;13:256-64).
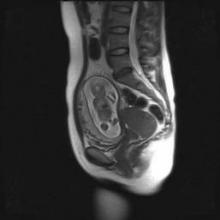
The children – 68 singletons and one set of twins – were born from pregnancies exposed to a total of 236 chemotherapy cycles. Exposure varied by the mother’s cancer type and its stage at diagnosis. In all, 34 mothers were treated with only chemotherapy, 27 had chemotherapy and surgery, 1 received chemotherapy and radiation, and 6 women were treated with all three modalities. Most of the children also had in utero exposure to multiple imaging studies, including MRI, ultrasound, echocardiography, CT, and mammography. Chemotherapy regimens included doxorubicin, epirubicin, idarubicin and daunorubicin.
Fetuses also were exposed to a variety of other drugs, including antibiotics, antiemetics, pain medications, colony stimulating factors, and anxiolytics.
Breast cancer was the most common disease type (35). There were 18 cases of hematologic cancers, 6 ovarian cancers, 4 cervical cancers, and 1 each of basal cell carcinoma, brain tumor, Ewing’s sarcoma, colorectal cancer, and nasopharyngeal cancer.
The mean gestational age at cancer diagnosis was 18 weeks, although fetuses ranged in age from 2 to 33 weeks when their mothers were diagnosed. About a third of the babies (23) were born at term.
Seven were born at 28-32 weeks, nine at 32-34 weeks, and 31 at 34-37 weeks. Weight for gestational age was below the 10th percentile in 14 children (21%).
Seven congenital anomalies were found in the group of 70 children (10%) – a rate not significantly different from that in the background population. There were only two major malformations, for a 2.9% rate. Malformations included the following:
• Hip subluxation, pectus excavatum and hemangioma, associated with chemotherapy only.
• Bilateral partial syndactyly, associated with chemotherapy plus radiotherapy.
• Bilateral small protuberance on one finger, and rectal atresia, associated with chemotherapy plus surgery.
• Bilateral double cartilage ring in a child exposed to chemotherapy, surgery and radiotherapy.
None of the children showed any congenital cardiac issues.
All of the children showed neurocognitive development that was within normal range, except for the set of twins, who were delivered by cesarean section at 32.5 weeks after a preterm premature rupture of membranes. These children were so delayed that they were not able to complete cognitive testing. Their mother developed an acute myeloid leukemia – one of the true "emergency" cancers diagnosed in pregnancy, Dr. Amant said. The babies had been exposed to idarubicin and cytosine arabinoside at 15.5, 21.5, 26.5, and 31.5 weeks’ gestation.
The boy, who weighed 1,640 g at birth, had a normal karyotype but, at 3 years, brain imaging showed a unilateral polymicrogyria in the left perisylvian area. He showed an early developmental delay; at age 9 years, he had the developmental capacity of a 12-month old.
The girl, who weighed 1,390 g at birth, also had an early developmental delay, but at age 9 years she attended school with support. Her parents refused brain imaging.
"The other 68 children did well," Dr. Amant said. "This doesn’t mean they were all normal in every way, but in any population you will see learning and developmental delay issues. We think the problem for the delayed children was not related to chemotherapy exposure, but more likely to their prematurity."
Dr. Amant saw a direct correlation between gestational age and intelligence quota. "When we controlled for age, gender, and country of birth, we found that the IQ score increased by almost 12 points for each additional month of gestation."
The U.S. Experience
Dr. Cardonick has found similar results. Her registry now contains information on 280 women who were enrolled over a 13-year period. The children born from these pregnancies have been assessed annually since birth. It also includes 70 controls – children whose mothers had cancer but who were not exposed to chemotherapy.
She published interim results of the registry in 2010 (Cancer J. 2010;16:76-82). At that point, it contained information on 231 women and 157 children. The most common malignancy was breast cancer (128); the mean gestational age at diagnosis was 13 weeks. About a third of the women (54) were advised to terminate their pregnancy; 12 did so.
Among those who continued both pregnancy and treatment, neonatal outcomes were generally good. There were nine premature deliveries related to preterm labor or premature rupture of membranes. The congenital anomaly rate born was 4%, which was in line with the normal background rate and slightly lower than that seen in Dr. Amant’s cohort.
The infants’ mean birth weight was 2,647 g, which was significantly less than the mean 2,873 g in the control group, but probably clinically irrelevant, Dr. Cardonick wrote in the paper.
She continues to follow these children annually. At this point, the children are a mean 5 years old; her oldest subject is 14 years. So far, the rate of neurocognitive issues in the group is no different than would be observed in any other group, and none of the children has developed any health problem that could be conclusively tied to intrauterine chemotherapy exposure.
Her experience stresses several key factors that must be considered in this situation. Her patients received chemotherapy at a mean of 20 weeks’ gestation – safely outside the critical early period. Only two women received chemotherapy before 10 weeks; both were treated before they knew they were pregnant. Both children born of these pregnancies were considered well. One with intrauterine exposure to cytarabine was developmentally normal at age 7 years. The other, who was exposed to oxaliplatin and capecitabine, was normal at age 2 years.
Treatment also was stopped a mean of 40 days before delivery, to allow the mother’s bone marrow to fully recover before giving birth.
A second U.S. study was reported at the 2011 meeting of the American Society of Clinical Oncology. A poster by Dr. Jennifer Litton and her colleagues examined physiological outcomes in 81 children exposed to chemotherapy for maternal breast cancer. The mothers had taken a standardized chemotherapy regimen of 5-fluorouracil, doxorubicin and cyclophosphamide (FAC) given during the second and third trimesters (J. Clin. Oncol. 2011;29[May 20 suppl.]:abstract 1099).
One child was born with Down syndrome, one with a club foot, and one with ureteral reflux. Three parents reported language delay in later follow-up surveys. Other reported health issues included 15 children with allergies and/or eczema, 2 with asthma, and 1 with absence seizures.
Dr. Litton, a breast oncologist at the University of Texas M.D. Anderson Cancer Center in Houston, also cowrote a 2010 review of breast cancer treatment in pregnancy, in which she discusses maternal and fetal outcomes from several cohorts, and the possible impact of intrauterine exposure to a variety of chemotherapy agents (Oncologist 2010;15:1238-47).
Risks Vary With Cancer Type
Breast cancer during pregnancy may be the simplest to treat. If the cancer is caught very early, it may be reasonable to delay treatment until the fetus has passed the critical first trimester, waiting until organs are formed and the risk of chemically induced damage is reduced, Dr. Temkin said. "It’s safe to do breast surgery during pregnancy and it’s safe to give chemotherapy after the first trimester."
But physicians can miss a new breast tumor during a prenatal exam, so some present at a more advanced stage, according to Dr. Amant, who is also the lead author of the Lancet’s breast cancer report (Lancet 2012;379:570-9).
Infiltrating ductal adenocarcinomas account for more than 70% of the breast cancers diagnosed during pregnancy. These can be aggressive, said Dr. Amant. Estrogen receptor status is probably no different in pregnant and nonpregnant women.
If the tumor is discovered early and is pathologically favorable, chemotherapy probably can be delayed until 14 weeks’ gestation, allowing nearly complete fetal organogenesis without worsening the mother’s outcome. Women also may elect an early termination if the pathology is unfavorable, or for other personal reasons, Dr. Temkin said. "I think a lot of it depends on when the cancer is diagnosed. Patients of mine who already have a diagnosis and then become pregnant almost always elect to terminate. But if the cancer is discovered when the pregnancy is farther along, most will continue, especially if the woman is highly emotionally invested," she noted.
Tougher Cancers, Tougher Choices
Treating gynecologic cancers during pregnancy often comes down to a choice between the mother’s health and maintenance of the pregnancy, Dr. Temkin said. "The standard of care for ovarian cancers is surgery or radiation to the pelvis, where the fetus is. Cervical cancer is treated with a hysterectomy or radiation, and neither treatment is compatible with keeping a pregnancy. Neoadjuvant therapy is not considered standard of care for these tumors. These are complex decisions for the patient: ‘Do I accept a different treatment [that might not be as effective] or maintain the pregnancy?’ "
In early cervical cancers without nodal spread, the most common tactic is close observation with periodic imaging to rule out spread; therapy is given after delivery, Dr. Phillippe Morice wrote in the Lancet section’s review on gynecologic malignancies (Lancet 2012;379:558-69).
"Delayed treatment until fetal maturation for patients with stage IA disease has an excellent prognosis and is now the standard of care," wrote Dr. Morice of the Institut de Cancérologie Gustave-Roussy in Villejuif, France.
Locally advanced disease is often not compatible with pregnancy. "The main treatment choice is either neoadjuvant chemotherapy or chemotherapy and radiotherapy. In pregnant patients, this approach means that the pregnancy must be ended before the initiation of therapy, but in exceptional cases in which surgery to end the pregnancy is not technically feasible ([that is], a bulky cervical tumor), radiation therapy can be delivered with the fetus in utero, resulting in a spontaneous abortion in about 3 weeks," he wrote.
Ovarian tumors can be surgically staged and – if it is of low malignant potential – can be laparoscopically removed, usually without endangering the pregnancy. Large tumors or those with aggressive pathology, like epithelial tumors, are much more difficult. Advanced or large tumors often have uterine and pelvic involvement, and treatment usually means a hysterectomy.
The literature contains reports of a very few women who have undergone chemotherapy to control peritoneal spread while keeping a pregnancy. However, despite giving birth to normally developed children, a number of these women died from recurrent disease, Dr. Morice noted.
Hematologic Cancers: True Emergency
Cancers of the blood are rare in pregnancy, occurring in only 1 of every 6,000. But when they do occur, they can be devastating, Dr. Benjamin Brenner wrote in the special series (Lancet 2012;379:580-7).
Pregnant patients with Hodgkin’s lymphoma generally do as well as their nonpregnant counterparts and can receive the same chemotherapy regimens, observing the first-trimester delay to favor the fetus.
Those who present with non-Hodgkin’s lymphoma are likely to have a very poor outlook. This disease is very rare in pregnant women, and symptoms can overlap with Hodgkin’s. Those factors, combined with a desire to avoid imaging, can delay diagnosis until the cancer is more advanced, said Dr. Brenner of the Rambam Health Care Campus, Haifa, Israel.
Acute leukemia is also rare, but demands urgent attention regardless of gestational stage, Dr. Brenner warned. "Patients diagnosed with acute leukemia during the first trimester are recommended to terminate the pregnancy, in view of the high risk of toxic effects on the fetus and mother, along with the expected need for further intensive treatment including stem-cell transplantation, which is absolutely contraindicated during gestation."
Talking It Out
Despite the emerging positive evidence, treating cancer during pregnancy can be a tough sell, Dr. Amant said. "Women have been told over and over to avoid taking so much as an aspirin. It’s very difficult to convince them that a fetus can not only survive a mother’s cancer treatment, but have a good chance of developing normally."
The stress of a cancer diagnosis during a desired pregnancy is very hard on patients, Dr. Temkin added. "Pregnancy is a time when many women come to grips with their own mortality as well as that of giving new life. Adding a diagnosis of cancer of top of that – especially in the face of a much-desired pregnancy – can be devastating."
These women are faced with two options: terminate the pregnancy and concentrate on their own treatment, or continue the pregnancy knowing that their unborn child will be exposed to the possible risks of radiation, chemotherapy, and surgery. Either option can "inflict terrible guilt on a pregnant woman. We can try to minimize that to some degree, but it’s important to know from the outset that what is the right solution for one patient is not right for the next."
Connecting with other women who have experienced the same situation can be of immense value, Dr. Cardonick said. She participates in an online support group called "Hope for Two."
The organization’s main goal is to link new patients with survivors who can help educate them as well as lend emotional support. Patients call in or fill out a secure online request for a personal match-up with a survivor, who is often a woman who has had the same type of cancer.
The website also contains links to news and medical articles, books, and financial assistance sources, and allows new patients to securely contact Dr. Cardonick’s pregnancy registry. "We keep in touch with the baby’s pediatrician and the mom every year, to see how things are going and [to] collect information," she said. "The best way to treat these women in the future depends on the information we continue to gather in the present."
None of the researchers interviewed for this article had any relevant financial disclosures. Dr. Litton noted that she had no financial disclosures for her 2011 ASCO poster.
Emerging data on pregnancy and cancer can now help women and their doctors chart a safer course between effective treatment and protecting the developing fetus.
Two registries – one in the United States and another in Europe – agree: It’s not only possible to save a pregnancy in many situations, but children born to these women appear to be largely unaffected by in utero chemotherapy exposure. The combined studies followed more than 200 exposed children for up to 18 years; neither one found any elevated risk of congenital anomaly or any kind of cognitive or developmental delay.
"This is practice-changing information," Dr. Frédéric Amant, primary author on the European paper, said in an interview. "Until now, physicians were reluctant to administer chemotherapy and usually opted for termination, or at least for a delay in treatment or premature delivery in order to get treatment going," he said.
Dr. Amant’s study leads off a special section on cancer in pregnancy, published in the March issue of Lancet Oncology. The paper examined evidence that both supports and questions the clinical wisdom of treating a disease that threatens two very different patients – an adult woman and the fetus she carries.
Every case is different, depending on the type of cancer, its grade and potential aggressiveness, the stage of pregnancy, and the woman’s own desires, said Dr. Elyce Cardonick, an ob.gyn. at Cooper University Hospital in Camden, N.J., and the lead investigator of the Pregnancy and Cancer Registry.
"With solid tumors you usually have time to do the surgery, get the pathologic diagnosis, and let the patient recover. But if there is leukemia, for instance, you have to move faster. The first question should be ‘Could we delay treatment for this patient if she was not pregnant?’ I don’t want to limit their treatment, but at the same time, it’s true that they might not be getting the most up-to-date treatment – the newest agent on the block – because you would want to go with something there is at least some experience with. But this doesn’t necessarily mean they are going to do worse."
Cancer occurs in about 1 in 1,000 pregnancies, said Dr. Sarah Temkin, a gynecologic oncologist at the University of Maryland, Baltimore. Many of her patients are referred after a routine screening during early pregnancy finds something abnormal, or when a woman with an existing cancer is incidentally found to be pregnant. But signs that might raise a red flag in other situations don’t necessarily alert physicians to danger in pregnant women, she said in an interview. Pregnancy could obfuscate some symptoms, which might be further downplayed in light of a mother’s relatively young age. Breast cancer is a prime example.
"There are two problems, especially for breast cancers, which are the most common ones we see in pregnancy. First, a woman’s breasts are changing anyway during that time. Breast cancer is so rare in women of earlier childbearing age that both the patient and the doctor tend to disregard any new lumps and bumps."
But despite its rarity, cancer in all forms appears to be increasing among pregnant women, she said. This is probably a direct relation to age. "Cancer rates increase with increasing age, and women are becoming mothers at older and older ages."
When cancer coincides with pregnancy, Dr. Temkin views the mother’s health as paramount. "The mother is the person with cancer, and she deserves whatever the standard of care is for that particular cancer – the best care that would be offered to her if she was not pregnant."
Chemotherapy and Fetal Outcomes
To examine long-term neurodevelopmental risks associated with maternal cancer treatment, Dr. Amant, a gynecologic oncologist at the Leuven (Belgium) Cancer Institute, and his colleagues, are following 70 children from the age of 18 months until 18 years. In the newly published interim analysis, the mean follow-up time is 22 months. All the children had intrauterine exposure to chemotherapy, radiation, oncologic surgery, or combinations of these.
The analysis, which also appeared in Lancet Oncology’s special issue, includes data on all the children, including 18 who are now older than 9 years (Lancet Oncol. 2012;13:256-64).
The children – 68 singletons and one set of twins – were born from pregnancies exposed to a total of 236 chemotherapy cycles. Exposure varied by the mother’s cancer type and its stage at diagnosis. In all, 34 mothers were treated with only chemotherapy, 27 had chemotherapy and surgery, 1 received chemotherapy and radiation, and 6 women were treated with all three modalities. Most of the children also had in utero exposure to multiple imaging studies, including MRI, ultrasound, echocardiography, CT, and mammography. Chemotherapy regimens included doxorubicin, epirubicin, idarubicin and daunorubicin.
Fetuses also were exposed to a variety of other drugs, including antibiotics, antiemetics, pain medications, colony stimulating factors, and anxiolytics.
Breast cancer was the most common disease type (35). There were 18 cases of hematologic cancers, 6 ovarian cancers, 4 cervical cancers, and 1 each of basal cell carcinoma, brain tumor, Ewing’s sarcoma, colorectal cancer, and nasopharyngeal cancer.
The mean gestational age at cancer diagnosis was 18 weeks, although fetuses ranged in age from 2 to 33 weeks when their mothers were diagnosed. About a third of the babies (23) were born at term.
Seven were born at 28-32 weeks, nine at 32-34 weeks, and 31 at 34-37 weeks. Weight for gestational age was below the 10th percentile in 14 children (21%).
Seven congenital anomalies were found in the group of 70 children (10%) – a rate not significantly different from that in the background population. There were only two major malformations, for a 2.9% rate. Malformations included the following:
• Hip subluxation, pectus excavatum and hemangioma, associated with chemotherapy only.
• Bilateral partial syndactyly, associated with chemotherapy plus radiotherapy.
• Bilateral small protuberance on one finger, and rectal atresia, associated with chemotherapy plus surgery.
• Bilateral double cartilage ring in a child exposed to chemotherapy, surgery and radiotherapy.
None of the children showed any congenital cardiac issues.
All of the children showed neurocognitive development that was within normal range, except for the set of twins, who were delivered by cesarean section at 32.5 weeks after a preterm premature rupture of membranes. These children were so delayed that they were not able to complete cognitive testing. Their mother developed an acute myeloid leukemia – one of the true "emergency" cancers diagnosed in pregnancy, Dr. Amant said. The babies had been exposed to idarubicin and cytosine arabinoside at 15.5, 21.5, 26.5, and 31.5 weeks’ gestation.
The boy, who weighed 1,640 g at birth, had a normal karyotype but, at 3 years, brain imaging showed a unilateral polymicrogyria in the left perisylvian area. He showed an early developmental delay; at age 9 years, he had the developmental capacity of a 12-month old.
The girl, who weighed 1,390 g at birth, also had an early developmental delay, but at age 9 years she attended school with support. Her parents refused brain imaging.
"The other 68 children did well," Dr. Amant said. "This doesn’t mean they were all normal in every way, but in any population you will see learning and developmental delay issues. We think the problem for the delayed children was not related to chemotherapy exposure, but more likely to their prematurity."
Dr. Amant saw a direct correlation between gestational age and intelligence quota. "When we controlled for age, gender, and country of birth, we found that the IQ score increased by almost 12 points for each additional month of gestation."
The U.S. Experience
Dr. Cardonick has found similar results. Her registry now contains information on 280 women who were enrolled over a 13-year period. The children born from these pregnancies have been assessed annually since birth. It also includes 70 controls – children whose mothers had cancer but who were not exposed to chemotherapy.
She published interim results of the registry in 2010 (Cancer J. 2010;16:76-82). At that point, it contained information on 231 women and 157 children. The most common malignancy was breast cancer (128); the mean gestational age at diagnosis was 13 weeks. About a third of the women (54) were advised to terminate their pregnancy; 12 did so.
Among those who continued both pregnancy and treatment, neonatal outcomes were generally good. There were nine premature deliveries related to preterm labor or premature rupture of membranes. The congenital anomaly rate born was 4%, which was in line with the normal background rate and slightly lower than that seen in Dr. Amant’s cohort.
The infants’ mean birth weight was 2,647 g, which was significantly less than the mean 2,873 g in the control group, but probably clinically irrelevant, Dr. Cardonick wrote in the paper.
She continues to follow these children annually. At this point, the children are a mean 5 years old; her oldest subject is 14 years. So far, the rate of neurocognitive issues in the group is no different than would be observed in any other group, and none of the children has developed any health problem that could be conclusively tied to intrauterine chemotherapy exposure.
Her experience stresses several key factors that must be considered in this situation. Her patients received chemotherapy at a mean of 20 weeks’ gestation – safely outside the critical early period. Only two women received chemotherapy before 10 weeks; both were treated before they knew they were pregnant. Both children born of these pregnancies were considered well. One with intrauterine exposure to cytarabine was developmentally normal at age 7 years. The other, who was exposed to oxaliplatin and capecitabine, was normal at age 2 years.
Treatment also was stopped a mean of 40 days before delivery, to allow the mother’s bone marrow to fully recover before giving birth.
A second U.S. study was reported at the 2011 meeting of the American Society of Clinical Oncology. A poster by Dr. Jennifer Litton and her colleagues examined physiological outcomes in 81 children exposed to chemotherapy for maternal breast cancer. The mothers had taken a standardized chemotherapy regimen of 5-fluorouracil, doxorubicin and cyclophosphamide (FAC) given during the second and third trimesters (J. Clin. Oncol. 2011;29[May 20 suppl.]:abstract 1099).
One child was born with Down syndrome, one with a club foot, and one with ureteral reflux. Three parents reported language delay in later follow-up surveys. Other reported health issues included 15 children with allergies and/or eczema, 2 with asthma, and 1 with absence seizures.
Dr. Litton, a breast oncologist at the University of Texas M.D. Anderson Cancer Center in Houston, also cowrote a 2010 review of breast cancer treatment in pregnancy, in which she discusses maternal and fetal outcomes from several cohorts, and the possible impact of intrauterine exposure to a variety of chemotherapy agents (Oncologist 2010;15:1238-47).
Risks Vary With Cancer Type
Breast cancer during pregnancy may be the simplest to treat. If the cancer is caught very early, it may be reasonable to delay treatment until the fetus has passed the critical first trimester, waiting until organs are formed and the risk of chemically induced damage is reduced, Dr. Temkin said. "It’s safe to do breast surgery during pregnancy and it’s safe to give chemotherapy after the first trimester."
But physicians can miss a new breast tumor during a prenatal exam, so some present at a more advanced stage, according to Dr. Amant, who is also the lead author of the Lancet’s breast cancer report (Lancet 2012;379:570-9).
Infiltrating ductal adenocarcinomas account for more than 70% of the breast cancers diagnosed during pregnancy. These can be aggressive, said Dr. Amant. Estrogen receptor status is probably no different in pregnant and nonpregnant women.
If the tumor is discovered early and is pathologically favorable, chemotherapy probably can be delayed until 14 weeks’ gestation, allowing nearly complete fetal organogenesis without worsening the mother’s outcome. Women also may elect an early termination if the pathology is unfavorable, or for other personal reasons, Dr. Temkin said. "I think a lot of it depends on when the cancer is diagnosed. Patients of mine who already have a diagnosis and then become pregnant almost always elect to terminate. But if the cancer is discovered when the pregnancy is farther along, most will continue, especially if the woman is highly emotionally invested," she noted.
Tougher Cancers, Tougher Choices
Treating gynecologic cancers during pregnancy often comes down to a choice between the mother’s health and maintenance of the pregnancy, Dr. Temkin said. "The standard of care for ovarian cancers is surgery or radiation to the pelvis, where the fetus is. Cervical cancer is treated with a hysterectomy or radiation, and neither treatment is compatible with keeping a pregnancy. Neoadjuvant therapy is not considered standard of care for these tumors. These are complex decisions for the patient: ‘Do I accept a different treatment [that might not be as effective] or maintain the pregnancy?’ "
In early cervical cancers without nodal spread, the most common tactic is close observation with periodic imaging to rule out spread; therapy is given after delivery, Dr. Phillippe Morice wrote in the Lancet section’s review on gynecologic malignancies (Lancet 2012;379:558-69).
"Delayed treatment until fetal maturation for patients with stage IA disease has an excellent prognosis and is now the standard of care," wrote Dr. Morice of the Institut de Cancérologie Gustave-Roussy in Villejuif, France.
Locally advanced disease is often not compatible with pregnancy. "The main treatment choice is either neoadjuvant chemotherapy or chemotherapy and radiotherapy. In pregnant patients, this approach means that the pregnancy must be ended before the initiation of therapy, but in exceptional cases in which surgery to end the pregnancy is not technically feasible ([that is], a bulky cervical tumor), radiation therapy can be delivered with the fetus in utero, resulting in a spontaneous abortion in about 3 weeks," he wrote.
Ovarian tumors can be surgically staged and – if it is of low malignant potential – can be laparoscopically removed, usually without endangering the pregnancy. Large tumors or those with aggressive pathology, like epithelial tumors, are much more difficult. Advanced or large tumors often have uterine and pelvic involvement, and treatment usually means a hysterectomy.
The literature contains reports of a very few women who have undergone chemotherapy to control peritoneal spread while keeping a pregnancy. However, despite giving birth to normally developed children, a number of these women died from recurrent disease, Dr. Morice noted.
Hematologic Cancers: True Emergency
Cancers of the blood are rare in pregnancy, occurring in only 1 of every 6,000. But when they do occur, they can be devastating, Dr. Benjamin Brenner wrote in the special series (Lancet 2012;379:580-7).
Pregnant patients with Hodgkin’s lymphoma generally do as well as their nonpregnant counterparts and can receive the same chemotherapy regimens, observing the first-trimester delay to favor the fetus.
Those who present with non-Hodgkin’s lymphoma are likely to have a very poor outlook. This disease is very rare in pregnant women, and symptoms can overlap with Hodgkin’s. Those factors, combined with a desire to avoid imaging, can delay diagnosis until the cancer is more advanced, said Dr. Brenner of the Rambam Health Care Campus, Haifa, Israel.
Acute leukemia is also rare, but demands urgent attention regardless of gestational stage, Dr. Brenner warned. "Patients diagnosed with acute leukemia during the first trimester are recommended to terminate the pregnancy, in view of the high risk of toxic effects on the fetus and mother, along with the expected need for further intensive treatment including stem-cell transplantation, which is absolutely contraindicated during gestation."
Talking It Out
Despite the emerging positive evidence, treating cancer during pregnancy can be a tough sell, Dr. Amant said. "Women have been told over and over to avoid taking so much as an aspirin. It’s very difficult to convince them that a fetus can not only survive a mother’s cancer treatment, but have a good chance of developing normally."
The stress of a cancer diagnosis during a desired pregnancy is very hard on patients, Dr. Temkin added. "Pregnancy is a time when many women come to grips with their own mortality as well as that of giving new life. Adding a diagnosis of cancer of top of that – especially in the face of a much-desired pregnancy – can be devastating."
These women are faced with two options: terminate the pregnancy and concentrate on their own treatment, or continue the pregnancy knowing that their unborn child will be exposed to the possible risks of radiation, chemotherapy, and surgery. Either option can "inflict terrible guilt on a pregnant woman. We can try to minimize that to some degree, but it’s important to know from the outset that what is the right solution for one patient is not right for the next."
Connecting with other women who have experienced the same situation can be of immense value, Dr. Cardonick said. She participates in an online support group called "Hope for Two."
The organization’s main goal is to link new patients with survivors who can help educate them as well as lend emotional support. Patients call in or fill out a secure online request for a personal match-up with a survivor, who is often a woman who has had the same type of cancer.
The website also contains links to news and medical articles, books, and financial assistance sources, and allows new patients to securely contact Dr. Cardonick’s pregnancy registry. "We keep in touch with the baby’s pediatrician and the mom every year, to see how things are going and [to] collect information," she said. "The best way to treat these women in the future depends on the information we continue to gather in the present."
None of the researchers interviewed for this article had any relevant financial disclosures. Dr. Litton noted that she had no financial disclosures for her 2011 ASCO poster.
Emerging data on pregnancy and cancer can now help women and their doctors chart a safer course between effective treatment and protecting the developing fetus.
Two registries – one in the United States and another in Europe – agree: It’s not only possible to save a pregnancy in many situations, but children born to these women appear to be largely unaffected by in utero chemotherapy exposure. The combined studies followed more than 200 exposed children for up to 18 years; neither one found any elevated risk of congenital anomaly or any kind of cognitive or developmental delay.
"This is practice-changing information," Dr. Frédéric Amant, primary author on the European paper, said in an interview. "Until now, physicians were reluctant to administer chemotherapy and usually opted for termination, or at least for a delay in treatment or premature delivery in order to get treatment going," he said.
Dr. Amant’s study leads off a special section on cancer in pregnancy, published in the March issue of Lancet Oncology. The paper examined evidence that both supports and questions the clinical wisdom of treating a disease that threatens two very different patients – an adult woman and the fetus she carries.
Every case is different, depending on the type of cancer, its grade and potential aggressiveness, the stage of pregnancy, and the woman’s own desires, said Dr. Elyce Cardonick, an ob.gyn. at Cooper University Hospital in Camden, N.J., and the lead investigator of the Pregnancy and Cancer Registry.
"With solid tumors you usually have time to do the surgery, get the pathologic diagnosis, and let the patient recover. But if there is leukemia, for instance, you have to move faster. The first question should be ‘Could we delay treatment for this patient if she was not pregnant?’ I don’t want to limit their treatment, but at the same time, it’s true that they might not be getting the most up-to-date treatment – the newest agent on the block – because you would want to go with something there is at least some experience with. But this doesn’t necessarily mean they are going to do worse."
Cancer occurs in about 1 in 1,000 pregnancies, said Dr. Sarah Temkin, a gynecologic oncologist at the University of Maryland, Baltimore. Many of her patients are referred after a routine screening during early pregnancy finds something abnormal, or when a woman with an existing cancer is incidentally found to be pregnant. But signs that might raise a red flag in other situations don’t necessarily alert physicians to danger in pregnant women, she said in an interview. Pregnancy could obfuscate some symptoms, which might be further downplayed in light of a mother’s relatively young age. Breast cancer is a prime example.
"There are two problems, especially for breast cancers, which are the most common ones we see in pregnancy. First, a woman’s breasts are changing anyway during that time. Breast cancer is so rare in women of earlier childbearing age that both the patient and the doctor tend to disregard any new lumps and bumps."
But despite its rarity, cancer in all forms appears to be increasing among pregnant women, she said. This is probably a direct relation to age. "Cancer rates increase with increasing age, and women are becoming mothers at older and older ages."
When cancer coincides with pregnancy, Dr. Temkin views the mother’s health as paramount. "The mother is the person with cancer, and she deserves whatever the standard of care is for that particular cancer – the best care that would be offered to her if she was not pregnant."
Chemotherapy and Fetal Outcomes
To examine long-term neurodevelopmental risks associated with maternal cancer treatment, Dr. Amant, a gynecologic oncologist at the Leuven (Belgium) Cancer Institute, and his colleagues, are following 70 children from the age of 18 months until 18 years. In the newly published interim analysis, the mean follow-up time is 22 months. All the children had intrauterine exposure to chemotherapy, radiation, oncologic surgery, or combinations of these.
The analysis, which also appeared in Lancet Oncology’s special issue, includes data on all the children, including 18 who are now older than 9 years (Lancet Oncol. 2012;13:256-64).
The children – 68 singletons and one set of twins – were born from pregnancies exposed to a total of 236 chemotherapy cycles. Exposure varied by the mother’s cancer type and its stage at diagnosis. In all, 34 mothers were treated with only chemotherapy, 27 had chemotherapy and surgery, 1 received chemotherapy and radiation, and 6 women were treated with all three modalities. Most of the children also had in utero exposure to multiple imaging studies, including MRI, ultrasound, echocardiography, CT, and mammography. Chemotherapy regimens included doxorubicin, epirubicin, idarubicin and daunorubicin.
Fetuses also were exposed to a variety of other drugs, including antibiotics, antiemetics, pain medications, colony stimulating factors, and anxiolytics.
Breast cancer was the most common disease type (35). There were 18 cases of hematologic cancers, 6 ovarian cancers, 4 cervical cancers, and 1 each of basal cell carcinoma, brain tumor, Ewing’s sarcoma, colorectal cancer, and nasopharyngeal cancer.
The mean gestational age at cancer diagnosis was 18 weeks, although fetuses ranged in age from 2 to 33 weeks when their mothers were diagnosed. About a third of the babies (23) were born at term.
Seven were born at 28-32 weeks, nine at 32-34 weeks, and 31 at 34-37 weeks. Weight for gestational age was below the 10th percentile in 14 children (21%).
Seven congenital anomalies were found in the group of 70 children (10%) – a rate not significantly different from that in the background population. There were only two major malformations, for a 2.9% rate. Malformations included the following:
• Hip subluxation, pectus excavatum and hemangioma, associated with chemotherapy only.
• Bilateral partial syndactyly, associated with chemotherapy plus radiotherapy.
• Bilateral small protuberance on one finger, and rectal atresia, associated with chemotherapy plus surgery.
• Bilateral double cartilage ring in a child exposed to chemotherapy, surgery and radiotherapy.
None of the children showed any congenital cardiac issues.
All of the children showed neurocognitive development that was within normal range, except for the set of twins, who were delivered by cesarean section at 32.5 weeks after a preterm premature rupture of membranes. These children were so delayed that they were not able to complete cognitive testing. Their mother developed an acute myeloid leukemia – one of the true "emergency" cancers diagnosed in pregnancy, Dr. Amant said. The babies had been exposed to idarubicin and cytosine arabinoside at 15.5, 21.5, 26.5, and 31.5 weeks’ gestation.
The boy, who weighed 1,640 g at birth, had a normal karyotype but, at 3 years, brain imaging showed a unilateral polymicrogyria in the left perisylvian area. He showed an early developmental delay; at age 9 years, he had the developmental capacity of a 12-month old.
The girl, who weighed 1,390 g at birth, also had an early developmental delay, but at age 9 years she attended school with support. Her parents refused brain imaging.
"The other 68 children did well," Dr. Amant said. "This doesn’t mean they were all normal in every way, but in any population you will see learning and developmental delay issues. We think the problem for the delayed children was not related to chemotherapy exposure, but more likely to their prematurity."
Dr. Amant saw a direct correlation between gestational age and intelligence quota. "When we controlled for age, gender, and country of birth, we found that the IQ score increased by almost 12 points for each additional month of gestation."
The U.S. Experience
Dr. Cardonick has found similar results. Her registry now contains information on 280 women who were enrolled over a 13-year period. The children born from these pregnancies have been assessed annually since birth. It also includes 70 controls – children whose mothers had cancer but who were not exposed to chemotherapy.
She published interim results of the registry in 2010 (Cancer J. 2010;16:76-82). At that point, it contained information on 231 women and 157 children. The most common malignancy was breast cancer (128); the mean gestational age at diagnosis was 13 weeks. About a third of the women (54) were advised to terminate their pregnancy; 12 did so.
Among those who continued both pregnancy and treatment, neonatal outcomes were generally good. There were nine premature deliveries related to preterm labor or premature rupture of membranes. The congenital anomaly rate born was 4%, which was in line with the normal background rate and slightly lower than that seen in Dr. Amant’s cohort.
The infants’ mean birth weight was 2,647 g, which was significantly less than the mean 2,873 g in the control group, but probably clinically irrelevant, Dr. Cardonick wrote in the paper.
She continues to follow these children annually. At this point, the children are a mean 5 years old; her oldest subject is 14 years. So far, the rate of neurocognitive issues in the group is no different than would be observed in any other group, and none of the children has developed any health problem that could be conclusively tied to intrauterine chemotherapy exposure.
Her experience stresses several key factors that must be considered in this situation. Her patients received chemotherapy at a mean of 20 weeks’ gestation – safely outside the critical early period. Only two women received chemotherapy before 10 weeks; both were treated before they knew they were pregnant. Both children born of these pregnancies were considered well. One with intrauterine exposure to cytarabine was developmentally normal at age 7 years. The other, who was exposed to oxaliplatin and capecitabine, was normal at age 2 years.
Treatment also was stopped a mean of 40 days before delivery, to allow the mother’s bone marrow to fully recover before giving birth.
A second U.S. study was reported at the 2011 meeting of the American Society of Clinical Oncology. A poster by Dr. Jennifer Litton and her colleagues examined physiological outcomes in 81 children exposed to chemotherapy for maternal breast cancer. The mothers had taken a standardized chemotherapy regimen of 5-fluorouracil, doxorubicin and cyclophosphamide (FAC) given during the second and third trimesters (J. Clin. Oncol. 2011;29[May 20 suppl.]:abstract 1099).
One child was born with Down syndrome, one with a club foot, and one with ureteral reflux. Three parents reported language delay in later follow-up surveys. Other reported health issues included 15 children with allergies and/or eczema, 2 with asthma, and 1 with absence seizures.
Dr. Litton, a breast oncologist at the University of Texas M.D. Anderson Cancer Center in Houston, also cowrote a 2010 review of breast cancer treatment in pregnancy, in which she discusses maternal and fetal outcomes from several cohorts, and the possible impact of intrauterine exposure to a variety of chemotherapy agents (Oncologist 2010;15:1238-47).
Risks Vary With Cancer Type
Breast cancer during pregnancy may be the simplest to treat. If the cancer is caught very early, it may be reasonable to delay treatment until the fetus has passed the critical first trimester, waiting until organs are formed and the risk of chemically induced damage is reduced, Dr. Temkin said. "It’s safe to do breast surgery during pregnancy and it’s safe to give chemotherapy after the first trimester."
But physicians can miss a new breast tumor during a prenatal exam, so some present at a more advanced stage, according to Dr. Amant, who is also the lead author of the Lancet’s breast cancer report (Lancet 2012;379:570-9).
Infiltrating ductal adenocarcinomas account for more than 70% of the breast cancers diagnosed during pregnancy. These can be aggressive, said Dr. Amant. Estrogen receptor status is probably no different in pregnant and nonpregnant women.
If the tumor is discovered early and is pathologically favorable, chemotherapy probably can be delayed until 14 weeks’ gestation, allowing nearly complete fetal organogenesis without worsening the mother’s outcome. Women also may elect an early termination if the pathology is unfavorable, or for other personal reasons, Dr. Temkin said. "I think a lot of it depends on when the cancer is diagnosed. Patients of mine who already have a diagnosis and then become pregnant almost always elect to terminate. But if the cancer is discovered when the pregnancy is farther along, most will continue, especially if the woman is highly emotionally invested," she noted.
Tougher Cancers, Tougher Choices
Treating gynecologic cancers during pregnancy often comes down to a choice between the mother’s health and maintenance of the pregnancy, Dr. Temkin said. "The standard of care for ovarian cancers is surgery or radiation to the pelvis, where the fetus is. Cervical cancer is treated with a hysterectomy or radiation, and neither treatment is compatible with keeping a pregnancy. Neoadjuvant therapy is not considered standard of care for these tumors. These are complex decisions for the patient: ‘Do I accept a different treatment [that might not be as effective] or maintain the pregnancy?’ "
In early cervical cancers without nodal spread, the most common tactic is close observation with periodic imaging to rule out spread; therapy is given after delivery, Dr. Phillippe Morice wrote in the Lancet section’s review on gynecologic malignancies (Lancet 2012;379:558-69).
"Delayed treatment until fetal maturation for patients with stage IA disease has an excellent prognosis and is now the standard of care," wrote Dr. Morice of the Institut de Cancérologie Gustave-Roussy in Villejuif, France.
Locally advanced disease is often not compatible with pregnancy. "The main treatment choice is either neoadjuvant chemotherapy or chemotherapy and radiotherapy. In pregnant patients, this approach means that the pregnancy must be ended before the initiation of therapy, but in exceptional cases in which surgery to end the pregnancy is not technically feasible ([that is], a bulky cervical tumor), radiation therapy can be delivered with the fetus in utero, resulting in a spontaneous abortion in about 3 weeks," he wrote.
Ovarian tumors can be surgically staged and – if it is of low malignant potential – can be laparoscopically removed, usually without endangering the pregnancy. Large tumors or those with aggressive pathology, like epithelial tumors, are much more difficult. Advanced or large tumors often have uterine and pelvic involvement, and treatment usually means a hysterectomy.
The literature contains reports of a very few women who have undergone chemotherapy to control peritoneal spread while keeping a pregnancy. However, despite giving birth to normally developed children, a number of these women died from recurrent disease, Dr. Morice noted.
Hematologic Cancers: True Emergency
Cancers of the blood are rare in pregnancy, occurring in only 1 of every 6,000. But when they do occur, they can be devastating, Dr. Benjamin Brenner wrote in the special series (Lancet 2012;379:580-7).
Pregnant patients with Hodgkin’s lymphoma generally do as well as their nonpregnant counterparts and can receive the same chemotherapy regimens, observing the first-trimester delay to favor the fetus.
Those who present with non-Hodgkin’s lymphoma are likely to have a very poor outlook. This disease is very rare in pregnant women, and symptoms can overlap with Hodgkin’s. Those factors, combined with a desire to avoid imaging, can delay diagnosis until the cancer is more advanced, said Dr. Brenner of the Rambam Health Care Campus, Haifa, Israel.
Acute leukemia is also rare, but demands urgent attention regardless of gestational stage, Dr. Brenner warned. "Patients diagnosed with acute leukemia during the first trimester are recommended to terminate the pregnancy, in view of the high risk of toxic effects on the fetus and mother, along with the expected need for further intensive treatment including stem-cell transplantation, which is absolutely contraindicated during gestation."
Talking It Out
Despite the emerging positive evidence, treating cancer during pregnancy can be a tough sell, Dr. Amant said. "Women have been told over and over to avoid taking so much as an aspirin. It’s very difficult to convince them that a fetus can not only survive a mother’s cancer treatment, but have a good chance of developing normally."
The stress of a cancer diagnosis during a desired pregnancy is very hard on patients, Dr. Temkin added. "Pregnancy is a time when many women come to grips with their own mortality as well as that of giving new life. Adding a diagnosis of cancer of top of that – especially in the face of a much-desired pregnancy – can be devastating."
These women are faced with two options: terminate the pregnancy and concentrate on their own treatment, or continue the pregnancy knowing that their unborn child will be exposed to the possible risks of radiation, chemotherapy, and surgery. Either option can "inflict terrible guilt on a pregnant woman. We can try to minimize that to some degree, but it’s important to know from the outset that what is the right solution for one patient is not right for the next."
Connecting with other women who have experienced the same situation can be of immense value, Dr. Cardonick said. She participates in an online support group called "Hope for Two."
The organization’s main goal is to link new patients with survivors who can help educate them as well as lend emotional support. Patients call in or fill out a secure online request for a personal match-up with a survivor, who is often a woman who has had the same type of cancer.
The website also contains links to news and medical articles, books, and financial assistance sources, and allows new patients to securely contact Dr. Cardonick’s pregnancy registry. "We keep in touch with the baby’s pediatrician and the mom every year, to see how things are going and [to] collect information," she said. "The best way to treat these women in the future depends on the information we continue to gather in the present."
None of the researchers interviewed for this article had any relevant financial disclosures. Dr. Litton noted that she had no financial disclosures for her 2011 ASCO poster.
Older Women May Not Need Radiation for Luminal A Breast Tumors
CHICAGO – Older breast cancer patients with the luminal A tumor subtype may be able to forgo whole breast radiation therapy if they are taking tamoxifen or other breast cancer hormone therapy.
Preliminary results from a randomized clinical trial of tamoxifen with and without radiation therapy showed that radiation therapy had minimal impact on the risk of developing ipsilateral breast tumor recurrence in patients aged 50 years and older with T1 and T2 node-negative breast cancer identified with luminal A disease based on 6-marker immunohistochemistry testing.
In contrast, radiation therapy appeared to decrease the risk of breast cancer relapse in patients with luminal B, human epidermal growth factor receptor 2 (HER2)–enriched, and basal tumor subtypes, according to radiation oncologist Dr. Fei-Fei Liu of Princess Margaret Hospital, the Ontario Cancer Institute, and the University of Toronto, all in Toronto. She discussed the findings in a press conference April 1 at the annual meeting of the American Association for Cancer Research.
Luminal A tumors – estrogen receptor (ER) or progesterone receptor (PR) positive, HER2-negative, and low Ki-67 (a nuclear marker for cell proliferation) – are associated with a relatively good prognosis compared with the other subtypes, she noted.
To determine the predictive value of tumor subtype for ipsilateral recurrence in this population, Dr. Liu and her colleagues performed molecular subtyping for ER, PR, Ki-67, HER2, EGFR, and cytokeratine 5/6 on 304 available tumor specimens from 769 women in a clinical trial. All had been randomized to treatment with tamoxifen and whole breast radiation or tamoxifen alone between December 1992 and June 2000.
Based on the subtyping results, the patients were classified as luminal A, luminal B, luminal HER2, HER2-enriched, basal-like, or triple-negative phenotype–non-basal and followed for a median of 10 years, she said.
In the overall group of 769 women, the recurrence rate at a median of 10 years was 13.8% in the tamoxifen-only group and 5.0% in the combination group, Dr. Liu reported, noting that, in a multivariate analysis, "patient age, tumor size, estrogen-receptor positive status, and combination tamoxifen/whole breast radiation therapy were all significant factors."
Of the 304 tissue microarrays, 145 came from patients treated with tamoxifen only and 159 from patients treated with tamoxifen plus radiotherapy. In this population, the best outcomes were observed in 133 patients with luminal A tumors; their rate of ipsilateral recurrence was statistically similar at 8% among those in the tamoxifen-only group and 4.6% in the tamoxifen plus radiation group, Dr. Liu reported.
The 103 women older than 60 years with luminal A tumors fared particularly well, with rates of 4.3% with tamoxifen alone and 6.0% with tamoxifen and radiotherapy. The respective rates for the 114 women with grade I-II luminal A tumors also were similar at 4.9% and 5.5%, she said.
In contrast, the ipsilateral recurrence rates for the tamoxifen only and tamoxifen plus radiation groups were, respectively, 16.1% and 3.9% in 82 patients with luminal B tumors (differentiated from luminal A tumors by Ki-67 expression greater than 14%), said Dr. Liu.
Further, although the number of HER2 (11), HER2-enriched (11), and basal-like tumors (16) were small, "we saw higher relapse rates in patients who did not undergo radiation therapy," she said.
Luminal A lymph-node negative breast cancer represents approximately 25% of all cases of newly diagnosed breast cancer in North America, according to Dr. Liu. In addition to sparing a large number of women unnecessary radiation exposures, unwanted side effects, and inconvenience, bypassing radiation therapy in early cases would save millions of health care dollars each year.
"We estimated a savings of $20 million annually in Ontario if radiation therapy were avoided in early luminal A [breast cancer]," she said. "Extrapolating the figures to the [United States] resulted in a savings of about $400 million per year."
Dr. Liu stressed that the data presented at the meeting are preliminary but noted that, if the findings are validated through the analysis of a larger number of tumor samples, "we would recommend adding Ki-67 to the current standard immunohistochemistry panel, and discussing the possibility of avoiding radiation with lymph node–negative patients in whom the luminal A subtype is identified, if they are taking tamoxifen or an equivalent medication, especially patients who are 60 years old or older."
Dr. Liu disclosed no conflicts of interest.
CHICAGO – Older breast cancer patients with the luminal A tumor subtype may be able to forgo whole breast radiation therapy if they are taking tamoxifen or other breast cancer hormone therapy.
Preliminary results from a randomized clinical trial of tamoxifen with and without radiation therapy showed that radiation therapy had minimal impact on the risk of developing ipsilateral breast tumor recurrence in patients aged 50 years and older with T1 and T2 node-negative breast cancer identified with luminal A disease based on 6-marker immunohistochemistry testing.
In contrast, radiation therapy appeared to decrease the risk of breast cancer relapse in patients with luminal B, human epidermal growth factor receptor 2 (HER2)–enriched, and basal tumor subtypes, according to radiation oncologist Dr. Fei-Fei Liu of Princess Margaret Hospital, the Ontario Cancer Institute, and the University of Toronto, all in Toronto. She discussed the findings in a press conference April 1 at the annual meeting of the American Association for Cancer Research.
Luminal A tumors – estrogen receptor (ER) or progesterone receptor (PR) positive, HER2-negative, and low Ki-67 (a nuclear marker for cell proliferation) – are associated with a relatively good prognosis compared with the other subtypes, she noted.
To determine the predictive value of tumor subtype for ipsilateral recurrence in this population, Dr. Liu and her colleagues performed molecular subtyping for ER, PR, Ki-67, HER2, EGFR, and cytokeratine 5/6 on 304 available tumor specimens from 769 women in a clinical trial. All had been randomized to treatment with tamoxifen and whole breast radiation or tamoxifen alone between December 1992 and June 2000.
Based on the subtyping results, the patients were classified as luminal A, luminal B, luminal HER2, HER2-enriched, basal-like, or triple-negative phenotype–non-basal and followed for a median of 10 years, she said.
In the overall group of 769 women, the recurrence rate at a median of 10 years was 13.8% in the tamoxifen-only group and 5.0% in the combination group, Dr. Liu reported, noting that, in a multivariate analysis, "patient age, tumor size, estrogen-receptor positive status, and combination tamoxifen/whole breast radiation therapy were all significant factors."
Of the 304 tissue microarrays, 145 came from patients treated with tamoxifen only and 159 from patients treated with tamoxifen plus radiotherapy. In this population, the best outcomes were observed in 133 patients with luminal A tumors; their rate of ipsilateral recurrence was statistically similar at 8% among those in the tamoxifen-only group and 4.6% in the tamoxifen plus radiation group, Dr. Liu reported.
The 103 women older than 60 years with luminal A tumors fared particularly well, with rates of 4.3% with tamoxifen alone and 6.0% with tamoxifen and radiotherapy. The respective rates for the 114 women with grade I-II luminal A tumors also were similar at 4.9% and 5.5%, she said.
In contrast, the ipsilateral recurrence rates for the tamoxifen only and tamoxifen plus radiation groups were, respectively, 16.1% and 3.9% in 82 patients with luminal B tumors (differentiated from luminal A tumors by Ki-67 expression greater than 14%), said Dr. Liu.
Further, although the number of HER2 (11), HER2-enriched (11), and basal-like tumors (16) were small, "we saw higher relapse rates in patients who did not undergo radiation therapy," she said.
Luminal A lymph-node negative breast cancer represents approximately 25% of all cases of newly diagnosed breast cancer in North America, according to Dr. Liu. In addition to sparing a large number of women unnecessary radiation exposures, unwanted side effects, and inconvenience, bypassing radiation therapy in early cases would save millions of health care dollars each year.
"We estimated a savings of $20 million annually in Ontario if radiation therapy were avoided in early luminal A [breast cancer]," she said. "Extrapolating the figures to the [United States] resulted in a savings of about $400 million per year."
Dr. Liu stressed that the data presented at the meeting are preliminary but noted that, if the findings are validated through the analysis of a larger number of tumor samples, "we would recommend adding Ki-67 to the current standard immunohistochemistry panel, and discussing the possibility of avoiding radiation with lymph node–negative patients in whom the luminal A subtype is identified, if they are taking tamoxifen or an equivalent medication, especially patients who are 60 years old or older."
Dr. Liu disclosed no conflicts of interest.
CHICAGO – Older breast cancer patients with the luminal A tumor subtype may be able to forgo whole breast radiation therapy if they are taking tamoxifen or other breast cancer hormone therapy.
Preliminary results from a randomized clinical trial of tamoxifen with and without radiation therapy showed that radiation therapy had minimal impact on the risk of developing ipsilateral breast tumor recurrence in patients aged 50 years and older with T1 and T2 node-negative breast cancer identified with luminal A disease based on 6-marker immunohistochemistry testing.
In contrast, radiation therapy appeared to decrease the risk of breast cancer relapse in patients with luminal B, human epidermal growth factor receptor 2 (HER2)–enriched, and basal tumor subtypes, according to radiation oncologist Dr. Fei-Fei Liu of Princess Margaret Hospital, the Ontario Cancer Institute, and the University of Toronto, all in Toronto. She discussed the findings in a press conference April 1 at the annual meeting of the American Association for Cancer Research.
Luminal A tumors – estrogen receptor (ER) or progesterone receptor (PR) positive, HER2-negative, and low Ki-67 (a nuclear marker for cell proliferation) – are associated with a relatively good prognosis compared with the other subtypes, she noted.
To determine the predictive value of tumor subtype for ipsilateral recurrence in this population, Dr. Liu and her colleagues performed molecular subtyping for ER, PR, Ki-67, HER2, EGFR, and cytokeratine 5/6 on 304 available tumor specimens from 769 women in a clinical trial. All had been randomized to treatment with tamoxifen and whole breast radiation or tamoxifen alone between December 1992 and June 2000.
Based on the subtyping results, the patients were classified as luminal A, luminal B, luminal HER2, HER2-enriched, basal-like, or triple-negative phenotype–non-basal and followed for a median of 10 years, she said.
In the overall group of 769 women, the recurrence rate at a median of 10 years was 13.8% in the tamoxifen-only group and 5.0% in the combination group, Dr. Liu reported, noting that, in a multivariate analysis, "patient age, tumor size, estrogen-receptor positive status, and combination tamoxifen/whole breast radiation therapy were all significant factors."
Of the 304 tissue microarrays, 145 came from patients treated with tamoxifen only and 159 from patients treated with tamoxifen plus radiotherapy. In this population, the best outcomes were observed in 133 patients with luminal A tumors; their rate of ipsilateral recurrence was statistically similar at 8% among those in the tamoxifen-only group and 4.6% in the tamoxifen plus radiation group, Dr. Liu reported.
The 103 women older than 60 years with luminal A tumors fared particularly well, with rates of 4.3% with tamoxifen alone and 6.0% with tamoxifen and radiotherapy. The respective rates for the 114 women with grade I-II luminal A tumors also were similar at 4.9% and 5.5%, she said.
In contrast, the ipsilateral recurrence rates for the tamoxifen only and tamoxifen plus radiation groups were, respectively, 16.1% and 3.9% in 82 patients with luminal B tumors (differentiated from luminal A tumors by Ki-67 expression greater than 14%), said Dr. Liu.
Further, although the number of HER2 (11), HER2-enriched (11), and basal-like tumors (16) were small, "we saw higher relapse rates in patients who did not undergo radiation therapy," she said.
Luminal A lymph-node negative breast cancer represents approximately 25% of all cases of newly diagnosed breast cancer in North America, according to Dr. Liu. In addition to sparing a large number of women unnecessary radiation exposures, unwanted side effects, and inconvenience, bypassing radiation therapy in early cases would save millions of health care dollars each year.
"We estimated a savings of $20 million annually in Ontario if radiation therapy were avoided in early luminal A [breast cancer]," she said. "Extrapolating the figures to the [United States] resulted in a savings of about $400 million per year."
Dr. Liu stressed that the data presented at the meeting are preliminary but noted that, if the findings are validated through the analysis of a larger number of tumor samples, "we would recommend adding Ki-67 to the current standard immunohistochemistry panel, and discussing the possibility of avoiding radiation with lymph node–negative patients in whom the luminal A subtype is identified, if they are taking tamoxifen or an equivalent medication, especially patients who are 60 years old or older."
Dr. Liu disclosed no conflicts of interest.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR CANCER RESEARCH
Major Finding: The rate of ipsilateral breast tumor recurrence in women older than 60 years with luminal A tumor subtypes was 4.3% among those taking tamoxifen only and 6.0% among those undergoing whole breast radiation therapy in addition to tamoxifen.
Data Source: Investigators presented preliminary results from microarray analyses of 304 patients in a randomized clinical trial of tamoxifen with and without radiation therapy.
Disclosures: Dr. Liu disclosed no conflicts of interest.
Breast Screening Linked to Cancer 'Overdiagnosis' in Norway
The introduction of widespread screening mammography in Norway was associated with an estimated 15%-25% "overdiagnosis" of breast cancer there, according to a report in the April 3 issue of the Annals of Internal Medicine.
This finding is consistent with those of previous studies in other countries, which estimated rates of overdiagnosis ranging from 0% to 54%, with randomized controlled trials tending to estimate it at approximately 30%, investigators said.
The result of this study in Norway adds to the evidence that "overdiagnosis and unnecessary treatment of nonfatal cancer creates a substantial ethical and clinical dilemma and may cast doubt on whether mammography screening programs should exist," said Dr. Mette Kalager of the department of epidemiology, Harvard School of Public Health, Boston, and her associates.
Screening mammography was uncommon in Norway until a national, state-funded program began in 1996. Screening mammography was then implemented gradually, in different geographic areas, over the course of 10 years. Since 2005, all women in Norway aged 50-69 years have been invited to participate in mammographic screening every 2 years, and approximately 77% of them do so.
"This staggered implementation allowed comparison of contemporaneous trends in breast cancer incidence in areas with and without mammography screening," as well as the comparison of current and historical trends in incidence. This in turn gave the researchers two analytic methods for calculating estimates of overdiagnosis.
They defined overdiagnosis as the percentage of cases of cancer that would not have become clinically apparent in a woman’s lifetime without screening. It refers to cases of breast cancer that would be diagnosed and treated without yielding any possible survival benefit – cases in which the tumor would never have progressed to a clinical stage or in which the woman would die from other causes before the breast cancer became evident.
The study population comprised 39,888 women diagnosed as having invasive breast cancer in 1996-2005, including 27,238 who were aged 50-79 years at diagnosis. A total of 7,793 women were diagnosed after the introduction of routine screening.
In fully adjusted analyses using the first method of estimating, 15%-20% of the cases of breast cancer found on screening mammography – that is, between 1,169 and 1,948 women – were overdiagnosed. In an analysis using the second method of estimating, 18%-25% of cases were overdiagnosed.
Thus, the overall rate of overdiagnosis in this study was 15%-25%, Dr. Kalager and her colleagues said (Ann. Intern. Med. 2012;156:491-9).
Moreover, the proportion of advanced-stage breast cancers decreased over time to the same degree among screened and unscreened women, while the proportion of stage I breast cancers markedly increased only among screened women. This indicates that the cancers being found on screening mammography were almost entirely early-stage, low-risk tumors.
"Our findings suggest that enhanced awareness is probably the reason for the reduction of late-stage cancer, not screening," the investigators noted.
Extrapolating their findings, they added that "after 10 years of biennial mammography screening, for every 2,500 women invited, 6-10 women have been overdiagnosed, 20 women are diagnosed with breast cancer ... and one death from breast cancer has been prevented.
"To put it differently, if 2,500 women are invited to undergo mammography screening over 10 years, 2,470-2,474 women will not be diagnosed with breast cancer, 2,499 will not die of breast cancer, but 6-10 women will be overdiagnosed," they said.
This study was supported by the Research Council of Norway and Frontier Science. Dr. Kalager and her coauthors had no relevant disclosures.
"Instead of focusing on the exact extent of overdiagnosis, it is time to agree that any amount of overdiagnosis is serious and to start dealing with this issue now," said Dr. Joann G. Elmore and Dr. Suzanne W. Fletcher.
One approach to cut back on overdiagnosis would be for mammographers to change their threshold for labeling a mammographic feature as "abnormal." They also could suggest observing certain lesions over time rather than immediately biopsying them.
"We have an ethical responsibility to alert women to this phenomenon [of overdiagnosis]. Most patient education aids do not even mention overdiagnosis, and most women are not aware of its possibility," they said.
Joann G. Elmore, M.D., is at the University of Washington, Seattle. She serves as medical editor for the patient education materials published by the nonprofit Informed Medical Decisions Foundation. Suzanne W. Fletcher, M.D., is at Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston. Dr Fletcher declared a 36-year professional interest in breast cancer screening and served on the U.S. Preventive Services Task Force in the early 1980s. These remarks were taken from their editorial accompanying Dr. Kalager’s report (Ann. Intern. Med. 2012;156:536-7).
"Instead of focusing on the exact extent of overdiagnosis, it is time to agree that any amount of overdiagnosis is serious and to start dealing with this issue now," said Dr. Joann G. Elmore and Dr. Suzanne W. Fletcher.
One approach to cut back on overdiagnosis would be for mammographers to change their threshold for labeling a mammographic feature as "abnormal." They also could suggest observing certain lesions over time rather than immediately biopsying them.
"We have an ethical responsibility to alert women to this phenomenon [of overdiagnosis]. Most patient education aids do not even mention overdiagnosis, and most women are not aware of its possibility," they said.
Joann G. Elmore, M.D., is at the University of Washington, Seattle. She serves as medical editor for the patient education materials published by the nonprofit Informed Medical Decisions Foundation. Suzanne W. Fletcher, M.D., is at Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston. Dr Fletcher declared a 36-year professional interest in breast cancer screening and served on the U.S. Preventive Services Task Force in the early 1980s. These remarks were taken from their editorial accompanying Dr. Kalager’s report (Ann. Intern. Med. 2012;156:536-7).
"Instead of focusing on the exact extent of overdiagnosis, it is time to agree that any amount of overdiagnosis is serious and to start dealing with this issue now," said Dr. Joann G. Elmore and Dr. Suzanne W. Fletcher.
One approach to cut back on overdiagnosis would be for mammographers to change their threshold for labeling a mammographic feature as "abnormal." They also could suggest observing certain lesions over time rather than immediately biopsying them.
"We have an ethical responsibility to alert women to this phenomenon [of overdiagnosis]. Most patient education aids do not even mention overdiagnosis, and most women are not aware of its possibility," they said.
Joann G. Elmore, M.D., is at the University of Washington, Seattle. She serves as medical editor for the patient education materials published by the nonprofit Informed Medical Decisions Foundation. Suzanne W. Fletcher, M.D., is at Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston. Dr Fletcher declared a 36-year professional interest in breast cancer screening and served on the U.S. Preventive Services Task Force in the early 1980s. These remarks were taken from their editorial accompanying Dr. Kalager’s report (Ann. Intern. Med. 2012;156:536-7).
The introduction of widespread screening mammography in Norway was associated with an estimated 15%-25% "overdiagnosis" of breast cancer there, according to a report in the April 3 issue of the Annals of Internal Medicine.
This finding is consistent with those of previous studies in other countries, which estimated rates of overdiagnosis ranging from 0% to 54%, with randomized controlled trials tending to estimate it at approximately 30%, investigators said.
The result of this study in Norway adds to the evidence that "overdiagnosis and unnecessary treatment of nonfatal cancer creates a substantial ethical and clinical dilemma and may cast doubt on whether mammography screening programs should exist," said Dr. Mette Kalager of the department of epidemiology, Harvard School of Public Health, Boston, and her associates.
Screening mammography was uncommon in Norway until a national, state-funded program began in 1996. Screening mammography was then implemented gradually, in different geographic areas, over the course of 10 years. Since 2005, all women in Norway aged 50-69 years have been invited to participate in mammographic screening every 2 years, and approximately 77% of them do so.
"This staggered implementation allowed comparison of contemporaneous trends in breast cancer incidence in areas with and without mammography screening," as well as the comparison of current and historical trends in incidence. This in turn gave the researchers two analytic methods for calculating estimates of overdiagnosis.
They defined overdiagnosis as the percentage of cases of cancer that would not have become clinically apparent in a woman’s lifetime without screening. It refers to cases of breast cancer that would be diagnosed and treated without yielding any possible survival benefit – cases in which the tumor would never have progressed to a clinical stage or in which the woman would die from other causes before the breast cancer became evident.
The study population comprised 39,888 women diagnosed as having invasive breast cancer in 1996-2005, including 27,238 who were aged 50-79 years at diagnosis. A total of 7,793 women were diagnosed after the introduction of routine screening.
In fully adjusted analyses using the first method of estimating, 15%-20% of the cases of breast cancer found on screening mammography – that is, between 1,169 and 1,948 women – were overdiagnosed. In an analysis using the second method of estimating, 18%-25% of cases were overdiagnosed.
Thus, the overall rate of overdiagnosis in this study was 15%-25%, Dr. Kalager and her colleagues said (Ann. Intern. Med. 2012;156:491-9).
Moreover, the proportion of advanced-stage breast cancers decreased over time to the same degree among screened and unscreened women, while the proportion of stage I breast cancers markedly increased only among screened women. This indicates that the cancers being found on screening mammography were almost entirely early-stage, low-risk tumors.
"Our findings suggest that enhanced awareness is probably the reason for the reduction of late-stage cancer, not screening," the investigators noted.
Extrapolating their findings, they added that "after 10 years of biennial mammography screening, for every 2,500 women invited, 6-10 women have been overdiagnosed, 20 women are diagnosed with breast cancer ... and one death from breast cancer has been prevented.
"To put it differently, if 2,500 women are invited to undergo mammography screening over 10 years, 2,470-2,474 women will not be diagnosed with breast cancer, 2,499 will not die of breast cancer, but 6-10 women will be overdiagnosed," they said.
This study was supported by the Research Council of Norway and Frontier Science. Dr. Kalager and her coauthors had no relevant disclosures.
The introduction of widespread screening mammography in Norway was associated with an estimated 15%-25% "overdiagnosis" of breast cancer there, according to a report in the April 3 issue of the Annals of Internal Medicine.
This finding is consistent with those of previous studies in other countries, which estimated rates of overdiagnosis ranging from 0% to 54%, with randomized controlled trials tending to estimate it at approximately 30%, investigators said.
The result of this study in Norway adds to the evidence that "overdiagnosis and unnecessary treatment of nonfatal cancer creates a substantial ethical and clinical dilemma and may cast doubt on whether mammography screening programs should exist," said Dr. Mette Kalager of the department of epidemiology, Harvard School of Public Health, Boston, and her associates.
Screening mammography was uncommon in Norway until a national, state-funded program began in 1996. Screening mammography was then implemented gradually, in different geographic areas, over the course of 10 years. Since 2005, all women in Norway aged 50-69 years have been invited to participate in mammographic screening every 2 years, and approximately 77% of them do so.
"This staggered implementation allowed comparison of contemporaneous trends in breast cancer incidence in areas with and without mammography screening," as well as the comparison of current and historical trends in incidence. This in turn gave the researchers two analytic methods for calculating estimates of overdiagnosis.
They defined overdiagnosis as the percentage of cases of cancer that would not have become clinically apparent in a woman’s lifetime without screening. It refers to cases of breast cancer that would be diagnosed and treated without yielding any possible survival benefit – cases in which the tumor would never have progressed to a clinical stage or in which the woman would die from other causes before the breast cancer became evident.
The study population comprised 39,888 women diagnosed as having invasive breast cancer in 1996-2005, including 27,238 who were aged 50-79 years at diagnosis. A total of 7,793 women were diagnosed after the introduction of routine screening.
In fully adjusted analyses using the first method of estimating, 15%-20% of the cases of breast cancer found on screening mammography – that is, between 1,169 and 1,948 women – were overdiagnosed. In an analysis using the second method of estimating, 18%-25% of cases were overdiagnosed.
Thus, the overall rate of overdiagnosis in this study was 15%-25%, Dr. Kalager and her colleagues said (Ann. Intern. Med. 2012;156:491-9).
Moreover, the proportion of advanced-stage breast cancers decreased over time to the same degree among screened and unscreened women, while the proportion of stage I breast cancers markedly increased only among screened women. This indicates that the cancers being found on screening mammography were almost entirely early-stage, low-risk tumors.
"Our findings suggest that enhanced awareness is probably the reason for the reduction of late-stage cancer, not screening," the investigators noted.
Extrapolating their findings, they added that "after 10 years of biennial mammography screening, for every 2,500 women invited, 6-10 women have been overdiagnosed, 20 women are diagnosed with breast cancer ... and one death from breast cancer has been prevented.
"To put it differently, if 2,500 women are invited to undergo mammography screening over 10 years, 2,470-2,474 women will not be diagnosed with breast cancer, 2,499 will not die of breast cancer, but 6-10 women will be overdiagnosed," they said.
This study was supported by the Research Council of Norway and Frontier Science. Dr. Kalager and her coauthors had no relevant disclosures.
FROM THE ANNALS OF INTERNAL MEDICINE
Major Finding: The estimated rate of overdiagnosis of breast cancer by screening mammography was 15%-25% in Norway.
Data Source: The investigators analyzed data on 39,888 women with invasive breast cancer diagnosed in 1996-2005, including 7,793 diagnosed after a national screening mammography program was introduced.
Disclosures: This study was supported by the Norwegian Research Council and Frontier Science. Dr. Kalager and her coauthors had no relevant disclosures.
ASCO: Stop Underdosing Obese Cancer Patients
Chemotherapy doses should be tailored for obese cancer patients based on their actual body weight, not their ideal body weight, according to a new practice guideline from the American Society of Clinical Oncology.
There is no evidence that full-weight-based chemotherapy doses cause greater toxicity than adjusted doses, and concerns about "overdosing" obese cancer patients are unfounded, a panel of experts wrote in a report published online April 2 in the Journal of Clinical Oncology.
A systematic review of the literature showed that many overweight and obese cancer patients continue to receive underdoses of intravenous and oral cytotoxic drugs because of "considerable uncertainty among physicians about optimal dose selection," even though research has confirmed that full-weight-based dosing is both safe and crucial to the patients’ survival.
"Many oncologists continue to use either ideal body weight or adjusted ideal body weight, or to cap the body surface area at, for example, 2.0 m2, rather than use actual body weight to calculate body surface area," said Dr. Jennifer J. Griggs of the University of Michigan, Ann Arbor, and her associates on the expert panel for ASCO’s new practice guideline.
As a result, chemotherapy dosing varies widely in overweight and obese patients, with as many as 40% receiving less than optimal dosing. This "may explain, in part, the significantly higher cancer mortality observed in overweight and obese individuals," they noted.
"With the incidence of obesity at an all-time high in the United States, as well as in other developed and developing nations, oncologists face this issue more than ever before," Dr. Griggs added in a press statement accompanying release of the guideline.
The ASCO guideline panel reviewed all the randomized clinical trials, meta-analyses, and clinical practice guidelines of other organizations concerning cytotoxic oral or IV chemotherapy dosing approaches for overweight or obese patients with cancer, excluding leukemias. Since there have been no prospective randomized studies directly comparing full-weight-based dose selection against other types of dose selection, they had to rely primarily on subgroup analyses and registry data.
Most of the studies concerned breast, ovarian, colon, and lung cancers, the authors said. As little data in the literature addressed dosing for novel agents such as tyrosine kinase inhibitors, immunotherapies such as interleukin-2 or interferon, or monoclonal antibodies, the guideline did not address these agents.
A summary of the guideline (J. Clin. Oncol. 2012 [doi:10.1200/JCO.2011.39.9436]) lists these key recommendations:
• Actual body weight should be used to select cytotoxic chemotherapy doses, regardless of obesity status. There is no evidence that either short- or long-term toxicity is increased with this approach.
• Use the same strategy in obese patients as in other patients for dose reductions, taking into account the type and severity of toxicity, any comorbid conditions, and whether the aim of treatment is cure or palliation. There is no evidence that greater dose reductions are needed for obese patients. Also, consider resuming the full-weight-based dose for subsequent chemotherapy cycles, especially if a possible cause of toxicity (such as impaired renal or liver function) has resolved.
• Consider fixed dosing only with select cytotoxic agents for which maximal dosing limits have been established, such as vincristine, carboplatin, or bleomycin.
• Calculate body surface area using any of the standard formulas currently available. There is no evidence to support using one formula over any other.
• Further research is needed into the pharmacokinetics and pharmacogenetics of chemotherapy dosing for obese patients, who have been excluded from many anticancer drug trials.
The guideline also emphasizes that physicians may need to fully discuss this issue with patients and caregivers, stressing that higher doses are needed in obese patients for the chemotherapy to be effective and reassuring them that toxicity is not expected to be any greater at proportionally higher doses.
"Communication with other health care providers is also warranted. Pharmacists and nursing professionals who are accustomed to limiting chemotherapy doses for obese patients should be informed of the existing evidence. IV and oral doses may be prepackaged for patients of normal weight, but appropriate dosing should be delivered, regardless of doses contained within a given vial. Arbitrary capping based on drug procurement is unacceptable (e.g., 1 vs. 1.5 vials)," the guideline stated.
Clinicians also should be aware that since rates of obesity are higher in black patients, Hispanic patients, and patients of lower socioeconomic status, these groups are harmed the most by underdosing and may benefit the most when full-weight-based dosing is adopted.
"This guideline should ease fears about administering chemotherapy based on actual body weight to otherwise healthy obese patients with cancer," Dr. Gary H. Lyman, cochair of the expert panel that drafted the guideline, said in a press statement.
"While chemotherapy dose for an obese patient may be larger than some physicians are accustomed to, they can rest assured that the risk of toxicity associated with chemotherapy dosing based on actual body weight is no greater in obese patients than in nonobese patients with cancer," said Dr. Lyman, a professor of medicine in the division of medical oncology at Duke University, Durham, N.C.
The full practice guideline, along with additional information on methodology and clinical resources, is available at ASCO’s website. For additional patient information, click here.
No financial conflicts of interest were reported.
Chemotherapy doses should be tailored for obese cancer patients based on their actual body weight, not their ideal body weight, according to a new practice guideline from the American Society of Clinical Oncology.
There is no evidence that full-weight-based chemotherapy doses cause greater toxicity than adjusted doses, and concerns about "overdosing" obese cancer patients are unfounded, a panel of experts wrote in a report published online April 2 in the Journal of Clinical Oncology.
A systematic review of the literature showed that many overweight and obese cancer patients continue to receive underdoses of intravenous and oral cytotoxic drugs because of "considerable uncertainty among physicians about optimal dose selection," even though research has confirmed that full-weight-based dosing is both safe and crucial to the patients’ survival.
"Many oncologists continue to use either ideal body weight or adjusted ideal body weight, or to cap the body surface area at, for example, 2.0 m2, rather than use actual body weight to calculate body surface area," said Dr. Jennifer J. Griggs of the University of Michigan, Ann Arbor, and her associates on the expert panel for ASCO’s new practice guideline.
As a result, chemotherapy dosing varies widely in overweight and obese patients, with as many as 40% receiving less than optimal dosing. This "may explain, in part, the significantly higher cancer mortality observed in overweight and obese individuals," they noted.
"With the incidence of obesity at an all-time high in the United States, as well as in other developed and developing nations, oncologists face this issue more than ever before," Dr. Griggs added in a press statement accompanying release of the guideline.
The ASCO guideline panel reviewed all the randomized clinical trials, meta-analyses, and clinical practice guidelines of other organizations concerning cytotoxic oral or IV chemotherapy dosing approaches for overweight or obese patients with cancer, excluding leukemias. Since there have been no prospective randomized studies directly comparing full-weight-based dose selection against other types of dose selection, they had to rely primarily on subgroup analyses and registry data.
Most of the studies concerned breast, ovarian, colon, and lung cancers, the authors said. As little data in the literature addressed dosing for novel agents such as tyrosine kinase inhibitors, immunotherapies such as interleukin-2 or interferon, or monoclonal antibodies, the guideline did not address these agents.
A summary of the guideline (J. Clin. Oncol. 2012 [doi:10.1200/JCO.2011.39.9436]) lists these key recommendations:
• Actual body weight should be used to select cytotoxic chemotherapy doses, regardless of obesity status. There is no evidence that either short- or long-term toxicity is increased with this approach.
• Use the same strategy in obese patients as in other patients for dose reductions, taking into account the type and severity of toxicity, any comorbid conditions, and whether the aim of treatment is cure or palliation. There is no evidence that greater dose reductions are needed for obese patients. Also, consider resuming the full-weight-based dose for subsequent chemotherapy cycles, especially if a possible cause of toxicity (such as impaired renal or liver function) has resolved.
• Consider fixed dosing only with select cytotoxic agents for which maximal dosing limits have been established, such as vincristine, carboplatin, or bleomycin.
• Calculate body surface area using any of the standard formulas currently available. There is no evidence to support using one formula over any other.
• Further research is needed into the pharmacokinetics and pharmacogenetics of chemotherapy dosing for obese patients, who have been excluded from many anticancer drug trials.
The guideline also emphasizes that physicians may need to fully discuss this issue with patients and caregivers, stressing that higher doses are needed in obese patients for the chemotherapy to be effective and reassuring them that toxicity is not expected to be any greater at proportionally higher doses.
"Communication with other health care providers is also warranted. Pharmacists and nursing professionals who are accustomed to limiting chemotherapy doses for obese patients should be informed of the existing evidence. IV and oral doses may be prepackaged for patients of normal weight, but appropriate dosing should be delivered, regardless of doses contained within a given vial. Arbitrary capping based on drug procurement is unacceptable (e.g., 1 vs. 1.5 vials)," the guideline stated.
Clinicians also should be aware that since rates of obesity are higher in black patients, Hispanic patients, and patients of lower socioeconomic status, these groups are harmed the most by underdosing and may benefit the most when full-weight-based dosing is adopted.
"This guideline should ease fears about administering chemotherapy based on actual body weight to otherwise healthy obese patients with cancer," Dr. Gary H. Lyman, cochair of the expert panel that drafted the guideline, said in a press statement.
"While chemotherapy dose for an obese patient may be larger than some physicians are accustomed to, they can rest assured that the risk of toxicity associated with chemotherapy dosing based on actual body weight is no greater in obese patients than in nonobese patients with cancer," said Dr. Lyman, a professor of medicine in the division of medical oncology at Duke University, Durham, N.C.
The full practice guideline, along with additional information on methodology and clinical resources, is available at ASCO’s website. For additional patient information, click here.
No financial conflicts of interest were reported.
Chemotherapy doses should be tailored for obese cancer patients based on their actual body weight, not their ideal body weight, according to a new practice guideline from the American Society of Clinical Oncology.
There is no evidence that full-weight-based chemotherapy doses cause greater toxicity than adjusted doses, and concerns about "overdosing" obese cancer patients are unfounded, a panel of experts wrote in a report published online April 2 in the Journal of Clinical Oncology.
A systematic review of the literature showed that many overweight and obese cancer patients continue to receive underdoses of intravenous and oral cytotoxic drugs because of "considerable uncertainty among physicians about optimal dose selection," even though research has confirmed that full-weight-based dosing is both safe and crucial to the patients’ survival.
"Many oncologists continue to use either ideal body weight or adjusted ideal body weight, or to cap the body surface area at, for example, 2.0 m2, rather than use actual body weight to calculate body surface area," said Dr. Jennifer J. Griggs of the University of Michigan, Ann Arbor, and her associates on the expert panel for ASCO’s new practice guideline.
As a result, chemotherapy dosing varies widely in overweight and obese patients, with as many as 40% receiving less than optimal dosing. This "may explain, in part, the significantly higher cancer mortality observed in overweight and obese individuals," they noted.
"With the incidence of obesity at an all-time high in the United States, as well as in other developed and developing nations, oncologists face this issue more than ever before," Dr. Griggs added in a press statement accompanying release of the guideline.
The ASCO guideline panel reviewed all the randomized clinical trials, meta-analyses, and clinical practice guidelines of other organizations concerning cytotoxic oral or IV chemotherapy dosing approaches for overweight or obese patients with cancer, excluding leukemias. Since there have been no prospective randomized studies directly comparing full-weight-based dose selection against other types of dose selection, they had to rely primarily on subgroup analyses and registry data.
Most of the studies concerned breast, ovarian, colon, and lung cancers, the authors said. As little data in the literature addressed dosing for novel agents such as tyrosine kinase inhibitors, immunotherapies such as interleukin-2 or interferon, or monoclonal antibodies, the guideline did not address these agents.
A summary of the guideline (J. Clin. Oncol. 2012 [doi:10.1200/JCO.2011.39.9436]) lists these key recommendations:
• Actual body weight should be used to select cytotoxic chemotherapy doses, regardless of obesity status. There is no evidence that either short- or long-term toxicity is increased with this approach.
• Use the same strategy in obese patients as in other patients for dose reductions, taking into account the type and severity of toxicity, any comorbid conditions, and whether the aim of treatment is cure or palliation. There is no evidence that greater dose reductions are needed for obese patients. Also, consider resuming the full-weight-based dose for subsequent chemotherapy cycles, especially if a possible cause of toxicity (such as impaired renal or liver function) has resolved.
• Consider fixed dosing only with select cytotoxic agents for which maximal dosing limits have been established, such as vincristine, carboplatin, or bleomycin.
• Calculate body surface area using any of the standard formulas currently available. There is no evidence to support using one formula over any other.
• Further research is needed into the pharmacokinetics and pharmacogenetics of chemotherapy dosing for obese patients, who have been excluded from many anticancer drug trials.
The guideline also emphasizes that physicians may need to fully discuss this issue with patients and caregivers, stressing that higher doses are needed in obese patients for the chemotherapy to be effective and reassuring them that toxicity is not expected to be any greater at proportionally higher doses.
"Communication with other health care providers is also warranted. Pharmacists and nursing professionals who are accustomed to limiting chemotherapy doses for obese patients should be informed of the existing evidence. IV and oral doses may be prepackaged for patients of normal weight, but appropriate dosing should be delivered, regardless of doses contained within a given vial. Arbitrary capping based on drug procurement is unacceptable (e.g., 1 vs. 1.5 vials)," the guideline stated.
Clinicians also should be aware that since rates of obesity are higher in black patients, Hispanic patients, and patients of lower socioeconomic status, these groups are harmed the most by underdosing and may benefit the most when full-weight-based dosing is adopted.
"This guideline should ease fears about administering chemotherapy based on actual body weight to otherwise healthy obese patients with cancer," Dr. Gary H. Lyman, cochair of the expert panel that drafted the guideline, said in a press statement.
"While chemotherapy dose for an obese patient may be larger than some physicians are accustomed to, they can rest assured that the risk of toxicity associated with chemotherapy dosing based on actual body weight is no greater in obese patients than in nonobese patients with cancer," said Dr. Lyman, a professor of medicine in the division of medical oncology at Duke University, Durham, N.C.
The full practice guideline, along with additional information on methodology and clinical resources, is available at ASCO’s website. For additional patient information, click here.
No financial conflicts of interest were reported.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Estrogen-Only HT Also Increases Breast Cancer Risk
CHICAGO – Long-term use of estrogen-only therapy increases the risk of postmenopausal women developing breast cancer, according to new data from the Nurses’ Health Study.
The finding, reported April 1 by Dr. Wendy Chen at the annual meeting of the American Association for Cancer Research, suggests that opting for progesterone-free hormone therapy for the treatment of menopause symptoms should not be considered the risk-free alternative to combination progesterone plus estrogen formulations.
Still, the absolute risks were small. During the study’s 1.57 million person-years of follow-up from 1980 through 2008, 5,631 incident invasive breast cancers were diagnosed and 884 of the women died of breast cancer.
To evaluate the breast cancer risk associated with long-term use of both combined and estrogen-only hormone therapy, Dr. Chen of Brigham and Women’s Hospital in Boston and her colleagues evaluated data collected over 28 years through the Nurses’ Health Study. Of the 121,700 study participants who were aged 30-55 years in 1976, women who used estrogen-only therapy for 10.0-14.9 years and for 15.0-19.9 years had, respectively, a 22% and 43% increased risk of developing breast cancer relative to those women not on hormone therapy (HT).
"Our data also confirmed the previously reported increased risk associated with combined hormone therapy," Dr. Chen stated, noting that women in the study who used progesterone plus estrogen for 10-14.9 years had an 88% increased risk of developing breast cancer relative to those not on HT and the risk increased to more than twofold in women using it for up to 20 years. Further, the risk of developing breast cancer does not appear to plateau over time, but rather continues to increase. "The longer women use [HT]. The higher their risk," she said.
In a separate analysis, the investigators restricted the study population to healthy, active postmenopausal women 50-79 years with an intact uterus – the same population observed in the Women’s Health Initiative. "What we saw was a decline in breast cancer risk among women using estrogen-only therapy for less than 10 years, but an increased risk among those women using estrogen for 15-20 years," Dr. Chen said.
Importantly, although breast cancer incidence was increased in the HT groups, "there was no increase in the risk of fatal breast cancer, either with combined or estrogen-only therapy," Dr. Chen stressed. "This is something we are continuing to investigate."
The findings have the potential to increase the confusion regarding HT and to perhaps reignite the hormone therapy debate, Dr. Chen acknowledged in an interview. However, they should be considered in their proper context. "While the relative risk of developing breast cancer in increased, the absolute risk associated with [HT] are low," she said.
The observed effects associated with HT were stronger for estrogen receptor–positive tumors and among thinner women, Dr. Chen noted, adding that the results were similar when limited to women who underwent regular breast cancer screening.
The study was funded by the National Cancer Institute. Dr. Chen disclosed no financial conflicts of interest.
CHICAGO – Long-term use of estrogen-only therapy increases the risk of postmenopausal women developing breast cancer, according to new data from the Nurses’ Health Study.
The finding, reported April 1 by Dr. Wendy Chen at the annual meeting of the American Association for Cancer Research, suggests that opting for progesterone-free hormone therapy for the treatment of menopause symptoms should not be considered the risk-free alternative to combination progesterone plus estrogen formulations.
Still, the absolute risks were small. During the study’s 1.57 million person-years of follow-up from 1980 through 2008, 5,631 incident invasive breast cancers were diagnosed and 884 of the women died of breast cancer.
To evaluate the breast cancer risk associated with long-term use of both combined and estrogen-only hormone therapy, Dr. Chen of Brigham and Women’s Hospital in Boston and her colleagues evaluated data collected over 28 years through the Nurses’ Health Study. Of the 121,700 study participants who were aged 30-55 years in 1976, women who used estrogen-only therapy for 10.0-14.9 years and for 15.0-19.9 years had, respectively, a 22% and 43% increased risk of developing breast cancer relative to those women not on hormone therapy (HT).
"Our data also confirmed the previously reported increased risk associated with combined hormone therapy," Dr. Chen stated, noting that women in the study who used progesterone plus estrogen for 10-14.9 years had an 88% increased risk of developing breast cancer relative to those not on HT and the risk increased to more than twofold in women using it for up to 20 years. Further, the risk of developing breast cancer does not appear to plateau over time, but rather continues to increase. "The longer women use [HT]. The higher their risk," she said.
In a separate analysis, the investigators restricted the study population to healthy, active postmenopausal women 50-79 years with an intact uterus – the same population observed in the Women’s Health Initiative. "What we saw was a decline in breast cancer risk among women using estrogen-only therapy for less than 10 years, but an increased risk among those women using estrogen for 15-20 years," Dr. Chen said.
Importantly, although breast cancer incidence was increased in the HT groups, "there was no increase in the risk of fatal breast cancer, either with combined or estrogen-only therapy," Dr. Chen stressed. "This is something we are continuing to investigate."
The findings have the potential to increase the confusion regarding HT and to perhaps reignite the hormone therapy debate, Dr. Chen acknowledged in an interview. However, they should be considered in their proper context. "While the relative risk of developing breast cancer in increased, the absolute risk associated with [HT] are low," she said.
The observed effects associated with HT were stronger for estrogen receptor–positive tumors and among thinner women, Dr. Chen noted, adding that the results were similar when limited to women who underwent regular breast cancer screening.
The study was funded by the National Cancer Institute. Dr. Chen disclosed no financial conflicts of interest.
CHICAGO – Long-term use of estrogen-only therapy increases the risk of postmenopausal women developing breast cancer, according to new data from the Nurses’ Health Study.
The finding, reported April 1 by Dr. Wendy Chen at the annual meeting of the American Association for Cancer Research, suggests that opting for progesterone-free hormone therapy for the treatment of menopause symptoms should not be considered the risk-free alternative to combination progesterone plus estrogen formulations.
Still, the absolute risks were small. During the study’s 1.57 million person-years of follow-up from 1980 through 2008, 5,631 incident invasive breast cancers were diagnosed and 884 of the women died of breast cancer.
To evaluate the breast cancer risk associated with long-term use of both combined and estrogen-only hormone therapy, Dr. Chen of Brigham and Women’s Hospital in Boston and her colleagues evaluated data collected over 28 years through the Nurses’ Health Study. Of the 121,700 study participants who were aged 30-55 years in 1976, women who used estrogen-only therapy for 10.0-14.9 years and for 15.0-19.9 years had, respectively, a 22% and 43% increased risk of developing breast cancer relative to those women not on hormone therapy (HT).
"Our data also confirmed the previously reported increased risk associated with combined hormone therapy," Dr. Chen stated, noting that women in the study who used progesterone plus estrogen for 10-14.9 years had an 88% increased risk of developing breast cancer relative to those not on HT and the risk increased to more than twofold in women using it for up to 20 years. Further, the risk of developing breast cancer does not appear to plateau over time, but rather continues to increase. "The longer women use [HT]. The higher their risk," she said.
In a separate analysis, the investigators restricted the study population to healthy, active postmenopausal women 50-79 years with an intact uterus – the same population observed in the Women’s Health Initiative. "What we saw was a decline in breast cancer risk among women using estrogen-only therapy for less than 10 years, but an increased risk among those women using estrogen for 15-20 years," Dr. Chen said.
Importantly, although breast cancer incidence was increased in the HT groups, "there was no increase in the risk of fatal breast cancer, either with combined or estrogen-only therapy," Dr. Chen stressed. "This is something we are continuing to investigate."
The findings have the potential to increase the confusion regarding HT and to perhaps reignite the hormone therapy debate, Dr. Chen acknowledged in an interview. However, they should be considered in their proper context. "While the relative risk of developing breast cancer in increased, the absolute risk associated with [HT] are low," she said.
The observed effects associated with HT were stronger for estrogen receptor–positive tumors and among thinner women, Dr. Chen noted, adding that the results were similar when limited to women who underwent regular breast cancer screening.
The study was funded by the National Cancer Institute. Dr. Chen disclosed no financial conflicts of interest.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION OF CANCER RESEARCH
Major Finding: Of the 121,700 study participants in the Nurses’ Health Study who were aged 30-55 years in 1976, women who used estrogen-only therapy for 10.0-14.9 years and for 15.0-19.9 years had, respectively, a 22% and 43% increased risk of developing breast cancer relative to those not on hormone therapy.
Data Source: The Nurses’ Health Study of data collected during 1980-2008 from 121,700 postmenopausal women aged 30-55 years in 1976.
Disclosures: Dr. Chen disclosed no financial conflicts of interest.
Some Triple-Negative Breast Cancers Express Androgen Receptor
ORLANDO – Triple-negative breast tumors are notorious for their ability to evade hormonal agents and targeted therapies. But a subset of these intractable tumors expresses androgen receptors, and may be vulnerable to antiandrogen drugs, investigators suggested at the symposium of the Society of Surgical Oncology.
An evaluation of cancerous and normal breast tissues from 94 patients with triple-negative breast tumors (lacking estrogen-, progesterone-, and HER2-receptor expression), showed that the androgen receptor (AR) was expressed in 23% of tumors, reported Dr. Barbara Pockaj of the Mayo Clinic in Scottsdale, Ariz., and colleagues.
AR–positive cancers occurred more frequently in older patients and were significantly associated with lymph node metastases, compared with AR-negative, triple-negative breast cancers in this small study, she said.
There was a trend toward higher tumor stage at diagnosis among patients with AR-positive tumors, but AR-positive and AR-negative patients did not differ significantly in overall or recurrence-free survival, said Dr. Pockaj.
Previous studies have suggested that 10%-43% of triple-negative breast cancers bear the androgen receptor, but the antibodies and methods used for characterizing the presence of the receptor varied significantly, making it difficult to nail down actual numbers, Dr. Pockaj said.
The investigators examined 177 tissue biopsy cores from 94 patients with triple-negative breast cancer to see whether AR-receptor expression correlated with patient and tumor factors and survival, and where expression of the receptors in different tissues from the same patients correlated with tumor progression.
The receptor was expressed in 88% of normal breast tissues in the samples, a proportion identical to that of the estrogen receptor in normal tissues from the same patients.
AR expression was detected in all 6 of 6 adjacent DCIS (ductal carcinoma in situ) samples from AR-positive patients, and in 9 of 15 DCIS samples from patients with AR-negative cancer.
All lymph node metastases from AR-positive patients were also positive, whereas no lymph node metastases from AR-negative patients were found to express the androgen receptor.
There were no significant differences between AR-positive and -negative patients in tumor grade, angiolymphatic invasion, TNM (tumor, node, metastasis) stage, or tumor size. In contrast, 16 of the 72 (22%) of the AR-negative patients had lymph node metastases, compared with 10 of 22 (46%) AR-positive patients (P = .033).
There were no significant differences in locoregional recurrences, overall survival, or disease-specific survival between positive and negative patients.
Among all 94 patients, however, the presence of lymph node metastases was associated with a significantly worse recurrence-free survival (hazard ratio, 5.502; P = .017). Chemotherapy significantly reduced that risk (HR, 0.099; P = .0004).
In multivariate analysis, the investigators found that AR expression was associated with older age (63 years vs. 57 years; P = .051) and with the presence of lymph nodes metastases (P = .033).
Although larger studies are needed, the data suggest that AR-positive, triple-negative breast cancer "has unique clinical behavior and may need different treatment," Dr. Pockaj said.
A phase II, open-label trial of the antiandrogen bicalutamide (Casodex) in patients with AR-positive, estrogen- and progesterone-receptor–negative, metastatic breast cancer is currently underway in eight U.S. cancer centers.
The current study was supported by the Translational Genomics Research Institute, Phoenix, and the Mayo Clinic, Scottsdale, Ariz. Dr. Pockaj is an employee of the Mayo Clinic.
ORLANDO – Triple-negative breast tumors are notorious for their ability to evade hormonal agents and targeted therapies. But a subset of these intractable tumors expresses androgen receptors, and may be vulnerable to antiandrogen drugs, investigators suggested at the symposium of the Society of Surgical Oncology.
An evaluation of cancerous and normal breast tissues from 94 patients with triple-negative breast tumors (lacking estrogen-, progesterone-, and HER2-receptor expression), showed that the androgen receptor (AR) was expressed in 23% of tumors, reported Dr. Barbara Pockaj of the Mayo Clinic in Scottsdale, Ariz., and colleagues.
AR–positive cancers occurred more frequently in older patients and were significantly associated with lymph node metastases, compared with AR-negative, triple-negative breast cancers in this small study, she said.
There was a trend toward higher tumor stage at diagnosis among patients with AR-positive tumors, but AR-positive and AR-negative patients did not differ significantly in overall or recurrence-free survival, said Dr. Pockaj.
Previous studies have suggested that 10%-43% of triple-negative breast cancers bear the androgen receptor, but the antibodies and methods used for characterizing the presence of the receptor varied significantly, making it difficult to nail down actual numbers, Dr. Pockaj said.
The investigators examined 177 tissue biopsy cores from 94 patients with triple-negative breast cancer to see whether AR-receptor expression correlated with patient and tumor factors and survival, and where expression of the receptors in different tissues from the same patients correlated with tumor progression.
The receptor was expressed in 88% of normal breast tissues in the samples, a proportion identical to that of the estrogen receptor in normal tissues from the same patients.
AR expression was detected in all 6 of 6 adjacent DCIS (ductal carcinoma in situ) samples from AR-positive patients, and in 9 of 15 DCIS samples from patients with AR-negative cancer.
All lymph node metastases from AR-positive patients were also positive, whereas no lymph node metastases from AR-negative patients were found to express the androgen receptor.
There were no significant differences between AR-positive and -negative patients in tumor grade, angiolymphatic invasion, TNM (tumor, node, metastasis) stage, or tumor size. In contrast, 16 of the 72 (22%) of the AR-negative patients had lymph node metastases, compared with 10 of 22 (46%) AR-positive patients (P = .033).
There were no significant differences in locoregional recurrences, overall survival, or disease-specific survival between positive and negative patients.
Among all 94 patients, however, the presence of lymph node metastases was associated with a significantly worse recurrence-free survival (hazard ratio, 5.502; P = .017). Chemotherapy significantly reduced that risk (HR, 0.099; P = .0004).
In multivariate analysis, the investigators found that AR expression was associated with older age (63 years vs. 57 years; P = .051) and with the presence of lymph nodes metastases (P = .033).
Although larger studies are needed, the data suggest that AR-positive, triple-negative breast cancer "has unique clinical behavior and may need different treatment," Dr. Pockaj said.
A phase II, open-label trial of the antiandrogen bicalutamide (Casodex) in patients with AR-positive, estrogen- and progesterone-receptor–negative, metastatic breast cancer is currently underway in eight U.S. cancer centers.
The current study was supported by the Translational Genomics Research Institute, Phoenix, and the Mayo Clinic, Scottsdale, Ariz. Dr. Pockaj is an employee of the Mayo Clinic.
ORLANDO – Triple-negative breast tumors are notorious for their ability to evade hormonal agents and targeted therapies. But a subset of these intractable tumors expresses androgen receptors, and may be vulnerable to antiandrogen drugs, investigators suggested at the symposium of the Society of Surgical Oncology.
An evaluation of cancerous and normal breast tissues from 94 patients with triple-negative breast tumors (lacking estrogen-, progesterone-, and HER2-receptor expression), showed that the androgen receptor (AR) was expressed in 23% of tumors, reported Dr. Barbara Pockaj of the Mayo Clinic in Scottsdale, Ariz., and colleagues.
AR–positive cancers occurred more frequently in older patients and were significantly associated with lymph node metastases, compared with AR-negative, triple-negative breast cancers in this small study, she said.
There was a trend toward higher tumor stage at diagnosis among patients with AR-positive tumors, but AR-positive and AR-negative patients did not differ significantly in overall or recurrence-free survival, said Dr. Pockaj.
Previous studies have suggested that 10%-43% of triple-negative breast cancers bear the androgen receptor, but the antibodies and methods used for characterizing the presence of the receptor varied significantly, making it difficult to nail down actual numbers, Dr. Pockaj said.
The investigators examined 177 tissue biopsy cores from 94 patients with triple-negative breast cancer to see whether AR-receptor expression correlated with patient and tumor factors and survival, and where expression of the receptors in different tissues from the same patients correlated with tumor progression.
The receptor was expressed in 88% of normal breast tissues in the samples, a proportion identical to that of the estrogen receptor in normal tissues from the same patients.
AR expression was detected in all 6 of 6 adjacent DCIS (ductal carcinoma in situ) samples from AR-positive patients, and in 9 of 15 DCIS samples from patients with AR-negative cancer.
All lymph node metastases from AR-positive patients were also positive, whereas no lymph node metastases from AR-negative patients were found to express the androgen receptor.
There were no significant differences between AR-positive and -negative patients in tumor grade, angiolymphatic invasion, TNM (tumor, node, metastasis) stage, or tumor size. In contrast, 16 of the 72 (22%) of the AR-negative patients had lymph node metastases, compared with 10 of 22 (46%) AR-positive patients (P = .033).
There were no significant differences in locoregional recurrences, overall survival, or disease-specific survival between positive and negative patients.
Among all 94 patients, however, the presence of lymph node metastases was associated with a significantly worse recurrence-free survival (hazard ratio, 5.502; P = .017). Chemotherapy significantly reduced that risk (HR, 0.099; P = .0004).
In multivariate analysis, the investigators found that AR expression was associated with older age (63 years vs. 57 years; P = .051) and with the presence of lymph nodes metastases (P = .033).
Although larger studies are needed, the data suggest that AR-positive, triple-negative breast cancer "has unique clinical behavior and may need different treatment," Dr. Pockaj said.
A phase II, open-label trial of the antiandrogen bicalutamide (Casodex) in patients with AR-positive, estrogen- and progesterone-receptor–negative, metastatic breast cancer is currently underway in eight U.S. cancer centers.
The current study was supported by the Translational Genomics Research Institute, Phoenix, and the Mayo Clinic, Scottsdale, Ariz. Dr. Pockaj is an employee of the Mayo Clinic.
FROM A SYMPOSIUM SPONSORED BY THE SOCIETY OF SURGICAL ONCOLOGY
Major Finding: The androgen receptor was expressed in 23% of triple-negative breast tumors.
Data Source: Investigators did a microarray analysis of cancerous and normal breast tissue from 94 patients with triple-negative breast tumors stained for the AR receptor.
Disclosures: The study was supported by the Translational Genomics Research Institute and the Mayo Clinic Arizona. Dr. Pockaj is an employee of the Mayo Clinic.