User login
Navigators improve medication adherence in HFrEF
PHILADELPHIA – Treatment guidelines are clear about optimal treatment of heart failure in patients with reduced ejection fraction (HFrEF), but adherence breakdowns often occur.
So, Brigham and Women’s Hospital in Boston implemented a navigator-administered patient outreach program that led to improved medication adherence over usual care, according to study results reported at the American Heart Association scientific sessions.
Although the study was done at a major academic center, the findings have implications for community practitioners, lead study author Akshay S. Desai, MD, MPH, said in an interview. “The impact of the intervention is clearly greater in those practitioners who manage heart failure and have the least support around them,” he said.
“Our sense is that the kind of population where this intervention would have the greater impact would be a community-dwelling heart failure population managed by community cardiologists, where the infrastructure to provide longitudinal heart failure care is less robust than may be in an academic center,” Dr. Desai said.
The study evaluated adherence in guideline-directed medical therapy (GDMT) at 3 months. “The navigator-led remote medication optimization strategy improved utilization and dosing of all categories of GDMP and was associated with a lower rate of adverse events,” Dr. Desai said. “The impact was more pronounced in patients followed by general practitioners than by a HF specialist.” In the outreach, health navigators contacted patients by phone and managed medications based on remote surveillance of labs, blood pressure, and symptoms under supervision of a pharmacist, nurse practitioner, and heart failure specialist.
The study included 1,028 patients with chronic HFrEF who’d visited a cardiologist at Brigham and Women’s in the year prior to the study: 197 patients and their providers consented to participate in the program with the remainder serving as the reference usual-care group. Most HF specialists at Brigham and Women’s declined to participate in the navigator-led program, Dr. Desai said.
Treating providers were approached for consent to adjust medical therapy according to a sequential, stepped titration algorithm modeled on the current American College of Cardiology/American Heart Association HF Guidelines. The study population did not include patients with end-stage HF, those with a severe noncardiac illness with a life expectancy of less than a year, and patients with a pattern of nonadherence. Baseline characteristics of the two groups were well balanced, Dr. Desai said.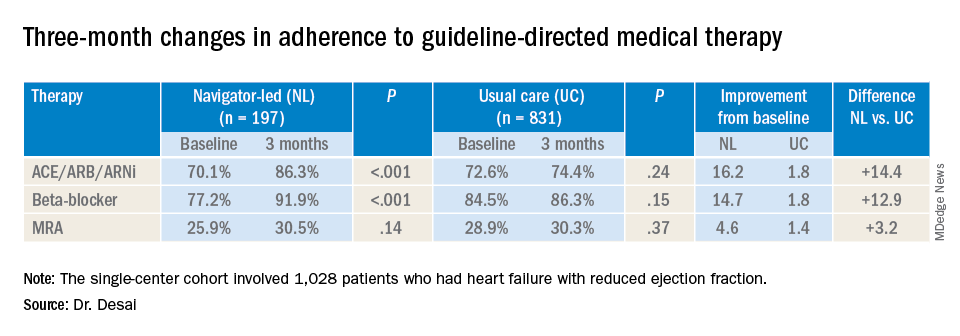
At baseline, 74% (759) participants were treated with ACE inhibitors/angiotensin receptor blockers/angiotensin-receptor neprilysin inhibitors (ACE/ARB/ARNi), 73% (746) with guideline-directed beta-blockers, and 29% (303) with mineralocorticoid receptor antagonists (MRAs), with 10% (107) and 11% (117) treated with target doses of ACE/ARB/ARNi and beta-blockers, respectively.
In the navigator-led group, beta-blocker adherence improved from 77.2% at baseline to 91.9% at 3 months (P less than 0.001) compared with an increase from 84.5% to 86.3% in the usual-care patients (P = 0.15), Dr. Desai said. ACE/ARB/ARNi adherence increased 16.2 percentage points to 86.3% (P less than 0.001) in the navigator-group versus 1.8 percentage points to 74.4% (P = 0.24) for usual care. In the MRA subgroup, 3-month adherence to GDMT was almost identical: 30.5% (P = 0.14) and 30.3% (P = 0.37) for the two treatment groups, respectively, although the navigator-led patients averaged a larger increase of 4.6 versus 1.4 percentage points from baseline.
Adverse event rates were similar in both groups, although the navigator group had “slightly higher rates” of hypotension and hyperkalemia but no serious events, Dr. Desai said. This group also had similarly higher rates of worsening renal function, but most were asymptomatic change in creatinine that was addressed with medication changes, he said. There were no hospitalizations for adverse events.
He said the navigator-led optimization has potential in a community setting because the referral nature of Brigham and Women’s HF population “reflects potentially a worst-case scenario for such a program.” The greatest impact was seen in patients managed by general cardiologists, he said. “If we were to move this forward, which we hope to do with scale, the impact might be greater in a community population where there are fewer specialists and less severe illnesses present.”
This study represents a proof of concept, Dr. Desai said in an interview. “What we would like to do is demonstrate that this can be done on a larger scale,” he said. “That might involve partnership with a payer or health care system to see if we can replicate these findings across a broader range of providers.”
Dr. Desai disclosed financial relationships with Novartis, AstraZeneca, Abbott, Boehringer-Ingelheim, Coston Scientific, Biofourmis, DalCor, Relypsa, Regeneron, and Alnylam. Novartis provided an unrestricted grant for the investigator-initiated trial.
SOURCE: Desai AS. AHA 2019 Featured Science session AOS.07.
PHILADELPHIA – Treatment guidelines are clear about optimal treatment of heart failure in patients with reduced ejection fraction (HFrEF), but adherence breakdowns often occur.
So, Brigham and Women’s Hospital in Boston implemented a navigator-administered patient outreach program that led to improved medication adherence over usual care, according to study results reported at the American Heart Association scientific sessions.
Although the study was done at a major academic center, the findings have implications for community practitioners, lead study author Akshay S. Desai, MD, MPH, said in an interview. “The impact of the intervention is clearly greater in those practitioners who manage heart failure and have the least support around them,” he said.
“Our sense is that the kind of population where this intervention would have the greater impact would be a community-dwelling heart failure population managed by community cardiologists, where the infrastructure to provide longitudinal heart failure care is less robust than may be in an academic center,” Dr. Desai said.
The study evaluated adherence in guideline-directed medical therapy (GDMT) at 3 months. “The navigator-led remote medication optimization strategy improved utilization and dosing of all categories of GDMP and was associated with a lower rate of adverse events,” Dr. Desai said. “The impact was more pronounced in patients followed by general practitioners than by a HF specialist.” In the outreach, health navigators contacted patients by phone and managed medications based on remote surveillance of labs, blood pressure, and symptoms under supervision of a pharmacist, nurse practitioner, and heart failure specialist.
The study included 1,028 patients with chronic HFrEF who’d visited a cardiologist at Brigham and Women’s in the year prior to the study: 197 patients and their providers consented to participate in the program with the remainder serving as the reference usual-care group. Most HF specialists at Brigham and Women’s declined to participate in the navigator-led program, Dr. Desai said.
Treating providers were approached for consent to adjust medical therapy according to a sequential, stepped titration algorithm modeled on the current American College of Cardiology/American Heart Association HF Guidelines. The study population did not include patients with end-stage HF, those with a severe noncardiac illness with a life expectancy of less than a year, and patients with a pattern of nonadherence. Baseline characteristics of the two groups were well balanced, Dr. Desai said.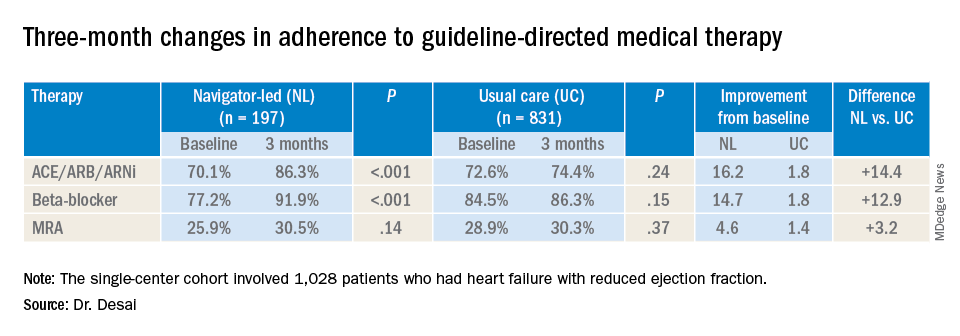
At baseline, 74% (759) participants were treated with ACE inhibitors/angiotensin receptor blockers/angiotensin-receptor neprilysin inhibitors (ACE/ARB/ARNi), 73% (746) with guideline-directed beta-blockers, and 29% (303) with mineralocorticoid receptor antagonists (MRAs), with 10% (107) and 11% (117) treated with target doses of ACE/ARB/ARNi and beta-blockers, respectively.
In the navigator-led group, beta-blocker adherence improved from 77.2% at baseline to 91.9% at 3 months (P less than 0.001) compared with an increase from 84.5% to 86.3% in the usual-care patients (P = 0.15), Dr. Desai said. ACE/ARB/ARNi adherence increased 16.2 percentage points to 86.3% (P less than 0.001) in the navigator-group versus 1.8 percentage points to 74.4% (P = 0.24) for usual care. In the MRA subgroup, 3-month adherence to GDMT was almost identical: 30.5% (P = 0.14) and 30.3% (P = 0.37) for the two treatment groups, respectively, although the navigator-led patients averaged a larger increase of 4.6 versus 1.4 percentage points from baseline.
Adverse event rates were similar in both groups, although the navigator group had “slightly higher rates” of hypotension and hyperkalemia but no serious events, Dr. Desai said. This group also had similarly higher rates of worsening renal function, but most were asymptomatic change in creatinine that was addressed with medication changes, he said. There were no hospitalizations for adverse events.
He said the navigator-led optimization has potential in a community setting because the referral nature of Brigham and Women’s HF population “reflects potentially a worst-case scenario for such a program.” The greatest impact was seen in patients managed by general cardiologists, he said. “If we were to move this forward, which we hope to do with scale, the impact might be greater in a community population where there are fewer specialists and less severe illnesses present.”
This study represents a proof of concept, Dr. Desai said in an interview. “What we would like to do is demonstrate that this can be done on a larger scale,” he said. “That might involve partnership with a payer or health care system to see if we can replicate these findings across a broader range of providers.”
Dr. Desai disclosed financial relationships with Novartis, AstraZeneca, Abbott, Boehringer-Ingelheim, Coston Scientific, Biofourmis, DalCor, Relypsa, Regeneron, and Alnylam. Novartis provided an unrestricted grant for the investigator-initiated trial.
SOURCE: Desai AS. AHA 2019 Featured Science session AOS.07.
PHILADELPHIA – Treatment guidelines are clear about optimal treatment of heart failure in patients with reduced ejection fraction (HFrEF), but adherence breakdowns often occur.
So, Brigham and Women’s Hospital in Boston implemented a navigator-administered patient outreach program that led to improved medication adherence over usual care, according to study results reported at the American Heart Association scientific sessions.
Although the study was done at a major academic center, the findings have implications for community practitioners, lead study author Akshay S. Desai, MD, MPH, said in an interview. “The impact of the intervention is clearly greater in those practitioners who manage heart failure and have the least support around them,” he said.
“Our sense is that the kind of population where this intervention would have the greater impact would be a community-dwelling heart failure population managed by community cardiologists, where the infrastructure to provide longitudinal heart failure care is less robust than may be in an academic center,” Dr. Desai said.
The study evaluated adherence in guideline-directed medical therapy (GDMT) at 3 months. “The navigator-led remote medication optimization strategy improved utilization and dosing of all categories of GDMP and was associated with a lower rate of adverse events,” Dr. Desai said. “The impact was more pronounced in patients followed by general practitioners than by a HF specialist.” In the outreach, health navigators contacted patients by phone and managed medications based on remote surveillance of labs, blood pressure, and symptoms under supervision of a pharmacist, nurse practitioner, and heart failure specialist.
The study included 1,028 patients with chronic HFrEF who’d visited a cardiologist at Brigham and Women’s in the year prior to the study: 197 patients and their providers consented to participate in the program with the remainder serving as the reference usual-care group. Most HF specialists at Brigham and Women’s declined to participate in the navigator-led program, Dr. Desai said.
Treating providers were approached for consent to adjust medical therapy according to a sequential, stepped titration algorithm modeled on the current American College of Cardiology/American Heart Association HF Guidelines. The study population did not include patients with end-stage HF, those with a severe noncardiac illness with a life expectancy of less than a year, and patients with a pattern of nonadherence. Baseline characteristics of the two groups were well balanced, Dr. Desai said.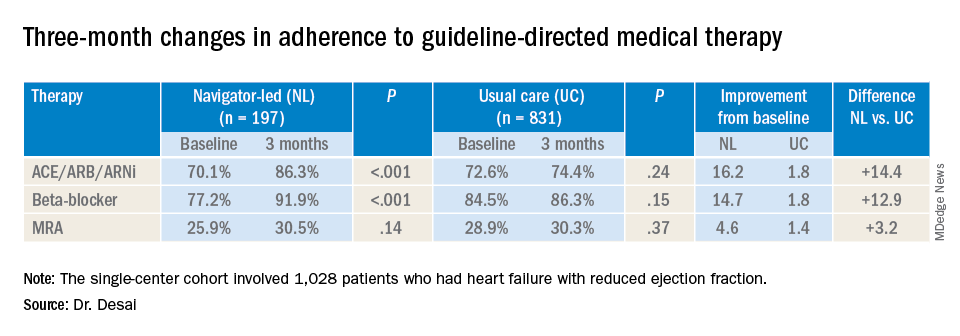
At baseline, 74% (759) participants were treated with ACE inhibitors/angiotensin receptor blockers/angiotensin-receptor neprilysin inhibitors (ACE/ARB/ARNi), 73% (746) with guideline-directed beta-blockers, and 29% (303) with mineralocorticoid receptor antagonists (MRAs), with 10% (107) and 11% (117) treated with target doses of ACE/ARB/ARNi and beta-blockers, respectively.
In the navigator-led group, beta-blocker adherence improved from 77.2% at baseline to 91.9% at 3 months (P less than 0.001) compared with an increase from 84.5% to 86.3% in the usual-care patients (P = 0.15), Dr. Desai said. ACE/ARB/ARNi adherence increased 16.2 percentage points to 86.3% (P less than 0.001) in the navigator-group versus 1.8 percentage points to 74.4% (P = 0.24) for usual care. In the MRA subgroup, 3-month adherence to GDMT was almost identical: 30.5% (P = 0.14) and 30.3% (P = 0.37) for the two treatment groups, respectively, although the navigator-led patients averaged a larger increase of 4.6 versus 1.4 percentage points from baseline.
Adverse event rates were similar in both groups, although the navigator group had “slightly higher rates” of hypotension and hyperkalemia but no serious events, Dr. Desai said. This group also had similarly higher rates of worsening renal function, but most were asymptomatic change in creatinine that was addressed with medication changes, he said. There were no hospitalizations for adverse events.
He said the navigator-led optimization has potential in a community setting because the referral nature of Brigham and Women’s HF population “reflects potentially a worst-case scenario for such a program.” The greatest impact was seen in patients managed by general cardiologists, he said. “If we were to move this forward, which we hope to do with scale, the impact might be greater in a community population where there are fewer specialists and less severe illnesses present.”
This study represents a proof of concept, Dr. Desai said in an interview. “What we would like to do is demonstrate that this can be done on a larger scale,” he said. “That might involve partnership with a payer or health care system to see if we can replicate these findings across a broader range of providers.”
Dr. Desai disclosed financial relationships with Novartis, AstraZeneca, Abbott, Boehringer-Ingelheim, Coston Scientific, Biofourmis, DalCor, Relypsa, Regeneron, and Alnylam. Novartis provided an unrestricted grant for the investigator-initiated trial.
SOURCE: Desai AS. AHA 2019 Featured Science session AOS.07.
REPORTING FROM AHA 2019
Low RAAS inhibitor dosing linked to MACE risk
Suboptimal dosing of renin-angiotensin-aldosterone system (RAAS) inhibitors to reduce the risk of hyperkalemia could increase the risk of major adverse cardiac events (MACE) and all-cause mortality in patients with chronic kidney disease (CKD) or heart failure.
Researchers reported the outcomes of an observational study that explored the real-world associations between RAAS inhibitor dose, hyperkalemia, and clinical outcomes.
RAAS inhibitors – such as ACE inhibitors, angiotensin receptor blockers, and mineralocorticoid receptor antagonists – are known to reduce potassium excretion and therefore increase the risk of high potassium levels.
Dr. Cecilia Linde, from the Karolinska University Hospital and Karolinska Institutet in Stockholm, and coauthors wrote that management of serum potassium levels often requires reducing the dosage of RAAS inhibitors or stopping them altogether. However, this is also associated with risks in patients with heart failure or CKD.
In this study, researchers looked at data from 100,572 people with nondialysis CKD and 13,113 with new-onset heart failure who were prescribed RAAS inhibitors during 2006-2015.
Overall, 58% of patients with CKD and 63% of patients with heart failure spent the majority of follow-up on prescribed optimal doses of RAAS inhibitors – defined as at least 50% of the guidelines-recommended dose.
Patients with hyperkalemia were more likely to have down-titrations or discontinue their RAAS inhibitors, and this increased with increasing hyperkalemia severity.
The study found consistently lower mortality rates among patients who spent most of their follow-up time on at least 50% of the guideline-recommended dose of RAAS inhibitors.
In patients with CKD, mortality rates were 7.2 deaths per 1,000 patient-years in those taking at least 50% of the recommended dose, compared with 57.7 deaths per 1,000 patient-years for those on suboptimal doses. The rates of MACE were 73 and 130 per 1,000 patient-years, respectively.
The differences were even more pronounced in patients with heart failure. Those taking at least 50% of the recommended dose had mortality rates of 12.5 per 1000 patient-years, compared with 141.7 among those on suboptimal doses. The rates of MACE were 148.5 and 290.4, respectively.
“The results highlight the potential negative impact of suboptimal RAASi dosing, indicate the generalizability of [European Society of Cardiology–recommended] RAASi doses in HF to CKD patients, and emphasize the need for strategies that allow patients to be maintained on appropriate therapy, avoiding RAASi dose modification or discontinuation,” the authors wrote.
The study was funded by AstraZeneca. One author was an employee and stockholder of AstraZeneca, and five authors declared funding and support from the pharmaceutical sector, including AstraZeneca.
SOURCE: Linde C et al. J Am Heart Assoc. 2019 Nov 12. doi: 10.1161/JAHA.119.012655.
Suboptimal dosing of renin-angiotensin-aldosterone system (RAAS) inhibitors to reduce the risk of hyperkalemia could increase the risk of major adverse cardiac events (MACE) and all-cause mortality in patients with chronic kidney disease (CKD) or heart failure.
Researchers reported the outcomes of an observational study that explored the real-world associations between RAAS inhibitor dose, hyperkalemia, and clinical outcomes.
RAAS inhibitors – such as ACE inhibitors, angiotensin receptor blockers, and mineralocorticoid receptor antagonists – are known to reduce potassium excretion and therefore increase the risk of high potassium levels.
Dr. Cecilia Linde, from the Karolinska University Hospital and Karolinska Institutet in Stockholm, and coauthors wrote that management of serum potassium levels often requires reducing the dosage of RAAS inhibitors or stopping them altogether. However, this is also associated with risks in patients with heart failure or CKD.
In this study, researchers looked at data from 100,572 people with nondialysis CKD and 13,113 with new-onset heart failure who were prescribed RAAS inhibitors during 2006-2015.
Overall, 58% of patients with CKD and 63% of patients with heart failure spent the majority of follow-up on prescribed optimal doses of RAAS inhibitors – defined as at least 50% of the guidelines-recommended dose.
Patients with hyperkalemia were more likely to have down-titrations or discontinue their RAAS inhibitors, and this increased with increasing hyperkalemia severity.
The study found consistently lower mortality rates among patients who spent most of their follow-up time on at least 50% of the guideline-recommended dose of RAAS inhibitors.
In patients with CKD, mortality rates were 7.2 deaths per 1,000 patient-years in those taking at least 50% of the recommended dose, compared with 57.7 deaths per 1,000 patient-years for those on suboptimal doses. The rates of MACE were 73 and 130 per 1,000 patient-years, respectively.
The differences were even more pronounced in patients with heart failure. Those taking at least 50% of the recommended dose had mortality rates of 12.5 per 1000 patient-years, compared with 141.7 among those on suboptimal doses. The rates of MACE were 148.5 and 290.4, respectively.
“The results highlight the potential negative impact of suboptimal RAASi dosing, indicate the generalizability of [European Society of Cardiology–recommended] RAASi doses in HF to CKD patients, and emphasize the need for strategies that allow patients to be maintained on appropriate therapy, avoiding RAASi dose modification or discontinuation,” the authors wrote.
The study was funded by AstraZeneca. One author was an employee and stockholder of AstraZeneca, and five authors declared funding and support from the pharmaceutical sector, including AstraZeneca.
SOURCE: Linde C et al. J Am Heart Assoc. 2019 Nov 12. doi: 10.1161/JAHA.119.012655.
Suboptimal dosing of renin-angiotensin-aldosterone system (RAAS) inhibitors to reduce the risk of hyperkalemia could increase the risk of major adverse cardiac events (MACE) and all-cause mortality in patients with chronic kidney disease (CKD) or heart failure.
Researchers reported the outcomes of an observational study that explored the real-world associations between RAAS inhibitor dose, hyperkalemia, and clinical outcomes.
RAAS inhibitors – such as ACE inhibitors, angiotensin receptor blockers, and mineralocorticoid receptor antagonists – are known to reduce potassium excretion and therefore increase the risk of high potassium levels.
Dr. Cecilia Linde, from the Karolinska University Hospital and Karolinska Institutet in Stockholm, and coauthors wrote that management of serum potassium levels often requires reducing the dosage of RAAS inhibitors or stopping them altogether. However, this is also associated with risks in patients with heart failure or CKD.
In this study, researchers looked at data from 100,572 people with nondialysis CKD and 13,113 with new-onset heart failure who were prescribed RAAS inhibitors during 2006-2015.
Overall, 58% of patients with CKD and 63% of patients with heart failure spent the majority of follow-up on prescribed optimal doses of RAAS inhibitors – defined as at least 50% of the guidelines-recommended dose.
Patients with hyperkalemia were more likely to have down-titrations or discontinue their RAAS inhibitors, and this increased with increasing hyperkalemia severity.
The study found consistently lower mortality rates among patients who spent most of their follow-up time on at least 50% of the guideline-recommended dose of RAAS inhibitors.
In patients with CKD, mortality rates were 7.2 deaths per 1,000 patient-years in those taking at least 50% of the recommended dose, compared with 57.7 deaths per 1,000 patient-years for those on suboptimal doses. The rates of MACE were 73 and 130 per 1,000 patient-years, respectively.
The differences were even more pronounced in patients with heart failure. Those taking at least 50% of the recommended dose had mortality rates of 12.5 per 1000 patient-years, compared with 141.7 among those on suboptimal doses. The rates of MACE were 148.5 and 290.4, respectively.
“The results highlight the potential negative impact of suboptimal RAASi dosing, indicate the generalizability of [European Society of Cardiology–recommended] RAASi doses in HF to CKD patients, and emphasize the need for strategies that allow patients to be maintained on appropriate therapy, avoiding RAASi dose modification or discontinuation,” the authors wrote.
The study was funded by AstraZeneca. One author was an employee and stockholder of AstraZeneca, and five authors declared funding and support from the pharmaceutical sector, including AstraZeneca.
SOURCE: Linde C et al. J Am Heart Assoc. 2019 Nov 12. doi: 10.1161/JAHA.119.012655.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Hydroxychloroquine prevents congenital heart block recurrence in anti-Ro pregnancies
ATLANTA – Hydroxychloroquine (Plaquenil) 400 mg/day starting by pregnancy week 10 reduces recurrence of congenital heart block in infants born to women with anti-Ro antibodies, according to an open-label, prospective study presented at the annual meeting of the American College of Rheumatology.
Among antibody-positive women who had a previous pregnancy complicated by congenital heart block (CHB), the regimen reduced recurrence in a subsequent pregnancy from the expected historical rate of 18% to 7.4%, a more than 50% drop. “Given the potential benefit of hydroxychloroquine” (HCQ) and its relative safety during pregnancy, “testing all pregnancies for anti-Ro antibodies, regardless of maternal health, should be considered,” concluded investigators led by rheumatologist Peter Izmirly, MD, associate professor of medicine at New York (N.Y.) University.
About 40% of women with systemic lupus erythematosus and nearly 100% of women with Sjögren’s syndrome, as well as about 1% of women in the general population, have anti-Ro antibodies. They can be present in completely asymptomatic women, which is why the authors called for general screening. Indeed, half of the women in the trial had no or only mild, undifferentiated rheumatic symptoms. Often, “women who carry anti-Ro antibodies have no idea they have them” until they have a child with CHB and are tested, Dr. Izmirly said.
The antibodies cross the placenta and interfere with the normal development of the AV node; about 18% of infants die and most of the rest require lifelong pacing. The risk of CHB in antibody-positive women is about 2%, but once a child is born with the condition, the risk climbs to about 18% in subsequent pregnancies.
Years ago, Dr. Izmirly and his colleagues had a hunch that HCQ might help because it disrupts the toll-like receptor signaling involved in the disease process. A database review he led added weight to the idea, finding that among 257 anti-Ro positive pregnancies, the rate of CHB was 7.5% among the 40 women who happened to take HCQ, versus 21.2% among the 217 who did not. “We wanted to see if we could replicate that prospectively,” he said.
The Preventive Approach to Congenital Heart Block with Hydroxychloroquine (PATCH) trial enrolled 54 antibody positive women with a previous CHB pregnancy. They were started on 400 mg/day HCQ by gestation week 10.
There were four cases of second- or third-degree CHB among the women (7.4%, P = 0.02), all detected by fetal echocardiogram around week 20.
Nine of the women were treated with IVIG and/or dexamethasone for lupus flares or fetal heart issues other than advanced block, which confounded the results. To analyze the effect in a purely HCQ cohort, the team recruited an additional nine women not treated with any other medication during pregnancy, one of whose fetus developed third-degree heart block.
In total, 5 of 63 pregnancies (7.9%) resulted in advanced block. Among the 54 women exposed only to HCQ, the rate of second- or third-degree block was again 7.4% (4 of 54, P = .02). HCQ compliance, assessed by maternal blood levels above 200 ng/mL at least once, was 98%, and cord blood confirmed fetal exposure to HCQ.
Once detected, CHB was treated with dexamethasone or IVIG. One case progressed to cardiomyopathy, and the pregnancy was terminated. Another child required pacing after birth. Other children reverted to normal sinus rhythm but had intermittent second-degree block at age 2.
Overall, “the safety in this study was excellent,” said rheumatologist and senior investigator Jill Buyon, MD, director of the division of rheumatology at New York University.
The complications – nine births before 37 weeks, one infant small for gestational age – were not unexpected in a rheumatic population. “We were very nervous about Plaquenil cardiomyopathy” in the pregnancy that was terminated, but there was no evidence of it on histology.
The children will have ocular optical coherence tomography at age 5 to check for retinal toxicity; the 12 who have been tested so far show no obvious signs. Dr. Izmirly said he doesn’t expect to see any problems. “We are just being super cautious.”
The audience had questions about why the trial didn’t have a placebo arm. He explained that CHB is a rare event – one in 15,000 pregnancies – and it took 8 years just to adequately power the single-arm study; recruiting more than 100 additional women for a placebo-controlled trial wasn’t practical.
Also, “there was no way” women were going to be randomized to placebo when HCQ seemed so promising; 35% of the enrollees had already lost a child to CHB. “Everyone wanted the drug,” Dr. Izmirly said.
The majority of women were white, and about half met criteria for lupus and/or Sjögren’s. Anti-Ro levels remained above 1,000 EU throughout pregnancy. Women were excluded if they were taking high-dose prednisone or any dose of fluorinated corticosteroids at baseline.
The National Institutes of Health funded the work. The investigators had no relevant disclosures.
SOURCE: Izmirly P et al. Arthritis Rheumatol. 2019;71(suppl 10). Abstract 1761.
ATLANTA – Hydroxychloroquine (Plaquenil) 400 mg/day starting by pregnancy week 10 reduces recurrence of congenital heart block in infants born to women with anti-Ro antibodies, according to an open-label, prospective study presented at the annual meeting of the American College of Rheumatology.
Among antibody-positive women who had a previous pregnancy complicated by congenital heart block (CHB), the regimen reduced recurrence in a subsequent pregnancy from the expected historical rate of 18% to 7.4%, a more than 50% drop. “Given the potential benefit of hydroxychloroquine” (HCQ) and its relative safety during pregnancy, “testing all pregnancies for anti-Ro antibodies, regardless of maternal health, should be considered,” concluded investigators led by rheumatologist Peter Izmirly, MD, associate professor of medicine at New York (N.Y.) University.
About 40% of women with systemic lupus erythematosus and nearly 100% of women with Sjögren’s syndrome, as well as about 1% of women in the general population, have anti-Ro antibodies. They can be present in completely asymptomatic women, which is why the authors called for general screening. Indeed, half of the women in the trial had no or only mild, undifferentiated rheumatic symptoms. Often, “women who carry anti-Ro antibodies have no idea they have them” until they have a child with CHB and are tested, Dr. Izmirly said.
The antibodies cross the placenta and interfere with the normal development of the AV node; about 18% of infants die and most of the rest require lifelong pacing. The risk of CHB in antibody-positive women is about 2%, but once a child is born with the condition, the risk climbs to about 18% in subsequent pregnancies.
Years ago, Dr. Izmirly and his colleagues had a hunch that HCQ might help because it disrupts the toll-like receptor signaling involved in the disease process. A database review he led added weight to the idea, finding that among 257 anti-Ro positive pregnancies, the rate of CHB was 7.5% among the 40 women who happened to take HCQ, versus 21.2% among the 217 who did not. “We wanted to see if we could replicate that prospectively,” he said.
The Preventive Approach to Congenital Heart Block with Hydroxychloroquine (PATCH) trial enrolled 54 antibody positive women with a previous CHB pregnancy. They were started on 400 mg/day HCQ by gestation week 10.
There were four cases of second- or third-degree CHB among the women (7.4%, P = 0.02), all detected by fetal echocardiogram around week 20.
Nine of the women were treated with IVIG and/or dexamethasone for lupus flares or fetal heart issues other than advanced block, which confounded the results. To analyze the effect in a purely HCQ cohort, the team recruited an additional nine women not treated with any other medication during pregnancy, one of whose fetus developed third-degree heart block.
In total, 5 of 63 pregnancies (7.9%) resulted in advanced block. Among the 54 women exposed only to HCQ, the rate of second- or third-degree block was again 7.4% (4 of 54, P = .02). HCQ compliance, assessed by maternal blood levels above 200 ng/mL at least once, was 98%, and cord blood confirmed fetal exposure to HCQ.
Once detected, CHB was treated with dexamethasone or IVIG. One case progressed to cardiomyopathy, and the pregnancy was terminated. Another child required pacing after birth. Other children reverted to normal sinus rhythm but had intermittent second-degree block at age 2.
Overall, “the safety in this study was excellent,” said rheumatologist and senior investigator Jill Buyon, MD, director of the division of rheumatology at New York University.
The complications – nine births before 37 weeks, one infant small for gestational age – were not unexpected in a rheumatic population. “We were very nervous about Plaquenil cardiomyopathy” in the pregnancy that was terminated, but there was no evidence of it on histology.
The children will have ocular optical coherence tomography at age 5 to check for retinal toxicity; the 12 who have been tested so far show no obvious signs. Dr. Izmirly said he doesn’t expect to see any problems. “We are just being super cautious.”
The audience had questions about why the trial didn’t have a placebo arm. He explained that CHB is a rare event – one in 15,000 pregnancies – and it took 8 years just to adequately power the single-arm study; recruiting more than 100 additional women for a placebo-controlled trial wasn’t practical.
Also, “there was no way” women were going to be randomized to placebo when HCQ seemed so promising; 35% of the enrollees had already lost a child to CHB. “Everyone wanted the drug,” Dr. Izmirly said.
The majority of women were white, and about half met criteria for lupus and/or Sjögren’s. Anti-Ro levels remained above 1,000 EU throughout pregnancy. Women were excluded if they were taking high-dose prednisone or any dose of fluorinated corticosteroids at baseline.
The National Institutes of Health funded the work. The investigators had no relevant disclosures.
SOURCE: Izmirly P et al. Arthritis Rheumatol. 2019;71(suppl 10). Abstract 1761.
ATLANTA – Hydroxychloroquine (Plaquenil) 400 mg/day starting by pregnancy week 10 reduces recurrence of congenital heart block in infants born to women with anti-Ro antibodies, according to an open-label, prospective study presented at the annual meeting of the American College of Rheumatology.
Among antibody-positive women who had a previous pregnancy complicated by congenital heart block (CHB), the regimen reduced recurrence in a subsequent pregnancy from the expected historical rate of 18% to 7.4%, a more than 50% drop. “Given the potential benefit of hydroxychloroquine” (HCQ) and its relative safety during pregnancy, “testing all pregnancies for anti-Ro antibodies, regardless of maternal health, should be considered,” concluded investigators led by rheumatologist Peter Izmirly, MD, associate professor of medicine at New York (N.Y.) University.
About 40% of women with systemic lupus erythematosus and nearly 100% of women with Sjögren’s syndrome, as well as about 1% of women in the general population, have anti-Ro antibodies. They can be present in completely asymptomatic women, which is why the authors called for general screening. Indeed, half of the women in the trial had no or only mild, undifferentiated rheumatic symptoms. Often, “women who carry anti-Ro antibodies have no idea they have them” until they have a child with CHB and are tested, Dr. Izmirly said.
The antibodies cross the placenta and interfere with the normal development of the AV node; about 18% of infants die and most of the rest require lifelong pacing. The risk of CHB in antibody-positive women is about 2%, but once a child is born with the condition, the risk climbs to about 18% in subsequent pregnancies.
Years ago, Dr. Izmirly and his colleagues had a hunch that HCQ might help because it disrupts the toll-like receptor signaling involved in the disease process. A database review he led added weight to the idea, finding that among 257 anti-Ro positive pregnancies, the rate of CHB was 7.5% among the 40 women who happened to take HCQ, versus 21.2% among the 217 who did not. “We wanted to see if we could replicate that prospectively,” he said.
The Preventive Approach to Congenital Heart Block with Hydroxychloroquine (PATCH) trial enrolled 54 antibody positive women with a previous CHB pregnancy. They were started on 400 mg/day HCQ by gestation week 10.
There were four cases of second- or third-degree CHB among the women (7.4%, P = 0.02), all detected by fetal echocardiogram around week 20.
Nine of the women were treated with IVIG and/or dexamethasone for lupus flares or fetal heart issues other than advanced block, which confounded the results. To analyze the effect in a purely HCQ cohort, the team recruited an additional nine women not treated with any other medication during pregnancy, one of whose fetus developed third-degree heart block.
In total, 5 of 63 pregnancies (7.9%) resulted in advanced block. Among the 54 women exposed only to HCQ, the rate of second- or third-degree block was again 7.4% (4 of 54, P = .02). HCQ compliance, assessed by maternal blood levels above 200 ng/mL at least once, was 98%, and cord blood confirmed fetal exposure to HCQ.
Once detected, CHB was treated with dexamethasone or IVIG. One case progressed to cardiomyopathy, and the pregnancy was terminated. Another child required pacing after birth. Other children reverted to normal sinus rhythm but had intermittent second-degree block at age 2.
Overall, “the safety in this study was excellent,” said rheumatologist and senior investigator Jill Buyon, MD, director of the division of rheumatology at New York University.
The complications – nine births before 37 weeks, one infant small for gestational age – were not unexpected in a rheumatic population. “We were very nervous about Plaquenil cardiomyopathy” in the pregnancy that was terminated, but there was no evidence of it on histology.
The children will have ocular optical coherence tomography at age 5 to check for retinal toxicity; the 12 who have been tested so far show no obvious signs. Dr. Izmirly said he doesn’t expect to see any problems. “We are just being super cautious.”
The audience had questions about why the trial didn’t have a placebo arm. He explained that CHB is a rare event – one in 15,000 pregnancies – and it took 8 years just to adequately power the single-arm study; recruiting more than 100 additional women for a placebo-controlled trial wasn’t practical.
Also, “there was no way” women were going to be randomized to placebo when HCQ seemed so promising; 35% of the enrollees had already lost a child to CHB. “Everyone wanted the drug,” Dr. Izmirly said.
The majority of women were white, and about half met criteria for lupus and/or Sjögren’s. Anti-Ro levels remained above 1,000 EU throughout pregnancy. Women were excluded if they were taking high-dose prednisone or any dose of fluorinated corticosteroids at baseline.
The National Institutes of Health funded the work. The investigators had no relevant disclosures.
SOURCE: Izmirly P et al. Arthritis Rheumatol. 2019;71(suppl 10). Abstract 1761.
REPORTING FROM ACR 2019
Mechanical circulatory support in PCI needs clearer guidance
PHILADELPHIA – Use of the Impella ventricular-assist device in patients with cardiogenic shock having percutaneous coronary interventions (PCI) has increased rapidly since its approval in 2008, but two studies comparing it with intra-aortic balloon pumps in PCI patients have raised questions about the safety, effectiveness, and cost of the ventricular-assist device, according to results of two studies presented at the American Heart Association scientific sessions.
The results of an observational analysis of 48,306 patients and a national real-world study of 28,304 patients may not be telling the complete story of the utility of ventricular assist in patients requiring mechanical circulatory support (MCS), one interventional cardiologist said in an interview. “It’s concerning; it’s sobering,” said Ranya N. Sweis, MD, of Northwestern University, Chicago. However, the data didn’t parse out patients who would have been routed to palliative care and otherwise wouldn’t have been candidates for PCI without MCS.
“What I take from it is that we need to get more randomized data,” she said. “Who are the patients that were doing worse? Who are the patients who really needed the Impella support for the PCI after cardiogenic shock?”
In the observational study, Amit P. Amin, MD, of Washington University, St. Louis, said that the use of MCS devices increased steadily to 32% of all PCI patients receiving MCS from 2008 to 2016 while use of intra-aortic balloon pump (IABP) declined, but that Impella was less likely to be used in critically ill patients. The study analyzed patients in the Premier Healthcare Database who had PCI with MCS at 432 hospitals from 2004 to 2016.
Outcomes in what Dr. Amin called “the Impella era,” showed significantly higher risks for death, acute kidney injury, and stroke, with odds ratios of 1.17, 1.91 and 3.34, respectively (P less than .001 for all). In the patient-level comparison of Impella versus IABP, Impella had a 24% higher risk of death (P less than .0001), 10% for bleeding (P = .0445), 8% for acute kidney injury (P = .0521) and 34% for stroke (P less than .0001). The findings were published simultaneously with the presentation (Circulation. 2019 Nov 17. doi: 10.1161/CIRCULATIONAHA.119.044007)
“The total length of stay, as well as the ICU length of stay, were actually lower with Impella use, by approximately a half day to 1 day,” Dr. Amin said. “Despite that, the total costs were approximately $15,000.”
Yet, the study found wide variation in the use of Impella among hospitals, some doing no cases with the device and others all of them, Dr. Amin said. The risk analysis also found wide variations in outcomes across hospitals using Impella. “We saw a 2.5-fold variation in bleeding across hospitals and a 1.5-fold variation in acute kidney injury, stroke and death,” he noted. The study found less variation in hospital stays and total cost of Impella, “perhaps related to the uniformly high device acquisition costs.”
“These data underscore the need for defining the appropriate use of mechanical circulatory support in patients undergoing PCI,” Dr. Amin said.
Dr. Sweis wasn’t surprised by the cost findings. “New technology is going to cost more,” she said in an interview. “I’m actually surprised that the cost wasn’t more significantly different just knowing the cost of some of these devices.
Patients who require MCS represent a small portion of PCI cases: 2%, according to Dr. Sweis. “It’s not like all PCI has increased because of MCS, and there’s a potential improvement in the length of stay so there are going to be cost savings that way.”
The national real-world study that Sanket S. Dhruva, MD, MHS, of the University of California San Francisco, reported on focused on Impella and IABP in PCI patients with acute MI complicated by cardiogenic shock (CS). The study used outcomes of patients with AMI-CS who had PCI from October 2015 to December 2017 in the National Cardiovascular Data Registry’s CathPCI and Chest Pain–MI registries. An estimated 4%-12% of AMIs present with CS.
Most patients in the study population had medical therapy only, but this study focused on the 1,768 who had Impella only and the 8,471 who had IABP only. The rates of in-hospital death and bleeding were 34.1% 16% in the IABP group, and 45% and 31.3% in the Impella group, Dr. Dhruva said. In this study population, the rate of Impella use increased from 3.5% in 2015 to 8.7% by the end of 2017 (P less than .001).
Dr. Dhruva acknowledged a number of limitations to the study findings, including residual confounding. However, the “robust propensity match” of 95% of the Impella-only patients and the results were consistent across multiple sensitivity analyses. “There may have been questions about the clinical severity of AMI-CS patients in the NCDR Registry,” he said. “However, the registry definition is similar to that used in the trials.”
The trial also failed to distinguish between the different types of Impella devices, but the results mostly pertain to the Impella 2.5 and CP because the 5.0 device requires a surgical cutdown, and the study excluded patients who received multiple devices.
“Better evidence and guidance are needed regarding the optimal management of patients with AMI-CS as well as the role of mechanical circulatory support devices in general and Impella in particular,” he said, adding that Impella has been on the U.S. market since 2008, but with limited randomized clinical trial evidence in cardiogenic shock.
The study population of patient’s with CS is “only a piece of the puzzle,” Dr. Sweis said. “We know that there are sick hearts that aren’t in shock right now, but you’re going to do triple-vessel intervention and use atherectomy. Those patients would not do very well during the procedure itself and it may not even be offered to them if there weren’t support.”
Impella is not going away, Dr. Sweis said. “It provides an option that a patient wouldn’t otherwise have. This is really stressing to me that we need to get rid of that variability in the safety related to these devices.”
Dr. Amin disclosed financial relationships with Terumo and GE Healthcare. Dr. Dhruva had no financial relationships to disclose. The study was supported in part by a Center of Excellence in Regulatory Science and Innovation grant from the Food and Drug Administration and the American College of Cardiology’s National Cardiovascular Data Registry.
PHILADELPHIA – Use of the Impella ventricular-assist device in patients with cardiogenic shock having percutaneous coronary interventions (PCI) has increased rapidly since its approval in 2008, but two studies comparing it with intra-aortic balloon pumps in PCI patients have raised questions about the safety, effectiveness, and cost of the ventricular-assist device, according to results of two studies presented at the American Heart Association scientific sessions.
The results of an observational analysis of 48,306 patients and a national real-world study of 28,304 patients may not be telling the complete story of the utility of ventricular assist in patients requiring mechanical circulatory support (MCS), one interventional cardiologist said in an interview. “It’s concerning; it’s sobering,” said Ranya N. Sweis, MD, of Northwestern University, Chicago. However, the data didn’t parse out patients who would have been routed to palliative care and otherwise wouldn’t have been candidates for PCI without MCS.
“What I take from it is that we need to get more randomized data,” she said. “Who are the patients that were doing worse? Who are the patients who really needed the Impella support for the PCI after cardiogenic shock?”
In the observational study, Amit P. Amin, MD, of Washington University, St. Louis, said that the use of MCS devices increased steadily to 32% of all PCI patients receiving MCS from 2008 to 2016 while use of intra-aortic balloon pump (IABP) declined, but that Impella was less likely to be used in critically ill patients. The study analyzed patients in the Premier Healthcare Database who had PCI with MCS at 432 hospitals from 2004 to 2016.
Outcomes in what Dr. Amin called “the Impella era,” showed significantly higher risks for death, acute kidney injury, and stroke, with odds ratios of 1.17, 1.91 and 3.34, respectively (P less than .001 for all). In the patient-level comparison of Impella versus IABP, Impella had a 24% higher risk of death (P less than .0001), 10% for bleeding (P = .0445), 8% for acute kidney injury (P = .0521) and 34% for stroke (P less than .0001). The findings were published simultaneously with the presentation (Circulation. 2019 Nov 17. doi: 10.1161/CIRCULATIONAHA.119.044007)
“The total length of stay, as well as the ICU length of stay, were actually lower with Impella use, by approximately a half day to 1 day,” Dr. Amin said. “Despite that, the total costs were approximately $15,000.”
Yet, the study found wide variation in the use of Impella among hospitals, some doing no cases with the device and others all of them, Dr. Amin said. The risk analysis also found wide variations in outcomes across hospitals using Impella. “We saw a 2.5-fold variation in bleeding across hospitals and a 1.5-fold variation in acute kidney injury, stroke and death,” he noted. The study found less variation in hospital stays and total cost of Impella, “perhaps related to the uniformly high device acquisition costs.”
“These data underscore the need for defining the appropriate use of mechanical circulatory support in patients undergoing PCI,” Dr. Amin said.
Dr. Sweis wasn’t surprised by the cost findings. “New technology is going to cost more,” she said in an interview. “I’m actually surprised that the cost wasn’t more significantly different just knowing the cost of some of these devices.
Patients who require MCS represent a small portion of PCI cases: 2%, according to Dr. Sweis. “It’s not like all PCI has increased because of MCS, and there’s a potential improvement in the length of stay so there are going to be cost savings that way.”
The national real-world study that Sanket S. Dhruva, MD, MHS, of the University of California San Francisco, reported on focused on Impella and IABP in PCI patients with acute MI complicated by cardiogenic shock (CS). The study used outcomes of patients with AMI-CS who had PCI from October 2015 to December 2017 in the National Cardiovascular Data Registry’s CathPCI and Chest Pain–MI registries. An estimated 4%-12% of AMIs present with CS.
Most patients in the study population had medical therapy only, but this study focused on the 1,768 who had Impella only and the 8,471 who had IABP only. The rates of in-hospital death and bleeding were 34.1% 16% in the IABP group, and 45% and 31.3% in the Impella group, Dr. Dhruva said. In this study population, the rate of Impella use increased from 3.5% in 2015 to 8.7% by the end of 2017 (P less than .001).
Dr. Dhruva acknowledged a number of limitations to the study findings, including residual confounding. However, the “robust propensity match” of 95% of the Impella-only patients and the results were consistent across multiple sensitivity analyses. “There may have been questions about the clinical severity of AMI-CS patients in the NCDR Registry,” he said. “However, the registry definition is similar to that used in the trials.”
The trial also failed to distinguish between the different types of Impella devices, but the results mostly pertain to the Impella 2.5 and CP because the 5.0 device requires a surgical cutdown, and the study excluded patients who received multiple devices.
“Better evidence and guidance are needed regarding the optimal management of patients with AMI-CS as well as the role of mechanical circulatory support devices in general and Impella in particular,” he said, adding that Impella has been on the U.S. market since 2008, but with limited randomized clinical trial evidence in cardiogenic shock.
The study population of patient’s with CS is “only a piece of the puzzle,” Dr. Sweis said. “We know that there are sick hearts that aren’t in shock right now, but you’re going to do triple-vessel intervention and use atherectomy. Those patients would not do very well during the procedure itself and it may not even be offered to them if there weren’t support.”
Impella is not going away, Dr. Sweis said. “It provides an option that a patient wouldn’t otherwise have. This is really stressing to me that we need to get rid of that variability in the safety related to these devices.”
Dr. Amin disclosed financial relationships with Terumo and GE Healthcare. Dr. Dhruva had no financial relationships to disclose. The study was supported in part by a Center of Excellence in Regulatory Science and Innovation grant from the Food and Drug Administration and the American College of Cardiology’s National Cardiovascular Data Registry.
PHILADELPHIA – Use of the Impella ventricular-assist device in patients with cardiogenic shock having percutaneous coronary interventions (PCI) has increased rapidly since its approval in 2008, but two studies comparing it with intra-aortic balloon pumps in PCI patients have raised questions about the safety, effectiveness, and cost of the ventricular-assist device, according to results of two studies presented at the American Heart Association scientific sessions.
The results of an observational analysis of 48,306 patients and a national real-world study of 28,304 patients may not be telling the complete story of the utility of ventricular assist in patients requiring mechanical circulatory support (MCS), one interventional cardiologist said in an interview. “It’s concerning; it’s sobering,” said Ranya N. Sweis, MD, of Northwestern University, Chicago. However, the data didn’t parse out patients who would have been routed to palliative care and otherwise wouldn’t have been candidates for PCI without MCS.
“What I take from it is that we need to get more randomized data,” she said. “Who are the patients that were doing worse? Who are the patients who really needed the Impella support for the PCI after cardiogenic shock?”
In the observational study, Amit P. Amin, MD, of Washington University, St. Louis, said that the use of MCS devices increased steadily to 32% of all PCI patients receiving MCS from 2008 to 2016 while use of intra-aortic balloon pump (IABP) declined, but that Impella was less likely to be used in critically ill patients. The study analyzed patients in the Premier Healthcare Database who had PCI with MCS at 432 hospitals from 2004 to 2016.
Outcomes in what Dr. Amin called “the Impella era,” showed significantly higher risks for death, acute kidney injury, and stroke, with odds ratios of 1.17, 1.91 and 3.34, respectively (P less than .001 for all). In the patient-level comparison of Impella versus IABP, Impella had a 24% higher risk of death (P less than .0001), 10% for bleeding (P = .0445), 8% for acute kidney injury (P = .0521) and 34% for stroke (P less than .0001). The findings were published simultaneously with the presentation (Circulation. 2019 Nov 17. doi: 10.1161/CIRCULATIONAHA.119.044007)
“The total length of stay, as well as the ICU length of stay, were actually lower with Impella use, by approximately a half day to 1 day,” Dr. Amin said. “Despite that, the total costs were approximately $15,000.”
Yet, the study found wide variation in the use of Impella among hospitals, some doing no cases with the device and others all of them, Dr. Amin said. The risk analysis also found wide variations in outcomes across hospitals using Impella. “We saw a 2.5-fold variation in bleeding across hospitals and a 1.5-fold variation in acute kidney injury, stroke and death,” he noted. The study found less variation in hospital stays and total cost of Impella, “perhaps related to the uniformly high device acquisition costs.”
“These data underscore the need for defining the appropriate use of mechanical circulatory support in patients undergoing PCI,” Dr. Amin said.
Dr. Sweis wasn’t surprised by the cost findings. “New technology is going to cost more,” she said in an interview. “I’m actually surprised that the cost wasn’t more significantly different just knowing the cost of some of these devices.
Patients who require MCS represent a small portion of PCI cases: 2%, according to Dr. Sweis. “It’s not like all PCI has increased because of MCS, and there’s a potential improvement in the length of stay so there are going to be cost savings that way.”
The national real-world study that Sanket S. Dhruva, MD, MHS, of the University of California San Francisco, reported on focused on Impella and IABP in PCI patients with acute MI complicated by cardiogenic shock (CS). The study used outcomes of patients with AMI-CS who had PCI from October 2015 to December 2017 in the National Cardiovascular Data Registry’s CathPCI and Chest Pain–MI registries. An estimated 4%-12% of AMIs present with CS.
Most patients in the study population had medical therapy only, but this study focused on the 1,768 who had Impella only and the 8,471 who had IABP only. The rates of in-hospital death and bleeding were 34.1% 16% in the IABP group, and 45% and 31.3% in the Impella group, Dr. Dhruva said. In this study population, the rate of Impella use increased from 3.5% in 2015 to 8.7% by the end of 2017 (P less than .001).
Dr. Dhruva acknowledged a number of limitations to the study findings, including residual confounding. However, the “robust propensity match” of 95% of the Impella-only patients and the results were consistent across multiple sensitivity analyses. “There may have been questions about the clinical severity of AMI-CS patients in the NCDR Registry,” he said. “However, the registry definition is similar to that used in the trials.”
The trial also failed to distinguish between the different types of Impella devices, but the results mostly pertain to the Impella 2.5 and CP because the 5.0 device requires a surgical cutdown, and the study excluded patients who received multiple devices.
“Better evidence and guidance are needed regarding the optimal management of patients with AMI-CS as well as the role of mechanical circulatory support devices in general and Impella in particular,” he said, adding that Impella has been on the U.S. market since 2008, but with limited randomized clinical trial evidence in cardiogenic shock.
The study population of patient’s with CS is “only a piece of the puzzle,” Dr. Sweis said. “We know that there are sick hearts that aren’t in shock right now, but you’re going to do triple-vessel intervention and use atherectomy. Those patients would not do very well during the procedure itself and it may not even be offered to them if there weren’t support.”
Impella is not going away, Dr. Sweis said. “It provides an option that a patient wouldn’t otherwise have. This is really stressing to me that we need to get rid of that variability in the safety related to these devices.”
Dr. Amin disclosed financial relationships with Terumo and GE Healthcare. Dr. Dhruva had no financial relationships to disclose. The study was supported in part by a Center of Excellence in Regulatory Science and Innovation grant from the Food and Drug Administration and the American College of Cardiology’s National Cardiovascular Data Registry.
REPORTING FROM AHA 2019
End ‘therapeutic nihilism’ in care of older diabetic patients, says expert
LOS ANGELES – In the opinion of Richard Pratley, MD, it’s time for diabetes treatment guidelines to evolve in light of accumulating data from cardiovascular outcome trials in type 2 diabetes.
“They have evolved for the general patient population, and this should apply to older individuals as well,” Dr. Pratley said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “My fear is, there is therapeutic nihilism, the idea that by the time someone is 75 years old, the horse is out of the barn and you’re not going to be able to impact outcomes with directed therapy. I don’t think that’s true. Our current treatment guidelines for the treatment of diabetes in older individuals remain focused on glycemic control. It’s not hyperglycemia that’s killing people; it’s heart disease and renal disease.”
According to data from the United Nations, about 12% of the global population is older than 60. By 2050, that number is expected to reach 20%, which will continue to drive an epidemic of diabetes in the near future. Dr. Pratley, medical director of AdventHealth Diabetes Institute in Orlando, pointed out that diabetes in older individuals is not a homogeneous condition. “There are many people in my clinic who had type 1 diabetes diagnosed as kids, but I also have patients who have adult-onset type 1 diabetes,” he said. “We also have type 2 patients who can be diagnosed in their 20s, 30s, or 40s, and there are people who are diagnosed in their 70s and 80s. Now we are learning that there are different subtypes of diabetes; so even type 2 diabetes is not a homogeneous condition. There are people who are more insulin resistant or have more of an insulin secretory defect, and there’s a special type of older-onset type 2 diabetes. When you consider all this in talking about diabetes treatments, about 30% of patients in the United States are diagnosed [when they are] over the age of 60, so this is an ongoing issue.”
Older adults with diabetes may have longstanding diabetes with associated microvascular and macrovascular complications, he continued, or they may have newly diagnosed diabetes with evidence of end organ complications at the time of presentation. Or, they may have newly diagnosed diabetes without evidence of complications. “Does this matter? It does,” Dr. Pratley said. “The things we worry about with all patients with diabetes are the microvascular complications, but I would argue that the macrovascular complications, particularly diabetic nephropathy, are things we should have a laser focus on, because they have high morbidity and mortality, especially in older individuals.”
There are more than 28 cardiovascular outcomes trials in patients with type 2 diabetes ongoing or completed, and involving eight classes of medications, with more than 200,000 planned participants, Dr. Pratley said. Of those participants, 90,000 are older than 65 years, and 30,000 are older than 75 years. “This is great,” he said. “Not only do these cardiovascular outcome studies give us a lot of information about the safety and efficacy of these drugs in the general population, we can now dig in to this specific patient population.” For example, in cardiovascular outcomes trials with dipeptidyl peptidase–4 (DPP-4) inhibitors, the mean age of patients was 65. About half of the patients were older than 65, and 10%-14% were older than 75.
Investigators in the SAVOR-TIMI 53 trial examined age in one of their subgroup analyses (Diabetes Care. 2015;38:1145-53). In that study with saxagliptin, among people older than 65 who received the study drug, the hazard ratio for major adverse cardiac events (MACE) was 0.92, compared with 1.15 for those younger than 65 (P value for interaction = .058). “So older people did great [on this drug],” Dr. Pratley said. “In fact, they had a bit of a decreased risk.” A similar association was seen in adults aged 75 years and older (HR, 1.01 in those younger than 75 years, vs. 0.95 in those aged 75 years and older; P value for interaction = .673). “This is telling us that saxagliptin is safe in the older population.”
In the EXAMINE trial, in which patients with type 2 diabetes who had had a recent acute coronary syndrome received either alogliptin or placebo, researchers conducted an analysis of patients older and younger than 65 (N Engl J Med. 2013;369:1327-35). They observed no significant interactions on the primary composite cardiovascular outcome in those younger than 65 (HR, 0.91) and those aged 65 and older (HR, 0.98).
Dr. Pratley noted that in cardiovascular outcome trials with sodium-glucose transporter 2 (SGLT2) inhibitors, the mean age of patients was 64, and 48%-50% of them were older than 65. In the EMPA-REG OUTCOME trial of empagliflozin, the hazard ratio for the primary cardiovascular outcome was 1.04 in patients younger than 65 and 0.71 in those aged 65 and older (P = .01; N Engl J Med, 2015;373:2117-28). “That was a significant interaction,” he said. In addition, the hazard ratio for cardiovascular death was 0.72 in those younger than 65, and 0.54 in those aged 65 and older (P = .21). “There was not a significant interaction here, but clearly there was some trending in the older patient population,” Dr. Pratley said.
In the LEADER study of liraglutide in patients with diabetes, the hazard ratio for the primary composite cardiovascular outcome was 0.87 in the overall population, 0.78 in patients younger than 60, and 0.90 in those aged 60 and older (P = 0.27; N Engl J Med. 2016;375:311-22). In a post hoc analysis that stratified LEADER patients into younger than 75 and 75 and older, the researchers observed a 31% reduction in the 75 and older population, compared with a 10% reduction in the younger population (P for interaction = .09; Ann Intern Med. 2019;170[6]:423-6). “This was driven largely by a decrease in nonfatal [myocardial infarction],” said Dr. Pratley, who was one of the study investigators. “But in patients who were 75 years and older, there was a 30% reduction in all-cause mortality in those treated with liraglutide, compared with 12% in those younger than 75 (P for interaction = .22). That interaction is not significant, but the theme here is that older populations do quite well.”
Based on such evidence, he said, In particular, SGLT2 inhibitors and certain GLP-1 receptor agonists may be associated with an additional benefit in older individuals with cardiovascular disease, “perhaps because they’re the ones at highest risk,” Dr. Pratley said. “But we need further studies to better identify those older individuals who may be at highest risk of adverse cardiovascular complications from diabetes and who might benefit from targeted therapies.”
Many questions remain unanswered in efforts to provide optimal care to older adults with diabetes. “One of the problems is being inclusive in the older patient population,” Dr. Pratley said. “We tried to do a study of frail older individuals looking at different treatments and policies. It was difficult to recruit frail older individuals, even though they routinely are treated with the drugs we study in healthier populations. We need to know how to enroll patients, and which investigators are going to do these trials. Who is going to support these trials? Pharma? The NIH?”
Then there’s the question of what appropriate outcomes are in older individuals. “I think we can agree that hemoglobin A1c is a surrogate of microvascular complications,” he said. “Do we need to be looking at outcomes like MACE, hospitalization for heart failure, death, progression of [chronic kidney disease], and perhaps cognitive function, physical function, sarcopenia, and quality of life?”
Dr. Pratley called for the development of a personalized approach to diabetes management that takes into account heterogeneity in disease pathogenesis, comorbidities, and patient preference.
“We need to change the focus to patient-important outcomes: dying, heart attack, strokes, and avoid therapeutic nihilism, which is still pervasive among many practitioners,” he said. “We also need to partner with primary care, because they take care of the majority of older individuals, and they need to understand how we’re evolving the goals of therapy. We need to educate them about the new guidelines and try to get them on board with some of the latest data that will help improve outcomes in our patients. We also need to understand the cost of diabetes and the cost effectiveness of interventions.”
He also recommends the development of a comprehensive evidence base for the use of drugs in older individuals. “I suggest pooled analyses within clinical development programs,” he said. “That’s been done for most development programs, but the phase 3 studies tend to enroll younger, healthier individuals. It would be good to do a meta-analysis across CVOTs [cardiovascular outcome trials] within different classes of medications.”
Dr. Pratley disclosed that all honoraria and fees he receives are directed to AdventHealth. These include serving on the advisory board or as consultant to AstraZeneca, GlaxoSmithKline, Glytec, Janssen, Ligand, Lilly, Merck, Mundipharma, Novo Nordisk, and Sanofi. He also has served as a speaker for AstraZeneca and Novo Nordisk, and has received research support from Lexicon, Ligand, Lilly, Merck, Novo Nordisk, and Sanofi. He receives no direct or indirect compensation.
LOS ANGELES – In the opinion of Richard Pratley, MD, it’s time for diabetes treatment guidelines to evolve in light of accumulating data from cardiovascular outcome trials in type 2 diabetes.
“They have evolved for the general patient population, and this should apply to older individuals as well,” Dr. Pratley said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “My fear is, there is therapeutic nihilism, the idea that by the time someone is 75 years old, the horse is out of the barn and you’re not going to be able to impact outcomes with directed therapy. I don’t think that’s true. Our current treatment guidelines for the treatment of diabetes in older individuals remain focused on glycemic control. It’s not hyperglycemia that’s killing people; it’s heart disease and renal disease.”
According to data from the United Nations, about 12% of the global population is older than 60. By 2050, that number is expected to reach 20%, which will continue to drive an epidemic of diabetes in the near future. Dr. Pratley, medical director of AdventHealth Diabetes Institute in Orlando, pointed out that diabetes in older individuals is not a homogeneous condition. “There are many people in my clinic who had type 1 diabetes diagnosed as kids, but I also have patients who have adult-onset type 1 diabetes,” he said. “We also have type 2 patients who can be diagnosed in their 20s, 30s, or 40s, and there are people who are diagnosed in their 70s and 80s. Now we are learning that there are different subtypes of diabetes; so even type 2 diabetes is not a homogeneous condition. There are people who are more insulin resistant or have more of an insulin secretory defect, and there’s a special type of older-onset type 2 diabetes. When you consider all this in talking about diabetes treatments, about 30% of patients in the United States are diagnosed [when they are] over the age of 60, so this is an ongoing issue.”
Older adults with diabetes may have longstanding diabetes with associated microvascular and macrovascular complications, he continued, or they may have newly diagnosed diabetes with evidence of end organ complications at the time of presentation. Or, they may have newly diagnosed diabetes without evidence of complications. “Does this matter? It does,” Dr. Pratley said. “The things we worry about with all patients with diabetes are the microvascular complications, but I would argue that the macrovascular complications, particularly diabetic nephropathy, are things we should have a laser focus on, because they have high morbidity and mortality, especially in older individuals.”
There are more than 28 cardiovascular outcomes trials in patients with type 2 diabetes ongoing or completed, and involving eight classes of medications, with more than 200,000 planned participants, Dr. Pratley said. Of those participants, 90,000 are older than 65 years, and 30,000 are older than 75 years. “This is great,” he said. “Not only do these cardiovascular outcome studies give us a lot of information about the safety and efficacy of these drugs in the general population, we can now dig in to this specific patient population.” For example, in cardiovascular outcomes trials with dipeptidyl peptidase–4 (DPP-4) inhibitors, the mean age of patients was 65. About half of the patients were older than 65, and 10%-14% were older than 75.
Investigators in the SAVOR-TIMI 53 trial examined age in one of their subgroup analyses (Diabetes Care. 2015;38:1145-53). In that study with saxagliptin, among people older than 65 who received the study drug, the hazard ratio for major adverse cardiac events (MACE) was 0.92, compared with 1.15 for those younger than 65 (P value for interaction = .058). “So older people did great [on this drug],” Dr. Pratley said. “In fact, they had a bit of a decreased risk.” A similar association was seen in adults aged 75 years and older (HR, 1.01 in those younger than 75 years, vs. 0.95 in those aged 75 years and older; P value for interaction = .673). “This is telling us that saxagliptin is safe in the older population.”
In the EXAMINE trial, in which patients with type 2 diabetes who had had a recent acute coronary syndrome received either alogliptin or placebo, researchers conducted an analysis of patients older and younger than 65 (N Engl J Med. 2013;369:1327-35). They observed no significant interactions on the primary composite cardiovascular outcome in those younger than 65 (HR, 0.91) and those aged 65 and older (HR, 0.98).
Dr. Pratley noted that in cardiovascular outcome trials with sodium-glucose transporter 2 (SGLT2) inhibitors, the mean age of patients was 64, and 48%-50% of them were older than 65. In the EMPA-REG OUTCOME trial of empagliflozin, the hazard ratio for the primary cardiovascular outcome was 1.04 in patients younger than 65 and 0.71 in those aged 65 and older (P = .01; N Engl J Med, 2015;373:2117-28). “That was a significant interaction,” he said. In addition, the hazard ratio for cardiovascular death was 0.72 in those younger than 65, and 0.54 in those aged 65 and older (P = .21). “There was not a significant interaction here, but clearly there was some trending in the older patient population,” Dr. Pratley said.
In the LEADER study of liraglutide in patients with diabetes, the hazard ratio for the primary composite cardiovascular outcome was 0.87 in the overall population, 0.78 in patients younger than 60, and 0.90 in those aged 60 and older (P = 0.27; N Engl J Med. 2016;375:311-22). In a post hoc analysis that stratified LEADER patients into younger than 75 and 75 and older, the researchers observed a 31% reduction in the 75 and older population, compared with a 10% reduction in the younger population (P for interaction = .09; Ann Intern Med. 2019;170[6]:423-6). “This was driven largely by a decrease in nonfatal [myocardial infarction],” said Dr. Pratley, who was one of the study investigators. “But in patients who were 75 years and older, there was a 30% reduction in all-cause mortality in those treated with liraglutide, compared with 12% in those younger than 75 (P for interaction = .22). That interaction is not significant, but the theme here is that older populations do quite well.”
Based on such evidence, he said, In particular, SGLT2 inhibitors and certain GLP-1 receptor agonists may be associated with an additional benefit in older individuals with cardiovascular disease, “perhaps because they’re the ones at highest risk,” Dr. Pratley said. “But we need further studies to better identify those older individuals who may be at highest risk of adverse cardiovascular complications from diabetes and who might benefit from targeted therapies.”
Many questions remain unanswered in efforts to provide optimal care to older adults with diabetes. “One of the problems is being inclusive in the older patient population,” Dr. Pratley said. “We tried to do a study of frail older individuals looking at different treatments and policies. It was difficult to recruit frail older individuals, even though they routinely are treated with the drugs we study in healthier populations. We need to know how to enroll patients, and which investigators are going to do these trials. Who is going to support these trials? Pharma? The NIH?”
Then there’s the question of what appropriate outcomes are in older individuals. “I think we can agree that hemoglobin A1c is a surrogate of microvascular complications,” he said. “Do we need to be looking at outcomes like MACE, hospitalization for heart failure, death, progression of [chronic kidney disease], and perhaps cognitive function, physical function, sarcopenia, and quality of life?”
Dr. Pratley called for the development of a personalized approach to diabetes management that takes into account heterogeneity in disease pathogenesis, comorbidities, and patient preference.
“We need to change the focus to patient-important outcomes: dying, heart attack, strokes, and avoid therapeutic nihilism, which is still pervasive among many practitioners,” he said. “We also need to partner with primary care, because they take care of the majority of older individuals, and they need to understand how we’re evolving the goals of therapy. We need to educate them about the new guidelines and try to get them on board with some of the latest data that will help improve outcomes in our patients. We also need to understand the cost of diabetes and the cost effectiveness of interventions.”
He also recommends the development of a comprehensive evidence base for the use of drugs in older individuals. “I suggest pooled analyses within clinical development programs,” he said. “That’s been done for most development programs, but the phase 3 studies tend to enroll younger, healthier individuals. It would be good to do a meta-analysis across CVOTs [cardiovascular outcome trials] within different classes of medications.”
Dr. Pratley disclosed that all honoraria and fees he receives are directed to AdventHealth. These include serving on the advisory board or as consultant to AstraZeneca, GlaxoSmithKline, Glytec, Janssen, Ligand, Lilly, Merck, Mundipharma, Novo Nordisk, and Sanofi. He also has served as a speaker for AstraZeneca and Novo Nordisk, and has received research support from Lexicon, Ligand, Lilly, Merck, Novo Nordisk, and Sanofi. He receives no direct or indirect compensation.
LOS ANGELES – In the opinion of Richard Pratley, MD, it’s time for diabetes treatment guidelines to evolve in light of accumulating data from cardiovascular outcome trials in type 2 diabetes.
“They have evolved for the general patient population, and this should apply to older individuals as well,” Dr. Pratley said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “My fear is, there is therapeutic nihilism, the idea that by the time someone is 75 years old, the horse is out of the barn and you’re not going to be able to impact outcomes with directed therapy. I don’t think that’s true. Our current treatment guidelines for the treatment of diabetes in older individuals remain focused on glycemic control. It’s not hyperglycemia that’s killing people; it’s heart disease and renal disease.”
According to data from the United Nations, about 12% of the global population is older than 60. By 2050, that number is expected to reach 20%, which will continue to drive an epidemic of diabetes in the near future. Dr. Pratley, medical director of AdventHealth Diabetes Institute in Orlando, pointed out that diabetes in older individuals is not a homogeneous condition. “There are many people in my clinic who had type 1 diabetes diagnosed as kids, but I also have patients who have adult-onset type 1 diabetes,” he said. “We also have type 2 patients who can be diagnosed in their 20s, 30s, or 40s, and there are people who are diagnosed in their 70s and 80s. Now we are learning that there are different subtypes of diabetes; so even type 2 diabetes is not a homogeneous condition. There are people who are more insulin resistant or have more of an insulin secretory defect, and there’s a special type of older-onset type 2 diabetes. When you consider all this in talking about diabetes treatments, about 30% of patients in the United States are diagnosed [when they are] over the age of 60, so this is an ongoing issue.”
Older adults with diabetes may have longstanding diabetes with associated microvascular and macrovascular complications, he continued, or they may have newly diagnosed diabetes with evidence of end organ complications at the time of presentation. Or, they may have newly diagnosed diabetes without evidence of complications. “Does this matter? It does,” Dr. Pratley said. “The things we worry about with all patients with diabetes are the microvascular complications, but I would argue that the macrovascular complications, particularly diabetic nephropathy, are things we should have a laser focus on, because they have high morbidity and mortality, especially in older individuals.”
There are more than 28 cardiovascular outcomes trials in patients with type 2 diabetes ongoing or completed, and involving eight classes of medications, with more than 200,000 planned participants, Dr. Pratley said. Of those participants, 90,000 are older than 65 years, and 30,000 are older than 75 years. “This is great,” he said. “Not only do these cardiovascular outcome studies give us a lot of information about the safety and efficacy of these drugs in the general population, we can now dig in to this specific patient population.” For example, in cardiovascular outcomes trials with dipeptidyl peptidase–4 (DPP-4) inhibitors, the mean age of patients was 65. About half of the patients were older than 65, and 10%-14% were older than 75.
Investigators in the SAVOR-TIMI 53 trial examined age in one of their subgroup analyses (Diabetes Care. 2015;38:1145-53). In that study with saxagliptin, among people older than 65 who received the study drug, the hazard ratio for major adverse cardiac events (MACE) was 0.92, compared with 1.15 for those younger than 65 (P value for interaction = .058). “So older people did great [on this drug],” Dr. Pratley said. “In fact, they had a bit of a decreased risk.” A similar association was seen in adults aged 75 years and older (HR, 1.01 in those younger than 75 years, vs. 0.95 in those aged 75 years and older; P value for interaction = .673). “This is telling us that saxagliptin is safe in the older population.”
In the EXAMINE trial, in which patients with type 2 diabetes who had had a recent acute coronary syndrome received either alogliptin or placebo, researchers conducted an analysis of patients older and younger than 65 (N Engl J Med. 2013;369:1327-35). They observed no significant interactions on the primary composite cardiovascular outcome in those younger than 65 (HR, 0.91) and those aged 65 and older (HR, 0.98).
Dr. Pratley noted that in cardiovascular outcome trials with sodium-glucose transporter 2 (SGLT2) inhibitors, the mean age of patients was 64, and 48%-50% of them were older than 65. In the EMPA-REG OUTCOME trial of empagliflozin, the hazard ratio for the primary cardiovascular outcome was 1.04 in patients younger than 65 and 0.71 in those aged 65 and older (P = .01; N Engl J Med, 2015;373:2117-28). “That was a significant interaction,” he said. In addition, the hazard ratio for cardiovascular death was 0.72 in those younger than 65, and 0.54 in those aged 65 and older (P = .21). “There was not a significant interaction here, but clearly there was some trending in the older patient population,” Dr. Pratley said.
In the LEADER study of liraglutide in patients with diabetes, the hazard ratio for the primary composite cardiovascular outcome was 0.87 in the overall population, 0.78 in patients younger than 60, and 0.90 in those aged 60 and older (P = 0.27; N Engl J Med. 2016;375:311-22). In a post hoc analysis that stratified LEADER patients into younger than 75 and 75 and older, the researchers observed a 31% reduction in the 75 and older population, compared with a 10% reduction in the younger population (P for interaction = .09; Ann Intern Med. 2019;170[6]:423-6). “This was driven largely by a decrease in nonfatal [myocardial infarction],” said Dr. Pratley, who was one of the study investigators. “But in patients who were 75 years and older, there was a 30% reduction in all-cause mortality in those treated with liraglutide, compared with 12% in those younger than 75 (P for interaction = .22). That interaction is not significant, but the theme here is that older populations do quite well.”
Based on such evidence, he said, In particular, SGLT2 inhibitors and certain GLP-1 receptor agonists may be associated with an additional benefit in older individuals with cardiovascular disease, “perhaps because they’re the ones at highest risk,” Dr. Pratley said. “But we need further studies to better identify those older individuals who may be at highest risk of adverse cardiovascular complications from diabetes and who might benefit from targeted therapies.”
Many questions remain unanswered in efforts to provide optimal care to older adults with diabetes. “One of the problems is being inclusive in the older patient population,” Dr. Pratley said. “We tried to do a study of frail older individuals looking at different treatments and policies. It was difficult to recruit frail older individuals, even though they routinely are treated with the drugs we study in healthier populations. We need to know how to enroll patients, and which investigators are going to do these trials. Who is going to support these trials? Pharma? The NIH?”
Then there’s the question of what appropriate outcomes are in older individuals. “I think we can agree that hemoglobin A1c is a surrogate of microvascular complications,” he said. “Do we need to be looking at outcomes like MACE, hospitalization for heart failure, death, progression of [chronic kidney disease], and perhaps cognitive function, physical function, sarcopenia, and quality of life?”
Dr. Pratley called for the development of a personalized approach to diabetes management that takes into account heterogeneity in disease pathogenesis, comorbidities, and patient preference.
“We need to change the focus to patient-important outcomes: dying, heart attack, strokes, and avoid therapeutic nihilism, which is still pervasive among many practitioners,” he said. “We also need to partner with primary care, because they take care of the majority of older individuals, and they need to understand how we’re evolving the goals of therapy. We need to educate them about the new guidelines and try to get them on board with some of the latest data that will help improve outcomes in our patients. We also need to understand the cost of diabetes and the cost effectiveness of interventions.”
He also recommends the development of a comprehensive evidence base for the use of drugs in older individuals. “I suggest pooled analyses within clinical development programs,” he said. “That’s been done for most development programs, but the phase 3 studies tend to enroll younger, healthier individuals. It would be good to do a meta-analysis across CVOTs [cardiovascular outcome trials] within different classes of medications.”
Dr. Pratley disclosed that all honoraria and fees he receives are directed to AdventHealth. These include serving on the advisory board or as consultant to AstraZeneca, GlaxoSmithKline, Glytec, Janssen, Ligand, Lilly, Merck, Mundipharma, Novo Nordisk, and Sanofi. He also has served as a speaker for AstraZeneca and Novo Nordisk, and has received research support from Lexicon, Ligand, Lilly, Merck, Novo Nordisk, and Sanofi. He receives no direct or indirect compensation.
EXPERT ANALYSIS FROM WCIRDC 2019
ENGAGE AF-TIMI: Insulin linked to greater risk for stroke, CV death, bleeding
LOS ANGELES – Patients with diabetes had significantly higher adjusted risk of bleeding, cardiovascular-related death, and poorer net outcomes, particularly those treated with insulin, a subanalysis of the ENGAGE AF-TIMI 48 trial has shown.
In addition, the pharmacokinetic and pharmacodynamic profile of the study drug, edoxaban – a novel oral anticoagulant drug and a direct factor Xa inhibitor – was generally similar in patients with and without diabetes.
“We know that atrial fibrillation is associated with a fivefold increased risk of stroke,” Anna Plitt, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “Type 2 diabetes is associated with a twofold increased risk of stroke, and longer duration of diabetes is associated with even higher ischemic event rates. The coexistence of [atrial fibrillation] and type 2 diabetes further increases thromboembolic risk.”
Dr. Plitt, a cardiology fellow at Mount Sinai Hospital, New York, noted that, although type 2 diabetes is characterized by a prothrombotic and inflammatory state, the mechanism of action by which hyperglycemia and/or insulin resistance leads to the development of atrial fibrillation (AFib) remains unknown. “Given the complex clinical interactions between AFib and type 2 diabetes, care for these patients remains challenging,” she said. “Recommendations for anticoagulation managements vary based on the presence of additional risk factors and which guidelines are followed.”
In the ENGAGE AF-TIMI 48 trial, 21,105 patients with documented AFib within the previous 12 months were randomized to standard-care warfarin or high-dose edoxaban (60 mg daily) or low-dose edoxaban (30 mg daily). The edoxaban dose was reduced by 50% if creatinine clearance reached 30-50 mL/min, patient weight reached 60 kg or less, or there was concomitant use of a P-glycoprotein inhibitor (N Engl J Med. 2013;369:2093-104). The median follow-up was 2.8 years, and the primary efficacy endpoint was stroke or systemic embolic events (SEEs). The primary safety endpoint was major bleeding, as defined by the International Society on Thrombosis and Haemostasis criteria.
The findings showed that edoxaban was noninferior to warfarin in preventing stroke/SEEs. It also significantly reduced major bleeding, cardiovascular death, and net outcomes. “Therefore, the higher dose of edoxaban was approved globally for treating patients with AFib,” Dr. Plitt said. “The lower-dose regimen was not approved because there was less protection from ischemic stroke, compared with warfarin.”
For the current subanalysis, Dr. Plitt and colleagues set out to further evaluate outcomes of patients enrolled in the ENGAGE AF-TIMI 48 trial, excluding those who were in the low-dose edoxaban group. The presence or absence of diabetes was determined by the local investigator at randomization. The investigators further stratified patients into insulin-treated and non–insulin treated groups and used multivariate Cox regression models to adjust for baseline characteristics across the groups stratified by diabetes status. Next, they analyzed edoxaban concentration, anti–factor Xa activity, and international normalized ratio data and compared outcomes of high-dose edoxaban with those of warfarin.
The primary endpoint and the primary safety endpoint of interest were the same as in the main ENGAGE AF-TIMI 48 trial. Key secondary endpoints included in the subanalysis were cardiovascular death, stroke/SEE, major adverse cardiovascular events (MACE, a composite of myocardial infarction, stroke, SEE, or death because of cardiovascular cause or bleeding), and all-cause death.
In all, 7,624 of the 21,105 patients in the ENGAGE AF-TIMI 48 trial had diabetes, for a rate of 36%. Most of the patients with diabetes did not require insulin (30%), while 6% did. There were fewer female patients with diabetes than without (37% vs. 39%, respectively). Of note was that history of prior stroke/transient ischemic attack was higher in the no-diabetes group than in the diabetes group (33% vs. 21%), as was congestive heart failure (63% vs. 48%).
The mean CHA2DS2-VASc score for predicting thromboembolic risk (0, low risk; greater than 1, high risk) was 4.6 in the diabetes group and 4.2 in the no-diabetes group. When diabetes was not included in the score, the mean CHA2DS2-VASc score was 3.6 in the diabetes group. “Because the trial entry criteria required a minimum CHADS2 score of 2, patients without diabetes were enriched with stroke risk factors other than diabetes,” Dr. Plitt said.
Adjusted outcomes from the subanalysis showed that the risk of stroke/SEE was similar between patients with and without diabetes (hazard ratio, 1.08). However, patients with diabetes were at higher adjusted risk for cardiovascular death than patients without diabetes (HR, 1.29), MACE (HR, 1.28), major bleed (HR, 1.28), and the net outcome of stroke, SEE, major bleed, or all-cause death (HR, 1.25).
The researchers also analyzed the pharmacodynamic and pharmacokinetic data of high-dose edoxaban, stratified by diabetes status. They found that the parameters were generally similar between patients with and without diabetes, including trough concentrations of edoxaban (34.3 and 37.2 ng/mL, respectively; P = .04), trough exogenous anti–factor Xa activity (0.59 and 0.68 IU/mL; P = .11), and the percentage change from baseline in the peak endogenous anti–factor Xa activity (P = .66). The percentage changes from baseline of the trough endogenous anti–factor Xa activity was slightly lower in patients with diabetes, compared with patients without diabetes (P less than .001). “However, these modest differences between the two groups are of unclear clinical significance,” Dr. Plitt said.
Results from the main ENGAGE AF-TIMI 48 showed that the rates of stroke/SEE were reduced by 13% on high-dose edoxaban. However, the subanalysis found no significant effect modification in the reduction in stroke/SEE with edoxaban, compared with warfarin, when stratified by diabetes status (reductions of 16% vs. 7% in the no-diabetes and diabetes groups, respectively; P for interaction = .54). The researchers also observed similar reductions with edoxaban in the risks of secondary outcomes when patients were stratified by diabetes status.
In another finding, patients with diabetes who were treated with insulin were at a higher adjusted risk for all outcomes, compared with those with diabetes who were not treated with insulin. This included stroke/SEE (HR, 1.44), cardiovascular-related death (HR, 1.83), MACE (HR, 1.78), major bleed (HR, 1.31), and net outcome (HR, 1.57).
Next, the researchers compared the study endpoints of high-dose edoxaban and warfarin, with and without insulin. “None of the efficacy, safety, or net outcomes demonstrated evidence of treatment effect modification related to the use of insulin among [patients with diabetes],” she said.
Dr. Plitt disclosed having received honoraria for educational activities from Bristol-Myers Squibb.
LOS ANGELES – Patients with diabetes had significantly higher adjusted risk of bleeding, cardiovascular-related death, and poorer net outcomes, particularly those treated with insulin, a subanalysis of the ENGAGE AF-TIMI 48 trial has shown.
In addition, the pharmacokinetic and pharmacodynamic profile of the study drug, edoxaban – a novel oral anticoagulant drug and a direct factor Xa inhibitor – was generally similar in patients with and without diabetes.
“We know that atrial fibrillation is associated with a fivefold increased risk of stroke,” Anna Plitt, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “Type 2 diabetes is associated with a twofold increased risk of stroke, and longer duration of diabetes is associated with even higher ischemic event rates. The coexistence of [atrial fibrillation] and type 2 diabetes further increases thromboembolic risk.”
Dr. Plitt, a cardiology fellow at Mount Sinai Hospital, New York, noted that, although type 2 diabetes is characterized by a prothrombotic and inflammatory state, the mechanism of action by which hyperglycemia and/or insulin resistance leads to the development of atrial fibrillation (AFib) remains unknown. “Given the complex clinical interactions between AFib and type 2 diabetes, care for these patients remains challenging,” she said. “Recommendations for anticoagulation managements vary based on the presence of additional risk factors and which guidelines are followed.”
In the ENGAGE AF-TIMI 48 trial, 21,105 patients with documented AFib within the previous 12 months were randomized to standard-care warfarin or high-dose edoxaban (60 mg daily) or low-dose edoxaban (30 mg daily). The edoxaban dose was reduced by 50% if creatinine clearance reached 30-50 mL/min, patient weight reached 60 kg or less, or there was concomitant use of a P-glycoprotein inhibitor (N Engl J Med. 2013;369:2093-104). The median follow-up was 2.8 years, and the primary efficacy endpoint was stroke or systemic embolic events (SEEs). The primary safety endpoint was major bleeding, as defined by the International Society on Thrombosis and Haemostasis criteria.
The findings showed that edoxaban was noninferior to warfarin in preventing stroke/SEEs. It also significantly reduced major bleeding, cardiovascular death, and net outcomes. “Therefore, the higher dose of edoxaban was approved globally for treating patients with AFib,” Dr. Plitt said. “The lower-dose regimen was not approved because there was less protection from ischemic stroke, compared with warfarin.”
For the current subanalysis, Dr. Plitt and colleagues set out to further evaluate outcomes of patients enrolled in the ENGAGE AF-TIMI 48 trial, excluding those who were in the low-dose edoxaban group. The presence or absence of diabetes was determined by the local investigator at randomization. The investigators further stratified patients into insulin-treated and non–insulin treated groups and used multivariate Cox regression models to adjust for baseline characteristics across the groups stratified by diabetes status. Next, they analyzed edoxaban concentration, anti–factor Xa activity, and international normalized ratio data and compared outcomes of high-dose edoxaban with those of warfarin.
The primary endpoint and the primary safety endpoint of interest were the same as in the main ENGAGE AF-TIMI 48 trial. Key secondary endpoints included in the subanalysis were cardiovascular death, stroke/SEE, major adverse cardiovascular events (MACE, a composite of myocardial infarction, stroke, SEE, or death because of cardiovascular cause or bleeding), and all-cause death.
In all, 7,624 of the 21,105 patients in the ENGAGE AF-TIMI 48 trial had diabetes, for a rate of 36%. Most of the patients with diabetes did not require insulin (30%), while 6% did. There were fewer female patients with diabetes than without (37% vs. 39%, respectively). Of note was that history of prior stroke/transient ischemic attack was higher in the no-diabetes group than in the diabetes group (33% vs. 21%), as was congestive heart failure (63% vs. 48%).
The mean CHA2DS2-VASc score for predicting thromboembolic risk (0, low risk; greater than 1, high risk) was 4.6 in the diabetes group and 4.2 in the no-diabetes group. When diabetes was not included in the score, the mean CHA2DS2-VASc score was 3.6 in the diabetes group. “Because the trial entry criteria required a minimum CHADS2 score of 2, patients without diabetes were enriched with stroke risk factors other than diabetes,” Dr. Plitt said.
Adjusted outcomes from the subanalysis showed that the risk of stroke/SEE was similar between patients with and without diabetes (hazard ratio, 1.08). However, patients with diabetes were at higher adjusted risk for cardiovascular death than patients without diabetes (HR, 1.29), MACE (HR, 1.28), major bleed (HR, 1.28), and the net outcome of stroke, SEE, major bleed, or all-cause death (HR, 1.25).
The researchers also analyzed the pharmacodynamic and pharmacokinetic data of high-dose edoxaban, stratified by diabetes status. They found that the parameters were generally similar between patients with and without diabetes, including trough concentrations of edoxaban (34.3 and 37.2 ng/mL, respectively; P = .04), trough exogenous anti–factor Xa activity (0.59 and 0.68 IU/mL; P = .11), and the percentage change from baseline in the peak endogenous anti–factor Xa activity (P = .66). The percentage changes from baseline of the trough endogenous anti–factor Xa activity was slightly lower in patients with diabetes, compared with patients without diabetes (P less than .001). “However, these modest differences between the two groups are of unclear clinical significance,” Dr. Plitt said.
Results from the main ENGAGE AF-TIMI 48 showed that the rates of stroke/SEE were reduced by 13% on high-dose edoxaban. However, the subanalysis found no significant effect modification in the reduction in stroke/SEE with edoxaban, compared with warfarin, when stratified by diabetes status (reductions of 16% vs. 7% in the no-diabetes and diabetes groups, respectively; P for interaction = .54). The researchers also observed similar reductions with edoxaban in the risks of secondary outcomes when patients were stratified by diabetes status.
In another finding, patients with diabetes who were treated with insulin were at a higher adjusted risk for all outcomes, compared with those with diabetes who were not treated with insulin. This included stroke/SEE (HR, 1.44), cardiovascular-related death (HR, 1.83), MACE (HR, 1.78), major bleed (HR, 1.31), and net outcome (HR, 1.57).
Next, the researchers compared the study endpoints of high-dose edoxaban and warfarin, with and without insulin. “None of the efficacy, safety, or net outcomes demonstrated evidence of treatment effect modification related to the use of insulin among [patients with diabetes],” she said.
Dr. Plitt disclosed having received honoraria for educational activities from Bristol-Myers Squibb.
LOS ANGELES – Patients with diabetes had significantly higher adjusted risk of bleeding, cardiovascular-related death, and poorer net outcomes, particularly those treated with insulin, a subanalysis of the ENGAGE AF-TIMI 48 trial has shown.
In addition, the pharmacokinetic and pharmacodynamic profile of the study drug, edoxaban – a novel oral anticoagulant drug and a direct factor Xa inhibitor – was generally similar in patients with and without diabetes.
“We know that atrial fibrillation is associated with a fivefold increased risk of stroke,” Anna Plitt, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “Type 2 diabetes is associated with a twofold increased risk of stroke, and longer duration of diabetes is associated with even higher ischemic event rates. The coexistence of [atrial fibrillation] and type 2 diabetes further increases thromboembolic risk.”
Dr. Plitt, a cardiology fellow at Mount Sinai Hospital, New York, noted that, although type 2 diabetes is characterized by a prothrombotic and inflammatory state, the mechanism of action by which hyperglycemia and/or insulin resistance leads to the development of atrial fibrillation (AFib) remains unknown. “Given the complex clinical interactions between AFib and type 2 diabetes, care for these patients remains challenging,” she said. “Recommendations for anticoagulation managements vary based on the presence of additional risk factors and which guidelines are followed.”
In the ENGAGE AF-TIMI 48 trial, 21,105 patients with documented AFib within the previous 12 months were randomized to standard-care warfarin or high-dose edoxaban (60 mg daily) or low-dose edoxaban (30 mg daily). The edoxaban dose was reduced by 50% if creatinine clearance reached 30-50 mL/min, patient weight reached 60 kg or less, or there was concomitant use of a P-glycoprotein inhibitor (N Engl J Med. 2013;369:2093-104). The median follow-up was 2.8 years, and the primary efficacy endpoint was stroke or systemic embolic events (SEEs). The primary safety endpoint was major bleeding, as defined by the International Society on Thrombosis and Haemostasis criteria.
The findings showed that edoxaban was noninferior to warfarin in preventing stroke/SEEs. It also significantly reduced major bleeding, cardiovascular death, and net outcomes. “Therefore, the higher dose of edoxaban was approved globally for treating patients with AFib,” Dr. Plitt said. “The lower-dose regimen was not approved because there was less protection from ischemic stroke, compared with warfarin.”
For the current subanalysis, Dr. Plitt and colleagues set out to further evaluate outcomes of patients enrolled in the ENGAGE AF-TIMI 48 trial, excluding those who were in the low-dose edoxaban group. The presence or absence of diabetes was determined by the local investigator at randomization. The investigators further stratified patients into insulin-treated and non–insulin treated groups and used multivariate Cox regression models to adjust for baseline characteristics across the groups stratified by diabetes status. Next, they analyzed edoxaban concentration, anti–factor Xa activity, and international normalized ratio data and compared outcomes of high-dose edoxaban with those of warfarin.
The primary endpoint and the primary safety endpoint of interest were the same as in the main ENGAGE AF-TIMI 48 trial. Key secondary endpoints included in the subanalysis were cardiovascular death, stroke/SEE, major adverse cardiovascular events (MACE, a composite of myocardial infarction, stroke, SEE, or death because of cardiovascular cause or bleeding), and all-cause death.
In all, 7,624 of the 21,105 patients in the ENGAGE AF-TIMI 48 trial had diabetes, for a rate of 36%. Most of the patients with diabetes did not require insulin (30%), while 6% did. There were fewer female patients with diabetes than without (37% vs. 39%, respectively). Of note was that history of prior stroke/transient ischemic attack was higher in the no-diabetes group than in the diabetes group (33% vs. 21%), as was congestive heart failure (63% vs. 48%).
The mean CHA2DS2-VASc score for predicting thromboembolic risk (0, low risk; greater than 1, high risk) was 4.6 in the diabetes group and 4.2 in the no-diabetes group. When diabetes was not included in the score, the mean CHA2DS2-VASc score was 3.6 in the diabetes group. “Because the trial entry criteria required a minimum CHADS2 score of 2, patients without diabetes were enriched with stroke risk factors other than diabetes,” Dr. Plitt said.
Adjusted outcomes from the subanalysis showed that the risk of stroke/SEE was similar between patients with and without diabetes (hazard ratio, 1.08). However, patients with diabetes were at higher adjusted risk for cardiovascular death than patients without diabetes (HR, 1.29), MACE (HR, 1.28), major bleed (HR, 1.28), and the net outcome of stroke, SEE, major bleed, or all-cause death (HR, 1.25).
The researchers also analyzed the pharmacodynamic and pharmacokinetic data of high-dose edoxaban, stratified by diabetes status. They found that the parameters were generally similar between patients with and without diabetes, including trough concentrations of edoxaban (34.3 and 37.2 ng/mL, respectively; P = .04), trough exogenous anti–factor Xa activity (0.59 and 0.68 IU/mL; P = .11), and the percentage change from baseline in the peak endogenous anti–factor Xa activity (P = .66). The percentage changes from baseline of the trough endogenous anti–factor Xa activity was slightly lower in patients with diabetes, compared with patients without diabetes (P less than .001). “However, these modest differences between the two groups are of unclear clinical significance,” Dr. Plitt said.
Results from the main ENGAGE AF-TIMI 48 showed that the rates of stroke/SEE were reduced by 13% on high-dose edoxaban. However, the subanalysis found no significant effect modification in the reduction in stroke/SEE with edoxaban, compared with warfarin, when stratified by diabetes status (reductions of 16% vs. 7% in the no-diabetes and diabetes groups, respectively; P for interaction = .54). The researchers also observed similar reductions with edoxaban in the risks of secondary outcomes when patients were stratified by diabetes status.
In another finding, patients with diabetes who were treated with insulin were at a higher adjusted risk for all outcomes, compared with those with diabetes who were not treated with insulin. This included stroke/SEE (HR, 1.44), cardiovascular-related death (HR, 1.83), MACE (HR, 1.78), major bleed (HR, 1.31), and net outcome (HR, 1.57).
Next, the researchers compared the study endpoints of high-dose edoxaban and warfarin, with and without insulin. “None of the efficacy, safety, or net outcomes demonstrated evidence of treatment effect modification related to the use of insulin among [patients with diabetes],” she said.
Dr. Plitt disclosed having received honoraria for educational activities from Bristol-Myers Squibb.
REPORTING FROM THE WCIRDC 2019
CvLPRIT: Complete revascularization benefits persist long term
The greater reduction in major adverse cardiovascular events with complete revascularization for ST-segment elevation myocardial infarction, compared with target-lesion only, persists for many years after the procedure, a study has found.
In the Journal of the American College of Cardiology, researchers report the outcomes of long-term follow-up of 272 patients admitted with ST-segment elevation myocardial infarction, who were enrolled in CvLPRIT (Complete Versus Lesion-Only Primary PCI Trial).
The trial randomized patients to complete revascularization or infarct-related artery revascularization only, with a median follow-up of 5.6 years after randomization.
Anthony H. Gershlick, MD, from the University of Leicester (England) and NIHR Leicester Biomedical Research Centre, and coauthors highlighted conflicting evidence on the relative benefit of complete revascularization, compared with revascularization focused on the culprit artery only.
“The aim of this study was, for the first time, to determine if there is a sustained benefit in favor of multivessel percutaneous coronary intervention [PCI] in the longer term,” they wrote.
In the group of patients who underwent complete revascularization, the composite major adverse cardiovascular event rate at 5.6 years was 43% lower than in the infarct-related artery revascularization group (24.0 vs. 37.7%; P = .0079), according to the intention-to-treat analysis.
The complete revascularization group also showed a significantly lower rate of the secondary composite endpoint of death or MI, which was 10% in the complete revascularization group and 18.5% in the target lesion group (hazard ratio, 0.47; P = .0175).
“Our data suggest that total revascularization, known to have benefits in various cohorts with coronary artery disease, should now probably be considered the standard of care in suitable patients with STEMI with multivessel disease,” they wrote.
However they did find that the rates of ischemia-driven revascularization were not significantly different between the two groups at the long-term follow-up.
The authors also did an analysis of outcomes from the end of the original 12-month study to the final follow-up point. This showed a nonsignificant trend toward a lower rate of major adverse cardiovascular events in the group who underwent complete revascularization; 17.1%, compared with 23.3% in the infarct-related artery revascularization group. The rates of the individual components of that primary endpoint also trended toward lower rates in individuals with complete revascularization.
Similarly, the rates of ischemia-driven revascularization were similar in both groups when analyzed after the 12-month mark, and the authors noted that the need for ischemia-driven revascularization was equally spread between infarct-related arteries and non–infarct-related arteries.
The authors commented that the event rate curves for the two groups remained separated even to the median follow-up point of 5.6 years, showing that the highly significant difference in major adverse cardiovascular event rates between the two groups persists.
“All of these data suggest that lower rates of events seen within 12 months do translate into longer-term benefit, predominantly through nonattenuation of benefit,” they wrote.
They speculated that the longer-term benefit of early complete revascularization could be the result of improvement in blood flow to areas around the original site of ischemia, and because it managed lesions in nontarget vessels in patients with disease in multiple arteries.
“Certainly, given that both the MRI and nuclear medicine substudies of CvLPRIT showed no difference between the groups in infarct size (at 1 week) and no difference in ischemic burden at 6 weeks, the benefit we have demonstrated does not appear to be explained simply in terms of ischemic burden being dealt with prophylactically in the complete group,” they wrote.
Commenting on the study’s limitations, the authors noted that the overall numbers of patients were small, and that the use of all-cause mortality rather than cardiovascular mortality may affect the interpretation of results.
The CvLPRIT study was funded by the British Heart Foundation, with support from the National Institute for Health Research Comprehensive Local Research Networks. No conflicts of interest were declared.
SOURCE: Gershlick A et al. J Am Coll Cardiol. 2019 Dec 16;74:3083-9.
Multivessel coronary artery disease is present in around half of all patients presenting with STEMI and is associated with worse outcomes. However the decision about whether to revascularize beyond the culprit lesions – including lesions that may be asymptomatic and cause no ischemia – has been a matter of debate.
This longer-term follow-up from the CvLPRIT trial, along with evidence from other studies, has confirmed that complete revascularization should be considered in STEMI patients with multivessel disease. However, we suggest an individualized approach, rather than one-size-fits-all. This should also take into account factors such as the patient’s age and comorbidities, to avoid futile complex procedures in very old or frail patients. It is also important not to underestimate the importance of revascularization of the target lesion only.
There also remain questions about the best timing for complete revascularization and how to select the nonculprit lesions for revascularization.
Guillaume Cayla, MD, and Benoit Lattuca, MD, are from the Service de cardiologie, CHU de Nimes, ACTION Study Group at the Université de Montpellier, Nimes, France. These comments are adapted from an accompanying editorial (J Am Coll Cardiol. 2019; 74:3095-8. doi. org/10.1016/j.jacc.2019.10.037). Both authors declared research grants and lecture or consultancy fees from the pharmaceutical sector.
Multivessel coronary artery disease is present in around half of all patients presenting with STEMI and is associated with worse outcomes. However the decision about whether to revascularize beyond the culprit lesions – including lesions that may be asymptomatic and cause no ischemia – has been a matter of debate.
This longer-term follow-up from the CvLPRIT trial, along with evidence from other studies, has confirmed that complete revascularization should be considered in STEMI patients with multivessel disease. However, we suggest an individualized approach, rather than one-size-fits-all. This should also take into account factors such as the patient’s age and comorbidities, to avoid futile complex procedures in very old or frail patients. It is also important not to underestimate the importance of revascularization of the target lesion only.
There also remain questions about the best timing for complete revascularization and how to select the nonculprit lesions for revascularization.
Guillaume Cayla, MD, and Benoit Lattuca, MD, are from the Service de cardiologie, CHU de Nimes, ACTION Study Group at the Université de Montpellier, Nimes, France. These comments are adapted from an accompanying editorial (J Am Coll Cardiol. 2019; 74:3095-8. doi. org/10.1016/j.jacc.2019.10.037). Both authors declared research grants and lecture or consultancy fees from the pharmaceutical sector.
Multivessel coronary artery disease is present in around half of all patients presenting with STEMI and is associated with worse outcomes. However the decision about whether to revascularize beyond the culprit lesions – including lesions that may be asymptomatic and cause no ischemia – has been a matter of debate.
This longer-term follow-up from the CvLPRIT trial, along with evidence from other studies, has confirmed that complete revascularization should be considered in STEMI patients with multivessel disease. However, we suggest an individualized approach, rather than one-size-fits-all. This should also take into account factors such as the patient’s age and comorbidities, to avoid futile complex procedures in very old or frail patients. It is also important not to underestimate the importance of revascularization of the target lesion only.
There also remain questions about the best timing for complete revascularization and how to select the nonculprit lesions for revascularization.
Guillaume Cayla, MD, and Benoit Lattuca, MD, are from the Service de cardiologie, CHU de Nimes, ACTION Study Group at the Université de Montpellier, Nimes, France. These comments are adapted from an accompanying editorial (J Am Coll Cardiol. 2019; 74:3095-8. doi. org/10.1016/j.jacc.2019.10.037). Both authors declared research grants and lecture or consultancy fees from the pharmaceutical sector.
The greater reduction in major adverse cardiovascular events with complete revascularization for ST-segment elevation myocardial infarction, compared with target-lesion only, persists for many years after the procedure, a study has found.
In the Journal of the American College of Cardiology, researchers report the outcomes of long-term follow-up of 272 patients admitted with ST-segment elevation myocardial infarction, who were enrolled in CvLPRIT (Complete Versus Lesion-Only Primary PCI Trial).
The trial randomized patients to complete revascularization or infarct-related artery revascularization only, with a median follow-up of 5.6 years after randomization.
Anthony H. Gershlick, MD, from the University of Leicester (England) and NIHR Leicester Biomedical Research Centre, and coauthors highlighted conflicting evidence on the relative benefit of complete revascularization, compared with revascularization focused on the culprit artery only.
“The aim of this study was, for the first time, to determine if there is a sustained benefit in favor of multivessel percutaneous coronary intervention [PCI] in the longer term,” they wrote.
In the group of patients who underwent complete revascularization, the composite major adverse cardiovascular event rate at 5.6 years was 43% lower than in the infarct-related artery revascularization group (24.0 vs. 37.7%; P = .0079), according to the intention-to-treat analysis.
The complete revascularization group also showed a significantly lower rate of the secondary composite endpoint of death or MI, which was 10% in the complete revascularization group and 18.5% in the target lesion group (hazard ratio, 0.47; P = .0175).
“Our data suggest that total revascularization, known to have benefits in various cohorts with coronary artery disease, should now probably be considered the standard of care in suitable patients with STEMI with multivessel disease,” they wrote.
However they did find that the rates of ischemia-driven revascularization were not significantly different between the two groups at the long-term follow-up.
The authors also did an analysis of outcomes from the end of the original 12-month study to the final follow-up point. This showed a nonsignificant trend toward a lower rate of major adverse cardiovascular events in the group who underwent complete revascularization; 17.1%, compared with 23.3% in the infarct-related artery revascularization group. The rates of the individual components of that primary endpoint also trended toward lower rates in individuals with complete revascularization.
Similarly, the rates of ischemia-driven revascularization were similar in both groups when analyzed after the 12-month mark, and the authors noted that the need for ischemia-driven revascularization was equally spread between infarct-related arteries and non–infarct-related arteries.
The authors commented that the event rate curves for the two groups remained separated even to the median follow-up point of 5.6 years, showing that the highly significant difference in major adverse cardiovascular event rates between the two groups persists.
“All of these data suggest that lower rates of events seen within 12 months do translate into longer-term benefit, predominantly through nonattenuation of benefit,” they wrote.
They speculated that the longer-term benefit of early complete revascularization could be the result of improvement in blood flow to areas around the original site of ischemia, and because it managed lesions in nontarget vessels in patients with disease in multiple arteries.
“Certainly, given that both the MRI and nuclear medicine substudies of CvLPRIT showed no difference between the groups in infarct size (at 1 week) and no difference in ischemic burden at 6 weeks, the benefit we have demonstrated does not appear to be explained simply in terms of ischemic burden being dealt with prophylactically in the complete group,” they wrote.
Commenting on the study’s limitations, the authors noted that the overall numbers of patients were small, and that the use of all-cause mortality rather than cardiovascular mortality may affect the interpretation of results.
The CvLPRIT study was funded by the British Heart Foundation, with support from the National Institute for Health Research Comprehensive Local Research Networks. No conflicts of interest were declared.
SOURCE: Gershlick A et al. J Am Coll Cardiol. 2019 Dec 16;74:3083-9.
The greater reduction in major adverse cardiovascular events with complete revascularization for ST-segment elevation myocardial infarction, compared with target-lesion only, persists for many years after the procedure, a study has found.
In the Journal of the American College of Cardiology, researchers report the outcomes of long-term follow-up of 272 patients admitted with ST-segment elevation myocardial infarction, who were enrolled in CvLPRIT (Complete Versus Lesion-Only Primary PCI Trial).
The trial randomized patients to complete revascularization or infarct-related artery revascularization only, with a median follow-up of 5.6 years after randomization.
Anthony H. Gershlick, MD, from the University of Leicester (England) and NIHR Leicester Biomedical Research Centre, and coauthors highlighted conflicting evidence on the relative benefit of complete revascularization, compared with revascularization focused on the culprit artery only.
“The aim of this study was, for the first time, to determine if there is a sustained benefit in favor of multivessel percutaneous coronary intervention [PCI] in the longer term,” they wrote.
In the group of patients who underwent complete revascularization, the composite major adverse cardiovascular event rate at 5.6 years was 43% lower than in the infarct-related artery revascularization group (24.0 vs. 37.7%; P = .0079), according to the intention-to-treat analysis.
The complete revascularization group also showed a significantly lower rate of the secondary composite endpoint of death or MI, which was 10% in the complete revascularization group and 18.5% in the target lesion group (hazard ratio, 0.47; P = .0175).
“Our data suggest that total revascularization, known to have benefits in various cohorts with coronary artery disease, should now probably be considered the standard of care in suitable patients with STEMI with multivessel disease,” they wrote.
However they did find that the rates of ischemia-driven revascularization were not significantly different between the two groups at the long-term follow-up.
The authors also did an analysis of outcomes from the end of the original 12-month study to the final follow-up point. This showed a nonsignificant trend toward a lower rate of major adverse cardiovascular events in the group who underwent complete revascularization; 17.1%, compared with 23.3% in the infarct-related artery revascularization group. The rates of the individual components of that primary endpoint also trended toward lower rates in individuals with complete revascularization.
Similarly, the rates of ischemia-driven revascularization were similar in both groups when analyzed after the 12-month mark, and the authors noted that the need for ischemia-driven revascularization was equally spread between infarct-related arteries and non–infarct-related arteries.
The authors commented that the event rate curves for the two groups remained separated even to the median follow-up point of 5.6 years, showing that the highly significant difference in major adverse cardiovascular event rates between the two groups persists.
“All of these data suggest that lower rates of events seen within 12 months do translate into longer-term benefit, predominantly through nonattenuation of benefit,” they wrote.
They speculated that the longer-term benefit of early complete revascularization could be the result of improvement in blood flow to areas around the original site of ischemia, and because it managed lesions in nontarget vessels in patients with disease in multiple arteries.
“Certainly, given that both the MRI and nuclear medicine substudies of CvLPRIT showed no difference between the groups in infarct size (at 1 week) and no difference in ischemic burden at 6 weeks, the benefit we have demonstrated does not appear to be explained simply in terms of ischemic burden being dealt with prophylactically in the complete group,” they wrote.
Commenting on the study’s limitations, the authors noted that the overall numbers of patients were small, and that the use of all-cause mortality rather than cardiovascular mortality may affect the interpretation of results.
The CvLPRIT study was funded by the British Heart Foundation, with support from the National Institute for Health Research Comprehensive Local Research Networks. No conflicts of interest were declared.
SOURCE: Gershlick A et al. J Am Coll Cardiol. 2019 Dec 16;74:3083-9.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Minimum transcatheter mitral valve intervention case load recommended
U.S. sites that perform transcatheter mitral valve interventions should treat a minimum of 20 such patients each year or at least 40 every 2 years, according to revised recommendations and requirements released on Dec. 16, 2019, by several U.S. cardiology and cardiac surgery societies.
The revised recommendations also for the first time address patient selection for using transcatheter mitral valve (MV) intervention in patients with mitral regurgitation (MR) secondary to heart failure and a left ventricular ejection fraction of 21%-49%, a patient target for transcatheter interventions approved by the Food and Drug Administration in March 2019. The FDA first approved the same transcatheter MV intervention system (MitraClip) in 2013 for patients with primary MR caused by an abnormality of the MV and a prohibitive risk for surgical MV repair or replacement, and the same societies had previously issued their recommendations based on that approval (J Am Coll Cardiol. 2014 Oct; 64[14]:1515-26).
The need for updated recommendations on the delivery of transcatheter MV interventions including the personnel and facilities required for a valid U.S. program was driven by “new transcatheter technology, new trial results, and the new FDA-approved indication” of secondary MR. “We did the update for patients with secondary MR,” said Robert O. Bonow, MD, professor of medicine at Northwestern University, Chicago, and chair of the committee that wrote the revised recommendations.
“Primary and secondary MR are like two different diseases. Primary MR is a disease of the MV leaflets. Secondary MR is a disease of heart failure, left ventricular dysfunction, and left ventricular enlargement.” That makes secondary MR an indication with a potentially huge upside, given how many patients have heart failure today, plus projections for steadily increasing numbers of patients as the geriatric population grows.
“Heart failure is a huge issue, and the numbers are growing, which is why we felt it was important to say which heart failure patients should be candidates. We did not endorse this for all patients, although MR is very common in heart failure,” with estimated prevalence rates as high as two-thirds of all heart failure patients, Dr. Bonow said.
The new recommendations spell out an approach to patient selection that aims to apply transcatheter MV intervention to patients who match those enrolled in the COAPT (Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients With Functional Mitral Regurgitation) trial, which randomized 614 patients with MR secondary to heart failure and found for that MV intervention cut the rate of heart failure hospitalization by about half during 2 years of follow-up, a statistically significant effect for the study’s primary endpoint (N Engl J Med. 2018 Dec 13;379[24]:2307-18). The new recommendations provide “a way to replicate the COAPT trial” in routine practice, Dr. Bonow said in an interview.”We thought it was important to try to replicate the COAPT results,” and a key step toward trying to accomplish that is to apply the multidisciplinary team concept to evaluating patients and determining their management strategy. Dr. Bonow coauthored a commentary that discussed how the COAPT results should influence routine practice (N Engl J Med. 2018 Dec 13;379[24]:2374-6).
“In this case, perhaps the most important member of the multidisciplinary team is the heart failure specialist, because secondary MR is a disease of heart failure and it’s important to also optimize medical therapy to reduce MR and prolong life,” he said. Treatment optimization before undertaking a transcatheter MV intervention involves not only drug treatment but also treatment with indicated devices, such as biventricular pacing, to optimize left ventricular size and function. The 2019 FDA approval of the transcatheter approach for treating MV disease specified that eligible patients had to continue to have significant MR despite receiving optimal drug and device treatment.
Treatment decisions for patients with MR must be highly individualized, and unlike transcatheter aortic valve replacement (TAVR), which occurs against a background of “really good results” for surgical aortic valve replacement, surgical treatment of MR “has never been shown to prolong life, although it can improve function,” Dr. Bonow said. In addition, open surgical repair or replacement of a faulty MV “is much better than the MitraClip for elimination a MV leak; usually with transcatheter intervention there is some residual leak. And other etiologies of MR, such as atrial fibrillation causing atrial enlargement and dilatation of the mitral annulus, generally have much better results with surgery than with a transcatheter intervention. For both primary and secondary MR, deciding when to use surgery and when to do a transcatheter intervention is very individualized,” concluded Dr. Bonow, and a fact that distinguishes transcatheter MV interventions from TAVR, which has been shown to have efficacy that’s comparable with surgical aortic valve replacement. The MitraClip system is currently the only device with U.S. marketing approval for transcatheter MV intervention, although other devices are in development.
Case volume requirements
The designation of a minimum transcatheter MV intervention case load of 20 procedures a year or 40 every 2 years reflected a “consensus among interventional cardiologists and cardiac surgeons of what the experience had to be for MV repair,” Dr. Bonow said. This number contrasts with a minimum case volume of 50 procedures/year or 100 every 2 years to maintain a TAVR program proposed in 2018 by a similar expert panel organized by U.S. cardiology and cardiac surgery societies (J Am Coll of Cardiol. 2019 Jan;73[3]:340-74). The new MV recommendations “follow a similar template [as the TAVR recommendations], but the numbers are what we thought would be best for optimal transcatheter MV expertise. MV interventions will likely increase, and we felt it would be best to define the transcatheter operators and are the right patients; the volume is unclear. There are a lot of heart failure patients, but we know from COAPT that not everyone is a candidate. The existing MV device does not fit all settings. We thought the numbers we selected were most appropriate, at least when we are starting.”
Dr. Bonow and coauthors who wrote the new recommendations will rely on payers, particularly the Centers for Medicare & Medicaid Services, to adopt the societal recommendations as part of their criteria for reimbursement and thereby give them teeth. In June 2019, CMS announced its Medicare coverage determination for TAVR, which included procedure minimums of 20 per year or 40 over 2 years for TAVR programs, a number that fell substantially below the 50 per year or 100 over 2 years that had been proposed by the societies. “We hope CMS will use our MV recommendations as a starting point,” but the final CMS coverage decision for transcatheter MV intervention could again differ from what the societies proposed, Dr. Bonow acknowledged.
In addition to strongly promoting a multidisciplinary team approach (and spelling out the members of the team) and shared decision making involvement of the patient with the team, the new recommendations also endorse participation of MV intervention programs in the Transcatheter Valve Therapy U.S. patient registry that’s maintained by two of the societies that helped organize the writing committee. The recommendations discuss the need to collect 30-day (and longer) outcomes data from transcatheter MV intervention programs through the registry as is now done for TAVR programs (N Engl J Med. 2019 Jun 27;380[26]:2541-50). Dr. Bonow declined to predict when 30-day outcomes data may start appearing for programs performing transcatheter MV interventions.
Dr. Bonow had no disclosures. The COAPT study was funded by Abbott, the company that markets the MitrClip clip delivery system.
SOURCE: Bonow RO et al. J Am Coll Cardiol. 2019 Dec 16. doi: 10.1016/j.jacc.2019.12.002.
U.S. sites that perform transcatheter mitral valve interventions should treat a minimum of 20 such patients each year or at least 40 every 2 years, according to revised recommendations and requirements released on Dec. 16, 2019, by several U.S. cardiology and cardiac surgery societies.
The revised recommendations also for the first time address patient selection for using transcatheter mitral valve (MV) intervention in patients with mitral regurgitation (MR) secondary to heart failure and a left ventricular ejection fraction of 21%-49%, a patient target for transcatheter interventions approved by the Food and Drug Administration in March 2019. The FDA first approved the same transcatheter MV intervention system (MitraClip) in 2013 for patients with primary MR caused by an abnormality of the MV and a prohibitive risk for surgical MV repair or replacement, and the same societies had previously issued their recommendations based on that approval (J Am Coll Cardiol. 2014 Oct; 64[14]:1515-26).
The need for updated recommendations on the delivery of transcatheter MV interventions including the personnel and facilities required for a valid U.S. program was driven by “new transcatheter technology, new trial results, and the new FDA-approved indication” of secondary MR. “We did the update for patients with secondary MR,” said Robert O. Bonow, MD, professor of medicine at Northwestern University, Chicago, and chair of the committee that wrote the revised recommendations.
“Primary and secondary MR are like two different diseases. Primary MR is a disease of the MV leaflets. Secondary MR is a disease of heart failure, left ventricular dysfunction, and left ventricular enlargement.” That makes secondary MR an indication with a potentially huge upside, given how many patients have heart failure today, plus projections for steadily increasing numbers of patients as the geriatric population grows.
“Heart failure is a huge issue, and the numbers are growing, which is why we felt it was important to say which heart failure patients should be candidates. We did not endorse this for all patients, although MR is very common in heart failure,” with estimated prevalence rates as high as two-thirds of all heart failure patients, Dr. Bonow said.
The new recommendations spell out an approach to patient selection that aims to apply transcatheter MV intervention to patients who match those enrolled in the COAPT (Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients With Functional Mitral Regurgitation) trial, which randomized 614 patients with MR secondary to heart failure and found for that MV intervention cut the rate of heart failure hospitalization by about half during 2 years of follow-up, a statistically significant effect for the study’s primary endpoint (N Engl J Med. 2018 Dec 13;379[24]:2307-18). The new recommendations provide “a way to replicate the COAPT trial” in routine practice, Dr. Bonow said in an interview.”We thought it was important to try to replicate the COAPT results,” and a key step toward trying to accomplish that is to apply the multidisciplinary team concept to evaluating patients and determining their management strategy. Dr. Bonow coauthored a commentary that discussed how the COAPT results should influence routine practice (N Engl J Med. 2018 Dec 13;379[24]:2374-6).
“In this case, perhaps the most important member of the multidisciplinary team is the heart failure specialist, because secondary MR is a disease of heart failure and it’s important to also optimize medical therapy to reduce MR and prolong life,” he said. Treatment optimization before undertaking a transcatheter MV intervention involves not only drug treatment but also treatment with indicated devices, such as biventricular pacing, to optimize left ventricular size and function. The 2019 FDA approval of the transcatheter approach for treating MV disease specified that eligible patients had to continue to have significant MR despite receiving optimal drug and device treatment.
Treatment decisions for patients with MR must be highly individualized, and unlike transcatheter aortic valve replacement (TAVR), which occurs against a background of “really good results” for surgical aortic valve replacement, surgical treatment of MR “has never been shown to prolong life, although it can improve function,” Dr. Bonow said. In addition, open surgical repair or replacement of a faulty MV “is much better than the MitraClip for elimination a MV leak; usually with transcatheter intervention there is some residual leak. And other etiologies of MR, such as atrial fibrillation causing atrial enlargement and dilatation of the mitral annulus, generally have much better results with surgery than with a transcatheter intervention. For both primary and secondary MR, deciding when to use surgery and when to do a transcatheter intervention is very individualized,” concluded Dr. Bonow, and a fact that distinguishes transcatheter MV interventions from TAVR, which has been shown to have efficacy that’s comparable with surgical aortic valve replacement. The MitraClip system is currently the only device with U.S. marketing approval for transcatheter MV intervention, although other devices are in development.
Case volume requirements
The designation of a minimum transcatheter MV intervention case load of 20 procedures a year or 40 every 2 years reflected a “consensus among interventional cardiologists and cardiac surgeons of what the experience had to be for MV repair,” Dr. Bonow said. This number contrasts with a minimum case volume of 50 procedures/year or 100 every 2 years to maintain a TAVR program proposed in 2018 by a similar expert panel organized by U.S. cardiology and cardiac surgery societies (J Am Coll of Cardiol. 2019 Jan;73[3]:340-74). The new MV recommendations “follow a similar template [as the TAVR recommendations], but the numbers are what we thought would be best for optimal transcatheter MV expertise. MV interventions will likely increase, and we felt it would be best to define the transcatheter operators and are the right patients; the volume is unclear. There are a lot of heart failure patients, but we know from COAPT that not everyone is a candidate. The existing MV device does not fit all settings. We thought the numbers we selected were most appropriate, at least when we are starting.”
Dr. Bonow and coauthors who wrote the new recommendations will rely on payers, particularly the Centers for Medicare & Medicaid Services, to adopt the societal recommendations as part of their criteria for reimbursement and thereby give them teeth. In June 2019, CMS announced its Medicare coverage determination for TAVR, which included procedure minimums of 20 per year or 40 over 2 years for TAVR programs, a number that fell substantially below the 50 per year or 100 over 2 years that had been proposed by the societies. “We hope CMS will use our MV recommendations as a starting point,” but the final CMS coverage decision for transcatheter MV intervention could again differ from what the societies proposed, Dr. Bonow acknowledged.
In addition to strongly promoting a multidisciplinary team approach (and spelling out the members of the team) and shared decision making involvement of the patient with the team, the new recommendations also endorse participation of MV intervention programs in the Transcatheter Valve Therapy U.S. patient registry that’s maintained by two of the societies that helped organize the writing committee. The recommendations discuss the need to collect 30-day (and longer) outcomes data from transcatheter MV intervention programs through the registry as is now done for TAVR programs (N Engl J Med. 2019 Jun 27;380[26]:2541-50). Dr. Bonow declined to predict when 30-day outcomes data may start appearing for programs performing transcatheter MV interventions.
Dr. Bonow had no disclosures. The COAPT study was funded by Abbott, the company that markets the MitrClip clip delivery system.
SOURCE: Bonow RO et al. J Am Coll Cardiol. 2019 Dec 16. doi: 10.1016/j.jacc.2019.12.002.
U.S. sites that perform transcatheter mitral valve interventions should treat a minimum of 20 such patients each year or at least 40 every 2 years, according to revised recommendations and requirements released on Dec. 16, 2019, by several U.S. cardiology and cardiac surgery societies.
The revised recommendations also for the first time address patient selection for using transcatheter mitral valve (MV) intervention in patients with mitral regurgitation (MR) secondary to heart failure and a left ventricular ejection fraction of 21%-49%, a patient target for transcatheter interventions approved by the Food and Drug Administration in March 2019. The FDA first approved the same transcatheter MV intervention system (MitraClip) in 2013 for patients with primary MR caused by an abnormality of the MV and a prohibitive risk for surgical MV repair or replacement, and the same societies had previously issued their recommendations based on that approval (J Am Coll Cardiol. 2014 Oct; 64[14]:1515-26).
The need for updated recommendations on the delivery of transcatheter MV interventions including the personnel and facilities required for a valid U.S. program was driven by “new transcatheter technology, new trial results, and the new FDA-approved indication” of secondary MR. “We did the update for patients with secondary MR,” said Robert O. Bonow, MD, professor of medicine at Northwestern University, Chicago, and chair of the committee that wrote the revised recommendations.
“Primary and secondary MR are like two different diseases. Primary MR is a disease of the MV leaflets. Secondary MR is a disease of heart failure, left ventricular dysfunction, and left ventricular enlargement.” That makes secondary MR an indication with a potentially huge upside, given how many patients have heart failure today, plus projections for steadily increasing numbers of patients as the geriatric population grows.
“Heart failure is a huge issue, and the numbers are growing, which is why we felt it was important to say which heart failure patients should be candidates. We did not endorse this for all patients, although MR is very common in heart failure,” with estimated prevalence rates as high as two-thirds of all heart failure patients, Dr. Bonow said.
The new recommendations spell out an approach to patient selection that aims to apply transcatheter MV intervention to patients who match those enrolled in the COAPT (Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients With Functional Mitral Regurgitation) trial, which randomized 614 patients with MR secondary to heart failure and found for that MV intervention cut the rate of heart failure hospitalization by about half during 2 years of follow-up, a statistically significant effect for the study’s primary endpoint (N Engl J Med. 2018 Dec 13;379[24]:2307-18). The new recommendations provide “a way to replicate the COAPT trial” in routine practice, Dr. Bonow said in an interview.”We thought it was important to try to replicate the COAPT results,” and a key step toward trying to accomplish that is to apply the multidisciplinary team concept to evaluating patients and determining their management strategy. Dr. Bonow coauthored a commentary that discussed how the COAPT results should influence routine practice (N Engl J Med. 2018 Dec 13;379[24]:2374-6).
“In this case, perhaps the most important member of the multidisciplinary team is the heart failure specialist, because secondary MR is a disease of heart failure and it’s important to also optimize medical therapy to reduce MR and prolong life,” he said. Treatment optimization before undertaking a transcatheter MV intervention involves not only drug treatment but also treatment with indicated devices, such as biventricular pacing, to optimize left ventricular size and function. The 2019 FDA approval of the transcatheter approach for treating MV disease specified that eligible patients had to continue to have significant MR despite receiving optimal drug and device treatment.
Treatment decisions for patients with MR must be highly individualized, and unlike transcatheter aortic valve replacement (TAVR), which occurs against a background of “really good results” for surgical aortic valve replacement, surgical treatment of MR “has never been shown to prolong life, although it can improve function,” Dr. Bonow said. In addition, open surgical repair or replacement of a faulty MV “is much better than the MitraClip for elimination a MV leak; usually with transcatheter intervention there is some residual leak. And other etiologies of MR, such as atrial fibrillation causing atrial enlargement and dilatation of the mitral annulus, generally have much better results with surgery than with a transcatheter intervention. For both primary and secondary MR, deciding when to use surgery and when to do a transcatheter intervention is very individualized,” concluded Dr. Bonow, and a fact that distinguishes transcatheter MV interventions from TAVR, which has been shown to have efficacy that’s comparable with surgical aortic valve replacement. The MitraClip system is currently the only device with U.S. marketing approval for transcatheter MV intervention, although other devices are in development.
Case volume requirements
The designation of a minimum transcatheter MV intervention case load of 20 procedures a year or 40 every 2 years reflected a “consensus among interventional cardiologists and cardiac surgeons of what the experience had to be for MV repair,” Dr. Bonow said. This number contrasts with a minimum case volume of 50 procedures/year or 100 every 2 years to maintain a TAVR program proposed in 2018 by a similar expert panel organized by U.S. cardiology and cardiac surgery societies (J Am Coll of Cardiol. 2019 Jan;73[3]:340-74). The new MV recommendations “follow a similar template [as the TAVR recommendations], but the numbers are what we thought would be best for optimal transcatheter MV expertise. MV interventions will likely increase, and we felt it would be best to define the transcatheter operators and are the right patients; the volume is unclear. There are a lot of heart failure patients, but we know from COAPT that not everyone is a candidate. The existing MV device does not fit all settings. We thought the numbers we selected were most appropriate, at least when we are starting.”
Dr. Bonow and coauthors who wrote the new recommendations will rely on payers, particularly the Centers for Medicare & Medicaid Services, to adopt the societal recommendations as part of their criteria for reimbursement and thereby give them teeth. In June 2019, CMS announced its Medicare coverage determination for TAVR, which included procedure minimums of 20 per year or 40 over 2 years for TAVR programs, a number that fell substantially below the 50 per year or 100 over 2 years that had been proposed by the societies. “We hope CMS will use our MV recommendations as a starting point,” but the final CMS coverage decision for transcatheter MV intervention could again differ from what the societies proposed, Dr. Bonow acknowledged.
In addition to strongly promoting a multidisciplinary team approach (and spelling out the members of the team) and shared decision making involvement of the patient with the team, the new recommendations also endorse participation of MV intervention programs in the Transcatheter Valve Therapy U.S. patient registry that’s maintained by two of the societies that helped organize the writing committee. The recommendations discuss the need to collect 30-day (and longer) outcomes data from transcatheter MV intervention programs through the registry as is now done for TAVR programs (N Engl J Med. 2019 Jun 27;380[26]:2541-50). Dr. Bonow declined to predict when 30-day outcomes data may start appearing for programs performing transcatheter MV interventions.
Dr. Bonow had no disclosures. The COAPT study was funded by Abbott, the company that markets the MitrClip clip delivery system.
SOURCE: Bonow RO et al. J Am Coll Cardiol. 2019 Dec 16. doi: 10.1016/j.jacc.2019.12.002.
SZC passes extension test for hyperkalemia
Treatment with sodium zirconium cyclosilicate (SZC) led to lasting improvement of hyperkalemia, according to results from an 11-month open-label extension study of the HARMONIZE randomized clinical trial.
SZC selectively binds potassium ions in the colon, reducing absorption and promoting excretion. In the original study, 248 patients with mild hyperkalemia were randomized to SZC or placebo. Within 48 hours, the drug returned potassium to normal and maintained those levels out to 4 weeks.
In the extension study, 123 patients with measured potassium levels of 3.5-6.2 mmol/L, 48 of whom had previously been assigned to placebo, received a 5- to 10-g dose of SZC once per day for up to 337 days. Median daily dose was 10 g, with a dose range of 2.5-15 g (Am J Nephrol. 2019;50[6]:473-480).
Just under 65% of patients completed the 11 months of the open-label extension study, with 88.3% of those achieving the primary endpoint of mean serum potassium levels of 5.1 mmol/L or lower, according to Simon D. Roger, MD, a nephrologist based in Gosford, Australia, and colleagues.
Most patients (83) were taking renin–angiotensin–aldosterone system inhibitors at baseline of the extension study; 78.3% continued a stable dose throughout the open-label phase, 8.4% increased the dose, and 3.6% discontinued.
Two-thirds of patients reported adverse events, most commonly gastrointestinal disorders (18.7%). Constipation was the most frequent (5.7%), followed by nausea, vomiting, and diarrhea (3.3% each).
Adverse events that occurred in 5% or more of participants included hypertension (12.2%), urinary tract infection (8.9%), and peripheral edema (8.1%). Hypertension severity was either mild (46.7%) or moderate (53.3%), and only one case was believed to be associated with the study medication. Thirteen percent of participants reported a total of 17 SMQ edema events. Eleven of the 16 patients had baseline risk factors for edema, leading the authors to conclude that causality between SZC and edema could not be established.
Serious adverse events occurred in 19.5% of participants, and 4.9% of participants discontinued SZC as a result.
SZC is approved for the treatment of hyperkalemia in the United States and Europe. The study was funded by AstraZeneca.
SOURCE: Roger S et al. Am J Nephrol;2019:50(6):473-80.
Treatment with sodium zirconium cyclosilicate (SZC) led to lasting improvement of hyperkalemia, according to results from an 11-month open-label extension study of the HARMONIZE randomized clinical trial.
SZC selectively binds potassium ions in the colon, reducing absorption and promoting excretion. In the original study, 248 patients with mild hyperkalemia were randomized to SZC or placebo. Within 48 hours, the drug returned potassium to normal and maintained those levels out to 4 weeks.
In the extension study, 123 patients with measured potassium levels of 3.5-6.2 mmol/L, 48 of whom had previously been assigned to placebo, received a 5- to 10-g dose of SZC once per day for up to 337 days. Median daily dose was 10 g, with a dose range of 2.5-15 g (Am J Nephrol. 2019;50[6]:473-480).
Just under 65% of patients completed the 11 months of the open-label extension study, with 88.3% of those achieving the primary endpoint of mean serum potassium levels of 5.1 mmol/L or lower, according to Simon D. Roger, MD, a nephrologist based in Gosford, Australia, and colleagues.
Most patients (83) were taking renin–angiotensin–aldosterone system inhibitors at baseline of the extension study; 78.3% continued a stable dose throughout the open-label phase, 8.4% increased the dose, and 3.6% discontinued.
Two-thirds of patients reported adverse events, most commonly gastrointestinal disorders (18.7%). Constipation was the most frequent (5.7%), followed by nausea, vomiting, and diarrhea (3.3% each).
Adverse events that occurred in 5% or more of participants included hypertension (12.2%), urinary tract infection (8.9%), and peripheral edema (8.1%). Hypertension severity was either mild (46.7%) or moderate (53.3%), and only one case was believed to be associated with the study medication. Thirteen percent of participants reported a total of 17 SMQ edema events. Eleven of the 16 patients had baseline risk factors for edema, leading the authors to conclude that causality between SZC and edema could not be established.
Serious adverse events occurred in 19.5% of participants, and 4.9% of participants discontinued SZC as a result.
SZC is approved for the treatment of hyperkalemia in the United States and Europe. The study was funded by AstraZeneca.
SOURCE: Roger S et al. Am J Nephrol;2019:50(6):473-80.
Treatment with sodium zirconium cyclosilicate (SZC) led to lasting improvement of hyperkalemia, according to results from an 11-month open-label extension study of the HARMONIZE randomized clinical trial.
SZC selectively binds potassium ions in the colon, reducing absorption and promoting excretion. In the original study, 248 patients with mild hyperkalemia were randomized to SZC or placebo. Within 48 hours, the drug returned potassium to normal and maintained those levels out to 4 weeks.
In the extension study, 123 patients with measured potassium levels of 3.5-6.2 mmol/L, 48 of whom had previously been assigned to placebo, received a 5- to 10-g dose of SZC once per day for up to 337 days. Median daily dose was 10 g, with a dose range of 2.5-15 g (Am J Nephrol. 2019;50[6]:473-480).
Just under 65% of patients completed the 11 months of the open-label extension study, with 88.3% of those achieving the primary endpoint of mean serum potassium levels of 5.1 mmol/L or lower, according to Simon D. Roger, MD, a nephrologist based in Gosford, Australia, and colleagues.
Most patients (83) were taking renin–angiotensin–aldosterone system inhibitors at baseline of the extension study; 78.3% continued a stable dose throughout the open-label phase, 8.4% increased the dose, and 3.6% discontinued.
Two-thirds of patients reported adverse events, most commonly gastrointestinal disorders (18.7%). Constipation was the most frequent (5.7%), followed by nausea, vomiting, and diarrhea (3.3% each).
Adverse events that occurred in 5% or more of participants included hypertension (12.2%), urinary tract infection (8.9%), and peripheral edema (8.1%). Hypertension severity was either mild (46.7%) or moderate (53.3%), and only one case was believed to be associated with the study medication. Thirteen percent of participants reported a total of 17 SMQ edema events. Eleven of the 16 patients had baseline risk factors for edema, leading the authors to conclude that causality between SZC and edema could not be established.
Serious adverse events occurred in 19.5% of participants, and 4.9% of participants discontinued SZC as a result.
SZC is approved for the treatment of hyperkalemia in the United States and Europe. The study was funded by AstraZeneca.
SOURCE: Roger S et al. Am J Nephrol;2019:50(6):473-80.
FROM AMERICAN JOURNAL OF NEPHROLOGY
Icosapent ethyl approved for cardiovascular risk reduction
Icosapent ethyl (Vascepa) has gained an indication from the Food and Drug Administration for reduction of cardiovascular events in patients with high triglycerides who are at high risk for cardiovascular events.
as an add-on to maximally tolerated statin therapy,” the agency said in an announcement.
The decision, announced on Dec. 13, was based primarily on results of REDUCE-IT (Reduction of Cardiovascular Events with Icosapent Ethyl-Intervention Trial), which tested icosapent ethyl in 8,179 patients with either established cardiovascular disease or diabetes and at least one additional cardiovascular disease risk factor. It showed that patients who received icosapent ethyl had a statistically significant 25% relative risk reduction in the trial’s primary, composite endpoint (N Engl J Med. 2019 Jan 3;380[1]:11-22).
In a November meeting, the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee voted unanimously for approval.
The agency notes that, in clinical trials, icosapent ethyl was linked to an increased risk of atrial fibrillation or atrial flutter requiring hospitalization, especially in patients with a history of either condition. The highly purified form of the ethyl ester of eicosapentaenoic acid was also associated with an increased risk of bleeding events, particularly in those taking blood-thinning drugs that increase the risk of bleeding, such as aspirin, clopidogrel, or warfarin.
The most common side effects reported in the clinical trials for icosapent ethyl were musculoskeletal pain, peripheral edema, atrial fibrillation, and arthralgia.
The complete indication is “as an adjunct to maximally tolerated statin therapy to reduce the risk of myocardial infarction, stroke, coronary revascularization, and unstable angina requiring hospitalization in adult patients with elevated triglyceride levels (at least 150 mg/dL) and established cardiovascular disease or diabetes mellitus and two or more additional risk factors for cardiovascular disease,” according to a statement from Amalin, which markets Vascepa.
The drug was approved in 2012 for the indication of cutting triglyceride levels once they reached at least 500 mg/dL.
Icosapent ethyl (Vascepa) has gained an indication from the Food and Drug Administration for reduction of cardiovascular events in patients with high triglycerides who are at high risk for cardiovascular events.
as an add-on to maximally tolerated statin therapy,” the agency said in an announcement.
The decision, announced on Dec. 13, was based primarily on results of REDUCE-IT (Reduction of Cardiovascular Events with Icosapent Ethyl-Intervention Trial), which tested icosapent ethyl in 8,179 patients with either established cardiovascular disease or diabetes and at least one additional cardiovascular disease risk factor. It showed that patients who received icosapent ethyl had a statistically significant 25% relative risk reduction in the trial’s primary, composite endpoint (N Engl J Med. 2019 Jan 3;380[1]:11-22).
In a November meeting, the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee voted unanimously for approval.
The agency notes that, in clinical trials, icosapent ethyl was linked to an increased risk of atrial fibrillation or atrial flutter requiring hospitalization, especially in patients with a history of either condition. The highly purified form of the ethyl ester of eicosapentaenoic acid was also associated with an increased risk of bleeding events, particularly in those taking blood-thinning drugs that increase the risk of bleeding, such as aspirin, clopidogrel, or warfarin.
The most common side effects reported in the clinical trials for icosapent ethyl were musculoskeletal pain, peripheral edema, atrial fibrillation, and arthralgia.
The complete indication is “as an adjunct to maximally tolerated statin therapy to reduce the risk of myocardial infarction, stroke, coronary revascularization, and unstable angina requiring hospitalization in adult patients with elevated triglyceride levels (at least 150 mg/dL) and established cardiovascular disease or diabetes mellitus and two or more additional risk factors for cardiovascular disease,” according to a statement from Amalin, which markets Vascepa.
The drug was approved in 2012 for the indication of cutting triglyceride levels once they reached at least 500 mg/dL.
Icosapent ethyl (Vascepa) has gained an indication from the Food and Drug Administration for reduction of cardiovascular events in patients with high triglycerides who are at high risk for cardiovascular events.
as an add-on to maximally tolerated statin therapy,” the agency said in an announcement.
The decision, announced on Dec. 13, was based primarily on results of REDUCE-IT (Reduction of Cardiovascular Events with Icosapent Ethyl-Intervention Trial), which tested icosapent ethyl in 8,179 patients with either established cardiovascular disease or diabetes and at least one additional cardiovascular disease risk factor. It showed that patients who received icosapent ethyl had a statistically significant 25% relative risk reduction in the trial’s primary, composite endpoint (N Engl J Med. 2019 Jan 3;380[1]:11-22).
In a November meeting, the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee voted unanimously for approval.
The agency notes that, in clinical trials, icosapent ethyl was linked to an increased risk of atrial fibrillation or atrial flutter requiring hospitalization, especially in patients with a history of either condition. The highly purified form of the ethyl ester of eicosapentaenoic acid was also associated with an increased risk of bleeding events, particularly in those taking blood-thinning drugs that increase the risk of bleeding, such as aspirin, clopidogrel, or warfarin.
The most common side effects reported in the clinical trials for icosapent ethyl were musculoskeletal pain, peripheral edema, atrial fibrillation, and arthralgia.
The complete indication is “as an adjunct to maximally tolerated statin therapy to reduce the risk of myocardial infarction, stroke, coronary revascularization, and unstable angina requiring hospitalization in adult patients with elevated triglyceride levels (at least 150 mg/dL) and established cardiovascular disease or diabetes mellitus and two or more additional risk factors for cardiovascular disease,” according to a statement from Amalin, which markets Vascepa.
The drug was approved in 2012 for the indication of cutting triglyceride levels once they reached at least 500 mg/dL.