User login
Address physical health risks of people with SMI
ROCKVILLE, MD. – The problem of medical comorbidities in people with serious mental illness (SMI) persists and must be addressed, researchers said at a National Institute on Mental Health conference on mental health services research. Part of that effort, they said, is a more careful consideration of risks tied to the off-label use of second-generation antipsychotics.
The researchers discussed strategies aimed at combating obesity and diabetes, as well as behaviors such as smoking and sedentary lifestyle.
“One of the things that jumps out is the tremendous need for evidence-based strategies to address these physical health problems that are common in general population but even more of a burden for people with serious mental illness,” said Susan T. Azrin, PhD, of the NIMH, in an interview.
A study published in 2015, estimated that people with schizophrenia, for example, might lose almost 30 years of life because of premature death. Individuals with serious mental illness also experience elevated morbidity from cardiovascular disease and cancer. The NIMH and other federal agencies have in recent years looked for ways to help people with SMI quit smoking, and better control their weight and cholesterol.
But approaches that sound promising for boosting physical fitness in this group of patients have not always proven successful. Joshua Breslau, PhD, ScD, of the Rand Corp. discussed findings from a 2014 paper where he and his colleagues reported somewhat disappointing results from a study of federal Primary and Behavioral Health Care Integration grants.
The researchers matched clinics receiving this funding with similar ones that did not. They found that people with mental illness treated at the clinics receiving the grants showed improvements in some indicators of physical health (diastolic blood pressure, total cholesterol, LDL cholesterol, and fasting plasma glucose) but not in others (systolic blood pressure, body mass index, HDL cholesterol, hemoglobin A1c, triglycerides, self-reported smoking). Dr. Breslau said he and his colleagues also found only limited benefits in quality of care for physical health conditions associated with the grant program. Still, he remains hopeful.
“There is some potential here,” Dr. Breslau said. “Sometimes, we are seeing positive effects, but it’s certainly not a slam-dunk.”
He noted that opening a new setting for primary care services could strain a workforce that’s already in short supply. In addition, he said, attempts to fold primary care services into mental health programs could, in some cases, result in replication of care of chronic conditions for certain patients with SMI.
We “may still not reach that portion of the target population that has the greatest need,” Dr. Breslau said in an interview. “The new services may turn out to be duplicative rather than filling a gap.”
In another session, Gail L. Daumit, MD, MHS, of Johns Hopkins University, Baltimore, discussed her plan to build on a past success in helping people with SMI lose weight.
In the ACHIEVE (Achieving Healthy Lifestyles In Psych Rehabilitation) trial, Dr. Daumit and her colleagues found that people enrolled in an intervention group lost an average of 3.2 kg more than did a control group after 18 months (N Engl J Med. 2013;368:1594-602). The intervention steps included alternating group and individual weight management sessions, on-site group physical activity three times weekly, and weigh-ins. The study had 291 patients who were randomized between the control and intervention groups.
that can be used more broadly. She’s seeking to scale up effective interventions to address cardiovascular risk factors in people with SMI.
“Our goal is not just to get process-of-care measures like ‘counseling was delivered,’ ‘a medicine was started,’ but to actually show impact on health outcomes,” Dr. Daumit said.
Risks tied to antipsychotics
People with SMI face cardiovascular risks not only from unhealthy behaviors but also from the medications used to treat their psychiatric conditions. The American Diabetes Association and American Psychiatric Association in 2004 released a consensus statement on the impact of antipsychotics such as clozapine, olanzapine, and risperidone on obesity and diabetes. It included guidelines for monitoring the metabolic status of patients both at baseline and after initiating treatment, including checking body mass index, waist circumference, blood pressure, fasting glucose, and fasting lipids.
Yet, substantial evidence suggests that the medical community still has not paid enough attention to the health risks of those medications, said Alisa Busch, MD, of Harvard Medical School, Boston.
“A slew of research has shown since then that we have done a very poor job in adhering to those monitoring guidelines,” Dr. Busch said.
A fellow panelist, Marcela Horvitz-Lennon, MD, MPH, of the Rand Corp., presented results from her study showing continued common use of second-generation antipsychotics for off-label use for treatment of anxiety, posttraumatic stress disorder, and dementia in people of all ages.
Consistent with previous research, Dr. Horvitz-Lennon and her colleagues found that off-label use of second-generation antipsychotics was common during 2008-2012 in the four states they studied. They looked at available data from fee-for-service Medicare, Medicaid, and dually (Medicaid-Medicare) covered adult beneficiaries in California, Georgia, Mississippi, and Oklahoma.
Throughout the study period, California had the highest rate of fee-for-service beneficiaries whose SGA use was consistently off label (44.6%). Georgia had the lowest rate of always off-label use (35.1%), while Mississippi (42%) and Oklahoma (36.3%) fell somewhere in the middle.
When second-generation antipsychotics have approved uses such as schizophrenia, the known profile of a medication gives some assurance that the benefit of the medications will exceed the risk for that patient, she said. “When the medication is used off label, the implication is that there is no good evidence that the benefits are there,” Dr. Horvitz-Lennon said. “Hence, the potential for harm is most likely exceeding that likely or unlikely benefit.”
Dr. Daumit, Dr. Breslau, and Dr. Horvitz-Lennon said they had no financial disclosures.
ROCKVILLE, MD. – The problem of medical comorbidities in people with serious mental illness (SMI) persists and must be addressed, researchers said at a National Institute on Mental Health conference on mental health services research. Part of that effort, they said, is a more careful consideration of risks tied to the off-label use of second-generation antipsychotics.
The researchers discussed strategies aimed at combating obesity and diabetes, as well as behaviors such as smoking and sedentary lifestyle.
“One of the things that jumps out is the tremendous need for evidence-based strategies to address these physical health problems that are common in general population but even more of a burden for people with serious mental illness,” said Susan T. Azrin, PhD, of the NIMH, in an interview.
A study published in 2015, estimated that people with schizophrenia, for example, might lose almost 30 years of life because of premature death. Individuals with serious mental illness also experience elevated morbidity from cardiovascular disease and cancer. The NIMH and other federal agencies have in recent years looked for ways to help people with SMI quit smoking, and better control their weight and cholesterol.
But approaches that sound promising for boosting physical fitness in this group of patients have not always proven successful. Joshua Breslau, PhD, ScD, of the Rand Corp. discussed findings from a 2014 paper where he and his colleagues reported somewhat disappointing results from a study of federal Primary and Behavioral Health Care Integration grants.
The researchers matched clinics receiving this funding with similar ones that did not. They found that people with mental illness treated at the clinics receiving the grants showed improvements in some indicators of physical health (diastolic blood pressure, total cholesterol, LDL cholesterol, and fasting plasma glucose) but not in others (systolic blood pressure, body mass index, HDL cholesterol, hemoglobin A1c, triglycerides, self-reported smoking). Dr. Breslau said he and his colleagues also found only limited benefits in quality of care for physical health conditions associated with the grant program. Still, he remains hopeful.
“There is some potential here,” Dr. Breslau said. “Sometimes, we are seeing positive effects, but it’s certainly not a slam-dunk.”
He noted that opening a new setting for primary care services could strain a workforce that’s already in short supply. In addition, he said, attempts to fold primary care services into mental health programs could, in some cases, result in replication of care of chronic conditions for certain patients with SMI.
We “may still not reach that portion of the target population that has the greatest need,” Dr. Breslau said in an interview. “The new services may turn out to be duplicative rather than filling a gap.”
In another session, Gail L. Daumit, MD, MHS, of Johns Hopkins University, Baltimore, discussed her plan to build on a past success in helping people with SMI lose weight.
In the ACHIEVE (Achieving Healthy Lifestyles In Psych Rehabilitation) trial, Dr. Daumit and her colleagues found that people enrolled in an intervention group lost an average of 3.2 kg more than did a control group after 18 months (N Engl J Med. 2013;368:1594-602). The intervention steps included alternating group and individual weight management sessions, on-site group physical activity three times weekly, and weigh-ins. The study had 291 patients who were randomized between the control and intervention groups.
that can be used more broadly. She’s seeking to scale up effective interventions to address cardiovascular risk factors in people with SMI.
“Our goal is not just to get process-of-care measures like ‘counseling was delivered,’ ‘a medicine was started,’ but to actually show impact on health outcomes,” Dr. Daumit said.
Risks tied to antipsychotics
People with SMI face cardiovascular risks not only from unhealthy behaviors but also from the medications used to treat their psychiatric conditions. The American Diabetes Association and American Psychiatric Association in 2004 released a consensus statement on the impact of antipsychotics such as clozapine, olanzapine, and risperidone on obesity and diabetes. It included guidelines for monitoring the metabolic status of patients both at baseline and after initiating treatment, including checking body mass index, waist circumference, blood pressure, fasting glucose, and fasting lipids.
Yet, substantial evidence suggests that the medical community still has not paid enough attention to the health risks of those medications, said Alisa Busch, MD, of Harvard Medical School, Boston.
“A slew of research has shown since then that we have done a very poor job in adhering to those monitoring guidelines,” Dr. Busch said.
A fellow panelist, Marcela Horvitz-Lennon, MD, MPH, of the Rand Corp., presented results from her study showing continued common use of second-generation antipsychotics for off-label use for treatment of anxiety, posttraumatic stress disorder, and dementia in people of all ages.
Consistent with previous research, Dr. Horvitz-Lennon and her colleagues found that off-label use of second-generation antipsychotics was common during 2008-2012 in the four states they studied. They looked at available data from fee-for-service Medicare, Medicaid, and dually (Medicaid-Medicare) covered adult beneficiaries in California, Georgia, Mississippi, and Oklahoma.
Throughout the study period, California had the highest rate of fee-for-service beneficiaries whose SGA use was consistently off label (44.6%). Georgia had the lowest rate of always off-label use (35.1%), while Mississippi (42%) and Oklahoma (36.3%) fell somewhere in the middle.
When second-generation antipsychotics have approved uses such as schizophrenia, the known profile of a medication gives some assurance that the benefit of the medications will exceed the risk for that patient, she said. “When the medication is used off label, the implication is that there is no good evidence that the benefits are there,” Dr. Horvitz-Lennon said. “Hence, the potential for harm is most likely exceeding that likely or unlikely benefit.”
Dr. Daumit, Dr. Breslau, and Dr. Horvitz-Lennon said they had no financial disclosures.
ROCKVILLE, MD. – The problem of medical comorbidities in people with serious mental illness (SMI) persists and must be addressed, researchers said at a National Institute on Mental Health conference on mental health services research. Part of that effort, they said, is a more careful consideration of risks tied to the off-label use of second-generation antipsychotics.
The researchers discussed strategies aimed at combating obesity and diabetes, as well as behaviors such as smoking and sedentary lifestyle.
“One of the things that jumps out is the tremendous need for evidence-based strategies to address these physical health problems that are common in general population but even more of a burden for people with serious mental illness,” said Susan T. Azrin, PhD, of the NIMH, in an interview.
A study published in 2015, estimated that people with schizophrenia, for example, might lose almost 30 years of life because of premature death. Individuals with serious mental illness also experience elevated morbidity from cardiovascular disease and cancer. The NIMH and other federal agencies have in recent years looked for ways to help people with SMI quit smoking, and better control their weight and cholesterol.
But approaches that sound promising for boosting physical fitness in this group of patients have not always proven successful. Joshua Breslau, PhD, ScD, of the Rand Corp. discussed findings from a 2014 paper where he and his colleagues reported somewhat disappointing results from a study of federal Primary and Behavioral Health Care Integration grants.
The researchers matched clinics receiving this funding with similar ones that did not. They found that people with mental illness treated at the clinics receiving the grants showed improvements in some indicators of physical health (diastolic blood pressure, total cholesterol, LDL cholesterol, and fasting plasma glucose) but not in others (systolic blood pressure, body mass index, HDL cholesterol, hemoglobin A1c, triglycerides, self-reported smoking). Dr. Breslau said he and his colleagues also found only limited benefits in quality of care for physical health conditions associated with the grant program. Still, he remains hopeful.
“There is some potential here,” Dr. Breslau said. “Sometimes, we are seeing positive effects, but it’s certainly not a slam-dunk.”
He noted that opening a new setting for primary care services could strain a workforce that’s already in short supply. In addition, he said, attempts to fold primary care services into mental health programs could, in some cases, result in replication of care of chronic conditions for certain patients with SMI.
We “may still not reach that portion of the target population that has the greatest need,” Dr. Breslau said in an interview. “The new services may turn out to be duplicative rather than filling a gap.”
In another session, Gail L. Daumit, MD, MHS, of Johns Hopkins University, Baltimore, discussed her plan to build on a past success in helping people with SMI lose weight.
In the ACHIEVE (Achieving Healthy Lifestyles In Psych Rehabilitation) trial, Dr. Daumit and her colleagues found that people enrolled in an intervention group lost an average of 3.2 kg more than did a control group after 18 months (N Engl J Med. 2013;368:1594-602). The intervention steps included alternating group and individual weight management sessions, on-site group physical activity three times weekly, and weigh-ins. The study had 291 patients who were randomized between the control and intervention groups.
that can be used more broadly. She’s seeking to scale up effective interventions to address cardiovascular risk factors in people with SMI.
“Our goal is not just to get process-of-care measures like ‘counseling was delivered,’ ‘a medicine was started,’ but to actually show impact on health outcomes,” Dr. Daumit said.
Risks tied to antipsychotics
People with SMI face cardiovascular risks not only from unhealthy behaviors but also from the medications used to treat their psychiatric conditions. The American Diabetes Association and American Psychiatric Association in 2004 released a consensus statement on the impact of antipsychotics such as clozapine, olanzapine, and risperidone on obesity and diabetes. It included guidelines for monitoring the metabolic status of patients both at baseline and after initiating treatment, including checking body mass index, waist circumference, blood pressure, fasting glucose, and fasting lipids.
Yet, substantial evidence suggests that the medical community still has not paid enough attention to the health risks of those medications, said Alisa Busch, MD, of Harvard Medical School, Boston.
“A slew of research has shown since then that we have done a very poor job in adhering to those monitoring guidelines,” Dr. Busch said.
A fellow panelist, Marcela Horvitz-Lennon, MD, MPH, of the Rand Corp., presented results from her study showing continued common use of second-generation antipsychotics for off-label use for treatment of anxiety, posttraumatic stress disorder, and dementia in people of all ages.
Consistent with previous research, Dr. Horvitz-Lennon and her colleagues found that off-label use of second-generation antipsychotics was common during 2008-2012 in the four states they studied. They looked at available data from fee-for-service Medicare, Medicaid, and dually (Medicaid-Medicare) covered adult beneficiaries in California, Georgia, Mississippi, and Oklahoma.
Throughout the study period, California had the highest rate of fee-for-service beneficiaries whose SGA use was consistently off label (44.6%). Georgia had the lowest rate of always off-label use (35.1%), while Mississippi (42%) and Oklahoma (36.3%) fell somewhere in the middle.
When second-generation antipsychotics have approved uses such as schizophrenia, the known profile of a medication gives some assurance that the benefit of the medications will exceed the risk for that patient, she said. “When the medication is used off label, the implication is that there is no good evidence that the benefits are there,” Dr. Horvitz-Lennon said. “Hence, the potential for harm is most likely exceeding that likely or unlikely benefit.”
Dr. Daumit, Dr. Breslau, and Dr. Horvitz-Lennon said they had no financial disclosures.
REPORTING FROM AN NIMH CONFERENCE
ADA underscores distinctions in youth, adult T1DM
Management of type 1 diabetes mellitus in children should include careful consideration of the unique features and challenges that differentiate it from T1DM in adults, according to a new position statement released by the American Diabetes Association.
The statement, published Aug. 10 in Diabetes Care, includes guidance on diagnosis, staging, screening, monitoring, treatment, nutrition, physical activity, and transition from pediatric to adult care.
With regard to diagnosis and staging, the recommendations emphasize the importance of distinguishing between T1DM, type 2 diabetes mellitus, and monogenic diabetes. It also asserts that a pediatric endocrinologist should be consulted before making a diagnosis when “isolated glycosuria or hyperglycemia is discovered in the setting of acute illness and in the absence of classic symptoms,” wrote Jane L. Chiang, MD, of McKinsey & Company and chief medical officer at Diasome Pharmaceuticals in Palo Alto, Calif., and coauthors.
The guidance also describes the three stages of type 1 diabetes development. Stage 1 is presymptomatic and features the presence of beta-cell autoimmunity. Stage 2, also presymptomatic, includes the presence of beta-cell autoimmunity with dysglycemia. Symptomatic disease from insulin deficiency begins in stage 3, and may include hyperglycemia, polyuria, polydipsia, weight loss, polyphagia, fatigue, and blurred vision. Perineal candidiasis is common in girls, and about one-third of cases present with diabetic ketoacidosis (DKA).
In patients with hyperglycemia symptoms, blood glucose, not hemoglobin A1c, should be used to diagnose acute onset of disease. Delays in diagnosis and insulin replacement therapy should be avoided and a definitive diagnosis made quickly, the authors added.
Because the current method of using HbA1c to diagnose diabetes was based on studies limited to adults, there is still debate over whether to use HbA1c to diagnose T1DM in children and adolescents, Dr. Chiang and colleagues noted. Additionally, physicians must take care to distinguish between diabetes types because of increased numbers of overweight children with T1DM, as well as frequent misdiagnosis of monogenic diabetes as T1DM.
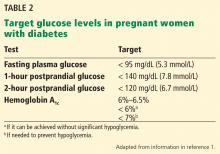
The position statement emphasizes the importance of insulin therapy as treatment for children with T1DM and recommends that most patients should be treated with either multiple injections of prandial and basal insulin, or with continuous subcutaneous insulin infusion. HbA1c should be measured at 3-month intervals to assess glycemic control, with a target HbA1c of less than 7.5%, the authors said. Also covered are recommendations for blood glucose monitoring, blood and urine ketone monitoring, and continuous glucose monitoring.
The importance of integrating an exercise and nutrition plan is also highlighted in the guidance. In addition to monitoring carbohydrate and caloric intake with the help of a dietitian, 60 minutes of moderate to vigorous activity daily are recommended as an exercise goal. Steps should also be taken to prevent hypoglycemia during and after exercise, the authors added.
Measures must also be taken to anticipate and address the unique behavioral and social challenges that accompany diabetes management in developing adolescents, the authors said. Social and family issues, peer relationships, and disordered eating should all be considered, and, starting at age 12 years, patients should be allowed time to speak in confidentiality with their health care provider, Dr. Chiang and colleagues said.
Additionally, as adolescents assert increased independence and autonomy, independent disease management should be facilitated, and issues such as depression and risky behaviors discussed.
The guidelines also discuss the importance of following the Centers for Disease Control and Prevention immunization schedule, and monitoring growth and weight gain. Patients with T1DM and their caregivers should also be sufficiently educated on comorbidities such as diabetic ketoacidosis, hypoglycemia, retinopathy, dyslipidemia, autoimmune diseases, and other complications.
Supportive environments such as diabetes camps, as well as technological advances, may be effective tools in encouraging diabetes self-management. Though there is no “optimal transition age” for the shift from pediatric to adult care, ADA recommends that providers begin transition preparation in the early adolescent years, and provide counseling on diabetes self-management.
“An ineffective transition from pediatric to adult diabetes care may contribute to fragmentation of health care and increased risk for adverse outcomes,” the authors said. “An individualized approach to transition timing is recommended, prioritizing the developmental needs and preferences of the patient.”
The authors reported relationships with Diasome Pharmaceuticals and numerous other companies.
SOURCE: Chiang J et al. Diabetes Care. 2018 Jul. doi: 10.2337/dci18-0023.
Management of type 1 diabetes mellitus in children should include careful consideration of the unique features and challenges that differentiate it from T1DM in adults, according to a new position statement released by the American Diabetes Association.
The statement, published Aug. 10 in Diabetes Care, includes guidance on diagnosis, staging, screening, monitoring, treatment, nutrition, physical activity, and transition from pediatric to adult care.
With regard to diagnosis and staging, the recommendations emphasize the importance of distinguishing between T1DM, type 2 diabetes mellitus, and monogenic diabetes. It also asserts that a pediatric endocrinologist should be consulted before making a diagnosis when “isolated glycosuria or hyperglycemia is discovered in the setting of acute illness and in the absence of classic symptoms,” wrote Jane L. Chiang, MD, of McKinsey & Company and chief medical officer at Diasome Pharmaceuticals in Palo Alto, Calif., and coauthors.
The guidance also describes the three stages of type 1 diabetes development. Stage 1 is presymptomatic and features the presence of beta-cell autoimmunity. Stage 2, also presymptomatic, includes the presence of beta-cell autoimmunity with dysglycemia. Symptomatic disease from insulin deficiency begins in stage 3, and may include hyperglycemia, polyuria, polydipsia, weight loss, polyphagia, fatigue, and blurred vision. Perineal candidiasis is common in girls, and about one-third of cases present with diabetic ketoacidosis (DKA).
In patients with hyperglycemia symptoms, blood glucose, not hemoglobin A1c, should be used to diagnose acute onset of disease. Delays in diagnosis and insulin replacement therapy should be avoided and a definitive diagnosis made quickly, the authors added.
Because the current method of using HbA1c to diagnose diabetes was based on studies limited to adults, there is still debate over whether to use HbA1c to diagnose T1DM in children and adolescents, Dr. Chiang and colleagues noted. Additionally, physicians must take care to distinguish between diabetes types because of increased numbers of overweight children with T1DM, as well as frequent misdiagnosis of monogenic diabetes as T1DM.
The position statement emphasizes the importance of insulin therapy as treatment for children with T1DM and recommends that most patients should be treated with either multiple injections of prandial and basal insulin, or with continuous subcutaneous insulin infusion. HbA1c should be measured at 3-month intervals to assess glycemic control, with a target HbA1c of less than 7.5%, the authors said. Also covered are recommendations for blood glucose monitoring, blood and urine ketone monitoring, and continuous glucose monitoring.
The importance of integrating an exercise and nutrition plan is also highlighted in the guidance. In addition to monitoring carbohydrate and caloric intake with the help of a dietitian, 60 minutes of moderate to vigorous activity daily are recommended as an exercise goal. Steps should also be taken to prevent hypoglycemia during and after exercise, the authors added.
Measures must also be taken to anticipate and address the unique behavioral and social challenges that accompany diabetes management in developing adolescents, the authors said. Social and family issues, peer relationships, and disordered eating should all be considered, and, starting at age 12 years, patients should be allowed time to speak in confidentiality with their health care provider, Dr. Chiang and colleagues said.
Additionally, as adolescents assert increased independence and autonomy, independent disease management should be facilitated, and issues such as depression and risky behaviors discussed.
The guidelines also discuss the importance of following the Centers for Disease Control and Prevention immunization schedule, and monitoring growth and weight gain. Patients with T1DM and their caregivers should also be sufficiently educated on comorbidities such as diabetic ketoacidosis, hypoglycemia, retinopathy, dyslipidemia, autoimmune diseases, and other complications.
Supportive environments such as diabetes camps, as well as technological advances, may be effective tools in encouraging diabetes self-management. Though there is no “optimal transition age” for the shift from pediatric to adult care, ADA recommends that providers begin transition preparation in the early adolescent years, and provide counseling on diabetes self-management.
“An ineffective transition from pediatric to adult diabetes care may contribute to fragmentation of health care and increased risk for adverse outcomes,” the authors said. “An individualized approach to transition timing is recommended, prioritizing the developmental needs and preferences of the patient.”
The authors reported relationships with Diasome Pharmaceuticals and numerous other companies.
SOURCE: Chiang J et al. Diabetes Care. 2018 Jul. doi: 10.2337/dci18-0023.
Management of type 1 diabetes mellitus in children should include careful consideration of the unique features and challenges that differentiate it from T1DM in adults, according to a new position statement released by the American Diabetes Association.
The statement, published Aug. 10 in Diabetes Care, includes guidance on diagnosis, staging, screening, monitoring, treatment, nutrition, physical activity, and transition from pediatric to adult care.
With regard to diagnosis and staging, the recommendations emphasize the importance of distinguishing between T1DM, type 2 diabetes mellitus, and monogenic diabetes. It also asserts that a pediatric endocrinologist should be consulted before making a diagnosis when “isolated glycosuria or hyperglycemia is discovered in the setting of acute illness and in the absence of classic symptoms,” wrote Jane L. Chiang, MD, of McKinsey & Company and chief medical officer at Diasome Pharmaceuticals in Palo Alto, Calif., and coauthors.
The guidance also describes the three stages of type 1 diabetes development. Stage 1 is presymptomatic and features the presence of beta-cell autoimmunity. Stage 2, also presymptomatic, includes the presence of beta-cell autoimmunity with dysglycemia. Symptomatic disease from insulin deficiency begins in stage 3, and may include hyperglycemia, polyuria, polydipsia, weight loss, polyphagia, fatigue, and blurred vision. Perineal candidiasis is common in girls, and about one-third of cases present with diabetic ketoacidosis (DKA).
In patients with hyperglycemia symptoms, blood glucose, not hemoglobin A1c, should be used to diagnose acute onset of disease. Delays in diagnosis and insulin replacement therapy should be avoided and a definitive diagnosis made quickly, the authors added.
Because the current method of using HbA1c to diagnose diabetes was based on studies limited to adults, there is still debate over whether to use HbA1c to diagnose T1DM in children and adolescents, Dr. Chiang and colleagues noted. Additionally, physicians must take care to distinguish between diabetes types because of increased numbers of overweight children with T1DM, as well as frequent misdiagnosis of monogenic diabetes as T1DM.
The position statement emphasizes the importance of insulin therapy as treatment for children with T1DM and recommends that most patients should be treated with either multiple injections of prandial and basal insulin, or with continuous subcutaneous insulin infusion. HbA1c should be measured at 3-month intervals to assess glycemic control, with a target HbA1c of less than 7.5%, the authors said. Also covered are recommendations for blood glucose monitoring, blood and urine ketone monitoring, and continuous glucose monitoring.
The importance of integrating an exercise and nutrition plan is also highlighted in the guidance. In addition to monitoring carbohydrate and caloric intake with the help of a dietitian, 60 minutes of moderate to vigorous activity daily are recommended as an exercise goal. Steps should also be taken to prevent hypoglycemia during and after exercise, the authors added.
Measures must also be taken to anticipate and address the unique behavioral and social challenges that accompany diabetes management in developing adolescents, the authors said. Social and family issues, peer relationships, and disordered eating should all be considered, and, starting at age 12 years, patients should be allowed time to speak in confidentiality with their health care provider, Dr. Chiang and colleagues said.
Additionally, as adolescents assert increased independence and autonomy, independent disease management should be facilitated, and issues such as depression and risky behaviors discussed.
The guidelines also discuss the importance of following the Centers for Disease Control and Prevention immunization schedule, and monitoring growth and weight gain. Patients with T1DM and their caregivers should also be sufficiently educated on comorbidities such as diabetic ketoacidosis, hypoglycemia, retinopathy, dyslipidemia, autoimmune diseases, and other complications.
Supportive environments such as diabetes camps, as well as technological advances, may be effective tools in encouraging diabetes self-management. Though there is no “optimal transition age” for the shift from pediatric to adult care, ADA recommends that providers begin transition preparation in the early adolescent years, and provide counseling on diabetes self-management.
“An ineffective transition from pediatric to adult diabetes care may contribute to fragmentation of health care and increased risk for adverse outcomes,” the authors said. “An individualized approach to transition timing is recommended, prioritizing the developmental needs and preferences of the patient.”
The authors reported relationships with Diasome Pharmaceuticals and numerous other companies.
SOURCE: Chiang J et al. Diabetes Care. 2018 Jul. doi: 10.2337/dci18-0023.
FROM DIABETES CARE
Key clinical point: Management of type 1 diabetes in children and adolescents should take into account the unique challenges of disease management in that age group, and facilitate an effective transition to adult care.
Major finding: The position statement emphasizes the importance of insulin therapy as treatment for children with T1DM and the importance of integrating an exercise and nutrition plan.
Study details: An analysis of numerous diabetes studies and clinical trials.
Disclosures: The authors reported relationships with Diasome Pharmaceuticals and numerous other companies.
Source: Chiang J et al. Diabetes Care. 2018 Jul. doi: 10.2337/dci18-0023.
Hospitalists target inpatient glycemic control
SHM benchmarks provide ‘objective format’ for improving outcomes
Physicians are trained to manage their patients’ diabetes and often do a meticulous job – one on one. But in order to maximize glycemic control outcomes throughout the hospital, you need a kind of diabetic epidemiology team to focus on the data, said Andjela Drincic, MD, an endocrinologist at Nebraska Medicine, the clinical partner of the University of Nebraska Medical Center in Omaha.
As medical director for diabetes stewardship, Dr. Drincic serves as the epidemiologic lead for her hospital, which has worked systematically to improve inpatient glycemic control since 2012 – with help from the Society of Hospital Medicine.
“You need a team and to set up a system that works, with protocols and some way of knowing if the protocols are succeeding,” Dr. Drincic said. “Quality improvement targets are never static.” She credited SHM’s glycemic control eQUIPS (Electronic Quality Improvement Program), an online quality improvement resource and collaborative of 104 participating hospitals, for providing the support and the data needed to drive glycemic QI efforts at Nebraska Medicine. SHM provided reporting metrics, quarterly benchmarking reports, a library of tools and resources, an implementation guide, educational webinars on demand and, for some participants, mentored implementation with the advice of a leading expert in the field.
One big reason for giving more attention to glycemic control in the hospital is patient safety, said Gregory Maynard, MD, MHM, clinical professor and chief quality officer at the University of California–Davis Medical Center and SHM’s project team leader for eQUIPS.
“Hyperglycemia in hospitalized patients is an extraordinarily common and growing problem, affecting up to 40%-50% of patients in the hospital,” he said. In 2012, 7.7 million hospital stays involved patients with diabetes, the seventh leading cause of death in the United States.1
Hyperglycemia is linked to elevated rates of medical complications, infections, wound complications, hospital mortality, length of stay, readmissions, and ICU admissions, along with other outcomes not directly related to diabetes. Hyperglycemia in hospitalized patients who have not been given a diagnosis of diabetes is, if anything, more dangerous. Add the related risk for hypoglycemia, and clinicians are challenged to keep their patients controlled within the zone between the extremes of hyper- and hypoglycemia. The American Diabetes Association recently issued recommendations with more relaxed glucose targets between 140 and 180 mg/dL for most patients in non–intensive care settings.2
“To not have a standardized way of managing hyperglycemia for your hospital seems like an enormous missed opportunity,” Dr. Maynard said. “If someone comes into the hospital with a chronic condition of diabetes that you ignore, just maintaining them in the hospital and sending them back out into the world without addressing the underlying condition is not good care. You have missed an important opportunity to alter the course of a serious chronic condition.”
Dr. Maynard said SHM recognized this opportunity when it established eQUIPS. “Hospitalists are often tasked with taking care of patients with glycemic issues because there may not be an endocrinologist readily accessible in the hospital,” he said. “We have seen through our benchmarking in eQUIPS incredible variability – with 10-fold differences in hyperglycemia and hypoglycemia rates between the best- and worst-performing sites. The biggest variable is whether the hospital systematically manages glycemic control. We have also shown that achieving high levels of glycemic control and low hypoglycemia rates concurrently is very possible.”
Reliable benchmarks
Nebraska Medicine enrolled in eQUIPS in 2012.
“We utilize SHM’s glucometrics (standardized analyses of inpatient glycemic control data).”3 said Dr. Drincic. “I was looking for a reliable glucometric system and some way to make comparisons with other hospitals when I came across the data Dr. Maynard published about SHM via a PubMed search. We needed outcomes that are validated in the literature and comparison groups.”
Nebraska Medicine has also received a certificate of distinction for inpatient diabetes care from the Joint Commission, and Dr. Drincic is active in PRIDE (Planning Research in Inpatient Diabetes), a national consortium of leading investigators in inpatient diabetes care formed to promote collaborative research. The PRIDE group meets yearly at the ADA conference, communicates regularly by email, and publishes articles.
“Once a year I present our glycemic control data to our administration and to the quality and safety committees at the hospital. I have been pleased with the level of support we have received,” Dr. Drincic said. “We needed a mandate to do this, but when I reported the impact on readmissions and other outcomes, I got the full support of administration. This would have been a lot harder without SHM.”
Engagement with hospitalists is another key to the glucose management project’s success, Dr. Drincic said. “We as endocrinologists think we know how to manage diabetes, but hospitalists have the daunting task of dealing with all of the patient’s medical issues. If we don’t have a strong collaboration, how can we change practice hospitalwide?” Rachel Thompson, MD, SFHM, Nebraska Medicine’s chief of hospital medicine, participates in the glucose management project, Dr. Drincic said.
“We occasionally are guests at hospitalist meetings to share new glucose treatment algorithms,” she said. “We’re also looking at collaborating on other quality initiatives, for example, studying how perioperative dexamethasone affects glycemic control. We built this relationship with hospitalists by establishing trust while trying to shed a reputation as ‘sugar police.’ I don’t want hospitalists saying ‘There she goes again’ whenever I come on the unit. We have tried to establish personal relationships and figure out what the hospitalists need, especially relative to EPIC (the hospital’s electronic medical record software).”
Dr. Thompson said her group’s recent growth to nearly 70 clinicians has increased its footprint hospitalwide and given hospitalists a greater opportunity to influence glycemic control. “We see up to a third of the patients in the hospital outside of the ICU. Glycemic control is something you learn as a hospitalist – It’s a very important frontline quality issue. In the patient list on EPIC every morning we have a field highlighting all patients with glycemic control issues,” she said.
“Poor glucose control is associated with poor outcomes for our patients. We need the right systems in place for patient safety. Moreover, if we are ignoring glycemic control when the patient is in the hospital, we’re sending the wrong message and setting a bad example for our patients when they return home.”
Lack of clear metrics
A significant defect in the infrastructure of many glucose management programs is the lack of clear metrics for outcomes, Dr. Maynard said. Nearly one-third of hospitals in the United States have no standardized metric to track the quality of their inpatient glycemic management, a sobering statistic considering that the first step in any QI initiative is to define and measure the problem at hand.
“I believe the main reason that glycemic control has been left off hospitals’ radar screens is that we still have not adopted national, publicly reported quality measures for glycemic control, although those were proposed recently by a government interagency work group,” Dr. Maynard said. “Until that happens, we’ll continue to see uneven response.”
The first step for frontline hospitalists is to learn and understand the basics of glucose control, for example, basal bolus insulin administration, and to stop writing orders for sliding scale insulin as the sole means of controlling hyperglycemia.
“Develop and adopt standards of practice for insulin administration in your hospital,” Dr. Maynard said. “Be part of the solution, not the problem. Once you get into the weeds – patients on steroids or on total parenteral nutrition – it can get tricky. But it’s important to get the basics right and move beyond inertia on this topic.”
The glycemic team at Nebraska Medicine includes, in addition to Dr. Drincic and Dr. Thompson, an endocrinology fellow, diabetes case managers, resource nurses, nurse leadership, pharmacists, inpatient care transitions coordinators, and representatives from pediatrics and critical care, all working to impact the overall quality of glycemic management in the hospital. Jon Knezevich, PharmD is diabetes stewardship pharmacy coordinator, and Shelly Lautenbaugh, RN, CDE, is diabetes lead care manager and diabetes coordinator for the Joint Commission certificate program. Diabetes stewardship also includes online and live training courses and a class in acute glucose management for the diabetes resource nurses, who bring the knowledge back to their units.
The glucose team’s job is to make sure patients are cared for safely, using appropriate policies and procedures, education, and training, Ms. Lautenbaugh said. “We have a mission as a hospital to transform people’s lives. We try to live our values, and everything follows from the focus on patient safety,” she added. “If our patients can receive extraordinary care and leave better informed about their condition than when they came in, and then we don’t see them again, we’ve achieved our ultimate goal.”
Hyperglycemia is most often not the primary reason why patients are hospitalized, Ms. Lautenbaugh said. “But we need to give them appropriate glucose management regardless. We’ve worked with bedside staff, nurse leadership, and teams to develop plans to raise our outcome scores. We have a lot of different outcomes we examine, and it’s always evolving.”
Quality metrics are incorporated into the electronic medical record, but those reports are not timely enough for day-to-day management, Dr. Knezevich said. “So we created a diabetes dashboard, constantly updated in real time to identify patients who are out of glycemic control.” The measures tracked include a mean patient day glucose score, percentage of readings within recommended limits, mean time between measured low readings and next documented reading or resolution of hypoglycemia, readmission rates, and diabetes nutrition assessments.
For hospitals with diabetes certificates, the Joint Commission also requires that every patient with hyperglycemia receives a clinic visit 30 days after discharge to make sure they are receiving appropriate follow-up care. Other facets of the Nebraska glycemic initiative include utilizing the hospital’s voluntary “Meds to Beds” program, which brings prescribed medications to the patient’s room at discharge. “We offer a diabetes discharge kit for patients who are self-pay, with all of the insulin and medical supplies they will need to get to the 30-day follow-up visit,” Dr. Knezevich said. “We can dream up amazing treatment regimens, but if they can’t afford the medications, what have we accomplished?”
SHM’s external benchmarks have provided an objective format for comparing and improving outcomes, Ms. Lautenbaugh said. “We like to see where we are and use the data to make significant improvements, but we’re also focused on internal assessments. If we make changes for a given metric, how does it affect performance in other areas?” One important metric is percentage of glucose readings within target range hospitalwide. “Our overall goal is 75%. It was 72% in April 2018, and we’ve raised it to 74.4%. It’s a small gain but it shows steady progress. Little steps make small but steady improvement,” she said.
“One area where we were not pleased was the occurrence of hypoglycemia,” Ms. Lautenbaugh said. “We did a root cause analysis of every hypoglycemic event, including several reports for patients who didn’t have diabetes at all. We had to weed out some that weren’t pertinent to our quality questions, but for those that are, the diabetes case manager calls the provider to make sure they were aware of the incident. We were able to identify the outliers in noncritical care, which we’re now able to tackle using a systematic approach.”
Get on the bus
Hospitalists are also integrally involved in a hospital glycemic improvement initiative at Orange Regional Medical Center (ORMC) in Middletown, N.Y.
The Glycemic Improvement Team (GIT) was formed in 2012 when a new hospital campus opened and EPIC was implemented as the hospital’s EMR. But glycemic control has taken on greater focus since 2015, when ORMC enrolled in eQUIPS, said Lorraine Porcaro, RN, the hospital’s diabetes clinical manager. The glycemic control team includes representatives from medicine, nursing, case management, laboratory, nutrition, pharmacy, wound care, and quality improvement.
Implementing the new EMR offered the opportunity to track a number of medical values in real time, Ms. Porcaro said. ORMC has focused its glycemic quality improvement efforts on hypoglycemia and hyperglycemia, with a recent emphasis on the need for improvements related to glucose reassessment 15 minutes post hypoglycemia treatment. More than a hundred “Diabetes Champions” have completed 16 hours of advanced training in diabetes and provide in-unit mentorship for other staff.
The ORMC team’s glycemic improvement “bus” is a rolling cart that goes from unit to unit supplying nurse education, reminders, copies of department-specific policies and protocols, and treats for staff. “It’s what we’re known for,” Ms. Porcaro said. Pens with the motto: “Don’t Miss the Bus! Retest in 15!” summarize the GIT’s current focus on post–hypoglycemia treatment retesting.
Hospitalists were part of the glycemic improvement process at ORMC from the beginning and are still involved, said Adrian Paraschiv, MD, FHM, a hospitalist and assistant director of the medical center, as well as the ORMC director of clinical information technology. ORMC initiated hospitalist coverage in 1998 and now has three HM groups, two of them represented on the glycemic improvement team.
“Like any hospital, we feel we should minimize hypoglycemic events,” Dr. Paraschiv explained. “This became important for other hospital departments, and we recognized we needed a major QI initiative to improve our outcomes hospitalwide. In the process, we noticed what other people were saying: Results from improving glycemic control included reduced length of stay, cost, and infections. That provided motivation for the hospital to support our initiative.”
Glucose management isn’t only about blood sugar, but whether the patient ate or not, their other blood work, the level of education for patient and staff, and a variety of other inputs, Dr. Paraschiv said. “All of these things were in the EMR but all over the place. EPIC had an incipient structure for pulling the data together, and we modified it to show everything that’s going on with the patient’s glycemic control on a single screen. We can build order sets and issue different reports.”
Today at ORMC, hypoglycemia is reassessed within 30 minutes more than 50% of the time. “It will never be at 100%, but we wanted to at least be at the national mean for eQUIPS hospitals. Our stretch goal was to be in the top quartile, and by the end of 2017, we realized that goal,” Ms. Porcaro said. Sometimes, because of changes in patients and staff, the GIT needs to repeat the education and review policies. “Since then, it’s been a matter of continuing staff education; sharing glucose data with stakeholders; talking about goals for ICU and non-ICU units; and, when needed, rolling out the bus.”
Participation in eQUIPS has made it possible to gather this information in one place and present it in a way that makes sense to physicians, Dr. Paraschiv said. “Dr. Maynard and SHM showed us how to put the data together to add value. Using these tools, we started looking at our processes, what needed to change, and what we are able to change. Now we’re examining what happens afterward. Can we use the electronic system to automatically alert physicians to make changes to the treatment regimen in real time? We continue to improve using upgrades to our EMR, such as an alert system with best practice advisories for the clinician. We now think we can actually achieve what we set out to achieve,” he said.
“Our idea was that we needed to market this program throughout the hospital – starting from the kitchen, meal delivery staff, IT, laboratory, medical and nursing staff,” Ms. Porcaro said. “The issue is multifactorial – it’s for the entire hospital. My heart is warmed when I see the woman who delivers the meals asking the patient: ‘Have you gotten your insulin shot?’ ”
References
1. Corvino L et al. “Management of diabetes and hyperglycemia in hospitalized patients.” Updated 2017 Oct 1 in De Groot LJ et al. editors. Endotext. South Dartmouth (MA): MDText.com 2000.
2. American Diabetes Association. Glycemic targets. Diabetes Care 2017 Jan;40(Suppl 1):S48-56.
3. Maynard G et al. “Design and implementation of a web-based reporting and benchmarking center for inpatient glucometrics.” J Diabetes Sci Technol. 2014 May 12;8(4):630-40.
SHM benchmarks provide ‘objective format’ for improving outcomes
SHM benchmarks provide ‘objective format’ for improving outcomes
Physicians are trained to manage their patients’ diabetes and often do a meticulous job – one on one. But in order to maximize glycemic control outcomes throughout the hospital, you need a kind of diabetic epidemiology team to focus on the data, said Andjela Drincic, MD, an endocrinologist at Nebraska Medicine, the clinical partner of the University of Nebraska Medical Center in Omaha.
As medical director for diabetes stewardship, Dr. Drincic serves as the epidemiologic lead for her hospital, which has worked systematically to improve inpatient glycemic control since 2012 – with help from the Society of Hospital Medicine.
“You need a team and to set up a system that works, with protocols and some way of knowing if the protocols are succeeding,” Dr. Drincic said. “Quality improvement targets are never static.” She credited SHM’s glycemic control eQUIPS (Electronic Quality Improvement Program), an online quality improvement resource and collaborative of 104 participating hospitals, for providing the support and the data needed to drive glycemic QI efforts at Nebraska Medicine. SHM provided reporting metrics, quarterly benchmarking reports, a library of tools and resources, an implementation guide, educational webinars on demand and, for some participants, mentored implementation with the advice of a leading expert in the field.
One big reason for giving more attention to glycemic control in the hospital is patient safety, said Gregory Maynard, MD, MHM, clinical professor and chief quality officer at the University of California–Davis Medical Center and SHM’s project team leader for eQUIPS.
“Hyperglycemia in hospitalized patients is an extraordinarily common and growing problem, affecting up to 40%-50% of patients in the hospital,” he said. In 2012, 7.7 million hospital stays involved patients with diabetes, the seventh leading cause of death in the United States.1
Hyperglycemia is linked to elevated rates of medical complications, infections, wound complications, hospital mortality, length of stay, readmissions, and ICU admissions, along with other outcomes not directly related to diabetes. Hyperglycemia in hospitalized patients who have not been given a diagnosis of diabetes is, if anything, more dangerous. Add the related risk for hypoglycemia, and clinicians are challenged to keep their patients controlled within the zone between the extremes of hyper- and hypoglycemia. The American Diabetes Association recently issued recommendations with more relaxed glucose targets between 140 and 180 mg/dL for most patients in non–intensive care settings.2
“To not have a standardized way of managing hyperglycemia for your hospital seems like an enormous missed opportunity,” Dr. Maynard said. “If someone comes into the hospital with a chronic condition of diabetes that you ignore, just maintaining them in the hospital and sending them back out into the world without addressing the underlying condition is not good care. You have missed an important opportunity to alter the course of a serious chronic condition.”
Dr. Maynard said SHM recognized this opportunity when it established eQUIPS. “Hospitalists are often tasked with taking care of patients with glycemic issues because there may not be an endocrinologist readily accessible in the hospital,” he said. “We have seen through our benchmarking in eQUIPS incredible variability – with 10-fold differences in hyperglycemia and hypoglycemia rates between the best- and worst-performing sites. The biggest variable is whether the hospital systematically manages glycemic control. We have also shown that achieving high levels of glycemic control and low hypoglycemia rates concurrently is very possible.”
Reliable benchmarks
Nebraska Medicine enrolled in eQUIPS in 2012.
“We utilize SHM’s glucometrics (standardized analyses of inpatient glycemic control data).”3 said Dr. Drincic. “I was looking for a reliable glucometric system and some way to make comparisons with other hospitals when I came across the data Dr. Maynard published about SHM via a PubMed search. We needed outcomes that are validated in the literature and comparison groups.”
Nebraska Medicine has also received a certificate of distinction for inpatient diabetes care from the Joint Commission, and Dr. Drincic is active in PRIDE (Planning Research in Inpatient Diabetes), a national consortium of leading investigators in inpatient diabetes care formed to promote collaborative research. The PRIDE group meets yearly at the ADA conference, communicates regularly by email, and publishes articles.
“Once a year I present our glycemic control data to our administration and to the quality and safety committees at the hospital. I have been pleased with the level of support we have received,” Dr. Drincic said. “We needed a mandate to do this, but when I reported the impact on readmissions and other outcomes, I got the full support of administration. This would have been a lot harder without SHM.”
Engagement with hospitalists is another key to the glucose management project’s success, Dr. Drincic said. “We as endocrinologists think we know how to manage diabetes, but hospitalists have the daunting task of dealing with all of the patient’s medical issues. If we don’t have a strong collaboration, how can we change practice hospitalwide?” Rachel Thompson, MD, SFHM, Nebraska Medicine’s chief of hospital medicine, participates in the glucose management project, Dr. Drincic said.
“We occasionally are guests at hospitalist meetings to share new glucose treatment algorithms,” she said. “We’re also looking at collaborating on other quality initiatives, for example, studying how perioperative dexamethasone affects glycemic control. We built this relationship with hospitalists by establishing trust while trying to shed a reputation as ‘sugar police.’ I don’t want hospitalists saying ‘There she goes again’ whenever I come on the unit. We have tried to establish personal relationships and figure out what the hospitalists need, especially relative to EPIC (the hospital’s electronic medical record software).”
Dr. Thompson said her group’s recent growth to nearly 70 clinicians has increased its footprint hospitalwide and given hospitalists a greater opportunity to influence glycemic control. “We see up to a third of the patients in the hospital outside of the ICU. Glycemic control is something you learn as a hospitalist – It’s a very important frontline quality issue. In the patient list on EPIC every morning we have a field highlighting all patients with glycemic control issues,” she said.
“Poor glucose control is associated with poor outcomes for our patients. We need the right systems in place for patient safety. Moreover, if we are ignoring glycemic control when the patient is in the hospital, we’re sending the wrong message and setting a bad example for our patients when they return home.”
Lack of clear metrics
A significant defect in the infrastructure of many glucose management programs is the lack of clear metrics for outcomes, Dr. Maynard said. Nearly one-third of hospitals in the United States have no standardized metric to track the quality of their inpatient glycemic management, a sobering statistic considering that the first step in any QI initiative is to define and measure the problem at hand.
“I believe the main reason that glycemic control has been left off hospitals’ radar screens is that we still have not adopted national, publicly reported quality measures for glycemic control, although those were proposed recently by a government interagency work group,” Dr. Maynard said. “Until that happens, we’ll continue to see uneven response.”
The first step for frontline hospitalists is to learn and understand the basics of glucose control, for example, basal bolus insulin administration, and to stop writing orders for sliding scale insulin as the sole means of controlling hyperglycemia.
“Develop and adopt standards of practice for insulin administration in your hospital,” Dr. Maynard said. “Be part of the solution, not the problem. Once you get into the weeds – patients on steroids or on total parenteral nutrition – it can get tricky. But it’s important to get the basics right and move beyond inertia on this topic.”
The glycemic team at Nebraska Medicine includes, in addition to Dr. Drincic and Dr. Thompson, an endocrinology fellow, diabetes case managers, resource nurses, nurse leadership, pharmacists, inpatient care transitions coordinators, and representatives from pediatrics and critical care, all working to impact the overall quality of glycemic management in the hospital. Jon Knezevich, PharmD is diabetes stewardship pharmacy coordinator, and Shelly Lautenbaugh, RN, CDE, is diabetes lead care manager and diabetes coordinator for the Joint Commission certificate program. Diabetes stewardship also includes online and live training courses and a class in acute glucose management for the diabetes resource nurses, who bring the knowledge back to their units.
The glucose team’s job is to make sure patients are cared for safely, using appropriate policies and procedures, education, and training, Ms. Lautenbaugh said. “We have a mission as a hospital to transform people’s lives. We try to live our values, and everything follows from the focus on patient safety,” she added. “If our patients can receive extraordinary care and leave better informed about their condition than when they came in, and then we don’t see them again, we’ve achieved our ultimate goal.”
Hyperglycemia is most often not the primary reason why patients are hospitalized, Ms. Lautenbaugh said. “But we need to give them appropriate glucose management regardless. We’ve worked with bedside staff, nurse leadership, and teams to develop plans to raise our outcome scores. We have a lot of different outcomes we examine, and it’s always evolving.”
Quality metrics are incorporated into the electronic medical record, but those reports are not timely enough for day-to-day management, Dr. Knezevich said. “So we created a diabetes dashboard, constantly updated in real time to identify patients who are out of glycemic control.” The measures tracked include a mean patient day glucose score, percentage of readings within recommended limits, mean time between measured low readings and next documented reading or resolution of hypoglycemia, readmission rates, and diabetes nutrition assessments.
For hospitals with diabetes certificates, the Joint Commission also requires that every patient with hyperglycemia receives a clinic visit 30 days after discharge to make sure they are receiving appropriate follow-up care. Other facets of the Nebraska glycemic initiative include utilizing the hospital’s voluntary “Meds to Beds” program, which brings prescribed medications to the patient’s room at discharge. “We offer a diabetes discharge kit for patients who are self-pay, with all of the insulin and medical supplies they will need to get to the 30-day follow-up visit,” Dr. Knezevich said. “We can dream up amazing treatment regimens, but if they can’t afford the medications, what have we accomplished?”
SHM’s external benchmarks have provided an objective format for comparing and improving outcomes, Ms. Lautenbaugh said. “We like to see where we are and use the data to make significant improvements, but we’re also focused on internal assessments. If we make changes for a given metric, how does it affect performance in other areas?” One important metric is percentage of glucose readings within target range hospitalwide. “Our overall goal is 75%. It was 72% in April 2018, and we’ve raised it to 74.4%. It’s a small gain but it shows steady progress. Little steps make small but steady improvement,” she said.
“One area where we were not pleased was the occurrence of hypoglycemia,” Ms. Lautenbaugh said. “We did a root cause analysis of every hypoglycemic event, including several reports for patients who didn’t have diabetes at all. We had to weed out some that weren’t pertinent to our quality questions, but for those that are, the diabetes case manager calls the provider to make sure they were aware of the incident. We were able to identify the outliers in noncritical care, which we’re now able to tackle using a systematic approach.”
Get on the bus
Hospitalists are also integrally involved in a hospital glycemic improvement initiative at Orange Regional Medical Center (ORMC) in Middletown, N.Y.
The Glycemic Improvement Team (GIT) was formed in 2012 when a new hospital campus opened and EPIC was implemented as the hospital’s EMR. But glycemic control has taken on greater focus since 2015, when ORMC enrolled in eQUIPS, said Lorraine Porcaro, RN, the hospital’s diabetes clinical manager. The glycemic control team includes representatives from medicine, nursing, case management, laboratory, nutrition, pharmacy, wound care, and quality improvement.
Implementing the new EMR offered the opportunity to track a number of medical values in real time, Ms. Porcaro said. ORMC has focused its glycemic quality improvement efforts on hypoglycemia and hyperglycemia, with a recent emphasis on the need for improvements related to glucose reassessment 15 minutes post hypoglycemia treatment. More than a hundred “Diabetes Champions” have completed 16 hours of advanced training in diabetes and provide in-unit mentorship for other staff.
The ORMC team’s glycemic improvement “bus” is a rolling cart that goes from unit to unit supplying nurse education, reminders, copies of department-specific policies and protocols, and treats for staff. “It’s what we’re known for,” Ms. Porcaro said. Pens with the motto: “Don’t Miss the Bus! Retest in 15!” summarize the GIT’s current focus on post–hypoglycemia treatment retesting.
Hospitalists were part of the glycemic improvement process at ORMC from the beginning and are still involved, said Adrian Paraschiv, MD, FHM, a hospitalist and assistant director of the medical center, as well as the ORMC director of clinical information technology. ORMC initiated hospitalist coverage in 1998 and now has three HM groups, two of them represented on the glycemic improvement team.
“Like any hospital, we feel we should minimize hypoglycemic events,” Dr. Paraschiv explained. “This became important for other hospital departments, and we recognized we needed a major QI initiative to improve our outcomes hospitalwide. In the process, we noticed what other people were saying: Results from improving glycemic control included reduced length of stay, cost, and infections. That provided motivation for the hospital to support our initiative.”
Glucose management isn’t only about blood sugar, but whether the patient ate or not, their other blood work, the level of education for patient and staff, and a variety of other inputs, Dr. Paraschiv said. “All of these things were in the EMR but all over the place. EPIC had an incipient structure for pulling the data together, and we modified it to show everything that’s going on with the patient’s glycemic control on a single screen. We can build order sets and issue different reports.”
Today at ORMC, hypoglycemia is reassessed within 30 minutes more than 50% of the time. “It will never be at 100%, but we wanted to at least be at the national mean for eQUIPS hospitals. Our stretch goal was to be in the top quartile, and by the end of 2017, we realized that goal,” Ms. Porcaro said. Sometimes, because of changes in patients and staff, the GIT needs to repeat the education and review policies. “Since then, it’s been a matter of continuing staff education; sharing glucose data with stakeholders; talking about goals for ICU and non-ICU units; and, when needed, rolling out the bus.”
Participation in eQUIPS has made it possible to gather this information in one place and present it in a way that makes sense to physicians, Dr. Paraschiv said. “Dr. Maynard and SHM showed us how to put the data together to add value. Using these tools, we started looking at our processes, what needed to change, and what we are able to change. Now we’re examining what happens afterward. Can we use the electronic system to automatically alert physicians to make changes to the treatment regimen in real time? We continue to improve using upgrades to our EMR, such as an alert system with best practice advisories for the clinician. We now think we can actually achieve what we set out to achieve,” he said.
“Our idea was that we needed to market this program throughout the hospital – starting from the kitchen, meal delivery staff, IT, laboratory, medical and nursing staff,” Ms. Porcaro said. “The issue is multifactorial – it’s for the entire hospital. My heart is warmed when I see the woman who delivers the meals asking the patient: ‘Have you gotten your insulin shot?’ ”
References
1. Corvino L et al. “Management of diabetes and hyperglycemia in hospitalized patients.” Updated 2017 Oct 1 in De Groot LJ et al. editors. Endotext. South Dartmouth (MA): MDText.com 2000.
2. American Diabetes Association. Glycemic targets. Diabetes Care 2017 Jan;40(Suppl 1):S48-56.
3. Maynard G et al. “Design and implementation of a web-based reporting and benchmarking center for inpatient glucometrics.” J Diabetes Sci Technol. 2014 May 12;8(4):630-40.
Physicians are trained to manage their patients’ diabetes and often do a meticulous job – one on one. But in order to maximize glycemic control outcomes throughout the hospital, you need a kind of diabetic epidemiology team to focus on the data, said Andjela Drincic, MD, an endocrinologist at Nebraska Medicine, the clinical partner of the University of Nebraska Medical Center in Omaha.
As medical director for diabetes stewardship, Dr. Drincic serves as the epidemiologic lead for her hospital, which has worked systematically to improve inpatient glycemic control since 2012 – with help from the Society of Hospital Medicine.
“You need a team and to set up a system that works, with protocols and some way of knowing if the protocols are succeeding,” Dr. Drincic said. “Quality improvement targets are never static.” She credited SHM’s glycemic control eQUIPS (Electronic Quality Improvement Program), an online quality improvement resource and collaborative of 104 participating hospitals, for providing the support and the data needed to drive glycemic QI efforts at Nebraska Medicine. SHM provided reporting metrics, quarterly benchmarking reports, a library of tools and resources, an implementation guide, educational webinars on demand and, for some participants, mentored implementation with the advice of a leading expert in the field.
One big reason for giving more attention to glycemic control in the hospital is patient safety, said Gregory Maynard, MD, MHM, clinical professor and chief quality officer at the University of California–Davis Medical Center and SHM’s project team leader for eQUIPS.
“Hyperglycemia in hospitalized patients is an extraordinarily common and growing problem, affecting up to 40%-50% of patients in the hospital,” he said. In 2012, 7.7 million hospital stays involved patients with diabetes, the seventh leading cause of death in the United States.1
Hyperglycemia is linked to elevated rates of medical complications, infections, wound complications, hospital mortality, length of stay, readmissions, and ICU admissions, along with other outcomes not directly related to diabetes. Hyperglycemia in hospitalized patients who have not been given a diagnosis of diabetes is, if anything, more dangerous. Add the related risk for hypoglycemia, and clinicians are challenged to keep their patients controlled within the zone between the extremes of hyper- and hypoglycemia. The American Diabetes Association recently issued recommendations with more relaxed glucose targets between 140 and 180 mg/dL for most patients in non–intensive care settings.2
“To not have a standardized way of managing hyperglycemia for your hospital seems like an enormous missed opportunity,” Dr. Maynard said. “If someone comes into the hospital with a chronic condition of diabetes that you ignore, just maintaining them in the hospital and sending them back out into the world without addressing the underlying condition is not good care. You have missed an important opportunity to alter the course of a serious chronic condition.”
Dr. Maynard said SHM recognized this opportunity when it established eQUIPS. “Hospitalists are often tasked with taking care of patients with glycemic issues because there may not be an endocrinologist readily accessible in the hospital,” he said. “We have seen through our benchmarking in eQUIPS incredible variability – with 10-fold differences in hyperglycemia and hypoglycemia rates between the best- and worst-performing sites. The biggest variable is whether the hospital systematically manages glycemic control. We have also shown that achieving high levels of glycemic control and low hypoglycemia rates concurrently is very possible.”
Reliable benchmarks
Nebraska Medicine enrolled in eQUIPS in 2012.
“We utilize SHM’s glucometrics (standardized analyses of inpatient glycemic control data).”3 said Dr. Drincic. “I was looking for a reliable glucometric system and some way to make comparisons with other hospitals when I came across the data Dr. Maynard published about SHM via a PubMed search. We needed outcomes that are validated in the literature and comparison groups.”
Nebraska Medicine has also received a certificate of distinction for inpatient diabetes care from the Joint Commission, and Dr. Drincic is active in PRIDE (Planning Research in Inpatient Diabetes), a national consortium of leading investigators in inpatient diabetes care formed to promote collaborative research. The PRIDE group meets yearly at the ADA conference, communicates regularly by email, and publishes articles.
“Once a year I present our glycemic control data to our administration and to the quality and safety committees at the hospital. I have been pleased with the level of support we have received,” Dr. Drincic said. “We needed a mandate to do this, but when I reported the impact on readmissions and other outcomes, I got the full support of administration. This would have been a lot harder without SHM.”
Engagement with hospitalists is another key to the glucose management project’s success, Dr. Drincic said. “We as endocrinologists think we know how to manage diabetes, but hospitalists have the daunting task of dealing with all of the patient’s medical issues. If we don’t have a strong collaboration, how can we change practice hospitalwide?” Rachel Thompson, MD, SFHM, Nebraska Medicine’s chief of hospital medicine, participates in the glucose management project, Dr. Drincic said.
“We occasionally are guests at hospitalist meetings to share new glucose treatment algorithms,” she said. “We’re also looking at collaborating on other quality initiatives, for example, studying how perioperative dexamethasone affects glycemic control. We built this relationship with hospitalists by establishing trust while trying to shed a reputation as ‘sugar police.’ I don’t want hospitalists saying ‘There she goes again’ whenever I come on the unit. We have tried to establish personal relationships and figure out what the hospitalists need, especially relative to EPIC (the hospital’s electronic medical record software).”
Dr. Thompson said her group’s recent growth to nearly 70 clinicians has increased its footprint hospitalwide and given hospitalists a greater opportunity to influence glycemic control. “We see up to a third of the patients in the hospital outside of the ICU. Glycemic control is something you learn as a hospitalist – It’s a very important frontline quality issue. In the patient list on EPIC every morning we have a field highlighting all patients with glycemic control issues,” she said.
“Poor glucose control is associated with poor outcomes for our patients. We need the right systems in place for patient safety. Moreover, if we are ignoring glycemic control when the patient is in the hospital, we’re sending the wrong message and setting a bad example for our patients when they return home.”
Lack of clear metrics
A significant defect in the infrastructure of many glucose management programs is the lack of clear metrics for outcomes, Dr. Maynard said. Nearly one-third of hospitals in the United States have no standardized metric to track the quality of their inpatient glycemic management, a sobering statistic considering that the first step in any QI initiative is to define and measure the problem at hand.
“I believe the main reason that glycemic control has been left off hospitals’ radar screens is that we still have not adopted national, publicly reported quality measures for glycemic control, although those were proposed recently by a government interagency work group,” Dr. Maynard said. “Until that happens, we’ll continue to see uneven response.”
The first step for frontline hospitalists is to learn and understand the basics of glucose control, for example, basal bolus insulin administration, and to stop writing orders for sliding scale insulin as the sole means of controlling hyperglycemia.
“Develop and adopt standards of practice for insulin administration in your hospital,” Dr. Maynard said. “Be part of the solution, not the problem. Once you get into the weeds – patients on steroids or on total parenteral nutrition – it can get tricky. But it’s important to get the basics right and move beyond inertia on this topic.”
The glycemic team at Nebraska Medicine includes, in addition to Dr. Drincic and Dr. Thompson, an endocrinology fellow, diabetes case managers, resource nurses, nurse leadership, pharmacists, inpatient care transitions coordinators, and representatives from pediatrics and critical care, all working to impact the overall quality of glycemic management in the hospital. Jon Knezevich, PharmD is diabetes stewardship pharmacy coordinator, and Shelly Lautenbaugh, RN, CDE, is diabetes lead care manager and diabetes coordinator for the Joint Commission certificate program. Diabetes stewardship also includes online and live training courses and a class in acute glucose management for the diabetes resource nurses, who bring the knowledge back to their units.
The glucose team’s job is to make sure patients are cared for safely, using appropriate policies and procedures, education, and training, Ms. Lautenbaugh said. “We have a mission as a hospital to transform people’s lives. We try to live our values, and everything follows from the focus on patient safety,” she added. “If our patients can receive extraordinary care and leave better informed about their condition than when they came in, and then we don’t see them again, we’ve achieved our ultimate goal.”
Hyperglycemia is most often not the primary reason why patients are hospitalized, Ms. Lautenbaugh said. “But we need to give them appropriate glucose management regardless. We’ve worked with bedside staff, nurse leadership, and teams to develop plans to raise our outcome scores. We have a lot of different outcomes we examine, and it’s always evolving.”
Quality metrics are incorporated into the electronic medical record, but those reports are not timely enough for day-to-day management, Dr. Knezevich said. “So we created a diabetes dashboard, constantly updated in real time to identify patients who are out of glycemic control.” The measures tracked include a mean patient day glucose score, percentage of readings within recommended limits, mean time between measured low readings and next documented reading or resolution of hypoglycemia, readmission rates, and diabetes nutrition assessments.
For hospitals with diabetes certificates, the Joint Commission also requires that every patient with hyperglycemia receives a clinic visit 30 days after discharge to make sure they are receiving appropriate follow-up care. Other facets of the Nebraska glycemic initiative include utilizing the hospital’s voluntary “Meds to Beds” program, which brings prescribed medications to the patient’s room at discharge. “We offer a diabetes discharge kit for patients who are self-pay, with all of the insulin and medical supplies they will need to get to the 30-day follow-up visit,” Dr. Knezevich said. “We can dream up amazing treatment regimens, but if they can’t afford the medications, what have we accomplished?”
SHM’s external benchmarks have provided an objective format for comparing and improving outcomes, Ms. Lautenbaugh said. “We like to see where we are and use the data to make significant improvements, but we’re also focused on internal assessments. If we make changes for a given metric, how does it affect performance in other areas?” One important metric is percentage of glucose readings within target range hospitalwide. “Our overall goal is 75%. It was 72% in April 2018, and we’ve raised it to 74.4%. It’s a small gain but it shows steady progress. Little steps make small but steady improvement,” she said.
“One area where we were not pleased was the occurrence of hypoglycemia,” Ms. Lautenbaugh said. “We did a root cause analysis of every hypoglycemic event, including several reports for patients who didn’t have diabetes at all. We had to weed out some that weren’t pertinent to our quality questions, but for those that are, the diabetes case manager calls the provider to make sure they were aware of the incident. We were able to identify the outliers in noncritical care, which we’re now able to tackle using a systematic approach.”
Get on the bus
Hospitalists are also integrally involved in a hospital glycemic improvement initiative at Orange Regional Medical Center (ORMC) in Middletown, N.Y.
The Glycemic Improvement Team (GIT) was formed in 2012 when a new hospital campus opened and EPIC was implemented as the hospital’s EMR. But glycemic control has taken on greater focus since 2015, when ORMC enrolled in eQUIPS, said Lorraine Porcaro, RN, the hospital’s diabetes clinical manager. The glycemic control team includes representatives from medicine, nursing, case management, laboratory, nutrition, pharmacy, wound care, and quality improvement.
Implementing the new EMR offered the opportunity to track a number of medical values in real time, Ms. Porcaro said. ORMC has focused its glycemic quality improvement efforts on hypoglycemia and hyperglycemia, with a recent emphasis on the need for improvements related to glucose reassessment 15 minutes post hypoglycemia treatment. More than a hundred “Diabetes Champions” have completed 16 hours of advanced training in diabetes and provide in-unit mentorship for other staff.
The ORMC team’s glycemic improvement “bus” is a rolling cart that goes from unit to unit supplying nurse education, reminders, copies of department-specific policies and protocols, and treats for staff. “It’s what we’re known for,” Ms. Porcaro said. Pens with the motto: “Don’t Miss the Bus! Retest in 15!” summarize the GIT’s current focus on post–hypoglycemia treatment retesting.
Hospitalists were part of the glycemic improvement process at ORMC from the beginning and are still involved, said Adrian Paraschiv, MD, FHM, a hospitalist and assistant director of the medical center, as well as the ORMC director of clinical information technology. ORMC initiated hospitalist coverage in 1998 and now has three HM groups, two of them represented on the glycemic improvement team.
“Like any hospital, we feel we should minimize hypoglycemic events,” Dr. Paraschiv explained. “This became important for other hospital departments, and we recognized we needed a major QI initiative to improve our outcomes hospitalwide. In the process, we noticed what other people were saying: Results from improving glycemic control included reduced length of stay, cost, and infections. That provided motivation for the hospital to support our initiative.”
Glucose management isn’t only about blood sugar, but whether the patient ate or not, their other blood work, the level of education for patient and staff, and a variety of other inputs, Dr. Paraschiv said. “All of these things were in the EMR but all over the place. EPIC had an incipient structure for pulling the data together, and we modified it to show everything that’s going on with the patient’s glycemic control on a single screen. We can build order sets and issue different reports.”
Today at ORMC, hypoglycemia is reassessed within 30 minutes more than 50% of the time. “It will never be at 100%, but we wanted to at least be at the national mean for eQUIPS hospitals. Our stretch goal was to be in the top quartile, and by the end of 2017, we realized that goal,” Ms. Porcaro said. Sometimes, because of changes in patients and staff, the GIT needs to repeat the education and review policies. “Since then, it’s been a matter of continuing staff education; sharing glucose data with stakeholders; talking about goals for ICU and non-ICU units; and, when needed, rolling out the bus.”
Participation in eQUIPS has made it possible to gather this information in one place and present it in a way that makes sense to physicians, Dr. Paraschiv said. “Dr. Maynard and SHM showed us how to put the data together to add value. Using these tools, we started looking at our processes, what needed to change, and what we are able to change. Now we’re examining what happens afterward. Can we use the electronic system to automatically alert physicians to make changes to the treatment regimen in real time? We continue to improve using upgrades to our EMR, such as an alert system with best practice advisories for the clinician. We now think we can actually achieve what we set out to achieve,” he said.
“Our idea was that we needed to market this program throughout the hospital – starting from the kitchen, meal delivery staff, IT, laboratory, medical and nursing staff,” Ms. Porcaro said. “The issue is multifactorial – it’s for the entire hospital. My heart is warmed when I see the woman who delivers the meals asking the patient: ‘Have you gotten your insulin shot?’ ”
References
1. Corvino L et al. “Management of diabetes and hyperglycemia in hospitalized patients.” Updated 2017 Oct 1 in De Groot LJ et al. editors. Endotext. South Dartmouth (MA): MDText.com 2000.
2. American Diabetes Association. Glycemic targets. Diabetes Care 2017 Jan;40(Suppl 1):S48-56.
3. Maynard G et al. “Design and implementation of a web-based reporting and benchmarking center for inpatient glucometrics.” J Diabetes Sci Technol. 2014 May 12;8(4):630-40.
What do you call a koala who is too sweet for its own good? Diabetic
SAN DIEGO – The 14-pound patient with the deep-pile complexion was lethargic, kept drinking a lot of water, and had a glucose level in the range of 600-700 mg/dL. He was nearly comatose by the time medical staff transferred him to a specialized facility.
The diagnosis: Diabetes. The treatment: Insulin. But multiple daily skin pricks were quite a challenge for Quincy the koala. After all, he requires up to 22 hours of shut-eye each day.
What to do? The veterinary staff at the San Diego Zoo turned to the experts – an endocrinologist and a manufacturer of continuous glucose monitors. Now, Quincy has his own CGM, and a medical team that is tracking his glucose levels in real time on their smartphones.
In fact, Athena Philis-Tsimikas, MD, of the Scripps Whittier Diabetes Institute, pulls out her phone and checks on him at least a couple times a day. She also gets alerts if his blood sugar drops too quickly.
“He is definitely another one of my patients,” she said in an interview. But he’s the only one who lives in trees and enjoys a nice eucalyptus smoothie.
Humans are hardly the only mammals who get diabetes
Veterinarians are quite familiar with diabetes. A wide variety of mammals from pigs and apes to horses and dolphins can develop an equivalent of the human condition. Dogs may be prescribed daily insulin shots, and cats even develop peripheral neuropathy and retinopathy like humans with diabetes.
So it’s not entirely surprising that a team at the Los Angeles Zoo diagnosed Quincy, a 3-year-old Queensland koala, with diabetes.
Quincy’s glucose levels should have been around 80-130 mg/dL, similar to the ideal levels in humans, said San Diego Zoo senior veterinarian Cora Singleton, DVM, in an interview. But tests prompted by his symptoms showed his levels were high, she said, and they stayed that way. According to her, that suggested he wasn’t just having a one-time elevation that animals can experience when they’re stressed.
Unfortunately, there are only a few scattered reports of diabetes in koalas, and “there’s not anything documented about treating a koala over a long term,” Dr. Singleton said. “We’re in uncharted territory here.”
So the Los Angeles Zoo sent Quincy down the California coast for more specialized treatment. The San Diego Zoo’s veterinary staff took in Quincy and treated him with glucose tests and insulin shots, Dr. Singleton said. “But we were looking a way for to get more information with less disturbance to Quincy.”
Someone mentioned the idea of a sensor. “We thought, ‘What a great idea,’” Dr. Singleton said. “It would be a way for us to get a lot of information and find out how his highs and lows are related.”
That’s when the team turned to local endocrinologist Dr. Tsimikas for a helping hand.
The key to koala calming: Eucalyptus smoothies
“They did reach out to us and asked what kind of sensors might be available. We connected them to Dexcom,” a CGM company that’s based in San Diego, Dr. Tsimikas said. “We knew the newest one was coming along and suggested they place that on him as a starting point.”
On June 1, a zoo team attached a Dexcom G6 Continuous Glucose Monitoring System to the koala’s side.
“He’s doing very well. He tolerates the CGM superbly,” Dr. Singleton said. And Quincy doesn’t react when sensors are applied, she said, although it helps that he gets to enjoy a eucalyptus smoothie during the procedure. “Put that in a big syringe, and he’ll volunteer for most anything,” she said.
Obesity can trigger diabetes in mammals other than humans. Could eucalyptus overindulgence explain Quincy’s case of diabetes? Nope.
According to Dr. Tsimikas, the ingredients of the eucalyptus smoothie are just pureed eucalyptus leaves that “go down fast and easy.” These naturally have a nice mix of carbohydrates, fat, and protein to better manage the koala’s sugars and other nutritional needs. If he is dropping his blood sugar values fast, there is another dextrose drink they give him in small amounts, which contains 5-10 g carbohydrates. This is enough to help bring his glucose values back up. It is similar to the treatment recommendations provided to humans with diabetes where they are told to take 15 g of carbohydrates such as honey, hard candies, or juice to prevent a severe hypoglycemic episode.
Dr. Singleton noted that Quincy appears to have the koala equivalent is type 1 diabetes mellitus (T1DM).
Dr. Tsimikas noted “We are not finding the typical antibodies that we find in human T1DM. Quincy is showing low insulin levels, which is why it more closely resembles T1DM. We will be doing further analysis and comparisons with nondiabetic koalas in the future to see if it can be better differentiated.
While he appears to have type 1 diabetes, it’s not clear why he developed it, Dr. Singleton said.
While Quincy is only 3 years old, he’s a full-fledged adult in koala terms. Koalas typically live up to their mid-teens, she said.
This speechless patient still manages to communicate
The San Diego Zoo’s veterinary staff is monitoring Quincy and trying to understand how his glucose levels and daily insulin shots affect him. His tiny size has ruled out use of an insulin pump: Although the insulin pumps have been getting smaller and lighter, they are still too large to attach to our tiny friend. Especially since he would need both the CGM device and the pump, there is not a lot of surface area on his body for attachment of all the devices, according to Dr. Tsimikas.
Since Quincy is so tiny, insulin doses must be minuscule to avoid sending him into hypoglycemia, Dr. Tsimikas said. She said the koala’s medical team is planning to try using a NovoPen Echo injector with a half-unit of insulin.
Dr. Singleton noted that for now, “he’s maintaining his body weight, and he has days when he feels spunky. Sometimes, when he knows it’s breakfast time, and he hears his caretakers coming up the doorway with his breakfast, he’ll be very active on his perch.”
But he has sluggish days, too, when he’ll try to sleep in. Dr. Singleton keeps an eye out for grogginess and signs of weakness and hypoglycemia or hyperglycemia like “a little wobble in his step.”
“The biggest thing I’ve learned from Quincy is the value of his particular nonverbal cues,” she said. “I’m starting to understand when he feels like his sugars are a little high or a little low. I imagine that doctors and parents have the same challenges with little patients, along with figuring out how you communicate that this is supposed to help them.”
Dr. Tsimikas agreed, noting that she sees similarities between Quincy and patients who are hospitalized and can’t easily communicate. Now, “we can track the folks who are on the CGM and intervene earlier than before,” said Dr. Tsimikas, who’s part of a clinical trial team testing CGM devices in two hospitals. “It’s almost like having another vital sign.
“It is only when we have all the data on all the other factors that can influence blood sugar, such as eating patterns, insulin dose and timing, and activity level that we can more accurately adjust the medical interventions.” This requires collaboration between all the groups involved in Quincy’s care. In koalas, the collaboration is with the veterinarian, koala zookeepers, dietitian, and the technology monitoring team. Whereas, for humans, we need parents, care providers, diabetes educators, dietitians, and physicians.
It’s not clear if Quincy will need his CGM for the rest of his life. If he’s stable on a specific insulin dose, Dr. Tsimikas said, he may not need it. But it sounds like eucalyptus smoothies will always be a vital part of his regimen.
In the name of thoroughness, take note that Quincy is not the first diabetic zoo animal whose care involved physicians from Scripps. “We have had several other consultations for animals with diabetes. Nearly 25 years ago, a roller-skating chimpanzee with diabetes was brought to the Scripps Whittier Institute labs for evaluation and treatment recommendations. A few years later, one of our medical directors, Alberto Hayek, MD, advised on the care of Lune, a diabetic baboon at the San Diego Zoo, for insulin management. This time we are making house calls to the zoo to treat Quincy in his home environment. Each animal experience offers opportunities to expand our knowledge about diabetes care and exchange approaches that we might not otherwise be aware of. This has been fun and rewarding. I am looking forward to seeing further outcomes from our interactions with Quincy,” according to Dr. Tsimikas.
Dr. Tsimikas reports that her center conducts research with Dexcom and Novo Nordisk. Dr. Singleton reports no relevant disclosures.
SAN DIEGO – The 14-pound patient with the deep-pile complexion was lethargic, kept drinking a lot of water, and had a glucose level in the range of 600-700 mg/dL. He was nearly comatose by the time medical staff transferred him to a specialized facility.
The diagnosis: Diabetes. The treatment: Insulin. But multiple daily skin pricks were quite a challenge for Quincy the koala. After all, he requires up to 22 hours of shut-eye each day.
What to do? The veterinary staff at the San Diego Zoo turned to the experts – an endocrinologist and a manufacturer of continuous glucose monitors. Now, Quincy has his own CGM, and a medical team that is tracking his glucose levels in real time on their smartphones.
In fact, Athena Philis-Tsimikas, MD, of the Scripps Whittier Diabetes Institute, pulls out her phone and checks on him at least a couple times a day. She also gets alerts if his blood sugar drops too quickly.
“He is definitely another one of my patients,” she said in an interview. But he’s the only one who lives in trees and enjoys a nice eucalyptus smoothie.
Humans are hardly the only mammals who get diabetes
Veterinarians are quite familiar with diabetes. A wide variety of mammals from pigs and apes to horses and dolphins can develop an equivalent of the human condition. Dogs may be prescribed daily insulin shots, and cats even develop peripheral neuropathy and retinopathy like humans with diabetes.
So it’s not entirely surprising that a team at the Los Angeles Zoo diagnosed Quincy, a 3-year-old Queensland koala, with diabetes.
Quincy’s glucose levels should have been around 80-130 mg/dL, similar to the ideal levels in humans, said San Diego Zoo senior veterinarian Cora Singleton, DVM, in an interview. But tests prompted by his symptoms showed his levels were high, she said, and they stayed that way. According to her, that suggested he wasn’t just having a one-time elevation that animals can experience when they’re stressed.
Unfortunately, there are only a few scattered reports of diabetes in koalas, and “there’s not anything documented about treating a koala over a long term,” Dr. Singleton said. “We’re in uncharted territory here.”
So the Los Angeles Zoo sent Quincy down the California coast for more specialized treatment. The San Diego Zoo’s veterinary staff took in Quincy and treated him with glucose tests and insulin shots, Dr. Singleton said. “But we were looking a way for to get more information with less disturbance to Quincy.”
Someone mentioned the idea of a sensor. “We thought, ‘What a great idea,’” Dr. Singleton said. “It would be a way for us to get a lot of information and find out how his highs and lows are related.”
That’s when the team turned to local endocrinologist Dr. Tsimikas for a helping hand.
The key to koala calming: Eucalyptus smoothies
“They did reach out to us and asked what kind of sensors might be available. We connected them to Dexcom,” a CGM company that’s based in San Diego, Dr. Tsimikas said. “We knew the newest one was coming along and suggested they place that on him as a starting point.”
On June 1, a zoo team attached a Dexcom G6 Continuous Glucose Monitoring System to the koala’s side.
“He’s doing very well. He tolerates the CGM superbly,” Dr. Singleton said. And Quincy doesn’t react when sensors are applied, she said, although it helps that he gets to enjoy a eucalyptus smoothie during the procedure. “Put that in a big syringe, and he’ll volunteer for most anything,” she said.
Obesity can trigger diabetes in mammals other than humans. Could eucalyptus overindulgence explain Quincy’s case of diabetes? Nope.
According to Dr. Tsimikas, the ingredients of the eucalyptus smoothie are just pureed eucalyptus leaves that “go down fast and easy.” These naturally have a nice mix of carbohydrates, fat, and protein to better manage the koala’s sugars and other nutritional needs. If he is dropping his blood sugar values fast, there is another dextrose drink they give him in small amounts, which contains 5-10 g carbohydrates. This is enough to help bring his glucose values back up. It is similar to the treatment recommendations provided to humans with diabetes where they are told to take 15 g of carbohydrates such as honey, hard candies, or juice to prevent a severe hypoglycemic episode.
Dr. Singleton noted that Quincy appears to have the koala equivalent is type 1 diabetes mellitus (T1DM).
Dr. Tsimikas noted “We are not finding the typical antibodies that we find in human T1DM. Quincy is showing low insulin levels, which is why it more closely resembles T1DM. We will be doing further analysis and comparisons with nondiabetic koalas in the future to see if it can be better differentiated.
While he appears to have type 1 diabetes, it’s not clear why he developed it, Dr. Singleton said.
While Quincy is only 3 years old, he’s a full-fledged adult in koala terms. Koalas typically live up to their mid-teens, she said.
This speechless patient still manages to communicate
The San Diego Zoo’s veterinary staff is monitoring Quincy and trying to understand how his glucose levels and daily insulin shots affect him. His tiny size has ruled out use of an insulin pump: Although the insulin pumps have been getting smaller and lighter, they are still too large to attach to our tiny friend. Especially since he would need both the CGM device and the pump, there is not a lot of surface area on his body for attachment of all the devices, according to Dr. Tsimikas.
Since Quincy is so tiny, insulin doses must be minuscule to avoid sending him into hypoglycemia, Dr. Tsimikas said. She said the koala’s medical team is planning to try using a NovoPen Echo injector with a half-unit of insulin.
Dr. Singleton noted that for now, “he’s maintaining his body weight, and he has days when he feels spunky. Sometimes, when he knows it’s breakfast time, and he hears his caretakers coming up the doorway with his breakfast, he’ll be very active on his perch.”
But he has sluggish days, too, when he’ll try to sleep in. Dr. Singleton keeps an eye out for grogginess and signs of weakness and hypoglycemia or hyperglycemia like “a little wobble in his step.”
“The biggest thing I’ve learned from Quincy is the value of his particular nonverbal cues,” she said. “I’m starting to understand when he feels like his sugars are a little high or a little low. I imagine that doctors and parents have the same challenges with little patients, along with figuring out how you communicate that this is supposed to help them.”
Dr. Tsimikas agreed, noting that she sees similarities between Quincy and patients who are hospitalized and can’t easily communicate. Now, “we can track the folks who are on the CGM and intervene earlier than before,” said Dr. Tsimikas, who’s part of a clinical trial team testing CGM devices in two hospitals. “It’s almost like having another vital sign.
“It is only when we have all the data on all the other factors that can influence blood sugar, such as eating patterns, insulin dose and timing, and activity level that we can more accurately adjust the medical interventions.” This requires collaboration between all the groups involved in Quincy’s care. In koalas, the collaboration is with the veterinarian, koala zookeepers, dietitian, and the technology monitoring team. Whereas, for humans, we need parents, care providers, diabetes educators, dietitians, and physicians.
It’s not clear if Quincy will need his CGM for the rest of his life. If he’s stable on a specific insulin dose, Dr. Tsimikas said, he may not need it. But it sounds like eucalyptus smoothies will always be a vital part of his regimen.
In the name of thoroughness, take note that Quincy is not the first diabetic zoo animal whose care involved physicians from Scripps. “We have had several other consultations for animals with diabetes. Nearly 25 years ago, a roller-skating chimpanzee with diabetes was brought to the Scripps Whittier Institute labs for evaluation and treatment recommendations. A few years later, one of our medical directors, Alberto Hayek, MD, advised on the care of Lune, a diabetic baboon at the San Diego Zoo, for insulin management. This time we are making house calls to the zoo to treat Quincy in his home environment. Each animal experience offers opportunities to expand our knowledge about diabetes care and exchange approaches that we might not otherwise be aware of. This has been fun and rewarding. I am looking forward to seeing further outcomes from our interactions with Quincy,” according to Dr. Tsimikas.
Dr. Tsimikas reports that her center conducts research with Dexcom and Novo Nordisk. Dr. Singleton reports no relevant disclosures.
SAN DIEGO – The 14-pound patient with the deep-pile complexion was lethargic, kept drinking a lot of water, and had a glucose level in the range of 600-700 mg/dL. He was nearly comatose by the time medical staff transferred him to a specialized facility.
The diagnosis: Diabetes. The treatment: Insulin. But multiple daily skin pricks were quite a challenge for Quincy the koala. After all, he requires up to 22 hours of shut-eye each day.
What to do? The veterinary staff at the San Diego Zoo turned to the experts – an endocrinologist and a manufacturer of continuous glucose monitors. Now, Quincy has his own CGM, and a medical team that is tracking his glucose levels in real time on their smartphones.
In fact, Athena Philis-Tsimikas, MD, of the Scripps Whittier Diabetes Institute, pulls out her phone and checks on him at least a couple times a day. She also gets alerts if his blood sugar drops too quickly.
“He is definitely another one of my patients,” she said in an interview. But he’s the only one who lives in trees and enjoys a nice eucalyptus smoothie.
Humans are hardly the only mammals who get diabetes
Veterinarians are quite familiar with diabetes. A wide variety of mammals from pigs and apes to horses and dolphins can develop an equivalent of the human condition. Dogs may be prescribed daily insulin shots, and cats even develop peripheral neuropathy and retinopathy like humans with diabetes.
So it’s not entirely surprising that a team at the Los Angeles Zoo diagnosed Quincy, a 3-year-old Queensland koala, with diabetes.
Quincy’s glucose levels should have been around 80-130 mg/dL, similar to the ideal levels in humans, said San Diego Zoo senior veterinarian Cora Singleton, DVM, in an interview. But tests prompted by his symptoms showed his levels were high, she said, and they stayed that way. According to her, that suggested he wasn’t just having a one-time elevation that animals can experience when they’re stressed.
Unfortunately, there are only a few scattered reports of diabetes in koalas, and “there’s not anything documented about treating a koala over a long term,” Dr. Singleton said. “We’re in uncharted territory here.”
So the Los Angeles Zoo sent Quincy down the California coast for more specialized treatment. The San Diego Zoo’s veterinary staff took in Quincy and treated him with glucose tests and insulin shots, Dr. Singleton said. “But we were looking a way for to get more information with less disturbance to Quincy.”
Someone mentioned the idea of a sensor. “We thought, ‘What a great idea,’” Dr. Singleton said. “It would be a way for us to get a lot of information and find out how his highs and lows are related.”
That’s when the team turned to local endocrinologist Dr. Tsimikas for a helping hand.
The key to koala calming: Eucalyptus smoothies
“They did reach out to us and asked what kind of sensors might be available. We connected them to Dexcom,” a CGM company that’s based in San Diego, Dr. Tsimikas said. “We knew the newest one was coming along and suggested they place that on him as a starting point.”
On June 1, a zoo team attached a Dexcom G6 Continuous Glucose Monitoring System to the koala’s side.
“He’s doing very well. He tolerates the CGM superbly,” Dr. Singleton said. And Quincy doesn’t react when sensors are applied, she said, although it helps that he gets to enjoy a eucalyptus smoothie during the procedure. “Put that in a big syringe, and he’ll volunteer for most anything,” she said.
Obesity can trigger diabetes in mammals other than humans. Could eucalyptus overindulgence explain Quincy’s case of diabetes? Nope.
According to Dr. Tsimikas, the ingredients of the eucalyptus smoothie are just pureed eucalyptus leaves that “go down fast and easy.” These naturally have a nice mix of carbohydrates, fat, and protein to better manage the koala’s sugars and other nutritional needs. If he is dropping his blood sugar values fast, there is another dextrose drink they give him in small amounts, which contains 5-10 g carbohydrates. This is enough to help bring his glucose values back up. It is similar to the treatment recommendations provided to humans with diabetes where they are told to take 15 g of carbohydrates such as honey, hard candies, or juice to prevent a severe hypoglycemic episode.
Dr. Singleton noted that Quincy appears to have the koala equivalent is type 1 diabetes mellitus (T1DM).
Dr. Tsimikas noted “We are not finding the typical antibodies that we find in human T1DM. Quincy is showing low insulin levels, which is why it more closely resembles T1DM. We will be doing further analysis and comparisons with nondiabetic koalas in the future to see if it can be better differentiated.
While he appears to have type 1 diabetes, it’s not clear why he developed it, Dr. Singleton said.
While Quincy is only 3 years old, he’s a full-fledged adult in koala terms. Koalas typically live up to their mid-teens, she said.
This speechless patient still manages to communicate
The San Diego Zoo’s veterinary staff is monitoring Quincy and trying to understand how his glucose levels and daily insulin shots affect him. His tiny size has ruled out use of an insulin pump: Although the insulin pumps have been getting smaller and lighter, they are still too large to attach to our tiny friend. Especially since he would need both the CGM device and the pump, there is not a lot of surface area on his body for attachment of all the devices, according to Dr. Tsimikas.
Since Quincy is so tiny, insulin doses must be minuscule to avoid sending him into hypoglycemia, Dr. Tsimikas said. She said the koala’s medical team is planning to try using a NovoPen Echo injector with a half-unit of insulin.
Dr. Singleton noted that for now, “he’s maintaining his body weight, and he has days when he feels spunky. Sometimes, when he knows it’s breakfast time, and he hears his caretakers coming up the doorway with his breakfast, he’ll be very active on his perch.”
But he has sluggish days, too, when he’ll try to sleep in. Dr. Singleton keeps an eye out for grogginess and signs of weakness and hypoglycemia or hyperglycemia like “a little wobble in his step.”
“The biggest thing I’ve learned from Quincy is the value of his particular nonverbal cues,” she said. “I’m starting to understand when he feels like his sugars are a little high or a little low. I imagine that doctors and parents have the same challenges with little patients, along with figuring out how you communicate that this is supposed to help them.”
Dr. Tsimikas agreed, noting that she sees similarities between Quincy and patients who are hospitalized and can’t easily communicate. Now, “we can track the folks who are on the CGM and intervene earlier than before,” said Dr. Tsimikas, who’s part of a clinical trial team testing CGM devices in two hospitals. “It’s almost like having another vital sign.
“It is only when we have all the data on all the other factors that can influence blood sugar, such as eating patterns, insulin dose and timing, and activity level that we can more accurately adjust the medical interventions.” This requires collaboration between all the groups involved in Quincy’s care. In koalas, the collaboration is with the veterinarian, koala zookeepers, dietitian, and the technology monitoring team. Whereas, for humans, we need parents, care providers, diabetes educators, dietitians, and physicians.
It’s not clear if Quincy will need his CGM for the rest of his life. If he’s stable on a specific insulin dose, Dr. Tsimikas said, he may not need it. But it sounds like eucalyptus smoothies will always be a vital part of his regimen.
In the name of thoroughness, take note that Quincy is not the first diabetic zoo animal whose care involved physicians from Scripps. “We have had several other consultations for animals with diabetes. Nearly 25 years ago, a roller-skating chimpanzee with diabetes was brought to the Scripps Whittier Institute labs for evaluation and treatment recommendations. A few years later, one of our medical directors, Alberto Hayek, MD, advised on the care of Lune, a diabetic baboon at the San Diego Zoo, for insulin management. This time we are making house calls to the zoo to treat Quincy in his home environment. Each animal experience offers opportunities to expand our knowledge about diabetes care and exchange approaches that we might not otherwise be aware of. This has been fun and rewarding. I am looking forward to seeing further outcomes from our interactions with Quincy,” according to Dr. Tsimikas.
Dr. Tsimikas reports that her center conducts research with Dexcom and Novo Nordisk. Dr. Singleton reports no relevant disclosures.
Maternal obesity plus diabetes lead to psychiatric disorders in offspring
Women who were obese and had diabetes before becoming pregnant were sixfold more likely to have children with psychiatric and neurodevelopmental disorders by age 11 years, as compared to women with normal body mass indexes (BMIs), based on results of a large, prospective, population-based, cohort study published in Pediatrics.
The risks to offspring whose mothers were obese and had pregestational diabetes mellitus (PGDM) were far greater than the risks seen when mothers had either condition alone or had gestational diabetes mellitus (GDM) in the study, reported Linghua Kong of the Karolinska Institute, Stockholm, and colleagues. The study is based on data from various national registries in Finland regarding 649,043 live births during 2004-2014 and data regarding psychiatric diagnoses from the Finnish Care Registers for Health Care.
Of the children in the cohort, 7.67% had mothers who were obese and 3.66% had mothers who were severely obese based on standard World Health Organization criteria; mothers had PGDM in 0.62% of the births and GDM in 15.7% of the births.
Overall, 5.4% of the children were diagnosed with a psychiatric disorder by age 11 years.
Compared with children born to mothers of normal weight (BMI less than 25 kg/m2), those born to mothers with severe maternal obesity alone (BMI greater than 35) had higher rates of developmental disorders or speech, language, motor, and scholastic skills (hazard ratio, 1.69; 95% confidence interval 1.54-1.86); ADHD and/or conduct disorder (HR, 1.88; 95% CI, 1.58-2.23); and psychosis and mood and anxiety disorders (HR, 1.67; 95% CI, 1.31-2.13). Increased risk of psychiatric disorders were only slightly statistically significant in the offspring of women with severe obesity and GDM.
The risks were significantly elevated, however, for children born to obese women who also had PGDM. The hazard ratio for autism spectrum disorder was 6.49 (95% CI, 3.08-13.69), and the HR for ADHD and/or conduct disorder was 6.03 (95% CI, 3.23-11.24). The risks were fourfold higher for mixed disorders of emotions and conduct, disorders of social function, and tics (HR, 4.29; 95% CI, 2.14-8.60).
Limitations of the study included basing results on shorter follow-up times for those born later in the study period, grouping of offspring’s disorder diagnoses, basing the definition of PGDM on insulin prescription, and using BMI measurements taken at only one time point during pregnancy.
The researchers were supported by the National Institute for Health and Welfare: Drugs and Pregnancy project, the Swedish Research Council, the regional agreement on medical training and clinical research between Stockholm County Council and Karolinska Institutet Stockholm County Council, the China Scholarship Council, and the Swedish Brain Foundation.
SOURCE: Kong L et al. Pediatrics. 2018 Sep;142(3):1-11.
Women who were obese and had diabetes before becoming pregnant were sixfold more likely to have children with psychiatric and neurodevelopmental disorders by age 11 years, as compared to women with normal body mass indexes (BMIs), based on results of a large, prospective, population-based, cohort study published in Pediatrics.
The risks to offspring whose mothers were obese and had pregestational diabetes mellitus (PGDM) were far greater than the risks seen when mothers had either condition alone or had gestational diabetes mellitus (GDM) in the study, reported Linghua Kong of the Karolinska Institute, Stockholm, and colleagues. The study is based on data from various national registries in Finland regarding 649,043 live births during 2004-2014 and data regarding psychiatric diagnoses from the Finnish Care Registers for Health Care.
Of the children in the cohort, 7.67% had mothers who were obese and 3.66% had mothers who were severely obese based on standard World Health Organization criteria; mothers had PGDM in 0.62% of the births and GDM in 15.7% of the births.
Overall, 5.4% of the children were diagnosed with a psychiatric disorder by age 11 years.
Compared with children born to mothers of normal weight (BMI less than 25 kg/m2), those born to mothers with severe maternal obesity alone (BMI greater than 35) had higher rates of developmental disorders or speech, language, motor, and scholastic skills (hazard ratio, 1.69; 95% confidence interval 1.54-1.86); ADHD and/or conduct disorder (HR, 1.88; 95% CI, 1.58-2.23); and psychosis and mood and anxiety disorders (HR, 1.67; 95% CI, 1.31-2.13). Increased risk of psychiatric disorders were only slightly statistically significant in the offspring of women with severe obesity and GDM.
The risks were significantly elevated, however, for children born to obese women who also had PGDM. The hazard ratio for autism spectrum disorder was 6.49 (95% CI, 3.08-13.69), and the HR for ADHD and/or conduct disorder was 6.03 (95% CI, 3.23-11.24). The risks were fourfold higher for mixed disorders of emotions and conduct, disorders of social function, and tics (HR, 4.29; 95% CI, 2.14-8.60).
Limitations of the study included basing results on shorter follow-up times for those born later in the study period, grouping of offspring’s disorder diagnoses, basing the definition of PGDM on insulin prescription, and using BMI measurements taken at only one time point during pregnancy.
The researchers were supported by the National Institute for Health and Welfare: Drugs and Pregnancy project, the Swedish Research Council, the regional agreement on medical training and clinical research between Stockholm County Council and Karolinska Institutet Stockholm County Council, the China Scholarship Council, and the Swedish Brain Foundation.
SOURCE: Kong L et al. Pediatrics. 2018 Sep;142(3):1-11.
Women who were obese and had diabetes before becoming pregnant were sixfold more likely to have children with psychiatric and neurodevelopmental disorders by age 11 years, as compared to women with normal body mass indexes (BMIs), based on results of a large, prospective, population-based, cohort study published in Pediatrics.
The risks to offspring whose mothers were obese and had pregestational diabetes mellitus (PGDM) were far greater than the risks seen when mothers had either condition alone or had gestational diabetes mellitus (GDM) in the study, reported Linghua Kong of the Karolinska Institute, Stockholm, and colleagues. The study is based on data from various national registries in Finland regarding 649,043 live births during 2004-2014 and data regarding psychiatric diagnoses from the Finnish Care Registers for Health Care.
Of the children in the cohort, 7.67% had mothers who were obese and 3.66% had mothers who were severely obese based on standard World Health Organization criteria; mothers had PGDM in 0.62% of the births and GDM in 15.7% of the births.
Overall, 5.4% of the children were diagnosed with a psychiatric disorder by age 11 years.
Compared with children born to mothers of normal weight (BMI less than 25 kg/m2), those born to mothers with severe maternal obesity alone (BMI greater than 35) had higher rates of developmental disorders or speech, language, motor, and scholastic skills (hazard ratio, 1.69; 95% confidence interval 1.54-1.86); ADHD and/or conduct disorder (HR, 1.88; 95% CI, 1.58-2.23); and psychosis and mood and anxiety disorders (HR, 1.67; 95% CI, 1.31-2.13). Increased risk of psychiatric disorders were only slightly statistically significant in the offspring of women with severe obesity and GDM.
The risks were significantly elevated, however, for children born to obese women who also had PGDM. The hazard ratio for autism spectrum disorder was 6.49 (95% CI, 3.08-13.69), and the HR for ADHD and/or conduct disorder was 6.03 (95% CI, 3.23-11.24). The risks were fourfold higher for mixed disorders of emotions and conduct, disorders of social function, and tics (HR, 4.29; 95% CI, 2.14-8.60).
Limitations of the study included basing results on shorter follow-up times for those born later in the study period, grouping of offspring’s disorder diagnoses, basing the definition of PGDM on insulin prescription, and using BMI measurements taken at only one time point during pregnancy.
The researchers were supported by the National Institute for Health and Welfare: Drugs and Pregnancy project, the Swedish Research Council, the regional agreement on medical training and clinical research between Stockholm County Council and Karolinska Institutet Stockholm County Council, the China Scholarship Council, and the Swedish Brain Foundation.
SOURCE: Kong L et al. Pediatrics. 2018 Sep;142(3):1-11.
FROM PEDIATRICS
Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic Syndrome Management
In this review, the authors discuss the similarities and differences between diabetic ketoacidosis and the hyperosmolar hyperglycemic state, providing clinical pearls and common pitfalls to help guide the clinician in the diagnosis and management.
Diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) are similar but distinct diabetic emergencies that are frequently encountered in the ED. Patients with DKA or HHS present with hyperglycemia and dehydration and frequently appear quite ill physically. In both syndromes, there is insufficient insulin levels to transport glucose into cells.
As previously noted, although DKA and HHS share similar characteristic signs and symptoms, they are two distinct conditions that must be differentiated in the clinical work-up. One characteristic that helps the emergency physician (EP) to distinguish between the two conditions is the patient age at symptom onset. Although both conditions can occur at any age, diabetic ketoacidosis typically develops in younger patients, less than 45 years, who have little or no endogenous insulin production, whereas HHS usually occurs in much older non-insulin-dependent patients (who are often greater than 60 years old). 1-3 This review discusses the similarities and differences in the etiology, diagnosis, and treatment of DKA and HHS to guide evaluation and simplify management, highlighting practical tips and clinical pearls. When applicable, information has been organized into groups of five to facilitate retention and recall.
The Etiology of DKA Vs HHS
The fundamental underlying issue in both DKA and HHS is an absolute or relative lack of insulin that results in an increase in counter-regulatory hormones, including glucagon, cortisol, and catecholamines.
Insulin has five main actions: (1) to drive glucose into cells; (2) to drive potassium into cells; (3) to create an anabolic environment; (4) to inhibit breakdown of fat; and (5) to block the breakdown of proteins. (Table 1).
Diabetic ketoacidosis typically develops in patients who lack significant endogenous insulin; this insufficiency of circulating insulin causes hyperglycemia and hyperkalemia, the creation of a catabolic state with high levels of both ketone bodies and free-fatty acids due to the breakdown of proteins and fats.
In contrast, HHS occurs in patients who produce a sufficient amount of insulin to drive potassium into cells and to inhibit the breakdown of proteins and fats; as such these patients are not ketoacidotic. However, patients with HHS do not produce enough insulin to drive glucose intracellularly. As the glucose levels increase, patients with HHS become increasingly hyperosmolar and dehydrated, resulting in further elevation of glucose levels, causing a perpetual cycle of increasing glucose and resultant hyperosmolarity and dehydration.1-3 It is important to appreciate that both hyperglycemic crises result in an osmotic diuresis leading to severe dehydration and urinary wasting of electrolytes.
Diagnosis and Workup
Laboratory Evaluation
In addition to hyperglycemia, another key finding in DKA is elevated anion gap metabolic acidosis resulting from ketoacid production. Laboratory evaluation will demonstrate a pH less than 7.3 and serum bicarbonate level less than 18 mEq/L; urinalysis will be positive for ketones.
Though HHS patients also present with hyperglycemia, laboratory evaluation will demonstrate no, or only mild, acidosis, normal pH (typically >7.3), bicarbonate level greater than 18 mEq/L, and a high-serum osmolality (>350 mOsm/kg). While urinalysis may show low or no ketones, patients with HHS do not develop the marked ketoacidosis seen in DKA. Moreover, glucose values are more elevated in patients with HHS, frequently exceeding 1,000 mg/dL.
Signs and Symptoms
Patients with either of these hyperglycemic crises often present with fatigue, polyuria, and polydipsia. They appear dehydrated on examination with dry mucous membranes, tachycardia, and in severe cases, hypotension. Patients with HHS often present with altered mental status, seizures, and even coma, while patients with DKA typically only experience changes in mental status in the most severe cases (Table 2). As many as one-third of patients with a hyperglycemic crisis will have an overlapping DKA/HHS syndrome.1-3 With respect to patient age, HHS tends to develop in older patients who have type 2 diabetes and several underlying comorbidities.2
Precipitating Causes of DKA and HHS
The five causes of DKA/HHS can be remembered as the “Five I’s”: (1) infection; (2) infarction; (3) infant (pregnancy), (4) indiscretion, and (5) [lack of] insulin (Table 3).
Infection. Infection is one of the most common precipitating factors in both DKA and HHS.1 During the history intake, the EP should ask the patient if he or she has had any recent urinary and respiratory symptoms, as positive responses prompt further investigation with urinalysis and chest radiography. A thorough dermatological examination should be performed to assess for visible signs of infection, particularly in the extremities and intertriginous areas.
When assessing patients with DKA or HHS for signs of infection, body temperature to assess for the presence of fever is not always a reliable indicator. This is because many patients with DKA/HHS develop tachypnea, which can affect the efficacy of an oral thermometer. In such cases, the rectal temperature is more sensitive for detecting fever. It should be noted, however, that some patients with severe infection or immunocompromised state—regardless of the presence or absence of tachypnea—may be normothermic or even hypothermic due to peripheral vasodilation—a poor prognostic sign.3 Blood and urine cultures should be obtained for all patients in whom infection is suspected.
Laboratory evaluation of patients with DKA may demonstrate a mild leukocytosis, a very common finding in DKA even in the absence of infection; leukocytosis is believed to result from elevated stress hormones such as cortisol and epinephrine.3
Infarction. Infarction is another important underlying cause of DKA/HHS and one that must not be overlooked. Screening for acute coronary syndrome through patient history, electrocardiography, and cardiac biomarkers should be performed in all patients older than age 40 years and in patients in whom there is any suggestion of myocardial ischemia.
A thorough neurological examination should be performed to assess for deficits indicative of stroke. Although neurological deficits can be due to severe hyperglycemia, most patients with focal neurological deficits from hyperglycemia also have altered mental status. Focal neurological deficits without a change in mental status are more likely to represent an actual stroke.4
Infant (Pregnancy). Pregnant patients are at an increased risk of developing DKA for several reasons, most notably due to the increased production of insulin-antagonistic hormones, which can lead to higher insulin resistance and thus increased insulin requirements during pregnancy.5 A pregnancy test is therefore indicated for all female patients of child-bearing age.
Indiscretion. Non-compliance with diet, such as taking in too many calories without appropriate insulin correction, and the ingestion of significant amounts of alcohol can lead to DKA. Eating disorders, particularly in young patients, may also contribute to recurrent cases.3
[Lack of] Insulin. In insulin-dependent diabetes, skipped insulin doses or insulin pump failure can trigger DKA/HHS. In fact, missed insulin doses are becoming a more frequent cause of DKA than infections.1
Both DKA and HHS are usually triggered by an underlying illness or event. Therefore, clinicians should always focus on identifying precipitating causes such as acute infection, stroke, or myocardial infarction, as some require immediate treatment. In fact, DKA or HHS is rarely the primary cause of death; patients are much more likely to die from the precipitating event that caused DKA or HHS.1,3
Assessing Disease Severity
Mental status and pH and serum bicarbonate levels help clinicians determine the extent of disease severity, classifying patients as having mild, moderate, or severe DKA (Table 4).2 Patients at the highest risk for poor outcomes include those at the extremes of age, who have severe comorbidities, who have underlying infection, and who are hypotensive and/or in a comatose state.3
Patients who have HHS are much more likely to present with altered mental status, including coma. There is a linear relationship between osmolality and degree of altered mental status. Thus, diabetic patients with major changes in mental status but without high serum osmolality warrant immediate workup for alternative causes of their altered mental status.3 In addition, seizures, especially focal seizures, are relatively common in severe cases of HHS. Finally, highly abnormal blood pressure, pulse, and respiratory rate can also provide additional clues regarding the severity of hyperglycemic crisis.
Arterial Blood Gas Assessment: To Stick or Not to Stick?
In the past, measuring arterial blood gases (ABG) has been considered a mainstay in the evaluation of patients with DKA. But does an arterial stick, which is associated with some risk, really add essential information? One study by Ma et al6 evaluated whether ABG results significantly alter how physicians manage patients with DKA. In the study, the authors evaluated 200 ED patients and found that ABG analysis only changed diagnosis in 1% of patients, altered treatment in 3.5% of patients, and changed disposition in only 1% of patients. Arterial stick partial pressure of oxygen and partial pressure of carbon dioxide altered treatment and disposition in only 1% of patients. Furthermore, the study results showed venous pH correlated very strongly with arterial pH (r = 0.95).6 These findings demonstrate that ABG measurements rarely affect or alter DKA management, and support the use of venous pH as an adequate substitute for ABG testing.
Euglycemia
Euglycemic DKA has been reported in patients with type 1 diabetes who had been fasting or vomiting or who had received exogenous insulin prior to presentation.1Euglycemia has also been reported in pregnant patients with type I diabetes.1 More recently, sodium glucose cotransporter 2 inhibitors (SGLT2) have been shown to cause euglycemic DKA. While the therapeutic mechanism of this drug class is to inhibit proximal tubular resorption of glucose, they can cause DKA by decreasing renal clearance of ketone bodies and increasing glucagon levels and promoting hepatic ketogenesis. Patients with DKA who are on SGLT2 inhibitors may present with only modestly elevated glucose levels (typically in the 200- to 300-mg/dL range), but have profound wide gap metabolic acidosis due to β-hydroxybutyrate acid and acetoacetate accumulation.7 When evaluating patients on SGLT2 inhibitors for DKA, EPs should not solely rely on glucose values but rather assess the patient’s overall clinical picture, including the physical examination, vital signs, and pH. Additionally, once resuscitation with intravenous (IV) fluids and insulin is initiated, it may take longer for patients who use SGLT2 inhibitors to clear ketoacids than patients with DKA who do not use these medications.8
Treatment
The goal of treatment for DKA and HHS is to correct volume deficits, hyperglycemia, and electrolyte abnormalities (Table 5). Three of the five therapies to manage DKA and HHS are mandatory: IV fluid resuscitation, IV insulin, and IV potassium. The other therapies, IV bicarbonate, and IV phosphate, should be considered, but are rarely required for DKA or HHS.
In general, management of HHS is less aggressive than that of DKA because HHS develops over a period of weeks—unlike DKA, which develops over only 1 to 2 days. Treatment of any underlying causes of HHS should occur simultaneously.
Intravenous Fluids
The goal of IV fluid therapy for patients with DKA is rehydration—not to “wash-out” ketones. Ketone elimination occurs through insulin-stimulated metabolism. When determining volume-replacement goals, it is helpful to keep in mind that patients with moderate-to-mild DKA typically have fluid deficiencies of 3 to 5 L, and patients with severe DKA have fluid deficiencies between 5 and 6 L. Patients with HHS present with significantly higher fluid deficiencies of around 9 to 12 L.
The initial goal of fluid management is to correct hypoperfusion with bolus fluids, followed by a more gradual repletion of remaining deficits. After bolus fluids are administered, the rate and type of subsequent IV fluid infusion varies depending on hemodynamics, hydration state, and serum sodium levels.2,3
Nonaggressive Vs Aggressive Fluid Management. One study by Adrogué et al9 compared the effects of managing DKA with aggressive vs nonaggressive fluid repletion. In the study, one group of patients received normal saline at 1,000 mL per hour for 4 hours, followed by normal saline at 500 mL per hour for 4 hours. The other group of patients received normal saline at a more modest rate of 500 mL per hour for 4 hours, followed by normal saline at 250 mL per hour for 4 hours. The authors found that patients in the less aggressive volume therapy group achieved a prompt and adequate recovery and maintained higher serum bicarbonate levels.9
Current recommendations for patients with DKA are to first treat patients with an initial bolus of 1,000 mL or 20 cc/kg of normal saline. Patients without profound dehydration should then receive 500 cc of normal saline per hour for the first 4 hours of treatment, after which the flow rate may be reduced to 250 cc per hour. For patients with mild DKA, therapy can start at 250 cc per hour with a smaller bolus dose or no bolus dose. Patients with profound dehydration and poor perfusion, should receive crystalloid fluids wide open until perfusion has improved. Overall, volume resuscitation in HHS is similar to DKA. However, the EP should be cautious with respect to total fluid volume and infusion rates to avoid fluid overload, since many patients with HHS are elderly and may have congestive heart failure.
Crystalloid Fluid Type for Initial Resuscitation. Normal saline has been the traditional crystalloid fluid of choice for managing DKA and HHS. Recent studies, however, have shown some benefit to using balanced solutions (Ringer’s lactate or PlasmaLyte) instead of normal saline. A recently published large study by Semler et al10 compared balanced crystalloid, in most cases lactated Ringers solution, to normal saline in critically ill adult patients, some of whom were diagnosed with DKA. The study demonstrated decreased mortality (from any cause) in the group who received balanced crystalloid fluid therapy and reduced need for renal-replacement therapy and reduced incidence of persistent renal dysfunction. The findings by Semler et al10 and findings from other smaller studies, calls into question whether normal saline is the best crystalloid to manage DKA and HHS.11,12 It remains to be seen what modification the American Diabetes Association (ADA) will make to its current recommendations for fluid therapy, which were last updated in 2009.
It appears that though the use of Ringers lactate or PlasmaLyte to treat DKA usually raises a patient’s serum bicarbonate level to 18 mEq/L at a more rapid rate than normal saline, the use of balanced solutions may result in longer time to lower blood glucose to 250 mg/dL.13 However, by using a balanced solution, the hyperchloremic metabolic acidosis often seen with normal saline treatment will be avoided.12
Half-Normal Saline. An initially normal or increased serum sodium level, despite significant hyperglycemia, suggests a substantial free-water deficit. Calculating a corrected serum sodium can help quantify the degree of free-water deficit.3 While isotonic fluids remain the standard for initial volume load, clinicians should consider switching patients to half-normal saline following initial resuscitation if the corrected serum sodium is elevated above normal. The simplest estimation to correct sodium levels in DKA is to expect a decrease in sodium levels at a rate of at least 2 mEq/L per 100-mg/dL increase in glucose levels above 100 mg/dL. For a more accurate calculation, providers can expect a drop in sodium of 1.6 mEq/L per 100 mg/dL increase of glucose up to a level of 400 mg/dL and then a fall of 2.4 mEq/L in sodium per every 100 mg/dL rise in glucose thereafter.14
Glucose. Patients with DKA require insulin therapy until ketoacidosis resolves. However, the average time to correct ketoacidosis from initiating treatment is about 12 hours compared to only 6 hours for correction of hyperglycemia. Since insulin therapy must be continued despite lower glucose levels, patients are at risk for developing hypoglycemia if glucose is not added to IV fluids. To prevent hypoglycemia and provide an energy source for ketone metabolism, patients should be switched to fluids containing dextrose when their serum glucose approaches 200 to 250 mg/dL.1,3 Typically, 5% dextrose in half-normal saline at 150 to 250 cc per hour is usually adequate to achieve this goal.
Insulin
As previously noted, insulin therapy is required to treat hyperglycemic crises from DKA and HHS. In DKA there is an absolute insulin deficiency, whereas in HHS, there is a relative insulin deficiency. In HHS, there is not enough endogenous insulin to move glucose into the cells, but there is enough insulin to block a catabolic state. That is why the breakdown of fats and proteins does not occur, and why ketoacidosis and hyperkalemia are not seen in HHS. On the other hand, glucose elevations do occur, and are usually more extreme in HHS than DKA. There are five major therapeutic actions of insulin in DKA (Table 5), and it is imperative to determine serum potassium before starting an insulin infusion as insulin will drive potassium into the cell, worsening hypokalemia and promoting the development of life-threatening arrhythmias, including ventricular fibrillation, ventricular tachycardia, and torsades de pointes. The electrocardiogram does not accurately predict severity of hypokalemia and should not be used as a substitute for direct potassium measurement.
Loading Dose and Drip Rate. When treating adult patients with DKA or HHS, the ADA recommends an IV push loading dose of 0.1 U/kg insulin, followed by an hourly maintenance dose of 0.1 U/kg. Alternatively, a continuous infusion of 0.16 U/kg/hr can be used without a bolus. The rationale behind a bolus is the rapid saturation of insulin receptors, followed by a drip to maintain saturation of receptors. However, a recent prospective observational cohort study by Goyal et al15 questions the utility of the initial insulin bolus. The study compared DKA patients who received an initial insulin bolus to those who did not. Both groups were similar at baseline and received equivalent IV fluids and insulin drips. They found no statistically significant differences in the incidence of hypoglycemia, rate of serum glucose change, anion gap change, or length of stay in the ED or hospital. The authors concluded that administration of an insulin bolus has no significant benefit to patients and does not change clinically relevant end-points.15 At this time, there is no proven benefit to giving DKA patients an IV insulin bolus; moreover, doing so may further increase hypoglycemia. The use of an insulin bolus is particularly not recommended for use in pediatric patients with DKA due to a higher incidence of hypoglycemia in this patient population.16
As with DKA, the ADA3 recommends giving HHS patients an insulin bolus of 0.1 U/ kg followed by a continuous infusion at 0.1 U/kg per hour. It is crucial to monitor patients closely to ensure glucose levels do not fall too rapidly. Glucose levels should be kept between 150 to 200 mg/dL for patients with DKA and 200 to 300 mg/dL for patients with HHS until the conditions resolve; this may necessitate lowering the infusion rate to 0.02 to 0.05 U/kg per hour. In addition to frequent glucose monitoring, a basic metabolic panel and venous pH should be obtained every 2 to 4 hours while a patient is on an insulin drip.3
Subcutaneous Vs Intravenous Insulin for DKA. Several small studies evaluating patients with mild-moderate DKA demonstrated similar outcomes when subcutaneous (SQ) insulin was used instead of IV insulin. However, SQ injections require more frequent dosing (every 1 to 2 hours) and still require close monitoring of blood glucose. This monitoring frequency is usually not feasible on a hospital floor, but may be feasible on step-down units, thus avoiding admission to the intensive care unit (ICU) for patients who do not otherwise require ICU-level of care.17 Subcutaneous insulin should not be given to patients with severe acidosis, hypotension, or altered mental status. The ADA consensus statement continues to recommend IV infusion of regular insulin as the preferred route due to its short half-life and easy titration.3
Determining When to Switch to Subcutaneous Insulin. Ideally, patients are not in the ED long enough to have their metabolic abnormalities corrected, as this usually requires several hours. In DKA, the insulin drip should continue until the blood glucose is less than 200 and at least two of the following conditions are met: the anion gap is less than 12, venous pH greater than 7.3, and serum bicarbonate >15. In HHS, osmolality and mental status should both return to normal prior to stopping the infusion. In both cases, subcutaneous insulin should be administered at least 1 to 2 hours before stopping the drip to prevent recurrent crisis.1,3
Refractory Acidosis. First and foremost, refractory acidosis should prompt a diligent source for dead gut, abscess, and underlying sepsis. While vomiting and diffuse abdominal pain are common in DKA and are related to ketoacidosis, these symptoms are atypical of HHS and should raise suspicion for underlying pathology.3 Additionally, a lower than expected bicarbonate level can also occur from resuscitation with large volumes of normal saline, resulting in a hyperchloremic non-gap metabolic acidosis.
Potassium
Both DKA and HHS patients have total body potassium deficits due to osmotic diuresis that require careful repletion. Deficits can be substantial: The average total whole body potassium deficit in DKA is 3 to 5 mEq/kg.2 Clinicians should exercise caution, however, since DKA patients may be hyperkalemic initially despite a total body potassium deficit. Early hyperkalemia is due to the transmembrane shift of potassium secondary to acidosis and insulin deficiency as well as hypertonicity. If initial potassium is greater than 5.2 mEq/L, potassium should not be administered but instead rechecked in 1 to 2 hours. If the potassium level is 4.0 to 5.2 mEq/L, then 10 mEq per hour is usually adequate. For levels between 3.3 and 4.0 mEq/L, administer potassium chloride at 20 mEq per hour. For levels less than 3.3 mEq/L, insulin should be held and potassium chloride should be aggressively repleted at 20 to 30 mEq per hour with continuous cardiac monitoring.1-3 Failure to recognize and act on critical potassium levels is a known cause of unexpected death in DKA. During the first hour of DKA onset, patients are more likely to die from hyperkalemia. Later, while the patient is “stabilizing” on an insulin infusion, potassium levels will fall as insulin drives potassium back into cells.
Bicarbonate
Bicarbonate has many theoretical benefits but also has potential risks (Table 6).
Phosphate
Since there is no proven benefit to giving phosphate to adult patients with DKA, it is rarely used, except in specific situations other than pediatric DKA. Similar to potassium, initial serum phosphate levels do not reflect total body phosphate levels due to transmembrane shifts.2,3 Phosphate repletionis most beneficial for patients who have cachexia, respiratory depression, anemia, cardiac dysfunction, or phosphate values lower than 1.0 to 1.5. If given, 20 to 30 mEq/L potassium phosphate (K2PO4) added to fluids is usually sufficient.3 Overly aggressive phosphate administration (>4.5 mmol/h or 1.5 mL/h potassium phosphate) can cause severe hypocalcemia and should be avoided.1,3 In pediatric patients, up to one-half of potassium requirements are often given as potassium phosphate, but this may vary by institution.
Conclusion
Both DKA and HHS are diabetic emergencies that must be approached and managed systematically to correct underlying dehydration and metabolic abnormalities. Patient care begins by determining the etiology of these conditions, especially HHS. Once the cause has been identified, patients should be treated with bolus fluids to obtain adequate perfusion, followed by IV fluid infusion. Clinicians should carefully monitor the serum sodium level of patients with DKA or HHS to determine the ideal amount and type of fluid required, and also should measure potassium levels prior to starting patients on insulin. (Tables 7 and 8 summarize important clinical pearls when treating patients with DKA or HHS.)
1. Nyenwe EA, Kitabchi AE. The evolution of diabetic ketoacidosis: an update of its etiology, pathogenesis and management. Metabolism. 2016;65(4):507-521. doi:10.1016/j.metabol.2015.12.007.
2. Fayfman M, Pasquel FJ, Umpierrez GE. Management of hyperglycemic crises: diabetic ketoacidosis and hyperglycemic hyperosmolar state. Med Clin North Am. 2017;101(3):587-606. doi:10.1016/j.mcna.2016.12.011.
3. Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009;32(7):1335-1343. doi:10.2337/dc09-9032.
4. Fugate JE, Rabinstein AA. Absolute and relative contraindications to IV rt-PA for acute ischemic stroke. Neurohospitalist. 2015;5(3):110-121. doi:10.1177/1941874415578532.
5. Kamalakannan D, Baskar V, Barton DM, Abdu TA. Diabetic ketoacidosis in pregnancy. Postgrad Med J. 2003;79(9):454-457.
6. Ma OJ, Rush MD, Godfrey MM, Gaddis G. Arterial blood gas results rarely influence emergency physician management of patients with suspected diabetic ketoacidosis. Acad Emerg Med. 2003;10(8):836-841.
7. Taylor S, Blau J, Rother K. SGLT2 Inhibitors may predispose to ketoacidosis. J Clin Endocrinol Metab. 2015;100(8):2849-2852. doi:10.1210/jc.2015-1884.
8. Kum-Nji JS, Gosmanov AR, Steinberg H, Dagogo-Jack S. Hyperglycemic, high anion-gap metabolic acidosis in patients receiving SGLT-2 inhibitors for diabetes management. J Diabetes Complications. 2017;31(3):611-614. doi:10.1016/j.jdiacomp.2016.11.004.
9. Adrogué HJ, Barrero J, Eknoyan G. Salutary effects of modest fluid replacement in the treatment of adults with diabetic ketoacidosis. Use in patients without extreme volume deficit. JAMA. 1989;262(15):2108-2013.
10. Semler MW, Self WH, Wanderer JP, et al; SMART Investigators and the Pragmatic Critical Care Research Group. Balanced crystalloid versus saline in critically ill adults. N Engl J Med. 2018;378(9):829-839. doi:10.1056/NEJMoa1711584.
11. Chua HR, Venkatesh B, Stachowski E, et al. Plasma-Lyte 148 vs 0.9% saline for fluid resuscitation in diabetic ketoacidosis. J Crit Care. 2012;27(2):138-145. doi:10.1016/j.jcrc.2012.01.007.
12. Mahler S, Conrad S, Wang H, Arnold T. Resuscitation with balanced electrolyte solution prevents hyperchloremic metabolic acidosis in patients with diabetic ketoacidosis. Am J Emerg Med. 2011;29(9):1194-1197. doi:10.1016/j.ajem.2010.07.015.
11. Van Zyl DG, Rheeder P, Delport E. Fluid management in diabetic-acidosis--Ringer’s lactate versus normal saline: a randomized controlled trial. QJM. 2012;105(4):337-343. doi:10.1093/qjmed/hcr226.
14. Penne EL, Thijssen S, Raimann JG, Levin NW, Kotanko P. Correction of serum sodium for glucose concentration in hemodialysis patients with poor glucose control. Diabetes Care. 2010;33(7):e91. doi:10.2337/dc10-0557.
15. Goyal N, Miller JB, Sankey SS, Mossallam U. Utility of initial bolus insulin in the treatment of diabetic ketoacidosis. J Emerg Med. 2010;38(4):422-427. doi:10.1016/j.jemermed.2007.11.033.
16. Wolfsdorf JI, Allgrove J, Craig ME, et al; International Society for Pediatric and Adolescent Diabetes. Diabetic ketoacidosis and hyperglycemic hyperosmolar state. Pediatr Diabetes. 2014;15(Suppl 20):154-179. doi:10.1111/pedi.12165.
17. Cohn BG, Keim SM, Watkins JW, Camargo CA. Does management of diabetic ketoacidosis with subcutaneous rapid-acting insulin reduce the need for intensive care unit admission? J Emerg Med. 2015;49(4):530-538. doi:10.1016/j.jemermed.2015.05.016.
18. Glaser N, Barnett P, McCaslin I, et al; Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. Risk factors for cerebral edema in children with diabetic ketoacidosis. The Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. N Engl J Med. 2001;344(4):264-269. doi:10.1056/NEJM200101253440404.
In this review, the authors discuss the similarities and differences between diabetic ketoacidosis and the hyperosmolar hyperglycemic state, providing clinical pearls and common pitfalls to help guide the clinician in the diagnosis and management.
In this review, the authors discuss the similarities and differences between diabetic ketoacidosis and the hyperosmolar hyperglycemic state, providing clinical pearls and common pitfalls to help guide the clinician in the diagnosis and management.
Diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) are similar but distinct diabetic emergencies that are frequently encountered in the ED. Patients with DKA or HHS present with hyperglycemia and dehydration and frequently appear quite ill physically. In both syndromes, there is insufficient insulin levels to transport glucose into cells.
As previously noted, although DKA and HHS share similar characteristic signs and symptoms, they are two distinct conditions that must be differentiated in the clinical work-up. One characteristic that helps the emergency physician (EP) to distinguish between the two conditions is the patient age at symptom onset. Although both conditions can occur at any age, diabetic ketoacidosis typically develops in younger patients, less than 45 years, who have little or no endogenous insulin production, whereas HHS usually occurs in much older non-insulin-dependent patients (who are often greater than 60 years old). 1-3 This review discusses the similarities and differences in the etiology, diagnosis, and treatment of DKA and HHS to guide evaluation and simplify management, highlighting practical tips and clinical pearls. When applicable, information has been organized into groups of five to facilitate retention and recall.
The Etiology of DKA Vs HHS
The fundamental underlying issue in both DKA and HHS is an absolute or relative lack of insulin that results in an increase in counter-regulatory hormones, including glucagon, cortisol, and catecholamines.
Insulin has five main actions: (1) to drive glucose into cells; (2) to drive potassium into cells; (3) to create an anabolic environment; (4) to inhibit breakdown of fat; and (5) to block the breakdown of proteins. (Table 1).
Diabetic ketoacidosis typically develops in patients who lack significant endogenous insulin; this insufficiency of circulating insulin causes hyperglycemia and hyperkalemia, the creation of a catabolic state with high levels of both ketone bodies and free-fatty acids due to the breakdown of proteins and fats.
In contrast, HHS occurs in patients who produce a sufficient amount of insulin to drive potassium into cells and to inhibit the breakdown of proteins and fats; as such these patients are not ketoacidotic. However, patients with HHS do not produce enough insulin to drive glucose intracellularly. As the glucose levels increase, patients with HHS become increasingly hyperosmolar and dehydrated, resulting in further elevation of glucose levels, causing a perpetual cycle of increasing glucose and resultant hyperosmolarity and dehydration.1-3 It is important to appreciate that both hyperglycemic crises result in an osmotic diuresis leading to severe dehydration and urinary wasting of electrolytes.
Diagnosis and Workup
Laboratory Evaluation
In addition to hyperglycemia, another key finding in DKA is elevated anion gap metabolic acidosis resulting from ketoacid production. Laboratory evaluation will demonstrate a pH less than 7.3 and serum bicarbonate level less than 18 mEq/L; urinalysis will be positive for ketones.
Though HHS patients also present with hyperglycemia, laboratory evaluation will demonstrate no, or only mild, acidosis, normal pH (typically >7.3), bicarbonate level greater than 18 mEq/L, and a high-serum osmolality (>350 mOsm/kg). While urinalysis may show low or no ketones, patients with HHS do not develop the marked ketoacidosis seen in DKA. Moreover, glucose values are more elevated in patients with HHS, frequently exceeding 1,000 mg/dL.
Signs and Symptoms
Patients with either of these hyperglycemic crises often present with fatigue, polyuria, and polydipsia. They appear dehydrated on examination with dry mucous membranes, tachycardia, and in severe cases, hypotension. Patients with HHS often present with altered mental status, seizures, and even coma, while patients with DKA typically only experience changes in mental status in the most severe cases (Table 2). As many as one-third of patients with a hyperglycemic crisis will have an overlapping DKA/HHS syndrome.1-3 With respect to patient age, HHS tends to develop in older patients who have type 2 diabetes and several underlying comorbidities.2
Precipitating Causes of DKA and HHS
The five causes of DKA/HHS can be remembered as the “Five I’s”: (1) infection; (2) infarction; (3) infant (pregnancy), (4) indiscretion, and (5) [lack of] insulin (Table 3).
Infection. Infection is one of the most common precipitating factors in both DKA and HHS.1 During the history intake, the EP should ask the patient if he or she has had any recent urinary and respiratory symptoms, as positive responses prompt further investigation with urinalysis and chest radiography. A thorough dermatological examination should be performed to assess for visible signs of infection, particularly in the extremities and intertriginous areas.
When assessing patients with DKA or HHS for signs of infection, body temperature to assess for the presence of fever is not always a reliable indicator. This is because many patients with DKA/HHS develop tachypnea, which can affect the efficacy of an oral thermometer. In such cases, the rectal temperature is more sensitive for detecting fever. It should be noted, however, that some patients with severe infection or immunocompromised state—regardless of the presence or absence of tachypnea—may be normothermic or even hypothermic due to peripheral vasodilation—a poor prognostic sign.3 Blood and urine cultures should be obtained for all patients in whom infection is suspected.
Laboratory evaluation of patients with DKA may demonstrate a mild leukocytosis, a very common finding in DKA even in the absence of infection; leukocytosis is believed to result from elevated stress hormones such as cortisol and epinephrine.3
Infarction. Infarction is another important underlying cause of DKA/HHS and one that must not be overlooked. Screening for acute coronary syndrome through patient history, electrocardiography, and cardiac biomarkers should be performed in all patients older than age 40 years and in patients in whom there is any suggestion of myocardial ischemia.
A thorough neurological examination should be performed to assess for deficits indicative of stroke. Although neurological deficits can be due to severe hyperglycemia, most patients with focal neurological deficits from hyperglycemia also have altered mental status. Focal neurological deficits without a change in mental status are more likely to represent an actual stroke.4
Infant (Pregnancy). Pregnant patients are at an increased risk of developing DKA for several reasons, most notably due to the increased production of insulin-antagonistic hormones, which can lead to higher insulin resistance and thus increased insulin requirements during pregnancy.5 A pregnancy test is therefore indicated for all female patients of child-bearing age.
Indiscretion. Non-compliance with diet, such as taking in too many calories without appropriate insulin correction, and the ingestion of significant amounts of alcohol can lead to DKA. Eating disorders, particularly in young patients, may also contribute to recurrent cases.3
[Lack of] Insulin. In insulin-dependent diabetes, skipped insulin doses or insulin pump failure can trigger DKA/HHS. In fact, missed insulin doses are becoming a more frequent cause of DKA than infections.1
Both DKA and HHS are usually triggered by an underlying illness or event. Therefore, clinicians should always focus on identifying precipitating causes such as acute infection, stroke, or myocardial infarction, as some require immediate treatment. In fact, DKA or HHS is rarely the primary cause of death; patients are much more likely to die from the precipitating event that caused DKA or HHS.1,3
Assessing Disease Severity
Mental status and pH and serum bicarbonate levels help clinicians determine the extent of disease severity, classifying patients as having mild, moderate, or severe DKA (Table 4).2 Patients at the highest risk for poor outcomes include those at the extremes of age, who have severe comorbidities, who have underlying infection, and who are hypotensive and/or in a comatose state.3
Patients who have HHS are much more likely to present with altered mental status, including coma. There is a linear relationship between osmolality and degree of altered mental status. Thus, diabetic patients with major changes in mental status but without high serum osmolality warrant immediate workup for alternative causes of their altered mental status.3 In addition, seizures, especially focal seizures, are relatively common in severe cases of HHS. Finally, highly abnormal blood pressure, pulse, and respiratory rate can also provide additional clues regarding the severity of hyperglycemic crisis.
Arterial Blood Gas Assessment: To Stick or Not to Stick?
In the past, measuring arterial blood gases (ABG) has been considered a mainstay in the evaluation of patients with DKA. But does an arterial stick, which is associated with some risk, really add essential information? One study by Ma et al6 evaluated whether ABG results significantly alter how physicians manage patients with DKA. In the study, the authors evaluated 200 ED patients and found that ABG analysis only changed diagnosis in 1% of patients, altered treatment in 3.5% of patients, and changed disposition in only 1% of patients. Arterial stick partial pressure of oxygen and partial pressure of carbon dioxide altered treatment and disposition in only 1% of patients. Furthermore, the study results showed venous pH correlated very strongly with arterial pH (r = 0.95).6 These findings demonstrate that ABG measurements rarely affect or alter DKA management, and support the use of venous pH as an adequate substitute for ABG testing.
Euglycemia
Euglycemic DKA has been reported in patients with type 1 diabetes who had been fasting or vomiting or who had received exogenous insulin prior to presentation.1Euglycemia has also been reported in pregnant patients with type I diabetes.1 More recently, sodium glucose cotransporter 2 inhibitors (SGLT2) have been shown to cause euglycemic DKA. While the therapeutic mechanism of this drug class is to inhibit proximal tubular resorption of glucose, they can cause DKA by decreasing renal clearance of ketone bodies and increasing glucagon levels and promoting hepatic ketogenesis. Patients with DKA who are on SGLT2 inhibitors may present with only modestly elevated glucose levels (typically in the 200- to 300-mg/dL range), but have profound wide gap metabolic acidosis due to β-hydroxybutyrate acid and acetoacetate accumulation.7 When evaluating patients on SGLT2 inhibitors for DKA, EPs should not solely rely on glucose values but rather assess the patient’s overall clinical picture, including the physical examination, vital signs, and pH. Additionally, once resuscitation with intravenous (IV) fluids and insulin is initiated, it may take longer for patients who use SGLT2 inhibitors to clear ketoacids than patients with DKA who do not use these medications.8
Treatment
The goal of treatment for DKA and HHS is to correct volume deficits, hyperglycemia, and electrolyte abnormalities (Table 5). Three of the five therapies to manage DKA and HHS are mandatory: IV fluid resuscitation, IV insulin, and IV potassium. The other therapies, IV bicarbonate, and IV phosphate, should be considered, but are rarely required for DKA or HHS.
In general, management of HHS is less aggressive than that of DKA because HHS develops over a period of weeks—unlike DKA, which develops over only 1 to 2 days. Treatment of any underlying causes of HHS should occur simultaneously.
Intravenous Fluids
The goal of IV fluid therapy for patients with DKA is rehydration—not to “wash-out” ketones. Ketone elimination occurs through insulin-stimulated metabolism. When determining volume-replacement goals, it is helpful to keep in mind that patients with moderate-to-mild DKA typically have fluid deficiencies of 3 to 5 L, and patients with severe DKA have fluid deficiencies between 5 and 6 L. Patients with HHS present with significantly higher fluid deficiencies of around 9 to 12 L.
The initial goal of fluid management is to correct hypoperfusion with bolus fluids, followed by a more gradual repletion of remaining deficits. After bolus fluids are administered, the rate and type of subsequent IV fluid infusion varies depending on hemodynamics, hydration state, and serum sodium levels.2,3
Nonaggressive Vs Aggressive Fluid Management. One study by Adrogué et al9 compared the effects of managing DKA with aggressive vs nonaggressive fluid repletion. In the study, one group of patients received normal saline at 1,000 mL per hour for 4 hours, followed by normal saline at 500 mL per hour for 4 hours. The other group of patients received normal saline at a more modest rate of 500 mL per hour for 4 hours, followed by normal saline at 250 mL per hour for 4 hours. The authors found that patients in the less aggressive volume therapy group achieved a prompt and adequate recovery and maintained higher serum bicarbonate levels.9
Current recommendations for patients with DKA are to first treat patients with an initial bolus of 1,000 mL or 20 cc/kg of normal saline. Patients without profound dehydration should then receive 500 cc of normal saline per hour for the first 4 hours of treatment, after which the flow rate may be reduced to 250 cc per hour. For patients with mild DKA, therapy can start at 250 cc per hour with a smaller bolus dose or no bolus dose. Patients with profound dehydration and poor perfusion, should receive crystalloid fluids wide open until perfusion has improved. Overall, volume resuscitation in HHS is similar to DKA. However, the EP should be cautious with respect to total fluid volume and infusion rates to avoid fluid overload, since many patients with HHS are elderly and may have congestive heart failure.
Crystalloid Fluid Type for Initial Resuscitation. Normal saline has been the traditional crystalloid fluid of choice for managing DKA and HHS. Recent studies, however, have shown some benefit to using balanced solutions (Ringer’s lactate or PlasmaLyte) instead of normal saline. A recently published large study by Semler et al10 compared balanced crystalloid, in most cases lactated Ringers solution, to normal saline in critically ill adult patients, some of whom were diagnosed with DKA. The study demonstrated decreased mortality (from any cause) in the group who received balanced crystalloid fluid therapy and reduced need for renal-replacement therapy and reduced incidence of persistent renal dysfunction. The findings by Semler et al10 and findings from other smaller studies, calls into question whether normal saline is the best crystalloid to manage DKA and HHS.11,12 It remains to be seen what modification the American Diabetes Association (ADA) will make to its current recommendations for fluid therapy, which were last updated in 2009.
It appears that though the use of Ringers lactate or PlasmaLyte to treat DKA usually raises a patient’s serum bicarbonate level to 18 mEq/L at a more rapid rate than normal saline, the use of balanced solutions may result in longer time to lower blood glucose to 250 mg/dL.13 However, by using a balanced solution, the hyperchloremic metabolic acidosis often seen with normal saline treatment will be avoided.12
Half-Normal Saline. An initially normal or increased serum sodium level, despite significant hyperglycemia, suggests a substantial free-water deficit. Calculating a corrected serum sodium can help quantify the degree of free-water deficit.3 While isotonic fluids remain the standard for initial volume load, clinicians should consider switching patients to half-normal saline following initial resuscitation if the corrected serum sodium is elevated above normal. The simplest estimation to correct sodium levels in DKA is to expect a decrease in sodium levels at a rate of at least 2 mEq/L per 100-mg/dL increase in glucose levels above 100 mg/dL. For a more accurate calculation, providers can expect a drop in sodium of 1.6 mEq/L per 100 mg/dL increase of glucose up to a level of 400 mg/dL and then a fall of 2.4 mEq/L in sodium per every 100 mg/dL rise in glucose thereafter.14
Glucose. Patients with DKA require insulin therapy until ketoacidosis resolves. However, the average time to correct ketoacidosis from initiating treatment is about 12 hours compared to only 6 hours for correction of hyperglycemia. Since insulin therapy must be continued despite lower glucose levels, patients are at risk for developing hypoglycemia if glucose is not added to IV fluids. To prevent hypoglycemia and provide an energy source for ketone metabolism, patients should be switched to fluids containing dextrose when their serum glucose approaches 200 to 250 mg/dL.1,3 Typically, 5% dextrose in half-normal saline at 150 to 250 cc per hour is usually adequate to achieve this goal.
Insulin
As previously noted, insulin therapy is required to treat hyperglycemic crises from DKA and HHS. In DKA there is an absolute insulin deficiency, whereas in HHS, there is a relative insulin deficiency. In HHS, there is not enough endogenous insulin to move glucose into the cells, but there is enough insulin to block a catabolic state. That is why the breakdown of fats and proteins does not occur, and why ketoacidosis and hyperkalemia are not seen in HHS. On the other hand, glucose elevations do occur, and are usually more extreme in HHS than DKA. There are five major therapeutic actions of insulin in DKA (Table 5), and it is imperative to determine serum potassium before starting an insulin infusion as insulin will drive potassium into the cell, worsening hypokalemia and promoting the development of life-threatening arrhythmias, including ventricular fibrillation, ventricular tachycardia, and torsades de pointes. The electrocardiogram does not accurately predict severity of hypokalemia and should not be used as a substitute for direct potassium measurement.
Loading Dose and Drip Rate. When treating adult patients with DKA or HHS, the ADA recommends an IV push loading dose of 0.1 U/kg insulin, followed by an hourly maintenance dose of 0.1 U/kg. Alternatively, a continuous infusion of 0.16 U/kg/hr can be used without a bolus. The rationale behind a bolus is the rapid saturation of insulin receptors, followed by a drip to maintain saturation of receptors. However, a recent prospective observational cohort study by Goyal et al15 questions the utility of the initial insulin bolus. The study compared DKA patients who received an initial insulin bolus to those who did not. Both groups were similar at baseline and received equivalent IV fluids and insulin drips. They found no statistically significant differences in the incidence of hypoglycemia, rate of serum glucose change, anion gap change, or length of stay in the ED or hospital. The authors concluded that administration of an insulin bolus has no significant benefit to patients and does not change clinically relevant end-points.15 At this time, there is no proven benefit to giving DKA patients an IV insulin bolus; moreover, doing so may further increase hypoglycemia. The use of an insulin bolus is particularly not recommended for use in pediatric patients with DKA due to a higher incidence of hypoglycemia in this patient population.16
As with DKA, the ADA3 recommends giving HHS patients an insulin bolus of 0.1 U/ kg followed by a continuous infusion at 0.1 U/kg per hour. It is crucial to monitor patients closely to ensure glucose levels do not fall too rapidly. Glucose levels should be kept between 150 to 200 mg/dL for patients with DKA and 200 to 300 mg/dL for patients with HHS until the conditions resolve; this may necessitate lowering the infusion rate to 0.02 to 0.05 U/kg per hour. In addition to frequent glucose monitoring, a basic metabolic panel and venous pH should be obtained every 2 to 4 hours while a patient is on an insulin drip.3
Subcutaneous Vs Intravenous Insulin for DKA. Several small studies evaluating patients with mild-moderate DKA demonstrated similar outcomes when subcutaneous (SQ) insulin was used instead of IV insulin. However, SQ injections require more frequent dosing (every 1 to 2 hours) and still require close monitoring of blood glucose. This monitoring frequency is usually not feasible on a hospital floor, but may be feasible on step-down units, thus avoiding admission to the intensive care unit (ICU) for patients who do not otherwise require ICU-level of care.17 Subcutaneous insulin should not be given to patients with severe acidosis, hypotension, or altered mental status. The ADA consensus statement continues to recommend IV infusion of regular insulin as the preferred route due to its short half-life and easy titration.3
Determining When to Switch to Subcutaneous Insulin. Ideally, patients are not in the ED long enough to have their metabolic abnormalities corrected, as this usually requires several hours. In DKA, the insulin drip should continue until the blood glucose is less than 200 and at least two of the following conditions are met: the anion gap is less than 12, venous pH greater than 7.3, and serum bicarbonate >15. In HHS, osmolality and mental status should both return to normal prior to stopping the infusion. In both cases, subcutaneous insulin should be administered at least 1 to 2 hours before stopping the drip to prevent recurrent crisis.1,3
Refractory Acidosis. First and foremost, refractory acidosis should prompt a diligent source for dead gut, abscess, and underlying sepsis. While vomiting and diffuse abdominal pain are common in DKA and are related to ketoacidosis, these symptoms are atypical of HHS and should raise suspicion for underlying pathology.3 Additionally, a lower than expected bicarbonate level can also occur from resuscitation with large volumes of normal saline, resulting in a hyperchloremic non-gap metabolic acidosis.
Potassium
Both DKA and HHS patients have total body potassium deficits due to osmotic diuresis that require careful repletion. Deficits can be substantial: The average total whole body potassium deficit in DKA is 3 to 5 mEq/kg.2 Clinicians should exercise caution, however, since DKA patients may be hyperkalemic initially despite a total body potassium deficit. Early hyperkalemia is due to the transmembrane shift of potassium secondary to acidosis and insulin deficiency as well as hypertonicity. If initial potassium is greater than 5.2 mEq/L, potassium should not be administered but instead rechecked in 1 to 2 hours. If the potassium level is 4.0 to 5.2 mEq/L, then 10 mEq per hour is usually adequate. For levels between 3.3 and 4.0 mEq/L, administer potassium chloride at 20 mEq per hour. For levels less than 3.3 mEq/L, insulin should be held and potassium chloride should be aggressively repleted at 20 to 30 mEq per hour with continuous cardiac monitoring.1-3 Failure to recognize and act on critical potassium levels is a known cause of unexpected death in DKA. During the first hour of DKA onset, patients are more likely to die from hyperkalemia. Later, while the patient is “stabilizing” on an insulin infusion, potassium levels will fall as insulin drives potassium back into cells.
Bicarbonate
Bicarbonate has many theoretical benefits but also has potential risks (Table 6).
Phosphate
Since there is no proven benefit to giving phosphate to adult patients with DKA, it is rarely used, except in specific situations other than pediatric DKA. Similar to potassium, initial serum phosphate levels do not reflect total body phosphate levels due to transmembrane shifts.2,3 Phosphate repletionis most beneficial for patients who have cachexia, respiratory depression, anemia, cardiac dysfunction, or phosphate values lower than 1.0 to 1.5. If given, 20 to 30 mEq/L potassium phosphate (K2PO4) added to fluids is usually sufficient.3 Overly aggressive phosphate administration (>4.5 mmol/h or 1.5 mL/h potassium phosphate) can cause severe hypocalcemia and should be avoided.1,3 In pediatric patients, up to one-half of potassium requirements are often given as potassium phosphate, but this may vary by institution.
Conclusion
Both DKA and HHS are diabetic emergencies that must be approached and managed systematically to correct underlying dehydration and metabolic abnormalities. Patient care begins by determining the etiology of these conditions, especially HHS. Once the cause has been identified, patients should be treated with bolus fluids to obtain adequate perfusion, followed by IV fluid infusion. Clinicians should carefully monitor the serum sodium level of patients with DKA or HHS to determine the ideal amount and type of fluid required, and also should measure potassium levels prior to starting patients on insulin. (Tables 7 and 8 summarize important clinical pearls when treating patients with DKA or HHS.)
Diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) are similar but distinct diabetic emergencies that are frequently encountered in the ED. Patients with DKA or HHS present with hyperglycemia and dehydration and frequently appear quite ill physically. In both syndromes, there is insufficient insulin levels to transport glucose into cells.
As previously noted, although DKA and HHS share similar characteristic signs and symptoms, they are two distinct conditions that must be differentiated in the clinical work-up. One characteristic that helps the emergency physician (EP) to distinguish between the two conditions is the patient age at symptom onset. Although both conditions can occur at any age, diabetic ketoacidosis typically develops in younger patients, less than 45 years, who have little or no endogenous insulin production, whereas HHS usually occurs in much older non-insulin-dependent patients (who are often greater than 60 years old). 1-3 This review discusses the similarities and differences in the etiology, diagnosis, and treatment of DKA and HHS to guide evaluation and simplify management, highlighting practical tips and clinical pearls. When applicable, information has been organized into groups of five to facilitate retention and recall.
The Etiology of DKA Vs HHS
The fundamental underlying issue in both DKA and HHS is an absolute or relative lack of insulin that results in an increase in counter-regulatory hormones, including glucagon, cortisol, and catecholamines.
Insulin has five main actions: (1) to drive glucose into cells; (2) to drive potassium into cells; (3) to create an anabolic environment; (4) to inhibit breakdown of fat; and (5) to block the breakdown of proteins. (Table 1).
Diabetic ketoacidosis typically develops in patients who lack significant endogenous insulin; this insufficiency of circulating insulin causes hyperglycemia and hyperkalemia, the creation of a catabolic state with high levels of both ketone bodies and free-fatty acids due to the breakdown of proteins and fats.
In contrast, HHS occurs in patients who produce a sufficient amount of insulin to drive potassium into cells and to inhibit the breakdown of proteins and fats; as such these patients are not ketoacidotic. However, patients with HHS do not produce enough insulin to drive glucose intracellularly. As the glucose levels increase, patients with HHS become increasingly hyperosmolar and dehydrated, resulting in further elevation of glucose levels, causing a perpetual cycle of increasing glucose and resultant hyperosmolarity and dehydration.1-3 It is important to appreciate that both hyperglycemic crises result in an osmotic diuresis leading to severe dehydration and urinary wasting of electrolytes.
Diagnosis and Workup
Laboratory Evaluation
In addition to hyperglycemia, another key finding in DKA is elevated anion gap metabolic acidosis resulting from ketoacid production. Laboratory evaluation will demonstrate a pH less than 7.3 and serum bicarbonate level less than 18 mEq/L; urinalysis will be positive for ketones.
Though HHS patients also present with hyperglycemia, laboratory evaluation will demonstrate no, or only mild, acidosis, normal pH (typically >7.3), bicarbonate level greater than 18 mEq/L, and a high-serum osmolality (>350 mOsm/kg). While urinalysis may show low or no ketones, patients with HHS do not develop the marked ketoacidosis seen in DKA. Moreover, glucose values are more elevated in patients with HHS, frequently exceeding 1,000 mg/dL.
Signs and Symptoms
Patients with either of these hyperglycemic crises often present with fatigue, polyuria, and polydipsia. They appear dehydrated on examination with dry mucous membranes, tachycardia, and in severe cases, hypotension. Patients with HHS often present with altered mental status, seizures, and even coma, while patients with DKA typically only experience changes in mental status in the most severe cases (Table 2). As many as one-third of patients with a hyperglycemic crisis will have an overlapping DKA/HHS syndrome.1-3 With respect to patient age, HHS tends to develop in older patients who have type 2 diabetes and several underlying comorbidities.2
Precipitating Causes of DKA and HHS
The five causes of DKA/HHS can be remembered as the “Five I’s”: (1) infection; (2) infarction; (3) infant (pregnancy), (4) indiscretion, and (5) [lack of] insulin (Table 3).
Infection. Infection is one of the most common precipitating factors in both DKA and HHS.1 During the history intake, the EP should ask the patient if he or she has had any recent urinary and respiratory symptoms, as positive responses prompt further investigation with urinalysis and chest radiography. A thorough dermatological examination should be performed to assess for visible signs of infection, particularly in the extremities and intertriginous areas.
When assessing patients with DKA or HHS for signs of infection, body temperature to assess for the presence of fever is not always a reliable indicator. This is because many patients with DKA/HHS develop tachypnea, which can affect the efficacy of an oral thermometer. In such cases, the rectal temperature is more sensitive for detecting fever. It should be noted, however, that some patients with severe infection or immunocompromised state—regardless of the presence or absence of tachypnea—may be normothermic or even hypothermic due to peripheral vasodilation—a poor prognostic sign.3 Blood and urine cultures should be obtained for all patients in whom infection is suspected.
Laboratory evaluation of patients with DKA may demonstrate a mild leukocytosis, a very common finding in DKA even in the absence of infection; leukocytosis is believed to result from elevated stress hormones such as cortisol and epinephrine.3
Infarction. Infarction is another important underlying cause of DKA/HHS and one that must not be overlooked. Screening for acute coronary syndrome through patient history, electrocardiography, and cardiac biomarkers should be performed in all patients older than age 40 years and in patients in whom there is any suggestion of myocardial ischemia.
A thorough neurological examination should be performed to assess for deficits indicative of stroke. Although neurological deficits can be due to severe hyperglycemia, most patients with focal neurological deficits from hyperglycemia also have altered mental status. Focal neurological deficits without a change in mental status are more likely to represent an actual stroke.4
Infant (Pregnancy). Pregnant patients are at an increased risk of developing DKA for several reasons, most notably due to the increased production of insulin-antagonistic hormones, which can lead to higher insulin resistance and thus increased insulin requirements during pregnancy.5 A pregnancy test is therefore indicated for all female patients of child-bearing age.
Indiscretion. Non-compliance with diet, such as taking in too many calories without appropriate insulin correction, and the ingestion of significant amounts of alcohol can lead to DKA. Eating disorders, particularly in young patients, may also contribute to recurrent cases.3
[Lack of] Insulin. In insulin-dependent diabetes, skipped insulin doses or insulin pump failure can trigger DKA/HHS. In fact, missed insulin doses are becoming a more frequent cause of DKA than infections.1
Both DKA and HHS are usually triggered by an underlying illness or event. Therefore, clinicians should always focus on identifying precipitating causes such as acute infection, stroke, or myocardial infarction, as some require immediate treatment. In fact, DKA or HHS is rarely the primary cause of death; patients are much more likely to die from the precipitating event that caused DKA or HHS.1,3
Assessing Disease Severity
Mental status and pH and serum bicarbonate levels help clinicians determine the extent of disease severity, classifying patients as having mild, moderate, or severe DKA (Table 4).2 Patients at the highest risk for poor outcomes include those at the extremes of age, who have severe comorbidities, who have underlying infection, and who are hypotensive and/or in a comatose state.3
Patients who have HHS are much more likely to present with altered mental status, including coma. There is a linear relationship between osmolality and degree of altered mental status. Thus, diabetic patients with major changes in mental status but without high serum osmolality warrant immediate workup for alternative causes of their altered mental status.3 In addition, seizures, especially focal seizures, are relatively common in severe cases of HHS. Finally, highly abnormal blood pressure, pulse, and respiratory rate can also provide additional clues regarding the severity of hyperglycemic crisis.
Arterial Blood Gas Assessment: To Stick or Not to Stick?
In the past, measuring arterial blood gases (ABG) has been considered a mainstay in the evaluation of patients with DKA. But does an arterial stick, which is associated with some risk, really add essential information? One study by Ma et al6 evaluated whether ABG results significantly alter how physicians manage patients with DKA. In the study, the authors evaluated 200 ED patients and found that ABG analysis only changed diagnosis in 1% of patients, altered treatment in 3.5% of patients, and changed disposition in only 1% of patients. Arterial stick partial pressure of oxygen and partial pressure of carbon dioxide altered treatment and disposition in only 1% of patients. Furthermore, the study results showed venous pH correlated very strongly with arterial pH (r = 0.95).6 These findings demonstrate that ABG measurements rarely affect or alter DKA management, and support the use of venous pH as an adequate substitute for ABG testing.
Euglycemia
Euglycemic DKA has been reported in patients with type 1 diabetes who had been fasting or vomiting or who had received exogenous insulin prior to presentation.1Euglycemia has also been reported in pregnant patients with type I diabetes.1 More recently, sodium glucose cotransporter 2 inhibitors (SGLT2) have been shown to cause euglycemic DKA. While the therapeutic mechanism of this drug class is to inhibit proximal tubular resorption of glucose, they can cause DKA by decreasing renal clearance of ketone bodies and increasing glucagon levels and promoting hepatic ketogenesis. Patients with DKA who are on SGLT2 inhibitors may present with only modestly elevated glucose levels (typically in the 200- to 300-mg/dL range), but have profound wide gap metabolic acidosis due to β-hydroxybutyrate acid and acetoacetate accumulation.7 When evaluating patients on SGLT2 inhibitors for DKA, EPs should not solely rely on glucose values but rather assess the patient’s overall clinical picture, including the physical examination, vital signs, and pH. Additionally, once resuscitation with intravenous (IV) fluids and insulin is initiated, it may take longer for patients who use SGLT2 inhibitors to clear ketoacids than patients with DKA who do not use these medications.8
Treatment
The goal of treatment for DKA and HHS is to correct volume deficits, hyperglycemia, and electrolyte abnormalities (Table 5). Three of the five therapies to manage DKA and HHS are mandatory: IV fluid resuscitation, IV insulin, and IV potassium. The other therapies, IV bicarbonate, and IV phosphate, should be considered, but are rarely required for DKA or HHS.
In general, management of HHS is less aggressive than that of DKA because HHS develops over a period of weeks—unlike DKA, which develops over only 1 to 2 days. Treatment of any underlying causes of HHS should occur simultaneously.
Intravenous Fluids
The goal of IV fluid therapy for patients with DKA is rehydration—not to “wash-out” ketones. Ketone elimination occurs through insulin-stimulated metabolism. When determining volume-replacement goals, it is helpful to keep in mind that patients with moderate-to-mild DKA typically have fluid deficiencies of 3 to 5 L, and patients with severe DKA have fluid deficiencies between 5 and 6 L. Patients with HHS present with significantly higher fluid deficiencies of around 9 to 12 L.
The initial goal of fluid management is to correct hypoperfusion with bolus fluids, followed by a more gradual repletion of remaining deficits. After bolus fluids are administered, the rate and type of subsequent IV fluid infusion varies depending on hemodynamics, hydration state, and serum sodium levels.2,3
Nonaggressive Vs Aggressive Fluid Management. One study by Adrogué et al9 compared the effects of managing DKA with aggressive vs nonaggressive fluid repletion. In the study, one group of patients received normal saline at 1,000 mL per hour for 4 hours, followed by normal saline at 500 mL per hour for 4 hours. The other group of patients received normal saline at a more modest rate of 500 mL per hour for 4 hours, followed by normal saline at 250 mL per hour for 4 hours. The authors found that patients in the less aggressive volume therapy group achieved a prompt and adequate recovery and maintained higher serum bicarbonate levels.9
Current recommendations for patients with DKA are to first treat patients with an initial bolus of 1,000 mL or 20 cc/kg of normal saline. Patients without profound dehydration should then receive 500 cc of normal saline per hour for the first 4 hours of treatment, after which the flow rate may be reduced to 250 cc per hour. For patients with mild DKA, therapy can start at 250 cc per hour with a smaller bolus dose or no bolus dose. Patients with profound dehydration and poor perfusion, should receive crystalloid fluids wide open until perfusion has improved. Overall, volume resuscitation in HHS is similar to DKA. However, the EP should be cautious with respect to total fluid volume and infusion rates to avoid fluid overload, since many patients with HHS are elderly and may have congestive heart failure.
Crystalloid Fluid Type for Initial Resuscitation. Normal saline has been the traditional crystalloid fluid of choice for managing DKA and HHS. Recent studies, however, have shown some benefit to using balanced solutions (Ringer’s lactate or PlasmaLyte) instead of normal saline. A recently published large study by Semler et al10 compared balanced crystalloid, in most cases lactated Ringers solution, to normal saline in critically ill adult patients, some of whom were diagnosed with DKA. The study demonstrated decreased mortality (from any cause) in the group who received balanced crystalloid fluid therapy and reduced need for renal-replacement therapy and reduced incidence of persistent renal dysfunction. The findings by Semler et al10 and findings from other smaller studies, calls into question whether normal saline is the best crystalloid to manage DKA and HHS.11,12 It remains to be seen what modification the American Diabetes Association (ADA) will make to its current recommendations for fluid therapy, which were last updated in 2009.
It appears that though the use of Ringers lactate or PlasmaLyte to treat DKA usually raises a patient’s serum bicarbonate level to 18 mEq/L at a more rapid rate than normal saline, the use of balanced solutions may result in longer time to lower blood glucose to 250 mg/dL.13 However, by using a balanced solution, the hyperchloremic metabolic acidosis often seen with normal saline treatment will be avoided.12
Half-Normal Saline. An initially normal or increased serum sodium level, despite significant hyperglycemia, suggests a substantial free-water deficit. Calculating a corrected serum sodium can help quantify the degree of free-water deficit.3 While isotonic fluids remain the standard for initial volume load, clinicians should consider switching patients to half-normal saline following initial resuscitation if the corrected serum sodium is elevated above normal. The simplest estimation to correct sodium levels in DKA is to expect a decrease in sodium levels at a rate of at least 2 mEq/L per 100-mg/dL increase in glucose levels above 100 mg/dL. For a more accurate calculation, providers can expect a drop in sodium of 1.6 mEq/L per 100 mg/dL increase of glucose up to a level of 400 mg/dL and then a fall of 2.4 mEq/L in sodium per every 100 mg/dL rise in glucose thereafter.14
Glucose. Patients with DKA require insulin therapy until ketoacidosis resolves. However, the average time to correct ketoacidosis from initiating treatment is about 12 hours compared to only 6 hours for correction of hyperglycemia. Since insulin therapy must be continued despite lower glucose levels, patients are at risk for developing hypoglycemia if glucose is not added to IV fluids. To prevent hypoglycemia and provide an energy source for ketone metabolism, patients should be switched to fluids containing dextrose when their serum glucose approaches 200 to 250 mg/dL.1,3 Typically, 5% dextrose in half-normal saline at 150 to 250 cc per hour is usually adequate to achieve this goal.
Insulin
As previously noted, insulin therapy is required to treat hyperglycemic crises from DKA and HHS. In DKA there is an absolute insulin deficiency, whereas in HHS, there is a relative insulin deficiency. In HHS, there is not enough endogenous insulin to move glucose into the cells, but there is enough insulin to block a catabolic state. That is why the breakdown of fats and proteins does not occur, and why ketoacidosis and hyperkalemia are not seen in HHS. On the other hand, glucose elevations do occur, and are usually more extreme in HHS than DKA. There are five major therapeutic actions of insulin in DKA (Table 5), and it is imperative to determine serum potassium before starting an insulin infusion as insulin will drive potassium into the cell, worsening hypokalemia and promoting the development of life-threatening arrhythmias, including ventricular fibrillation, ventricular tachycardia, and torsades de pointes. The electrocardiogram does not accurately predict severity of hypokalemia and should not be used as a substitute for direct potassium measurement.
Loading Dose and Drip Rate. When treating adult patients with DKA or HHS, the ADA recommends an IV push loading dose of 0.1 U/kg insulin, followed by an hourly maintenance dose of 0.1 U/kg. Alternatively, a continuous infusion of 0.16 U/kg/hr can be used without a bolus. The rationale behind a bolus is the rapid saturation of insulin receptors, followed by a drip to maintain saturation of receptors. However, a recent prospective observational cohort study by Goyal et al15 questions the utility of the initial insulin bolus. The study compared DKA patients who received an initial insulin bolus to those who did not. Both groups were similar at baseline and received equivalent IV fluids and insulin drips. They found no statistically significant differences in the incidence of hypoglycemia, rate of serum glucose change, anion gap change, or length of stay in the ED or hospital. The authors concluded that administration of an insulin bolus has no significant benefit to patients and does not change clinically relevant end-points.15 At this time, there is no proven benefit to giving DKA patients an IV insulin bolus; moreover, doing so may further increase hypoglycemia. The use of an insulin bolus is particularly not recommended for use in pediatric patients with DKA due to a higher incidence of hypoglycemia in this patient population.16
As with DKA, the ADA3 recommends giving HHS patients an insulin bolus of 0.1 U/ kg followed by a continuous infusion at 0.1 U/kg per hour. It is crucial to monitor patients closely to ensure glucose levels do not fall too rapidly. Glucose levels should be kept between 150 to 200 mg/dL for patients with DKA and 200 to 300 mg/dL for patients with HHS until the conditions resolve; this may necessitate lowering the infusion rate to 0.02 to 0.05 U/kg per hour. In addition to frequent glucose monitoring, a basic metabolic panel and venous pH should be obtained every 2 to 4 hours while a patient is on an insulin drip.3
Subcutaneous Vs Intravenous Insulin for DKA. Several small studies evaluating patients with mild-moderate DKA demonstrated similar outcomes when subcutaneous (SQ) insulin was used instead of IV insulin. However, SQ injections require more frequent dosing (every 1 to 2 hours) and still require close monitoring of blood glucose. This monitoring frequency is usually not feasible on a hospital floor, but may be feasible on step-down units, thus avoiding admission to the intensive care unit (ICU) for patients who do not otherwise require ICU-level of care.17 Subcutaneous insulin should not be given to patients with severe acidosis, hypotension, or altered mental status. The ADA consensus statement continues to recommend IV infusion of regular insulin as the preferred route due to its short half-life and easy titration.3
Determining When to Switch to Subcutaneous Insulin. Ideally, patients are not in the ED long enough to have their metabolic abnormalities corrected, as this usually requires several hours. In DKA, the insulin drip should continue until the blood glucose is less than 200 and at least two of the following conditions are met: the anion gap is less than 12, venous pH greater than 7.3, and serum bicarbonate >15. In HHS, osmolality and mental status should both return to normal prior to stopping the infusion. In both cases, subcutaneous insulin should be administered at least 1 to 2 hours before stopping the drip to prevent recurrent crisis.1,3
Refractory Acidosis. First and foremost, refractory acidosis should prompt a diligent source for dead gut, abscess, and underlying sepsis. While vomiting and diffuse abdominal pain are common in DKA and are related to ketoacidosis, these symptoms are atypical of HHS and should raise suspicion for underlying pathology.3 Additionally, a lower than expected bicarbonate level can also occur from resuscitation with large volumes of normal saline, resulting in a hyperchloremic non-gap metabolic acidosis.
Potassium
Both DKA and HHS patients have total body potassium deficits due to osmotic diuresis that require careful repletion. Deficits can be substantial: The average total whole body potassium deficit in DKA is 3 to 5 mEq/kg.2 Clinicians should exercise caution, however, since DKA patients may be hyperkalemic initially despite a total body potassium deficit. Early hyperkalemia is due to the transmembrane shift of potassium secondary to acidosis and insulin deficiency as well as hypertonicity. If initial potassium is greater than 5.2 mEq/L, potassium should not be administered but instead rechecked in 1 to 2 hours. If the potassium level is 4.0 to 5.2 mEq/L, then 10 mEq per hour is usually adequate. For levels between 3.3 and 4.0 mEq/L, administer potassium chloride at 20 mEq per hour. For levels less than 3.3 mEq/L, insulin should be held and potassium chloride should be aggressively repleted at 20 to 30 mEq per hour with continuous cardiac monitoring.1-3 Failure to recognize and act on critical potassium levels is a known cause of unexpected death in DKA. During the first hour of DKA onset, patients are more likely to die from hyperkalemia. Later, while the patient is “stabilizing” on an insulin infusion, potassium levels will fall as insulin drives potassium back into cells.
Bicarbonate
Bicarbonate has many theoretical benefits but also has potential risks (Table 6).
Phosphate
Since there is no proven benefit to giving phosphate to adult patients with DKA, it is rarely used, except in specific situations other than pediatric DKA. Similar to potassium, initial serum phosphate levels do not reflect total body phosphate levels due to transmembrane shifts.2,3 Phosphate repletionis most beneficial for patients who have cachexia, respiratory depression, anemia, cardiac dysfunction, or phosphate values lower than 1.0 to 1.5. If given, 20 to 30 mEq/L potassium phosphate (K2PO4) added to fluids is usually sufficient.3 Overly aggressive phosphate administration (>4.5 mmol/h or 1.5 mL/h potassium phosphate) can cause severe hypocalcemia and should be avoided.1,3 In pediatric patients, up to one-half of potassium requirements are often given as potassium phosphate, but this may vary by institution.
Conclusion
Both DKA and HHS are diabetic emergencies that must be approached and managed systematically to correct underlying dehydration and metabolic abnormalities. Patient care begins by determining the etiology of these conditions, especially HHS. Once the cause has been identified, patients should be treated with bolus fluids to obtain adequate perfusion, followed by IV fluid infusion. Clinicians should carefully monitor the serum sodium level of patients with DKA or HHS to determine the ideal amount and type of fluid required, and also should measure potassium levels prior to starting patients on insulin. (Tables 7 and 8 summarize important clinical pearls when treating patients with DKA or HHS.)
1. Nyenwe EA, Kitabchi AE. The evolution of diabetic ketoacidosis: an update of its etiology, pathogenesis and management. Metabolism. 2016;65(4):507-521. doi:10.1016/j.metabol.2015.12.007.
2. Fayfman M, Pasquel FJ, Umpierrez GE. Management of hyperglycemic crises: diabetic ketoacidosis and hyperglycemic hyperosmolar state. Med Clin North Am. 2017;101(3):587-606. doi:10.1016/j.mcna.2016.12.011.
3. Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009;32(7):1335-1343. doi:10.2337/dc09-9032.
4. Fugate JE, Rabinstein AA. Absolute and relative contraindications to IV rt-PA for acute ischemic stroke. Neurohospitalist. 2015;5(3):110-121. doi:10.1177/1941874415578532.
5. Kamalakannan D, Baskar V, Barton DM, Abdu TA. Diabetic ketoacidosis in pregnancy. Postgrad Med J. 2003;79(9):454-457.
6. Ma OJ, Rush MD, Godfrey MM, Gaddis G. Arterial blood gas results rarely influence emergency physician management of patients with suspected diabetic ketoacidosis. Acad Emerg Med. 2003;10(8):836-841.
7. Taylor S, Blau J, Rother K. SGLT2 Inhibitors may predispose to ketoacidosis. J Clin Endocrinol Metab. 2015;100(8):2849-2852. doi:10.1210/jc.2015-1884.
8. Kum-Nji JS, Gosmanov AR, Steinberg H, Dagogo-Jack S. Hyperglycemic, high anion-gap metabolic acidosis in patients receiving SGLT-2 inhibitors for diabetes management. J Diabetes Complications. 2017;31(3):611-614. doi:10.1016/j.jdiacomp.2016.11.004.
9. Adrogué HJ, Barrero J, Eknoyan G. Salutary effects of modest fluid replacement in the treatment of adults with diabetic ketoacidosis. Use in patients without extreme volume deficit. JAMA. 1989;262(15):2108-2013.
10. Semler MW, Self WH, Wanderer JP, et al; SMART Investigators and the Pragmatic Critical Care Research Group. Balanced crystalloid versus saline in critically ill adults. N Engl J Med. 2018;378(9):829-839. doi:10.1056/NEJMoa1711584.
11. Chua HR, Venkatesh B, Stachowski E, et al. Plasma-Lyte 148 vs 0.9% saline for fluid resuscitation in diabetic ketoacidosis. J Crit Care. 2012;27(2):138-145. doi:10.1016/j.jcrc.2012.01.007.
12. Mahler S, Conrad S, Wang H, Arnold T. Resuscitation with balanced electrolyte solution prevents hyperchloremic metabolic acidosis in patients with diabetic ketoacidosis. Am J Emerg Med. 2011;29(9):1194-1197. doi:10.1016/j.ajem.2010.07.015.
11. Van Zyl DG, Rheeder P, Delport E. Fluid management in diabetic-acidosis--Ringer’s lactate versus normal saline: a randomized controlled trial. QJM. 2012;105(4):337-343. doi:10.1093/qjmed/hcr226.
14. Penne EL, Thijssen S, Raimann JG, Levin NW, Kotanko P. Correction of serum sodium for glucose concentration in hemodialysis patients with poor glucose control. Diabetes Care. 2010;33(7):e91. doi:10.2337/dc10-0557.
15. Goyal N, Miller JB, Sankey SS, Mossallam U. Utility of initial bolus insulin in the treatment of diabetic ketoacidosis. J Emerg Med. 2010;38(4):422-427. doi:10.1016/j.jemermed.2007.11.033.
16. Wolfsdorf JI, Allgrove J, Craig ME, et al; International Society for Pediatric and Adolescent Diabetes. Diabetic ketoacidosis and hyperglycemic hyperosmolar state. Pediatr Diabetes. 2014;15(Suppl 20):154-179. doi:10.1111/pedi.12165.
17. Cohn BG, Keim SM, Watkins JW, Camargo CA. Does management of diabetic ketoacidosis with subcutaneous rapid-acting insulin reduce the need for intensive care unit admission? J Emerg Med. 2015;49(4):530-538. doi:10.1016/j.jemermed.2015.05.016.
18. Glaser N, Barnett P, McCaslin I, et al; Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. Risk factors for cerebral edema in children with diabetic ketoacidosis. The Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. N Engl J Med. 2001;344(4):264-269. doi:10.1056/NEJM200101253440404.
1. Nyenwe EA, Kitabchi AE. The evolution of diabetic ketoacidosis: an update of its etiology, pathogenesis and management. Metabolism. 2016;65(4):507-521. doi:10.1016/j.metabol.2015.12.007.
2. Fayfman M, Pasquel FJ, Umpierrez GE. Management of hyperglycemic crises: diabetic ketoacidosis and hyperglycemic hyperosmolar state. Med Clin North Am. 2017;101(3):587-606. doi:10.1016/j.mcna.2016.12.011.
3. Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009;32(7):1335-1343. doi:10.2337/dc09-9032.
4. Fugate JE, Rabinstein AA. Absolute and relative contraindications to IV rt-PA for acute ischemic stroke. Neurohospitalist. 2015;5(3):110-121. doi:10.1177/1941874415578532.
5. Kamalakannan D, Baskar V, Barton DM, Abdu TA. Diabetic ketoacidosis in pregnancy. Postgrad Med J. 2003;79(9):454-457.
6. Ma OJ, Rush MD, Godfrey MM, Gaddis G. Arterial blood gas results rarely influence emergency physician management of patients with suspected diabetic ketoacidosis. Acad Emerg Med. 2003;10(8):836-841.
7. Taylor S, Blau J, Rother K. SGLT2 Inhibitors may predispose to ketoacidosis. J Clin Endocrinol Metab. 2015;100(8):2849-2852. doi:10.1210/jc.2015-1884.
8. Kum-Nji JS, Gosmanov AR, Steinberg H, Dagogo-Jack S. Hyperglycemic, high anion-gap metabolic acidosis in patients receiving SGLT-2 inhibitors for diabetes management. J Diabetes Complications. 2017;31(3):611-614. doi:10.1016/j.jdiacomp.2016.11.004.
9. Adrogué HJ, Barrero J, Eknoyan G. Salutary effects of modest fluid replacement in the treatment of adults with diabetic ketoacidosis. Use in patients without extreme volume deficit. JAMA. 1989;262(15):2108-2013.
10. Semler MW, Self WH, Wanderer JP, et al; SMART Investigators and the Pragmatic Critical Care Research Group. Balanced crystalloid versus saline in critically ill adults. N Engl J Med. 2018;378(9):829-839. doi:10.1056/NEJMoa1711584.
11. Chua HR, Venkatesh B, Stachowski E, et al. Plasma-Lyte 148 vs 0.9% saline for fluid resuscitation in diabetic ketoacidosis. J Crit Care. 2012;27(2):138-145. doi:10.1016/j.jcrc.2012.01.007.
12. Mahler S, Conrad S, Wang H, Arnold T. Resuscitation with balanced electrolyte solution prevents hyperchloremic metabolic acidosis in patients with diabetic ketoacidosis. Am J Emerg Med. 2011;29(9):1194-1197. doi:10.1016/j.ajem.2010.07.015.
11. Van Zyl DG, Rheeder P, Delport E. Fluid management in diabetic-acidosis--Ringer’s lactate versus normal saline: a randomized controlled trial. QJM. 2012;105(4):337-343. doi:10.1093/qjmed/hcr226.
14. Penne EL, Thijssen S, Raimann JG, Levin NW, Kotanko P. Correction of serum sodium for glucose concentration in hemodialysis patients with poor glucose control. Diabetes Care. 2010;33(7):e91. doi:10.2337/dc10-0557.
15. Goyal N, Miller JB, Sankey SS, Mossallam U. Utility of initial bolus insulin in the treatment of diabetic ketoacidosis. J Emerg Med. 2010;38(4):422-427. doi:10.1016/j.jemermed.2007.11.033.
16. Wolfsdorf JI, Allgrove J, Craig ME, et al; International Society for Pediatric and Adolescent Diabetes. Diabetic ketoacidosis and hyperglycemic hyperosmolar state. Pediatr Diabetes. 2014;15(Suppl 20):154-179. doi:10.1111/pedi.12165.
17. Cohn BG, Keim SM, Watkins JW, Camargo CA. Does management of diabetic ketoacidosis with subcutaneous rapid-acting insulin reduce the need for intensive care unit admission? J Emerg Med. 2015;49(4):530-538. doi:10.1016/j.jemermed.2015.05.016.
18. Glaser N, Barnett P, McCaslin I, et al; Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. Risk factors for cerebral edema in children with diabetic ketoacidosis. The Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. N Engl J Med. 2001;344(4):264-269. doi:10.1056/NEJM200101253440404.
Metformin and Long-Acting Insulin Don’t Help Slow Diabetes in Young People
The only 2 medicines currently approved for young people with type 2 diabetes—long-acting insulin and metformin—do not slow the progression of diabetes in young people, according to a study funded in part by the National Institute of Diabetes and Digestive and Kidney Diseases.
A substudy of the Restoring Insulin Secretion (RISE) study, the RISE Pediatric Medication Study looked at the effects of insulin and metformin in 91 patients aged 10 to 19 years. The participants were randomly assigned to 1 of 2 treatment groups. The first received 3 months of glargine, a long-acting insulin, followed by 9 months of metformin. The second group received only metformin for 12 months. The participants were followed for 3 more months after treatment ended. The pediatric study found that beta-cell function declined in both groups during treatment and worsened after treatment ended.
Researchers also compared the pediatric participants with their adult counterparts in 2 other RISE trials and found the young people had more insulin resistance and other signs of disease progression at the same stage in the disease. Moreover, at baseline, the younger patients responded to the severe insulin resistance with a greater insulin response than did the adults, which the researchers say may be a reason for their more rapid loss of beta-cell function.
However, the study also found modest improvement in blood glucose with metformin in both groups. But metformin alone is not a long-term solution for many youth, said Dr. Kristen Nadeau, principal investigator for the pediatric study. Their findings underscore the “urgent and growing need,” she says, for more options.
The only 2 medicines currently approved for young people with type 2 diabetes—long-acting insulin and metformin—do not slow the progression of diabetes in young people, according to a study funded in part by the National Institute of Diabetes and Digestive and Kidney Diseases.
A substudy of the Restoring Insulin Secretion (RISE) study, the RISE Pediatric Medication Study looked at the effects of insulin and metformin in 91 patients aged 10 to 19 years. The participants were randomly assigned to 1 of 2 treatment groups. The first received 3 months of glargine, a long-acting insulin, followed by 9 months of metformin. The second group received only metformin for 12 months. The participants were followed for 3 more months after treatment ended. The pediatric study found that beta-cell function declined in both groups during treatment and worsened after treatment ended.
Researchers also compared the pediatric participants with their adult counterparts in 2 other RISE trials and found the young people had more insulin resistance and other signs of disease progression at the same stage in the disease. Moreover, at baseline, the younger patients responded to the severe insulin resistance with a greater insulin response than did the adults, which the researchers say may be a reason for their more rapid loss of beta-cell function.
However, the study also found modest improvement in blood glucose with metformin in both groups. But metformin alone is not a long-term solution for many youth, said Dr. Kristen Nadeau, principal investigator for the pediatric study. Their findings underscore the “urgent and growing need,” she says, for more options.
The only 2 medicines currently approved for young people with type 2 diabetes—long-acting insulin and metformin—do not slow the progression of diabetes in young people, according to a study funded in part by the National Institute of Diabetes and Digestive and Kidney Diseases.
A substudy of the Restoring Insulin Secretion (RISE) study, the RISE Pediatric Medication Study looked at the effects of insulin and metformin in 91 patients aged 10 to 19 years. The participants were randomly assigned to 1 of 2 treatment groups. The first received 3 months of glargine, a long-acting insulin, followed by 9 months of metformin. The second group received only metformin for 12 months. The participants were followed for 3 more months after treatment ended. The pediatric study found that beta-cell function declined in both groups during treatment and worsened after treatment ended.
Researchers also compared the pediatric participants with their adult counterparts in 2 other RISE trials and found the young people had more insulin resistance and other signs of disease progression at the same stage in the disease. Moreover, at baseline, the younger patients responded to the severe insulin resistance with a greater insulin response than did the adults, which the researchers say may be a reason for their more rapid loss of beta-cell function.
However, the study also found modest improvement in blood glucose with metformin in both groups. But metformin alone is not a long-term solution for many youth, said Dr. Kristen Nadeau, principal investigator for the pediatric study. Their findings underscore the “urgent and growing need,” she says, for more options.
Diabetes and pregnancy: Risks and opportunities
A 29-year-old nulliparous woman presents for a routine checkup. She has hypertension and type 2 diabetes mellitus. Her current medications are chlorpropamide 500 mg daily, metformin 500 mg twice a day, lisinopril 40 mg daily, simvastatin 40 mg daily, and aspirin 81 mg daily. Her body mass index is 37 kg/m2 and her blood pressure is 130/80 mm Hg. Her hemoglobin A1c level is 7.8% and her low-density lipoprotein cholesterol 90 mg/dL.
She is considering pregnancy. How would you counsel her?
DEFINING DIABETES IN PREGNANCY
Diabetes in pregnant women, both gestational and pregestational, is the most common medical complication associated with pregnancy.1
- Gestational diabetes is defined as diabetes that is diagnosed during the second or third trimester of pregnancy and that is not clearly pregestational.2
- Pregestational diabetes exists before pregnancy and can be either type 1 or type 2.
Most cases of diabetes diagnosed during the first trimester reflect pregestational diabetes, as gestational diabetes occurs when insulin resistance increases in the later trimesters.
Type 1 diabetes involves autoimmune destruction of pancreatic islet cells, leading to insulin deficiency and the need for insulin therapy. Type 2 diabetes is characterized by insulin resistance rather than overall insulin deficiency. Type 2 diabetes tends to be associated with comorbidities such as obesity and hypertension, which are independent risk factors for adverse perinatal outcomes.3,4
Gestational diabetes accounts for most cases of diabetes during pregnancy. Although both pregestational and gestational diabetes increase the risk of maternal and fetal complications, pregestational diabetes is associated with significantly greater risks.1
IMPACT OF DIABETES ON THE MOTHER
Pregnancy increases the risk of maternal hypoglycemia, especially during the first trimester in patients with type 1 diabetes, as insulin sensitivity increases in early pregnancy.1 Pregnant women with diabetes may also have an altered counterregulatory response and less hypoglycemic awareness.1 Insulin resistance rises during the second and early third trimesters, increasing the risk of hyperglycemia in women with diabetes.1
Glycemic control during pregnancy is usually easier to achieve in patients with type 2 diabetes than with type 1, but it may require much higher insulin doses.
Because pregnancy is inherently a ketogenic state, women with type 1 diabetes are at higher risk of diabetic ketoacidosis, particularly during the second and third trimesters.1 There are reports of euglycemic diabetic ketoacidosis in pregnant women with either gestational or pregestational diabetes.5
Diabetes is associated with a risk of preeclampsia 4 times higher than in nondiabetic women.6 Other potential pregnancy-related complications include infections, polyhydramnios, spontaneous abortion, and cesarean delivery.1,7 The risk of pregnancy loss is similar in women with either type 1 or type 2 diabetes (2.6% and 3.7%, respectively), but the causes are different.8 Although preexisting diabetic complications such as retinopathy, nephropathy, and gastroparesis can be exacerbated during pregnancy,1 only severe gastroparesis and advanced renal disease are considered relative contraindications to pregnancy.
IMPACT OF DIABETES ON THE FETUS
Fetal complications of maternal diabetes include embryopathy (fetal malformations) and fetopathy (overgrowth, ie, fetus large for gestational age, and increased risk of fetal death or distress). Maternal hyperglycemia is associated with diabetic embryopathy, resulting in major birth defects in 5% to 25% of pregnancies and spontaneous abortions in 15% to 20%.9,10 There is a 2- to 6-fold increase in risk of congenital malformations.6
The most common diabetes-associated congenital malformations affect the cardiovascular system. Congenital heart disease includes tetralogy of Fallot, transposition of the great vessels, septal defects, and anomalous pulmonary venous return. Other relatively common defects involve the fetal central nervous system, spine, orofacial system, kidneys, urogenital system, gastrointestinal tract, and skeleton.11
The risk of fetopathy is proportional to the degree of maternal hyperglycemia. Excess maternal glucose and fatty acid levels can lead to fetal hyperglycemia and overgrowth, which increases fetal oxygen requirements. Erythropoietin levels rise, causing an increase in red cell mass, with subsequent hyperviscosity within the placenta and higher risk of fetal death.
Other complications include intrauterine growth restriction, prematurity, and preterm delivery. Fetal macrosomia (birth weight > 90th percentile or 4 kg, approximately 8 lb, 13 oz) occurs in 27% to 62% of children born to mothers with diabetes, a rate 10 times higher than in patients without diabetes. It contributes to shoulder dystocia (risk 2 to 4 times higher in diabetic pregnancies) and cesarean delivery.6 Infants born to mothers with diabetes also have higher risks of neonatal hypoglycemia, erythrocytosis, hyperbilirubinemia, hypocalcemia, respiratory distress, cardiomyopathy, and death, as well as for developing diabetes, obesity, and other adverse cardiometabolic outcomes later in life.11
GET GLUCOSE UNDER CONTROL BEFORE PREGNANCY
Nearly half of pregnancies in the general population are unplanned,15 so preconception diabetes assessment needs to be part of routine medical care for all reproductive-age women. Because most organogenesis occurs during the first 5 to 8 weeks after fertilization—potentially before a woman realizes she is pregnant—achieving optimal glycemic control before conception is necessary to improve pregnancy outcomes.1
EVERY VISIT IS AN OPPORTUNITY
Every medical visit with a reproductive-age woman with diabetes is an opportunity for counseling about pregnancy. Topics that need to be discussed include the risks of unplanned pregnancy and of poor metabolic control, and the benefits of improved maternal and fetal outcomes with appropriate pregnancy planning and diabetes management.
Referral to a registered dietitian for individualized counseling about proper nutrition, particularly during pregnancy, has been associated with positive outcomes.16 Patients with diabetes and at high risk of pregnancy complications should be referred to a clinic that specializes in high-risk pregnancies.
Practitioners also should emphasize the importance of regular exercise and encourage patients to maintain or achieve a medically optimal weight before conception. Ideally, this would be a normal body mass index; however, this is not always possible.
In women who are planning pregnancy or are not on effective contraception, medications should be reviewed for potential teratogenicity. If needed, discuss alternative medications or switch to safer ones. However, these changes should not interrupt diabetes treatment.
In addition, ensure that the patient is up to date on age- and disease-appropriate preventive care (eg, immunizations, screening for sexually transmitted disease and malignancy). Counseling and intervention for use of tobacco, alcohol, and recreational drugs are also important. As with any preconception counseling, the patient (and her partner, if possible) should be advised to avoid travel to areas where Zika virus is endemic, and informed about the availability of expanded carrier genetic screening through her obstetric provider.
Finally, pregnant women with diabetes benefit from screening for diabetic complications including hypertension, retinopathy, cardiovascular disease, neuropathy, and nephropathy.
ASSESSING RISKS
Blood pressure
Chronic (preexisting) hypertension is defined as a systolic pressure 140 mm Hg or higher or a diastolic pressure 90 mm Hg or higher, or both, that antedates pregnancy or is present before the 20th week of pregnancy.3 Chronic hypertension has been reported in up to 5% of pregnant women and is associated with increased risk of preterm delivery, superimposed preeclampsia, low birth weight, and perinatal death.3
Reproductive-age women with diabetes and high blood pressure benefit from lifestyle and behavioral modifications.17 If drug therapy is needed, antihypertensive drugs that are safe for the fetus should be used. Treatment of mild or moderate hypertension during pregnancy reduces the risk of progression to severe hypertension but may not improve obstetric outcomes.
Diabetic retinopathy
Diabetic retinopathy can significantly worsen during pregnancy: the risk of progression is double that in the nonpregnant state.18 Women with diabetes who are contemplating pregnancy should have a comprehensive eye examination before conception, and any active proliferative retinopathy needs to be treated. These patients may require ophthalmologic monitoring and treatment during pregnancy. (Note: laser photocoagulation is not contraindicated during pregnancy.)
Cardiovascular disease
Cardiovascular physiology changes dramatically during pregnancy. Cardiovascular disease, especially when superimposed on diabetes, can increase the risk of maternal death. Thus, evaluation for cardiovascular risk factors as well as cardiovascular system integrity before conception is important. Listen for arterial bruits and murmurs, and assess peripheral pulses. Consideration should be given to obtaining a preconception resting electrocardiogram in women with diabetes who are over age 35 or who are suspected of having cardiovascular disease.16
Neurologic disorders
Peripheral neuropathy, the most common neurologic complication of diabetes, is associated with injury and infection.19
Autonomic neuropathy is associated with decreased cardiac responsiveness and orthostatic hypotension.19 Diabetic gastroparesis alone can precipitate serious complications during pregnancy, including extreme hypoglycemia and hyperglycemia, increased risk of diabetic ketoacidosis, weight loss, malnutrition, frequent hospitalizations, and increased requirement for parenteral nutrition.20
Although diabetic neuropathy does not significantly worsen during pregnancy, women with preexisting gastroparesis should be counseled on the substantial risks associated with pregnancy. Screening for neuropathy should be part of all diabetic preconception examinations.
Renal complications
Pregnancy in women with diabetes and preexisting renal dysfunction increases their risk of accelerated progression of diabetic kidney disease.21 Preexisting renal dysfunction also increases the risk of pregnancy-related complications, such as stillbirth, intrauterine growth restriction, gestational hypertension, preeclampsia, and preterm delivery.19,21,22 Further, the risk of pregnancy complications correlates directly with the severity of renal dysfunction.22
Psychiatric disorders
Emotional wellness is essential for optimal diabetes management. It is important to recognize the emotional impact of diabetes in pregnant women and to conduct routine screening for depression, anxiety, stress, and eating disorders.16
LABORATORY TESTS TO CONSIDER
Hemoglobin A1c. The general consensus is to achieve the lowest hemoglobin A1c level possible that does not increase the risk of hypoglycemia. The American Diabetes Association (ADA) recommends that, before attempting to conceive, women should lower their hemoglobin A1c to below 6.5%.1
Thyroid measures. Autoimmune thyroid disease is the most common autoimmune disorder associated with diabetes and has been reported in 35% to 40% of women with type 1 diabetes.23 Recommendations are to check thyroid-stimulating hormone and thyroid peroxidase antibody levels before conception or early in pregnancy in all women with diabetes.1,24 Overt hypothyroidism should be treated before conception, given that early fetal brain development depends on maternal thyroxine.
Renal function testing. Preconception assessment of renal function is important for counseling and risk stratification. This assessment should include serum creatinine level, estimated glomerular filtration rate, and urinary albumin excretion.21
Celiac screening. Because women with type 1 diabetes are more susceptible to autoimmune diseases, they should be screened for celiac disease before conception, with testing for immunoglobulin A (IgA) and tissue transglutaminase antibodies, with or without IgA endomysial antibodies.16,25,26 An estimated 6% of patients with type 1 diabetes have celiac disease vs 1% of the general population.25 Celiac disease is 2 to 3 times more common in women, and asymptomatic people with type 1 diabetes are considered at increased risk for celiac disease.26
The association between type 1 diabetes and celiac disease most likely relates to the overlap in human leukocyte antigens of the diseases. There is no established link between type 2 diabetes and celiac disease.25
Undiagnosed celiac disease increases a woman’s risk of obstetric complications such as preterm birth, low birth weight, and stillbirth.26 The most likely explanation for these adverse effects is nutrient malabsorption, which is characteristic of celiac disease. Adherence to a gluten-free diet before and during gestation may reduce the risk of preterm delivery by as much as 20%.26
Vitamin B12 level. Celiac disease interferes with the absorption of vitamin B12-instrinsic factor in the ileum, which can lead to vitamin B12 deficiency. Therefore, baseline vitamin B12 levels should be checked before conception in women with celiac disease. Levels should also be checked in women taking metformin, which also decreases vitamin B12 absorption. Of note, increased folate levels due to taking supplements can potentially mask vitamin B12 deficiency.
MEDICATIONS TO REVIEW FOR PREGNANCY INTERACTIONS
Diabetic medications
Insulin is the first-line pharmacotherapy for pregnant patients with type 1, type 2, or gestational diabetes. Insulin does not cross the placenta to a measurable extent, and most insulin preparations have been classified as category B,1 meaning no risks to the fetus have been found in humans.
Insulin dosing during pregnancy is not static. Beginning around mid-gestation, insulin requirements increase,28,29 but after 32 weeks the need may decrease. These changes require practitioners to closely monitor blood glucose throughout pregnancy.
Both basal-bolus injections and continuous subcutaneous infusion are reasonable options during pregnancy.30 However, the need for multiple and potentially painful insulin injections daily can lead to poor compliance. This inconvenience has led to studies using oral hypoglycemic medications instead of insulin for patients with gestational and type 2 diabetes.
Metformin is an oral biguanide that decreases hepatic gluconeogenesis and intestinal glucose absorption while peripherally increasing glucose utilization and uptake. Metformin does not pose a risk of hypoglycemia because its mechanism of action does not involve increased insulin production.7
Metformin does cross the placenta, resulting in umbilical cord blood levels higher than maternal levels. Nevertheless, studies support the efficacy and short-term safety of metformin use during a pregnancy complicated by gestational or type 2 diabetes.7,31 Moreover, metformin has been associated with a lower risk of neonatal hypoglycemia and maternal weight gain than insulin.32 However, this agent should be used with caution, as long-term data are not yet available, and it may slightly increase the risk of premature delivery.
Glyburide is another oral hypoglycemic medication that has been used during pregnancy. This second-generation sulfonylurea enhances the release of insulin from the pancreas by binding beta islet cell ATP-calcium channel receptors. Compared with other sulfonylureas, glyburide has the lowest rate of maternal-to-fetal transfer, with umbilical cord plasma concentrations 70% of maternal levels.33 Although some trials support the efficacy and short-term safety of glyburide treatment for gestational diabetes,34 recent studies have associated glyburide use during pregnancy with a higher rate of neonatal hypoglycemia, neonatal respiratory distress, macrosomia, and neonatal intensive care unit admissions than insulin and metformin.1,35
Patients treated with oral agents should be informed that these drugs cross the placenta, and that although no adverse effects on the fetus have been demonstrated, long-term safety data are lacking. In addition, oral agents are ineffective in type 1 diabetes and may be insufficient to overcome the insulin resistance in type 2 diabetes.
Antihypertensive drugs
All antihypertensive drugs cross the placenta, but several have an acceptable safety profile in pregnancy, including methyldopa, labetalol, clonidine, prazosin, and nifedipine. Hydralazine and labetalol are short-acting, come in intravenous formulations, and can be used for urgent blood pressure control during pregnancy. Diltiazem may be used for heart rate control during pregnancy, and it has been shown to lower blood pressure and proteinuria in pregnant patients with underlying renal disease.36,37 The ADA recommends against chronic use of diuretics during pregnancy because of potential reductions in maternal plasma volume and uteroplacental perfusion.1
Angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), and direct renin inhibitors are contraindicated during pregnancy because of the risk of fetal defects, particularly in the renal system.21,38 Although there is evidence to question the association between first semester exposure and fetotoxicity,39 we avoid these drugs during pregnancy and switch to a different agent in women planning pregnancy.
Other drugs
Statins are contraindicated in pregnancy because they interfere with the development of the fetal nervous system.21 Although preliminary data from a small study did not identify safety risks associated with pravastatin use after 12 weeks of gestation,40 we recommend discontinuing statins in women attempting pregnancy.
Aspirin. The US Preventive Services Task Force41 recommends low-dose aspirin (81 mg/day) after 12 weeks of gestation for women with type 1 or type 2 diabetes, as well as those with renal disease or chronic hypertension, to prevent preeclampsia. Of note, higher doses need to be used with caution during pregnancy because fetal abnormalities have been reported, such as disruption of fetal vasculature (mesenteric vessels), gastroschisis, and small intestinal atresia.16
Folate supplementation (0.6–4 mg/day) is recommended in women with celiac disease to prevent neural tube defects in the offspring, and the US Preventive Services Task Force recommends 0.4 mg daily of folic acid supplementation for all women planning or capable of pregnancy.42–44 Higher doses, ranging from 0.6 to 5 mg/day, have been proposed for patients with diabetes,13 and we recommend at least 1 mg for this group, based on data suggesting that higher doses further reduce the risk of neural tube defects.43
IS BREASTFEEDING AFFECTED?
Maternal diabetes, insulin therapy, and oral hypoglycemic agents are not contraindications to breastfeeding. The US Preventive Services Task Force recommends interventions by primary care physicians to promote and support breastfeeding.45 Breastfeeding is encouraged based on various short- and long-term health benefits for both breastfed infants and breastfeeding mothers. Breastfeeding decreases a woman’s insulin requirements and increases the risk for hypoglycemia, especially in patients with insulin-dependent type 1 diabetes.1
Additionally, insulin sensitivity increases immediately following delivery of the placenta.1 Therefore, it is prudent to adjust insulin doses postpartum, especially while a patient is breastfeeding, or to suggest high-carbohydrate snacks before feeds.9,29
Antihypertensive drugs considered safe to use during lactation include captopril, enalapril, quinapril, labetalol, propranolol, nifedipine, and hydralazine.21,46 Methyldopa is not contraindicated, but it causes fatigue and worsened postpartum depression and should not be used as first-line therapy. Diuretics and ARBs are not recommended during lactation.21 Both metformin and glyburide enter breast milk in small enough amounts that they are not contraindicated during breastfeeding.16 The Lactmed database (www.toxnet.nlm.nih.gov) provides information about drugs and breastfeeding.
WHAT ABOUT CONTRACEPTIVES?
The ADA recommends contraception for women with diabetes because, just as in women without diabetes, the risks of unplanned pregnancy outweigh those of contraceptives.1
We recommend low-dose combination estrogen-progestin oral contraceptives to normotensive women under age 35 with diabetes but without underlying microvascular disease. For women over age 35 or for those with microvascular disease, additional options include intrauterine devices or progestin implants. We prefer not to use injectable depot medroxyprogesterone acetate because of its side effects of insulin resistance and weight gain.47
CASE DISCUSSION: NEXT STEPS
Our patient’s interest in family planning presents an opportunity for preconception counseling. We recommend a prenatal folic acid supplement, diet and regular exercise for weight loss, and screening tests including a comprehensive metabolic panel, hemoglobin A1c, thyroid-stimulating hormone, and dilated eye examination. We make sure she is up to date on her indicated health maintenance (eg, immunizations, disease screening), and we review her medications for potential teratogens. She denies any recreational drug use. Also, she has no plans for long-distance travel.
Our counseling includes discussions of pregnancy risks associated with pregestational diabetes and suboptimal glycemic control. We encourage her to use effective contraception until she is “medically optimized” for pregnancy—ie, until her hemoglobin A1c is lower than 6.5% and she has achieved a medically optimal weight. If feasible, a reduction of weight (7% or so) through lifestyle modification should be attempted, and if her hemoglobin A1c remains elevated, adding insulin would be recommended.
Pregnant patients or patients contemplating pregnancy are usually motivated to modify their behavior, making this a good time to reinforce lifestyle modifications. Many patients benefit from individualized counseling by a registered dietitian to help achieve the recommended weight and glycemic control.
Our physical examination in this patient includes screening for micro- and macrovascular complications of diabetes, and the test results are negative. Patients with active proliferative retinopathy should be referred to an ophthalmologist for assessment and treatment.
We review her medications for potential teratogenic effects and stop her ACE inhibitor (lisinopril) and statin (simvastatin). We switch her from a first-generation sulfonylurea (chlorpropamide) to glyburide, a second-generation sulfonylurea. Second-generation sulfonylureas are considered more “fetus-friendly” because first-generation sulfonylureas cross the placenta more easily and can cause fetal hyperinsulinemia, leading to macrosomia and neonatal hypoglycemia.7
The management of diabetes during pregnancy leans toward insulin use, given the lack of information regarding long-term outcomes with oral agents. If insulin is needed, it is best to initiate it before the patient conceives, and then to stop other diabetes medications. We would not make any changes to her aspirin or metformin use.
Educating the patient and her family about prevention, recognition, and treatment of hypoglycemia is important to prevent and manage the increased risk of hypoglycemia with insulin therapy and in early pregnancy.1 Consideration should be given to providing ketone strips as well as education on diabetic ketoacidosis prevention and detection.1 If the patient conceives, begin prenatal care early to allow adequate planning for care of her disease and evaluation of the fetus. Because of the complexity of insulin management in pregnancy, the ADA recommends referral, if possible, to a center offering team-based care, including an obstetrician specialized in high-risk pregnancies, an endocrinologist, and a dietitian.1
- American Diabetes Association. 13. Management of diabetes in pregnancy: standards of medical care in diabetes—2018. Diabetes Care 2018; 41(suppl 1):S137–S143. doi:10.2337/dc18-S013
- American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2018. Diabetes Care 2018; 41(suppl 1):S13–S27. doi:10.2337/dc18-S002
- Lawler J, Osman M, Shelton JA, Yeh J. Population-based analysis of hypertensive disorders in pregnancy. Hypertens Pregnancy 2007; 26(1):67–76. doi:10.1080/10641950601147945
- Marchi J, Berg M, Dencker A, Olander EK, Begley C. Risks associated with obesity in pregnancy, for the mother and baby: a systematic review of reviews. Obes Rev 2015; 16(8):621–638. doi:10.1111/obr.12288
- Garrison EA, Jagasia S. Inpatient management of women with gestational and pregestational diabetes in pregnancy. Curr Diab Rep 2014; 14(2):457. doi:10.1007/s11892-013-0457-x
- Ballas J, Moore TR, Ramos GA. Management of diabetes in pregnancy. Curr Diab Rep 2012; 12(1):33–42. doi:10.1007/s11892-011-0249-0
- Ryu RJ, Hays KE, Hebert MF. Gestational diabetes mellitus management with oral hypoglycemic agents. Semin Perinatol 2014; 38(8):508–515. doi:10.1053/j.semperi.2014.08.012
- Cundy T, Gamble G, Neale L, et al. Differing causes of pregnancy loss in type 1 and type 2 diabetes. Diabetes Care 2007; 30(10):2603–2607. doi:10.2337/dc07-0555
- Castorino K, Jovanovic L. Pregnancy and diabetes management: advances and controversies. Clin Chem 2011; 57(2):221–230. doi:10.1373/clinchem.2010.155382
- Hammouda SA, Hakeem R. Role of HbA1c in predicting risk for congenital malformations. Prim Care Diabetes 2015; 9(6):458–464. doi:10.1016/j.pcd.2015.01.004
- Chen CP. Congenital malformations associated with maternal diabetes. Taiwanese J Obstet Gynecol 2005; 44(1):1–7. doi:10.1016/S1028-4559(09)60099-1
- International Association of Diabetes and Pregnancy Study Groups Consensus Panel, Metzger BE, Gabbe SG, Persson B, et al. International Association of Diabetes and Pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 2010; 33(3):676–682. doi:10.2337/dc09-1848
- Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care 2013; 36(5):1384–1395. doi:10.2337/dc12-2480
- HAPO Study Cooperative Research Group; Metzger BE, Lowe LP, Dyer AR, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 2008; 358(19):1991–2002. doi:10.1056/NEJMoa0707943
- Finer LB, Zolna MR. Shifts in intended and unintended pregnancies in the United States, 2001–2008. Am J Public Health 2014; 104(suppl 1):S43–S48. doi:10.2105/AJPH.2013.301416
- Kitzmiller JL, Block JM, Brown FM, et al. Managing preexisting diabetes for pregnancy: summary of evidence and consensus recommendations for care. Diabetes Care 2008; 31(5):1060–1079. doi:10.2337/dc08-9020
- Webster LM, Conti-Ramsden F, Seed PT, Webb AJ, Nelson-Piercy C, Chappell LC. Impact of antihypertensive treatment on maternal and perinatal outcomes in pregnancy complicated by chronic hypertension: a systematic review and meta-analysis. J Am Heart Assoc 2017; 6(5).pii:e005526. doi:10.1161/JAHA.117.005526
- Chew EY, Mills JL, Metzger BE, et al. Metabolic control and progression of retinopathy: the Diabetes in Early Pregnancy Study. Diabetes Care 1995; 18(5):631–637. pmid:8586000
- American Diabetes Association. Standards of medical care in diabetes—2016. Diabetes Care 2016; 39 (suppl 1):S1–S109.
- Hawthorne, G. Maternal complications in diabetic pregnancy. Best Pract Res Clin Obstet Gynaecol 2011; 25(1):77–90. doi:10.1016/j.bpobgyn.2010.10.015
- Ringholm L, Damm JA, Vestgaard M, Damm P, Mathiesen ER. Diabetic nephropathy in women with preexisting diabetes: from pregnancy planning to breastfeeding. Curr Diab Rep 2016; 16(2):12. doi:10.1007/s11892-015-0705-3
- Zhang JJ, Ma XX, Hao L, Liu LJ, Lv JC, Zhang H. A systematic review and meta-analysis of outcomes of pregnancy in CKD and CKD outcomes in pregnancy. Clin J Am Soc Nephrol 2015; 10(11):1964–1978. doi:10.2215/CJN.09250914
- Umpierrez GE, Latif KA, Murphy MB, et al. Thyroid dysfunction in patients with type 1 diabetes: a longitudinal study. Diabetes Care 2003; 26(4):1181–1185. pmid:12663594
- Alexander EK, Pearce EN, Brent GA, et al. 2017 Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and the Postpartum. Thyroid 2017; 27(3):315–389. doi:10.1089/thy.2016.0457
- Akirov A, Pinhas-Hamiel O. Co-occurrence of type 1 diabetes mellitus and celiac disease. World J Diabetes 2015; 6(5):707–714. doi:10.4239/wjd.v6.i5.707
- Saccone G, Berghella V, Sarno L, et al. Celiac disease and obstetric complications: a systematic review and metaanalysis. Am J Obstet Gynecol 2016; 214(2):225–234. doi:10.1016/j.ajog.2015.09.080
- Feghali M, Venkataramanan R, Caritis S. Pharmacokinetics of drugs in pregnancy. Semin Perinatol 2015; 39(7):512–519. doi:10.1053/j.semperi.2015.08.003
- de Valk HW, Visser GH. Insulin during pregnancy, labour and delivery. Best Pract Res Clin Obstet Gynaecol 2011; 25(1):65–76. doi:10.1016/j.bpobgyn.2010.10.002
- Morello CM. Pharmacokinetics and pharmacodynamics of insulin analogs in special populations with type 2 diabetes mellitus. Int J Gen Med 2011; 4:827–835. doi:10.2147/IJGM.S26889
- Farrar D, Tuffnell DJ, West J, West HM. Continuous subcutaneous insulin infusion versus multiple daily injections of insulin for pregnant women with diabetes. Cochrane Database Syst Rev 2016; (6):CD005542. doi:10.1002/14651858.CD005542.pub2
- Charles B, Norris R, Xiao X, Hague W. Population pharmacokinetics of metformin in late pregnancy. Ther Drug Monit 2006; 28(1):67–72. pmid:16418696
- Balsells M, García-Patterson A, Solà I, Roqué M, Gich I, Corcoy R. Glibenclamide, metformin, and insulin for the treatment of gestational diabetes: a systematic review and meta-analysis. BMJ 2015; 350:h102. doi:10.1136/bmj.h102
- Hebert MF, Ma X, Naraharisetti SB, et al; Obstetric-Fetal Pharmacology Research Unit Network. Are we optimizing gestational diabetes treatment with glyburide? The pharmacologic basis for better clinical practice. Clin Pharmacol Ther 2009; 85(6):607–614. doi:10.1038/clpt.2009.5
- Langer O, Conway DL, Berkus MD, Xenakis EM, Gonzales O. A comparison of glyburide and insulin in women with gestational diabetes mellitus. N Engl J Med 2000; 343(16):1134–1138. doi:10.1056/NEJM200010193431601
- Camelo Castillo W, Boggess K, Stürmer T, Brookhart MA, Benjamin DK Jr, Jonsson Funk M. Association of adverse pregnancy outcomes with glyburide vs insulin in women with gestational diabetes. JAMA Pediatr 2015; 169:452–458. doi:10.1001/jamapediatrics.2015.74
- Gowda RM, Khan IA, Mehta NJ, Vasavada BC, Sacchi TJ. Cardiac arrhythmias in pregnancy: clinical and therapeutic considerations. Int J Cardiol 2003; 88(2):129–133. pmid:12714190
- Khandelwal M, Kumanova M, Gaughan JP, Reece EA. Role of diltiazem in pregnant women with chronic renal disease. J Matern Fetal Neonatal Med 2002; 12(6):408–412. doi:10.1080/jmf.12.6.408.412
- Magee LA, Abalos E, von Dadelszen P, Sibai B, Easterling T, Walkinshaw S; CHIPS Study Group. How to manage hypertension in pregnancy effectively. Br J Clin Pharmacol 2011; 72(3):394–401. doi:10.1111/j.1365-2125.2011.04002.x
- Cooper WO, Hernandez-Diaz S, Arbogast PG, et al. Major congenital malformations after first-trimester exposure to ACE inhibitors. N Engl J Med 2006; 354(23):2443–2451. doi:10.1056/NEJMoa055202
- Costantine MM, Cleary K, Hebert MF, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Obstetric-Fetal Pharmacology Research Units Network. Safety and pharmacokinetics of pravastatin used for the prevention of preeclampsia in high-risk pregnant women: a pilot randomized controlled trial. Am J Obstet Gynecol 2016; 214(6):720.e1–720.e17. doi:10.1016/j.ajog.2015.12.038
- LeFevre ML; US Preventive Services Task Force. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: US Preventive Services Task Force recommendation statement. Ann Intern Med 2014; 161(11):819–826. doi:10.7326/M14-1884
- Curry SJ, Grossman DC, Whitlock EP, Cantu A. Behavioral counseling research and evidence-based practice recommendations: US Preventive Services Task Force perspectives. Ann Intern Med 2014; 160(6):407–413. doi:10.7326/M13-2128
- Wald N, Law M, Morris J, Wald D. Quantifying the effect of folic acid. Lancet 2001; 358(9298):2069–2073. pmid:11755633
- US Preventive Services Task Force; Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Folic acid supplementation for the prevention of neural tube defects: US Preventive Services Task Force recommendation statement. JAMA 2017; 317(2):183–189. doi:10.1001/jama.2016.19438
- US Preventive Services Task Force; Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Primary care interventions to support breastfeeding: US Preventive Services Task Force recommendation statement. JAMA 2016; 316(16):1688–1693. doi:10.1001/jama.2016.14697
- Newton ER, Hale TW. Drugs in breast milk. Clin Obstet Gynecol 2015; 58(4):868–884. doi:10.1097/GRF.0000000000000142
- Xiang AH, Kawakubo M, Kjos SL, Buchanan TA. Long-acting injectable progestin contraception and risk of type 2 diabetes in Latino women with prior gestational diabetes mellitus. Diabetes Care 2006; 29(3):613–617. pmid:16505515
A 29-year-old nulliparous woman presents for a routine checkup. She has hypertension and type 2 diabetes mellitus. Her current medications are chlorpropamide 500 mg daily, metformin 500 mg twice a day, lisinopril 40 mg daily, simvastatin 40 mg daily, and aspirin 81 mg daily. Her body mass index is 37 kg/m2 and her blood pressure is 130/80 mm Hg. Her hemoglobin A1c level is 7.8% and her low-density lipoprotein cholesterol 90 mg/dL.
She is considering pregnancy. How would you counsel her?
DEFINING DIABETES IN PREGNANCY
Diabetes in pregnant women, both gestational and pregestational, is the most common medical complication associated with pregnancy.1
- Gestational diabetes is defined as diabetes that is diagnosed during the second or third trimester of pregnancy and that is not clearly pregestational.2
- Pregestational diabetes exists before pregnancy and can be either type 1 or type 2.
Most cases of diabetes diagnosed during the first trimester reflect pregestational diabetes, as gestational diabetes occurs when insulin resistance increases in the later trimesters.
Type 1 diabetes involves autoimmune destruction of pancreatic islet cells, leading to insulin deficiency and the need for insulin therapy. Type 2 diabetes is characterized by insulin resistance rather than overall insulin deficiency. Type 2 diabetes tends to be associated with comorbidities such as obesity and hypertension, which are independent risk factors for adverse perinatal outcomes.3,4
Gestational diabetes accounts for most cases of diabetes during pregnancy. Although both pregestational and gestational diabetes increase the risk of maternal and fetal complications, pregestational diabetes is associated with significantly greater risks.1
IMPACT OF DIABETES ON THE MOTHER
Pregnancy increases the risk of maternal hypoglycemia, especially during the first trimester in patients with type 1 diabetes, as insulin sensitivity increases in early pregnancy.1 Pregnant women with diabetes may also have an altered counterregulatory response and less hypoglycemic awareness.1 Insulin resistance rises during the second and early third trimesters, increasing the risk of hyperglycemia in women with diabetes.1
Glycemic control during pregnancy is usually easier to achieve in patients with type 2 diabetes than with type 1, but it may require much higher insulin doses.
Because pregnancy is inherently a ketogenic state, women with type 1 diabetes are at higher risk of diabetic ketoacidosis, particularly during the second and third trimesters.1 There are reports of euglycemic diabetic ketoacidosis in pregnant women with either gestational or pregestational diabetes.5
Diabetes is associated with a risk of preeclampsia 4 times higher than in nondiabetic women.6 Other potential pregnancy-related complications include infections, polyhydramnios, spontaneous abortion, and cesarean delivery.1,7 The risk of pregnancy loss is similar in women with either type 1 or type 2 diabetes (2.6% and 3.7%, respectively), but the causes are different.8 Although preexisting diabetic complications such as retinopathy, nephropathy, and gastroparesis can be exacerbated during pregnancy,1 only severe gastroparesis and advanced renal disease are considered relative contraindications to pregnancy.
IMPACT OF DIABETES ON THE FETUS
Fetal complications of maternal diabetes include embryopathy (fetal malformations) and fetopathy (overgrowth, ie, fetus large for gestational age, and increased risk of fetal death or distress). Maternal hyperglycemia is associated with diabetic embryopathy, resulting in major birth defects in 5% to 25% of pregnancies and spontaneous abortions in 15% to 20%.9,10 There is a 2- to 6-fold increase in risk of congenital malformations.6
The most common diabetes-associated congenital malformations affect the cardiovascular system. Congenital heart disease includes tetralogy of Fallot, transposition of the great vessels, septal defects, and anomalous pulmonary venous return. Other relatively common defects involve the fetal central nervous system, spine, orofacial system, kidneys, urogenital system, gastrointestinal tract, and skeleton.11
The risk of fetopathy is proportional to the degree of maternal hyperglycemia. Excess maternal glucose and fatty acid levels can lead to fetal hyperglycemia and overgrowth, which increases fetal oxygen requirements. Erythropoietin levels rise, causing an increase in red cell mass, with subsequent hyperviscosity within the placenta and higher risk of fetal death.
Other complications include intrauterine growth restriction, prematurity, and preterm delivery. Fetal macrosomia (birth weight > 90th percentile or 4 kg, approximately 8 lb, 13 oz) occurs in 27% to 62% of children born to mothers with diabetes, a rate 10 times higher than in patients without diabetes. It contributes to shoulder dystocia (risk 2 to 4 times higher in diabetic pregnancies) and cesarean delivery.6 Infants born to mothers with diabetes also have higher risks of neonatal hypoglycemia, erythrocytosis, hyperbilirubinemia, hypocalcemia, respiratory distress, cardiomyopathy, and death, as well as for developing diabetes, obesity, and other adverse cardiometabolic outcomes later in life.11
GET GLUCOSE UNDER CONTROL BEFORE PREGNANCY
Nearly half of pregnancies in the general population are unplanned,15 so preconception diabetes assessment needs to be part of routine medical care for all reproductive-age women. Because most organogenesis occurs during the first 5 to 8 weeks after fertilization—potentially before a woman realizes she is pregnant—achieving optimal glycemic control before conception is necessary to improve pregnancy outcomes.1
EVERY VISIT IS AN OPPORTUNITY
Every medical visit with a reproductive-age woman with diabetes is an opportunity for counseling about pregnancy. Topics that need to be discussed include the risks of unplanned pregnancy and of poor metabolic control, and the benefits of improved maternal and fetal outcomes with appropriate pregnancy planning and diabetes management.
Referral to a registered dietitian for individualized counseling about proper nutrition, particularly during pregnancy, has been associated with positive outcomes.16 Patients with diabetes and at high risk of pregnancy complications should be referred to a clinic that specializes in high-risk pregnancies.
Practitioners also should emphasize the importance of regular exercise and encourage patients to maintain or achieve a medically optimal weight before conception. Ideally, this would be a normal body mass index; however, this is not always possible.
In women who are planning pregnancy or are not on effective contraception, medications should be reviewed for potential teratogenicity. If needed, discuss alternative medications or switch to safer ones. However, these changes should not interrupt diabetes treatment.
In addition, ensure that the patient is up to date on age- and disease-appropriate preventive care (eg, immunizations, screening for sexually transmitted disease and malignancy). Counseling and intervention for use of tobacco, alcohol, and recreational drugs are also important. As with any preconception counseling, the patient (and her partner, if possible) should be advised to avoid travel to areas where Zika virus is endemic, and informed about the availability of expanded carrier genetic screening through her obstetric provider.
Finally, pregnant women with diabetes benefit from screening for diabetic complications including hypertension, retinopathy, cardiovascular disease, neuropathy, and nephropathy.
ASSESSING RISKS
Blood pressure
Chronic (preexisting) hypertension is defined as a systolic pressure 140 mm Hg or higher or a diastolic pressure 90 mm Hg or higher, or both, that antedates pregnancy or is present before the 20th week of pregnancy.3 Chronic hypertension has been reported in up to 5% of pregnant women and is associated with increased risk of preterm delivery, superimposed preeclampsia, low birth weight, and perinatal death.3
Reproductive-age women with diabetes and high blood pressure benefit from lifestyle and behavioral modifications.17 If drug therapy is needed, antihypertensive drugs that are safe for the fetus should be used. Treatment of mild or moderate hypertension during pregnancy reduces the risk of progression to severe hypertension but may not improve obstetric outcomes.
Diabetic retinopathy
Diabetic retinopathy can significantly worsen during pregnancy: the risk of progression is double that in the nonpregnant state.18 Women with diabetes who are contemplating pregnancy should have a comprehensive eye examination before conception, and any active proliferative retinopathy needs to be treated. These patients may require ophthalmologic monitoring and treatment during pregnancy. (Note: laser photocoagulation is not contraindicated during pregnancy.)
Cardiovascular disease
Cardiovascular physiology changes dramatically during pregnancy. Cardiovascular disease, especially when superimposed on diabetes, can increase the risk of maternal death. Thus, evaluation for cardiovascular risk factors as well as cardiovascular system integrity before conception is important. Listen for arterial bruits and murmurs, and assess peripheral pulses. Consideration should be given to obtaining a preconception resting electrocardiogram in women with diabetes who are over age 35 or who are suspected of having cardiovascular disease.16
Neurologic disorders
Peripheral neuropathy, the most common neurologic complication of diabetes, is associated with injury and infection.19
Autonomic neuropathy is associated with decreased cardiac responsiveness and orthostatic hypotension.19 Diabetic gastroparesis alone can precipitate serious complications during pregnancy, including extreme hypoglycemia and hyperglycemia, increased risk of diabetic ketoacidosis, weight loss, malnutrition, frequent hospitalizations, and increased requirement for parenteral nutrition.20
Although diabetic neuropathy does not significantly worsen during pregnancy, women with preexisting gastroparesis should be counseled on the substantial risks associated with pregnancy. Screening for neuropathy should be part of all diabetic preconception examinations.
Renal complications
Pregnancy in women with diabetes and preexisting renal dysfunction increases their risk of accelerated progression of diabetic kidney disease.21 Preexisting renal dysfunction also increases the risk of pregnancy-related complications, such as stillbirth, intrauterine growth restriction, gestational hypertension, preeclampsia, and preterm delivery.19,21,22 Further, the risk of pregnancy complications correlates directly with the severity of renal dysfunction.22
Psychiatric disorders
Emotional wellness is essential for optimal diabetes management. It is important to recognize the emotional impact of diabetes in pregnant women and to conduct routine screening for depression, anxiety, stress, and eating disorders.16
LABORATORY TESTS TO CONSIDER
Hemoglobin A1c. The general consensus is to achieve the lowest hemoglobin A1c level possible that does not increase the risk of hypoglycemia. The American Diabetes Association (ADA) recommends that, before attempting to conceive, women should lower their hemoglobin A1c to below 6.5%.1
Thyroid measures. Autoimmune thyroid disease is the most common autoimmune disorder associated with diabetes and has been reported in 35% to 40% of women with type 1 diabetes.23 Recommendations are to check thyroid-stimulating hormone and thyroid peroxidase antibody levels before conception or early in pregnancy in all women with diabetes.1,24 Overt hypothyroidism should be treated before conception, given that early fetal brain development depends on maternal thyroxine.
Renal function testing. Preconception assessment of renal function is important for counseling and risk stratification. This assessment should include serum creatinine level, estimated glomerular filtration rate, and urinary albumin excretion.21
Celiac screening. Because women with type 1 diabetes are more susceptible to autoimmune diseases, they should be screened for celiac disease before conception, with testing for immunoglobulin A (IgA) and tissue transglutaminase antibodies, with or without IgA endomysial antibodies.16,25,26 An estimated 6% of patients with type 1 diabetes have celiac disease vs 1% of the general population.25 Celiac disease is 2 to 3 times more common in women, and asymptomatic people with type 1 diabetes are considered at increased risk for celiac disease.26
The association between type 1 diabetes and celiac disease most likely relates to the overlap in human leukocyte antigens of the diseases. There is no established link between type 2 diabetes and celiac disease.25
Undiagnosed celiac disease increases a woman’s risk of obstetric complications such as preterm birth, low birth weight, and stillbirth.26 The most likely explanation for these adverse effects is nutrient malabsorption, which is characteristic of celiac disease. Adherence to a gluten-free diet before and during gestation may reduce the risk of preterm delivery by as much as 20%.26
Vitamin B12 level. Celiac disease interferes with the absorption of vitamin B12-instrinsic factor in the ileum, which can lead to vitamin B12 deficiency. Therefore, baseline vitamin B12 levels should be checked before conception in women with celiac disease. Levels should also be checked in women taking metformin, which also decreases vitamin B12 absorption. Of note, increased folate levels due to taking supplements can potentially mask vitamin B12 deficiency.
MEDICATIONS TO REVIEW FOR PREGNANCY INTERACTIONS
Diabetic medications
Insulin is the first-line pharmacotherapy for pregnant patients with type 1, type 2, or gestational diabetes. Insulin does not cross the placenta to a measurable extent, and most insulin preparations have been classified as category B,1 meaning no risks to the fetus have been found in humans.
Insulin dosing during pregnancy is not static. Beginning around mid-gestation, insulin requirements increase,28,29 but after 32 weeks the need may decrease. These changes require practitioners to closely monitor blood glucose throughout pregnancy.
Both basal-bolus injections and continuous subcutaneous infusion are reasonable options during pregnancy.30 However, the need for multiple and potentially painful insulin injections daily can lead to poor compliance. This inconvenience has led to studies using oral hypoglycemic medications instead of insulin for patients with gestational and type 2 diabetes.
Metformin is an oral biguanide that decreases hepatic gluconeogenesis and intestinal glucose absorption while peripherally increasing glucose utilization and uptake. Metformin does not pose a risk of hypoglycemia because its mechanism of action does not involve increased insulin production.7
Metformin does cross the placenta, resulting in umbilical cord blood levels higher than maternal levels. Nevertheless, studies support the efficacy and short-term safety of metformin use during a pregnancy complicated by gestational or type 2 diabetes.7,31 Moreover, metformin has been associated with a lower risk of neonatal hypoglycemia and maternal weight gain than insulin.32 However, this agent should be used with caution, as long-term data are not yet available, and it may slightly increase the risk of premature delivery.
Glyburide is another oral hypoglycemic medication that has been used during pregnancy. This second-generation sulfonylurea enhances the release of insulin from the pancreas by binding beta islet cell ATP-calcium channel receptors. Compared with other sulfonylureas, glyburide has the lowest rate of maternal-to-fetal transfer, with umbilical cord plasma concentrations 70% of maternal levels.33 Although some trials support the efficacy and short-term safety of glyburide treatment for gestational diabetes,34 recent studies have associated glyburide use during pregnancy with a higher rate of neonatal hypoglycemia, neonatal respiratory distress, macrosomia, and neonatal intensive care unit admissions than insulin and metformin.1,35
Patients treated with oral agents should be informed that these drugs cross the placenta, and that although no adverse effects on the fetus have been demonstrated, long-term safety data are lacking. In addition, oral agents are ineffective in type 1 diabetes and may be insufficient to overcome the insulin resistance in type 2 diabetes.
Antihypertensive drugs
All antihypertensive drugs cross the placenta, but several have an acceptable safety profile in pregnancy, including methyldopa, labetalol, clonidine, prazosin, and nifedipine. Hydralazine and labetalol are short-acting, come in intravenous formulations, and can be used for urgent blood pressure control during pregnancy. Diltiazem may be used for heart rate control during pregnancy, and it has been shown to lower blood pressure and proteinuria in pregnant patients with underlying renal disease.36,37 The ADA recommends against chronic use of diuretics during pregnancy because of potential reductions in maternal plasma volume and uteroplacental perfusion.1
Angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), and direct renin inhibitors are contraindicated during pregnancy because of the risk of fetal defects, particularly in the renal system.21,38 Although there is evidence to question the association between first semester exposure and fetotoxicity,39 we avoid these drugs during pregnancy and switch to a different agent in women planning pregnancy.
Other drugs
Statins are contraindicated in pregnancy because they interfere with the development of the fetal nervous system.21 Although preliminary data from a small study did not identify safety risks associated with pravastatin use after 12 weeks of gestation,40 we recommend discontinuing statins in women attempting pregnancy.
Aspirin. The US Preventive Services Task Force41 recommends low-dose aspirin (81 mg/day) after 12 weeks of gestation for women with type 1 or type 2 diabetes, as well as those with renal disease or chronic hypertension, to prevent preeclampsia. Of note, higher doses need to be used with caution during pregnancy because fetal abnormalities have been reported, such as disruption of fetal vasculature (mesenteric vessels), gastroschisis, and small intestinal atresia.16
Folate supplementation (0.6–4 mg/day) is recommended in women with celiac disease to prevent neural tube defects in the offspring, and the US Preventive Services Task Force recommends 0.4 mg daily of folic acid supplementation for all women planning or capable of pregnancy.42–44 Higher doses, ranging from 0.6 to 5 mg/day, have been proposed for patients with diabetes,13 and we recommend at least 1 mg for this group, based on data suggesting that higher doses further reduce the risk of neural tube defects.43
IS BREASTFEEDING AFFECTED?
Maternal diabetes, insulin therapy, and oral hypoglycemic agents are not contraindications to breastfeeding. The US Preventive Services Task Force recommends interventions by primary care physicians to promote and support breastfeeding.45 Breastfeeding is encouraged based on various short- and long-term health benefits for both breastfed infants and breastfeeding mothers. Breastfeeding decreases a woman’s insulin requirements and increases the risk for hypoglycemia, especially in patients with insulin-dependent type 1 diabetes.1
Additionally, insulin sensitivity increases immediately following delivery of the placenta.1 Therefore, it is prudent to adjust insulin doses postpartum, especially while a patient is breastfeeding, or to suggest high-carbohydrate snacks before feeds.9,29
Antihypertensive drugs considered safe to use during lactation include captopril, enalapril, quinapril, labetalol, propranolol, nifedipine, and hydralazine.21,46 Methyldopa is not contraindicated, but it causes fatigue and worsened postpartum depression and should not be used as first-line therapy. Diuretics and ARBs are not recommended during lactation.21 Both metformin and glyburide enter breast milk in small enough amounts that they are not contraindicated during breastfeeding.16 The Lactmed database (www.toxnet.nlm.nih.gov) provides information about drugs and breastfeeding.
WHAT ABOUT CONTRACEPTIVES?
The ADA recommends contraception for women with diabetes because, just as in women without diabetes, the risks of unplanned pregnancy outweigh those of contraceptives.1
We recommend low-dose combination estrogen-progestin oral contraceptives to normotensive women under age 35 with diabetes but without underlying microvascular disease. For women over age 35 or for those with microvascular disease, additional options include intrauterine devices or progestin implants. We prefer not to use injectable depot medroxyprogesterone acetate because of its side effects of insulin resistance and weight gain.47
CASE DISCUSSION: NEXT STEPS
Our patient’s interest in family planning presents an opportunity for preconception counseling. We recommend a prenatal folic acid supplement, diet and regular exercise for weight loss, and screening tests including a comprehensive metabolic panel, hemoglobin A1c, thyroid-stimulating hormone, and dilated eye examination. We make sure she is up to date on her indicated health maintenance (eg, immunizations, disease screening), and we review her medications for potential teratogens. She denies any recreational drug use. Also, she has no plans for long-distance travel.
Our counseling includes discussions of pregnancy risks associated with pregestational diabetes and suboptimal glycemic control. We encourage her to use effective contraception until she is “medically optimized” for pregnancy—ie, until her hemoglobin A1c is lower than 6.5% and she has achieved a medically optimal weight. If feasible, a reduction of weight (7% or so) through lifestyle modification should be attempted, and if her hemoglobin A1c remains elevated, adding insulin would be recommended.
Pregnant patients or patients contemplating pregnancy are usually motivated to modify their behavior, making this a good time to reinforce lifestyle modifications. Many patients benefit from individualized counseling by a registered dietitian to help achieve the recommended weight and glycemic control.
Our physical examination in this patient includes screening for micro- and macrovascular complications of diabetes, and the test results are negative. Patients with active proliferative retinopathy should be referred to an ophthalmologist for assessment and treatment.
We review her medications for potential teratogenic effects and stop her ACE inhibitor (lisinopril) and statin (simvastatin). We switch her from a first-generation sulfonylurea (chlorpropamide) to glyburide, a second-generation sulfonylurea. Second-generation sulfonylureas are considered more “fetus-friendly” because first-generation sulfonylureas cross the placenta more easily and can cause fetal hyperinsulinemia, leading to macrosomia and neonatal hypoglycemia.7
The management of diabetes during pregnancy leans toward insulin use, given the lack of information regarding long-term outcomes with oral agents. If insulin is needed, it is best to initiate it before the patient conceives, and then to stop other diabetes medications. We would not make any changes to her aspirin or metformin use.
Educating the patient and her family about prevention, recognition, and treatment of hypoglycemia is important to prevent and manage the increased risk of hypoglycemia with insulin therapy and in early pregnancy.1 Consideration should be given to providing ketone strips as well as education on diabetic ketoacidosis prevention and detection.1 If the patient conceives, begin prenatal care early to allow adequate planning for care of her disease and evaluation of the fetus. Because of the complexity of insulin management in pregnancy, the ADA recommends referral, if possible, to a center offering team-based care, including an obstetrician specialized in high-risk pregnancies, an endocrinologist, and a dietitian.1
A 29-year-old nulliparous woman presents for a routine checkup. She has hypertension and type 2 diabetes mellitus. Her current medications are chlorpropamide 500 mg daily, metformin 500 mg twice a day, lisinopril 40 mg daily, simvastatin 40 mg daily, and aspirin 81 mg daily. Her body mass index is 37 kg/m2 and her blood pressure is 130/80 mm Hg. Her hemoglobin A1c level is 7.8% and her low-density lipoprotein cholesterol 90 mg/dL.
She is considering pregnancy. How would you counsel her?
DEFINING DIABETES IN PREGNANCY
Diabetes in pregnant women, both gestational and pregestational, is the most common medical complication associated with pregnancy.1
- Gestational diabetes is defined as diabetes that is diagnosed during the second or third trimester of pregnancy and that is not clearly pregestational.2
- Pregestational diabetes exists before pregnancy and can be either type 1 or type 2.
Most cases of diabetes diagnosed during the first trimester reflect pregestational diabetes, as gestational diabetes occurs when insulin resistance increases in the later trimesters.
Type 1 diabetes involves autoimmune destruction of pancreatic islet cells, leading to insulin deficiency and the need for insulin therapy. Type 2 diabetes is characterized by insulin resistance rather than overall insulin deficiency. Type 2 diabetes tends to be associated with comorbidities such as obesity and hypertension, which are independent risk factors for adverse perinatal outcomes.3,4
Gestational diabetes accounts for most cases of diabetes during pregnancy. Although both pregestational and gestational diabetes increase the risk of maternal and fetal complications, pregestational diabetes is associated with significantly greater risks.1
IMPACT OF DIABETES ON THE MOTHER
Pregnancy increases the risk of maternal hypoglycemia, especially during the first trimester in patients with type 1 diabetes, as insulin sensitivity increases in early pregnancy.1 Pregnant women with diabetes may also have an altered counterregulatory response and less hypoglycemic awareness.1 Insulin resistance rises during the second and early third trimesters, increasing the risk of hyperglycemia in women with diabetes.1
Glycemic control during pregnancy is usually easier to achieve in patients with type 2 diabetes than with type 1, but it may require much higher insulin doses.
Because pregnancy is inherently a ketogenic state, women with type 1 diabetes are at higher risk of diabetic ketoacidosis, particularly during the second and third trimesters.1 There are reports of euglycemic diabetic ketoacidosis in pregnant women with either gestational or pregestational diabetes.5
Diabetes is associated with a risk of preeclampsia 4 times higher than in nondiabetic women.6 Other potential pregnancy-related complications include infections, polyhydramnios, spontaneous abortion, and cesarean delivery.1,7 The risk of pregnancy loss is similar in women with either type 1 or type 2 diabetes (2.6% and 3.7%, respectively), but the causes are different.8 Although preexisting diabetic complications such as retinopathy, nephropathy, and gastroparesis can be exacerbated during pregnancy,1 only severe gastroparesis and advanced renal disease are considered relative contraindications to pregnancy.
IMPACT OF DIABETES ON THE FETUS
Fetal complications of maternal diabetes include embryopathy (fetal malformations) and fetopathy (overgrowth, ie, fetus large for gestational age, and increased risk of fetal death or distress). Maternal hyperglycemia is associated with diabetic embryopathy, resulting in major birth defects in 5% to 25% of pregnancies and spontaneous abortions in 15% to 20%.9,10 There is a 2- to 6-fold increase in risk of congenital malformations.6
The most common diabetes-associated congenital malformations affect the cardiovascular system. Congenital heart disease includes tetralogy of Fallot, transposition of the great vessels, septal defects, and anomalous pulmonary venous return. Other relatively common defects involve the fetal central nervous system, spine, orofacial system, kidneys, urogenital system, gastrointestinal tract, and skeleton.11
The risk of fetopathy is proportional to the degree of maternal hyperglycemia. Excess maternal glucose and fatty acid levels can lead to fetal hyperglycemia and overgrowth, which increases fetal oxygen requirements. Erythropoietin levels rise, causing an increase in red cell mass, with subsequent hyperviscosity within the placenta and higher risk of fetal death.
Other complications include intrauterine growth restriction, prematurity, and preterm delivery. Fetal macrosomia (birth weight > 90th percentile or 4 kg, approximately 8 lb, 13 oz) occurs in 27% to 62% of children born to mothers with diabetes, a rate 10 times higher than in patients without diabetes. It contributes to shoulder dystocia (risk 2 to 4 times higher in diabetic pregnancies) and cesarean delivery.6 Infants born to mothers with diabetes also have higher risks of neonatal hypoglycemia, erythrocytosis, hyperbilirubinemia, hypocalcemia, respiratory distress, cardiomyopathy, and death, as well as for developing diabetes, obesity, and other adverse cardiometabolic outcomes later in life.11
GET GLUCOSE UNDER CONTROL BEFORE PREGNANCY
Nearly half of pregnancies in the general population are unplanned,15 so preconception diabetes assessment needs to be part of routine medical care for all reproductive-age women. Because most organogenesis occurs during the first 5 to 8 weeks after fertilization—potentially before a woman realizes she is pregnant—achieving optimal glycemic control before conception is necessary to improve pregnancy outcomes.1
EVERY VISIT IS AN OPPORTUNITY
Every medical visit with a reproductive-age woman with diabetes is an opportunity for counseling about pregnancy. Topics that need to be discussed include the risks of unplanned pregnancy and of poor metabolic control, and the benefits of improved maternal and fetal outcomes with appropriate pregnancy planning and diabetes management.
Referral to a registered dietitian for individualized counseling about proper nutrition, particularly during pregnancy, has been associated with positive outcomes.16 Patients with diabetes and at high risk of pregnancy complications should be referred to a clinic that specializes in high-risk pregnancies.
Practitioners also should emphasize the importance of regular exercise and encourage patients to maintain or achieve a medically optimal weight before conception. Ideally, this would be a normal body mass index; however, this is not always possible.
In women who are planning pregnancy or are not on effective contraception, medications should be reviewed for potential teratogenicity. If needed, discuss alternative medications or switch to safer ones. However, these changes should not interrupt diabetes treatment.
In addition, ensure that the patient is up to date on age- and disease-appropriate preventive care (eg, immunizations, screening for sexually transmitted disease and malignancy). Counseling and intervention for use of tobacco, alcohol, and recreational drugs are also important. As with any preconception counseling, the patient (and her partner, if possible) should be advised to avoid travel to areas where Zika virus is endemic, and informed about the availability of expanded carrier genetic screening through her obstetric provider.
Finally, pregnant women with diabetes benefit from screening for diabetic complications including hypertension, retinopathy, cardiovascular disease, neuropathy, and nephropathy.
ASSESSING RISKS
Blood pressure
Chronic (preexisting) hypertension is defined as a systolic pressure 140 mm Hg or higher or a diastolic pressure 90 mm Hg or higher, or both, that antedates pregnancy or is present before the 20th week of pregnancy.3 Chronic hypertension has been reported in up to 5% of pregnant women and is associated with increased risk of preterm delivery, superimposed preeclampsia, low birth weight, and perinatal death.3
Reproductive-age women with diabetes and high blood pressure benefit from lifestyle and behavioral modifications.17 If drug therapy is needed, antihypertensive drugs that are safe for the fetus should be used. Treatment of mild or moderate hypertension during pregnancy reduces the risk of progression to severe hypertension but may not improve obstetric outcomes.
Diabetic retinopathy
Diabetic retinopathy can significantly worsen during pregnancy: the risk of progression is double that in the nonpregnant state.18 Women with diabetes who are contemplating pregnancy should have a comprehensive eye examination before conception, and any active proliferative retinopathy needs to be treated. These patients may require ophthalmologic monitoring and treatment during pregnancy. (Note: laser photocoagulation is not contraindicated during pregnancy.)
Cardiovascular disease
Cardiovascular physiology changes dramatically during pregnancy. Cardiovascular disease, especially when superimposed on diabetes, can increase the risk of maternal death. Thus, evaluation for cardiovascular risk factors as well as cardiovascular system integrity before conception is important. Listen for arterial bruits and murmurs, and assess peripheral pulses. Consideration should be given to obtaining a preconception resting electrocardiogram in women with diabetes who are over age 35 or who are suspected of having cardiovascular disease.16
Neurologic disorders
Peripheral neuropathy, the most common neurologic complication of diabetes, is associated with injury and infection.19
Autonomic neuropathy is associated with decreased cardiac responsiveness and orthostatic hypotension.19 Diabetic gastroparesis alone can precipitate serious complications during pregnancy, including extreme hypoglycemia and hyperglycemia, increased risk of diabetic ketoacidosis, weight loss, malnutrition, frequent hospitalizations, and increased requirement for parenteral nutrition.20
Although diabetic neuropathy does not significantly worsen during pregnancy, women with preexisting gastroparesis should be counseled on the substantial risks associated with pregnancy. Screening for neuropathy should be part of all diabetic preconception examinations.
Renal complications
Pregnancy in women with diabetes and preexisting renal dysfunction increases their risk of accelerated progression of diabetic kidney disease.21 Preexisting renal dysfunction also increases the risk of pregnancy-related complications, such as stillbirth, intrauterine growth restriction, gestational hypertension, preeclampsia, and preterm delivery.19,21,22 Further, the risk of pregnancy complications correlates directly with the severity of renal dysfunction.22
Psychiatric disorders
Emotional wellness is essential for optimal diabetes management. It is important to recognize the emotional impact of diabetes in pregnant women and to conduct routine screening for depression, anxiety, stress, and eating disorders.16
LABORATORY TESTS TO CONSIDER
Hemoglobin A1c. The general consensus is to achieve the lowest hemoglobin A1c level possible that does not increase the risk of hypoglycemia. The American Diabetes Association (ADA) recommends that, before attempting to conceive, women should lower their hemoglobin A1c to below 6.5%.1
Thyroid measures. Autoimmune thyroid disease is the most common autoimmune disorder associated with diabetes and has been reported in 35% to 40% of women with type 1 diabetes.23 Recommendations are to check thyroid-stimulating hormone and thyroid peroxidase antibody levels before conception or early in pregnancy in all women with diabetes.1,24 Overt hypothyroidism should be treated before conception, given that early fetal brain development depends on maternal thyroxine.
Renal function testing. Preconception assessment of renal function is important for counseling and risk stratification. This assessment should include serum creatinine level, estimated glomerular filtration rate, and urinary albumin excretion.21
Celiac screening. Because women with type 1 diabetes are more susceptible to autoimmune diseases, they should be screened for celiac disease before conception, with testing for immunoglobulin A (IgA) and tissue transglutaminase antibodies, with or without IgA endomysial antibodies.16,25,26 An estimated 6% of patients with type 1 diabetes have celiac disease vs 1% of the general population.25 Celiac disease is 2 to 3 times more common in women, and asymptomatic people with type 1 diabetes are considered at increased risk for celiac disease.26
The association between type 1 diabetes and celiac disease most likely relates to the overlap in human leukocyte antigens of the diseases. There is no established link between type 2 diabetes and celiac disease.25
Undiagnosed celiac disease increases a woman’s risk of obstetric complications such as preterm birth, low birth weight, and stillbirth.26 The most likely explanation for these adverse effects is nutrient malabsorption, which is characteristic of celiac disease. Adherence to a gluten-free diet before and during gestation may reduce the risk of preterm delivery by as much as 20%.26
Vitamin B12 level. Celiac disease interferes with the absorption of vitamin B12-instrinsic factor in the ileum, which can lead to vitamin B12 deficiency. Therefore, baseline vitamin B12 levels should be checked before conception in women with celiac disease. Levels should also be checked in women taking metformin, which also decreases vitamin B12 absorption. Of note, increased folate levels due to taking supplements can potentially mask vitamin B12 deficiency.
MEDICATIONS TO REVIEW FOR PREGNANCY INTERACTIONS
Diabetic medications
Insulin is the first-line pharmacotherapy for pregnant patients with type 1, type 2, or gestational diabetes. Insulin does not cross the placenta to a measurable extent, and most insulin preparations have been classified as category B,1 meaning no risks to the fetus have been found in humans.
Insulin dosing during pregnancy is not static. Beginning around mid-gestation, insulin requirements increase,28,29 but after 32 weeks the need may decrease. These changes require practitioners to closely monitor blood glucose throughout pregnancy.
Both basal-bolus injections and continuous subcutaneous infusion are reasonable options during pregnancy.30 However, the need for multiple and potentially painful insulin injections daily can lead to poor compliance. This inconvenience has led to studies using oral hypoglycemic medications instead of insulin for patients with gestational and type 2 diabetes.
Metformin is an oral biguanide that decreases hepatic gluconeogenesis and intestinal glucose absorption while peripherally increasing glucose utilization and uptake. Metformin does not pose a risk of hypoglycemia because its mechanism of action does not involve increased insulin production.7
Metformin does cross the placenta, resulting in umbilical cord blood levels higher than maternal levels. Nevertheless, studies support the efficacy and short-term safety of metformin use during a pregnancy complicated by gestational or type 2 diabetes.7,31 Moreover, metformin has been associated with a lower risk of neonatal hypoglycemia and maternal weight gain than insulin.32 However, this agent should be used with caution, as long-term data are not yet available, and it may slightly increase the risk of premature delivery.
Glyburide is another oral hypoglycemic medication that has been used during pregnancy. This second-generation sulfonylurea enhances the release of insulin from the pancreas by binding beta islet cell ATP-calcium channel receptors. Compared with other sulfonylureas, glyburide has the lowest rate of maternal-to-fetal transfer, with umbilical cord plasma concentrations 70% of maternal levels.33 Although some trials support the efficacy and short-term safety of glyburide treatment for gestational diabetes,34 recent studies have associated glyburide use during pregnancy with a higher rate of neonatal hypoglycemia, neonatal respiratory distress, macrosomia, and neonatal intensive care unit admissions than insulin and metformin.1,35
Patients treated with oral agents should be informed that these drugs cross the placenta, and that although no adverse effects on the fetus have been demonstrated, long-term safety data are lacking. In addition, oral agents are ineffective in type 1 diabetes and may be insufficient to overcome the insulin resistance in type 2 diabetes.
Antihypertensive drugs
All antihypertensive drugs cross the placenta, but several have an acceptable safety profile in pregnancy, including methyldopa, labetalol, clonidine, prazosin, and nifedipine. Hydralazine and labetalol are short-acting, come in intravenous formulations, and can be used for urgent blood pressure control during pregnancy. Diltiazem may be used for heart rate control during pregnancy, and it has been shown to lower blood pressure and proteinuria in pregnant patients with underlying renal disease.36,37 The ADA recommends against chronic use of diuretics during pregnancy because of potential reductions in maternal plasma volume and uteroplacental perfusion.1
Angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), and direct renin inhibitors are contraindicated during pregnancy because of the risk of fetal defects, particularly in the renal system.21,38 Although there is evidence to question the association between first semester exposure and fetotoxicity,39 we avoid these drugs during pregnancy and switch to a different agent in women planning pregnancy.
Other drugs
Statins are contraindicated in pregnancy because they interfere with the development of the fetal nervous system.21 Although preliminary data from a small study did not identify safety risks associated with pravastatin use after 12 weeks of gestation,40 we recommend discontinuing statins in women attempting pregnancy.
Aspirin. The US Preventive Services Task Force41 recommends low-dose aspirin (81 mg/day) after 12 weeks of gestation for women with type 1 or type 2 diabetes, as well as those with renal disease or chronic hypertension, to prevent preeclampsia. Of note, higher doses need to be used with caution during pregnancy because fetal abnormalities have been reported, such as disruption of fetal vasculature (mesenteric vessels), gastroschisis, and small intestinal atresia.16
Folate supplementation (0.6–4 mg/day) is recommended in women with celiac disease to prevent neural tube defects in the offspring, and the US Preventive Services Task Force recommends 0.4 mg daily of folic acid supplementation for all women planning or capable of pregnancy.42–44 Higher doses, ranging from 0.6 to 5 mg/day, have been proposed for patients with diabetes,13 and we recommend at least 1 mg for this group, based on data suggesting that higher doses further reduce the risk of neural tube defects.43
IS BREASTFEEDING AFFECTED?
Maternal diabetes, insulin therapy, and oral hypoglycemic agents are not contraindications to breastfeeding. The US Preventive Services Task Force recommends interventions by primary care physicians to promote and support breastfeeding.45 Breastfeeding is encouraged based on various short- and long-term health benefits for both breastfed infants and breastfeeding mothers. Breastfeeding decreases a woman’s insulin requirements and increases the risk for hypoglycemia, especially in patients with insulin-dependent type 1 diabetes.1
Additionally, insulin sensitivity increases immediately following delivery of the placenta.1 Therefore, it is prudent to adjust insulin doses postpartum, especially while a patient is breastfeeding, or to suggest high-carbohydrate snacks before feeds.9,29
Antihypertensive drugs considered safe to use during lactation include captopril, enalapril, quinapril, labetalol, propranolol, nifedipine, and hydralazine.21,46 Methyldopa is not contraindicated, but it causes fatigue and worsened postpartum depression and should not be used as first-line therapy. Diuretics and ARBs are not recommended during lactation.21 Both metformin and glyburide enter breast milk in small enough amounts that they are not contraindicated during breastfeeding.16 The Lactmed database (www.toxnet.nlm.nih.gov) provides information about drugs and breastfeeding.
WHAT ABOUT CONTRACEPTIVES?
The ADA recommends contraception for women with diabetes because, just as in women without diabetes, the risks of unplanned pregnancy outweigh those of contraceptives.1
We recommend low-dose combination estrogen-progestin oral contraceptives to normotensive women under age 35 with diabetes but without underlying microvascular disease. For women over age 35 or for those with microvascular disease, additional options include intrauterine devices or progestin implants. We prefer not to use injectable depot medroxyprogesterone acetate because of its side effects of insulin resistance and weight gain.47
CASE DISCUSSION: NEXT STEPS
Our patient’s interest in family planning presents an opportunity for preconception counseling. We recommend a prenatal folic acid supplement, diet and regular exercise for weight loss, and screening tests including a comprehensive metabolic panel, hemoglobin A1c, thyroid-stimulating hormone, and dilated eye examination. We make sure she is up to date on her indicated health maintenance (eg, immunizations, disease screening), and we review her medications for potential teratogens. She denies any recreational drug use. Also, she has no plans for long-distance travel.
Our counseling includes discussions of pregnancy risks associated with pregestational diabetes and suboptimal glycemic control. We encourage her to use effective contraception until she is “medically optimized” for pregnancy—ie, until her hemoglobin A1c is lower than 6.5% and she has achieved a medically optimal weight. If feasible, a reduction of weight (7% or so) through lifestyle modification should be attempted, and if her hemoglobin A1c remains elevated, adding insulin would be recommended.
Pregnant patients or patients contemplating pregnancy are usually motivated to modify their behavior, making this a good time to reinforce lifestyle modifications. Many patients benefit from individualized counseling by a registered dietitian to help achieve the recommended weight and glycemic control.
Our physical examination in this patient includes screening for micro- and macrovascular complications of diabetes, and the test results are negative. Patients with active proliferative retinopathy should be referred to an ophthalmologist for assessment and treatment.
We review her medications for potential teratogenic effects and stop her ACE inhibitor (lisinopril) and statin (simvastatin). We switch her from a first-generation sulfonylurea (chlorpropamide) to glyburide, a second-generation sulfonylurea. Second-generation sulfonylureas are considered more “fetus-friendly” because first-generation sulfonylureas cross the placenta more easily and can cause fetal hyperinsulinemia, leading to macrosomia and neonatal hypoglycemia.7
The management of diabetes during pregnancy leans toward insulin use, given the lack of information regarding long-term outcomes with oral agents. If insulin is needed, it is best to initiate it before the patient conceives, and then to stop other diabetes medications. We would not make any changes to her aspirin or metformin use.
Educating the patient and her family about prevention, recognition, and treatment of hypoglycemia is important to prevent and manage the increased risk of hypoglycemia with insulin therapy and in early pregnancy.1 Consideration should be given to providing ketone strips as well as education on diabetic ketoacidosis prevention and detection.1 If the patient conceives, begin prenatal care early to allow adequate planning for care of her disease and evaluation of the fetus. Because of the complexity of insulin management in pregnancy, the ADA recommends referral, if possible, to a center offering team-based care, including an obstetrician specialized in high-risk pregnancies, an endocrinologist, and a dietitian.1
- American Diabetes Association. 13. Management of diabetes in pregnancy: standards of medical care in diabetes—2018. Diabetes Care 2018; 41(suppl 1):S137–S143. doi:10.2337/dc18-S013
- American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2018. Diabetes Care 2018; 41(suppl 1):S13–S27. doi:10.2337/dc18-S002
- Lawler J, Osman M, Shelton JA, Yeh J. Population-based analysis of hypertensive disorders in pregnancy. Hypertens Pregnancy 2007; 26(1):67–76. doi:10.1080/10641950601147945
- Marchi J, Berg M, Dencker A, Olander EK, Begley C. Risks associated with obesity in pregnancy, for the mother and baby: a systematic review of reviews. Obes Rev 2015; 16(8):621–638. doi:10.1111/obr.12288
- Garrison EA, Jagasia S. Inpatient management of women with gestational and pregestational diabetes in pregnancy. Curr Diab Rep 2014; 14(2):457. doi:10.1007/s11892-013-0457-x
- Ballas J, Moore TR, Ramos GA. Management of diabetes in pregnancy. Curr Diab Rep 2012; 12(1):33–42. doi:10.1007/s11892-011-0249-0
- Ryu RJ, Hays KE, Hebert MF. Gestational diabetes mellitus management with oral hypoglycemic agents. Semin Perinatol 2014; 38(8):508–515. doi:10.1053/j.semperi.2014.08.012
- Cundy T, Gamble G, Neale L, et al. Differing causes of pregnancy loss in type 1 and type 2 diabetes. Diabetes Care 2007; 30(10):2603–2607. doi:10.2337/dc07-0555
- Castorino K, Jovanovic L. Pregnancy and diabetes management: advances and controversies. Clin Chem 2011; 57(2):221–230. doi:10.1373/clinchem.2010.155382
- Hammouda SA, Hakeem R. Role of HbA1c in predicting risk for congenital malformations. Prim Care Diabetes 2015; 9(6):458–464. doi:10.1016/j.pcd.2015.01.004
- Chen CP. Congenital malformations associated with maternal diabetes. Taiwanese J Obstet Gynecol 2005; 44(1):1–7. doi:10.1016/S1028-4559(09)60099-1
- International Association of Diabetes and Pregnancy Study Groups Consensus Panel, Metzger BE, Gabbe SG, Persson B, et al. International Association of Diabetes and Pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 2010; 33(3):676–682. doi:10.2337/dc09-1848
- Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care 2013; 36(5):1384–1395. doi:10.2337/dc12-2480
- HAPO Study Cooperative Research Group; Metzger BE, Lowe LP, Dyer AR, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 2008; 358(19):1991–2002. doi:10.1056/NEJMoa0707943
- Finer LB, Zolna MR. Shifts in intended and unintended pregnancies in the United States, 2001–2008. Am J Public Health 2014; 104(suppl 1):S43–S48. doi:10.2105/AJPH.2013.301416
- Kitzmiller JL, Block JM, Brown FM, et al. Managing preexisting diabetes for pregnancy: summary of evidence and consensus recommendations for care. Diabetes Care 2008; 31(5):1060–1079. doi:10.2337/dc08-9020
- Webster LM, Conti-Ramsden F, Seed PT, Webb AJ, Nelson-Piercy C, Chappell LC. Impact of antihypertensive treatment on maternal and perinatal outcomes in pregnancy complicated by chronic hypertension: a systematic review and meta-analysis. J Am Heart Assoc 2017; 6(5).pii:e005526. doi:10.1161/JAHA.117.005526
- Chew EY, Mills JL, Metzger BE, et al. Metabolic control and progression of retinopathy: the Diabetes in Early Pregnancy Study. Diabetes Care 1995; 18(5):631–637. pmid:8586000
- American Diabetes Association. Standards of medical care in diabetes—2016. Diabetes Care 2016; 39 (suppl 1):S1–S109.
- Hawthorne, G. Maternal complications in diabetic pregnancy. Best Pract Res Clin Obstet Gynaecol 2011; 25(1):77–90. doi:10.1016/j.bpobgyn.2010.10.015
- Ringholm L, Damm JA, Vestgaard M, Damm P, Mathiesen ER. Diabetic nephropathy in women with preexisting diabetes: from pregnancy planning to breastfeeding. Curr Diab Rep 2016; 16(2):12. doi:10.1007/s11892-015-0705-3
- Zhang JJ, Ma XX, Hao L, Liu LJ, Lv JC, Zhang H. A systematic review and meta-analysis of outcomes of pregnancy in CKD and CKD outcomes in pregnancy. Clin J Am Soc Nephrol 2015; 10(11):1964–1978. doi:10.2215/CJN.09250914
- Umpierrez GE, Latif KA, Murphy MB, et al. Thyroid dysfunction in patients with type 1 diabetes: a longitudinal study. Diabetes Care 2003; 26(4):1181–1185. pmid:12663594
- Alexander EK, Pearce EN, Brent GA, et al. 2017 Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and the Postpartum. Thyroid 2017; 27(3):315–389. doi:10.1089/thy.2016.0457
- Akirov A, Pinhas-Hamiel O. Co-occurrence of type 1 diabetes mellitus and celiac disease. World J Diabetes 2015; 6(5):707–714. doi:10.4239/wjd.v6.i5.707
- Saccone G, Berghella V, Sarno L, et al. Celiac disease and obstetric complications: a systematic review and metaanalysis. Am J Obstet Gynecol 2016; 214(2):225–234. doi:10.1016/j.ajog.2015.09.080
- Feghali M, Venkataramanan R, Caritis S. Pharmacokinetics of drugs in pregnancy. Semin Perinatol 2015; 39(7):512–519. doi:10.1053/j.semperi.2015.08.003
- de Valk HW, Visser GH. Insulin during pregnancy, labour and delivery. Best Pract Res Clin Obstet Gynaecol 2011; 25(1):65–76. doi:10.1016/j.bpobgyn.2010.10.002
- Morello CM. Pharmacokinetics and pharmacodynamics of insulin analogs in special populations with type 2 diabetes mellitus. Int J Gen Med 2011; 4:827–835. doi:10.2147/IJGM.S26889
- Farrar D, Tuffnell DJ, West J, West HM. Continuous subcutaneous insulin infusion versus multiple daily injections of insulin for pregnant women with diabetes. Cochrane Database Syst Rev 2016; (6):CD005542. doi:10.1002/14651858.CD005542.pub2
- Charles B, Norris R, Xiao X, Hague W. Population pharmacokinetics of metformin in late pregnancy. Ther Drug Monit 2006; 28(1):67–72. pmid:16418696
- Balsells M, García-Patterson A, Solà I, Roqué M, Gich I, Corcoy R. Glibenclamide, metformin, and insulin for the treatment of gestational diabetes: a systematic review and meta-analysis. BMJ 2015; 350:h102. doi:10.1136/bmj.h102
- Hebert MF, Ma X, Naraharisetti SB, et al; Obstetric-Fetal Pharmacology Research Unit Network. Are we optimizing gestational diabetes treatment with glyburide? The pharmacologic basis for better clinical practice. Clin Pharmacol Ther 2009; 85(6):607–614. doi:10.1038/clpt.2009.5
- Langer O, Conway DL, Berkus MD, Xenakis EM, Gonzales O. A comparison of glyburide and insulin in women with gestational diabetes mellitus. N Engl J Med 2000; 343(16):1134–1138. doi:10.1056/NEJM200010193431601
- Camelo Castillo W, Boggess K, Stürmer T, Brookhart MA, Benjamin DK Jr, Jonsson Funk M. Association of adverse pregnancy outcomes with glyburide vs insulin in women with gestational diabetes. JAMA Pediatr 2015; 169:452–458. doi:10.1001/jamapediatrics.2015.74
- Gowda RM, Khan IA, Mehta NJ, Vasavada BC, Sacchi TJ. Cardiac arrhythmias in pregnancy: clinical and therapeutic considerations. Int J Cardiol 2003; 88(2):129–133. pmid:12714190
- Khandelwal M, Kumanova M, Gaughan JP, Reece EA. Role of diltiazem in pregnant women with chronic renal disease. J Matern Fetal Neonatal Med 2002; 12(6):408–412. doi:10.1080/jmf.12.6.408.412
- Magee LA, Abalos E, von Dadelszen P, Sibai B, Easterling T, Walkinshaw S; CHIPS Study Group. How to manage hypertension in pregnancy effectively. Br J Clin Pharmacol 2011; 72(3):394–401. doi:10.1111/j.1365-2125.2011.04002.x
- Cooper WO, Hernandez-Diaz S, Arbogast PG, et al. Major congenital malformations after first-trimester exposure to ACE inhibitors. N Engl J Med 2006; 354(23):2443–2451. doi:10.1056/NEJMoa055202
- Costantine MM, Cleary K, Hebert MF, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Obstetric-Fetal Pharmacology Research Units Network. Safety and pharmacokinetics of pravastatin used for the prevention of preeclampsia in high-risk pregnant women: a pilot randomized controlled trial. Am J Obstet Gynecol 2016; 214(6):720.e1–720.e17. doi:10.1016/j.ajog.2015.12.038
- LeFevre ML; US Preventive Services Task Force. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: US Preventive Services Task Force recommendation statement. Ann Intern Med 2014; 161(11):819–826. doi:10.7326/M14-1884
- Curry SJ, Grossman DC, Whitlock EP, Cantu A. Behavioral counseling research and evidence-based practice recommendations: US Preventive Services Task Force perspectives. Ann Intern Med 2014; 160(6):407–413. doi:10.7326/M13-2128
- Wald N, Law M, Morris J, Wald D. Quantifying the effect of folic acid. Lancet 2001; 358(9298):2069–2073. pmid:11755633
- US Preventive Services Task Force; Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Folic acid supplementation for the prevention of neural tube defects: US Preventive Services Task Force recommendation statement. JAMA 2017; 317(2):183–189. doi:10.1001/jama.2016.19438
- US Preventive Services Task Force; Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Primary care interventions to support breastfeeding: US Preventive Services Task Force recommendation statement. JAMA 2016; 316(16):1688–1693. doi:10.1001/jama.2016.14697
- Newton ER, Hale TW. Drugs in breast milk. Clin Obstet Gynecol 2015; 58(4):868–884. doi:10.1097/GRF.0000000000000142
- Xiang AH, Kawakubo M, Kjos SL, Buchanan TA. Long-acting injectable progestin contraception and risk of type 2 diabetes in Latino women with prior gestational diabetes mellitus. Diabetes Care 2006; 29(3):613–617. pmid:16505515
- American Diabetes Association. 13. Management of diabetes in pregnancy: standards of medical care in diabetes—2018. Diabetes Care 2018; 41(suppl 1):S137–S143. doi:10.2337/dc18-S013
- American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2018. Diabetes Care 2018; 41(suppl 1):S13–S27. doi:10.2337/dc18-S002
- Lawler J, Osman M, Shelton JA, Yeh J. Population-based analysis of hypertensive disorders in pregnancy. Hypertens Pregnancy 2007; 26(1):67–76. doi:10.1080/10641950601147945
- Marchi J, Berg M, Dencker A, Olander EK, Begley C. Risks associated with obesity in pregnancy, for the mother and baby: a systematic review of reviews. Obes Rev 2015; 16(8):621–638. doi:10.1111/obr.12288
- Garrison EA, Jagasia S. Inpatient management of women with gestational and pregestational diabetes in pregnancy. Curr Diab Rep 2014; 14(2):457. doi:10.1007/s11892-013-0457-x
- Ballas J, Moore TR, Ramos GA. Management of diabetes in pregnancy. Curr Diab Rep 2012; 12(1):33–42. doi:10.1007/s11892-011-0249-0
- Ryu RJ, Hays KE, Hebert MF. Gestational diabetes mellitus management with oral hypoglycemic agents. Semin Perinatol 2014; 38(8):508–515. doi:10.1053/j.semperi.2014.08.012
- Cundy T, Gamble G, Neale L, et al. Differing causes of pregnancy loss in type 1 and type 2 diabetes. Diabetes Care 2007; 30(10):2603–2607. doi:10.2337/dc07-0555
- Castorino K, Jovanovic L. Pregnancy and diabetes management: advances and controversies. Clin Chem 2011; 57(2):221–230. doi:10.1373/clinchem.2010.155382
- Hammouda SA, Hakeem R. Role of HbA1c in predicting risk for congenital malformations. Prim Care Diabetes 2015; 9(6):458–464. doi:10.1016/j.pcd.2015.01.004
- Chen CP. Congenital malformations associated with maternal diabetes. Taiwanese J Obstet Gynecol 2005; 44(1):1–7. doi:10.1016/S1028-4559(09)60099-1
- International Association of Diabetes and Pregnancy Study Groups Consensus Panel, Metzger BE, Gabbe SG, Persson B, et al. International Association of Diabetes and Pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 2010; 33(3):676–682. doi:10.2337/dc09-1848
- Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care 2013; 36(5):1384–1395. doi:10.2337/dc12-2480
- HAPO Study Cooperative Research Group; Metzger BE, Lowe LP, Dyer AR, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 2008; 358(19):1991–2002. doi:10.1056/NEJMoa0707943
- Finer LB, Zolna MR. Shifts in intended and unintended pregnancies in the United States, 2001–2008. Am J Public Health 2014; 104(suppl 1):S43–S48. doi:10.2105/AJPH.2013.301416
- Kitzmiller JL, Block JM, Brown FM, et al. Managing preexisting diabetes for pregnancy: summary of evidence and consensus recommendations for care. Diabetes Care 2008; 31(5):1060–1079. doi:10.2337/dc08-9020
- Webster LM, Conti-Ramsden F, Seed PT, Webb AJ, Nelson-Piercy C, Chappell LC. Impact of antihypertensive treatment on maternal and perinatal outcomes in pregnancy complicated by chronic hypertension: a systematic review and meta-analysis. J Am Heart Assoc 2017; 6(5).pii:e005526. doi:10.1161/JAHA.117.005526
- Chew EY, Mills JL, Metzger BE, et al. Metabolic control and progression of retinopathy: the Diabetes in Early Pregnancy Study. Diabetes Care 1995; 18(5):631–637. pmid:8586000
- American Diabetes Association. Standards of medical care in diabetes—2016. Diabetes Care 2016; 39 (suppl 1):S1–S109.
- Hawthorne, G. Maternal complications in diabetic pregnancy. Best Pract Res Clin Obstet Gynaecol 2011; 25(1):77–90. doi:10.1016/j.bpobgyn.2010.10.015
- Ringholm L, Damm JA, Vestgaard M, Damm P, Mathiesen ER. Diabetic nephropathy in women with preexisting diabetes: from pregnancy planning to breastfeeding. Curr Diab Rep 2016; 16(2):12. doi:10.1007/s11892-015-0705-3
- Zhang JJ, Ma XX, Hao L, Liu LJ, Lv JC, Zhang H. A systematic review and meta-analysis of outcomes of pregnancy in CKD and CKD outcomes in pregnancy. Clin J Am Soc Nephrol 2015; 10(11):1964–1978. doi:10.2215/CJN.09250914
- Umpierrez GE, Latif KA, Murphy MB, et al. Thyroid dysfunction in patients with type 1 diabetes: a longitudinal study. Diabetes Care 2003; 26(4):1181–1185. pmid:12663594
- Alexander EK, Pearce EN, Brent GA, et al. 2017 Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and the Postpartum. Thyroid 2017; 27(3):315–389. doi:10.1089/thy.2016.0457
- Akirov A, Pinhas-Hamiel O. Co-occurrence of type 1 diabetes mellitus and celiac disease. World J Diabetes 2015; 6(5):707–714. doi:10.4239/wjd.v6.i5.707
- Saccone G, Berghella V, Sarno L, et al. Celiac disease and obstetric complications: a systematic review and metaanalysis. Am J Obstet Gynecol 2016; 214(2):225–234. doi:10.1016/j.ajog.2015.09.080
- Feghali M, Venkataramanan R, Caritis S. Pharmacokinetics of drugs in pregnancy. Semin Perinatol 2015; 39(7):512–519. doi:10.1053/j.semperi.2015.08.003
- de Valk HW, Visser GH. Insulin during pregnancy, labour and delivery. Best Pract Res Clin Obstet Gynaecol 2011; 25(1):65–76. doi:10.1016/j.bpobgyn.2010.10.002
- Morello CM. Pharmacokinetics and pharmacodynamics of insulin analogs in special populations with type 2 diabetes mellitus. Int J Gen Med 2011; 4:827–835. doi:10.2147/IJGM.S26889
- Farrar D, Tuffnell DJ, West J, West HM. Continuous subcutaneous insulin infusion versus multiple daily injections of insulin for pregnant women with diabetes. Cochrane Database Syst Rev 2016; (6):CD005542. doi:10.1002/14651858.CD005542.pub2
- Charles B, Norris R, Xiao X, Hague W. Population pharmacokinetics of metformin in late pregnancy. Ther Drug Monit 2006; 28(1):67–72. pmid:16418696
- Balsells M, García-Patterson A, Solà I, Roqué M, Gich I, Corcoy R. Glibenclamide, metformin, and insulin for the treatment of gestational diabetes: a systematic review and meta-analysis. BMJ 2015; 350:h102. doi:10.1136/bmj.h102
- Hebert MF, Ma X, Naraharisetti SB, et al; Obstetric-Fetal Pharmacology Research Unit Network. Are we optimizing gestational diabetes treatment with glyburide? The pharmacologic basis for better clinical practice. Clin Pharmacol Ther 2009; 85(6):607–614. doi:10.1038/clpt.2009.5
- Langer O, Conway DL, Berkus MD, Xenakis EM, Gonzales O. A comparison of glyburide and insulin in women with gestational diabetes mellitus. N Engl J Med 2000; 343(16):1134–1138. doi:10.1056/NEJM200010193431601
- Camelo Castillo W, Boggess K, Stürmer T, Brookhart MA, Benjamin DK Jr, Jonsson Funk M. Association of adverse pregnancy outcomes with glyburide vs insulin in women with gestational diabetes. JAMA Pediatr 2015; 169:452–458. doi:10.1001/jamapediatrics.2015.74
- Gowda RM, Khan IA, Mehta NJ, Vasavada BC, Sacchi TJ. Cardiac arrhythmias in pregnancy: clinical and therapeutic considerations. Int J Cardiol 2003; 88(2):129–133. pmid:12714190
- Khandelwal M, Kumanova M, Gaughan JP, Reece EA. Role of diltiazem in pregnant women with chronic renal disease. J Matern Fetal Neonatal Med 2002; 12(6):408–412. doi:10.1080/jmf.12.6.408.412
- Magee LA, Abalos E, von Dadelszen P, Sibai B, Easterling T, Walkinshaw S; CHIPS Study Group. How to manage hypertension in pregnancy effectively. Br J Clin Pharmacol 2011; 72(3):394–401. doi:10.1111/j.1365-2125.2011.04002.x
- Cooper WO, Hernandez-Diaz S, Arbogast PG, et al. Major congenital malformations after first-trimester exposure to ACE inhibitors. N Engl J Med 2006; 354(23):2443–2451. doi:10.1056/NEJMoa055202
- Costantine MM, Cleary K, Hebert MF, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Obstetric-Fetal Pharmacology Research Units Network. Safety and pharmacokinetics of pravastatin used for the prevention of preeclampsia in high-risk pregnant women: a pilot randomized controlled trial. Am J Obstet Gynecol 2016; 214(6):720.e1–720.e17. doi:10.1016/j.ajog.2015.12.038
- LeFevre ML; US Preventive Services Task Force. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: US Preventive Services Task Force recommendation statement. Ann Intern Med 2014; 161(11):819–826. doi:10.7326/M14-1884
- Curry SJ, Grossman DC, Whitlock EP, Cantu A. Behavioral counseling research and evidence-based practice recommendations: US Preventive Services Task Force perspectives. Ann Intern Med 2014; 160(6):407–413. doi:10.7326/M13-2128
- Wald N, Law M, Morris J, Wald D. Quantifying the effect of folic acid. Lancet 2001; 358(9298):2069–2073. pmid:11755633
- US Preventive Services Task Force; Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Folic acid supplementation for the prevention of neural tube defects: US Preventive Services Task Force recommendation statement. JAMA 2017; 317(2):183–189. doi:10.1001/jama.2016.19438
- US Preventive Services Task Force; Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Primary care interventions to support breastfeeding: US Preventive Services Task Force recommendation statement. JAMA 2016; 316(16):1688–1693. doi:10.1001/jama.2016.14697
- Newton ER, Hale TW. Drugs in breast milk. Clin Obstet Gynecol 2015; 58(4):868–884. doi:10.1097/GRF.0000000000000142
- Xiang AH, Kawakubo M, Kjos SL, Buchanan TA. Long-acting injectable progestin contraception and risk of type 2 diabetes in Latino women with prior gestational diabetes mellitus. Diabetes Care 2006; 29(3):613–617. pmid:16505515
KEY POINTS
- Aim for a hemoglobin A1c of 6.5% or lower, if it is attainable without increasing the risk of hypoglycemia.
- Avoid teratogenic drugs in sexually active women of childbearing age unless the patient uses effective contraception.
- Because about half of pregnancies are unplanned, it is important to routinely discuss family planning and provide preconception counseling that includes reducing risks associated with pregnancy.
- Screen for diabetic end-organ damage, especially retinopathy and nephropathy.
HbA1c cutpoint predicts pediatric T1DM within a year
ORLANDO – Among children with genetic risks for type 1 diabetes and autoantibodies against pancreatic islet cells, a hemoglobin A1c at or above 5.6% strongly predicts the onset of type 1 diabetes within a year, according to investigators from The Environmental Determinants of Diabetes in the Young (TEDDY) study.
The risk is even greater if other factors – age at A1c test, month of A1c test, continent of residence, and the z-score for one antibody in particular, IA2A, a tyrosine phosphatase antigen protein – are taken into account, with an area under the curve (AUC) of about 0.97. The study team is developing an online risk calculator for clinicians so they can simply plug in the numbers.
But the 5.6% cutpoint works well even by itself, with an AUC of about 0.86. Among the children with genetic risk factors and islet cell autoantibodies who hit that mark in the study, the median time to diagnosis of type 1 diabetes mellitus (T1DM) was 7.1 months.
The point of the work is to catch disease onset early to prevent children from going into diabetic ketoacidosis.
The ultimate goal of TEDDY is to identify infectious agents, dietary factors, and other environmental agents that either trigger or protect against T1DM in genetically susceptible children, to develop strategies to prevent, delay, or even reverse T1DM. For more than a decade, the consortium has been following more than 8,000 children who screened positive at birth for genetic anomalies in the human leukocyte antigen region on their 6th chromosome, a major risk factor for T1DM. The team is following them to find out what puts them over the edge; A1c seems to be key.
Catching the disease early is a goal. Until now, the TEDDY team has used the development of pancreatic islet cell autoantibodies to trigger oral glucose tolerance tests (OGTTs) every 6 months.
The problem is that islet antibodies “are great at saying that you are going to get diabetes but not when. We have kids who have been multiple antibody positive now for 6, 7, 8 years” but who still haven’t developed T1DM. In the meantime, their parents have been dragging them in for OGTTs every 6 months for years, said lead investigator and TEDDY study coordinator Michael Killian, of the Pacific Northwest Research Institute, Seattle.
With the A1c cutpoint, it should be safe to hold off on direct glycemic surveillance until A1c levels reach 5.6%, and even safer when the full risk prediction model with 1A2A z-scores and other factors are available. Once children hit the parameters, it’s near certain they will develop T1DM within a year, so the findings should reduce the number of OGTT tests to just two or three. In the end, “we’ll get better compliance” with testing and still “catch these kids early,” Mr. Killian said at the annual scientific sessions of the American Diabetes Association.
Rare is the newborn who is screened for diabetes risk at birth, and even rarer is the child who is followed for autoantibodies. If the findings hold out, however, such early action could be the future.
“We envision a time” when newborns are screened for T1DM risk and followed for autoantibodies. Glycemic surveillance will kick in if they hit A1c levels of 5.6%, said William Hagopian, MD, PhD, clinical associate professor at the University of Washington, Seattle, and a TEDDY principal investigator.
Among the 8,000-plus children followed, 456 had persistent islet autoantibodies and at least three A1c tests in the prior 12 months; 104 progressed to T1DM and 352 did not. The mean age to islet autoantibody seroconversion was 43 months, and mean age to T1DM diagnosis was 73 months. The team ran a receiver operating curve analysis to identify the optimum A1c cutpoint, 5.6%.
The month of testing mattered, because “glycemia is higher in the winter, lower in the summer, and insulin sensitivity is lower in the winter, and higher in the summer,” Dr. Hagopian said. It probably has something to do with what the stresses of early human evolution bred into the genes.
The IA2A autoantibody z-score is the only number that will be cumbersome to plug into the upcoming online risk calculator. It’s the number of standard deviations off your reference lab’s mean. “You have to talk to the lab that does your IA2As to know what the standard deviation is,” Dr. Hagopian said.
The investigators had no disclosures. TEDDY is supported by the National Institutes of Health, among other entities.
SOURCE: Killian M et al. ADA 2018, Abstract 162-LB
ORLANDO – Among children with genetic risks for type 1 diabetes and autoantibodies against pancreatic islet cells, a hemoglobin A1c at or above 5.6% strongly predicts the onset of type 1 diabetes within a year, according to investigators from The Environmental Determinants of Diabetes in the Young (TEDDY) study.
The risk is even greater if other factors – age at A1c test, month of A1c test, continent of residence, and the z-score for one antibody in particular, IA2A, a tyrosine phosphatase antigen protein – are taken into account, with an area under the curve (AUC) of about 0.97. The study team is developing an online risk calculator for clinicians so they can simply plug in the numbers.
But the 5.6% cutpoint works well even by itself, with an AUC of about 0.86. Among the children with genetic risk factors and islet cell autoantibodies who hit that mark in the study, the median time to diagnosis of type 1 diabetes mellitus (T1DM) was 7.1 months.
The point of the work is to catch disease onset early to prevent children from going into diabetic ketoacidosis.
The ultimate goal of TEDDY is to identify infectious agents, dietary factors, and other environmental agents that either trigger or protect against T1DM in genetically susceptible children, to develop strategies to prevent, delay, or even reverse T1DM. For more than a decade, the consortium has been following more than 8,000 children who screened positive at birth for genetic anomalies in the human leukocyte antigen region on their 6th chromosome, a major risk factor for T1DM. The team is following them to find out what puts them over the edge; A1c seems to be key.
Catching the disease early is a goal. Until now, the TEDDY team has used the development of pancreatic islet cell autoantibodies to trigger oral glucose tolerance tests (OGTTs) every 6 months.
The problem is that islet antibodies “are great at saying that you are going to get diabetes but not when. We have kids who have been multiple antibody positive now for 6, 7, 8 years” but who still haven’t developed T1DM. In the meantime, their parents have been dragging them in for OGTTs every 6 months for years, said lead investigator and TEDDY study coordinator Michael Killian, of the Pacific Northwest Research Institute, Seattle.
With the A1c cutpoint, it should be safe to hold off on direct glycemic surveillance until A1c levels reach 5.6%, and even safer when the full risk prediction model with 1A2A z-scores and other factors are available. Once children hit the parameters, it’s near certain they will develop T1DM within a year, so the findings should reduce the number of OGTT tests to just two or three. In the end, “we’ll get better compliance” with testing and still “catch these kids early,” Mr. Killian said at the annual scientific sessions of the American Diabetes Association.
Rare is the newborn who is screened for diabetes risk at birth, and even rarer is the child who is followed for autoantibodies. If the findings hold out, however, such early action could be the future.
“We envision a time” when newborns are screened for T1DM risk and followed for autoantibodies. Glycemic surveillance will kick in if they hit A1c levels of 5.6%, said William Hagopian, MD, PhD, clinical associate professor at the University of Washington, Seattle, and a TEDDY principal investigator.
Among the 8,000-plus children followed, 456 had persistent islet autoantibodies and at least three A1c tests in the prior 12 months; 104 progressed to T1DM and 352 did not. The mean age to islet autoantibody seroconversion was 43 months, and mean age to T1DM diagnosis was 73 months. The team ran a receiver operating curve analysis to identify the optimum A1c cutpoint, 5.6%.
The month of testing mattered, because “glycemia is higher in the winter, lower in the summer, and insulin sensitivity is lower in the winter, and higher in the summer,” Dr. Hagopian said. It probably has something to do with what the stresses of early human evolution bred into the genes.
The IA2A autoantibody z-score is the only number that will be cumbersome to plug into the upcoming online risk calculator. It’s the number of standard deviations off your reference lab’s mean. “You have to talk to the lab that does your IA2As to know what the standard deviation is,” Dr. Hagopian said.
The investigators had no disclosures. TEDDY is supported by the National Institutes of Health, among other entities.
SOURCE: Killian M et al. ADA 2018, Abstract 162-LB
ORLANDO – Among children with genetic risks for type 1 diabetes and autoantibodies against pancreatic islet cells, a hemoglobin A1c at or above 5.6% strongly predicts the onset of type 1 diabetes within a year, according to investigators from The Environmental Determinants of Diabetes in the Young (TEDDY) study.
The risk is even greater if other factors – age at A1c test, month of A1c test, continent of residence, and the z-score for one antibody in particular, IA2A, a tyrosine phosphatase antigen protein – are taken into account, with an area under the curve (AUC) of about 0.97. The study team is developing an online risk calculator for clinicians so they can simply plug in the numbers.
But the 5.6% cutpoint works well even by itself, with an AUC of about 0.86. Among the children with genetic risk factors and islet cell autoantibodies who hit that mark in the study, the median time to diagnosis of type 1 diabetes mellitus (T1DM) was 7.1 months.
The point of the work is to catch disease onset early to prevent children from going into diabetic ketoacidosis.
The ultimate goal of TEDDY is to identify infectious agents, dietary factors, and other environmental agents that either trigger or protect against T1DM in genetically susceptible children, to develop strategies to prevent, delay, or even reverse T1DM. For more than a decade, the consortium has been following more than 8,000 children who screened positive at birth for genetic anomalies in the human leukocyte antigen region on their 6th chromosome, a major risk factor for T1DM. The team is following them to find out what puts them over the edge; A1c seems to be key.
Catching the disease early is a goal. Until now, the TEDDY team has used the development of pancreatic islet cell autoantibodies to trigger oral glucose tolerance tests (OGTTs) every 6 months.
The problem is that islet antibodies “are great at saying that you are going to get diabetes but not when. We have kids who have been multiple antibody positive now for 6, 7, 8 years” but who still haven’t developed T1DM. In the meantime, their parents have been dragging them in for OGTTs every 6 months for years, said lead investigator and TEDDY study coordinator Michael Killian, of the Pacific Northwest Research Institute, Seattle.
With the A1c cutpoint, it should be safe to hold off on direct glycemic surveillance until A1c levels reach 5.6%, and even safer when the full risk prediction model with 1A2A z-scores and other factors are available. Once children hit the parameters, it’s near certain they will develop T1DM within a year, so the findings should reduce the number of OGTT tests to just two or three. In the end, “we’ll get better compliance” with testing and still “catch these kids early,” Mr. Killian said at the annual scientific sessions of the American Diabetes Association.
Rare is the newborn who is screened for diabetes risk at birth, and even rarer is the child who is followed for autoantibodies. If the findings hold out, however, such early action could be the future.
“We envision a time” when newborns are screened for T1DM risk and followed for autoantibodies. Glycemic surveillance will kick in if they hit A1c levels of 5.6%, said William Hagopian, MD, PhD, clinical associate professor at the University of Washington, Seattle, and a TEDDY principal investigator.
Among the 8,000-plus children followed, 456 had persistent islet autoantibodies and at least three A1c tests in the prior 12 months; 104 progressed to T1DM and 352 did not. The mean age to islet autoantibody seroconversion was 43 months, and mean age to T1DM diagnosis was 73 months. The team ran a receiver operating curve analysis to identify the optimum A1c cutpoint, 5.6%.
The month of testing mattered, because “glycemia is higher in the winter, lower in the summer, and insulin sensitivity is lower in the winter, and higher in the summer,” Dr. Hagopian said. It probably has something to do with what the stresses of early human evolution bred into the genes.
The IA2A autoantibody z-score is the only number that will be cumbersome to plug into the upcoming online risk calculator. It’s the number of standard deviations off your reference lab’s mean. “You have to talk to the lab that does your IA2As to know what the standard deviation is,” Dr. Hagopian said.
The investigators had no disclosures. TEDDY is supported by the National Institutes of Health, among other entities.
SOURCE: Killian M et al. ADA 2018, Abstract 162-LB
FROM ADA 2018
Key clinical point: Among children with genetic risks for type 1 diabetes and autoantibodies against pancreatic islet cells, a hemoglobin A1c at or above 5.6% strongly predicts the onset of type 1 diabetes within a year.
Major finding: Among the children with genetic risk factors and islet cell autoantibodies who hit that mark, the median time to diagnosis was 7.1 months.
Study details: The findings are from more than 400 children in The Environmental Determinants of Diabetes in the Young (TEDDY) cohort.
Disclosures: The investigators had no disclosures. TEDDY is supported by the National Institutes of Health, among other entities.
Source: Killian M et al. ADA 2018, Abstract 162-LB.
Diabetes, hypertension, smoking may raise risk for late-onset epilepsy
Hypertension, diabetes, and smoking in midlife are potentially modifiable risk factors for late-onset epilepsy, according to a study that also found an increased risk with the apolipoprotein E4 (APOE4) genotype and in black individuals.
Emily L. Johnson, MD, of Johns Hopkins University, Baltimore, and her coauthors analyzed data from 10,420 participants in the Atherosclerosis Risk in Communities prospective cohort study and found 596 who developed late-onset epilepsy (LOE), defined as recurrent unprovoked seizures starting at 60 years or older.
The study, published online July 23 in JAMA Neurology, showed that individuals with hypertension at baseline had a 30% higher risk of LOE, those who smoked had a 9% higher risk, and those with diabetes had a 45% higher risk. However, the increased risk associated with smoking was evident only in women, who had a 27% higher risk.
Participants with incident stroke had a 3.38-fold higher risk of LOE, and those with dementia had a 2.56-fold higher risk, Dr. Johnson and her colleagues reported.
“The association of LOE with vascular and lifestyle risk factors persisted after participants with diagnosis of clinical stroke or dementia were included or censored, suggesting that these risk factors may contribute to LOE even in the absence of dementia or clinical stroke,” the investigators wrote.
However, higher levels of physical activity decreased the risk by 10%, and moderate alcohol consumption – defined as 1-7 standard drinks per week – was associated with a 28% reduction.
Race and geographic location both influenced the risk of LOE; black participants showed a 66% higher risk, compared with whites, and black participants in Mississippi and North Carolina had a higher risk than did North Carolina white participants. The highest risk of LOE was seen in black participants with diabetes.
“The reasons for the different incidences of LOE by race/ethnicity may be owing to differing effects of comorbidities, such as diabetes, for which we found a significantly higher effect in black individuals than in white individuals,” the authors wrote.
Individuals who had one APOE4 allele showed a 46% higher risk, and those with two alleles showed a 2.57-fold higher risk.
“The APOE4 genotype is the major genetic risk factor for Alzheimer’s disease, which is associated with epilepsy; however, no prior association between APOE4 and LOE has previously been shown,” the authors reported.
The researchers noted that their findings suggested that lifestyle modifications earlier in life could mitigate some of the risk factors associated with LOE, and could also help identify patients at higher risk for the disease.
No funding was declared. One author declared consultancy and investigator positions with private industry.
SOURCE: Johnson E et al. JAMA Neurol, 2018 July 23. doi: 10.1001/jamaneurol.2018.1935.
Hypertension, diabetes, and smoking in midlife are potentially modifiable risk factors for late-onset epilepsy, according to a study that also found an increased risk with the apolipoprotein E4 (APOE4) genotype and in black individuals.
Emily L. Johnson, MD, of Johns Hopkins University, Baltimore, and her coauthors analyzed data from 10,420 participants in the Atherosclerosis Risk in Communities prospective cohort study and found 596 who developed late-onset epilepsy (LOE), defined as recurrent unprovoked seizures starting at 60 years or older.
The study, published online July 23 in JAMA Neurology, showed that individuals with hypertension at baseline had a 30% higher risk of LOE, those who smoked had a 9% higher risk, and those with diabetes had a 45% higher risk. However, the increased risk associated with smoking was evident only in women, who had a 27% higher risk.
Participants with incident stroke had a 3.38-fold higher risk of LOE, and those with dementia had a 2.56-fold higher risk, Dr. Johnson and her colleagues reported.
“The association of LOE with vascular and lifestyle risk factors persisted after participants with diagnosis of clinical stroke or dementia were included or censored, suggesting that these risk factors may contribute to LOE even in the absence of dementia or clinical stroke,” the investigators wrote.
However, higher levels of physical activity decreased the risk by 10%, and moderate alcohol consumption – defined as 1-7 standard drinks per week – was associated with a 28% reduction.
Race and geographic location both influenced the risk of LOE; black participants showed a 66% higher risk, compared with whites, and black participants in Mississippi and North Carolina had a higher risk than did North Carolina white participants. The highest risk of LOE was seen in black participants with diabetes.
“The reasons for the different incidences of LOE by race/ethnicity may be owing to differing effects of comorbidities, such as diabetes, for which we found a significantly higher effect in black individuals than in white individuals,” the authors wrote.
Individuals who had one APOE4 allele showed a 46% higher risk, and those with two alleles showed a 2.57-fold higher risk.
“The APOE4 genotype is the major genetic risk factor for Alzheimer’s disease, which is associated with epilepsy; however, no prior association between APOE4 and LOE has previously been shown,” the authors reported.
The researchers noted that their findings suggested that lifestyle modifications earlier in life could mitigate some of the risk factors associated with LOE, and could also help identify patients at higher risk for the disease.
No funding was declared. One author declared consultancy and investigator positions with private industry.
SOURCE: Johnson E et al. JAMA Neurol, 2018 July 23. doi: 10.1001/jamaneurol.2018.1935.
Hypertension, diabetes, and smoking in midlife are potentially modifiable risk factors for late-onset epilepsy, according to a study that also found an increased risk with the apolipoprotein E4 (APOE4) genotype and in black individuals.
Emily L. Johnson, MD, of Johns Hopkins University, Baltimore, and her coauthors analyzed data from 10,420 participants in the Atherosclerosis Risk in Communities prospective cohort study and found 596 who developed late-onset epilepsy (LOE), defined as recurrent unprovoked seizures starting at 60 years or older.
The study, published online July 23 in JAMA Neurology, showed that individuals with hypertension at baseline had a 30% higher risk of LOE, those who smoked had a 9% higher risk, and those with diabetes had a 45% higher risk. However, the increased risk associated with smoking was evident only in women, who had a 27% higher risk.
Participants with incident stroke had a 3.38-fold higher risk of LOE, and those with dementia had a 2.56-fold higher risk, Dr. Johnson and her colleagues reported.
“The association of LOE with vascular and lifestyle risk factors persisted after participants with diagnosis of clinical stroke or dementia were included or censored, suggesting that these risk factors may contribute to LOE even in the absence of dementia or clinical stroke,” the investigators wrote.
However, higher levels of physical activity decreased the risk by 10%, and moderate alcohol consumption – defined as 1-7 standard drinks per week – was associated with a 28% reduction.
Race and geographic location both influenced the risk of LOE; black participants showed a 66% higher risk, compared with whites, and black participants in Mississippi and North Carolina had a higher risk than did North Carolina white participants. The highest risk of LOE was seen in black participants with diabetes.
“The reasons for the different incidences of LOE by race/ethnicity may be owing to differing effects of comorbidities, such as diabetes, for which we found a significantly higher effect in black individuals than in white individuals,” the authors wrote.
Individuals who had one APOE4 allele showed a 46% higher risk, and those with two alleles showed a 2.57-fold higher risk.
“The APOE4 genotype is the major genetic risk factor for Alzheimer’s disease, which is associated with epilepsy; however, no prior association between APOE4 and LOE has previously been shown,” the authors reported.
The researchers noted that their findings suggested that lifestyle modifications earlier in life could mitigate some of the risk factors associated with LOE, and could also help identify patients at higher risk for the disease.
No funding was declared. One author declared consultancy and investigator positions with private industry.
SOURCE: Johnson E et al. JAMA Neurol, 2018 July 23. doi: 10.1001/jamaneurol.2018.1935.
FROM JAMA NEUROLOGY
Key clinical point:
Major finding: Midlife diabetes is associated with a 45% higher risk of late-onset epilepsy.
Study details: A prospective cohort study in 10,420 individuals in the Atherosclerosis Risk in Communities study.
Disclosures: No funding was declared. One author declared consultancy and investigator positions with private industry.
Source: Johnson E et al. JAMA Neurol. 2018 Jul 23. doi: 10.1001/jamaneurol.2018.1935.