User login
Intensive treatment for T2D pays off in the long run
ORLANDO – Intensified multifactorial treatment proved cost effective over time in type 2 diabetes patients in the practice-changing Steno-2 study, according to 21-year follow-up data from the randomized Danish study.
Cumulative direct health care costs from the start of the trial in 1993 through 2014 were about $13 million in 24 patients in the intensive treatment group who were available for follow-up, and about $12.3 million in 42 patients in the conventional treatment group. The difference in costs between the groups was not statistically significant, Joachim Gaede reported at the annual scientific sessions of the American Diabetes Association.
Costs per patient-year during 1996-2014, however, were significantly lower in the intensive treatment group ($9,648 vs. $10, 681, respectively), said Mr. Gaede, a graduate student in the medicine program at the University of Copenhagen.
Furthermore, patients in the intensified treatment group lived a median of 7.9 years longer than did those who were in the conventional treatment group, suggesting that while costs might be higher early on, investing in early intensified treatment of all known modifiable risk factors in high-risk patients will prolong life and still save money over time thanks to reduced complication-related costs, he noted.
Steno-2 was an open, parallel group study initiated in 1993 to compare conventional multifactorial treatment of type 2 diabetes mellitus (T2DM) with an intensified approach over an 8-year period. Enrollment included 160 patients with high-risk type 2 diabetes. After the primary composite cardiovascular endpoint was assessed, the trial continued as an observational study, with all patients given the intensified, multifactorial treatment that consisted of lifestyle measures and medications targeting hyperglycemia, hypertension, hypercholesterolemia, and hypercoagulation.
Reports from the study over the years led to changes in treatment guidelines to promote more intensive multifactorial treatment, Mr. Gaede said. For example, the initial results reported in 1999 showed a 50% relative risk reduction in kidney, eye, and nerve complications after 4 years with intensive versus conventional treatment; a 2003 report showed a 53% relative risk reduction in MI, stroke, and amputation after 8 years; and a 2008 report demonstrated a 46% relative risk reduction in death after 13 years. Finally, in 2016 a 7.9-year gain in lifespan after 21 years with intensive versus conventional treatment was reported.
In this video interview, Mr. Gaede, junior lead study author, discusses the Steno-2 study findings and the current cost analysis data.
“The bottom line is that ... you can actually, as a patient, be treated at a specialized diabetes clinic ... and, in the long run, it doesn’t cost you anything” more, he said, explaining that the up-front costs of intensive treatment are offset by the money saved because of the reduced complications over time.
Mr. Gaede reported having no disclosures.
sworcester@frontlinemedcom.com
SOURCE: Gaede J et al. ADA 2018, Abstract 162-OR.
ORLANDO – Intensified multifactorial treatment proved cost effective over time in type 2 diabetes patients in the practice-changing Steno-2 study, according to 21-year follow-up data from the randomized Danish study.
Cumulative direct health care costs from the start of the trial in 1993 through 2014 were about $13 million in 24 patients in the intensive treatment group who were available for follow-up, and about $12.3 million in 42 patients in the conventional treatment group. The difference in costs between the groups was not statistically significant, Joachim Gaede reported at the annual scientific sessions of the American Diabetes Association.
Costs per patient-year during 1996-2014, however, were significantly lower in the intensive treatment group ($9,648 vs. $10, 681, respectively), said Mr. Gaede, a graduate student in the medicine program at the University of Copenhagen.
Furthermore, patients in the intensified treatment group lived a median of 7.9 years longer than did those who were in the conventional treatment group, suggesting that while costs might be higher early on, investing in early intensified treatment of all known modifiable risk factors in high-risk patients will prolong life and still save money over time thanks to reduced complication-related costs, he noted.
Steno-2 was an open, parallel group study initiated in 1993 to compare conventional multifactorial treatment of type 2 diabetes mellitus (T2DM) with an intensified approach over an 8-year period. Enrollment included 160 patients with high-risk type 2 diabetes. After the primary composite cardiovascular endpoint was assessed, the trial continued as an observational study, with all patients given the intensified, multifactorial treatment that consisted of lifestyle measures and medications targeting hyperglycemia, hypertension, hypercholesterolemia, and hypercoagulation.
Reports from the study over the years led to changes in treatment guidelines to promote more intensive multifactorial treatment, Mr. Gaede said. For example, the initial results reported in 1999 showed a 50% relative risk reduction in kidney, eye, and nerve complications after 4 years with intensive versus conventional treatment; a 2003 report showed a 53% relative risk reduction in MI, stroke, and amputation after 8 years; and a 2008 report demonstrated a 46% relative risk reduction in death after 13 years. Finally, in 2016 a 7.9-year gain in lifespan after 21 years with intensive versus conventional treatment was reported.
In this video interview, Mr. Gaede, junior lead study author, discusses the Steno-2 study findings and the current cost analysis data.
“The bottom line is that ... you can actually, as a patient, be treated at a specialized diabetes clinic ... and, in the long run, it doesn’t cost you anything” more, he said, explaining that the up-front costs of intensive treatment are offset by the money saved because of the reduced complications over time.
Mr. Gaede reported having no disclosures.
sworcester@frontlinemedcom.com
SOURCE: Gaede J et al. ADA 2018, Abstract 162-OR.
ORLANDO – Intensified multifactorial treatment proved cost effective over time in type 2 diabetes patients in the practice-changing Steno-2 study, according to 21-year follow-up data from the randomized Danish study.
Cumulative direct health care costs from the start of the trial in 1993 through 2014 were about $13 million in 24 patients in the intensive treatment group who were available for follow-up, and about $12.3 million in 42 patients in the conventional treatment group. The difference in costs between the groups was not statistically significant, Joachim Gaede reported at the annual scientific sessions of the American Diabetes Association.
Costs per patient-year during 1996-2014, however, were significantly lower in the intensive treatment group ($9,648 vs. $10, 681, respectively), said Mr. Gaede, a graduate student in the medicine program at the University of Copenhagen.
Furthermore, patients in the intensified treatment group lived a median of 7.9 years longer than did those who were in the conventional treatment group, suggesting that while costs might be higher early on, investing in early intensified treatment of all known modifiable risk factors in high-risk patients will prolong life and still save money over time thanks to reduced complication-related costs, he noted.
Steno-2 was an open, parallel group study initiated in 1993 to compare conventional multifactorial treatment of type 2 diabetes mellitus (T2DM) with an intensified approach over an 8-year period. Enrollment included 160 patients with high-risk type 2 diabetes. After the primary composite cardiovascular endpoint was assessed, the trial continued as an observational study, with all patients given the intensified, multifactorial treatment that consisted of lifestyle measures and medications targeting hyperglycemia, hypertension, hypercholesterolemia, and hypercoagulation.
Reports from the study over the years led to changes in treatment guidelines to promote more intensive multifactorial treatment, Mr. Gaede said. For example, the initial results reported in 1999 showed a 50% relative risk reduction in kidney, eye, and nerve complications after 4 years with intensive versus conventional treatment; a 2003 report showed a 53% relative risk reduction in MI, stroke, and amputation after 8 years; and a 2008 report demonstrated a 46% relative risk reduction in death after 13 years. Finally, in 2016 a 7.9-year gain in lifespan after 21 years with intensive versus conventional treatment was reported.
In this video interview, Mr. Gaede, junior lead study author, discusses the Steno-2 study findings and the current cost analysis data.
“The bottom line is that ... you can actually, as a patient, be treated at a specialized diabetes clinic ... and, in the long run, it doesn’t cost you anything” more, he said, explaining that the up-front costs of intensive treatment are offset by the money saved because of the reduced complications over time.
Mr. Gaede reported having no disclosures.
sworcester@frontlinemedcom.com
SOURCE: Gaede J et al. ADA 2018, Abstract 162-OR.
REPORTING FROM ADA 2018
Better stent technology needed for diabetes patients
PARIS – Interventional cardiologists are hopeful that a new generation of investigational coronary stents designed specifically for use in diabetes patients will improve upon the relatively poor current outcomes of percutaneous coronary intervention in that population.
The operative word here is “abluminal.” Both of the novel drug-eluting stents featured at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions position their antirestenosis drugs abluminally: that is, aimed toward the vessel wall surface, not the lumen.
“The hypothesis is that ,” explained Luca Testa, MD, PhD, head of the coronary revascularization unit at San Donato Hospital in Milan.
There is a major unmet need for improved stent technology that addresses the special needs of diabetes patients, who tend to have more diffuse and rapidly progressive coronary artery disease (CAD) with longer lesions. Target lesion revascularization rates at 5 years of follow-up in diabetes patients with current generation drug-eluting stents (DES) remain high, at 20% or more. And diabetes patients are roughly 3.5-fold more likely to have nonfocal, diffuse coronary lesions than are nondiabetic patients with CAD, the cardiologist noted.
The sense of urgency surrounding this unmet need stems from the ongoing worldwide epidemic of diabetes. The global prevalence of diabetes was estimated at 382 million in 2013 and is projected to climb to nearly 600 million by 2035. Diabetes patients are two to four times more likely to develop CAD than are those without the disease. Because of the current suboptimal results with percutaneous coronary intervention (PCI), many of them are being referred for coronary artery bypass surgery.
Dr. Testa presented the 1-year results of the ongoing en-ABL e-Registry, a 5-year, multicenter, prospective, all-comers registry of 859 diabetic and 1,641 nondiabetic CAD patients who received the Abluminus DES at 31 centers in India. The novel stent, developed by Envision Scientific of India, is coated with sirolimus on the abluminal side. The device is actually both a DES and a drug-coated balloon. The balloon, including its proximal and distal ends, are also sirolimus coated to maximize exposure of diseased artery to the drug. The balloon needs to be inflated in position for at least 30 seconds to deliver its portion of sirolimus. The stent is composed of a biodegradable polymer matrix that is metabolized within 6-8 months.
The primary endpoint at 1 year of follow-up was the composite of cardiac death, target vessel MI, and target lesion or vessel revascularization. The rate was 3.12% in the diabetic population, which wasn’t significantly different from the 2.1% rate in nondiabetic patients. Of note, the rate was 5.17% in the 138 insulin-dependent diabetes patients, compared with 2.76% in 721 non–insulin-dependent patients.
Among diabetes patients, the composite endpoint occurred in 2.82% of those who underwent primary PCI with the Abluminus DES for an acute MI, 3.96% of those treated for lesions in small vessels 2.75 mm or less in diameter, 3.75% in diabetes patients treated for long lesions, and 4.18% in the subgroup with long lesions in small vessels.
On the basis of these encouraging results, Dr. Testa has been named the principal investigator for the new prospective, multicenter, observational DEDICATE registry, restricted to diabetic patients treated with the Abluminus DES.
Also getting underway is a randomized, investigator-initiated, multicenter, single-blind pilot study involving 165 diabetes patients assigned 2:1 to the Abluminus DES or the Xience everolimus-eluting stent, widely considered the current gold standard DES. The study, known as the ABILITY trial, has as its primary endpoint the in-stent neointimal volume as measured by optical coherence tomography 6 months post PCI. The medical director of the study is Antonio Colombo, MD, director of the cardiac catheterization laboratory and the interventional cardiology unit at San Raffaele Hospital in Milan.
Elsewhere at EuroPCR 2018, officials at Alvimedica Medical Technologies announced that the company’s abluminal stent, known as the Cre8 EVO, will be pitted against the everolimus-eluting stent in a 55-center trial of 3,040 diabetes patients. The hypothesis of the Diab8 trial, based on preliminary data from pilot studies, is that the abluminal stent will show clinical superiority – not merely equivalence – at 1 year.
The Cre8 EVO stent utilizes a proprietary, polymer-free, drug-release technology involving reservoirs located on the stent’s outer surface that direct the controlled release of a mixture of sirolimus and fatty acids that the company calls the amphilimus formulation. The drug mixture is designed to enhance tissue permeation and sirolimus bioavailability. The body of the stent is cobalt, which was used based upon a conviction that polymers are more proinflammatory.
Dr. Colombo is also the principal investigator of the Diab8 trial, sponsored by Alvimedica.
Dr. Testa reported having no financial conflicts regarding his work on the en-ABL e-Registry, funded by a nonprofit Italian cardiovascular research foundation.
PARIS – Interventional cardiologists are hopeful that a new generation of investigational coronary stents designed specifically for use in diabetes patients will improve upon the relatively poor current outcomes of percutaneous coronary intervention in that population.
The operative word here is “abluminal.” Both of the novel drug-eluting stents featured at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions position their antirestenosis drugs abluminally: that is, aimed toward the vessel wall surface, not the lumen.
“The hypothesis is that ,” explained Luca Testa, MD, PhD, head of the coronary revascularization unit at San Donato Hospital in Milan.
There is a major unmet need for improved stent technology that addresses the special needs of diabetes patients, who tend to have more diffuse and rapidly progressive coronary artery disease (CAD) with longer lesions. Target lesion revascularization rates at 5 years of follow-up in diabetes patients with current generation drug-eluting stents (DES) remain high, at 20% or more. And diabetes patients are roughly 3.5-fold more likely to have nonfocal, diffuse coronary lesions than are nondiabetic patients with CAD, the cardiologist noted.
The sense of urgency surrounding this unmet need stems from the ongoing worldwide epidemic of diabetes. The global prevalence of diabetes was estimated at 382 million in 2013 and is projected to climb to nearly 600 million by 2035. Diabetes patients are two to four times more likely to develop CAD than are those without the disease. Because of the current suboptimal results with percutaneous coronary intervention (PCI), many of them are being referred for coronary artery bypass surgery.
Dr. Testa presented the 1-year results of the ongoing en-ABL e-Registry, a 5-year, multicenter, prospective, all-comers registry of 859 diabetic and 1,641 nondiabetic CAD patients who received the Abluminus DES at 31 centers in India. The novel stent, developed by Envision Scientific of India, is coated with sirolimus on the abluminal side. The device is actually both a DES and a drug-coated balloon. The balloon, including its proximal and distal ends, are also sirolimus coated to maximize exposure of diseased artery to the drug. The balloon needs to be inflated in position for at least 30 seconds to deliver its portion of sirolimus. The stent is composed of a biodegradable polymer matrix that is metabolized within 6-8 months.
The primary endpoint at 1 year of follow-up was the composite of cardiac death, target vessel MI, and target lesion or vessel revascularization. The rate was 3.12% in the diabetic population, which wasn’t significantly different from the 2.1% rate in nondiabetic patients. Of note, the rate was 5.17% in the 138 insulin-dependent diabetes patients, compared with 2.76% in 721 non–insulin-dependent patients.
Among diabetes patients, the composite endpoint occurred in 2.82% of those who underwent primary PCI with the Abluminus DES for an acute MI, 3.96% of those treated for lesions in small vessels 2.75 mm or less in diameter, 3.75% in diabetes patients treated for long lesions, and 4.18% in the subgroup with long lesions in small vessels.
On the basis of these encouraging results, Dr. Testa has been named the principal investigator for the new prospective, multicenter, observational DEDICATE registry, restricted to diabetic patients treated with the Abluminus DES.
Also getting underway is a randomized, investigator-initiated, multicenter, single-blind pilot study involving 165 diabetes patients assigned 2:1 to the Abluminus DES or the Xience everolimus-eluting stent, widely considered the current gold standard DES. The study, known as the ABILITY trial, has as its primary endpoint the in-stent neointimal volume as measured by optical coherence tomography 6 months post PCI. The medical director of the study is Antonio Colombo, MD, director of the cardiac catheterization laboratory and the interventional cardiology unit at San Raffaele Hospital in Milan.
Elsewhere at EuroPCR 2018, officials at Alvimedica Medical Technologies announced that the company’s abluminal stent, known as the Cre8 EVO, will be pitted against the everolimus-eluting stent in a 55-center trial of 3,040 diabetes patients. The hypothesis of the Diab8 trial, based on preliminary data from pilot studies, is that the abluminal stent will show clinical superiority – not merely equivalence – at 1 year.
The Cre8 EVO stent utilizes a proprietary, polymer-free, drug-release technology involving reservoirs located on the stent’s outer surface that direct the controlled release of a mixture of sirolimus and fatty acids that the company calls the amphilimus formulation. The drug mixture is designed to enhance tissue permeation and sirolimus bioavailability. The body of the stent is cobalt, which was used based upon a conviction that polymers are more proinflammatory.
Dr. Colombo is also the principal investigator of the Diab8 trial, sponsored by Alvimedica.
Dr. Testa reported having no financial conflicts regarding his work on the en-ABL e-Registry, funded by a nonprofit Italian cardiovascular research foundation.
PARIS – Interventional cardiologists are hopeful that a new generation of investigational coronary stents designed specifically for use in diabetes patients will improve upon the relatively poor current outcomes of percutaneous coronary intervention in that population.
The operative word here is “abluminal.” Both of the novel drug-eluting stents featured at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions position their antirestenosis drugs abluminally: that is, aimed toward the vessel wall surface, not the lumen.
“The hypothesis is that ,” explained Luca Testa, MD, PhD, head of the coronary revascularization unit at San Donato Hospital in Milan.
There is a major unmet need for improved stent technology that addresses the special needs of diabetes patients, who tend to have more diffuse and rapidly progressive coronary artery disease (CAD) with longer lesions. Target lesion revascularization rates at 5 years of follow-up in diabetes patients with current generation drug-eluting stents (DES) remain high, at 20% or more. And diabetes patients are roughly 3.5-fold more likely to have nonfocal, diffuse coronary lesions than are nondiabetic patients with CAD, the cardiologist noted.
The sense of urgency surrounding this unmet need stems from the ongoing worldwide epidemic of diabetes. The global prevalence of diabetes was estimated at 382 million in 2013 and is projected to climb to nearly 600 million by 2035. Diabetes patients are two to four times more likely to develop CAD than are those without the disease. Because of the current suboptimal results with percutaneous coronary intervention (PCI), many of them are being referred for coronary artery bypass surgery.
Dr. Testa presented the 1-year results of the ongoing en-ABL e-Registry, a 5-year, multicenter, prospective, all-comers registry of 859 diabetic and 1,641 nondiabetic CAD patients who received the Abluminus DES at 31 centers in India. The novel stent, developed by Envision Scientific of India, is coated with sirolimus on the abluminal side. The device is actually both a DES and a drug-coated balloon. The balloon, including its proximal and distal ends, are also sirolimus coated to maximize exposure of diseased artery to the drug. The balloon needs to be inflated in position for at least 30 seconds to deliver its portion of sirolimus. The stent is composed of a biodegradable polymer matrix that is metabolized within 6-8 months.
The primary endpoint at 1 year of follow-up was the composite of cardiac death, target vessel MI, and target lesion or vessel revascularization. The rate was 3.12% in the diabetic population, which wasn’t significantly different from the 2.1% rate in nondiabetic patients. Of note, the rate was 5.17% in the 138 insulin-dependent diabetes patients, compared with 2.76% in 721 non–insulin-dependent patients.
Among diabetes patients, the composite endpoint occurred in 2.82% of those who underwent primary PCI with the Abluminus DES for an acute MI, 3.96% of those treated for lesions in small vessels 2.75 mm or less in diameter, 3.75% in diabetes patients treated for long lesions, and 4.18% in the subgroup with long lesions in small vessels.
On the basis of these encouraging results, Dr. Testa has been named the principal investigator for the new prospective, multicenter, observational DEDICATE registry, restricted to diabetic patients treated with the Abluminus DES.
Also getting underway is a randomized, investigator-initiated, multicenter, single-blind pilot study involving 165 diabetes patients assigned 2:1 to the Abluminus DES or the Xience everolimus-eluting stent, widely considered the current gold standard DES. The study, known as the ABILITY trial, has as its primary endpoint the in-stent neointimal volume as measured by optical coherence tomography 6 months post PCI. The medical director of the study is Antonio Colombo, MD, director of the cardiac catheterization laboratory and the interventional cardiology unit at San Raffaele Hospital in Milan.
Elsewhere at EuroPCR 2018, officials at Alvimedica Medical Technologies announced that the company’s abluminal stent, known as the Cre8 EVO, will be pitted against the everolimus-eluting stent in a 55-center trial of 3,040 diabetes patients. The hypothesis of the Diab8 trial, based on preliminary data from pilot studies, is that the abluminal stent will show clinical superiority – not merely equivalence – at 1 year.
The Cre8 EVO stent utilizes a proprietary, polymer-free, drug-release technology involving reservoirs located on the stent’s outer surface that direct the controlled release of a mixture of sirolimus and fatty acids that the company calls the amphilimus formulation. The drug mixture is designed to enhance tissue permeation and sirolimus bioavailability. The body of the stent is cobalt, which was used based upon a conviction that polymers are more proinflammatory.
Dr. Colombo is also the principal investigator of the Diab8 trial, sponsored by Alvimedica.
Dr. Testa reported having no financial conflicts regarding his work on the en-ABL e-Registry, funded by a nonprofit Italian cardiovascular research foundation.
REPORTING FROM EUROPCR 2018
Diabetes patients pushed into high-deductible plans
ORLANDO – The proportion of diabetes patients enrolled in high-deductible health plans jumped from 10% in 2005 to about 50% in 2014, according to a review of insurance data for 63 million Americans under age 65 years.
Diabetes patients often don’t have a choice. To cut costs, high-deductible plans are increasingly the only ones employers offer.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
While that may be adequate for healthy people, it’s quite another issue for people with chronic conditions, especially ones with low income. Out-of-pocket expenses can be thousands of dollars more than with traditional health plans, and the extra costs aren’t always offset by lower premiums.
The trend is concerning, said senior investigator J. Frank Wharam, MB, MPH, an associate professor of population medicine at Harvard Medical School, Boston. He explained the problem, and what’s being done about it, in an interview at the annual scientific sessions of the American Diabetes Association.
aotto@mdedge.com
SOURCE: Garabedian LF et al. ADA 2018. Abstract 175-OR.
ORLANDO – The proportion of diabetes patients enrolled in high-deductible health plans jumped from 10% in 2005 to about 50% in 2014, according to a review of insurance data for 63 million Americans under age 65 years.
Diabetes patients often don’t have a choice. To cut costs, high-deductible plans are increasingly the only ones employers offer.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
While that may be adequate for healthy people, it’s quite another issue for people with chronic conditions, especially ones with low income. Out-of-pocket expenses can be thousands of dollars more than with traditional health plans, and the extra costs aren’t always offset by lower premiums.
The trend is concerning, said senior investigator J. Frank Wharam, MB, MPH, an associate professor of population medicine at Harvard Medical School, Boston. He explained the problem, and what’s being done about it, in an interview at the annual scientific sessions of the American Diabetes Association.
aotto@mdedge.com
SOURCE: Garabedian LF et al. ADA 2018. Abstract 175-OR.
ORLANDO – The proportion of diabetes patients enrolled in high-deductible health plans jumped from 10% in 2005 to about 50% in 2014, according to a review of insurance data for 63 million Americans under age 65 years.
Diabetes patients often don’t have a choice. To cut costs, high-deductible plans are increasingly the only ones employers offer.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
While that may be adequate for healthy people, it’s quite another issue for people with chronic conditions, especially ones with low income. Out-of-pocket expenses can be thousands of dollars more than with traditional health plans, and the extra costs aren’t always offset by lower premiums.
The trend is concerning, said senior investigator J. Frank Wharam, MB, MPH, an associate professor of population medicine at Harvard Medical School, Boston. He explained the problem, and what’s being done about it, in an interview at the annual scientific sessions of the American Diabetes Association.
aotto@mdedge.com
SOURCE: Garabedian LF et al. ADA 2018. Abstract 175-OR.
REPORTING FROM ADA 2018
Obesity didn’t just happen overnight
Is it possible to get more exercise and still gain weight? In America it is.
The steady increase in obesity prevalence among adults in the United States has been exceeded over the last decade by the percentage of adults who are getting the recommended amount of exercise, according to the National Center for Health Statistics.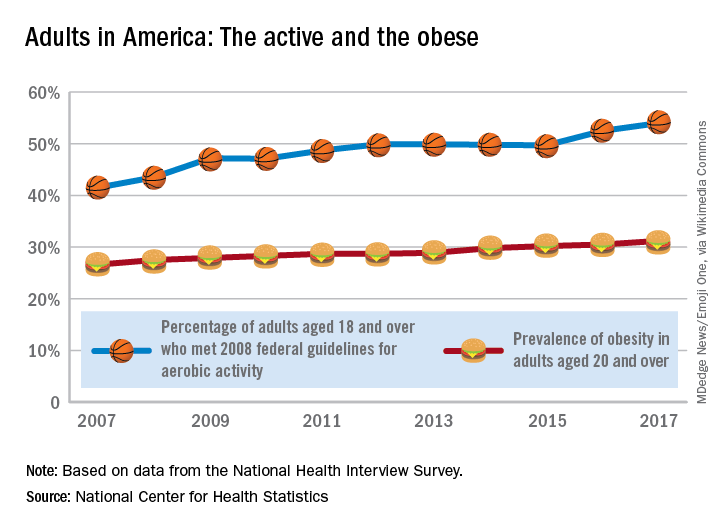
The 2008 guideline, “Physical Activity Guidelines for Americans” recommends that “adults perform at least 150 minutes a week of moderate-intensity aerobic physical activity, 75 minutes a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity, performed in episodes of at least 10 minutes and preferably should be spread throughout the week,” the NCHS noted.
Is it possible to get more exercise and still gain weight? In America it is.
The steady increase in obesity prevalence among adults in the United States has been exceeded over the last decade by the percentage of adults who are getting the recommended amount of exercise, according to the National Center for Health Statistics.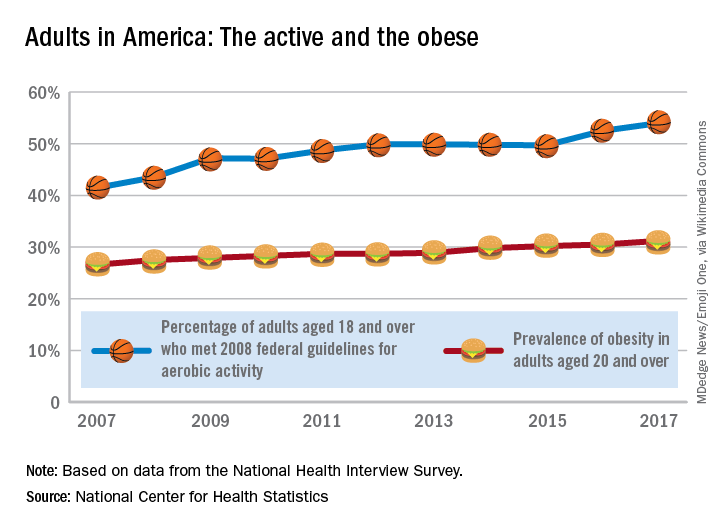
The 2008 guideline, “Physical Activity Guidelines for Americans” recommends that “adults perform at least 150 minutes a week of moderate-intensity aerobic physical activity, 75 minutes a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity, performed in episodes of at least 10 minutes and preferably should be spread throughout the week,” the NCHS noted.
Is it possible to get more exercise and still gain weight? In America it is.
The steady increase in obesity prevalence among adults in the United States has been exceeded over the last decade by the percentage of adults who are getting the recommended amount of exercise, according to the National Center for Health Statistics.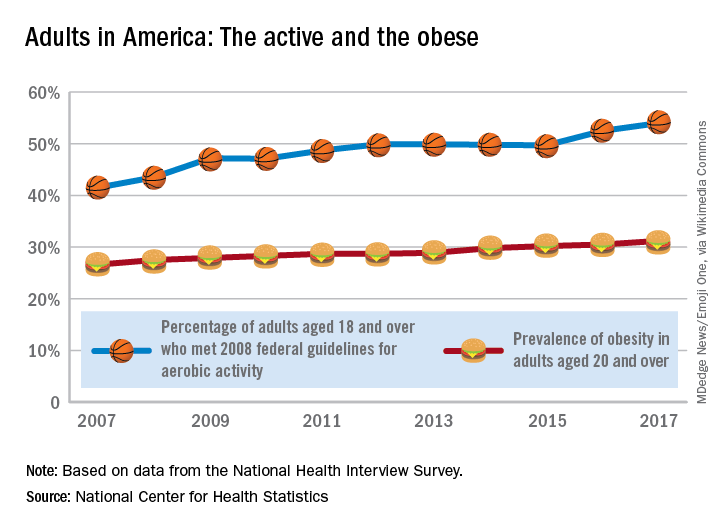
The 2008 guideline, “Physical Activity Guidelines for Americans” recommends that “adults perform at least 150 minutes a week of moderate-intensity aerobic physical activity, 75 minutes a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity, performed in episodes of at least 10 minutes and preferably should be spread throughout the week,” the NCHS noted.
Research provides more evidence of a maternal diabetes/autism link
ORLANDO – Longer-term data are providing more evidence of a possible link between maternal diabetes and autism spectrum disorder in their children.
Anny Xiang, PhD, and coathors with Kaiser Permanente of Southern California sought to further understand the possible effect of maternal T1D on offspring’s development of autism spectrum disorder (ASD) by expanding the cohort and timeline of their earlier work (JAMA. 2015;313(14):1425-1434).
Across the cohort, 1.3% of children were diagnosed with autism spectrum disorder (ASD). The rate was barely different, at 1.5%, for those whose mothers developed gestational diabetes after 26 weeks. But rates of ASD were higher – 3.1%, 2.5%, 2.1% – among those whose mothers had T1D, T2D, and gestational diabetes that developed at 26 weeks or earlier, respectively. The findings were adjusted for co-founders such as birth year, age at delivery, eduction level and income, Dr. Xiang said at the annual scientific sessions of the American Diabetes Association.
Compared to offspring of mothers without diabetes, ASD was more common in the children of mothers with T1D (adjusted HR=2.36, 95% CI, 1.36-4.12) mothers with type 2 diabetes (AHR= 1.45, 95% CI, 1.24-1.70) and gestational diabetes mellitus that developed by 26 weeks gestation (1.30, 95% CI, 1.12-1.51).
The numbers remained similar after they were adjusted for smoking during pregnancy and prepregnancy BMI, statistics which were available for about 36% of the subjects, according to the findings which were published simultaneously in JAMA (June 23, 2018. doi:10.1001/jama.2018.7614).
Possible explanations for the link between ASD and maternal diabetes include maternal glycemic control, prematurity, and levels of neonatal hypoglycemia, Dr. Xiang said.
The results do not take into account any paternal risks for offspring developing ASD, which also includes diabetes, Dr. Xiang said, noting that two previous studies linked diabetes in fathers to ASD, although to a lesser extent than diabetes in mothers. (Epidemiology. 2010 Nov;21(6):805-8; Pediatrics. 2009 Aug;124(2):687-94)
The study also doesn’t take breastfeeding into account, Dr. Xiang noted. A 2016 study found that women with T2D were less likely to breastfeed (J Matern Fetal Neonatal Med. 2016;29(15):2513-8), and some research has suggested that breastfeeding may be protective against the development of ASD in children (Nutrition 2012;28(7-8):e27-32).
In addition, the study doesn’t track maternal glucose levels over time.
Session co-chair Peter Damm, MD, professor of obstetrics at the University of Copenhagen, said in an interview that he is impressed by the study. He cautioned, however, that it does not prove a connection.“This not a proof, but it seems likely, or like a possibility,” he said.
One possible explanation for a diabetes/ASD connection is the fact that the fetal brain is evolving throughout pregnancy unlike other body organs, which simply grow after developing in the first trimester, he said. As a result, glucose levels may affect the brain’s development in a unique way compared to other organs.
He also noted that the impact may be reduced when pregnancy is further along, potentially explaining why researchers didn’t connect late-developing gestational diabetes to ASD.
There’s still a “low risk” of ASD even in children born to mothers with diabetes, he said. “You shouldn’t scare anyone with this.”
The study was funded in part by Kaiser Permanente Southern California Direct Community Benefit funds. The study authors and Dr. Damm report no relevant disclosures.
SOURCE: Xiang A, et al. ADA 2018 Abstract OR-117.
ORLANDO – Longer-term data are providing more evidence of a possible link between maternal diabetes and autism spectrum disorder in their children.
Anny Xiang, PhD, and coathors with Kaiser Permanente of Southern California sought to further understand the possible effect of maternal T1D on offspring’s development of autism spectrum disorder (ASD) by expanding the cohort and timeline of their earlier work (JAMA. 2015;313(14):1425-1434).
Across the cohort, 1.3% of children were diagnosed with autism spectrum disorder (ASD). The rate was barely different, at 1.5%, for those whose mothers developed gestational diabetes after 26 weeks. But rates of ASD were higher – 3.1%, 2.5%, 2.1% – among those whose mothers had T1D, T2D, and gestational diabetes that developed at 26 weeks or earlier, respectively. The findings were adjusted for co-founders such as birth year, age at delivery, eduction level and income, Dr. Xiang said at the annual scientific sessions of the American Diabetes Association.
Compared to offspring of mothers without diabetes, ASD was more common in the children of mothers with T1D (adjusted HR=2.36, 95% CI, 1.36-4.12) mothers with type 2 diabetes (AHR= 1.45, 95% CI, 1.24-1.70) and gestational diabetes mellitus that developed by 26 weeks gestation (1.30, 95% CI, 1.12-1.51).
The numbers remained similar after they were adjusted for smoking during pregnancy and prepregnancy BMI, statistics which were available for about 36% of the subjects, according to the findings which were published simultaneously in JAMA (June 23, 2018. doi:10.1001/jama.2018.7614).
Possible explanations for the link between ASD and maternal diabetes include maternal glycemic control, prematurity, and levels of neonatal hypoglycemia, Dr. Xiang said.
The results do not take into account any paternal risks for offspring developing ASD, which also includes diabetes, Dr. Xiang said, noting that two previous studies linked diabetes in fathers to ASD, although to a lesser extent than diabetes in mothers. (Epidemiology. 2010 Nov;21(6):805-8; Pediatrics. 2009 Aug;124(2):687-94)
The study also doesn’t take breastfeeding into account, Dr. Xiang noted. A 2016 study found that women with T2D were less likely to breastfeed (J Matern Fetal Neonatal Med. 2016;29(15):2513-8), and some research has suggested that breastfeeding may be protective against the development of ASD in children (Nutrition 2012;28(7-8):e27-32).
In addition, the study doesn’t track maternal glucose levels over time.
Session co-chair Peter Damm, MD, professor of obstetrics at the University of Copenhagen, said in an interview that he is impressed by the study. He cautioned, however, that it does not prove a connection.“This not a proof, but it seems likely, or like a possibility,” he said.
One possible explanation for a diabetes/ASD connection is the fact that the fetal brain is evolving throughout pregnancy unlike other body organs, which simply grow after developing in the first trimester, he said. As a result, glucose levels may affect the brain’s development in a unique way compared to other organs.
He also noted that the impact may be reduced when pregnancy is further along, potentially explaining why researchers didn’t connect late-developing gestational diabetes to ASD.
There’s still a “low risk” of ASD even in children born to mothers with diabetes, he said. “You shouldn’t scare anyone with this.”
The study was funded in part by Kaiser Permanente Southern California Direct Community Benefit funds. The study authors and Dr. Damm report no relevant disclosures.
SOURCE: Xiang A, et al. ADA 2018 Abstract OR-117.
ORLANDO – Longer-term data are providing more evidence of a possible link between maternal diabetes and autism spectrum disorder in their children.
Anny Xiang, PhD, and coathors with Kaiser Permanente of Southern California sought to further understand the possible effect of maternal T1D on offspring’s development of autism spectrum disorder (ASD) by expanding the cohort and timeline of their earlier work (JAMA. 2015;313(14):1425-1434).
Across the cohort, 1.3% of children were diagnosed with autism spectrum disorder (ASD). The rate was barely different, at 1.5%, for those whose mothers developed gestational diabetes after 26 weeks. But rates of ASD were higher – 3.1%, 2.5%, 2.1% – among those whose mothers had T1D, T2D, and gestational diabetes that developed at 26 weeks or earlier, respectively. The findings were adjusted for co-founders such as birth year, age at delivery, eduction level and income, Dr. Xiang said at the annual scientific sessions of the American Diabetes Association.
Compared to offspring of mothers without diabetes, ASD was more common in the children of mothers with T1D (adjusted HR=2.36, 95% CI, 1.36-4.12) mothers with type 2 diabetes (AHR= 1.45, 95% CI, 1.24-1.70) and gestational diabetes mellitus that developed by 26 weeks gestation (1.30, 95% CI, 1.12-1.51).
The numbers remained similar after they were adjusted for smoking during pregnancy and prepregnancy BMI, statistics which were available for about 36% of the subjects, according to the findings which were published simultaneously in JAMA (June 23, 2018. doi:10.1001/jama.2018.7614).
Possible explanations for the link between ASD and maternal diabetes include maternal glycemic control, prematurity, and levels of neonatal hypoglycemia, Dr. Xiang said.
The results do not take into account any paternal risks for offspring developing ASD, which also includes diabetes, Dr. Xiang said, noting that two previous studies linked diabetes in fathers to ASD, although to a lesser extent than diabetes in mothers. (Epidemiology. 2010 Nov;21(6):805-8; Pediatrics. 2009 Aug;124(2):687-94)
The study also doesn’t take breastfeeding into account, Dr. Xiang noted. A 2016 study found that women with T2D were less likely to breastfeed (J Matern Fetal Neonatal Med. 2016;29(15):2513-8), and some research has suggested that breastfeeding may be protective against the development of ASD in children (Nutrition 2012;28(7-8):e27-32).
In addition, the study doesn’t track maternal glucose levels over time.
Session co-chair Peter Damm, MD, professor of obstetrics at the University of Copenhagen, said in an interview that he is impressed by the study. He cautioned, however, that it does not prove a connection.“This not a proof, but it seems likely, or like a possibility,” he said.
One possible explanation for a diabetes/ASD connection is the fact that the fetal brain is evolving throughout pregnancy unlike other body organs, which simply grow after developing in the first trimester, he said. As a result, glucose levels may affect the brain’s development in a unique way compared to other organs.
He also noted that the impact may be reduced when pregnancy is further along, potentially explaining why researchers didn’t connect late-developing gestational diabetes to ASD.
There’s still a “low risk” of ASD even in children born to mothers with diabetes, he said. “You shouldn’t scare anyone with this.”
The study was funded in part by Kaiser Permanente Southern California Direct Community Benefit funds. The study authors and Dr. Damm report no relevant disclosures.
SOURCE: Xiang A, et al. ADA 2018 Abstract OR-117.
REPORTING FROM ADA 2018
Key clinical point: Children of mothers with various forms of diabetes – including type 1 diabetes (T1D) – could be at higher risk of autism.
Major finding: Autism spectrum disorder (ASD) was more common in the children of mothers with T1D (adjusted HR=2.36, 95% CI, 1.36-4.12) type 2 diabetes (AHR= 1.45, 95% CI, 1.24-1.70) and gestational diabetes that developed by 26 weeks gestation (1.30, 95% CI, 1.12-1.51).
Study details: Retrospective analysis of 419,425 children born at Kaiser Permanente Southern California hospitals from 1995-2012 (51% boys).
Disclosures: The study was funded in part by Kaiser Permanente Southern California Direct Community Benefit funds. The study authors report no relevant disclosures.
Source: Xiang A, et al. ADA 2018 Abstract OR-117.
Eversense CGM shown safe, accurate for 180 days in adolescents
ORLANDO – The Eversense continuous glucose monitoring (CGM) system, recently approved for use in adults with diabetes, also provides safe, durable, and accurate monitoring in the pediatric population, according to findings from a prospective single-arm study of 30 children and 6 adults.
Study subjects, who were all over age 11 years, with an average of 14 years, had the fully implantable sensor inserted at day 0 and removed at day 180, and the mean absolute relative difference (MARD) between sensor and true laboratory glucose values showed high device accuracy, Ronnie Aronson, MD, reported at the annual scientific sessions of the American Diabetes Association.
“Anything under 10% is considered good, and ours was 9.4% – and it didn’t deteriorate throughout the duration, so at 180 days it was still at 9.4%; every accuracy measure we looked at showed similar high levels of accuracy,” Dr. Aronson, founder and chief medical officer of LMC Diabetes & Endocrinology in Ontario, Canada said in a video interview.
The sensor, which is roughly 1.5 cm long, is coated with a material that fluoresces when exposed to glucose; the sensor uses the amount of light emitted to calculate blood glucose levels. Patients use an adhesive patch, changed daily, to attach a “smart” transmitter that overlies the area where the sensor is implanted. This rechargeable transmitter sends blood glucose levels to the mobile app every 5 minutes, and also powers the sensor. The Food and Drug Administration approved it for use in adults on June 21.
The system was highly rated by study participants, he said. “What makes it stand out is that it’s implanted, it’s there for at least 180 days, it’s accurate for 180 days,” the transmitter can be taken on and off, and the results can be seen very easily on a smart phone or Apple Watch.
Dr. Aronson said he also hopes to study the device in younger patients and for longer durations.
Dr. Aronson is an advisor for Novo Nordisk and Sanofi. He also receives research support from AstraZeneca, Eli Lilly, Valeant, Janssen, and Senseonics.
SOURCE: Aronson R et al. ADA 2018 Abstract 13-OR.
ORLANDO – The Eversense continuous glucose monitoring (CGM) system, recently approved for use in adults with diabetes, also provides safe, durable, and accurate monitoring in the pediatric population, according to findings from a prospective single-arm study of 30 children and 6 adults.
Study subjects, who were all over age 11 years, with an average of 14 years, had the fully implantable sensor inserted at day 0 and removed at day 180, and the mean absolute relative difference (MARD) between sensor and true laboratory glucose values showed high device accuracy, Ronnie Aronson, MD, reported at the annual scientific sessions of the American Diabetes Association.
“Anything under 10% is considered good, and ours was 9.4% – and it didn’t deteriorate throughout the duration, so at 180 days it was still at 9.4%; every accuracy measure we looked at showed similar high levels of accuracy,” Dr. Aronson, founder and chief medical officer of LMC Diabetes & Endocrinology in Ontario, Canada said in a video interview.
The sensor, which is roughly 1.5 cm long, is coated with a material that fluoresces when exposed to glucose; the sensor uses the amount of light emitted to calculate blood glucose levels. Patients use an adhesive patch, changed daily, to attach a “smart” transmitter that overlies the area where the sensor is implanted. This rechargeable transmitter sends blood glucose levels to the mobile app every 5 minutes, and also powers the sensor. The Food and Drug Administration approved it for use in adults on June 21.
The system was highly rated by study participants, he said. “What makes it stand out is that it’s implanted, it’s there for at least 180 days, it’s accurate for 180 days,” the transmitter can be taken on and off, and the results can be seen very easily on a smart phone or Apple Watch.
Dr. Aronson said he also hopes to study the device in younger patients and for longer durations.
Dr. Aronson is an advisor for Novo Nordisk and Sanofi. He also receives research support from AstraZeneca, Eli Lilly, Valeant, Janssen, and Senseonics.
SOURCE: Aronson R et al. ADA 2018 Abstract 13-OR.
ORLANDO – The Eversense continuous glucose monitoring (CGM) system, recently approved for use in adults with diabetes, also provides safe, durable, and accurate monitoring in the pediatric population, according to findings from a prospective single-arm study of 30 children and 6 adults.
Study subjects, who were all over age 11 years, with an average of 14 years, had the fully implantable sensor inserted at day 0 and removed at day 180, and the mean absolute relative difference (MARD) between sensor and true laboratory glucose values showed high device accuracy, Ronnie Aronson, MD, reported at the annual scientific sessions of the American Diabetes Association.
“Anything under 10% is considered good, and ours was 9.4% – and it didn’t deteriorate throughout the duration, so at 180 days it was still at 9.4%; every accuracy measure we looked at showed similar high levels of accuracy,” Dr. Aronson, founder and chief medical officer of LMC Diabetes & Endocrinology in Ontario, Canada said in a video interview.
The sensor, which is roughly 1.5 cm long, is coated with a material that fluoresces when exposed to glucose; the sensor uses the amount of light emitted to calculate blood glucose levels. Patients use an adhesive patch, changed daily, to attach a “smart” transmitter that overlies the area where the sensor is implanted. This rechargeable transmitter sends blood glucose levels to the mobile app every 5 minutes, and also powers the sensor. The Food and Drug Administration approved it for use in adults on June 21.
The system was highly rated by study participants, he said. “What makes it stand out is that it’s implanted, it’s there for at least 180 days, it’s accurate for 180 days,” the transmitter can be taken on and off, and the results can be seen very easily on a smart phone or Apple Watch.
Dr. Aronson said he also hopes to study the device in younger patients and for longer durations.
Dr. Aronson is an advisor for Novo Nordisk and Sanofi. He also receives research support from AstraZeneca, Eli Lilly, Valeant, Janssen, and Senseonics.
SOURCE: Aronson R et al. ADA 2018 Abstract 13-OR.
REPORTING FROM ADA 2018
Key clinical point: The Eversense fully implantable continuous glucose monitoring device is safe and accurate in adolescents.
Major finding: The MARD between sensor and true laboratory glucose values showed high device accuracy, at 9.4% over 180 days.
Study details: A prospective single-arm study of 30 children and 6 adults.
Disclosures: Dr. Aronson is an advisor for Novo Nordisk and Sanofi. He also receives research support from AstraZeneca, Eli Lilly, Valeant, Janssen, and Senseonics.
Source: Aronson R et al. ADA Abstract 13-OR.
Switch back to human insulin a viable money saver
ORLANDO – It’s safe to switch many Medicare beneficiaries with type 2 diabetes to human insulins to save money on analogues, according to a review of 14,635 members of CareMore, a Medicare Advantage company based in Cerritos, Calif.
The company noticed that it’s spending on analogue insulins had ballooned to over $3 million a month by the end of 2014, in the wake of a more than 300% price increase in analogue insulins in recent years, while copays on analogues rose from nothing to $37.50. In 2015, it launched a program to switch type 2 patients to less costly human insulins. Physicians were counseled to stop secretagogues and move patients to premixed insulins at 80% of their former total daily analogue dose, two-thirds at breakfast, and one-third a dinner, with appropriate follow-up.
Analogue insulins fell from 90% of all insulins dispensed to 30%, with a corresponding rise in human insulin prescriptions. Total plan spending on analogues fell to about a half million dollars a month by the end of 2016. Spending on human insulins rose to just under a million dollars. The risk of patients falling into the Medicare Part D coverage gap – where they assume a greater proportion of their drug costs – was reduced by 55% (P less than .001).
“A lot of money was saved as a result of this intervention,” said lead investigator Jin Luo, MD, an internist and health services researcher at Brigham and Women’s Hospital, Boston.
Mean hemoglobin A1c rose 0.14 % from a baseline of 8.46% in 2014 (P less than 0.01), “but we do not believe that this is clinically important because this value falls within the biological within-subject variation of most modern HbA1c assays,” he said at the annual scientific sessions of the American Diabetes Association.
Meanwhile, there was no statistically significant change in the rate of hospitalizations or emergency department visits for hypoglycemia or hyperglycemia.
“Patients with type 2 diabetes and their clinical providers should strongly consider human insulin as a clinically viable and cost effective option,” Dr. Luo said.
“My personal clinical opinion is that if I have a patient who is really hard to control, and after four or five different regimens, we finally settle on an analogue regimen that [keeps] them under control” and out of the hospital, “I’m not going to switch them just because a health plan tells me I should. They are just too brittle, and I’m not comfortable doing that. Whereas if I have a patient who’d be fine with either option, and I’m not really worried about hypoglycemia, I’ll switch them,” he said.
There was no industry funding. Dr. Luo is a consultant for Alosa Health and Health Action International.
SOURCE: Luo J et al. 2018 American Diabetes Association scientific session abstract 4-OR
ORLANDO – It’s safe to switch many Medicare beneficiaries with type 2 diabetes to human insulins to save money on analogues, according to a review of 14,635 members of CareMore, a Medicare Advantage company based in Cerritos, Calif.
The company noticed that it’s spending on analogue insulins had ballooned to over $3 million a month by the end of 2014, in the wake of a more than 300% price increase in analogue insulins in recent years, while copays on analogues rose from nothing to $37.50. In 2015, it launched a program to switch type 2 patients to less costly human insulins. Physicians were counseled to stop secretagogues and move patients to premixed insulins at 80% of their former total daily analogue dose, two-thirds at breakfast, and one-third a dinner, with appropriate follow-up.
Analogue insulins fell from 90% of all insulins dispensed to 30%, with a corresponding rise in human insulin prescriptions. Total plan spending on analogues fell to about a half million dollars a month by the end of 2016. Spending on human insulins rose to just under a million dollars. The risk of patients falling into the Medicare Part D coverage gap – where they assume a greater proportion of their drug costs – was reduced by 55% (P less than .001).
“A lot of money was saved as a result of this intervention,” said lead investigator Jin Luo, MD, an internist and health services researcher at Brigham and Women’s Hospital, Boston.
Mean hemoglobin A1c rose 0.14 % from a baseline of 8.46% in 2014 (P less than 0.01), “but we do not believe that this is clinically important because this value falls within the biological within-subject variation of most modern HbA1c assays,” he said at the annual scientific sessions of the American Diabetes Association.
Meanwhile, there was no statistically significant change in the rate of hospitalizations or emergency department visits for hypoglycemia or hyperglycemia.
“Patients with type 2 diabetes and their clinical providers should strongly consider human insulin as a clinically viable and cost effective option,” Dr. Luo said.
“My personal clinical opinion is that if I have a patient who is really hard to control, and after four or five different regimens, we finally settle on an analogue regimen that [keeps] them under control” and out of the hospital, “I’m not going to switch them just because a health plan tells me I should. They are just too brittle, and I’m not comfortable doing that. Whereas if I have a patient who’d be fine with either option, and I’m not really worried about hypoglycemia, I’ll switch them,” he said.
There was no industry funding. Dr. Luo is a consultant for Alosa Health and Health Action International.
SOURCE: Luo J et al. 2018 American Diabetes Association scientific session abstract 4-OR
ORLANDO – It’s safe to switch many Medicare beneficiaries with type 2 diabetes to human insulins to save money on analogues, according to a review of 14,635 members of CareMore, a Medicare Advantage company based in Cerritos, Calif.
The company noticed that it’s spending on analogue insulins had ballooned to over $3 million a month by the end of 2014, in the wake of a more than 300% price increase in analogue insulins in recent years, while copays on analogues rose from nothing to $37.50. In 2015, it launched a program to switch type 2 patients to less costly human insulins. Physicians were counseled to stop secretagogues and move patients to premixed insulins at 80% of their former total daily analogue dose, two-thirds at breakfast, and one-third a dinner, with appropriate follow-up.
Analogue insulins fell from 90% of all insulins dispensed to 30%, with a corresponding rise in human insulin prescriptions. Total plan spending on analogues fell to about a half million dollars a month by the end of 2016. Spending on human insulins rose to just under a million dollars. The risk of patients falling into the Medicare Part D coverage gap – where they assume a greater proportion of their drug costs – was reduced by 55% (P less than .001).
“A lot of money was saved as a result of this intervention,” said lead investigator Jin Luo, MD, an internist and health services researcher at Brigham and Women’s Hospital, Boston.
Mean hemoglobin A1c rose 0.14 % from a baseline of 8.46% in 2014 (P less than 0.01), “but we do not believe that this is clinically important because this value falls within the biological within-subject variation of most modern HbA1c assays,” he said at the annual scientific sessions of the American Diabetes Association.
Meanwhile, there was no statistically significant change in the rate of hospitalizations or emergency department visits for hypoglycemia or hyperglycemia.
“Patients with type 2 diabetes and their clinical providers should strongly consider human insulin as a clinically viable and cost effective option,” Dr. Luo said.
“My personal clinical opinion is that if I have a patient who is really hard to control, and after four or five different regimens, we finally settle on an analogue regimen that [keeps] them under control” and out of the hospital, “I’m not going to switch them just because a health plan tells me I should. They are just too brittle, and I’m not comfortable doing that. Whereas if I have a patient who’d be fine with either option, and I’m not really worried about hypoglycemia, I’ll switch them,” he said.
There was no industry funding. Dr. Luo is a consultant for Alosa Health and Health Action International.
SOURCE: Luo J et al. 2018 American Diabetes Association scientific session abstract 4-OR
REPORTING FROM ADA 2018
Key clinical point:
Major finding: Mean HbA1c rose just 0.14% from a baseline of 8.46% (P less than 0.01).
Study details: A review of 14,635 members Medicare patients with type 2 diabetes.
Disclosures: There was no industry funding. The lead investigator is a consultant for Alosa Health and Health Action International.
Source: Luo J et al. ADA 2018, Abstract 4-OR
T1D neuropathy declines as glycemic control improves
ORLANDO – Rates of diabetic peripheral neuropathy (DPN) in U.S. patients with type 1 diabetes (T1D) may have dipped, possibly because of improving clinical care, a new study suggests. Researchers also found evidence that nonglycemic factors may play important roles in the development of the condition.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
There are differences between DPN in T1D and type 2 diabetes: Lifetime incidence in T1D is believed to be 45%, lower than in T2D. However, a 2016 report noted that, “whereas treating hyperglycemia in type 1 DM can significantly reduce the incidence of neuropathy by up to 60 to 70%, glucose control in type 2 DM has only a marginal 5 to 7% reduction in the development of neuropathy.” (F1000Research 2016, 5(F1000 Faculty Rev):738)
Still, DPN is believed to be very common in T1D. According to the new study, previous research has suggested that the DPN rate in this population could be as high as 35%.
For the new study, researchers examined self-reports of DPN from 5,058 patients across 62 sites via the T1D Exchange Registry. All patients were at least 18 years of age and had at least 5 years of T1D. Their mean age was 39 years, the duration of diabetes was 22 years, and their average hemoglobin A1c was 8.1. Over half (56%) were women, and most (88%) were white were white.
A preliminary analysis found that just 10% of the patients had signs of DPN, according to their self-reports. In part, the difference between this number and previous estimates of DPN prevalence may be because previous studies relied on symptoms, exams, and electrophysiologic testing, said study researcher Kara Mizokami-Stout, MD, of the University of Michigan, in an interview.
However, study researcher Rodica Pop-Busui, MD, PhD, noted in an interview that one strength of the new study is that it’s “a broad sample of patients with type 1 diabetes as they are currently treated in clinical care across the United States.”
Versus those without DPN, those with the condition were more likely to be older (mean 52 vs. 37 years), female (61% vs. 55%), and had T1D for a longer period (mean 32 vs. 21 years). They were also poorer and had less education. (All P less than .001)
The DPN group also had slightly higher systolic blood pressure (mean 126 vs. 123), higher triglycerides (117 vs. 95) and more than double the rate of tobacco use (9% vs. 4%), all P less than .001.
Also, cardiovascular disease was more common (26% vs. 6%) even though this group used statins (64% vs. 31%) and ACE inhibitors/ARBs (45% vs. 23%) at much higher levels, all P less than .001.
Researchers also found that this with DPN had higher HbA1c even after controlling for various confounders (8.4% vs. 8.1%, P less than .01).
“We have the ability to prevent neuropathy, and we should do that to our advantage, targeting glycemic control as best as possible without increasing the risk of hypoglycemia,” Dr. Mizokami-Stout said. Targeting nonglycemic factors is also crucial, she said.
The study was funded by the Helmsley Charitable Trust. Dr. Mizokami-Stout and Dr. Pop-Busui report no relevant disclosures. Some of the other authors report various disclosures.
SOURCE: Mizokami-Stout K, et al. ADA 2018, Abstract 62-OR.
ORLANDO – Rates of diabetic peripheral neuropathy (DPN) in U.S. patients with type 1 diabetes (T1D) may have dipped, possibly because of improving clinical care, a new study suggests. Researchers also found evidence that nonglycemic factors may play important roles in the development of the condition.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
There are differences between DPN in T1D and type 2 diabetes: Lifetime incidence in T1D is believed to be 45%, lower than in T2D. However, a 2016 report noted that, “whereas treating hyperglycemia in type 1 DM can significantly reduce the incidence of neuropathy by up to 60 to 70%, glucose control in type 2 DM has only a marginal 5 to 7% reduction in the development of neuropathy.” (F1000Research 2016, 5(F1000 Faculty Rev):738)
Still, DPN is believed to be very common in T1D. According to the new study, previous research has suggested that the DPN rate in this population could be as high as 35%.
For the new study, researchers examined self-reports of DPN from 5,058 patients across 62 sites via the T1D Exchange Registry. All patients were at least 18 years of age and had at least 5 years of T1D. Their mean age was 39 years, the duration of diabetes was 22 years, and their average hemoglobin A1c was 8.1. Over half (56%) were women, and most (88%) were white were white.
A preliminary analysis found that just 10% of the patients had signs of DPN, according to their self-reports. In part, the difference between this number and previous estimates of DPN prevalence may be because previous studies relied on symptoms, exams, and electrophysiologic testing, said study researcher Kara Mizokami-Stout, MD, of the University of Michigan, in an interview.
However, study researcher Rodica Pop-Busui, MD, PhD, noted in an interview that one strength of the new study is that it’s “a broad sample of patients with type 1 diabetes as they are currently treated in clinical care across the United States.”
Versus those without DPN, those with the condition were more likely to be older (mean 52 vs. 37 years), female (61% vs. 55%), and had T1D for a longer period (mean 32 vs. 21 years). They were also poorer and had less education. (All P less than .001)
The DPN group also had slightly higher systolic blood pressure (mean 126 vs. 123), higher triglycerides (117 vs. 95) and more than double the rate of tobacco use (9% vs. 4%), all P less than .001.
Also, cardiovascular disease was more common (26% vs. 6%) even though this group used statins (64% vs. 31%) and ACE inhibitors/ARBs (45% vs. 23%) at much higher levels, all P less than .001.
Researchers also found that this with DPN had higher HbA1c even after controlling for various confounders (8.4% vs. 8.1%, P less than .01).
“We have the ability to prevent neuropathy, and we should do that to our advantage, targeting glycemic control as best as possible without increasing the risk of hypoglycemia,” Dr. Mizokami-Stout said. Targeting nonglycemic factors is also crucial, she said.
The study was funded by the Helmsley Charitable Trust. Dr. Mizokami-Stout and Dr. Pop-Busui report no relevant disclosures. Some of the other authors report various disclosures.
SOURCE: Mizokami-Stout K, et al. ADA 2018, Abstract 62-OR.
ORLANDO – Rates of diabetic peripheral neuropathy (DPN) in U.S. patients with type 1 diabetes (T1D) may have dipped, possibly because of improving clinical care, a new study suggests. Researchers also found evidence that nonglycemic factors may play important roles in the development of the condition.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
There are differences between DPN in T1D and type 2 diabetes: Lifetime incidence in T1D is believed to be 45%, lower than in T2D. However, a 2016 report noted that, “whereas treating hyperglycemia in type 1 DM can significantly reduce the incidence of neuropathy by up to 60 to 70%, glucose control in type 2 DM has only a marginal 5 to 7% reduction in the development of neuropathy.” (F1000Research 2016, 5(F1000 Faculty Rev):738)
Still, DPN is believed to be very common in T1D. According to the new study, previous research has suggested that the DPN rate in this population could be as high as 35%.
For the new study, researchers examined self-reports of DPN from 5,058 patients across 62 sites via the T1D Exchange Registry. All patients were at least 18 years of age and had at least 5 years of T1D. Their mean age was 39 years, the duration of diabetes was 22 years, and their average hemoglobin A1c was 8.1. Over half (56%) were women, and most (88%) were white were white.
A preliminary analysis found that just 10% of the patients had signs of DPN, according to their self-reports. In part, the difference between this number and previous estimates of DPN prevalence may be because previous studies relied on symptoms, exams, and electrophysiologic testing, said study researcher Kara Mizokami-Stout, MD, of the University of Michigan, in an interview.
However, study researcher Rodica Pop-Busui, MD, PhD, noted in an interview that one strength of the new study is that it’s “a broad sample of patients with type 1 diabetes as they are currently treated in clinical care across the United States.”
Versus those without DPN, those with the condition were more likely to be older (mean 52 vs. 37 years), female (61% vs. 55%), and had T1D for a longer period (mean 32 vs. 21 years). They were also poorer and had less education. (All P less than .001)
The DPN group also had slightly higher systolic blood pressure (mean 126 vs. 123), higher triglycerides (117 vs. 95) and more than double the rate of tobacco use (9% vs. 4%), all P less than .001.
Also, cardiovascular disease was more common (26% vs. 6%) even though this group used statins (64% vs. 31%) and ACE inhibitors/ARBs (45% vs. 23%) at much higher levels, all P less than .001.
Researchers also found that this with DPN had higher HbA1c even after controlling for various confounders (8.4% vs. 8.1%, P less than .01).
“We have the ability to prevent neuropathy, and we should do that to our advantage, targeting glycemic control as best as possible without increasing the risk of hypoglycemia,” Dr. Mizokami-Stout said. Targeting nonglycemic factors is also crucial, she said.
The study was funded by the Helmsley Charitable Trust. Dr. Mizokami-Stout and Dr. Pop-Busui report no relevant disclosures. Some of the other authors report various disclosures.
SOURCE: Mizokami-Stout K, et al. ADA 2018, Abstract 62-OR.
REPORTING FROM ADA 2018
Key clinical point: Diabetic peripheral neuropathy (DPN) may be on the decline in type 1 diabetes (T1D), and nonglycemic factors may be crucial.
Major finding: 10% of subjects showed signs of DPN via self-report, and those with DPN had much higher rates of cardiovascular disease.
Study details: Analysis of 5,058 patients across 62 sites via the T1D Exchange Registry.
Disclosures: The study was funded by the Helmsley Charitable Trust. Some of the authors report various disclosures.
Source: Mizokami-Stout K, et al. ADA 2018, Abstract 62-OR.
Average glucose, A1c discordance is common, highlights ADAG equation concerns
ORLANDO – Significant discordance exists between average glucose and hemoglobin A1c (HbA1c) measures in patients with certain comorbidities, according to findings from a retrospective chart review.
For example, there was a complete lack of correlation between average glucose (AG) and A1c measures in patients with advanced renal dysfunction and non-alcoholic fatty liver disease, (NAFLD) Jordan E. Perlman, MD, reported at the annual scientific sessions of the American Diabetes Association.
Unweighted averages of self-monitored blood glucose (SMBG) and continuous glucose monitor (CGM) readings were calculated based on downloads from 1,039 patients who had been prescribed insulin for diabetes mellitus between January 2011 and October 2016 and who had a comorbid condition proven or hypothesized to invalidate A1c, including anemia, chronic kidney disease (CKD), abnormal liver function tests (LFTs), and NAFLD. Predicted AG was also derived from paired A1c using the equation established by the A1c Derived Average Glucose (ADAG) Study Group in a 2013 re-analysis of its 2008 report, which excluded patients with comorbidities.
The averages calculated using downloads were then compared with the averages derived using the ADAG equation to assess concordance.
“The term ‘discordant’ refers to averages that differ by more than 15%,” Dr. Perlman explained.
She and her colleagues found that CGM, compared with SMBG, decreased the odds of discordance after controlling for diabetes type (odds ratio, 0.39).
Additionally, having type 2 vs. type 1 diabetes mellitus increased the odds of discordance, as did renal dysfunction.
“Having CKD stage 3b or worse increases the odds of ADAG discordance (OR, 2.04),” she said. “The relationship demonstrates statistical significance at a P value of 0.004. Unfortunately, we did not have enough patients to analyze stage 4 or 5 CKD alone.”
Poor linear correlation was clearly seen between AG and A1c in patients with NAFLD, she noted.
“The relationship doesn’t reach statistical significance, but the odds ratio of 1.6 is difficult to ignore. The wide confidence interval (0.67-3.58) leads us to believe that this particular analysis is probably underpowered,” Dr. Perlman said.
Factors assessed and found to have no significant effect on ADAG discordance included abnormal LFTs, age, body mass index, and hemoglobin, including by gender.
“These important data suggest that any patient on insulin who comes to diabetes clinic has an automatic 33.5% chance of mismatch between their A1c and average glucose, and this is before you know anything else about them. To go a step further, it seems excluding comorbidities doesn’t really improve the percent discordance,” she said, adding that this suggests comorbidities have less impact than previously thought. “This makes us wonder if maybe there is a problem with our test and not the person having the test.”
It remains unclear what is acceptable in terms of discordance, Dr. Perlman said, noting that using ADAG to interpret A1c yields a wide range of estimated AG.
“Comorbidities alone do not explain this variation,” she said. “Clinicians should not rely on A1c alone to make treatment decisions because it is unclear when discordance gains clinical relevance.”
This study is limited by the retrospective study design and a number of factors, such as the difficulties of confirming or excluding comorbidities based on a single encounter and the limitless potential for unestablished confounders of A1c and AG, Dr. Perlman noted.
Also, fingersticks inflate discordance.
“A better assessment of ADAG would be to measure only CGM averages in comorbities, though this may need to be a prospective trial as only 17% of our patients who have identified comorbidities use CGM,” she said.
Dr. Perlman concluded that fingersticks and CGM can provide important confirmation of A1c, but said this applies only at the population level and not to individual patients.
“For individual patients, any level of A1c can translate to a large range of average glucoses. We see this even in our concordant patients,” she said.
Further, while discordance is increased by some comorbidities, it also occurs absent of comorbidities at a rate of 28.7%.
she said.
Dr. Perlman reported having no disclosures. Senior author Irl B. Hirsch, MD, professor of medicine at the University of Washington, Seattle, disclosed financial relationships diabetes drug and device manufacturers Abbot, ADOCIA, Bigfoot Biomedical, Roche, and Medtronic MiniMed.
SOURCE: Perlman J et al., ADA 2018 Abstract 12-OR.
ORLANDO – Significant discordance exists between average glucose and hemoglobin A1c (HbA1c) measures in patients with certain comorbidities, according to findings from a retrospective chart review.
For example, there was a complete lack of correlation between average glucose (AG) and A1c measures in patients with advanced renal dysfunction and non-alcoholic fatty liver disease, (NAFLD) Jordan E. Perlman, MD, reported at the annual scientific sessions of the American Diabetes Association.
Unweighted averages of self-monitored blood glucose (SMBG) and continuous glucose monitor (CGM) readings were calculated based on downloads from 1,039 patients who had been prescribed insulin for diabetes mellitus between January 2011 and October 2016 and who had a comorbid condition proven or hypothesized to invalidate A1c, including anemia, chronic kidney disease (CKD), abnormal liver function tests (LFTs), and NAFLD. Predicted AG was also derived from paired A1c using the equation established by the A1c Derived Average Glucose (ADAG) Study Group in a 2013 re-analysis of its 2008 report, which excluded patients with comorbidities.
The averages calculated using downloads were then compared with the averages derived using the ADAG equation to assess concordance.
“The term ‘discordant’ refers to averages that differ by more than 15%,” Dr. Perlman explained.
She and her colleagues found that CGM, compared with SMBG, decreased the odds of discordance after controlling for diabetes type (odds ratio, 0.39).
Additionally, having type 2 vs. type 1 diabetes mellitus increased the odds of discordance, as did renal dysfunction.
“Having CKD stage 3b or worse increases the odds of ADAG discordance (OR, 2.04),” she said. “The relationship demonstrates statistical significance at a P value of 0.004. Unfortunately, we did not have enough patients to analyze stage 4 or 5 CKD alone.”
Poor linear correlation was clearly seen between AG and A1c in patients with NAFLD, she noted.
“The relationship doesn’t reach statistical significance, but the odds ratio of 1.6 is difficult to ignore. The wide confidence interval (0.67-3.58) leads us to believe that this particular analysis is probably underpowered,” Dr. Perlman said.
Factors assessed and found to have no significant effect on ADAG discordance included abnormal LFTs, age, body mass index, and hemoglobin, including by gender.
“These important data suggest that any patient on insulin who comes to diabetes clinic has an automatic 33.5% chance of mismatch between their A1c and average glucose, and this is before you know anything else about them. To go a step further, it seems excluding comorbidities doesn’t really improve the percent discordance,” she said, adding that this suggests comorbidities have less impact than previously thought. “This makes us wonder if maybe there is a problem with our test and not the person having the test.”
It remains unclear what is acceptable in terms of discordance, Dr. Perlman said, noting that using ADAG to interpret A1c yields a wide range of estimated AG.
“Comorbidities alone do not explain this variation,” she said. “Clinicians should not rely on A1c alone to make treatment decisions because it is unclear when discordance gains clinical relevance.”
This study is limited by the retrospective study design and a number of factors, such as the difficulties of confirming or excluding comorbidities based on a single encounter and the limitless potential for unestablished confounders of A1c and AG, Dr. Perlman noted.
Also, fingersticks inflate discordance.
“A better assessment of ADAG would be to measure only CGM averages in comorbities, though this may need to be a prospective trial as only 17% of our patients who have identified comorbidities use CGM,” she said.
Dr. Perlman concluded that fingersticks and CGM can provide important confirmation of A1c, but said this applies only at the population level and not to individual patients.
“For individual patients, any level of A1c can translate to a large range of average glucoses. We see this even in our concordant patients,” she said.
Further, while discordance is increased by some comorbidities, it also occurs absent of comorbidities at a rate of 28.7%.
she said.
Dr. Perlman reported having no disclosures. Senior author Irl B. Hirsch, MD, professor of medicine at the University of Washington, Seattle, disclosed financial relationships diabetes drug and device manufacturers Abbot, ADOCIA, Bigfoot Biomedical, Roche, and Medtronic MiniMed.
SOURCE: Perlman J et al., ADA 2018 Abstract 12-OR.
ORLANDO – Significant discordance exists between average glucose and hemoglobin A1c (HbA1c) measures in patients with certain comorbidities, according to findings from a retrospective chart review.
For example, there was a complete lack of correlation between average glucose (AG) and A1c measures in patients with advanced renal dysfunction and non-alcoholic fatty liver disease, (NAFLD) Jordan E. Perlman, MD, reported at the annual scientific sessions of the American Diabetes Association.
Unweighted averages of self-monitored blood glucose (SMBG) and continuous glucose monitor (CGM) readings were calculated based on downloads from 1,039 patients who had been prescribed insulin for diabetes mellitus between January 2011 and October 2016 and who had a comorbid condition proven or hypothesized to invalidate A1c, including anemia, chronic kidney disease (CKD), abnormal liver function tests (LFTs), and NAFLD. Predicted AG was also derived from paired A1c using the equation established by the A1c Derived Average Glucose (ADAG) Study Group in a 2013 re-analysis of its 2008 report, which excluded patients with comorbidities.
The averages calculated using downloads were then compared with the averages derived using the ADAG equation to assess concordance.
“The term ‘discordant’ refers to averages that differ by more than 15%,” Dr. Perlman explained.
She and her colleagues found that CGM, compared with SMBG, decreased the odds of discordance after controlling for diabetes type (odds ratio, 0.39).
Additionally, having type 2 vs. type 1 diabetes mellitus increased the odds of discordance, as did renal dysfunction.
“Having CKD stage 3b or worse increases the odds of ADAG discordance (OR, 2.04),” she said. “The relationship demonstrates statistical significance at a P value of 0.004. Unfortunately, we did not have enough patients to analyze stage 4 or 5 CKD alone.”
Poor linear correlation was clearly seen between AG and A1c in patients with NAFLD, she noted.
“The relationship doesn’t reach statistical significance, but the odds ratio of 1.6 is difficult to ignore. The wide confidence interval (0.67-3.58) leads us to believe that this particular analysis is probably underpowered,” Dr. Perlman said.
Factors assessed and found to have no significant effect on ADAG discordance included abnormal LFTs, age, body mass index, and hemoglobin, including by gender.
“These important data suggest that any patient on insulin who comes to diabetes clinic has an automatic 33.5% chance of mismatch between their A1c and average glucose, and this is before you know anything else about them. To go a step further, it seems excluding comorbidities doesn’t really improve the percent discordance,” she said, adding that this suggests comorbidities have less impact than previously thought. “This makes us wonder if maybe there is a problem with our test and not the person having the test.”
It remains unclear what is acceptable in terms of discordance, Dr. Perlman said, noting that using ADAG to interpret A1c yields a wide range of estimated AG.
“Comorbidities alone do not explain this variation,” she said. “Clinicians should not rely on A1c alone to make treatment decisions because it is unclear when discordance gains clinical relevance.”
This study is limited by the retrospective study design and a number of factors, such as the difficulties of confirming or excluding comorbidities based on a single encounter and the limitless potential for unestablished confounders of A1c and AG, Dr. Perlman noted.
Also, fingersticks inflate discordance.
“A better assessment of ADAG would be to measure only CGM averages in comorbities, though this may need to be a prospective trial as only 17% of our patients who have identified comorbidities use CGM,” she said.
Dr. Perlman concluded that fingersticks and CGM can provide important confirmation of A1c, but said this applies only at the population level and not to individual patients.
“For individual patients, any level of A1c can translate to a large range of average glucoses. We see this even in our concordant patients,” she said.
Further, while discordance is increased by some comorbidities, it also occurs absent of comorbidities at a rate of 28.7%.
she said.
Dr. Perlman reported having no disclosures. Senior author Irl B. Hirsch, MD, professor of medicine at the University of Washington, Seattle, disclosed financial relationships diabetes drug and device manufacturers Abbot, ADOCIA, Bigfoot Biomedical, Roche, and Medtronic MiniMed.
SOURCE: Perlman J et al., ADA 2018 Abstract 12-OR.
REPORTING FROM ADA 2018
Key clinical point: AG and A1c discordance is common, thus professional consensus regarding acceptable discordance is needed before ADAG equation use is broadened.
Major finding: CKD stage 3b or worse increases the odds of ADAG discordance (OR, 2.04).
Study details: A retrospective review of 1,039 patient charts.
Disclosures: Dr. Perlman reported having no disclosures. Senior author Irl B. Hirsch, MD, disclosed financial relationships diabetes drug and device manufacturers Abbot, ADOCIA, Bigfoot Biomedical, Roche, and Medtronic MiniMed.
Source: Perlman J et al. ADA 2018 Abstract 12-OR.
Patients going without as insulin prices skyrocket
ORLANDO – About a quarter of diabetes patients use less insulin than prescribed because they can’t afford it, and they have worse glycemic control because of it, according to a survey of patients at the Yale Diabetes Center in New Haven, Conn.
The soaring cost of insulin – especially analogues – has been in the news following a more than 300% increase from 2004-2018. The cash price for a 10 mL vial of insulin lispro (Humalog), for example, has climbed from $59 to $320. The American Diabetes Association recently released a white paper on the issue, citing a “lack of transparency throughout the insulin supply chain” that obscures the reasons for the surge. It’s working with other groups to ensure affordable access.
Six questions were key: In the past 12 months, did you, because of cost, use less insulin than prescribed; try to stretch out your insulin; take smaller doses of insulin than prescribed; stop insulin; not fill an insulin prescription; or not start insulin?
Fifty-one patients answered “yes” to at least one of those questions, signaling to investigators that they were using less insulin than prescribed because they couldn’t afford it. Compared with other patients, they were three times more likely to have HbA1c levels above 9%, controlling for age, sex, diabetes duration, and income (P = 0.03).
“One in four patients were using less of an essential medication because it costs too much for them to take the prescribed amount,” said investigator Darby Herkert, who participated in the study as an undergraduate at Yale. “It’s having a tangible health effect.”
The problem was greatest among people making less than $100,000 dollars a year, and was not associated with race or the type of diabetes they had. Employer health coverage was not protective, and patients who were covered by a mix of government and employer insurance were at greater risk of underuse, as were those who were unable to work.
The situation is probably common in the United States, Ms. Herkert noted at the American Diabetes Association scientific sessions meeting. “New Haven is a demographic microcosm of the U.S.”
“These results highlight an urgent need to address high insulin prices,” she said. This may be done through greater transparency in pricing, advocacy for patients who can’t afford their prescription, use of alternative insulin options for some patients, and assistance programs,” she said.
The work was funded in part by the National Institutes of Health. The investigators had no disclosures.
SOURCE: Herkert D et al. ADA 2018 abstract 2-OR
ORLANDO – About a quarter of diabetes patients use less insulin than prescribed because they can’t afford it, and they have worse glycemic control because of it, according to a survey of patients at the Yale Diabetes Center in New Haven, Conn.
The soaring cost of insulin – especially analogues – has been in the news following a more than 300% increase from 2004-2018. The cash price for a 10 mL vial of insulin lispro (Humalog), for example, has climbed from $59 to $320. The American Diabetes Association recently released a white paper on the issue, citing a “lack of transparency throughout the insulin supply chain” that obscures the reasons for the surge. It’s working with other groups to ensure affordable access.
Six questions were key: In the past 12 months, did you, because of cost, use less insulin than prescribed; try to stretch out your insulin; take smaller doses of insulin than prescribed; stop insulin; not fill an insulin prescription; or not start insulin?
Fifty-one patients answered “yes” to at least one of those questions, signaling to investigators that they were using less insulin than prescribed because they couldn’t afford it. Compared with other patients, they were three times more likely to have HbA1c levels above 9%, controlling for age, sex, diabetes duration, and income (P = 0.03).
“One in four patients were using less of an essential medication because it costs too much for them to take the prescribed amount,” said investigator Darby Herkert, who participated in the study as an undergraduate at Yale. “It’s having a tangible health effect.”
The problem was greatest among people making less than $100,000 dollars a year, and was not associated with race or the type of diabetes they had. Employer health coverage was not protective, and patients who were covered by a mix of government and employer insurance were at greater risk of underuse, as were those who were unable to work.
The situation is probably common in the United States, Ms. Herkert noted at the American Diabetes Association scientific sessions meeting. “New Haven is a demographic microcosm of the U.S.”
“These results highlight an urgent need to address high insulin prices,” she said. This may be done through greater transparency in pricing, advocacy for patients who can’t afford their prescription, use of alternative insulin options for some patients, and assistance programs,” she said.
The work was funded in part by the National Institutes of Health. The investigators had no disclosures.
SOURCE: Herkert D et al. ADA 2018 abstract 2-OR
ORLANDO – About a quarter of diabetes patients use less insulin than prescribed because they can’t afford it, and they have worse glycemic control because of it, according to a survey of patients at the Yale Diabetes Center in New Haven, Conn.
The soaring cost of insulin – especially analogues – has been in the news following a more than 300% increase from 2004-2018. The cash price for a 10 mL vial of insulin lispro (Humalog), for example, has climbed from $59 to $320. The American Diabetes Association recently released a white paper on the issue, citing a “lack of transparency throughout the insulin supply chain” that obscures the reasons for the surge. It’s working with other groups to ensure affordable access.
Six questions were key: In the past 12 months, did you, because of cost, use less insulin than prescribed; try to stretch out your insulin; take smaller doses of insulin than prescribed; stop insulin; not fill an insulin prescription; or not start insulin?
Fifty-one patients answered “yes” to at least one of those questions, signaling to investigators that they were using less insulin than prescribed because they couldn’t afford it. Compared with other patients, they were three times more likely to have HbA1c levels above 9%, controlling for age, sex, diabetes duration, and income (P = 0.03).
“One in four patients were using less of an essential medication because it costs too much for them to take the prescribed amount,” said investigator Darby Herkert, who participated in the study as an undergraduate at Yale. “It’s having a tangible health effect.”
The problem was greatest among people making less than $100,000 dollars a year, and was not associated with race or the type of diabetes they had. Employer health coverage was not protective, and patients who were covered by a mix of government and employer insurance were at greater risk of underuse, as were those who were unable to work.
The situation is probably common in the United States, Ms. Herkert noted at the American Diabetes Association scientific sessions meeting. “New Haven is a demographic microcosm of the U.S.”
“These results highlight an urgent need to address high insulin prices,” she said. This may be done through greater transparency in pricing, advocacy for patients who can’t afford their prescription, use of alternative insulin options for some patients, and assistance programs,” she said.
The work was funded in part by the National Institutes of Health. The investigators had no disclosures.
SOURCE: Herkert D et al. ADA 2018 abstract 2-OR
REPORTING FROM ADA 2018
Key clinical point: because of it.
Major finding: Compared with other patients, they were three times more likely to have hemoglobin A1c levels above 9%, controlling for age, sex, diabetes duration, and income (P = 0.03).
Study details: A single-center survey of 199 patients with type 1 or type 2 diabetes.
Disclosures: The work was funded in part by the National Institutes of Health. The investigators had no disclosures.
Source: Herkert D et al. ADA 2018, Abstract 2-OR











