User login
Inexperience Diagnosing Syphilis Adding to Higher Rates
With rates of syphilis rising quickly in the United States and elsewhere, clinicians are having to up their game when it comes to diagnosing and treating an infection that they may not be paying enough attention to.
More than 200,000 cases of syphilis were reported in the United States in 2022, which is the highest number since 1950 and is a 17.3% increase over 2021, according to the latest figures from the Centers for Disease Control and Prevention (CDC). The rate of infection has increased almost every year since a historic low in 2001.
And the trend is not limited to the United States. Last year, the infection rate in the United Kingdom hit a 50-year high, said David Mabey, BCh, DM, from the London School of Hygiene and Tropical Medicine. Syphilis and other sexually transmitted infections are also a major problem in low- and middle-income countries, he added, although good data are not always available.
Many of today’s healthcare professionals have little experience with the disease, shared Ina Park, MD, a sexually transmitted infections specialist at the University of California at San Francisco. “An entire generation of physicians — including myself — did not see any cases until we were well out of our training,” Dr. Park reported. “We’re really playing catch-up.”
A Centuries-Old Ailment
Dr. Park offered some advice on the challenges of diagnosing what can be an elusive infection at the Conference on Retroviruses and Opportunistic Infections (CROI) 2024 Annual Meeting in Denver. That advice boiled down to one simple rule: “Test, test, test.”
Because syphilis can mimic so many other conditions and can have long periods of latency, it can be easily missed or even misdiagnosed by experienced physicians, said Dr. Park. Clinicians need to keep it front of mind and have a lower threshold for testing, even if there are no obvious symptoms.
Following the CDC’s new recommendations for syphilis screening will help, she noted; every sexually active patient aged between 15 and 44 years who lives in a county with a syphilis infection rate of 4.6 per 100,000 people or higher should get the test. And clinicians should remain vigilant, even in areas with a lower prevalence. “If you can’t account for new symptoms in a sexually active patient, order a test,” said Dr. Park.
Complicated Cases
The lack of experience with syphilis affects not just diagnosis but also treatment, particularly for complex cases, said Khalil Ghanem, MD, PhD, from the Johns Hopkins University School of Medicine in Baltimore. “When you don’t have to deal with something for a while, you forget how to deal with it,” he added.
At CROI, Dr. Ghanem offered suggestions for how to navigate complicated cases of ocular syphilis, otic syphilis, and neurosyphilis, and how to interpret test results when a patient’s antigen titers are being “unruly.”
With potential ocular or otic syphilis, you shouldn’t wait for a specialist like an ophthalmologist to weigh in but instead refer the patient directly to the emergency department because of the risk that the symptoms may become irreversible and result in permanent blindness or deafness. “You don’t want to dilly-dally with those conditions,” Dr. Ghanem said.
Closely monitoring a patient’s rapid plasma regain and venereal disease research laboratory antigen levels is the only way to manage syphilis and to determine whether the infection is responding to treatment, he noted, but sometimes those titers “don’t do what you think they should be doing” and fail to decline or even go up after treatment.
“You don’t know if they went up because the patient was re-infected, or they developed neurosyphilis, or there was a problem at the lab,” he said. “It can be challenging to interpret.”
To decipher confusing test results, Dr. Ghanem recommended getting a detailed history to understand whether a patient is at risk for reinfection, whether there are signs of neurosyphilis or other complications, whether pregnancy is possible, and so on. “Based on the answers, you can determine what the most rational approach to treatment would be,” he shared.
Drug Shortages
Efforts to get the infection under control have become more complicated. Last summer, Pfizer announced that it had run out of penicillin G benzathine (Bicillin), an injectable, long-acting drug that is one of the main treatments for syphilis and the only one that can be given to pregnant people. Supplies for children ran out at the end of June 2023, and supplies for adults were gone by the end of September.
Because Pfizer is the only company that manufactures penicillin G benzathine, there is no one to pick up the slack in the short-term, so the shortage is expected to continue until at least the middle of 2024.
In response, the US Food and Drug Administration has temporarily allowed the use of benzylpenicillin benzathine (Extencilline), a French formulation that has not been approved in the United States, until supplies of penicillin G benzathine are stabilized.
The shortage has shone a spotlight on the important issue of a lack of alternatives for the treatment of syphilis during pregnancy, which increases the risk for congenital syphilis. “Hopefully, this pushes the National Institutes of Health and others to step up their game on studies for alternative drugs for use in pregnancy,” Dr. Ghanem said.
A version of this article appeared on Medscape.com.
With rates of syphilis rising quickly in the United States and elsewhere, clinicians are having to up their game when it comes to diagnosing and treating an infection that they may not be paying enough attention to.
More than 200,000 cases of syphilis were reported in the United States in 2022, which is the highest number since 1950 and is a 17.3% increase over 2021, according to the latest figures from the Centers for Disease Control and Prevention (CDC). The rate of infection has increased almost every year since a historic low in 2001.
And the trend is not limited to the United States. Last year, the infection rate in the United Kingdom hit a 50-year high, said David Mabey, BCh, DM, from the London School of Hygiene and Tropical Medicine. Syphilis and other sexually transmitted infections are also a major problem in low- and middle-income countries, he added, although good data are not always available.
Many of today’s healthcare professionals have little experience with the disease, shared Ina Park, MD, a sexually transmitted infections specialist at the University of California at San Francisco. “An entire generation of physicians — including myself — did not see any cases until we were well out of our training,” Dr. Park reported. “We’re really playing catch-up.”
A Centuries-Old Ailment
Dr. Park offered some advice on the challenges of diagnosing what can be an elusive infection at the Conference on Retroviruses and Opportunistic Infections (CROI) 2024 Annual Meeting in Denver. That advice boiled down to one simple rule: “Test, test, test.”
Because syphilis can mimic so many other conditions and can have long periods of latency, it can be easily missed or even misdiagnosed by experienced physicians, said Dr. Park. Clinicians need to keep it front of mind and have a lower threshold for testing, even if there are no obvious symptoms.
Following the CDC’s new recommendations for syphilis screening will help, she noted; every sexually active patient aged between 15 and 44 years who lives in a county with a syphilis infection rate of 4.6 per 100,000 people or higher should get the test. And clinicians should remain vigilant, even in areas with a lower prevalence. “If you can’t account for new symptoms in a sexually active patient, order a test,” said Dr. Park.
Complicated Cases
The lack of experience with syphilis affects not just diagnosis but also treatment, particularly for complex cases, said Khalil Ghanem, MD, PhD, from the Johns Hopkins University School of Medicine in Baltimore. “When you don’t have to deal with something for a while, you forget how to deal with it,” he added.
At CROI, Dr. Ghanem offered suggestions for how to navigate complicated cases of ocular syphilis, otic syphilis, and neurosyphilis, and how to interpret test results when a patient’s antigen titers are being “unruly.”
With potential ocular or otic syphilis, you shouldn’t wait for a specialist like an ophthalmologist to weigh in but instead refer the patient directly to the emergency department because of the risk that the symptoms may become irreversible and result in permanent blindness or deafness. “You don’t want to dilly-dally with those conditions,” Dr. Ghanem said.
Closely monitoring a patient’s rapid plasma regain and venereal disease research laboratory antigen levels is the only way to manage syphilis and to determine whether the infection is responding to treatment, he noted, but sometimes those titers “don’t do what you think they should be doing” and fail to decline or even go up after treatment.
“You don’t know if they went up because the patient was re-infected, or they developed neurosyphilis, or there was a problem at the lab,” he said. “It can be challenging to interpret.”
To decipher confusing test results, Dr. Ghanem recommended getting a detailed history to understand whether a patient is at risk for reinfection, whether there are signs of neurosyphilis or other complications, whether pregnancy is possible, and so on. “Based on the answers, you can determine what the most rational approach to treatment would be,” he shared.
Drug Shortages
Efforts to get the infection under control have become more complicated. Last summer, Pfizer announced that it had run out of penicillin G benzathine (Bicillin), an injectable, long-acting drug that is one of the main treatments for syphilis and the only one that can be given to pregnant people. Supplies for children ran out at the end of June 2023, and supplies for adults were gone by the end of September.
Because Pfizer is the only company that manufactures penicillin G benzathine, there is no one to pick up the slack in the short-term, so the shortage is expected to continue until at least the middle of 2024.
In response, the US Food and Drug Administration has temporarily allowed the use of benzylpenicillin benzathine (Extencilline), a French formulation that has not been approved in the United States, until supplies of penicillin G benzathine are stabilized.
The shortage has shone a spotlight on the important issue of a lack of alternatives for the treatment of syphilis during pregnancy, which increases the risk for congenital syphilis. “Hopefully, this pushes the National Institutes of Health and others to step up their game on studies for alternative drugs for use in pregnancy,” Dr. Ghanem said.
A version of this article appeared on Medscape.com.
With rates of syphilis rising quickly in the United States and elsewhere, clinicians are having to up their game when it comes to diagnosing and treating an infection that they may not be paying enough attention to.
More than 200,000 cases of syphilis were reported in the United States in 2022, which is the highest number since 1950 and is a 17.3% increase over 2021, according to the latest figures from the Centers for Disease Control and Prevention (CDC). The rate of infection has increased almost every year since a historic low in 2001.
And the trend is not limited to the United States. Last year, the infection rate in the United Kingdom hit a 50-year high, said David Mabey, BCh, DM, from the London School of Hygiene and Tropical Medicine. Syphilis and other sexually transmitted infections are also a major problem in low- and middle-income countries, he added, although good data are not always available.
Many of today’s healthcare professionals have little experience with the disease, shared Ina Park, MD, a sexually transmitted infections specialist at the University of California at San Francisco. “An entire generation of physicians — including myself — did not see any cases until we were well out of our training,” Dr. Park reported. “We’re really playing catch-up.”
A Centuries-Old Ailment
Dr. Park offered some advice on the challenges of diagnosing what can be an elusive infection at the Conference on Retroviruses and Opportunistic Infections (CROI) 2024 Annual Meeting in Denver. That advice boiled down to one simple rule: “Test, test, test.”
Because syphilis can mimic so many other conditions and can have long periods of latency, it can be easily missed or even misdiagnosed by experienced physicians, said Dr. Park. Clinicians need to keep it front of mind and have a lower threshold for testing, even if there are no obvious symptoms.
Following the CDC’s new recommendations for syphilis screening will help, she noted; every sexually active patient aged between 15 and 44 years who lives in a county with a syphilis infection rate of 4.6 per 100,000 people or higher should get the test. And clinicians should remain vigilant, even in areas with a lower prevalence. “If you can’t account for new symptoms in a sexually active patient, order a test,” said Dr. Park.
Complicated Cases
The lack of experience with syphilis affects not just diagnosis but also treatment, particularly for complex cases, said Khalil Ghanem, MD, PhD, from the Johns Hopkins University School of Medicine in Baltimore. “When you don’t have to deal with something for a while, you forget how to deal with it,” he added.
At CROI, Dr. Ghanem offered suggestions for how to navigate complicated cases of ocular syphilis, otic syphilis, and neurosyphilis, and how to interpret test results when a patient’s antigen titers are being “unruly.”
With potential ocular or otic syphilis, you shouldn’t wait for a specialist like an ophthalmologist to weigh in but instead refer the patient directly to the emergency department because of the risk that the symptoms may become irreversible and result in permanent blindness or deafness. “You don’t want to dilly-dally with those conditions,” Dr. Ghanem said.
Closely monitoring a patient’s rapid plasma regain and venereal disease research laboratory antigen levels is the only way to manage syphilis and to determine whether the infection is responding to treatment, he noted, but sometimes those titers “don’t do what you think they should be doing” and fail to decline or even go up after treatment.
“You don’t know if they went up because the patient was re-infected, or they developed neurosyphilis, or there was a problem at the lab,” he said. “It can be challenging to interpret.”
To decipher confusing test results, Dr. Ghanem recommended getting a detailed history to understand whether a patient is at risk for reinfection, whether there are signs of neurosyphilis or other complications, whether pregnancy is possible, and so on. “Based on the answers, you can determine what the most rational approach to treatment would be,” he shared.
Drug Shortages
Efforts to get the infection under control have become more complicated. Last summer, Pfizer announced that it had run out of penicillin G benzathine (Bicillin), an injectable, long-acting drug that is one of the main treatments for syphilis and the only one that can be given to pregnant people. Supplies for children ran out at the end of June 2023, and supplies for adults were gone by the end of September.
Because Pfizer is the only company that manufactures penicillin G benzathine, there is no one to pick up the slack in the short-term, so the shortage is expected to continue until at least the middle of 2024.
In response, the US Food and Drug Administration has temporarily allowed the use of benzylpenicillin benzathine (Extencilline), a French formulation that has not been approved in the United States, until supplies of penicillin G benzathine are stabilized.
The shortage has shone a spotlight on the important issue of a lack of alternatives for the treatment of syphilis during pregnancy, which increases the risk for congenital syphilis. “Hopefully, this pushes the National Institutes of Health and others to step up their game on studies for alternative drugs for use in pregnancy,” Dr. Ghanem said.
A version of this article appeared on Medscape.com.
Biological Sex Differences: Key to Understanding Long COVID?
Letícia Soares was infected with COVID-19 in April 2020, in the final year of postdoctoral studies in disease ecology at a Canadian University. What started with piercing migraines and severe fatigue in 2020 soon spiraled into a myriad of long COVID symptoms: Gastrointestinal issues, sleep problems, joint and muscle pain, along with unexpected menstrual changes.
After an absence of menstrual bleeding and its usual signs, she later suffered from severe periods and symptoms that worsened her long COVID condition. “It just baffled me,” said Soares, now 39. “It was debilitating.”
Cases like Soares’s are leading scientists to spend more time trying to understand the biological sex disparity in chronic illnesses such as long COVID that until recently have all but been ignored. According to the Centers for Disease Control and Prevention, long COVID affects nearly twice as many women as men.
What’s more, up to two thirds of female patients with long COVID report an increase in symptoms related to menstruation, which suggests a possible link between sex hormone fluctuations and immune dysfunction in the illness.
“These illnesses are underfunded and understudied relative to their disease burdens,” said Beth Pollack, a research scientist at the Massachusetts Institute of Technology, Cambridge, Massachusetts, who studies complex chronic illnesses.
Addressing knowledge gaps, especially around sex differences, could significantly improve our understanding of complex chronic illnesses, said Pollack, who coauthored a 2023 literature review of female reproductive health impacts of long COVID.
Emerging ‘Menstrual Science’ Could Be Key
There is a critical need, she said, for studies on these illnesses to include considerations of sex differences, hormones, reproductive phases, and reproductive conditions. This research could potentially inform doctors and other clinicians or lead to treatments, both for reproductive symptoms and for the illnesses themselves.
Pollack noted that reproductive symptoms are prevalent across a group of infection-associated chronic illnesses she studies, all of which disproportionately affect women. These associated conditions, traditionally studied in isolation, share pathologies like reproductive health concerns, signaling a need for focused research on their shared mechanisms.
Recognizing this critical gap, “menstrual science” is emerging as a pivotal area of study, aiming to connect these dots through focused research on hormonal influences.
Researchers at the University of Melbourne, Melbourne, Australia, for example, are studying whether hormones play a role in causing or worsening the symptoms of long COVID. By comparing hormone levels in people with these conditions with those in healthy people and by tracking how symptoms change with hormone levels over time and across menstrual cycles, scientists hope to find patterns that could help diagnose these conditions more easily and lead to new treatments. They’re also examining how hormonal life phases such as puberty, pregnancy, or perimenopause and hormone treatments like birth control might affect these illnesses.
How Gender and Long COVID Intertwine
The pathologies of long COVID, affecting at least 65 million people worldwide, currently focus on four hypotheses: Persistent viral infection, reactivation of dormant viruses (such as common herpes viruses), inflammation-related damage to tissues and organs, and autoimmunity (the body attacking itself).
It’s this last reason that holds some of the most interesting clues on biological sex differences, said Akiko Iwasaki, PhD, a Yale University, New Haven, Connecticut, immunologist who has led numerous research breakthroughs on long COVID since the start of the pandemic. Women have two X chromosomes, for example, and although one is inactivated, the inactivation is incomplete.
Some cells still express genes from the “inactivated genes” on the X chromosome, Iwasaki said. Those include key immune genes, which trigger a more robust response to infections and vaccinations but also predispose them to autoimmune reactions. “It comes at the cost of triggering too much immune response,” Iwasaki said.
Sex hormones also factor in. Testosterone, which is higher in males, is immunosuppressive, so it can dampen immune responses, Iwasaki said. That may contribute to making males more likely to get severe acute infections of COVID-19 but have fewer long-term effects.
Estrogen, on the other hand, is known to enhance the immune response. It can increase the production of antibodies and the activation of T cells, which are critical for fighting off infections. This heightened immune response, however, might also contribute to the persistent inflammation observed in long COVID, where the immune system continues to react even after the acute infection has resolved.
Sex-Specific Symptoms and Marginalized Communities
Of the more than 200 symptoms long haulers experience, Iwasaki said, several are also sex-specific. A recent draft study by Iwasaki and another leading COVID researcher, David Putrino, PhD, at Mount Sinai Health System in New York City, shows hair loss as one of the most female-dominant symptoms and sexual dysfunction among males.
In examining sex differences, another question is why long COVID rates in the trans community are disproportionately high. One of the reasons Iwasaki’s lab is looking at testosterone closely is because anecdotal evidence from female-to-male trans individuals indicates that testosterone therapy improved their long COVID symptoms significantly. It also raises the possibility that hormone therapy could help.
However, patients and advocates say it’s also important to consider socioeconomic factors in the trans community. “We need to start at this population and social structure level to understand why trans people over and over are put in harm’s way,” said JD Davids, a trans patient-researcher with long COVID and the cofounder and codirector of Strategies for High Impact and its Long COVID Justice project.
For trans people, said Davids, risk factors for both severe COVID and long COVID include being part of low-income groups, belonging to marginalized racial and ethnic communities, and living in crowded environments such as shelters or prisons.
The disproportionate impact of long COVID on marginalized communities, especially when seen through the lens of historical medical neglect, also demands attention, said Iwasaki. “Women used to be labeled hysteric when they complained about these kinds of symptoms.”
Where It All Leads
The possibility of diagnosing long COVID with a simple blood test could radically change some doctors’ false perceptions that it is not a real condition, Iwasaki said, ensuring it is recognized and treated with the seriousness it deserves.
“I feel like we need to get there with long COVID. If we can order a blood test and say somebody has a long COVID because of these values, then suddenly the diseases become medically explainable,” Iwasaki added. This advancement is critical for propelling research forward, she said, refining treatment approaches — including those that target sex-specific hormone, immunity, and inflammation issues — and improving the well-being of those living with long COVID.
This hope resonates with scientists like Pollack, who recently led the first National Institutes of Health-sponsored research webinar on less studied pathologies in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and long COVID, and with the experiences of individuals like Soares, who navigates through the unpredictable nature of both of these conditions with resilience.
“This illness never ceases to surprise me in how it changes my body. I feel like it’s a constant adaptation,” said Soares. Now living in Salvador, Brazil, her daily life has dramatically shifted to the confines of her home.
“It’s how I have more predictability in my symptoms,” she said, pointing out the pressing need for the scientific advancements that Iwasaki envisions and a deepening of our understanding of the disease’s impacts on patients’ lives.
A version of this article appeared on Medscape.com.
Letícia Soares was infected with COVID-19 in April 2020, in the final year of postdoctoral studies in disease ecology at a Canadian University. What started with piercing migraines and severe fatigue in 2020 soon spiraled into a myriad of long COVID symptoms: Gastrointestinal issues, sleep problems, joint and muscle pain, along with unexpected menstrual changes.
After an absence of menstrual bleeding and its usual signs, she later suffered from severe periods and symptoms that worsened her long COVID condition. “It just baffled me,” said Soares, now 39. “It was debilitating.”
Cases like Soares’s are leading scientists to spend more time trying to understand the biological sex disparity in chronic illnesses such as long COVID that until recently have all but been ignored. According to the Centers for Disease Control and Prevention, long COVID affects nearly twice as many women as men.
What’s more, up to two thirds of female patients with long COVID report an increase in symptoms related to menstruation, which suggests a possible link between sex hormone fluctuations and immune dysfunction in the illness.
“These illnesses are underfunded and understudied relative to their disease burdens,” said Beth Pollack, a research scientist at the Massachusetts Institute of Technology, Cambridge, Massachusetts, who studies complex chronic illnesses.
Addressing knowledge gaps, especially around sex differences, could significantly improve our understanding of complex chronic illnesses, said Pollack, who coauthored a 2023 literature review of female reproductive health impacts of long COVID.
Emerging ‘Menstrual Science’ Could Be Key
There is a critical need, she said, for studies on these illnesses to include considerations of sex differences, hormones, reproductive phases, and reproductive conditions. This research could potentially inform doctors and other clinicians or lead to treatments, both for reproductive symptoms and for the illnesses themselves.
Pollack noted that reproductive symptoms are prevalent across a group of infection-associated chronic illnesses she studies, all of which disproportionately affect women. These associated conditions, traditionally studied in isolation, share pathologies like reproductive health concerns, signaling a need for focused research on their shared mechanisms.
Recognizing this critical gap, “menstrual science” is emerging as a pivotal area of study, aiming to connect these dots through focused research on hormonal influences.
Researchers at the University of Melbourne, Melbourne, Australia, for example, are studying whether hormones play a role in causing or worsening the symptoms of long COVID. By comparing hormone levels in people with these conditions with those in healthy people and by tracking how symptoms change with hormone levels over time and across menstrual cycles, scientists hope to find patterns that could help diagnose these conditions more easily and lead to new treatments. They’re also examining how hormonal life phases such as puberty, pregnancy, or perimenopause and hormone treatments like birth control might affect these illnesses.
How Gender and Long COVID Intertwine
The pathologies of long COVID, affecting at least 65 million people worldwide, currently focus on four hypotheses: Persistent viral infection, reactivation of dormant viruses (such as common herpes viruses), inflammation-related damage to tissues and organs, and autoimmunity (the body attacking itself).
It’s this last reason that holds some of the most interesting clues on biological sex differences, said Akiko Iwasaki, PhD, a Yale University, New Haven, Connecticut, immunologist who has led numerous research breakthroughs on long COVID since the start of the pandemic. Women have two X chromosomes, for example, and although one is inactivated, the inactivation is incomplete.
Some cells still express genes from the “inactivated genes” on the X chromosome, Iwasaki said. Those include key immune genes, which trigger a more robust response to infections and vaccinations but also predispose them to autoimmune reactions. “It comes at the cost of triggering too much immune response,” Iwasaki said.
Sex hormones also factor in. Testosterone, which is higher in males, is immunosuppressive, so it can dampen immune responses, Iwasaki said. That may contribute to making males more likely to get severe acute infections of COVID-19 but have fewer long-term effects.
Estrogen, on the other hand, is known to enhance the immune response. It can increase the production of antibodies and the activation of T cells, which are critical for fighting off infections. This heightened immune response, however, might also contribute to the persistent inflammation observed in long COVID, where the immune system continues to react even after the acute infection has resolved.
Sex-Specific Symptoms and Marginalized Communities
Of the more than 200 symptoms long haulers experience, Iwasaki said, several are also sex-specific. A recent draft study by Iwasaki and another leading COVID researcher, David Putrino, PhD, at Mount Sinai Health System in New York City, shows hair loss as one of the most female-dominant symptoms and sexual dysfunction among males.
In examining sex differences, another question is why long COVID rates in the trans community are disproportionately high. One of the reasons Iwasaki’s lab is looking at testosterone closely is because anecdotal evidence from female-to-male trans individuals indicates that testosterone therapy improved their long COVID symptoms significantly. It also raises the possibility that hormone therapy could help.
However, patients and advocates say it’s also important to consider socioeconomic factors in the trans community. “We need to start at this population and social structure level to understand why trans people over and over are put in harm’s way,” said JD Davids, a trans patient-researcher with long COVID and the cofounder and codirector of Strategies for High Impact and its Long COVID Justice project.
For trans people, said Davids, risk factors for both severe COVID and long COVID include being part of low-income groups, belonging to marginalized racial and ethnic communities, and living in crowded environments such as shelters or prisons.
The disproportionate impact of long COVID on marginalized communities, especially when seen through the lens of historical medical neglect, also demands attention, said Iwasaki. “Women used to be labeled hysteric when they complained about these kinds of symptoms.”
Where It All Leads
The possibility of diagnosing long COVID with a simple blood test could radically change some doctors’ false perceptions that it is not a real condition, Iwasaki said, ensuring it is recognized and treated with the seriousness it deserves.
“I feel like we need to get there with long COVID. If we can order a blood test and say somebody has a long COVID because of these values, then suddenly the diseases become medically explainable,” Iwasaki added. This advancement is critical for propelling research forward, she said, refining treatment approaches — including those that target sex-specific hormone, immunity, and inflammation issues — and improving the well-being of those living with long COVID.
This hope resonates with scientists like Pollack, who recently led the first National Institutes of Health-sponsored research webinar on less studied pathologies in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and long COVID, and with the experiences of individuals like Soares, who navigates through the unpredictable nature of both of these conditions with resilience.
“This illness never ceases to surprise me in how it changes my body. I feel like it’s a constant adaptation,” said Soares. Now living in Salvador, Brazil, her daily life has dramatically shifted to the confines of her home.
“It’s how I have more predictability in my symptoms,” she said, pointing out the pressing need for the scientific advancements that Iwasaki envisions and a deepening of our understanding of the disease’s impacts on patients’ lives.
A version of this article appeared on Medscape.com.
Letícia Soares was infected with COVID-19 in April 2020, in the final year of postdoctoral studies in disease ecology at a Canadian University. What started with piercing migraines and severe fatigue in 2020 soon spiraled into a myriad of long COVID symptoms: Gastrointestinal issues, sleep problems, joint and muscle pain, along with unexpected menstrual changes.
After an absence of menstrual bleeding and its usual signs, she later suffered from severe periods and symptoms that worsened her long COVID condition. “It just baffled me,” said Soares, now 39. “It was debilitating.”
Cases like Soares’s are leading scientists to spend more time trying to understand the biological sex disparity in chronic illnesses such as long COVID that until recently have all but been ignored. According to the Centers for Disease Control and Prevention, long COVID affects nearly twice as many women as men.
What’s more, up to two thirds of female patients with long COVID report an increase in symptoms related to menstruation, which suggests a possible link between sex hormone fluctuations and immune dysfunction in the illness.
“These illnesses are underfunded and understudied relative to their disease burdens,” said Beth Pollack, a research scientist at the Massachusetts Institute of Technology, Cambridge, Massachusetts, who studies complex chronic illnesses.
Addressing knowledge gaps, especially around sex differences, could significantly improve our understanding of complex chronic illnesses, said Pollack, who coauthored a 2023 literature review of female reproductive health impacts of long COVID.
Emerging ‘Menstrual Science’ Could Be Key
There is a critical need, she said, for studies on these illnesses to include considerations of sex differences, hormones, reproductive phases, and reproductive conditions. This research could potentially inform doctors and other clinicians or lead to treatments, both for reproductive symptoms and for the illnesses themselves.
Pollack noted that reproductive symptoms are prevalent across a group of infection-associated chronic illnesses she studies, all of which disproportionately affect women. These associated conditions, traditionally studied in isolation, share pathologies like reproductive health concerns, signaling a need for focused research on their shared mechanisms.
Recognizing this critical gap, “menstrual science” is emerging as a pivotal area of study, aiming to connect these dots through focused research on hormonal influences.
Researchers at the University of Melbourne, Melbourne, Australia, for example, are studying whether hormones play a role in causing or worsening the symptoms of long COVID. By comparing hormone levels in people with these conditions with those in healthy people and by tracking how symptoms change with hormone levels over time and across menstrual cycles, scientists hope to find patterns that could help diagnose these conditions more easily and lead to new treatments. They’re also examining how hormonal life phases such as puberty, pregnancy, or perimenopause and hormone treatments like birth control might affect these illnesses.
How Gender and Long COVID Intertwine
The pathologies of long COVID, affecting at least 65 million people worldwide, currently focus on four hypotheses: Persistent viral infection, reactivation of dormant viruses (such as common herpes viruses), inflammation-related damage to tissues and organs, and autoimmunity (the body attacking itself).
It’s this last reason that holds some of the most interesting clues on biological sex differences, said Akiko Iwasaki, PhD, a Yale University, New Haven, Connecticut, immunologist who has led numerous research breakthroughs on long COVID since the start of the pandemic. Women have two X chromosomes, for example, and although one is inactivated, the inactivation is incomplete.
Some cells still express genes from the “inactivated genes” on the X chromosome, Iwasaki said. Those include key immune genes, which trigger a more robust response to infections and vaccinations but also predispose them to autoimmune reactions. “It comes at the cost of triggering too much immune response,” Iwasaki said.
Sex hormones also factor in. Testosterone, which is higher in males, is immunosuppressive, so it can dampen immune responses, Iwasaki said. That may contribute to making males more likely to get severe acute infections of COVID-19 but have fewer long-term effects.
Estrogen, on the other hand, is known to enhance the immune response. It can increase the production of antibodies and the activation of T cells, which are critical for fighting off infections. This heightened immune response, however, might also contribute to the persistent inflammation observed in long COVID, where the immune system continues to react even after the acute infection has resolved.
Sex-Specific Symptoms and Marginalized Communities
Of the more than 200 symptoms long haulers experience, Iwasaki said, several are also sex-specific. A recent draft study by Iwasaki and another leading COVID researcher, David Putrino, PhD, at Mount Sinai Health System in New York City, shows hair loss as one of the most female-dominant symptoms and sexual dysfunction among males.
In examining sex differences, another question is why long COVID rates in the trans community are disproportionately high. One of the reasons Iwasaki’s lab is looking at testosterone closely is because anecdotal evidence from female-to-male trans individuals indicates that testosterone therapy improved their long COVID symptoms significantly. It also raises the possibility that hormone therapy could help.
However, patients and advocates say it’s also important to consider socioeconomic factors in the trans community. “We need to start at this population and social structure level to understand why trans people over and over are put in harm’s way,” said JD Davids, a trans patient-researcher with long COVID and the cofounder and codirector of Strategies for High Impact and its Long COVID Justice project.
For trans people, said Davids, risk factors for both severe COVID and long COVID include being part of low-income groups, belonging to marginalized racial and ethnic communities, and living in crowded environments such as shelters or prisons.
The disproportionate impact of long COVID on marginalized communities, especially when seen through the lens of historical medical neglect, also demands attention, said Iwasaki. “Women used to be labeled hysteric when they complained about these kinds of symptoms.”
Where It All Leads
The possibility of diagnosing long COVID with a simple blood test could radically change some doctors’ false perceptions that it is not a real condition, Iwasaki said, ensuring it is recognized and treated with the seriousness it deserves.
“I feel like we need to get there with long COVID. If we can order a blood test and say somebody has a long COVID because of these values, then suddenly the diseases become medically explainable,” Iwasaki added. This advancement is critical for propelling research forward, she said, refining treatment approaches — including those that target sex-specific hormone, immunity, and inflammation issues — and improving the well-being of those living with long COVID.
This hope resonates with scientists like Pollack, who recently led the first National Institutes of Health-sponsored research webinar on less studied pathologies in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and long COVID, and with the experiences of individuals like Soares, who navigates through the unpredictable nature of both of these conditions with resilience.
“This illness never ceases to surprise me in how it changes my body. I feel like it’s a constant adaptation,” said Soares. Now living in Salvador, Brazil, her daily life has dramatically shifted to the confines of her home.
“It’s how I have more predictability in my symptoms,” she said, pointing out the pressing need for the scientific advancements that Iwasaki envisions and a deepening of our understanding of the disease’s impacts on patients’ lives.
A version of this article appeared on Medscape.com.
Poor Quality of Cancer Content on Social Media
This transcript has been edited for clarity.
I’m delighted to talk about a very interesting topic in this commentary. This is an area that we generally don’t discuss, but it’s one that’s obviously very topical, which includes the question of social media.
The paper I’m referring to is entitled, “More Than a Song and Dance”: Exploration of Patient Perspectives and Educational Quality of Gynecologic Cancer Content on TikTok. The paper was published in Gynecologic Oncology in 2023.
They had a total of 466.7 million views. They looked at 430 of the 500 top posts that were eligible, looked at 11 central themes, did an objective analysis of educational content based on published strategy for looking at this.
What they found, unfortunately but not surprisingly, overall was that the educational quality and reliability were quite poor. They also noticed considerable differences in disparities based on racial background and really emphasized in their analysis not only how common it is for individuals to look at this content on TikTok but also concerns about what it is that the public, patients, and their families are actually seeing.
This, of course, specifically relates to gynecologic cancers, but almost certainly relates to other cancers as well. Clearly, this is a topic that needs to be discussed widely. It’s very complex and very controversial, but when you think about the information that might be provided to our patients and their families going to social media, it’s important that we understand what they’re seeing, what they’re hearing, what they’re viewing, and the impact this might have on their care and outcomes.
I encourage you to read this very interesting paper if you have an interest in this topic. Again, it was recently published in Gynecologic Oncology. I thank you for your attention.
Dr. Markman is professor, Department of Medical Oncology and Therapeutics Research, City of Hope, Duarte, California; president of Medicine & Science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed ties with GlaxoSmithKline and AstraZeneca.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I’m delighted to talk about a very interesting topic in this commentary. This is an area that we generally don’t discuss, but it’s one that’s obviously very topical, which includes the question of social media.
The paper I’m referring to is entitled, “More Than a Song and Dance”: Exploration of Patient Perspectives and Educational Quality of Gynecologic Cancer Content on TikTok. The paper was published in Gynecologic Oncology in 2023.
They had a total of 466.7 million views. They looked at 430 of the 500 top posts that were eligible, looked at 11 central themes, did an objective analysis of educational content based on published strategy for looking at this.
What they found, unfortunately but not surprisingly, overall was that the educational quality and reliability were quite poor. They also noticed considerable differences in disparities based on racial background and really emphasized in their analysis not only how common it is for individuals to look at this content on TikTok but also concerns about what it is that the public, patients, and their families are actually seeing.
This, of course, specifically relates to gynecologic cancers, but almost certainly relates to other cancers as well. Clearly, this is a topic that needs to be discussed widely. It’s very complex and very controversial, but when you think about the information that might be provided to our patients and their families going to social media, it’s important that we understand what they’re seeing, what they’re hearing, what they’re viewing, and the impact this might have on their care and outcomes.
I encourage you to read this very interesting paper if you have an interest in this topic. Again, it was recently published in Gynecologic Oncology. I thank you for your attention.
Dr. Markman is professor, Department of Medical Oncology and Therapeutics Research, City of Hope, Duarte, California; president of Medicine & Science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed ties with GlaxoSmithKline and AstraZeneca.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I’m delighted to talk about a very interesting topic in this commentary. This is an area that we generally don’t discuss, but it’s one that’s obviously very topical, which includes the question of social media.
The paper I’m referring to is entitled, “More Than a Song and Dance”: Exploration of Patient Perspectives and Educational Quality of Gynecologic Cancer Content on TikTok. The paper was published in Gynecologic Oncology in 2023.
They had a total of 466.7 million views. They looked at 430 of the 500 top posts that were eligible, looked at 11 central themes, did an objective analysis of educational content based on published strategy for looking at this.
What they found, unfortunately but not surprisingly, overall was that the educational quality and reliability were quite poor. They also noticed considerable differences in disparities based on racial background and really emphasized in their analysis not only how common it is for individuals to look at this content on TikTok but also concerns about what it is that the public, patients, and their families are actually seeing.
This, of course, specifically relates to gynecologic cancers, but almost certainly relates to other cancers as well. Clearly, this is a topic that needs to be discussed widely. It’s very complex and very controversial, but when you think about the information that might be provided to our patients and their families going to social media, it’s important that we understand what they’re seeing, what they’re hearing, what they’re viewing, and the impact this might have on their care and outcomes.
I encourage you to read this very interesting paper if you have an interest in this topic. Again, it was recently published in Gynecologic Oncology. I thank you for your attention.
Dr. Markman is professor, Department of Medical Oncology and Therapeutics Research, City of Hope, Duarte, California; president of Medicine & Science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed ties with GlaxoSmithKline and AstraZeneca.
A version of this article appeared on Medscape.com.
Long-Term Follow-Up Emphasizes HPV Vaccination Importance
This transcript has been edited for clarity.
I want to briefly discuss a critically important topic that cannot be overly emphasized. It is the relevance, the importance, the benefits, and the outcome of HPV vaccination.
The paper I’m referring to was published in Pediatrics in October 2023. It’s titled, “Ten-Year Follow-up of 9-Valent Human Papillomavirus Vaccine: Immunogenicity, Effectiveness, and Safety.”
Let me emphasize that we’re talking about a 10-year follow-up. In this particular paper and analysis, 301 boys — I emphasize boys — were included and 971 girls at 40 different sites in 13 countries, who received the 9-valent vaccine, which includes HPV 16, 18, and seven other types.
Most importantly, there was not a single case. Not one. Let me repeat this: There was not a single case of high-grade intraepithelial neoplasia, or worse, or condyloma in either males or females. There was not a single case in over 1000 individuals with a follow-up of more than 10 years.
It is difficult to overstate the magnitude of the benefit associated with HPV vaccination for our children and young adults on their risk of developing highly relevant, life-changing, potentially deadly cancers.
For those of you who are interested in this topic — which should include almost all of you, if not all of you — I encourage you to read this very important follow-up paper, again, demonstrating the simple, overwhelming magnitude of the benefit of HPV vaccination. I thank you for your attention.
Dr. Markman is a professor in the department of medical oncology and therapeutics research, City of Hope, Duarte, California, and president of medicine and science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed ties with GlaxoSmithKline; AstraZeneca.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I want to briefly discuss a critically important topic that cannot be overly emphasized. It is the relevance, the importance, the benefits, and the outcome of HPV vaccination.
The paper I’m referring to was published in Pediatrics in October 2023. It’s titled, “Ten-Year Follow-up of 9-Valent Human Papillomavirus Vaccine: Immunogenicity, Effectiveness, and Safety.”
Let me emphasize that we’re talking about a 10-year follow-up. In this particular paper and analysis, 301 boys — I emphasize boys — were included and 971 girls at 40 different sites in 13 countries, who received the 9-valent vaccine, which includes HPV 16, 18, and seven other types.
Most importantly, there was not a single case. Not one. Let me repeat this: There was not a single case of high-grade intraepithelial neoplasia, or worse, or condyloma in either males or females. There was not a single case in over 1000 individuals with a follow-up of more than 10 years.
It is difficult to overstate the magnitude of the benefit associated with HPV vaccination for our children and young adults on their risk of developing highly relevant, life-changing, potentially deadly cancers.
For those of you who are interested in this topic — which should include almost all of you, if not all of you — I encourage you to read this very important follow-up paper, again, demonstrating the simple, overwhelming magnitude of the benefit of HPV vaccination. I thank you for your attention.
Dr. Markman is a professor in the department of medical oncology and therapeutics research, City of Hope, Duarte, California, and president of medicine and science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed ties with GlaxoSmithKline; AstraZeneca.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I want to briefly discuss a critically important topic that cannot be overly emphasized. It is the relevance, the importance, the benefits, and the outcome of HPV vaccination.
The paper I’m referring to was published in Pediatrics in October 2023. It’s titled, “Ten-Year Follow-up of 9-Valent Human Papillomavirus Vaccine: Immunogenicity, Effectiveness, and Safety.”
Let me emphasize that we’re talking about a 10-year follow-up. In this particular paper and analysis, 301 boys — I emphasize boys — were included and 971 girls at 40 different sites in 13 countries, who received the 9-valent vaccine, which includes HPV 16, 18, and seven other types.
Most importantly, there was not a single case. Not one. Let me repeat this: There was not a single case of high-grade intraepithelial neoplasia, or worse, or condyloma in either males or females. There was not a single case in over 1000 individuals with a follow-up of more than 10 years.
It is difficult to overstate the magnitude of the benefit associated with HPV vaccination for our children and young adults on their risk of developing highly relevant, life-changing, potentially deadly cancers.
For those of you who are interested in this topic — which should include almost all of you, if not all of you — I encourage you to read this very important follow-up paper, again, demonstrating the simple, overwhelming magnitude of the benefit of HPV vaccination. I thank you for your attention.
Dr. Markman is a professor in the department of medical oncology and therapeutics research, City of Hope, Duarte, California, and president of medicine and science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed ties with GlaxoSmithKline; AstraZeneca.
A version of this article appeared on Medscape.com.
RNA Vaccines: Risk for Heavy Menstrual Bleeding Clarified
Cases of menstrual disorders, particularly unusually heavy menstrual bleeding, have been reported following RNA vaccination against COVID-19.
In France, this safety signal has been confirmed and added to the product characteristics summaries and vaccine leaflets for mRNA vaccines in October 2022. However, few studies have accurately measured this risk to date.
To address this gap in research, the French scientific interest group in the epidemiology of health products, ANSM-Cnam EPI-PHARE, conducted a study to assess the risk for heavy menstrual bleeding requiring hospitalization after COVID-19 vaccination in France.
“This study provides new evidence supporting the existence of an increased risk for heavy menstrual bleeding following COVID-19 vaccination with mRNA vaccines,” wrote the authors.
Study Details
The study included all women aged 15-50 years who were diagnosed with heavy menstrual bleeding in the hospital between May 12, 2021, and August 31, 2022. Participants were identified in the National Health Data System, and the study population totaled 4610 women.
Each participant was randomly matched with as many as 30 women who had not been hospitalized for abnormal genital bleeding and had similar characteristics in terms of age, department of residence, social deprivation index of the commune of residence, and contraceptive method.
Women who had a recent pregnancy, hysterectomy, or coagulation disorder within the specified time frames were excluded.
At the time of the study, 71% of cases and 70% of controls had received at least one dose of the COVID-19 vaccine. Among vaccinated participants, 68% and 66%, respectively, received a vaccination dose (first or second dose). An mRNA vaccine (Comirnaty or Spikevax) was the last vaccine for 99.8% of the population.
Increased Risk
Compared with control women, those hospitalized for heavy menstrual bleeding were more likely to have received their last dose of mRNA vaccine (Comirnaty or Spikevax) in the previous 1-3 months. This association was observed for vaccination doses (odds ratio [OR], 1.20), indicating a 20% increased risk, but it was not found for booster doses (OR, 1.07).
This association was particularly notable for women residing in socially disadvantaged communities (OR, 1.28) and women not using hormonal contraception (OR, 1.28).
The risk did not appear to be increased beyond 3 months after vaccination. Researchers noted that the increased risk may have occurred earlier, considering the likely interval between initial symptoms and hospitalization.
Assuming a causal relationship, the estimated number of cases attributable to vaccination was 8 cases per million vaccinated women, totaling 103 cases among all women aged 15-50 years who were vaccinated in France between May 12, 2021, and August 31, 2022.
As of the study date and in the 3 years before the study, none of the authors had any conflicts of interest with pharmaceutical companies.
This article was translated from the Medscape French edition. A version of this article appeared on Medscape.com.
Cases of menstrual disorders, particularly unusually heavy menstrual bleeding, have been reported following RNA vaccination against COVID-19.
In France, this safety signal has been confirmed and added to the product characteristics summaries and vaccine leaflets for mRNA vaccines in October 2022. However, few studies have accurately measured this risk to date.
To address this gap in research, the French scientific interest group in the epidemiology of health products, ANSM-Cnam EPI-PHARE, conducted a study to assess the risk for heavy menstrual bleeding requiring hospitalization after COVID-19 vaccination in France.
“This study provides new evidence supporting the existence of an increased risk for heavy menstrual bleeding following COVID-19 vaccination with mRNA vaccines,” wrote the authors.
Study Details
The study included all women aged 15-50 years who were diagnosed with heavy menstrual bleeding in the hospital between May 12, 2021, and August 31, 2022. Participants were identified in the National Health Data System, and the study population totaled 4610 women.
Each participant was randomly matched with as many as 30 women who had not been hospitalized for abnormal genital bleeding and had similar characteristics in terms of age, department of residence, social deprivation index of the commune of residence, and contraceptive method.
Women who had a recent pregnancy, hysterectomy, or coagulation disorder within the specified time frames were excluded.
At the time of the study, 71% of cases and 70% of controls had received at least one dose of the COVID-19 vaccine. Among vaccinated participants, 68% and 66%, respectively, received a vaccination dose (first or second dose). An mRNA vaccine (Comirnaty or Spikevax) was the last vaccine for 99.8% of the population.
Increased Risk
Compared with control women, those hospitalized for heavy menstrual bleeding were more likely to have received their last dose of mRNA vaccine (Comirnaty or Spikevax) in the previous 1-3 months. This association was observed for vaccination doses (odds ratio [OR], 1.20), indicating a 20% increased risk, but it was not found for booster doses (OR, 1.07).
This association was particularly notable for women residing in socially disadvantaged communities (OR, 1.28) and women not using hormonal contraception (OR, 1.28).
The risk did not appear to be increased beyond 3 months after vaccination. Researchers noted that the increased risk may have occurred earlier, considering the likely interval between initial symptoms and hospitalization.
Assuming a causal relationship, the estimated number of cases attributable to vaccination was 8 cases per million vaccinated women, totaling 103 cases among all women aged 15-50 years who were vaccinated in France between May 12, 2021, and August 31, 2022.
As of the study date and in the 3 years before the study, none of the authors had any conflicts of interest with pharmaceutical companies.
This article was translated from the Medscape French edition. A version of this article appeared on Medscape.com.
Cases of menstrual disorders, particularly unusually heavy menstrual bleeding, have been reported following RNA vaccination against COVID-19.
In France, this safety signal has been confirmed and added to the product characteristics summaries and vaccine leaflets for mRNA vaccines in October 2022. However, few studies have accurately measured this risk to date.
To address this gap in research, the French scientific interest group in the epidemiology of health products, ANSM-Cnam EPI-PHARE, conducted a study to assess the risk for heavy menstrual bleeding requiring hospitalization after COVID-19 vaccination in France.
“This study provides new evidence supporting the existence of an increased risk for heavy menstrual bleeding following COVID-19 vaccination with mRNA vaccines,” wrote the authors.
Study Details
The study included all women aged 15-50 years who were diagnosed with heavy menstrual bleeding in the hospital between May 12, 2021, and August 31, 2022. Participants were identified in the National Health Data System, and the study population totaled 4610 women.
Each participant was randomly matched with as many as 30 women who had not been hospitalized for abnormal genital bleeding and had similar characteristics in terms of age, department of residence, social deprivation index of the commune of residence, and contraceptive method.
Women who had a recent pregnancy, hysterectomy, or coagulation disorder within the specified time frames were excluded.
At the time of the study, 71% of cases and 70% of controls had received at least one dose of the COVID-19 vaccine. Among vaccinated participants, 68% and 66%, respectively, received a vaccination dose (first or second dose). An mRNA vaccine (Comirnaty or Spikevax) was the last vaccine for 99.8% of the population.
Increased Risk
Compared with control women, those hospitalized for heavy menstrual bleeding were more likely to have received their last dose of mRNA vaccine (Comirnaty or Spikevax) in the previous 1-3 months. This association was observed for vaccination doses (odds ratio [OR], 1.20), indicating a 20% increased risk, but it was not found for booster doses (OR, 1.07).
This association was particularly notable for women residing in socially disadvantaged communities (OR, 1.28) and women not using hormonal contraception (OR, 1.28).
The risk did not appear to be increased beyond 3 months after vaccination. Researchers noted that the increased risk may have occurred earlier, considering the likely interval between initial symptoms and hospitalization.
Assuming a causal relationship, the estimated number of cases attributable to vaccination was 8 cases per million vaccinated women, totaling 103 cases among all women aged 15-50 years who were vaccinated in France between May 12, 2021, and August 31, 2022.
As of the study date and in the 3 years before the study, none of the authors had any conflicts of interest with pharmaceutical companies.
This article was translated from the Medscape French edition. A version of this article appeared on Medscape.com.
Is Your Patient With PCOS at Risk for Suicide?
Women with polycystic ovary syndrome (PCOS) may be as much as eight times more likely to attempt suicide than are those without the disorder, according to a new study published in the Annals of Internal Medicine on February 5.
The results point to the importance of mental health screening for all patients who may have syndrome, the researchers concluded.
“If we can know such conditions earlier in our clinical practice, we may reduce the subsequence risk and bad consequences,” said Mu-Hong Chen, MD, PhD, an attending psychiatrist at the Department of Psychiatry at Taipei Veterans General Hospital in Taiwan, a coauthor of the study.
PCOS affects as many as 15% of reproductive-age women in the United States, or approximately six million people. The condition is associated with an increased risk for metabolic disorders, like diabetes and metabolic syndrome, and cardiovascular problems, like hypertension and stroke. The disorder is associated with infertility, weight gain, hirsutism, and skin changes. Evidence also shows that these changes can lead to poorer self-image and mental health conditions like depression and anxiety.
Dr. Chen and his coauthors compared the records of nearly 19,000 women between ages 12 and 64 years who had a PCOS diagnosis with a matched control group of 189,600 women and girls without PCOS using data from 1997 to 2012 in the Taiwan National Health Insurance Research Database. Cohorts were matched by age, income, urbanization level, and mental health conditions.
Older women with PCOS had slightly lower risk compared with younger women, but the risk was higher compared with older women without PCOS. Studies in other countries have shown similar results.
Adolescents with PCOS had more than five times the risk for attempted suicide than did the control group (hazard ratio [HR], 5.38; 95% CI, 3.93-7.3). Those between ages 20 and 40 years had more than nine times the risk for attempted suicide (HR, 9.15; 95% CI, 8.03-10.42), and those older than 40 years had the lowest risk (HR, 3.75; 95% CI, 2.23-6.28).
The number of women with PCOS in the study was likely underreported, and those who were included likely had more serious cases, according to Ricardo Azziz, MD, MPH, MBA, professor in the Department of Obstetrics & Gynecology and the Department of Medicine at the University of Alabama at Birmingham.
The findings, “speak to the fact that women with PCOS do have a greater incidence of mental health disorders and do require clinicians and patients themselves and their families to be aware of these risks,” said Dr. Azziz, former CEO of the American Society for Reproductive Medicine.
Clinicians should ask their patients with PCOS about suicide risk and mental health, according to Dr. Azziz.
“It’s not infrequent that those of us in clinical practice see patients who are significantly depressed, and we need to ask the right questions,” he said.
Though he was only aware of a few patients with PCOS who have attempted suicide, he said that clinicians should be prepared to refer these patients to another professional who can address mental health concerns if they express any signs of distress.
“Simply asking and inviting patients to speak about this will allow physicians to identify patients who may need to be referred,” Dr. Azziz said.
The study was funded by grants from the Taipei Veterans General Hospital, Yen Tjing Ling Medical Foundation, and the Ministry of Science and Technology of Taiwan.
The study authors report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Women with polycystic ovary syndrome (PCOS) may be as much as eight times more likely to attempt suicide than are those without the disorder, according to a new study published in the Annals of Internal Medicine on February 5.
The results point to the importance of mental health screening for all patients who may have syndrome, the researchers concluded.
“If we can know such conditions earlier in our clinical practice, we may reduce the subsequence risk and bad consequences,” said Mu-Hong Chen, MD, PhD, an attending psychiatrist at the Department of Psychiatry at Taipei Veterans General Hospital in Taiwan, a coauthor of the study.
PCOS affects as many as 15% of reproductive-age women in the United States, or approximately six million people. The condition is associated with an increased risk for metabolic disorders, like diabetes and metabolic syndrome, and cardiovascular problems, like hypertension and stroke. The disorder is associated with infertility, weight gain, hirsutism, and skin changes. Evidence also shows that these changes can lead to poorer self-image and mental health conditions like depression and anxiety.
Dr. Chen and his coauthors compared the records of nearly 19,000 women between ages 12 and 64 years who had a PCOS diagnosis with a matched control group of 189,600 women and girls without PCOS using data from 1997 to 2012 in the Taiwan National Health Insurance Research Database. Cohorts were matched by age, income, urbanization level, and mental health conditions.
Older women with PCOS had slightly lower risk compared with younger women, but the risk was higher compared with older women without PCOS. Studies in other countries have shown similar results.
Adolescents with PCOS had more than five times the risk for attempted suicide than did the control group (hazard ratio [HR], 5.38; 95% CI, 3.93-7.3). Those between ages 20 and 40 years had more than nine times the risk for attempted suicide (HR, 9.15; 95% CI, 8.03-10.42), and those older than 40 years had the lowest risk (HR, 3.75; 95% CI, 2.23-6.28).
The number of women with PCOS in the study was likely underreported, and those who were included likely had more serious cases, according to Ricardo Azziz, MD, MPH, MBA, professor in the Department of Obstetrics & Gynecology and the Department of Medicine at the University of Alabama at Birmingham.
The findings, “speak to the fact that women with PCOS do have a greater incidence of mental health disorders and do require clinicians and patients themselves and their families to be aware of these risks,” said Dr. Azziz, former CEO of the American Society for Reproductive Medicine.
Clinicians should ask their patients with PCOS about suicide risk and mental health, according to Dr. Azziz.
“It’s not infrequent that those of us in clinical practice see patients who are significantly depressed, and we need to ask the right questions,” he said.
Though he was only aware of a few patients with PCOS who have attempted suicide, he said that clinicians should be prepared to refer these patients to another professional who can address mental health concerns if they express any signs of distress.
“Simply asking and inviting patients to speak about this will allow physicians to identify patients who may need to be referred,” Dr. Azziz said.
The study was funded by grants from the Taipei Veterans General Hospital, Yen Tjing Ling Medical Foundation, and the Ministry of Science and Technology of Taiwan.
The study authors report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Women with polycystic ovary syndrome (PCOS) may be as much as eight times more likely to attempt suicide than are those without the disorder, according to a new study published in the Annals of Internal Medicine on February 5.
The results point to the importance of mental health screening for all patients who may have syndrome, the researchers concluded.
“If we can know such conditions earlier in our clinical practice, we may reduce the subsequence risk and bad consequences,” said Mu-Hong Chen, MD, PhD, an attending psychiatrist at the Department of Psychiatry at Taipei Veterans General Hospital in Taiwan, a coauthor of the study.
PCOS affects as many as 15% of reproductive-age women in the United States, or approximately six million people. The condition is associated with an increased risk for metabolic disorders, like diabetes and metabolic syndrome, and cardiovascular problems, like hypertension and stroke. The disorder is associated with infertility, weight gain, hirsutism, and skin changes. Evidence also shows that these changes can lead to poorer self-image and mental health conditions like depression and anxiety.
Dr. Chen and his coauthors compared the records of nearly 19,000 women between ages 12 and 64 years who had a PCOS diagnosis with a matched control group of 189,600 women and girls without PCOS using data from 1997 to 2012 in the Taiwan National Health Insurance Research Database. Cohorts were matched by age, income, urbanization level, and mental health conditions.
Older women with PCOS had slightly lower risk compared with younger women, but the risk was higher compared with older women without PCOS. Studies in other countries have shown similar results.
Adolescents with PCOS had more than five times the risk for attempted suicide than did the control group (hazard ratio [HR], 5.38; 95% CI, 3.93-7.3). Those between ages 20 and 40 years had more than nine times the risk for attempted suicide (HR, 9.15; 95% CI, 8.03-10.42), and those older than 40 years had the lowest risk (HR, 3.75; 95% CI, 2.23-6.28).
The number of women with PCOS in the study was likely underreported, and those who were included likely had more serious cases, according to Ricardo Azziz, MD, MPH, MBA, professor in the Department of Obstetrics & Gynecology and the Department of Medicine at the University of Alabama at Birmingham.
The findings, “speak to the fact that women with PCOS do have a greater incidence of mental health disorders and do require clinicians and patients themselves and their families to be aware of these risks,” said Dr. Azziz, former CEO of the American Society for Reproductive Medicine.
Clinicians should ask their patients with PCOS about suicide risk and mental health, according to Dr. Azziz.
“It’s not infrequent that those of us in clinical practice see patients who are significantly depressed, and we need to ask the right questions,” he said.
Though he was only aware of a few patients with PCOS who have attempted suicide, he said that clinicians should be prepared to refer these patients to another professional who can address mental health concerns if they express any signs of distress.
“Simply asking and inviting patients to speak about this will allow physicians to identify patients who may need to be referred,” Dr. Azziz said.
The study was funded by grants from the Taipei Veterans General Hospital, Yen Tjing Ling Medical Foundation, and the Ministry of Science and Technology of Taiwan.
The study authors report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Polycystic Ovary Syndrome Associated With Midlife Memory, Thinking Problems
TOPLINE:
People with polycystic ovary syndrome (PCOS) may score lower on cognitive tests than people without the condition, a research showed. They also may have worse integrity of brain tissue as evident on an MRI.
METHODOLOGY:
- Researchers used data from the Coronary Artery Risk Development in Young Adults Women’s Study; individuals were 18-30 years old at the beginning of the study and were followed over 30 years.
- A little over 900 women were included in the study, of which 66 had PCOS, which was defined as having elevated androgen levels or self-reported hirsutism and irregular menstrual cycles more than 32 days apart.
- Study participants completed tests measuring verbal learning and memory, processing speed and executive function, attention and cognitive control, and semantics and attention.
- Researchers analyzed brain white matter integrity for 291 of the individuals, including 25 with PCOS, who underwent MRI.
TAKEAWAY:
- Individuals with PCOS had worse memory, attention, and verbal ability scores than those without the disorder.
- MRI scans showed that those with PCOS had lower white matter integrity, an indicator of cognitive deficits, including poorer decision-making abilities.
- Those in the PCOS group were more likely to be White and have diabetes than those in the control group.
IN PRACTICE:
“This report of midlife cognition in PCOS raises a new concern about another potential comorbidity for individuals with this common disorder; given that up to 10% of women may be affected by PCOS, these results have important implications for public health at large,” the authors concluded.
SOURCE:
Heather G. Huddleston, MD, director of the PCOS Clinic at the UCSF Health, San Francisco, California, is the lead author of the study published in Neurology.
LIMITATIONS:
PCOS was determined on the basis of serum androgen levels and self-reporting of hirsutism and oligomenorrhea, so some cases may have been misclassified without the official diagnosis of a clinician.
DISCLOSURES:
The authors did not report any relevant financial conflicts. The study was funded by a grant from the University of California, San Francisco, California.
A version of this article appeared on Medscape.com.
TOPLINE:
People with polycystic ovary syndrome (PCOS) may score lower on cognitive tests than people without the condition, a research showed. They also may have worse integrity of brain tissue as evident on an MRI.
METHODOLOGY:
- Researchers used data from the Coronary Artery Risk Development in Young Adults Women’s Study; individuals were 18-30 years old at the beginning of the study and were followed over 30 years.
- A little over 900 women were included in the study, of which 66 had PCOS, which was defined as having elevated androgen levels or self-reported hirsutism and irregular menstrual cycles more than 32 days apart.
- Study participants completed tests measuring verbal learning and memory, processing speed and executive function, attention and cognitive control, and semantics and attention.
- Researchers analyzed brain white matter integrity for 291 of the individuals, including 25 with PCOS, who underwent MRI.
TAKEAWAY:
- Individuals with PCOS had worse memory, attention, and verbal ability scores than those without the disorder.
- MRI scans showed that those with PCOS had lower white matter integrity, an indicator of cognitive deficits, including poorer decision-making abilities.
- Those in the PCOS group were more likely to be White and have diabetes than those in the control group.
IN PRACTICE:
“This report of midlife cognition in PCOS raises a new concern about another potential comorbidity for individuals with this common disorder; given that up to 10% of women may be affected by PCOS, these results have important implications for public health at large,” the authors concluded.
SOURCE:
Heather G. Huddleston, MD, director of the PCOS Clinic at the UCSF Health, San Francisco, California, is the lead author of the study published in Neurology.
LIMITATIONS:
PCOS was determined on the basis of serum androgen levels and self-reporting of hirsutism and oligomenorrhea, so some cases may have been misclassified without the official diagnosis of a clinician.
DISCLOSURES:
The authors did not report any relevant financial conflicts. The study was funded by a grant from the University of California, San Francisco, California.
A version of this article appeared on Medscape.com.
TOPLINE:
People with polycystic ovary syndrome (PCOS) may score lower on cognitive tests than people without the condition, a research showed. They also may have worse integrity of brain tissue as evident on an MRI.
METHODOLOGY:
- Researchers used data from the Coronary Artery Risk Development in Young Adults Women’s Study; individuals were 18-30 years old at the beginning of the study and were followed over 30 years.
- A little over 900 women were included in the study, of which 66 had PCOS, which was defined as having elevated androgen levels or self-reported hirsutism and irregular menstrual cycles more than 32 days apart.
- Study participants completed tests measuring verbal learning and memory, processing speed and executive function, attention and cognitive control, and semantics and attention.
- Researchers analyzed brain white matter integrity for 291 of the individuals, including 25 with PCOS, who underwent MRI.
TAKEAWAY:
- Individuals with PCOS had worse memory, attention, and verbal ability scores than those without the disorder.
- MRI scans showed that those with PCOS had lower white matter integrity, an indicator of cognitive deficits, including poorer decision-making abilities.
- Those in the PCOS group were more likely to be White and have diabetes than those in the control group.
IN PRACTICE:
“This report of midlife cognition in PCOS raises a new concern about another potential comorbidity for individuals with this common disorder; given that up to 10% of women may be affected by PCOS, these results have important implications for public health at large,” the authors concluded.
SOURCE:
Heather G. Huddleston, MD, director of the PCOS Clinic at the UCSF Health, San Francisco, California, is the lead author of the study published in Neurology.
LIMITATIONS:
PCOS was determined on the basis of serum androgen levels and self-reporting of hirsutism and oligomenorrhea, so some cases may have been misclassified without the official diagnosis of a clinician.
DISCLOSURES:
The authors did not report any relevant financial conflicts. The study was funded by a grant from the University of California, San Francisco, California.
A version of this article appeared on Medscape.com.
Restricted Abortion Access Tied to Mental Health Harm
, which revoked a woman’s constitutional right to an abortion, new research shows.
This could be due to a variety of factors, investigators led by Benjamin Thornburg, Johns Hopkins Bloomberg School of Public Health, Baltimore, noted. These include fear about the imminent risk of being denied an abortion, uncertainty around future limitations on abortion and other related rights such as contraception, worry over the ability to receive lifesaving medical care during pregnancy, and a general sense of violation and powerlessness related to loss of the right to reproductive autonomy.
The study was published online on January 23, 2024, in JAMA.
Mental Health Harm
In June 2022, the US Supreme Court overturned Roe vs Wade, removing federal protections for abortion rights. Thirteen states had “trigger laws” that immediately banned or severely restricted abortion — raising concerns this could negatively affect mental health.
The researchers used data from the Household Pulse Survey to estimate changes in anxiety and depression symptoms after vs before the Dobbs decision in nearly 160,000 adults living in 13 states with trigger laws compared with roughly 559,000 adults living in 37 states without trigger laws.
The mean age of respondents was 48 years, and 51% were women. Anxiety and depression symptoms were measured via the Patient Health Questionnaire-4 (PHQ-4).
In trigger states, the mean PHQ-4 score at baseline (before Dobbs) was 3.51 (out of 12) and increased to 3.81 after the Dobbs decision. In nontrigger states, the mean PHQ-4 score at baseline was 3.31 and increased to 3.49 after Dobbs.
Living in a trigger state was associated with a small but statistically significant worsening (0.11-point; P < .001) in anxiety/depression symptoms following the Dobbs decision vs living in a nontrigger state, the investigators report.
Women aged 18-45 years faced greater worsening of anxiety and depression symptoms following Dobbs in trigger vs nontrigger states, whereas men of a similar age experienced minimal or negligible changes.
Implications for Care
In an accompanying editorial, Julie Steinberg, PhD, with University of Maryland in College Park, notes the study results provide “emerging evidence that at an individual level taking away reproductive autonomy (by not having legal access to an abortion) may increase symptoms of anxiety and depression in all people and particularly females of reproductive age.”
These results add to findings from two other studies that examined abortion restrictions and mental health outcomes. Both found that limiting access to abortion was associated with more mental health symptoms among females of reproductive age than among others,” Dr. Steinberg pointed out.
“Together these findings highlight the need for clinicians who practice in states where abortion is banned to be aware that female patients of reproductive age may be experiencing significantly more distress than before the Dobbs decision,” Dr. Steinberg added.
The study received no specific funding. The authors had no relevant conflicts of interest. Dr. Steinberg reported serving as a paid expert scientist on abortion and mental health in seven cases challenging abortion policies.
A version of this article appeared on Medscape.com.
, which revoked a woman’s constitutional right to an abortion, new research shows.
This could be due to a variety of factors, investigators led by Benjamin Thornburg, Johns Hopkins Bloomberg School of Public Health, Baltimore, noted. These include fear about the imminent risk of being denied an abortion, uncertainty around future limitations on abortion and other related rights such as contraception, worry over the ability to receive lifesaving medical care during pregnancy, and a general sense of violation and powerlessness related to loss of the right to reproductive autonomy.
The study was published online on January 23, 2024, in JAMA.
Mental Health Harm
In June 2022, the US Supreme Court overturned Roe vs Wade, removing federal protections for abortion rights. Thirteen states had “trigger laws” that immediately banned or severely restricted abortion — raising concerns this could negatively affect mental health.
The researchers used data from the Household Pulse Survey to estimate changes in anxiety and depression symptoms after vs before the Dobbs decision in nearly 160,000 adults living in 13 states with trigger laws compared with roughly 559,000 adults living in 37 states without trigger laws.
The mean age of respondents was 48 years, and 51% were women. Anxiety and depression symptoms were measured via the Patient Health Questionnaire-4 (PHQ-4).
In trigger states, the mean PHQ-4 score at baseline (before Dobbs) was 3.51 (out of 12) and increased to 3.81 after the Dobbs decision. In nontrigger states, the mean PHQ-4 score at baseline was 3.31 and increased to 3.49 after Dobbs.
Living in a trigger state was associated with a small but statistically significant worsening (0.11-point; P < .001) in anxiety/depression symptoms following the Dobbs decision vs living in a nontrigger state, the investigators report.
Women aged 18-45 years faced greater worsening of anxiety and depression symptoms following Dobbs in trigger vs nontrigger states, whereas men of a similar age experienced minimal or negligible changes.
Implications for Care
In an accompanying editorial, Julie Steinberg, PhD, with University of Maryland in College Park, notes the study results provide “emerging evidence that at an individual level taking away reproductive autonomy (by not having legal access to an abortion) may increase symptoms of anxiety and depression in all people and particularly females of reproductive age.”
These results add to findings from two other studies that examined abortion restrictions and mental health outcomes. Both found that limiting access to abortion was associated with more mental health symptoms among females of reproductive age than among others,” Dr. Steinberg pointed out.
“Together these findings highlight the need for clinicians who practice in states where abortion is banned to be aware that female patients of reproductive age may be experiencing significantly more distress than before the Dobbs decision,” Dr. Steinberg added.
The study received no specific funding. The authors had no relevant conflicts of interest. Dr. Steinberg reported serving as a paid expert scientist on abortion and mental health in seven cases challenging abortion policies.
A version of this article appeared on Medscape.com.
, which revoked a woman’s constitutional right to an abortion, new research shows.
This could be due to a variety of factors, investigators led by Benjamin Thornburg, Johns Hopkins Bloomberg School of Public Health, Baltimore, noted. These include fear about the imminent risk of being denied an abortion, uncertainty around future limitations on abortion and other related rights such as contraception, worry over the ability to receive lifesaving medical care during pregnancy, and a general sense of violation and powerlessness related to loss of the right to reproductive autonomy.
The study was published online on January 23, 2024, in JAMA.
Mental Health Harm
In June 2022, the US Supreme Court overturned Roe vs Wade, removing federal protections for abortion rights. Thirteen states had “trigger laws” that immediately banned or severely restricted abortion — raising concerns this could negatively affect mental health.
The researchers used data from the Household Pulse Survey to estimate changes in anxiety and depression symptoms after vs before the Dobbs decision in nearly 160,000 adults living in 13 states with trigger laws compared with roughly 559,000 adults living in 37 states without trigger laws.
The mean age of respondents was 48 years, and 51% were women. Anxiety and depression symptoms were measured via the Patient Health Questionnaire-4 (PHQ-4).
In trigger states, the mean PHQ-4 score at baseline (before Dobbs) was 3.51 (out of 12) and increased to 3.81 after the Dobbs decision. In nontrigger states, the mean PHQ-4 score at baseline was 3.31 and increased to 3.49 after Dobbs.
Living in a trigger state was associated with a small but statistically significant worsening (0.11-point; P < .001) in anxiety/depression symptoms following the Dobbs decision vs living in a nontrigger state, the investigators report.
Women aged 18-45 years faced greater worsening of anxiety and depression symptoms following Dobbs in trigger vs nontrigger states, whereas men of a similar age experienced minimal or negligible changes.
Implications for Care
In an accompanying editorial, Julie Steinberg, PhD, with University of Maryland in College Park, notes the study results provide “emerging evidence that at an individual level taking away reproductive autonomy (by not having legal access to an abortion) may increase symptoms of anxiety and depression in all people and particularly females of reproductive age.”
These results add to findings from two other studies that examined abortion restrictions and mental health outcomes. Both found that limiting access to abortion was associated with more mental health symptoms among females of reproductive age than among others,” Dr. Steinberg pointed out.
“Together these findings highlight the need for clinicians who practice in states where abortion is banned to be aware that female patients of reproductive age may be experiencing significantly more distress than before the Dobbs decision,” Dr. Steinberg added.
The study received no specific funding. The authors had no relevant conflicts of interest. Dr. Steinberg reported serving as a paid expert scientist on abortion and mental health in seven cases challenging abortion policies.
A version of this article appeared on Medscape.com.
FROM JAMA
Time to rethink endometrial ablation: A gyn oncology perspective on the sequelae of an overused procedure
CASE New patient presents with a history of endometrial hyperplasia
A 51-year-old patient (G2P2002) presents to a new gynecologist’s office after moving from a different state. In her medical history, the gynecologist notes that 5 years ago she underwent dilation and curettage and endometrial ablation procedures for heavy menstrual bleeding (HMB). Ultrasonography performed prior to those procedures showed a slightly enlarged uterus, a simple left ovarian cyst, and a non ̶ visualized right ovary. The patient had declined a 2-step procedure due to concerns with anesthesia, and surgical pathology at the time of ablation revealed hyperplasia without atypia. The patient’s medical history was otherwise notable for prediabetes (recent hemoglobin A1c [HbA1c] measurement, 6.0%) and obesity (body mass index, 43 kg/m2). Pertinent family history included her mother’s diagnosis of endometrial cancer at age 36. Given the patient’s diagnosis of endometrial hyperplasia, she was referred to gynecologic oncology, but she ultimately declined hysterectomy, stating that she was happy with the resolution of her abnormal bleeding. At the time of her initial gynecologic oncology consultation, the consultant suggested lifestyle changes to combat prediabetes and obesity to reduce the risk of endometrial cancer, as future signs of cancer, namely bleeding, may be masked by the endometrial ablation. The patient was prescribed metformin given these medical comorbidities.
At today’s appointment, the patient notes continued resolution of bleeding since the procedure. She does, however, note a 6-month history of vasomotor symptoms and one episode of spotting 3 months ago. Three years ago she was diagnosed with type 2 diabetes mellitus, and her current HbA1c is 6.9%. She has gained 10 lb since being diagnosed with endometrial cancer 5 years ago, and she has continued to take metformin.
An in-office endometrial biopsy is unsuccessful due to cervical stenosis. The treating gynecologist orders a transvaginal ultrasound, which reveals a small left ovarian cyst and a thickened endometrium (measuring 10 mm). Concerned that these findings could represent endometrial cancer, the gynecologist refers the patient to gynecologic oncology for further evaluation.
Sequelae and complications following endometrial ablation are often managed by a gynecologic oncologist. Indeed, a 2018 poll of Society of Gynecologic Oncology (SGO) members revealed that 93.8% of respondents had received such a referral, and almost 20% of respondents were managing more than 20 patients with post-ablation complications in their practices.1 These complications, including hematometra, post-ablation tubal sterilization syndrome, other pain syndromes associated with retrograde menstruation, and thickened endometrium with scarring leading to an inability to sample the endometrium to investigate post-ablation bleeding are symptoms and findings that often lead to further surgery, including hysterectomy.2 General gynecologists faced with these complications may refer patients to gynecologic oncology given an inability to sample the post-ablation endometrium or anticipated difficulties with hysterectomy. A recent meta-analysis revealed a 12.4% hysterectomy rate 5 years after endometrial ablation. Among these patients, the incidence of endometrial cancer ranged from 0% to 1.6%.3
In 2023, endometrial cancer incidence continues to increase, as does the incidence of obesity in women of all ages. Endometrial cancer mortality rates are also increasing, and these trends disproportionately affects non-Hispanic Black women.4 As providers and advocates work to narrow these disparities, gynecologic oncologists are simultaneously noting increased referrals for very likely benign conditions.5 Patients referred for post-ablation bleeding are a subset of these, as most patients who undergo endometrial ablation will not develop cancer. Considering the potential bottlenecks created en route to a gynecologic oncology evaluation, it seems prudent to minimize practices, like endometrial ablation, that may directly or indirectly prevent timely referral of patients with cancer to a gynecologic oncologist.
In this review we focus on the current use of endometrial ablation, associated complications, the incidence of treatment failure, and patient selection. Considering these issues in the context of the current endometrial cancer landscape, we posit best practices aimed at optimizing patient outcomes, and empowering general gynecologists to practice cancer prevention and to triage their surgical patients.
- Before performing endometrial ablation, consider whether alternatives such as hysterectomy or insertion of a progestin-containing IUD would be appropriate.
- Clinical management of patients with abnormal bleeding with indications for endometrial ablation should be guidelinedriven.
- Post-ablation bleeding or pain does not inherently require referral to oncology.
- General gynecologists can perform hysterectomy in this setting if appropriate.
- Patients with endometrial hyperplasia at endometrial ablation should be promptly offered hysterectomy. If atypia is not present, this hysterectomy, too, can be performed by a general gynecologist if appropriate, as the chance for malignancy is minimal.
Continue to: Current use of endometrial ablation in the US...
Current use of endometrial ablation in the US
In 2015, more than 500,000 endometrial ablations were performed in the United States.Given the ability to perform in-office ablation, this number is growing and potentially underestimated each year.6 In 2022, the global endometrial ablation market was valued at $3.4 billion, a figure projected to double in 10 years.7 The procedure has evolved as different devices and approaches have developed, offering patients different means to manage bleeding without hysterectomy. The minimally invasive procedure, performed in premenopausal patients with heavy menstrual bleeding (HMB) due to benign causes who have completed childbearing, has been associated with faster recovery times and fewer short-term complications compared with more invasive surgery.8 There are several non-resectoscope ablative devices approved by the US Food and Drug Administration (FDA), and each work to destroy the endometrial lining via thermal or cryoablation. Endometrial ablation can be performed in premenopausal patients with HMB due to benign causes who have completed childbearing.
Recently, promotional literature has begun to report on so-called overuse of hysterectomy, despite decreasing overall hysterectomy rates. This reporting proposes and applies “appropriateness criteria,” accounting for the rate of preoperative counseling regarding alternatives to hysterectomy, as well as the rate of “unsupportive” final pathology.9 The adoption of endometrial ablation and increasing market value of such vendors suggest that this campaign is having its desired effect. From the oncology perspective, we are concerned the pendulum could swing too far away from hysterectomy, a procedure that definitively cures abnormal uterine bleeding, toward endometrial ablation without explicit acknowledgement of the trade-offs involved.
Endometrial ablation complications: Late-onset procedure failure
A number of post-ablation syndromes may present at least 1 month following the procedure. Collectively known as late-onset endometrial ablation failure (LOEAF), these syndromes are characterized by recurrent vaginal bleeding, and/or new cyclic pelvic pain.10 It is difficult to measure the true incidence of LOEAF. Thomassee and colleagues examined a Canadian retrospective cohort of 437 patients who underwent endometrial ablation; 20.8% reported post-ablation pelvic pain after a median 301 days.11 The subsequent need for surgical intervention, often hysterectomy, is a surrogate for LOEAF.
It should be noted that LOEAF is distinct from post-ablation tubal sterilization syndrome (PATSS), which describes cornual menstrual bleeding impeded by the ligated proximal fallopian tube.12 Increased awareness of PATSS, along with the discontinuation of Essure (a permanent hysteroscopic sterilization device) in 2018, has led some surgeons to advocate for concomitant salpingectomy at the time of endometrial ablation.13 The role of opportunistic salpingectomy in primary prevention of epithelial ovarian cancer is well described, and while we strongly support this practice at the time of endometrial ablation, we do not feel that it effectively prevents LOEAF.14
The post-ablation inability to adequately sample the endometrium is also considered a LOEAF. A prospective study of 57 women who underwent endometrial ablation assessed post-ablation sampling feasibility via transvaginal ultrasonography, saline infusion sonohysterography (SIS), and in-office endometrial biopsies. In 23% of the cohort, endometrial sampling failed, and the authors noted decreased reliability of pathologic assessment.15 One systematic review, in which authors examined the incidence of endometrial cancer following endometrial ablation, characterized 38 cases of endometrial cancer and reported a post-ablation endometrial sampling success rate of 89%. This figure was based on a self-selected sample of 18 patients; cases in which endometrial sampling was thought to be impossible were excluded. The study also had a 30% missing data rate and several other biases.16
In the previously mentioned poll of SGO members,1 84% of the surveyed gynecologic oncologists managing post-ablation patients reported that endometrial sampling following endometrial ablation was “moderately” or “extremely” difficult. More than half of the survey respondents believed that hysterectomy was required for accurate diagnosis.1 While we acknowledge the likely sampling bias affecting the survey results, we are not comforted by any data that minimizes this diagnostic challenge.
Appropriate patient selection and contraindications
The ideal candidate for endometrial ablation is a premenopausal patient with HMB who does not desire future fertility. According to the FDA, absolute contraindications include pregnancy or desired fertility, prior ablation, current IUD in place, inadequate preoperative endometrial assessment, known or suspected malignancy, active infection, or unfavorable anatomy.17
What about patients who may be at increased risk for endometrial cancer?
There is a paucity of data regarding the safety of endometrial ablation in patients at increased risk for developing endometrial cancer in the future. The American College of Obstetricians and Gynecologists (ACOG) 2007 practice bulletin on endometrial ablation (no longer accessible online) alludes to this concern and other contraindications,18 but there are no established guidelines. Currently, no ACOG practice bulletin or committee opinion lists relative contraindications to endometrial ablation, long-term complications (except risks associated with future pregnancy), or risk of subsequent hysterectomy. The risk that “it may be harder to detect endometrial cancer after ablation” is noted on ACOG’s web page dedicated to frequently asked questions (FAQs) regarding abnormal uterine bleeding.19 It is not mentioned on their web page dedicated to the FAQs regarding endometrial ablation.20
In the absence of high-quality published data on established contraindications for endometrial ablation, we advocate for the increased awareness of possible relative contraindications—namely well-established risk factors for endometrial cancer (TABLE 1).For example, in a pooled analysis of 24 epidemiologic studies, authors found that the odds of developing endometrial cancer was 7 times higher among patients with a body mass index (BMI) ≥ 40 kg/m2, compared with controls (odds ratio [OR], 7.14; 95% confidence interval [CI], 6.33–8.06).21 Additionally, patients with Lynch syndrome, a history of extended tamoxifen use, or those with a history of chronic anovulation or polycystic ovary syndrome are at increased risk for endometrial cancer.22-24 If the presence of one or more of these factors does not dissuade general gynecologists from performing an endometrial ablation (even armed with a negative preoperative endometrial biopsy), we feel they should at least prompt thoughtful guideline-driven pause.
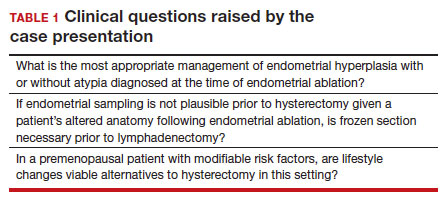
Continue to: Hysterectomy—A disincentivized option...
Hysterectomy—A disincentivized option
The annual number of hysterectomies performed by general gynecologists has declined over time. One study by Cadish and colleagues revealed that recent residency graduates performed only 3 to 4 annually.25 These numbers partly reflect the decreasing number of hysterectomies performed during residency training. Furthermore, other factors—including the increasing rate of placenta accreta spectrum, the focus on risk stratification of adnexal masses via the ovarian-adnexal reporting and data classification system (O-RADs), and the emphasis on minimally invasive approaches often acquired in subspecialty training—have likely contributed to referral patterns to such specialists as minimally invasive gynecologic surgeons and gynecologic oncologists.26 This trend is self-actualizing, as quality metrics funnel patients to high-volume surgeons, and general gynecologists risk losing hysterectomy privileges.
These factors lend themselves to a growing emphasis on endometrial ablation. Endometrial ablations can be performed in several settings, including in the hospital, in outpatient clinics, and more and more commonly, in ambulatory surgery centers. This increased access to endometrial ablation in the ambulatory surgery setting has corresponded with an annual endometrial ablation market value growth rate of 5% to 7%.27 These rates are likely compounded by payer reimbursement policies that promote endometrial ablation and other alternatives to hysterectomy that are cost savings in the short term.28 While the actual payer models are unavailable to review, they may not consider the costs of LOEAFs, including subsequent hysterectomy up to 5 years after initial ablation procedures. Provocatively, they almost certainly do not consider the costs of delayed care of patients with endometrial cancer vying for gynecologic oncology appointment slots occupied by post-ablation patients.
We urge providers, patients, and advocates to question who benefits from the uptake of ablation procedures: Patients? Payors? Providers? And how will the field of gynecology fare if hysterectomy skills and privileges are supplanted by ablation?
Post-ablation bleeding: Management by the gyn oncologist
Patients with post-ablation bleeding, either immediately or years later, are sometimes referred to a gynecologic oncologist given the possible risk for cancer and need for surgical staging if cancer is found on the hysterectomy specimen. In practice, assuming normal preoperative ultrasonography and no other clinical or radiologic findings suggestive of malignancy (eg, computed tomography findings concerning for metastases, abnormal cervical cytology, etc.), the presence of cancer is extremely unlikely to be determined at the time of surgery. Frozen section is not generally performed on the endometrium; intraoperative evaluation of even the unablated endometrium is notoriously unreliable; and histologic assessment of the ablated endometrium is limited by artifact (FIGURE 1). The abnormalities caused by ablation further impede selection of a representative focus, obfuscating any actionable result.
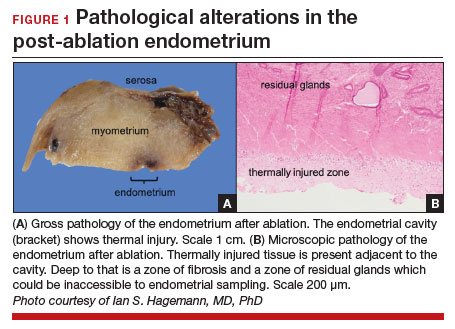
Some surgeons routinely bivalve the excised uterus prior to fixation to assess presence of tumor, tumor size, and the degree of myometrial invasion.29 A combination of factors may compel surgeons to perform lymphadenectomy if not already performed, or if sentinel lymph node mapping was unsuccessful. But this practice has not been studied in patients with post-ablation bleeding, and applying these principles relies on a preoperative diagnosis establishing the presence and grade of a cancer. Furthermore, the utility of frozen section and myometrial assessment to decide whether or not to proceed with lymphadenectomy is less relevant in the era of molecular classification guiding adjuvant therapy. In summary, assuming no pathologic or radiologic findings suggestive of cancer, gynecologic oncologists are unlikely to perform lymphadenectomy at the time of hysterectomy in these post-ablation cases, which therefore can safely be performed by general gynecologists.
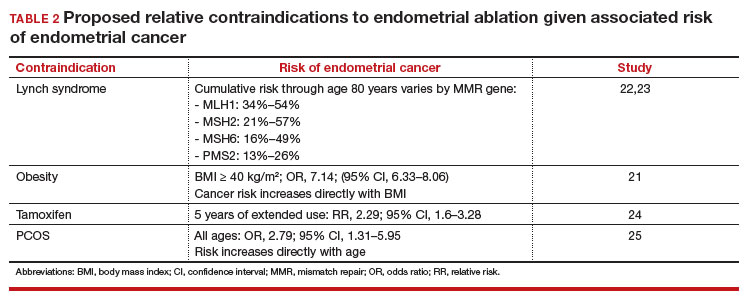
Our recommendations
Consider the LNG-IUD as an alternative to ablation. A recent randomized controlled trial by Beelen and colleagues compared the effectiveness of LNG-releasing IUDs with endometrial ablation in patients with HMB. While the LNG-IUD was inferior to endometrial ablation, quality-of-life measures were similar up to 2 years.31 Realizing that the hysterectomy rate following endometrial ablation increases significantly beyond that time point (2 years), this narrative may be incomplete. A 5- to 10-year follow-up time-frame may be a more helpful gauge of long-term outcomes. This prolonged time-frame also may allow study of the LNG-IUD’s protective effects on the endometrium in the prevention of endometrial hyperplasia and cancer.
Consider hysterectomy. A 2021 Cochrane review revealed that, compared with endometrial ablation, minimally invasive hysterectomy is associated with higher quality-of-life metrics, higher self-reported patient satisfaction, and similar rates of adverse events.32 While patient autonomy is paramount, the developing step-wise approach from endometrial ablation to hysterectomy, and its potential effects on the health care system at a time when endometrial cancer incidence and mortality rates are rising, is troubling.
Postablation, consider hysterectomy by the general gynecologist. Current trends appear to disincentivize general gynecologists from performing hysterectomy either for HMB or LOEAF. We would offer reassurance that they can safely perform this procedure. Referral to oncology may not be necessary since, in the absence of an established diagnosis of cancer, a lymphadenectomy is not typically required. A shift away from referral for these patients can preserve access to oncology for those women, especially minority women, with an explicit need for oncologic care.
In FIGURE 2, we propose a management algorithm for the patient who presents with post–ablation bleeding. We acknowledge that the evidence base for our management recommendations is limited. Still, we hope providers, ACOG, and other guidelines-issuing organizations consider them as they adapt their own practices and recommendations. We believe this is one of many steps needed to improve outcomes for patients with gynecologic cancer, particularly those in marginalized communities disproportionately impacted by current trends.
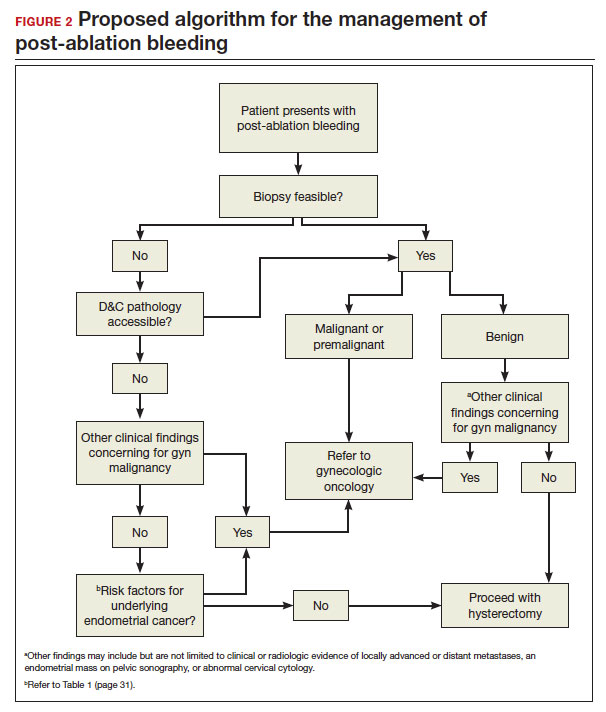
CASE Resolution
After reviewing the relevant documentation and examining the patient, the gynecologic oncology consultant contacts the referring gynecologist. They review the low utility of frozen section and the overall low risk of cancer on the final hysterectomy specimen if the patient were to undergo hysterectomy. The consultant clarifies that there is no other concern for surgical complexity beyond the skill of the referring provider, and they discuss the possibility of referral to a minimally invasive specialist for the surgery.
Ultimately, the patient undergoes uncomplicated laparoscopic hysterectomy performed by the original referring gynecologist. Final pathology reveals inactive endometrium with ablative changes and cornual focus of endometrial hyperplasia without atypia. ●
Acknowledgement
The authors acknowledge Ian Hagemann, MD, PhD, for his review of the manuscript.
- Chen H, Saiz AM, McCausland AM, et al. Experience of gynecologic oncologists regarding endometrial cancer after endometrial ablation. J Clin Oncol. 2018;36:e17566-e.
- McCausland AM, McCausland VM. Long-term complications of endometrial ablation: cause, diagnosis, treatment, and prevention. J Minim Invasive Gynecol. 2007;14:399-406.
- Oderkerk TJ, Beelen P, Bukkems ALA, et al. Risk of hysterectomy after endometrial ablation: a systematic review and meta-analysis. Obstet Gynecol. 2023;142:51-60.
- Clarke MA, Devesa SS, Hammer A, et al. Racial and ethnic differences in hysterectomy-corrected uterine corpus cancer mortality by stage and histologic subtype. JAMA Oncol. 2022;8:895-903.
- Barber EL, Rossi EC, Alexander A, et al. Benign hysterectomy performed by gynecologic oncologists: is selection bias altering our ability to measure surgical quality? Gynecol Oncol. 2018;151:141-144.
- Wortman M. Late-onset endometrial ablation failure. Case Rep Womens Health. 2017;15:11-28.
- Insights FM. Endometrial Ablation Market Outlook.Accessed July 26, 2023. https://www.futuremarketinsights.com/reports/endometrial-ablation -market
- Famuyide A. Endometrial ablation. J Minim Invasive Gynecol. 2018;25:299-307.
- Corona LE, Swenson CW, Sheetz KH, et al. Use of other treatments before hysterectomy for benign conditions in a statewide hospital collaborative. Am J Obstet Gynecol. 2015;212:304.e1-e7.
- Wortman M, Cholkeri A, McCausland AM, et al. Late-onset endometrial ablation failure—etiology, treatment, and prevention. J Minim Invasive Gynecol. 2015;22:323-331.
- Thomassee MS, Curlin H, Yunker A, et al. Predicting pelvic pain after endometrial ablation: which preoperative patient characteristics are associated? J Minim Invasive Gynecol. 2013;20:642-647.
- Townsend DE, McCausland V, McCausland A, et al. Post-ablation-tubal sterilization syndrome. Obstet Gynecol. 1993;82:422-424.
- Greer Polite F, DeAgostino-Kelly M, Marchand GJ. Combination of laparoscopic salpingectomy and endometrial ablation: a potentially underused procedure. J Gynecol Surg. 2021;37:89-91.
- Hanley GE, Pearce CL, Talhouk A, et al. Outcomes from opportunistic salpingectomy for ovarian cancer prevention. JAMA Network Open. 2022;5:e2147343-e.
- Ahonkallio SJ, Liakka AK, Martikainen HK, et al. Feasibility of endometrial assessment after thermal ablation. Eur J Obstet Gynecol Reprod Biol. 2009;147:69-71.
- Tamara JO, Mileen RDvdK, Karlijn MCC, et al. Endometrial cancer after endometrial ablation: a systematic review. Int J Gynecol Cancer. 2022;32:1555.
- US Food and Drug Administration. Endometrial ablation for heavy menstrual bleeding.Accessed July 26, 2023. https://www.fda.gov/medical-devices /surgery-devices/endometrial-ablation-heavy-menstrual-bleeding
- ACOG Practice Bulletin. Clinical management guidelines for obstetriciangynecologists. Number 81, May 2007. Obstet Gynecol. 2007;109:1233-1248.
- The American College of Obstetricians and Gynecologists. Abnormal uterine bleeding frequently asked questions. Accessed July 26, 2023. https://www.acog .org/womens-health/faqs/abnormal-uterine-bleeding
- The American College of Obstetricians and Gynecologists. Endometrial ablation frequently asked questions. Accessed November 28, 2023. https://www.acog. org/womens-health/faqs/endometrial-ablation#:~:text=Can%20I%20still%20 get%20pregnant,should%20not%20have%20this%20procedure
- Setiawan VW, Yang HP, Pike MC, et al. Type I and II endometrial cancers: have they different risk factors? J Clin Oncol. 2013;31:2607-2618.
- National Comprehensive Cancer Network. Lynch Syndrome (Version 2.2023). Accessed November 15, 2023. https://www.nccn.org/professionals /physician_gls/pdf/genetics_colon.pdf
- Bonadona V, Bonaïti B, Olschwang S, et al. Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA. 2011;305: 2304-2310.
- Fleming CA, Heneghan HM, O’Brien D, et al. Meta-analysis of the cumulative risk of endometrial malignancy and systematic review of endometrial surveillance in extended tamoxifen therapy. Br J Surg. 2018;105:1098-1106.
- Barry JA, Azizia MM, Hardiman PJ. Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2014;20:748-758.
- Cadish LA, Kropat G, Muffly TM. Hysterectomy volume among recent obstetrics and gynecology residency graduates. Urogynecology. 2021;27.
- Blank SV, Huh WK, Bell M, et al. Doubling down on the future of gynecologic oncology: the SGO future of the profession summit report. Gynecol Oncol. 2023;171:76-82.
- Reports MI. Global endometrial ablation market growth, trends and forecast 2023 to 2028 by types, by application, by regions and by key players like Boston Scientific, Hologic, Olympus, Minerva Surgical. Accessed July 30, 2023. https://www.marketinsightsreports.com/single-report/061612632440/global -endometrial-ablation-market-growth-trends-and-forecast-2023-to-2028-by -types-by-application-by-regions-and-by-key-players-like-boston-scientific -hologic-olympus-minerva-surgical
- London R, Holzman M, Rubin D, et al. Payer cost savings with endometrial ablation therapy. Am J Manag Care. 1999;5:889-897.
- Mariani A, Dowdy SC, Cliby WA, et al. Prospective assessment of lymphatic dissemination in endometrial cancer: a paradigm shift in surgical staging. Gynecol Oncol. 2008;109:11-18.
- Beelen P, van den Brink MJ, Herman MC, et al. Levonorgestrel-releasing intrauterine system versus endometrial ablation for heavy menstrual bleeding. Am J Obstet Gynecol. 2021;224:187.e1-e10.
- Bofill Rodriguez M, Lethaby A, Fergusson RJ. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding. Cochrane Database Syst Rev. 2021;2:Cd000329.
CASE New patient presents with a history of endometrial hyperplasia
A 51-year-old patient (G2P2002) presents to a new gynecologist’s office after moving from a different state. In her medical history, the gynecologist notes that 5 years ago she underwent dilation and curettage and endometrial ablation procedures for heavy menstrual bleeding (HMB). Ultrasonography performed prior to those procedures showed a slightly enlarged uterus, a simple left ovarian cyst, and a non ̶ visualized right ovary. The patient had declined a 2-step procedure due to concerns with anesthesia, and surgical pathology at the time of ablation revealed hyperplasia without atypia. The patient’s medical history was otherwise notable for prediabetes (recent hemoglobin A1c [HbA1c] measurement, 6.0%) and obesity (body mass index, 43 kg/m2). Pertinent family history included her mother’s diagnosis of endometrial cancer at age 36. Given the patient’s diagnosis of endometrial hyperplasia, she was referred to gynecologic oncology, but she ultimately declined hysterectomy, stating that she was happy with the resolution of her abnormal bleeding. At the time of her initial gynecologic oncology consultation, the consultant suggested lifestyle changes to combat prediabetes and obesity to reduce the risk of endometrial cancer, as future signs of cancer, namely bleeding, may be masked by the endometrial ablation. The patient was prescribed metformin given these medical comorbidities.
At today’s appointment, the patient notes continued resolution of bleeding since the procedure. She does, however, note a 6-month history of vasomotor symptoms and one episode of spotting 3 months ago. Three years ago she was diagnosed with type 2 diabetes mellitus, and her current HbA1c is 6.9%. She has gained 10 lb since being diagnosed with endometrial cancer 5 years ago, and she has continued to take metformin.
An in-office endometrial biopsy is unsuccessful due to cervical stenosis. The treating gynecologist orders a transvaginal ultrasound, which reveals a small left ovarian cyst and a thickened endometrium (measuring 10 mm). Concerned that these findings could represent endometrial cancer, the gynecologist refers the patient to gynecologic oncology for further evaluation.
Sequelae and complications following endometrial ablation are often managed by a gynecologic oncologist. Indeed, a 2018 poll of Society of Gynecologic Oncology (SGO) members revealed that 93.8% of respondents had received such a referral, and almost 20% of respondents were managing more than 20 patients with post-ablation complications in their practices.1 These complications, including hematometra, post-ablation tubal sterilization syndrome, other pain syndromes associated with retrograde menstruation, and thickened endometrium with scarring leading to an inability to sample the endometrium to investigate post-ablation bleeding are symptoms and findings that often lead to further surgery, including hysterectomy.2 General gynecologists faced with these complications may refer patients to gynecologic oncology given an inability to sample the post-ablation endometrium or anticipated difficulties with hysterectomy. A recent meta-analysis revealed a 12.4% hysterectomy rate 5 years after endometrial ablation. Among these patients, the incidence of endometrial cancer ranged from 0% to 1.6%.3
In 2023, endometrial cancer incidence continues to increase, as does the incidence of obesity in women of all ages. Endometrial cancer mortality rates are also increasing, and these trends disproportionately affects non-Hispanic Black women.4 As providers and advocates work to narrow these disparities, gynecologic oncologists are simultaneously noting increased referrals for very likely benign conditions.5 Patients referred for post-ablation bleeding are a subset of these, as most patients who undergo endometrial ablation will not develop cancer. Considering the potential bottlenecks created en route to a gynecologic oncology evaluation, it seems prudent to minimize practices, like endometrial ablation, that may directly or indirectly prevent timely referral of patients with cancer to a gynecologic oncologist.
In this review we focus on the current use of endometrial ablation, associated complications, the incidence of treatment failure, and patient selection. Considering these issues in the context of the current endometrial cancer landscape, we posit best practices aimed at optimizing patient outcomes, and empowering general gynecologists to practice cancer prevention and to triage their surgical patients.
- Before performing endometrial ablation, consider whether alternatives such as hysterectomy or insertion of a progestin-containing IUD would be appropriate.
- Clinical management of patients with abnormal bleeding with indications for endometrial ablation should be guidelinedriven.
- Post-ablation bleeding or pain does not inherently require referral to oncology.
- General gynecologists can perform hysterectomy in this setting if appropriate.
- Patients with endometrial hyperplasia at endometrial ablation should be promptly offered hysterectomy. If atypia is not present, this hysterectomy, too, can be performed by a general gynecologist if appropriate, as the chance for malignancy is minimal.
Continue to: Current use of endometrial ablation in the US...
Current use of endometrial ablation in the US
In 2015, more than 500,000 endometrial ablations were performed in the United States.Given the ability to perform in-office ablation, this number is growing and potentially underestimated each year.6 In 2022, the global endometrial ablation market was valued at $3.4 billion, a figure projected to double in 10 years.7 The procedure has evolved as different devices and approaches have developed, offering patients different means to manage bleeding without hysterectomy. The minimally invasive procedure, performed in premenopausal patients with heavy menstrual bleeding (HMB) due to benign causes who have completed childbearing, has been associated with faster recovery times and fewer short-term complications compared with more invasive surgery.8 There are several non-resectoscope ablative devices approved by the US Food and Drug Administration (FDA), and each work to destroy the endometrial lining via thermal or cryoablation. Endometrial ablation can be performed in premenopausal patients with HMB due to benign causes who have completed childbearing.
Recently, promotional literature has begun to report on so-called overuse of hysterectomy, despite decreasing overall hysterectomy rates. This reporting proposes and applies “appropriateness criteria,” accounting for the rate of preoperative counseling regarding alternatives to hysterectomy, as well as the rate of “unsupportive” final pathology.9 The adoption of endometrial ablation and increasing market value of such vendors suggest that this campaign is having its desired effect. From the oncology perspective, we are concerned the pendulum could swing too far away from hysterectomy, a procedure that definitively cures abnormal uterine bleeding, toward endometrial ablation without explicit acknowledgement of the trade-offs involved.
Endometrial ablation complications: Late-onset procedure failure
A number of post-ablation syndromes may present at least 1 month following the procedure. Collectively known as late-onset endometrial ablation failure (LOEAF), these syndromes are characterized by recurrent vaginal bleeding, and/or new cyclic pelvic pain.10 It is difficult to measure the true incidence of LOEAF. Thomassee and colleagues examined a Canadian retrospective cohort of 437 patients who underwent endometrial ablation; 20.8% reported post-ablation pelvic pain after a median 301 days.11 The subsequent need for surgical intervention, often hysterectomy, is a surrogate for LOEAF.
It should be noted that LOEAF is distinct from post-ablation tubal sterilization syndrome (PATSS), which describes cornual menstrual bleeding impeded by the ligated proximal fallopian tube.12 Increased awareness of PATSS, along with the discontinuation of Essure (a permanent hysteroscopic sterilization device) in 2018, has led some surgeons to advocate for concomitant salpingectomy at the time of endometrial ablation.13 The role of opportunistic salpingectomy in primary prevention of epithelial ovarian cancer is well described, and while we strongly support this practice at the time of endometrial ablation, we do not feel that it effectively prevents LOEAF.14
The post-ablation inability to adequately sample the endometrium is also considered a LOEAF. A prospective study of 57 women who underwent endometrial ablation assessed post-ablation sampling feasibility via transvaginal ultrasonography, saline infusion sonohysterography (SIS), and in-office endometrial biopsies. In 23% of the cohort, endometrial sampling failed, and the authors noted decreased reliability of pathologic assessment.15 One systematic review, in which authors examined the incidence of endometrial cancer following endometrial ablation, characterized 38 cases of endometrial cancer and reported a post-ablation endometrial sampling success rate of 89%. This figure was based on a self-selected sample of 18 patients; cases in which endometrial sampling was thought to be impossible were excluded. The study also had a 30% missing data rate and several other biases.16
In the previously mentioned poll of SGO members,1 84% of the surveyed gynecologic oncologists managing post-ablation patients reported that endometrial sampling following endometrial ablation was “moderately” or “extremely” difficult. More than half of the survey respondents believed that hysterectomy was required for accurate diagnosis.1 While we acknowledge the likely sampling bias affecting the survey results, we are not comforted by any data that minimizes this diagnostic challenge.
Appropriate patient selection and contraindications
The ideal candidate for endometrial ablation is a premenopausal patient with HMB who does not desire future fertility. According to the FDA, absolute contraindications include pregnancy or desired fertility, prior ablation, current IUD in place, inadequate preoperative endometrial assessment, known or suspected malignancy, active infection, or unfavorable anatomy.17
What about patients who may be at increased risk for endometrial cancer?
There is a paucity of data regarding the safety of endometrial ablation in patients at increased risk for developing endometrial cancer in the future. The American College of Obstetricians and Gynecologists (ACOG) 2007 practice bulletin on endometrial ablation (no longer accessible online) alludes to this concern and other contraindications,18 but there are no established guidelines. Currently, no ACOG practice bulletin or committee opinion lists relative contraindications to endometrial ablation, long-term complications (except risks associated with future pregnancy), or risk of subsequent hysterectomy. The risk that “it may be harder to detect endometrial cancer after ablation” is noted on ACOG’s web page dedicated to frequently asked questions (FAQs) regarding abnormal uterine bleeding.19 It is not mentioned on their web page dedicated to the FAQs regarding endometrial ablation.20
In the absence of high-quality published data on established contraindications for endometrial ablation, we advocate for the increased awareness of possible relative contraindications—namely well-established risk factors for endometrial cancer (TABLE 1).For example, in a pooled analysis of 24 epidemiologic studies, authors found that the odds of developing endometrial cancer was 7 times higher among patients with a body mass index (BMI) ≥ 40 kg/m2, compared with controls (odds ratio [OR], 7.14; 95% confidence interval [CI], 6.33–8.06).21 Additionally, patients with Lynch syndrome, a history of extended tamoxifen use, or those with a history of chronic anovulation or polycystic ovary syndrome are at increased risk for endometrial cancer.22-24 If the presence of one or more of these factors does not dissuade general gynecologists from performing an endometrial ablation (even armed with a negative preoperative endometrial biopsy), we feel they should at least prompt thoughtful guideline-driven pause.
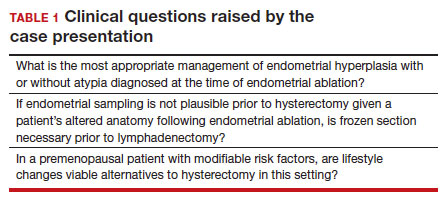
Continue to: Hysterectomy—A disincentivized option...
Hysterectomy—A disincentivized option
The annual number of hysterectomies performed by general gynecologists has declined over time. One study by Cadish and colleagues revealed that recent residency graduates performed only 3 to 4 annually.25 These numbers partly reflect the decreasing number of hysterectomies performed during residency training. Furthermore, other factors—including the increasing rate of placenta accreta spectrum, the focus on risk stratification of adnexal masses via the ovarian-adnexal reporting and data classification system (O-RADs), and the emphasis on minimally invasive approaches often acquired in subspecialty training—have likely contributed to referral patterns to such specialists as minimally invasive gynecologic surgeons and gynecologic oncologists.26 This trend is self-actualizing, as quality metrics funnel patients to high-volume surgeons, and general gynecologists risk losing hysterectomy privileges.
These factors lend themselves to a growing emphasis on endometrial ablation. Endometrial ablations can be performed in several settings, including in the hospital, in outpatient clinics, and more and more commonly, in ambulatory surgery centers. This increased access to endometrial ablation in the ambulatory surgery setting has corresponded with an annual endometrial ablation market value growth rate of 5% to 7%.27 These rates are likely compounded by payer reimbursement policies that promote endometrial ablation and other alternatives to hysterectomy that are cost savings in the short term.28 While the actual payer models are unavailable to review, they may not consider the costs of LOEAFs, including subsequent hysterectomy up to 5 years after initial ablation procedures. Provocatively, they almost certainly do not consider the costs of delayed care of patients with endometrial cancer vying for gynecologic oncology appointment slots occupied by post-ablation patients.
We urge providers, patients, and advocates to question who benefits from the uptake of ablation procedures: Patients? Payors? Providers? And how will the field of gynecology fare if hysterectomy skills and privileges are supplanted by ablation?
Post-ablation bleeding: Management by the gyn oncologist
Patients with post-ablation bleeding, either immediately or years later, are sometimes referred to a gynecologic oncologist given the possible risk for cancer and need for surgical staging if cancer is found on the hysterectomy specimen. In practice, assuming normal preoperative ultrasonography and no other clinical or radiologic findings suggestive of malignancy (eg, computed tomography findings concerning for metastases, abnormal cervical cytology, etc.), the presence of cancer is extremely unlikely to be determined at the time of surgery. Frozen section is not generally performed on the endometrium; intraoperative evaluation of even the unablated endometrium is notoriously unreliable; and histologic assessment of the ablated endometrium is limited by artifact (FIGURE 1). The abnormalities caused by ablation further impede selection of a representative focus, obfuscating any actionable result.
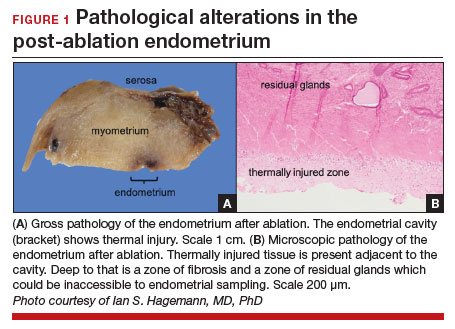
Some surgeons routinely bivalve the excised uterus prior to fixation to assess presence of tumor, tumor size, and the degree of myometrial invasion.29 A combination of factors may compel surgeons to perform lymphadenectomy if not already performed, or if sentinel lymph node mapping was unsuccessful. But this practice has not been studied in patients with post-ablation bleeding, and applying these principles relies on a preoperative diagnosis establishing the presence and grade of a cancer. Furthermore, the utility of frozen section and myometrial assessment to decide whether or not to proceed with lymphadenectomy is less relevant in the era of molecular classification guiding adjuvant therapy. In summary, assuming no pathologic or radiologic findings suggestive of cancer, gynecologic oncologists are unlikely to perform lymphadenectomy at the time of hysterectomy in these post-ablation cases, which therefore can safely be performed by general gynecologists.
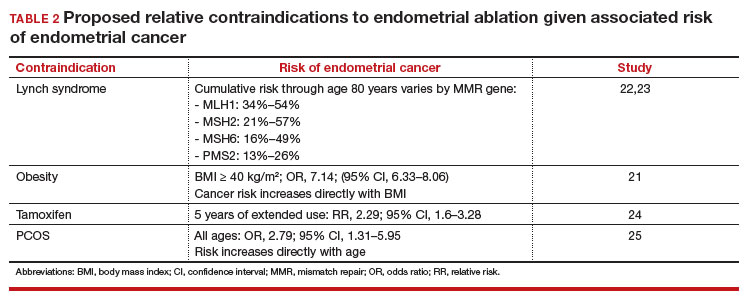
Our recommendations
Consider the LNG-IUD as an alternative to ablation. A recent randomized controlled trial by Beelen and colleagues compared the effectiveness of LNG-releasing IUDs with endometrial ablation in patients with HMB. While the LNG-IUD was inferior to endometrial ablation, quality-of-life measures were similar up to 2 years.31 Realizing that the hysterectomy rate following endometrial ablation increases significantly beyond that time point (2 years), this narrative may be incomplete. A 5- to 10-year follow-up time-frame may be a more helpful gauge of long-term outcomes. This prolonged time-frame also may allow study of the LNG-IUD’s protective effects on the endometrium in the prevention of endometrial hyperplasia and cancer.
Consider hysterectomy. A 2021 Cochrane review revealed that, compared with endometrial ablation, minimally invasive hysterectomy is associated with higher quality-of-life metrics, higher self-reported patient satisfaction, and similar rates of adverse events.32 While patient autonomy is paramount, the developing step-wise approach from endometrial ablation to hysterectomy, and its potential effects on the health care system at a time when endometrial cancer incidence and mortality rates are rising, is troubling.
Postablation, consider hysterectomy by the general gynecologist. Current trends appear to disincentivize general gynecologists from performing hysterectomy either for HMB or LOEAF. We would offer reassurance that they can safely perform this procedure. Referral to oncology may not be necessary since, in the absence of an established diagnosis of cancer, a lymphadenectomy is not typically required. A shift away from referral for these patients can preserve access to oncology for those women, especially minority women, with an explicit need for oncologic care.
In FIGURE 2, we propose a management algorithm for the patient who presents with post–ablation bleeding. We acknowledge that the evidence base for our management recommendations is limited. Still, we hope providers, ACOG, and other guidelines-issuing organizations consider them as they adapt their own practices and recommendations. We believe this is one of many steps needed to improve outcomes for patients with gynecologic cancer, particularly those in marginalized communities disproportionately impacted by current trends.
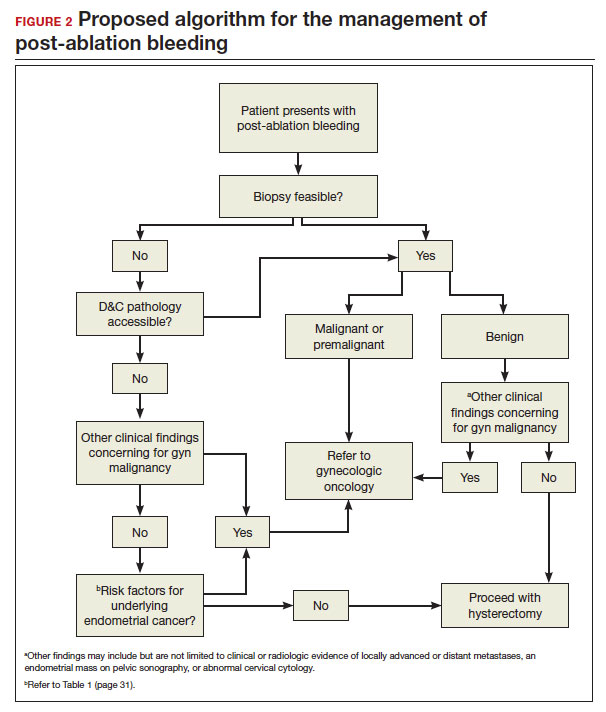
CASE Resolution
After reviewing the relevant documentation and examining the patient, the gynecologic oncology consultant contacts the referring gynecologist. They review the low utility of frozen section and the overall low risk of cancer on the final hysterectomy specimen if the patient were to undergo hysterectomy. The consultant clarifies that there is no other concern for surgical complexity beyond the skill of the referring provider, and they discuss the possibility of referral to a minimally invasive specialist for the surgery.
Ultimately, the patient undergoes uncomplicated laparoscopic hysterectomy performed by the original referring gynecologist. Final pathology reveals inactive endometrium with ablative changes and cornual focus of endometrial hyperplasia without atypia. ●
Acknowledgement
The authors acknowledge Ian Hagemann, MD, PhD, for his review of the manuscript.
CASE New patient presents with a history of endometrial hyperplasia
A 51-year-old patient (G2P2002) presents to a new gynecologist’s office after moving from a different state. In her medical history, the gynecologist notes that 5 years ago she underwent dilation and curettage and endometrial ablation procedures for heavy menstrual bleeding (HMB). Ultrasonography performed prior to those procedures showed a slightly enlarged uterus, a simple left ovarian cyst, and a non ̶ visualized right ovary. The patient had declined a 2-step procedure due to concerns with anesthesia, and surgical pathology at the time of ablation revealed hyperplasia without atypia. The patient’s medical history was otherwise notable for prediabetes (recent hemoglobin A1c [HbA1c] measurement, 6.0%) and obesity (body mass index, 43 kg/m2). Pertinent family history included her mother’s diagnosis of endometrial cancer at age 36. Given the patient’s diagnosis of endometrial hyperplasia, she was referred to gynecologic oncology, but she ultimately declined hysterectomy, stating that she was happy with the resolution of her abnormal bleeding. At the time of her initial gynecologic oncology consultation, the consultant suggested lifestyle changes to combat prediabetes and obesity to reduce the risk of endometrial cancer, as future signs of cancer, namely bleeding, may be masked by the endometrial ablation. The patient was prescribed metformin given these medical comorbidities.
At today’s appointment, the patient notes continued resolution of bleeding since the procedure. She does, however, note a 6-month history of vasomotor symptoms and one episode of spotting 3 months ago. Three years ago she was diagnosed with type 2 diabetes mellitus, and her current HbA1c is 6.9%. She has gained 10 lb since being diagnosed with endometrial cancer 5 years ago, and she has continued to take metformin.
An in-office endometrial biopsy is unsuccessful due to cervical stenosis. The treating gynecologist orders a transvaginal ultrasound, which reveals a small left ovarian cyst and a thickened endometrium (measuring 10 mm). Concerned that these findings could represent endometrial cancer, the gynecologist refers the patient to gynecologic oncology for further evaluation.
Sequelae and complications following endometrial ablation are often managed by a gynecologic oncologist. Indeed, a 2018 poll of Society of Gynecologic Oncology (SGO) members revealed that 93.8% of respondents had received such a referral, and almost 20% of respondents were managing more than 20 patients with post-ablation complications in their practices.1 These complications, including hematometra, post-ablation tubal sterilization syndrome, other pain syndromes associated with retrograde menstruation, and thickened endometrium with scarring leading to an inability to sample the endometrium to investigate post-ablation bleeding are symptoms and findings that often lead to further surgery, including hysterectomy.2 General gynecologists faced with these complications may refer patients to gynecologic oncology given an inability to sample the post-ablation endometrium or anticipated difficulties with hysterectomy. A recent meta-analysis revealed a 12.4% hysterectomy rate 5 years after endometrial ablation. Among these patients, the incidence of endometrial cancer ranged from 0% to 1.6%.3
In 2023, endometrial cancer incidence continues to increase, as does the incidence of obesity in women of all ages. Endometrial cancer mortality rates are also increasing, and these trends disproportionately affects non-Hispanic Black women.4 As providers and advocates work to narrow these disparities, gynecologic oncologists are simultaneously noting increased referrals for very likely benign conditions.5 Patients referred for post-ablation bleeding are a subset of these, as most patients who undergo endometrial ablation will not develop cancer. Considering the potential bottlenecks created en route to a gynecologic oncology evaluation, it seems prudent to minimize practices, like endometrial ablation, that may directly or indirectly prevent timely referral of patients with cancer to a gynecologic oncologist.
In this review we focus on the current use of endometrial ablation, associated complications, the incidence of treatment failure, and patient selection. Considering these issues in the context of the current endometrial cancer landscape, we posit best practices aimed at optimizing patient outcomes, and empowering general gynecologists to practice cancer prevention and to triage their surgical patients.
- Before performing endometrial ablation, consider whether alternatives such as hysterectomy or insertion of a progestin-containing IUD would be appropriate.
- Clinical management of patients with abnormal bleeding with indications for endometrial ablation should be guidelinedriven.
- Post-ablation bleeding or pain does not inherently require referral to oncology.
- General gynecologists can perform hysterectomy in this setting if appropriate.
- Patients with endometrial hyperplasia at endometrial ablation should be promptly offered hysterectomy. If atypia is not present, this hysterectomy, too, can be performed by a general gynecologist if appropriate, as the chance for malignancy is minimal.
Continue to: Current use of endometrial ablation in the US...
Current use of endometrial ablation in the US
In 2015, more than 500,000 endometrial ablations were performed in the United States.Given the ability to perform in-office ablation, this number is growing and potentially underestimated each year.6 In 2022, the global endometrial ablation market was valued at $3.4 billion, a figure projected to double in 10 years.7 The procedure has evolved as different devices and approaches have developed, offering patients different means to manage bleeding without hysterectomy. The minimally invasive procedure, performed in premenopausal patients with heavy menstrual bleeding (HMB) due to benign causes who have completed childbearing, has been associated with faster recovery times and fewer short-term complications compared with more invasive surgery.8 There are several non-resectoscope ablative devices approved by the US Food and Drug Administration (FDA), and each work to destroy the endometrial lining via thermal or cryoablation. Endometrial ablation can be performed in premenopausal patients with HMB due to benign causes who have completed childbearing.
Recently, promotional literature has begun to report on so-called overuse of hysterectomy, despite decreasing overall hysterectomy rates. This reporting proposes and applies “appropriateness criteria,” accounting for the rate of preoperative counseling regarding alternatives to hysterectomy, as well as the rate of “unsupportive” final pathology.9 The adoption of endometrial ablation and increasing market value of such vendors suggest that this campaign is having its desired effect. From the oncology perspective, we are concerned the pendulum could swing too far away from hysterectomy, a procedure that definitively cures abnormal uterine bleeding, toward endometrial ablation without explicit acknowledgement of the trade-offs involved.
Endometrial ablation complications: Late-onset procedure failure
A number of post-ablation syndromes may present at least 1 month following the procedure. Collectively known as late-onset endometrial ablation failure (LOEAF), these syndromes are characterized by recurrent vaginal bleeding, and/or new cyclic pelvic pain.10 It is difficult to measure the true incidence of LOEAF. Thomassee and colleagues examined a Canadian retrospective cohort of 437 patients who underwent endometrial ablation; 20.8% reported post-ablation pelvic pain after a median 301 days.11 The subsequent need for surgical intervention, often hysterectomy, is a surrogate for LOEAF.
It should be noted that LOEAF is distinct from post-ablation tubal sterilization syndrome (PATSS), which describes cornual menstrual bleeding impeded by the ligated proximal fallopian tube.12 Increased awareness of PATSS, along with the discontinuation of Essure (a permanent hysteroscopic sterilization device) in 2018, has led some surgeons to advocate for concomitant salpingectomy at the time of endometrial ablation.13 The role of opportunistic salpingectomy in primary prevention of epithelial ovarian cancer is well described, and while we strongly support this practice at the time of endometrial ablation, we do not feel that it effectively prevents LOEAF.14
The post-ablation inability to adequately sample the endometrium is also considered a LOEAF. A prospective study of 57 women who underwent endometrial ablation assessed post-ablation sampling feasibility via transvaginal ultrasonography, saline infusion sonohysterography (SIS), and in-office endometrial biopsies. In 23% of the cohort, endometrial sampling failed, and the authors noted decreased reliability of pathologic assessment.15 One systematic review, in which authors examined the incidence of endometrial cancer following endometrial ablation, characterized 38 cases of endometrial cancer and reported a post-ablation endometrial sampling success rate of 89%. This figure was based on a self-selected sample of 18 patients; cases in which endometrial sampling was thought to be impossible were excluded. The study also had a 30% missing data rate and several other biases.16
In the previously mentioned poll of SGO members,1 84% of the surveyed gynecologic oncologists managing post-ablation patients reported that endometrial sampling following endometrial ablation was “moderately” or “extremely” difficult. More than half of the survey respondents believed that hysterectomy was required for accurate diagnosis.1 While we acknowledge the likely sampling bias affecting the survey results, we are not comforted by any data that minimizes this diagnostic challenge.
Appropriate patient selection and contraindications
The ideal candidate for endometrial ablation is a premenopausal patient with HMB who does not desire future fertility. According to the FDA, absolute contraindications include pregnancy or desired fertility, prior ablation, current IUD in place, inadequate preoperative endometrial assessment, known or suspected malignancy, active infection, or unfavorable anatomy.17
What about patients who may be at increased risk for endometrial cancer?
There is a paucity of data regarding the safety of endometrial ablation in patients at increased risk for developing endometrial cancer in the future. The American College of Obstetricians and Gynecologists (ACOG) 2007 practice bulletin on endometrial ablation (no longer accessible online) alludes to this concern and other contraindications,18 but there are no established guidelines. Currently, no ACOG practice bulletin or committee opinion lists relative contraindications to endometrial ablation, long-term complications (except risks associated with future pregnancy), or risk of subsequent hysterectomy. The risk that “it may be harder to detect endometrial cancer after ablation” is noted on ACOG’s web page dedicated to frequently asked questions (FAQs) regarding abnormal uterine bleeding.19 It is not mentioned on their web page dedicated to the FAQs regarding endometrial ablation.20
In the absence of high-quality published data on established contraindications for endometrial ablation, we advocate for the increased awareness of possible relative contraindications—namely well-established risk factors for endometrial cancer (TABLE 1).For example, in a pooled analysis of 24 epidemiologic studies, authors found that the odds of developing endometrial cancer was 7 times higher among patients with a body mass index (BMI) ≥ 40 kg/m2, compared with controls (odds ratio [OR], 7.14; 95% confidence interval [CI], 6.33–8.06).21 Additionally, patients with Lynch syndrome, a history of extended tamoxifen use, or those with a history of chronic anovulation or polycystic ovary syndrome are at increased risk for endometrial cancer.22-24 If the presence of one or more of these factors does not dissuade general gynecologists from performing an endometrial ablation (even armed with a negative preoperative endometrial biopsy), we feel they should at least prompt thoughtful guideline-driven pause.
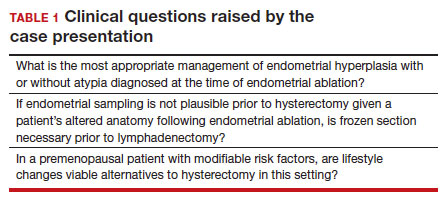
Continue to: Hysterectomy—A disincentivized option...
Hysterectomy—A disincentivized option
The annual number of hysterectomies performed by general gynecologists has declined over time. One study by Cadish and colleagues revealed that recent residency graduates performed only 3 to 4 annually.25 These numbers partly reflect the decreasing number of hysterectomies performed during residency training. Furthermore, other factors—including the increasing rate of placenta accreta spectrum, the focus on risk stratification of adnexal masses via the ovarian-adnexal reporting and data classification system (O-RADs), and the emphasis on minimally invasive approaches often acquired in subspecialty training—have likely contributed to referral patterns to such specialists as minimally invasive gynecologic surgeons and gynecologic oncologists.26 This trend is self-actualizing, as quality metrics funnel patients to high-volume surgeons, and general gynecologists risk losing hysterectomy privileges.
These factors lend themselves to a growing emphasis on endometrial ablation. Endometrial ablations can be performed in several settings, including in the hospital, in outpatient clinics, and more and more commonly, in ambulatory surgery centers. This increased access to endometrial ablation in the ambulatory surgery setting has corresponded with an annual endometrial ablation market value growth rate of 5% to 7%.27 These rates are likely compounded by payer reimbursement policies that promote endometrial ablation and other alternatives to hysterectomy that are cost savings in the short term.28 While the actual payer models are unavailable to review, they may not consider the costs of LOEAFs, including subsequent hysterectomy up to 5 years after initial ablation procedures. Provocatively, they almost certainly do not consider the costs of delayed care of patients with endometrial cancer vying for gynecologic oncology appointment slots occupied by post-ablation patients.
We urge providers, patients, and advocates to question who benefits from the uptake of ablation procedures: Patients? Payors? Providers? And how will the field of gynecology fare if hysterectomy skills and privileges are supplanted by ablation?
Post-ablation bleeding: Management by the gyn oncologist
Patients with post-ablation bleeding, either immediately or years later, are sometimes referred to a gynecologic oncologist given the possible risk for cancer and need for surgical staging if cancer is found on the hysterectomy specimen. In practice, assuming normal preoperative ultrasonography and no other clinical or radiologic findings suggestive of malignancy (eg, computed tomography findings concerning for metastases, abnormal cervical cytology, etc.), the presence of cancer is extremely unlikely to be determined at the time of surgery. Frozen section is not generally performed on the endometrium; intraoperative evaluation of even the unablated endometrium is notoriously unreliable; and histologic assessment of the ablated endometrium is limited by artifact (FIGURE 1). The abnormalities caused by ablation further impede selection of a representative focus, obfuscating any actionable result.
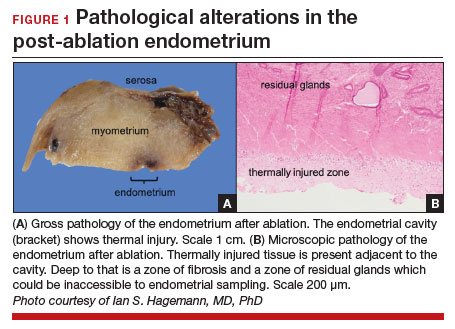
Some surgeons routinely bivalve the excised uterus prior to fixation to assess presence of tumor, tumor size, and the degree of myometrial invasion.29 A combination of factors may compel surgeons to perform lymphadenectomy if not already performed, or if sentinel lymph node mapping was unsuccessful. But this practice has not been studied in patients with post-ablation bleeding, and applying these principles relies on a preoperative diagnosis establishing the presence and grade of a cancer. Furthermore, the utility of frozen section and myometrial assessment to decide whether or not to proceed with lymphadenectomy is less relevant in the era of molecular classification guiding adjuvant therapy. In summary, assuming no pathologic or radiologic findings suggestive of cancer, gynecologic oncologists are unlikely to perform lymphadenectomy at the time of hysterectomy in these post-ablation cases, which therefore can safely be performed by general gynecologists.
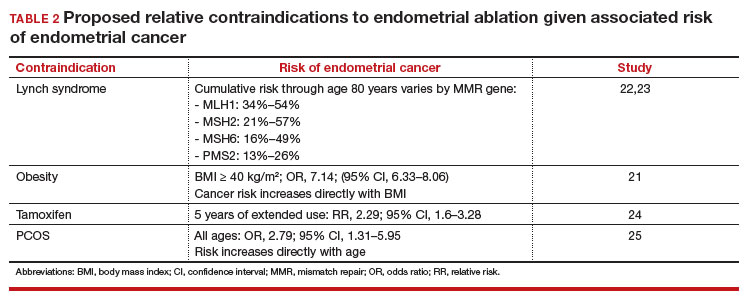
Our recommendations
Consider the LNG-IUD as an alternative to ablation. A recent randomized controlled trial by Beelen and colleagues compared the effectiveness of LNG-releasing IUDs with endometrial ablation in patients with HMB. While the LNG-IUD was inferior to endometrial ablation, quality-of-life measures were similar up to 2 years.31 Realizing that the hysterectomy rate following endometrial ablation increases significantly beyond that time point (2 years), this narrative may be incomplete. A 5- to 10-year follow-up time-frame may be a more helpful gauge of long-term outcomes. This prolonged time-frame also may allow study of the LNG-IUD’s protective effects on the endometrium in the prevention of endometrial hyperplasia and cancer.
Consider hysterectomy. A 2021 Cochrane review revealed that, compared with endometrial ablation, minimally invasive hysterectomy is associated with higher quality-of-life metrics, higher self-reported patient satisfaction, and similar rates of adverse events.32 While patient autonomy is paramount, the developing step-wise approach from endometrial ablation to hysterectomy, and its potential effects on the health care system at a time when endometrial cancer incidence and mortality rates are rising, is troubling.
Postablation, consider hysterectomy by the general gynecologist. Current trends appear to disincentivize general gynecologists from performing hysterectomy either for HMB or LOEAF. We would offer reassurance that they can safely perform this procedure. Referral to oncology may not be necessary since, in the absence of an established diagnosis of cancer, a lymphadenectomy is not typically required. A shift away from referral for these patients can preserve access to oncology for those women, especially minority women, with an explicit need for oncologic care.
In FIGURE 2, we propose a management algorithm for the patient who presents with post–ablation bleeding. We acknowledge that the evidence base for our management recommendations is limited. Still, we hope providers, ACOG, and other guidelines-issuing organizations consider them as they adapt their own practices and recommendations. We believe this is one of many steps needed to improve outcomes for patients with gynecologic cancer, particularly those in marginalized communities disproportionately impacted by current trends.
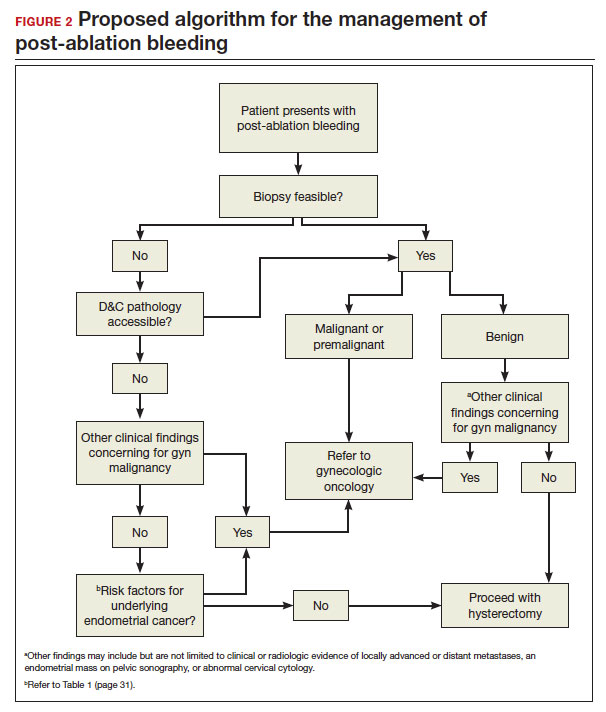
CASE Resolution
After reviewing the relevant documentation and examining the patient, the gynecologic oncology consultant contacts the referring gynecologist. They review the low utility of frozen section and the overall low risk of cancer on the final hysterectomy specimen if the patient were to undergo hysterectomy. The consultant clarifies that there is no other concern for surgical complexity beyond the skill of the referring provider, and they discuss the possibility of referral to a minimally invasive specialist for the surgery.
Ultimately, the patient undergoes uncomplicated laparoscopic hysterectomy performed by the original referring gynecologist. Final pathology reveals inactive endometrium with ablative changes and cornual focus of endometrial hyperplasia without atypia. ●
Acknowledgement
The authors acknowledge Ian Hagemann, MD, PhD, for his review of the manuscript.
- Chen H, Saiz AM, McCausland AM, et al. Experience of gynecologic oncologists regarding endometrial cancer after endometrial ablation. J Clin Oncol. 2018;36:e17566-e.
- McCausland AM, McCausland VM. Long-term complications of endometrial ablation: cause, diagnosis, treatment, and prevention. J Minim Invasive Gynecol. 2007;14:399-406.
- Oderkerk TJ, Beelen P, Bukkems ALA, et al. Risk of hysterectomy after endometrial ablation: a systematic review and meta-analysis. Obstet Gynecol. 2023;142:51-60.
- Clarke MA, Devesa SS, Hammer A, et al. Racial and ethnic differences in hysterectomy-corrected uterine corpus cancer mortality by stage and histologic subtype. JAMA Oncol. 2022;8:895-903.
- Barber EL, Rossi EC, Alexander A, et al. Benign hysterectomy performed by gynecologic oncologists: is selection bias altering our ability to measure surgical quality? Gynecol Oncol. 2018;151:141-144.
- Wortman M. Late-onset endometrial ablation failure. Case Rep Womens Health. 2017;15:11-28.
- Insights FM. Endometrial Ablation Market Outlook.Accessed July 26, 2023. https://www.futuremarketinsights.com/reports/endometrial-ablation -market
- Famuyide A. Endometrial ablation. J Minim Invasive Gynecol. 2018;25:299-307.
- Corona LE, Swenson CW, Sheetz KH, et al. Use of other treatments before hysterectomy for benign conditions in a statewide hospital collaborative. Am J Obstet Gynecol. 2015;212:304.e1-e7.
- Wortman M, Cholkeri A, McCausland AM, et al. Late-onset endometrial ablation failure—etiology, treatment, and prevention. J Minim Invasive Gynecol. 2015;22:323-331.
- Thomassee MS, Curlin H, Yunker A, et al. Predicting pelvic pain after endometrial ablation: which preoperative patient characteristics are associated? J Minim Invasive Gynecol. 2013;20:642-647.
- Townsend DE, McCausland V, McCausland A, et al. Post-ablation-tubal sterilization syndrome. Obstet Gynecol. 1993;82:422-424.
- Greer Polite F, DeAgostino-Kelly M, Marchand GJ. Combination of laparoscopic salpingectomy and endometrial ablation: a potentially underused procedure. J Gynecol Surg. 2021;37:89-91.
- Hanley GE, Pearce CL, Talhouk A, et al. Outcomes from opportunistic salpingectomy for ovarian cancer prevention. JAMA Network Open. 2022;5:e2147343-e.
- Ahonkallio SJ, Liakka AK, Martikainen HK, et al. Feasibility of endometrial assessment after thermal ablation. Eur J Obstet Gynecol Reprod Biol. 2009;147:69-71.
- Tamara JO, Mileen RDvdK, Karlijn MCC, et al. Endometrial cancer after endometrial ablation: a systematic review. Int J Gynecol Cancer. 2022;32:1555.
- US Food and Drug Administration. Endometrial ablation for heavy menstrual bleeding.Accessed July 26, 2023. https://www.fda.gov/medical-devices /surgery-devices/endometrial-ablation-heavy-menstrual-bleeding
- ACOG Practice Bulletin. Clinical management guidelines for obstetriciangynecologists. Number 81, May 2007. Obstet Gynecol. 2007;109:1233-1248.
- The American College of Obstetricians and Gynecologists. Abnormal uterine bleeding frequently asked questions. Accessed July 26, 2023. https://www.acog .org/womens-health/faqs/abnormal-uterine-bleeding
- The American College of Obstetricians and Gynecologists. Endometrial ablation frequently asked questions. Accessed November 28, 2023. https://www.acog. org/womens-health/faqs/endometrial-ablation#:~:text=Can%20I%20still%20 get%20pregnant,should%20not%20have%20this%20procedure
- Setiawan VW, Yang HP, Pike MC, et al. Type I and II endometrial cancers: have they different risk factors? J Clin Oncol. 2013;31:2607-2618.
- National Comprehensive Cancer Network. Lynch Syndrome (Version 2.2023). Accessed November 15, 2023. https://www.nccn.org/professionals /physician_gls/pdf/genetics_colon.pdf
- Bonadona V, Bonaïti B, Olschwang S, et al. Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA. 2011;305: 2304-2310.
- Fleming CA, Heneghan HM, O’Brien D, et al. Meta-analysis of the cumulative risk of endometrial malignancy and systematic review of endometrial surveillance in extended tamoxifen therapy. Br J Surg. 2018;105:1098-1106.
- Barry JA, Azizia MM, Hardiman PJ. Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2014;20:748-758.
- Cadish LA, Kropat G, Muffly TM. Hysterectomy volume among recent obstetrics and gynecology residency graduates. Urogynecology. 2021;27.
- Blank SV, Huh WK, Bell M, et al. Doubling down on the future of gynecologic oncology: the SGO future of the profession summit report. Gynecol Oncol. 2023;171:76-82.
- Reports MI. Global endometrial ablation market growth, trends and forecast 2023 to 2028 by types, by application, by regions and by key players like Boston Scientific, Hologic, Olympus, Minerva Surgical. Accessed July 30, 2023. https://www.marketinsightsreports.com/single-report/061612632440/global -endometrial-ablation-market-growth-trends-and-forecast-2023-to-2028-by -types-by-application-by-regions-and-by-key-players-like-boston-scientific -hologic-olympus-minerva-surgical
- London R, Holzman M, Rubin D, et al. Payer cost savings with endometrial ablation therapy. Am J Manag Care. 1999;5:889-897.
- Mariani A, Dowdy SC, Cliby WA, et al. Prospective assessment of lymphatic dissemination in endometrial cancer: a paradigm shift in surgical staging. Gynecol Oncol. 2008;109:11-18.
- Beelen P, van den Brink MJ, Herman MC, et al. Levonorgestrel-releasing intrauterine system versus endometrial ablation for heavy menstrual bleeding. Am J Obstet Gynecol. 2021;224:187.e1-e10.
- Bofill Rodriguez M, Lethaby A, Fergusson RJ. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding. Cochrane Database Syst Rev. 2021;2:Cd000329.
- Chen H, Saiz AM, McCausland AM, et al. Experience of gynecologic oncologists regarding endometrial cancer after endometrial ablation. J Clin Oncol. 2018;36:e17566-e.
- McCausland AM, McCausland VM. Long-term complications of endometrial ablation: cause, diagnosis, treatment, and prevention. J Minim Invasive Gynecol. 2007;14:399-406.
- Oderkerk TJ, Beelen P, Bukkems ALA, et al. Risk of hysterectomy after endometrial ablation: a systematic review and meta-analysis. Obstet Gynecol. 2023;142:51-60.
- Clarke MA, Devesa SS, Hammer A, et al. Racial and ethnic differences in hysterectomy-corrected uterine corpus cancer mortality by stage and histologic subtype. JAMA Oncol. 2022;8:895-903.
- Barber EL, Rossi EC, Alexander A, et al. Benign hysterectomy performed by gynecologic oncologists: is selection bias altering our ability to measure surgical quality? Gynecol Oncol. 2018;151:141-144.
- Wortman M. Late-onset endometrial ablation failure. Case Rep Womens Health. 2017;15:11-28.
- Insights FM. Endometrial Ablation Market Outlook.Accessed July 26, 2023. https://www.futuremarketinsights.com/reports/endometrial-ablation -market
- Famuyide A. Endometrial ablation. J Minim Invasive Gynecol. 2018;25:299-307.
- Corona LE, Swenson CW, Sheetz KH, et al. Use of other treatments before hysterectomy for benign conditions in a statewide hospital collaborative. Am J Obstet Gynecol. 2015;212:304.e1-e7.
- Wortman M, Cholkeri A, McCausland AM, et al. Late-onset endometrial ablation failure—etiology, treatment, and prevention. J Minim Invasive Gynecol. 2015;22:323-331.
- Thomassee MS, Curlin H, Yunker A, et al. Predicting pelvic pain after endometrial ablation: which preoperative patient characteristics are associated? J Minim Invasive Gynecol. 2013;20:642-647.
- Townsend DE, McCausland V, McCausland A, et al. Post-ablation-tubal sterilization syndrome. Obstet Gynecol. 1993;82:422-424.
- Greer Polite F, DeAgostino-Kelly M, Marchand GJ. Combination of laparoscopic salpingectomy and endometrial ablation: a potentially underused procedure. J Gynecol Surg. 2021;37:89-91.
- Hanley GE, Pearce CL, Talhouk A, et al. Outcomes from opportunistic salpingectomy for ovarian cancer prevention. JAMA Network Open. 2022;5:e2147343-e.
- Ahonkallio SJ, Liakka AK, Martikainen HK, et al. Feasibility of endometrial assessment after thermal ablation. Eur J Obstet Gynecol Reprod Biol. 2009;147:69-71.
- Tamara JO, Mileen RDvdK, Karlijn MCC, et al. Endometrial cancer after endometrial ablation: a systematic review. Int J Gynecol Cancer. 2022;32:1555.
- US Food and Drug Administration. Endometrial ablation for heavy menstrual bleeding.Accessed July 26, 2023. https://www.fda.gov/medical-devices /surgery-devices/endometrial-ablation-heavy-menstrual-bleeding
- ACOG Practice Bulletin. Clinical management guidelines for obstetriciangynecologists. Number 81, May 2007. Obstet Gynecol. 2007;109:1233-1248.
- The American College of Obstetricians and Gynecologists. Abnormal uterine bleeding frequently asked questions. Accessed July 26, 2023. https://www.acog .org/womens-health/faqs/abnormal-uterine-bleeding
- The American College of Obstetricians and Gynecologists. Endometrial ablation frequently asked questions. Accessed November 28, 2023. https://www.acog. org/womens-health/faqs/endometrial-ablation#:~:text=Can%20I%20still%20 get%20pregnant,should%20not%20have%20this%20procedure
- Setiawan VW, Yang HP, Pike MC, et al. Type I and II endometrial cancers: have they different risk factors? J Clin Oncol. 2013;31:2607-2618.
- National Comprehensive Cancer Network. Lynch Syndrome (Version 2.2023). Accessed November 15, 2023. https://www.nccn.org/professionals /physician_gls/pdf/genetics_colon.pdf
- Bonadona V, Bonaïti B, Olschwang S, et al. Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA. 2011;305: 2304-2310.
- Fleming CA, Heneghan HM, O’Brien D, et al. Meta-analysis of the cumulative risk of endometrial malignancy and systematic review of endometrial surveillance in extended tamoxifen therapy. Br J Surg. 2018;105:1098-1106.
- Barry JA, Azizia MM, Hardiman PJ. Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2014;20:748-758.
- Cadish LA, Kropat G, Muffly TM. Hysterectomy volume among recent obstetrics and gynecology residency graduates. Urogynecology. 2021;27.
- Blank SV, Huh WK, Bell M, et al. Doubling down on the future of gynecologic oncology: the SGO future of the profession summit report. Gynecol Oncol. 2023;171:76-82.
- Reports MI. Global endometrial ablation market growth, trends and forecast 2023 to 2028 by types, by application, by regions and by key players like Boston Scientific, Hologic, Olympus, Minerva Surgical. Accessed July 30, 2023. https://www.marketinsightsreports.com/single-report/061612632440/global -endometrial-ablation-market-growth-trends-and-forecast-2023-to-2028-by -types-by-application-by-regions-and-by-key-players-like-boston-scientific -hologic-olympus-minerva-surgical
- London R, Holzman M, Rubin D, et al. Payer cost savings with endometrial ablation therapy. Am J Manag Care. 1999;5:889-897.
- Mariani A, Dowdy SC, Cliby WA, et al. Prospective assessment of lymphatic dissemination in endometrial cancer: a paradigm shift in surgical staging. Gynecol Oncol. 2008;109:11-18.
- Beelen P, van den Brink MJ, Herman MC, et al. Levonorgestrel-releasing intrauterine system versus endometrial ablation for heavy menstrual bleeding. Am J Obstet Gynecol. 2021;224:187.e1-e10.
- Bofill Rodriguez M, Lethaby A, Fergusson RJ. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding. Cochrane Database Syst Rev. 2021;2:Cd000329.
Elagolix curbs heavy bleeding linked to uterine leiomyomas
Uterine leiomyomas are common in premenopausal women, and 60% experience heavy menstrual bleeding, but nonsurgical options as an alternative to hysterectomy are limited, wrote Eric Brown, MD, of Gyn-Care, Atlanta, Georgia, and colleagues.
Elagolix sodium, an oral, short-acting nonpeptide, gonadotropin-releasing hormone antagonist, has been approved by the Food and Drug Administration at a dose of 300 mg twice daily with add-back therapy for up to 24 months of use. However, this treatment protocol is contraindicated or not preferable for some patients, the researchers said.
In a study published in Obstetrics & Gynecology , the researchers randomized 54 women to 150 mg of oral elagolix once daily, and 28 to a placebo for 6 months to investigate the safety and efficacy of the lower dose. The study population included women aged 18-51 years with a history of heavy menstrual bleeding association with uterine leiomyomas. Approximately two-thirds (65.9%) were Black.
The primary endpoint was the proportion of patients who met the criteria of menstrual blood loss volume less than 80 mL during the final month of treatment and menstrual blood loss volume reduction of 50% or more from baseline to the final month of treatment.
After 6 months, nearly half (49.4%) of the elagolix group met the study endpoint compared with 23.3% of the placebo group (P = .035).
Elagolix patients showed significantly greater reductions in both mean and median menstrual blood loss volumes compared with the placebo patients over the study period, and significant differences between the groups in the mean reduction of menstrual blood loss were evident after 1 month of treatment (P < .05 for months 1, 2, 3, and 5).
Results were similar in a further sensitivity analysis in which patients with incomplete final month data were considered nonresponders; 44.4% of elagolix patients and 21.4% of patients met the primary endpoint.
Overall, 51.9% of elagolix patients and 39.3% of placebo patients reported adverse events; the most common were headache and hot flush. Three patients (5.6%) in the elagolix group discontinued the drug because of adverse events. No serious or severe adverse events were reported in the elagolix group; both cases of reported serious adverse events (COVID-19 and an enlarged uvula) occurred in placebo patients.
Patient-reported outcomes were significantly greater in the elagolix patients, based on symptom severity score, 5 of 6 Uterine Fibroid Symptom and Quality of Life (UFS-QOL) health-related quality of life subscales, and the HRQOL total score at the end of the study.
The findings were limited by several factors including the small study population and lenient eligibility criteria that may have led to a higher placebo response rate, and the study did not monitor bone mineral density, the researchers noted.
However, the results suggest that elagolix at a 150-mg dose was well tolerated, with a safety profile similar to that seen in women who took the drug for endometriosis pain, and may be an option for women with contraindications to other therapy or for those who prefer once-daily dosing, they concluded.
The study was funded by AbbVie. Lead author Dr. Brown had no additional financial conflicts to disclose, but several coauthors disclosed relationships with AbbVie and other companies.
Uterine leiomyomas are common in premenopausal women, and 60% experience heavy menstrual bleeding, but nonsurgical options as an alternative to hysterectomy are limited, wrote Eric Brown, MD, of Gyn-Care, Atlanta, Georgia, and colleagues.
Elagolix sodium, an oral, short-acting nonpeptide, gonadotropin-releasing hormone antagonist, has been approved by the Food and Drug Administration at a dose of 300 mg twice daily with add-back therapy for up to 24 months of use. However, this treatment protocol is contraindicated or not preferable for some patients, the researchers said.
In a study published in Obstetrics & Gynecology , the researchers randomized 54 women to 150 mg of oral elagolix once daily, and 28 to a placebo for 6 months to investigate the safety and efficacy of the lower dose. The study population included women aged 18-51 years with a history of heavy menstrual bleeding association with uterine leiomyomas. Approximately two-thirds (65.9%) were Black.
The primary endpoint was the proportion of patients who met the criteria of menstrual blood loss volume less than 80 mL during the final month of treatment and menstrual blood loss volume reduction of 50% or more from baseline to the final month of treatment.
After 6 months, nearly half (49.4%) of the elagolix group met the study endpoint compared with 23.3% of the placebo group (P = .035).
Elagolix patients showed significantly greater reductions in both mean and median menstrual blood loss volumes compared with the placebo patients over the study period, and significant differences between the groups in the mean reduction of menstrual blood loss were evident after 1 month of treatment (P < .05 for months 1, 2, 3, and 5).
Results were similar in a further sensitivity analysis in which patients with incomplete final month data were considered nonresponders; 44.4% of elagolix patients and 21.4% of patients met the primary endpoint.
Overall, 51.9% of elagolix patients and 39.3% of placebo patients reported adverse events; the most common were headache and hot flush. Three patients (5.6%) in the elagolix group discontinued the drug because of adverse events. No serious or severe adverse events were reported in the elagolix group; both cases of reported serious adverse events (COVID-19 and an enlarged uvula) occurred in placebo patients.
Patient-reported outcomes were significantly greater in the elagolix patients, based on symptom severity score, 5 of 6 Uterine Fibroid Symptom and Quality of Life (UFS-QOL) health-related quality of life subscales, and the HRQOL total score at the end of the study.
The findings were limited by several factors including the small study population and lenient eligibility criteria that may have led to a higher placebo response rate, and the study did not monitor bone mineral density, the researchers noted.
However, the results suggest that elagolix at a 150-mg dose was well tolerated, with a safety profile similar to that seen in women who took the drug for endometriosis pain, and may be an option for women with contraindications to other therapy or for those who prefer once-daily dosing, they concluded.
The study was funded by AbbVie. Lead author Dr. Brown had no additional financial conflicts to disclose, but several coauthors disclosed relationships with AbbVie and other companies.
Uterine leiomyomas are common in premenopausal women, and 60% experience heavy menstrual bleeding, but nonsurgical options as an alternative to hysterectomy are limited, wrote Eric Brown, MD, of Gyn-Care, Atlanta, Georgia, and colleagues.
Elagolix sodium, an oral, short-acting nonpeptide, gonadotropin-releasing hormone antagonist, has been approved by the Food and Drug Administration at a dose of 300 mg twice daily with add-back therapy for up to 24 months of use. However, this treatment protocol is contraindicated or not preferable for some patients, the researchers said.
In a study published in Obstetrics & Gynecology , the researchers randomized 54 women to 150 mg of oral elagolix once daily, and 28 to a placebo for 6 months to investigate the safety and efficacy of the lower dose. The study population included women aged 18-51 years with a history of heavy menstrual bleeding association with uterine leiomyomas. Approximately two-thirds (65.9%) were Black.
The primary endpoint was the proportion of patients who met the criteria of menstrual blood loss volume less than 80 mL during the final month of treatment and menstrual blood loss volume reduction of 50% or more from baseline to the final month of treatment.
After 6 months, nearly half (49.4%) of the elagolix group met the study endpoint compared with 23.3% of the placebo group (P = .035).
Elagolix patients showed significantly greater reductions in both mean and median menstrual blood loss volumes compared with the placebo patients over the study period, and significant differences between the groups in the mean reduction of menstrual blood loss were evident after 1 month of treatment (P < .05 for months 1, 2, 3, and 5).
Results were similar in a further sensitivity analysis in which patients with incomplete final month data were considered nonresponders; 44.4% of elagolix patients and 21.4% of patients met the primary endpoint.
Overall, 51.9% of elagolix patients and 39.3% of placebo patients reported adverse events; the most common were headache and hot flush. Three patients (5.6%) in the elagolix group discontinued the drug because of adverse events. No serious or severe adverse events were reported in the elagolix group; both cases of reported serious adverse events (COVID-19 and an enlarged uvula) occurred in placebo patients.
Patient-reported outcomes were significantly greater in the elagolix patients, based on symptom severity score, 5 of 6 Uterine Fibroid Symptom and Quality of Life (UFS-QOL) health-related quality of life subscales, and the HRQOL total score at the end of the study.
The findings were limited by several factors including the small study population and lenient eligibility criteria that may have led to a higher placebo response rate, and the study did not monitor bone mineral density, the researchers noted.
However, the results suggest that elagolix at a 150-mg dose was well tolerated, with a safety profile similar to that seen in women who took the drug for endometriosis pain, and may be an option for women with contraindications to other therapy or for those who prefer once-daily dosing, they concluded.
The study was funded by AbbVie. Lead author Dr. Brown had no additional financial conflicts to disclose, but several coauthors disclosed relationships with AbbVie and other companies.
FROM OBSTETRICS & GYNECOLOGY