User login
Implementing enhanced recovery protocols for gynecologic surgery
“Enhanced Recovery After Surgery” (ERAS) practices and protocols have been increasingly refined and adopted for the field of gynecology, and there is hope among gynecologic surgeons – and some recent evidence – that, with the ERAS movement, we are improving patient recoveries and outcomes and minimizing the need for opioids.
This applies not only to open surgeries but also to the minimally invasive procedures that already are prized for significant reductions in morbidity and length of stay. The overarching and guiding principle of ERAS is that any surgery – whether open or minimally invasive, major or minor – places stress on the body and is associated with risks and morbidity.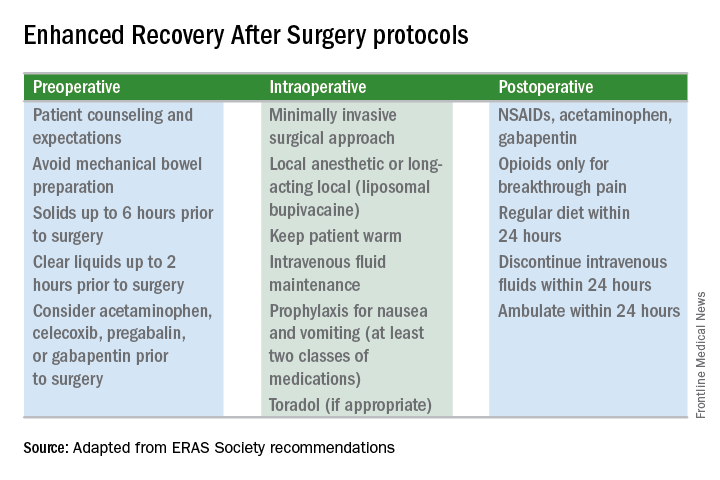
Enhanced recovery protocols are multidisciplinary, perioperative approaches designed to lessen the body’s stress response to surgery. The protocols and pathways offer us a menu of small changes that, in the aggregate, can lead to large and demonstrable benefits – especially when these small changes are chosen across the preoperative, intraoperative, and postoperative arenas and then standardized in one’s practice. Among the major components of ERAS practices and protocols are limiting preoperative fasting, employing multimodal analgesia, encouraging early ambulation and early postsurgical feeding, and creating culture shift that includes greater emphasis on patient expectations.
In our practice, we are incorporating ERAS practices not only in hopes of reducing the stress of all surgeries before, during, and after, but also with the goal of achieving a postoperative opioid-free hysterectomy, myomectomy, and extensive endometriosis surgery. (All of our advanced procedures are performed laparoscopically or robotically.)
Over the past 7 or so years, we have adopted a multimodal approach to pain control that includes a bundle of preoperative analgesics – acetaminophen, pregabalin, and celecoxib (we call it “TLC” for Tylenol, Lyrica, and Celebrex) – and the use of liposomal bupivacaine in our robotic surgeries. We are now turning toward ERAS nutritional changes, most of which run counter to traditional paradigms for surgical care. And in other areas, such as dedicated preoperative counseling, we continue to refine and improve our practices.
Improved Outcomes
The ERAS mindset notably intersected gynecology with the publication in 2016 of a two-part series of guidelines for gynecology/oncology surgery from the ERAS Society. The 8-year-old society has its roots in a study group of European surgeons and others who decided to examine surgical practices and the concept of multimodal surgical care put forth in the 1990s by Henrik Kehlet, MD, PhD, then a professor at the University of Copenhagen.
The first set of recommendations addressed pre- and intraoperative care (Gynecol Oncol. 2016 Feb;140[2]:313-22), and the second set addressed postoperative care (Gynecol Oncol. 2016 Feb;140[2]:323-32). Similar evidence-based recommendations were previously written for colonic resections, rectal and pelvic surgery, and other surgical specialties.
Most of the published outcomes of enhanced recovery protocols come from colorectal surgery. As noted in the ERAS Society gynecology/oncology guidelines, the benefits include an average reduction in length of stay of 2.5 days and a decrease in complications by as much as 50%.
There is growing evidence, however, that ERAS programs are also beneficial for patients undergoing laparoscopic surgery, and outcomes from gynecology – including minimally invasive surgery – are also being reported.
For instance, a retrospective case-control study of 55 consecutive gynecologic oncology patients treated at the University of California, San Francisco, with laparoscopic or robotic surgery and an enhanced recovery pathway – and 110 historical control patients matched on the basis of age and surgery type – found significant improvements in recovery time, decreased pain despite reduced opioid use, and overall lower hospital costs (Obstet Gynecol. 2016 Jul;128[1]:138-44).
The enhanced recovery pathway included patient education, multimodal antiemetics, multimodal analgesia, and balanced fluid administration. Early catheter removal, ambulation, and feeding were also components. Analgesia included routine preoperative gabapentin, diclofenac, and acetaminophen; routine postoperative gabapentin, NSAIDs, and acetaminophen; and transversus abdominis plane blocks in 32 of the ERAS patients.
ERAS patients were significantly more likely to be discharged on day 1 (91%, compared with 60% in the control group). Opioid use decreased by 30%, and pain scores on postoperative day 1 were significantly lower.
Another study looking at the effect of enhanced recovery implementation in gynecologic surgeries at the University of Virginia, Charlottesville, (gynecologic oncology, urogynecology, and general gynecology) similarly reported benefits for vaginal and minimally invasive procedures, as well as for open procedures (Obstet Gynecol. 2016 Sep;128[3]:457-66).
In the minimally invasive group, investigators compared 324 patients before ERAS implementation with 249 patients afterward and found that the median length of stay was unchanged (1 day). However, intraoperative and postoperative opioid consumption decreased significantly and – even though actual pain scores improved only slightly – patient satisfaction scores improved markedly among post-ERAS patients. Patients gave higher marks, for instance, to questions regarding pain control (“how well your pain was controlled”) and teamwork (“staff worked together to care for you”).
Reducing Opioids
New opioid use that persists after a surgical procedure is a postsurgical complication that we all should be working to prevent. It has been estimated that 6% of surgical patients – even those who’ve had relatively minor surgical procedures – will become long-term opioid users, developing a dependence on the drugs prescribed to them for postsurgical pain.
This was shown last year in a national study of insurance claims data from between 2013 and 2014; investigators identified adults without opioid use in the year prior to surgery (including hysterectomy) and found that 5.9%-6.5% were filling opioid prescriptions 90-180 days after their surgical procedure. The incidence in a nonoperative control cohort was 0.4% (JAMA Surg. 2017 Jun 21;152[6]:e170504). Notably, this prolonged use was greatest in patients with prior pain conditions, substance abuse, and mental health disorders – a finding that may have implications for the counseling we provide prior to surgery.
It’s not clear what the optimal analgesic regimen is for minimally invasive or other gynecologic surgeries. What is clearly recommended, however, is that the approach be multifaceted. In our practice, we believe that the preoperative use of acetaminophen, pregabalin, and celecoxib plays an important role in reducing postoperative pain and opioid use. But we also have striven to create a practice-wide culture shift (throughout the operating and recovery rooms), for instance, that encourages using the least amounts of narcotics possible and using the shortest-acting formulations possible.
Transversus abdominis plane (TAP) blocks are also often part of ERAS protocols; they have been shown in at least two randomized controlled trials of abdominal hysterectomy to reduce intraoperative fentanyl requirements and to reduce immediate postoperative pain scores and postoperative morphine requirements (Anesth Analg. 2008 Dec;107[6]:2056-60; J Anaesthesiol Clin Pharmacol. 2014 Jul-Sep;30[3]:391-6).
More recently, liposomal bupivacaine, which is slowly released over several days, has gained traction as a substitute for standard bupivacaine and other agents in TAP blocks. In one recent retrospective study, abdominal incision infiltration with liposomal bupivacaine was associated with less opioid use (with no change in pain scores), compared with bupivacaine hydrochloride after laparotomy for gynecologic malignancies (Obstet Gynecol. 2016 Nov;128[5]:1009-17). It’s significantly more expensive, however, making it likely that the formulation is being used more judiciously in minimally invasive gynecologic surgery than in open surgeries.
Because of costs, we currently are restricted to using liposomal bupivacaine in our robotic surgeries only. In our practice, the single 20 mL vial (266 mg of liposomal bupivacaine) is diluted with 20 mL of normal saline, but it can be further diluted without loss of efficacy. With a 16-gauge needle, the liposomal bupivacaine is distributed across the incisions (usually 20 mL in the umbilicus with a larger incision and 10 mL in each of the two lateral incisions). Patients are counseled that they may have more discomfort after 3 days, but by this point most are mobile and feeling relatively well with a combination of NSAIDs and acetaminophen.
With growing visibility of the problem of narcotic dependence in the United States, patients seem increasingly receptive and even eager to limit or avoid the use of opioids. Patients should be counseled that minimizing or avoiding opioids may also speed recovery. Narcotics cause gut motility to slow down, which may hinder mobilization. Early mobilization (within 24 hours) is among the enhanced recovery elements that the ERAS Society guidelines say is “of particular value” for minimally invasive surgery, along with maintenance of normothermia and normovolemia with maintenance of adequate cardiac output.
Selecting Steps
Our practice is also trying to reduce preoperative bowel preparation and preoperative fasting, both of which have been found to be stressful for the body without evidence of benefit. These practices can lead to insulin resistance and hyperglycemia, which are associated with increased morbidity and length of stay.
It is now recommended that clear fluids be allowed up to 2 hours before surgery and solids up to 6 hours before. Some health systems and practices also recommend presurgical carbohydrate loading (for example, 10 ounces of apple juice 2 hours before surgery) – another small change on the ERAS menu – to further reduce postoperative insulin resistance and help the body cope with its stress response to surgery.
Along with nutritional changes are also various measures aimed at optimizing the body’s functionality before surgery (“prehabilitation”), from walking 30 minutes a day to abstaining from alcohol for patients who drink heavily.
Throughout the country, enhanced recovery protocols are taking shape in gynecologic surgery. ERAS was featured in an aptly titled panel session at the 2017 annual meeting of the American Association of Gynecologic Laparoscopists: “Outpatient Hysterectomy, ERAS, and Same-Day Discharge: The Next Big Thing in Gyn Surgery.” Others are applying ERAS to scheduled cesarean sections. And in our practice, I believe that if we continue making small changes, we will reach our goal of opioid-free recoveries and a better surgical experience for our patients.
Kirsten Sasaki, MD, is an associate of the Advanced Gynecologic Surgery Institute. She reported that she has no disclosures relevant to this Master Class.
“Enhanced Recovery After Surgery” (ERAS) practices and protocols have been increasingly refined and adopted for the field of gynecology, and there is hope among gynecologic surgeons – and some recent evidence – that, with the ERAS movement, we are improving patient recoveries and outcomes and minimizing the need for opioids.
This applies not only to open surgeries but also to the minimally invasive procedures that already are prized for significant reductions in morbidity and length of stay. The overarching and guiding principle of ERAS is that any surgery – whether open or minimally invasive, major or minor – places stress on the body and is associated with risks and morbidity.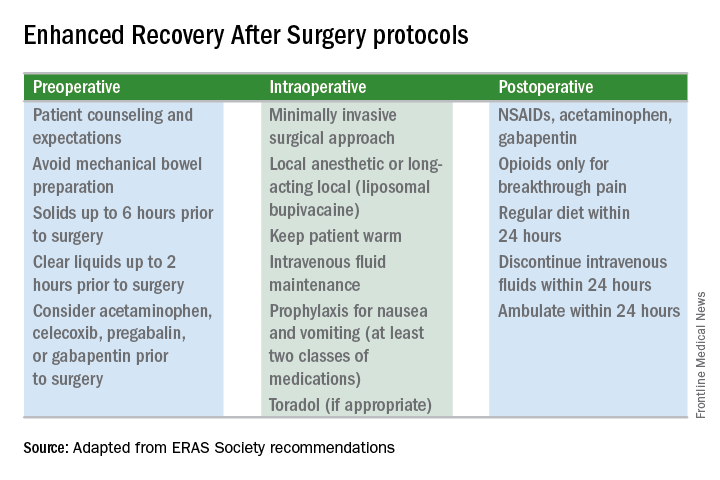
Enhanced recovery protocols are multidisciplinary, perioperative approaches designed to lessen the body’s stress response to surgery. The protocols and pathways offer us a menu of small changes that, in the aggregate, can lead to large and demonstrable benefits – especially when these small changes are chosen across the preoperative, intraoperative, and postoperative arenas and then standardized in one’s practice. Among the major components of ERAS practices and protocols are limiting preoperative fasting, employing multimodal analgesia, encouraging early ambulation and early postsurgical feeding, and creating culture shift that includes greater emphasis on patient expectations.
In our practice, we are incorporating ERAS practices not only in hopes of reducing the stress of all surgeries before, during, and after, but also with the goal of achieving a postoperative opioid-free hysterectomy, myomectomy, and extensive endometriosis surgery. (All of our advanced procedures are performed laparoscopically or robotically.)
Over the past 7 or so years, we have adopted a multimodal approach to pain control that includes a bundle of preoperative analgesics – acetaminophen, pregabalin, and celecoxib (we call it “TLC” for Tylenol, Lyrica, and Celebrex) – and the use of liposomal bupivacaine in our robotic surgeries. We are now turning toward ERAS nutritional changes, most of which run counter to traditional paradigms for surgical care. And in other areas, such as dedicated preoperative counseling, we continue to refine and improve our practices.
Improved Outcomes
The ERAS mindset notably intersected gynecology with the publication in 2016 of a two-part series of guidelines for gynecology/oncology surgery from the ERAS Society. The 8-year-old society has its roots in a study group of European surgeons and others who decided to examine surgical practices and the concept of multimodal surgical care put forth in the 1990s by Henrik Kehlet, MD, PhD, then a professor at the University of Copenhagen.
The first set of recommendations addressed pre- and intraoperative care (Gynecol Oncol. 2016 Feb;140[2]:313-22), and the second set addressed postoperative care (Gynecol Oncol. 2016 Feb;140[2]:323-32). Similar evidence-based recommendations were previously written for colonic resections, rectal and pelvic surgery, and other surgical specialties.
Most of the published outcomes of enhanced recovery protocols come from colorectal surgery. As noted in the ERAS Society gynecology/oncology guidelines, the benefits include an average reduction in length of stay of 2.5 days and a decrease in complications by as much as 50%.
There is growing evidence, however, that ERAS programs are also beneficial for patients undergoing laparoscopic surgery, and outcomes from gynecology – including minimally invasive surgery – are also being reported.
For instance, a retrospective case-control study of 55 consecutive gynecologic oncology patients treated at the University of California, San Francisco, with laparoscopic or robotic surgery and an enhanced recovery pathway – and 110 historical control patients matched on the basis of age and surgery type – found significant improvements in recovery time, decreased pain despite reduced opioid use, and overall lower hospital costs (Obstet Gynecol. 2016 Jul;128[1]:138-44).
The enhanced recovery pathway included patient education, multimodal antiemetics, multimodal analgesia, and balanced fluid administration. Early catheter removal, ambulation, and feeding were also components. Analgesia included routine preoperative gabapentin, diclofenac, and acetaminophen; routine postoperative gabapentin, NSAIDs, and acetaminophen; and transversus abdominis plane blocks in 32 of the ERAS patients.
ERAS patients were significantly more likely to be discharged on day 1 (91%, compared with 60% in the control group). Opioid use decreased by 30%, and pain scores on postoperative day 1 were significantly lower.
Another study looking at the effect of enhanced recovery implementation in gynecologic surgeries at the University of Virginia, Charlottesville, (gynecologic oncology, urogynecology, and general gynecology) similarly reported benefits for vaginal and minimally invasive procedures, as well as for open procedures (Obstet Gynecol. 2016 Sep;128[3]:457-66).
In the minimally invasive group, investigators compared 324 patients before ERAS implementation with 249 patients afterward and found that the median length of stay was unchanged (1 day). However, intraoperative and postoperative opioid consumption decreased significantly and – even though actual pain scores improved only slightly – patient satisfaction scores improved markedly among post-ERAS patients. Patients gave higher marks, for instance, to questions regarding pain control (“how well your pain was controlled”) and teamwork (“staff worked together to care for you”).
Reducing Opioids
New opioid use that persists after a surgical procedure is a postsurgical complication that we all should be working to prevent. It has been estimated that 6% of surgical patients – even those who’ve had relatively minor surgical procedures – will become long-term opioid users, developing a dependence on the drugs prescribed to them for postsurgical pain.
This was shown last year in a national study of insurance claims data from between 2013 and 2014; investigators identified adults without opioid use in the year prior to surgery (including hysterectomy) and found that 5.9%-6.5% were filling opioid prescriptions 90-180 days after their surgical procedure. The incidence in a nonoperative control cohort was 0.4% (JAMA Surg. 2017 Jun 21;152[6]:e170504). Notably, this prolonged use was greatest in patients with prior pain conditions, substance abuse, and mental health disorders – a finding that may have implications for the counseling we provide prior to surgery.
It’s not clear what the optimal analgesic regimen is for minimally invasive or other gynecologic surgeries. What is clearly recommended, however, is that the approach be multifaceted. In our practice, we believe that the preoperative use of acetaminophen, pregabalin, and celecoxib plays an important role in reducing postoperative pain and opioid use. But we also have striven to create a practice-wide culture shift (throughout the operating and recovery rooms), for instance, that encourages using the least amounts of narcotics possible and using the shortest-acting formulations possible.
Transversus abdominis plane (TAP) blocks are also often part of ERAS protocols; they have been shown in at least two randomized controlled trials of abdominal hysterectomy to reduce intraoperative fentanyl requirements and to reduce immediate postoperative pain scores and postoperative morphine requirements (Anesth Analg. 2008 Dec;107[6]:2056-60; J Anaesthesiol Clin Pharmacol. 2014 Jul-Sep;30[3]:391-6).
More recently, liposomal bupivacaine, which is slowly released over several days, has gained traction as a substitute for standard bupivacaine and other agents in TAP blocks. In one recent retrospective study, abdominal incision infiltration with liposomal bupivacaine was associated with less opioid use (with no change in pain scores), compared with bupivacaine hydrochloride after laparotomy for gynecologic malignancies (Obstet Gynecol. 2016 Nov;128[5]:1009-17). It’s significantly more expensive, however, making it likely that the formulation is being used more judiciously in minimally invasive gynecologic surgery than in open surgeries.
Because of costs, we currently are restricted to using liposomal bupivacaine in our robotic surgeries only. In our practice, the single 20 mL vial (266 mg of liposomal bupivacaine) is diluted with 20 mL of normal saline, but it can be further diluted without loss of efficacy. With a 16-gauge needle, the liposomal bupivacaine is distributed across the incisions (usually 20 mL in the umbilicus with a larger incision and 10 mL in each of the two lateral incisions). Patients are counseled that they may have more discomfort after 3 days, but by this point most are mobile and feeling relatively well with a combination of NSAIDs and acetaminophen.
With growing visibility of the problem of narcotic dependence in the United States, patients seem increasingly receptive and even eager to limit or avoid the use of opioids. Patients should be counseled that minimizing or avoiding opioids may also speed recovery. Narcotics cause gut motility to slow down, which may hinder mobilization. Early mobilization (within 24 hours) is among the enhanced recovery elements that the ERAS Society guidelines say is “of particular value” for minimally invasive surgery, along with maintenance of normothermia and normovolemia with maintenance of adequate cardiac output.
Selecting Steps
Our practice is also trying to reduce preoperative bowel preparation and preoperative fasting, both of which have been found to be stressful for the body without evidence of benefit. These practices can lead to insulin resistance and hyperglycemia, which are associated with increased morbidity and length of stay.
It is now recommended that clear fluids be allowed up to 2 hours before surgery and solids up to 6 hours before. Some health systems and practices also recommend presurgical carbohydrate loading (for example, 10 ounces of apple juice 2 hours before surgery) – another small change on the ERAS menu – to further reduce postoperative insulin resistance and help the body cope with its stress response to surgery.
Along with nutritional changes are also various measures aimed at optimizing the body’s functionality before surgery (“prehabilitation”), from walking 30 minutes a day to abstaining from alcohol for patients who drink heavily.
Throughout the country, enhanced recovery protocols are taking shape in gynecologic surgery. ERAS was featured in an aptly titled panel session at the 2017 annual meeting of the American Association of Gynecologic Laparoscopists: “Outpatient Hysterectomy, ERAS, and Same-Day Discharge: The Next Big Thing in Gyn Surgery.” Others are applying ERAS to scheduled cesarean sections. And in our practice, I believe that if we continue making small changes, we will reach our goal of opioid-free recoveries and a better surgical experience for our patients.
Kirsten Sasaki, MD, is an associate of the Advanced Gynecologic Surgery Institute. She reported that she has no disclosures relevant to this Master Class.
“Enhanced Recovery After Surgery” (ERAS) practices and protocols have been increasingly refined and adopted for the field of gynecology, and there is hope among gynecologic surgeons – and some recent evidence – that, with the ERAS movement, we are improving patient recoveries and outcomes and minimizing the need for opioids.
This applies not only to open surgeries but also to the minimally invasive procedures that already are prized for significant reductions in morbidity and length of stay. The overarching and guiding principle of ERAS is that any surgery – whether open or minimally invasive, major or minor – places stress on the body and is associated with risks and morbidity.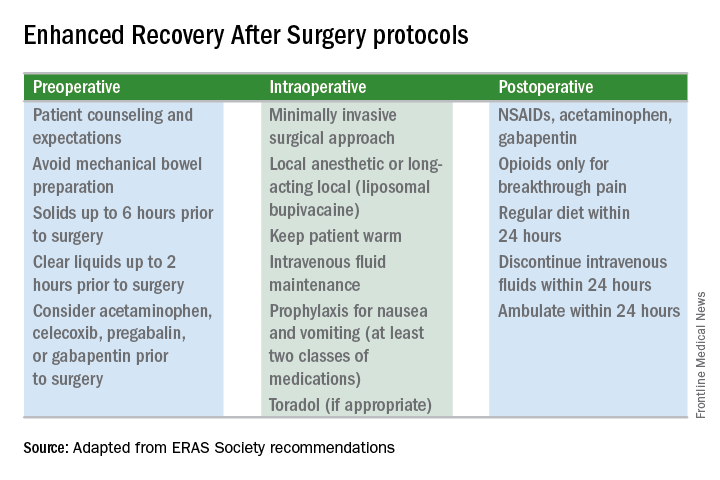
Enhanced recovery protocols are multidisciplinary, perioperative approaches designed to lessen the body’s stress response to surgery. The protocols and pathways offer us a menu of small changes that, in the aggregate, can lead to large and demonstrable benefits – especially when these small changes are chosen across the preoperative, intraoperative, and postoperative arenas and then standardized in one’s practice. Among the major components of ERAS practices and protocols are limiting preoperative fasting, employing multimodal analgesia, encouraging early ambulation and early postsurgical feeding, and creating culture shift that includes greater emphasis on patient expectations.
In our practice, we are incorporating ERAS practices not only in hopes of reducing the stress of all surgeries before, during, and after, but also with the goal of achieving a postoperative opioid-free hysterectomy, myomectomy, and extensive endometriosis surgery. (All of our advanced procedures are performed laparoscopically or robotically.)
Over the past 7 or so years, we have adopted a multimodal approach to pain control that includes a bundle of preoperative analgesics – acetaminophen, pregabalin, and celecoxib (we call it “TLC” for Tylenol, Lyrica, and Celebrex) – and the use of liposomal bupivacaine in our robotic surgeries. We are now turning toward ERAS nutritional changes, most of which run counter to traditional paradigms for surgical care. And in other areas, such as dedicated preoperative counseling, we continue to refine and improve our practices.
Improved Outcomes
The ERAS mindset notably intersected gynecology with the publication in 2016 of a two-part series of guidelines for gynecology/oncology surgery from the ERAS Society. The 8-year-old society has its roots in a study group of European surgeons and others who decided to examine surgical practices and the concept of multimodal surgical care put forth in the 1990s by Henrik Kehlet, MD, PhD, then a professor at the University of Copenhagen.
The first set of recommendations addressed pre- and intraoperative care (Gynecol Oncol. 2016 Feb;140[2]:313-22), and the second set addressed postoperative care (Gynecol Oncol. 2016 Feb;140[2]:323-32). Similar evidence-based recommendations were previously written for colonic resections, rectal and pelvic surgery, and other surgical specialties.
Most of the published outcomes of enhanced recovery protocols come from colorectal surgery. As noted in the ERAS Society gynecology/oncology guidelines, the benefits include an average reduction in length of stay of 2.5 days and a decrease in complications by as much as 50%.
There is growing evidence, however, that ERAS programs are also beneficial for patients undergoing laparoscopic surgery, and outcomes from gynecology – including minimally invasive surgery – are also being reported.
For instance, a retrospective case-control study of 55 consecutive gynecologic oncology patients treated at the University of California, San Francisco, with laparoscopic or robotic surgery and an enhanced recovery pathway – and 110 historical control patients matched on the basis of age and surgery type – found significant improvements in recovery time, decreased pain despite reduced opioid use, and overall lower hospital costs (Obstet Gynecol. 2016 Jul;128[1]:138-44).
The enhanced recovery pathway included patient education, multimodal antiemetics, multimodal analgesia, and balanced fluid administration. Early catheter removal, ambulation, and feeding were also components. Analgesia included routine preoperative gabapentin, diclofenac, and acetaminophen; routine postoperative gabapentin, NSAIDs, and acetaminophen; and transversus abdominis plane blocks in 32 of the ERAS patients.
ERAS patients were significantly more likely to be discharged on day 1 (91%, compared with 60% in the control group). Opioid use decreased by 30%, and pain scores on postoperative day 1 were significantly lower.
Another study looking at the effect of enhanced recovery implementation in gynecologic surgeries at the University of Virginia, Charlottesville, (gynecologic oncology, urogynecology, and general gynecology) similarly reported benefits for vaginal and minimally invasive procedures, as well as for open procedures (Obstet Gynecol. 2016 Sep;128[3]:457-66).
In the minimally invasive group, investigators compared 324 patients before ERAS implementation with 249 patients afterward and found that the median length of stay was unchanged (1 day). However, intraoperative and postoperative opioid consumption decreased significantly and – even though actual pain scores improved only slightly – patient satisfaction scores improved markedly among post-ERAS patients. Patients gave higher marks, for instance, to questions regarding pain control (“how well your pain was controlled”) and teamwork (“staff worked together to care for you”).
Reducing Opioids
New opioid use that persists after a surgical procedure is a postsurgical complication that we all should be working to prevent. It has been estimated that 6% of surgical patients – even those who’ve had relatively minor surgical procedures – will become long-term opioid users, developing a dependence on the drugs prescribed to them for postsurgical pain.
This was shown last year in a national study of insurance claims data from between 2013 and 2014; investigators identified adults without opioid use in the year prior to surgery (including hysterectomy) and found that 5.9%-6.5% were filling opioid prescriptions 90-180 days after their surgical procedure. The incidence in a nonoperative control cohort was 0.4% (JAMA Surg. 2017 Jun 21;152[6]:e170504). Notably, this prolonged use was greatest in patients with prior pain conditions, substance abuse, and mental health disorders – a finding that may have implications for the counseling we provide prior to surgery.
It’s not clear what the optimal analgesic regimen is for minimally invasive or other gynecologic surgeries. What is clearly recommended, however, is that the approach be multifaceted. In our practice, we believe that the preoperative use of acetaminophen, pregabalin, and celecoxib plays an important role in reducing postoperative pain and opioid use. But we also have striven to create a practice-wide culture shift (throughout the operating and recovery rooms), for instance, that encourages using the least amounts of narcotics possible and using the shortest-acting formulations possible.
Transversus abdominis plane (TAP) blocks are also often part of ERAS protocols; they have been shown in at least two randomized controlled trials of abdominal hysterectomy to reduce intraoperative fentanyl requirements and to reduce immediate postoperative pain scores and postoperative morphine requirements (Anesth Analg. 2008 Dec;107[6]:2056-60; J Anaesthesiol Clin Pharmacol. 2014 Jul-Sep;30[3]:391-6).
More recently, liposomal bupivacaine, which is slowly released over several days, has gained traction as a substitute for standard bupivacaine and other agents in TAP blocks. In one recent retrospective study, abdominal incision infiltration with liposomal bupivacaine was associated with less opioid use (with no change in pain scores), compared with bupivacaine hydrochloride after laparotomy for gynecologic malignancies (Obstet Gynecol. 2016 Nov;128[5]:1009-17). It’s significantly more expensive, however, making it likely that the formulation is being used more judiciously in minimally invasive gynecologic surgery than in open surgeries.
Because of costs, we currently are restricted to using liposomal bupivacaine in our robotic surgeries only. In our practice, the single 20 mL vial (266 mg of liposomal bupivacaine) is diluted with 20 mL of normal saline, but it can be further diluted without loss of efficacy. With a 16-gauge needle, the liposomal bupivacaine is distributed across the incisions (usually 20 mL in the umbilicus with a larger incision and 10 mL in each of the two lateral incisions). Patients are counseled that they may have more discomfort after 3 days, but by this point most are mobile and feeling relatively well with a combination of NSAIDs and acetaminophen.
With growing visibility of the problem of narcotic dependence in the United States, patients seem increasingly receptive and even eager to limit or avoid the use of opioids. Patients should be counseled that minimizing or avoiding opioids may also speed recovery. Narcotics cause gut motility to slow down, which may hinder mobilization. Early mobilization (within 24 hours) is among the enhanced recovery elements that the ERAS Society guidelines say is “of particular value” for minimally invasive surgery, along with maintenance of normothermia and normovolemia with maintenance of adequate cardiac output.
Selecting Steps
Our practice is also trying to reduce preoperative bowel preparation and preoperative fasting, both of which have been found to be stressful for the body without evidence of benefit. These practices can lead to insulin resistance and hyperglycemia, which are associated with increased morbidity and length of stay.
It is now recommended that clear fluids be allowed up to 2 hours before surgery and solids up to 6 hours before. Some health systems and practices also recommend presurgical carbohydrate loading (for example, 10 ounces of apple juice 2 hours before surgery) – another small change on the ERAS menu – to further reduce postoperative insulin resistance and help the body cope with its stress response to surgery.
Along with nutritional changes are also various measures aimed at optimizing the body’s functionality before surgery (“prehabilitation”), from walking 30 minutes a day to abstaining from alcohol for patients who drink heavily.
Throughout the country, enhanced recovery protocols are taking shape in gynecologic surgery. ERAS was featured in an aptly titled panel session at the 2017 annual meeting of the American Association of Gynecologic Laparoscopists: “Outpatient Hysterectomy, ERAS, and Same-Day Discharge: The Next Big Thing in Gyn Surgery.” Others are applying ERAS to scheduled cesarean sections. And in our practice, I believe that if we continue making small changes, we will reach our goal of opioid-free recoveries and a better surgical experience for our patients.
Kirsten Sasaki, MD, is an associate of the Advanced Gynecologic Surgery Institute. She reported that she has no disclosures relevant to this Master Class.
In the Evolving Mystery of BV, an Innovative Oral Treatment Emerges
Click Here to Read the Supplement
Topics include:
- BV terminology and treatment over time
- Current understanding of BV etiology
- BV consequences
- BV treatments
- Future research needs in BV
Author:
Steven E. Chavoustie, MD, FACOG, CCRP
University of Miami
Miller School of Medicine
Miami, Florida
Click Here to Read the Supplement
Topics include:
- BV terminology and treatment over time
- Current understanding of BV etiology
- BV consequences
- BV treatments
- Future research needs in BV
Author:
Steven E. Chavoustie, MD, FACOG, CCRP
University of Miami
Miller School of Medicine
Miami, Florida
Click Here to Read the Supplement
Topics include:
- BV terminology and treatment over time
- Current understanding of BV etiology
- BV consequences
- BV treatments
- Future research needs in BV
Author:
Steven E. Chavoustie, MD, FACOG, CCRP
University of Miami
Miller School of Medicine
Miami, Florida
Protocols to reduce opioid use and shorten length of stay
While originally pioneered by European anesthesiologists and surgeons in Europe in the 1990s, enhanced recovery after surgery (ERAS) programs, also known as enhanced recovery protocols or fast-track surgery, have now gained popularity across the surgical spectrum within the United States. The goal of these programs is to utilize multidisciplinary and multimodal interventions to minimize the physiologic changes associated with surgery and thereby enhance the perioperative experience – reduced morbidity and mortality, shorter length of stay, less postoperative opioid use, and faster resumption to normal activity, at a decreased cost of care.
1. Enhanced patient education, including managing expectations.
2. Decreased perioperative fasting periods.
3. Blood volume and temperature maintenance intraoperatively.
4. Postoperative mobilization early and often.
5. Multimodal pain relief and nausea/vomiting prophylaxis.
6. Use of postoperative drains and catheters only as long as required.
Today, I have asked Kirsten Sasaki, MD, to discuss some of these ERAS concepts. I have asked Dr. Sasaki to especially focus on decreasing opioid utilization. For a thorough discussion on ERAS recommendations using an evidence-based approach, one can review two excellent papers by Nelson et al. (Gynecol Oncol. 2016 Feb;140[2]:313-22; Gynecol Oncol. 2016 Feb;140[2]:323-32).
Dr. Sasaki completed her internship and residency at Tufts Medical Center, Boston. Dr. Sasaki then went on to become our second fellow at the Fellowship in Minimally Invasive Gynecologic Surgery in affiliation with AAGL and Society of Reproductive Surgeons at Advocate Lutheran General Hospital, Park Ridge, Ill. As a Fellow, Dr. Sasaki was recognized for her excellent teaching and research capabilities. Ultimately, however, it was her tremendous surgical skills and surgical sense that led me to invite her to join my practice in 2014.
Dr. Miller is a clinical associate professor at the University of Illinois in Chicago and past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in metropolitan Chicago and the director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill. He has no disclosures relevant to this Master Class.
While originally pioneered by European anesthesiologists and surgeons in Europe in the 1990s, enhanced recovery after surgery (ERAS) programs, also known as enhanced recovery protocols or fast-track surgery, have now gained popularity across the surgical spectrum within the United States. The goal of these programs is to utilize multidisciplinary and multimodal interventions to minimize the physiologic changes associated with surgery and thereby enhance the perioperative experience – reduced morbidity and mortality, shorter length of stay, less postoperative opioid use, and faster resumption to normal activity, at a decreased cost of care.
1. Enhanced patient education, including managing expectations.
2. Decreased perioperative fasting periods.
3. Blood volume and temperature maintenance intraoperatively.
4. Postoperative mobilization early and often.
5. Multimodal pain relief and nausea/vomiting prophylaxis.
6. Use of postoperative drains and catheters only as long as required.
Today, I have asked Kirsten Sasaki, MD, to discuss some of these ERAS concepts. I have asked Dr. Sasaki to especially focus on decreasing opioid utilization. For a thorough discussion on ERAS recommendations using an evidence-based approach, one can review two excellent papers by Nelson et al. (Gynecol Oncol. 2016 Feb;140[2]:313-22; Gynecol Oncol. 2016 Feb;140[2]:323-32).
Dr. Sasaki completed her internship and residency at Tufts Medical Center, Boston. Dr. Sasaki then went on to become our second fellow at the Fellowship in Minimally Invasive Gynecologic Surgery in affiliation with AAGL and Society of Reproductive Surgeons at Advocate Lutheran General Hospital, Park Ridge, Ill. As a Fellow, Dr. Sasaki was recognized for her excellent teaching and research capabilities. Ultimately, however, it was her tremendous surgical skills and surgical sense that led me to invite her to join my practice in 2014.
Dr. Miller is a clinical associate professor at the University of Illinois in Chicago and past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in metropolitan Chicago and the director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill. He has no disclosures relevant to this Master Class.
While originally pioneered by European anesthesiologists and surgeons in Europe in the 1990s, enhanced recovery after surgery (ERAS) programs, also known as enhanced recovery protocols or fast-track surgery, have now gained popularity across the surgical spectrum within the United States. The goal of these programs is to utilize multidisciplinary and multimodal interventions to minimize the physiologic changes associated with surgery and thereby enhance the perioperative experience – reduced morbidity and mortality, shorter length of stay, less postoperative opioid use, and faster resumption to normal activity, at a decreased cost of care.
1. Enhanced patient education, including managing expectations.
2. Decreased perioperative fasting periods.
3. Blood volume and temperature maintenance intraoperatively.
4. Postoperative mobilization early and often.
5. Multimodal pain relief and nausea/vomiting prophylaxis.
6. Use of postoperative drains and catheters only as long as required.
Today, I have asked Kirsten Sasaki, MD, to discuss some of these ERAS concepts. I have asked Dr. Sasaki to especially focus on decreasing opioid utilization. For a thorough discussion on ERAS recommendations using an evidence-based approach, one can review two excellent papers by Nelson et al. (Gynecol Oncol. 2016 Feb;140[2]:313-22; Gynecol Oncol. 2016 Feb;140[2]:323-32).
Dr. Sasaki completed her internship and residency at Tufts Medical Center, Boston. Dr. Sasaki then went on to become our second fellow at the Fellowship in Minimally Invasive Gynecologic Surgery in affiliation with AAGL and Society of Reproductive Surgeons at Advocate Lutheran General Hospital, Park Ridge, Ill. As a Fellow, Dr. Sasaki was recognized for her excellent teaching and research capabilities. Ultimately, however, it was her tremendous surgical skills and surgical sense that led me to invite her to join my practice in 2014.
Dr. Miller is a clinical associate professor at the University of Illinois in Chicago and past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in metropolitan Chicago and the director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill. He has no disclosures relevant to this Master Class.
FDA issues safety measures for all gadolinium-based contrast agents for MRI
A US Food & Drug Administration (FDA) Drug Safety Communication concerning a New Class Warning for all gadolinium-based contrast agents (GBCAs) for magnetic resonance imaging (MRI) has been released. Gadolinium has been found to remain in patients’ bodies, including the brain, for months to years.1
The FDA concluded that the benefit of all approved GBCAs outweighs any potential risks because gadolinium retention has not been directly linked to adverse health effects in patients with normal kidney function. To date, the only known adverse health effect related to gadolinium retention is a rare condition called nephrogenic systemic fibrosis that occurs in a small subgroup of patients with preexisting kidney failure. However, the FDA has recently received reports of adverse events involving multiple organ systems in patients with normal kidney function.1
After a review by the Medical Imaging Drugs Advisory Committee, the FDA is requiring several actions1:
- the development of a new Patient Medication Guide for GBCAs
- a requirement that every patient must read educational information before receiving a GBCA
- manufacturers of GBCAs must conduct human and animal studies to further assess the safety of these contrast agents.
FDA recommendations for your practice
The FDA advises that health care professionals should consider the retention characteristics of each agent when choosing a GBCA for patients who might be of higher risk for gadolinium retention.1,2 These patients include1:
- those requiring multiple lifetime doses
- pregnant women
- children
- patients with inflammatory conditions.
There are 2 types of GBCAs based on chemical structure: linear and macrocyclic. Linear GBCAs result in more retention and retention for a longer time than macrocyclic GBCAs.2 A list of FDA-approved GBCAs with their chemical structures is found here: https://www.fda.gov/Drugs/DrugSafety/ucm589213.htm.2
Recommendations also state that repeated GBCA imaging studies be minimized when possible, particularly closely spaced MRI studies. However, necessary GBCA MRI scans should not be avoided or deferred.1
Report adverse effects
Health care professionals and patients are encouraged to report adverse effects or side effects related to the use of GBCAs to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program found here: https://www.accessdata.fda.gov/scripts/medwatch/index.cfm?action=reporting.home.
- US Food & Drug Administration. Safety: Gadolinium-based Contrast Agents (GBCAs): Drug Safety Communication - Retained in Body; New Class Warnings. https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm589580.htm. Published December 19, 2017. Accessed January 10, 2018.
- US Food & Drug Administration. Drugs: FDA Drug Safety Communication: FDA warns that gadolinium-based contrast agents (GBCAs) are retained in the body; requires new class warning. https://www.fda.gov/Drugs/DrugSafety/ucm589213.htm. Published December 19, 2017. Accessed January 10, 2018.
A US Food & Drug Administration (FDA) Drug Safety Communication concerning a New Class Warning for all gadolinium-based contrast agents (GBCAs) for magnetic resonance imaging (MRI) has been released. Gadolinium has been found to remain in patients’ bodies, including the brain, for months to years.1
The FDA concluded that the benefit of all approved GBCAs outweighs any potential risks because gadolinium retention has not been directly linked to adverse health effects in patients with normal kidney function. To date, the only known adverse health effect related to gadolinium retention is a rare condition called nephrogenic systemic fibrosis that occurs in a small subgroup of patients with preexisting kidney failure. However, the FDA has recently received reports of adverse events involving multiple organ systems in patients with normal kidney function.1
After a review by the Medical Imaging Drugs Advisory Committee, the FDA is requiring several actions1:
- the development of a new Patient Medication Guide for GBCAs
- a requirement that every patient must read educational information before receiving a GBCA
- manufacturers of GBCAs must conduct human and animal studies to further assess the safety of these contrast agents.
FDA recommendations for your practice
The FDA advises that health care professionals should consider the retention characteristics of each agent when choosing a GBCA for patients who might be of higher risk for gadolinium retention.1,2 These patients include1:
- those requiring multiple lifetime doses
- pregnant women
- children
- patients with inflammatory conditions.
There are 2 types of GBCAs based on chemical structure: linear and macrocyclic. Linear GBCAs result in more retention and retention for a longer time than macrocyclic GBCAs.2 A list of FDA-approved GBCAs with their chemical structures is found here: https://www.fda.gov/Drugs/DrugSafety/ucm589213.htm.2
Recommendations also state that repeated GBCA imaging studies be minimized when possible, particularly closely spaced MRI studies. However, necessary GBCA MRI scans should not be avoided or deferred.1
Report adverse effects
Health care professionals and patients are encouraged to report adverse effects or side effects related to the use of GBCAs to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program found here: https://www.accessdata.fda.gov/scripts/medwatch/index.cfm?action=reporting.home.
A US Food & Drug Administration (FDA) Drug Safety Communication concerning a New Class Warning for all gadolinium-based contrast agents (GBCAs) for magnetic resonance imaging (MRI) has been released. Gadolinium has been found to remain in patients’ bodies, including the brain, for months to years.1
The FDA concluded that the benefit of all approved GBCAs outweighs any potential risks because gadolinium retention has not been directly linked to adverse health effects in patients with normal kidney function. To date, the only known adverse health effect related to gadolinium retention is a rare condition called nephrogenic systemic fibrosis that occurs in a small subgroup of patients with preexisting kidney failure. However, the FDA has recently received reports of adverse events involving multiple organ systems in patients with normal kidney function.1
After a review by the Medical Imaging Drugs Advisory Committee, the FDA is requiring several actions1:
- the development of a new Patient Medication Guide for GBCAs
- a requirement that every patient must read educational information before receiving a GBCA
- manufacturers of GBCAs must conduct human and animal studies to further assess the safety of these contrast agents.
FDA recommendations for your practice
The FDA advises that health care professionals should consider the retention characteristics of each agent when choosing a GBCA for patients who might be of higher risk for gadolinium retention.1,2 These patients include1:
- those requiring multiple lifetime doses
- pregnant women
- children
- patients with inflammatory conditions.
There are 2 types of GBCAs based on chemical structure: linear and macrocyclic. Linear GBCAs result in more retention and retention for a longer time than macrocyclic GBCAs.2 A list of FDA-approved GBCAs with their chemical structures is found here: https://www.fda.gov/Drugs/DrugSafety/ucm589213.htm.2
Recommendations also state that repeated GBCA imaging studies be minimized when possible, particularly closely spaced MRI studies. However, necessary GBCA MRI scans should not be avoided or deferred.1
Report adverse effects
Health care professionals and patients are encouraged to report adverse effects or side effects related to the use of GBCAs to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program found here: https://www.accessdata.fda.gov/scripts/medwatch/index.cfm?action=reporting.home.
- US Food & Drug Administration. Safety: Gadolinium-based Contrast Agents (GBCAs): Drug Safety Communication - Retained in Body; New Class Warnings. https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm589580.htm. Published December 19, 2017. Accessed January 10, 2018.
- US Food & Drug Administration. Drugs: FDA Drug Safety Communication: FDA warns that gadolinium-based contrast agents (GBCAs) are retained in the body; requires new class warning. https://www.fda.gov/Drugs/DrugSafety/ucm589213.htm. Published December 19, 2017. Accessed January 10, 2018.
- US Food & Drug Administration. Safety: Gadolinium-based Contrast Agents (GBCAs): Drug Safety Communication - Retained in Body; New Class Warnings. https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm589580.htm. Published December 19, 2017. Accessed January 10, 2018.
- US Food & Drug Administration. Drugs: FDA Drug Safety Communication: FDA warns that gadolinium-based contrast agents (GBCAs) are retained in the body; requires new class warning. https://www.fda.gov/Drugs/DrugSafety/ucm589213.htm. Published December 19, 2017. Accessed January 10, 2018.
Alopecia tied to nearly fivefold increase in fibroids in African American women
based on data from more than 400,000 women.
In a study published in JAMA Dermatology, researchers reviewed data from 487,104 black women seen at a single center between Aug. 1, 2013, and Aug. 1, 2017. Overall, 14% of women with central centrifugal cicatricial alopecia (CCCA) also had a history of uterine fibroids, compared with 3% percent of black women without CCCA.
“Alopecia is more than just a cosmetic problem. … It could signal an increased risk of developing other conditions,” corresponding author Crystal Aguh, MD, of Johns Hopkins University in Baltimore said in an interview. “To our knowledge, this is the first time that an association has been noted between these two conditions. We believe that the fact that both are related to excess scarring and fibrous tissue deposition may reflect similarities in how both [conditions] develop, but this is still unknown.”
Overall, 62 of 447 women who met criteria for CCCA also had fibroids, representing a nearly fivefold increase in fibroid risk for women with CCCA.
“I was definitely surprised by the findings,” said Dr. Aguh. “I thought it would be interesting to look at any possible correlation between the two diseases, but did not expect to see such a large difference between black women with and without this form of hair loss,” she noted.
As fibroids are often asymptomatic, “physicians should screen their patients with CCCA for symptoms of fibroids such as painful menstrual cycles, heavy bleeding, unexplained anemia, or difficulty conceiving,” said Dr. Aguh. “In those patients who may not know they have fibroids, early recognition that allows for treatment will be especially beneficial.”
The findings were limited by the retrospective nature of the study. “I believe that larger studies are warranted to help us fully understand how these two conditions are connected,” Dr. Aguh said.
Lead author Yemisi Dina of Meharry Medical College, Nashville, Tenn., is supported in part by a grant from the National Institutes of Health. The other researchers had no financial conflicts to disclose.
SOURCE: Dina Y et al. JAMA Dermatol. 2017 Dec 27. doi: 10.1001/jamadermatol.2017.5163
based on data from more than 400,000 women.
In a study published in JAMA Dermatology, researchers reviewed data from 487,104 black women seen at a single center between Aug. 1, 2013, and Aug. 1, 2017. Overall, 14% of women with central centrifugal cicatricial alopecia (CCCA) also had a history of uterine fibroids, compared with 3% percent of black women without CCCA.
“Alopecia is more than just a cosmetic problem. … It could signal an increased risk of developing other conditions,” corresponding author Crystal Aguh, MD, of Johns Hopkins University in Baltimore said in an interview. “To our knowledge, this is the first time that an association has been noted between these two conditions. We believe that the fact that both are related to excess scarring and fibrous tissue deposition may reflect similarities in how both [conditions] develop, but this is still unknown.”
Overall, 62 of 447 women who met criteria for CCCA also had fibroids, representing a nearly fivefold increase in fibroid risk for women with CCCA.
“I was definitely surprised by the findings,” said Dr. Aguh. “I thought it would be interesting to look at any possible correlation between the two diseases, but did not expect to see such a large difference between black women with and without this form of hair loss,” she noted.
As fibroids are often asymptomatic, “physicians should screen their patients with CCCA for symptoms of fibroids such as painful menstrual cycles, heavy bleeding, unexplained anemia, or difficulty conceiving,” said Dr. Aguh. “In those patients who may not know they have fibroids, early recognition that allows for treatment will be especially beneficial.”
The findings were limited by the retrospective nature of the study. “I believe that larger studies are warranted to help us fully understand how these two conditions are connected,” Dr. Aguh said.
Lead author Yemisi Dina of Meharry Medical College, Nashville, Tenn., is supported in part by a grant from the National Institutes of Health. The other researchers had no financial conflicts to disclose.
SOURCE: Dina Y et al. JAMA Dermatol. 2017 Dec 27. doi: 10.1001/jamadermatol.2017.5163
based on data from more than 400,000 women.
In a study published in JAMA Dermatology, researchers reviewed data from 487,104 black women seen at a single center between Aug. 1, 2013, and Aug. 1, 2017. Overall, 14% of women with central centrifugal cicatricial alopecia (CCCA) also had a history of uterine fibroids, compared with 3% percent of black women without CCCA.
“Alopecia is more than just a cosmetic problem. … It could signal an increased risk of developing other conditions,” corresponding author Crystal Aguh, MD, of Johns Hopkins University in Baltimore said in an interview. “To our knowledge, this is the first time that an association has been noted between these two conditions. We believe that the fact that both are related to excess scarring and fibrous tissue deposition may reflect similarities in how both [conditions] develop, but this is still unknown.”
Overall, 62 of 447 women who met criteria for CCCA also had fibroids, representing a nearly fivefold increase in fibroid risk for women with CCCA.
“I was definitely surprised by the findings,” said Dr. Aguh. “I thought it would be interesting to look at any possible correlation between the two diseases, but did not expect to see such a large difference between black women with and without this form of hair loss,” she noted.
As fibroids are often asymptomatic, “physicians should screen their patients with CCCA for symptoms of fibroids such as painful menstrual cycles, heavy bleeding, unexplained anemia, or difficulty conceiving,” said Dr. Aguh. “In those patients who may not know they have fibroids, early recognition that allows for treatment will be especially beneficial.”
The findings were limited by the retrospective nature of the study. “I believe that larger studies are warranted to help us fully understand how these two conditions are connected,” Dr. Aguh said.
Lead author Yemisi Dina of Meharry Medical College, Nashville, Tenn., is supported in part by a grant from the National Institutes of Health. The other researchers had no financial conflicts to disclose.
SOURCE: Dina Y et al. JAMA Dermatol. 2017 Dec 27. doi: 10.1001/jamadermatol.2017.5163
FROM JAMA DERMATOLOGY
Key clinical point: Dermatologists should screen patients with central centrifugal cicatricial alopecia for potential fibroids.
Major finding: Women with CCCA were nearly five times more likely to have fibroids, compared with controls.
Data source: The data come from a review of 487,104 black women seen at a single center between Aug. 1, 2013, and Aug. 1, 2017.
Disclosures: Lead author Yemisi Dina of Meharry Medical College, Nashville, Tenn., is supported in part by a grant from the National Institutes of Health. The other researchers had no financial conflicts to disclose.
Source: Dina Y et al. JAMA Dermatol. 2017 Dec 27. doi: 10.1001/jamadermatol.2017.5163.
Teens with PID underscreened for HIV, syphilis
CHICAGO – Adolescents with pelvic inflammatory disease (PID) were unlikely to be screened for HIV or syphilis, and many didn’t receive an appropriate antibiotic regimen, according to a recent study reported at the annual meeting of the American Academy of Pediatrics.
Patients who were sent home rather than admitted were especially likely to miss screening, as were Hispanic patients and those with private insurance.
The Centers for Disease Control and Prevention strongly recommends that all women diagnosed with PID be tested for HIV, and that high-risk individuals also be tested for syphilis, wrote Amanda Jichlinski, MD, and her coauthors at Children’s National Health System, Washington.
The study, presented during a poster session, used data from the national Pediatric Health Information System database from 2010 to 2015. A total of 10,698 records with a diagnostic code for PID were included; patients were females aged 12-21 years seen in a pediatric emergency department.
In addition to the primary outcome of syphilis and HIV testing, the authors also looked at whether antibiotic administration for PID was in line with CDC recommendations – and it wasn’t. “Fewer than half of patients in the ED received antibiotic regimens adherent to CDC guidelines,” wrote Dr. Jichlinski and her coauthors.
Forty-six percent of patients received ceftriaxone and doxycycline, 21% received ceftriaxone and azithromycin, and 6% received ceftriaxone and metronidazole. Ceftriaxone monotherapy was given to 15% of patients. One in 10 patients with a PID diagnosis received no antibiotic at all; 2% of patients received some other regimen.
The researchers used multivariable analysis to examine separately which patient and hospital characteristics were associated with an increased likelihood of testing for both HIV and syphilis. With white, non-Hispanic adolescents used as the referent, Hispanic females with PID were less likely to receive screening for either HIV or syphilis (adjusted odds ratio, 0.8 for both; 95% confidence interval, 0.7-1.0 for both).
In contrast, black non-Hispanic females were screened more often; the aOR for HIV screening was 1.4 (95% CI, 1.2-1.6), and the aOR for syphilis screening was 1.8 (95% CI, 1.6-2.0) for this group of adolescents.
Patients were dichotomized into older (17-21 years of age; n = 4,737, 44%) and younger (12-16 years of age; n = 5,961, 56%) age groups; younger patients were slightly more likely to receive HIV (aOR, 1.2) and syphilis (aOR, 1.1) screening.
Just under a third of patients in the study were seen in a hospital with fewer than 300 beds, and these facilities were more likely to screen for HIV (aOR, 1.4) and syphilis (aOR, 1.1) than the larger hospitals.
By far the largest predictor of whether HIV and syphilis screening was done, though, was a hospital admission. Patients who were admitted (n = 4,043, 38%) were 7 times more likely to be screened for HIV and 4.6 times more likely to be screened for syphilis than those who were sent home from the emergency department.
Although the large, nationally representative study had many strengths, Dr. Jichlinski and her coauthors acknowledged that the data they were provided couldn’t account for medication that was prescribed, rather than administered in the emergency department. Also, the results may not be generalizable to adolescents treated in nonpediatric emergency departments or other facilities, such as urgent care centers.
“Adolescents with PID are underscreened for HIV and syphilis,” wrote Dr. Jichlinski and her coauthors. They called for pediatricians to receive more education about management of PID in adolescents. From a practical perspective, the investigators also suggested incorporating order sets for sexually transmitted infection testing and antibiotic administration into electronic medical records; in this way, a PID diagnosis code would trigger simplified testing and treatment choices.
Dr. Jichlinski reported no conflicts of interest. Dr. Monika Goyal, MD, senior author on the study, reported funding support by the National Institute of Child Health and Human Development. Dr. Goyal also holds an appointment at the George Washington University, Washington.
SOURCE: Jichlinski A et al. AAP 2017 Abstract 5, AAP Section on Emergency Medicine.
CHICAGO – Adolescents with pelvic inflammatory disease (PID) were unlikely to be screened for HIV or syphilis, and many didn’t receive an appropriate antibiotic regimen, according to a recent study reported at the annual meeting of the American Academy of Pediatrics.
Patients who were sent home rather than admitted were especially likely to miss screening, as were Hispanic patients and those with private insurance.
The Centers for Disease Control and Prevention strongly recommends that all women diagnosed with PID be tested for HIV, and that high-risk individuals also be tested for syphilis, wrote Amanda Jichlinski, MD, and her coauthors at Children’s National Health System, Washington.
The study, presented during a poster session, used data from the national Pediatric Health Information System database from 2010 to 2015. A total of 10,698 records with a diagnostic code for PID were included; patients were females aged 12-21 years seen in a pediatric emergency department.
In addition to the primary outcome of syphilis and HIV testing, the authors also looked at whether antibiotic administration for PID was in line with CDC recommendations – and it wasn’t. “Fewer than half of patients in the ED received antibiotic regimens adherent to CDC guidelines,” wrote Dr. Jichlinski and her coauthors.
Forty-six percent of patients received ceftriaxone and doxycycline, 21% received ceftriaxone and azithromycin, and 6% received ceftriaxone and metronidazole. Ceftriaxone monotherapy was given to 15% of patients. One in 10 patients with a PID diagnosis received no antibiotic at all; 2% of patients received some other regimen.
The researchers used multivariable analysis to examine separately which patient and hospital characteristics were associated with an increased likelihood of testing for both HIV and syphilis. With white, non-Hispanic adolescents used as the referent, Hispanic females with PID were less likely to receive screening for either HIV or syphilis (adjusted odds ratio, 0.8 for both; 95% confidence interval, 0.7-1.0 for both).
In contrast, black non-Hispanic females were screened more often; the aOR for HIV screening was 1.4 (95% CI, 1.2-1.6), and the aOR for syphilis screening was 1.8 (95% CI, 1.6-2.0) for this group of adolescents.
Patients were dichotomized into older (17-21 years of age; n = 4,737, 44%) and younger (12-16 years of age; n = 5,961, 56%) age groups; younger patients were slightly more likely to receive HIV (aOR, 1.2) and syphilis (aOR, 1.1) screening.
Just under a third of patients in the study were seen in a hospital with fewer than 300 beds, and these facilities were more likely to screen for HIV (aOR, 1.4) and syphilis (aOR, 1.1) than the larger hospitals.
By far the largest predictor of whether HIV and syphilis screening was done, though, was a hospital admission. Patients who were admitted (n = 4,043, 38%) were 7 times more likely to be screened for HIV and 4.6 times more likely to be screened for syphilis than those who were sent home from the emergency department.
Although the large, nationally representative study had many strengths, Dr. Jichlinski and her coauthors acknowledged that the data they were provided couldn’t account for medication that was prescribed, rather than administered in the emergency department. Also, the results may not be generalizable to adolescents treated in nonpediatric emergency departments or other facilities, such as urgent care centers.
“Adolescents with PID are underscreened for HIV and syphilis,” wrote Dr. Jichlinski and her coauthors. They called for pediatricians to receive more education about management of PID in adolescents. From a practical perspective, the investigators also suggested incorporating order sets for sexually transmitted infection testing and antibiotic administration into electronic medical records; in this way, a PID diagnosis code would trigger simplified testing and treatment choices.
Dr. Jichlinski reported no conflicts of interest. Dr. Monika Goyal, MD, senior author on the study, reported funding support by the National Institute of Child Health and Human Development. Dr. Goyal also holds an appointment at the George Washington University, Washington.
SOURCE: Jichlinski A et al. AAP 2017 Abstract 5, AAP Section on Emergency Medicine.
CHICAGO – Adolescents with pelvic inflammatory disease (PID) were unlikely to be screened for HIV or syphilis, and many didn’t receive an appropriate antibiotic regimen, according to a recent study reported at the annual meeting of the American Academy of Pediatrics.
Patients who were sent home rather than admitted were especially likely to miss screening, as were Hispanic patients and those with private insurance.
The Centers for Disease Control and Prevention strongly recommends that all women diagnosed with PID be tested for HIV, and that high-risk individuals also be tested for syphilis, wrote Amanda Jichlinski, MD, and her coauthors at Children’s National Health System, Washington.
The study, presented during a poster session, used data from the national Pediatric Health Information System database from 2010 to 2015. A total of 10,698 records with a diagnostic code for PID were included; patients were females aged 12-21 years seen in a pediatric emergency department.
In addition to the primary outcome of syphilis and HIV testing, the authors also looked at whether antibiotic administration for PID was in line with CDC recommendations – and it wasn’t. “Fewer than half of patients in the ED received antibiotic regimens adherent to CDC guidelines,” wrote Dr. Jichlinski and her coauthors.
Forty-six percent of patients received ceftriaxone and doxycycline, 21% received ceftriaxone and azithromycin, and 6% received ceftriaxone and metronidazole. Ceftriaxone monotherapy was given to 15% of patients. One in 10 patients with a PID diagnosis received no antibiotic at all; 2% of patients received some other regimen.
The researchers used multivariable analysis to examine separately which patient and hospital characteristics were associated with an increased likelihood of testing for both HIV and syphilis. With white, non-Hispanic adolescents used as the referent, Hispanic females with PID were less likely to receive screening for either HIV or syphilis (adjusted odds ratio, 0.8 for both; 95% confidence interval, 0.7-1.0 for both).
In contrast, black non-Hispanic females were screened more often; the aOR for HIV screening was 1.4 (95% CI, 1.2-1.6), and the aOR for syphilis screening was 1.8 (95% CI, 1.6-2.0) for this group of adolescents.
Patients were dichotomized into older (17-21 years of age; n = 4,737, 44%) and younger (12-16 years of age; n = 5,961, 56%) age groups; younger patients were slightly more likely to receive HIV (aOR, 1.2) and syphilis (aOR, 1.1) screening.
Just under a third of patients in the study were seen in a hospital with fewer than 300 beds, and these facilities were more likely to screen for HIV (aOR, 1.4) and syphilis (aOR, 1.1) than the larger hospitals.
By far the largest predictor of whether HIV and syphilis screening was done, though, was a hospital admission. Patients who were admitted (n = 4,043, 38%) were 7 times more likely to be screened for HIV and 4.6 times more likely to be screened for syphilis than those who were sent home from the emergency department.
Although the large, nationally representative study had many strengths, Dr. Jichlinski and her coauthors acknowledged that the data they were provided couldn’t account for medication that was prescribed, rather than administered in the emergency department. Also, the results may not be generalizable to adolescents treated in nonpediatric emergency departments or other facilities, such as urgent care centers.
“Adolescents with PID are underscreened for HIV and syphilis,” wrote Dr. Jichlinski and her coauthors. They called for pediatricians to receive more education about management of PID in adolescents. From a practical perspective, the investigators also suggested incorporating order sets for sexually transmitted infection testing and antibiotic administration into electronic medical records; in this way, a PID diagnosis code would trigger simplified testing and treatment choices.
Dr. Jichlinski reported no conflicts of interest. Dr. Monika Goyal, MD, senior author on the study, reported funding support by the National Institute of Child Health and Human Development. Dr. Goyal also holds an appointment at the George Washington University, Washington.
SOURCE: Jichlinski A et al. AAP 2017 Abstract 5, AAP Section on Emergency Medicine.
REPORTING FROM AAP 2017
Key clinical point:
Major finding: Hispanic females were least likely to be screened (adjusted OR, 0.8), compared with non-Hispanic white females.
Study details: Retrospective study of 10,698 adolescent patients with PID from a national database.
Disclosures: The study was funded in part by the National Institute of Child Health and Development. The authors had no relevant financial disclosures.
Source: Jichlinski A et al. AAP 2017 Abstract 5, AAP Section on Emergency Medicine
Is mannitol a good alternative agent for evaluating ureteral patency after gynecologic surgery?
EXPERT COMMENTARY
Although the incidence of lower urinary tract and ureteral injury following gynecologic surgery is low, intraoperative identification of ureteral patency can prevent serious long-term sequelae. Since the indigo carmine shortage in 2014, US surgeons have searched for multiple alternative agents. Intravenous methylene blue is suboptimal due to its systemic adverse effects and the length of time for dye excretion in the urine.
Grimes and colleagues conducted a study to determine if there was any significant difference in surgeon satisfaction among 4 different alternatives to indigo carmine for intraoperative ureteral patency evaluation.
Related article:
Farewell to indigo carmine
Details of the study
The investigators conducted a randomized clinical trial of 130 women undergoing benign gynecologic or pelvic reconstructive surgery. Four different regimens were used for intraoperative ureteral evaluation: 1) oral phenazopyridine 200 mg, 2) intravenous sodium fluorescein 25 mg, 3) mannitol bladder distention, and 4) normal saline bladder distention.
Study outcomes. The primary outcome was surgeon satisfaction based on a 0 to 100 point visual analog scale rating (with 0 indicating strong agreement, 100 indicating disagreement). Secondary outcomes included ease of ureteral jet visualization, time to surgeon confidence of ureteral patency, and occurrence of adverse events over 6 weeks.
Surgeon satisfaction rating. The investigators found statistically significant physician satisfaction with the use of mannitol as a bladder distention medium over oral phenazopyridine, and slightly better satisfaction compared with the use of intravenous sodium fluorescein or normal saline distention. The median (range) visual analog scores for ureteral patency were phenazopyridine, 48 (0–83); sodium fluorescein 20 (0–82); mannitol, 0 (0–44); and normal saline, 23 (3–96) (P<.001).
There was no difference across the 4 groups in the timing to surgeon confidence of ureteral patency, length of cystoscopy (on average, 3 minutes), and development of postoperative urinary tract infections (UTIs).
Most dissatisfaction related to phenazopyridine is the fact that the resulting orange-stained urine can obscure the bladder mucosa.
One significant adverse event was a protocol deviation in which 1 patient received an incorrect dose of IV sodium fluorescein (500 mg) instead of the recommended 25-mg dose.
Related article:
Alternative options for visualizing ureteral patency during intraoperative cystoscopy
Study strengths and weaknesses
The strength of this study is in its randomized design and power. Its major weakness is surgeon bias, since the surgeons could not possibly be blinded to the method used.
The study confirms the problem that phenazopyridine makes the urine so orange that bladder mucosal lesions and de novo hematuria could be difficult to detect. Recommending mannitol as a hypertonic distending medium (as it is used in hysteroscopy procedures), however, may be premature. Prior studies have shown increased postoperative UTIs when 50% and 10% dextrose was used versus normal saline for cystoscopy.1,2 Since the Grimes study protocol did not include postoperative urine collection for cultures, more research on UTIs after mannitol use would be needed before surgeons confidently could use it routinely.
In our practice, surgeons prefer that intravenous sodium fluorescein be administered just prior to cystoscopy and oral phenazopyridine en route to the operating room. I agree that a major disadvantage to phenazopyridine is the heavy orange staining that obscures visualization.
Finally, this study did not account for cost of the various methods; standard normal saline would be cheapest, followed by phenazopyridine.
This study showed that surgeon satisfaction was greatest with the use of mannitol as a distending medium for intraoperative evaluation of ureteral patency compared with oral phenazopyridine, intravenous sodium fluorescein, and normal saline distention. However, time to surgeon confidence of ureteral patency was similar with all 4 methods. More data are needed related to UTIs and the cost of mannitol compared with the other 3 methods.
-- Cheryl B. Iglesia, MD
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Narasimhulu DM, Prabakar C, Tang N, Bral P. 50% dextrose versus normal saline as distention media during cystoscopy for assessment of ureteric patency. Eur J Obstet Gynecol Reprod Biol. 2016;199:38–41.
- Siff LN, Unger CA, Jelovsek JE, Paraiso MF, Ridgeway BM, Barber MD. Assessing ureteral patency using 10% dextrose cystoscopy fluid: evaluation of urinary tract infection rates. Am J Obstet Gynecol. 2016;215(1):74.e1–e6.
EXPERT COMMENTARY
Although the incidence of lower urinary tract and ureteral injury following gynecologic surgery is low, intraoperative identification of ureteral patency can prevent serious long-term sequelae. Since the indigo carmine shortage in 2014, US surgeons have searched for multiple alternative agents. Intravenous methylene blue is suboptimal due to its systemic adverse effects and the length of time for dye excretion in the urine.
Grimes and colleagues conducted a study to determine if there was any significant difference in surgeon satisfaction among 4 different alternatives to indigo carmine for intraoperative ureteral patency evaluation.
Related article:
Farewell to indigo carmine
Details of the study
The investigators conducted a randomized clinical trial of 130 women undergoing benign gynecologic or pelvic reconstructive surgery. Four different regimens were used for intraoperative ureteral evaluation: 1) oral phenazopyridine 200 mg, 2) intravenous sodium fluorescein 25 mg, 3) mannitol bladder distention, and 4) normal saline bladder distention.
Study outcomes. The primary outcome was surgeon satisfaction based on a 0 to 100 point visual analog scale rating (with 0 indicating strong agreement, 100 indicating disagreement). Secondary outcomes included ease of ureteral jet visualization, time to surgeon confidence of ureteral patency, and occurrence of adverse events over 6 weeks.
Surgeon satisfaction rating. The investigators found statistically significant physician satisfaction with the use of mannitol as a bladder distention medium over oral phenazopyridine, and slightly better satisfaction compared with the use of intravenous sodium fluorescein or normal saline distention. The median (range) visual analog scores for ureteral patency were phenazopyridine, 48 (0–83); sodium fluorescein 20 (0–82); mannitol, 0 (0–44); and normal saline, 23 (3–96) (P<.001).
There was no difference across the 4 groups in the timing to surgeon confidence of ureteral patency, length of cystoscopy (on average, 3 minutes), and development of postoperative urinary tract infections (UTIs).
Most dissatisfaction related to phenazopyridine is the fact that the resulting orange-stained urine can obscure the bladder mucosa.
One significant adverse event was a protocol deviation in which 1 patient received an incorrect dose of IV sodium fluorescein (500 mg) instead of the recommended 25-mg dose.
Related article:
Alternative options for visualizing ureteral patency during intraoperative cystoscopy
Study strengths and weaknesses
The strength of this study is in its randomized design and power. Its major weakness is surgeon bias, since the surgeons could not possibly be blinded to the method used.
The study confirms the problem that phenazopyridine makes the urine so orange that bladder mucosal lesions and de novo hematuria could be difficult to detect. Recommending mannitol as a hypertonic distending medium (as it is used in hysteroscopy procedures), however, may be premature. Prior studies have shown increased postoperative UTIs when 50% and 10% dextrose was used versus normal saline for cystoscopy.1,2 Since the Grimes study protocol did not include postoperative urine collection for cultures, more research on UTIs after mannitol use would be needed before surgeons confidently could use it routinely.
In our practice, surgeons prefer that intravenous sodium fluorescein be administered just prior to cystoscopy and oral phenazopyridine en route to the operating room. I agree that a major disadvantage to phenazopyridine is the heavy orange staining that obscures visualization.
Finally, this study did not account for cost of the various methods; standard normal saline would be cheapest, followed by phenazopyridine.
This study showed that surgeon satisfaction was greatest with the use of mannitol as a distending medium for intraoperative evaluation of ureteral patency compared with oral phenazopyridine, intravenous sodium fluorescein, and normal saline distention. However, time to surgeon confidence of ureteral patency was similar with all 4 methods. More data are needed related to UTIs and the cost of mannitol compared with the other 3 methods.
-- Cheryl B. Iglesia, MD
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
EXPERT COMMENTARY
Although the incidence of lower urinary tract and ureteral injury following gynecologic surgery is low, intraoperative identification of ureteral patency can prevent serious long-term sequelae. Since the indigo carmine shortage in 2014, US surgeons have searched for multiple alternative agents. Intravenous methylene blue is suboptimal due to its systemic adverse effects and the length of time for dye excretion in the urine.
Grimes and colleagues conducted a study to determine if there was any significant difference in surgeon satisfaction among 4 different alternatives to indigo carmine for intraoperative ureteral patency evaluation.
Related article:
Farewell to indigo carmine
Details of the study
The investigators conducted a randomized clinical trial of 130 women undergoing benign gynecologic or pelvic reconstructive surgery. Four different regimens were used for intraoperative ureteral evaluation: 1) oral phenazopyridine 200 mg, 2) intravenous sodium fluorescein 25 mg, 3) mannitol bladder distention, and 4) normal saline bladder distention.
Study outcomes. The primary outcome was surgeon satisfaction based on a 0 to 100 point visual analog scale rating (with 0 indicating strong agreement, 100 indicating disagreement). Secondary outcomes included ease of ureteral jet visualization, time to surgeon confidence of ureteral patency, and occurrence of adverse events over 6 weeks.
Surgeon satisfaction rating. The investigators found statistically significant physician satisfaction with the use of mannitol as a bladder distention medium over oral phenazopyridine, and slightly better satisfaction compared with the use of intravenous sodium fluorescein or normal saline distention. The median (range) visual analog scores for ureteral patency were phenazopyridine, 48 (0–83); sodium fluorescein 20 (0–82); mannitol, 0 (0–44); and normal saline, 23 (3–96) (P<.001).
There was no difference across the 4 groups in the timing to surgeon confidence of ureteral patency, length of cystoscopy (on average, 3 minutes), and development of postoperative urinary tract infections (UTIs).
Most dissatisfaction related to phenazopyridine is the fact that the resulting orange-stained urine can obscure the bladder mucosa.
One significant adverse event was a protocol deviation in which 1 patient received an incorrect dose of IV sodium fluorescein (500 mg) instead of the recommended 25-mg dose.
Related article:
Alternative options for visualizing ureteral patency during intraoperative cystoscopy
Study strengths and weaknesses
The strength of this study is in its randomized design and power. Its major weakness is surgeon bias, since the surgeons could not possibly be blinded to the method used.
The study confirms the problem that phenazopyridine makes the urine so orange that bladder mucosal lesions and de novo hematuria could be difficult to detect. Recommending mannitol as a hypertonic distending medium (as it is used in hysteroscopy procedures), however, may be premature. Prior studies have shown increased postoperative UTIs when 50% and 10% dextrose was used versus normal saline for cystoscopy.1,2 Since the Grimes study protocol did not include postoperative urine collection for cultures, more research on UTIs after mannitol use would be needed before surgeons confidently could use it routinely.
In our practice, surgeons prefer that intravenous sodium fluorescein be administered just prior to cystoscopy and oral phenazopyridine en route to the operating room. I agree that a major disadvantage to phenazopyridine is the heavy orange staining that obscures visualization.
Finally, this study did not account for cost of the various methods; standard normal saline would be cheapest, followed by phenazopyridine.
This study showed that surgeon satisfaction was greatest with the use of mannitol as a distending medium for intraoperative evaluation of ureteral patency compared with oral phenazopyridine, intravenous sodium fluorescein, and normal saline distention. However, time to surgeon confidence of ureteral patency was similar with all 4 methods. More data are needed related to UTIs and the cost of mannitol compared with the other 3 methods.
-- Cheryl B. Iglesia, MD
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Narasimhulu DM, Prabakar C, Tang N, Bral P. 50% dextrose versus normal saline as distention media during cystoscopy for assessment of ureteric patency. Eur J Obstet Gynecol Reprod Biol. 2016;199:38–41.
- Siff LN, Unger CA, Jelovsek JE, Paraiso MF, Ridgeway BM, Barber MD. Assessing ureteral patency using 10% dextrose cystoscopy fluid: evaluation of urinary tract infection rates. Am J Obstet Gynecol. 2016;215(1):74.e1–e6.
- Narasimhulu DM, Prabakar C, Tang N, Bral P. 50% dextrose versus normal saline as distention media during cystoscopy for assessment of ureteric patency. Eur J Obstet Gynecol Reprod Biol. 2016;199:38–41.
- Siff LN, Unger CA, Jelovsek JE, Paraiso MF, Ridgeway BM, Barber MD. Assessing ureteral patency using 10% dextrose cystoscopy fluid: evaluation of urinary tract infection rates. Am J Obstet Gynecol. 2016;215(1):74.e1–e6.
Questions value of ACOG/SMFM guidelines
FOR THE MANAGEMENT OF LABOR, PATIENCE IS A VIRTUE
ROBERT L. BARBIERI, MD (EDITORIAL; AUGUST 2017)
Questions value of ACOG/SMFM guidelines
The labor management guidelines recommended by the American College of Obstetricians and Gynecologists (ACOG) and the Society of Maternal-Fetal Medicine (SMFM) are terrible. Now retired, I trained in 1959–1963. In my career as an obstetrician, my primary cesarean delivery rate was 10% or less, and part of that was external pressure from people who did not know how to deliver a baby. Persistent occiput posterior position is a problem of inadequate flexion of the head, often due to ineffective contractions earlier. In such a situation, “pit” early! Rotate the head if you must, and teach residents how, please. The guidelines do not discuss the exhausted mother who goes home after a long labor or hours of pushing. I have interviewed new obstetricians in my community as early as 1980 who did not know what deep transverse arrest was. There, I am done voicing my disgust with obstetrics as it is practiced today.
James Honig, MD
Merritt Island, Florida
Managing difficult labor scenarios
I concur with Dr. Barbieri’s views on labor management that watchful waiting and giving the patient adequate time to progress naturally is the key to increase the chances of vaginal delivery. After all, labor is a physiologic process and should progress naturally. Having said that, I would like to know Dr. Barbieri’s views on handling certain circumstances in which patients these days land in the labor room, including 1) postdatedpregnancy with reduced fetal movements and not in labor; 2) full-term/postterm pregnancy with free-floating head and poor Bishop score; 3) full-term pregnancy with niggling pains for more than 1 week; and many such conditions that place you in the dilemma of whether to induce, knowing that chances of failure are high.
Manju Hotchandani, MD
New Delhi, India
Midwives always use patience to guide labor
As a Certified Nurse-Midwife since 1985 (now retired), “patience” in managing labor has always been my guide, as it has been for my midwifery colleagues. This is another example of ACOG finally acknowledging the truths we women have always known, without crediting the wisdom of midwives over the centuries. Lamaze International’s 6 Healthy Birth Practices also must have been their guide. “Evolving concepts of normal labor progress,” as though this was new information, would be humorous if it were not so frustrating!
Marsha Kelly, CNM
Charlotte, North Carolina
Dr. Barbieri responds
The readers of OBG
Every clinician involved in the birth process is deeply committed to a safe delivery for both mother and baby. Clinicians guide the birth process based on the unique characteristics and needs of each woman. Dr. Honig advocates for the active management of the labor process, while Ms. Kelly advocates for less intervention. Both approaches to labor management may be optimal depending on the unique clinical needs of each woman. Dr. Hotchandani inquires about managing common obstetric presentations. In my practice, induction is recommended for all women postterm who report consistently reduced fetal movement with the goal of reducing the risk of sudden intrauterine fetal demise. For healthy women at term with painful contractions and reassuring fetal status, but no cervical change, we support and counsel the patient and offer therapeutic rest with morphine. For women at term with a floating head and poor Bishop score, we would not intervene, until 41 weeks’ gestation when we would initiate gentle cervical ripening with mechanical or pharmacologic treatment.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
FOR THE MANAGEMENT OF LABOR, PATIENCE IS A VIRTUE
ROBERT L. BARBIERI, MD (EDITORIAL; AUGUST 2017)
Questions value of ACOG/SMFM guidelines
The labor management guidelines recommended by the American College of Obstetricians and Gynecologists (ACOG) and the Society of Maternal-Fetal Medicine (SMFM) are terrible. Now retired, I trained in 1959–1963. In my career as an obstetrician, my primary cesarean delivery rate was 10% or less, and part of that was external pressure from people who did not know how to deliver a baby. Persistent occiput posterior position is a problem of inadequate flexion of the head, often due to ineffective contractions earlier. In such a situation, “pit” early! Rotate the head if you must, and teach residents how, please. The guidelines do not discuss the exhausted mother who goes home after a long labor or hours of pushing. I have interviewed new obstetricians in my community as early as 1980 who did not know what deep transverse arrest was. There, I am done voicing my disgust with obstetrics as it is practiced today.
James Honig, MD
Merritt Island, Florida
Managing difficult labor scenarios
I concur with Dr. Barbieri’s views on labor management that watchful waiting and giving the patient adequate time to progress naturally is the key to increase the chances of vaginal delivery. After all, labor is a physiologic process and should progress naturally. Having said that, I would like to know Dr. Barbieri’s views on handling certain circumstances in which patients these days land in the labor room, including 1) postdatedpregnancy with reduced fetal movements and not in labor; 2) full-term/postterm pregnancy with free-floating head and poor Bishop score; 3) full-term pregnancy with niggling pains for more than 1 week; and many such conditions that place you in the dilemma of whether to induce, knowing that chances of failure are high.
Manju Hotchandani, MD
New Delhi, India
Midwives always use patience to guide labor
As a Certified Nurse-Midwife since 1985 (now retired), “patience” in managing labor has always been my guide, as it has been for my midwifery colleagues. This is another example of ACOG finally acknowledging the truths we women have always known, without crediting the wisdom of midwives over the centuries. Lamaze International’s 6 Healthy Birth Practices also must have been their guide. “Evolving concepts of normal labor progress,” as though this was new information, would be humorous if it were not so frustrating!
Marsha Kelly, CNM
Charlotte, North Carolina
Dr. Barbieri responds
The readers of OBG
Every clinician involved in the birth process is deeply committed to a safe delivery for both mother and baby. Clinicians guide the birth process based on the unique characteristics and needs of each woman. Dr. Honig advocates for the active management of the labor process, while Ms. Kelly advocates for less intervention. Both approaches to labor management may be optimal depending on the unique clinical needs of each woman. Dr. Hotchandani inquires about managing common obstetric presentations. In my practice, induction is recommended for all women postterm who report consistently reduced fetal movement with the goal of reducing the risk of sudden intrauterine fetal demise. For healthy women at term with painful contractions and reassuring fetal status, but no cervical change, we support and counsel the patient and offer therapeutic rest with morphine. For women at term with a floating head and poor Bishop score, we would not intervene, until 41 weeks’ gestation when we would initiate gentle cervical ripening with mechanical or pharmacologic treatment.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
FOR THE MANAGEMENT OF LABOR, PATIENCE IS A VIRTUE
ROBERT L. BARBIERI, MD (EDITORIAL; AUGUST 2017)
Questions value of ACOG/SMFM guidelines
The labor management guidelines recommended by the American College of Obstetricians and Gynecologists (ACOG) and the Society of Maternal-Fetal Medicine (SMFM) are terrible. Now retired, I trained in 1959–1963. In my career as an obstetrician, my primary cesarean delivery rate was 10% or less, and part of that was external pressure from people who did not know how to deliver a baby. Persistent occiput posterior position is a problem of inadequate flexion of the head, often due to ineffective contractions earlier. In such a situation, “pit” early! Rotate the head if you must, and teach residents how, please. The guidelines do not discuss the exhausted mother who goes home after a long labor or hours of pushing. I have interviewed new obstetricians in my community as early as 1980 who did not know what deep transverse arrest was. There, I am done voicing my disgust with obstetrics as it is practiced today.
James Honig, MD
Merritt Island, Florida
Managing difficult labor scenarios
I concur with Dr. Barbieri’s views on labor management that watchful waiting and giving the patient adequate time to progress naturally is the key to increase the chances of vaginal delivery. After all, labor is a physiologic process and should progress naturally. Having said that, I would like to know Dr. Barbieri’s views on handling certain circumstances in which patients these days land in the labor room, including 1) postdatedpregnancy with reduced fetal movements and not in labor; 2) full-term/postterm pregnancy with free-floating head and poor Bishop score; 3) full-term pregnancy with niggling pains for more than 1 week; and many such conditions that place you in the dilemma of whether to induce, knowing that chances of failure are high.
Manju Hotchandani, MD
New Delhi, India
Midwives always use patience to guide labor
As a Certified Nurse-Midwife since 1985 (now retired), “patience” in managing labor has always been my guide, as it has been for my midwifery colleagues. This is another example of ACOG finally acknowledging the truths we women have always known, without crediting the wisdom of midwives over the centuries. Lamaze International’s 6 Healthy Birth Practices also must have been their guide. “Evolving concepts of normal labor progress,” as though this was new information, would be humorous if it were not so frustrating!
Marsha Kelly, CNM
Charlotte, North Carolina
Dr. Barbieri responds
The readers of OBG
Every clinician involved in the birth process is deeply committed to a safe delivery for both mother and baby. Clinicians guide the birth process based on the unique characteristics and needs of each woman. Dr. Honig advocates for the active management of the labor process, while Ms. Kelly advocates for less intervention. Both approaches to labor management may be optimal depending on the unique clinical needs of each woman. Dr. Hotchandani inquires about managing common obstetric presentations. In my practice, induction is recommended for all women postterm who report consistently reduced fetal movement with the goal of reducing the risk of sudden intrauterine fetal demise. For healthy women at term with painful contractions and reassuring fetal status, but no cervical change, we support and counsel the patient and offer therapeutic rest with morphine. For women at term with a floating head and poor Bishop score, we would not intervene, until 41 weeks’ gestation when we would initiate gentle cervical ripening with mechanical or pharmacologic treatment.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Unnecessary laparotomy: $625,000 award
Unnecessary laparotomy: $625,000 award
A woman in her 20s reported cramping and rectal bleeding to her ObGyn. Pelvic and rectal examinations were normal. Her family physician's exam and a gastroenterologist's rectal exam and colonoscopy were all normal. A radiologist (Dr. A) identified a 3-cm by 6-cm mass on transvaginal ultrasonography. A computed tomography (CT) scan read by another radiologist (Dr. B) confirmed the mass. After receiving the radiologists' reports, the ObGyn told the patient that she had a small tumor that needed immediate removal. No mass was found during exploratory laparotomy.
Three years postsurgery, after trying to conceive, the patient underwent exploratory laparoscopy to evaluate her fallopian tubes. A surgeon found significant pelvic adhesions occluding the left fallopian tube. He lysed the adhesions and resected the left fallopian tube.
PATIENT'S CLAIM: The patient sued the ObGyn and both radiologists, alleging that the unnecessary surgeries resulted in reduced fertility.
Postoperatively, the ObGyn told the patient that the surgery, performed for "nothing," was the radiologists' fault, and that she would have no trouble conceiving. He later blamed her fallopian tube damage on a diagnosis of chlamydia that was successfully treated years earlier with no evidence of reinfection.
The ObGyn disregarded Dr. A's recommendation for a CT scan with rectal contrast; instead he ordered oral contrast. The ObGyn also ignored Dr. B's recommendation for magnetic resonance imaging (MRI).
The mass misidentified by the radiologists was described in 2 different places on the anterior wall of the bowel, both outside the purview of a gynecologist. Given the uncertain diagnosis, referral to a general surgeon was mandated; exploratory laparotomy was not indicated. The ObGyn never referred the patient to a general surgeon for evaluation or sent records or films to the surgeon whom he claimed to have consulted before surgery. The general surgeon denied that any such discussion occurred. The surgeon's first contact with the patient occurred when he was called into the operating room because the ObGyn could not find a mass; the patient was under anesthesia and her abdomen was open.
DEFENDANTS' DEFENSE: The ObGyn claimed that he had developed a plan with the general surgeon before surgery: if the mass was a uterine fibroid, he would remove it, but if the mass was mesenteric, the surgeon would operate.
The ObGyn was justified in performing surgery based on the patient's complaints and the radiologists' findings.
The radiologists contended that, since neither of them expressed certainty, both requested further studies, and neither suggested surgery, their treatment was consistent with the standard of care.
VERDICT: A $625,000 Pennsylvania verdict was returned, finding the ObGyn 100% liable.
Both ureters injured during TAH
A 49-year-old woman underwent total abdominal hysterectomy (TAH) for removal of a uterine fibroid performed by her gynecologist and a surgical assistant. The patient had limited urine output immediately after surgery, no urinary output overnight, and abdominal pain. The gynecologist ordered a urology consultation. A CT scan showed bilateral ureteral obstruction; an interventional radiology study confirmed a blockage due to severance of both ureters. A nephrostomy was performed and, 6 weeks later, the ureters were reimplanted.
PATIENT'S CLAIM: The severing of both ureters was a negligent surgical error. While the risk of injuring a single ureter is a recognized complication of TAH, it is unacceptable that both ureters were severed.
DEFENDANTS' DEFENSE: Standard of care was met: bilateral ureteral injury is a known risk of TAH. Before surgery, the patient was fully informed of the risks and signed a consent agreement. There was no intraoperative evidence that the ureters had been damaged. The injuries were detected as soon as medically possible and timely and successfully treated.
VERDICT: An Illinois defense verdict was returned.
Failure to detect breast cancer: $21.9M verdict against radiologist
A woman went to a diagnostic imaging service for ultrasonography (US) after an earlier US was suspicious for a breast mass. She had a history of left breast pain and swelling that had been treated with antibiotics. The radiologist interpreted the second ultrasound as showing no masses; he noted skin thickening and a lymph node abnormality.
Nine months after initial US, the patient had a breast biopsy performed in another state. She was diagnosed with stage 3 breast cancer.
PATIENT'S CLAIM: The radiologist failed to properly interpret the findings of the second ultrasound.
PHYSICIAN'S DEFENSE: The radiologist contended that he was not liable because the technologist failed to place the transducer over the breast lump. The first US films were not provided for comparison.
VERDICT: A $21.9 million Florida verdict was returned.
Vesicovaginal fistula after hysterectomy
A 39-year-old woman with a history of 4 cesarean deliveries and an enlarged fibroid uterus underwent TAH. She subsequently developed urinary incontinence.
PATIENT'S CLAIM: The ObGyn used an inappropriate dissection technique to remove the uterus, causing a bladder injury. He also sutured the vaginal cuff to the bladder, causing the formation of a vesicovaginal fistula. Repair surgeries were unsuccessful and the patient now is permanently incontinent.
PHYSICIAN'S DEFENSE: The standard of care was met. The patient had a pre-existing bladder weakness due to the size of her uterus and prior surgeries. The bladder injury is a known complication of the surgery. The vaginal cuff adhered to the bladder due to postsurgical scarring or fibrosis.
VERDICT: A Michigan defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Unnecessary laparotomy: $625,000 award
A woman in her 20s reported cramping and rectal bleeding to her ObGyn. Pelvic and rectal examinations were normal. Her family physician's exam and a gastroenterologist's rectal exam and colonoscopy were all normal. A radiologist (Dr. A) identified a 3-cm by 6-cm mass on transvaginal ultrasonography. A computed tomography (CT) scan read by another radiologist (Dr. B) confirmed the mass. After receiving the radiologists' reports, the ObGyn told the patient that she had a small tumor that needed immediate removal. No mass was found during exploratory laparotomy.
Three years postsurgery, after trying to conceive, the patient underwent exploratory laparoscopy to evaluate her fallopian tubes. A surgeon found significant pelvic adhesions occluding the left fallopian tube. He lysed the adhesions and resected the left fallopian tube.
PATIENT'S CLAIM: The patient sued the ObGyn and both radiologists, alleging that the unnecessary surgeries resulted in reduced fertility.
Postoperatively, the ObGyn told the patient that the surgery, performed for "nothing," was the radiologists' fault, and that she would have no trouble conceiving. He later blamed her fallopian tube damage on a diagnosis of chlamydia that was successfully treated years earlier with no evidence of reinfection.
The ObGyn disregarded Dr. A's recommendation for a CT scan with rectal contrast; instead he ordered oral contrast. The ObGyn also ignored Dr. B's recommendation for magnetic resonance imaging (MRI).
The mass misidentified by the radiologists was described in 2 different places on the anterior wall of the bowel, both outside the purview of a gynecologist. Given the uncertain diagnosis, referral to a general surgeon was mandated; exploratory laparotomy was not indicated. The ObGyn never referred the patient to a general surgeon for evaluation or sent records or films to the surgeon whom he claimed to have consulted before surgery. The general surgeon denied that any such discussion occurred. The surgeon's first contact with the patient occurred when he was called into the operating room because the ObGyn could not find a mass; the patient was under anesthesia and her abdomen was open.
DEFENDANTS' DEFENSE: The ObGyn claimed that he had developed a plan with the general surgeon before surgery: if the mass was a uterine fibroid, he would remove it, but if the mass was mesenteric, the surgeon would operate.
The ObGyn was justified in performing surgery based on the patient's complaints and the radiologists' findings.
The radiologists contended that, since neither of them expressed certainty, both requested further studies, and neither suggested surgery, their treatment was consistent with the standard of care.
VERDICT: A $625,000 Pennsylvania verdict was returned, finding the ObGyn 100% liable.
Both ureters injured during TAH
A 49-year-old woman underwent total abdominal hysterectomy (TAH) for removal of a uterine fibroid performed by her gynecologist and a surgical assistant. The patient had limited urine output immediately after surgery, no urinary output overnight, and abdominal pain. The gynecologist ordered a urology consultation. A CT scan showed bilateral ureteral obstruction; an interventional radiology study confirmed a blockage due to severance of both ureters. A nephrostomy was performed and, 6 weeks later, the ureters were reimplanted.
PATIENT'S CLAIM: The severing of both ureters was a negligent surgical error. While the risk of injuring a single ureter is a recognized complication of TAH, it is unacceptable that both ureters were severed.
DEFENDANTS' DEFENSE: Standard of care was met: bilateral ureteral injury is a known risk of TAH. Before surgery, the patient was fully informed of the risks and signed a consent agreement. There was no intraoperative evidence that the ureters had been damaged. The injuries were detected as soon as medically possible and timely and successfully treated.
VERDICT: An Illinois defense verdict was returned.
Failure to detect breast cancer: $21.9M verdict against radiologist
A woman went to a diagnostic imaging service for ultrasonography (US) after an earlier US was suspicious for a breast mass. She had a history of left breast pain and swelling that had been treated with antibiotics. The radiologist interpreted the second ultrasound as showing no masses; he noted skin thickening and a lymph node abnormality.
Nine months after initial US, the patient had a breast biopsy performed in another state. She was diagnosed with stage 3 breast cancer.
PATIENT'S CLAIM: The radiologist failed to properly interpret the findings of the second ultrasound.
PHYSICIAN'S DEFENSE: The radiologist contended that he was not liable because the technologist failed to place the transducer over the breast lump. The first US films were not provided for comparison.
VERDICT: A $21.9 million Florida verdict was returned.
Vesicovaginal fistula after hysterectomy
A 39-year-old woman with a history of 4 cesarean deliveries and an enlarged fibroid uterus underwent TAH. She subsequently developed urinary incontinence.
PATIENT'S CLAIM: The ObGyn used an inappropriate dissection technique to remove the uterus, causing a bladder injury. He also sutured the vaginal cuff to the bladder, causing the formation of a vesicovaginal fistula. Repair surgeries were unsuccessful and the patient now is permanently incontinent.
PHYSICIAN'S DEFENSE: The standard of care was met. The patient had a pre-existing bladder weakness due to the size of her uterus and prior surgeries. The bladder injury is a known complication of the surgery. The vaginal cuff adhered to the bladder due to postsurgical scarring or fibrosis.
VERDICT: A Michigan defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Unnecessary laparotomy: $625,000 award
A woman in her 20s reported cramping and rectal bleeding to her ObGyn. Pelvic and rectal examinations were normal. Her family physician's exam and a gastroenterologist's rectal exam and colonoscopy were all normal. A radiologist (Dr. A) identified a 3-cm by 6-cm mass on transvaginal ultrasonography. A computed tomography (CT) scan read by another radiologist (Dr. B) confirmed the mass. After receiving the radiologists' reports, the ObGyn told the patient that she had a small tumor that needed immediate removal. No mass was found during exploratory laparotomy.
Three years postsurgery, after trying to conceive, the patient underwent exploratory laparoscopy to evaluate her fallopian tubes. A surgeon found significant pelvic adhesions occluding the left fallopian tube. He lysed the adhesions and resected the left fallopian tube.
PATIENT'S CLAIM: The patient sued the ObGyn and both radiologists, alleging that the unnecessary surgeries resulted in reduced fertility.
Postoperatively, the ObGyn told the patient that the surgery, performed for "nothing," was the radiologists' fault, and that she would have no trouble conceiving. He later blamed her fallopian tube damage on a diagnosis of chlamydia that was successfully treated years earlier with no evidence of reinfection.
The ObGyn disregarded Dr. A's recommendation for a CT scan with rectal contrast; instead he ordered oral contrast. The ObGyn also ignored Dr. B's recommendation for magnetic resonance imaging (MRI).
The mass misidentified by the radiologists was described in 2 different places on the anterior wall of the bowel, both outside the purview of a gynecologist. Given the uncertain diagnosis, referral to a general surgeon was mandated; exploratory laparotomy was not indicated. The ObGyn never referred the patient to a general surgeon for evaluation or sent records or films to the surgeon whom he claimed to have consulted before surgery. The general surgeon denied that any such discussion occurred. The surgeon's first contact with the patient occurred when he was called into the operating room because the ObGyn could not find a mass; the patient was under anesthesia and her abdomen was open.
DEFENDANTS' DEFENSE: The ObGyn claimed that he had developed a plan with the general surgeon before surgery: if the mass was a uterine fibroid, he would remove it, but if the mass was mesenteric, the surgeon would operate.
The ObGyn was justified in performing surgery based on the patient's complaints and the radiologists' findings.
The radiologists contended that, since neither of them expressed certainty, both requested further studies, and neither suggested surgery, their treatment was consistent with the standard of care.
VERDICT: A $625,000 Pennsylvania verdict was returned, finding the ObGyn 100% liable.
Both ureters injured during TAH
A 49-year-old woman underwent total abdominal hysterectomy (TAH) for removal of a uterine fibroid performed by her gynecologist and a surgical assistant. The patient had limited urine output immediately after surgery, no urinary output overnight, and abdominal pain. The gynecologist ordered a urology consultation. A CT scan showed bilateral ureteral obstruction; an interventional radiology study confirmed a blockage due to severance of both ureters. A nephrostomy was performed and, 6 weeks later, the ureters were reimplanted.
PATIENT'S CLAIM: The severing of both ureters was a negligent surgical error. While the risk of injuring a single ureter is a recognized complication of TAH, it is unacceptable that both ureters were severed.
DEFENDANTS' DEFENSE: Standard of care was met: bilateral ureteral injury is a known risk of TAH. Before surgery, the patient was fully informed of the risks and signed a consent agreement. There was no intraoperative evidence that the ureters had been damaged. The injuries were detected as soon as medically possible and timely and successfully treated.
VERDICT: An Illinois defense verdict was returned.
Failure to detect breast cancer: $21.9M verdict against radiologist
A woman went to a diagnostic imaging service for ultrasonography (US) after an earlier US was suspicious for a breast mass. She had a history of left breast pain and swelling that had been treated with antibiotics. The radiologist interpreted the second ultrasound as showing no masses; he noted skin thickening and a lymph node abnormality.
Nine months after initial US, the patient had a breast biopsy performed in another state. She was diagnosed with stage 3 breast cancer.
PATIENT'S CLAIM: The radiologist failed to properly interpret the findings of the second ultrasound.
PHYSICIAN'S DEFENSE: The radiologist contended that he was not liable because the technologist failed to place the transducer over the breast lump. The first US films were not provided for comparison.
VERDICT: A $21.9 million Florida verdict was returned.
Vesicovaginal fistula after hysterectomy
A 39-year-old woman with a history of 4 cesarean deliveries and an enlarged fibroid uterus underwent TAH. She subsequently developed urinary incontinence.
PATIENT'S CLAIM: The ObGyn used an inappropriate dissection technique to remove the uterus, causing a bladder injury. He also sutured the vaginal cuff to the bladder, causing the formation of a vesicovaginal fistula. Repair surgeries were unsuccessful and the patient now is permanently incontinent.
PHYSICIAN'S DEFENSE: The standard of care was met. The patient had a pre-existing bladder weakness due to the size of her uterus and prior surgeries. The bladder injury is a known complication of the surgery. The vaginal cuff adhered to the bladder due to postsurgical scarring or fibrosis.
VERDICT: A Michigan defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Product Update: MyoSure MANUAL; Rivanna's Accuro 3D; PeriGen; Instavit
HYSTEROSCOPY TISSUE REMOVAL DEVICE
Hologic, Inc, has introduced the MyoSure® MANUAL Tissue Removal Device for resecting and removing tissue during in-office hysteroscopic intrauterine procedures. When used with the MyoSure hysteroscope, the MyoSure MANUAL device has a fully integrated vacuum that does not require external suction and can be operated using a 1-L saline bag. The clear tissue trap allows for visual co
This new Hologic product joins the MyoSure suite of gynecologic surgical products that includes the MyoSure, MyoSure REACH, MyoSure XL, and MyoSure LITE devices.
FOR MORE INFORMATION, VISIT: http://myosure.com/
SPINAL NAVIGATION TECHNOLOGY FOR EPIDURAL ANESTHESIA
The Accuro® 3D image-guided spinal navigation technology by Rivanna Medical® is a handheld, lightweight, untethered ultrasound-based system designed to help apply spinal and epidural anesthesia. Ultrasonography is the imaging modality of choice for epidurals in expectant mothers who must avoid the radiation involved in other imaging procedures, according to Rivanna Medical.
In a recent trial, Accuro identified the appropriate epidural injection sites along the lower spine and calculated the depth to the epidural space. Actual epidural depth was confirmed by measuring needle penetration during successful epidural delivery by anesthesia providers. Accuro predicted this depth within an average of 0.61 cm, reports Rivanna Medical. In addition, Accuro identified the appropriate spinal interspace for needle insertion in 94% of patients and enabled 87% success in first-attempt epidural administration.
FOR MORE INFORMATION, VISIT: https://rivannamedical.com/
SOFTWARE AND HUB HELP IDENTIFY CRITICALLY ILL L&D PATIENTS
PeriGen, Inc, a software-solutions company, has launched PeriWatch™ HUB™, new perinatal software and a dashboard for labor and delivery (L&D) units.
PeriGen says that its PeriWatch modules provide state-of-the-art L&D documentation and fetal surveillance coupled with analytics and an electronic critical-condition dashboard for hospital maternity units.
HUB is an intelligent perinatal dashboard designed to facilitate the timely recognition of maternity patients who develop critical illness. Using PeriGen’s proprietary algorithms, it prioritizes patients based on physician-chosen threshold settings for vital signs, labor progress, and fetal heart rate patterns, and consolidates that data into an easy-to-read interactive dashboard.
FOR MORE INFORMATION, VISIT: http://perigen.com/
ORAL SPRAY VITAMINS: ALTERNATIVE TO PILLS
Instavit® Spray Vitamins offer an alternative to patients who have difficulty swallowing pills. Instavit says that its oral vitamins, sprayed directly into the mouth, are sugar-free, tasty, gluten-free, and contain zero calories. The sprays are manufactured to the highest standard in cGMP, FDA approved facilities in the United States. Each Instavit spray provides an exact and measured amount of liquid, allowing for correct dosing and also permitting individualization of intake. A 14-oz spray bottle contains about 28 doses.
The Instavit line includes: “Prenatal Care,” “Vitamin B12,” “Instant Energy,” “Vitamin D,” “Daily Health,” “Sweet Dreams,” “Immune Strength,” “Clearer Thinking,” and “Instavit for Kids.” Instavit products are available in retail stores in North America.
FOR MORE INFORMATION, VISIT: http://www.instavit.com/
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
HYSTEROSCOPY TISSUE REMOVAL DEVICE
Hologic, Inc, has introduced the MyoSure® MANUAL Tissue Removal Device for resecting and removing tissue during in-office hysteroscopic intrauterine procedures. When used with the MyoSure hysteroscope, the MyoSure MANUAL device has a fully integrated vacuum that does not require external suction and can be operated using a 1-L saline bag. The clear tissue trap allows for visual co
This new Hologic product joins the MyoSure suite of gynecologic surgical products that includes the MyoSure, MyoSure REACH, MyoSure XL, and MyoSure LITE devices.
FOR MORE INFORMATION, VISIT: http://myosure.com/
SPINAL NAVIGATION TECHNOLOGY FOR EPIDURAL ANESTHESIA
The Accuro® 3D image-guided spinal navigation technology by Rivanna Medical® is a handheld, lightweight, untethered ultrasound-based system designed to help apply spinal and epidural anesthesia. Ultrasonography is the imaging modality of choice for epidurals in expectant mothers who must avoid the radiation involved in other imaging procedures, according to Rivanna Medical.
In a recent trial, Accuro identified the appropriate epidural injection sites along the lower spine and calculated the depth to the epidural space. Actual epidural depth was confirmed by measuring needle penetration during successful epidural delivery by anesthesia providers. Accuro predicted this depth within an average of 0.61 cm, reports Rivanna Medical. In addition, Accuro identified the appropriate spinal interspace for needle insertion in 94% of patients and enabled 87% success in first-attempt epidural administration.
FOR MORE INFORMATION, VISIT: https://rivannamedical.com/
SOFTWARE AND HUB HELP IDENTIFY CRITICALLY ILL L&D PATIENTS
PeriGen, Inc, a software-solutions company, has launched PeriWatch™ HUB™, new perinatal software and a dashboard for labor and delivery (L&D) units.
PeriGen says that its PeriWatch modules provide state-of-the-art L&D documentation and fetal surveillance coupled with analytics and an electronic critical-condition dashboard for hospital maternity units.
HUB is an intelligent perinatal dashboard designed to facilitate the timely recognition of maternity patients who develop critical illness. Using PeriGen’s proprietary algorithms, it prioritizes patients based on physician-chosen threshold settings for vital signs, labor progress, and fetal heart rate patterns, and consolidates that data into an easy-to-read interactive dashboard.
FOR MORE INFORMATION, VISIT: http://perigen.com/
ORAL SPRAY VITAMINS: ALTERNATIVE TO PILLS
Instavit® Spray Vitamins offer an alternative to patients who have difficulty swallowing pills. Instavit says that its oral vitamins, sprayed directly into the mouth, are sugar-free, tasty, gluten-free, and contain zero calories. The sprays are manufactured to the highest standard in cGMP, FDA approved facilities in the United States. Each Instavit spray provides an exact and measured amount of liquid, allowing for correct dosing and also permitting individualization of intake. A 14-oz spray bottle contains about 28 doses.
The Instavit line includes: “Prenatal Care,” “Vitamin B12,” “Instant Energy,” “Vitamin D,” “Daily Health,” “Sweet Dreams,” “Immune Strength,” “Clearer Thinking,” and “Instavit for Kids.” Instavit products are available in retail stores in North America.
FOR MORE INFORMATION, VISIT: http://www.instavit.com/
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
HYSTEROSCOPY TISSUE REMOVAL DEVICE
Hologic, Inc, has introduced the MyoSure® MANUAL Tissue Removal Device for resecting and removing tissue during in-office hysteroscopic intrauterine procedures. When used with the MyoSure hysteroscope, the MyoSure MANUAL device has a fully integrated vacuum that does not require external suction and can be operated using a 1-L saline bag. The clear tissue trap allows for visual co
This new Hologic product joins the MyoSure suite of gynecologic surgical products that includes the MyoSure, MyoSure REACH, MyoSure XL, and MyoSure LITE devices.
FOR MORE INFORMATION, VISIT: http://myosure.com/
SPINAL NAVIGATION TECHNOLOGY FOR EPIDURAL ANESTHESIA
The Accuro® 3D image-guided spinal navigation technology by Rivanna Medical® is a handheld, lightweight, untethered ultrasound-based system designed to help apply spinal and epidural anesthesia. Ultrasonography is the imaging modality of choice for epidurals in expectant mothers who must avoid the radiation involved in other imaging procedures, according to Rivanna Medical.
In a recent trial, Accuro identified the appropriate epidural injection sites along the lower spine and calculated the depth to the epidural space. Actual epidural depth was confirmed by measuring needle penetration during successful epidural delivery by anesthesia providers. Accuro predicted this depth within an average of 0.61 cm, reports Rivanna Medical. In addition, Accuro identified the appropriate spinal interspace for needle insertion in 94% of patients and enabled 87% success in first-attempt epidural administration.
FOR MORE INFORMATION, VISIT: https://rivannamedical.com/
SOFTWARE AND HUB HELP IDENTIFY CRITICALLY ILL L&D PATIENTS
PeriGen, Inc, a software-solutions company, has launched PeriWatch™ HUB™, new perinatal software and a dashboard for labor and delivery (L&D) units.
PeriGen says that its PeriWatch modules provide state-of-the-art L&D documentation and fetal surveillance coupled with analytics and an electronic critical-condition dashboard for hospital maternity units.
HUB is an intelligent perinatal dashboard designed to facilitate the timely recognition of maternity patients who develop critical illness. Using PeriGen’s proprietary algorithms, it prioritizes patients based on physician-chosen threshold settings for vital signs, labor progress, and fetal heart rate patterns, and consolidates that data into an easy-to-read interactive dashboard.
FOR MORE INFORMATION, VISIT: http://perigen.com/
ORAL SPRAY VITAMINS: ALTERNATIVE TO PILLS
Instavit® Spray Vitamins offer an alternative to patients who have difficulty swallowing pills. Instavit says that its oral vitamins, sprayed directly into the mouth, are sugar-free, tasty, gluten-free, and contain zero calories. The sprays are manufactured to the highest standard in cGMP, FDA approved facilities in the United States. Each Instavit spray provides an exact and measured amount of liquid, allowing for correct dosing and also permitting individualization of intake. A 14-oz spray bottle contains about 28 doses.
The Instavit line includes: “Prenatal Care,” “Vitamin B12,” “Instant Energy,” “Vitamin D,” “Daily Health,” “Sweet Dreams,” “Immune Strength,” “Clearer Thinking,” and “Instavit for Kids.” Instavit products are available in retail stores in North America.
FOR MORE INFORMATION, VISIT: http://www.instavit.com/
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.