User login
Tumor heterogeneity: a central foe in the war on cancer
A major challenge to effective cancer treatment is the astounding level of heterogeneity that tumors display on many different fronts. Here, we discuss how a deeper appreciation of this heterogeneity and its impact is driving research efforts to better understand and tackle it and a radical rethink of treatment paradigms.
A complex and dynamic disease
The nonuniformity of cancer has long been appreciated, reflected most visibly in the variation of response to the same treatment across patients with the same type of tumor (inter-tumor heterogeneity). The extent of tumor heterogeneity is being fully realized only now, with the advent of next-generation sequencing technologies. Even within the same tumor, there can be significant heterogeneity from cell to cell (intra-tumor heterogeneity), yielding substantial complexity in cancer.
Heterogeneity reveals itself on many different levels. Histologically speaking, tumors are composed of a nonhomogenous mass of cells that vary in type and number. In terms of their molecular make-up, there is substantial variation in the types of molecular alterations observed, all the way down to the single cell level. In even more abstract terms, beyond the cancer itself, the microenvironment in which it resides can be highly heterogeneous, composed of a plethora of different supportive and tumor-infiltrating normal cells.
Heterogeneity can manifest spatially, reflecting differences in the composition of the primary tumor and tumors at secondary sites or across regions of the same tumor mass and temporally, at different time points across a tumor’s natural history. Evocative of the second law of thermodynamics, cancers generally become more diverse and complex over time.1-3
A tale of 2 models
It is widely accepted that the transformation of a normal cell into a malignant one occurs with the acquisition of certain “hallmark” abilities, but there are myriad ways in which these can be attained.
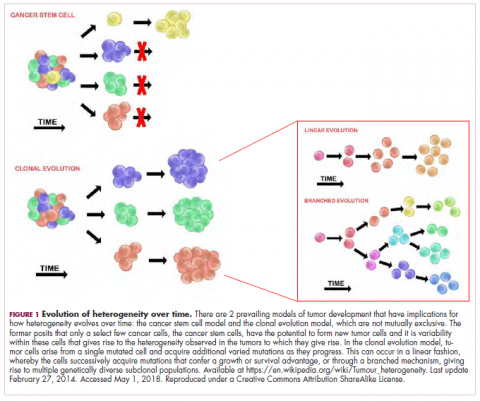
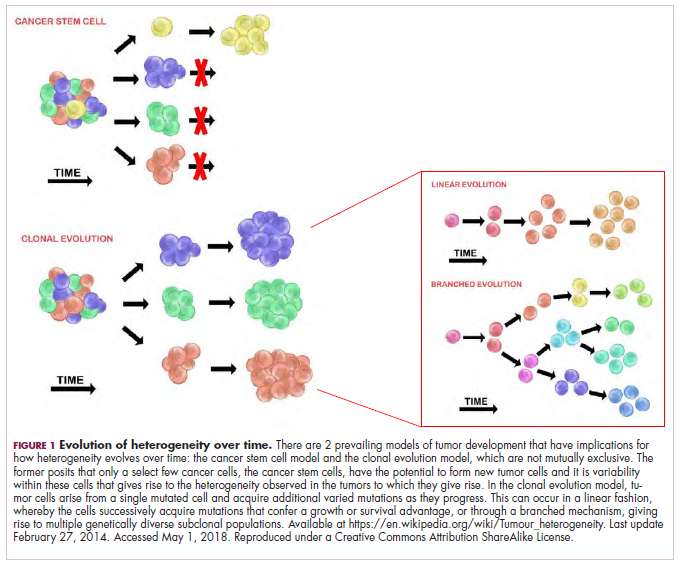
The clonal evolution model
As cells divide, they randomly acquire mutations as a result of DNA damage. The clonal evolution model posits that cancer develops as the result of a multistep accumulation of a series of “driver” mutations that confer a promalignant advantage to the cell and ultimately fuel a cancerous hallmark.
This evolution can occur in a linear fashion, whereby the emergence of a new driver mutation conveys such a potent evolutionary advantage that it outcompetes all previous clones. There is limited evidence for linear evolution in most advanced human cancers; instead, they are thought to evolve predominantly through a process of branching evolution, in which multiple clones can diverge in parallel from a common ancestor through the acquisition of different driver mutations. This results in common clonal mutations that form the trunk of the cancer’s evolutionary tree and are shared by all cells and subclonal mutations, which make up the branches and differ from cell to cell.
More recently, several other mechanisms of clonal evolution have been proposed, including neutral evolution, a type of branching evolution in which there are no selective pressures and evolution occurs by random mutations occurring over time that lead to genetic drift, and punctuated evolution, in which there are short evolutionary bursts of hypermutation.4,5
The CSC model
This model posits that the ability to form and sustain a cancer is restricted to a single cell type – the cancer stem cells – which have the unique capacity for self-renewal and differentiation. Although the forces of evolution are still involved in this model, they act on a hierarchy of cells, with stem cells sitting at the top. A tumor is derived from a single stem cell that has acquired a mutation, and the heterogeneity observed results both from the differentiation and the accumulation of mutations in CSCs.
Accumulated experimental evidence suggests that these models are not mutually exclusive and that they can all contribute to heterogeneity in varied amounts across different tumor types. What is clear is that heterogeneity and evolution are intricately intertwined in cancer development.1,2,6
An unstable genome
Heterogeneity and evolution are fueled by genomic alterations and the genome instability that they foster. This genome instability can range from single base pair substitutions to a doubling of the entire genome and results from both exposure to exogenous mutagens (eg, chemicals and ultraviolet radiation) and genomic alterations that have an impact on important cellular processes (eg, DNA repair or replication).
Among the most common causes of genome instability are mutations in the DNA mismatch repair pathway proteins or in the proofreading polymerase enzymes. Genome instability is often associated with unique mutational signatures – characteristic combinations of mutations that arose as the result of the specific biological processes underlying them.7
Genome-wide analyses have begun to reveal these mutational signatures across the spectrum of human cancers. The Wellcome Sanger Institute’s Catalogue of Somatic Mutations in Cancer (COSMIC) database has generated a set of 30 mutational signatures based on analysis of almost 11,000 exomes and more than 1,000 whole genomes spanning 40 different cancer types, some of which have been linked with specific mutagenic processes, such as tobacco, UV radiation, and DNA repair deficiency (Table 1).8
Fueling resistance
Arguably, heterogeneity presents one of the most significant barriers to effective cancer therapy, and this has become increasingly true in the era of personalized medicine in which targeted therapies take aim at specific molecular abnormalities.
It is vital that drugs target the truncal alterations that are present in all cancer cells to ensure that the entire cancer is eradicated. However, it is not always possible to target these alterations, for example, at the present time tumor suppressor proteins like p53 are not druggable.
Even when truncal alterations have been targeted successfully, such as epidermal growth factor receptor (EGFR) mutations and anaplastic lymphoma kinase (ALK) chromosomal rearrangements in non–small-cell lung cancer (NSCLC) and BRAF mutations in melanoma, the long-term efficacy of these drugs is almost invariably limited by the development of resistance.
Tumor heterogeneity and the clonal evolution it fuels are central drivers of resistance. Because tumors are dynamic and continue to evolve, anticancer treatments can act as a strong selective pressure and drive the emergence of drug-resistant subclones that allow the tumor to persist. In fact, study findings have revealed that small populations of resistant cells may be present before treatment. Thus, resistance may also occur as a result of the outgrowth of preexisting treatment-resistant cells that suddenly find that they acquire a survival advantage in the presence of a drug.1,6
Tackling heterogeneity
Despite extensive clinical documentation of the existence of heterogeneity and its underlying mechanisms across a range of tumor types, the development of novel clinical trial designs and therapeutic strategies that account for its effects have only recently begun to be explored.
For the most part, this was because of a lack of effective methods for evaluating intratumor heterogeneity. Multiregion biopsies, in which tissue derived from multiple different regions of a single tumor mass or from distinct cancerous lesions within the same patient, give a snapshot of tumor heterogeneity at a single point in time. The repeated longitudinal sampling required to gain a deeper appreciation of tumor heterogeneity over the course of tumor evolution is often not possible because of the morbidity associated with repeated surgical procedures.
Liquid biopsies, in which DNA sequencing can be performed on tumor components that are found circulating in the blood of cancer patients (including circulating tumor cells and cell-free circulating tumor DNA) have rapidly gained traction in the past several decades and offer an unprecedented opportunity for real-time assessment of evolving tumor heterogeneity.
They have proved to be highly sensitive and specific, with a high degree of concordance with tissue biopsy, they can identify both clonal and subclonal mutations, and they can detect resistance substantially earlier than radiographic imaging, which could permit earlier intervention.10,11 The first liquid biopsy-based companion diagnostic test was approved by the US Food and Drug Administration in 2016, for the detection of EGFR mutations associated with NSCLC.
Yet, even liquid biopsy alone is not able to fully dissect the extent of tumor heterogeneity, especially because it is limited in its ability to assess spatial heterogeneity. Truly effective assessment of tumor heterogeneity is likely to require a combination of liquid biopsy, carefully selected tumor tissue biopsies, imaging diagnostics, and biomarkers.
The ongoing TRACERx (Tracking cancer evolution through therapy [Rx]) trials are evaluating a combination of approaches to follow tumor evolution across the course of treatment. The study in NSCLC began in 2014 with a target enrollment of 842 patients and will follow patients over 6 years. Preliminary data from the first 100 patients were recently published and demonstrated that increased intratumor heterogeneity correlated with increased risk of recurrence or death.12
If patients consent, the TRACERx trials also feed into the PEACE (Posthumous evaluation of advanced cancer environment) trials, which are collecting postmortem biopsies to further evaluate tumor heterogeneity and evolution. TRACERx trials in several other cancer types are now also underway.
Cutting off the source
The main therapeutic strategies for overcoming tumor heterogeneity are focused on the mechanisms of resistance that it drives. It is becoming increasingly apparent that rationally designed combinations of drugs are likely to be required and might need to be administered early in the course of disease to prevent resistance.
However, according to mathematical modeling studies, combinations of at least 3 drugs may be necessary.13 In many cases, this is unlikely to be feasible owing to the unavailability of drugs for certain targets and issues of toxicity, as well as the high cost.
An alternative strategy is to use immunotherapy, because a single treatment can target multiple neoantigens simultaneously. Although immunotherapy has proved to be a highly effective treatment paradigm in multiple tumor types, resistance still arises through varied mechanisms with tumor heterogeneity at their core.14,15
A promising avenue for drug development is to cut off the source of tumor heterogeneity – genomic instability and the mutagenic processes that foster it (Table 2). This is exemplified by the success of poly(ADP-ribose) polymerase (PARP) inhibitors in patients with breast cancer susceptibility (BRCA1/2) gene mutations.
Both germline and somatic mutations in the BRCA1/2 genes are observed in 10% to 15% of patients with ovarian cancer and a substantial number of patients with other types of cancer, including breast, pancreatic, and prostate cancers.16,17
These genes play a central role in the homologous recombination (HR) pathway of DNA repair, which repairs double-strand breaks in DNA. PARP inhibitors target a different DNA repair pathway, base excision repair, which repairs single-strand breaks. The use of PARP inhibitors in patients with BRCA1/2 mutations is designed to create irreparable damage to the DNA repair processes and drive an unsustainable level of genome instability that leads to cell death, whereas normal cells without HR deficiency can survive.18
A growing number of PARP inhibitors are now approved for use in the United States for the treatment of ovarian cancer. In January, olaparib became the first PARP inhibitor approved for patients with BRCA1/2-mutant breast cancer, based on data from the OlympiAD trial in which 302 patients were randomized to receive olaparib 300 mg twice daily or physician’s choice of chemotherapy. Olaparib improved progression-free survival from 4.2 months to 7.0 months (hazard ratio, 0.58; P = .0009), and the most common adverse events included anemia, nausea, fatigue, and vomiting.19
Tumors with other defects in HR have also shown susceptibility to PARP inhibition, shifting interest toward identifying and treating these tumors as a group, independent of histology – about a quarter of all tumors display HR deficiency.20 This novel strategy of targeting mutational processes across a range of tumor types has also been exploited in the development of immunotherapies.
Patients with defects in the mismatch repair (MMR) pathway and microsatellite instability (MSI) – multiple alterations in the length of microsatellite markers within the DNA – are more sensitive to immunotherapy, likely because they are predisposed to a high level of somatic mutations that can serve as neoantigens to provoke a strong anti-tumor immune response.
In 2017, 2 immune checkpoint inhibitors were approved for use in patients with MSI-high or defective MMR (dMMR) cancers. The indication for pembrolizumab (Keytruda) was independent of tumor histology, the first approval of its kind. It was based on the results of 5 clinical trials in which 149 patients with MSI-H or dMMR cancers were given pembrolizumab 200 mg every 3 weeks or 10 mg/kg every 2 weeks for a maximum of 24 months. The overall response rate was 39.6%, including 11 complete responses and 48 partial responses.21
A new paradigm
Treatment of a tumor is one of the major selective pressures that shapes its evolution and recent evidence has emerged that these selective pressures can be highly dynamic. Study findings have shown that there is a cost associated with evolution of resistant subclones and, if the selective pressure of therapy is removed, that cost may become too high, such that resistant subclones are then outcompeted by drug-sensitive ones. There have been reports of reversal of drug resistance when drug treatment is interrupted.
The current treatment paradigm is to try to eliminate tumors by hitting them hard and fast with the maximum tolerated dose (MTD) of a drug. However, there is increasing appreciation that this may be inadvertently fostering more rapid disease progression because it selects for the emergence of resistant cells and eliminates all their competitors (Figure 2).
This is driving a potential paradigm shift, in which researchers are applying concepts from evolutionary biology and the control of invasive species to the treatment of cancer. Instead of completely eliminating a cancer, a strategy of adaptive therapy could be used to set up competition between different subclones and keep tumor growth in check by exploiting the high cost of resistance.22
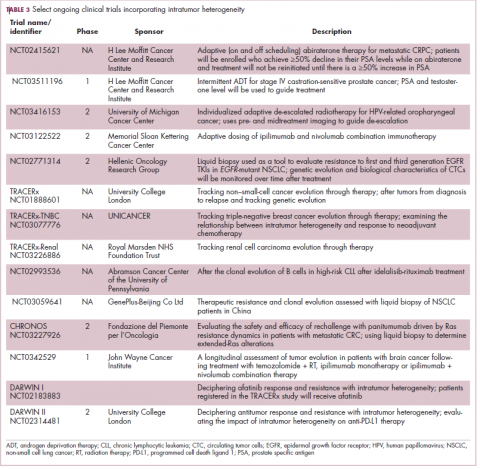
Adaptive therapy involves the use of treatment holidays, intermittent dosing schedules or reduced drug doses, rather than using the MTD. Adaptive therapy was tested recently in mice with triple-negative and estrogen receptor-positive breast cancer. The standard maximum dose of chemotherapy was compared with adaptive therapy with either reduced doses or skipped doses as the tumor responded. Tumor growth initially decreased with all 3 treatment scenarios, but then regrew when chemotherapy was stopped or doses were skipped. However, adaptive therapy with lower doses resulted in long-term stabilization of the tumor where treatment was eventually able to be withdrawn.23 Clinical trials of several different types of adaptive therapy strategies are ongoing (Table 3).
1. Dagogo-Jack I, Shaw AT. Tumour heterogeneity and resistance to cancer therapies. Nat Rev Clin Oncol. 2018;15(2):81-94.
2. Dzobo K, Senthebane DA, Thomford NE, Rowe A, Dandara C, Parker MI. Not everyone fits the mold: intratumor and intertumor heterogeneity and innovative cancer drug design and development. OMICS. 2018;22(1):17-34.
3. McGranahan N, Swanton C. Clonal heterogeneity and tumor evolution: past, present, and the future. Cell. 2017;168(4):613-628.
4. Davis A, Gao R, Navin N. Tumor evolution: linear, branching, neutral or punctuated? Biochim Biophys Acta. 2017;1867(2):151-161.
5. Amirouchene-Angelozzi N, Swanton C, Bardelli A. Tumor evolution as a therapeutic target. Cancer Discov. Published online first July 20, 2017. Accessed May 23, 2018. doi: 10.1158/2159-8290.CD-17-0343
6. Wu D, Wang DC, Cheng Y, et al. Roles of tumor heterogeneity in the development of drug resistance: a call for precision therapy. Semin Cancer Biol. 2017;42:13-19.
7. Ferguson LR, Chen H, Collins AR, et al. Genomic instability in human cancer: molecular insights and opportunities for therapeutic attack and prevention through diet and nutrition. Semin Cancer Biol. 2015;35(suppl):S5-S24.
8. Forbes SA, Beare D, Gunasekaran P, et al. COSMIC: exploring the world’s knowledge of somatic mutations in human cancer. Nucleic Acids Res. 2015;43(Database issue):D805-811.
9. Rosenthal R, McGranahan N, Herrero J, Swanton C. Deciphering genetic intratumor heterogeneity and its impact on cancer evolution. Ann Rev Cancer Biol. 2017;1(1):223-240.
10. Esposito A, Criscitiello C, Locatelli M, Milano M, Curigliano G. Liquid biopsies for solid tumors: understanding tumor heterogeneity and real time monitoring of early resistance to targeted therapies. Pharmacol Ther. 2016;157:120-124.
11. Venesio T, Siravegna G, Bardelli A, Sapino A. Liquid biopsies for monitoring temporal genomic heterogeneity in breast and colon cancers. Pathobiology. 2018;85(1-2):146-154.
12. Jamal-Hanjani M, Wilson GA, McGranahan N, et al. Tracking the evolution of non–small-cell lung cancer. New Engl J Med. 2017;376(22):2109-2121.
13. Bozic I, Reiter JG, Allen B, et al. Evolutionary dynamics of cancer in response to targeted combination therapy. Elife. 2013;2:e00747.
14. Zugazagoitia J, Guedes C, Ponce S, Ferrer I, Molina-Pinelo S, Paz-Ares L. Current challenges in cancer treatment. Clin Ther. 2016;38(7):1551-1566.
15. Ventola CL. Cancer immunotherapy, Part 3: challenges and future trends. PT. 2017;42(8):514-521.
16. Cavanagh H, Rogers KMA. The role of BRCA1 and BRCA2 mutations in prostate, pancreatic and stomach cancers. Hered Cancer Clin Pract. 2015;13:16.
17. Moschetta M, George A, Kaye SB, Banerjee S. BRCA somatic mutations and epigenetic BRCA modifications in serous ovarian cancer. Ann Oncol. 2016;27(8):1449-1455.
18. Brown JS, O’Carrigan B, Jackson SP, Yap TA. Targeting DNA repair in cancer: beyond PARP inhibitors. Cancer Discov. 2017;7(1):20-37.
19. Robson M, Im S-A, Senkus E, et al. Olaparib for Metastatic Breast Cancer in Patients with a Germline BRCA Mutation. New England Journal of Medicine. 2017;377(6):523-533.
20. Williers H, Pfaffle HN, Zou L. Targeting homologous recombination repair in cancer: molecular targets and clinical applications. In: Kelley M, Fishel M, eds. DNA repair in cancer therapy. 2nd ed: Academic Press; 2016:119-160.
21. U.S. Food and Drug Administration. FDA grants accelerated approval to pembrolizumab for first tissue/site agnostic indication. 2017; https://www.fda.gov/Drugs/InformationOnDrugs/ ApprovedDrugs/ucm560040.htm. Accessed May 1st,, 2018.
22. Gallaher JA, Enriquez-Navas PM, Luddy KA, Gatenby RA, Anderson ARA. Adaptive Therapy For Heterogeneous Cancer: Exploiting Space And Trade-Offs In Drug Scheduling. bioRxiv. 2017.
23. Enriquez-Navas PM, Kam Y, Das T, et al. Exploiting evolutionary principles to prolong tumor control in preclinical models of breast cancer. Sci Transl Med. 2016;8(327):327ra24.
A major challenge to effective cancer treatment is the astounding level of heterogeneity that tumors display on many different fronts. Here, we discuss how a deeper appreciation of this heterogeneity and its impact is driving research efforts to better understand and tackle it and a radical rethink of treatment paradigms.
A complex and dynamic disease
The nonuniformity of cancer has long been appreciated, reflected most visibly in the variation of response to the same treatment across patients with the same type of tumor (inter-tumor heterogeneity). The extent of tumor heterogeneity is being fully realized only now, with the advent of next-generation sequencing technologies. Even within the same tumor, there can be significant heterogeneity from cell to cell (intra-tumor heterogeneity), yielding substantial complexity in cancer.
Heterogeneity reveals itself on many different levels. Histologically speaking, tumors are composed of a nonhomogenous mass of cells that vary in type and number. In terms of their molecular make-up, there is substantial variation in the types of molecular alterations observed, all the way down to the single cell level. In even more abstract terms, beyond the cancer itself, the microenvironment in which it resides can be highly heterogeneous, composed of a plethora of different supportive and tumor-infiltrating normal cells.
Heterogeneity can manifest spatially, reflecting differences in the composition of the primary tumor and tumors at secondary sites or across regions of the same tumor mass and temporally, at different time points across a tumor’s natural history. Evocative of the second law of thermodynamics, cancers generally become more diverse and complex over time.1-3
A tale of 2 models
It is widely accepted that the transformation of a normal cell into a malignant one occurs with the acquisition of certain “hallmark” abilities, but there are myriad ways in which these can be attained.
The clonal evolution model
As cells divide, they randomly acquire mutations as a result of DNA damage. The clonal evolution model posits that cancer develops as the result of a multistep accumulation of a series of “driver” mutations that confer a promalignant advantage to the cell and ultimately fuel a cancerous hallmark.
This evolution can occur in a linear fashion, whereby the emergence of a new driver mutation conveys such a potent evolutionary advantage that it outcompetes all previous clones. There is limited evidence for linear evolution in most advanced human cancers; instead, they are thought to evolve predominantly through a process of branching evolution, in which multiple clones can diverge in parallel from a common ancestor through the acquisition of different driver mutations. This results in common clonal mutations that form the trunk of the cancer’s evolutionary tree and are shared by all cells and subclonal mutations, which make up the branches and differ from cell to cell.
More recently, several other mechanisms of clonal evolution have been proposed, including neutral evolution, a type of branching evolution in which there are no selective pressures and evolution occurs by random mutations occurring over time that lead to genetic drift, and punctuated evolution, in which there are short evolutionary bursts of hypermutation.4,5
The CSC model
This model posits that the ability to form and sustain a cancer is restricted to a single cell type – the cancer stem cells – which have the unique capacity for self-renewal and differentiation. Although the forces of evolution are still involved in this model, they act on a hierarchy of cells, with stem cells sitting at the top. A tumor is derived from a single stem cell that has acquired a mutation, and the heterogeneity observed results both from the differentiation and the accumulation of mutations in CSCs.
Accumulated experimental evidence suggests that these models are not mutually exclusive and that they can all contribute to heterogeneity in varied amounts across different tumor types. What is clear is that heterogeneity and evolution are intricately intertwined in cancer development.1,2,6
An unstable genome
Heterogeneity and evolution are fueled by genomic alterations and the genome instability that they foster. This genome instability can range from single base pair substitutions to a doubling of the entire genome and results from both exposure to exogenous mutagens (eg, chemicals and ultraviolet radiation) and genomic alterations that have an impact on important cellular processes (eg, DNA repair or replication).
Among the most common causes of genome instability are mutations in the DNA mismatch repair pathway proteins or in the proofreading polymerase enzymes. Genome instability is often associated with unique mutational signatures – characteristic combinations of mutations that arose as the result of the specific biological processes underlying them.7
Genome-wide analyses have begun to reveal these mutational signatures across the spectrum of human cancers. The Wellcome Sanger Institute’s Catalogue of Somatic Mutations in Cancer (COSMIC) database has generated a set of 30 mutational signatures based on analysis of almost 11,000 exomes and more than 1,000 whole genomes spanning 40 different cancer types, some of which have been linked with specific mutagenic processes, such as tobacco, UV radiation, and DNA repair deficiency (Table 1).8
Fueling resistance
Arguably, heterogeneity presents one of the most significant barriers to effective cancer therapy, and this has become increasingly true in the era of personalized medicine in which targeted therapies take aim at specific molecular abnormalities.
It is vital that drugs target the truncal alterations that are present in all cancer cells to ensure that the entire cancer is eradicated. However, it is not always possible to target these alterations, for example, at the present time tumor suppressor proteins like p53 are not druggable.
Even when truncal alterations have been targeted successfully, such as epidermal growth factor receptor (EGFR) mutations and anaplastic lymphoma kinase (ALK) chromosomal rearrangements in non–small-cell lung cancer (NSCLC) and BRAF mutations in melanoma, the long-term efficacy of these drugs is almost invariably limited by the development of resistance.
Tumor heterogeneity and the clonal evolution it fuels are central drivers of resistance. Because tumors are dynamic and continue to evolve, anticancer treatments can act as a strong selective pressure and drive the emergence of drug-resistant subclones that allow the tumor to persist. In fact, study findings have revealed that small populations of resistant cells may be present before treatment. Thus, resistance may also occur as a result of the outgrowth of preexisting treatment-resistant cells that suddenly find that they acquire a survival advantage in the presence of a drug.1,6
Tackling heterogeneity
Despite extensive clinical documentation of the existence of heterogeneity and its underlying mechanisms across a range of tumor types, the development of novel clinical trial designs and therapeutic strategies that account for its effects have only recently begun to be explored.
For the most part, this was because of a lack of effective methods for evaluating intratumor heterogeneity. Multiregion biopsies, in which tissue derived from multiple different regions of a single tumor mass or from distinct cancerous lesions within the same patient, give a snapshot of tumor heterogeneity at a single point in time. The repeated longitudinal sampling required to gain a deeper appreciation of tumor heterogeneity over the course of tumor evolution is often not possible because of the morbidity associated with repeated surgical procedures.
Liquid biopsies, in which DNA sequencing can be performed on tumor components that are found circulating in the blood of cancer patients (including circulating tumor cells and cell-free circulating tumor DNA) have rapidly gained traction in the past several decades and offer an unprecedented opportunity for real-time assessment of evolving tumor heterogeneity.
They have proved to be highly sensitive and specific, with a high degree of concordance with tissue biopsy, they can identify both clonal and subclonal mutations, and they can detect resistance substantially earlier than radiographic imaging, which could permit earlier intervention.10,11 The first liquid biopsy-based companion diagnostic test was approved by the US Food and Drug Administration in 2016, for the detection of EGFR mutations associated with NSCLC.
Yet, even liquid biopsy alone is not able to fully dissect the extent of tumor heterogeneity, especially because it is limited in its ability to assess spatial heterogeneity. Truly effective assessment of tumor heterogeneity is likely to require a combination of liquid biopsy, carefully selected tumor tissue biopsies, imaging diagnostics, and biomarkers.
The ongoing TRACERx (Tracking cancer evolution through therapy [Rx]) trials are evaluating a combination of approaches to follow tumor evolution across the course of treatment. The study in NSCLC began in 2014 with a target enrollment of 842 patients and will follow patients over 6 years. Preliminary data from the first 100 patients were recently published and demonstrated that increased intratumor heterogeneity correlated with increased risk of recurrence or death.12
If patients consent, the TRACERx trials also feed into the PEACE (Posthumous evaluation of advanced cancer environment) trials, which are collecting postmortem biopsies to further evaluate tumor heterogeneity and evolution. TRACERx trials in several other cancer types are now also underway.
Cutting off the source
The main therapeutic strategies for overcoming tumor heterogeneity are focused on the mechanisms of resistance that it drives. It is becoming increasingly apparent that rationally designed combinations of drugs are likely to be required and might need to be administered early in the course of disease to prevent resistance.
However, according to mathematical modeling studies, combinations of at least 3 drugs may be necessary.13 In many cases, this is unlikely to be feasible owing to the unavailability of drugs for certain targets and issues of toxicity, as well as the high cost.
An alternative strategy is to use immunotherapy, because a single treatment can target multiple neoantigens simultaneously. Although immunotherapy has proved to be a highly effective treatment paradigm in multiple tumor types, resistance still arises through varied mechanisms with tumor heterogeneity at their core.14,15
A promising avenue for drug development is to cut off the source of tumor heterogeneity – genomic instability and the mutagenic processes that foster it (Table 2). This is exemplified by the success of poly(ADP-ribose) polymerase (PARP) inhibitors in patients with breast cancer susceptibility (BRCA1/2) gene mutations.
Both germline and somatic mutations in the BRCA1/2 genes are observed in 10% to 15% of patients with ovarian cancer and a substantial number of patients with other types of cancer, including breast, pancreatic, and prostate cancers.16,17
These genes play a central role in the homologous recombination (HR) pathway of DNA repair, which repairs double-strand breaks in DNA. PARP inhibitors target a different DNA repair pathway, base excision repair, which repairs single-strand breaks. The use of PARP inhibitors in patients with BRCA1/2 mutations is designed to create irreparable damage to the DNA repair processes and drive an unsustainable level of genome instability that leads to cell death, whereas normal cells without HR deficiency can survive.18
A growing number of PARP inhibitors are now approved for use in the United States for the treatment of ovarian cancer. In January, olaparib became the first PARP inhibitor approved for patients with BRCA1/2-mutant breast cancer, based on data from the OlympiAD trial in which 302 patients were randomized to receive olaparib 300 mg twice daily or physician’s choice of chemotherapy. Olaparib improved progression-free survival from 4.2 months to 7.0 months (hazard ratio, 0.58; P = .0009), and the most common adverse events included anemia, nausea, fatigue, and vomiting.19
Tumors with other defects in HR have also shown susceptibility to PARP inhibition, shifting interest toward identifying and treating these tumors as a group, independent of histology – about a quarter of all tumors display HR deficiency.20 This novel strategy of targeting mutational processes across a range of tumor types has also been exploited in the development of immunotherapies.
Patients with defects in the mismatch repair (MMR) pathway and microsatellite instability (MSI) – multiple alterations in the length of microsatellite markers within the DNA – are more sensitive to immunotherapy, likely because they are predisposed to a high level of somatic mutations that can serve as neoantigens to provoke a strong anti-tumor immune response.
In 2017, 2 immune checkpoint inhibitors were approved for use in patients with MSI-high or defective MMR (dMMR) cancers. The indication for pembrolizumab (Keytruda) was independent of tumor histology, the first approval of its kind. It was based on the results of 5 clinical trials in which 149 patients with MSI-H or dMMR cancers were given pembrolizumab 200 mg every 3 weeks or 10 mg/kg every 2 weeks for a maximum of 24 months. The overall response rate was 39.6%, including 11 complete responses and 48 partial responses.21
A new paradigm
Treatment of a tumor is one of the major selective pressures that shapes its evolution and recent evidence has emerged that these selective pressures can be highly dynamic. Study findings have shown that there is a cost associated with evolution of resistant subclones and, if the selective pressure of therapy is removed, that cost may become too high, such that resistant subclones are then outcompeted by drug-sensitive ones. There have been reports of reversal of drug resistance when drug treatment is interrupted.
The current treatment paradigm is to try to eliminate tumors by hitting them hard and fast with the maximum tolerated dose (MTD) of a drug. However, there is increasing appreciation that this may be inadvertently fostering more rapid disease progression because it selects for the emergence of resistant cells and eliminates all their competitors (Figure 2).
This is driving a potential paradigm shift, in which researchers are applying concepts from evolutionary biology and the control of invasive species to the treatment of cancer. Instead of completely eliminating a cancer, a strategy of adaptive therapy could be used to set up competition between different subclones and keep tumor growth in check by exploiting the high cost of resistance.22
Adaptive therapy involves the use of treatment holidays, intermittent dosing schedules or reduced drug doses, rather than using the MTD. Adaptive therapy was tested recently in mice with triple-negative and estrogen receptor-positive breast cancer. The standard maximum dose of chemotherapy was compared with adaptive therapy with either reduced doses or skipped doses as the tumor responded. Tumor growth initially decreased with all 3 treatment scenarios, but then regrew when chemotherapy was stopped or doses were skipped. However, adaptive therapy with lower doses resulted in long-term stabilization of the tumor where treatment was eventually able to be withdrawn.23 Clinical trials of several different types of adaptive therapy strategies are ongoing (Table 3).
A major challenge to effective cancer treatment is the astounding level of heterogeneity that tumors display on many different fronts. Here, we discuss how a deeper appreciation of this heterogeneity and its impact is driving research efforts to better understand and tackle it and a radical rethink of treatment paradigms.
A complex and dynamic disease
The nonuniformity of cancer has long been appreciated, reflected most visibly in the variation of response to the same treatment across patients with the same type of tumor (inter-tumor heterogeneity). The extent of tumor heterogeneity is being fully realized only now, with the advent of next-generation sequencing technologies. Even within the same tumor, there can be significant heterogeneity from cell to cell (intra-tumor heterogeneity), yielding substantial complexity in cancer.
Heterogeneity reveals itself on many different levels. Histologically speaking, tumors are composed of a nonhomogenous mass of cells that vary in type and number. In terms of their molecular make-up, there is substantial variation in the types of molecular alterations observed, all the way down to the single cell level. In even more abstract terms, beyond the cancer itself, the microenvironment in which it resides can be highly heterogeneous, composed of a plethora of different supportive and tumor-infiltrating normal cells.
Heterogeneity can manifest spatially, reflecting differences in the composition of the primary tumor and tumors at secondary sites or across regions of the same tumor mass and temporally, at different time points across a tumor’s natural history. Evocative of the second law of thermodynamics, cancers generally become more diverse and complex over time.1-3
A tale of 2 models
It is widely accepted that the transformation of a normal cell into a malignant one occurs with the acquisition of certain “hallmark” abilities, but there are myriad ways in which these can be attained.
The clonal evolution model
As cells divide, they randomly acquire mutations as a result of DNA damage. The clonal evolution model posits that cancer develops as the result of a multistep accumulation of a series of “driver” mutations that confer a promalignant advantage to the cell and ultimately fuel a cancerous hallmark.
This evolution can occur in a linear fashion, whereby the emergence of a new driver mutation conveys such a potent evolutionary advantage that it outcompetes all previous clones. There is limited evidence for linear evolution in most advanced human cancers; instead, they are thought to evolve predominantly through a process of branching evolution, in which multiple clones can diverge in parallel from a common ancestor through the acquisition of different driver mutations. This results in common clonal mutations that form the trunk of the cancer’s evolutionary tree and are shared by all cells and subclonal mutations, which make up the branches and differ from cell to cell.
More recently, several other mechanisms of clonal evolution have been proposed, including neutral evolution, a type of branching evolution in which there are no selective pressures and evolution occurs by random mutations occurring over time that lead to genetic drift, and punctuated evolution, in which there are short evolutionary bursts of hypermutation.4,5
The CSC model
This model posits that the ability to form and sustain a cancer is restricted to a single cell type – the cancer stem cells – which have the unique capacity for self-renewal and differentiation. Although the forces of evolution are still involved in this model, they act on a hierarchy of cells, with stem cells sitting at the top. A tumor is derived from a single stem cell that has acquired a mutation, and the heterogeneity observed results both from the differentiation and the accumulation of mutations in CSCs.
Accumulated experimental evidence suggests that these models are not mutually exclusive and that they can all contribute to heterogeneity in varied amounts across different tumor types. What is clear is that heterogeneity and evolution are intricately intertwined in cancer development.1,2,6
An unstable genome
Heterogeneity and evolution are fueled by genomic alterations and the genome instability that they foster. This genome instability can range from single base pair substitutions to a doubling of the entire genome and results from both exposure to exogenous mutagens (eg, chemicals and ultraviolet radiation) and genomic alterations that have an impact on important cellular processes (eg, DNA repair or replication).
Among the most common causes of genome instability are mutations in the DNA mismatch repair pathway proteins or in the proofreading polymerase enzymes. Genome instability is often associated with unique mutational signatures – characteristic combinations of mutations that arose as the result of the specific biological processes underlying them.7
Genome-wide analyses have begun to reveal these mutational signatures across the spectrum of human cancers. The Wellcome Sanger Institute’s Catalogue of Somatic Mutations in Cancer (COSMIC) database has generated a set of 30 mutational signatures based on analysis of almost 11,000 exomes and more than 1,000 whole genomes spanning 40 different cancer types, some of which have been linked with specific mutagenic processes, such as tobacco, UV radiation, and DNA repair deficiency (Table 1).8
Fueling resistance
Arguably, heterogeneity presents one of the most significant barriers to effective cancer therapy, and this has become increasingly true in the era of personalized medicine in which targeted therapies take aim at specific molecular abnormalities.
It is vital that drugs target the truncal alterations that are present in all cancer cells to ensure that the entire cancer is eradicated. However, it is not always possible to target these alterations, for example, at the present time tumor suppressor proteins like p53 are not druggable.
Even when truncal alterations have been targeted successfully, such as epidermal growth factor receptor (EGFR) mutations and anaplastic lymphoma kinase (ALK) chromosomal rearrangements in non–small-cell lung cancer (NSCLC) and BRAF mutations in melanoma, the long-term efficacy of these drugs is almost invariably limited by the development of resistance.
Tumor heterogeneity and the clonal evolution it fuels are central drivers of resistance. Because tumors are dynamic and continue to evolve, anticancer treatments can act as a strong selective pressure and drive the emergence of drug-resistant subclones that allow the tumor to persist. In fact, study findings have revealed that small populations of resistant cells may be present before treatment. Thus, resistance may also occur as a result of the outgrowth of preexisting treatment-resistant cells that suddenly find that they acquire a survival advantage in the presence of a drug.1,6
Tackling heterogeneity
Despite extensive clinical documentation of the existence of heterogeneity and its underlying mechanisms across a range of tumor types, the development of novel clinical trial designs and therapeutic strategies that account for its effects have only recently begun to be explored.
For the most part, this was because of a lack of effective methods for evaluating intratumor heterogeneity. Multiregion biopsies, in which tissue derived from multiple different regions of a single tumor mass or from distinct cancerous lesions within the same patient, give a snapshot of tumor heterogeneity at a single point in time. The repeated longitudinal sampling required to gain a deeper appreciation of tumor heterogeneity over the course of tumor evolution is often not possible because of the morbidity associated with repeated surgical procedures.
Liquid biopsies, in which DNA sequencing can be performed on tumor components that are found circulating in the blood of cancer patients (including circulating tumor cells and cell-free circulating tumor DNA) have rapidly gained traction in the past several decades and offer an unprecedented opportunity for real-time assessment of evolving tumor heterogeneity.
They have proved to be highly sensitive and specific, with a high degree of concordance with tissue biopsy, they can identify both clonal and subclonal mutations, and they can detect resistance substantially earlier than radiographic imaging, which could permit earlier intervention.10,11 The first liquid biopsy-based companion diagnostic test was approved by the US Food and Drug Administration in 2016, for the detection of EGFR mutations associated with NSCLC.
Yet, even liquid biopsy alone is not able to fully dissect the extent of tumor heterogeneity, especially because it is limited in its ability to assess spatial heterogeneity. Truly effective assessment of tumor heterogeneity is likely to require a combination of liquid biopsy, carefully selected tumor tissue biopsies, imaging diagnostics, and biomarkers.
The ongoing TRACERx (Tracking cancer evolution through therapy [Rx]) trials are evaluating a combination of approaches to follow tumor evolution across the course of treatment. The study in NSCLC began in 2014 with a target enrollment of 842 patients and will follow patients over 6 years. Preliminary data from the first 100 patients were recently published and demonstrated that increased intratumor heterogeneity correlated with increased risk of recurrence or death.12
If patients consent, the TRACERx trials also feed into the PEACE (Posthumous evaluation of advanced cancer environment) trials, which are collecting postmortem biopsies to further evaluate tumor heterogeneity and evolution. TRACERx trials in several other cancer types are now also underway.
Cutting off the source
The main therapeutic strategies for overcoming tumor heterogeneity are focused on the mechanisms of resistance that it drives. It is becoming increasingly apparent that rationally designed combinations of drugs are likely to be required and might need to be administered early in the course of disease to prevent resistance.
However, according to mathematical modeling studies, combinations of at least 3 drugs may be necessary.13 In many cases, this is unlikely to be feasible owing to the unavailability of drugs for certain targets and issues of toxicity, as well as the high cost.
An alternative strategy is to use immunotherapy, because a single treatment can target multiple neoantigens simultaneously. Although immunotherapy has proved to be a highly effective treatment paradigm in multiple tumor types, resistance still arises through varied mechanisms with tumor heterogeneity at their core.14,15
A promising avenue for drug development is to cut off the source of tumor heterogeneity – genomic instability and the mutagenic processes that foster it (Table 2). This is exemplified by the success of poly(ADP-ribose) polymerase (PARP) inhibitors in patients with breast cancer susceptibility (BRCA1/2) gene mutations.
Both germline and somatic mutations in the BRCA1/2 genes are observed in 10% to 15% of patients with ovarian cancer and a substantial number of patients with other types of cancer, including breast, pancreatic, and prostate cancers.16,17
These genes play a central role in the homologous recombination (HR) pathway of DNA repair, which repairs double-strand breaks in DNA. PARP inhibitors target a different DNA repair pathway, base excision repair, which repairs single-strand breaks. The use of PARP inhibitors in patients with BRCA1/2 mutations is designed to create irreparable damage to the DNA repair processes and drive an unsustainable level of genome instability that leads to cell death, whereas normal cells without HR deficiency can survive.18
A growing number of PARP inhibitors are now approved for use in the United States for the treatment of ovarian cancer. In January, olaparib became the first PARP inhibitor approved for patients with BRCA1/2-mutant breast cancer, based on data from the OlympiAD trial in which 302 patients were randomized to receive olaparib 300 mg twice daily or physician’s choice of chemotherapy. Olaparib improved progression-free survival from 4.2 months to 7.0 months (hazard ratio, 0.58; P = .0009), and the most common adverse events included anemia, nausea, fatigue, and vomiting.19
Tumors with other defects in HR have also shown susceptibility to PARP inhibition, shifting interest toward identifying and treating these tumors as a group, independent of histology – about a quarter of all tumors display HR deficiency.20 This novel strategy of targeting mutational processes across a range of tumor types has also been exploited in the development of immunotherapies.
Patients with defects in the mismatch repair (MMR) pathway and microsatellite instability (MSI) – multiple alterations in the length of microsatellite markers within the DNA – are more sensitive to immunotherapy, likely because they are predisposed to a high level of somatic mutations that can serve as neoantigens to provoke a strong anti-tumor immune response.
In 2017, 2 immune checkpoint inhibitors were approved for use in patients with MSI-high or defective MMR (dMMR) cancers. The indication for pembrolizumab (Keytruda) was independent of tumor histology, the first approval of its kind. It was based on the results of 5 clinical trials in which 149 patients with MSI-H or dMMR cancers were given pembrolizumab 200 mg every 3 weeks or 10 mg/kg every 2 weeks for a maximum of 24 months. The overall response rate was 39.6%, including 11 complete responses and 48 partial responses.21
A new paradigm
Treatment of a tumor is one of the major selective pressures that shapes its evolution and recent evidence has emerged that these selective pressures can be highly dynamic. Study findings have shown that there is a cost associated with evolution of resistant subclones and, if the selective pressure of therapy is removed, that cost may become too high, such that resistant subclones are then outcompeted by drug-sensitive ones. There have been reports of reversal of drug resistance when drug treatment is interrupted.
The current treatment paradigm is to try to eliminate tumors by hitting them hard and fast with the maximum tolerated dose (MTD) of a drug. However, there is increasing appreciation that this may be inadvertently fostering more rapid disease progression because it selects for the emergence of resistant cells and eliminates all their competitors (Figure 2).
This is driving a potential paradigm shift, in which researchers are applying concepts from evolutionary biology and the control of invasive species to the treatment of cancer. Instead of completely eliminating a cancer, a strategy of adaptive therapy could be used to set up competition between different subclones and keep tumor growth in check by exploiting the high cost of resistance.22
Adaptive therapy involves the use of treatment holidays, intermittent dosing schedules or reduced drug doses, rather than using the MTD. Adaptive therapy was tested recently in mice with triple-negative and estrogen receptor-positive breast cancer. The standard maximum dose of chemotherapy was compared with adaptive therapy with either reduced doses or skipped doses as the tumor responded. Tumor growth initially decreased with all 3 treatment scenarios, but then regrew when chemotherapy was stopped or doses were skipped. However, adaptive therapy with lower doses resulted in long-term stabilization of the tumor where treatment was eventually able to be withdrawn.23 Clinical trials of several different types of adaptive therapy strategies are ongoing (Table 3).
1. Dagogo-Jack I, Shaw AT. Tumour heterogeneity and resistance to cancer therapies. Nat Rev Clin Oncol. 2018;15(2):81-94.
2. Dzobo K, Senthebane DA, Thomford NE, Rowe A, Dandara C, Parker MI. Not everyone fits the mold: intratumor and intertumor heterogeneity and innovative cancer drug design and development. OMICS. 2018;22(1):17-34.
3. McGranahan N, Swanton C. Clonal heterogeneity and tumor evolution: past, present, and the future. Cell. 2017;168(4):613-628.
4. Davis A, Gao R, Navin N. Tumor evolution: linear, branching, neutral or punctuated? Biochim Biophys Acta. 2017;1867(2):151-161.
5. Amirouchene-Angelozzi N, Swanton C, Bardelli A. Tumor evolution as a therapeutic target. Cancer Discov. Published online first July 20, 2017. Accessed May 23, 2018. doi: 10.1158/2159-8290.CD-17-0343
6. Wu D, Wang DC, Cheng Y, et al. Roles of tumor heterogeneity in the development of drug resistance: a call for precision therapy. Semin Cancer Biol. 2017;42:13-19.
7. Ferguson LR, Chen H, Collins AR, et al. Genomic instability in human cancer: molecular insights and opportunities for therapeutic attack and prevention through diet and nutrition. Semin Cancer Biol. 2015;35(suppl):S5-S24.
8. Forbes SA, Beare D, Gunasekaran P, et al. COSMIC: exploring the world’s knowledge of somatic mutations in human cancer. Nucleic Acids Res. 2015;43(Database issue):D805-811.
9. Rosenthal R, McGranahan N, Herrero J, Swanton C. Deciphering genetic intratumor heterogeneity and its impact on cancer evolution. Ann Rev Cancer Biol. 2017;1(1):223-240.
10. Esposito A, Criscitiello C, Locatelli M, Milano M, Curigliano G. Liquid biopsies for solid tumors: understanding tumor heterogeneity and real time monitoring of early resistance to targeted therapies. Pharmacol Ther. 2016;157:120-124.
11. Venesio T, Siravegna G, Bardelli A, Sapino A. Liquid biopsies for monitoring temporal genomic heterogeneity in breast and colon cancers. Pathobiology. 2018;85(1-2):146-154.
12. Jamal-Hanjani M, Wilson GA, McGranahan N, et al. Tracking the evolution of non–small-cell lung cancer. New Engl J Med. 2017;376(22):2109-2121.
13. Bozic I, Reiter JG, Allen B, et al. Evolutionary dynamics of cancer in response to targeted combination therapy. Elife. 2013;2:e00747.
14. Zugazagoitia J, Guedes C, Ponce S, Ferrer I, Molina-Pinelo S, Paz-Ares L. Current challenges in cancer treatment. Clin Ther. 2016;38(7):1551-1566.
15. Ventola CL. Cancer immunotherapy, Part 3: challenges and future trends. PT. 2017;42(8):514-521.
16. Cavanagh H, Rogers KMA. The role of BRCA1 and BRCA2 mutations in prostate, pancreatic and stomach cancers. Hered Cancer Clin Pract. 2015;13:16.
17. Moschetta M, George A, Kaye SB, Banerjee S. BRCA somatic mutations and epigenetic BRCA modifications in serous ovarian cancer. Ann Oncol. 2016;27(8):1449-1455.
18. Brown JS, O’Carrigan B, Jackson SP, Yap TA. Targeting DNA repair in cancer: beyond PARP inhibitors. Cancer Discov. 2017;7(1):20-37.
19. Robson M, Im S-A, Senkus E, et al. Olaparib for Metastatic Breast Cancer in Patients with a Germline BRCA Mutation. New England Journal of Medicine. 2017;377(6):523-533.
20. Williers H, Pfaffle HN, Zou L. Targeting homologous recombination repair in cancer: molecular targets and clinical applications. In: Kelley M, Fishel M, eds. DNA repair in cancer therapy. 2nd ed: Academic Press; 2016:119-160.
21. U.S. Food and Drug Administration. FDA grants accelerated approval to pembrolizumab for first tissue/site agnostic indication. 2017; https://www.fda.gov/Drugs/InformationOnDrugs/ ApprovedDrugs/ucm560040.htm. Accessed May 1st,, 2018.
22. Gallaher JA, Enriquez-Navas PM, Luddy KA, Gatenby RA, Anderson ARA. Adaptive Therapy For Heterogeneous Cancer: Exploiting Space And Trade-Offs In Drug Scheduling. bioRxiv. 2017.
23. Enriquez-Navas PM, Kam Y, Das T, et al. Exploiting evolutionary principles to prolong tumor control in preclinical models of breast cancer. Sci Transl Med. 2016;8(327):327ra24.
1. Dagogo-Jack I, Shaw AT. Tumour heterogeneity and resistance to cancer therapies. Nat Rev Clin Oncol. 2018;15(2):81-94.
2. Dzobo K, Senthebane DA, Thomford NE, Rowe A, Dandara C, Parker MI. Not everyone fits the mold: intratumor and intertumor heterogeneity and innovative cancer drug design and development. OMICS. 2018;22(1):17-34.
3. McGranahan N, Swanton C. Clonal heterogeneity and tumor evolution: past, present, and the future. Cell. 2017;168(4):613-628.
4. Davis A, Gao R, Navin N. Tumor evolution: linear, branching, neutral or punctuated? Biochim Biophys Acta. 2017;1867(2):151-161.
5. Amirouchene-Angelozzi N, Swanton C, Bardelli A. Tumor evolution as a therapeutic target. Cancer Discov. Published online first July 20, 2017. Accessed May 23, 2018. doi: 10.1158/2159-8290.CD-17-0343
6. Wu D, Wang DC, Cheng Y, et al. Roles of tumor heterogeneity in the development of drug resistance: a call for precision therapy. Semin Cancer Biol. 2017;42:13-19.
7. Ferguson LR, Chen H, Collins AR, et al. Genomic instability in human cancer: molecular insights and opportunities for therapeutic attack and prevention through diet and nutrition. Semin Cancer Biol. 2015;35(suppl):S5-S24.
8. Forbes SA, Beare D, Gunasekaran P, et al. COSMIC: exploring the world’s knowledge of somatic mutations in human cancer. Nucleic Acids Res. 2015;43(Database issue):D805-811.
9. Rosenthal R, McGranahan N, Herrero J, Swanton C. Deciphering genetic intratumor heterogeneity and its impact on cancer evolution. Ann Rev Cancer Biol. 2017;1(1):223-240.
10. Esposito A, Criscitiello C, Locatelli M, Milano M, Curigliano G. Liquid biopsies for solid tumors: understanding tumor heterogeneity and real time monitoring of early resistance to targeted therapies. Pharmacol Ther. 2016;157:120-124.
11. Venesio T, Siravegna G, Bardelli A, Sapino A. Liquid biopsies for monitoring temporal genomic heterogeneity in breast and colon cancers. Pathobiology. 2018;85(1-2):146-154.
12. Jamal-Hanjani M, Wilson GA, McGranahan N, et al. Tracking the evolution of non–small-cell lung cancer. New Engl J Med. 2017;376(22):2109-2121.
13. Bozic I, Reiter JG, Allen B, et al. Evolutionary dynamics of cancer in response to targeted combination therapy. Elife. 2013;2:e00747.
14. Zugazagoitia J, Guedes C, Ponce S, Ferrer I, Molina-Pinelo S, Paz-Ares L. Current challenges in cancer treatment. Clin Ther. 2016;38(7):1551-1566.
15. Ventola CL. Cancer immunotherapy, Part 3: challenges and future trends. PT. 2017;42(8):514-521.
16. Cavanagh H, Rogers KMA. The role of BRCA1 and BRCA2 mutations in prostate, pancreatic and stomach cancers. Hered Cancer Clin Pract. 2015;13:16.
17. Moschetta M, George A, Kaye SB, Banerjee S. BRCA somatic mutations and epigenetic BRCA modifications in serous ovarian cancer. Ann Oncol. 2016;27(8):1449-1455.
18. Brown JS, O’Carrigan B, Jackson SP, Yap TA. Targeting DNA repair in cancer: beyond PARP inhibitors. Cancer Discov. 2017;7(1):20-37.
19. Robson M, Im S-A, Senkus E, et al. Olaparib for Metastatic Breast Cancer in Patients with a Germline BRCA Mutation. New England Journal of Medicine. 2017;377(6):523-533.
20. Williers H, Pfaffle HN, Zou L. Targeting homologous recombination repair in cancer: molecular targets and clinical applications. In: Kelley M, Fishel M, eds. DNA repair in cancer therapy. 2nd ed: Academic Press; 2016:119-160.
21. U.S. Food and Drug Administration. FDA grants accelerated approval to pembrolizumab for first tissue/site agnostic indication. 2017; https://www.fda.gov/Drugs/InformationOnDrugs/ ApprovedDrugs/ucm560040.htm. Accessed May 1st,, 2018.
22. Gallaher JA, Enriquez-Navas PM, Luddy KA, Gatenby RA, Anderson ARA. Adaptive Therapy For Heterogeneous Cancer: Exploiting Space And Trade-Offs In Drug Scheduling. bioRxiv. 2017.
23. Enriquez-Navas PM, Kam Y, Das T, et al. Exploiting evolutionary principles to prolong tumor control in preclinical models of breast cancer. Sci Transl Med. 2016;8(327):327ra24.
FDA database reveals many rheumatic and musculoskeletal adverse events on immunotherapies
AMSTERDAM – Mining of the Food and Drug Administration adverse events database revealed a more substantial risk of rheumatic and musculoskeletal events on checkpoint inhibitor therapy than has been previously reported, according to Xerxes N. Pundole, PhD, an instructor in the research faculty at the University of Texas MD Anderson Cancer Center, Houston.
In a video interview, Dr. Pundole summarized data he presented at the European Congress of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
So far, according to Dr. Pundole, there have been a relatively limited number of reports in the medical literature of inflammatory rheumatic or musculoskeletal events from checkpoint inhibitors. However, other inflammatory conditions, such as colitis and pneumonitis, are known to occur commonly with these agents. The FDA adverse event database provided an opportunity to evaluate how often rheumatic and musculoskeletal events are reported in the real world.
In this interview, Dr. Pundole explained that rheumatic and musculoskeletal events do occur at higher rates than would be expected in patients not treated with a checkpoint inhibitor. With data from more than 30,000 unique patients, the relative risks of some of these adverse events, such as polymyositis, were more than doubled, although the event rates were not evenly distributed.
Specifically, rheumatic and musculoskeletal adverse events were far less common with the cytotoxic T-lymphocyte antigen 4 checkpoint inhibitor ipilimumab (Yervoy) relative to programmed cell death protein 1 inhibitors, particularly nivolumab (Opdivo).
In another notable finding, a demographic stratification of the FDA database found elderly men to be overrepresented among patients developing adverse events related to musculoskeletal inflammation.
Overall, his data do support a relationship between checkpoint inhibitors and a greater risk of rheumatic and musculoskeletal adverse events than has been previously reported, but he noted that these data provide no specific guidance for those who already have RA or another inflammatory condition.
“Can you identify these adverse events early on to keep the patients on immune checkpoint inhibitor therapy and not have to stop their cancer treatment? That’s a question,” Dr. Pundole said. However, he suggested that the FDA data support clinician awareness of the problem and the studies that will establish strategies for preserving the benefit-to-risk ratio of checkpoint inhibitors in patients who are at greater risk of adverse events relative to immune function because of a preexisting inflammatory condition.
SOURCE: Pundole XN et al. Ann Rheum Dis. 2018;77(Suppl 2):147-148. Abstract OP0197.
AMSTERDAM – Mining of the Food and Drug Administration adverse events database revealed a more substantial risk of rheumatic and musculoskeletal events on checkpoint inhibitor therapy than has been previously reported, according to Xerxes N. Pundole, PhD, an instructor in the research faculty at the University of Texas MD Anderson Cancer Center, Houston.
In a video interview, Dr. Pundole summarized data he presented at the European Congress of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
So far, according to Dr. Pundole, there have been a relatively limited number of reports in the medical literature of inflammatory rheumatic or musculoskeletal events from checkpoint inhibitors. However, other inflammatory conditions, such as colitis and pneumonitis, are known to occur commonly with these agents. The FDA adverse event database provided an opportunity to evaluate how often rheumatic and musculoskeletal events are reported in the real world.
In this interview, Dr. Pundole explained that rheumatic and musculoskeletal events do occur at higher rates than would be expected in patients not treated with a checkpoint inhibitor. With data from more than 30,000 unique patients, the relative risks of some of these adverse events, such as polymyositis, were more than doubled, although the event rates were not evenly distributed.
Specifically, rheumatic and musculoskeletal adverse events were far less common with the cytotoxic T-lymphocyte antigen 4 checkpoint inhibitor ipilimumab (Yervoy) relative to programmed cell death protein 1 inhibitors, particularly nivolumab (Opdivo).
In another notable finding, a demographic stratification of the FDA database found elderly men to be overrepresented among patients developing adverse events related to musculoskeletal inflammation.
Overall, his data do support a relationship between checkpoint inhibitors and a greater risk of rheumatic and musculoskeletal adverse events than has been previously reported, but he noted that these data provide no specific guidance for those who already have RA or another inflammatory condition.
“Can you identify these adverse events early on to keep the patients on immune checkpoint inhibitor therapy and not have to stop their cancer treatment? That’s a question,” Dr. Pundole said. However, he suggested that the FDA data support clinician awareness of the problem and the studies that will establish strategies for preserving the benefit-to-risk ratio of checkpoint inhibitors in patients who are at greater risk of adverse events relative to immune function because of a preexisting inflammatory condition.
SOURCE: Pundole XN et al. Ann Rheum Dis. 2018;77(Suppl 2):147-148. Abstract OP0197.
AMSTERDAM – Mining of the Food and Drug Administration adverse events database revealed a more substantial risk of rheumatic and musculoskeletal events on checkpoint inhibitor therapy than has been previously reported, according to Xerxes N. Pundole, PhD, an instructor in the research faculty at the University of Texas MD Anderson Cancer Center, Houston.
In a video interview, Dr. Pundole summarized data he presented at the European Congress of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
So far, according to Dr. Pundole, there have been a relatively limited number of reports in the medical literature of inflammatory rheumatic or musculoskeletal events from checkpoint inhibitors. However, other inflammatory conditions, such as colitis and pneumonitis, are known to occur commonly with these agents. The FDA adverse event database provided an opportunity to evaluate how often rheumatic and musculoskeletal events are reported in the real world.
In this interview, Dr. Pundole explained that rheumatic and musculoskeletal events do occur at higher rates than would be expected in patients not treated with a checkpoint inhibitor. With data from more than 30,000 unique patients, the relative risks of some of these adverse events, such as polymyositis, were more than doubled, although the event rates were not evenly distributed.
Specifically, rheumatic and musculoskeletal adverse events were far less common with the cytotoxic T-lymphocyte antigen 4 checkpoint inhibitor ipilimumab (Yervoy) relative to programmed cell death protein 1 inhibitors, particularly nivolumab (Opdivo).
In another notable finding, a demographic stratification of the FDA database found elderly men to be overrepresented among patients developing adverse events related to musculoskeletal inflammation.
Overall, his data do support a relationship between checkpoint inhibitors and a greater risk of rheumatic and musculoskeletal adverse events than has been previously reported, but he noted that these data provide no specific guidance for those who already have RA or another inflammatory condition.
“Can you identify these adverse events early on to keep the patients on immune checkpoint inhibitor therapy and not have to stop their cancer treatment? That’s a question,” Dr. Pundole said. However, he suggested that the FDA data support clinician awareness of the problem and the studies that will establish strategies for preserving the benefit-to-risk ratio of checkpoint inhibitors in patients who are at greater risk of adverse events relative to immune function because of a preexisting inflammatory condition.
SOURCE: Pundole XN et al. Ann Rheum Dis. 2018;77(Suppl 2):147-148. Abstract OP0197.
REPORTING FROM THE EULAR 2018 CONGRESS
MRD-negative status signals better outcomes in CAR T–treated ALL
CHICAGO – Minimal residual disease (MRD)–negative complete remission was strongly associated with improved survival outcomes in patients with B-cell acute lymphocytic leukemia (ALL) who received CD19 chimeric antigen receptor (CAR) T cells, results of a retrospective study showed.
Allogeneic hematopoietic stem cell transplant (HSCT) appeared to improve both disease-free and overall survival in those patients who had achieved MRD-negative complete remission, according to results of the study, which were presented at the annual meeting of the American Society of Clinical Oncology.
“Based upon our interaction testing, the potential benefit [of transplant] appears to exist in both good-risk and bad-risk patients as identified through multivariate modeling,” said study investigator Kevin Anthony Hay, MD, of Fred Hutchinson Cancer Research Center, Seattle.
In a comment on the results, Sarah Cooley, MD, noted that the benefits of allogeneic transplant were apparent regardless of whether the patients met criteria for the good-risk subgroup, which was defined by levels of lactate dehydrogenase (LDH) and platelets along with exposure to fludarabine as part of the conditioning regimen.
“I think this suggests that the goal at this point is to get patients to an MRD-negative state and to potentially curative transplant,” said Dr. Cooley, director of investigator-initiated research at Masonic Medical Center at the University of Minnesota, Minneapolis.
The retrospective analysis by Dr. Hay and his colleagues included 53 adults with relapsed or refractory ALL who had bone marrow or extramedullary disease at baseline and had received CD19 CAR T cells at or under the maximum tolerated dose at least 1 year prior to this analysis. Of that group, 45 (85%) achieved MRD-negative complete remission.
Those patients who did achieve MRD-negative complete remission had an improved median disease-free survival at 7.6 months versus 0.8 months (P less than .0001) and improved overall survival at 20.0 months versus 5.0 months (P = 0.014).
Most of the MRD-negative patients who relapsed did so within the first 6 months, an observation that led investigators to consider whether factors exist that could predict better outcomes.
In a multivariate analysis, they found three variables associated with disease free survival: higher LDH prior to lymphodepletion (hazard ratio, 1.39), along with higher platelet count prior to lymphodepletion and incorporation of fludarabine into the regimen, with hazard ratios of 0.65 and 0.34, respectively.
Using those three characteristics, investigators grouped patients as “good risk” if they had normal LDH, platelet count at or above 100 prior to lymphodepletion that included fludarabine. The 24-month disease-free survival for good-risk patients was 78%, and overall survival was 86%.
The role of allogeneic HSCT after ALL patients achieved MRD-negative complete remission with CAR T-cell therapy was one of the “major questions in the field,” Dr. Hay said.
In this analysis, Dr. Hay and colleagues found that patients who underwent transplant in MRD-negative complete remission had a 24-month disease free survival and overall survival of 61% and 72%, respectively, both of which were significantly higher than in patients with MRD-negative complete remission who had no transplant.
The disease-free survival benefit was not specific to the good-risk group, according to Dr. Hay, who said an interaction test demonstrated no significant interaction between risk group and allogeneic HSCT after CAR T-cell infusion (P = 0.53).
“This is a very important finding that should be further [studied] in an appropriately designed clinical trial,” Dr. Hay said during an oral presentation of the study results.
Dr. Hay and several coauthors reported financial disclosures related to Juno Therapeutics. Other disclosures reported by study coauthors included Cell Medica, Celgene, Eureka Therapeutics, Genentech/Roche, Gilead Sciences, Kite Pharma, Novartis, and others.
SOURCE: Hay KA. ASCO 2018, Abstract 7005.
CHICAGO – Minimal residual disease (MRD)–negative complete remission was strongly associated with improved survival outcomes in patients with B-cell acute lymphocytic leukemia (ALL) who received CD19 chimeric antigen receptor (CAR) T cells, results of a retrospective study showed.
Allogeneic hematopoietic stem cell transplant (HSCT) appeared to improve both disease-free and overall survival in those patients who had achieved MRD-negative complete remission, according to results of the study, which were presented at the annual meeting of the American Society of Clinical Oncology.
“Based upon our interaction testing, the potential benefit [of transplant] appears to exist in both good-risk and bad-risk patients as identified through multivariate modeling,” said study investigator Kevin Anthony Hay, MD, of Fred Hutchinson Cancer Research Center, Seattle.
In a comment on the results, Sarah Cooley, MD, noted that the benefits of allogeneic transplant were apparent regardless of whether the patients met criteria for the good-risk subgroup, which was defined by levels of lactate dehydrogenase (LDH) and platelets along with exposure to fludarabine as part of the conditioning regimen.
“I think this suggests that the goal at this point is to get patients to an MRD-negative state and to potentially curative transplant,” said Dr. Cooley, director of investigator-initiated research at Masonic Medical Center at the University of Minnesota, Minneapolis.
The retrospective analysis by Dr. Hay and his colleagues included 53 adults with relapsed or refractory ALL who had bone marrow or extramedullary disease at baseline and had received CD19 CAR T cells at or under the maximum tolerated dose at least 1 year prior to this analysis. Of that group, 45 (85%) achieved MRD-negative complete remission.
Those patients who did achieve MRD-negative complete remission had an improved median disease-free survival at 7.6 months versus 0.8 months (P less than .0001) and improved overall survival at 20.0 months versus 5.0 months (P = 0.014).
Most of the MRD-negative patients who relapsed did so within the first 6 months, an observation that led investigators to consider whether factors exist that could predict better outcomes.
In a multivariate analysis, they found three variables associated with disease free survival: higher LDH prior to lymphodepletion (hazard ratio, 1.39), along with higher platelet count prior to lymphodepletion and incorporation of fludarabine into the regimen, with hazard ratios of 0.65 and 0.34, respectively.
Using those three characteristics, investigators grouped patients as “good risk” if they had normal LDH, platelet count at or above 100 prior to lymphodepletion that included fludarabine. The 24-month disease-free survival for good-risk patients was 78%, and overall survival was 86%.
The role of allogeneic HSCT after ALL patients achieved MRD-negative complete remission with CAR T-cell therapy was one of the “major questions in the field,” Dr. Hay said.
In this analysis, Dr. Hay and colleagues found that patients who underwent transplant in MRD-negative complete remission had a 24-month disease free survival and overall survival of 61% and 72%, respectively, both of which were significantly higher than in patients with MRD-negative complete remission who had no transplant.
The disease-free survival benefit was not specific to the good-risk group, according to Dr. Hay, who said an interaction test demonstrated no significant interaction between risk group and allogeneic HSCT after CAR T-cell infusion (P = 0.53).
“This is a very important finding that should be further [studied] in an appropriately designed clinical trial,” Dr. Hay said during an oral presentation of the study results.
Dr. Hay and several coauthors reported financial disclosures related to Juno Therapeutics. Other disclosures reported by study coauthors included Cell Medica, Celgene, Eureka Therapeutics, Genentech/Roche, Gilead Sciences, Kite Pharma, Novartis, and others.
SOURCE: Hay KA. ASCO 2018, Abstract 7005.
CHICAGO – Minimal residual disease (MRD)–negative complete remission was strongly associated with improved survival outcomes in patients with B-cell acute lymphocytic leukemia (ALL) who received CD19 chimeric antigen receptor (CAR) T cells, results of a retrospective study showed.
Allogeneic hematopoietic stem cell transplant (HSCT) appeared to improve both disease-free and overall survival in those patients who had achieved MRD-negative complete remission, according to results of the study, which were presented at the annual meeting of the American Society of Clinical Oncology.
“Based upon our interaction testing, the potential benefit [of transplant] appears to exist in both good-risk and bad-risk patients as identified through multivariate modeling,” said study investigator Kevin Anthony Hay, MD, of Fred Hutchinson Cancer Research Center, Seattle.
In a comment on the results, Sarah Cooley, MD, noted that the benefits of allogeneic transplant were apparent regardless of whether the patients met criteria for the good-risk subgroup, which was defined by levels of lactate dehydrogenase (LDH) and platelets along with exposure to fludarabine as part of the conditioning regimen.
“I think this suggests that the goal at this point is to get patients to an MRD-negative state and to potentially curative transplant,” said Dr. Cooley, director of investigator-initiated research at Masonic Medical Center at the University of Minnesota, Minneapolis.
The retrospective analysis by Dr. Hay and his colleagues included 53 adults with relapsed or refractory ALL who had bone marrow or extramedullary disease at baseline and had received CD19 CAR T cells at or under the maximum tolerated dose at least 1 year prior to this analysis. Of that group, 45 (85%) achieved MRD-negative complete remission.
Those patients who did achieve MRD-negative complete remission had an improved median disease-free survival at 7.6 months versus 0.8 months (P less than .0001) and improved overall survival at 20.0 months versus 5.0 months (P = 0.014).
Most of the MRD-negative patients who relapsed did so within the first 6 months, an observation that led investigators to consider whether factors exist that could predict better outcomes.
In a multivariate analysis, they found three variables associated with disease free survival: higher LDH prior to lymphodepletion (hazard ratio, 1.39), along with higher platelet count prior to lymphodepletion and incorporation of fludarabine into the regimen, with hazard ratios of 0.65 and 0.34, respectively.
Using those three characteristics, investigators grouped patients as “good risk” if they had normal LDH, platelet count at or above 100 prior to lymphodepletion that included fludarabine. The 24-month disease-free survival for good-risk patients was 78%, and overall survival was 86%.
The role of allogeneic HSCT after ALL patients achieved MRD-negative complete remission with CAR T-cell therapy was one of the “major questions in the field,” Dr. Hay said.
In this analysis, Dr. Hay and colleagues found that patients who underwent transplant in MRD-negative complete remission had a 24-month disease free survival and overall survival of 61% and 72%, respectively, both of which were significantly higher than in patients with MRD-negative complete remission who had no transplant.
The disease-free survival benefit was not specific to the good-risk group, according to Dr. Hay, who said an interaction test demonstrated no significant interaction between risk group and allogeneic HSCT after CAR T-cell infusion (P = 0.53).
“This is a very important finding that should be further [studied] in an appropriately designed clinical trial,” Dr. Hay said during an oral presentation of the study results.
Dr. Hay and several coauthors reported financial disclosures related to Juno Therapeutics. Other disclosures reported by study coauthors included Cell Medica, Celgene, Eureka Therapeutics, Genentech/Roche, Gilead Sciences, Kite Pharma, Novartis, and others.
SOURCE: Hay KA. ASCO 2018, Abstract 7005.
REPORTING FROM ASCO 2018
Key clinical point:
Major finding: Patients who achieved MRD-negative complete remission had an improved median disease-free survival at 7.6 months versus 0.8 months (P less than .0001)
Study details: A retrospective analysis including 53 patients with ALL who had bone marrow or extramedullary disease at baseline and had received CD19 CAR T cells at or under the maximum tolerated dose at least 1 year prior to this analysis.
Disclosures: Researchers reported financial ties to Juno Therapeutics, Cell Medica, Celgene, Eureka Therapeutics, Genentech/Roche, Gilead Sciences, Kite Pharma, Novartis, and others.
Source: Hay KA. ASCO 2018, Abstract 7005.
New ‘immune checkpoint’ vaccine shows promise in treating colorectal cancer
A novel vaccine may provide a breakthrough treatment option in colorectal and other cancers.
“We [researchers] at the Peter MacCallum Cancer Centre in Melbourne, Australia, have developed a new, DNA-based vaccine, which we call TetMYB, for the treatment of MYB-overexpressing cancers such as colorectal, adenoid cystic carcinoma, and breast cancer, to name a few,” Toan Pham, MD, of the Peter MacCallum Cancer Centre, said in a media briefing in advance of the annual Digestive Disease Week® conference.
The immunotherapy approach described by Dr. Pham involves combining the TetMYB vaccine, which boosts the immune system, and an antibody, BGB-A317, that helps enhance the effectiveness of the vaccine.
“The research we are presenting at DDW involves testing this approach in mouse models, which we had previously published. In our studies, tumors in the mice responded very well to the treatment and cancer was cured in about half of them,” stated Dr. Pham.
The study is really composed of two smaller studies that looked at colonic adenoma, induced using tamoxifen-enriched feed, in a total of 22 mice. The mice were split into two study groups: 15 in a prophylactic study and 7 in a therapeutic pilot study.
In the prophylactic study, eight treatment mice received three TetMYB vaccinations at weeks 7, 9, and 11. Tamoxifen was given to the treatment and control mice at week 13.
The seven mice in the therapeutic pilot study were given tamoxifen at week 9 and subsequently monitored via colonoscopy weekly. Once the presence of adenoma was identified, mice received six doses of TetMYB and four doses of anti-PD1 antibody.
In both the prophylactic and therapeutic study, the mice survival rates were higher than expected. In the prophylactic study, the treatment groups’ median survival time was 356 days, nearly double the control group (183 days). More impressively, all mice in the therapeutic group were alive at 235 days.
“The mice were only expected to live for a couple of days or weeks. But, about 50% of them, they lived for more than 2 years,” said Dr. Pham. “Additionally, when the cured mice from the original study were later rechallenged with the same treatment, it was immediately rejected, thus proving there is an immune memory induced by the vaccine.”
With the positive results of the mouse trial, Dr. Pham spoke to the ongoing human clinical trial and the future of this vaccine.
“Currently, we are conducting a first-in-human phase 1 clinical trial,” stated Dr. Pham. “The next phase of evolution for our vaccine, which I will also be presenting at DDW, is testing our vaccine as an anti-adenoma vaccine.” Adenomas account for nearly 80% of bowel cancers, according to Dr. Pham.
Should the safety data from the phase 1 trial prove the vaccine to be safe, a follow-up clinical trial looking at high-risk populations would be the next step.
A novel vaccine may provide a breakthrough treatment option in colorectal and other cancers.
“We [researchers] at the Peter MacCallum Cancer Centre in Melbourne, Australia, have developed a new, DNA-based vaccine, which we call TetMYB, for the treatment of MYB-overexpressing cancers such as colorectal, adenoid cystic carcinoma, and breast cancer, to name a few,” Toan Pham, MD, of the Peter MacCallum Cancer Centre, said in a media briefing in advance of the annual Digestive Disease Week® conference.
The immunotherapy approach described by Dr. Pham involves combining the TetMYB vaccine, which boosts the immune system, and an antibody, BGB-A317, that helps enhance the effectiveness of the vaccine.
“The research we are presenting at DDW involves testing this approach in mouse models, which we had previously published. In our studies, tumors in the mice responded very well to the treatment and cancer was cured in about half of them,” stated Dr. Pham.
The study is really composed of two smaller studies that looked at colonic adenoma, induced using tamoxifen-enriched feed, in a total of 22 mice. The mice were split into two study groups: 15 in a prophylactic study and 7 in a therapeutic pilot study.
In the prophylactic study, eight treatment mice received three TetMYB vaccinations at weeks 7, 9, and 11. Tamoxifen was given to the treatment and control mice at week 13.
The seven mice in the therapeutic pilot study were given tamoxifen at week 9 and subsequently monitored via colonoscopy weekly. Once the presence of adenoma was identified, mice received six doses of TetMYB and four doses of anti-PD1 antibody.
In both the prophylactic and therapeutic study, the mice survival rates were higher than expected. In the prophylactic study, the treatment groups’ median survival time was 356 days, nearly double the control group (183 days). More impressively, all mice in the therapeutic group were alive at 235 days.
“The mice were only expected to live for a couple of days or weeks. But, about 50% of them, they lived for more than 2 years,” said Dr. Pham. “Additionally, when the cured mice from the original study were later rechallenged with the same treatment, it was immediately rejected, thus proving there is an immune memory induced by the vaccine.”
With the positive results of the mouse trial, Dr. Pham spoke to the ongoing human clinical trial and the future of this vaccine.
“Currently, we are conducting a first-in-human phase 1 clinical trial,” stated Dr. Pham. “The next phase of evolution for our vaccine, which I will also be presenting at DDW, is testing our vaccine as an anti-adenoma vaccine.” Adenomas account for nearly 80% of bowel cancers, according to Dr. Pham.
Should the safety data from the phase 1 trial prove the vaccine to be safe, a follow-up clinical trial looking at high-risk populations would be the next step.
A novel vaccine may provide a breakthrough treatment option in colorectal and other cancers.
“We [researchers] at the Peter MacCallum Cancer Centre in Melbourne, Australia, have developed a new, DNA-based vaccine, which we call TetMYB, for the treatment of MYB-overexpressing cancers such as colorectal, adenoid cystic carcinoma, and breast cancer, to name a few,” Toan Pham, MD, of the Peter MacCallum Cancer Centre, said in a media briefing in advance of the annual Digestive Disease Week® conference.
The immunotherapy approach described by Dr. Pham involves combining the TetMYB vaccine, which boosts the immune system, and an antibody, BGB-A317, that helps enhance the effectiveness of the vaccine.
“The research we are presenting at DDW involves testing this approach in mouse models, which we had previously published. In our studies, tumors in the mice responded very well to the treatment and cancer was cured in about half of them,” stated Dr. Pham.
The study is really composed of two smaller studies that looked at colonic adenoma, induced using tamoxifen-enriched feed, in a total of 22 mice. The mice were split into two study groups: 15 in a prophylactic study and 7 in a therapeutic pilot study.
In the prophylactic study, eight treatment mice received three TetMYB vaccinations at weeks 7, 9, and 11. Tamoxifen was given to the treatment and control mice at week 13.
The seven mice in the therapeutic pilot study were given tamoxifen at week 9 and subsequently monitored via colonoscopy weekly. Once the presence of adenoma was identified, mice received six doses of TetMYB and four doses of anti-PD1 antibody.
In both the prophylactic and therapeutic study, the mice survival rates were higher than expected. In the prophylactic study, the treatment groups’ median survival time was 356 days, nearly double the control group (183 days). More impressively, all mice in the therapeutic group were alive at 235 days.
“The mice were only expected to live for a couple of days or weeks. But, about 50% of them, they lived for more than 2 years,” said Dr. Pham. “Additionally, when the cured mice from the original study were later rechallenged with the same treatment, it was immediately rejected, thus proving there is an immune memory induced by the vaccine.”
With the positive results of the mouse trial, Dr. Pham spoke to the ongoing human clinical trial and the future of this vaccine.
“Currently, we are conducting a first-in-human phase 1 clinical trial,” stated Dr. Pham. “The next phase of evolution for our vaccine, which I will also be presenting at DDW, is testing our vaccine as an anti-adenoma vaccine.” Adenomas account for nearly 80% of bowel cancers, according to Dr. Pham.
Should the safety data from the phase 1 trial prove the vaccine to be safe, a follow-up clinical trial looking at high-risk populations would be the next step.
REPORTING FROM DDW
Is cancer immunotherapy more effective in men than women?
Cancer immunotherapy using checkpoint inhibitors may achieve greater mortality reductions in men than they do in women, new research has suggested.
In a meta-analysis and systematic review published in Lancet Oncology, researchers analyzed 20 randomized, controlled trials of immune checkpoint inhibitors that included detail on overall survival and patients’ sex; altogether, these studies involved 11,351 patients with advanced or metastatic cancers.
They found that while men treated with checkpoint inhibitors had a significant 28% reduced risk of death, compared with male controls, the survival benefit in women was smaller (14% reduced risk of death, compared with female controls).
Fabio Conforti, MD, from the European Institute of Oncology, Milan, and coauthors commented that the magnitude of the difference between the effect seen men and that in women was clinically significant.
“The pooled reduction of risk of death was double the size for male patients than for female patients – a difference that is similar to the size of the difference in survival benefit observed between patients with non–small cell lung cancer with PD-L1 positive (greater than 1%) tumors versus negative tumors, who were treated with anti-PD-1,” they wrote.
This difference between the benefit seen men and that in women was evident across all the subgroups in the study, which included subgroups based on cancer histotype, line of treatment, drugs used, and type of control.
However there was greater heterogeneity in the magnitude of the effect of checkpoint inhibitors on mortality in men than there was in women. The authors suggested this could be explained by the fact that the drugs have lower efficacy in women and this may therefore reduce the variability of results when compared with those in men.
The authors also looked at whether the studies that compared immunotherapies with nonimmunological therapies might show a different effect, but they still found a significantly higher benefit in men, compared with women.
The overall study population was two-thirds male and one-third female. The checkpoint inhibitors used were ipilimumab, tremelimumab, nivolumab, and pembrolizumab, and the trials were conducted in patients with melanoma, non–small cell lung cancer, head and neck cancer, renal cell carcinoma, urothelial tumors, gastric tumors, and mesothelioma.
Men have almost double the risk of mortality from cancer than do women, the authors said, with the greatest differences seen in melanoma, lung cancer, larynx cancer, esophagus cancer, and bladder cancer.
“This male-biased mortality is hypothesized to reflect differences not only in behavioral and biological factors, including causes of cancer and hormonal regulation, but also in the immune system.”
Despite this, sex is rarely taken into account when new therapeutic approaches are tested, the authors said.
They also commented on the fact that there was a relatively low number of women included in each trial, an issue that was recognized as far back as the 1990s as a major problem in medical trials.
“Our results further highlight this problem, showing clinically relevant differences in the efficacy of two important classes of immunological drugs, namely anti–CTLA-4 and anti–PD-1 antibodies, when compared with controls in male and female patients with advanced solid tumors,” they wrote.
They noted that they couldn’t exclude the possibility that the effect may be the result of other variables that were distributed differently between the sexes. However, they also qualified this by saying that variables known to affect the efficacy of immune checkpoint inhibitors, such as PD-L1 expression and mutation status, were not likely to explain the results.
Given their findings, the authors said a patient’s sex should be taken into account when weighing the risks and benefits of checkpoint inhibitors given the magnitude of benefit was sex-dependent. They also called for future immunotherapy studies to include more women.
No funding or conflicts of interest were declared.
SOURCE: Conforti F et al. Lancet Oncol. 2018 May 16. doi: 10.1016/S1470-2045(18)30261-4.
While cancer immunotherapy represents one of the most significant clinical advances in cancer treatment in the past decade, the basic but important clinical question about different effects between men and woman has not been addressed until now. The authors of this study are to be congratulated on such a comprehensive and well-conducted analysis, but the data does not completely support their final conclusion that checkpoint inhibitors benefit men more than women.
There are a large number of baseline characteristics of solid tumors that might differ between men and women and that have also been reported to impact the outcomes of patients treated with checkpoint inhibitors. Some of these may be lifestyle or behavioral characteristics – such as different smoking habits between men and women with non–small cell lung cancer – or differences in the distribution of oncogenic driver mutations between men and women.
We should therefore be cautious in jumping to conclusions and changing the current standard of care with respect to checkpoint inhibitors. In particular, we should not be denying treatment to women who are otherwise indicated for checkpoint inhibitors, based on these findings.
Omar Abdel-Rahman, MD, is from the clinical oncology department of the faculty of medicine at Ain Shams University in Cairo and from the Tom Baker Cancer Centre in Calgary. These comments are taken from an accompanying editorial (Lancet Oncol. 2018 May 16. doi: 10.1016/S1470-2045[18]30270-5.) No conflicts of interest were declared.
While cancer immunotherapy represents one of the most significant clinical advances in cancer treatment in the past decade, the basic but important clinical question about different effects between men and woman has not been addressed until now. The authors of this study are to be congratulated on such a comprehensive and well-conducted analysis, but the data does not completely support their final conclusion that checkpoint inhibitors benefit men more than women.
There are a large number of baseline characteristics of solid tumors that might differ between men and women and that have also been reported to impact the outcomes of patients treated with checkpoint inhibitors. Some of these may be lifestyle or behavioral characteristics – such as different smoking habits between men and women with non–small cell lung cancer – or differences in the distribution of oncogenic driver mutations between men and women.
We should therefore be cautious in jumping to conclusions and changing the current standard of care with respect to checkpoint inhibitors. In particular, we should not be denying treatment to women who are otherwise indicated for checkpoint inhibitors, based on these findings.
Omar Abdel-Rahman, MD, is from the clinical oncology department of the faculty of medicine at Ain Shams University in Cairo and from the Tom Baker Cancer Centre in Calgary. These comments are taken from an accompanying editorial (Lancet Oncol. 2018 May 16. doi: 10.1016/S1470-2045[18]30270-5.) No conflicts of interest were declared.
While cancer immunotherapy represents one of the most significant clinical advances in cancer treatment in the past decade, the basic but important clinical question about different effects between men and woman has not been addressed until now. The authors of this study are to be congratulated on such a comprehensive and well-conducted analysis, but the data does not completely support their final conclusion that checkpoint inhibitors benefit men more than women.
There are a large number of baseline characteristics of solid tumors that might differ between men and women and that have also been reported to impact the outcomes of patients treated with checkpoint inhibitors. Some of these may be lifestyle or behavioral characteristics – such as different smoking habits between men and women with non–small cell lung cancer – or differences in the distribution of oncogenic driver mutations between men and women.
We should therefore be cautious in jumping to conclusions and changing the current standard of care with respect to checkpoint inhibitors. In particular, we should not be denying treatment to women who are otherwise indicated for checkpoint inhibitors, based on these findings.
Omar Abdel-Rahman, MD, is from the clinical oncology department of the faculty of medicine at Ain Shams University in Cairo and from the Tom Baker Cancer Centre in Calgary. These comments are taken from an accompanying editorial (Lancet Oncol. 2018 May 16. doi: 10.1016/S1470-2045[18]30270-5.) No conflicts of interest were declared.
Cancer immunotherapy using checkpoint inhibitors may achieve greater mortality reductions in men than they do in women, new research has suggested.
In a meta-analysis and systematic review published in Lancet Oncology, researchers analyzed 20 randomized, controlled trials of immune checkpoint inhibitors that included detail on overall survival and patients’ sex; altogether, these studies involved 11,351 patients with advanced or metastatic cancers.
They found that while men treated with checkpoint inhibitors had a significant 28% reduced risk of death, compared with male controls, the survival benefit in women was smaller (14% reduced risk of death, compared with female controls).
Fabio Conforti, MD, from the European Institute of Oncology, Milan, and coauthors commented that the magnitude of the difference between the effect seen men and that in women was clinically significant.
“The pooled reduction of risk of death was double the size for male patients than for female patients – a difference that is similar to the size of the difference in survival benefit observed between patients with non–small cell lung cancer with PD-L1 positive (greater than 1%) tumors versus negative tumors, who were treated with anti-PD-1,” they wrote.
This difference between the benefit seen men and that in women was evident across all the subgroups in the study, which included subgroups based on cancer histotype, line of treatment, drugs used, and type of control.
However there was greater heterogeneity in the magnitude of the effect of checkpoint inhibitors on mortality in men than there was in women. The authors suggested this could be explained by the fact that the drugs have lower efficacy in women and this may therefore reduce the variability of results when compared with those in men.
The authors also looked at whether the studies that compared immunotherapies with nonimmunological therapies might show a different effect, but they still found a significantly higher benefit in men, compared with women.
The overall study population was two-thirds male and one-third female. The checkpoint inhibitors used were ipilimumab, tremelimumab, nivolumab, and pembrolizumab, and the trials were conducted in patients with melanoma, non–small cell lung cancer, head and neck cancer, renal cell carcinoma, urothelial tumors, gastric tumors, and mesothelioma.
Men have almost double the risk of mortality from cancer than do women, the authors said, with the greatest differences seen in melanoma, lung cancer, larynx cancer, esophagus cancer, and bladder cancer.
“This male-biased mortality is hypothesized to reflect differences not only in behavioral and biological factors, including causes of cancer and hormonal regulation, but also in the immune system.”
Despite this, sex is rarely taken into account when new therapeutic approaches are tested, the authors said.
They also commented on the fact that there was a relatively low number of women included in each trial, an issue that was recognized as far back as the 1990s as a major problem in medical trials.
“Our results further highlight this problem, showing clinically relevant differences in the efficacy of two important classes of immunological drugs, namely anti–CTLA-4 and anti–PD-1 antibodies, when compared with controls in male and female patients with advanced solid tumors,” they wrote.
They noted that they couldn’t exclude the possibility that the effect may be the result of other variables that were distributed differently between the sexes. However, they also qualified this by saying that variables known to affect the efficacy of immune checkpoint inhibitors, such as PD-L1 expression and mutation status, were not likely to explain the results.
Given their findings, the authors said a patient’s sex should be taken into account when weighing the risks and benefits of checkpoint inhibitors given the magnitude of benefit was sex-dependent. They also called for future immunotherapy studies to include more women.
No funding or conflicts of interest were declared.
SOURCE: Conforti F et al. Lancet Oncol. 2018 May 16. doi: 10.1016/S1470-2045(18)30261-4.
Cancer immunotherapy using checkpoint inhibitors may achieve greater mortality reductions in men than they do in women, new research has suggested.
In a meta-analysis and systematic review published in Lancet Oncology, researchers analyzed 20 randomized, controlled trials of immune checkpoint inhibitors that included detail on overall survival and patients’ sex; altogether, these studies involved 11,351 patients with advanced or metastatic cancers.
They found that while men treated with checkpoint inhibitors had a significant 28% reduced risk of death, compared with male controls, the survival benefit in women was smaller (14% reduced risk of death, compared with female controls).
Fabio Conforti, MD, from the European Institute of Oncology, Milan, and coauthors commented that the magnitude of the difference between the effect seen men and that in women was clinically significant.
“The pooled reduction of risk of death was double the size for male patients than for female patients – a difference that is similar to the size of the difference in survival benefit observed between patients with non–small cell lung cancer with PD-L1 positive (greater than 1%) tumors versus negative tumors, who were treated with anti-PD-1,” they wrote.
This difference between the benefit seen men and that in women was evident across all the subgroups in the study, which included subgroups based on cancer histotype, line of treatment, drugs used, and type of control.
However there was greater heterogeneity in the magnitude of the effect of checkpoint inhibitors on mortality in men than there was in women. The authors suggested this could be explained by the fact that the drugs have lower efficacy in women and this may therefore reduce the variability of results when compared with those in men.
The authors also looked at whether the studies that compared immunotherapies with nonimmunological therapies might show a different effect, but they still found a significantly higher benefit in men, compared with women.
The overall study population was two-thirds male and one-third female. The checkpoint inhibitors used were ipilimumab, tremelimumab, nivolumab, and pembrolizumab, and the trials were conducted in patients with melanoma, non–small cell lung cancer, head and neck cancer, renal cell carcinoma, urothelial tumors, gastric tumors, and mesothelioma.
Men have almost double the risk of mortality from cancer than do women, the authors said, with the greatest differences seen in melanoma, lung cancer, larynx cancer, esophagus cancer, and bladder cancer.
“This male-biased mortality is hypothesized to reflect differences not only in behavioral and biological factors, including causes of cancer and hormonal regulation, but also in the immune system.”
Despite this, sex is rarely taken into account when new therapeutic approaches are tested, the authors said.
They also commented on the fact that there was a relatively low number of women included in each trial, an issue that was recognized as far back as the 1990s as a major problem in medical trials.
“Our results further highlight this problem, showing clinically relevant differences in the efficacy of two important classes of immunological drugs, namely anti–CTLA-4 and anti–PD-1 antibodies, when compared with controls in male and female patients with advanced solid tumors,” they wrote.
They noted that they couldn’t exclude the possibility that the effect may be the result of other variables that were distributed differently between the sexes. However, they also qualified this by saying that variables known to affect the efficacy of immune checkpoint inhibitors, such as PD-L1 expression and mutation status, were not likely to explain the results.
Given their findings, the authors said a patient’s sex should be taken into account when weighing the risks and benefits of checkpoint inhibitors given the magnitude of benefit was sex-dependent. They also called for future immunotherapy studies to include more women.
No funding or conflicts of interest were declared.
SOURCE: Conforti F et al. Lancet Oncol. 2018 May 16. doi: 10.1016/S1470-2045(18)30261-4.
FROM LANCET ONCOLOGY
Key clinical point: Checkpoint inhibitors are linked with greater mortality reductions in men than in women.
Major finding: Checkpoint inhibitors are associated with a 28% reduction in cancer mortality in men and 14% in women.
Study details: Systematic review and meta-analysis of 20 randomized, controlled trials involving 11,351 patients.
Disclosures: No funding or conflicts of interest were declared.
Source: Conforti F et al. Lancet Oncol. 2018 May 16. doi: 10.1016/S1470-2045(18)30261-4.
Low microbiota diversity linked to poor survival after transplant
SALT LAKE CITY – A multicenter study confirmed that diversity of gut microbiota is associated with better survival after allogeneic hematopoietic cell transplantation (HCT), while low diversity and the predominance of pathogenic bacteria are linked to graft versus host disease (GVHD).
Lower calorie intake and exposure to broad-spectrum antibiotics were both associated with lower diversity, the study found.
“One of the striking findings early on was this association between diversity in the gut and overall survival,” said Jonathan Peled, MD, PhD, noting that his research group also saw that high gut diversity was associated with lower rates of GVHD-related mortality.
“The first question that I want to ask today is ‘Are the patterns of microbiota injury that have been described in single-center studies and their association with clinical outcomes consistent across geography?’” Dr. Peled said during a top abstracts session at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
To answer this, Dr. Peled and his associates at Memorial Sloan Kettering Cancer Center (MSKCC), New York, teamed up with a research group at Duke University, Durham, N.C., and with investigators in Regensburg, Germany. The international group devised a study that would use centralized sequencing and analysis to examine patient fecal samples from all three centers.
In all, 5,310 samples were obtained from 1,034 HCT patients. MSKCC contributed most of the samples (n = 908, 87.8%), with Regensburg contributing 79 (7.6%) and Duke contributing 47 (4.5%).
The most common malignancies treated were acute myeloid leukemia, myelodysplastic syndrome, and non-Hodgkin lymphoma. The balance of graft sources and conditioning intensity varied between centers, but overall, more than three-quarters of grafts were from peripheral blood stem cells and just over half of patients received myeloablative conditioning.
The centralized microbiota profiling involved extracting bacterial DNA, and then using polymerase chain reaction to amplify 16sRNA for sequencing and subsequent taxonomic identification.
“Samples can be segregated into clusters according to microbiota composition,” said Dr. Peled, a medical oncologist at MSKCC. The investigators used an algorithm called t-distributed stochastic neighbor embedding, or tSNE, to help detect patterns in microbiota composition and diversity before and throughout the HCT process. Visualizations using tSNE allow for two-dimensional representations of complicated associations and interrelatedness in data.
“Color-coded by diversity and time, we see that these early samples tend to be more diverse,” in the tSNE analyses, Dr. Peled said. The later clusters, he said, show evidence of lower diversity and injury.
Individual samples can also be coded in a way that shows clusters by abundance of various bacterial taxa, Dr. Peled said. “The early, diverse cluster tends to be dominated, or filled, by anaerobic commensals such as Firmicutes and Clostridia, which we and others have found are associated with good outcomes after transplant.”
The lower-diversity states seen later, after transplant, tend to be dominated by a variety of pathogenic bacteria, Dr. Peled said. These include Enterococcus and Proteobacteria, a phylum that includes Klebsiella and Escherichia coli species. This predominance has been associated with subsequent bacteremia, he said.
“Patients tend to enter transplant with a relatively diverse flora, and a frequent event in the posttransplant samples is domination by these pathobiomes,” Dr. Peled said. “In some cases, almost the entire composition of the gut is [composed] of a single species.” This loss of diversity and single-species domination was seen across the three geographically diverse research sites, he said.
This decimation of diversity is linked to poor transplant outcomes. In particular, Dr. Peled said, an enterococcus-dominated gut had previously been associated with higher risk for acute GVHD and with gastrointestinal GVHD.
Here, the multisite data showed that at Regensburg, higher enterococcus abundance on days 7-14 post HCT was associated with increased risk of GI GVHD. At MSKCC, enterococcus domination was associated with a hazard ratio of 1.4 for acute GVHD (P = .008). The MSKCC group used data from 503 patients, defining domination as at least 30% relative abundance in any sample from post-HCT days 7-21.
Patients at both MSKCC and Regensburg had a better chance of overall survival if they had high intestinal microbial diversity around the period of neutrophil engraftment, as seen in a sample collected within 7 days of post-HCT day 14. At MSKCC, data for 651 patients showed a statistically significant association (P = .006); this finding was reproduced at Regensburg, which also saw a significant association (P = .015) for the 59 patients studied, Dr. Peled reported.
Increased treatment-related mortality was seen for patients who had low microbial diversity following neutrophil engraftment as well. Of 372 MSKCC patients who had samples available 7-50 days after engraftment, high diversity was associated with better overall survival, and with lower treatment-related mortality (P = .03 for both).
Dr. Peled and his collaborators also divided patients into quartiles by amount of biodiversity. They found that comparing the highest to the lowest biodiversity quartile showed significantly overall survival benefits for the highest-diversity group (P = .007).
The problem starts before transplant, Dr. Peled explained. The researchers found that compared with healthy controls at MSKCC and data from the Human Microbiome Project, HCT patients entered their transplant with significantly less gut biodiversity.
The second question to be addressed is “What are the key environmental determinants of intestinal microbiota composition?” said Dr. Peled.
“Peri-HCT exposure to broad-spectrum antibiotics is associated with lower intestinal microbial diversity,” he said. For 5,936 samples taken from 976 patients receiving allogeneic HCT, the most significant difference in diversity between those with and without broad-spectrum antibiotic exposure was seen at day 15 post transplant (P = .008).
Higher calorie intake was also associated with greater diversity (P less than .001). Higher dietary fiber intake was associated with higher abundance of Blautia, a genus considered to be a healthy commensal microorganism, Dr. Peled said.
“Conditioning intensity is associated with the magnitude of diversity loss, and with distinct microbiome configurations,” said Dr. Peled. Using 4,311 samples from 908 patients, a myeloablative conditioning regimen (n = 508) was associated with significantly less diversity when compared with reduced intensity (n = 316) and nonmyeloablative regimens (n = 84; P =.002 and P less than .001, respectively).
To answer a third question – What is the natural history of recovery from microbiota injury after HCT? – the investigators looked at trends over time for 28 allogeneic HCT recipients. With a total of 294 samples for analysis, Dr. Peled and his group found that “diversity increases, but often to a configuration distinct from the pre-HCT state.” It took some patients nearly a year to return to their pretransplant level of diversity.
Patients in the subset of those who go on to develop lower gastrointestinal GVHD have an intestinal microbiota composition that is distinct from those patients whose GVHD exclusively involved the upper gastrointestinal tract, the skin, or the liver (P = .019), Dr. Peled said.
He and his team are currently enrolling patients for a phase 2 randomized clinical trial (NCT03078010) that will explore strategies to deescalate the use of broad-spectrum antibiotics for febrile neutropenia in patients with allogeneic HCT. The trial will randomize patients to receive either piperacillin-tazobactam, the current standard of care at MSKCC, or cefepime with deescalation to aztreonam with vancomycin, the microbiota-sparing strategy. The trial will examine the abundance of Clostridiales and Blautia species, gut biodiversity, the rate of GVHD, bacteremia, and survival rates.
The research presented was funded by the Parker Institute for Cancer Immunotherapy, the Sawiris Foundation, Empire Clinical Research Investigator Program, and Seres Therapeutics. Dr. Peled reported that he has intellectual property rights and research funding through Seres Therapeutics
SOURCE: Peled J et al. 2018 BMT Tandem Meetings, Abstract 3.
SALT LAKE CITY – A multicenter study confirmed that diversity of gut microbiota is associated with better survival after allogeneic hematopoietic cell transplantation (HCT), while low diversity and the predominance of pathogenic bacteria are linked to graft versus host disease (GVHD).
Lower calorie intake and exposure to broad-spectrum antibiotics were both associated with lower diversity, the study found.
“One of the striking findings early on was this association between diversity in the gut and overall survival,” said Jonathan Peled, MD, PhD, noting that his research group also saw that high gut diversity was associated with lower rates of GVHD-related mortality.
“The first question that I want to ask today is ‘Are the patterns of microbiota injury that have been described in single-center studies and their association with clinical outcomes consistent across geography?’” Dr. Peled said during a top abstracts session at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
To answer this, Dr. Peled and his associates at Memorial Sloan Kettering Cancer Center (MSKCC), New York, teamed up with a research group at Duke University, Durham, N.C., and with investigators in Regensburg, Germany. The international group devised a study that would use centralized sequencing and analysis to examine patient fecal samples from all three centers.
In all, 5,310 samples were obtained from 1,034 HCT patients. MSKCC contributed most of the samples (n = 908, 87.8%), with Regensburg contributing 79 (7.6%) and Duke contributing 47 (4.5%).
The most common malignancies treated were acute myeloid leukemia, myelodysplastic syndrome, and non-Hodgkin lymphoma. The balance of graft sources and conditioning intensity varied between centers, but overall, more than three-quarters of grafts were from peripheral blood stem cells and just over half of patients received myeloablative conditioning.
The centralized microbiota profiling involved extracting bacterial DNA, and then using polymerase chain reaction to amplify 16sRNA for sequencing and subsequent taxonomic identification.
“Samples can be segregated into clusters according to microbiota composition,” said Dr. Peled, a medical oncologist at MSKCC. The investigators used an algorithm called t-distributed stochastic neighbor embedding, or tSNE, to help detect patterns in microbiota composition and diversity before and throughout the HCT process. Visualizations using tSNE allow for two-dimensional representations of complicated associations and interrelatedness in data.
“Color-coded by diversity and time, we see that these early samples tend to be more diverse,” in the tSNE analyses, Dr. Peled said. The later clusters, he said, show evidence of lower diversity and injury.
Individual samples can also be coded in a way that shows clusters by abundance of various bacterial taxa, Dr. Peled said. “The early, diverse cluster tends to be dominated, or filled, by anaerobic commensals such as Firmicutes and Clostridia, which we and others have found are associated with good outcomes after transplant.”
The lower-diversity states seen later, after transplant, tend to be dominated by a variety of pathogenic bacteria, Dr. Peled said. These include Enterococcus and Proteobacteria, a phylum that includes Klebsiella and Escherichia coli species. This predominance has been associated with subsequent bacteremia, he said.
“Patients tend to enter transplant with a relatively diverse flora, and a frequent event in the posttransplant samples is domination by these pathobiomes,” Dr. Peled said. “In some cases, almost the entire composition of the gut is [composed] of a single species.” This loss of diversity and single-species domination was seen across the three geographically diverse research sites, he said.
This decimation of diversity is linked to poor transplant outcomes. In particular, Dr. Peled said, an enterococcus-dominated gut had previously been associated with higher risk for acute GVHD and with gastrointestinal GVHD.
Here, the multisite data showed that at Regensburg, higher enterococcus abundance on days 7-14 post HCT was associated with increased risk of GI GVHD. At MSKCC, enterococcus domination was associated with a hazard ratio of 1.4 for acute GVHD (P = .008). The MSKCC group used data from 503 patients, defining domination as at least 30% relative abundance in any sample from post-HCT days 7-21.
Patients at both MSKCC and Regensburg had a better chance of overall survival if they had high intestinal microbial diversity around the period of neutrophil engraftment, as seen in a sample collected within 7 days of post-HCT day 14. At MSKCC, data for 651 patients showed a statistically significant association (P = .006); this finding was reproduced at Regensburg, which also saw a significant association (P = .015) for the 59 patients studied, Dr. Peled reported.
Increased treatment-related mortality was seen for patients who had low microbial diversity following neutrophil engraftment as well. Of 372 MSKCC patients who had samples available 7-50 days after engraftment, high diversity was associated with better overall survival, and with lower treatment-related mortality (P = .03 for both).
Dr. Peled and his collaborators also divided patients into quartiles by amount of biodiversity. They found that comparing the highest to the lowest biodiversity quartile showed significantly overall survival benefits for the highest-diversity group (P = .007).
The problem starts before transplant, Dr. Peled explained. The researchers found that compared with healthy controls at MSKCC and data from the Human Microbiome Project, HCT patients entered their transplant with significantly less gut biodiversity.
The second question to be addressed is “What are the key environmental determinants of intestinal microbiota composition?” said Dr. Peled.
“Peri-HCT exposure to broad-spectrum antibiotics is associated with lower intestinal microbial diversity,” he said. For 5,936 samples taken from 976 patients receiving allogeneic HCT, the most significant difference in diversity between those with and without broad-spectrum antibiotic exposure was seen at day 15 post transplant (P = .008).
Higher calorie intake was also associated with greater diversity (P less than .001). Higher dietary fiber intake was associated with higher abundance of Blautia, a genus considered to be a healthy commensal microorganism, Dr. Peled said.
“Conditioning intensity is associated with the magnitude of diversity loss, and with distinct microbiome configurations,” said Dr. Peled. Using 4,311 samples from 908 patients, a myeloablative conditioning regimen (n = 508) was associated with significantly less diversity when compared with reduced intensity (n = 316) and nonmyeloablative regimens (n = 84; P =.002 and P less than .001, respectively).
To answer a third question – What is the natural history of recovery from microbiota injury after HCT? – the investigators looked at trends over time for 28 allogeneic HCT recipients. With a total of 294 samples for analysis, Dr. Peled and his group found that “diversity increases, but often to a configuration distinct from the pre-HCT state.” It took some patients nearly a year to return to their pretransplant level of diversity.
Patients in the subset of those who go on to develop lower gastrointestinal GVHD have an intestinal microbiota composition that is distinct from those patients whose GVHD exclusively involved the upper gastrointestinal tract, the skin, or the liver (P = .019), Dr. Peled said.
He and his team are currently enrolling patients for a phase 2 randomized clinical trial (NCT03078010) that will explore strategies to deescalate the use of broad-spectrum antibiotics for febrile neutropenia in patients with allogeneic HCT. The trial will randomize patients to receive either piperacillin-tazobactam, the current standard of care at MSKCC, or cefepime with deescalation to aztreonam with vancomycin, the microbiota-sparing strategy. The trial will examine the abundance of Clostridiales and Blautia species, gut biodiversity, the rate of GVHD, bacteremia, and survival rates.
The research presented was funded by the Parker Institute for Cancer Immunotherapy, the Sawiris Foundation, Empire Clinical Research Investigator Program, and Seres Therapeutics. Dr. Peled reported that he has intellectual property rights and research funding through Seres Therapeutics
SOURCE: Peled J et al. 2018 BMT Tandem Meetings, Abstract 3.
SALT LAKE CITY – A multicenter study confirmed that diversity of gut microbiota is associated with better survival after allogeneic hematopoietic cell transplantation (HCT), while low diversity and the predominance of pathogenic bacteria are linked to graft versus host disease (GVHD).
Lower calorie intake and exposure to broad-spectrum antibiotics were both associated with lower diversity, the study found.
“One of the striking findings early on was this association between diversity in the gut and overall survival,” said Jonathan Peled, MD, PhD, noting that his research group also saw that high gut diversity was associated with lower rates of GVHD-related mortality.
“The first question that I want to ask today is ‘Are the patterns of microbiota injury that have been described in single-center studies and their association with clinical outcomes consistent across geography?’” Dr. Peled said during a top abstracts session at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
To answer this, Dr. Peled and his associates at Memorial Sloan Kettering Cancer Center (MSKCC), New York, teamed up with a research group at Duke University, Durham, N.C., and with investigators in Regensburg, Germany. The international group devised a study that would use centralized sequencing and analysis to examine patient fecal samples from all three centers.
In all, 5,310 samples were obtained from 1,034 HCT patients. MSKCC contributed most of the samples (n = 908, 87.8%), with Regensburg contributing 79 (7.6%) and Duke contributing 47 (4.5%).
The most common malignancies treated were acute myeloid leukemia, myelodysplastic syndrome, and non-Hodgkin lymphoma. The balance of graft sources and conditioning intensity varied between centers, but overall, more than three-quarters of grafts were from peripheral blood stem cells and just over half of patients received myeloablative conditioning.
The centralized microbiota profiling involved extracting bacterial DNA, and then using polymerase chain reaction to amplify 16sRNA for sequencing and subsequent taxonomic identification.
“Samples can be segregated into clusters according to microbiota composition,” said Dr. Peled, a medical oncologist at MSKCC. The investigators used an algorithm called t-distributed stochastic neighbor embedding, or tSNE, to help detect patterns in microbiota composition and diversity before and throughout the HCT process. Visualizations using tSNE allow for two-dimensional representations of complicated associations and interrelatedness in data.
“Color-coded by diversity and time, we see that these early samples tend to be more diverse,” in the tSNE analyses, Dr. Peled said. The later clusters, he said, show evidence of lower diversity and injury.
Individual samples can also be coded in a way that shows clusters by abundance of various bacterial taxa, Dr. Peled said. “The early, diverse cluster tends to be dominated, or filled, by anaerobic commensals such as Firmicutes and Clostridia, which we and others have found are associated with good outcomes after transplant.”
The lower-diversity states seen later, after transplant, tend to be dominated by a variety of pathogenic bacteria, Dr. Peled said. These include Enterococcus and Proteobacteria, a phylum that includes Klebsiella and Escherichia coli species. This predominance has been associated with subsequent bacteremia, he said.
“Patients tend to enter transplant with a relatively diverse flora, and a frequent event in the posttransplant samples is domination by these pathobiomes,” Dr. Peled said. “In some cases, almost the entire composition of the gut is [composed] of a single species.” This loss of diversity and single-species domination was seen across the three geographically diverse research sites, he said.
This decimation of diversity is linked to poor transplant outcomes. In particular, Dr. Peled said, an enterococcus-dominated gut had previously been associated with higher risk for acute GVHD and with gastrointestinal GVHD.
Here, the multisite data showed that at Regensburg, higher enterococcus abundance on days 7-14 post HCT was associated with increased risk of GI GVHD. At MSKCC, enterococcus domination was associated with a hazard ratio of 1.4 for acute GVHD (P = .008). The MSKCC group used data from 503 patients, defining domination as at least 30% relative abundance in any sample from post-HCT days 7-21.
Patients at both MSKCC and Regensburg had a better chance of overall survival if they had high intestinal microbial diversity around the period of neutrophil engraftment, as seen in a sample collected within 7 days of post-HCT day 14. At MSKCC, data for 651 patients showed a statistically significant association (P = .006); this finding was reproduced at Regensburg, which also saw a significant association (P = .015) for the 59 patients studied, Dr. Peled reported.
Increased treatment-related mortality was seen for patients who had low microbial diversity following neutrophil engraftment as well. Of 372 MSKCC patients who had samples available 7-50 days after engraftment, high diversity was associated with better overall survival, and with lower treatment-related mortality (P = .03 for both).
Dr. Peled and his collaborators also divided patients into quartiles by amount of biodiversity. They found that comparing the highest to the lowest biodiversity quartile showed significantly overall survival benefits for the highest-diversity group (P = .007).
The problem starts before transplant, Dr. Peled explained. The researchers found that compared with healthy controls at MSKCC and data from the Human Microbiome Project, HCT patients entered their transplant with significantly less gut biodiversity.
The second question to be addressed is “What are the key environmental determinants of intestinal microbiota composition?” said Dr. Peled.
“Peri-HCT exposure to broad-spectrum antibiotics is associated with lower intestinal microbial diversity,” he said. For 5,936 samples taken from 976 patients receiving allogeneic HCT, the most significant difference in diversity between those with and without broad-spectrum antibiotic exposure was seen at day 15 post transplant (P = .008).
Higher calorie intake was also associated with greater diversity (P less than .001). Higher dietary fiber intake was associated with higher abundance of Blautia, a genus considered to be a healthy commensal microorganism, Dr. Peled said.
“Conditioning intensity is associated with the magnitude of diversity loss, and with distinct microbiome configurations,” said Dr. Peled. Using 4,311 samples from 908 patients, a myeloablative conditioning regimen (n = 508) was associated with significantly less diversity when compared with reduced intensity (n = 316) and nonmyeloablative regimens (n = 84; P =.002 and P less than .001, respectively).
To answer a third question – What is the natural history of recovery from microbiota injury after HCT? – the investigators looked at trends over time for 28 allogeneic HCT recipients. With a total of 294 samples for analysis, Dr. Peled and his group found that “diversity increases, but often to a configuration distinct from the pre-HCT state.” It took some patients nearly a year to return to their pretransplant level of diversity.
Patients in the subset of those who go on to develop lower gastrointestinal GVHD have an intestinal microbiota composition that is distinct from those patients whose GVHD exclusively involved the upper gastrointestinal tract, the skin, or the liver (P = .019), Dr. Peled said.
He and his team are currently enrolling patients for a phase 2 randomized clinical trial (NCT03078010) that will explore strategies to deescalate the use of broad-spectrum antibiotics for febrile neutropenia in patients with allogeneic HCT. The trial will randomize patients to receive either piperacillin-tazobactam, the current standard of care at MSKCC, or cefepime with deescalation to aztreonam with vancomycin, the microbiota-sparing strategy. The trial will examine the abundance of Clostridiales and Blautia species, gut biodiversity, the rate of GVHD, bacteremia, and survival rates.
The research presented was funded by the Parker Institute for Cancer Immunotherapy, the Sawiris Foundation, Empire Clinical Research Investigator Program, and Seres Therapeutics. Dr. Peled reported that he has intellectual property rights and research funding through Seres Therapeutics
SOURCE: Peled J et al. 2018 BMT Tandem Meetings, Abstract 3.
REPORTING FROM THE 2018 BMT TANDEM MEETINGS
Key clinical point:
Major finding: High microbiota diversity post transplant was associated with better overall survival at two sites (P = .006 and P = .015).
Study details: Multicenter study of 5,310 fecal samples obtained from 1,034 hematopoietic cell transplant recipients.
Disclosures: The research presented was funded by the Parker Institute for Cancer Immunotherapy, the Sawiris Foundation, Empire Clinical Research Investigator Program, and Seres Therapeutics. Dr. Peled reported that he has intellectual property rights and research funding through Seres Therapeutics.
Source: Peled J et al. 2018 BMT Tandem Meetings, Abstract 3.
Outpatient CAR T infusions feasible using liso-cel
SALT LAKE CITY – A CD19-directed 4-1BB chimeric antigen receptor (CAR) T cell product showed efficacy and a low rate of cytokine release syndrome and neurotoxicity in patients with aggressive lymphomas and poor prognoses, raising the possibility of outpatient administration and fewer hospitalization days in this high-risk group.
A total of 86 patients who received inpatient infusions of lisocabtagene maraleucel (liso-cel, also known as JCAR017) had a mean 15.6 days of hospitalization, compared with 9.3 days for 8 outpatient recipients, said Jeremy Abramson, MD, speaking at a top abstracts session of the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
As of October 2017, eight patients had received liso-cel infusion as outpatients with at least 28 days of postinfusion data, Dr. Abramson said.
Although all but one required hospital admission, at a median of 5 days postinfusion (range, 4-22 days), there had been no intensive care unit admissions, and no outpatient recipients had experienced severe cytokine release syndrome (CRS) or neurotoxicity. All admitted patients presented with fever.
Among the study population, “Cytokine release syndrome was only seen in 35% of our entire dataset,” with neurologic toxicity seen in 19% of participants, Dr. Abramson said. “The majority of subjects had no CRS and no toxicity,” he said. Severe CRS occurred in 1% of the study population, and severe neurotoxicity in 12%. There were no deaths related to either complication.
Dr. Abramson reported these results from the TRANSCEND NHL 001 trial, a seamless design phase 1 pivotal trial of liso-cel enrolling patients with relapsed and refractory aggressive B cell non-Hodgkin lymphoma (NHL). Liso-cel delivers CD19-directed CD4 and CD8 CAR T cells in a 1:1 ratio, said Dr. Abramson, director of the lymphoma program at the Massachusetts General Hospital Cancer Center, Boston.
A total of 91 patients were randomized to one of the three dose-finding cohorts of the multicenter trial of liso-cel. One cohort received 5 x 107 cells in a single dose; a second cohort received the same number of cells but in two doses administered 14 days apart; the third cohort received a single dose of 1 x 108 cells.
The seamless trial design then moved to dose expansion, using the two single doses established in the dose-finding phase of the study. Ultimately, Dr. Abramson said, the third and pivotal diffuse large B-cell lymphoma (DLBCL) cohort received the higher single dose, since a dose-response relationship was seen in the earlier cohorts. No increase in cytokine release syndrome or neurotoxicity has been seen with the higher dose in patients evaluated to date.
Patients (median age, 61 years) were eligible to participate in the trial if they had relapsed or refractory DLBCL, primary mediastinal B-cell lymphoma, grade 3B follicular lymphoma, or mantle cell lymphoma. Patients with a failed prior allogeneic stem cell transplant or secondary central nervous system involvement were eligible, but all patients had to have an Eastern Cooperative Oncology Group (ECOG) performance status of 0-2.
As the trial moved to the core pivotal phase, eligibility requirements shifted slightly to include patients with ECOG status 0 or 1, and lymphoma diagnoses narrowed to include only DLBCL not otherwise specified (NOS), transformed follicular lymphoma, and high-grade B-cell lymphoma with double- and triple-hit cytogenetics. The core group was nearing completion of accrual at the time of the presentation, which presented preliminary results from this phase of the trial.
Among the 88 evaluable patients in the initial population with DLBCL receiving any of three dose levels, the best overall response rate (ORR) was 74% (95% confidence interval, 63%-83%); 52% of these patients achieved complete response (CR; 95% CI, 41%-63%).
For patients receiving the higher dose of liso-cel, the ORR was 81% (95% CI, 62%-94%), with a 63% CR rate (95% CI, 42%-81%), bearing out the dose-response rate that had been seen earlier in the trial, Dr. Abramson said.
The median duration of response in all TRANSCEND patients was 9.2 months; the median duration of remission has not been reached, he said. “We see evidence of durable response at 3 months in all our high-risk subsets, and that includes double- and triple-hit lymphomas, double-expresser lymphomas, patients who’ve never achieved prior complete remission, and patients with refractory disease.”
“The overall results are similarly encouraging,” Dr. Abramson said, with 86% of all patients alive at 6 months. Among the complete responders, 94% are alive at the 6-month mark. “The median duration of complete responders has not been reached in this cohort,” he said.
These results are notable, Dr. Abramson said, since about 90% of study participants have at least one disease risk factor that would predict median overall survival of 3-6 months.
During the period after leukapheresis while the CAR T cells were in production, patients could have ongoing treatment, but received PET scans to confirm disease before continuing enrollment in the trial and receiving liso-cel. The time from apheresis to product release for the pivotal cohort is now under 21 days, he said.
The study was supported by Juno Therapeutics, which plans to market liso-cel. Dr. Abramson reported ties with Celgene, Gilead, Seattle Genetics, Novartis, and Genentech.
SOURCE: Abramson J et al. Abstract 5.
SALT LAKE CITY – A CD19-directed 4-1BB chimeric antigen receptor (CAR) T cell product showed efficacy and a low rate of cytokine release syndrome and neurotoxicity in patients with aggressive lymphomas and poor prognoses, raising the possibility of outpatient administration and fewer hospitalization days in this high-risk group.
A total of 86 patients who received inpatient infusions of lisocabtagene maraleucel (liso-cel, also known as JCAR017) had a mean 15.6 days of hospitalization, compared with 9.3 days for 8 outpatient recipients, said Jeremy Abramson, MD, speaking at a top abstracts session of the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
As of October 2017, eight patients had received liso-cel infusion as outpatients with at least 28 days of postinfusion data, Dr. Abramson said.
Although all but one required hospital admission, at a median of 5 days postinfusion (range, 4-22 days), there had been no intensive care unit admissions, and no outpatient recipients had experienced severe cytokine release syndrome (CRS) or neurotoxicity. All admitted patients presented with fever.
Among the study population, “Cytokine release syndrome was only seen in 35% of our entire dataset,” with neurologic toxicity seen in 19% of participants, Dr. Abramson said. “The majority of subjects had no CRS and no toxicity,” he said. Severe CRS occurred in 1% of the study population, and severe neurotoxicity in 12%. There were no deaths related to either complication.
Dr. Abramson reported these results from the TRANSCEND NHL 001 trial, a seamless design phase 1 pivotal trial of liso-cel enrolling patients with relapsed and refractory aggressive B cell non-Hodgkin lymphoma (NHL). Liso-cel delivers CD19-directed CD4 and CD8 CAR T cells in a 1:1 ratio, said Dr. Abramson, director of the lymphoma program at the Massachusetts General Hospital Cancer Center, Boston.
A total of 91 patients were randomized to one of the three dose-finding cohorts of the multicenter trial of liso-cel. One cohort received 5 x 107 cells in a single dose; a second cohort received the same number of cells but in two doses administered 14 days apart; the third cohort received a single dose of 1 x 108 cells.
The seamless trial design then moved to dose expansion, using the two single doses established in the dose-finding phase of the study. Ultimately, Dr. Abramson said, the third and pivotal diffuse large B-cell lymphoma (DLBCL) cohort received the higher single dose, since a dose-response relationship was seen in the earlier cohorts. No increase in cytokine release syndrome or neurotoxicity has been seen with the higher dose in patients evaluated to date.
Patients (median age, 61 years) were eligible to participate in the trial if they had relapsed or refractory DLBCL, primary mediastinal B-cell lymphoma, grade 3B follicular lymphoma, or mantle cell lymphoma. Patients with a failed prior allogeneic stem cell transplant or secondary central nervous system involvement were eligible, but all patients had to have an Eastern Cooperative Oncology Group (ECOG) performance status of 0-2.
As the trial moved to the core pivotal phase, eligibility requirements shifted slightly to include patients with ECOG status 0 or 1, and lymphoma diagnoses narrowed to include only DLBCL not otherwise specified (NOS), transformed follicular lymphoma, and high-grade B-cell lymphoma with double- and triple-hit cytogenetics. The core group was nearing completion of accrual at the time of the presentation, which presented preliminary results from this phase of the trial.
Among the 88 evaluable patients in the initial population with DLBCL receiving any of three dose levels, the best overall response rate (ORR) was 74% (95% confidence interval, 63%-83%); 52% of these patients achieved complete response (CR; 95% CI, 41%-63%).
For patients receiving the higher dose of liso-cel, the ORR was 81% (95% CI, 62%-94%), with a 63% CR rate (95% CI, 42%-81%), bearing out the dose-response rate that had been seen earlier in the trial, Dr. Abramson said.
The median duration of response in all TRANSCEND patients was 9.2 months; the median duration of remission has not been reached, he said. “We see evidence of durable response at 3 months in all our high-risk subsets, and that includes double- and triple-hit lymphomas, double-expresser lymphomas, patients who’ve never achieved prior complete remission, and patients with refractory disease.”
“The overall results are similarly encouraging,” Dr. Abramson said, with 86% of all patients alive at 6 months. Among the complete responders, 94% are alive at the 6-month mark. “The median duration of complete responders has not been reached in this cohort,” he said.
These results are notable, Dr. Abramson said, since about 90% of study participants have at least one disease risk factor that would predict median overall survival of 3-6 months.
During the period after leukapheresis while the CAR T cells were in production, patients could have ongoing treatment, but received PET scans to confirm disease before continuing enrollment in the trial and receiving liso-cel. The time from apheresis to product release for the pivotal cohort is now under 21 days, he said.
The study was supported by Juno Therapeutics, which plans to market liso-cel. Dr. Abramson reported ties with Celgene, Gilead, Seattle Genetics, Novartis, and Genentech.
SOURCE: Abramson J et al. Abstract 5.
SALT LAKE CITY – A CD19-directed 4-1BB chimeric antigen receptor (CAR) T cell product showed efficacy and a low rate of cytokine release syndrome and neurotoxicity in patients with aggressive lymphomas and poor prognoses, raising the possibility of outpatient administration and fewer hospitalization days in this high-risk group.
A total of 86 patients who received inpatient infusions of lisocabtagene maraleucel (liso-cel, also known as JCAR017) had a mean 15.6 days of hospitalization, compared with 9.3 days for 8 outpatient recipients, said Jeremy Abramson, MD, speaking at a top abstracts session of the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
As of October 2017, eight patients had received liso-cel infusion as outpatients with at least 28 days of postinfusion data, Dr. Abramson said.
Although all but one required hospital admission, at a median of 5 days postinfusion (range, 4-22 days), there had been no intensive care unit admissions, and no outpatient recipients had experienced severe cytokine release syndrome (CRS) or neurotoxicity. All admitted patients presented with fever.
Among the study population, “Cytokine release syndrome was only seen in 35% of our entire dataset,” with neurologic toxicity seen in 19% of participants, Dr. Abramson said. “The majority of subjects had no CRS and no toxicity,” he said. Severe CRS occurred in 1% of the study population, and severe neurotoxicity in 12%. There were no deaths related to either complication.
Dr. Abramson reported these results from the TRANSCEND NHL 001 trial, a seamless design phase 1 pivotal trial of liso-cel enrolling patients with relapsed and refractory aggressive B cell non-Hodgkin lymphoma (NHL). Liso-cel delivers CD19-directed CD4 and CD8 CAR T cells in a 1:1 ratio, said Dr. Abramson, director of the lymphoma program at the Massachusetts General Hospital Cancer Center, Boston.
A total of 91 patients were randomized to one of the three dose-finding cohorts of the multicenter trial of liso-cel. One cohort received 5 x 107 cells in a single dose; a second cohort received the same number of cells but in two doses administered 14 days apart; the third cohort received a single dose of 1 x 108 cells.
The seamless trial design then moved to dose expansion, using the two single doses established in the dose-finding phase of the study. Ultimately, Dr. Abramson said, the third and pivotal diffuse large B-cell lymphoma (DLBCL) cohort received the higher single dose, since a dose-response relationship was seen in the earlier cohorts. No increase in cytokine release syndrome or neurotoxicity has been seen with the higher dose in patients evaluated to date.
Patients (median age, 61 years) were eligible to participate in the trial if they had relapsed or refractory DLBCL, primary mediastinal B-cell lymphoma, grade 3B follicular lymphoma, or mantle cell lymphoma. Patients with a failed prior allogeneic stem cell transplant or secondary central nervous system involvement were eligible, but all patients had to have an Eastern Cooperative Oncology Group (ECOG) performance status of 0-2.
As the trial moved to the core pivotal phase, eligibility requirements shifted slightly to include patients with ECOG status 0 or 1, and lymphoma diagnoses narrowed to include only DLBCL not otherwise specified (NOS), transformed follicular lymphoma, and high-grade B-cell lymphoma with double- and triple-hit cytogenetics. The core group was nearing completion of accrual at the time of the presentation, which presented preliminary results from this phase of the trial.
Among the 88 evaluable patients in the initial population with DLBCL receiving any of three dose levels, the best overall response rate (ORR) was 74% (95% confidence interval, 63%-83%); 52% of these patients achieved complete response (CR; 95% CI, 41%-63%).
For patients receiving the higher dose of liso-cel, the ORR was 81% (95% CI, 62%-94%), with a 63% CR rate (95% CI, 42%-81%), bearing out the dose-response rate that had been seen earlier in the trial, Dr. Abramson said.
The median duration of response in all TRANSCEND patients was 9.2 months; the median duration of remission has not been reached, he said. “We see evidence of durable response at 3 months in all our high-risk subsets, and that includes double- and triple-hit lymphomas, double-expresser lymphomas, patients who’ve never achieved prior complete remission, and patients with refractory disease.”
“The overall results are similarly encouraging,” Dr. Abramson said, with 86% of all patients alive at 6 months. Among the complete responders, 94% are alive at the 6-month mark. “The median duration of complete responders has not been reached in this cohort,” he said.
These results are notable, Dr. Abramson said, since about 90% of study participants have at least one disease risk factor that would predict median overall survival of 3-6 months.
During the period after leukapheresis while the CAR T cells were in production, patients could have ongoing treatment, but received PET scans to confirm disease before continuing enrollment in the trial and receiving liso-cel. The time from apheresis to product release for the pivotal cohort is now under 21 days, he said.
The study was supported by Juno Therapeutics, which plans to market liso-cel. Dr. Abramson reported ties with Celgene, Gilead, Seattle Genetics, Novartis, and Genentech.
SOURCE: Abramson J et al. Abstract 5.
REPORTING FROM THE 2018 BMT TANDEM MEETINGS
Key clinical point:
Major finding: High-risk lymphoma patients had more than 6 fewer inpatient days with outpatient CAR T infusion.
Study details: Seamless phase 1 trial initially evaluating 91 patients with relapsed/refractory diffuse large B cell lymphoma.
Disclosures: Juno Therapeutics sponsored the study. Dr. Abramson reported ties with Celgene, Gilead, Seattle Genetics, Novartis, and Genentech.
Source: Abramson J et al. Abstract 5.
Cancer groups offer guidance on immune-related adverse events
The American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) have released new guidelines designed to help clinicians manage the unique and sometimes severe side effects associated with cancer immunotherapy agents.
These guidelines meet a growing need to help practicing clinicians identify and best manage immune-related adverse events, according to Bryan J. Schneider, MD, of the University of Michigan Comprehensive Cancer Center, and vice chair of the NCCN Panel on Management of Immunotherapy-Related Toxicities.
“The mechanism of action of these anticancer therapies is so much different from anything that we’re used to,” Dr. Schneider said in an interview.
Critical need for guidance
The ASCO and NCCN guidelines are “critically important” to ensure uniform management of common immune-related adverse events, according to Stephen M. Ansell, MD, PhD, professor of medicine and chair of the Lymphoma Group at Mayo Clinic, Rochester, Minn.
“I think it also specifically highlights a few side effects that many people may not necessarily think about, from eye toxicities to thyroid effects, or the type of things that the average oncologist who is now using this in their practice quite regularly may not necessarily think about,” Dr. Ansell said. “Those kind of effects are now clearly outlined with clear guidance about what should be done, and I think that allows oncologists a resource to go and look at this carefully so that they do the right thing.”
The spectrum of adverse effects associated with checkpoint inhibitors is markedly different from what is seen with cytotoxic chemotherapy, the guidelines note. Most often, the side effects are seen in the skin, GI tract, and lungs, as well as the endocrine, adrenal, nervous, thyroid, pituitary, musculoskeletal, cardiovascular, ocular, and hematologic systems.
Stepwise approach
Side effects of checkpoint inhibitors are typically mild, but they can be severe and sometimes life-threatening, according to ASCO and NCCN.
If immune-related adverse events are mild (i.e., grade 1), treatment can continue with close monitoring, according to the guidelines. By contrast, moderate to severe immune-related adverse events can lead to severe declines in organ function and quality of life, or even fatal outcomes, so early detection and proper management are needed.
Grade 2 toxicities warrant suspending immune checkpoint inhibitor treatment, and resuming it once symptoms subside to grade 1 or less, according to the guidelines. Grade 3 toxicities should also prompt suspension of treatment, plus initiation of high-dose corticosteroids tapered over at least 4-6 weeks.
For most toxicities that reach grade 4, permanent discontinuation of checkpoint inhibitors is recommended.
A thoughtful discussion of potential risks and benefits is needed before using immune checkpoint inhibitors in patients who have autoimmune disease or prior organ transplant, according to the guidelines.
Vigilance required
Checkpoint inhibitors have been approved by the Food and Drug Administration to treat a variety of cancers, including melanoma, lung cancer, and Hodgkin lymphoma, as well as lung, liver, kidney, and bladder cancers.
Clinicians managing patients on checkpoint inhibitors should always be vigilant because immune-related adverse event symptoms can be subtle, according to Julie Brahmer, MD, of The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins in Baltimore.
“Everyone has to work as a team, which includes being educated on possible side effects to immunotherapy prior to prescribing it,” said Dr. Brahmer, chair of the ASCO panel and vice chair of the NCCN panel that developed the guidelines.
The guidelines were published Feb. 14 in two documents that are similar in content, but different in format. The ASCO guideline was published in the Journal of Clinical Oncology (doi: 10.1200/JCO.2017.77.6385) and the NCCN Clinical Practice Guidelines in Oncology were posted on the NCCN website.
While the first edition of the guidelines focuses specifically on immune checkpoint inhibitors, an update anticipated for 2019 will include guidance on chimeric antigen receptor (CAR) T-cell therapy, which is associated with several important side effects, notably cytokine release syndrome.
The American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) have released new guidelines designed to help clinicians manage the unique and sometimes severe side effects associated with cancer immunotherapy agents.
These guidelines meet a growing need to help practicing clinicians identify and best manage immune-related adverse events, according to Bryan J. Schneider, MD, of the University of Michigan Comprehensive Cancer Center, and vice chair of the NCCN Panel on Management of Immunotherapy-Related Toxicities.
“The mechanism of action of these anticancer therapies is so much different from anything that we’re used to,” Dr. Schneider said in an interview.
Critical need for guidance
The ASCO and NCCN guidelines are “critically important” to ensure uniform management of common immune-related adverse events, according to Stephen M. Ansell, MD, PhD, professor of medicine and chair of the Lymphoma Group at Mayo Clinic, Rochester, Minn.
“I think it also specifically highlights a few side effects that many people may not necessarily think about, from eye toxicities to thyroid effects, or the type of things that the average oncologist who is now using this in their practice quite regularly may not necessarily think about,” Dr. Ansell said. “Those kind of effects are now clearly outlined with clear guidance about what should be done, and I think that allows oncologists a resource to go and look at this carefully so that they do the right thing.”
The spectrum of adverse effects associated with checkpoint inhibitors is markedly different from what is seen with cytotoxic chemotherapy, the guidelines note. Most often, the side effects are seen in the skin, GI tract, and lungs, as well as the endocrine, adrenal, nervous, thyroid, pituitary, musculoskeletal, cardiovascular, ocular, and hematologic systems.
Stepwise approach
Side effects of checkpoint inhibitors are typically mild, but they can be severe and sometimes life-threatening, according to ASCO and NCCN.
If immune-related adverse events are mild (i.e., grade 1), treatment can continue with close monitoring, according to the guidelines. By contrast, moderate to severe immune-related adverse events can lead to severe declines in organ function and quality of life, or even fatal outcomes, so early detection and proper management are needed.
Grade 2 toxicities warrant suspending immune checkpoint inhibitor treatment, and resuming it once symptoms subside to grade 1 or less, according to the guidelines. Grade 3 toxicities should also prompt suspension of treatment, plus initiation of high-dose corticosteroids tapered over at least 4-6 weeks.
For most toxicities that reach grade 4, permanent discontinuation of checkpoint inhibitors is recommended.
A thoughtful discussion of potential risks and benefits is needed before using immune checkpoint inhibitors in patients who have autoimmune disease or prior organ transplant, according to the guidelines.
Vigilance required
Checkpoint inhibitors have been approved by the Food and Drug Administration to treat a variety of cancers, including melanoma, lung cancer, and Hodgkin lymphoma, as well as lung, liver, kidney, and bladder cancers.
Clinicians managing patients on checkpoint inhibitors should always be vigilant because immune-related adverse event symptoms can be subtle, according to Julie Brahmer, MD, of The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins in Baltimore.
“Everyone has to work as a team, which includes being educated on possible side effects to immunotherapy prior to prescribing it,” said Dr. Brahmer, chair of the ASCO panel and vice chair of the NCCN panel that developed the guidelines.
The guidelines were published Feb. 14 in two documents that are similar in content, but different in format. The ASCO guideline was published in the Journal of Clinical Oncology (doi: 10.1200/JCO.2017.77.6385) and the NCCN Clinical Practice Guidelines in Oncology were posted on the NCCN website.
While the first edition of the guidelines focuses specifically on immune checkpoint inhibitors, an update anticipated for 2019 will include guidance on chimeric antigen receptor (CAR) T-cell therapy, which is associated with several important side effects, notably cytokine release syndrome.
The American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) have released new guidelines designed to help clinicians manage the unique and sometimes severe side effects associated with cancer immunotherapy agents.
These guidelines meet a growing need to help practicing clinicians identify and best manage immune-related adverse events, according to Bryan J. Schneider, MD, of the University of Michigan Comprehensive Cancer Center, and vice chair of the NCCN Panel on Management of Immunotherapy-Related Toxicities.
“The mechanism of action of these anticancer therapies is so much different from anything that we’re used to,” Dr. Schneider said in an interview.
Critical need for guidance
The ASCO and NCCN guidelines are “critically important” to ensure uniform management of common immune-related adverse events, according to Stephen M. Ansell, MD, PhD, professor of medicine and chair of the Lymphoma Group at Mayo Clinic, Rochester, Minn.
“I think it also specifically highlights a few side effects that many people may not necessarily think about, from eye toxicities to thyroid effects, or the type of things that the average oncologist who is now using this in their practice quite regularly may not necessarily think about,” Dr. Ansell said. “Those kind of effects are now clearly outlined with clear guidance about what should be done, and I think that allows oncologists a resource to go and look at this carefully so that they do the right thing.”
The spectrum of adverse effects associated with checkpoint inhibitors is markedly different from what is seen with cytotoxic chemotherapy, the guidelines note. Most often, the side effects are seen in the skin, GI tract, and lungs, as well as the endocrine, adrenal, nervous, thyroid, pituitary, musculoskeletal, cardiovascular, ocular, and hematologic systems.
Stepwise approach
Side effects of checkpoint inhibitors are typically mild, but they can be severe and sometimes life-threatening, according to ASCO and NCCN.
If immune-related adverse events are mild (i.e., grade 1), treatment can continue with close monitoring, according to the guidelines. By contrast, moderate to severe immune-related adverse events can lead to severe declines in organ function and quality of life, or even fatal outcomes, so early detection and proper management are needed.
Grade 2 toxicities warrant suspending immune checkpoint inhibitor treatment, and resuming it once symptoms subside to grade 1 or less, according to the guidelines. Grade 3 toxicities should also prompt suspension of treatment, plus initiation of high-dose corticosteroids tapered over at least 4-6 weeks.
For most toxicities that reach grade 4, permanent discontinuation of checkpoint inhibitors is recommended.
A thoughtful discussion of potential risks and benefits is needed before using immune checkpoint inhibitors in patients who have autoimmune disease or prior organ transplant, according to the guidelines.
Vigilance required
Checkpoint inhibitors have been approved by the Food and Drug Administration to treat a variety of cancers, including melanoma, lung cancer, and Hodgkin lymphoma, as well as lung, liver, kidney, and bladder cancers.
Clinicians managing patients on checkpoint inhibitors should always be vigilant because immune-related adverse event symptoms can be subtle, according to Julie Brahmer, MD, of The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins in Baltimore.
“Everyone has to work as a team, which includes being educated on possible side effects to immunotherapy prior to prescribing it,” said Dr. Brahmer, chair of the ASCO panel and vice chair of the NCCN panel that developed the guidelines.
The guidelines were published Feb. 14 in two documents that are similar in content, but different in format. The ASCO guideline was published in the Journal of Clinical Oncology (doi: 10.1200/JCO.2017.77.6385) and the NCCN Clinical Practice Guidelines in Oncology were posted on the NCCN website.
While the first edition of the guidelines focuses specifically on immune checkpoint inhibitors, an update anticipated for 2019 will include guidance on chimeric antigen receptor (CAR) T-cell therapy, which is associated with several important side effects, notably cytokine release syndrome.
ERV expression may predict response to immune checkpoint blockade in ccRCC, other solid tumors
SAN FRANCISCO – The (ccRCC), according to findings from an analysis of nearly 5,000 tumor samples.
Similar associations may exist in other solid tumors, Shridar Ganesan, MD, reported at the ASCO-SITC Clinical Immuno-Oncology Symposium.
Merkel cell carcinoma, for example, has a high response rate despite its relatively low mutation burden. This is explained by the presence of infection with the Merkel cell polyomavirus in a low mutation burden subset, he said, noting that expression of the virus likely leads to expression of antigens that makes the disease both highly immunogenic and responsive to immune checkpoint therapy.
Expression of exogenous viruses is associated with response to immune checkpoint therapy in other cancers with low mutation burden, such as Epstein-Barr virus-positive gastric cancer, natural killer lymphoma, and Hodgkin disease.
“Intriguingly, renal cell carcinoma also has a relatively higher response rate to immune checkpoint therapy than would be anticipated by its relatively low mutation burden. However, this has no evidence of exogenous virus infection. Therefore, we turned our attention to endogenous retroviruses, which are an abundant potential stimulant of innate immunity in cancer,” he said.
Endogenous retroviruses (ERVs) now comprise about 5-8% of the human genome, and almost all of them have mutations that disable key coding genes of the retrovirus, meaning most cannot produce all the proteins necessary for viral replication.
“They’re essentially genomic fossils,” Dr. Ganesan said, adding that they all are silenced epigenetically in most normal adult tissues, both by DNA methylation and histone methylation. “However, inappropriate expression of endogenous retroviruses has been reported by multiple groups in some cancers and has been associated with evidence of immune activation. One can imagine that endogenous retroviral expression can be immunogenic both by expression of some [open reading frames] that are not disabled ... or just the viral RNA itself, which can be detected by cytoplasmic sensors ... and activate innate immunity,” he said.
To assess whether ERV expression corresponds with evidence of immune checkpoint activation in cancer, he and his colleagues conducted a pan-cancer analysis of more than 4,900 tumors across 21 cancer types using data from the Cancer Genome Atlas (TCGA).
“When we did this for about 66 annotated endogenous retroviruses in the TCGA database, we could see that different cancers had different amounts of retrovirus associated with immune activation ... in fact the strongest signal seen in this analysis was in clear cell renal cell carcinoma,” he said.
Signals were also seen in estrogen receptor–positive/human epidermal growth factor receptor 2-negative breast cancer, head and neck squamous cell carcinoma, and colon cancer.
A variety of ERVs were upregulated in RCC; different panels were associated with different cancer types. But two – ERVK.2 and ERV3.2 – were consistently upregulated across all the tumor types.
A closer look at ERV expression showed three clear clusters: extremely-high, intermediate, and low expression of ERV, and the very-high expression cluster had increased expression of numerous checkpoint genes, including CD8A, PD1, CTLA4, and LAG3 among others, compared with the low expression cluster.
This leads to the question of why a subset of RCCs have ERV expression.
In an attempt to answer that question, a transcript analysis was conducted to determine which transcripts are differentially regulated between the high and low ERV-expressing groups, and gene ontology analysis was performed.
“The results were quite striking. If you look at the modules that are differentially expressed between the high-ERV and the low-ERV groups, what pops up is really a lot of histone methyltransferase modules and chromatin regulation modules, ” he said, noting that this makes sense because of the silencing of ERV expression by histone methylation and DNA methylation, and suggests that “there is some deep abnormality in chromatin modulation in this subset of RCCs.
“This is intriguing, because RCCs are known to have mutations in chromatin modifying genes,” he said.
A look into whether the high-ERV–expressing group was enriched in any of these mutations showed some enrichment of BAP1 in the high- vs. low-expressing group, and that is currently being looked at further, he noted.
The next question was whether ERV expression correlated with response to immune checkpoint blockade in ccRCC, and this was looked at in a nonrandomized group of 15 patients with metastatic ccRCC who were treated with single-agent immune checkpoint therapy who had either clearly documented partial response or progressive disease. In 13 patient samples for which RNA expression of ERV3.2 was successfully measured by quantitative real-time polymerase chain reaction using two primer sets, ERV3.2 expression was significantly higher in responders vs. nonresponders in both primer sets (P less than .05 and .005).
“In summary, we have shown that expression of ERVs correlates with immune activation and increased expression of immune checkpoint genes in a subset of ccRCC, and perhaps several other solid tumor classes, and the expression of ERV3.2 is perhaps associated with response to PD1 blockade in this small preliminary cohort of ccRCC patients,” he said, noting that abnormal expression of ERV may be a biomarker of immune checkpoint therapy response in some cancers with a low mutation burden. “Mechanisms underlying ERV expression need to be investigated and may reflect underlying chromatin alterations or epigenetic abnormalities.”
Dr. Ganesan reported that his spouse is employed by Merck and that he is a consultant and/or advisory board member for Novartis, Roche, and Inspirata. He also holds patents with Inspirata.
sworcester@frontlinemedcom.com
SOURCE: Panda A et al., ASCO-SITC, Abstract #104.
SAN FRANCISCO – The (ccRCC), according to findings from an analysis of nearly 5,000 tumor samples.
Similar associations may exist in other solid tumors, Shridar Ganesan, MD, reported at the ASCO-SITC Clinical Immuno-Oncology Symposium.
Merkel cell carcinoma, for example, has a high response rate despite its relatively low mutation burden. This is explained by the presence of infection with the Merkel cell polyomavirus in a low mutation burden subset, he said, noting that expression of the virus likely leads to expression of antigens that makes the disease both highly immunogenic and responsive to immune checkpoint therapy.
Expression of exogenous viruses is associated with response to immune checkpoint therapy in other cancers with low mutation burden, such as Epstein-Barr virus-positive gastric cancer, natural killer lymphoma, and Hodgkin disease.
“Intriguingly, renal cell carcinoma also has a relatively higher response rate to immune checkpoint therapy than would be anticipated by its relatively low mutation burden. However, this has no evidence of exogenous virus infection. Therefore, we turned our attention to endogenous retroviruses, which are an abundant potential stimulant of innate immunity in cancer,” he said.
Endogenous retroviruses (ERVs) now comprise about 5-8% of the human genome, and almost all of them have mutations that disable key coding genes of the retrovirus, meaning most cannot produce all the proteins necessary for viral replication.
“They’re essentially genomic fossils,” Dr. Ganesan said, adding that they all are silenced epigenetically in most normal adult tissues, both by DNA methylation and histone methylation. “However, inappropriate expression of endogenous retroviruses has been reported by multiple groups in some cancers and has been associated with evidence of immune activation. One can imagine that endogenous retroviral expression can be immunogenic both by expression of some [open reading frames] that are not disabled ... or just the viral RNA itself, which can be detected by cytoplasmic sensors ... and activate innate immunity,” he said.
To assess whether ERV expression corresponds with evidence of immune checkpoint activation in cancer, he and his colleagues conducted a pan-cancer analysis of more than 4,900 tumors across 21 cancer types using data from the Cancer Genome Atlas (TCGA).
“When we did this for about 66 annotated endogenous retroviruses in the TCGA database, we could see that different cancers had different amounts of retrovirus associated with immune activation ... in fact the strongest signal seen in this analysis was in clear cell renal cell carcinoma,” he said.
Signals were also seen in estrogen receptor–positive/human epidermal growth factor receptor 2-negative breast cancer, head and neck squamous cell carcinoma, and colon cancer.
A variety of ERVs were upregulated in RCC; different panels were associated with different cancer types. But two – ERVK.2 and ERV3.2 – were consistently upregulated across all the tumor types.
A closer look at ERV expression showed three clear clusters: extremely-high, intermediate, and low expression of ERV, and the very-high expression cluster had increased expression of numerous checkpoint genes, including CD8A, PD1, CTLA4, and LAG3 among others, compared with the low expression cluster.
This leads to the question of why a subset of RCCs have ERV expression.
In an attempt to answer that question, a transcript analysis was conducted to determine which transcripts are differentially regulated between the high and low ERV-expressing groups, and gene ontology analysis was performed.
“The results were quite striking. If you look at the modules that are differentially expressed between the high-ERV and the low-ERV groups, what pops up is really a lot of histone methyltransferase modules and chromatin regulation modules, ” he said, noting that this makes sense because of the silencing of ERV expression by histone methylation and DNA methylation, and suggests that “there is some deep abnormality in chromatin modulation in this subset of RCCs.
“This is intriguing, because RCCs are known to have mutations in chromatin modifying genes,” he said.
A look into whether the high-ERV–expressing group was enriched in any of these mutations showed some enrichment of BAP1 in the high- vs. low-expressing group, and that is currently being looked at further, he noted.
The next question was whether ERV expression correlated with response to immune checkpoint blockade in ccRCC, and this was looked at in a nonrandomized group of 15 patients with metastatic ccRCC who were treated with single-agent immune checkpoint therapy who had either clearly documented partial response or progressive disease. In 13 patient samples for which RNA expression of ERV3.2 was successfully measured by quantitative real-time polymerase chain reaction using two primer sets, ERV3.2 expression was significantly higher in responders vs. nonresponders in both primer sets (P less than .05 and .005).
“In summary, we have shown that expression of ERVs correlates with immune activation and increased expression of immune checkpoint genes in a subset of ccRCC, and perhaps several other solid tumor classes, and the expression of ERV3.2 is perhaps associated with response to PD1 blockade in this small preliminary cohort of ccRCC patients,” he said, noting that abnormal expression of ERV may be a biomarker of immune checkpoint therapy response in some cancers with a low mutation burden. “Mechanisms underlying ERV expression need to be investigated and may reflect underlying chromatin alterations or epigenetic abnormalities.”
Dr. Ganesan reported that his spouse is employed by Merck and that he is a consultant and/or advisory board member for Novartis, Roche, and Inspirata. He also holds patents with Inspirata.
sworcester@frontlinemedcom.com
SOURCE: Panda A et al., ASCO-SITC, Abstract #104.
SAN FRANCISCO – The (ccRCC), according to findings from an analysis of nearly 5,000 tumor samples.
Similar associations may exist in other solid tumors, Shridar Ganesan, MD, reported at the ASCO-SITC Clinical Immuno-Oncology Symposium.
Merkel cell carcinoma, for example, has a high response rate despite its relatively low mutation burden. This is explained by the presence of infection with the Merkel cell polyomavirus in a low mutation burden subset, he said, noting that expression of the virus likely leads to expression of antigens that makes the disease both highly immunogenic and responsive to immune checkpoint therapy.
Expression of exogenous viruses is associated with response to immune checkpoint therapy in other cancers with low mutation burden, such as Epstein-Barr virus-positive gastric cancer, natural killer lymphoma, and Hodgkin disease.
“Intriguingly, renal cell carcinoma also has a relatively higher response rate to immune checkpoint therapy than would be anticipated by its relatively low mutation burden. However, this has no evidence of exogenous virus infection. Therefore, we turned our attention to endogenous retroviruses, which are an abundant potential stimulant of innate immunity in cancer,” he said.
Endogenous retroviruses (ERVs) now comprise about 5-8% of the human genome, and almost all of them have mutations that disable key coding genes of the retrovirus, meaning most cannot produce all the proteins necessary for viral replication.
“They’re essentially genomic fossils,” Dr. Ganesan said, adding that they all are silenced epigenetically in most normal adult tissues, both by DNA methylation and histone methylation. “However, inappropriate expression of endogenous retroviruses has been reported by multiple groups in some cancers and has been associated with evidence of immune activation. One can imagine that endogenous retroviral expression can be immunogenic both by expression of some [open reading frames] that are not disabled ... or just the viral RNA itself, which can be detected by cytoplasmic sensors ... and activate innate immunity,” he said.
To assess whether ERV expression corresponds with evidence of immune checkpoint activation in cancer, he and his colleagues conducted a pan-cancer analysis of more than 4,900 tumors across 21 cancer types using data from the Cancer Genome Atlas (TCGA).
“When we did this for about 66 annotated endogenous retroviruses in the TCGA database, we could see that different cancers had different amounts of retrovirus associated with immune activation ... in fact the strongest signal seen in this analysis was in clear cell renal cell carcinoma,” he said.
Signals were also seen in estrogen receptor–positive/human epidermal growth factor receptor 2-negative breast cancer, head and neck squamous cell carcinoma, and colon cancer.
A variety of ERVs were upregulated in RCC; different panels were associated with different cancer types. But two – ERVK.2 and ERV3.2 – were consistently upregulated across all the tumor types.
A closer look at ERV expression showed three clear clusters: extremely-high, intermediate, and low expression of ERV, and the very-high expression cluster had increased expression of numerous checkpoint genes, including CD8A, PD1, CTLA4, and LAG3 among others, compared with the low expression cluster.
This leads to the question of why a subset of RCCs have ERV expression.
In an attempt to answer that question, a transcript analysis was conducted to determine which transcripts are differentially regulated between the high and low ERV-expressing groups, and gene ontology analysis was performed.
“The results were quite striking. If you look at the modules that are differentially expressed between the high-ERV and the low-ERV groups, what pops up is really a lot of histone methyltransferase modules and chromatin regulation modules, ” he said, noting that this makes sense because of the silencing of ERV expression by histone methylation and DNA methylation, and suggests that “there is some deep abnormality in chromatin modulation in this subset of RCCs.
“This is intriguing, because RCCs are known to have mutations in chromatin modifying genes,” he said.
A look into whether the high-ERV–expressing group was enriched in any of these mutations showed some enrichment of BAP1 in the high- vs. low-expressing group, and that is currently being looked at further, he noted.
The next question was whether ERV expression correlated with response to immune checkpoint blockade in ccRCC, and this was looked at in a nonrandomized group of 15 patients with metastatic ccRCC who were treated with single-agent immune checkpoint therapy who had either clearly documented partial response or progressive disease. In 13 patient samples for which RNA expression of ERV3.2 was successfully measured by quantitative real-time polymerase chain reaction using two primer sets, ERV3.2 expression was significantly higher in responders vs. nonresponders in both primer sets (P less than .05 and .005).
“In summary, we have shown that expression of ERVs correlates with immune activation and increased expression of immune checkpoint genes in a subset of ccRCC, and perhaps several other solid tumor classes, and the expression of ERV3.2 is perhaps associated with response to PD1 blockade in this small preliminary cohort of ccRCC patients,” he said, noting that abnormal expression of ERV may be a biomarker of immune checkpoint therapy response in some cancers with a low mutation burden. “Mechanisms underlying ERV expression need to be investigated and may reflect underlying chromatin alterations or epigenetic abnormalities.”
Dr. Ganesan reported that his spouse is employed by Merck and that he is a consultant and/or advisory board member for Novartis, Roche, and Inspirata. He also holds patents with Inspirata.
sworcester@frontlinemedcom.com
SOURCE: Panda A et al., ASCO-SITC, Abstract #104.
REPORTING FROM THE CLINICAL IMMUNO-ONCOLOGY SYMPOSIUM
Key clinical point: ERV3.2 expression is associated with immune checkpoint blockade response in ccRCC.
Major finding: ERV3.2 expression was significantly higher in responders vs. nonresponders in two primer sets (P less than .05 and.005).
Study details: A pan-cancer analysis of more 4,900 tumors.
Disclosures: Dr. Ganesan reported that his spouse is employed by Merck and that he is a consultant and/or advisory board member for Novartis, Roche, and Inspirata. He also holds patents with Inspirata
Source: Panda A et al. ASCO-SITC, Abstract #104.
Two biomarkers predict immunotherapy response for NSCLC
Two biomarkers were correlated with poor outcomes for patients with non–small cell lung cancer (NSCLC) who were treated with immune checkpoint inhibitors, according to the results of a multicenter retrospective study.
Furthermore, these two biomarkers – derived neutrophil to lymphocyte ratio (dNLR) and lactate dehydrogenase (LDH) – could make up a lung immune prognostic index (LIPI) to help predict response to immune checkpoint inhibitor therapy, Laura Mezquita, MD, of the Institut Gustave Roussy in Villejuif, France, and her associates reported in JAMA Oncology.
The median overall survival for the population evaluated was 10.1 months (95% CI, 9.0-11.7 months), and the population’s median progression-free survival was 4.0 months (95% confidence interval, 3.4-5.0 months).
Overall survival was independently associated with both a dNLR greater than three (HR, 2.22) and an LDH level greater than the upper limit of normal (HR, 2.51), they reported.
The researchers sought to examine dNLR and LDH after previously reported data had shown that those biomarkers predict immunotherapy response for other types of disease.
“We hypothesized that the combination of baseline dNLR and LDH could be correlated with resistance to ICI [immune checkpoint inhibitor] therapy ... and could be used to develop a long immune prognostic index,” Dr. Mezquita and her associates wrote.
The researchers examined whether, at baseline, patients had a dNLR greater than three or an LDH level greater than the upper limit of normal. They then derived the LIPI by categorizing patients based on whether they met both biomarker criteria (“poor”), only one (“intermediate”), or neither (“good”), and analyzed the results accordingly.
Researchers evaluated 431 patients using the LIPI: 15% of these patients were in the poor group, 48% were in the intermediate group, and 38% were in the good group.
Patients in the poor group experienced worse median overall survival (4.8 months) and progression-free survival (2 months) than did those who had an LIPI considered intermediate (OS, 10 months; PFS, 3.7 months) or good (OS, 16.5 months; PFS, 6.3 months), according to Dr. Mezquita and her associates.
The investigators noted that the retrospective nature of the study and unknown clinical and pathological data may have limited these findings, but they concluded that LIPI with PD-L1 expression ought to be explored in future prospective trials and that LIPI could be used for patient stratification in future randomized trials.
The researchers reported no disclosures.
SOURCE: Mezquita L et al. Jama Oncol. 2018 Jan 11. doi: 10.1001/jamaoncol.2017.4771.
Two biomarkers were correlated with poor outcomes for patients with non–small cell lung cancer (NSCLC) who were treated with immune checkpoint inhibitors, according to the results of a multicenter retrospective study.
Furthermore, these two biomarkers – derived neutrophil to lymphocyte ratio (dNLR) and lactate dehydrogenase (LDH) – could make up a lung immune prognostic index (LIPI) to help predict response to immune checkpoint inhibitor therapy, Laura Mezquita, MD, of the Institut Gustave Roussy in Villejuif, France, and her associates reported in JAMA Oncology.
The median overall survival for the population evaluated was 10.1 months (95% CI, 9.0-11.7 months), and the population’s median progression-free survival was 4.0 months (95% confidence interval, 3.4-5.0 months).
Overall survival was independently associated with both a dNLR greater than three (HR, 2.22) and an LDH level greater than the upper limit of normal (HR, 2.51), they reported.
The researchers sought to examine dNLR and LDH after previously reported data had shown that those biomarkers predict immunotherapy response for other types of disease.
“We hypothesized that the combination of baseline dNLR and LDH could be correlated with resistance to ICI [immune checkpoint inhibitor] therapy ... and could be used to develop a long immune prognostic index,” Dr. Mezquita and her associates wrote.
The researchers examined whether, at baseline, patients had a dNLR greater than three or an LDH level greater than the upper limit of normal. They then derived the LIPI by categorizing patients based on whether they met both biomarker criteria (“poor”), only one (“intermediate”), or neither (“good”), and analyzed the results accordingly.
Researchers evaluated 431 patients using the LIPI: 15% of these patients were in the poor group, 48% were in the intermediate group, and 38% were in the good group.
Patients in the poor group experienced worse median overall survival (4.8 months) and progression-free survival (2 months) than did those who had an LIPI considered intermediate (OS, 10 months; PFS, 3.7 months) or good (OS, 16.5 months; PFS, 6.3 months), according to Dr. Mezquita and her associates.
The investigators noted that the retrospective nature of the study and unknown clinical and pathological data may have limited these findings, but they concluded that LIPI with PD-L1 expression ought to be explored in future prospective trials and that LIPI could be used for patient stratification in future randomized trials.
The researchers reported no disclosures.
SOURCE: Mezquita L et al. Jama Oncol. 2018 Jan 11. doi: 10.1001/jamaoncol.2017.4771.
Two biomarkers were correlated with poor outcomes for patients with non–small cell lung cancer (NSCLC) who were treated with immune checkpoint inhibitors, according to the results of a multicenter retrospective study.
Furthermore, these two biomarkers – derived neutrophil to lymphocyte ratio (dNLR) and lactate dehydrogenase (LDH) – could make up a lung immune prognostic index (LIPI) to help predict response to immune checkpoint inhibitor therapy, Laura Mezquita, MD, of the Institut Gustave Roussy in Villejuif, France, and her associates reported in JAMA Oncology.
The median overall survival for the population evaluated was 10.1 months (95% CI, 9.0-11.7 months), and the population’s median progression-free survival was 4.0 months (95% confidence interval, 3.4-5.0 months).
Overall survival was independently associated with both a dNLR greater than three (HR, 2.22) and an LDH level greater than the upper limit of normal (HR, 2.51), they reported.
The researchers sought to examine dNLR and LDH after previously reported data had shown that those biomarkers predict immunotherapy response for other types of disease.
“We hypothesized that the combination of baseline dNLR and LDH could be correlated with resistance to ICI [immune checkpoint inhibitor] therapy ... and could be used to develop a long immune prognostic index,” Dr. Mezquita and her associates wrote.
The researchers examined whether, at baseline, patients had a dNLR greater than three or an LDH level greater than the upper limit of normal. They then derived the LIPI by categorizing patients based on whether they met both biomarker criteria (“poor”), only one (“intermediate”), or neither (“good”), and analyzed the results accordingly.
Researchers evaluated 431 patients using the LIPI: 15% of these patients were in the poor group, 48% were in the intermediate group, and 38% were in the good group.
Patients in the poor group experienced worse median overall survival (4.8 months) and progression-free survival (2 months) than did those who had an LIPI considered intermediate (OS, 10 months; PFS, 3.7 months) or good (OS, 16.5 months; PFS, 6.3 months), according to Dr. Mezquita and her associates.
The investigators noted that the retrospective nature of the study and unknown clinical and pathological data may have limited these findings, but they concluded that LIPI with PD-L1 expression ought to be explored in future prospective trials and that LIPI could be used for patient stratification in future randomized trials.
The researchers reported no disclosures.
SOURCE: Mezquita L et al. Jama Oncol. 2018 Jan 11. doi: 10.1001/jamaoncol.2017.4771.
FROM JAMA ONCOLOGY
Key clinical point:
Major finding: Median OS was 4.8 months and median PFS was 2.0 months for patients with advanced NSCLC who had both a dNLR greater than three and an LDH level greater than the upper limit of normal.
Study details: A multicenter retrospective study which included a test cohort, validation cohort, and control cohort.
Disclosures: No conflict of interest disclosures.
Source: Mezquita L et al. Jama Oncol. 2018 Jan 11. doi: 10.1001/jamaoncol.2017.4771.