User login
Atypical Keratotic Nodule on the Knuckle
The Diagnosis: Atypical Mycobacterial Infection
The history of rapid growth followed by shrinkage as well as the craterlike clinical appearance of our patient’s lesion were suspicious for the keratoacanthoma variant of squamous cell carcinoma (SCC). Periodic acid–Schiff green staining was negative for fungal or bacterial organisms, and the biopsy findings of keratinocyte atypia and irregular epidermal proliferation seemed to confirm our suspicion for well-differentiated SCC (Figure 1). Our patient subsequently was scheduled for Mohs micrographic surgery. Fortunately, a sample of tissue had been sent for panculture—bacterial, fungal, and mycobacterial—to rule out infectious etiologies, given the history of possible traumatic inoculation, and returned positive for Mycobacterium marinum infection prior to the surgery. Mohs surgery was canceled, and he was referred to an infectious disease specialist who started antibiotic treatment with azithromycin, ethambutol, and rifabutin. After 1 month of treatment the lesion substantially improved (Figure 2), further supporting the diagnosis of M marinum infection over SCC.

The differential diagnosis also included sporotrichosis, leishmaniasis, and chromoblastomycosis. Sporotrichosis lesions typically develop as multiple nodules and ulcers along a path of lymphatic drainage and can exhibit asteroid bodies and cigar-shaped yeast forms on histology. Chromoblastomycosis may display pseudoepitheliomatous hyperplasia and granulomatous inflammation; however, pathognomonic pigmented Medlar bodies also likely would be present.1 Leishmaniasis has a wide variety of presentations; however, it typically occurs in patients with exposure to endemic areas outside of the United States. Although leishmaniasis may demonstrate pseudoepitheliomatous hyperplasia, ulceration, and mixed inflammation on histology, it also likely would show amastigotes within dermal macrophages.2

Atypical mycobacterial infections initially may be misdiagnosed as SCC due to their tendency to induce irregular acanthosis in the form of pseudoepitheliomatous hyperplasia as well as mild keratinocyte atypia secondary to inflammation.3,4 Our case is unique because it occurred with M marinum infection specifically. The histopathologic findings of M marinum infections are variable and may additionally include granulomas, most commonly suppurative; intraepithelial abscesses; small vessel proliferation; dermal fibrosis; multinucleated giant cells; and transepidermal elimination.4,5 Periodic acid–Schiff, Ziehl-Neelsen (acid-fast bacilli), and Fite staining may be used to distinguish M marinum infection from SCC but have low sensitivities (approximately 30%). Culture remains the most reliable test, with a sensitivity of nearly 80%.5-7 In our patient, a Periodic acid–Schiff stain was obtained prior to receiving culture results, and acid-fast bacilli and Fite staining were added after the culture returned positive; however, all 3 stains failed to highlight any mycobacteria.
The primary risk factor for infection with M marinum is contact with aquatic environments or marine animals, and most cases involve the fingers or the hand.6 After we reached the diagnosis and further discussed the patient’s history, he recalled fishing for and cleaning raw shrimp around the time that he had a splinter. The Infectious Diseases Society of America recommends a treatment course extending 1 to 2 months after clinical symptoms resolve with ethambutol in addition to clarithromycin or azithromycin.8 If the infection is near a joint, rifampin should be empirically added to account for a potentially deeper infection. Imaging should be obtained to evaluate for joint space involvement, with magnetic resonance imaging being the preferred modality. If joint space involvement is confirmed, surgical debridement is indicated. Surgical debridement also is indicated for infections that fail to respond to antibiotic therapy.8
This case highlights M marinum infection as a potential mimicker of SCC, particularly if the biopsy is relatively superficial, as often occurs when obtained via the common shave technique. The distinction is critical, as M marinum infection is highly treatable and inappropriate surgery on the typical hand and finger locations may subject patients to substantial morbidity, such as the need for a skin graft, reduced mobility from scarring, or risk for serious wound infection.9 For superficial biopsies of an atypical squamous process, pathologists also may consider routinely recommending tissue culture, especially for hand and finger locations or when a history of local trauma is reported, instead of recommending complete excision or repeat biopsy alone.
- Elewski BE, Hughey LC, Hunt KM, et al. Fungal diseases. In: Bolognia J, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:1329-1363.
- Bravo FG. Protozoa and worms. In: Bolognia J, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:1470-1502.
- Zayour M, Lazova R. Pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2011;33:112-122; quiz 123-126. doi:10.1097 /DAD.0b013e3181fcfb47
- Li JJ, Beresford R, Fyfe J, et al. Clinical and histopathological features of cutaneous nontuberculous mycobacterial infection: a review of 13 cases. J Cutan Pathol. 2017;44:433-443. doi:10.1111/cup.12903
- Abbas O, Marrouch N, Kattar MM, et al. Cutaneous non-tuberculous mycobacterial infections: a clinical and histopathological study of 17 cases from Lebanon. J Eur Acad Dermatol Venereol. 2011;25:33-42. doi:10.1111/j.1468-3083.2010.03684.x
- Johnson MG, Stout JE. Twenty-eight cases of Mycobacterium marinum infection: retrospective case series and literature review. Infection. 2015;43:655-662. doi:10.1007/s15010-015-0776-8
- Aubry A, Mougari F, Reibel F, et al. Mycobacterium marinum. Microbiol Spectr. 2017;5. doi:10.1128/microbiolspec.TNMI7-0038-2016
- Griffith DE, Aksamit T, Brown-Elliott BA, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175:367-416. doi:10.1164/rccm.200604-571ST
- Alam M, Ibrahim O, Nodzenski M, et al. Adverse events associated with Mohs micrographic surgery: multicenter prospective cohort study of 20,821 cases at 23 centers. JAMA Dermatol. 2013;149:1378-1385. doi:10.1001/jamadermatol.2013.6255
The Diagnosis: Atypical Mycobacterial Infection
The history of rapid growth followed by shrinkage as well as the craterlike clinical appearance of our patient’s lesion were suspicious for the keratoacanthoma variant of squamous cell carcinoma (SCC). Periodic acid–Schiff green staining was negative for fungal or bacterial organisms, and the biopsy findings of keratinocyte atypia and irregular epidermal proliferation seemed to confirm our suspicion for well-differentiated SCC (Figure 1). Our patient subsequently was scheduled for Mohs micrographic surgery. Fortunately, a sample of tissue had been sent for panculture—bacterial, fungal, and mycobacterial—to rule out infectious etiologies, given the history of possible traumatic inoculation, and returned positive for Mycobacterium marinum infection prior to the surgery. Mohs surgery was canceled, and he was referred to an infectious disease specialist who started antibiotic treatment with azithromycin, ethambutol, and rifabutin. After 1 month of treatment the lesion substantially improved (Figure 2), further supporting the diagnosis of M marinum infection over SCC.

The differential diagnosis also included sporotrichosis, leishmaniasis, and chromoblastomycosis. Sporotrichosis lesions typically develop as multiple nodules and ulcers along a path of lymphatic drainage and can exhibit asteroid bodies and cigar-shaped yeast forms on histology. Chromoblastomycosis may display pseudoepitheliomatous hyperplasia and granulomatous inflammation; however, pathognomonic pigmented Medlar bodies also likely would be present.1 Leishmaniasis has a wide variety of presentations; however, it typically occurs in patients with exposure to endemic areas outside of the United States. Although leishmaniasis may demonstrate pseudoepitheliomatous hyperplasia, ulceration, and mixed inflammation on histology, it also likely would show amastigotes within dermal macrophages.2

Atypical mycobacterial infections initially may be misdiagnosed as SCC due to their tendency to induce irregular acanthosis in the form of pseudoepitheliomatous hyperplasia as well as mild keratinocyte atypia secondary to inflammation.3,4 Our case is unique because it occurred with M marinum infection specifically. The histopathologic findings of M marinum infections are variable and may additionally include granulomas, most commonly suppurative; intraepithelial abscesses; small vessel proliferation; dermal fibrosis; multinucleated giant cells; and transepidermal elimination.4,5 Periodic acid–Schiff, Ziehl-Neelsen (acid-fast bacilli), and Fite staining may be used to distinguish M marinum infection from SCC but have low sensitivities (approximately 30%). Culture remains the most reliable test, with a sensitivity of nearly 80%.5-7 In our patient, a Periodic acid–Schiff stain was obtained prior to receiving culture results, and acid-fast bacilli and Fite staining were added after the culture returned positive; however, all 3 stains failed to highlight any mycobacteria.
The primary risk factor for infection with M marinum is contact with aquatic environments or marine animals, and most cases involve the fingers or the hand.6 After we reached the diagnosis and further discussed the patient’s history, he recalled fishing for and cleaning raw shrimp around the time that he had a splinter. The Infectious Diseases Society of America recommends a treatment course extending 1 to 2 months after clinical symptoms resolve with ethambutol in addition to clarithromycin or azithromycin.8 If the infection is near a joint, rifampin should be empirically added to account for a potentially deeper infection. Imaging should be obtained to evaluate for joint space involvement, with magnetic resonance imaging being the preferred modality. If joint space involvement is confirmed, surgical debridement is indicated. Surgical debridement also is indicated for infections that fail to respond to antibiotic therapy.8
This case highlights M marinum infection as a potential mimicker of SCC, particularly if the biopsy is relatively superficial, as often occurs when obtained via the common shave technique. The distinction is critical, as M marinum infection is highly treatable and inappropriate surgery on the typical hand and finger locations may subject patients to substantial morbidity, such as the need for a skin graft, reduced mobility from scarring, or risk for serious wound infection.9 For superficial biopsies of an atypical squamous process, pathologists also may consider routinely recommending tissue culture, especially for hand and finger locations or when a history of local trauma is reported, instead of recommending complete excision or repeat biopsy alone.
The Diagnosis: Atypical Mycobacterial Infection
The history of rapid growth followed by shrinkage as well as the craterlike clinical appearance of our patient’s lesion were suspicious for the keratoacanthoma variant of squamous cell carcinoma (SCC). Periodic acid–Schiff green staining was negative for fungal or bacterial organisms, and the biopsy findings of keratinocyte atypia and irregular epidermal proliferation seemed to confirm our suspicion for well-differentiated SCC (Figure 1). Our patient subsequently was scheduled for Mohs micrographic surgery. Fortunately, a sample of tissue had been sent for panculture—bacterial, fungal, and mycobacterial—to rule out infectious etiologies, given the history of possible traumatic inoculation, and returned positive for Mycobacterium marinum infection prior to the surgery. Mohs surgery was canceled, and he was referred to an infectious disease specialist who started antibiotic treatment with azithromycin, ethambutol, and rifabutin. After 1 month of treatment the lesion substantially improved (Figure 2), further supporting the diagnosis of M marinum infection over SCC.

The differential diagnosis also included sporotrichosis, leishmaniasis, and chromoblastomycosis. Sporotrichosis lesions typically develop as multiple nodules and ulcers along a path of lymphatic drainage and can exhibit asteroid bodies and cigar-shaped yeast forms on histology. Chromoblastomycosis may display pseudoepitheliomatous hyperplasia and granulomatous inflammation; however, pathognomonic pigmented Medlar bodies also likely would be present.1 Leishmaniasis has a wide variety of presentations; however, it typically occurs in patients with exposure to endemic areas outside of the United States. Although leishmaniasis may demonstrate pseudoepitheliomatous hyperplasia, ulceration, and mixed inflammation on histology, it also likely would show amastigotes within dermal macrophages.2

Atypical mycobacterial infections initially may be misdiagnosed as SCC due to their tendency to induce irregular acanthosis in the form of pseudoepitheliomatous hyperplasia as well as mild keratinocyte atypia secondary to inflammation.3,4 Our case is unique because it occurred with M marinum infection specifically. The histopathologic findings of M marinum infections are variable and may additionally include granulomas, most commonly suppurative; intraepithelial abscesses; small vessel proliferation; dermal fibrosis; multinucleated giant cells; and transepidermal elimination.4,5 Periodic acid–Schiff, Ziehl-Neelsen (acid-fast bacilli), and Fite staining may be used to distinguish M marinum infection from SCC but have low sensitivities (approximately 30%). Culture remains the most reliable test, with a sensitivity of nearly 80%.5-7 In our patient, a Periodic acid–Schiff stain was obtained prior to receiving culture results, and acid-fast bacilli and Fite staining were added after the culture returned positive; however, all 3 stains failed to highlight any mycobacteria.
The primary risk factor for infection with M marinum is contact with aquatic environments or marine animals, and most cases involve the fingers or the hand.6 After we reached the diagnosis and further discussed the patient’s history, he recalled fishing for and cleaning raw shrimp around the time that he had a splinter. The Infectious Diseases Society of America recommends a treatment course extending 1 to 2 months after clinical symptoms resolve with ethambutol in addition to clarithromycin or azithromycin.8 If the infection is near a joint, rifampin should be empirically added to account for a potentially deeper infection. Imaging should be obtained to evaluate for joint space involvement, with magnetic resonance imaging being the preferred modality. If joint space involvement is confirmed, surgical debridement is indicated. Surgical debridement also is indicated for infections that fail to respond to antibiotic therapy.8
This case highlights M marinum infection as a potential mimicker of SCC, particularly if the biopsy is relatively superficial, as often occurs when obtained via the common shave technique. The distinction is critical, as M marinum infection is highly treatable and inappropriate surgery on the typical hand and finger locations may subject patients to substantial morbidity, such as the need for a skin graft, reduced mobility from scarring, or risk for serious wound infection.9 For superficial biopsies of an atypical squamous process, pathologists also may consider routinely recommending tissue culture, especially for hand and finger locations or when a history of local trauma is reported, instead of recommending complete excision or repeat biopsy alone.
- Elewski BE, Hughey LC, Hunt KM, et al. Fungal diseases. In: Bolognia J, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:1329-1363.
- Bravo FG. Protozoa and worms. In: Bolognia J, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:1470-1502.
- Zayour M, Lazova R. Pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2011;33:112-122; quiz 123-126. doi:10.1097 /DAD.0b013e3181fcfb47
- Li JJ, Beresford R, Fyfe J, et al. Clinical and histopathological features of cutaneous nontuberculous mycobacterial infection: a review of 13 cases. J Cutan Pathol. 2017;44:433-443. doi:10.1111/cup.12903
- Abbas O, Marrouch N, Kattar MM, et al. Cutaneous non-tuberculous mycobacterial infections: a clinical and histopathological study of 17 cases from Lebanon. J Eur Acad Dermatol Venereol. 2011;25:33-42. doi:10.1111/j.1468-3083.2010.03684.x
- Johnson MG, Stout JE. Twenty-eight cases of Mycobacterium marinum infection: retrospective case series and literature review. Infection. 2015;43:655-662. doi:10.1007/s15010-015-0776-8
- Aubry A, Mougari F, Reibel F, et al. Mycobacterium marinum. Microbiol Spectr. 2017;5. doi:10.1128/microbiolspec.TNMI7-0038-2016
- Griffith DE, Aksamit T, Brown-Elliott BA, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175:367-416. doi:10.1164/rccm.200604-571ST
- Alam M, Ibrahim O, Nodzenski M, et al. Adverse events associated with Mohs micrographic surgery: multicenter prospective cohort study of 20,821 cases at 23 centers. JAMA Dermatol. 2013;149:1378-1385. doi:10.1001/jamadermatol.2013.6255
- Elewski BE, Hughey LC, Hunt KM, et al. Fungal diseases. In: Bolognia J, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:1329-1363.
- Bravo FG. Protozoa and worms. In: Bolognia J, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:1470-1502.
- Zayour M, Lazova R. Pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2011;33:112-122; quiz 123-126. doi:10.1097 /DAD.0b013e3181fcfb47
- Li JJ, Beresford R, Fyfe J, et al. Clinical and histopathological features of cutaneous nontuberculous mycobacterial infection: a review of 13 cases. J Cutan Pathol. 2017;44:433-443. doi:10.1111/cup.12903
- Abbas O, Marrouch N, Kattar MM, et al. Cutaneous non-tuberculous mycobacterial infections: a clinical and histopathological study of 17 cases from Lebanon. J Eur Acad Dermatol Venereol. 2011;25:33-42. doi:10.1111/j.1468-3083.2010.03684.x
- Johnson MG, Stout JE. Twenty-eight cases of Mycobacterium marinum infection: retrospective case series and literature review. Infection. 2015;43:655-662. doi:10.1007/s15010-015-0776-8
- Aubry A, Mougari F, Reibel F, et al. Mycobacterium marinum. Microbiol Spectr. 2017;5. doi:10.1128/microbiolspec.TNMI7-0038-2016
- Griffith DE, Aksamit T, Brown-Elliott BA, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175:367-416. doi:10.1164/rccm.200604-571ST
- Alam M, Ibrahim O, Nodzenski M, et al. Adverse events associated with Mohs micrographic surgery: multicenter prospective cohort study of 20,821 cases at 23 centers. JAMA Dermatol. 2013;149:1378-1385. doi:10.1001/jamadermatol.2013.6255
A 75-year-old man presented with a lesion on the knuckle of 5 months’ duration. He reported that the lesion initially grew very quickly before shrinking down to its current size. He denied any bleeding or pain but thought he may have had a splinter in the area around the time the lesion appeared. He reported spending a lot of time outdoors and noted several recent insect and tick bites. He also owned a boat and frequently went fishing. He previously had been treated for actinic keratoses but had no history of skin cancer and no family history of melanoma. Physical examination revealed a 2-cm erythematous nodule with central hyperkeratosis overlying the metacarpophalangeal joint of the right index finger. A shave biopsy was performed.

Meningococcal B vaccine protects against gonorrhea
PARIS – All the way back in 1907, The Lancet published an article on a gonorrhea vaccine trial. Today, after continuous research throughout the intervening 110-plus years, scientists may finally have achieved success. Sébastien Fouéré, MD, discussed the details at a press conference that focused on the highlights of the Dermatology Days of Paris conference. Dr. Fouéré is the head of the genital dermatology and sexually transmitted infections unit at Saint-Louis Hospital, Paris.
Twin bacteria
Although the gonorrhea vaccine has long been the subject of research, Dr. Fouéré views 2017 as a turning point. This was when the results of a study led by Helen Petousis-Harris, PhD, were published.
“She tried to formalize the not completely indisputable results published by Cuba, where it seemed there were fewer gonococci in individuals vaccinated against meningococcal group B,” he noted.
Dr. Petousis-Harris, an immunologist, conducted a retrospective case-control study involving 11 clinics in New Zealand. The participants were aged 15-30 years, were eligible to receive the meningococcal B vaccine, and had been diagnosed with gonorrhea, chlamydia, or both. The researchers found that receiving the meningococcal B vaccine in childhood provides around 30% protection against Neisseria gonorrhoeae infections.
“It’s not perhaps a coincidence that a meningococcal B vaccine would be protective against gonorrhea,” Dr. Fouéré pointed out. He considers this protection logical, even expected, insofar as “meningococcus and gonococcus are almost twins.” There is 90% and 100% homology between membrane proteins of the two bacteria.
Vaccine is effective
Two retrospective case-control studies confirm that the vaccine is protective. One of the studies, carried out by an Australian team, found that the effectiveness was 32%, quite close to that reported by Petousis-Harris. In the other study, a U.S. team brought to light a dose-response relationship. while a complete vaccination series (two MenB-4C doses) was 40% effective.
Prospective studies are in progress, which will provide a higher level of evidence. The ANRS DOXYVAC trial has been underway since January 2021. The participants are men who have sex with men, who are highly exposed to the risk of sexually transmitted infections, and who presented with at least one STI in the year before their participation in the study. “The study is being conducted by Jean-Michel Molina of Saint-Louis Hospital. What they’re trying to do is protect our cohort of pre-exposure prophylaxis patients with meningococcal vaccine,” explained Dr. Fouéré.
Initial findings demonstrated the efficacy of a meningococcal B vaccine in reducing the risk of gonorrhea and the efficacy of doxycycline as preventive intervention for STIs when taken within 72 hours after sexual intercourse. In light of these results, a decision was made at the end of October to discontinue the trial and to recommend providing both interventions to all ANRS DOXYVAC participants. The follow-up of the participants will continue until the end of 2023. The results that led to stopping the study in its current form will be presented in early 2023.
This article was translated from the Medscape French edition. A version of this article appeared on Medscape.com.
PARIS – All the way back in 1907, The Lancet published an article on a gonorrhea vaccine trial. Today, after continuous research throughout the intervening 110-plus years, scientists may finally have achieved success. Sébastien Fouéré, MD, discussed the details at a press conference that focused on the highlights of the Dermatology Days of Paris conference. Dr. Fouéré is the head of the genital dermatology and sexually transmitted infections unit at Saint-Louis Hospital, Paris.
Twin bacteria
Although the gonorrhea vaccine has long been the subject of research, Dr. Fouéré views 2017 as a turning point. This was when the results of a study led by Helen Petousis-Harris, PhD, were published.
“She tried to formalize the not completely indisputable results published by Cuba, where it seemed there were fewer gonococci in individuals vaccinated against meningococcal group B,” he noted.
Dr. Petousis-Harris, an immunologist, conducted a retrospective case-control study involving 11 clinics in New Zealand. The participants were aged 15-30 years, were eligible to receive the meningococcal B vaccine, and had been diagnosed with gonorrhea, chlamydia, or both. The researchers found that receiving the meningococcal B vaccine in childhood provides around 30% protection against Neisseria gonorrhoeae infections.
“It’s not perhaps a coincidence that a meningococcal B vaccine would be protective against gonorrhea,” Dr. Fouéré pointed out. He considers this protection logical, even expected, insofar as “meningococcus and gonococcus are almost twins.” There is 90% and 100% homology between membrane proteins of the two bacteria.
Vaccine is effective
Two retrospective case-control studies confirm that the vaccine is protective. One of the studies, carried out by an Australian team, found that the effectiveness was 32%, quite close to that reported by Petousis-Harris. In the other study, a U.S. team brought to light a dose-response relationship. while a complete vaccination series (two MenB-4C doses) was 40% effective.
Prospective studies are in progress, which will provide a higher level of evidence. The ANRS DOXYVAC trial has been underway since January 2021. The participants are men who have sex with men, who are highly exposed to the risk of sexually transmitted infections, and who presented with at least one STI in the year before their participation in the study. “The study is being conducted by Jean-Michel Molina of Saint-Louis Hospital. What they’re trying to do is protect our cohort of pre-exposure prophylaxis patients with meningococcal vaccine,” explained Dr. Fouéré.
Initial findings demonstrated the efficacy of a meningococcal B vaccine in reducing the risk of gonorrhea and the efficacy of doxycycline as preventive intervention for STIs when taken within 72 hours after sexual intercourse. In light of these results, a decision was made at the end of October to discontinue the trial and to recommend providing both interventions to all ANRS DOXYVAC participants. The follow-up of the participants will continue until the end of 2023. The results that led to stopping the study in its current form will be presented in early 2023.
This article was translated from the Medscape French edition. A version of this article appeared on Medscape.com.
PARIS – All the way back in 1907, The Lancet published an article on a gonorrhea vaccine trial. Today, after continuous research throughout the intervening 110-plus years, scientists may finally have achieved success. Sébastien Fouéré, MD, discussed the details at a press conference that focused on the highlights of the Dermatology Days of Paris conference. Dr. Fouéré is the head of the genital dermatology and sexually transmitted infections unit at Saint-Louis Hospital, Paris.
Twin bacteria
Although the gonorrhea vaccine has long been the subject of research, Dr. Fouéré views 2017 as a turning point. This was when the results of a study led by Helen Petousis-Harris, PhD, were published.
“She tried to formalize the not completely indisputable results published by Cuba, where it seemed there were fewer gonococci in individuals vaccinated against meningococcal group B,” he noted.
Dr. Petousis-Harris, an immunologist, conducted a retrospective case-control study involving 11 clinics in New Zealand. The participants were aged 15-30 years, were eligible to receive the meningococcal B vaccine, and had been diagnosed with gonorrhea, chlamydia, or both. The researchers found that receiving the meningococcal B vaccine in childhood provides around 30% protection against Neisseria gonorrhoeae infections.
“It’s not perhaps a coincidence that a meningococcal B vaccine would be protective against gonorrhea,” Dr. Fouéré pointed out. He considers this protection logical, even expected, insofar as “meningococcus and gonococcus are almost twins.” There is 90% and 100% homology between membrane proteins of the two bacteria.
Vaccine is effective
Two retrospective case-control studies confirm that the vaccine is protective. One of the studies, carried out by an Australian team, found that the effectiveness was 32%, quite close to that reported by Petousis-Harris. In the other study, a U.S. team brought to light a dose-response relationship. while a complete vaccination series (two MenB-4C doses) was 40% effective.
Prospective studies are in progress, which will provide a higher level of evidence. The ANRS DOXYVAC trial has been underway since January 2021. The participants are men who have sex with men, who are highly exposed to the risk of sexually transmitted infections, and who presented with at least one STI in the year before their participation in the study. “The study is being conducted by Jean-Michel Molina of Saint-Louis Hospital. What they’re trying to do is protect our cohort of pre-exposure prophylaxis patients with meningococcal vaccine,” explained Dr. Fouéré.
Initial findings demonstrated the efficacy of a meningococcal B vaccine in reducing the risk of gonorrhea and the efficacy of doxycycline as preventive intervention for STIs when taken within 72 hours after sexual intercourse. In light of these results, a decision was made at the end of October to discontinue the trial and to recommend providing both interventions to all ANRS DOXYVAC participants. The follow-up of the participants will continue until the end of 2023. The results that led to stopping the study in its current form will be presented in early 2023.
This article was translated from the Medscape French edition. A version of this article appeared on Medscape.com.
CDC reports uptick in invasive Strep A infections
Clinicians in the United States are reporting more cases of invasive group A streptococcal infection (iGAS) in children, according to an alert from the Centers for Disease Control and Prevention. These infections are rare but can be deadly, and they can affect adults as well as children.
including those with recent or co-occurring viral respiratory infections, the agency advised in a Dec. 22 alert.
In some cases, iGAS manifests as persistent or worsening symptoms after a patient with a known viral infection initially starts to show signs of improvement, according to the agency.
In November, the CDC was notified about a possible increase in cases of pediatric iGAS at a hospital in Colorado. Since then, two surveillance systems – the Infectious Diseases Society of America’s Emerging Infections Network and the CDC’s Active Bacterial Core Surveillance System – have detected potential increases in pediatric iGAS cases in other states.
The uptick has coincided with “increased circulation of respiratory syncytial virus (RSV), influenza viruses, SARS-CoV-2, and other respiratory viruses,” the advisory stated. “While the overall number of cases has remained relatively low and iGAS infections remain rare in children, [the] CDC is investigating these reports.”
Not just strep throat
Group A Streptococcus bacteria can cause strep throat and infections in skin and soft tissue. The pathogens also can lead to uncommon but severe diseases, such as sepsis, streptococcal toxic shock syndrome, and necrotizing fasciitis, according to the CDC. The severe illnesses “are associated with high mortality rates and require immediate treatment, including appropriate antibiotic therapy,” the agency said.
Groups at higher risk for iGAS include people aged 65 years or older, American Indian and Alaska Native populations, residents of long-term care facilities, those with wounds or skin disease, people who inject drugs, and people experiencing homelessness.
People with medical conditions such as diabetes, cancer, immunosuppression, and chronic kidney, heart, or respiratory disease also are at increased risk.
Invasive strep A infections initially decreased during the COVID-19 pandemic amid measures to reduce the spread of disease, such as masking and social distancing. But since September, monthly cases have exceeded those in 2020 and 2021. “It is too early to determine whether this rise is beyond what would be expected for pre-COVID” seasonal patterns, the CDC said.
Recommendations
Because iGAS can occur after the flu or chickenpox, health care providers should offer influenza and varicella vaccinations to all eligible people who are not up to date with their vaccines.
In addition, clinicians should educate patients about symptoms of iGAS that require urgent medical attention, including necrotizing fasciitis, cellulitis, and toxic shock syndrome.
They also should obtain cultures for suspected cases of iGAS as clinically indicated, follow guidelines for the diagnosis and treatment of strep throat, and be aware of alternative ways to treat strep throat in children amid a shortage of amoxicillin suspension.
Researchers have reported more cases of iGAS in the United Kingdom this year, as well. According to the UK Health Security Agency, 74 deaths, including 16 children, in England have been attributed to iGAS since September.
“We know that this is concerning for parents, but I want to stress that while we are seeing an increase in cases in children, this remains very uncommon,” UKHSA Deputy Director Colin Brown said in a news release. “There are lots of winter bugs circulating that can make your child feel unwell that mostly aren’t cause for alarm. However, make sure you talk to a health professional if your child is getting worse after a bout of scarlet fever, a sore throat, or respiratory infection.”
A fever that doesn’t resolve, dehydration, extreme tiredness, and difficulty breathing are signs to watch out for, Dr. Brown said.
A version of this article first appeared on Medscape.com.
Clinicians in the United States are reporting more cases of invasive group A streptococcal infection (iGAS) in children, according to an alert from the Centers for Disease Control and Prevention. These infections are rare but can be deadly, and they can affect adults as well as children.
including those with recent or co-occurring viral respiratory infections, the agency advised in a Dec. 22 alert.
In some cases, iGAS manifests as persistent or worsening symptoms after a patient with a known viral infection initially starts to show signs of improvement, according to the agency.
In November, the CDC was notified about a possible increase in cases of pediatric iGAS at a hospital in Colorado. Since then, two surveillance systems – the Infectious Diseases Society of America’s Emerging Infections Network and the CDC’s Active Bacterial Core Surveillance System – have detected potential increases in pediatric iGAS cases in other states.
The uptick has coincided with “increased circulation of respiratory syncytial virus (RSV), influenza viruses, SARS-CoV-2, and other respiratory viruses,” the advisory stated. “While the overall number of cases has remained relatively low and iGAS infections remain rare in children, [the] CDC is investigating these reports.”
Not just strep throat
Group A Streptococcus bacteria can cause strep throat and infections in skin and soft tissue. The pathogens also can lead to uncommon but severe diseases, such as sepsis, streptococcal toxic shock syndrome, and necrotizing fasciitis, according to the CDC. The severe illnesses “are associated with high mortality rates and require immediate treatment, including appropriate antibiotic therapy,” the agency said.
Groups at higher risk for iGAS include people aged 65 years or older, American Indian and Alaska Native populations, residents of long-term care facilities, those with wounds or skin disease, people who inject drugs, and people experiencing homelessness.
People with medical conditions such as diabetes, cancer, immunosuppression, and chronic kidney, heart, or respiratory disease also are at increased risk.
Invasive strep A infections initially decreased during the COVID-19 pandemic amid measures to reduce the spread of disease, such as masking and social distancing. But since September, monthly cases have exceeded those in 2020 and 2021. “It is too early to determine whether this rise is beyond what would be expected for pre-COVID” seasonal patterns, the CDC said.
Recommendations
Because iGAS can occur after the flu or chickenpox, health care providers should offer influenza and varicella vaccinations to all eligible people who are not up to date with their vaccines.
In addition, clinicians should educate patients about symptoms of iGAS that require urgent medical attention, including necrotizing fasciitis, cellulitis, and toxic shock syndrome.
They also should obtain cultures for suspected cases of iGAS as clinically indicated, follow guidelines for the diagnosis and treatment of strep throat, and be aware of alternative ways to treat strep throat in children amid a shortage of amoxicillin suspension.
Researchers have reported more cases of iGAS in the United Kingdom this year, as well. According to the UK Health Security Agency, 74 deaths, including 16 children, in England have been attributed to iGAS since September.
“We know that this is concerning for parents, but I want to stress that while we are seeing an increase in cases in children, this remains very uncommon,” UKHSA Deputy Director Colin Brown said in a news release. “There are lots of winter bugs circulating that can make your child feel unwell that mostly aren’t cause for alarm. However, make sure you talk to a health professional if your child is getting worse after a bout of scarlet fever, a sore throat, or respiratory infection.”
A fever that doesn’t resolve, dehydration, extreme tiredness, and difficulty breathing are signs to watch out for, Dr. Brown said.
A version of this article first appeared on Medscape.com.
Clinicians in the United States are reporting more cases of invasive group A streptococcal infection (iGAS) in children, according to an alert from the Centers for Disease Control and Prevention. These infections are rare but can be deadly, and they can affect adults as well as children.
including those with recent or co-occurring viral respiratory infections, the agency advised in a Dec. 22 alert.
In some cases, iGAS manifests as persistent or worsening symptoms after a patient with a known viral infection initially starts to show signs of improvement, according to the agency.
In November, the CDC was notified about a possible increase in cases of pediatric iGAS at a hospital in Colorado. Since then, two surveillance systems – the Infectious Diseases Society of America’s Emerging Infections Network and the CDC’s Active Bacterial Core Surveillance System – have detected potential increases in pediatric iGAS cases in other states.
The uptick has coincided with “increased circulation of respiratory syncytial virus (RSV), influenza viruses, SARS-CoV-2, and other respiratory viruses,” the advisory stated. “While the overall number of cases has remained relatively low and iGAS infections remain rare in children, [the] CDC is investigating these reports.”
Not just strep throat
Group A Streptococcus bacteria can cause strep throat and infections in skin and soft tissue. The pathogens also can lead to uncommon but severe diseases, such as sepsis, streptococcal toxic shock syndrome, and necrotizing fasciitis, according to the CDC. The severe illnesses “are associated with high mortality rates and require immediate treatment, including appropriate antibiotic therapy,” the agency said.
Groups at higher risk for iGAS include people aged 65 years or older, American Indian and Alaska Native populations, residents of long-term care facilities, those with wounds or skin disease, people who inject drugs, and people experiencing homelessness.
People with medical conditions such as diabetes, cancer, immunosuppression, and chronic kidney, heart, or respiratory disease also are at increased risk.
Invasive strep A infections initially decreased during the COVID-19 pandemic amid measures to reduce the spread of disease, such as masking and social distancing. But since September, monthly cases have exceeded those in 2020 and 2021. “It is too early to determine whether this rise is beyond what would be expected for pre-COVID” seasonal patterns, the CDC said.
Recommendations
Because iGAS can occur after the flu or chickenpox, health care providers should offer influenza and varicella vaccinations to all eligible people who are not up to date with their vaccines.
In addition, clinicians should educate patients about symptoms of iGAS that require urgent medical attention, including necrotizing fasciitis, cellulitis, and toxic shock syndrome.
They also should obtain cultures for suspected cases of iGAS as clinically indicated, follow guidelines for the diagnosis and treatment of strep throat, and be aware of alternative ways to treat strep throat in children amid a shortage of amoxicillin suspension.
Researchers have reported more cases of iGAS in the United Kingdom this year, as well. According to the UK Health Security Agency, 74 deaths, including 16 children, in England have been attributed to iGAS since September.
“We know that this is concerning for parents, but I want to stress that while we are seeing an increase in cases in children, this remains very uncommon,” UKHSA Deputy Director Colin Brown said in a news release. “There are lots of winter bugs circulating that can make your child feel unwell that mostly aren’t cause for alarm. However, make sure you talk to a health professional if your child is getting worse after a bout of scarlet fever, a sore throat, or respiratory infection.”
A fever that doesn’t resolve, dehydration, extreme tiredness, and difficulty breathing are signs to watch out for, Dr. Brown said.
A version of this article first appeared on Medscape.com.
FDA approves first-in-class drug for HIV
The U.S. Food and Drug Administration has approved the medication lenacapavir (Sunlenca) for adults living with multidrug resistant HIV-1 infection. .
“Following today’s decision from the FDA, lenacapavir helps to fill a critical unmet need for people with complex prior treatment histories and offers physicians a long-awaited twice-yearly option for these patients who otherwise have limited therapy choices,” said site principal investigator Sorana Segal-Maurer, MD, a professor of clinical medicine at Weill Cornell Medicine, New York, in a statement.
HIV drug regimens generally consist of two or three HIV medicines combined in a daily pill. In 2021, the FDA approved the first injectable complete drug regimen for HIV-1, Cabenuva, which can be administered monthly or every other month. Lenacapavir is administered only twice annually, but it is also combined with other antiretrovirals. The injections and oral tablets of lenacapavir are estimated to cost $42,250 in the first year of treatment and then $39,000 annually in the subsequent years, Reuters reported.
Lenacapavir is the first of a new class of drug called capsid inhibitors to be FDA-approved for treating HIV-1. The drug blocks the HIV-1 virus’s protein shell and interferes with essential steps of the virus’s evolution. The approval, announced today, was based on a multicenter clinical trial of 72 patients with multidrug resistant HIV-1 infection. After a year of the medication, 30 (83%) of the 36 patients randomly assigned to take lenacapavir, in combination with other HIV medications, had undetectable viral loads.
“Today’s approval ushers in a new class of antiretroviral drugs that may help patients with HIV who have run out of treatment options,” said Debra Birnkrant, MD, director of the division of antivirals in the FDA’s Center for Drug Evaluation and Research, in a press release. “The availability of new classes of antiretroviral medications may possibly help these patients live longer, healthier lives.”
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved the medication lenacapavir (Sunlenca) for adults living with multidrug resistant HIV-1 infection. .
“Following today’s decision from the FDA, lenacapavir helps to fill a critical unmet need for people with complex prior treatment histories and offers physicians a long-awaited twice-yearly option for these patients who otherwise have limited therapy choices,” said site principal investigator Sorana Segal-Maurer, MD, a professor of clinical medicine at Weill Cornell Medicine, New York, in a statement.
HIV drug regimens generally consist of two or three HIV medicines combined in a daily pill. In 2021, the FDA approved the first injectable complete drug regimen for HIV-1, Cabenuva, which can be administered monthly or every other month. Lenacapavir is administered only twice annually, but it is also combined with other antiretrovirals. The injections and oral tablets of lenacapavir are estimated to cost $42,250 in the first year of treatment and then $39,000 annually in the subsequent years, Reuters reported.
Lenacapavir is the first of a new class of drug called capsid inhibitors to be FDA-approved for treating HIV-1. The drug blocks the HIV-1 virus’s protein shell and interferes with essential steps of the virus’s evolution. The approval, announced today, was based on a multicenter clinical trial of 72 patients with multidrug resistant HIV-1 infection. After a year of the medication, 30 (83%) of the 36 patients randomly assigned to take lenacapavir, in combination with other HIV medications, had undetectable viral loads.
“Today’s approval ushers in a new class of antiretroviral drugs that may help patients with HIV who have run out of treatment options,” said Debra Birnkrant, MD, director of the division of antivirals in the FDA’s Center for Drug Evaluation and Research, in a press release. “The availability of new classes of antiretroviral medications may possibly help these patients live longer, healthier lives.”
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved the medication lenacapavir (Sunlenca) for adults living with multidrug resistant HIV-1 infection. .
“Following today’s decision from the FDA, lenacapavir helps to fill a critical unmet need for people with complex prior treatment histories and offers physicians a long-awaited twice-yearly option for these patients who otherwise have limited therapy choices,” said site principal investigator Sorana Segal-Maurer, MD, a professor of clinical medicine at Weill Cornell Medicine, New York, in a statement.
HIV drug regimens generally consist of two or three HIV medicines combined in a daily pill. In 2021, the FDA approved the first injectable complete drug regimen for HIV-1, Cabenuva, which can be administered monthly or every other month. Lenacapavir is administered only twice annually, but it is also combined with other antiretrovirals. The injections and oral tablets of lenacapavir are estimated to cost $42,250 in the first year of treatment and then $39,000 annually in the subsequent years, Reuters reported.
Lenacapavir is the first of a new class of drug called capsid inhibitors to be FDA-approved for treating HIV-1. The drug blocks the HIV-1 virus’s protein shell and interferes with essential steps of the virus’s evolution. The approval, announced today, was based on a multicenter clinical trial of 72 patients with multidrug resistant HIV-1 infection. After a year of the medication, 30 (83%) of the 36 patients randomly assigned to take lenacapavir, in combination with other HIV medications, had undetectable viral loads.
“Today’s approval ushers in a new class of antiretroviral drugs that may help patients with HIV who have run out of treatment options,” said Debra Birnkrant, MD, director of the division of antivirals in the FDA’s Center for Drug Evaluation and Research, in a press release. “The availability of new classes of antiretroviral medications may possibly help these patients live longer, healthier lives.”
A version of this article first appeared on Medscape.com.
AAP offers new guidance on child exploitation and sex trafficking
In a new updated report, the American Academy of Pediatrics urges pediatricians to understand signs of exploitation and labor/sex trafficking and learn how to support children and adolescents who are targeted.
“It’s incredibly scary when you encounter someone you worry is a victim, and you don’t know how to help them, and they’re not saying what’s going on,” pediatrician and report coauthor Dana Kaplan, MD, of Staten Island (N.Y.) University Hospital, said in an interview. “Every case is so unique and different: There’s no algorithm of ‘If A, then B, then C.’ You have to approach each person as an individual, and it takes time to make sure you’re thinking things through about how to provide what’s needed.”
The AAP published the clinical report, which is intended to provide guidance to pediatricians, in the January 2023 issue of Pediatrics. The organization previously tackled this topic in a 2017 clinical report, and Dr. Kaplan said the new report includes updated recommendations.
As the new report notes, there aren’t reliable estimates of exploited children in the United States, although millions are thought to be trafficked and subjected to forced labor around the world. “By virtue of their young age, children and adolescents are vulnerable to manipulation and exploitation, because they have limited life experiences, a need for attachment and acceptance, an immature prefrontal cortex ... and limited options for action,” the report says.
Dr. Kaplan puts it this way: “By the nature of being a child, you’re vulnerable.”
Still, health care professionals often aren’t trained in regard to human trafficking, the report says, even though it’s clear that they “must remain alert for the possibility.”
Dr. Kaplan, who has special training in child abuse and often sees children at risk, cautioned that children usually don’t directly say that they need help. “That’s generally not the case. They don’t articulate what’s going on around them as unsafe, or concerning, or dangerous. If you go and see a doctor for 10 minutes, are you going to tell them everything?
Instead, clinicians must often rely on their own observations. The report lists multiple possible signs of exploitation.
- The patient is accompanied by a domineering adult who does not allow the child to answer questions or accompanied by an unrelated adult. Inconsistent information is provided by the patient or companion. There’s a delay in seeking medical care.
- The patient has multiple sexually transmitted infections, previous pregnancy or termination, and/or frequent visits for emergency contraception. There are signs of prior sexual abuse, assault, or other maltreatment.
- The patient is withdrawn, fearful, hostile, or has a suspicious demeanor. The patient is constantly checking his or her phone and appears anxious or afraid.
What should clinicians do if they suspect exploitation? The report recommends that health care organizations develop guidelines for workers to follow. For her part, Dr. Kaplan advises colleagues to let patients lead conversations and not dig too deeply into their lives.
“Don’t turn into an investigator. This is not [Law & Order] SVU,” she said. “Stay focused on what you’re trained to do – provide health care.”
That doesn’t mean clinicians should ignore signs of trouble. It’s crucial to develop trust with the patient over time, she said, and turn to a specialist in your community or institution if you have suspicions.
And be careful to not portray victims as perpetrators. The new report emphasizes that “it’s important for health care providers to emphasize to authorities that the patient is a victim of exploitation who needs services rather than a juvenile offender.”
The report also highlights the importance of creating an environment that supports clinicians themselves: “Self-care for the clinician is critical in preventing and addressing secondary traumatic stress. A work environment that fosters peer support, encourages open discussion of work-related stress, and implements reasonable work-life balance policies can help protect providers from secondary stress and its consequences.”
Resources for clinicians include the National Human Trafficking Hotline, the federal Office of Trafficking in Persons, and the Centers for Disease Control and Prevention’s domestic refugee screening guidelines.
The study has no external funding. The authors report no disclosures.
In a new updated report, the American Academy of Pediatrics urges pediatricians to understand signs of exploitation and labor/sex trafficking and learn how to support children and adolescents who are targeted.
“It’s incredibly scary when you encounter someone you worry is a victim, and you don’t know how to help them, and they’re not saying what’s going on,” pediatrician and report coauthor Dana Kaplan, MD, of Staten Island (N.Y.) University Hospital, said in an interview. “Every case is so unique and different: There’s no algorithm of ‘If A, then B, then C.’ You have to approach each person as an individual, and it takes time to make sure you’re thinking things through about how to provide what’s needed.”
The AAP published the clinical report, which is intended to provide guidance to pediatricians, in the January 2023 issue of Pediatrics. The organization previously tackled this topic in a 2017 clinical report, and Dr. Kaplan said the new report includes updated recommendations.
As the new report notes, there aren’t reliable estimates of exploited children in the United States, although millions are thought to be trafficked and subjected to forced labor around the world. “By virtue of their young age, children and adolescents are vulnerable to manipulation and exploitation, because they have limited life experiences, a need for attachment and acceptance, an immature prefrontal cortex ... and limited options for action,” the report says.
Dr. Kaplan puts it this way: “By the nature of being a child, you’re vulnerable.”
Still, health care professionals often aren’t trained in regard to human trafficking, the report says, even though it’s clear that they “must remain alert for the possibility.”
Dr. Kaplan, who has special training in child abuse and often sees children at risk, cautioned that children usually don’t directly say that they need help. “That’s generally not the case. They don’t articulate what’s going on around them as unsafe, or concerning, or dangerous. If you go and see a doctor for 10 minutes, are you going to tell them everything?
Instead, clinicians must often rely on their own observations. The report lists multiple possible signs of exploitation.
- The patient is accompanied by a domineering adult who does not allow the child to answer questions or accompanied by an unrelated adult. Inconsistent information is provided by the patient or companion. There’s a delay in seeking medical care.
- The patient has multiple sexually transmitted infections, previous pregnancy or termination, and/or frequent visits for emergency contraception. There are signs of prior sexual abuse, assault, or other maltreatment.
- The patient is withdrawn, fearful, hostile, or has a suspicious demeanor. The patient is constantly checking his or her phone and appears anxious or afraid.
What should clinicians do if they suspect exploitation? The report recommends that health care organizations develop guidelines for workers to follow. For her part, Dr. Kaplan advises colleagues to let patients lead conversations and not dig too deeply into their lives.
“Don’t turn into an investigator. This is not [Law & Order] SVU,” she said. “Stay focused on what you’re trained to do – provide health care.”
That doesn’t mean clinicians should ignore signs of trouble. It’s crucial to develop trust with the patient over time, she said, and turn to a specialist in your community or institution if you have suspicions.
And be careful to not portray victims as perpetrators. The new report emphasizes that “it’s important for health care providers to emphasize to authorities that the patient is a victim of exploitation who needs services rather than a juvenile offender.”
The report also highlights the importance of creating an environment that supports clinicians themselves: “Self-care for the clinician is critical in preventing and addressing secondary traumatic stress. A work environment that fosters peer support, encourages open discussion of work-related stress, and implements reasonable work-life balance policies can help protect providers from secondary stress and its consequences.”
Resources for clinicians include the National Human Trafficking Hotline, the federal Office of Trafficking in Persons, and the Centers for Disease Control and Prevention’s domestic refugee screening guidelines.
The study has no external funding. The authors report no disclosures.
In a new updated report, the American Academy of Pediatrics urges pediatricians to understand signs of exploitation and labor/sex trafficking and learn how to support children and adolescents who are targeted.
“It’s incredibly scary when you encounter someone you worry is a victim, and you don’t know how to help them, and they’re not saying what’s going on,” pediatrician and report coauthor Dana Kaplan, MD, of Staten Island (N.Y.) University Hospital, said in an interview. “Every case is so unique and different: There’s no algorithm of ‘If A, then B, then C.’ You have to approach each person as an individual, and it takes time to make sure you’re thinking things through about how to provide what’s needed.”
The AAP published the clinical report, which is intended to provide guidance to pediatricians, in the January 2023 issue of Pediatrics. The organization previously tackled this topic in a 2017 clinical report, and Dr. Kaplan said the new report includes updated recommendations.
As the new report notes, there aren’t reliable estimates of exploited children in the United States, although millions are thought to be trafficked and subjected to forced labor around the world. “By virtue of their young age, children and adolescents are vulnerable to manipulation and exploitation, because they have limited life experiences, a need for attachment and acceptance, an immature prefrontal cortex ... and limited options for action,” the report says.
Dr. Kaplan puts it this way: “By the nature of being a child, you’re vulnerable.”
Still, health care professionals often aren’t trained in regard to human trafficking, the report says, even though it’s clear that they “must remain alert for the possibility.”
Dr. Kaplan, who has special training in child abuse and often sees children at risk, cautioned that children usually don’t directly say that they need help. “That’s generally not the case. They don’t articulate what’s going on around them as unsafe, or concerning, or dangerous. If you go and see a doctor for 10 minutes, are you going to tell them everything?
Instead, clinicians must often rely on their own observations. The report lists multiple possible signs of exploitation.
- The patient is accompanied by a domineering adult who does not allow the child to answer questions or accompanied by an unrelated adult. Inconsistent information is provided by the patient or companion. There’s a delay in seeking medical care.
- The patient has multiple sexually transmitted infections, previous pregnancy or termination, and/or frequent visits for emergency contraception. There are signs of prior sexual abuse, assault, or other maltreatment.
- The patient is withdrawn, fearful, hostile, or has a suspicious demeanor. The patient is constantly checking his or her phone and appears anxious or afraid.
What should clinicians do if they suspect exploitation? The report recommends that health care organizations develop guidelines for workers to follow. For her part, Dr. Kaplan advises colleagues to let patients lead conversations and not dig too deeply into their lives.
“Don’t turn into an investigator. This is not [Law & Order] SVU,” she said. “Stay focused on what you’re trained to do – provide health care.”
That doesn’t mean clinicians should ignore signs of trouble. It’s crucial to develop trust with the patient over time, she said, and turn to a specialist in your community or institution if you have suspicions.
And be careful to not portray victims as perpetrators. The new report emphasizes that “it’s important for health care providers to emphasize to authorities that the patient is a victim of exploitation who needs services rather than a juvenile offender.”
The report also highlights the importance of creating an environment that supports clinicians themselves: “Self-care for the clinician is critical in preventing and addressing secondary traumatic stress. A work environment that fosters peer support, encourages open discussion of work-related stress, and implements reasonable work-life balance policies can help protect providers from secondary stress and its consequences.”
Resources for clinicians include the National Human Trafficking Hotline, the federal Office of Trafficking in Persons, and the Centers for Disease Control and Prevention’s domestic refugee screening guidelines.
The study has no external funding. The authors report no disclosures.
FROM PEDIATRICS
How to have a safer and more joyful holiday season
This holiday season, I am looking forward to spending some time with family, as I have in the past. As I have chatted with others, many friends are looking forward to events that are potentially larger and potentially returning to prepandemic type gatherings.
Gathering is important and can bring joy, sense of community, and love to the lives of many. Unfortunately, the risks associated with gathering are not over. as our country faces many cases of respiratory syncytial virus (RSV), COVID-19, and influenza at the same time.
During the first week of December, cases of influenza were rising across the country1 and were rising faster than in previous years. Although getting the vaccine is an important method of influenza prevention and is recommended for everyone over the age of 6 months with rare exception, many have not gotten their vaccine this year.
Influenza
Thus far, “nearly 50% of reported flu-associated hospitalizations in women of childbearing age have been in women who are pregnant.” We are seeing this at a time with lower-than-average uptake of influenza vaccine leaving both the pregnant persons and their babies unprotected. In addition to utilizing vaccines as prevention, isolating when ill, cleaning surfaces, and practicing good hand hygiene can all decrease transmission.
RSV
In addition to rises of influenza, there are currently high rates of RSV in various parts of the country. Prior to 2020, RSV typically started in the fall and peaked in the winter months. However, since the pandemic, the typical seasonal pattern has not returned, and it is unclear when it will. Although RSV hits the very young, the old, and the immunocompromised the most, RSV can infect anyone. Unfortunately, we do not currently have a vaccine for everyone against this virus. Prevention of transmission includes, as with flu, isolating when ill, cleaning surfaces, and washing hands.2
COVID-19
Of course, the effects of the COVID-19 pandemic are also still here as well. During the first week of December, the CDC reported rising cases of COVID across the country. Within the past few months, there have been several developments, though, for protection. There are now bivalent vaccines available as either third doses or booster doses approved for all persons over 6 months of age. As of the first week of December, only 13.5% of those aged 5 and over had received an updated booster.
There is currently wider access to rapid testing, including at-home testing, which can allow individuals to identify if COVID positive. Additionally, there is access to medication to decrease the likelihood of severe disease – though this does not take the place of vaccinations.
If anyone does test positive for COVID, they should follow the most recent quarantine guidelines including wearing a well-fitted mask when they do begin returning to activities.3
With rising cases of all three of these viruses, some may be asking how we can safely gather. There are several things to consider and do to enjoy our events. The first thing everyone can do is to receive updated vaccinations for both influenza and COVID-19 if eligible. Although it may take some time to be effective, vaccination is still one of our most effective methods of disease prevention and is important this winter season. Vaccinations can also help decrease the risk of severe disease.
Although many have stopped masking, as cases rise, it is time to consider masking particularly when community levels of any of these viruses are high. Masks help with preventing and spreading more than just COVID-19. Using them can be especially important for those going places such as stores and to large public gatherings and when riding on buses, planes, or trains.
In summary
Preventing exposure by masking can help keep individuals healthy prior to celebrating the holidays with others. With access to rapid testing, it makes sense to consider testing prior to gathering with friends and family. Most importantly, although we all are looking forward to spending time with our loved ones, it is important to stay home if not feeling well. Following these recommendations will allow us to have a safer and more joyful holiday season.
Dr. Wheat is a family physician at Erie Family Health Center and program director of Northwestern University’s McGaw Family Medicine residency program, both in Chicago. Dr. Wheat serves on the editorial advisory board of Family Practice News. You can contact her at fpnews@mdedge.com.
References
1. Centers for Disease Control and Prevention. Influenza (flu). [Online] Dec. 1, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/flu/index.htm.
2. Respiratory syncytial virus. Respiratory syncytial virus infection (RSV). [Online] Oct. 28, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/rsv/index.html.
3. COVID-19. [Online] Dec. 7, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/coronavirus/2019-ncov/index.html.
This holiday season, I am looking forward to spending some time with family, as I have in the past. As I have chatted with others, many friends are looking forward to events that are potentially larger and potentially returning to prepandemic type gatherings.
Gathering is important and can bring joy, sense of community, and love to the lives of many. Unfortunately, the risks associated with gathering are not over. as our country faces many cases of respiratory syncytial virus (RSV), COVID-19, and influenza at the same time.
During the first week of December, cases of influenza were rising across the country1 and were rising faster than in previous years. Although getting the vaccine is an important method of influenza prevention and is recommended for everyone over the age of 6 months with rare exception, many have not gotten their vaccine this year.
Influenza
Thus far, “nearly 50% of reported flu-associated hospitalizations in women of childbearing age have been in women who are pregnant.” We are seeing this at a time with lower-than-average uptake of influenza vaccine leaving both the pregnant persons and their babies unprotected. In addition to utilizing vaccines as prevention, isolating when ill, cleaning surfaces, and practicing good hand hygiene can all decrease transmission.
RSV
In addition to rises of influenza, there are currently high rates of RSV in various parts of the country. Prior to 2020, RSV typically started in the fall and peaked in the winter months. However, since the pandemic, the typical seasonal pattern has not returned, and it is unclear when it will. Although RSV hits the very young, the old, and the immunocompromised the most, RSV can infect anyone. Unfortunately, we do not currently have a vaccine for everyone against this virus. Prevention of transmission includes, as with flu, isolating when ill, cleaning surfaces, and washing hands.2
COVID-19
Of course, the effects of the COVID-19 pandemic are also still here as well. During the first week of December, the CDC reported rising cases of COVID across the country. Within the past few months, there have been several developments, though, for protection. There are now bivalent vaccines available as either third doses or booster doses approved for all persons over 6 months of age. As of the first week of December, only 13.5% of those aged 5 and over had received an updated booster.
There is currently wider access to rapid testing, including at-home testing, which can allow individuals to identify if COVID positive. Additionally, there is access to medication to decrease the likelihood of severe disease – though this does not take the place of vaccinations.
If anyone does test positive for COVID, they should follow the most recent quarantine guidelines including wearing a well-fitted mask when they do begin returning to activities.3
With rising cases of all three of these viruses, some may be asking how we can safely gather. There are several things to consider and do to enjoy our events. The first thing everyone can do is to receive updated vaccinations for both influenza and COVID-19 if eligible. Although it may take some time to be effective, vaccination is still one of our most effective methods of disease prevention and is important this winter season. Vaccinations can also help decrease the risk of severe disease.
Although many have stopped masking, as cases rise, it is time to consider masking particularly when community levels of any of these viruses are high. Masks help with preventing and spreading more than just COVID-19. Using them can be especially important for those going places such as stores and to large public gatherings and when riding on buses, planes, or trains.
In summary
Preventing exposure by masking can help keep individuals healthy prior to celebrating the holidays with others. With access to rapid testing, it makes sense to consider testing prior to gathering with friends and family. Most importantly, although we all are looking forward to spending time with our loved ones, it is important to stay home if not feeling well. Following these recommendations will allow us to have a safer and more joyful holiday season.
Dr. Wheat is a family physician at Erie Family Health Center and program director of Northwestern University’s McGaw Family Medicine residency program, both in Chicago. Dr. Wheat serves on the editorial advisory board of Family Practice News. You can contact her at fpnews@mdedge.com.
References
1. Centers for Disease Control and Prevention. Influenza (flu). [Online] Dec. 1, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/flu/index.htm.
2. Respiratory syncytial virus. Respiratory syncytial virus infection (RSV). [Online] Oct. 28, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/rsv/index.html.
3. COVID-19. [Online] Dec. 7, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/coronavirus/2019-ncov/index.html.
This holiday season, I am looking forward to spending some time with family, as I have in the past. As I have chatted with others, many friends are looking forward to events that are potentially larger and potentially returning to prepandemic type gatherings.
Gathering is important and can bring joy, sense of community, and love to the lives of many. Unfortunately, the risks associated with gathering are not over. as our country faces many cases of respiratory syncytial virus (RSV), COVID-19, and influenza at the same time.
During the first week of December, cases of influenza were rising across the country1 and were rising faster than in previous years. Although getting the vaccine is an important method of influenza prevention and is recommended for everyone over the age of 6 months with rare exception, many have not gotten their vaccine this year.
Influenza
Thus far, “nearly 50% of reported flu-associated hospitalizations in women of childbearing age have been in women who are pregnant.” We are seeing this at a time with lower-than-average uptake of influenza vaccine leaving both the pregnant persons and their babies unprotected. In addition to utilizing vaccines as prevention, isolating when ill, cleaning surfaces, and practicing good hand hygiene can all decrease transmission.
RSV
In addition to rises of influenza, there are currently high rates of RSV in various parts of the country. Prior to 2020, RSV typically started in the fall and peaked in the winter months. However, since the pandemic, the typical seasonal pattern has not returned, and it is unclear when it will. Although RSV hits the very young, the old, and the immunocompromised the most, RSV can infect anyone. Unfortunately, we do not currently have a vaccine for everyone against this virus. Prevention of transmission includes, as with flu, isolating when ill, cleaning surfaces, and washing hands.2
COVID-19
Of course, the effects of the COVID-19 pandemic are also still here as well. During the first week of December, the CDC reported rising cases of COVID across the country. Within the past few months, there have been several developments, though, for protection. There are now bivalent vaccines available as either third doses or booster doses approved for all persons over 6 months of age. As of the first week of December, only 13.5% of those aged 5 and over had received an updated booster.
There is currently wider access to rapid testing, including at-home testing, which can allow individuals to identify if COVID positive. Additionally, there is access to medication to decrease the likelihood of severe disease – though this does not take the place of vaccinations.
If anyone does test positive for COVID, they should follow the most recent quarantine guidelines including wearing a well-fitted mask when they do begin returning to activities.3
With rising cases of all three of these viruses, some may be asking how we can safely gather. There are several things to consider and do to enjoy our events. The first thing everyone can do is to receive updated vaccinations for both influenza and COVID-19 if eligible. Although it may take some time to be effective, vaccination is still one of our most effective methods of disease prevention and is important this winter season. Vaccinations can also help decrease the risk of severe disease.
Although many have stopped masking, as cases rise, it is time to consider masking particularly when community levels of any of these viruses are high. Masks help with preventing and spreading more than just COVID-19. Using them can be especially important for those going places such as stores and to large public gatherings and when riding on buses, planes, or trains.
In summary
Preventing exposure by masking can help keep individuals healthy prior to celebrating the holidays with others. With access to rapid testing, it makes sense to consider testing prior to gathering with friends and family. Most importantly, although we all are looking forward to spending time with our loved ones, it is important to stay home if not feeling well. Following these recommendations will allow us to have a safer and more joyful holiday season.
Dr. Wheat is a family physician at Erie Family Health Center and program director of Northwestern University’s McGaw Family Medicine residency program, both in Chicago. Dr. Wheat serves on the editorial advisory board of Family Practice News. You can contact her at fpnews@mdedge.com.
References
1. Centers for Disease Control and Prevention. Influenza (flu). [Online] Dec. 1, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/flu/index.htm.
2. Respiratory syncytial virus. Respiratory syncytial virus infection (RSV). [Online] Oct. 28, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/rsv/index.html.
3. COVID-19. [Online] Dec. 7, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/coronavirus/2019-ncov/index.html.
Ohio measles outbreak grows, fueled by vaccine hesitancy
The Ohio measles outbreak continues to expand, with cases now totaling 81 – a 37% increase in the course of just 2 weeks.
. Most of the children infected were unvaccinated but were old enough to get the measles, mumps, and rubella (MMR) shot, which is 97% effective at preventing measles.
“I think these are individuals who are making a decision not to protect their children against vaccine-preventable diseases, and some of them are making a specific decision not to use the MMR vaccine,” Columbus Public Health Commissioner Mysheika W. Roberts, MD, told JAMA.
She said that parents’ refusal to vaccinate their children was due to a misconception that the vaccine causes autism.
“We’re sounding the alarm that if your child is of age and not vaccinated, they should get vaccinated ASAP,” Dr. Roberts said, noting that she hasn’t seen that happening more.
Health officials have predicted the outbreak, which started in November, will last at least several months. Measles is so contagious that 9 out of 10 unvaccinated people in a room will become infected if exposed.
All of the infections have been in children. According to the Columbus Public Health measles dashboard, of the 81 confirmed cases:
- 29 children have been hospitalized.
- 22 cases are among children under 1 year old.
- No deaths have been reported.
Dr. Roberts said the hospitalized children have had symptoms including dehydration, diarrhea, and pneumonia. Some have had to go to the intensive care unit.
Measles infection causes a rash and a fever that can spike beyond 104° F. Sometimes, the illness can lead to brain swelling, brain damage, and even death, the CDC says.
One of the most recent cases was an infant too young to be vaccinated who lives 45 miles away from where the outbreak began, the Dayton Daily News reported. That’s the first case in Clark County in more than 20 years. At least 10% of kindergartners’ parents in the region’s elementary schools opted out of vaccines because of religious or moral objections.
“We knew this was coming. It was a matter of when, not if,” Yamini Teegala, MD, chief medical officer at Rocking Horse Community Health Center in Springfield, told the Dayton Daily News.
This is the second measles outbreak this year. Minnesota tallied 22 cases since June in an unrelated outbreak, JAMA reported.
A version of this article first appeared on WebMD.com.
The Ohio measles outbreak continues to expand, with cases now totaling 81 – a 37% increase in the course of just 2 weeks.
. Most of the children infected were unvaccinated but were old enough to get the measles, mumps, and rubella (MMR) shot, which is 97% effective at preventing measles.
“I think these are individuals who are making a decision not to protect their children against vaccine-preventable diseases, and some of them are making a specific decision not to use the MMR vaccine,” Columbus Public Health Commissioner Mysheika W. Roberts, MD, told JAMA.
She said that parents’ refusal to vaccinate their children was due to a misconception that the vaccine causes autism.
“We’re sounding the alarm that if your child is of age and not vaccinated, they should get vaccinated ASAP,” Dr. Roberts said, noting that she hasn’t seen that happening more.
Health officials have predicted the outbreak, which started in November, will last at least several months. Measles is so contagious that 9 out of 10 unvaccinated people in a room will become infected if exposed.
All of the infections have been in children. According to the Columbus Public Health measles dashboard, of the 81 confirmed cases:
- 29 children have been hospitalized.
- 22 cases are among children under 1 year old.
- No deaths have been reported.
Dr. Roberts said the hospitalized children have had symptoms including dehydration, diarrhea, and pneumonia. Some have had to go to the intensive care unit.
Measles infection causes a rash and a fever that can spike beyond 104° F. Sometimes, the illness can lead to brain swelling, brain damage, and even death, the CDC says.
One of the most recent cases was an infant too young to be vaccinated who lives 45 miles away from where the outbreak began, the Dayton Daily News reported. That’s the first case in Clark County in more than 20 years. At least 10% of kindergartners’ parents in the region’s elementary schools opted out of vaccines because of religious or moral objections.
“We knew this was coming. It was a matter of when, not if,” Yamini Teegala, MD, chief medical officer at Rocking Horse Community Health Center in Springfield, told the Dayton Daily News.
This is the second measles outbreak this year. Minnesota tallied 22 cases since June in an unrelated outbreak, JAMA reported.
A version of this article first appeared on WebMD.com.
The Ohio measles outbreak continues to expand, with cases now totaling 81 – a 37% increase in the course of just 2 weeks.
. Most of the children infected were unvaccinated but were old enough to get the measles, mumps, and rubella (MMR) shot, which is 97% effective at preventing measles.
“I think these are individuals who are making a decision not to protect their children against vaccine-preventable diseases, and some of them are making a specific decision not to use the MMR vaccine,” Columbus Public Health Commissioner Mysheika W. Roberts, MD, told JAMA.
She said that parents’ refusal to vaccinate their children was due to a misconception that the vaccine causes autism.
“We’re sounding the alarm that if your child is of age and not vaccinated, they should get vaccinated ASAP,” Dr. Roberts said, noting that she hasn’t seen that happening more.
Health officials have predicted the outbreak, which started in November, will last at least several months. Measles is so contagious that 9 out of 10 unvaccinated people in a room will become infected if exposed.
All of the infections have been in children. According to the Columbus Public Health measles dashboard, of the 81 confirmed cases:
- 29 children have been hospitalized.
- 22 cases are among children under 1 year old.
- No deaths have been reported.
Dr. Roberts said the hospitalized children have had symptoms including dehydration, diarrhea, and pneumonia. Some have had to go to the intensive care unit.
Measles infection causes a rash and a fever that can spike beyond 104° F. Sometimes, the illness can lead to brain swelling, brain damage, and even death, the CDC says.
One of the most recent cases was an infant too young to be vaccinated who lives 45 miles away from where the outbreak began, the Dayton Daily News reported. That’s the first case in Clark County in more than 20 years. At least 10% of kindergartners’ parents in the region’s elementary schools opted out of vaccines because of religious or moral objections.
“We knew this was coming. It was a matter of when, not if,” Yamini Teegala, MD, chief medical officer at Rocking Horse Community Health Center in Springfield, told the Dayton Daily News.
This is the second measles outbreak this year. Minnesota tallied 22 cases since June in an unrelated outbreak, JAMA reported.
A version of this article first appeared on WebMD.com.
FROM JAMA
Children and COVID: New-case counts offer dueling narratives
New COVID-19 cases in children jumped by 66% during the first 2 weeks of December after an 8-week steady period lasting through October and November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
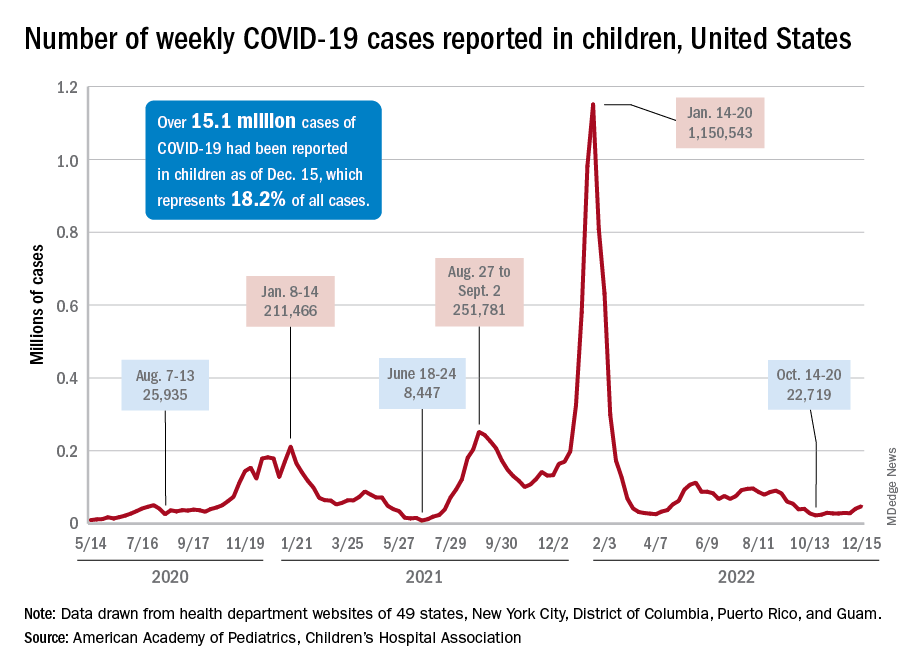
and totaling less than 29,000 for the week of Nov. 25 to Dec. 1. That increase of almost 19,000 cases is the largest over a 2-week period since late July, the AAP and CHA said in their weekly COVID report based on data collected from state and territorial health department websites.
[This publication has been following the AAP/CHA report since the summer of 2020 and continues to share the data for the sake of consistency, but it must be noted that a number of states are no longer updating their public COVID dashboards. As a result, there is now a considerable discrepancy between the AAP/CHA weekly figures and those reported by the Centers for Disease Control and Prevention, which has no such limitations on state data.]
The situation involving new cases over the last 2 weeks is quite different from the CDC’s perspective. The agency does not publish a weekly count, instead offering cumulative cases, which stood at almost 16.1 million as of Dec. 14. Calculating a 2-week total puts the new-case count for Dec. 1-14 at 113,572 among children aged 0-17 years. That is higher than the AAP/CHA count (88,629) for roughly the same period, but it is actually lower than the CDC’s figure (161,832) for the last 2 weeks of November.
The CDC data, in other words, suggest that new cases have gone down in the last 2 weeks, while the AAP and CHA, with their somewhat limited perspective, announced that new cases have gone up.
One COVID-related measure from the CDC that is not contradicted by other sources is hospitalization rates, which had climbed from 0.16 new admissions in children aged 0-17 years with confirmed COVID per 100,000 population on Oct. 22 to 0.29 per 100,000 on Dec. 9. Visits to the emergency department with diagnosed COVID, meanwhile, have been fairly steady so far through December in children, according to the CDC.
New COVID-19 cases in children jumped by 66% during the first 2 weeks of December after an 8-week steady period lasting through October and November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
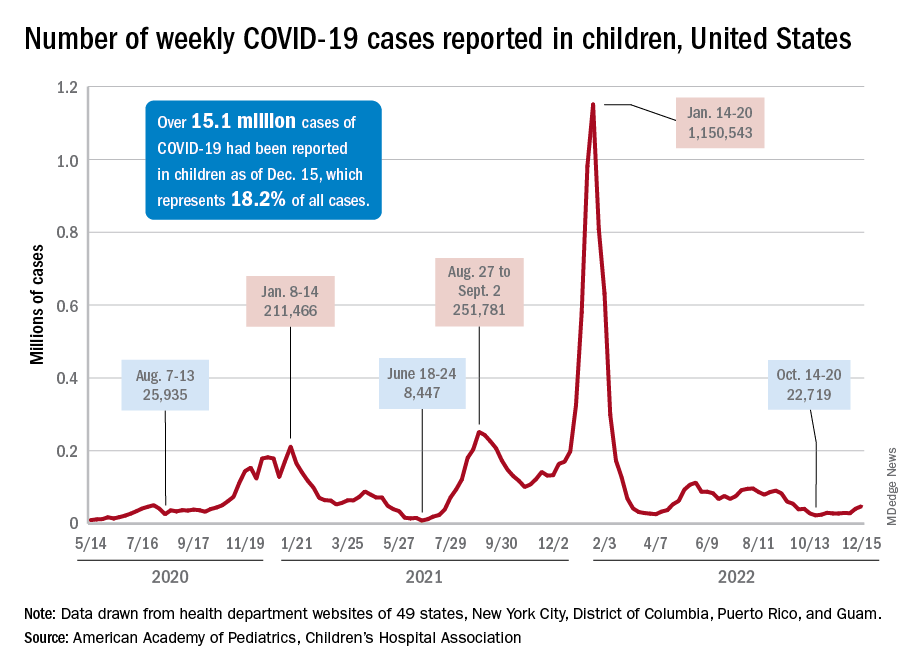
and totaling less than 29,000 for the week of Nov. 25 to Dec. 1. That increase of almost 19,000 cases is the largest over a 2-week period since late July, the AAP and CHA said in their weekly COVID report based on data collected from state and territorial health department websites.
[This publication has been following the AAP/CHA report since the summer of 2020 and continues to share the data for the sake of consistency, but it must be noted that a number of states are no longer updating their public COVID dashboards. As a result, there is now a considerable discrepancy between the AAP/CHA weekly figures and those reported by the Centers for Disease Control and Prevention, which has no such limitations on state data.]
The situation involving new cases over the last 2 weeks is quite different from the CDC’s perspective. The agency does not publish a weekly count, instead offering cumulative cases, which stood at almost 16.1 million as of Dec. 14. Calculating a 2-week total puts the new-case count for Dec. 1-14 at 113,572 among children aged 0-17 years. That is higher than the AAP/CHA count (88,629) for roughly the same period, but it is actually lower than the CDC’s figure (161,832) for the last 2 weeks of November.
The CDC data, in other words, suggest that new cases have gone down in the last 2 weeks, while the AAP and CHA, with their somewhat limited perspective, announced that new cases have gone up.
One COVID-related measure from the CDC that is not contradicted by other sources is hospitalization rates, which had climbed from 0.16 new admissions in children aged 0-17 years with confirmed COVID per 100,000 population on Oct. 22 to 0.29 per 100,000 on Dec. 9. Visits to the emergency department with diagnosed COVID, meanwhile, have been fairly steady so far through December in children, according to the CDC.
New COVID-19 cases in children jumped by 66% during the first 2 weeks of December after an 8-week steady period lasting through October and November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
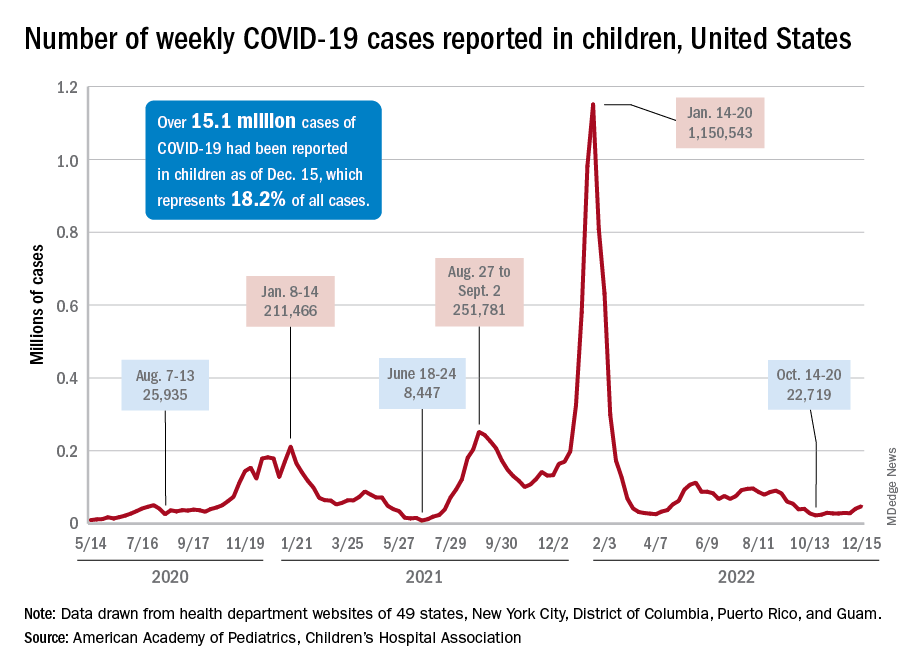
and totaling less than 29,000 for the week of Nov. 25 to Dec. 1. That increase of almost 19,000 cases is the largest over a 2-week period since late July, the AAP and CHA said in their weekly COVID report based on data collected from state and territorial health department websites.
[This publication has been following the AAP/CHA report since the summer of 2020 and continues to share the data for the sake of consistency, but it must be noted that a number of states are no longer updating their public COVID dashboards. As a result, there is now a considerable discrepancy between the AAP/CHA weekly figures and those reported by the Centers for Disease Control and Prevention, which has no such limitations on state data.]
The situation involving new cases over the last 2 weeks is quite different from the CDC’s perspective. The agency does not publish a weekly count, instead offering cumulative cases, which stood at almost 16.1 million as of Dec. 14. Calculating a 2-week total puts the new-case count for Dec. 1-14 at 113,572 among children aged 0-17 years. That is higher than the AAP/CHA count (88,629) for roughly the same period, but it is actually lower than the CDC’s figure (161,832) for the last 2 weeks of November.
The CDC data, in other words, suggest that new cases have gone down in the last 2 weeks, while the AAP and CHA, with their somewhat limited perspective, announced that new cases have gone up.
One COVID-related measure from the CDC that is not contradicted by other sources is hospitalization rates, which had climbed from 0.16 new admissions in children aged 0-17 years with confirmed COVID per 100,000 population on Oct. 22 to 0.29 per 100,000 on Dec. 9. Visits to the emergency department with diagnosed COVID, meanwhile, have been fairly steady so far through December in children, according to the CDC.
Vaccinating pregnant women protects infants against severe RSV infection
An investigational vaccine against respiratory syncytial virus (RSV) in pregnant women has been shown to help protect infants against severe disease, according to the vaccine’s manufacturer.
Pfizer recently announced that in the course of a randomized, double-blind, placebo-controlled phase 3 study, the vaccine RSVpreF had an almost 82% efficacy against severe RSV infection in infants from birth through the first 90 days of life, according to a company press release.
The vaccine also had a 69% efficacy against severe disease through the first 6 months of life. A total of 7,400 women had received a single dose of 120 mcg RSVpreF in the late second or third trimester of their pregnancy. There were no signs of safety issues for the mothers or infants.
Due to the good results, the enrollment in the study was halted on the recommendation of the study’s Data Monitoring Committee after achieving a primary endpoint. The company plans to apply for marketing authorization to the U.S. Food and Drug Administration by the end of 2022 and to other regulatory agencies in 2023.
“The directness of the strategy, to vaccinate expectant mothers during pregnancy so that their newborn is then later protected, is new and a very interesting approach,” commented Prof. Ortwin Adams, MD, head of virologic diagnostics at the Institute for Virology of the University Hospital of Düsseldorf (Germany) to the Science Media Centre (SMC).
In terms of the RSV vaccination strategy presented, “the unborn child has taken center stage from the outset.” Because the vaccination route is the placental transfer of antibodies from mother to child (“passive immunity”), “... the medical points of contact for this vaccination will be the gynecologists, not the pediatricians,” Dr. Adams said.
“This concept imitates the natural process, since the mother normally passes immune defenses she acquired through infections to the child via the umbilical cord and her breast milk before and after birth. This procedure is long-proven and practiced worldwide, especially in nonindustrialized countries, for a variety of diseases, including tetanus, whooping cough (pertussis), and viral flu (influenza),” explained Markus Rose, MD, PhD, head of Pediatric Pulmonology at the Olgahospital, Stuttgart, Germany.
The development of an RSV vaccine had ground to a halt for many decades: A tragedy in the 1960s set the whole field of research back. Using the model of the first polio vaccine, scientists had manufactured an experimental vaccine with inactivated viruses. However, tests showed that the vaccine did not protect the children vaccinated, but it actually infected them with RSV, they then fell ill, and two children died. Today, potential RSV vaccines are first tested on adults and not on children.
Few treatment options
RSV causes seasonal epidemics, can lead to bronchiolitis and pneumonia in infants, and is one of the main causes of hospital stays in young children. Monoclonal antibodies are currently the only preventive option, since there is still no vaccine. Usually, 60%-70% of infants and nearly all children younger than 2 years are infected with RSV, but the virus can also trigger pneumonia in adults.
“RSV infections constitute a major public health challenge: It is the most dangerous respiratory virus for young infants, it is also a threat to the chronically ill and immunocompromised of all ages, and [it] is the second most common cause of death worldwide (after malaria) in young children,” stated Dr. Rose.
Recently, pandemic-related measures (face masks, more intense disinfection) meant that the “normal” RSV infections in healthy adults, which usually progress like a mild cold, were prevented, and mothers were unable to pass on as much RSV immune defense to their children. “This was presumably responsible in part for the massive wave of RSV infections in fall and winter of 2021/22,” explained Dr. Rose.
Thomas Mertens, MD, PhD, chair of the Standing Committee on Vaccination at the Robert Koch Institute (STIKO) and former director of the Institute for Virology at Ulm University Hospital, Germany, also noted: “It would be an important and potentially achievable goal to significantly reduce the incidence rate of hospitalizations. In this respect, RSV poses a significant problem for young children, their parents, and the burden on pediatric clinics.”
Final evaluation pending
“I am definitely finding the data interesting, but the original data are needed,” Dr. Mertens said. Once the data are published at a conference or published in a peer-reviewed journal, physicians will be able to better judge the data for themselves, he said.
Dr. Rose characterized the new vaccine as “novel,” including in terms of its composition. Earlier RSV vaccines used the so-called postfusion F protein as their starting point. But it has become known in the meantime that the key to immunogenicity is the continued prefusion state of the apical epitope: Prefusion F-specific memory B cells in adults naturally infected with RSV produce potent neutralizing antibodies.
The new vaccine is bivalent and protects against both RSV A and RSV B.
To date, RSV vaccination directly in young infants have had only had a weak efficacy and were sometimes poorly tolerated. The vaccine presented here is expected to be tested in young adults first, then in school children, then young children.
Through successful vaccination of the entire population, the transfer of RS viruses to young children could be prevented. “To what extent this, or any other RSV vaccine still to be developed on the same basis, will also be effective and well tolerated in young infants is still difficult to assess,” said Dr. Rose.
Dr. Mertens emphasized that all of the study data now needs to be seen as quickly as possible: “This is also a general requirement for transparency from the pharmaceutical companies, which is also rightly criticized.”
This article was originally published in Medscape’s German edition and a version appeared on Medscape.com.
An investigational vaccine against respiratory syncytial virus (RSV) in pregnant women has been shown to help protect infants against severe disease, according to the vaccine’s manufacturer.
Pfizer recently announced that in the course of a randomized, double-blind, placebo-controlled phase 3 study, the vaccine RSVpreF had an almost 82% efficacy against severe RSV infection in infants from birth through the first 90 days of life, according to a company press release.
The vaccine also had a 69% efficacy against severe disease through the first 6 months of life. A total of 7,400 women had received a single dose of 120 mcg RSVpreF in the late second or third trimester of their pregnancy. There were no signs of safety issues for the mothers or infants.
Due to the good results, the enrollment in the study was halted on the recommendation of the study’s Data Monitoring Committee after achieving a primary endpoint. The company plans to apply for marketing authorization to the U.S. Food and Drug Administration by the end of 2022 and to other regulatory agencies in 2023.
“The directness of the strategy, to vaccinate expectant mothers during pregnancy so that their newborn is then later protected, is new and a very interesting approach,” commented Prof. Ortwin Adams, MD, head of virologic diagnostics at the Institute for Virology of the University Hospital of Düsseldorf (Germany) to the Science Media Centre (SMC).
In terms of the RSV vaccination strategy presented, “the unborn child has taken center stage from the outset.” Because the vaccination route is the placental transfer of antibodies from mother to child (“passive immunity”), “... the medical points of contact for this vaccination will be the gynecologists, not the pediatricians,” Dr. Adams said.
“This concept imitates the natural process, since the mother normally passes immune defenses she acquired through infections to the child via the umbilical cord and her breast milk before and after birth. This procedure is long-proven and practiced worldwide, especially in nonindustrialized countries, for a variety of diseases, including tetanus, whooping cough (pertussis), and viral flu (influenza),” explained Markus Rose, MD, PhD, head of Pediatric Pulmonology at the Olgahospital, Stuttgart, Germany.
The development of an RSV vaccine had ground to a halt for many decades: A tragedy in the 1960s set the whole field of research back. Using the model of the first polio vaccine, scientists had manufactured an experimental vaccine with inactivated viruses. However, tests showed that the vaccine did not protect the children vaccinated, but it actually infected them with RSV, they then fell ill, and two children died. Today, potential RSV vaccines are first tested on adults and not on children.
Few treatment options
RSV causes seasonal epidemics, can lead to bronchiolitis and pneumonia in infants, and is one of the main causes of hospital stays in young children. Monoclonal antibodies are currently the only preventive option, since there is still no vaccine. Usually, 60%-70% of infants and nearly all children younger than 2 years are infected with RSV, but the virus can also trigger pneumonia in adults.
“RSV infections constitute a major public health challenge: It is the most dangerous respiratory virus for young infants, it is also a threat to the chronically ill and immunocompromised of all ages, and [it] is the second most common cause of death worldwide (after malaria) in young children,” stated Dr. Rose.
Recently, pandemic-related measures (face masks, more intense disinfection) meant that the “normal” RSV infections in healthy adults, which usually progress like a mild cold, were prevented, and mothers were unable to pass on as much RSV immune defense to their children. “This was presumably responsible in part for the massive wave of RSV infections in fall and winter of 2021/22,” explained Dr. Rose.
Thomas Mertens, MD, PhD, chair of the Standing Committee on Vaccination at the Robert Koch Institute (STIKO) and former director of the Institute for Virology at Ulm University Hospital, Germany, also noted: “It would be an important and potentially achievable goal to significantly reduce the incidence rate of hospitalizations. In this respect, RSV poses a significant problem for young children, their parents, and the burden on pediatric clinics.”
Final evaluation pending
“I am definitely finding the data interesting, but the original data are needed,” Dr. Mertens said. Once the data are published at a conference or published in a peer-reviewed journal, physicians will be able to better judge the data for themselves, he said.
Dr. Rose characterized the new vaccine as “novel,” including in terms of its composition. Earlier RSV vaccines used the so-called postfusion F protein as their starting point. But it has become known in the meantime that the key to immunogenicity is the continued prefusion state of the apical epitope: Prefusion F-specific memory B cells in adults naturally infected with RSV produce potent neutralizing antibodies.
The new vaccine is bivalent and protects against both RSV A and RSV B.
To date, RSV vaccination directly in young infants have had only had a weak efficacy and were sometimes poorly tolerated. The vaccine presented here is expected to be tested in young adults first, then in school children, then young children.
Through successful vaccination of the entire population, the transfer of RS viruses to young children could be prevented. “To what extent this, or any other RSV vaccine still to be developed on the same basis, will also be effective and well tolerated in young infants is still difficult to assess,” said Dr. Rose.
Dr. Mertens emphasized that all of the study data now needs to be seen as quickly as possible: “This is also a general requirement for transparency from the pharmaceutical companies, which is also rightly criticized.”
This article was originally published in Medscape’s German edition and a version appeared on Medscape.com.
An investigational vaccine against respiratory syncytial virus (RSV) in pregnant women has been shown to help protect infants against severe disease, according to the vaccine’s manufacturer.
Pfizer recently announced that in the course of a randomized, double-blind, placebo-controlled phase 3 study, the vaccine RSVpreF had an almost 82% efficacy against severe RSV infection in infants from birth through the first 90 days of life, according to a company press release.
The vaccine also had a 69% efficacy against severe disease through the first 6 months of life. A total of 7,400 women had received a single dose of 120 mcg RSVpreF in the late second or third trimester of their pregnancy. There were no signs of safety issues for the mothers or infants.
Due to the good results, the enrollment in the study was halted on the recommendation of the study’s Data Monitoring Committee after achieving a primary endpoint. The company plans to apply for marketing authorization to the U.S. Food and Drug Administration by the end of 2022 and to other regulatory agencies in 2023.
“The directness of the strategy, to vaccinate expectant mothers during pregnancy so that their newborn is then later protected, is new and a very interesting approach,” commented Prof. Ortwin Adams, MD, head of virologic diagnostics at the Institute for Virology of the University Hospital of Düsseldorf (Germany) to the Science Media Centre (SMC).
In terms of the RSV vaccination strategy presented, “the unborn child has taken center stage from the outset.” Because the vaccination route is the placental transfer of antibodies from mother to child (“passive immunity”), “... the medical points of contact for this vaccination will be the gynecologists, not the pediatricians,” Dr. Adams said.
“This concept imitates the natural process, since the mother normally passes immune defenses she acquired through infections to the child via the umbilical cord and her breast milk before and after birth. This procedure is long-proven and practiced worldwide, especially in nonindustrialized countries, for a variety of diseases, including tetanus, whooping cough (pertussis), and viral flu (influenza),” explained Markus Rose, MD, PhD, head of Pediatric Pulmonology at the Olgahospital, Stuttgart, Germany.
The development of an RSV vaccine had ground to a halt for many decades: A tragedy in the 1960s set the whole field of research back. Using the model of the first polio vaccine, scientists had manufactured an experimental vaccine with inactivated viruses. However, tests showed that the vaccine did not protect the children vaccinated, but it actually infected them with RSV, they then fell ill, and two children died. Today, potential RSV vaccines are first tested on adults and not on children.
Few treatment options
RSV causes seasonal epidemics, can lead to bronchiolitis and pneumonia in infants, and is one of the main causes of hospital stays in young children. Monoclonal antibodies are currently the only preventive option, since there is still no vaccine. Usually, 60%-70% of infants and nearly all children younger than 2 years are infected with RSV, but the virus can also trigger pneumonia in adults.
“RSV infections constitute a major public health challenge: It is the most dangerous respiratory virus for young infants, it is also a threat to the chronically ill and immunocompromised of all ages, and [it] is the second most common cause of death worldwide (after malaria) in young children,” stated Dr. Rose.
Recently, pandemic-related measures (face masks, more intense disinfection) meant that the “normal” RSV infections in healthy adults, which usually progress like a mild cold, were prevented, and mothers were unable to pass on as much RSV immune defense to their children. “This was presumably responsible in part for the massive wave of RSV infections in fall and winter of 2021/22,” explained Dr. Rose.
Thomas Mertens, MD, PhD, chair of the Standing Committee on Vaccination at the Robert Koch Institute (STIKO) and former director of the Institute for Virology at Ulm University Hospital, Germany, also noted: “It would be an important and potentially achievable goal to significantly reduce the incidence rate of hospitalizations. In this respect, RSV poses a significant problem for young children, their parents, and the burden on pediatric clinics.”
Final evaluation pending
“I am definitely finding the data interesting, but the original data are needed,” Dr. Mertens said. Once the data are published at a conference or published in a peer-reviewed journal, physicians will be able to better judge the data for themselves, he said.
Dr. Rose characterized the new vaccine as “novel,” including in terms of its composition. Earlier RSV vaccines used the so-called postfusion F protein as their starting point. But it has become known in the meantime that the key to immunogenicity is the continued prefusion state of the apical epitope: Prefusion F-specific memory B cells in adults naturally infected with RSV produce potent neutralizing antibodies.
The new vaccine is bivalent and protects against both RSV A and RSV B.
To date, RSV vaccination directly in young infants have had only had a weak efficacy and were sometimes poorly tolerated. The vaccine presented here is expected to be tested in young adults first, then in school children, then young children.
Through successful vaccination of the entire population, the transfer of RS viruses to young children could be prevented. “To what extent this, or any other RSV vaccine still to be developed on the same basis, will also be effective and well tolerated in young infants is still difficult to assess,” said Dr. Rose.
Dr. Mertens emphasized that all of the study data now needs to be seen as quickly as possible: “This is also a general requirement for transparency from the pharmaceutical companies, which is also rightly criticized.”
This article was originally published in Medscape’s German edition and a version appeared on Medscape.com.
Systematic review supports preferred drugs for HIV in youths
A systematic review of observational studies and clinical trials found dolutegravir and raltegravir to be safe and effective for treating teens and children living with HIV.
Effectiveness was higher across dolutegravir studies, the authors reported. After 12 months of treatment and observation, viral suppression levels were greater than 70% in most studies assessing dolutegravir. Viral suppression with raltegravir after 12 months varied between 42% and 83%.
“Our findings support the use of these two integrase inhibitors as part of WHO-recommended regimens for treating HIV,” said lead study author Claire Townsend, PhD, an epidemiologist and consultant to the World Health Organization HIV department in Geneva. “They were in line with what has been reported in adults and provide reassurance for the continued use of these two drugs in children and adolescents.”
The study was published in the Journal of the International AIDS Society.
Tracking outcomes for WHO guidelines
Integrase inhibitors, including dolutegravir and raltegravir, have become leading first- and second-line treatments in patients with HIV, largely owing to their effectiveness and fewer side effects, compared with other antiretroviral treatments.
Monitoring short- and long-term health outcomes of these widely used drugs is critical, the authors wrote. This is especially the case for dolutegravir, which has recently been approved in pediatric formulations. The review supported the development of the 2021 WHO consolidated HIV guidelines.
Dr. Townsend and colleagues searched the literature and screened trial registries for relevant studies conducted from January 2009 to March 2021. Among more than 4,000 published papers and abstracts, they identified 19 studies that met their review criteria relating to dolutegravir or raltegravir in children or adolescents aged 0-19 years who are living with HIV, including two studies that reported data on both agents.
Data on dolutegravir were extracted from 11 studies that included 2,330 children and adolescents in 1 randomized controlled trial, 1 single-arm trial, and 9 cohort studies. Data on raltegravir were extracted from 10 studies that included 649 children and adolescents in 1 randomized controlled trial, 1 single-arm trial, and 8 cohort studies.
The median follow-up in the dolutegravir studies was 6-36 months. Six studies recruited participants from Europe, three studies were based in sub-Saharan Africa, and two studies included persons from multiple geographic regions.
Across all studies, grade 3/4 adverse events were reported in 0%-50% of cases. Of these adverse events, very few were drug related, and no deaths were attributed to either dolutegravir or raltegravir.
However, Dr. Townsend cautioned that future research is needed to fill in evidence gaps “on longer-term safety and effectiveness of dolutegravir and raltegravir in children and adolescents,” including “research into adverse outcomes such as weight gain, potential metabolic changes, and neuropsychiatric adverse events, which have been reported in adults.”
The researchers noted that the small sample size of many of the studies contributed to variability in the findings and that most studies were observational, providing important real-world data but making their results less robust compared with data from randomized controlled studies with large sample sizes. They also noted that there was a high risk of bias (4 studies) and unclear risk of bias (5 studies) among the 15 observational studies included in their analysis.
“This research is particularly important because it supports the WHO recommendation that dolutegravir, which has a particularly high barrier of resistance to the HIV virus, be synchronized in adults and children as the preferred first-line and second-line treatment against HIV,” said Natella Rakhmanina, MD, PhD, director of HIV Services & Special Immunology at the Children’s National Hospital in Washington, D.C. Dr. Rakhmanina was not associated with the study.
Dr. Rakhmanina agreed that the safety profile of both drugs is “very good.” The lack of serious adverse events was meaningful, she highlighted, because “good tolerability is very important, particularly in children” as it means that drug compliance and viral suppression are achievable.
Two authors reported their authorship on two studies included in the review, as well as grant funding from ViiV Healthcare/GlaxoSmithKline, the marketing authorization holder for dolutegravir.
A version of this article first appeared on Medscape.com.
A systematic review of observational studies and clinical trials found dolutegravir and raltegravir to be safe and effective for treating teens and children living with HIV.
Effectiveness was higher across dolutegravir studies, the authors reported. After 12 months of treatment and observation, viral suppression levels were greater than 70% in most studies assessing dolutegravir. Viral suppression with raltegravir after 12 months varied between 42% and 83%.
“Our findings support the use of these two integrase inhibitors as part of WHO-recommended regimens for treating HIV,” said lead study author Claire Townsend, PhD, an epidemiologist and consultant to the World Health Organization HIV department in Geneva. “They were in line with what has been reported in adults and provide reassurance for the continued use of these two drugs in children and adolescents.”
The study was published in the Journal of the International AIDS Society.
Tracking outcomes for WHO guidelines
Integrase inhibitors, including dolutegravir and raltegravir, have become leading first- and second-line treatments in patients with HIV, largely owing to their effectiveness and fewer side effects, compared with other antiretroviral treatments.
Monitoring short- and long-term health outcomes of these widely used drugs is critical, the authors wrote. This is especially the case for dolutegravir, which has recently been approved in pediatric formulations. The review supported the development of the 2021 WHO consolidated HIV guidelines.
Dr. Townsend and colleagues searched the literature and screened trial registries for relevant studies conducted from January 2009 to March 2021. Among more than 4,000 published papers and abstracts, they identified 19 studies that met their review criteria relating to dolutegravir or raltegravir in children or adolescents aged 0-19 years who are living with HIV, including two studies that reported data on both agents.
Data on dolutegravir were extracted from 11 studies that included 2,330 children and adolescents in 1 randomized controlled trial, 1 single-arm trial, and 9 cohort studies. Data on raltegravir were extracted from 10 studies that included 649 children and adolescents in 1 randomized controlled trial, 1 single-arm trial, and 8 cohort studies.
The median follow-up in the dolutegravir studies was 6-36 months. Six studies recruited participants from Europe, three studies were based in sub-Saharan Africa, and two studies included persons from multiple geographic regions.
Across all studies, grade 3/4 adverse events were reported in 0%-50% of cases. Of these adverse events, very few were drug related, and no deaths were attributed to either dolutegravir or raltegravir.
However, Dr. Townsend cautioned that future research is needed to fill in evidence gaps “on longer-term safety and effectiveness of dolutegravir and raltegravir in children and adolescents,” including “research into adverse outcomes such as weight gain, potential metabolic changes, and neuropsychiatric adverse events, which have been reported in adults.”
The researchers noted that the small sample size of many of the studies contributed to variability in the findings and that most studies were observational, providing important real-world data but making their results less robust compared with data from randomized controlled studies with large sample sizes. They also noted that there was a high risk of bias (4 studies) and unclear risk of bias (5 studies) among the 15 observational studies included in their analysis.
“This research is particularly important because it supports the WHO recommendation that dolutegravir, which has a particularly high barrier of resistance to the HIV virus, be synchronized in adults and children as the preferred first-line and second-line treatment against HIV,” said Natella Rakhmanina, MD, PhD, director of HIV Services & Special Immunology at the Children’s National Hospital in Washington, D.C. Dr. Rakhmanina was not associated with the study.
Dr. Rakhmanina agreed that the safety profile of both drugs is “very good.” The lack of serious adverse events was meaningful, she highlighted, because “good tolerability is very important, particularly in children” as it means that drug compliance and viral suppression are achievable.
Two authors reported their authorship on two studies included in the review, as well as grant funding from ViiV Healthcare/GlaxoSmithKline, the marketing authorization holder for dolutegravir.
A version of this article first appeared on Medscape.com.
A systematic review of observational studies and clinical trials found dolutegravir and raltegravir to be safe and effective for treating teens and children living with HIV.
Effectiveness was higher across dolutegravir studies, the authors reported. After 12 months of treatment and observation, viral suppression levels were greater than 70% in most studies assessing dolutegravir. Viral suppression with raltegravir after 12 months varied between 42% and 83%.
“Our findings support the use of these two integrase inhibitors as part of WHO-recommended regimens for treating HIV,” said lead study author Claire Townsend, PhD, an epidemiologist and consultant to the World Health Organization HIV department in Geneva. “They were in line with what has been reported in adults and provide reassurance for the continued use of these two drugs in children and adolescents.”
The study was published in the Journal of the International AIDS Society.
Tracking outcomes for WHO guidelines
Integrase inhibitors, including dolutegravir and raltegravir, have become leading first- and second-line treatments in patients with HIV, largely owing to their effectiveness and fewer side effects, compared with other antiretroviral treatments.
Monitoring short- and long-term health outcomes of these widely used drugs is critical, the authors wrote. This is especially the case for dolutegravir, which has recently been approved in pediatric formulations. The review supported the development of the 2021 WHO consolidated HIV guidelines.
Dr. Townsend and colleagues searched the literature and screened trial registries for relevant studies conducted from January 2009 to March 2021. Among more than 4,000 published papers and abstracts, they identified 19 studies that met their review criteria relating to dolutegravir or raltegravir in children or adolescents aged 0-19 years who are living with HIV, including two studies that reported data on both agents.
Data on dolutegravir were extracted from 11 studies that included 2,330 children and adolescents in 1 randomized controlled trial, 1 single-arm trial, and 9 cohort studies. Data on raltegravir were extracted from 10 studies that included 649 children and adolescents in 1 randomized controlled trial, 1 single-arm trial, and 8 cohort studies.
The median follow-up in the dolutegravir studies was 6-36 months. Six studies recruited participants from Europe, three studies were based in sub-Saharan Africa, and two studies included persons from multiple geographic regions.
Across all studies, grade 3/4 adverse events were reported in 0%-50% of cases. Of these adverse events, very few were drug related, and no deaths were attributed to either dolutegravir or raltegravir.
However, Dr. Townsend cautioned that future research is needed to fill in evidence gaps “on longer-term safety and effectiveness of dolutegravir and raltegravir in children and adolescents,” including “research into adverse outcomes such as weight gain, potential metabolic changes, and neuropsychiatric adverse events, which have been reported in adults.”
The researchers noted that the small sample size of many of the studies contributed to variability in the findings and that most studies were observational, providing important real-world data but making their results less robust compared with data from randomized controlled studies with large sample sizes. They also noted that there was a high risk of bias (4 studies) and unclear risk of bias (5 studies) among the 15 observational studies included in their analysis.
“This research is particularly important because it supports the WHO recommendation that dolutegravir, which has a particularly high barrier of resistance to the HIV virus, be synchronized in adults and children as the preferred first-line and second-line treatment against HIV,” said Natella Rakhmanina, MD, PhD, director of HIV Services & Special Immunology at the Children’s National Hospital in Washington, D.C. Dr. Rakhmanina was not associated with the study.
Dr. Rakhmanina agreed that the safety profile of both drugs is “very good.” The lack of serious adverse events was meaningful, she highlighted, because “good tolerability is very important, particularly in children” as it means that drug compliance and viral suppression are achievable.
Two authors reported their authorship on two studies included in the review, as well as grant funding from ViiV Healthcare/GlaxoSmithKline, the marketing authorization holder for dolutegravir.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE INTERNATIONAL AIDS SOCIETY


