User login
Liver transplantation is on the rise for patients with severe alcoholic hepatitis
More transplant centers are offering liver transplantation as a viable therapeutic option for patients with severe alcoholic hepatitis who do not respond to steroid treatment.
“Alcoholic hepatitis is a disease caused by drinking alcohol. Excessive alcohol consumption causes fat to build up in your liver cells, as well as inflammation and scarring of the liver,” stated Saroja Bangaru, MD, chief resident at the University of Texas, Dallas. “Severe alcoholic hepatitis has an extremely high mortality and steroids are really the mainstay of therapy. Some alcoholic hepatitis patients do not respond to steroids and a significant percentage of them will die within 3 months. For these patients, liver transplantation is a therapeutic option.”
Dr. Bangaru and her colleagues conducted a survey that gathered data from 45 transplant centers in the United States and found that an increasing number have changed this practice and now offer liver transplantation to patients with severe alcoholic hepatitis.
The survey revealed that 51.1% of the 45 clinics offered liver transplantation to patients who had not yet been sober for 6 months, and 47.8% of transplant centers reported performing at least one liver transplant for severe alcoholic hepatitis. Just over a third (34.8%) of these centers had conducted three to five liver transplants, while only 8.9% of clinics performed at least six transplants. It is of note that most clinics have transplanted livers in fewer than five patients with severe alcoholic hepatitis, Dr. Bangaru said at the annual Digestive Disease Week®.
Patients experienced positive outcomes from these transplants, with almost 75% of surveyed clinics reporting 1-year survival rates of more than 90%, and 15% reporting 1-year survival rates of 80%-90%.
A factor that may have contributed to such positive outcomes was good patient selection based on liver transplant criteria for severe alcoholic hepatitis. More than 85% of center directors believed that liver transplant candidates should have a strong social support system, absence of severe psychiatric disorders, and a completed psychosocial evaluation, among other criteria.
Dr. Bangaru pointed out that the change in treating patients who have not abstained from alcohol is a break from traditional medical practice. “Historically, transplant centers would not consider a liver transplantation as an option unless a patient had abstained from drinking alcohol for 6 months. This rule was due to a concern that the patient would return to drinking after transplant as well as a perceived high risk that patients who continued drinking would miss medical appointments, fail to take their immunosuppressants and medications, and that this would lead to eventual graft failure.”
Another compounding issue was that patients were not counseled on their alcohol consumption habits, leading to further issues with transplantation. “Not infrequently, patients receive a diagnosis of severe alcoholic hepatitis during their initial visit and no one had previously told them to stop drinking. Since their presentation was preceded by active alcohol consumption, they would essentially be rendered ineligible for a transplant at that time,” she said.
Despite the history surrounding liver transplants in patients with severe alcoholic hepatitis, Dr. Bangaru hopes the shift in practice will improve the lives of more patients. “Because this practice of transplantation is being increasingly accepted and demonstrating positive outcomes, the hope is that more patients will be evaluated for transplantation and that transplant centers will improve their posttransplant support to ensure patients have great success after transplantation.”
Digestive Disease Week® is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
More transplant centers are offering liver transplantation as a viable therapeutic option for patients with severe alcoholic hepatitis who do not respond to steroid treatment.
“Alcoholic hepatitis is a disease caused by drinking alcohol. Excessive alcohol consumption causes fat to build up in your liver cells, as well as inflammation and scarring of the liver,” stated Saroja Bangaru, MD, chief resident at the University of Texas, Dallas. “Severe alcoholic hepatitis has an extremely high mortality and steroids are really the mainstay of therapy. Some alcoholic hepatitis patients do not respond to steroids and a significant percentage of them will die within 3 months. For these patients, liver transplantation is a therapeutic option.”
Dr. Bangaru and her colleagues conducted a survey that gathered data from 45 transplant centers in the United States and found that an increasing number have changed this practice and now offer liver transplantation to patients with severe alcoholic hepatitis.
The survey revealed that 51.1% of the 45 clinics offered liver transplantation to patients who had not yet been sober for 6 months, and 47.8% of transplant centers reported performing at least one liver transplant for severe alcoholic hepatitis. Just over a third (34.8%) of these centers had conducted three to five liver transplants, while only 8.9% of clinics performed at least six transplants. It is of note that most clinics have transplanted livers in fewer than five patients with severe alcoholic hepatitis, Dr. Bangaru said at the annual Digestive Disease Week®.
Patients experienced positive outcomes from these transplants, with almost 75% of surveyed clinics reporting 1-year survival rates of more than 90%, and 15% reporting 1-year survival rates of 80%-90%.
A factor that may have contributed to such positive outcomes was good patient selection based on liver transplant criteria for severe alcoholic hepatitis. More than 85% of center directors believed that liver transplant candidates should have a strong social support system, absence of severe psychiatric disorders, and a completed psychosocial evaluation, among other criteria.
Dr. Bangaru pointed out that the change in treating patients who have not abstained from alcohol is a break from traditional medical practice. “Historically, transplant centers would not consider a liver transplantation as an option unless a patient had abstained from drinking alcohol for 6 months. This rule was due to a concern that the patient would return to drinking after transplant as well as a perceived high risk that patients who continued drinking would miss medical appointments, fail to take their immunosuppressants and medications, and that this would lead to eventual graft failure.”
Another compounding issue was that patients were not counseled on their alcohol consumption habits, leading to further issues with transplantation. “Not infrequently, patients receive a diagnosis of severe alcoholic hepatitis during their initial visit and no one had previously told them to stop drinking. Since their presentation was preceded by active alcohol consumption, they would essentially be rendered ineligible for a transplant at that time,” she said.
Despite the history surrounding liver transplants in patients with severe alcoholic hepatitis, Dr. Bangaru hopes the shift in practice will improve the lives of more patients. “Because this practice of transplantation is being increasingly accepted and demonstrating positive outcomes, the hope is that more patients will be evaluated for transplantation and that transplant centers will improve their posttransplant support to ensure patients have great success after transplantation.”
Digestive Disease Week® is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
More transplant centers are offering liver transplantation as a viable therapeutic option for patients with severe alcoholic hepatitis who do not respond to steroid treatment.
“Alcoholic hepatitis is a disease caused by drinking alcohol. Excessive alcohol consumption causes fat to build up in your liver cells, as well as inflammation and scarring of the liver,” stated Saroja Bangaru, MD, chief resident at the University of Texas, Dallas. “Severe alcoholic hepatitis has an extremely high mortality and steroids are really the mainstay of therapy. Some alcoholic hepatitis patients do not respond to steroids and a significant percentage of them will die within 3 months. For these patients, liver transplantation is a therapeutic option.”
Dr. Bangaru and her colleagues conducted a survey that gathered data from 45 transplant centers in the United States and found that an increasing number have changed this practice and now offer liver transplantation to patients with severe alcoholic hepatitis.
The survey revealed that 51.1% of the 45 clinics offered liver transplantation to patients who had not yet been sober for 6 months, and 47.8% of transplant centers reported performing at least one liver transplant for severe alcoholic hepatitis. Just over a third (34.8%) of these centers had conducted three to five liver transplants, while only 8.9% of clinics performed at least six transplants. It is of note that most clinics have transplanted livers in fewer than five patients with severe alcoholic hepatitis, Dr. Bangaru said at the annual Digestive Disease Week®.
Patients experienced positive outcomes from these transplants, with almost 75% of surveyed clinics reporting 1-year survival rates of more than 90%, and 15% reporting 1-year survival rates of 80%-90%.
A factor that may have contributed to such positive outcomes was good patient selection based on liver transplant criteria for severe alcoholic hepatitis. More than 85% of center directors believed that liver transplant candidates should have a strong social support system, absence of severe psychiatric disorders, and a completed psychosocial evaluation, among other criteria.
Dr. Bangaru pointed out that the change in treating patients who have not abstained from alcohol is a break from traditional medical practice. “Historically, transplant centers would not consider a liver transplantation as an option unless a patient had abstained from drinking alcohol for 6 months. This rule was due to a concern that the patient would return to drinking after transplant as well as a perceived high risk that patients who continued drinking would miss medical appointments, fail to take their immunosuppressants and medications, and that this would lead to eventual graft failure.”
Another compounding issue was that patients were not counseled on their alcohol consumption habits, leading to further issues with transplantation. “Not infrequently, patients receive a diagnosis of severe alcoholic hepatitis during their initial visit and no one had previously told them to stop drinking. Since their presentation was preceded by active alcohol consumption, they would essentially be rendered ineligible for a transplant at that time,” she said.
Despite the history surrounding liver transplants in patients with severe alcoholic hepatitis, Dr. Bangaru hopes the shift in practice will improve the lives of more patients. “Because this practice of transplantation is being increasingly accepted and demonstrating positive outcomes, the hope is that more patients will be evaluated for transplantation and that transplant centers will improve their posttransplant support to ensure patients have great success after transplantation.”
Digestive Disease Week® is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
REPORTING FROM DDW
Alcohol abuse untreated in HCV patients, including HIV coinfected
Nearly 4% of Veterans Affairs patients who screened positive for unhealthy alcohol use were infected with hepatitis C virus, and 64% of these patients were diagnosed with alcohol use disorder, according to the results of a large database analysis.
Despite the fact that alcohol use at all levels can compound the adverse effects of HCV and lead to heightened risks of mortality, particularly among those coinfected with HIV, the majority of these patients did not receive specialty addiction treatment, according to Mandy D. Owens, PhD, and her colleagues at the VA Puget Sound Health Care System, Seattle.
In their study, published in Drug and Alcohol Dependence, the researchers queried the national VA health care system database, which is made up of 139 large facilities and more than 900 clinics throughout the United States, for all patients with a documented outpatient appointment between October 2009 and May 2013 to identify those with one or more with positive screens on the AUDIT-C (Alcohol Use Disorders Identification Test-Consumption) questionnaire. Those with AUDIT-C scores greater than or equal to 5 were considered positive, and each positive screen was tracked for up to 1 year to assess alcohol-related care outcomes. The four alcohol-related care outcomes measured were: receipt of brief intervention, specialty addiction treatment, alcohol use disorder (AUD) pharmacotherapy, and a composite measure of receiving any of these services.
Patients also were compared across HCV status in the entire sample of patients with positive screening as well as in the subsample with a clinically documented AUD.
During the study period, 830,825 VA patients screened positive for unhealthy alcohol use. Among those, 31,841 (3.8%) patients had a documented diagnosis for HCV, and of these 20,320 (64%) had an AUD. Two-thirds of these AUD patients did not receive specialty addiction treatment, and more than 90% did not receive pharmacotherapy that is approved by the Food and Drug Administration to treat AUD, according to the researchers. “These rates are concerning given the negative impact alcohol use can have on HCV,” they wrote.
They reiterated the importance of the 2016 change in policy adopted by the VA Health System, which updated its treatment guidelines to recommend that all patients with HCV be considered for treatment, regardless of substance use, and explicitly stated that alcohol use and length of abstinence should not be disqualifiers for receiving HCV treatment.
“All patients with HCV should be receiving evidence-based alcohol-related care given the risks of alcohol use in this population, particularly among those coinfected with HIV,” the researchers concluded.
The research was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism. The authors reported that they had no conflicts of interest.
SOURCE: Owens MD et al. Drug Alcohol Depend. 2018;188:79-85.
Nearly 4% of Veterans Affairs patients who screened positive for unhealthy alcohol use were infected with hepatitis C virus, and 64% of these patients were diagnosed with alcohol use disorder, according to the results of a large database analysis.
Despite the fact that alcohol use at all levels can compound the adverse effects of HCV and lead to heightened risks of mortality, particularly among those coinfected with HIV, the majority of these patients did not receive specialty addiction treatment, according to Mandy D. Owens, PhD, and her colleagues at the VA Puget Sound Health Care System, Seattle.
In their study, published in Drug and Alcohol Dependence, the researchers queried the national VA health care system database, which is made up of 139 large facilities and more than 900 clinics throughout the United States, for all patients with a documented outpatient appointment between October 2009 and May 2013 to identify those with one or more with positive screens on the AUDIT-C (Alcohol Use Disorders Identification Test-Consumption) questionnaire. Those with AUDIT-C scores greater than or equal to 5 were considered positive, and each positive screen was tracked for up to 1 year to assess alcohol-related care outcomes. The four alcohol-related care outcomes measured were: receipt of brief intervention, specialty addiction treatment, alcohol use disorder (AUD) pharmacotherapy, and a composite measure of receiving any of these services.
Patients also were compared across HCV status in the entire sample of patients with positive screening as well as in the subsample with a clinically documented AUD.
During the study period, 830,825 VA patients screened positive for unhealthy alcohol use. Among those, 31,841 (3.8%) patients had a documented diagnosis for HCV, and of these 20,320 (64%) had an AUD. Two-thirds of these AUD patients did not receive specialty addiction treatment, and more than 90% did not receive pharmacotherapy that is approved by the Food and Drug Administration to treat AUD, according to the researchers. “These rates are concerning given the negative impact alcohol use can have on HCV,” they wrote.
They reiterated the importance of the 2016 change in policy adopted by the VA Health System, which updated its treatment guidelines to recommend that all patients with HCV be considered for treatment, regardless of substance use, and explicitly stated that alcohol use and length of abstinence should not be disqualifiers for receiving HCV treatment.
“All patients with HCV should be receiving evidence-based alcohol-related care given the risks of alcohol use in this population, particularly among those coinfected with HIV,” the researchers concluded.
The research was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism. The authors reported that they had no conflicts of interest.
SOURCE: Owens MD et al. Drug Alcohol Depend. 2018;188:79-85.
Nearly 4% of Veterans Affairs patients who screened positive for unhealthy alcohol use were infected with hepatitis C virus, and 64% of these patients were diagnosed with alcohol use disorder, according to the results of a large database analysis.
Despite the fact that alcohol use at all levels can compound the adverse effects of HCV and lead to heightened risks of mortality, particularly among those coinfected with HIV, the majority of these patients did not receive specialty addiction treatment, according to Mandy D. Owens, PhD, and her colleagues at the VA Puget Sound Health Care System, Seattle.
In their study, published in Drug and Alcohol Dependence, the researchers queried the national VA health care system database, which is made up of 139 large facilities and more than 900 clinics throughout the United States, for all patients with a documented outpatient appointment between October 2009 and May 2013 to identify those with one or more with positive screens on the AUDIT-C (Alcohol Use Disorders Identification Test-Consumption) questionnaire. Those with AUDIT-C scores greater than or equal to 5 were considered positive, and each positive screen was tracked for up to 1 year to assess alcohol-related care outcomes. The four alcohol-related care outcomes measured were: receipt of brief intervention, specialty addiction treatment, alcohol use disorder (AUD) pharmacotherapy, and a composite measure of receiving any of these services.
Patients also were compared across HCV status in the entire sample of patients with positive screening as well as in the subsample with a clinically documented AUD.
During the study period, 830,825 VA patients screened positive for unhealthy alcohol use. Among those, 31,841 (3.8%) patients had a documented diagnosis for HCV, and of these 20,320 (64%) had an AUD. Two-thirds of these AUD patients did not receive specialty addiction treatment, and more than 90% did not receive pharmacotherapy that is approved by the Food and Drug Administration to treat AUD, according to the researchers. “These rates are concerning given the negative impact alcohol use can have on HCV,” they wrote.
They reiterated the importance of the 2016 change in policy adopted by the VA Health System, which updated its treatment guidelines to recommend that all patients with HCV be considered for treatment, regardless of substance use, and explicitly stated that alcohol use and length of abstinence should not be disqualifiers for receiving HCV treatment.
“All patients with HCV should be receiving evidence-based alcohol-related care given the risks of alcohol use in this population, particularly among those coinfected with HIV,” the researchers concluded.
The research was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism. The authors reported that they had no conflicts of interest.
SOURCE: Owens MD et al. Drug Alcohol Depend. 2018;188:79-85.
FROM DRUG AND ALCOHOL DEPENDENCE
Key clinical point: Alcohol-use disorder therapy is underdelivered to patients with HCV who would benefit.
Major finding: Only 27% of patients with HCV plus alcohol-abuse disorder received AUD therapy.
Study details: National VA health care system database of 830,825 patients who screened positive for unhealthy alcohol use.
Disclosures: The research was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism. The authors reported that they had no conflicts of interest.
Source: Owens MD et al. Drug Alcohol Depend. 2018;188:79-85.
FDA approves Doptelet for liver disease patients undergoing procedures
Doptelet (avatrombopag) is the first drug to be approved by the Food and Drug Administration for thrombocytopenia in adults with chronic liver disease who are scheduled to undergo a medical or dental procedure, the FDA announced in a statement.
“Patients with chronic liver disease who have low platelet counts and require a procedure are at increased risk of bleeding,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Doptelet was demonstrated to safely increase the platelet count. This drug may decrease or eliminate the need for platelet transfusions, which are associated with risk of infection and other adverse reactions.”
The safety and efficacy of two different doses of Doptelet administered orally over 5 days, as compared with placebo, was studied in the ADAPT trials (ADAPT-1 and ADAPT-2) involving 435 patients with chronic liver disease and severe thrombocytopenia who were scheduled to undergo a procedure that would typically require platelet transfusion. At both dose levels of Doptelet, a higher proportion of patients had increased platelet counts and did not require platelet transfusion or any rescue therapy on the day of the procedure and up to 7 days following the procedure as compared with those treated with placebo.
The most common side effects reported by clinical trial participants who received Doptelet were fever, stomach (abdominal) pain, nausea, headache, fatigue and edema in the hands or feet. People with chronic liver disease and people with certain blood clotting conditions may have an increased risk of developing blood clots when taking Doptelet, the FDA said in a press release announcing the approval.
The FDA granted the Doptelet approval to AkaRx.
Doptelet (avatrombopag) is the first drug to be approved by the Food and Drug Administration for thrombocytopenia in adults with chronic liver disease who are scheduled to undergo a medical or dental procedure, the FDA announced in a statement.
“Patients with chronic liver disease who have low platelet counts and require a procedure are at increased risk of bleeding,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Doptelet was demonstrated to safely increase the platelet count. This drug may decrease or eliminate the need for platelet transfusions, which are associated with risk of infection and other adverse reactions.”
The safety and efficacy of two different doses of Doptelet administered orally over 5 days, as compared with placebo, was studied in the ADAPT trials (ADAPT-1 and ADAPT-2) involving 435 patients with chronic liver disease and severe thrombocytopenia who were scheduled to undergo a procedure that would typically require platelet transfusion. At both dose levels of Doptelet, a higher proportion of patients had increased platelet counts and did not require platelet transfusion or any rescue therapy on the day of the procedure and up to 7 days following the procedure as compared with those treated with placebo.
The most common side effects reported by clinical trial participants who received Doptelet were fever, stomach (abdominal) pain, nausea, headache, fatigue and edema in the hands or feet. People with chronic liver disease and people with certain blood clotting conditions may have an increased risk of developing blood clots when taking Doptelet, the FDA said in a press release announcing the approval.
The FDA granted the Doptelet approval to AkaRx.
Doptelet (avatrombopag) is the first drug to be approved by the Food and Drug Administration for thrombocytopenia in adults with chronic liver disease who are scheduled to undergo a medical or dental procedure, the FDA announced in a statement.
“Patients with chronic liver disease who have low platelet counts and require a procedure are at increased risk of bleeding,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Doptelet was demonstrated to safely increase the platelet count. This drug may decrease or eliminate the need for platelet transfusions, which are associated with risk of infection and other adverse reactions.”
The safety and efficacy of two different doses of Doptelet administered orally over 5 days, as compared with placebo, was studied in the ADAPT trials (ADAPT-1 and ADAPT-2) involving 435 patients with chronic liver disease and severe thrombocytopenia who were scheduled to undergo a procedure that would typically require platelet transfusion. At both dose levels of Doptelet, a higher proportion of patients had increased platelet counts and did not require platelet transfusion or any rescue therapy on the day of the procedure and up to 7 days following the procedure as compared with those treated with placebo.
The most common side effects reported by clinical trial participants who received Doptelet were fever, stomach (abdominal) pain, nausea, headache, fatigue and edema in the hands or feet. People with chronic liver disease and people with certain blood clotting conditions may have an increased risk of developing blood clots when taking Doptelet, the FDA said in a press release announcing the approval.
The FDA granted the Doptelet approval to AkaRx.
Where the latest HCV drug combos fit in
MAUI, HAWAII – The addition of the two latest treatment regimens to receive approval for hepatitis C essentially closes the circle on treatment of this disease, Steven L. Flamm, MD, declared at the Gastroenterology Updates, IBD, Liver Disease meeting.
“We now have good options available for all the hepatitis C scenarios you will ever see in your practice,” said Dr. Flamm, professor of medicine and chief of the hepatology program at Northwestern University, Chicago.
Moreover, this wide range of highly effective, well-tolerated therapies is having a major clinical impact.
“We’re already seeing a decline in the number of patients who are listed for liver transplantation with hepatitis C as the indication with UNOS [the United Organ Sharing database],” the gastroenterologist noted, citing a study presented at the 2017 annual meeting of the American Association for the Study of Liver Disease that showed that the proportion of patients who join the transplant wait-list with hepatitis C as their qualifying diagnosis has fallen by 35% since approval of the direct-acting antiviral (DAA) regimens in late 2013.
What’s special about the two newest DAA treatment regimens – sofosbuvir/velpatasvir/voxilaprevir (Vosevi) and glecaprevir/pibrentasvir (Mavyret) – is that they are pangenotypic, they are effective in prior treatment failures, they don’t need to be accompanied by ribavirin, and there is no need for baseline pretreatment resistance-associated substitution testing, Dr. Flamm noted.
“So if you have a patient sitting in front of you with any genotype of hepatitis C infection who has failed on NS5a-inhibitor therapy, you can tell them in general their chance of getting an SVR [sustained viral response] with sofosbuvir/velpatasvir/voxilaprevir is about 97%. And you can give it without worrying about what resistances they might have to begin with,” he said.
His copanelist Norah Terrault, MD, agreed that these two regimens are important additions.
“Glecaprevir/pibrentasvir is the first pangenic 8-week regimen for noncirrhotics. This is a major advance. And now having sofosbuvir/velpatasvir/voxilaprevir for treatment-experienced patients, that’s another strong advance,” commented Dr. Terrault, professor of medicine and director of the Viral Hepatitis Center at the University of California, San Francisco.
Dr. Flamm said the biggest remaining challenge in the treatment of hepatitis C is to gain improved access to therapy.
“The public-aid patients make up 30%-35% of patients with hepatitis C in my part of the country, and they still can’t get therapy unless they have cirrhosis. We can’t even treat people who have stage 2 fibrosis if they’re public-aid patients in Illinois. So we can’t achieve the goal of eliminating hepatitis C,” Dr. Flamm said.
He reported having no financial conflicts regarding his presentation.
Encourage your patients to visit AGA’s new online GI Patient Center to learn more about digestive diseases, including HCV, at gastro.org/patient.
MAUI, HAWAII – The addition of the two latest treatment regimens to receive approval for hepatitis C essentially closes the circle on treatment of this disease, Steven L. Flamm, MD, declared at the Gastroenterology Updates, IBD, Liver Disease meeting.
“We now have good options available for all the hepatitis C scenarios you will ever see in your practice,” said Dr. Flamm, professor of medicine and chief of the hepatology program at Northwestern University, Chicago.
Moreover, this wide range of highly effective, well-tolerated therapies is having a major clinical impact.
“We’re already seeing a decline in the number of patients who are listed for liver transplantation with hepatitis C as the indication with UNOS [the United Organ Sharing database],” the gastroenterologist noted, citing a study presented at the 2017 annual meeting of the American Association for the Study of Liver Disease that showed that the proportion of patients who join the transplant wait-list with hepatitis C as their qualifying diagnosis has fallen by 35% since approval of the direct-acting antiviral (DAA) regimens in late 2013.
What’s special about the two newest DAA treatment regimens – sofosbuvir/velpatasvir/voxilaprevir (Vosevi) and glecaprevir/pibrentasvir (Mavyret) – is that they are pangenotypic, they are effective in prior treatment failures, they don’t need to be accompanied by ribavirin, and there is no need for baseline pretreatment resistance-associated substitution testing, Dr. Flamm noted.
“So if you have a patient sitting in front of you with any genotype of hepatitis C infection who has failed on NS5a-inhibitor therapy, you can tell them in general their chance of getting an SVR [sustained viral response] with sofosbuvir/velpatasvir/voxilaprevir is about 97%. And you can give it without worrying about what resistances they might have to begin with,” he said.
His copanelist Norah Terrault, MD, agreed that these two regimens are important additions.
“Glecaprevir/pibrentasvir is the first pangenic 8-week regimen for noncirrhotics. This is a major advance. And now having sofosbuvir/velpatasvir/voxilaprevir for treatment-experienced patients, that’s another strong advance,” commented Dr. Terrault, professor of medicine and director of the Viral Hepatitis Center at the University of California, San Francisco.
Dr. Flamm said the biggest remaining challenge in the treatment of hepatitis C is to gain improved access to therapy.
“The public-aid patients make up 30%-35% of patients with hepatitis C in my part of the country, and they still can’t get therapy unless they have cirrhosis. We can’t even treat people who have stage 2 fibrosis if they’re public-aid patients in Illinois. So we can’t achieve the goal of eliminating hepatitis C,” Dr. Flamm said.
He reported having no financial conflicts regarding his presentation.
Encourage your patients to visit AGA’s new online GI Patient Center to learn more about digestive diseases, including HCV, at gastro.org/patient.
MAUI, HAWAII – The addition of the two latest treatment regimens to receive approval for hepatitis C essentially closes the circle on treatment of this disease, Steven L. Flamm, MD, declared at the Gastroenterology Updates, IBD, Liver Disease meeting.
“We now have good options available for all the hepatitis C scenarios you will ever see in your practice,” said Dr. Flamm, professor of medicine and chief of the hepatology program at Northwestern University, Chicago.
Moreover, this wide range of highly effective, well-tolerated therapies is having a major clinical impact.
“We’re already seeing a decline in the number of patients who are listed for liver transplantation with hepatitis C as the indication with UNOS [the United Organ Sharing database],” the gastroenterologist noted, citing a study presented at the 2017 annual meeting of the American Association for the Study of Liver Disease that showed that the proportion of patients who join the transplant wait-list with hepatitis C as their qualifying diagnosis has fallen by 35% since approval of the direct-acting antiviral (DAA) regimens in late 2013.
What’s special about the two newest DAA treatment regimens – sofosbuvir/velpatasvir/voxilaprevir (Vosevi) and glecaprevir/pibrentasvir (Mavyret) – is that they are pangenotypic, they are effective in prior treatment failures, they don’t need to be accompanied by ribavirin, and there is no need for baseline pretreatment resistance-associated substitution testing, Dr. Flamm noted.
“So if you have a patient sitting in front of you with any genotype of hepatitis C infection who has failed on NS5a-inhibitor therapy, you can tell them in general their chance of getting an SVR [sustained viral response] with sofosbuvir/velpatasvir/voxilaprevir is about 97%. And you can give it without worrying about what resistances they might have to begin with,” he said.
His copanelist Norah Terrault, MD, agreed that these two regimens are important additions.
“Glecaprevir/pibrentasvir is the first pangenic 8-week regimen for noncirrhotics. This is a major advance. And now having sofosbuvir/velpatasvir/voxilaprevir for treatment-experienced patients, that’s another strong advance,” commented Dr. Terrault, professor of medicine and director of the Viral Hepatitis Center at the University of California, San Francisco.
Dr. Flamm said the biggest remaining challenge in the treatment of hepatitis C is to gain improved access to therapy.
“The public-aid patients make up 30%-35% of patients with hepatitis C in my part of the country, and they still can’t get therapy unless they have cirrhosis. We can’t even treat people who have stage 2 fibrosis if they’re public-aid patients in Illinois. So we can’t achieve the goal of eliminating hepatitis C,” Dr. Flamm said.
He reported having no financial conflicts regarding his presentation.
Encourage your patients to visit AGA’s new online GI Patient Center to learn more about digestive diseases, including HCV, at gastro.org/patient.
EXPERT ANALYSIS FROM GUILD 2018
Class III obesity increases risk of acute on chronic liver failure in cirrhotic patients
Class III obesity was significantly, independently associated with acute on chronic liver failure (ACLF) in patients with decompensated cirrhosis, and patients with both class III obesity and acute on chronic liver failure also had a significant risk of renal failure, according to a recent retrospective analysis of two databases publised in the Journal of Hepatology.
Vinay Sundaram, MD, from Cedars-Sinai Medical Center in Los Angeles, and his colleagues evaluated 387,884 patients who were in the United Network for Organ Sharing (UNOS) during 2005-2016; were class I or II obese (body mass index 30-39 kg/m2), class III obese (BMI greater than or equal to 40), or not obese (BMI less than 30); and were on a wait list for liver transplantation.
They used the definition of ACLF outlined in the CANONIC (Consortium Acute on Chronic Liver Failure in Cirrhosis) study, which defined it as having “a single hepatic decompensation, such as ascites, hepatic encephalopathy, variceal bleed, or bacterial infection, and one of the following organ failures: single renal failure, single nonrenal organ failure with renal dysfunction or hepatic encephalopathy, or two nonrenal organ failures,” and confirmed the results in the Nationwide Inpatient Sample (NIS) databases by using diagnostic coding algorithms to identify factors such as hepatic decompensation, obesity, and ACLF in that study population.
Dr. Sundarem and his colleagues identified 116,704 patients (30.1%) with acute on chronic liver failure in both the UNOS and NIS databases. At the time of liver transplantation, there was a significant association between ACLF and class I and class II obesity (hazard ratio, 1.12; 95% confidence interval, 1.05-1.19; P less than .001) and class III obesity (HR, 1.24; 95% CI, 1.09-1.41; P less than .001). Other predictors of ACLF in this population were increased age (HR, 1.01 per year; 95% CI, 1.00-1.01; P = .037), hepatitis C virus (HR, 1.25; 95% CI, 1.16-1.35; P less than .001) and hepatitis C combined with alcoholic liver disease (HR, 1.18; 95% CI, 1.06-1.30; P = .002). Regarding organ failure, “renal insufficiency was similar among the three groups,” with increasing obesity class associated with a greater prevalence of renal failure.
“Given the heightened risk of renal failure among obese patients with cirrhosis, we suggest particularly careful management of this fragile population regarding diuretic usage, avoidance of nephrotoxic agents, and administration of an adequate albumin challenge in the setting of acute kidney injury,” the researchers wrote.
The researchers encouraged “an even greater emphasis on weight reduction” for class III obese patients. They noted the association between class III obesity and ACLF is likely caused by an “obesity-related chronic inflammatory state” and said future prospective studies should seek to describe the inflammatory pathways for each condition to predict risk of ACLF in these patients.
The authors reported having no financial disclosures.
SOURCE: Sundarem V et al. J Hepatol. 2018 April 27. doi: 10.1016/j.jhep.2018.04.016.
Class III obesity was significantly, independently associated with acute on chronic liver failure (ACLF) in patients with decompensated cirrhosis, and patients with both class III obesity and acute on chronic liver failure also had a significant risk of renal failure, according to a recent retrospective analysis of two databases publised in the Journal of Hepatology.
Vinay Sundaram, MD, from Cedars-Sinai Medical Center in Los Angeles, and his colleagues evaluated 387,884 patients who were in the United Network for Organ Sharing (UNOS) during 2005-2016; were class I or II obese (body mass index 30-39 kg/m2), class III obese (BMI greater than or equal to 40), or not obese (BMI less than 30); and were on a wait list for liver transplantation.
They used the definition of ACLF outlined in the CANONIC (Consortium Acute on Chronic Liver Failure in Cirrhosis) study, which defined it as having “a single hepatic decompensation, such as ascites, hepatic encephalopathy, variceal bleed, or bacterial infection, and one of the following organ failures: single renal failure, single nonrenal organ failure with renal dysfunction or hepatic encephalopathy, or two nonrenal organ failures,” and confirmed the results in the Nationwide Inpatient Sample (NIS) databases by using diagnostic coding algorithms to identify factors such as hepatic decompensation, obesity, and ACLF in that study population.
Dr. Sundarem and his colleagues identified 116,704 patients (30.1%) with acute on chronic liver failure in both the UNOS and NIS databases. At the time of liver transplantation, there was a significant association between ACLF and class I and class II obesity (hazard ratio, 1.12; 95% confidence interval, 1.05-1.19; P less than .001) and class III obesity (HR, 1.24; 95% CI, 1.09-1.41; P less than .001). Other predictors of ACLF in this population were increased age (HR, 1.01 per year; 95% CI, 1.00-1.01; P = .037), hepatitis C virus (HR, 1.25; 95% CI, 1.16-1.35; P less than .001) and hepatitis C combined with alcoholic liver disease (HR, 1.18; 95% CI, 1.06-1.30; P = .002). Regarding organ failure, “renal insufficiency was similar among the three groups,” with increasing obesity class associated with a greater prevalence of renal failure.
“Given the heightened risk of renal failure among obese patients with cirrhosis, we suggest particularly careful management of this fragile population regarding diuretic usage, avoidance of nephrotoxic agents, and administration of an adequate albumin challenge in the setting of acute kidney injury,” the researchers wrote.
The researchers encouraged “an even greater emphasis on weight reduction” for class III obese patients. They noted the association between class III obesity and ACLF is likely caused by an “obesity-related chronic inflammatory state” and said future prospective studies should seek to describe the inflammatory pathways for each condition to predict risk of ACLF in these patients.
The authors reported having no financial disclosures.
SOURCE: Sundarem V et al. J Hepatol. 2018 April 27. doi: 10.1016/j.jhep.2018.04.016.
Class III obesity was significantly, independently associated with acute on chronic liver failure (ACLF) in patients with decompensated cirrhosis, and patients with both class III obesity and acute on chronic liver failure also had a significant risk of renal failure, according to a recent retrospective analysis of two databases publised in the Journal of Hepatology.
Vinay Sundaram, MD, from Cedars-Sinai Medical Center in Los Angeles, and his colleagues evaluated 387,884 patients who were in the United Network for Organ Sharing (UNOS) during 2005-2016; were class I or II obese (body mass index 30-39 kg/m2), class III obese (BMI greater than or equal to 40), or not obese (BMI less than 30); and were on a wait list for liver transplantation.
They used the definition of ACLF outlined in the CANONIC (Consortium Acute on Chronic Liver Failure in Cirrhosis) study, which defined it as having “a single hepatic decompensation, such as ascites, hepatic encephalopathy, variceal bleed, or bacterial infection, and one of the following organ failures: single renal failure, single nonrenal organ failure with renal dysfunction or hepatic encephalopathy, or two nonrenal organ failures,” and confirmed the results in the Nationwide Inpatient Sample (NIS) databases by using diagnostic coding algorithms to identify factors such as hepatic decompensation, obesity, and ACLF in that study population.
Dr. Sundarem and his colleagues identified 116,704 patients (30.1%) with acute on chronic liver failure in both the UNOS and NIS databases. At the time of liver transplantation, there was a significant association between ACLF and class I and class II obesity (hazard ratio, 1.12; 95% confidence interval, 1.05-1.19; P less than .001) and class III obesity (HR, 1.24; 95% CI, 1.09-1.41; P less than .001). Other predictors of ACLF in this population were increased age (HR, 1.01 per year; 95% CI, 1.00-1.01; P = .037), hepatitis C virus (HR, 1.25; 95% CI, 1.16-1.35; P less than .001) and hepatitis C combined with alcoholic liver disease (HR, 1.18; 95% CI, 1.06-1.30; P = .002). Regarding organ failure, “renal insufficiency was similar among the three groups,” with increasing obesity class associated with a greater prevalence of renal failure.
“Given the heightened risk of renal failure among obese patients with cirrhosis, we suggest particularly careful management of this fragile population regarding diuretic usage, avoidance of nephrotoxic agents, and administration of an adequate albumin challenge in the setting of acute kidney injury,” the researchers wrote.
The researchers encouraged “an even greater emphasis on weight reduction” for class III obese patients. They noted the association between class III obesity and ACLF is likely caused by an “obesity-related chronic inflammatory state” and said future prospective studies should seek to describe the inflammatory pathways for each condition to predict risk of ACLF in these patients.
The authors reported having no financial disclosures.
SOURCE: Sundarem V et al. J Hepatol. 2018 April 27. doi: 10.1016/j.jhep.2018.04.016.
FROM THE JOURNAL OF HEPATOLOGY
Key clinical point: Patients with a BMI greater than or equal to 40 kg/m2 with decompensated cirrhosis are at greater risk of developing acute on chronic liver failure.
Major finding: Class III obesity carried a hazard ratio of 1.24 in the UNOS database and an odds ratio of 1.30 in the NIS database at the time of liver transplantation.
Data source: A retrospective cohort database study of 116,704 patients with acute on chronic liver failure listed during 2005-2016.
Disclosures: The authors reported having no financial disclosures.
Source: Sundaram V et al. J Hepatol. 2018 Apr 27. doi: 10.1016/j.jhep.2018.04.016.
Very few infants born to HCV-infected mothers receive testing
Despite the increasing prevalence of hepatitis C virus (HCV) infection in pregnant women, infants exposed to the disease are screened at a very low rate, Catherine A. Chappell, MD, and her associates wrote in Pediatrics.
During 2006-2014, 87,924 women gave birth at the Magee-Womens Hospital at the University of Pittsburgh Medical Center, of whom 1,043 had HCV. Over this time, the HCV prevalence rate increased 60%, from 1,026 cases per 100,000 women to 1,637 cases per 100,000 women. Women with HCV were more likely to be white, have Medicaid, have opiate use disorder, have other substance use disorders, and be under the age of 30 years.
Infants born to HCV-infected women are significantly more likely to be preterm and of low birth weight.
An additional 32 infants who did not receive well child care did receive HCV testing. A total of nine infants, seven in the well child group and two in the non-well child group, tested positive for HCV.
“Of the infants tested with conclusive results, the HCV transmission rate was 8.4%, with 7.2% having chronic HCV infection,” which is in line with previous reports, according to the researchers.
“Because of the poor rates of pediatric HCV screening described, future researchers should focus on interventions to increase screening in infants who are at risk for perinatal HCV acquisition by including technology to improve the transfer of maternal HCV status to the pediatric record and increase pediatric provider awareness regarding HCV screening guidelines,” the investigators concluded.
SOURCE: Chappell CA et al. Pediatrics. 2018 May 2. doi: 10.1542/peds.2017-3273.
Despite the increasing prevalence of hepatitis C virus (HCV) infection in pregnant women, infants exposed to the disease are screened at a very low rate, Catherine A. Chappell, MD, and her associates wrote in Pediatrics.
During 2006-2014, 87,924 women gave birth at the Magee-Womens Hospital at the University of Pittsburgh Medical Center, of whom 1,043 had HCV. Over this time, the HCV prevalence rate increased 60%, from 1,026 cases per 100,000 women to 1,637 cases per 100,000 women. Women with HCV were more likely to be white, have Medicaid, have opiate use disorder, have other substance use disorders, and be under the age of 30 years.
Infants born to HCV-infected women are significantly more likely to be preterm and of low birth weight.
An additional 32 infants who did not receive well child care did receive HCV testing. A total of nine infants, seven in the well child group and two in the non-well child group, tested positive for HCV.
“Of the infants tested with conclusive results, the HCV transmission rate was 8.4%, with 7.2% having chronic HCV infection,” which is in line with previous reports, according to the researchers.
“Because of the poor rates of pediatric HCV screening described, future researchers should focus on interventions to increase screening in infants who are at risk for perinatal HCV acquisition by including technology to improve the transfer of maternal HCV status to the pediatric record and increase pediatric provider awareness regarding HCV screening guidelines,” the investigators concluded.
SOURCE: Chappell CA et al. Pediatrics. 2018 May 2. doi: 10.1542/peds.2017-3273.
Despite the increasing prevalence of hepatitis C virus (HCV) infection in pregnant women, infants exposed to the disease are screened at a very low rate, Catherine A. Chappell, MD, and her associates wrote in Pediatrics.
During 2006-2014, 87,924 women gave birth at the Magee-Womens Hospital at the University of Pittsburgh Medical Center, of whom 1,043 had HCV. Over this time, the HCV prevalence rate increased 60%, from 1,026 cases per 100,000 women to 1,637 cases per 100,000 women. Women with HCV were more likely to be white, have Medicaid, have opiate use disorder, have other substance use disorders, and be under the age of 30 years.
Infants born to HCV-infected women are significantly more likely to be preterm and of low birth weight.
An additional 32 infants who did not receive well child care did receive HCV testing. A total of nine infants, seven in the well child group and two in the non-well child group, tested positive for HCV.
“Of the infants tested with conclusive results, the HCV transmission rate was 8.4%, with 7.2% having chronic HCV infection,” which is in line with previous reports, according to the researchers.
“Because of the poor rates of pediatric HCV screening described, future researchers should focus on interventions to increase screening in infants who are at risk for perinatal HCV acquisition by including technology to improve the transfer of maternal HCV status to the pediatric record and increase pediatric provider awareness regarding HCV screening guidelines,” the investigators concluded.
SOURCE: Chappell CA et al. Pediatrics. 2018 May 2. doi: 10.1542/peds.2017-3273.
FROM PEDIATRICS
Treatment of HCV in special populations
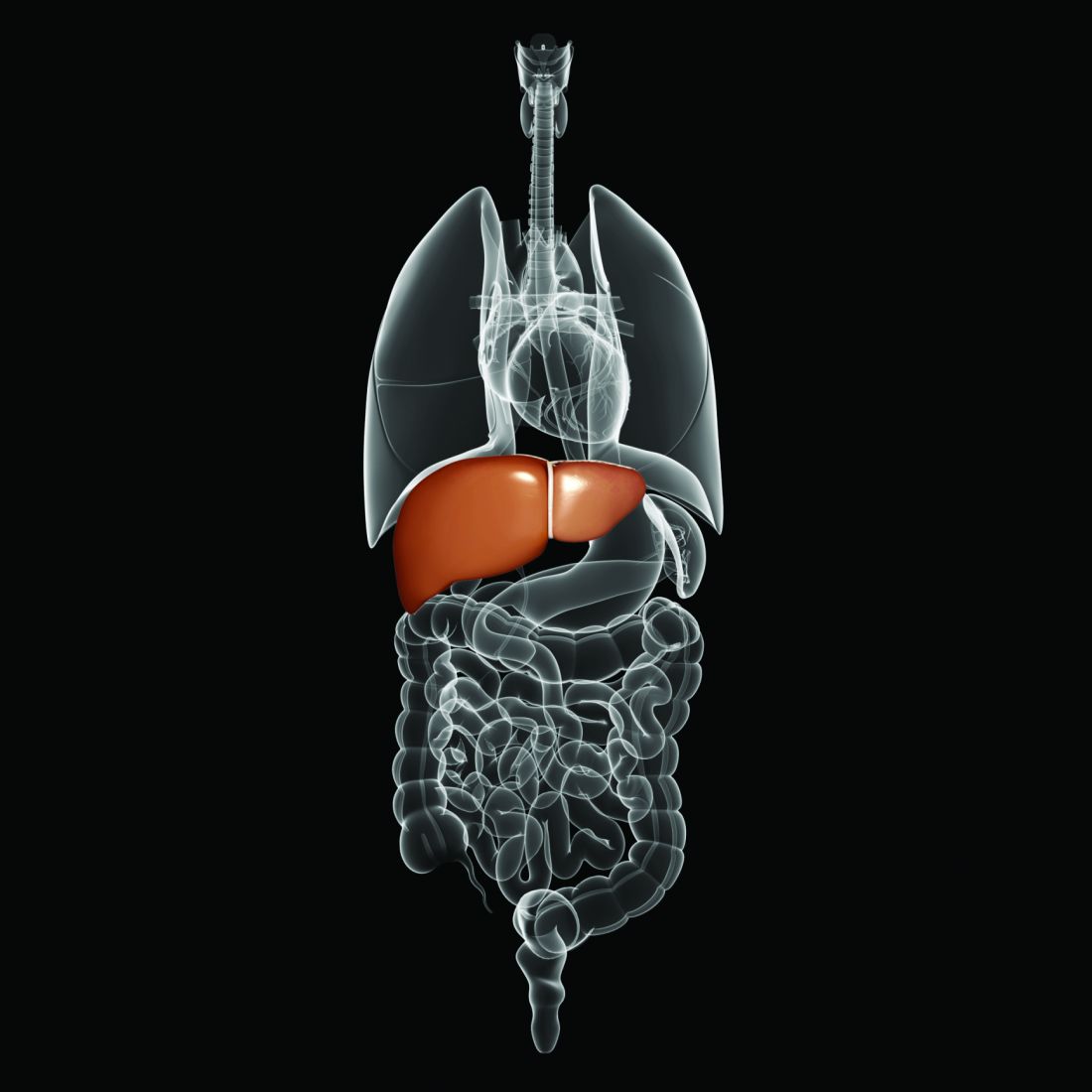
MAUI, HAWAII – Treatment of acute rather than chronic hepatitis C infection is well worth considering in selected circumstances, Norah Terrault, MD, asserted at the Gastroenterology Updates, IBD, Liver Disease meeting.
This is not at present guideline-recommended therapy. Current American Association for the Study of Liver Disease/Infectious Diseases Society of America guidance states that while there is emerging data to support treatment of acute hepatitis C, the evidence isn’t yet sufficiently robust to support a particular regimen or duration. The guidelines currently recommend waiting 6 months to see if the acute infection resolves spontaneously, as happens in a minority of cases, or becomes chronic, at which point it becomes guideline-directed treatment time. But Dr. Terrault believes persuasive evidence to back treatment of acute hepatitis C infection (HCV) is forthcoming, and she noted that the guidelines leave the door ajar by stating, “There are instances wherein a clinician may decide that the benefits of early treatment outweigh waiting for possible spontaneous clearance.”
Treatment of acute HCV
Dr. Terrault deems treatment of acute HCV warranted in circumstances in which there is significant danger of transmission from the acutely infected individual to others. For example, health care providers with a needlestick HCV infection, injecting drug users, and men with acute HCV/HIV coinfection. She also treats acute HCV in patients with underlying chronic liver disease.
“Clearly, I wouldn’t want those individuals to have any worsening of their liver function, so I would treat them acutely,” explained Dr. Terrault, professor of medicine and director of the Viral Hepatitis Center at the University of California, San Francisco.
She cited as particularly impressive the results of the SWIFT-C trial presented by Suzanna Naggie, MD, of Duke University, Durham, N.C., at the 2017 AASLD annual meeting. In this modest-size, National Institutes of Health–sponsored, multicenter study of HIV-infected men with acute HCV coinfection, the sustained viral response (SVR) rate with 8 weeks of ledipasvir/sofosbuvir (Harvoni) was 100%, regardless of their baseline HCV RNA level.
“I think this is remarkable. They cleared virus quite late and yet they went on to achieve HCV eradication. It highlights how little we really know about the treatment of individuals in this phase and that relying on HCV RNA levels may not tell the whole story. I think this is important data to suggest maybe when we treat acute hepatitis C we can use a shorter duration of treatment for that population. There are also other small studies testing 8 weeks of treatment in non–HIV-infected individuals with acute hepatitis C in which they also showed very high SVR rates,” the hepatologist said.
Copanelist Steven L. Flamm, MD, said that when he encounters a patient with acute HCV he, too, is prepared to offer treatment – he finds the available supporting evidence sufficiently compelling – but he often encounters a problem.
“Sometimes I’m blocked by insurance companies because this isn’t officially approved,” noted Dr. Flamm, professor of medicine and chief of the hepatology program at Northwestern University, Chicago.
“You’re right,” Dr. Terrault commented, “we have to make a pretty compelling argument to the insurer as to why we’re treating. But ‘treat to prevent transmission to others’ usually is successful in our hands.”
HCV in patients with end-stage renal disease
The product labeling for sofosbuvir (Sovaldi) says the drug’s safety and efficacy haven’t been established in patients with severe renal impairment or end-stage renal disease. However, a small multicenter study presented at the 2017 AASLD meeting demonstrated that 12 weeks of ledipasvir/sofosbuvir achieved a 100% SVR rate in patients with genotype 1 HCV and severe renal impairment, including some on dialysis, with no clinically meaningful change in estimated glomerular filtration rate or any signal of cardiac arrhythmia.
“The serum drug levels went up significantly, but reassuringly they saw no meaningful safety signals,” according to Dr. Terrault. “This, I think, is initial reassuring information that we were all very much waiting for.”
Still, as the AASLD/IDSA guidelines point out, ledipasvir/sofosbuvir is not a recommended option for HCV treatment in end-stage renal disease.
“In general, I think glecapravir/pibrentasvir [Mavyret] has become the go-to drug for patients who have renal dysfunction because it’s a pangenic regimen, it doesn’t require use of sofosbuvir, and there’s no dose adjustment. But I would say you could encounter situations where you might want to use sofosbuvir, and for me that situation is typically those direct-acting, antiviral-experienced patients who have failed other therapies and you really need to use sofosbuvir/velpatasvir/voxilaprevir [Vosevi] as your last or rescue therapy,” the hepatologist continued.
HCV in liver transplant recipients
“In the years before the direct-acting antivirals, treating transplant patients was always very challenging,” Dr. Terrault recalled. “They had very low response rates to therapy. That’s all gone away. Now we can say that liver transplant recipients who require treatment have response rates that are the same as in individuals who have not had a transplant. These patients are now being treated earlier and earlier after their transplant because you can do it safely.”
She pointed to a study presented at the 2017 AASLD meeting by Kosh Agarwal, MD, of Kings College London. It involved 79 adults with recurrent genotypes 1-4 HCV infection post–liver transplant who were treated with sofosbuvir/velpatasvir (Epclusa) for 12 weeks with a total SVR rate of 96%.
“The nice thing about sofosbuvir/velpatasvir is there are no drug-drug interactions with immunosuppressive drugs. Now it’s very easy to take care of these patients. The SVR rates are excellent,” Dr. Terrault observed.
The other combination that’s been studied specifically in liver transplant recipients, and in kidney transplant recipients as well, is glecapravir/pibrentasvir. In the MAGELLAN-2 study of 100 such patients with genotypes 1-6 HCV, the SVR rate was 99% with no drug-related adverse events leading to discontinuation.
Persons who inject drugs
The Centers for Disease Control and Prevention and the World Health Organization want HCV eradicated by 2030. If that’s going to happen, physicians will have to become more comfortable treating the disease in injectable drug users, a population with a high prevalence of HCV. Several studies have now shown that very high SVR rates can be achieved with direct-acting antiviral regimens as short as 8 weeks in these individuals, even if they are concurrently injecting drugs.
“There is increasing evidence that we should be doing more treatment in persons who inject drugs. Many of these individuals have very early disease and their response rates are excellent,” according to Dr. Terrault.
Moreover, their reinfection rates “are not outrageous,” she said: 1% or less in individuals who stopped injecting drugs decades prior to anti-HCV treatment, 5%-10% over the course of 3-5 years in those who continue injecting drugs after achieving SVR, and about 2% in those on methadone substitution therapy.
“These are very acceptable levels of reinfection if our goal is to move toward elimination of hepatitis C in this population,” she said.
She reported having no financial conflicts regarding her presentation.
MAUI, HAWAII – Treatment of acute rather than chronic hepatitis C infection is well worth considering in selected circumstances, Norah Terrault, MD, asserted at the Gastroenterology Updates, IBD, Liver Disease meeting.
This is not at present guideline-recommended therapy. Current American Association for the Study of Liver Disease/Infectious Diseases Society of America guidance states that while there is emerging data to support treatment of acute hepatitis C, the evidence isn’t yet sufficiently robust to support a particular regimen or duration. The guidelines currently recommend waiting 6 months to see if the acute infection resolves spontaneously, as happens in a minority of cases, or becomes chronic, at which point it becomes guideline-directed treatment time. But Dr. Terrault believes persuasive evidence to back treatment of acute hepatitis C infection (HCV) is forthcoming, and she noted that the guidelines leave the door ajar by stating, “There are instances wherein a clinician may decide that the benefits of early treatment outweigh waiting for possible spontaneous clearance.”
Treatment of acute HCV
Dr. Terrault deems treatment of acute HCV warranted in circumstances in which there is significant danger of transmission from the acutely infected individual to others. For example, health care providers with a needlestick HCV infection, injecting drug users, and men with acute HCV/HIV coinfection. She also treats acute HCV in patients with underlying chronic liver disease.
“Clearly, I wouldn’t want those individuals to have any worsening of their liver function, so I would treat them acutely,” explained Dr. Terrault, professor of medicine and director of the Viral Hepatitis Center at the University of California, San Francisco.
She cited as particularly impressive the results of the SWIFT-C trial presented by Suzanna Naggie, MD, of Duke University, Durham, N.C., at the 2017 AASLD annual meeting. In this modest-size, National Institutes of Health–sponsored, multicenter study of HIV-infected men with acute HCV coinfection, the sustained viral response (SVR) rate with 8 weeks of ledipasvir/sofosbuvir (Harvoni) was 100%, regardless of their baseline HCV RNA level.
“I think this is remarkable. They cleared virus quite late and yet they went on to achieve HCV eradication. It highlights how little we really know about the treatment of individuals in this phase and that relying on HCV RNA levels may not tell the whole story. I think this is important data to suggest maybe when we treat acute hepatitis C we can use a shorter duration of treatment for that population. There are also other small studies testing 8 weeks of treatment in non–HIV-infected individuals with acute hepatitis C in which they also showed very high SVR rates,” the hepatologist said.
Copanelist Steven L. Flamm, MD, said that when he encounters a patient with acute HCV he, too, is prepared to offer treatment – he finds the available supporting evidence sufficiently compelling – but he often encounters a problem.
“Sometimes I’m blocked by insurance companies because this isn’t officially approved,” noted Dr. Flamm, professor of medicine and chief of the hepatology program at Northwestern University, Chicago.
“You’re right,” Dr. Terrault commented, “we have to make a pretty compelling argument to the insurer as to why we’re treating. But ‘treat to prevent transmission to others’ usually is successful in our hands.”
HCV in patients with end-stage renal disease
The product labeling for sofosbuvir (Sovaldi) says the drug’s safety and efficacy haven’t been established in patients with severe renal impairment or end-stage renal disease. However, a small multicenter study presented at the 2017 AASLD meeting demonstrated that 12 weeks of ledipasvir/sofosbuvir achieved a 100% SVR rate in patients with genotype 1 HCV and severe renal impairment, including some on dialysis, with no clinically meaningful change in estimated glomerular filtration rate or any signal of cardiac arrhythmia.
“The serum drug levels went up significantly, but reassuringly they saw no meaningful safety signals,” according to Dr. Terrault. “This, I think, is initial reassuring information that we were all very much waiting for.”
Still, as the AASLD/IDSA guidelines point out, ledipasvir/sofosbuvir is not a recommended option for HCV treatment in end-stage renal disease.
“In general, I think glecapravir/pibrentasvir [Mavyret] has become the go-to drug for patients who have renal dysfunction because it’s a pangenic regimen, it doesn’t require use of sofosbuvir, and there’s no dose adjustment. But I would say you could encounter situations where you might want to use sofosbuvir, and for me that situation is typically those direct-acting, antiviral-experienced patients who have failed other therapies and you really need to use sofosbuvir/velpatasvir/voxilaprevir [Vosevi] as your last or rescue therapy,” the hepatologist continued.
HCV in liver transplant recipients
“In the years before the direct-acting antivirals, treating transplant patients was always very challenging,” Dr. Terrault recalled. “They had very low response rates to therapy. That’s all gone away. Now we can say that liver transplant recipients who require treatment have response rates that are the same as in individuals who have not had a transplant. These patients are now being treated earlier and earlier after their transplant because you can do it safely.”
She pointed to a study presented at the 2017 AASLD meeting by Kosh Agarwal, MD, of Kings College London. It involved 79 adults with recurrent genotypes 1-4 HCV infection post–liver transplant who were treated with sofosbuvir/velpatasvir (Epclusa) for 12 weeks with a total SVR rate of 96%.
“The nice thing about sofosbuvir/velpatasvir is there are no drug-drug interactions with immunosuppressive drugs. Now it’s very easy to take care of these patients. The SVR rates are excellent,” Dr. Terrault observed.
The other combination that’s been studied specifically in liver transplant recipients, and in kidney transplant recipients as well, is glecapravir/pibrentasvir. In the MAGELLAN-2 study of 100 such patients with genotypes 1-6 HCV, the SVR rate was 99% with no drug-related adverse events leading to discontinuation.
Persons who inject drugs
The Centers for Disease Control and Prevention and the World Health Organization want HCV eradicated by 2030. If that’s going to happen, physicians will have to become more comfortable treating the disease in injectable drug users, a population with a high prevalence of HCV. Several studies have now shown that very high SVR rates can be achieved with direct-acting antiviral regimens as short as 8 weeks in these individuals, even if they are concurrently injecting drugs.
“There is increasing evidence that we should be doing more treatment in persons who inject drugs. Many of these individuals have very early disease and their response rates are excellent,” according to Dr. Terrault.
Moreover, their reinfection rates “are not outrageous,” she said: 1% or less in individuals who stopped injecting drugs decades prior to anti-HCV treatment, 5%-10% over the course of 3-5 years in those who continue injecting drugs after achieving SVR, and about 2% in those on methadone substitution therapy.
“These are very acceptable levels of reinfection if our goal is to move toward elimination of hepatitis C in this population,” she said.
She reported having no financial conflicts regarding her presentation.
MAUI, HAWAII – Treatment of acute rather than chronic hepatitis C infection is well worth considering in selected circumstances, Norah Terrault, MD, asserted at the Gastroenterology Updates, IBD, Liver Disease meeting.
This is not at present guideline-recommended therapy. Current American Association for the Study of Liver Disease/Infectious Diseases Society of America guidance states that while there is emerging data to support treatment of acute hepatitis C, the evidence isn’t yet sufficiently robust to support a particular regimen or duration. The guidelines currently recommend waiting 6 months to see if the acute infection resolves spontaneously, as happens in a minority of cases, or becomes chronic, at which point it becomes guideline-directed treatment time. But Dr. Terrault believes persuasive evidence to back treatment of acute hepatitis C infection (HCV) is forthcoming, and she noted that the guidelines leave the door ajar by stating, “There are instances wherein a clinician may decide that the benefits of early treatment outweigh waiting for possible spontaneous clearance.”
Treatment of acute HCV
Dr. Terrault deems treatment of acute HCV warranted in circumstances in which there is significant danger of transmission from the acutely infected individual to others. For example, health care providers with a needlestick HCV infection, injecting drug users, and men with acute HCV/HIV coinfection. She also treats acute HCV in patients with underlying chronic liver disease.
“Clearly, I wouldn’t want those individuals to have any worsening of their liver function, so I would treat them acutely,” explained Dr. Terrault, professor of medicine and director of the Viral Hepatitis Center at the University of California, San Francisco.
She cited as particularly impressive the results of the SWIFT-C trial presented by Suzanna Naggie, MD, of Duke University, Durham, N.C., at the 2017 AASLD annual meeting. In this modest-size, National Institutes of Health–sponsored, multicenter study of HIV-infected men with acute HCV coinfection, the sustained viral response (SVR) rate with 8 weeks of ledipasvir/sofosbuvir (Harvoni) was 100%, regardless of their baseline HCV RNA level.
“I think this is remarkable. They cleared virus quite late and yet they went on to achieve HCV eradication. It highlights how little we really know about the treatment of individuals in this phase and that relying on HCV RNA levels may not tell the whole story. I think this is important data to suggest maybe when we treat acute hepatitis C we can use a shorter duration of treatment for that population. There are also other small studies testing 8 weeks of treatment in non–HIV-infected individuals with acute hepatitis C in which they also showed very high SVR rates,” the hepatologist said.
Copanelist Steven L. Flamm, MD, said that when he encounters a patient with acute HCV he, too, is prepared to offer treatment – he finds the available supporting evidence sufficiently compelling – but he often encounters a problem.
“Sometimes I’m blocked by insurance companies because this isn’t officially approved,” noted Dr. Flamm, professor of medicine and chief of the hepatology program at Northwestern University, Chicago.
“You’re right,” Dr. Terrault commented, “we have to make a pretty compelling argument to the insurer as to why we’re treating. But ‘treat to prevent transmission to others’ usually is successful in our hands.”
HCV in patients with end-stage renal disease
The product labeling for sofosbuvir (Sovaldi) says the drug’s safety and efficacy haven’t been established in patients with severe renal impairment or end-stage renal disease. However, a small multicenter study presented at the 2017 AASLD meeting demonstrated that 12 weeks of ledipasvir/sofosbuvir achieved a 100% SVR rate in patients with genotype 1 HCV and severe renal impairment, including some on dialysis, with no clinically meaningful change in estimated glomerular filtration rate or any signal of cardiac arrhythmia.
“The serum drug levels went up significantly, but reassuringly they saw no meaningful safety signals,” according to Dr. Terrault. “This, I think, is initial reassuring information that we were all very much waiting for.”
Still, as the AASLD/IDSA guidelines point out, ledipasvir/sofosbuvir is not a recommended option for HCV treatment in end-stage renal disease.
“In general, I think glecapravir/pibrentasvir [Mavyret] has become the go-to drug for patients who have renal dysfunction because it’s a pangenic regimen, it doesn’t require use of sofosbuvir, and there’s no dose adjustment. But I would say you could encounter situations where you might want to use sofosbuvir, and for me that situation is typically those direct-acting, antiviral-experienced patients who have failed other therapies and you really need to use sofosbuvir/velpatasvir/voxilaprevir [Vosevi] as your last or rescue therapy,” the hepatologist continued.
HCV in liver transplant recipients
“In the years before the direct-acting antivirals, treating transplant patients was always very challenging,” Dr. Terrault recalled. “They had very low response rates to therapy. That’s all gone away. Now we can say that liver transplant recipients who require treatment have response rates that are the same as in individuals who have not had a transplant. These patients are now being treated earlier and earlier after their transplant because you can do it safely.”
She pointed to a study presented at the 2017 AASLD meeting by Kosh Agarwal, MD, of Kings College London. It involved 79 adults with recurrent genotypes 1-4 HCV infection post–liver transplant who were treated with sofosbuvir/velpatasvir (Epclusa) for 12 weeks with a total SVR rate of 96%.
“The nice thing about sofosbuvir/velpatasvir is there are no drug-drug interactions with immunosuppressive drugs. Now it’s very easy to take care of these patients. The SVR rates are excellent,” Dr. Terrault observed.
The other combination that’s been studied specifically in liver transplant recipients, and in kidney transplant recipients as well, is glecapravir/pibrentasvir. In the MAGELLAN-2 study of 100 such patients with genotypes 1-6 HCV, the SVR rate was 99% with no drug-related adverse events leading to discontinuation.
Persons who inject drugs
The Centers for Disease Control and Prevention and the World Health Organization want HCV eradicated by 2030. If that’s going to happen, physicians will have to become more comfortable treating the disease in injectable drug users, a population with a high prevalence of HCV. Several studies have now shown that very high SVR rates can be achieved with direct-acting antiviral regimens as short as 8 weeks in these individuals, even if they are concurrently injecting drugs.
“There is increasing evidence that we should be doing more treatment in persons who inject drugs. Many of these individuals have very early disease and their response rates are excellent,” according to Dr. Terrault.
Moreover, their reinfection rates “are not outrageous,” she said: 1% or less in individuals who stopped injecting drugs decades prior to anti-HCV treatment, 5%-10% over the course of 3-5 years in those who continue injecting drugs after achieving SVR, and about 2% in those on methadone substitution therapy.
“These are very acceptable levels of reinfection if our goal is to move toward elimination of hepatitis C in this population,” she said.
She reported having no financial conflicts regarding her presentation.
EXPERT ANALYSIS FROM GUILD 2018
Alpha fetoprotein boosted detection of early-stage liver cancer
For patients with cirrhosis, adding serum alpha fetoprotein testing to ultrasound significantly boosted its ability to detect early-stage hepatocellular carcinoma, according to the results of a systematic review and meta-analysis reported in the May issue of Gastroenterology.
Used alone, ultrasound detected only 45% of early-stage hepatocellular carcinomas (95% confidence interval, 30%-62%), reported Kristina Tzartzeva, MD, of the University of Texas, Dallas, with her associates. Adding alpha fetoprotein (AFP) increased this sensitivity to 63% (95% CI, 48%-75%; P = .002). Few studies evaluated alternative surveillance tools, such as CT or MRI.
Diagnosing liver cancer early is key to survival and thus is a central issue in cirrhosis management. However, the best surveillance strategy remains uncertain, hinging as it does on sensitivity, specificity, and cost. The American Association for the Study of Liver Diseases and the European Association for the Study of the Liver recommend that cirrhotic patients undergo twice-yearly ultrasound to screen for hepatocellular carcinoma (HCC), but they disagree about the value of adding serum biomarker AFP testing. Meanwhile, more and more clinics are using CT and MRI because of concerns about the unreliability of ultrasound. “Given few direct comparative studies, we are forced to primarily rely on indirect comparisons across studies,” the reviewers wrote.
To do so, they searched MEDLINE and Scopus and identified 32 studies of HCC surveillance that comprised 13,367 patients, nearly all with baseline cirrhosis. The studies were published from 1990 to August 2016.
Ultrasound detected HCC of any stage with a sensitivity of 84% (95% CI, 76%-92%), but its sensitivity for detecting early-stage disease was less than 50%. In studies that performed direct comparisons, ultrasound alone was significantly less sensitive than ultrasound plus AFP for detecting all stages of HCC (relative risk, 0.80; 95% CI, 0.72-0.88) and early-stage disease (0.78; 0.66-0.92). However, ultrasound alone was more specific than ultrasound plus AFP (RR, 1.08; 95% CI, 1.05-1.09).
Four studies of about 900 patients evaluated cross-sectional imaging with CT or MRI. In one single-center, randomized trial, CT had a sensitivity of 63% for detecting early-stage disease, but the 95% CI for this estimate was very wide (30%-87%) and CT did not significantly outperform ultrasound (Aliment Pharmacol Ther. 2013;38:303-12). In another study, MRI and ultrasound had significantly different sensitivities of 84% and 26% for detecting (usually) early-stage disease (JAMA Oncol. 2017;3[4]:456-63).
“Ultrasound currently forms the backbone of professional society recommendations for HCC surveillance; however, our meta-analysis highlights its suboptimal sensitivity for detection of hepatocellular carcinoma at an early stage. Using ultrasound in combination with AFP appears to significantly improve sensitivity for detecting early HCC with a small, albeit statistically significant, trade-off in specificity. There are currently insufficient data to support routine use of CT- or MRI-based surveillance in all patients with cirrhosis,” the reviewers concluded.
The National Cancer Institute and Cancer Prevention Research Institute of Texas provided funding. None of the reviewers had conflicts of interest.
SOURCE: Tzartzeva K et al. Gastroenterology. 2018 Feb 6. doi: 10.1053/j.gastro.2018.01.064.
For patients with cirrhosis, adding serum alpha fetoprotein testing to ultrasound significantly boosted its ability to detect early-stage hepatocellular carcinoma, according to the results of a systematic review and meta-analysis reported in the May issue of Gastroenterology.
Used alone, ultrasound detected only 45% of early-stage hepatocellular carcinomas (95% confidence interval, 30%-62%), reported Kristina Tzartzeva, MD, of the University of Texas, Dallas, with her associates. Adding alpha fetoprotein (AFP) increased this sensitivity to 63% (95% CI, 48%-75%; P = .002). Few studies evaluated alternative surveillance tools, such as CT or MRI.
Diagnosing liver cancer early is key to survival and thus is a central issue in cirrhosis management. However, the best surveillance strategy remains uncertain, hinging as it does on sensitivity, specificity, and cost. The American Association for the Study of Liver Diseases and the European Association for the Study of the Liver recommend that cirrhotic patients undergo twice-yearly ultrasound to screen for hepatocellular carcinoma (HCC), but they disagree about the value of adding serum biomarker AFP testing. Meanwhile, more and more clinics are using CT and MRI because of concerns about the unreliability of ultrasound. “Given few direct comparative studies, we are forced to primarily rely on indirect comparisons across studies,” the reviewers wrote.
To do so, they searched MEDLINE and Scopus and identified 32 studies of HCC surveillance that comprised 13,367 patients, nearly all with baseline cirrhosis. The studies were published from 1990 to August 2016.
Ultrasound detected HCC of any stage with a sensitivity of 84% (95% CI, 76%-92%), but its sensitivity for detecting early-stage disease was less than 50%. In studies that performed direct comparisons, ultrasound alone was significantly less sensitive than ultrasound plus AFP for detecting all stages of HCC (relative risk, 0.80; 95% CI, 0.72-0.88) and early-stage disease (0.78; 0.66-0.92). However, ultrasound alone was more specific than ultrasound plus AFP (RR, 1.08; 95% CI, 1.05-1.09).
Four studies of about 900 patients evaluated cross-sectional imaging with CT or MRI. In one single-center, randomized trial, CT had a sensitivity of 63% for detecting early-stage disease, but the 95% CI for this estimate was very wide (30%-87%) and CT did not significantly outperform ultrasound (Aliment Pharmacol Ther. 2013;38:303-12). In another study, MRI and ultrasound had significantly different sensitivities of 84% and 26% for detecting (usually) early-stage disease (JAMA Oncol. 2017;3[4]:456-63).
“Ultrasound currently forms the backbone of professional society recommendations for HCC surveillance; however, our meta-analysis highlights its suboptimal sensitivity for detection of hepatocellular carcinoma at an early stage. Using ultrasound in combination with AFP appears to significantly improve sensitivity for detecting early HCC with a small, albeit statistically significant, trade-off in specificity. There are currently insufficient data to support routine use of CT- or MRI-based surveillance in all patients with cirrhosis,” the reviewers concluded.
The National Cancer Institute and Cancer Prevention Research Institute of Texas provided funding. None of the reviewers had conflicts of interest.
SOURCE: Tzartzeva K et al. Gastroenterology. 2018 Feb 6. doi: 10.1053/j.gastro.2018.01.064.
For patients with cirrhosis, adding serum alpha fetoprotein testing to ultrasound significantly boosted its ability to detect early-stage hepatocellular carcinoma, according to the results of a systematic review and meta-analysis reported in the May issue of Gastroenterology.
Used alone, ultrasound detected only 45% of early-stage hepatocellular carcinomas (95% confidence interval, 30%-62%), reported Kristina Tzartzeva, MD, of the University of Texas, Dallas, with her associates. Adding alpha fetoprotein (AFP) increased this sensitivity to 63% (95% CI, 48%-75%; P = .002). Few studies evaluated alternative surveillance tools, such as CT or MRI.
Diagnosing liver cancer early is key to survival and thus is a central issue in cirrhosis management. However, the best surveillance strategy remains uncertain, hinging as it does on sensitivity, specificity, and cost. The American Association for the Study of Liver Diseases and the European Association for the Study of the Liver recommend that cirrhotic patients undergo twice-yearly ultrasound to screen for hepatocellular carcinoma (HCC), but they disagree about the value of adding serum biomarker AFP testing. Meanwhile, more and more clinics are using CT and MRI because of concerns about the unreliability of ultrasound. “Given few direct comparative studies, we are forced to primarily rely on indirect comparisons across studies,” the reviewers wrote.
To do so, they searched MEDLINE and Scopus and identified 32 studies of HCC surveillance that comprised 13,367 patients, nearly all with baseline cirrhosis. The studies were published from 1990 to August 2016.
Ultrasound detected HCC of any stage with a sensitivity of 84% (95% CI, 76%-92%), but its sensitivity for detecting early-stage disease was less than 50%. In studies that performed direct comparisons, ultrasound alone was significantly less sensitive than ultrasound plus AFP for detecting all stages of HCC (relative risk, 0.80; 95% CI, 0.72-0.88) and early-stage disease (0.78; 0.66-0.92). However, ultrasound alone was more specific than ultrasound plus AFP (RR, 1.08; 95% CI, 1.05-1.09).
Four studies of about 900 patients evaluated cross-sectional imaging with CT or MRI. In one single-center, randomized trial, CT had a sensitivity of 63% for detecting early-stage disease, but the 95% CI for this estimate was very wide (30%-87%) and CT did not significantly outperform ultrasound (Aliment Pharmacol Ther. 2013;38:303-12). In another study, MRI and ultrasound had significantly different sensitivities of 84% and 26% for detecting (usually) early-stage disease (JAMA Oncol. 2017;3[4]:456-63).
“Ultrasound currently forms the backbone of professional society recommendations for HCC surveillance; however, our meta-analysis highlights its suboptimal sensitivity for detection of hepatocellular carcinoma at an early stage. Using ultrasound in combination with AFP appears to significantly improve sensitivity for detecting early HCC with a small, albeit statistically significant, trade-off in specificity. There are currently insufficient data to support routine use of CT- or MRI-based surveillance in all patients with cirrhosis,” the reviewers concluded.
The National Cancer Institute and Cancer Prevention Research Institute of Texas provided funding. None of the reviewers had conflicts of interest.
SOURCE: Tzartzeva K et al. Gastroenterology. 2018 Feb 6. doi: 10.1053/j.gastro.2018.01.064.
FROM GASTROENTEROLOGY
Key clinical point: Ultrasound unreliably detects hepatocellular carcinoma, but adding alpha fetoprotein increases its sensitivity.
Major finding: Used alone, ultrasound detected only 47% of early-stage cases. Adding alpha fetoprotein increased this sensitivity to 63% (P = .002).
Study details: Systematic review and meta-analysis of 32 studies comprising 13,367 patients and spanning from 1990 to August 2016.
Disclosures: The National Cancer Institute and Cancer Prevention Research Institute of Texas provided funding. None of the researchers had conflicts of interest.
Source: Tzartzeva K et al. Gastroenterology. 2018 Feb 6. doi: 10.1053/j.gastro.2018.01.064.
Heavy drinking did not worsen clinical outcomes from drug-induced liver injury
Heavy drinking was not associated with higher proportions of liver-related deaths or liver transplantation among patients with drug-induced liver injury (DILI), according to the results of a prospective multicenter cohort study reported in the May issue of Clinical Gastroenterology and Hepatology.
Anabolic steroids were the most common cause of DILI among heavy drinkers, defined as men who averaged more than three drinks a day or women who averaged more than two drinks daily, said Lara Dakhoul, MD, of Indiana University, Indianapolis, and her associates. There also was no evidence that heavy alcohol consumption increased the risk of liver injury attributable to isoniazid exposure, the researchers wrote in.
Although consuming alcohol significantly increases the risk of acetaminophen-induced liver injury, there is much less clarity about the relationship between drinking and hepatotoxicity from drugs such as duloxetine or antituberculosis medications, the researchers noted. In fact, one recent study found that drinking led to less severe liver injury among individuals with DILI. To better elucidate these links, the investigators studied 1,198 individuals with confirmed or probable DILI who enrolled in the DILI Network study (DILIN) between 2004 and 2016. At enrollment, all participants were asked if they consumed alcohol, and those who reported drinking within the past 12 months were offered a shortened version of the Skinner Alcohol Dependence Scale to collect details on alcohol consumption, including type, amount, and frequency.
In all, 601 persons reported consuming at least one alcoholic drink in the preceding year, of whom 348 completed the Skinner questionnaire. A total of 80 individuals reported heavy alcohol consumption. Heavy drinkers were typically in their early 40s, while nondrinkers tended to be nearly 50 years old (P less than .01). Heavy drinkers were also more often men (63%) while nondrinkers were usually women (65%; P less than .01). Heavy drinkers were significantly more likely to have DILI secondary to anabolic steroid exposure (13%) than were nondrinkers (2%; P less than .001). However, latency, pattern of liver injury, peak enzyme levels, and patterns of recovery from steroid hepatotoxicity were similar regardless of alcohol history.
A total of eight patients with DILI died of liver-related causes or underwent liver transplantation, and proportions of patients with these outcomes were similar regardless of alcohol history. These eight patients had no evidence of hepatitis C virus infection, but three appeared to have underlying alcoholic liver disease with superimposed acute-on-chronic liver failure. Heavy drinkers did not have significantly higher DILI severity scores than nondrinkers, but they did have significantly higher peak serum levels of alanine aminotransferase (1,323 U/L vs. 754, respectively; P = .02) and significantly higher levels of bilirubin (16.1 vs. 12.7 mg/dL; P = .03).
The two fatal cases of DILI among heavy drinkers involved a 44-year-old man with underlying alcoholic cirrhosis and steatohepatitis who developed acute-on-chronic liver failure 11 days after starting niacin, and a 76-year-old man with chronic obstructive pulmonary disease and bronchitis flare who developed severe liver injury and skin rash 6 days after starting azithromycin.
The study was not able to assess whether heavy alcohol consumption contributed to liver injury from specific agents, the researchers said. Additionally, a substantial number of drinkers did not complete the Skinner questionnaire, and those who did might have underestimated or underreported their own alcohol consumption. “Counterbalancing these issues are the [study’s] unique strengths, such as prospective design, larger sample size, well-characterized DILI phenotype, and careful, structured adjudication of causality and severity,” the researchers wrote.
Funders included the National Institute of Diabetes and Digestive and Kidney Diseases and the National Cancer Institute. Dr. Dakhoul had no conflicts of interest. On coinvestigator disclosed ties to numerous pharmaceutical companies.
SOURCE: Dakhoul L et al. Clin Gastro Hepatol. 2018 Jan 3. doi: 10.1016/j.cgh.2017.12.036.
Heavy drinking was not associated with higher proportions of liver-related deaths or liver transplantation among patients with drug-induced liver injury (DILI), according to the results of a prospective multicenter cohort study reported in the May issue of Clinical Gastroenterology and Hepatology.
Anabolic steroids were the most common cause of DILI among heavy drinkers, defined as men who averaged more than three drinks a day or women who averaged more than two drinks daily, said Lara Dakhoul, MD, of Indiana University, Indianapolis, and her associates. There also was no evidence that heavy alcohol consumption increased the risk of liver injury attributable to isoniazid exposure, the researchers wrote in.
Although consuming alcohol significantly increases the risk of acetaminophen-induced liver injury, there is much less clarity about the relationship between drinking and hepatotoxicity from drugs such as duloxetine or antituberculosis medications, the researchers noted. In fact, one recent study found that drinking led to less severe liver injury among individuals with DILI. To better elucidate these links, the investigators studied 1,198 individuals with confirmed or probable DILI who enrolled in the DILI Network study (DILIN) between 2004 and 2016. At enrollment, all participants were asked if they consumed alcohol, and those who reported drinking within the past 12 months were offered a shortened version of the Skinner Alcohol Dependence Scale to collect details on alcohol consumption, including type, amount, and frequency.
In all, 601 persons reported consuming at least one alcoholic drink in the preceding year, of whom 348 completed the Skinner questionnaire. A total of 80 individuals reported heavy alcohol consumption. Heavy drinkers were typically in their early 40s, while nondrinkers tended to be nearly 50 years old (P less than .01). Heavy drinkers were also more often men (63%) while nondrinkers were usually women (65%; P less than .01). Heavy drinkers were significantly more likely to have DILI secondary to anabolic steroid exposure (13%) than were nondrinkers (2%; P less than .001). However, latency, pattern of liver injury, peak enzyme levels, and patterns of recovery from steroid hepatotoxicity were similar regardless of alcohol history.
A total of eight patients with DILI died of liver-related causes or underwent liver transplantation, and proportions of patients with these outcomes were similar regardless of alcohol history. These eight patients had no evidence of hepatitis C virus infection, but three appeared to have underlying alcoholic liver disease with superimposed acute-on-chronic liver failure. Heavy drinkers did not have significantly higher DILI severity scores than nondrinkers, but they did have significantly higher peak serum levels of alanine aminotransferase (1,323 U/L vs. 754, respectively; P = .02) and significantly higher levels of bilirubin (16.1 vs. 12.7 mg/dL; P = .03).
The two fatal cases of DILI among heavy drinkers involved a 44-year-old man with underlying alcoholic cirrhosis and steatohepatitis who developed acute-on-chronic liver failure 11 days after starting niacin, and a 76-year-old man with chronic obstructive pulmonary disease and bronchitis flare who developed severe liver injury and skin rash 6 days after starting azithromycin.
The study was not able to assess whether heavy alcohol consumption contributed to liver injury from specific agents, the researchers said. Additionally, a substantial number of drinkers did not complete the Skinner questionnaire, and those who did might have underestimated or underreported their own alcohol consumption. “Counterbalancing these issues are the [study’s] unique strengths, such as prospective design, larger sample size, well-characterized DILI phenotype, and careful, structured adjudication of causality and severity,” the researchers wrote.
Funders included the National Institute of Diabetes and Digestive and Kidney Diseases and the National Cancer Institute. Dr. Dakhoul had no conflicts of interest. On coinvestigator disclosed ties to numerous pharmaceutical companies.
SOURCE: Dakhoul L et al. Clin Gastro Hepatol. 2018 Jan 3. doi: 10.1016/j.cgh.2017.12.036.
Heavy drinking was not associated with higher proportions of liver-related deaths or liver transplantation among patients with drug-induced liver injury (DILI), according to the results of a prospective multicenter cohort study reported in the May issue of Clinical Gastroenterology and Hepatology.
Anabolic steroids were the most common cause of DILI among heavy drinkers, defined as men who averaged more than three drinks a day or women who averaged more than two drinks daily, said Lara Dakhoul, MD, of Indiana University, Indianapolis, and her associates. There also was no evidence that heavy alcohol consumption increased the risk of liver injury attributable to isoniazid exposure, the researchers wrote in.
Although consuming alcohol significantly increases the risk of acetaminophen-induced liver injury, there is much less clarity about the relationship between drinking and hepatotoxicity from drugs such as duloxetine or antituberculosis medications, the researchers noted. In fact, one recent study found that drinking led to less severe liver injury among individuals with DILI. To better elucidate these links, the investigators studied 1,198 individuals with confirmed or probable DILI who enrolled in the DILI Network study (DILIN) between 2004 and 2016. At enrollment, all participants were asked if they consumed alcohol, and those who reported drinking within the past 12 months were offered a shortened version of the Skinner Alcohol Dependence Scale to collect details on alcohol consumption, including type, amount, and frequency.
In all, 601 persons reported consuming at least one alcoholic drink in the preceding year, of whom 348 completed the Skinner questionnaire. A total of 80 individuals reported heavy alcohol consumption. Heavy drinkers were typically in their early 40s, while nondrinkers tended to be nearly 50 years old (P less than .01). Heavy drinkers were also more often men (63%) while nondrinkers were usually women (65%; P less than .01). Heavy drinkers were significantly more likely to have DILI secondary to anabolic steroid exposure (13%) than were nondrinkers (2%; P less than .001). However, latency, pattern of liver injury, peak enzyme levels, and patterns of recovery from steroid hepatotoxicity were similar regardless of alcohol history.
A total of eight patients with DILI died of liver-related causes or underwent liver transplantation, and proportions of patients with these outcomes were similar regardless of alcohol history. These eight patients had no evidence of hepatitis C virus infection, but three appeared to have underlying alcoholic liver disease with superimposed acute-on-chronic liver failure. Heavy drinkers did not have significantly higher DILI severity scores than nondrinkers, but they did have significantly higher peak serum levels of alanine aminotransferase (1,323 U/L vs. 754, respectively; P = .02) and significantly higher levels of bilirubin (16.1 vs. 12.7 mg/dL; P = .03).
The two fatal cases of DILI among heavy drinkers involved a 44-year-old man with underlying alcoholic cirrhosis and steatohepatitis who developed acute-on-chronic liver failure 11 days after starting niacin, and a 76-year-old man with chronic obstructive pulmonary disease and bronchitis flare who developed severe liver injury and skin rash 6 days after starting azithromycin.
The study was not able to assess whether heavy alcohol consumption contributed to liver injury from specific agents, the researchers said. Additionally, a substantial number of drinkers did not complete the Skinner questionnaire, and those who did might have underestimated or underreported their own alcohol consumption. “Counterbalancing these issues are the [study’s] unique strengths, such as prospective design, larger sample size, well-characterized DILI phenotype, and careful, structured adjudication of causality and severity,” the researchers wrote.
Funders included the National Institute of Diabetes and Digestive and Kidney Diseases and the National Cancer Institute. Dr. Dakhoul had no conflicts of interest. On coinvestigator disclosed ties to numerous pharmaceutical companies.
SOURCE: Dakhoul L et al. Clin Gastro Hepatol. 2018 Jan 3. doi: 10.1016/j.cgh.2017.12.036.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Heavy alcohol consumption was not associated with worse outcomes of drug-induced liver toxicity.
Major finding: Proportions of patients with liver-related deaths and liver transplantation were statistically similar regardless of alcohol consumption history (P = .18).
Study details: Prospective study of 1,198 individuals with probable drug-induced liver injury.
Disclosures: Funders included the National Institute of Diabetes and Digestive and Kidney Diseases and the National Cancer Institute. Dr. Dakhoul had no conflicts. One coinvestigator disclosed ties to numerous pharmaceutical companies.
Source: Dakhoul L et al. Clin Gastro Hepatol. 2018 Jan 3. doi: 10.1016/j.cgh.2017.12.036.
Hep B therapy: Indefinite or FINITE for e-negative patients?
LAS VEGAS – Current guidelines recommend indefinite continuation of antiviral therapy in chronic hepatitis B patients who are hepatitis B e-antigen (HBeAg)-negative. But emerging data suggest that this may not always be the case.
“It’s very provocative data, though not at the guideline level,” W. Ray Kim, MD, said in a presentation at the inaugural Perspectives in Digestive Diseases meeting held by Global Academy for Medical Education.
“There are patients who really have begged to go off treatment because they are sick of taking the medication for year after year after year,” said Dr. Kim, professor of medicine, gastroenterology and hepatology, Stanford (Calif.) University.
In light of new data, taking them off medication might be “something to consider” in noncirrhotic patients if they are completely suppressed, have normal ALT, and have a low level of quantitative hepatitis B surface antigen (HBsAg), Dr. Kim told attendees.
The most current Association for the Advancement of the Study of Liver Diseases guidelines state that unless there is a competing rationale, antiviral therapy should be continued indefinitely for noncirrhotic adults with HBeAg‐negative immune‐active chronic hepatitis B.
They do also say that treatment discontinuation “may be considered” for individuals with proven loss of HBsAg. “However, there is currently insufficient evidence to definitively guide treatment decisions for such persons,” the guidelines say.
Evidence has emerged since those guideline statements were written. Most recently, German investigators published results of the FINITE study showing some long-term responses after stopping tenofovir disoproxil fumarate (TDF) in noncirrhotic, HBeAg-negative patients.
In that prospective, controlled study, 62% of patients who stopped TDF therapy (n = 13) stayed off therapy to week 144 of treatment follow-up. Four of the patients achieved HBsAg loss, and median HBsAg change was –0.59log10IU/mL vs. 0.21log10IU/mL in patients who stayed on TDF therapy.
Investigators said that result demonstrated the potential of stopping long-term TDF treatment and seeing either HBsAg loss or sustained virologic response.
Before that, a retrospective study from investigators in Taiwan showed that age plus level of HBsAg were associated with HBV relapse after entecavir treatment in HBeAg-negative patients. According to investigators, those results suggested HBsAg levels could be used to guide timing of entecavir cessation.
If antiviral therapy is stopped in an HBeAg-negative patient, that patient should be monitored every 3 month for a year for recurrent viremia, ALT flares, and hepatic decompensation, Dr. Kim said at the meeting.
Even before stopping, “there are a number of factors to consider, including biological relapse, flare, hepatic decompensation,” he said.
On the other hand, there is the burden of continued therapy, financial concerns of continuing treatment due not only to medication costs but also long-term monitoring, as well as patient and provider preference, he noted in his presentation.
Global Academy and this news organization are owned by the same parent company.
Dr. Kim reported serving as a consultant to Gilead.
LAS VEGAS – Current guidelines recommend indefinite continuation of antiviral therapy in chronic hepatitis B patients who are hepatitis B e-antigen (HBeAg)-negative. But emerging data suggest that this may not always be the case.
“It’s very provocative data, though not at the guideline level,” W. Ray Kim, MD, said in a presentation at the inaugural Perspectives in Digestive Diseases meeting held by Global Academy for Medical Education.
“There are patients who really have begged to go off treatment because they are sick of taking the medication for year after year after year,” said Dr. Kim, professor of medicine, gastroenterology and hepatology, Stanford (Calif.) University.
In light of new data, taking them off medication might be “something to consider” in noncirrhotic patients if they are completely suppressed, have normal ALT, and have a low level of quantitative hepatitis B surface antigen (HBsAg), Dr. Kim told attendees.
The most current Association for the Advancement of the Study of Liver Diseases guidelines state that unless there is a competing rationale, antiviral therapy should be continued indefinitely for noncirrhotic adults with HBeAg‐negative immune‐active chronic hepatitis B.
They do also say that treatment discontinuation “may be considered” for individuals with proven loss of HBsAg. “However, there is currently insufficient evidence to definitively guide treatment decisions for such persons,” the guidelines say.
Evidence has emerged since those guideline statements were written. Most recently, German investigators published results of the FINITE study showing some long-term responses after stopping tenofovir disoproxil fumarate (TDF) in noncirrhotic, HBeAg-negative patients.
In that prospective, controlled study, 62% of patients who stopped TDF therapy (n = 13) stayed off therapy to week 144 of treatment follow-up. Four of the patients achieved HBsAg loss, and median HBsAg change was –0.59log10IU/mL vs. 0.21log10IU/mL in patients who stayed on TDF therapy.
Investigators said that result demonstrated the potential of stopping long-term TDF treatment and seeing either HBsAg loss or sustained virologic response.
Before that, a retrospective study from investigators in Taiwan showed that age plus level of HBsAg were associated with HBV relapse after entecavir treatment in HBeAg-negative patients. According to investigators, those results suggested HBsAg levels could be used to guide timing of entecavir cessation.
If antiviral therapy is stopped in an HBeAg-negative patient, that patient should be monitored every 3 month for a year for recurrent viremia, ALT flares, and hepatic decompensation, Dr. Kim said at the meeting.
Even before stopping, “there are a number of factors to consider, including biological relapse, flare, hepatic decompensation,” he said.
On the other hand, there is the burden of continued therapy, financial concerns of continuing treatment due not only to medication costs but also long-term monitoring, as well as patient and provider preference, he noted in his presentation.
Global Academy and this news organization are owned by the same parent company.
Dr. Kim reported serving as a consultant to Gilead.
LAS VEGAS – Current guidelines recommend indefinite continuation of antiviral therapy in chronic hepatitis B patients who are hepatitis B e-antigen (HBeAg)-negative. But emerging data suggest that this may not always be the case.
“It’s very provocative data, though not at the guideline level,” W. Ray Kim, MD, said in a presentation at the inaugural Perspectives in Digestive Diseases meeting held by Global Academy for Medical Education.
“There are patients who really have begged to go off treatment because they are sick of taking the medication for year after year after year,” said Dr. Kim, professor of medicine, gastroenterology and hepatology, Stanford (Calif.) University.
In light of new data, taking them off medication might be “something to consider” in noncirrhotic patients if they are completely suppressed, have normal ALT, and have a low level of quantitative hepatitis B surface antigen (HBsAg), Dr. Kim told attendees.
The most current Association for the Advancement of the Study of Liver Diseases guidelines state that unless there is a competing rationale, antiviral therapy should be continued indefinitely for noncirrhotic adults with HBeAg‐negative immune‐active chronic hepatitis B.
They do also say that treatment discontinuation “may be considered” for individuals with proven loss of HBsAg. “However, there is currently insufficient evidence to definitively guide treatment decisions for such persons,” the guidelines say.
Evidence has emerged since those guideline statements were written. Most recently, German investigators published results of the FINITE study showing some long-term responses after stopping tenofovir disoproxil fumarate (TDF) in noncirrhotic, HBeAg-negative patients.
In that prospective, controlled study, 62% of patients who stopped TDF therapy (n = 13) stayed off therapy to week 144 of treatment follow-up. Four of the patients achieved HBsAg loss, and median HBsAg change was –0.59log10IU/mL vs. 0.21log10IU/mL in patients who stayed on TDF therapy.
Investigators said that result demonstrated the potential of stopping long-term TDF treatment and seeing either HBsAg loss or sustained virologic response.
Before that, a retrospective study from investigators in Taiwan showed that age plus level of HBsAg were associated with HBV relapse after entecavir treatment in HBeAg-negative patients. According to investigators, those results suggested HBsAg levels could be used to guide timing of entecavir cessation.
If antiviral therapy is stopped in an HBeAg-negative patient, that patient should be monitored every 3 month for a year for recurrent viremia, ALT flares, and hepatic decompensation, Dr. Kim said at the meeting.
Even before stopping, “there are a number of factors to consider, including biological relapse, flare, hepatic decompensation,” he said.
On the other hand, there is the burden of continued therapy, financial concerns of continuing treatment due not only to medication costs but also long-term monitoring, as well as patient and provider preference, he noted in his presentation.
Global Academy and this news organization are owned by the same parent company.
Dr. Kim reported serving as a consultant to Gilead.
EXPERT ANALYSIS FROM PERSPECTIVES IN DIGESTIVE DISEASES