User login
MD-IQ only
All patients with VTE have a high risk of recurrence
Recurrence risk is significant among all patients with venous thromboembolism (VTE), though recurrence is most frequent in patients with cancer-related VTE, according to a nationwide Danish study.
Ida Ehlers Albertsen, MD, of Aalborg (Denmark) University Hospital and her coauthors followed 73,993 patients who were diagnosed with incident VTE during January 2000–December 2015. The patients’ VTEs were classified as either cancer-related, unprovoked (occurring in patients without any provoking factors), or provoked (occurring in patients with one or more provoking factors, such as recent major surgery, recent fracture/trauma, obesity, or hormone replacement therapy).
The researchers found similar risks of recurrence among patients with unprovoked and provoked VTE at 6-month follow-up, with rates per 100 person-years of 6.80 and 6.92, respectively. By comparison, the recurrence rate for cancer-related VTE at 6 months was 9.06. The findings were reported in the American Journal of Medicine.
However, at 10-year follow-up the rates were 3.70 for cancer-related VTE, 2.84 for unprovoked VTE, and 2.22 for provoked VTE, which reinforces the belief that “unprovoked venous thromboembolism is associated with long-term higher risk of recurrence than provoked venous thromboembolism.”
Additionally, at 10-year follow-up, the absolute recurrence risk of cancer-related VTE and unprovoked VTE were both at approximately 20%, with recurrence risk of provoked VTE at just above 15%. Compared with the recurrence risk of provoked VTE at 10-year follow-up, the hazard ratios of cancer-related VTE and unprovoked VTE recurrence risk were 1.23 (95% confidence interval, 1.13-1.33) and 1.18 (95% CI, 1.13-1.24), respectively.
The coauthors observed several challenges in comparing their study to previous analyses on recurrent risk, noting that the definition of provoked VTE “varies throughout the literature” and that the majority of VTE studies “provide cumulative incidence proportions and not the actual rates.” They also stated that indefinite or extended therapy for all VTE patients comes with its own potential complications, even with the improved safety of non–vitamin K antagonist oral anticoagulants, writing that “treatment should be given to patients where the benefits outweigh the risks.”
Despite the differences in recurrence rates at 6-month and 10-year follow-up, the coauthors suggested that enough risk was present in all types to warrant additional studies and reconsider how VTE patients are categorized.
“A high recurrence risk in all types of venous thromboembolism indicates that further research is needed to optimize risk stratification for venous thromboembolism patients,” they wrote.
The study was partially funded by a grant from the Obel Family Foundation. Some authors reported financial disclosures related to Janssen, Bayer, Roche, and others.
SOURCE: Albertsen IE et al. Am J Med. 2018 Sep;131(9):1067-74.e4.
Recurrence risk is significant among all patients with venous thromboembolism (VTE), though recurrence is most frequent in patients with cancer-related VTE, according to a nationwide Danish study.
Ida Ehlers Albertsen, MD, of Aalborg (Denmark) University Hospital and her coauthors followed 73,993 patients who were diagnosed with incident VTE during January 2000–December 2015. The patients’ VTEs were classified as either cancer-related, unprovoked (occurring in patients without any provoking factors), or provoked (occurring in patients with one or more provoking factors, such as recent major surgery, recent fracture/trauma, obesity, or hormone replacement therapy).
The researchers found similar risks of recurrence among patients with unprovoked and provoked VTE at 6-month follow-up, with rates per 100 person-years of 6.80 and 6.92, respectively. By comparison, the recurrence rate for cancer-related VTE at 6 months was 9.06. The findings were reported in the American Journal of Medicine.
However, at 10-year follow-up the rates were 3.70 for cancer-related VTE, 2.84 for unprovoked VTE, and 2.22 for provoked VTE, which reinforces the belief that “unprovoked venous thromboembolism is associated with long-term higher risk of recurrence than provoked venous thromboembolism.”
Additionally, at 10-year follow-up, the absolute recurrence risk of cancer-related VTE and unprovoked VTE were both at approximately 20%, with recurrence risk of provoked VTE at just above 15%. Compared with the recurrence risk of provoked VTE at 10-year follow-up, the hazard ratios of cancer-related VTE and unprovoked VTE recurrence risk were 1.23 (95% confidence interval, 1.13-1.33) and 1.18 (95% CI, 1.13-1.24), respectively.
The coauthors observed several challenges in comparing their study to previous analyses on recurrent risk, noting that the definition of provoked VTE “varies throughout the literature” and that the majority of VTE studies “provide cumulative incidence proportions and not the actual rates.” They also stated that indefinite or extended therapy for all VTE patients comes with its own potential complications, even with the improved safety of non–vitamin K antagonist oral anticoagulants, writing that “treatment should be given to patients where the benefits outweigh the risks.”
Despite the differences in recurrence rates at 6-month and 10-year follow-up, the coauthors suggested that enough risk was present in all types to warrant additional studies and reconsider how VTE patients are categorized.
“A high recurrence risk in all types of venous thromboembolism indicates that further research is needed to optimize risk stratification for venous thromboembolism patients,” they wrote.
The study was partially funded by a grant from the Obel Family Foundation. Some authors reported financial disclosures related to Janssen, Bayer, Roche, and others.
SOURCE: Albertsen IE et al. Am J Med. 2018 Sep;131(9):1067-74.e4.
Recurrence risk is significant among all patients with venous thromboembolism (VTE), though recurrence is most frequent in patients with cancer-related VTE, according to a nationwide Danish study.
Ida Ehlers Albertsen, MD, of Aalborg (Denmark) University Hospital and her coauthors followed 73,993 patients who were diagnosed with incident VTE during January 2000–December 2015. The patients’ VTEs were classified as either cancer-related, unprovoked (occurring in patients without any provoking factors), or provoked (occurring in patients with one or more provoking factors, such as recent major surgery, recent fracture/trauma, obesity, or hormone replacement therapy).
The researchers found similar risks of recurrence among patients with unprovoked and provoked VTE at 6-month follow-up, with rates per 100 person-years of 6.80 and 6.92, respectively. By comparison, the recurrence rate for cancer-related VTE at 6 months was 9.06. The findings were reported in the American Journal of Medicine.
However, at 10-year follow-up the rates were 3.70 for cancer-related VTE, 2.84 for unprovoked VTE, and 2.22 for provoked VTE, which reinforces the belief that “unprovoked venous thromboembolism is associated with long-term higher risk of recurrence than provoked venous thromboembolism.”
Additionally, at 10-year follow-up, the absolute recurrence risk of cancer-related VTE and unprovoked VTE were both at approximately 20%, with recurrence risk of provoked VTE at just above 15%. Compared with the recurrence risk of provoked VTE at 10-year follow-up, the hazard ratios of cancer-related VTE and unprovoked VTE recurrence risk were 1.23 (95% confidence interval, 1.13-1.33) and 1.18 (95% CI, 1.13-1.24), respectively.
The coauthors observed several challenges in comparing their study to previous analyses on recurrent risk, noting that the definition of provoked VTE “varies throughout the literature” and that the majority of VTE studies “provide cumulative incidence proportions and not the actual rates.” They also stated that indefinite or extended therapy for all VTE patients comes with its own potential complications, even with the improved safety of non–vitamin K antagonist oral anticoagulants, writing that “treatment should be given to patients where the benefits outweigh the risks.”
Despite the differences in recurrence rates at 6-month and 10-year follow-up, the coauthors suggested that enough risk was present in all types to warrant additional studies and reconsider how VTE patients are categorized.
“A high recurrence risk in all types of venous thromboembolism indicates that further research is needed to optimize risk stratification for venous thromboembolism patients,” they wrote.
The study was partially funded by a grant from the Obel Family Foundation. Some authors reported financial disclosures related to Janssen, Bayer, Roche, and others.
SOURCE: Albertsen IE et al. Am J Med. 2018 Sep;131(9):1067-74.e4.
FROM THE AMERICAN JOURNAL OF MEDICINE
Key clinical point:
Major finding: At 10-year follow-up, recurrence rates per 100 person-years were 3.70 for patients with cancer-related VTE, 2.84 for patients with unprovoked VTE, and 2.22 for patients with provoked VTE.
Study details: An observational cohort study of 73,993 Danish patients with incident venous thromboembolism during January 2000–December 2015.
Disclosures: The study was partially funded by a grant from the Obel Family Foundation. Some authors reported financial disclosures related to Janssen, Bayer, Roche, and others.
Source: Albertsen IE et al. Am J Med. 2018 Sep;131(9):1067-74.e4.
EHR-guided strategy reduces postop VTE events
BOSTON – Avoiding could result in a reduction in VTE rates, a speaker said at the annual clinical congress of the American College of Surgeons.
The VTE rate dropped by about one-quarter in the trauma care pathway at the University of Pittsburgh Medical Center (UPMC) after implementation of algorithms to risk-stratify patients and guide nursing staff, said Matthew D. Neal, MD, FACS, the Roberta G. Simmons Assistant Professor of Surgery at the University of Pittsburgh.
By incorporating algorithms into the electronic health record (EHR), UPMC was able to realize a “dramatic” 72% reduction in missed doses, from 4,331 missed doses in 2014 to 1,193 in 2015, Dr. Neal told attendees in a session focused on hot topics in surgical patient safety.
That decrease in missed doses has translated into a decreased rate of VTE, from an already relatively low rate of 1.5% in 2015, to 1.1% in 2017, representing a 26.7% reduction, according to data Dr. Neal shared in his podium presentation.
“This has been a sustainable event for us, largely linked to the implementation of an EHR-guided risk assessment pathway to guide the implementation of VTE prophylaxis,” he said.
The change was safe, he added, noting that, since utilization of this pathway, there have been no significant increases in the rate of bleeding events among patients who have mandatory orders.
These results corroborate those of some previous investigations, including one key study from the Johns Hopkins Hospital that described the adoption of a mandatory computerized clinical decision support tool to improve adherence to best practices for VTE prophylaxis.
After incorporation of the tool in the computerized order entry system, there was a significant increase in VTE prophylaxis, translating into a significant drop in preventable harm from VTE, from 1.0% to 0.17% (P = .04), investigators reported in JAMA Surgery.
Reducing missed doses is one of the major contributing factors to decreased VTE rates, according to Dr. Neal.
Missed doses of enoxaparin correlate with increased incidence of deep vein thrombosis (DVT) in trauma and general surgery patients, according to results of one prospective study Dr. Neal described. In that study of 202 patients, reported in JAMA Surgery, DVTs were seen in 23.5% of patients with missed doses, compared with 4.8 for patients with no missed doses (P < .01).
“We need to understand how to risk assess and how to utilize our EHR as a tool,” Dr. Neal told attendees.
Dr. Neal reported disclosures related to Janssen Pharmaceuticals, CSL Behring, Accriva Diagnostics, and Haemonetics, as well as a U.S. patent for a treatment of infectious and inflammatory disorders, and laboratory funding from the National Institutes of Health, Department of Defense, and the Biomedical Advanced Research and Development Authority.
SOURCE: Neal MD. Presentation at the American College of Surgeons Clinical Congress. 2018 Oct 25.
BOSTON – Avoiding could result in a reduction in VTE rates, a speaker said at the annual clinical congress of the American College of Surgeons.
The VTE rate dropped by about one-quarter in the trauma care pathway at the University of Pittsburgh Medical Center (UPMC) after implementation of algorithms to risk-stratify patients and guide nursing staff, said Matthew D. Neal, MD, FACS, the Roberta G. Simmons Assistant Professor of Surgery at the University of Pittsburgh.
By incorporating algorithms into the electronic health record (EHR), UPMC was able to realize a “dramatic” 72% reduction in missed doses, from 4,331 missed doses in 2014 to 1,193 in 2015, Dr. Neal told attendees in a session focused on hot topics in surgical patient safety.
That decrease in missed doses has translated into a decreased rate of VTE, from an already relatively low rate of 1.5% in 2015, to 1.1% in 2017, representing a 26.7% reduction, according to data Dr. Neal shared in his podium presentation.
“This has been a sustainable event for us, largely linked to the implementation of an EHR-guided risk assessment pathway to guide the implementation of VTE prophylaxis,” he said.
The change was safe, he added, noting that, since utilization of this pathway, there have been no significant increases in the rate of bleeding events among patients who have mandatory orders.
These results corroborate those of some previous investigations, including one key study from the Johns Hopkins Hospital that described the adoption of a mandatory computerized clinical decision support tool to improve adherence to best practices for VTE prophylaxis.
After incorporation of the tool in the computerized order entry system, there was a significant increase in VTE prophylaxis, translating into a significant drop in preventable harm from VTE, from 1.0% to 0.17% (P = .04), investigators reported in JAMA Surgery.
Reducing missed doses is one of the major contributing factors to decreased VTE rates, according to Dr. Neal.
Missed doses of enoxaparin correlate with increased incidence of deep vein thrombosis (DVT) in trauma and general surgery patients, according to results of one prospective study Dr. Neal described. In that study of 202 patients, reported in JAMA Surgery, DVTs were seen in 23.5% of patients with missed doses, compared with 4.8 for patients with no missed doses (P < .01).
“We need to understand how to risk assess and how to utilize our EHR as a tool,” Dr. Neal told attendees.
Dr. Neal reported disclosures related to Janssen Pharmaceuticals, CSL Behring, Accriva Diagnostics, and Haemonetics, as well as a U.S. patent for a treatment of infectious and inflammatory disorders, and laboratory funding from the National Institutes of Health, Department of Defense, and the Biomedical Advanced Research and Development Authority.
SOURCE: Neal MD. Presentation at the American College of Surgeons Clinical Congress. 2018 Oct 25.
BOSTON – Avoiding could result in a reduction in VTE rates, a speaker said at the annual clinical congress of the American College of Surgeons.
The VTE rate dropped by about one-quarter in the trauma care pathway at the University of Pittsburgh Medical Center (UPMC) after implementation of algorithms to risk-stratify patients and guide nursing staff, said Matthew D. Neal, MD, FACS, the Roberta G. Simmons Assistant Professor of Surgery at the University of Pittsburgh.
By incorporating algorithms into the electronic health record (EHR), UPMC was able to realize a “dramatic” 72% reduction in missed doses, from 4,331 missed doses in 2014 to 1,193 in 2015, Dr. Neal told attendees in a session focused on hot topics in surgical patient safety.
That decrease in missed doses has translated into a decreased rate of VTE, from an already relatively low rate of 1.5% in 2015, to 1.1% in 2017, representing a 26.7% reduction, according to data Dr. Neal shared in his podium presentation.
“This has been a sustainable event for us, largely linked to the implementation of an EHR-guided risk assessment pathway to guide the implementation of VTE prophylaxis,” he said.
The change was safe, he added, noting that, since utilization of this pathway, there have been no significant increases in the rate of bleeding events among patients who have mandatory orders.
These results corroborate those of some previous investigations, including one key study from the Johns Hopkins Hospital that described the adoption of a mandatory computerized clinical decision support tool to improve adherence to best practices for VTE prophylaxis.
After incorporation of the tool in the computerized order entry system, there was a significant increase in VTE prophylaxis, translating into a significant drop in preventable harm from VTE, from 1.0% to 0.17% (P = .04), investigators reported in JAMA Surgery.
Reducing missed doses is one of the major contributing factors to decreased VTE rates, according to Dr. Neal.
Missed doses of enoxaparin correlate with increased incidence of deep vein thrombosis (DVT) in trauma and general surgery patients, according to results of one prospective study Dr. Neal described. In that study of 202 patients, reported in JAMA Surgery, DVTs were seen in 23.5% of patients with missed doses, compared with 4.8 for patients with no missed doses (P < .01).
“We need to understand how to risk assess and how to utilize our EHR as a tool,” Dr. Neal told attendees.
Dr. Neal reported disclosures related to Janssen Pharmaceuticals, CSL Behring, Accriva Diagnostics, and Haemonetics, as well as a U.S. patent for a treatment of infectious and inflammatory disorders, and laboratory funding from the National Institutes of Health, Department of Defense, and the Biomedical Advanced Research and Development Authority.
SOURCE: Neal MD. Presentation at the American College of Surgeons Clinical Congress. 2018 Oct 25.
AT THE ACS CLINICAL CONGRESS
Rivaroxaban gains indication for prevention of major cardiovascular events in CAD/PAD
when taken with aspirin, Janssen Pharmaceuticals announced on October 11.
The Food and Drug Administration’s approval was based on a review of the 27,000-patient COMPASS trial, which showed last year that a low dosage of rivaroxaban (Xarelto) plus aspirin reduced the combined rate of cardiovascular disease events by 24% in patients with coronary artery disease and by 28% in participants with peripheral artery disease, compared with aspirin alone. (N Engl J Med. 2017 Oct 5;377[14]:1319-30)
The flip side to the reduction in COMPASS’s combined primary endpoint was a 51% increase in major bleeding. However, that bump did not translate to increases in fatal bleeds, intracerebral bleeds, or bleeding in other critical organs.
COMPASS (Cardiovascular Outcomes for People Using Anticoagulation Strategies) studied two dosages of rivaroxaban, 2.5 mg and 5 mg twice daily, and it was the lower dosage that did the trick. Until this approval, that formulation wasn’t available; Janssen announced the coming of the 2.5-mg pill in its release.
The new prescribing information states specifically that Xarelto 2.5 mg is indicated, in combination with aspirin, to reduce the risk of major cardiovascular events, cardiovascular death, MI, and stroke in patients with chronic coronary artery disease or peripheral artery disease.
This is the sixth indication for rivaroxaban, a factor Xa inhibitor that was first approved in 2011. It is also the first indication for cardiovascular prevention for any factor Xa inhibitor. Others on the U.S. market are apixaban (Eliquis), edoxaban (Savaysa), and betrixaban (Bevyxxa).
COMPASS was presented at the 2017 annual congress of the European Society of Cardiology. At that time, Eugene Braunwald, MD, of Harvard Medical School and Brigham and Women’s Hospital in Boston, commented that the trial produced “unambiguous results that should change guidelines and the management of stable coronary artery disease.” He added that the results are “an important step for thrombocardiology.”
when taken with aspirin, Janssen Pharmaceuticals announced on October 11.
The Food and Drug Administration’s approval was based on a review of the 27,000-patient COMPASS trial, which showed last year that a low dosage of rivaroxaban (Xarelto) plus aspirin reduced the combined rate of cardiovascular disease events by 24% in patients with coronary artery disease and by 28% in participants with peripheral artery disease, compared with aspirin alone. (N Engl J Med. 2017 Oct 5;377[14]:1319-30)
The flip side to the reduction in COMPASS’s combined primary endpoint was a 51% increase in major bleeding. However, that bump did not translate to increases in fatal bleeds, intracerebral bleeds, or bleeding in other critical organs.
COMPASS (Cardiovascular Outcomes for People Using Anticoagulation Strategies) studied two dosages of rivaroxaban, 2.5 mg and 5 mg twice daily, and it was the lower dosage that did the trick. Until this approval, that formulation wasn’t available; Janssen announced the coming of the 2.5-mg pill in its release.
The new prescribing information states specifically that Xarelto 2.5 mg is indicated, in combination with aspirin, to reduce the risk of major cardiovascular events, cardiovascular death, MI, and stroke in patients with chronic coronary artery disease or peripheral artery disease.
This is the sixth indication for rivaroxaban, a factor Xa inhibitor that was first approved in 2011. It is also the first indication for cardiovascular prevention for any factor Xa inhibitor. Others on the U.S. market are apixaban (Eliquis), edoxaban (Savaysa), and betrixaban (Bevyxxa).
COMPASS was presented at the 2017 annual congress of the European Society of Cardiology. At that time, Eugene Braunwald, MD, of Harvard Medical School and Brigham and Women’s Hospital in Boston, commented that the trial produced “unambiguous results that should change guidelines and the management of stable coronary artery disease.” He added that the results are “an important step for thrombocardiology.”
when taken with aspirin, Janssen Pharmaceuticals announced on October 11.
The Food and Drug Administration’s approval was based on a review of the 27,000-patient COMPASS trial, which showed last year that a low dosage of rivaroxaban (Xarelto) plus aspirin reduced the combined rate of cardiovascular disease events by 24% in patients with coronary artery disease and by 28% in participants with peripheral artery disease, compared with aspirin alone. (N Engl J Med. 2017 Oct 5;377[14]:1319-30)
The flip side to the reduction in COMPASS’s combined primary endpoint was a 51% increase in major bleeding. However, that bump did not translate to increases in fatal bleeds, intracerebral bleeds, or bleeding in other critical organs.
COMPASS (Cardiovascular Outcomes for People Using Anticoagulation Strategies) studied two dosages of rivaroxaban, 2.5 mg and 5 mg twice daily, and it was the lower dosage that did the trick. Until this approval, that formulation wasn’t available; Janssen announced the coming of the 2.5-mg pill in its release.
The new prescribing information states specifically that Xarelto 2.5 mg is indicated, in combination with aspirin, to reduce the risk of major cardiovascular events, cardiovascular death, MI, and stroke in patients with chronic coronary artery disease or peripheral artery disease.
This is the sixth indication for rivaroxaban, a factor Xa inhibitor that was first approved in 2011. It is also the first indication for cardiovascular prevention for any factor Xa inhibitor. Others on the U.S. market are apixaban (Eliquis), edoxaban (Savaysa), and betrixaban (Bevyxxa).
COMPASS was presented at the 2017 annual congress of the European Society of Cardiology. At that time, Eugene Braunwald, MD, of Harvard Medical School and Brigham and Women’s Hospital in Boston, commented that the trial produced “unambiguous results that should change guidelines and the management of stable coronary artery disease.” He added that the results are “an important step for thrombocardiology.”
Obesity paradox extends to PE patients
SAN ANTONIO – compared with those who are not obese, according to results of a retrospective analysis covering 13 years and nearly 2 million PE discharges.
The obese patients in the analysis had a lower mortality risk, despite receiving more thrombolytics and mechanical intubation, said investigator Zubair Khan, MD, an internal medicine resident at the University of Toledo (Ohio) Medical Center.
“Surprisingly, the mortality of PE was significantly less in obese patients,” Dr. Khan said in a podium presentation at the annual meeting of the American College of Chest Physicians. “When we initiated the study, we did not expect this result.”
The association between obesity and lower mortality, sometimes called the “obesity paradox,” has been observed in studies of other chronic health conditions including stable heart failure, coronary artery disease, unstable angina, MI, and also in some PE studies, Dr. Khan said.
The study by Dr. Khan and his colleagues, based on the National Inpatient Sample (NIS) database, included adults with a primary discharge diagnosis of PE between 2002 and 2014. They included 1,959,018 PE discharges, of which 312,770 (16%) had an underlying obesity diagnosis.
Obese PE patients had more risk factors and more severe disease but had an overall mortality of 2.2%, compared with 3.7% in PE patients without obesity (P less than .001), Dr. Khan reported.
Hypertension was significantly more prevalent in the obese PE patients (65% vs. 50.5%; P less than .001), as was chronic lung disease and chronic liver disease, he noted in his presentation.
Obese patients more often received thrombolytics (3.6% vs. 1.9%; P less than .001) and mechanical ventilation (5.8% vs. 4%; P less than .001), and more frequently had cardiogenic shock (0.65% vs. 0.45%; P less than .001), he said.
The obese PE patients were more often female, black, and younger than 65 years of age, it was reported.
Notably, the prevalence of obesity in PE patients more than doubled over the course of the study period, from 10.2% in 2002 to 22.6% in 2014, Dr. Khan added.
The paradoxically lower mortality in obese patients might be explained by increased levels of endocannabinoids, which have shown protective effects in rat and mouse studies, Dr. Khan told attendees at the meeting.
“I think it’s a rich area for more and further research, especially in basic science,” Dr. Khan said.
Dr. Khan and his coauthors disclosed that they had no relationships relevant to the study.
SOURCE: Khan Z et al. CHEST. 2018 Oct. doi: 10.1016/j.chest.2018.08.919.
SAN ANTONIO – compared with those who are not obese, according to results of a retrospective analysis covering 13 years and nearly 2 million PE discharges.
The obese patients in the analysis had a lower mortality risk, despite receiving more thrombolytics and mechanical intubation, said investigator Zubair Khan, MD, an internal medicine resident at the University of Toledo (Ohio) Medical Center.
“Surprisingly, the mortality of PE was significantly less in obese patients,” Dr. Khan said in a podium presentation at the annual meeting of the American College of Chest Physicians. “When we initiated the study, we did not expect this result.”
The association between obesity and lower mortality, sometimes called the “obesity paradox,” has been observed in studies of other chronic health conditions including stable heart failure, coronary artery disease, unstable angina, MI, and also in some PE studies, Dr. Khan said.
The study by Dr. Khan and his colleagues, based on the National Inpatient Sample (NIS) database, included adults with a primary discharge diagnosis of PE between 2002 and 2014. They included 1,959,018 PE discharges, of which 312,770 (16%) had an underlying obesity diagnosis.
Obese PE patients had more risk factors and more severe disease but had an overall mortality of 2.2%, compared with 3.7% in PE patients without obesity (P less than .001), Dr. Khan reported.
Hypertension was significantly more prevalent in the obese PE patients (65% vs. 50.5%; P less than .001), as was chronic lung disease and chronic liver disease, he noted in his presentation.
Obese patients more often received thrombolytics (3.6% vs. 1.9%; P less than .001) and mechanical ventilation (5.8% vs. 4%; P less than .001), and more frequently had cardiogenic shock (0.65% vs. 0.45%; P less than .001), he said.
The obese PE patients were more often female, black, and younger than 65 years of age, it was reported.
Notably, the prevalence of obesity in PE patients more than doubled over the course of the study period, from 10.2% in 2002 to 22.6% in 2014, Dr. Khan added.
The paradoxically lower mortality in obese patients might be explained by increased levels of endocannabinoids, which have shown protective effects in rat and mouse studies, Dr. Khan told attendees at the meeting.
“I think it’s a rich area for more and further research, especially in basic science,” Dr. Khan said.
Dr. Khan and his coauthors disclosed that they had no relationships relevant to the study.
SOURCE: Khan Z et al. CHEST. 2018 Oct. doi: 10.1016/j.chest.2018.08.919.
SAN ANTONIO – compared with those who are not obese, according to results of a retrospective analysis covering 13 years and nearly 2 million PE discharges.
The obese patients in the analysis had a lower mortality risk, despite receiving more thrombolytics and mechanical intubation, said investigator Zubair Khan, MD, an internal medicine resident at the University of Toledo (Ohio) Medical Center.
“Surprisingly, the mortality of PE was significantly less in obese patients,” Dr. Khan said in a podium presentation at the annual meeting of the American College of Chest Physicians. “When we initiated the study, we did not expect this result.”
The association between obesity and lower mortality, sometimes called the “obesity paradox,” has been observed in studies of other chronic health conditions including stable heart failure, coronary artery disease, unstable angina, MI, and also in some PE studies, Dr. Khan said.
The study by Dr. Khan and his colleagues, based on the National Inpatient Sample (NIS) database, included adults with a primary discharge diagnosis of PE between 2002 and 2014. They included 1,959,018 PE discharges, of which 312,770 (16%) had an underlying obesity diagnosis.
Obese PE patients had more risk factors and more severe disease but had an overall mortality of 2.2%, compared with 3.7% in PE patients without obesity (P less than .001), Dr. Khan reported.
Hypertension was significantly more prevalent in the obese PE patients (65% vs. 50.5%; P less than .001), as was chronic lung disease and chronic liver disease, he noted in his presentation.
Obese patients more often received thrombolytics (3.6% vs. 1.9%; P less than .001) and mechanical ventilation (5.8% vs. 4%; P less than .001), and more frequently had cardiogenic shock (0.65% vs. 0.45%; P less than .001), he said.
The obese PE patients were more often female, black, and younger than 65 years of age, it was reported.
Notably, the prevalence of obesity in PE patients more than doubled over the course of the study period, from 10.2% in 2002 to 22.6% in 2014, Dr. Khan added.
The paradoxically lower mortality in obese patients might be explained by increased levels of endocannabinoids, which have shown protective effects in rat and mouse studies, Dr. Khan told attendees at the meeting.
“I think it’s a rich area for more and further research, especially in basic science,” Dr. Khan said.
Dr. Khan and his coauthors disclosed that they had no relationships relevant to the study.
SOURCE: Khan Z et al. CHEST. 2018 Oct. doi: 10.1016/j.chest.2018.08.919.
REPORTING FROM CHEST 2018
Key clinical point: The obesity paradox observed in other chronic conditions held true in this study of patients with pulmonary embolism (PE).
Major finding: Obese PE patients had more risk factors and more severe disease, but an overall mortality of 2.2% vs 3.7% in nonobese PE patients.
Study details: Retrospective analysis of the National Inpatient Sample (NIS) database including almost 2 million individuals with a primary discharge diagnosis of PE.
Disclosures: Study authors had no disclosures.
Source: Khan Z et al. CHEST. 2018 Oct. doi: 10.1016/j.chest.2018.08.919.
No significant VTE risk for women taking noncyclic COCs
Women who use combined oral contraceptives (COC) without hormone-free or low-dose hormone intervals have a slightly elevated, but not statistically significant, risk of venous thromboembolism (VTE), compared with women who use cyclic COCs, according to research published in JAMA Internal Medicine.
Jie Li, PhD, from the Center for Drug Evaluation and Research, and colleagues performed a retrospective cohort study of 733,007 women aged 18-50 years in the Sentinel Distributed Database from 2007 to 2015 who received low-dose extended and continuous cycle (210,691 women; mean age, 30 years) COCs or cyclic COCs (522,316 women; mean age, 29 years). Continuous cycle COCs were defined as an 84/7 cycle or a 365/0 cycle, while cyclic COCs were 21/7 cycles.
The researchers noted some baseline differences between the two groups, with gynecologic conditions occurring in 40% of the noncyclic group, compared with 32% in the cyclic group; cardiovascular and metabolic conditions occurring in 7% of noncyclic women, compared with 5% of cyclic women; inflammatory disease occurring in 3% of noncyclic women, compared with 2% of cyclic women; and a slightly higher rate of health care services use in the noncyclic group, compared with the cyclic group.
Dr. Li and associates found 228 cases of VTE in the noncyclic group and 297 cases in the cyclic group, with an incidence rate of 1.54 (95% confidence interval, 1.34-1.74) per 1,000 person-years for noncyclic users and 0.83 (95% CI, 0.74-0.93) per 1,000 person-years for cyclic users (crude hazard ratio, 1.84; 95% CI, 1.53-2.21).
However, propensity score matching lowered the incidence rate to 1.44 (95% CI, 1.24-1.64) per 1,000 person-years for the noncyclic group and raised it to 1.09 (95% CI, 0.92-1.27) per 1,000 person-years for the cyclic group, for an adjusted hazard ratio of 1.32 (95% CI, 1.07-1.64), which does not show “strong evidence” of VTE risk based on a small absolute risk difference of 0.27 cases per 1,000 persons, the researchers said. They added that there might be residual or unmeasured confounding, perhaps for potential concurrent medication use or incompletely measured covariates.
“Accordingly, we do not recommend selective prescribing of COCs based on the cyclic and continuous/extended type,” Dr. Li and colleagues wrote. “Clinicians should prescribe COCs based on patients’ individual risk factors and preferences.”
The Sentinel Initiative is funded by a contract from the Department of Health and Human Services. The authors reported no relevant conflicts of interest.
SOURCE: Li J et al. JAMA Intern Med. 2018 Oct 1. doi: 10.1001/jamainternmed.2018.4251.
Women who use combined oral contraceptives (COC) without hormone-free or low-dose hormone intervals have a slightly elevated, but not statistically significant, risk of venous thromboembolism (VTE), compared with women who use cyclic COCs, according to research published in JAMA Internal Medicine.
Jie Li, PhD, from the Center for Drug Evaluation and Research, and colleagues performed a retrospective cohort study of 733,007 women aged 18-50 years in the Sentinel Distributed Database from 2007 to 2015 who received low-dose extended and continuous cycle (210,691 women; mean age, 30 years) COCs or cyclic COCs (522,316 women; mean age, 29 years). Continuous cycle COCs were defined as an 84/7 cycle or a 365/0 cycle, while cyclic COCs were 21/7 cycles.
The researchers noted some baseline differences between the two groups, with gynecologic conditions occurring in 40% of the noncyclic group, compared with 32% in the cyclic group; cardiovascular and metabolic conditions occurring in 7% of noncyclic women, compared with 5% of cyclic women; inflammatory disease occurring in 3% of noncyclic women, compared with 2% of cyclic women; and a slightly higher rate of health care services use in the noncyclic group, compared with the cyclic group.
Dr. Li and associates found 228 cases of VTE in the noncyclic group and 297 cases in the cyclic group, with an incidence rate of 1.54 (95% confidence interval, 1.34-1.74) per 1,000 person-years for noncyclic users and 0.83 (95% CI, 0.74-0.93) per 1,000 person-years for cyclic users (crude hazard ratio, 1.84; 95% CI, 1.53-2.21).
However, propensity score matching lowered the incidence rate to 1.44 (95% CI, 1.24-1.64) per 1,000 person-years for the noncyclic group and raised it to 1.09 (95% CI, 0.92-1.27) per 1,000 person-years for the cyclic group, for an adjusted hazard ratio of 1.32 (95% CI, 1.07-1.64), which does not show “strong evidence” of VTE risk based on a small absolute risk difference of 0.27 cases per 1,000 persons, the researchers said. They added that there might be residual or unmeasured confounding, perhaps for potential concurrent medication use or incompletely measured covariates.
“Accordingly, we do not recommend selective prescribing of COCs based on the cyclic and continuous/extended type,” Dr. Li and colleagues wrote. “Clinicians should prescribe COCs based on patients’ individual risk factors and preferences.”
The Sentinel Initiative is funded by a contract from the Department of Health and Human Services. The authors reported no relevant conflicts of interest.
SOURCE: Li J et al. JAMA Intern Med. 2018 Oct 1. doi: 10.1001/jamainternmed.2018.4251.
Women who use combined oral contraceptives (COC) without hormone-free or low-dose hormone intervals have a slightly elevated, but not statistically significant, risk of venous thromboembolism (VTE), compared with women who use cyclic COCs, according to research published in JAMA Internal Medicine.
Jie Li, PhD, from the Center for Drug Evaluation and Research, and colleagues performed a retrospective cohort study of 733,007 women aged 18-50 years in the Sentinel Distributed Database from 2007 to 2015 who received low-dose extended and continuous cycle (210,691 women; mean age, 30 years) COCs or cyclic COCs (522,316 women; mean age, 29 years). Continuous cycle COCs were defined as an 84/7 cycle or a 365/0 cycle, while cyclic COCs were 21/7 cycles.
The researchers noted some baseline differences between the two groups, with gynecologic conditions occurring in 40% of the noncyclic group, compared with 32% in the cyclic group; cardiovascular and metabolic conditions occurring in 7% of noncyclic women, compared with 5% of cyclic women; inflammatory disease occurring in 3% of noncyclic women, compared with 2% of cyclic women; and a slightly higher rate of health care services use in the noncyclic group, compared with the cyclic group.
Dr. Li and associates found 228 cases of VTE in the noncyclic group and 297 cases in the cyclic group, with an incidence rate of 1.54 (95% confidence interval, 1.34-1.74) per 1,000 person-years for noncyclic users and 0.83 (95% CI, 0.74-0.93) per 1,000 person-years for cyclic users (crude hazard ratio, 1.84; 95% CI, 1.53-2.21).
However, propensity score matching lowered the incidence rate to 1.44 (95% CI, 1.24-1.64) per 1,000 person-years for the noncyclic group and raised it to 1.09 (95% CI, 0.92-1.27) per 1,000 person-years for the cyclic group, for an adjusted hazard ratio of 1.32 (95% CI, 1.07-1.64), which does not show “strong evidence” of VTE risk based on a small absolute risk difference of 0.27 cases per 1,000 persons, the researchers said. They added that there might be residual or unmeasured confounding, perhaps for potential concurrent medication use or incompletely measured covariates.
“Accordingly, we do not recommend selective prescribing of COCs based on the cyclic and continuous/extended type,” Dr. Li and colleagues wrote. “Clinicians should prescribe COCs based on patients’ individual risk factors and preferences.”
The Sentinel Initiative is funded by a contract from the Department of Health and Human Services. The authors reported no relevant conflicts of interest.
SOURCE: Li J et al. JAMA Intern Med. 2018 Oct 1. doi: 10.1001/jamainternmed.2018.4251.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Continuous or extended cycle combined oral contraceptive (COC) use was associated with a slightly elevated, but not statistically significant, risk of venous thromboembolism.
Major finding: The adjusted hazard ratio for women taking continuous/extended COCs was 1.32 (95% confidence interval, 1.07-1.74), compared with women taking noncyclic COCs, but the absolute risk difference between the two groups was low (0.27 per 1,000 persons).
Study details: A retrospective cohort study of 210,691 women with continuous/extended COC use and 522,316 women with cyclic COC use.
Disclosures: The Sentinel Initiative is funded by a contract from the Department of Health and Human Services. The authors reported no relevant conflicts of interest.
Source: Li J et al. JAMA Intern Med. 2018 Oct 1. doi:10.1001/jamainternmed.2018.4251.
A new, simple, inexpensive DVT diagnostic aid
NEW ORLEANS – Both the neutrophil-to-lymphocyte ratio and the platelet-to-lymphocyte ratio proved to be better predictors of the presence or absence of deep vein thrombosis than the ubiquitous D-dimer test in a retrospective study, Jason Mouabbi, MD, reported at the annual meeting of the American College of Physicians.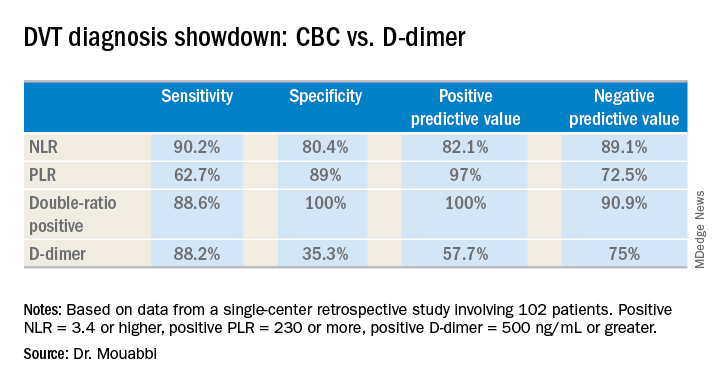
What’s more, both the neutrophil-to-lymphocyte ratio (NLR) and the platelet-to-lymphocyte ratio (PLR) can be readily calculated from the readout of a complete blood count (CBC) with differential. A CBC costs an average of $16, and everybody that comes through a hospital emergency department gets one. In contrast, the average charge for a D-dimer test is about $231 nationwide, and depending upon the specific test used the results can take up to a couple of hours to come back, noted Dr. Mouabbi of St. John Hospital and Medical Center in Detroit.
“The NLR and PLR ratios offer a new, powerful, affordable, simple, and readily available tool in the hands of clinicians to help them in the diagnosis of DVT,” he said. “The NLR can be useful to rule out DVT when it’s negative, whereas PLR can be useful in ruling DVT when positive.”
Investigators in a variety of fields are looking at the NLR and PLR as emerging practical, easily obtainable biomarkers for systemic inflammation. And DVT is thought to be an inflammatory process, he explained.
Dr. Mouabbi presented a single-center retrospective study of 102 matched patients who presented with lower extremity swelling and had a CBC drawn, as well as a D-dimer test, on the same day they underwent a lower extremity Doppler ultrasound evaluation. In 51 patients, the ultrasound revealed the presence of DVT and anticoagulation was started. In the other 51 patients, the ultrasound exam was negative and they weren’t anticoagulated. Since the study purpose was to assess the implications of a primary elevation of NLR and/or PLR, patients with rheumatic diseases, inflammatory bowel disease, recent surgery, chronic renal or liver disease, inherited thrombophilia, infection, or other possible secondary causes of altered ratios were excluded from the study.
A positive NLR was considered 3.4 or higher, a positive PLR was a ratio of 230 or more, and a positive D-dimer level was 500 ng/mL or greater. The NLR and PLR collectively outperformed the D-dimer test in terms of sensitivity, specificity, positive predictive value, and negative predictive value.
In addition, 89% of the DVT group were classified as “double-positive,” meaning they were both NLR and PLR positive. That combination provided the best diagnostic value of all, since none of the controls were double-positive and only 2% were PLR positive.
While the results are encouraging, before NLR and PLR can supplant D-dimer in patients with suspected DVT in clinical practice a confirmatory prospective study should be carried out, according to Dr. Mouabbi. Ideally it should include the use of the Wells score, which is part of most diagnostic algorithms as a preliminary means of categorizing DVT probability as low, moderate, or high. However, the popularity of the Wells score has fallen off in the face of reports that the results are subjective and variable. Indeed, the Wells score was included in the electronic medical record of so few participants in Dr. Mouabbi’s study that he couldn’t evaluate its utility.
He reported having no financial conflicts regarding his study, which was conducted free of commercial support.
NEW ORLEANS – Both the neutrophil-to-lymphocyte ratio and the platelet-to-lymphocyte ratio proved to be better predictors of the presence or absence of deep vein thrombosis than the ubiquitous D-dimer test in a retrospective study, Jason Mouabbi, MD, reported at the annual meeting of the American College of Physicians.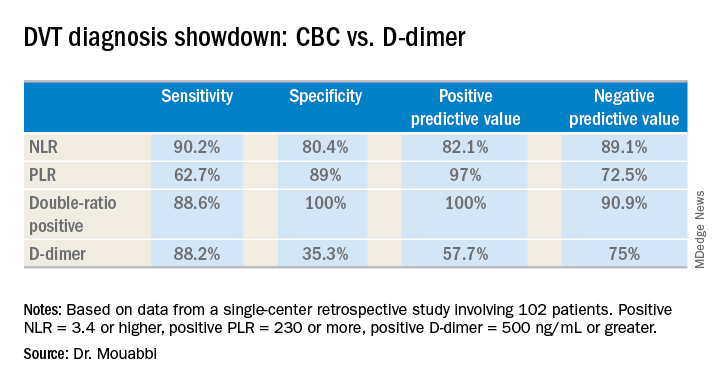
What’s more, both the neutrophil-to-lymphocyte ratio (NLR) and the platelet-to-lymphocyte ratio (PLR) can be readily calculated from the readout of a complete blood count (CBC) with differential. A CBC costs an average of $16, and everybody that comes through a hospital emergency department gets one. In contrast, the average charge for a D-dimer test is about $231 nationwide, and depending upon the specific test used the results can take up to a couple of hours to come back, noted Dr. Mouabbi of St. John Hospital and Medical Center in Detroit.
“The NLR and PLR ratios offer a new, powerful, affordable, simple, and readily available tool in the hands of clinicians to help them in the diagnosis of DVT,” he said. “The NLR can be useful to rule out DVT when it’s negative, whereas PLR can be useful in ruling DVT when positive.”
Investigators in a variety of fields are looking at the NLR and PLR as emerging practical, easily obtainable biomarkers for systemic inflammation. And DVT is thought to be an inflammatory process, he explained.
Dr. Mouabbi presented a single-center retrospective study of 102 matched patients who presented with lower extremity swelling and had a CBC drawn, as well as a D-dimer test, on the same day they underwent a lower extremity Doppler ultrasound evaluation. In 51 patients, the ultrasound revealed the presence of DVT and anticoagulation was started. In the other 51 patients, the ultrasound exam was negative and they weren’t anticoagulated. Since the study purpose was to assess the implications of a primary elevation of NLR and/or PLR, patients with rheumatic diseases, inflammatory bowel disease, recent surgery, chronic renal or liver disease, inherited thrombophilia, infection, or other possible secondary causes of altered ratios were excluded from the study.
A positive NLR was considered 3.4 or higher, a positive PLR was a ratio of 230 or more, and a positive D-dimer level was 500 ng/mL or greater. The NLR and PLR collectively outperformed the D-dimer test in terms of sensitivity, specificity, positive predictive value, and negative predictive value.
In addition, 89% of the DVT group were classified as “double-positive,” meaning they were both NLR and PLR positive. That combination provided the best diagnostic value of all, since none of the controls were double-positive and only 2% were PLR positive.
While the results are encouraging, before NLR and PLR can supplant D-dimer in patients with suspected DVT in clinical practice a confirmatory prospective study should be carried out, according to Dr. Mouabbi. Ideally it should include the use of the Wells score, which is part of most diagnostic algorithms as a preliminary means of categorizing DVT probability as low, moderate, or high. However, the popularity of the Wells score has fallen off in the face of reports that the results are subjective and variable. Indeed, the Wells score was included in the electronic medical record of so few participants in Dr. Mouabbi’s study that he couldn’t evaluate its utility.
He reported having no financial conflicts regarding his study, which was conducted free of commercial support.
NEW ORLEANS – Both the neutrophil-to-lymphocyte ratio and the platelet-to-lymphocyte ratio proved to be better predictors of the presence or absence of deep vein thrombosis than the ubiquitous D-dimer test in a retrospective study, Jason Mouabbi, MD, reported at the annual meeting of the American College of Physicians.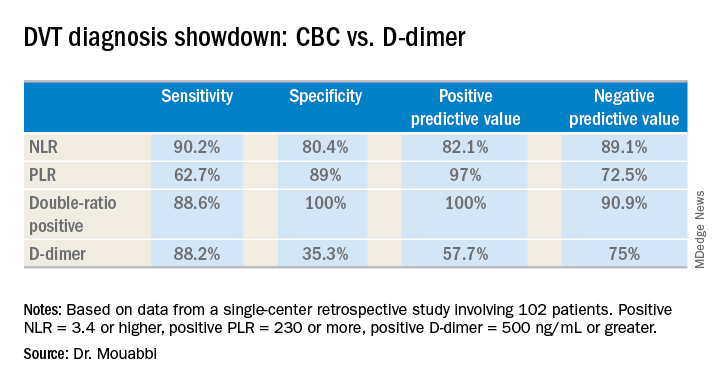
What’s more, both the neutrophil-to-lymphocyte ratio (NLR) and the platelet-to-lymphocyte ratio (PLR) can be readily calculated from the readout of a complete blood count (CBC) with differential. A CBC costs an average of $16, and everybody that comes through a hospital emergency department gets one. In contrast, the average charge for a D-dimer test is about $231 nationwide, and depending upon the specific test used the results can take up to a couple of hours to come back, noted Dr. Mouabbi of St. John Hospital and Medical Center in Detroit.
“The NLR and PLR ratios offer a new, powerful, affordable, simple, and readily available tool in the hands of clinicians to help them in the diagnosis of DVT,” he said. “The NLR can be useful to rule out DVT when it’s negative, whereas PLR can be useful in ruling DVT when positive.”
Investigators in a variety of fields are looking at the NLR and PLR as emerging practical, easily obtainable biomarkers for systemic inflammation. And DVT is thought to be an inflammatory process, he explained.
Dr. Mouabbi presented a single-center retrospective study of 102 matched patients who presented with lower extremity swelling and had a CBC drawn, as well as a D-dimer test, on the same day they underwent a lower extremity Doppler ultrasound evaluation. In 51 patients, the ultrasound revealed the presence of DVT and anticoagulation was started. In the other 51 patients, the ultrasound exam was negative and they weren’t anticoagulated. Since the study purpose was to assess the implications of a primary elevation of NLR and/or PLR, patients with rheumatic diseases, inflammatory bowel disease, recent surgery, chronic renal or liver disease, inherited thrombophilia, infection, or other possible secondary causes of altered ratios were excluded from the study.
A positive NLR was considered 3.4 or higher, a positive PLR was a ratio of 230 or more, and a positive D-dimer level was 500 ng/mL or greater. The NLR and PLR collectively outperformed the D-dimer test in terms of sensitivity, specificity, positive predictive value, and negative predictive value.
In addition, 89% of the DVT group were classified as “double-positive,” meaning they were both NLR and PLR positive. That combination provided the best diagnostic value of all, since none of the controls were double-positive and only 2% were PLR positive.
While the results are encouraging, before NLR and PLR can supplant D-dimer in patients with suspected DVT in clinical practice a confirmatory prospective study should be carried out, according to Dr. Mouabbi. Ideally it should include the use of the Wells score, which is part of most diagnostic algorithms as a preliminary means of categorizing DVT probability as low, moderate, or high. However, the popularity of the Wells score has fallen off in the face of reports that the results are subjective and variable. Indeed, the Wells score was included in the electronic medical record of so few participants in Dr. Mouabbi’s study that he couldn’t evaluate its utility.
He reported having no financial conflicts regarding his study, which was conducted free of commercial support.
REPORTING FROM ACP INTERNAL MEDICINE
Key clinical point:
Major finding: The neutrophil-to-lymphocyte ratio was better than the D-dimer test at helping to rule out DVT, while the platelet-to-lymphocyte ratio bested the D-dimer at ruling in DVT.
Study details: A retrospective study of 102 patients with suspected DVT.
Disclosures: Dr. Mouabbi reported no financial conflicts regarding his study, which was conducted free of commercial support.
VTE risk after bariatric surgery should be assessed
SEATTLE – Preop thromboelastometry can identify patients who need extra according to a prospective investigation of 40 patients at Conemaugh Memorial Medical Center in Johnstown, Pa.
Enoxaparin 40 mg twice daily just wasn’t enough for people who were hypercoagulable before surgery. The goal of the study was to find the best way to prevent venous thromboembolism (VTE) after weight loss surgery. At present, there’s no consensus on prophylaxis dosing, timing, duration, or even what agent to use for these patients. Conemaugh uses postop enoxaparin, a low-molecular-weight heparin. Among many other options, some hospitals opt for preop dosing with traditional heparin, which is less expensive.
The Conemaugh team turned to thromboelastometry (TEM) to look at the question of VTE risk in bariatric surgery patients. The test gauges coagulation status by measuring elasticity as a small blood sample clots over a few minutes. The investigators found that patients who were hypercoagulable before surgery were likely to be hypercoagulable afterwards. The finding argues for baseline TEM testing to guide postop anticoagulation.
The problem is that bariatric services don’t often have access to TEM equipment, and insurance doesn’t cover the $60 test. In this instance, the Lake Erie College of Osteopathic Medicine in Erie, Pa., had the equipment and covered the testing for the study.
The patients had TEM at baseline and then received 40 mg of enoxaparin about 4 hours after surgery – mostly laparoscopic gastric bypasses – and a second dose about 12 hours after the first. TEM was repeated about 2 hours after the second dose.
At baseline, 2 (5%) of the patients were hypocoagulable, 15 (37.5%) were normal, and 23 (57.5%) were hypercoagulable. On postop TEM, 17 patients (42.5%) were normal and 23 (57.5%) were hypercoagulable: “These 23 were inadequately anticoagulated,” said lead investigator Daniel Urias, MD, a general surgery resident at the medical center.
“There was an association between being normal at baseline and being normal postop, and being hypercoagulable at baseline and hypercoagulable postop. We didn’t anticipate finding such similarity between the numbers. Our suspicion that baseline status plays a major role is holding true,” Dr. Urias said at the World Congress of Endoscopic Surgery hosted by SAGES & CAGS.
When patients test hypercoagulable at baseline, “we are [now] leaning towards [enoxaparin] 60 mg twice daily,” he said.
Ultimately, anticoagulation TEM could be used to titrate patients into the normal range. For best outcomes, it’s likely that “obese patients require goal-directed therapy instead of weight-based or fixed dosing,” he said, but nothing is going to happen until insurance steps up.
The patients did not have underlying coagulopathies, and 33 (82.5%) were women; the average age was 44 years and average body mass index was 43.6 kg/m2. The mean preop Caprini score was 4, indicating moderate VTE risk. Surgery lasted about 200 minutes. Patients were out of bed and walking on postop day 0.
The investigators had no relevant disclosures.
SOURCE: Urias D et al. World Congress of Endoscopic Surgery hosted by SAGES & CAGS abstract S023.
SEATTLE – Preop thromboelastometry can identify patients who need extra according to a prospective investigation of 40 patients at Conemaugh Memorial Medical Center in Johnstown, Pa.
Enoxaparin 40 mg twice daily just wasn’t enough for people who were hypercoagulable before surgery. The goal of the study was to find the best way to prevent venous thromboembolism (VTE) after weight loss surgery. At present, there’s no consensus on prophylaxis dosing, timing, duration, or even what agent to use for these patients. Conemaugh uses postop enoxaparin, a low-molecular-weight heparin. Among many other options, some hospitals opt for preop dosing with traditional heparin, which is less expensive.
The Conemaugh team turned to thromboelastometry (TEM) to look at the question of VTE risk in bariatric surgery patients. The test gauges coagulation status by measuring elasticity as a small blood sample clots over a few minutes. The investigators found that patients who were hypercoagulable before surgery were likely to be hypercoagulable afterwards. The finding argues for baseline TEM testing to guide postop anticoagulation.
The problem is that bariatric services don’t often have access to TEM equipment, and insurance doesn’t cover the $60 test. In this instance, the Lake Erie College of Osteopathic Medicine in Erie, Pa., had the equipment and covered the testing for the study.
The patients had TEM at baseline and then received 40 mg of enoxaparin about 4 hours after surgery – mostly laparoscopic gastric bypasses – and a second dose about 12 hours after the first. TEM was repeated about 2 hours after the second dose.
At baseline, 2 (5%) of the patients were hypocoagulable, 15 (37.5%) were normal, and 23 (57.5%) were hypercoagulable. On postop TEM, 17 patients (42.5%) were normal and 23 (57.5%) were hypercoagulable: “These 23 were inadequately anticoagulated,” said lead investigator Daniel Urias, MD, a general surgery resident at the medical center.
“There was an association between being normal at baseline and being normal postop, and being hypercoagulable at baseline and hypercoagulable postop. We didn’t anticipate finding such similarity between the numbers. Our suspicion that baseline status plays a major role is holding true,” Dr. Urias said at the World Congress of Endoscopic Surgery hosted by SAGES & CAGS.
When patients test hypercoagulable at baseline, “we are [now] leaning towards [enoxaparin] 60 mg twice daily,” he said.
Ultimately, anticoagulation TEM could be used to titrate patients into the normal range. For best outcomes, it’s likely that “obese patients require goal-directed therapy instead of weight-based or fixed dosing,” he said, but nothing is going to happen until insurance steps up.
The patients did not have underlying coagulopathies, and 33 (82.5%) were women; the average age was 44 years and average body mass index was 43.6 kg/m2. The mean preop Caprini score was 4, indicating moderate VTE risk. Surgery lasted about 200 minutes. Patients were out of bed and walking on postop day 0.
The investigators had no relevant disclosures.
SOURCE: Urias D et al. World Congress of Endoscopic Surgery hosted by SAGES & CAGS abstract S023.
SEATTLE – Preop thromboelastometry can identify patients who need extra according to a prospective investigation of 40 patients at Conemaugh Memorial Medical Center in Johnstown, Pa.
Enoxaparin 40 mg twice daily just wasn’t enough for people who were hypercoagulable before surgery. The goal of the study was to find the best way to prevent venous thromboembolism (VTE) after weight loss surgery. At present, there’s no consensus on prophylaxis dosing, timing, duration, or even what agent to use for these patients. Conemaugh uses postop enoxaparin, a low-molecular-weight heparin. Among many other options, some hospitals opt for preop dosing with traditional heparin, which is less expensive.
The Conemaugh team turned to thromboelastometry (TEM) to look at the question of VTE risk in bariatric surgery patients. The test gauges coagulation status by measuring elasticity as a small blood sample clots over a few minutes. The investigators found that patients who were hypercoagulable before surgery were likely to be hypercoagulable afterwards. The finding argues for baseline TEM testing to guide postop anticoagulation.
The problem is that bariatric services don’t often have access to TEM equipment, and insurance doesn’t cover the $60 test. In this instance, the Lake Erie College of Osteopathic Medicine in Erie, Pa., had the equipment and covered the testing for the study.
The patients had TEM at baseline and then received 40 mg of enoxaparin about 4 hours after surgery – mostly laparoscopic gastric bypasses – and a second dose about 12 hours after the first. TEM was repeated about 2 hours after the second dose.
At baseline, 2 (5%) of the patients were hypocoagulable, 15 (37.5%) were normal, and 23 (57.5%) were hypercoagulable. On postop TEM, 17 patients (42.5%) were normal and 23 (57.5%) were hypercoagulable: “These 23 were inadequately anticoagulated,” said lead investigator Daniel Urias, MD, a general surgery resident at the medical center.
“There was an association between being normal at baseline and being normal postop, and being hypercoagulable at baseline and hypercoagulable postop. We didn’t anticipate finding such similarity between the numbers. Our suspicion that baseline status plays a major role is holding true,” Dr. Urias said at the World Congress of Endoscopic Surgery hosted by SAGES & CAGS.
When patients test hypercoagulable at baseline, “we are [now] leaning towards [enoxaparin] 60 mg twice daily,” he said.
Ultimately, anticoagulation TEM could be used to titrate patients into the normal range. For best outcomes, it’s likely that “obese patients require goal-directed therapy instead of weight-based or fixed dosing,” he said, but nothing is going to happen until insurance steps up.
The patients did not have underlying coagulopathies, and 33 (82.5%) were women; the average age was 44 years and average body mass index was 43.6 kg/m2. The mean preop Caprini score was 4, indicating moderate VTE risk. Surgery lasted about 200 minutes. Patients were out of bed and walking on postop day 0.
The investigators had no relevant disclosures.
SOURCE: Urias D et al. World Congress of Endoscopic Surgery hosted by SAGES & CAGS abstract S023.
REPORTING FROM SAGES 2018
Key clinical point: Preoperative thromboelastometry identifies patients who need extra anticoagulation against venous thromboembolism following bariatric surgery.
Major finding: Baseline and postop coagulation were similar: 37.5% vs. 42.5% were normal and 57.5% vs 57.5% were hypercoagulable.
Study details: Prospective study of 40 bariatric surgery patients.
Disclosures: The investigators did not have any relevant disclosures. The Lake Erie College of Osteopathic Medicine paid for the testing.
Source: Urias D et al. World Congress of Endoscopic Surgery hosted by SAGES & CAGS abstract S023.
The ‘holy grail’ of thrombosis prevention
SAN DIEGO – The “holy grail” of thrombosis prevention is the ability to determine the risk of recurrence with or without continuation of anticoagulant treatment, according to Philip S. Wells, MD.
“Very little data exists for the comparison of active treatment to placebo in the acute and long-term phases of treatment,” he said at the biennial summit of the Thrombosis & Hemostasis Societies of North America. “With low molecular weight heparin, vitamin K antagonists, and direct-acting oral anticoagulants, the relative risk reduction is about 90% in the acute phase and 80%-85% in the extended phase. After discontinuing anticoagulants, the absolute risk of recurrence varies depending on VTE category.”
Dr. Wells, chair and chief of the department of medicine at The Ottawa Hospital and the University of Ottawa, said that after 3 months of anticoagulation the chance of recurrence in postsurgical VTE patients is less than 1% per year. After 3 months of anticoagulant use in nonsurgical patients with provoked risk factors, it is around 4%. This includes medical patients, trauma victims, pregnant women, and patients wearing a plaster cast.
In patients who survive an unprovoked VTE, after 3-6 months of anticoagulant therapy their overall recurrence risk is 10% in the first year and 30% after 5 years. The risk of recurrence is 50% higher if a patient experiences a second unprovoked VTE, and the risk of fatality is 50% higher if the initial event was a pulmonary embolism (PE), he said.
According to the ongoing prospective Austrian Study on Recurrent Venous Thromboembolism, the risk of recurrent VTE is 20% in men and 6% in women (N Engl J Med. 2004 Jun 17;350[25]:2558-63). A multicenter prospective study in Canada yielded similar results. It found that the risk of recurrent VTE is 19% in men versus 9% in women (CMAJ 2008;179[5]:417-26).
That Canadian prospective study, led by Marc Rodger, MD, described the development of the HERDOO2 clinical decision rule for determining a patient’s risk for a recurrent VTE. This includes hyperpigmentation, edema, or redness in either leg (signs of postthrombotic syndrome), D-dimer level of 250 mcg/L or greater while on warfarin, body mass index of 30 kg/m2 or greater, and age of 65 years or older.
If patients have zero or one risk factor, the annual risk of VTE after 6 months of treatment is 1.6%, while two or more risk factors bumps the annual risk of VTE to 14.1%, according to the researchers.
In a subsequent study to validate the HERDOO2, researchers found that the risk of recurrent major VTE was 3.0% in low-risk women who discontinued oral anticoagulants (OACs), 8.1% in high-risk women and men who discontinued OACs, 1.6% in high-risk women and men who continued OACs, and 7.4% in high-risk women who discontinued OACs (BMJ 2017;356:j1065).
“I think the HERDOO2 rule is working pretty well to determine a low-risk group of women, and it’s not an unreasonable tool to be using,” Dr. Wells said.
Other variables that might help clinicians predict a patient’s VTE recurrence include the presence of recurrent venous obstruction (adjusted HR 1.32), and older age (HR 1.01 for every 1 year increase).
D-dimer levels can also be helpful. “If the serial D-dimers are positive, stay on anticoagulants,” Dr. Wells advised. “If they’re negative, discontinue anticoagulants and have the D-dimer levels repeated monthly for 3 months. If positive or positive conversions, return to OAC therapy.”
In one study, the annual risk of a VTE was 3% in the negative D-dimer patients, compared with 6.1% in those who had a history of an unprovoked VTE (Blood 2014;124:196-203).
In a separate study of 319 patients with two negative D-dimer results who did not restart anticoagulation therapy, the rate of recurrent VTE was 6.7% per patient-year (Ann Intern Med 2015;162:27-34). It was 9.7% per patient-year in men, compared with 5.4% per patient-year in women.
Dr. Wells emphasized the importance of shared decision-making with the patient when devising a strategy for long-term anticoagulation following a VTE. “We don’t have a lot of good tools, but [trying to elicit] patient preference is the right thing to try and do,” he said. “Physicians should present an unbiased perspective to patients regarding their treatment, including the benefits and harms, effect on quality of life, and cost.”
Dr. Wells also shared his current clinical approach. In women with an unprovoked VTE, he applies the HERDOO2 rule. If there’s a low recurrence risk, he discontinues the anticoagulant. If there’s a non-low recurrence risk he continues with the anticoagulant unless there’s a high risk for bleeding. Men with an unprovoked VTE receive indefinite anticoagulant therapy, but if the index event is a deep vein thrombosis (DVT), Dr. Wells applies a bleeding risk tool to help him determine management going forward. If the patient has a high risk of bleeding, he does not use an anticoagulant.
“If there is a high risk of bleeding it’s best of stay off anticoagulant therapy,” he said. “If there is an intermediate risk of bleeding and the index event was a DVT, the patient could stay off anticoagulants. I think we have a long way to go to developing tools that actually enable us to reach these points with each patient in discussions we have with them about continuing anticoagulants.”
Dr. Wells reported having received research support from BMS/Pfizer and honoraria from Bayer AG, Janssen, Pfizer, and Daiichi Sankyo. He is a member of the scientific advisory board for Bayer AG and Pfizer.
SAN DIEGO – The “holy grail” of thrombosis prevention is the ability to determine the risk of recurrence with or without continuation of anticoagulant treatment, according to Philip S. Wells, MD.
“Very little data exists for the comparison of active treatment to placebo in the acute and long-term phases of treatment,” he said at the biennial summit of the Thrombosis & Hemostasis Societies of North America. “With low molecular weight heparin, vitamin K antagonists, and direct-acting oral anticoagulants, the relative risk reduction is about 90% in the acute phase and 80%-85% in the extended phase. After discontinuing anticoagulants, the absolute risk of recurrence varies depending on VTE category.”
Dr. Wells, chair and chief of the department of medicine at The Ottawa Hospital and the University of Ottawa, said that after 3 months of anticoagulation the chance of recurrence in postsurgical VTE patients is less than 1% per year. After 3 months of anticoagulant use in nonsurgical patients with provoked risk factors, it is around 4%. This includes medical patients, trauma victims, pregnant women, and patients wearing a plaster cast.
In patients who survive an unprovoked VTE, after 3-6 months of anticoagulant therapy their overall recurrence risk is 10% in the first year and 30% after 5 years. The risk of recurrence is 50% higher if a patient experiences a second unprovoked VTE, and the risk of fatality is 50% higher if the initial event was a pulmonary embolism (PE), he said.
According to the ongoing prospective Austrian Study on Recurrent Venous Thromboembolism, the risk of recurrent VTE is 20% in men and 6% in women (N Engl J Med. 2004 Jun 17;350[25]:2558-63). A multicenter prospective study in Canada yielded similar results. It found that the risk of recurrent VTE is 19% in men versus 9% in women (CMAJ 2008;179[5]:417-26).
That Canadian prospective study, led by Marc Rodger, MD, described the development of the HERDOO2 clinical decision rule for determining a patient’s risk for a recurrent VTE. This includes hyperpigmentation, edema, or redness in either leg (signs of postthrombotic syndrome), D-dimer level of 250 mcg/L or greater while on warfarin, body mass index of 30 kg/m2 or greater, and age of 65 years or older.
If patients have zero or one risk factor, the annual risk of VTE after 6 months of treatment is 1.6%, while two or more risk factors bumps the annual risk of VTE to 14.1%, according to the researchers.
In a subsequent study to validate the HERDOO2, researchers found that the risk of recurrent major VTE was 3.0% in low-risk women who discontinued oral anticoagulants (OACs), 8.1% in high-risk women and men who discontinued OACs, 1.6% in high-risk women and men who continued OACs, and 7.4% in high-risk women who discontinued OACs (BMJ 2017;356:j1065).
“I think the HERDOO2 rule is working pretty well to determine a low-risk group of women, and it’s not an unreasonable tool to be using,” Dr. Wells said.
Other variables that might help clinicians predict a patient’s VTE recurrence include the presence of recurrent venous obstruction (adjusted HR 1.32), and older age (HR 1.01 for every 1 year increase).
D-dimer levels can also be helpful. “If the serial D-dimers are positive, stay on anticoagulants,” Dr. Wells advised. “If they’re negative, discontinue anticoagulants and have the D-dimer levels repeated monthly for 3 months. If positive or positive conversions, return to OAC therapy.”
In one study, the annual risk of a VTE was 3% in the negative D-dimer patients, compared with 6.1% in those who had a history of an unprovoked VTE (Blood 2014;124:196-203).
In a separate study of 319 patients with two negative D-dimer results who did not restart anticoagulation therapy, the rate of recurrent VTE was 6.7% per patient-year (Ann Intern Med 2015;162:27-34). It was 9.7% per patient-year in men, compared with 5.4% per patient-year in women.
Dr. Wells emphasized the importance of shared decision-making with the patient when devising a strategy for long-term anticoagulation following a VTE. “We don’t have a lot of good tools, but [trying to elicit] patient preference is the right thing to try and do,” he said. “Physicians should present an unbiased perspective to patients regarding their treatment, including the benefits and harms, effect on quality of life, and cost.”
Dr. Wells also shared his current clinical approach. In women with an unprovoked VTE, he applies the HERDOO2 rule. If there’s a low recurrence risk, he discontinues the anticoagulant. If there’s a non-low recurrence risk he continues with the anticoagulant unless there’s a high risk for bleeding. Men with an unprovoked VTE receive indefinite anticoagulant therapy, but if the index event is a deep vein thrombosis (DVT), Dr. Wells applies a bleeding risk tool to help him determine management going forward. If the patient has a high risk of bleeding, he does not use an anticoagulant.
“If there is a high risk of bleeding it’s best of stay off anticoagulant therapy,” he said. “If there is an intermediate risk of bleeding and the index event was a DVT, the patient could stay off anticoagulants. I think we have a long way to go to developing tools that actually enable us to reach these points with each patient in discussions we have with them about continuing anticoagulants.”
Dr. Wells reported having received research support from BMS/Pfizer and honoraria from Bayer AG, Janssen, Pfizer, and Daiichi Sankyo. He is a member of the scientific advisory board for Bayer AG and Pfizer.
SAN DIEGO – The “holy grail” of thrombosis prevention is the ability to determine the risk of recurrence with or without continuation of anticoagulant treatment, according to Philip S. Wells, MD.
“Very little data exists for the comparison of active treatment to placebo in the acute and long-term phases of treatment,” he said at the biennial summit of the Thrombosis & Hemostasis Societies of North America. “With low molecular weight heparin, vitamin K antagonists, and direct-acting oral anticoagulants, the relative risk reduction is about 90% in the acute phase and 80%-85% in the extended phase. After discontinuing anticoagulants, the absolute risk of recurrence varies depending on VTE category.”
Dr. Wells, chair and chief of the department of medicine at The Ottawa Hospital and the University of Ottawa, said that after 3 months of anticoagulation the chance of recurrence in postsurgical VTE patients is less than 1% per year. After 3 months of anticoagulant use in nonsurgical patients with provoked risk factors, it is around 4%. This includes medical patients, trauma victims, pregnant women, and patients wearing a plaster cast.
In patients who survive an unprovoked VTE, after 3-6 months of anticoagulant therapy their overall recurrence risk is 10% in the first year and 30% after 5 years. The risk of recurrence is 50% higher if a patient experiences a second unprovoked VTE, and the risk of fatality is 50% higher if the initial event was a pulmonary embolism (PE), he said.
According to the ongoing prospective Austrian Study on Recurrent Venous Thromboembolism, the risk of recurrent VTE is 20% in men and 6% in women (N Engl J Med. 2004 Jun 17;350[25]:2558-63). A multicenter prospective study in Canada yielded similar results. It found that the risk of recurrent VTE is 19% in men versus 9% in women (CMAJ 2008;179[5]:417-26).
That Canadian prospective study, led by Marc Rodger, MD, described the development of the HERDOO2 clinical decision rule for determining a patient’s risk for a recurrent VTE. This includes hyperpigmentation, edema, or redness in either leg (signs of postthrombotic syndrome), D-dimer level of 250 mcg/L or greater while on warfarin, body mass index of 30 kg/m2 or greater, and age of 65 years or older.
If patients have zero or one risk factor, the annual risk of VTE after 6 months of treatment is 1.6%, while two or more risk factors bumps the annual risk of VTE to 14.1%, according to the researchers.
In a subsequent study to validate the HERDOO2, researchers found that the risk of recurrent major VTE was 3.0% in low-risk women who discontinued oral anticoagulants (OACs), 8.1% in high-risk women and men who discontinued OACs, 1.6% in high-risk women and men who continued OACs, and 7.4% in high-risk women who discontinued OACs (BMJ 2017;356:j1065).
“I think the HERDOO2 rule is working pretty well to determine a low-risk group of women, and it’s not an unreasonable tool to be using,” Dr. Wells said.
Other variables that might help clinicians predict a patient’s VTE recurrence include the presence of recurrent venous obstruction (adjusted HR 1.32), and older age (HR 1.01 for every 1 year increase).
D-dimer levels can also be helpful. “If the serial D-dimers are positive, stay on anticoagulants,” Dr. Wells advised. “If they’re negative, discontinue anticoagulants and have the D-dimer levels repeated monthly for 3 months. If positive or positive conversions, return to OAC therapy.”
In one study, the annual risk of a VTE was 3% in the negative D-dimer patients, compared with 6.1% in those who had a history of an unprovoked VTE (Blood 2014;124:196-203).
In a separate study of 319 patients with two negative D-dimer results who did not restart anticoagulation therapy, the rate of recurrent VTE was 6.7% per patient-year (Ann Intern Med 2015;162:27-34). It was 9.7% per patient-year in men, compared with 5.4% per patient-year in women.
Dr. Wells emphasized the importance of shared decision-making with the patient when devising a strategy for long-term anticoagulation following a VTE. “We don’t have a lot of good tools, but [trying to elicit] patient preference is the right thing to try and do,” he said. “Physicians should present an unbiased perspective to patients regarding their treatment, including the benefits and harms, effect on quality of life, and cost.”
Dr. Wells also shared his current clinical approach. In women with an unprovoked VTE, he applies the HERDOO2 rule. If there’s a low recurrence risk, he discontinues the anticoagulant. If there’s a non-low recurrence risk he continues with the anticoagulant unless there’s a high risk for bleeding. Men with an unprovoked VTE receive indefinite anticoagulant therapy, but if the index event is a deep vein thrombosis (DVT), Dr. Wells applies a bleeding risk tool to help him determine management going forward. If the patient has a high risk of bleeding, he does not use an anticoagulant.
“If there is a high risk of bleeding it’s best of stay off anticoagulant therapy,” he said. “If there is an intermediate risk of bleeding and the index event was a DVT, the patient could stay off anticoagulants. I think we have a long way to go to developing tools that actually enable us to reach these points with each patient in discussions we have with them about continuing anticoagulants.”
Dr. Wells reported having received research support from BMS/Pfizer and honoraria from Bayer AG, Janssen, Pfizer, and Daiichi Sankyo. He is a member of the scientific advisory board for Bayer AG and Pfizer.
EXPERT ANALYSIS FROM THSNA 2018









