User login
Official Newspaper of the American College of Surgeons
Will AI or robotics steal your job?
NEW YORK – Artificial intelligence is currently linked to specific problem solving and is not some form of Terminator model capable of handling multiple tasks with autonomy. In other words, each time you hear the term “AI,” it is a computer solving a specific problem or task using algorithms “and not ‘thinking’ like you and me,” said Ido Weinberg, MD, assistant professor, Harvard Medical School, Boston.
AI is present in daily life – everything from cellphones to the Alexa voice interface on a smart speaker. That AI system, however, is amassing data, learning about you, and using that data intelligently, Dr. Weinberg said at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
AI in health care make sense, he said, because the health sector is a vast consumer market with potential for financial gain. Repetition, which is common in the health sector, is one of the foundations required for using AI and robotics. If a task can be repeated, then it means a machine can do it, said Dr. Weinberg.
The spread of AI and robotics one day may improve health care accessibility in remote areas where physicians with the appropriate training may not be available.
AI is already at work in the health care industry. “Pulmonary nodule detection can be done better with machines than by people, pathological identification and scanning of various slides can be done better by a machine than by a humans,” he said.
Artificial intelligence also can be designed to detect emotion by assessing various cues in phrasing, key words, and tone. These AI functions already are being used by sales reps on the phone to defuse and control interactions with customers and complainants. AI also can be implemented in interactions with people, which is an important part of dealing with patients, Dr. Weinberg said. Drug discovery is a key area where AI is flourishing, as well.
Luckily, in terms of physicians keeping their jobs, there are barriers to the use of AI to replace clinicians, Dr. Weinberg pointed out. Health care is not a monolith, and every specialty is different, meaning AI would have to be tailored to each task and specialty for each unique field. Quick proliferation of AI across the board is unlikely, especially when the varying roles of nurses and physician assistants are included.
Although robots in science fiction stories and films often are capable of multitasking a variety of needs, robots at present are much more limited in real life. In surgical situations, for example, they can perform specifically tailored tasks but cannot extend beyond those defined parameters as a real surgeon can, according to Dr. Weinberg, and this lack of flexibility is a severe limitation on the expansion of AI into health care.
Despite these limitations, Dr. Weinberg urged attendees to consider how AI can be used to facilitate their work.
“Believe in the roadblocks, but be a fast adopter – an early adopter – and understand where AI can currently augment you and make you better and more productive,” he said. “And keep doing procedures; AI and robotics currently have a problem with most of those,” Dr. Weinberg concluded.
Dr. Weinberg reported no conflicts relevant to his talk.
NEW YORK – Artificial intelligence is currently linked to specific problem solving and is not some form of Terminator model capable of handling multiple tasks with autonomy. In other words, each time you hear the term “AI,” it is a computer solving a specific problem or task using algorithms “and not ‘thinking’ like you and me,” said Ido Weinberg, MD, assistant professor, Harvard Medical School, Boston.
AI is present in daily life – everything from cellphones to the Alexa voice interface on a smart speaker. That AI system, however, is amassing data, learning about you, and using that data intelligently, Dr. Weinberg said at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
AI in health care make sense, he said, because the health sector is a vast consumer market with potential for financial gain. Repetition, which is common in the health sector, is one of the foundations required for using AI and robotics. If a task can be repeated, then it means a machine can do it, said Dr. Weinberg.
The spread of AI and robotics one day may improve health care accessibility in remote areas where physicians with the appropriate training may not be available.
AI is already at work in the health care industry. “Pulmonary nodule detection can be done better with machines than by people, pathological identification and scanning of various slides can be done better by a machine than by a humans,” he said.
Artificial intelligence also can be designed to detect emotion by assessing various cues in phrasing, key words, and tone. These AI functions already are being used by sales reps on the phone to defuse and control interactions with customers and complainants. AI also can be implemented in interactions with people, which is an important part of dealing with patients, Dr. Weinberg said. Drug discovery is a key area where AI is flourishing, as well.
Luckily, in terms of physicians keeping their jobs, there are barriers to the use of AI to replace clinicians, Dr. Weinberg pointed out. Health care is not a monolith, and every specialty is different, meaning AI would have to be tailored to each task and specialty for each unique field. Quick proliferation of AI across the board is unlikely, especially when the varying roles of nurses and physician assistants are included.
Although robots in science fiction stories and films often are capable of multitasking a variety of needs, robots at present are much more limited in real life. In surgical situations, for example, they can perform specifically tailored tasks but cannot extend beyond those defined parameters as a real surgeon can, according to Dr. Weinberg, and this lack of flexibility is a severe limitation on the expansion of AI into health care.
Despite these limitations, Dr. Weinberg urged attendees to consider how AI can be used to facilitate their work.
“Believe in the roadblocks, but be a fast adopter – an early adopter – and understand where AI can currently augment you and make you better and more productive,” he said. “And keep doing procedures; AI and robotics currently have a problem with most of those,” Dr. Weinberg concluded.
Dr. Weinberg reported no conflicts relevant to his talk.
NEW YORK – Artificial intelligence is currently linked to specific problem solving and is not some form of Terminator model capable of handling multiple tasks with autonomy. In other words, each time you hear the term “AI,” it is a computer solving a specific problem or task using algorithms “and not ‘thinking’ like you and me,” said Ido Weinberg, MD, assistant professor, Harvard Medical School, Boston.
AI is present in daily life – everything from cellphones to the Alexa voice interface on a smart speaker. That AI system, however, is amassing data, learning about you, and using that data intelligently, Dr. Weinberg said at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
AI in health care make sense, he said, because the health sector is a vast consumer market with potential for financial gain. Repetition, which is common in the health sector, is one of the foundations required for using AI and robotics. If a task can be repeated, then it means a machine can do it, said Dr. Weinberg.
The spread of AI and robotics one day may improve health care accessibility in remote areas where physicians with the appropriate training may not be available.
AI is already at work in the health care industry. “Pulmonary nodule detection can be done better with machines than by people, pathological identification and scanning of various slides can be done better by a machine than by a humans,” he said.
Artificial intelligence also can be designed to detect emotion by assessing various cues in phrasing, key words, and tone. These AI functions already are being used by sales reps on the phone to defuse and control interactions with customers and complainants. AI also can be implemented in interactions with people, which is an important part of dealing with patients, Dr. Weinberg said. Drug discovery is a key area where AI is flourishing, as well.
Luckily, in terms of physicians keeping their jobs, there are barriers to the use of AI to replace clinicians, Dr. Weinberg pointed out. Health care is not a monolith, and every specialty is different, meaning AI would have to be tailored to each task and specialty for each unique field. Quick proliferation of AI across the board is unlikely, especially when the varying roles of nurses and physician assistants are included.
Although robots in science fiction stories and films often are capable of multitasking a variety of needs, robots at present are much more limited in real life. In surgical situations, for example, they can perform specifically tailored tasks but cannot extend beyond those defined parameters as a real surgeon can, according to Dr. Weinberg, and this lack of flexibility is a severe limitation on the expansion of AI into health care.
Despite these limitations, Dr. Weinberg urged attendees to consider how AI can be used to facilitate their work.
“Believe in the roadblocks, but be a fast adopter – an early adopter – and understand where AI can currently augment you and make you better and more productive,” he said. “And keep doing procedures; AI and robotics currently have a problem with most of those,” Dr. Weinberg concluded.
Dr. Weinberg reported no conflicts relevant to his talk.
REPORTING FROM THE VEITHSYMPOSIUM
Open enrollment: HealthCare.gov busier in week 2
but the gap has closed since week 1, according to the Centers for Medicare & Medicaid Services.
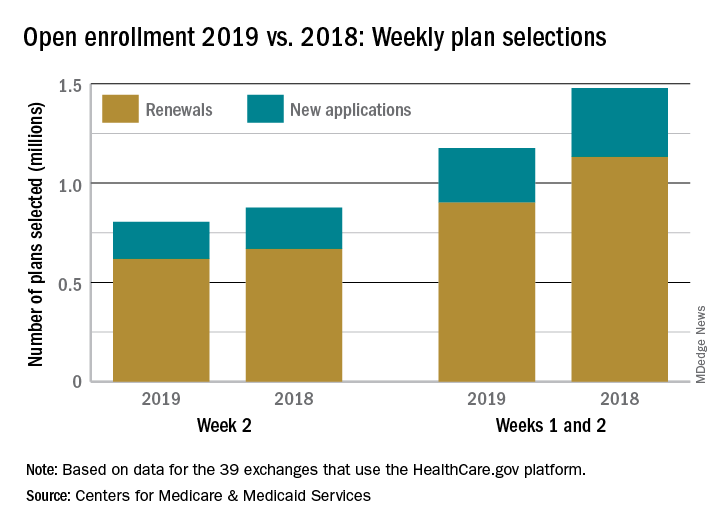
With almost 805,000 plans selected this year during the second week (Nov. 4-10) of open enrollment, the total for the 2019 coverage year stands at nearly 1.18 million for the 39 states that use the HealthCare.gov platform, which is down 20.4% from the 1.48 million plans selected through the first 2 weeks of last year’s enrollment period. After week 1, this year’s total enrollment was down by 38%, compared with last year, CMS data show.
Consumers renewing their insurance plans account for the majority selected for 2019 coverage – 619,000 in week 2 and 901,000 for weeks 1 and 2 (close to 77% in each case) – with the rest coming from new consumers – 186,000 in week 2 and 275,000 overall. The figures reported in the weekly enrollment snapshot could change later since they represent selections only and not “consumers who have paid premiums to effectuate their enrollment,” CMS said.
but the gap has closed since week 1, according to the Centers for Medicare & Medicaid Services.
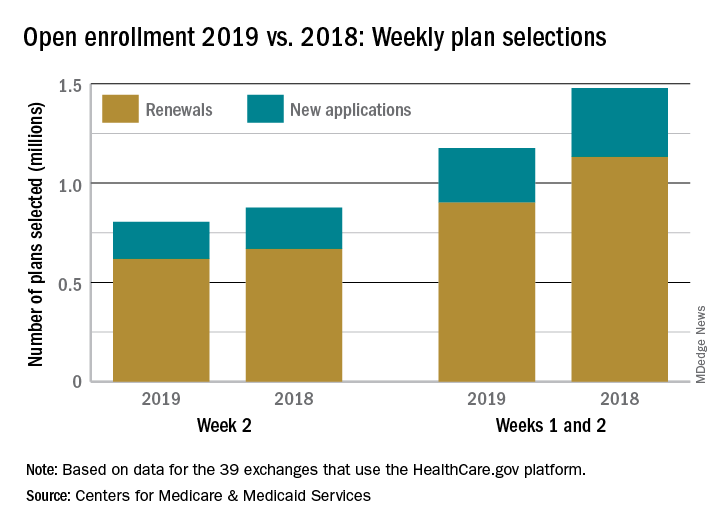
With almost 805,000 plans selected this year during the second week (Nov. 4-10) of open enrollment, the total for the 2019 coverage year stands at nearly 1.18 million for the 39 states that use the HealthCare.gov platform, which is down 20.4% from the 1.48 million plans selected through the first 2 weeks of last year’s enrollment period. After week 1, this year’s total enrollment was down by 38%, compared with last year, CMS data show.
Consumers renewing their insurance plans account for the majority selected for 2019 coverage – 619,000 in week 2 and 901,000 for weeks 1 and 2 (close to 77% in each case) – with the rest coming from new consumers – 186,000 in week 2 and 275,000 overall. The figures reported in the weekly enrollment snapshot could change later since they represent selections only and not “consumers who have paid premiums to effectuate their enrollment,” CMS said.
but the gap has closed since week 1, according to the Centers for Medicare & Medicaid Services.
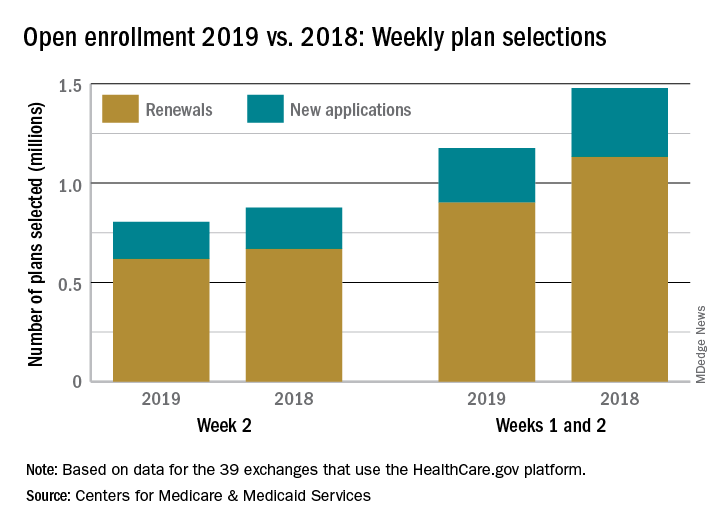
With almost 805,000 plans selected this year during the second week (Nov. 4-10) of open enrollment, the total for the 2019 coverage year stands at nearly 1.18 million for the 39 states that use the HealthCare.gov platform, which is down 20.4% from the 1.48 million plans selected through the first 2 weeks of last year’s enrollment period. After week 1, this year’s total enrollment was down by 38%, compared with last year, CMS data show.
Consumers renewing their insurance plans account for the majority selected for 2019 coverage – 619,000 in week 2 and 901,000 for weeks 1 and 2 (close to 77% in each case) – with the rest coming from new consumers – 186,000 in week 2 and 275,000 overall. The figures reported in the weekly enrollment snapshot could change later since they represent selections only and not “consumers who have paid premiums to effectuate their enrollment,” CMS said.
VQI-VVR registry data eyed for guiding development of ethical standards
NEW YORK – Registry data can be used to craft guidance for determining the appropriateness of procedures at vein centers, based on data presented by Thomas W. Wakefield, MD at the 2018 Veith Symposium.
The Vascular Quality Initiative Varicose Vein Registry (VQI-VVR), initiated in 2014 by the Society for Vascular Surgery in conjunction with the American Venous Forum, captures procedures that are performed in vein centers, office-based practices, and ambulatory or inpatient settings. The VVR looks at ablation and phlebectomy techniques and captures data including patient demographics, history, procedure data, plus early and late office-based and patient-reported follow-up in order to benchmark and improve outcomes and develop best practices and to help meet vein center certification requirements. The VVR includes 39 centers and more than 23,000 procedures.
Dr. Wakefield, who heads the VVR, used this registry as a means to illustrate how VQIs could be used to establish whether “the expected health benefit exceeds the expected negative consequences by a sufficiently wide margin that the procedure is worth doing.” This can be considered to be “appropriateness, which is part of ethical treatment.” Dr. Wakefield is the Stanley Professor of Vascular Surgery at the University of Michigan and section head, vascular surgery, University of Michigan Cardiovascular Center, Ann Arbor.
Data from the VQI registry (of which the VVR is a component) are now being used to generate appropriateness reports, said Dr. Wakefield.
The VQI represents a large comprehensive database of long-term data to define appropriate care. In addition, the VQI infrastructure is already geared to producing these reports both at a center and at a surgeon level. One disadvantage of the VVR registry, however, is low participation – only the 39 centers – and that it doesn’t capture cosmetic procedures and lesser (C1) disease. Further, it’s “likely the VQI participants are the ‘good actors,’ ” he added.
Targets for appropriateness include the proportion of patients undergoing ablation C2 or C4 disease or greater, the mean number of ablations per patient, the mean number of ablations per limb, and the proportion of perforated ablations for greater than C4 disease. Plotting out the data for these procedures at the center level can be assessed against current thinking on best practices in the various areas. For example, “the mean number of ablations per patient has been suggested at 1.8 to be about the right number,” and he used the graph of the center performance in this area to show that most of the centers were below this objective.
In an even more appropriate example of how this kind of data could be used to determine appropriateness, Dr. Wakefield described how perforated ablations should be performed for greater than C4 disease, but not for C2 disease. He described how, according to the actual data in the registry, there have been 870 total perforated treatments recorded, 38% for C2 disease, and of these 332 procedures, almost half of these were performed at one center only, with two other centers reporting 30 such procedures. “So clearly there are three centers that are doing perforated ablations for patients that are outside the guidelines,” Dr. Wakefield pointed out.
In future, payer demand is likely to demand that each treating physician provide evidence of the appropriateness of procedures performed, as well as appropriate patient selection and adherence to best practices, and good outcomes, which is part of what a society-based registry such as the VVR can provide.
“I believe the VQI-VVR is well-positioned to meet these needs. And if we ask the question ‘can VQI be used as a benchmark for setting ethical standards,’ I think it can certainly be used to help set appropriate standards, and since appropriateness is one part of ethical standards, I believe it has a role,” he concluded.
Dr. Wakefield reported that he had no disclosures.
NEW YORK – Registry data can be used to craft guidance for determining the appropriateness of procedures at vein centers, based on data presented by Thomas W. Wakefield, MD at the 2018 Veith Symposium.
The Vascular Quality Initiative Varicose Vein Registry (VQI-VVR), initiated in 2014 by the Society for Vascular Surgery in conjunction with the American Venous Forum, captures procedures that are performed in vein centers, office-based practices, and ambulatory or inpatient settings. The VVR looks at ablation and phlebectomy techniques and captures data including patient demographics, history, procedure data, plus early and late office-based and patient-reported follow-up in order to benchmark and improve outcomes and develop best practices and to help meet vein center certification requirements. The VVR includes 39 centers and more than 23,000 procedures.
Dr. Wakefield, who heads the VVR, used this registry as a means to illustrate how VQIs could be used to establish whether “the expected health benefit exceeds the expected negative consequences by a sufficiently wide margin that the procedure is worth doing.” This can be considered to be “appropriateness, which is part of ethical treatment.” Dr. Wakefield is the Stanley Professor of Vascular Surgery at the University of Michigan and section head, vascular surgery, University of Michigan Cardiovascular Center, Ann Arbor.
Data from the VQI registry (of which the VVR is a component) are now being used to generate appropriateness reports, said Dr. Wakefield.
The VQI represents a large comprehensive database of long-term data to define appropriate care. In addition, the VQI infrastructure is already geared to producing these reports both at a center and at a surgeon level. One disadvantage of the VVR registry, however, is low participation – only the 39 centers – and that it doesn’t capture cosmetic procedures and lesser (C1) disease. Further, it’s “likely the VQI participants are the ‘good actors,’ ” he added.
Targets for appropriateness include the proportion of patients undergoing ablation C2 or C4 disease or greater, the mean number of ablations per patient, the mean number of ablations per limb, and the proportion of perforated ablations for greater than C4 disease. Plotting out the data for these procedures at the center level can be assessed against current thinking on best practices in the various areas. For example, “the mean number of ablations per patient has been suggested at 1.8 to be about the right number,” and he used the graph of the center performance in this area to show that most of the centers were below this objective.
In an even more appropriate example of how this kind of data could be used to determine appropriateness, Dr. Wakefield described how perforated ablations should be performed for greater than C4 disease, but not for C2 disease. He described how, according to the actual data in the registry, there have been 870 total perforated treatments recorded, 38% for C2 disease, and of these 332 procedures, almost half of these were performed at one center only, with two other centers reporting 30 such procedures. “So clearly there are three centers that are doing perforated ablations for patients that are outside the guidelines,” Dr. Wakefield pointed out.
In future, payer demand is likely to demand that each treating physician provide evidence of the appropriateness of procedures performed, as well as appropriate patient selection and adherence to best practices, and good outcomes, which is part of what a society-based registry such as the VVR can provide.
“I believe the VQI-VVR is well-positioned to meet these needs. And if we ask the question ‘can VQI be used as a benchmark for setting ethical standards,’ I think it can certainly be used to help set appropriate standards, and since appropriateness is one part of ethical standards, I believe it has a role,” he concluded.
Dr. Wakefield reported that he had no disclosures.
NEW YORK – Registry data can be used to craft guidance for determining the appropriateness of procedures at vein centers, based on data presented by Thomas W. Wakefield, MD at the 2018 Veith Symposium.
The Vascular Quality Initiative Varicose Vein Registry (VQI-VVR), initiated in 2014 by the Society for Vascular Surgery in conjunction with the American Venous Forum, captures procedures that are performed in vein centers, office-based practices, and ambulatory or inpatient settings. The VVR looks at ablation and phlebectomy techniques and captures data including patient demographics, history, procedure data, plus early and late office-based and patient-reported follow-up in order to benchmark and improve outcomes and develop best practices and to help meet vein center certification requirements. The VVR includes 39 centers and more than 23,000 procedures.
Dr. Wakefield, who heads the VVR, used this registry as a means to illustrate how VQIs could be used to establish whether “the expected health benefit exceeds the expected negative consequences by a sufficiently wide margin that the procedure is worth doing.” This can be considered to be “appropriateness, which is part of ethical treatment.” Dr. Wakefield is the Stanley Professor of Vascular Surgery at the University of Michigan and section head, vascular surgery, University of Michigan Cardiovascular Center, Ann Arbor.
Data from the VQI registry (of which the VVR is a component) are now being used to generate appropriateness reports, said Dr. Wakefield.
The VQI represents a large comprehensive database of long-term data to define appropriate care. In addition, the VQI infrastructure is already geared to producing these reports both at a center and at a surgeon level. One disadvantage of the VVR registry, however, is low participation – only the 39 centers – and that it doesn’t capture cosmetic procedures and lesser (C1) disease. Further, it’s “likely the VQI participants are the ‘good actors,’ ” he added.
Targets for appropriateness include the proportion of patients undergoing ablation C2 or C4 disease or greater, the mean number of ablations per patient, the mean number of ablations per limb, and the proportion of perforated ablations for greater than C4 disease. Plotting out the data for these procedures at the center level can be assessed against current thinking on best practices in the various areas. For example, “the mean number of ablations per patient has been suggested at 1.8 to be about the right number,” and he used the graph of the center performance in this area to show that most of the centers were below this objective.
In an even more appropriate example of how this kind of data could be used to determine appropriateness, Dr. Wakefield described how perforated ablations should be performed for greater than C4 disease, but not for C2 disease. He described how, according to the actual data in the registry, there have been 870 total perforated treatments recorded, 38% for C2 disease, and of these 332 procedures, almost half of these were performed at one center only, with two other centers reporting 30 such procedures. “So clearly there are three centers that are doing perforated ablations for patients that are outside the guidelines,” Dr. Wakefield pointed out.
In future, payer demand is likely to demand that each treating physician provide evidence of the appropriateness of procedures performed, as well as appropriate patient selection and adherence to best practices, and good outcomes, which is part of what a society-based registry such as the VVR can provide.
“I believe the VQI-VVR is well-positioned to meet these needs. And if we ask the question ‘can VQI be used as a benchmark for setting ethical standards,’ I think it can certainly be used to help set appropriate standards, and since appropriateness is one part of ethical standards, I believe it has a role,” he concluded.
Dr. Wakefield reported that he had no disclosures.
REPORTING FROM THE 2018 VEITH SYMPOSIUM
Change is upon us
It shouldn’t be a surprise. Although we don’t necessarily welcome change, change is a constant in our world. Nothing new here – it has always been so. Most of us dread change, because of our natural apprehension of the unknown. New ideas and ways of functioning that disrupt the status quo require effort, adjustment, and learning with no guarantee of success.
In my lifetime alone, ways of communicating with one another have undergone so many changes that it’s dizzying to contemplate. When I was a child in rural Oregon, our means of communicating with friends and family was the “party line” (by which was meant, not the political party, but the community’s telephone connection). We didn’t have a separate phone number, but rather a ring that was specific to our family. Most people on the line knew each other’s ring and could surreptitiously listen in if curiosity got the best of them. Privacy was not a big consideration.
Fast forward just over a half-century, and our system of communication is barely recognizable: 24/7 connectivity on hand-held electronic devices to any part of the world, SMS, Skype, Facebook, texting. Instantaneous worldwide communication is a given from anywhere, even the golf course.
Yes, there are hazards in this convenience. Recent events have demonstrated the lack of privacy and security of our communications, and what you see is not necessarily what it appears to be. It has become abundantly clear just how fragile the process of exchanging valid information can be. And yet, who would wish to erase all of this convenience to go back to the old days before the Internet? I doubt seriously that many surgeons would exchange the old world of limited access to information and communication for our era of immersive connectivity.
A comparable progression has occurred in our methods of professional learning and moving our corpus of knowledge forward. For the past half-century and more, new techniques, knowledge, and ideas have been presented in meetings of established societies and published in peer-reviewed journals. Unfortunately, not all who might benefit from these new ideas have access to them. If you belong to the society, can afford the time and money to attend the meeting, and work in an institution that subscribes to online access to all of the major journals, you can read them. Surgeons in independent practice in rural, remote communities likely do not have that luxury. ACS Surgery News has had many functions but one of the most important has been to serve surgeons in those remote communities as well as for others who simply wanted the convenience of ready access to new information all in one place.
Unfortunately, print publications are becoming more expensive to produce and mail, and advertising dollars to subsidize them are shrinking. Thus, Tyler Hughes and I, the coeditors of ACS Surgery News, were informed that our publication will cease production after the December 2018 issue. We and the ACS leadership huddled to find a way to continue what we all believe is a benefit to our ACS Fellows, particularly those who practice in small rural hospitals. The answer was right in front of us: The ACS Communities, to which all Fellows have online access. So that is our plan: Tyler and I will continue to write our “homespun” commentaries, and our editorial board will contribute concise articles that summarize the “latest and greatest” presentations at meetings they attend or from recently published articles in major journals across the spectrum of general surgery and surgical specialties. If readers have questions or comments, they will be able to communicate with the authors for clarification. We hope that this structure and content will benefit our surgical colleagues. Look for our new ACS Communities presence in January 2019.
Dr. Deveney is professor of surgery emerita in the department of surgery at Oregon Health & Science University, Portland. She is the coeditor of ACS Surgery News.
It shouldn’t be a surprise. Although we don’t necessarily welcome change, change is a constant in our world. Nothing new here – it has always been so. Most of us dread change, because of our natural apprehension of the unknown. New ideas and ways of functioning that disrupt the status quo require effort, adjustment, and learning with no guarantee of success.
In my lifetime alone, ways of communicating with one another have undergone so many changes that it’s dizzying to contemplate. When I was a child in rural Oregon, our means of communicating with friends and family was the “party line” (by which was meant, not the political party, but the community’s telephone connection). We didn’t have a separate phone number, but rather a ring that was specific to our family. Most people on the line knew each other’s ring and could surreptitiously listen in if curiosity got the best of them. Privacy was not a big consideration.
Fast forward just over a half-century, and our system of communication is barely recognizable: 24/7 connectivity on hand-held electronic devices to any part of the world, SMS, Skype, Facebook, texting. Instantaneous worldwide communication is a given from anywhere, even the golf course.
Yes, there are hazards in this convenience. Recent events have demonstrated the lack of privacy and security of our communications, and what you see is not necessarily what it appears to be. It has become abundantly clear just how fragile the process of exchanging valid information can be. And yet, who would wish to erase all of this convenience to go back to the old days before the Internet? I doubt seriously that many surgeons would exchange the old world of limited access to information and communication for our era of immersive connectivity.
A comparable progression has occurred in our methods of professional learning and moving our corpus of knowledge forward. For the past half-century and more, new techniques, knowledge, and ideas have been presented in meetings of established societies and published in peer-reviewed journals. Unfortunately, not all who might benefit from these new ideas have access to them. If you belong to the society, can afford the time and money to attend the meeting, and work in an institution that subscribes to online access to all of the major journals, you can read them. Surgeons in independent practice in rural, remote communities likely do not have that luxury. ACS Surgery News has had many functions but one of the most important has been to serve surgeons in those remote communities as well as for others who simply wanted the convenience of ready access to new information all in one place.
Unfortunately, print publications are becoming more expensive to produce and mail, and advertising dollars to subsidize them are shrinking. Thus, Tyler Hughes and I, the coeditors of ACS Surgery News, were informed that our publication will cease production after the December 2018 issue. We and the ACS leadership huddled to find a way to continue what we all believe is a benefit to our ACS Fellows, particularly those who practice in small rural hospitals. The answer was right in front of us: The ACS Communities, to which all Fellows have online access. So that is our plan: Tyler and I will continue to write our “homespun” commentaries, and our editorial board will contribute concise articles that summarize the “latest and greatest” presentations at meetings they attend or from recently published articles in major journals across the spectrum of general surgery and surgical specialties. If readers have questions or comments, they will be able to communicate with the authors for clarification. We hope that this structure and content will benefit our surgical colleagues. Look for our new ACS Communities presence in January 2019.
Dr. Deveney is professor of surgery emerita in the department of surgery at Oregon Health & Science University, Portland. She is the coeditor of ACS Surgery News.
It shouldn’t be a surprise. Although we don’t necessarily welcome change, change is a constant in our world. Nothing new here – it has always been so. Most of us dread change, because of our natural apprehension of the unknown. New ideas and ways of functioning that disrupt the status quo require effort, adjustment, and learning with no guarantee of success.
In my lifetime alone, ways of communicating with one another have undergone so many changes that it’s dizzying to contemplate. When I was a child in rural Oregon, our means of communicating with friends and family was the “party line” (by which was meant, not the political party, but the community’s telephone connection). We didn’t have a separate phone number, but rather a ring that was specific to our family. Most people on the line knew each other’s ring and could surreptitiously listen in if curiosity got the best of them. Privacy was not a big consideration.
Fast forward just over a half-century, and our system of communication is barely recognizable: 24/7 connectivity on hand-held electronic devices to any part of the world, SMS, Skype, Facebook, texting. Instantaneous worldwide communication is a given from anywhere, even the golf course.
Yes, there are hazards in this convenience. Recent events have demonstrated the lack of privacy and security of our communications, and what you see is not necessarily what it appears to be. It has become abundantly clear just how fragile the process of exchanging valid information can be. And yet, who would wish to erase all of this convenience to go back to the old days before the Internet? I doubt seriously that many surgeons would exchange the old world of limited access to information and communication for our era of immersive connectivity.
A comparable progression has occurred in our methods of professional learning and moving our corpus of knowledge forward. For the past half-century and more, new techniques, knowledge, and ideas have been presented in meetings of established societies and published in peer-reviewed journals. Unfortunately, not all who might benefit from these new ideas have access to them. If you belong to the society, can afford the time and money to attend the meeting, and work in an institution that subscribes to online access to all of the major journals, you can read them. Surgeons in independent practice in rural, remote communities likely do not have that luxury. ACS Surgery News has had many functions but one of the most important has been to serve surgeons in those remote communities as well as for others who simply wanted the convenience of ready access to new information all in one place.
Unfortunately, print publications are becoming more expensive to produce and mail, and advertising dollars to subsidize them are shrinking. Thus, Tyler Hughes and I, the coeditors of ACS Surgery News, were informed that our publication will cease production after the December 2018 issue. We and the ACS leadership huddled to find a way to continue what we all believe is a benefit to our ACS Fellows, particularly those who practice in small rural hospitals. The answer was right in front of us: The ACS Communities, to which all Fellows have online access. So that is our plan: Tyler and I will continue to write our “homespun” commentaries, and our editorial board will contribute concise articles that summarize the “latest and greatest” presentations at meetings they attend or from recently published articles in major journals across the spectrum of general surgery and surgical specialties. If readers have questions or comments, they will be able to communicate with the authors for clarification. We hope that this structure and content will benefit our surgical colleagues. Look for our new ACS Communities presence in January 2019.
Dr. Deveney is professor of surgery emerita in the department of surgery at Oregon Health & Science University, Portland. She is the coeditor of ACS Surgery News.
Growing the pool of academic vascular surgeons
NEW YORK – Strategies for growing the pool of academic vascular surgeons might help avert the expected scarcity of physicians in this specialty, according to Peter K. Henke, MD, a professor of vascular surgery at the University of Michigan, Ann Arbor.
Dr. Henke recounted in a video interview key messages he delivered at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. He argued for going back to basics to enlist residents and fellows completing their training to stay in the specialty and consider an academic position.
Many of these steps are known, such as verifying that mentors are available to encourage skill acquisition and providing adequate time to achieve an acceptable balance of research and clinical work.
However, a successful program would not solely focus on luring young and promising junior faculty, he said. A supportive atmosphere requires collaboration and support to flow both up and down the ranks of seniority where everyone benefits.As an example, he singled out midlevel faculty as vulnerable when programs are not developed to ensure support is equally distributed. He explained that midlevel faculty members denied the encouragement available to surgeons just initiating their career can feel abandoned when they are skilled but not yet leaders in their program.
The Society of Vascular Surgery is pursing several initiatives to address the projected shortage within this specialty, according to Dr. Henke, but he argues that leaders of academic programs have a role to play in helping make the specialty attractive, particularly for those considering an academic career.
NEW YORK – Strategies for growing the pool of academic vascular surgeons might help avert the expected scarcity of physicians in this specialty, according to Peter K. Henke, MD, a professor of vascular surgery at the University of Michigan, Ann Arbor.
Dr. Henke recounted in a video interview key messages he delivered at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. He argued for going back to basics to enlist residents and fellows completing their training to stay in the specialty and consider an academic position.
Many of these steps are known, such as verifying that mentors are available to encourage skill acquisition and providing adequate time to achieve an acceptable balance of research and clinical work.
However, a successful program would not solely focus on luring young and promising junior faculty, he said. A supportive atmosphere requires collaboration and support to flow both up and down the ranks of seniority where everyone benefits.As an example, he singled out midlevel faculty as vulnerable when programs are not developed to ensure support is equally distributed. He explained that midlevel faculty members denied the encouragement available to surgeons just initiating their career can feel abandoned when they are skilled but not yet leaders in their program.
The Society of Vascular Surgery is pursing several initiatives to address the projected shortage within this specialty, according to Dr. Henke, but he argues that leaders of academic programs have a role to play in helping make the specialty attractive, particularly for those considering an academic career.
NEW YORK – Strategies for growing the pool of academic vascular surgeons might help avert the expected scarcity of physicians in this specialty, according to Peter K. Henke, MD, a professor of vascular surgery at the University of Michigan, Ann Arbor.
Dr. Henke recounted in a video interview key messages he delivered at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. He argued for going back to basics to enlist residents and fellows completing their training to stay in the specialty and consider an academic position.
Many of these steps are known, such as verifying that mentors are available to encourage skill acquisition and providing adequate time to achieve an acceptable balance of research and clinical work.
However, a successful program would not solely focus on luring young and promising junior faculty, he said. A supportive atmosphere requires collaboration and support to flow both up and down the ranks of seniority where everyone benefits.As an example, he singled out midlevel faculty as vulnerable when programs are not developed to ensure support is equally distributed. He explained that midlevel faculty members denied the encouragement available to surgeons just initiating their career can feel abandoned when they are skilled but not yet leaders in their program.
The Society of Vascular Surgery is pursing several initiatives to address the projected shortage within this specialty, according to Dr. Henke, but he argues that leaders of academic programs have a role to play in helping make the specialty attractive, particularly for those considering an academic career.
REPORTING FROM VEITHSYMPOSIUM
Drug-coated balloon advantage persists in femoral artery disease
NEW YORK – John Laird, MD, of the Adventist Heart Institute, St. Helena, Calif., presented the data at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
The data were drawn from the IN.PACT trial. In this trial, 331 patients were randomized to a paclitaxel-coated DCB device or standard percutaneous balloon angioplasty (PCBA), Dr. Laird explained.
The 5-year results are consistent with those previously reported at 1, 2, and 3 years. According to Dr. Laird, DCB continues to show an advantage for major outcomes over PCBA, and adverse events remain low.
Three DCB devices now available in the United States for dilatation of narrowed SFA. Although all have been associated with a reduced risk of target lesion revascularization relative to standard PCBA, the long-term follow-up presented from IN.PACT by Dr. Laird are the first to document 5-year outcomes.
In a video interview, Dr. Laird reported that there have been no thrombotic events since the 3-year results were presented.
Overall, he explains that the long-term outcomes provide additional confirmation that DCB is a safe procedure that reduces the need for stenting in SFA occlusions. Although he believes there might be clinically significant differences between available DCB devices, he concludes that DCB can be considered the first-line therapy for treating occluded femoral-popliteal arteries.
NEW YORK – John Laird, MD, of the Adventist Heart Institute, St. Helena, Calif., presented the data at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
The data were drawn from the IN.PACT trial. In this trial, 331 patients were randomized to a paclitaxel-coated DCB device or standard percutaneous balloon angioplasty (PCBA), Dr. Laird explained.
The 5-year results are consistent with those previously reported at 1, 2, and 3 years. According to Dr. Laird, DCB continues to show an advantage for major outcomes over PCBA, and adverse events remain low.
Three DCB devices now available in the United States for dilatation of narrowed SFA. Although all have been associated with a reduced risk of target lesion revascularization relative to standard PCBA, the long-term follow-up presented from IN.PACT by Dr. Laird are the first to document 5-year outcomes.
In a video interview, Dr. Laird reported that there have been no thrombotic events since the 3-year results were presented.
Overall, he explains that the long-term outcomes provide additional confirmation that DCB is a safe procedure that reduces the need for stenting in SFA occlusions. Although he believes there might be clinically significant differences between available DCB devices, he concludes that DCB can be considered the first-line therapy for treating occluded femoral-popliteal arteries.
NEW YORK – John Laird, MD, of the Adventist Heart Institute, St. Helena, Calif., presented the data at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
The data were drawn from the IN.PACT trial. In this trial, 331 patients were randomized to a paclitaxel-coated DCB device or standard percutaneous balloon angioplasty (PCBA), Dr. Laird explained.
The 5-year results are consistent with those previously reported at 1, 2, and 3 years. According to Dr. Laird, DCB continues to show an advantage for major outcomes over PCBA, and adverse events remain low.
Three DCB devices now available in the United States for dilatation of narrowed SFA. Although all have been associated with a reduced risk of target lesion revascularization relative to standard PCBA, the long-term follow-up presented from IN.PACT by Dr. Laird are the first to document 5-year outcomes.
In a video interview, Dr. Laird reported that there have been no thrombotic events since the 3-year results were presented.
Overall, he explains that the long-term outcomes provide additional confirmation that DCB is a safe procedure that reduces the need for stenting in SFA occlusions. Although he believes there might be clinically significant differences between available DCB devices, he concludes that DCB can be considered the first-line therapy for treating occluded femoral-popliteal arteries.
REPORTING FROM VEITHSYMPOSIUM
Single-port robotic sacrocolpopexy has same learning curve as multiport
LAS VEGAS – according to Israeli investigators.
Multiport sacrocolpopexy is common, but the single-port approach hasn’t really caught on yet. That’s likely to change, however, with ongoing development of the da Vinci robotic platform, said lead investigator Emad Matanes, MD, of the Rambam Medical Center, Haifa, Israel.
The medical center recently has been switching over to the single-port approach, and Dr. Matanes and his colleagues wanted to share their experience with surgeons considering doing the same.
They compared their first 52 multiport cases during Dec. 2011-Dec. 2012 to their first 52 single-port cases during Aug. 2015-Aug. 2017.
It took about 15 cases with either approach for operative times to stabilize, dropping from an average of 222 minutes to 161 minutes after the first 15 single-port cases, and from 224 to 198 minutes after the first 15 multiport cases (J Minim Invasive Gynecol. 2018 Nov-Dec;25[7]:S47-S8).
With both, “we reached our steady state after the first 15. Both approaches are feasible, and for both, surgery times improve after 15 cases,” Dr. Matanes said at the American Association of Gynecologic Laparoscopists Global Congress.
Overall, the single-port approach proved about 20 minutes quicker, due to shorter docking and anesthesia times.
There wasn’t a single prolapse recurrence in either group, even after the first few cases. There was slightly less postoperative pain with single-port surgery (visual analogue scale sore 1.5 vs. 2 points), and slightly less estimated blood loss (38 mL vs. 54 mL), but neither difference was statistically significant.
There were no statistically significant differences between women in the two groups. Their average age was 58 years, mean body mass index was 28 kg/m2, and most women had a preoperative Pelvic Organ Prolapse Quantification score of 3.
There was no outside funding, and Dr. Matanes didn’t disclose any relevant financial disclosures.
LAS VEGAS – according to Israeli investigators.
Multiport sacrocolpopexy is common, but the single-port approach hasn’t really caught on yet. That’s likely to change, however, with ongoing development of the da Vinci robotic platform, said lead investigator Emad Matanes, MD, of the Rambam Medical Center, Haifa, Israel.
The medical center recently has been switching over to the single-port approach, and Dr. Matanes and his colleagues wanted to share their experience with surgeons considering doing the same.
They compared their first 52 multiport cases during Dec. 2011-Dec. 2012 to their first 52 single-port cases during Aug. 2015-Aug. 2017.
It took about 15 cases with either approach for operative times to stabilize, dropping from an average of 222 minutes to 161 minutes after the first 15 single-port cases, and from 224 to 198 minutes after the first 15 multiport cases (J Minim Invasive Gynecol. 2018 Nov-Dec;25[7]:S47-S8).
With both, “we reached our steady state after the first 15. Both approaches are feasible, and for both, surgery times improve after 15 cases,” Dr. Matanes said at the American Association of Gynecologic Laparoscopists Global Congress.
Overall, the single-port approach proved about 20 minutes quicker, due to shorter docking and anesthesia times.
There wasn’t a single prolapse recurrence in either group, even after the first few cases. There was slightly less postoperative pain with single-port surgery (visual analogue scale sore 1.5 vs. 2 points), and slightly less estimated blood loss (38 mL vs. 54 mL), but neither difference was statistically significant.
There were no statistically significant differences between women in the two groups. Their average age was 58 years, mean body mass index was 28 kg/m2, and most women had a preoperative Pelvic Organ Prolapse Quantification score of 3.
There was no outside funding, and Dr. Matanes didn’t disclose any relevant financial disclosures.
LAS VEGAS – according to Israeli investigators.
Multiport sacrocolpopexy is common, but the single-port approach hasn’t really caught on yet. That’s likely to change, however, with ongoing development of the da Vinci robotic platform, said lead investigator Emad Matanes, MD, of the Rambam Medical Center, Haifa, Israel.
The medical center recently has been switching over to the single-port approach, and Dr. Matanes and his colleagues wanted to share their experience with surgeons considering doing the same.
They compared their first 52 multiport cases during Dec. 2011-Dec. 2012 to their first 52 single-port cases during Aug. 2015-Aug. 2017.
It took about 15 cases with either approach for operative times to stabilize, dropping from an average of 222 minutes to 161 minutes after the first 15 single-port cases, and from 224 to 198 minutes after the first 15 multiport cases (J Minim Invasive Gynecol. 2018 Nov-Dec;25[7]:S47-S8).
With both, “we reached our steady state after the first 15. Both approaches are feasible, and for both, surgery times improve after 15 cases,” Dr. Matanes said at the American Association of Gynecologic Laparoscopists Global Congress.
Overall, the single-port approach proved about 20 minutes quicker, due to shorter docking and anesthesia times.
There wasn’t a single prolapse recurrence in either group, even after the first few cases. There was slightly less postoperative pain with single-port surgery (visual analogue scale sore 1.5 vs. 2 points), and slightly less estimated blood loss (38 mL vs. 54 mL), but neither difference was statistically significant.
There were no statistically significant differences between women in the two groups. Their average age was 58 years, mean body mass index was 28 kg/m2, and most women had a preoperative Pelvic Organ Prolapse Quantification score of 3.
There was no outside funding, and Dr. Matanes didn’t disclose any relevant financial disclosures.
REPORTING FROM THE AAGL GLOBAL CONGRESS
What are the barriers to solving the upcoming vascular surgeon shortage?
NEW YORK – Increasing the number of 0+5 integrated vascular surgery residency programs would help to alleviate a projected shortage of vascular surgeons, according to William D. Jordan, Jr., MD, professor of surgery, Emory University, Atlanta.*
“Ultimately the question is whether the workforce pipeline is large enough,” Dr. Jordan said at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. “When you consider that there are little more than 600 vascular trainees right now, and almost 600 planned retirements over the next 5 years, the answer to the question is no. Our workforce pipeline is not big enough.”
Dr. Jordan pointed out that, in addition, if one considers the current geographic distribution of vascular surgeons across the country, and go with the new standard that 1.4 surgeons are needed per 100,000 population, there is not a single state in the country that matches up to that goal. “So we are clearly going to have a shortage,” he commented. The only way to fill that shortage is to produce more vascular surgeons. But how does the change to a 0+5 residency program model impact that need?
In a survey conducted by the Association of Program Directors in Vascular Surgery in 2016, regarding challenges as perceived by the trainees, the top two concerns expressed were regarding competing specialties and physician burnout. Statistics bear out the concern regarding competing specialties, for example, there is an increase of 85% in interventional cardiology trainees being produced and a nearly 50% increase in interventional radiology trainees. However, in vascular, it is only 18%. With regard to the goals of those vascular trainees, 90% indicated that they wanted to be attached to some academic or teaching environment. “They don’t want to be the lone wolf out there,” Dr. Jordan said, and this is from concerns regarding workload, mentorship, and camaraderie, as well as regulatory and administrative obligations that are steadily increasing and can be handled more easily in a large institution. This will not fill the need for vascular surgeons in community hospitals, creating a shortage of distribution as well as actual numbers.
One key problem with current training is the fact that the new form of student comes with almost no real surgical skills and there is a dearth of vascular surgery cases available to fully accommodate many of them throughout their training career. This is a problem exacerbated by some residency review committees, which are loathe to give vascular surgery cases to new trainees.
Integrated vascular surgery residency programs have grown and there is a substantially greater interest in them, receiving even more applicants than orthopedics or neurosurgery. U.S. interest exceeds the number of 0+5 positions available. One way to deal with the projected 31% deficit in vascular surgeons by 2025 would thus be to increase the number of these training positions. The financial accommodations to do this would be large, but perhaps the creation of an independent vascular surgery specialty board would facilitate dealing with that issue, he concluded.
Dr. Jordan reported no disclosures relevant to his talk.
Correction, 11/19/18: An earlier version of this article misidentified the speaker in the session. The speaker was William D. Jordan, Jr., MD.
NEW YORK – Increasing the number of 0+5 integrated vascular surgery residency programs would help to alleviate a projected shortage of vascular surgeons, according to William D. Jordan, Jr., MD, professor of surgery, Emory University, Atlanta.*
“Ultimately the question is whether the workforce pipeline is large enough,” Dr. Jordan said at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. “When you consider that there are little more than 600 vascular trainees right now, and almost 600 planned retirements over the next 5 years, the answer to the question is no. Our workforce pipeline is not big enough.”
Dr. Jordan pointed out that, in addition, if one considers the current geographic distribution of vascular surgeons across the country, and go with the new standard that 1.4 surgeons are needed per 100,000 population, there is not a single state in the country that matches up to that goal. “So we are clearly going to have a shortage,” he commented. The only way to fill that shortage is to produce more vascular surgeons. But how does the change to a 0+5 residency program model impact that need?
In a survey conducted by the Association of Program Directors in Vascular Surgery in 2016, regarding challenges as perceived by the trainees, the top two concerns expressed were regarding competing specialties and physician burnout. Statistics bear out the concern regarding competing specialties, for example, there is an increase of 85% in interventional cardiology trainees being produced and a nearly 50% increase in interventional radiology trainees. However, in vascular, it is only 18%. With regard to the goals of those vascular trainees, 90% indicated that they wanted to be attached to some academic or teaching environment. “They don’t want to be the lone wolf out there,” Dr. Jordan said, and this is from concerns regarding workload, mentorship, and camaraderie, as well as regulatory and administrative obligations that are steadily increasing and can be handled more easily in a large institution. This will not fill the need for vascular surgeons in community hospitals, creating a shortage of distribution as well as actual numbers.
One key problem with current training is the fact that the new form of student comes with almost no real surgical skills and there is a dearth of vascular surgery cases available to fully accommodate many of them throughout their training career. This is a problem exacerbated by some residency review committees, which are loathe to give vascular surgery cases to new trainees.
Integrated vascular surgery residency programs have grown and there is a substantially greater interest in them, receiving even more applicants than orthopedics or neurosurgery. U.S. interest exceeds the number of 0+5 positions available. One way to deal with the projected 31% deficit in vascular surgeons by 2025 would thus be to increase the number of these training positions. The financial accommodations to do this would be large, but perhaps the creation of an independent vascular surgery specialty board would facilitate dealing with that issue, he concluded.
Dr. Jordan reported no disclosures relevant to his talk.
Correction, 11/19/18: An earlier version of this article misidentified the speaker in the session. The speaker was William D. Jordan, Jr., MD.
NEW YORK – Increasing the number of 0+5 integrated vascular surgery residency programs would help to alleviate a projected shortage of vascular surgeons, according to William D. Jordan, Jr., MD, professor of surgery, Emory University, Atlanta.*
“Ultimately the question is whether the workforce pipeline is large enough,” Dr. Jordan said at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. “When you consider that there are little more than 600 vascular trainees right now, and almost 600 planned retirements over the next 5 years, the answer to the question is no. Our workforce pipeline is not big enough.”
Dr. Jordan pointed out that, in addition, if one considers the current geographic distribution of vascular surgeons across the country, and go with the new standard that 1.4 surgeons are needed per 100,000 population, there is not a single state in the country that matches up to that goal. “So we are clearly going to have a shortage,” he commented. The only way to fill that shortage is to produce more vascular surgeons. But how does the change to a 0+5 residency program model impact that need?
In a survey conducted by the Association of Program Directors in Vascular Surgery in 2016, regarding challenges as perceived by the trainees, the top two concerns expressed were regarding competing specialties and physician burnout. Statistics bear out the concern regarding competing specialties, for example, there is an increase of 85% in interventional cardiology trainees being produced and a nearly 50% increase in interventional radiology trainees. However, in vascular, it is only 18%. With regard to the goals of those vascular trainees, 90% indicated that they wanted to be attached to some academic or teaching environment. “They don’t want to be the lone wolf out there,” Dr. Jordan said, and this is from concerns regarding workload, mentorship, and camaraderie, as well as regulatory and administrative obligations that are steadily increasing and can be handled more easily in a large institution. This will not fill the need for vascular surgeons in community hospitals, creating a shortage of distribution as well as actual numbers.
One key problem with current training is the fact that the new form of student comes with almost no real surgical skills and there is a dearth of vascular surgery cases available to fully accommodate many of them throughout their training career. This is a problem exacerbated by some residency review committees, which are loathe to give vascular surgery cases to new trainees.
Integrated vascular surgery residency programs have grown and there is a substantially greater interest in them, receiving even more applicants than orthopedics or neurosurgery. U.S. interest exceeds the number of 0+5 positions available. One way to deal with the projected 31% deficit in vascular surgeons by 2025 would thus be to increase the number of these training positions. The financial accommodations to do this would be large, but perhaps the creation of an independent vascular surgery specialty board would facilitate dealing with that issue, he concluded.
Dr. Jordan reported no disclosures relevant to his talk.
Correction, 11/19/18: An earlier version of this article misidentified the speaker in the session. The speaker was William D. Jordan, Jr., MD.
REPORTING FROM THE VEITHSYMPOSIUM
A bovine arch predicts worse outcomes with type B aortic dissections
NEW YORK – The presence of a bovine arch predicts higher mortality in patients with a type B aortic dissection (TBAD), according to a study presented by Jan S. Brunkwall, MD, at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
The bovine arch is a congenital interruption in the evolution of the arch, and is a misnomer because it does not actually reflect the arch branching pattern found in cattle. It represents the most common variation of the aortic arch, with a prevalence of 1%-41%, depending on the literature, according to a study published by Dr. Brunkwall, chairman of the department of vascular and endovascular surgery at the University of Cologne (Germany), and his colleagues (Eur J Vasc Endovasc Surg. 2018; 55:385-391).
In order to assess the effect of the bovine arch on survival, Dr. Brunkwall and his colleagues performed a retrospective cohort analysis of patients with TBAD admitted at two centers. CT angiograms (CTAs) of patients referred because of aortic dissection were also reevaluated with regard to the presence of a bovine arch.
A total of 154 patients with TBAD and 168 with type A aortic dissection were assessed, and 110 oncologic patients who had undergone a chest CTA for disease staging during the study period acted as a control group.
There was an overall prevalence of 17.6% for bovine arch variants, with no statistical difference in prevalence between patients with a dissection and those in the control group, or between patients with a type A or type B dissection. However, mortality was 34.5% in patients with TBAD who had a bovine arch versus 16% in patients without a bovine arch. This was a significant difference (P =.04), according to Dr. Brunkwall.
Multivariate analysis showed that the presence of a bovine arch with TBAD was an independent predictor of mortality. “The reason for the high mortality cannot be explained by our data,” said Dr. Brunkwall, “but there has been a suggestion that the shear stress is different and higher in patients with a bovine arch leading to a stiffer aorta and more endothelial damage.”
Dr. Brunkwall reported that he had no disclosures.
NEW YORK – The presence of a bovine arch predicts higher mortality in patients with a type B aortic dissection (TBAD), according to a study presented by Jan S. Brunkwall, MD, at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
The bovine arch is a congenital interruption in the evolution of the arch, and is a misnomer because it does not actually reflect the arch branching pattern found in cattle. It represents the most common variation of the aortic arch, with a prevalence of 1%-41%, depending on the literature, according to a study published by Dr. Brunkwall, chairman of the department of vascular and endovascular surgery at the University of Cologne (Germany), and his colleagues (Eur J Vasc Endovasc Surg. 2018; 55:385-391).
In order to assess the effect of the bovine arch on survival, Dr. Brunkwall and his colleagues performed a retrospective cohort analysis of patients with TBAD admitted at two centers. CT angiograms (CTAs) of patients referred because of aortic dissection were also reevaluated with regard to the presence of a bovine arch.
A total of 154 patients with TBAD and 168 with type A aortic dissection were assessed, and 110 oncologic patients who had undergone a chest CTA for disease staging during the study period acted as a control group.
There was an overall prevalence of 17.6% for bovine arch variants, with no statistical difference in prevalence between patients with a dissection and those in the control group, or between patients with a type A or type B dissection. However, mortality was 34.5% in patients with TBAD who had a bovine arch versus 16% in patients without a bovine arch. This was a significant difference (P =.04), according to Dr. Brunkwall.
Multivariate analysis showed that the presence of a bovine arch with TBAD was an independent predictor of mortality. “The reason for the high mortality cannot be explained by our data,” said Dr. Brunkwall, “but there has been a suggestion that the shear stress is different and higher in patients with a bovine arch leading to a stiffer aorta and more endothelial damage.”
Dr. Brunkwall reported that he had no disclosures.
NEW YORK – The presence of a bovine arch predicts higher mortality in patients with a type B aortic dissection (TBAD), according to a study presented by Jan S. Brunkwall, MD, at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
The bovine arch is a congenital interruption in the evolution of the arch, and is a misnomer because it does not actually reflect the arch branching pattern found in cattle. It represents the most common variation of the aortic arch, with a prevalence of 1%-41%, depending on the literature, according to a study published by Dr. Brunkwall, chairman of the department of vascular and endovascular surgery at the University of Cologne (Germany), and his colleagues (Eur J Vasc Endovasc Surg. 2018; 55:385-391).
In order to assess the effect of the bovine arch on survival, Dr. Brunkwall and his colleagues performed a retrospective cohort analysis of patients with TBAD admitted at two centers. CT angiograms (CTAs) of patients referred because of aortic dissection were also reevaluated with regard to the presence of a bovine arch.
A total of 154 patients with TBAD and 168 with type A aortic dissection were assessed, and 110 oncologic patients who had undergone a chest CTA for disease staging during the study period acted as a control group.
There was an overall prevalence of 17.6% for bovine arch variants, with no statistical difference in prevalence between patients with a dissection and those in the control group, or between patients with a type A or type B dissection. However, mortality was 34.5% in patients with TBAD who had a bovine arch versus 16% in patients without a bovine arch. This was a significant difference (P =.04), according to Dr. Brunkwall.
Multivariate analysis showed that the presence of a bovine arch with TBAD was an independent predictor of mortality. “The reason for the high mortality cannot be explained by our data,” said Dr. Brunkwall, “but there has been a suggestion that the shear stress is different and higher in patients with a bovine arch leading to a stiffer aorta and more endothelial damage.”
Dr. Brunkwall reported that he had no disclosures.
REPORTING FROM VEITHSYMPOSIUM
Dr. Mary Edwards Walker Inspiring Women in Surgery Award presented to Dr. Lee
The American College of Surgeons (ACS) presented the Dr. Mary Edwards Walker Inspiring Women in Surgery Award to Yeu-Tsu Margaret Lee, MD, FACS, at the Convocation at Clinical Congress 2018 in Boston, MA. This award was established by the ACS Women in Surgery Committee (WiSC) and is presented annually at the Clinical Congress to recognize an individual’s significant contributions to the advancement of women in surgery.
Dr. Lee is from Honolulu, HI, and was born in Xian, China, in 1936. During her childhood, four of her siblings died from illness, motivating Dr. Lee to become a physician. Her family was forced to flee to Taiwan after the Chinese Civil War, and she immigrated to the U.S. in 1955, graduated from Harvard Medical School, Boston, in 1961, and has worked as a general surgeon and a surgical oncologist for more than 50 years. In the early 1980s, she was a tenured associate professor of surgery, University of Southern California (USC), Los Angeles, and head physician, Los Angeles County-USC Medical Center, but chose to pursue a different path.
In 1983, Dr. Lee moved to Hawaii, worked at Tripler Army Medical Center, Honolulu, as chief, surgical oncology section of general surgical services, and joined the U.S. Army Corps. She was deployed to Iraq during Operation Desert Storm and treated many U.S. soldiers as well as Iraqi prisoners of war. She served on a team of surgeons that performed more than 125 operations in a 400-bed hospital in northern Saudi Arabia. Dr. Lee received several accolades in the military, including an “A” Proficiency Designator from the Army Medical Department and a Certificate of Achievement. After retiring from the Army as a colonel, she became professor of surgery, University of Hawaii at Manoa, Honolulu, where she was the only woman surgeon for most of her career.
Dr. Lee has participated in medical missions to Ghana, Honduras, Cambodia, Laos, the Philippines, and other underserved countries. She has made many international trips to promote friendship and medical exchanges. Notably, in 1995, she was the leader of a Women Surgeons Delegation to Russia and Romania. The trip was a Citizen Ambassador Program sponsored by People to People International, which was established by President Dwight D. Eisenhower. From 2000 to 2017, Dr. Lee taught surgery for a month, four times a year, at the Tzu-Chi University School of Medicine, Hualien, Taiwan.
Dr. Lee was one of 21 women surgeons in attendance at a networking breakfast at the 1981 Clinical Congress—led by ACS Past-President Patricia Numann, MD, FACS—which proved to be the genesis of the Association of Women Surgeons (AWS). She has been a supporter of the association, in time and talent, since its inception, and her presence at the AWS meetings, her academic career at teaching hospitals, and her research publications provide women surgeons and medical students from around the world an example of what women can achieve in the field.
Because her home is in Hawaii, midway between the East and West, she hopes to function as a “bridge,” contributing to global understanding and promoting communication, collaboration, and goodwill, and continues to work in the areas of medical education, international health, and world peace.
Committed to improving the care of the surgical patient, Dr. Lee is an outstanding leader and role model for surgeons everywhere. Her contributions to academic medicine in surgery, in the military, and in surgical volunteerism worldwide have made a lasting impression on the surgical profession. Her passion, endless energy, and dedication to the ACS and to women in surgery are without equal.
The American College of Surgeons (ACS) presented the Dr. Mary Edwards Walker Inspiring Women in Surgery Award to Yeu-Tsu Margaret Lee, MD, FACS, at the Convocation at Clinical Congress 2018 in Boston, MA. This award was established by the ACS Women in Surgery Committee (WiSC) and is presented annually at the Clinical Congress to recognize an individual’s significant contributions to the advancement of women in surgery.
Dr. Lee is from Honolulu, HI, and was born in Xian, China, in 1936. During her childhood, four of her siblings died from illness, motivating Dr. Lee to become a physician. Her family was forced to flee to Taiwan after the Chinese Civil War, and she immigrated to the U.S. in 1955, graduated from Harvard Medical School, Boston, in 1961, and has worked as a general surgeon and a surgical oncologist for more than 50 years. In the early 1980s, she was a tenured associate professor of surgery, University of Southern California (USC), Los Angeles, and head physician, Los Angeles County-USC Medical Center, but chose to pursue a different path.
In 1983, Dr. Lee moved to Hawaii, worked at Tripler Army Medical Center, Honolulu, as chief, surgical oncology section of general surgical services, and joined the U.S. Army Corps. She was deployed to Iraq during Operation Desert Storm and treated many U.S. soldiers as well as Iraqi prisoners of war. She served on a team of surgeons that performed more than 125 operations in a 400-bed hospital in northern Saudi Arabia. Dr. Lee received several accolades in the military, including an “A” Proficiency Designator from the Army Medical Department and a Certificate of Achievement. After retiring from the Army as a colonel, she became professor of surgery, University of Hawaii at Manoa, Honolulu, where she was the only woman surgeon for most of her career.
Dr. Lee has participated in medical missions to Ghana, Honduras, Cambodia, Laos, the Philippines, and other underserved countries. She has made many international trips to promote friendship and medical exchanges. Notably, in 1995, she was the leader of a Women Surgeons Delegation to Russia and Romania. The trip was a Citizen Ambassador Program sponsored by People to People International, which was established by President Dwight D. Eisenhower. From 2000 to 2017, Dr. Lee taught surgery for a month, four times a year, at the Tzu-Chi University School of Medicine, Hualien, Taiwan.
Dr. Lee was one of 21 women surgeons in attendance at a networking breakfast at the 1981 Clinical Congress—led by ACS Past-President Patricia Numann, MD, FACS—which proved to be the genesis of the Association of Women Surgeons (AWS). She has been a supporter of the association, in time and talent, since its inception, and her presence at the AWS meetings, her academic career at teaching hospitals, and her research publications provide women surgeons and medical students from around the world an example of what women can achieve in the field.
Because her home is in Hawaii, midway between the East and West, she hopes to function as a “bridge,” contributing to global understanding and promoting communication, collaboration, and goodwill, and continues to work in the areas of medical education, international health, and world peace.
Committed to improving the care of the surgical patient, Dr. Lee is an outstanding leader and role model for surgeons everywhere. Her contributions to academic medicine in surgery, in the military, and in surgical volunteerism worldwide have made a lasting impression on the surgical profession. Her passion, endless energy, and dedication to the ACS and to women in surgery are without equal.
The American College of Surgeons (ACS) presented the Dr. Mary Edwards Walker Inspiring Women in Surgery Award to Yeu-Tsu Margaret Lee, MD, FACS, at the Convocation at Clinical Congress 2018 in Boston, MA. This award was established by the ACS Women in Surgery Committee (WiSC) and is presented annually at the Clinical Congress to recognize an individual’s significant contributions to the advancement of women in surgery.
Dr. Lee is from Honolulu, HI, and was born in Xian, China, in 1936. During her childhood, four of her siblings died from illness, motivating Dr. Lee to become a physician. Her family was forced to flee to Taiwan after the Chinese Civil War, and she immigrated to the U.S. in 1955, graduated from Harvard Medical School, Boston, in 1961, and has worked as a general surgeon and a surgical oncologist for more than 50 years. In the early 1980s, she was a tenured associate professor of surgery, University of Southern California (USC), Los Angeles, and head physician, Los Angeles County-USC Medical Center, but chose to pursue a different path.
In 1983, Dr. Lee moved to Hawaii, worked at Tripler Army Medical Center, Honolulu, as chief, surgical oncology section of general surgical services, and joined the U.S. Army Corps. She was deployed to Iraq during Operation Desert Storm and treated many U.S. soldiers as well as Iraqi prisoners of war. She served on a team of surgeons that performed more than 125 operations in a 400-bed hospital in northern Saudi Arabia. Dr. Lee received several accolades in the military, including an “A” Proficiency Designator from the Army Medical Department and a Certificate of Achievement. After retiring from the Army as a colonel, she became professor of surgery, University of Hawaii at Manoa, Honolulu, where she was the only woman surgeon for most of her career.
Dr. Lee has participated in medical missions to Ghana, Honduras, Cambodia, Laos, the Philippines, and other underserved countries. She has made many international trips to promote friendship and medical exchanges. Notably, in 1995, she was the leader of a Women Surgeons Delegation to Russia and Romania. The trip was a Citizen Ambassador Program sponsored by People to People International, which was established by President Dwight D. Eisenhower. From 2000 to 2017, Dr. Lee taught surgery for a month, four times a year, at the Tzu-Chi University School of Medicine, Hualien, Taiwan.
Dr. Lee was one of 21 women surgeons in attendance at a networking breakfast at the 1981 Clinical Congress—led by ACS Past-President Patricia Numann, MD, FACS—which proved to be the genesis of the Association of Women Surgeons (AWS). She has been a supporter of the association, in time and talent, since its inception, and her presence at the AWS meetings, her academic career at teaching hospitals, and her research publications provide women surgeons and medical students from around the world an example of what women can achieve in the field.
Because her home is in Hawaii, midway between the East and West, she hopes to function as a “bridge,” contributing to global understanding and promoting communication, collaboration, and goodwill, and continues to work in the areas of medical education, international health, and world peace.
Committed to improving the care of the surgical patient, Dr. Lee is an outstanding leader and role model for surgeons everywhere. Her contributions to academic medicine in surgery, in the military, and in surgical volunteerism worldwide have made a lasting impression on the surgical profession. Her passion, endless energy, and dedication to the ACS and to women in surgery are without equal.