User login
VIDEO: Outpatient hysterectomies offer advantages for surgeons, patients
NATIONAL HARBOR, MD. – Moving hysterectomy and advanced gynecologic procedures to the ambulatory surgical environment is better for patients, surgeons, and the health care system, Richard B. Rosenfield, MD, who is in private practice in Portland, Ore., said at the AAGL Global Congress.
“We’ve been basically proving this model over the last decade by performing advanced laparoscopic surgery in the outpatient environment, and we do this for a number of reasons,” Dr. Rosenfield said in an interview. “The patients get to go home the same day, which they typically enjoy, we avoid the hospital-acquired infections, which is great, and in addition to that, the physicians tend to really appreciate the efficiency of an outpatient center.”
But with the focus on value-based payment under federal health programs, there should also be a greater focus on getting more high-volume surgeons to perform their procedures, he said. The idea is to lower the hospital readmissions, complications, and infections that could arise during procedures by less experienced surgeons and redirect the cost savings toward payments for surgeons with better outcomes, Dr. Rosenfield said. But this should be coupled with training and mentoring for lower-volume surgeons, he said.
Dr. Rosenfield reported having no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
NATIONAL HARBOR, MD. – Moving hysterectomy and advanced gynecologic procedures to the ambulatory surgical environment is better for patients, surgeons, and the health care system, Richard B. Rosenfield, MD, who is in private practice in Portland, Ore., said at the AAGL Global Congress.
“We’ve been basically proving this model over the last decade by performing advanced laparoscopic surgery in the outpatient environment, and we do this for a number of reasons,” Dr. Rosenfield said in an interview. “The patients get to go home the same day, which they typically enjoy, we avoid the hospital-acquired infections, which is great, and in addition to that, the physicians tend to really appreciate the efficiency of an outpatient center.”
But with the focus on value-based payment under federal health programs, there should also be a greater focus on getting more high-volume surgeons to perform their procedures, he said. The idea is to lower the hospital readmissions, complications, and infections that could arise during procedures by less experienced surgeons and redirect the cost savings toward payments for surgeons with better outcomes, Dr. Rosenfield said. But this should be coupled with training and mentoring for lower-volume surgeons, he said.
Dr. Rosenfield reported having no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
NATIONAL HARBOR, MD. – Moving hysterectomy and advanced gynecologic procedures to the ambulatory surgical environment is better for patients, surgeons, and the health care system, Richard B. Rosenfield, MD, who is in private practice in Portland, Ore., said at the AAGL Global Congress.
“We’ve been basically proving this model over the last decade by performing advanced laparoscopic surgery in the outpatient environment, and we do this for a number of reasons,” Dr. Rosenfield said in an interview. “The patients get to go home the same day, which they typically enjoy, we avoid the hospital-acquired infections, which is great, and in addition to that, the physicians tend to really appreciate the efficiency of an outpatient center.”
But with the focus on value-based payment under federal health programs, there should also be a greater focus on getting more high-volume surgeons to perform their procedures, he said. The idea is to lower the hospital readmissions, complications, and infections that could arise during procedures by less experienced surgeons and redirect the cost savings toward payments for surgeons with better outcomes, Dr. Rosenfield said. But this should be coupled with training and mentoring for lower-volume surgeons, he said.
Dr. Rosenfield reported having no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
AT AAGL 2017
VIDEO: Bariatric experts discuss recent experience with gastric balloon devices
Two experts on bariatric surgery spoke at the Minimally Invasive Surgery Symposium, held in Las Vegas. Jaime Ponce, MD, FACS, and John Morton, MD, FACS, discussed several different types of gastric balloon devices and the factors guiding their use for patients. Dr. Morton suggested that the balloon devices could serve as an intermediate treatment between medications and surgery.

Two experts on bariatric surgery spoke at the Minimally Invasive Surgery Symposium, held in Las Vegas. Jaime Ponce, MD, FACS, and John Morton, MD, FACS, discussed several different types of gastric balloon devices and the factors guiding their use for patients. Dr. Morton suggested that the balloon devices could serve as an intermediate treatment between medications and surgery.

Two experts on bariatric surgery spoke at the Minimally Invasive Surgery Symposium, held in Las Vegas. Jaime Ponce, MD, FACS, and John Morton, MD, FACS, discussed several different types of gastric balloon devices and the factors guiding their use for patients. Dr. Morton suggested that the balloon devices could serve as an intermediate treatment between medications and surgery.

VIDEO: Regionalized STEMI care slashes in-hospital mortality
ANAHEIM, CALIF. – An American Heart Association program aimed at streamlining care of patients with ST-elevation MI resulted in a dramatic near-halving of in-hospital mortality, compared with STEMI patients treated in hospitals not participating in the project, James G. Jollis, MD, reported at the American Heart Association scientific sessions.
He presented the results of the STEMI ACCELERATOR 2 study, which involved 12 participating metropolitan regions across the United States, 132 percutaneous coronary intervention–capable hospitals, and 946 emergency medical services agencies. The ACCELERATOR 2 program entailed regional implementation of a structured STEMI care plan in which EMS personnel were trained to obtain prehospital ECGs and to activate cardiac catheterization labs prior to hospital arrival, bypassing the emergency department when appropriate.
Key elements of the project, which was part of the AHA’s Mission: Lifeline program, included having participating hospitals measure their performance of key processes and send that information as well as patient outcome data to the National Cardiovascular Data Registry’s ACTION–Get With The Guidelines registry. The hospitals in turn received quarterly feedback reports containing blinded hospital comparisons.
Dr. Jollis and his coinvestigators worked to obtain buy-in from local stakeholders, organize regional leadership, and help in drafting a central regional STEMI plan featuring prespecified treatment protocols.
The STEMI ACCELERATOR 2 study was carried out in 2015-2017, during which 10,730 patients with STEMI were transported directly to participating hospitals with PCI capability.
The primary study outcome was the change from the first to the final quarter of the study in the proportion of EMS-transported patients with a time from first medical contact to treatment in the cath lab of 90 minutes or less. This improved significantly, from 67% at baseline to 74% in the final quarter. Nine of the 12 participating regions reduced their time from first medical contact to treatment in the cath lab, and eight reached the national of goal of having 75% of STEMI patients treated within 90 minutes.
The other key time-to-care measures improved, too: At baseline, only 38% of patients had a time from first medical contact to cath lab activation of 20 minutes or less; by the final quarter, this figure had climbed to 56%. That’s an important metric, as evidenced by the study finding that in-hospital mortality occurred in 4.5% of patients with a time from first medical contact to cath lab activation of more than 20 minutes, compared with 2.2% in those with a time of 20 minutes or less.
Also, the proportion of patients who spent 20 minutes or less in the emergency department improved from 33% to 43%.
In-hospital mortality improved from 4.4% in the baseline quarter to 2.3% in the final quarter. No similar improvement in in-hospital mortality occurred in a comparison group of 22,651 STEMI patients treated at hospitals not involved in ACCELERATOR 2.
A significant reduction in the rate of in-hospital congestive heart failure occurred in the ACCELERATOR 2 centers, from 7.4% at baseline to 5.0%. In contrast, stroke, cardiogenic shock, and major bleeding rates were unchanged over time.
The ACCELERATOR 2 model of emergency cardiovascular care is designed to be highly generalizable, according to Dr. Jollis.
“This study supports the implementation of regionally coordinated systems across the United States to abort heart attacks, save lives, and enable heart attack victims to return to their families and productive lives,” he said.
The ACCELERATOR 2 operations manual – essentially a blueprint for organizing a regional STEMI system of care – is available gratis.
Dr. Allen, a cardiologist at the University of Colorado, Denver, said the ACCELERATOR 2 model has been successful because it is consistent with a fundamental principle of implementation science as described by Carolyn Clancy, MD, Executive in Charge at the Veterans Health Affairs Administration, who has said it’s a matter of making the right thing to do the easy thing to do.
Gregg C. Fonarow, MD, founder of the Get With the Guidelines program, predicted that the success of this program will lead to a ramping up of efforts to regionalize and coordinate STEMI care across the country. “I hope and anticipate that the AHA will take and run with the ACCELERATOR 2 model and adopt this into Mission: Lifeline, hoping to make this the standard approach to further improving care and outcomes in these patients,” said Dr. Fonarow, professor and cochief of cardiology at the University of California, Los Angeles, in a video interview.
Simultaneous with his presentation at the AHA conference, the results of STEMI ACCELERATOR 2 were published online in Circulation (2017 Nov 14; doi: 0.1161/CIRCULATIONAHA.117.032446).
The trial was sponsored by research and educational grants from AstraZeneca and The Medicines Company. Dr. Jollis reported having no financial conflicts of interest.
ANAHEIM, CALIF. – An American Heart Association program aimed at streamlining care of patients with ST-elevation MI resulted in a dramatic near-halving of in-hospital mortality, compared with STEMI patients treated in hospitals not participating in the project, James G. Jollis, MD, reported at the American Heart Association scientific sessions.
He presented the results of the STEMI ACCELERATOR 2 study, which involved 12 participating metropolitan regions across the United States, 132 percutaneous coronary intervention–capable hospitals, and 946 emergency medical services agencies. The ACCELERATOR 2 program entailed regional implementation of a structured STEMI care plan in which EMS personnel were trained to obtain prehospital ECGs and to activate cardiac catheterization labs prior to hospital arrival, bypassing the emergency department when appropriate.
Key elements of the project, which was part of the AHA’s Mission: Lifeline program, included having participating hospitals measure their performance of key processes and send that information as well as patient outcome data to the National Cardiovascular Data Registry’s ACTION–Get With The Guidelines registry. The hospitals in turn received quarterly feedback reports containing blinded hospital comparisons.
Dr. Jollis and his coinvestigators worked to obtain buy-in from local stakeholders, organize regional leadership, and help in drafting a central regional STEMI plan featuring prespecified treatment protocols.
The STEMI ACCELERATOR 2 study was carried out in 2015-2017, during which 10,730 patients with STEMI were transported directly to participating hospitals with PCI capability.
The primary study outcome was the change from the first to the final quarter of the study in the proportion of EMS-transported patients with a time from first medical contact to treatment in the cath lab of 90 minutes or less. This improved significantly, from 67% at baseline to 74% in the final quarter. Nine of the 12 participating regions reduced their time from first medical contact to treatment in the cath lab, and eight reached the national of goal of having 75% of STEMI patients treated within 90 minutes.
The other key time-to-care measures improved, too: At baseline, only 38% of patients had a time from first medical contact to cath lab activation of 20 minutes or less; by the final quarter, this figure had climbed to 56%. That’s an important metric, as evidenced by the study finding that in-hospital mortality occurred in 4.5% of patients with a time from first medical contact to cath lab activation of more than 20 minutes, compared with 2.2% in those with a time of 20 minutes or less.
Also, the proportion of patients who spent 20 minutes or less in the emergency department improved from 33% to 43%.
In-hospital mortality improved from 4.4% in the baseline quarter to 2.3% in the final quarter. No similar improvement in in-hospital mortality occurred in a comparison group of 22,651 STEMI patients treated at hospitals not involved in ACCELERATOR 2.
A significant reduction in the rate of in-hospital congestive heart failure occurred in the ACCELERATOR 2 centers, from 7.4% at baseline to 5.0%. In contrast, stroke, cardiogenic shock, and major bleeding rates were unchanged over time.
The ACCELERATOR 2 model of emergency cardiovascular care is designed to be highly generalizable, according to Dr. Jollis.
“This study supports the implementation of regionally coordinated systems across the United States to abort heart attacks, save lives, and enable heart attack victims to return to their families and productive lives,” he said.
The ACCELERATOR 2 operations manual – essentially a blueprint for organizing a regional STEMI system of care – is available gratis.
Dr. Allen, a cardiologist at the University of Colorado, Denver, said the ACCELERATOR 2 model has been successful because it is consistent with a fundamental principle of implementation science as described by Carolyn Clancy, MD, Executive in Charge at the Veterans Health Affairs Administration, who has said it’s a matter of making the right thing to do the easy thing to do.
Gregg C. Fonarow, MD, founder of the Get With the Guidelines program, predicted that the success of this program will lead to a ramping up of efforts to regionalize and coordinate STEMI care across the country. “I hope and anticipate that the AHA will take and run with the ACCELERATOR 2 model and adopt this into Mission: Lifeline, hoping to make this the standard approach to further improving care and outcomes in these patients,” said Dr. Fonarow, professor and cochief of cardiology at the University of California, Los Angeles, in a video interview.
Simultaneous with his presentation at the AHA conference, the results of STEMI ACCELERATOR 2 were published online in Circulation (2017 Nov 14; doi: 0.1161/CIRCULATIONAHA.117.032446).
The trial was sponsored by research and educational grants from AstraZeneca and The Medicines Company. Dr. Jollis reported having no financial conflicts of interest.
ANAHEIM, CALIF. – An American Heart Association program aimed at streamlining care of patients with ST-elevation MI resulted in a dramatic near-halving of in-hospital mortality, compared with STEMI patients treated in hospitals not participating in the project, James G. Jollis, MD, reported at the American Heart Association scientific sessions.
He presented the results of the STEMI ACCELERATOR 2 study, which involved 12 participating metropolitan regions across the United States, 132 percutaneous coronary intervention–capable hospitals, and 946 emergency medical services agencies. The ACCELERATOR 2 program entailed regional implementation of a structured STEMI care plan in which EMS personnel were trained to obtain prehospital ECGs and to activate cardiac catheterization labs prior to hospital arrival, bypassing the emergency department when appropriate.
Key elements of the project, which was part of the AHA’s Mission: Lifeline program, included having participating hospitals measure their performance of key processes and send that information as well as patient outcome data to the National Cardiovascular Data Registry’s ACTION–Get With The Guidelines registry. The hospitals in turn received quarterly feedback reports containing blinded hospital comparisons.
Dr. Jollis and his coinvestigators worked to obtain buy-in from local stakeholders, organize regional leadership, and help in drafting a central regional STEMI plan featuring prespecified treatment protocols.
The STEMI ACCELERATOR 2 study was carried out in 2015-2017, during which 10,730 patients with STEMI were transported directly to participating hospitals with PCI capability.
The primary study outcome was the change from the first to the final quarter of the study in the proportion of EMS-transported patients with a time from first medical contact to treatment in the cath lab of 90 minutes or less. This improved significantly, from 67% at baseline to 74% in the final quarter. Nine of the 12 participating regions reduced their time from first medical contact to treatment in the cath lab, and eight reached the national of goal of having 75% of STEMI patients treated within 90 minutes.
The other key time-to-care measures improved, too: At baseline, only 38% of patients had a time from first medical contact to cath lab activation of 20 minutes or less; by the final quarter, this figure had climbed to 56%. That’s an important metric, as evidenced by the study finding that in-hospital mortality occurred in 4.5% of patients with a time from first medical contact to cath lab activation of more than 20 minutes, compared with 2.2% in those with a time of 20 minutes or less.
Also, the proportion of patients who spent 20 minutes or less in the emergency department improved from 33% to 43%.
In-hospital mortality improved from 4.4% in the baseline quarter to 2.3% in the final quarter. No similar improvement in in-hospital mortality occurred in a comparison group of 22,651 STEMI patients treated at hospitals not involved in ACCELERATOR 2.
A significant reduction in the rate of in-hospital congestive heart failure occurred in the ACCELERATOR 2 centers, from 7.4% at baseline to 5.0%. In contrast, stroke, cardiogenic shock, and major bleeding rates were unchanged over time.
The ACCELERATOR 2 model of emergency cardiovascular care is designed to be highly generalizable, according to Dr. Jollis.
“This study supports the implementation of regionally coordinated systems across the United States to abort heart attacks, save lives, and enable heart attack victims to return to their families and productive lives,” he said.
The ACCELERATOR 2 operations manual – essentially a blueprint for organizing a regional STEMI system of care – is available gratis.
Dr. Allen, a cardiologist at the University of Colorado, Denver, said the ACCELERATOR 2 model has been successful because it is consistent with a fundamental principle of implementation science as described by Carolyn Clancy, MD, Executive in Charge at the Veterans Health Affairs Administration, who has said it’s a matter of making the right thing to do the easy thing to do.
Gregg C. Fonarow, MD, founder of the Get With the Guidelines program, predicted that the success of this program will lead to a ramping up of efforts to regionalize and coordinate STEMI care across the country. “I hope and anticipate that the AHA will take and run with the ACCELERATOR 2 model and adopt this into Mission: Lifeline, hoping to make this the standard approach to further improving care and outcomes in these patients,” said Dr. Fonarow, professor and cochief of cardiology at the University of California, Los Angeles, in a video interview.
Simultaneous with his presentation at the AHA conference, the results of STEMI ACCELERATOR 2 were published online in Circulation (2017 Nov 14; doi: 0.1161/CIRCULATIONAHA.117.032446).
The trial was sponsored by research and educational grants from AstraZeneca and The Medicines Company. Dr. Jollis reported having no financial conflicts of interest.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: The in-hospital mortality rate of STEMI patients dropped from 4.4% in the baseline quarter to 2.3% in the final quarter of a study that examined the impact of introducing regionalized STEMI care.
Data source: This was a prospective study of an intervention that involved implementation of regionalized STEMI care in a dozen U.S. metropolitan areas.
Disclosures: The study was sponsored by research and educational grants from AstraZeneca and The Medicines Company. The presenter reported having no financial conflicts of interest.
VIDEO: Innovative technology is opening doors for vaginal hysterectomy
NATIONAL HARBOR, MD. – Innovative tools for vaginal hysterectomy were in the spotlight during a surgical demonstration at the AAGL Global Congress.
“I think it’s really compelling that we use the technologies that the AAGL is known for investigating and teaching each other,” said Charles Rardin, MD, director of the robotic surgery program at Women & Infants Hospital, Providence, R.I. “It’s nice to see a renewed interest in some newer technologies and applying them to vaginal hysterectomy.”
The presentation of new tools comes as the number of vaginal hysterectomies have decreased and laparoscopic procedures are on the rise. The rate of vaginal hysterectomy in the United States has fallen from 24.8% in 1998 to 16.7% in 2010, according to the Nationwide Inpatient Sample from the Agency for Healthcare Research and Quality.
Surgeons demonstrated new tools with the intent of showing physicians that the benefits some associate with laparoscopic procedures, such as having easier access or a better sense of the uterus, can be associated with vaginal hysterectomy as well.
Advanced tools, such as a self-retaining retractor and 3-D camera systems, could make it easier to teach students by allowing more mobility and easier visual access, Dr. Rardin said in a video interview.
The tutorial ended with a demonstration of the natural orifice transluminal endoscopic surgery tool that allows laparoscopic tools to be introduced through the vaginal pathway.
All the tools exhibited at AAGL are currently available.
Dr. Rardin reported having no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
NATIONAL HARBOR, MD. – Innovative tools for vaginal hysterectomy were in the spotlight during a surgical demonstration at the AAGL Global Congress.
“I think it’s really compelling that we use the technologies that the AAGL is known for investigating and teaching each other,” said Charles Rardin, MD, director of the robotic surgery program at Women & Infants Hospital, Providence, R.I. “It’s nice to see a renewed interest in some newer technologies and applying them to vaginal hysterectomy.”
The presentation of new tools comes as the number of vaginal hysterectomies have decreased and laparoscopic procedures are on the rise. The rate of vaginal hysterectomy in the United States has fallen from 24.8% in 1998 to 16.7% in 2010, according to the Nationwide Inpatient Sample from the Agency for Healthcare Research and Quality.
Surgeons demonstrated new tools with the intent of showing physicians that the benefits some associate with laparoscopic procedures, such as having easier access or a better sense of the uterus, can be associated with vaginal hysterectomy as well.
Advanced tools, such as a self-retaining retractor and 3-D camera systems, could make it easier to teach students by allowing more mobility and easier visual access, Dr. Rardin said in a video interview.
The tutorial ended with a demonstration of the natural orifice transluminal endoscopic surgery tool that allows laparoscopic tools to be introduced through the vaginal pathway.
All the tools exhibited at AAGL are currently available.
Dr. Rardin reported having no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
NATIONAL HARBOR, MD. – Innovative tools for vaginal hysterectomy were in the spotlight during a surgical demonstration at the AAGL Global Congress.
“I think it’s really compelling that we use the technologies that the AAGL is known for investigating and teaching each other,” said Charles Rardin, MD, director of the robotic surgery program at Women & Infants Hospital, Providence, R.I. “It’s nice to see a renewed interest in some newer technologies and applying them to vaginal hysterectomy.”
The presentation of new tools comes as the number of vaginal hysterectomies have decreased and laparoscopic procedures are on the rise. The rate of vaginal hysterectomy in the United States has fallen from 24.8% in 1998 to 16.7% in 2010, according to the Nationwide Inpatient Sample from the Agency for Healthcare Research and Quality.
Surgeons demonstrated new tools with the intent of showing physicians that the benefits some associate with laparoscopic procedures, such as having easier access or a better sense of the uterus, can be associated with vaginal hysterectomy as well.
Advanced tools, such as a self-retaining retractor and 3-D camera systems, could make it easier to teach students by allowing more mobility and easier visual access, Dr. Rardin said in a video interview.
The tutorial ended with a demonstration of the natural orifice transluminal endoscopic surgery tool that allows laparoscopic tools to be introduced through the vaginal pathway.
All the tools exhibited at AAGL are currently available.
Dr. Rardin reported having no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
AT AAGL 2017
VIDEO: MISS 2017– Hot topics, innovations, debates
Philip R. Schauer, MD, FACS, discusses innovations, hot topics, and controversies covered in the sessions of this year’s Minimally Invasive Surgery Symposium, held in Las Vegas. In addition to highlighting what’s new this year, Dr. Schauer also spoke about plans for next year’s meeting and what makes the MISS unique and valuable to attendees.

Philip R. Schauer, MD, FACS, discusses innovations, hot topics, and controversies covered in the sessions of this year’s Minimally Invasive Surgery Symposium, held in Las Vegas. In addition to highlighting what’s new this year, Dr. Schauer also spoke about plans for next year’s meeting and what makes the MISS unique and valuable to attendees.

Philip R. Schauer, MD, FACS, discusses innovations, hot topics, and controversies covered in the sessions of this year’s Minimally Invasive Surgery Symposium, held in Las Vegas. In addition to highlighting what’s new this year, Dr. Schauer also spoke about plans for next year’s meeting and what makes the MISS unique and valuable to attendees.

VIDEO: New vaccines target global infections
LAS VEGAS – There are now vaccines for two infectious diseases that “are not purely dermatologic, but have a great impact on many patients around the world,” Kenneth J. Tomecki, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
The recent development of a vaccine to protect against malaria, with an efficacy around 40%, “is something we should all be proud of,” said Dr. Tomecki of the Cleveland Clinic. Another advance is that there is now also a vaccine for Ebola that is so effective, it is being stockpiled in African countries in preparation for future Ebola outbreaks, he added.
Dr. Tomecki had no financial conflicts to disclose.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – There are now vaccines for two infectious diseases that “are not purely dermatologic, but have a great impact on many patients around the world,” Kenneth J. Tomecki, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
The recent development of a vaccine to protect against malaria, with an efficacy around 40%, “is something we should all be proud of,” said Dr. Tomecki of the Cleveland Clinic. Another advance is that there is now also a vaccine for Ebola that is so effective, it is being stockpiled in African countries in preparation for future Ebola outbreaks, he added.
Dr. Tomecki had no financial conflicts to disclose.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – There are now vaccines for two infectious diseases that “are not purely dermatologic, but have a great impact on many patients around the world,” Kenneth J. Tomecki, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
The recent development of a vaccine to protect against malaria, with an efficacy around 40%, “is something we should all be proud of,” said Dr. Tomecki of the Cleveland Clinic. Another advance is that there is now also a vaccine for Ebola that is so effective, it is being stockpiled in African countries in preparation for future Ebola outbreaks, he added.
Dr. Tomecki had no financial conflicts to disclose.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SDEF LAS VEGAS DERMATOLOGY SEMINAR
VIDEO: Consider combining treatments when body sculpting
LAS VEGAS – Currently, there are available treatments that are effective in contouring the body, Christopher B. Zachary, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
Some devices can help patients looking for reductions of trouble spots, such as around the abdomen, and are safe and effective, said Dr. Zachary of the University of California, Irvine. However, they are not a realistic option for obese or overweight patients, he added.
In addition, other treatments can be combined with body sculpting devices to optimize results, particularly when removing fat in the submental area, he noted.
Dr. Zachary disclosed relationships with Solta, Zeltiq, Sciton, DUSA, Zimmer, Cutera, Alma, and Amway.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Currently, there are available treatments that are effective in contouring the body, Christopher B. Zachary, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
Some devices can help patients looking for reductions of trouble spots, such as around the abdomen, and are safe and effective, said Dr. Zachary of the University of California, Irvine. However, they are not a realistic option for obese or overweight patients, he added.
In addition, other treatments can be combined with body sculpting devices to optimize results, particularly when removing fat in the submental area, he noted.
Dr. Zachary disclosed relationships with Solta, Zeltiq, Sciton, DUSA, Zimmer, Cutera, Alma, and Amway.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Currently, there are available treatments that are effective in contouring the body, Christopher B. Zachary, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
Some devices can help patients looking for reductions of trouble spots, such as around the abdomen, and are safe and effective, said Dr. Zachary of the University of California, Irvine. However, they are not a realistic option for obese or overweight patients, he added.
In addition, other treatments can be combined with body sculpting devices to optimize results, particularly when removing fat in the submental area, he noted.
Dr. Zachary disclosed relationships with Solta, Zeltiq, Sciton, DUSA, Zimmer, Cutera, Alma, and Amway.
SDEF and this news organization are owned by the same parent company.
AT SDEF LAS VEGAS DERMATOLOGY SEMINAR
VIDEO: Hone aesthetic technique with upper face first
LAS VEGAS – For those starting to use toxins and fillers, “my first advice is to get a good education,” Christopher B. Zachary, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
“Know … how to evaluate your patient, know where the problems are, know what the danger zones are, understand your anatomy,” advised Dr. Zachary of the University of California, Irvine.
, he noted. Procedures on the upper face, such as the treatment for crow’s feet or a brow lift, can be “a home run,” while the lower face is much more complicated, he said in the video interview.
Dr. Zachary disclosed relationships with companies including Solta, Zeltiq, Sciton, DUSA, Zimmer, Cutera, Alma, and Amway.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – For those starting to use toxins and fillers, “my first advice is to get a good education,” Christopher B. Zachary, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
“Know … how to evaluate your patient, know where the problems are, know what the danger zones are, understand your anatomy,” advised Dr. Zachary of the University of California, Irvine.
, he noted. Procedures on the upper face, such as the treatment for crow’s feet or a brow lift, can be “a home run,” while the lower face is much more complicated, he said in the video interview.
Dr. Zachary disclosed relationships with companies including Solta, Zeltiq, Sciton, DUSA, Zimmer, Cutera, Alma, and Amway.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – For those starting to use toxins and fillers, “my first advice is to get a good education,” Christopher B. Zachary, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
“Know … how to evaluate your patient, know where the problems are, know what the danger zones are, understand your anatomy,” advised Dr. Zachary of the University of California, Irvine.
, he noted. Procedures on the upper face, such as the treatment for crow’s feet or a brow lift, can be “a home run,” while the lower face is much more complicated, he said in the video interview.
Dr. Zachary disclosed relationships with companies including Solta, Zeltiq, Sciton, DUSA, Zimmer, Cutera, Alma, and Amway.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SDEF LAS VEGAS DERMATOLOGY SEMINAR
VIDEO: U.S. hypertension guidelines reset threshold to 130/80 mm Hg
ANAHEIM, CALIF. – Thirty million Americans became hypertensive overnight on Nov. 13 with the introduction of new high blood pressure guidelines from the American College of Cardiology and American Heart Association.
That happened by resetting the definition of adult hypertension from the long-standing threshold of 140/90 mm Hg to a blood pressure at or above 130/80 mm Hg, a change that jumps the U.S. adult prevalence of hypertension from roughly 32% to 46%. Nearly half of all U.S. adults now have hypertension, bringing the total national hypertensive population to a staggering 103 million.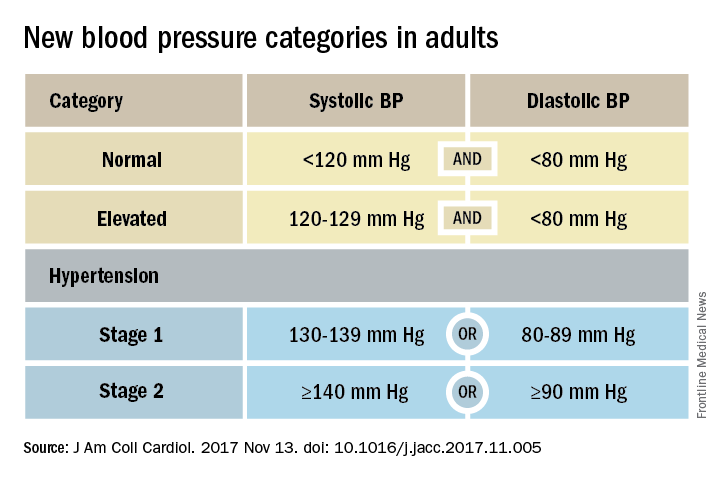
Goal is to transform care
But the new guidelines (J Am Coll Cardiol. 2017 Nov 13. doi: 10.1016/j.jacc.2017.11.005) for preventing, detecting, evaluating, and managing adult hypertension do lots more than just shake up the epidemiology of high blood pressure. With 106 total recommendations, the guidelines seek to transform every aspect of blood pressure in American medical practice, starting with how it’s measured and stretching to redefine applications of medical systems to try to ensure that every person with a blood pressure that truly falls outside the redefined limits gets a comprehensive package of interventions.
Many of these are “seismic changes,” said Lawrence J. Appel, MD. He particularly cited as seismic the new classification of stage 1 hypertension as a pressure at or above 130/80 mm Hg, the emphasis on using some form of out-of-office blood pressure measurement to confirm a diagnosis, the use of risk assessment when deciding whether to treat certain patients with drugs, and the same blood pressure goal of less than 130/80 mm Hg for all hypertensives, regardless of age, as long as they remain ambulatory and community dwelling.
One goal for all adults
“The systolic blood pressure goal for older people has gone from 140 mm Hg to 150 mm Hg and now to 130 mm Hg in the space of 2-3 years,” commented Dr. Appel, professor of epidemiology at Johns Hopkins University in Baltimore and not involved in the guideline-writing process.
In fact, the guidelines simplified the treatment goal all around, to less than 130/80 mm Hg for patients with diabetes, those with chronic kidney disease, and the elderly; that goal remains the same for all adults.
“It will be clearer and easier now that everyone should be less than 130/80 mm Hg. You won’t need to remember a second target,” said Sandra J. Taler, MD, a nephrologist and professor of medicine at the Mayo Clinic in Rochester, Minn., and a member of the guidelines task force.
“Some people may be upset that we changed the rules on them. They had normal blood pressure yesterday, and today it’s high. But it’s a good awakening, especially for using lifestyle interventions,” Dr. Taler said in an interview.
Preferred intervention: Lifestyle, not drugs
Lifestyle optimization is repeatedly cited as the cornerstone of intervention for everyone, including those with elevated blood pressure with a systolic pressure of 120-129 mm Hg, and as the only endorsed intervention for patients with hypertension of 130-139 mm Hg but below a 10% risk for a cardiovascular disease event during the next 10 years on the American College of Cardiology’s online risk calculator. The guidelines list six lifestyle goals: weight loss, following a DASH diet, reducing sodium, enhancing potassium, 90-150 min/wk of physical activity, and moderate alcohol intake.
Team-based care essential
The guidelines also put unprecedented emphasis on using a team-based management approach, which means having nurses, nurse practitioners, pharmacists, dietitians, and other clinicians, allowing for more frequent and focused care. Dr. Whelton and others cited in particular the VA Health System and Kaiser-Permanente as operating team-based and system-driven blood pressure management programs that have resulted in control rates for more than 90% of hypertensive patients. The team-based approach is also a key in the Target:BP program that the American Heart Association and American Medical Association founded. Target:BP will be instrumental in promoting implementation of the new guidelines, Dr. Carey said. Another systems recommendation is that every patient with hypertension should have a “clear, detailed, and current evidence-based plan of care.”
“Using nurse practitioners, physician assistants, and pharmacists has been shown to improve blood pressure levels,” and health systems that use this approach have had “great success,” commented Donald M. Lloyd-Jones, MD, professor and chairman of preventive medicine at Northwestern University in Chicago and not part of the guidelines task force. Some systems have used this approach to achieve high levels of blood pressure control. Now that financial penalties and incentives from payers also exist to push for higher levels of blood pressure control, the alignment of financial and health incentives should result in big changes, Dr. Lloyd-Jones predicted in a video interview.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
ANAHEIM, CALIF. – Thirty million Americans became hypertensive overnight on Nov. 13 with the introduction of new high blood pressure guidelines from the American College of Cardiology and American Heart Association.
That happened by resetting the definition of adult hypertension from the long-standing threshold of 140/90 mm Hg to a blood pressure at or above 130/80 mm Hg, a change that jumps the U.S. adult prevalence of hypertension from roughly 32% to 46%. Nearly half of all U.S. adults now have hypertension, bringing the total national hypertensive population to a staggering 103 million.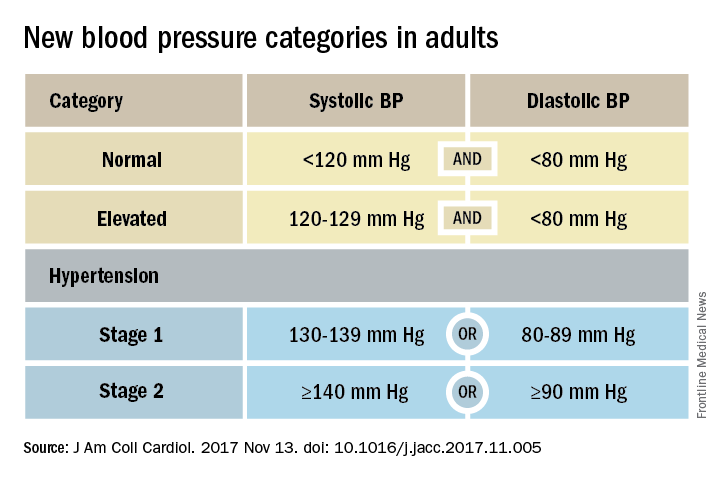
Goal is to transform care
But the new guidelines (J Am Coll Cardiol. 2017 Nov 13. doi: 10.1016/j.jacc.2017.11.005) for preventing, detecting, evaluating, and managing adult hypertension do lots more than just shake up the epidemiology of high blood pressure. With 106 total recommendations, the guidelines seek to transform every aspect of blood pressure in American medical practice, starting with how it’s measured and stretching to redefine applications of medical systems to try to ensure that every person with a blood pressure that truly falls outside the redefined limits gets a comprehensive package of interventions.
Many of these are “seismic changes,” said Lawrence J. Appel, MD. He particularly cited as seismic the new classification of stage 1 hypertension as a pressure at or above 130/80 mm Hg, the emphasis on using some form of out-of-office blood pressure measurement to confirm a diagnosis, the use of risk assessment when deciding whether to treat certain patients with drugs, and the same blood pressure goal of less than 130/80 mm Hg for all hypertensives, regardless of age, as long as they remain ambulatory and community dwelling.
One goal for all adults
“The systolic blood pressure goal for older people has gone from 140 mm Hg to 150 mm Hg and now to 130 mm Hg in the space of 2-3 years,” commented Dr. Appel, professor of epidemiology at Johns Hopkins University in Baltimore and not involved in the guideline-writing process.
In fact, the guidelines simplified the treatment goal all around, to less than 130/80 mm Hg for patients with diabetes, those with chronic kidney disease, and the elderly; that goal remains the same for all adults.
“It will be clearer and easier now that everyone should be less than 130/80 mm Hg. You won’t need to remember a second target,” said Sandra J. Taler, MD, a nephrologist and professor of medicine at the Mayo Clinic in Rochester, Minn., and a member of the guidelines task force.
“Some people may be upset that we changed the rules on them. They had normal blood pressure yesterday, and today it’s high. But it’s a good awakening, especially for using lifestyle interventions,” Dr. Taler said in an interview.
Preferred intervention: Lifestyle, not drugs
Lifestyle optimization is repeatedly cited as the cornerstone of intervention for everyone, including those with elevated blood pressure with a systolic pressure of 120-129 mm Hg, and as the only endorsed intervention for patients with hypertension of 130-139 mm Hg but below a 10% risk for a cardiovascular disease event during the next 10 years on the American College of Cardiology’s online risk calculator. The guidelines list six lifestyle goals: weight loss, following a DASH diet, reducing sodium, enhancing potassium, 90-150 min/wk of physical activity, and moderate alcohol intake.
Team-based care essential
The guidelines also put unprecedented emphasis on using a team-based management approach, which means having nurses, nurse practitioners, pharmacists, dietitians, and other clinicians, allowing for more frequent and focused care. Dr. Whelton and others cited in particular the VA Health System and Kaiser-Permanente as operating team-based and system-driven blood pressure management programs that have resulted in control rates for more than 90% of hypertensive patients. The team-based approach is also a key in the Target:BP program that the American Heart Association and American Medical Association founded. Target:BP will be instrumental in promoting implementation of the new guidelines, Dr. Carey said. Another systems recommendation is that every patient with hypertension should have a “clear, detailed, and current evidence-based plan of care.”
“Using nurse practitioners, physician assistants, and pharmacists has been shown to improve blood pressure levels,” and health systems that use this approach have had “great success,” commented Donald M. Lloyd-Jones, MD, professor and chairman of preventive medicine at Northwestern University in Chicago and not part of the guidelines task force. Some systems have used this approach to achieve high levels of blood pressure control. Now that financial penalties and incentives from payers also exist to push for higher levels of blood pressure control, the alignment of financial and health incentives should result in big changes, Dr. Lloyd-Jones predicted in a video interview.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
ANAHEIM, CALIF. – Thirty million Americans became hypertensive overnight on Nov. 13 with the introduction of new high blood pressure guidelines from the American College of Cardiology and American Heart Association.
That happened by resetting the definition of adult hypertension from the long-standing threshold of 140/90 mm Hg to a blood pressure at or above 130/80 mm Hg, a change that jumps the U.S. adult prevalence of hypertension from roughly 32% to 46%. Nearly half of all U.S. adults now have hypertension, bringing the total national hypertensive population to a staggering 103 million.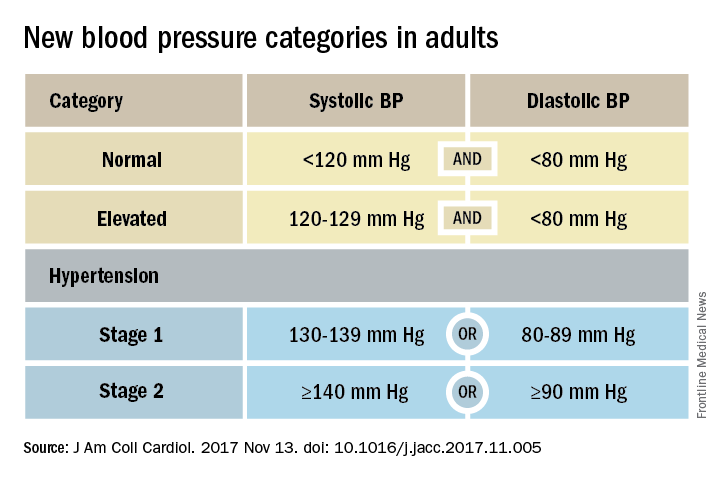
Goal is to transform care
But the new guidelines (J Am Coll Cardiol. 2017 Nov 13. doi: 10.1016/j.jacc.2017.11.005) for preventing, detecting, evaluating, and managing adult hypertension do lots more than just shake up the epidemiology of high blood pressure. With 106 total recommendations, the guidelines seek to transform every aspect of blood pressure in American medical practice, starting with how it’s measured and stretching to redefine applications of medical systems to try to ensure that every person with a blood pressure that truly falls outside the redefined limits gets a comprehensive package of interventions.
Many of these are “seismic changes,” said Lawrence J. Appel, MD. He particularly cited as seismic the new classification of stage 1 hypertension as a pressure at or above 130/80 mm Hg, the emphasis on using some form of out-of-office blood pressure measurement to confirm a diagnosis, the use of risk assessment when deciding whether to treat certain patients with drugs, and the same blood pressure goal of less than 130/80 mm Hg for all hypertensives, regardless of age, as long as they remain ambulatory and community dwelling.
One goal for all adults
“The systolic blood pressure goal for older people has gone from 140 mm Hg to 150 mm Hg and now to 130 mm Hg in the space of 2-3 years,” commented Dr. Appel, professor of epidemiology at Johns Hopkins University in Baltimore and not involved in the guideline-writing process.
In fact, the guidelines simplified the treatment goal all around, to less than 130/80 mm Hg for patients with diabetes, those with chronic kidney disease, and the elderly; that goal remains the same for all adults.
“It will be clearer and easier now that everyone should be less than 130/80 mm Hg. You won’t need to remember a second target,” said Sandra J. Taler, MD, a nephrologist and professor of medicine at the Mayo Clinic in Rochester, Minn., and a member of the guidelines task force.
“Some people may be upset that we changed the rules on them. They had normal blood pressure yesterday, and today it’s high. But it’s a good awakening, especially for using lifestyle interventions,” Dr. Taler said in an interview.
Preferred intervention: Lifestyle, not drugs
Lifestyle optimization is repeatedly cited as the cornerstone of intervention for everyone, including those with elevated blood pressure with a systolic pressure of 120-129 mm Hg, and as the only endorsed intervention for patients with hypertension of 130-139 mm Hg but below a 10% risk for a cardiovascular disease event during the next 10 years on the American College of Cardiology’s online risk calculator. The guidelines list six lifestyle goals: weight loss, following a DASH diet, reducing sodium, enhancing potassium, 90-150 min/wk of physical activity, and moderate alcohol intake.
Team-based care essential
The guidelines also put unprecedented emphasis on using a team-based management approach, which means having nurses, nurse practitioners, pharmacists, dietitians, and other clinicians, allowing for more frequent and focused care. Dr. Whelton and others cited in particular the VA Health System and Kaiser-Permanente as operating team-based and system-driven blood pressure management programs that have resulted in control rates for more than 90% of hypertensive patients. The team-based approach is also a key in the Target:BP program that the American Heart Association and American Medical Association founded. Target:BP will be instrumental in promoting implementation of the new guidelines, Dr. Carey said. Another systems recommendation is that every patient with hypertension should have a “clear, detailed, and current evidence-based plan of care.”
“Using nurse practitioners, physician assistants, and pharmacists has been shown to improve blood pressure levels,” and health systems that use this approach have had “great success,” commented Donald M. Lloyd-Jones, MD, professor and chairman of preventive medicine at Northwestern University in Chicago and not part of the guidelines task force. Some systems have used this approach to achieve high levels of blood pressure control. Now that financial penalties and incentives from payers also exist to push for higher levels of blood pressure control, the alignment of financial and health incentives should result in big changes, Dr. Lloyd-Jones predicted in a video interview.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM THE AHA SCIENTIFIC SESSIONS
VIDEO: ERAS for minimally invasive surgery
Stacy A. Brethauer, MD, FACS, discusses the role of Enhanced Recovery After Surgery (ERAS) in minimally invasive surgical procedures. The goal of the ERAS approach is to minimize surgical stress on the patient, reduce length of stay, and reduce the use of opioids in the recovery phase. Dr. Brethauer discusses a pilot program, the Energy project, which will be conducted in more than 30 institutions for a year to look at an ERAS protocol designed to work with minimally invasive surgical procedures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Stacy A. Brethauer, MD, FACS, discusses the role of Enhanced Recovery After Surgery (ERAS) in minimally invasive surgical procedures. The goal of the ERAS approach is to minimize surgical stress on the patient, reduce length of stay, and reduce the use of opioids in the recovery phase. Dr. Brethauer discusses a pilot program, the Energy project, which will be conducted in more than 30 institutions for a year to look at an ERAS protocol designed to work with minimally invasive surgical procedures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Stacy A. Brethauer, MD, FACS, discusses the role of Enhanced Recovery After Surgery (ERAS) in minimally invasive surgical procedures. The goal of the ERAS approach is to minimize surgical stress on the patient, reduce length of stay, and reduce the use of opioids in the recovery phase. Dr. Brethauer discusses a pilot program, the Energy project, which will be conducted in more than 30 institutions for a year to look at an ERAS protocol designed to work with minimally invasive surgical procedures.