User login
VIDEO: Evidence mounts for pulmonary embolism benefit from catheter thrombolysis
TORONTO – Catheter-directed thrombolysis of pulmonary embolism using an ultrasound-assisted device led to significantly better outcomes in patients hospitalized for pulmonary embolism, compared with conventional systemic thrombolytic treatment, in a propensity score–adjusted analysis of nearly 3,400 patients.
Catheter-directed thrombolysis (CDT) “represents an opportunity to locally treat pulmonary embolism with significant thrombus burden with lower bleeding complications,” Abhishek Mishra, MD, said at the CHEST annual meeting. “I think we are underusing CDT,” said Dr. Mishra, a cardiovascular disease physician at Guthrie Robert Packer Hospital in Sayre, Pa.
Although one CDT device, the EKOS endovascular system that uses ultrasound to facilitate pulmonary embolism (PE) thrombolysis, received Food & Drug Administration approval for U.S. marketing in 2014, the trials that have compared it with systemic thrombolysis have been small, noted Dr. Mishra, and none have looked at whether CDT improves patient survival, compared with standard treatments. The largest report on CDT treatment of PE came from a single-arm, uncontrolled study with 150 patients who received ultrasound-facilitated CDT (JACC Cardiovasc Interv. 2015 Aug;8[10]:1382-92).
To better document the incremental benefit from CDT, Dr. Mishra and his associates used data collected by the Nationwide Readmissions Database during 2013 and 2014, both before and after a CDT device became available for U.S. use. From among 4,426 patients hospitalized with a primary diagnosis of PE and treated with thrombolytic therapy, they used propensity score matching to compare 2,256 patients treated with systemic thrombolysis with 1,128 matched patients treated with CDT using tissue plasminogen activator.
The analysis showed that in-hospital death was 15% in the systemic patients and 6% in the CDT group, a relative risk reduction of 63%, and 30-day readmissions occurred in 11% of the systemic patients and in 8% of those treated with CDT, a 30% relative risk reduction. Both were statistically significant differences for the study’s two primary endpoints, Dr. Mishra reported at the meeting. Rates of intracerebral hemorrhage and gastrointestinal bleeds were both numerically lower with CDT, and significantly lower for gastrointestinal bleeds.
The researchers also ran a multivariate analysis on their data that showed CDT was linked with significant relative reductions of about 60% for both in-hospital death and 30-day readmissions, compared with patients on systemic therapy. The results Dr. Mishra reported also appeared in a published report (Am J Cardiol. 2017 Nov 1;120[9]:1653-61).
These findings help buttress the case for using CDT for at least some PE patients. “The key is which patients need it. What is the best way to stratify patients?” commented Victor F. Tapson, MD, a pulmonologist at Cedars-Sinai Medical Center in Los Angeles.
“Patients with PE and a normal right ventricle generally don’t need anything more aggressive than anticoagulation, and really sick patients with massive PE need systemic thrombolytics. Intermediate-risk patients” are best suited to CDT, but “the problem is that intermediate-risk patients are heterogeneous,” Dr. Tapson said in a video interview. Future studies should establish a more specific subgroup of intermediate-risk patients who benefit from routinely employed CDT, he suggested.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
BY MITCHEL L. ZOLER
Frontline Medical News
BY MITCHEL L. ZOLER
Frontline Medical News
BY MITCHEL L. ZOLER
Frontline Medical News
TORONTO – Catheter-directed thrombolysis of pulmonary embolism using an ultrasound-assisted device led to significantly better outcomes in patients hospitalized for pulmonary embolism, compared with conventional systemic thrombolytic treatment, in a propensity score–adjusted analysis of nearly 3,400 patients.
Catheter-directed thrombolysis (CDT) “represents an opportunity to locally treat pulmonary embolism with significant thrombus burden with lower bleeding complications,” Abhishek Mishra, MD, said at the CHEST annual meeting. “I think we are underusing CDT,” said Dr. Mishra, a cardiovascular disease physician at Guthrie Robert Packer Hospital in Sayre, Pa.
Although one CDT device, the EKOS endovascular system that uses ultrasound to facilitate pulmonary embolism (PE) thrombolysis, received Food & Drug Administration approval for U.S. marketing in 2014, the trials that have compared it with systemic thrombolysis have been small, noted Dr. Mishra, and none have looked at whether CDT improves patient survival, compared with standard treatments. The largest report on CDT treatment of PE came from a single-arm, uncontrolled study with 150 patients who received ultrasound-facilitated CDT (JACC Cardiovasc Interv. 2015 Aug;8[10]:1382-92).
To better document the incremental benefit from CDT, Dr. Mishra and his associates used data collected by the Nationwide Readmissions Database during 2013 and 2014, both before and after a CDT device became available for U.S. use. From among 4,426 patients hospitalized with a primary diagnosis of PE and treated with thrombolytic therapy, they used propensity score matching to compare 2,256 patients treated with systemic thrombolysis with 1,128 matched patients treated with CDT using tissue plasminogen activator.
The analysis showed that in-hospital death was 15% in the systemic patients and 6% in the CDT group, a relative risk reduction of 63%, and 30-day readmissions occurred in 11% of the systemic patients and in 8% of those treated with CDT, a 30% relative risk reduction. Both were statistically significant differences for the study’s two primary endpoints, Dr. Mishra reported at the meeting. Rates of intracerebral hemorrhage and gastrointestinal bleeds were both numerically lower with CDT, and significantly lower for gastrointestinal bleeds.
The researchers also ran a multivariate analysis on their data that showed CDT was linked with significant relative reductions of about 60% for both in-hospital death and 30-day readmissions, compared with patients on systemic therapy. The results Dr. Mishra reported also appeared in a published report (Am J Cardiol. 2017 Nov 1;120[9]:1653-61).
These findings help buttress the case for using CDT for at least some PE patients. “The key is which patients need it. What is the best way to stratify patients?” commented Victor F. Tapson, MD, a pulmonologist at Cedars-Sinai Medical Center in Los Angeles.
“Patients with PE and a normal right ventricle generally don’t need anything more aggressive than anticoagulation, and really sick patients with massive PE need systemic thrombolytics. Intermediate-risk patients” are best suited to CDT, but “the problem is that intermediate-risk patients are heterogeneous,” Dr. Tapson said in a video interview. Future studies should establish a more specific subgroup of intermediate-risk patients who benefit from routinely employed CDT, he suggested.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
TORONTO – Catheter-directed thrombolysis of pulmonary embolism using an ultrasound-assisted device led to significantly better outcomes in patients hospitalized for pulmonary embolism, compared with conventional systemic thrombolytic treatment, in a propensity score–adjusted analysis of nearly 3,400 patients.
Catheter-directed thrombolysis (CDT) “represents an opportunity to locally treat pulmonary embolism with significant thrombus burden with lower bleeding complications,” Abhishek Mishra, MD, said at the CHEST annual meeting. “I think we are underusing CDT,” said Dr. Mishra, a cardiovascular disease physician at Guthrie Robert Packer Hospital in Sayre, Pa.
Although one CDT device, the EKOS endovascular system that uses ultrasound to facilitate pulmonary embolism (PE) thrombolysis, received Food & Drug Administration approval for U.S. marketing in 2014, the trials that have compared it with systemic thrombolysis have been small, noted Dr. Mishra, and none have looked at whether CDT improves patient survival, compared with standard treatments. The largest report on CDT treatment of PE came from a single-arm, uncontrolled study with 150 patients who received ultrasound-facilitated CDT (JACC Cardiovasc Interv. 2015 Aug;8[10]:1382-92).
To better document the incremental benefit from CDT, Dr. Mishra and his associates used data collected by the Nationwide Readmissions Database during 2013 and 2014, both before and after a CDT device became available for U.S. use. From among 4,426 patients hospitalized with a primary diagnosis of PE and treated with thrombolytic therapy, they used propensity score matching to compare 2,256 patients treated with systemic thrombolysis with 1,128 matched patients treated with CDT using tissue plasminogen activator.
The analysis showed that in-hospital death was 15% in the systemic patients and 6% in the CDT group, a relative risk reduction of 63%, and 30-day readmissions occurred in 11% of the systemic patients and in 8% of those treated with CDT, a 30% relative risk reduction. Both were statistically significant differences for the study’s two primary endpoints, Dr. Mishra reported at the meeting. Rates of intracerebral hemorrhage and gastrointestinal bleeds were both numerically lower with CDT, and significantly lower for gastrointestinal bleeds.
The researchers also ran a multivariate analysis on their data that showed CDT was linked with significant relative reductions of about 60% for both in-hospital death and 30-day readmissions, compared with patients on systemic therapy. The results Dr. Mishra reported also appeared in a published report (Am J Cardiol. 2017 Nov 1;120[9]:1653-61).
These findings help buttress the case for using CDT for at least some PE patients. “The key is which patients need it. What is the best way to stratify patients?” commented Victor F. Tapson, MD, a pulmonologist at Cedars-Sinai Medical Center in Los Angeles.
“Patients with PE and a normal right ventricle generally don’t need anything more aggressive than anticoagulation, and really sick patients with massive PE need systemic thrombolytics. Intermediate-risk patients” are best suited to CDT, but “the problem is that intermediate-risk patients are heterogeneous,” Dr. Tapson said in a video interview. Future studies should establish a more specific subgroup of intermediate-risk patients who benefit from routinely employed CDT, he suggested.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT CHEST 2017
Key clinical point:
Major finding: Catheter-directed thrombolysis cut in-hospital mortality by 63%, compared with conventional systemic thrombolysis.
Data source: The National Readmission Database, which included 4,426 patients hospitalized during 2013 and 2014 with primary pulmonary embolism and treated with thrombolysis.
Disclosures: Dr. Mishra had no disclosures. Dr. Tapson has been a consultant to and had received research funding from Ekos/BTG, a company that markets a catheter-directed thrombolysis device. He has also ties to Daiichi Sankyo, Inari, Janssen, and Portola.
VIDEO: Revised guidelines raise lung cancer screening age ceiling
TORONTO – A proposed change to CHEST’s lung cancer screening guideline calls for raising the upper age for screening recent cigarette smokers to 77 years of age from 74 years of age.
This proposal is part of draft guideline that was unveiled during the CHEST annual meeting but is still subject to tweaking by peer review until formal release in early 2018. The draft also offers expanded guidance on how to implement screening, containing three times as many recommendations as the current lung cancer screening guidelines (Chest. 2013 May; 143[5 Suppl]:e78S-e92S).
“We want screening to expand in a safe and effective way,” said Peter J. Mazzone, MD, chair of the expert panel that is preparing the revision for CHEST and a pulmonologist at the Cleveland Clinic. “We are less restrictive with these guidelines” than in the 2013 version.
Dr. Mazzone cited two major changes that will produce modest broadening of the criteria that determine which patients can appropriately get screening. The clearest change was the age range, which expanded from 55-74 years of age set in 2013 to reflect the age criterion for enrollment in the National Lung Screening Trial (New Engl J Med. 2011 Aug 4; 365[5]:395-409). Dr. Mazzone explained, though it remains short of the 80-year old ceiling recommended by the U.S. Preventive Services Task Force.
The second, subtler change eased back on the outright ban that the 2013 guidelines placed on screening anyone who falls outside the target age range and smoking history (at least 30 pack years and either being a current smoker or having recently quit within the past 15 years) and who is without severe comorbidities.
The guidelines from 2013 said that screening people who fell outside these limits “should not be performed.” In contrast, the new draft guideline simply said that people who fall outside of the age and smoking-history criteria but who are still considered high risk for lung cancer based on a risk-prediction calculator should not “routinely” undergo screening. Additionally, exceptions could be made for certain patients whose high risk appears to warrant screening, Dr. Mazzone and others from the expert panel noted.
The revision specified that a high-risk person outside of the core criteria might still be a reasonable candidate for screening if this person tallies at least a 1.51% risk of developing lung cancer during the next 6 years according to the PLCOM2012 risk calculator (New Engl J Med. 2013 Feb 21; 368[8]:728-36).
“Some of the evidence allowed us to be a little more flexible,” though not to the point of “opening screening widely” to people who fall outside the core target population; rather, clinicians get to have a little more discretion, said Dr. Mazzone, who directs the Cleveland Clinic’s Lung Cancer Program. “We hope this will lead to more patients being screened in a high quality way,” he said in an interview. The panel strove to “look beyond the National Lung Screening Trial and find other groups of patients who could benefit” from screening. “We say that other high-risk people should not, on the whole, be screened” but that clinicians could consider individuals as appropriate for screening on a case-by-case basis.
The revision “fills in the outline” for screening that was established in the 2013 guidelines, said Gerard A. Silvestri, MD, a member of the revision panel, in a video interview. The updated guideline better detailed who benefits the most from screening and who benefits less, as well as the potential complications screening may cause, said Dr. Silvestri, a professor of medicine and lung cancer pulmonologist at the Medical University of South Carolina in Charleston.
“The sweet spot for screening is patients with a medium lung cancer risk without many comorbidities. We are trying to come up with individualized risk profiling,” explained Dr. Silvestri during the CHEST session. He noted that, in the screening program he runs in Charleston, every person who contacts the program and is interested in screening undergoes risk profiling. Are there people with a risk profile that justifies screening but fall outside the proposed criteria? “Absolutely,” Dr. Silvestri said.
People considering screening also need to recognize its potential harms, noted Renda Soylemez Wiener, MD, another member of the expert panel who spoke at the meeting. She cited five potential harms: death or complications from a biopsy of a screen-detected nodule, surgery for a screen-detected lesion that turns out to be benign, the psychosocial impact of finding a lung nodule, over diagnosis, and the cumulative radiation exposure from serial low-dose chest CT scans. “All of these dangers are real and may be magnified or mitigated as low-dose CT screening is implemented in real world practice,” said Dr. Wiener, a pulmonologist at Boston University.
In addition to four evidence-based recommendations that help define who is and isn’t an appropriate screening candidate, the revised guideline also included 11 mostly consensus-based “suggestions” about how screening programs should ideally operate. These covered issues such as identifying symptomatic patients who require diagnosis rather than screening, having strategies to encourage compliance with annual screening, including smoking cessation treatments in screening programs, and having strategies that minimize overtreatment of potentially indolent cancers.
The goal of these suggestions is to help in the design of high-quality screening programs, said Dr. Mazzone. “It’s not just who you screen but also how you screen.”
On Twitter @mitchelzoler
M. Patricia Rivera, MD, FCCP, comments: The revised ACCP screening guidelines recommend expanding the screening age from 55-74 years (age criterion used in the National Lung Screening Trial) to 55-77 years. While this may be interpreted as raising the screening age ceiling, the new recommendation is in line with the age range approved by Medicare. We should also keep in mind that after modeling studies to predict the benefits and harms of screening programs using different screening intervals, age ranges, and smoking histories (duration and time since quitting), the USPSTF concluded in their final recommendation that screening adults aged 55-80 years with same smoking history and time since quitting used in the National Lung Screening Trial (NLST) had a reasonable balance of benefits and harms. Implementing lung cancer screening has been challenging, and studies have reported many patient-, provider-, and system-based barriers including conflicting upper age range recommendations.
While age and smoking history are important in identifying individuals at risk for lung cancer, development of lung cancer is likely multifactorial and several other risk factors need to be considered. The ACCP's revised guidelines provide flexibility when evaluating patients who do not meet the age and smoking history criteria for screening but who have a high risk for developing lung cancer based on risk prediction models. Following publication of the NLST results, secondary analysis of the data using a risk prediction model that takes into account additional risk factors for the development of lung cancer (race, COPD, and family history of lung cancer, among others) suggests risk prediction modeling may be helpful at identifying the individuals who are at highest risk for developing lung cancer. As pointed out by Dr. Mazzone and Dr. Silvestri, the ACCP lung cancer screening guidelines promote the expansion of lung cancer screening in a safe and effective way and encourage individualized risk profiling to aid in the selection of all individuals who will benefit from lung cancer screening.
M. Patricia Rivera, MD, FCCP, comments: The revised ACCP screening guidelines recommend expanding the screening age from 55-74 years (age criterion used in the National Lung Screening Trial) to 55-77 years. While this may be interpreted as raising the screening age ceiling, the new recommendation is in line with the age range approved by Medicare. We should also keep in mind that after modeling studies to predict the benefits and harms of screening programs using different screening intervals, age ranges, and smoking histories (duration and time since quitting), the USPSTF concluded in their final recommendation that screening adults aged 55-80 years with same smoking history and time since quitting used in the National Lung Screening Trial (NLST) had a reasonable balance of benefits and harms. Implementing lung cancer screening has been challenging, and studies have reported many patient-, provider-, and system-based barriers including conflicting upper age range recommendations.
While age and smoking history are important in identifying individuals at risk for lung cancer, development of lung cancer is likely multifactorial and several other risk factors need to be considered. The ACCP's revised guidelines provide flexibility when evaluating patients who do not meet the age and smoking history criteria for screening but who have a high risk for developing lung cancer based on risk prediction models. Following publication of the NLST results, secondary analysis of the data using a risk prediction model that takes into account additional risk factors for the development of lung cancer (race, COPD, and family history of lung cancer, among others) suggests risk prediction modeling may be helpful at identifying the individuals who are at highest risk for developing lung cancer. As pointed out by Dr. Mazzone and Dr. Silvestri, the ACCP lung cancer screening guidelines promote the expansion of lung cancer screening in a safe and effective way and encourage individualized risk profiling to aid in the selection of all individuals who will benefit from lung cancer screening.
M. Patricia Rivera, MD, FCCP, comments: The revised ACCP screening guidelines recommend expanding the screening age from 55-74 years (age criterion used in the National Lung Screening Trial) to 55-77 years. While this may be interpreted as raising the screening age ceiling, the new recommendation is in line with the age range approved by Medicare. We should also keep in mind that after modeling studies to predict the benefits and harms of screening programs using different screening intervals, age ranges, and smoking histories (duration and time since quitting), the USPSTF concluded in their final recommendation that screening adults aged 55-80 years with same smoking history and time since quitting used in the National Lung Screening Trial (NLST) had a reasonable balance of benefits and harms. Implementing lung cancer screening has been challenging, and studies have reported many patient-, provider-, and system-based barriers including conflicting upper age range recommendations.
While age and smoking history are important in identifying individuals at risk for lung cancer, development of lung cancer is likely multifactorial and several other risk factors need to be considered. The ACCP's revised guidelines provide flexibility when evaluating patients who do not meet the age and smoking history criteria for screening but who have a high risk for developing lung cancer based on risk prediction models. Following publication of the NLST results, secondary analysis of the data using a risk prediction model that takes into account additional risk factors for the development of lung cancer (race, COPD, and family history of lung cancer, among others) suggests risk prediction modeling may be helpful at identifying the individuals who are at highest risk for developing lung cancer. As pointed out by Dr. Mazzone and Dr. Silvestri, the ACCP lung cancer screening guidelines promote the expansion of lung cancer screening in a safe and effective way and encourage individualized risk profiling to aid in the selection of all individuals who will benefit from lung cancer screening.
TORONTO – A proposed change to CHEST’s lung cancer screening guideline calls for raising the upper age for screening recent cigarette smokers to 77 years of age from 74 years of age.
This proposal is part of draft guideline that was unveiled during the CHEST annual meeting but is still subject to tweaking by peer review until formal release in early 2018. The draft also offers expanded guidance on how to implement screening, containing three times as many recommendations as the current lung cancer screening guidelines (Chest. 2013 May; 143[5 Suppl]:e78S-e92S).
“We want screening to expand in a safe and effective way,” said Peter J. Mazzone, MD, chair of the expert panel that is preparing the revision for CHEST and a pulmonologist at the Cleveland Clinic. “We are less restrictive with these guidelines” than in the 2013 version.
Dr. Mazzone cited two major changes that will produce modest broadening of the criteria that determine which patients can appropriately get screening. The clearest change was the age range, which expanded from 55-74 years of age set in 2013 to reflect the age criterion for enrollment in the National Lung Screening Trial (New Engl J Med. 2011 Aug 4; 365[5]:395-409). Dr. Mazzone explained, though it remains short of the 80-year old ceiling recommended by the U.S. Preventive Services Task Force.
The second, subtler change eased back on the outright ban that the 2013 guidelines placed on screening anyone who falls outside the target age range and smoking history (at least 30 pack years and either being a current smoker or having recently quit within the past 15 years) and who is without severe comorbidities.
The guidelines from 2013 said that screening people who fell outside these limits “should not be performed.” In contrast, the new draft guideline simply said that people who fall outside of the age and smoking-history criteria but who are still considered high risk for lung cancer based on a risk-prediction calculator should not “routinely” undergo screening. Additionally, exceptions could be made for certain patients whose high risk appears to warrant screening, Dr. Mazzone and others from the expert panel noted.
The revision specified that a high-risk person outside of the core criteria might still be a reasonable candidate for screening if this person tallies at least a 1.51% risk of developing lung cancer during the next 6 years according to the PLCOM2012 risk calculator (New Engl J Med. 2013 Feb 21; 368[8]:728-36).
“Some of the evidence allowed us to be a little more flexible,” though not to the point of “opening screening widely” to people who fall outside the core target population; rather, clinicians get to have a little more discretion, said Dr. Mazzone, who directs the Cleveland Clinic’s Lung Cancer Program. “We hope this will lead to more patients being screened in a high quality way,” he said in an interview. The panel strove to “look beyond the National Lung Screening Trial and find other groups of patients who could benefit” from screening. “We say that other high-risk people should not, on the whole, be screened” but that clinicians could consider individuals as appropriate for screening on a case-by-case basis.
The revision “fills in the outline” for screening that was established in the 2013 guidelines, said Gerard A. Silvestri, MD, a member of the revision panel, in a video interview. The updated guideline better detailed who benefits the most from screening and who benefits less, as well as the potential complications screening may cause, said Dr. Silvestri, a professor of medicine and lung cancer pulmonologist at the Medical University of South Carolina in Charleston.
“The sweet spot for screening is patients with a medium lung cancer risk without many comorbidities. We are trying to come up with individualized risk profiling,” explained Dr. Silvestri during the CHEST session. He noted that, in the screening program he runs in Charleston, every person who contacts the program and is interested in screening undergoes risk profiling. Are there people with a risk profile that justifies screening but fall outside the proposed criteria? “Absolutely,” Dr. Silvestri said.
People considering screening also need to recognize its potential harms, noted Renda Soylemez Wiener, MD, another member of the expert panel who spoke at the meeting. She cited five potential harms: death or complications from a biopsy of a screen-detected nodule, surgery for a screen-detected lesion that turns out to be benign, the psychosocial impact of finding a lung nodule, over diagnosis, and the cumulative radiation exposure from serial low-dose chest CT scans. “All of these dangers are real and may be magnified or mitigated as low-dose CT screening is implemented in real world practice,” said Dr. Wiener, a pulmonologist at Boston University.
In addition to four evidence-based recommendations that help define who is and isn’t an appropriate screening candidate, the revised guideline also included 11 mostly consensus-based “suggestions” about how screening programs should ideally operate. These covered issues such as identifying symptomatic patients who require diagnosis rather than screening, having strategies to encourage compliance with annual screening, including smoking cessation treatments in screening programs, and having strategies that minimize overtreatment of potentially indolent cancers.
The goal of these suggestions is to help in the design of high-quality screening programs, said Dr. Mazzone. “It’s not just who you screen but also how you screen.”
On Twitter @mitchelzoler
TORONTO – A proposed change to CHEST’s lung cancer screening guideline calls for raising the upper age for screening recent cigarette smokers to 77 years of age from 74 years of age.
This proposal is part of draft guideline that was unveiled during the CHEST annual meeting but is still subject to tweaking by peer review until formal release in early 2018. The draft also offers expanded guidance on how to implement screening, containing three times as many recommendations as the current lung cancer screening guidelines (Chest. 2013 May; 143[5 Suppl]:e78S-e92S).
“We want screening to expand in a safe and effective way,” said Peter J. Mazzone, MD, chair of the expert panel that is preparing the revision for CHEST and a pulmonologist at the Cleveland Clinic. “We are less restrictive with these guidelines” than in the 2013 version.
Dr. Mazzone cited two major changes that will produce modest broadening of the criteria that determine which patients can appropriately get screening. The clearest change was the age range, which expanded from 55-74 years of age set in 2013 to reflect the age criterion for enrollment in the National Lung Screening Trial (New Engl J Med. 2011 Aug 4; 365[5]:395-409). Dr. Mazzone explained, though it remains short of the 80-year old ceiling recommended by the U.S. Preventive Services Task Force.
The second, subtler change eased back on the outright ban that the 2013 guidelines placed on screening anyone who falls outside the target age range and smoking history (at least 30 pack years and either being a current smoker or having recently quit within the past 15 years) and who is without severe comorbidities.
The guidelines from 2013 said that screening people who fell outside these limits “should not be performed.” In contrast, the new draft guideline simply said that people who fall outside of the age and smoking-history criteria but who are still considered high risk for lung cancer based on a risk-prediction calculator should not “routinely” undergo screening. Additionally, exceptions could be made for certain patients whose high risk appears to warrant screening, Dr. Mazzone and others from the expert panel noted.
The revision specified that a high-risk person outside of the core criteria might still be a reasonable candidate for screening if this person tallies at least a 1.51% risk of developing lung cancer during the next 6 years according to the PLCOM2012 risk calculator (New Engl J Med. 2013 Feb 21; 368[8]:728-36).
“Some of the evidence allowed us to be a little more flexible,” though not to the point of “opening screening widely” to people who fall outside the core target population; rather, clinicians get to have a little more discretion, said Dr. Mazzone, who directs the Cleveland Clinic’s Lung Cancer Program. “We hope this will lead to more patients being screened in a high quality way,” he said in an interview. The panel strove to “look beyond the National Lung Screening Trial and find other groups of patients who could benefit” from screening. “We say that other high-risk people should not, on the whole, be screened” but that clinicians could consider individuals as appropriate for screening on a case-by-case basis.
The revision “fills in the outline” for screening that was established in the 2013 guidelines, said Gerard A. Silvestri, MD, a member of the revision panel, in a video interview. The updated guideline better detailed who benefits the most from screening and who benefits less, as well as the potential complications screening may cause, said Dr. Silvestri, a professor of medicine and lung cancer pulmonologist at the Medical University of South Carolina in Charleston.
“The sweet spot for screening is patients with a medium lung cancer risk without many comorbidities. We are trying to come up with individualized risk profiling,” explained Dr. Silvestri during the CHEST session. He noted that, in the screening program he runs in Charleston, every person who contacts the program and is interested in screening undergoes risk profiling. Are there people with a risk profile that justifies screening but fall outside the proposed criteria? “Absolutely,” Dr. Silvestri said.
People considering screening also need to recognize its potential harms, noted Renda Soylemez Wiener, MD, another member of the expert panel who spoke at the meeting. She cited five potential harms: death or complications from a biopsy of a screen-detected nodule, surgery for a screen-detected lesion that turns out to be benign, the psychosocial impact of finding a lung nodule, over diagnosis, and the cumulative radiation exposure from serial low-dose chest CT scans. “All of these dangers are real and may be magnified or mitigated as low-dose CT screening is implemented in real world practice,” said Dr. Wiener, a pulmonologist at Boston University.
In addition to four evidence-based recommendations that help define who is and isn’t an appropriate screening candidate, the revised guideline also included 11 mostly consensus-based “suggestions” about how screening programs should ideally operate. These covered issues such as identifying symptomatic patients who require diagnosis rather than screening, having strategies to encourage compliance with annual screening, including smoking cessation treatments in screening programs, and having strategies that minimize overtreatment of potentially indolent cancers.
The goal of these suggestions is to help in the design of high-quality screening programs, said Dr. Mazzone. “It’s not just who you screen but also how you screen.”
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM CHEST 2017
VIDEO: Light-based scar treatments improve more than just cosmetic appearance
LAS VEGAS – Clinicians can offer patients with scarring the potential for more comprehensive improvement thanks to progress in light-based devices and technologies, Kristen M. Kelly, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
“Not only can we improve these scars from a cosmetic appearance ... but we can also greatly improve the symptoms that patients have,” such as scar-related stinging, discomfort, and movement restrictions or contractures, said Dr. Kelly of the University of California, Irvine.
In addition, combining light-based therapies with medications applied after the treatments can optimize results, she said.
Dr. Kelly disclosed relationships with multiple companies including Allergan, MundiPharma, Syneron-Candela, Light Sciences Oncology, Novartis, Sciton, and ThermiRF.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – Clinicians can offer patients with scarring the potential for more comprehensive improvement thanks to progress in light-based devices and technologies, Kristen M. Kelly, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
“Not only can we improve these scars from a cosmetic appearance ... but we can also greatly improve the symptoms that patients have,” such as scar-related stinging, discomfort, and movement restrictions or contractures, said Dr. Kelly of the University of California, Irvine.
In addition, combining light-based therapies with medications applied after the treatments can optimize results, she said.
Dr. Kelly disclosed relationships with multiple companies including Allergan, MundiPharma, Syneron-Candela, Light Sciences Oncology, Novartis, Sciton, and ThermiRF.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – Clinicians can offer patients with scarring the potential for more comprehensive improvement thanks to progress in light-based devices and technologies, Kristen M. Kelly, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
“Not only can we improve these scars from a cosmetic appearance ... but we can also greatly improve the symptoms that patients have,” such as scar-related stinging, discomfort, and movement restrictions or contractures, said Dr. Kelly of the University of California, Irvine.
In addition, combining light-based therapies with medications applied after the treatments can optimize results, she said.
Dr. Kelly disclosed relationships with multiple companies including Allergan, MundiPharma, Syneron-Candela, Light Sciences Oncology, Novartis, Sciton, and ThermiRF.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SDEF LAS VEGAS DERMATOLOGY SEMINAR
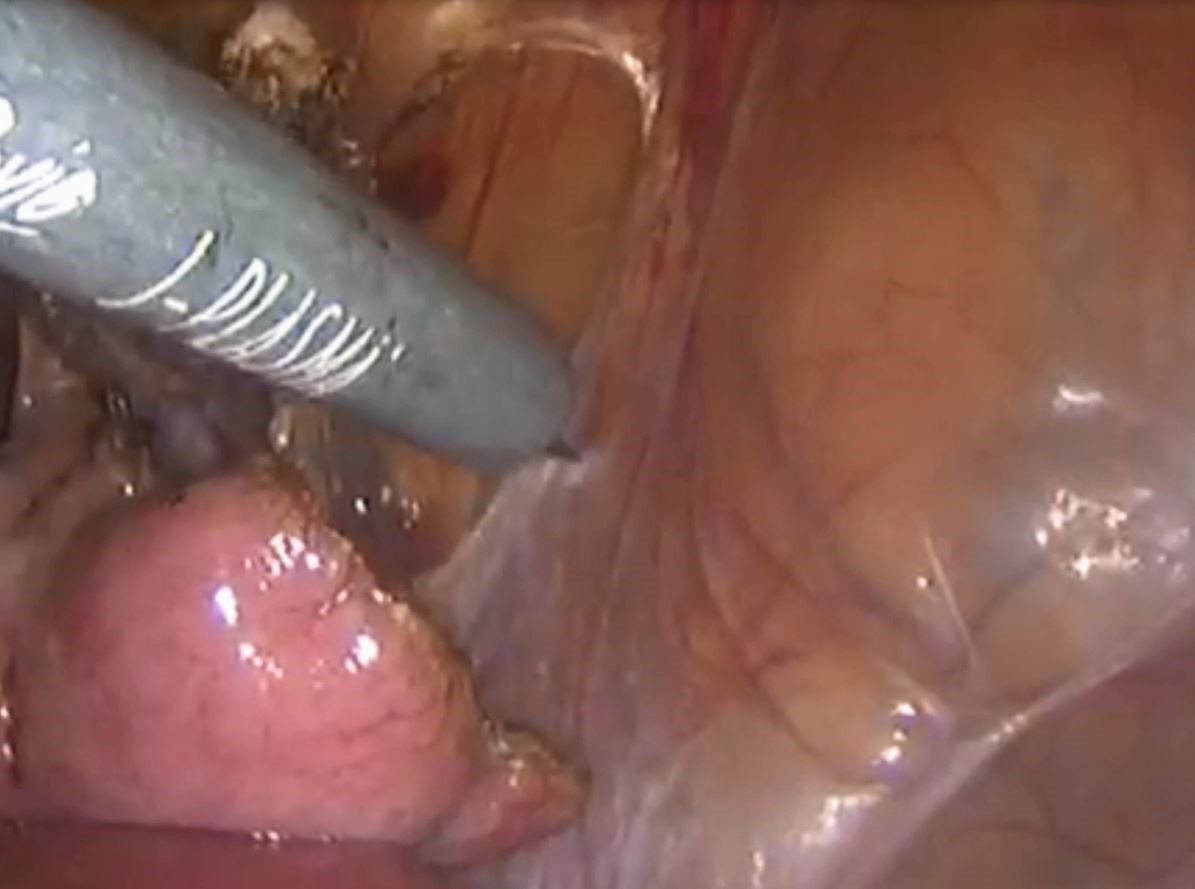
Laparoscopic management of chronic pelvic pain utilizing J-Plasma



VIDEO: MBSAQIP data looks at sleeve gastrectomy outcomes
Surgeon Matthew A. Hutter, MD, FACS, discusses the first report from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) focused on laparoscopic sleeve gastrectomy. The study (Ann Surg. 2016;264[3]:464-73) looked at outcomes, methods, and complications of this procedure based on a database of nearly 190,000 patients, more than 1,600 surgeons, and 720 centers. Dr. Hutter said that is high-quality data that offers surgeons good information on the procedure.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Surgeon Matthew A. Hutter, MD, FACS, discusses the first report from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) focused on laparoscopic sleeve gastrectomy. The study (Ann Surg. 2016;264[3]:464-73) looked at outcomes, methods, and complications of this procedure based on a database of nearly 190,000 patients, more than 1,600 surgeons, and 720 centers. Dr. Hutter said that is high-quality data that offers surgeons good information on the procedure.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Surgeon Matthew A. Hutter, MD, FACS, discusses the first report from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) focused on laparoscopic sleeve gastrectomy. The study (Ann Surg. 2016;264[3]:464-73) looked at outcomes, methods, and complications of this procedure based on a database of nearly 190,000 patients, more than 1,600 surgeons, and 720 centers. Dr. Hutter said that is high-quality data that offers surgeons good information on the procedure.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
A Peek at Our November 2017 Issue
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO: New PsA guideline expected in 2018
SAN DIEGO – For the first time, a forthcoming evidence-based guideline for the management of psoriatic arthritis recommends tumor necrosis factor inhibitor biologics as first-line therapy.
“Guidelines that have been around for the last several years have been skirting around the fact that there’s really no evidence that methotrexate works for PsA,” Dafna D. Gladman, MD, said during a press briefing at the annual meeting of the American College of Rheumatology. “So it’s refreshing and reassuring that when you do an appropriate, evidence-based approach, you finally find the truth in front of you, and you have TNF inhibitors as the first-line treatment. Obviously, they’re not for everybody. There are patients in whom we cannot use TNF inhibitors, either because they don’t like needles, or because they have contraindications to getting these particular needles, but at least we have a recommendation for the use of these drugs as a first-line treatment.”
“At first, I wasn’t a big fan of the idea of the GRADE guidelines because the number of questions blows up so fast, [but] it really makes you focus on what the most common [clinical] settings are,” said another core oversight team member, Alexis Ogdie, MD, a rheumatologist at the University of Pennsylvania, Philadelphia. “These guidelines also reveal the major gap of no head-to-head studies. I think we’ve known that, but this really called that out as important. When we’re making a treatment decision between [drugs] A and B, we need those studies to be able to better understand how to treat our patients, rather than using the data from one trial to make a decision. ... For my patients, I’m excited that I can now use a TNF inhibitor as a first-line agent. When we have patients come in with very severe disease, occasionally they also have severe psoriasis, so we’ve been able to use TNF inhibitors as first-line treatment in some of our patients in Pennsylvania. This differs state by state. But the exciting thing is that they get better so fast and you don’t have to tell them to wait 12 weeks for methotrexate to work.”
The ACR/NPF guideline is currently under peer review and is expected to be published in Arthritis & Rheumatology, Arthritis Care & Research, and the Journal of Psoriasis and Psoriatic Arthritis in the spring or summer of 2018. It focuses on common PsA patients, not exceptional cases. It includes recommendations on the management of patients with active PsA that is defined by the patients’ self-report and judged by the examining clinician to be caused by PsA, based on the on the presence of at least one of the following: actively inflamed joints; dactylitis; enthesitis; axial disease; active skin and/or nail involvement; and/or extra-articular manifestations such as uveitis or inflammatory bowel disease. Authors of the guideline considered cost as one of many possible factors affecting the use of the recommendations, but explicit cost-effectiveness analyses were not conducted. Also, since the NPF and the American Academy of Dermatology are concurrently developing a psoriasis treatment guideline, the treatment of skin psoriasis was not included in the guideline.
According to the guideline’s principal investigator Jasvinder Singh, MD, professor of medicine and epidemiology at the University of Alabama at Birmingham, the guideline will include 80 recommendations, 75 (94%) that are rated as “conditional,” and 5 (6%) that are rated as “strong,” based on the quality of evidence in the existing medical literature. “Most of our treatment guidelines rely on very low-to-moderate quality evidence, which means that there needs to be an active discussion between the physician and the patient with regard to which treatment to choose,” said Dr. Singh, who is also a staff rheumatologist at the Birmingham Veterans Affairs Medical Center and who led development of the 2012 and 2015 ACR treatment guidelines for RA. “When you’re not choosing the preferred treatment, there are defined specific recommendations under which that second treatment may be preferred over the first treatment.”
During a separate session at the meeting, Dr. Singh unveiled a few of the draft recommendations. One calls for using a treat-to-target strategy over not using one. In the setting of immunizing patients who are receiving a biologic, another recommendation calls for clinicians to start the indicated biologic and administer killed vaccines (as indicated) in patients with active PsA rather than delaying the biologic to give the killed vaccines. In addition, delaying the start of the indicated biologic is recommended over not delaying in order to administer a live attenuated vaccine in patients with active PsA. When patients continue to have with active PsA despite being on a TNF inhibitor, the draft guideline recommends switching to a different TNF inhibitor rather than an IL-17 inhibitor, an IL-12/IL-23 inhibitor, abatacept (Orencia), tofacitinib (Xeljanz), or adding methotrexate. If PsA is still active, the guideline recommends switching to an IL-17 inhibitor instead of an IL-12/IL-23 inhibitor, abatacept, or tofacitinib. If PsA is still active, the guideline recommends switching to an IL-12/IL-23 inhibitor over abatacept or tofacitinib.
The guideline also includes suggestions for nonpharmacologic treatments, including recommending low-impact exercise over high-impact exercise, occupational therapy, physical therapy, and weight loss. It also includes a strong recommendation to provide smoking cessation advice to patients.
Dr. Singh acknowledged significant research gaps in the current PsA medical literature, including no head-to-head comparisons of treatments. He said that the field also could benefit from specific studies for enthesitis, axial disease, and arthritis mutilans; randomized trials of nonpharmacologic interventions; more trials of monotherapy vs. combination therapy; vaccination trials for live attenuated vaccines; trials and registry studies of patients with common comorbidities, and studies of NSAIDs and glucocorticoids, to define their role.
Possible topics for future PsA guidelines, he continued, include treatment options for patients for whom biologic medication is not an option; use of therapies in pregnancy and conception; incorporation of high-quality cost or cost-effectiveness analysis into recommendations; and the role of other comorbidities, such as fibromyalgia, hepatitis, depression/anxiety, malignancy, and cardiovascular disease.
“Evidence-based medicine needs to be practiced, even in situations where it’s difficult to get a drug,” Dr. Gladman said. “One of the things we hope will happen in the near future is that companies will start doing head-to-head studies, to help us support evidence-based recommendations in the future.”
None of the speakers reported having relevant financial disclosures.
SAN DIEGO – For the first time, a forthcoming evidence-based guideline for the management of psoriatic arthritis recommends tumor necrosis factor inhibitor biologics as first-line therapy.
“Guidelines that have been around for the last several years have been skirting around the fact that there’s really no evidence that methotrexate works for PsA,” Dafna D. Gladman, MD, said during a press briefing at the annual meeting of the American College of Rheumatology. “So it’s refreshing and reassuring that when you do an appropriate, evidence-based approach, you finally find the truth in front of you, and you have TNF inhibitors as the first-line treatment. Obviously, they’re not for everybody. There are patients in whom we cannot use TNF inhibitors, either because they don’t like needles, or because they have contraindications to getting these particular needles, but at least we have a recommendation for the use of these drugs as a first-line treatment.”
“At first, I wasn’t a big fan of the idea of the GRADE guidelines because the number of questions blows up so fast, [but] it really makes you focus on what the most common [clinical] settings are,” said another core oversight team member, Alexis Ogdie, MD, a rheumatologist at the University of Pennsylvania, Philadelphia. “These guidelines also reveal the major gap of no head-to-head studies. I think we’ve known that, but this really called that out as important. When we’re making a treatment decision between [drugs] A and B, we need those studies to be able to better understand how to treat our patients, rather than using the data from one trial to make a decision. ... For my patients, I’m excited that I can now use a TNF inhibitor as a first-line agent. When we have patients come in with very severe disease, occasionally they also have severe psoriasis, so we’ve been able to use TNF inhibitors as first-line treatment in some of our patients in Pennsylvania. This differs state by state. But the exciting thing is that they get better so fast and you don’t have to tell them to wait 12 weeks for methotrexate to work.”
The ACR/NPF guideline is currently under peer review and is expected to be published in Arthritis & Rheumatology, Arthritis Care & Research, and the Journal of Psoriasis and Psoriatic Arthritis in the spring or summer of 2018. It focuses on common PsA patients, not exceptional cases. It includes recommendations on the management of patients with active PsA that is defined by the patients’ self-report and judged by the examining clinician to be caused by PsA, based on the on the presence of at least one of the following: actively inflamed joints; dactylitis; enthesitis; axial disease; active skin and/or nail involvement; and/or extra-articular manifestations such as uveitis or inflammatory bowel disease. Authors of the guideline considered cost as one of many possible factors affecting the use of the recommendations, but explicit cost-effectiveness analyses were not conducted. Also, since the NPF and the American Academy of Dermatology are concurrently developing a psoriasis treatment guideline, the treatment of skin psoriasis was not included in the guideline.
According to the guideline’s principal investigator Jasvinder Singh, MD, professor of medicine and epidemiology at the University of Alabama at Birmingham, the guideline will include 80 recommendations, 75 (94%) that are rated as “conditional,” and 5 (6%) that are rated as “strong,” based on the quality of evidence in the existing medical literature. “Most of our treatment guidelines rely on very low-to-moderate quality evidence, which means that there needs to be an active discussion between the physician and the patient with regard to which treatment to choose,” said Dr. Singh, who is also a staff rheumatologist at the Birmingham Veterans Affairs Medical Center and who led development of the 2012 and 2015 ACR treatment guidelines for RA. “When you’re not choosing the preferred treatment, there are defined specific recommendations under which that second treatment may be preferred over the first treatment.”
During a separate session at the meeting, Dr. Singh unveiled a few of the draft recommendations. One calls for using a treat-to-target strategy over not using one. In the setting of immunizing patients who are receiving a biologic, another recommendation calls for clinicians to start the indicated biologic and administer killed vaccines (as indicated) in patients with active PsA rather than delaying the biologic to give the killed vaccines. In addition, delaying the start of the indicated biologic is recommended over not delaying in order to administer a live attenuated vaccine in patients with active PsA. When patients continue to have with active PsA despite being on a TNF inhibitor, the draft guideline recommends switching to a different TNF inhibitor rather than an IL-17 inhibitor, an IL-12/IL-23 inhibitor, abatacept (Orencia), tofacitinib (Xeljanz), or adding methotrexate. If PsA is still active, the guideline recommends switching to an IL-17 inhibitor instead of an IL-12/IL-23 inhibitor, abatacept, or tofacitinib. If PsA is still active, the guideline recommends switching to an IL-12/IL-23 inhibitor over abatacept or tofacitinib.
The guideline also includes suggestions for nonpharmacologic treatments, including recommending low-impact exercise over high-impact exercise, occupational therapy, physical therapy, and weight loss. It also includes a strong recommendation to provide smoking cessation advice to patients.
Dr. Singh acknowledged significant research gaps in the current PsA medical literature, including no head-to-head comparisons of treatments. He said that the field also could benefit from specific studies for enthesitis, axial disease, and arthritis mutilans; randomized trials of nonpharmacologic interventions; more trials of monotherapy vs. combination therapy; vaccination trials for live attenuated vaccines; trials and registry studies of patients with common comorbidities, and studies of NSAIDs and glucocorticoids, to define their role.
Possible topics for future PsA guidelines, he continued, include treatment options for patients for whom biologic medication is not an option; use of therapies in pregnancy and conception; incorporation of high-quality cost or cost-effectiveness analysis into recommendations; and the role of other comorbidities, such as fibromyalgia, hepatitis, depression/anxiety, malignancy, and cardiovascular disease.
“Evidence-based medicine needs to be practiced, even in situations where it’s difficult to get a drug,” Dr. Gladman said. “One of the things we hope will happen in the near future is that companies will start doing head-to-head studies, to help us support evidence-based recommendations in the future.”
None of the speakers reported having relevant financial disclosures.
SAN DIEGO – For the first time, a forthcoming evidence-based guideline for the management of psoriatic arthritis recommends tumor necrosis factor inhibitor biologics as first-line therapy.
“Guidelines that have been around for the last several years have been skirting around the fact that there’s really no evidence that methotrexate works for PsA,” Dafna D. Gladman, MD, said during a press briefing at the annual meeting of the American College of Rheumatology. “So it’s refreshing and reassuring that when you do an appropriate, evidence-based approach, you finally find the truth in front of you, and you have TNF inhibitors as the first-line treatment. Obviously, they’re not for everybody. There are patients in whom we cannot use TNF inhibitors, either because they don’t like needles, or because they have contraindications to getting these particular needles, but at least we have a recommendation for the use of these drugs as a first-line treatment.”
“At first, I wasn’t a big fan of the idea of the GRADE guidelines because the number of questions blows up so fast, [but] it really makes you focus on what the most common [clinical] settings are,” said another core oversight team member, Alexis Ogdie, MD, a rheumatologist at the University of Pennsylvania, Philadelphia. “These guidelines also reveal the major gap of no head-to-head studies. I think we’ve known that, but this really called that out as important. When we’re making a treatment decision between [drugs] A and B, we need those studies to be able to better understand how to treat our patients, rather than using the data from one trial to make a decision. ... For my patients, I’m excited that I can now use a TNF inhibitor as a first-line agent. When we have patients come in with very severe disease, occasionally they also have severe psoriasis, so we’ve been able to use TNF inhibitors as first-line treatment in some of our patients in Pennsylvania. This differs state by state. But the exciting thing is that they get better so fast and you don’t have to tell them to wait 12 weeks for methotrexate to work.”
The ACR/NPF guideline is currently under peer review and is expected to be published in Arthritis & Rheumatology, Arthritis Care & Research, and the Journal of Psoriasis and Psoriatic Arthritis in the spring or summer of 2018. It focuses on common PsA patients, not exceptional cases. It includes recommendations on the management of patients with active PsA that is defined by the patients’ self-report and judged by the examining clinician to be caused by PsA, based on the on the presence of at least one of the following: actively inflamed joints; dactylitis; enthesitis; axial disease; active skin and/or nail involvement; and/or extra-articular manifestations such as uveitis or inflammatory bowel disease. Authors of the guideline considered cost as one of many possible factors affecting the use of the recommendations, but explicit cost-effectiveness analyses were not conducted. Also, since the NPF and the American Academy of Dermatology are concurrently developing a psoriasis treatment guideline, the treatment of skin psoriasis was not included in the guideline.
According to the guideline’s principal investigator Jasvinder Singh, MD, professor of medicine and epidemiology at the University of Alabama at Birmingham, the guideline will include 80 recommendations, 75 (94%) that are rated as “conditional,” and 5 (6%) that are rated as “strong,” based on the quality of evidence in the existing medical literature. “Most of our treatment guidelines rely on very low-to-moderate quality evidence, which means that there needs to be an active discussion between the physician and the patient with regard to which treatment to choose,” said Dr. Singh, who is also a staff rheumatologist at the Birmingham Veterans Affairs Medical Center and who led development of the 2012 and 2015 ACR treatment guidelines for RA. “When you’re not choosing the preferred treatment, there are defined specific recommendations under which that second treatment may be preferred over the first treatment.”
During a separate session at the meeting, Dr. Singh unveiled a few of the draft recommendations. One calls for using a treat-to-target strategy over not using one. In the setting of immunizing patients who are receiving a biologic, another recommendation calls for clinicians to start the indicated biologic and administer killed vaccines (as indicated) in patients with active PsA rather than delaying the biologic to give the killed vaccines. In addition, delaying the start of the indicated biologic is recommended over not delaying in order to administer a live attenuated vaccine in patients with active PsA. When patients continue to have with active PsA despite being on a TNF inhibitor, the draft guideline recommends switching to a different TNF inhibitor rather than an IL-17 inhibitor, an IL-12/IL-23 inhibitor, abatacept (Orencia), tofacitinib (Xeljanz), or adding methotrexate. If PsA is still active, the guideline recommends switching to an IL-17 inhibitor instead of an IL-12/IL-23 inhibitor, abatacept, or tofacitinib. If PsA is still active, the guideline recommends switching to an IL-12/IL-23 inhibitor over abatacept or tofacitinib.
The guideline also includes suggestions for nonpharmacologic treatments, including recommending low-impact exercise over high-impact exercise, occupational therapy, physical therapy, and weight loss. It also includes a strong recommendation to provide smoking cessation advice to patients.
Dr. Singh acknowledged significant research gaps in the current PsA medical literature, including no head-to-head comparisons of treatments. He said that the field also could benefit from specific studies for enthesitis, axial disease, and arthritis mutilans; randomized trials of nonpharmacologic interventions; more trials of monotherapy vs. combination therapy; vaccination trials for live attenuated vaccines; trials and registry studies of patients with common comorbidities, and studies of NSAIDs and glucocorticoids, to define their role.
Possible topics for future PsA guidelines, he continued, include treatment options for patients for whom biologic medication is not an option; use of therapies in pregnancy and conception; incorporation of high-quality cost or cost-effectiveness analysis into recommendations; and the role of other comorbidities, such as fibromyalgia, hepatitis, depression/anxiety, malignancy, and cardiovascular disease.
“Evidence-based medicine needs to be practiced, even in situations where it’s difficult to get a drug,” Dr. Gladman said. “One of the things we hope will happen in the near future is that companies will start doing head-to-head studies, to help us support evidence-based recommendations in the future.”
None of the speakers reported having relevant financial disclosures.
AT ACR 2017
VIDEO: Consider depression in patients with psoriasis
LAS VEGAS – When treating patients with psoriasis, “it is very important for us to treat the entire patient,” and consider the comorbidities, including depression, associated with psoriasis, Jeffrey M. Sobell, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
Depression can be a particular concern for younger patients with more severe psoriasis, said Dr. Sobell of Tufts University, Boston.
When he sees patients aged 18-35 years with significant psoriasis in his practice, he has made it a habit to ask them about depression “and if they’ve ever had thoughts of hurting themselves,” and arranges for mental health follow-up visits for patients about whom he is concerned. “It’s something that’s hard to talk about, but so important,” he said.
Dr. Sobell disclosed relationships with multiple companies including AbbVie, Amgen, Celgene, Eli Lilly, Janssen, Merck, Novartis, Regeneron, Sanofi, and Sun Pharma.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – When treating patients with psoriasis, “it is very important for us to treat the entire patient,” and consider the comorbidities, including depression, associated with psoriasis, Jeffrey M. Sobell, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
Depression can be a particular concern for younger patients with more severe psoriasis, said Dr. Sobell of Tufts University, Boston.
When he sees patients aged 18-35 years with significant psoriasis in his practice, he has made it a habit to ask them about depression “and if they’ve ever had thoughts of hurting themselves,” and arranges for mental health follow-up visits for patients about whom he is concerned. “It’s something that’s hard to talk about, but so important,” he said.
Dr. Sobell disclosed relationships with multiple companies including AbbVie, Amgen, Celgene, Eli Lilly, Janssen, Merck, Novartis, Regeneron, Sanofi, and Sun Pharma.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – When treating patients with psoriasis, “it is very important for us to treat the entire patient,” and consider the comorbidities, including depression, associated with psoriasis, Jeffrey M. Sobell, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
Depression can be a particular concern for younger patients with more severe psoriasis, said Dr. Sobell of Tufts University, Boston.
When he sees patients aged 18-35 years with significant psoriasis in his practice, he has made it a habit to ask them about depression “and if they’ve ever had thoughts of hurting themselves,” and arranges for mental health follow-up visits for patients about whom he is concerned. “It’s something that’s hard to talk about, but so important,” he said.
Dr. Sobell disclosed relationships with multiple companies including AbbVie, Amgen, Celgene, Eli Lilly, Janssen, Merck, Novartis, Regeneron, Sanofi, and Sun Pharma.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SDEF LAS VEGAS DERMATOLOGY SEMINAR