User login
VIDEO: Does genitourinary syndrome of menopause capture all the symptoms?
PHILADELPHIA – Genitourinary syndrome of menopause (GSM) replaced vulvovaginal atrophy in 2014 as a way to describe the changes to the genital and urinary tracts after menopause, but preliminary research shows it may be missing some symptoms.
In 2015, Amanda Clark, MD, a urogynecologist at the Kaiser Center for Health Research in Portland, Ore., and her colleagues surveyed women aged 55 years and older about their vulvar, vaginal, urinary, and sexual symptoms within 2 weeks of a well-woman visit to their primary care physician or gynecologist in the Kaiser system. In total, 1,533 provided valid data.
The researchers then used factor analysis to see if the symptoms matched up with GSM. If GSM is a true syndrome and only a single syndrome, then all of the factors would fit together in a one-factor model, Dr. Clark explained at the annual meeting of the North American Menopause Society. Instead, the researchers found that a three-factor model – with vulvovaginal symptoms of irritation and pain in one group, urinary symptoms in another group, and vaginal discharge and odor in a third group – fit best with the symptoms reported in their survey.
“This work is very preliminary and needs to be replicated in many other samples and looked at carefully,” Dr. Clark said in an interview. “But what we think is that genitourinary syndrome of menopause is a starting point.”
The study was funded by a Pfizer Independent Grant for Learning & Change and the North American Menopause Society. Dr. Clark reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mschneider@frontlinemedcom.com
On Twitter @maryellenny
PHILADELPHIA – Genitourinary syndrome of menopause (GSM) replaced vulvovaginal atrophy in 2014 as a way to describe the changes to the genital and urinary tracts after menopause, but preliminary research shows it may be missing some symptoms.
In 2015, Amanda Clark, MD, a urogynecologist at the Kaiser Center for Health Research in Portland, Ore., and her colleagues surveyed women aged 55 years and older about their vulvar, vaginal, urinary, and sexual symptoms within 2 weeks of a well-woman visit to their primary care physician or gynecologist in the Kaiser system. In total, 1,533 provided valid data.
The researchers then used factor analysis to see if the symptoms matched up with GSM. If GSM is a true syndrome and only a single syndrome, then all of the factors would fit together in a one-factor model, Dr. Clark explained at the annual meeting of the North American Menopause Society. Instead, the researchers found that a three-factor model – with vulvovaginal symptoms of irritation and pain in one group, urinary symptoms in another group, and vaginal discharge and odor in a third group – fit best with the symptoms reported in their survey.
“This work is very preliminary and needs to be replicated in many other samples and looked at carefully,” Dr. Clark said in an interview. “But what we think is that genitourinary syndrome of menopause is a starting point.”
The study was funded by a Pfizer Independent Grant for Learning & Change and the North American Menopause Society. Dr. Clark reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mschneider@frontlinemedcom.com
On Twitter @maryellenny
PHILADELPHIA – Genitourinary syndrome of menopause (GSM) replaced vulvovaginal atrophy in 2014 as a way to describe the changes to the genital and urinary tracts after menopause, but preliminary research shows it may be missing some symptoms.
In 2015, Amanda Clark, MD, a urogynecologist at the Kaiser Center for Health Research in Portland, Ore., and her colleagues surveyed women aged 55 years and older about their vulvar, vaginal, urinary, and sexual symptoms within 2 weeks of a well-woman visit to their primary care physician or gynecologist in the Kaiser system. In total, 1,533 provided valid data.
The researchers then used factor analysis to see if the symptoms matched up with GSM. If GSM is a true syndrome and only a single syndrome, then all of the factors would fit together in a one-factor model, Dr. Clark explained at the annual meeting of the North American Menopause Society. Instead, the researchers found that a three-factor model – with vulvovaginal symptoms of irritation and pain in one group, urinary symptoms in another group, and vaginal discharge and odor in a third group – fit best with the symptoms reported in their survey.
“This work is very preliminary and needs to be replicated in many other samples and looked at carefully,” Dr. Clark said in an interview. “But what we think is that genitourinary syndrome of menopause is a starting point.”
The study was funded by a Pfizer Independent Grant for Learning & Change and the North American Menopause Society. Dr. Clark reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mschneider@frontlinemedcom.com
On Twitter @maryellenny
AT NAMS 2017
VIDEO: IBD epidemiology provides clues into disease underpinnings
ORLANDO – The incidence of Crohn’s disease and ulcerative colitis has stabilized in the Western world, but is rising rapidly in newly industrialized countries, according to a systematic review of population-based studies.
The findings could provide important new insights into the environmental, genetic, and microbiome-related factors and interactions that form the underpinnings of IBD, Gilaad Kaplan, MD, of the University of Calgary (Alta.) said at the World Congress of Gastroenterology at ACG 2017.
In turn, that information could lead to approaches to reduce IBD incidence, he said in a video interview.
It has been known that Crohn’s disease and ulcerative colitis are “modern diseases of modern times,” but few studies have addressed the epidemiology of IBD in newly industrialized countries in Asia, Africa, and South America, he said.
“We see a pattern that as newly industrialized countries transition toward a westernized society, IBD emerges and its incidence rises, and there are many different explanations for that,” he said, noting that in part, the increase is due to improved health care infrastructure and advances in adoption of medical technology that lead to better identification of new cases.
“But probably one of the most important factors is that there are environmental exposures linked to the westernization of society that are creating this pressure that’s driving incidence of IBD up in many of the countries of the world,” he said. “I think if we do a lot more research focused on how environment influences microbiome, we might start to see things we could do that could potentially stem the tide of IBD.”
Dr. Kaplan reported having no relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – The incidence of Crohn’s disease and ulcerative colitis has stabilized in the Western world, but is rising rapidly in newly industrialized countries, according to a systematic review of population-based studies.
The findings could provide important new insights into the environmental, genetic, and microbiome-related factors and interactions that form the underpinnings of IBD, Gilaad Kaplan, MD, of the University of Calgary (Alta.) said at the World Congress of Gastroenterology at ACG 2017.
In turn, that information could lead to approaches to reduce IBD incidence, he said in a video interview.
It has been known that Crohn’s disease and ulcerative colitis are “modern diseases of modern times,” but few studies have addressed the epidemiology of IBD in newly industrialized countries in Asia, Africa, and South America, he said.
“We see a pattern that as newly industrialized countries transition toward a westernized society, IBD emerges and its incidence rises, and there are many different explanations for that,” he said, noting that in part, the increase is due to improved health care infrastructure and advances in adoption of medical technology that lead to better identification of new cases.
“But probably one of the most important factors is that there are environmental exposures linked to the westernization of society that are creating this pressure that’s driving incidence of IBD up in many of the countries of the world,” he said. “I think if we do a lot more research focused on how environment influences microbiome, we might start to see things we could do that could potentially stem the tide of IBD.”
Dr. Kaplan reported having no relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – The incidence of Crohn’s disease and ulcerative colitis has stabilized in the Western world, but is rising rapidly in newly industrialized countries, according to a systematic review of population-based studies.
The findings could provide important new insights into the environmental, genetic, and microbiome-related factors and interactions that form the underpinnings of IBD, Gilaad Kaplan, MD, of the University of Calgary (Alta.) said at the World Congress of Gastroenterology at ACG 2017.
In turn, that information could lead to approaches to reduce IBD incidence, he said in a video interview.
It has been known that Crohn’s disease and ulcerative colitis are “modern diseases of modern times,” but few studies have addressed the epidemiology of IBD in newly industrialized countries in Asia, Africa, and South America, he said.
“We see a pattern that as newly industrialized countries transition toward a westernized society, IBD emerges and its incidence rises, and there are many different explanations for that,” he said, noting that in part, the increase is due to improved health care infrastructure and advances in adoption of medical technology that lead to better identification of new cases.
“But probably one of the most important factors is that there are environmental exposures linked to the westernization of society that are creating this pressure that’s driving incidence of IBD up in many of the countries of the world,” he said. “I think if we do a lot more research focused on how environment influences microbiome, we might start to see things we could do that could potentially stem the tide of IBD.”
Dr. Kaplan reported having no relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE 13TH WORLD CONGRESS OF GASTROENTEROLOGY
VIDEO: Mechanical colonoscope enhancements improve adenoma detection
ORLANDO – Mechanical enhancements to existing colonoscopes may be better than optical enhancements for improving adenoma detection, according to findings from a meta-analysis of data from 240 studies.
“Even though colonoscopy is felt to be our best test compared to others … we also recognize that we do not see every square inch of the colon,” Seth Gross, MD, of New York University Langone Medical Center said in a video interview at the World Congress of Gastroenterology at ACG 2017.
There has been a “tremendous drive” to improve the ability to inspect blind spots in the colon, and also to better recognize subtle precancerous lesions in visible areas of the colon, but it has been unclear whether optical or mechanical enhancements will better achieve that goal, Dr. Gross said.
Based on the findings of his meta-analysis, it appears that mechanical enhancements, including integrated balloons and single-use caps with finger-like projections or discs that clip on to the colonoscope to engage the colon wall and flatten areas to allow access to areas behind folds, are most effective.
The preliminary data should lead to more clinical questions about what can be done to improve exams, he said.
In fact, one four-arm study looking at standard colonoscopy vs. colonoscopy with various mechanical enhancements was just completed, and others looking at “deep learning” and computer assistance are underway.
The latter technology is intriguing, as “not every polyp that we’re missing is behind a fold,” Dr. Gross noted.
Preliminary findings from a study out of China demonstrated the feasibility of such computer assistance, and the researchers are now working on a prospective study of real-time cases to see if that type of integrated learning with computer assistance can improve polyp detection.
“Sometimes it’s just these subtle mucosal changes that we have to train our eye to identify,” he said. “So imagine having another set of eyes … where there’s a computer sort of highlighting an area that we should focus on.”
Dr. Gross reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Mechanical enhancements to existing colonoscopes may be better than optical enhancements for improving adenoma detection, according to findings from a meta-analysis of data from 240 studies.
“Even though colonoscopy is felt to be our best test compared to others … we also recognize that we do not see every square inch of the colon,” Seth Gross, MD, of New York University Langone Medical Center said in a video interview at the World Congress of Gastroenterology at ACG 2017.
There has been a “tremendous drive” to improve the ability to inspect blind spots in the colon, and also to better recognize subtle precancerous lesions in visible areas of the colon, but it has been unclear whether optical or mechanical enhancements will better achieve that goal, Dr. Gross said.
Based on the findings of his meta-analysis, it appears that mechanical enhancements, including integrated balloons and single-use caps with finger-like projections or discs that clip on to the colonoscope to engage the colon wall and flatten areas to allow access to areas behind folds, are most effective.
The preliminary data should lead to more clinical questions about what can be done to improve exams, he said.
In fact, one four-arm study looking at standard colonoscopy vs. colonoscopy with various mechanical enhancements was just completed, and others looking at “deep learning” and computer assistance are underway.
The latter technology is intriguing, as “not every polyp that we’re missing is behind a fold,” Dr. Gross noted.
Preliminary findings from a study out of China demonstrated the feasibility of such computer assistance, and the researchers are now working on a prospective study of real-time cases to see if that type of integrated learning with computer assistance can improve polyp detection.
“Sometimes it’s just these subtle mucosal changes that we have to train our eye to identify,” he said. “So imagine having another set of eyes … where there’s a computer sort of highlighting an area that we should focus on.”
Dr. Gross reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Mechanical enhancements to existing colonoscopes may be better than optical enhancements for improving adenoma detection, according to findings from a meta-analysis of data from 240 studies.
“Even though colonoscopy is felt to be our best test compared to others … we also recognize that we do not see every square inch of the colon,” Seth Gross, MD, of New York University Langone Medical Center said in a video interview at the World Congress of Gastroenterology at ACG 2017.
There has been a “tremendous drive” to improve the ability to inspect blind spots in the colon, and also to better recognize subtle precancerous lesions in visible areas of the colon, but it has been unclear whether optical or mechanical enhancements will better achieve that goal, Dr. Gross said.
Based on the findings of his meta-analysis, it appears that mechanical enhancements, including integrated balloons and single-use caps with finger-like projections or discs that clip on to the colonoscope to engage the colon wall and flatten areas to allow access to areas behind folds, are most effective.
The preliminary data should lead to more clinical questions about what can be done to improve exams, he said.
In fact, one four-arm study looking at standard colonoscopy vs. colonoscopy with various mechanical enhancements was just completed, and others looking at “deep learning” and computer assistance are underway.
The latter technology is intriguing, as “not every polyp that we’re missing is behind a fold,” Dr. Gross noted.
Preliminary findings from a study out of China demonstrated the feasibility of such computer assistance, and the researchers are now working on a prospective study of real-time cases to see if that type of integrated learning with computer assistance can improve polyp detection.
“Sometimes it’s just these subtle mucosal changes that we have to train our eye to identify,” he said. “So imagine having another set of eyes … where there’s a computer sort of highlighting an area that we should focus on.”
Dr. Gross reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE WORLD CONGRESS OF GASTROENTEROLOGY
VIDEO: What’s next in women’s health policy?
PHILADELPHIA – The Affordable Care Act (ACA) largely has delivered on its promises to expand access to care for women, but those benefits are in jeopardy because of actions by the Trump administration, one health policy expert said.
President Trump’s announcement that he plans to end the ACA’s cost-sharing reduction payments, which help subsidize the cost of insurance for low-income Americans, combined with new federal regulations expanding religious exemptions to the health law’s contraception mandate, would make it harder for women to obtain health care, said Michael Policar, MD, MPH, a clinical professor of obstetrics, gynecology, and reproductive sciences at the University of California, San Francisco.
In an interview at the annual meeting of the North American Menopause Society, Dr. Policar said it’s unclear whether these executive actions actually will go into effect because they are being challenged in court. But Dr. Policar said his concern is that this is just the “leading edge of more proposals and more changes” to come from the administration, which could target family planning funding.
Dr. Policar reported that he is a litigation consultant for Bayer.
PHILADELPHIA – The Affordable Care Act (ACA) largely has delivered on its promises to expand access to care for women, but those benefits are in jeopardy because of actions by the Trump administration, one health policy expert said.
President Trump’s announcement that he plans to end the ACA’s cost-sharing reduction payments, which help subsidize the cost of insurance for low-income Americans, combined with new federal regulations expanding religious exemptions to the health law’s contraception mandate, would make it harder for women to obtain health care, said Michael Policar, MD, MPH, a clinical professor of obstetrics, gynecology, and reproductive sciences at the University of California, San Francisco.
In an interview at the annual meeting of the North American Menopause Society, Dr. Policar said it’s unclear whether these executive actions actually will go into effect because they are being challenged in court. But Dr. Policar said his concern is that this is just the “leading edge of more proposals and more changes” to come from the administration, which could target family planning funding.
Dr. Policar reported that he is a litigation consultant for Bayer.
PHILADELPHIA – The Affordable Care Act (ACA) largely has delivered on its promises to expand access to care for women, but those benefits are in jeopardy because of actions by the Trump administration, one health policy expert said.
President Trump’s announcement that he plans to end the ACA’s cost-sharing reduction payments, which help subsidize the cost of insurance for low-income Americans, combined with new federal regulations expanding religious exemptions to the health law’s contraception mandate, would make it harder for women to obtain health care, said Michael Policar, MD, MPH, a clinical professor of obstetrics, gynecology, and reproductive sciences at the University of California, San Francisco.
In an interview at the annual meeting of the North American Menopause Society, Dr. Policar said it’s unclear whether these executive actions actually will go into effect because they are being challenged in court. But Dr. Policar said his concern is that this is just the “leading edge of more proposals and more changes” to come from the administration, which could target family planning funding.
Dr. Policar reported that he is a litigation consultant for Bayer.
AT NAMS 2017
VIDEO: Rethinking deep brain stimulation for depression
SAN DIEGO – Earlier this month, an article in Lancet Psychiatry reported the results of a prospective, randomized, sham-controlled trial that tested deep brain stimulation of the Brodmann area 25 within the subcallosal cingulate white matter in 90 patients with treatment-resistant depression. Unfortunately, the study showed no significant benefit at 6 months.
The approach had shown promise in some previous open-label studies, which prompted the multicenter trial (Lancet Psychiatry. 2017 Oct 4. doi: 10.1016/S2215-0366(17)30371-1).
Although the 6-month results were disappointing, the open-label phase of the study told a different story. At 2 years, 48% of patients in the stimulation group achieved an antidepressant response, higher than what would be expected from treatment as usual in this difficult population.
In this video interview at the annual meeting of the American Neurological Association, Helen Mayberg, MD, one of the study authors and professor of psychiatry, neurology, and radiology at Emory University, Atlanta, discusses these long-term results and their implications, as well as lessons learned and how they might inform future research.
SAN DIEGO – Earlier this month, an article in Lancet Psychiatry reported the results of a prospective, randomized, sham-controlled trial that tested deep brain stimulation of the Brodmann area 25 within the subcallosal cingulate white matter in 90 patients with treatment-resistant depression. Unfortunately, the study showed no significant benefit at 6 months.
The approach had shown promise in some previous open-label studies, which prompted the multicenter trial (Lancet Psychiatry. 2017 Oct 4. doi: 10.1016/S2215-0366(17)30371-1).
Although the 6-month results were disappointing, the open-label phase of the study told a different story. At 2 years, 48% of patients in the stimulation group achieved an antidepressant response, higher than what would be expected from treatment as usual in this difficult population.
In this video interview at the annual meeting of the American Neurological Association, Helen Mayberg, MD, one of the study authors and professor of psychiatry, neurology, and radiology at Emory University, Atlanta, discusses these long-term results and their implications, as well as lessons learned and how they might inform future research.
SAN DIEGO – Earlier this month, an article in Lancet Psychiatry reported the results of a prospective, randomized, sham-controlled trial that tested deep brain stimulation of the Brodmann area 25 within the subcallosal cingulate white matter in 90 patients with treatment-resistant depression. Unfortunately, the study showed no significant benefit at 6 months.
The approach had shown promise in some previous open-label studies, which prompted the multicenter trial (Lancet Psychiatry. 2017 Oct 4. doi: 10.1016/S2215-0366(17)30371-1).
Although the 6-month results were disappointing, the open-label phase of the study told a different story. At 2 years, 48% of patients in the stimulation group achieved an antidepressant response, higher than what would be expected from treatment as usual in this difficult population.
In this video interview at the annual meeting of the American Neurological Association, Helen Mayberg, MD, one of the study authors and professor of psychiatry, neurology, and radiology at Emory University, Atlanta, discusses these long-term results and their implications, as well as lessons learned and how they might inform future research.
AT ANA 2017
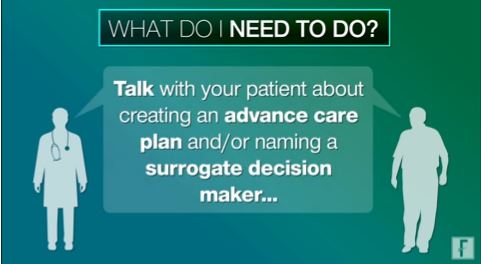
MACRA Monday: Advance care plan
If you haven’t started reporting quality data for the Merit-Based Incentive Payment System (MIPS), there’s still time to avoid a 4% cut to your Medicare payments.
Under the Pick Your Pace approach being offered this year, the Centers for Medicare & Medicaid Services allows clinicians to test the system by reporting on one quality measure for one patient through paper-based claims. Be sure to append a Quality Data Code (QDC) to the claim form for care provided up to Dec. 31, 2017, in order to avoid a penalty in payment year 2019.
Consider this measure:
Measure #47: Care Plan
This measure is aimed at capturing the percentage of patients aged 65 years and older who have a documented advance care plan in their medical records.
What you need to do: Discuss with the patient the creation of an advance care plan or the naming of a surrogate decision maker and then document that in the medical record. If the patient does not wish to make a plan or is unable to name a decision maker, document that along with the fact that the issue of advance care planning was discussed.
Eligible cases include patients aged 65 years or older on the date of the encounter and a patient encounter during the performance period. Applicable codes include (CPT or HCPCS): 99201, 99202, 99203, 99204, 99205,99212, 99213, 99214, 99215, 99218, 99219, 99220, 99221, 99222, 99223, 99231, 99232, 99233, 99234, 99235, 99236, 99291, 99304, 99305, 99306, 99307, 99308, 99309, 99310, 99324, 99325, 99326, 99327, 99328, 99334, 99335, 99336, 99337, 99341, 99342, 99343, 99344, 99345, 99347, 99348, 99349, 99350, G0402, G0438, G0439.
To get credit under MIPS, be sure to include a Quality Data Code that shows that you successfully performed the measure or had a good reason for not doing so. For instance, CPT II 1123F indicates that advance care planning was discussed and documented, and an advance care plan or surrogate decision maker was documented in the medical record. On the other hand, CPT II 1124F should be used if advance care planning was discussed and documented in the medical record, but the patient did not wish or was not able to name a surrogate decision maker or provide an advance care plan.
CMS has a full list of measures available for claims-based reporting at qpp.cms.gov. The American Medical Association has also created a step-by-step guide for reporting on one quality measure.
Certain clinicians are exempt from reporting and do not face a penalty under MIPS:
- Those who enrolled in Medicare for the first time during a performance period.
- Those who have Medicare Part B–allowed charges of $30,000 or less.
- Those who have 100 or fewer Medicare Part B patients.
- Those who are significantly participating in an Advanced Alternative Payment Model (APM).
If you haven’t started reporting quality data for the Merit-Based Incentive Payment System (MIPS), there’s still time to avoid a 4% cut to your Medicare payments.
Under the Pick Your Pace approach being offered this year, the Centers for Medicare & Medicaid Services allows clinicians to test the system by reporting on one quality measure for one patient through paper-based claims. Be sure to append a Quality Data Code (QDC) to the claim form for care provided up to Dec. 31, 2017, in order to avoid a penalty in payment year 2019.
Consider this measure:
Measure #47: Care Plan
This measure is aimed at capturing the percentage of patients aged 65 years and older who have a documented advance care plan in their medical records.
What you need to do: Discuss with the patient the creation of an advance care plan or the naming of a surrogate decision maker and then document that in the medical record. If the patient does not wish to make a plan or is unable to name a decision maker, document that along with the fact that the issue of advance care planning was discussed.
Eligible cases include patients aged 65 years or older on the date of the encounter and a patient encounter during the performance period. Applicable codes include (CPT or HCPCS): 99201, 99202, 99203, 99204, 99205,99212, 99213, 99214, 99215, 99218, 99219, 99220, 99221, 99222, 99223, 99231, 99232, 99233, 99234, 99235, 99236, 99291, 99304, 99305, 99306, 99307, 99308, 99309, 99310, 99324, 99325, 99326, 99327, 99328, 99334, 99335, 99336, 99337, 99341, 99342, 99343, 99344, 99345, 99347, 99348, 99349, 99350, G0402, G0438, G0439.
To get credit under MIPS, be sure to include a Quality Data Code that shows that you successfully performed the measure or had a good reason for not doing so. For instance, CPT II 1123F indicates that advance care planning was discussed and documented, and an advance care plan or surrogate decision maker was documented in the medical record. On the other hand, CPT II 1124F should be used if advance care planning was discussed and documented in the medical record, but the patient did not wish or was not able to name a surrogate decision maker or provide an advance care plan.
CMS has a full list of measures available for claims-based reporting at qpp.cms.gov. The American Medical Association has also created a step-by-step guide for reporting on one quality measure.
Certain clinicians are exempt from reporting and do not face a penalty under MIPS:
- Those who enrolled in Medicare for the first time during a performance period.
- Those who have Medicare Part B–allowed charges of $30,000 or less.
- Those who have 100 or fewer Medicare Part B patients.
- Those who are significantly participating in an Advanced Alternative Payment Model (APM).
If you haven’t started reporting quality data for the Merit-Based Incentive Payment System (MIPS), there’s still time to avoid a 4% cut to your Medicare payments.
Under the Pick Your Pace approach being offered this year, the Centers for Medicare & Medicaid Services allows clinicians to test the system by reporting on one quality measure for one patient through paper-based claims. Be sure to append a Quality Data Code (QDC) to the claim form for care provided up to Dec. 31, 2017, in order to avoid a penalty in payment year 2019.
Consider this measure:
Measure #47: Care Plan
This measure is aimed at capturing the percentage of patients aged 65 years and older who have a documented advance care plan in their medical records.
What you need to do: Discuss with the patient the creation of an advance care plan or the naming of a surrogate decision maker and then document that in the medical record. If the patient does not wish to make a plan or is unable to name a decision maker, document that along with the fact that the issue of advance care planning was discussed.
Eligible cases include patients aged 65 years or older on the date of the encounter and a patient encounter during the performance period. Applicable codes include (CPT or HCPCS): 99201, 99202, 99203, 99204, 99205,99212, 99213, 99214, 99215, 99218, 99219, 99220, 99221, 99222, 99223, 99231, 99232, 99233, 99234, 99235, 99236, 99291, 99304, 99305, 99306, 99307, 99308, 99309, 99310, 99324, 99325, 99326, 99327, 99328, 99334, 99335, 99336, 99337, 99341, 99342, 99343, 99344, 99345, 99347, 99348, 99349, 99350, G0402, G0438, G0439.
To get credit under MIPS, be sure to include a Quality Data Code that shows that you successfully performed the measure or had a good reason for not doing so. For instance, CPT II 1123F indicates that advance care planning was discussed and documented, and an advance care plan or surrogate decision maker was documented in the medical record. On the other hand, CPT II 1124F should be used if advance care planning was discussed and documented in the medical record, but the patient did not wish or was not able to name a surrogate decision maker or provide an advance care plan.
CMS has a full list of measures available for claims-based reporting at qpp.cms.gov. The American Medical Association has also created a step-by-step guide for reporting on one quality measure.
Certain clinicians are exempt from reporting and do not face a penalty under MIPS:
- Those who enrolled in Medicare for the first time during a performance period.
- Those who have Medicare Part B–allowed charges of $30,000 or less.
- Those who have 100 or fewer Medicare Part B patients.
- Those who are significantly participating in an Advanced Alternative Payment Model (APM).
VIDEO: AF ablation boosts survival in heart failure patients
BARCELONA – In patients with heart failure with reduced ejection fraction who also have atrial fibrillation, catheter ablation of the arrhythmia produced significantly improved long-term survival and a significant reduction in heart failure hospitalizations, in results from a multicenter randomized trial with more than 350 patients.
During 5-year follow-up, heart failure patients who underwent an ablative procedure for their atrial fibrillation (AF) had a statistically significant 37% lower rate of the combined primary endpoint of all-cause death or hospitalization for worsening heart failure, compared with control patients managed by standard medical therapy, Nassir F. Marrouche, MD, said at the annual congress of the European Society of Cardiology. The results also showed significant reductions from ablation, compared with controls, for the individual secondary endpoints of all-cause mortality, heart failure hospitalizations, cardiovascular mortality, and cardiovascular hospitalizations, said Dr. Marrouche, a professor of medicine and electrophysiologist at the University of Utah in Salt Lake City.
“Catheter ablation of atrial fibrillation is already done in heart failure patients, but now we have added information that this treatment may not just improve AF symptoms but also lead to a significant improvement in prognosis,” said Johannes Brachmann, MD, a coinvestigator on the study and professor and chief of cardiology at Coburg (Germany) Hospital.
The CASTLE-AF (Catheter Ablation vs. Standard Conventional Treatment in Patients With LV Dysfunction and AF) trial was investigator initiated and run at 31 centers in nine countries. The study randomized patients with paroxysmal or persistent AF and heart failure with a left ventricular ejection fraction of 35% or less. All patients also had to have failed treatment with, been intolerant of, or refused treatment with at least one antiarrhythmic drug, and they had to have been implanted with either an implantable cardioverter defibrillator or a cardiac resynchronization therapy and defibrillation device. The researchers randomized 179 patients to catheter ablation by pulmonary vein isolation, and 184 patients to either a standard rate or rhythm-control regimen plus anticoagulation to prevent ischemic stroke.
The ablation procedure also cut the average AF burden by more than half, compared with medical therapy throughout the 5-year follow-up, Dr. Marrouche reported.
The results “support the need to monitor patients with heart failure for atrial fibrillation,” Dr. Brachmann said in a video interview. This means broader use of monitoring technologies to diagnose AF in heart failure patients, such as implanted loop recorders or implanted rhythm devices.
The prevalence of atrial fibrillation in patients with heart failure with reduced ejection fraction can run 30% or higher. In patients with NYHA class IV heart failure, the AF prevalence is about 50%, Dr. Brachmann said.
CASTLE AF was funded by Biotronik. Dr. Marrouche has been a consultant to and received research funding from Biotronik and from several other companies. Dr. Brachmann has been a speaker for and has received research funding from Biotronik and from Abbott and Medtronic.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
The results of several studies have shown that patients with both atrial fibrillation and heart failure have about a 40% increased mortality, compared with heart failure patients without atrial fibrillation.
Five prior randomized controlled trials assessed the impact of AF ablation, compared with rate or rhythm control, in heart failure patients. But unlike CASTLE AF, all the prior studies used freedom from AF as the primary endpoint.
Enrolled patients were symptomatic from AF. Would asymptomatic patients get the same benefits? All enrolled patients had failed prior antiarrhythmic treatment or were intolerant or unwilling to take it. Does this mean the trial enrolled patients who generally were unresponsive to antiarrhythmic drugs, thereby skewing the results toward worse outcomes in control patients? Also, the 5-week run-in period used before randomization may have shifted enrollment toward patients well suited to ablation. The enrolled patients were also relatively young (averaging 64 years of age), and about 60% were New York Heart Association functional class II. A minority had longstanding AF. Were these younger and healthier patients better able to tolerate ablation? And can centers with less experience performing ablations have similar results?
The CASTLE AF results suggest that the time has come to offer AF ablation to patients with heart failure with reduced ejection fraction and AF, but we must be careful to select patients who are similar to the ones enrolled in this trial.
Carina Blomström-Lundqvist, MD, an electrophysiologist at Uppsala (Sweden) University Hospital, made these comments as designated discussant for the report. She has received research funding from Medtronic and Cardiome, and she has received honoraria from Biotronik, Bayer, Bristol-Myers Squibb, Medtronic, Merck, Pfizer, and Sanofi.
The results of several studies have shown that patients with both atrial fibrillation and heart failure have about a 40% increased mortality, compared with heart failure patients without atrial fibrillation.
Five prior randomized controlled trials assessed the impact of AF ablation, compared with rate or rhythm control, in heart failure patients. But unlike CASTLE AF, all the prior studies used freedom from AF as the primary endpoint.
Enrolled patients were symptomatic from AF. Would asymptomatic patients get the same benefits? All enrolled patients had failed prior antiarrhythmic treatment or were intolerant or unwilling to take it. Does this mean the trial enrolled patients who generally were unresponsive to antiarrhythmic drugs, thereby skewing the results toward worse outcomes in control patients? Also, the 5-week run-in period used before randomization may have shifted enrollment toward patients well suited to ablation. The enrolled patients were also relatively young (averaging 64 years of age), and about 60% were New York Heart Association functional class II. A minority had longstanding AF. Were these younger and healthier patients better able to tolerate ablation? And can centers with less experience performing ablations have similar results?
The CASTLE AF results suggest that the time has come to offer AF ablation to patients with heart failure with reduced ejection fraction and AF, but we must be careful to select patients who are similar to the ones enrolled in this trial.
Carina Blomström-Lundqvist, MD, an electrophysiologist at Uppsala (Sweden) University Hospital, made these comments as designated discussant for the report. She has received research funding from Medtronic and Cardiome, and she has received honoraria from Biotronik, Bayer, Bristol-Myers Squibb, Medtronic, Merck, Pfizer, and Sanofi.
The results of several studies have shown that patients with both atrial fibrillation and heart failure have about a 40% increased mortality, compared with heart failure patients without atrial fibrillation.
Five prior randomized controlled trials assessed the impact of AF ablation, compared with rate or rhythm control, in heart failure patients. But unlike CASTLE AF, all the prior studies used freedom from AF as the primary endpoint.
Enrolled patients were symptomatic from AF. Would asymptomatic patients get the same benefits? All enrolled patients had failed prior antiarrhythmic treatment or were intolerant or unwilling to take it. Does this mean the trial enrolled patients who generally were unresponsive to antiarrhythmic drugs, thereby skewing the results toward worse outcomes in control patients? Also, the 5-week run-in period used before randomization may have shifted enrollment toward patients well suited to ablation. The enrolled patients were also relatively young (averaging 64 years of age), and about 60% were New York Heart Association functional class II. A minority had longstanding AF. Were these younger and healthier patients better able to tolerate ablation? And can centers with less experience performing ablations have similar results?
The CASTLE AF results suggest that the time has come to offer AF ablation to patients with heart failure with reduced ejection fraction and AF, but we must be careful to select patients who are similar to the ones enrolled in this trial.
Carina Blomström-Lundqvist, MD, an electrophysiologist at Uppsala (Sweden) University Hospital, made these comments as designated discussant for the report. She has received research funding from Medtronic and Cardiome, and she has received honoraria from Biotronik, Bayer, Bristol-Myers Squibb, Medtronic, Merck, Pfizer, and Sanofi.
BARCELONA – In patients with heart failure with reduced ejection fraction who also have atrial fibrillation, catheter ablation of the arrhythmia produced significantly improved long-term survival and a significant reduction in heart failure hospitalizations, in results from a multicenter randomized trial with more than 350 patients.
During 5-year follow-up, heart failure patients who underwent an ablative procedure for their atrial fibrillation (AF) had a statistically significant 37% lower rate of the combined primary endpoint of all-cause death or hospitalization for worsening heart failure, compared with control patients managed by standard medical therapy, Nassir F. Marrouche, MD, said at the annual congress of the European Society of Cardiology. The results also showed significant reductions from ablation, compared with controls, for the individual secondary endpoints of all-cause mortality, heart failure hospitalizations, cardiovascular mortality, and cardiovascular hospitalizations, said Dr. Marrouche, a professor of medicine and electrophysiologist at the University of Utah in Salt Lake City.
“Catheter ablation of atrial fibrillation is already done in heart failure patients, but now we have added information that this treatment may not just improve AF symptoms but also lead to a significant improvement in prognosis,” said Johannes Brachmann, MD, a coinvestigator on the study and professor and chief of cardiology at Coburg (Germany) Hospital.
The CASTLE-AF (Catheter Ablation vs. Standard Conventional Treatment in Patients With LV Dysfunction and AF) trial was investigator initiated and run at 31 centers in nine countries. The study randomized patients with paroxysmal or persistent AF and heart failure with a left ventricular ejection fraction of 35% or less. All patients also had to have failed treatment with, been intolerant of, or refused treatment with at least one antiarrhythmic drug, and they had to have been implanted with either an implantable cardioverter defibrillator or a cardiac resynchronization therapy and defibrillation device. The researchers randomized 179 patients to catheter ablation by pulmonary vein isolation, and 184 patients to either a standard rate or rhythm-control regimen plus anticoagulation to prevent ischemic stroke.
The ablation procedure also cut the average AF burden by more than half, compared with medical therapy throughout the 5-year follow-up, Dr. Marrouche reported.
The results “support the need to monitor patients with heart failure for atrial fibrillation,” Dr. Brachmann said in a video interview. This means broader use of monitoring technologies to diagnose AF in heart failure patients, such as implanted loop recorders or implanted rhythm devices.
The prevalence of atrial fibrillation in patients with heart failure with reduced ejection fraction can run 30% or higher. In patients with NYHA class IV heart failure, the AF prevalence is about 50%, Dr. Brachmann said.
CASTLE AF was funded by Biotronik. Dr. Marrouche has been a consultant to and received research funding from Biotronik and from several other companies. Dr. Brachmann has been a speaker for and has received research funding from Biotronik and from Abbott and Medtronic.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
BARCELONA – In patients with heart failure with reduced ejection fraction who also have atrial fibrillation, catheter ablation of the arrhythmia produced significantly improved long-term survival and a significant reduction in heart failure hospitalizations, in results from a multicenter randomized trial with more than 350 patients.
During 5-year follow-up, heart failure patients who underwent an ablative procedure for their atrial fibrillation (AF) had a statistically significant 37% lower rate of the combined primary endpoint of all-cause death or hospitalization for worsening heart failure, compared with control patients managed by standard medical therapy, Nassir F. Marrouche, MD, said at the annual congress of the European Society of Cardiology. The results also showed significant reductions from ablation, compared with controls, for the individual secondary endpoints of all-cause mortality, heart failure hospitalizations, cardiovascular mortality, and cardiovascular hospitalizations, said Dr. Marrouche, a professor of medicine and electrophysiologist at the University of Utah in Salt Lake City.
“Catheter ablation of atrial fibrillation is already done in heart failure patients, but now we have added information that this treatment may not just improve AF symptoms but also lead to a significant improvement in prognosis,” said Johannes Brachmann, MD, a coinvestigator on the study and professor and chief of cardiology at Coburg (Germany) Hospital.
The CASTLE-AF (Catheter Ablation vs. Standard Conventional Treatment in Patients With LV Dysfunction and AF) trial was investigator initiated and run at 31 centers in nine countries. The study randomized patients with paroxysmal or persistent AF and heart failure with a left ventricular ejection fraction of 35% or less. All patients also had to have failed treatment with, been intolerant of, or refused treatment with at least one antiarrhythmic drug, and they had to have been implanted with either an implantable cardioverter defibrillator or a cardiac resynchronization therapy and defibrillation device. The researchers randomized 179 patients to catheter ablation by pulmonary vein isolation, and 184 patients to either a standard rate or rhythm-control regimen plus anticoagulation to prevent ischemic stroke.
The ablation procedure also cut the average AF burden by more than half, compared with medical therapy throughout the 5-year follow-up, Dr. Marrouche reported.
The results “support the need to monitor patients with heart failure for atrial fibrillation,” Dr. Brachmann said in a video interview. This means broader use of monitoring technologies to diagnose AF in heart failure patients, such as implanted loop recorders or implanted rhythm devices.
The prevalence of atrial fibrillation in patients with heart failure with reduced ejection fraction can run 30% or higher. In patients with NYHA class IV heart failure, the AF prevalence is about 50%, Dr. Brachmann said.
CASTLE AF was funded by Biotronik. Dr. Marrouche has been a consultant to and received research funding from Biotronik and from several other companies. Dr. Brachmann has been a speaker for and has received research funding from Biotronik and from Abbott and Medtronic.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT THE ESC CONGRESS 2017
Key clinical point:
Major finding: AF ablation was linked to a 37% 5-year reduction in mortality and heart failure hospitalization, compared with standard treatment.
Data source: CASTLE AF, a multicenter randomized trial with 363 patients.
Disclosures: CASTLE AF was funded by Biotronik. Dr. Marrouche has been a consultant to and received research funding from Biotronik and from several other companies. Dr. Brachmann has been a speaker for and has received research funding from Biotronik and from Abbott and Medtronic.
W. Curt LaFrance Jr, MD
VIDEO: Intermittent furosemide during acute HFpEF favors kidneys
DALLAS – Patients with heart failure with preserved ejection fraction who were hospitalized for acute decompensation had a significantly smaller rise in serum creatinine when treated with intermittent, bolus doses of furosemide, compared with patients who received a continuous furosemide infusion in a single-center, randomized trial with 90 patients.
Intermittent furosemide also resulted in many fewer episodes of worsening renal function. In the trial, 12% of patients who received bolus furosemide doses developed worsening renal function during hospitalization compared with 36% of patients treated with a continuous furosemide infusion, Kavita Sharma, MD, said at the annual scientific meeting of the Heart Failure Society of America.
While acknowledging that this finding is preliminary because it was made in a relatively small, single-center study, “I’d be cautious about continuous infusion” in acute decompensated patients with heart failure with preserved ejection fraction (HFpEF); “bolus is preferred,” Dr. Sharma said in a video interview.
Results from the prior Diuretic Optimization Strategies Evaluation (DOSE) trial, published in 2011, had shown no significant difference in renal function in hospitalized heart failure patients randomized to receive either bolus or continuous furosemide, but that study largely enrolled patients with heart failure with reduced ejection fraction (HFrEF) (N Engl J Med. 2011 Mar 3;364[9]:797-805).
“When patients with HFpEF are hospitalized with acute heart failure there is a high rate of kidney injury, that often results in slowing diuresis leading to longer hospital stays. With adjustment for changes in blood pressure and volume of diuresis we saw a fourfold increase in worsening renal failure [with continuous infusion], so you should think twice before using continuous dosing,” said Dr. Sharma, a heart failure cardiologist at Johns Hopkins Medicine in Baltimore.
She presented results from Diuretics and Dopamine in Heart Failure With Preserved Ejection Fraction (ROPA-DOP), which randomized 90 hospitalized heart failure patients with a left ventricular ejection fraction of at least 50% and an estimated glomerular filtration rate of more than 15 mL/min/1.73 m2. The enrolled patients averaged 66 years old, 61% were women, their average body mass index was 41 kg/m2, and their average estimated glomerular filtration rate was 58 mL/min/1.73 m2.
The study’s primary endpoint was percent change in creatinine during hospitalization, which rose by an average 5% in the patients who received intermittent bolus furosemide and by an average 16% in patient who received a continuous infusion, a statistically significant difference. In a regression analysis that controlled for between-group differences in patient’s age, sex, race, body mass index, smoking status, changes in systolic blood pressure, heart rate, fluid balance after 72 hours, and other variables, patients treated with continuous furosemide infusion averaged an 11% greater increase in serum creatinine, Dr. Sharma reported. After similar adjustments, the secondary endpoint rate of worsening renal function was more than four times more likely to occur in the patients on continuous infusion compared with those who received intermittent bolus treatment, she said.
A second aspect of the ROPA-DOP trial randomized the same patients to received either low dose (3 mcg/kg per min) dopamine or placebo during hospitalization. The results showed that low-dose dopamine had no significant impact on either change in creatinine levels or on the incidence of worsening renal function compared with placebo, though dopamine treatment did link with a nonsignificant trend toward somewhat greater diuresis. These results were consistent with prior findings in the Renal Optimization Strategies Evaluation (ROSE) trial (JAMA. 2013 Nov 18;310[23]:2533-43), which used a mixed population of patients with HFpEF or HFrEF but predominantly patients with HFrEF, Dr. Sharma noted.
“It was a neutral finding [for dopamine in ROPA-DOP], and while there was no harm from dopamine there was clearly no benefit,” she said. It is possible that HFpEF patients with right ventricular dysfunction secondary to pulmonary hypertension might benefit from low-dose dopamine, but this needs further study, Dr. Sharma said.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
In the Diuretic Optimization Strategies Evaluation (DOSE) trial, we enrolled heart failure patients with a mix of reduced ejection fraction and preserved ejection fraction. The DOSE results showed no relationship between ejection fraction and the response to furosemide treatment by intermittent bolus or by continuous infusion in patients hospitalized with acute decompensated heart failure. The results also showed that continuous infusion was no better than intermittent bolus treatment, and following our report in 2011 (N Engl J Med. 2011 Mar 3;364[9]:797-805), many centers that had previously relied on continuous furosemide switched to use of bolus doses primarily because continuous infusion is much less convenient.
But it is important to keep in mind that trial results focus on averages and populations of patients. Anecdotally, we see some acute heart failure patients who seem to respond better to continuous infusion, and so some clinicians switch patients who do not respond well to bolus treatment to continuous infusion. In DOSE, we only tested the efficacy of the initial strategy; we have no evidence on whether or not changing the dosing strategy helps patients who do not respond adequately to an initial strategy of intermittent bolus doses.
G. Michael Felker, MD , professor of medicine at Duke University, Durham, N.C., made these comments in an interview. He has been a consultant to Amgen, Bristol-Myers Squibb, GlaxoSmithKline, Medtronic, MyoKardia, Novartis, Stealth, and Trevena.
In the Diuretic Optimization Strategies Evaluation (DOSE) trial, we enrolled heart failure patients with a mix of reduced ejection fraction and preserved ejection fraction. The DOSE results showed no relationship between ejection fraction and the response to furosemide treatment by intermittent bolus or by continuous infusion in patients hospitalized with acute decompensated heart failure. The results also showed that continuous infusion was no better than intermittent bolus treatment, and following our report in 2011 (N Engl J Med. 2011 Mar 3;364[9]:797-805), many centers that had previously relied on continuous furosemide switched to use of bolus doses primarily because continuous infusion is much less convenient.
But it is important to keep in mind that trial results focus on averages and populations of patients. Anecdotally, we see some acute heart failure patients who seem to respond better to continuous infusion, and so some clinicians switch patients who do not respond well to bolus treatment to continuous infusion. In DOSE, we only tested the efficacy of the initial strategy; we have no evidence on whether or not changing the dosing strategy helps patients who do not respond adequately to an initial strategy of intermittent bolus doses.
G. Michael Felker, MD , professor of medicine at Duke University, Durham, N.C., made these comments in an interview. He has been a consultant to Amgen, Bristol-Myers Squibb, GlaxoSmithKline, Medtronic, MyoKardia, Novartis, Stealth, and Trevena.
In the Diuretic Optimization Strategies Evaluation (DOSE) trial, we enrolled heart failure patients with a mix of reduced ejection fraction and preserved ejection fraction. The DOSE results showed no relationship between ejection fraction and the response to furosemide treatment by intermittent bolus or by continuous infusion in patients hospitalized with acute decompensated heart failure. The results also showed that continuous infusion was no better than intermittent bolus treatment, and following our report in 2011 (N Engl J Med. 2011 Mar 3;364[9]:797-805), many centers that had previously relied on continuous furosemide switched to use of bolus doses primarily because continuous infusion is much less convenient.
But it is important to keep in mind that trial results focus on averages and populations of patients. Anecdotally, we see some acute heart failure patients who seem to respond better to continuous infusion, and so some clinicians switch patients who do not respond well to bolus treatment to continuous infusion. In DOSE, we only tested the efficacy of the initial strategy; we have no evidence on whether or not changing the dosing strategy helps patients who do not respond adequately to an initial strategy of intermittent bolus doses.
G. Michael Felker, MD , professor of medicine at Duke University, Durham, N.C., made these comments in an interview. He has been a consultant to Amgen, Bristol-Myers Squibb, GlaxoSmithKline, Medtronic, MyoKardia, Novartis, Stealth, and Trevena.
DALLAS – Patients with heart failure with preserved ejection fraction who were hospitalized for acute decompensation had a significantly smaller rise in serum creatinine when treated with intermittent, bolus doses of furosemide, compared with patients who received a continuous furosemide infusion in a single-center, randomized trial with 90 patients.
Intermittent furosemide also resulted in many fewer episodes of worsening renal function. In the trial, 12% of patients who received bolus furosemide doses developed worsening renal function during hospitalization compared with 36% of patients treated with a continuous furosemide infusion, Kavita Sharma, MD, said at the annual scientific meeting of the Heart Failure Society of America.
While acknowledging that this finding is preliminary because it was made in a relatively small, single-center study, “I’d be cautious about continuous infusion” in acute decompensated patients with heart failure with preserved ejection fraction (HFpEF); “bolus is preferred,” Dr. Sharma said in a video interview.
Results from the prior Diuretic Optimization Strategies Evaluation (DOSE) trial, published in 2011, had shown no significant difference in renal function in hospitalized heart failure patients randomized to receive either bolus or continuous furosemide, but that study largely enrolled patients with heart failure with reduced ejection fraction (HFrEF) (N Engl J Med. 2011 Mar 3;364[9]:797-805).
“When patients with HFpEF are hospitalized with acute heart failure there is a high rate of kidney injury, that often results in slowing diuresis leading to longer hospital stays. With adjustment for changes in blood pressure and volume of diuresis we saw a fourfold increase in worsening renal failure [with continuous infusion], so you should think twice before using continuous dosing,” said Dr. Sharma, a heart failure cardiologist at Johns Hopkins Medicine in Baltimore.
She presented results from Diuretics and Dopamine in Heart Failure With Preserved Ejection Fraction (ROPA-DOP), which randomized 90 hospitalized heart failure patients with a left ventricular ejection fraction of at least 50% and an estimated glomerular filtration rate of more than 15 mL/min/1.73 m2. The enrolled patients averaged 66 years old, 61% were women, their average body mass index was 41 kg/m2, and their average estimated glomerular filtration rate was 58 mL/min/1.73 m2.
The study’s primary endpoint was percent change in creatinine during hospitalization, which rose by an average 5% in the patients who received intermittent bolus furosemide and by an average 16% in patient who received a continuous infusion, a statistically significant difference. In a regression analysis that controlled for between-group differences in patient’s age, sex, race, body mass index, smoking status, changes in systolic blood pressure, heart rate, fluid balance after 72 hours, and other variables, patients treated with continuous furosemide infusion averaged an 11% greater increase in serum creatinine, Dr. Sharma reported. After similar adjustments, the secondary endpoint rate of worsening renal function was more than four times more likely to occur in the patients on continuous infusion compared with those who received intermittent bolus treatment, she said.
A second aspect of the ROPA-DOP trial randomized the same patients to received either low dose (3 mcg/kg per min) dopamine or placebo during hospitalization. The results showed that low-dose dopamine had no significant impact on either change in creatinine levels or on the incidence of worsening renal function compared with placebo, though dopamine treatment did link with a nonsignificant trend toward somewhat greater diuresis. These results were consistent with prior findings in the Renal Optimization Strategies Evaluation (ROSE) trial (JAMA. 2013 Nov 18;310[23]:2533-43), which used a mixed population of patients with HFpEF or HFrEF but predominantly patients with HFrEF, Dr. Sharma noted.
“It was a neutral finding [for dopamine in ROPA-DOP], and while there was no harm from dopamine there was clearly no benefit,” she said. It is possible that HFpEF patients with right ventricular dysfunction secondary to pulmonary hypertension might benefit from low-dose dopamine, but this needs further study, Dr. Sharma said.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
DALLAS – Patients with heart failure with preserved ejection fraction who were hospitalized for acute decompensation had a significantly smaller rise in serum creatinine when treated with intermittent, bolus doses of furosemide, compared with patients who received a continuous furosemide infusion in a single-center, randomized trial with 90 patients.
Intermittent furosemide also resulted in many fewer episodes of worsening renal function. In the trial, 12% of patients who received bolus furosemide doses developed worsening renal function during hospitalization compared with 36% of patients treated with a continuous furosemide infusion, Kavita Sharma, MD, said at the annual scientific meeting of the Heart Failure Society of America.
While acknowledging that this finding is preliminary because it was made in a relatively small, single-center study, “I’d be cautious about continuous infusion” in acute decompensated patients with heart failure with preserved ejection fraction (HFpEF); “bolus is preferred,” Dr. Sharma said in a video interview.
Results from the prior Diuretic Optimization Strategies Evaluation (DOSE) trial, published in 2011, had shown no significant difference in renal function in hospitalized heart failure patients randomized to receive either bolus or continuous furosemide, but that study largely enrolled patients with heart failure with reduced ejection fraction (HFrEF) (N Engl J Med. 2011 Mar 3;364[9]:797-805).
“When patients with HFpEF are hospitalized with acute heart failure there is a high rate of kidney injury, that often results in slowing diuresis leading to longer hospital stays. With adjustment for changes in blood pressure and volume of diuresis we saw a fourfold increase in worsening renal failure [with continuous infusion], so you should think twice before using continuous dosing,” said Dr. Sharma, a heart failure cardiologist at Johns Hopkins Medicine in Baltimore.
She presented results from Diuretics and Dopamine in Heart Failure With Preserved Ejection Fraction (ROPA-DOP), which randomized 90 hospitalized heart failure patients with a left ventricular ejection fraction of at least 50% and an estimated glomerular filtration rate of more than 15 mL/min/1.73 m2. The enrolled patients averaged 66 years old, 61% were women, their average body mass index was 41 kg/m2, and their average estimated glomerular filtration rate was 58 mL/min/1.73 m2.
The study’s primary endpoint was percent change in creatinine during hospitalization, which rose by an average 5% in the patients who received intermittent bolus furosemide and by an average 16% in patient who received a continuous infusion, a statistically significant difference. In a regression analysis that controlled for between-group differences in patient’s age, sex, race, body mass index, smoking status, changes in systolic blood pressure, heart rate, fluid balance after 72 hours, and other variables, patients treated with continuous furosemide infusion averaged an 11% greater increase in serum creatinine, Dr. Sharma reported. After similar adjustments, the secondary endpoint rate of worsening renal function was more than four times more likely to occur in the patients on continuous infusion compared with those who received intermittent bolus treatment, she said.
A second aspect of the ROPA-DOP trial randomized the same patients to received either low dose (3 mcg/kg per min) dopamine or placebo during hospitalization. The results showed that low-dose dopamine had no significant impact on either change in creatinine levels or on the incidence of worsening renal function compared with placebo, though dopamine treatment did link with a nonsignificant trend toward somewhat greater diuresis. These results were consistent with prior findings in the Renal Optimization Strategies Evaluation (ROSE) trial (JAMA. 2013 Nov 18;310[23]:2533-43), which used a mixed population of patients with HFpEF or HFrEF but predominantly patients with HFrEF, Dr. Sharma noted.
“It was a neutral finding [for dopamine in ROPA-DOP], and while there was no harm from dopamine there was clearly no benefit,” she said. It is possible that HFpEF patients with right ventricular dysfunction secondary to pulmonary hypertension might benefit from low-dose dopamine, but this needs further study, Dr. Sharma said.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point:
Major finding: Serum creatinine rose by an average 5% with intermittent bolus furosemide and by 16% with continuous infusion.
Data source: ROPA-DOP, a single-center randomized trial with 90 patients.
Disclosures: Dr. Sharma had no disclosures.