User login
ESC: New review yields reassuring digoxin data
LONDON – The best-quality available evidence demonstrates that digoxin reduces hospital admissions and has no effect upon all-cause mortality in patients with heart failure with or without atrial fibrillation, Dr. Dipak Kotecha reported at the annual congress of the European Society of Cardiology.
His meta-analysis of all observational and randomized controlled studies published since 1960 included 41 studies with 260,335 digoxin-treated patients, roughly 1 million controls, and more than 4 million person-years of follow-up.
What was unique about this meta-analysis is Dr. Kotecha and coworkers assessed each study in terms of its degree of bias due to confounding by indication and other limitations using two standardized bias scoring systems: the Cochrane Collaboration’s risk of bias tool for randomized controlled trials and the Risk of Bias Assessment tool for Non-randomized Studies (RoBANS).
The level of bias varied greatly among the observational studies. Moreover, the higher an observational study’s bias score, the greater the reported association between digoxin and mortality. In contrast, the seven randomized controlled trials all scored very low on bias and carried a consistent message that digoxin had a neutral effect on mortality, according to Dr. Kotecha of the University of Birmingham (England).
He noted that digoxin was first introduced into clinical cardiology back in 1785 in the form of digitalis. And although digoxin has seen widespread use for heart rate control and symptom reduction in patients with heart failure and/or atrial fibrillation over the years, prescriptions for the venerable drug have markedly declined recently in response to observational studies reporting a link with increased mortality. That purported association, he asserted, is highly dubious.
“Our comprehensive systematic review would suggest that confounding is the main reason why observational studies continue to show increases in mortality associated with digoxin. And this suggests that digoxin should continue to be considered as a treatment option to avoid hospital admissions in patients with heart failure and to achieve heart rate control in those with atrial fibrillation until better randomized data become available,” the cardiologist explained.
“I think that there’s one further important point to make here, and that’s that observational data, particularly when there are systematic differences in the two groups, should not be used to determine clinical efficacy. Propensity matching does not replace a randomized controlled trial in the assessment of efficacy,” he emphasized. “We’ve shown that observational data should be taken with extreme caution because digoxin is a second-line therapy and, like most of us, I tend to give digoxin to patients who are sicker, so we’re bound to see an increase in mortality and hospitalizations in those patients.”
Across all 41 studies, digoxin was associated with a small but clinically meaningful 8% reduction in the rate of all-cause hospitalization.
Asked what data are available regarding optimal dosing of digoxin, the cardiologist replied that the data are limited. “What data there are would suggest lower digoxin doses are better and higher doses tend to cause mortality. So our suggestion would be to continue using low digoxin doses, in combination if necessary with other drugs,” he said.
All of the randomized controlled trials have focused on patients with heart failure, alone or with comorbid atrial fibrillation. None have evaluated the impact of digoxin in patients with atrial fibrillation without heart failure. Given that atrial fibrillation is an emerging modern epidemic and a large chunk of digoxin-prescribing today is for rate control in such patients, this lack of high-quality data constitutes a major unmet need, Dr. Kotecha observed.
The RATE-AF trial, designed to advance knowledge in this area, is due to begin next year. The study, based at the University of Birmingham, will enroll patients with atrial fibrillation without heart failure who need rate control, randomizing them to a beta-blocker or digoxin.
Dr. Kotecha reported having no financial conflicts regarding his meta-analysis, which was funded by a grant from the university’s Arthur Thompson Trust.
Simultaneously with his presentation at the ESC congress, the meta-analysis was published online (BMJ 2105;351:h4451 doi:10.1136/bmj.h4451).
LONDON – The best-quality available evidence demonstrates that digoxin reduces hospital admissions and has no effect upon all-cause mortality in patients with heart failure with or without atrial fibrillation, Dr. Dipak Kotecha reported at the annual congress of the European Society of Cardiology.
His meta-analysis of all observational and randomized controlled studies published since 1960 included 41 studies with 260,335 digoxin-treated patients, roughly 1 million controls, and more than 4 million person-years of follow-up.
What was unique about this meta-analysis is Dr. Kotecha and coworkers assessed each study in terms of its degree of bias due to confounding by indication and other limitations using two standardized bias scoring systems: the Cochrane Collaboration’s risk of bias tool for randomized controlled trials and the Risk of Bias Assessment tool for Non-randomized Studies (RoBANS).
The level of bias varied greatly among the observational studies. Moreover, the higher an observational study’s bias score, the greater the reported association between digoxin and mortality. In contrast, the seven randomized controlled trials all scored very low on bias and carried a consistent message that digoxin had a neutral effect on mortality, according to Dr. Kotecha of the University of Birmingham (England).
He noted that digoxin was first introduced into clinical cardiology back in 1785 in the form of digitalis. And although digoxin has seen widespread use for heart rate control and symptom reduction in patients with heart failure and/or atrial fibrillation over the years, prescriptions for the venerable drug have markedly declined recently in response to observational studies reporting a link with increased mortality. That purported association, he asserted, is highly dubious.
“Our comprehensive systematic review would suggest that confounding is the main reason why observational studies continue to show increases in mortality associated with digoxin. And this suggests that digoxin should continue to be considered as a treatment option to avoid hospital admissions in patients with heart failure and to achieve heart rate control in those with atrial fibrillation until better randomized data become available,” the cardiologist explained.
“I think that there’s one further important point to make here, and that’s that observational data, particularly when there are systematic differences in the two groups, should not be used to determine clinical efficacy. Propensity matching does not replace a randomized controlled trial in the assessment of efficacy,” he emphasized. “We’ve shown that observational data should be taken with extreme caution because digoxin is a second-line therapy and, like most of us, I tend to give digoxin to patients who are sicker, so we’re bound to see an increase in mortality and hospitalizations in those patients.”
Across all 41 studies, digoxin was associated with a small but clinically meaningful 8% reduction in the rate of all-cause hospitalization.
Asked what data are available regarding optimal dosing of digoxin, the cardiologist replied that the data are limited. “What data there are would suggest lower digoxin doses are better and higher doses tend to cause mortality. So our suggestion would be to continue using low digoxin doses, in combination if necessary with other drugs,” he said.
All of the randomized controlled trials have focused on patients with heart failure, alone or with comorbid atrial fibrillation. None have evaluated the impact of digoxin in patients with atrial fibrillation without heart failure. Given that atrial fibrillation is an emerging modern epidemic and a large chunk of digoxin-prescribing today is for rate control in such patients, this lack of high-quality data constitutes a major unmet need, Dr. Kotecha observed.
The RATE-AF trial, designed to advance knowledge in this area, is due to begin next year. The study, based at the University of Birmingham, will enroll patients with atrial fibrillation without heart failure who need rate control, randomizing them to a beta-blocker or digoxin.
Dr. Kotecha reported having no financial conflicts regarding his meta-analysis, which was funded by a grant from the university’s Arthur Thompson Trust.
Simultaneously with his presentation at the ESC congress, the meta-analysis was published online (BMJ 2105;351:h4451 doi:10.1136/bmj.h4451).
LONDON – The best-quality available evidence demonstrates that digoxin reduces hospital admissions and has no effect upon all-cause mortality in patients with heart failure with or without atrial fibrillation, Dr. Dipak Kotecha reported at the annual congress of the European Society of Cardiology.
His meta-analysis of all observational and randomized controlled studies published since 1960 included 41 studies with 260,335 digoxin-treated patients, roughly 1 million controls, and more than 4 million person-years of follow-up.
What was unique about this meta-analysis is Dr. Kotecha and coworkers assessed each study in terms of its degree of bias due to confounding by indication and other limitations using two standardized bias scoring systems: the Cochrane Collaboration’s risk of bias tool for randomized controlled trials and the Risk of Bias Assessment tool for Non-randomized Studies (RoBANS).
The level of bias varied greatly among the observational studies. Moreover, the higher an observational study’s bias score, the greater the reported association between digoxin and mortality. In contrast, the seven randomized controlled trials all scored very low on bias and carried a consistent message that digoxin had a neutral effect on mortality, according to Dr. Kotecha of the University of Birmingham (England).
He noted that digoxin was first introduced into clinical cardiology back in 1785 in the form of digitalis. And although digoxin has seen widespread use for heart rate control and symptom reduction in patients with heart failure and/or atrial fibrillation over the years, prescriptions for the venerable drug have markedly declined recently in response to observational studies reporting a link with increased mortality. That purported association, he asserted, is highly dubious.
“Our comprehensive systematic review would suggest that confounding is the main reason why observational studies continue to show increases in mortality associated with digoxin. And this suggests that digoxin should continue to be considered as a treatment option to avoid hospital admissions in patients with heart failure and to achieve heart rate control in those with atrial fibrillation until better randomized data become available,” the cardiologist explained.
“I think that there’s one further important point to make here, and that’s that observational data, particularly when there are systematic differences in the two groups, should not be used to determine clinical efficacy. Propensity matching does not replace a randomized controlled trial in the assessment of efficacy,” he emphasized. “We’ve shown that observational data should be taken with extreme caution because digoxin is a second-line therapy and, like most of us, I tend to give digoxin to patients who are sicker, so we’re bound to see an increase in mortality and hospitalizations in those patients.”
Across all 41 studies, digoxin was associated with a small but clinically meaningful 8% reduction in the rate of all-cause hospitalization.
Asked what data are available regarding optimal dosing of digoxin, the cardiologist replied that the data are limited. “What data there are would suggest lower digoxin doses are better and higher doses tend to cause mortality. So our suggestion would be to continue using low digoxin doses, in combination if necessary with other drugs,” he said.
All of the randomized controlled trials have focused on patients with heart failure, alone or with comorbid atrial fibrillation. None have evaluated the impact of digoxin in patients with atrial fibrillation without heart failure. Given that atrial fibrillation is an emerging modern epidemic and a large chunk of digoxin-prescribing today is for rate control in such patients, this lack of high-quality data constitutes a major unmet need, Dr. Kotecha observed.
The RATE-AF trial, designed to advance knowledge in this area, is due to begin next year. The study, based at the University of Birmingham, will enroll patients with atrial fibrillation without heart failure who need rate control, randomizing them to a beta-blocker or digoxin.
Dr. Kotecha reported having no financial conflicts regarding his meta-analysis, which was funded by a grant from the university’s Arthur Thompson Trust.
Simultaneously with his presentation at the ESC congress, the meta-analysis was published online (BMJ 2105;351:h4451 doi:10.1136/bmj.h4451).
AT THE ESC CONGRESS 2015
Key clinical point: Digoxin remains safe and effective in patients with heart failure and/or atrial fibrillation, according to a major new review.
Major finding: Using digoxin in patients with heart failure and/or atrial fibrillation reduces all-cause hospitalizations by 8% and has no impact on mortality.
Data source: A meta-analysis of all studies of the impact of digoxin on death and clinical outcomes published since 1960, including 41 studies with more than a quarter million digoxin-treated patients, 1 million controls, and more than 4 million person-years of follow-up.
Disclosures: The presenter reported having no financial conflicts regarding this study, funded by a university grant.
VIDEO: Spironolactone a game changer in resistant hypertension
LONDON – Spironolactone is far and away the most effective therapy for resistant hypertension, according to the findings of the first randomized clinical trial comparing the aldosterone antagonist with other active agents.
“The result in favor of spironolactone is unequivocal: Spironolactone is the most effective treatment for resistant hypertension, and these results should influence treatment guidelines globally,” Dr. Bryan Williams said in presenting the PATHWAY-2 (Optimum Treatment for Drug-Resistant Hypertension) trial findings at the annual congress of the European Society of Cardiology.
Indeed, on the basis of the drug’s performance – a mean reduction in home systolic blood pressure of 8.7 mm Hg, compared with reductions of 4.03 and 4.48 mm Hg for doxazosin and bisoprolol, respectively, in the 314-patient crossover study – no one should any longer be categorized as having treatment-resistant hypertension unless they’ve first failed to achieve blood pressure control on spironolactone. And that will be a surprisingly small group, the chair of medicine at University College London said in an interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LONDON – Spironolactone is far and away the most effective therapy for resistant hypertension, according to the findings of the first randomized clinical trial comparing the aldosterone antagonist with other active agents.
“The result in favor of spironolactone is unequivocal: Spironolactone is the most effective treatment for resistant hypertension, and these results should influence treatment guidelines globally,” Dr. Bryan Williams said in presenting the PATHWAY-2 (Optimum Treatment for Drug-Resistant Hypertension) trial findings at the annual congress of the European Society of Cardiology.
Indeed, on the basis of the drug’s performance – a mean reduction in home systolic blood pressure of 8.7 mm Hg, compared with reductions of 4.03 and 4.48 mm Hg for doxazosin and bisoprolol, respectively, in the 314-patient crossover study – no one should any longer be categorized as having treatment-resistant hypertension unless they’ve first failed to achieve blood pressure control on spironolactone. And that will be a surprisingly small group, the chair of medicine at University College London said in an interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LONDON – Spironolactone is far and away the most effective therapy for resistant hypertension, according to the findings of the first randomized clinical trial comparing the aldosterone antagonist with other active agents.
“The result in favor of spironolactone is unequivocal: Spironolactone is the most effective treatment for resistant hypertension, and these results should influence treatment guidelines globally,” Dr. Bryan Williams said in presenting the PATHWAY-2 (Optimum Treatment for Drug-Resistant Hypertension) trial findings at the annual congress of the European Society of Cardiology.
Indeed, on the basis of the drug’s performance – a mean reduction in home systolic blood pressure of 8.7 mm Hg, compared with reductions of 4.03 and 4.48 mm Hg for doxazosin and bisoprolol, respectively, in the 314-patient crossover study – no one should any longer be categorized as having treatment-resistant hypertension unless they’ve first failed to achieve blood pressure control on spironolactone. And that will be a surprisingly small group, the chair of medicine at University College London said in an interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ESC CONGRESS 2015
ESC: Aldosterone blockade fails to fly for early MI in ALBATROSS
LONDON – Aldosterone blockade with oral spironolactone showed a disappointing lack of clinical benefit when initiated in the first hours after an acute MI without heart failure in the large, randomized ALBATROSS trial.
ALBATROSS did, however, flash a silver lining under one wing: A whopping 80% reduction in 6-month mortality in a prespecified subgroup analysis restricted to the 1,229 participants with ST-elevation MI, Dr. Gilles Montalescot reported at the annual congress of the European Society of Cardiology.
Although this finding is intriguing, hypothesis-generating, and definitely warrants a confirmatory study, he continued, mortality was nevertheless merely a secondary endpoint in ALBATROSS (Aldosterone Lethal Effects Blockade in Acute Myocardial Infarction Treated With or Without Reperfusion to Improve Outcome and Survival at Six Months Follow-up).
In contrast, the primary composite outcome was negative, so the takeaway message is clear: “The results of the ALBATROSS study do not warrant the extension of aldosterone blockade to MI patients without heart failure,” said Dr. Montalescot, professor of cardiology at the University of Paris.
ALBATROSS was a multicenter French trial that randomly assigned 1,603 acute MI patients to standard therapy alone or with added mineralocorticoid antagonist therapy started within the first 2 days of their coronary event. Often the aldosterone antagonist was begun in the ambulance en route to the hospital.
The primary endpoint was a composite of death, resuscitated cardiac arrest, ventricular fibrillation or tachycardia, heart failure, or an indication for an implantable cardioverter defibrillator. There were 194 such events, and they occurred at a similar rate in the patients who got 25 mg/day of spironolactone and those who did not.
The rationale for ALBATROSS was sound, according to the cardiologist. Aldosterone is a stress hormone released in acute MI. It has deleterious cardiac effects, including arrhythmias, heart failure, and a dose-dependent increase in mortality, so it makes good sense to block it as soon as possible in MI patients. In the EPHESUS trial, the aldosterone antagonist eplerenone, when started 3-14 days post MI in patients with early heart failure, significantly reduced mortality (N Engl J Med. 2003 Apr 3;348[14]:1309-2), with the bulk of the benefit occurring in patients in whom the drug was started 3-7 days post MI.
Last year, Dr. Montalescot and his coinvestigators published the REMINDER study, in which 1,012 ST-elevation MI (STEMI) patients without heart failure were randomized to eplerenone or placebo within the first 24 hours. The study showed a significant reduction in levels of brain natriuretic peptide or N-terminal pro-BNP in the eplerenone arm (Eur Heart J. 2014 Sep 7;35[34]:2295-302), but that’s not a clinical endpoint. ALBATROSS was the first study to look at the clinical impact of commencing mineralocorticoid antagonist therapy prior to day 3 post MI.
Discussant Dr. John McMurray, professor of cardiology at the University of Glasgow, said that ALBATROSS was simply underpowered and thus leaves unanswered the clinically important question of whether early initiation of aldosterone blockade post MI in patients without heart failure confers clinical benefit. The investigators projected a total of 269 events in the composite endpoint but got only 194 because the study participants were so well treated and contemporary medical and interventional therapies are quite effective.
He dismissed the sharp reduction seen in 6-month mortality with spironolactone in the STEMI patients as “just implausible – we don’t know of any treatments in medicine that reduce mortality by 80%.”
Noting that there were only 28 deaths in the study, Dr. McMurray asserted that “a subgroup analysis on such a small number of events is never going to give you a reliable result.” Moreover, he added, “subgroup analysis is even more treacherous when the overall trial is underpowered.”
Dr. Montalescot replied that, while he considers the signal of a mortality benefit for aldosterone blockade in STEMI patients worthy of pursuit in a large randomized trial, the prospects for mounting such a study are poor. The medications are now available as generics, so there is no commercial incentive. The French Ministry of Health, which funded ALBATROSS, isn’t prepared to back a follow-up study. The best hope is that eventually one of the pharmaceutical companies developing third-generation aldosterone antagonists, now in phase II studies, will become interested, he said.
Dr. Montalescot said that, while he receives research grants and consulting fees from numerous pharmaceutical companies, these commercial relationships aren’t relevant to the government-funded ALBATROSS trial.
LONDON – Aldosterone blockade with oral spironolactone showed a disappointing lack of clinical benefit when initiated in the first hours after an acute MI without heart failure in the large, randomized ALBATROSS trial.
ALBATROSS did, however, flash a silver lining under one wing: A whopping 80% reduction in 6-month mortality in a prespecified subgroup analysis restricted to the 1,229 participants with ST-elevation MI, Dr. Gilles Montalescot reported at the annual congress of the European Society of Cardiology.
Although this finding is intriguing, hypothesis-generating, and definitely warrants a confirmatory study, he continued, mortality was nevertheless merely a secondary endpoint in ALBATROSS (Aldosterone Lethal Effects Blockade in Acute Myocardial Infarction Treated With or Without Reperfusion to Improve Outcome and Survival at Six Months Follow-up).
In contrast, the primary composite outcome was negative, so the takeaway message is clear: “The results of the ALBATROSS study do not warrant the extension of aldosterone blockade to MI patients without heart failure,” said Dr. Montalescot, professor of cardiology at the University of Paris.
ALBATROSS was a multicenter French trial that randomly assigned 1,603 acute MI patients to standard therapy alone or with added mineralocorticoid antagonist therapy started within the first 2 days of their coronary event. Often the aldosterone antagonist was begun in the ambulance en route to the hospital.
The primary endpoint was a composite of death, resuscitated cardiac arrest, ventricular fibrillation or tachycardia, heart failure, or an indication for an implantable cardioverter defibrillator. There were 194 such events, and they occurred at a similar rate in the patients who got 25 mg/day of spironolactone and those who did not.
The rationale for ALBATROSS was sound, according to the cardiologist. Aldosterone is a stress hormone released in acute MI. It has deleterious cardiac effects, including arrhythmias, heart failure, and a dose-dependent increase in mortality, so it makes good sense to block it as soon as possible in MI patients. In the EPHESUS trial, the aldosterone antagonist eplerenone, when started 3-14 days post MI in patients with early heart failure, significantly reduced mortality (N Engl J Med. 2003 Apr 3;348[14]:1309-2), with the bulk of the benefit occurring in patients in whom the drug was started 3-7 days post MI.
Last year, Dr. Montalescot and his coinvestigators published the REMINDER study, in which 1,012 ST-elevation MI (STEMI) patients without heart failure were randomized to eplerenone or placebo within the first 24 hours. The study showed a significant reduction in levels of brain natriuretic peptide or N-terminal pro-BNP in the eplerenone arm (Eur Heart J. 2014 Sep 7;35[34]:2295-302), but that’s not a clinical endpoint. ALBATROSS was the first study to look at the clinical impact of commencing mineralocorticoid antagonist therapy prior to day 3 post MI.
Discussant Dr. John McMurray, professor of cardiology at the University of Glasgow, said that ALBATROSS was simply underpowered and thus leaves unanswered the clinically important question of whether early initiation of aldosterone blockade post MI in patients without heart failure confers clinical benefit. The investigators projected a total of 269 events in the composite endpoint but got only 194 because the study participants were so well treated and contemporary medical and interventional therapies are quite effective.
He dismissed the sharp reduction seen in 6-month mortality with spironolactone in the STEMI patients as “just implausible – we don’t know of any treatments in medicine that reduce mortality by 80%.”
Noting that there were only 28 deaths in the study, Dr. McMurray asserted that “a subgroup analysis on such a small number of events is never going to give you a reliable result.” Moreover, he added, “subgroup analysis is even more treacherous when the overall trial is underpowered.”
Dr. Montalescot replied that, while he considers the signal of a mortality benefit for aldosterone blockade in STEMI patients worthy of pursuit in a large randomized trial, the prospects for mounting such a study are poor. The medications are now available as generics, so there is no commercial incentive. The French Ministry of Health, which funded ALBATROSS, isn’t prepared to back a follow-up study. The best hope is that eventually one of the pharmaceutical companies developing third-generation aldosterone antagonists, now in phase II studies, will become interested, he said.
Dr. Montalescot said that, while he receives research grants and consulting fees from numerous pharmaceutical companies, these commercial relationships aren’t relevant to the government-funded ALBATROSS trial.
LONDON – Aldosterone blockade with oral spironolactone showed a disappointing lack of clinical benefit when initiated in the first hours after an acute MI without heart failure in the large, randomized ALBATROSS trial.
ALBATROSS did, however, flash a silver lining under one wing: A whopping 80% reduction in 6-month mortality in a prespecified subgroup analysis restricted to the 1,229 participants with ST-elevation MI, Dr. Gilles Montalescot reported at the annual congress of the European Society of Cardiology.
Although this finding is intriguing, hypothesis-generating, and definitely warrants a confirmatory study, he continued, mortality was nevertheless merely a secondary endpoint in ALBATROSS (Aldosterone Lethal Effects Blockade in Acute Myocardial Infarction Treated With or Without Reperfusion to Improve Outcome and Survival at Six Months Follow-up).
In contrast, the primary composite outcome was negative, so the takeaway message is clear: “The results of the ALBATROSS study do not warrant the extension of aldosterone blockade to MI patients without heart failure,” said Dr. Montalescot, professor of cardiology at the University of Paris.
ALBATROSS was a multicenter French trial that randomly assigned 1,603 acute MI patients to standard therapy alone or with added mineralocorticoid antagonist therapy started within the first 2 days of their coronary event. Often the aldosterone antagonist was begun in the ambulance en route to the hospital.
The primary endpoint was a composite of death, resuscitated cardiac arrest, ventricular fibrillation or tachycardia, heart failure, or an indication for an implantable cardioverter defibrillator. There were 194 such events, and they occurred at a similar rate in the patients who got 25 mg/day of spironolactone and those who did not.
The rationale for ALBATROSS was sound, according to the cardiologist. Aldosterone is a stress hormone released in acute MI. It has deleterious cardiac effects, including arrhythmias, heart failure, and a dose-dependent increase in mortality, so it makes good sense to block it as soon as possible in MI patients. In the EPHESUS trial, the aldosterone antagonist eplerenone, when started 3-14 days post MI in patients with early heart failure, significantly reduced mortality (N Engl J Med. 2003 Apr 3;348[14]:1309-2), with the bulk of the benefit occurring in patients in whom the drug was started 3-7 days post MI.
Last year, Dr. Montalescot and his coinvestigators published the REMINDER study, in which 1,012 ST-elevation MI (STEMI) patients without heart failure were randomized to eplerenone or placebo within the first 24 hours. The study showed a significant reduction in levels of brain natriuretic peptide or N-terminal pro-BNP in the eplerenone arm (Eur Heart J. 2014 Sep 7;35[34]:2295-302), but that’s not a clinical endpoint. ALBATROSS was the first study to look at the clinical impact of commencing mineralocorticoid antagonist therapy prior to day 3 post MI.
Discussant Dr. John McMurray, professor of cardiology at the University of Glasgow, said that ALBATROSS was simply underpowered and thus leaves unanswered the clinically important question of whether early initiation of aldosterone blockade post MI in patients without heart failure confers clinical benefit. The investigators projected a total of 269 events in the composite endpoint but got only 194 because the study participants were so well treated and contemporary medical and interventional therapies are quite effective.
He dismissed the sharp reduction seen in 6-month mortality with spironolactone in the STEMI patients as “just implausible – we don’t know of any treatments in medicine that reduce mortality by 80%.”
Noting that there were only 28 deaths in the study, Dr. McMurray asserted that “a subgroup analysis on such a small number of events is never going to give you a reliable result.” Moreover, he added, “subgroup analysis is even more treacherous when the overall trial is underpowered.”
Dr. Montalescot replied that, while he considers the signal of a mortality benefit for aldosterone blockade in STEMI patients worthy of pursuit in a large randomized trial, the prospects for mounting such a study are poor. The medications are now available as generics, so there is no commercial incentive. The French Ministry of Health, which funded ALBATROSS, isn’t prepared to back a follow-up study. The best hope is that eventually one of the pharmaceutical companies developing third-generation aldosterone antagonists, now in phase II studies, will become interested, he said.
Dr. Montalescot said that, while he receives research grants and consulting fees from numerous pharmaceutical companies, these commercial relationships aren’t relevant to the government-funded ALBATROSS trial.
AT THE ESC CONGRESS 2015
Key clinical point: Giving aldosterone antagonists to acute MI patients without heart failure doesn’t improve clinical outcomes.
Major finding: The 6-month rate of a multipronged composite clinical endpoint was closely similar, regardless of whether patients with acute MI without heart failure were placed on spironolactone within the first couple of days post-MI.
Data source: ALBATROSS was an open-label, multicenter French study in which 1,603 patients were randomized to 6 months of aldosterone blockade or not within the first hours after an acute MI without heart failure.
Disclosures: The investigator-initiated ALBATROSS trial was funded by the French Ministry of Health.
VIDEO: Europeans adopt 1-hour ED chest pain triage
LONDON – The positive findings of the Biomarkers in Acute Cardiovascular Care (BACC) study reinforce a key change contained in the brand-new European Society of Cardiology guidelines for management of patients with acute coronary syndrome without ST-segment elevation: namely, that it’s appropriate to assess such patients using two measurements of a validated high-sensitivity cardiac troponin assay taken just 1 hour apart, according to Dr. Kurt Huber.
The BACC results are the evidence-based icing on the cake in support of the new recommendation in the guidelines, released at the annual congress of the European Society of Cardiology. The BACC study, which included 1,045 patients who presented to a university emergency department with acute chest pain suggestive of an acute coronary syndrome without ST-segment elevation, was the latest of several studies to show that most such patients can either be safely sent home from the ED or ruled-in for acute MI in just 1 hour when evaluated using a high-sensitivity troponin assay backed by a validated patient-management algorithm. The result means reduced pressure on overcrowded EDs and less patient anxiety because of delayed diagnosis, Dr. Huber, director of cardiology and emergency medicine at Wilhelminen Hospital in Vienna, observed during an interview at the meeting.
The BACC study, presented by Dr. Dirk Westermann of the University Heart Center Hamburg (Germany), utilized a high-sensitivity cardiac troponin I assay. The 1-hour algorithm had a 99.7% negative predictive value for acute MI. A total of 53% of patients were ruled out or in for MI at the 1-hour mark; the rest required further evaluation.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LONDON – The positive findings of the Biomarkers in Acute Cardiovascular Care (BACC) study reinforce a key change contained in the brand-new European Society of Cardiology guidelines for management of patients with acute coronary syndrome without ST-segment elevation: namely, that it’s appropriate to assess such patients using two measurements of a validated high-sensitivity cardiac troponin assay taken just 1 hour apart, according to Dr. Kurt Huber.
The BACC results are the evidence-based icing on the cake in support of the new recommendation in the guidelines, released at the annual congress of the European Society of Cardiology. The BACC study, which included 1,045 patients who presented to a university emergency department with acute chest pain suggestive of an acute coronary syndrome without ST-segment elevation, was the latest of several studies to show that most such patients can either be safely sent home from the ED or ruled-in for acute MI in just 1 hour when evaluated using a high-sensitivity troponin assay backed by a validated patient-management algorithm. The result means reduced pressure on overcrowded EDs and less patient anxiety because of delayed diagnosis, Dr. Huber, director of cardiology and emergency medicine at Wilhelminen Hospital in Vienna, observed during an interview at the meeting.
The BACC study, presented by Dr. Dirk Westermann of the University Heart Center Hamburg (Germany), utilized a high-sensitivity cardiac troponin I assay. The 1-hour algorithm had a 99.7% negative predictive value for acute MI. A total of 53% of patients were ruled out or in for MI at the 1-hour mark; the rest required further evaluation.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LONDON – The positive findings of the Biomarkers in Acute Cardiovascular Care (BACC) study reinforce a key change contained in the brand-new European Society of Cardiology guidelines for management of patients with acute coronary syndrome without ST-segment elevation: namely, that it’s appropriate to assess such patients using two measurements of a validated high-sensitivity cardiac troponin assay taken just 1 hour apart, according to Dr. Kurt Huber.
The BACC results are the evidence-based icing on the cake in support of the new recommendation in the guidelines, released at the annual congress of the European Society of Cardiology. The BACC study, which included 1,045 patients who presented to a university emergency department with acute chest pain suggestive of an acute coronary syndrome without ST-segment elevation, was the latest of several studies to show that most such patients can either be safely sent home from the ED or ruled-in for acute MI in just 1 hour when evaluated using a high-sensitivity troponin assay backed by a validated patient-management algorithm. The result means reduced pressure on overcrowded EDs and less patient anxiety because of delayed diagnosis, Dr. Huber, director of cardiology and emergency medicine at Wilhelminen Hospital in Vienna, observed during an interview at the meeting.
The BACC study, presented by Dr. Dirk Westermann of the University Heart Center Hamburg (Germany), utilized a high-sensitivity cardiac troponin I assay. The 1-hour algorithm had a 99.7% negative predictive value for acute MI. A total of 53% of patients were ruled out or in for MI at the 1-hour mark; the rest required further evaluation.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ESC CONGRESS 2015
VIDEO: Napping – a novel nondrug antihypertensive therapy
LONDON – A regular midday nap is associated with clinically meaningful reductions in blood pressure in hypertensive patients, according to a prospective observational study presented at the annual congress of the European Society of Cardiology.
The midday nappers in the 386-patient study averaged 5 mm Hg lower daytime and 8 mm Hg lower nighttime systolic blood pressure, compared with non-nappers, Dr. Manolis Kallistratos said in a video interview.
Sleep during nap time was associated with bigger blood pressure reductions than simply resting. Sawing logs for 60 minutes or more brought the most benefits, according to Dr. Kallistratos, head of the hypertension division at Asklepieion Voula General Hospital in Athens.
Nappers also had significantly less arterial stiffness as reflected in a lower pulse wave velocity, as well as a smaller average left atrial diameter indicative of less structural heart damage, the cardiologist noted.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LONDON – A regular midday nap is associated with clinically meaningful reductions in blood pressure in hypertensive patients, according to a prospective observational study presented at the annual congress of the European Society of Cardiology.
The midday nappers in the 386-patient study averaged 5 mm Hg lower daytime and 8 mm Hg lower nighttime systolic blood pressure, compared with non-nappers, Dr. Manolis Kallistratos said in a video interview.
Sleep during nap time was associated with bigger blood pressure reductions than simply resting. Sawing logs for 60 minutes or more brought the most benefits, according to Dr. Kallistratos, head of the hypertension division at Asklepieion Voula General Hospital in Athens.
Nappers also had significantly less arterial stiffness as reflected in a lower pulse wave velocity, as well as a smaller average left atrial diameter indicative of less structural heart damage, the cardiologist noted.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LONDON – A regular midday nap is associated with clinically meaningful reductions in blood pressure in hypertensive patients, according to a prospective observational study presented at the annual congress of the European Society of Cardiology.
The midday nappers in the 386-patient study averaged 5 mm Hg lower daytime and 8 mm Hg lower nighttime systolic blood pressure, compared with non-nappers, Dr. Manolis Kallistratos said in a video interview.
Sleep during nap time was associated with bigger blood pressure reductions than simply resting. Sawing logs for 60 minutes or more brought the most benefits, according to Dr. Kallistratos, head of the hypertension division at Asklepieion Voula General Hospital in Athens.
Nappers also had significantly less arterial stiffness as reflected in a lower pulse wave velocity, as well as a smaller average left atrial diameter indicative of less structural heart damage, the cardiologist noted.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ESC CONGRESS 2015
‘Troubling’ trend in narcotic prescribing for ankylosing spondylitis
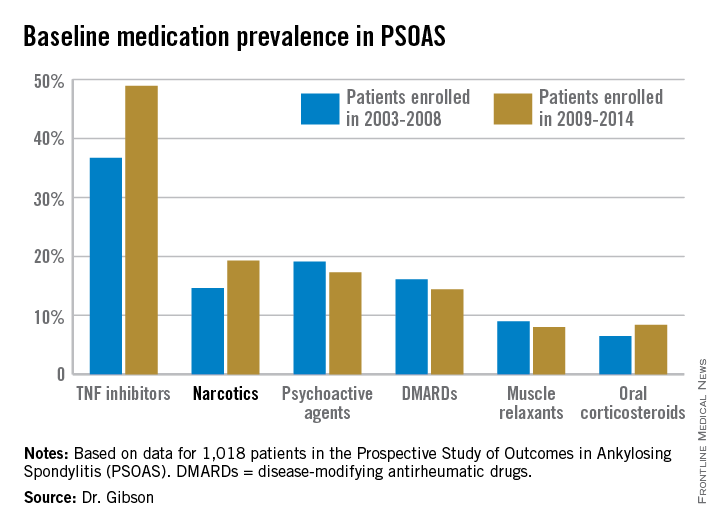
DENVER – Even as prescribing of tumor necrosis factor inhibitors for patients with ankylosing spondylitis climbed in the last half-dozen years, patients’ use of prescription narcotics increased as well.
This was the unexpected finding of a comprehensive analysis of trends in medication use over a 12-year period among 1,018 ankylosing spondylitis patients participating in the ongoing multicenter Prospective Study of Outcomes in Ankylosing Spondylitis (PSOAS), Dr. Mary C. Gibson reported at the annual meeting of the Spondyloarthritis Research and Treatment Network.
“Even with treatment with TNF inhibitors, patients are often requiring additional pain control with narcotic medications. This could reflect inadequate pain control from directed therapy or a trend toward change in pain control use in general practice,” observed Dr. Gibson of the University of Texas, Houston.
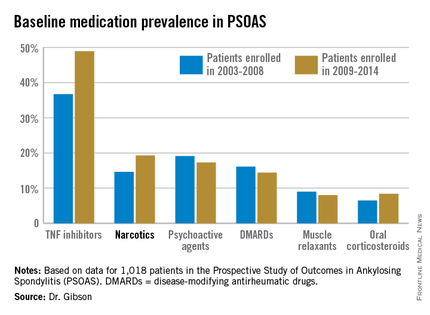
The patients enrolled in PSOAS during 2003-2014 are being followed longitudinally. They were recruited from community practice settings as well as academic centers. Dr. Gibson analyzed their medication use at the time of their baseline enrollment visit on a year-by-year basis, then stepped back to look at broader trends, comparing baseline medication use for patients enrolled in 2003-2008 to those enrolled during 2009-2014.
Not surprisingly, significantly more patients entered the study on a TNF inhibitor during the enrollment years 2009-2014 than during the first half of the study period: 49% compared with 37% during 2003-2008. What came as a surprise, however, was the time trend in narcotic use: 14.6% of ankylosing spondylitis patients in the 2003-2008 cohort were on narcotics, compared with 19.3% who enrolled since then.
“That’s a little bit troubling,” said Dr. John D. Reveille, professor and vice chair of rheumatology at the University of Texas, Houston, and head of PSOAS.
Oxycodone use nearly tripled between the first and second half of the study period: 1.1% were on the drug at enrollment in 2003-2008 compared with 3.1% in 2009-2014.
Of note, baseline use of oxycodone peaked in the enrollment class of 2012, 5.6% of whom were on the medication when they joined PSOAS. For narcotics overall, the peak year was 2008: over 27% of patients who enrolled in the study that year were on narcotic therapy at the time.
The use of NSAIDs – a guideline-recommended first-line therapy in ankylosing spondylitis – trended lower over time, albeit not significantly so. Among patients who enrolled in PSOAS during 2003-2008, over 70% were on NSAID therapy, compared with 66% of those who enrolled later.
There was no significant change over time in the use of DMARDs, psychoactive medications, muscle relaxants, or corticosteroids.
PSOAS is sponsored by the National Institutes of Health. Dr. Gibson reported having no financial conflicts.
DENVER – Even as prescribing of tumor necrosis factor inhibitors for patients with ankylosing spondylitis climbed in the last half-dozen years, patients’ use of prescription narcotics increased as well.
This was the unexpected finding of a comprehensive analysis of trends in medication use over a 12-year period among 1,018 ankylosing spondylitis patients participating in the ongoing multicenter Prospective Study of Outcomes in Ankylosing Spondylitis (PSOAS), Dr. Mary C. Gibson reported at the annual meeting of the Spondyloarthritis Research and Treatment Network.
“Even with treatment with TNF inhibitors, patients are often requiring additional pain control with narcotic medications. This could reflect inadequate pain control from directed therapy or a trend toward change in pain control use in general practice,” observed Dr. Gibson of the University of Texas, Houston.
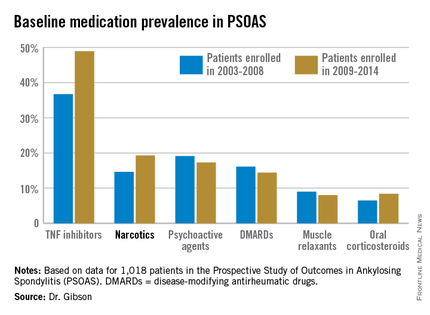
The patients enrolled in PSOAS during 2003-2014 are being followed longitudinally. They were recruited from community practice settings as well as academic centers. Dr. Gibson analyzed their medication use at the time of their baseline enrollment visit on a year-by-year basis, then stepped back to look at broader trends, comparing baseline medication use for patients enrolled in 2003-2008 to those enrolled during 2009-2014.
Not surprisingly, significantly more patients entered the study on a TNF inhibitor during the enrollment years 2009-2014 than during the first half of the study period: 49% compared with 37% during 2003-2008. What came as a surprise, however, was the time trend in narcotic use: 14.6% of ankylosing spondylitis patients in the 2003-2008 cohort were on narcotics, compared with 19.3% who enrolled since then.
“That’s a little bit troubling,” said Dr. John D. Reveille, professor and vice chair of rheumatology at the University of Texas, Houston, and head of PSOAS.
Oxycodone use nearly tripled between the first and second half of the study period: 1.1% were on the drug at enrollment in 2003-2008 compared with 3.1% in 2009-2014.
Of note, baseline use of oxycodone peaked in the enrollment class of 2012, 5.6% of whom were on the medication when they joined PSOAS. For narcotics overall, the peak year was 2008: over 27% of patients who enrolled in the study that year were on narcotic therapy at the time.
The use of NSAIDs – a guideline-recommended first-line therapy in ankylosing spondylitis – trended lower over time, albeit not significantly so. Among patients who enrolled in PSOAS during 2003-2008, over 70% were on NSAID therapy, compared with 66% of those who enrolled later.
There was no significant change over time in the use of DMARDs, psychoactive medications, muscle relaxants, or corticosteroids.
PSOAS is sponsored by the National Institutes of Health. Dr. Gibson reported having no financial conflicts.
DENVER – Even as prescribing of tumor necrosis factor inhibitors for patients with ankylosing spondylitis climbed in the last half-dozen years, patients’ use of prescription narcotics increased as well.
This was the unexpected finding of a comprehensive analysis of trends in medication use over a 12-year period among 1,018 ankylosing spondylitis patients participating in the ongoing multicenter Prospective Study of Outcomes in Ankylosing Spondylitis (PSOAS), Dr. Mary C. Gibson reported at the annual meeting of the Spondyloarthritis Research and Treatment Network.
“Even with treatment with TNF inhibitors, patients are often requiring additional pain control with narcotic medications. This could reflect inadequate pain control from directed therapy or a trend toward change in pain control use in general practice,” observed Dr. Gibson of the University of Texas, Houston.
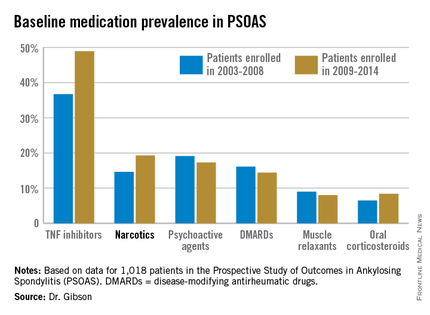
The patients enrolled in PSOAS during 2003-2014 are being followed longitudinally. They were recruited from community practice settings as well as academic centers. Dr. Gibson analyzed their medication use at the time of their baseline enrollment visit on a year-by-year basis, then stepped back to look at broader trends, comparing baseline medication use for patients enrolled in 2003-2008 to those enrolled during 2009-2014.
Not surprisingly, significantly more patients entered the study on a TNF inhibitor during the enrollment years 2009-2014 than during the first half of the study period: 49% compared with 37% during 2003-2008. What came as a surprise, however, was the time trend in narcotic use: 14.6% of ankylosing spondylitis patients in the 2003-2008 cohort were on narcotics, compared with 19.3% who enrolled since then.
“That’s a little bit troubling,” said Dr. John D. Reveille, professor and vice chair of rheumatology at the University of Texas, Houston, and head of PSOAS.
Oxycodone use nearly tripled between the first and second half of the study period: 1.1% were on the drug at enrollment in 2003-2008 compared with 3.1% in 2009-2014.
Of note, baseline use of oxycodone peaked in the enrollment class of 2012, 5.6% of whom were on the medication when they joined PSOAS. For narcotics overall, the peak year was 2008: over 27% of patients who enrolled in the study that year were on narcotic therapy at the time.
The use of NSAIDs – a guideline-recommended first-line therapy in ankylosing spondylitis – trended lower over time, albeit not significantly so. Among patients who enrolled in PSOAS during 2003-2008, over 70% were on NSAID therapy, compared with 66% of those who enrolled later.
There was no significant change over time in the use of DMARDs, psychoactive medications, muscle relaxants, or corticosteroids.
PSOAS is sponsored by the National Institutes of Health. Dr. Gibson reported having no financial conflicts.
AT THE 2015 SPARTAN ANNUAL MEETING
Key clinical point: The use of prescription narcotics by patients with ankylosing spondylitis has gone up during the past 12 years, even as their use of tumor necrosis factor inhibitor therapy has grown.
Major finding: Among a large cohort of patients with ankylosing spondylitis, 14.6% were on prescription narcotic therapy during 2003-2008, compared with 19.3% in 2009-2014.
Data source: Analysis of 1,018 patients with ankylosing spondylitis, from PSOAS – a prospective, multicenter, longitudinal cohort study.
Disclosures: The ongoing PSOAS study is funded by the National Institutes of Health. The presenter reported having no conflicts of interest.
In Diabetic Foot Ulcers, Use 50% Rule to Gauge Need for Advanced Therapies
VANCOUVER – When diabetic foot ulcer healing has stalled despite 4 weeks of optimal standard therapy, it’s time to seriously consider resorting to advanced therapies, according to Dr. Afsaneh Alavi of the University of Toronto.
Advanced therapy options include negative pressure wound therapy, hyperbaric oxygen, artificial skin substitutes, growth factors, collagen-based dressings, and electromagnetic therapy.
“You hear a lot about advanced therapy for diabetic foot ulcers. It’s expensive. But it can be cost-effective if used properly. It’s our duty to see who is the best person to receive this therapy,” she said at the World Congress of Dermatology.
A useful rule of thumb, the dermatologist added, is that if a healable ulcer isn’t 50% smaller at week 4 despite optimal care, it’s time to consider moving on to advanced therapies. As was shown in a well-conducted, 203-patient, randomized, prospective controlled clinical trial, a wound that hasn’t met that threshold is unlikely to be healed at 12 weeks (Diabetes Care. 2003 Jun;26(6):1879-82).
Two caveats: advanced therapy is appropriate only for healable diabetic foot ulcers, meaning those in patients with adequate peripheral circulation as defined by measurements of transcutaneous oxygen pressure, toe pressure brachial index, and Doppler studies.
“Eighty percent of diabetic patients have noncompressible arteries and therefore the ankle brachial index is not an accurate test to evaluate their circulation,” according to Dr. Avali.
The other caveat regarding advanced therapy is that appropriate candidates should have a wound edge that’s sharp, not migrating, she continued.
The 4-week cutoff for seeing substantial progress in wound healing with standard therapy before turning to advanced therapies is based in part upon an influential study of 2,517 patients with diabetic neuropathic foot ulcers who received one of three advanced biological therapies. On average, patients started advanced biological therapy within 28 days following their first visit to a specialized wound clinic. Prolonged time to initiation of advanced treatment was associated with significantly longer time to healing (Arch Dermatol. 2010 Aug;146(8):857-62).
While thinking about local wound care in a patient with a diabetic foot ulcer, Dr. Avali said it’s also important to take a step back and make sure hypertension and other conventional cardiovascular risk factors are well controlled and also to take a close look at the HbA1c. In a study of 183 patients with diabetic wounds treated at a specialized academic wound center, for every 1.0% increase in HbA1c above the mean level of 8.0%, the wound-area healing rate was reduced by 0.028 cm2 per day. The implication is that HbA1c may be a key biomarker that’s useful in predicting wound-healing rate in patients with diabetic ulcers (J. Invest Dermatol. 2011 Oct;131(10):2121-7).
She reported serving as a consultant to Acelity and Smith & Nephew.
VANCOUVER – When diabetic foot ulcer healing has stalled despite 4 weeks of optimal standard therapy, it’s time to seriously consider resorting to advanced therapies, according to Dr. Afsaneh Alavi of the University of Toronto.
Advanced therapy options include negative pressure wound therapy, hyperbaric oxygen, artificial skin substitutes, growth factors, collagen-based dressings, and electromagnetic therapy.
“You hear a lot about advanced therapy for diabetic foot ulcers. It’s expensive. But it can be cost-effective if used properly. It’s our duty to see who is the best person to receive this therapy,” she said at the World Congress of Dermatology.
A useful rule of thumb, the dermatologist added, is that if a healable ulcer isn’t 50% smaller at week 4 despite optimal care, it’s time to consider moving on to advanced therapies. As was shown in a well-conducted, 203-patient, randomized, prospective controlled clinical trial, a wound that hasn’t met that threshold is unlikely to be healed at 12 weeks (Diabetes Care. 2003 Jun;26(6):1879-82).
Two caveats: advanced therapy is appropriate only for healable diabetic foot ulcers, meaning those in patients with adequate peripheral circulation as defined by measurements of transcutaneous oxygen pressure, toe pressure brachial index, and Doppler studies.
“Eighty percent of diabetic patients have noncompressible arteries and therefore the ankle brachial index is not an accurate test to evaluate their circulation,” according to Dr. Avali.
The other caveat regarding advanced therapy is that appropriate candidates should have a wound edge that’s sharp, not migrating, she continued.
The 4-week cutoff for seeing substantial progress in wound healing with standard therapy before turning to advanced therapies is based in part upon an influential study of 2,517 patients with diabetic neuropathic foot ulcers who received one of three advanced biological therapies. On average, patients started advanced biological therapy within 28 days following their first visit to a specialized wound clinic. Prolonged time to initiation of advanced treatment was associated with significantly longer time to healing (Arch Dermatol. 2010 Aug;146(8):857-62).
While thinking about local wound care in a patient with a diabetic foot ulcer, Dr. Avali said it’s also important to take a step back and make sure hypertension and other conventional cardiovascular risk factors are well controlled and also to take a close look at the HbA1c. In a study of 183 patients with diabetic wounds treated at a specialized academic wound center, for every 1.0% increase in HbA1c above the mean level of 8.0%, the wound-area healing rate was reduced by 0.028 cm2 per day. The implication is that HbA1c may be a key biomarker that’s useful in predicting wound-healing rate in patients with diabetic ulcers (J. Invest Dermatol. 2011 Oct;131(10):2121-7).
She reported serving as a consultant to Acelity and Smith & Nephew.
VANCOUVER – When diabetic foot ulcer healing has stalled despite 4 weeks of optimal standard therapy, it’s time to seriously consider resorting to advanced therapies, according to Dr. Afsaneh Alavi of the University of Toronto.
Advanced therapy options include negative pressure wound therapy, hyperbaric oxygen, artificial skin substitutes, growth factors, collagen-based dressings, and electromagnetic therapy.
“You hear a lot about advanced therapy for diabetic foot ulcers. It’s expensive. But it can be cost-effective if used properly. It’s our duty to see who is the best person to receive this therapy,” she said at the World Congress of Dermatology.
A useful rule of thumb, the dermatologist added, is that if a healable ulcer isn’t 50% smaller at week 4 despite optimal care, it’s time to consider moving on to advanced therapies. As was shown in a well-conducted, 203-patient, randomized, prospective controlled clinical trial, a wound that hasn’t met that threshold is unlikely to be healed at 12 weeks (Diabetes Care. 2003 Jun;26(6):1879-82).
Two caveats: advanced therapy is appropriate only for healable diabetic foot ulcers, meaning those in patients with adequate peripheral circulation as defined by measurements of transcutaneous oxygen pressure, toe pressure brachial index, and Doppler studies.
“Eighty percent of diabetic patients have noncompressible arteries and therefore the ankle brachial index is not an accurate test to evaluate their circulation,” according to Dr. Avali.
The other caveat regarding advanced therapy is that appropriate candidates should have a wound edge that’s sharp, not migrating, she continued.
The 4-week cutoff for seeing substantial progress in wound healing with standard therapy before turning to advanced therapies is based in part upon an influential study of 2,517 patients with diabetic neuropathic foot ulcers who received one of three advanced biological therapies. On average, patients started advanced biological therapy within 28 days following their first visit to a specialized wound clinic. Prolonged time to initiation of advanced treatment was associated with significantly longer time to healing (Arch Dermatol. 2010 Aug;146(8):857-62).
While thinking about local wound care in a patient with a diabetic foot ulcer, Dr. Avali said it’s also important to take a step back and make sure hypertension and other conventional cardiovascular risk factors are well controlled and also to take a close look at the HbA1c. In a study of 183 patients with diabetic wounds treated at a specialized academic wound center, for every 1.0% increase in HbA1c above the mean level of 8.0%, the wound-area healing rate was reduced by 0.028 cm2 per day. The implication is that HbA1c may be a key biomarker that’s useful in predicting wound-healing rate in patients with diabetic ulcers (J. Invest Dermatol. 2011 Oct;131(10):2121-7).
She reported serving as a consultant to Acelity and Smith & Nephew.
EXPERT ANALYSIS FROM WCD 2015
In diabetic foot ulcers, use 50% rule to gauge need for advanced therapies
VANCOUVER – When diabetic foot ulcer healing has stalled despite 4 weeks of optimal standard therapy, it’s time to seriously consider resorting to advanced therapies, according to Dr. Afsaneh Alavi of the University of Toronto.
Advanced therapy options include negative pressure wound therapy, hyperbaric oxygen, artificial skin substitutes, growth factors, collagen-based dressings, and electromagnetic therapy.
“You hear a lot about advanced therapy for diabetic foot ulcers. It’s expensive. But it can be cost-effective if used properly. It’s our duty to see who is the best person to receive this therapy,” she said at the World Congress of Dermatology.
A useful rule of thumb, the dermatologist added, is that if a healable ulcer isn’t 50% smaller at week 4 despite optimal care, it’s time to consider moving on to advanced therapies. As was shown in a well-conducted, 203-patient, randomized, prospective controlled clinical trial, a wound that hasn’t met that threshold is unlikely to be healed at 12 weeks (Diabetes Care. 2003 Jun;26(6):1879-82).
Two caveats: advanced therapy is appropriate only for healable diabetic foot ulcers, meaning those in patients with adequate peripheral circulation as defined by measurements of transcutaneous oxygen pressure, toe pressure brachial index, and Doppler studies.
“Eighty percent of diabetic patients have noncompressible arteries and therefore the ankle brachial index is not an accurate test to evaluate their circulation,” according to Dr. Avali.
The other caveat regarding advanced therapy is that appropriate candidates should have a wound edge that’s sharp, not migrating, she continued.
The 4-week cutoff for seeing substantial progress in wound healing with standard therapy before turning to advanced therapies is based in part upon an influential study of 2,517 patients with diabetic neuropathic foot ulcers who received one of three advanced biological therapies. On average, patients started advanced biological therapy within 28 days following their first visit to a specialized wound clinic. Prolonged time to initiation of advanced treatment was associated with significantly longer time to healing (Arch Dermatol. 2010 Aug;146(8):857-62).
While thinking about local wound care in a patient with a diabetic foot ulcer, Dr. Avali said it’s also important to take a step back and make sure hypertension and other conventional cardiovascular risk factors are well controlled and also to take a close look at the HbA1c. In a study of 183 patients with diabetic wounds treated at a specialized academic wound center, for every 1.0% increase in HbA1c above the mean level of 8.0%, the wound-area healing rate was reduced by 0.028 cm2 per day. The implication is that HbA1c may be a key biomarker that’s useful in predicting wound-healing rate in patients with diabetic ulcers (J. Invest Dermatol. 2011 Oct;131(10):2121-7).
She reported serving as a consultant to Acelity and Smith & Nephew.
VANCOUVER – When diabetic foot ulcer healing has stalled despite 4 weeks of optimal standard therapy, it’s time to seriously consider resorting to advanced therapies, according to Dr. Afsaneh Alavi of the University of Toronto.
Advanced therapy options include negative pressure wound therapy, hyperbaric oxygen, artificial skin substitutes, growth factors, collagen-based dressings, and electromagnetic therapy.
“You hear a lot about advanced therapy for diabetic foot ulcers. It’s expensive. But it can be cost-effective if used properly. It’s our duty to see who is the best person to receive this therapy,” she said at the World Congress of Dermatology.
A useful rule of thumb, the dermatologist added, is that if a healable ulcer isn’t 50% smaller at week 4 despite optimal care, it’s time to consider moving on to advanced therapies. As was shown in a well-conducted, 203-patient, randomized, prospective controlled clinical trial, a wound that hasn’t met that threshold is unlikely to be healed at 12 weeks (Diabetes Care. 2003 Jun;26(6):1879-82).
Two caveats: advanced therapy is appropriate only for healable diabetic foot ulcers, meaning those in patients with adequate peripheral circulation as defined by measurements of transcutaneous oxygen pressure, toe pressure brachial index, and Doppler studies.
“Eighty percent of diabetic patients have noncompressible arteries and therefore the ankle brachial index is not an accurate test to evaluate their circulation,” according to Dr. Avali.
The other caveat regarding advanced therapy is that appropriate candidates should have a wound edge that’s sharp, not migrating, she continued.
The 4-week cutoff for seeing substantial progress in wound healing with standard therapy before turning to advanced therapies is based in part upon an influential study of 2,517 patients with diabetic neuropathic foot ulcers who received one of three advanced biological therapies. On average, patients started advanced biological therapy within 28 days following their first visit to a specialized wound clinic. Prolonged time to initiation of advanced treatment was associated with significantly longer time to healing (Arch Dermatol. 2010 Aug;146(8):857-62).
While thinking about local wound care in a patient with a diabetic foot ulcer, Dr. Avali said it’s also important to take a step back and make sure hypertension and other conventional cardiovascular risk factors are well controlled and also to take a close look at the HbA1c. In a study of 183 patients with diabetic wounds treated at a specialized academic wound center, for every 1.0% increase in HbA1c above the mean level of 8.0%, the wound-area healing rate was reduced by 0.028 cm2 per day. The implication is that HbA1c may be a key biomarker that’s useful in predicting wound-healing rate in patients with diabetic ulcers (J. Invest Dermatol. 2011 Oct;131(10):2121-7).
She reported serving as a consultant to Acelity and Smith & Nephew.
VANCOUVER – When diabetic foot ulcer healing has stalled despite 4 weeks of optimal standard therapy, it’s time to seriously consider resorting to advanced therapies, according to Dr. Afsaneh Alavi of the University of Toronto.
Advanced therapy options include negative pressure wound therapy, hyperbaric oxygen, artificial skin substitutes, growth factors, collagen-based dressings, and electromagnetic therapy.
“You hear a lot about advanced therapy for diabetic foot ulcers. It’s expensive. But it can be cost-effective if used properly. It’s our duty to see who is the best person to receive this therapy,” she said at the World Congress of Dermatology.
A useful rule of thumb, the dermatologist added, is that if a healable ulcer isn’t 50% smaller at week 4 despite optimal care, it’s time to consider moving on to advanced therapies. As was shown in a well-conducted, 203-patient, randomized, prospective controlled clinical trial, a wound that hasn’t met that threshold is unlikely to be healed at 12 weeks (Diabetes Care. 2003 Jun;26(6):1879-82).
Two caveats: advanced therapy is appropriate only for healable diabetic foot ulcers, meaning those in patients with adequate peripheral circulation as defined by measurements of transcutaneous oxygen pressure, toe pressure brachial index, and Doppler studies.
“Eighty percent of diabetic patients have noncompressible arteries and therefore the ankle brachial index is not an accurate test to evaluate their circulation,” according to Dr. Avali.
The other caveat regarding advanced therapy is that appropriate candidates should have a wound edge that’s sharp, not migrating, she continued.
The 4-week cutoff for seeing substantial progress in wound healing with standard therapy before turning to advanced therapies is based in part upon an influential study of 2,517 patients with diabetic neuropathic foot ulcers who received one of three advanced biological therapies. On average, patients started advanced biological therapy within 28 days following their first visit to a specialized wound clinic. Prolonged time to initiation of advanced treatment was associated with significantly longer time to healing (Arch Dermatol. 2010 Aug;146(8):857-62).
While thinking about local wound care in a patient with a diabetic foot ulcer, Dr. Avali said it’s also important to take a step back and make sure hypertension and other conventional cardiovascular risk factors are well controlled and also to take a close look at the HbA1c. In a study of 183 patients with diabetic wounds treated at a specialized academic wound center, for every 1.0% increase in HbA1c above the mean level of 8.0%, the wound-area healing rate was reduced by 0.028 cm2 per day. The implication is that HbA1c may be a key biomarker that’s useful in predicting wound-healing rate in patients with diabetic ulcers (J. Invest Dermatol. 2011 Oct;131(10):2121-7).
She reported serving as a consultant to Acelity and Smith & Nephew.
EXPERT ANALYSIS FROM WCD 2015
Offloading is key to diabetic foot ulcer management
VANCOUVER – Offloading of plantar pressures is the key component of successful management of plantar diabetic foot ulcers, Dr. Afsaneh Alavi asserted at the World Congress of Dermatology.
“Debridement to remove the callous is the most important part of local wound care, but debridement without offloading afterwards will rebuild callous,” explained Dr. Alavi, a University of Toronto dermatologist.
Many options exist in terms of offloading devices. The total contact cast is recognized as the gold standard. It reduces pressures by 90%. Yet a national survey of more than 900 foot clinics found that less than 2% of centers utilized total contact casts for the majority of their patients with plantar diabetic foot ulcers. Only 15% of centers utilized another highly effective option, the removable cast walker, in the majority of patients (Diabetes Care. 2008 Nov; 31(11): 2118–2119). Cost is believed to be a major issue. Other options include custom orthotic inserts and forefoot and heel relief shoes.
The diabetic foot ulcer recurrence rate is extremely high: up to 83% within the first year.
“Counsel patients to use therapeutic shoes and insoles, engage in self-inspection, and get professional foot care. Shoes should be worn at all times, even in the house. Patients typically spend 30%-40% of their time at home,” Dr. Alavi continued.
The pathophysiology of diabetic foot ulcers is a vicious circle of immunopathy, neuropathy, and angiopathy. Callous formation secondary to sensory and motor neuropathy leads to subcutaneous bleeding, ulcer formation, and deeper infection, sometimes with life- or limb-threatening osteomyelitis.
“Detection of this chain of events at the stage of callous formation would make a huge difference,” according to the dermatologist. She pointed out that “Most of our health care system is focused more on management than prevention. We spend more on amputations due to diabetic foot ulcers than for prevention.”
Although many methods of callous removal are available, including autolytic therapy with hydrogels, whirlpools, and wet-to-dry dressings, Dr. Alavi said the best method is sharp surgical debridement. She highlighted a retrospective 12-week study of topical wound treatments in 310 diabetic foot ulcers and 366 chronic venous leg ulcers which found that venous leg ulcers showed a 34% greater median wound surface area reduction following office visits with surgical debridement compared with no surgical debridement. Serial surgical debridement in patients with diabetic foot ulcers was also associated with a 2.35-fold increased likelihood of wound closure (Wound Repair Regen. 2009 May-June;17(3):306-11).
She noted that it has been estimated that by 2030, at least 10% of the world’s adult population -- some 550 million people -- will have diabetes. And a diabetic individual’s lifetime risk of developing diabetic foot ulcers is up to 25%. The 5-year mortality rate following amputation related to a diabetic foot ulcer is nearly 50%, about the same as following diagnosis of colon cancer.
Dr. Alavi reported serving as a consultant to Acelity and Smith & Nephew.
VANCOUVER – Offloading of plantar pressures is the key component of successful management of plantar diabetic foot ulcers, Dr. Afsaneh Alavi asserted at the World Congress of Dermatology.
“Debridement to remove the callous is the most important part of local wound care, but debridement without offloading afterwards will rebuild callous,” explained Dr. Alavi, a University of Toronto dermatologist.
Many options exist in terms of offloading devices. The total contact cast is recognized as the gold standard. It reduces pressures by 90%. Yet a national survey of more than 900 foot clinics found that less than 2% of centers utilized total contact casts for the majority of their patients with plantar diabetic foot ulcers. Only 15% of centers utilized another highly effective option, the removable cast walker, in the majority of patients (Diabetes Care. 2008 Nov; 31(11): 2118–2119). Cost is believed to be a major issue. Other options include custom orthotic inserts and forefoot and heel relief shoes.
The diabetic foot ulcer recurrence rate is extremely high: up to 83% within the first year.
“Counsel patients to use therapeutic shoes and insoles, engage in self-inspection, and get professional foot care. Shoes should be worn at all times, even in the house. Patients typically spend 30%-40% of their time at home,” Dr. Alavi continued.
The pathophysiology of diabetic foot ulcers is a vicious circle of immunopathy, neuropathy, and angiopathy. Callous formation secondary to sensory and motor neuropathy leads to subcutaneous bleeding, ulcer formation, and deeper infection, sometimes with life- or limb-threatening osteomyelitis.
“Detection of this chain of events at the stage of callous formation would make a huge difference,” according to the dermatologist. She pointed out that “Most of our health care system is focused more on management than prevention. We spend more on amputations due to diabetic foot ulcers than for prevention.”
Although many methods of callous removal are available, including autolytic therapy with hydrogels, whirlpools, and wet-to-dry dressings, Dr. Alavi said the best method is sharp surgical debridement. She highlighted a retrospective 12-week study of topical wound treatments in 310 diabetic foot ulcers and 366 chronic venous leg ulcers which found that venous leg ulcers showed a 34% greater median wound surface area reduction following office visits with surgical debridement compared with no surgical debridement. Serial surgical debridement in patients with diabetic foot ulcers was also associated with a 2.35-fold increased likelihood of wound closure (Wound Repair Regen. 2009 May-June;17(3):306-11).
She noted that it has been estimated that by 2030, at least 10% of the world’s adult population -- some 550 million people -- will have diabetes. And a diabetic individual’s lifetime risk of developing diabetic foot ulcers is up to 25%. The 5-year mortality rate following amputation related to a diabetic foot ulcer is nearly 50%, about the same as following diagnosis of colon cancer.
Dr. Alavi reported serving as a consultant to Acelity and Smith & Nephew.
VANCOUVER – Offloading of plantar pressures is the key component of successful management of plantar diabetic foot ulcers, Dr. Afsaneh Alavi asserted at the World Congress of Dermatology.
“Debridement to remove the callous is the most important part of local wound care, but debridement without offloading afterwards will rebuild callous,” explained Dr. Alavi, a University of Toronto dermatologist.
Many options exist in terms of offloading devices. The total contact cast is recognized as the gold standard. It reduces pressures by 90%. Yet a national survey of more than 900 foot clinics found that less than 2% of centers utilized total contact casts for the majority of their patients with plantar diabetic foot ulcers. Only 15% of centers utilized another highly effective option, the removable cast walker, in the majority of patients (Diabetes Care. 2008 Nov; 31(11): 2118–2119). Cost is believed to be a major issue. Other options include custom orthotic inserts and forefoot and heel relief shoes.
The diabetic foot ulcer recurrence rate is extremely high: up to 83% within the first year.
“Counsel patients to use therapeutic shoes and insoles, engage in self-inspection, and get professional foot care. Shoes should be worn at all times, even in the house. Patients typically spend 30%-40% of their time at home,” Dr. Alavi continued.
The pathophysiology of diabetic foot ulcers is a vicious circle of immunopathy, neuropathy, and angiopathy. Callous formation secondary to sensory and motor neuropathy leads to subcutaneous bleeding, ulcer formation, and deeper infection, sometimes with life- or limb-threatening osteomyelitis.
“Detection of this chain of events at the stage of callous formation would make a huge difference,” according to the dermatologist. She pointed out that “Most of our health care system is focused more on management than prevention. We spend more on amputations due to diabetic foot ulcers than for prevention.”
Although many methods of callous removal are available, including autolytic therapy with hydrogels, whirlpools, and wet-to-dry dressings, Dr. Alavi said the best method is sharp surgical debridement. She highlighted a retrospective 12-week study of topical wound treatments in 310 diabetic foot ulcers and 366 chronic venous leg ulcers which found that venous leg ulcers showed a 34% greater median wound surface area reduction following office visits with surgical debridement compared with no surgical debridement. Serial surgical debridement in patients with diabetic foot ulcers was also associated with a 2.35-fold increased likelihood of wound closure (Wound Repair Regen. 2009 May-June;17(3):306-11).
She noted that it has been estimated that by 2030, at least 10% of the world’s adult population -- some 550 million people -- will have diabetes. And a diabetic individual’s lifetime risk of developing diabetic foot ulcers is up to 25%. The 5-year mortality rate following amputation related to a diabetic foot ulcer is nearly 50%, about the same as following diagnosis of colon cancer.
Dr. Alavi reported serving as a consultant to Acelity and Smith & Nephew.
EXPERT ANALYSIS FROM WCD 2015
Exercise boosts medication’s benefits in ankylosing spondylitis
DENVER – Recreational exercise and tumor necrosis factor–inhibitor therapy provide synergistic improvement in the functional status of patients with ankylosing spondylitis, according to an analysis from the multicenter Prospective Study of Outcomes in Ankylosing Spondylitis (PSOAS).
Among 683 PSOAS participants prospectively followed for up to 12 years, those who consistently engaged in moderate recreational exercise, defined as at least 120 minutes of exercise per week, had significantly lower, more favorable Bath Ankylosing Spondylitis Functional Index (BASFI) scores during years 1-5 than did those who exercised less, even after controlling for baseline function and other potential confounders in a multivariate analysis, Dr. Lianne S. Gensler said at the annual meeting of the Spondyloarthritis Research and Treatment Network.
Additionally, a significant interaction was observed between exercise time and anti-TNF therapy. BASFI scores improved through 5 years of follow-up in TNF inhibitor users regardless of their exercise status, but the impact on functional status was “strikingly” greater in those patients on a TNF inhibitor who engaged in at least 120 minutes of exercise per week, according to Dr. Gensler of the University of California, San Francisco.
“This suggests that it’s not simply taking a TNF inhibitor that’s going to promote long-term function. These patients should also be exercising to synergize and get the best out of their therapy,” she emphasized.
The PSOAS cohort included averaged 43 years of age at baseline, with a mean 19-year disease duration and an average of 2.1 comorbid conditions. In a multivariate longitudinal analysis, several factors emerged as significant predictors of more pronounced functional impairment over time: being age 40 or older at baseline was associated with a 25% increased risk, opiate use was associated with a 12% increase in risk, a baseline Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) score of at least 40 conferred a 19% increase in risk, as did a modified Stoke Ankylosing Spondylitis Spinal Score of 4 or greater.
Dr. Gensler drew a sharp distinction between the effects of moderate recreational exercise and occupational physical activity in ankylosing spondylitis patients. In an earlier landmark study involving 397 members of the PSOAS cohort with at least a 20-year history of ankylosing spondylitis, investigators mapped the patients’ work histories, the physical activities their work entailed, and the time they spent at each activity. Jobs that involved repeated bending, stretching, twisting, and vibration exposure were associated with worse BASFI scores and greater radiographic disease severity (Arthritis Rheum. 2008 Jun 15;59[6]:822-32).
Taking a step back to summarize what’s known today about what affects outcomes in ankylosing spondylitis patients, Dr. Gensler listed in the ‘bad’ column smoking, ongoing inflammation, baseline damage to the spine, certain occupational activities involving biomechanical stress, adiposity, and low socioeconomic status.
What’s good for patients with ankylosing spondylitis is physical therapy and back exercises – both will receive favorable marks in soon-to-be-published American College of Rheumatology guidelines on the management of ankylosing spondylitis that Dr. Gensler worked on – as well as TNF-inhibitor therapy, NSAIDs, and recreational exercise, which wasn’t addressed in the former guidelines.
Dr. Gensler reported receiving research funds from or serving as a consultant to AbbVie, Amgen, Celgene, Janssen, and UCB.
DENVER – Recreational exercise and tumor necrosis factor–inhibitor therapy provide synergistic improvement in the functional status of patients with ankylosing spondylitis, according to an analysis from the multicenter Prospective Study of Outcomes in Ankylosing Spondylitis (PSOAS).
Among 683 PSOAS participants prospectively followed for up to 12 years, those who consistently engaged in moderate recreational exercise, defined as at least 120 minutes of exercise per week, had significantly lower, more favorable Bath Ankylosing Spondylitis Functional Index (BASFI) scores during years 1-5 than did those who exercised less, even after controlling for baseline function and other potential confounders in a multivariate analysis, Dr. Lianne S. Gensler said at the annual meeting of the Spondyloarthritis Research and Treatment Network.
Additionally, a significant interaction was observed between exercise time and anti-TNF therapy. BASFI scores improved through 5 years of follow-up in TNF inhibitor users regardless of their exercise status, but the impact on functional status was “strikingly” greater in those patients on a TNF inhibitor who engaged in at least 120 minutes of exercise per week, according to Dr. Gensler of the University of California, San Francisco.
“This suggests that it’s not simply taking a TNF inhibitor that’s going to promote long-term function. These patients should also be exercising to synergize and get the best out of their therapy,” she emphasized.
The PSOAS cohort included averaged 43 years of age at baseline, with a mean 19-year disease duration and an average of 2.1 comorbid conditions. In a multivariate longitudinal analysis, several factors emerged as significant predictors of more pronounced functional impairment over time: being age 40 or older at baseline was associated with a 25% increased risk, opiate use was associated with a 12% increase in risk, a baseline Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) score of at least 40 conferred a 19% increase in risk, as did a modified Stoke Ankylosing Spondylitis Spinal Score of 4 or greater.
Dr. Gensler drew a sharp distinction between the effects of moderate recreational exercise and occupational physical activity in ankylosing spondylitis patients. In an earlier landmark study involving 397 members of the PSOAS cohort with at least a 20-year history of ankylosing spondylitis, investigators mapped the patients’ work histories, the physical activities their work entailed, and the time they spent at each activity. Jobs that involved repeated bending, stretching, twisting, and vibration exposure were associated with worse BASFI scores and greater radiographic disease severity (Arthritis Rheum. 2008 Jun 15;59[6]:822-32).
Taking a step back to summarize what’s known today about what affects outcomes in ankylosing spondylitis patients, Dr. Gensler listed in the ‘bad’ column smoking, ongoing inflammation, baseline damage to the spine, certain occupational activities involving biomechanical stress, adiposity, and low socioeconomic status.
What’s good for patients with ankylosing spondylitis is physical therapy and back exercises – both will receive favorable marks in soon-to-be-published American College of Rheumatology guidelines on the management of ankylosing spondylitis that Dr. Gensler worked on – as well as TNF-inhibitor therapy, NSAIDs, and recreational exercise, which wasn’t addressed in the former guidelines.
Dr. Gensler reported receiving research funds from or serving as a consultant to AbbVie, Amgen, Celgene, Janssen, and UCB.
DENVER – Recreational exercise and tumor necrosis factor–inhibitor therapy provide synergistic improvement in the functional status of patients with ankylosing spondylitis, according to an analysis from the multicenter Prospective Study of Outcomes in Ankylosing Spondylitis (PSOAS).
Among 683 PSOAS participants prospectively followed for up to 12 years, those who consistently engaged in moderate recreational exercise, defined as at least 120 minutes of exercise per week, had significantly lower, more favorable Bath Ankylosing Spondylitis Functional Index (BASFI) scores during years 1-5 than did those who exercised less, even after controlling for baseline function and other potential confounders in a multivariate analysis, Dr. Lianne S. Gensler said at the annual meeting of the Spondyloarthritis Research and Treatment Network.
Additionally, a significant interaction was observed between exercise time and anti-TNF therapy. BASFI scores improved through 5 years of follow-up in TNF inhibitor users regardless of their exercise status, but the impact on functional status was “strikingly” greater in those patients on a TNF inhibitor who engaged in at least 120 minutes of exercise per week, according to Dr. Gensler of the University of California, San Francisco.
“This suggests that it’s not simply taking a TNF inhibitor that’s going to promote long-term function. These patients should also be exercising to synergize and get the best out of their therapy,” she emphasized.
The PSOAS cohort included averaged 43 years of age at baseline, with a mean 19-year disease duration and an average of 2.1 comorbid conditions. In a multivariate longitudinal analysis, several factors emerged as significant predictors of more pronounced functional impairment over time: being age 40 or older at baseline was associated with a 25% increased risk, opiate use was associated with a 12% increase in risk, a baseline Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) score of at least 40 conferred a 19% increase in risk, as did a modified Stoke Ankylosing Spondylitis Spinal Score of 4 or greater.
Dr. Gensler drew a sharp distinction between the effects of moderate recreational exercise and occupational physical activity in ankylosing spondylitis patients. In an earlier landmark study involving 397 members of the PSOAS cohort with at least a 20-year history of ankylosing spondylitis, investigators mapped the patients’ work histories, the physical activities their work entailed, and the time they spent at each activity. Jobs that involved repeated bending, stretching, twisting, and vibration exposure were associated with worse BASFI scores and greater radiographic disease severity (Arthritis Rheum. 2008 Jun 15;59[6]:822-32).
Taking a step back to summarize what’s known today about what affects outcomes in ankylosing spondylitis patients, Dr. Gensler listed in the ‘bad’ column smoking, ongoing inflammation, baseline damage to the spine, certain occupational activities involving biomechanical stress, adiposity, and low socioeconomic status.
What’s good for patients with ankylosing spondylitis is physical therapy and back exercises – both will receive favorable marks in soon-to-be-published American College of Rheumatology guidelines on the management of ankylosing spondylitis that Dr. Gensler worked on – as well as TNF-inhibitor therapy, NSAIDs, and recreational exercise, which wasn’t addressed in the former guidelines.
Dr. Gensler reported receiving research funds from or serving as a consultant to AbbVie, Amgen, Celgene, Janssen, and UCB.
EXPERT ANALYSIS FROM THE 2015 SPARTAN ANNUAL MEETING